The World Health Organization (WHO) defines a Sustainable Healthcare System as 'a system that improves, maintains or restores health, while minimizing negative impacts on the environment and leveraging opportunities to restore and improve it, to the benefit of the health and well-being of current and future generations





i.















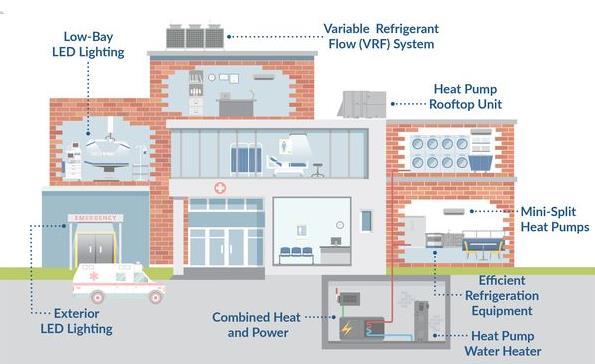
Energy-efficient hospitals and clinics















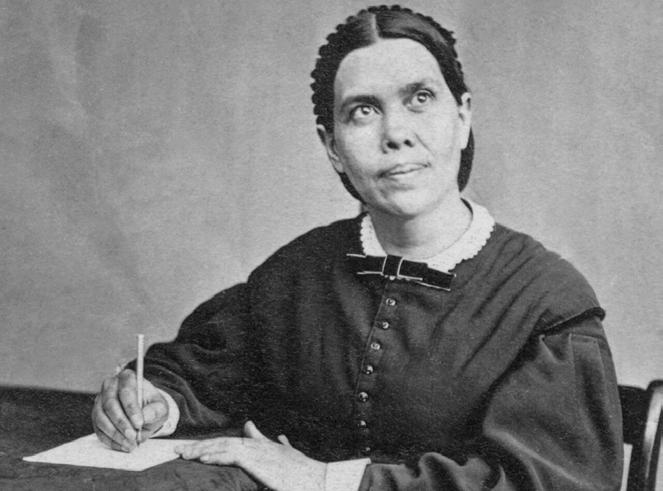
Dr Katia Reinert PhD, RN, MSN, FNP-BC, PHCNS-BC
Health Ministries Associate Director
Seventh-Day Adventist Church World Headquarter
Arthur Schopenhauer

Health is not everything, but without health, everything is nothing.
Physical
• Covid-19
• Cardiovascular diseases
• Heart attacks
• HTN
• stroke
Mental/Emotional
• Depression
• Anxiety
• Insomnia
• Generalized distress
• Burnout
1. https://www.unicamillus.org/covid -19 -the -devasting -impact-of-the -pandemic -on -nurses -working -lives/
2. Archives of Psychiatric Nursing , Volume 41 , December 2022

Consensus Report | 2021
National Academies of Sciences


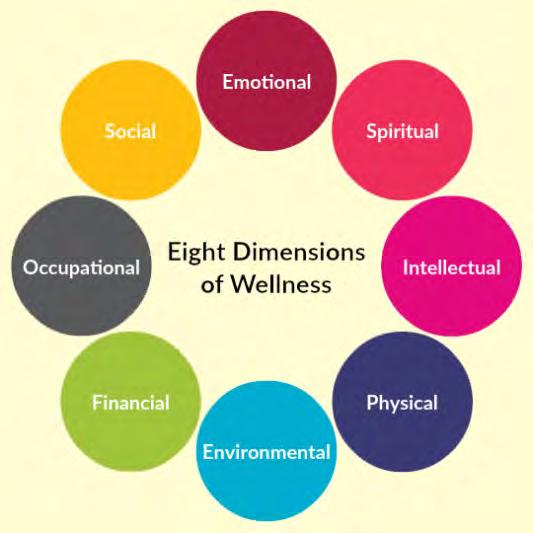
Nurses' well-being impacts their whole health:
• Physical
• Mental
• Emotional: joy and professional satisfaction
• Spiritual: meaning in their work
• Social: engagement with their job
• “ Is a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community.”
• Common m ental health issues in nurses:
• stress
• compassion fatigue
• burnout [35-45%]
• SUD [10%]
• depression and suicide [>general population]
Adriaenssens et al., 2015; da Silva et al., 2016; Gómez-Urquiza et al., 2016, 2017; Mark and Smith, 2012; McVicar, 2003. https://www.ncbi.nlm.nih.gov/books/NBK573902/
• perceptions of the quality of care they receive
Healthcare Organizations
• impacts turnover rates and the costs of hiring and training new nurses


“Ensuring nurse’s well-being is essential for the health and safety of , the functioning of health systems, and the financial health of health care organizations.”
THE FUTURE OF NURSING 2020Consensus Report 2021

Definition of Health ...a state of complete physical, mental and social well being and not merely the absence of disease.”
“The
ability of all people within the community to reach full mental, spiritual, and physical potential by living safety with vigor and purpose; meeting personal needs; meeting community responsibilities; adapting to change; and having trusting and caring relationships.”
Mayor ’s Task Force, Lincoln, Nebraska, USA

“The
integration of an individual’s emotional, intellectual, physical, social, spiritual, and vocational dimensions into positive beliefs and meaningful activities that enhance human functioning and quality of life. It includes an openness to change, capacity to deal with stress and personal view of self-worth .”
ANA/HMA, 2017












“An integrative
concept
that characterizes quality of life with respect to an individual’s health
and work-related environmental, organizational, and psychosocial factors.
Well-being is the experience of positive perceptions and the presence of constructive conditions at work and beyond that enables workers to thrive and achieve their full potential.”
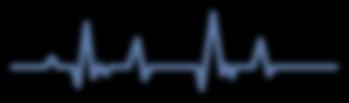
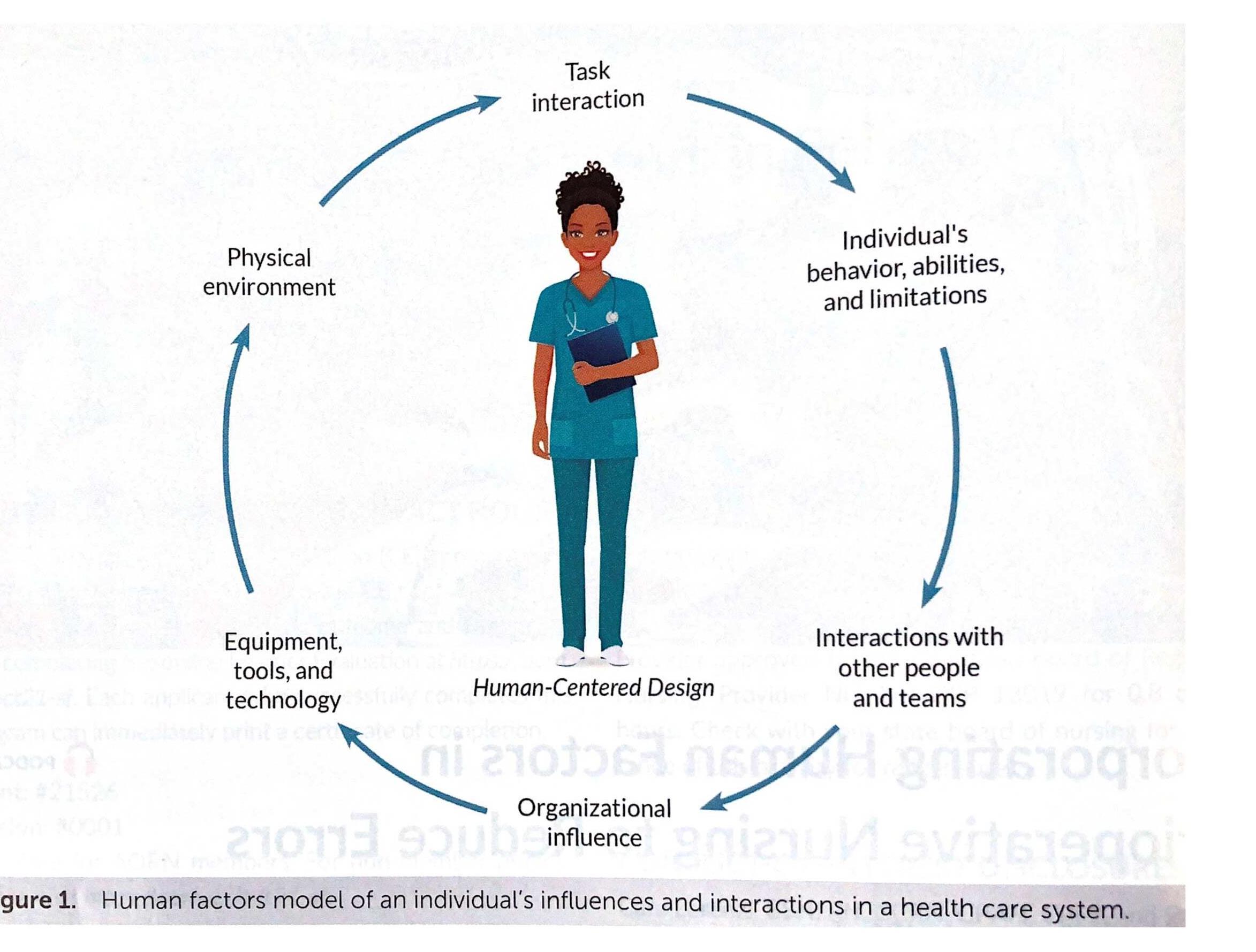
The systems model of clinician burnout and professional well- being

