






It’s a critical time to talk about lungs.
While we are still having the conversation about smoking harm, 30 years of ongoing public health campaigns have made enormous inroads into smoking cessation rates. However, now vaping is catching the attention of doctors, public health experts, law enforcers and policy makers and causing great worry.

It is no longer a sneaky fag behind the school shed, vaping has become all-pervasive in schools, workplaces and in entertainment precincts, and like tobacco, it has become big business. Simply reference the WA Health Department’s first (an only) seizure of illegal vapes.
While it has been the first in a months-long campaign, it was a doozy – 15 tonnes of vapes were seized from a warehouse in Perth's north-east in August, estimated to be worth $10 million. This alone should ring warning bells for politicians and law enforcers.
As for the health industry, the notion that something which smells like Fruit Tingles can’t be harmful has been well and truly debunked by the scientists.
Doctors are warning that e-cigarette and vaping-associated lung injury (EVALI) is a real threat now, and that’s without having to wait for medium-to-long-term data to come in. Dr Sina Keihani has written a fascinating (and sobering) clinical update on page 47. If this discretionary pollution of our lungs isn’t enough, there is the deteriorating state of the planet, and for us in Australia, on the brink of another fire season, that is of increasing concern.
I am lucky to be close enough to magical tracts of city bushland to take regular walks. Now these landscapes are just beginning to unfurl their spring colours. As I drove out of stunning Bold Park this morning, the radio news reported that fire protection officers were already concerned about the forecast predicting drier spring and the heavy fire load of our bush.
At best, and I use the term loosely, it means more burn-offs and at worst bushfires. With every bad fire season, a bad asthma season is heralded. At least we have a better understanding, thanks to local doctors GP Dr Tom Brett and respiratory physician Dr John Blakey what inhalers emit less harmful greenhouse gases.
Everything is connected, nothing just happens. It might have been a dippy hippy saying when I was a girl, but we all have to adopt conscious living. Our lungs and the planet’s lungs need us to.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
Doctors are warning that e-cigarette and vaping-associated lung injury (EVALI) is a real threat now
12 Close-up: Dr Femi Oshin

16 GPs could be the answer to ADHD logjam

22 AI: to boldly go…

32 Multi-faceted research targets MS LIFESTYLE
58 Dr Peter Burke’s new book, The Silk Merchant's Son
59 WASO mood music
60 Rediscovering our beauty
61 Wine review: Arlewood Estate – Dr Craig Drummond
62 Artist Rachel Coad’s new passion
1 Editorial: Every breath we take – Jan Hallam
4 News & views
6 In brief
20 RACGP boss heads bush
27 ChatGPT beware – Dr Fangli Hu
28
43 Trust – Dr Joe Kosterich
57 Lung health scorecard
Dr Helen Mead from Perth Children’s Hospital has won the Nikola Estate doctors dozen in our monthly competition.

This month on page Dr Craig Drummond reviews the exciting red wines from Arlewood Estate. See his review on page 61.
To win the wine, use the QR code on this page or go to www.mforum.com.au and hit the competitions tab.
PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au

EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au


Journalist Eric Martin 08 9203 5222 eric@mforum.com.au


Clinical Editor Dr Joe Kosterich 0417 998 697 joe@mforum.com.au






Marketing Rhiannon Arnold rhiannon@mforum.com.au


Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory
Andrew Bowyer 08 9203 5222 andrew@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222
Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au
OUR


The Shire of Murray, which has its administrative base in Pinjarra, has established a multi-agency steering committee to undertake a health and social needs analysis so it can help identify a long-term solution to health care provision for its 18,000 residents.

Shire President, Councillor David Bolt, said the Murray Health Futures Steering Committee had representatives from the Shire, South Metropolitan Health Service, WA Primary Health Alliance and Peel Development Commission.
“With the population expected to grow from 18,000 today to around 71,000 by 2051 – comprising a higher proportion of older residents than Perth – now is the time to identify a suitable long-term solution for future generations,” Cr Bolt said.
“The steering committee will explore opportunities and develop a business case for government consideration. As part of this project, we will be undertaking a health and social needs analysis. This will inform our submission to government, ensuring our proposed solution meets the needs of the people in and around Murray.”
Statistics show, people living in Murray have more longterm health conditions (37%) – such as arthritis, heart disease and lung conditions – than Greater Perth (30%). They also tend to have limited access to public transport.
The health and social needs analysis will begin midAugust and will include broad community and industry
Australia will take part in an global study into community-based health care that will explore the outcomes, experiences and satisfaction of patients with chronic diseases who are treated in GP practices.
Australia is one of 20 countries participating in the inaugural Patient-Reported Indicator Survey (PaRIS) Health Survey, an initiative of the Organisation for Economic Cooperation and Development (OECD).
For the first time, patients across the world living with a chronic condition are being asked to share their experiences so that healthcare providers can better understand their needs and in turn, improve care.
The Australian Commission on Safety and Quality in Health Care is implementing the survey here with ORIMA Research, on behalf of the Department of Health and Aged Care. The survey takes about 20 minutes to complete and examines:
• measures of physical and mental health
consultation through surveys and workshops, and the assessment of official health data.
Residents and health service providers in Murray and the surrounding areas are invited to complete an online survey accessible from the council’s website between 16 August and 22 September.
“We are also inviting residents and service providers from neighbouring local government areas to participate, as we acknowledge our solution may also be of benefit to them,” Cr Bolt said.
“So, if you are in Mandurah, Boddington, Waroona, or Serpentine and Jarrahdale, we also welcome your feedback.”
• experiences of GP consultations
• how health information is communicated.
GP practices across Australia are invited to sign up for the PaRIS Health Survey, open until October 31. 2023. Patients of GP practices who register can take part in the survey.
With nearly half of all Australians having one or more prevalent chronic conditions, Australian patients will have a lot to contribute. The online survey is available in English, Chinese Simplified, Punjabi, Vietnamese, Arabic, Greek and Italian. Support is also available for patients who need help to complete the survey.
Gambling and its impact on health is big news. Curtin University researchers are refining their inquiry to the effect gambling advertising has on 16 to 17-year-old West Australians in a series of workshops. Healthway is funding the Young
Voices on Gambling project, which will ask participants to document their day-to-day interface with gambling advertising and then have their say at workshops that will be held through to the end of the year.
Project co-ordinator Louise Francis from Curtin’s School of Population Health said many gambling promotions are visible to children and young people and research shows that they find these ads appealing and have high brand awareness.
“We’ll work with study participants to document what ads they see and their thoughts on the advertising and the marketing strategies used by the gambling industry. These young citizen scientists will then collaborate with us on recommendations for policy to reduce gambling-related harm in the community,” she said.
It is expected that Healthway will receive the report by mid-next year.
continued on Page 6
Every winter virus season is unique, especially influenza trends. Wellestablished global influenza surveillance systems aim to gauge, predict, report and ultimately provide guidance for protection (vaccine development) for the upcoming influenza season.
The ongoing COVID-19 pandemic adds another layer of complexity in making an accurate clinical diagnosis of winter respiratory illness, necessitating a robust, multiplex respiratory PCR assay to enable accurate and timely diagnosis and pathogen-directed specific therapy.
The 2022 Special Report COVID-19 U.S. Impact on Antimicrobial Resistance by the Centers for Disease Control and Prevention (CDC) found the impact of the pandemic on alarming trends in antibiotic resistance and on antibiotic prescribing practices. This is attributed to the pandemic, which pushed healthcare facilities and health departments in the US near their breaking points, with a significant increase in antimicrobial use and difficulties in following infection prevention and control guidance.
Resistant hospital-onset infections and deaths increased by at least 15% during the first year of the pandemic, 2019 versus 2020. The increase in hospital onset-infections due to resistant pathogens varied from 13% for MRSA, 32-35% for ESBL-producing Enterobacterales, carbapenem-resistant Enterobacterales and multi-drug resistant P.aeruginosa to 78% increase for carbapenem-resistant Acinetobacter sp.
The pandemic also impacted antibiotic prescribing, where antibiotics were often the first treatment prescribed for any febrile pulmonary illness, which often turned out to be COVID-19, a viral illness where antibiotics had no effect. The importance of preserving and prolonging the efficacy of the currently available antibiotics by being responsible antibiotic stewards is emphasised.
The Australian Influenza Surveillance report #08, 2023, noted 174,898 laboratory-confirmed influenza cases, with 162 influenza-associated deaths
By Dr Sudha Pottumarthy-Boddu MBBS FRCPA D(ABMM)Dr Sudha Pottumarthy-Boddu has a distinguished career in microbiology with extensive experience in the US New Zealand and Australia. Sudha is a Diplomate of the American Board of Medical Microbiology, and a member of both the Antimicrobial Stewardship Committees and Infection Prevention and Control Committees at multiple St John of God hospitals in WA.

identified in the year-to-date in the NNDSS (National Notifiable Diseases Surveillance System). Of the laboratoryconfirmed influenza notifications
Australia-wide in 2023, 62.64% were influenza A, with influenza B accounting for 35.19% of notifications (the rest being mixed infections or untyped).
This is in contrast to the reported influenza season notifications of 2022 (National 2022 Influenza Season Summary), where influenza B accounted for only 0.2% of influenza notifications, the majority being influenza A (82.7%). Unlike influenza A viruses, which are also found in several different animals (ducks, chickens, pigs, whales etc.), influenza B viruses circulate widely only among humans.

Influenza notifications in WA from January 1 to July 23, 2023, reflect trends not dissimilar to the national data. Of the 15,280 influenza notifications during this period, 75% were influenza A, 24% influenza B and 1% untyped (Surveillance and Disease Control Program, Communicable Disease Control
Directorate). The trend data of PCR positive influenza detections at PathWest 2022-2023, also depicts the continuing presence of circulating influenza B virus throughout this year-to-date, differing from that in 2022 (Fig 1).
Given the ongoing influenza notifications in Australia in 2023, in the face of resumed worldwide travel and limited social restrictions, the trends of winter respiratory illnesses continue to evolve over the season. The use of the multiplex respiratory PCR assay allows for an accurate and timely diagnosis of respiratory viral illness, early administration of appropriate antivirals if indicated, and at the same time limits the unnecessary use of antibiotics.
Acknowledgements: We thank Cara Minney-Smith, Kritu Panta, Avram Levy and staff of the Microbial Surveillance Unit at PathWest Laboratory Medicine, Perth, WA, for providing influenza subtyping data.
– References available on request
WA faculty chair of the RACGP Dr Ramya Raman has been selected to be a part of a 15-person Australian delegation to the Australia India Youth Dialogue this month. The five-day exchange aims to raise and discuss the geo-political relationship between the two countries.
Little Green Farmer CEO and founder Fleta Solomon is moving to a part-time executive director role and long-time COO Paul Long has stepped into the role. Ms Solomon will focus on external communications, market positioning, environmental, social and corporate governance (ESG) and branding.
The federal government has announced a $114.2 million boost to universities for an extra 80 news commonwealth supported medical places (CSPs) for rural-trained medical students, as well as $82 million capital funding for new regional training facilities.

St John of God Mt Lawley Hospital is first hospital in WA to undergo and pass NSQHS short notice accreditation (24 hours), with full compliance to the eight core standards.
Members of the Claremont community came together to celebrate Bethesda Health Care’s milestone 80th anniversary.
Opening in 1943 with 14-beds, Bethesda is now an 86-bed surgical and specialist palliative care hospital with nine state-of-the-art operating theatres, a community palliative care service and a recent historical expansion to a second site mental health hospital in Cockburn.
The anniversary was recognised at the hospital’s annual Celebration Day, which recognises the achievements of the organisation and Length of Service awards. This year, 34 staff were acknowledged for their length of service. Chef Steven Taylor, pictured here with Bethesda chairman Dominic Bourke) has been with Bethesda for 30 years and and Surgical Ward Manager Sally Winfield and Hotel Services Manager Rohitha Siriwardena were jointly awarded the Matron Beryl Hill Exemplary Professional Practice Award.
continued from Page 4
GP Dr Brett Montgomery and respiratory physician Dr John Blakey have done an analysis of inhaler devices on the market to illustrate those that are kinder to the environment. Their research was published in the Australian Journal of General Practice
With the number of people using the devices for asthma and COPD, Australians use millions of inhalers each year. Apart from the pollution emitted from their manufacture, transportation and disposal, some pressurised inhalers’ propellants use hydrofluorocarbons, which, while ozone safe, are still potent greenhouse gases.
They have found that inhalers other than metered-dose inhalers were kinder on the environment. There is now a wide array of dry powder inhalers on the Australian market and a soft mist inhaler which are free of the HFC propellant gases that make MDIs so polluting.
You can read the full article at https://www1.racgp.org. au/ajgp/2022/december/respiratory-inhalers-and-theenvironment
continued on Page 10

Defence departments attract a lot of funding, but the US Department of Defense (USDD) is pushing some back and to the Perron Institute in WA for researchers who are working on a drug for Amyotrophic Lateral Sclerosis (ALS) the commonest form of motor neurone disease.
The USDD grant of $760,000 is a welcome addition to funding secured for the research.
Principal Investigator Dr Sarah Rea, from the Perron Institute and Murdoch University's Centre for Molecular Medicine and Innovative Therapeutics (CMMIT) said her team would be investigating the mislocalisation and abnormal aggregation of a protein called TDP43 in surviving neurons.

Co-investigators are Dr Loren Flynn (Perron Institute and CMMIT), Professor Anthony Akkari (Perron Institute and CMMIT), Professor Sue Fletcher (Murdoch University), Professor Brad Turner (Florey Institute) and Associate Professor Rakesh Veedu (Perron Institute and CMMIT).
“Delivery into the central nervous system remains a critical problem for the development of effective neurodegenerative disease therapeutics, and we now have three major grants allowing us to attack this issue from multiple avenues.
“The ongoing support of the Perron institute, the Racing for MNDi Foundation and the WA Health Department has provided the support needed to progress the project and secure this substantial funding,” Dr Rea said.
MAJOR PARTNER BACK

CRS utilises body plethysmography machines - the gold standard in respirator y testing available to all patients
In one session, CLFT can help assess the functioning of your patient’s air ways, lung capacity and gas exchange to differentiate diagnosis and determine severity and progression of respirator y disease This includes assessment of:
SPIROMETRY: used to assess airway calibre and ventilatory capacity. Assists in determining obstructive or restrictive ventilatory defects and identifying any reversibility.
Conditions include but are not limited to: Asthma, COPD, Emphysema, Bronchiectasis, Fibrotic diseases.
DLCO (Gas Transfer): used to assess the integrity of the blood-gas interface as well as estimating the volume of lung that is ventilated for gas exchange. A precise but nonspecific measurement of the transfer to the blood gas barrier, and the complex interactions between the lung parenchyma and the pulmonary vasculature.
STATIC LUNG VOLUMES: Utilizes body plethysmography, the lung volume gold standard, to measure all gas in the lung including unventilated volume. It can confirm a restrictive defect or identify gas trapping and / or hyperinflation.
MAXIMAL RESPIRATORY PRESSURES: Assessment of respiratory muscle strength. Useful for identifying and monitoring respiratory muscle weakness such as in neuromuscular disorders.

Available
MANNITOL CHALLENGE: Changes the osmolarity of the airways such that any inflammatory cells present will release mediators and cause bronchoconstriction. Useful and calibrated test that is specific for Asthma but not sensitive.
FeNO: (Fractional Expired Nitric Oxide): Higher in the presence of inflammation in the airways. Useful aid in asthma diagnosis and over time in titration of ICS dosage and efficacy.
SIX MINUTE WALK TEST: Assesses patient’s levels of oxygen desaturation or otherwise and walking capacity with chronic lung disease.



continued from Page 6
Australians living with one of 200 chronic conditions may be eligible to participate in a global study into the impact of medicinal cannabis treatment on health economic outcomes and quality of life for patients suffering from chronic health conditions.
The QUEST Global study, led by Curtin University and sponsored by medicinal cannabis supplier Little Green Pharma (LGP) and HIF health insurer, will assess whether medicinal cannabis reduces the economic impact of chronic disease, by reducing both the number of medications a patient requires and their need for health-care services.
Lead researcher Associate Professor Richard Norman, from the Curtin School of Population Health, said QUEST Global aims to address real health challenges faced by many people living with chronic conditions such as pain, anxiety, insomnia and mood, development or movement disorders.
“Using medicinal cannabis as a treatment option may help to improve their outcomes and reduce their level of suffering and this study
is an opportunity to quantify this,” A/Prof Norman said.
“As part of the study, participants can access pharmaceutical-grade cannabis oils and flower medications made locally, as well as consult affordable, independent doctors who are experienced medical cannabis prescribers.
“We hope to gain more information about the benefits of using medicinal cannabis to treat chronic conditions and how we can make these types of medications more economical.”
Following on from the unveiling of the statue of Perth nurse Lieutenant Colonel Vivian Bullwinkel AO MBE ARRC ED FNM FRCNA, the Australian College of Nursing (ACN) has announced that 21 scholarships in perpetuity, known as the ACN Bullwinkel Scholarships, will be granted to honour the memory and sacrifice of the 21 nurses who were massacred at Radji Beach on Bangka Island, Indonesia, in February 1942, along with the sole survivor Lt Col Vivian Bullwinkel.
The scholarships will be for ACN Institute of Leadership and Post
Graduate courses. Sponsors include Aspen Medical, Bupa, Serco, Leidos and Boeing and the Federal Government has matched funding with a grant of $1 million.
Nominations for the $10,000 scholarships open in September 2023 and successful candidates will be announced on February 16 – the anniversary of the massacre 82 years ago.
Details on the ACN website.
The Pharmaceutical Benefits Advisory Committee (PBAC) announced in August that Keytruda (pembrolizumab) will be recommended for subsidy on the Pharmaceutical Benefits Scheme (PBS) for early-stage triple negative breast cancer (TNBC).
Keytruda is one of the first immunotherapies that has shown to be effective for early-stage TNBC. When combined with chemotherapy after surgery, it can reduce the risk of cancer recurrence when compared to chemotherapy alone.
Around 15% of breast cancer diagnoses are triple negative. In Australia, that equates to about 3000 new cases each year.
“In preparation for transition and closure, WAGPET wrote this e-book about delivering GP training and workforce (AGPT program) 2001-23 – no topic unaddressed, courageous, honest – lots of wonderful and painful memories, lessons we learned, and lessons yet to learn, especially about the kryptonite that must be addressed if we are ever to be serious about closing the gap for our Aboriginal and rural, remote, and disadvantaged outer urban communities,” Dr Bell says.
When this is translated to GP training in WA, which has been one of the state’s, indeed the country’s most pressing need, the turbulent 1980s and 90s of disruptive primary care policy were replace by two decades of a single training organisation – WA GP Education and Training (WAGPET) – which was under the leadership of Dr Janice Bell for 18 of those 20 years. With training returning to the colleges – and all the complexity that is involved with it – it has left

WAGPET to windup, with its highly experienced staff moving to various aspects of the new training system. But before the doors closed, the organisation has produced a book, Being There
Dr Bell describes it as a “message stick” to the funders and organisations that are now responsible for GP RG training.
“We hope people will enjoy it, and – like us – appreciate the magnificence, adaptability, generosity, and ingenuity of our communities and the profession that serves them.”
You can access an electronic copy of Being There from the WAGPET website at www.wagpet.com.au/about/ being-there
WA has always done things a little differently – we have had to, being a vast land mass with vastly different health needs within it.2001-2023



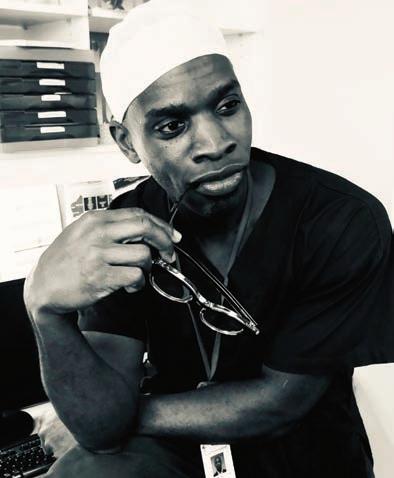
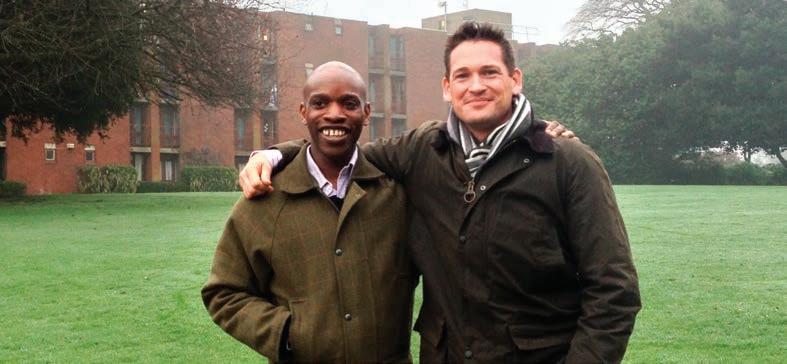
Dr Femi Oshin didn’t take a direct route to medicine, but an engineering degree has certainly helped the vascular surgeon in his area of passion – diabetic foot disease in rural and remote communities.
By Ara JansenIn Nigeria, doctors, engineers and teachers are prized professions. In Dr Femi Oshin, his family got all three.

