WWW.PHYSICIANOUTLOOK.COM PUBLICATION DEDICATED SOLELY TO PHYSICIANS AND THEIR PATIENTS Cover art by Kaitlin Walsh of Lyon Road Art 2022: THE YEAR WE START ANEW VOLUME 10 | 2022

D



WWW.PHYSICIANOUTLOOK.COM | 3 P H O T O B Y T I M M O S S H O L D E R O N U N S P L A S H Diversity elevates everyone's talents CONECT WITH US TODAY! VISIT US AT WWW HISPANICOUTLOOK COM EMAIL: INFO@HISPANIICOUTLOOK COM PHONE: (201) 587-8800 S E R V I N G T H E H I S P A N I C C O M M U N I T Y S I N C E 1 9 9 0 P H O T O B Y T I M M O S S H O L D E R O N U N S P L A S H Diversity elevates everyone's talents CONECT WITH US TODAY! VISIT US AT WWW HISPANICOUTLOOK COM EMAIL: INFO@HISPANIICOUTLOOK COM PHONE: (201) 587-8800 S E R V I N G T H E H I S P A N I C C O M M U N I T Y S I N C E 1 9 9 0
IMilitary and Medicine
THANKFUL FOR THEIR SERVICE
Written by Marlene Wüst-Smith, M.D.
t takes a special kind of person and supportive network to commit to the selfless service required of those who join the military. As a physician, I can relate. But to simultaneously embark on the path to serve BOTH in healthcare AND for our country? That takes commitment and dedication to the next level.
This issue of Physician Outlook is dedicated to those in uniform who don BOTH the white coat and military fatigues, altruistically giving of themselves to protect not just our freedom but also our health, sacrificing precious time with their loved ones (and themselves) in the process.
We owe a debt of GRATITUDE to our active duty Military and our Veterans, not a $6 BILLION debt from unpaid medical bills! Learn about www. EndVeteranMedicalDebt.com by reading Jerry Ashton’s article “A Look at V.A. Hospitals.” Ashton (a Navy Veteran and former debt collector) remains on the Board of #RIPMedical -

Debt, the well-respected charity that he co-founded in 2014. Jerry’s latest project, an organization called Let’s Rethink This (www.LetsReThinkThis. com) is shining a much needed spotlight on the medical debt burden that plagues our nation’s protectors and proposing solutions to collectively help relieve that debt by working with the Veterans Administration and its network of hospitals. Physician Outlook is proud to be one of the Impact Organizations being highlighted by LRT and partnering with Ashton and his team to help #EndVetMedDebt.
Nurses at the bedside of our patients are the true backbone of our healthcare system. I had the pleasure of personally meeting Bronze Star recipient Nurse Colonel Olga Rodriguez (now retired), a fellow Latina in medicine, at the annual www.Free2Care.org conference in Austin Texas this fall. She is an “old school” Syracuse University trained nurse who is passionate about patient safety and Nursing Edu -
cation, focusing on the importance of bedside and field Nursing.
In an article titled “We Need Our Bedside Nurses,” Dr. Linda Hodges, a civilian Critical Care physician (who works in ICUs across the country) discusses the alarming trend of registered nurses wanting to leave the bedside, pondering “what nursing would be like if we made the bedside job one that doesn’t need escaping from.” The best nurses (and physicians) are walking away from what has become a malignant system.
Perhaps the most fascinating story you will read in this issue is “Military in Medicine” which spotlights the career of (Retired) Colonel Kevin C. O’Connor, a Family Practice physician who calls himself the “Forrest Gump” of Military Medicine. He has some fantastic ideas about how to solve the physician shortage, and a great appreciation for physician-led, coordinated and collaborative team-based care. He has some pretty influential connections to share these
FROM THE PUBLISHER
BY KAITLIN WALSH 4 | 2022 VOLUME 10
ARTWORK
ideas with, and I am blessed to consider Kevin a friend and colleague, so thankful that he “gets” the importance that primary care plays in the world of medicine and population health.
Authentic Medicine
Why is the system malignant? As former Army Major and Emergency Room Physician Dr. Natalie Newman points out in “Dollars and Sins” (an article that first appeared on Dr. Doug Farrago’s blog www.AuthenticMedicine.com) that one cannot “fake it until you make it in medicine. The art and science of medicine is simply too complex, as is the human body.” Everyone wants to be “a doctor” these days without going to medical school or doing a residency, and that is just plain dangerous. Legislation cannot replace education. What most young nurses don’t realize is that profit-motivated puppeteers are purposefully taking advantage of their lack of experience and naïveté. Obtaining a Doctorate in Nursing is NOT the solution to solving the physician shortage. The more obvious solution to addressing projected shortages is to “grow more doctors,” something I have previously written about.
However, we need to ensure that pre-medical students do not become disillusioned along the path. In his article “Misgivings about Medicine,” high school student Jack McGowan, an aspiring future doctor, writes about how he ALMOST abandoned his childhood dream when he learned about the greedy Private Equity firms that have infiltrated Emergency Medicine and other fields. Fortunately for our future, he remains undeterred in his plans to become a physician after learning that grassroots physician groups are working together to expose the corruption and actively planning ways to “take back medicine.”
Sh!T Following the COVID Storm
It has been two long years since the onset of the worldwide COVID-19 pandemic. We are simultaneously weary and wishful as we have adapted to what has become “the new normal.” This issue features two COVID-related pieces.
Neurologist Dr. Ayushi Chugh’s beautiful poem reminds us of the importance of self-care and positive mindsets, reminding us that COVID-created thunderstorms will eventually be followed by sunshine to brighten the relentless “Coronaceous-Colored Sky.”
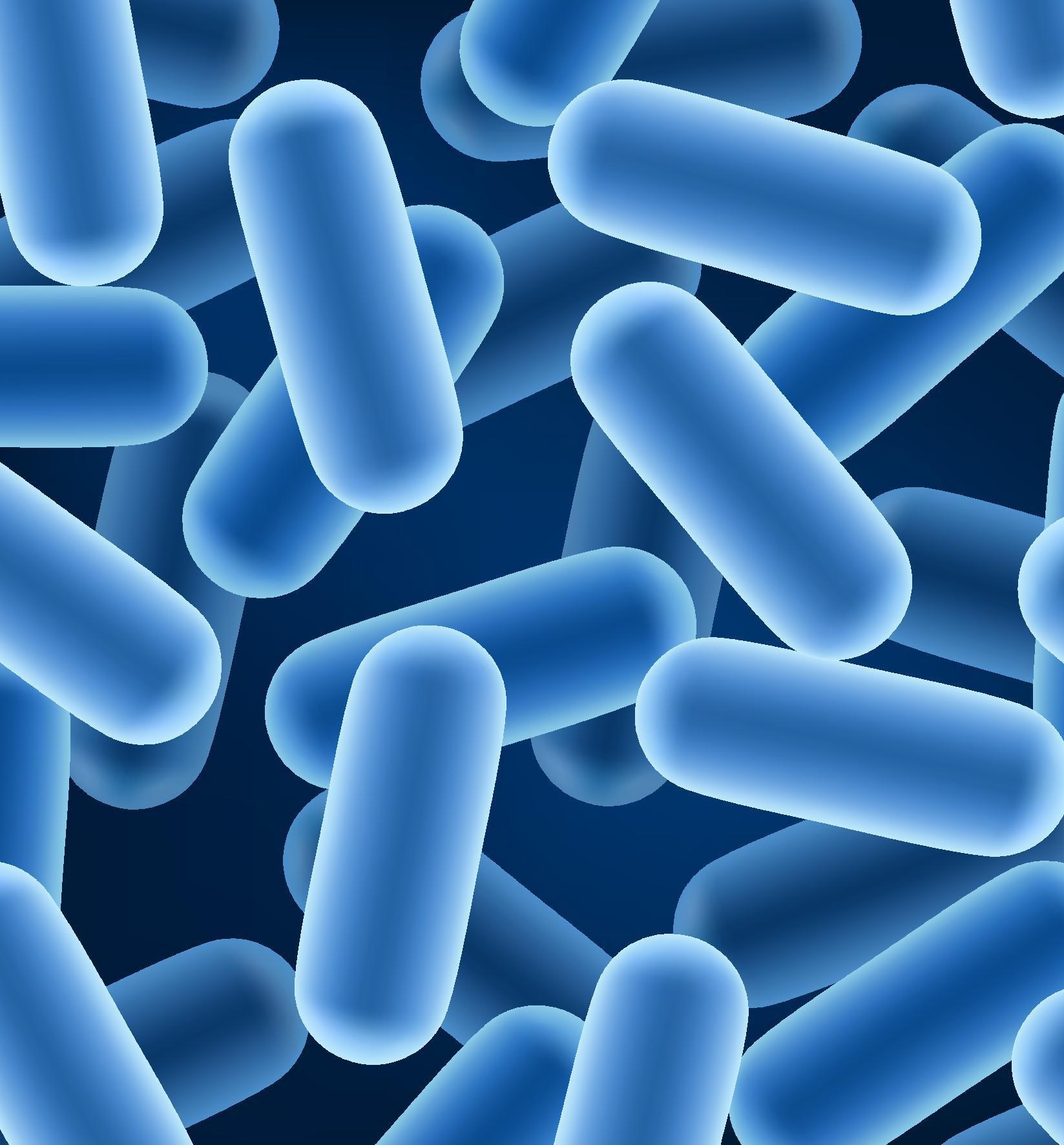
If you have ever wondered why the novel coronavirus disproportionately affects some individuals and not others (regardless of vaccination status), the key could be hidden in the person’s “microbiome signature.” Gastroenterologist Dr. Sabine Hazan (author of the best-selling book “Let’s Talk Sh!T” book) continues to study the role of a diverse and protective microbiome in predicting the clinical severity of COVID-19 disease. As reported by Trial Site News, the case series authored by Hazan and published in the peer-reviewed journal Case Reports in Gastroenterology features 6 members of the same household in which she happened to have some pre-pandemic stool analyses. Results from this family and other patients she has studied support her hypothesis of the protective importance of having a diverse, Bifidobacterium-rich microbiome.
Alternatively dubbed “Hurricane Hazan” and the “Queen of Sh!t,” Dr. Hazan continues to perform cutting-edge research through her FDA-approved COVID-19 prevention and treatment clinical trials. She is currently working on studies that will develop non-invasive baseline testing that could predict an individual’s SARS-CoV-2 susceptibility, perhaps allowing time for individuals to make dietary interventions with preor probiotics.
Left and Right Brain Connections
As we celebrate our 2nd birthday as a magazine, our readers will notice that Physician Outlook is taking on a more active role as a quasi- “corpus callosum” by acting as connectors, as synaptic neural bridges between the many severed connections we are experiencing between the left and right hemispheres of society, particularly within the scientific community.
My faith in medicine becomes restored when I hear physicians amicably and heatedly discuss controversial medical topics on podcasts such as
“The VPZD Show.” Dr. Zubin Damania (aka ZDoggMD) and Dr. Vinay Prasad have been named the “Click and Clack” of medicine, and discuss difficult topics with a sense of humor and a healthy sprinkling of swear-words. They are part of a movement Dr. Damania has called “the alt-Middle” and we at Physician Outlook invite all who are open-minded and tolerant to become a part of our complementary “Corpus Callosum Crew.”
As a publication Physician Outlook does not censor, avoids picking sides, and actively seeks to represent a spectrum of points of view. We respect transparency and truth-telling, and firmly believe that the answer to solving divisive issues in education, economics, in politics—in medicine—is to engage in true, meaningful, non-judgmental and peaceful nuanced discourse.
Collaborative problem solving, something that Dr. Diana Blum touches on in her article “Respectful Debate Amongst Doctors,” is at the core of the patient-physician relationship, and as physicians we need to model the kind of tolerance and respect we want to see reflected in the world and in our patients.
Dr. Marlene Wüst-Smith Publisher & Founder

WWW.PHYSICIANOUTLOOK.COM | 5
☤



6 | 2022 VOLUME 10

For more inFormation, visit https://www.doc-related.com/ https
 By
By
Olga
C. Rodriguez,
DNP, MSN, RN, CPHQ
THE DOCTOR’S BAG HOW TO DEMYSTIFY DPC FOR EMPLOYER GROUPS
By Kyle Rickner, MD
CIVILIAN VS. MILITARY HEALTHCARE EXPERIENCE
By Roxanne Bruce,
MBA, DrBA, FACHT

FAMILIES FISHER HOUSE FOUNDATION
By Madison Smith, PSU’22
BEDSIDE RNS: WE NEED YOU!
By Linda Hodges, MD
“The safety of the people shall be the highest law.”Marcus Tullius Cicero-Roman statesman, lawyer, and philosopher-first century BC
#ENDVETMEDICALDEBT: A LOOK AT VA HOSPITALS
By Jerry Ashton, Veteran and Founder of Let’s Rethink This
DOLLARS AND SINS:
By Natalie Newman, MD
EMERGENCY: BREAKDOWN IN COMMUNICATION
By Elizabeth Egan, SBU ‘24
The recent attacks in Texas and a hospital in North Carolina highlight the importance and obligation to keep your patients and staff safe. I thought you might be interested in a webinar about the latest revolution in video security hosted by one of our innovative partners, Verkada.
THE DIFFICULTY IN COMING HOME: WHAT DOCTORS AND SOLDIERS HAVE IN COMMON
By Susan Hart Gaines, CPCC, MS
Verkada’s hybrid cloud solution provides organizations with scalable, easy-tomanage, and secure video security that could benefit those for whom you are

LET’S TALK SH!T: A CASE SERIES CONNECTION BETWEEN MICROBIOME & COVID-19
By Sabine Hazan, MD
You’ll get a YETI Tumbler just for attending and they will provide you with a free camera to try out, and the webinar itself is incredibly informative and entertaining
PLEASURES AND PASTIMES CORONACEOUS COLORED SKY
By Ayushi Chugh, MD,
Find out how your peers are using Verkada, by signing up for an upcoming
THE VPZD SHOW
By Marlene Wüst-Smith, MD

36. 40. 44. 46. 48. 50. 51.
WWW.PHYSICIANOUTLOOK.COM | 41
22. 24. 26. 32.
2022 | VOL. 10 CONTENTS PHYSICIAN OUTLOOK MAGAZINE
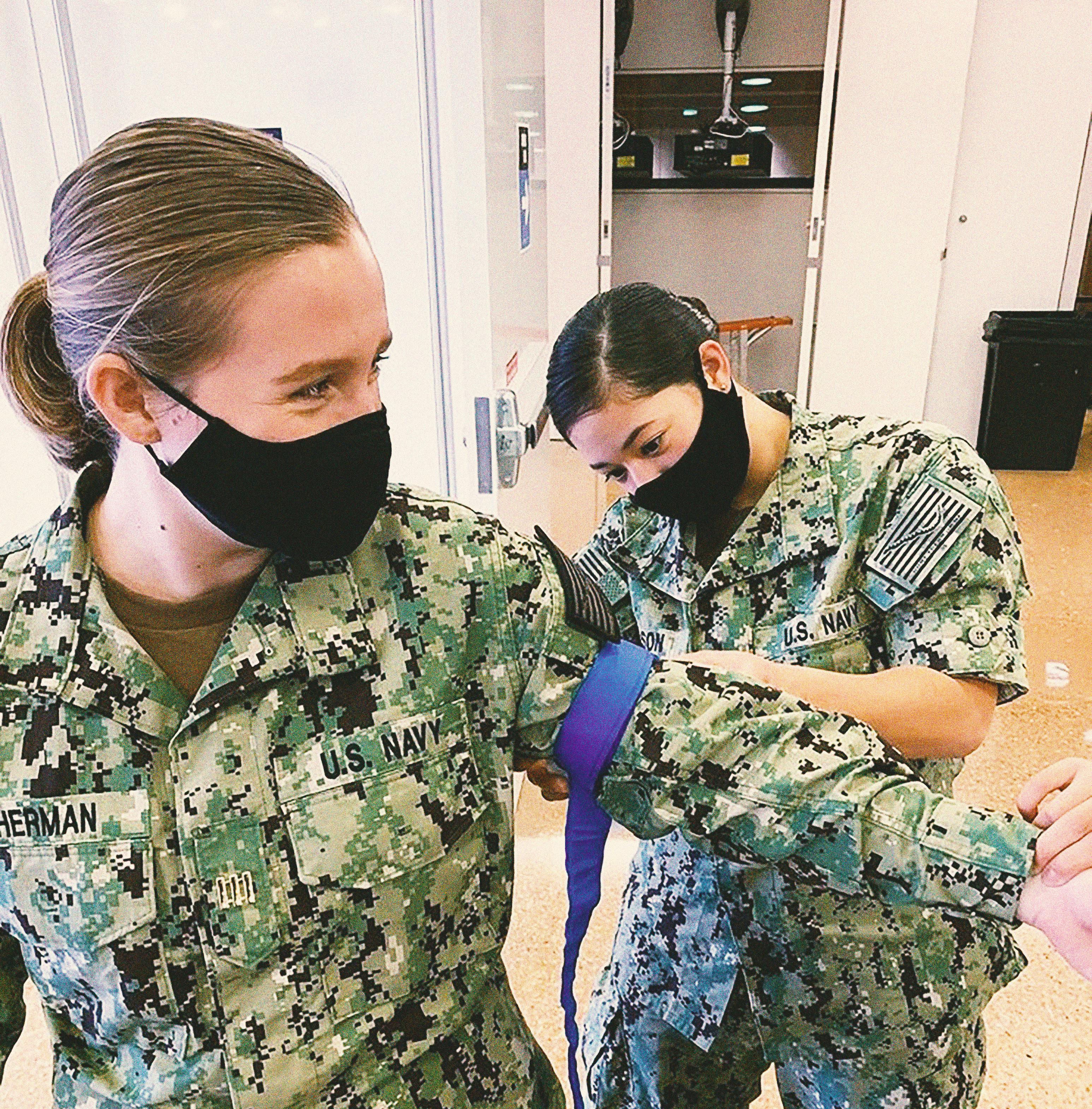
ROTC
MY JOURNEY INTO MEDICINE
Written by Sophia M. Sherman, U.S. Navy, MIDN1/C
8 | 2022 VOLUME 10
FUTURE PHYSICIAN/NAVAL OFFICER

Igrew up with aspirations of working in the medical field, but I had no idea I would first be serving in the Navy on the way to achieving that dream. Once I began considering going into the military, it seemed like a great fit. I had always cared about helping people and serving a larger community to do good in such a hectic world, and I realized those ideals carried over between both the medical and military fields.
I did not have much interest in attending the Naval Academy, and ROTC was the perfect option for me to pursue my degree at university of my choice and receive a commission into the Navy. I decided to attend the University of North Carolina at Chapel Hill because it was exactly the place I envisioned myself- a top-rated academic program with a variety of opportunities for research and experience in the medical field with a beautiful campus and diversity of experiences. I also knew it was a place where the academic rigor would well prepare me for the challenges I would inevitably face both in my military and medical pursuits.
I had applied for the Naval ROTC scholarship prior to my acceptance at UNC, and once I had received it, I was placed in UNC’s battalion where it covers the entirety of my tuition as well as providing monthly stipends and a book allowance each semester. This financial assistance allowed me to attend UNC, and I am incredibly grateful for this opportunity to graduate with my bachelor’s in biology without taking out any loans.
Since I joined the battalion in addition to our normal responsibilities, I have been able to interact with service members currently in the Navy Medical Corps and listen to their advice and experiences which has only increased my interest in pursuing an MD. Upon graduation, I will commission to begin a 5 year long active

duty commitment and I have been selected to enter the Submarine Warfare Community. From there, I will hopefully laterally transfer into the Medical Corps or separately apply for medical school following my commitment and applying for the Health Profession Scholarship Program with the Navy to continue my Naval career as a physician.
I have not quite decided yet if my position in the military will be for the entirely of my career, but I will certainly be considering staying in and continuing to serve as a doctor.
While it is a long, challenging path ahead of me, the ROTC program and my time at UNC has opened many doors into the medical community that I am so excited to enter. ☤


WWW.PHYSICIANOUTLOOK.COM | 9
FMisgivings About Medicine
A PROSPECTIVE PRE-MED STUDENT SPEAKS OUT
Written by Jack McGowan
or the past few years I have spent much of my free time outside of high school and my two part-time jobs immersing myself in the field of medicine, as I have dreamt of becoming a doctor for as long as I can remember.
In fact, when I was discovered to have Type 1 diabetes in November of 2019, the diagnosis did not devastate me nor deter me from my conviction for my chosen career path. It was as if my childhood fascination with the inner workings of the human body had eerily served as a form of foreshadowing, allowing me to swiftly bypass through the Kübler-Ross stages that I should have experienced as a freshman in high school when I

found out I had developed a life-altering chronic illness.
I simultaneously found myself at both the “bargaining” and “acceptance” phases shortly after my diagnosis, and have continued to practice these two virtues in my daily approach to life.
There was no denying what was going on: it was clearly irrefutable that seemingly overnight my once precisely functioning pancreas had to be replaced by crude approximations of self-administered exogenous insulin to manage the wild fluctuations in my blood sugar. Instead of wallowing in self-pity about my body’s betrayal, I was able to pivot my mindset to appreciate the complexity and precision
of God’s handiwork. Most of us take for granted how remarkably efficient a human body is when it works well.
I was more irate and angry at the COVID-19 pandemic and the way it was being managed than I was at the diabetes itself and how it had turned my world upside down. Anger is one of those emotions that can be all-consuming, and I made a conscious decision to not let it become a dominating factor in my life.
I HAVE experienced feeling depressed and discouraged, but surprisingly, the sadness and melancholy that enveloped me had nothing to do with my diagnosis or the pandemic. The despondency I
10 | 2022 VOLUME 10

felt was a direct result of discovering the current state of the medical profession. It was “perfect” timing (insert sarcastic tone) I might add, as I had just gone through the arduous task of completing and submitting 11 college applications as a prospective pre-med student.
I will never forget the moment that I started questioning my dream of becoming a doctor. I was working on an article for Physician Outlook Magazine (where I had been volunteering as a content intern). I was assigned to write about Dr. Luke Lin, an inspiring ER doctor who was the cover artist for Volume 6. After reaching out to him I wanted to learn more about Emergency Medicine. I have been shadowing an Orthope -
dic Surgeon, and although I love the Operating Room and the idea of being able to restore patients with musculoskeletal issues to normal function, I also was attracted to the field of Emergency Medicine as it is more diverse and requires a more broad base of medical knowledge and has that “adrenaline appeal” for me.
During my research I came across an Emergency Room Reddit post that included a link to a YouTube video titled “The Harsh Future of ER Doctors” that was sobering. It described the plight of “Bernard,” an ER doctor with extensive training (4 years of undergraduate education, 4 years of medical school, and a 3-5 year residency/fellow -
ship) who suddenly finds himself JOBLESS. I couldn’t believe that what I was watching could possibly be happening, and started doing some deeper research. I interviewed Dr. Mitch Li, founder of Take Medicine Back, PBLLC which is an advocacy organization that provides education and advocacy to the public regarding the corporate takeover of modern medicine. This corporatization has led to the financial exploitation of patients and the erosion of trust between healthcare providers and patients.
I learned about the growing trend of private equity firms “buying up” Emergency Medicine training programs with profit-making as the primary goal, with little to no regard for the ethical and moral obligations that make medicine the trusted and respected career that it is (or rather was). These programs essentially skimp on training and education, choosing instead to “fast track” doctors with a goal of making the most money in the least amount of time.
I know that healthcare is a business, and can understand that businesses must employ basic economic strategies to survive and thrive, but I cannot support nor turn a blind eye to the predatory practices that for-profit private equity firms are sneaking into the business of medicine. These PE firms are allowing young undertrained Physician Assistants and Nurse Practitioners to literally “practice” medicine unsupervised as if they were doctors, which undermines the integrity of both the specialty and the position. Physicians being trained at these PE-backed emergency medicine programs are often poorly prepared as the programs are not designed to create quality doctors. Simply put, PE firms “pump out” doctors as if they were being mass produced in a factory
WWW.PHYSICIANOUTLOOK.COM | 11
PHOTO BY MAT NAPO ON UNSPLASH
to make as much money in as little time as possible. This may work for manufacturers producing tangible products but has no place in medical education and in patient care.
There are two victims of this criminal practice: unsuspecting patients who are being financially exploited while getting substandard care, as well as the physicians who are being short-changed in their education and training. The trend is not just affecting ER doctors; these profit-driven investment firms are swooping in to purchase and “run” Dermatology, Plastic Surgery and Radiology groups.
I am often asked if I doing this research affected my plans to pursue medicine as a career. Did I still want to be a doctor? The answer is a resounding “yes.” When I myself became a patient as a freshman in high school, lost in an unfamiliar new world of Type 1 diabetes, It was my physicians who guided me through the dark tunnel towards the light. I personally experienced the importance of well-trained care teams who put ME, the patient, not profits, as the top priority. My care team at the Childrens Hospital of Philadelphia is physician-led and includes endocrinologists, nurses, nutritionists and pediatric residents. They have made an incredible difference in my life, and I plan to do the same for many other people’s lives. I am so grateful that as I am embarking on this long journey I am doing so with my eyes wide open, and with connections to and knowledge of grass-roots groups that are dedicated to maintaining the integrity of a profession that is rooted in a pledge to “Primum No Nocere.” Part of “Doing No Harm” is to continue to educate myself about the dark and dangerous side of medicine, and to advocate for much needed transparency and change. ☤

36 | 2022 VOLUME 10 12 | 2022 VOLUME 10
WWW.PHYSICIANOUTLOOK.COM | 13 history. God’s FHCP eduretired Seneca Pre-MedPROGRAM 3+4 B.S.-
 Written by Marlene Wüst-Smith, M.D.
Written by Marlene Wüst-Smith, M.D.
Medicine and the Military SPOTLIGHT ON FAMILY PRACTICE PHYSICIAN U.S. ARMY RETIRED COLONEL KEVIN O’CONNOR, D.O., F.A.A.F. P. PHOTO CREDIT: THE GW MEDICAL FACULTY ASSOCIATES 14 | 2022 VOLUME 10
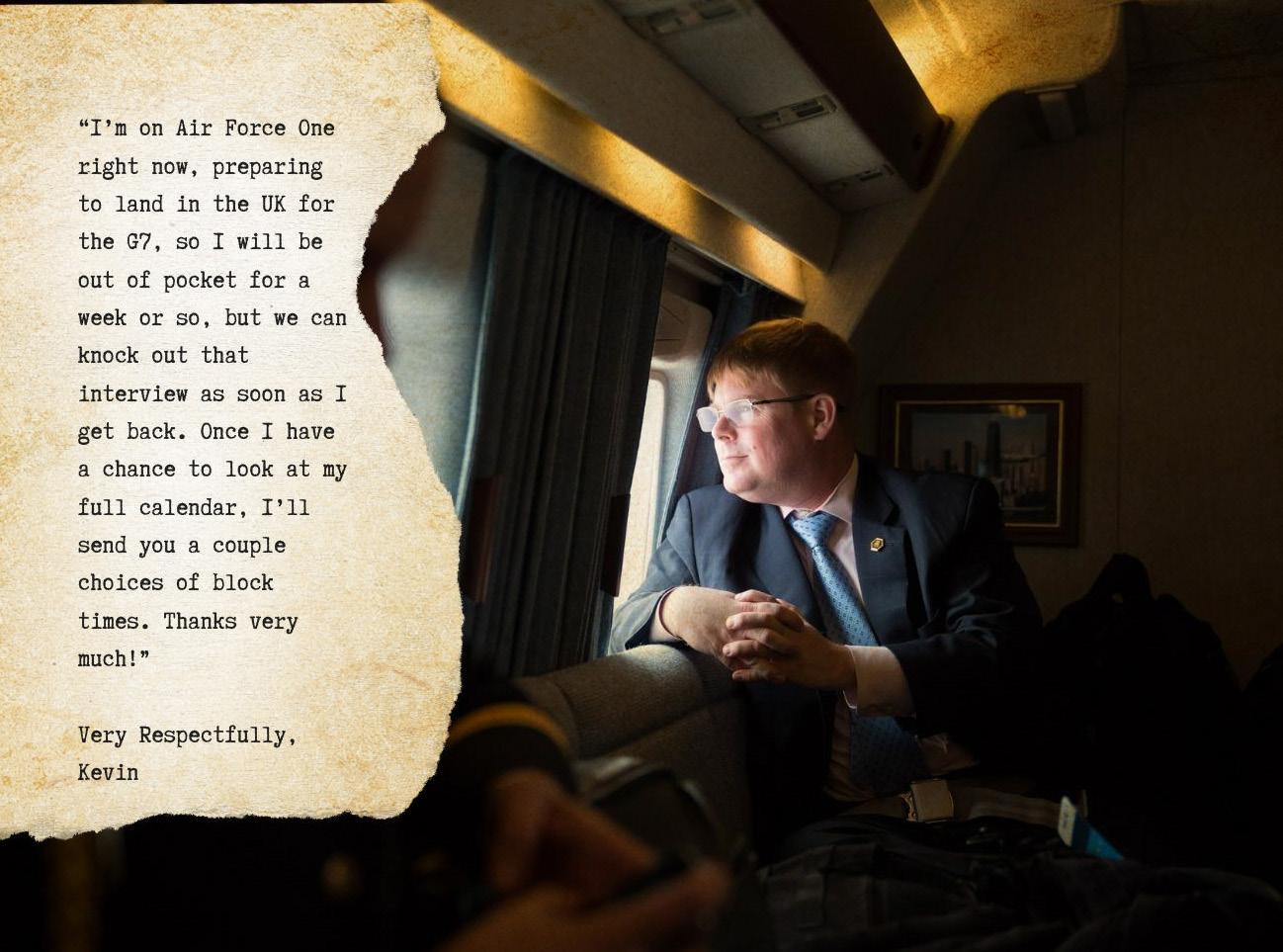
Doctors are very busy people, and our staff at Physician Outlook sometimes has trouble scheduling mutually convenient times when researching and fact-checking articles. We had an especially tough time coordinating with one Family Practice physician who is featured in our Military and Medicine issue, but as can be garnered from his email response above (dated June 9, 2021), he had some compelling reasons for being difficult to pin down:
“Kevin,” the author of this email, is Dr. Kevin O’Connor, F.A.A.F.P., a physician who we’ve wanted to feature in Physician Outlook Magazine since he became the Medical Director for the Franciscan Health Care Professions
Program (FHCP) at Saint Bonaventure University, where I have the privilege of working my “day job” as the Medical Director for the Center for Student Wellness.
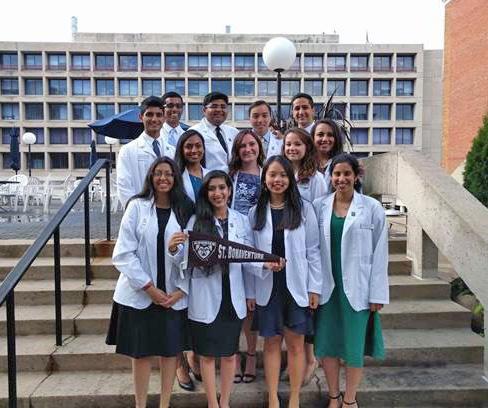
The combined-degree FHCP program fosters talented and dedicated young adults through the field of medicine. Bright, motivated high school students are guaranteed provisional entry into medical school upon admission to the university, and by the time they are college sophomores they are officially accepted into the medical school where they will receive their D.O. or M.D.
Early-admission and combined-degree programs afford pre-med students the opportunity to become more well-rounded hu -
man beings while they are undergraduates, without the pressure of having to apply to and interview at many different medical schools.
Dr. O’Connor is a 1988 graduate of St. Bonaventure University, in rural Allegany, New York, where he majored in Biology with a minor in Theology; a 1992 graduate of the New York Institute of Technology College of Osteopathic Medicine in Old Westbury, New York; a 1995 graduate of a Family Medicine residency at (Hackensack Meridian Health) Mountainside Hospital in Montclair, New Jersey, (where he served as Chief Resident his last year), and he currently holds a faculty appointment at George Washington University Hospital in Washington, D.C.
WWW.PHYSICIANOUTLOOK.COM | 15
PHOTO CREDIT DAVID LIENEMANN
SPOILER ALERT
He’s Kind of A Big Deal