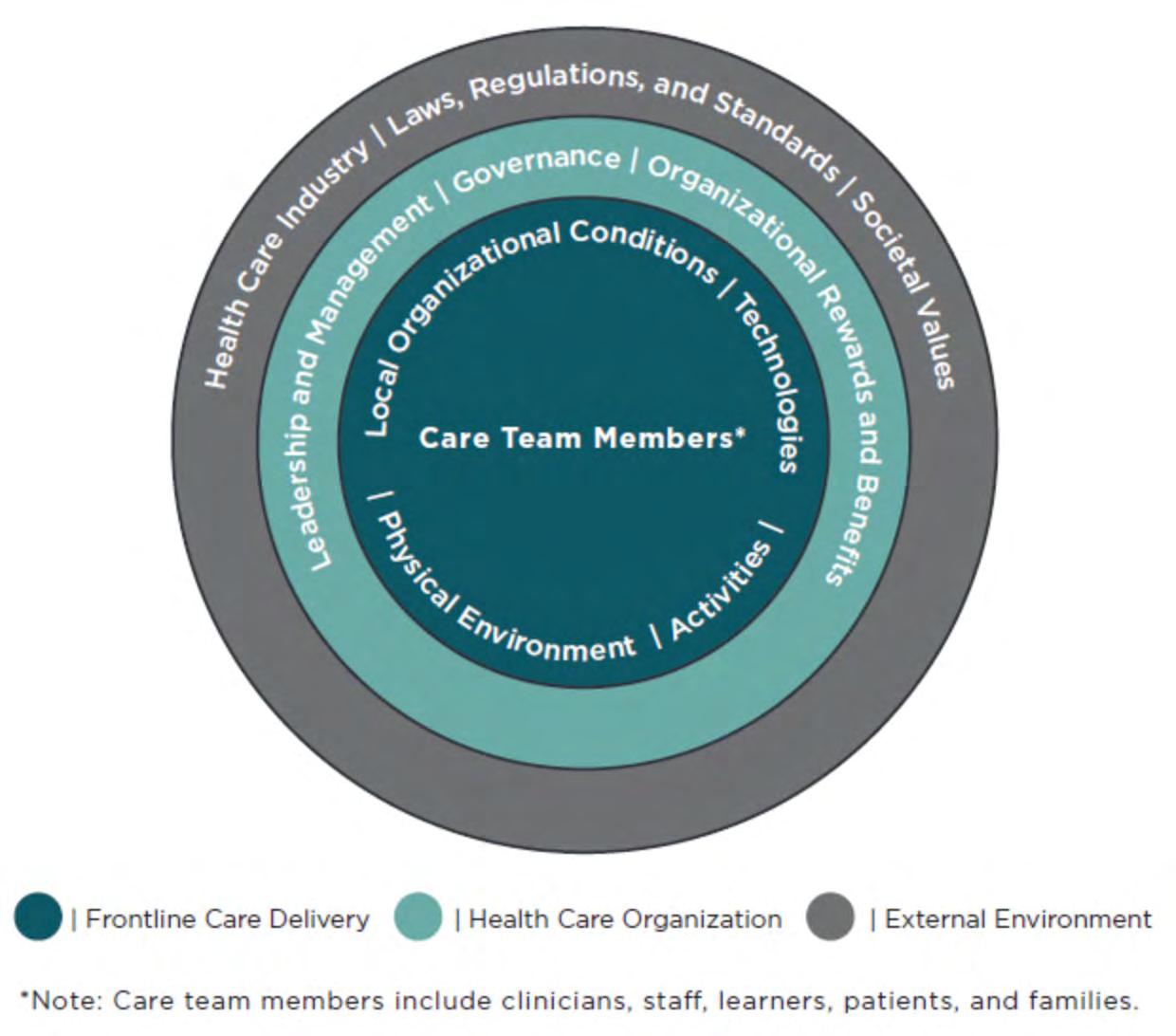
The three levels of the systems model of clinician burnout and professional well-being.

Deliberate expenditure of energy and time to perform those activities required for well - being and good health, including rest and relaxation.

“There is a time for everything, and a season for every activity under the heavens.”
King Solomon. Ecclesiastes 3:1 [NIV]

“The ability of individuals, families and communities to promote health, prevent disease, maintain health, and cope with illness and disability with or without the support of a health - care provider.”

Making healthy lifestyle choices being physically active and eating healthily
Avoiding unhealthy lifestyle habits avoiding smoking and alcohol consumption

Making responsible use of prescription and non-prescription medicines

Global Self-care Federation

Self-recognition of symptoms
Self-monitoring

Self-management
assessing and addressing symptoms, in partnership with a healthcare professional where necessary
checking for signs of deterioration or improvement
managing symptoms of disease, either alone, in partnership with healthcare professionals, or alongside other people with the same health condition.
The body’s nonspecific response to any increased demand placed upon it.
• Foot tapping/pacing
• Overeating
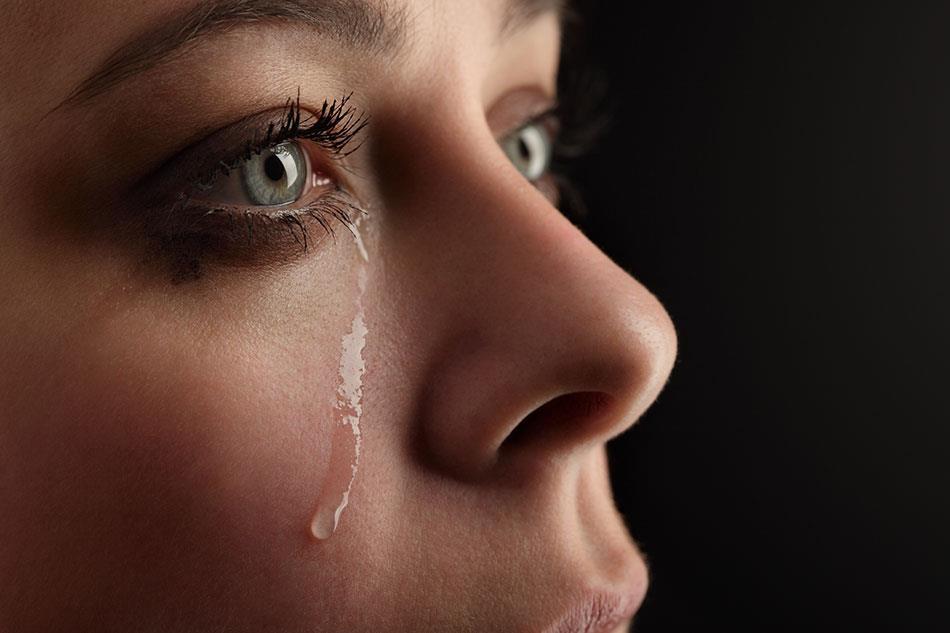
• Feeling fearful/Crying
• Fatigue/low energy levels
• Jittery feelings
• Palpitations
• Sweating
• Irritability/emotional instability
• Insomnia/nightmares
• Negative thougths
• Temper outbursts
• Nervous Tic
• Clearing throat
• Gritting teeth
• Feeling lonely
• Queasy stomach
• Vomiting/diarrhea
• Headache/backache
• Hives/rash
• Constipation
• Depression
• Forgetfulness


He that can take rest is greater than he that can take cities.
Benjamin Franklin
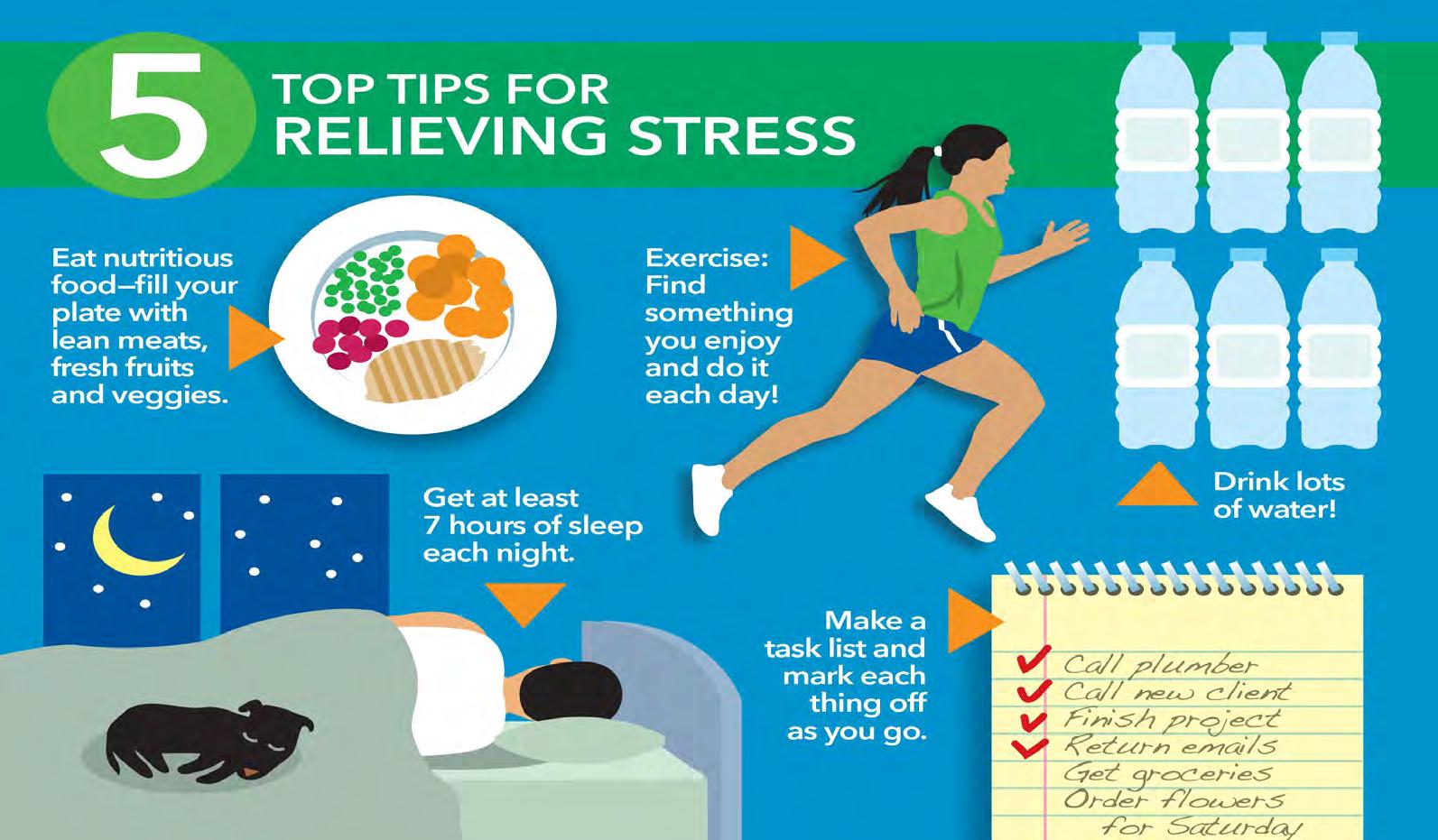
• Sleep 7-8 hrs/day
• Before 10pm is ideal
• Time for a phone call and to listen
• Sit down to eat without multitasking
• Smell the flowers, look the colors
• Time for yourself
• Time with God

• Creation – God rested on the 7th day (a full day)
• Exodus 20:8-11 – Reminder
"Remember the Sabbath day by keeping it holy. Six days you shall labor and do all your work, but the seventh day is a Sabbath to the LORD your God. On it you shall not do any work, neither you, nor your son or daughter, nor your manservant or maidservant, nor your animals, nor the alien within your gates. For in six days the LORD made the heavens and the earth, the sea, and all that is in them, but he rested on the seventh day. Therefore the LORD blessed the Sabbath day and made it holy.
• Sanctuary of rest – spiritual rest
“If you keep your feet from breaking the Sabbath and from doing as you please on my holy day, if you call the Sabbath a delight and the LORD's holy day honorable, and if you honor it by not going your own way and not doing as you please or speaking idle words, then you will find your joy in the LORD , and I will cause you to ride on the heights of the land and to feast on the inheritance of your father Jacob. The mouth of the LORD has spoken.” Isaiah 58:13-15
“ Celebrating the Sabbath is more than the absence of work, it is not just a day off to catch up on television and errands. It is the presence of something that arises when we consecrate a period of time to listen to what is most deeply beautiful, nourishing or true.
It is time consecrated with our attention, our mindfulness, honoring those quiet forces of grace or spirit that sustain and heal us…During the Sabbath, we set aside a sanctuary in time, disconnect from the frenzy of consumption and accomplishment, and consecrate our day as an offering for healing all beings”.
Wayne Mueller – Restoring the Sacred Rhythm of Life