Femi is a vascular surgeon and medical co-director of the Hospital Logistics and Acute Access Division at Royal Perth Hospital as well as being a transplant to Perth. Femi – or Olufemi to his mum – holds degrees in both engineering and medicine. The former it turns out has been hugely helpful for a doctor.
An excellent high school student, but when it came down to the final exams, 17-year-old Femi didn’t perform as well as he’d hoped. He’d been provisionally accepted into several medical schools but his exam results didn’t stack up. Instead, he went into engineering at the University of Liverpool, focusing on tissue engineering and material science.
The work was interesting. He investigated all sorts of cutting-edge ideas such as regenerating or replacing body parts such as lenses in the eye, and hip and knee joints. There were lots of lessons from the aerospace industry to create advanced materials and in some instances, this was coupled with cell
technology to create biomaterials that restore or augment biological tissue function.
“It was fascinating,” says Femi. “And closely aligned to medicine. Turns out, a lot of the things I did have been very applicable to what I am doing now. We’ve been using engineering solutions on some of the problems we have in vascular surgery.
“I have been involved in research looking at people who have lost body parts through diabetes, and what materials we can use to regenerate lost tissue. I work with some extremely talented engineers and they love that we can talk the same language.”
Femi completed his engineering degree and obtained his medical degree in 1999. Partway through his postgraduate medical training, he took two years out to focus on research and was awarded his doctorate. He completed vascular training in his late-30s after 10 years in the surgical training program in the United Kingdom.

Born in Ethiopia to Nigerian parents, Femi’s father worked for the Nigerian foreign service. The family moved around a lot and his youngest brother was born in France. When Femi was six, the family moved to the UK. A British education was highly prized, so the family settled in London for the children’s education.
“I always had an interest in medicine and wanted to help people, particularly through surgery as I like doing things with my hands and being precise. I remember when we were growing up, my dad drew a picture of the human body and the digestive system, and I was totally fascinated. I always had that curiosity, things like that were easy
to understand and medicine seemed like a natural progression.
“There was never any other path for me. Even when I didn’t get in at first, I always knew I was going to get there. As an immigrant, the desire and drive to succeed is palpable.”
In 2017, Femi found his way to Perth as part of a fellowship and at the urging of a friend – a vet – who lives here and loves it. Within a few days of arriving, Femi declared the place was a lot better than he thought it would be and perhaps it was a place to settle long term.
It was initially understood as part of the fellowship that Femi would return to the UK, but he gave up his permanent job there to stay in Perth. Six years later Femi has successfully completed the Australian Fellowship exams to have his qualifications recognised and considers this home.
He’s gone through the same set of exams four times to achieve his end goal and is extremely happy to be done with them. Femi credits resilience, hard work and the strong belief he would get through, which kept him going while juggling work, two highly active children, a marriage breakdown and COVID.
“It has been tough, but I still get up and am pleased to go to work and know that I am making a difference. I miss family and friends in the UK, but I have made some incredible friends here who have become family, and have met people who have been incredibly supportive. There’s a lot to be thankful for.”
What has become one of Femi’s biggest interests and professional passions has been delivering equitable health care to Aboriginal people in rural and remote areas. He admits it poses huge challenges on several fronts, including from inside the health system, through to public perception.
“The ability to have a more sanguine approach to this very complex problem is really important and helps me avoid taking setbacks personally. I understand there are different agendas and potential solutions for this issue. Navigating this to make progress to improve outcomes for Aboriginal people is going to take effort, of course, but I believe we are going to get there.”
And Femi is well placed to be part of that difference, which includes creating the WA Foot Collaborative Annual Meeting in 2019. The threeday conference brought together like-minded health professionals, specialist speakers from all over the world and patient advocacy groups such as Diabetes WA to focus on foot complications because of diabetes.
In an Australian first, the conference also featured a hands-on multidisciplinary cadaveric course to teach core skills in the surgical management of diabetic foot complications.
continued on Page 15


continued from Page 13
“I want to continue to push the boundaries in this area of Aboriginal health care and diabetic foot disease. As part of the tireless work with Kimberley Aboriginal Medical Services (KAMS), WACHS and Diabetes WA, we have managed to get a full-time podiatrist based in Broome. That’s been a huge game changer and Broome, in my view, is a regional hub for diabetic foot care in the Kimberley.”
Working with the podiatrist in situ makes it much easier for Femi to decide if someone needs surgery. Patients arrive on Thursday, he operates on a Friday and, where possible, they go home over the weekend.
“These patients are no longer coming to Perth fearful and not knowing what’s going to happen to them. Because they already know me, there’s a bit of a comfort in that. Nothing like word of mouth to spread the word that it might not be as bad as you think and the mob in Perth will look after you. I’m very excited about the ongoing development of the relationship with regional communities.
“There is enough going on that this could be a full-time job for me. One thing we have been exploring and thinking a lot about is how we could deliver this service at other sites. Along with other like-minded people we could make this the norm and part of sustainable change.”
Femi says one of the great lessons of COVID was leveraging technology – the use of telehealth – especially in remote areas and regional centres. His approach to diabetic foot care has embraced this and it has made all the difference in building patient-doctor relationships, which otherwise would never have happened for him in Perth.
“I can still work with patients who can’t come to see me in person, I can work around the times that work for them and build those relationships. We can also fix some problems without them having to come to hospital, rather than them coming to hospital only to find out they didn’t need to come.
“It’s not unusual for patients from remote communities with diabetic foot disease to end up in Perth. But if we can work with someone who knows them, like a podiatrist, then maybe we don’t have to bring them down. Between us, they are still getting the knowledge to help the problem. The more we can leverage local expertise, the more we can provide them with access to specialist knowledge.”

While Femi doesn’t formally teach, he certainly believes in helping others to learn. He’s not a fan of didactic learning because, in his experience, teaching doctors to be great clinicians is only part of the job. Teaching them to be able to reflect on what they do and how they do it is also important. Fostering and encouraging compassion and connection should be equally prized.
“I also tell junior colleagues there’s always something to learn in the ordinary. I remind people they have taken the Hippocratic Oath for a reason – and it must mean something. Doctors are scholars, teachers and scientists and that is an immense privilege.”
A natural runner, you’ll also find Femi at the gym or chasing after his kids and the dog as his way of keeping in shape. He likes to paint and draw during quieter moments and has a passion for home improvement, which apparently, he’s quite good at.
Luckily, he also doesn’t like mess and is very ordered, so he tidily finishes the jobs he starts. He finds it therapeutic and is another outlet where he can enjoy using his hands. Largely self-taught, he couldn’t
afford to pay a tradesman to do fix-it jobs while he was studying and training. He says the affinity his children have for drawing and building Lego seems to echo their dad’s love for home improvement and working with his hands.
Femi’s mother went to Le Cordon Bleu while they lived in France, so he definitely grew up with a solid basic knowledge of how to cook. In Liverpool, many of his university friends missed their Sunday dinners at home, so Femi took it upon himself to cater for them. They paid for the ingredients, he channelled his mum’s skills and sometimes turned a small profit at the end of the night.
Since moving to Australia, Femi has added improved barbecuing skills to his repertoire. Now all his exams are done, he’s enjoyed finding time to entertain again and teaching his sons the appropriate use of cutlery.
Saturdays at the Oshins are given over to rugby and athletics, the boys are learning to play chess and have discovered board games. There’s also always Lego, crafts and Harry Potter on audio book.
Femi’s partner Kirsty is a social worker. The pair met online and Femi said he was really into wine – accompanying the comment with a photo of his fledgling wine collection. While Kirsty’s wine knowledge was more advanced, it’s now a shared interest. They’ve been in their house for nearly two years and continue to work on the renovations together.

The increasingly desperate plea from parents and doctors alike for better access to child developmental care has reached crisis point. When will this ‘train wreck in slow motion’ finally be offered a lifeline?
By Suzanne HarrisonThe emotional toll on mother-ofthree Amanda* and her family has at times felt insurmountable. With a 12-year-old daughter in dire need of medical intervention to help with ADHD and related behavioural problems, a teenage son also requiring developmental assistance, a full-time legal job and being regularly called in to her daughter’s school, it felt they had nowhere to turn.
But it wasn’t just a feeling. It was real. After a GP diagnosed Amanda’s daughter with ADHD, her family really did have nowhere to turn. It’s a sad reality that accessing paediatric specialist care has never been more difficult. Tragically, to the point recently where a 14-yearold South-West boy took his own life while waiting for ADHD treatment.
With wait times of up to 18 months regularly reported (Amanda confirms she, too, was told this), parents said to be travelling interstate to access appointments and, in WA, GPs unable to fully contribute on the frontline, the call to implement drastic measures for change is becoming significantly louder.
After speaking with parents and doctors on this issue, it’s not an exaggeration to say that despair is the overriding condition in both camps.
“There was so much friction at home,” says Amanda, who spent many months calling medical offices every week, desperate for a cancellation or some glimmer of hope. She even accepted a place at a medical centre in Mandurah, which didn’t eventuate (Amanda then lived in Perth’s northern coastal suburbs).
“There was an orchestra going on in her head,” she says of her daughter’s experience, “But no conductor there to co-ordinate it all.
“All you can do is sit on the phone every Monday morning … while she goes to school, using all her energy just to get to ground level. She had no capacity to take in information. She would come home every day and explode. You can’t make progress. And all you want is to get a prescription.”
Finally, Amanda bit the bullet and turned to a friend in the medical
fraternity, begging her to help find an appointment with a specialist who could prescribe medication to her daughter.
“It is very stressful. Everyone is impacted. Before you start, you think there is a solution. But then, it’s out of your reach for no reason,” she said.
Stories like Amanda’s have been widely reported, with both a current (WA) parliamentary inquiry soon due to release a report and the Senate’s Barriers to consistent, timely and best practice assessment of attention deficit hyperactivity disorder (ADHD) underway. Paediatricians and GPs have submitted detailed proposals to both.
Despite the stress, Amanda was one of the luckier ones. She can afford to pay for a private psychiatrist or paediatrician (who can prescribe medication), and she had a friend with contacts. However, this kind of ‘in’, too, has reportedly come to an end.
“Off the record?” says one unnamed specialist, not long ago, “if you knew people, it could be done. Now, you can’t, no matter whether you’re connected or not.”
According to Perth-based paediatrician Lana Bell, “It’s a train wreck in slow motion. We’ve been talking about this for 10 years.
“Even if you can afford to go private, you can’t see someone. I run a private clinic two days a week and if someone is sick or we’re understaffed, I have to cancel the clinic.”
Dr Bell said she has tried to bring in overseas specialists but was plagued with visa problems. She and her colleagues have made representations, but they seem to have fallen on deaf ears.
“Unless parents make it a political issue, I don’t think anything will change,” she said.
While conditions such as ADHD are not new, there is a true increase (in ADHD/neurodivergent diagnoses) a time, she says, when we have a workforce that can’t cope, adding that there is no lack of interest from students wanting to fill the gaps if there were more training positions available.
This would require greater communication and a more collaborative effort within the entire health sector.
For example, a spokesperson from Curtin University – a major provider of undergraduate and graduateentry level therapy courses, which includes paediatric training alongside other major fields of practice (Curtin does not offer specialised paediatric training) – says every therapy student requires significant hours of field work experience as part of their qualifications.
“For every extra therapy student enrolled, the university needs to ensure that up to 1,000 hours of field work is available across the four years of the student’s training,” the spokesperson said.
“To increase the number of students enrolling in therapy courses, all universities, WA healthcare providers and the entire sector would need to work together to determine how those extra field work placements would be created. Curtin has commenced preliminary discussions with the sector to help map a plan for the future.”
Curtin has recorded “steady and growing enrolments” across therapy courses (including speech pathology, occupational therapy, physiotherapy, social work and nursing) in recent years. On another note, the average wait time for speech pathologists in WA is also reportedly over 12 months.
GP and director of The Garden Family Medical Clinic in Murdoch, Dr Andrew Leech, says that as far as he is aware, no developmental paediatrician is seeing
continued on Page 18

“Unless parents make it a political issue, I don’t think anything will change.”
continued from Page 17
new patients (privately). The public system is out to a 30-month wait, with 7,000 children on the waitlist.
“I can't imagine the impact this has on families waiting,” said Dr Leech. “The ripple effect is huge – socially, emotionally, financially and so on.”
Dr Leech has worked with another two GPs via the Royal Australian College of GPs (RACGP) to offer ideas. In May, he presented to the state parliamentary inquiry.
These include increased education and training of GPs, increased multi-disciplinary teams in an ECHO-style format (a Queensland model), increased prescribing and diagnosing rights, and increased access to paediatricians by doing the leg work (screening tools, history, examination, bloods and so on) with less requirement for paediatric involvement but still in collaboration.
“The ultimate goal would have GPs run relatively straightforward cases (about half of developmental paediatrics) independently, and for paediatricians to be freed up to deal with the complex cases,” Dr Leech adds.
Dr James Best , Chair of the RACGP’s Specific Interests Child and Young Persons’ Health Group, says most parents can’t afford hundreds of dollars for a private paediatric appointment (then there is the cost of any medication) so they use GPs. The GP then has to refer them to a psychologist or paediatrician, and that leads to wait lists.

“It’s getting worse for GPs and carers. We saw a situation in WA recently where a young person with ADHD had suicided and that wouldn’t have been a case in isolation.”
GPs, he adds, are there as a rescue, in a system that’s not changing and will only get worse.
“Make the choice of doing general
practice more attractive. ADHD, autism, while always being with us, is being diagnosed more. My practice is dominated by this. And then you have to turn around and tell parents they will need $700 for an ADHD diagnosis.
“The main way to fix this is at the medical student level. Getting overseas doctors is a way they are trying to rectify the problem, but it’s not going to fix it.”
A statement released by the RACGP in June this year called for expanded roles for GPs in the diagnosis and treatment of ADHD to improve affordability and access to care for patients.
In its submission to the Senate inquiry, it said Australia needed consistent rules
across all states and territories on which clinicians could diagnose and prescribe stimulant medications for patients, funding to support effective shared models of care, and appropriate funding for long consultations.
“Long waits for specialists and high costs are a significant barrier for patients living with ADHD, particularly adult patients who do not have access to diagnosis via a paediatrician,” it said.

“Most public sector mental health services do not provide ADHD services, resulting in an overreliance on private sector care and services.”
RACGP president Dr Nicole Higgins said costs, potentially in the thousands of dollars that might include interstate travel, show that not only is access too hard,

but that people are desperate for health care in this area.
The recently published ADHD clinical guidelines have given GPs a comprehensive, evidence-based resource to guide the diagnosis and management of ADHD.
Guidelines support
“With appropriate support, GPs can step up to help patients, psychiatrists, and paediatricians to diagnose and manage ADHD. This will require appropriate training, funding, regulatory change for prescribing and the development of shared-care arrangements between GPs and other health professionals,” she said.
Dr Higgins said GPs could play a more active role in sharedcare arrangements, but were hampered by rules on diagnosis and prescription of stimulant medication that varied by jurisdiction.
In Queensland, GPs can diagnose ADHD and initiate stimulant medication prescriptions for patients aged between four and 18; on NSW, GPs can diagnose and initiate prescription for patients six
to 18-years with permission from the Ministry of Health.
As discussed in the RACGP submission, trials and pilots where GPs work with paediatricians and psychiatrists to upskill in ADHD treatment – and diagnose and manage patients – are underway or proposed in WA, Queensland, NSW, and Victoria, but each state operates under different rules, which need to be brought into line.
“At the moment, it’s a postcode lottery. Patients would benefit from consistent rules across all states and territories describing the clinicians that are authorised to diagnose and prescribe stimulant medications,” Dr Higgins said. “This should include GPs.”

A government spokesperson for the WA parliamentary inquiry into access delays to child developmental services said the inquiry will be solutions-focused to deliver meaningful findings for the children of WA.
“We understand the important role these services play in child development and are committed
to addressing the challenges facing the service in the context of global workforce shortages,” they told Medical Forum
For Amanda’s daughter, medication has been a game changer.
“Now we can have a reasonable conversation with her, and there’s not so much disjointed behaviour. The medication helps her make strategies.”
Amanda will be keeping a particularly close eye on the parliamentary inquiry.
“If you could just go to your local GP who knows you, and they could write a prescription for medication, that would go 100 miles,” she said.
“People are genuinely just trying to get their kids on track. There are so many hurdles, and that’s concerning when it’s about a child.”
ED: The members of the WA Select Committee are Sally Talbot (Chair), Donna Faragher and Samantha Rowe. *Amanda is not her real name
Whether it's for knees, hips, hands, arms, legs or shoulders, St John of God Mt Lawley Hospital orthopaedic services provide care from pre-surgery through to rehabilitation to get your patients moving.
Upper limb (shoulder, elbow, wrist and hand) surgery and trauma
Shoulder and upper limb surgery, knee surgery and replacement, and sports injuries
Dr Michael Perret Hand and upper limb surgery and trauma









To learn more about our specialists’ expertise and specialties, scan the QR code. Email GP.MtLawley@sjog.org.au • visit sjog.org.au/mtlawley and search ‘orthopaedic surgery’.

While Robyn Kruk is yet to submit her final report into regulatory settings for overseas practitioners, her interim report has already set the wheels of change in motion.
Ahpra in April flagged it would play its part in cutting red tape and costs to help alleviate nationwide health-care workforce shortages.
In August, the RACGP announced it would simplify its processes for IMGs to get more GPs into communities that need them sooner. The college has committed to make its assessment and accreditation processes easier for applicants, while maintaining safety and quality.
RACGP President Dr Nicole Higgins said IMGs were an important part of Australia’s general practice workforce and the college was considering measures including simplifying assessments and reducing the minimum time for IMG training.
“However, we are warning strongly against Ms Kruk’s recommendation that comparability assessments – which determine if a specialist IMG is competent and safe to practise in Australia – are transitioned to the Australian Medical Council,” she said.

When the GP college president and vice-president headed West to listen to members, they discovered innovation and determination.
Jan Hallam reports
“The inquiry into the ‘Dr Death’ case at Bundaberg Base Hospital made clear the risks to patient safety when specialist colleges don’t have responsibility for assessing specialist IMGs. We cannot risk this happening again.
“Also, training and comparability assessments must consider where IMGs work, because practising in a rural area is very different to an urban area. Rural doctors need to have the right skills and ability to work independently because there is often less support available. They also need cultural safety training.
“We largely support the report’s other recommendations, including a single portal for applications, the removal of labour market testing for employers sponsoring visas for priority practitioners, broadening age exemptions for permanent skilled visas to include key practitioners, and continued workforce support and demand modelling.”
The RACGP statement comes hard on the heels of a visit to WA by Dr Higgins and college vicepresident Dr Bruce Willett, where she and WA faculty chair Dr Ramya Raman visited GPs working in the Geraldton region to hear firsthand their specific needs.

