
APRIL 2024
122
CONTINUOUS POSITIVE AIRWAY PRESSURE: IS IT STILL THE GOLD STANDARD?
A THOUGHTFUL ANALYSIS WITH THE ADVENT OF ORAL APPLIANCE THERAPY
MARTIN DENBAR, DDS
Reprinted with permission from the American Academy of Dental Sleep Medicine
128
TRENDING CULTURAL DRIVERS OF SMOKELESS TOBACCO FOR RECENT REFUGEE AND IMMIGRANTS AS KNOWLEDGE, ATTITUDES, AND BEHAVIOR DETERMINANTS:
A SOUTH TEXAS ORAL HEALTH NETWORK COLLABORATIVE STUDY
MOSHTAGH R. FAROKHI, DDS, MPH, MAGD, FICD, FPFA
JONATHAN A. GELFOND, PHD, MD
SAIMA KARIMI KHAN, DDS
MELANIE V. TAVERNA, MSDH, RDH, FADHA, MAADH FOZIA A. ALI MD
CAITLIN E. SANGDAHL
RAHMA MUNGIA, BDS, MSC, DDPHRCS
141
ASK THE POWERS CENTER
RADE PARAVINA, DDS, MS, PHD
142
ETHICS CORNER: UNDERSTANDING THE TRANSGENDER PATIENT
DONALD F. COHEN, DDS
Reprinted with permission from the American Dental Association
TDA Texas Dental Journal
2024 TDA MEETING





















114 Texas Dental Journal | Vol 141 | No. 3
BOOTH 221
BOOTH 226
BOOTH 209
BOOTH 210
Anesthesia Education & Safety Foundation
Two ways to register: Call us at 214-384-0796 or e-mail us at sedationce@aol.com Visit us on the web: www.sedationce.com
NOW Available: In-Office ACLS & PALS renewals; In-Office Emergency Program Live Programs Available Throughout Texas
Two ways to Register for our Continuing Education Programs: e-mail us at sedationce@aol.com or call us at 214-384-0796
OUR GOAL: To teach safe and effective anesthesia techniques and management of medical emergencies in an understandable manner. WHO WE ARE: We are licensed and practicing dentists in Texas who understand your needs, having provided anesthesia continuing education courses for 34 years. The new anesthesia guidelines were recently approved by the Texas State Board of Dental Examiners. As practicing dental anesthesiologists and educators, we have established continuing education programs to meet these needs.
New TSBDE Requirement of Pain Management
Two programs available (satisfies rules 104.1 and 111.1)
Live Webcast (counts as in-class CE) or Online (at your convenience)
All programs can be taken individually or with a special discount pricing (ask Dr. Canfield) for a bundle of 2 programs:
Principles of Pain Management
Fulfills rule 104.1 for all practitioners
Use and Abuse of Prescription M edications and Provider Prescription Program Fulfills rules 104.1 and 111.1
SEDATION & EMERGENCY PROGRAMS:
Nitrous Oxide/Oxygen Conscious Sedation Course for Dentists:
Credit: 18 hours lecture/participation (you must complete the online portion prior to the clinical part)
Level 1 Initial Minimal Sedation Permit Courses:
*Hybrid program consisting of Live Lecture and online combination
Credit: 20 hours lecture with 20 clinical experiences
SEDATION REPERMIT PROGRAMS: LEVELS 1 and 2
(ONLINE, LIVE WEBCAST AND IN CLASS)
ONLINE LEVEL 3 AND 4 SEDATION REPERMIT AVAILABLE! (Parenteral Review) Level 3 or Level 4 Anesthesia Programs (In Class, Webcast and Online available): American Heart Association Advanced Cardiac Life Support (ACLS) and Pediatric Advanced Life Support (PALS) Initial and Renewal Programs
NOTE: ACLS or PALS Renewal can be completed by itself at any combined program Combined ACLS-PALS-BLS and Level 2, 3 and 4
Program
WEBCASTING and ONLINE RENEWALS AVAILABLE! Live and archived webcasting to your computer in the comfort of your home. Here are the distinct advantages of the webcast (contact us at 214-384-0796 to see which courses are available for webcast):
1. You can receive continuing education credit for simultaneous live lecture CE hours.
2. There is no need to travel to the program location. You can stay at home or in your office to view and listen to the course.
3. There may be a post-test after the online course concludes, so you will receive immediate CE credit for attendance
4. With the webcast, you can enjoy real-time interaction with the course instructor, utilizing a question and answer format
OUR MISSION STATEMENT: To provide affordable, quality anesthesia education with knowledgeable and experienced instructors, both in a clinical and academic manner while being a valuable resource to the practitioner after the programs. Courses are designed to meet the needs of the dental profession at all levels.
Our continuing education programs fulfill the TSBDE Rule 110 practitioner requirement in the process to obtain selected Sedation permits. AGD Codes for all programs: 341 Anesthesia & Pain Control; 342 Conscious Sedation; 343 Oral Sedation This is only a partial listing of sedation courses. Please consult our www.sedationce.com for updates and new programs. Two ways to Register: e-mail us at sedationce@aol.com or call us at 214-384-0796
www.tda.org | April 2024 115
Approved PACE Program Provider FAGD/MAGD Credit. Approval does not imply acceptance by a state of provincial board of dentistry or AGD endorsement. 8/1/2018 to 7/31/2022. Provider ID# 217924
HIGHLIGHTS
A THOUGHTFUL ANALYSIS WITH THE ADVENT OF ORAL APPLIANCE THERAPY
Martin Denbar, DDS
Reprinted with permission from the American Academy of Dental Sleep Medicine.
128 TRENDING CULTURAL DRIVERS OF SMOKELESS TOBACCO FOR RECENT REFUGEE AND
STUDY
Moshtagh R. Farokhi, DDS, MPH, MAGD, FICD, FPFA
Jonathan A. Gelfond, PhD, MD
Saima Karimi Khan, DDS
Melanie V. Taverna, MSDH, RDH, FADHA, MAADH
Fozia A. Ali MD
Caitlin E. Sangdahl
Rahma Mungia, BDS, MSc, DDPHRCS 141 ASK THE POWERS CENTER
Rade Paravina, DDS, MS, PHD 142 ETHICS CORNER: UNDERSTANDING
Donald F. Cohen, DDS
Reprinted with permission from the American Dental Association.
Value for Your Profession: Accepting Credit Card Payments is Getting Increasingly Expensive. Here’s What You Want to Know—and
It’s
about the cover
Many Texans were lucky enough to experience the total solar eclipse on April 8, 2024, which occurs when the Moon passes between the Sun and Earth, completely blocking the face of the Sun.1 The eclipse began in North America at Mazatlan, Mexico, and started darkening Texas at Eagle Pass. Weather across the state was spotty, but people near the middle of the path of the total solar eclipse enjoyed a duration of over 4 minutes.2 The next total eclipse across the United States will be on August 23, 2044, according to NASA.
Resources
1. 2024 Total Solar Eclipse. [cited 2024 Apr 18]; Available from URL: https://science.nasa.gov/ eclipses/future-eclipses/eclipse-2024/ 2. Great Texan Eclipses! Annular eclipse of Oct 14 2023 and total eclipse of Apr 8 2024. [cited 2024 Apr 18]; Available from URL: https://www. greatamericaneclipse.com/eclipse-maps-andglobe/texas
Editorial Staff
Jacqueline M. Plemons, DDS, MS, Editor
Juliana Robledo, DDS, Associate Editor
Nicole Scott, Managing Editor
Barbara Donovan, Art Director
Lee Ann Johnson, CAE, Director of Member Services
Editorial Advisory Board
Ronald C. Auvenshine, DDS, PhD
Barry K. Bartee, DDS, MD
Patricia L. Blanton, DDS, PhD
William C. Bone, DDS
Phillip M. Campbell, DDS, MSD
Michaell A. Huber, DDS
Arthur H. Jeske, DMD, PhD
Larry D. Jones, DDS
Paul A. Kennedy, Jr., DDS, MS
Scott R. Makins, DDS, MS
Daniel Perez, DDS
William F. Wathen, DMD
Robert C. White, DDS
Leighton A. Wier, DDS
Douglas B. Willingham, DDS
The Texas Dental Journal is a peer-reviewed publication. Established February 1883 • Vol 141 | No. 3
Texas Dental Association
1946 S IH-35 Ste 400, Austin, TX 78704-3698
Phone: 512-443-3675 • FAX: 512-443-3031
Email: tda@tda.org • Website: www.tda.org
Texas Dental Journal (ISSN 0040-4284) is published monthly except January-February and August-September, which are combined issues, by the Texas Dental Association, 1946 S IH-35, Austin, TX, 78704-3698, 512-443-3675. PeriodicalsPostage Paid at Austin, Texas and at additional mailing offices. POSTMASTER: Send address changes to TEXAS DENTAL JOURNAL, 1946 S IH 35 Ste 400, Austin, TX 78704. Copyright 2023 Texas Dental Association. All rights reserved. Annual subscriptions: Texas Dental Association members $17. Instate ADA Affiliated $49.50 + tax, Out-of-state ADA Affiliated $49.50. In-state Non-ADA Affiliated $82.50 + tax, Out-of-state Non-ADA Affiliated $82.50. Single issue price: $6 ADA Affiliated, $17 Non-ADA Affiliated. For in-state orders, add 8.25% sales tax.
Contributions: Manuscripts and news items of interest to the membership of the society are solicited. Electronic submissions are required. Manuscripts should be typewritten, double spaced, and the original copy should be submitted. For more information, please refer to the Instructions for Contributors statement included in the online September Annual Membership Directory or on the TDA website: tda.org. All statements of opinion and of supposed facts are published on authority of the writer under whose name they appear and are not to be regarded as the views of the Texas Dental Association, unless such statements have been adopted by the Association. Articles are accepted with the understanding that they have not been published previously. Authors must disclose any financial or other interests they may have in products or services described in their articles.
Advertisements: Publication of advertisements in this journal does not constitute a guarantee or endorsement by the Association of the quality of value of such product or of the claims made.
116 Texas Dental Journal | Vol 141 | No. 3
contents
FEATURES 122
POSITIVE AIRWAY PRESSURE: IS IT STILL
GOLD STANDARD?
CONTINUOUS
THE
IMMIGRANTS AS KNOWLEDGE, ATTITUDES,
BEHAVIOR DETERMINANTS:
HEALTH NETWORK COLLABORATIVE
AND
A SOUTH TEXAS ORAL
THE TRANSGENDER PATIENT
120
121
Notice 140 Official
TDA House
Delegates 148
160
164 Classifieds 170 Index to Advertisers
In Memoriam
2025 Proposed Budget
Call to the 2024
of
Oral and Maxillofacial Pathology: Case of the Month
How to Find Out What
Costing You.








THE 11 TH LINDA C. NIESSEN GERIATRIC DENTISTRY SYMPOSIUM SUCCESSFUL DENTAL MANAGEMENT OF GERIATRIC PATIENTS: TIPS & TOOLS
MAY 31, 2024 8:30 AM TO 4:30 PM (CST) Texas A&M School of Dentistry - Room 605 - Dallas, TX Linda C Niessen, DMD, MPH, MPP Professor and Dean Kansas City University College of Dental Medicine Vice Provost for Oral Health Affairs Event Organizer Helena Tapias Perdigon, DDS, MS Clinical Associate Professor Texas A&M School of Dentistry Comprehensive Dentistry Department REGISTER ONLINE: https://www.eventbrite.com/e/11th-annual-linda-niessen-geriatric-symposiumregistration-853674773227 for additional information and to register, please scan this QR code: Questions? Contact Dr. Helena Tapias: 214.828.8940 or htapias@tamu.edu Randy F. Huffines DDS, FRCSEd Director of Geriatric Dentistry Quillen Medical Center Johnson City, TN 7 Hours CE credits provided through Texas A&M University School of Dentistry Office of Continuing Education
FRIDAY,

JKJ Pathology
Oral Pathology Laboratory
John E Kacher, DDS
¥ Available for consultation by phone or email
¥ Color histology images on all reports
¥ Expedited specimen shipping with tracking numbers
¥ Reports available online through secure web interface Professional, reliable service with hightechnology solutions so that you can better serve your patients. Call or email for free kits or consultation. jkjpathology.com 281-292-7954 (T) 281-292-7372 (F) johnkacher@jkjpathology.com Protecting

Board of Directors Texas Dental Association
PRESIDENT Cody C. Graves, DDS 325-648-2251, drc@centex.net
PRESIDENT-ELECT Georganne P. McCandless, DDS 281-516-2700, gmccandl@yahoo.com
PAST PRESIDENT Duc “Duke” M. Ho, DDS • 281-395-2112, ducmho@sbcglobal.net
VICE PRESIDENT, SOUTHWEST Richard M. Potter, DDS 210-673-9051, rnpotter@att.net
VICE PRESIDENT, NORTHWEST Summer Ketron Roark, DDS 806-793-3556, summerketron@gmail.com
VICE PRESIDENT, NORTHEAST Jodi D. Danna, DDS 972-377-7800, jodidds1@gmail.com
VICE PRESIDENT, SOUTHEAST Shailee J. Gupta, DDS 512-879-6225, sgupta@stdavidsfoundation.org
SENIOR DIRECTOR, SOUTHWEST Krystelle Anaya, DDS 915-855-1000, krystelle.barrera@gmail.com
SENIOR DIRECTOR, NORTHWEST Stephen A. Sperry, DDS 806-794-8124, stephenasperry@gmail.com
SENIOR DIRECTOR, NORTHEAST Mark A. Camp, DDS 903-757-8890, macamp1970@yahoo.com
SENIOR DIRECTOR, SOUTHEAST Laji J. James, DDS 281-870-9270, lajijames@yahoo.com
DIRECTOR, SOUTHWEST Melissa Uriegas, DDS 956-369-9235, meluriegas@gmail.com
DIRECTOR, NORTHWEST Adam S. Awtrey, DDS 314-503-4457, awtrey.adam@gmail.com
DIRECTOR, NORTHEAST Drew M. Vanderbrook, DDS 214-821-5200, vanderbrookdds@gmail.com
DIRECTOR, SOUTHEAST Matthew J. Heck, DDS 210-393-6606, matthewjheckdds@gmail.com
SECRETARY-TREASURER* Carmen P. Smith, DDS 214-503-6776, drprincele@gmail.com
SPEAKER OF THE HOUSE* John W. Baucum III, DDS 361-855-3900, jbaucum3@gmail.com
PARLIAMENTARIAN** Glen D. Hall, DDS 325-698-7560, abdent78@gmail.com
EDITOR** Jacqueline M. Plemons, DDS, MS 214-369-8585, drplemons@yahoo.com
LEGAL COUNSEL Carl R. Galant
*Non-voting member • **Non-voting





























