




Chief Executive Officer
Megan N. Schagrin, MBA, CAE, CFRE
Ext. 212, mschagrin@saem.org
Director, Finance & Operations
Doug Ray, MSA Ext. 208, dray@saem.org
Manager, Accounting
Edwina Zaccardo
Ext. 216, ezaccardo@saem.org
Director, IT
Anthony Macalindong
Ext. 217, amacalindong@saem.org
Specialist, IT Support
Dawud Lawson
Ext. 225, dlawson@saem.org
Director, Governance
Erin Campo
Ext. 201, ecampo@saem.org
Manager, Governance
Juana Vazquez
Ext. 228, jvazquez@saem.org
Director, Communications & Publications
Laura Giblin
Ext. 219, lgiblin@saem.org
Sr. Manager, Communications & Publications
Stacey Roseen
Ext. 207, sroseen@saem.org
Manager, Digital Marketing & Communications
Raf Rokita
Ext. 244, rrokita@saem.org
Sr. Director, Foundation and Business Development
Melissa McMillian, CAE, CNP Ext. 203, mmcmillian@saem.org
Sr. Manager, Development for the SAEM Foundation
Julie Wolfe
Ext. 230, jwolfe@saem.org
Manager, Educational Course Development
Kayla Belec Roseen Ext. 206, kbelec@saem.org
Manager, Exhibits and Sponsorships
Bill Schmitt Ext. 204, wschmitt@saem.org
Director, Membership & Meetings
Holly Byrd-Duncan, MBA Ext. 210, hbyrdduncan@saem.org
Sr. Manager, Membership
George Greaves Ext. 211, ggreaves@saem.org
Sr. Manager, Education
Andrea Ray Ext. 214, aray@saem.org
Sr. Coordinator, Membership & Meetings
Monica Bell, CMP Ext. 202, mbell@saem.org
Specialist, Membership Recruitment
Krystle Ansay Ext. 239, kansay@saem.org
Meeting Planner
Kar Corlew Ext. 218, kcorlew@saem.org
AEM Editor in Chief
Jeffrey Kline, MD AEMEditor@saem.org
AEM E&T Editor in Chief Susan Promes, MD AEMETeditor@saem.org
AEM/AEM E&T Peer Review Coordinator
Taylor Bowen tbowen@saem.org aem@saem.org aemet@saem.org
Associate Editor, RAMS
Aaron R. Kuzel, DO, MBA aaron.kuzel@louisville.edu
Angela M. Mills, MD President
Columbia University, Vagelos College of Physicians and Surgeons
Wendy C. Coates, MD President Elect Los Angeles County HarborUCLA Medical Center
Members-at-Large
Pooja Agrawal, MD, MPH
Yale University School of Medicine
Jeffrey P. Druck, MD University of Colorado School of Medicine
Julianna J. Jung, MD
Johns Hopkins University School of Medicine
Michelle D. Lall, MD, MHS Emory University
Ali S. Raja, MD, MBA, MPH Secretary Treasurer Massachusetts General Hospital / Harvard Medical School
Amy H. Kaji, MD, PhD
Immediate Past President Harbor-UCLA Medical Center
Ava E. Pierce, MD UT Southwestern Medical Center, Dallas
Jody A. Vogel, MD, MSc, MSW Stanford University Department of Emergency Medicine
Resident Member
Wendy W. Sun, MD Yale University School of Medicine
3 A Special President’s Comments
SAEM in 2022: Continuing to Lead the Way in Innovating and Shaping Academic EM
6 Spotlight
Guided by Grace, Compassion, and Empath – An Interview With Dr. Joseph “Adrian” Tyndall, MD, MPH
10 SAEMF Funding Opportunities
11 Apply for Supplemental Funding
11
12 Medical Students: Apply by January 31 for Your SAEMF Emergency Medicine Interest Group Grant
13 Donor Perspectives: Michelle Lall, MD, MHS
34 Global EM
How the COVID-19 Pandemic Highlighted the Need for More EM Specialists in Brazil
36 NIH Office of Emergency Care Research
NIH Training Grant Focus: The Research Career Development Award
38 Opinion
Isolating Patients During Disease Outbreak: We Can Do Better
40 Perspective
Post-Roe Emergency Medicine Education Considerations
42 Prehospital Care
Improving Continuity of Care through EMS Assessment of Social Determinants of Health
44 Profile
A Conversation With Dr. Lance Becker on Building an Academic Research Program
46 Research
What Federal Funding Program Officers Want You to Know
48 Research
The Importance of Educators to Clinical Research
50 Research Focus on Medical Student and Resident Research
52 Sex & Gender
The Role of Sex in Autoimmune Diseases
54 Wellness
Winter Well-Being: Combating Seasonal Affective Disorder
56 Wellness
Self-Compassion: Treating Yourself Like You Treat Your Friends
58 Briefs & Bullet Points
- SAEM23 Updates - SAEM News
- Educational Courses - SAEM Foundation
- SAEM23 Journals
60 Academic Announcements
62 Now Hiring

As we ring in a new year, I want to express my deep gratitude to our SAEM members and staff for all that has been accomplished as a society this past year. SAEM continues to break new records and lead the way in innovating and shaping academic emergency medicine. Our success as a Society is because of YOU, our members, who come together as a community working within our academies, committees, and interest groups to produce a tremendous amount of content, new products, and services for our membership.
Over this past year, SAEM has broken several records, including achieving a new membership high of 8,268 reached in June of this year — a 27% increase over the past five years! Among those we welcomed into our membership were four new faculty
groups, eight new residency groups, and three new medical student groups.
SAEM22, held this past May in New Orleans, realized our highest attendance ever for an SAEM Annual Meeting with over 3,500 attendees and approximately 1,300 unique presenters with hundreds of abstracts and didactics providing education and cutting-edge research. In addition, SAEM hosted its largest SonoGames competition to date with over 1,000 spectators.
SAEM’s fundraising efforts in 2022 were highly successful, leading to a new record
continued on Page 4

A special “President’s Comments” from Dr. Angela M. Mills, SAEM PresidentAngela M. Mills, MD Columbia University Vagelos 2022–2023 President, SAEM
PRESIDENT'S COMMENTS continued from Page 3
in grant funding of over $850,000 in education and research grants to SAEM members — the largest singleyear investment in SAEM Foundation’s history. Because of the great work by the SAEM Foundation and generous donations from all of you, we were also able to:
• fund two investigators through the Emerging Infectious Diseases and Preparedness Grants this year that will help keep EM prepared for the next national crisis;
• establish SAEMF’s first donor-funded geriatric emergency medicine focused grant;
• increase the Medical Toxicology Foundation/SAEMF Grant from $10,000 to $20,000;
• announce a new funding opportunity for the SAEMF Advanced Research Methodology Evaluation and Design in Medical Education (ARMED MedEd) Pilot Training Grant
SAEM Publications Make an Impact
This year saw our journals thriving, with Academic Emergency Medicine (AEM) achieving its highest impact factor yet of 5.22 and AEM Education & Training accepted into the Emerging Sources Citation Index. In addition, we published our second Guideline for Reasonable and Appropriate Care in the Emergency Department (GRACE) publication: LowRisk, Recurrent Abdominal Pain in the Emergency Department as well as the
Look for the SAEM Foundation to:
• announce a new funding opportunity for clinical operations research;
• SAEM Career Roadmap, a resource for our members at every level of their career in academic emergency medicine.
• A Reason for Research, a guide for medical students, residents, and junior faculty interested in pursuing an academic career in emergency medicine research.
• Stop the Stigma EM: A Toolkit for Individuals, Educators and Institutions Addressing Workforce Issues
Head On
SAEM’s new Workforce Development Committee began to define the evolving landscape and workforce of academic EM and develop a multiyear plan to address where SAEM can uniquely support dynamic changes in the workforce.
• award a new $10,000 SAEMF Geriatric Emergency Medicine Research Catalyst Grant (made possible through a generous donation from Michelle Blanda, MD);
• introduce a new New Vice Chairs’ Challenge;
• host a live and in person EMF-SAEMF Grantee Workshop.
In research and educational course developments:
• SAEM Master Educator course will launch its inaugural cohort at SAEM23;
• eLEAD (Emerging Leader Development Program) will graduate its inaugural cohort;
• ARMED will host its first winter workshop in the new state-of-the-art training center at SAEM headquarters;
• The Chair Development Program (CDP) will celebrate its 10th anniversary cycle;
• SAEM Research Committee will publish an electronic guidebook with updated resources and a roadmap to give researchers relevant information and education on obtaining federal funding.
Continued diversity, equity, inclusion Initiatives will include:
• a comprehensive vision statement to be issued by the new, all-EM DEI Task Force;
• formal DEI training developed by the SAEM Equity and Inclusion Committee for all SAEM staff;
• a new Outstanding Department Award for Excellence and Innovation in Diversity, Equity, and Inclusion award to honor an emergency department that has shown significant support for diversity, equity, and inclusion;
• a new RAMS URiM Resident Education/Innovation Award to provide financial assistance to underrepresented residents demonstrating leadership skills and innovation in emergency medicine.
Our Society has continued to be deliberate in advancing diversity, equity, and inclusion (DEI) within both SAEM and our specialty, including the development of a DEI Curriculum for our members, as well as leadership of a new all-EM DEI Task Force with member and staff representation from SAEM, RAMS, AACEM, and our sister emergency medicine organizations: AAEM, AAEM/ RSA, ABEM, ACEP, ACOEP, CORD, and EMRA. In addition, at SAEM23 in May, SAEM held a successful consensus conference on diversity, equity and inclusion to develop a research agenda for addressing racism in emergency medicine.



In the month of October, SAEM hosted its largest campaign yet: #StopTheStigmaEM Month. This first-ever Stop the Stigma

EM awareness campaign was led by the SAEM Wellness Committee in collaboration with an all-EM Mental Health Collaborative. The campaign focused on breaking down barriers to mental health care in emergency medicine. Successful efforts included a robust use of social media, an in-person session at ACEP, free Zoom gatherings, and other activities to get folks engaged, sharing stories, and talking about the importance of our mental health.

SAEM continues to lead as the premier organization for developing and supporting academic leaders. This year we launched the Emerging Leader Development Program (eLEAD) receiving 50 applicants — the largest number of applications for any SAEM course ever! We graduated our inaugural Advanced Research Methodology Evaluation and Design (ARMED) MedEd class at

SAEM22 and kicked off the sixth cycle of the Advanced Research Methodology Evaluation and Design (ARMED) course, welcoming a cohort of 24 future medical researchers and clinicians.
As I reflect on 2022, I am incredibly proud of all that our Society has accomplished — breaking many records while leading and innovating in academic emergency medicine. As we enter this new year, I urge you to explore the educational content and many resources available to you as an SAEM member and take advantage of the numerous opportunities SAEM offers to learn, grow, lead, and flourish.
ABOUT DR. MILLS: Angela M. Mills, MD, is the J. E. Beaumont professor and chair of the department of emergency medicine at Columbia University Vagelos College of Physicians & Surgeons and chief of emergency services for NewYorkPresbyterian –Columbia
One of the most powerful things you can do to help break down barriers to mental health is to talk openly about your personal mental health journey. Share your story and help stop the stigma.

Joseph (Adrian) Tyndall, MD, MPH is the executive vice president for health affairs and professor and dean of the Morehouse School of Medicine since July 1, 2021. Prior to Morehouse School of Medicine, Dr. Tyndall served for 13 years as chair and professor in the department of emergency medicine at the University of Florida (UF) College of Medicine from January 2008, until his departure from UF in 2021. He was the first person of color to serve as chair of an academic department in the college of medicine’s history and only the second African American to be named chair of an academic emergency medicine department at a United States medical school. Dr. Tyndall represented the UF College of Medicine as the senior medical school representative to the Council for Faculty and Academic Societies of the Association of American Medical Colleges (AAMC) from 2014 to 2018 and was named a fellow of the Council of Deans of the AAMC. In August of 2018, he was appointed to the role of interim dean of the College of Medicine at UF and then subsequently to the position of associate vice president for strategic and academic affairs for UF Health in 2021. Dr. Tyndall served for more than a decade on the board of directors of the UF Health Hospital System and was chair of the board of trustees for the UF Health Proton Therapy Institute during his tenure as interim dean.
Dr. Tyndall’s extensive record of service on boards, committees, and foundations include his service on the board of directors of the Florida College of Emergency Physicians from 2011 through 2021, serving as president from 2018 to 2019. Within SAEM, he has served on the SAEM Development Committee, the SAEM Foundation (SAEMF) Board of Trustees, and as a member of the Association of Academic Chairs of Emergency Medicine (AACEM), the Academy for Women in Academic Emergency Medicine (AWAEM), and the Academy for Diversity and Inclusion in Emergency Medicine (ADIEM). Dr. Tyndall is currently president on the board of trustees for the Society for Academic Emergency Medicine Foundation, emergency medicine’s national foundation supporting education and research in emergency care. He has been a member of the SAEMF since 2018, serving on its major gifts committee since 2021. Dr. Tyndall is also currently a member of the board of directors of the Grady Health System in Atlanta Georgia, and is an appointed member of the administrative board of the Council of Deans of the Association of American Medical Colleges.
Dr. Tyndall is a graduate of the University of Maryland School of Medicine and the emergency medicine residency program at the University of Maryland Medical System. He received a master’s degree in health services management and health policy from Columbia University, New York, New York. He started his academic career in Brooklyn, New York where he served in several roles including residency program director at the Brooklyn Hospital Center.
Dr. Tyndall is a member of the Alpha Omega Alpha Honor Society and the Gold Humanism Honor Society and an editor of the 10th edition of Rosen’s Emergency Medicine: Concepts and Clinical Practice.
When you were a child, what did you want to “grow up” to be? Growing up, I always wanted to be either a musician or scientist. I spent my childhood years listening to some of the greatest classical and jazz pianists of our modern times and honing my skills on the piano and fantasizing playing concerts. But I also was enthralled by the “How and Why Wonder Books,” a series of illustrated books published in the 60s and 70s that were designed to teach science and history to children. I spent my time trying to think up crazy science experiments that I wanted to conduct. Wanting to become a physician came much later. Why did you choose academic emergency medicine and who or what influenced your decision?
Emergency medicine became a natural choice because of my early experiences. I spent time as a nursing assistant and emergency medicine technician at the George Washington University’s (GWU) Department of Emergency Medicine. The people there influenced me because of the passion they had for the work they were doing, as well as the great skill and humanity with which they pursued it. Their ability to cope admirably under the severest of circumstances, to handle human tragedy with grace, and always showing compassion and empathy at every instance — I wanted to be that. The GWU Emergency Department was the place where I was introduced to academic emergency medicine and clinical teaching. It was the place where I learned a lot about life in my late teens. What was pivotal to my decision to pursue academic emergency medicine was my experiences at the University of Maryland and the mentorship I received there from all leadership but especially the late Dr. Elizabeth Tso who was one of the three original emergency physicians, along with Robert Barish and Brian Browne, who started emergency medicine at the University of Maryland. Many can say that Dr. Tso was a mentor. She was the mother of my career.
I have always maintained a system of values in treating and leading others and leading organizations as well as a reliance on deep personal Christian faith handed to me by my grandmother and mother. I have always been struck by how closely the construct of values-based leadership is aligned to my upbringing, my tendencies and instincts in how I approach the work I do. I have relied heavily on values of self-reflection, true self confidence, balance, and humility to guide my behaviors, my disposition towards others and my effort to always self-improve. In the sometimes highly competitive nature of academic
medicine, where the primacy of ambition and hubris sometimes seems as the inevitable pathway to success, I have always yielded to having others go first, and in many aspects of my career, it may not have been an obvious winning strategy. Although Black and African Americans compose 13 percent of the nation, they account for only four percent of the physician workforce. Clearly much work remains to be done to align the diversity of the health care workforce with the racial and ethnic backgrounds of patients, especially in the field of emergency medicine…

What do you believe is the biggest obstacle to achieving substantial diversity in the EM workforce?
The biggest obstacle to achieving substantial diversity in the EM work force is a common and transcending denominator across medicine and science. There simply is not enough equity in opportunity for underrepresented populations in the US. Our education systems also need to be reframed. The barriers are many and begin at the root causes of societal inequities that are determined by both persistent economic and political determinants. The disparities in the opportunity trajectory occurs very early on. If those trajectories cannot be influenced at early stages, the divergence in opportunities and outcomes is inevitable. Achieving substantial diversity in the health care, scientific and emergency medicine work force means shifting the curve by creating opportunities to influence the trajectory for more people of color and greater ethnic diversity for as far back as is practical for us to do.
In your experience, how far have we come (i.e., what are some positive steps/signs you’ve seen)? How far do we still have to go? Do you believe we will ever “get there?
There has been some progress. For a long time, I was the only active African American chair of an academic emergency department. Now, there are more African American chairs of emergency medicine than ever before and delightfully, the national academy inducted several this past year. However, the major economic and political equation for many people of color in this country remains unchanged. Black men in medicine have remained a persistent crisis even if the needle has been ever slightly nudged these last few years and other ethnic underrepresented groups have been persistently challenged in making progress. Will things change? I believe and hope that it will. The U.S. is marching inevitably towards greater diversity,
continued on Page 8
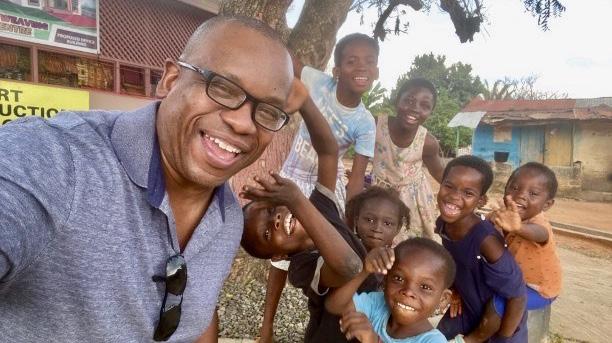
Morehouse school of medicine convocation Dr. Tyndall spending a moment with children in Kumasi Ghanacontinued from Page 7
and we know more than we have ever known before, the importance of diversity for all of society in every framework of health, from discovery to clinical care. This is why places like Morehouse School of Medicine and so many other schools of medicine and institutions of higher learning invest in pipeline and pathway programs that go as far back as middle school to shift the curve. However, meaningful and lasting impact means that society must muster the economic and political will to reach back even further, and invest sustainably to change our communities, especially those marginalized, with an understanding of the costs that resulted from past wrongs, especially in our African American communities.
What is the first thing that comes to mind when you think of SAEM? SAEMF?
Straightaway, I think about research, teaching, and acknowledgement of academic excellence.
As a graduating medical student, I received the Medical Student Excellence in Emergency Medicine Award. This was the first time I had heard of SAEM and it is something that I have always remained exceptionally proud of.
How did you become involved with SAEM and, subsequently, the SAEM Foundation (SAEMF)?
My first true introduction to SAEM happened when I first became a faculty member and was asked to become the student clerkship director at my first job in academic medicine at the Brooklyn Hospital Center. Attending SAEM meetings back then felt like being part of an extended family of kindred spirits who cared deeply for the same things I cared about, which was medical student education. I subsequently became involved in the Council of Residency Directors (CORD) and attended my first “Navigating the Academic Waters of Emergency Medicine” — probably the most influential academic meeting I had ever attended to date in my early career. There, I met many of my closest colleagues and friends including the late Dr. Leon Haley Jr. who encouraged me to get more involved in organized SAEM activity. I found myself navigating various interest groups, and committees, but as I reflect 20 years ago, my early sojourn, while not completely aimless, was more about seeking opportunity, contacts, and interests, rather than a guided, mentored or focused approach. I eventually joined the development committee of SAEM when I became a department chair because I had a keen interest in supporting the careers of others. The SAEM development committee eventually became absorbed into the SAEM Foundation.
You are considered a trailblazer who has carved out new career pathways for emergency medicine chairs to follow after they complete their chair role. How have the leadership


roles you’ve held within SAEM and SAEMF contributed to you becoming the inspiring leader you are today?
We are the sum total of our experiences, and I would say that it has been more about the relationships that I developed and what I learned from others in SAEM that prepared me for the work I am doing today. At SAEM, I was taught about mentorship, grantsmanship, and the imperative of the academic mission.

