Rotary negotiation and roto-reciprocation
Dr. Reid Pullen
Unlocking the power of dental lasers in endodontics
Dr. Fernando J. Meza
Management of acute hemorrhage in the anterior maxillary region from an aberrant blood vessel
Drs. Lanka Mahesh, et al.



Drs. Hunter Bennett and Nate Dewsnup
Exploring

The for Specialists PROMOTING EXCELLENCE IN ENDODONTICS Implants / Lasers n 4 CE Credits Available in This Issue* Summer 2024 Vol 17 No 2 endopracticeus.com
the true value of partnership





SmartLite
EndoActivator™
up
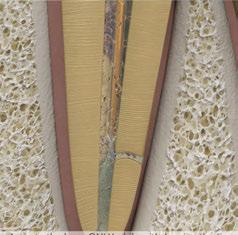
idea of clean Untreated Treated with SmartLite
EndoActivator™ ENJOY ENDO
here to learn more about the effective cleaning power of the SmartLite Pro EndoActivator™
irrigants produces a surface with more opened dentinal tubules,
for better obturation of lateral and accessory canals.2 1. Kanter V, Weldon E, Nair U, et al. A quantitative and qualitative analysis of ultrasonic versus sonic endodontic systems on canal cleanliness and obturation.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(6):809-813.doi:10.1016/j.tripleo. 2011.06.002 2. Internal data on file. For more information contact Consumables-Data-Requests@dentsplysirona.com
Pro
Shake
your
Pro
Scan
More effective cleaning in just 90 seconds1 Activating
allowing
Summer 2024 n Volume 17 Number 2
Editorial Advisors
Dennis G. Brave, DDS
David C. Brown, BDS, MDS, MSD
L. Stephen Buchanan, DDS, FICD, FACD
Gary B. Carr, DDS
Arnaldo Castellucci, MD, DDS
Gordon J. Christensen, DDS, MSD, PhD
Stephen Cohen, MS, DDS, FACD, FICD
Samuel O. Dorn, DDS
Josef Dovgan, DDS, MS
Luiz R. Fava, DDS
Robert Fleisher, DMD
Marcela Fridland, DDS
Gerald N. Glickman, DDS, MS
Jeffrey W Hutter, DMD, MEd
Syngcuk Kim, DDS, PhD
Kenneth A. Koch, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, DICOI
Joshua Moshonov, DMD
Richard Mounce, DDS
Yosef Nahmias, DDS, MS
David L. Pitts, DDS, MDSD
Louis E. Rossman, DMD
Stephen F. Schwartz, DDS, MS
Ken Serota, DDS, MMSc
E Steve Senia, DDS, MS, BS
Michael Tagger, DMD, MS
Martin Trope, BDS, DMD
Peter Velvart, DMD
Rick Walton, DMD, MS
John West, DDS, MSD
CE Quality Assurance Board
Bradford N. Edgren, DDS, MS, FACD
Fred Stewart Feld, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FADI, DICOI, DADIA
Justin D. Moody, DDS, DABOI, DICOI
Lisa Moler (Publisher)
Mali Schantz-Feld, MA, CDE (Managing Editor)
Lou Shuman, DMD, CAGS

Last Act With A File
Root canals systems can be microscopic tortuous pathways, and below the orifice, their anatomy is obscure at best. Because of this, endodontists, have taken many wrong turns on the lonely way to the apex. The difficulties of conefitting are a great example.
Conefitting is a common challenge in RCT (one of the main drivers of early Thermafil® acceptance by the GP community), and most clinicians think it is because apical regions of canals are so small that gutta-percha cones have trouble traversing to length. Au contraire. While the last three millimeters of the apical region is very small, current manufacturing standards mean that we can easily fit cones into canal shapes smaller than 15-.03 when the canal is unobstructed by debris. The problem is that after instrumentation, canals are always obstructed by debris, albeit a very tiny bit of debris when it’s done carefully. It requires mental imaging skills to understand the huge impact of this miniscule impediment, but it is contained in a very tiny space, and as such, it constitutes a soft tissue blockage of sorts.
You might think that this debris can be pushed aside or out the end of the canal with the master cone, but fitting gutta-percha points is like trying to push a noodle up a pipe, so any slight irregularity in a canal wall or crust left near the terminus will make it an impossible procedure. This lack of patency is the culprit in 99% of all conefitting difficulties, yet academics continue to debate whether the use of patency instruments is safe. That is nonsensical to me.
Ironically, even some of those clinicians who understand the safety and importance of patency procedures endure conefitting frustration when their final patency procedures are done in the presence of NaOCl. NaOCl is essential for disinfection and dissolution of pulp tissue remnants, but it does nothing to hard tissue particles, so the debris remains clumped near the terminus.
When an acidic irrigant like EDTA is used during patency procedures instead of bleach, these mineralized particles melt into solution, and after that, the same exact GP cone that could not be coached to length drops there immediately, delivering perfectly crisp tugback. Remember, the slightest scrape of a file on a canal wall, even gauging, recreates a smear layer that must be removed again before obturation. I call this procedural concept, “Last Act With A File” (LAWAF), and with my nerd in full bloom, I say it to myself as a mantra after completing instrumentation of all canals. “Irrigate with EDTA, slip a file to and through the terminus of the canal, and the GP fits to length.” The solution is super simple and works every time.
In 1975, McComb and Smith recommended that dentists do all instrumentation with 17% EDTA. In 1987, Baumgartner confirmed the basis for that recommendation, and in 2002, Ralan Wong showed the problem to be hugely magnified by the use of rotary files. When using rotary files, the ground dentin and pulp debris created is not a layer; it fills the entire canal and any adjacent lateral recesses in 1.5 seconds. Most of us continued to apply Schilder’s irrigation concepts despite the fact that all the tools have changed, creating vastly different dynamics between our instruments and our irrigants. Should we worry about carrying EDTA through the ends of canals with patency files? Re-engage your mental imaging powers, and you will see that patency files displace irrigants from apical regions; they don’t carry aqueous solutions anywhere.
Remember, instrument with EDTA, use the LAWAF procedure to finish, irrigate effectively with NaOCl, stuff that root canal system, and I’ll see you at the apex.
L. Stephen Buchanan, DDS, FICD, FACD, Dipl. ABE, has been lecturing and teaching hands-on endodontic continuing education courses for over 30 years, both in his state-of-the-art training facility in Santa Barbara, California, as well as in dental schools and at meetings around the world. He currently serves as a part-time faculty member in the endodontic departments at the University of the Pacific’s Arthur Dugoni School of Dentistry and the University of California at Los Angeles as well as being the Endodontic Advisory Board Member to the Academy of General Dentistry. He is a Diplomate of the American Board of Endodontists and a Fellow of the International and American College of Dentists. Dr. Buchanan also maintains a private practice limited to Endodontics in Santa Barbara, California.
1 endopracticeus.com Volume 17 Number 2 INTRODUCTION
© MedMark, LLC 2024. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Endodontic Practice US or the publisher.
ISSN number 2372-6245

Drs. Hunter Bennett and Nate Dewsnup
Exploring the true value of partnership — in business and in life
Cover image of Drs. Bennett and Dewsnup courtesy of Specialized Dental Partners.
CLINICAL
Management of acute hemorrhage in the anterior maxillary region from an aberrant blood vessel
Drs. Lanka Mahesh, Gregori M. Kurtzman, Sagarika Shukla, and Zara Dhawan discuss management of a surgical complication
PUBLISHER’S PERSPECTIVE My Rx for summer Lisa Moler, Founder/CEO, MedMark Media............................... 6

CASE REPORT
Single visit regenerative endodontics using the GentleWave® Procedure: a pediatric case report
Dr. Lauren Tink treats an anxious pediatric patient using an efficient treatment .......................16

CONTINUING EDUCATION Rotary negotiation and roto-reciprocation: a new hybridized shaping technique
Dr. Reid Pullen introduces a protocol for shaping and finishing root canals ................... 20
2 Endodontic Practice US Volume 17 Number 2 TABLE OF CONTENTS
8 11 COVER STORY
The All-In-One Obturation Solution.
Minimally Invasive, Light-Cured Obturation. Simply fill the canal and light-cure. OdneFill flows into complex endodontic structures (isthmuses, deltas, C-shapes) and provides gap-free root canal sealing without compaction.

Join our Priority Access Program! Participation is limited. Scan the QR-code to find out more.
M-EF-0030-V1.0-ADV-EN-240 odne.co
Clinical case, Albert Einstein Medical Center
No gutta-percha. No sealer.
Dr. Albert (Ace) Goerig discusses the many ways to improve the quality of your personal and practice life

Endo education with a giveback twist
Daniel Lewis discusses a program that brings needed resources to underserved patients
Thomas Terronez
Drs. Joel Small and Edwin McDonald





4 Endodontic Practice US Volume 17 Number 2 TABLE OF CONTENTS
The
PRACTICE MANAGEMENT
intangible value of practice success
..................................... 28
HUMANITARIAN EFFORTS
................ 31 PRODUCT PROFILE Bio-C Sealer ION+ A new class of calcium silicate 32
VIRAL Cybersecurity — a necessity, not a luxury
GOING
your practice data safe from cyberattacks ................................... 34 INDUSTRY NEWS ........................ 36 SMALL TALK What I know now (that I wish I knew then!)
offers some guidance on keeping
share how to cultivate effective leadership qualities ......................................................... 38 SOUND ADVICE Specialized: the Specialists Podcast Specialized Dental Partners continues to amplify the voices of specialists and industry insiders .........................................................40 Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business WATCH DocTalk Dental video interviews with KOLs LEARN through live and archived webinars RECEIVE news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media www.endopracticeus.com *Paid subscribers can earn 4 continuing education credits per issue by passing the 2 CE article quizzes online at https://endopracticeus.com/category/continuing-education/ 23 CONTINUING EDUCATION Unlocking the power of dental lasers in endodontics
Fernando Meza discusses uses of lasers in the endodontic practice
Dr.

800 - 605 - 3437 | Specialty1partners.com YOUR SPECIALTY IS OUR SPECIALTY . The Only Doctor-Founded, Doctor-Led Specialty Partnership Organization.
a partnership of specialists and we are all specialty strong.” Dr. Joanne Jensen Endodontic Artistry
“It’s
My Rx for summer
How many times have you written prescriptions for your patients? Even after they leave your office, you strive to ease their pain, head off their infections, and get them back to healthy lives. I’m not a dentist, but I have played one for almost 20 years now! So, for this summer issue, it’s my turn to write a prescription — to encourage ongoing mental and physical health for our dedicated readers.
My Rx for a productive and rejuvenating summer
Vitamin D: Take some time to get out in the sun and soak up the relaxing rays! Change out of your scrubs and breathe some fresh air — and don’t forget your hat and sunscreen. You will return to work revitalized and ready to tackle any patient.
 Moler Founder/Publisher, MedMark Media
Moler Founder/Publisher, MedMark Media
Get moving: Even if you don’t have time to get to the beach or take a longer vacation, exercise is one of the best ways to relieve tension and clear your mind. The CDC recommends 150 minutes of moderate-intensity physical activity per week. You don’t even need to join a gym — a daily walk will keep that blood flowing. Breaking the time up into 30 minutes a day for 5 days is very doable and can become a healthy habit.
Give your mind some thought: Every day, take some time for mindful thought or meditation. It doesn’t have to be the same time every day, or even done in the same way. Just pick a comfortable spot, close your eyes, breathe deeply, and focus on your breathing. Picture the beach, a mountain trail, or any spot that brings you peace. Taking a few minutes can reduce stress, ease frustration, and open the door to serenity.
Read, watch television, or listen to music: Having a way to unwind first thing in the morning or before bed can calm your mind and body.
Eat healthy, but give yourself a treat: We all know the drill — eat healthy fruits, vegetables and grains, go big on the protein and low on fats and sugars. But, as with all things under heaven, there is a time for ice cream and cake too (in moderation).
Build a trusted team, in and out of the office: Having support people to boost you when you are sad and laugh with you when you are happy can make life a warmer, more welcoming place.
Forgive yourself! One of my main mantras throughout this journey of life is to give yourself a break. Everyone makes mistakes, and no matter what some people think, no one is perfect. Every mistake is an opportunity to learn from and grow.
Keep learning: Whether you are in the office or on vacation, take MedMark specialty publications with you! Keep learning new concepts so when you return to work, you can expand your patients’ options for care.
In this summer issue, our Cover Story explores beneficial partnerships — in business and in life, Drs. Hunter Bennett and Nate Dewsnup find a balanced long-term practice strategy with the support of Specialized Dental Partners. Our CE by Dr. Fernando Meza shines a light on the power of dental lasers in the endodontic practice. Dr. Reid Pullen’s CE describes a hybridized technique for shaping and finishing root canals, and Drs. Lanka Mahesh, Gregori M. Kurtzman, Sagarika Shukla, and Zara Dhawan manage a challenging acute hemorrhage during an implant procedure. Even if your summer is busy with patients, there are plenty of ways to keep a healthy outlook on life. Journalist Charles Bowden once said, “Summertime is always the best of what might be.” Try a few of my Rx recommendations, and you will feel that endless summer in your hearts and minds for all future seasons.
To your best success,
Lisa Moler
Published by

Publisher Lisa Moler lmoler@medmarkmedia.com
Managing Editor
Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com Tel: (727) 515-5118
National Account Manager Adrienne Good agood@medmarkmedia.com Tel: (623) 340-4373
Sales Assistant & Client Services
Melissa Minnick melissa@medmarkmedia.com
Creative Director/Production Manager Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius emedia@medmarkmedia.com
Social Media Manager Felicia Vaughn felicia@medmarkmedia.com
Digital Marketing & Sales Administrator Sharif Rod sharif@medmarkmedia.com
Website Support Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC 15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260 Tel: (480) 621-8955 Toll-free: (866) 579-9496 www.medmarkmedia.com www.endopracticeus.com
Subscription Rate
1 year (4 issues) $149 https://endopracticeus.com/subscribe/
6 Endodontic Practice US Volume 17 Number 2 PUBLISHER’S PERSPECTIVE
Lisa


Drs. Hunter Bennett and Nate Dewsnup
Exploring the true value of partnership — in business and in life
Dr. Hunter Bennett likes to think one step ahead.
A native of Arizona, Dr. Bennett got his first job at a practice in the Grand Canyon State, and initially thought he’d never leave — until he started a friendship with the endodontist he was replacing at the practice, Dr. Nate Dewsnup, who had moved to another practice in Florida.
It was the potential of a partnership with Dewsnup that got Bennett the most excited about the future. The two endodontists — and eventual friends — started talking about what they wanted out of a practice and how to build a long-term career strategy that felt balanced.
After about 2 years in the Arizona practice, Bennett, who by then was looking to make a move and wanted a partner, made the decision to join forces with Dewsnup in Florida, who had also been looking to team up with the right endodontist.
The two now practice together at Bonita Endodontics in Southwest Florida, which has been a model of great partnership from day one. Bennett said, “Partnering with Nate gave me the ability to grow like I wanted.”
And grow they did. After just a few years in the practice, Bennett and Dewsnup were suddenly busier than they ever thought they’d be. Dewsnup said, “We were up to our eyeballs doing root canals, but we still had to handle all of that back-office stuff,
like payroll, 401ks, and onboarding new associates. It was kind of overwhelming.”
“We had decision fatigue,” said Bennett. “Things like PTO, holidays, and hiring would end up falling into my lap or Nate’s lap, and it became too much. As successful as we were, I remember a lot of days just wanting to walk out of the office at 5:00 p.m. and just lie down because I was so worn out.”
Both doctors agreed that they needed help — but weren’t sure about the next step to take. Bennett had a contact at Specialized Dental Partners (SDP) and brought up the idea of partnering with them to Dewsnup. However, it was initially a hard sell, as both were suspicious of working with DSOs and feared ceding control of their practice.
“When I first heard about it, I was an absolute hard no, just because of things that I’d heard about DSOs,” said Dewsnup.
“That was the biggest fear. Are they going to take away all my autonomy and be looking over my shoulder telling me what I can and can’t do? Or are they going to put quotas on things and say, you’ve got to do this many root canals, or you can’t do a root canal that way anymore. And so that made me nervous.”
However, after taking about 6 months to do research and talk with a representative from SDP, both Bennett and Dewsnup realized that having the right partner for the practice might be
8 Endodontic Practice US Volume 17 Number 2 COVER STORY
just what they needed to continue to grow and thrive.
Dewsnup said, “We had gotten to a point where we didn’t know what we were going to do if we kept growing, and we could only go so far alone. How much bigger can we get without really having the wheels come off?”
Partnering with Specialized Dental made me feel like I could go back to focusing on what I do best, which is taking care of patients and doing root canals.”
— Dr. Nate Dewsnup
The pair spoke with several DSOs, but only Specialized Dental Partners offered them the support resources they needed with the empathy and personal connection that mattered even more.
“As we talked with other groups, it became clear to me right away that they weren’t the right fit for us as a partnership. But talking to the guys in SDP, you could just tell the quality of character. It was a good fit from the beginning. It just felt right,” said Dewsnup.
Representatives from Specialized Dental made Bennett and Dewsnup feel heard — and helped them see how a partnership could help them build toward future goals, while improving their work processes and easing administrative burdens right away.
Dewsnup said, “Partnering with Specialized made me feel like I could go back to focusing on what I do best, which is taking care of patients and doing root canals.”
Bennett agreed and said that partnering with SDP allowed the endodontists to grow more strategically, by providing structure and advice for tasks like hiring new associates or adding technology, while still giving them the autonomy to run the business as they see fit.
But even more than the infrastructure that SDP offered, Bennett said the deciding factor in choosing them was about the people, especially when it comes to the support team.
“They’re always bending over backwards to accommodate what we need and what we do. And that’s something that I’ve really appreciated. I’ve never been disappointed with an interaction with someone from the support team. That’s probably one of my favorite parts, to be honest.”
Dewsnup added that he really appreciated SDP’s willingness to help the doctors as they have navigated challenges in the practice.

