






I have to admit that I’m more a warm weather person, having recently returned from a three-month road trip up north to escape Perth’s winter.
Within a few hours of returning I was lamenting the sudden drop in temperature and contemplating booking a one-way fare up to Broome.
Meanwhile several of my friends were frolicking around in Italy and posting photos on social media of another glorious European summer.
Except that in some parts of southern Europe, it was anything but glorious, with extreme temperatures in several cities reaching just shy of 50°C.
The Cerberus heatwave – named by the Italian Meteorological Society after the three-headed monster that features in Dante's Inferno – caused a rush of heat-related hospital casualties.
And as I write this, a couple of weeks into Spring, Sydney is having a 35°C day, its highest September temperature on record – only days after the Bureau of Meteorology officially declared an El Niño weather event – the first in eight years.
El Niño largely affects eastern Australia, but also brings an increased risk of extreme heat across large parts of the country. Every event is different, so it is unclear exactly how the climate system will react.
It’s expected to be a major influence on our weather and climate, increasing the risk of heatwaves, droughts and bushfires – and the impacts may well become more severe with climate change.

And that is going to affect all aspects of our lives, but especially the health system.
Perhaps I should be looking at flights down to Albany instead?
Talking of important issues, don’t miss this month’s sobering interview with Myanmar former health minister Dr Zhao Wai Sao, who discusses the health crisis in his country with Eric Martin.
Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
SYNDICATION AND REPRODUCTION
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers
than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
El Nino largely affects eastern Australia, but also brings an increased risk of extreme heat across large parts of the country
12 Sports medicine spotlight on women

16 Evolving world of trans medicine
22 Getting hip about early care
30 Myanmar medicos on the frontline
LIFESTYLE
62 Sisters take control
63 3drops expertly mixed
– Dr Louis Papaelias

64 Singing career comes home
1 Editorial: Bracing for summer

– Cathy O’Leary
4 News & views
8 In brief
26 Taking on eating disorders … together
34 Close-up: Dr Andrew Leech

45 Actions not words needed
– Dr Joe Kosterich
The winner of the Castelli Estate doctors dozen from the August wine competition is Dr Mark Strahan from South Perth Hospital.

This month we have more premium wine in the offing, this time from 3drops in the Great Southern. Read what impressed our reviewer, Dr Louis Papaelias, on page 63.
For your chance to win, use the QR code on this page or go to www.mforum.com.au and hit the competitions tab.
PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au

EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au

Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au





Journalist Eric Martin 08 9203 5222 eric@mforum.com.au
Clinical Editor Dr Joe Kosterich 0417 998 697 joe@mforum.com.au

Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager

Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory Andrew Bowyer 08 9203 5222 andrew@mforum.com.au





CONTACT MEDICAL FORUM Suite 3/8 Howlett Street, North Perth WA 6006 Phone: 08 9203 5222
Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au OUR PRINTER’S ACCREDITATIONS
Australia’s world-first national collaborative to safely reduce rates of preterm and early term birth held its final session in Brisbane for more than 260 obstetricians, midwives, GPs, sonographers, neonatologists, consumers and quality improvement experts from more than 63 maternity hospitals.

The two-day Every Week Counts National Preterm Birth Prevention Collaborative learning session included presentations on a midwifery continuity model of care for women having a First Nations baby. Other topics included cervical length measurement, the importance of continuity of care, pathways for women with highrisk pregnancies, and quit smoking strategies for pregnant women.
Being born too soon is the single greatest cause of death in young children and one of the major causes of lifelong disability, including cerebral palsy, blindness, deafness and behavioural and learning problems at school age.
The Royal Australasian College of Physicians says that the Australian Government should be increasing access to bariatric surgeries to help reduce rates of diabetes and obesity.
The college says that many patients are being forced to wait years to access bariatric surgery and cannot afford to pay through the private system.
RACP President Dr Jacqueline Small said prevention measures were important, but attention should also be given to improving access to treatments for people who are living with obesity, such bariatric surgery and effective medicines.
“The Federal Government should also increase the PBS subsidies for obesity and diabetes medicines to ensure that treatment for these often-linked conditions isn’t limited by individual affordability,” she said.
The RACP submission to the Federal Inquiry into Diabetes also called for:
• Early involvement of physicians in team-based care for patients at risk of hospitalisation through innovative care pathways
• Introduce national regulations to restrict marketing of unhealthy diets to children
• Fully fund the effective implementation of the National
Each year more than 26,000 Australian babies are born preterm, while the rate of preterm birth for Aboriginal mothers is almost double that of non-Aboriginal mothers. The collaborative is jointly run by the Australian Preterm Birth Prevention Alliance, Women’s Healthcare Australasia, the Institute for Healthcare Improvement, Safer Care Victoria, and WA’s Women and Infants Research Foundation.
• Mandate the Health Star Rating System for all packaged foods
• Implement a tax on sugarsweetened drinks.
A new cold-stored platelet product that could reduce bleeding during complex heart surgery and potentially triple the existing product shelf life has been transfused to Australia’s first patients as part of a world-first trial.
Currently platelets in Australia are stored at room temperature with gentle agitation, based on evidence from the 1970s, and have a shelf-life of only seven days. The Chilled Platelet Study is the first international clinical trial to test if platelets stored at 4°C are better at reducing blood loss during complex cardiac surgery than room temperature platelets.
The US Department of Defence funded clinical trial is being led by the University of Pittsburgh and in Australia by Australian Red Cross Lifeblood and the University of WA.
The RCT will involve 1000 complex cardiac surgery patients across Australia and the US. In Australia, the study is open to patients from Fiona Stanley Hospital and Sir Charles Gairdner Hospital,
and will use platelets collected at Lifeblood’s Perth Donor Centre.
The Royal Australian College of General Practitioners has welcomed a recent 100% exam pass rate for Aboriginal and Torres Strait Islander GPs in training as a phenomenal achievement.
It comes following the recent results of the College’s Clinical Competency Exam, designed to assess clinical competence and readiness for independent practice as a specialist GP.
The latest CCE exams show Aboriginal and Torres Strait Islander GPs in training are excelling, with 100% of self-identified candidates passing the exam.
RACGP Aboriginal and Torres Strait Islander Health Council Chair Dr Karen Nicholls said that not only are Aboriginal and Torres Strait Islander GPs in training passing this exam, they were achieving very strong results.
RACGP Aboriginal and Torres Strait Islander Health Censor Dr Olivia O’Donoghue said she was focused
continued on Page 8



A recent article in The Conversation has stirred the pot by questioning the value of diagnosing and treating gestational diabetes in pregnant women. Bond University Professor of Medicine Paul Glasziou and University of Queensland Clinical Professorial Research Fellow Jenny Doust cited one in six pregnant women now diagnosed with the condition – a doubling of cases since new criteria was developed in 2010. They argued the glucose test used was unreliable, some women were tested too early, and the thresholds were too low. Their article referred to findings from a recent randomised controlled trial – the Treatment of Booking Gestational Diabetes Mellitus (TOBOGM) study published in The New England of Journal of Medicine – suggesting it showed no benefit from testing and treating women with risk factors early in pregnancy.
Medical Forum asked one of the authors of the TOBOGM paper, Perth endocrinologist Dr Emily Gianatti, to respond. She expressed concern that women and their health care providers, after reading this article may choose not to have or offer testing or treatment for gestational diabetes, despite there being clear evidence that it benefits women and their babies, and made these points:

Significant evidence exists that shows treatment of gestational diabetes benefits women and their babies particularly in reducing risk of fetal overgrowth, serious perinatal outcomes including shoulder dystocia, and hypertensive disorders of pregnancy. A diagnosis of gestational diabetes also identifies women and babies who are at greater risk, beyond pregnancy, of diabetes and overweight, allowing for targeted support and intervention.
There has been a significant increase in recent decades in the incidence of gestational diabetes in Australia, in part related to changes in diagnostic practices as acknowledged by the authors of the article, but also due to increasing risk factors for gestational diabetes in our society.
Overweight and obesity are known risk factors for gestational diabetes, with rates in Australian women increasing from 49.4% in 1995 to 59.7% in 2018. Ethnicity is also a known risk factor with the incidence of gestational diabetes being higher among Asian, Indian subcontinent, Aboriginal, Torres Strait Islander, Pacific Islander, Maori, Middle Eastern and nonwhite African women. In recent decades there has been significant change in Australia in where migrant women were born, with a majority now from Asian countries. The average maternal age at birth also continues to rise with the incidence of gestational diabetes rising also with mother’s age.
The authors highlighted results of
the recently published GEMS study. In this study pregnant women were randomly assigned at 24-32 weeks pregnancy to be evaluated for gestational diabetes by a 75g twohour oral glucose tolerance test using lower (WHO 2013 criteria) or higher (current NZ criteria) glycaemic criteria for diagnosis.
As the authors assert there was no difference between the groups in relation to incidence of large-for-gestational-age infants. Importantly, neonatal hypoglycaemia was detected and treated more frequently among the infants in the lower glycaemic criteria group. This is most likely due an increased percentage of infants born to a mother with a diagnosis of gestational diabetes who therefore are identified as requiring screening for hypoglycaemia according to hospital protocols.
Some infants born to mothers in the higher glycaemic criteria group may have had undetected hypoglycaemia that was not treated. Neonatal hypoglycaemia is associated with later adverse neurodevelopment. In addition, in a pre-specified subgroup analysis, women whose glucose levels fell between the two groups (fasting glucose 5.1- <5.5 mmol/L, 1-hour glucose >=10 mmol/L or 2-hour glucose 8.5 - <9.0 mmol/L) were compared according to whether they were treated. Those who were treated had better outcomes overall with fewer babies that were LGAs while the number needed to treat to prevent one LGA baby was four.
The authors highlighted the results of the TOBOGM study, an international, multi-site, randomised controlled trial assessing the impact of diagnosing and treating gestational diabetes early in pregnancy (<20 weeks) in women who had risk factors for diabetes. Contrary to the authors’ comments, this study showed early treatment of gestational diabetes before 20 weeks' gestation led to lower incidence of the primary outcome of composite of adverse neonatal outcomes (birth <37 weeks, birth trauma, birth weight >4500g, respiratory distress (distress warranting >=4 hours of supplemental oxygen, continuous positive airway pressure or intermittent positive pressure ventilation in the first day of life), phototherapy, stillbirth or neonatal death or shoulder dystocia).
Over one in 20 babies avoided a group of severe birth complications, respiratory distress was almost halved, the number of days needed in neonatal intensive care or special care unit were down by 40% and severe perineal injury was reduced by three quarters. More study is required to determine how these findings should be translated to clinical care.
The authors raise an important point that a diagnosis of gestational diabetes does impact women’s experience of pregnancy, and health care professionals providing care to these women need to provide empathic, woman-centred care.
Most women will not require continued on Page 8
Low back pain is the leading global cause of disability(1). A range of treatments include manual and physical therapies, opioids, non-opioid painkillers, medicinal cannabis, spinal injections, and nerve ablation. Spinal surgery is often sought when these treatments fail, but the benefits must be carefully weighed against the risks.
Elective spinal surgery rates have been increasing over the last 20 years in Australia(2), a trend also seen in the US and Europe(3,4,5,6), with the increase disproportionally greater among privately insured patients. During 2012–18, 83% of spine procedures in Australia were performed in the private sector (7)
Suggested reasons for increased spinal surgeries include the ageing population, the advent of newer technologies for performing procedures, the increased availability of imaging, ineffectiveness of other treatments, and surgeon preference(8).
A review of the evidence for spinal surgery as a treatment for low back pain found that spinal surgery has a role in alleviating radicular pain and disability resulting from neural compression, or where back pain relates to cancer, infection, or gross instability. However, spinal surgery for all other forms of back pain is unsupported by clinical data, and the broader evidence base for spinal surgery in the management of low back pain is poor and suggests it is ineffective(9). The lack of high-quality evidence for the effectiveness of many spinal procedures(10) means there are no clear clinical practice guidelines, no consensus on the indications for spinal surgery, and considerable practice variation(8)
Negative outcomes for spinal surgery patients can be catastrophic, such as paraplegia, incontinence, and severe and/or chronic pain.
Spinal surgery was the most common type of procedure involved in wrong site surgery, and 60% of neurosurgery malpractice claims involved spinal surgery, in US studies(4). MDA National’s claims data shows that claims related to spinal surgery are costly, with 78% of incurred costs for claims against neurosurgeons from 2005-2019 related to spinal surgery.
Common themes in claims and complaints which can be addressed by clinicians are:
Poor choice of patient or procedure
Referrals to surgeons and decisions to operate should be made according to current evidence-based clinical thresholds, for example the Low Back Pain Clinical Care Standard(11), Therapeutic Guidelines(12), or Choosing Wisely(13). Caution is advised in proceeding to surgery for patients with comorbidities, psychological components of chronic pain and on workers compensation(14,15,16)
Patients should be informed about the risks and alternative treatment options, preferably using a procedure-specific consent form and with thorough documentation in the medical record. Surgeons should try to ensure that patients have realistic expectations and are not rushed into providing consent(17,18,19,20)
Protocols should be followed to help with accurate intraoperative localisation, prevention of wrong site surgery, patient positioning that minimises compromise of nerves, and equipment checks(21,22,23,24)
Recovery room staff, other treating health professionals and patients should be informed about signs and symptoms to be concerned about and how to contact the surgeon urgently if issues arise. Surgeons should be alert to minimising delays in responding to potential complications(25)
References
1. To view the references visit: www.mdanational.com.au/advice-and-support/Library/Articles-and-Case-Studies/2023/09/Spinal-Surgery
continued from Page 4
on boosting Aboriginal and Torres Strait Islander GP numbers, and while progress is being made, more work needed to be done.
“Numbers of self-identified Aboriginal and Torres Strait Islander trainees have been steadily increasing. The RACGP currently has 60 GPs in training and 124 Fellows. The aim is for greater than 3% representation across training and for Fellows.”
A RACGP analysis of all three Fellowship exams – the CCE, Applied Knowledge Test and Key Feature Problem – showed that since 2018, success in these assessments for Aboriginal and Torres Strait Islander GPs in training had markedly improved. Pass rates across all exams had increased from 46% in 2017 to 75% in 2022.

continued from Page 6
pharmacotherapy and in these cases less frequent monitoring of blood glucose levels is appropriate. Ongoing food diaries are not required in most patients and it is not usual practice for babies to be separated from mother for monitoring of blood glucose levels as compared to treatment of severe hypoglycaemia not responding to first line treatments.
It is expected that over time clinical guidelines will change in response to new findings. However women and their treating health care professionals can remain confident that diagnosing and treating gestational diabetes remains important in reducing risk for women and their babies.
Silverchain has launched a GP Education Series in WA, with the first session looking at managing comorbidities in patients.
The series of free interactive and practical education sessions are aimed at GPs, practice managers and specialists and will discuss ways to provide effective integrated care. It kicks off with its first session on October 18, focusing on management of chronic and complex diseases.
Each event for the series will feature presentations from industry and Silverchain experts to help GPs, clinicrelated staff and specialists to build their expertise across a range of health topics. Presentations for each event will be followed by a panel discussion.
Silverchain Medical Director Dr Sayanta Jana said the series would also provide insights on the services available for referral and the best referrer pathways.
Leading blood cancer researcher Professor
Chan
Cheah has been named Cancer Council WA’s 2023 Cancer Researcher of the Year. A clinical haematologist at Sir Charles Gairdner Hospital, he founded Blood Cancer Research WA in 2016, and since then it has enrolled 800 people with lymphoma and other blood cancers into clinical trials.

“These sessions are designed around the multi-faceted needs of our major referrers, our external GP networks, who play a major part in the health system to support our Silverchain clients in primary care, community care and home care environments,” Dr Jana said.
The panel for the first session, “When Chronic Disease and Mental Illness Coexist”, comprises Dr Stefan Schutte Head of Psychiatry, St John of God Midland Public and Private Hospitals, Dr Michael Christmass, Consultant Addiction Medicine, Fiona Stanley Hospital and Next Step Drug and Alcohol Services and Jaclyn Geraghty, manager of Silverchain’s Primary Care and Chronic Disease program.
The event will be held at the Joondalup Resort in Connolly and includes a two-course dinner and refreshments. Register by October 6 by visiting silverchain.org.au/gp-education-series or email ReferrerEngagement@silverchain.org.au
Perth Radiological Clinic recently notched up 75 years of operation. PRC is WA’s oldest private radiological practice, established in 1948.
Rockingham General Hospital has a new hospital liaison GP, Dr Alison Soerensen
Anti-bullying champion and former head of TKI’s Health Promotion and Education research program Professor Donna Cross was inducted into the WA Science Hall of Fame.
Several Telethon Kids Institute researchers took out top gongs in the recent Premier’s Science Awards, including leading paediatric anaesthetist Professor Britta Regli-von UngernSternberg, who was named joint winner of the Mid-Career Scientist of the Year. PhD student Denby Evans, from the Wal-yan Respiratory Research Centre, was named Student Scientist of the Year in recognition of her research into the lung health of pre-term babies.

Available across Perth: Nedlands, Leeming, Joondalup and Mandurah
Appointments
For any additional information, testing advice, clinical questions: Contact the Respiratory Services Manager Paul Guy 0418 307 524 or paul.guy@sleepcrs.net.au
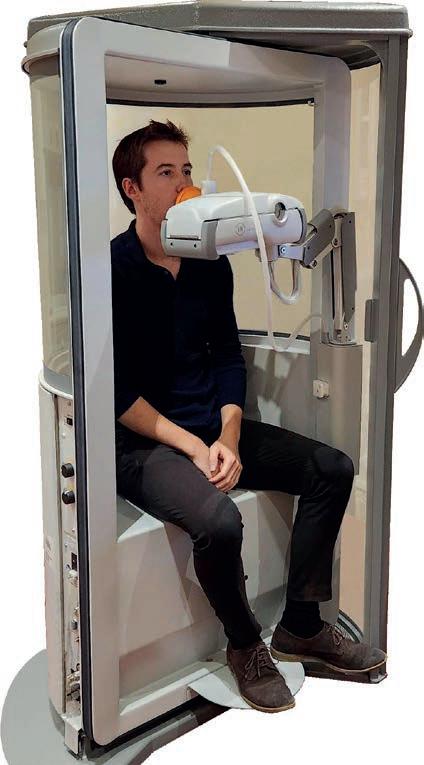
CRS utilises body plethysmography machines - the gold standard in respirator y testing available to all patients.
In one session, CLFT can help assess the functioning of your patient’s air ways, lung capacity and gas exchange, to differentiate diagnosis and determine severity and progression of respirator y disease
Conditions include but are not limited to: Asthma, COPD, Emphysema, Bronchiectasis, Fibrotic diseases.
This includes assessment of:
SPIROMETRY: used to assess airway calibre and ventilatory capacity. Assists in determining obstructive or restrictive ventilatory defects and identifying any reversibility.
DLCO (Gas Transfer): used to assess the integrity of the blood-gas interface as well as estimating the volume of lung that is ventilated for gas exchange. A precise but nonspecific measurement of the transfer to the blood gas barrier, and the complex interactions between the lung parenchyma and the pulmonary vasculature.
STATIC LUNG VOLUMES: Utilizes body plethysmography, the lung volume gold standard, to measure all gas in the lung including unventilated volume. It can confirm a restrictive defect or identify gas trapping and / or hyperinflation.
MAXIMAL RESPIRATORY PRESSURES: Assessment of respiratory muscle strength. Useful for identifying and monitoring respiratory muscle weakness such as in neuromuscular disorders.

MANNITOL CHALLENGE: Changes the osmolarity of the airways such that any inflammatory cells present will release mediators and cause bronchoconstriction. Useful and calibrated test that is specific for Asthma but not sensitive.
FeNO: (Fractional Expired Nitric Oxide): Higher in the presence of inflammation in the airways. Useful aid in asthma diagnosis and over time in titration of ICS dosage and efficacy.
SIX MINUTE WALK TEST: Assesses patient’s levels of oxygen desaturation or otherwise and walking capacity with chronic lung disease.
NASAL RESISTANCE: Objective measurement of nasal obstruction and determining reversible vascular or fixed anatomical causes of resistance.



All eyes have been on women’s elite sports this year, with the frenzy over the Matildas in the Women’s World Cup and a string of women’s worldleague events in cycling, tennis, rugby, golf and cricket.