• God’s time
• Worship and praise time
• Communion with Him (nature, reading, praying)
• Family’s time
• Spend time together with loved ones


• Vacations
• Time to laugh
• Play
• Lounge
• Consider new ideas
• Dream
• Re - create
Fremingham study
• Since 1965 (men and women)
• All women (45-64) had no CAD
• Followed them for 24 years, and found that
• “a lack of vacations was predictive of an increased incidence of heart disease”
Pittsburg University
• 12,000 men high risk for CAD
• Those with regular vacations had lower risk of death
• Solitude
• Align priorities, hopes and aspirations
• Time for personal refilling
• Need intentional planning
• Snooze more
• More sleep (daily / weekly)
Minimize
• Watch multitasking - do one thing at a time
• Decrease the weekend TO DO list and keep the Sabbath as God created it to be.
• Be careful of excessive work – “put the glass down”
• Take yearly vacations

• Healthy lifestyle (eating, sleeping, boundaries)
• Exercise regularly
• Share feelings
• Manage time efficiently
• Avoid arguments or quarrels
• Minimize expose to things that cause distress
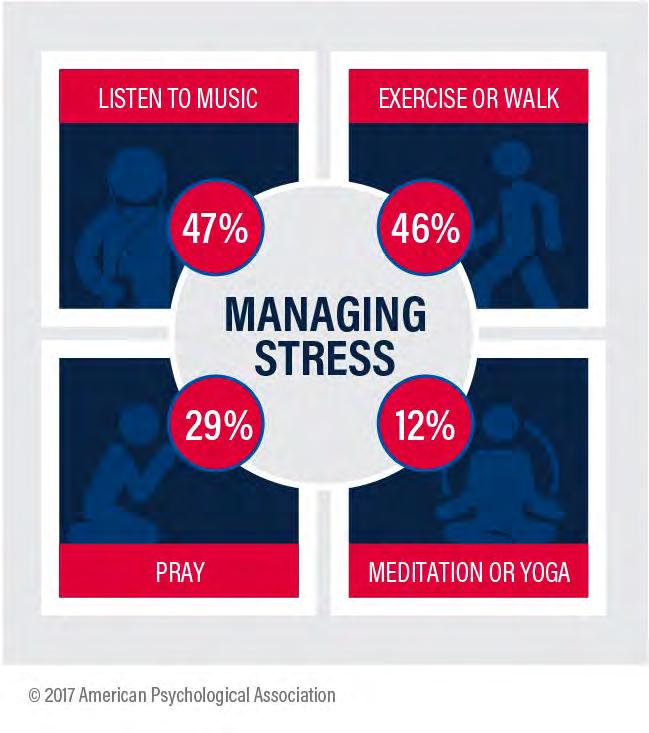
• Practice relaxation techniques daily
• Take deep breaths
• Develop and maintain a positive attitude
• Improve your laugh life
• Help someone
• Balance work and play
• Plan some “me” time daily
• Make a gratitude list daily
• Reward yourself
• Surround yourself with cheery people, not negative
• Set realistic goals for yourself
• Be flexible (events , people)
• Forgive yourself for mistakes
• See professional help if needed
• Set time for Spiritual/Religious Contemplation
• Journaling
• Music
• Hot bath/Massage
• Hobby (art, scrap booking, traveling)
• Take time to rest (daily, weekly, yearly)
• Relaxation and deep breathing
• Relationships
• Humor and laughter
Connect with someone .
• Laugh with someone.
• Share with someone.
• Be of service to someone.
• Practice compassion and forgiveness on a regular basis.
• Remember to take the ego out of any situation.


• Read
• Pray
• Meditate
• Journal your experience

• Personal reflection and prayer
• Exercise
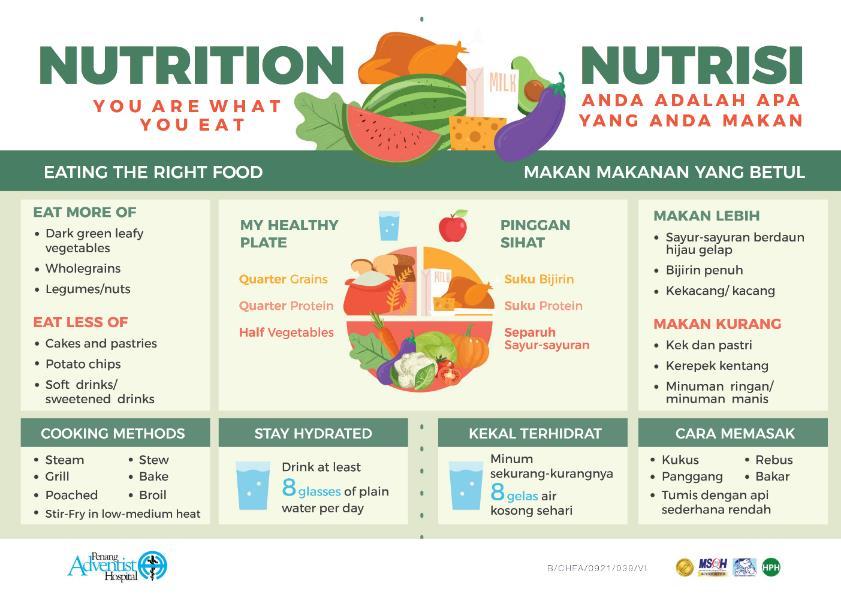
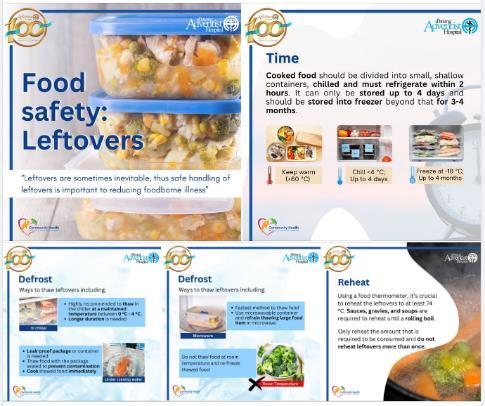
• Nutritious meals
• Family and friends
• Worship
• Study
• Work
• Service to others
• Rest
• Play

God, grant me: - the serenity things I cannot change - the courage things I can, and - the wisdom difference. Amen.

Dr Katia Reinert
PhD, RN, MSN, FNP-BC, PHCNS-BC
Health Ministries Associate Director
Seventh-Day Adventist Church World Headquarter


“The integration of an individual’s emotional, intellectual, physical, social, spiritual, and vocational dimensions into positive beliefs and meaningful activities that enhance human functioning and quality of life. It includes an openness to change, capacity to deal with stress and personal view of self-worth.”
ANA/HMA, 2017
• Nutrition
• Rest
• Exercise
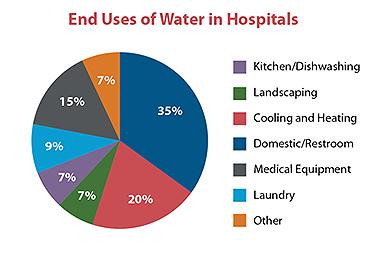
• Clean Water
• Adequate Housing
• Access to health exams



• How we think or process information
• Self Concept
• Rational Thought
• EQ | reframing

•
• Joy • Fear
• Disgust
• Sadness
• Anger

• Healthy Relationships
• Social Support
• Friends
• Family
• Fait h Community
1. What gives meaning and purpose in your life
2. Religious/spiritual practices
• Prayer | Holy book readings
• Worship
• Spiritual Virtues
• Gratitude
• Forgiveness
• Altruism
• Integrity
• Compassion

“Many of the diseases from which [people] suffer are the result of mental depression.

Grief, anxiety, discontent, remorse, guilt, distrust all tend to break down the life forces and to invite decay and death. White, E. Ministry of Healing, p. 241 (1905)
Suicide
Kidney Disease
Illicit Drug Use

Heart Disease
Tobacco Use
Influenza & Pneumonia
U.S.
All Races
Cancer
Diet & Activity Patterns
Stroke
Motor Vehicles
External & Internal Stress
Meaningless Existence
Sexual Behavior
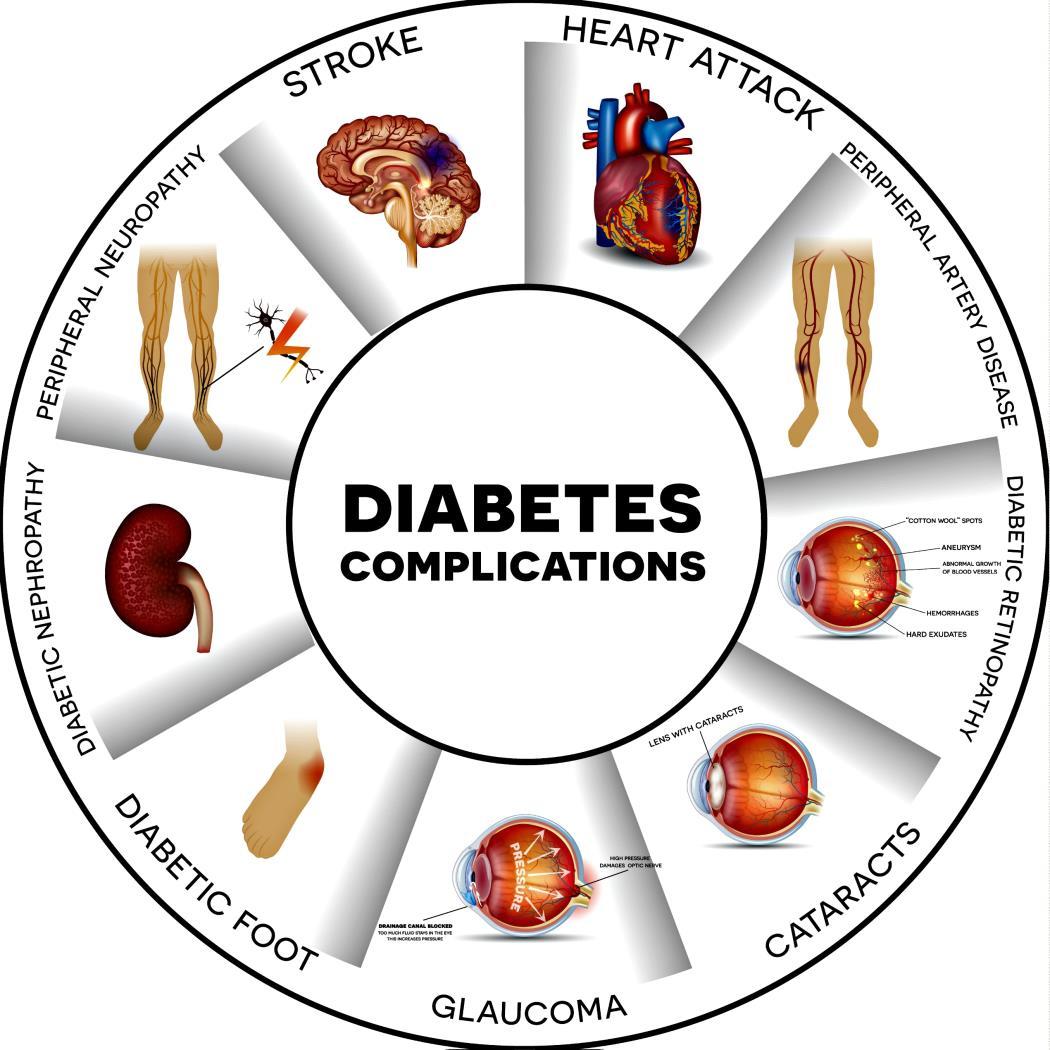
Diabetes
Anger & Frustration
Powerlessness Loneliness
Low Self Esteem or Self Worth
Economic Disparity
Alcohol & Substance Abuse