As founder and publisher of Physician Outlook Magazine, I love highlighting the stories of interesting doctors as a way of inspiring others to carry the healthcare baton into the future, and to also show some much-needed love and respect to a profession that for many has become increasingly devalued. Dr. O’Connor’s story is an inspiring one that needs to be told.
Dr. O’Connor was indeed on Air Force One on his way to London for
the G7 Summit (and not delusional! ) when we were playing email and phone “tag” last summer.
“Physician-in-Chief” to the “Commander-in-Chief”
In January of 2021, retired Colonel Kevin O’Connor, D.O., was honored to be officially commissioned as the “P2P,” or the “Physician to the President,” by President Biden. He is supported by the White House Medical Unit (WHMU) which provides
24/7 worldwide emergency action response and comprehensive medical care to President Biden, Vice President Harris, and their families.
The WHMU (pronounced “WHAM-u”) is responsible for tactical coordination with the U.S. Secret Service and the White House Military Office to create and execute detailed medical contingency plans. This unit is also responsible for providing emergency care to the many pre-pandemic annual visitors to the
16 | 2022 VOLUME 10
PHOTO CREDIT DAVID LIENEMANN
White House, including dignitaries from other countries. For the past two years, the WHMU has also been instrumental in the White House COVID-19 mitigation strategy.
Being appointed to the role of the nation’s “First Physician” probably did not come as a big surprise to Dr. O’Connor, who has been providing primary care for the Biden family since 2009, when he was appointed as “P2VP” or “Physician to the Vice President.” O’Connor was physician for the “Second Family” for the two terms of the Obama presidency, and after leaving office in 2017, Vice President Biden asked Dr. O’Connor to stay on as the family’s primary care Family Physician.
Simply Extraordinary: “The Forrest Gump of Military Medicine”
Dr. O’Connor is one of the most down-to-earth, unassuming “badass” doctors I have ever had the pleasure of interviewing. He has jumped out of airplanes, visited more than 75 countries, has served in top secret Special Ops missions, and has helped to change the way life-threatening injuries and their resultant wounds are managed in active combat situations, to name just a few of his accomplishments.
In an American Academy of Family Physicians article titled “FP Reflects on Service on Front Lines of Family Medicine,” Dr. O’Connor jokingly referred to himself as “the Forrest Gump of Military Medicine … a simple man who just found himself in extraordinary circumstances and didn’t screw up.”
Dr. O’Connor’s curriculum vitae is impressive. During his tenure with the Army, he served as a Family Physician, a flight surgeon, an instructor and a hyperbaric medical officer for some of the nation’s most elite units, including the 82nd Airborne Division, the 75th Ranger Regiment as well as serving in a special mis-

sions unit within the United States Army Special Operations Command. O’Connor was also instrumental in re-designing Department of Defense trauma procedures to develop innovative strategies for addressing the unique needs of wounded Soldiers in hostile, non-permissive combat settings.
Politics: Proudly Non-Partisan
Dr. O’Connor was selected into the WHMU in 2006 during the BushCheney Administration. He was part of a team that provided urgent, immediate and emergency medical care as needed to the President, the Vice President and their families on nights and weekends, and
WWW.PHYSICIANOUTLOOK.COM | 17
PHOTO CREDIT DAVID LIENEMANN
on any trips outside of Washington D.C. In 2009, Dr. O’Connor’s original plan had been to stay on as a “utility player” for only 6 months, as an average WHMU tour of duty is typically 3 years. His heart was still overseas with the war fighters, and he wanted to return to his friends in Special Operations.
Six months ended up turning into the entire eight years of the Obama administration after he was asked by then Vice President Biden to become the Second Family’s personal physician. It was the excellent care and support that O’Connor provided to Biden’s beloved mother Jean that sealed his fate. O’Connor was just beginning his time with President Biden when she fell at her home in Delaware on a weekend in March of 2009, breaking her hip. O’Connor responded up to Delaware, coordinated her admission to the University of Pennsylvania Hospital in nearby Philadelphia, where she was operated on by Dr. Samir Mehta, the Chief of the Division of Orthopedic Trauma and Fracture Care at Penn Medicine.
 DDr. Samir Mehta Chief of Ortho at Penn Med
DDr. Samir Mehta Chief of Ortho at Penn Med
““Dr. O’Connor is the consummate professional.
It was a very collaborative relationship. In some of these unique patient care scenarios, doctors sometimes start to cross into another specialties’ expertise. That was not the case with Kevin at all. He “let me be” the orthopod, and I very much appreciated that. He is absolutely the kind of physician I would want to care for a family member (or the President of the United States).
r. O’Connor left the WHMU in 2017 after having served in that unit for 11 ½ years, retiring from the Army to enter civilian life and practice Family and Executive Medicine. At their request, he continued to provide primary medical care to the Biden family privately through his office at GW Medical Faculty Associates, where he was hired as Founding Director of Executive Medicine.
We could all take a lesson from how Dr. O’Connor practices medicine and fulfills his obligations free of partisanship. In fact, several years ago when he was interviewed by his medical school alma mater (New York Institute of Technology, College of Osteopathic Medicine, ’92) he is coyly quoted as saying
“(Biden) never once asked me if I was a Republican or a Democrat, and I never asked him ... although I (was) pretty sure he was a Democrat.”
“On-Call” 24/7, For Years at a Time
According to an AMA article, taking night or weekend calls increases the odds of burnout by 3 to 9% for each additional night or weekend that a physician is on call.
The role of a White House physician in a pandemic: 24-7, 365 days per year, for years at a time.
Dr. O’Connor does not seem “burnt out,” and takes his unrelenting schedule in stride. When asked if he ever gets any sleep at night, he winks: “Yes, with one eye open.”
”
18 | 2022 VOLUME 10
PHOTO CREDIT DAVID LIENEMANN
He credits the highly supported, well-organized, team-based care model at the WHMU for allowing him to do his job. He works with a coordinated, highly talented, handpicked group of White House physicians, nurses, physician assistants, medics, corpsmen, logisticians and other essential personnel that support the Unit.
The WHMU is truly a model for how all of healthcare should be functioning.
Returning to his Franciscan Roots as a Civilian
When asked by St. Bonaventure University, his undergraduate alma mater, to serve as the Medical Director of the Franciscan Health Care Professions Program in early 2020, Dr. O’Connor eagerly embraced the opportunity. He describes it as an honor to be able to return to his “academic home” and put into practice through the FHCP and its collaboration with the School of Health Professions the Franciscan values of selflessness, benevolence and charity.
He fondly recalls his time on campus where he served as Class President, helping to implement the campus’ newly founded student-run Medical Emergency Response Team (MERT), and ultimately receiving his military commission as a Distinguished Military Graduate through the ROTC program.
O’Connor’s military career began serendipitously shortly after he arrived at St. Bonaventure. He was a baby-faced, long-haired teenage freshman from New Jersey who chose to enroll in a Military Science Basic ARMY ROTC elective “as a goof,” with the intention of meeting new people and getting some exercise. The syllabus for the Military Science curriculum explained that students would
be taught the fundamentals of leadership and decision-making, skills that he thought would come in handy as a future doctor (he came in as a biology major). The opportunity to engage in individual fitness and unit training utilizing a combination of classroom instruction and hands-on exercises that included land navigation, rappelling and survival skills sounded fun. This elective (that he had initially picked on a “whim”) ended up becoming one of his favorite classes and became a life-altering pivotal touchpoint for O’Connor.
When a recruiter presented to his freshmen class the opportunity to become a cadet and receive a “full ride” 3-year college scholarship through the Army Reserve Officers’ Training Corps (ROTC), O’Connor became intrigued. He had grown up in an average, middle class household not far from the Jersey shore. His father was a homicide detective and mom a homemaker. He had a younger sister that would also soon be college-bound.
A career in law enforcement is not known for its generous pay, and it was understood that his father’s “cop” salary was not going to finance putting two kids through college. Besides, Kevin aspired to go to medical school, which would be very expensive. He had planned on taking out student loans to pay for his education, but the ROTC scholarship sounded too good to be true.
After hearing about all the outstanding benefits of enlisting and realizing how much he loved the culture of the Army, O’Connor asked his Military Instructor what the next step was…what he needed to do. The recruiter’s answer: “Cut your hair and submit your application.”
The rest, as they say, is history.
The Gift of Military Medicine
What started out as a 4-year commitment to serve his country as a way of paying for college culminated into the opportunity of a lifetime for O’Connor. After being accepted into medical school at the New York
WWW.PHYSICIANOUTLOOK.COM | 19
PHOTO CREDIT: ST. BONAVENTURE UNIVERSITY AND GEORGE WASHINGTON UNIVERSITY MEDICAL SCHOOL

Institute of Technology’s College of Osteopathic Medicine he applied to The Health Professions Scholarship Program, not sure at first if he would be funded. It turns out that getting into medical school is much harder than being granted an HPSP award (to read more about Dr. O’Connor’s story applying to medical school please subscribe to Physician Outlook and look for “the scoop” at www.PhysicianOutlook.com).
By the time he completed his civilian Family Practice residency in 1995, O’Connor had signed three separate four-year contracts and “owed” the Army 12 years of service. The truth, however, Dr. O’Connor admits is that he has never felt burdened by any sort of “debt”—in fact, he is forever grateful for the gift of being given the opportunity to serve his country and to fulfill his life-long dream of becoming a servant leader, a physician and a Soldier. “I would have paid them for the opportunities of a lifetime afforded to me throughout my tenure.”
He loved the military so much that he would spend a total of 29 years (22 years in Active Duty) serving our country before retiring as a Colonel.
A Divine Calling: Physician, Teacher, Mentor
Becoming a physician allows those who are called to “do well,” as one “does good,” O’Connor is quoted as saying (when describing the Franciscan Health Care Program at St. Bonaventure University).
“It
answers both the community’s call for workforce development and God’s call to always care for those who are suffering.”
O’Connor is passionate about education and remains very active at George Washington University, teaching and mentoring medical students (some of whom come to GW through the St. Bonaventure’s FHCP combined-degree program). He is very proud of St. Bonaventure’s commitment to veteran education and advancement through the Military Aligned Students Program championed by retired Master Sergeant Francisco Morales. Both Morales and O’Connor were inducted into the Seneca Battalion ROTC Hall of Fame in 2019.
When asked (during an interview with fellow veteran Dr. Humayum “Hank” Chaudry of the FSMB) if there was a specific mentor or role model who inspired him to choose Family Medicine as a specialty, O’Connor’s answer is insightful: “nobody, and everybody.” Dr. O’Connor reflected that he liked ALL of his rotations in medical school, but he didn’t love any one specialty so much that he was willing to give up all the rest.
As a Fellow of the American Academy of Family Physicians, O’Connor found his perfect niche. The practice of Family Medicine best suits his personality and
ego. He has never felt the need to be “the last word” in any medical situation and appreciates the opportunity to collaborate and ask for help when the situation calls for it.
In his mentoring role with medical students, Dr. O’Connor offers sage advice that is reminiscent of Robert Fulghum’s famous essay “Everything I Need To Know I Learned in Kindergarten,” when children have unabashed zeal for learning new things every day. He recommends to third-year medical students that they identify those times when they approach life as they did when they were 5 years old and to ask parents, siblings, spouse, significant others, friends, and neighbors: “Over the past year, when was I good to be around … when was my ‘best self’?”
Living His Best Life
Dr. O’Connor has found a career that allows him to feel his “best self” ALL the time.
It was inspirational to hear his story first-hand, and an honor that he agreed to be featured exclusively in Physician Outlook. He is usually a very private person who grants very few interviews. His love for St. Bonaventure University and the guiding principles of our shared Franciscan-influenced faith created a mutually trusting relationship.
We clearly have a shared passion for longitudinal patient relationships that value the role of physician as leader of a healthcare team.
That the leader of the free world happens to call him “Doc” and ALSO understands the important role physicians play in healthcare? That is what I call…divine serendipity. ☤
For information about the Franciscan Health Care Professions Program at St. Bonaventure University, contact the Pre-Medicine Admissions Liaison, Chris Scheppner, at 716 375-2413 and/ or Monica Thomas, PhD, Faculty Director at 716 375-2656.
St. Joseph’s Oratory, built in 1927, served as a quiet place for O’Connor to reflect and pray before exams as an SBU student between 1984-1988
20 | 2022 VOLUME 10
PHOTO CREDIT: ST. BONAVENTURE UNIVERSITY

PHOTO CREDIT DAVID LIENEMANN
The Military
NEEDS NURSES TOO
Written by Elizabeth Egan and Olga Rodriguez
Olga C. Rodriguez, DNP, MSN, RN, CPHQ is currently the Executive Director of Clinical Services for the nursing and allied health Travel Division of Career Staff Unlimited.
Olga completed her undergraduate and graduate studies in Nursing at Syracuse University. Early in her career, Olga chose critical care as her specialty and cardiology as a subspecialty. Her first nursing position was with the Veterans Administration Medical Center in Syracuse, NY which culminated in being selected (two years out of her bachelor’s degree) to the position of Critical Care Education Specialist and Coordinator for the medical center. She pursued a master’s in adult critical care and administration, and soon after graduation she joined the US Army Reserves as an officer and proudly served overseas in Korea, Germany, Hawaii (considered over-

seas by the US Army), Japan, and Iraq. Stateside assignments included: Moncrief Community Hospital, FT Jackson, SC: Walter Reed Medical and Research Center, DC, Ft Benning, GA, and Ft Sam Houston, TX.
In all of her assignments, she held managerial and leadership positions ranging from unit manager to Executive Officer for an Infantry Brigade as well as Commander of the Medical Detachment for the Hawaii National Guard. Her love for field nursing and working alongside the combat soldier resulted in her being recognized as an expert in the management of combat support hospitals. She is the recipient of the Bronze Star and numerous military awards, ribbons, and badges. She retired from the military in the rank of Colonel. In her civilian professional life, Olga has focused her work on teaching hospitals and some community hospitals. Leader-
ship positions she has held include executive nursing and allied health services such as respiratory therapy, pharmacy, nutrition care, laboratory services, and clinical support services.
Healthcare Quality and Patient Safety are the drivers for patient care and outcomes for her. As a consultant, she has been involved with regulatory and federal agencies and has developed expertise often sought out by healthcare entities experiencing challenges with The Joint Commission, Centers for Medicare and Medicaid, Office of Inspector General (OIG), Department of Justice (DOJ), and departments of health. Since she retired from the US Army, Olga has worked as a consultant in Clinical operations, Quality and Performance Improvement, Critical Care, Behavioral Health, and Regulatory Compliance. Olga has held leadership positions as a CNO,
22 | 2022 VOLUME 10
PHOTO BY CANVA

VP, Hospital Administrator, and COO in the US and overseas.
Olga is an active member of the American Organization of Nurse Leaders (AONL), American Association of Critical Care Nursing (AACN), Society of Critical Care Medicine (SCCM), and National Association of Healthcare Quality (NAHQ).
As a member of these organizations, she has held leadership positions (president, present-elect, treasurer, secretary, and committee chair) at the local and state chapter level. At the national level, she has been involved with task forces and Foundation activities (AONE and AACN). As a champion of life-long learning, Olga is currently pursuing her Doctorate of Nursing Practice (DNP) in Nursing Leadership with Florida Southern College. Olga is an avid tennis player and enjoys mentoring aspiring leaders in healthcare.


☤
PHOTO CREDITS: OLGA RODRIGUEZ
PHOTO CREDITS: OLGA RODRIGUEZ
How To Demystify DPC
FOR EMPLOYER GROUPS
Written by Kyle Rickner, M.D. Family Practice Physician CEO and Founder of Primary Health Partners

At 8 a.m. a few weeks ago I received a text from one of my patients, John, about some abdominal pain. By noon, we were face-to-face in my office, figuring out the next steps for treatment of an umbilical hernia that would not reduce. He was in surgery by 10 a.m. the next day, and back to work within the week.
Would that process have been as smooth in our traditional healthcare system? Most likely not.
Especially when you factor in that John was actually a few hours
outside of town when he first reached out. But as a Direct Primary Care Physician, I’m able to meet my patients where they’re at – in the exact moment that they need care. Sometimes that’s in the form of an urgent text, or a virtual visit. Or even a last-minute office visit. Because I’ve capped the number of patients I take on – considerably fewer than the healthcare industry’s expected average – I was able to make room for John.
Within minutes of John’s diagnosis that day, I was on the phone with
a surgeon who is also a “preferred provider” through his employer. The surgeon was able to see him that same afternoon. He recommended immediate intervention and scheduled surgery for the next morning.
We’re all familiar with the runaround that can often come with traditional healthcare – it can be challenging at times. For patients. For us physicians. For employers.
The Employer’s Perspective
“John’s experience is exactly the kind of care I want for my

24 | 2022 VOLUME 10
employees. He didn’t go to the emergency room, he didn’t go to a non-preferred surgeon, he didn’t inadvertently create a claim on my health plan that would have cost double or triple what it should have. Catching John in the moment he needed care, like only Direct Primary Care can, didn’t just save me time and money in the short term…HE got the very best care experience available. As a small business owner, I was spared the compounding effects of an expense that unexpected large claims create for my business’ health plan for years to come.
What Does it Cost?
Primary Health Partners charges a very reasonable membership fee (currently $79/month for adults 18 and above, and $49/
month for children from birth through age 17). Most families also purchase inexpensive High Deductible Health Plans for major medical needs that they purchase through the Healthcare Marketplace or through an employer. Most patients do not ever have to file insurance claims through their HDHP because as a DPC we are able to meet most of their needs through virtual visits and in-office care.
How to De-mystify DPC?
So how do we actually demystify costs for employer groups? How do we even get in the door in the first place?
We begin by providing worldclass care for our patients.
Then, THEY tell their stories. WE tell their stories.
Relentlessly.
To anyone who will listen. ☤
Dr. Kyle Rickner is a Board-Certified Family Practice Physician who graduated from Southern Nazarene University in his native home state of Oklahoma, and from Case Western Reserve School of Medicine in Ohio. He completed a Residency at Great Plains Family Medicine in Oklahoma City, and then began his career as a physician in the U.S. Army where he served at Fort Bragg in North Carolina as a staff physician and as a battalion surgeon in the 82nd Airborne division. After retiring from the military, he practiced in both private group practices and corporate medicine settings before discovering the magic of the Direct Primary Care model, where he is able to continue to innovate, restore the doctor-patient relationship and participate in IRB-approved clinical research.
Primary Health Partners is a multi-site Direct Primary Care practice based in Edmond, Oklahoma.
Like many other DPC practices, this model of care is bringing common sense to the chaos of medicine by championing a TRULY affordable provider-to-patient relationship. Dr. Kyle Rickner (one of the practice’s founders) and the team of physicians and other providers who work at Primary Health Partners help patients and employers achieve desired health outcomes through a transparent, patient-centered approach. The team at Primary Health Partners cares for thousands of patients on behalf of their employer partners through a nationwide affiliate network.
Learn more by visiting www.primary-healthpartners.com

Civilian Vs. Military Healthcare Experience
MUSINGS OF A SOLDIER’S SPOUSE
Written by Roxanne Bruce, MBA, DrBA, FACHT

Ihave had my fair share of trips to Emergency Rooms and the differences between military hospitals and civilian hospitals were a real eye opener for me.
In 2009 we were stationed in San Antonio, Texas. I was new to cockroaches and the little bugs were all over the apartment we rented. We had put baby gates up in the kitchen and
every night we sprayed pesticide in an attempt to rid the kitchen of the bugs. In San Antonio, I had the unexpected “privilege” of having to visit a military emergency room, and firsthand got to experience the big differences between military medicine and civilian medicine.
While washing dishes in our little apartment kitchen, I fell. We don’t know if I blacked out or how long I was uncon-
scious, but the last thing I remembered was that I was in the kitchen washing dishes, having left my kids in the living room watching television. When I woke up and found myself on the kitchen floor, I had two pairs of scared-looking eyeballs staring at me through the baby gate. I was home alone with a 2-yearold, a 1-year-old and a 3-month-old (who was crying from his bassinette).
26 | 2022 VOLUME 10
PHOTO CREDIT ROXANNE BRUCE
I immediately called my husband (who was on duty) and let him know what happened; we both assumed that I had somehow poisoned myself with the bug spray.
He rushed back from the base and together we loaded the children in the car, and he dropped me off at the base’s Emergency Room. I was put in a “room” (curtained off area) and the nurses and doctors were there within minutes. They had a small machine with them that took my blood from a finger, and spit out results almost instantly. We talked about what I had experienced, and the doctor performed a few bedside neurologic function tests. At first he thought that perhaps I had passed out from “heat stroke” since we had come from a cooler climate and the temperature change was drastic. For safety reasons, he ordered an MRI of my brain.
It was about the time that they brought me back to my room from Radiology that my husband got back to the hospital. He was trying to get answers from the nurses, and within a few minutes the ER doctor peeked his head in. He repeated a few more neurologic tests, having me touch my finger to my nose, balance on one foot, turn around and sit down. The doctor sighed and said “If you had come in with a broken bone, or an open wound, I would be the right doctor for you. I am worried from some spots that I see on your brain MRI that what you may have Multiple Sclerosis and I am putting in a referral for you to see a specialist.”
That started my Multiple Sclerosis journey and the multi-state, multi-hospital, multi-doctor adventure to living with a chronic illness. It was the first time that I had been seen in an ER where the doctor was able to run tests without delay. I had a similar trip to a civilian hospital in New Hampshire almost a year later with a very different experience.
My husband was in the process of retiring from the US Army, and I had moved myself and our children to our new home in New Hampshire while he finished up his tour of duty in Texas. I started a job, hired a nanny and life was going smoothly and without stress, at first. Then, as inexplicably as the first time, some strange neurologic symp -
toms started happening again. At the time I still did not have a confirmed diagnosis of MS and since we had just moved, I didn’t have a doctor yet. I knew that being home alone with 3 toddlers and no idea of what was going on wasn’t safe, so off to the ER I went.
I swung though a McDonald’s drive through, picked up 3 “Happy Meals” and headed to the local community Emergency Room. The nurses took me back to and examination room and I waited. And waited. And waited some more. The ER did not appear to be crowded, but it seemed like an eternity before an ER doctor finally came in to see me. He ordered a handful of blood tests and then left without performing much of an exam. After waiting some more, a phlebotomy team came in to draw some blood. I was thankful for the kind nurses who sat with my kids while I had a brain scan. After my scan I returned to my room, and I sat and waited for results with three children who were tired and cranky. After hours of waiting I was eventually sent home without results.
The ER doctor and discharge nurse told me that I would be getting a call with my results, and that someone would also help me to schedule follow-up appointments. After a week of not hearing anything I called to get my own results, and no one had any information about who I needed to follow up with. I ended up coordinating my own care, eventually finding a PCP who accepted our insurance, and then got on a wait-list to see the only neurologist in the area who had any expertise with Multiple Sclerosis.
The civilian experience of finding out what was wrong with me took weeks vs. the military experience which took just a few mere hours.
There is nothing wrong with either kind of emergency room; in fact the medical staff at every Emergency Room I have ever been treated at has been wonderful. The biggest differences for me have been the consistent experience at civilian hospitals of having to “hurry up and wait” for results, the lack of coordination of care, and of course—the extraordinarily large, uncovered bills. Military hospitals universally accept military insurance. Civilian hospitals—not so much. ☤
WWW.PHYSICIANOUTLOOK.COM | 27