When it comes to research in sport and exercise medicine, women have largely been left on the sidelines. Female athletes, their coaches and physicians have relied mostly on anecdotal reports and science focused on male athletes to navigate performance and injury in women’s elite sport.
Dr Carmel Goodman, sport and exercise medicine physician and chief medical officer for the Western Australian Institute of Sport (WAIS), says the research on female athletes is starting to catch up only now.
“Men’s sport has always been rated as much more important than women’s sport. It’s only been as women’s sport has become more popular that the money and interest has gone into research,” she said.
Dr Goodman has worked with elite athletes over her expansive three-decade career, including being a long-time physician for the Hockeyroos and Rowing Australia and a team doctor at the Olympic and Commonwealth Games since 2000.
Emerging research is uncovering how the menstrual cycle is a significant factor on physical performance, psychological stress, mental focus, and rates of injury among elite female athletes.

Most of the research in sport and exercise medicine has been geared towards men, but attention in women’s sport is changing the game.
Kathy Skantzos reports
“We know that athletes are performing at their worst a few days premenstrual because they’re feeling fatigued,” Dr Goodman said.
Hormonal changes at various times of the menstrual cycle, particularly during the premenstrual and menstrual phases, can alter mood, motivation, focus and sleep, and can bring on cramps, pain, inflammation, muscle soreness, stress, and fatigue.
Every elite female football player involved in a 2021 interviewbased study said changes in their menstrual cycle negatively impacted their competitive performance, noting fatigue, impaired strength, lower confidence and reduced focus, particularly during menstruation.
A 2022 systematic review with meta-analysis showed changes in motivation and competitiveness during the menstrual cycle and better outcomes in the ovulation phase compared to follicular and luteal phases. The review showed an increase in mood disturbance in the premenstrual phase (versus mid-cycle), decreased vigour during menses (versus luteal phase), increased menstrual symptoms in the follicular phase (versus ovulation), increased fatigue and decreased sleep quality in the luteal phase (versus follicular).
Female athletes reported their sport performance was particularly worse during the early follicular and late luteal phases. During the luteal phase (post-ovulation before the next cycle begins), after oestrogen levels peak and then drop as progesterone levels rise, women can typically feel more mentally and physically tired, with higher progesterone causing low energy and low mood.
A 2021 study in Medicine & Science in Sport & Exercise found that in a 20-minute cycling time trial, active women had lower performance and higher fatigue during the luteal phase.
Tracking menstrual cycles has only recently been introduced to leading sports institutes to help female athletes, their coaches and medical practitioners understand how to avoid injury and fatigue and improve performance.
tracking as part of its injury reporting system earlier this year as a recent addition to Australia-wide medical records.
“It’s only been the last four or five months that the menstrual cycle tracking has been added to dayto-day tracking. Prior to that we never tracked the female menstrual cycle,” Dr Goodman says.
WAIS uses the menstrual tracking data to modify training and reduce injury.
“Every new female athlete that comes to WAIS needs to record their menstrual cycle and every few months when they do their medical review, we see if it correlates with injury and illness, and we share that information with the coaches who are advised to reduce vigorous exercise when hormonal symptoms arise to avoid injury.
“We’re recognising more and more that mental and physical performance is certainly affected at different times of the menstrual cycle and that is something that has previously not been taken into account.”
Research published in the BMJ suggests women have higher rates of concussion compared with men, and Dr Goodman adds that women can take longer to recover.
“We don’t know if it’s related to hormonal changes because no one has done enough research to determine it,” Dr Goodman said.
A preliminary study showed that while progesterone is shown to be neuroprotective against concussion, women injured during the luteal phase of their menstrual cycle, when progesterone is highest, had worse post-concussion symptoms possibly due to the sudden drop in the hormone after injury.
As well as concussion, women athletes are more prone to anterior cruciate ligament (ACL) tears at certain times of their menstrual cycle and Dr Goodman said this was another line of inquiry.
For elite female cyclists, who now
have European grand tours on their competitive calendar, saddle sores and UTIs are common in greater number than male cyclists.
Dr Goodman says around 40% of female athletes are on the pill for contraceptive reasons, and about 60% are taking it to control their cycle and reduce the severity of premenstrual symptoms.
“We can modify training but that doesn’t help us when it’s competition time. What we can do is make sure they are not in their menstrual or premenstrual phase at the time of major competition,” she said.
Using the contraceptive pill to reduce premenstrual symptoms, such as fatigue, cramps and muscular pains, can be beneficial during competitions and elite training if symptoms impact athletic performance.
“For women who get significant menstrual cramps and pains, the pill has been used to decrease those symptoms,” Dr Goodman said.
A 2020 meta-analysis in Sports Medicine that found oral contraceptives “might result in slightly inferior exercise performance on average when compared to naturally menstruating women” but stated that “effects tended to be trivial and variable across studies”.
While Dr Goodman says hormonal fluctuations in the menstrual cycle “absolutely can” impact athletic performance, she notes the complexity and variability of the menstrual cycle between individual women, which can show up differently in their athletic performance.
“Performance, fatigue and injury seem to be heightened during premenstrual or follicular stage of their cycle, but it’s important to note that all women are impacted differently by their individual cycle,” she says.
High-performance athletes push themselves hard, but some can
continued on Page 15
“Men’s sport has always been rated as much more important than women’s sport.”
At Perth Radiological Clinic your musculosketal (MSK) investigations are reported locally by Perth’s largest team of musculoskeletal and spinal radiology experts.
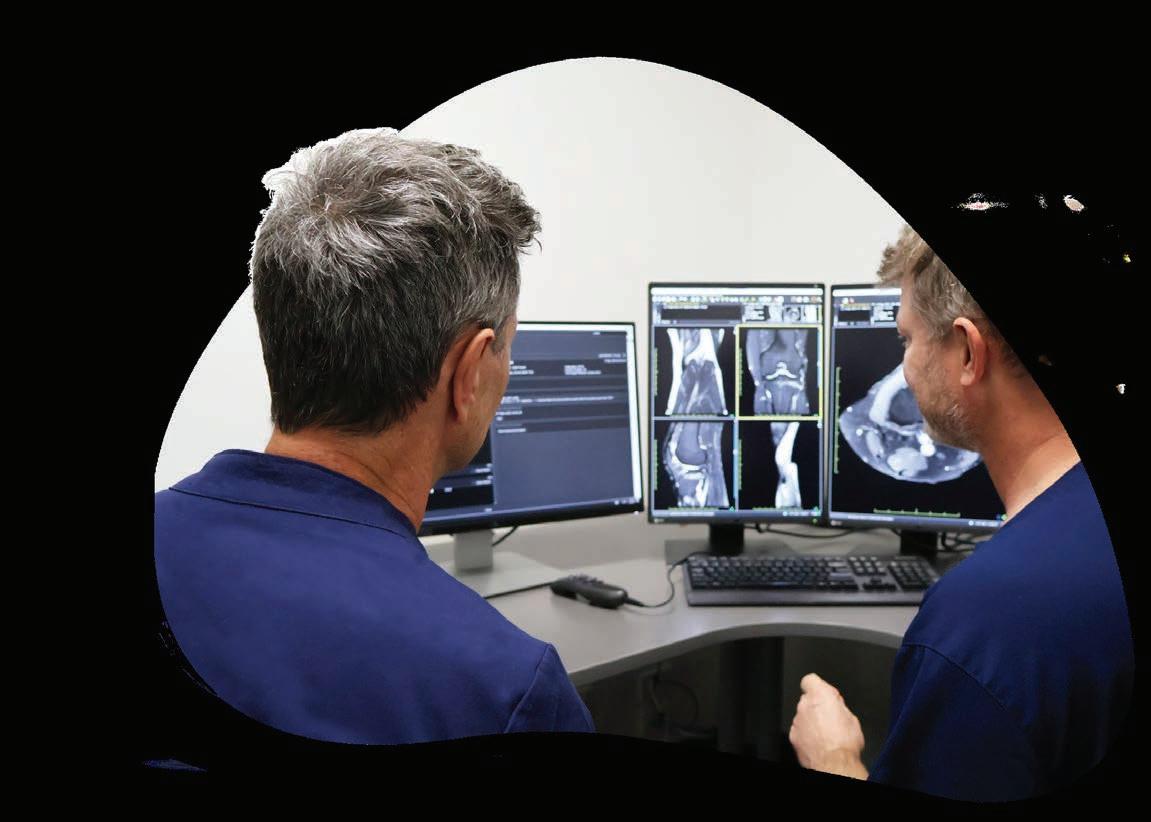
• Rapid access to high quality scans and image guided injections.
• MRI appointments available evenings and weekends.
• Fast report turnaround times delivered by Perth’s largest team of musculoskeletal and spinal radiology experts.

• Radiologists available to discuss the imaging and interventional requirements
PRC MSK sub-specialist, Dr Matt Prentice saysOur rapid turnaround reports expedite the path to appropriate treatment, can rule out serious pathology or help differentiate acute injury from chronic non traumatic conditions.
Please contact your customer relations team for more information or email assist@perthradclinic.com.au
continued from Page 13
train so intensely that it can cause them to stop menstruating altogether, a condition called RED-S (relative energy deficiency in sport). Symptoms include periods stopping or becoming irregular, reduced performance, mood changes, and recurrent illnesses and injuries including stress fractures.
Almost 80% of elite and pre-elite female athletes in a 2020 Australian research study demonstrated at least one symptom consistent with RED-S, and almost 40% experienced at least two symptoms.
A combination of physical and mental stressors, such as personal conflicts, relationships, bullying, and busyness outside of training, can add to overtraining.
“Overtraining isn’t only training at a high level but it’s everything else that’s going on in an athlete’s life at the time,” Dr Goodman said.
“This is partly because elite athletes, by nature, are driven and competitive in many areas of their life. They are trying to achieve as much success at a school or university level as they are at a sporting level. They are pushing themselves to achieve all the time.”
WAIS has three in-house psychologists regularly checking in on the mental health of athletes and coaches are advised to reduce training loads if necessary.

“I often see athletes presenting with fatigue, which is not only a decrease in performance but general life fatigue and that is a combination of a lot of factors. That’s when looking into their menstrual tracking and see if their cycle is playing a part,” Dr Goodman says.
Young female athletes also are vulnerable to eating disorders, with Dr Goodman saying that at least 90% of the eating disorders WAIS sees are in women.
“We see eating disorders presenting much more frequently and at a much younger age than we have ever had before. We’re seeing
girls as young as 11 or 12 presenting with disordered eating,” she said.
WAIS has refined its eating disorder policy which now requires coaches to speak to medical staff or a nutritionist if they believe weight is impacting an athlete’s sporting performance rather than approaching the athlete directly about their weight.
“Nobody is allowed to comment to an athlete about their weight nor advise them how to lose weight. We’re trying to educate coaches and all those involved with a female athlete that they can’t be told they need to lose weight,” she said.
“Previously, coaches persuading athletes to lose weight may have contributed to eating disorders, so we’re very focused on preventing and managing eating disorders. It is probably the biggest single issue I see at the moment in female athletes.”
Dr Goodman believes more research will have a positive impact on women athletes’ performances.
“As we do more research into what’s happening during women’s hormonal cycles and in their brains, their mental health as well as physical performance will improve,” she said.
The AIS launched the Female Performance & Health Initiative in late 2019, aiming to improve female athlete performance, health and
support systems. In 2022, the AIS conducted a landmark camp in collaboration with the National Women’s Rugby League to study the correlations between sport performance and female health, including the influence of the menstrual cycle and hormonal contraceptives on injury prevention, energy levels, recovery and sleep.
Women athletes all over the world have come forward to talk about period pain being a major cause of discomfort that affects performance. Chloe Dalton, GWS Giants AFLW player and founder of The Female Athlete Project, has reported she suffers nausea and pain every month due to her period. Sprinter Dina Asher-Smith spoke up at the 2022 European Championships about being unable to complete a race due to period pain.
“More people need to actually research it from a sports science perspective," Asher-Smith told the BBC. “It’s absolutely huge and people don’t always talk about it either. Sometimes you see girls who are so consistent and yet behind the scenes they’ve been really struggling. I feel like if it was a men’s issue, we’d have a million different ways to combat things, but with women there just needs to be more funding.”
The Australian Professional Association for Trans Health released standards guidelines earlier this year. WA dermatologist Dr Ahmed Kazmi has been working with trans patients and urges doctors to move beyond the headlines.
 Eric Martin reports
Eric Martin reports
Though transgender people have existed down through the ages, the origins of the modern transgender healthcare debate can potentially be traced back to the 18th century Irish philosopher, George Berkley, his theory of ‘subjective idealism,’ and its ideas about how we create reality through the modality of our minds.
Bishop Berkley followed in the footsteps of some of the great philosophical thinkers, yet his theories caused conflict with proponents of Descartes’ ‘natural philosophy’, where matter and form construct the true reality, and the subsequent debate has continued to split the epistemological approach to science, and the trans debate, nearly 300 years later.
Despite the timeless nature of trans identity, the medical need is here and now, and controversial studies such as the one released by Sydney’s Westmead Children’s Hospital in 2021, have involved Australia in the international debate, highlighting the conflict that exists nationally.
Given the necessity for more discussion on the topic, Medical Forum spoke with dermatologist, Dr Ahmed Kazmi, who recently gave the first presentation on transgender medicine to this year’s
Australian Dermatology Annual Conference, delivering content that has been subsequently requested for their curriculum. He also spoke to local doctors at the Annual Perth Urology Clinic Masterclass.
“I tend to see people already on gender affirming hormonal therapy who develop subsequent skin problems. But I teach a lot on the subject just because I find it a lovely intersection of a lot of disciplines of medicine,” Dr Kazmi said.
“And I feel like we're trying to establish health advocacy for a group that's traditionally had a raw deal – it makes me feel proud to be able to contribute towards trying to improve their health outcomes.”
He said the health authorities should get credit for establishing facilities such as the paediatric service at the Perth Children's Hospital, and the adult service at Royal Perth Hospital.
“For a long time there has been nothing, but now, almost every major city in Australia has some state-backed service of some description for both paediatrics and adults,” he said.
“There's still a lot of finding feet and trying to see what the best
arrangement of services is, but at least there is a home for where this health care is happening.
“As there aren’t many surgical options in Perth yet, many people still end up going abroad. But it’s slowly growing, especially as medical interest increases, and more doctors become aware that there are now options. Lots of GPs that are quite keen to join and prescribe gender-affirming hormones.
“They're also trying to get allied health professional input too, such as speech and language therapists that specialise in transgender voice and gender affirming voice therapies. Things are really changing, but it's still like a boat that's being navigated through uncharted waters.”
Dr Kazmi said that the level of transgender care provided was broadly similar in most countries that he had worked in, though there was always a split in terms of approach due to the impact of people’s different worldviews.
“There are certain areas of medicine where it's black and white and all of your personal upbringing and political and religious views don't play a role, no one gets ethical about rhinitis or about
atopic dermatitis. And then in some areas, bits start to bleed in, such as when it’s about service allocation, or Aboriginal health, and you can see people's personal opinions have an influence.
“But areas of medicine like transgender are extremely polarising. The conflict that's created and the conversation around these issues have been the same anywhere because there are the same varying mixes of political and religious views.
“People speak about it like it's some kind of fad or fashion, when transgender people have existed since the dawn of humanity. As long as there have been cisgender people and heterosexual people, there have been queer people and trans people.
“I think some doctors are a bit black and white with transgender medicine and they don't seem to understand the sort of psychosexual, psychosocial nuance and the complexity of it all.
“If there's one thing I could say to communicate, it's that the aspect of transgender medicine that I find most overlooked by clinicians and the public is the relationship between transgender identity and being neurodivergent or neurodiverse.”
Dr Kazmi said that while official numbers might show that around 35% of children on the spectrum were potentially transitioning, in his anecdotal experience, that number was closer to 100%.
“I would say nearly 100% of my transgender patients have either significant psychological psychiatric morbidity and/or neurodiversity. Almost all of them have ADHD or autistic spectrum disorder or learning difficulties or Tourette's, something in that spectrum, or epilepsy or dyslexia, or serious anxiety, depression, or OCD –and often the two are different manifestations of the same thing,” he explained.
“We're only just beginning to understand the overlap with neurodiversity. But that helps explain why people find it difficult to engage with this group and why they often get mislabelled as ‘weird’ or ‘confused’ – those are the type of pejorative words I hear a lot about trans people.
“The other thing that I find interesting is that people always assume that transgender medicine is just about sex changes. Yet if you look at trans men, almost none of them will undergo phalloplasty or some form of gender reassignment surgery. They may well have a mastectomy, or top surgery, but they didn’t just suddenly stitch
up their vagina and then ask for a replacement.
“I don't know the statistics, but although most trans women will want to have full surgery, many end up not, especially in Australia because it's so difficult to access.”
Dr Kazmi explained that there was a common misconception that transgender meant someone was just ‘trapped’ in the wrong gender, and that they wanted to exactly mirror what societal norms have set for a cis man or a cis woman.
“If this person identifies as a trans woman, we expect they're going to want breasts, no body hair and to wear a dress. And then, when we find out that actually loads of people are somewhere in the middle, or they want to use she/ her pronouns, but they don't mind having a beard, I don't know why, but that sets people off,” he said.
“They're like, ‘Oh, hang on a minute, that's not the rules of the game. You're allowed to transition, but only if you exactly match what we think a female should look like’.”
In terms of defining gender as referring to either a biological, physiological trait or as a selfrealised or socially constructed
continued on Page 18
Dr Shane LaBianca, from Perth Urological Clinic, said that in WA, transgender patients only had access to aftercare because there was no surgical care as such here.

“We don't do transgender surgery in terms of gender affirmation, except for orchidectomy: testicular removal for trans females is the only operation we perform,” Dr LaBianca said. “I have probably no more than a dozen patients who've had full gender affirming surgery, and maybe another dozen patients in a year who have come to see me to have an orchidectomy, for example.
“Similarly, there's only a handful of patients in WA who've had female-to-male surgery and full reconstruction, they have generally had that done in the US and tend to follow-up with their surgeons there as well.
“But in aftercare, it's often more complicated.”
Dr LaBianca pointed out that this was often influenced by the enormous variation of what transgender people wanted, a factor that was not limited to the cisgender ideal of what society expected a man or a woman to be.
“People have surgery done in lots of different places, and what they come back with varies considerably depending on their own desires, on how they want to have surgery, what they want to have done, who has performed the surgery, and where it's been performed,” he said.
continued on Page 21
continued from Page 17
concept, Dr Kazmi believed that it depended on the individual.
“People get sex and gender mixed up. For example, you'll see some discuss gender in terms of genitals and procreation – as we see on television people going, ‘You’ve got a penis, therefore you're a man, what's complicated about that?’. Yet there are people born intersex, with ovaries and a penis,” he said. “Generally, in medical terms, we tend to discuss sex as being a phenotype or a genotype, and it's attributed to someone. It's imparted to them at birth based on what they look like, what their genitals are, and therefore what we assume is their karyotype is based solely on their genes. Whereas gender, we're understanding, is much more socially constructed.”
He noted that even if society comes to some kind of middle ground, where we recognise that
the growing mind may be subject to change and that many of these behaviours are on the ‘normal’ spectrum, it was vital to ensure that boundary markers were established for beginning treatment.
“People will recount, ‘Oh, I used to dress up in girls’ clothes when I was six. Doesn't mean I'm trans.’ Sure you didn't, but I don't think you referred to yourself using female pronouns; I don't think you hated your name; I don't think you tried removing your own breasts when you went through puberty, and maintained that for six months, one year, three years, or five years,” Dr Kazmi said.
“There's a definite difference between those people and somebody saying, ‘Mommy, I think I'm a girl’ or ‘I think I'm a boy’ when they're three. Those aren't the people rushing to try and be put on hormones, and that is an important distinction to make for the public and for doctors.
Lessons abound
“We must apply the same common
GenesisCare at Hollywood offers access to radiation oncology consultations, treatment, and access to allied health support services. We offer modern evidence-based techniques and technology combined with compassionate care – aiming to deliver the best possible patient experience and outcomes.
We offer patients:

• Personalised treatment plans, striving for minimal wait times
• Tattoo-free technology
• Access to a wide range of allied health services (including exercise physiology), accommodation, and transportation packages
• For patients who are eligible for Medicare, approximately 80 to 90% of radiation therapy treatment costs are often covered by Medicare rebates

• Private health insurance is not required for radiation therapy
• A multidisciplinary team of supportive clinical professionals
*For radiation treatment patients. Based on patient survey results Oct 2021–2022.
genesiscare.com
sense that we would in other areas. For example, there's lots of standards that apply for a teenage girl wanting to go on the contraceptive pill without her parents’ knowledge. Even if she's under the age of legal consent, we'll say, ‘OK, well, she's more likely to come to harm from pregnancy and she's more likely to come to harm from an STI, therefore…’
“So, if we can apply that for the termination of a pregnancy, contraception or accepting a surgical procedure, why is that not relevant here?
“People always seem worried that children or adolescents may undergo the process and then have remorse. But all I've seen are adults who were unfairly put through a puberty that they spend the rest of their lives trying to reverse.”
Education was the most important thing that doctors can access to improve their patients’ outcomes, he said.
“No one is ignorant, but this is a growing, evolving area of medicine. There are huge risks associated with hormone therapy, such as the increased risk of malignancy, increased risk of DVT, and increased cardiovascular risk. We don't have a good enough data set to know how much that risk translates to actual harm – that will only become more evident over time.”