What do you believe are the biggest challenges academic emergency medicine (EM) faces moving forward?
The face of medicine and health care is changing, and the pace of change is accelerating. This is occurring across all domains, from fundamental discovery and the role of personalized medicine and ancestral genomics in therapeutics all the way to precision public health and the evolution of health care delivery and advancement of technology that will allow for delivery at scale. The role of emergency medicine must also evolve in this context as we continually assess the scope and breadth of our clinical impact as well as the education and research imperatives that will drive that impact. The biggest challenge is to evolve fast enough to remain relevant. Much (not all) of what we do today, the world will one day be able to do differently and more efficiently in both diagnostic and therapeutic categories. The good news is that emergency medicine is no stranger to rapid evolution. The training and the opportunities I received over 25 years ago are very different from today’s offerings.
How do you feel SAEM and SAEMF is addressing these challenges and contributing to building the pipeline of future EM research and education leaders?
SAEM and SAEMF is driving innovation through the creation of critical opportunities for future researchers, educators, and leaders to pursue ideas that we believe can fundamentally translate to EM practice and impact. The foundation has grown significantly over time, but the critical need, both now and in the future is to scale our ability to support even more funding for more ideas and to ensure that the opportunities become available to greater diversity of individuals.
In 2022, SAEMF made the largest single-year investment in research and education grant funding in its history. What made this possible?
2022 was a phenomenal year for the foundation but I believe it was made possible through deliberate strategic planning around philanthropy, focused partnerships, a record of outstanding stewardship as well as careful and sustained success in the investments of the corpus. People also stepped up. Most of the donors to the SAEMF come from SAEM past and present membership. To continue these successes, we have to accelerate a culture of giving. Keeping this momentum will get us even closer to a critical mass of sustainable funding.
You've been a long-time donor to SAEMF’s Annual Alliance, which is a big reason SAEMF has grown to one of the foremost sources of EM grant funding. Why do you feel it’s so important to support SAEMF year after year?
You only need look at countless examples of how the funding opportunities from the SAEMF has helped to initiate and support successful careers of many. If we are serious about opening the doors of academic medicine to an even more diverse group of people who have a serious focus in emergency care, then we must expand and create even more sustainable opportunities to launch careers. Continuous support is fundamental. It would be great to have someone, or some entity, step forward and triple our endowment, and while that could happen, it will take work and cultivation over time.
Under your leadership, SAEMF has been expanding its partnerships with other organizations concerned about EM research and education. Why and how are these partnerships key to our future successes in EM research and education? What can SAEM members do to help in this area?


I think we all understand that when there is common cause, collaboration is always the superior strategy. The key is finding common cause and ensuring that they align with our interests. I have always felt that seeking out others who care deeply about the same things we care about, would be fundamentally beneficial to pursue. Emergency medicine does not have to do it alone; we never really have. In the past, we were more resistant collaborations, especially with industry, because of conflicts and influences we wished to avoid and loss of control and influence. Learning to navigate these partnerships as a mature entity will be critical to SAEMF’s future growth. Adopting and maturing our philosophy around partnership and collaboration will be key in developing greater opportunities to fund our missions.
Stigma is a leading barrier to mental health care for emergency physicians. Many fear that treatment for mental illness could jeopardize their careers or their licenses to practice. What would you say are the key challenges to addressing this stigma?
Mental health care for emergency physicians is a critical issue that has been exacerbated by the COVID-19 pandemic and tragically underlined by disproportionate rates of burnout and death by suicide in emergency medicine. Broadly and fundamentally, the key challenges to addressing the stigma lie within our education, regulatory, and health systems — all of which are far from optimally designed to allow learners, providers, and physicians to focus on key aspects of caring for the mental and emotional aspects of the human condition and the promotion of well-being.
What do you think the EM specialty and/or SAEM can do to address stress and improve physician well-being?
Influence, advocacy, and education are key starting points. Emergency medicine can contribute through teaching and mentorship and innovation, to challenges that reside at the individual level, starting early in medical education with the reinforcement of adaptive coping skills and the extinguishing of stigma in accessing mental health services. Organizationally, emergency medicine can advocate and influence the redesign and optimization of health care clinical systems that will allow for improved working conditions, reducing unnecessary burdens in care environments while promoting greater clinician well-being.
What can be done to create a sense of safety for EM physicians and medical trainees that would encourage them to ask for help or self-report when they’re struggling with their mental health?
Creating an environment that allows both mentor and mentees to freely express vulnerabilities. Focus on mental health as a preventative strategy rather than an intervention.
What's the one thing few people know about you?
I have perfect pitch as an amateur musician
What is your guiltiest pleasure (book, movie, music, show, food, etc.)?
A good science fiction novel if I could find the time
Who would play you in the movie of your life and what would that movie be called?

Title: Unlikely Path and Sydney Poitier
Name three people, living or deceased, whom you would invite to your dream dinner party?
1. Dr. Martin Luther King Jr.
2. Art Tatum, an American jazz pianist who is widely regarded as one of the greatest in his field
3. Moses Tyndall, my paternal grandfather who died in 1937
One quote I live by is:
“without faith, nothing is possible”
Bolstering Funding for Geriatric Emergency Medicine Research through the New SAEMF Geriatric Emergency Medicine Research Catalyst Grant
Please consider helping to make this new funding mechanism available for future years!
Michelle Blanda, MD
SAEMF is pleased to announce that Michelle Blanda, MD, has made possible a new SAEMF research grant to recognize the incredible work of those who have been involved in building the Academy for Geriatric Emergency Medicine (AGEM) and to encourage more geriatric emergency medicine (GEM) research and discovery. This grant, which will be offered for the first time with the 2023 grants cycle, will:
• Fund the work of one early career investigator with a project focused on GEM
• Address research questions leading to improved emergency care and quality of life of older patients
• Allow for preliminary data collection, analysis, or collection of pilot data that will further support greater research endeavors
• Complement the GEMSSTAR matching funds program by providing seed funding for applicants who desire to eventually apply to the NIA’s program
See saemfoundation.org for details, then apply beginning May 1, 2023.
Dr. Blanda, a longtime SAEM member and an SAEMF Board of Trustees member, has supported the early growth of SAEMF in her role as the Chair of the Annual Gifts Committee. As SAEMF announced its new Naming Opportunities initiative to build a reliable source of funding for emergency medicine grants, Dr. Blanda was the first donor to step forward and show interest. Her generous gift is making possible the first two years of this GEM-focus funding opportunity.
A Named Grant commitment of $10,000 will ensure that one future year of the grant is fully-funded. If you are interested in supporting, but are not yet ready to fund at the Named Grant level, we invite you to support the effort to make even more future grants possible by providing an Annual Alliance gift or multi-year pledge of any amount to help fund future years of this grant*. SAEM members often find satisfaction in uniting behind causes like this one. SAEMF would be pleased to recognize group commitments totalling $10,000 to fund additional years of this grant. Please contact us for more information. Or, to donate, visit www.saem.org/donate and note that your gift is to support GEM research.
*If there are not sufficient funds raised to support additional years of the GEM Grant, SAEMF’s Board of Trustees will apply funds to the area of greatest need with a GEM focus, for example the GEMSSTAR grant, on an annual basis.
The National Institute on Aging (NIA) offers a grant called the Grants for Early Medical/Surgical Specialists’ Transition to Aging Research (GEMSSTAR) Program. The GEMSSTAR program uses an NIA-funded small research project (R03) mechanism. As part of the R03 application, investigators may include a Professional Development Plan (PDP) to run concomitantly with the R03 award which is to be supported through non-R03 funds.
In order to support emergency medicine GEMSSTAR applicants in their PDP, matching grant funding of $25,000 is provided by SAEM Foundation (SAEMF) and Emergency Medicine Foundation (EMF), who jointly created a special GEMSSTAR for Emergency Medicine Supplemental Funding Program.
Donate to help make more funding for geriatric emergency medicine research and education projects.
• A maximum of $25,000 will be provided over two years if selected to receive this award.
• The program has a separate application process from the NIA R03. See the grant announcement for more information and to apply. For questions about the NIA R03, view the GEMSSTAR FAQs.
• Applicants for the GEMSSTAR for Emergency Medicine Supplemental Funding Program must have applied to the NIA GEMSSTAR program prior to applying for SAEMF’s/EMF’s supplemental award.
• Only NIA GEMSSTAR funding recipients are eligible to receive the GEMSSTAR for Emergency Medicine Supplemental Funding Program.
• Applications due by 5 pm, CT on February 15, 2023.
Apply by January 20, 2023 for the EMF/SAEMF Medical Student Research Grant
The Emergency Medicine Foundation (EMF) and Society for Academic Emergency Medicine Foundation (SAEMF) partner each year to award stipends to encourage medical students (our future emergency medicine researchers and educators) to engage in and to be exposed to emergency medicine research. We applaud the 2022 grantees and wish them all the best as they move forward with their research training. See the grant announcement for more information about how to apply for these important grants.
• A maximum of $5,000.
• Up to four awards.
• Application may be made by either a specific medical student or by an Emergency Medicine residency program wishing to sponsor a medical student research project.
• Applications due by 5 pm, CT on January 20, 2023.


The Warren Alpert Medical School of Brown University for “Feasibility and Barriers to Implementation of an Emergency Department Community Health
Worker-Peer Recovery Specialist Program for Patients with Substance Use Disorders”

Sara Lin
Vanderbilt University
School of Medicine for “Examining Insurance Status and Presentation to Percutaneous Coronary Intervention
Capable Facility for Patients with STElevation Myocardial Infarction”
Grant McDaniel, MS
University of Toledo for “Using Simulation to Assess Bag Valve Mask Performance in Stressed Emergency Medicine Residents and Physicians”
SAEMF recognizes the valuable role of emergency medicine medical student interest groups (EMIGs), and awards $500 grants to support the educational activities of these groups. EMIG grant goals are:

• To promote the growth of emergency medicine education at the medical student level
• To identify new educational methodologies advancing undergraduate education in emergency medicine, and
• To support the educational endeavors of an EMIG. Given these broad goals, there are few limitations on the nature of eligible proposals. Proposals should focus on educational activities or projects related to undergraduate education in emergency medicine. See the grant announcement for more information and to apply.
• The award is provided for one year.
• Awardees may apply for subsequent year/s of funding on a competitive basis.
• Grant monies may be used for supplies, consultation, and seed money. Faculty salary support is excluded
• Applications due by 5 pm, CT on January 31, 2023.

Alexa Curt and Raylin Xu
Harvard Medical School for "Pediatric Emergency Bootcamp: Targeted Procedural and Simulation Skills for the Developing Physician"
Jasmanpreet Kaur and Amanda Schoonover


Michigan State University College of Human Medicine for “'Stop The Bleed' Events: A Missed Opportunity for the Inclusion of Firearm Safety and Education in U.S. Medical Schools"
Carter Griest

The Perelman School of Medicine at the University of Pennsylvania for "Advanced Cardiac Life Support (ACLS) and Related Clinical Skills Session for Preclinical Students"
Kristina Gueco and Shaylyn Fahey

Virginia Tech Carilion School of Medicine Pilot for "CPR/AED Education and Outreach Project for Local Nepalese Community"
Harry Fillmore and Thomas Heisler
Columbia University Vagelos College of Physicians and Surgeons for "First Responder Competition"
Julia Horiates
East Carolina University, I-TEAM Day: Interprofessional Triage for "Emergency Assessment, and Management Day"
How has your engagement with SAEM and the SAEMF impacted your professional or personal life?
SAEM has helped me to find my "niche" in academic emergency medicine and to hone my skills as a leader.

What compelled you to support the SAEMF? Why do you feel now is the right time to support more grants?
As EM physicians, we are the frontline of so many aspects of medicine including research and education. Now is the time as we continue to strive for improved acute care and equity in EM.
What impact do you hope your donation will have?
I hope my donation will improve equity and inclusion not only for EM physicians but for our patients as well.
Is there an important moment, person or special occasion that influenced your decision?
Reading the stories of those who have been awarded grants and the amazing work that they are doing influenced me to donate.
Do you have any sentiments to share with others who may be considering a gift? There is no donation too small. Let's continue to make EM research a priority.
What did you aspire to be when you were a child?
A teacher or 911 dispatcher
Who is your favorite musician? Queen
What is your hobby? Triathlon
to Dr. Lall and all of our Annual Alliance donors. You can join her and the rest of the Annual Alliance, a community of academic emergency medicine leaders, as they connect, network, and influence the future of emergency medicine. It's easy: donate online today or download the pledge form and your gift will help fund future researchers, educators, and leaders. Thank you!
Join the Annual Alliance, a community of academic emergency medicine leaders as they connect, network, and influence the future of emergency medicine. It's easy: donate online today or download the pledge form and your gift will help fund future researchers, educators, and leaders through:
1. Essential, relevant funding sources through our flagship grant portfolio



2. New funding opportunities like those featured in this issue of SAEM Pulse
3. Mentorship and professional development opportunities like the Resident Reviewers Program A gift of any amount will help make these initiatives, and more, possible this year. When you donate, SAEMF will honor you as part of the Annual Alliance. With SAEM23 right around the corner, consider these donor recognition thank yous that our donors enjoy*:

• A sedan escorts you from the airport to your hotel


• VIP Lounge access…a.k.a. the source for bottomless coffee cups
• Connecting with colleagues at the Coffee & Networking breakfast
*See the Annual Alliance Recognition chart for details of recognition by level
We are grateful for the support of our Annual Alliance donors. Thank you if you have joined or renewed support — if not, please do so today.
“SAEMF is driving innovation through the creation of critical opportunities for future researchers, educators, and leaders to pursue ideas that we believe can fundamentally translate to EM practice and impact. The SAEMF has grown significantly over time, but the critical need, both now and in the future, is to scale our ability to support even more funding for more ideas and to ensure that the opportunities become available to greater diversity of individuals.”
- Joseph Adrian Tyndall, MD, MPH SAEMF President, 2022-23Your gift now will count towards participation in the Chairs’ Challenge, the new Vice Chairs' Challenge, and the Academy, Committee, Interest Group Challenge that take place later this year. Give once and you are done!
Join now to take advantage of 2023 benefits. It's easy: donate online today or download the pledge form and your gift will help fund future researchers, educators, and leaders.
Stigma is defined as a mark of disgrace associated with a particular attribute or condition. Stigmas are insidious and pervasive in society — they are negative determinants of health affecting many patients who seek care in our emergency departments. Public stigmas are social stereotypes based on a defining characteristic that often result in discrimination. They significantly impact how patients feel about themselves and their health. Self-stigma is the internalization of public stigmas, resulting in emotional responses such as shame, guilt, or denial of a health condition. Self-stigma makes it difficult for patients to fulfill social expectations
in their lives, decreases self-esteem, lowers self-worth, and can promote behaviors that are detrimental to health. These consequences lead to a lack of public empathy and understanding of those stigmatized.
Self-stigma is most commonly experienced by patients suffering from mental illness, and numerous studies have demonstrated the prevalence of self-stigma in this population. Patients with mental health conditions remain

“Self-stigma makes it difficult for patients to fulfill social expectations in their lives, decreases self-esteem, lowers self-worth, and can promote behaviors that are detrimental to health.”
heavily stigmatized in society, and they are susceptible to self-stigma that can result in extreme behavioral and emotional responses. In a meta-analysis, Livingston and Boyd determined that 36% of patients with serious mental illness experienced self-stigma that can significantly threaten their well-being. For instance, self-stigma negatively impacts health maintenance behaviors such as seeking routine medical care or being medication compliant. These behaviors increase symptom burden, worsen conditions, and exacerbate the selfstigma that patients experience.
The association between public stigma, self-stigma, and negative health consequences is evident. We propose a conceptual framework that demonstrates a cyclical nature of stigma: self-stigma causes negative health consequences, these consequences exacerbate
societal lack of understanding of some patients, lack of understanding promotes stereotypes and public stigmas, and belief in societal stereotypes augments self-stigma. (Figure 1) Though other “cycles” of stigma have been described in the literature, we believe our cause-andeffect model to be unique. We will briefly address each element in our conceptual framework and then summarize several practical interventions for emergency providers to use to disrupt this cycle of stigma.