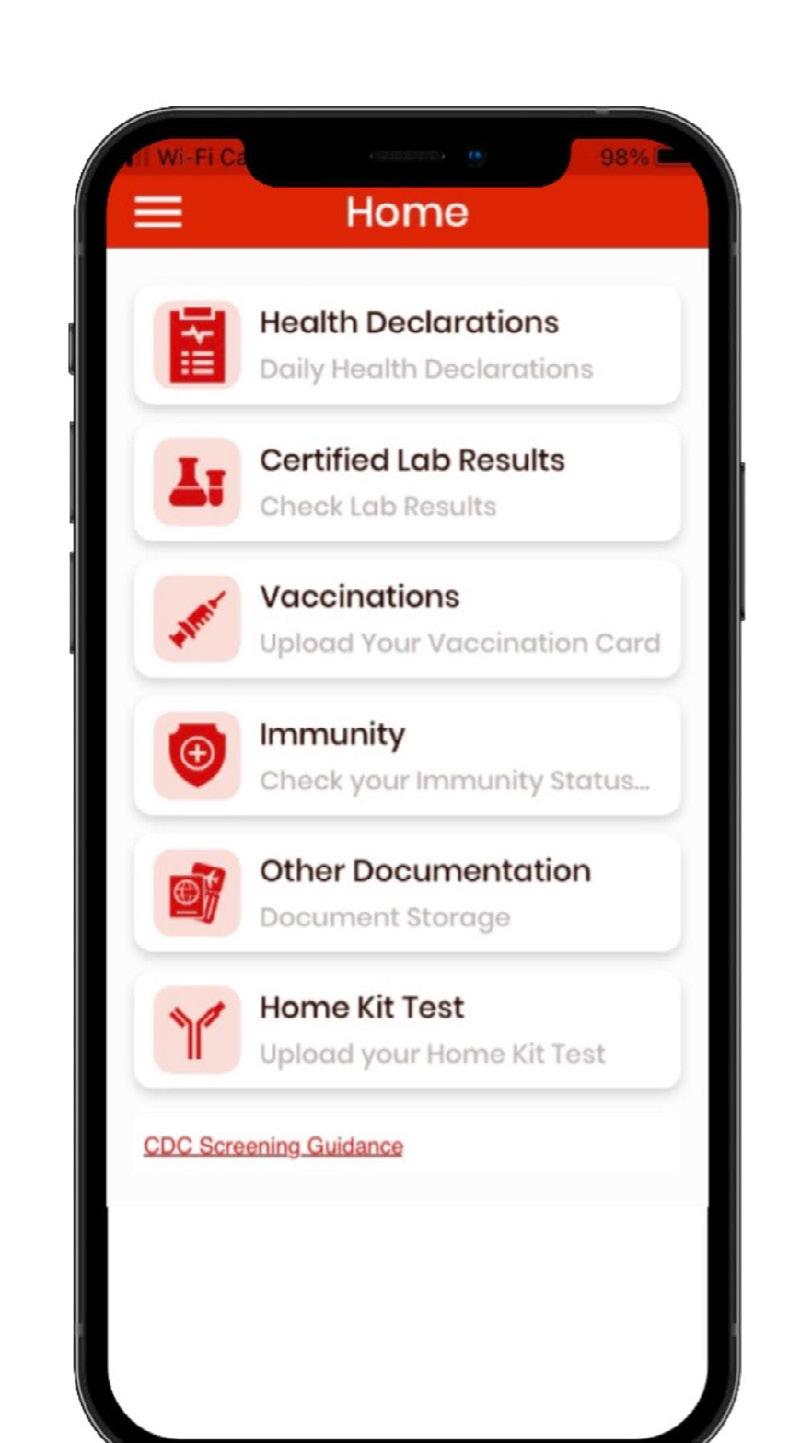
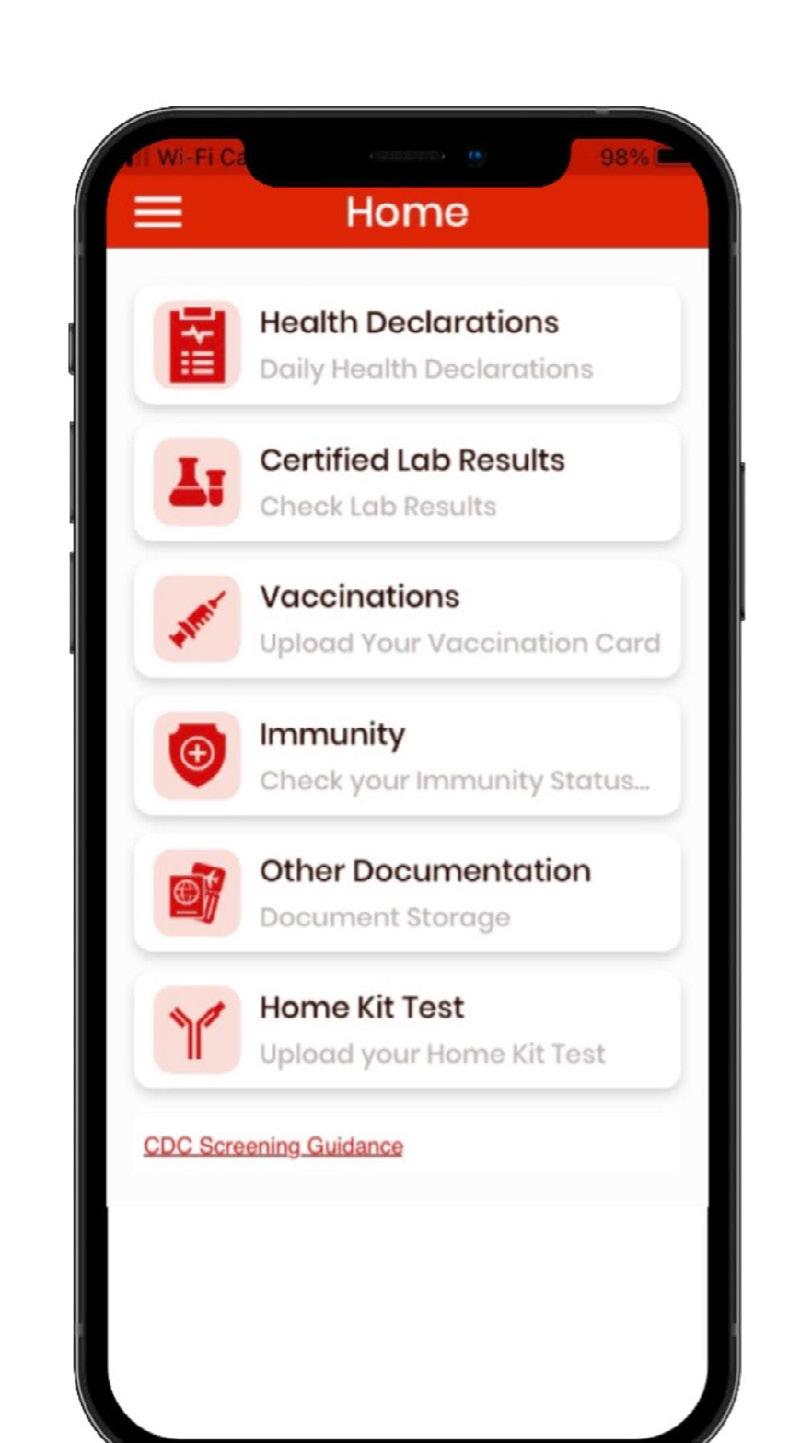
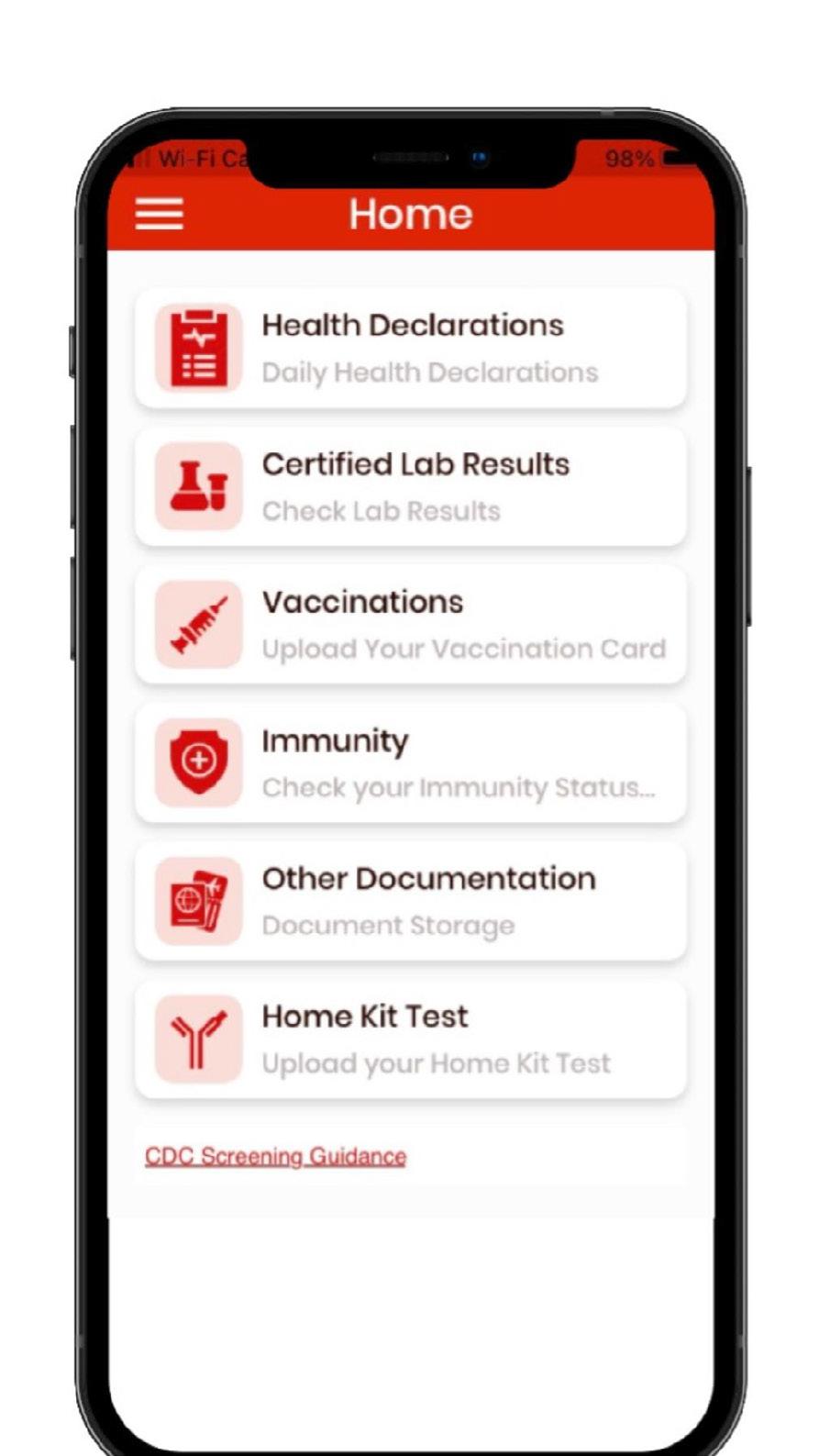
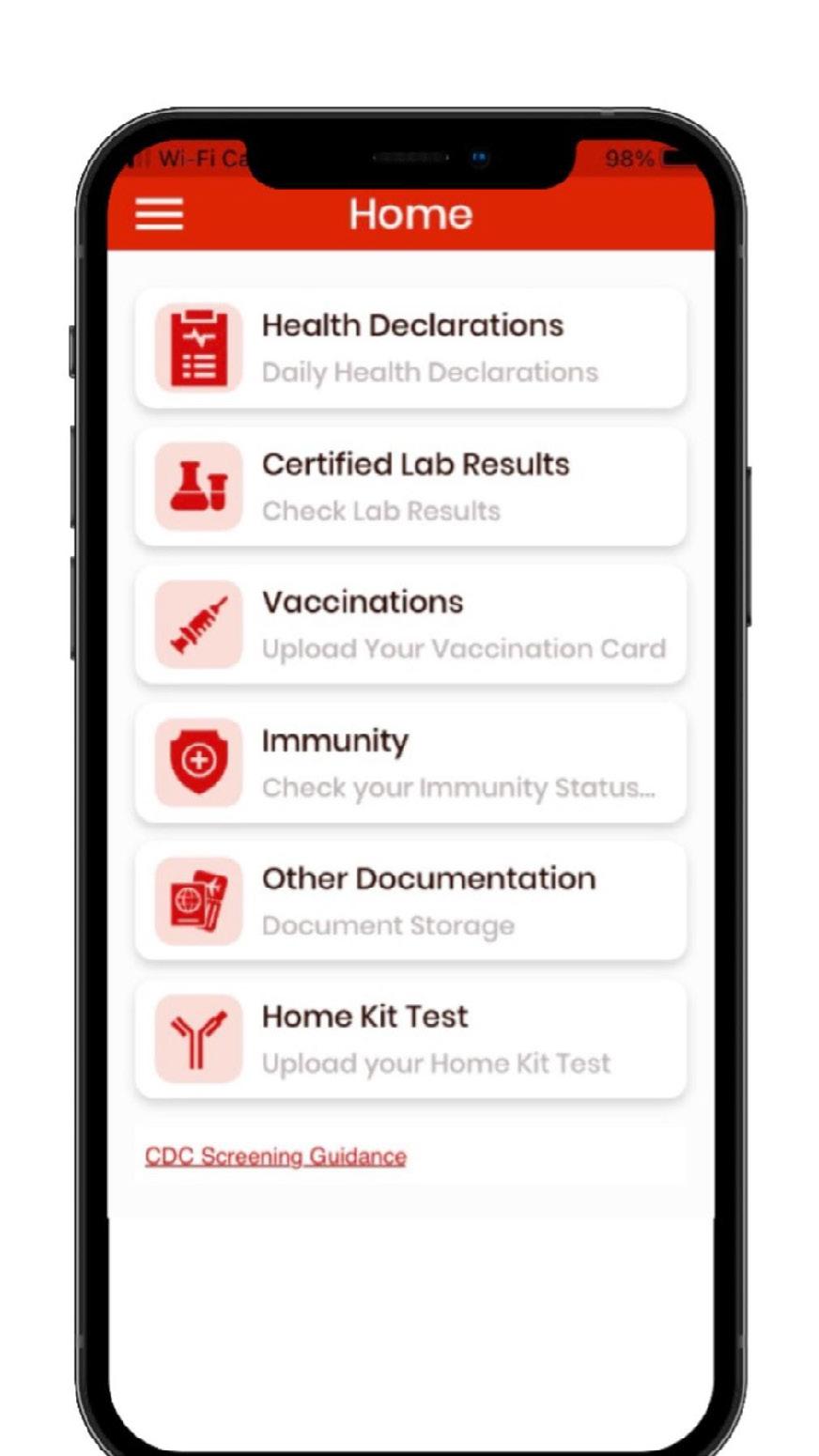
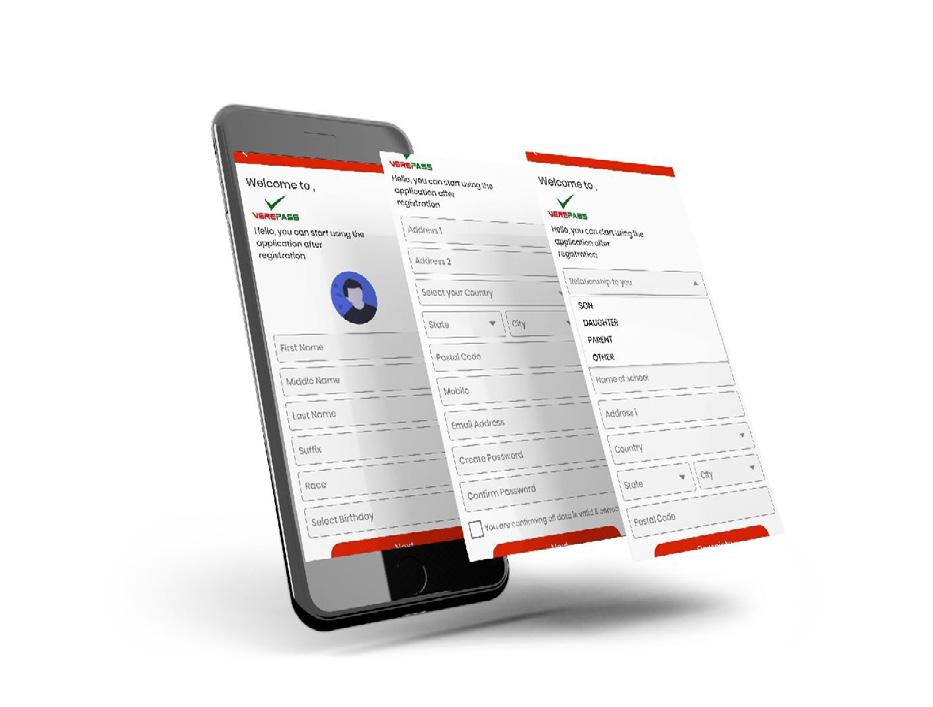
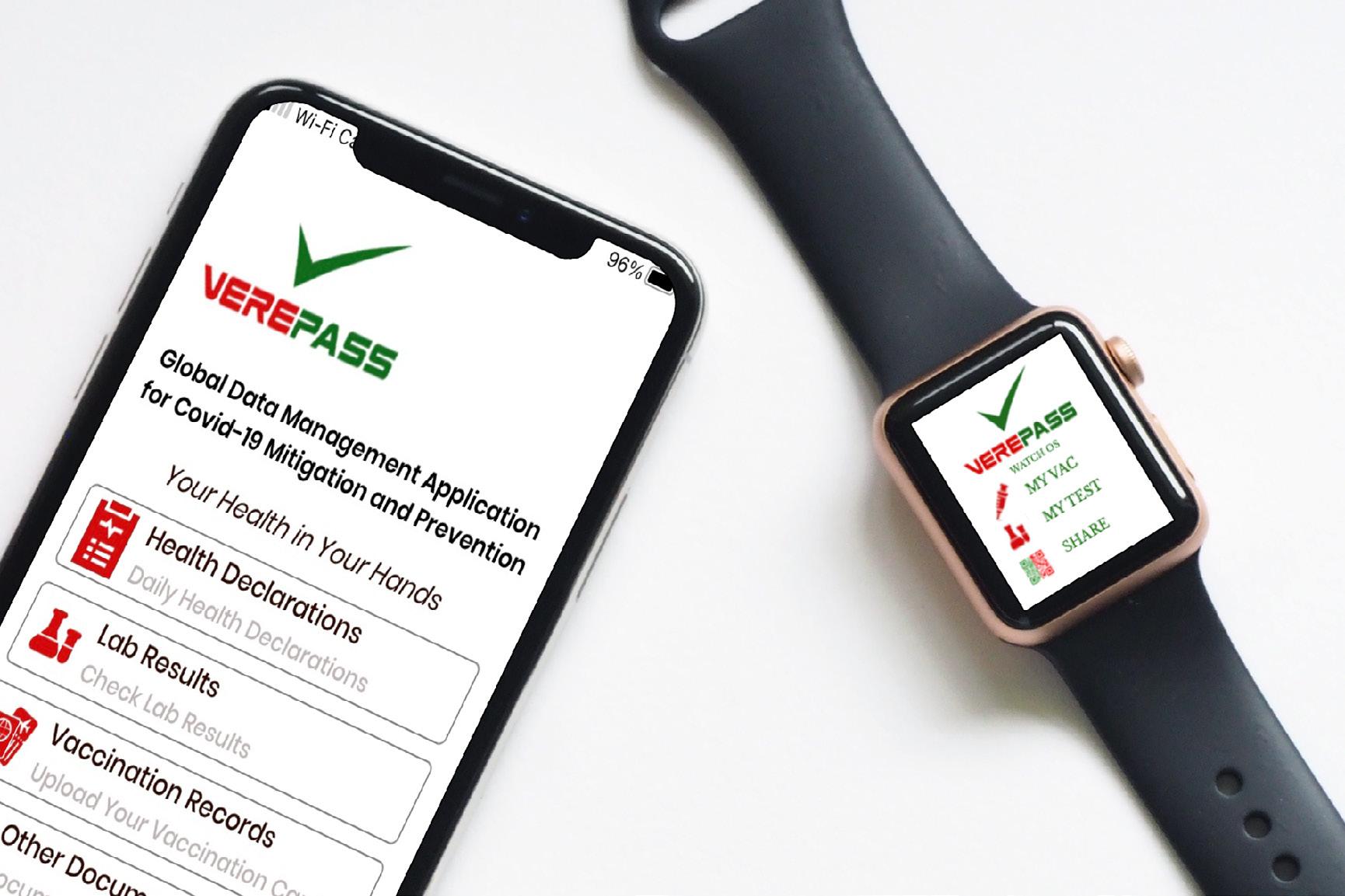
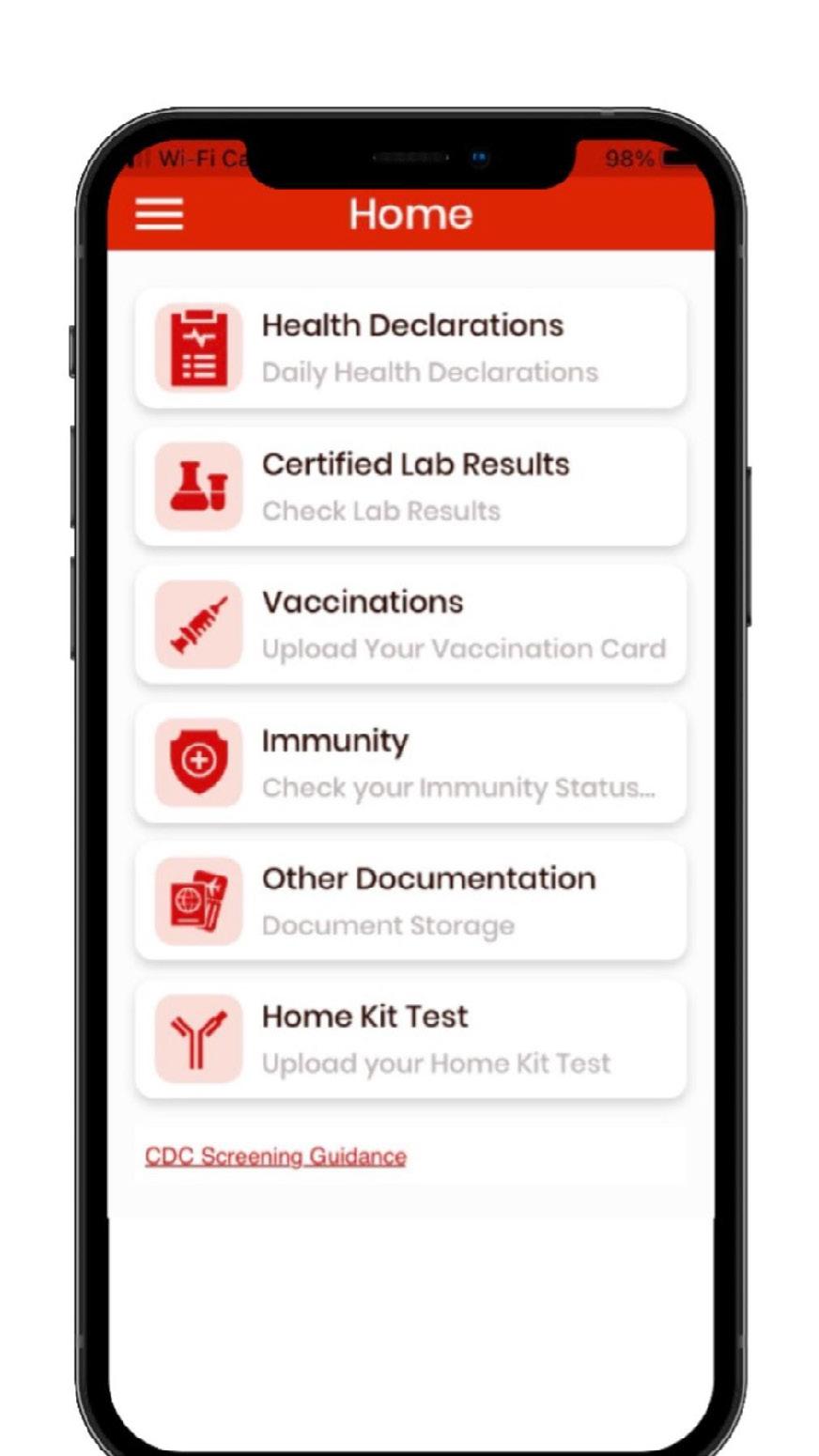
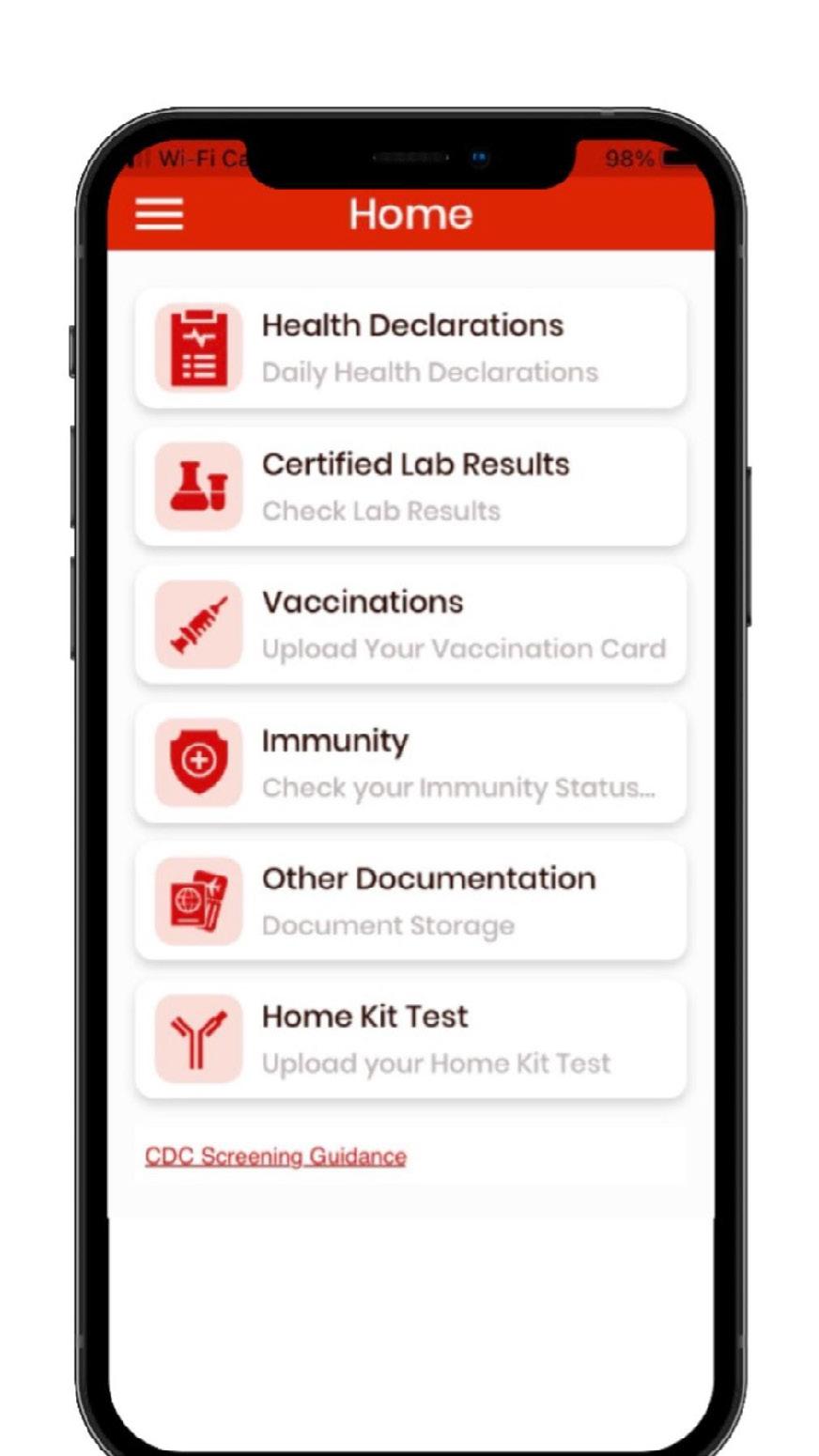
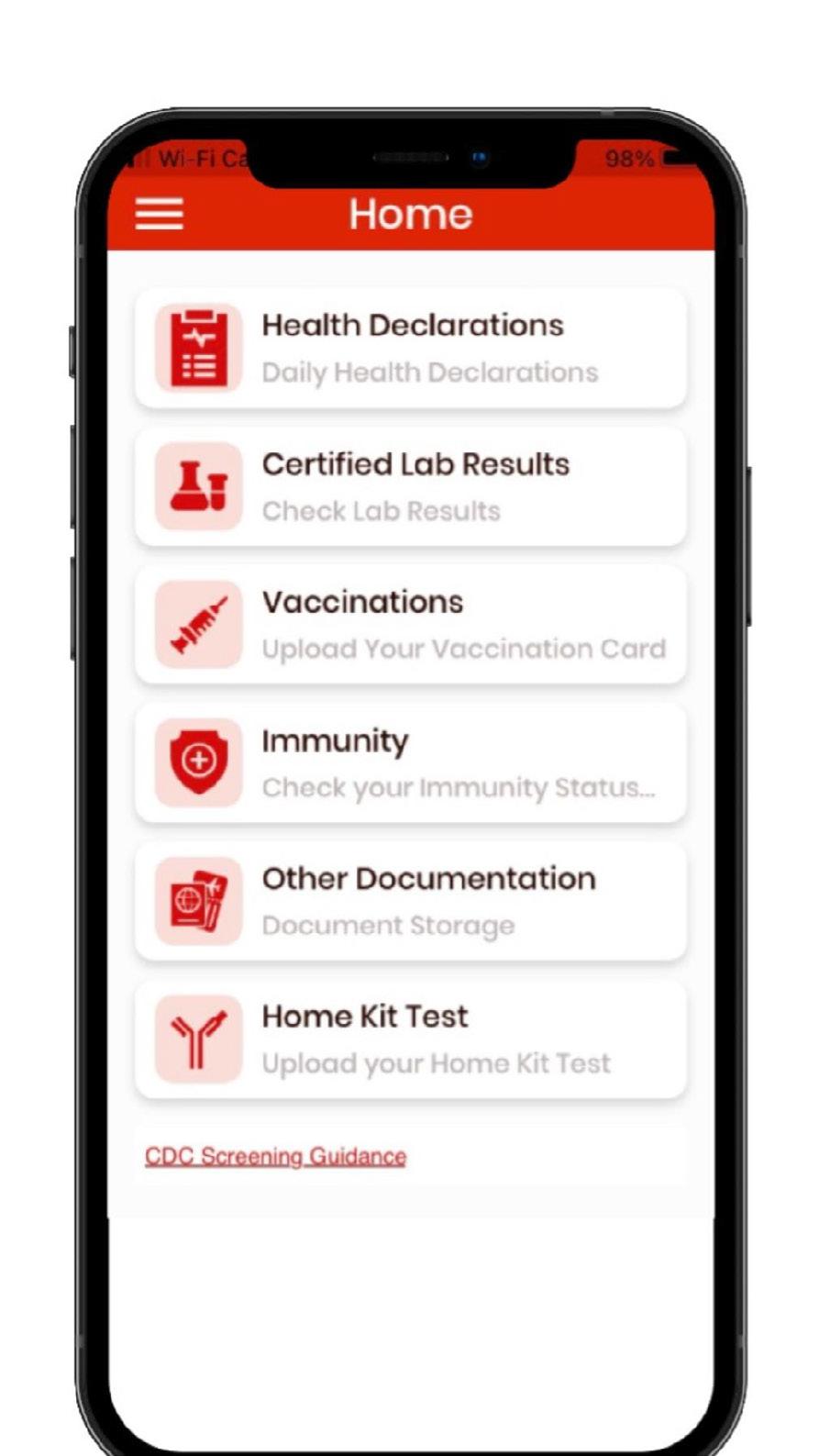
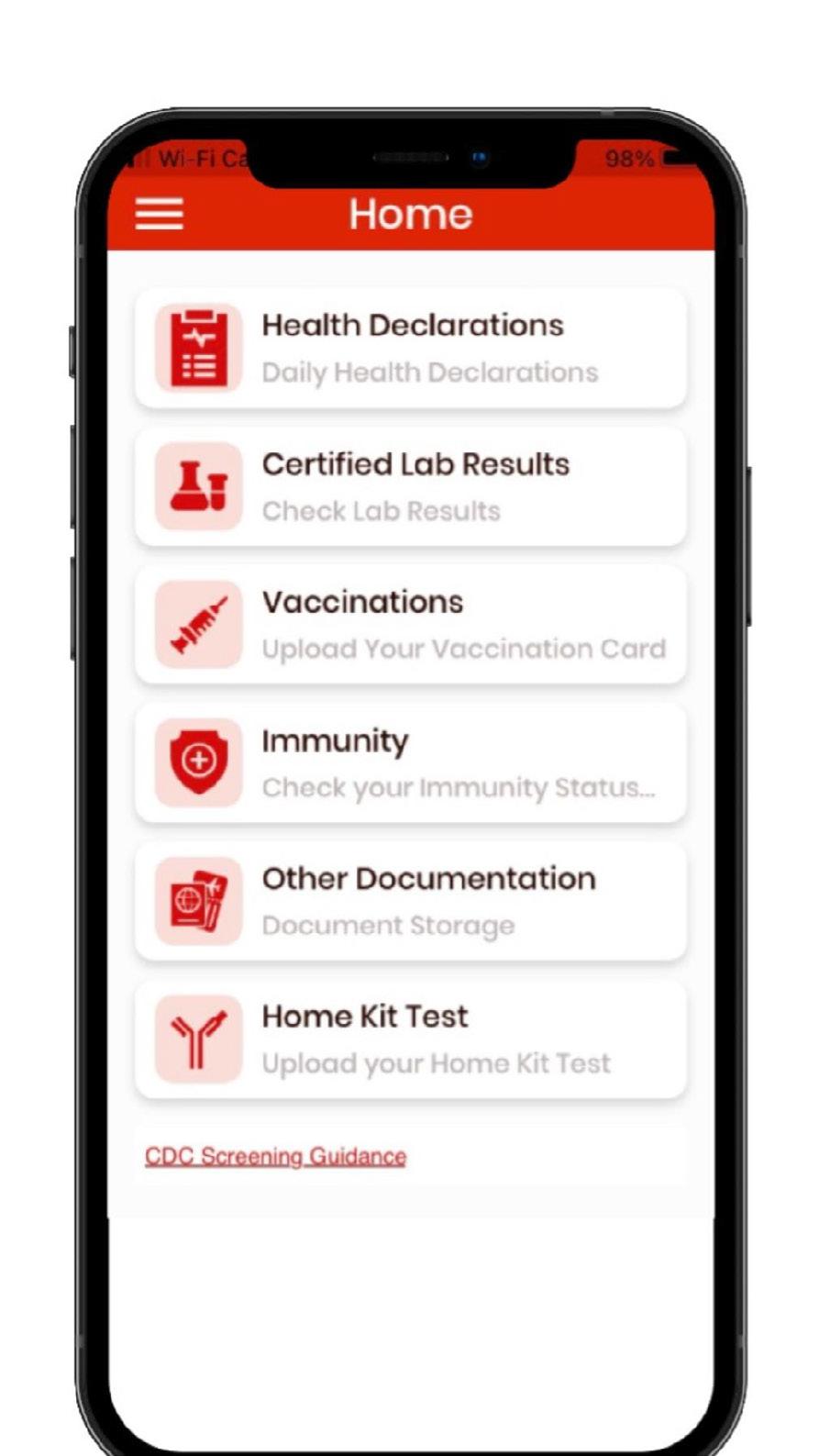
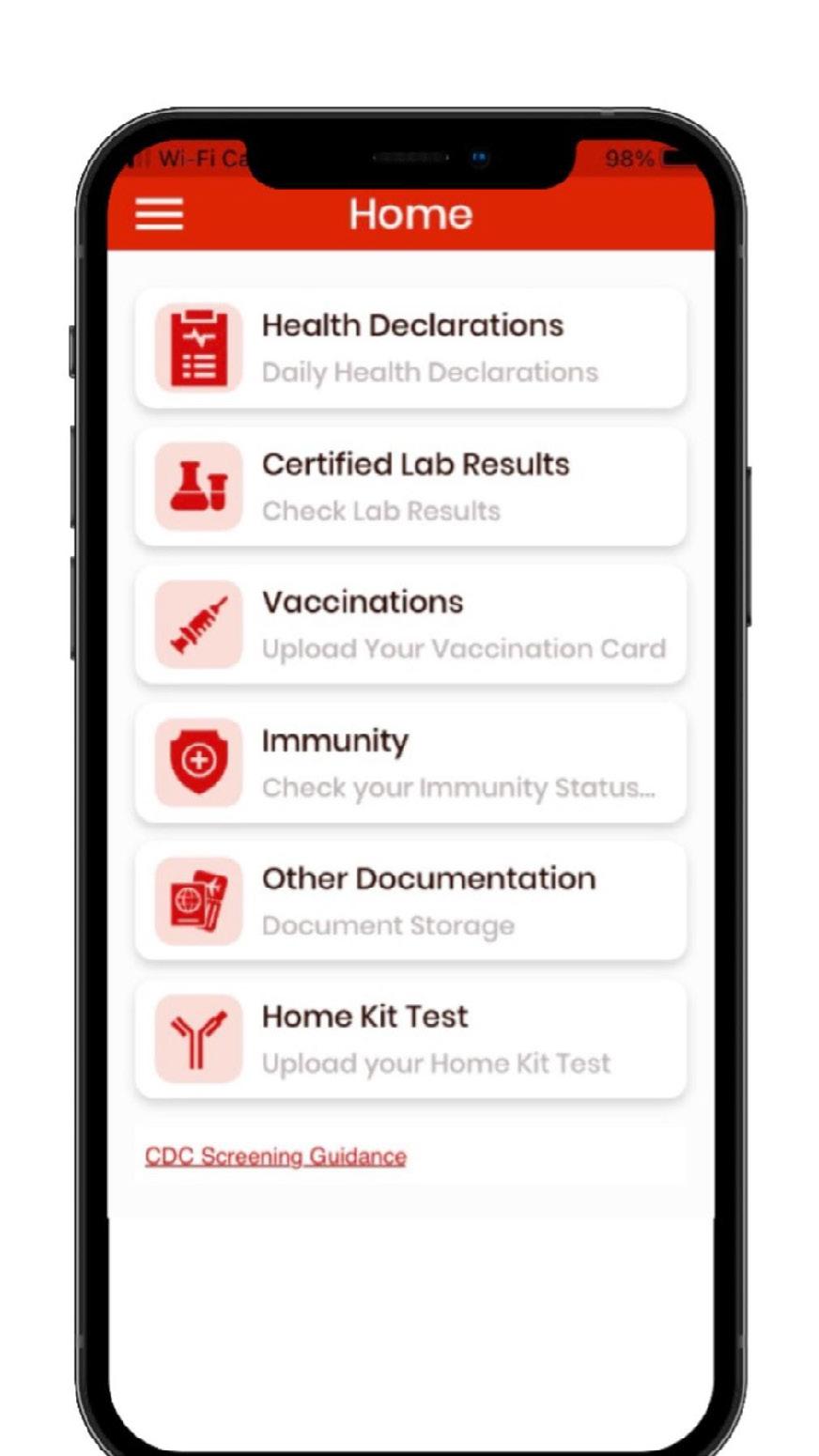
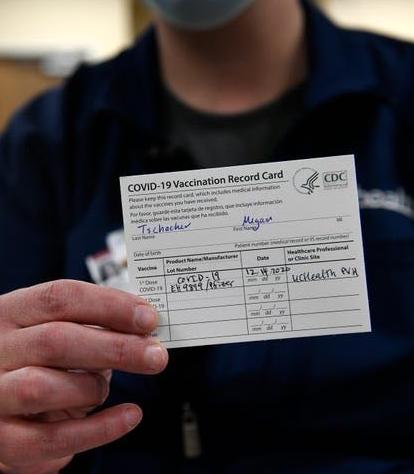
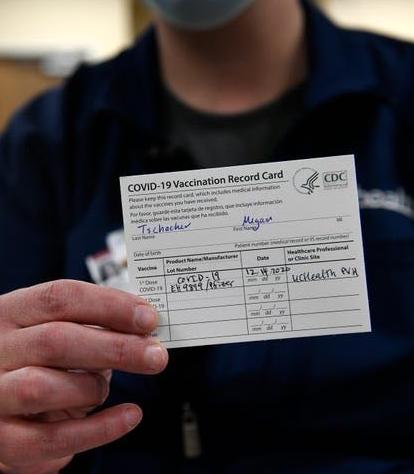
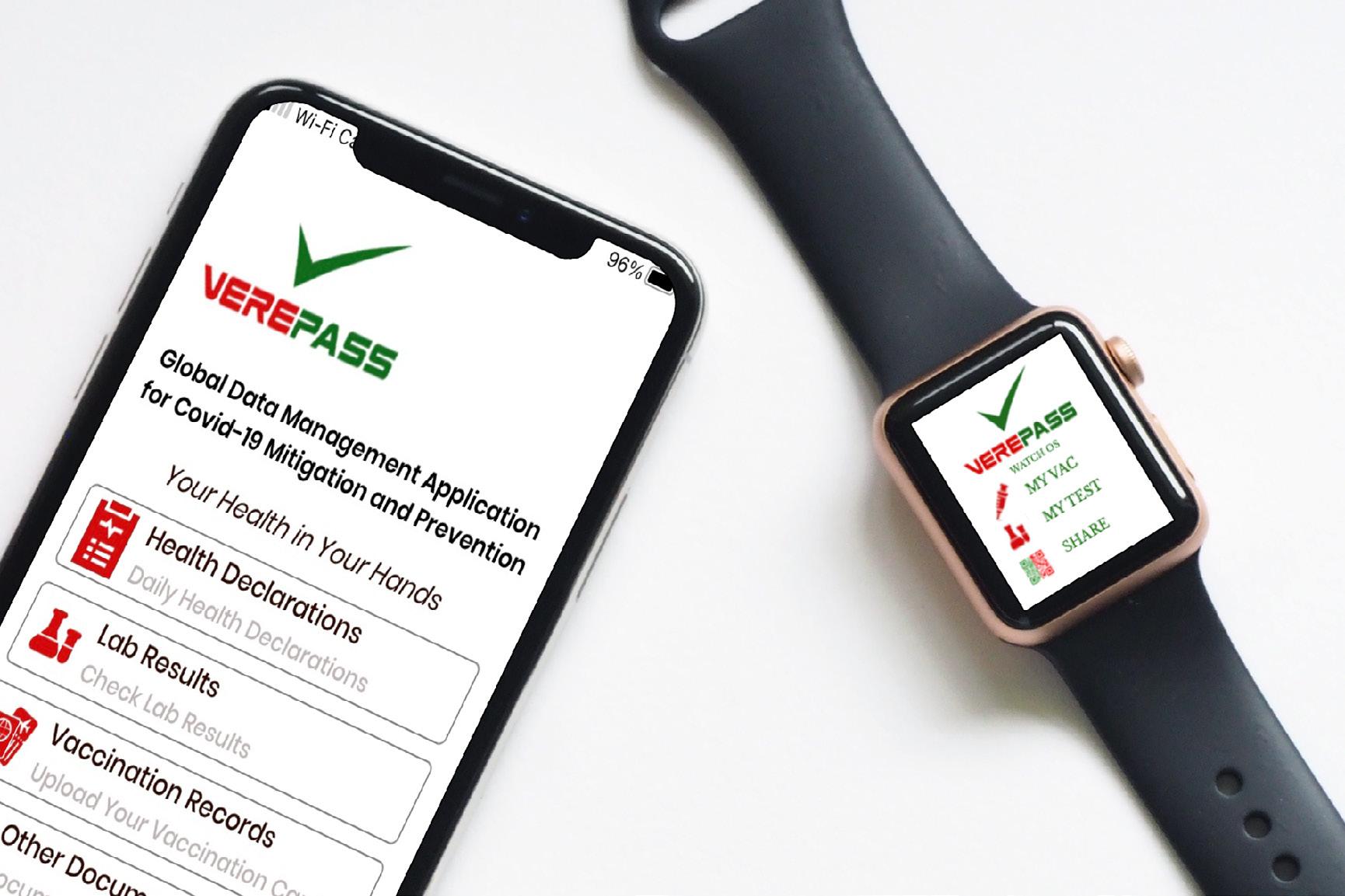
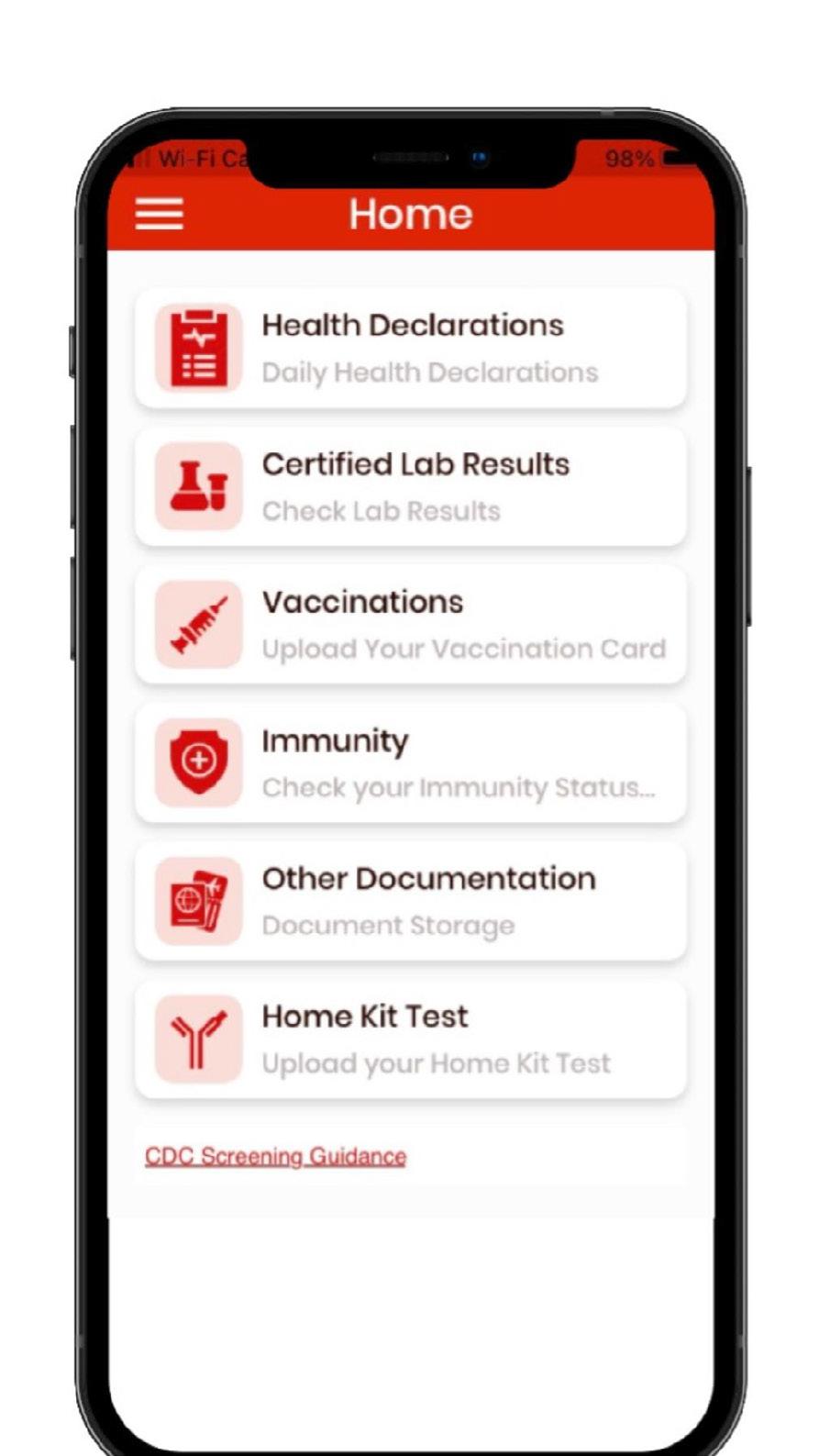
Full Suite of COIVD-19 related services
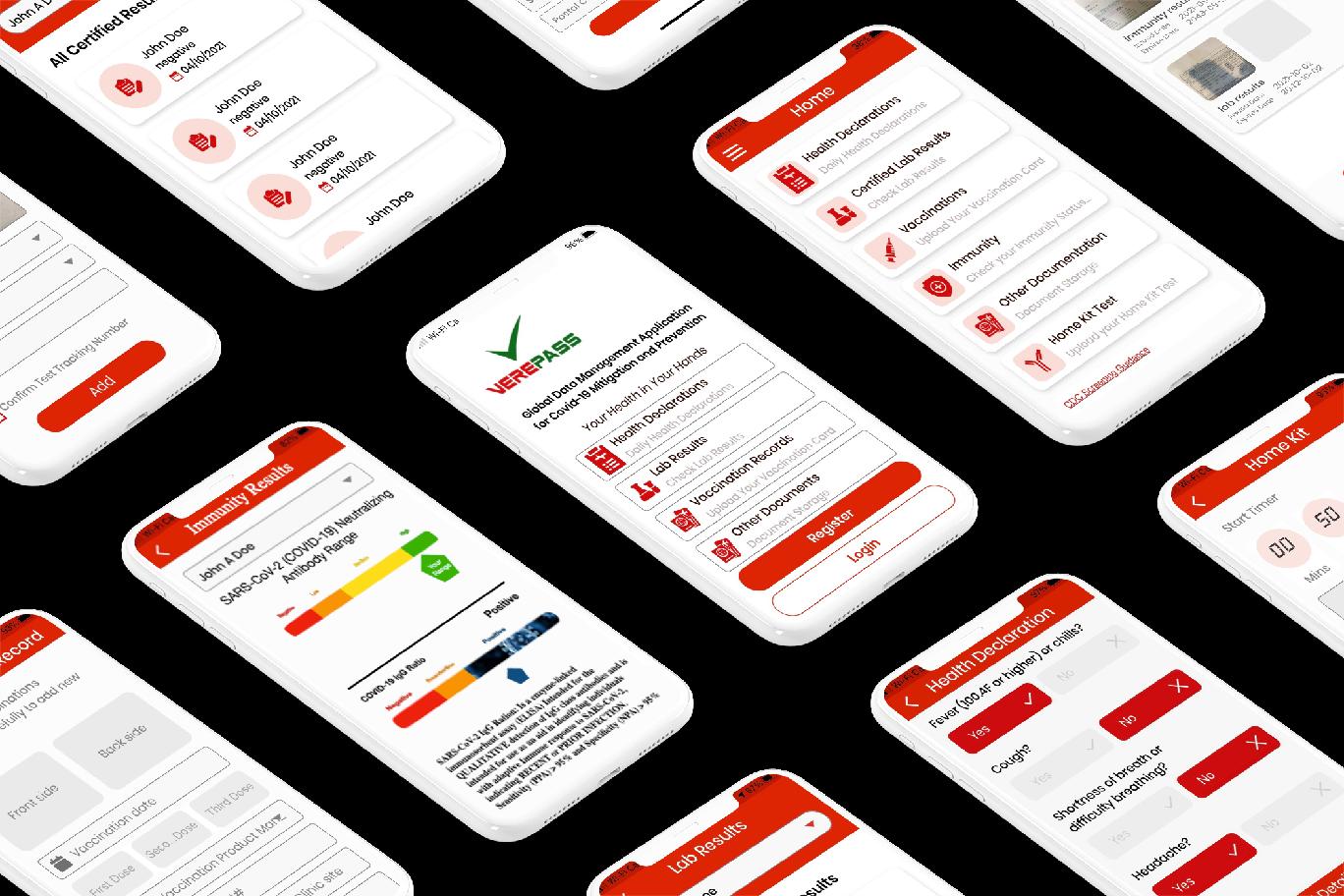
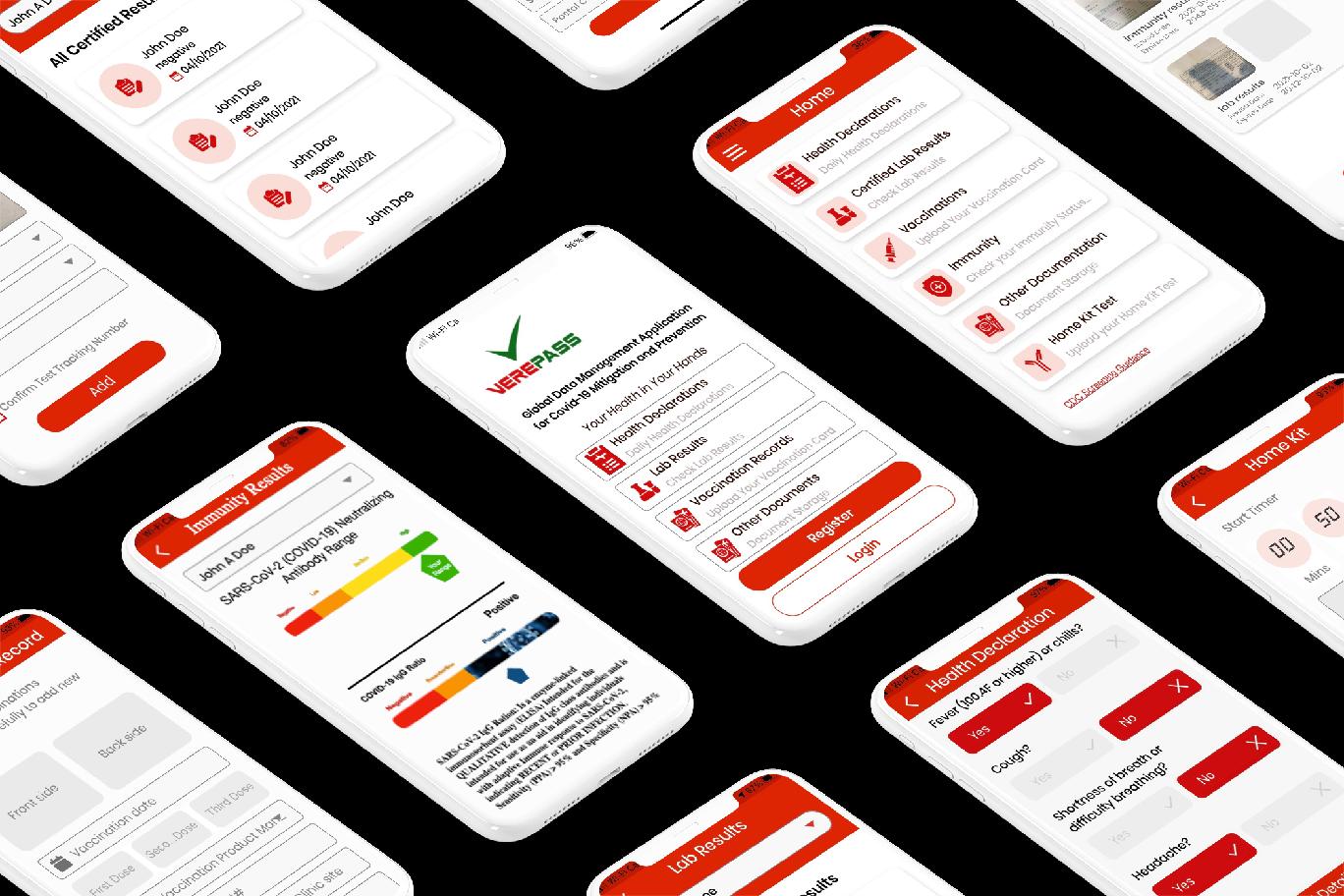