Sex steroids, such as estrogen or testosterone, are commonly prescribed as a part of hormone replacement therapy for transgender patients and these enzymes are known to metabolise several commonly prescribed drugs, including anti-HIV agents like protease inhibitors and other antiretrovirals, the antidepressant bupropion, the opioid analgesic methadone, and even drugs as ordinary as acetaminophen.
Research in cisgender adults already shows that genetic variability in these enzymes can impact an individual’s response to these drugs and continued ignorance may lead to unintended side effects in transgender individuals when prescribing treatments.
“But again, we've known these risks for HRT in women. We know these risks for the contraceptive pill. Yet we just say to the patient, ‘These are the pros, these are the cons. It will protect you against this but increase the risk of that. Do you want to proceed?’ And you go for it. I think we need to really toe the exact same line with genderaffirming hormonal therapy.”
Access to gender-affirming interventions in Australia typically follows one of two pathways –either a formal assessment and approval by a mental health professional, or by informed consent, where a decision to commence gender-affirming hormones was shared between a primary care general practitioner and a trans individual – without mandating a formal mental health review.
“No one's saying that you need to be an expert in this area, but you should know how to take the history for that patient,” Dr Kazmi said.
“You should be able to screen them. You should know where to refer them, if that is something that they want to do.”
In March this year, the Australian Informed Consent Standards of Care for Gender Affirming Hormone Therapy by the Australian Professional Association for Trans Health (AusPATH) was released. It is intended to assist and enable clinicians across Australia to meet the medical gender affirmation needs of their non-binary patients. The standards state that informed consent models of hormone prescribing “resist the notion that a doctor can determine the validity of a person’s gender, and instead centre the trans person in the decision-making process, whilst ensuring that the patient understands and can consent to the potential impacts that gender affirming hormone therapy may have on their body and life.” Importantly, they also stipulated that when trans people attend clinical services seeking medical care, it is important to avoid pathologising the trans experience: “Being trans is not a mental illness, it is an aspect of human variation, and hormones and surgery are not necessarily desired by all trans people.”
Talk to us about expanding your services into Albany and the Great Southern, a region with a growing population of over 60,000.
Call our Practice Manager Latrice Porter on 0439 520 183 or email latrice@gsspecialistcentre.com www.gsspecialistcentre.com
Great Southern Specialist Centre (GSSC) supports the delivery of coordinated access to specialist medical services by offering facilities and professional support for specialists.

We are currently looking to attract services from the following specialties to address areas of need:
• Paediatrics
• Pain Specialist
• Gynaecology
• Dermatology
• Neurology
• Psychiatry
GSSC offers a variety of service level options to suit your needs. Our centrally located modern facilities provide spacious consulting rooms along with a dedicated team of administrative and clinical staff who will work with your team to ensure your clinic runs efficiently.
Scan the QR code to find out more about GSSC

Direct Admission for cardiac and respiratory patients (Call the FREE PAS HOTLINE on 1800 668 681) which allows your patients to have immediate individualized care as they may if they present in a public ED.
Mount Hospital prides itself on being one of the leading providers of private cardiac care in the state. Shortly after its opening, Mount Hospital performed the first private heart bypass surgery in 1986. Since then, Mount Hospital’s cardiac service has grown. We provide integrated cardiology care incorporating diagnostic, therapeutic and procedural services in our state-of-the-art catheter lab.
Mount has opened the first private hybrid operating theatre in WA. We have performed over 700 open heart surgeries in total and are the lead TAVI program in WA.
Mount Hospital has the largest private ICU/CCU in WA with 24/7 Specialist & Registrar Cover.
Mount Hospital’s extensive multidisciplinary team offers a comprehensive rehabilitation programs for inpatients.
continued from Page 17
“There are many transgender people who don't want to go to the next step involving surgical procedures.
“So, a lot of the time, it's a case of re-establishing the doctorpatient relationship with someone who's newly presented, in terms of determining their medical history and what their ongoing issues are. There's no single picture in terms of what we see, there's a lot of variation.
“But in terms of urology, a lot of the things we see are similar whether you're male or female, but they're just slightly more complicated because of what's happened in the past.
“Essentially, the principles are all the same. There's not a lot of difference whether you're looking at a reconstructed female or a cisgender female, and it’s largely the identical structure in terms of how you approach the problems.”
Dr LaBianca pointed out that one of the issues with developing greater medical expertise in WA was the small number of people who were interested in gender readjustment surgery.
“Many surgeons will not deal with members of the transgender community, they just say, ‘I'm not interested in that, I don't see those patients here.’ Similarly, they might not work with certain cancers, and that's reasonable,” he said.
“Because of the low case numbers here in WA, it's difficult to establish good systems and pathways. Until we see the case numbers, we’re not going to have many specialists interested, therefore we're not going to have the expertise, and it will remain with generalists like me to be involved.”
Dr LaBianca noted that much like other conditions, where there could be only four cases each year, rather than attracting a specialist, it was more likely to foster a network of medical professionals who had some experience connected to its management and treatment.
“Having a trans health network of
interested individuals like myself, GPs, endocrinologists, etc, and having some way of coordinating care through that network, rather than necessarily going to one specific person, is probably the best way to manage transgender healthcare here in WA,” he said.
“Patients will essentially go to see someone who's a liaison in that network, who can point them in the right direction, and if they've got the right people who are receptive, that's all that really matters.
“A lot of it is just awareness and making sure that GPs understand who the right contact people are and where to go, and we need to get better at getting that information out there, because a lot of the time, patients hit a roadblock when their GP doesn't know anything about transgender healthcare.
“Yet it's the same for any area of medicine – you may not know the answer, but you need to know where to find it, and that's probably more important than knowing all the information.”
Like Dr Ahmed Kazmi, Dr LaBianca also noted he saw a high number of neurodivergent individuals presenting for treatment.
“Disorders such as autism are common among the trans population. There's also a lot of psychological ill health, depression, and other psychological illnesses, which can be challenging to deal with if they present comorbidly,” he said.
“It’s essential to have staff members and teams that are aware of the distinctions that different individuals present with, and how to deal with those in a clinical environment.
“Yet I think a lot of people just don't want to take the time to appreciate those things, which can make it quite difficult for patients when they need care – just the same as everyone else.”
Dr LaBianca explained that there were two aspects to providing the necessary follow-up, which required little that was outside a qualified medical practitioner’s clinical expertise, but noted the need for consideration of the
patient’s potential physiological changes when prescribing.
“Post-surgical care is often quite significant because the patient may have had their surgery done in Southeast Asia and has been discharged within a short period of time, and therefore perhaps don't feel they've had the support they needed post-operatively,” he said.
“This could be for aspects that such as wound healing, infection, problems with stenosis. And then you've got the longer-term complications we sometimes see that tend to approximate CIS gender pathologies.
“So male trans females tend to have issues with bladder infections and urethral complications and may have problems with sexual dysfunction, just as female members of the CIS gender population may as they age.
“The reverse are the trans males who are on anti-oestrogens and female hormones. As they get older, it is possible that with the adjustments in their hormone levels – and depending on how much surgery they've had – changes can also potentially occur within their natural organs.
“As such, you need to deal with patients according to their chosen gender, but also according to their underlying anatomy, depending on what that is. Just having an open approach and thinking about the problem logically is usually all you need – it's not rocket science.
“And then you just need to take it back to basic principles and most of the time, it's solvable.”
Dr LaBianca said that if GPs or specialists were looking to connect with the unofficial trans health network in Perth, the best way to start was by reaching out to a fellow GP, social worker or psychologist already established in the field.
“And they're well-advertised. There are a couple of GP practices in the city linked to sexual health services, and others like Miranda and Alexander Heights that have developed a strong affiliation with transgender care,” he said.
Every year, more than 19,000 Australians – many of them elderly –fracture their hip. Now revised guidelines are aimed at ensuring they get more timely treatment.
 By Cathy O’Leary
By Cathy O’Leary
WA geriatrician Dr Hannah Seymour knows only too well that time can be the enemy when treating people who break their hip, particularly when facing geographical barriers.
Based at Fiona Stanley Hospital, her experience of working closely with older patients who have had a hip fracture means Dr Seymour understands that prompt surgery reduces pain, speeds recovery and reduces time spent in hospital.
Yet as hip fracture surgery can only be performed at larger hospitals with suitable facilities, some people in regional and remote areas have to be transferred long distances. In 2022, 14% of hip fracture patients in Australia were transferred from another hospital for their surgery.
However, updated guides for the care of hip fractures are now calling for hospitals to move more quickly to get patients into theatre – and up walking after their surgery.
The Australian Commission on Safety and Quality in Health Care (ACSQHC) launched a revised national clinical care standard for hip fracture in September at the binational Hip Fest 2023 conference, hosted by the Australian and New Zealand Hip Fracture Registry.
The standard was first launched in September 2016 to guide consumers, clinicians and health services on delivering appropriate care to people with a hip fracture. The revised standard reduces the recommended maximum time to surgery, along with other improvements for better care.
The commission said many people with a hip fracture were waiting longer than was optimal for surgery, despite some hospitals making big improvements in the past few years.
Australia’s ageing population made improvements to hip fracture care even more important, as most fractures occur in people aged over 65 who are more vulnerable to complications.
Hip fracture significantly increases an older person’s risk of death, with one in four people dying within 12 months. Of those who survive,
many lose their ability to live independently or return to their former lifestyle.
The updated standard for hospitals has reduced the maximum time to surgery from 48 hours to 36 hours, in line with international guidelines. For the first time, this explicitly includes patients who need to be transferred to a hospital that can perform the surgery.
The revised standard calls on healthcare services to build effective systems and networks with other facilities to ensure coordinated transfer and help all patients receive timely surgery. For Dr Seymour, this change in the standard will be a key driver to improve time to surgery for all patients.
“Nationally, we haven’t reduced our average time to surgery and are failing patients. It is disappointing and needs to change because frail, older people are lying in hospitals in pain for longer than they need to be.
“We know that it is possible to reduce the time to surgery if you have the right systems in place,” she said.
“We’ve shown in WA that it often takes just as long for a patient being transferred for surgery from a hospital 45 minutes away by car, as it does for someone flown in from hundreds of kilometres away. It doesn’t matter where you transfer from, all patients are waiting, even if they are just down the road.”
Dr Seymour has long advocated for older people needing a transfer to a larger hospital for hip surgery. WA Health has streamlined interhospital transfer, so there are now clear arrangements for hospitals in smaller WA towns to know where they need to transfer the patient.
The ACSQHC’s acting chief medical officer, emergency physician Associate Professor Carolyn Hullick , said there was an urgent need for health services to offer better care for
people with a hip fracture, using the framework in the updated standard.
“Anyone who has seen someone live through a hip fracture knows it’s much more than a broken bone,” she said. “People with a hip fracture tend to be older, frail and more vulnerable, so it is critical the fracture is repaired quickly to reduce pain and get them on the road to recovery and back to independence.
“The data is sobering, as an Australian with a hip fracture is almost four times more likely to die within a year than someone of the same age who isn’t injured. This has an immense personal toll on individuals and families, in addition to the burden on our health system of around $600 million each year.”
Much has improved since the Hip Fracture Clinical Care Standard was introduced in 2016, according to ANZHFR annual reports, with 91% of hospitals performing hip fracture surgery in Australia participating to help improve their hip fracture care.
An evaluation of the standard in 2020 found that 98% of respondents reported that the standard improved care when implemented by their organisation; and 96% of respondents said the standard was relevant to their practice.
But while some hospitals had substantially reduced their time to surgery, there was still marked variation.
In 2022, the average time to surgery ranged from 16 to 92 hours, with the longest waiting times for people being transferred for surgery. About 78% of patients had surgery within 48 hours.
Geriatrician Professor Jacqueline Close, Co-Chair of the ANZHFR and the expert advisory group for the standard, believes the updated standard will be a lever for change.


“The Hip Fracture Clinical Care Standard sets expectations for how every patient should be cared for, while allowing for treatment to be tailored to the individual,” she said.
“The adage ‘don’t let the sun set twice before hip
continued on Page 25

continued from Page 23
fracture repair’ has merit. No one wants to see their mum or dad fasting and in pain waiting for surgery; and shorter time to surgery is associated with fewer complications, better recovery and survival.
“It is also more cost efficient to manage these patients well. Every day surgery is delayed, two days are added to the length of stay. The sooner you operate, the quicker patients can get walking and go home.”
Professor Close said the registry data showed Australia could do better in several key areas of hip fracture care. “The evidence tells us the sooner you are supported to get out of bed, the better your functional recovery. Last year, fewer than half of patients walked on the first day after hip fracture surgery.
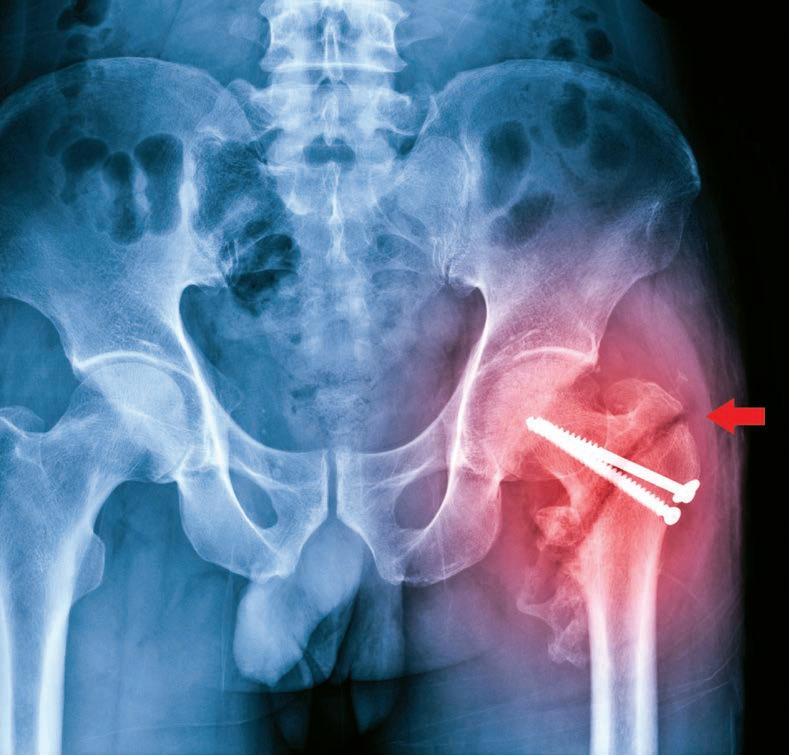
“Also, only one third (32%) of patients leave hospital on bone protection medication for osteoporosis to prevent another fracture. We absolutely can and should do better,” she said.
For 85-year-old Esperance grandmother Jill Bower, it was a relief to know she was in good hands when she arrived by ambulance at Esperance Hospital after fracturing her hip. The ED team swung into action to transfer Jill from the coastal town to Fiona Stanley nearly 700km away, with the Royal Flying Doctor Service.
“At Esperance they gave me the nerve block in my groin for pain before they moved me, which was great,” she said. “Early the next morning they put me on the RFDS flight, and I arrived in Perth by midday. I went straight to Fiona Stanley Hospital because they’d been warned – so I got a bed straight away, I didn’t have to wait.”
The whole process meant that Jill had surgery less than 48 hours after presenting to Esperance Hospital. The next day, she began her recovery under the care of Dr Seymour.
“They got me up the day after surgery on a tall frame and I felt good. Later they changed me onto
a four-wheel walker and had me walking up the hallways once a day, using the side rails to keep me moving.”
Jill completed her recovery in two smaller hospitals where she was able to build up her strength before heading home to Esperance on a regional flight.
Dr Seymour said that for a patient like Jill, Esperance was too small a place for surgery at the local hospital, but staff could deliver a nerve block and knew which hospital to call.
“The patient is put on our surgery list when they call, so are in the queue based on the time of fracture,” she said.
“Established communication channels are now in place, and much of the time we can operate in that 36-hour window because we have a system with transfer protocols and straight-to-ward arrangements.
“We have a partnership with the RFDS who know that Fiona Stanley Hospital wants to operate promptly
and that the patient is already on their list, even though they aren’t physically in the hospital.”
The WA Country Health Service team also worked hard with their emergency departments to ensure staff were well-trained to deliver a nerve block prior to moving patients, ensuring effective pain relief.
Dr Seymour said it was encouraging that 90% of hip fracture patients nationally now received nerve blocks before surgery, but sometimes only in the operating theatre. She supports the increased emphasis in the revised standard on patients receiving nerve blocks before transfer to decrease pain during transportation.
A one-stop eating disorders clinic will be opening in Perth in December, due to the commitment of a dedicated band of local clinicians.
 By Suzanne Harrison
By Suzanne Harrison
Based on the core belief that food is medicine, Perth is now home to the Esus Centre (esus is Latin for ‘eating’) a multi-disciplinary centre dedicated to treating, managing, and over time, providing integrated research into eating disorders (EDs).
Opening in early December in Subiaco, the motivation to develop Esus was to provide a better model of care for an increasingly prevalent health issue, which drew together Dr Urvashnee (Vash) Singh, a psychiatrist specialising in EDs, Dr Susan Cann, a general practitioner with an interest in EDs, and Kerry Mairs, a clinical psychologist also specialising in EDs. This small yet determined Perthbased group started out with a shared goal to provide a place where treatment was across the board – not siloed over various locations – where there was a welcoming, central focus for patients and their families, and step-up, step-down treatment. It is mostly directed at early intervention.
“The reason why we have come together really is driven by working in the field and understanding what the limitations are,” says Dr Singh. “What we are about is early intervention, picking up on emerging EDs and dealing with that quickly, which will involve intensive treatment programs, and others that are less intensive day programs, plus a consultation arm.”
It was the clinicians’ unique decision to elongate their already long work hours to build Esus, travel to observe and learn about the advances in ED care in other countries, wear many hats as not only medical professionals but business founders, and utilise their own funds to create Esus.
Finding an appropriate building, negotiating with the landlord, dealing with fit-out, finding staff – this has all come down to the hard work of the three, alongside project manager Jennifer Paterson, with the result being primarily a ‘day hospital’ (its official definition) offering regular and ongoing programs, GPs who deal with EDs (including Dr Cann), psychiatry, psychology, and allied health services, such as dietetic, occupational therapy, physical therapy, and social workers.
Esus’ day programs cater for ages 16-plus, but any age can access
outpatient specialist services required for an ED.
Esus is also a place to gather information about EDs – and program, patients and outcomes will be evaluated for future information and research, providing greater understanding for generations to come. In other words, Esus offers a one-stop-shop treatment and work-in-progress research centre.
Seated in one of Dr Singh’s treatment rooms in Nedlands prior to opening, Ms Mairs, Dr Cann, Dr Singh, and Ms Paterson form a powerhouse of experience and an impressive intent to do better. The only one involved who isn’t a clinician is Ms Paterson. She does, however, have recent lived experience of helping her daughter navigate through an ED and, thankfully, come out the other side.
It’s obvious upon meeting, the four have forged a bond during this exhaustive process. There is a relaxed rapport as they agree on their vision and model of care, and what they learnt when travelling together to London for an ED conference to research how EDs are now being tackled in other parts of the world.
Their collaboration forms the ideal multi-pronged approach to what is clearly a perfect storm of a disorder, triggered by various factors and/or other personal interactions which is best treated with input from different areas of expertise.
The new centre could not be arriving at a better time. According to the Butterfly Foundation, a national charity which also coordinates the National Eating Disorders Collaboration (NEDC) for the Commonwealth Government, more than one million Australians were affected by EDs in 2022. Women and girls are more likely than men and boys to suffer from an ED or disordered eating, though over a third of people with EDs are male, but the foundation believes this could be much higher, as their experiences may be overlooked or misdiagnosed.
The foundation says types of EDs include anorexia nervosa, bulimia nervosa, binge eating, and avoidant/restrictive food intake disorder, among several others. Globally, 55 million people
experience an ED every year, similar in numbers to substance abuse and higher than autism spectrum or bipolar disorder. In 2022, the total social and economic cost of EDs in Australia was estimated at $80.1 billion.
The cause of the onset of an ED is not just one thing. As the NEDC explains, “the elements that contribute to the development of an eating disorder are complex, and involve a range of biological, psychological and sociocultural factors”.
An individual’s susceptibility is best understood as an interaction between these factors, and the presence of risk factors will vary from person to person.
“Compelling evidence from family and twin studies indicates that a strong genetic component influences the development of eating disorders, in particular anorexia nervosa,” the NEDC said. “There are biological and genetic, psychological and behavioural, and socio-cultural factors which may increase the vulnerability to developing an eating disorder.” Therefore, it is how EDs are approached, understood, researched, and treated that will make much-needed changes, particularly when there is still so much misunderstanding in the greater community. Having a centre such as Esus will make major inroads into doing just that.
For successful treatment of an ED, it is vital that comorbidities also be considered. EDs are “frequently associated with other psychological and physical disorders, such as depression, anxiety disorders, substance abuse and personality disorders”, the Butterfly Foundation adds.
“What I’ve found about EDs is that they are where these two things meet (the mental and the physical), and we can’t continue to ignore that,” Ms Mairs says. “Esus has the ability to do this, all in one centre.
“The home-style kitchen at Esus, for example, really sets us apart. All our day program (patients) will have supportive eating … whatever is on site at Esus, the patient needs to be made to feel at home.”
Esus brings related practitioners
continued on Page 29

continued from Page 27
into one system for treating ED patients as well as educating and informing their families, removing the need for them to chase information from various areas.
“There’s a sense of everything and everyone adding value (for patients) and collaborating for the most beneficial outcome,” Dr Singh says. And WA needs more services, says Dr Cann.

