STANDARDS
PUSH TOWARDS UNIVERSAL ACCESS TO MYOPIA MANAGEMENT FOR AUSSIE KIDS


MORE AUSTRALIAN OPHTHALMOLOGISTS SEEK THE SECURITY OF PRIVATE GROUP PRACTICE
A new snapshot into the "financial health" of private medical practices in Australia has shown the profits of ophthalmology and other non-GP specialist businesses in Australia have continued to increase over time, averaging around $216,000 in 2020-21, and are more profitable than other non-medical enterprises in legal, finance, accountancy, construction and agriculture.
The 2022 report entitled: ‘ANZ— Melbourne Institute health sector report – Trends in the structure and financial health of private medical practices in Australia’, by University of Melbourne health economist Professor Anthony Scott, has also confirmed more ophthalmologists and other specialists are seeking the security of private group practice in the face of inflationary pressures.
The findings come as no surprise to the Australian Society of Ophthalmologists vice president Dr Peter Sumich who said group private practice is becoming the norm as the cost of running practices increases.
“No longer does a sole ophthalmologist wish to take individual responsibility for the growing overheads which include IT, human resources, technology, insurances and leasing costs,” he said.
“Furthermore, group practice provides the opportunity to share care across subspecialties and during holiday periods. Group practices often provide regional services as an offshoot which is a good model for delivering more remote care.”
In his report, Scott assessed
the growth trajectory of doctors in Australia and the financial performance of GP and non-GP specialist businesses, the latter which includes ophthalmology.
He found medical business profits rose by an average of 2.4% per year for GPs and 5.4% per year for non-GP specialists before the COVID-19 pandemic.
Non-GP specialist business entities had the highest median gross profit (defined as turnover minus costs from Business Activity Statements) in 2020–21 ($216,468), followed by GP businesses ($144,485). The next closest were legal businesses which have slightly lower profits than GP businesses ($124,131). Finance, accountancy, construction and agriculture businesses generally have much lower median gross profits per business.
Gross profit margins (profits as a percentage of turnover) generally follow the same pattern. However, businesses in the financial sector had higher gross profit margins per business (37.5%) than GP businesses (35.8%).
continued page 8
OPTOMETRY AMONG TOP BULK BILLING HEALTH PROFESSIONS
The latest Medicare utilisation figures show the rate of bulk billed optometry services in Australia has remained high and stable compared to other health disciplines such as GPs, however Medicare items are insufficient to cover the true costs of providing quality eyecare, advocates say.
The Federal Government released its quarterly Medicare statistics (September quarter 2022-23) which show 94.3% of optometry services were bulk billed in the quarter, which is consistent with statistics back to 2014-15 when there was a noticeable drop from the 97% rate.
Optometry Australia (OA) interim CEO Ms Skye Cappuccio said optometry has long been one of the

highest bulk-billing professions.
“There are a number of reasons for this, including perceptions –perhaps not fully founded – about the willingness of patients to pay out-of-pocket costs for optometric care. Removal of the ‘cap’ on fees optometrists could charge for Medicare-subsidised services (which OA was successful in securing in 2015) did result in a small drop in bulk billing,” she said.
“Whilst bulk-billing for Medicare-subsidised services remains high, anecdotal evidence suggests that more practices are billing privately for services not covered by Medicare.”
When an optometry patient was charged an out-of-pocket cost, the
average amount paid was $34. For specialists, which include ophthalmologists, the data unsurprisingly showed the minority of patients were bulk billed at a rate of 30.6%. In the 5.9 million services that involved billing a patient, the average out-of-pocket cost was $101 per service.

GPs have been particularly concerned about their diminishing ability to provide bulk billed care. GP non-referred attendances were bulk billed 83.4% of the time in the latest figures. This is significantly lower than the corresponding 2021-22 quarter at 89.6% and the peak in the 2019-20 June quarter at 92.5%.
“[GP] practices are under strain, continued page 8
businesses performance after investing in premium lens technology manufactured by Rodenstock.
page 42


IN THIS ISSUE
EDITORIAL
MY 2023 PREDICTIONS
Five topics come to mind when I think of issues that will shape the 2023 ophthalmic agenda: a changing optometric workforce, waiting lists, dry AMD, axial length and artificial intelligence (AI).
In 2023, expect plenty of activity in the practice ownership space, brought about by changes at either end of the optometry career spectrum. Many experienced optometrists are moving into retirement and corporate-style groups are presenting themselves as a good exit strategy option.

COLOURFUL COLLECTION
SPECIALISED SERVICE
Equally, the sector is expected to have more graduates entering the industry than previously. Anecdotally, several early-career optometrists are being attracted to independent ownership, creating another succession pathway for existing owners. If the independent market is to maintain its foothold, structured business-related education and advice for emerging practice owners will be crucial.

Surgical waiting lists were a major problem in 2022, with cataract surgery one of the worst offenders. Expect more elective surgery ‘blitzs’ and the call to go out to the private sector.
While myopia management interventions have made headlines of late, there will be a push towards the more accurate measurement of axial length to monitor progression. This will form part of a new Standard of Care being developed to ensure children have universal access to appropriate management plans.
YEAR AHEAD
In macular disease, the first approved treatment for geographic atrophy (dry AMD) could be available locally this year. While good news, more thought needs to be given to how this will be rolled out to patients.

Finally, I expect AI to further realise its potential. With several eye screening systems TGA-approved, studies are investigating real-world implementation to overcome the tyranny of distance in Australia. And whether the technology is eventually incorporated into metro eye clinics is an interesting proposition.


We hope you enjoy the first edition of Insight for 2023, and look forward to further serving the ophthalmic community throughout the year.
MYLES HUME Editor
Pentacam®
The indispensable tool for contact lens fitting
Cornea Scleral Profile

Pentacam® Scheimpflug technology has long been renowned for accurate corneal surface data. Combined with non-invasive scleral topography and sagittal height data, CSP delivers accurate parameters to simplify fitting of scleral contact lenses.

The Pentacam® and Pentacam® HR models can accurately perform CSP by capturing five scans which are automatically combined to create one cornea scleral map.
NEW Pentacam® AXL WAVE & CSP Pro
To optimise workflow, the newest model Pentacam® AXL Wave with CSP Pro enables single scans exceeding 20mm in diameter, improving efficiency and reproducibility.

UPFRONT
Just as Insight went to print, AHPRA, invited practitioners, stakeholders and the community to provide feedback on its review of healthcare professional’s accreditation arrangements for the next five years. With consultation ending 14 February, Ahpra stated accreditation was a core regulatory function in the supply of new qualified, safe and competent health practitioners. The review will be completed by May 2023.
WEIRD
The eyes can help scientists measure human consciousness and awareness, a new study has found. When people were shown clear images, their eye movements showed a distinct pattern indicating awareness, but with progressively dimmer images, the pattern changed. The eye-tracking may help research into the amorphous dividing line between consciousness and unconsciousness, a state most obvious as people awake from sleep.
WONDERFUL
US eye doctor Dr Diane Hilal-Campo has developed her own range of eye-friendly cosmetic products after spending decades treating female patients struggling with dry eye and other painful conditions caused by makeup and beauty treatments. Her range includes a lash and brow serum, mascara and liquid eye liner, which don’t include ingredients like prostaglandins, acetyl hexapeptide and benzalkonium chloride.
WACKY
Researchers have discovered that fruit flies can’t move their eyes relative to their head, so to overcome this they move their retinas instead. Using a fluorescent molecule that binds to muscle fibers, the scientists initially found the insect has two muscles attached to each of their retinas –allowing the retina to move both back and forth, and up and down.
IN OTHER NEWS the landmark L iGHT study – that ultimately recommended selective laser trabeculoplasty (SLT) as a first-line glaucoma intervention – has published six-year results. “After six years of treatment and monitoring, SLT safely offers IOP control without the need for medical or surgical treatment in more than 70% of eyes with ocular hypertension and open-angle glaucoma, while also demonstrating reduced progression rates and a reduced
need for glaucoma and cataract surgery,” the study said. FINALLY, Lumibird Medical has launched its next generation YAG/SLT laser, the Tango Reflex Neo, by Ellex. A fully integrated Q-switched Nd:YAG and frequency doubled Nd:YAG laser for anterior segment YAG and glaucoma indications, Tango Reflex Neo features second-generation Reflex technology with True Coaxial Illumination (TCI), designed to enhance visualisation of anterior and posterior segments.
Published by: 379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766 www.primecreative.com.au
Chief Operating Officer Christine Clancy christine.clancy@primecreative.com.au
Group Managing Editor Sarah Baker sarah.baker@primecreative.com.au
Editor Myles Hume myles.hume@primecreative.com.au
Journalist Rhiannon Bowman rhiannon.bowman@primecreative.com.au
Commissioning Editor, Healthcare Education Jeff Megahan Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager Salma Kennedy salma.kennedy@primecreative.com.au
EARLY CHILDHOOD VISION

2009
2016,
WHAT'S ON
16 – 19 FEBRUARY
The congress, in Queenstown, will be expanded to incorporate a broader range of glaucoma science and encourage connection with translational scientists. anzgsconference@conceptevents. com.au
9 – 10 MARCH
The 38th annual ANZ Cornea Society and Eye Banking Meeting is taking place at DoubleTree by Hilton on Perth’s waterfront. 38cornea@lei.org.au
Design Production Manager Michelle Weston michelle.weston@primecreative.com.au
Head of Design Blake Storey
Art Director Bea Barthelson Subscriptions
T: 03 9690 8766 subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright – No part of this publication be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.

ADMIN COMPLEXITIES 'CONTINUE TO RAMP UP'
continued from page 3
“Non-GP specialists saw profits of almost 49% of turnover and for GPs this was 36%,” Scott added.
While profits are increasing, so too are expenses, which could be leading more medical entities to consolidate. The report found the total number of doctors in a solo private practice has fallen by 0.5% between 2013 and 2020, while the number in group private practices has increased by 28.9%
Further, the proportion of non-GP specialists working in group private practice has increased three times faster (12%) compared to GPs (4%) in the seven years to 2020 – equivalent to an average increase of 4% per year.
When it comes to the proportion of all doctors who are in private group medical practice, ophthalmologists rank among the highest, well over 70%.
Mr James Thiedeman, CEO of Australia’s largest private ophthalmology network the Vision Eye Institute, told Insight many doctors are choosing to join group practices once they complete their training, to allow them to focus on clinical care and “outsource” the extensive administrative burdens.

“If you ask any doctor if they prefer to spend time on patient care or paperwork, you can be pretty confident what the answer will be,” he said.
“Doctors understandably want to ‘doctor’, not administer. That said, the reality is administrative demands
on clinical staff continue to grow; as complexities around funding arrangements, accreditation and regulation, people and culture and stakeholder relationship management continue to ramp up.”
Through scale, Thiedeman said large providers can also pass on the benefits of lower operating costs and access to in-house dedicated professional experts in areas like people and culture, marketing, quality and risk, and cyber security.
“It’s not surprising more and more medical specialists are increasingly choosing to align themselves with larger group practices,” he said.
“The latest data from ANZ-Melbourne Institute show ophthalmology is only second behind general practice with approximately 70% of all ophthalmologists in private practice choosing to delivering care from a group practice. My prediction is this will grow further and the scale of group practices with continue to increase.”
OPERATIONAL CHALLENGES
In the report, Scott points to many pressures facing the health sector, including sharp falls in healthcare utilisation during the COVID pandemic, the freeze on Medicare indexation between 2014-18, increasing competition among doctors and a drop in private health insurance membership between 2015-20 due to out-of-pocket costs rising faster than wages.
“How the private medical sector is responding to these pressures is a key issue because the structure and operation
of the market can influence overall health expenditures, access and quality of care, out-of-pocket costs and employment in the sector,” Scott said.
Looking to the future, the report stated the long-term trend toward further consolidation of non-GP specialist private practices could continue as the number of doctors keeps increasing.
“There is also uncertainty around whether increasing inflation could lead to higher business costs through higher interest rates and upward pressure on the wages of employees. A tight fiscal environment could limit the growth in Medicare revenue and further increase Medicare and tax compliance pressures,” the report concluded.
The private medical sector could also flexibly respond to future challenges through reducing costs and improving efficiency.
“Being able to manage medical businesses more efficiently through new technology and improvements in management and organisation (such as efficient business structures) is becoming more important as cost pressures continue," the report said.
Consolidation and cost cutting can improve the efficiency of medical businesses but also has potential implications for patients in terms of access to care, choice and out-of-pocket costs which need to be monitored."
REBATES A DECADE BEHIND WHERE THEY SHOULD BE
continued from page 3
and many are making the difficult but necessary decision to stop bulk billing some or all of their patients and move to a private or mixed billing model,” Royal Australian College of General Practitioners president Dr Nicole Higgins said.
“This follows many years of under-investment in general practice care including the six year-long Medicare rebate freeze.”

Optometry was first included on the Medicare Benefits Schedule (MBS) in 1975. But since 1997, adjustments to the optometric MBS have continued to significantly lag beshind CPI, Optometry Australia said in June 2022 when
indexation was increased by a “modest”
1.6%.
This came after a freeze in indexation for optometry between 2013 and 2019, plus a 5% cut to MBS rebates introduced by the government in 2015, which OA says has resulted in Medicare rebates in real terms being a decade behind where they should be today.
Cappuccio said the lengthy freeze on indexation of Medicare items, and inadequate indexation that isn’t aligned to increasing costs to provide healthcare, mean that many optometry Medicare items are insufficient to address the true costs of providing quality optometric care.
“We continue to advocate for fairer
indexation. We also encourage and support practices to charge fair fees that cover the true cost of providing such care – and have extensive resources online to assist members in making this transition,” she said.
In the latest quarter, there were 2.6 million optometry services provided, which is the fifth highest number since records began in 2009-10.
The figure is considerably higher compared to 1.9 million optometry services provided in the corresponding 2021-22 quarter (when COVID limited public access to optometry), and the 2.3 million services provided in the 2018-19 September quarter (pre pandemic).
OF THE MARKET CAN INFLUENCE OVERALL HEALTH EXPENDITURES, ACCESS AND QUALITY OF CARE, OUT-OF-POCKET COSTS AND EMPLOYMENT IN THE SECTOR”
ANTHONY SCOTT, UNIVERSITY OF MELBOURNE
PEAK BODY CONSIDERS SOUTHERN UNIFICATION
A new southern alliance between Optometry Victoria South Australia (OV/ SA), Optometry Tasmania (OTas) and the national body Optometry Australia (OA) is being explored to drive greater efficiencies and better use of member funds.
News of the potential amalgamation came as the national body appointed optometrists Mr Theo Charalambous and Mr Albert Lee to its board as deputy president and treasurer, respectively.
Charalambous has extensive experience as a franchise owner of OPSM practices based in Pakenham, Berwick, Brighton and South Yarra. He also partners in a private practice, Hastings Optical. Lee is a clinical optometrist and owner of an independent, full-scope optometry practice based in Rockdale, NSW.

Their appointments follow the departure of Ms Fiona Moore (former deputy president), Ms Tori Halsey (former treasurer), and Mr Rob Howie who stepped down from the board at OA’s annual general meeting on 25 November 2022.
Sydney optometrist Ms Margaret Lam
retained the national presidency, while other new board members include Mr Lee Baumwol, Mr Kevin Sun and Mr Shuvagata Bose.
Regarding the potential unification of OV/ SA, OA and OTas, OV/SA president Ms Elise Pocknee-Clem and OTas president Mr John Kingshott confirmed that discussions “are currently exploratory”, and no structural details have yet been decided on.
OV/SA, OTas, and OA are currently three separate entities, with individual optometrist members of their respective state divisions. As state divisions, OV/SA and OTas are member organisations of OA.
According to a report on the OA website, the goal of a potential unification is to create a more streamlined single entity to deliver more efficient use of member funds and reduce duplication and administrative burden. The organisations say the benefits of such an approach have been evidence in the 2019 amalgamation between Optometry Victoria and Optometry South Australia.
Theo Charalambous, Optometry Australia deputy presidentThe boards of OV/SA and OTas have reportedly expressed confidence that if an amalgamation occurred, OA would continue to provide members in Victoria, South Australia, and Tasmania with the same direct services it already provides to OV/SA and OTas members.

They also confirmed that OA will continue to function as the peak national body for optometrists, while continuing to provide services to members based in NSW, ACT, Queensland, Northern Territory, and Western Australia, as per agreements with those state divisions.
The decision on amalgamation will ultimately be left up to the members of each state organisation.
“While our talks are still early, our boards wanted to be transparent by informing you that these discussions are underway. We will keep you updated and provide you with opportunity to input," Kingshott said to members.
Discussions have continued in recent months, with plans for a possible amalgamation to occur in 2023, OA stated.

COMPLAINTS AGAINST OPTOMETRISTS RISING
Complaints against Australian optometrists are on the rise, with health regulator Ahpra receiving ‘notifications’ about 17 more optometrists than this time last year – a 38% increase.
The latest optometry complaints data from the Australian Health Practitioner Regulation Agency (Ahpra) was released in its 2021/22 annual report on Tuesday 22 November.
It shows there were 68 notifications lodged against 61 optometrists, including data from the NSW Health Professional Councils Authority and Queensland’s Office of the Health Ombudsman (OHO). This compares with 38 complaints against 44 optometrists in 2019/20.
This means 0.9% of the Australian optometry profession had received complaints, compared to 0.7% the previous year.
The increase is part of a broader trend among all health professions regulated by Ahpra, with 6.5% more complaints in 2021/22 than 2020/21. The overall percentage (1.6-1.7%) of health practitioners with a notification stayed around the same, however.
In terms of the 33 optometry cases that were closed in 2020/21, 42% resulted in no further action, significantly down from 74% the year before.
Fifteen per cent of closed cases this year resulted in conditions being imposed on their registration and 42% were referred to another body or retained by a health complaints entity.
Criminal complaints were lodged in four optometry cases in 2021/22; two related to advertising breaches, one about title protection and another about practice protection.
In terms of why patients complained about optometrists, clinical care was the most common reason (57%), followed by breach of non-offence provision (9%), documentation (9%), communication (6%), behaviour (3%), confidentiality (3%) and other (14%).
The majority of all complaints were made by a patient, relative or member of the public (74%), followed by a health complaints entity (11%), board-initiated (3%), employer (3%), another practitioner (3%) and other (6%).
The annual report figures show the number of registered optometrists continues to increase, up 3.4% from the year prior to 6,500. Feminisation of the Australian optometry workforce continues, with 57.6% now identifying as female.
Ahpra CEO Mr Martin Fletcher said overall there was a steady increase in notifications raising concerns about the conduct, performance or impairment of a

OF OUR REGULATORY PROCESSES, ACCESS TO SUPPORT FOR BOTH PRACTITIONERS AND NOTIFIERS AND IMPROVING OUR COMMUNICATION”
registered health practitioners.
However, more than 60% did not require regulatory action, with practitioners or their employers taking steps to resolve the issue. More than 70% of the notifications closed were done so within six months on average.
Ahpra also received 925 notifications about lack of appropriate professional boundaries (63% increase). The increase can partly be attributed to new concern types relating to sexism, sexual harassment or gendered violence in healthcare, and expectations of practitioners to maintain respectful, professional practise.
“We recognise the significant stress for both practitioners and notifiers when a concern is raised with us. While there are significant challenges, we continue to focus on improving the timeliness of our regulatory processes, access to support for both practitioners and notifiers and improving our communication throughout,” Fletcher said.
In June, Ahpra updated the shared Code of conduct which sets out the expectations for 12 regulated professions, including optometry.
It also revised regulatory principles underpinning its decision making, making it clear that public protection is its paramount objective.
CALL FOR RETURN TO ‘OPTING IN’ ON DRIVER LICENCES TO LIFT ORGAN AND TISSUE DONATION RATES

Transplant Australia is concerned about the hidden residual effect of the COVID-19 pandemic on Australia’s organ and tissue donation system and has called for a retuning of the ‘yes’ donor option within state-based driver licence systems.
The peak body has also welcomed the Federal Government’s decision to consult the sector in the adoption of a new National Strategy for Organ Donation, Retrieval and Transplantation.
A key component of the strategy, according to Transplant Australia, will be increasing the number of Australians registered as organ donors as evidence shows a direct correlation between registration rates and family consent rates at the time of donation.
But the organisation also wanted federal, state and territory governments to work
together under the proposed new national strategy to return the option to say “yes” to organ donation when applying for or renewing a driver’s licence.
“The year 2018 was a record-breaking year for donation in Australia with 554 donors saving the lives of 1,544 Australians. It represented the hard work of the DonateLife Network and the Organ and Tissue Authority over the past decade in reforming donation across Australia,” Transplant Australia CEO Mr Chris Thomas said.
“Unfortunately, donation since then has been severely impacted by the COVID pandemic. In 2021 the number of donors was 421 compared to the record of 554. Unfortunately for those waiting, 2022 had about the same number of donors. (359 donors to the end of October).”
In terms of eye donations, the latest data showed in 2021 there were 1,472 donors, up by 154 compared to 2020. As a result, there were 2,413 corneal transplants, which was 6% more than 2020 when 2,277 were performed.
“Despite significant success the one key area yet to change in donation is the overall family consent rate which fell to 56% in 2021,” Thomas said.
“There is a strong correlation between consent and registration – if a person is registered to be a donor, in nine out of 10 cases families will support that decision. This drops to four out of 10 when there is no knowledge of their wishes.”
In South Australia, where registration is still part of the driver’s licence, Thomas said 73% of the population is registered, with the family consent rate also 73%.

“WE CONTINUE TO FOCUS ON IMPROVING THE TIMELINESS
MARTIN FLETCHER, AHPRAAustralia could achieve a 75% family consent rate within five years.


SWAROVSKI AND ESSILORLUXOTTICA ANNOUNCE 10-YEAR LICENSE DEAL
Luxury label Swarovski has signed a new exclusive license agreement EssilorLuxottica who will design, manufacture and distribute Swarovski Eyewear globally potentially for the next decade.
The agreement will be effective until December 31, 2028, with an automatic renewal option of an additional five years. The first collection as part of the deal will be developed under the leadership of Swarovski Creative Director Ms Giovanna Engelbert and launched in time for the FW23 season.
According to a statement, the agreement combines Swarovski’s creativity and savoir-faire with the knowledge, innovation, and expertise of EssilorLuxottica.
The partnership is said to build on Swarovski’s “luxury credentials” alongside its commitment to eyewear as a key fashion accessory.

Mr Alexis Nasard, CEO of Swarovski, said the company was pleased to evolve its eyewear business with EssilorLuxottica.
“This is in-line with our LUXignite strategy, and is a natural partnership for us, forged from a shared passion for beautiful design coupled with impeccable quality and savoir-faire,” he said.
Mr Francesco Milleri, chairman and CEO of EssilorLuxottica, added: “We are excited to embark on this journey with Swarovski, a brand known for its artful design and incredible attention to detail. We have always seen each pair of frames as a piece of art to be worn, which makes Swarovski and its story such a wonderful fit.”
Swarovski Eyewear, which features designs inspired by the brand’s jewellery families, brings an additional facet to Swarovski’s customer offering, and complements its jewellery, home décor and accessories collections.
INDEPENDENT ACQUIRES ASSETS OF OVERSEAS CHAIN IN LIQUIDATION
An independent practice in Bondi Junction has acquired unspecified assets following the closure of an overseas-owned optical chain’s Australian stores.
Carolina Lemke Berlin, the Israeli owned optical network which had set up stores in Australia several years ago, has exited the Australian market closing its three stores in Sydney and one in Melbourne.