118 Texas Dental Journal | Vol 141 | No. 3
patients, limiting your liability
your



www.tda.org | April 2024 119 DQ2676 (2.23) Scan the QR code to learn more about partnering with DentaQuest! PROMOTING DENTAL PROVIDER DIVERSITY TO IMPROVE THE ORAL HEALTH OF ALL WELCOME TO PREVENTISTRY ®
in memoriam
Those in the dental community who have recently passed
Joseph J Dusek
Houston
7/29/49–6/7/23
Good Fellow: 2002
Life: 2014
Harvey W Fodell
Houston
12/1/30–12/28/23
Good Fellow: 1983
Life: 1995
Fifty Year: 2008
Robert L Ellis
Houston
9/6/28–11/16/23
Good Fellow: 1983
Life: 1993
Fifty Year: 2008
Herbert E Eubanks Jr
Houston
9/14/30–8/5/23
Good Fellow: 1981
Life: 1995
Fifty Year: 2007
William H Greenlee
Dallas
6/19/32–2/20/24
Good Fellow: 1985
Life: 1997
Fifty Year: 2008
Jeran J Hooten
Austin
10/9/42–2/13/24
Good Fellow: 1996
Life: 2007
Fifty Year: 2016
James R Mellard
New Braunfels
9/20/52–2/29/24
Good Fellow: 2008
Life: 2017
Clarence E Musslewhite Jr
Houston
6/20/30–1/9/24
Good Fellow: 1980
Life: 1995
Fifty Year: 2005
Paul L Pearce
Llano
6/23/30–2/19/24
Good Fellow: 2010
Life: 2007
Charles B Schmidt Jr
Spring
11/4/29–2/20/24
Good Fellow: 1982
Life: 1994
Fifty Year: 2005
Harold L Smith
Tyler
2/13/23–10/13/23
Good Fellow: 1976
Life: 1988
Fifty Year: 2002
Harry G Wilson Jr
San Antonio
12/28/38–11/16/23
Good Fellow: 1991
Life: 2003
Fifty Year: 2016
James H Wooham
Ingram
11/10/45–2/17/24
Good Fellow: 1997 Life: 2010
120 Texas Dental Journal | Vol 141 | No.3
Notice

Texas Dental Association Delegates
Per the TDA Bylaws, “The proposed annual budget shall be submitted by the Board of Directors to the members of the House of Delegates at least thirty (30) days prior to the opening of the annual session of the House of Delegates.”
Thus, the 2025 Proposed Budget, including a financial report from TDA Secretary-Treasurer Dr Carmen Smith, will be available on tda.org no later than April 15, 2024.
We are pleased to announce...
Hulen Dental
Mark Malone, D.D.S. has acquired the practice of have acquired the practice of Houston, Texas Fort Worth, Texas We are pleased to have represented all parties in these transitions. & David C. Sun, D.D.S.
Veronica Y. Chen, D.D.S.
Jini P. Kuruvilla, D.D.S.
Practices For Sale
MULTI-MILLION DOLLAR PRACTICE OPPORTUNITY: Large GP located north of Houston is available with real estate. The office is in a stand-alone building with 8 ops and is in excellent condition, with digital x-rays, Pano, and paperless charts. The office operates 45 hours per week with 3 clinicians. There is over 6,500+ active patients, 70% Medicaid & 30% PPO/FFS, with an average of 96 new patients per month. Opportunity ID: TX-01979
FANTASTIC GROWTH POTENTIAL: Cypress GP in a busy retail center with great visibility and foot traffic. This 3,000 sq. ft. office has 8 ops, 6 of which are equipped with 2 additional plumbed and ready for expansion. The office is all digital with paperless patient files and Open Dental operating software. With over 1,200 active FFS/PPO patients, this practice has the location and potential to be a huge collecting office with the right motivated purchaser. Opportunity ID: TX-01929
ROOM FOR GROWTH WITH POSSIBLE IMMEDIATE MERGER OPTION: Fort Worth GP located in the retail level of a live/work/play community. The office has 3 ops fully equipped with digital x-ray, Pan and paperless patient files; 2 additional ops are available. The office is in excellent condition with newer equipment. The practice currently operates on 4 doctor days and one hygiene day per week. This practice has over 2,000 active patients that are a blend of 20% FFS, 65% PPO, & 15% Medicaid. Opportunity ID: TX-01913
FANTASTIC RETAIL LOCATION: Plano GP in a highly visible retail center. This practice operates with the owner and 1 PT associate, is open 7 days a week and provides regular dental care as well as emergency services. The practice has over 1,750 active patients who are ~20% FFS, ~70% PPO, and less than 10% Medicaid. The office has 4 fully equipped ops and is in excellent condition. This is a great opportunity for growth by capitalizing on the existing patient base and expanding services. Opportunity ID: TX-01829
www.tda.org | April 2024 121 Since 1968
Go to our website or call to request information on other available practice opportunities! 800.232.3826 Practice Sales & Purchases Over $3.2 Billion www.AFTCO.net

Continuous Positive Airway Pressure: Is It Still the Gold Standard?
A Thoughtful Analysis With the Advent of Oral Appliance Therapy
Martin Denbar, DDS
Austin Apnea & Snoring Therapy; Diplomate, American Board of Dental Sleep Medicine; Assistant Clinical Professor (non-principled) Texas A&M School of Medicine
Adapted and printed with permission from the American Academy of Dental Sleep Medicine. Available from: www.jdsm.org. The views presented in this paper do not necessarily reflect those of the JDSM/AADSM.
It can be said that the term ‘gold standard’ is assumed to mean near perfection.
But what is the definition of this term and how should it be applied to the field of airway management? Segen’s Medical Dictionary defines gold standard as “a method or procedure that is widely recognized as the best available.” McGraw-Hill Concise Dictionary of Modern Medicine defines it as “the best or most successful diagnostic or therapeutic modality for a condition against which new tests or results and protocols are compared.” An excellent conceptual analysis article in the Frontiers of Psychology stated that “the phrase “gold standard” is often used to characterize an object or procedure described as unequivocally the best in its genre, against which all others should be compared”.1 Analysis of the use of this term should be updated when describing continuous positive airway pressure (CPAP) and its role in treatment of obstructive sleep apnea (OSA) when compared with the use of an oral appliance.2
From a practical viewpoint, for any therapy to be successful it should be affordable, have a high patient compliance rate, easy to use, have minimal or comparable adverse effects, and customizable to meet the unique needs of each patient. Any product, test, or procedure that is considered the gold standard should score above all competing therapies, in this instance oral appliance therapy (OAT), for each of the aforementioned criteria. Let’s review the comparisons.
122 Texas Dental Journal | Vol 141 | No. 3
LETTER TO THE EDITOR reprint
How does CPAP compare to OAT when considering affordability? There have been few real comparisons because of the infancy of the field of OAT. One recent analysis stated, “A cost analysis of these two OSA treatment options presented at the 2021 Virtual Annual Meeting of the American Academy of Dental Sleep Medicine attempts a true head-to-head cost comparison. This analysis, based on Medicare fee schedules, suggests that CPAP may be cheaper initially, but that OAT comes with fewer costs over time.”3,4 Of course, there are fees being charged that are significantly higher than the Medicare rate at this time, but as more dental providers enter this field and insurance carriers begin to allow for in-network medical credentialling for dentists with reasonable contracted reimbursement schedules, costs will become more standardized, validating the aforementioned quote even more so.
How does CPAP compare with OAT as far as patient compliance is concerned? Significant numbers of studies have shown that OAT is much more accepted than CPAP by the patient. No matter how good a therapy is, it has to be used if treatment outcomes are to be successful.5-15 Also, research has shown that if the oral appliance is not as effective as CPAP for a given patient but worn every night versus sporadically as can be the case with CPAP, the resulting