Speaking to Medical Forum at its conclusion, Dr Raman said the visit reinforced the college’s position on comparability assessments.
“Candidates must be able to competently and safely practice anywhere within Australia, and that includes rural and remote areas,” she said. “There are certain locations which are much further away from support – for both patient and doctor (and their
families). The college plays a role in ensuring that support.”
In Geraldton, the college delegation visited two local GP practices as well the Rural Clinical School.
“We had some really useful conversations with local GP teams especially around strategies that they had adopted through COVID, including negotiating bloc funding from the local health service to provide after-hours care and aged care, which reduced the number of presentations to hospital,” Dr Raman said.
“Their model of care showed how we can improve health outcomes and reduce hospital admissions by turning our dial to general practice and primary care. It's a small example, but it's a very costefficient solution at a local level.
“And these stories are very powerful because without us going to Geraldton and speaking with GP teams, we may never have heard about them.
“These are the sort of solutions we want our health policy makers to
listen to. If we can show how GPs are at the centre of some of these local solutions for health service provision, it will have an enormous impact on our health system.”
Dr Raman said workforce was the most critical need for the Geraldton teams.
“There are some very committed general practitioners and physicians and, and of course medical students who are coming through the pipeline, but the issue is just not a shortage of GPs,” she said. “It’s also practice nurses and allied health support within the practices.
“We need to make rural practice attractive, but it’s also about ensuring families have support, and that means schools for doctors’ children, work for their partners, and suitable housing. These are the elements that ensure a doctor will stay on.
“It was also heartening to hear from medical students who were in Geraldton, particularly those who originally came from a rural area, say they were renewing their term for another year because they enjoyed the teaching and the medicine.
“That was very reassuring because it’s a sign that they would most likely return when they are qualified. It was also incredibly valuable for Nicole and Bruce to see how well our Rural Clinical School integrates into communities. WA’s RCS, which embeds all three universities, is unique.”
Before they returned East, Dr Higgins and Dr Willett met urban doctors and several member functions, and also visited the team at Debarl Yerrigan in East Perth, which is taking on GP registrars.

The launch of OpenAI’s ChatGPT in November 2022 propelled the technology to the forefront of the collective consciousness, and the impact of the statements issued earlier this year by experts and industry leaders –one signed by none other than Elon Musk – asking for development to be put on hold, has ensured that AI is one of the hottest issues of our times.
In July, the RACGP issued a statement calling for greater government oversight of the Australian AI industry, with President Dr Nicole Higgins declaring that “Australia’s GPs need to be empowered to adopt AI, that is responsibly developed and regulated, so we can improve our patients lives.”
Yet despite the hype, AI still seems remote to many in the medical community where the opportunity for practical applications that assist clinicians in diagnosis and treatment daily may be hard to quantify.
In fact, experts have criticised the slow approach that Australia has adopted, stating that the “national conversation on AI in health care has for now remained niche and low in priority.”
“With AI’s many opportunities and risks, one would think the national gaze would be firmly fixed on it,” Enrico Coiera, an NRMHC investigator from the Centre for Health Informatics at Macquarie University, said in an article published earlier this month in Perspectives.
“However, Australia lags most developed nations in its engagement with AI in health care and has done so for many years. The policy space is embryonic, with focus mostly on limited safety regulation of AI embedded in clinical devices and avoidance of general-purpose technologies such as ChatGPT.
“There is currently no national framework for an AI-ready workforce, overall regulation of safety, industry development, or targeted research investment.”
Medical Forum spoke to Director of the WA Data Science Innovation Hub, Mr Alex Jenkins , after last month’s 2023 Data & AI for Business Conference & Exhibition, held in Perth, to ask what’s happening with AI in the medical field.

“Part of my role is to ensure that we promote and advocate for the people doing the work, so that the public have some visibility into this research. For example, there is a local medical company using AI for the diagnosis of coronary disease and they are doing some amazing work,” he said.
“There is also a medical imaging platform under development, which is being designed to operate inside a health facility to run AI and machine learning experiments.”
While there are an ever-increasing number of platforms being released, much of the development research is driven globally.
“There have been some eyeopening advances over the past few years, but probably the biggest impact in the field of life sciences so far has been Alphafold, an AI that solves the protein-folding issues,” he said.
“Protein folding, or understanding how that sequence of amino acids
is structured in 3D, based on all the intermolecular forces, has been an active and open problem for 40 years.
“It is an important aspect of biochemistry for drug discovery and pharmacology, and it used to take a single PhD student about three years to figure out the structure of one single protein – it now takes about 15 seconds for Alphafold to find it.
“Three years to 15 seconds. And to the best of my knowledge, we had less than 200,000 experimentally verified protein structures around 2016, which went to 2 million and then 200 million in the space of a couple of years – so you can see the significance.
“This is a problem that we have been trying to solve with computers for over 30 years using traditional algorithms, and there is such a complex interplay of all the different molecular forces that we have never been able to crack until now.”
Alex explained that AI was driven by a type of software called a neural network, loosely inspired by the human brain and the way neurons worked together.
“It’s important to say it's only inspired by the way that human cognition works because we don't have a great picture of that,” he clarified.
“And it is a much-simplified model of a neuron, but it is a parallel way of computing, and it requires an incredible amount of computing power, much more computing power than traditional software would require.
“You can think of traditional programming like baking a cake by following a recipe: you have a specific set of ingredients and a specific set of steps, and you must follow the steps, very linear, very predetermined, and then you have a cake at the end of it.
“With AI, we do not explicitly tell the algorithm what to do. It must learn the association or the representation of what we are doing from the data, from reward outcomes, or from correlations that we signal are important.
“Some of the best outcomes in AI occur when we get a data scientist to cross-pollinate their input with that of a biochemist or an engineer, or a geologist. And if you look globally, that is where amazing things are happening in AI.
“Health is a massive area for that development because it requires such a significant level of exploration – the real deep-domain specific problems that AI excels at.”
Alex said that the other application for AI, which was “extremely promising” in health, was synthetic data, and then promptly asked if I had seen one of the artificial intelligence models that create images from text?
“So that might seem like a toy, it is all a bit of fun. But those same algorithms that create these photorealistic pictures from nothing can be used to create synthetic data, be it a fake MRI or fake tabular data, that is statistically representative of the original data set,” he said.
“You can immediately see the application in how we share health data, bypassing the current issues around privacy and ensuring people's privacy is protected. It is exceedingly difficult sometimes for researchers to access medical data, and rightly so, and this just sidesteps the whole issue by using what is effectively an anonymous data set.
“If you look at the individual records within these data sets, they are all nonsense. But if you look at it as a whole, you'll find the same statistical correlations as the original data set.”
Once the synthetic data was there, multiple teams around the world could work on the same problem, with no need for specific knowledge of a patient.
“Just think about how much data is locked up inside a hospital system or medical imaging facilities, it would be astonishing if we could open this up for everyone to have a look at,” he said.
“These techniques have only really started to mature recently, and our organisation is going to run a hackathon with the WA Department of Health in October, to use these synthetic datasets.
continued on Page 25
Have your patients been exposed?

At Perth Radiological Clinic your chest imaging investigations are reported locally by WA’s most experienced team of subspecialist respiratory radiologists.
• Comprehensive experience including teaching hospital consultant radiologist appointments, and involvement in multidisciplinary team meetings across Perth.




• RANZCR registered experts in occupational dust lung disease (RANZCR EODLD register).
• Expertise in all types of chest disease including malignancy, interstitial lung disease, occupational lung diseases, lung cancer screening, vascular diseases and trauma.

• Our low dose silica CT scans, complying with work safe legislation, are performed at multiple locations across Perth and reported by PRC’s subspecialist respiratory team.
• Appointments available within 24 hours at multiple convenient clinic locations.
PRC Specialist Chest Radiologist, Dr Stephen Melsom says -



If diagnosed early, particularly before symptoms develop, the progression of silicosis can be slowed
Dr Priority Line 9599 3929 perthradclinic.com.au
continued from Page 23
“We are going to give them to these bright young PhDs and professionals, to test if their conclusions from the synthetic data mirrored those in the real data.
“There's already researchers in King's College London that have been using it to create synthetic MRIs of brains, which have exciting potential.”
He explained that the concept of a hackathon was to take a problem, then take a data set from that problem, and open it up to a wider community of professionals with fresh eyes.
“Usually, they are software developers or people who have experience with data science. We just did a hackathon with fire and emergency services, and it is a wonderful way to get innovative ideas and new types of solutions to old problems.”
Alex explained that development in AI was often fast-tracked through the open-source community.
“When it happens out in the open, it is astonishing how fast it happens. Problems just seem to drop week by week. It is a new way of doing science, it seems, and if we can open up health data in a comparable way, we expect research outcomes to accelerate,” he said.
“The other interesting concept under development is the idea of using an AI-based preclinical analysis to speed things up. Currently, people are required to fill in this enormous form about their personal details and medical history when they visit a new GP.
“Why not have an AI facilitate that process and then ask about their ailment, such as what they have done and how they are feeling, and then – without making a clinical judgment – the AI could summarise the patient’s symptoms and specific aspects of why the patient has presented, so that the doctor does not have ask the simple questions?
“One way for doctors to think of the use of AI is to consider how a doctor goes through this enormous amount of training, then might
work for 10 to 15 years before they are called a real expert in the field.
“Now, if you can imagine, not just having 20 years of training in one field but having 20,000 hours of training or 20,000 years, or even 100,000 years, across multiple fields – the range of ailments that could be screened is vast, including rare diseases.
“It is like a second opinion from someone who is extraordinarily experienced across all medical domains – a clinical assistant that could accelerate what a clinician is able to achieve and the number of patients that they're able to see over time.”
Alex said a surprise has emerged with the uptake of ChatGPT that people were finding it useful as a self-psychotherapy tool.
“That’s intriguing because they tell things to a computer with no fear of judgment from the ‘person’ on the other side of that conversation,” he said.
“And while there are no official recommendations for that, I think it is a fascinating area for development that we will see emerge, but it is obviously no substitute for human relationships.
“Which comes back to the point that, even though it seems to be useful for psychotherapy, much of the job of a GP is to work with patients and make a judgment about their situation.
“Whether they're telling the truth or if there's some information that's being withheld or maybe there's a domestic situation: those are the things that an AI is not going to be able to pick up, but they are critically important parts of being a doctor.”

ALSO OFFERING: Spine Focused Physiotherapy Treatment






Referral
GUARANTEED ACCESS TO A SURGEON ALL YEAR ROUND
 Dr Paul Taylor
A/Prof Greg Cunningham
Dr Andrew Miles
Dr Paul Taylor
A/Prof Greg Cunningham
Dr Andrew Miles
Many will have by now heard of — or even experimented with — ChatGPT, the artificial intelligencedriven language processing tool designed to generate humanlike text responses when given prompts or asked questions.
Based on a deep learning architecture known as the Transformer, ChatGPT has been trained on huge amounts of internet text data to learn language patterns and respond coherently on various topics.
This advanced language model can support multiple languages and be used for chatbots, text generation, text summarisation, machine translation and more.
Since its release in November 2022, ChatGPT has rapidly become ubiquitous in many areas of our lives, with far-reaching potential implications for productivity and information accessibility, but it has also raised concerns about job displacement and data security. But research from Professor Wei Wang, Dr Jun Wen and I have found that it could also end up impacting health.
There is currently a significant controversy about the potential influence of ChatGPT on academic research and publishing: some researchers believe ChatGPT is a helpful instrument for academic innovation, while others argue it stifles creativity and even undermines academic integrity and ethics.
Its use is particularly debatable in health research, where there is argument over whether ChatGPT is revolutionary or risky.
On one hand, ChatGPT offers potential benefits for healthcare research, which often involves processing and analysing large volumes of literature and data — a time-consuming and tedious task.
Here ChatGPT has emerged as a more efficient and automated solution to enable researchers to quickly retrieve, filter, and extract valuable information.
These insights or critical knowledge could help provide new ideas and directions for healthcare research and produce reliable results to inform healthcare policymakers, researchers, practitioners, and patients.
In addition, ChatGPT can serve as a supporting tool in study design, statistical analysis, and grammar checking, thereby improving writing quality and reducing researchers’ busy workloads.
However, despite some promising possibilities, ChatGPT also poses significant risks and challenges.
Firstly, ChatGPT’s information is lagging. Its current knowledge is primarily based on data prior to September 2021. This lack of new data can be a serious impediment in a rapidly changing field such as health.
Up-to-date data enables researchers to understand trends in disease prevalence and identify new risk factors and intervention options to optimise healthcare delivery resulting in the best possible health outcomes for patients.
An over-reliance on outdated data in ChatGPT can divert researchers from the right direction, resulting in time and other resources being unnecessarily wasted and even potentially serious consequences for individuals and public health.
ChatGPT is also powerful in acquiring and summarising information from the Internet, but its generated answers are not necessarily factual.

Its developer, OpenAI, admits the program “sometimes writes plausible sounding, but incorrect or nonsensical answers”, a
phenomenon common in large language models and known as “artificial hallucination”.
These inaccurate responses aren’t easy to discern, and the difficulty of identification is further compounded by unclear information sources and made-up references. Thus, there is danger when ChatGPT is applied to rigorous research.
As a key driver of progress and innovation, research plays a critical role in the development of society. It can offer reliable evidence for clinical practice (disease diagnosis, prevention, and treatment) and guidance for public health policy formulation and resource allocation to improve health outcomes and build more functional systems.
Inaccurate ChatGPT-generated information could undermine the reliability and validity of health studies, leading to academic mishaps, misinformed medical decisions and policymaking, or even compromised health outcomes and unbalanced healthcare networks.
The spread of misinformation is damaging, but it would be particularly so in health research as having such erroneous knowledge widely disseminated and adopted in academic research will mislead the public and impair health literacy, thus causing more long-term negative effects on public health.
As with any new technology, there are benefits and drawbacks to using ChatGPT. Until the potential risks are addressed, ChatGPT may be best used as an auxiliary tool that can enhance efficiency and spark inspiration, but we need to carefully consider how we apply it, especially in evidence-based research pertaining to our health.
Data is the bedrock of medical and health research, so it needs to be accurate. ECU researcher Fangli Hu needs more convincing that ChatGPT is the answer.
Some WA pharmacists have started prescribing for ‘uncomplicated’ UTIs. RACGP WA and AMA (WA) heads – Dr Ramya Raman and Dr Michael Page – respond to questions from Medical Forum.

MF: How could this program impact on patient safety?
Patient safety must come first and hence we are concerned regarding this program. Due to the potential harms, the RACGP and AMA (WA) have not endorsed this trial. However, through our advocacy to date we have endeavoured to improve the safety of the program.
There is no such thing as a simple diagnosis of UTI or any other medical condition. People present to pharmacy with symptoms, not a diagnosis. GPs train for over 10 years before diagnosing patients and do ongoing training over our entire working life for many more years. Medical training cannot be reduced to algorithms and flowcharts when diagnosing medical conditions.
Pharmacists are valued by GPs, practice teams and their communities and they play a vital role in our primary care system. However, they are not trained to diagnose or prescribe medications.
The best practice for UTI diagnosis involves history taking and patient assessment and then urine dipstick testing as a minimum to determine if what the patient is presenting with is a UTI or something else. That is why the College and the AMA have recommended this process is a part of this trial and any future trials in WA or across Australia.
The RACGP advocated for the inclusion of referral to a medical practitioner and pharmacists involved in the program are encouraged to advise their patients about the importance of having a GP as part of follow-up care.

Antimicrobial resistance is a top global health threat and should be top of mind when implementing this pilot. Over-prescribing antibiotics through this initiative could significantly impact the health of our communities. Taking into account WA resistance patterns, nitrofurantoin will be considered as first-line therapy in the program, trimethoprim second line choice and cefalexin has been excluded.
Where neither nitrofurantoin nor trimethoprim is appropriate, the patient should be referred to a medical practitioner for management. Pharmacists will have the challenge of separating their prescribing decisions from the influence of pecuniary interests. Evaluation of patient health outcomes is essential.
MF: How does it impact on privacy issues?
Disclosing confidential medical information in a crowded retail setting is far from ideal. When you visit your GP, you are taken to a separate room away from the waiting room so that you feel comfortable talking candidly about your health and personal circumstances including, where necessary, your sexual history.
continued on Page 31
Infectious disease specialist and clinical microbiologist Dr Jonathan Chambers was one of the doctors who was consulted by WA Health before the decision was made to go ahead with the pharmacy prescribing trial. This is his take.

There is no consistent agreed definition of an uncomplicated urinary tract infection. An uncomplicated UTI generally refers to an infection that occurs in the lower urinary tract (bladder and urethra) of pre-menopausal adult women, without any evidence of systemic infection, pyelonephritis (or history of pyelonephritis/ urosepsis), pregnancy, underlying complicating medical condition or recurrent urinary tract infections. This type of UTI is characterised by mild to moderate symptoms localised to the lower urinary tract, such as dysuria, frequency, urgency, and suprapubic discomfort. It occurs in otherwise healthy individuals and is typically caused by Escherichia coli (E.coli) in approximately +90% of cases.
Many these patients will recover with no antibiotic therapy. However, a proportion may go on to develop a complicated infection which
may be prevented with antibiotics.
Empiric antibiotic recommendations for uncomplicated UTI reflect the prevailing patterns of E.coli resistance in the community. This typically aims for an effective antibiotic >80% of the time based on prevailing resistance patterns.
At present in Western Australia, Nitrofurantoin remains susceptible in roughly 90-95% of cases.
Nitrofurantoin given in short courses 100mg PO QID for five days (or as directed by international/national/ local guidelines) for uncomplicated urinary tract infections in healthy premenopausal adult women is safe and effective.
Unlike other antibiotics there is minimal impact on the patients commensal flora outside of the urinary tract, low rates of C.difficile and similar rates of severe adverse drug reactions compared to other antibiotics. Importantly this is arguably the cheapest and best

antibiotic to use to preserve our other critical antimicrobials for other more severe infections.
Alternatives such as Trimethoprim are no longer testing reliably susceptible >80 % of the time in the local context for E.coli. Whilst it is still recommended in Australian guidelines this may not continue without certain caveats.
I believe it is important to perform urine culture and susceptibilities in patients in whom this drug is used to confirm it is likely to be effective. Antibiotics like ciprofloxacin, norfloxacin, amoxicillin/clavulanic acid, and cephalexin aren't recommended first-line due to being overly broad spectrum with a similar efficacy for uncomplicated UTIs.
Investigation/Management:
1. Patient history: Gather information about the patient's symptoms, medical history, current medications, allergies, recent sexual activity, and any previous UTIs.
continued on Page 31



continued from Page 28
However, registered pharmacies providing the service must have an area suitable to maintain confidentiality of the consultation as per the Structured Administration and Supply Arrangement (SASA) which outlines the criteria and conditions for ‘Pharmacist Initiated Treatment of Urinary Tract Infection’.
MF: Is the treating pharmacist obliged to notify a person’s GP/ or WA Health about the treatment they have given?
A patient must be provided with a service summary, and this can then be provided to their primary health provider.
The RACGP strongly advocated for the inclusion of “referral to a medical practitioner” as part of the pharmacist supplementary information. Presentations of acute issues provide an opportunity for preventive healthcare and pharmacists are encouraged to highlight to patients the importance of having a GP.
MF: If a person suffers a reaction to a medication, or it is the wrong medication, what happens next? This would be an adverse outcome and should be registered in the
same way any adverse events for pilots and trials are recorded.
This is an aspect of the trial that we are particularly concerned about. If a person suffers a reaction to the medication, or is given the wrong medication, they will then have to book a GP visit or, if it is after-hours or requires urgent attention, their local emergency department. The left hand won’t know what the right hand is doing. If a patient visits their pharmacy for a suspected UTI and ends up suffering from complications, the GP may be left in the dark. This fragments care and can lead to poor health outcomes.
MF: Is there any evidence to suggest GP access is a problem for women with UTIs?
Depending on where you live, some patients are having difficulties
continued from Page 29
2. Physical examination: Conduct a quick physical examination to assess for signs of infection and any abnormalities in the genital and urinary areas.
3. Urine sample: Collect a midstream urine sample for urinalysis and urine culture to confirm the presence of infection and identify the causative organism.
Urine dipstick and culture aid the diagnosis. It is this author’s opinion that a positive urine is required to diagnose a urinary tract infection in the context of compatible
symptoms. Negative results suggest alternative diagnoses, like Mycoplasma genitalium or Chlamydia/Gonococcalassociated urethritis or even sinister non-infective causes. Accurate antibiotic susceptibility data is crucial for optimal future empirical recommendations. It will also identify other common urinary pathogens that may require different approaches.
Non-Antibiotic Therapy:
• Avoid dehydration in addition to Increasing fluid intake to maintain clear and frequent urination
• Simple analgesics such as ibuprofen or paracetamol
accessing timely general practice care. That is because we are facing a maldistribution of GPs in Western Australia and indeed in communities across Australia. The proper solution is boosting general practice care and ensuring all patients, irrespective of their postcode, can access highquality general practice care when they need it.
Reliance upon another workforce who are also currently under strain and experiencing workforce shortages, and introducing multiple providers duplicating the same services adds to health system complexity, duplicates or fragments care, creates patient confusion and directs patients away from the essential coordinated medical care. This compounds the problem of GP access rather than fixing it.
MF: Does the pharmacist charge the patient for the consult on top of the medication? Is this any more cost effective than a GP consult?
This is not covered by Medicare, so the patient is likely to have to pay. As part of this trial, pharmacists are obligated to make sure patients understand the costs involved when offering the service.
• There is minimal high-quality evidence to recommend cranberry supplements, urinary alkalinisation (contraindicated with Nitrofurantoin) and probiotics
Follow-Up:
If symptoms persist or worsen, consider further investigation to rule out underlying complications. If that patient becomes unwell with fevers and/or severe back pain and/or Nausea/vomiting may need referral to an emergency department for parenteral therapy.
The prevalence of multiple sclerosis (MS) has increased in every world region from 2013 to 2020, with a person diagnosed every five minutes, according to MS Australia CEO Rohan Greenland.