“We’ve been through some spots where we’re like, man, how are we going to get through this? And all we have to do is reach out and ask a question, and the people on the other side are more than willing to talk it through because they care. It’s a group of really good people, and that continues to be true. It just makes me more confident in what we decided to do.”
Even though both endodontists are years away from retirement age, they both agreed that partnering with SDP was a smart long-term strategy for them — and the practice.
Dewsnup said, “This was a really exciting opportunity. I felt like this is the future of our specialty and dentistry in general — so why not get on the train early and take advantage of that potential for growth early on?
Bennett added that lifestyle choices were another big reason it made sense to partner now — as opposed to closer to retirement. He spoke about wanting to have more time to enjoy his life and his family outside of work.
“A lot of it was lifestyle choice, too. I just don’t want to keep running like this, and I want to have more time. I want to delegate some of these headaches.”
In the several years since their partnership with SDP began, both doctors say that life at the practice has become more streamlined and predictable.
Bennett stated that before partnering with SDP, day-to-day issues could quickly turn chaotic. “One thing that was probably the most mentally exhausting in the practice was being really busy all day and then sort of putting everything on the back burner and either dealing with it after work or on Fridays.”
“SDP helped us hire a new office manager to act in more of a managerial role. And that honestly for me has been really, really

9 endopracticeus.com Volume 17 Number 2 COVER STORY
Dr. Nathan Dewsnup with a patient
Dr. Timothy Jernberg (right), Dr. Nathan Dewsnup (middle), and Dr. Hunter Bennett (right)

helpful to find someone that could handle that load. Now, you delegate it, and it goes away.”
However, Bennett stresses that the partners are still in charge of all major decisions — they’re just now relieved of some of the busy work of running a practice. Bennett said, “They’re not telling us what to do. It’s more like an advisory role so we can get things done.”
For both endodontists, having the support of SDP to handle the back-office work has made them better leaders. Dewsnup said, “I’ve realized I am still the leader in the practice. Hunter’s still the leader in the practice; it’s still our practice. We have teammates in place now who take a lot of that off our plates, but ultimately, it’s still us. We have to make the decisions. We have to be a positive influence on the team.”
More than anything, Dewsnup and Bennett said that partnering with SDP has helped them take stock of their priorities and position themselves more effectively for the future.
Bennett said, “It’s made me just step back and say, not what do I want next year or the year after, but what do I want in 20 years? And now because of Specialized Dental Partners and how I’ve positioned myself financially, I’m trying to just build for my kids and build for my family in a way to free myself up emotionally and financially in a way that I can sort of be the best of me.”
Bennett added that partnering with SDP also helps them better realize the possibilities of integrated care — and how to incorporate that care model into their practice as they grow.
“Nate and I just met with a local periodontist, and we said we would love to have a periodontist in our practice at some point. We’d love to have a surgeon. And so that’s something that we’re considering and working out because it’s a great service for the patients.”

“While we haven’t implemented it yet, I see huge benefits to that with time. I do think it’s where things are heading in our industry.”
Overall, the two partners have really appreciated the value of expanding that partnership with the support of Specialized Dental Partners and can’t wait to see how it will continue to help them become successful in their business — and in life.
Dewsnup noted that the partnership with SDP has re-invigorated him to keep building on what they’ve accomplished so far.
“It’s just re-energized me a little bit. It was getting a little bit stale, doing root canals the way that we were and just kind of grinding. But now I’m not just working for the practice. It’s like I’ve got a group of partners throughout the entire country who are counting on me and what we do at Bonita Endodontics. And I’m also kind of competitive. So, when I hear about other partners who are doing things a certain way, I’m like, oh man, I want to learn about that, and I want to incorporate that into what I do. I want to make sure we’re still at the top of our game.”

Want to hear more? Scan the QR code and catch the full conversation with Drs. Dewsnup and Bennett on the Specialized Podcast. EP
10 Endodontic Practice US Volume 17 Number 2 COVER STORY
Bonita Endodontics team
Bonita Endodontics team member greets a patient
Management of acute hemorrhage in the anterior maxillary region from an aberrant blood vessel
Drs. Lanka Mahesh, Gregori M. Kurtzman, Sagarika Shukla, and Zara Dhawan discuss management of a surgical complication
Abstract
Implant placement for missing teeth has become a routine procedure to establish the functional and esthetic needs of the patient. And just like any surgical procedure, complications like bleeding, infection, etc., can occur during implant placement as well. Bleeding from the alveolar antral artery (AAA) is one such complication which causes bleeding, and any clinician should be prepared for its management. Authors will discuss one such case and the management of this complication. CBCT is a very important diagnostic tool which should be used for every case possible.
Introduction
Implant placement has become a common procedure when one has to rehabilitate missing teeth functionally and esthet-

Lanka Mahesh, BDS, MBA, completed a bachelor’s degree in dental surgery and a diploma in hospital administration and is currently pursuing a PhD in Integrated Implantology. He has published over 225 articles and authored several textbooks. He practices in a private specialized implant practice at The Specialist Clinic in New Delhi, India and can be reached at drlanka. mahesh@gmail.com.

Gregori Kurtzman, DDS, is in private general dental practice in Silver Spring, Maryland. He is a former Assistant Clinical Professor at University of Maryland in the department of Restorative Dentistry and Endodontics and a former AAID Implant Maxi-Course assistant program director at Howard University College of Dentistry. He has lectured internationally on the topics of restorative dentistry, endodontics and implant surgery, removable and fixed prosthetics, and periodontics. He has over 870 published articles, as well as several ebooks and textbook chapters. He can be reached at dr_kurtzman@maryland-implants.com.


Sagarika Shukla, MDS, has a degree in periodontics with a special interest in facial esthetics. She is in private practice at The Specialist Clinic in New Delhi, India.
Zara Dhawan, BDS, is in private practice at The Specialist Clinic in New Delhi, India. She graduated from the School of Dental Sciences, Sharda University, Uttar Pradesh, India, in 2020.
ically. With better understanding and advances in technology, many procedures are available to rehabilitate the maxillary arch, and clinicians have many options of bypassing the sinus such as zygoma implants, the All-on-4 technique, indirect sinus lifts or graftless solutions, and short implants. However, each aforementioned technique is not as predictable as a direct sinus lift, especially in cases of a severely atrophic maxilla.1,2 Short implants have less bone-to-implant contact and have more chances of failure in load-bearing areas. In a meta-analysis by Papaspyridakos, et al.,3 authors stated that short implants (≤6 mm) have less predictable survival rates compared to longer implants (>6 mm) after periods of 1-5 years in function. When it comes to an indirect sinus lift, the procedure does not increase the height of maxillary sinus sufficiently,4 leaving a direct sinus lift a predictable treatment choice. However, many patients are anxious about maxillary sinus grafting and the complications which follow the surgery, hence procedures like All-on-4 were developed which can rehabilitate the entire arch along with bypassing the sinus. In this type of clinical situation, knowledge of anatomy and the arterial blood supply becomes paramount. Structure wise, the maxillary sinus (MS) is pyramidal in shape and largest of the paranasal sinuses.5 The anterior wall of the MS is formed by the facial surface of the maxilla and is internally grooved by the canalis sinuosus (which houses the anterior superior alveolar nerve and vessels).5 It receives blood supply via the maxillary artery and its branches. In this article, the artery of interest is alveolar antral artery (AAA), which is an anastomosis of the posterior superior alveolar artery (PSAA) and the infraorbital artery (IOA).6 As the name suggests, it appears on the maxillary facial plate near to or in close approximation with maxillary second premolar and first molar area, a position from where it takes a U-turn, roughly paralleling the sinus floor. Not much has been reported regarding this artery in the literature as it goes undetected, and the clinician only comes to know when it interferes during osteotomy (10%-30% of cases) or any complication.7,8 It has higher detection rates in males due to larger diameters, as well as in narrower maxillary sinuses <14 mm in width. The immediate complication is bleeding, which can be called as the “gateway complication” further leading to a series of complications that impact treatment prognosis and outcome and or abortion of the surgical procedure.6,9
The vertical distance of the artery from the alveolar ridge varies in patients depending upon the resorption of the ridge. Solar, et al.,10 reported a range of 15 mm - 25 mm of vertical
11 endopracticeus.com Volume 17 Number 2 CLINICAL
positioning of the artery in alveolar bone in a mixed dentate/ edentulous population. However, a more reliable measurement, which had been found to be mean of 7.66 mm, could be found via CBCT, where ridge resorption would not influence the vertical distance.11 Park, et al.,12 found this height to be between 7.71 mm - 8.01 mm, and suggested a lateral window of 8 mm for visualization, instrumentation, and graft placement if the sinus lift is to be performed. Studies have shown that the artery has an average diameter of 1.5 mm,13 and that a diameter of < 0.5 mm does not indicate any significant bleeding that would interfere with surgery.14 However, Testori, et al.,15 suggested that a small caliber vessel on CBCT, may correspond to a much larger caliber vessel clinically.
Case report
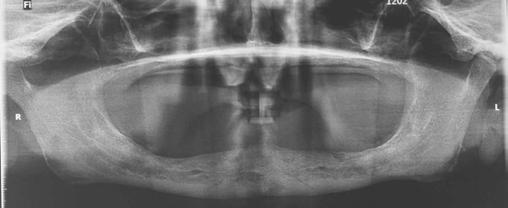
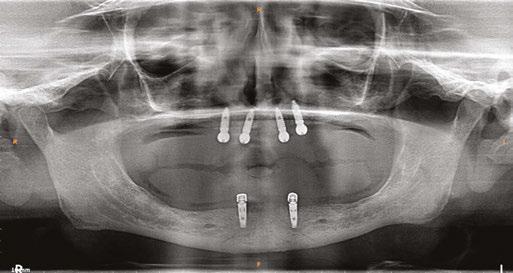
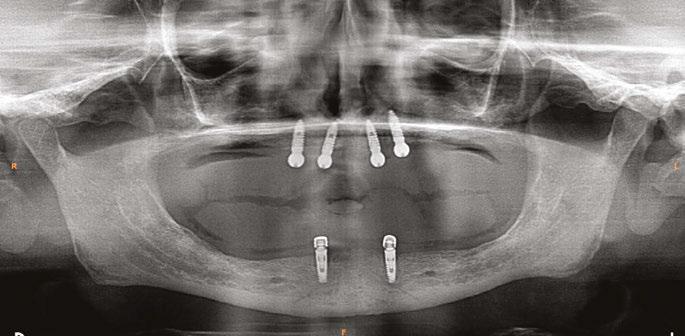
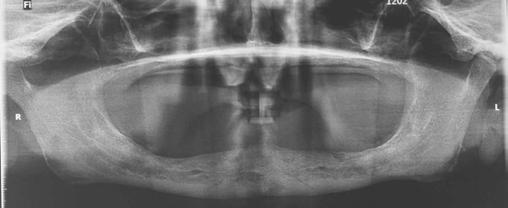
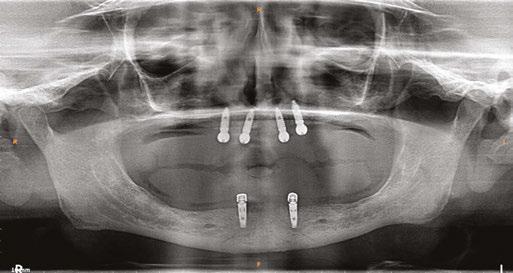
A 59-year-old male reported to the dental office with missing maxillary teeth due to poor oral hygiene. Treatment planning was done for all on four implant placements followed by prosthesis. A complete medical history was obtained and was negative for any significant medical problems. The patient denied being allergic to any medication as well. The patient agreed to the implant placement and was advised to have an orthopantomogram (Figure 1).
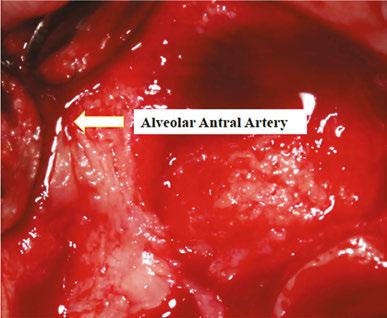
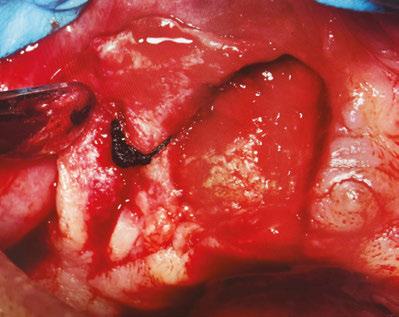
On the day of the surgery, before commencing the procedure under strict asepsis, the patient was asked to rinse with 0.12% chlorhexidine gluconate mouthwash (Peridex™; 3M™). Local anesthesia with a vasoconstrictor was infiltrated buccally and palatally into the posterior and anterior maxilla on both the sides using S-blades (straight) (Zabby, India). The incision was made
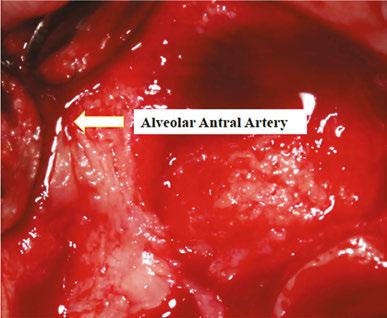
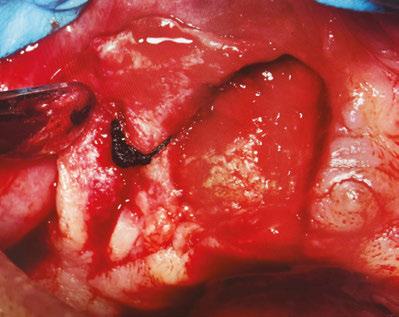
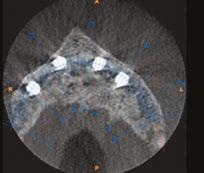
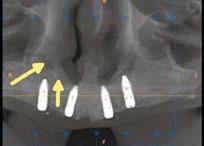
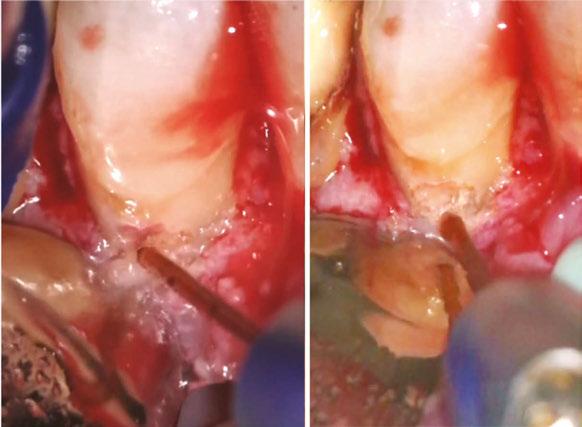
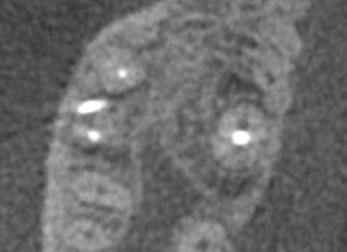
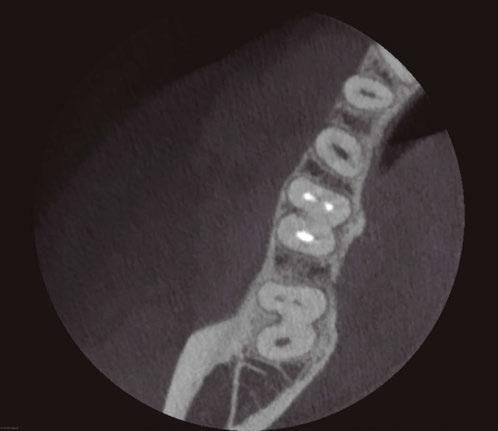
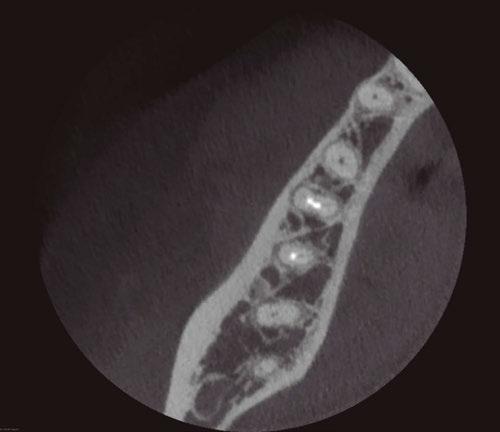
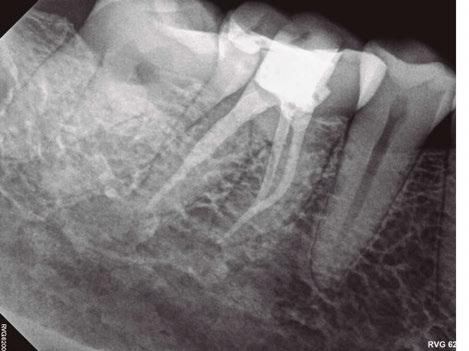
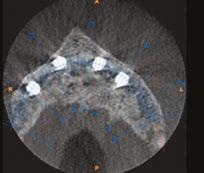
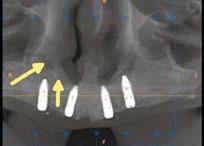
on the crest of the ridge in the region of teeth Nos. 15-25. While creating the incision, bleeding was noticed in the region of tooth No. 15 which intensified during the flap reflection (Figure 2). Bleeding was pulsatile, indicating an arterial bleed. Initially attempts to control bleeding included a pressure pack and ice pack, and the bleeder was isolated, and the vessel ligated (Figure 3). The bleeding could be controlled, and the procedure was completed by placing four Bioner implants (Bioner, Spain), size 4/10 mm. Sutures were placed, and patient was kept on basic medication for pain and infection control. Immediately after the surgery, the patient was advised to get a CBCT. As shown in Figure 4, a coronal view and Figure 4B (yellow arrows), the position of the artery can be seen.
In the follow-up sessions, the patient was comfortable, but did complain of mild swelling which subsided within 4-5 days. A post-op CBCT showed excellent recovery, bone width, and proper implant placement (Figure 5).
Discussion
Encountering a, AAA complication during an All-on-4 procedure in the region of teeth Nos. 14 and 15 has not been reported so far, however literature reports bleeding complications from AAA during sinus-lift procedures. Another complication that occurs is infection in about 3% of the cases, and in 1% of the cases loss of graft,16 and this usually happens after hematoma formation. In simple terms, the larger the vessels, the more the bleeding will occur. According to Ella, et al.,17 the risk involving AAA in osteotomies can be >10%, whereas according to authors Chan and Wang18 and Elian, et al.,8 it is 20%. Authors Jensen, et al.,19 have reported severe bleeding in sinus elevation surgery through a transcrestal approach, wherein bleeding led to swelling and consecutive hospitalization for 3 days, after which, normal functioning was regained. Hence management of the complication plays an important part for the clinician.
The first and foremost solution is the application of pressure pack and ice pack to control the bleeding along with topical thrombin. Other products such as SURGICEL® Absorbable Hemostat, SURGICEL™ Powder (Surgicel; Johnson & Johnson Co., Somerville, New Jersey), and bone wax can also be used. Usually because of bleeding at the surgical sight, pin-
12 Endodontic Practice US Volume 17 Number 2 CLINICAL
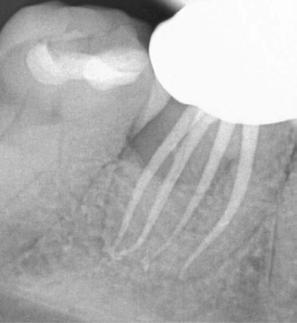
Figure 1: Pre-op panoramic radiograph
Figure 2 (left): Alveolar antral artery (AAA). Figure 3 (center): The artery has been ligated with suture. Figures 4A and 4B (right): CBCT post-implant placement and position of the artery coronally (top). 4B. Showing the position of alveolar antral artery (AAA) in relation to implant placement as indicated by the yellow arrows (bottom)