treatment outcome between the two therapies is comparable.16-38
When considering ease of use of a particular therapy, the simplest answer is how comfortable and therefore compliant a patient is. In most studies to date, OAT has a much higher patient compliance and preferability rating than CPAP.15-20
The next issue is the adverse effects of using oral appliances versus CPAP. Almost every form of therapy has some degree of adverse effects. The real question is what the risk versus benefits are for the patient. One of the major adverse effects of wearing an oral appliance is the effect on a patient’s bite.21,27 There are very few major lifealtering or life-threatening issues when dealing with an occlusion that would justify nontreatment because sleep apnea is a life-threatening condition for the patient and potentially others (for example, falling asleep at the wheel and causing a car accident).22 Most dental issues can be managed with conservative titration techniques.21 CPAP-induced adverse effects are also a major issue when dealing with patient compliance. If patient compliance is affected by the presence of adverse effects, it would appear that CPAPinduced adverse effects have a greater effect than those caused by an oral appliance because OAT has a much higher acceptance and compliance rate.23-26
When reviewing the issue of customization for CPAP versus OAT to fit the patient’s needs, there can be a significant difference between the two therapies. Positive airway pressure devices come in different models depending on the needs of the patient, but they still involve headgear and/or a chin strap of some type and potentially
high air pressures, which can result in diminished compliance.29 Also, few if any patients have ever experienced wearing any form of face mask, whether while sleeping or awake, during their lifetime.
However, there are more than 100 different types of oral appliances to choose from, and some appliances can be easily modified to fit the patient’s unique dental needs.28 Most patients have either worn braces with or without a retainer, an athletic mouthguard, or an appliance for bruxism. Having an oral appliance is very familiar to patients’ past experiences with the aforementioned dental appliances.
Wearing a conventional CPAP device over an oral appliance (type 1 therapy) does improve the therapeutic result, but many patients still have to deal with the CPAP headgear/chin strap issue.31,32,37 With the advent of the Airway Management, TAP-PAP Interface, a customized chairside attachment connecting a CPAP device to the oral appliance without any headgear and chin strap (type 2 therapy), patients can experience even more comfort and freedom of movement even in the most severe cases of OSA.33-36 However, there are significant numbers of patients with severe OSA who have had success with type 1 therapy.39 Experienced dentists using either type 1 or type 2 therapy have with consistency successfully treated patients with an apnea-hypopnea index from 20 to 144 events/hour and nadirs down to 45%, having a full complement of teeth, and a partially edentulous or fully edentulous situation. Therefore, type 1 and type 2 combination therapy could really be considered the new gold standard.30-31,37,39 Oral appliances allow for more treatment flexibility and thereby enhance the efficacy of CPAP by creating the best of both worlds,
www.tda.org | April 2024 123
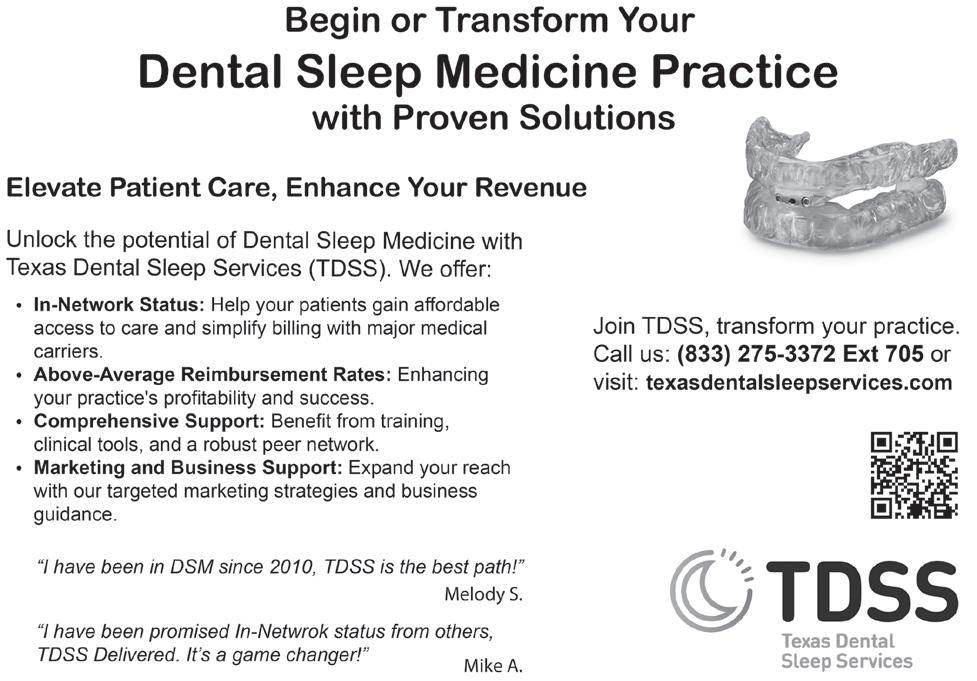
Oral appliance therapy (OAT)
reduced therapeutic pressures and minimal mandibular advancement. Also, this treatment modality reduces most adverse effects created by either individual therapy, resulting in a higher compliance rate.
It can be said that there have been no high-level studies using combination therapy with or without a TAP-PAP Interface. Almost all higher level studies are performed through dental or medical schools or other professional organizations, but there will continue to be a lack of studies until these entities decide to perform the needed research.39 Hundreds if not thousands of patients have already been successfully treated with either type 1 or type 2 therapy and studies have been performed, mostly at a lower level or with limited numbers of patients. Although few in number, some private practices have a wealth of well-documented information with more than 10 to 20 years of follow-up treatment data. It would be a significant loss to let this existing information go to waste.
In conclusion, the term ‘gold standard’ can be reconsidered when referring to CPAP therapy with the advent of OAT. Although new to most physicians and dentists, combination therapy has been available and used for more than 20 years and is really the new gold standard when considering all the issues discussed. Both therapies are needed, can coexist, and should be used to derive the most therapeutic and least invasive treatment for the patient.
CITATION
Denbar M. Continuous positive airway pressure: Is it still the gold standard? A thoughtful analysis with the advent of oral appliance therapy. J Dent Sleep Med. 2023;10(4).
REFERENCES
1. Brodsky SL, Lichtenstein B. The gold standard and the Pyrite Principle: Toward a supplemental frame of reference. Front Psychol. 31 March 2020.
2. Duggna PF. Time to abolish “gold standard”. BMJ.1992;304 (6841):1568-1569.
3. Rapaport L. Which costs more: CPAP or oral appliance therapy? Sleep Review. Jan 18, 2022. Accessed September 13, 2023. https://sleepreviewmag.com/ sleep-treatments/therapy-devices/ oral-appliances/costs-cpap-oralappliance-therapy/
4. de Vries GE, Hoekema A, Vermeulen KM, et al. Clinicaland cost-effectiveness of a mandibular advancement device versus continuous positive airway pressure in moderate obstructive sleep apnea, J Clin Sleep Med. 2019;15(10):1477-1485.
5. Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: A flattened curve. J Otolaryngol Head Neck Surg. 2016; 45: 43.
6. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245–258.
7. Aarab G, Lobbezoo F, Heymans MW, Hamburger HL, Naeije M. Longterm follow-up of a randomized controlled trial of oral appliance therapy in obstructive sleep apnea. Respiration. 2011;82(2):162-168.
8. Ferguson KA, Ono T, Lowe A, Keenan SP, Fleetham JA. A randomized crossover study of an oral appliance vs nasal-continuous positive airway pressure in the treatment of mild-moderate obstructive sleep apnea. Chest. 1996; 109(5):1269-1275.
9. Randerath WJ, Heise M, Hinz R, Ruehle K-H. An individually adjustable oral appliance vs continuous positive airway pressure in mild-to-moderate obstructive sleep apnea syndrome. Chest. 2002; 122(2):569-575.
10. Tan YK, L’Estrange PR, Luo YM, et al. Mandibular advancement splints and continuous positive airway pressure in patients with obstructive sleep apnoea: A randomized cross-over trial, Eur J Orthod. 2002;24(3):239-249.
11. Salepci B, Caglayan B, Kiral N, et al. CPAP adherence of patients with obstructive sleep apnea. Respir Care. 2013;58(9):1467-1473
12. Summer J, Singh A. Oral appliances for sleep apnea. Sleep Foundation. September 30, 2022. Accessed September 13, 2023. https://www. sleepfoundation.org/sleep-apnea/ oral-appliance-for-sleep-apnea
13. Radmand R, Chiang H, Di Giosia M, et al. Defining and measuring compliance with oral appliance therapy. J Dent Sleep Med 2021;8(3).
14. Obstructive sleep apnea: Study finds excellent agreement between subjective and objective compliance with oral appliance therapy. Science News. American Academy of Dental Sleep Medicine, June 13, 2011.
15. Basyuni S, Barabas M, Quinnell T. An update on mandibular advancement devices for the treatment of obstructive sleep apnoea hypopnoea syndrome. J Thorac Dis. 2018;10(Suppl 1):S48-S56.
16. Phillips CL, Grunstein RR, Darendeliler MA, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive
124 Texas Dental Journal | Vol 141 | No. 3
sleep apnea: A randomized controlled trial. Am J Respir Crit Care Med. 2013; 187(8):879-887.
17. Sutherland K, Phillips CL, Cistulli PA. Efficacy versus effectiveness in the treatment of obstructive sleep apnea: CPAP and oral appliances. J Dent Sleep Med. 2015;2(4):175–181.
18. Sutherland K, Cistulli PA. Oral appliance therapy for obstructive sleep apnoea: State of the art. J Clin Med. 2019;8(12):2121.
19. Li W, Xiao L, Hu J. The comparison of CPAP and oral appliances in treatment of patients with OSA: A systematic review and meta-analysis. Respir Care. 2013;58(7):1184-1195.
20. Kalonia N, Raghav P, Amit K, Sharma P. Effect of mandibular advancement through oral appliance therapy on quality of life in obstructive sleep apnea: A scoping review. Indian J Sleep Med. 2021;16(4):125–130.
21. Sheats RD, Schell TG, Blanton AO, Braga PM. Management of side effects of oral appliance therapy for sleep-disordered breathing. J Dent Sleep Med. 2017;4(4):111-125.
22. Jean-Louis G, Zizi F, Clark LT, Brown CD, McFarlane SI. Obstructive sleep apnea and cardiovascular disease: Role of the metabolic syndrome and its components. J Clin Sleep Med. 2008;4(3):261–272.
23. Ghadiri M, Grunstein RR. Clinical side effects of continuous positive airway pressure in patients with obstructive sleep apnoea. Respirology. 2020;25(6):593-602.
24. Koutsourelakis E, Vagiakis E, Perraki M, et al. Nasal inflammation in sleep apnoea patients using CPAP and effect of heated humidification. Eur Respir J. 2011;37(3):587-594.
25. Brown LK. Up, down, or no change: Weight gain as an unwanted side
effect of CPAP for obstructive sleep apnea. J Clin Sleep Med. 2020;16(suppl_1):21S–22S.
26. Rotty M-C, Suehs CM, Mallet J-P, Martinez C, Borel J-C. Mask sideeffects in long-term CPAP-patients impact adherence and sleepiness: the InterfaceVent real-life study. Respir Res. 2021;22(1):17.
27. Fritsch KM, Iseli A, Russi EW, Bloch KE. Side effects of mandibular advancement devices for sleep apnea treatment. Am J Respir Crit Care Med. 2001;164(5):813-818.
28. Burhenne M. Sleep apnea oral appliances: Types, uses, and how they work. August 7, 2023. Accessed September 13, 2023. https://askthedentist.com/sleepapnea-oral-appliance/
29. Summer J, Singh A. What are the different types of CPAP machines? Sleep Foundation. August 31, 2023. Accessed September 13, 2023
30. Custom TAP-PAP. Airway Management. Accessed September 13, 2023. https://tapintosleep.com/ products/tap-pap-cs/
31. El-Solh AA, Moitheennazima B, Akinnusi ME, Churder PM, Lafornara AM. Combined oral appliance and positive airway pressure therapy for obstructive sleep apnea: A pilot study. Sleep Breath. 2011;15(2):203-208.
32. Upadhyay R, Dubey A, Kant S, Singh BP. Management of severe obstructive sleep apnea using mandibular advancement devices with auto continuous positive airway pressures. Lung India. 2015;32(2):158–161.
33. Prehn RS, Swick T. A descriptive report of combination therapy (custom face mask for CPAP integrated with a mandibular advancement splint) for longterm treatment of OSA with literature review. J Dent Sleep Med.
2017;4(2):29–36.
34. Denbar MA. A case study involving the combination treatment of an oral appliance and an auto-titrating CPAP unit. Sleep Breath. 2002 Sep;6(3):125-128.
35 Denbar MA, Essick GK, Schram P. Hybrid Therapy, A case study using hybrid therapy Sleep to treat a soon to be deployed soldier with obstructive and central sleep apnea. Sleep Review. June 2012.
36. Sanders AE, Denbar MA, White J, et al. Dental clinicians observations of combination therapy in PAP intolerant patients. Sleep Review. March 9, 2015,
37. Liu H-W, Chen Y-J, Lai Y-C, et al. Combining MAD and CPAP as an effective strategy for treating patients with severe sleep apnea intolerant to high-pressure PAP and unresponsive to MAD. PLoS One. 2017;12(10):e0187032.
38. Uniken Venema JAM, Doff MHJ, Sokolova D, Wijkstra PJ, van der Hoeven, JH, Stegenga B, Hoekema A. LONG-TERM OBSTRUCTIVE SLEEP APNEA THERAPY; A 10-YEAR FOLLOW-UP OF MANDIBULAR ADVANCEMENT DEVICE AND CONTINUOUS POSITIVE AIRWAY PRESSURE, JDSM. Abstracts, Issue 6.3
39. Tanaka Y, Adame JM, Kaplan A, Almeida FR. The simultaneous use of positive airway pressure and oral appliance therapy with and without connector: A preliminary study. J Dent Sleep Med. 2022;9(1).
SUBMISSION AND CORRESPONDENCE
INFORMATION: Submitted for publication June 7, 2023; Accepted for publication August 21, 2023.
Correspondence: Martin Denbar, DDS; Email: drmdenbar@tx-dss.com
DISCLOSURE STATEMENT
The author has no relevant conflicts of interest to disclose.
www.tda.org | April 2024 125











126 Texas Dental Journal | Vol 141 | No. 3 1. Do you have or have you considered an exit strategy? 2. How long do you plan on being a practice owner? If your health allows, would you like to continue practicing after that point? 3. Do you know what your practice is worth today? How do you know? When was your last Practice Valuation done? 4. Have you met with a financial planner and have a documented plan? Have you established a liquid financial resources target that will enable you to retire with your desired lifestyle/level of income? Henry Schein Dental Practice Transitions has your best interests has your best in mind throughout your career. Schedule a complime a complimentary consultation with your local Transition Sales Consultant today! If you answered no or do not know to any of these questions, let’s have a conversation! As a Practice Owner, You Should be Able to Answer the Following Questions: C ll: 866-335-2947 © 2024 Henry Schein, Inc. No copying without permission. Not responsible for typographical errors. 23PT2801 www.henryscheinDPT.com 866-335-2947 n C C n n B Y














www.tda.org | April 2024 127 Content on the Texas Health Steps Online Provider Education website has been accredited by the UTHSCSA Dental School Office of Continuing Dental Education, the Texas Medical Association, American Nurses Credentialing Center, National Commission for Health Education Credentialing, Texas State Board of Social Worker Examiners, and Accreditation Council for Pharmacy Education. Continuing Education for multiple disciplines will be provided for some online content. Join 250,000+ professionals who get free Continuing Education (CE) with Texas Health Steps Online Provider Education. Choose from a wide range of courses developed by trusted Texas experts, for dental experts like you. Courses such as caries risk assessment and dental quality measures are available 24/7. Texas Health Steps is health care for children from birth through age 20 who have Medicaid. Learn more at TXHealthSteps.com Practical dental CE, at your pace.