Lack of Information Or Education
Firearms
Hopelessness & Emotional Despair
Pollutants & Toxic Agents
Alzheimer’s Disease

Infectious Agents
Chronic Lung Disease
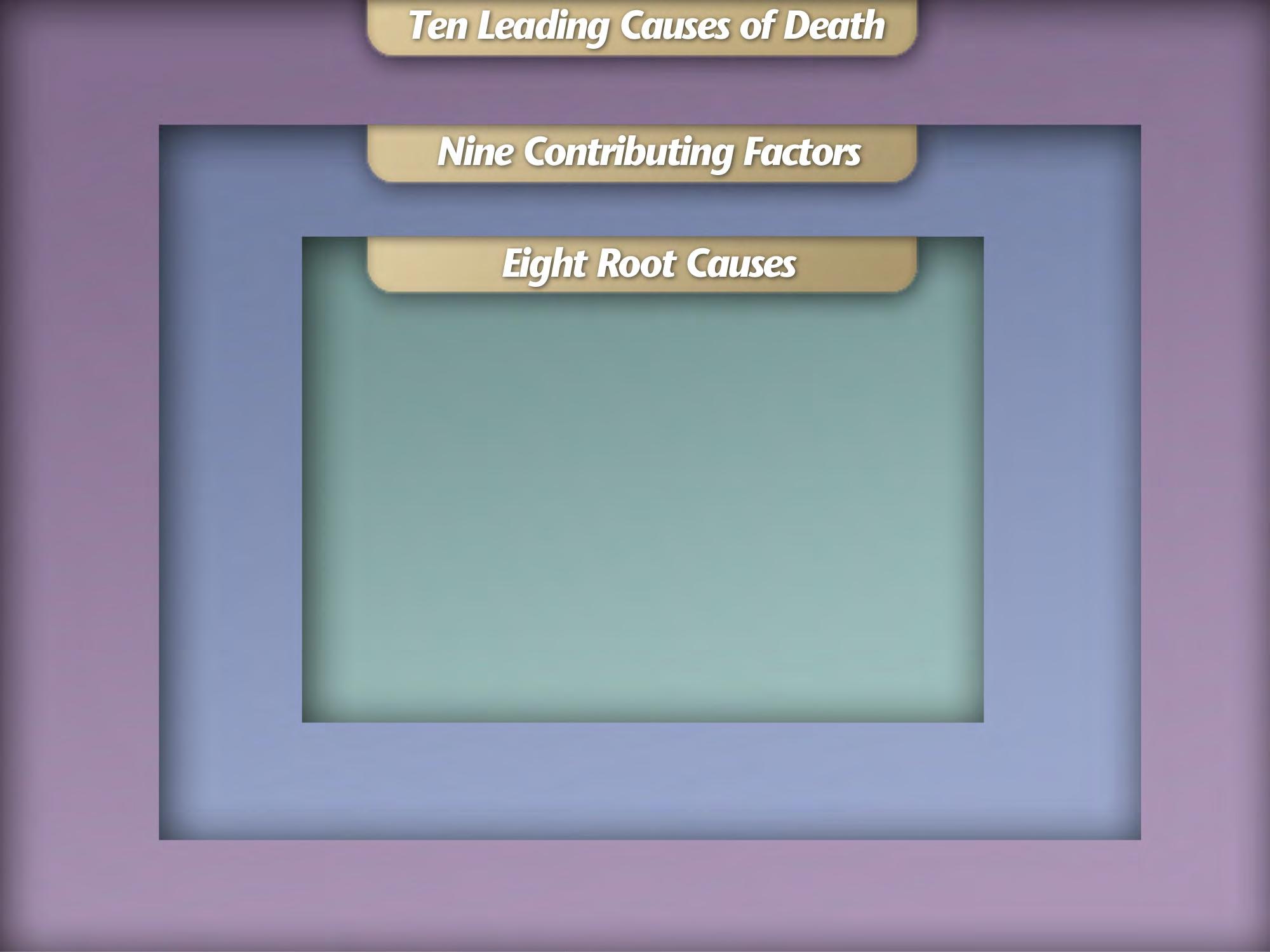
Accidents
Cummings, CREATION Life Discovery
https://www.adventhealth.com/adventhealthpress/creation-life-discovery

“... And wellness is more than health. Wellness is being mentally fit, physically robust, spiritually vital, and socially comfortable.
It is being able to face accidents, aging, and illness with a positive outlook.
Most of all, it is trusting that God has a “better idea” for living, and that he is eager to help us experience full Life.”
Des Cummings, Ph.D., CREATION Life Discovery AdventHealth, Florida Hospital


I have come that they may have LIFE to the FULL.

the experience of wholeness, salvation, or shalom
• integration of the spiritual, physical, psychological, emotional, and social aspects



• may be experienced in the presence or absence of disease or injury (ANA/HMA, 2017)

Redefining health as wholeness expands the understanding of healing , and all activities and efforts surrounding the achievement of optimal health.
The process of integrating the body, mind, and spirit to bring about wholeness, health, and a sense of spiritual well-being.
ANA/HMA 2017.
Cure
Cure
Cure
Cure
Cure
Cure
Cure
Cure may occur without healing; healing may occur without cure.
Cure separates body from soul; healing embraces the whole.
Cure addresses disease; healing addresses illness.
Cure isolates; healing incorporates.
Cure costs; healing enhances.
Cure combats illness; healing fosters wellness.
Cure fosters function; healing fosters purpose.
Cure
Cure
Cure
Cure
Cure
Cure
Cure
Cure alters what is; healing offers what might be .
Cure is an act; healing is a process.
Cure acts upon another; healing shares with a sister, a brother.
Cure manages; healing touches.
Cure seeks to conquer pain; healing seeks to transcend pain .
Cure ignores grief; healing assumes grief.
Cure rejects death and views it as a defeat; healing includes death among the blessed outcomes of care.


• anxiety
• fear
• loneliness
• caregiver role strain
• spiritual distress
• spiritual well-being
• decisional conflict
• hopelessness
• H sources of hope , strength, comfort, meaning, peace, love, and connection
• O the role of organized religion for the patient
• P personal spirituality and practices
• E effects on medical care and endof-life decisions
The practical expression of presence , guidance, and interventions, individual or communal, to support, nurture, or encourage an individual’s or group’s ability to achieve:
- wholeness
- health
- personal, spiritual, religious, and social well-being
- integration of body, mind, and spirit
- a sense of connection to self, others, and a higher power
Practical expressions
• presence
• guidance
• interventions Purpose to enhance
• support
• nurture
• encouragement
Healing rather than cure
• companioning
• facilitate healing
• ministry of presence
• active listening
• e motional support
• s cripture and sacred readings
• prayers and rituals
• silence
• lament
• laughter
• reminiscing, storytelling, journaling
• appropriate referral
• relaxation techniques
• Arts
• hope instillation
• decision - making support




The greatest disease today is not TB or leprosy; it is being unwanted, unloved, and uncared for. We can cure physical diseases with medicine, but the only cure for loneliness, despair, and hopelessness is LOVE .

Lord, make me an instrument of your peace: where there is hatred, let me sow love; where there is injury, pardon; where there is doubt, faith; where there is despair, hope; where there is darkness, light; where there is sadness, joy.
O divine Master, grant that I may not so much seek to be consoled as to console, to be understood as to understand, to be loved as to love. For it is in giving that we receive, it is in pardoning that we are pardoned, and it is in dying that we will awake to see your face and sit at the Table with you in your Kingdom. Amen.
Chief Nursing Officer, Penang General Hospital
Chairman