The effects of self-stigma represent significant risks to patient welfare. Selfstigma is the negativity and internalized shame that patients have about their health condition; it largely results from public stigma and manifests differently in patients based on circumstances and settings. Self-stigma is common and
measurable. The Internalized Stigma
Mental Illness Inventory-29 assesses markers of self-stigma across several domains including isolation, stereotype endorsement, discrimination experience, stigma resistance, and social withdrawal. This tool is useful for providers when discussing stigma and screening patients for referral to outpatient providers. Though self-stigma is often associated with mental health issues, it can present with many other social and health conditions. For instance, two groups who commonly experience self-stigma include those who are food insecure and patients with substance use disorders; for these individuals, self-stigma can lead to low utilization of food stamps or failure to seek addiction treatment.
continued on Page 19
“Self-stigma is the negativity and internalized shame that patients have about their health condition; it largely results from public stigma and manifests differently in patients based on circumstances and settings.”Figure 1

continued from Page 17
Self-stigma clearly causes negative health consequences. Patients with selfstigma may feel embarrassed about their conditions, leading to harmful actions (or inactions) that might worsen their health. For example, after examining data from over 300 patients who suffer from a variety of mental disorders including schizophrenia, depression, and anxiety, researchers found a significant negative correlation between self-stigma and the continuation of mental health services; specifically, individuals with higher levels of self-stigma were more likely to stop taking their medications. Further, this study found a positive correlation between self-stigma and medication compliance. Therefore, patients who experience a regression in their condition or struggle with chronic treatment regimens should be screened for selfstigma as a potential etiology.
Mental illness is heavily stigmatized in society, and a lack of understanding regarding mental health conditions can manifest in a variety of hurtful stereotypes that perpetuate public stigma. Society stigmatizes patients who purposely neglect their health or appear to irresponsibly exacerbate their conditions. Unfortunately, the negative health consequences caused by selfstigma may be misattributed to poor self-control or inadequate self-sufficiency. This lack of understanding leads to a lack of empathy, indifference, and stereotyping. Furthermore, disorders such as depression, schizophrenia, and bipolar disorder can result in a variety of circumstances that society further stigmatizes, such as the inability to maintain a job or engage in fulfilling relationships.
Taken together, there is an apparent cycle of stigma that is dangerous,
particularly for patients with mental illness. Public stigma towards mental illness leads to internalized stigma for those affected. This self-stigma leads to negative health repercussions such as failure to take medications. The behavior of patients who are not being adequately treated perpetuates a further lack of understanding in society. Society then responds by taking actions that exacerbate the problem, such as stereotyping and providing inadequate treatment for mental illness. Discrimination, lack of community support, and public stigma become easily internalized by those with mental illness who have low self-esteem, resulting in damaging self-stigma. It is a vicious cycle that rapidly repeats.
Stigma is a complex problem without a quick solution. That said, emergency providers can initiate interventions and help patients access appropriate outpatient care. Simply creating space and taking the time to understand why a patient experienced adverse health consequences can have an impact. The initial steps are to listen to patients, discern the trajectories of their conditions, explore if they are experiencing selfstigma and its effects, and assess their insights about the role of self-stigma in their lives. The goal of any treatment regimen is to change the stigmatizing beliefs of the patient and develop coping skills for those affected by self-stigma. This includes caregivers as well as patients. Resources exist to combat this problem for both groups, and treatment plans take time and persistence to execute effectively.
Referrals to outpatient providers are generally warranted. Therapists can help improve communication between patients and family members by teaching listening skills and thoughtful responses to alleviate anxiety. Self-stigma debunking and other treatment goals can be achieved
through cognitive behavioral therapy, selfaffirmations, and peer support groups. Since a reduction in self-esteem is one of the main consequences of self-stigma, interventions that specifically address self-esteem maintenance or renewal are key. For example, emergency providers can encourage patients to download apps such as I Am that provide free, daily positive affirmations to users. The National Alliance on Mental Health has resources for programming and stigma-reduction activities that can benefit patients who are struggling. Structured, intensive outpatient programs are available as well. For example, the Ontario Central Local Health Integration Network developed a two-week, inperson program called Understanding Stigma to increase patient awareness of self-stigma and teach coping skills. Ending Self-Stigma is another groupbased treatment approach that meets longitudinally and focuses on coping mechanisms through cognitive therapy.
There is a cyclical relationship between self-stigma, its adverse health consequences, a resultant lack of understanding by society, and harmful stereotyping that promotes stigma. Emergency providers should identify patients with self-stigma and refer them to appropriate outpatient resources. Treatment options are aimed at reducing self-stigma and its effects. Interventions such as those described can interrupt the cycle of stigma, creating a positive feedback loop where individuals increase their self-esteem, treat their conditions, achieve positive goals, and slowly eliminate the effects of self-stigma.
Radhika Shah is an undergraduate student at Stanford University.

Michael A. Gisondi, MD is an associate professor and vice chair of education in the department of emergency medicine at Stanford University. He is the principal of The Precision Education and Assessment Research Lab (The PEARL) at Stanford.

“Since a reduction in self-esteem is one of the main consequences of self-stigma, interventions that specifically address selfesteem maintenance or renewal are key.”
BEHAVIORAL & PSYCHOLOGICAL EM

A flipped classroom is a teaching technique that involves using pre-class assignments to introduce content followed by using classroom time to engage with learners and explore topics in more depth. This reverses the standard model of classroom instruction in which topics are introduced in class followed by at-home assignments to reinforce concepts (Figure 1). Preclass assignments may consist of a variety of activities including but not limited to videos, reading assignments, or interactive modules. The flipped classroom has been increasingly used and studied as an alternative to traditional lecture methods.

The principal advantage of the flipped classroom model is that more time is spent exploring material using an
active rather than a passive learning strategy. Students can review preclass content as many times as they need before class and then practice applying principles and deepening their understanding while in class under the guidance of an instructor. Studies of
this teaching technique show increased student participation and increased instructor engagement. Additionally, this technique can lead to higher student satisfaction and favorable instructor evaluation of the learning experience. Kraut et al. (2019) suggest that a flipped
classroom can be particularly effective in enhancing procedural learning, discussion of critical thinking, and higher order medical decision making.
Disadvantages of the flipped classroom lie in the increased time requirement for both instructors and students. There is additional work for instructors to create or curate pre-class materials as well as to prepare for moderation of in-class activities. Students need to allot time to complete pre-class assignments in order to participate effectively in class. Also, learners may have different levels of understanding of the material that can lead to imbalanced participation during in-class discussions. Lastly, there is no clear consensus that the flipped classroom improves student learning, rather, studies have concluded that it is not inferior to traditional lecture methods when evaluating student retention of knowledge.
Define session-specific learning objectives. The learning objectives will drive the rest of the session components and discussion. While the main goal for the class may be broad, such as understanding a common chief complaint or a procedure, these objectives should be designed to answer specific questions or clarify specific points. Objectives should also be attainable within the available pre-class and in-class time. Create pre-class components. These can be sourced from existing FOAMed resources, published flipped classroom activities, or created from the ground up using instructor curated resources such as articles, book chapters, videos, blog posts, etc. Keep in mind the amount of time required to complete pre-class activities, and ideally time them to be less than 25 minutes for maximal student participation. Make sure to send out materials with ample time for completion before the session.
Create in-class components.
Decide how to structure the in-class
Figure 2. An example of a flipped classroom design. Pre-class assignments curated by the instructor may include articles, videos, or other resources that students may work through at their own pace. In-class components can be designed to be simulations, small group discussions, or other facilitator-guided methods. Post-class assessments may be used to further reinforce concepts or evaluate overall efficacy.

activities in a way that promotes interaction and discussion. Examples include oral board examination style cases, simulations, problem-based learning or team-based learning, and small group discussions to name a few. Consider the number of instructors or facilitators needed for the session. The bulk of learning through the flipped classroom comes from the application of pre-class content, so there should also be adequate time allotted for generating questions and exploring solutions to problems.
Use assessment tools.
Consider using assessments to gauge understanding of topics covered during the session. For example, this could consist of pre- and post-tests to evaluate students’ knowledge growth. Alternatively, students could be surveyed on how effective the session was in achieving the learning objectives.
Conclusion
The flipped classroom is an alternative to traditional lecture-based instruction that allows students to apply knowledge and explore concepts in the classroom after completing pre-class assignments. Sessions are designed to facilitate interaction and discussion rather than passive learning and may be particularly effective in teaching procedures and
developing clinical reasoning skills. While adequate preparation time is a must for both instructors and students, the flipped classroom can be an engaging method to use with learners to diversify and enhance their learning
Dr. Anand is a first-year medical education fellow and clinical instructor in the Virginia Commonwealth University Department of Emergency Medicine.

Dr. Schneider is a second-year medical education fellow and clinical instructor in the Virginia Commonwealth University Department of Emergency Medicine.
Dr. Lewis is an associate professor at the Virginia Commonwealth University School of Medicine where he serves as the emergency medicine clerkship director and assistant residency program director.


Clerkship Directors in Emergency Medicine (CDEM) represents the interests of undergraduate medical educators in emergency medicine. It serves as a unified voice for EM clerkship directors and medical student educators and provides a forum for them to communicate, share ideas, and generate solutions to common problems. For more information, visit the CDEM webpage
Membership in SAEM's academies and interest groups is free. To participate in one more groups: 1.) log into SAEM.org; 2.) click “My Participation” in the upper navigation bar; and 3) click “Update (+/-) Academies or Interest Groups.”
Increasing diversity and inclusion within medicine is an ongoing challenge that leading professional organizations have wrestled with for more than forty years. Recently, the Association of American Medical Colleges (AAMC), Society for Academic Emergency Medicine (SAEM), American College of Emergency Physicians (ACEP), and others have taken action to underscore efforts that promote diversity. However, the challenges Black people experience in navigating everyday interactions in health care and forging successful, longlasting careers are often overlooked. One such challenge is overcoming imposter syndrome, a term coined by psychologists Dr. Pauline Clance and Dr. Suzanne Imes, which describes a psychological occurrence in which individuals doubt their skills, talents, or accomplishments and has a persistent
internalized fear of being exposed as a fraud, despite external evidence of their competence. While imposter syndrome was first conceptualized as occurring in high-achieving women, what is often overlooked is how imposter syndrome is also rooted in racism and other hierarchical systems. As this phenomenon becomes more widely recognized, the focus has been on how individuals can develop skills to overcome it.
In the field of medicine, imposter syndrome is nothing new. A 2022 Stanford study found that U.S. physicians were at a 30% increased risk of reporting imposter syndrome compared to all other U.S. nonphysicians and at an 80% increased risk relative to people with a doctoral or professional degree in another field.
Symptoms like emotional exhaustion and questioning one’s accomplishments were more common among women, young and unmarried physicians, as well as those who practice in an academic medical facility or within the Veterans Health Administration. Additionally, Black people are often more vulnerable to this feeling. Black physicians in medicine are unfortunately set up to feel imposter syndrome within the cultural context, environment, and institutional shortcomings of the medical system.
When discussing imposter syndrome, the onus is often placed on the individual feeling like an imposter. In her 1978 paper, Dr. Clance describes the characteristics of individuals who experience “impostorism” — this includes traits such as feeling the need to be special, fear of failure,

denial of ability, and fear and guilt about success. In that same paper, which highlights individual behaviors and personality traits, individual and group psychotherapy is highly recommended to work through imposter syndrome. The value of talking about imposter syndrome amongst recognized peers should not be understated; however, progress can be halted if one is still immersed in an environment entrenched in bias. The individualization of imposter syndrome can inadvertently dismiss the systemic bias and cultural contexts that are essential to how it presents in Black scholars.
While the culture of medical institutions varies drastically, they greatly influence
perceptions of imposter syndrome. Such perceptions present early in medical training with identity cues that signal who belongs and who does not. For example, individuals from marginalized groups only see images of white male figures heralded as intellects in the halls of their academic institutions. Many Black people can attest to being mistaken for ancillary hospital staff rather than recognized as a physician. Similarly, women physicians are often referred to as nurses due to individual inherent gender biases. For Black women, these intersectional identities compound their experiences of discrimination in the health care setting. Other ways institutions can influence perceptions of imposter syndrome

include incivility rates, which are “low intensity” behaviors demonstrated by being mildly but consistently rude, discourteous, or impolite. These include being talked over, called the wrong name repeatedly, translated for, having ideas discounted, etc. When microaggressions like these occur, they should be treated as an opportunity to be addressed and corrected rather than ignored under the guise of antiquity, also known as “that’s just the way it has always been.” When people repeatedly deal with these transgressions, it’s no wonder that the feeling of being an imposter starts to creep up.
continued on Page 24
“While imposter syndrome was first conceptualized as occurring in highachieving women, what is often overlooked is how imposter syndrome is also rooted in racism and other hierarchical systems.”
continued from Page 23
Bias in perceived intelligence and merit is another factor that can lead to Black people feeling fearful of their success — another symptom of imposter syndrome. The field of medicine is one that naturally attracts lifelong learners and is known to have rigorously high standards requiring a high level of conventional intelligence. Many assume that those who can navigate multiple standardized tests, complex academic training, and various clinical roadblocks are brilliant. Yet, the assumption of lower intelligence and lack of merit is often ascribed to Black physicians. Words like affirmative action and diversity quotas are thrown around to justify the questioning of their credentials. Rarely do racial majorities in medicine or men find themselves being questioned, but rather their voices are heralded and affirmed. Black physicians can find themselves feeling less heard and seen and can themselves start to deny or question their own abilities.
The harm caused by biased narratives and lack of representation aside, imposter syndrome is given a chance to grow when there are no opportunities to thrive in the environment. It is known that advancing within the medical field is met with more barriers for Black people, whether in the form of a lack of mentorship, sponsorship, or guidance. It can feel like a losing battle to be held to higher standards in order to be considered for advancement while simultaneously facing doubts and questions about merit. When Black scholars are promoted, they can find that these feelings grow stronger due to isolation and lack of representation. Following the summer of 2020, many Black scholars found themselves being promoted to higher positions to re-energize diversification. For many, these changes served to be Band-Aid solutions as they still found themselves the subject of discrimination, being
silenced when speaking out, and being figureheads for committees without real authority or protected time and money to do the job effectively.

It is time to stop misdiagnosing imposter syndrome. As described by social psychologist Jennifer Jordan, instead of presenting it imposter syndrome as a problem that arises within individuals, the focus must shift to the environment, context, and interactions that lead people to question their own worth. Institutions should first acknowledge imposter syndrome as a systemic issue, then begin dismantling it by deemphasizing the perceived inadequacies of the individual and simultaneously addressing systemic factors which create unfavorable environments for Black physicians. This can be accomplished by creating environments that decrease selfdoubt and reaffirm contributions from those traditionally prone to feeling like imposters. Pairing Black trainees and physicians with mentors who can help early career professionals navigate career challenges can help achieve this aim. From its inception, the profession of medicine was intended to exclude women and Black people. Institutions must be deliberate in undergoing acts that truly achieve inclusion. Organizations must redefine traditional notions of successful leadership models to avoid sexism, ableism, heterosexism, and other forms of discrimination. Creating an organizational culture that values the representation of Black physicians and intentionally seeks to place them in leadership roles with the requisite support and authority is imperative. It is also critical to reframe workplace values that are often rooted in racism, such as professionalism, to emphasize the unique and valuable characteristics of Black women physicians. Dismantling this heavily ingrained culture will take deliberate, intentional actions to avoid the continued misdiagnosing of imposter syndrome.
Dr. Adeleye is a PGY-2 resident at the Baylor College of Medicine Emergency Medicine Residency. @md_mide

Dr. Wilson is a PGY-2 resident at Baylor College of Medicine Emergency Medicine Residency. @AskABlackDoc
Dr. Bradby is the program director at East Carolina University Emergency Medicine Residency and president-elect of SAEM’s Academy for Diversity and Inclusion in Emergency Medicine (ADIEM). @NotSoLilMD

The Academy for Diversity & Inclusion in Emergency Medicine (ADIEM) works towards the goal of diversifying the physician workforce at all levels, eliminating disparities in health care and outcomes, and insuring that all emergency physicians are delivering culturally competent care. Membership in SAEM's academies and interest groups is free. To participate in one more groups: 1.) log into SAEM.org; 2.) click “My Participation” in the upper navigation bar; and 3) click “Update (+/-) Academies or Interest Groups.”

Drug overdose fatalities involving opioids continued to rise in 2021 with 71,238 deaths in the United States. The emergency department (ED) serves as a critical safety-net and window of opportunity for this population and must be integrated into multidisciplinary research aimed at finding solutions for those living with opioid use disorder (OUD). Furthermore, certain populations face higher burdens of OUD risk, such as American Indian, Alaskan Native, and non-Hispanic Black individuals. However, one potential high-risk population that intersects all groups is the lesbian, gay, bisexual, trans, queer+ (LGBTQ+) community.
There remains a substantial literature gap in examining the burden of overdose faced by the LGBTQ+ community. There needs to be more quantitative and qualitative research exploring behaviors, patterns, outcomes, and interventions targeted at LGBTQ+ folks living with OUD. In 2019, just before the global COVID-19 outbreak, Canadian researchers issued a call for action on overdose among LGBTQ+ people in North America. Interdisciplinary solutions are needed to provide support, alleviate

continued on Page 27

“While most OUD prevention research currently focuses on integrating behavioral and primary health care, a third specialty should be considered more thoroughly: emergency medicine.”