sswhitedental.com/try-exacttaperh-dc © 2024 SS White. All rights reserved. SS White, the SS White logo and ExactTap erH DC are regis te red tr ade marks of SS White Dental. Market research and test s tu dies availa bl e upon request. That feeling when you perform a root canal treatment for a patient is powerful — especially when you not only resolve their pain but prevent further discomfor t in the process. Instill your patients ® . Creating RCT, saving your patient s from enduring more pain and leaving their tooth stronger, for longer. TFW you complete a pain-free root canal procedure.
pointing the exact bleeding spot becomes difficult, but if that can be isolated, then electrocautery/chemocautery or ligation can be done. As aforementioned, if the vessel is large, and bleeding cannot be controlled, the procedure should be aborted, and patient should be hospitalized.
Use of piezoelectric devices safely bypasses the vessels as it only cuts the bony surface, avoiding any chance of vessel rupture. The only disadvantage is that it is a time-consuming method, but better when it comes to any complication or aborting the procedure. In a surgical double-window technique described by Maridati, et al.,20 an osteotomy is made above and below the vessel, leaving a thin bridge of bone holding the vessel intact. However, this is a difficult technique to follow and does not work in terms of instrumentation, implant placement, and septated sinuses.6 The simplest of the methods to avoid this complication is detection which is best achieved with CBCT, however even with CBCT, AAA can be detected in only 50% of the cases,22 perhaps because the vessel is too small to be detected by CBCT, which does not mean that there is an absent vessel, or anastomosis does not exist. Cadaveric studies have shown that anastomosis is present 100% of the time,23 but it goes undetected or unreported, simply because many clinicians assume that the anastomosis does not exist or use basic radiographic techniques for the implant placement.
In the case discussed here, authors encountered a small vessel wherein the bleeding was easily controlled with pressure packs and ice packs. The site of implant placement is a safe zone, and such a bleeding complication usually occurs during sinus-lift procedures and not in the anterior region. A simple detection could have helped clinicians to plan osteotomy better. Fortunately, the vessel was not big, and the bleeding could be controlled by ligation. Otherwise the implant placement may have had to be postponed. This proves that CBCT is an excellent tool and should be used more often for the case planning and detection of pathologies.21
Conclusion
Dental radiographs are an important tool in accurate diagnosis and treatment planning.21 Imaging is also the most common and important investigation carried out before any dental procedure that requires surgical or corrective intervention.21 Thus, accuracy of the X-ray, whether it is an intraoral periapical radiograph (IOPA) or an orthopantomogram (OPG) becomes paramount. However, these investigative tools provide a 2D
image of a 3D object and are subject to false positive errors. Also, patients should be counselled and motivated to receive the proper imaging for the procedure. Above all, the surgeon must anticipate and effectively manage complications encountered during the surgery.
REFERENCES
1. Chipaila N, Marini R, Sfasciotti GL, Cielo A, Bonanome L, Monaco A. Graftless sinus augmentation technique with contextual placement of implants: a case report. J Med Case Rep. 2014 Dec 17;8:437.
2. Bedrossian E, Rangert B, Stumpel L, Indresano T. Immediate function with the zygomatic implant: a graftless solution for the patient with mild to advanced atrophy of the maxilla. Int J Oral Maxillofac Implants. 2006 Nov-Dec;21(6):937-942.
3. Papaspyridakos P, De Souza A, Vazouras K, Gholami H, Pagni S, Weber HP. Survival rates of short dental implants (≤6 mm) compared with implants longer than 6 mm in posterior jaw areas: A meta-analysis. Clin Oral Implants Res. 2018 Oct;29 Suppl 16:8-20.
4. Balaji SM. Direct v/s Indirect sinus lift in maxillary dental implants. Ann Maxillofac Surg. 2013 Jul;3(2):148-153.
5. Standring S., ed. Gray’s anatomy: the anatomical basis of clinical practice. 41st ed. London: Elsevier Health Sciences; 2015.
6. Yang D, Lee N. A Simple Method of Managing the Alveolar Antral Artery during Sinus Lift Surgery. Int J Otolaryngology Head Neck Surg. 2021;10(3):131-146.
7. Lee CY. Brisk, prolonged pulsatile hemorrhage during the sinus graft procedure: a case report with discussion on intra-operative hemostatic management. Implant Dent. 2010 Jun;19(3):189-195.
8. Elian N, Wallace S, Cho SC, Jalbout ZN, Froum S. Distribution of the maxillary artery as it relates to sinus floor augmentation. Int J Oral Maxillofac Implants. 2005 Sep-Oct; 20(5):784-787.
9. Varela-Centelles P, Loira M, González-Mosquera A, Romero-Mendez A, Seoane J, GarcíaPola MJ, Seoane-Romero JM. Study of factors influencing preoperative detection of alveolar antral artery by CBCT in sinus floor elevation. Sci Rep. 2020 Jul 2;10(1):10820.
10. Solar P, Geyerhofer U, Traxler H, Windisch A, Ulm C, Watzek G. Blood supply to the maxillary sinus relevant to sinus floor elevation procedures. Clin Oral Implants Res. 1999 Feb;10(1):34-44.
11. Varela-Centelles P, Loira-Gago M, Gonzalez-Mosquera A, Seoane-Romero JM, Garcia-Martin JM, Seoane J. Distance of the alveolar antral artery from the alveolar crest. Related factors and surgical considerations in sinus floor elevation. Med Oral Patol Oral Cir Bucal. 2016 Nov 1;21(6):e758-e765.
12. Park WH, Choi SY, Kim CS. Study on the position of the posterior superior alveolar artery in relation to the performance of the maxillary sinus bone graft procedure in a Korean population. J Korean Assoc Oral Maxillofac Surg. 2012;38(2):71-77.
13. Kim JH, Ryu JS, Kim KD, Hwang SH, Moon HS. A radiographic study of the posterior superior alveolar artery. Implant Dent. 2011 Aug;20(4):306-310.
14. Rysz M, Ciszek B, Rogowska M, Krajewski R. Arteries of the anterior wall of the maxilla in sinus lift surgery. Int J Oral Maxillofac Surg. 2014 Sep;43(9):1127-30.
15. Testori T, Rosano G, Taschieri S, Del Fabbro M. Ligation of an unusually large vessel during maxillary sinus floor augmentation. A case report. Eur J Oral Implantol. 2010 Autumn;3(3):255-258.
16. Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants. 2009;24 Suppl:237-259.
17. Ella B, Sédarat C, Noble Rda C, Normand E, Lauverjat Y, Siberchicot F, Caix P, Zwetyenga N. Vascular connections of the lateral wall of the sinus: surgical effect in sinus augmentation. Int J Oral Maxillofac Implants. 2008 Nov-Dec;23(6):1047-1052.
18. Chan HL, Wang HL. Sinus pathology and anatomy in relation to complications in lateral window sinus augmentation. Implant Dent. 2011 Dec;20(6):406-412.
19. Jensen SS, Eriksen J, Schiodt M. Severe bleeding after sinus floor elevation using the transcrestal technique: a case report. Eur J Oral Implantol. 2012 Autumn;5(3):287-291.
20. Maridati P, Stoffella E, Speroni S, Cicciu M, Maiorana C. Alveolar antral artery isolation during sinus lift procedure with the double window technique. Open Dent J. 2014 May 30;8:95-103.
21. Shukla S, Chug A, Afrashtehfar KI. Role of Cone Beam Computed Tomography in Diagnosis and Treatment Planning in Dentistry: An Update. J Int Soc Prev Community Dent. 2017 Nov;7(Suppl 3):S125-S136.
22. Ilgüy D, Ilgüy M, Dolekoglu S, Fisekcioglu E. Evaluation of the posterior superior alveolar artery and the maxillary sinus with CBCT. Braz Oral Res. 2013 Sep-Oct;27(5):431-437.
23. Bernardi S, Mummolo S, Ciavarelli LM, Li Vigni M, Continenza MA, Marzo G. Cone beam computed tomography investigation of the antral artery anastomosis in a population of Central Italy. Folia Morphol (Warsz). 2016;75(2):149-153.
14 Endodontic Practice US Volume 17 Number 2 CLINICAL
EP
Figure 5: Panoramic radiograph following implant placement
Large Practice Sales Brings Multiple Bidders For The Highest Value in IDSO Partnerships
















“I was about to sign an offer I had in hand for $8 million from an IDSO I really liked. Chip convinced me to go through the LPS process to see my other options. LPS delivered nine bidders and the $8 million became $11 million from the same group!”
-Dr. T.S., Tennesee
“So glad I met you guys. You changed my life. My partner is great and I am still amazed how you achieved 3.9x collections for my practice.” -Dr. S.L, Indiana
“I never could have achieved this value or completed this deal without you.Thank you for everything.”
Achieved
Our clients are happy to talk to you about their LPS experience. Why IDSO Partnership? Millions in Cash at Closing Full Autonomy in Clinical & Business Reduced Administration Burden Higher Reimbursement Rates
Costs in Clinical & Business
& Marketing Support
Gains in Retained Ownership LPS vs. Do-It-Yourself & Small Advisors Six to Ten or More Bidders Highest EBITDA Calculation Full Knowledge of Risks & Rewards Most Tax Efficient Structures Complete Accounting, Legal & Closing No Fee Unless the Transaction Closes Paid Only By Our Client, Not Both Sides LPS Large Practice Sales Monetizing Larger Dental Practices FindMySilentPartner.com 877-437-3353 Endo@LargePracticeSales.com
-Dr. J.N., Maryland
12.2x EBITDA in 2023
Lower
Recruiting
Upside
Single visit regenerative endodontics using the GentleWave ® Procedure: a pediatric case report
Dr. Lauren Tink treats an anxious pediatric patient using an efficient treatment
Introduction
Recent advancements in endodontic techniques have revolutionized our ability to manage pediatric patients with complex cases. Traditionally, cases with wide open apices presented significant challenges. These cases often required multiple visits in order to achieve optimal outcomes.
However, contemporary approaches have provided more efficient treatment options, leading to improved clinical results and patient satisfaction.
Apexification has been the treatment of choice for teeth with open apices, aiming to induce the formation of an artificial apical barrier. While effective, apexification has its limitations as there is no potential for further root development.1 The emergence of regenerative endodontics has offered a paradigm shift in the management of these cases.2 This technique not only addresses the underlying pathology but also allows for continued root growth, ultimately leading to a more functional and resilient dentition.3
The implementation of traditional pulpal regeneration protocols in pediatric patients can be challenging, especially in cases with limited cooperation. Conventional approaches often require multiple visits,4 increasing the burden on both the patient and the clinician.
Single visit regenerative endodontics, coupled with advanced disinfection techniques, have emerged as a promising solution. This approach requires fewer visits, allows for enhanced disinfection, and promotes optimal blood clot formation in the canal. By eliminating the need for multiple visits, single visit regenerative endodontics offers a patient-centered approach that prioritizes both clinical outcomes and patient comfort.