The Sydney stores were located in Westfield Bondi Junction, Westfield Miranda, and World Square in George Street.
Tracton Optometrists in Bondi Junction, Sydney – established by Mr Daniel and Ms Michelle Tracton last year – have emerged as the buyers of the three closed Sydney stores’ assets.
“This decision made sense for us. The Carolina Lemke store in Bondi Junction was a mere 150 metres away from our new practice,” Tracton said.
“When they closed the stores, patients of all three sites were at a loose end,
looking for a new place for their eyecare and eyewear. We are very happy to give these patients continuity of care in our practice, especially as we approach the busy optical period,” he said.
Carolina Lemke is part of the Hoodies group of four companies: Hoodies, Top Ten, Carolina Lemke and Accessories London. It was acquired over a decade ago by Castro Model Ltd.
Carolina Lemke, which also operates stores in Europe, the UK and the US, did not respond to Insight’s request for comment.
NOVARTIS EYES SALE OF OPHTHALMOLOGY BUSINESS
Pharmaceutical giant Novartis is reportedly weighing up the sale of its ophthalmology and respiratory units.

A Bloomberg reported stated the company – which has operations in Australia – is seeking to raise funds from the possible sale to invest in cutting-edge medicines. The ophthalmology unit could alone fetch about US$5 billion (AU$7.5 billion).

Novartis has a significant presence in ophthalmology, with one of the first approved anti-VEGFs for macular disease, Lucentis (ranibizumab), available on the Pharmaceutical Benefits Scheme (PBS) since 2007. The therapy – which has seven indications in Australia – is now the eighth most expensive drug on the PBS, costing the government around $220 million annually.
The company subsequently developed
the longer-acting (Beovu) which was ultimately listed on the PBS as a second-line anti-VEGF therapy for neovascular age-related macular degeneration in October 2021, and also secured approval of Australia’s first gene therapy, Luxturna (voretigene neparvovec), in August 2020.
However, it was unclear which therapies would be sold as part of the ophthalmology portfolio.
In August, Novartis said it intended to spin off its generics unit Sandoz to focus on five core areas (hematology, solid tumours, immunology, neuroscience and cardiovascular) and strengthen its technology platforms, including gene therapy, cell therapy, radioligand therapy, targeted protein degradation and xRNA.
The company also spun off its Alcon eyecare business in 2019.
RODENSTOCK SELLING EYEWEAR BUSINESS
Rodenstock Group is selling its eyewear business to Italian frames company De Rigo, as the German firm intensifies its focus on ophthalmic lens technology.
The transaction is expected to be completed towards the end of the second quarter of 2023, with Rodenstock Australia general manager Mr Tim McCann stating the company would ensure a smooth transition of Porsche Design Eyewear and Rodenstock-branded frames into the hands of De Rigo’s Australia and New Zealand subsidiary.
De Rigo is described as a family-owned global market leader in the design, production, and distribution of high-quality eyewear.
“With lenses being a key focus for Rodenstock for a long time and B.I.G. VISION doing great things for us, and De Rigo being at the peak of the game when it comes to eyewear, it makes for a perfect arrangement for De Rigo to take over the Rodenstock eyewear division,” McCann said.
“For our Australian customers, we will ensure everything transitions as smoothly
as possible and we are working towards building a really close relationship between Rodenstock and De Rigo locally.”
De Rigo Vision Australia general manager Ms Angelina Chee added: “We are very excited to have these premium, quality eyewear brands join our stable and to be working with Rodenstock on the transition.”
Eyewear frames have been a part of the Rodenstock business since its foundation in 1877. McCann said the company founder Josef Rodenstock designed the original frame which was the first patented product of its kind in the world.
According to a statement from Rodenstock Group, the introduction of its B.I.G. VISION for all initiative in 2020, and launch of its B.I.G. NORM technology in early 2022, reinforced its capabilities in developing market leading technologies and setting industry benchmarks.
Having carefully examined different options, Rodenstock management made the “strategic decision” to sell its eyewear business, embarking on another major
For more information, speak to your local Rodenstock Account Manager.
step on its “transformational path to become a leading med-tech company in vision care”.
Rodenstock will continue to invest in R&D, as well as product and service portfolio.

“This strategic move serves our overarching goal of continuing Rodenstock’s growth as a med-tech company through innovation, commercial execution, and digitalisation,” Rodenstock CEO Mr Anders Hedegaard said.
“Rodenstock’s strong and growing pipeline of innovation and the ability to reinvent itself and thus drive the industry transformation is and has always been our biggest asset combined with the highest level of service for our customers and partners."

Mr Maurizio Dessolis, executive vice chairman of De Rigo Vision, added: “Rodenstock and De Rigo are trusted partners, and we look forward to expanding this partnership in the future and to support the continued growth of the eyewear business.”
Go
Follow:
NOVATEARS®
PBS
Listed
OMEGA-3 AVAILABLE NOW*
For Evaporative Dry Eye & Meibomian Gland Dysfunction




Innovative water-free mode of action

*Please note: NovaTears ® + Omega-3 is not PBS listed
NovaTears® is a unique preservative-free eye lubricant, which acts as a lipid layer substitute and evaporative barrier for improved tear film stability and quality.

Clinically validated with significant improvement in signs and symptoms with Evaporative Dry Eye Disease and Meibomian Gland Dysfunction patients1,2
Lipid layer deficiency Apply NovaTears®

STREAMLINED AUTHORITY CODE 6172 – NovaTears® only
Spreads quickly and easily on the lipid layer
PBS Information: Authority Required (STREAMLINED): Severe dry eye syndrome in patients who are sensitive to preservatives in multi-dose eye drops.

References: 1. Steven, Philipp, et al. “Semifluorinated Alkane Eye Drops for Treatment of Dry Eye Disease – A Prospective, Multicenter Noninterventional Study.” Journal of Ocular Pharmacology and Therapeutics 31 (8), 498-503 (2015). 2. Steven, Philipp, et al. “Semifluorinated Alkane Eye Drops for Treatment of Dry Eye Disease Due to Meibomian Gland Disease.” Journal of Ocular Pharmacology and Therapeutics. 33(9), 678-685 (2017). Sponsored by Novaliq GmbH. NovaTears ® Eye Drops (Perfluorohexyloctane 100% v/v, 3mL) are for the lubrication and relief of dry and irritated eyes. Do not use NovaTears ® with contact lenses. If using any other eye medication, allow at least 15 minutes between using the other product and applying NovaTears ®. NovaTears ® should not be used in children under 18 years. NovaTears ® should not be used while pregnant or breastfeeding. AFT Pharmaceuticals Pty Ltd, Sydney. ABN 29105636413.
For more information: 1800 238 742 www.aftpharm.com mydryeyes.com.au
‘MORE IS MORE’
Camilla collection to colour the eyewear scene


Australian luxury label Camilla has turned to Sunshades Eyewear to bring its iconic designs to life in its first eyewear collection. Insight goes behind the scenes to discover the value the new range will create for optical practices.
As a three-practice independent optometry business, Central Coast Eyecare in NSW places significant value on having access to luxury eyewear brands that help set the family-owned practice apart. Through its long-term supplier relationship with Sunshades Eyewear, labels like Oroton and Gucci have been best-sellers among its patients who would have otherwise travelled long distances to Sydney to touch and feel brands of such vintage.
“On the Central Coast and places like Bathurst where I grew up, we’ve had many chain and department stores close or reduce in size, so the ability for people to get their hands on high-end branded products is decreasing,” says Mrs Lisa Hooper, operations manager for the business’ locations in Erina, Gosford and Killarney Vale.
“As an independent optometry business, it’s important we have a point-of-difference with the eyewear we stock that can also act as an entry point for many people seeking out those iconic brands; they may not be able to obtain the clutch or the handbag, but the sunglass or optical frame is more realistic option.”

With this in mind, Hooper is excited about the latest luxury brand to join the comprehensive Sunshades Eyewear stable. The Sydney-based company has secured the license to design, manufacture and distribute the first eyewear collection for Camilla, founded by one of Australia’s foremost fashion designers Ms Camilla Franks in 2004.
The brand, originally known for its bright kaftan designs, is revered globally for its artistic, innovative and intricate designs inspired by trips to exotic countries (at the time of writing Camilla and her team were visiting Egypt). It has grown into a global print house with a presence in 55 countries and loyal following, branching out into ready-to-wear garments,
accessories such as jewellery, belts, clutches, as well as shoes and homewares.
Camilla’s entrance into the eyewear sphere is a unique proposition for independent optometry practices like Central Coast Eyewear (ProVision) who are excited to see the brand’s mission to “colour the world” translated into an eyewear collection. In fact, Hooper says her practice’s frame displays are arranged by colour, not by brand, and can see the range filling an important gap in the practice.
“I’m most excited by the use of colour – that’s the essence of Camilla. It’s just beautiful works of art,” she says.

“Camilla has such strong brand recognition, it will be a real drawcard and certain demographics just love their ranges. When it comes to choosing what to display, I’ll be packing in as much colour. The fact that we can now access a brand of this calibre in independent optometry practices is fantastic and I can’t wait – I’ve even left two windows vacant for [promotional materials] once we have the range in stock.”
CAMILLA CHOOSES A TRUSTED PARTNER
As a luxury label, Camilla has been interested in an eyewear collection for some time and it perhaps comes as no surprise that it has turned to fellow Sydneysiders, Sunshades Eyewear, who are experts in executing the end-to-end frame design, manufacture and distribution of licenced brands.
Sunshades Eyewear creative director Mr Hamish Tame, who has helped oversee the creation of the new collection, says both entities believe it’s the right time for Camilla’s arrival on the eyewear scene.
“In 2020/21, Sunshades Eyewear were looking at opportunities for the domestic optometry market – there was this demand for higher-end, European brands that incorporate a lot of colour and play with textures, but they do it in a very European way that doesn’t always translate to the needs of the Australian market,” he explains.
“We went back to Camilla and said this is how we think we can take the essence of your brand – that celebration of ‘more is more’ – to create something unique, and they were into the idea. It almost felt like the perfect dating partnership in that we were very familiar with one another and our offices are located just around the corner. It ticks all the right boxes for what we expect to be a great product in the local optometry market and internationally as well.”
For Tame’s design team, it’s been a fascinating creative process working with Camilla. Typically, they find themselves paring back designs for a more minimalistic feel, but Camilla has challenged them capture the founder’s free-spirit, wanderlust soul and adventurous heart by creating gilded frames studded with glittering accents and exotic details that are brought to life with vibrant colour, bold design and playful prints.
“It’s exciting to work with someone with such a love of product – the force of Camilla is that she loves to celebrate colour, life and travel, and you can’t help but be intoxicated by that,” Tame explains.
“That’s why the brand feels so special, because they’ve managed to create a unique perspective on design that not many international brands out there can achieve in the same way.”
As a result, the respective Camilla and Sunshades Eyewear design teams have collaborated to create a collection comprising around 120 pieces, evenly split between optical and sunglasses pieces. It’s a relatively large collection on par with other Australian brands like Oroton. For independent practices, Tame says the Camilla collection offers something for everyone. It’s segmented into three groups, with “unicorn” pieces offering colour, shapes and embellishments for people who want to stand out, mid-tier pieces that might incorporate an interesting acetate with a more classic design, and the core range of classic styles that are more subdued while still offering a point-of-difference.
“There’s a lot of analysis and ranging architecture that goes into producing something desirable and that, when it enters the optometry store, actually turns and sells and is a worthwhile commercial proposition,” Tame says.
For metropolitan independents – where many practices have a more boutique offering – Tame expects Camilla’s more expressive unicorn pieces to sit nicely alongside other Sunshades Eyewear-supplied brands like Cartier, Gucci and Balenciaga, offering similar levels of luxury at a more affordable price point.
“And when you think of regional areas like some of our great optometrists in Tamworth or the NSW South Coast, Camilla’s classic designs are sitting above brands like Ray-Ban, Vogue or Ted Baker. It can be more aspirational, but still classical,” he says.
“The great thing about Camilla is it’s not single-minded in terms of offering one solution to a particular type of customer. It’s more about what range you can tailor to that specific optical practice: are they seeking something that sits in that luxury sphere, or maybe something that becomes the pinnacle piece in their store?”
‘A RANGE FOR THE HUMANS OF THE WORLD’

When creating the eyewear range, Sunshades Eyewear has been tasked with committing to Camilla’s brand values: vibrant, free and diverse, always unexpected, and artisan spirit.
For founder Ms Camilla Franks, sunglasses and spectacles are the cherry on top of every great look.
“More is more, and I love having fun with accessories. Everyone’s invited to the Camilla party, so there’s a style of frame for every personality,” she says.
“Maximalist, minimalist, urbanist or adventurer, this is a range for the humans of the world. It’s for lovers of exploration, of late night escapades, and sojourns through ancient cities.”
Franks says “this is fashion for your face”. She believes the eyewear range is as unique as Camilla’s other collections and just like its garments, they will elicit a feeling when people place the eyewear on their face.
“The signature Camilla DNA is core to every project I work on and is imbued within this range of shades,” she explains.
“Elements like bedazzled arms, charms, and playful colours are evocative of joy. Everything I design is created with love, to make you smile. I hope you enjoy soaking up mother nature’s golden rays with a pair of my sunglasses this summer and beyond.”
LOCAL MINDSET, GLOBAL REACH

Sunshades Eyewear prides itself on being much more than a wholesaler. The company has been trusted with producing eyewear for other iconic Australasian brands such as Oroton and Karen Walker, providing creative direction through its in-house design team and high quality manufacturing through its eight factory partners.
In the case of Camilla, Sunshades Eyewear has engaged the services of a factory that has a more than 35-year relationship with that specialises in more boutique collections and understands the importance of intricate details, as well as look, feel and weight.

The company also has a comprehensive network of optical practices (independent and corporate) across Australia, and can help practices tailor their frame ranges for their demographics. Practices like Central Coast Eyecare also value the assistance they get with sales strategies and innovative promotional offers. And many of the sunglass ranges it produces can be found in fast-fashion/department stores like David Jones.

As such, the company has grown into an Australian eyewear powerhouse with global reach. However, many of the founding principles embedded by Ms Bette Lasse, the mother of current CEO Mr Rodney Grunseit who established the company in 1969, continue to drive the company today.
“When brands like Camilla partner with us, they get both ends of the spectrum; someone who can take their product to a global network of stores, but who’s also that family-owned company that’s nearby to help build genuine, friendly business relationships,” Tame explains.
“While we’re all about supporting the Australian fashion industry and working with like-minded people, it’s equally important for us to create product that resonates with an Australian consumer. We’re ensuring we partner with the most-forward thinking brands that offer a unique perspective and have a great brand following.”
Tame says once the Camilla eyewear collection is launched and established in Australia, Sunshades Eyewear plans to take it to global markets through its distributor partners.
“The focus for now is to ensure we make this work for Australia first, because we have generally found that if we can achieve that, then the success follows overseas.”

"I’M MOST EXCITED BY THE USE OF COLOUR – THAT’S THE ESSENCE OF CAMILLA. IT’S JUST BEAUTIFUL WORKS OF ART.”
LISA HOOPER CENTRAL COAST EYECARE
THE CASE FOR A universal
STANDARD OF MYOPIA MANAGEMENT
With a large proportion of Australian and New Zealand eyecare professionals still prescribing vision correction-only for progressing myopic children, it’s hoped a new recommended Standard of Care will provide a valuable framework for practitioners to band together to tackle this looming public health crisis.
WHAT DOES THE STANDARD OF CARE LOOK LIKE?
For the practice setting, the Child Myopia Working Group recommended the following key elements be included when managing a patient’s myopia:
1. Us e a myopia management program for patients with pre myopia or myopia based on the best available evidence.
2. Explain to patients and their parents or carers what myopia is and discuss the increased risks to long term ocular health associated with myopia.
3. Dis cuss, formulate, and implement an agreed management plan with the parent or carer and patient (child), including discussion of the evidence-based available myopia management options to mitigate axial length elongation; risks (lifestyle and family history) of myopia progression; provision of verbal and written information describing the risks and benefits of treatment, duration of treatment, review frequency, when to cease treatment and rebound effects.
4. Document a review/recall for patients with myopia that demonstrate progression.
5. Monitor the impact of treatment.
6. Recognise personal limitations and refer patients to a suitable optometrist or ophthalmologist if the required myopia management services cannot be provided.
The Australia and New Zealand Child Myopia Working Group –comprising a high-powered line-up of eyecare professionals from across the region – was established in 2018 with a clear mandate: to deliver a recommended Standard of Care for myopia management in children living in Oceania.
Why there’s a priority to implement such an initiative boils down to the fact that each year of delayed progression substantially reduces the likelihood of a myopic child developing high myopia in adulthood – a situation that could lead to potentially blinding conditions such as myopic maculopathy, glaucoma, cataract and retinal detachment.
By setting a new Standard of Care, it’s hoped a critical mass of optometrists in Australia and New Zealand will move away from mere vision correction towards a comprehensive myopia management program.
By doing this – and changing how myopia is managed with intervention starting as soon as possible – it's thought that only then can the true public health benefits of reducing its onset and impact be attainable.
In November 2022, the ANZ Myopia Working Group completed the first stage of its mission and published a recommended Standard of Care in the ‘The Australia and New Zealand Child Myopia Report 2022/23-Reducing the Risk to Vision’, which is an adjunct report to the inaugural 2018 Child Myopia Report.

At its core, the Standard of Care describes the overarching elements eyecare professionals need to implement without prescribing how or when to employ specific options or techniques. This latest report also highlights shifting trends, and awareness and understanding of myopia during the past four years.
The group recommended a shift from not only correcting vision but to also include a discussion between the eyecare practitioner and the parents and carers that explains what myopia is, lifestyle factors that may impact myopia, and the increased risks to long-term ocular health.
It also recommended discussing with caregivers the available and increasing number of approaches to manage myopia and slow its progression.
Since 2019, the profession’s peak body Optometry Australia has undertaken a review of the Entry-Level Competency Standards for Australian optometrists.
The ANZ Child Myopia Working Group report said these competency standards don’t provide management techniques or protocols of specific diseases such as myopia, as these should be available to the profession through avenues other than the Entry-Level Competency Standards. Optometry Australia recognises that best practice for myopia management, supported by the contemporary evidence base, should be followed.
Mr Jagrut Lallu is a New Zealand optometrist and founding member of the ANZ Myopia Working Group. He says for Australia and New Zealand, the forecast rate of myopia by 2050 is estimated to be 55%, with an estimated 36% of the population currently affected.
“Furthermore, Australia is expected to have 4.1 million high myopes and New Zealand over 600,000 high myopes by 2050, unless myopia management is implemented by everyone,” he says.
“These forecasts highlight the scale of the problem that is facing the profession given Australia in 2020 had an estimated 1.1 million, and New Zealand over 200,000, high myopes.”
Given the seriousness of the myopia problem, the industry-wide adoption of a Standard of Care could prove significant in this major public health problem, according to internationally-renowned paediatric ophthalmologist Professor Ian Flitcroft, who supports the ANZ Myopia Working Group’s recommended standard.
“I have long advocated for a change in the Standard of Care for myopic children away from simple refractive correction to a comprehensive program of myopia management,” Flitcroft, who practises at Children’s Health Ireland in Dublin among other positions.
“I therefore sincerely hope that the Australia and New Zealand Child Myopia Working Group’s recommended Standard of Care for myopia management will be embraced by the region. If so, it will help bring about more informed
discussions in the practice setting with parents or carers, helping them to consider the available options that can be used to manage myopia and what may work best for their child.
“Most importantly, setting a new Standard of Care is critical to moving myopia management from a service offered by a minority of eyecare practitioners to being universally available. Only then will the full public health benefits of reducing the prevalence and impact of myopia be achievable. Now is the time for optometrists, ophthalmologists, parents and carers, educators and other healthcare professionals to collaborate effectively on behalf of the children for whom we have the privilege to care.”
In its report, the ANZ Myopia Working Group highlights the importance of children having regular eye exams as part of a child’s regular health checks, akin to dental visits. The group wants to encourage all parents and carers across Australia and New Zealand to have their children’s eyes examined by an optometrist before starting school and regularly thereafter.

“By doing so, this will enable every child diagnosed with myopia to be managed with the recommended Standard of Care,” NSW-based paediatric ophthalmologist and ANZ Myopia Working Group member Dr Loren Rose says.
“A myopia management Standard of Care is critical, given that each year of delay in developing myopia substantially reduces the chance of a child developing high myopia in adulthood.”
Mr Joe Tanner is the professional services manager for CooperVision ANZ which supported the ANZ Myopia Working Group and its report.
“It is time to change how myopia is managed with intervention starting as soon as possible. We call on the profession to adopt the recommended Standard of Care to ensure myopia management is universally practised and available to every child,” he says.
WHAT’S CHANGED SINCE 2018
As Flitcroft explains, there has been progress during the past four years in terms of raising much-needed awareness of myopia and how to manage it.
The optometry profession’s understanding of myopia also continues to advance, he says, with the latest evidence and data continually informing best practice.
“However, the coronavirus pandemic has had a significant impact on the
AUSTRALIA AND NEW ZEALAND CHILD MYOPIA WORKING GROUP MEMBERS:
• Dr Rasha Alt aie , Ophthalmologist, Vice President of the Cornea and Contact Lens Society of New Zealand, Auckland, New Zealand.
• Luke Arundel , Optometrist, Chief Clinical Officer, Optometry Australia, Melbourne, Australia.