DIVERSITY
continued from Page 25
suffering, and to address the root causes of addiction within the LGBTQ+ community.
While most OUD prevention research currently focuses on integrating behavioral and primary health care, a third specialty should be considered more thoroughly: emergency medicine. Especially because the volume of patients in need of emergency care for OUD consistently overwhelms the ED. Perhaps upstream solutions targeting psychosocial stressors, housing instability, access to preventative health services, and systemic mistreatment of marginalized communities can reduce this burden; however, targeting “downstream” bottlenecks in emergency care could improve opportunities for sustainable progress, enhance access to resources, and optimize care.
It is important to note that LGBTQ+ people of color (POC) are further subject to additional social stressors stemming from experiences of racism, heterosexism, and/or cissexism. Starting from a young age, LGBTQ+ people live everyday with discrimination,

marginalization, and victimization based on their sexual and gender minority status. The Fenway Institute in Boston recently reported on the higher prevalence of substance use disorders amongst LGBTQ+ persons. The higher prevalence of OUD, among LGBTQ+ people should be considered within a model of minority stress. Given minority stress theory’s emphasis on the detrimental impact of cumulative stress on well-being, researchers have posited that these multiple experiences of social stressors may leave LGBTQ+ POC especially vulnerable to adverse health outcomes, such as OUD and overdose.
Leveraging the ED could help alleviate burdens of OUD for LGBTQ+ populations. To make way for solutions to drive improved outcomes, we must bolster the body of evidence-based research that examines interdisciplinary interventions at the intersection of OUD in the LGBTQ+ community in the ED. Optimizing emergency care will not only improve outcomes for those most burdened by OUD, but will also help to alleviate the tension placed on our most vulnerable health care resource, the ED. This vision will require additional resources and funding to examine the specific characteristics and health care
utilization patterns of the LGBTQ+ community who engage in opioid use and remain at risk for overdose. Unless this data is gathered, published, and disseminated, this population will continue to face elevated adverse health outcomes as compared to their cisheterosexual counterparts.
Jonathan Berger is a toxicology research project manager at the Icahn School of Medicine at Mount Sinai in the department of emergency medicine. He received his MPH in healthcare policy and management from Columbia University Mailman School of Public Health.

Dr. Manini is a professor of emergency medicine at the Icahn School of Medicine at Mount Sinai and practices clinically at Elmhurst Hospital Center. Dr. Manini is director of the toxicology research core in the emergency medicine research division and associate program director of the T32 training program focused on emergency care research.

“To make way for solutions to drive improved outcomes, we must bolster the body of evidence-based research that examines interdisciplinary interventions at the intersection of OUD in the LGBTQ+ community in the ED.”
One of the senior faculty in your department elicits input from you and two other residents on a manuscript. He provides each of you with a specific part of the manuscript to work on, with the requirement that you write no more than 300 words each. After the manuscript is completed, your faculty member has written a 5,000-word article. He tells you and your classmates that because you contributed a minimal amount to the article, under ICJME guidance, you will not be listed as authors. He will mention your names in the acknowledgments. You speak with your fellow residents and are upset; you were specifically asked to limit the size of your contribution, which your faculty member now tells you is not significant enough to merit authorship. Your faculty member is already a tenured professor; the three of you were interested in having an article for your CV to help start an academic career. Is what your faculty member did ethical?
Authorship of articles in academic medicine has undergone a slow evolution. Frequently, department chairs or other senior faculty members would be routinely listed as authors on papers, regardless of their degree of involvement. On other papers, multiple faculty members would be listed, to
be able to credit them with authorship, even if their contributions were minimal as well. This gamesmanship with assigning authors to academic papers took on an additional unsavory dimension when it became public that pharmaceutical companies would assign a well-known physician author to
a scientific paper that was ghostwritten by a technical writer to bring more attention to the article.
The International Committee of Medical Journal Editors (ICJME) released guidelines that specifically define the criteria that should be

used to determine authorship, require manuscripts to define each author’s role in the performance of the study or preparation of the manuscript, the appropriate number of authors that should be listed, and acknowledgement of any financial or other conflicts of interest. The role of these guidelines is to make the publication more transparent, by helping to demonstrate that the authors listed did contribute meaningfully to the paper and to make clear any potential conflicts that could cast doubt on the impartiality of the results being reported.
The ICJME authorship criteria do not specify any rigid values that are required for authorship. They do, however, give guidance as to what should be done to qualify as an author:
• Contribute to the intellectual content of the work through concept and study design, data acquisition, and/or data analysis
• Draft, critically review, or revise the manuscript
• Approve the final version of the manuscript for submission
There is no question that the ICJME guidelines do not create any ethical conflict in publication; to the contrary, the guidelines have been widely adopted and are a demonstration of the rigor and selectivity of the journal. By disrupting a longstanding practice through which many physicians over the years may have manipulated to burnish their CVs and achieve academic promotions, the use of the ICJME guidelines has been an ethical boon to publishing.
What the faculty member did to the residents is a different matter altogether. While the resident’s contributions did not meet ICJME guidelines for inclusion as authors, by limiting their contributions, it seems that the faculty member ensured a priori that the residents could not possibly qualify for authorship. In the news industry, there was once a well-known
practice known as “bigfooting” in which a lesser-known journalist would break and write a story and then be forced by the editors to turn the information over to a more famous journalist to present the story, often without crediting the lessfamous journalist who did all the legwork. Attaching a marquee name to the story was done to elicit more readership or viewership. Similarly, academic bigfooting involves listing a senior, well-known figure as a lead author to increase likelihood of publication and citation.
Is this ethical? There are several issues. First, the senior faculty member obviously knew that the limitations he put the residents under in terms of length of their submissions would likely preclude them from meeting authorship criteria. Therefore, he needed to be clear with the residents ahead of time that this would be a project that may get them academic writing practice but would not result in authorship credit. By not explaining this ahead of time, he created misunderstanding and hard feelings. At least some of the residents may have inquired about writing a longer piece
to earn authorship credit. The faculty member should also have included mentoring in this assignment. Lastly, the faculty member should ensure that he attributes in the final work any direct quotes he uses from the resident’s contributions.


Academic authorship has become more rigorous, with fair assignment of authorship becoming a much higher priority than it has been historically. However, there are still potential pitfalls, particularly involving senior faculty members with junior members or residents, and care must be taken to avoid an ethical misstep
Dr. Maloney is an associate professor of medicine, Case Western Reserve University, Cleveland, Ohio and medical director, emergency department, Louis Stokes Cleveland VA Medical Center

“By disrupting a longstanding practice through which many physicians over the years may have manipulated to burnish their CVs and achieve academic promotions, the use of the ICJME guidelines has been an ethical boon to publishing.”
 By Ashley Voroba, MD,
By Ashley Voroba, MD,
on behalf of the SAEM
I gave birth to my daughter at the end of my second year of residency. For the first 13 months of her life, I pumped breastmilk. It was the hardest thing I have ever had to do. I had no clue about breastfeeding or pumping before I did it. The extent of my training was less than one hour of didactic teaching in medical school and about the same amount throughout all of residency, mostly focused on medications and procedures that are contraindicated in breastfeeding. I received no guidance from my obstetrician about breastfeeding, other than that I should do it. In those 13 months, I learned more about breastfeeding, breast pumps, breastmilk storage, milk supply, and medications safety than I ever knew
Faculty Development Committeeexisted. For most of my information I relied heavily on forums and fellow emergency medicine residents and attendings who had experience with breastfeeding. There was a lot of trial and error. Now I find myself an unexpected breastfeeding and pumping
expert and advocate, especially as it relates to residents.
In June 2022, the American Academy of Pediatrics (AAP) updated their recommendations on breastfeeding to align with the World Health Organization (WHO) recommendations which suggest
“Pump breaks are medically necessary to prevent mastitis and decrease in supply. You are providing food for your child. Pump breaks are not optional.”
breastfeeding exclusively from birth to six months, and continued breastfeeding from two years and beyond. In honor of these changes, I’d like to share my top 10 tips for on-shift breast pumping for the busy emergency medicine residents.
1. Don’t let residency dictate your breastfeeding goals
The decision to breastfeed or not, and for how long, is completely up to the person making the milk. There will be challenges. There will be barriers to overcome. There will be bad days. There will be uncomfortable conversations. Don’t let someone else make the decision for your family.
2. Strategize with your team at the beginning of the shift how and when you will take your pump breaks
It’s always a good policy to have a brief chat with your attending and your onshift coresidents about the breaks you will take during the shift. Over time, as your colleagues get used to your pump schedule, this discussion will be less necessary. A good time to pump is during a lull, after seeing a few patients in a row, or after discharging a few patients. At my current shop, we take critical patients in a round-robin fashion, and I typically urge residents to take their breaks after our “hit,” when we are not “up” for another critical patient.
3. Don’t ask, tell
While we are on the topic of discussing your break schedule with the team, remember that this is not an ask. Pump breaks are medically necessary to prevent mastitis and decrease in supply. You are providing food for your child. Pump breaks are not optional.
4. When you can, take pump breaks early
This will give you “money in the bank” for later in the shift when things get hectic and you have to delay a pump break.
5. Multitask if you can
The space where you pump on shift should have a computer and a phone. One way to not feel like you are falling behind on shift is to chart, place orders, review results, call consults, write discharge papers and other EMR-related tasks while pumping. If you need to add
extra pumps to your day, try pumping while driving to and from shift. If you find that you can’t multitask during your pump breaks, that’s okay too. Relax and pump.
6. Consider a portable pump
There are so many pumps on the market that allow you to pump on the go, without being attached to the wall. This could be an option that allows you more time on the floor and less time in the pump room. Remember that not everyone responds well to these pumps, so the default assumption should always be that you will need to take breaks to pump.
7. Eat and hydrate
It sounds basic, but how many times have you gone the whole shift without drinking water or eating a real meal? It’s essential while breastfeeding to keep up your water and calorie intake. Breastfeeding expends a lot of energy and you need to replenish.
8. Find your tribe and enlist help
You are not alone in this task. Join Dr. Milk on Facebook. Seek out attendings and fellow residents who have walked this road. They can be a wealth of information, support, and can help you advocate for yourself when needed. Have your partner wash pump parts and prepare them for the next shift.
9. Don’t quit on your worst day
This is a marathon, not a sprint. And there will be bad days. Give yourself grace. Reassess your goals. Press on.
The Accreditation Council for Graduate Medical Education (ACGME) Common Program Requirements states that “Sites must provide private and clean locations where residents may lactate and store the milk within a refrigerator. These locations should be in close proximity to clinical responsibilities. It would be helpful to have additional support within these locations that may assist the resident with the continued care of patients, such as a computer and a phone. While space is important, the time required for lactation is also critical for the well-being of the resident and the resident's family.”

While breastfeeding on shift while a resident has been one of the hardest challenges of my life, it is something I wanted to do and am grateful I was able to do. If on-shift breastfeeding is something you’d like to do as well, know that it is possible, even in residency, and that your EM colleagues will advocate for you, cheer you up, and cheer you on.
Dr. Ashley Voroba is an emergency medicine physician and the ultrasound director at St. Barnabas Hospital in Bronx, NY
10. Know your rights“It’s essential while breastfeeding to keep up your water and calorie intake. Breastfeeding expends a lot of energy and you need to replenish.”

The “wellness” conundrum poses a challenge to health care; what makes one person well is very different from that which makes the next person feel equally well. Most approaches to wellbeing have been a series of narrowly focused point solutions that lack evidence.
Lifestyle Medicine (LM) has successfully changed the well-being landscape. The American College of Lifestyle Medicine has defined LM as the use of evidence-based lifestyle therapeutic interventions, including a whole-food, plant-predominant eating pattern, regular physical activity, restorative sleep, stress management, avoidance of risky substances, and
positive social connection. Clinicians certified in LM help people intentionally replace unhealthy behaviors with positive ones by identifying those behaviors that a person can easily integrate into their daily life. This approach to lifestyle addresses
underlying causes of disease, not just symptoms — supporting overall wellbeing while preventing, treating, and often reversing chronic disease.
When is it too late to bring LM into one’s life? It is never too late! A skilled
“A skilled LM provider assesses the patient’s current state and meets them there, creating simple, feasible goals to move the patient towards a healthier state.”
LM provider assesses the patient’s current state and meets them there, creating simple, feasible goals to move the patient towards a healthier state. The goal is nonpharmacologic intervention. The simpler and more personalized the goal, the more sustainable it becomes.
Briefly, the six pillars of LM can be interpreted in the context of older patients:
1. Nutrition: Plant-based diets have anti-inflammatory effects, reduce cardiovascular disease, and impact the onset of many common malignancies. For patients suffering from constipation, nutritional adjustments can provide the motility enhancement needed.

2. Exercise: Moderate exercise in one’s routine reduces cardiovascular disease, obesity, diabetes, and improves brain health among other things. For older adults, it allows them to maintain independent living for longer, improve balance, and provides strength to be functional with ADLs (activities of daily living).
3. Sleep: Understanding healthy sleeping habits may prevent insomnia or changes in sleep-wake cycles experienced by many older adults as well as allow them to reduce the deleterious sleep aids often trialed. Poor sleep quantity/quality is linked to the development of Alzheimer’s disease and other forms of dementia.
4. Stress management: The ability to cope and manage stress is a lifelong skill that allows people to return to their “pre-event” status after an acute issue. Maintaining a sense of purpose can be critical for older adults.
5. Avoiding risky substances: Alcohol can be especially dangerous in older adults as their metabolism changes. Older adults are more likely to fall, leading to devastating consequences, and suffer from unrecognized alcohol withdrawal upon losing access to drinks in acute scenarios, compounding lifethreatening situations.
6. Social connectedness: Older adults who stay connected with their community have increased longevity and better brain health. Social constructs facilitate the goals in all the above pillars.
Aging with LM promotes not only longevity but vitality alongside that longevity. We all know age alone means nothing, functional age means everything. Awareness and education are core to the LM mission. We have a unique opportunity to introduce LM during our care in the emergency department (ED). Challenge: The next time you are left with an unrevealing workup, spend a few minutes outlining the positive changes the patient might make in one of these six pillars to prevent a similar trip to the ED. It is possible that you could identify simple, feasible goals to move the patient to a healthier state.
Dr. Harrison is dual board certified in emergency medicine and lifestyle medicine. After years in education as an assistant professor and assistant residency director at Yale School of Medicine, she now directs her passion for teaching toward educating her emergency medicine colleagues and local community about lifestyle medicine.

Dr. Mulcare is fellowship trained in geriatric emergency medicine and clinical assistant professor of emergency medicine at Weill Cornell, New York. She has held several educational leadership roles at NYP/Weill Cornell. She is currently chief medical officer for Summus, the leading virtual specialty care platform.
The Academy of Geriatric Emergency Medicine (AGEM) works to improve the clinical care of older patients, prepare trainees to care for older patients, and advance the geriatric EM research agenda. Joining AGEM is free! Just log into your member profile. Click “My Account” in the upper right navigation bar. Click the “Update (+/-) Academies and Interest Groups” button on the left side. Select the box next to the academy you wish to join. Click “save.”

 By Marcos Campos, MD; Lucas da Matta, MD; and Anjni Joiner, DO, MPH on behalf of the SAEM Global Emergency Medicine Academy
By Marcos Campos, MD; Lucas da Matta, MD; and Anjni Joiner, DO, MPH on behalf of the SAEM Global Emergency Medicine Academy
During my first year as an internal medicine resident working in the emergency department in Brazil, I experienced firsthand the emotional and physical toll that the COVID-19 pandemic brought to health care providers. The combination of fear and doubt in caring for patients with respiratory failure coupled with hospital capacity issues, staffing, and resource shortages, and the all-too-frequent deaths followed by the inevitable difficult family conversations, gave me an appreciation for some of the intricacies and challenges involved with
emergency medicine. I've witnessed other colleagues working in these settings develop anxiety, depression, and substance use disorders while living through the chaos of providing critical care in the Brazilian health system during the pandemic. The Brazilian public health system, the largest in the world, had its breaking points tested over the last few years. With emergency medicine still in its infancy in Brazil, there are few emergency medicine specialties and specialties such as internal medicine has been forced to fill this gap and become part of the front lines of the pandemic.
Sistema Único de Saúde (SUS), or the Unified Health System, is the Brazilian government-run health care system. As the largest public health care system in the world, coverage is available to the entire population of Brazil, over 220 million people. SUS provides multiple services, from community-based primary care, to heart transplants, as well as epidemiological surveillance programs and professional training. The system aims to improve the health of
citizens, particularly those with vulnerable backgrounds, but the sheer size and scale of the health care system leads to inherent challenges, particularly with respect to emergency care provision.
The first emergency medicine residency in Brazil was only created in 1996. It was a full 18 years later that the second one was opened. In fact, emergency medicine was only recognized as a medical specialty in Brazil in 2015. Despite a demonstrated need for dedicated emergency medicine physicians, there are still only 11 emergency medicine training centers in a country of over 200 million, highlighting the slow acceptance of this field amongst the greater medical community.
The slow growth of emergency medicine specialists does not reflect the pace of new doctors in the country. In fact, over the last 50 years, the rate of growth of Brazilian doctors has increased almost four times that of the general Brazilian population. New graduates of medical schools are projected to reach 16 per 100,000 inhabitants in the near future, increasing the overall ratio of physicians above the 3.5 physicians per thousand inhabitants of Organization for Economic Co-operation and Development (OECD) countries.
These newly graduated physicians are often placed unsupervised in emergency settings, including emergency departments, where approximately 25% of all doctors are new graduates. These physicians have typically not completed residency training in any area, as residency training is not required to work in primary care or emergency departments. They are also most often the physicians that staff ambulances in the physician-led national ambulance service (Serviço de Atendimento Móvel de Urgência - SAMU).
Despite this influx of new doctors, due to the low proportion of emergency medicine physicians, residents from different specialties across the country, including my internal medicine, were floated over to cover ICU and COVIDdedicated emergency rooms during the
pandemic. This change has not only impaired residency training for their specific specialties, but the combination of new graduates and nonemergency medicine residents with little to no oversight greatly impacts the quality of care.