Trending
Cultural Drivers of Smokeless Tobacco
Attitudes, and Behavior Determinants: A South Texas Oral Health Network Collaborative Study
128 Texas Dental Journal | Vol 141 | No. 3
Knowledge,
for Recent Refugee and Immigrants as
AUTHORS
Moshtagh R. Farokhi, DDS, MPH, MAGD, FICD, FPFA
Corresponding Author, Professor/Clinical, The University of Texas Health Science Center at San Antonio, School of Dentistry, San Antonio, Texas; Department of Comprehensive Dentistry, Dental Director, The San Antonio Refugee Health Clinic, 7703 Floyd Curl Drive, San Antonio, Texas; Office: 210.567.4589; Email: farokhi@ uthscsa.edu
Jonathan A. Gelfond, PhD, MD
Professor, The University of Texas Health Science Center at San Antonio, Joe and Teresa Long School of Medicine, Department of Population Health Sciences, San Antonio, Texas
Saima Karimi Khan, DDS
Dentist, Lucent Dental Group, Private Practice Dentistry, Duncanville, Texas
Melanie V. Taverna, MSDH, RDH, FADHA, MAADH
Assistant Professor, The University of Texas Health Science Center at San Antonio, School of Dentistry, Department of Periodontics, Division of Dental Hygiene, San Antonio, Texas
Fozia A. Ali, MD
Professor/Clinical, The University of Texas Health Science Center at San Antonio, Joe and Teresa Long School of Medicine, Department of Family and Community Medicine, San Antonio, Texas
Caitlin E. Sangdahl
Practice-Based Research Network Coordinator, Supporting Older Adults through Research Network (SOARNet), South Texas Oral Health Network (STOHN). Institute for Integration of Medicine and Science, Health Science Center at San Antonio, San Antonio, Texas
Rahma Mungia, BDS, MSc, DDPHRCS
Associate Professor, The University of Texas Health Science Center at San Antonio, School of Dentistry, Department of Periodontics, San Antonio, Texas
ACKNOWLEDGEMENTS: This study was conducted by the South Texas Oral Health Network (STOHN), supported by the National Center for Advancing Translation Sciences, National Institutes of Health, through Grant UL1TR002645. This study was approved by the University of Texas Health San Antonio Institutional Review Board as an Exempt Study. All participants gave written or verbal consent to participate. The content is solely the authors’ responsibility and does not necessarily represent the official views of the NIH. All authors affirm that they have no financial affiliation (employment, direct payment, stock holdings, retainers, consultantships, patent-licensing arrangements, or honoraria) or involvement with any commercial organization with a direct financial interest in the subject or materials discussed in this manuscript, nor have any such arrangements existed in the past three years. The authors deny any conflicts of interest related to this study. We also acknowledge the work of Ms Anusha Kuchibhotla and Ms Kayla Hernandez, interns from the South Texas Oral Health Network. We want to acknowledge Ms Marissa Mexquitic, who was instrumental in this study’s IRB acquisition and all related administrative tasks.
FUNDING STATEMENT: The study described was supported by the Institute for Integration of Medicine & Science Community Engagement Small Projects Grant, UT Health San Antonio.
DISCLOSURE STATEMENT: The authors declare no conflict of interest.
DATA AVAILABILITY: The data that support the findings of this study are openly available at the South Texas Oral Health Network (STOHN) website: https://iims. uthscsa.edu/ce/wp-content/uploads/sites/18/2023/08/SmokelessTobaccoCEGr_DATA_ LABELS_2023-08-02_0932.xlsx
ABSTRACT
Objectives: Smokeless tobacco (SLT) use is a phenomenon that is detrimental to the health of adults worldwide and dramatically impacts the health of resettled populations. The prevalence of SLT has exponentially grown as a public health threat for the refugee and immigrant populations and is worthy of addressing. This research study examined the SLT cultural drivers of the Texas immigrant and refugee community, which led to their knowledge, perception, awareness, and cessation practices.
Methods: A convenience sample of refugee and immigrant community members resettled in San Antonio was recruited from the local Health Clinic and Center. Ninety-four consented participants completed a 29item survey that gathered participants’ demographics, SLT history, beliefs, knowledge, perceptions of the risk, awareness, availability of SLT, and cessation practices influenced by their culture.
Results: Of the 94 participants, 87.2% identified as Asian or natives of Afghanistan, Myanmar, and Pakistan. 70% reported SLT as a ‘feel good’ or recreational use, while 33% used it to relieve stress. Thirty-five percent stated they continuously use or have the desire to use SLT first thing in the morning. 86.2% perceived SLT products as unsafe for their health, 83% believed that it caused oral cancer and periodontal disease, and 76.6% were aware that SLT contains nicotine. 63.8% wished to stop using them, and 36.2% attempted to quit unsuccessfully but were unsuccessful. 54% sought cessation assistance from a family member, 32% from a friend, and only 12% from a healthcare provider.
Conclusion: SLT use is culturally prevalent within the immigrant and refugee populations. Participants’ quit attempts likely failed due to a lack of professional cessation support that was taxing due to language, interpretation, and literacy barriers. Healthcare providers are well-positioned to offer cessation interventions and reduce SLT use to achieve community well-being pathways.
Keywords
Culture, Oral Health, Health Belief Model, Refugees, Tobacco Use Cessation, Smokeless Tobacco Use
www.tda.org | April 2024 129
INTRODUCTION
Smokeless tobacco (SLT) use is a health determinant for millions of adults globally, especially those from Southeast Asian ethnic backgrounds.1 Evidence-based tobacco interventions are established pathways to prevent tobacco-related cancer.2,3 Of the 5.7 million adults (2.3%) who consume SLT products in the U.S., individuals of Asian ethnicity have the highest percentage (6.8%) of use.5,6 The 2016 U.S. Behavioral Risk Factor Surveillance System reports males (7.4%) are more likely to use SLT products than females (1.3%) in Texas.7
SLT use varies from inhaling to chewing products, where moist tobacco is placed between cheeks, lips, gums, and nasal cavities.8 Dry snuff powder originates from cured or fermented tobacco leaves.9 Dipping tobacco is shredded leaves that are easily pinched and placed inside the mouth. Snus is the moist tobacco placed behind the upper lip as loose or portioned sachets resembling miniature tea bags.10
Betel quid (Gutka) combines powdered tobacco, areca nut, slaked lime, and catechu.11 Mawa is areca nut, tobacco, and slaked lime, khaini is used with slaked lime, and Chimo is a syrup or paste from Venezuela.12,13 Naswar (Nass) is a dip used by Afghans made from sun-dried, powdered tobacco (N. rustica), ash, oil, flavoring agents (e.g., cardamom, menthol), coloring agents (indigo), and, in some areas, slaked lime placed in the oral cavity to achieve a euphoric sensation.14
Health consequences of SLT use, like cigarette smoking, include impairments in brain neurology that change cognitive and neurobehavioral functions.15 Tobacco-specific nitrosamines are tobacco alkaloids from curing,
fermentation, and aging as the most abundant carcinogens in chewing tobacco and snuff SLT products.16
Oral health consequences of SLT use include oral carcinomas and malignant disorders presenting as leukoplakia and erythroplakia.17 Snuff and betel leaf are risk factors for oral cavity cancer.18 SLT use is a predisposing risk factor for tooth decay, tooth loss, and periodontal disease.19,20
Resettlement depends on individuals choosing to move from their native land to live permanently in a foreign country (immigrants) or if they are forced to move (refugees).21 As the resettlements increase due to global conflicts, refugee patients seeking care present with a higher incidence of SLT-related oral lesions.22
Cultural implications of SLT use include activities between family and friends, where traditions, spiritual values, and religious beliefs are formed, SLT use is influenced by accessibility and affordability, except for lower socioeconomic South Asian populations that use SLT products to suppress hunger and boredom.14,23-26 In Saudi Arabia, the use of Shammah (SLT) is culturally and socially bonding family and friends, and in Venezuela, chimó (SLT) is a traditional practice from the pre-Columbian Indian era.27,28 Religion either prohibits SLT use or condones it as a stress-coping mechanism.29
Healthcare providers should be aware of cultural drivers leading to family and peers as primary SLT cessation support. We hypothesized that SLT cessation interventions are feasible when the providers 1) understand their refugee and immigrant patients’ cultural drivers and perspectives promoting SLT use and 2) recognize patient barriers deterring the cessation process.
METHODS
The Institutional Review Board (IRB) approved this study as HSC20220274EX for this study. The study was funded by a small grant from the Institute for Integration of Medicine and Science (IIMS) Community Engagement Small Project. Verbal and written consent for the study was obtained from all participants.
Participants
Participants were members of San Antonio’s local refugee and immigrant populations, such as any refugee or immigrant community member 18 years and older who used SLT as a lifetime or current practice and consented to participate. Participants were compensated with a $20 gift card for their time.
Ninety-four (n=94) participants were recruited from the San Antonio Refugee Health Clinic and El-Bari Community Health Center, where providers delivered healthcare to this local refugee and immigrant population. The study coordinators visited site-specific Health Fairs to recruit participants with assistance from certified interpreters to address language and health literacy barriers. Random participants were approached and asked about SLT product use. Participants who currently or had previously used SLT and consented were informed about the IRB protocol and surveyed.
Survey Design
The quantitative survey design included a 29-question multiple-choice, dichotomous, validated survey (Table 1).23 The survey design was a deliberate act to tackle participants’ reading and comprehension since they either spoke English as a second language or used an interpreter to complete
130 Texas Dental Journal | Vol 141 | No. 3
Table 1: THE VALIDATED SURVEY

Risk and Prevalence of Oral Cancer and Oral Leucoplakia of Smokeless Tobacco Use in Bangladesh
About You:
A1. Are you? Male Female
A2. How old are you? __________Years old
A3. What is your father’s job if he is working?
A4. What is your mother’s job if she is working? Smokeless Tobacco Habits:
B1. Have you ever used smokeless tobacco, such as Pan with Jarda, Gul, Pan Masala etc., even just a small amount?
Yes (If yes, then what brand or type of smokeless tobacco you used
No
[If you tried smokeless tobacco, then answer the next questions. Otherwise, go to B15.]
B2. How old were you when you first tried using smokeless tobacco?
I have never tried using smokeless tobacco
7 years old or younger
8 or 9 years old
10 or 11 years old
12 or 13 years old
14 or 15 years old
B3. During the past 30 days, how many days did you use smokeless tobacco?
0 days
1 or 2 days
3 to 5 days
6 to 9 days
10 to 19 days
20 to 29 days
All 30 days.
B4. How many times did you usually use smokeless tobacco per day, in the past 30 days?
I did not use smokeless tobacco during the past 30 days
Less than once per day
Once per day
2 to 5 times per day
6 to 10 times per day
11 to 20 times per day
More than 20 times per day.
B5. Do you ever use smokeless tobacco or feel like using smokeless tobacco first thing in the morning?
No, I don’t use or feel like using smokeless tobacco first thing in the morning
Yes, I sometimes use or feel like using smokeless tobacco first thing in the morning
Yes, I always use or feel like using smokeless tobacco first thing in the morning.
B6. How soon after you use smokeless tobacco, do you start to feel a strong desire to use it again that is hard to ignore?
I never feel a strong desire to use it again after
using smokeless tobacco
Within 60 minutes
1 to 2 hours
More than 2 hours to 4 hours
More than 4 hours but less than one full day 1 to 3 days 4 days or more.
B7. Why do you use smokeless tobacco? (You can have more than one answer for this question)
Taste
Smell
Pleasure
To feel better/good/Happy Because my friend is using it
Don’t Know.
Other reason (Please Specify)
B8. Do you want to stop using smokeless tobacco now?
I don’t use smokeless tobacco now Yes No
B9. During the past 12 months, did you ever try to stop using smokeless tobacco?
I did not use smokeless tobacco during the past 12 months
I tried, but not successful
Yes No
B10. If you have tried to stop, but are not successful, why?
B11. Have you ever received help or advice to help you stop using smokeless tobacco? (If necessary, you can give more than one answer)
Yes, from a program or professional Yes, from a friend
Yes, from a family member
No
B12. The last time you used smokeless tobacco during the past 30 days, how did you get it? (If necessary, you can give more than one answer)
I did not use smokeless tobacco during the past 30 days
I bought it in a store or shop in the school canteen
I bought it from a street vendor outside the school gate
I got it from someone else
I bought it from a store near to my house
I bought it from a store on the way to school I got it some other way. If you are willing to state how, please do
B13. During the past 30 days, did anyone refuse to sell you smokeless tobacco because of your age?
I did not try to buy smokeless tobacco during the past 30 days
Yes, someone refused to sell me smokeless tobacco because of my age
No, my age did not keep me from buying smokeless tobacco.
B14. During the past 30 days, did you see any health warnings on smokeless tobacco packages?
Yes, but I didn’t think much of them. Yes, and they led me to think about quitting smokeless tobacco or not starting smokeless tobacco.
No.
B15. If one of your best friends offered you smokeless tobacco, would you use it?
Definitely not
Probably not
Probably yes
Definitely yes
B16. Once someone has started using smokeless tobacco, do you think it would be difficult for them to quit?
Definitely not
Probably not
Probably yes
Definitely yes
Health Effects of Smokeless Tobacco Use:
C1. Do you think smokeless tobacco use is: Good for your health
Neither good nor bad for your health
Not good for your health
Don’t Know
C2. Are there benefits of smokeless tobacco to your body and health?
Yes, please name them
No
C3. Does smokeless tobacco cause less harm to your health compared to smoking tobacco?
Yes No
Don’t Know.
C4. Does smokeless tobacco cause white patches in the mouth?
Yes No
Don’t Know.
C5. Can smokeless tobacco cause oral cancer?
Yes No
Don’t Know
C6. Does smokeless tobacco cause gum disease (Gum disease is an infection of the gum that surrounds and supports your teeth)?
Yes No
Don’t Know
C7. Does smokeless tobacco cause heart disease?
Yes No
Don’t Know.
C8. Does smokeless tobacco contain nicotine? (Nicotine is a chemical that is present in cigarettes that makes people addicted)?
Yes No
Don’t Know.
www.tda.org | April 2024 131
survey questions. The survey was also planned with the cultural and linguistic assistance of refugee and immigrant community interpreters as an online REDCap30 web-based link. The design generated a culturally appropriate health-literate and plain language survey with illustrative aptitude.31 The survey gathered participants’ sociodemographic data, history of SLT use, types of SLT products, beliefs, knowledge, perceptions about SLT use, awareness, availability, and SLT cessation practices. The survey blended the cultural and behavioral attitudes, intentions, or motivational factors influencing behavior toward SLT use, adapted from the worldview of Social Cognitive Theory (SCT) and the Health Belief Model (HBM).32,33
The SCT model emphasizes internal and external influences by which individuals acquire and maintain behavior.32 SCT considers whether behavioral action will occur with expectations that shape whether an individual will engage in a specific behavior and why they engage in that behavior.
For this study, SCT questions related to the effect of social environment on the individual’s health behavior, such as using SLT products, enabled researchers to understand cultural and external factors that affect someone’s decision to use SLT.23 Environmental influences were trended as questions about cultural and religious appeals, social norms, peer pressure, recreational use, and stress. Environmental determinants of health indicated the availability and accessibility of SLT products and exposure to SLT advertisements.
The HBM model construction includes the perceived quitting benefits from a health or social perspective, perceived barriers or potential obstacles to
quitting, and perceived self-efficacy as the self-ability to stop smoking.33 HBM derives components of healthrelated behavior that influence strategies promoting healthy behaviors by preventing and treating health conditions.33 The HBM model also includes the decision-making process of accepting a recommended health action as internal (e.g., wheezing, difficulty swallowing) or external factors (e.g., culturally influenced advice from friends). Finally, this model braces an individual’s confidence in their ability to succeed.
For this study, HBM survey questions were related to understanding motives to partake in SLT use, and reasons for unsuccessful SLT quit attempts.23 Questions about the harmful effects of SLT measured participants’ perceived susceptibility, and items asking about
barriers determined reasoning for SLT use. Questions about attitude refer to the degree to which a person has a favorable or unfavorable evaluation of the behavior of interest.
Analysis
The study’s primary goal was to identify the perspectives of recently resettled refugee and immigrant SLT users. Percentages summarized categorical variables, and continuous outcomes defined the medians and interquartile ranges (25th and 75th percentiles). The hypothesis tested was that the characteristics of SLT users would vary by ethnicity. This was assessed using Chi-square tests for categorical variables and Kruskal-Wallis nonparametric tests for continuous outcomes. All testing was two-sided at a significance level of p=.05.