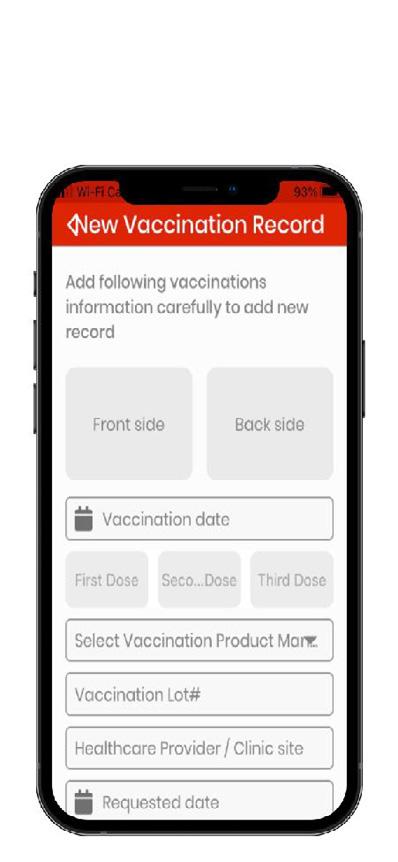
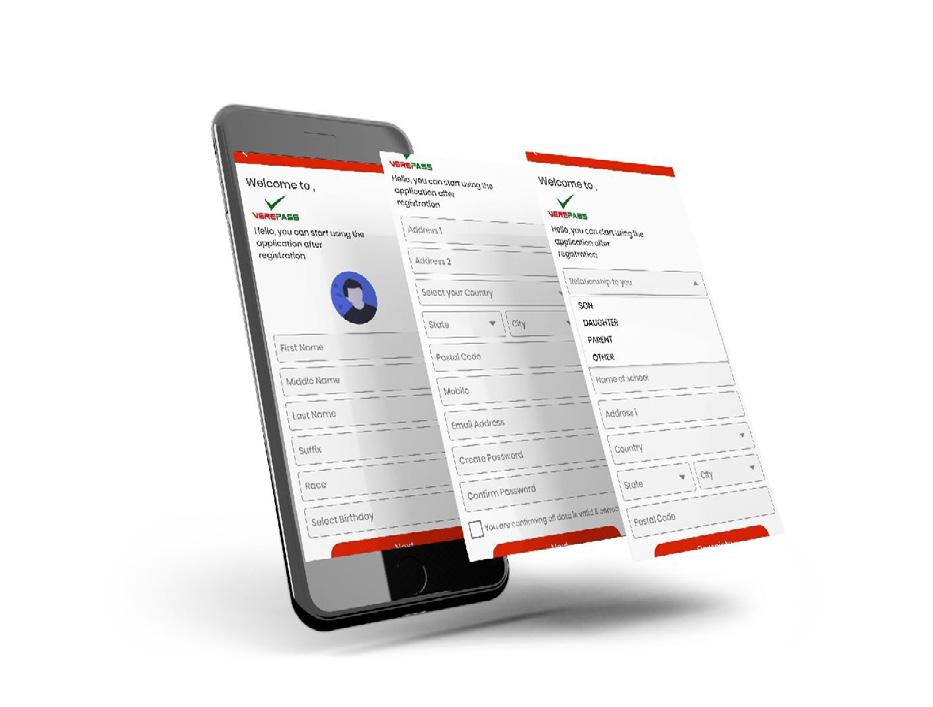
What is Verepass
Full Suite of COIVD-19 related services erepass
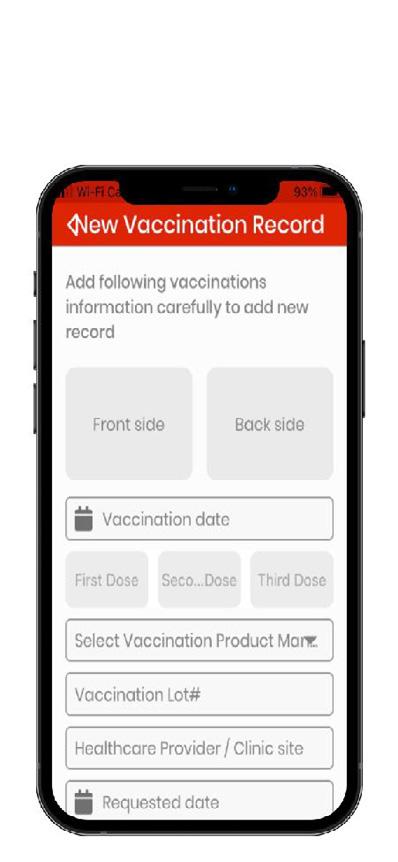
The only approach to ensure and comply with all COVID mandates
The only approach to ensure and comply with all COVID mandates
is a never-before-seen revolutionary global application that includes simple ease of use features to help you use your data effortlessly and enjoy life safely.
is a never-before-seen revolutionary global application that includes ortlessly and enjoy life safely.
expedites turnaround times of COVID-19 test results and allows large population customers, including municipalities, state and federal governments, universities, corporations, and others, to manage their COVID-19 compliance and health of their entire workforce, constituent, student, or customer populations.
expedites turnaround times of COVID-19 test results and allows large population customers, including municipalities, state and federal governments, universities, corporations, and others, to manage their COVID-19 compliance and health of their entire workforce, constituent, student, or customer populations.
is a mobile application (Android & IOS) as well as a Progressive Web Application (PWA) which means no matter where you are, users will always have access
is a mobile application (Android & IOS) as well as a Progressive Web Application (PWA) which means no matter where you are, users will always have access
is HIPAA, ePHI and GDPR compliant.
the only application which validates a users vaccine strength and durability for antibodies (validating vaccine compliance) and informed booster
the only application which validates a users vaccine strength and durability for antibodies (validating vaccine compliance) and informed booster

Version 1.0
Version 1.0


Vaccination Record Management
Vaccination Record Mangement
Your card is always with you
Vaccine Validation
Vaccine Durability
Vaccine Strength
Understand your vulnerability










pass
life safer & easier Aids in Recovery Opens Business Travel Testing Verepass A Full Suite of services to understand and mange your COVID-19 Risk. verepass.com
Makes
pass
life safer & easier Aids in Recovery Opens Business Travel Testing Verepass A Full Suite of services to understand and mange your COVID-19 Risk. verepass.com
Makes
28 | 2022 VOLUME 10
Record Mangement
always with you
Validation
Durability
Strength
vulnerability
Verepass