“Our model is really recovery focused and aimed at early intervention with a holistic approach. Our understanding of EDs shows us it is possible to reverse the disorder and return a patient to their full potential,” she says.
Because of the need for a new model of care, the clinicians agree there has been a hugely positive reaction to Esus’s opening and work is being done to collaboratively work with the public sector.
The centre also comes a few months after the federal government announced its latest 10-year strategy on EDs, developed by the NEDC and described as a “call to action and a roadmap for people who care about Australia’s reaction to and are responsible for improving Australia’s reaction to eating disorders”.
It is designed to guide sector and policy development for the next decade and is based on information gathered not only from clinicians, researchers, public health experts and community providers, but also those with lived experience.
This last cohort involved is a breakthrough, as for many of those living with an ED (or the families of those with an ED) there is often suffering in silence. Misunderstanding, old beliefs and lack of information to the broader community has resulted in an element of shame surrounding EDs. The Butterfly Foundation says that “stigmatising views” still surround EDs, with one in four Australians believing EDs are a choice and view them as a “sign of weakness”.
Ms Paterson knows this only too well, making her involvement
in Esus not only invaluable, but reflective of the government’s new 10year approach. She has also moved beyond the silence and spoke candidly to Medical Forum about her daughter, Ruby, and her struggles with anorexia nervosa.
“When we got the diagnosis, we thought, what are we going to do?” she says. “We looked at all the options – do we sell the house and go to NSW, the US? But we realised, this is our home, and we are going to use what we’ve got here.”
But without a single entity such as Esus, the family was run off their feet visiting separate clinics, a situation that could be avoided with an integrated service. (She is quick to point out she’s a proponent of the supportive nature of the Eating Disorders Families Australia – EDFA – and the work that they do, and later became involved in fundraising and information-sharing with the parent-founded group).

Terrified for her daughter, Ms Paterson gave up her then new job and looked after Ruby full-time. She regularly slept in her daughter’s bedroom to make sure she wasn’t sneaking out to go for a run, as like many anorexia nervosa sufferers, exercise can become obsessive.
Mealtimes were carefully managed and prepared. The entire family had to change their mindset to focus on ensuring Ruby’s recovery.
Ruby did visit hospital but didn’t recover; she was angry she was being forced to eat. Pointed in the direction of a different GP,
Ms Paterson says that changed everything. This GP empowered Ruby.
“She was someone who would hold our hand, but she also said, ‘you’ve got this’.”
“Although services were limited, we knew the only way forward was to give it all we had. It was an unimaginable journey from community-based care to family-based therapy then repeated hospitalisations, a day program, weight restoration and finally – recovery,” Ms Paterson told the EDFA in a personal carers’ story.
It took two years, and now Ruby has finished school, is studying in the East and doing well.
“We got in quickly and we got out quickly. Everything revolved around Ruby. EDs are so sneaky. We had to set a lot of boundaries, and if the clinicians were not on the same page, ED sufferers will work out ways to falsify their weight, for example. Our strategy was to get rid of that ED voice and not back out.”
Yet Ms Paterson says they were lucky she could focus so much attention on Ruby. She also had a supportive family and could access private care when needed. For many other ED sufferers, clearly not enough is being done, and “we need to think differently”.
COVID was not kind to people with the potential to suffer from an ED, either. The Butterfly Foundation reports a 63% increase in calls to its helpline compared with the year prior to the onset of the pandemic. Of course, disrupted social support networks and access to treatment and support were an additional stressor.
“We have been inundated by patients since COVID,” says Dr Singh. “Systems are stressed. Schools are stressed. The launch of Esus is as a huge positive because there is a sense that we are being left behind (in WA particularly). Esus allows everyone to add value – it’s collaborative and therefore benefits everyone.”
During his recent visit to Australia, Dr Zhao Wai Sao, Myanmar’s former Health Minister in Aung San Su Kyi’s government before the military coup in February 2021, spoke exclusively to Medical Forum about the health crisis in his country.

The world watched on as doctors and nurses took the lead in the peaceful uprising and protests that occurred throughout Myanmar as a response to the 2021 coup, before the violent crackdown by the military forced ordinary Myanma to take up arms.

Caught between the two regimes, the British-trained orthopaedic surgeon Dr Sao was smuggled out of Myanmar by his relatives in Australia and he has spent the past two years raising awareness around the globe of the plight of his countrymen.
“The condition of our central health care was not good. We began reforming the system from 2011 after the partial democratisation, which started in 2008. But before that, the Myanmar healthcare situation equated to $1 per person per year and we had the second lowest healthcare ranking in the world,” Dr Sao said.
“Since 2008, we started to collaborate with the Australian College of Emergency Medicine and the Royal College of Surgeons. It was fantastic, I had a scholarship program in 2010 and it helped us to begin developing primary trauma care and emergency medicine in Myanmar.
“And then in 2016, Aung San Su Kyi and her NLD party won, bringing up expenditure and enacting reform in cooperation with all the healthcare workers, the doctors and nurses, and all the Myanmar people.
“During the first and second COVID wave in Myanmar, we had little mortality, and I believe that in Asia – and even the world – we were
one of the few countries who controlled COVID exceptionally.
“It was because the democratic government, healthcare workers and the people of Myanmar were working together. Aung San Suu Kyi was leading our communication and participation with the public during the pandemic, showing people how to wash their hands and mouth.”
At the time, Dr Sao oversaw COVID control for the government, first for the Yangon region, then for the Jago region as well.
“That's why I was very involved in phase one and wave one and two. At that time, we calculated just how much oxygen we were going to need and established a COVID control and quarantine centre.
“We had a systematic way of mitigating and then controlling COVID, even though during the pandemic Myanmar had a shortage of manpower, with only one third of the Sustainable Development Goals. But with that manpower, we were controlling COVID. You can imagine how they people were working – 24 hours a day, seven days a week.
“We had already planned, engaged, and paid for about 20 million Indian vaccines through two projects, one backed by the WHO for developing countries, and then through donations. At the time of the coup, we were maybe the fifth or sixth country in terms of the global vaccination drive.
“But as the WHO pointed out, this was not the time to have a conflict, the pandemic was already challenging enough.”
Dr Sao found himself in the difficult position where his overwhelming concern for the people of Myanmar – and enabling them to be vaccinated – forced him to cooperate with the junta, juggling the world and his people’s perception of that collaboration, as well the limitations of operating within that environment.
“Before the coup, I was close to the junta, including BrigadierGeneral Min Aung Hlaing, and as senior Tatmadaw (military) their family were my patients. I even operated on them because I'm an orthopaedic surgeon, I performed knee replacement surgery for the generals, their wives, and their families,” he said.
“But the thing is, I know which is right and which is wrong. I also thought about what would happen if I stood with the people, what would happen if I walked with the military? Which is the best path to save the most people’s lives?”
In fact, Dr Sao’s experience was like a microcosm of the situation facing doctors and nurses across Myanmar, who suddenly found themselves forced to take sides.
“We all knew that, historically, the military’s mindset makes them very difficult to work with. And if we worked with the military, we could not get the kind of support we needed to succeed with COVID control and then healthcare,” Dr Sao said.
“We did not want to go back to 1988, and we did not want to go back to $1 per person per year.”
Doctors and healthcare workers were a rallying point for citizens, able to eloquently express their opposition to the junta and share that rationale, acting as unofficial spokespeople for community resistance.
“In Myanmar culture, there are five respected individuals and professions: the Buddha and then monks, parents, teachers and doctors,” Dr Sao said. “On day one and day two we were waiting to see what would happen, but by day three, doctors from Mandalay started a second demonstration. We couldn’t accept a coup of this kind during the pandemic.”
It was a decision that had ongoing ramifications for doctors and healthcare workers, leading to their continued persecution.
“The military were not happy with the healthcare workers and doctors and nurses who were leading the protests and the crackdown started targeting them; doctors, nurses and then ambulance staff were arrested and tortured,” he said.
“One of my university students was shot and killed, these are the human faces, the human stories behind what's happening in Myanmar.
“Up to now, 85 doctors, nurses and medical and nursing students have been killed, as well as some 900 doctors, nurses and healthcare workers detained. Some of them are still in jail.
“About 40,000 healthcare workers, doctors, and nurses joined the CDM, or about 80% of the healthcare workforce. But, after two and a half years, some of them cannot continue because of the difficulties and the risk to their families inside the city – and those people beg you to know that working with the military is a very difficult situation they cannot overcome.
“Yet we still have 25,000 healthcare workers with the CDM, even though most have not received a salary for two and a half years.”
Throughout that time, those doctors and nurse have been in battlefield triage situations, and because of the trauma involved, Dr Sao holds deep concerns for the
long-term impact on the mental health of Myanmar.
“Combat medical care is very important now with fighting all over Myanmar, everywhere there is armed struggle and revolution – the whole country is a war zone. There is a host of different war injuries, including gunshot wounds,” he said.
“These injuries need physical and mental rehabilitation. I'm very concerned about that because in Myanmar, as a Buddhist country, mental health was not that much of an issue, the suicide rate was relatively low, but now that rate is increasing because of the stress and brutality associated with the revolution.”
Dr Sao explained that to discuss healthcare in Myanmar within the context of the uprising, it was necessary to divide the country into three regions.
“One is the region under the control of the military, such as major cities, another region is a conflict area where there is an armed struggle; and the other area is under revolutionary or ethnic revolutionary organisation control. Population-wise, because of the cities, the military control is much higher,” he said.
“But within the conflict area, we have an ethnic health organisation that has been there for many years, joined by the CDM doctors and nurses. Actually, there are 4000 doctors and nurses who are working with the revolution in Enugu.
“There are 66 secondary hospitals where we can operate. Some are station hospitals with 25 beds, and some are township hospitals with 50 beds, but half of the hospitals we built during the revolutionary time – in just two and a half years.
“We also have 258 mobile and frontier hospitals where they are working. But delivering proper healthcare is very difficult. Hospitals in the military controlled area have problems with human resource shortages, with workers fleeing to the countryside to join the revolution.”
Dr Sao said Myanmar was an ethnically diverse country with nine major tribes and over 100 spoken dialects but has been
continued on Page 33



continued from Page 31
heavily influenced by its time as a British colony, before gaining independence in 1947.
“At that time, the ethnic leaders, under the guidance of the national hero Aung San, the father of Aung San Suu Kyi, agreed to establish the future State as a federal and democratic country to reflect and fairly represent that diversity,” he said.
“But that never happened because Aung San was killed and then the Majority Bamar group took power and then there was the military coup. That's why a federal democracy never eventuated and that is a reason why we have had civil war since – that’s more than 70 years, the longest civil war in the world.”
Each ethnic group has been fighting with the military for many years, and each one has their own, independent health organisation.
“I'm retiring age, yet I have seen only one side of the Myanmar healthcare system,” Dr Sao noted.
“Because I am from the Burmese side, the central government side, I have never seen the care they are delivering in ethnic organisations, in the Kachin, Karen and Karenni areas, or the Mon and Chin.
“But now we understand and know each other because we have been forced to work together. The military are not discriminating when it comes to ethnicity, they attack everybody equally.
“We are working and sharing with the ethnic organisations and early during the revolution we formed a collective, a COVID taskforce currently led by Dr Cynthia Mong, who is well known for her philanthropic efforts and is working in refugee camps on the Thai border with the Mayo Clinic.
“Before the coup we already had 1 million refugees in the Rohingya area, about 1.5 million refugees in the Kachin, Karen, Karenni, and some of the Rakhine areas, but now that has increased to 4 million.
Historically, Myanmar’s healthcare system was highly centralised, with training and resources concentrated in the cities, meaning
that doctors from every corner of the country may have trained together. Now, they were reforging those relationships as they united against the junta.
But the challenges are enormous.
“The general secretary of ASEAN remarked on February 23 that the UN and other organisations were providing no real support for the refugees, no support for vaccination, and none for primary healthcare,” Dr Sao said.

“ASEAN also noted that humanitarian aid and immunisation programs were being weaponised by the military. For two and a half years there has been no immunisation of our children –not just for COVID, but the key vaccinations that will protect them and enable them to go through life safely.
“We even proposed to the UN to have a third party to monitor and evaluate, and to establish a humanitarian corridor, but that never eventuated.”
The price paid by the people of Myanmar for the conflict is not just the current political turmoil, the lives destroyed and the physical destruction of the nation’s infrastructure, but the potential impact of a future health crisis as the next generation comes of age without access to basic healthcare.
“Communicable disease outbreaks of polio, measles, and Japanese encephalitis, all these things could impact not only Myanmar but our neighbouring region – that's very much a concern,” Dr Sao said.
“We had a 90-95% vaccination coverage before the pandemic, but now this is only 20-25% –that's alarming. We have even
been forced to trial a pilot project we bought from the black market, just because it was available, but it was a very small amount and not enough.
“Before the coup, we had an elected parliament and a real government, but we did not have any money. But people from the Myanmar diaspora donated and supported us, that was the way that we survived and were able to continue developing.
“But now it’s an even more challenging situation – our doctors and nurses have been working without salary for two and half years.
“On the junta’s side, the defence budget has gone up and the health budget has gone down. Similarly, when healthcare aid is sent through the military, we cannot get it.”
Dr Sao pointed out that material and moral support was critical –even now.
“Almost anyone can do that – just talking with me and giving me a chance to share about Myanmar; this is you standing with us, Australian doctors and nurses standing in solidarity with the people,” he said.
“And now we have developed a federal medical school, nursing school and a certificate program training program, Australian doctors can help with that area using technology to support the online training program.
“Then there's also the Myanmar diaspora; the doctors from the diaspora have the details, they have people that they can contact who can get these supplies through. These are the areas where you can help us a lot.
“I'm sure we will win. We will win because we are fighting for the future against a brutal military regime, but after, we will need support – that's when the rebuilding really starts.
“Our revolution is not like in 1988 or 1962. We are fighting not only for democracy, but also for federalism and the chance to embrace the opportunity to live together as a country.”
 By Ara Jansen
By Ara Jansen
Recently Dr Andrew Leech lost a patient. He posted how he felt about it on a popular business networking platform. While that might seem a little odd, Andrew wanted to remind people and other doctors that it was OK to grieve and feel sad for the loss of a patient, especially one with whom you have worked closely.
“I don’t mind being vulnerable,” says Andrew, who was recently named RACGP WA GP of the Year. “I want to be open and transparent and describe the challenges that doctors have, as much as we can, in a public space. Sharing the story wasn’t about courting controversy but to bring to light issues of being human.
“Some of our patients die and you are at the forefront of their lives. It’s OK to feel grief. We have emotions too and it’s important to talk about them and get support.
“We are in such a privileged position where we are part of the journey and death is challenging. I felt really moved in that situation and I felt quite emotional about this patient. In so many cases we are at the other end of that – we are doctors and should keep ourselves apart from that. It was a reminder that we are all human. That person was special to me and that’s a very special part of the job. I’m grateful to be able to work with patients that way.”
Born and raised in Melbourne, Andrew is an only child. As the only kid in the house, he learnt to keep himself entertained and regularly reminds his daughters, Charlotte and Isabelle, if they ever cry boredom. His first step into university was for a Bachelor of Science at the University of Melbourne. Then Andrew decided he wanted to do medicine and flew across the country to Notre Dame Fremantle. He later received a Diploma in Child Health from the University of Sydney.
“It was challenging,” Andrew recalls. “Notre Dame was just starting and part of their process was doing an interview. My grades were fine and I convinced them I would make a great doctor. I got a place and moved across the country.
Bold move
“To be honest, I’d never really even heard of Perth, and I’d never been here or had friends here. It was one of the hardest things I have ever done. I lived at UWA and eventually found my feet and made friends.
“My parents always told me to take every opportunity and I have lived by that throughout my career so far. It has opened up so many things for me.”
His mother and father remain a strong influence in his life. “I’m very connected to them and they have given me a lot of great advice and values around life and spirituality.”
Andrew has lived in Perth for almost 10 years and considers it home, though he will probably always have a piece of his heart in Melbourne. He met his wife Tanya here. His daughters were born in Perth.