132 Texas Dental Journal | Vol 141 | No. 3
Areca Nut 23.4% n=22 Chewing Tobacco 12.8% n=12 Dissolvable Tobacco 1.1% n=1 Snuff Tobacco 28.7% n=27 Dip Tobacco 27.7% n=26
Paan/Betel Quid/
Table 2. PARTICIPANT SOCIODEMOGRAPHICS
Characteristic
Smokeless Use Yes
Education
No education at all Less than a high school diploma
High school diploma or GED
Some college Associate degree
Bachelor’s degree Graduate degree
Household Size
Income
Up-to (> or = to) $25,000
$25,001-$50,000
$50,001-$100,000
Over $100,000
Prefer not to answer
1n (%): Median (IQR)
2Kruskal-Wallis rank sum test: Pearson’s Chi-squared test
RESULTS
Sociodemographic data for the 94 participants trended an age range of 1978 years, where the majority (87%,n=82) were males compared to 13% (n=12) females. 87.2% self-identified as Asian or natives of Afghanistan, Myanmar,
and Pakistan. Participant’s highest level of education obtained varied by their ethnicity (p=.002). 31% (n=29, 36% Asians vs. 0% Latino and 0% Non-Latino White) had completed less than a high school education. Considering higher education, they received associate’s (2.1%, n=2), bachelor’s (15%, n=14), and
graduate degrees (11%, n=10). Most had annual incomes less than or equal to $25,000 (57%, n=54). Asian participants reported the lowest income level (64%, n=51) compared to 25% for Latinos, mainly from Venezuela, and 0% for nonLatino whites (p=.014, Table 2).
www.tda.org | April 2024 133
Age Unknown
Gender Female Male
Overall N = 941 94 (100%) 36 (31, 44) 1 12 (13%) 82 (87%) 17
29
18
4
2
14
10
5.00
54
17
8
7
8
Asian N = 801 80 (100%) 36 (31, 44) 0 6 (7.5%) 74 (92%) 17 (21%) 29 (36%) 15 (19%) 2
1
10
6
5.00
51
14
5
6
4
Latinos N = 121 12 (100%) 38 (34, 48) 1 6 (50%) 6 (50%) 0 (0%) 0 (0%) 3
1 (8.3%) 1
3 (25%) 4
5.00
3
3
2
1
3
Non-Latino/ White N = 21 2 (100%) 34 (32, 37) 0 0 (0%) 2 (100%) 0 (0%) 0 (0%) 0 (0%) 0 (0%) 0 (0%) 4.00 (3.50,
0 (0%) 0 (0%) 1 (50%) 0 (0%) 1 (50%) p-value2 0.8 <0.001 0.002 0.8 0.014
(18%)
(31%)
(19%)
(4.3%)
(2.1%)
(15%)
(11%)
(3.00, 6.00)
(57%)
(18%)
(8.5%)
(7.4%)
(8.5%)
(2.5%)
(1.3%)
(12%)
(7.5%)
(3.00, 7.00)
(64%)
(18%)
(6.2%)
(7.5%)
(5.0%)
(25%)
(8.3%)
(33%)
(5.00, 5.25)
(25%)
(25%)
(17%)
(8.3%)
(25%)
4.50)
Table 3. PARTICIPANT REPORTED DRIVERS OF SLT USE
Characteristic/
Recreational
Cultural Drivers
Socialization
1n (%)
2Pearson’s Chi-squared test
Smokeless Tobacco (SLT) Use and Beliefs According to the Survey
The frequency of SLT use was highest among the Asian refugee population, or 100% of the participants reported using SLT at some point. More than half (52%, n=49) used SLT every day monthly. SLT use during the past 30 days before the survey ranged from 2-5 times daily (30%, n=28) to 6-10 times a day (16%, n=15), and 29.8% (n=28) had not used any SLT products in the past 30 days.
SLT Types of product use and dependence indicated that snuff tobacco (28.7%, n=27), dip tobacco (27.7%, n=26), Paan/betel quid/areca nut (23.4%, n=22), and chewing tobacco (12.8%, n=13), were most frequently forms used (Figure 1). SLT dependence rates were limited to 20.2% (n=19) of participants who reported a strong desire to use SLT within a 60-minute window of waking up. Many participants (76.6%, n=72) started using SLT at 15 years or older, and 3.2% (n=3) reported first-time use at 7 years or younger.
Drivers of SLT use reported by the participants were to 1) to feel good or happy (34%, n=32), 2) use it as recreation (35%, n=33), 3) cope with stress (33%, n=31), 4) taste (18%, n=17), and because of peer pressure (12% n=Table 3 ). Participants reported that cultural drivers, including family (8.5%, n=8), social purposes (17%, n=16), and overall culture (7.4%, n=7, p=0.001), influenced their decision to use. Meanwhile, 9.6% (n=9) of the participants used SLT for the smell, and 11% (n=10) used it for curiosity (Table 3).
134 Texas Dental Journal | Vol 141 | No. 3
Drivers Taste Smell Feel Happy
Family Use
Other including loneliness
No Unknown Overall N = 941 17 (18%) 9 (9.6%) 32 (34%) 33 (35%) 8 (8.5%) 16 (17%) 11 (12%) 7 (7.4%) 31 (33%) 10 (11%) 4 (4.3%) 8 (8.5%) 8 (100%) 86 Asian N = 801 14 (18%) 8 (10%) 31 (39%) 30 (38%) 5 (6.2%) 15 (19%) 8 (10%) 3 (3.8%) 25 (31%) 7 (8.8%) 3 (3.8%) 4 (5.0%) 4 (100%) 76 Latinos N = 121 2 (17%) 1 (8.3%) 1 (8.3%) 2 (17%) 3 (25%) 1 (8.3%) 2 (17%) 4 (33%) 4 (33%) 3 (25%) 1 (8.3%) 4 (33%) 4 (100%) 8 Non-Latino/ White N = 21 1 (50%) 0 (0%) 0 (0%) 1 (50%) 0 (0%) 0 (0%) 1 (50%) 0 (0%) 2 (100%) 0 (0%) 0 (0%) 0 (0%) 0 (NA%) 2 p-value2 0.5 0.9 0.069 0.3 0.086 0.5 0.2 0.001 0.12 0.2 0.7 0.004
Friends/peer Cultural Reason Stress Curious Don’t Know
Other Reason
Knowledge, risks, and perception for most participants (86.2%, n=81) was that SLT products were unsafe for their health, caused changes in their mouth (87.2%, n=82)), and caused oral cancer and gum disease (83%, n=78). When comparing SLT to smoking other tobacco use, 60.2% (n=56) perceived it to be less harmful, and a vast majority (76.6%, n=72) understood that the SLT products contained nicotine. The immigrants and refugees of Asian ethnicity were most likely to use SLT products despite an increased awareness (89%, n=71) of their harmful effects and because of cultural norms.
Awareness, availability, and warning statements indicated that participants purchased SLT products within the past 30 days at a convenience store or gas station (48%, n=45) or at a supermarket (22.3%, n=22). 46.8% (n=44) were aware of positive advertising to promote tobacco products at the point of sale, and 43.6% (n=41) did not recall any advertisements or promotions at the point of purchase. More than half (59.6%, n=56) did not notice any health warning statement on SLT packages, and 21% (n=17) reported having seen warning labels but did not think much of them.
STL cessation practices indicated that 63.8% (n=60) desired to stop using SLT, and 22.3% 9n=21) no longer used SLT. 36.2% (n=34) attempted to quit using SLT on their own unsuccessfully, 26.6% (n=25) did not quit at all, and 19% (n=18) stopped using SLT products within the past 12 months of the survey.
Reasons for unsuccessful cessation practices included increased levels of stress, anxiety, loneliness, addiction, and peer pressure as family or friends’ cultural offers. Most who attempted to quit SLT use received support from
their family (54%) and friends (32%). Only 12% received an intervention from a healthcare provider, and 1.1% from a health program. 45% percent believed that once someone started using SLT, quitting attempts would be difficult. 50% of non-Latino White (50%) and 51% of Asian participants reported that SLT was hard to quit, relative to the 0% of Latino participants (p<.001).
DISCUSSION
This study found that the most significant SLT use was among South Asians and presented as a cultural norm for predominantly male participants (100%), supported by research, even though some females prefer the SLT form of tobacco, as did the immigrant Venezuelan females for this study.34,35
We found that the prevalence of SLT use by participants was rooted in easy access to the products at nearby ethnic convenience stores, gas stations, or supermarkets catering to their purchasing needs, also reported by research.26 However, participant SLT use escalated due to their desire to feel happy or cope with stress and loneliness as determinants of health as supported by similar research highlighting immigrants’ cultural beliefs about using tobacco products (e.g., aiding digestion or sleep effectiveness).26
Our study found that participants’ dependence on SLT products, culturally acceptable SLT use, and stressors were risk factors inhibiting quitting. The dependent nature of SLT products explained why participants continued using them even though they understood the adverse health effects. Finally, culture and religion as recreation and social interactions influenced the profound use of SLT as supported by research from Pakistan, indicating
family, friends, and peer pressure significantly impacted SLT use.28-29,36
The limitations of this study include the self-reported survey and the proportion of Afghan participants as the dominant Asians, even though this composition is scaled to the current resettled population in Texas. Participants included individuals who considered Venezuela (Latinos), Afghanistan, Pakistan, and Myanmar (Asians) as their native lands and resettled in San Antonio. Considering the results may not precisely scale to other cities, the resettled population represents the global community using SLT products. Finally, our study trended frequent forms of Naswar (Afghans), Paan (Burmese), and Betel Quid (Pakistanis) for the current refugee and immigrant population served in San Antonio.
Clinical relevance connects oral to overall health outcomes as tobacco cessation intervention is prioritized by professional associations, including the American Academy of Family Physicians, and the American Dental Education Association, where providers are called to intervene.37,38 Healthcare providers should connect their vulnerable patients’ social, cultural, and addictive nature of SLT use with tailored interventions.
Providers should examine their refugee/immigrant patient SLT use by considering their limited access to care due to oral health literacy, financial, transportation, and interpretation challenges upon resettlement in the U.S.39 It was discouraging to realize that practitioners and community intervention programs played an insignificant role for this population’s SLT quit attempts.
www.tda.org | April 2024 135
Based on this study and supportive current research, future interventions should focus on tailored, culturally sensitive intervention approaches endorsed by the WHO.40 SLT interventions should focus on 1) resettlement-induced stressors and cultural norms combating SLT cessation, 2) the role that underlying trauma, loneliness, stress, and anxiety play in SLT quitting attempts and relapse challenges, 3) assessing the patient’s level of health literacy preinterventions, and 4) addressing patient barriers to quitting realizing that SLT tobacco cessation protocols are further complicated for refugee patients requiring time and interpretation services for cessation interventions.
CONCLUSION
This effort aims to empower providers to enhance their vulnerable resettled patient SLT cessation practices as participants either did not have access to professional support or were not offered tailored cessations.
Practitioners must aim for more upstream early cessation interventions in contrast to the traditional downstream late-stage cancer detection approach.29 The critical role of friends and family in supporting the use and the quitting process of SLT should not be underestimated. Cultural norms and easy access to SLT products intertwined with literacy and language barriers are trials providers encounter engaging with their newly resettled patients.
REFERENCES
1. Singh PK. Smokeless tobacco use and public health in countries of South-East Asia region. Indian J Cancer. 2014 Dec;51 Suppl 1: S1-2.
2. National Cancer Institute and Centers for Disease Control and Prevention. Smokeless Tobacco and Public Health: A Global Perspective. Bethesda, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Institutes of Health, National Cancer Institute. 2014; NIH Publication No. 14-7983.
3. Hecht SS, Hatsukami DK. Smokeless tobacco and cigarette smoking: chemical mechanisms and cancer prevention. Nat Rev Cancer. 2022 Mar;22(3):143-155.
4. Hatsukami D, Zeller M, Gupta P, et al. Smokeless Tobacco, and Public Health: A Global Perspective. 2014. The National Institute of Health Publication No. 14-7983.
5. Cornelius ME, Loretan CG, Wang TW, et al. Tobacco Product Use Among Adults - United States, 2020. MMWR Morb Mortal Wkly Rep. 2022 Mar 18;71(11):397-405.
6. Han BH, Wyatt LC, Sherman SE, et al. Prevalence and Correlates of Cultural Smokeless Tobacco Products among South Asian Americans in New York City. J Community Health. 2019 Jun;44(3):479-486.
7. Hu SS, Wang TW, Homa DM, et al. Cigarettes, Smokeless Tobacco, and E-Cigarettes: State-Specific Use Patterns Among U.S. Adults, 2017-2018. Am J Prev Med. 2022 Jun;62(6):930-942.
8. Chagué F, Guenancia C, Gudjoncik A, et al. Smokeless tobacco, sport and the heart. Arch Cardiovasc Dis. 2015 Jan;108(1):75-83.
9. Titova, OE., Baron JA, Michaëlsson, K, et al. Swedish snuff (snus) and risk of cardiovascular disease and mortality: a prospective cohort study of middle-aged and older individuals. BMC Med. 2021:19, 111.
10. Clarke E, Thompson K, Weaver S, et al. Snus: a compelling harm reduction alternative to cigarettes. Harm Reduct J. 2019; 16: 62.
11. Patidar KA, Parwani R, Wanjari SP, et al. Various terminologies associated with areca nut and tobacco chewing: A review. J Oral Maxillofac Pathol. 2015 JanApr;19(1):69-76.
12. Chadda R, Sengupta S. Tobacco use by Indian adolescents. Tob Induc Dis. 2002 Jun 15;1(2):111-119.
13. Gonzalez-Rivas JP, Santiago RJG, Mechanick JI, et al. Chimo, a Smokeless Tobacco Preparation, is Associated with a Lower Frequency of Hypertension in Subjects with Type 2 Diabetes. Int. J. Cardiovas. Sci. 2017;30(5): 373-379.
14. Nakhaei Moghaddam T, Mobaraki F, Darvish Moghaddam MR, et al. A review on the addictive materials paan masala (Paan Parag) and Nass (Naswar). SciMedicine Journal. 2019; 1(2): p. 64-73.
15. Nadar MS, Hasan AM, Alsaleh M. The negative impact of chronic tobacco smoking on adult neuropsychological function: a cross-sectional study. BMC Public Health. 2021;21, 1278.
16. Richter P, Hodge K, Stanfill S, et al. Surveillance of moist snuff: total nicotine, moisture, pH, un-ionized nicotine, and tobacco-specific nitrosamines. Nicotine Tob Res. 2008 Nov;10(11):1645-52.
17. Muthukrishnan A, Warnakulasuriya S. Oral health consequences of smokeless tobacco use. Indian J Med Res. 2018 Jul;148(1):35-40.
136 Texas Dental Journal | Vol 141 | No. 3
18. Khan SZ, Farooq A, Masood M, et al. Smokeless tobacco use and risk of oral cavity cancer. Turk J Med Sci. 2020 Apr 9;50(1):291-297.
19. Centers for Disease Control and Prevention. Factsheet: Smokeless Tobacco: Health Effects. December 2016. Available from: https://www. cdc.gov/tobacco/data_statistics/ fact_sheets/smokeless/health_ effects/index.htm.
20. Kamath KP, Mishra S, Anand PS. Smokeless tobacco use as a risk factor for periodontal disease. Front Public Health. 2014; Oct 20;2:195.
21. The United Nations Commission of Refugees. Available from: https:// www.unhcr.org/what-refugee.
22. Dreher A, Langlotz S, Matzat J, Parsons C. Immigration, Political Ideologies and the Polarization of American Politics. CESifo WP 8789. Munich 2020.
23. Ullah MZ, Lim JN, Ha MA, et al. Smokeless tobacco use: pattern of use, knowledge, and perceptions among rural Bangladeshi adolescents. PeerJ. 2018 Aug 21;6:e5463.
24. Rollins K, Lewis C, Edward Smith T, et al. Development of a Culturally Appropriate Smokeless Tobacco Cessation Program for American Indians. J Health Dispar Res Pract. 2018 Spring;11(1):45-55.
25. Auluck A, Hislop G, Poh C, et al. Areca nut and betel quid chewing among South Asian immigrants to Western countries and its implications for oral cancer screening. Rural Remote Health. 2009 Apr-Jun;9(2):1118.
26. Blank M, Deshpande L, Balster RL. Availability and characteristics of betel products in the U.S. J Psychoactive Drugs. 2008 Sep;40(3):309-313.
27. Moafa I, Crutzen R, van den Borne B, et al. Towards a better understanding of the psychosocial determinants associated with adults’ use of smokeless tobacco in the Jazan Region of Saudi Arabia: a qualitative study. BMC Public Health. 2022 Apr 13;22(1):732.
28. Kamen-Kaye D. Chimó: an unusual form of tobacco in Venezuela. Bot Mus Lealf Harv Univ. 1971 Jan 20; 23:1-59.
29. Farhadmollashahi L. Sociocultural reasons for smokeless tobacco use behavior. Int J High Risk Behav Addict. 2014; Jun 1;3(2): e20002.
30. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377-381.
31. Shohet L, Renaud L. Critical analysis on best practices in health literacy. Can J Public Health. 2006 MayJun;97 Suppl 2(Suppl 2):S10-3.
32. Bandura A. Health promotion from the perspective of social cognitive theory. Psychol. Health. 1998;13(4):623–649.
33. Pribadi ET, Devy SR. Application of the Health Belief Model on the intention to stop smoking behavior among young adult women. J Public Health Res. 2020 Jul 2;9(2):1817.
34. Hussain A, Zaheer S, and Shafique K. Individual, social and environmental determinants of smokeless tobacco and betel quid use amongst adolescents of Karachi: a school-based crosssectional survey. BMC Public Health. 2017; 17(1): 913.
35. Pampel F, Khlat M, Bricard D, et. al. Smoking Among Immigrant Groups in the United States: Prevalence, Education Gradients, and Male-toFemale Ratios. Nicotine Tob Res. 2020 Apr 17;22(4):532-538.
36. Mukherjea A, Morgan PA, Snowden LR, et al. Social and cultural influences on tobacco-related health disparities among South Asians in the USA. Tob Control. 2012 Jul;21(4):422-428.
37. American Association of Family Physicians. Ask and Act Tobacco Cessation Program. Available from: https://www.aafp.org/ family-physician/patient-care/careresources/tobacco-and-nicotine/ ask-act.html.
38. American Dental Association Position on Tobacco Cessation. Available from: https://www.ada. org/about/governance/currentpolicies#tobacco.
39. Farokhi MR, Muck A, Lozano-Pineda J, et al. Using Interprofessional Education to Promote Oral Health Literacy in a Faculty-Student Collaborative Practice. J Dent Educ. 2018 Oct;82(10):1091-1097.
40. World Health Organization (WHO) monograph on tobacco cessation and oral health integration. Geneva: World Health Organization; 2017. License: CC BY-NC-SA 3.0 IGO. Available from: https://www. who.int/publications/i/item/whomonograph-on-tobacco-cessationand-oral-health-integration.
www.tda.org | April 2024 137
OFFICIAL CALL TO THE 2024 TEXAS
DENTAL ASSOCIATION HOUSE OF DELEGATES
HOUSE OF DELEGATES:
In accordance with Chapter IV, Section 70, paragraph A-1 of the Texas Dental Association (TDA) Bylaws, this is the official call for the 154th Annual Session of the Texas Dental Association House of Delegates. All sessions of the House will be in the Hemisfair C-3 Ballroom of the Henry B. Gonzalez Convention Center, 900 E. Market Street, San Antonio, Texas. The opening session of the House will convene at 8:00 AM on Thursday, May 16, 2024. The second meeting of the House will be at 1:30 PM on Friday, May 17, 2024. The third meeting of the House will be at 8:00 AM on Saturday, May 18, 2024, followed by the fourth meeting at 10:00 AM until close of business.
Please see the TDA Meeting website for details and additional information (www.tdameeting.com).
Component Societies are urged to certify an accurate list of Delegates and Alternates to fill each of their seats on the floor of the TDA House of Delegates.
FINANCIAL FORUM:
The TDA Secretary-Treasurer will facilitate a question-and-answer financial forum at 10:00 AM, or 15 minutes after adjournment of the first meeting of the House of Delegates, on Thursday, May 16, 2024, open to all members who are present in the Hemisfair C-3 Ballroom of the Henry B. Gonzalez Convention Center, 900 E. Market Street, San Antonio, Texas (same room as the House of Delegates meetings).
Reference Committee hearings will follow the financial forum.
REFERENCE COMMITTEE
HEARINGS: Reference Committee hearings will be combined and facilitated to follow the financial forum at approximately 10:30 AM on Thursday, May 16, 2024, and open to all members who are present in the Hemisfair C-3 Ballroom of the Henry B. Gonzalez Convention Center, 900 E. Market Street, San Antonio, Texas (same room as the House of Delegates meetings). Hearings will conclude when no further testimony is presented.
Combined Topics:
• Administration, Budget, Building, House of Delegates, Membership Processing
• President’s Address, Miscellaneous Matters, Component Societies, Subsidiaries, Strategic Planning, Annual Session
• Dental Education, Dental Economics, Health and Dental Care Programs
• Legislative, Legal and Governmental Affairs
• Constitution, Bylaws, Ethics & Peer Review
The agenda for the Reference Committee hearings will be included in the Reference Committee section of the House Documents.
REFERENCE COMMITTEE
REPORTS: Reference Committee Reports will be made available in PDF format to the members of the House of Delegates (reports may be downloaded from any location with Internet access). Printed copies will not be provided.
TDA CANDIDATES FORUM:
The TDA “Meet the Candidates Forum” will be held on Friday, May 17, 2024, from 10:30 AM to 11:30 AM in the in the
Hemisfair C-3 Ballroom of the Henry B. Gonzalez Convention Center, 900 E. Market Street, San Antonio, Texas (same room as the House of Delegates meetings). There will not be an ADA candidates forum this year due to scheduling conflicts.
DIVISIONAL CAUCUSES:
Divisional Caucuses (Northwest, Northeast, Southwest, Southeast) will be facilitated at 5:30 PM on Friday, May 17, 2024, in the Convention Center and open to all current members— please see the TDA website for details and additional information. (Room assignments: SE-303C; SW-304A; NE304B; NW-304C).
DELEGATE MATERIALS:
In accordance with TDA Bylaws, the House documents will be available 30 days prior to the Annual Session of the House of Delegates. The supplements to the House documents, containing the agenda and subsequent reports, will be sent after the March 2024 TDA Board of Directors meeting. The minutes of the TDA Board shall be posted on the members’ side of the TDA website and made available to the general TDA membership once the minutes are approved by the TDA Board of Directors in accordance with Policy 26-2018-H. Delegates and alternates will receive all House Documents in PDF format. Printed copies of the House Documents will not be provided. Wireless internet access will not be available in the House chamber—please download all House materials on a fully charged laptop or device prior to attendance (charging stations will be centrally located in the meeting rooms).
138 Texas Dental Journal | Vol 141 | No. 3
Ask the Powers Center
UTHealth Houston School of Dentistry
John M. Powers, PhD, Center for Biomaterials & Biomimetics
By Rade D. Paravina, DDS, MS, PhD