• J agrut Lallu , Optometrist, Past President of the Cornea and Contact Lens Society of New Zealand, Hamilton, New Zealand.
• Mar garet Lam , Optometrist, National President, Optometry Australia and National President of the Cornea and Contact Lens Society of Australia, Sydney, Australia.
• Dr L oren Rose , Paediatric Ophthalmologist, Senior Clinical Lecturer Macquarie University, Sydney and Canberra, Australia.
• Andr ew Sangster , Optometrist, Board Member of The Orthokeratology Society of Oceania, Wellington, New Zealand.
• Chair –Scientia Professor Fiona Stapleton , Head, Eye Research Group, School of Optometry and Vision Science UNSW, Sydney, Australia.
progression of child myopia in those populations who endured extended lockdowns, bringing the issue of myopia to the attention of a wider audience than ever before,” he says.
To demonstrate this, the report highlights a large Chinese study that found myopia prevalence rose significantly in young school children during the COVID-19 pandemic. It reported an almost 400% increase in six-year-olds, a substantial myopic shift (approximately −0.30 dioptres) that hasn’t been seen in any other year-to-year comparison.
The evidence of the protective effect of time outdoors also continues to expand and Optometry Australia now recommends children spend at least 90 minutes per day outside to help prevent myopic development and progression.
Ethnic and geographical differences in terms of myopia prevalence also need to be acknowledged as influencing factors, as does the urban or rural environment in which an individual resides, the report states.
For example, myopia prevalence differences exist between people living in south Asia (which includes Bangladesh, Bhutan, India, the Maldives, Nepal, Pakistan and, more recently, Afghanistan), compared to south Asian populations living outside the region. Myopia rates for Indians living in Singapore are more aligned with rates for the Singaporean Chinese population than for Indians in India. Similarly, south Asian children living in Australia and England are approximately five times more likely to be myopic than their counterparts living in Nepal or India.
“At age 15, around 40% of migrant south Asians develop myopia, compared to 9% of indigenous south Asians,” the report says.
“It is estimated that children living in predominantly urban environments have 2.6 times greater chance of developing myopia than those living in rural environments. Regions that have undergone rapid economic transition, south and east Asia for example, have also experienced a rapid rise in rates of myopia.”
“SETTING A NEW STANDARD OF CARE IS CRITICAL TO MOVING MYOPIA MANAGEMENT FROM A SERVICE OFFERED BY A MINORITY OF EYECARE PRACTITIONERS TO BEING UNIVERSALLY AVAILABLE.”
— PROF IAN FLITCROFT
2 UNIQUE TECHNOLOGIES
ONE REASON TO SAY YES TO PRECISION1 ™ CONTACT LENSES



ALWAYS FOLLOW THE DIRECTIONS FOR USE.
† Based on lens movement, centration, and rotation at initial fitting.
* Based on a survey in which 94% of eye care professionals in Germany, Italy, Austria, Switzerland, and the US who agreed/strongly agreed with the statement ‘The lenses are as easy to fit as spherical lenses.’ (n=50).
Based on 98.7% of eyes with lens oscillation with blink of ≤5° while wearing PRECISION1 for Astigmatism contact lenses


References: 1. Cummings S, Giedd B, Pearson C. Clinical performance of a new daily disposable spherical contact lens. (DDT2) Lens with Smart Surface study; Alcon data on file, 2019. 3. Tucker B, Leveillee E, Bauman E, Subbaraman L. Characterization of the Surface Properties of a Novel Daily Disposable Silicone Hydrogel Contact Lens. Poster presented at the American Academy of Optometry Annual Conference, October 23-26; Orlando FL. 4. IDDrop Comparative Study DACP and BioTrue ONEday Report; Alcon data on file, 2019. 5. IDDrop Comparative Study Oasys 1 Day and TruEye; Alcon data on file, 2019. 6. Alcon data on file, 2021. In a clinical trial to assess comfort and vision over 16 hours of wear with PRECISION1™ sphere contact lenses where n=35. [IIT #59917981]. 7. Alcon data on file, 2021. In a clinical trial to assess comfort and vision over 16 hours of wear with PRECISION1™ for Astigmatism contact lenses where n=30. [IIT #64882539]. 8. Alcon data on file, 2020. Clinical Performance of a Daily Disposable Toric Silicone Hydrogel Contact Lens [CLA306-C003] n=78 eyes. 9. Alcon Data on File, 2021. PRECISION1™ for Astigmatism PEaCEEurope Regional Report REF-12902. 10. Alcon Data on File 2021. PRECISION1 for



Finding your niche
WITH A SPECIALTY CONTACT LENS CLINIC
There’s no denying more chair time is a prerequisite of fitting specialty contact lenses in Australia, but when the practitioner's skills are highly sought-after and they've built a supportive network with product suppliers and peers, there is no limit to the lives that can be changed.
Most of Custom Eyecare Newcastle’s specialty contact lens patients are directly referred by optometrists and ophthalmologists in the surrounding area. The fact other eyecare professionals are happy to send their patients to a potential nearby competitor is a reflection of the reputation the practice has built over several years.
Some come from further afield, explains optometrist and managing director Ms Heidi Hunter.
“Some of my patients come from Armidale and Tamworth; they drive four or five hours to come down for their specialty contact lens fitting,” she says.
In an optometry landscape where independents are increasingly required to differentiate, Hunter is among a selection of Australian optometrists who have found their niche in specialty contact lens fitting.
She believes there’s several advantages to offering such a service but in Newcastle and the surrounding area specifically, fulfilling an unmet need is the greatest benefit.

“For some reason, Newcastle and Lake Macquarie has a much higher incidence of keratoconus than the national average, so for me, the main reason to upskill and specialise in this area, is that there was a need, and it was about looking after people properly,” she says.
“I used to work in the rooms of a corneal specialist, so I got exposure to lots of interesting corneal disease patients, and realised they needed looking after by a local optometrist. It didn’t start out as an area of interest, but it has grown into an area of specific interest.”
Hunter believes there’s demand for more specialty contact lens

practitioners that give better access to patients.
“When I used to work in the rooms of a corneal specialist, I realised that a lot of Newcastle keratoconus patients were being sent to Sydney for specialty contact lens fitting. That’s a two-hour drive, a lot of expense, dealing with Sydney parking and Sydney traffic, where there isn’t any reason that an optometrist couldn’t do it locally,” she says.
“At Custom Eyecare Newcastle, we have gone above and beyond in terms of learning to fit all types of specialty lenses – scleral, hybrids and rigid – absolutely everything. We offer the full suite of lenses whereas a lot of the other optometrists in our area that do fit keratoconus patients, most of them will just be fit into a conventional RGP.”
But learning to fit all types of speciality lenses is not achieved overnight.
Especially at the beginning, Hunter found the learning curve is steep, so she sought as much support as she could get.
“Most of the learning comes from either educating yourself, or simply experience, so if you don’t put in the hard yards to educate yourself, and you don’t see enough patients, I think it would be quite difficult to develop your skills,” she explains.
Peer support can come from groups including the Cornea and Contact Lens Society of Australia (CCLSA) and the Orthokeratology Society of Oceania (OSO).
Hunter is a national board member of CCLSA whose CEO is the well-respected specialty contact lens fitter Mr Alan Saks. OSO is an Australian-based group led by president Mr Gavin Boneham (principal optometrist at Boneham Optometrist in Sydney’s CBD) and secretary
Ms Celia Bloxsom (principal optometrist at Eyeconic Optometry Southport on the Gold Coast).
“CCLSA and OSO run bootcamps in Australia and New Zealand, as both organisations teach beginners about orthokeratology, including how to kickstart your learning, how to find patients, what equipment you need, and what to look for when you’ve just started using a corneal topographer but don’t yet have enough experience. If you haven’t had enough throughput of patients to really develop your skills, these bootcamps are incredible for learning,” Hunter, who was formerly on the OSO board, says.
A corneal topographer is a must-have, not a nice-to-have, in Hunter’s opinion.
“I honestly think you can’t do anything without a corneal topographer. As I explain to patients, it’s akin to a surveyor mapping out the hills and valleys in a landscape; a corneal topographer maps out the hills and valleys in the surface of your eye and that’s what we’re trying to fit a lens around. In the case of ortho-k, if you don’t have a corneal topographer, it’s difficult to work out where the lens is sitting overnight,” she says.
“We also have an anterior OCT in our practice. You don’t need an anterior OCT for ortho-k fitting or for simple straightforward keratoconus fitting, but when you start to get into hybrids and sclerals, certainly it’s an advantage.”
Hunter estimates hybrid lenses make up about 10% of her specialty contact lens fittings. She says they’re ideal for patients who have mild keratoconus, or those who can’t deal with the discomfort of rigid lenses.
“Hybrid lenses are much more comfortable because the edge of
the lens is hidden in the soft skirt. They’re good for patients who have keratoconus in only one eye because adapting to a hard lens in one eye is quite difficult. A hard lens can feel like a little piece of eggshell on the surface of your eye, while you’re getting used to it,” she says.
According to Hunter, the best way to stay informed about hybrid lenses and product developments from suppliers such as Gelflex and Capricornia in Australia, and Corneal Lens Corporation (CLC) – New Zealand’s largest contact lens manufacturer – is to attend conferences.
“The CCLSA runs a conference and trade show every second year, which industry attends. On the off year, the OSO runs their conference and again, it’s attached to an industry trade show. Whether it’s equipment suppliers or specialty contact lens suppliers – anybody that has anything to do with specialty contact lenses will attend one of these two events because that’s where their customers are,” Hunter says.
“I love being able to say to patients that these lenses are manufactured by an Australian lab, so they understand this isn’t something that’s bought in a box from China.”
When considering the business case for branching into specialty contact lens fitting, Hunter suggests weighing up whether there is going to be enough demand for speciality contact lens fitting in the immediate area, or whether another nearby practice is already providing the service, or whether patients are driving four hours to attend the ‘nearest’ optometrist who can fit custom lenses.
“There is scope. In cities like Melbourne, Sydney, or Brisbane, there’s plenty of optometrists that fit custom contact lenses. From a patient’s perspective, I wouldn’t think there’s a lack of choice. But if you’re in a regional area, where are keratoconus patients going for specialty contact lens fitting?” she asks.
Hunter recommends optometrists consider how contact lens prescribing – beyond daily disposables and the like – can set their practice apart.

“I THINK IT’S A NICHE AND A POINT-OF-DIFFERENCE THAT A CORPORATE PRACTICE IS NEVER GOING TO BE ABLE TO ENCROACH ON.” HEIDI HUNTER
“Corporate practices don’t tend to do specialty contact lens fitting because it doesn’t fit with their practice model. I spend an hour with a new keratoconic patient. If I worked in a corporate practice that had a half-hour appointment schedule, I just can’t do it in 30 minutes,” she says.
“I spend a lot of time outside of hours ordering lenses and answering emails back and forth with the lab to try and customise and refine the fit. I don’t know if there is the scope in a busy corporate practice to be able to take this on, and with more and more practices being owned by corporates, I think it’s a niche and a point-of-difference that a corporate practice is never going to be able to encroach on.”
While it may require more chair time, the difference that time makes can be immeasurable, in Hunter’s experience.
“My typical patient would be somebody who, because of their eye condition or corneal disease, has gotten to the stage that they’re about to lose their driver licence because they no longer meet the visual requirements for the RMS standards – and for lots of people that runs the risk of losing their job,” she says.
“When you get to the stage that they’ve already contemplated early retirement because they’ve lost their vision, and with a specialty contact lens, you can get them better vision than they’ve had for the last 20 years, that’s the stuff I love. It makes such a big difference in a patient’s life by literally just restoring their sight back to something that’s reasonable or incredible in some cases.”
TEST YOUR LIMITS
For optometrist and practice owner Mr David Foresto, the biggest advantage of going above and beyond soft contact lenses to fit specialty lenses is the clinical challenge itself.


“I feel if you really want to get the most out of your career you need to be willing to take on difficult cases and put your energy into helping the people who need it the most. Yes, you can enhance people’s lives with regular glasses and soft contact lenses, but custom and complex contact lenses aren’t just life enhancing, they are life changing,” he says.
Beyond the clinical challenge, is another off-set advantage.
“A practice built around addressing people’s needs is more economically secure than one built on wants or trends. Businesses based on refraction and low-cost optical products will be the first to be replaced by technology in the future.”
Foresto, who established Advanced Optometry (formerly Foresto EyeQ) in 2015, says incorporating specialty contact lenses into an existing practice requires analytical thinking and planning.

“You have to educate yourself first before taking on new clinical

“A CORNEAL TOPOGRAPHER IS ABSOLUTELY NECESSARY FOR FITTING CUSTOM LENSES. THERE REALLY IS NO DEBATE ABOUT THAT.”
DAVID FORESTO ADVANCED OPTOMETRY
services. That means attending contact lens conferences, reading articles and staying up-to-date with new technology,” Foresto, who has been a guest lecturer at Queensland University of Technology for a

“Once you have formed a good basis of knowledge, then taking on some of the more basic custom lens fits is appropriate, but you need to always be willing to stop what you’re doing if a case becomes more complicated than you thought it would be and refer the patient onwards.
“You can easily find your own orthokeratology and high astigmatism patients for custom lenses first before you put yourself out there for more complex referrals.”

While most custom lens patients at Advanced Optometry have keratoconus or corneal grafts, Foresto says there are outliers.
For example, fitting orthokeratology for myopia control has “taken off to levels I never would have imagined when I first graduated”. He also fits lenses for babies from four weeks of age, which, sadly, there remains some need for despite how good the surgical options for various congenital eye diseases have become.
Foresto’s practice in Brisbane has invested in the latest diagnostic equipment, some of it essential, in his opinion.
“A corneal topographer is absolutely necessary for fitting custom lenses. There really is no debate about that. An anterior segment OCT is also necessary if you are fitting sclerals,” he says.
“As far as the investment side of these devices is concerned, we have three topographers, and we would have paid those off many times each by now easily. We also have a wavefront aberrometer. I don’t think this is strictly necessary however we use it every day and I really do believe it leads to better visual outcomes than ever before.”
For custom lens fitting troubleshooting and support, Foresto says there are several options.
“I think optometry Facebook groups are very helpful for practitioners needing some clinical support. Australian Optoms, SiCo and Scleral Lens Practitioners are all great resources filled with generally helpful practitioners. I also think CCLSA does a great job of bringing the contact lens community together, so getting along to their CPD events really helps build your network of people to call on if you need help.”
A MENTOR TO MANY
A keratoconus patient who works in a hospital in Perth is adamant he would be on a different career trajectory if not for the help of optometrist Mr Damon Ezekiel.

“He said I’m not allowed to retire because without me, he can’t hold down a job, or drive. He keeps telling me he would be weaving baskets if it wasn’t for what I do. What a difference you can make to someone’s life,” Ezekiel says.
“These patients cannot see without what we do with specialty rigid lenses.”
Ezekiel has been fitting custom contact lenses his entire professional life. From a purely business revenue perspective, he says some
practitioners see one particular downside to fitting specialty contact lenses – but there is an upside.

“There is a lot of chair time involved in treating keratoconic, post-graft, post-surgical patients. The great thing is, patients come in who’ve been elsewhere, and no one can help them – and you can. The look on their face when they say, ‘I can see’, and ‘Is this what normal vision is like?’, because they can now drive a car, they can hold down a job,” he says.
“Yes, there is a lot of chair time but the upside of that is, you chat to patients, you find out more about them and their family. They know they’re not just a number that’s coming in and out, getting a pair of reading glasses or whatever. You’re doing something that not many people do and they’re exceptionally loyal because they can’t go down the road to get this, they can’t go on the internet and get anything that we’re supplying. It’s the quality of life that you can give them which is just
Ezekiel is owner and manager of Ezekiel Eyes, a third-generation optometry practice in Perth, Western Australia. His father, Don Ezekiel, was a pioneer in developing specialty contact lenses in Australia.
“Getting lenses from London in those days took forever so my father went over to London, learnt how to make lenses, bought a lathe, came back and set up Gelflex, which he’s now sold,” Ezekiel says.
“I learned from him because you don’t do many rigid lenses going through university. Now, I have lots of optometrists and students sitting-in because they’re wanting to know what we do and how we do it. Masters optometry students from Sydney and Melbourne come in, and students from the University of Western Australia program now, as well."
When he was speaking at conferences in Sydney and Auckland earlier this year, Ezekiel tells those interested in the field to find a mentor; there’s no need to reinvent the wheel.
“We’ve spent thousands of dollars making mistakes. I’m more than happy for anyone interested to come and sit in with me,” Ezekiel says, explaining an optometrist from Orange recently flew over to sit in and observe for a few days.
“Ninety-nine percent of patients are more than happy to have someone sit in, because they know their eyes are not normal, and they’re helping other optometrists learn, so they can then continue the tradition of helping more patients like them, to see.”
Along with a corneal topographer, Ezekiel is one of only a handful of practitioners in Australia with a scleral topographer, to measure the profile of the sclera.
“THERE IS A LOT OF CHAIR TIME INVOLVED IN TREATING KERATOCONIC, POST-GRAFT, POST-SURGICAL PATIENTS.”
DAMON EZEKIEL EZEKIEL EYESA corneal topographer is considered a 'must-have' device for a specialty contact lens clinic.
“It’s only $30,000. By comparison, a Medmont is about $26,000; an OCT can be $70,000 to $100,000, so a scleral topographer is ‘affordable’. But if you’re going to do the job right, you need a corneal topographer, bottom line. I also have 10, 12, 15 different trial sets, depending on who walks into my room. You need to have all that sort of armoury.”
Ezekiel, who is also president of The International Society of Contact Lens Specialists, a non-profit organisation comprised of distinguished contact lens practitioners and educators, says networking at industry events is a prime opportunity to discuss cases with colleagues and learn from their experience, but this can also be done with suppliers.
“I order the occasional lens from the UK, France or the US, depending on what the patient needs, if I know I can’t get it locally. But local labs like Gelflex, Capricornia and CLC have really good technical advice. They know their designs well and if you need extra edge lift, for example, you ring up and they can talk you through the nuances depending on what that design is,” he says.
If a problem still needs a solution, Ezekiel has the answer: “There’s plenty of fellows within the CCLSA that I’m sure would be more than happy, like myself, to take emails and phone calls and have a chat.”
Lately, he has noticed more comfortably-fitting scleral lenses are performing particularly well, especially among WA’s ‘fly-in, fly-out’ mining and agricultural workforce, who are operating in harsh environmental conditions which affects their lenses, with dust, dirt and grit.
“They’re a little tricky to fit but one patient, who sent me a video showing the environment he works in, used to wear smaller lenses now wears big scleral lenses, and he can do whatever he wants without his vision affected. Another patient, a farmer, used to put eye drops in 17
times a day. Now he wears bigger scleral lenses and he can do anything – dust, wind, doesn’t matter. Scleral lenses have undergone huge change,” Ezekiel says.
The future of custom contact lenses is also brimming with opportunity, as technology advances.
“Now you can take the corneal topography in a scleral profile and send that directly to a lathe and you can specify how much clearance you want, as in a tear layer between the back of the lens and the front of the eyes, so there’s lots of really amazing stuff taking place.”
Is the warm weather and luxurious beaches of Far North Queensland calling you?




George & Matilda Eyecare is currently recruiting Optometrist to join our team in Airlie Beach, Innisfail & Atherton. Reach out to our HR Team at opportunities@georgeandmatilda.com.au to find out more.
 Local and interstate students and practising optometrists often sit-in on specialty contact lens fittings at Damon Ezekiel's practice in Perth.
Local and interstate students and practising optometrists often sit-in on specialty contact lens fittings at Damon Ezekiel's practice in Perth.
Pentacam:
THE CENTREPIECE IN A SPECIALTY CONTACT LENS CLINIC
The iconic OCULUS Pentacam has found a home among specialty contact lens practitioners largely thanks to its advanced software for scleral contact lens fitting. The company has made significant upgrades to the technology, with Queensland optometrist TREVOR WILLIAMS one of Australia’s early adopters.
Orthokeratology (ortho-K) provided the gateway for Mr Trevor Williams’ interest in advanced contact lens fitting. The owner-optometrist of his namesake independent practice, in the Brisbane suburb of Coorparoo, enjoys the clinical satisfaction of improving patients’ lives through customised contact lenses, which brings the added benefit of differentiation.
With a service based on exceptional clinical care underpinned by investment in advanced diagnostic technology, two years ago Williams expanded his specialty contact lens offering by taking the plunge into scleral contact lenses for patients with keratoconus, post-LASIK ectasia and other conditions with abnormal corneas.
He had owned an advanced corneal topographer for some time, but to prescribe scleral lenses he required new hardware that could accurately map the anterior shape of the eye, across the cornea and all the way to the sclera, ensuring the lens can vault over the cornea.
To support his scleral lens service, he sought an earlier model of the OCULUS Pentacam – a German made, multifunctional anterior segment tomographer, supplied by Designs For Vision in Australia and New Zealand. Although popular among anterior segment ophthalmologists, it’s also found a home among specialty contact lens practitioners.

That’s largely because OCULUS developed an optional software module called the Cornea Scleral Profile (CSP) Report – originally available on the Pentacam and Pentacam HR models – to capture scleral topography in a non-invasive fashion. Together with sagittal height data and scleral angles, this is said to provide eyecare professionals with the necessary parameters for fitting scleral lenses.
The original CSP Report requires the practitioner to capture five scans – a central corneal scan and four scleral scans (inferior, superior, nasal, temporal) – which the software merges into one overall cornea and sclera map.
When he started using the software, Williams was impressed with its ability to create custom fit scleral contact lenses, often without the need for multiple trial fits. However, he noted some inefficiencies due to the need to stitch together multiple scans, and often he required assistance to keep the patient’s eye lids open.
But that all changed in a few months when Williams – an optometrist of more than 30 years – upgraded from the Pentacam Basic to the Pentacam AXL Wave and began using OCULUS’ upgraded software, CSP Pro. It provides more coverage in a single scan – up to 22mm diameter with a speculum – which is faster by avoiding the need to create a mosaic of the scans. Hence, it offers a better user experience and more reproducible data for the practitioner.
The software upgrade is available on OCULUS’ Pentacam AXL Wave, which became available in Australia in mid-2020. The fourth-generation system is the company’s most advanced Pentacam to date and is the first to combine Scheimpflug tomography with axial length, total wavefront, refraction and retroillumination.
Hearing the benefits CSP Pro could bring to his scleral lens fitting service, Williams made it a priority to have the Pentacam AXL Wave installed in his practice in September 2022, the first in Queensland.

“I’m now able to obtain much more efficient and accurate measurements of the cornea and sclera. With the CSP Pro it’s usually a case of one scan and you’re done, if the lids are wide enough apart or you use the speculum. But it still has the ability for you to stitch together multiple scans, if required,” he says.
“It’s nice and simple for the patient and myself – it’s been a welcome addition to the practice.”
With CSP Pro, Williams says he’s able to obtain high quality data that’s translating into accurate scleral lenses.
“Previously, there were times where it could take three or four lenses to get a good fit and a happy patient but now with the excellent elevation data from the CSP Pro software it’s usually done in one or two goes.”
Another impressive feature of the Pentacam and CSP software, according to Williams, is its ability to take measurements independent of the tear film.
“With my existing placido topographer, which is a great instrument, you must take several measurements to make sure the results are repeatable, due to the variability in the
tear film quality between blinks. With the Pentacam AXL Wave, you are measuring the true corneal surface, not the tear film.”
“Unlike other scleral profilometers, fluorescein is not required to image the sclera. And because you’re able to work from a longer distance compared to a small cone topographer, it’s not so intimidating for children, while still being able to capture a wide scan.”
In terms of other features, the Pentacam data is capable of being exported directly to the contact lens laboratory’s design software and Williams hopes this will become more readily available in Australia in the future.
He also likes the simplicity of the display and readings. This makes it easy to interpret findings and educate patients on their conditions and the need to invest in scleral lenses.

“I show patients their cross-sectional scans to demonstrate the warped shape of their cornea. Advanced keratoconus patients, in particular, are often gobsmacked and then I can show them why a normal lens is not going to sit correctly, and why there’s the need for a large scleral lens to vault over their distorted cornea.”
MANY DEVICES IN ONE
As the owner-optometrist of an eyecare-led practice, the Pentacam AXL Wave is an example of how Williams carefully selects the latest diagnostic technology to provide a premium level of care.