Lack of emergency medicine specialists notwithstanding, emergency departments are ubiquitous throughout Brazil, but remain staffed by nonemergency medicine physicians. Spurred by the pandemic, which highlighted the obvious need for increased emergency medicine specialty training, Brazilian doctors have developed a renewed interest in emergency medicine as a specialty. Recently, many students and doctors have personally invested in extracurricular courses focused on emergency care, including training and optimization of care for patients with COVID-19 in emergency settings. Structured emergency training for nonemergency medicine residents and medical students is a viable shortterm solution. However, in the long term, we need to increase the number of quality emergency medicine residencies and continue to encourage new graduates to enter the field. Organized, direct
investments in emergency centers and emergency medicine training programs can help to address the growing gap in emergency care in Brazil.
Dr. Campos is a second-year internal medicine resident at State University of São Paulo, Botucatu City, Brazil. He is also a contributor to the Global Emergency Medicine Innovation & Implementation (GEMINI) Research Center from Duke University, NC.

Dr. da Matta is a first-year emergency medicine resident at Duke University Medical Center, NC. He earned his MD from the Federal University of Minas Gerais, Brazil.

Dr. Joiner is an assistant professor of emergency medicine at Duke University Medical Center in Durham, NC. She has an interest in improving access to emergency care in low-resource settings.
The Global Emergency Medicine Academy (GEMA) focuses on improvement of the worldwide delivery of emergency medical care. Membership in SAEM's academies and interest groups is free. To participate in one more groups: 1.) log into SAEM.org; 2.) click “My Participation” in the upper navigation bar; and 3) click “Update (+/-) Academies or Interest Groups.”

“Organized, direct investments in emergency centers and emergency medicine training programs can help to address the growing gap in emergency care in Brazil.”
 By Jeremy Brown, MD
By Jeremy Brown, MD
There are dozens of different grant types at the National Institutes of Health (NIH) and they make up an alphabetic smorgasbord. There are U01 grants and U10 grants and UG3/UH3 grants, P01 grants and P20 grants, R01 and R21 and R33 and R56 grants, and on and on. But in this month’s column we will learn about another of the alphabetic grant types, known as the K awards. And K awards are special because they are training awards, in which the principal investigator is a mentee as well as a researcher. These K awards are known as Research Career Development Awards.
Not surprisingly, there are many kinds of K awards — at least twenty. But for emergency physicians, the most used is the K23, with about 36 awards to emergency medicine (EM) physicians over the last decade. The K08 is a distant second, with 16 awards over the same period. But it is possible to think of these two K grants as differing
only in one important aspect: for the K23 grants, the focus is on clinical research, while for K08 grants, the focus is on basic research. (Just to keep it confusing, note that Agency for Healthcare Research and Quality (AHRQ), a federal research funding agency that is not part of the NIH, also has a K08 award, but that one has a clinical focus. Got it?)
The NIH K23 supports “the career development of individuals with a clinical doctoral degree, who have the potential to develop into productive, clinical investigators, and who have made a commitment to focus their research endeavors on patient-oriented research.” These individuals may be
residents, but are more likely to be early EM faculty, perhaps a few years after completion of their residency or fellowship.
During the award, the principal investigator (PI) pursues a specific training program, but the makeup of that program will vary. One might obtain a master’s degree in public health or take a few courses in statistics or the ethics of clinical research, while another might work with a named mentor and complete courses for a PhD. The training component and the clinical research you undertake is yours to decide.
In general, the application is judged on two points: Is there a good
“...there is a golden rule when applying to the NIH for any kind of grant: always, always talk to the program officer.”
mentoring plan, and is there a good clinical research plan? Both need to be addressed in the application, and both are equally important to your success. One way of thinking about the application is to use a “gap-based” approach, in which the candidate describes her existing skill set and expertise, and outlines what skills and expertise she still needs to obtain to become an expert in their field. This does not have to involve taking courses
or obtaining a degree; but the needs must be clearly articulated and relevant.
The way the K23 awards are managed varies among the many institutes and centers that make up the NIH, and you should carefully read the notices that each publishes. Just as importantly, you should contact the program officer who runs the training programs at each institute. They will be an invaluable source of important information and can make
all the difference to the chances of success. In fact, there is a golden rule when applying to the NIH for any kind of grant: always, always talk to the program officer. Another tip is to find a K award that was successful and read it. You can find the abstracts on the NIH RePORTER website, and then ask the PI if he or she might share the complete application with you. The time spent tracking down a successful K application is more than offset by the tips you will learn when you read it.
The K23 awards offer significant salary support — typically up to $100,000 (plus fringe benefits) for each of the 3-5 years of the award; you will use that to buy protected time for your research and education. That’s a lot of tax-payer money, but all those taxpayers ask of you is that at the end of your award, you will use your expertise to improve their health. And that seems like a good deal.
You can learn more about the National Institutes of Health here

Dr. Brown is the director of the Office of Emergency Care Research (OECR) where he leads efforts to coordinate emergency care research funding opportunities across NIH. Additionally, Jeremy is the primary contact for the NINDS Exploratory and Efficacy FOAs and serves as NIH's representative in government-wide efforts to improve emergency care throughout the country. He is also the medical officer for the SIREN emergency care research network which is supported by both NINDS and NHLBI. Jeremy.brown@nih.gov

“The NIH K23 supports “the career development of individuals with a clinical doctoral degree, who have the potential to develop into productive, clinical investigators, and who have made a commitment to focus their research endeavors on patient-oriented research.”
The pandemic uprooted and brought changes and new challenges to every aspect of our lives. We were faced with a problem that we were not prepared for and did not completely understand. We went into lock down and isolation, not just in our homes, but also in our hospitals. Patients were being admitted for COVID-19 as well as the normal medical issues we see daily. We were scared for ourselves and our patients, and our patients were scared for themselves and their families. Fast forward two years after the beginning, and while as health care providers we became more used to the daily life of COVID-19, our patients were still left isolated, scared, and alone. We need to do better.
During the early portion of the pandemic, hospitals across the nation did the right thing by isolating patients and limiting visitors into the hospitals
while we tried to get control of the pandemic. There was also the issue of conserving personal protective equipment (PPE) for our health care

“Patients who were critically ill in our emergency departments and our intensive care units were not allowed the human decency to have their loved ones visit with them while they struggled to live, or while some took their last breaths.”
providers while there was an ongoing shortage across the country. However, as it became clearer that COVID-19 was going to become a daily part of our lives, and PPE stores became replenished, we left these isolation protocols and visitation policies in place. At times we had policies in place that allowed no visitors in our hospitals. Patients who were critically ill in our emergency departments and our intensive care units were not allowed the human decency to have their loved ones visit with them while they struggled to live, or while some took their last breaths. We spoke with family members by telephone and explained to them the seriousness of the patient’s illness and were invariably met with the question “Can I come see him?” and we had to tell them “unfortunately at this time we are not allowing visitors.”
All providers have seen the firsthand effects that isolation can have on patients in the hospital and know this as inherently
true, but there is also data to back this up. A 2017 study of 1,506 patients in three Canadian hospitals isolated for respiratory illness were studied compared to non-isolated patients which demonstrated that those on isolation precautions for respiratory illnesses stayed 17% longer (95% CI: 9%, 25%), stayed 9% longer than expected (95% CI: 3%, 15%), and had 23% higher cost of care (95% CI: 14%, 32%). Furthermore, a 2018 meta-analysis of 26 papers showed a marked trend for isolated patients to exhibit higher levels of depression, the pooled standardized mean difference being 1.28 (95% CI 0.47 to 2.09) and anxiety 1.45 (95% CI 0.56 to 2.34). These studies help highlight the importance visitors have on the outcomes of patients who are hospitalized.
We all want what is best for our patients, those around them, and the community. There is undoubtedly a fine balance between isolating patients to

control disease spread and allowing visitors to see their loved ones to improve patient outcomes. I believe we had the right approach early in the global pandemic but should have adjusted our visitor policies once we had a better idea of how the virus is transmitted and how to limit spread. I believe that to best serve our patients, we need to reflect on this so we can be better prepared in the future to adapt our policies when we have another outbreak such as this. Next time, we need to do better.
Dr. Hyde is a Minnesota native and current chief resident at Ascension St. John Hospital Emergency Medicine Program in Detroit, Michigan. His interests include wilderness medicine and the patient care experience.

“There is undoubtedly a fine balance between isolating patients to control disease spread and allowing visitors to see their loved ones to improve patient outcomes.”
On June 24, 2022, the United States Supreme Court overturned Roe v. Wade, resulting in new restriction laws on abortion across the country. This change had significant implications for pregnant patients and the role of clinicians across the country, including emergency clinicians. The Guttermacher Institute estimates 26 states will ultimately have bans on abortion; 11 states currently have made abortions illegal at conception. It is estimated that one in three women ages 15 to 44 live in states where abortion is banned or mostly banned, according to United States (U.S.) census data. The emergency department (ED) has a crucial role in reproductive care — providing postexposure prophylaxis, emergency contraception, and care for new pregnancy or risk of pregnancy
loss. Our newly released article on Academic Emergency Medicine titled Post-Roe emergency medicine: Policy, clinical, training, and individual implications for emergency clinicians details the multifactorial implications of this new era in the ED. In this abbreviated summary, we highlight new educational considerations that emergency medicine (EM) residency programs can incorporate to ensure trainees are prepared for their new role in providing reproductive care.
The emergency department serves as a critical access point for reproductive care, especially for patients that may have barriers to accessing routine care. We see 900,000 ED visits each year for early pregnancy loss, excluding ectopic pregnancy or other pregnancy complications. Prior to
1973, pregnant people in the United States had complications such as hemorrhage, sepsis, pelvic injury, and death from unsafe abortions. We now need to expand our core obstetric EM content to include complications of self-managed or unsafe abortions, high risk pregnancies, and pregnancy related complications previously managed with abortions and delayed prenatal care. We must define what new medical knowledge, procedural expertise and communication skills will be needed to care for these patients. As demonstrated in our paper, these new laws affect multiple Accreditation Council for Graduate Medical Education (ACGME) core competencies: patient care, medical knowledge, interpersonal communication, professionalism, practice-based learning and

improvement and systems-based practice. Additionally, we may need to consider expanding our procedural competencies depending on the practice setting, geographic location, and local needs of the patient population to include management of uterine hemorrhage (e.g. from self-managed abortion), IUD insertion for emergency contraception, medication abortion, and medications for management of miscarriage. It may be important to update department policies to offer surgical options in the ED with our obstetrics and gynecology colleagues.

As we prepare to increasingly manage complications of abortions, we also need to be knowledgeable of current reproductive care guidelines to provide appropriate care and education to patients. It may be beneficial to understand our patients’ unmet needs related to reproductive health and provide education and resources accordingly.
A study by Liles et al. demonstrated that while many ED providers referred patients for contraception, there was
no universal standard for contraceptive counseling and management. In this study, ED providers had incorrect understanding of the efficacy, risks, and eligibility associated with contraceptive methods. Another study by Alexander et al. demonstrated that approximately 55% of women wanted to receive contraception and information about contraception in the ED. As the ED may now serve as a timely and critical point of access for contraception counseling and management, it may be important to incorporate this topic into existing resident education as well as develop institutionally specific protocols for implementation. Similarly, it may be important to consider basic prenatal screening (e.g. sexually transmitted disease, basic labs, and type and screen) in the ED for new diagnosis of pregnancy and ensure referral to obstetric care, especially if there are significant barriers to accessing routine care.
Despite uncertainty and constantly evolving policies impacting access to
reproductive care, the ED will continue to serve as a place for patients to seek care. We can prepare for these changes by recognizing ways that we can advance our medical knowledge and procedural competency to best serve our patients.
Table 1 reprinted with permission from the December 2022 issue of Academic Emergency Medicine Journal
Dr. Rodriguez is a current emergency medicine resident at Harvard’s Affiliated Emergency Medicine Residency program at Massachusetts General Hospital (MGH) and Brigham and Women’s (BWH). She is also on the board of SAEM AWAEM, as the resident member.


Dr. Samuels-Kalow is an associate professor at Harvard Medical School and an attending physician in adult and pediatric emergency medicine at Massachusetts General Hospital (MGH). Her work focuses on developing interventions to reduce disparities in emergency care and designing strategies to use the emergency department visit to address adverse social determinants of health.
Dr. Zeidan is an assistant professor at Emory University School of Medicine and adjunct professor in the Rollins School of Public Health. She is codirector of the Georgia Human Rights Clinic and cofounder of the Society of Asylum Medicine.

The Academy for Women in Academic Emergency Medicine works to promote the recruitment, retention, advancement and leadership of women in academic emergency medicine. Joining AWAEM is free! Just log in to your member profile. Click “My Account” in the upper right navigation bar. Click the “Update (+/-) Academies and Interest Groups” button on the left side. Select the box next to the academy you wish to join. Click “save.”
“We now need to expand our core obstetric EM content to include complications of self-managed or unsafe abortions, high risk pregnancies, and pregnancy related complications previously managed with abortions and delayed prenatal care.”
Seasoned with diesel fumes and CaviCide, my interviewing skills and ability to build quick rapport with my patients were two things I took great pride in when I started medical school. Yet, the transition from emergency medical technician (EMT) to medical student did not come without a great deal of turbulence and discomfort for me. In each of my interactions with standardized patients, something felt…off. I initially chalked this up to nerves, but after some introspection, I discovered that the fluidity and sense of ease of my interview characteristically began to drop off as I started taking the social history, when I became much more awkward. Despite knowing the significant impact of social determinants
of health (SDOH) on health outcomes and the usefulness of that information in the development of a differential diagnosis, I still squirmed as I asked patients about their home life and education status. Why was this so? Why was there such a difference in how I felt interviewing patients now versus out in the field?
In the field of emergency medical services (EMS), asking the patient about their SDOH is largely unnecessary, as we have the privilege of observing these factors at almost every call. We see people’s neighborhoods — those with a Trader Joe’s down the street and those with a Dollar General as the only grocery store nearby. We see the degrees on the walls and the hallways
full of pictures of their support systems. We see the excess stairs leading up to the front entrance and the dusty car, indicating that this person may have trouble with mobility. We see the pile of bills on the kitchen table and cockroaches on the floor. We see, hear, and smell it all. To be invited into patients’ homes, in any state, is an honor, a window into their lives, and is a unique aspect of the profession. What if this could be harnessed to improve the health and lives of the people served by the emergency department (ED)?
Overutilization of EMS and EDs is an ongoing issue, and combined with an ever-increasing number of bureaucratic tasks, physicians must ultimately spend less time with each

patient to meet demands. Considering also that physicians do not work out in the field like EMS, the patient’s SDOH may never be adequately addressed in favor of mitigating the chief complaint in that limited window of time. Still, the ED is the prime link in the chain of health care services patients encounter for connecting them with the appropriate resources they need, whether that be housing, food, or some other social support. It would be beneficial, then, if EMS had the capability to objectively report observations from the scene regarding SDOH and share these observations via the electronic health record (EHR) to ED physicians and social workers.
Thus, a brief, standardized SDOH screener for transporting EMS agencies could provide invaluable information to the hospital staff responsible for identifying resources for patients. When SDOH are identified and confronted, ED utilization decreases and health outcomes are improved. While not all social determinants could be reasonably addressed, nor should it replace the communicating with the patient about their social history, this screener

could allow EMS personnel the ability to note whether there were obvious health hazards (e.g., animal urine/feces everywhere inside), access to electricity, or environmental obstacles to mobility (e.g., hoarding conditions, staircases patients are unable to navigate, etc.), to name a few. First responders witness the spectrum of the human experience every day; utilizing their eyes and ears to improve health and wellness via a screener is a viable option. This is the basis of many community paramedicine programs; however, for jurisdictions without this resource, patients (especially those who utilize emergency services frequently) may never have their SDOH addressed.
The design and implementation of such a screener to improve continuity of care would require several things to be taken into consideration such as ensuring the interoperability between the EMS and hospital EHR systems; structuring items to ensure objectivity of responses, as to not promote prejudice or discrimination; and educating EMS and ED personnel on implicit bias and the impact of SDOH on health and wellbeing. Solutions for these considerations and specifics on screener
design are outside the scope of the article, which is simply serving to propose a possible method by which continuity of care and health outcomes for emergency patients can be improved.
While we may not personally be involved in the creation of societal structures that affect the health of our patients, we still have a duty to address them. One of the ways we can accomplish that is to leverage EMS' ability to literally meet people where they are. If a description of vehicular damage in a trauma patient is important to the receiving ED, would it not also be important to know that the patient in diabetic ketoacidosis does not have the ability to refrigerate their insulin due to lack of electricity?
Mel Ebeling is a secondyear medical student at The University of Alabama at Birmingham Heersink School of Medicine and a practicing emergency medical technician (EMT) in the fire service. mebeling@uab.edu

“To be invited into patients’ homes, in any state, is an honor, a window into their lives, and is a unique aspect of the profession. What if this could be harnessed to improve the health and lives of the people served by the emergency department?”