Quo vadis, esthetic dentistry?
Part II: Composite resin overtreatment and social media appeal
Ronaldo Hirata DDS, MS, PhD, Leandro Augusto Hilgert DDS, MS, PhD, Camila S. Sampaio DDS, MS, PhD, Oswaldo Scopin de Andrade DDS, MS, PhD, Ginger Melo DDS, MS, André V. Ritter DDS, MS, MBA, PhD
Read the article in full at: https://onlinelibrary.wiley.com/doi/10.1111/jerd.13162
This article presents case reports highlighting over-treatments with resin composites, often misconceived as minimally invasive procedures.
Clinical Considerations
Tooth-colored restorative materials, such as ceramics and composites, have found widespread application to correct problems related to tooth color, shape, and alignment. When composite resin is used, these procedures can be done in a very conservative, cost-effective, and timely fashion. However, it is noteworthy that contemporary dental esthetic expectations are based on standards propagated by social media and other marketing and communications platforms. The abuse of and addiction to social media impacts can lead to unrealistic esthetic expectations and standards for both patients and dentists.
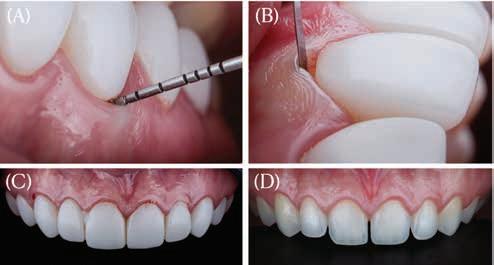
Conclusions
After a critical discussion on ceramic veneers published in part 1 of this 2-part series, this article directs attention toward what has become a trendy fashion, i.e., the use of direct composite resins as “non-prep” veneers in clinical situations that arguably required no restorative intervention at all. We further explore how social media influences the decisionmaking processes of both professionals and patients.
www.tda.org | April 2024 139
Professor, Department of Restorative Dentistry and Prosthodontics; Director, John M. Powers, PhD, Center for Biomaterials & Biomimetics (PCBB); Ralph C. Cooley, DDS, Distinguished Professor in Biomaterials; Vice President, American Academy of Esthetic Dentistry (AAED); Editor-in-Chief, Journal of Esthetic and Restorative Dentistry (JERD, Wiley, Impact Factor 3.2)
Case : (A, B) Overcountoured resin composites that were triggering gum inflammation in the patient. (C) Previous set of resin composite restorations involving pre molar to pre molar. (D) Removal of the patient’s resin restorations, revealing the natural, exquisite shades of her teeth.