Over the years he’s invested in the OCT, ultra-widefield retinal camera, visual fields system, corneal topographers, optical biometer, and an
advanced dispensing measurement system.
With the Pentacam AXL Wave being the latest addition to the practice’s equipment armoury, Williams says it has superseded some other instrumentation, proving to be a key space saver in the clinic. It performs autorefraction, aberrometry, retroillumination of the crystalline lens or IOL, axial length, anterior and posterior corneal measurements and scleral profilometry.
But he’s discovered an unexpected benefit for his practice. Using both the retroillumination function together with tomography, he’s able to show patients their cataracts or posterior capsular opacification. It even gives a Pentacam Nuclear Sclerosis Score (PNS) and he’s able to demonstrate to patients their level of cataract.
“I’m routinely showing patients their PNS cataract grading score,” he says.
“It also performs axial length automatically which I use for myopia management. I also think it’s really important to exclude subtle keratoconus in potential ortho-K patients and the fact that the Pentacam measures the posterior cornea as well, you’ll pick up some keratoconics earlier than if you used a placido topographer.
“All in all, the Pentacam AXL Wave has been a great investment for my practice, and has brought about greater efficiencies and accuracy with my scleral lens fitting that I don’t think would be possible on any other device.”

Proven by 7 years of clinical data to significantly slow myopic progression with no rebound effect

Supported by the Brilliant Futures™ myopia management program



Further information at childmyopia.com and coopervision.net.au / coopervision.co.nz
*95-100% of children expressed a preference for contact lenses over glasses at each visit over 36 months. †’How much do you like wearing your contact lenses?’ 87/97 (90%) Top box ‘I like contact lenses the best’ Subjective response at 60 months. ‡Compared to a single-vision, 1-day lens over a three-year period; rate of progression maintained out to 6 years. On average, there was no indication that accumulated treatment effect gained following 3 or 6 years of MiSight® 1 day wear was lost during a 12-month cessation study in children aged 8-15 at initiation of treatment. Instead, eye growth reverted to expected, age average myopic progression rates. References: 1. Sulley A et al. Wearer experience and subjective responses with dual focus compared to spherical, single vision soft contact lenses in children during a 3-year clinical trial. AAO 2019 Poster Presentation. 2. CooperVision® data on file, 2019. 3. Chamberlain P et al. A 3-year randomized clinical trial of MiSight® lenses for myopia control. Optom Vis Sci 2019;96:556–567. 4. Chamberlain P et al. Myopia Progression in Children wearing Dual-Focus Contact Lenses: 6-year findings. Optom Vis Sci 2020;97(E-abstract):200038. 5. Chamberlain P et al. Myopia progression on cessation of Dual-Focus contact lens wear: MiSight 1 day 7 year findings. Optom Vis Sci 2021;98:E-abstract 210049.
6. Hammond D et al. Myopia Control Treatment Gains are Retained after Termination of Dual-focus Contact Lens Wear with no Evidence of a Rebound Effect. Optom Vis Sci 2021;98:E-abstract 215130. For instructions for use refer to https://coopervision.net.au/patient-instruction. MiSight®, Brilliant Futures™ and CooperVision® are registered trademarks of the Cooper Companies, Inc. and its subsidiaries. EMVCOO0841 ©2022 CooperVision.

PRODUCT SHOWCASE Contact Lens

HOMEGROWN COMPANY PRIDES ITSELF ON PRODUCT AND SERVICE
Founded in 1987, Capricornia
Contact Lens designs and manufactures lenses for irregular corneas, astigmatism, presbyopia, orthokeratology (two options), prosthetic lenses and all conceivable lens designs in between.
The company says its commitment to ISO regulatory compliance underpins its consistent and reliable quality in service and product; Capricornnia has just completed its third consecutive quality audit with zero non-conformances.
“We believe we have the speediest and most reliable delivery times with many lenses despatched on the day of ordering,” the company says, noting some of its key products are:
• Mark’ennovy – custom made to order, monthly disposables in an extensive range of fit and power, including BHVI EDOF and MYLO (TGA-registered for myopia management).
• SEED – Quality Japanes e daily disposable lenses with a wide power range, also including BHVI EDOF technology.
• RoseK – offering the complete range of RoseK lens designs. Whether practitioners are experienced or starting out in the specialist lens world, Capricornia is encouraging them to get in touch to discuss how it can assist them and their patients.

Email: info@capcl.com.au
A SOLUTION FOR A RANGE OF CONTACT LENS TYPES
Ote Clean, available through Contact Lens Centre Australia (CLCA), is an optimal daily contact lens cleaner suitable for all plasma-coated lenses, including rigid gas permeable lenses and soft contacts. Its deep cleaning ability is designed to help the wearer see clearly without irritating their eyes.
Ote Clean is described as the best option to care for lenses, providing thorough daily cleaning. Ote Clean removes proteins and lipids, is alcohol based and contains no animal or toxic substances.

Active ingredients: non-ionic cleaning agents.
Preservative: polyhexanide biguanide.

Email: admin@clcaustralia.com.au
HP-OCT OFFERS ACCURATE TOPOGRAPHY MAPS, UNAFFECTED BY TEAR FILM
Cylite is an Australian-based company developing the next generation of diagnostic OCTs for optometry and ophthalmology. The company’s Hyperparallel OCT (HP-OCT) is described as a world-first, capturing accurate volumetric data of the eye, with particular advantages in the anterior segment.
“Scanning at an industry-leading 302,400 A-scans per second, the technology simultaneously images across a wide area of the eye with minimal motion artefacts, allowing the production of highly accurate and repeatable elevation and curvature maps of the cornea, ideal for contact lens fitting,” Cylite states.
According to the company, being OCT-based, its three-dimensional images of the anterior segment are not affected by artefacts caused by poor tear film, therefore can be used to produce various highly accurate topography maps of the anterior and posterior corneal surface. Additionally, the device produces valuable pachymetry and epithelial thickness maps.

Furthermore, for those clinicians utilising ortho-K for myopia management, axial length can also be captured in the same scan.
Email: info@cyliteoptics.com
A TRULY PORTABLE – AND UNIQUE –TOPOGRAPHER
The OCULUS Easygraph corneal topographer offers the ideal solution for practices with limited space, mounting directly on to most slit lamp brands. The Easygraph is light and compact and therefore allows practitioners with multiple practices to move it between sites, making it a portable – and unique – topographer, according to supplier Designs For Vision.

Using the same precise measuring technology as its larger sibling, the Keratograph 5M, it measures topography and true keratometry which aids in finding the right base curve in quick time. Numerous analyses and display formats support the quantitative classification of the cornea, including refractive power comparison for pre and post ortho-K, and keratoconus screening and staging, with the ability to compare up to four maps over time to identify progression.
The optional Contact Lens Fitting module simulates fluorescein fits, and links to the databases of several contact lens manufacturers, adding confidence and trust to your contact lens consultations.
Email: cameron.loveless@paragoncare.com.au
PRODUCT SHOWCASE Contact Lens

A NEW LEVEL OF ACCURACY FOR SCLERAL TOPOGRAPHY

MYOPIA CONTROL LENS AVAILABLE TO MORE PATIENTS
CooperVision MiSight 1 day contact lenses are now available in higher prescriptions. The expanded range covers -0.25D to -10.00D (0.50D steps after -6.00D)— which means that MiSight 1 day now covers 99.97% of prescriptions for Asian children – and 99.97% for Caucasian children – who have myopia and less than 1D of astigmatism.¹ The diopter extension for this innovative, specially designed lens will allow even more children to benefit from myopia management.

MiSight 1 day contact lenses are backed by the longest-running soft contact lens study among children.
Reference
1. CVI Data on file, 2022. SERE coverage of childhood myopia prescriptions with MiSight 1 day for 104,810 eyes in Asia (China, Korea) and 116,336 eyes in Europe and USA aged 8-18 years.
Email: hello@au.coopervision.com
OPTOPOL REVO SD-OCT 'A MUST HAVE' FOR CONTACT LENS FITTING
Optopol REVO
SD-OCT has a built-in anterior lens allowing the user to perform anterior segment imaging without installing an additional lens or forehead adapter. Now practitioners can display the whole anterior segment using a radial scan to view 18mm wide 6mm deep for various angles. This is a standard feature in any of the five REVO models.

T-OCT is a pioneering way to provide detailed corneal curvature maps by using posterior dedicated OCT. Anterior, posterior surfaces and corneal thickness provide the True Net Curvature information. With the net power, a precise understanding of the patient’s corneal condition is generated easily and free of errors associated with modelling of posterior surface. The REVO T-OCT module provides axial maps, tangential maps, total mower map, height maps, epithelium and corneal thickness maps.
Practitioners can customise their favoured view by selecting various maps and display options. Fully Automatic Capture with examination time of up to 0.2 sec makes testing simple. The T-OCT follow-up feature offers the ability to compare corneal topography changes over time in LASIK, keratoconus and contact lens wearers.
Email: sales@optimed.com.au
Pentacam, utilising Scheimpflug technology, has long been relied upon for accurate corneal surface data for contact lens fitting. OCULUS took this further by developing the cornea scleral profile (CSP) to also capture scleral topography in a non-invasive way. Together with sagittal height data, this provides users with all necessary parameters for fitting scleral lenses.
Supplied by Designs For Vision, the Pentacam and Pentacam HR models can accurately preform CSP by capturing five scans which are automatically combined to create one cornea scleral map. However, for the ultimate user experience and reproducible data, the newest model, Pentacam AXL Wave, offers CSP Pro. This allows capture of more than 20 mm diameter in a single scan – described as a clear industry stand out – with both CSP Report and CSP Pro software able to link to the databases of several contact lens manufacturers, allowing for easy data transfer to the appropriate external lens calculator.
Email: cameron.loveless@paragoncare.com.au
TRIPLE ACTION TARGETS ALL LAYERS OF THE TEAR FILM

Cationorm (cationic nanoemulsion) is a preservative-free, hydrating and lubricating emulsion eye drop which protects the eye surface, relieving the discomfort and irritation of persistent dry eye caused by prolonged use of contact lenses, or environmental conditions.1
Its triple action repairs the lipid layer to reduce evaporation by lubricating and stabilising the tear film, and restores the moisture balance in the muco-aqueous layer of the tear film. It also forms a barrier to lock in moisture, giving dry eyes the time they need to heal. 2,3,4,5
Administered as one drop, up to four-times daily in the affected eye, Cationorm is suitable for use with contact lenses, 6 and gentle enough to use every day.7
PBS information: Cationorm Multi Dose (10mL). Authority Required (STREAMLINED) 6172. Refer to PBS Schedule for full authority information. Cationorm (30 x 0.4mL) is not listed on the PBS. References available upon request. Learn more, visit Cationorm.com.au. Email: orders@goodopticalservices.com.au.

DISCOVER HOW
TRIPLE ACTION TARGETS ALL LAYERS OF THE TEAR FILM:








PAEDIATRIC VISION SCREENING IN AUSTRALIA StEPS towards national
The pursuit of an Australia-wide early childhood vision screening program has been a passion project for Professor Frank Martin throughout his career, and one that has endured many false starts.

But this goal may finally be realised by 2030, with the potential nationwide roll out of the successful NSW Statewide Eyesight Preschooler Screening (StEPS) program – with modifications – thanks to a major push from the eye health sector and an appetite from the Federal Government.
Martin, a Sydney-based paediatric ophthalmologist, presented on this topic to close out the RANZCO Congress in Brisbane in The Council Lecture where he reviewed the status of pre-schooler vision screening in Australia and charted a path towards a national program.
Martin – whose various roles include visiting ophthalmologist at The Sydney Children’s Hospitals Network at Westmead and Randwick, Sydney Eye Hospital and his private practice at Sydney Ophthalmic Specialists – became interested in this topic in the 1960s when working alongside Professor Fred Hollows before later accompanying him in western NSW in 1978 for the National Trachoma and Eye Health Program.
Years later in 1982, he provided a paper on the epidemiology of strabismus that discovered amblyopia was significantly more common in the non-Aboriginal population than Aboriginal, and concluded the need for an early childhood screening program.
Despite this, it would take several decades for a breakthrough.
This came when Martin met Associate Professor Elizabeth Murphy, senior advisor for child and family health in NSW Ministry of Health who advocated for hearing screening of newborns. The pair had discussions about a similar approach for vision. Eventually, the NSW Government granted funding for a preschool vision screening program in 2007, with Murphy chair of an implementation reference group, and Martin the ophthalmology representative.
StEPS was born: a program that commenced in 2008 and continues today. At its core, it provides an outreach vision screening service to 4-year-olds at their preschools, childcare centres and community health centres.
“I thought things were moving along nicely, because in 2009 the Commonwealth commissioned the Murdoch Children’s Research Institute in Melbourne to prepare a report on early childhood vision screening.
“I represented RANZCO and all eyecare stakeholders were represented – and the report came to the recommendation there was a need for vision screening for all children, but the government ultimately didn’t implement the recommendation," Martin said.
NSW MODEL TO BECOME NATIONAL BLUEPRINT
With the absence of a national program still 13 years later, in The Council Lecture Martin broke down the siloed nature of child vision screening programs across Australia in 2022.
These vary from no formal vision screening program in the Northern Territory, and screening of 5- to 7-years-olds in Queensland and 3.5to 4.5-year-olds in Victoria, through to the NSW StEPS program for 4-year-olds. While there are differences in the age of testing, they can also vary significantly in terms of testing settings, the types of tests conducted and overall participation rates, which were not known in Western Australia and as low as 60% in Victoria.

In essence, Martin said the NSW StEPS program is the only established pre-schooler vision screening program in Australia. Today, the program operates in 15 NSW Local Health Districts (eight in metro Sydney and seven in regional NSW), visiting early childhood care centres, with nurses and lay-screeners preforming testing with the HOTV logMAR vision chart.
Since 2009, 96.4% of 4-year-old children have been offered screening through what constitutes a universal program.
StEPS was born out of an election commitment in 2007 of $14.2 million over four years. An implementation group was formed comprising NSW Health, the state education department, rural and metropolitan nurses, early childhood nurses, ophthalmology, optometry, orthoptics. They debated:
- How StEPS should be administered

The fragmented nature of early childhood vision screening across Australia could be overcome if the eye health sector can implement a new nationwide program by 2030. The topic is close to the heart of PROF FRANK MARTIN, as outlined in his Council Lecture presentation.Prof Frank Martin examining a child in his rooms in Sydney.
- Who should perform the screening
- Where should screening be performed
- Age at which screening occurs
- What ocular problems should be screened for
- What vision tests should be used
- Referral criteria and the pathway
“Having such a diverse group led to quite acrimonious discussion at times, but with good final outcomes,” Martin said.
While NSW Health administered the program, a unique feature allowed each Local Health District (LDH) the autonomy to run StEPS as suited to their area.
Screeners underwent rigorous training that was orthoptist-led, and included two training modules through the Higher Education Training Institute, four hours minimum of onsite practical training, assessment for competency after three months, and reassessment annually.

Martin said: “The evidence showed you could test most 4-year-olds’ vision accurately using quality testing. Also at that age, the conditions that threaten vision can’t be detected by surveillance or the child’s behaviour – children can have extremely poor vision and not complain, so it goes unnoticed by their parents. At this age, children are also young enough for treatment to commence during a critical period of brain development.
“But it was what type of vision tests that should be used that generated the most discussion. Some wanted colour vison testing and convergence testing, but we agreed on visual acuity because if this is affected, there’s got to be a reason. It could be amblyopia, a refractive problem, or another issue. There was rapid agreement that the HOTV logMAR chart should be used at 6m, but where not possible, at 3m.”
When it comes to screening results and referral criteria, the StEPS program follows international guidelines whereby 6/9 (right and left) is considered a ‘pass’, and 6/9-1 or 6/9-2 in either eye is a ‘borderline pass’ where parents are informed vision is within normal limits but will require reassessment after one year. A result of 6/9-3 or worse in either eye but better than 6/18 is referred to an eye health professional. 6/18 or worse in either eye is deemed a high priority referral and children are also referred if vision is within normal limits but there are other findings or they’re unable to do the test. In these cases, children can be referred to one of eight StEPS Paediatric Ophthalmic Outpatient Clinics (POOCs) located in metro hospitals, a GP, optometrist, ophthalmologist, or community orthoptist.
The dedicated POOCs are unique to the program, in addition to ‘catch up clinics’ for children who might have been away when the screeners visited their care centre. There are also StEPS coordinators who have the major
responsibility of following up with families to ensure high priority referrals are seen within a timely manner.
PROVEN VALUE
As expected, the NSW Government was keen to understand the ROI with StEPS. University of Technology (UTS) Sydney won the tender to conduct an independent evaluation, which assessed the program’s appropriateness, effectiveness, efficiency, cost-effectiveness and whether it was implemented as intended.
“The evaluation report [published in 2018] came to the conclusion the model is unique to Australia and internationally, and is one of the largest, most systematically implemented and evidence-based vision screening programs available,” Martin said.
Specifically, the report said that use of an age-appropriate gold standard visual acuity test (HOVT logMAR) and ‘catch up clinics’ were appropriate. It also found that, despite local implementation variation, this was not associated with a difference in referral or outcome patterns. In terms of effectiveness, Martin said the report was favourable, achieving a high rate of vision screening in the target population; between 2009 and 2016, 96.4% of NSW 4-year-olds were offered the program, with 75.6% uptake. The availability of ‘catch up clinics’ had the greatest impact on screening rates at 19.3%.

With an overall referral rate of 9.4%, StEPS was also found to have a negligible number of false positive referrals and, according to Martin, an additional unforeseen advantage was previously undetected autism spectrum disorder and/or developmental delays in some children.
The annual cost of the program is $3.9 million, based on 2016/17 data.
“This translates to less than $50 for every child, and if screening was increased to 100% would be round $38 per child. The independent evaluation concluded StEPS was similarly cost effective to other prevention programs and represented good value for money," Martin said.
PROGRESS TO A NATIONAL VISION SCREENING PROGRAM

How the Australian ophthalmic sector can implement the StEPS model country-wide is currently the focus of peak eye health body Vision 2020 Australia, whose member organisations include RANZCO, Optometry Australia and Orthoptics Australia.
Martin said Vision 2020 had established a child screening working group, with many of the same arguments emerging as per StEPS in 2009.
“They came to the conclusion there’s a need for a program and developed a national screening framework for 3.5- to 5-year-olds,” Martin said.“It will have universal access, there will be minimum standards for vision screening, they have addressed the issue of post-screening pathways and the model is to be based on StEPS.”
Momentum has been gathering in the literature too, with at least two studies published on how to deploy StEPS nationally. RANZCO has also been active. Outgoing president Professor Nitin Verma met with previous Federal Health Minister Mr Greg Hunt last year who tasked the college to develop a plan to eliminate avoidable blindness by 2030. RANZCO subsequently launched Vision 2030 and beyond, highlighting the need for a national paediatric vision screening program.
“So how do we achieve this? We need to consider the NSW StEPS model to be the national model with some modifications. It needs to be a collaborative effort with all stakeholders involved,” Martin concluded.
“It will depend on advocacy and implementation in each state and territory. With advocacy, Vision 2020 have a very good record and are committed to seeing this through. Implementation will be the role for RANZCO as the leader in collaborative eyecare.
“The minster and college have set the goal of 2030, and let’s hope by then a national pre-schooler vision screening program will be available to all Australian children.”
“WE NEED TO CONSIDER THE NSW StEPS MODEL TO BE THE NATIONAL MODEL WITH SOME MODIFICATIONS”
— PROF FRANK MARTIN

Gene therapies present
AS MANY CHALLENGES AS OPPORTUNITIES
Gene therapies represent the next frontier in ophthalmology, with a multitude of drug development programs progressing towards market clearance off the back of the breakthrough approval of Luxturna for RPE-65-mediated inherited retinal dystrophies (approved in Australia in August 2020).
These next-generation, potential one-time therapies aren’t limited to inherited retinal diseases either. Programs are looking into more-complicated-to-treat conditions like neovascular age-related macular degeneration (AMD) and geographic atrophy where the defect isn’t always necessarily down to one genetic fault.
With so much happening in this space, it can be challenging to remain abreast of the most promising techniques that fall under the gene therapy umbrella. There are also major challenges to address in terms of patient safety, drug delivery systems and scalability.
Moorfields Eye Hospital London consultant retinal surgeon Professor James Bainbridge demystified many of these issues in the Retina Update at the recent RANZCO Congress in Brisbane, offering a bird’s eye view of the gene therapy landscape.
He’s well accomplished in the area himself, performing the world’s first retinal gene therapy in 2007 and winning awards for his work developing such therapies for Leber congenital amaurosis.
HOW GENE THERAPY IS BEING APPLIED IN OPHTHALMOLOGY
Bainbridge commenced his RANZCO presentation by outlining the three main gene therapy techniques being tested in ophthalmology – each with their benefits and drawbacks. In essence, gene defects can be addressed by:
1. C ompensating by supplementation (Luxturna, the first and only approved gene therapy in ophthalmology)
2. C ompensating by silencing
3. C orrection by gene editing, which offers the most promise.
Ultimately, gene therapies are developed according to the impact of the gene defect on the protein that it encodes.