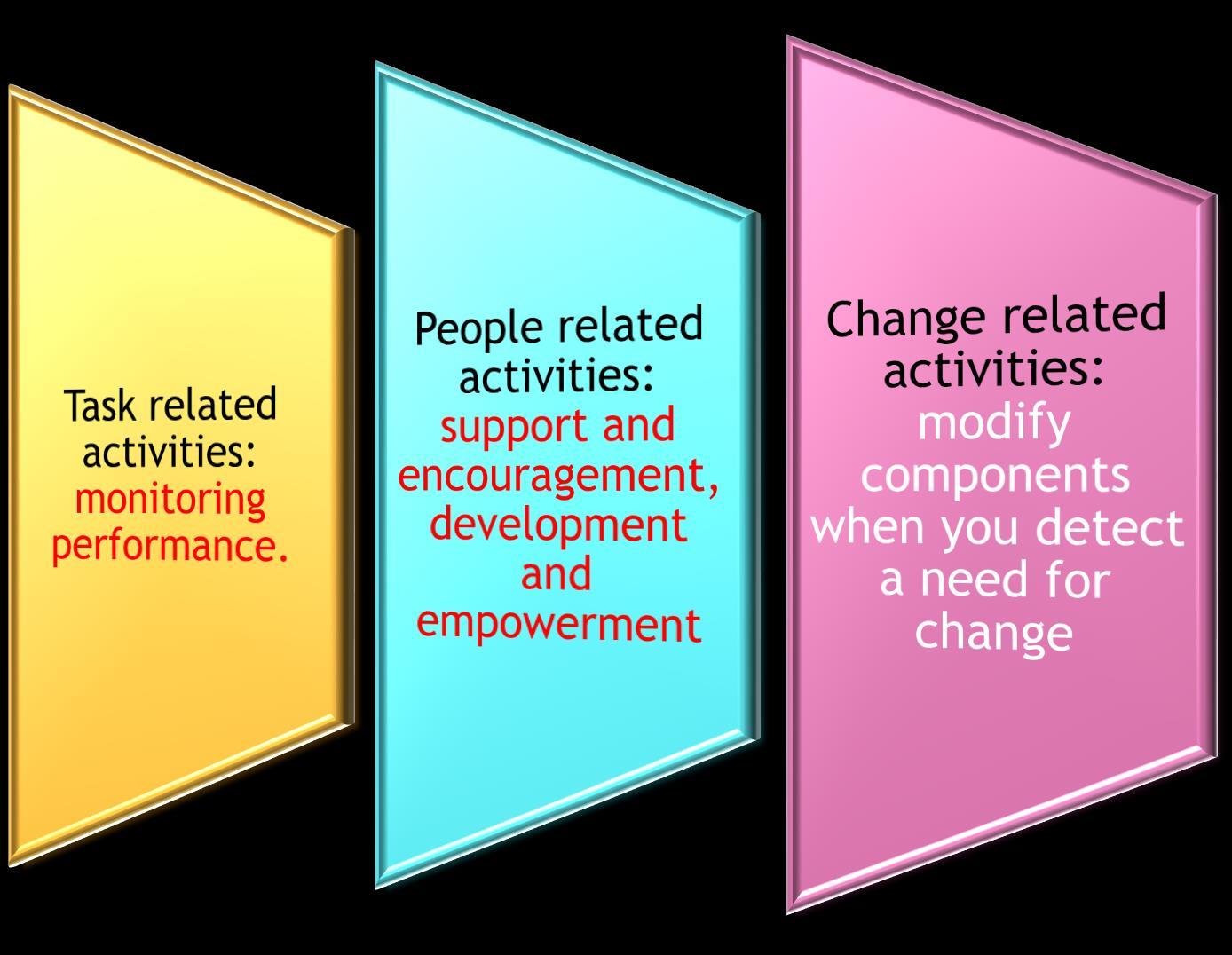
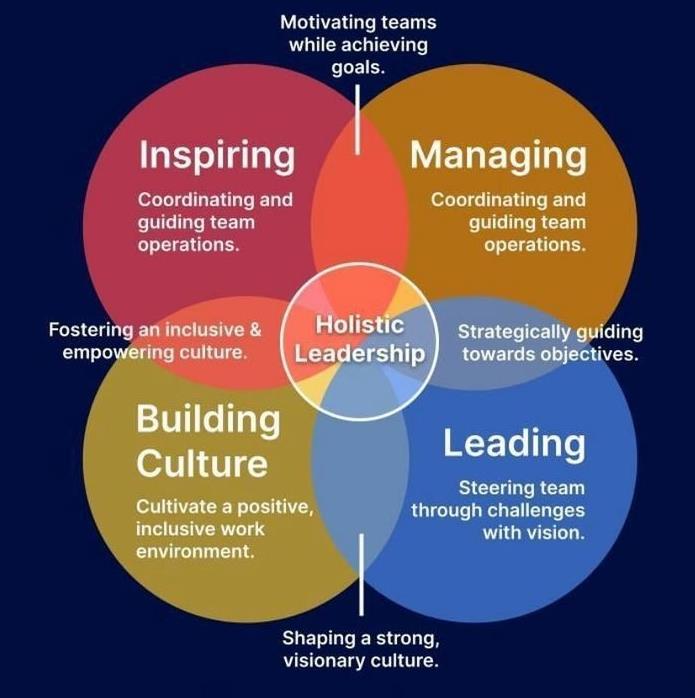
Leadership






Principle
1. Focus on the situation, issue, or behavior, not on the person.

2. Maintain the self-confidence and self-esteem of others.
3. Maintain Professional relationships with your employees, peers, and managers.
4. Take initiative to make things better.
5. Lead by example.




Problem solving helps to acquire knowledge obtains information explaining the nature of the problem and recommends possible solutions evaluate and select the application of the best without rejecting them in a possible appeal of the original. It approaches issues when solving problems that are often used is the empirical method, intuition, research process and the scientific method modified

How complete, neat and tidy your work is.
Your initiative to complete your task
The effective punctuality in time upon completing your task.
Able to communicate verbally, written command and effective use of politeness and being humble. Good Communication command
Visionary, committed, able to lead, to the objectives of organizations.
Able to use resources to plan, arrange, divide, carryout duties to meet organization objectives.
A Calm Person, able to control mental and physical state is any directive commanded. Able to be punctual on time management.
Able to contribute good ideas, make changes in quality and organization productivity.
Able to create harmony environment, friendly and comfortable and able to adjust in all situation.


“To ‘be in charge’ is certainly not only to carry out the proper measures yourself but to see that everyone else does so too.”
Florence Nightingale
“A true leader has the confidence to stand alone, the courage to make tough decisions, and the compassion to listen to the needs of others. He does not set out to be a leader, but becomes one by the quality of his action and the integrity of his intent.”
Douglas Mac Arthur (1880-1946) United States Army General
• Know yourself • Current Challenges at work • Element of Leadership • Management Conflict
• How to motivate



• 50-60%
• 60-70%
• 70-80%

• 80-90%
• 90-100%








• It will never work. What do you dislike about it?
• My way is better. What makes that seem the best option?
• It’s impossible. What would it take to make it possible?
• I can’t. What difference would it make if you could?
• You can’t do that. What would happen if we did?
• That is not the What would be the best way best way for you?
• It’s too expensive. Compared to what?




















Ensure the health and well-being of nurses by actively developing and enforcing policies, practices, and a supportive work environment that promotes their overall health.
THANK YOU







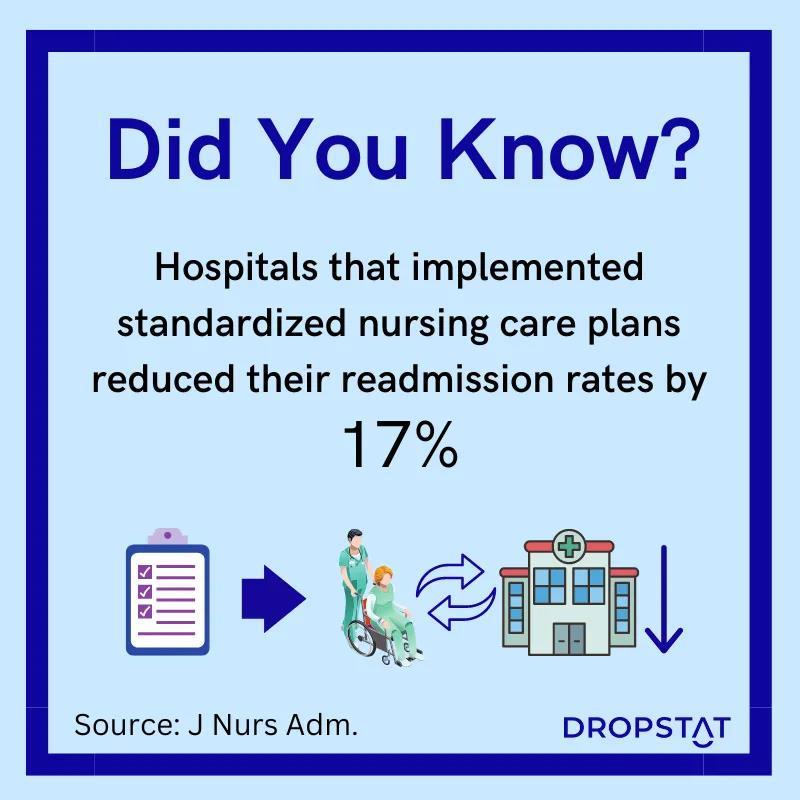
The Nursing Process / NCP – a systematic approach to nursing which comprises of a series of steps which, most commonly, are referred to assessing, planning, implementing and evaluating.
(Roper 1990)
An organized, systematic, and rational method of planning and providing individualized and holistic nursing care.
(Kozier 1995)

Nursing Process is said to be highly humanistic
Because the plan of care is developed and implemented in such a way that the total need of the patient (physical, mental, social and spiritual) is given great consideration.
Thus, it is also believed to be highly effective in promoting quality care, efficiency and patient satisfaction.
(Alfaro-LeFerve 1994)


A REMEMBER.....





EVALUATE IMPLEMENT

PLAN NURSING


TYPES OF DATA
Subjective Data - described by the patient e.g. : itching, pain, feelings of worry, values, beliefs, attitudes and perception of personal health status
Data Objective - signs detectable by an observer and can be measured against an accepted standard - can be seen, heard, felt or smelled and obtained by observation or physical examination

Nurse interprets assessment data , identifies patient’s strengths and health problems and formulates diagnostic statements.

Diagnosing refers to the reasoning process or the clinical act of identifying problems.
Diagnosis is a statement or conclusion regarding a nature of a Phenomenon or problem.
Nursing Diagnosis is the clinical judgment of the patient’s response to the health problem he or she suffers which can be either actual or potential.







A Nursing Diagnosis is a statement of nursing judgment and refers to a condition that nurses are licensed to treat.



A Medical Diagnosis is made by a Doctor and refers to a condition that only a Doctor can treat.

Nursing Diagnosisdescribes a patient’s phycical, psychologic sociocultural, and spiritual responses to an illness or a health problem.

Medical Diagnosis refers to disease processes –specific pathophysiologic responses that are fairly uniform from one patient to another.
Basic - 2 parts of statement

1. Problem: statement of the client’s responses
2. Etiology: factors contributing to or probable causes of the response
The 2 parts are joined by the word related to rather than due to. Due to implies that one part causes or is responsible for the other part.
Related to implies a relationship


Short term goals
Long term goals

Cognitive goals


Psychomotor goals

Specific Measurable Attainable Relevant Time Bound Nurse and patient develop patient goals/desired outcomes and nursing interventions to prevent or reduce the patients’ health problems.
Affective goals
Goals Must be (SMART)

• The nurse implements the nursing interventions and documents the care provided.
• Setting your plans in motion and delegating responsibilities for each step.
• Communication is essential to the nursing process.

Independent ( Nurse initiated ) - any action the nurse can initiate without direct supervision
Dependent ( Physician initiated ) -nursing actions requiring Doctor orders
Collaborative - nursing actions performed jointly with other health care team members



The final phase of the nursing process in which the nurse determines the patients progress toward goal achievement and the effectiveness of the nursing care plan. The plan may be continued, modified or terminated.