The latest data from MS Australia and the University of Tasmania’s Menzies Institute for Medical Research shows that the neurological disease, affecting mostly young to middle-aged women, rose in Australia by 30% over four years, from 25,607 in 2017 to 33,335 in 2021.
The data, published in Health Economic Impact of Multiple Sclerosis in Australia in 2021, shows the number of people living with MS more than doubled from 2010 to 2017, with an increase of 4,324 people. Consequently, the prevalence of MS in Australia has risen considerably. There were 131 people living with MS per 100,000 people in Australia in 2021, up from 103.7 per 100,000 people in 2017.
MS Australia has funded 22 new MS-focused projects this year, injecting over $3 million to address the sharp rise in cases, including studies that examine family genetics, the impact of diet on brain health, and cellular repair and regeneration.
MS Australia is ramping up research to find out more about the neurological disease to combat the sharp surge in prevalence.
“MS is extraordinarily complex, and we need to cover much ground to advance our understanding of the disease and to devise better approaches to combat it,” Mr Greenland said.
“We’ll be hitting MS from every direction with these research projects to ensure we go further and faster towards better treatments and prevention of the disease.”
Commonly adult onset, diagnosed usually between the ages of 20 and 40 and mostly in women, MS is the neurodegenerative disease identified by demyelinating lesions in the brain and spinal cord. High inflammation is thought to cause the death the myelinating cells, oligodendrocytes.
Symptoms include visual impairment, sensory disturbances, cognitive problems, sexual dysfunction, motor dysfunction and weakness, bowel or bladder continence, fatigue, sleep disturbance, anxiety and depression, and can result in marked declines in both physical and psychosocial health-related quality of life.
Lifestyle factors, such as smoking, low sun exposure and consequently low vitamin D levels, and being overweight increase the risk of developing MS. New research from Curtin University and Deakin’s Institute for Physical Activity and Nutrition (IPAN) is showing the link between diet and MS.
One of the interim report authors, Professor Bruce Taylor, principal research fellow at the Menzies Institute for Medical Research and clinical neurologist at the Royal Hobart Hospital, said the rise in MS incidence and prevalence over the past decade was concerning.

“MS is a rapidly progressive neurodegenerative disease which results in an accumulation of disability. People think of MS as a disease of young women but that’s when it starts and once you’ve got MS you’ve got it for life,” he told Medical Forum
As well as genetics, he said there were several epigenetic factors that played a role in developing MS.
Research has shown that the risk of MS is significantly increased if someone has had early adolescent obesity, which is also on the rise.
“If we could reduce adolescent obesity, we could potentially reduce 50% of cases of MS,” Prof Taylor said. “And the incidence of MS is higher in Tasmania compared to northern Queensland due to the role sun exposure plays in getting sufficient vitamin D.
“We think people aren’t getting as much sun – since the 1980s ‘slip, slop, slap’ message – and we know less sun exposure reduces vitamin D in your system which has a direct impact on the immune system.”
Being female increases the likelihood of MS by three times compared with men, and women who put off pregnancy until their later reproductive years increase their risk due to pregnancy’s immunology protective factors.
“Every pregnancy reduces the risk of developing MS by 50%, and women are having less children and later,” he said.
Then exposure to the Epstein-Barr Virus (EBV), which includes 90% of the population, is clearly linked to MS.
“It’s the obligatory risk factor for getting MS,” Prof Taylor said. “We’ve known this link between EBV and MS for many years. The risk of having MS without EBV approaches zero, and with the virus it’s 99.99% so it is a major risk factor.
“If a vaccine for EBV were developed, it could significantly reduce the numbers of MS.”
He said that genetic makeup and genomic host-pathogen interaction added complexity to risk factors for the disease and how these risk factors interacted was also complicated.
“We know smoking interacts with genetics, EBV exposure interacts with genes as does obesity,” Prof Taylor said.
Research at IPAN and Curtin University is investigating the largely
unknown role of diet – including ultra-processed foods, fish and dairy products – in the onset of MS.
Professor Lucinda Black , who is leading the MS Australiafunded research through the MS Nutrition Research Team, started looking into diet and MS in 2016 at Curtin University with a fellowship from MSWA.

Previous research led by Prof Black showed a healthy Mediterraneanstyle diet – including chicken, fish, eggs, vegetables, legumes, and some unprocessed red meat – was associated with reduced likelihood of the first clinical diagnosis of demyelination in the brain and spinal cord (FCD), while ultra-processed foods and a pro-inflammatory diet were associated with higher likelihood of FCD.
There was a lot of confusion about diet and MS, and many different diets were marketed to people with the disease that might restrict certain food groups or foods that could help their symptoms.
“There isn’t enough high-quality, conclusive evidence to support any of the special diets for people with MS,” Prof Black said. “We’re aiming to generate high-quality evidence about the link between diet and risk of MS, whether diet can help prevent MS, and for those with MS what is the best diet for their condition."
“What we’ve found so far, using data from Australia, is that a healthy diet overall is linked to a lower likelihood of getting MS, and we’ve seen that same pattern in the American study,” she said.
The Australian data shows that consuming a moderate amount of unprocessed red meat and oily fish in accordance with the Australian Dietary Guidelines (ADG) is linked to a lower risk of getting MS, and higher consumption of ultraprocessed foods increases the likelihood of MS.
“Most Australians don’t eat enough fruit or vegetables, young adult women generally don’t eat enough unprocessed red meat, we all probably don’t eat enough oily fish, so it’s about following the
continued on Page 35

continued from Page 33
ADG and not necessarily going on a restricted diet.”
Prof Black’s team is also developing an online nutrition education program tailored for, and codesigned with, individuals with MS. “We’re talking to people with MS about their attitudes and behaviours around diet and getting their input in all our research projects. What they’ve asked for is education around diet that’s relevant to them, not necessarily information that’s relevant to the general population.” However, Prof Black said diet was only part of a bigger picture alongside research into physical activity, stress, sleep, mental health, vitamin D status, and other environmental risk factors.
Dr Eleonor Dunlop, from the Curtin School of Population Health, is an MS Australia Postdoctoral Fellow and Accredited Practising Dietitian working alongside Prof Black. She is looking at the role of diet in children with MS, which is rare but the incidence in increasing.
The research, which draws on a study conducted in Canada led by Professor Helen Tremlett at the University of British Columbia, could lead to the creation of evidencebased dietary advice for children at high risk of developing MS.
Meanwhile, MS Australia is also funding research at Edith Cowan University that aims to understand how motor neuron behaviour contributes to muscle weakness.

The research is led by Dr Christopher Latella, from ECU’s School of Medical and Health Sciences, and builds on evidence suggesting a problem with serotonin and noradrenaline in the nervous system of people with MS. However, it is not yet known if the spinal motor neurons are also affected. The research is looking into the motor neuron firing of persistent inward currents and will record the electrical activity of leg muscles to determine the firing of nerve cells during voluntary muscle contractions.
“There’s been some evidence to
suggest that certain centres in the brain might become dysfunctional and those centres in particular are responsible for the release of specific neurotransmitters such as serotonin and noradrenaline, Dr Latella said.
“Those centres of the brain also have important interruptions with the spinal cord, in particular nerves that control muscles.”
He will investigate whether changes in the properties of the motor neurons influence performance of tasks like walking and standing in people living with MS.
“Both serotonin and noradrenaline are important for this system to work properly, so if both are disrupted in MS, it might be one of the contributors to muscle weakness and fatigue, and we know that’s quite prevalent in people with MS.”
Research led by Associate Professor Jennifer Rodger from UWA and the Perron Institute will use repetitive transcranial magnetic stimulation (rTMS) to generate small electrical pulses in the brain to explore if this can improve the survival of the myelin-producing oligodendrocytes. The project could open the door for treatments that maximise the survival of oligodendrocytes.
From the University of Sydney, Associate Professor Laura Piccio is studying the role of TREM2 proteins, located on microglia in the phagocytosis of myelin debris, and remyelination. Preliminary results suggest the activation of TREM2 could enhance myelin debris clearance and remyelination.
While Prof Taylor said a cure is likely to be far off, MS Australia’s funding towards the new studies is taking steps to find better treatments, preventions, and understand the disease affecting 2.5 million people worldwide.
“At this stage a cure looks difficult,” Prof Taylor said, “though our treatments have made a huge difference for the prognosis of people with MS.
While newer treatments have made a difference, prognosis is still serious for primary progressive MS (PPMS), affecting 10-15% of people with MS, where there is a gradual worsening of neurologic symptoms and an accumulation of disability.
“We hope that in the next 10 years we will have an effective treatment for progressive MS, and if we had that we will be able to turn it into a much more benign disease,” Prof Taylor said.
Nia Parker, from Down Syndrome WA, urges the local medical community to be aware of this heartbreaking disorder and help find some answers.
Down syndrome is the most common cause of genetic intellectual disability, occurring in approximately 1/800-1000 live births.
The medical profession, and society in general, has come a long way in terms of attitudes to education and opportunity for those living with an intellectual disability and many adults with Down syndrome now live independently – working and integrating fully into the mainstream community.

Imagine then, how devastating it is to see this independence, confidence and skills disappear over a short period of time –sometimes in as little as 6-12 months, with no explanation as to why a 25-year-old, who has a job, catches public transport and plays basketball, has suddenly lost the ability to self care, takes an hour to eat a bowl of cereal and whispers (if they speak at all).
These are just a few of the many symptoms of Down Syndrome Regression Disorder (DSRD). The first paper discussing this condition was published in the 1940s, but little since until five years ago when the level of interest sharply increased. The condition was described by a variety of names, but an international group of researchers collaborated to reach a consensus on nomenclature, diagnostic criteria and testing (published July 2022, Frontiers in Neurology).
The Down Syndrome Association of Western Australia (DSWA) has established a support group for parents who have a teen or adults showing signs of regression. Most have seen a GP, some have been prescribed anti-depression/antianxiety medication or referred to a psychiatrist, others to a neurologist, but most are just told that it’s “probably early onset dementia” and given little hope for meaningful treatment or change.

Perth Children’s Hospital has a T21 clinic, but when a child reaches 18 and too old to attend, there is no adult centre for Down syndrome providing specialist care, so each patient sees their own GP who has possibly never heard of this condition and therefore unaware of how to approach the situation.
DSRD is a cluster condition, with diagnosis by elimination. Many people with Down syndrome suffer from autoimmune disorders, so often the first point of call is to rule out any of these conditions. Unfortunately, at this time there are no definitive biomarkers for DSRD. Some will show changes on cerebral MRI, others won’t, some will show anomalies in CSF taken by spinal tap, others won’t.
Globally, treatments currently being offered include lorazepam (an antianxiety medication which treats catatonia and other symptoms),
IVIg (an immune regulating therapy) and tofacitinib (a type of drug which suppresses the immune system). There are documented cases where one or more of these treatments have yielded remarkable improvements in symptoms, even after regression has been present for many years.
A multidisciplinary clinical trial of these three treatments began in July this year in the US. Research into DSRD is hopefully going to provide some answers as to the cause of this condition, as well as consensus on diagnostic tools and first-line treatment. Until then, the message is that the devastating loss of skills and the onset and development of unusual behaviours such as catatonia and increased OCD may not be the signs of early onset dementia, but rather the manifestation of Down Syndrome Regression Disorder.
DSRD has a devastating impact on the person with Down syndrome and their families, carers and immediate community. Watching a person who has created a meaningful place in society, working and contributing, suddenly lose their spark, their skills and the love and energy they bring is heart breaking.
For the young person, you can see their frustration, often manifesting in aggression directed toward parents and carers, they withdraw, lose their jobs, stop leaving the house, and in many cases stop communicating.
For parents and carers who have spent a lifetime supporting their child to have a meaningful life, it is not only heartbreaking but exhausting. Parents are returning to carrying out tasks such as dressing and bathing, being desperately concerned as their family member won’t eat and experiences rapid weight loss, and frustrated that everything that has worked so far, is gone.
The impact on families is devastating, parents are physically, mentally and emotionally
exhausted, being left with feelings of hopelessness and loneliness. More broadly, siblings, other family and close friends are also affected, struggling to understand, having difficulty now communicating with a person that, to date, they have been deeply connected with.
The needs of the person with Down syndrome increases dramatically, family members may have given up work, some have had to change their lives completely to support their family member, and many have struggled with the impact on their own mental health. It is a crisis for all involved.
At DSWA, we are bringing together families who are experiencing some symptoms of regression to provide support and open discussion, enabling us to collect information from the families that have self-identified these regressive behaviours.
In doing so, DSWA is collating data from each family, and as more families reach out, it is the intention that we will have a big enough cohort to attract funding for research in this area, here in WA.
GenesisCare at Hollywood offers access to radiation oncology consultations, treatment, and access to allied health support services. We offer modern evidence-based techniques and technology combined with compassionate care – aiming to deliver the best possible patient experience and outcomes.
At present there is a small study being undertaken at the Mater Institute in Queensland but otherwise there is very little activity around DSRD in Australia. The DSWA DSRD support group has recently received requests from families in both Queensland and Tasmania to join the group.
It is DSWA’s goal to raise awareness of DSRD and to seek professional and financial support for research into the condition to assist with diagnosis and treatment. To read our case studies, view our small data set or review the documents (including journal articles and webinars), please reach out to chair@downsyndromewa.org.au or view our website, www.downsyndrome.org.au/wa
ED: Nia Parker is chair of DSWA.
• Personalised treatment plans, striving for minimal wait times
• Tattoo-free technology
• Access to a wide range of allied health services (including exercise physiology), accommodation, and transportation packages
• For patients who are eligible for Medicare, approximately 80 to 90% of radiation therapy treatment costs are often covered by Medicare rebates
• Private health insurance is not required for radiation therapy
• A multidisciplinary team of supportive clinical professionals
We offer patients: *For radiation treatment patients. Based on patient survey results Oct 2021–2022.

genesiscare.com

Bethesda Clinic is a voluntary, adult only, 75 bed clinic that provides multidisciplinary clinical services to aid recovery from mental health issues through inpatient and day patient programs.
Services Bethesda Clinic provides:
Inpatient care and therapy programs managed by a multidisciplinary team. Day patient therapy programs in the Wellness and Recovery Centre. Psychiatric and psychological services for those experiencing mental health issues.
Specialties:
DVA-accredited Trauma Recovery for veterans, military and first responder communities. The first designated women’s-only ward in Western Australia, providing a safe recovery environment.

Alcohol and other drug use.
General mental health.
How to refer to Bethesda Clinic:
Download the referral direct from our website bethesdaclinic.org.au/referrals
Find us on HealthLink: Bethesda Clinic
Contact Bethesda’s Triage Officer on (08) 6378 4999 or BC.Triage@bethesda.org.au
Bethesda Clinic
1 Honour Way, Cockburn Central WA 6164
Phone (08) 6378 4900
bethesdaclinic.org.au
Every Australian deserves to live in a community that is safe and free from harm. Sadly, as a surgeon, working in a major trauma centre in Southwest Sydney, each day I see a range of patients where alcohol use has significantly contributed to their injuries.
Victims of domestic and family violence horrendously injured with facial fractures. Permanent resultant disfiguring scarring.
Road crash incidents where alcohol use is a significant contributor to the crash, with resultant death or serious injuries to other vulnerable road users.
E-scooter riders, often intoxicated, with horrific facial and skull fractures.
Every surgical specialty is required in the treatment of victims of alcohol-related presentations.
Neurosurgeons decompress skulls fractured in injuries sustained because the person was intoxicated or caused by others affected by alcohol. The brain injuries that follow are often lifelong in terms of their destruction of quality of life for the patient and those around the patient.
Orthopaedic surgeons treat the fractured arms and legs, often defence injuries, or injuries sustained because of the impaired judgment or reaction time of the alcohol-affected patient. The plastic surgeons repair complex skin, soft tissue wounds and tendon damage.
This burden of largely preventable injury often adds greatly to the demand for services within already overladen emergency departments and surgical services, which are still struggling to cope with the backlog of surgical cases from three years of the COVID-19 pandemic.
More chronic patterns of liver disease, cancers of the oesophagus and colon, acute and chronic
pancreatitis, anaemia and neuropathy are often seen by surgeons treating patients that have years of alcohol use.
Urgent action by the federal government to tax alcoholic beverages proportional to the alcohol content is long overdue. Clear messaging identifying the over 200 health conditions associated with alcohol use is paramount.
At a state and territory level, regulatory authorities must introduce and enforce effective controls related to liquor outlet density and hours of trade. Packaged liquor outlets, particularly those with online sales and courier deliveries, need to have online age verification, ID checks upon delivery, and trade restrictions for the hours between 10pm and 10am.
These long overdue measures are essential to reduce the billions of dollars spent each year treating alcohol-related harm in Australia.
The advocacy of the surgeon is magnified by working in partnership with other health and community groups. It is often those who experience harms from alcohol who are least able to advocate for change, such as women and children subject to family violence. Many in the community adversely affected by the profitable and wellresourced alcohol and hospitality industry depend on coalitions committed to effective alcohol control policy.
For this reason, the Royal Australasian College of Surgeons is a member of Alcohol Change Australia, a group of health and community organisations from across Australia working together to prevent and reduce alcohol harm among Australian individuals, families, and communities.
When alcohol products are responsible for 15 deaths and
over 390 hospitalisations in Australia every day, change is urgently needed. Alcohol Change Australia is calling on the Australian Government to take action in five key areas to reduce the harms caused by alcohol:
1. Protect the community from alcohol marketing
2. Address cheap alcohol that fuels harm
3. Empower the community by raising awareness of the harms caused by alcohol
4. Support alcohol-free pregnancies
5. Create healthy public policy free of industry influence
The more alcohol that is sold, the more the alcohol industry profits, and the more people in our communities experience harm. We must act to put people ahead of alcohol industry profits. To keep people healthy and well, the Australian Government must take more responsibility for regulating alcohol products and introduce these proven measures that reduce harms from alcohol products. We know what works to reduce harm. What is needed is strong government action.
Dr John Crozier is a vascular and trauma surgeon. He is a member of the Alcohol Change Australia executive as the representative for the Royal Australasian College of Surgeons. For more information on Alcohol Change Australia, seet www.alcoholchangeaus.org.au.

Sleep – both quantity and quality – is under the microscope. CEO of member health fund HIF Justin James commissioned a sleep survey and was alarmed at the findings.