In the case of ‘supplementation’ – the simplest and most common approach – Bainbridge said the patient’s condition can be improved by simply providing synthetic copies of the healthy gene to the cells that need them. This does not correct the gene defect, but establishes a
sustained separate expression system inside the cell that compensates for the deficiency.
This approach has enjoyed a rapid rise, with the first proof-of-concept recorded in 2000 before the first in-human delivery in 2007 and eventually market approval in the US by 2017.
In contrast, therapies based on ‘silencing’ are designed for when a gene defect produces a protein that has an abnormal toxic function. Protection might be offered by blocking or interfering with the RNA.
“However, these approaches must both silence the toxic gene efficiently and specifically, if they’re to avoid harm by interfering with the expression of the healthy gene. And this combination of efficiency, expression and specificity presents a serious challenge.”
Gene editing, which encompasses the famous CRISP-Cas9 platform that exploits an ancient bacteria anti-viral system, has become more feasible in recent years. This form of therapy offers the most potential by correcting the exact genetic fault to permanently produce a healthy protein.
While this shows the most promise, issues remain with the two methods being applied.
The non-homologous end joining approach involves cutting out the target defect, before the DNA strands join back together – while this is efficient it can be imprecise. The alternative method, homology directed repair, allows for pasting of a new sequence into the double stranded breaks to correct for an existing defect or to add a new one –however this process is inefficient and doesn’t work particularly well in the non-dividing cells of the eye.
CHALLENGES TO OVERCOME
To realise the potential of gene therapies, Bainbridge pointed to several challenges that need addressing.
For example, the supplementation of large genes will depend on new vector systems, while optimal safety and efficacy will demand improved control of both genetic dosing and harmful inflammatory responses. There’s also the need to avoid off-target effects and overcome inefficiencies in the techniques.
To compensate a gene defect through supplementation, the working copy of the gene needs to be delivered through a special vehicle, most commonly the adeno-associated viral vector. Viruses are highly
Gene therapies are one of the most exciting prospects in modern medicine, but as more treatments progress through clinical trials, the sector will need to grapple with issues around safety, delivery systems and health system expenditure, says PROF JAMES BAINBRIDGE.
evolved for this function to deliver the gene, and can be disabled to prevent the spreading of infection.
“Viral vector systems can efficiently deliver genes of a certain size to target surviving photoreceptor or RPE cells, if the vector is delivered closely in contact with those cells, for example by subretinal injection. This is conventionally achieved using a pars plana vitrectomy approach, but alternative routes are being explored,” he said.
“In addition to single gene defects, similar vectors are being used in trials to establish sustained local expression of therapeutic proteins in complex acquired diseases, principally AMD. These include expression of aflibercept for neovascular AMD and expression of compliment factor I in geographic atrophy.”
But Bainbridge said currently available vectors that can target photoreceptor cells have limited capacity and cannot accommodate larger genes like those involved in Stargardt disease and Usher syndrome, or indeed some of the gene editing components necessary for CRISPR-Cas9.
“So alternative strategies are needed for this,” he said.
“It’s also perhaps not surprising that the delivery of billions of copies of viruses into the eye causes inflammation and this has been anticipated. This does appear to present a risk of harm.
“For example, there’s increasing awareness of inflammatory events following injection subretinally of Luxturna and this is just one example. A recent report with 12 patients receiving Luxturna, according to the appropriate methods, showed a number developed vitritis and a number developed areas of atrophy which are not limited to the bleb itself but appear to evolve in areas outside the bleb.”
Bainbridge said the exact mechanism of this was not clear, but seemed to relate to a sub-acute or chronic immune process. To date, there doesn’t appear to be evidence that it actually causes harm in terms of the overall functional effect, but there is a likelihood it could in the longer term.
“So this is something which needs to be addressed. And in terms of safety of the vector itself this could include modifying the capsid (the protective protein shell), or perhaps the route of delivery can be changed and consideration of alternative immune suppression techniques is going to be important.”
With this in mind, Bainbridge said intravitreal injection remained an attractive opportunity for gene therapy delivery – even though this method has had difficulty targeting the outer retina. But there are potential methods to modify the capsid to make this possible in small experimental models at present.
GENE THERAPY DELIVERY MECHANISMS
Nevertheless, gene therapies still rely on being delivered in the subretinal space, which is conventionally done by a transvitreal approach. According to Bainbridge, this is efficient and offers the ability to accurately target the therapy, but has the disadvantage of being invasive.
“In terms of scalability in the long term, it’s difficult to imagine how this can be performed cheaply and easily for everybody that might benefit – so there are alternative ways to try to deliver genes to the subretinal space,” he said.
These include a transscleral approach which is performed in
conjunction with a cannula that can be inserted anteriorly and fed posteriorly behind the macula with a needle that is inserted through the choroid and into the subretinal space, avoiding the side effects of vitrectomy.
But Bainbridge said this approach introduced other concerns; for example, it might be difficult to target the macula if that is what’s required.
The other alternative is suprachoroidal or transchoroidal that involves delivery of a therapy to the suprachoroidal space using microneedles past anterior to the pars plana.
“This is potentially scalable but not targeted, and has uncertain systemic dissemination and immunogenicity. This pathway may prove to be a viable alternative for the treatment of acquired retinal diseases where cell specificity is not a priority. Trials of this device are ongoing with the use of Regenxbio’s product in AMD. This demonstrates widespread expression in preclinical models and is being investigated in patients.”
The final challenge that must be addressed to allow broader use of gene therapies relates to the design of clinical trials to evaluate their impact. Bainbridge believes they must adopt reliable and relevant outcome measures that demonstrate improved quality
the challenge of confidently measuring rod function and understanding how children in a reliable manner while performance and learning effects.
“We need relevant, sensitive patient reported outcomes that includes quality of life. We also
especially where we might see improvements and function which
“We also need to consider whether it’s feasible and ethically acceptable to include sham injection, or some form of placebo control. And finally, we need to consider how we can get rapid outcomes: where we expect an improvement in function we hope this can be measured quickly with confidence, but in many of these conditions we rely on slowing or arresting of degeneration that may become evident only after many years.
“Ideally, we would have some sort of surrogate measure that might be easy to measure, such as imaging, or electrophysiology, but this is going to take some time to develop.”
AN EXCITING PROSPECT
In summary, Bainbridge said there has been significant progress in the gene therapy space, with supplementation for deficiencies now a reality. Meanwhile, silencing can improve the affected site temporarily, and the prospect of gene editing to not just compensate for gene defects, but to correct them in vivo, is “a really exciting prospect”.

“Having said that, there are major challenges to be faced, including targeting and dosing of these new products, managing and understanding some of the immune responses, optimising some of the surgical delivery techniques for safety, efficiency and upscaling, and, finally, optimising trial design in order to be able to make these improvements rapidly and reliably,” Bainbridge concluded.

WHAT THE EYES
tell us about the brain
PROF HELEN DANESH-MEYER was ranked by Ophthalmologist magazine as one of the top 100 most influential people in the world of ophthalmology in 2022. Several aspects of her research have influenced and altered clinical management strategies, particularly in the field of neuro-ophthalmology.
As early as 1986, a team at the University of Southern California undertook a post-mortem study in deceased patients with Alzheimer’s disease and observed that eight of their 10 samples demonstrated varying levels of optic nerve degeneration.
But due to the study’s very small sample size, and limited post-mortem histological methods, determining the relevance of this observation had to wait 20 years, when in 2006, Professor Helen Danesh-Meyer’s research team reported the first study on this topic in living patients.
“We started the efforts a few years earlier with the Heidelberg Retina Tomograph (HRT), a scanning laser ophthalmoscope. At the time, the HRT was the only technology available that could quantitatively image the optic nerve,” she said.

“We correlated optic nerve measurements and retinal nerve fibre layer with cognitive function and risk of Alzheimer’s disease in 90 participants. Our study found a clear dose-response relationship between optic nerve head thinning and lower cognitive function, including a threefold excess of Alzheimer’s disease and patients with extreme thinning. Importantly, this was in the absence of any measurable optic nerve visual dysfunction.”
The fascinating insight is an example of the way in which technological advances have opened opportunities for novel ocular biomarkers into brain function and disease, which was the focus of Danesh-Meyer’s Dame Ida Mann Memorial Lecture at RANZCO’s 53rd Congress in Brisbane in late 2022.
Ultimately, her team’s work helped establish the concept of optic nerve biomarkers and their ability to give insight into central nervous system injury. But it also raised new questions about whether future advances in technology would support the clinical translation of their findings, given the inherent limitations of HRT.
The answer was ‘yes’.
ABOUT THE SPEAKER
“More than a decade after the publication of our group’s results, a team lead by Moorfields Eye Hospital combined OCT, and serial cognitive testing in over 32,000 participants in the UK Biobank population study. Their findings confirmed our observations,” Danesh-Meyer explained.
“Thinner retinal nerve fibres were associated with worse cognitive function, but they also made an additional intriguing observation. Retinal nerve fibre layer thinning is associated with a doubling of risk of future cognitive decline.”
Further research from her team and others has generalised these observations showing that the link between the optic nerve biomarkers and cognitive decline are not an isolated example.
“Accumulating data also show that ocular biomarkers are an indicator of a wide range of neurodegenerative diseases. Such findings will be useful in clinical trials of novel agents in neurodegenerative conditions and have already been incorporated into some trials.”
M ultimodal imaging of the optic nerve is advancing the diagnosis and management of patients with a range of neuro ocular conditions. But Danesh-Meyer believes a challenge in the coming years will be to identify imaging and other biomarker signatures that are specific to neuro ocular conditions.

EYE TRACKING AND CONCUSSION
According to Danesh-Meyer, recent advances in software and hardware technology have opened major opportunities for examining the efferent visual system.
“Over the past three years Dr Matthew McDonald, a PhD student in my group, has built a state-of-the-art eye tracking system using 3D printed glasses. The device is compact and mobile and allows a patient’s gaze to be mapped with high precision and accuracy,” she said.
Professor Helen Danesh-Meyer is the first female Professor of Ophthalmology in New Zealand and is Sir William and Lady Stevenson Professor of Ophthalmology Chair at the New Zealand National Eye Centre, University of Auckland.
As a neuro-ophthalmologist, she pioneered quantitative evaluation of the optic nerve and its morphological changes using many optic nerve imaging modalities such as OCT.
Several aspects of her research have influenced and altered clinical management strategies in the international arena, in particular her work on imaging of the retinal nerve fibre layer and chiasmal compression.
Over the last 20 years, Danesh-Meyer has established the Optic Nerve Research Laboratory at the University of Auckland which investigates mechanisms of injury and repair in the optic nerve head and retina.

Examining the issue of concussion, McDonald worked with Matai Medical Research Institute (Gisborne, NZ) to recruit 40 high school rugby players who were tested at the beginning and end of the season, as well as following any concussion.
Each player also wore a mouthguard accelerometer, which allowed McDonald to quantify the amount of force sustained to their heads throughout a season.
Initial pre- and post-concussion eye tracking results were striking, demonstrating micro saccadic intrusions invisible to the human eye, occurring in less than 20 milliseconds, but a characteristic of concussion.


“These gives us a glimpse into the omnipause neuron function and the pathology that occurs with concussion,” Danesh-Meyer said.
Given that the US National Institute of Health recently acknowledged a causal link between concussion and chronic traumatic encephalopathy, such readily available tools for diagnosing and managing concussion are likely to play a major role both in amateur and professional sports in years to come, she said.
DISEASE PROGNOSIS
There’s also evidence to suggest that the eye has a role in prognosis. In 2006, together with collaborators from Wills Eye Hospital, and Dr Peter Savino, Danesh-Meyer’s team reported the first study to compare structure function correlation of retinal nerve fibre layer thinning in patients with chiasmal compression, taking advantage of the newly available OCT at the time.




They found that temporal and nasal quadrants showed thinning of nearly 50% in patients with complete bitemporal hemianopias.

However, in some patients there is a glaring mismatch between a normal-appearing OCT and a dense bitemporal defect, dismissed in some instances as poor scanning technique, or the unsuitability of OCT in neuropathy, she explained.
“Rather than interpreting our results as artefacts we believed the mismatch told the meaningful biological story, something essential about the nature of compressive optic neuropathies,” she said.
“We hypothesised that our findings demonstrated that compression
at the chiasm was analogous to one’s arm falling asleep; after sitting on it for a period of time, function is lost, but structure remains intact. So, if we freed the compression, such as with pituitary surgery, the function should improve. To us, this interpretation explained why the OCT was measuring a normal retinal nerve fibre layer and the presence of a complete bitemporal loss.”
Along with neurosurgeons in Auckland, and at Wills Eye Hospital, Danesh-Meyer and her team designed a prospective study to test if OCT could predict recovery of vision following chiasmal compression.
“Remarkably, we found that the degree of recovery of visual dysfunction was related to the thickness of the retinal nerve fibre layer as a measure of OCT,” she said.
“We had identified a biomarker that predicted degree of visual recovery after surgical intervention. In particular, patients with a complete bitemporal defect, who had recovery of greater than 10 decibels, had an OCT thickness of greater than 75 micrometres.”
To investigate the temporal pattern of visual recovery following pituitary tumour resection in eyes with and without preoperative retinal nerve fibre layer (RNFL) thinning, they then conducted a 10-year prospective study of 230 patients in collaboration with the neurosurgical department at the University of Melbourne.
“We found that eyes with normal retinal nerve fibre layer thickness at baseline experienced most of the recovery within the first six weeks. However, eyes with a thin RNFL had whatever recovery they were going to have at a much slower rate,” Danesh-Meyer said.

“We’ve subsequently extended this work and developed a multivariable risk prediction model, which has now been widely adopted for patients counselling and prognostication, making a real-world impact.”
DYNAMIC INJURY
While advances in imaging have allowed visibility of detail previously invisible to the naked eye, Danesh-Meyer said there is another invisible world to be visualised: tiny motion.
“Our assumption about aetiology of disease has been dominated by
what we see in static 3D because that is what available technology can resolve. But perhaps this paradigm needs to be challenged,” she said.
“We now have tools to see the brain in motion. Eulerian magnification relies on computation rather than optics, and it is already having an impact on biology, structural analysis, and mechanical engineering – and it is poised to make a major contribution to clinical neuroscience.”
Dr Samantha Holdsworth at the University of Auckland has recently taken this technology and applied it to MRI to create a new imaging processing tool called Amplified MRI, to study eye brain connections.

“Our initial focus is to develop a non-invasive technique to measure intracranial pressure, and we are working towards being able to incorporate a four-minute amplified MRI (aMRI) sequence that will accurately estimate intracranial pressure,” Danesh-Meyer said.
“Motion maps from patients pre and post lumbar puncture are allowing us to build a computational model that predicts brain pressure. We are also using this technology to help understand how microscopic movements impact different eye and brain diseases.”
Danesh-Meyer and her team are applying aMRI to two conditions where the translaminar pressure gradient plays a significant role –glaucoma and idiopathic intracranial hypertension (IIH) – and shared some preliminary unpublished data at RANZCO.
“In patients with IIH, there are three interesting observations post lumbar puncture. First, the optic nerve sheath diameter is visibly smaller. Second, the sheath is more collapsible. And third, the entire optic nerve seems more mobile in the orbit following lumbar puncture,” she said.
“In glaucoma, it appears there’s no significant difference between pre and post IOP but we need to recruit a few more patients to confirm this. However, in the orbit, there seems some intriguing observations. In one case, a patient had an IOP of 27 millimetres of mercury prior to treatment, and then we applied latanoprost and brimonidine to lower the IOP to 15. The pre-treatment eye with high pressure shows significant greater anterior posterior movement while, in contrast to IIH, the diameter of the sheath is greater after drops. We’re still to unravel the full implications of these findings so watch this space.”
In closing, Danesh-Meyer highlighted Ida Mann’s scientific collaborations with leading authorities worldwide across multiple fields, including Nobel Prize winning pathologist Sir Howard Florey and biochemist Sir Hans Adolf Krebs.
“As I have observed through my own research experiences, diverse collaborations enrich perspectives and help maximise the scope and impact of scientific discoveries,” she concluded.
“Visual science is increasingly a global team sport, or in the words of Ida, ‘We use research in order to answer the age-old question: what makes you get what you get, when you get it, and why?’. And nothing could be more rewarding than that.”
Many technological advances have opened opportunities for novel ocular biomarkers into brain function and disease.
And into

practice
Adrian Vecchio | The Eye Collective by Russo Optometry
“We show every patient their image and talk to them about the health of their eyes. We find the optomap invaluable for educating our patients.”
FOR A PREMIUM SERVICE Premium lenses
More independent optometry practices are upping their businesses performance by investing in premium lens technology. Insight speaks to two practices that have recently made Rodenstock lenses and equipment the focal point of their ophthalmic lens offering.


Wangaratta Eyecare, based in the namesake regional Victorian town, experienced the biggest change in its business eight years ago when it relocated to the main intersection in town. Suddenly, the practice was attracting patients prepared to pay $700 for a frame, significantly more than their previous location.
“We knew people were already happy to invest in beautiful frames, so why not give them the option of having the best lenses?” says Ms Roxy Akers, who owns and operates the practice with her optometrist husband Paul. “We were having some issues with our previous lens brand and wanted to do better by our patients, so we knew it was time to start offering something different, something customised.”
A frames sales rep visited the store one day and began talking about Rodenstock’s DNEye Scanner, which has been helping independent Australian optical practices differentiate their businesses since 2018. At its core, the device is an aberrometer, topographer, pachymeter, and additionally a tonometer. Within a matter of seconds, it takes more than 7,000 measurements of 80 parameters to create “a biometric model of the eye” that is then cleverly used to calculate the final lens.
These premium, tier one lenses are known as B.I.G. EXACT in the recently revamped Rodenstock portfolio. The DNEye device has also helped the lens manufacturer create a new tier two lens, B.I.G. NORM, which leverages artificial intelligence to analyse data from more than 500,000 DNEye scans to put measurements from the subjective refraction – sphere, cylinder, axis, and addition – to much greater use in lens designs.
Akers was impressed by what she was hearing. She did her research and eventually decided to trial the Rodenstock DNEye Scanner 2 for six months before making it a permanent fixture in the practice in 2022. Wangaratta Eyecare also invested in the Rodenstock ImpressionIST dispensing measurement system that offers precise, 3D video measurement without the need for a jig.
Now, many satisfied patients are walking out the door with complete spectacles in excess of $1000.
“I believe we’ve got the most customised lens on the market by going with Rodenstock – no one is putting that amount of intelligence into their lenses here. We’re now able to offer something that local patients can’t get anywhere else,” Akers explains.
“Before investing, we ran the numbers to justify the return on investment we were very comfortable with where it all sat, but you don’t know how people will respond with a significant increase in the lens cost, but once we have taken them through the DNEye journey people are understanding the value they’re getting.”
She continues: “Our previous premium option, particularly in the multifocal, is some way off what we’re able to offer now, so we’ve jumped to a whole new level in terms of lens products, and some people might think ‘this is going to be interesting, do you think you can sell that?’, but we haven’t looked back. People have taken it up and run with it.”
Akers and her husband also own two other regional Victorian practices, Alpine Eyecare in Myrtleford and Eyes of Bright in Bright. ImpressionIST towers were installed in those practices too, and they hope to one day rollout the DNEye Scanner to these businesses.
This is because they’ve seen what the DNEye Scanner has done for their Wangaratta practice. Shortly after embedding the Rodenstock lens portfolio, the store recorded its strongest ever month in terms of revenue. Seeing such a quick result is validation for a major purchasing decision, which is now helping the practice differentiate from the two corporate practices and other independent in town.
For now, patients examined at the Bright and Myrtleford practices can access Rodenstock’s B.I.G. NORM lenses, which Akers says is still a cut above what they were offering previously.
But word is also getting out in the broader community about the new DNEye technology and some patients from Bright have been happy to make the one-hour drive to Wangaratta to be scanned for B.I.G. EXACT lenses. Once their appointment is complete, they can collect their high precision specs from their nearby store.
While Akers has been impressed by the product itself, she’s also been
complimentary of the service provided. It’s been a big adjustment switching to an entirely new lens manufacturer for the practice team, with new terminology, features and equipment to operate.
Implementing the DNEye Scanner into the practice’s pre-test workflow (the business also recently purchased a new ultra-widefield camera) has been a small adjustment, with any additional time more than offset with the uptake of B.I.G. EXACT lenses.
“Our staff have been amazing – they’ve been 100% on board with the change, which is significant as we had been using the previous lens products for the past 10-15 years. We made the big decision to shut all three stores for a full day of training for everyone because we knew our staff would need to feel really supported to get their head around such a new concept,” Akers says.
“I’ve also had to call [Rodenstock Australia's national sales and professional services manager] Nicola Peaper to troubleshoot a problem and she was so helpful – having people readily available who know the product so well makes a huge difference. And they’ve done refresher training sessions since; the product is comprehensive and there’s lots of things you can adjust, change and customise.”
In addition to this, when Wangaratta Eyecare had an issue with the DNEye Scanner, Rodenstock Australia general manager Mr Tim McCann personally drove a replacement system down from Sydney (14-hour round-trip). Akers and her husband Paul were also invited to Munich to visit Rodenstock’s headquarters and lens laboratory and witness the manufacturing process.
A PREMIUM LENS THAT REFLECTS QUALITY SERVICE
In May 2022, when optometrist A/Prof Richard Vojlay acquired Collin & Kirk Optometrists, an iconic practice located in the Melbourne suburb of Thornbury, he was quick to implement his own optometric philosophy. Ninety-minute consultations, routine dilation and OCT on every patient, and state-of-the-art diagnostic technology define his offering centred on clinical excellence.
It was a significant gear-shift for the practice that was established in 1940 and somewhat lagged behind the times under the previous owner in terms of technology, frames and lenses.
But Vojlay wasn’t done yet. Now offering a premium-level eye exam, he needed a lens portfolio that reflected his service. When he took over the practice, the lens offering was fairly standard, with patients measured with a pupillary distance (PD) rule and marked with a texta. This level of service was perhaps a reflection of the suburb’s demographic some years ago, but Thornbury has changed and more double-income, young professionals are moving into the area after being priced out of inner-city suburbs.
As a starting point, the new owner of Collin & Kirk Optometrists made it a priority to find a high-tech dispensing measuring system. After canvassing the market, he was most impressed by the Rodenstock ImpressionIST. Then Vojlay was shown Rodenstock’s flagship DNEye Scanner 2, to complement the ImpressionIST tower.

Despite being a significant investment, he “didn’t blink” once shown the value both instruments could bring to his practice.
measuring system that doesn’t require a jig on the frame to measure PD, heights, wrap, vertex distance and pantoscopic tilt. The ImpressionIST is easy-to-use, very accurate and patients are impressed with the level of the technology.”
For Collin & Kirk Optometrists, offering a premium lens like B.I.G. EXACT has been a welcome surprise for many of the existing patient base who have readily upgraded their spectacles.
When it comes to discussing lens options, he says patients put faith in the practice staff and a lot of it comes down to them feeling confident and educated in their choice. The Rodenstock system allows the practice to demonstrate the difference.
“With Rodenstock lenses, we’re able to present the very best option for patients and advise them about how they can obtain the best quality of vision – then we leave it up to them to decide. While it might not be for everyone, many patients offered a standard product previously are seeing the value in a thinner lens that’s customised to them and with better lens coatings,” Vojlay explains.
In his practice, patient’s often remark “it’s just so clear” when delivering the latest multifocal lenses.

“And when combined with a quality frame, I know the patient is going to feel very comfortable in their new spectacles. I’d much rather the patient had one pair of high-quality glasses every five years, rather than a low-quality pair that fall apart after 12 months. I hate repairing glasses –it’s a pain for the patient and for us as it takes up valuable time,” he says.
At the end of the day, Vojlay says it’s important for practices like his to remember it’s a long-term relationship being built with the patient.
“High quality services and spectacles are crucial to building loyalty, trust, and word of mouth referrals, particularly for independent practices," he says.
“AS I’M OFFERING THE BEST POSSIBLE CONSULTATION, I WANTED TO MATCH THAT SERVICE WITH STATE-OFTHE-ART LENS DESIGNS AND A PRECISE USER-FRIENDLY MEASURING SYSTEM” — A/PROF RICHARD VOJLAY

WHAT THE OPHTHALMIC WORLD CAN EXPECT IN
Ophthalmic surgery wait times, further consolidation of the optometry market and new therapies for macular disease and myopia were among the standout issues in 2022, so what will 2023 have in store? Prominent figures within the Australian ophthalmic sector offer their predictions for the year ahead.