Recognize health problems accurately.
Anticipate complications. Initiate actions to ensure safe, appropriate and timely nursing care. Practice critical thinking






Our Nurses, Our Future: The Economic Power of CARE

What are the risk factors for these causes?
3 + 1
Source: Statistics on Causes of Death, Malaysia, 2023, Department of Statistics Malaysia


Can you guess how many adults in Malaysia are living with obesity?
Can you guess how many adults in Malaysia are living with 3 NCDs?
Source:
half a million


Source: Michaelidou M, Pappachan JM, Jeeyavudeen MS. Management of diabesity: Current concepts. World J Diabetes. 2023 Apr 15;14(4):396-411.
doi: 10.4239/wjd.v14.i4.396. PMID: 37122433; PMCID: PMC10130896


Source:
Source: National Health and Morbidity
Think about it...
What are the effects of these NCDs on our healthcare system?
Think about it...
How can we overcome these health challenges in Malaysia?
What are the benefits of overcoming these health challenges?
What physician sees:
in hospital
Patients in community
• Mild or no symptoms
• Self-prescription
• Take prescriptions elsewhere
• Potential spreader of communicable diseases
What is the role of those who step in here?
“Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”
(WHO Const., 1946, para 1)
Reference: World Health Organization (WHO). (1946). Constitution of the World Health Organization. https://apps.who.int/gb/bd/PDF/bd47/EN/constitution-en.pdf
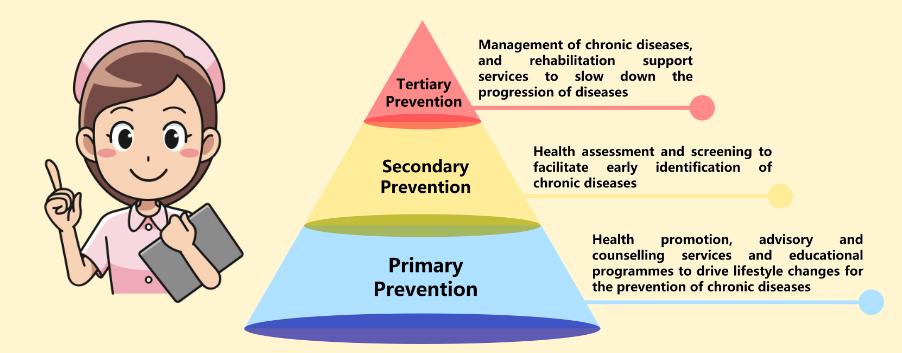
Primary healthcare is the first point of contact for individuals and families in a continuing healthcare process which entails the provision of accessible, comprehensive, continuing, co-ordinated and person-centred care in the context of family and community. It contributes to the health of the population through health promotion, disease prevention, disease management and supportive care.
(WHO, 2024)
Source: Goodman, R. A., Bunnell, R., & Posner, S. F. (2014). What is “community health”? Examining the meaning of an evolving field in public health. Preventive medicine, 67, S58-S61. https://doi.org/10.1016%2Fj.ypmed.2014.07.028
Introducing the concept of Primary Healthcare . . .
“…the
process of working collaboratively with and through groups of people affiliated by geographic proximity, special interest, or similar situations to address issues affecting the well-being of those people.”
(National Institutes of Health, 2016)
Source: National Institutes of Health. (2016, September 9). Community engagement. https://www.nih.gov/health-information/nih-clinical-research-trialsyou/community-engagement
Public Policy
Community
Organization
Interpersonal
Cultural values, norms
Environment, ethos
Social network
Knowledge, attitude, skills -
Follow healthy lifestyle
Individual
Korom, B., Malloy, M., Remmers, C. et al. “It’s about being healthy”; a novel approach to the socio-ecological model using family perspectives within the Latinx community. BMC Public Health 23, 86 (2023). https://doi.org/10.1186/s12889-023-15005-2
• Family history
• Genetic inheritance
• Epigenetic changes
• Environment exposure-based
Genetic factors • Air pollution • Weather changes • Sunlight (UV radiation)
Environmental factors
• Toxic materialbased mutations
• Age • Gender • Race • Ethnicity • Education • Income
Source: Budreviciute, A., Damiati, S., Sabir, D. K., Onder, K., Schuller-Goetzburg, P., Plakys, G., Katileviciute, A., Khoja, S., & Kodzius, R. (2020). Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Frontiers in Public Health, 8. https://doi.org/10.3389/fpubh.2020.574111
Factors of selfmanagement
• Tobacco use
• Alcohol use
• Physical activity
• Person’s weight
• Food choice
• Dental health care
• Medications
• Blood pressure
• Lipids
• Glucose
• Viruses
• Obesity
• Stress
Source: Budreviciute, A., Damiati, S., Sabir, D. K., Onder, K., Schuller-Goetzburg, P., Plakys, G., Katileviciute, A., Khoja, S., & Kodzius, R. (2020). Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Frontiers in Public Health, 8. https://doi.org/10.3389/fpubh.2020.574111
• HPH is initiated by the World Health Organization.
• The mission of the HPH network is to improve the quality of health care for the hospital patients and their family members, as well as hospital staff through evidencebased health promotion services.
• Standard 1: Demonstrating organizational commitment for HPH
• Standard 2: Ensuring access to the service
• Standard 3: Enhancing peoplecentered health care and user involvement
• Standard 4: Creating a healthy workplace and healthy setting
• Standard 5: Promoting health in the wider society
Adventist Health Philosophy (AHP) emphasizes concepts necessary for the development of whole-person health, which includes the perspective of:
• BODY (physical, financial)
• MIND (mental, emotional)
• SPIRIT (spiritual wellbeing of the individual)

Services
Patient’s Services Community Staff
Counseling
- Wellness Nutrition Counseling
- Diabetes Counseling
- Diabeties Foot Counseling
- Lactation Counseling
Program & Classes
- Diabetes Initial Assessment
- Weight Management Program
- Breathe Free Class (Smoking Cessation)
- Antenatal Class
Patient Family Education Material
- E-booklet, leaflet, flyer
Support Group
- Diabetes Malaysia
- Rainbow Touch (Cancer)
Kangaroo Club (Breastfeeding mother)
Public Awareness Events
- World Heart Day
- World Diabetes Day
- World Breastfeeding Week
- World No Tobacco Day
- Online Education Program
School Project
- Health Talks
- Campaign Corporate
- Health Talks
- Health Screening
- Cooking Demonstration
- Weight Loss Program
Workplace Wellness
- Stress Assessment
- Get Your Body Fit
- Cook & Bond
- Interest Class
- PAH 10k Step Challenge
Staff Health Talk
Team composition:
• Occupational Health Doctor
• Public Health Doctor
• Nurses
• Nutritionist
• Diabetes Educator
• Mental Health Educator
• Lactation Educator
Support Group:
• Diabetes Support Group
• Kangaroo Breastfeeding Support Group
• Cancer Support Group


• Give out pamphlet/education health brochures to patients’ friends & family
• Clinical nurses can provide basic health information to patients & refer patients to Community Health Dept health educators



Nutrition counseling, lactation counseling, diabetes counseling, and weight management program


Education materials with various languages (Bahasa Malaysia, English, Mandarin) based on the composition of the local population.


Different delivery method on health education to ensure access to the service and enhance people-centered health care and user involvement




HealthEducationBooth












Benefits of coordinating together with Community Health to achieve a healthier, greener community
• More preventive health services, fewer patients in hospital
⚬ Reduces healthcare burden
• Supporting a healthier community overall
• Implement knowledge in personal life - promote health among nurses and the community

Kidd, M. R. (2018). Why strengthening primary health care is essential to achieving universal health coverage. CMAJ : Canadian Medical Association
Journal, 190(15), E463. https://doi.org/10.1503/cmaj.170784
Sources:
• Samuel, R., Zaini, N. H., Hassan, W. H. W., Talib, A. N., & Ramly, F. A. (2021, March). Nurses’ perspective of work-related stressors. In IOP Conference Series: Earth and Environmental Science (Vol. 704, No. 1, p. 012026). IOP Publishing.
• Muhamad Robat, R., Mohd Fauzi, M. F., Mat Saruan, N. A., Mohd Yusoff, H., & Harith, A. A. (2021). Why so stressed? A comparative study on stressors and stress between hospital and non-hospital nurses. BMC nursing, 20, 1-10.
• Atefi, N., Abdullah, K. L., & Wong, L. P. (2016). Job satisfaction of Malaysian registered nurses: A qualitative study. Nursing in critical care, 21(1), 8-17.

• Understand nursing burnout
• Adjust staffing
• Salary adjustment
• Nursing appreciation
• Supportive work environment with work-life balance
• Promote self-care and wellness












• Workplace Wellness Activities to improve health and wellbeing
• Mental health resources

For nurses’ wellbeing:

• Training & Learning Opportunities for empowerment






For nurses’ wellbeing:
• Building Resilience and Support Networks
- Invest in resilience-building programs for coping mechanisms
- Foster support networks and peer monitoring

















http://www.free-powerpoint-templates-design.com









Overview

Nurses are essential to healthcare systems worldwide.
Investing in nursing education impacts patient care and system efficiency.
Objective
Explore how investing in nursing education is crucial for the future of healthcare. .







Patient Care: Direct care, treatment, and emotional support for patients
Healthcare System Impact: Contribution to improved health outcomes, patient satisfaction, and system efficiency.
Diverse Roles: From bedside care to advanced practice and leadership positions.


Patient Care: Provide direct care, treatment, and emotional support.

Key person in managing chronic conditions and providing preventive care.





Healthcare System Impact:
o Enhance health outcomes, patient satisfaction, and operational efficiency.
o Serve as a bridge between patients and the healthcare system.



o Include bedside care, advanced practice roles, and leadership positions.
o Engage in specialized fields such as paediatrics, geriatrics, and critical care.