Sleep is one of the three key pillars of health, alongside diet and exercise, but if we’re honest about it can we really say we’re getting the amount or quality we need?
We commissioned CoreData WA to survey 2,000 Australians (including more than 1,000 HIF members) and found a clear link between poor health, lower disposable income and quality of sleep.
The HIF Sleep Index Survey found most Australians were in sleep deficit – especially on workdays. The average Australian views eight hours sleep as 'ideal' each day/ night.
However, most are getting far less – especially workers and students, with one in four (25%) people who are either working or studying sleeping no more than six hours on days when they work. Those not currently in employment, like retirees and stay-at-home parents, are getting 7.4 hours on a typical day.
And while nearly two in three (65%) Australians prioritise sleep, few are consistent with their bedtime routine (25%), or sleep pattern (i.e. when they go to bed and wake up each day) (16%) because they are getting distracted and losing track of time (41%) or just finding it hard to maintain consistency, despite trying (30%).
Other key survey findings include:
• Digital relaxation is hampering sleep
More than 46% read on a device, listen to music or a podcast and/ or watch a show on a device in the hour immediately before they go to sleep. However, those reading on a device before bed are much more likely to wake up feeling like they didn't get enough sleep.
• 4.8 million Australians are using a sleep app, monitor or wearable
Nearly a quarter of Australian
adults (24%) are using these devices, typically to check how long they slept (50%) but also to review their deep/light sleep (35%) or how often they woke up (28%). Sleep apps and wearables are slightly more common among those who say they don't get enough sleep (26%) than those who get an ideal amount (21%), but there are no differences in sleep quality or scores between users and non-users.
The survey also found four distinct groups, or personas, that Australians typically fall into when it comes to sleep. HIF will be using these to create tools to help support members in getting a better night’s sleep.
The Sleep Index Survey found those with no disposable income are significantly more likely to have a low sleep score (23% vs 9% of those with at least some disposable income). They are also almost twice as likely to not have enough sleep than others (31% vs 17%) and sleep quality is more often poor (58% vs 42%).
According to a 2021 report by the Sleep Health Foundation, during the 2019-20 financial year poor sleep cost the Australian economy $14.4 billion, equating to roughly 0.73% of Australian GDP.

It also found that the non-financial costs relating to the loss of well-
being totalled an additional $36.6 billion.
That’s a huge cost to bear and it’s not accounting for that fact this represented 3.2% of the Australian burden of disease for that year. And then there’s the cost to our mental health of not getting quality and lengthy shut eye. Sleep is considered key in preventing mental health disorders in otherwise healthy people with no history of mental illness, and there is also a growing amount of evidence on the importance of sleep in the prevention and management of psychiatric disorders.
We had expert input into the survey from Dr Jennifer Walsh, Director of the Centre for Sleep Science at the University of WA, Dr Kathleen Maddison, a fellow at the Centre for Sleep Science. Michael Gradisar, Professor, Director and Clinical Psychologist at the Child and Adolescent Sleep Clinic at WINK Sleep, and David Beard, an accredited exercise physiologist at the Australasian Society of Lifestyle Medicine.
Dr Walsh said the survey results showed there was still a long way to go in educating Australians about sleep.
We’ve been doing that for our members for some time, but the Sleep Index Survey has allowed us to identify common routines and practices that may be hindering them from getting the recommended hours of sleep a night - and determine what we, as a private health insurer, can do to help them.
It’s time for Australians to get serious because sleep is the one thing we are continually sacrificing, but at what cost?
As National Carers Week 2023 begins in October, it’s timely to acknowledge and celebrate WA’s hidden health workforce, says Richard Newman from Carers WA.

There are 2.65 million unpaid family and friend carers in Australia – an estimated 320,000 in WA, and they’re just those we know about.
Caring is an essential form of unpaid work that supports our aged, disability, health, mental health, and palliative care systems. However, many unpaid carers go unrecognised for their efforts.
According to research by Deloitte, in 2020 alone, unpaid carers dedicated a 2.2 billion hours of care, with an annual replacement value estimated at $77.9 billion.
These carers are our Hidden Health Workforce and without them, our health service would face immeasurable challenges. That is why it’s imperative that these carers receive the supports they need to maintain their own health and wellbeing while continuing to care for their loved ones.
Carer identification is our biggest challenge. The term ‘carer’ is used across all spectrums of service provision, often describing paid formal support workers. But there is another cohort.
Those people looking after a loved one with disability, a mental health challenge, a chronic health condition, a terminal illness, an alcohol or other drug dependency, or who are frail aged.
Unfortunately, these individuals are often unaware that they are carers, primarily seeing themselves in their relationship role first, such as a partner, parent, child, sibling, relative or friend. They do not realise that what they are doing is over and above the responsibilities usual with those roles.
The unpaid caring role can be relentless, typically requiring round-the-clock attention, with no annual leave, personal leave, or superannuation contributions.
Without support, these carers can face significant struggles and are usually reluctant to ask for help until they reach crisis. These are often the people who present to their GP with their own health issues, which are frequently brought on by exhaustion.
In such cases, GPs are in the best position to identify these carers and can play a critical role in recognising their challenges and offering supports. Referring carers to Carers WA will help ensure they receive the supports and services they need to flourish in their caring role and live a rewarding, healthy and fulfilling life.
Carers WA, works in collaboration with Carer Gateway. We are a non-profit, community-based organisation and registered charity dedicated to improving the lives of unpaid carers living in WA.
We have a variety of communitybased supports and services, but we also offer hospital-based supports. Our Prepare to Care Hospital Program is available to support carers when their loved one is admitted.
Our hospital team delivers education to clinical staff, focusing on carer recognition and engagement, and provide resources that carers can use to navigate the hospital system. By ensuring the carer is well supported on discharge, hospital readmissions of the patient are less likely.
The Prepare to Care Hospital Program helps public hospitals meet accreditation requirements for Standard 2 of the Safety and Quality Health Service Standards (Partnering with Consumers) and comply with both the federal and WA Carers Recognition Acts.
In WA, the Carers Recognition Act recognises the role of carers in the community and as key partners in the delivery of care. It includes the
WA Carers Charter which outlines how carers are to be treated and how they are to be involved in delivering services that affect them and their caring role.
The WA Act requires Department of Health, public hospitals and the Disability Services Commission, and non-government services funded by these agencies to comply with the WA Carers Charter.
The four principles of the Western Australian Carers Charter are:
1. Carers must be treated with respect and dignity.
2. The role of carers must be recognised by including carers in the assessment, planning, delivery and review of services that impact on them and the role of carers.
3. The views and needs of carers must be taken into account along with the views, needs and best interests of people receiving care when decisions are made that impact on carers and the role of carers.
4. Complaints made by carers in relation to services that impact on them, and the role of carers must be given due attention and consideration.
Unpaid family and friend carers play a crucial role in WA’s health-care system. Their tireless dedication and countless hours of care provided to loved ones are invaluable.
Although the identification of unpaid carers remains a challenge, through community- and hospitalbased initiatives like the Prepare to Care Hospital Program, unpaid carers can also receive support, leading to reduced hospital readmissions and better care outcomes.
Mr Newman is CEO of Carers WA. National Carers Week: October 15-21. If you, or somebody you know, is a carer and needs support, contact Carers WA. Visit carerswa.asn.au or phone 1300 227 377.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
Trust takes a long time to build up but can be lost quickly. Generally, doctors fare well when the public is surveyed on who they trust.
It was with interest then that I heard Dr Eric Reinhart, who is a political anthropologist, psychoanalyst and medical resident say, “In my view the biggest obstacle to health in the US today is the lack of trust the public holds for medical care, for public health systems and ultimately for the government”.

Yes, our health and political systems are different to the US. However, we too are more polarised than ever and, like it or not, we often follow trends which first appear in the US. While I hope to be wrong, it would not surprise me if the next survey showed a decrease in trust for the medical profession.
It is claimed that Sweden was successfully able to negotiate COVID without lockdowns or draconian measures because there is two-way trust. The people generally trust that the government has the public (rather than its own) best interests at heart and the government trusted the people to behave in a sensible manner without coercion.
Most people when asked will say they trust their doctor (or lawyer) but not necessarily “the doctors” or “the lawyers”. When we have a personal relationship, we can form a view as to whether a person is trustworthy. While not correct 100% of the time, most people are usually right and can learn if wrong. It is harder to trust an amorphous group especially when the errors or sins of even one member of said group can cast aspersions across all.
Part of building trust is humility and empathy. This means conceding that you don’t know everything and are open to the view that you could be wrong. It also means understanding how others feel. While this may not deter you from a course of action, it shows that you are aware of different perspectives and have considered them in making a decision.
We have seen elements in our profession become increasingly dogmatic and tin-eared to views they do not hold. This reflects poorly on the entire profession especially when played out in the public square.
It has been said by many that half of what we learn in medical school was wrong but we don’t know which half. Thus humility and being open to new ideas which contradict our current thinking is critical both to advancing medicine and to building and maintaining public trust.
Part of building trust is humility and empathy. This means conceding that you don’t know everything and are open to the view that you could be wrong. It also means understanding how others feel.


Small airways are those less than 2mm in diameter and by definition, the bronchioles. Resistance in these airways is normally low and are sites of laminar rather than turbulent flow.
From a surface area point of view, the small airways are several-fold greater in surface area than the larger airways. Collateral ventilation can exist. Small airways have surfactant on their surface compared to large airways and have a different immunological response.
If the surface properties change these airways readily collapse. Small airway closure is the main reason for gas trapping.
Small airways, when they narrow, are too small to make an audible sound. Compared to larger airway obstruction, there is no obvious wheeze. Instead, with relative airway collapse occurring on expiration, a ball valve effect occurs, and the main physiological effect is air trapping.
This leads to over stretching of the chest wall leading to a sensation of chest tightness. As the chest is already hyperexpanded at the initiation of inspiration, the work of breathing is increased, and breathlessness ensues. Cough can be an added feature due to airway nerve stimulation.
Wheeze either never occurs or is a relatively late feature as larger airways are recruited into the pathological process.
Consequently, patients with small airway obstruction are underdiagnosed and their severity both acutely and longer term is usually underestimated. It is important to ask patients to describe the order in which their symptoms occur and the extent to which wheeze is a primary feature or not.
Being at the distal end of the respiratory tree, small airways’ function is not easily measured. Peak flow is very insensitive, being much more influenced by the immediate expiratory air flow from larger airways. FEV1 is again more influenced by large airway emptying than small airways.
Once air trapping occurs spirometry can also be misleading with FVC being a more sensitive measure than FEV1 while the FEV1/FVC ratio can worsen as the patient improves. FEF25-75 although helpful has significant testto-test variability. The shape of the flow volume loop can be indicative of small airway disease (fig.A).

Frequency Oscillation Testing is a relatively new measurement and is used during tidal breathing. It measures the transit of low-frequency sound waves to provide information on airway resistance at the large airway and simultaneously, and independently, at the small airway level. The test requires no formal input from the patient and in our experience is very sensitive to small airways disease.
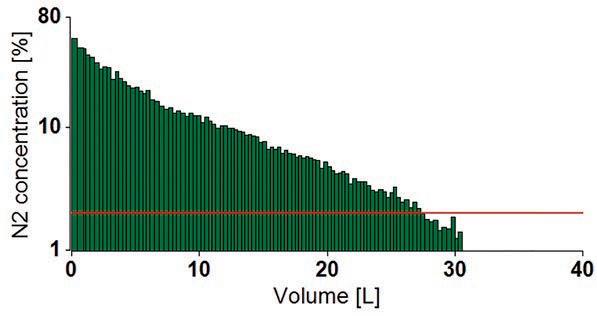
Small airways disease states are generally overlooked in respiratory health
They can be diagnosed and managed more effectively Certain inhalation devices can deliver medication to small airways.
Single breath nitrogen washout curves provide information on the relative gas emptying of the small airways, while multiple nitrogen washout testing (fig.B) and related Lung Clearance Index provide information on the heterogeneity of small-to-medium airway gas emptying. In our hands, this latter test can often be the only abnormality in early disease.
CT scanning can provide information on air trapping (byproduct of small airway closure) and with sophisticated computer algorithms one can map out which parts of the lung have gas trapping and is then very helpful if interventional treatments such as airway valves or surgery are being considered.
Other techniques (e.g. nuclear medicine and more sophisticated pulmonary physiology assessments) are feasible but more complex and not necessarily more informative.
(Small airway) asthma, bronchiolitis, bronchiolitis obliterans, emphysema and hypersensitivity pneumonitis are the primary disease groups. However, only asthma and emphysema are common and the use of the term COPD as an overarching term and the description of an Asthma-COPD overlap syndrome only serve to confuse having a more precise definition.
In emphysema, which is the primary small airway obstructive disease labelled as COPD, the gas transfer is usually reduced, while in small airways asthma, the opposite is the case, with gas transfer intact or increased as this disease does not impact on the alveolar space and gas transfer.
Many patients with this latter entity do not have a significant (if any) smoking history, describe significant variability, have trigger factors peculiar to asthma and/or have a history of childhood asthma/bronchitis.

There is a logic in trying to deliver medication to the small airways. However, MDI devices are limited in the particle sizes they can successfully deliver to the airways. Propellant based systems (pMDI) can, overall, only generate particles of approximately 5u in diameter. Drypowder devices are limited in the size of particles they can be disaggregated to. Standard nebulisers produce particles too large to penetrate to small airways, but newer mesh nebulisers and ultrasonic nebulisers can accommodate this.
There are currently several MDI devices/systems that can deliver to the small airways. These are the 3M concept that dissolves steroid medications into the propellant, the Respimat device – a vaporisation system – and the more recent-to-market Modulite, an aerosphere propellant system. Each has their strengths and weaknesses.
Author competing interests – nil.
By Mr Peter Ammon Foot Ankle & Knee Surgery


Dermatologist-led cosmetic medicine service

Doctor-delivered treatments, for GP-referred patients
Laser modalities for
Rosacea
Acne
Hyperpigmentation
Lentigos, melasma etc.
Vascular Lesions
Tattoo removal
Hair removal
Birthmarks (pigmented & vascular)
Rejuvenation/ageing
Hair loss service
Comprehensive medical service for alopecia and patterned hair loss
Injectables for medical indications
Wrinkle relaxers
Fillers for loss of facial volume
Emphasis on ‘natural look’
Axillary Hyperhidrosis
Referrals accepted by Healthlink, Email, Fax, Post or Phone
Post: Karrinyup Dermatology, 5 Cheddar Place, Karrinyup WA 6018
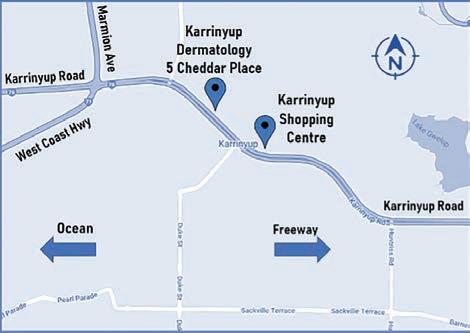
Phone: (08) 9245 3376 Fax: (08) 9245 5033
Healthlink: karrinyd
Email: admin@karrinyupdermatology.com.au
As a specialist Dermatology Clinic, we continue to accept GP referrals for all general dermatology presentations.

There is no denying the exponential popularity of e-cigarette use in Australia, particularly among adolescents. These devices are misleadingly considered as ‘less harmful’ alternatives to conventional cigarettes.
As a smoking cessation tool, nicotine-containing products may have a role in risk reduction for active smokers. Conversely there is good evidence they encourage the initiation of cigarette smoking in the uninitiated.
The explosion of youth use and flurry of acute toxicities over the past few years swamps any potential harm reduction that may accompany adults switching to e-cigarettes, in my opinion.
While the overall health effects of e-cigarettes are limited, pulmonary toxicity is established. At the cellular level, studies have shown increased oxidative stress, endothelial cell dysfunction and impaired host defence with functional changes in macrophages and neutrophils.
E-cigarettes have become more popular
A new pathology called EVALI has been described Vigilance is required.
Clinically, several lung injury patterns have been recognised albeit, the long-term sequelae remain unknown at present.
E-cigarettes are well-established causes of hypersensitivity pneumonitis and bronchiolitis obliterans. A new recognised pathology, EVALI, emerged in 2019 with thousands of hospitalisations and many deaths over the following couple of years, now on the decline.
This entity is a result of acute lung injury and should be considered in any patient with atypical pneumonia picture. Presentation can be very similar – dyspnoea, fevers, cough the main symptoms. Many patients will also have GI symptoms and chest pains. Inflammatory markers are high. Radiology from published series are as below:
Proposed Diagnostic Criteria:
Pulmonary inflammation
Oxidative stress
Protease-mediated lung tissue damage
Increased airway hyper-reactivity
Increased airway resistance
Decreased antimicrobial activity
Down regulation of host defence genes
Increased resistance of bacteria to antimicrobial factors
High levels of particle deposition
Increased epithelial necrosis and cytotoxicity
Direct mucociliary dysfunction
Acquired cystic fibrosis transmembrane conductance regulator dysfunction,
Increased mucus viscosity and reduced Airway Surface Liquid height leading to impaired mucociliary clearance
• Use of e-cigarettes in the previous 90 days
• Lung opacities on imaging
• Confirmed – exclusion of lung infection
• Probable – other cause of disease (infection) may be present but is not thought to be sole cause of underlying lung injury
• Absence of a plausible alternative diagnosis.
The optimal treatment is not known. Antibiotic cover is usually initiated in the case of co-existing bacterial infection with or without the addition of antivirals. Steroids have been used in serious cases, with unknown benefits at this stage.
EVALI is a serious illness and case series show follow-up of ongoing morbidity in the majority of
patients. Prevention is paramount, particularly with patients having co-morbidities such as asthma, and while there has not been a single implicated constituent, avoiding THC containing products is recommended.
Fortunately, the reported incidences of EVALI have been decreasing. Nevertheless, one cannot negate other worrying risks in counselling patients.
Nicotine has been found in majority of products in use in the US, although it is illegal to be sold here in Australia without a script, we know many of these devices are obtained from overseas. These devices are not approved for smoking cessation. The blood nicotine levels achieved have been shown to be similar to conventional cigarettes.
Short-term data on cardiovascular effects have shown mixed results. Carcinogen levels in the blood have been lower and long-term lung cancer risk probably lower than conventional cigarettes. However, direct testing has shown a huge variance depending on the product tested.
Secondhand exposure studies have been scarce. We know from European registration documents that the big tobacco companies own the great majority of the e-cigarette manufacturing (The Australian article in November 2022 cited four out of the top five brands).
Even though the medium-long term data is yet to emerge, as a medical community, we need to be ever vigilant, I believe, in interpreting the reports and tactics which will undoubtably continue to come our way.
Author competing interests – nil