Lauren Tink, DMD, was born and raised in Montreal, Canada. She attended McGill University and earned her doctoral degree in 2014. Following graduation, Dr. Tink moved to New York City and furthered her training at NYU Lutheran Medical Center’s Advanced Education in General Dentistry residency program. Subsequently, she attended Nova Southeastern University where she earned her postdoctorate degree in Endodontics. During her training at Nova, Dr. Tink participated in a surgical externship in Barcelona, Spain at the Universitat Internacional de Catalunya, performing a variety of specialized surgical procedures. She is currently in private practice at Weston Endodontic Care in Weston, Florida.
Disclosure: Dr. Tink reports no financial or other interests regarding any of the products mentioned in this article.




Figure 3 (left): Preoperative CBCT scan of tooth No. 20 showing evidence of a wide open apex. Figure 4 (right): Bleeding noted in the canal immediately after removing the GentleWave platform
In this case report, we present a 10-year-old patient with a wide open apex and a dens evaginatus.5 This case was successfully managed with single visit regenerative endodontics using the GentleWave® System (Sonendo®).6 The outcomes demonstrate not only the feasibility but also the efficacy of this approach in achieving favorable clinical and radiographic results in pediatric patients.
Case report
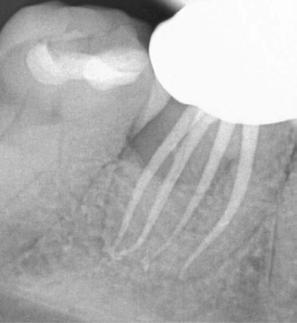
A 10-year-old female patient with a history of swelling and pain associated with tooth No. 20 was referred to our office. The patient exhibited severe dental anxiety. Upon clinical evaluation, a dens evaginatus was noted on the occlusal surface of the tooth (Figure 1). The tooth was sensitive to percussion, palpation, and bite stick while cold testing yielded no response. A periapical radiograph and CBCT scan (Carestream 9600) revealed a wide open apex and evidence of apical periodontitis, leading to the
16 Endodontic Practice US Volume 17 Number 2 CASE REPORT
Figure 1 (left): Dens evaginatus noted on the occlusal surface. Figure 2 (right): Preoperative periapical radiograph of tooth No. 20 showing evidence of apical periodontitis and a wide open apex
ZenSeal™
Calcium Silicate-Based Bioceramic Root Canal Sealer BUY 3 ZenSeal
or
Less Waste per Application Efficiency



High Flowability to Fill Complex Canals
With high flowability, ZenSeal has excellent flow into accessory canals.
Excellent Sealability with Zero Shrinkage ZenSeal adheres tightly to dentin and gutta percha with zero shrinkage.
Simplified Root Canal Procedure
Provides a simplified root canal procedure, including single cone technique.



The opinions expressed are those of Dr. Paola López Kerr Dental is a medical device manufacturer and does not dispense medical advice. Clinicians should use their own professional judgment in treating their patients. *Promotional goods must be of equal or lesser value and may not be combined with any other offers. Purchase must be made on one invoice between 6/1/24 and 7/30/24, unless otherwise noted. Redeem by 8/30/24. To receive your promotional goods, email or fax a copy of your authorized invoice noting promo code ZS62024 and product(s) desired to: kerrpromo@kerrdental.com or FAX: 888.727.2614 Limit to 3 redemptions. Incomplete submissions will not be processed. Allow 8 weeks for delivery. Offer valid in the 50 United States and the District of Columbia only. Promotions are subject to change or cancellation without notice. Offer void if purchased product is returned. Note that you may have an obligation under federal, state or local law to reflect discounts on product given pursuant to this promotion on any cost report forms submitted to a federal or state government or private payer who provides reimbursement for that product. 1-800-KERR-123 | kerrdental.com For more information Scan the QR Code or visit kerrdental.com/Zenseal Valid:
June 1 - July 30, 2024 | Promo Code: ZS62024
your financial goals.
money by getting more out
to meet
Save more
of each syringe.
©2023 Kerr Corporation. All trademarks are property of Kerr Corporation. All Rights Reserved. MKT-23-0769 Rev 0
GET 1 FREE
BUY 1 ZenSeal Kit, GET 10
Files FREE!*
Kits,
Packs of Hand




diagnosis of a necrotic pulp and symptomatic apical periodontitis of tooth No. 20 (Figures 2 and 3).
Given the presence of a wide open apex, traditional root canal therapy was not possible in this case. Treatment options such as apexification and regenerative endodontics were discussed along with the risks and benefits of both modalities. With apexification, placing the apical plug would present a challenge since there would be a risk of extruding the material past the apex. In addition, this option would present no opportunity for increasing the root width and length. For these reasons, it was determined that pulpal regeneration would be the ideal approach. The goals of the pulpal regeneration procedure would include facilitating root formation while eliminating apical periodontitis and achieving an asymptomatic and functional outcome for the patient. Traditionally, pulpal regeneration would be completed over the course of two visits with interim calcium hydroxide or triple antibiotic paste. However, this 10-year-old patient was severely anxious. Her parents requested for her to be treated under IV sedation. By maintaining the traditional protocol for pulpal regeneration, the patient would have to undergo IV sedation twice at two separate visits.


a
barrier forming mid-root
scan showed no evidence of apical periodontitis (Figure 10). Thickening of the radicular walls was noted, and a calcific barrier was noted to be forming mid-root. She will continue to be recalled in another 6 months to continue monitoring the healing of this case.
Summary
An alternative approach of single visit regenerative endodontics was employed utilizing the GentleWave system to facilitate disinfection and blood clot formation. After the IV was placed, local anesthesia was administered using 3% mepivacaine. No vasoconstrictor was used so as not to inhibit blood flow to the tooth. After isolating with a rubber dam, the tooth was accessed. A necrotic pulp was noted. No endodontic files were used for instrumentation. Flowable dam material (EndoSequence®, Brasseler USA) was used to build a platform and create a seal for the GentleWave CleanFlow™ procedure instrument (Sonendo). The full GentleWave cycle was run using NaOCl and EDTA as irrigants with a final water flush. Once the platform was removed, bleeding was immediately noted in the canal (Figure 4). A microsuction tip was used to control the bleeding to below the level of the CEJ. A piece of collagen tape (HeliCote® Collagen Dressing by Integra Miltex) was placed over the blood clot (Figure 5). Bioceramic putty (EndoSequence BC RRM Fast Set Putty) was placed on top of the collagen tape (Figures 6 and 7). The chamber was then etched and bonded and restored using Luxacore build up material (LuxaCore Z Dual Cure) and light-cured resin composite (Clearfil Majesty™ Composite, Kuraray) (Figures 8 and 9).
The patient was recalled 6 months later and showed promising results. She was asymptomatic and functional. The CBCT
In conclusion, this case report highlights the successful management of an anxious pediatric patient with a wide open apex using single visit regenerative endodontics, incorporating the GentleWave procedure. By circumventing the need for multiple visits and integrating advanced disinfection techniques, this approach not only expedited treatment but also optimized disinfection and facilitated blood clot formation in the canal. The favorable clinical and radiographic outcomes observed underscore the efficacy and feasibility of single visit regenerative endodontics as a patient-centered approach for addressing challenging cases in pediatric patients with limited cooperation and severe dental anxiety.
REFERENCES:
1. Rafter M. Apexification: a review Dent Traumatol. 2005 Feb;21(1):1-8.
2. Diogenes A, Ruparel NB, Shiloah Y, Hargreaves KM. Regenerative endodontics: A way forward. J Am Dent Assoc. 2016 May;147(5):372-380.
3. Lin J, Zeng Q, Wei X, Zhao W, Cui M, Gu J, Lu J, Yang M, Ling J. Regenerative Endodontics Versus Apexification in Immature Permanent Teeth with Apical Periodontitis: A Prospective Randomized Controlled Study. J Endod. 2017 Nov;43(11):1821-1827.
4. American Association of Endodontists. AAE Clinical Considerations for a Regenerative Procedure: Revised 5/18/2021. https://www.aae.org/specialty/wp-content/uploads/sites/2/2021/08/ ClinicalConsiderationsApprovedByREC062921.pdf. Accessed May 17, 2024.
5. Lerdrungroj K, Banomyong D, Songtrakul K, Porkaew P, Nakornchai S. Current Management of Dens Evaginatus Teeth Based on Pulpal Diagnosis. J Endod. 2023 Oct;49(10):1230-1237.
6. Sigurdsson A, Garland RW, Le KT, Woo SM. 12-month Healing Rates after Endodontic Therapy Using the Novel GentleWave System: A Prospective Multicenter Clinical Study. J Endod. 2016 Jul;42(7):1040-1048.
18 Endodontic Practice US Volume 17 Number 2 CASE REPORT
Figure 5 (left): Collagen tape was placed directly over the blood clot. Figure 6 (center left): Bioceramic putty was placed directly over the collagen tape. Figure 7 (center right): Periapical radiograph showing the placement of the bioceramic putty in the canal. Figure 8 (right): Restored access
Figure 9 (left): Immediate postoperative periapical radiograph of tooth No. 20. Figure 10 (right): 6-month recall CBCT scan showing no evidence of apical periodontitis and
calcific
EP
How to submit an article to Endodontic Practice US
Endodontic Practice US is a peer-reviewed, quarterly publication containing articles by leading authors from around the world. Endodontic Practice US is designed to be read by specialists in Endodontics, Periodontics, Oral Surgery, and Prosthodontics.
Submitting articles
Endodontic Practice US requires original, unpublished article submissions on endodontic topics, multidisciplinary dentistry, clinical cases, practice management, technology, clinical updates, literature reviews, and continuing education.
Typically, clinical articles and case studies range between 1,500 and 2,400 words. Authors can include up to 15 illustrations. Manuscripts should be double-spaced, and all pages should be numbered. Endodontic Practice US reserves the right to edit articles for clarity and style as well as for the limitations of space available.
Articles are classified as either clinical, continuing education, technology, or research reports. Clinical articles and continuing education articles typically include case presentations, technique reports, or literature reviews on a clinical topic. Research reports state the problem and the objective, describe the materials and methods (so they can be duplicated and their validity judged), report the results accurately and concisely, provide discussion of the findings, and offer conclusions that can be drawn from the research. Under a separate heading, research reports provide a statement of the research’s clinical implications and relevance to endodontics. Continuing education articles also include three to four educational aims and objectives, a short “expected outcomes” paragraph, and a 10-question, multiple-choice quiz with the correct answers indicated. Questions and answers should be in the order of appearance in the text, and verbatim. Product trade names cited in the text must be accompanied by a generic term and include the manufacturer, city, and country in parentheses.
Additional items to include:
• Include full name, academic degrees, and institutional affiliations and locations
• If presented as part of a meeting, please state the name, date, and location of the meeting
• Sources of support in the form of grants, equipment, products, or drugs must be disclosed
• Full contact details for the corresponding author must be included
• Short author bio and author headshot
Pictures/images/tables
Illustrations should be clearly identified, numbered in sequential order, and accompanied by a caption. Digital images must be high resolution, 300 dpi minimum, and at least 90 mm wide. We can accept digital images in all image formats (preferring .tif or jpeg).
Ensure that each table is cited in the text. Number tables consecutively, and provide a brief title and caption (if appropriate) for each.
Disclosure of AI use
Authors must disclose any AI used in researching, writing, or creating their articles. This includes a language model, machine learning, or similar technologies to create or assist with this submission. If AI was used, please provide a description of the AI-generated content and the name, model or tool used, and manufacturer. If AI was used, please confirm that you take responsibility for the integrity of the content that you are submitting.
References
References must appear in the text as numbered superscripts (not footnotes) and should be listed at the end of the article in their order of appearance in the text. The majority of references should be less than 10 years old. Provide inclusive page numbers, volume and issue numbers, date of publication, and all authors’ names. References should be submitted in American Medical Association style. For example:
Journals: (Print)
White LW. Pearls from Dr. Larry White. Int J Orthod Milwaukee. 2016;27(1):7-8. (Online)
Author(s). Article title. Journal Name. Year; vol(issue#):inclusive pages. URL. Accessed [date].
Or in the case of a book: Pedetta F. New Straight Wire. Quintessence Publishing; 2017.
Website:
Author or name of organization if no author is listed. Title or name of the organization if no title is provided. Name of website. URL. Accessed Month Day, Year. Example of Date: Accessed June 12, 2011.
Author’s name: (Single) (Multiple) Doe JF Doe JF, Roe JP
Permissions
Written permission must be obtained by the author for material that has been published in copyrighted material; this includes tables, figures, pictures, and quoted text that exceeds 150 words. Signed release forms are required for photographs of identifiable persons.
Disclosure of financial interest
Authors must disclose any financial interest they (or family members) have in products mentioned in their articles. They must also disclose any developmental or research relationships with companies that manufacture products by signing a “Conflict of Interest Declaration” form after their article is accepted. Any commercial or financial interest will be acknowledged in the article.
Manuscript review and extra issues
All clinical and continuing education manuscripts are peer-reviewed and accepted, accepted with modification, or rejected at the discretion of the editorial review board. Authors are responsible for meeting review board requirements for final approval and publication of manuscripts. If additional issues are desired, they must be ordered from the publisher when the page proofs are reviewed by the authors. The publisher does not stock back issues. Reprints can be purchased after the issue is published.
Proofing
Page proofs will be supplied to authors for corrections and/or final sign off. Changes should be limited to those that are essential for correctness and clarity.
Articles should be submitted to: Mali Schantz-Feld, managing editor, at mali@medmarkmedia.com
19 endopracticeus.com Volume 17 Number 2 AUTHOR GUIDELINES
Rotary negotiation and roto-reciprocation: a new hybridized shaping technique
Dr. Reid Pullen introduces a protocol for shaping and finishing root canals
The goal of endodontic therapy is to remove the diseased pulp and seal the root canal system to prevent recontamination.1 To accomplish this, we must first locate all the canals, get down the canals (full negotiation), and then shape and clean the canal system.2 This involves removing the diseased pulp tissue and clearing the microbial field encased in biofilm as much as possible. This is accomplished through a chemo-mechanical approach using antibacterial irrigants coupled with hand and nickel-titanium shaping files.3
With this process in mind, a new paradigm in endodontics has occurred. With the advent of rotary negotiation files like the ProTaper Ultimate™ Slider (Dentsply Sirona) and the miniKUT 15/03 and 15/05 (Plan B Dental), clinicians can now utilize a faster approach to negotiating to the apex. Rotary negotiation is defined as negotiating down the length of the root without the use of a hand file. Roto-reciprocation can be defined as a technique where both rotary and reciprocation are employed to shape and clean the canals. This article will discuss the extremely efficient technique of both rotary negotiation using the ProTaper Ultimate Slider and roto-reciprocation using the ProTaper Gold™ S1 and WaveOne® Gold Primary to shape and finish the canals.
The ProTaper Ultimate system, introduced to the market in 2021, was designed by Cliff Ruddle, John West, and Pierre Machtou, and was created as the next evolution to the ProTaper series. It was designed to cut a minimally invasive shape and preserve pericervical dentin. In this file system, the Slider was born. This employed a newer concept of rotary negotiation. The initial testing4 with ProTaper Ultimate Slider showed that endodontists were 63% successful at negotiating down to the apex without the use of a hand file. I wanted to personally test 1) If the Slider was first successful at negotiating down to patency (the Slider had to exit out the foramen with a “long” reading on the EAL to be counted as a success), and 2) if it was safe to do so (was there a high separation rate — could the Slider ledge?).