140 Texas Dental Journal | Vol 141 | No. 3

Free Dental Practice Valuation Take the 1st step in selling your dental practice. Contact us to receive a free practice valuation. Terry Watson, D.D.S. Jeremy Brown, J.D. Frank Brown, J.D., LL.M. WatsonBrownSales.com 469-222-3200 * Call us for details on this offer.
ethics corner
TDA Council on Ethics and Judicial Affairs
understanding the transgender patient
Donald F. Cohen, DDS
This article is reprinted from The Journal of the American Dental Association and may not be copied, distributed, or modified without written permission from the American Dental Association. The article was reprinted with permission from The Journal of the American Dental Association (JADA) and published in The Journal of the American Dental Association (JADA), Volume 151, Issue 1, Daniel Cohen, Ethical Moment Understanding the transgender patient, Copyright American Dental Association (2020). ©2020 American Dental Association (ADA). Reprinted with permission from the ADA. All rights reserved.
QI have been contacted by one of my male patients who informed me that he is transitioning to female. The patient is a long-standing patient with a long relationship with my staff. What, if any, are the ethical considerations in preparing my staff, and how can we work to ensure the comfort of all involved?
AA transgender person is defined as a person who identifies differently than their assigned sex at birth.1 In 2016, the Williams Institute at the University of California, Los Angeles, stated that there are 1.4 million people (0.6% of US adults) who identify as transgender in the United States.2
According to the American Dental Association Principles of Ethics and Code of Professional Conduct (ADA Code), the profession makes a commitment to society that its members will adhere to high ethical standards of conduct.3 Applying the principles set forth in the ADA Code as well as the advisory opinions will help guide you and your staff members. Under Section 1, the principle Patient Autonomy (“selfgovernance”), “the dentist has a duty to respect the patient’s rights to self-determination and confidentiality.”3
To best reflect respect for patient autonomy and when communicating with the patient, one should use the patient’s preferred name and appropriate pronouns. The patient’s gender identity should be recorded in the chart or electronic record, and the office staff members should be made aware of the preferred gender identity. If you are not aware of which pronoun to use for a patient, you can ask the patient for their preferred pronouns. If this is uncomfortable, referring to the patient by their proper name is appropriate. This level of respect will enable “the patient to become involved in treatment decisions.”3
142 Texas Dental Journal | Vol 141 | No. 3
In Section 2, the principle Nonmaleficence (“do no harm”) is another principle to take into consideration. Under this principle, “The dentist has a duty to refrain from harming the patient.”3 This implies that we as professionals commit to being competent by means of minimizing any harm to our patients. Harm can take many forms, including barriers to care, limiting access to care, discrimination, perpetuation of stigma, and avoiding discussing potential risks.
Considering your own attitude and assessing your knowledge and acceptance of gender nonconforming patients is important to avoid harming patients and to better enable you to prepare your staff members for your expectation of their behavior and conduct. If you are uncomfortable or unsure of how to proceed or if this impacts oral health care in any way, this principle would obligate you to seek a consultation or make a referral.3
In Section 3, the principle Beneficence (“do good”) is also relevant. Under this principle, “The dentist has a duty to promote the patient’s welfare.”3
This section of the ADA Code addresses the removal of barriers to health care for all patients. Oral health care as well as health care in general must be positive, helpful, and nonjudgmental. Dentists “shall conduct themselves in such a manner as to maintain or elevate the esteem of the profession.”3
Creating a welcoming environment for all patients will create a nonbiased atmosphere and will support transgender patients, contributing to overall well-being.
Cultural sensitivity training on issues affecting transgender patients—including how to ensure a welcoming environment to all of our patients, how to develop an understanding of a patient’s gender identity and preferred name and pronoun usage, and how to be nonjudgmental in the provision of care—improves the patient experience.1
You and your staff should consider how to be sensitive by understanding people’s gender identities, which, as mentioned earlier, may be as simple as using the proper gender-neutral pronoun. This 1 change can improve the patient experience, as the patient will feel respected.4 A 2019 study found that study participants “reported greater satisfaction and less anxiety when referred to by their chosen name and pronouns.”5
In Section 4 of the ADA Code, the principle Justice (“fairness”) is directly on point. Under this principle, “The dentist has the duty to treat people fairly.”
In fact, Section 4.A. Patient Selection of the ADA Code was amended in 2018 with the following addition: “…[D]entists shall not refuse to accept patients into their practice or deny dental service to patients because of the patient’s race, creed, color, gender, sexual orientation, gender identity, national origin or disability (emphasis added).”3 This principle should be reiterated with staff members so that they understand the importance of the obligation.
The patient’s gender identity should be recorded in the chart or electronic record, and the office staff members should be made aware of the preferred gender identity. If you are not aware of which pronoun to use for a patient, you can ask the patient for their preferred pronouns. If this is uncomfortable, referring to the patient by their proper name is appropriate.
www.tda.org | April 2024 143
Finally, in Section 5, the principle Veracity (“truthfulness”) should be considered:
This principle expresses the concept that professionals have a duty to be honest and trustworthy in their dealing with people. Under this principle, the dentist’s primary obligations include respecting the position of trust inherent in the dentist-patient relationship, communicating truthfully and without deception, and maintaining intellectual integrity.3
Truthful communication is the best way to ensure trust; therefore, if there is any aspect of the patient’s transition that may impact their oral health care, this should be discussed.
In a 2018 editorial published in The Journal of the American Dental Association, Ludwig and Morrison concisely summarized the important role dentists play in the care of transgender patients, stating, “As dentists and dental specialists, we should continually aim for progress in our field such that we can provide comprehensive and compassionate care to all, including those patients identifying as transgender.”6 The ADA Code serves as a guide to remind you and your staff members that a transgender patient is a patient like any other and is entitled to respect, appropriate care and treatment, truthful communication, and privacy and confidentiality.
Dr Cohen is retired from oral and maxillofacial surgery and is an assistant professor, School of Dentistry, The University of Texas Health Science Center at Houston, Houston, TX. Dr Cohen is a member of the American Dental Association Council on Ethics, Bylaws and Judicial Affairs. Address correspondence to the American Dental Association Council on Ethics, Bylaws and Judicial Affairs, 211 E. Chicago Ave, Chicago, IL 60611.
Disclosure
Dr Cohen did not report any disclosures.
Ethical Moment is prepared by individual members of the American Dental Association Council on Ethics, Bylaws and Judicial Affairs (CEBJA) or guests of CEBJA, in cooperation with The Journal of the American Dental Association. Its purpose is to promote awareness of the American Dental Association Principles of Ethics and Code of Professional Conduct. Readers are invited to submit questions to CEBJA at 211 E. Chicago Ave., Chicago, IL 60611, email ethics@ada.org.
The views expressed are those of the author and do not necessarily reflect the opinions of the American Dental Association Council on Ethics, Bylaws and Judicial Affairs or official policy of the ADA.
References
1. Hann M, Ivester R, Denton GD. Bioethics in practice: ethical issues in the care of transgender patients. Ochsner J. 2017;17(2):144-145.
2. Flores AR, Herman JL, Gates GJ, Brown TNT. How Many Adults Identify as Transgender in the United States? Los Angeles, CA: The Williams Institute; 2016.
3. American Dental Association. American Dental Association principles of ethics and code of professional conduct, with official advisory opinions revised to November 2018. Available at: https://www.ada.org/w/media/ADA/Member%20 Center/Ethics/Code_Of_Ethics_Book_With_Advisory_Opinions_Revised_to_November_2018.pdf?la=en. Accessed October 12, 2019.
4. Deutsch MB, ed. Guidelines for the primary and gender-affirming care of transgender nonbinary people. Available at: https://transcare.ucsf.edu/guidelines. Accessed December 4, 2019.
5. Macdonald DW, Grossoehme DH, Mazzola A, Pestian T, Schwartz SB. “I just want to be treated like a normal person”: Oral health care experiences of transgender adolescents and young adults. JADA. 2019;150(9):748-754.
6. Ludwig DC, Morrison SD. Should dental care make a transition? JADA. 2018;149(2):79-80.
144 Texas Dental Journal | Vol 141 | No. 3

www.tda.org | April 2024 145
LAW OFFICES OF MARK J. HANNA
 Former General Counsel, Texas Dental Association
Former General Counsel, Texas Dental Association
• Representation Before the Texas State Board of Dental Examiners
• Medicaid Audits and Administrative Hearings
• Employment Issues—Texas Workforce Commission Hearings
• Administrative (SOAH) Hearings and Counsel
• Professional Recovery Network (PRN) Compliance
• Employment/Associateship Contract Reviews
• Practice Acquisition and Sales
• Business Organizations, PAs, PCs, and PLLCs
• Civil Litigation

146 Texas Dental Journal | Vol 141 | No. 3
2414 Exposition Blvd., Suite A1 • Austin, Texas 78703 • Phone: 512-477-6200 • Fax: 512-477-1188 • Email: mhanna@markjhanna.com Not Board Certified by the Texas Board of Legal Specialization Mark J. Hanna JD
EXPERIENCED LEGAL REPRESENTATION FOR TEXAS DENTISTS CONTACT YOUR LOCAL DENTAL SUPPLY FOR THE E-VAC TIP The Original E-VAC Tip • Inexpensive • Disposable • Non-Toxic • 100 Tips/Pk PROTECT YOUR PATIENT FROM PAINFUL TISSUE PLUGS • PROTECT YOUR EQUIPMENT FROM COSTLY REPAIRS E-VAC INC.© Phone: (509) 448-2602 • EMAIL:kenevac hotmail.com Made in USA FDA Registered


•
•
•
•
•


•
www.tda.org | April 2024 147 713.486.4411 go.uth.edu/Pathology • Complimentary biopsy kits • Delivery via FedEx, local courier or USPS • Diagnosis within two business days of receiving most biopsy specimens.
UT M.D. Anderson Cancer Center and UTHealth Medical School available for consultations as needed.
•
Affiliated with UT School of Dentistry at Houston. Our Pathologists: Specializing in:
Conventional biopsy testing
Cytopathology
Histochemistry
Immunohistochemistry
Direct immunofluorescence testing
Jerry E. Bouquot, DDS, MSD Ngozi N. Nwizu, BDS, MMSc, PhD
MCNA Dental is a provider-centered organization committed to helping dentists serve Medicaid and CHIP enrollees. We provide dentists with leading-edge technology and superb customer service support to reduce missed appointments and encourage patients to seek timely dental care. Visit our website at www.mcnatx.net for more information.
Kalu U.E. Ogbureke, BDS, DMSc, JD, MSc Nadarajah Vigneswaran, DMD, DrMedDent
ORAL and
maxillofacial pathology
case of the month
AUTHORS

Ajay Shakya
Post-doctoral Fellow, Department of Biomedical Sciences, Texas A&M University School of Dentistry; Intern, Maxradpath
Karan Dharia Director, Maxradpath
CALCIFICATIONS WITHIN ORAL AND MAXILLOFACIAL

SOFT TISSUES:
A DENTIST’S GUIDE TO DETECTION
Introduction
Cone Beam Computerized Tomography (CBCT) is an increasingly popular imaging technology used in dentistry. Cone-beam computed tomography (CBCT) is commonly used for comprehensive dental imaging and skull diagnosis, providing a wider field of view beyond the specific area of interest.1 CBCT has the ability to detect calcification in delicate soft tissue structures.2–6 Calcifications in the head and neck region can have various causes and implications, ranging from age-related to pathological or idiopathic.5 While many calcifications are asymptomatic and incidental findings, some require intervention or ongoing monitoring due to their clinical implications or association with systemic diseases.2,5 Dental professionals should have a thorough understanding of the significance of different types of calcifications. Depending on their location, characteristics, and impact on nearby structures, these calcifications may or may not necessitate referral, intervention, additional imaging, or long-term monitoring.2 Accurately identifying soft tissue calcifications requires knowledge of their common anatomical sites, distribution patterns, and morphologies, which aids in determining their tissue of origin. In this regard, cone-beam computed

Madhu Shrestha Clinical Assistant Professor, Department of Diagnostic Sciences, Texas A&M University School of Dentistry
tomography (CBCT) is particularly valuable as it enables a threedimensional and precise assessment of mineralized structures.7 Thorough examination of CBCT images, both within and outside the specific area of interest, is imperative since calcifications are commonly discovered incidentally.8,9 It is the duty of dental practitioners to identify, diagnose, treat, or make appropriate referrals for the management of any pathologies detected on radiographic images. This paper aims to provide practitioners with an understanding of the differential diagnosis of soft tissue radiopacities observed on dental radiographs. To accomplish this, a comprehensive knowledge of the anatomical structures in the head and neck region is crucial.
148 Texas Dental Journal | Vol 141 | No. 3
Abstract
Cone Beam Computerized Tomography (CBCT) can detect calcifications in soft tissue structures. While many calcifications are asymptomatic, some require intervention or monitoring due to their clinical implications. Dental professionals should understand the significance of different types of calcifications and their anatomical locations. CBCT enables precise 3-dimensional assessment of mineralized structures, making it valuable for identifying soft tissue calcifications. Thorough examination of CBCT images is essential as calcifications are often found incidentally. Dental practitioners are responsible for identifying, diagnosing, treating, or referring for the management of detected pathologies. This paper aims to enhance practitioners’ understanding of the differential diagnosis of soft tissue radiopacities observed on dental radiographs using anatomical knowledge of the head and neck region.

www.tda.org | April 2024 149
Various anatomical landmarks seen in a radiograph
1. Stylohyoid complex
The stylohyoid complex (SHC) consists of the styloid process (SP), the stylohyoid ligament (SHL), and the lesser horn of the hyoid bone.10 Positioned in front of the stylomastoid foramen, the SHC extends from the temporal bone’s styloid process (SP) to the hyoid bone (Figure 1). The SHL connects the SP to the lesser horn of the hyoid bone, and the ligament cannot be visualized on radiographs unless it undergoes ossification. The precise etiology of SHL calcification remains uncertain, various predisposing factors have been suggested: congenital factor, ligament stiffening with age, tonsillectomy, and head and neck trauma.11 Clinically, calcification of the stylohyoid ligament complex can result in facial pain, throat discomfort, otalgia, dysphagia, headache, or vertigo. Eagle syndrome is a condition that can occur when calcified stylohyoid ligaments (CSL) are present along with elongated styloid processes (ESP). Patients with this syndrome may experience sensations of a foreign body in the throat, odynophagia, dysphagia, as well as neck or facial pain.10,11 The close proximity of the SHC to the internal carotid artery can compromise cerebrovascular perfusion, resulting in symptoms such as dizziness, headache, syncope, and temporary visual loss.12 Therefore, it is crucial for dentists to accurately diagnose and assist patients in managing this condition.