Almost until the last minute, Andrew was undecided about becoming a
GP as he enjoyed all his rotations and found each of them interesting. He had a feeling paediatrics might be his specialty and moved back to Melbourne for a while to pursue it. While he started working as a GP in Melbourne, he’s been back in Perth since 2015. What eventually moved him to become a GP was continuity of care. It’s also one of thing he prides his clinic for working hard at. He loves that he can treat whole families or generations from the same family.
“When I was doing paediatrics, you’d be getting to know someone, successfully working with them and then you would never see them again. I think it’s really important to cultivate a connection with a patient over time. I think that’s what moved me into becoming a GP with an interest in paediatrics – 60-70% of my patients are children and young people now.”
Andrew’s initial idea for The Garden Family Medical Clinic in Murdoch was a one-stop-shop for child and paediatric health, but he realised that excluded the rest of the family and he didn’t want to lose them from the circle of care.
The Garden opened just over a year ago and has 16 doctors and six nurses. The space is cheerful, childfriendly and features a much-used garden courtyard and internal green
walls. His one brief when fitting out the space was to not make it look like a medical clinic.
“As a bystander and an educator, I pick up so many things – primarily it’s about the emotions and feelings about how we should care for people. I think GPs need to be invited to be inspired, and together we can do so many things better and help how we work to evolve.
“It doesn’t come cheap but part of that is to create a climate of vibrant and compassionate care no matter where the patient comes from and that they feel welcomed with quality of care.”
Andrew’s wife Tanya is a nurse who also works at The Garden. Her influence – and working closely with the other staff – has improved the clinic and reminds Andrew to always be collaborative.
“We want people who work here to feel valued and respected and to use their own experience to help us all learn.”
He maintains one of the most powerful things a doctor can do is listen. In more vulnerable patients, they often need someone to just hear them. In younger patients, looking out for their mental health is vital.
continued on Page 37







continued from Page 35
“The connection you create with young people is one of the most important things to set up early. It’s a wise investment, because the more they can talk to you, the more they will trust you. Sometimes that may save their life; it’s happened over and over again,” he says.
“The world is tough for teens, and I want to be here to help them. Being able to talk to them in their own language – I’ve definitely learnt some new lingo – is also hugely valuable in order to connect.”
He’s currently writing a book on child mental health.
With his own daughters in upper primary school, he’s also putting those skills to work at home. “They are the core of my universe. In everything I do, I have them in my heart. I can’t emphasise that enough. Coming home to family is the most important part of my life.” Andrew’s parents have recently moved to Perth as well.
Being the only male in a house of three females and an apparently feral collection of eight Barbies, Andrew recently felt it was time to get reinforcements. He braved a toy store and bought the last Ken on the shelf.
“I didn’t know how embarrassing that would be!” He’s now been pressganged into playing Barbies and sometimes is convinced to be a real live Ken to his daughters’ lifesized Barbies.
When they’re not in Barbieland, the Leeches – along with labradoodle Monty – spend a lot of time outdoors. A good dose of green is really calming for the whole family. The chance to walk in nature creates mindfulness and encourages easy conversation. Game nights and jigsaw puzzles are also big in their home – Monopoly, Scrabble, Uno and Avocado Smash are all favourites. For fitness, Andrew enjoys cycling and going to the gym. He also teaches a regular spin class.
“It makes my patients laugh. They think it’s hilarious. It’s my escape and I feel so much better after doing it. I love the energy of it and teaching
the class guarantees I’ll show up! I’ve made the commitment, so I’ll be there.
“We have a bit of a disco atmosphere, but people don’t like me singing in class. If I start singing, they all ask me to stop. Clearly, I can’t sing.” Apparently, he’s also a terrible cook and can’t follow a recipe.
While Andrew takes the practice of medicine seriously, he believes there’s always room for laughter, honest connection and a bit of fun. It’s part of why he started a Teddy Bear Hospital.


Once a year, teddies, bunnies, the odd dinosaur and all precious stuffed friends are welcomed at the clinic where staff and Notre Dame medical


student volunteers do everything from stitches to injections or use the MRI machine, delightfully made from a large cardboard box with a skateboard rolling the patient inside of it.
By participating, kids can learn about the types of treatments they might encounter at the doctor’s or in hospital. They treated 120 friends at the most recent hospital and raised more than $1000 for Fair Game Australia. The money allows the WA-based not-for-profit to rehome 200 pieces of pre-loved sports equipment which improves access to sport and fitness activities in WA’s remote, regional and underserviced communities.
Chronic pain can be debilitating and have adverse effects on work, sleep and relationships often leading to comorbidities such as, depression, sleep disturbances and fatigue resulting in worsened health and negative societal and financial impact.

An increased reliance on pain medications and the concurrent disorders associated with chronic pain places individuals at a higher risk of developing a substance use disorder.
Risk factors for Substance use Disorders:
Recurrent and easy access to substances
Stress and financial difficulties
Any mental illness
PTSD and trauma.
Signs & symptoms of a substance use disorder:
Frequent requests for early prescription refills
Social withdrawal or neglecting responsibilities
Physical changes; weight, poor hygiene or skin problems
Taking higher doses or more frequently than prescribed Patient requesting prescriptions on first visit, “doctor shopping”
Changes in mood or behaviour; agitation, irritability and mood swings
Defensive or evasive when questioned about medications.
If you suspect that a patient may have a substance use disorder, please refer them to Fresh Start, or a suitable specialist.
Referral forms can be found on our website www.freshstart.org.au or call our clinic on 08 9381 1333
“One in five Australian adults are estimated to live with chronic pain.”
(Commonwealth of Australia, Department of health, 2021)

WA’s abortion reform bill was passed by State Parliament last month, and here sexual health expert Dr Alison Creagh reminds doctors of some amended rules around medical abortions.
From 1 August 2023, any doctor in Western Australia has been able to prescribe the medical abortion medications MS-2 Step (mifepristone and misoprostol), and they are no longer required to complete an online training course every three years.

In addition, pharmacists no longer need to be authorised to dispense these medications.
These changes are likely to significantly improve access to medical abortion for patients. However, it is important that each practitioner new to medical abortion think about their own process to minimise the risk of
complications. It is recommended to seek support from those with significant experience, and/or who have completed some training. Online training, while no longer a requirement, is still available at no cost from the drug manufacturer. More information is available at www.ms2step.com.au.




For those hoping to offer medical abortion soon, it is important to consider:
• Will I offer ’very early’ abortions (before the pregnancy tissue can be seen on ultrasound in the uterine cavity)? If so, how will I make sure the patient is
well-informed about the risk of ectopic pregnancy?
• How will I make sure the patient has all the information they need to make an informed choice of procedure, how to take the medications, and what to do if any difficulties occur?
• How will I ensure that the patient understands the followup process, and the risk of complications?
• How will I ensure that follow-up is completed?

There are resources about abortion for patients and for health professionals, including:
continued on Page 41

Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
 Bresnehan
Bresnehan
It is certainly pleasing to see an increase in the number of medical students interested in rural medicine in the latest 2023 Medical Schools Outcome Database (MSOD) National Data Report. It shows that the efforts of medical schools and interest groups to expose medical students to rural practice is paying off in some ways.
However, other findings from the survey are frustrating to medical students, like myself, who are looking to enter general practice in a few years’ time. The General Practice Students Network (GPSN) is a national network of 4,000 plus aspiring students who also want to become GPs and we continue to tell policy makers what needs to be invested in – but are our voices being heard?
In early 2023, the GPSN called on policy makers to invest in the quality of medical school general practice placements and to support more peer-to- peer initiatives.
Medical students are aware of the current uncertainty within general
practice and are not immune to the media coverage that general practice has been attracting. Therefore, while it is disappointing, it is not surprising there has been a small drop in final year medical students preferencing general practice as their specialty of choice.
continued from Page 39
• King Edward Memorial Hospital – WNHS pregnancy choices and abortion care service (booklets for medical practitioners and patients)
• The SHQ patient resource – I’m Pregnant: What Are My Options?
• And for more information about assessment, management, and referral for unintended pregnancy and abortion, the following recently reviewed pathways are available from HealthPathways
WA: Unintended Pregnancy and Abortion; Medical Abortion; and Follow-up After Abortion.
Sexual Health Quarters (SHQ) also has a course on medical abortion prescribing in development. Those interested should contact clinic.ed@shq.org.au.
Dr Alison Creagh is Medical Educator at Sexual Health Quarters.

ED: The Abortion Legislation Reform Bill 2023 was passed by the WA Parliament on September 20, to streamline access to abortion and bring WA's regulations in line with other states.
But how do you start reversing this declining trend? How do you increase the profile and attractiveness of general practice to the future medical workforce?
continued on Page 43
Key changes included removing the need for women to be referred for an abortion by a doctor; no longer requiring women to undergo mandatory counselling; and moving provisions out of WA's criminal code. Additional requirements that are imposed on late-term abortions will also be applied from 23 weeks, rather than 20 weeks currently. Doctors with a conscientious objection to abortion will need to refer women to a doctor who offers it.
Bethesda Clinic is a voluntary, adult only, 75 bed clinic that provides multidisciplinary clinical services to aid recovery from mental health issues through inpatient and day patient programs.
Services Bethesda Clinic provides:
Inpatient care and therapy programs managed by a multidisciplinary team. Day patient therapy programs in the Wellness and Recovery Centre. Psychiatric and psychological services for those experiencing mental health issues.
Specialties:
DVA-accredited Trauma Recovery for veterans, military and first responder communities. The first designated women’s-only ward in Western Australia, providing a safe recovery environment.

Alcohol and other drug use.
General mental health.
How to refer to Bethesda Clinic:
Download the referral direct from our website bethesdaclinic.org.au/referrals
Find us on HealthLink: Bethesda Clinic
Contact Bethesda’s Triage Officer on (08) 6378 4999 or BC.Triage@bethesda.org.au
Bethesda Clinic
1 Honour Way, Cockburn Central WA 6164
Phone (08) 6378 4900
bethesdaclinic.org.au
continued from Page 41
The answer is to listen to future GPs, to the students coming up through the pipeline. We know and see the barriers and have effective solutions, so start investing in the most valuable resource within general practice – its future practitioners!
Our members continually tell us the importance of quality early exposure to general practice at the beginning of their journey, and this work needs to be done before hospital training. Our GPSN members want to connect with general practice, understand it, and be supported in professional peer exchange with existing GPs early on in their medical school experience.
We all know that early positive impressions of general practice will go a long way to increasing the number of medical students becoming GPs. GPSN members want an opportunity to get to know general practice and GPs early in
their first few years of training.
Professor Richard Murray, the Dean of Medicine and Dentistry at James Cook University, recently said that general practices have a tougher time compared with teaching hospitals.



We agree and believe medical schools need to be more hands on and connected with their GP partners when it comes to

the general practice placement experience. This means a change in how medical schools, general practice, and students are supported.

While the GP specialty is at a crossroads, we understand that GPSN has a role to play in strengthening access to primary care in Australia and working with our sector peak partners to uplift the GP specialty. GPSN wants to play a role, and we want to challenge the preconceptions of medical students about the specialty of general practice. But the perspectives of medical students must be listened to, otherwise policy makers will continue to invest in initiatives that miss the mark. Isn’t it time for a new approach to addressing Australia’s GP shortage?
ED: Sarah Bresnehan is the national chair of the General Practice Students Network.

Whether it's for knees, hips, hands, arms, legs or shoulders, St John of God Mt Lawley Hospital orthopaedic services provide care from pre-surgery through to rehabilitation to get your patients moving.
elbow,
Dr
Shoulder and upper limb surgery, knee surgery and replacement, and sports injuries






Hand and upper limb surgery and trauma
To learn more about our specialists’ expertise and specialties, scan the QR code. Email GP.MtLawley@sjog.org.au • visit sjog.org.au/mtlawley and search ‘orthopaedic surgery’.




Adora Fertility provides affordable IVF without compromising on quality. By referring your patient to one of our highly qualified specialists, they will receive a tailored approach to their fertility treatment plans with medications sensitive to their needs. Out-of-pocket costs are typically less than $2,000 for a fully stimulated IVF cycle. Give your patients the best chance of conception without the financial sacrifice.
Our range of fertility treatment options has expanded to include our newly launched, Known Donor Program. As part of this program, patients can access affordable fertility treatment with donated sperm, eggs or embryos from a donor known to the patient. By facilitating sperm, egg and embryo donation in this way, we know that we can help more people grow their families in more ways.

Part of me is reluctant to go down this path as views are polarised. The other part says it is important for the exact same reason. Having spent three weeks this year in far flung regions of Australia doing Indigenous health checks, I have some observations.
Here is the easy bit. The Clontarf Foundation and Shooting Stars do a phenomenal job in many schools providing guidance and support to Indigenous boys (Clontarf) and girls (Shooting Stars). The aim is to develop improved self-esteem and confidence assisting them to participate in education, employment and society in a positive way. This has the capacity to help break the poverty and welfare cycle for the next generation. International data shows that better education is strongly correlated with better health.
Not every child will succeed (like all ethnicities and backgrounds) but these programs make a real difference. I would encourage you to check out the respective websites.
One case really struck me. In the north of WA is an Indigenous child with a cochlear implant put in at age three. Somehow, there has not been follow-up. As I was informed, there is no classroom supports in place. While not metropolitan Perth, it is not a remote community either. This is a reasonable size rural town. What are country health services doing? What is the education department doing? They have the capacity and resources to help children like this. There is money in the system and what is required is routine. This is but one example.
We can all agree on two issues. Firstly, the health outcomes of Indigenous people are less than that of the general population. Secondly, the billions that have been spent over the past 50 years have not brought about improvement. Too much has been wasted on bureaucracies in capital cities.
In medical practice, we can offer advice but the patient needs to action it to get any benefit. We can provide support, guidance and assistance but not do it for them. On a community basis the principle is similar. We know what needs to happen to improve Indigenous health. It won’t happen unless communities and individuals action it. Society can provide support, guidance and assistance but can’t do it for them. External imposition will not fix Indigenous health, or indeed any health issue. It must be a partnership.
We already have the capacity to do better. Governments have the money. We have the knowledge. Action not words is what is missing.
In medical practice, we can offer advice but the patient needs to action it to get any benefit. We can provide support, guidance and assistance but not do it for them.

The prospect of spinal surgery has long sent shockwaves of fear and trepidation through patients and referring practitioners. Invasive surgery, long recovery times and the concern about needing repeated procedures in the future come to mind.
Safely visualising delicate neural structures often meant extensive surgery. In recent years, advancements in optical and camera technology have miniaturised the equipment commonly used for procedures such as arthroscopy and laparoscopy allowing them to be usefully employed in spine surgery.
Key-hole spinal surgery, known as spinal endoscopy, has long been trialled but with varying success internationally. It has been spurred on though by the successful adoption of endoscopic and arthroscopic procedures in other surgical disciplines. Who remembers the last patient who underwent an open cholecystectomy or ACL reconstruction? All are now done with key-hole laparoscopic or arthroscopic techniques.
Access to the spine is challenging with limited safe working corridors previously limiting the useful introduction of key-hole equipment that was often quite large. Device technology has reached the point where this can be achieved safely.
While most disc prolapses causing sciatica self-resolve over six weeks, those with persistent neuropathic pain or ‘sciatica’ are difficult to manage, often progressing to needing analgesia that impairs daily function.
The prospect of open surgery that comes with an 8 to 12-week recovery period before returning to normal work duties is also undesirable especially in the typical young working demographic. The desire to improve the current standard of surgical treatment often offered to these patients is clear.

At the forefront of innovation stands endoscopic spinal surgery. This approach represents a monumental shift in the field of sciatica treatment, offering a streamlined path to recovery while minimising the invasive nature of traditional open surgeries.
Essentially, key-hole surgery involves making a tiny (typically 8mm) incision, through which specialised instruments and a miniature camera are inserted. The camera provides real-time visualisation of the surgical site
and, given the high-quality optics achieved, it is superior to a typical image from an operating room microscope (once considered the gold standard).
By accessing the affected area through such a small opening, the disruption to surrounding muscles and tissues is dramatically reduced, resulting in diminished post-operative pain, scarring, and an expedited return to normal activities.
1. Recovery: Perhaps the most remarkable advantage of
Endoscopic key-hole spine surgery is increasingly being employed to treat problems previously only open surgery could address
Modern spinal endoscopes utilise new technology, this is not universally adopted or available everywhere, yet
Patients need careful expectation management, not all pathology can be addressed with key-hole techniques.
endoscopic spinal surgery is its ability to significantly accelerate the recovery timeline. With minimal tissue damage and reduced trauma, patients return to their normal activities sooner, compared to conventional open surgeries.
2. Minimal scarring: Whilst the cosmetic scaring is inherently reduced, this often isn’t a concern on the back. Minimising the scar tissue generated within the muscles and around deeper neural structures is vital in
returning to maximal function quickly.
3. Post-operative pain: Postoperative pain is a substantial concern for patients undergoing surgery. With keyhole spinal surgery, patients experience less pain and less dependence on opioid analgesia after their surgery, most don’t require this at all.
4. Shorter hospital stays: Patients undergoing endoscopic discectomy for sciatica will typically be cleared by physiotherapy the day of their surgery and spend less than 24 hours in hospital.
5. Patient outcomes: Patient reported outcomes scores relating to pain relief and return to function have been extensively researched and reported to show that effective treatment can be achieved utilising these endoscopic techniques.

Like all advances in medical technology, they come at a cost. The equipment is specialised and costly, and it is not available at every hospital in WA. Further, the
procedure requires specialised training and accreditation to be able to perform. The burden of this training and development of experience in the technique ultimately falls on the hospitals and surgeons with a significant cost. As such it has not been widely adopted among all practitioners.
In navigating the decision, our guidance plays a pivotal role in steering patients toward the most suitable treatments. Endoscopic key-hole spinal surgery will likely allow more patients to undergo effective treatment of their sciatica pain and with a recovery that is more acceptable to them.
Like most medical treatments, managing expectation is key. This treatment may not be appropriate for all. As innovation and advancement continues, the aim will be to further adopt keyhole techniques to reduce the invasiveness of all surgery, improve outcomes and drive safety.
Author competing interests – nil
. H i p, k ne e , s houlde r, foot , a n k le a nd t ra um a
. P riv a tely in s u red , DVA , Wo rke rs Compen sa tion a nd M VA p a tient s welcome d
. Medico L e g a l ass e ss ment s

P R OF PI E R S YAT E S
Hi p , K n ee & Tr aum a
P ri ma r y & R e v i s i o n
A r t h r o pl as t y
Hi p Res u rfac i n g
M R B E NJAM I N W I TT E
Kn ee Su rge r y
A CL & S po r t s I nj ur i e s
Kn ee & Hip Rep l acemen t
M e d i co L ega l
MR TH O MA S B UC H E R

H ip & Kne e - P rim a r y & R e v i s i o n

ACL a n d Tra u m a
Glut ea l Te ndo n R e co n s t r u c ti o n
MR ANDR E W M A T T I N



S hou l de r, El b o w & Wr i s t
Kn e e , Sh o ul der Rep l acemen t
S po r t s inj ur i e s
Tr a u m a
MR SI M O N W A L L

H ip & K ne e - Pr im a r y &
R e v i s i o n
A CL and Tra um a
Ili za r o v F ra m e s
A/P R OF G A R ET H P R OSS E R
Hi p , Knee & Traum a



Pr i ma r y & R e v i s i o n
You n g Adu lt Hi p
Hi p R esu r fac in g
M R S AT Y EN GO H I L
Kn e e & S ho ul d e r
A CL & S po r t s I nj u rie s
A r t h r op l as t y & Tr aum a
M R LI-O N L A M
Kn e e , S ho ul d e r & Hi p
U n i C ompa r tm e nt a l Kne e
Kn e e and S hou l de r
A r t h r osco p y
A CL and Tr au m a
A/P ROF CH RI S TO P HE R JO N E S
Hi p & Knee Re pl ace m en t
- Pr i ma r y & R e v i s i o n
C ompu t er ass i s t ed S urge r y
Hi p Res u rfac in g
Traum a
MR DANIE L MAR S HA L L




Hi p , Kn e e , F oo t & An kl e
An kle R ep l ac e m en t
Robo t Ass i s te d A r t h r o pl as t y
Traum a
T HE H I G H L Y
AN TI C I PA T E D
AR R I V A L O F
D A N I E L
M A R SHA L L
BS C , M BBS ,
F A O R T H A
F R ANC S ( O R TH O )
My nam e i s M r D an iel Ma r s h a ll , the n ewe s t a d d iti o n t o O r th o p a e d i cs WA te a m b as e d a t St John of G o d Mu rdoch Hos pit a l .
My spec i a li s t tr a ini ng i nc lu d e s l o we r li mb su r g e r y, h i p a n d kn ee a r th ro pl as t y, with a pa r ti cu l ar f ocus o n l o wer li m b d e f o rmit y co r re c ti o n a n d f oo t & ank l e su r g e r y.
I h ave re c e n t l y retur n e d f rom t h e L o we r Li m b l eng t h e n i ng & R e cons tru c ti o n Sur ge r y Fe ll o w sh i p i n S yd n ey, as well as the Hi p a n d Kne e A r t h rop l as t y Fell o w sh ip a t t h e ren o wne d R oya l D evon and E xe t e r Hosp it a l i n U K , re cogn i s e d as on e of t h e Wor l d ’ s l ead in g h ip un it s
My wife Maggie and I take pride in our role as parents to our wonderful two year old daughter. It brings us great joy to have the opportunity to settle back down in our beloved hometown of Perth, where I will wholeheartedly dedicate myself to Orthopaedics and optimising patient care
My sp e c i a li s t sk ill s we re ob t a in ed w hen tr a i n i ng i n WA and N S W as we ll as i n te r n a ti ona l f e ll o w sh ip s an d v i s it a ti ons , in c lu d e comp l e x p roc e du res o f t h e f oo t and ank l e , t o t a l an kle a r t h rop l as t y, m i n i ma l l y i nvas i ve f oo t and ank l e su r g e r y, de f o r m it y co r rec ti on us i n g int ra m edu ll a r y and c i rcu l a r f r ame d ev i ces , robo ti cass i s t ed pa r ti a l kn e e , t o t a l kne e a r t h rop l as t y an d t o t a l h i p a r th ro pl as t y.
I am tr a in ed i n th e ROS A and MA KO robo t f o r h i p and k n e e a r th ro pl as t y p roc e du res .
I a m d e d i ca te d t o p ro v i d in g h i g h-q ua lit y o r t hopa e d i c ca re t o red u ce pa i n a n d rega i n f u nc ti on , wit h t h e g oa l t o i m p ro ve pa tie n t ’ s q ua lit y of li f e I l ook f or w a rd t o p ro v i d i ng o r t hopaed i c ca re t o you r pa ti en t s .

Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

First we had ‘the global military industrial complex’. Then it was ‘Big Pharma’. Is the ‘rotator cuff repair industry’ next? Tongue in cheek, but there is no denying there are big multinational companies relentlessly marketing implants and devices to orthopaedic surgeons.
Any number of GPs will have had a patient who has had a poor result from rotator cuff repair surgery. The reluctance to refer is understandable. So how do we make a sensible decision as to who should and should not have a rotator cuff repair?
I always fall back on two criteria in orthopaedic decision-making – pain and function. We are not dealing with life and death decisions, and we all took an oath to ‘do no harm’ (for a good read see Hippocrasy: How Doctors are Betraying Their Oath, by orthopaedic surgeon Ian Harris).
The
There is a high incidence of asymptomatic rotator cuff tears in older age. A low estimate based on ultrasound studies is 10% of people in their 60s, 20% in their 70s and 40% in their 80s. The actual numbers may be higher.
Furthermore, post-operative studies have historically shown that many people who have had rotator cuff repair surgery have a good result, even when the repair has
Rotator cuff tears are common and not all require surgery
There are cases for operating and for conservative treatment depending on individual circumstances
A rational approach leads to the best outcome for the patient.
failed. It begs the question – if the surgery succeeds without achieving its primary objective, would the patient’s condition have improved regardless? Did the surgery just buy time, or was it the acromioplasty/ spur removal that did the job?
As much as anecdotal evidence is poor science, I can say that I have seen many elderly patients with symptomatic rotator cuff tears settle over time with conservative treatment. The emphasis is on ‘over time’. Things don’t happen quickly with orthopaedic rehab.
On the flip side, what are the risks of doing nothing?
In a nutshell, the pain might continue, function may not improve, and we might ‘miss the boat’ in terms of repair. Tendons retract, muscles atrophy and the fixable may become unfixable. This is a big problem as there are no good alternatives once the tear becomes irreparable. ‘The bail-out’ may be
shoulder replacement. Outcomes for a successful early repair will be vastly better in a high-functioning patient.
There is too much dogma about orthopaedic surgery online today: All impingement can be treated non-operatively. All ACL tears can be treated with physio. The truth is rarely ever black and white in medicine, that’s why we talk about the ‘art’ of medicine. There is nothing conservative about not operating on a young patient with a full thickness rotator cuff tear. In fact, it would be radical at the very least, but probably negligent. So here is the algorithm I use.
1. Is it fixable? MRI allows us to pick winners. A big, retracted tear with atrophic muscle is a nonstarter. Acute tears will do much better. There is a grey zone in the middle; acute on chronic.

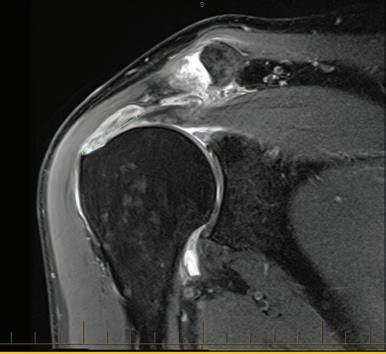
2. Biological age – 80 doesn’t rule you out if you look 60 and the corollary.
3. Comorbidities – diabetes is a big one. It comes with increased risks of infection, frozen shoulder and poor tendon revascularisation. Same for smokers.
4. Pain and function – night pain and loss of sleep will test your sanity. Pseudo paralysis from a big acute tear is catastrophic. These factors might push us towards surgery.
5. Patient expectations – even if I think we are heading to surgery, a short period of non-operative treatment might help decision making. Partial tears or those not retracted can be rescanned in six months without significant risk.
My final point, more than any other operation, the success of rotator cuff repair surgery depends on good rehab. It’s an unforgiving operation. Patients need a clear understanding of the rehab timeline and targets, and ‘constructive feedback’ if they are not meeting those targets!
Author competing interests – nil

The different knee imaging modalities all have strengths and weaknesses. The initial and subsequent investigations are similar depending on whether the presentation is acute or chronic. In almost all circumstances imaging of the knee should begin with an X-ray. This may avoid the need for costly advanced imaging and can direct appropriate further imaging or referral. X-ray is good at assessing the bony structures including assessment for a fracture, an arthropathy, or a bone lesion (Fig.1). X-ray also has a role in identifying calcified or ossified loose bodies and structures which can be difficult to detect and characterise on MRI.
X-ray is unable to accurately assess the soft tissues, but sometimes secondary signs of internal derangement may be seen, such as the secondary signs of an anterior cruciate ligament (ACL) tear, or a large joint effusion in the setting of trauma. Although other imaging may be required, X-ray is a complementary test.

X-ray is a good initial investigation
Ultrasound has a limited role in imaging of the knee, particularly in the setting of trauma. MRI is the preferred modality for assessing the knee following X-ray. It is good at assessing the cruciate and collateral ligaments, menisci, articular cartilage, and bone marrow.
Ultrasound has a limited role in knee imaging. Ultrasound can assess for tendinopathy, especially the extensor mechanism, and for the presence of a joint effusion, Baker’s cyst, distended bursa, parameniscal cyst, or mass. It has a limited role in assessing collateral ligaments.
Because of incomplete or inadequate visualisation, ultrasound is not recommended to assess the cartilage, menisci, and cruciate ligaments. The entire meniscus cannot be visualised on ultrasound and it is difficult to differentiate intrasubstance meniscal degeneration from a tear. Ultrasound is unable to visualise and assess the ACL. In trauma, ultrasound is of limited utility.
CT (non-arthrographic) also has a limited role in knee imaging. The spatial resolution of CT is excellent, providing more bony detail than an X-ray. This makes CT ideal for fracture characterisation and for fracture detection when X-ray is normal, but the clinical features suggest a fracture.
CT can also demonstrate in more detail the degree of joint space narrowing and other features
of osteoarthritis. Like X-ray, assessment of the soft tissues is limited. CT is unable to assess the ACL and menisci.
MRI is the preferred modality for assessing the knee following X-ray. It is good at assessing the cruciate and collateral ligaments, menisci, articular cartilage, and bone marrow.
A normal ACL and a complete ACL tear can be diagnosed with high accuracy. On MRI, the normal ACL is a low signal intensity structure extending from the posterior inner lateral femoral condyle to the tibial plateau anteriorly (Fig.2A). On the sagittal images the ligament is parallel to the intercondylar notch/ Blumensaat line.
The MRI findings of an acute complete ACL tear are discontinuity, increased signal intensity, mass-like tissue at the expected location of the ACL, and abnormal orientation. The combination of discontinuity and abnormal orientation has a 100% positive predictive value (Fig.2B).
On MRI, we often see secondary findings associated with an acute complete ACL tear. These have low sensitivity but high specificity and may help when there is diagnostic uncertainty. On MRI these secondary findings include osseous injuries such as marrow contusions or impaction fractures, which are typically located at the anterior lateral femoral condyle and posterior lateral tibial plateau (Fig.2C).



Diagnosing a partial thickness ACL tear is more difficult than a complete tear. Secondary findings are often absent and differentiating partial and complete ACL tears can be difficult.
Figure 2A: Normal ACL on a sagittal MRI image
Figure 2B: Complete ACL tear with discontinuity and abnormal orientation
Figure 2C: Impaction fracture at the lateral femoral condyle anteriorly and bone bruise/trabecular microfracture at the lateral tibial plateau posteriorly secondary to a complete ACL tear
On MRI, the menisci are low signal intensity triangular shaped structures on coronal and sagittal images (Fig.3A). On MRI, a meniscal tear is diagnosed by identifying increased signal intensity extending to an articular surface (superior/femoral, inferior/tibial, or the apex) or abnormal morphology of the meniscus with no history of previous surgery to the meniscus (Fig.3).

Where the abnormality is found on at least two slices (consecutively in the same plane or the same region on different planes) there is a high likelihood that a tear will be found at arthroscopy. MRI has excellent sensitivity and specificity for primary meniscal tears but diagnostic performance decreases after surgery. Post-operative MRI can be challenging because post-operative changes can mimic a meniscal tear.
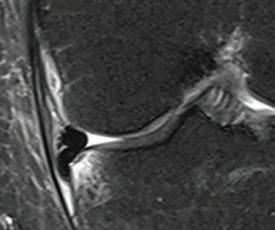
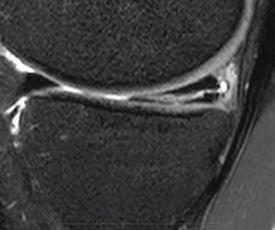

MRI is very sensitive in detecting bone marrow oedema but sometimes fracture lines can be difficult to visualise. Calcification and ossification can also be difficult to visualise or interpret on MRI. In these settings, both X-ray and CT are complementary.
CT arthrogram is an alternative to MRI in patients unable to access MRI or have a contraindication to MRI. In elderly patients, a simple X-ray may suffice and avoid the need for the procedure.
CT arthrography involves scanning the knee following injection of iodinated contrast into the joint. This is uncomfortable and has a very small risk of infection. Although MRI is the preferred modality, a good quality CT arthrogram is an accurate method for detecting ACL and meniscal tears. Poor coating of the menisci with contrast and chondrocalcinosis of the menisci can reduce the accuracy of the scan to diagnose or exclude a meniscal tear.
– References on request
Author competing interest – nil
By Mr Peter Ammon Foot Ankle & Knee Surgery



At BreastScreen WA (BSWA), women from the age of 40 are eligible for annual screening mammograms if they meet one of the following criteria:
- One or more 1st degree relatives (mother, sister, daughter, father, brother, son) with breast cancer before the age of 50;
- One or more 1st degree relatives with cancer in both breasts (diagnosed at any age);
- Two or more 1st degree relatives with breast cancer (diagnosed at any age);
- Past personal history of breast cancer;
- Past personal history of ovarian cancer;


- Past personal history of a biopsy proven borderline lesion (Atypical Ductal Hyperplasia, Lobular Neoplasia (LCIS, ALH))
Between 10% to 15% of women are currently rescreened annually at BreastScreen WA.

Only a limited past history and family history can be obtained by the radiographer at the time of the woman’s screening examination. BreastScreen WA may not be aware of important second degree relative family history information that could warrant a woman attending for annual screening.
A breast cancer risk assessment and risk management decision support tool recommended by Cancer Australia is available for GPs and women called iPrevent https://www.petermac.org/iprevent. iPrevent is a RACGP accepted clinical resource that can help women derive the benefits of screening mammography, by helping determine their risk and appropriate screening interval. Information on Annual Screening can also be found at https://www.breastscreen.health.wa.gov.au/Breast-health/Annual-screening .
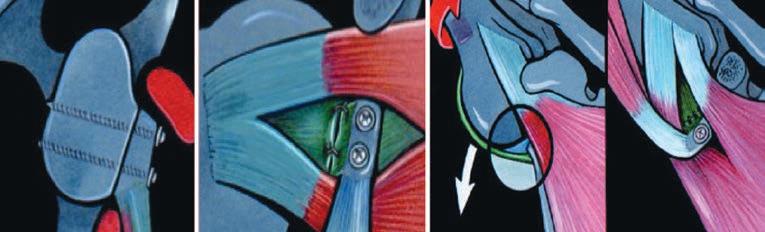 By Dr William Blakeney, Orthopaedic Surgeon, Subiaco
By Dr William Blakeney, Orthopaedic Surgeon, Subiaco

Recurrent shoulder dislocation is a common presentation to hospitals and general practice. About 95% of shoulder dislocations are anterior. Chronic traumatic anterior shoulder instability is defined as recurrent instability that has required glenohumeral reduction. Recurrent episodes may include further dislocations, symptomatic subluxations or apprehension.
It is caused by three anatomical lesions: (i) a capsulo-ligamentous and labral lesion (Bankart); (ii) anterior glenoid bone loss and (iii) a humeral head impaction (Hill–Sachs) lesion. These need to be assessed to decide on the surgical strategy.
It is also important to assess patient risk factors. Proven risk factors for recurrence are young age (under 20–25 years); bone loss; competitive, contact and overhead sports; and hyperlaxity.
There is continuous debate as to the indications for different treatment options, such as arthroscopic stabilisation (with and without remplissage); free bone block procedures, and coracoid transfer surgery with its most common technique, the Latarjet procedure. Arthroscopic stabilisation is performed by releasing the capsule-ligamentous complex and freshening up the insertion of the labrum. Capsule and labrum are then repaired with suture anchors to create an anatomical reconstruction.
According to recent surveys, the majority of surgeons would use this procedure as the initial repair procedure. High patient satisfaction has been documented, but there is evidence of a high
recurrent dislocation rate over time, associated with risk factors.
The procedure consists of transfer of the coracoid to the anterior surface of the scapula and fixed with two screws. The coracoacromial ligament stump is repaired to the anterior capsule. The procedure is intricate and has a serious learning curve. It has been standardised and broken up into key manoeuvres and stages, to prevent complications. The Latarjet procedure has the lowest rate of dislocation recurrence of all surgical options.
Postoperative stability is attributed to a triple effect:
i. Bone augmentation by the coracoid process
ii. Sling effect by the conjoint tendon and hammock effect of the lower portion of the subscapularis
iii. Capsular repair with the coracoacromial ligament stump
There is increasing evidence that for patients with risk factors, arthroscopic stabilisation techniques have higher failure rates than the Latarjet procedure
Patients at the highest risk of failure are young patients and those with bone loss. The amount of bone loss deemed significant continues to decrease
All surgeries have satisfactory rates of return to sport across all sports, as well as high patient satisfaction, but more patients return after a Latarjet procedure and they do so sooner.
Most studies have shown a high return to sport following stabilisation surgery. Comparative studies have all shown significantly higher rates of return to sport, quicker return and lower rates of redislocation with the Latarjet procedure compared to arthroscopic stabilisation. These results have been replicated in sport-specific studies looking at soccer, rugby and AFL. For this reason, most surgeons are doing a Latarjet procedure as the first option in contact sport athletes.
Risks factors for development of arthritis include increased number of dislocations, older age at the time of dislocation, high-energy sports and alcoholism. There is no evidence for differences in osteoarthritis rates between arthroscopic stabilisation and Latarjet procedure, as long as there are no technical errors. Poor anchor placement and lateral graft overhang are both associated with increased risk.
In my practice, the Latarjet procedure is the first-line treatment for the majority of patients. With the increasing evidence of high rates of recurrence following arthroscopic stabilisation, there are fewer and fewer patients for whom this is indicated.
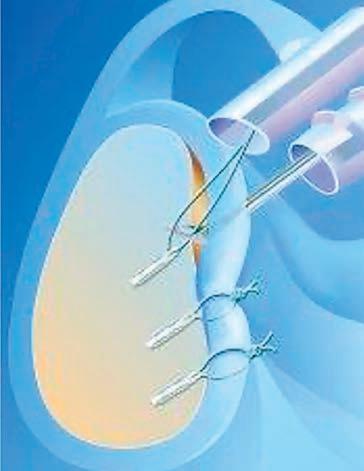
– References on request
Author competing interests – nil
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
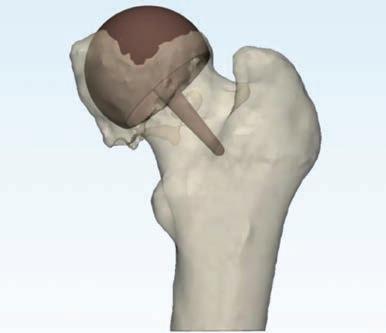 By A/Prof Piers Yates, Orthopaedic Surgeon, Murdoch
By A/Prof Piers Yates, Orthopaedic Surgeon, Murdoch

Hip resurfacing was developed in England during the 1990s for younger, active patients with hip arthritis as an alternative to conventional hip replacement. The original expectation was that this would give 10 years of high activity, however, the results have far exceeded this, with many patients now at over 20 years.
Although the best-performing resurfacing implants have been available for more than 20 years, only 3% of patients undergoing hip replacement in Australia end up with a resurfacing – 1020% of patients requiring a hip replacement are suitable.

This procedure allows return to any activity including impact sport, running, surfing etc. and several high-profile athletes have even been able to return to competitive

Metal on metal hip resurfacing is ideal for many active, younger, male patients with hip arthritis

Patient, implant and surgeon selection is important for good results
Ceramic resurfacing is a promising option for young active females with hip arthritis.
professional sport after surgery, including boxer Anthony Mundine and tennis player Andy Murray. Compared to normal hip replacements, the femoral bone is preserved for the future, and if does eventually fail, revision of the cup component is usually not needed, making for a quick and easy revision and recovery.