Verepass
Verepass
Verepass
Verepass
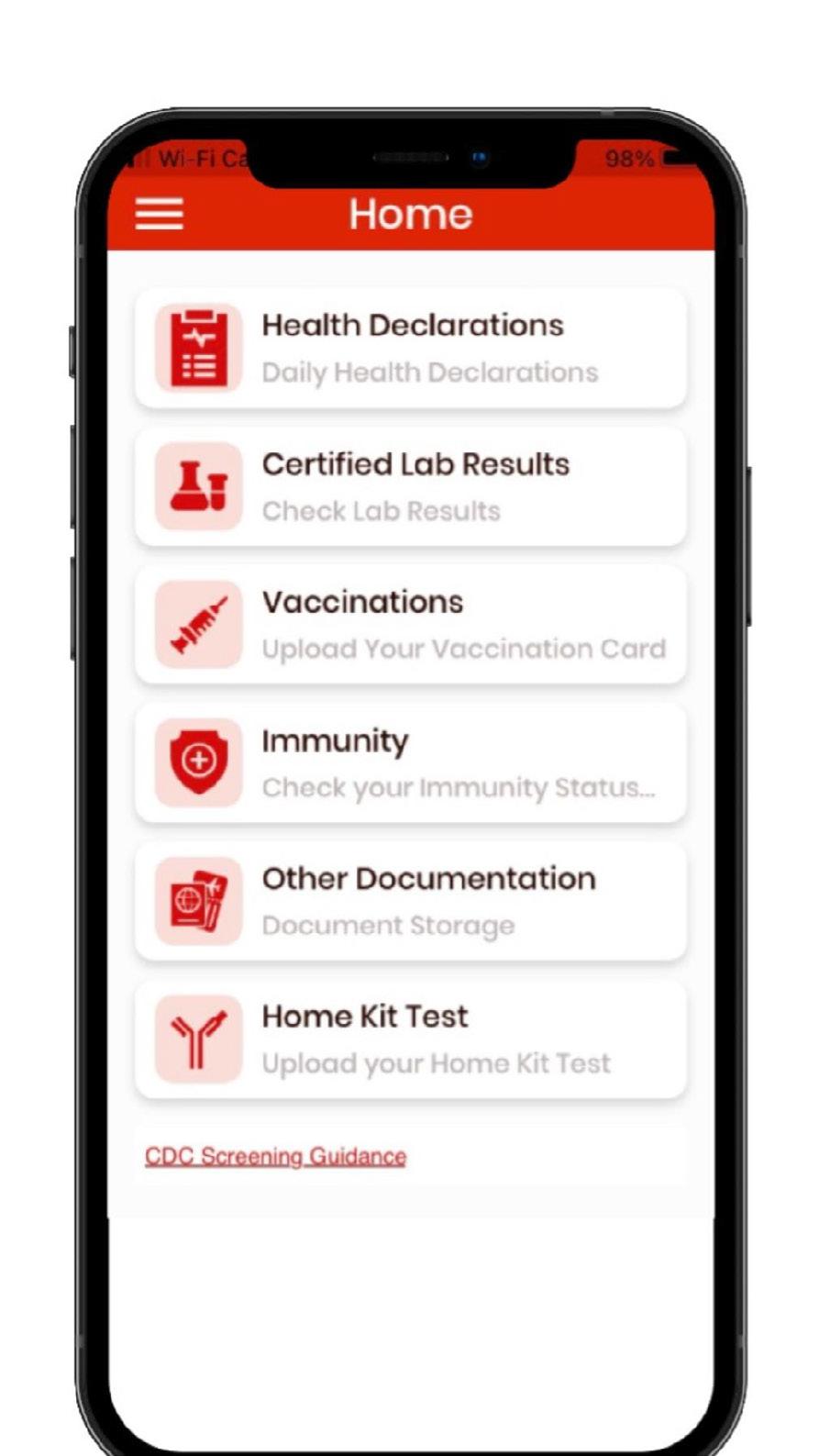
Daily Health Declaration
Daily Health Declaration
Certified Lab Results Rapid
Track & Monitor COVID like Symptoms
Track & Monitor COVID like Symptoms
Vaccination Management
Vaccination Management
Vaccination Records Always Available
Vaccination Records Always Available
Verepass
Built-in Health Algorithms
Built-in Health Algorithms
Early Identification of Possible Exposure
Early Identification of Possible Exposure
All of Your Lab Results

Email, QR-Code, Print
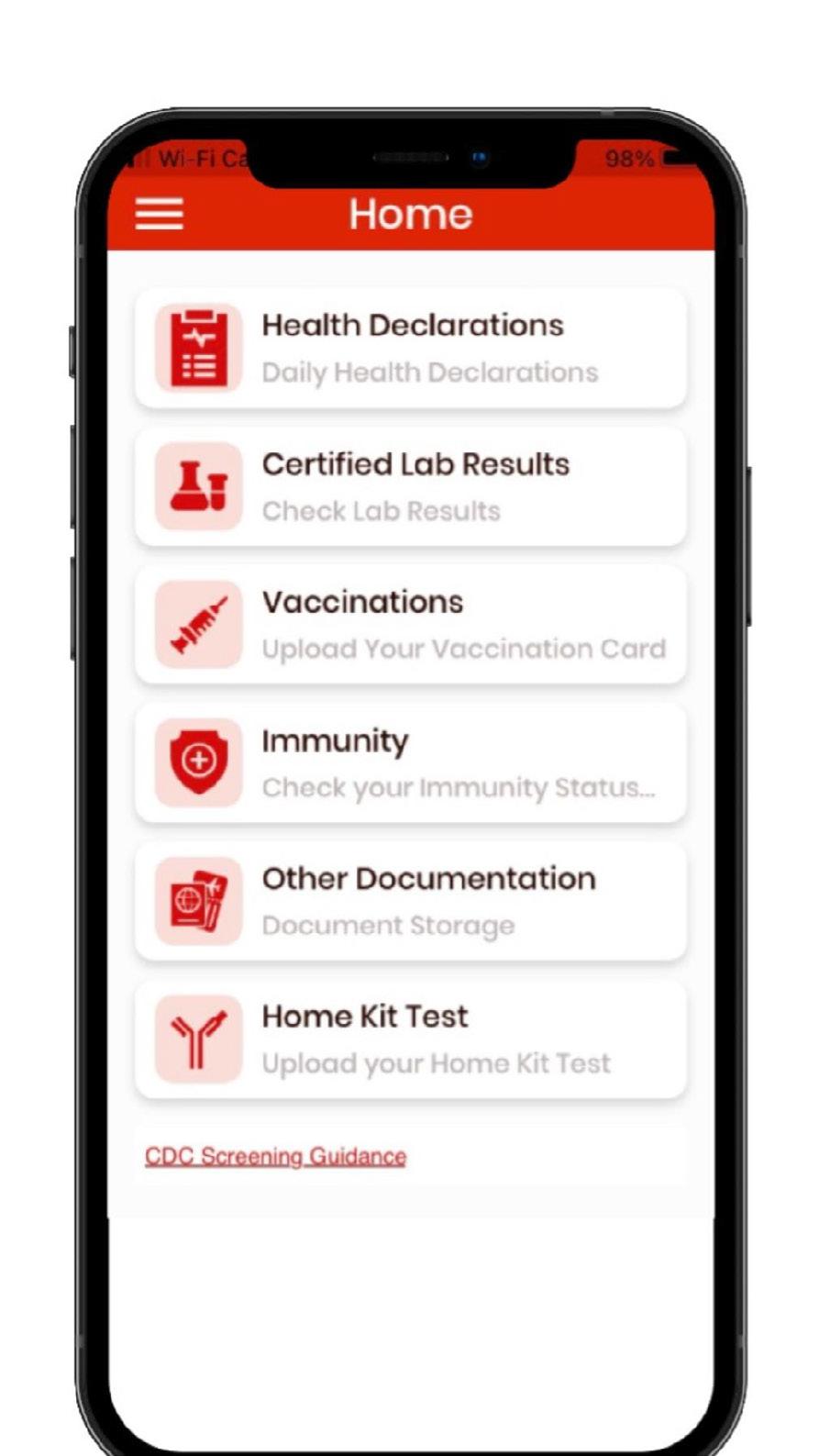
Email, QR-Code, Print
Email, QR-Code, Print
Verepass
Built-in Vaccine Management Algorithms
Built-in Vaccine Management Algorithms
Daily Health Declaration
Email, QR-Code, Print
Email, QR-Code, Print
Self Declaration Application

Self Declaration Application


Schools
Emergency Use Authorized (EUA)
Universally Accepted GOLD STANDARD
Verepass
Home Tests





All Verepass Test provide Self Collection
Rapid Antigen Test Results Certified in 30 mins
PCR Test Results < 24 hrs from SHIPPING
All Verepass testing Insurance Reimbursable
Email, QR-Code, Print


“Test when you want.”

Track & Monitor COVID like Symptoms
Vaccination Management
* Meets or Exceeds Vaccine Requirement Proof
* Meets or Exceeds Vaccine Requirement Proof
Vaccination Records Always Available
“Your Card is Always With You”
“Your Card is Always With You”
Email, QR-Code, Print
Built-in Health Algorithms






Early Identification of Possible Exposure



Email, QR-Code, Print


Self Declaration Application Schools







one set of login credentials across
Add & Manage Multiple USERs


“Your Card is Always With You”
Built-in Vaccine Management Algorithms
* Meets or Exceeds Vaccine Requirement Proof
ss
ss
Other Documents
Other Documents

ss
Other Documents
All of your COVID documents
Work COVID Policy cation
Email, QR-Code, Print
Treatment Record (Prior/Post COVID)
Coming
Antigen PCR
Rapid Antigen PCR
ften or when
Travel Schools Business Entertainment
Test o
needed
Fire Department Coffee

I was a Damage Controlman in the Navy which is the rate that trains the ship in firefighting and works to maintain the firefighting equipment. I was always fascinated by medicine. When I got out of the Navy, Rockford Fire hired me and trained me as a paramedic. I memorized my SMO’s, Standing Medical Orders, front and back so that I could make quick and confident decisions in the field.
I always thought if someone was calling us to help them in a medical emergency, I wanted to do everything possible to help. The medical field can sometimes require you to think fast with little time to decide. It’s an opportunity to help someone in what can be the scariest time in their life, from the first responders to the ongoing care. I’m thankful for all those who answer the call to take care of someone and do their best to give the person the best chance for a positive outcome that could change their lives and those around them.
Luke Schneider
CEO
|
FOUNDER FIRE DEPT. COFFEE
811 W Riverside Blvd., Rockford, IL 61103

HIGH-QUALITY, HANDCRAFTED COFFEE, RUN BY FIREFIGHTERS.
HIGH-QUALITY, HANDCRAFTED COFFEE, RUN BY FIREFIGHTERS.
Each small batch of Fire Department Co ee is freshly roasted in the U.S.A. Enjoy our range of roasts, from our family to yours.
Each small batch of Fire Department Co ee is freshly roasted in the U.S.A. Enjoy our range of roasts, from our family to yours.
Fire Dept. Co ee gives back to help sick and injured firefighters.
Fire Dept. Co ee gives back to help sick and injured firefighters.
16 | 2022 VOLUME 10
RAISE A MUG FOR OUR FELLOW FIREFIGHTERS
FIREDEPTCOFFEE.COM
RAISE A MUG FOR OUR FELLOW FIREFIGHTERS
FIREDEPTCOFFEE.COM
30 | 2022 VOLUME 10

WWW.PHYSICIANOUTLOOK.COM | 31 I’m the week look Spotlight

A Look at Veteran Medical Debt
Written by Jerry Ashton
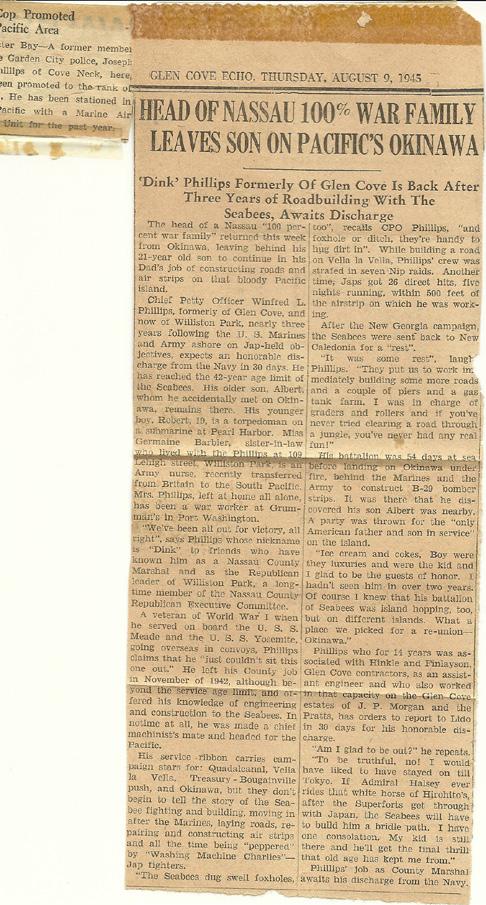
BILLION AND RISING OUR COUNTRY’S VETERANS DESERVE BETTER PHOTO CREDIT: JERRY ASHTON 32 | 2022 VOLUME 10
$6
Oppressive medical debt plagues many Americans--even those who have “good insurance” through an employer. Were you aware that even our nation’s veterans and Active Duty military are carrying a huge amount of unpaid (and unpayable) debt on their backs and shoulders?
We at Let’s Rethink This (LRT) are honored that Physician Outlook is making available its platform –and its audience – to learn more about America’s shame in allowing hundreds of thousands of active duty and veteran users of the VA system to be both financially and emotionally crippled and what to do about it.
And what better, singular group could better relate to the need for this broken system to be rethought than physicians, nurses and concerned members of the healthcare community? Whether you have a role in the VA delivery system or a civilian serving veterans at a public hospital, you are unwitting (unaware?) accomplices in bringing about the $6 billion in unpaid medical bills that the VA has refused to pay…or forgive…up to this point.
Sorry, kid. You fixed ‘em. The VA broke ‘em. Who is responsible for the “do no harm” part?
By The Numbers
Currently, there are fewer than 4,500 active-duty physicians tasked with overseeing the healthcare needs of America’s 1.4 million active duty, 330,000 members in the reserves and/or retired along with a veteran population of approximately 18 million. This takes place at 1,293 healthcare facilities, including 171 VA Medical Centers and 1,112 outpatient sites. The annual budget is $50 billion.
According to USA Today, of those 18 million veterans, more than 5 million veterans have at least one

disability, 1.2 million live in poverty, and 77% of veterans aged 18 to 64 are employed or looking for work. At the end of 2018, an estimated 37,878 veterans were homeless.
How can any of this be?
Military veterans, contrary to popular misconception, do not get free healthcare from the Dept. of Veterans Affairs. If a health issue isn’t related to military service or is not the result of their being more than 50 percent disabled – the vet can be held responsible for co-pays.
If the veteran has the misfortune of requiring the services of a civilian hospital emergency ward for a non-service-related injury or illness, they are also on the hook as they might need to meet a deductible or pay co-insurance – or did not get a pre-authorization to get service in a non-VA setting. If as a civilian, you feel you are dealing with uncaring insurers – try jumping through military hoops!
For example, in 2019, a federal appeals court in Virginia ruled that the VA would be required to reimburse veterans for $6.5 billion in unpaid emergency medical bills.
Good luck on that happening anytime soon. If ever.
What to do?
Lots, starting now. This is just the first shot across your consciousness prow. Visit www.endveteranmedicaldebt.com. Check out “Our Newspaper” at LRT for the latest news, articles and interviews.
Want a free copy of my chapter titled “No Thank You for Your Service” in the recently released End Medical Debt: COVID Recovery Edition to deep dive into the problem? Write me personally: jerry@letsrethinkthis.com ☤
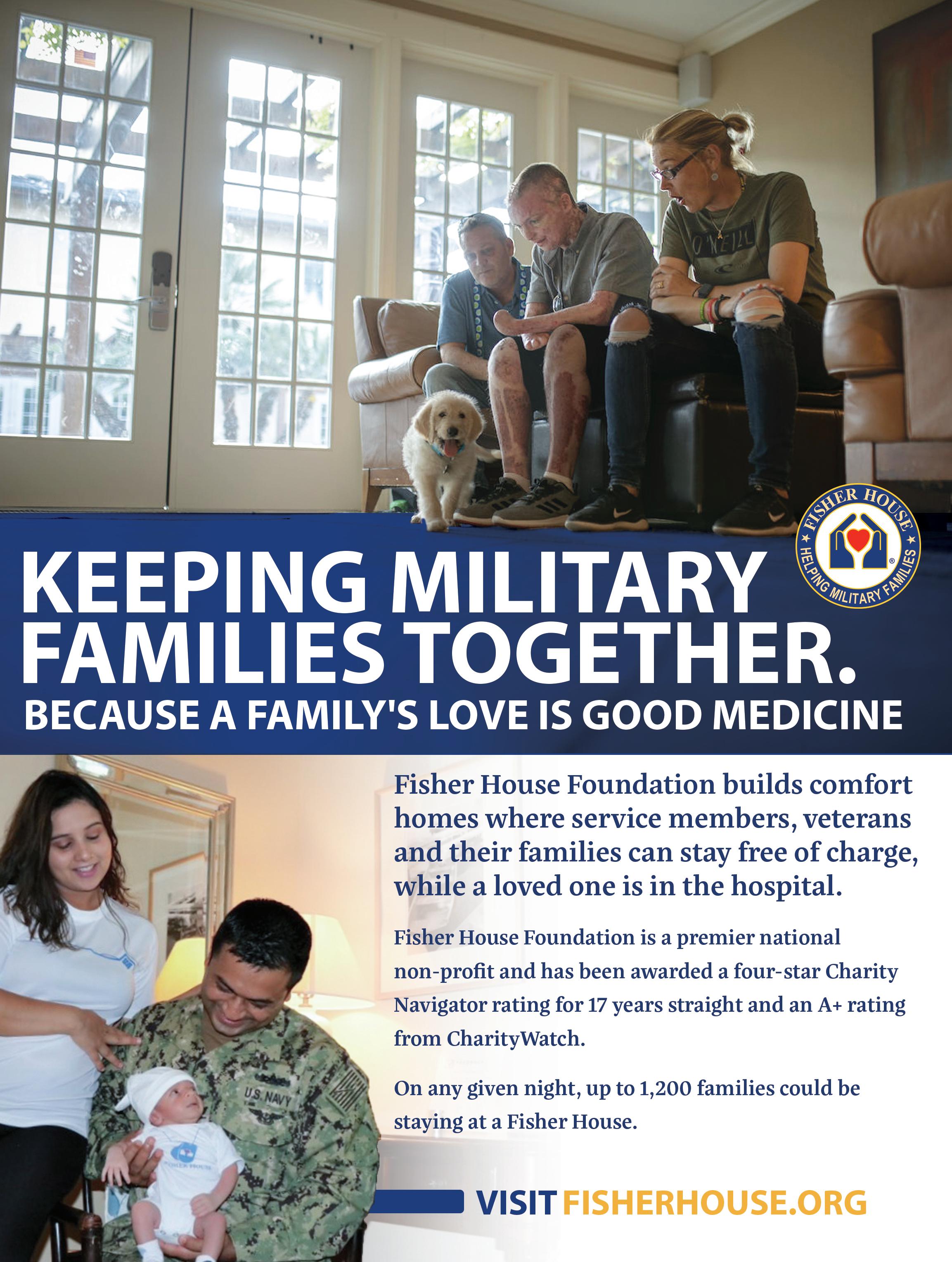
A Home Away From Home for Military Families
FISHER HOUSE FOUNDATION
Written by Madison Smith, PSU’22

For the past 3 decades, the Fisher House program has provided “a home away from home” for families of patients receiving medical care at major military and VA medical centers. These homes offer completely free, temporary lodging to Military and Veterans’ families, allowing them to be close to their loved ones during a medical crisis and focus on what’s important—the healing process.
As of March of 2021 there were 91 Fisher Houses located in the United States, Germany and the United Kingdom. 27,000 families were served in 2021 (since inception in the 1970’s FHF has served more than 430,000 families).
Fisher Houses range in size between 5,000 and 16,800 square feet, and have 7 to 21 private suites that are professionally furnished and decorat-
ed to accommodate anywhere from 16 to 42 family members at a given time. Fisher Houses feature common kitchens, dining and living room to encourage families to be able to support one another. Although they have grown in size and square footage, and the number of families that can be accommodated at a given time, each house is designed so that there is a sense of community and support amongst the guests and staff who are all in desperate need of peaceful rest and respite from the stress of their loved one’s illness, injury or death.
Once construction is completed, the Fisher House Foundation gifts the Fisher Houses to the Department of Defense and the Veterans Administration, who co-manage the Houses.
Fisher House Foundation has several other major programs:
Hero Programs—Allows donated frequent flyer miles and hotel points to be used to bring family members to the bedside of injured or ill service members. Over 70,000 airline tickets provided by Hero Miles to service members and their families (worth nearly $105 million). For times when a Fisher House is unavailable, the Hotels for Heroes program steps in and provides hotel rooms for families eligible to stay in a Fisher House using donated hotel points. Fisher House partners with Hilton, Wyndham, Marriott, Choice and Best Western hotel chains.
Chairman’s Award—in partnership with the Military Times Foundation, the Fisher House Foundation annually recognizes innovative programs for military and veteran communities, awarding $250,000 that is divided among the top applying nonprofits. Each award winner also receives an advertising package from Military Times valued at $30,000.
Scholarships—A grant program that provides scholarships to children and spouses of military families, as well as the children of fallen and disabled veterans. 15,000 students have received $27,000,000 in scholarship awards.
Physician Outlook Magazine is proud to be working with the Fisher House Foundation, providing complimentary advertising and amplification of the good work that they do for our nation’s heroes. We will be featuring some of the families that have been served in future issues and online. ☤
For more information, and to make a tax-deductible contribution (cash, miles, hotel points), visit www.FisherHouse.org or contact them at:
Fisher House Foundation
12300 Twinbrook Parkway, Ste. 410 Rockville, Maryland 20852 888-294-8560 info@fisherhouse.org
34 | 2022 VOLUME 10
PHOTO BY BERMIX STUDIO ON UNSPLASH

UNDERAPPRECIATED HEROES
Bedside
NURSES ARE THE HEART OF HEALTHCARE
Written by Linda Hodges, D.O.., Intensivist
RNs--WE Need You
ARTWORK BY KAITLIN WALSH 36 | 2022 VOLUME 10
As a critical care physician, I would be nearly paralyzed in my job without quality ICU nurses. Could I fumble my way through many situations? Sure. I mean, I’m an expert at pushing the “silence” button on the pumps when they are screaming at me. But, could I make it even half a day without my highly skilled co-workers? Not a chance.
I have so many thoughts about RNs, but let me say that I am 100% biased. In the ICU, the RNs are generally kick-ass. So kick-ass, in fact, that I feel sorrow when I see them leave the ICU for administrative or higher educational aspirations (NP, CRNA, etc). I’ll admit, that may be selfish - I should be happy for anyone to pursue “more” for themselves. But, I see more and more going this route, not to merely pursue higher aspirations, but to escape the grind of the bedside and the micromanaging of their careers.
I can’t help but wonder what nursing would be like if we made the bedside job one that doesn’t need escaping from. (This was an issue BEFORE the pandemic....) I’d love to hear an RN tell me he/she is going to XYZ school because it’s always been a dream....not because “I can’t do this forever.” The great RNs I’ve worked with give of themselves 100% - it’s important to THEM to do the very best they can, to be the most educated they can be at doing their bedside jobs. So, when those same RNs walk away from the bedside as an escape from a malignant system, it’s so sad.
I’ve done a lot of locum work during my career and have had privileges at over thirty facilities. Just in the past two years alone, I’ve staffed five ICUs. The ICU is a unique place because it’s not a unit where casual relationships develop
between physicians and staff. It’s a place where people on every level of the work force come together during times of ultimate craziness to save a life, to get a family member to the bedside before a loved one passes, to ensure medications are obtained from pharmacy as quickly as possible, to track down needed supplies for a bedside procedure, to figure out the most efficient way of doing something that needs to be done for a patient - and, so, so much more. It’s a place where trust is critical and knowing the skills of your coworkers is paramount. However, another crucial aspect of this relationship is knowing the hearts of these nurses - knowing why they do what they do. And, in my eleven years of practicing critical care medicine, it’s become quite clear that the best care is given through
a symbiotic relationship amongst everyone involved with giving that care. Personally, I don’t see how this can exist without truly knowing one another.
In the ICU, an RN that can recognize subtle changes happening within a patient, and know exactly what those changes mean, is invaluable to both the health and outcomes of patients but also to me and the rest of the treatment team. No physician can be everywhere at once, which is why the bedside nurse not only provides care, but also serves as the eyes and ears of the team. And, as with any skill, this severity recognition only gets better with experience.
So, seeing bedside RNs leave so early in their careers saddens me.
Every single place I’ve worked, I’ve seen RNs be denied negotiating power and leave - only to be
ARTWORK BY JACQUELINE PFLAUM-CARLSON


replaced by travel nurses making significantly more than the initial RN was asking for. It is perplexing that any system would let a quality RN leave only to take their chances with a traveling RN who (with the agency fees) is costing the facility significantly more. Don’t get me wrong - I’ve worked with some awesome travel RNs too....But what if there was a system where travel RNs weren’t needed??
What if there was a system that fostered an environment where great bedside RNs were so valued that they’d never WANT to leave the bedside, unless it truly was a dream to pursue another career? We’d have the absolute best, long-career RNs training our younger RNs. We’d have an environment that didn’t require escape....a feeling that is contagious and spreads like wildfire. It seems like young RNs come onto the scene already with the knowledge that it’s not a sustainable, life-long career from the get-go. I realize
this isn’t as simple as I’m making it. Because...the exact same thing happens with physicians and has happened to me.
This is a system problem, not just an isolated facility problem. I don’t pretend to understand the nuances of nursing administration or what goes into these decisions. And, there are a lot of reasons people feel the need to move on. But what I do know is that the sense of not being valued and appreciated leads to more people leaving than anything else....especially when one is giving their all and their intentions are pure of heart. I know this because I’ve worked at a lot of hospitals....and the conversations between the nurses are the same at all of them - literally 100% the same.
I’ve heard dozens of conversations between young RNs in the ICU who were thrown into patient care with suboptimal bedside training. (Not saying it was inadequate training, but certainly
“Kick ass” bedside nurses need to be paid and appreciated more…not replaced by travel nurses
not optimal for a newly certified RN in a high intensity unit.) They comment how they hear about the money their travel colleagues are making and that seems to be the answer to the inevitable burnout. They are tired of administrative overreach at a facility to which they’ve been loyal for years. I hear about flexible scheduling, only to have that flexibility taken away with staffing shortages and passive-aggressive, public comments in meetings about being a “team player” - so they work extra without time for self-care. These are all conversations I’ve heard over and over - from Georgia to Wisconsin. They do not feel heard or valued.
I genuinely hope someday this changes and RNs feel that a bedside career can be rewarding and lifelong, if it’s what they want for themselves. (If they want moreby all means...GO FOR IT!) But, if the decision to leave the bedside is a result of a broken system that promotes burnout and loathing for a job they once loved, it needs looking into. Because I need good beside nurses to do my job optimally. I need my team! ☤

38 | 2022 VOLUME 10


BECOME A MEMBER VISIT FREE2CARE.ORG TODAY!
Dollars And Sins
THE TRUTH BEHIND NPS REPLACING PHYSICIANS
Written by Natalie Newman, M.D., Emergency Room Physician

“Concerning Trends in Primary Care Physician Demand and Compensation.” was the title of the article, and “Merritt Hawkins report shows skyrocketing demand for nurse practitioners while the demand for family physicians dropped.” was the subtitle. This sobering article (authored by Dr. Seger Morris, summarized the fact that physicians ARE INDEED being replaced by non-physician providers).
“Nurse practitioners (NPs) topped the list of Merritt Hawkins’ most requested search engagements for the first time, underscoring the accelerating demand for these professionals. In 27 previous years, the top position has always been held by physicians.”
I submit that the demand is not due to patient requests or necessity, but corporate medicine (backed by private equity) preferentially seeking out and hiring cheaper NPs for positions for which they may not be fully or appropriately qualified….all to save costs and increase profits.
In an article titled “How to Discourage a Doctor,”² author Dr. Richard Gunderman further clarifies more reasons why demand may have increased– because the cor-
40 | 2022 VOLUME 10
PHOTO CREDIT BY CANVA
porate practice of medicine (CPOM) has a specific agenda.
The pandemic conveniently provided the CPOM with a “Eureka” moment; delivering an unexpected opportunity for them to remove physicians from the medical landscape without drawing much attention. Who would question the quality of care for anyone when so many patients with COVID were dying? A great smokescreen for hiding substandard care in other areas.
Additionally, COVID led to a financial boon for the CPOM that has persisted for two years, to their delight. It is also my opinion that the significant majority of patients do not demand NPs, as the marketing campaign, “We Choose NPs” by the American Association of Nurse Practitioners (AANP) would have you believe. Patient choice is almost completely removed in today’s health care scenario. Patients are forced, by the corporate practice of medicine and insurance companies, to take what is given to them while they are gouged financially. Being charged the same price they would pay if they had seen an actual physician rather than a facsimile purported to be “equivalent.” Common sense dictates that when given a choice, laypeople will choose physicians, especially if they are being charged the same for the service.
Primary care physicians (Family Medicine, Internal Medicine and Pediatrics) have the most difficult job in medicine because they manage the entire body and all of its systems. When damage is done to children, it is even more reprehensible. Children are not little adults and they are not always “easy”.
These con artists do their utmost to convince everyone else that NPP (non-physician provider) practice is “just as good” care provided by physicians.

 PHOTO CREDIT: DR. NATALIE NEWMAN
PHOTO CREDIT: DR. NATALIE NEWMAN
Bulls**t.
If it were, they would also use NPPs to provide primary care to their own families and/or children. The majority of them don’t. Their hypocrisy is lost on them. This is the s**t that occurs when ego overrides common sense. When gluttony is prioritized over safety. When one aspires to be a parasitic “Pimp or Ho”² rather than a healthcare professional or executive with integrity.
Bottom line: Primary care physicians are irreplaceable
As with all businesses, when medicine became corporatized, the expectation was to ensure that profits would be plentiful. The Cartel and Pimps needed it to “rain Benjamins.” The higher the net yield, the happier the shareholders. It never was about quality of care or health care at all. Although unintentional, the “Future of Nursing” campaign, of which Full Practice Authority (FPA) is an integral part, aligned nicely with the goals of the business of medicine. Both entities desired to remove physicians from their natural leadership position in the medical hierarchy.
For Pete’s sake, there was ready money to be had. For NPs seeking pay parity and equivalence by professional misappropriation (aka identity theft), physicians were obstructive. In the way. For the corporate practice of medicine, physicians’ pesky ethics not only obstructed their greedy pursuance of financial gain, they were also just too damn expensive. The CPOM had no desire to pay for expertise, their wish was to simply increase the profit margin by any means necessary.
So physicians had to go. And go they have. Family Medicine Physicians. Internists. Pediatricians. Anesthesiologists. Hospitalists.