There are an estimated 29 million nurses and 2.2 million midwives worldwide.
WHO estimates a shortage of 4.5 million nurses and 0.31 million midwives by the year 2030

In the U.S., The National Council of State Boards of Nursing (NCSBN) together with the National Forum of State Nursing Workforce Centers reported that Nursing is the nation's largest healthcare profession, with nearly 4.7 million registered nurses (RNs) nationwide. Of all licensed RNs, 89% are employed in nursing. The median age of RNs is 46 years. More than one-quarter of registered nurses report that they plan to leave nursing or retire over the next five years.
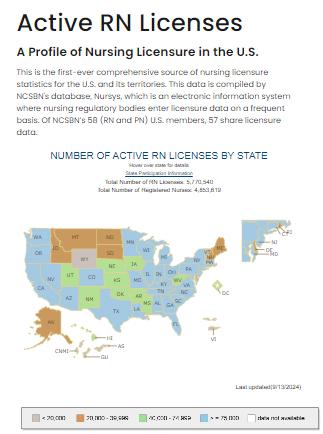
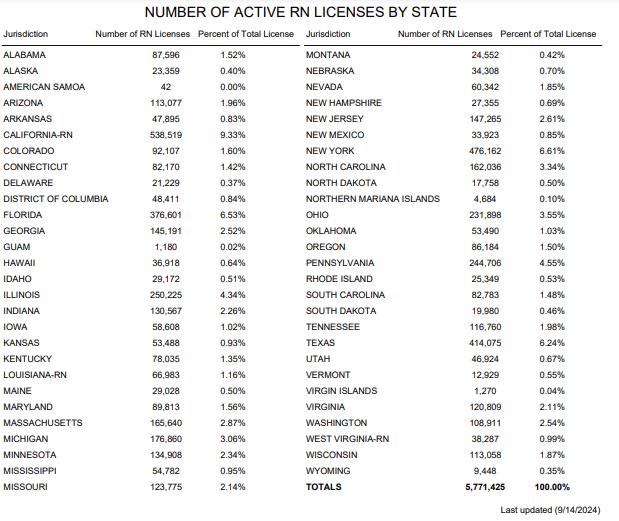
Taken from NNDLicenseStatisticsMap as of December 31, 2023
5,643,150

5,771,425

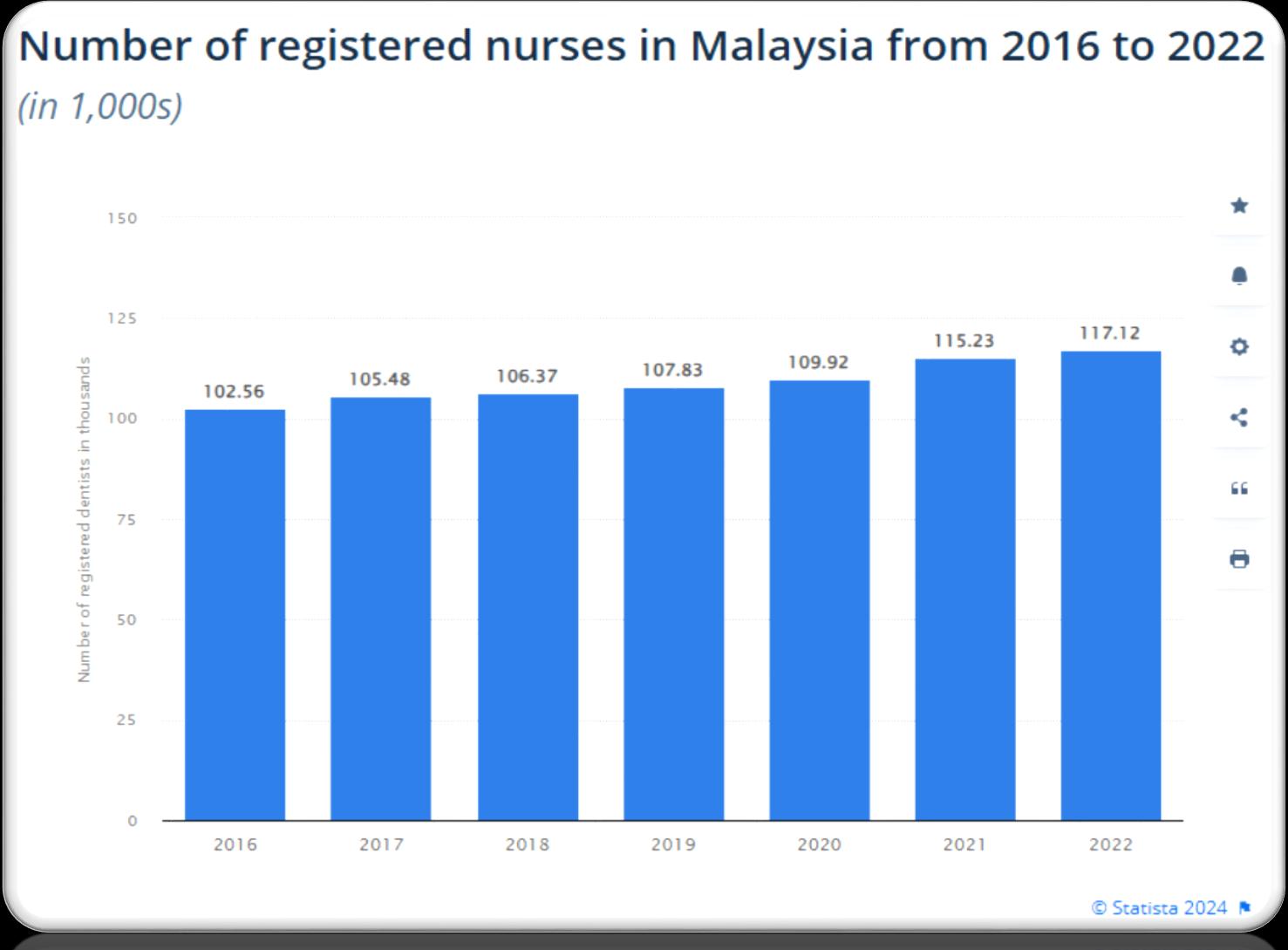




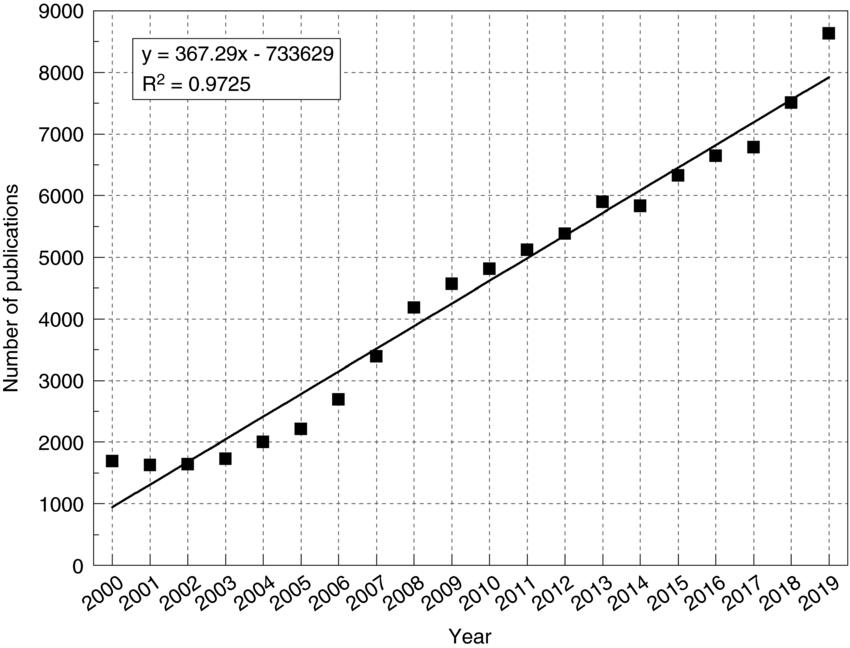
The nursing workforce has been experiencing steady growth due to increasing healthcare demands and efforts to address nursing shortages. Globally, the number of nurses is expected to continue rising, driven by factors such as an aging population, advancements in medical technology, and increased focus on preventive care. However, growth rates can vary by region. Developed countries generally see moderate growth with a focus on specialization and advanced practice roles, while developing countries may experience more rapid increases due to expanding healthcare access and investments in healthcare infrastructure.
Levels of education (Diploma, Bachelor’s, Master’s, Doctorate).
As of 2022, 71.7% of the RN workforce earned a baccalaureate or higher degree as their highest level of nursing education.

Diploma in Nursing

Bachelor’s Degree

Master’s Degree

Doctorate
In 2022, 17.4% of the nation’s registered nurses held a master’s degree and 2.7% held a doctoral degree as their highest educational preparation

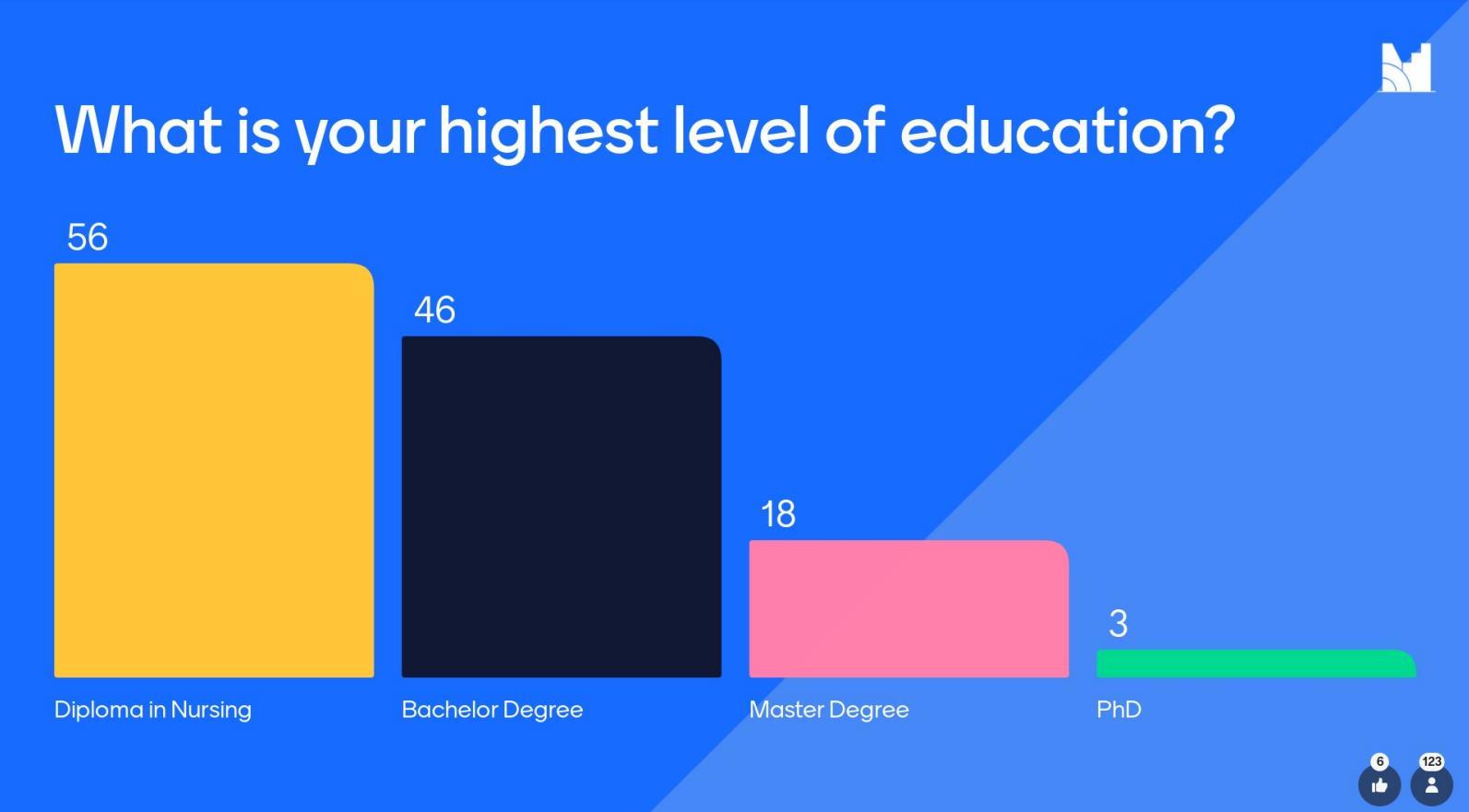
Captured from live participants
Nurses work in a variety of specialized roles, reflecting the diverse needs of patients and healthcare settings.
Settings:
Nurses practice in a range of healthcare settings:
Hospitals
Clinics
Community Health
Long-Term Care Facilities .