 By Daniel Jourdan, MD and Jonathan Gong, MD on behalf of the SAEM Faculty Development Committee and SAEM Research Committee
By Daniel Jourdan, MD and Jonathan Gong, MD on behalf of the SAEM Faculty Development Committee and SAEM Research Committee
Lance Becker, MD, is the chair for the department of emergency medicine at North Shore University Hospital and Long Island Jewish Medical Center at Northwell Health. He is a professor at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, and the Institute of Bioelectronic Medicine at the Feinstein Institutes for Medical Research, and the Dorothy and Jack Kupferberg Professor of Emergency Medicine. Dr. Becker is an elected member of the National Academy of Medicine and specializes in translational research on cardiac arrest. He has close to 300 research publications. His cardiac arrest research evaluates methods to advance life-saving therapies for cardiac arrest while protecting against brain death. He has mentored numerous young investigators in research over three decades.
Dr. Jonathan Gong: Dr. Becker, how did you initially get into research?
Dr. Lance Becker: There’s this book called “The Accidental Tourist.” My book would have been called the “The Accidental Researcher.” I felt that in the area of cardiac arrest, there was a lot that we did not know. I had the good fortune of being around mentors who helped me publish some papers and get some grants, and then suddenly I had some money coming in. I was able to get some protected time for my research. I started a laboratory on
resuscitation science because I was convinced that it was not enough to just do better CPR. We needed to fundamentally revolutionize the way that we thought about resuscitation and the human body and cells, and that led me to mitochondria. Emergency medicine is so rich with research opportunities and so many research targets that people know very little about.
Dr. Jonathan Gong: Was there a specific case or patient that sparked all this interest?
Dr. Lance Becker: I thought that I had a horrible dark cloud because I knew that my survival rates for the cardiac arrests that I took care of were not very good. I don’t know the exact numbers, but I would have 10 cases and maybe one that survived. Reading literature from Seattle that survival rates were 20% did not jive with my reality. I did not think that 20% was real, so I measured it for the city of Chicago and it ended up being 1.8%. So the statistics that we were teaching people across the country were off by a factor of 10. That
is when I realized that there is so much more that we can really do. I started on the population side of that, and as I read more, I had colleagues that drew me in. I got involved with the American Heart Association and became the chair of the BLS Subcommittee. I had the chance to rewrite the resuscitation guidelines for the United States and helped form an international liaison committee. At that point, I had the chance to redraft the world’s basic life support guidelines. The process transformed my life. Then I really got involved in mentoring a new generation of researchers. I had the chance to be involved in education and teaching both directly at the bedside, and via teaching things with papers that we would write. It reinvigorated my own passion about how important it is for the world that emergency medicine figure out important science. There has never been a better opportunity than today for young people to make discoveries.
Dr. Jonathan Gong: You mentioned you had a few mentors earlier in your career. What were some of the things that you looked to them for and how did they help shape your direction of research?
Dr. Lance Becker: I was really lucky, and I really owe my career to my mentors. I found so many people able and willing to mentor me, and many were from emergency medicine, but many were from cardiology and from surgery. When you communicate with somebody about something that is an idea, it's probably one of the most exciting things. I remember meeting one of the giants of cardiac resuscitation. After his talk, I asked him about a slide that he had shown. He said, “I'm not really sure about that” and then he handed me his box of slides (no PowerPoint in those times). He said “Well, just look through these and tell me what you think and let me know if you would make them any better.” This person was the top leader in the field, Mickey Eisenberg, who basically invented how to get CPR into the community. He had just given me all the slides from his entire talk. That sort of welcoming thing I had from people from all over the world, and they would reach out and help me. Fundamentally, we formed our own community, and these are people who stay with you. Even though I moved from Chicago to Philadelphia, and then to New York, the mentors that you have are people who stay with you for life. They are your second family.
Dr. Jonathan Gong: How did you balance your clinical responsibilities as you were developing your research career?

Dr. Lance Becker: It is very time-consuming and challenging and you have to be into it because you love it and know that you are not going to get paid for most of your time. In the beginning, for every hour you spend trying to pursue research, it's just something you do because you love it. I don't have a lot of secrets other than I don't believe in work-life balance. I believe in work-life integration and what I mean by that is the way you set things up in your life. I did it late at night for years and I would do it every day, but you figure out a way to integrate it into your life. I made sacrifices with my career like making less money than my colleagues and where I lived. There is no real game book on how to do this. I have so many more rejected grants and rejected papers than probably any of you out there. I am still writing NIH grants and I'm putting three in this next cycle. I counted my NIH grants just the other day and I had 49 rejected NIH grants.
Dr. Daniel Jourdan: How do you find and develop a niche?
Dr. Lance Becker: I don't want to say that it's completely at random, but I think you have to follow your heart. There are so many niches in emergency medicine that if there's nothing that interests you, go find another specialty. The area of critically ill patients is just ripe with emergency medicine, whether it's cardiac arrest, sepsis, stroke, or critical care. We are also the safety net for the entire country in terms of being sure that people have equitable access to care. The whole area of justice and health care in access to health care in disparities, in trying to right some of the wrongs of people who have difficulty, or are being taken advantage of in some way, I think that that whole area is what is called social emergency medicine, societal emergency medicine, and population health. The whole area of prehospital (EMS) care is just beginning to open and the future will involve much more care at home. I hope that emergency medicine will be the specialty that oversees the appropriate use of home health care to avoid a hospital admission. The whole area of women's health is just really undergoing a transformation. Finally, the topic of climate change and health of humans on our planet, is tied up with our existence as a species, and a new area of research.
I think, again, emergency medicine can be at the forefront.
Dr. Daniel Jourdan: For a resident who is interested in an academic career, what advice beyond just getting involved in research would you give?
Dr. Lance Becker: For residents and young faculty, I would suggest putting yourself in the right environment so that you get support. What are your resources going to be in terms of both collaborators and mentors? Maybe people could work for you to make some of the work easier. Do you have opportunities for that? One of the things that we do well in emergency medicine is we network. In emergency medicine, you can network with nearly any of the top people, the gurus of the field, just by sending them an e-mail and saying, “I need advice.” Part of my success is because I developed a supportive research infrastructure. For example, we developed a research associates program that would take young people, train them in research, and they could then help faculty with projects to ensure completion. Everyone benefits from programs like this. Despite all the challenges of pandemics, societal unrest, overcrowding, disparities, and lack of resources, emergency medicine has so many important discoveries to contribute to medicine. There has never been a time with so many opportunities for discovery in emergency care.
Dr. Jourdan is a PGY-3 in the combined emergency medicine/ internal medicine residency program at Henry Ford Hospital. He currently holds the position of member-at-large on the SAEM RAMS Board.
Dr. Gong is the director of the critical care division at Long Island Jewish Medical Center, Department of Emergency Medicine. He currently holds positions in both the department of pulmonary, critical care and sleep medicine and the department of emergency medicine, and is an assistant professor of emergency medicine at the Donald and Barbara Zucker School of Medicine. His research currently focuses on improving care of the critically ill, with specific focus on sepsis syndromes.

While there has been significant growth in emergency medicine (EM) sponsored federal research in the past decade, emergency medicine remains underrepresented in federal research funding relative to other medical specialties. Although many emergency physicians are engaged in research, obtaining large-scale funding to build independent research programs in emergency care is challenging.
As a first step to increasing emergency care research and the number of federally funded investigators, we facilitated a panel discussion with program officers (POs) from the National Institutes of Health (NIH) and the National Science Foundation (NSF). The objective for the session was to learn how to effectively engage with POs to optimize the success of grant applications. The panel of program officers included:
Henry Ahn, MBA, MS, Small Business Innovation Research (SBIR) and Small Business Technology Transfer (STTR) program officer at NSF
Kristen Huntley, PhD, addiction medicine team leader in the Center for the Clinical Trials Network (CCTN) of the NIH National Institute on Drug Abuse (NIDA)
Jane Scott, ScD, MSN, director of the Office of Research Training and Career Development of the Division of Cardiovascular Sciences in the NIH National Heart, Lung, and Blood Institute (NHLBI)
Jeremy Brown, MD, director of the Office of Emergency Care Research working within the NIH National Institute on Neurologic Disorders (NINDS)

NIH is just one source of federal research funding. The NSF, Patient Centered Outcomes Research Institute (PCORI), Centers for Disease Control and Prevention (CDC), and the Department of Defense (DOD) are other sources of federal funding for emergency care research. For NSF SBIR/STTR, the emphasis is on startups and very early-stage companies. If a company is developing innovative technology
with commercial potential, there is a fit somewhere within the NSF SBIR/STTR program regardless of the topic. NSF will not fund clinical trials but much of the research and development work from the very beginning (with preliminary evidence that the technology has the potential to work) through the preclinical trial stage would be considered appropriate.
The NIH is composed of 27 institutes and centers; each operates independently and differently. A key component of a successful application is to understand the structure and approach to funding in the institute or center through which you would like to obtain support for your research. It is important to review the website (search by institute) and weekly NIH publications to identify potential grant topic areas of interest to each Institute.
The Institutes that currently provide the largest amount of grant support for emergency care research include NHLBI, NINDS, NIDA, and the National Institute on Aging (NIA).
Establishing an independently funded research program requires a stepwise approach and is a multiyear process. Generally, it takes six to eight years of NIH research training to become a competitive NIH R01 independent investigator. Investigators often participate in multiple rigorous predoctoral and postdoctoral scientific training programs such as a National Research Service Award (NRSA) Institutional Training Grant (T32), Clinical and Translational Science Award (CTSA) Institutional NRSA (TL1), CTSA Institutional Career Development Awards (KL2) and individual K awards for postdocs and junior faculty that should, over the five years of the K award, transition mentored scientists to independent NIH investigators. The NIH has a research training website for reference.
It is important to read the strategic plan for each NIH institute prior to meeting with the PO. With a clear understanding of the strategic plan for the Institute, one can easily describe how the proposed project may support or advance the strategic research initiatives on the institute. As an example, if an investigator is interested in the cardiovascular side effects of chemotherapy, the topic may be better served with NHLBI if the primary endpoint is cardiovascular instead of the National Cancer Institute which may be focused on the cancer treatment.
The NIH RePORTER is an excellent resource to review current awards and ensure your planned approach to the topic area and investigation is novel and innovative. The RePORTER is an excellent way to familiarize oneself with investigations as it may take several years for research results to be published.
Effective communication with the PO can be very helpful during the grant application and review processes. The PO wants to engage with researchers and is available to assist you with understanding the priorities of the Institute and to provide helpful guidance related to the application. Early, effective communication with the PO is essential to help ensure a successful grant application. Prepare for your call with a PO. Think through which institute might be interested in your research,
and whether other institutes might also be interested. If you have specific aims and a biosketch, send them to the PO in advance of the call.
The Notice of Special Interest in Emergency Care Research is a list of research topics from several NIH institutes about research areas they are looking to fund. Although the notice officially expired in September 2022, the institutes may still be interested in related proposals and this list can be a good jumping-off place.
The Office of Emergency Care Research sits within NINDS but is a transNIH office where EM researchers can get help connecting with the correct PO based on their research. This office does not offer funding opportunities but can help you connect with the right institute. The Office of Emergency Care Research can help connect you with the right people for early exploratory ideas that still need to be prepared for a clinical trial.
When is the right time to reach out to a PO and when is the right time to start the initial communications?
Henry Ahn: The wrong time to reach out is when you have a proposal pending as our policy does not allow POs to discuss anything over the phone at that stage. The right time is any other time when you have any questions. The best way to start at the NSF is to submit a project to the project pitch portal where you can get feedback on which topic fits best and start putting together your proposal.
Jeremy Brown: The time to reach out is very early. Have a one-page specific aims, which can include one primary and two secondary aims, the approximate project cost, and with that, send the PO an email to start the conversation.
Jane Scott: With the specific aims, please also send a CV or a biosketch because this helps POs understand where you are in the process of becoming an independent investigator.
Kristen Huntley: Having the specific aims page can make the initial call more productive and will give the program officer time to review and think about your project and provide more in-depth feedback. Use your mentors, too, they’re vital.
I am a researcher from Canada. Do you welcome or are you interested in international collaborations?
Jane Scott: Part of the answer depends on what the mechanism of funding is. Historically at the NIH, international work has gone through Fogarty International Center.
Jeremy Brown: The primary grant can sometimes be totally foreign. If you can justify the need for an international collaboration (e.g., malaria research), that would be looked upon better than if one happens to have a colleague in Canada. NIH has used Canadian sites for clinical trials in the past if they can provide certain expertise, but not as the primary investigator.
Henry Ahn: In NSF, there is a specific office that deals with international collaboration, but the SBIR program requires that the grant funds stay within the country
Dr. Duanmu is an assistant professor and codirector of the ultrasound fellowship at the Stanford University Emergency Department. Her research interests include critical care ultrasound, clinical trials and ultrasound curriculum development and competency assessment.

Dr. Chang is vice chair of research and associate professor of emergency medicine at Columbia University, where he holds the Tushar Shah and Sarah Zion Endowed Chair in Emergency Medicine. Trained as a psychologist and emergency physician, his research focuses on neuropsychiatric emergencies and clinician health

Dr. Govindarajan is an associate professor at the Stanford University Emergency Department. Her research goals are to identify best prehospital practices in acute stroke care. AHRQ supports her work, and she is working with the CDC on developing best practices for US ambulance systems.

Dr. Vogel is an associate professor and vice chair for academic affairs in the department of emergency medicine at Stanford University. She currently serves as memberat-large on the SAEM Board of Directors.

 By James H. Paxton, MD, on behalf of the SAEM Research Committee
By James H. Paxton, MD, on behalf of the SAEM Research Committee
SAEM is home to a broad range of academic emergency physicians, including educators and researchers with a diverse background of experiences and training. This makes our organization a unique forum for talented academics to collaborate and synergize efforts to advance our specialty. The Advanced Research Methodology Evaluation and Design (ARMED) and Advanced Research Methodology Evaluation and Design in Medical Education (ARMED MedEd) training programs are two great examples of SAEM bringing together clinical researchers and educators to benefit SAEM members. These programs illustrate the importance of educators in the training of future
researchers and underscore the potential benefits of collaboration between educators and researchers in emergency medicine.
Health professions education (HPE) research is perhaps the most intuitive arena in which the unique skill sets characterizing educators and researchers complement one another. Clinical researchers are accustomed to utilizing a hypothesis-testing framework to arrive at simple, generalizable findings that can be applied broadly across a variety of domains and contexts. In fact, reproducibility of results is often considered to be a key determinant of the success of a clinical research protocol, with the expectation that an experiment conducted under the same
conditions should always yield the same outcomes. While this may appear to be true in well-designed clinical trials, the complexity of factors influencing educational outcomes often undermines our efforts to generalize findings.
In fact, the effectiveness of a teaching intervention may depend upon factors that would usually not be considered in the context of a clinical trial, such as the enthusiasm or communication skills of the person providing the intervention, differences in learning styles, and other educator (or learner) specific characteristics. These differences can make an effective educational intervention in one context ineffective in another context, underscoring the need to study not only the outcomes of the
intervention but also the ways in which various aspects of the intervention’s implementation can influence those outcomes. Thus, education researchers must often seek to simultaneously understand not just whether, but why, an educational intervention works.
The ideal randomized controlled trial is one in which all conditions other than the intervention of interest are the same between the control and intervention groups, but in the real world, things are rarely that simple. Confounders and other unmeasured factors are often cited when a medical intervention appears to work well in one clinical context and not in another. But such discrepancies in clinical outcomes between trials may suggest the need for further investigation into the reasons why the intervention failed, including patient-, provider- and researcher-specific factors. Individuals trained in HPE research may be uniquely qualified to help identify such factors; after all, clinical trials invariably involve some degree of teaching and training, whether the learner is the patient, the clinician, or the research team member executing the intervention. Improved attention to this educational process (including whether and why it failed) could be expected to standardize (and perhaps improve) outcomes for otherwise welldesigned clinical trials.
While training in clinical research skills can provide a foundation for conducting educational research, such basic skills are seldom adequate. Innovative clinical interventions are often developed by basic and translational scientists before being tested by clinical researchers, but HPE researchers are often required to both develop and test their interventions. Clinical trials generally utilize well-defined and easily quantifiable outcomes, with standardized measurement tools. But educational interventions may be assessed according to less easily defined (or even quantified) criteria, such as motivation, satisfaction, empathy, wellbeing, and resilience. Managing such challenges requires the development of
a specialized skill set — one that clinical researchers could benefit from as well.

In my experience, including educators in a research project always adds value, whether the educator is an HPE researcher or not. In addition to the potential for better training of patients, clinicians, and research team members, educators can also help to improve awareness of a clinical research study within the department and mobilize medical student and / or resident support. After all, participation in a clinical research project may help residents to complete their scholarly activity requirement for graduation. Educators (including education researchers) are also likely to have specific medical, technical, or statistical expertise that other members of the research team are lacking. These additional resources of manpower, time, and expertise could mean the difference between a successful clinical trial and a failed one, especially for investigators at resource-poor institutions.
Although educators and clinical researchers may have similar skill sets, they can have very different expertise. Each of these groups has a lot to offer the other, and it may be argued that these two areas of inquiry are inextricably linked, even outside of HPE research. After all, the conduct of

high-quality clinical research requires an understanding of educational factors that impact learning and behavior, just as effective education is informed and refined by high-quality research. However educators and researchers choose to collaborate, the combination of these two “halves” of SAEM’s academic mission offer the promise of a whole far greater than the sum of its parts
Dr. Paxton is an associate professor of emergency medicine at Wayne State University School of Medicine (Detroit, MI) and director of clinical research at Detroit Receiving Hospital. He is an active clinical researcher and educator, serving as core academic faculty at both Sinai-Grace Hospital and Detroit Receiving Hospital EM residencies. He is also chair of the SAEM Research Committee and a member of the SAEM ByLaws Committee. Dr. Paxton has been involved in the development of many educational programs within SAEM, including the Advanced Research Methodology Evaluation and Design (ARMED) program, and the SAEM Research Learning Series (RLS).
“Health professions education (HPE) research is perhaps the most intuitive arena in which the unique skill sets characterizing educators and researchers complement one another.”

Research Spotlight is a new initiative by the SAEM Research Committee to highlight research presented by students and residents at SAEM regional and national meetings. Full abstracts for all of the projects highlighted below can be found in the SAEM22 Annual Meeting Abstract Supplement.
Chase Richard and Daniel Weingrow
First author Chase Richard, MD, MBA is a chief resident at the UCLA Ronald Reagan Olive View emergency medicine program. He obtained his

medical degree from the Perelman School of Medicine at the University of Pennsylvania, and his master's in business administration from the Stanford Graduate School of Business.
Dr. Richard's academic interests include technological innovation and implementation, and EDI recruitment,
retention, and educational initiatives.
Author Conclusion: This study is the first of its kind to use rapid EEG and AI-assisted diagnostics in the ED. ED physicians were more likely to give ASM before they received EEG results. AI interpretation and EEG Fellows had agreement in 92% (34/37) of cases. Most rewarding aspect of my work on this project: Creating a protocol that was achieved institutional adoption and beginning the research required to improve patient safety and outcomes.
John Forrester, DO; Allison Cohen, MD; Timmy Li, PhD; Ajay Puri, MD; Nicholas Bielawa, Pettet, MD; Mathew Nelson, DO; Daniel Rolston, MD
First author John Forrester, DO, is a PGY-3 resident physician in emergency medicine at North Shore University Hospital in Manhasset, NY. He holds interests in cardiovascular disease, point-of-care ultrasound, and clinical research, and is pursuing a career in emergency and critical care medicine.