Hip resurfacing has excellent results for osteoarthritis at over 20 years, with over 95% survival of implants at 10 years in many series, and >88% survival at 20 years on the Australian National Joint Registry. New data even suggests that patients with hip resurfacing live longer than those with conventional hips, even when adjusted for health differences!

continued on Page 59




Nearly every person will have a scar in their lifetime – 100 million new scars occur each year in the developed world alone. A scar is always the result of some form of injury and can be a painful reminder of trauma suffered.
Improving scars is challenging. Most people know that there is no way to ‘erase’ a scar and may seek advice from a plastic surgeon to try to revise them. Occasionally, there will be valid reasons why scars are less than optimal, such as delayed healing, wound infection or dehiscence. If so, the answer could be as simple as cutting out the scar and starting again.
CO2 laser is a game-changer in the treatment of problematic scarring
Many types of scarring can benefit from CO2 laser; especially tight, raised and itchy scars
Improving scarring can require a multi-modal approach, combining laser with surgery.
But what if the wound healing was uncomplicated and the closure technique was adequate? What if the scars are too large to excise or the patient has keloids?
The risks of intervening in such situations are fraught with risk and many clinicians are rightly loath to make a bad situation worse. Patients are often disappointed with this response, even if it is based on sound reasoning, it doesn’t help their problematic scar.
CO2 laser has been used for many decades treating various cutaneous conditions such as ablating skin lesions and resurfacing wrinkles and rhinophyma. However, its use in treatment of scarring was limited as the continuous laser beam delivery method meant the entire surface area treated was ablated, and the open wound had to heal from deeper structures.
EOSedge is the first general X-ray system of its kind in WA with a high-resolution photon-counting detector remarkably improving image quality.
Fully functional 2D/3D biplanar X-ray imaging in seconds

Open design to suit an extensive range of patients

Up to 80% reduced radiation dose with Flex Dose

This was very risky in scars, as the deeper dermal appendages from which skin re-epithelialises are far fewer, increasing chances of delayed healing, infection, pigmentation change and worse scarring.
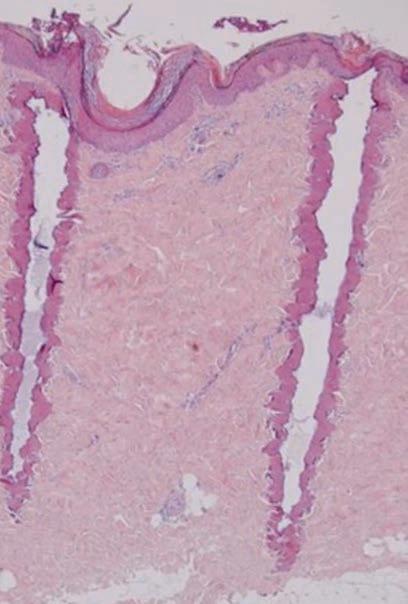
All of this changed with the invention of fractional CO2 laser delivery in the mid-2000s, whereby laser beam energy is delivered in tiny columns called micro-thermal zones (MTZs) to the scar, leaving undamaged adjacent epithelium (see image). This allows rapid reepithelialisation of the treated areas within days, while still allowing the laser energy to penetrate and stimulate remodelling of scar collagen.
Plastic surgeons specialising in burns were early adopters of this new fractionally delivered CO2 laser treatment, as patients with extensive hypertrophic scars have few reconstructive options.
Large series data and several RCTs have shown that CO2 laser can improve scarring clinically in terms of appearance and function and at a histological level can alter RNA and change dermal architecture towards that of normal skin. Most clinicians now agree that hypertrophic burn scars are improved by CO2 laser treatment. But what about other types of scarring?
Post-surgical hypertrophic – most surgical scars look reasonable up to six weeks post-operatively and then proliferate in vascularity and thickness until six months. After this, scars remodel for 12-18 months and hopefully leave a flat
pale line. For surgical or traumatic scars which persist in hypertrophy or are itchy and/or sore during remodelling, CO2 laser can help flatten and relieve symptoms.
Keloid scars – in our experience CO2 laser provides excellent relief of itch and pain in most keloids and will improve scar thickness in around 50% of cases. Relief of symptoms is often temporary, however, and many patients request repeat treatment every three to six months. In very large keloids, or those which are impacting on
continued from Page 57
The operation is more difficult than a standard hip replacement, and the early recovery takes longer. But although the incision is longer and the operation more invasive, patients recover very quickly with a short hospital stay.
Previous concerns over metal ion release and potential tissue damage are now well understood, and of very low risk in 2023. To minimise this risk, it is important to use one
of the two proven implants (Adept or Birmingham), select patients carefully, and use a surgeon that regularly carries out this procedure.
New technology has allowed safer and more accurate placement of both the acetabular and femoral components. On the femoral side, my practice has developed patientspecific templating, which produces a 3D printed sterile template that defines preparation of the bone. We expect this to further improve the results in the future.
function, surgical excision followed by repeated sessions of CO2 laser can slow the return of the keloid growth. This requires careful risk counselling with the patient, as keloids can always worsen with surgery.
Tight scars – scars over functional and mobile areas of the body (e.g. hands, feet, joints) may look flat but feel tight and restrictive to the patient. When the scar is too extensive to remove or realign with local flaps or z-plasties, CO2 laser is a good option to loosen scars. This probably works as a combination of micro-perforations of the scar with MTZs followed by remodelling (many patients feel increased scar pliability immediately post-laser). A combination of laser and surgical revision can effectively treat restrictive and raised scarring, releasing tension and stimulating collagen to remodel simultaneously. In summary, the treatment of scarring has progressed over the past 15 years and CO2 laser is now firmly inside the modern toolbox for scar treatment.
ED: Dr Douglas, Dr Rea and Dr GoodwinWalters are all specialist plastic and burns surgeons.
Author competing interests – nil
A ceramic version is undergoing clinical trial at Murdoch hospital, which is especially suited to female patients in whom metal on metal resurfacing has traditionally been limited due to component size and higher rates of metal reactions. Results are out to more than three years with excellent outcomes.
Author competing interests –Consulting contract with MatOrtho.
Brain aneurysms have an estimated prevalence of 1-3% and are thin-walled outpouchings of cerebral arteries, commonly occurring at arterial branching points around the circle of Willis. Risk factors include hypertension, cigarette smoking, a family history of brain aneurysms and certain inherited connective tissue disorders. Many occur in people with none of these risk factors.
For many patients, the existence of a brain aneurysm is unknown until they suffer a subarachnoid haemorrhage (SAH) due to rupture of the aneurysm – a devastating event with a prehospital mortality rate of ~12%. The mean age of occurrence is around 52 years –much lower than ischaemic stroke.
The case-fatality of SAH remains up to 35-45% and approximately 30% of patients survive with severe neurological and/or neurocognitive deficits. An unruptured brain aneurysm can occasionally present with neurological deficits due to its mass effect on the brain or cranial nerves. These are more often discovered incidentally on CT or MRI performed to investigate unrelated neurological complaints.
Elective treatment of a brain aneurysm is effective in preventing rupture but carries a periprocedural risk, which must be weighed against the estimated risk of rupture in management decisions.
The incidence of aneurysmal SAH in the entire population is about 10 in 100,000 person years. Based on this it is estimated that 1000 to 3000 in 100,000 people have an unruptured brain aneurysm. Extrapolating this generates an estimated rupture risk for an incidentally discovered unruptured intracranial aneurysm of 0.3 to 1% per year.
No successfully completed randomised controlled trial comparing conservative management with elective treatment has been done and it is unlikely one will be.
Several observational studies examined the rate of rupture in
Almost all aneurysms can be treated with minimally invasive endovascular techniques.
patients for whom a decision was made to manage their aneurysm conservatively. These studies therefore exclude the cohort of patients for whom a decision was made by neurointerventionists and neurosurgeons to treat unruptured aneurysms electively.
The PHASES meta-analysis of the larger of these studies provides some estimate of the rupture risk of different aneurysms and guidance on factors influencing it. Overall estimates of rupture rates in these observational studies are believed to be conservative, reflective of the study designs best described as audits of conservative management.
The rupture risk assessment is undertaken in a specialist clinic and based on several patientand aneurysm-related factors (e.g. age, hypertension, smoking, family history, history of previous aneurysmal SAH). The aneurysm location with the brain arterial network, size, morphology and documented growth on serial imaging form part of the rupturerisk calculation.
Aneurysm occlusion can be performed by a minimally invasive endovascular procedure, or open craniotomy and aneurysm clipping. Due to the proven lower risk of a poor neurological outcome, endovascular treatment has progressively replaced open craniotomy.
Open clipping and endovascular treatments are equally effective in preventing future aneurysm rupture. There is a higher rate of retreatment need following endovascular treatment, which varies depending on the aneurysm anatomy and the endovascular devices used, and this
is reducing over time with the rapid advances in device technology.
The recent CURES randomised trial demonstrated a lower rate of peri-procedural neurological complication with endovascular treatment, and a lower rate of needing a second stage treatment with open craniotomy and clipping. The statistically significant safety benefits of elective endovascular treatment over elective clipping were also recently demonstrated in a German registry of over 90,000 treatments. Open craniotomy and clipping represent a better option in a minority of patients. In WA, 80-90% of intracranial aneurysm treatments are now performed using endovascular techniques.
Endovascular treatment of intracranial aneurysms in WA is performed by a team of five interventional neuroradiologists at Sir Charles Gairdner Hospital working within the Neurological Intervention and Imaging Service of Western Australia (NIISWA). This is a state-wide service providing neurointerventional procedures to the tertiary hospitals.
Patients with incidental aneurysms can be referred directly to NIISWA by email or via the Central Referral System. Following in-house triaging, patients are seen by a consultant in our outpatient clinic for a discussion regarding management strategy. Cases appropriate for elective endovascular treatment are worked up, counselled, consented, and scheduled for treatment at SCGH. Complex cases are discussed in a multi-disciplinary team meeting and, if appropriate, referred to neurosurgical colleagues for consideration of neurosurgical clipping.
Treatment methods include endosaccular aneurysm coiling, with or without endoluminal balloon or stent assistance; endoluminal stent-only treatment with flow diverting devices; and intrasaccular occlusion devices.
Most patients are premedicated with antiplatelets. Some need to remain on antiplatelets for three

The time has come for the structure of medicine as we know it to change.
People are sicker than ever before, and while we may be living longer, are we actually living better?
When I was working in general practice, so many patients were living with chronic issues and on multiple medications they didn’t even know the names of, much less know what they were taking them for.
This relinquishment of power into the hands of the doctor, with the old school “doctor knows best” approach to healing, is no longer serving anyone.
For patients, this system only serves to keep them stuck – stuck in a disempowered state; stuck in understanding their illness or symptoms from a limited vantage point, in which the impacts of their mind, their emotions and their soul are sidelined.
When people are not routinely encouraged to understand how their life situation may be contributing to their health status, they miss the deeper messages the presence of an illness or symptom is attempting to bring to their awareness.
That by changing that job, leaving that relationship, addressing their loneliness, finding a purpose for their life are the things that may in fact
help reduce or eliminate the physical issues they face.
Similarly for the doctors who treat them – this system is no longer working. The system where doctors are placed in a position where all the risk and responsibility are in their hands only serves to create a level of pressure and over-responsibility that cannot be maintained.
So what is the alternative?
I believe that an approach in which we restore responsibility into the hands of the patient is the way to both empower the patient and reduce the burden on the doctor, by creating a more equal partnership in the creation of health. We need to be focusing more on providing patients with all their options, and then supporting them to choose what feels right for them and their own bodies.
This approach would require us to cultivate a level of self-awareness to avoid unintentionally speaking through our prejudiced viewpoints, which we all carry.
When people are sick, they are vulnerable. And when any professional speaks without enough self-awareness to know what their own biases are, and to remove them from influencing patient choices, they can unintentionally have a damaging effect on the person in front of them.
We are not here to tell others what path to follow. We are here to serve as healers. As guides to help people connect with themselves, and simply to use the knowledge we have obtained through our training to educate them as best we can. It is through this approach that we may start to see a shift in the state of health of the community. When people are informed and empowered, they have a chance to heal.
Other modalities are already employing these philosophies, and as respected leaders within our communities it is up to us to cease to judge them. To do so is simply a result of buying into the collective conditioned ego of our profession. Naturopaths, energy healers, acupuncturists, hypnotherapists – the list is endless, are not our enemies but our allies in the facilitation of healing.
We may convince ourselves that there are more “sham” healers to be found in the modalities indicated, though I ask you to reflect on the fact that even among doctors, there are those who fail to act in the patient’s best interest.
We need to keep up with our changing world. An old-school approach will no longer work. Let’s become doctors who heal.
Author competing interests – nil.
to six months post procedure. Patients generally spend one night in hospital and can resume normal activities including driving, the week after discharge.
A recent five-year audit of our results demonstrated a 5.9% rate of any complication including minor and transient issues, a 2.9% rate of any complication leading to a new deficit at 90 days, and a 0.5% rate of procedure related major disability or death.
Most patients have a single followup cerebral angiogram six months
after treatment. Many are followed up with MRI alone. Aneurysm recurrence has reduced over the past 30 years. In the five-year audit of our elective aneurysm treatment, 94% of patients required just a single elective endovascular procedure. All patients with brain aneurysms (regardless of treatment method) are offered long term follow-up with periodic MRI to look for new aneurysm formation.
With the increasing availability and use of cross-sectional brain imaging, most GPs will encounter patients with incidental intracranial aneurysms
in their practice. Awareness of the craft groups involved, referral pathways and knowledge of the risk assessment process outlined in this article may allow GPs to provide a sounding board for patients before and after they meet with the specialist, as well as manage the modifiable able risk factors for aneurysm growth and rupture.
ED: Dr Kabra is a consultant at the Neurological Intervention and Imaging Service of Western Australia (NIISWA) – References on request
It may have taken them a lifetime, but Hayley and Mandy McElhinney are finally working together. The Perth-born sisters have written and are starring in a darkly hilarious and emotional two-hander called Dirty Birds for Black Swan State Theatre Company.

You’ll probably recognise younger sister Hayley from her impressive acting CV, including more recently Mystery Road: Origins, Doctor Doctor and How to Please a Woman Sydney-based Mandy sports an equally successful list of work in shows such as Wakefield, The Glass Menagerie and the much-loved Rhonda and Ketut
“Mandy and I have wanted to work together for so long,” says Hayley, who now lives in Perth after working in Sydney and Los Angeles for almost two decades. “Things finally lined up and it’s interesting that the first time we step on stage together is in Perth. It feels pretty special that it’s happening here.”
The sisters had spent a long time looking for the right play or waiting for someone to ask them to work together but neither happened. During COVID, the sisters spent a lot of time on Zoom and came up with the same idea – they needed to write their own play.
“We approached Kate Champion from Black Swan and she encouraged us to keep going with the writing and to rely on each other.
“The story is many things. It’s mysterious because it’s not linear, however, the show could have only been created by us because it is about us. The characters are two women trying to figure out who they are by exploring their cultural background. They’re like bower birds trying on different personas because being themselves is excruciatingly difficult.”
The McElhinneys have mined their childhood and years of collective introspection about their Irish heritage to explore their characters’ innate longing and struggle to be themselves. It’s not exactly autobiographical but they’ve certainly drawn plenty from their lives.
The characters constantly change clothes and accents, like two children playing dress-ups in their loungeroom. They find it impossible to be themselves, run from it, dissociate and find themselves alienated and incredibly lonely.
“You can’t survive that way because it stops you really connecting and you’re not being authentic.
There’s no sense of inner strength because you are constantly trying to be other than yourself. Hopefully the characters find a way to be something new – which is themselves.”
The 2023 Logie nominee says the sisters like playing the clown and we should consider Dirty Birds a bit like Chekov injected with some Monty Python buffoonery.
“We’re making a show that we would want to watch – a lot of laughs, beauty and sadness but nothing too pretentious. I’m hoping a lot of people relate to the idea of trying to be a perfect woman, which really is impossible.”
Daughters of a cray fisherman, the sisters grew up living in a caravan. With no artists in their family, Hayley says it’s pretty amazing the sisters ended up in the arts.
“Because of not having any opportunities presented to us, we became incredibly grateful for the ones that did and we became pretty ambitious. We’re grateful we have each other. We have always been really close and a bit freaky in often knowing each other’s thoughts without talking to each other.”
continued on Page 64
are exploring their childhood in a highly personal play which sees them working together for the first time.
The approach to 3drops takes a scenic route west of Mt Barker along the Muir Highway heading towards Manjimup. Just before the West Cape Howe winery, a left turn onto St Werburgh’s Rd follows a picturesque drive through rolling hills studded with prosperous farmland and attractive bush. This is premium wine country where the continentality of the climate favours the production of quality wines capable of great delicacy of flavour.
The 3drops property was purchased 50 years ago with the original planting of 8ha of vines on Wragg Rd in 1999. This was expanded by a further 6.5ha in 2002. The 6ha Patterson’s vineyard on St Werburgh’s Rd was purchased in 2007. Its 40-year-old vines consistently yield high quality pinot noir, chardonnay and shiraz.


Interestingly there is also a strong focus on high quality olive oil, with owner John Bradbury in charge of its production. His wife Jo manages the wine business. Ray Williams is the viticulturalist. He has skilfully managed the vineyards for the past 24 years. Rob Diletti has been consistently and expertly making the wine since 2003.
All-in-all a very satisfying tasting. All wines are bursting in flavour showing lovely fruit and the deft touch of the winemaker. If forced to pick a favourite, I’ll go for the pinot. ‘Three drops’ by the way represents three very important liquids – rainwater, wine and olive oil.
From the Wragg Rd vineyard. Spring flowers, with citrus and honeysuckle aromas Crisp and lively. Not in the least bit aggressive. Very good balance and length. A joy to drink even at such a young age. Can age for 10 years if you wish. (12% alcohol, $27)
From the Wragg Rd vineyard, 80% Cabernet Sauvignon and 20% Cabernet Franc. Again, like the previous wines, pristine fruit aromas shine through. Blackcurrants, plums and a touch of tobacco. Fine-grained tannins interplay with fruit richness. This makes for a very approachable cabernet style. No doubt the cabernet franc component fills out and softens the wine adding complexity. (13.5% alcohol, $29)
From the Patterson vineyard. Straw coloured with volumes of peach and grapefruit mingling with nuttiness and vanillan. The cool climate gives a delicious freshness to the wine. Quite mouth-filling. Flavoursome and well balanced. Very approachable right now, but will easily age a for a few years. A complete package. (13% alcohol, $32)
From the Patterson vineyard. Shimmering red translucent in colour. The nose is quite seductive. Redolent of cherries and spice aromas that carry through to a crisp expansive mouth-feel held together in a background of fine quality oak. Really delicious and it will age no doubt but very hard to resist right now. (13% alcohol, $38)

 By Ara Jansen
By Ara Jansen
Life has come full circle for opera singer Rachelle Durkin. After starting her career in Perth, she spent almost two decades in New York and is now well settled back in Western Australia.
The soprano has been living in Busselton for the past few years with her husband and young son. Rachelle started her career in Perth at WAAPA. After winning the prestigious National Council Auditions in Manhattan, she earned a place in the Lindemann Young Artist Development Program at the Metropolitan Opera, better known as The Met, where she worked her way up to leading roles.
“New York was amazing,” says Rachelle. “I was young when I arrived there and worked consistently at The Met. I grew up quickly and was witness to four presidencies, 9/11, Hurricane Sandy, the Black Lives Matter movement and COVID.”
continued from Page 62
Then it was time to bring her family home, put her son into school and reconnect with the sand and surf. She’s also become artist patron of Albany-based arts organisation Breaksea.
In late October, Rachelle is starring in La Bohéme at His Majesty’s Theatre for WA Opera. She also joins other WAO stars for Opera in Kalgoorlie in November and Opera in Margaret River in December.
“I’m enjoying living near the beach and it’s nice to have family around, for the first time in a while. I’ve been doing a lot of hiking and walking. I just love being outside and I get antsy being indoors for too long now. I love to travel for work and also recently went to Albany, Denmark and Walpole. I’ve not been there since I was a kid. I’ve loved getting to know WA again.”
In La Bohéme, Rachelle plays Musetta, whose most famous aria is Musetta’s Waltz, which she sings
in Café Momus to her bohemian friends, hoping to reclaim the attention of her occasional boyfriend Marcello.
“This version has a contemporary edge and is set loosely in the 1920s, so we’re going to play with that. It’s going to be a nice challenge to find the calmness in her and look at her in a different light, instead of just playing her as over the top and for quick laughs.”
Rachelle is looking forward to working with Matt Ward, who is co-directing the opera to explore this different portrayal of Musetta. Having performed the part numerous times, she knows the libretto off by heart so her concentration this time will be on aspects such as how she shapes the character.
For more information on La Bohéme at www.waopera.asn.au/shows/ events/la-boheme
“Being able to set the tone has been one of the biggest joys of working on Dirty Birds. It’s an environment which is both respectful and vigorous. It’s one of the joys of getting older and being in this position – being able to create a work and create the environment you make it in.”
Working together has been such a treat. Because of their extensive acting experience and sometimes working in environments which weren’t the best, they also have a shared desire to foster a positive work environment to create in.
Dirty Birds is at Heath Ledger Theatre
from November 18 – December 10
Soprano Rachelle Durkin spent two decades working in New York. Now she’s living back home and Australian audiences are getting the benefit of all that experience.
MURDOCH
Wexford Medical Centre
Suite 30, Level 2
3 Barry Marshall Parade, Murdoch
Available within SJOG Campus
Specialist consulting rooms with professional practice management.
Contact: manager@murdochsp.com.au
Hollywood Medical Centre Suite 36, First Floor, 85 Monash Avenue, Nedlands

87sq m – fully fitted, large reception, 2 consulting, 2 treatment & 2 store rooms.
Contact: Kah-Lim 0400 066 160 kahlimtay@gmail.com
CANNINGTON
GP practice for sale in Cannington:
Established for past 30 years in Cannington on Albany highway right across Carousel shopping Centre. Excellent opportunity. Current owner need to move due to changes in their business model and also moving to another state. Great negotiable deal. Call 0408 928 916 for confidential inquiry.