Respiratory issues are a major cause of morbidity in young children. Especially common in winter, they can make up as many as one in three presentations to a GP practice. Common respiratory issues include influenza, asthma, croup, bronchiolitis and pneumonia.
While sleepless nights as a result of these illness can be disruptive for both children and their parents, minor illnesses can boost children’s immune system. We reduce respiratory issues by reducing transmission by handwashing, covering coughs/ sneezes, limiting contact when sick and vaccination. However, some children are “sick all the time”, which is a common presenting complaint. For children to be nasally congested, snorty and coughing continuously or having frequently recurring episodes is not ideal. Often there can be a few common ENT implications in children who are frequently sick that need to be considered as part of their overall assessment.
Otitis media (OM) can often be an associated issue in children who are frequently sick with respiratory issues. The respiratory system is closely linked to the middle ears via the eustachian tubes. OM is one of the most common reasons why young children present to GPs and winter is peak season. Approximately 75% of children have at least one episode of OM by school age. Those between 6-18 months of age are at a higher risk. Common types of OM are acute OM (AOM) or OM with effusion (OME)
AOM causes pain, fever, and occasionally perforation. The child will be irritable and sleep may be disrupted. Treatment is usually symptomatic control with adequate pain relief and oral antibiotic may be required. Symptoms may take one to two weeks to resolve. Recurring middle ear infections of three episodes or more in six months may warrant further assessment.
Respiratory infections are common in young children
Some children who are “sick all the time” may have underlying ENT issues
Consider paediatric ENT referral in chronically unwell children.
The presenting symptoms very often vary according to the severity and also age of presentation.
Tonsils and/or adenoid hypertrophy are usually the main causes of OSD in children. A comprehensive history to explore symptoms with parents and a detailed examination will usually suffice for diagnosis. A polysomnography can be considered as an investigation in certain patients.
OME or “glue ear” is accumulation of fluid in the middle ear. These children may have hearing loss, speech delay, learning difficulties and imbalance. Children with OME tend not to present with the acute infective symptoms as in AOM.
Common predisposing factors for children with OM are daycare attendance, frequent upper respiratory tract infections, exposure to cigarette smoke, bottle feeding and use of pacifiers.
Children with excessive middleear infections not responding to conservative measures will need to be reviewed by a paediatric ENT surgeon. An audiological assessment will be part of the examination. Surgery such as grommet insertion and/ or adenoidectomy may be recommended.
Children with enlarged adenoid and/or tonsils can be chronically or frequently nasally congested with a runny nose. These children appear “sick all the time”! In addition, they may also have associated obstructive sleep symptoms.
Obstructive sleep disorder (OSD) is a range of presenting symptoms from heavy breathing/snoring to sleep apnoea where some children can have pauses in breathing. Symptoms can include mouth breathing, sleeping in unusual positions, nightmares/night terrors, bedwetting, waking up tired and also daytime issues with behaviour or concentration. Some children can have difficulty with swallowing or fussy with certain foods.
Children frequently unwell with URTIs may end up with sore throats (viral or bacterial in origin). Treatment starts with symptomatic relief such as analgesia and adequate fluid rehydration. Sometimes bacterial tonsillitis occurs and needs treatment with antibiotics.
Symptoms of tonsillitis can include sore throat, difficulty swallowing, bad breath, fever, cervical lymphadenopathy and also disrupted sleep. If a child has recurrent tonsillitis, it will be recommended to have a GP review to determine its severity.
There are guidelines as to the frequency of tonsillitis to warrant an ENT assessment. Also, there should be consideration for other factors such as frequency of use of antibiotics, time off school and also time taken off work by parents to look after the child with tonsillitis.
Our GPs are generally well versed in ENT issues in children. However, some children who are chronically unwell or going through frequent cycles of illnesses, a paediatric ENT assessment may be considered in their overall care. Sometimes, it may just be the answer as to why some children are sick, irritable and grumpy all the time!
Author competing interest – nil

Insomnia and mental health is a complex dance. Insomnia disorder, characterised by difficulty falling asleep and/or staying asleep, accompanied by daytime impairment, affects 10-15% of the adult population in Australia (although 30% have symptoms of insomnia at any one time). This number jumps to over half in mental health populations.
Insomnia used to be considered a mere symptom of mental disorders. Indeed, it is the most commonly appearing symptom in the DSM-V. Insomnia, however, is not just a benign symptom but a potent causal factor across the spectrum of mental health diagnoses that increases first episode risk, relapse risk and symptom severity.
A recent Lancet review considered the link between suboptimal sleep
and psychiatric disorders, and found that, typically, the strongest pathway was poor sleep causing the psychiatric problems and not the other way around. When insomnia takes hold, even if it was precipitated by a mental health condition, it develops its own set of maintaining processes that don’t necessarily resolve upon treatment of the coexisting mental health concern.
By way of example, insomnia is the most common residual symptom in remitted depression, and treating the insomnia with CBT-I in this case reduces risk of depressive relapse.
In addition to being a risk factor for mental ill-health, insomnia may also be a marker of disrupted neuroplasticity and dysregulation of neurobiological mechanisms involved in various mental conditions. Recent research
suggests that insomnia treatment with CBT-I may normalise sleep processes, neuro inflammation and brain plasticity.
Insomnia can be screened for quickly by clinical interview or brief self-report measures such as the widely used Insomnia Severity Index (ISI). Scores above 10 on the ISI suggest Insomnia Disorder (86% sensitivity; 88% specificity).This is a link to online ISI: https://qxmd.com/ calculate/calculator_820/insomniaseverity-index-isi
The effectiveness of cognitive behaviour therapy-insomnia (CBT-I), particularly in the longterm, and the minimal adverse effects of this treatment have resulted in it being recommended as the first-line treatment for
Bulk Billing available for all diagnostic imaging
– urgent patients seen within 24 hours
EOSedge is the first general X-ray system of its kind in WA with a high-resolution photon-counting detector remarkably improving image quality.
Fully functional 2D/3D biplanar X-ray imaging in seconds

Open design to suit an extensive range of patients

Up to 80% reduced radiation dose with Flex Dose

Insomnia Disorder is common in the context of mental health disorders and increases disorder risk, severity, and relapse. The causal neurobiological pathway may be disruption in neuroplasticity
Cognitive Behaviour TherapyInsomnia (CBT-I) is the recommended first-line treatment and has a beneficial impact not just for insomnia but on coexisting mental health conditions
Screening and treatment of insomnia and other sleep disorders represents an opportunity to optimise outcomes in patients with mental health disturbance.
primary insomnia in Australian and international guidelines.
CBT-I is short-term, structured therapy that helps people change behaviours and thoughts that impact on their ability to sleep well. Typically, 4-8 sessions are required, and these can often occur before, after or be interweaved with other
psychological therapies.
Treatment revolves around patients understanding and harnessing the two-process model of sleep regulation (homeostatic sleep drive and circadian rhythm) as well as the impact of arousal on sleep. Intervention often includes patients adjusting their current sleep and/or daytime routine, (e.g. spending less time in bed overnight for 1-4 weeks), learning to reduce anxiety about sleep, working to maximise daytime energy, and better manage stress.
About 80% of those treated with CBT-I will benefit and those benefits are long lasting, even when mental health comorbidities are present. CBT-I can also work well combined with sleeping tablets and can support patients to taper their sleeping tablet use.
Much exciting research is raising understanding of the impact insomnia treatment has beyond insomnia. For example, CBT-I has been shown to amplify antidepressant response, reduce risk of mania in bipolar patients, amplify the effectiveness of psychological therapies for PTSD, reduce psychotic symptoms, and improve
mood, anxiety and quality of life.
Additionally, treating insomnia comorbid with Obstructive Sleep Apnoea (OSA) can benefit the OSA, both directly and via improved adherence to CPAP. This is relevant to mental health as OSA carries increased risk for depression.
Insomnia treatment can support engagement with broader psychological therapy. In the clinic, we notice that clients find seeking treatment for insomnia less stigmatising than for other mental health concerns. CBT-I can function as a good introduction to the process of seeing a clinical psychologist. Clients sometimes opt to address other mental health concerns after attending for CBTInsomnia that they would not have attended for the co-existing mental health concern in the first instance. CBT-I can directly and indirectly empower patients to better manage their mental health.
– References available on request
Author competing interests – nil


Almost 15% of the Australian population meet the diagnostic criteria for chronic insomnia. That is, when given sufficient opportunity for sleep, they have had difficulty falling asleep or staying asleep on at least three nights/week for at least three months.
This sleep disturbance results in clinically significant daytime symptoms such as mood disturbance, fatigue/exhaustion or impaired occupational, academic, behavioural or social functioning. For perspective, approximately three times as many Australians are living with chronic insomnia than those living with diabetes.
There are effective treatment options for insomnia. Cognitive behavioural therapy for insomnia (CBTi) is the first line treatment, in many cases, including when medical or psychiatric comorbidities are present. When performed under the guidance of a trained sleep psychologist there is high-quality evidence that CBTi results in positive outcomes in the majority of cases.
Recent diversification in treatment modalities to include telehealth, group therapy sessions and online tools has improved accessibility, nevertheless it remains difficult for many patients to access when they need it. For this reason, and possibly also due to lack of awareness of the effectiveness of CBTi or perceived expense of treatment, 90% of patients presenting to primary care providers with insomnia are offered pharmacotherapies.
However, potential adverse effects from conventional pharmacological treatments for insomnia including dependence, tolerance, abuse potential, daytime sedation, cognitive impairment and falls risk, preclude their use in some people, even for short-term use. Patients, clinicians and researchers are seeking alternative therapeutic options and cannabis, or its cannabinoid constituents, has been proposed as a possibility.
There is evidence in the medical literature that cannabis has been used for its soporific properties dating back to 1839. In Australia in 2022, insomnia and sleep disorders were the third and fourth most common reasons, after pain and anxiety, for the prescription of cannabinoid-based medicines.
Of those who use cannabis (sourced via prescribed or illicit means) for medicinal purposes, 55% are using it treat their insomnia. This upsurge in use of cannabinoid-based medicines for the treatment of insomnia contrasts with the evolution of other pharmaceutical products
for insomnia, as it has preceded high-quality clinical evidence for its efficacy, effectiveness and safety. One of the biggest challenges in using cannabinoids to treat insomnia is identifying the appropriate cannabinoid or cannabinoid formulation. The cannabis plant contains over 100 phytocannabinoids (referred to as cannabinoids), with Δ9tetrahydrocannabinol (THC), cannabidiol (CBD) and cannabinol (CBN) being the most wellrecognised and investigated.
THC is known for its intoxicating effects and typically drives the

Chronic insomnia is a common sleep disorder, affecting approximately 15% of Australians
As an alternative to existing pharmacological and nonpharmacological treatments, cannabinoids are being increasingly used to treat insomnia
Evidence to support the routine use of cannabinoids, or the most effective formulation, for treating insomnia is currently limited.
recreational use of cannabis. CBD and CBN are non-intoxicating and when combined with THC may moderate its intoxicating and psychological effects.
Emerging evidence suggests that each cannabinoid can induce different therapeutic effects and varying doses of the same cannabinoid can have opposing effects. The route of administration also affects response with onset of action significantly more rapid with inhalation (eg. smoked or vaporised) than oral consumption (eg. oils
or capsules) although no study has quantified this in relation to measures of sleep.

Research to date which has investigated the effects of orally consumed cannabinoids on sleep in patients with insomnia or insomnia symptoms, but no other comorbidities, is limited.
Early work (<1985) with basic sleep outcome measures found that 1030mg THC reduced time taken to fall asleep but did not increase sleep duration, and 160mg CBD increased sleep duration but not time to fall asleep. Since 2021 four randomised placebo-controlled trials have been conducted (all within Australia).


Three studies have used formulations including THC. One study showed improvement in a number of subjective and objective sleep outcomes when participants took 20:2:1mg THC:CBN:CBD (or a half dose) compared to placebo for two weeks. The other two studies reported either no improvement in sleep outcomes with two weeks of dosing (10:15mg THC:CBD) or an increase in the time taken to fall asleep following one night of dosing (10:200mg THC: CBD).
The most recent study identified no improvement in sleep outcomes with two weeks of 150mg CBD dosing (the maximum daily dose under Schedule 3 access) compared to placebo.
Based on the limited clinical evidence available, it may be that higher doses of THC, perhaps with small amounts of CBD, has better effect on sleep than formulations with higher concentrations of CBD. However, due to the vast differences in study designs and sleep outcome measures used, it is impossible to draw strong conclusions about the most effective formulations and dosing from the evidence currently available. The emerging evidence is encouraging, but there’s more research to be done.
ED: Dr Walsh is also research fellow at the WA Sleep Disorders Research Institute, SCGH



Author competing interests –Dr Walsh has received research funding from Zelira Therapeutics and Incannex Healthcare Ltd.


Chronic obstructive pulmonary disease (COPD) is among the world’s leading causes of mortality. Identifying strategies to prevent and control COPD onset and progression is an ongoing public health priority.
Flavonoids, bioactive compounds found in plant-based foods and beverages such as fruits, vegetables, tea, cocoa, red wine, and berries, have been linked with pulmonary-protective benefits.
While the respiratory tract it is primarily responsible for the exchange of oxygen and carbon dioxide between the external environment and the blood stream, it also performs important barrier and immune system functions.
Throughout life, the human lung is exposed to pollutants and infectious organisms in the ambient air, making it vulnerable to injury and disease. Gradually, over time, exposure to noxious substances, such as tobacco smoke and air pollution, causes lung tissue destruction, inflammation and narrowing of the airways, leading to COPD. One in 20 Australians aged 45 and over have COPD and those with COPD have a higher risk of other chronic diseases, such as cardiovascular disease and cancer.
In addition to vitamins, minerals and macro-nutrients, the human diet contains a wide variety of other compounds, including flavonoids. At least several hundred flavonoids are found in the foods we eat.

Sources of flavonoids are quite diverse ranging from nuts, seeds, wholegrains and legumes to fruits, herbs, and vegetables, and also include oils, tea, wine, and beer.
Based on chemical structure, flavonoids can be classified into six major subclasses including flavonols, flavones, flavanones,
Flavonoids are bioactive compounds found in foods and beverage such as tea, cocoa, red wine, nuts and berries
Flavonoids have demonstrated anti-inflammatory and antioxidative properties as well as pulmonary protective benefits
Emerging research links long-term consumption of dietary flavonoids with lower risk of COPD.
isoflavones, flavan-3-ols, and anthocyanins. Isoflavones are typically found in soy products, flavanones are mostly found in citrus fruits and anthocyanins are found in berries and red wine. Black and green tea, dark chocolate and apples are high in flavan-3-ols while flavanols are more ubiquitous and are found in many different plantbased foods.
The ability of flavonoids to modulate pulmonary health is dependent on their absorption and subsequent interaction with the processes involved in pulmonary pathophysiology. Flavonoids, or rather their in-vivo metabolites, act as signaling molecules, inducing protective enzymes, resulting in anti-inflammatory and anti-oxidant benefits.
That flavonoids may protect against COPD by inhibiting oxidative stress and inflammation has been demonstrated in cigarette smokeinduced COPD rodent models. Furthermore, flavonoids have been identified as synolytic agents inducing apoptosis and the removal of senescent cells which appears to further contribute to their pulmonary-protective properties. Although several studies have shown that higher habitual dietary flavonoid intakes are favourably associated with pulmonary function parameters, such as forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1), until last year, studies investigating their association with COPD incidence were missing.
In our recent work, published in European Respiratory Journal, we examined flavonoid intake and the incident of COPD in >50,000 participants from the Danish Diet, Cancer and Health study. Over 23 years of follow-up, we observed participants with the highest total flavonoid intakes had a 20% lower risk of COPD than those with the lowest intakes; a 6–22% lower risk was observed for each flavonoid subclass investigated. Furthermore, higher flavonoid intakes appeared to lessen, but not negate, the high risk of COPD associated with smoking.
continued on Page 55


A globally acknowledged variation exists in the management of ductal carcinoma in situ (DCIS), including the prescribing of adjuvant radiation therapy (RT). Adjuvant RT following breast conserving surgery (BCS) for women with DCIS reduces local recurrence risk of DCIS and invasive malignancy, however not all DCIS behaves the same.
Previous predictive tools and clinical treatment recommendations were based on clinical and pathological prognostic factors such as grade, size and margins. A new DCIS precision medicine tool is a biosignature that uses individual tumour biology in conjunction with clinical and pathologic risk factors and provides a validated score for women receiving BCS that assesses 10-year risk of DCIS recurrence and development of invasive breast cancer with and without adjuvant RT. The tool has level two clinical evidence and provides personalised information for women to allow for more informed treatment decisions. Testing is conducted exclusively at the PreludeDx laboratory in California, USA. Through an international partnership women in Australia can now access this option.
Patients accessing this precision medicine tool are asked to
A new assessment tool aims to allow for better informed decision making by patients
Management of DCIS varies across jurisdictions
Please note that this precision medicine tool for DCIS breast cancer patients has not been approved by the TGA.
participate in the AUS-PREDICT Registry. This prospective study is collecting treatment decision and outcome data (up to 10 years post treatment) on 1,500 Australian women and will allow us to inform the future management of patients with DCIS. Treating physicians’ are asked to complete treatment recommendation forms before and after receiving test reports to capture surgical, radiation, and hormonal treatment recommendations and patient preferences.
An interim analysis was performed on the first 232 patients treated at 40 sites who had definitive BCS and subsequent testing via the tool. The median age of patients was 63 years, 17% were 50 or younger, nuclear grade was high in 52% and
tumour size was 2.5cm or greater for 16%. Results were graded via a Score of (DS) Low Risk (DS ≤ 3) for 65% of women and 35% were DS Elevated Risk (DS >3). This interim analysis demonstrates a 45% change in treatment recommendations to add or safely omit radiation therapy based on results via the tool in 232 patients. There are currently >700 patients now recruited to the AUS-PREDICT registry (June 2023), with a further analysis underway.
The integration of this precision medicine tool into clinical decision processes has had a substantial impact on recommendations aimed at optimal management of women with DCIS to prevent over or under treatment. This precision medicine tool offers additional biological information for women with DCIS (of any clinical pathology grade) to help inform a personalised treatment plan.
– References available on request. Author competing interests
Dr Zissiadis is a Radiation Oncologist at GenesisCare and Principle Investigator of the Aus-Predict Registry Study. The prospective registry study, AUS-Predict, is a collaboration between PreludeDx and GenesisCare, following the impact of the precision medicine test on outcomes and treatment decisions in DCIS.
continued from Page 54
1) Clinicians are encouraged to prioritise smoking cessation for COPD prevention.
2) Low intakes of flavonoids do not cause dietary deficiency diseases, such as scurvy (vitamin C deficiency) or beriberi (vitamin B1 deficiency), rather their consumption appears to promote long-term health and protection against non-communicable
disease, with emerging evidence linking them to lower risk of COPD.
3) Promotion of dietary patterns, rich in a variety of fruits and vegetables, limited in ultra processed/discretionary foods, and sufficient in other foods groups (i.e., dairy, wholegrains and lean meats), in accordance with the Australian Dietary Guidelines, should provide plenty of flavonoids as well as a balanced intake of other health promoting factors (e.g. fibre,
etc.,) and is recommended for patients looking to optimise their nutrition for general long-term health.
4) Those with existing COPD can be referred to a dietitian for nutrition support.
ED: Dr Parmenter is from the Nutrition Innovation Institute at Edith Cowan University, and Dr Bondonno is from the Danish Cancer Society, Copenhagen
Author competing interests – nil
 Arjuna Somanathan, Radiologists
Arjuna Somanathan, Radiologists
Silicosis is one of the oldest known causes of occupational lung disease referring to a spectrum of preventable pulmonary disease caused by the inhalation of free crystalline silica. Written record of lung disease related to inhalation of silica dates to ancient Egypt and Greece.
Despite its long and welldocumented history, the prevalence and impact of silicosis in Australia remains largely unknown. Safe Work Australia estimates up to 1.45 million Australian workers are employed in industries with potential for silica exposure, suggesting the impact is potentially very significant. These industries include (but are not limited to) stone masonry, mining and hydraulic fracturing, sandblasting, foundry work, construction, demolition and earth moving.
Silica is one of the most abundant minerals on earth, existing in crystalline and amorphous forms. Silica is found in varying concentrations in the natural and man-made environment with marble containing low levels of silica (2-5%) as an example, and engineered stone containing up to 97% silica. Substandard industry safety and hygiene practices have, in the past, exposed workers in the aforementioned industries to unacceptably high levels of environmental silica.
Screening with low-dose CT is mandated by law in WA with chest x-ray and conventional high-resolution CT not acceptable surrogates
Imaging for silicosis must be performed at imaging providers capable of meeting the legislated dose requirements and with radiologists experienced in reporting thoracic imaging

Early CT findings of silicosis are not highly specific. Providing clinical information regarding occupational exposure, history of other pre-existing pulmonary disease (e.g. asthma, previous tuberculosis) smoking history and any intercurrent illness is vital for accurate interpretation of these studies.