Limited resources for nursing schools and programs
Lack of qualified instructors
Keeping up with rapidly changing healthcare technology and practices
Financial burden on nursing students
Funding: Limited resources for nursing schools and programs



Many nursing schools struggle with inadequate funding.
Ability to provide up-to-date equipment, maintain facilities, and offer competitive salaries to faculty were affected
Inadequate funding impacts not only the infrastructure but also the quality of education and training
Faculty Shortage: Lack of qualified instructors.

A significant shortage of qualified nursing instructors compounds the challenges in nursing education


The advanced education and experience required to become a nursing educator mean that there are fewer individuals qualified to take on this role.
This results in larger class sizes, less individualized attention for students, and a greater strain on existing faculty members.
Curriculum Gaps: Keeping up with rapidly changing healthcare technology and practices.
New technologies and practices emerging at a rapid pace

Nursing Schools need to continuously update their programs to reflect current standards and innovations, which requires both time and resources that are not always readily available.




The financial burden on nursing students is a critical issue. Nursing education often requires significant financial investment, leading to substantial student debt




These approaches include the integration of virtual reality simulations, fostering interdisciplinary collaboration, utilizing real-world case studies, implementing telehealth platforms, and establishing mentorship programs.
Nursing education is at the forefront of preparing healthcare professionals to meet the demands of a rapidly evolving healthcare landscape


Simulation Training: Use of high-fidelity simulations to enhance practical skills.
Online and Hybrid Learning: Flexibility and accessibility of nursing education.
Interdisciplinary Training: Collaborations with other healthcare professionals for comprehensive learning.
Continuing Education: Emphasis on lifelong learning and professional development.

Simulation Training: Use of high-fidelity simulations to enhance practical skills.
Simulation training has revolutionized how nursing students gain practical skills.

High-fidelity simulations—using advanced mannequins and computer programs—allow students to practice and refine their skills in a controlled, risk-free environment.













Online and Hybrid Learning: Flexibility and accessibility of nursing education.


The flexibility and accessibility offered by online and hybrid learning models have made nursing education more attainable

Interdisciplinary Training: Collaborations with other healthcare professionals for comprehensive learning. collaboration between nursing students and other healthcare professionals, such as physicians, pharmacists, and social workers fosters a holistic understanding of patient care and emphasizes the importance of teamwork in healthcare settings.


Continuing Education: Emphasis on lifelong learning and professional development.

The emphasis on lifelong learning and professional development is critical in nursing education. Healthcare is a rapidly evolving field, and continuous education ensures that nurses stay current with the latest advancements, best practices, and regulatory changes.
By fostering a culture of lifelong learning, nursing education helps professionals adapt to new challenges and maintain high standards of patient care throughout their careers




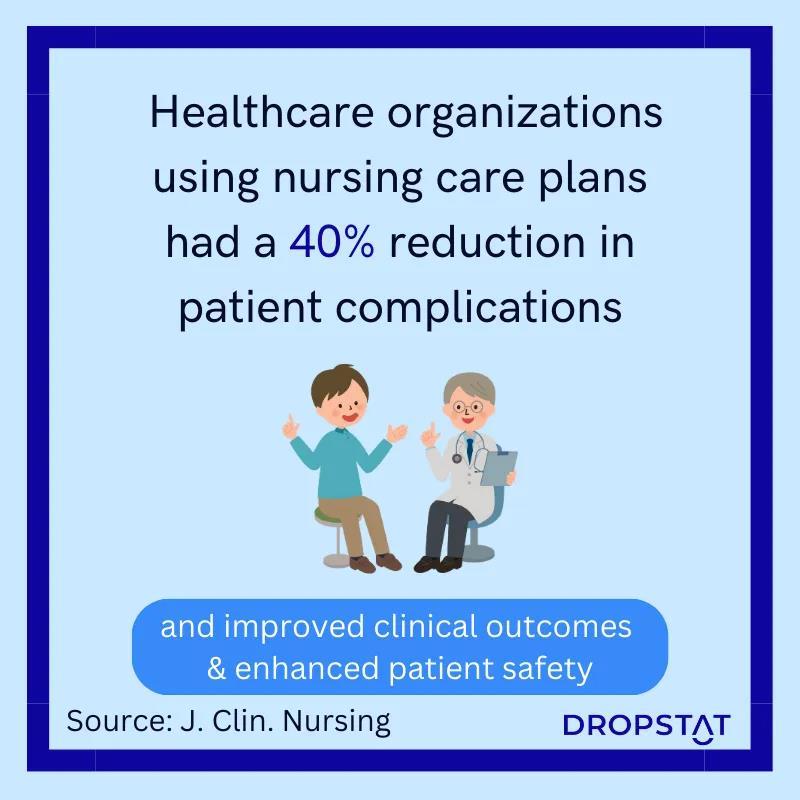
Better-trained nurses lead to higher quality care.
Well-trained nurses are equipped with advanced knowledge and skills, enabling them to provide higher quality care.

They are better prepared to assess, plan, implement, and evaluate patient care effectively

Increased Workforce Capacity: Addressing the nursing shortage and improving care delivery.

By expanding educational programs and increasing enrolment, we can produce more qualified nurses to meet the growing demand
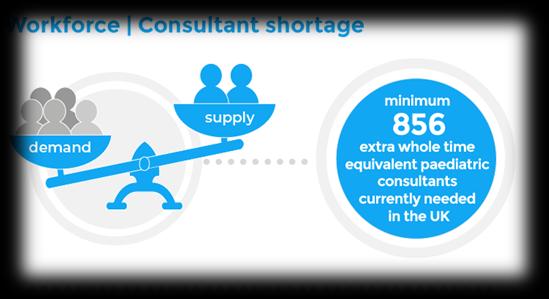

A larger and well-trained nursing workforce ensures that healthcare facilities can operate more efficiently, manage patient loads effectively, and deliver consistent, highquality care across various settings.
Enhanced Professional Growth: Better career opportunities and job satisfaction.

Enhanced educational opportunities lead to better career prospects, including advanced practice roles, specialized certifications, and leadership positions

Nurses can expand their expertise, stay current with industry trends, and pursue career advancement. This not only boosts job satisfaction but also fosters a more engaged and motivated workforce, which is crucial for retaining talented professionals in the field.
Healthcare Innovation: Nurses as leaders in advancing healthcare practices and technologies.


Investing in education empowers nurses to become leaders in healthcare innovation. Educated nurses are better positioned to contribute to research, implement evidencebased practices, and drive improvements in patient care.
As leaders in healthcare innovation, nurses can influence policy, champion new approaches to care, and help shape the future of the healthcare system.



Policy Advocacy
Promote Funding
Advocate for Increased Resources
Support Legislation:


Partnerships Collaborations Strengthen Institutional and Healthcare Partnerships
Industry Engagement

Community Engagement
Scholarships and Grants
Financial Support
Provide Scholarships and Grants

Raise Awareness
Engage in Awareness Campaigns
Organize Fundraising Efforts





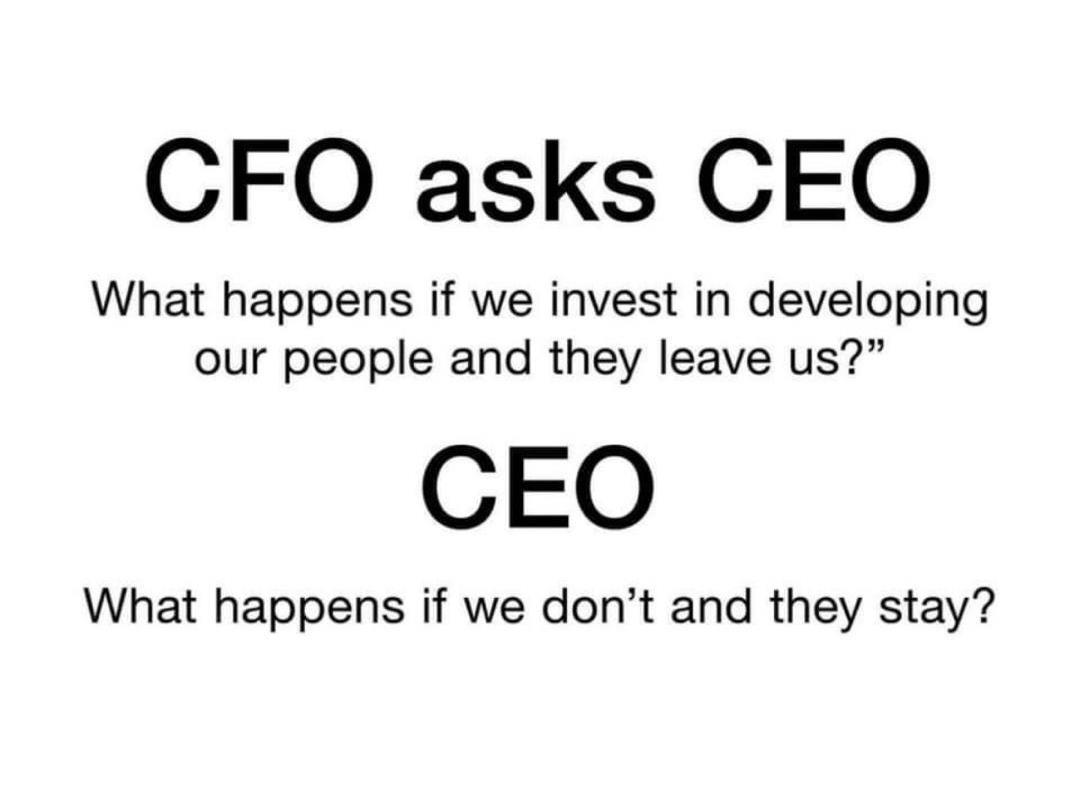
Investing in nursing education is fundamental to shaping a brighter future for healthcare. By prioritizing and supporting the education of our nursing workforce, we ensure enhanced patient care, expanded workforce capacity, and a continued drive for innovation in healthcare practices.

Well-educated nurses contribute to higher quality patient outcomes, address critical workforce shortages, and lead advancements in healthcare technologies and practices. They are essential not only in delivering exceptional care but also in shaping the future of healthcare systems.
It is crucial to maintain our commitment to this vital investment. This involves advocating for increased funding, supporting innovative educational approaches, and creating environments that nurture professional growth.