Full or part time GP to join our amazing team in idyllic location of Broome. 5 consult rooms, 3 treatment bays and 2 FTE Practice Nurses. Awesome team environment with an easy-going atmosphere. Private-mixed billing clinic. No on-call. Emergency department located directly next to our clinic with onsite and visiting specialists. We have onsite pathology.
Remuneration: 65% of billings on an Independent Contractor Agreement. Enquiries to Katrina Dow, Practice Manager – 08 9192 2022 or practicemanager@broomemedical.com.au
MENORA / DIANELLA
Visiting GP position
Commencing April 2023
Due to the retirement of our visiting GP, Masonic Care WA is looking for a Practitioner interested in visiting three retirement villages in the Menora and Dianella areas. Consulting rooms provided at no cost
Assistance available for bookings at no cost
Hours and days to suit
Opportunity for growth to other sites
If interested please contact Emma Benjamin emma@mcwa.net.au
ALKIMOS
Jupiter Health Alkimos
A wonderful and exciting opportunity for a VR-GP has arisen to join our experienced, friendly and supportive team. We are a modern purpose-built practice based in the heart of a growing community, with 7 consult rooms and a large treatment room.
•Mixed Billing
•Pathology onsite
•Excellent reputation with patients
•Modern, well-maintained equipment
•Established and expanding patient demographic
•Close-knit and supportive team culture
•Allied health rooms available onsite
•Open 6 days a week (Sunday-Friday)
•Efficient admin and nursing staff
•Own dedicated consulting room
•Free parking
For more information or expressions of interest please send an email to Emma at p.manager@jupiterhealthalkimos.com.au
Duncraig Medical Centre GP required

Full time patient load available.
Flexible hours seven days
Excellent remuneration –$200 to $300 per hour.
Predominantly private billing practice
Modern fully computerised practice (Best Practice)
Please contact Michael on 0403 927 934 or michael@duncraigmedicalcentre.com.au
PEEL
Thinking of a sea change?
An opportunity for a full time Doctor Is available at our busy group practice. Email your CV to robyn@peelwoodmedical.com.au
COMO
Opening for VR GP - F/time or P/time
Full Private List available now from retiring GPs FRACGP essential
Up to 70% private billings
BENTLEY
Burton Street Family Practice
Unrestricted VR GP required for well-established privately-owned mixed-billing practice
GPs required
We are seeking expressions of interest from GPs who are interested in providing primary health care to the Martu and Nyiyaparli people of the Western Desert. About the Opportunity: Puntukurnu
Aboriginal Medical Service (PAMS) is seeking General Practitioners with a sense of adventure and deep respect for Aboriginal peoples and their cultures to provide on-the-ground leadership of this project.

This opportunity is available for practice within either Newman or remote communities of Jigalong, Parnngurr, Punmu and Kunawarritji (or both) on a permanent residential (Newman) or on a fly in fly out rotation. We are looking for suitable practitioners, wherein conditions of engagement are flexible and negotiable!
Reporting to the Senior Medical Officer (located in Perth and our remote communities), the General Practitioners are responsible for provision of culturally safe General Practitioner services within a comprehensive primary health care framework to the communities within which PAMS operates.
Please call 0421 610 173 or email cara.sheppard@puntukurnu.com
HARVEY
Family Friendly Medical Group – GP Positions
•DPA Area’s and MMM5 Available
•FSP GP’s are welcome to apply
•Busy & well established Medical Group with 3 Locations in the South West of WA (Harvey, Waroona & Dalyellup)


•Fully computerized and accredited modern practice with nursing and admin support
•Well supported with large team of experienced GP’s
•Situated in the beautiful South West Region surrounded by coast and forest and close to tourist areas in the south of WA
•Only 1 ½ hrs from Perth
•Family friendly working hours and no on call or hospital cover required
•65 – 70% of billings depending on experience
Please forward CV and enquiries to Kylie Wilson kyliew@harveymed.com.au
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs. Enjoy working for a doctor-owned, non-corporate, well supported, and accredited practice.
Please contact the Practice Manager on 6165 2444 or email: reception@comogp.com.au
With an interest in all areas of general practice, you are expected to share our mission to provide high-quality care for the whole family in a coordinated fashion. Serving a diverse patient demographic, we aim to manage chronic illness to avoid complications and acute issues and reduce the need for hospital presentation and admission.
You are provided clinical autonomy and supported by a strong team of Australian trained GPs, nursing and administrative staff. AGPAL and WAGPET accredited, we offer the opportunity to be involved in teaching medical students and GP registrars.
Please apply to burtonst@burtonst.com.au or call 08 9458 4558

MADDINGTON
CHURCHLANDS
Seeking a locum GP who is able to work Tuesdays, Thursday and Fridays for the months of June, July and August
No afterhours consulting
Remuneration is negotiable
Herdsman Medical Centre is a busy, family orientated, accredited Practice Well Equipped Treatment Room Clinipath adjacent Privately Owned/Mixed Billing
Friendly Registered Nurses and Experienced Administration Support For further information please Email: karen@herdsmanmedical.com.au
OPPORTUNITY FOR GPS AT MEDICAL CENTRE IN MADDINGTON
Secure your future with a partnership in or part ownership of a new venture in Maddington commencing in January 2023. Alternatively choose to remain selfemployed retaining an above average percentage of your billings. Either way we will make it a high earning opportunity for you with the option of becoming a partner or becoming part owner.
For more information or expression of interest please contact us via our email at bvmc@bigpond.net.au or call our Practice Manager on 0416 193 399
GLEN FORREST
Glen Forrest Medical Centre
GP Position
The doctors at our practice enjoy clinical autonomy and practising on their own terms. There are no KPI’s or numbers of patients per hour. Our friendly, supportive administration team are there to assist with in-house IT and management of accounts. We use Best Practice software. We have a purposebuilt treatment room and separate procedure room for Mirena’s etc with a great team of nurses to support you.
Glen Forrest Medical Centre provides quality and comprehensive care to our patients including minor surgical procedures, women’s health (Mirena/ Implanon/IUCD), men’s health, IV fluids, iron infusions, mental health, paediatrics, adolescent health, complex medical comorbidities and palliative care. Please contact Maria Clark on 08 9298 8555 or email mariac@gfmc.com.au

Ocean Village Medical Centre is privately billing medical practice located in the heart of Wembley Downs. We are looking for an experienced General Practitioner to add to our growing practice.
Complimented by a team of high-quality Doctors, Experienced Practice Nurses, Allied Health and Admin team to support your practice, we offer a friendly working environment, modern facilities and an established patient base. Our ideal GP will be an all-rounder with the ability to take on new patients and offer morning and afternoon appointments to accommodate needs of our community with attractive remuneration on offer for the successful candidate.
If you are interested, please email your CV to pmgr@ovmc.com.au or phone Jess for a confidential discussion on 0418 927 010
GP FT/PT
Edgewater Medical Centre is an accredited, mixed billing, medical practice in Edgewater, Western Australia and seeking a General Practitioner to join our friendly, patient focused team. Work place:
You will be working with a dedicated and professional team of administration, nursing and health staff supporting GPs within this busy practice, providing a full range of medical services. The focus is on personal care, attention and expertise.
Role:
As an experienced GP, this role will allow you to provide high quality primary health care services to the community, in keeping with best practice standards.
Essentials:
•Applied knowledge, skills and experience in general practice
•Unrestricted VR GP qualification
•Full Australian Work Rights
What’s in it for you:
ATWELL
Require VR GP’s Unrestricted for Part-time Positions:
As an experienced GP, this role will allow you to provide high quality primary health care services to the community, in keeping with best practice standards.
Essentials:
•Applied knowledge, skills and experience in general practice
•Unrestricted VR GP qualification
•Full Australian Work Rights
What’s in it for you:
•Supportive and Experienced Admin team
•Doctor owned practice
•Nurse Support
•Onsite Pathology
•Flexible arrangements
•AGPAL Accredited Practice
•Located near FSH and SJOG Murdoch
•Mixed Billing (mainly Private)
JOONDALUP
Candlewood Medical Centre has an exciting opportunity for a General Practitioner to join our very well established, Privately owned and very busy accredited practice which provides quality medical care to the community for over 30 Years.
You will join a wonderfully passionate, friendly, and supporting Team, in a warm and welcoming environment.
As part of the Candlewood team, you will have a great work, life balance and will have the flexibility to work either FullTime or Part-Time, - Weekend and After Hour appointments are also available as we are open 7 days per week.
Locum General Practitioners are also very welcome
Benefits:
• very large existing and loyal patient base, with great patient demographics.
• Mixed Billing Weekdays & Private Billing only on Weekends- very competitive high remuneration potential available.
• Supported by a dedicated Practice Management, IT and long-standing Nursing and Administration Staff.
•Accredited Teaching Practice.
• On Site services including Allied Health, Pharmacist and Pathology.



• Highly reputable and established clinic within the community and surrounding suburbs.
•A committed Team of 7 GP’s and Nurse Practitioner.
•Great Location and Free Parking
•5 minutes’ drive from the beautiful local beaches and 30-minute drive from Perth CBD.
For more information, contact Practice Manager -Karon Hay on 08 9300 0999 email: candlewoodmedical@outlook.com
PERTH
Breast Clinic seeking VR GP
Perth Breast Clinic is seeking an enthusiastic VR GP to join our expert team of breast physicians, 1 – 2 days per week.
Located in the Mount Hospital Medical Centre, Perth Breast Clinic offers a comprehensive service for women, from breast screening and diagnosis through assessment of symptoms, diagnosis and management of breast cancer and benign breast disease. The clinic is led by our specialist breast physicians who work as part of a multidisciplinary team comprising radiologists, surgeons, pathologists, oncologists, nursing and support staff.
We offer
•Comprehensive training and mentorship by highly experienced breast physicians

•Flexible work hours, 1-2 days per week
•Mixed billing, low service fee
•Onsite parking
Requirements
•AHPRA registration / Medical Indemnity insurance
•Previous experience in women’s health
•Advanced communication skills
For further information, please contact Tasha Pratt by email tasha.pratt@healthscope.com.au or phone 0477 961 871
75% OF BILLINGS!!
Taking over existing patient base in brand new purpose-built surgery in Burswood. Looking for VR GPs and non-VR GP’s on a full time/part-time basis for weekday and Saturday afternoon (DWS) sessions.
Fully computerised with on-site pathology and RN support.
Please contact Dr Ang on 9472 9306 or Email: info@thewalkingp.com.au
•State of the art equipment, technology & facilities
•Supportive team
•Doctor owned practice
•Nurse Support
•Onsite Pathology
•No call outs– Week Day 8-5 roster
•Free parking onsite
•Flexible arrangements
•70% of billings
•Initial Guaranteed payment of $150.00 per hour in first 3 months For a confidential discussion, please contact Cecelia – (08) 9306 1899 or CeceliaC@edgewatermedical.com.au
If you are interested please contact our Practice Manager for further information on 9332 5556 or email: adminmetrogp@metrogp.com.au
BULL CREEK
Bull Creek Medical – VR GP opportunity

We are seeking full time or part time VR GP to join our friendly team. It is a mixed billing well established practice providing quality health care for many years.
It is located closer to world class public and private hospitals and near by top public and private schools. Flexible working hours and terms and conditions are negotiable.
If you are interested in this exciting opportunity, contact practice manager via email: admin_pm@bullcreekmedical.com or call on 08 9332 0488
MetroGP Requires a VR GP
Unrestricted for Part-time Position: As an experienced GP, this role will allow you to provide high quality primary health care services to the community, in keeping with best practice standards.
Essentials:
•Applied knowledge, skills and experience in general practice
•Unrestricted VR GP qualification
•Full Australian Work Rights
What’s in it for you:
•Supportive and Experienced Admin team
•Doctor owned practice
•Nurse Support
•Onsite Pathology
•Flexible arrangements
•AGPAL Accredited Practice
•Located near FSH and SJOG Murdoch
•Mixed Billing (mainly Private)
If you are interested please contact our Practice Manager for further information on 9332 5556 or email: adminmetrogp@metrogp.com.au
GREENWOOD
Kingsley Family Practice
We are seeking a part time or full time GP to join our well established, busy practice.
You will work in a highly equipped AGPAL accredited practice, alongside GPs with extensive specialised skills, including skin cancer surgery (including flaps and grafts), cosmetic medicine, ultrasoundguided musculoskeletal PRP injections, IUD insertion, ENT operating microscope use, and much more.
The practice itself is highly equipped, including on-site ECG, spirometry, ABI machine, ultrasound, digital dermoscopy imaging, ambulatory BP monitoring and a full time chronic disease management nurse.
Mixed billing, offering our GPs 70%. All appointments privately billed on Saturdays.
For more information please email kingsleypractice@gmail.com or call our Practice Manager Tracy Weare on (08) 9342 0471
Shenton Avenue Medical Centre has a great opportunity for a General Practitioner to join a very well established practice.

•Wonderful, friendly staff.
•Experienced doctors.
•Very large existing and loyal patient base.
•Mixed billing practice.
•75% of billings.
•Non-Corporate.
•On-site services including Pathology, Physiotherapy, Podiatry, Dietitian
•Fully accredited practice.
If you are interested in this exciting opportunity please contact Phil at phil@medibizz.com.au
Contact Andrew, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert
The role would suit a new Fellow or GP who wants to curate their own patient base with a guaranteed minimum offered for 3 months.
Work in a fantastic environment – a non-judgemental, respectful and safe space with a supportive nursing and admin team.
Enjoy an innovative, modern practice with the latest equipment and software (BestPractice).

Choose your hours – our clinic is open from 8am to 7pm Monday-Friday, 8-1pm Saturdays.
Get to know your colleagues with quarterly team-building activities Sub specialise – for the right applicant, we’re happy to support your special interest.
Central location - 15 minutes from the CBD, extensive parking available.
Contact: PracticeManager@balcattafamilypractice.com.au or call Debbie on 08 6478 3955
Northbridge Medical Centre is looking for a VR General Practitioner to join our well-established private billing medical practice located between Perth CBD and Mt Lawley
Ownedandoperatedbydoctors
Highpatientload
TakingoverexistingpatientbasefromrelocatingGPs
FullTimeorPartTimePositionavailablenow 65%billingswithminimumof$150/hour forthefirst6months
Joiningateamof6Doctorswithsupportive Nursing,ManagementandMarketingteam AGPALaccredited,wellequippedandfully computerizedwithBestPracticesoftware Doctor’sparkingavailable
Requirement: MBBSorequivalent,Vocational Registration/Fellowship,currentAHPRAregistration
Ifyouarelookingtopracticequalitymedicineina supportiveenvironment, please contact Dr Alex Koh on 0408 037 290 foraconfidentialconversationor email at Alex@northbridgemedical.com.au
Join our friendly Health Services team to provide quality care and make a difference in Curtin Community’s health and well-being at our Bentley campus.
Part-time and full-time contractor/temp opportunities available
Excellent working conditions and room facilities Administrative and Nursing support provided
JOB REFERENCE
Are you a caring and experienced General Practitioner? Join our friendly and collaborative team of general practitioners, nurses, medical receptionists, and a Practice Manager to make a difference to our Curtin Community’s health and well-being within our busy Medical Centre at our Bentley campus.
Our Medical Centre is a well-established and fully equipped practice with a total of 7 consulting rooms, a procedure room, treatment, and onsite pathology. The Centre is open Monday to Friday between 8:30 am and 4:30 pm. It is well-served by public transport and has ample parking.
We offer mixed billing (70% bulkbill) with flexible consulting hours. Our GPs are fully supported by a practice manager, registered nurses, administration staff and a mental health nurse practitioner. Our Medical Centre has high volumes of patient demands and full-appointment books during semesters. This is a large and diverse patient base offering lots of interesting work, plus walk-ins, opportunities for Healthcare Plans Health Assessments, and procedures.
BENEFITS
70% of the billing/mixed billing
Work full-time or part-time with flexible hours. You choose!
Excellent working conditions and room facilities
Walk into a full & immediate patient base, OR create your own, with walk-in presentations
Best Practice software in use throughout the practice
REQUIREMENTS
MBBS or equivalent
Current AHPRA registration as a General Practitioner
Vocationally Registered (VR)
No restrictions
To learn more about this opportunity, please contact Nandita Nadkar, Team Leader on 08 9266 7345.
For more information about our university, please visit www.curtin.edu.au
Applications close: 15 December 2023
Enjoy the perfect blend of professional fulfillment and an enviable coastal lifestyle. Our well-equipped and staffed clinic offers the resources and support you need to provide topquality care to our diverse patient community.
Collaborate with like-minded professionals in a vibrant and inclusive environment that encourages growth and learning. Outside of work, immerse yourself in the breathtaking natural beauty of Albany’s coastline, with pristine beaches and lush landscapes waiting to be explored.
Enjoy the benefits that working and living in regional WA offers, and a work-life balance that allows you to embrace the wonders of coastal living. A perfect opportunity for a GP, GP Obstetrician or GP Anaesthetist!
Apply now and embark on an extraordinary career journey in Albany, Western Australia.

Perth and suburbs



At Perth Cardiovascular Institute we believe in providing more than just a diagnostic imaging service. Our team are committed to delivering an excellent patient experience along with clinically robust findings in a timely manner.
Senior staff perform as leaders and assist with training, mentoring and development of less experienced team members. Much of our time is dedicated to ensure our trainees develop superior skillsets to tackle even the most difficult of cases. We foster an environment that promotes asking questions, seeking feedback and sharing of knowledge.
We have world class, internationally renowned cardiologists within our group that support and develop individuals. Our cardiologists are approachable to discuss patient findings and encourage and enable team members to manage patients. In completing our daily duties we go above and beyond expectation with clients repeatedly providing outstanding feedback from their contact with us.
If you wish to know more about the role, feel aligned to the way we do things and are excited by the unique opportunity Perth Cardio offers then we would be thrilled to hear from you.

Please contact Adam Lunghi on Phone (08) 6314 6881 or info@perthcardio.com.au
or Terry MacKinley (Practice Manager) on (08) 9845 9000

We are seeking a skilled and passionate cosmetic doctor/aesthetic physician to join our team at a cosmetic service co-located with a large dermatology practice in Karrinyup.
This is a fantastic opportunity to work in a thriving and rapidly growing service with strong demand.
Attractive remuneration package: We believe in recognising the value of Excellent working relationship with onsite Dermatologists: You will have
Support, clinical advice, and cross referrals:
Advanced training opportunities: While we require you to have FRACGP or equivalent
Are you a passionate GPseeking a fulfilling opportunity in a amazing coastal town?
Look no further! Join our dedicated team in Denmark, Western Australia, and experience the perfect blend of a rewarding career and a tranquil lifestyle.
Ourclinicprovidesasupportiveenvironmentwith modernfacilitiesandadvancedresourcestodeliver excellentpatientcare.Collaboratewithateamof skilledprofessionalswhoshareyourcommitment tohealthcareexcellence.
InDenmark,you’lldiscoveravibrantcommunity surroundedbybreathtakingnaturalbeauty.Explore pristinebeaches,lushforests,andenjoyoutdoor activitiesinthisidylliccoastalsetting.Benefitfrom ahealthywork-lifebalanceandembracetherelaxed paceofacoastaltownwhilemakingapositive impactonpatients’lives.
Apply now to embark on an incredible GP journey in Denmark, Western Australia.
CONTACT recruitment@denmarkmedicalcentre.com.au or Terry MacKinley (Practice Manager) on (08) 9848 4111

Freo Street Doctor is a highly rewarding and unique work environment – A well respected mobile medical service supporting the needs of disadvantaged and vulnerable people.

BENEFITS INCLUDE:
Complexandchallengingpatientcases
Workinacloseteam,alongsidearegisterednurseandoutreachworker Administrativesupportforbillingandclinicalcoordination
Enjoythesatisfactionofdeliveringanessentialservicethatistrustedbypatients andthebroadercommunitytoprovideanenduringpositiveimpact Noschedule8drugsorneedleexchangeoffered
AhighqualityandRACGPaccreditedservice,supportedbyarobustClinicalGovernanceFramework.
Hillarys Medical Centre is a very busy practice located 15mins from the Perth CBD along the coast. We have a strong focus on family & preventive health medicine.


We are a team of 10 doctors with excellent administrative and nursing support staff. We have been in Hillarys for 20 years with dedicated GP owners. We pride ourselves with providing exceptional health care to our community of Hillarys.
We have a modern purpose built well equipped 3 bed treatment room and 10 consulting rooms with quality equipment as well as a spacious staff & meeting room. We are also able to offer secure remote access and secure onsite parking. Pathology & Pharmacy are within our complex.

There is a high-income potential as we are mainly a private billing practice. We would also encourage doctors to develop their own special interests
Our patient base is varied as well as a strong family base practice including women’s & mens health, skin cancer medicine, iron infusions, aviation medicine and more. Our nurses are committed to support for care plans & health assessments.
We are a 7 day a week (Mon to Thur 8am to 7pm, Fri 8am to 6pm, weekends 8.30 to 12.30pm) we have a variety of sessions available and the opportunity to share a Saturday roster with your fellow GP colleagues, with nursing support.
We would require:
Current unrestricted registration with AHPRA as a general practitioner

Current medical indemnity insurance
Full Australian working rights and No DPA restrictions