42 | 2022 VOLUME 10

W W W . P H Y S I C I A N O U T L O O K . C O M M E D I C I N E I S O U R H O U S E , A N D W E A R E T A K I N G I T B A C K !
EMERGENCY: BREAKDOWN IN COMMUNICATION
LWritten by Elizabeth Eagan
. Bradley Schwartz went to the emergency room expecting care. He woke up a month later to the news he had lost vision in one eye and would lose all four limbs.
It was a beautiful Saturday afternoon in 2004, the day before Mother’s Day and Schwartz’s wife’s birthday. Schwartz, an attorney well-versed in healthcare (he grew up in a medical family and specialized in personal injury defense and insurance litigation) felt extremely fatigued and was experiencing a worsening headache throughout the day, to the point where his wife decided an ambulance was needed. It was not until midnight that the cause for his 105-degree fever, multi-organ failure, and septic shock was discovered. Schwartz did not receive antibiotics for 6-1/2 hours. By that time he had gone into septic shock, resulting in disseminated intravascular coagulation which severely compromised blood flow to his eye and extremities.
So, what went wrong? It started with how his history was taken and later communicated to ER staff. Paramedics on the scene at his home asked if he had anything to drink the night before. The Schwartz’s had hosted a wine tasting party, so he answered “yes.” His history as relayed by the transporting paramedics to the ER staff was that they had “an otherwise healthy 37-year-old man who had been drinking alcohol the night before who now had fatigue and a headache.” The ambulance crew had been called in the early evening, resulting in Schwartz arriving at his local hospital’s Emergency Room during a shift change. It was a holiday weekend and “spring fever” was in the air; the nurses and doctors who were working gave the impression that they really didn’t want to be there. It took a while for anyone to examine him.
Schwartz was triaged as a low-priority patient, and a tragic comedy of errors unfolded, including negligence on the part of his care team, who did not promptly nor thoroughly examine him nor take an independent thorough history.

Labs were drawn as per protocol shortly after his arrival in the ER but were not resulted nor reviewed in a timely manner. Had standard protocol been followed, Mr. Schwartz’s diagnosis (bacterial meningitis) would have been suspected. Cultures would have been drawn, a lumbar puncture would have been performed, and he would have been promptly started on broad-spectrum antibiotics. Instead, his blood test results went unseen for hours.
He became a victim of malpractice due to a series of avoidable breakdowns in communication and failure to follow standard established protocols.
After surviving the anger and eventual acceptance that follows a devastating injury, Schwartz began using his legal expertise and knowledge of hospital systems to benefit others and now focuses on medical negligence, amputee support, meningitis awareness, sepsis prevention, and elimination of medical error.
Medical error is the 3rd leading cause of death in the United States and patient advocates can help save lives. It became Brad Schwartz’s personal mission to make sure every patient’s voice is heard because in his case, it wasn’t.
It soon became his goal to prevent others from enduring the same systemic failures that almost took his life. Recognizing that many clinicians were leaving their practice to become Independent Patient Advocates, he founded Greater National Advocates, a nonprofit foundation determined to make these advocates known and available to everyone. From his perspective, an independent advocate by his side in the ER would have saved his limbs, so he started GNANOW.ORG, an online directory that connects patients and loved ones to immediate support.
For more information visit www.gnanow.org/about or get listed now at www.gnanow.org/advocates
44 | 2022 VOLUME 10
The Difficulty In Coming Home
WHAT DOCTORS AND SOLDIERS HAVE IN COMMON
Written by Susan Hart Gaines
PHOTO CREDIT: SERHII BOBYK VIA SHUTTERSTOCK 46 | 2022 VOLUME 10
When I was married to a physician, dinner was often delayed. When he finally came home, I was hungry if I hadn’t already eaten with the kids. Our dog would greet him with her whole body of yearning and relief, tail wagging furiously, whining, smiling, crying. She was the embodiment of what I felt but could not express. So I watched with jealousy as our dog received from my husband what I craved: pure connection and love. I didn’t know how to ask — plus, how could I?
Just as he’d signed up to be a doctor; I’d taken a vow to be married to that life. So we’d have a drink and chat. Sometimes he’d tell me a story about a particularly heartbreaking or mysterious case, stories from the front. For those moments, his story would be a bridge between us. But most of the time, he kept his stories locked away with the understatement of the year: “It was a normal day.” We kept it light, while I secretly tried to get to the heart of it, to the meat of his life, to draw something out that felt real, emotional, something to bring him home, to our kids and to me.
This inability to really be home started in residency. Of course, the degree to which physicians are able to completely turn off the lights at work depends on one’s specialty and personality. I’m sure plenty of doctors can leave work at work. But doctoring isn’t just any work. It’s messy work and doesn’t always adhere to the confines of 15-minute appointments. It’s human life — and death.
Soldiers of war experience this too. And even military personnel who are not on the battlefield. I have a friend who has been in the military since she was 17. She is the picture of courage and grit: a sharpshooter and a quick study, she masters every job she’s given by the military. She’s now looking to get out. This decision demands more courage than anything she’s ever done. Faced with this, she is paralyzed, dogged by the tasks she needs to do to complete the transition, including looking for jobs and taking classes offered by the military. By the time she gets home, she
is exhausted and overwhelmed. “So, I just sit on the couch and watch TV,” she says.
That faraway look. Home but not home.
What makes soldiers and doctors good at their jobs are also the very things that make it hard to leave work at work. My former husband was, and is, very good at his job, especially when it comes to compassion and care for his patients. At work, he gives his all. He sits with grieving families, helping them understand what’s happening with their loved ones and even crying with them as they die.
To ask one more thing of him when he’d given every ounce of his soul all day seemed selfish and childish. So I tried to be civilized and grown-up, swallowing my need for love, to be seen and cared for the way his patients were. By the end of the day, he was so drained; he must have felt that no story he could tell me could bridge the huge divide between the battlefield of the hospital and the home we shared. This is what many doctors do: go back and forth between the battlefield and whatever “home” they’ve created. They are soldiers in everyday life.
But who is that soldier or doctor when they come home from work?
My military friend’s inaction is tearing her up. If she waits long enough, the decision to stay will not really be a decision at all; it will happen by default. Signing out is a defiance of all that she knows. “So why leave at all?” I ask. “What’s the risk of staying?”
“That I won’t know myself,” she says. “That I won’t be myself. Everything is prescribed here: even how to talk.” Many doctors face a similar risk of losing themselves. Within the hospital or clinic walls, you know exactly how to act, what’s expected of you. But once you leave, like many others in medicine, you may struggle to be home, to even know what actually gives you pleasure anymore, or how to truly relax. The identity of soldier or physician — or many other job titles — comes at a cost; there
is the risk of becoming so identified with the job, that you don’t know what you are when you are not being a doctor.
The more you work, the more entangled you become with the job and the harder it is to really come home — to the place where connection to friends, family, spouses begins. And for un-partnered, you may fall asleep with your charts on your chest, with no one to even give you a hard time about it. For some doctors, my former spouse included, returning home is to face a hollow feeling, a deep sense of loneliness, even when surrounded by people who love them most.
The chasm between your identity and the essence of who you are grows wider and wider, until the only place you feel at home is at work.
Eventually, the cost of not knowing oneself is too big. After all, knowing oneself isn’t a “nice to have” quality. It is a profoundly human desire. To feel at home in one’s own heart is one of the highest callings of being human. For soldiers and physicians, death comes with the territory. But the hardest part of all may be this: To face the messy business of living. Becoming a marksman for your own deepest held values, your most powerful callings of the heart may be the greatest challenge you’ll ever face. And the most important. The commitment to oneself, to venture into that uncharted world of You, is the real work of grit and courage. This is the work of coming home. ☤
republished with permission. First published by www.KevinMD.com on January 11, 2022
https://www.kevinmd.com/blog/2022/01/ the-difficulty-in-coming-home-what-doctorsand-soldiers-have-in-common.html

WWW.PHYSICIANOUTLOOK.COM | 47
www.wildhartcoaching.com WILD HART COACHING
Case Series Explores
CONNECTION BETWEEN MICROBIOME & COVID-19
Written by TrialSiteNews Staff
Recently, a Southern California physician and clinical investigator leading several formal clinical trials regulated by the U.S. Food and Drug Administration (FDA) had a case series published in Case Reports in Gastroenterology.¹ An expert in an emerging field of microbiome research, Dr. Sabine Hazan recently reported on a case series showcasing the potential association of SARS-CoV-2, the virus that causes COVID-19, and the microbiome. While this is not a randomized controlled trial, this case series nonetheless offers more data suggesting the possibility of some association between gut health (the microbiome) and COVID-19.
TrialSite recently chronicled research led by the Chinese University of Hong Kong (CUHK) Center for Gut Microbiota Research indi -
cating² that the gut microbiome composition could possibly be associated with a person’s risk of developing long COVID months after initial SARS-CoV-2 infection.
Enter ProgenaBiome
Dr. Sabine Hazan runs a medical clinic out of Malibu, California, and a clinical trial site in Ventura California known as Ventura Clinical Trials. She also runs Ventura-based ProgenaBiome, a genetic sequencing research laboratory dedicated to continuing important research correlating microbes to diseases.
Recently, Dr. Hazan reported the results of a case series involving a 19-year-old man (the index patient) with Crohn’s disease. Back in May 2020, the young man, his 62-year-old father, and 14-year old sister all tested positive for SARS-
CoV-2. Importantly the trio shared the household with the 50-year old mother with a history of asthma as well as a healthy brother and sister-in-law—both are married, reside in the home. All of them remained COVID-19 negative.
Dr. Hazan observed that the index patient and his mother underwent microbiome analysis in May 2019 followed by the brother and sister-in-law by November 2020.
Observations
The physician-microbiome-focused scientist reported that she and the team observed significant differences between the fecal microbiota of the SARS-CoV-2-positive son and those of his healthy family members.
Hazan reports the following differences in Bacterial phylum, class,
48 | 2022 VOLUME 10
PHOTO CREDIT BY INGRAM IMAGES

order, family, genus level with the increased relative abundance of Bacteroidetes and reductions or deletions in bacterial diversity, especially associated with the Bifidobacterium family.
The author notes in the published, peer-reviewed manuscript that the unique investigation could indicate a novel exploratory direction for the prevention or treatment of SARS-CoV-2 infections. ☤
(re-published with permission. First appeared online @ www.TrialSiteNews.com on February 9, 2022)
1. Hazan S: Pre-Existing Microbiome Signature in a SARS-CoV-2 Discordant Family. Case Rep Gastroenterol 2022:15-22. doi: 10.1159/000520625
LINK FOR WEB VERSION : https://www. karger.com/Article/Abstract/520625#
2. Liu Q, Mak JWY, Su Q, et al Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome Gut 2022;71:544-552.
LINK FOR WEB VERSION: https://trialsitenews.com/chuk-study-adds-to-evidencethat-gut-microbiome-associates-withlong-covid/




WWW.PHYSICIANOUTLOOK.COM | 49
Coronaceous
COLORED SKY
Written by Ayushi Chugh, MD
When our skies are forever Gray
When our days are forever Blue
Some of us wear Red inside,
Red like those hearts revived
Under a Covid colored sky
Storm chasers don’t follow sunsets
Yet kowtow to honor setbacks
Embrace new growth mindset
Like your shadow has your back
Times when soul feels bare
And nothing feels Whole
Step away for self-care
Momentarily for that common goal
For in that moment you froze
Not that your love was flawed
No love lost since the heart you chose
Couldn’t beat on half hearted roads

Relentless spirits sway
Into wisps of doubt
World may question this dare
Of chasing rainbows amidst clouds
To adorn a coronaceous colored sky
This Pandora’s box is abysmal
Refill your cup and heal my friend
For the Road ahead be dismal
Under a Covid colored firmament
And Believe after every thunderstorm
There follows an orange firesky
That salutes as your own Sun, Brings sunshine, to a Coronaceous colored sky ☤
-Ayushi Chugh, MD Neurologist, Poet
50 | 2022 VOLUME 10
PHOTO
CREDIT BY CANVA
The VPZD Show
THE “CLICK AND CLACK” OF MEDICINE
Written by Marlene Wüst-Smith, M.D.
An entertaining fast-paced relatively new podcast that started airing in late 2021, the VPZD Show, features two very funny smart well-read, well-trained physicians who dare to challenge today’s “status quo.” They have been dubbed the “Click and Clack” (of NPR “Car Talk” fame) and are two of the very few un-censored voices in healthcare.
Dr. Zubin Damania, aka ZDOGGMD, is a Stanford/UCSF trained doc-
tor who leads a passionate tribe of healthcare professionals towards an “Alt-Middle” vision of what healthcare SHOULD look like. His medical and entertainment show “ZDoggMD Show” reaches millions of listeners weekly with in-depth interviews, “merciless and uncensored satire” and takedowns of “pseudoscientific nonsense” that can be found on Locals, Facebook and YouTube.
Vinay Prasad MD MPH is a hematologist-oncologist and Asso -
ciate Professor in the Department of Epidemiology and Biostatistics at the University of California San Francisco. He runs the VKPrasad lab at UCSF, which studies cancer drugs, health policy, clinical trials and what he calls “better decision making.” He hosts a podcast called Plenary Session, runs a YouTube Channel VinayPrasadMDMPH, and has a very active Twitter account @ VPrasadMDMPH. ☤
WWW.PHYSICIANOUTLOOK.COM | 51
PODCASTS WORTH LISTENING TO
LRespectful Debate Amongst Doctors
WHY IT REMAINS IMPORTANT
Written by Diana Blum, MD
ately, I find myself wondering, “how it is that physicians are increasingly condemning open debate, even when nuance can make the difference between life and death decisions?” Or…”how is it that we find ourselves justifying correlations for causations, and in doing so, subjugating the importance of the scientific method?”
I have been pondering questions like these over the past year as I watched the pandemic unfold and affect my family, friends, and patients. Finding myself caring for folks on all sides of the polit-

ical spectrum, I felt compelled to understand how the “science” was being discussed. I couldn’t help but notice that, across the whole range of mass media, there was an obvious politicization of narratives. Disappointingly, even physician “experts” towed the party lines, depending on which network they appeared.
We are sadly living through a rise in “othering,” which is bringing out our primitive reflexes and distracting us from our shared humanity — the common ground we need to stand together, move forward, and heal. I hope to dis -
cuss these important but sensitive topics here with my Hippocratic oath-abiding colleagues, and I am grateful for your willingness to consider my perspective with an open mind.
Among the pandemic-era themes gaining traction within the medical community is a renewed emphasis on “social determinants” of health, and how these factors ultimately impact diseases. Let me be clear: I don’t disagree with my fellow physicians who are advocating that these variables should be considered as highly relevant factors in any analysis of well-be -
THE LAST WORD
52 | 2022 VOLUME 10

ing outcomes. It’s reasonable to extrapolate that, by increasing our understanding of these issues, we can adjust how we practice medicine in ways that better address the needs of our patients.
However, in our zeal to deliver equity in medical outcomes, we owe it to the very populations we are trying to help to NOT fall into the trap of mistaking correlations for causations. It shouldn’t be anathema for us to simultaneously recognize the need to address disparate outcomes across patient populations, while also considering – as we were all trained to do
– other relevant factors, including a patient’s genetics or personal responsibility, that affect a patient’s health.
One of the reasons I joined FAIR in Medicine was to help address the growing erosion of ethical standards in medical education and delivery of medical care. Physicians are held to a higher standard than most other healthcare professionals because we are trained with a deep grounding in biomedical science and understanding of disease pathophysiology. Without these educational underpinnings, we can’t expect
other health care “providers” to reliably formulate proper differential diagnosis, work ups and treatment plans. Bending medical education to follow prevalent cultural movements will further escalate the growing trend of deadly unintended consequences we are already witnessing. Meanwhile, instead of addressing root causes of our failing healthcare system — including profit motives in health care, 3rd party waste, and clinician shortages — our medical institutions seem to be more focused on emphasizing language manipulation, which will fail to achieve meaningful change in health outcome gaps.
I propose we embrace our roots as scientists and healers and honor the oath we took by speaking up for excellence in education while elevating objectivity and transparency in scientific research. I have faith that we can do this without compromising the empathy and compassion all our patients deserve. ☤
References
https://www.fairforall.org/fair-in-medicine/
https://www.patientsatrisk.com/
https://www.ama-assn.org/system/files/ ama-aamc-equity-guide.pdf

WWW.PHYSICIANOUTLOOK.COM | 53
PHOTO CREDIT INGRAM IMAGES
POSSIBLE PICTURES: PHOTO CREDIT: DR. BLUM
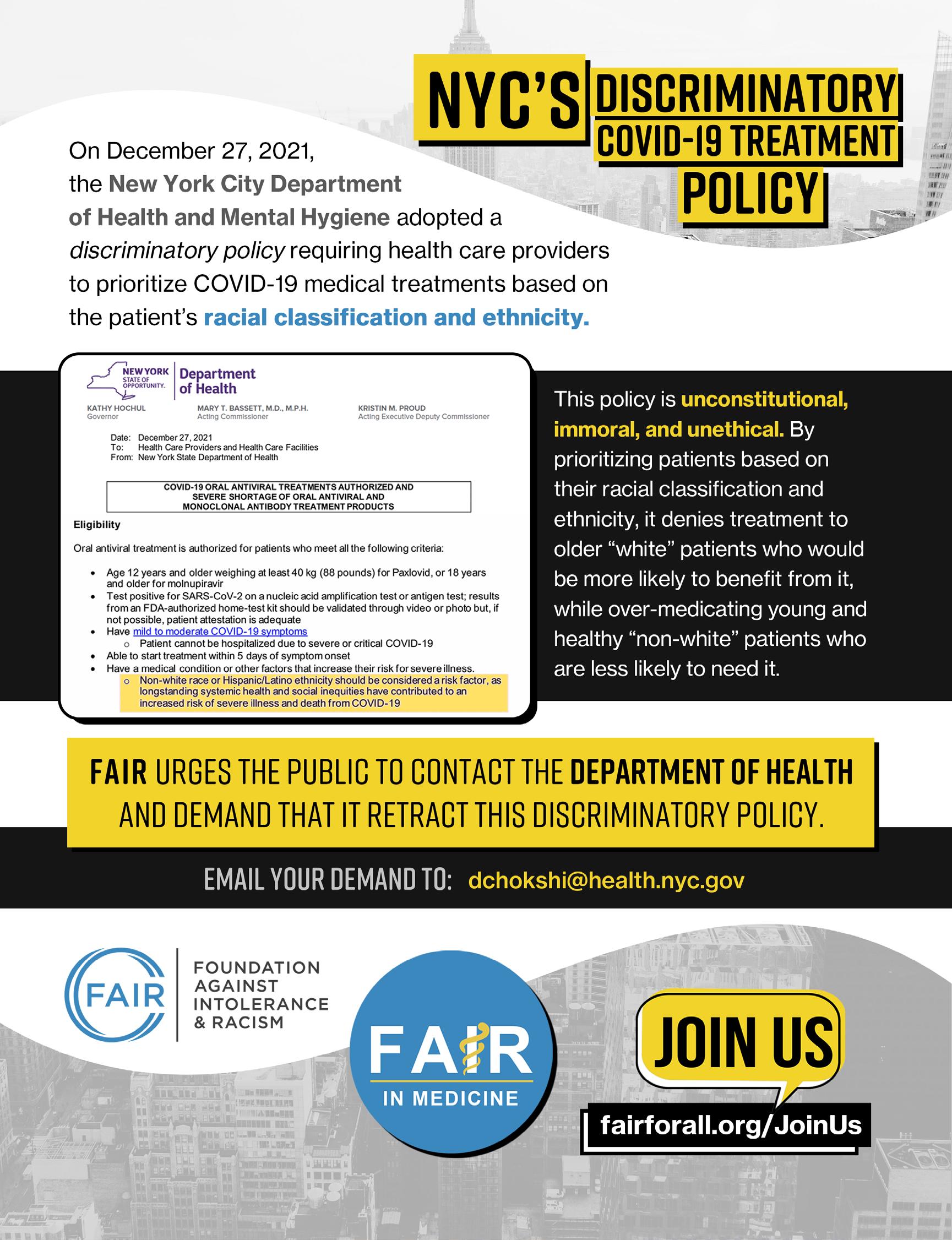
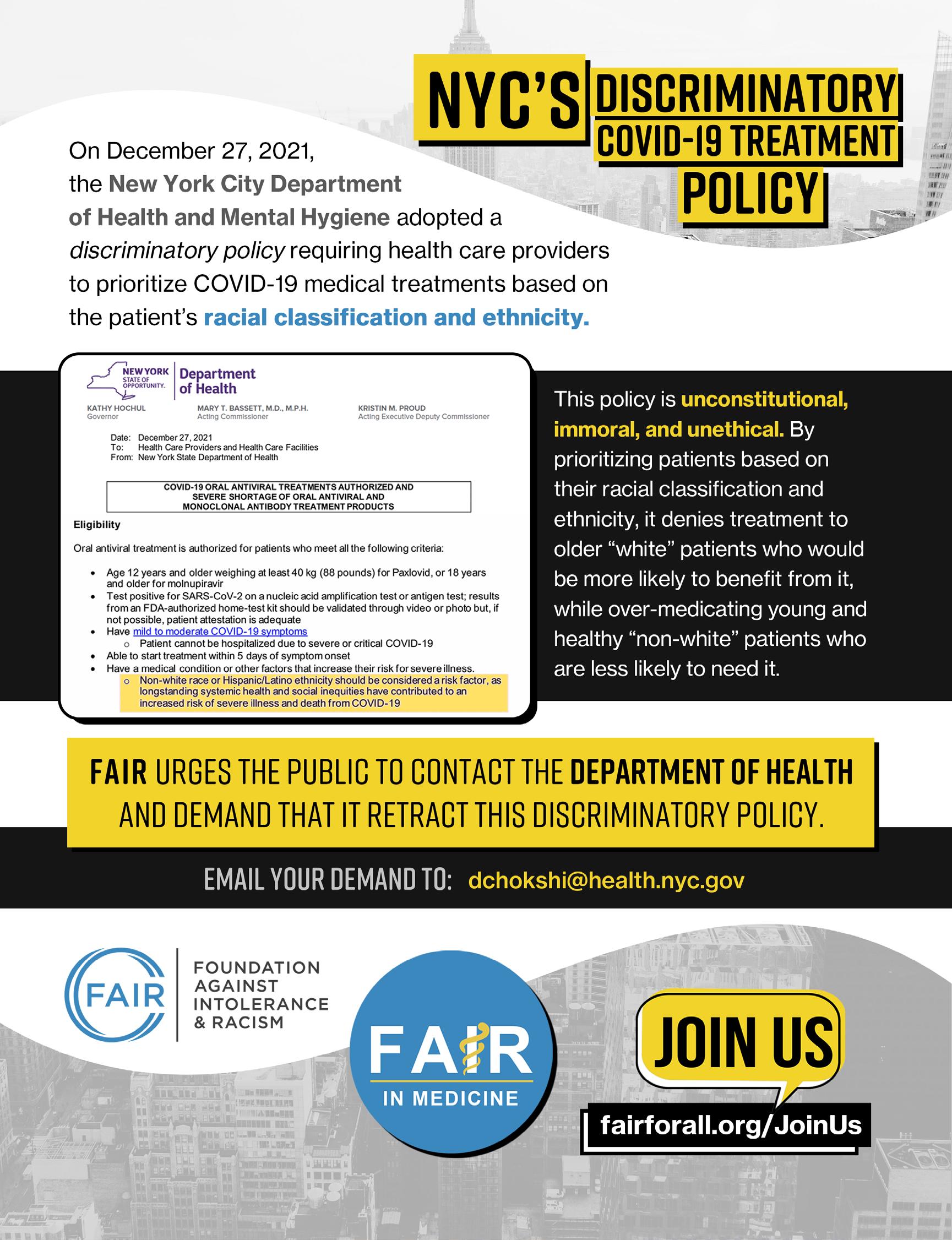
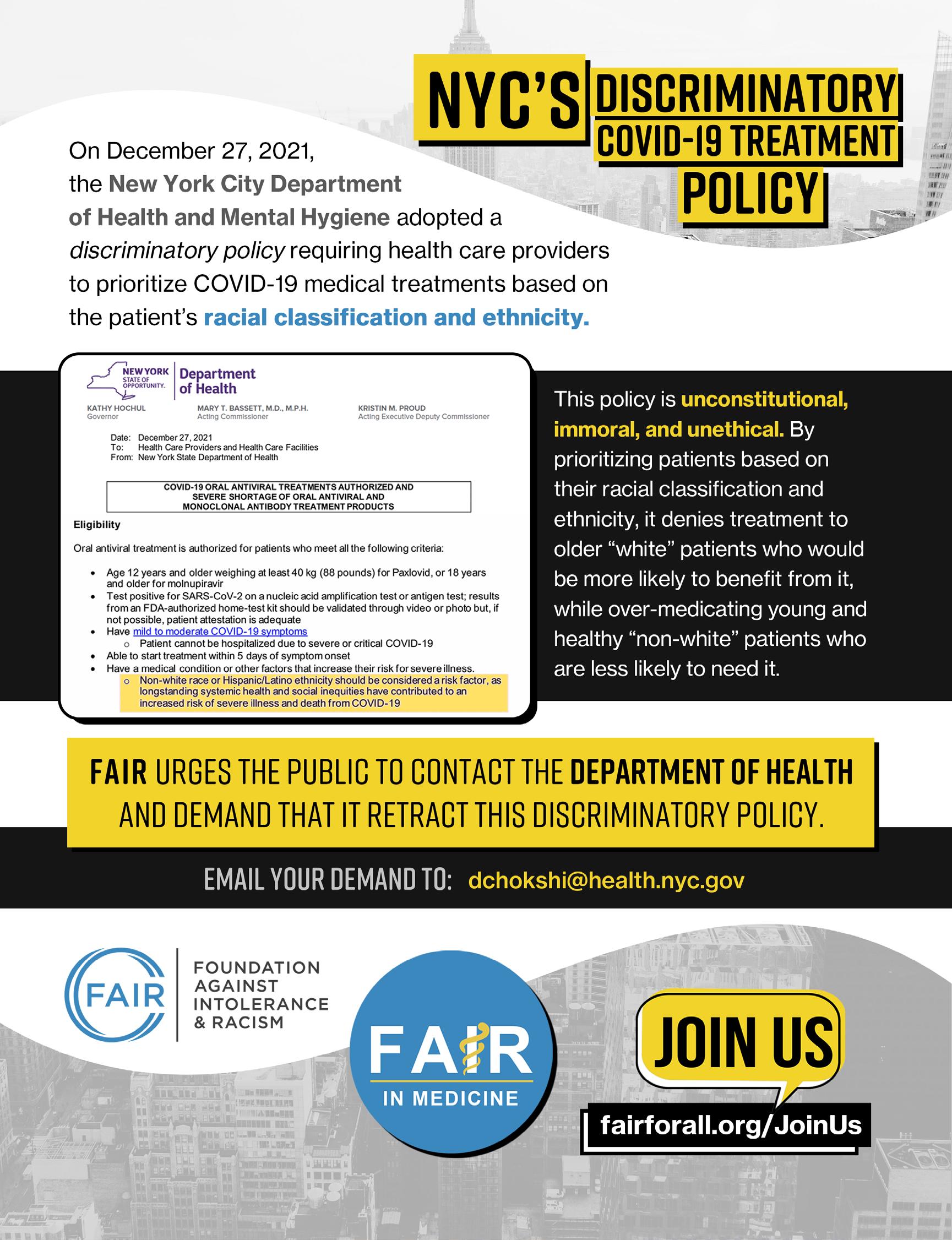
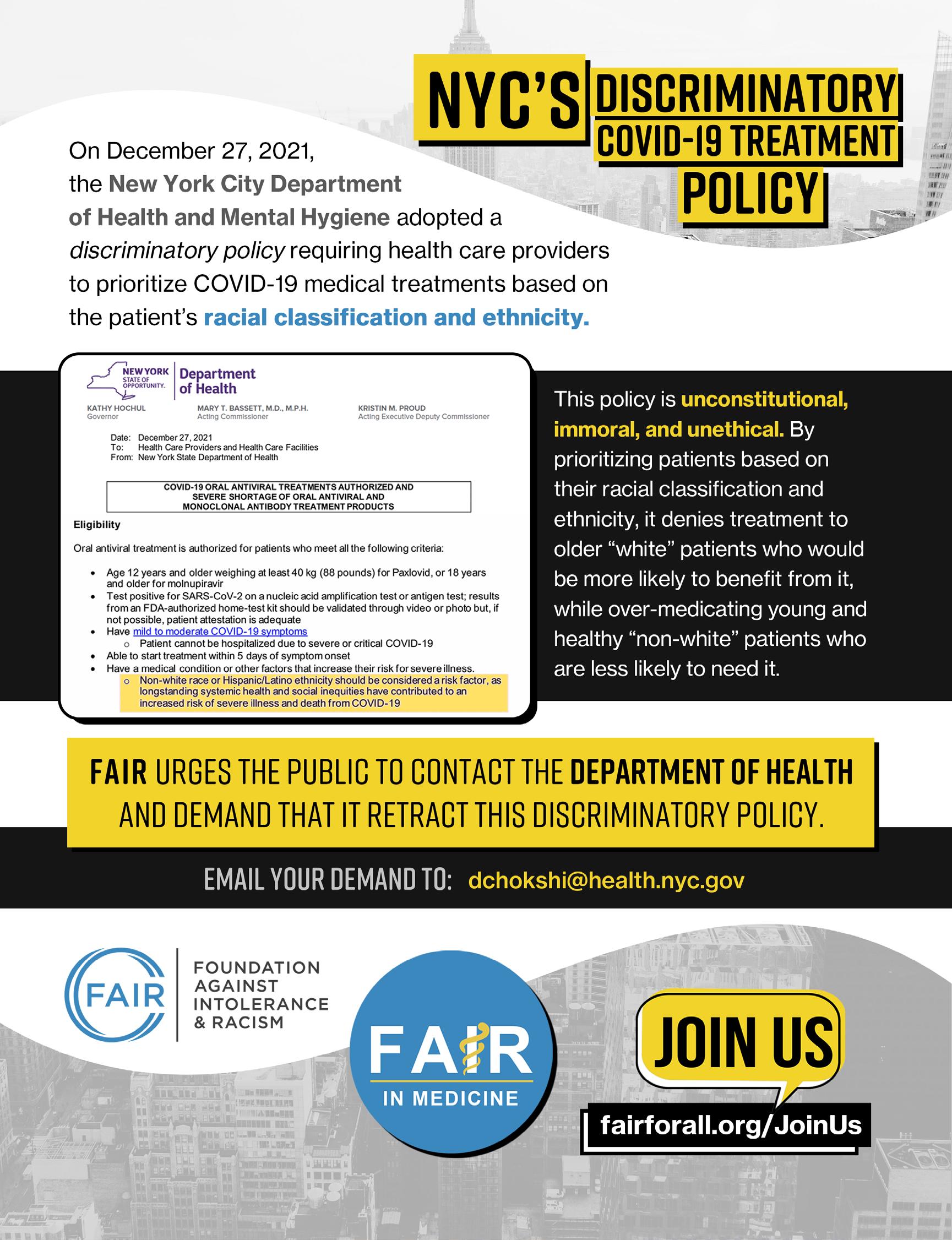


Coffee with a Mission
Coffee with a Mission
I’m not a veteran and I always make that clear.
I’m not a veteran and I always make that clear.