Acute silicosis, (silicoproteinosis), is rare and refers to development of pulmonary symptoms within a few weeks to a few years following exposure to very high concentrations of crystalline silica. It follows a rapidly progressive course with very poor prognosis.
Chronic silicosis refers to the ‘classic’ silicosis historically seen in early-mid 20th century miners developing respiratory symptoms 10-30 years after initial exposure to, relatively, low levels of silica. The surging popularity of engineered stone in Australian households since the turn of the century has led to the emergence of accelerated silicosis, typically affecting younger workers after a short period (5-10 years) of exposure to high levels of crystalline silica. Patients with accelerated silicosis are at
When inhaled, crystalline silica travels to the depths of the small airways where it interacts with the aqueous media found in the distal airways and alveoli to generate free radicals and activate alveolar macrophages, amongst others, to produce pro-inflammatory cytokines leading to an inflammatory cascade ultimately progressing to pulmonary injury and fibrosis.
Silicosis can be classified as ‘acute’, ‘accelerated’ or ‘chronic’.
Examples of work activities that can generate respirable silica dust particles include:
during fabrication and installation of composite (engineered or manufactured) stone countertops
excavation, earth moving and drilling plant operations
clay and stone processing machine operations
paving and surfacing
mining, quarrying and mineral ore treating processes
tunnelling
construction
labouring activities
brick, concrete or stone cutting; especially using dry methods
abrasive blasting
foundry casting
angle grinding, jack hammering and chiselling of concrete or masonry
Fig.1:
(A) 'Normal' chest x-ray in a stonemason in their 40's presenting with a new cough.
(B) Low dose CT (LDCT) demonstrating innumerable diffuse centrilobular nodules in the same patient.
(C) Magnified view of LDCT in (B) with innumerable "ground glass" attenuation nodule spread throughout the lung parenchyma (arrows).
hydraulic fracturing of gas and oil wells
pottery making
Source: SafeWork Australia
increased risk of developing progressive massive fibrosis and other complications of silicosis with poor prognosis and no specific treatment options.
The emergence of accelerated silicosis cases in Australia led to the formation of the National Dust Disease Taskforce which in 2021 delivered its comprehensive final report outlining its strategic approach to the prevention,
early identification, control and management of silicosis and other occupational respiratory diseases. One of the recommendations outlined in the report was the use of low dose CT screening, over the historically used chest x-ray (CXR), and in January 2021 legislation was passed for low dose CT scan (LDCT) to replace chest x-ray in Western Australia as the radiological screening test of occupational exposure to silica.

CT scans for the purposes of silica screening in WA are performed without intravenous contrast and at very low doses. They are required by legislation to have a dose of <1millisievert(mSv) for the entire study. This dose is equal to approximately six months of background radiation, considerably less than a standard high-resolution CT (HRCT).
The studies must be read by a radiologist with dedicated experience in thoracic imaging including the imaging of interstitial lung disease, with each report including a standardised
With World Lung Cancer Day in August, the Lung Foundation Australia released its annual scorecard, which celebrates vital wins and highlights where action is still needed.
Lung Foundation Australia CEO Mark Brooke said while the Federal Government’s commitment to a national lung cancer screening program was a massive step forward, there was still much work to be done in having lung cancer and lung disease equitably recognised.
“We know the lung cancer screening program will save thousands of lives. If Australians with lung cancer are diagnosed at Stage I, their five-year survival rate nears 70%,” Mr Brooke said.
“It’s wonderful that we’ve slightly increased the number of specialty nurses to 47 this year, but we know the more investment in these vital services, the greater the benefits and savings on the health care system in the long run – 100 nurses would reach 44% of lung cancer patients and save $18 million.”
In May, Health Minister Mark Butler announced $263.8 million from 202324 to implement a national screening program to start by July 2025.
“At risk Australians will be able to get a lung scan every two
classification and the total dose of the study. Imaging providers must have the latest CT scanners, software and dedicated low-dose protocols to facilitate high-quality studies at the mandated dose of <1mSv.
If these services are not available locally, CXR and/or HRCT are not acceptable screening substitutes and LDCT screening must be performed at a facility capable of providing the service.
Screening intervals are 2-5 years depending on level of exposure, with engineered stone workers screened every two years due to their higher risk of silicosis.
It is vital for clinicians to be mindful that patients who have left their exposure prone industries prior to 2021 will not be covered by current legislation and LDCT screening for silicosis should be considered in patients with a history of silica exposure when presenting with respiratory symptoms.
Author competing interests – nil
years,” Minister Butler said. “We are committed to continuing to invest in research to improve health outcomes of all Australians.”
GP Peter Burke’s passion for Western Australian history and his third book leads us on the arduous journey to the monastery of New Norcia.
 By Ara Jansen
By Ara Jansen
Dr Peter Burke says the early days of the Swan River Settlement are one of the most documented colonies in the world.
Because at the time it was so far from, well anywhere, people wrote copious journals and letters which they sent home to Europe. That has given the author plenty of source material for this third historical fiction novel.
Peter specialises in a fresh retelling of the stories that Western Australians thought they knew. His previous books have told stories of the pearlers of Broome and the C.Y. O’Connor tragedy.
His new book, The Silk Merchant’s Son, is a cracking read about the Spanish Benedictine monastery at New Norcia. Peter says while most
people are probably loosely aware of how European missionaries found their way in Perth and then New Norcia, his book both fills in some holes and adds a good dose of fiction.
You can easily imagine these mismatched and misguided Catholic missionaries trudging inland in clothes wildly ill-suited to the blazing sun of WA, and who didn’t share one common language between them.
Joining this group is a French linguistics professor Fabrice Cleriquot who is dispatched from home with a box of silkworms to stop him bringing further disgrace upon his family and who is charged with holding the purse strings for this ecclesiastical adventure. He’s also witness to the folly of his travelling companions who
make presumptuous attempts to rescue the original inhabitants from themselves.
The idea for Peter’s book first took hold when he got absorbed in the true story of French monk Dom Léandre Fonteinne who set out towards New Norcia in February 1846.
“He came out here and in his own words, was ‘totally unfit for being a priest’,” says Peter. “He was a great gossip and wrote constant letters about the 28 missionaries and gave lots of behind the scenes accounts of the famous people we know about. He’s the sort of fellow who would be elected straight off for a reality TV show today!
“Apart from Fonteinne’s gossipy letters, Ursula Frayne wrote to
Dublin about her battles with the cranky bishop, and Dom Salvado wrote his famous memoirs. Miraculously all these remain in print, so I had plenty to go on regarding the historical characters. Then I added in some fictional characters who are sceptics, to provide some pushback and humour.
Apart from being a fascinating read about early history, one of the other aspects which makes The Silk Merchant’s Son interesting is the duality of humour and compassion evident throughout the book.

“I am a fan of irony and the book is meant to be a bit funny. A lot of WA history makes people a bit glassyeyed so I hope I have written a book with heart and humour. You don’t want so much history that it stifles the story, but enough that you are intrigued by the characters.”
In his day job as a doctor, Peter divides his time as a GP in the
Murdoch University medical clinic and in the hospitals of the Kimberley over summer. It’s the time in the Kimberley when he’s not on call that gives Peter space to think, plot, research and write his books. He has never been tempted to author a medical story.
Another aspect which attracted Peter to the story was its contemporary resonance. With the evidence of colonialism right there on the page, it gently demands you think, consider and contemplate. The author was able to inject a little bit of 2023 into the story by having some of the characters ask tough questions about colonisation and colonialism.
“I love getting lots of little bits of information and turning it into something that gets people to read something they would not have otherwise read. My aim is to seduce them into becoming interested in WA history.”
Music, feeling and memories often go hand-in-hand. The West Australian Symphony Orchestra’s performances help tie those things together with their Choose Your Vibe series.
Music helps catalogue our memories, especially for certain times in our lives. A significant summer, your first concert or your first kiss are all quite possibly linked to a song, an annoying jingle or a piece of music. This year for the first time, WASO has bundled their performances into Choose Your Vibe categories. Ravel might be your ticket to adventure, Beethoven’s Violin Concerto could be the soother you need or find a date and swoon with Dvorak. The idea is that certain pieces evoke specific emotional reactions in listeners and personal memories, and this way you can choose how you want to feel. Consider it musical medicine.
WASO violinist Jane Serrangeli has performed with the orchestra for 30 years and has also performed in aged care and nursing homes as part of a string quartet in WASO’s Music for the Ages series. She says it’s a wonderful opportunity to travel the world and across time through music as they can perform
everything from a gentle classical piece through to some ragtime by Scott Joplin or the perennial sing along O sole mio.
“We can create a program which guides people through a series of emotions,” says Serrangeli. “We encourage them to sing or just hum along. At one concert I played, there was a gentleman with tears streaming down his face. It’s moving to be able to bring that kind of joy to someone.
“I love the way that when we start to play it fills the room with colour, energy and emotions. It can be calming, quite exciting or passionate and that can rekindle memories.”
For her own musical memories, Serrangeli clearly remembers her first concert, the first time she played pieces or played them publicly. Subsequent performances, she hopes, have brought greater depth to the performances – along with an ever-growing catalogue of wonderful memories of playing.
Dr Susanna Fleck has been a WASO chorister for more than 10 years and has sung for as long as she can remember, starting with her school choir. Having worked in various countries around the
world she has often connected with her local community and found a home through the power of singing, inextricably tying certain choir memories to different places.
“It’s such an amazing thing do to,” says Fleck about singing. “It’s difficult to describe why, but it’s using your body and your voice as an instrument. All your feelings, emotions and memories are coming out through your voice. I have a lot of wonderful memories of the things I have sung and when I have done them before.
“Singing definitely makes me happy and it’s really empowering when everything comes together when singing as a group. I will sing for as long as I can, and I always want to be involved in music. I enjoy the beauty of music and love to be moved by music. Some performances are almost life changing, it’s beautiful.”
– Ara JansenCurate music to match your feelings and memories by customising a subscription package with WASO. Their Choose Your Vibe packages return in 2024.
When Carrie Cox starts thinking about writing a book, it’s usually because an idea or an issue has caught her attention.


In the case of her newly released third novel, Storylines, it was issues about the human condition and several gnawing ideas – how we cover up and hide our own stories to fit society’s standards, expectations and how social media is bombarding and controlling our notions of what beauty is and how that makes us vulnerable.
“I was thinking a lot about what beauty is,” says Cox, a Perth author and journalist. “What makes a person beautiful? And why? It sent me down this rabbit hole on the philosophy of beauty and its history and to what degree it’s subjective. “We live in an Instagram world and that influences people’s decisions and perceptions. Running tandem to the idea of beauty is the modern notion of vulnerability. Social media is encouraging us to be so much more vulnerable, but doing so doesn’t mean the world will handle you with kid gloves.”
All these ideas, information and themes swirled around in her brain until they coalesced into Storylines. Told from the perspective of 30-something Nessa, she is hiding from the world and running
a wellness retreat after a horrific car accident has left her face scarred. She’s choosing to keep the world at arm’s length and while her circle is small, there are people trying to break down those walls.
“I wanted to amplify the idea of a person for whom navigating mainstream life from the aesthetic point of view is a tricky proposition.”
While not a major influence on the book, but still important, has been Cox’s own journey with facial scarring because of the removal of skin cancers, which she covers up daily. Once again amplified for the sake of the book, is Nessa’s lengthy and gruelling morning make-up routine.
“Most women have their hair and make-up routines and sometimes all I can do is whack on enough concealer to show up in the world and not draw attention to myself. I find that can be really tedious – and yet I do it.
“It’s not about vanity but it’s about being able to have a free an open conversation while people are not looking at my scars. Nessa is trying to do the same thing, so people get past it and engage with her.”
Cox is fascinated about how people perceive themselves and each other, and she wanted to explore this by choosing to use Nessa as the narrator in the first person, a voice which can often be highly distorted. Throw in the age of filters and social media misrepresentation and it might just be hard to find the true you.
Cox stresses it’s not a story about an ugly duckling becoming a swan, but how being pushed into vulnerable situations, forces Nessa to face her worth.
“Our contemporary society demands a lot about how we should look. This story amplifies the idea of having an aesthetically challenging face and how that might change the way we walk through life.
“Far from becoming enlightened, I think we have created a world the exact opposite of that. What’s on the inside is harder to find and we’re more likely to make snap judgments about people based on their sound bite as what they look like.”
Storylines is out now through Affirm Press (RRP $34.99).
wereally see ourselves in her latest novel called Storylines.
Arlewood Estate is located at Forest Grove in the Karridale subregion of Margaret River. It was originally planted in 1999 but didn’t find its way into the hands of Gary Gossati and family until 2009 when they purchased it as a run-down vineyard. They have dedicated themselves to restoring their six hectares to produce high-quality, intense fruit from well-cared for vines and they have done this very successfully.
Gary follows a long family tradition, with his great grandfather having run a wine co-operative in Valtellina, a region in Lombardi, on the Swiss border in Northern Italy. He has recently planted some Nebbiolo, the premium red grape of Northern Italy, at Arlewood. Their flagship wines are the La Bratta Rosso (red) and Bianco (white), La Bratta being his mother’s village. They are produced in the best vintages, from their best fruit.

Wines from this southerly Margaret River subregion experience the cooling ocean winds resulting in higher acidity and often leaner, more delicate styles and the two red wines reviewed reflect this.
Gourmet Traveller Wine magazine in 2020 awarded Arlewood the Best Small Cellar Door in Australia. Their La Bratta Wine and Chocolate Experience is a unique matching and not to be missed.

Sauvignon (rrp $40)
From a cooler vintage, this is a medium-bodied wine showing redcurrant, violets and dried herbs on the nose. The palate is ‘leafy’ with flavours of redcurrant and red cherry. Tannins are fine and linear, oak integrated and not overt, despite the 24 months in quality barriques. A slatey mineral mouth-feel. This is a more delicate, lighter fruit weight style of Cab Sav. Definitely needs time ‘in the glass’ to open up and show its true qualities. Initially I thought it was a bit ‘fruit thin’, but not so with time, with new flavours emerging , and giving it a nice chocolate finish. With its firm acidity, will cellar for up to 12 years.

Arlewood’s high premium flagship wine and from the exemplary 2018 vintage. It is an interesting blend of Cabernet Franc (47%), Merlot (42%), with 6% Nebbiolo and 5% Cabernet Sauvignon added. Very selected fruit and a limited production of only 360 dozen bottles. A wine of elegance and delicacy. Attractive ruby colour, rustic aromatics, blackcurrant-leaf, with hints of green pepper. Palate is savoury and mouthfilling. Blackberry, leafy, caraway seed flavours. Nice fine ‘grippy’ tannins. The Cab Franc characters come through strongly. Complex, balanced with a long finish. Will reward another 10 years. A wine of contemplation.
Known for her arresting portraits, painter Rachel Coad has released her first graphic novel, featuring two unlikely characters and a legendary New York venue.
 By Ara Jansen
By Ara Jansen
An octopus in jeans and a snake walk into a bar. Actually, it’s more like they slide into the legendary New York music club CBGBs.
Strawberry the octopus and Ray the snake are the characters in New York City Glow, the latest project from award-winning portrait painter Rachel Coad. Known for her large, emotional portraits, this is her first graphic novel or as she likes to call it, “a long comic”.
The story is an almost true account of the 1977 New York City blackout. Ray the snake is a sad, lonely, middle aged insurance salesman who wants a better life. Strawberry is a special octopus who can’t control her glow and finds herself in constant trouble. She has a prison record and an FBI file to prove it.
The unlikely pair embark on a road trip to New York City, where they rub shoulders with rock royalty and things get electric – in more ways than one. While she wasn’t exhibiting during COVID, the celebrated artist returned to one of her childhood loves – comics. A life-long fan of Mad Magazine, The Far Side’s Gary Larson and an avid comic reader, Rachel remembers drawing her own stories as a child. Even her Year 12 leaving project was a comic.
When she became a full-time painter in 2003, Rachel left behind her graphic design and illustrative work, but 10 years ago decided to get back into illustration with no plans for what would emerge.

“I started playing around with children’s picture books and enjoyed making up stories and characters,” she explains. “I pitched a couple of ideas, but they never went anywhere. The next story was about an octopus, which started as a silent graphic novel.”
She doesn’t quite know why she felt a bit shy about adding dialogue and a story, but when a critique from a trusted comic expert encouraged her to add a narrative in words, she dived in.
“I was surprised how that helped develop the characters. As soon as I gave them voices and they interacted, things changed again. It was a bit of a process.”
Each panel in the book is handinked and lovingly detailed, with
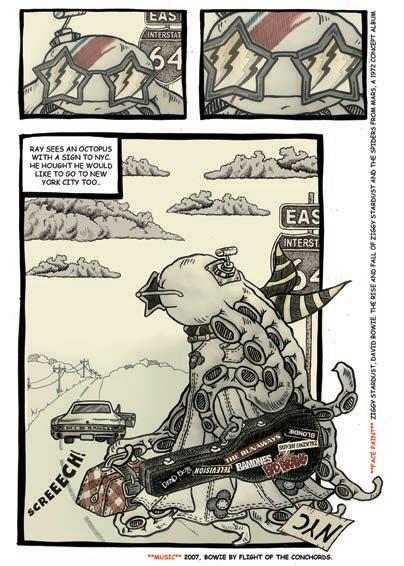

the elements put together using Photoshop. Rachel loves the mix of both mediums, which offers a different way to work from her oil on canvas works.
“I love life drawing and painting. I love ink and paper. Using Photoshop for the comic allows me to add another element.”
Like her paintings, New York City Glow has a matte feel, rather than screaming bright day glo colours. Each of the panels are intricately detailed, which demands the reader stop and examine them as closely as reading the words.
The graphic novel also gave Rachel a chance to indulge and explore her love for music. Influential punk band The Ramones make an appearance in the equally
notorious bar that closed in 2006 and the comic even comes with a suggested soundtrack.
“I love all kinds of music and am always playing something when I am in the studio. I love going down rabbit holes and finding obscure bands and I love emotive songs. These characters – a snake and an octopus – take their world quite seriously so I have some full-on songs to go with them. I find that amazing and sweet and a nice way to create a bit of atmosphere.”
In a rare self-portrait which she shared on Instagram, Rachel inserted herself into an old-style advertisement wearing a classic Ramones T-shirt as her nod to the graphic novel. The painting was selected for the Salon des Refusés 2023, the alternative Archibald and Wynne Prize.
“I started with the characters, a place and a time. I didn’t really have an end game. I just love doing it and it works as something creative I can now do in between my painting. I would love this to become a 50/50 thing with painting. That’s the plan because I really loved doing this project.”
You’ll be able to see Rachel’s work and both her painting and illustration spaces as part of Margaret River Regional Open Studios from September 9. New York City Glow is out now through Upswell Publishing. See more at www.coadoperations.com
MURDOCH
Wexford Medical Centre
Suite 30, Level 2
3 Barry Marshall Parade, Murdoch
Available within SJOG Campus
Specialist consulting rooms with professional practice management.
Contact: manager@murdochsp.com.au
Hollywood Medical Centre Suite 36, First Floor, 85 Monash Avenue, Nedlands

87sq m – fully fitted, large reception, 2 consulting, 2 treatment & 2 store rooms.