Reid V. Pullen, DDS, graduated from USC Dental School in 1999. He completed an advanced education in general dentistry in 2000 while serving in the Army Dental Corps in Landstuhl, Germany. He graduated from the Long Beach VA Endodontic Residency in 2006 and opened a private practice in Brea, California, in 2007. Dr. Pullen founded and runs Rootcanalacademy. com and The 2 Day Root Camp Boot Camp. Dr. Pullen became a Diplomate of the American Board of Endodontics in 2013.
Disclosure: Dr. Pullen is a Key Opinion Leader for Dentsply. He did not receive any financial compensation for this article.
Educational aims and objectives
This self-instructional course for dentists aims to discuss an efficient technique for rotary negotiation and roto-reciprocation.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online at endopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Summarize some history of the equipment used in the technique.
• Provide details on the implementation of the technique.
• Realize how to mitigate certain issues that may occur during the process.
• Identify some additional technologies for activated disinfection.


For over a year, I kept track of every canal for which I used the ProTaper Ultimate Slider and recorded if it negotiated to patency, how many passes it took (I stopped after 3 passes), and if it separated or ledged. After testing 1,357 canals, I was able to negotiate to patency and achieve a working length by attaching the EAL clip directly to the Slider, in 1,088 canals. This is an 80.2% success rate. In this sample, I separated 4 Sliders and ledged zero canals (in my clinical opinion, the file will separate prior to ledging the canal). This is a .2947% file separation rate. Of course, any file separation is contraindicated, especially at the beginning of treatment. What I encountered was that in the four separation events, I was able to either bypass or push the separated Slider to the “side” and still reach working length. In only one case, the Slider was right at working length and I was “stuck” and unable to achieve patency. Also, all four
20 Endodontic Practice US Volume 17 Number 2 CONTINUING EDUCATION
2 CE CREDITS
Figure 1: ProTaper Ultimate Slider
Figure 3: WaveOne Gold Primary
Figure 2: ProTaper Gold Shaper 1


times, I pushed on the Slider attempting to achieve full negotiation, and yet, the directions for use clearly state to employ a passive shaping technique. In other words, if the file binds or “hits a brick wall” DO NOT push and instead remove it, irrigate, and negotiate to patency using traditional hand files. I also noted that if the Slider does not advance to working length in two shaping passes, then the chance of it reaching on the third is rare. So after this period of testing (once I reach 1,500 canals), I will only try the Slider in 2 passes, and if I am unable to reach patency, then I will use a No. 8 or No. 10 K hand file with a 45° apical bend and negotiate in the traditional method.

After conducting research with the ProTaper Ultimate Slider and successfully negotiating to patency 80% of the time, I then experimented with a hybridized shaping system consisting of using the ProTaper Gold Shaper 1 (Dentspy Sirona) to prepare the middle 1/3 shape, and then following that with reciprocation using the WaveOne Gold Primary (Dentsply Sirona) to finish the apical shape. If a canal had a larger foramen than a No. 25 (tip size of the WaveOne Gold Primary), then I would “upshape” or “plus it” to a WaveOne Gold Medium (No. 35 tip).
In performing this technique on over 1,000 cases, I quickly realized the extreme efficiency of this technique. In most cases, I shaped the canal system so fast that I had plenty of time to use activated disinfection, either SWEEPS laser irrigation (LightWalker® laser, Fotona) or the sonic SmartLite Pro EndoActivator™ (18,000 cycle per minute) (Dentsply Sirona). This technique has reduced my shaping fatigue, has increased my shaping efficiency, and has made clinical endodontics more enjoyable (after 18 years of private endodontic practice, it is imperative that we continue to enjoy the process).
In closing, the ProTaper Ultimate Slider has completely changed the way I negotiate to the apex. In over 1,300 cases I have been successful at reaching the apex and beyond 80% of the time. In the majority of these cases, I am able to negotiate to
patency, achieve an accurate working length, and an open glide path (three key endodontic pillars) in seconds. I then follow this up with a hybridized roto-reciprocation technique using the ProTaper Gold S1 to shape the middle third and then the WaveOne Gold Primary to shape the apical third. This roto-reciprocation technique also shapes the majority of canals in just minutes. I now have plenty of time to activate and enhance irrigation with different devices on the market or let the sodium hypochlorite or Triton (Brasseler USA) soak in the canals while I am diagnosing and anesthetizing another patient. All in all, I have been using this new hybridized roto-reciprocation technique for the last year and a half, and it has increased my shaping efficiency, simplified my technique, and has made root canal therapy enjoyable.
REFERENCES
1. Ørstavik D.Materials used for root canal obturation: technical, biological and clinical testing. Endod Topics. 2006; 12(1):25-38.
2. Schilder H. Cleaning and shaping the root canal. Dent Clin North Am. 1974 Apr;18(2): 269-296.
3. Nair PN. Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med. 2004 Nov 1;15(6):348-381.
4. Internal study. Dentsply Sirona. 2021.
21 endopracticeus.com Volume 17 Number 2 CONTINUING EDUCATION
Figure 4 (left): Preoperative image of tooth No. 15. Figure 5 (right): Postoperative image. Rotary negotiation with Roto-reciprocation in all 3 canals with lengths from 25-28 mm and the ProTaper Ultimate Slider advanced to WL within 2 passes
EP
Figure 6 (left): Preoperative image of tooth No. 30. Figure 7 (right): Postoperative image. Rotary negotiation with Roto-reciprocation in all 4 canals and the ProTaper Ultimate Slider advanced to WL within 2 passes without the use of a hand file
Continuing Education Quiz
Rotary negotiation and roto-reciprocation: a new hybridized shaping technique PULLEN
1. To accomplish the goals of endodontic therapy, we must first ____.
a. locate all the canals
b. get down the canals (full negotiation)
c. shape and clean the canal system
d. all of the above
2. Removing the diseased pulp tissue and clearing the microbial field encased in biofilm as much as possible is accomplished through a chemo-mechanical approach using antibacterial irrigants coupled with _______.
a. hand and nickel-titanium shaping files
b. laser dopler flowmetry
c. Hertwig’s protocol
d. endodontic broaches
3. is defined as negotiating down the length of the root without the use of a hand file.
a. Rotary negotiation
b. Roto-reciprocation
c. File fatigue
d. Hedstrom protocol
4. _________ can be defined as a technique where both rotary and reciprocation are employed to shape and clean the canals.
a. Rotary reciprocation
b. Roto-reciprocation
c. Dual reciprocation
d. Masterfile reciprocation
5. The ProTaper Ultimate system, introduced to the market in 2021, was created as the next evolution to the ProTaper series. It was designed to _______.
a. cut a minimally invasive shape
b. preserve pericervical dentin
c. never separate
d. both a and b
6. The initial testing with ProTaper Ultimate Slider showed that endodontists were successful at negotiating down to the apex without the use of a hand file.
a. 45%
b. 56%
c. 63%
d. 84%
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://endopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://endopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 070
Date Published: June 21, 2024
Expiration Date: June 21, 2027
7. If the file binds or “hits a brick wall” DO NOT push and instead remove it, irrigate, and negotiate to patency using traditional hand files.
a. True
b. False
8. (The author wrote) After this period of testing (after the author reached 1,500 canals), I will only try the Slider in 2 passes, and if I am unable to reach patency, then I will use a No. 8 or No. 10 K hand file with a and negotiate in the traditional method.
a. 35° apical bend
b. 45° apical bend
c. 55° apical bend
d. 65° apical bend
9. In most cases, the author shaped the canal system so fast that he had plenty of time to use _______.
a. activated disinfection
b. calcium hydroxide
c. sodium hypochlorite
d. chlorhexidine
10. In the majority of these types of cases, the author is able to ______.
a. negotiate to patency
b. achieve an accurate working length
c. open a glide path in seconds
d. all of the above
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
22 Endodontic Practice US Volume 17 Number 2 CONTINUING EDUCATION
CE
2
CREDITS
Unlocking the power of dental lasers in endodontics
Dr.
Fernando J.
Meza discusses uses of lasers in the endodontic practice
Efficient endodontic interventions are crucial for maintaining dental wellness and securing the lasting integrity of natural teeth. Root canal therapies, a prevalent endodontic solution undergone by over half of the world’s population, according to a study titled “Prevalence of root canal treatment worldwide: A systematic review and meta-analysis,” are tailored to rectify concerns within the dental pulp, to alleviate discomfort and avert additional issues.1 Despite the annual treatment of over 15 million root canals as reported by the American Association of Endodontists, dental experts face a myriad of complexities in endodontic procedures, highlighting the significance of precise and innovative treatment methodologies.2
Difficulties linked with conventional endodontic treatments commonly center on attaining comprehensive disinfection of the root canal network and securely sealing the treated tooth to forestall recontamination. The complex structure of root canals, characterized by their curved and confined pathways, presents a notable challenge for achieving thorough cleansing and shaping, even for seasoned practitioners. Furthermore, the presence of microbes within the root canal system necessitates a meticulous and holistic strategy to eradicate bacteria and forestall the resurgence of infection.
In addressing these hurdles, the adoption of dental laser technology has brought about a revolutionary shift, enhancing the availability of high-quality care. Through leveraging laser energy, various dental procedures are executed with unmatched precision and effectiveness, thereby enhancing the standard of our treatments. Laser technology enables pinpoint targeting and elimination of infected tissue, debris, and bacteria from the complex root canal system, even in the most intricate anatomical arrangements. Such precision significantly reduces the likelihood of complications and enhances the overall success rates of endodontic interventions.
Beyond their efficacy in cleaning and disinfection, dental lasers offer advantages in terms of patient comfort and recovery — the minimally invasive nature of laser-based endodontic treat-
Fernando J. Meza, DMD, earned a bachelor’s degree in psychology from Vanderbilt University before graduating from the University of Connecticut School of Dental Medicine in 2002 and earning a certificate in endodontics from Temple University School of Dentistry in 2004. During his residency, Dr. Meza researched the BIOLASE Waterlase all-tissue laser’s capabilities to disinfect bacterially infected roots. The research was published in the Journal of the American Dental Association (JADA) in July 2007.
Disclosure: Dr. Meza has lectured for BIOLASE in hands-on courses and provides in-office training to endodontists and endodontic residents in the U.S. and Canada.
Educational aims and objectives
This self-instructional course for dentists aims to identify the various uses of the dental laser in endodontic practice.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online at endopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Identify some of the challenges of root canal therapy that may not be effectively addressed by traditional treatment.
• Realize the efficiencies of the laser in the processes of irrigation and disinfection.
• Identify other protocols besides RCT for which the laser can be an effective tool.
2
CE CREDITS
ments results in less postoperative pain and faster healing times.3 Patients experience reduced discomfort during and after the procedure, contributing to a more positive dental experience.
As we delve into the advantages of dental lasers in root canal treatment, it becomes evident that their versatility extends beyond traditional endodontic approaches leading to more conservative applications in certain instances. For example, the laser can be employed to assist with pulp tissue ablation, pulpal hemostasis, and decontamination of infected dentin in direct and indirect pulp cap procedures. This type of procedure may be useful in younger patients presenting with carious lesions with asymptomatic irreversible pulpitis where the pulpal tissue is more resilient.
Paradigm shift: lasers versus traditional drills
Traditional endodontic procedures, while successful, pose concerns as the intricacies of the treatment process often make it time-consuming for both the clinician and the patient. The need for multiple visits may be decreased since laser-assisted endodontics offers efficiencies in the search for difficult-to-find calcified canals and difficult to disinfect complex anatomies. More often than not, laser-assisted endodontics provides a more predictable one-visit treatment which is an advantage for both the patient and the provider.
Leveraging the principles of cavitation and acoustic streaming, dental lasers have demonstrated a remarkable improvement in disinfection efficacy. Recognizing the potential for better outcomes, and the superiority of lasers in terms of cleanliness and
23 endopracticeus.com Volume 17 Number 2 CONTINUING EDUCATION
disinfection, I found it imperative to incorporate laser technology into our practice with the Waterlase iPlus™.4
Since adopting the laser over 3 years ago, the advanced technology has surpassed our expectations. Beyond the evident improvements in cleaning and disinfecting canals, the technical aspects of the procedure have become more manageable. Laser activation of irrigants plays a pivotal role by efficiently removing debris, facilitating easier access for instruments to reach targeted areas within the tooth. This dual benefit has not only streamlined our process, making it more straightforward but also elevates the overall quality of disinfection for the patient. Incorporating the laser has resulted in shorter visits, in terms of time spent in the chair, and the possibility of reducing the number of required visits, which has demonstrated the efficiency brought about by laser-assisted root canal procedures. The newfound simplicity in the process, coupled with enhanced disinfection, signifies a positive shift in the overall treatment approach.
Irrigation and disinfection