Dad was the youngest of 16 - 14 boys, 2 girls. 3 of the boys served in WWI and my uncle Perce was awarded a Silver Star for action in France with the USA 77th Division. 5 siblings served in WWII, my dad with the Marines who spent 20+ months in the Pacific. 1, uncle Dink fought in both wars and ran into his son while landing under fire in Okinawa, who was also a USN CB.
Dad was the youngest of 16 - 14 boys, 2 girls. 3 of the boys served in WWI and my uncle Perce was awarded a Silver Star for action in France with the USA 77th Division. 5 siblings served in WWII, my dad with the Marines who spent 20+ months in the Pacific. 1, uncle Dink fought in both wars and ran into his son while landing under fire in Okinawa, who was also a USN CB.
I had my right eye removed at age 7, and so couldn’t serve in uniform. I ended up trading green coffee on Wall Street, lived in Brasil for several years and then came back and was the CEO of a Brasilian Agr Group’s global HQ which happened to be down the block from the US Marines’ MCRD HQ on Long Island, NY. I befriended the Marines there and did what I could to support them and their families and when I retired from trading in 2005 (and never having an opportunity to serve as my family had) I went to them and asked for help to get a deployment to Iraq.
I had my right eye removed at age 7, and so couldn’t serve in uniform. I ended up trading green coffee on Wall Street, lived in Brasil for several years and then came back and was the CEO of a Brasilian Agr Group’s global HQ which happened to be down the block from the US Marines’ MCRD HQ on Long Island, NY. I befriended the Marines there and did what I could to support them and their families and when I retired from trading in 2005 (and never having an opportunity to serve as my family had) I went to them and asked for help to get a deployment to Iraq.
In 2008 at age 55, I deployed to Iraq as part of the OIF LOGCAP (logistical support mission) and then volunteered to forward deploy and was sent to FOB Warrior, Kirkuk. It was there, seeing firsthand what a great job our men and women do - and in such miserable conditions - that the idea for Military Java Group was born.
TIn 2008 at age 55, I deployed to Iraq as part of the OIF LOGCAP (logistical support mission) and then volunteered to forward deploy and was sent to FOB Warrior, Kirkuk. It was there, seeing firsthand what a great job our men and women do - and in such miserable conditions - that the idea for Military Java Group was born.
That’s me on a very rare day off - ergo the shorts - LOL!
That’s me on a very rare day off - ergo the shorts - LOL!
~ Matt Phillips, Founder/President of Jarhead Java
he beautiful water color image on the cover of a Soldier in uniform hugging his son goodbye is the handiwork of Kaitlin Walsh, a talented professional independent artist who is the spouse of a retired Air Force military-trained Dentist and Physician, Dr. Martin Walsh. Her online gallery, www.LyonRoadArt.com truly represents the intersection of art and anatomy. As a young child Walsh exhibited an immense fascination with art and medicine, and focused her studies on both disciplines. She received a graduate degree in Biomedical Visualization from Chicago’s University of Illinois after taking pre-medical courses and art classes during her college years. She launched her studio in 2015, naming it “Lyon Road Art” in memory of the street address of the tiny apartment in Northern California where she and her husband spent the stressful first year of their marriage. Martin started his dental residency the day after their wedding, while also serving as an active duty officer in the Air Force, leaving Kaitlin to fend for herself in a new environment thousands of miles away from friends and family. It was in that tiny apartment on Lyon Road that Kaitlin went into very pre-term labor, and in that home that she spent months alone creating art as an outlet for the stress of having a precariously fragile very preterm son who would spend months in a Neonatal ICU.
~ Matt Phillips, Founder/President of Jarhead Java
Share a mug. Support a cause.
One of the things that distinguishes Physician Outlook Magazine from other publications is our desire to put beauty and “the human” back in the center of all interactions in healthcare. We do this by highlighting the artwork of healthcare workers, their families and their patients. We are honored to feature Kaitlin’s work throughout this issue, and encourage our readers and subscribers to visit her gallery. Her attention to anatomic detail and the beauty of her work has made her a well-known “famous” fixture within the Anatomical Art community. We look forward to continue to feature her art in issues to come.
Martin Walsh, DDS, MD is originally from Racine, Wisconsin. He attended Marquette University for his undergraduate studies where he majored in Biomedical Sciences, graduating in 2008. He then attended Marquette University School of Dentistry on an Air Force Health Professions Scholarship and received his DDS in 2011. After dental school he earned his M.D. by completing an Oral and Maxillofacial Surgery Residency at the David Grant Medical Center at the Travis Air Force Base, California where he served as an active duty officer.

And, we’ll donate 50% of our profits to the Semper Fi & America’s Fund to assist our wounded heroes. Great coffee for a great cause.
And, we’ll donate 50% of our profits to the Semper Fi & America’s Fund to assist our wounded heroes. Great coffee for a great cause.
Find our family of high-quality coffee products at MilitaryJavaGroup.com, MCX, DeCA, and Amazon.
Find our family of high-quality coffee products at MilitaryJavaGroup.com, MCX, DeCA, and Amazon.
In 2015, after residency, the family moved to Nebraska where Marty was stationed at Offutt Air Force Base in Omaha. There Dr. Walsh practiced Oral and Maxillofacial Surgery and was a faculty member for the Offutt
Air Force Base Advanced Education in General Dentistry (AEGD) Residency until he retired from the military in 2019. While he enjoyed serving his country and exploring the nation, the Walsh family is thrilled to be back “home” in Madison, Wisconsin with their three very healthy children, where Dr. Walsh works as a Maxillofacial Surgeon.
WWW.PHYSICIANOUTLOOK.COM | 27
MP1129_Share a Mug 5x6.indd 1 2/10/22 5:06 PM WWW.PHYSICIANOUTLOOK.COM | 27
Share a mug. Support a cause.
MP1129_Share a Mug 5x6.indd 1 2/10/22 5:06 PM
Giving Control Back to You

Want to contain the costs of your healthcare plan?

We can show you how. Employers everywhere are frustrated with the astronomical costs of healthcare, and rightfully so. Many accept annual rate increases in defeat. But there is a better way.
Through our FairCo$t Health Plan, we will help you identify ways to reduce the costs of healthcare, thereby reducing the cost of your insurance. You’ll become an active manager of your health plan instead of a victim of the system.
Our team at Mitigate Partners is committed to delivering employer-built healthcare vs. insurer-built healthcare. And we don’t take this responsibility lightly. We protect your money like it’s our own, serving as the fiduciary and steward of your health plan dollars.
Let us show you how to take control. Reach any of the
mitigatepartners.com Let us “UBER” your health plan before it gets “KODAKED”.
Mitigate Partners at
Coffee with a Mission
I’m not a veteran and I always make that clear.
Dad was the youngest of 16 - 14 boys, 2 girls. 3 of the boys served in WWI and my uncle Perce was awarded a Silver Star for action in France with the USA 77th Division. 5 siblings served in WWII, my dad with the Marines who spent 20+ months in the Pacific. 1, uncle Dink fought in both wars and ran into his son while landing under fire in Okinawa, who was also a USN CB.
I had my right eye removed at age 7, and so couldn’t serve in uniform. I ended up trading green coffee on Wall Street, lived in Brasil for several years and then came back and was the CEO of a Brasilian Agr Group’s global HQ which happened to be down the block from the US Marines’ MCRD HQ on Long Island, NY. I befriended the Marines there and did what I could to support them and their families and when I retired from trading in 2005 (and never having an opportunity to serve as my family had) I went to them and asked for help to get a deployment to Iraq.
In 2008 at age 55, I deployed to Iraq as part of the OIF LOGCAP (logistical support mission) and then volunteered to forward deploy and was sent to FOB Warrior, Kirkuk. It was there, see ing firsthand what a great job our men and women do - and in such miserable conditions - that the idea for Military Java Group was born.
That’s me on a very rare day off - ergo the shorts - LOL!
~ Matt Phillips, Founder/President of Jarhead Java


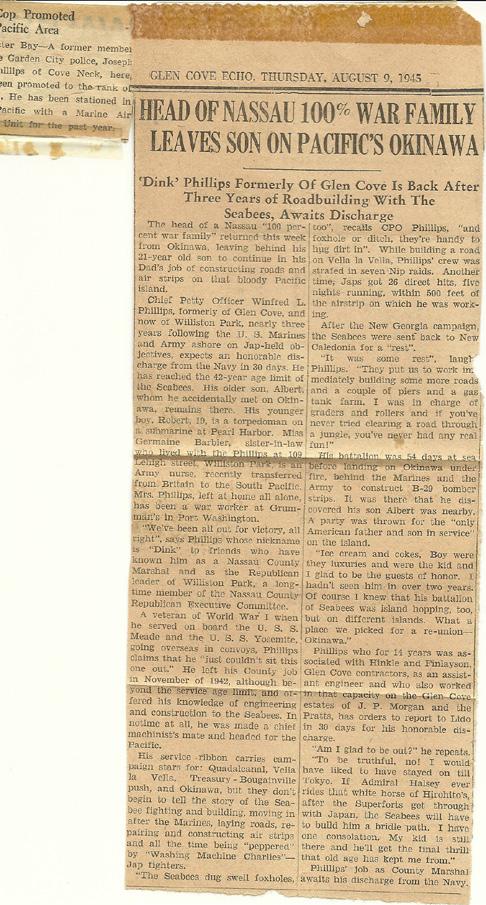

Share a mug. Support a cause. And, we’ll donate 50% of our profits to the Semper Fi & America’s Fund to assist our wounded heroes. Great coffee for a great cause. Find our family of high-quality coffee products at MilitaryJavaGroup.com, MCX, DeCA, and Amazon. MP1129_Share a Mug 5x6.indd 1 2/10/22 5:06 PM

Respectful Debate Amongst Doctors
Why It Is Still Important

Lately, I find myself wondering “how it is that physicians are increasingly condemning open debate, even when nuance can make the difference between life and death decisions?” Or “how is it that we find ourselves justifying correlations for causation, and in doing so, subjugating the importance of the scientific method?”
I have been pondering questions like these over the past year as I watched the pandemic unfold and affect my family, friends, and patients. Finding myself caring for folks on all sides of the political spectrum, I felt compelled to understand how the “science” was being discussed. I couldn’t help but notice that, across the whole range of mass media, there was an obvious politicization of narratives. Disappointingly, even physician “experts” towed the party lines, depending on which network they appeared.
We are sadly living through a rise in “othering,” which is bringing out our primitive reflexes and distracting us from our shared humanity — the common ground we need to stand together, move forward, and heal. I hope to discuss these important but sensitive topics here with my Hippocratic oath-abiding colleagues, and I am grateful for your willingness to consider my perspective with an open-mind.
Among the pandemic-era themes gaining traction within the medical community is a renewed emphasis on “social determinants” of health, and how these factors ultimately impact diseases. Let me be clear: I don’t disagree with my fellow physicians who are advocating that these variables should be considered as highly relevant factors in any analysis of well-being outcomes. It’s reasonable to extrapolate that,
as we were all trained to do other relevant factors, including a patient’s

pathophysiology. Without these educational underpinnings, we can’t expect other health care “providers” to reliably formulate proper differential diagnosis, work ups and treatment plans. Bending medical education to follow prevalent cultural movements will further escalate the growing trend of deadly unintended consequences we are already witnessing. Meanwhile, instead of addressing root causes of our failing healthcare system — including profit motives in health care, 3rd party waste, and clinician shortages — our medical institutions seem to be more focused on emphasizing language manipulation, which will fail to achieve meaningful change in health outcome gaps.
I propose we embrace our roots as scientists and healers and honor the oath we took by speaking up for excellence in education while elevating objectivity and transparency in scientific research. I have faith that we can do this without compromising the empathy and compassion all our patients deserve.

42 | 2022 VOLUME 10
10 | 2022 VOLUME 10



Publisher: Marlene Wüst-Smith, MD Editor in Chief: Alicia Roselli Managing Editor: Roxanne Bruce, MBA, DrBA Assistant to the Publisher: Jill Labecki, VP of Advertising: Pamela Ferman Director of Art and Production: Tobias Sarrio, Ricardo Castillo (current issue) Marketing/Copyright Editor/Journalism/Social Media Interns: Dana Bushery, Pennsylvania State University, Hannah Bushery, Hofstra University ,Elizabeth Egan, St. Bonaventure University and Madison Smith, Pennsylvania State University
Publisher: Marlene Wüst-Smith, MD Editor in Chief: Alicia Roselli Managing Editor: Roxanne Bruce, MBA, DrBA VP of Advertising: Pamela Ferman Director of Art and Production: Tobias Sarrio Marketing/Copyright Editor/Journalism/Social Media Interns: Riley Snowden, Pennsylvania State University Contributing Authors: Marlene J. Wüst-Smith, MD, Sophia M. Sherman, MIDN 4/c, Linda Hodges, MD, Kyle Rickner, Roxanne Bruce, MBA, DrBA, FACHT, Jerry Ashton, Jack McGowan, Olga C. Rodriguez, DNP©, MSN, RN, CPHQ, Riley Snowden, Elizabeth Eagan, Eden Courville, Annahieta Kalantari, DO, Kaitlin Walsh, Susan Hart Gaines, Diana Blum, MD Cover Art: Kaitlin Walsh of Lyon Road Art
Contributing Authors: Jerry Ashton, Patient Advocate & Founder of LRT, Roxanne Bruce, MBA, DrBA, FACHT, Ayushi Chugh, MD, Elizabeth Egan, SBU ’24, Susan Hart Gaines, CPCC, MS, Sabine Hazan, MD via TrialSiteNews, Linda Hodges, MD, Jack McGowan, HS Senior, Natalie Newman, MD, Kyle Rickner, MD, Olga C. Rodriguez, DNP, MSN, RN, CPHQ, Sophia M. Sherman, UNC-Chapel Hill ‘22,MIDN 1/C , Madison Smith, PSU’22, Marlene Wüst-Smith, MD
Cover Artist: Kaitlin Walsh, Lyon Road Art; Photography: David Lienemann
Published by “PhysicianOutlook Publishing” Editorial policy: PhysicianOutlook magazine is a national magazine dedicated to empowering physicians and their patients to improve the world of medicine together. Editorial decisions are based on the editor’s judgement of the quality of the writing, the timeliness of the content, and the potential interest to the readers of the PhysicianOutlook magazine. The magazine may publish articles dealing with controversial issues. The views expressed herein are of the authors and/or those interviewed, and may not reflect the official policy of the magazine. PhysicianOutlook neither agrees, nor disagrees with those ideas expressed, and no endorsement of those views should be inferred, unless specifically identified as officially endorsed by the magazine.
“Letters to the Editor” email: rbruce@physicianoutlook.com
Information on advertising, subscriptions, and job board email: hello@physicianoutlook.com
“PhysicianOutlook” is a registered trademark.
Published By “Physician Outlook Publishing” Editorial Policy Physician Outlook Magazine is a national magazine dedicated to empowering physicians and their patients to improve the world of medicine together. Editorial decisions are based on the editor’s judgement of the quality of the writing, the timeliness of the content and the potential interest to the readers of The Physician Outlook Magazine. The magazine may publish articles dealing with controversial issues. The views expressed herein are those of the authors and/or those interviewed and might not reflect the official policy of the magazine. Physician Outlook neither agrees nor disagrees with those ideas expressed, and no endorsement of those views should be inferred unless specifically identified as officially endorsed by the magazine.
Letters to the Editor Email: rbruce@physicianoutlook.com
Information on Advertising, Subscriptions, Job Board Email: hello@physicianoutlook.com “Physician Outlook is a registered trademark”
WWW.PHYSICIANOUTLOOK.COM | 59
WWW.PHYSICIANOUTLOOK.COM | 43
SUBMIT YOUR ART SUBSCRIBE

SUBMIT AN ARTICLE ISSN
2768-6019
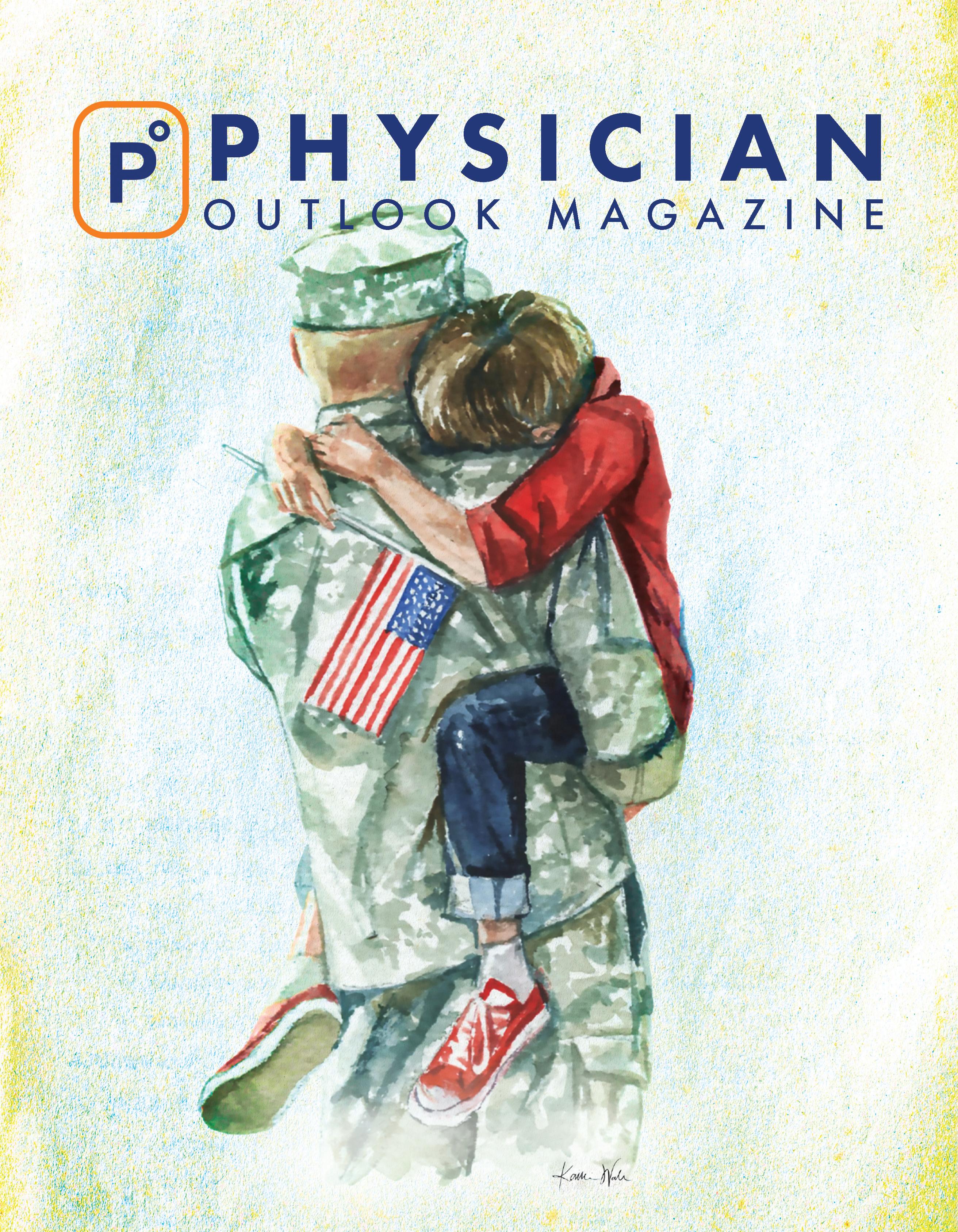










 By
By



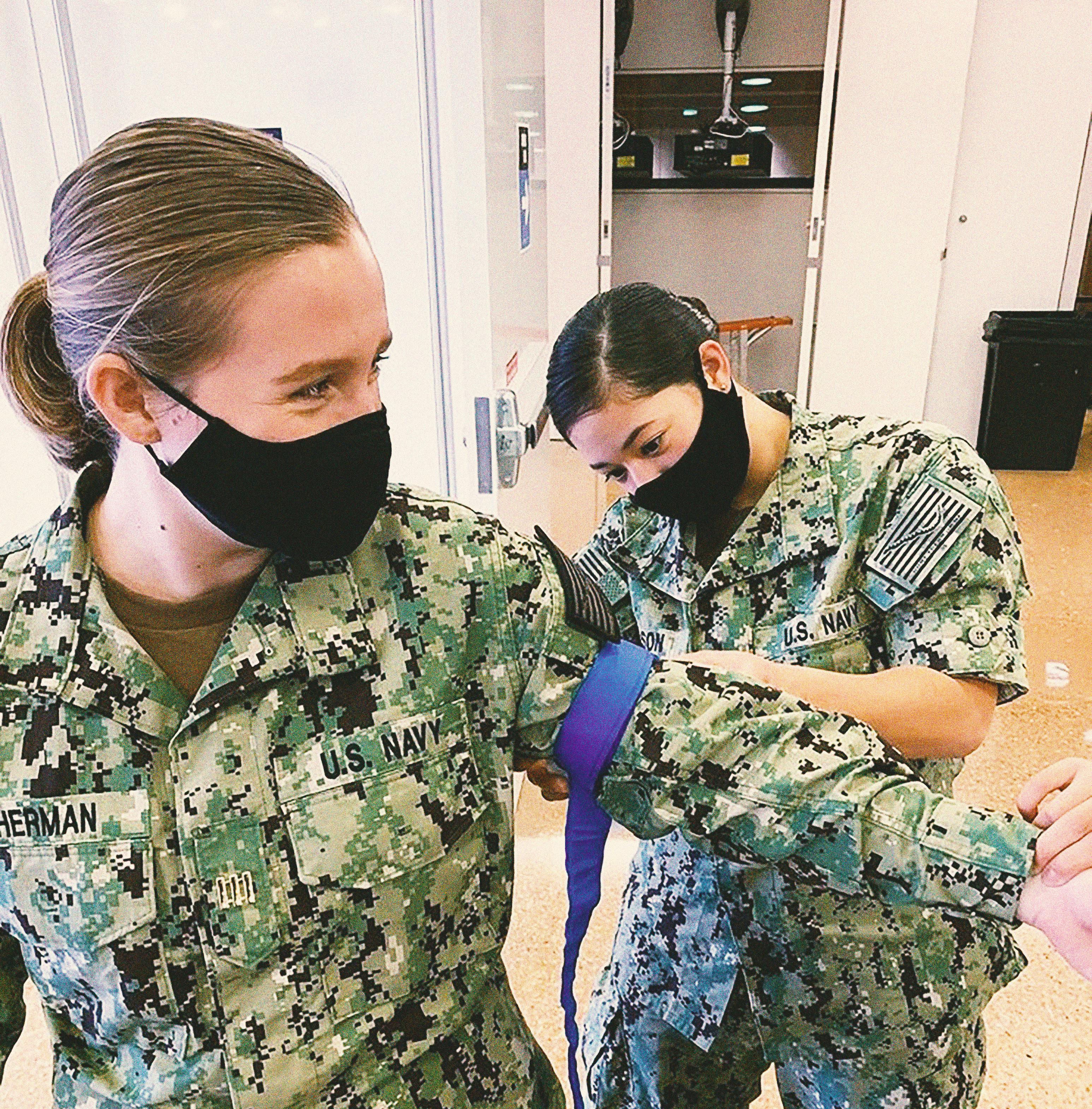







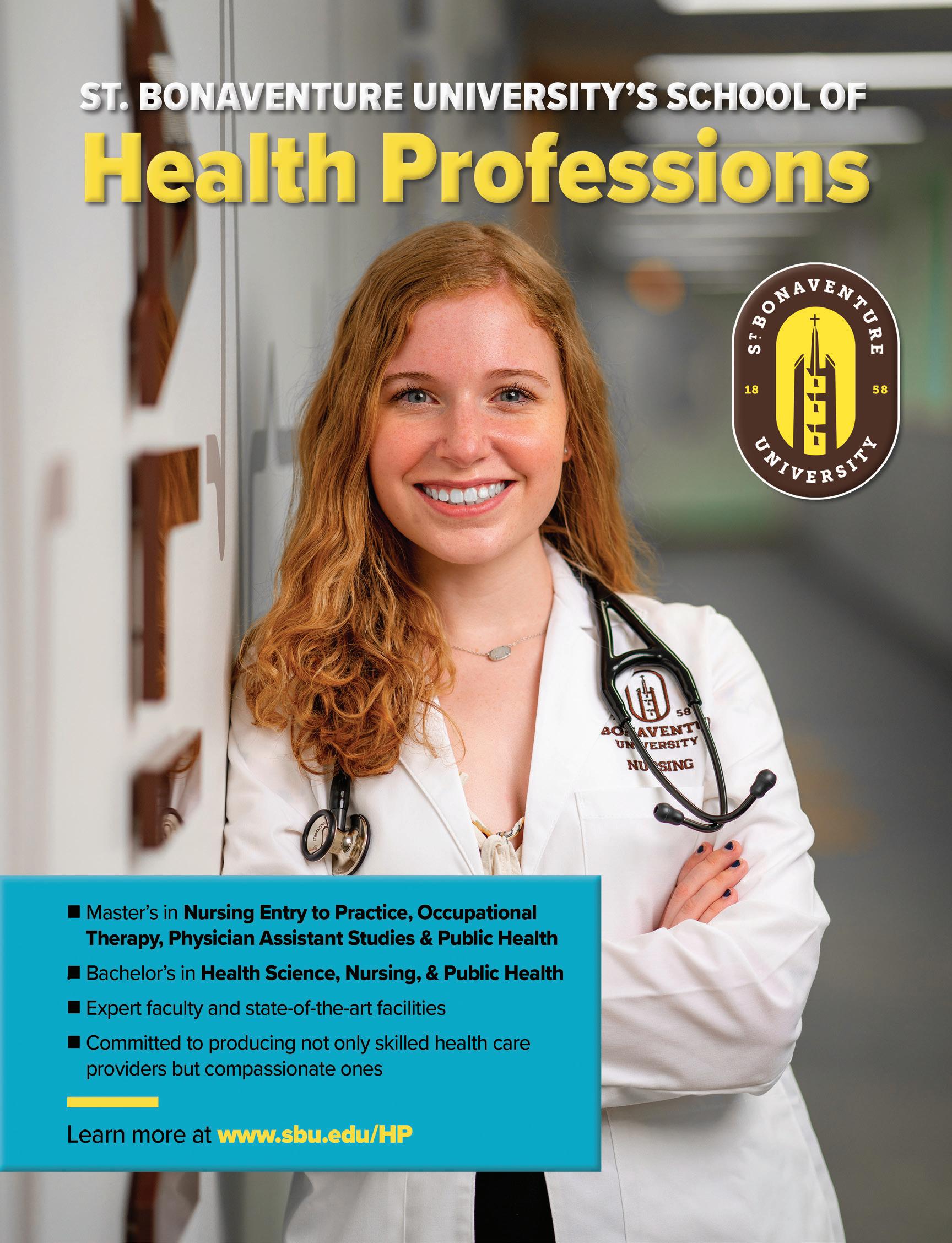
 Written by Marlene Wüst-Smith, M.D.
Written by Marlene Wüst-Smith, M.D.
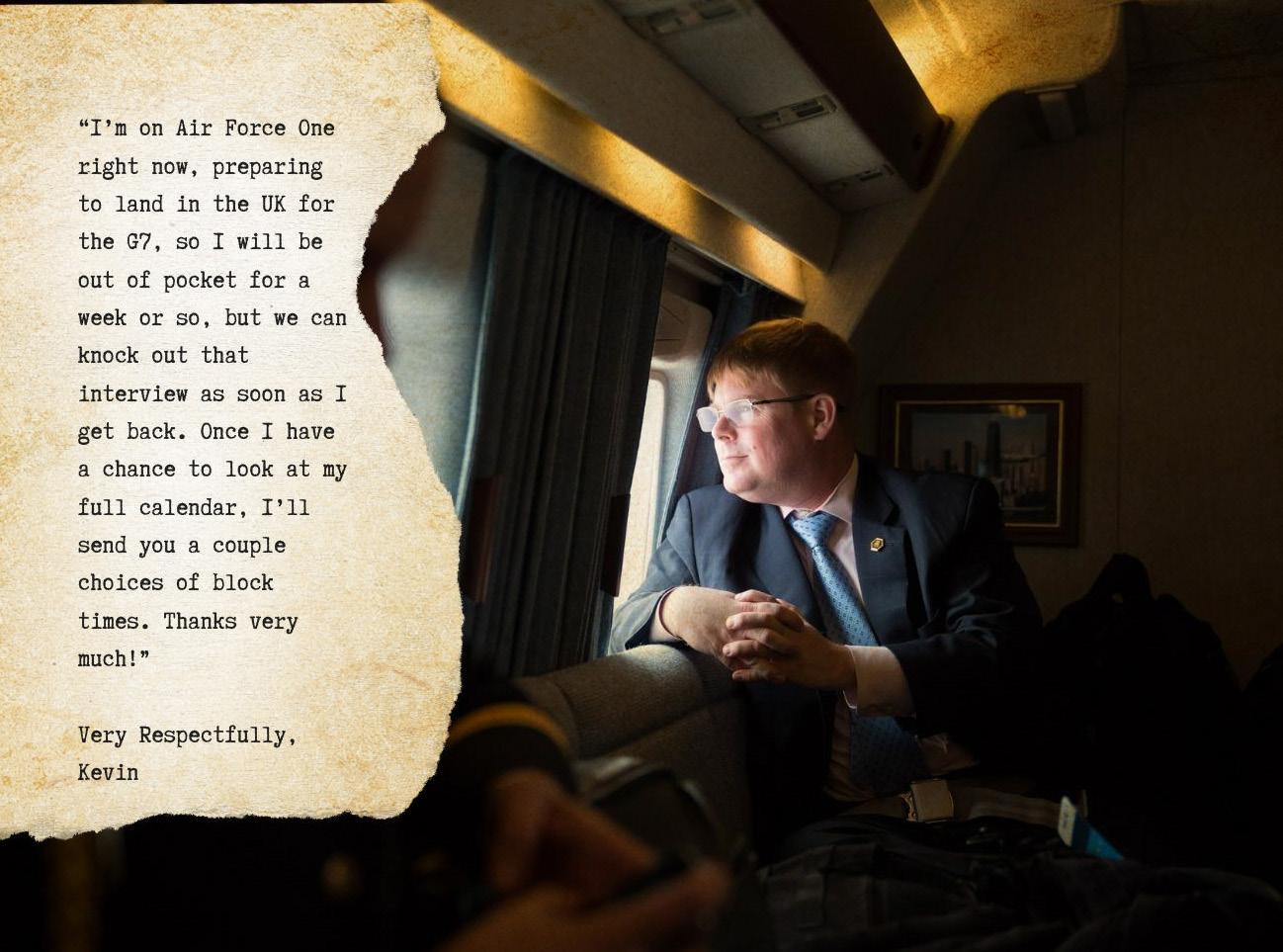