ORGANISATION:
Australian Society of Ophthalmologists, vice president
AREA OF INTEREST: Ophthalmology

The pressing issues in ophthalmology are the public hospital waiting lists, the aggressive tactics of health insurers and inflationary pressures on costs.
As we watch GPs come to their moment of reckoning with bulk billing, it becomes apparent that private billing is the only logical way forward. Ophthalmology reached this point over 20 years ago. Optometry will remain conflicted here as retail tends to dominate the business model.
The Medical Costs Finder website is launching in April and this will shake up the surgical space when fees become public. Expect to see a few practices champion their discount basement model whilst the majority continue business as normal trading on reputation, service and quality.
SKYE CAPPUCCIO
ORGANISATION:
Optometry Australia, interim CEO



REA OF INTEREST: Optometry
When Optometry Australia embarked on its Optometry 2040 project, we harnessed proven futures studies techniques and broad sector consultation to determine preferred and plausible futures for optometry.
In 2023 we remain focused on pursuing this vision. One element is our Big Data project, focused on filling a data gap and building a large-scale national dataset to provide a macro view of why people access optometry and what consultation outcomes are achieved. Effective use of this data will deliver informed advocacy and practice-level improvements and support research to guide better system design.
Another critical element is ensuring optometrists can work to their fullness of scope, and that our highly skilled workforce is used most effectively to ensure community eyecare needs are met. We do this through education, peer-to-peer development, and ongoing advocacy for greater uptake of collaborative care models, and for further development of clinical scope. Alongside these priorities, our commitment to supporting members with breadth of CPD, professional information and direct professional guidance, remains unwavering.
AMANDA TROTMAN
ORGANISATION: Optical Distributors and Manufacturers Association of Australia (ODMA), acting CEO
AREA OF INTEREST: Industry
For instrumentation, further development of OCT technology will feature, especially with AI. With the release of myopia-specific lenses, measuring eye length will be important in progression monitoring.
ODMA’s challenge is to adapt and remain relevant to members while helping grow the independent practice market segment, which is crucial to many of our member distributors given the further corporatisation of the market.
I’m personally committed to keeping ODMA at the forefront of live event offerings; these platforms provide a time efficient way for purchasers of optical equipment, supplies and eyewear to connect with suppliers face-to-face.
The industry is also watching for new disruptors and the potential impacts on all facets of the industry.
In most supplier encounters, I’m hearing commitments to sustainability such as the use of recycled materials – from frames through to lens cloths. I’m sure we will see more sustainable practices promoted by eyewear companies, from materials used to frames production. For example, Silhouette’s recent announcement that its production of rimless eyewear is now CO 2 neutral.

ORGANISATION:
Vision Eye Institute, CEO
REA OF INTEREST: Ophthalmology – private
As we’ve witnessed in pathology, diagnostic imaging, oncology, fertility and other medical specialities, we will continue to see consolidation in the private ophthalmic sector. Being part of a holistic ophthalmic care service along with better access to clinical resources, technology and management know-how is drawing more ophthalmologists into larger scale networks.
The last few years have shown how effectively the public and private healthcare systems can work together when the parameters are right. Expect to see more public-private partnerships and the private sector assisting with lengthy public hospital elective surgery waiting lists for the benefit of the community.
Attracting and retaining skilled, energetic staff will continue to be a challenge for VEI, and indeed all healthcare providers into 2023 and beyond. VEI continues to create an environment in which our staff can focus on direct patient care activities as we deploy technology to manage many of the more repetitive, transactional patient tasks.
As always VEI and Vision Hospital Group have some exciting growth initiatives launching in 2023.
APRIL PETRUSMA
ORGANISATION:
Optical Dispensers Australia (ODA), CEO

AREA OF INTEREST:
Optical dispensing
This year will see a rise in qualified optical dispenser numbers thanks to the influx of students undertaking the Cert IV in Optical Dispensing Certificate over the past two years. This was because of government training initiatives and subsidies during COVID to encourage upskilling and traineeships. We’re now seeing those students graduate and take their skills back into the workplace. From here, it’s important employers, and the industry alike, keep them engaged and encourage professional development to cement a lifelong career.
The ODA voluntary CPD program has proven popular in its inaugural year and will be bigger in 2023. The 2022 program was heavily focused on web-based content but the new program will have more face-to-face options throughout the year and across multiple locations.
This year will see the first biennial Optical Dispensers Australia Conference and National Excellence Awards in Sydney 28-29 April. Created by dispensers for dispensers, the event is an Australian-first with a two-day program complemented by a dedicated trade space, together with an evening recognising the achievements of outstanding dispensers and Cert IV graduates.
AP PLY THE BRAKES
ORGANISATION:
ProVision, CEO
REA OF INTEREST:
Optometry – independent
Independent optometry has a great opportunity in 2023 to build on the recent shift in consumer behaviour. With more consumers shopping local, there’s an opportunity for community-based alignment and differentiated patient messaging. Improved digital engagement and a sharper focus on optimising the patient experience will help strengthen patient relationships and increase the value perception of local independents. Integrating sustainable business practices and eco-friendly products will be important as consumers seek more from retailers here.
To combat the economic head winds and market pressures expected in 2023, ProVision will support member practices with solutions that aid in cost and time efficiencies and profit optimisation. The availability of services (new and existing) that strengthen the future position of practices has never been more important – and connecting with practices through networking and a broader education offering will build a greater appreciation of how these services support future growth.
Key stakeholder engagement will also be key – more supplier collaboration is planned and nurturing the pool of interested practice buyers will serve us well.

PBS information: this product
Before prescribing please review full Product Information available via www.aspenpharma.com.au/products or call 1300 659 646


This medicinal product is subject to additional monitoring in Australia. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events at https://www.tga.gov.au reporting-problems.
EIKANCE 0.01% EYE DROPS (atropine sulfate monohydrate 0.01%). Indication: To slow the progression of myopia in children aged 4 to 14 years. May be initiated in children when myopia progresses ≥-1.0 D per year. Contraindications: Presence of angle closure glaucoma or where angle closure glaucoma is suspected. In glaucoma susceptible patients, an estimation of the depth of the angle of the anterior chamber should be performed prior to the initiation of therapy. Known hypersensitivity to any ingredient of the product. Precautions: Risk-benefit should be considered when the following medical problems exist: Keratoconus - atropine may produce fixed dilated pupils, Synechiae - atropine may increase the risk of adherence of the iris to lens. Use in Children: atropine sulfate monohydrate should not be used in children who have previously had severe systemic reaction to atropine. Use with great caution in children with Down’s syndrome, spastic paralysis, or brain damage. Limited clinical evidence is available for the longterm safety in children and adolescents. Regular eye health clinical reviews recommended during long-term treatment, including the monitoring of anterior segment development, intraocular pressure, retinal health and myopia progression. Consider careful monitoring of anterior segment development with prolonged use in very young children. EIKANCE 0.01% eye drops should not be used in children less than 4 years of age. If children experience photophobia or glare, they may be offered polychromatic glasses or sunglasses. If children experience poor visual acuity, consider progressive glasses. Discontinuation may lead to a rebound in myopia. EIKANCE 0.01% eye drops are not indicated for use in the elderly. Possible effect on the ability to drive or use machinery due to poor visual acuity should be evaluated, particularly at the commencement of treatment. Pregnancy: Category A. Lactation: distributed into breast milk in very small amounts. Interactions: systemic absorption of ophthalmic atropine may potentiate anticholinergic effects of concomitant anticholinergics. If significant systemic absorption of ophthalmic atropine occurs, interactions may occur with antimyasthenics, potassium citrate, potassium supplements, CNS depressants, such as antiemetic agents, phenothiazines, or barbiturates. Concurrent use may interfere with anti-glaucoma agents, echothiophate, carbachol, physostigmine, pilocarpine. Adverse Effects: photophobia, blurred vision, poor visual acuity, allergy, local irritation, headache, fatigue. See full PI for other ophthalmic and systemic AEs. Dosage and administration: Treatment should be supervised by a paediatric ophthalmologist. Instil one drop into the eye as required for treatment. Minimise the risk of systemic absorption, by applying gentle pressure to the tear duct for one minute after application. Should be administered as one drop to each eye at night. The maximum benefit of treatment may not be achieved with less than a 2 year continued administration period. The duration of administration should be based on regular clinical assessment. Each container is for single use, discard after administration of dose. (Based on PI dated 25 November 2021) References:
Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma.com.au Trademarks are owned by

DR KATE GIFFORD
ORGANISATION:
Optometrist, professional educator, clinician-scientist, Myopia Profile founder
AREA OF INTEREST: Myopia

The last year has shown enormous growth in research knowledge, industry solutions and practitioner engagement with myopia management in children. 2022 saw the return of the International Myopia Conference (IMC). Last held in 2019, this was the biggest yet and we’re seeing more clinicians and industry engaging with what was traditionally a research conference. The release of new products in Australia in 2022 has been met with more data on existing treatments, with more of both expected in 2023.
The opportunities in such an exciting, evolving field are obvious. New product releases and wider release of current treatments will continue to grow the landscape. The challenges are keeping abreast of innovations, both in science and practice. Staying up-to-date is key in confident communication with parents, and Myopia Profile will continue to work hard on providing this support to ECPs through our educational and clinical resources.
In 2023, we can look forward to the publication of Volume 3 of the International Myopia Institute reports. These will include new papers on emerging topics and updates on previous reports.
DR RACHEL DAVID
ORGANISATION:
Private Healthcare Australia, CEO
A REA OF INTEREST: Private health insurance
The private health insurance sector has experienced nine consecutive quarters of membership growth and a record 14.37 million Australians now have private health cover. The Australian public clearly believes private health insurance is value for money. In recent years we’ve seen sustained positive growth in both ‘hospital’ and ‘extras’ coverage with a record 14.36 million people eligible to receive benefits for optical, dental, physiotherapy and other allied health services.
While the COVID-19 pandemic produced challenges in terms of accessing healthcare, health funds committed to return savings accumulated as a consequence of the pandemic lockdowns to members. No other health sector group made the commitment not to profit from the pandemic.
Since the start of the pandemic, more than $2 billion has been returned to customers through cash backs and premium deferrals in a process overseen by three regulators.
In 2023 health funds will keep working to provide value for members and advocate for sensible healthcare reform to keep health inflation under control and premiums affordable for Australian families.
DR KATHY CHAPMAN
ORGANISATION: Macular Disease Foundation ustralia (MDFA)
AREA OF INTEREST: Macular disease
MDFA’s successful advocacy leading to the rejection by both major parties of the proposal to cut the MBS rebate by 69% for intravitreal injections leaves us asking the question: where next in 2023?
Lifting the threat of the proposed rebate cut was a great relief to many in our community. Yet significant questions remain. What can be done to help people persevere with eye injections? How can eye injections become more affordable? And how can I access treatment closer to home?
MDFA has commissioned PwC to model these potential benefits. With answers to each of these questions, we will better understand the impact of these problems. Our “where next?” will then become a mission to work with federal and state/territory governments, professional organisations, and others to find solutions to these problems. We look forward to sharing these results with the eye health community in 2023.
One of our other important activities this year will be awarding the next round of research grants. MDFA is the largest non-government funder of research into macular disease. This year we are involving community members with the goal of ensuring research we fund has both scientific and community merit and value.
DR BEN ASHBY

ORGANISATION:
Specsavers ANZ, director of optometry


AREA OF INTEREST: Optometry – corporate
Specsavers’ mission has always been to make eyecare accessible and affordable, and recent years have shown the impact of this strategy on the early detection of avoidable blindness. This has protected the vision of thousands of our patients in their 40s, 50s, 60s and beyond. In 2023 we’re excited to broaden this strategy for
The year ahead will see new development opportunities for our professionals seeking to elevate their careers. We’ll also launch initiatives for our people, planet and communities through our sustainability agenda, impacting everything from the products we offer to our work with long-time partner, The Fred Hollows Foundation, in caring for First Nations patients.
Building on our ‘Great Place to Work’ status, we’ll continue building workplace cultures and supporting our team members to thrive.
For many of our customers, the economic headwinds suggest it’ll be a difficult year. Specsavers will be there for local communities with affordable quality eyecare and eyewear, providing great service, to change lives through better sight and hearing.
ROSE
Plus, general manager
Local independent optometry has recovered well during 2022 post-COVID-19 disruptions, so even with the potential for a return of mask mandates, clinical in-person service should be able to
For me, over the course of 2022, it was very satisfying to see how our national digital advertising and SEO efforts provided strong appointment booking growth for our co-branded and branded
In 2023, I look forward to further expanding our national advertising efforts in the digital space. As a branded group, by organising these efforts through our National Office, Eyecare Plus can increase our overall patient brand awareness while our locally owned practices continue to operate as they are accustomed.

With the help of our Marketing Plus team, our members can continue to focus on their specific local area advertising, while our National Office covers the national digital advertising and their website SEO to increase their new patient acquisition.
MITCHELL ANJOU

ORGANISATION:
The University of Melbourne’s Indigenous Eye Health Unit (IEHU), deputy director



















AREA OF INTEREST:
Aboriginal and Torres Strait Island eye health
2023 looms as an important year in Australia’s history as a referendum will determine the establishment of a First Nations Voice to Parliament.
IEHU will be starting 2023 acknowledging the retirement of Professor Hugh Taylor AC, who established the group in 2008, as he accepts an emeritus appointment within the university. IEHU has made significant changes over the past year including recasting our Advisory Board to be chaired and have a majority of Aboriginal and Torres Strait Islander people. The IEHU staff of 17 is now just under 50% First Nations people and we will begin shifting power within the group in 2023.
The Indigenous eye health sector has some important challenges ahead including collectively re-engaging with the new government to support sector proposals and activities.
First Nations leadership will be an emerging strength in the sector in 2023 through the activities of NEGATSIEH and FNEHA, including the National Aboriginal and Torres Strait Islander Eye Health Conference 2023 – to be held in Western Sydney in May.

RICHARD WYLIE
ORGANISATION:
Glaucoma Australia, CEO
REA OF INTEREST:
One of the prevailing themes in the health sector in 2023 (whether we like it or not) will be of budget repair at the state and federal levels. Specifically, how government can drive efficiencies in the health system and bring the exponential growth of the NDIS under control. Glaucoma Australia is here to play its part.
We will continue to run community-based programs aimed at identifying people with glaucoma (or those at elevated risk) as soon as possible. To provide ‘wrap around’ education and support to those who have been diagnosed. To be a trusted partner for healthcare professionals by “extending their care” beyond consultations with their patients. To continue to invest in cutting edge Australian-based medical research, to further confirm Australia’s status as a global centre of excellence in glaucoma diagnostic and treatment innovation. Finally, to be an influential advocate for those living with glaucoma in Australia. There is still much to be done to support those who are living with the day-to-day challenges of glaucoma sight loss.
MATTEO ACCORNERO

DR AMANDA FRENCH


ORGANISATION:
Orthoptics Australia, president
A REA OF INTEREST: Orthoptics
It seems 2023 will be about looking to the future with a refocus on strengthening the eye healthcare workforce and meeting
A key focus for Orthoptics Australia is beginning implementation of our 2023-2026 strategic plan with a vision to “support orthoptists to provide excellence and equity in eye health care”. Our strategic priorities are aligned with areas of current focus within the eyecare and broader allied health sector including, understanding allied health workforce distribution and demand through implementation of a national minimum dataset and working towards equity of access to healthcare services, particularly in regional and rural Australia.
The new RANZCO Vision 2030 and beyond plan will play a role in shaping the future eyecare workforce and Orthoptics Australia is looking forward to working with RANZCO to support its realisation. For orthoptists, our priorities are to foster strategic connections within eyecare and the community – and to promote the value of orthoptic practice in areas of specialty and where efficiencies can be gained through optimising orthoptic-led service delivery.
OPSM’s Clarifye digital eye exam experience to appointments and records management.
CARLY ILES
ORGANISATION:
Vision 2020 Australia, acting CEO

REA OF INTEREST:
Eye health and vision peak body


As we find ourselves in a post-pandemic environment, this year is important for our sector. Growing wait lists, particularly around cataract surgery, is a significant issue if we are to ensure that all Australians are getting the eyecare they need, when they need it. This is equally pertinent for children’s eye health and making inroads to progressing a national screening framework.
Advocating for innovation in cross care collaboration and addressing workforce issues are also at the forefront of our endeavours. We will be looking to increase our state-level advocacy efforts to improve health systems, especially in the first quarter of the year with the NSW election.
Ensuring the needs of people who are blind or have vision loss are better supported through the NDIS review process is an important priority, as is continuing to strengthen our allyship with First Nations partners to continue to close the eye health gap for Aboriginal and Torres Strait Islander people.
ORGANISATION:

Centre for Eye Research Australia CERA), managing director

AREA OF INTEREST: Eye research

In 2023 we will continue our work towards improving access to clinical trials by building stronger relationships throughout the wider ophthalmic community.
We recently launched a joint strategy with the Royal Victorian Eye and Ear Hospital, and together we are moving towards our shared vision of a research-active hospital campus.
The VENTURE natural history study, a collaboration between CERA and the University of Melbourne, is helping us give people with inherited retinal diseases the opportunity to participate in clinical trials for new treatments.


We are also planning to expand our clinical trials footprint to increase access to research opportunities. There are so many potential therapies emerging for previously untreatable conditions like retinitis pigmentosa and dry age-related macular degeneration. Working with community optometrists, ophthalmologists and other advocacy groups is the best way we can make sure patients see the benefits from our research as soon as possible.
MARK WYMOND



At the completion of this article, the reader should be able to improve their glaucoma management.
Including:
• Know how the classes of glaucoma medications induces/ exacerbates Ocular surface disease (OSD)
• Recognise the symptoms of OSD and chronic ocular inflammation in glaucoma patients

• Know the benefits, and limitations, of SLT
• Know the benefits, and drawbacks, of preservative-free preparations for glaucoma
• Know when the glaucoma patient and OSD should be referred for MIGS.
KEEPING THE OCULAR SURFACE HEALTHY IN THE GLAUCOMA PATIENT
Although topical glaucoma therapies are a proven strategy to lower IOP, their negative impact on the ocular surface can’t be overlooked. DR ROHAN GUPTA and A/PROF CHAMEEN SAMARAWICKRAMA argue for a more preventative approach, from prioritising ocular surface disease detection and the use of preservative-free therapies and lubricants, to surgical interventions.
Glaucoma remains the leading cause of irreversible blindness in the world, affecting 1.5-3.4% of Australians over the age of 40.1 The majority of these patients are treated with topical therapy to lower their intraocular pressure (IOP).

Unfortunately, many topical therapies used in the management of glaucoma can initiate and/ or exacerbate ocular surface disease (OSD). OSD in glaucoma patients can result in increased morbidity, reduced quality of life, poorer quality of vision and reduced compliance with glaucoma therapy leading to disease progression. 2 As such, it is important for clinicians to minimise the symptoms of OSD in glaucoma patients as much as possible.
In this article, we will outline the pathogensis and impact of OSD in glaucoma patients; methods to diagnose and monitor OSD; and strategies to manage OSD in glaucoma patients. Based on the results of the LiGHT Trial from the UK, 3 we will also discuss the need for a paradigm shift in the initial management of glaucoma, with a focus on using selective laser trabeculoplasty (SLT) as a first line treatment for open angle glaucoma and ocular hypertension to reduce the ocular toxicity of topical glaucoma therapy.
PATHOGENESIS OF OCULAR SURFACE DISEASE IN GLAUCOMA PATIENTS
OSD is a multifactorial disorder involving tear production, tear film quality, conjunctival and corneal epithelial status, and lacrimal and
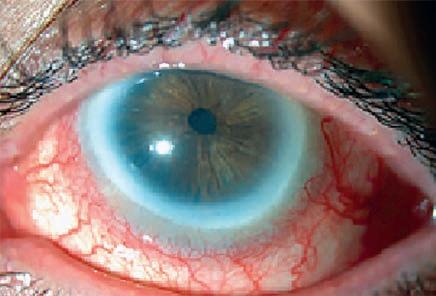
meibomian gland function. OSD can occur as a result of various factors including aging, hormone imbalance, systemic comorbidities, systemic medications, environmental exposure and drop toxicity. OSD is estimated to occur in 10-25% of the general population, however, this number increases to 50-60% in glaucoma patients on topical IOP lowering therapy. 4
The mechanism for OSD in glaucoma patients relates to changes in various inflammatory pathways. Long-term topical glaucoma therapy upregulates the production of several proinflammatory mediators including IgE and Class II antigen HLA-DR, resulting in reduced density of goblet cells, meibomian gland dysfunction, squamous metaplasia of the conjunctival epithelium and conjunctival and corneal desquamation. 5
The consequence of these changes is a reduction in tear quantity and quality resulting in symptomatic OSD.
Glaucoma medications can cause/exacerbate OSD either as a direct consequence of their active ingredient or from added preservatives. The four main classes of topical therapy for IOP lowering are prostaglandin analogues, beta blockers, alpha agonists and carbonic anhydrase inhibitors. Each of these classes of medications induces/exacerbates OSD via a different pathway.
• Prostaglandin analogues are associated with obstructive meibomian gland dysfunction.
Dr Rohan Gupta (MBBS (Hons), MMed (Ophth Sci), Grad Dip (Refrac Surg), FRANZCO) Cataract, Refractive and Glaucoma Surgeon Nexus Eyecare, Sydney Lindfield Eyecare, Sydney


A/Prof Chameen Samarawickrama
BSc(Med) MBBS, PhD, FRANZCO
NHMRC Investigator Fellow Director, Translational Ocular Research and Immunology Consortium (TORIC) Westmead Institute for Medical Research | Save Sight Institute Sydney University Nexus Eyecare, Blacktown and Norwest
• B eta blockers reduce basal tear turnover rate by acting on beta receptors in the lacrimal gland.
• Alpha agonists induce ocular allergy and upregulate IgE.
• Carbonic anhydrase inhibitors decrease the viability of the corneal epithelial cells resulting in apoptosis.
• Preservatives used to prevent microbial contamination include benzalkonium chloride (BAK), oxychloro complex and polyquaternium1. These substances initiate/exacerbate OSD by inducing squamous metaplasia of the conjunctival epithelium and destabilising the conjunctival goblet cells resulting in tear film instability. 5
The relationship between ocular inflammation and topical glaucoma therapy is dose-dependant, thus patients on multiple topical therapies for
prolonged periods are more likely to develop symptomatic OSD. This is particularly relevant to patients with ocular hypertension, as 49% of these patients will be on two or more topical therapies within five years of diagnosis. 4 Additionally, patients with primary open angle glaucoma (POAG) have been shown to have a lower basal tear turnover rate compared to normal controls, further increasing their risk of developing OSD.
IMPACT OF OSD IN GLAUCOMA PATIENTS
Symptoms of OSD and chronic ocular inflammation include burning, irritation, itching, tearing, and decreased visual acuity. These symptoms can occur as early as three months after starting topical therapy.6 The negative impact on quality of life of these symptoms can result in many patients being non-compliant with topical therapy. Studies have shown that compliance with topical therapy among glaucoma patients is often less than 50%, with OSD side-effects of topical therapy reported as one of the primary reasons.7
Additionally, the decrease in visual quality caused by OSD is compounded in glaucoma patients who already suffer from reduced contrast sensitivity, causing greater negative impact on their visual function, quality of life and increasing falls risk.
From a surgical glaucoma perspective, chronic OSD causes scarring of the conjunctiva and tenons, resulting in higher bleb failure rates in patients undergoing glaucoma filtering surgery.6
DIAGNOSING AND MONITORING OSD
The diagnosis of OSD is obtained through
both subjective and objective measurements. Subjective measurements include a thorough history specifically asking about foreign body sensation, redness, epiphora and/or a feeling of tired/heavy eyes. Patients should also be asked if they have visual fluctuations which improve with blinking, symptoms which are worse in the morning or evening and checking for other risk factors such as a history contact lens wear, snoring or systemic inflammatory conditions which may exacerbate OSD.