Author Conclusion: Our analysis demonstrates that VExUS scoring, previously used as a marker for venous congestion, may help identify ED patients with sepsis who are more likely to be volume unresponsive and at risk for adverse events due to excess fluid administration.
Most rewarding aspect of my work on this project: The opportunity to deepen my understanding of point-ofcare ultrasound, develop my skills as a clinical researcher, and provide this information to the emergency medicine community.

Abigail Alorda, MD, Etta Conteh, David Lebowitz, MD, and Tracy MacIntosh, MD, MPH, MS
First author Abigail Alorda, MD, is a second year emergency medicine resident at University of Central Florida/ HCA Florida Healthcare GME in Greater Orlando/ Osceola.

Author conclusion: In this national ED study, there was no statistically significant correlation between the use of chemical restraints among patients who presented to the ED with agitation or aggression and patient race/ethnicity.
Most rewarding aspect of my work on this project: Being able to share this information not only at a national level but also with my patients and colleagues to help continue to bring awareness to the topics of health inequities and racial bias in medicine.
John ForresterAutoimmune (AI) disease is a result of the inability of the body’s immune system to protect itself from selfantigens. Among the multiple factors that contribute, such as environmental triggers and human leukocyte antigens, the role of biological sex is crucial in the development of autoimmunity.

Females have a more robust immune system than males in both humoral and cellular immunity. Additionally, sex hormones influence the propensity of AI conditions, with estrogen and progesterone stimulating immune effects and androgens largely suppressing them through autoimmune regulator (AIRE) expression that prevents autoreactive T cells. For this reason, females are more at risk of developing AI conditions, and currently, 80% of
individuals with AI diseases are female. Sex chromosomes also play a large role in the sex bias of autoimmunity, as the X chromosome contains many immune-related genes, including CD40 ligand, tyrosine-protein kinase BTK,
and chemokine CXCR3, among others. Lastly, immunity in the gut microbiota is influenced in a sex-specific manner, as seen by many animal models for type 1 diabetes, where male microbiota seems to play a protective role.
“...it is vital to understand the current therapies used to treat both acute and chronic manifestations of AI conditions and whether these treatments have been studied based on sex differences.”
Three AI conditions where sex differences are prominent include systemic lupus erythematosus (SLE), Sjogren syndrome, and rheumatoid arthritis. A combination of hormonal and genetic factors contributes to the varying disease incidence, severity, and response to treatment.

Sjogren’s syndrome consists of the AI destruction of exocrine glands, including lacrimal and salivary. It has the highest female-to-male ratio for the incidence of all AI diseases (16:1). Many females are at the highest risk during their childbearing years, as an increase in estrogen and prolactin levels are linked to disease incidence. The highest disease prevalence is seen in ages 40-60. Estrogen and prolactin both increase the anti-Ro and anti-La autoantibodies. Studies have also shown an increase in CD40L expression in the lip biopsies of patients with Sjogren syndrome.
SLE is a multifactorial inflammatory condition targeting multiple organ systems through auto-antibody complexes that cause tissue injury. Pre-menopausal women have the highest rates compared to men (7:1). Like Sjogren’s, lupus is also seen as a “woman’s disease” for this reason. The ratio of female to male is reduced in pre-adolescents and post-menopausal women when the difference in estrogen levels is reduced. E2 influences immune function and production is accelerated
through the estrogen receptor ERα, which converts androgens to ER. Moreover, estrogen activates the CD40L on CD4+ cells on the inactivated X chromosome, which increases the interaction between B and T cells. These hormonal and genetic factors contribute to the predominance of Raynaud’s phenomenon, malar rash, and arthritis in females. Conversely, SLE in males presents later in life, and genetic factors play a significant role in disease formation, as many males have concomitant Klinefelter syndrome. There is not as much evidence to suggest the role of hormonal regulation and activation in males.
While SLE incidences are highest in pre-menopausal women, cases of rheumatoid arthritis peak in middle-aged women (3:1 prevalence over males). In contrast to SLE, there is not a clear relationship between increased E2 and progesterone and the development of RA. Studies do not show an increased incidence of RA with hormonal contraception or hormone replacement therapy, and pregnancy seems to decrease the incidence risk. Research suggests that androgens have a protective role in the development of the severity of RA. Moreover, a polymorphism in the CYB5A gene for androgen synthesis in females was associated with an increased risk of RA. Males usually have less severe symptoms of RA and
respond better to androgen replacement therapy as an adjuvant treatment than females.
These three AI conditions encompass a few examples of a strong female bias within autoimmunity due to genetics, hormones, and environmental factors For this reason, it is essential to continue to further research sex-specific therapies that can reduce the complications of these conditions. Furthermore, it is vital to understand the severity of acute manifestations of AI conditions that often present in the ED, including pericarditis and acute glomerulonephritis in SLE, atlantoaxial dislocation and vasculitis in RA, and interstitial pneumonia in Sjogren’s syndrome. In the future, it is vital to understand the current therapies used to treat both acute and chronic manifestations of AI conditions and whether these treatments have been studied based on sex differences.
Miloni Shah is a fourth-year medical student at Wayne State University School of Medicine applying for internal medicine residency and has an interest in sex and genderbased medicine within rheumatology.
@milshah27

 By Wendy W. Sun, MD; Amanda J. Deutsch, MD; and Vytas P. Karalius, MD, MPH; Michelle D. Lall MD, MHS; Mia L. Karamatsu, MD; and Amanda M. Ritchie, MD on behalf of the SAEM Wellness Committee
By Wendy W. Sun, MD; Amanda J. Deutsch, MD; and Vytas P. Karalius, MD, MPH; Michelle D. Lall MD, MHS; Mia L. Karamatsu, MD; and Amanda M. Ritchie, MD on behalf of the SAEM Wellness Committee
Seasonal Affective Disorder (SAD) was first described by Dr. Norman Rosenthal in 1984 as changes in mood that occur in a predictable pattern with the changes of the seasons, most frequently during the fall and winter months when the days get shorter. Epidemiology studies suggest that SAD affects approximately 6% of the U.S. population and correlates with latitude (e.g. 9.7% in New Hampshire and 1.4% in Florida). SAD could include symptoms of major depressive disorder as well as additional symptoms such as oversleeping, craving carbohydrates, weight gain, and desire to withdraw
socially/ “hibernate”. The “winter blues” are a less severe form of SAD. The current mainstays of treatment for SAD include light therapy (LT), psychotherapy (Cognitive Behavioral Therapy), and medications, with 60-80% of folks affected by SAD benefiting from LT (guidelines in table) However, physical exercise and other activities that decrease stress and increase well-being could be helpful as well.
Here is what some of our SAEM Wellness Committee Members do for their well-being in the winter to fend off SAD:
Exercise and Movement
• Participate in shared fitness activities for something to look forward to (e.g., volleyball league, Peloton with friends, running group)
• Download and use yoga apps like 26 & 2, Bikram, hot yoga and other fun fitness activity apps
• Strategically schedule breaks between Zoom meetings to take advantage of the outdoors (e.g., skiing a run between meetings)
• Go outside, especially during warmer days
Connectedness

• Build buddy and accountability systems
• Pause to reach out to friends not seen in a while
• Volunteer and give back to the community
• Visit family/friends who live in warmer places with longer daylight
Food
• Gather over food
• Make and enjoy warm soups and stews
Light
• Place a light box in work areas (helpful when wrapping up notes)
• Optimize light by moving a desk closer to a window
• Take a 5–10-minute break during work to step outside and enjoy the sunshine

• Put bedroom lights on a timer to simulate dawn when waking up (several smart lamps, smart light bulbs, and alarm clocks provide these features and can easily be paired with a phone via Bluetooth)
• Partake in plant retail therapy
If you find yourself with SAD or the winter blues, know that you are not alone. As emergency physicians, it is important to remember that, like anyone else, we are human and vulnerable to mental illness. These seasonal mood changes are not a reflection of our character or ability, so let’s remember to normalize these harder and sometimes literally darker moments in the fall and winter seasons. Please find available mental health resources here. Let’s continue to #StoptheStigmaEM
Dr. Sun is a chief resident at YaleNew Haven Health, Immediatepast president of SAEM RAMS, resident member on the SAEM Board of Directors, and AWAEM Wellness Committee cochair.
Dr. Deutsch is a clinical instructor and physician wellness fellow at Stanford Emergency Medicine.



Dr. Karalius is a clinical instructor and medical education scholarship fellow at Stanford University.
Dr. Lall is an associate professor at Emory University, an AWAEM past president, and is currently serving a second term as a member-at-large on the SAEM Board of Directors.
Dr. Karamatsu is an assistant professor and pediatric emergency medicine well-being champion at Stanford University. She is also AWAEM’s Wellness Committee cochair.


Dr. Ritchie is a second-year emergency medicine/internal medicine resident at Louisiana State University.

 By Amanda J. Deutsch, MD and Al’ai Alvarez, MD on behalf of the SAEM Wellness Committee
By Amanda J. Deutsch, MD and Al’ai Alvarez, MD on behalf of the SAEM Wellness Committee
Once during residency, in response to overhearing me berate myself for a mistake, a coresident confronted me with a compelling question: “You would never say that to a friend or to one of us if we made a mistake, so why would you say that to yourself; why would you treat yourself that way?”
She was right. I was being unkind to myself. I was judging myself. I was not practicing self-compassion. In other words, I was not treating myself with the same kindness and compassion with which I would treat a friend going through a rough time. Unfortunately, lack of self-compassion not uncommon; according to Dr. Kristen Neff, “data suggests that the vast majority of people are more compassionate to
others than to themselves.”
The core components of selfcompassion are self-kindness, common humanity, and mindfulness. While our default is to avoid discomfort, these core components help teach us to face moments of suffering through the lens of self-compassion. Self-kindness reminds us to be less critical of ourselves and our shortcomings. With the understanding of our common humanity, we recognize the imperfectness or the “perfect works-in-progress” that all of us are. Do you know anyone who has never made a mistake, failed, fallen short, or humiliated themselves? After all, to be human is to be imperfect. With mindfulness, we face all of our emotions, even the momentary painful
thoughts, to allow us to be open, aware, and present with our experiences. The mindfulness component enables us to observe our moments of suffering without going down the rabbit hole of exaggerating or overidentifying with these emotions.
The myths surrounding selfcompassion are what create obstacles to the practice of self-compassion. These myths include, but are not limited to the idea that self-compassion is a form of self-pity, will make you weak, is selfish, will make you lazy, will be an excuse for indulgence, and will take away that driver of criticism that has gotten you to where you are in your career (you know, the one that that pushed you to get into medical school
and drove you to excel throughout the long hours of a shift and numerous missed holidays, birthdays, and weddings). But these myths keep you from partaking in the benefits of selfcompassion. Acknowledging these myths is critical to developing an openness to the practice of self-compassion.
Self-compassion is an inner source of strength that makes people stronger and more courageous in difficulties, not weaker for facing them. Self-compassion researchers, Drs. Kristin Neff and Christopher Germer found that selfcompassionate people are more likely to practice perspective-taking rather than focus on their own distress. Selfcompassionate people are more likely to have better mental health by ruminating less about their own hardships. Research also shows that being compassionate to yourself enables you to give more to others. Moreover, self-compassionate people tend to be more caring and supportive in romantic relationships and more likely to be forgiving towards others. Self-compassion helps you focus on long-term health and well-being, instead of short-term pleasure. Unsurprisingly, the research shows that self-compassionate people engage more in exercising, eating well, drinking less, and even visiting the doctor more regularly. (When was the last time you booked your own primary care visit or dental check-up?) Lastly, self-compassionate people take great personal responsibility by admitting mistakes rather than blaming others for them and maintaining high standards while not beating themselves up for failures. This means that through selfcompassion, you can fear failure less and develop the ability to persist and try again, despite facing disappointment.
This is a growth mindset, and selfcompassion is critical to developing this mindset. Being self-compassionate will still allow you to apply for those grants, strive for promotion, go that extra distance, and keep pushing yourself. It will not make you weaker or lesser. Selfcompassion, however, will help you set boundaries to take care of yourself and protect your well-being.
One study refers to self-valuation, a form of self-compassion, using the selfvaluation test — a four-question scale to measure self-compassion in physicians with burnout and sleep impairment. Unsurprisingly, each one-point score higher in self-valuation is associated with a one-point decrease in burnout and lower sleep impairment scores. Having self-compassion pays off in the long run; however, as physicians, we as a group have lower self-valuation scores than workers in other fields. As we begin to understand the impact of the pandemic, we must start practicing ways to prioritize ourselves, starting with something small like being kind to ourselves. This is how we can sustainably continue to help others.
Another important aspect of selfcompassion is the ability to practice selfappreciation. Think of a time when you received a compliment about something you did. How did you respond? Often, we don’t know what to say or feel flustered by the acknowledgment. Accepting our positive traits is often more challenging than knowing our

flaws. We must let go of the fear that we might disappoint someone whenever we receive a compliment. Self-compassion acknowledges our high expectations and appreciates the work we are doing to achieve them. Go ahead and practice admiring the positive qualities your friends and colleagues see in you.
As we begin a new year, gift yourself a daily habit of self-compassion. The first step is self-awareness. Start with this quiz. If you score low, like many of us do, know this is a practice and you can work to improve — even if you sneak a few leftover holiday cookies or pie slices too.
During this season of kindness, and of giving to and thinking of others, let’s remember to treat ourselves to the gift of self-compassion
Dr. Deutsch is a clinical instructor and physician wellness fellow at Stanford Emergency Medicine.

Dr. Alvarez is director of wellbeing at Stanford Emergency Medicine and chair of the SAEM Wellness Committee. @alvarezzzy

“The myths surrounding selfcompassion are what create obstacles to the practice of selfcompassion.”
Closing January 11!
IGNITE! is a fun and fast-paced competition held each year at the SAEM Annual Meeting. Each IGNITE! talk is five minutes in length with 20 automatically advancing slides. Because of its unique format, IGNITE! talks are highly energetic, captivating, and engaging. Speakers are selected from all levels of training and from all parts of the country. A panel of judges selects a “Best of IGNITE!” winner from each IGNITE! session. An “Audience Choice Award” is also given at each session based on audience polling. Submit your IGNITE! proposal for SAEM23 by January 11, 2023. Questions? Contact education@saem.org
Innovations present novel ideas and approaches that enhance undergraduate and graduate medical education at all levels. These may include topics such as faculty development, wellness, and operations. Innovations are presented in either an oral format (seven-minute presentation) or a tabletop (hands-on) format, bringing diverse leaders together to cultivate and promote new ideas and advances. Submit your innovations proposal for SAEM23 by January 11, 2023. Questions? Contact education@saem.org
Each year, the SAEM Program Committee looks for enthusiastic and responsible medical students from around the country to work directly with SAEM leadership, through the Medical Student Ambassador (MSA) Program, to assist in the planning, coordination, and execution of SAEM’s Annual Meeting. Benefits include a waiver of your SAEM23 registration fee, a letter of commendation for your files, and an impressive addition to your CV. Submit your MSA application by January 11, 2023, to be considered for this one-of-akind opportunity!
SAEM is accepting submissions of original high-quality, image-based educational cases relevant to the practice
of emergency medicine for presentation in the SAEM Annual Meeting Clinical Images Exhibit. Submissions are selected based on their educational merit, relevance to emergency medicine, image quality, the case history, and appropriateness for public display. Accepted submissions will be displayed at SAEM23. Images that are accepted for display and have patient consent sign-off, will also be featured on Academic Life in Emergency Medicine’s (ALiEM) wide-reaching blog. Submit your clinical images by January 11, 2023. Questions? Contact education@saem.org
Registration is now open for SAEM23, to be held May 16–19, 2023 at the JW Marriott in Austin, Texas. We can’t wait to welcome you with an expansive lineup of expert educational content, ground-breaking research, cutting edge innovation, energetic events, career development opportunities, and a chance to connect in person with your friends and colleagues! For early bird pricing, register by March 14! Visit the SAEM23 website for all the latest annual meeting news and information.
Laura Oh, MD
Registration for team events is open. Pull your teams together for Dodgeball, SonoGames and SimWars and sign up today!
January 15 Is the Deadline to Apply for the Master Educator Course!
SAEM is accepting applications for the new Master Educator course. This year-long program is designed for early-career and mid-career faculty who desire to strengthen their conceptual understanding of educational theory and practice, their ability to design and implement educational programs of the highest quality, and their effectiveness as educators in the classroom and at the bedside. The course is intended for faculty who already have some experience and expertise in medical education but want to take their skills to the next level. Apply by January 15, 2023.
Associate Professor at Emory University