As touched on earlier, the traditional approach to root canal procedures involved rinsing the canal system using a conventional syringe. However, based on extensive studies,5 it is well-established that irrigant delivery using this method may not effectively6 reach the entirety of the root canal system. This limitation prompted the need for improvements in the irrigation process. Sonic and ultrasonic devices were introduced as enhancements to the conventional syringe method. While these devices represented progress, they still fell short7 of achieving optimal distribution of bactericidal irrigating solutions throughout the root canal system. The introduction of laser technology marked a transformative leap in addressing this challenge and improving patient outcomes.
Dental lasers have revolutionized root canal procedures by elevating the activation of irrigants to an unprecedented level. Through the laser’s unique capabilities, including cavitation, shockwaves, and shear forces, it facilitates the dissolution, fragmentation, and thorough debridement of tissues. This innovative approach addresses the common dilemma of leaving tissue remnants behind.
There is a compelling anticipation that the advanced irrigation technique facilitated by the laser will lead to enhanced success rates for our patients. This assertion underscores the potential of laser technology to contribute to the continued improvement of outcomes in root canal procedures.
When approaching root canal cleaning and disinfection with the laser, first we instrument the canals using less tapered files to conserve tooth structure. After instrumentation, we place the dental laser tip loosely at the mid-root in a wet canal, only activating the laser while withdrawing the tip from the canal in a circular motion at a rate of 1 mm per second.
The energy from the Waterlase forms a vapor bubble at the laser tip within the irrigation solution. When the bubble collapses, a pressure wave and additional cavitation bubbles are created, cleaning the canal walls, removing the smear layer, disrupting biofilm, and extending to reach lateral canals into the apical regions. Dentinal tubules are opened by more effective smear layer removal especially when agitating with 17% EDTA solution, facilitating a deeper dentinal cleaning. LAI with YSGG used to activate EDTA was shown8 to leave only <8% of residual debris, while needle irrigation was shown9 to leave 40% of residue. Although some bacteria may remain in the tubules, this will be treated during the disinfection step of the dental laser process.
I like to refer to this deeper cleaning of the dentinal tubules as “deep disinfection.” You can think of the prior steps as the debridement phase of endodontic treatment where vital or necrotic tissue, and smear layer removal generated from instrumentation are removed. Bulk disinfection of the main canal is also established in this phase, but it’s the next step in “deep disinfection,” where the laser really shines due to tip placement in the canal.
Again, I start by placing the laser tip at the mid-root and slowly withdraw the tip once activated at 1 mm/sec and repeat 3 to 4 times per canal. This is done with a final 3% NaOCl solution. To gauge the effectiveness of disinfection, I point to two studies: first when applied inside of the canal, laser-assisted irrigation with NaOCl reaches more than twice10 as deep into the tubules than NaOCl alone. Secondly, the laser tip into the canal with either
24 Endodontic Practice US Volume 17 Number 2 CONTINUING EDUCATION
Figure 1: Polishing Geristore restoration. A flame-shaped diamond bur is being used to polish the class V subcrestal Geristore restoration. Additional images show a polished restoration with full-thickness flap reflected
Figure 2: RFPT5 Sulcular flap and reflection on tooth No. 28. An RFPT5 tip positioned distal to tooth No. 28 is being used for a sulcular incision. Reflection of the full-thickness flap using a molt exposing the external invasive resorptive tissue is shown
2.5% NaOCl or 2% chlorhexidine reduced 4-week-old e. faecalis colonies by more than 99.9%.11 Always take great care not to bind the tip in the canal and stick to the recommended protocols and settings.
In addition to the system that is used in my practice, various other types of lasers have demonstrated efficacy in endodontic procedures. Among them, the Er: YAG (erbium-doped yttrium aluminum garnet) laser and the Nd: YAG (neodymium-doped yttrium aluminum garnet) laser are notable. The Er: YAG laser operates at a wavelength of 2940 nm, effectively removing soft and hard tissues with minimal thermal damage. Its ability to efficiently ablate dentin and enamel makes it suitable for root canal preparation and debridement. Similarly, the Nd: YAG laser, operating at a wavelength of 1064 nm, has shown promise in disinfection and debris removal within the root canal system. These lasers offer alternative options for endodontic treatment, providing clinicians with versatile tools to enhance cleaning, disinfection, and overall treatment outcomes. Integrating these advanced laser technologies into endodontic protocols can further optimize patient care by addressing challenges such as residual debris and microbial presence within the root canal system, ultimately leading to improved success rates and patient satisfaction.
A spectrum of possibilities
The Waterlase iPlus unit uses a versatile Erbium, Chromium: YSGG 2780 nm wavelength, and has a notable distinction in power, reaching up to 10 Watts. This versatile wavelength developed for dentistry specifically, along with its elevated power opens up a multitude of applications, allowing for not only irrigation but also enabling proficiency in soft tissue surgery and hard tissue surgery. This expanded capability establishes its utility in both routine and complex endodontic surgical procedures.
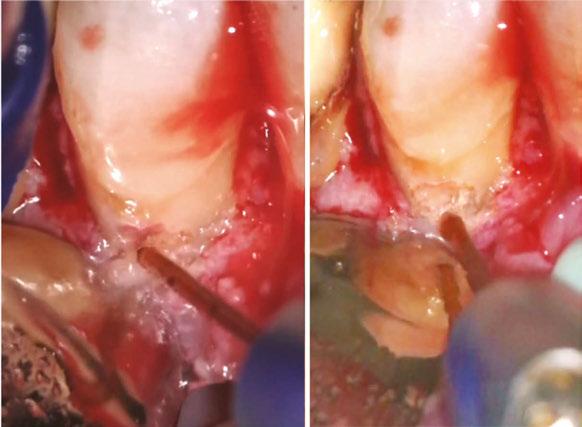

Beyond conventional root canal procedures, we also employ the laser for soft tissue surgeries, such as gingivectomy, gingivoplasty, crown lengthening, and precise incisions of flaps during endodontic surgeries. Additionally, the laser finds its utility in osteotomy, involving the judicious removal of bone and chronic apical granulation tissue during endodontic surgery. One of the benefits of the 2780 nm wavelength is deeper penetration into tissues and just the right amount of laser thermal effect to induce hemostasis while cutting at the same time.
In intricate cases, such as root resection, the laser enables precise cutting of the root tip from infected cases and debridement of the infected bone behind the resected root. Furthermore, when addressing certain resorption defects characterized by external resorptive tissue and persistent bleeding, the laser proves invaluable. It can ablate tissue minimally invasively and ensures remarkable hemostasis, mitigating the challenges commonly encountered during such procedures.
Additionally, laser-assisted vital pulp therapy techniques hold promise for preserving the vitality of dental pulp and promoting natural healing.12 The precision of lasers enables
targeted stimulation of the vital pulp with simultaneous precise disinfection and control of hemostasis as inflamed layers of the pulp are removed. This innovative approach marks a paradigm shift from traditional endodontic treatments. Laser applications in carious lesions leading to direct or indirect pulp caps, taking preoperative symptoms into account, could be approached in a whole new way, and in some instances eliminate the need for root canal procedures.
Lasers leading the way
As lasers continue to improve, their role in improving patient outcomes becomes increasingly prominent. From enhanced disinfection and tissue preservation to reduced postoperative discomfort, lasers contribute to a more positive overall patient experience. The future of endodontic practice is intricately tied to the continued refinement and integration of laser technology, promising a landscape where advanced techniques and improved outcomes redefine the standards of care in the field of endodontics.
25 endopracticeus.com Volume 17 Number 2 CONTINUING EDUCATION
Figure 4: Inspection and ablation of external resorptive tissue with an MZ6-14 tip, tooth No. 28. A micromirror is showing remaining resorptive tissue on the cervical portion of the resorptive cavity of tooth No. 28. Other images show an MZ6-14 tip ablating the remaining external resorptive tissue and dentin
Figure 3: Ablation of external resorptive tissue with an MZ6-14 tip, tooth No. 28 . An MZ614 tip is shown adjacent to the external resorptive tissue that has invaded and demineralized the buccal aspect of tooth No. 28 root dentin
Providers have an obligation to learn about any technology that will benefit the patients we care for. If it’s reasonable, effective, and affordable, there is no reason not to incorporate it into everyday endodontic treatment and expanded functions. The integration of lasers not only addresses current challenges but also paves the way for a brighter and more patient-centric approach to endodontics, where innovation meets precision for the benefit of both clinicians and those seeking the highest quality dental care.
REFERENCES
1. León-López M, Cabanillas-Balsera D, Martín-González J, Montero-Miralles P, Saúco-Márquez JJ, Segura-Egea JJ. Prevalence of root canal treatment worldwide: A systematic review and meta-analysis. Int Endod J. 2022 Nov;55(11):1105-1127.
2. American Association of Endodontists. Root Canal Explained. https://www.aae.org/ patients/root-canal-treatment/what-is-a-root-canal/root-canal-explained/. Accessed May 2, 2024.
3. Fahim SZ, Ghali RM, Hashem AA, Farid MM. The efficacy of 2780 nm Er,Cr;YSGG and 940 nm Diode Laser in root canal disinfection: A randomized clinical trial. Clin Oral Investig. 2024 Feb 26;28(3):175.
4. Biolase. Waterlase iPlus Premier Edition. https://www.biolase.com/products/dental-lasers-all-tissue/waterlase-iplus/. Accessed May 29, 2024.
5. Boutsioukis C, Arias-Moliz MT. Present status and future directions - irrigants and irrigation methods. Int Endod J. 2022 May;55 Suppl 3(Suppl 3):588-612.
6. Ali A, Bhosale A, Pawar S, Kakti A, Bichpuriya A, Agwan MA. Current Trends in Root Canal Irrigation. Cureus. 2022 May 8;14(5):e24833.
7. Raducka M, Piszko A, Piszko PJ, Jawor N, Dobrzyński M, Grzebieluch W, Mikulewicz M, Skośkiewicz-Malinowska K. Narrative Review on Methods of Activating Irrigation Liquids for Root Canal Treatment. Applied Sciences. 2023; 13(13):7733.
8. Kuştarcı A, Er K, Siso SH, Aydın H, Harorlı H, Arslan D, Kirmali O. Efficacy of Laser-Activated Irrigants in Calcium Hydroxide Removal from the Artificial Grooves in Root Canals: An Ex Vivo Study. Photomed Laser Surg. 2016 May;34(5):205-210.
9. Meire MA, Havelaerts S, De Moor RJ. Influence of lasing parameters on the cleaning efficacy of laser-activated irrigation with pulsed erbium lasers. Lasers Med Sci. 2016 May;31(4):653-658.
10. Wang X, Cheng X, Liu X, Wang Z, Wang J, Guo C, Zhang Y, He W. Bactericidal Effect of Various Laser Irradiation Systems on Enterococcus faecalis Biofilms in Dentinal Tubules: A Confocal Laser Scanning Microscopy Study. Photomed Laser Surg. 2018 Sep;36(9):472-479.
11. Aydin S, Taşdemir T, Buruk K, Celik D. Efficacy of Erbium, Chromium-doped Yttrium, Scandium, Gallium and Garnet Laser-activated Irrigation Compared with Passive Ultrasonic Irrigation, Conventional Irrigation, and Photodynamic Therapy against Enterococcus faecalis. J Contemp Dent Prac. January 2020;21(1):11-16.
12. Cengiz E, Yilmaz HG. Efficacy of Erbium, Chromium-doped:Yttrium, Scandium, Gallium, and Garnet Laser Irradiation Combined with Resin-based Tricalcium Silicate and Calcium Hydroxide on Direct Pulp Capping: A Randomized Clinical Trial. J Endod. 2016 Mar;42(3):351-355.

26 Endodontic Practice US Volume 17 Number 2 CONTINUING EDUCATION
EP *Not a subscriber yet? Get started today at Endopracticeus.com/subscribe! endopracticeus.com/continuing-education/ Don’t Forget to Take the CE Quiz Online!* Our Streamlined Dashboard Makes It Easy... ONE CLICK to your personal CE dashboard EASILY find completed course certificates FOCUSED on the content that matters to you DISCOVER more topics with webinar courses
Continuing Education Quiz
Unlocking the power of dental lasers in endodontics MEZA
1 Laser technology enables pinpoint targeting and elimination of _______ from the complex root canal system, even in the most intricate anatomical arrangements.
a. infected tissue
b. debris
c. bacteria
d. all of the above
2. More often than not, laser-assisted endodontics provides a more predictable ________ treatment which is an advantage for both the patient and the provider.
a. one-visit
b. two-visit
c. less expensive
d. none of the above
3. Through the laser’s unique capabilities, including cavitation, shockwaves, and shear forces, it facilitates the dissolution, fragmentation, and thorough debridement of tissues.
a. True
b. False
4. After instrumentation, the author places the dental laser tip loosely at the mid-root in a wet canal, only activating the laser while withdrawing the tip from the canal in a circular motion at a rate of _______ per second.
a. 1 mm
b. 2 mm
c. 3 mm
d. 4 mm
5. Dentinal tubules are opened by more effective smear layer removal especially when agitating with a _________, facilitating a deeper dentinal cleaning.
a. sodium hypochlorite solution
b. saline solution
c. 17% EDTA solution
d. 5% EDTA solution
6. To gauge the effectiveness of disinfection, I point to two studies: first when applied inside of the canal, laser-assisted irrigation with NaOCl reaches more than ______ as deep into the tubules than NaOCl alone.
a. twice
b. three times
c. four times
d. five times
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://endopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://endopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 070
Date Published: June 21, 2024
Expiration Date: June 21, 2027
7. Secondly, the laser tip into the canal with either 2.5% NaOCl or 2% chlorhexidine reduced 4-week-old e. faecalis colonies by more than
_______.
a. 52%
b. 64%
c. 76%
d. 99.9%
8. The Waterlase iPlus unit uses a versatile Erbium, Chromium: YSGG 2780 nm wavelength, and has a notable distinction in power, reaching up to ________.
a. 5 watts
b. 7 watts
c. 10 watts
d. 15 watts
9. The laser finds its utility in osteotomy, involving the judicious removal of _________ during endodontic surgery.
a. bone
b. chronic apical granulation tissue
c. blood
d. both a and b
10. The laser in endodontics can ablate tissue minimally invasively and ensures remarkable hemostasis, mitigating the challenges commonly encountered during such procedures.
a. True
b. False
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
27 endopracticeus.com Volume 17 Number 2 CONTINUING EDUCATION
2 CE
CREDITS
The intangible value of practice success
Dr. Albert (Ace) Goerig discusses the many ways to improve the quality of your personal and practice life
I’ve written frequently about how most endodontists in typical practices can add hundreds of thousands of dollars to their bottom line. We have a highly successful system, and it works. However, tangible “raw” dollars are only half the story. The intangible value is often overlooked. Here are some of the key intangibles that come into your practice and life when financial success takes a big leap forward.
Elimination of financial worries
Whether it is education debt, practice debt, mortgages, consumer debt, or anxiety about saving for future needs, financial stress is a 24-7 burden. When you significantly increase your practice income, you can immediately start paying off your obligations quickly and forever. Debt-free equals stress-free because all income previously diverted to debt service payments become 100% discretionary cash flow without any emotional overhead. If your goal is to save for the future, an extra $200k per year lets you save incredibly fast.

Escape from the daily grind mindset
Practice ownership has its challenges. Doctors have a big investment, and with that comes a necessary level of oversight, team management, and attention to business details. Sometimes every day can feel like a grind, especially when your income falls short of expectations or goals. Boosting your income changes your daily mindset. While it doesn’t eliminate your responsibilities, it gives you the satisfying context of heightened success that tells you that your efforts are worthwhile, meaningful, and rewarded.