SUBJECTIVE MEASUREMENTS
Quality of life questionnaires are a useful tool to help standardise responses so that the severity of OSD can be monitored from visit to visit. 8 Two such questionnaires are the Ocular Surface Disease Index (OSDI) and the Glaucoma Quality of Life-15 (GQL-15) form. The OSDI is composed of 12 questions, used to measure ocular discomfort, visual function and environmental triggers, with higher scores corresponding to worsening OSD. The GQL-15 is composed of 15 questions aimed at measuring the impact of glaucomatous optic neuropathy on daily visual function, with lower scores corresponding to worsening disease.
OBJECTIVE MEASUREMENTS
Objective measurements of OSD are obtained through clinical examination and various newer technologies. Factors that should be assessed include eyelid position, tear meniscus, tear film quality, tear quantity (Schirmer’s test), tear film break-up time (TBUT; less than 10 seconds being abnormal), meibomian gland dysfunction and any ocular surface staining with fluorescein.
Clinical examination can be augmented by several new technologies such as tear osmolarity
testers and ocular surface analysers which measure lipid layer thickness (LLT), capture blink dynamics, and image meibomian gland structures. These technologies can be helpful in diagnosing OSD and monitoring progression. 8 They can also be used to perform baseline tests before initiating topical glaucoma therapy.
MANAGEMENT OF OSD IN GLAUCOMA PATIENTS
OSD in glaucoma patients occurs as a consequence of their topical therapy and the traditional approach to managing OSD in glaucoma patients has been reactive (that is: treating symptoms of OSD after they arise). However, with the results of the LiGHT Trial, the advances in minimally invasive glaucoma surgery (MIGS) and the abundance of preservative-free glaucoma medications on the market, there is an argument to be made for a more preventative approach, which utilises therapies other than preserved topical therapy to lower IOP while maintaining ocular surface health. Below, we have outlined a step-wise approach to managing glaucoma and keeping the ocular surface healthy.
1. Non-invasive procedural intervention: SLT SLT is a non-invasive treatment which can be performed in clinic. It utilises short pulses of low-energy light to heat the trabecular meshwork resulting in a mild and transient inflammatory response which reduces trabecular resistance and increases aqueous outflow thereby reducing intraocular pressure without the need for topical therapy or as a supplementary treatment to reduce drop burden.
The LiGHT trial – this was a recently published multicentre randomised control trial in the Lancet,
which compared SLT with topical therapy as a first line treatment in patients with primary open angle glaucoma and ocular hypertension. The results showed that three years after a single SLT treatment, 78% of patients were able to maintain adequate IOP control without the need for topical therapy.
The patients who received SLT had better IOP control at more visits (93·0%) compared to the eye drops group (91·3%) and had a lower rate of progression to glaucoma surgery. 3 From an OSD perspective, patients in the SLT arm reported significantly less adverse symptoms compared to patients receiving topical therapy (30 events vs 150 aesthetic side effects/allergic reactions). 3
The results from SLT can last for up to four years, and the procedure can be repeated, however, the IOP lowering becomes less effective with successive treatments. The main benefits of SLT are that it reduces drop burden, thereby reducing OSD symptoms; removes the risk of non-compliance; reduces IOP fluctuations which can occur with topical therapy; and removes the challenges of cognitive impairment and failing grip strength which are common amongst older patients with glaucoma.7
The main limitations of SLT are that it cannot be used in all forms of glaucoma (specifically uveitic and angle closure glaucoma) and in more severe cases, it may be insufficient. The IOP lowering
effects also wear off after time, however, this ‘limitation’ is offset by the improved quality of life during the period the laser is effective. There is also an initial upfront cost, however, this is typically less than the cost of topical therapy over a three-year period, especially if patients also require additional lubricating drops to offset the symptoms of OSD. 3
2. Reducing preservative burden SLT cannot be used in all forms of glaucoma and may be insufficient in achieving IOP lowering in some patients. In these instances, topical therapy needs to be used. Conventional topical glaucoma therapies typically contain added preservatives to prevent microbial contamination of the bottle. The preservative BAK is the most commonly used preservative in ophthalmic preparations, and reducing exposure to BAK has been shown to reduce the severity of OSD and increase compliance with topical therapy.7 Reducing BAK exposure can be achieved through the use of preservative-free or preservative reduced medications, or by prescribing glaucoma medications which contain alternative preservatives that are less damaging to the ocular surface. Studies comparing the efficacy of BAK-preserved and preservative-free preparations showed no difference in the amount or duration of IOP reduction. 9
Reducing the preservative burden has been
shown to significantly reduce OSD in glaucoma patients and aid with compliance. There are some drawbacks with preservative-free preparations. Preservative-free drops have a theoretical increased risk of contamination, however, this risk can be mitigated by prescribing single use medications. Cost can be a barrier, with many preservative-free preparations being more expensive than their preserved counterparts. In these instances, patients, especially those who have evidence of pre-existing OSD, should be educated on the potential benefits of a preservative-free preparation. For many of these patients, an improved quality of life may justify the extra expense.
3. Improving ocular surface
As mentioned earlier, glaucoma medications can cause OSD as a result of their active ingredient. In patients who have OSD despite the use of preservative-free medications or in whom a preservative-free option is not suitable, strategies to improve ocular surface health should be employed to minimise the symptoms to OSD and reduce the risk of non-compliance. The mainstay of treatment includes the use of intensive preservative-free lubricants to provide symptomatic relief. Co-existing lid margin disease and meibomian gland dysfunction should also be addressed with hot compress and
PBS Information: Xalatan (latanoprost 0.005% eye drops, 2.5 mL) is listed on the PBS as antiglaucoma preparations and miotics.
Before prescribing please review Product Information available via www.aspenpharma.com.au/products or call 1300 659 646.
Minimum Product Information: XALATAN® (Latanoprost 50 μg/mL) Eye Drops. Indication: Reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension. Contraindications: Hypersensitivity to ingredients. Precautions: Change in eye colour due to increased iris pigmentation, heterochromia; eyelid skin darkening; eyelash and vellus hair changes; aphakia; pseudophakia; macular oedema; other types of glaucoma; contact lenses; severe or brittle asthma; herpetic keratitis; driving or using machines; elderly; children; lactation. Pregnancy: Category (B3)

Interactions: other prostaglandins, thiomersal. See PI for details. Adverse Effects: Iris hyperpigmentation; eye irritation (burning, grittiness, itching, stinging and foreign body sensation); eyelash and vellus hair changes (increased length, thickness, pigmentation and number of eyelashes); mild to moderate ocular hyperaemia; punctate keratitis; punctate epithelial erosions; blepharitis; eye pain; excessive tearing; conjunctivitis; blurred vision; eyelid oedema, localised skin reaction on eyelids; myalgia, arthralgia; dizziness; headache; skin rash; eczema; bronchitis; upper respiratory tract infection; abnormal liver function. Uncommon: Iritis, uveitis; keratitis; macular oedema; photophobia; chest pain; asthma; dyspnoea. Rare: periorbital and lid changes resulting in deepening of the eyelid sulcus; corneal calcification. See PI for details and other AEs. Dosage and Administration: One eye drop in the affected eye(s) once daily. Other eye drops should be administered at least 5 minutes apart. (Based on PI dated 2 March 2021)
References: 1. NHMRC Guidelines for the screening, prognosis, diagnosis, management and prevention of glaucoma 2010 2. Australian Commission on Safety and Quality in Healthcare Active Ingredient Prescribing Guide - list of medicines for brand consideration December 2020
Aspen Australia includes Aspen Pharmacare Australia Pty Ltd (ABN 51 096 236 985) and Aspen Pharma Pty Ltd (ABN 88 004 118 594). All sales and marketing requests to: Aspen Pharmacare Pty Ltd, 34-36 Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma. com.au Trademarks are owned by or licensed to the Aspen group of companies. © 2021 Aspen group of companies or its licensor. All rights reserved. Prepared: June 2021 AF05768 ASP2528
If clinically necessary for the treatment of your patient, prescribe by brand and disallow brand substitution2
✔
A first choice for glaucoma management1
massage, lid wipes +/- oral tetracycline.
Studies have shown that the use of topical lubricants in glaucoma patients improved mean OSDI scores, increased goblet cell density, improved TBUT, reduced lid margin inflammation and improved conjunctival injection.10
In more severe cases of OSD that are resistant to the above treatment options, topical cyclosporine 0.05% twice daily can also be considered. One study showed that a six-month course of topical cyclosporine in glaucoma patients on long-term therapy significantly improved corneal sensitivity and partially reversed surface toxicity from preserved glaucoma medications.11

4. Surgical intervention (MIGS)
With the advent and widespread adoption of MIGS over the past 10 years, surgical intervention for managing OSD in glaucoma patients is now a viable and relatively safe option.

Trabecular bypass devices, such as the iStent and Hydrus stent, can be inserted at the time of cataract surgery or as a standalone procedure in pseudophakic eyes, to reduce the need for topical therapy. Long-term data on these devices shows that at three years postoperatively, patients who underwent combined cataract and MIGS achieved 37% reduction in IOP and 68% reduction in topical therapy requirements, while patients who underwent a standalone MIGS achieved a 42% IOP reduction and 88% reduction in topical therapy requirements.12
Unlike traditional filtration surgery, which carries a higher risk of complications, MIGS procedures are relatively safe and appropriate for patients with mild-moderate glaucoma who have
significant OSD from topical therapy. It should be noted that MIGS is still an intraocular surgery, and it therefore carries increased risk compared with non-invasive therapies. MIGS should only be considered after conservative therapies have failed.
Other surgical technologies are also on the horizon for managing OSD in glaucoma patients, specifically, a sustained-release bimatoprost implant. Although not available in Australia at present, the device is in Phase 3 trials. This device is injected intracamerally to provide a non-pulsatile, sustained release of bimatoprost over a 90-day period. The IOP lowering effects are comparable to those of topical bimatoprost, without the ocular surface toxicity of topical therapy.13
CONCLUSION
OSD is common condition among glaucoma patients which can limit their quality of life and reduce their compliance with treatment. OSD is caused/exacerbated by topical glaucoma medications via both the preservatives and the active ingredient.
SLT has been shown to be an effective treatment for IOP reduction and should be considered as a first line treatment in patients with open angle glaucoma and ocular hypertension. For patients in whom topical therapy is required, efforts should be made to limit the preservative burden. Symptomatic relief can be provided by lubricants and topical cyclosporin. It is important to manage any co-existing lid margin disease. In recalcitrant cases, surgical intervention can also be employed in the form of MIGS to help lower IOP and reduce drop burden.
REFERENCES:
1. Keel S, Xie J, Foreman J, Lee PY, Alwan M, Fahy ET, et al. Prevalence of glaucoma in the Australian National Eye Health Survey. British Journal of Ophthalmology. 2018;103(2):191–5
2. Mylla B oso AL, Gasperi E, Fernandes L, Costa VP, Alves M. Impact of Ocular Surface Disease Treatment in Patients with Glaucoma. Clin Ophthalmol. 2020;14:103-111
3. Gazzard G, Konstantakopoulou K, Garway-Heath D, Garg A, et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. Lancet. 2019;393(10180):1505-1516
4. Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma. 2008;17:350–355
5. Zhang X, Vadoothker S, Munir WM, Saeedi O. Ocular Surface Disease and Glaucoma Medications: A Clinical Approach. Eye Contact Lens. 2019;45(1):11-18
6. Saade CE , Lari HB, Berezina TL, Fechtner RD, Khouri AS. Topical glaucoma therapy and ocular surface disease: A prospective, controlled cohort study. Can J Ophthalmol. 2015;50(2):132–136
7. Tsai JC, McClure CA, Ramos SE, et al. Compliance barriers in glaucoma: a systematic classification. J Glaucoma. 2003;12:393–398
8. Mathews PM, Ramulu PY, Friedman DS, Utine CA, Akpek EK. Evaluation of ocular surface disease in patients with glaucoma. Ophthalmology. 2013;120(11):2241–2248
9. Ramli N, Supramaniam G, Samsudin A, Juana A, Zahari M, Choo MM. Ocular surface disease in glaucoma: Effet of polypharmacy and preservatives. Optom Vis Sci. 2015;92(9):e222–e226
10. Aragona P, Papa V, Micali A, Santocono M, Milazzo G. Long term treatment with sodium hyaluronate-containing artificial tears reduces ocular surface damage in patients with dry eye. Br J Ophthalmol. 2002;86(2):181–184
11. Saini M, Dhiman R Dada T, Tandon R, Vanathi M. Topical cyclosporine to control ocular surface disease in patients with chronic glaucoma after long-term usage of topical ocular hypotensive medications. Eye (Lond) 2015;29(6):808–814
12. Hengerer FH, Auffarth GU, Riffel C, Conrad-Hengerer I. Second-generation trabecular micro-bypass stents as standalone treatment for glaucoma: a 36-month prospective study. Adv Ther. 2019;36(7):1606–17
13. Craven E.R., Walters T., Christie W.C., Day D.G., Lewis R.A., Goodkin M.L., et al. 24-Month Phase I/II Clinical Trial of Bimatoprost Sustained-Release Implant (Bimatoprost SR) in
NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
"COMPLIANCE WITH TOPICAL THERAPY AMONG GLAUCOMA PATIENTS IS OFTEN LESS THAN 50%, WITH OSD SIDE-EFFECTS OF TOPICAL THERAPY REPORTED AS ONE OF THE PRIMARY REASONS.7"FIGURE 5. iStent MIGS devices as viewed with gonioscopy.



When it comes to innovation, there’s no comparison.
OF A SPORTS VISION OPTOMETRIST Inside the world
come to me. Obviously, if they fail a short screening, they come to me, and we do a full workup here.”
“Here” is Gerry’s appropriately named Brisbane practice, Eyeman Optometrists, which includes a sports facility where athletes can perform drills specific to their sport and optometrists can observe.
“For the amateur but keen sportsperson, which is more of what I do than professional athletes, that’s what we do here. Patients of any age can come and put in contact lenses and face a cricket ball, a soccer ball or football. If a patient wants contact lenses for golf, we can put them in, and swing a golf club in our onsite facility,” he explains.
In February 2022, Eyeman Optometrists was affected by floods, which forced the practice to close for a week, but it hasn’t slowed demand. Gerry, who has a degree in optometry and completed a Masters in Sports Vision, works with junior through to elite athletes.


He was recently invited to work with the Brisbane Bullets (NBL) after the team’s strength and conditioning coach, Mr Stewart Briggs, requested his services.

His career has taken him Australia-wide as a consultant, conducting vision screenings for other sporting organisations like the Australian Institute of Sport, Cricket Australia, Cricket Umpires Australia, Queensland Cricket, the NRL, AFL and Fox Sports.
In Gerry’s experienced opinion, convergence is one of, if not the most, important visual skills for any sport where the ball is coming towards a player. He says there are three or four players on the Brisbane Bullets basketball team with poor binocular control and convergence.
“Binocular vision –because that gives you a spatial understanding of where you are, and where things are relative to you – that remains the biggest and most important skill in sport,” he says.
the gym – not in a consulting room – it sparked an online conversation about his atypical approach to vision assessment.
As Gerry explained in the post, after 30 years working with elite athletes, he finds it best working in their environment, making the testing specific and to their needs. Hence, all testing and training is done where the athletes are, typically in gyms.
“At the end of the day, if you are testing these players under the same conditions – under fatigue conditions – you’ve got a much better way of understanding what their vision and eyes are doing in a game,” says Gerry, nicknamed ‘The Eyeman’ by former AFL player Justin Leppitsch because he couldn’t remember Gerry’s name.
“Any patient, whether it be a sportsperson or not, who sits in your chair is hypersensitive to what their eyes are doing. They’ll be more likely to try harder to get results right or, if they’re not fatigued, they’re less likely to show any sort of compensation that’s breaking down.
“That’s why I’m quite adamant that I need to go to them, not them
Gerry says a sport like basketball has less acuity demand due to smaller court size and close proximity of players. Therefore, he is not overly concerned about minor visual acuity issues. Instead, he focuses on depth perception, binocular performance and ocular health.
Despite working with elite athletes in the AFL, NBL and other competitions to help them gain an edge, it is helping young kids improve their vision and sporting skills where optometrist PATRICK GERRY feels e can make the biggest difference.Patrick Gerry takes vision screening to the sport – wherever that may be. Here, he is vision screening junior cricket academy players in a shipping container. Optometrist Patrick Gerry with Brisbane Bullets NBL basketballer Lual Diing.
“We’ve got a squad of 12 or 14 players at the Bullets, I’m not going to change all of them. I’m just going to work with those who have a definite problem.”
He recently introduced proprioceptive training after the Bullet’s CEO spoke to him about one player who is amblyopic. The approach focuses on the use of somatosensory signals in the absence of information from other modalities such as vision.

“The player has learned ways to adapt but the coaching staff were worried about certain things he was doing. It was a really great conversation. I predicted what I thought he was doing to compensate, and that correlated with their observations of him adjusting to errors,” Gerry says.
“I suggested trying proprioceptive training. There’s nothing new about this technique, but if you follow basketball, players have often worn glasses that blocked their vision inferiorly so they couldn’t see the ball while dribbling. You’re trying to teach people to have skill acquisition without direction of vision. So, this is more about skill development.”
In the case of the Bullets player with amblyopia, Gerry says he wears glasses, or goggles, where the central superior visual field is blocked out, but he can still see peripherally and inferiorly. He can wear them on the court; but has limited vision of the board and basket.
“We’re teaching him to be aware of his surroundings and shoot with a confidence of feel, not relying on his vision per se.”
Gerry says sportspeople have experimented with this kind of concept for years.
“Some people like it, some don’t. Tiger Woods is famous for his dad forcing him to play golf, even though it was dark, to make Tiger learn to feel the distance, not rely on what he saw,” he explains.
“When you’re dealing with an elite athlete, and you’re trying to change a skill, you are untraining them, and this takes much longer than to train them. For example, if you’re right-handed and I wanted to teach you to change your writing skill with your right hand, it would be more difficult than to teach you to write with your left.”
Gerry points to cricket as another example.
“If a coach tries to teach a kid to play a good shot and he plays it badly but still gets four runs, what has he learned from it? He’s learnt nothing. He still thinks he can play a bad shot but get four runs – all that matters to him is the four – whereas what we want people to do, by blocking out their vision, is to feel what their muscles are doing.”
FROM WORST TO FIRST
As a father of two teenage boys, Gerry knows how much sport plays a big part in kids’ lives. His best advice to optometrists interested in furthering their skills in sports vision is to simply talk to patients and find out which play sports.
“Typically, a patient in their mid to late 40s or early 50s comes in and they have a child who plays sport,” he says.
“The parent may have astigmatism that needs correction. You have a conversation about the impact on their vision. You can ask if their child wears
contact lenses for sport. They might say they coach an under 14s team. You can ask if they’ve considered having all the kids’ vision screened.”
Like the NBL player’s vision screening in the gym, sometimes these conversations take place at kid’s sporting grounds, rather than in his consulting rooms.
He points to an occasion at his local rugby club where a child constantly dropped the ball.
“I spoke to his dad and said, ‘It’s none of my business and I’ll understand if you tell me to go jump in the lake, but your son’s just not catching the ball, I reckon he’s got some eye problems’. He said he’d taken his son to the shopping centre optometrist, and everything was okay. I asked him to give me five seconds and to show him something.”

By demonstrating the son had a vision issue, Gerry could then explain how he could correct the boy’s vision, and how that would then transfer to his sporting skills.
“This kid was getting put in the wrong positions on the field and getting dragged whenever he made a mistake. I saw him being belittled for no reason, so I made it my goal to correct his vision. He transferred into the kids’ team I coach in 2022 and played unbelievably well – he won best and fairest. He went from being the pariah who got three to five minutes a game to playing all bar 10 minutes in the grand final,” Gerry says.
“He had a really large exophoria so he had no depth perception, none. We fixed that with exercises and prisms – no contact lenses, no glasses – and taught him where to look when he caught.”
When someone’s making the same mistake repeatedly, and they’re copping feedback from people, they change the way they should do things.
“This young player was just looking at the wrong place. His eyes were never on the ball, they were always behind the ball. It took a while – over two rugby seasons – to correct his eyes and get him looking in front of the ball so he could give himself more time – and he never played wing again,” he says.
For a young optometrist who wants to get into sports vision, Gerry says it’s about having the right conversation and an understanding and confidence they can diagnose and correct the issue.
“ANY PATIENT, WHETHER IT BE A SPORTSPERSON OR NOT, WHO SITS IN YOUR CHAIR IS HYPERSENSITIVE TO WHAT THEIR EYES ARE DOING” — PATRICK GERRYFloods in February 2022 forced Eyeman Optometrists to close for a week.
DISPENSING FOR PAEDIATRIC PATIENTS – PART 2
IN THE SECOND PART IN A SERIES ON DISPENSING FOR CHILDREN, ELIZABETH CASSIDY OUTLINES PRACTICAL TIPS, AND HOW THE STORE CAN BE DESIGNED TO ELEVATE THE EXPERIENCE FOR BOTH CHILD AND PARENT.

Part one of this series on paediatric dispensing tips focused on communication techniques and frame selection. Part two covers considerations for lenses, measurements and collection.
LENSES
With lenses for paediatric dispenses, impact resistance should be a priority. Even if the parent says their child takes care of their glasses, they will be around other kids who may not be as careful – and we want to reduce the possibility for injury.