What unique benefits does the eLEAD program provide for participants?
The eLEAD program participants work in small groups with emergency medicine leaders - chairs, deans, presidents of national EM organizations, who have decades of experience and insight into what makes an outstanding leader. Many of the class participants are mid-career -- some feel "stuck," some are facing major career branching points, some have been elevated to leadership roles they don't feel quite qualified for. The eLEAD program provides a safe haven for discussion, learning, and growth through a combination of small group teaching, peer to peer mentoring, and reflection.
So far, how has eLEAD impacted your work and career trajectory?
The eLEAD program has given me the courage to change, to try new things even though I might fail. The supportive course directors and peers give invaluable advice for how to work through difficult scenarios. I value the quality time the eLEAD course allows us to set aside monthly to pause for development and reflection.
Who is the ideal candidate for this program, and why would you recommend it to them?
The ideal candidate for the program is an emerging leader with prior leadership responsibilities either in their home institution or through national EM organizations. The candidate should be willing to commit to the process, be vulnerable and sincere, and be a generous listener and supporter of their classmates.
I would recommend this course as the best leadership course I have ever taken.
The year-long Emerging Leader Development (eLead) course provides emerging leaders in academic emergency medicine with a structured, longitudinal experience designed to develop foundational leadership skills, cultivate a meaningful career network, and build a bridge to countless opportunities in their field. Apply today, and visit the eLEAD website for details.
Accepting Applications for AEM E&T Fellow Editor-in-Training Academic Emergency Medicine Education and Training (AEM E&T) journal is accepting applications for its 2023–2024 Fellow Editor-in-Training program. This one-of-a-kind opportunity is open to any SAEM member who is a current resident and who will start a medical education fellowship in the summer of 2023 OR is a current fellow in a two-year medical education fellowship program. The fellow appointment to the editorial board of AEM E&T is intended to mentor a medical education fellow in the process of peer review, editing, and publishing of education research manuscripts. Application deadline is February 17, 2023.
Call for Resident Members to Serve on the Editorial Board of AEM Applications are now being accepted for the resident appointment to the editorial board of Academic Emergency Medicine (AEM) journal for the 2023-2024 term. The 12-month resident appointment is intended to introduce the resident to the process of peer review, editing, and publishing of medical research manuscripts and will provide the resident with an experience that will enhance his/ her career in emergency medicine and in scientific publication. Application deadline is February 17, 2023.
SAEM introduced the Outstanding Department Award for Excellence and Innovation in Diversity, Equity, and Inclusion this year to honor an emergency department (ED) that has shown significant support for diversity,
equity, and inclusion (DEI). With so many exceptional programs underway, this award will showcase EDs that are advancing DEI through their organizational initiatives that address the recruitment, development, and advancement of its physicians, promoting equity, diversity, opportunity, and inclusion. The brief nomination packet won’t require too much time to assemble. Apply by January 15, 2023!
2022 has been an extraordinary year for SAEM, but we’re just getting started! It’s
going to be an amazing 2023 for SAEM and we hope you’ll share in our success by renewing your SAEM membership today. Renewing is easy. Just log into your member account and click the «Pay Dues» button. While you’re there, take a few minutes to update your member profile. New features for membership profiles now allow you to add your pronouns, fellowships, and related demographical information to keep the community and your fellow colleagues in the know! For the most comprehensive guide to SAEM’s member benefits, be sure to check out our updated SAEM Membership Guide!
“This grant was transformative for me. I had pursued multiple different career development programs since graduating (the UCLA Medical Education Fellowship, the Stanford Faculty Development program, etc.), but, I had never had formal training in medical education research. Being allowed protected time to obtain a Master of Health Professions Education degree and focusing on medical education research methods and working with my mentor Dr. Wendy Coates has been a wonderful experience. Since getting this additional training, I feel much more well rounded as a scholarly educator and am going to be able to give back so much more for the rest of my career.” – Ryan Pedigo, MD, MHPE, Associate Residency Program Director, Harbor-UCLA Medical Center; Assistant Professor of Emergency Medicine, David Geffen School of Medicine at UCLA and SAEMF Education Research Grant Recipient
Your gift now will count towards participation in the Chairs’ Challenge and the Academy, Committee, Interest Group Challenge that take place later this year. Give once and you are done!
It’s easy to become a Mentor level donor with an annual monthly gift of just $83.
Join now to take advantage of 2023 benefits. It's easy: donate online today or download the pledge form and your gift will help fund future researchers, educators, and leaders.
Thanks for considering a gift to fund emergency medicine’s future!

Kabir Yadav, MDCM, MC, MSHS, vice chair for academic affairs at Harbor-UCLA Medical Center and investigator for The Lundquist Institute, had been promoted to professor of clinical emergency medicine at UCLA (retroactive to July 2020). He has served in the role of vice chair for academic affairs since 2018, and will now serve as vice chair for research and academic affairs starting this year. After completing a NIH KL2 Career Development Award and a master's degree in translational science at George Washington University, Dr. Yadav became one of the first board-certified clinical informaticists in the country. He is core faculty at the UCLA Clinical and Translational Research Center for both the community engaged research program and biomedical informatics. He has been funded through PCORI, NIH, CDC, and foundations to leverage technology and implementation science to perform collaborative health services research focused on improving patient and provider decision making, and partners with the community to do mutually meaningful research with an emphasis on social determinants of health.

Roland C. Merchant, MD, MPH, ScD, vice chair of research in the department of emergency medicine, Icahn School of Medicine at Mount Sinai, was awarded a five-year National Institute on Drug Abuse (NIDA) R01 grant to support his research, “Evaluation of a Persuasive Health Communication Intervention Designed to Increase HIV/HCV Screening Among Emergency Departments Patients Who Currently, Formerly or Never Injected Drugs.” The project involves evaluating the efficacy of a persuasive communication health intervention designed to increase HIV and hepatitis C screening among adult emergency department patients who initially declined to be tested for these infections.
Kavita Babu, MD, professor of emergency medicine, University of Massachusetts Chan Medical School and Roland C. Merchant, MD, of the Icahn School of Medicine at Mount Sinai were awarded a two-year National Institute on Drug Abuse UG3 grant to support their research, "Sentanyl II: A Multi-State Analysis of

Fentanyl/Analogs, Naloxone, and Clinical Features of NonFatal Opioid Overdose." The project entails understanding how response to naloxone administration after an opioid overdose is affected by fentanyls and other opioids, alcohol, and other illicit and pharmaceutical substances.

Ian B. K. Martin, MD, MBA, professor with tenure and system chairman in the department of emergency medicine at Medical College of Wisconsin (MCW) and emergency physician-in-chief for the Froedtert & the MCW health network, has been selected as one of six fellows for the prestigious 2022-2023 Association of American Medical Colleges (AAMC) Council of Deans (COD) Fellowship Program. Dr. Martin was chosen from an exceptionally talented applicant pool that comprised the largest number of applications to date. The year-long AAMC COD Fellowship Program was created to enhance the development of future leaders in academic medicine.
Jeffrey Glassberg, MD, has been promoted to full professor with tenure, Department of Emergency Medicine, Icahn School of Medicine at Mount Sinai. Dr. Glassberg leads the Mount Sinai Sickle Cell Program, which has over 1,000 patients, two clinical sites, and 14 employees. He has received over $25 million in federal research funding to support his work on gene therapy cures, “BayesianAdaptive Clinical Trials, Management of Acute and Chronic Sickle Cell Pain and Implementation Science.”

Ethan Cowan, MD, professor of emergency medicine, Icahn School of Medicine at Mount Sinai, received a UG3 grant from the National Institute on Drug Abuse (NIDA), National Institutes of Health (NIH) to support his research, entitled, “Safety and Efficacy of High Dose Buprenorphine Induction in Fentanyl Positive Emergency Department Patients.” The project will take place in two phases. The first phase will determine the safety, tolerability, and feasibility of high dose buprenorphine induction. In the second phase, a multicenter randomized controlled trial will examine preliminary efficacy. Dr. Cowan, along with Dr.
 Dr. Kabir Yadav
Dr. Roland C. Merchant
Dr. Kavita Babu
Dr. Ian B. K. Martin
Dr. Jeffrey Glassberg
Dr. Kabir Yadav
Dr. Roland C. Merchant
Dr. Kavita Babu
Dr. Ian B. K. Martin
Dr. Jeffrey Glassberg
Susie Hoffman, Columbia University, also received a two-year National Institute of Mental Health (NIMH) R34 grant entitled, "PrEP-ED: PrEP Services in the Emergency Department for Hard-to-Reach Populations.” The first phase will identify patient preferences through a discrete-choice experiment. The second phase involves implementing and optimizing the PrEP program. The third phase is a pilot implementationeffectiveness type two randomized controlled trial.

Azita G. Hamedani, MD, MPH, MBA, founding and former chair of the BerbeeWalsh Department of Emergency Medicine at the University of Wisconsin School of Medicine and Public Health, has been named to the Wisconsin Endowed Chair of Leadership in Emergency Medicine. In her honor, the endowed chair held by the chair of emergency medicine at UW-Madison, will now be known as the Azita G. Hamedani Distinguished Chair of Emergency Medicine. This change honors Dr. Hamedani's transformational accomplishments as chair, establishing and building emergency medicine at the University of Wisconsin.
The SAEM Pulse Academic Announcements section publishes academic appointments, promotions, retirements, grant awards, research announcements, published papers, etc. Send your content (50-75 words max) to newsletter@saem.org. The next content deadline is February 1, 2023 for the March-April 2023 issue.

Jane Scott, ScD, MSN, renowned and respected for her work as a leader in emergency medicine research funding and training, has announced her retirement. Dr. Scott began her career in the emergency care setting as a nurse at the Duke University Emergency Department in the Hillsborough, NC volunteer EMS squad and then as a nurse practitioner at the Johns Hopkins emergency department. She presented her first research abstract in 1981 at the University Association of Emergency Medicine meeting, which was followed by publications in numerous emergency care publications. After obtaining a doctorate from Hopkins School of Public Health, Dr. Scott joined the Agency for Healthcare Research and Quality (AHRQ) as a program officer. In 1995 she joined the University of Maryland National Study Center for Trauma and EMS followed by serving as research director of the program in trauma at the R Adams Cowley Shock Trauma Center. In 2005 Dr. Scott joined the National Institutes of Health (NIH) as director of the Office of Research Training and Career Development, Division of Cardiovascular Sciences at the National Heart, Lung, and Blood Institute (NHLBI). In 2008 she created the NHLBI K12 program in emergency care research, which she managed until her retirement, working extensively with the emergency medicine researchers at the eight training programs that have trained over 50 K12 scholars.
Dr. Scott has served on the SAEM Research Committee, ACEP-SAEM Federal Research Funding Workgroup, and as faculty at the EMF-SAEMF Grantee Workshop for over eight years. She has educated and mentored countless SAEM members on the K12 programs, presented at numerous SAEM annual meetings, worked closely with program officers on NIH-related matters, and taught many of our investigators how to become independently funded.
Dr. Azita G. Hamedani Dr. Jane ScottThe George Washington University Medical Faculty Associates, an independent nonprofit academic clinical practice group affiliated with The George Washington University, is seeking full-time academic Emergency Medicine physicians. The Department of Emergency Medicine provides staffing for the emergency units of George Washington University Hospital, United Medical Center, the Walter Reed National Military Medical Center, and the Washington DC Veterans Administration Medical Center. The Department’s educational programs include a four-year residency and ten fellowship programs.
Responsibilities include providing clinical and consultative service; teaching fellows, residents, and medical students; and maintaining an active research program. These non-tenure track appointments will be made at a rank (instructor/assistant/associate/full professor) and salary commensurate with experience.
Basic Qualifications: Applicants must be American Board of Emergency Medicine or American Osteopathic Board of Emergency Medicine certified or have completed a residency certified by the Accreditation Council for Graduate Medical Education or American Osteopathic Association, and be eligible for licensure in the District of Columbia, at the time of appointment.

Application Procedure: Complete the online faculty application at http://www.gwu.jobs/postings/97288 and upload a CV and cover letter. Review of applications will begin November 10, 2022, and will continue until positions are filled. Only complete applications will be considered. Employment offers are contingent on the satisfactory outcome of a standard background screening.
The George Washington University and the George Washington University Medical Faculty Associates are Equal Employment Opportunity/Affirmative Action employers that do not unlawfully discriminate in any of its programs or activities on the basis of race, color, religion, sex, national origin, age, disability, veteran status, sexual orientation, gender identity or expression, or on any other basis prohibited by applicable law.
The University of California, Davis, School of Medicine, Department of Emergency Medicine is conducting a faculty search at the Assistant/Associate/Professors in the Adjunct or In-Residence track.
Applicants must possess a doctoral degree in health, epidemiology, or another related discipline. An applicant completing their doctoral degree must have proof of completion prior to hiring. Additional training during a formal post-doctoral fellowship or substantial prior research experience in the field is preferrable. A track record of independent funding is also highly desirable, as is a research focus in clinical medicine or clinical epidemiology. We especially welcome applicants whose research, teaching, and community outreach demonstrably attest to their commitment to inclusion of under-represented and/or non-majority individuals.
The UC Davis Department of Emergency Medicine provides comprehensive emergency services to a large local urban and referral population as a Level One Trauma Center, Comprehensive Stroke Center, and EMS base station. The Department of Emergency Medicine has a strong research infrastructure and consistently ranks near the top nationally in NIH funding. Primarily, the candidate will be expected to develop and maintain an active research portfolio that is externally funded. Secondarily, the candidate will be expected to participate in Departmental education, administrative, and mentorship activities commensurate to academic rank.
For full consideration, please consult the link below for apply by dates. This recruitment will be open until filled through June 30, 2023. To apply please upload the following: letter of interest, curriculum vitae, and a statement of contributions to diversity to: https://recruit.ucdavis.edu/apply/JPF05194. All files should be in PDF format.
UC Davis commits to inclusion excellence by advancing equity, diversity and inclusion in all that we do. We are an Affirmative Action/Equal Opportunity employer, and particularly encourage applications from members of historically underrepresented racial/ethnic groups, women, individuals with disabilities, veterans, LGBTQ community members, and others who demonstrate the ability to help us achieve our vision of a diverse and inclusive community
Under Federal law, the University of California may employ only individuals who are legally able to work in the United States as established by providing documents as specified in the Immigration Reform and Control Act of 1986. Certain UCD positions funded by federal contracts or sub-contracts require the selected candidate to pass an E-Verify check. More information is available at http://www.uscis.gov/e-verify
UC Davis is a smoke & tobacco-free campus (http://breathefree.ucdavis.edu/). If you need accommodation due to a disability, please contact the recruiting department. For additional information:

Erik Laurin, M.D., Professor and Search Committee Chair, (eglaurin@ucdavis.edu) UC Davis Department of Emergency Medicine 2315 Stockton Boulevard, PSSB 2100, Sacramento, CA 95817
The University of California is an affirmative action/equal opportunity employer.

The University of California, Davis, School of Medicine, D epart ment of Emergency Medicine is conducting a faculty search for emergency medicine physicians as Assistant/Associate/Full Professors in either a (HSCP) clinician/educator or (Clin X) clinician/researcher track




Requirements include MD/DO degree or equivalent, Board Certification or eligibility in Emergency Medicine, valid CA Medical License or eligibility for licensure, experience teaching medical students, residents, and fellows, the ability to work cooperatively and collegi ally within a divers e environment, and the ability to adhere to policies and procedures. Fell owship training with at least one year of post-traini ng clinical experience is desired. We especially welcome applicants whose research, teaching, and community outreach de monstrably attest to their commitment to diversity and inclusion of historically marginalized communities into thei r respective area of specialization within their discipline.

The Emergency Depart ment provides comprehensive emergency services to a large local urban and referral population as a Level One Trauma Center, paramedic base station, and t raining cent er The fully accredited residency trai ning program i n Emergency Medicine at UC Davis Medical Center began almost two decades ago and currently has 60 residents All f aculty me mbers are required to provide bot h bedside and didactic teaching to residents, medical st udents, and others rotating through the Emergency Depart ment. The successful candidate will show a commit ment to educating and ment oring a diverse student body t o expand opport unities and enhance personal growt h, retenti on, and academic s uccess.
For full consideration, please consult the link below for apply by dates. This recruitment will be open until filled through June 30 , 202 3 To apply please upload the following: letter of interest, curriculum vi tae, and a statement of contri butions to diversity to: htt ps://recruit ucdavis edu/apply/JPF05194 All files should be in PDF format.
This position may, at ti mes, require the incumbent to work with or be in areas where hazardous materials and/or infectious diseases are present. Specific hazards of the position may include, but are not limited to, treating patients with Hepatitis B, HIV, other infectious dis eases, and also patients who may inflict physical harm
UC Davis commits t o inclusion excellence by advancing equity, diversity and inclusion in all that we do. We are an Affirmative Action/Equal Opportunity e mployer, and particularly encourage applications from me mbers of historically marginalized racial/et hnic groups, women, i ndividuals wit h disabilities, veterans, LGBTQIA+ community me mbe rs, and others who demonstrate t he ability to help us achieve our vision of a diverse and inclusive commun ity
Under Federal law, the University of California may employ only individuals who are legally able t o work in the United States as established by providi ng docu ments as s pecified in the Immigration Reform and Control Act of 1986. Certai n UCD positions funded by federal contracts or sub-contracts require the selected candi date to pass an E-Verify check. More information is available at http://www.uscis gov/e-verif y
UC Davis is a smoke & tobacco-free campus (ht tp://breat hefree.ucdavis edu/) If you need accommodation due to a disability, please contact the recruiting depart ment For additi onal informati on:
Erik Laurin, M.D., Professor and Search Committee Chai r, (eglaurin@ucdavis edu)
UC Davis Department of Emergency Medicine
2315 Stockton Boulevard, PSSB 2100, Sac ramento, CA 95817
The University of California is an affirmative action/equal opportunity employer

Emergency Medicine
Emergency Medicine

is currently accepting applications for July 2023 from individuals who wish to pursue fellowship training in emergency care research. Clinical and health services research tracks are available. This NHLBI-funded T32 program will provide qualified candidates with:
Outstanding Mentorship
Multidisciplinary Research Training

Career and Leadership Development
Masters of Science in Clinical Research
2-3 years of salary support
Lynne D. Richardson, MD, FACEP, Program Director
Alex Manini, MD, MS , Associate Program Director
Roland Merchant, MD, MPH, ScD, Associate Program Director
Ethan Cowan MD, MSc, Assistant Director
Cindy Clesca, MA, Program Administrator
For more information, please contact us at ERTP@mountsinai.org or 212-824-8057, or to apply online click here
The Icahn School of Medicine at Mount Sinai is located in New York City. Our top-ranked Emergency Medicine Research Division is comprised of talented investigators conducting high quality research in a supportive, collegial atmosphere that promotes scholarly inquiry and mutual respect. We value diversity of all kinds.