Albert Goerig, DDS, MS, is a Diplomate of the American Board of Endodontics and a sought-after speaker who has lectured extensively on the field of endodontics and practice success throughout the United States, Canada, and abroad. He is the author of more than 100 published articles and contributing author to numerous endodontic textbooks. Dr. Goerig has a private endodontic practice in Olympia, Washington, in the top 1% nationwide for practice profitability. He has almost 40 years of experience as an endodontic educator and practice coach to over 1,000 endodontists. www.endomastery.com | 1-800-482-7563 | info@endomastery.com
Confidence to innovate and reinvest
Many doctors have goals that require innovation or reinvestments to improve the practice. For example, those may include enhanced team training, updating technology and equipment, renovating the office, or even building the facility of your dreams. Without the financial flexibility of high profitability, doctors often feel constrained. Financial growth in the practice gives doctors choices, sometimes for the very first time, to envision and achieve exactly the kind of practice environment that would make every day in the office an absolute joy.
Team performance and retention
Having a great team is a key factor in practice enjoyment and success. In highly successful practices, team members know they are working in a high-performance environment, and they know their individual performance needs to rise to that standard. Higher profitability also gives you the financial health to ensure you can always hire, train, and retain the best team possible. It makes a huge difference when every day is spent alongside an empowered and productive team who is having fun.
Work-life balance
Endodontists are among the worst of all dental specialists when it comes to taking time off. We often feel we must be available for referrers every day. There is also the general mindset that
28 Endodontic Practice US Volume 17 Number 2 PRACTICE MANAGEMENT
to earn more income, you must work more. In fact, daily teamwork and clinical efficiency are bigger drivers of income than hours worked. Highly productive practices mean fewer days worked per week and per year while earning more, and doctors get proper rest and relaxation for long-term health and to avoid burnout.
Lifestyle freedom
“Lifestyle” is an umbrella term that covers everything from how much you spend on a bottle of wine to what school your children attend, and everything in between. It includes things that are absolutely essential (like living expenses) and absolutely discretionary (like art or travel). There is no wrong lifestyle, except if you don’t have choices that are meaningful and enjoyable for you. Economics is ultimately a tool for making lifestyle choices, and so a more profitable practice can immensely enhance your options.
Family goals and legacy
Family goals are more than just lifestyle but also planning for great family unity and individual goals for everyone. How do you give your kids formative experiences to shape their outlook? How do you create special experiences that keep you close to your spouse? Great economics are a key part of the family
Independent practice owners have a largely untapped opportunity to unlock an incredible level of life success based on improved practice success.”
equation. Even more, highly profitable doctors can create generational wealth that becomes a vital and enduring legacy for the family or to dedicate to philanthropic goals.
It’s easy to understand each of these intangible benefits at face value. However, what is so important to appreciate is when all these benefits start to occur at the same time in your life. It is transformational and unbelievably uplifting. You will feel like a different person and the best version of yourself that you could ever imagine. Independent practice owners have a largely untapped opportunity to unlock an incredible level of life success based on improved practice success. If you would like to learn more, Endo Mastery offers a complimentary practice analysis.
For more information, visit www.endomastery.com, or call 1-800-482-7563.
Endodontic Practice US Webinars
LEARN about the lastest techniques and technology from industry leaders with our free live and archived educational webinars. Our online seminars are a convenient way to access great information and upskill. Check out our most recent webinars:
• The Science and Clinical Evidence Behind A ModernDay Disinfection and Debridement Technology with host Dr. Derek Peek
• Diagnosis & Cracked Teeth – How CBCT can change your practice with host Dr. Judy McIntyre
• Complete Endodontic Success: From Root Canals to Patient Reviews with host Dr. Ryan M. Walsh

30 Endodontic Practice US Volume 17 Number 2 PRACTICE MANAGEMENT
EP
WATCH
at https://endopracticeus.com/webinars/ Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com
NOW
Endo education with a giveback twist
Daniel Lewis discusses a program that brings needed resources to underserved patients
From recordkeeping to materials and techniques, clinicians are always searching for efficiency in a dental practice. Similarly, continued education and humanitarian efforts are highly valued by the dental community, and clinicians are often participating in both.
So, when Dr. Sonia Chopra saw the need for both endodontic education and access to endodontic care in her Charlotte, North Carolina community, she found an efficient way to address them at the same time through her E-school giveback program.
“In my practice I see two things. Number one, patients who come in and can’t afford treatment. And they have to either defer treatment, or they have to extract their tooth because that’s the only thing they can [afford to] do,” says Dr. Chopra. “I also see patients who come in, and not that they were mistreated, but you can tell that there’s still a lack of education in the dental world.”
The gap in training is no fault of the dentists — without resources they’ve been left underserving their patients. “I talk to dentists all the time, and they just want more help because they maybe only did 2 to 3 root canals before they graduated,” Chopra says. “They maybe had a crash course for a couple weeks before they got out of dental school.”
To address the need for education and the needs of the patients, Dr. Chopra adapted her already widely respected E-school program to incorporate a live element — general dentists are able to hone their endo skills, while patients receive treatment they need at a small fraction of the normal cost. “They are so grateful,” she says of the patients in this program. “They just can’t believe that something like this exists, and I feel like more of it should exist.”


Receiving a root canal through this program saved many patients from tooth extractions, which would be the only other financially viable alternative. “There’s a lot of practices around me who take Medicaid, but they can’t find an endo provider to

take Medicaid,” Chopra says. “Or maybe one of my normal patients has insurance maxed out so they can’t afford it, and we tell them about the program and they’re ecstatic to be a part of it.” When it comes to the course, Dr. Chopra says dentists love the training without the sales pitch. “This is completely unbiased. It’s not associated with any one company. I do like to promote the products I use because I’m so used to using them over a decade or so, but I don’t push anyone to buy a certain product ... [Dentists] are excited about the type of education they get because they don’t have to just work on extracted teeth in a course that’s provided by a company that just wants them to buy their products,” Dr. Chopra says. “They’re just really happy to have that type of clinical experience because working on extracted teeth doesn’t translate well to real-world endo, and this gives them that experience but also makes them feel safe and secure to really learn the true tips and tricks that are needed to perform these treatments.”
Roughly 20 patients can be seen throughout each session of the course, totaling some $50,000 in donated dentistry. “We do a free consult on them, a free cone beam, we do the treatment, and the buildup as well,” Dr. Chopra explains. “We’re doing a lot for just that one tooth.” Several sessions of the E-school live program are held each year, with the next coming in September 2024. For more information, visit https://drsoniachopra. com/e-school-live/.
31 endopracticeus.com Volume 17 Number 2 HUMANITARIAN EFFORTS
EP
Daniel Lewis is a longtime news producer turned dental industry storyteller for Ultradent Products. He’s interviewed people on every continent plus the international space station and can usually be found eating carbohydrates in the company of his dog.
Dr. Chopra with clincians from her E-school live program getting hands-on experience
Bio-C Sealer ION+
A new class of calcium silicate
BIO-C SEALER ION+ is an innovative premixed bioceramic sealer, patented new material, used for root canal filling and internal resorption treatment. It is based on a new class of calcium silicate, which has unique crystalline structure and chemical composition, different from traditional calcium-silicate materials.
To obtain this new bioceramic, a mixture of silicon, magnesium, and calcium oxides is used, replacing aluminum oxide with magnesium oxide in its composition. Previous studies have shown the effectiveness of materials releasing magnesium ions in treating bone defects, promoting osteogenic differentiation and significant mineral deposition. Magnesium ions stimulate an increase in alkaline phosphatase in osteoblasts and enhance intercellular junctions, indicating a positive correlation with cellular activity.

BIO-C SEALER ION+ functions by releasing these ions in a chemically balanced environment created by an alkaline pH. Upon contact with body fluids, it forms a silica-rich gel layer on its surface, facilitating enzymatic changes that influence cellular differentiation and promote tissue formation. It aids in the repair and regeneration of tissue-bone and dentin-pulp complexes.
In clinical practice, BIO-C SEALER ION+ offers a practical, easy, and efficient procedure. It is conveniently packaged in premixed syringes with disposable intracanal tips. To preserve its physical properties, each syringe contains a small quantity of 0.5 g and is accompanied by a metallized pouch containing silica gel that protects the product from moisture.
5 reasons to choose BIO-C® SEALER ION
1. Resin-free and eugenol-free material: BIO-C® SEALER ION does not contain resin, making it easy to clean the pulp chamber only with water. It is also biocompatible,

causing no postoperative pain. And being eugenol-free, it does not negatively interact with other root canal procedures such as post cementation.
2. Excellent flowability: With a flow of approximately 24 mm and micronized particles smaller than 2 µm, BIO-C® SEALER ION has excellent viscosity. It efficiently penetrates different branches of the complex root canal system and easily reaches the dentinal tubules, promoting a hermetic and three-dimensional filling.
3. Compatible with cold or warm technique: BIO-C® SEALER ION remains stable at the maximum temperature reached by equipment during root canal filling techniques that involve heating gutta percha (up to 392ºF). Unlike other sealers that degrade at temperatures close to 291.2ºF, it maintains its integrity.
4. Low solubility: With a solubility of less than 3%, BIO-C® SEALER ION prevents bacterial reinfection by ensuring a homogenous filling without gaps after setting. This increases the chances of successful treatment.
5. No tooth staining: BIO-C® SEALER ION contains zirconium oxide as a radiopaquer, allowing for excellent radiographic evaluation (≥ 7.0 mm Al) by the dentist, and unlike other products on the market that contain bismuth oxide, it does not cause tooth staining.
32 Endodontic Practice US Volume 17 Number 2 PRODUCT PROFILE
This information was provided by Angelus.
Figure 1: Bio-C Sealer Ion+ Syringe with translucent intracanal tip
EP
Figures 2 and 3: Clinical case kindly provided by Professor André Michelotto (Curitiba/PR - Brazil). 2. Initial CBCT. 3. CBCT after 7 months postoperative
Cybersecurity — a necessity, not a luxury
Thomas Terronez offers some guidance on keeping your practice data safe from cyberattacks
In today’s digital age, cybersecurity breaches are a major concern for businesses of all types and sizes — and your dental practice is no exception. The recent Change Healthcare breach was a wake-up call for the healthcare industry, proving that no organization is immune to cyberattacks. As a dental IT and cybersecurity expert with over 20 years in the trenches, I’ve seen firsthand the challenges practices face when it comes to protecting patient data. In this guide, I’ll dive deep into the specific risks targeting dental practices and share actionable strategies to strengthen your defenses.
Navigating the cybersecurity minefield
You might think your small practice is an unlikely target for hackers. Think again. Cybercriminals see dental offices as easy marks, thanks to your valuable patient data. Plus, the rise of high-tech dentistry has made practices even more reliant on IT systems, expanding your attack surface. The numbers don’t lie — cyberattacks on healthcare organizations, including dental practices, have skyrocketed in recent years. Ransomware, phishing scams, data breaches — the threats are real and growing.
Exposing your practice’s weak spots

• Weak security appliances: Outdated firewalls or bargain-basement security tools? They’re no match for today’s sophisticated cyber threats. Investing in strong perimeter defenses is non-negotiable.
So what makes dental practices so vulnerable? Here are some of the chinks in your armor:
• On-premise servers: Still relying on in-house servers? They’re a hacker’s dream if not properly secured and maintained. It’s like leaving your front door wide open.
• Elevated workstation settings: Your workstations need elevated security settings to run your practice management, EHR, and imaging software. Convenient, but risky if not configured correctly. One wrong move, and you’re exposed.

With over 20 years of experience in dental IT, Thomas Terronez is one of the nation’s renowned dental technology leaders. Thomas’ mission is to lead dental organizations through operational and scaling challenges by leveraging technology. He has a forward-thinking outlook and is solution-focused, which has led him to work with the top dental vendors on evolving and developing the technology infrastructure for the industry’s future. He is the founder and CEO of Medix Dental IT, the leading dental IT company focused on emerging and current dental organization needs. Presently, Thomas consults with dental groups, software companies and DSOs across the country on technology strategy. Additionally, Thomas serves as an ongoing Business Scaling Mentor program at Stanford University, where he guides mentees on entrepreneurship and innovation.
• Insufficient staff training: Your team is your first line of defense — or your weakest link. Without proper cybersecurity training, they’re easy prey for social engineering attacks like phishing. And with most workstations having full server access, one slip-up can bring down the whole network.
• Small IT vendors: Local IT shops play a vital role in keeping your practice humming. But they may lack the specialized expertise to implement ironclad cybersecurity measures. Don’t confuse general IT support with the kind of in-depth security know-how you need.
Shoring up your defenses
Ready to bullet-proof your practice against cyber threats? Here’s your action plan:
• Embrace the Cloud: Making the leap to cloud-based software is a smart security move. Let the experts handle the heavy lifting while you reap the benefits of enhanced protection, from encryption to real-time monitoring. Just be sure to vet providers carefully.
• Invest in the best: When it comes to security tech, you get what you pay for. Spring for enterprise-grade firewalls from trusted names like Cisco, SonicWall, or Fortinet. Activate advanced threat protection to stay ahead of emerging dangers. Endpoint detection and response (EDR) solutions add an extra layer of defense.
34 Endodontic Practice US Volume 17 Number 2 GOING VIRAL
• Train your team: Empower your staff to be your greatest security asset with regular cybersecurity training. From spotting phishing red flags to following data handling best practices, make security second nature for your whole team.
Cybercriminals see dental offices as easy marks, thanks to your valuable patient data.”
• Partner with pros: Join forces with an IT firm that specializes in the unique security needs of dental practices. They bring the deep expertise to tackle HIPAA compliance, data encryption, and more. You focus on patient care; they focus on keeping your data safe.
• Trust but verify: Regular security audits are like dental checkups for your network. They reveal hidden vulnerabilities and keep your defenses in fighting shape. Hire ethical hackers to really put your security through its paces.
• Back it up: Robust data backups are your lifeline in the face of threats like ransomware. Back up religiously to a secure offsite location, encrypt everything, and test your restore process regularly.
• Eyes on the prize: 24/7 security monitoring is like having a watchdog on patrol around the clock. Partner with a cybersecurity firm to keep tabs on your network, detect threats in real-time, and respond swiftly to minimize damage.
Cybersecurity is a never-ending battle, but with the right weapons in your arsenal, you can keep your practice safe and your patients’ trust intact. It takes commitment, vigilance, and ongoing effort, but it’s an investment in your practice’s future that you can’t afford to skrimp on. The cost of a breach — financial, legal, reputational — far outweighs the cost of prevention.
You’ve got enough on your plate keeping your patients smiling. Let the security experts help carry the load when it comes to locking down your data. Stay informed, stay alert, and keep putting your patients first — just don’t neglect the vital work of guarding their most sensitive information.
If you have any questions, need advice, or want to tighten up your practice’s cybersecurity game plan, I’m always ready to lend an ear and share some battle-tested wisdom. In this day and age, cybersecurity is a necessity, not a luxury. An ounce of prevention is worth a megabyte of cure. EP

DocTalk Dental
LEARN through our interactive and captivating DocTalk Dental live interview series. DocTalk Dental is your source for thought leader interviews in endodontics. This series provides insightful and delightful conversations with top dental professionals. Each episode led by Lisa Moler, CEO and Founder of MedMark Media, takes a deep-dive into a different and intriguing area of dentistry.
• Simplifying Irrigation with Dr. Allen Ali Nasseh
• How To Leverage Your Dental Practice Real Estate
• Triton: All-In-One Irrigation Solution
• Demystifying Private Equity and SDSOs
WATCH NOW at https://endopracticeus.com/doctalk-dental/

35 endopracticeus.com Volume 17 Number 2 GOING VIRAL
Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com

DEXIS announces AI enhancements to dental implant workflow plus new integration for 40,000+ users
Earlier this year, DEXIS launched its dental implant ecosystem so clinicians can manage their entire implant workflow, from diagnosis to delivery, with one integrated toolset. To enhance workflow efficiencies, DEXIS announced the release of a new intraoral scanning update, DEXIS™IS ScanFlow v.1.0.10. The update includes a new series of guided workflows, enhancements to its AI capabilities, and an integration with DEXIS Imaging Suite software version 10.
The IS ScanFlow integration allows DEXIS 10 users to launch IS ScanFlow directly from the DEXIS Imaging Suite and manage a more complete patient imaging history in one location for informed decision-making. This integration will be available to the over 40,000 users of DEXIS Imaging Suite version 10 to advance and streamline their workflows. The IS ScanFlow software update maintains high-speed scanning, a user-friendly interface, precise data capture, and an open, flexible system. Early adopters have provided positive feedback, highlighting the system’s ease of use and its ability to reliably capture accurate data.
To learn more, visit https://www.dexis.com
Ultradent
announces acquisition
of Ease-InShields™ laser protection
Ultradent has announced the acquisition of Ease-In-Shields™ from ViewMax Solutions, LLC. Ease-In-Shields provides unique eye protection for laser and curing light users, with their double patented shape, allowing the shields to fit into most loupe and eyewear shapes for maximum safety. Ease-In-Shields’ polycarbonate construction makes them both light and strong, less prone to fogging, and unlike other laser filter inserts in the market, offering total protective coverage as certified by Laservision USA’s Safety Laboratories.
For more information, call 800-552-5512 or visit ultradent.com.