Polycarbonate and Trivex are highly resistant materials and if kids fall over or have flying objects hit their glasses, the lens will stay in one piece.
At this stage, it’s common to be faced with conflicting needs from optical considerations, the child and the parent. Typically, these fall into four categories: Fashion – You may have a child or parent focused on the frame style. This is beneficial because kids are more likely to wear a frame they like. Remember, durability and fashion aren’t mutually exclusive.
Comfort – Children are unlikely to wear uncomfortable frames. Fortunately, modern frames and lenses are designed to be comfortable, as long as the frame dispensed is appropriate for the child’s anatomy.
Safety – This is a critical issue with impact resistance, but UV safety is especially important. Studies have shown up to 80% of an individual’s UV exposure occurs before the age of 18. In Australia, we’ve learned to be sun-safe, but the research shows only 32% of children are wearing sunglasses protection. In paediatric dispenses, photochromic lenses are the most common recommendation, as it reduces the need for the child to be swapping glasses.
Price – Some price-conscious parents may not wish to pay for the child’s first choice, or the highest quality lens. The duality of communication is essential here. As dispensers, we must ensure our customers are treated with respect and understanding, while giving quality care and advice.
MEASUREMENTS
Taking measurements can be difficult with paediatrics, and I have seen a range
of methods. Below are two specific measurements, pupillary distance (PD) and heights.
For older children, using a pupillometer is ideal, or an appropriate digital device. But for younger children or babies, the only option may be turning to the PD ruler. Here, we would be measuring from inner to outer canthus. This isn’t the most accurate method but is better than guessing where their PDs are. When frame selecting, choose one that ensures their PDs are as close to the geometric centres as possible. This helps to reduce extra unnecessary thickness, weight, aberrations, and will likely have a better fit.
Heights should also not be underestimated. Ideally, centre of rotation rule heights should be taken for single vision lenses, or if not possible, then having their eyes as close to the lens’ geometric centre will reduce the need to take this measurement. For bifocals, set the seg higher than normal – on pupil centre – so the child looks through the near seg when reading. Taking heights for very young children may be difficult, however a pre-marked demo lens or height gauge may be easier. This way you can observe the child over time, compared to getting them to stay still and focus.
COLLECTION
On collection, as with any dispense, we should ensure the correct fit and the specs work as intended.
Humour and keeping the tone light and simple is a great start. Use rhymes, rules and questions to reinforce understanding.
Humour and a light tone can be useful upon collection to ensure the child remembers how to care for their spectacles.
Remember for many paediatric dispenses, this may be the first time, so don’t assume prior knowledge, and it’s useful to repeat to existing wearers. It is easy to forget in the business of dispensing that children can’t always explain how they feel or what they see. Be patient, allow them to speak up and ask questions. Parents often tell children to just get used to the glasses as they don’t know what could indicate a problem. Therefore take time to check all aspects of the glasses on collection.
KIDS CORNER
A special area of the store for paediatric dispenses can change the experience for both the child and parent, including a colourful display that has mirrors at different heights. Also consider parents may be coming in with multiple children, so a toy box can be helpful. Finally, small gifts such as balloons or stickers can brighten their mood, especially if they’re unhappy about needing specs.
Overall, paediatric dispenses require extra care, patience and kindness. But nothing beats having families return and request the same dispenser. Providing a special service is a good investment for the future and families will often recommend your service to close ones.
ABOUT THE AUTHOR: Elizabeth Cassidy, who started working in optics in 2015, is an optical trainer and compliance officer for the Australasian College of Optical Dispensing (ACOD). She has completed a Cert IV in optical dispensing and a Cert IV in Teaching and Assessing. She has worked at numerous practices across Australia, as a senior dispenser and training other staff.
“PROVIDING A SPECIAL SERVICE IS A GOOD INVESTMENT FOR THE FUTURE AND FAMILIES WILL OFTEN RECOMMEND YOUR SERVICE TO CLOSE ONES”
FROM DISPENSER TO THE OWNER OF THREE PRACTICES
MEMBER PROFILE
Name: Belinda Musitano
Position: Director, Eyes@ Optometry (Australind, Dalyellup, Falcon), qualified optical dispenser



Location: Western Australia
Years in industry: 26
1. What initially attracted you to a career in optical dispensing, and how did you enter the
I deferred from university due to my family moving interstate and needing to pay for my living expenses. I was planning to do physiotherapy and always had an interest in the health sector. When looking for a job I applied for health-related positions. After studying Human Biology in Year 11 and 12 and physics, an optical job suited my interests. Initially I was employed in reception, but at the end of the year my employer offered me to attend TAFE for the Cert IV in Optical Dispensing. I jumped at the chance and never looked back.
2. What are your main career highlights?
I’ve had an interesting and varied path in the world of optics. I was managing an independent practice with three full time optometrists at 20 years old. Looking back, that responsibility at such a young age was a great achievement. I then moved into territory management with Transitions Optical and then Sola Optical. I loved being on the road, offering training and support to practices. I opened my own practice at the age of 25 in 2005, which felt exciting and risky in equal measure. Fast forward to today, and I now have three practices, 14 employees (including four optometrists), across the south west in WA. I’ve won Business Person of the Year for the local business awards twice, and was runner up once. I’ve also won multiple small business awards, including Small Business of the Year from 2018-2022.
3. What are your strengths as an optical dispenser and what excites you about your job?
The ability to sit down, build strong rapport and really uncover the patient’s needs makes me a great dispenser. I’m excited every time I speak to patients and have them realise something that might improve their life through vision. This also builds patient loyalty and trust. Recently I saw a 12-year-old girl – new to my practice –
who was a high hyperope (+5.00). I mentioned contact lenses could be great for her dancing. Her mother remarked this has never been presented as an option before. She ordered new glasses and I booked her for a trial of daily wear lenses. She’s returned, now wearing contact lenses for dancing, so happy and confident, and her mother was grateful for the recommendation that’s made such a difference. I love we have the power to make a difference for our communities and, hence, I’ve created programs to give back and assist those less fortunate. This includes my Vision For Learning program (which includes school screenings and free glasses for children), as well as a Salvation Army clinic annually to provide glasses for those in need in my local area.
4. If you could provide advice to yourself at the beginning of your optical dispensing career, what would you say?

Ask more questions and really get to know the needs of your patient. Don’t be scared to make recommendations, and don’t pre-judge what they are going to spend.
5. What do you see as the key opportunities and challenges facing the future of optical dispensing in Australia?
The biggest challenge is ongoing training and support. Especially as a practice owner who doubles as an optical dispenser, it’s nearly impossible to find practice management advice. Some current buying groups only wish to have optometrist-owned practices as part of their

groups. I find it extremely hard to find specific training for my team.
The key opportunity for optical dispensing is that it offers an exciting and varied career path. It allows you to make a real difference in people’s lives by offering a product that works perfectly for them.
6. How do you ensure your skills and knowledge stay up-to-date and current in such a fast moving industry?
I look to several areas to keep up-to-date with knowledge. This includes:
• Attending trade fairs at every opportunity
• S ubscribing to and reading industry journals and publications
• H aving an active peer network of professionals to have discussions with
• S igning up to Optical Dispensers Australia
7. Why did you become a member of Optical Dispensers Australia, and what value do you see in the organisation?
I became a member after feeling frustrated with the lack of organisation, knowledge, tools, and training available over the years. An organisation like ODA was well overdue and I’m excited for what it may bring to our industry.
8. What would you say to others thinking of joining Optical Dispensers Australia?
There is an amazing selection of tools, webinars, and training opportunities. If you’re looking for support and knowledge, I would highly encourage you to check it out.
A NEW FRONTIER IN TREATING INHERITED RETINAL DISEASES
CENTRE FOR EYE RESEARCH AUSTRALIA SENIOR RESEARCHER AND UNIT MANAGER FLEUR O’HARE SHARES HOW POTENTIAL TREATMENTS FOR INCURABLE RARE INHERITED RETINAL DISEASES ARE CLOSER THAN EVER BEFORE.

The Retinal Gene Therapy Unit at the Centre for Eye Research Australia, in collaboration with the Eye and Ear Hospital in East Melbourne and the University of Melbourne, are poised to expand our portfolio of retinal gene therapy trials.
With a significant number of clinical trials underway for inherited retinal diseases (IRDs) internationally, research institutes across Australia are now being tapped on the shoulder to be involved at an ever-increasing rate.

Part of my role is to select the clinical trials that show the greatest promise, engage with stakeholders, and work to get the trials off the ground locally. The biggest challenge for us is finding people with the specific gene variants for a particular therapy.
IRDs, which are caused by at least one faulty gene, are the largest cause of legal blindness in working-aged Australians, affecting up to 1 in 3,000 individuals.
There are now more than 300 known genes linked with IRD, and this number is increasing with gains in our understanding and gene discovery.
Historically, genetic testing has not been offered routinely to people with IRDs, owing to the fact there was no known cure for their disease.
Now, with the advent of improved genetic testing technologies and the growing number of retinal gene therapy clinical trials on the horizon, the desire to have genetic testing is growing in this patient population.
There is now also a high chance of being able to identify the gene change associated with a person’s IRD through genetic testing. From there, it can be determined if they might be suitable for upcoming clinical trials.
Knowing this genetic information allows researchers to help identify and inform people about clinical trials targeting their specific retinal disease, and also provide more nuanced prognoses.
Much of my research over the years has focused on understanding the characteristics of individual IRDs and learning more about genotype-
This has helped us to better understand how these diseases differ in their onset, symptoms, disease pattern and rate of progression. Our observational and longitudinal research work, namely the VENTURE study (Victorian Evolution of Inherited Retinal Diseases Natural History Registry), has also been incredibly helpful in preparing for this era of retinal gene therapy by identifying the people who might be able to benefit from new treatments.
We now have a better understanding of the course and journey of some of these retinal degenerative diseases, which helps us to understand how retinal gene therapy might work in changing the course of these diseases over time.
I am also passionate about ensuring people who consider being involved in clinical trials are fully informed about the benefit-to-risk ratio for these therapies, and orthoptists have a key role in patient education and managing the expectations around the potential results.
We also have a pivotal role in
multimodal tools (i.e. retinal imaging and retinal sensitivity measures).
Ultimately, there are no guarantees with participating in experimental research. However, the future looks promising for retinal gene therapy and other IRD treatments. It is giving hope to over 15,000 people in Australia affected with these devastating conditions.
If you would like to get in contact with CERA's IRD team to learn more about its research, email eyestudy@cera.org.au
ABOUT THE AUTHOR: Fleur O’Hare is the Unit Manager of the Retinal Gene Therapy Unit at the Centre for Eye Research Australia. An orthoptist with over 20 years of clinical and academic experience, she has completed post-graduate studies in research, genetics and health promotion. She is passionate about enhancing support, education and advocacy needs of individuals with inherited retinal disease and their families.
ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community. Visit: orthoptics.org.au

“THE BIGGEST CHALLENGE IS FINDING PEOPLE WITH THE SPECIFIC GENE VARIANTS FOR A PARTICULAR THERAPY”Senior researcher and orthoptist Fleur O’Hare with a patient at the Centre for Eye Research Australia. Image: CERA
HEALTHCARE WORKERS ASSISTING IN EMERGENCIES
VERY EARLY ONE MORNING YOU ARE ON A QUIET ROAD. YOU HEAR AN ENGINE ROARING THEN A SCREECH AND THE SOUND OF SCRAPING METAL AND GLASS BREAKING. AVANT’S RUANNE BRELL DISCUSSES YOUR OBLIGATIONS IF YOU STOP TO HELP.
If you are confronted with an emergency where someone needs medical care, as a healthcare practitioner you have an ethical obligation to try help and provide assistance where safe to do so.
If you do provide assistance, you should continue to do so until this is no longer required.
CAN YOU CHOOSE NOT TO GET INVOLVED?
It’s not usually an option to ignore an emergency – particularly if you are asked to help. In some jurisdictions, laws reinforce the ethical obligation, making it an offence or professional breach to ‘callously’ or unreasonably fail to provide assistance.
However, there is no absolute obligation to assist. The law, and the professional codes of conduct, expect you will also need to consider:
• Your own safety – you are never expected to put yourself in harm’s way
• The safety of any patients in your care
• Your skills and experience
• Your capacity to assist – including whether you are impaired by alcohol or drugs
• The other options for assistance. So, if the scenario above took place outside your practice before your first patient arrived and you heard someone
calling out there’s been an accident, as a health practitioner you may be expected to go and see if you could help.
However, consider if it is 3am on a dark remote road with no mobile reception and you have narrowly escaped the accident yourself. You might be fine to stop but it also might be reasonable to drive to a nearby police station for help, especially if you would put yourself in danger by going to investigate.
WHAT IF YOU ARE UNABLE TO HELP
In Avant’s experience, most practitioners do want to try help if they can. The questions we hear are more likely to be about whether they are liable if something goes wrong.
In all Australian states and territories, there are legal protections known as ‘Good Samaritan’ provisions. These mean that if you attempt to help in an emergency with no expectation of payment or reward, you generally cannot be sued personally, as long as you act in good faith and exercise reasonable care.
CAN YOU ASSIST IF YOU HAVE BEEN DRINKING?
Now consider that the scene takes place as you are leaving a bar to walk home at closing time.
The Good Samaritan protections generally do not apply if you are impaired by drugs or alcohol, but unfortunately there is no definitive answer to whether
‘Good Samaritan’ provisions mean that if health professionals help in an emergency with no expectation of payment or reward, they generally cannot be sued personally.
you can still assist if you have had one or two drinks. You will need to decide if you are fit to assist based on the nature of the emergency, how impaired you are, and who else can help.
Avant generally advises that in this situation you identify yourself and explain that you have been drinking and may be impaired.
AN EMERGENCY OUTSIDE YOUR AREA OF EXPERTISE
At an accident site, you are not expected to provide expert medical treatment or diagnose and treat issues outside your area of expertise.
If someone had sustained an eye injury in the accident you may be able to take the lead on dealing with that issue. Even if a situation is beyond your experience, any assistance is likely to be better than nothing at all, and any healthcare training better than none. If you have first aid skills or can liaise with emergency services, that may make a difference in the outcome. Your clinical experience may also mean you are the calmest person in attendance.
However, always be honest about your level of expertise and how recent your experience is.
AFTER AN ACCIDENT
You might be asked to make a statement to police after an accident. This doesn’t mean that your care is being criticised or questioned. We recommend you make a note about the event as soon as possible afterwards.
Even if you are very experienced, an accident scene is likely to be chaotic and distressing. Make sure you also take care of yourself and contact your indemnity provider if you need advice and support.

Disclaimer: The information in this article does not constitute legal advice or other professional advice and should not be relied upon as such. It is intended only to provide a summary and general overview on matters of interest and it is not intended to be comprehensive. You should seek legal or other professional advice before acting or relying on any of its content. The information in this article is current to 5 December 2022.
ABOUT THE AUTHOR: RUANNE BRELL is a senior legal advisor in the Advocacy, Education and Research team at Avant with almost 20 years’ experience in health and medical law.

“EVEN IF A SITUATION IS BEYOND YOUR EXPERIENCE, ANY ASSISTANCE IS LIKELY TO BE BETTER THAN NOTHING AT ALL, AND ANY HEALTHCARE TRAINING BETTER THAN NONE”
IT’S TIME FOR A MORE PROACTIVE APPROACH FOR GLAUCOMA SUSPECTS
stop smoking, and eat a healthy diet. We even give them an Amsler grid to monitor for distortion at home. The reason we do this? To reduce their risk of vision loss from AMD.
So why not do the same for our glaucoma suspect patients in addition to monitoring? Why do we not encourage them to cut down on smoking, eat a healthy balanced diet, and do more exercise and meditation? It is not as if evidence does not exist.
Population-based studies have confirmed that smoking is associated with higher IOP and increased risk of glaucoma.4-6 There is similar compelling data for higher intake of vegetables and fruit significantly reducing the odds of glaucoma risk by 47% to 79%.7-9 Increased moderate physical activity has been demonstrated to lower IOP10 and slow down the rate of glaucomatous field loss.11 Mindfulness meditation 45 to 60 minutes daily reduces IOP and improves quality of and is highly accepted by patients.13
considered to be at risk of glaucoma, or ‘glaucoma suspects’.2 Of these, around 12.5% will go on to develop glaucoma within the standard two-year interval for routine eye examinations.3
The reason glaucoma suspects are labelled as such is because we are not certain who will remain stable and who will progress to develop vision loss from glaucoma. Thus, the current approach to managing glaucoma suspects is to monitor every six to 24 months depending on the intraocular pressure (IOP) and level of risk, and to intervene only when structural or functional progression has occurred. This is a reactive approach, where we only act when there is progression. But is this the best approach when looking through the lens of a glaucoma suspect patient? The obvious question is: why do we wait until progression has occurred before we intervene?
Let’s take the example of age-related macular degeneration (AMD). When we see patients with drusen or early signs of AMD, do we just ask them to go away and come back for a review in 24 months? No. We proactively tell them to wear UV-protection sunglasses,
My personal observation is that the overwhelming majority of glaucoma and glaucoma suspect patients want information on natural ways to reduce risk. We should therefore discuss these lifestyle changes with our glaucoma suspect (and glaucoma) patients given that there is a lot of upside and very little downside.
The role of nutritional supplements for neuroprotection is more controversial given the financial expense and the fact that the dosages are usually well above the recommended daily allowance. Among those that have been evaluated in human clinical studies for glaucoma, ginkgo biloba extract and nicotinamide, are probably the two that stand out the most.14-16 At present, we do not know if consumption of these supplements will definitely reduce the risk of developing glaucoma over the long term, and we do not know what the ideal dosages should be. We also do not know if there are any adverse long-term effects, although the increased risk of bleeding with ginkgo biloba extract is probably overstated based on data from meta-analyses and systematic reviews.17, 18
However, the concept of taking supplements for neuroprotection makes sense to most glaucoma suspect patients, particularly those who are at higher risk.
My personal opinion is that we should proactively discuss supplements with our patients if they are open to it. Encourage them to seek further advice from other healthcare professionals if they are considering supplements. Arm them with clear, unbiased information about the potential risks and benefits, and empower them to decide on the best option based on their circumstances.

Critics will say there is no evidence to support this proactive glaucoma approach. However, there is already enough evidence to warrant open two-way discussion with patients. Let’s not wait for the perfect evidence to be published first before we proactively educate patients about proactively managing their glaucoma risk.
Acting in the best interests of our patients should be at the core of our clinical practice. In my opinion as a glaucoma suspect myself, just waiting passively for glaucoma progression to occur is not good practice – proactive glaucoma management is.
NOTE: The opinions expressed in this article are the author's own. References will appear in the online version of this article.
ABOUT THE AUTHOR
Name: Dr Brian Ang

Qualifications: FRANZCO, FRCOphth, FRCSEd
Affiliations: Royal Victorian Eye & Ear Hospital, Melbourne Eye Specialists and Geelong Eye Centre
Position: Glaucoma specialist
Location: Melbourne
Years in profession: 13
MY PERSONAL OBSERVATION IS THAT THE MAJORITY OF GLAUCOMA SUSPECT PATIENTS WANT INFORMATION ON NATURAL WAYS TO REDUCE RISK.Research shows increased moderate physical activity has been demonstrated to lower IOP and slow down the rate of glaucomatous field loss.
2023 CALENDAR
FEBRUARY
MIDO
Milan, Italy
4 – 6 February mido.com
ANZGS CONGRESS
Queenstown, New Zealand
16 – 19 February
anzgsconference.com
APAC ACADEMY OF OPHTHALMOLOGY CONGRESS
Kuala Lumpur, Malaysia
23 – 26 February
2023.apaophth.org
MARCH
ANZ CORNEA SOCIETY AND EYE BANK MEETING
Perth, Australia
9 – 10 March
rybooking.com/events landing/922238
CONGRESS ON CONTROVERSIES IN OPHTHALMOLOGY
Lisbon, Portugal 24 – 25 March cophy.comtecmed.com
APRIL
AUSTRALIAN VISION CONVENTION
Gold Coast, Australia
1 – 2 April events@optometryqldnt.org.au
SILMO SINGAPORE
Singapore
12 – 14 April www.silmosingapore.com
ARVO 2023
New Orleans, US 23 – 27 April arvo.org/annual-meeting
MAY
ANZSRS MEETING
Melbourne, Australia 20 – 21 May ranzco.edu/events/2023
JUNE
ASO EXPO 2023
Sydney, Australia
2 – 4 June asoeye.org
WORLD GLAUCOMA CONGRESS
Rome, Italy
28 June – 1 July worldglaucomacongress.org
To list an event in our calendar email: myles.hume@primecreative.com.au
JULY
AUSCRS 2023
Port Douglas, Australia 26 – 29 July auscrs.org.au/2023-conference
SEPTEMBER
O=MEGA23 & WORLD CONGRESS OF OPTOMETRY
Melbourne, Australia
8 – 10 September omega-event.org
OCTOBER
RANZCO SCIENTIFIC CONGRESS
Perth, Australia 20 – 24 October ranzco.edu/events
Optometrist Joint Venture Partnership opportunity – Kings Meadows, TAS
Specsavers has a fantastic opportunity on offer for an optometrist looking to take the next step in their career. Join an established, market-leading brand with state-of-the-art equipment including OCT, at our new store soon to open in Kings Meadows, Tasmania! King’s Meadows is a suburb in the south of Launceston. It offers a central location and is only a short 10-minute drive from the city centre. It’s a welldeveloped suburb with a greater number of shops than any other suburb within Launceston, making it the largest commercial district in Launceston outside of the CBD. This is a great chance to be part of a new store team!
Optometrist opportunity - Specsavers Karingal, VIC
A full-time optometrist opportunity is now available at our Specsavers Karingal store. This newly refurbished, six-test room store is decked out with fully automated, new equipment including phoropter, Tonoreff II and has two pre-test rooms, both of which have OCT machines. Work with a vibrant, committed, experienced and loyal team with a fantastic team culture. Free onsite car-parking is available and there is easy access to Peninsula Link. The store is offering an attractive salary with a sign-on bonus of up to $20,000.
Interested in seeing Australia? $180,000 for the growing Mobile Optometrist Role Specsavers is growing our community-based Mobile
Optometry Team nationally, With home-based locations in Perth and Melbourne along with longer term fly-in-fly-out roles available. With an amazing $180,000 package on offer, you will experience a wide variety of cases, while being able to explore different regions of Australia. These roles would suit optometrists who has the desire and flexibility to travel.
Interested in relocating to NZ?
Specsavers has a range of opportunities for NZ optometrists looking to return home. From North to South, we have fantastic opportunities for optometrists at all levels. And, as a Specsavers optometrist, you’ll have the chance to advance your skills and become part of a business that is focused on transforming eye health outcomes in New Zealand.
Be equipped with the latest ophthalmic equipment (including OCT in every store for use with every patient) and develop your clinical experience across a range of interesting conditions and an evergrowing patient base. You’ll also have the support of an experienced dispensing and pre-testing team, the mentorship of store partners and access to an exemplary professional development program. There’s no place like home – so if you’re ready to return, let us help you.
LET’S
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Kimberley Forbes on +61 (0) 429 566 846 or E kimberley.forbes@specsavers.com
Australia Optometrist employment enquiries: Marie Stewart – Recruitment Consultant marie.stewart@specsavers.com or 0408 084 134
Locum employment enquiries: Matthew Cooney matthew.cooney@specsavers.com or 0447 276 483
New Zealand employment enquiries: Chris Rickard –Recruitment Consultant chris.rickard@specsavers.com or 0275 795 499
Graduate employment enquiries: apac.graduateteam@specsavers.com
People
ON THE MOVE
new CEO. In mid-2022, the board asked Jones, then merchandise manager, to assume the CEO role in an acting capacity following the resignation of Ms Frances Mirabelli, who had commenced as CEO in February 2022. “Tony has led the team in the interim CEO role over the past six months demonstrating a strong commitment to the values of ProVision,” chair Rowena Beckenham said. “He possesses a unique skillset that we believe will support the culture of the business for staff and members, and champion the ongoing strategic initiatives of the group.”






when Beckenham, of Beckenham Optometrist in Avalon Beach, NSW, was unanimously elected. Bluntish will remain on the board, alongside Beckenham (chair), Ms Bernie Eastwood, Mr Brett Jenkinson, Mr Andrew Koch and Ms Leah Meulendjiks. DO



SEE YOURSELF DOING WHAT YOU LOVE
WORKING AT OPSM MEANS YOU’RE PART OF SOMETHING BIGGER.
At OPSM, we are obsessed with eye care and offering our customers the confidence in how they see the world. Our advanced technology enables us to look deeper to ensure we give the best care to every customer. When you join OPSM, you work with world class technology including the Optos Daytona ultra wide field scanner. You have many opportunities for continuing professional development through financially supported industry training, mentoring, graduate induction, peer learning communities and product training. You are rewarded with a competitive salary and bonus scheme to recognise your contribution. You have career flexibility through our extensive store network. Most importantly, you can make a real difference in the way people see the world not only from your consulting room but also by participating in our OneSight outreach program. #DoWhatYouLove
INTERESTED IN PAVING YOUR OWN PATH? PLEASE CONTACT