 DDr. Samir Mehta Chief of Ortho at Penn Med
DDr. Samir Mehta Chief of Ortho at Penn Med
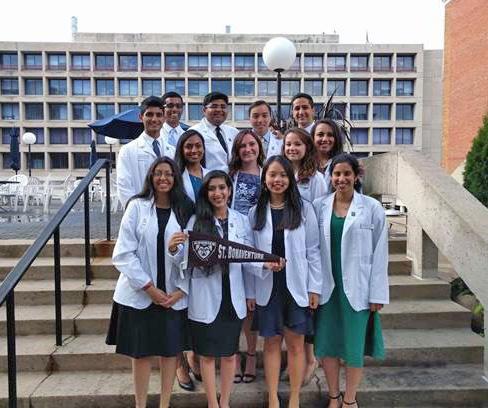










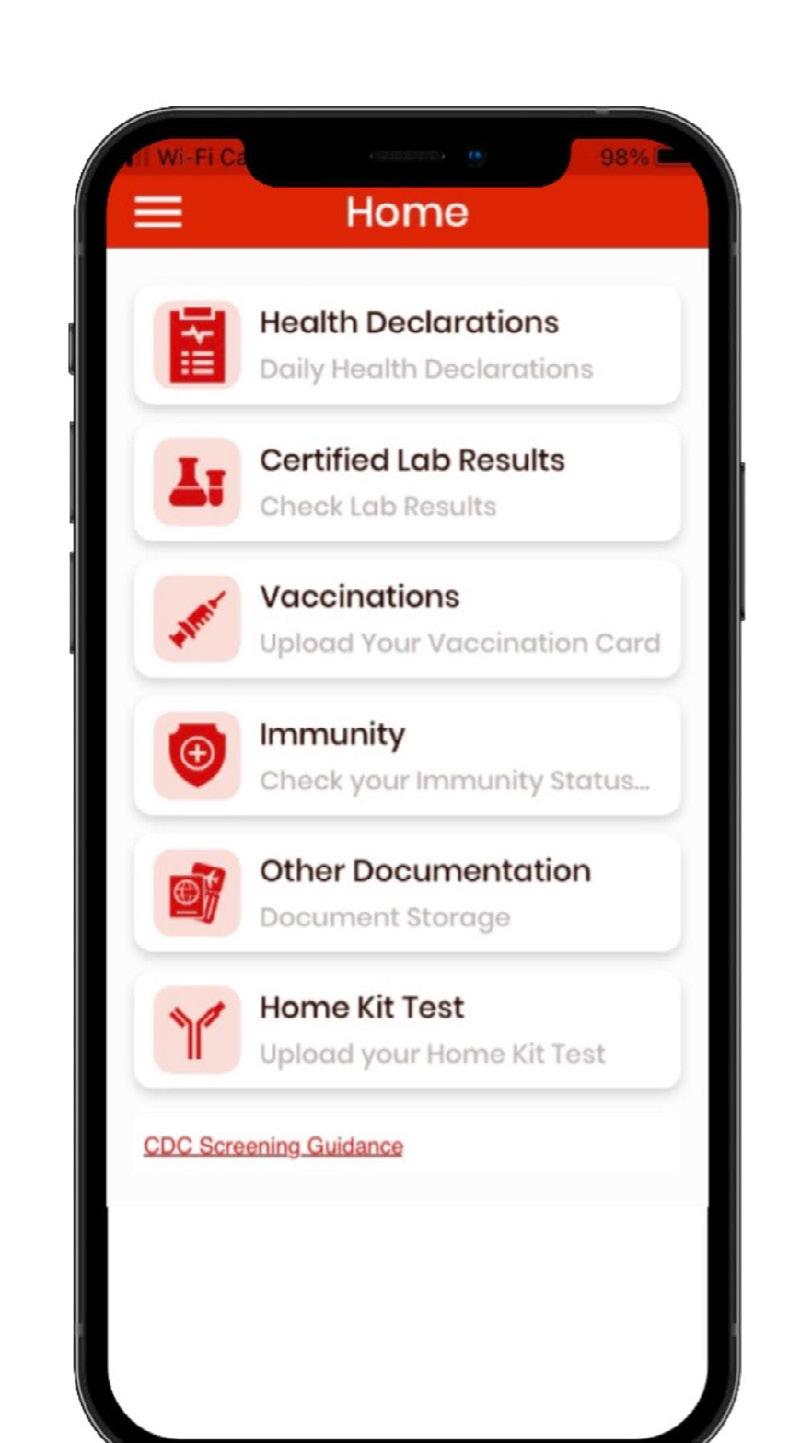
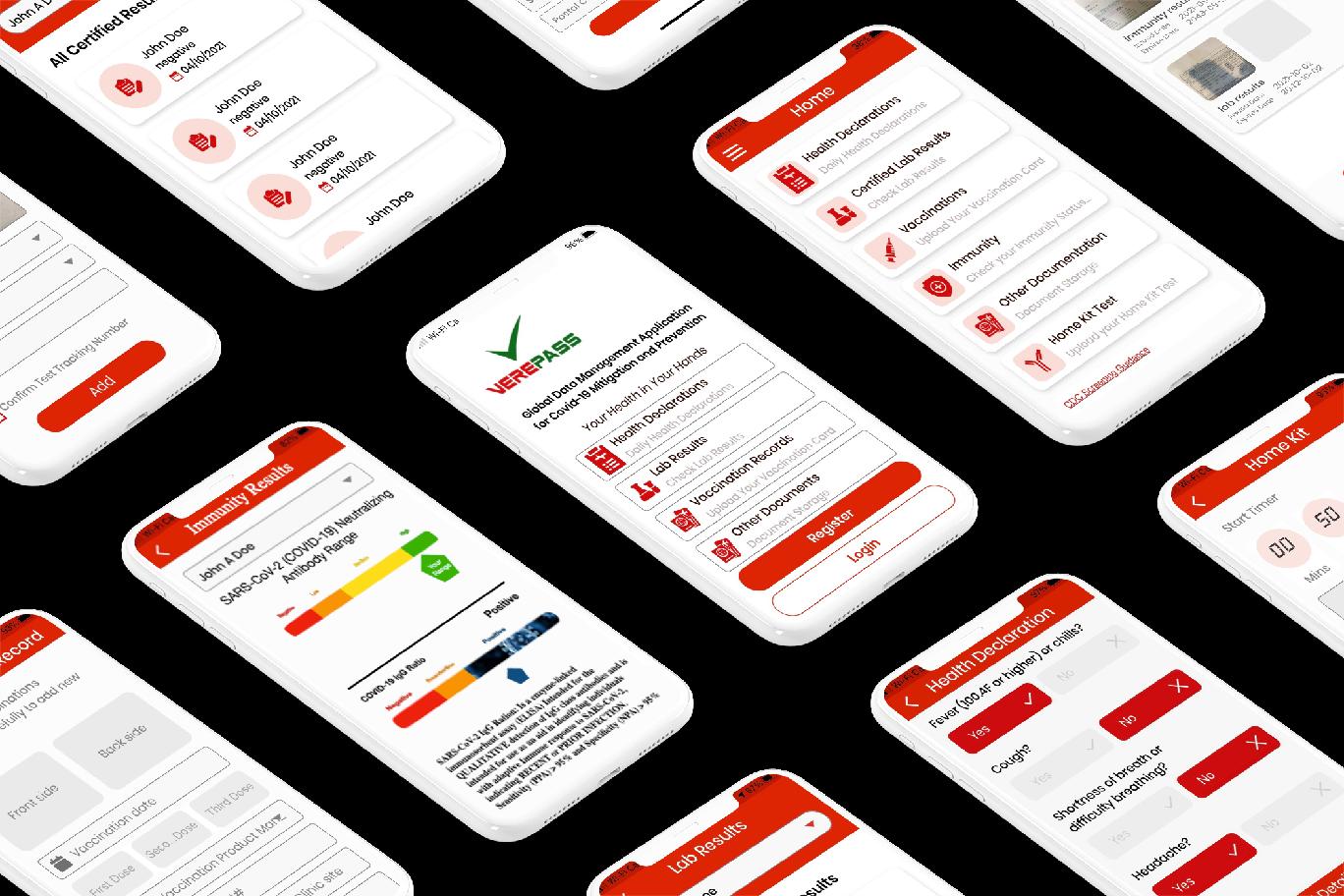

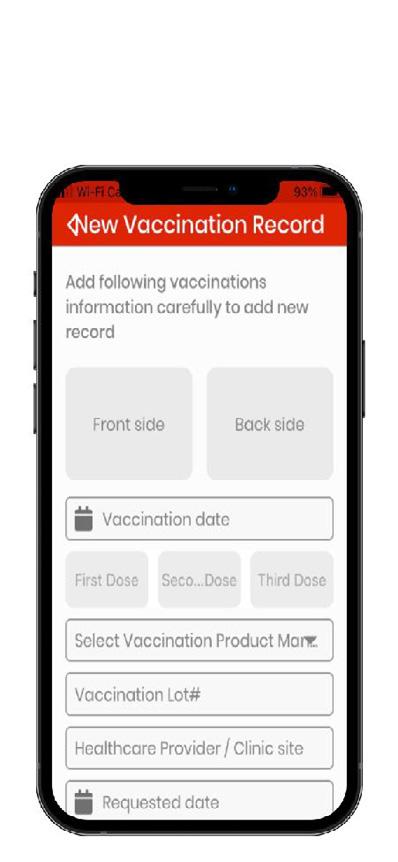






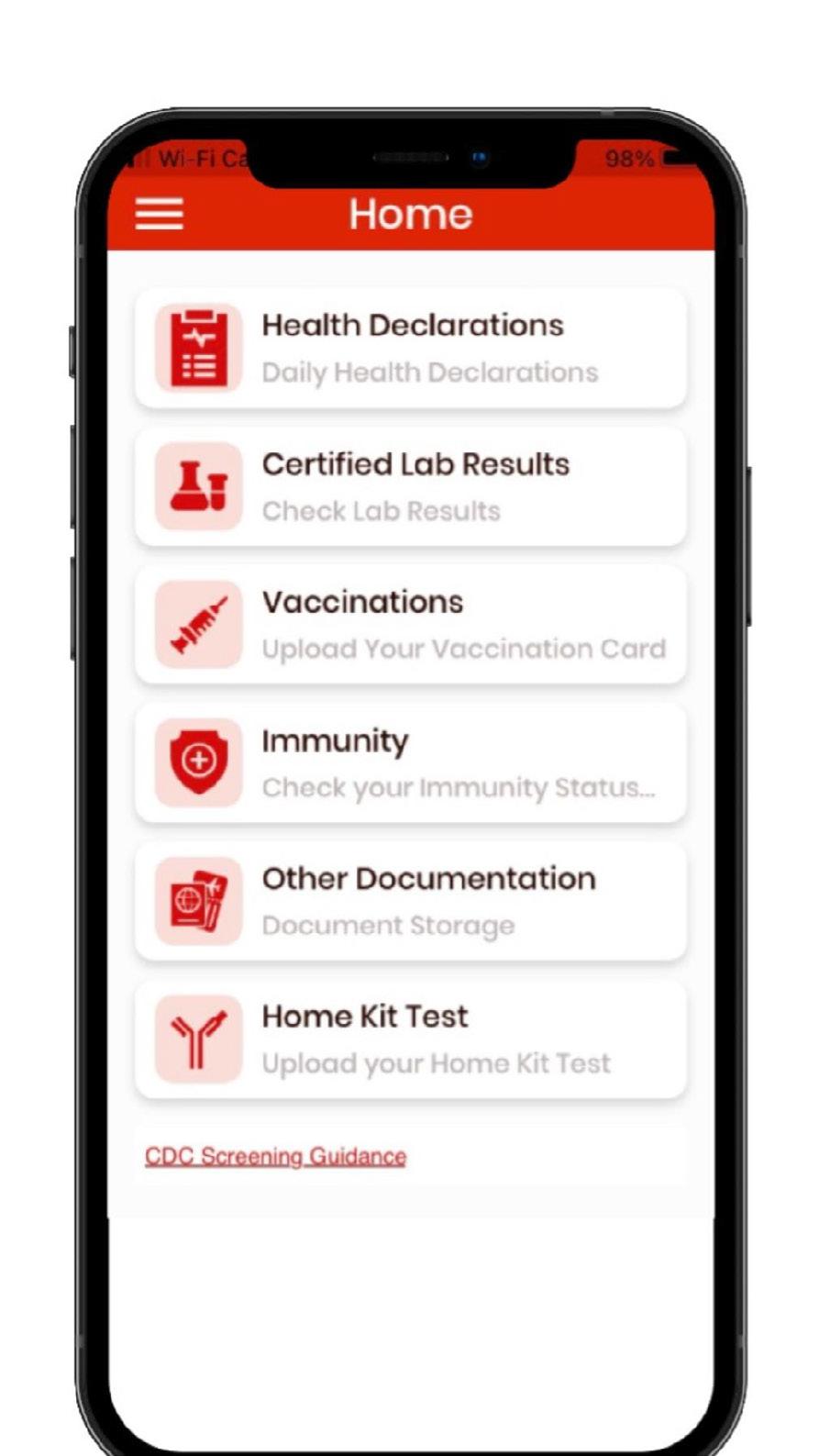
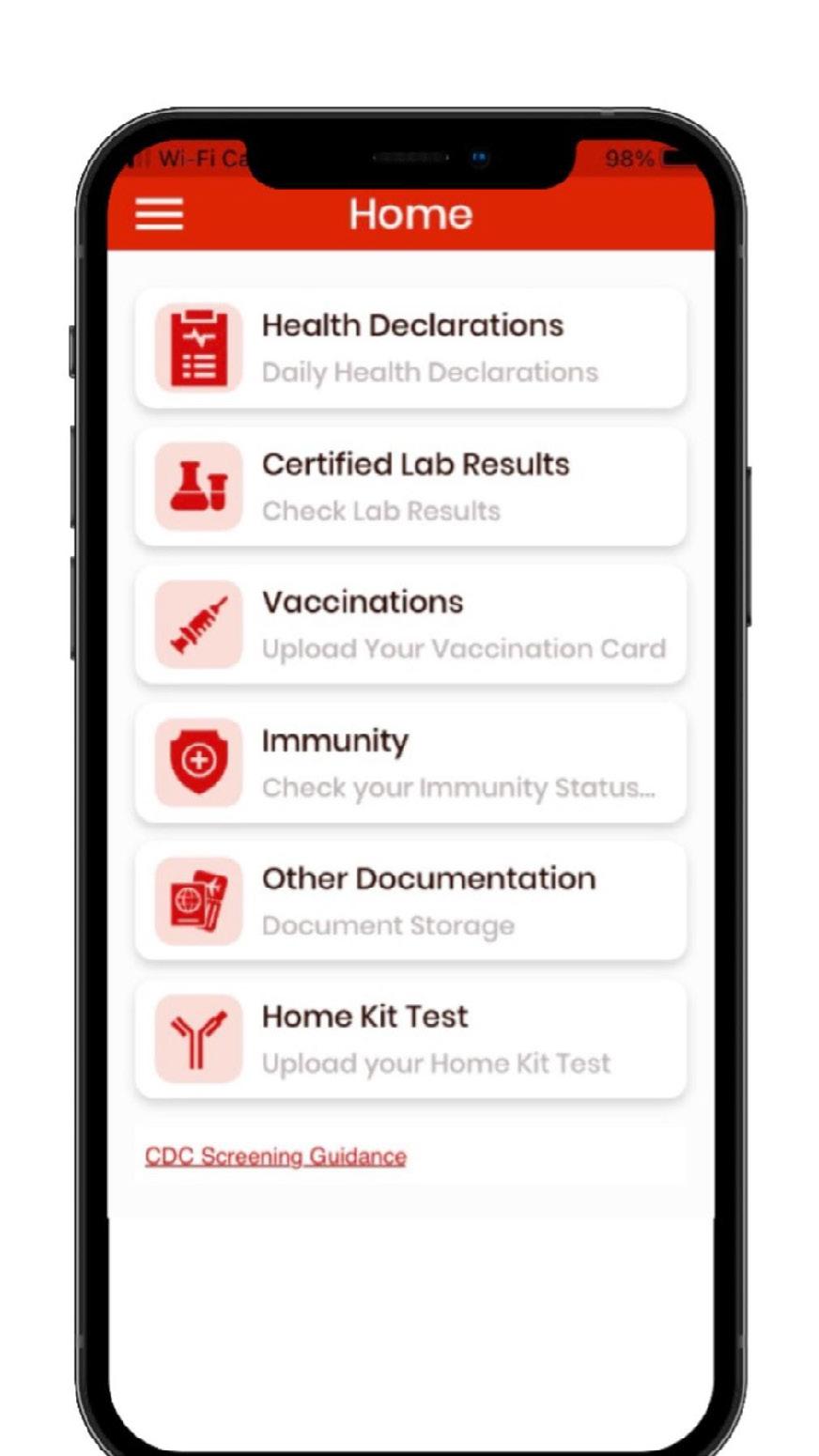
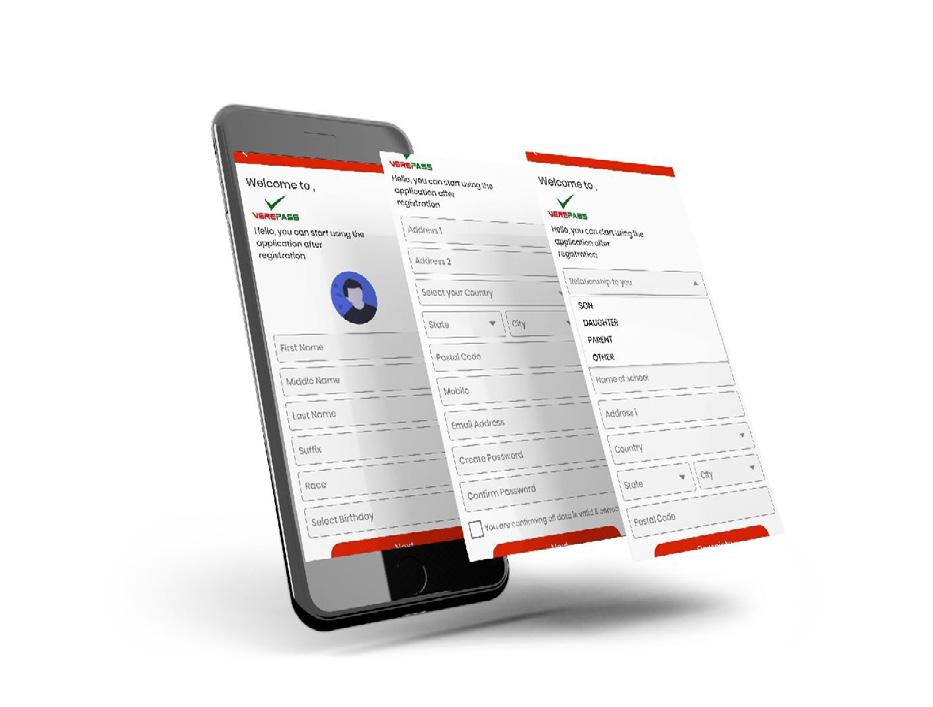


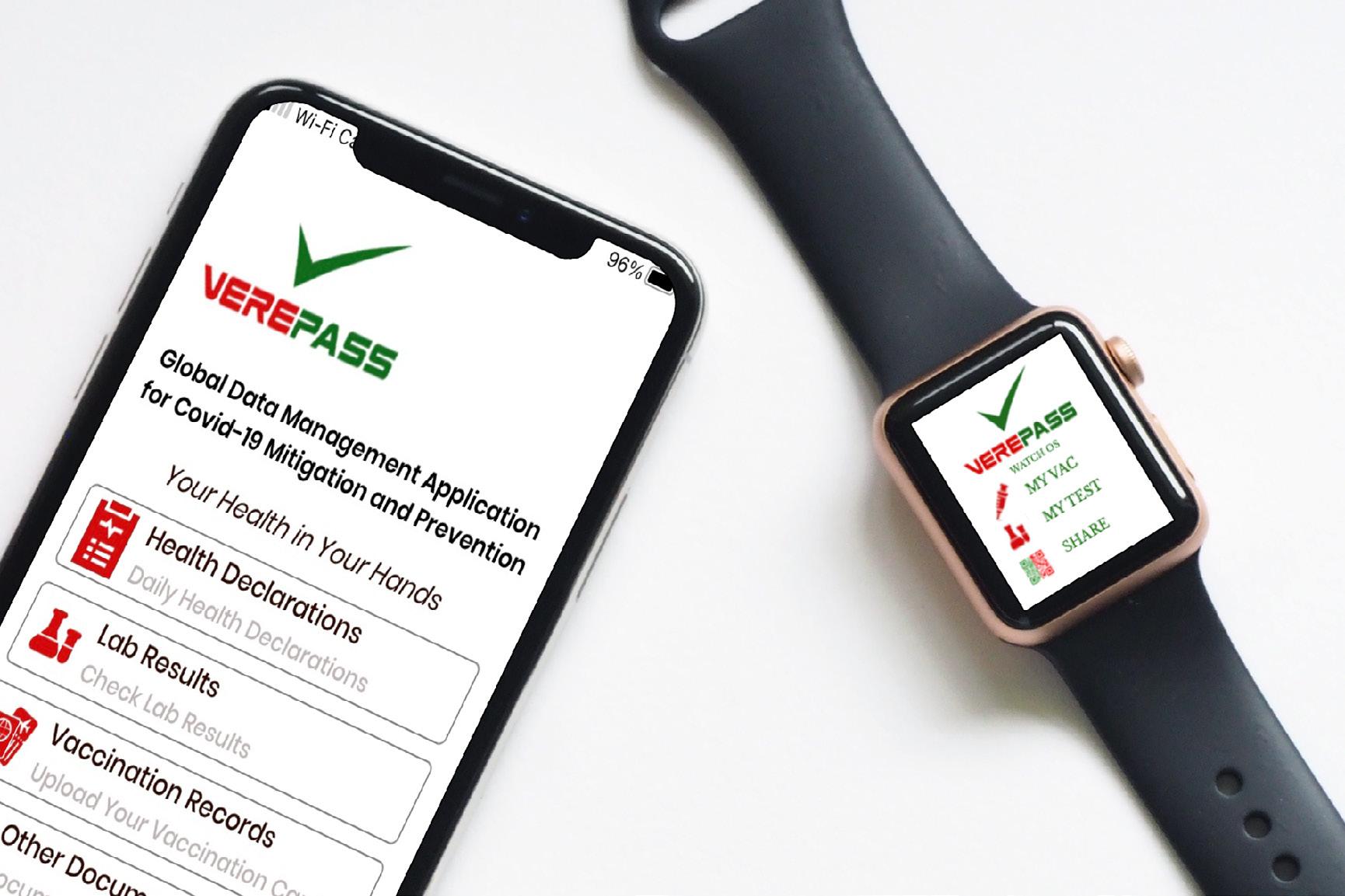










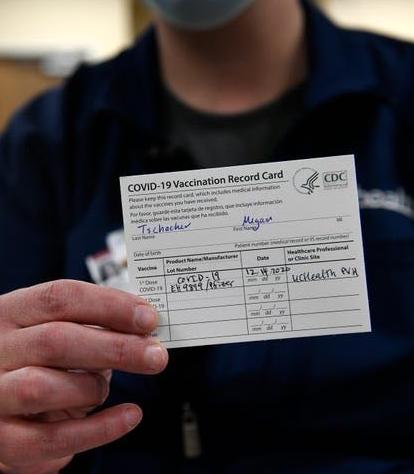






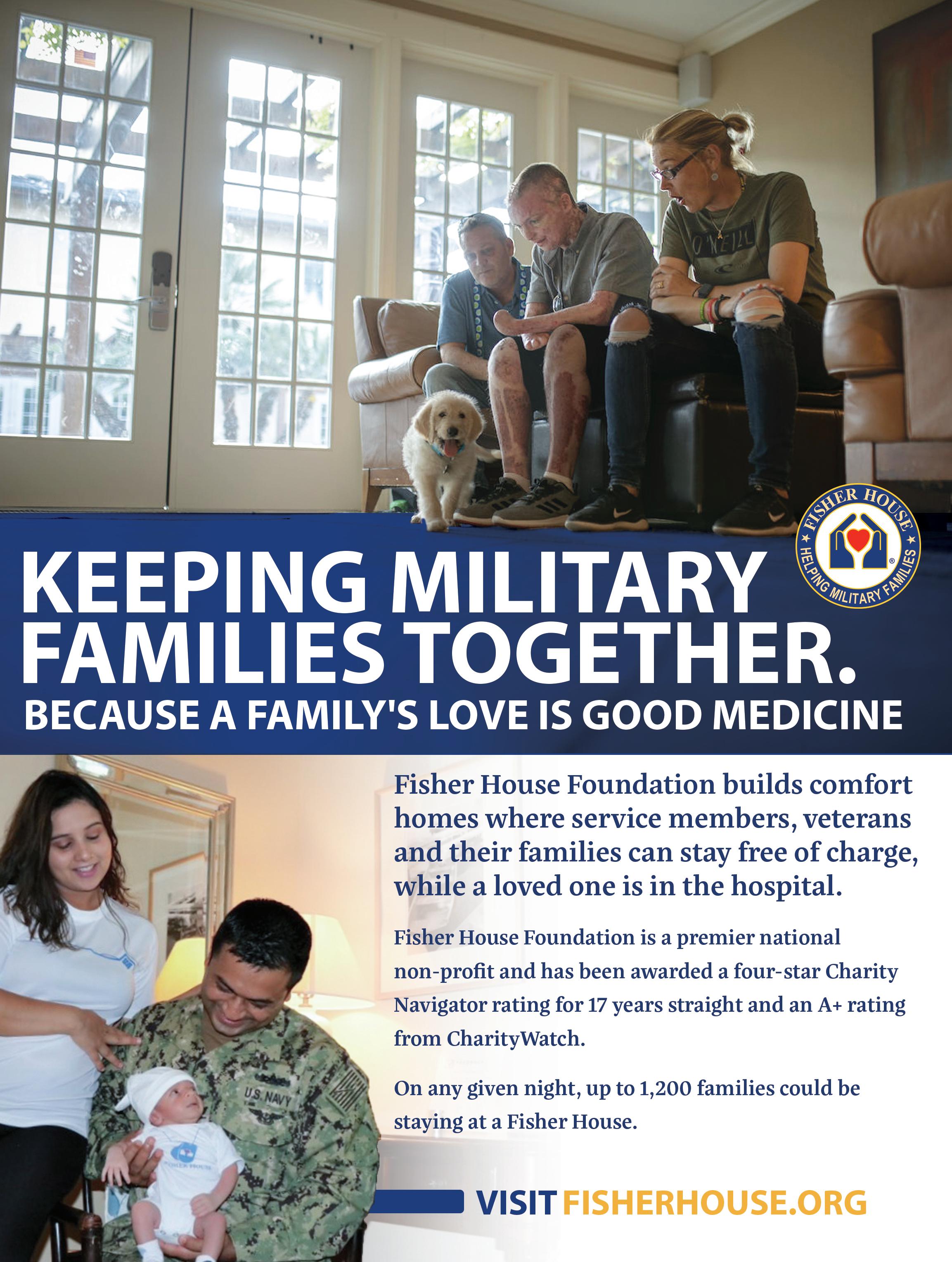







 PHOTO CREDIT: DR. NATALIE NEWMAN
PHOTO CREDIT: DR. NATALIE NEWMAN