Full or part time GP to join our amazing team in idyllic location of Broome. 5 consult rooms, 3 treatment bays and 2 FTE Practice Nurses. Awesome team environment with an easy-going atmosphere. Private-mixed billing clinic. No on-call. Emergency department located directly next to our clinic with onsite and visiting specialists. We have onsite pathology.
Remuneration: 65% of billings on an Independent Contractor Agreement. Enquiries to Katrina Dow, Practice Manager – 08 9192 2022 or practicemanager@broomemedical.com.au
MENORA / DIANELLA
Visiting GP position
Commencing April 2023
Due to the retirement of our visiting GP, Masonic Care WA is looking for a Practitioner interested in visiting three retirement villages in the Menora and Dianella areas. Consulting rooms provided at no cost Assistance available for bookings at no cost
Hours and days to suit
Opportunity for growth to other sites
ALKIMOS
Jupiter Health Alkimos
A wonderful and exciting opportunity for a VR-GP has arisen to join our experienced, friendly and supportive team. We are a modern purpose-built practice based in the heart of a growing community, with 7 consult rooms and a large treatment room.
•Mixed Billing
•Pathology onsite
•Excellent reputation with patients
•Modern, well-maintained equipment
•Established and expanding patient demographic
•Close-knit and supportive team culture
CANNINGTON
GP practice for sale in Cannington:
Established for past 30 years in Cannington on Albany highway right across Carousel shopping Centre. Excellent opportunity. Current owner need to move due to changes in their business model and also moving to another state. Great negotiable deal. Call 0408 928 916 for confidential inquiry.
Exmouth Health Professionals


– Ningaloo Reef
Full time, part time or locum GP required for private billing practice. Direct flights from Melbourne now available.
Multi practitioner clinic. Plenty of time for surfing, diving and fishing! Please contact clinic@exmouthhealth.com.au
If interested please contact Emma Benjamin emma@mcwa.net.au
•Allied health rooms available onsite
•Open 6 days a week (Sunday-Friday)
•Efficient admin and nursing staff
•Own dedicated consulting room
•Free parking
For more information or expressions of interest please send an email to Emma at p.manager@jupiterhealthalkimos.com.au
PEEL
Contact: Kah-Lim 0400 066 160 kahlimtay@gmail.com COMO
Thinking of a sea change?
An opportunity for a full time Doctor Is available at our busy group practice. Email your CV to robyn@peelwoodmedical.com.au
BENTLEY
Burton Street Family Practice
Unrestricted VR GP required for well-established privately-owned mixed-billing practice
Opening for VR GP - F/time or P/time
Full Private List available now from retiring GPs FRACGP essential
Up to 70% private billings
GPs required
We are seeking expressions of interest from GPs who are interested in providing primary health care to the Martu and Nyiyaparli people of the Western Desert. About the Opportunity: Puntukurnu
Aboriginal Medical Service (PAMS) is seeking General Practitioners with a sense of adventure and deep respect for Aboriginal peoples and their cultures to provide on-the-ground leadership of this project.

This opportunity is available for practice within either Newman or remote communities of Jigalong, Parnngurr, Punmu and Kunawarritji (or both) on a permanent residential (Newman) or on a fly in fly out rotation. We are looking for suitable practitioners, wherein conditions of engagement are flexible and negotiable!
Reporting to the Senior Medical Officer (located in Perth and our remote communities), the General Practitioners are responsible for provision of culturally safe General Practitioner services within a comprehensive primary health care framework to the communities within which PAMS operates.
Please call 0421 610 173 or email cara.sheppard@puntukurnu.com
HARVEY
Family Friendly Medical Group
– GP Positions
•DPA Area’s and MMM5 Available
•FSP GP’s are welcome to apply
•Busy & well established Medical Group with 3 Locations in the South West of WA (Harvey, Waroona & Dalyellup)

•Fully computerized and accredited modern practice with nursing and admin support
•Well supported with large team of experienced GP’s
•Situated in the beautiful South West Region surrounded by coast and forest and close to tourist areas in the south of WA
•Only 1 ½ hrs from Perth
•Family friendly working hours and no on call or hospital cover required
•65 – 70% of billings depending on experience
Please forward CV and enquiries to Kylie Wilson kyliew@harveymed.com.au
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs.
Enjoy working for a doctor-owned, non-corporate, well supported, and accredited practice.
Please contact the Practice Manager on 6165 2444 or email: reception@comogp.com.au
With an interest in all areas of general practice, you are expected to share our mission to provide high-quality care for the whole family in a coordinated fashion. Serving a diverse patient demographic, we aim to manage chronic illness to avoid complications and acute issues and reduce the need for hospital presentation and admission.
You are provided clinical autonomy and supported by a strong team of Australian trained GPs, nursing and administrative staff. AGPAL and WAGPET accredited, we offer the opportunity to be involved in teaching medical students and GP registrars.
Please apply to burtonst@burtonst.com.au or call 08 9458 4558
MADDINGTON
CHURCHLANDS
Seeking a locum GP who is able to work Tuesdays, Thursday and Fridays for the months of June, July and August
No afterhours consulting
Remuneration is negotiable
Herdsman Medical Centre is a busy, family orientated, accredited Practice Well Equipped Treatment Room Clinipath adjacent

Privately Owned/Mixed Billing
Friendly Registered Nurses and Experienced Administration Support For further information please Email: karen@herdsmanmedical.com.au
OPPORTUNITY FOR GPS AT MEDICAL CENTRE IN MADDINGTON
Secure your future with a partnership in or part ownership of a new venture in Maddington commencing in January 2023. Alternatively choose to remain selfemployed retaining an above average percentage of your billings. Either way we will make it a high earning opportunity for you with the option of becoming a partner or becoming part owner.
For more information or expression of interest please contact us via our email at bvmc@bigpond.net.au or call our Practice Manager on 0416 193 399
GLEN FORREST
Glen Forrest Medical Centre
GP Position
The doctors at our practice enjoy clinical autonomy and practising on their own terms. There are no KPI’s or numbers of patients per hour. Our friendly, supportive administration team are there to assist with in-house IT and management of accounts. We use Best Practice software. We have a purposebuilt treatment room and separate procedure room for Mirena’s etc with a great team of nurses to support you.
Glen Forrest Medical Centre provides quality and comprehensive care to our patients including minor surgical procedures, women’s health (Mirena/ Implanon/IUCD), men’s health, IV fluids, iron infusions, mental health, paediatrics, adolescent health, complex medical comorbidities and palliative care. Please contact Maria Clark on 08 9298 8555 or email mariac@gfmc.com.au

Ocean Village Medical Centre is privately billing medical practice located in the heart of Wembley Downs.
We are looking for an experienced General Practitioner to add to our growing practice.
Complimented by a team of high-quality Doctors, Experienced Practice Nurses, Allied Health and Admin team to support your practice, we offer a friendly working environment, modern facilities and an established patient base. Our ideal GP will be an all-rounder with the ability to take on new patients and offer morning and afternoon appointments to accommodate needs of our community with attractive remuneration on offer for the successful candidate.
If you are interested, please email your CV to pmgr@ovmc.com.au or phone Jess for a confidential discussion on 0418 927 010
GP FT/PT
Edgewater Medical Centre is an accredited, mixed billing, medical practice in Edgewater, Western Australia and seeking a General Practitioner to join our friendly, patient focused team. Work place:
You will be working with a dedicated and professional team of administration, nursing and health staff supporting GPs within this busy practice, providing a full range of medical services. The focus is on personal care, attention and expertise.
Role:
As an experienced GP, this role will allow you to provide high quality primary health care services to the community, in keeping with best practice standards.
Essentials:
•Applied knowledge, skills and experience in general practice
•Unrestricted VR GP qualification
•Full Australian Work Rights
What’s in it for you:
•State of the art equipment, technology & facilities

•Supportive team
•Doctor owned practice
•Nurse Support
Hatherley Medical Centre
– Full-Time GP
We are seeking a Full-Time General Practitioner to join our non-corporate 5 doctor practice.
Located centrally, close to Murdoch Hospital and Murdoch University.
Established for over 30 years with an expanding well accepted Private Billing patient base.

Stand-alone Fully Accredited Medical Centre with garden outlook from large consulting rooms supported by all services. Please contact Sharon – Practice Manager on 9310 4400 or email admin@hatherleymedical.com.au for further details.
JOONDALUP
Candlewood Medical Centre has an exciting opportunity for a General Practitioner to join our very well established, Privately owned and very busy accredited practice which provides quality medical care to the community for over 30 Years.
You will join a wonderfully passionate, friendly, and supporting Team, in a warm and welcoming environment.
As part of the Candlewood team, you will have a great work, life balance and will have the flexibility to work either FullTime or Part-Time, - Weekend and After Hour appointments are also available as we are open 7 days per week.
Locum General Practitioners are also very welcome
Benefits:
• very large existing and loyal patient base, with great patient demographics.
• Mixed Billing Weekdays & Private Billing only on Weekends- very competitive high remuneration potential available.
• Supported by a dedicated Practice Management, IT and long-standing Nursing and Administration Staff.
•Accredited Teaching Practice.
• On Site services including Allied Health, Pharmacist and Pathology.
• Highly reputable and established clinic within the community and surrounding suburbs.
•A committed Team of 7 GP’s and Nurse Practitioner.
•Great Location and Free Parking
•5 minutes’ drive from the beautiful local beaches and 30-minute drive from Perth CBD.
For more information, contact Practice Manager -Karon Hay on 08 9300 0999 email: candlewoodmedical@outlook.com
General Practitioner – Wesley Medical General Practitioners (Healthcare & Medical) Contract/Temp

New opportunity for a caring GP to join our team at Wesley Medical, a private medical center in the heart of Perth CBD. Our practice opened in October 2022 with an ultra-modern, friendly and comfortable environment.
We are currently seeking a dedicated and experienced GP who is passionate about providing high quality care within a supportive and collaborative team environment in a modern and fully equipped treatment room with a dedicated nurse.
Opportunity for career advancement.
Access to onsite pathology services and pharmacy located next door. Sessional, part time opportunities available. Choose the days and hours you want to work. No weekend.
If you are interested in this exciting opportunity, call Jenny on (08) 6556 8888 for any queries or email your resume to jenny.chan@wesleymedical.com.au
BULL CREEK
Bull Creek Medical – VR GP opportunity

We are seeking full time or part time VR GP to join our friendly team.
It is a mixed billing well established practice providing quality health care for many years.


It is located closer to world class public and private hospitals and near by top public and private schools.
Flexible working hours and terms and conditions are negotiable.
If you are interested in this exciting opportunity, contact practice manager via email: admin_pm@bullcreekmedical.com or call on 08 9332 0488
•Onsite Pathology
•No call outs– Week Day 8-5 roster
•Free parking onsite
•Flexible arrangements
•70% of billings
•Initial Guaranteed payment of $150.00 per hour in first 3 months
For a confidential discussion, please contact Cecelia – (08) 9306 1899 or CeceliaC@edgewatermedical.com.au
Tandara Medical Group in Gosnells offers a practice where doctors are inspired by their peers and supported by a long-standing Practice Manager, Jacky, who has 35 years’ experience managing GP clinics.
Jacky’s passion for efficiently operating a patient and doctor centric clinic, has largely contributed to the success of this welcoming clinic in operation for over 25 years.
•Mixed Billing – with 70% billings
•Huge patient demand
•Upfront payment
•Full clinical & billing autonomy
•Permanent & locums VR GPs welcome •25mins from CBD
Please contact Máire Haughey on maire.haughey@partneredhealth.com.au 0427 951 285
MetroGP Requires a VR GP
Unrestricted for Part-time Position: As an experienced GP, this role will allow you to provide high quality primary health care services to the community, in keeping with best practice standards.
Essentials:
•Applied knowledge, skills and experience in general practice
•Unrestricted VR GP qualification
•Full Australian Work Rights
What’s in it for you:
•Supportive and Experienced Admin team
•Doctor owned practice
•Nurse Support
•Onsite Pathology
•Flexible arrangements
•AGPAL Accredited Practice
•Located near FSH and SJOG Murdoch
•Mixed Billing (mainly Private)
If you are interested please contact our Practice Manager for further information on 9332 5556 or email: adminmetrogp@metrogp.com.au
We are seeking a part time or full time GP to join our well established, busy practice.
You will work in a highly equipped AGPAL accredited practice, alongside GPs with extensive specialised skills, including skin cancer surgery (including flaps and grafts), cosmetic medicine, ultrasoundguided musculoskeletal PRP injections, IUD insertion, ENT operating microscope use, and much more.
The practice itself is highly equipped, including on-site ECG, spirometry, ABI machine, ultrasound, digital dermoscopy imaging, ambulatory BP monitoring and a full time chronic disease management nurse.
Mixed billing, offering our GPs 70%. All appointments privately billed on Saturdays.
For more information please email kingsleypractice@gmail.com or call our Practice Manager Tracy Weare on (08) 9342 0471
Shenton Avenue Medical Centre has a great opportunity for a General Practitioner to join a very well established practice.

•Wonderful, friendly staff.
•Experienced doctors.
•Very large existing and loyal patient base.
•Mixed billing practice.
•75% of billings.
•Non-Corporate.
•On-site services including Pathology, Physiotherapy, Podiatry, Dietitian
•Fully accredited practice.
If you are interested in this exciting opportunity please contact Phil at phil@medibizz.com.au
Contact Andrew, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert
The role would suit a new Fellow or GP who wants to curate their own patient base with a guaranteed minimum offered for 3 months.
Work in a fantastic environment – a non-judgemental, respectful and safe space with a supportive nursing and admin team.
Enjoy an innovative, modern practice with the latest equipment and software (BestPractice).
Choose your hours – our clinic is open from 8am to 7pm Monday-Friday, 8-1pm Saturdays.
Get to know your colleagues with quarterly team-building activities Sub specialise – for the right applicant, we’re happy to support your special interest.
Central location - 15 minutes from the CBD, extensive parking available.
Contact: PracticeManager@balcattafamilypractice.com.au or call Debbie on 08 6478 3955
With over 50 years’ experience in the industry, SHP is a Continuing Medical Education (CME) approved provider, giving our Doctors and staff opportunities to broaden their knowledge and to advance their career through regular training and development.
If you’re looking to practice quality medicine in a professional and supportive environment, contact us to learn more about our doctor opportunities. Contact Natalie Tuivaga Natalie.Tuivaga@scs.com.au.
We are seeking expressions of interest for full-time or part-time roles in general practice or general practice and travel medicine combined to join our busy (CBD) Hay Street practice. We provide dedicated in-house training to support our clinicians.
If you are looking to work with a leading and innovative team, on a full-time or part-time basis, contact us to learn more, available for immediate start.
Contact: Natalie Tuivaga – Business Development to apply: Natalie.Tuivaga@scs.com.au
sonichealthplus.com.au/

Join our friendly Health Services team to provide quality care and make a difference in Curtin Community’s health and well-being at our Bentley campus.
Part-time and full-time contractor/temp opportunities available
Excellent working conditions and room facilities
Administrative and Nursing support provided
JOB REFERENCE
Are you a caring and experienced General Practitioner? Join our friendly and collaborative team of general practitioners, nurses, medical receptionists, and a Practice Manager to make a difference to our Curtin Community’s health and well-being within our busy Medical Centre at our Bentley campus.
Our Medical Centre is a well-established and fully equipped practice with a total of 7 consulting rooms, a procedure room, treatment, and onsite pathology. The Centre is open Monday to Friday between 8:30 am and 4:30 pm. It is well-served by public transport and has ample parking.
We offer mixed billing (70% bulkbill) with flexible consulting hours. Our GPs are fully supported by a practice manager, registered nurses, administration staff and a mental health nurse practitioner. Our Medical Centre has high volumes of patient demands and full-appointment books during semesters. This is a large and diverse patient base offering lots of interesting work, plus walk-ins, opportunities for Healthcare Plans Health Assessments, and procedures.
BENEFITS
70% of the billing/mixed billing
Work full-time or part-time with flexible hours. You choose!
Excellent working conditions and room facilities
Walk into a full & immediate patient base, OR create your own, with walk-in presentations
Best Practice software in use throughout the practice
REQUIREMENTS
MBBS or equivalent
Current AHPRA registration as a General Practitioner
Vocationally Registered (VR)
No restrictions
To learn more about this opportunity, please contact Nandita Nadkar, Team Leader on 08 9266 7345.
For more information about our university, please visit www.curtin.edu.au
Applications close: 15 December 2023
Enjoy the perfect blend of professional fulfillment and an enviable coastal lifestyle. Our well-equipped and staffed clinic offers the resources and support you need to provide topquality care to our diverse patient community.
Collaborate with like-minded professionals in a vibrant and inclusive environment that encourages growth and learning. Outside of work, immerse yourself in the breathtaking natural beauty of Albany’s coastline, with pristine beaches and lush landscapes waiting to be explored.
Enjoy the benefits that working and living in regional WA offers, and a work-life balance that allows you to embrace the wonders of coastal living. A perfect opportunity for a GP, GP Obstetrician or GP Anaesthetist!
Apply now and embark on an extraordinary career journey in Albany, Western Australia.

Perth and suburbs



At Perth Cardiovascular Institute we believe in providing more than just a diagnostic imaging service. Our team are committed to delivering an excellent patient experience along with clinically robust findings in a timely manner.
Senior staff perform as leaders and assist with training, mentoring and development of less experienced team members. Much of our time is dedicated to ensure our trainees develop superior skillsets to tackle even the most difficult of cases. We foster an environment that promotes asking questions, seeking feedback and sharing of knowledge.
We have world class, internationally renowned cardiologists within our group that support and develop individuals. Our cardiologists are approachable to discuss patient findings and encourage and enable team members to manage patients. In completing our daily duties we go above and beyond expectation with clients repeatedly providing outstanding feedback from their contact with us.
If you wish to know more about the role, feel aligned to the way we do things and are excited by the unique opportunity Perth Cardio offers then we would be thrilled to hear from you.

Please contact Adam Lunghi on Phone (08) 6314 6881 or info@perthcardio.com.au
or Terry MacKinley (Practice Manager) on (08) 9845 9000

We are seeking a skilled and passionate cosmetic doctor/aesthetic physician to join our team at a cosmetic service co-located with a large dermatology practice in Karrinyup.
This is a fantastic opportunity to work in a thriving and rapidly growing service with strong demand.
Attractive remuneration package: We believe in recognising the value of Excellent working relationship with onsite Dermatologists: You will have

Support, clinical advice, and cross referrals:
Advanced training opportunities: While we require you to have FRACGP or equivalent
Are you a passionate GPseeking a fulfilling opportunity in a amazing coastal town?
Look no further! Join our dedicated team in Denmark, Western Australia, and experience the perfect blend of a rewarding career and a tranquil lifestyle.
Our clinic provides a supportive environment with modern facilities and advanced resources to deliver excellent patient care. Collaborate with a team of skilled professionals who share your commitment to healthcare excellence.
In Denmark, you’ll discover a vibrant community surrounded by breathtaking natural beauty. Explore pristine beaches, lush forests, and enjoy outdoor activities in this idyllic coastal setting. Benefit from a healthy work-life balance and embrace the relaxed pace of a coastal town while making a positive impact on patients’ lives.
Apply now to embark on an incredible GP journey in Denmark, Western Australia.
Freo Street Doctor is a highly rewarding and unique work environment – A well respected mobile medical service supporting the needs of disadvantaged and vulnerable people.

BENEFITS INCLUDE:
Complex and challenging patient cases
Work in a close team, alongside a registered nurse and outreach worker
Administrative support for billing and clinical coordination
Enjoy the satisfaction of delivering an essential service that is trusted by patients and the broader community to provide an enduring positive impact
No schedule 8 drugs or needle exchange offered A high quality and RACGP accredited service, supported by a robust Clinical Governance Framework.
FOR MORE INFORMATION: Contact Freo Street Doctor: Phone: (08) 9432 0480
Fax: (08) 9339 8355 Email: freostreetdoctor@blackswanhealth.com.au Or contact Human Resources: Employment@blackswanhealth.com.au
Hillarys Medical Centre is a very busy practice located 15mins from the Perth CBD along the coast. We have a strong focus on family & preventive health medicine.

We are a team of 10 doctors with excellent administrative and nursing support staff. We have been in Hillarys for 20 years with dedicated GP owners. We pride ourselves with providing exceptional health care to our community of Hillarys.
We have a modern purpose built well equipped 3 bed treatment room and 10 consulting rooms with quality equipment as well as a spacious staff & meeting room. We are also able to offer secure remote access and secure onsite parking. Pathology & Pharmacy are within our complex.

There is a high-income potential as we are mainly a private billing practice. We would also encourage doctors to develop their own special interests
Our patient base is varied as well as a strong family base practice including women’s & mens health, skin cancer medicine, iron infusions, aviation medicine and more. Our nurses are committed to support for care plans & health assessments.
We are a 7 day a week (Mon to Thur 8am to 7pm, Fri 8am to 6pm, weekends 8.30 to 12.30pm) we have a variety of sessions available and the opportunity to share a Saturday roster with your fellow GP colleagues, with nursing support.
We would require:
Current unrestricted registration with AHPRA as a general practitioner

Current medical indemnity insurance
Full Australian working rights and No DPA restrictions

We respect your time is precious. Humphrey Homes’ integrated model of architecture, building and interior design ensures you realise your vision with unrivalled efficiency, construction quality and budget control. To learn how our approach makes the process seamless and enjoyable, contact Dean Humphrey for an informal chat.