Odne to launch priority access program for endodontics

Odne Inc., announced the appointment of Joe Werner as Director of Strategic Accounts. With over 20 years of experience in the dental industry, Werner brings a wealth of expertise in key areas such as Key Opinion Leader (KOL) development, endodontics, relationship management, and navigating the dynamic landscape of Dental Service Organizations (DSOs). In April, Odne launched its Priority Access Program to the endodontic specialist community. Odne’s Priority Access Program (PAP) will enable a selected group of endodontic specialists to receive first access to the clinical use of Odne’s innovative technology platform for root canal obturation: OdneFill and OdneCure. The Priority Access Program Associates will form the core of Odne’s scientific community, transforming endodontics. One initiative of the PAP is to perform a clinical case registry, collecting further scientific knowledge on the clinical use of Odne’s devices.
OdneFill is the first FDA-cleared light-curing, injectable endodontic obturation material. OdneFill is a hydrogel, a class of biomaterials known for their excellent biocompatibility and hydrophilicity. Due to its water-like viscosity and the ultra-high hydrophilicity in its uncured state, it can flow into complex endodontic structures, such as isthmuses, deltas, and C-shaped canals. Once cured with OdneCure, the corresponding micro-laser curing device, it provides gap-free root canal sealing and long-term obturation.
For more information, visit www.odne.co

RevenueWell and Rectangle Health partner to simplify the payments experience
RevenueWell, a patient experience software and digital marketing services partner for dental practices, announced a new partnership with Rectangle Health, a healthcare-care focused financial technology company providing software solutions to healthcare organizations. Through this partnership, RevenueWell has launched a comprehensive, yet simple solution for dental practices to collect and process payments both online and in-practice. Through RevenueWell’s integration with Bridge™ Payments, practices also have access to Rectangle Health’s Practice Management Bridge Platform® to fully manage their merchant account. With this new integration, practice teams will improve their on-the-job efficiency and get paid sooner. Meanwhile, patients have more flexibility to pay for their dental care in line with what they expect from healthcare providers and businesses.
To learn more, visit revenuewell.com.
36 Endodontic Practice US Volume 17 Number 2 INDUSTRY NEWS
Joe Werner
Endodontic Practice US


Implants/Lasers n 4 CE CreditsAvailable inThis Issue* Summer2024 Vol17 No2 endopracticeus.com Drs. Hunter Bennett and Nate Dewsnup Exploringthetruevalueofpartnership Rotarynegotiationand roto-reciprocation Dr.ReidPullen Unlockingthepowerofdental lasers in endodontics 1 year print $149 1 year digital only $79 Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com Address the Endodontic Complexities You Face Everyday with... 3 EASY WAYS TO SUBSCRIBE VISIT www.endopracticeus.com EMAIL subscriptions@medmarkmedia.com CALL 1.866.579.9496 SUBSCRIBERS BENEFIT FROM: 16 continuing education credits per year Clinical articles enhanced by high-quality photography Analysis of the latest groundbreaking developments in dentistry Technology reviews of the latest products Practice management advice on how to make endodontics more profitable Real-life profiles of successful endodontic practices
4 Issues • • • • • • • • • • • • 16 CEUs
What
I know now (that I wish I knew then!)
Drs. Joel Small and Edwin McDonald share how to cultivate effective leadership qualities
If you were approached by a young endodontist just starting out who was seeking your advice on keys to success, what would you share with them? Here are some of my suggestions that I learned the hard way — from experience.
The
shift from “ME” to “WE”
The challenges we encounter in academia require a high degree of self-management to be successful. Thriving in this environment is a solo endeavor. In other words, our success is determined by what we know, what we do, and how well we do it. Once we leave the academic environment to begin clinical practice, we must undergo a major shift in our mindset from self-manager to team leader, and as a team leader, our success is now determined more by what others know, what they do, and how well they do it. These others are the group of individuals that make up our practice team.
To successfully transition to a team leader, we must learn a new skill set, new communication skills, deep listening skills, motivational skills, emotional intelligence, etc. Unfortunately, none of these skills are taught in our dental schools or residency programs, so many of us struggle with these essential interpersonal skills that are now so vital to our success in this new environment. Over time, our deficiencies in these vital areas may become a major hindrance to developing our practice culture and a peak performing team.
The fine line between being the boss and being a member of the team
One of the most challenging lessons to learn as we transition from academia to clinical practice is that we are both the boss as well as being a member of the practice team. Let’s face it — our team cannot work without us, and we cannot work efficiently without the team. The question is how do we position ourselves to be effective in both capacities? Some would say that we should have an arm’s length relationship with the staff, fearing that becoming too close with our team members is an invitation to being taken advantage of. My response to this approach is that


Drs. Joel C. Small and Edwin (Mac) McDonald have a total of over 75 years of dental practice experience. Both doctors are trained and certified Executive Leadership Coaches. They have joined forces to create Line of Sight Coaching, a business dedicated to helping their fellow dentists discover a better and more enjoyable way to create and lead a highly productive clinical dental practice. Through their work, clients experience a better work/life balance, find more joy in their work, and develop a strong practice culture and brand that positively impact their bottom line. To receive their free ebook, 7 Surprising Steps to Grow Your Practice Through Leadership, go to www.lineofsightcoaching.com.
there will always be those who wish to take advantage of us. We prevent this from happening by setting strict boundaries that protect us from these attempts. Dealing with staff is no different. We must embed ourselves within our teams so that we can feel the pulse of the team and respond accordingly based on their needs and the perceived needs of the practice. We do this while maintaining personal boundaries that prevent us from being abused.
The problem, as I see it, with maintaining an arm’s length relationship with the staff is that we become unapproachable and never hear their needs or receive valuable feedback that potentially could make our team more cohesive, more efficient, and more productive. Smaller organizations like dental practices exist in feedback rich environments, and we do ourselves and our team a great disservice if we fail to acknowledge and appreciate this valuable feedback.
Our knowledge and technical skills are NOT the driving forces to our success
The academic environment prioritizes knowledge and technical skill as the keys to success, and this is as it should be in institutions of higher learning. In a practice environment, however, our IQ and technical skills become secondary drivers of success.
The vast majority of dental schools and residency programs provide an exceptional education for their students who are required to meet a very high standard of proficiency. Upon entering clinical practice, these same high standards of proficiency become what I refer to as table stakes, or the price of admission. In other words, we are expected to have and maintain this basic skill set, or we become irrelevant. Maintaining these high standards of knowledge and skill no longer distinguishes us from our fellow doctors with the same skill set or provides us with a sustainable competitive advantage in the dental marketplace. Our IQ becomes secondary to what Daniel Golman in his seminal book Emotional Intelligence refers to as our EQ, a measure of our capacity to be aware of, control, and express our emotions, and to handle interpersonal relationships judiciously and empathetically. In simpler terms, EQ is a measure of our ability to effectively engage with others, and this is where the rubber meets the road. Today’s effective leaders and successful practitioners are no longer authoritarians. They are instead exceptional influencers, and influence is a function of one’s ability to communicate in a manner that is engaging, compassionate, and motivating. These are the skills that set us apart from our competition and create a sustainable competitive advantage. Furthermore, doctors who have a high degree of emotional intelligence (EQ) are the ones who create exceptional practice cultures and peak performing teams.
These are just a few of the things that experience has taught me. I know I share these same thoughts and experiences with many of you. Hopefully, they will resonate with our younger colleagues as they begin their journey into private practice.
38 Endodontic Practice US Volume 17 Number 2 SMALL TALK
EP

ROOTED IN EXCELLENCE SAVE 30-50% ON NITI FILES & BIOCERMICS ROOTED IN EXCELLENCE We Put Our Customers at the Apex of All That We Do. SAVE 30-50% ON NITI FILES & BIOCERMICS www.endodirect.com 17% EDTA (16 Ounces): $34.99 ProShape™ HT: $24.95 (6/Pack) EndoCeramic™ Sealer: $65 2G Syringe + 20 MW Tips Minimal Waste Tips: $58 (50/Pack) ProShape™ Cyclone: $24.95 (6/Pack)
Specialized: the Specialists Podcast
Specialized Dental Partners continues to amplify the voices of specialists and industry insiders
The Specialized Podcast, formerly the Endo Files, is a show for endodontists looking to gain insights, education, and inspiration from their peers. Each episode features a rich conversation between industry experts, highlighting personal perspectives on the specialty including clinical best practices, hot topics, work-life balance, innovative technologies, and so much more!
From harnessing mental toughness to thriving in the demanding field of specialty dentistry, to the importance of giving back and investing your time to support the next generation of leaders, Seasons 1 and 2 covered myriad topics appealing to specialists in every stage of their career.

New for Season 3, Specialized will be hosted by a rotating line-up of experts, each bringing a distinct perspective to the table! You’ll hear dynamic conversations led by Dr. Jeremy Young, Dr. Brett Gilbert, and longtime industry insider and seasoned podcast host, Kim Livesay Brownell.
ICYMI: highlights from Season 2
• Financial Success Strategies for Dentists and Specialists with Doug Fettig
• Does Dentistry Have a Diversity Problem? Recent Graduates Discuss Cultural Competency in the Field

• How to Scale Your Social Media and Supercharge your Referral Relationships with Dr. Brian Baliwas
• AI’s Role in Dentistry: Insights from Dr. Tung Bui
• Under One Roof: How Integrated Care Can Revolutionize Dentistry with Dr. Kate Quinlin
• A Conversation with the Dean of Harvard’s School of Dental Medicine, Dr. William Giannobile
• Securing Your Spot: Insider Tips for Standout Residency Applications with Dr. Adham Azim
• Building a Successful Practice: Exploring the Path to Partnership with Dr. Diwakar Kinra
• From Fear to Fulfillment: Dr. Jeremy Young’s Journey Back from a Life-Altering Diagnosis
• Elevating Endodontics: A Paradigm-Changing Journey with Dr. Vladana Babcic Tal
• Exploring Innovations in Endodontics with Dr. Ali Nasseh
• Advice for Current Residents from New Associate, Dr. Allen Abrishami
• And more!
If you’re looking to differentiate yourself and your practice, to stay up to date on the latest happenings in the field, and to connect with other specialists on a personal level, The Specialized podcast is an excellent resource to add to your toolkit.
The podcast is brought to you by Specialized Dental Partners and is available for free on all major podcast platforms, including Apple Podcasts, Spotify, and Google Podcasts. Scan the QR code and subscribe today, so you never miss an episode! EP

40 Endodontic Practice US Volume 17 Number 2 SOUND ADVICE
Dr. Nathan Dewsnup and Dr. Hunter Bennett from Bonita Endodontics in Bonita Springs, Florida in the Season 3 kickoff of Specialized
“As a woman in Endodontics,

Specialized Dental Partners


We’re proud to champion Dr. Savani and more than 300 elite dental specialists in our growing network. Since 2018, we’ve helped our partners focus on delivering exceptional patient care, while our business experts provide customized solutions to help streamline practice management. Find out how our powerhouse community of endodontists, periodontists, and oral and maxillofacial surgeons work together to champion your long-term prosperity.
Formerly US Endo Partners Scan to catch the whole story Endodontist partner in Sacramento, CA by
than ever before in my career.” I feel more supported
Champion of Specialists
specializeddental.com


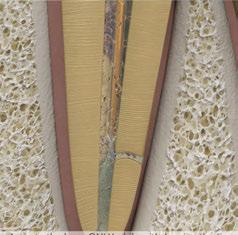
WATERLASE PREMIER EDITION FEATURES
Innovative modular software design
Onboard virtual protocol guides
Step-by-step clinical technique animations for predictable results
WiFi connectivity and remote diagnostics
Start-up and shutdown step-by-step wizards make set-up and daily maintenance a breeze
Waterlase iPlus Premier Edition effectively fights endodontic infection while opening dentinal tubules and removing smear layer in the canal. It’s revolutionary modular design allows you to focus solely on the procedures that matter most to you, with minimal investment.
WATERLASE ENDODONTIC PROCEDURES
Rapid Endo™ root canal therapy
Pulpotomy
Pulp Cap
Apicoectomy
MINIMALLY INVASIVE ENDODONTICS
Improve efficiency within your workflow
More productivity and less fatigue
Less post-op patient discomfort




To Learn More Visit biolase.com/endo biolase.com 833.BIOLASE NEW ©2024 BIOLASE, Inc. All rights reserved. *References are available at www.biolase.com/Waterlase-iPlus Case images courtesy of Dr. Gary Glassman. BEFORE AFTER BEFORE AFTER











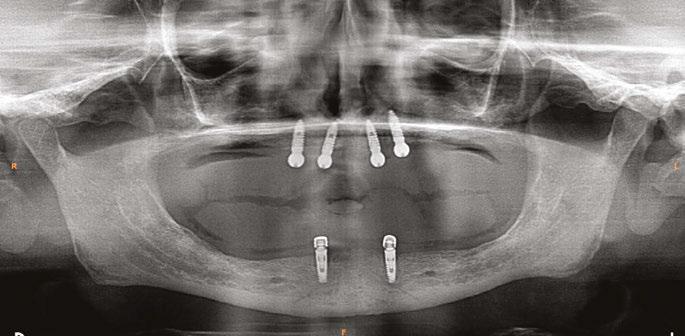


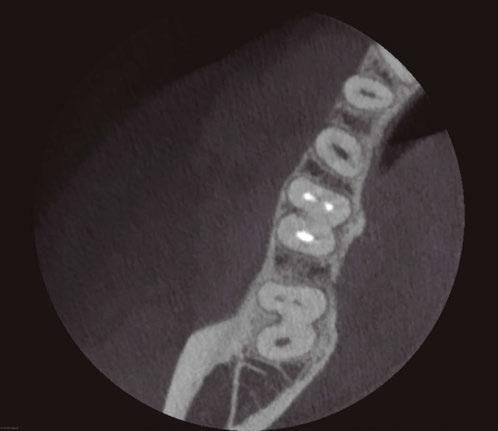
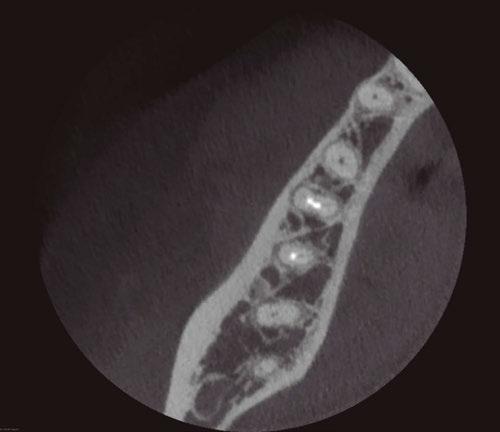

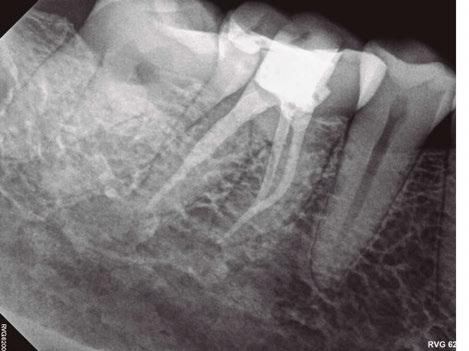



 Moler Founder/Publisher, MedMark Media
Moler Founder/Publisher, MedMark Media