2. Carotid artery
The carotid artery plays a vital role in supplying blood to the brain. Atherosclerotic conditions affecting the carotid artery can lead to neural ischemia, potentially resulting in a cerebrovascular accident or stroke.13 The risks associated with carotid artery calcification are more prevalent among older individuals and can be influenced by various factors, including hypercholesterolemia, obesity, physical inactivity, cigarette smoking, sleep apnea, head and neck radiation therapy, and male gender. These calcifications are typically located at the lower border of the third cervical vertebra and extend throughout the fourth cervical vertebra, approximately 1.5 to 2.5 cm inferior-posterior to the angle of the mandible.14 On axial projections of CBCT imaging, carotid artery calcifications typically appear as single or multiple “rice grains,” linear or curvilinear homogeneous opacifications located antero-laterally to the anterior tubercle of the transverse process (Figure 2). Before referring or initiating any medical treatment for carotid artery calcification, it is essential to consider the patient’s age, medical history, and current cardiovascular status. Calcifications when seen in veins are called phleboliths. Calcifications can also be seen on atrio-ventricular malformations.
150 Texas Dental Journal | Vol 141 | No. 3
Figure 1. Stylohyoid ligament (Sagittal section)
Figure 2. Carotid calcification (Axial section)

3. Triticeous cartilage
Triticeous cartilages (TC) are paired, ovalshaped structures that contribute to a complex of anatomical structures within the laryngeal skeleton region.15 Positioned centrally in the lateral thyrohyoid ligament between the superior horn of the thyroid cartilage and the major horn of the hyoid bone at the level of the third and fourth cervical vertebrae (C3-C4),the triticeous cartilage does not serve a known clinical function (Figure 3).16 However, when it becomes calcified, it can be mistaken for calcification in the carotid artery or other dystrophic calcifications in soft tissues. Given that calcified carotid atheromas pose a risk factor for stroke, it is vital for clinicians to distinguish between a calcified triticeous cartilage and a calcified carotid atheroma. On a panoramic radiograph, calcified Triticeous Cartilage (CTC) may appear as a faint, solitary opacification with a smooth, well-defined corticated border located just below the tip of the greater cornu of the hyoid bone (GCHB).17 On axial projections of CBCT imaging, CTC presents as a single ovoid homogeneous dense opacification resembling a “rice grain.”5 It is consistently positioned medio-posterior to the most distal part of the GCHB and is found within the superficial soft tissues of the lateral pre-vertebral space.
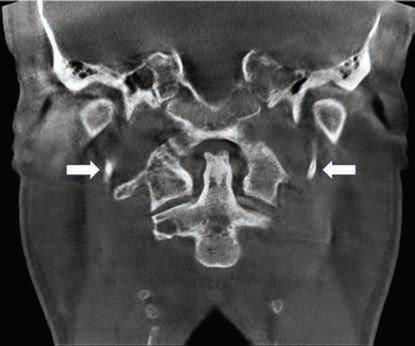
4. Thyroid cartilage
The thyroid cartilage, which is the largest and uppermost among the laryngeal cartilages, is situated directly beneath the hyoid bone.18 The triticeous cartilage is held in place by the thyrohyoid membrane, as well as the median and lateral thyrohyoid ligaments. The calcification of the thyroid cartilage is a progressive process that commonly begins at the posterior border, lower margin, and inferior horn of the cartilage.19 When observed on CBCT imaging, it often manifests as a non-continuous perpendicular extension in an anteroinferior direction from the terminal end of the greater cornu of the hyoid bone (Figure 4).15
www.tda.org | April 2024 151
Figure 3. Triticeous cartilage (Sagittal section)
Figure 4. Thyroid cartilage (Coronal section)
5. Sialoliths
A sialolith is a condition characterized by the accumulation of calcified material within the ducts or glandular tissue of the salivary glands. It ranks as one of the most prevalent conditions impacting the salivary glands, with viral parotitis (mumps) being the only disorder that occurs more frequently. Among the major salivary glands, the submandibular gland (Figure 5) is the most frequently affected (80%), followed by the parotid gland (19%), while calcifications in the sublingual gland are rare (1%).20,21 Sialoliths can also occur in minor salivary glands, primarily in the upper lip and buccal mucosa.22 In the submandibular gland, sialoliths typically form in the proximal portion of Wharton’s duct. On the other hand, calcifications in the parotid gland are usually found in Stenson’s duct. Parotid stones are smaller and often present as multiple calcifications. Cone beam computed tomography (CBCT) has shown exceptional accuracy in diagnosing sialolithiasis of the salivary glands, with a sensitivity and specificity of 99%. This underscores the valuable role of CBCT as a diagnostic tool for this condition.23
6. Lymph nodes
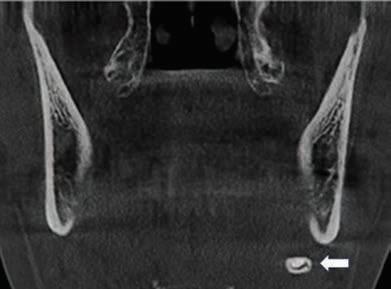
Calcification of lymph nodes in the head and neck area can be identified through conventional or CBCT imaging. Although typically asymptomatic, a healthcare professional may be able to detect calcified lymph nodes by palpation. It is possible for a single lymph node or multiple nodes to exhibit calcification. Dentists commonly come across calcified lymph nodes in regions such as the submandibular, submental, preauricular, and cervical areas.4,6 Radiographically, calcified lymph nodes typically appear as distinct, irregularly shaped opacities. Their irregular shape, often described as “cauliflower-like,” is a characteristic feature on radiographs (Figure 6).24 Differentiating between calcifications of lymph nodes and a sialolith in the submandibular duct or gland is essential. One distinguishing factor is that calcified lymph nodes are often observed in multiple numbers, whereas submandibular sialoliths are usually solitary.25 Currently, there are no specific treatment recommendations for calcified lymph nodes, and the primary approach involves acknowledging their presence and monitoring them through radiographic and clinical assessments.

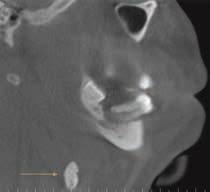


152 Texas Dental Journal | Vol 141 | No. 3
Figure 5. Sialolith in the submandibular gland (Coronal section)
Figure 6A.
Figure 6B.
Figure 6C.
Figure 6D.

7. Tonsilloliths
Tonsilloliths, commonly referred to as tonsil stones, are calcified formations that develop within enlarged tonsillar crypts.26 These crypts become filled with bacteria and organic debris, leading to the formation of these calcified structures.27,28 Tonsilloliths arise from dystrophic calcification occurring within the crypts of the palatine tonsils, which is a consequence of chronic inflammation. Usually, tonsilloliths are solitary and found on one side, although there are instances where they may appear as multiple or bilateral formations. They are composed of calcium salts such as hydroxyapatite or calcium carbonate apatite, along with oxalates, magnesium salts, and ammonium radicals.26 Tonsilloliths are usually small in size. The exact cause and underlying mechanisms of tonsilloliths formation remain unknown. Tonsilloliths commonly affect young adults who have a prolonged history of recurring sore throat. Individuals with tonsilloliths may either be asymptomatic or experience persistent throat irritation, an unpleasant taste and odor, ear pain (otalgia), or a feeling of having a foreign object in the throat.29 Tonsilloliths can range in size from a few millimeters to several centimeters. CBCT imaging reveals tonsilloliths as multiple clustered, ovoid, and densely opaque structures situated superficially to the lateral oropharyngeal airway space, resembling the shape of “rice grains”. When panoramic radiography reveals multiple opaque lesions with indistinct borders superimposed on the palatal uvula and the ramus, tonsilloliths should be considered as the primary differential diagnosis.30 A correct diagnosis helps avoid unnecessary further evaluations, including radiography and clinical examinations (Figure 7).26

8. Choroid plexus
The choroid plexuses (ChPs) are complex structures formed by specialized epithelial cells and fibroblasts in a vascular network, and are located within the lateral, third, and fourth brain ventricles.31 They perform various functions such as producing cerebrospinal fluid (CSF), secreting hormones and growth factors, eliminating toxins, regulating the sleep-wake cycle, supporting the generation of new neurons, and controlling inflammation. As people age, the choroid plexus tends to accumulate natural calcifications, primarily in the ventricular atria. Pathological processes like previous infections, inflammation, hemorrhage, and imbalances in calcium and phosphate levels can lead to premature or excessive mineralization of the choroid plexus. Therefore, it would be useful to know the typical time range for calcification to differentiate between normal physiology and abnormal conditions. The occurrence of choroid plexus calcification rises with age, although there is limited research available regarding calcifications in children. Choroid plexus calcifications are typically found in the atria of the lateral ventricles and are less common in the third and fourth ventricles or in individuals under the age of 9.32 Assessing ChPs changes associated with brain disorders using neuroimaging techniques may be a crucial step in effectively targeting these conditions for treatment (Figure 8).31
www.tda.org | April 2024 153
Figure 7. Pharyngeal tonsilloliths
Figure 8. Choroid plexus (Axial section)
9. Pineal calcification
The pineal gland, a cone-shaped organ located between the two cerebral hemispheres, plays a role in regulating the circadian rhythm by secreting the hormone melatonin.33 Following an initial growth phase, the size of the pineal gland typically stabilizes after the first 1-2 years of life. It is present in approximately two-thirds of adults and tends to increase in size with age.34 To identify the pineal gland and associated calcification on CBCT scans, it appears as a midline calcification in the posterior cranial fossa, positioned posteriorly and superiorly to the sella turcica.35 Pineal calcification is often incidentally found during large-FOV CBCT scans.35 While isolated pineal calcifications are usually harmless, they may indicate the presence of tumors if there is concurrent enlargement of the gland.36 Calcified deposits within the pineal gland predominantly comprise calcium and magnesium salts, giving rise to multiple concentrically calcified regions distributed throughout the gland, with larger aggregates located at the center.37 Calcifications larger than 1 cm or found in patients younger than 9 years old should be investigated further as they may indicate underlying tumors.38,39 It is essential to perform a thorough clinical and biochemical evaluation, and additional imaging may be required to exclude the early manifestation of a pineal tumor (Figure 8).
10. Falx cerebri

The dura mater, the thickest among the meningeal membranes, serves as a barrier within the intracranial structures and offers mechanical support.40 The falx cerebri is a dura fold that has a vertical shape resembling a sickle. It is positioned within the longitudinal fissure, between the cerebral hemispheres, and extends downward from the superior sagittal sinus. Calcification of the falx cerebri is uncommon in children but becomes more prevalent as age advances. Thus, if diffuse calcifications are detected in the dura of a young individual, it is important to consider conditions such as Gorlin-Goltz syndrome, meningioma, consequences of epidural or subdural hemorrhage, or disturbances in calcium-phosphate balance.40 In such cases, it is advisable to refer the patient for further evaluation and examination. In adults, calcification of the falx cerebri is frequently encountered. However, it can be mistaken for signs of recent intracranial bleeding. Generally, calcification of the falx cerebri is an incidental finding with no clinical significance, and the need for differential diagnosis arises only in a few cases.40,41 The use of CT scans with “bone windows” helps visualize the calcification of the falx cerebri more clearly (Figure 10).

154 Texas Dental Journal | Vol 141 | No. 3
Figure 9. Pineal calcification (Sagittal section)
Figure 10. Falx cerebri

11. Clinoid process
The interclinoid ligament links the anterior and posterior clinoid processes.42 Calcification of this ligament has been observed in studies conducted through autopsies and radiographic imaging. The calcification of interclinoid ligaments can present additional risks during surgical procedures conducted at the skull base, such as aneurysm treatment. It is essential to have knowledge about the existence and properties of these structures to facilitate surgical planning. Mineralized interclinoid ligaments have been observed in individuals of all age groups.43 The clinical importance of mineralized interclinoid ligaments is mainly due to their proximity to the paraclinoid internal carotid artery and cavernous sinus.43 In certain instances, the calcification of the interclinoid ligament has been misinterpreted as an aneurysm in the para-posterior communicating artery.44 The reported detection rate of calcified interclinoid ligaments is approximately 39% for partially calcified ligaments and 8% for fully calcified ligaments (Figure 11).45
12. Vertebral arteries
The vertebral arteries originate from the subclavian artery and supply blood to the occipital lobes and posterior cranial fossa.46 The variable and tortuous nature of the vertebral artery can pose challenges in identification, diagnosis, and may contribute to various pathologies.47 Vascular calcification refers to the deposition of calcium and phosphate in blood vessels.48 It is a significant contributor to approximately 90% of atherosclerotic lesions.49 The presence of calcified atheromatous plaque in the vertebral arteries is less commonly encountered due to the anatomic location of the vertebral arteries obscured by the cervical vertebrae.50 Panoramic radiographs cannot detect extracranial vertebral artery calcifications, unlike carotid artery calcifications. CBCT volumetric imaging enables the three-dimensional visualization of the neck, including the cervical vertebrae, foramina, and their calcified contents. Although the vessels themselves may not be directly visible in non-contrast CBCT reconstructions, the location and radiographic features of calcifications within the vessels can be used to diagnose calcified atheromas.51 Referral to a medical specialist upon detecting calcifications in CBCT reconstructions can help prevent major strokes (Figure 12).

www.tda.org | April 2024 155
Figure 11. Petroclinoid ligament calcification
Figure 12. Vertebral arteries
13. Antrolith
An antrolith is a calcified mass that develops in the maxillary sinus, formed by the buildup of mineral salts around a central core. The core can consist of various substances such as a blood clot, bone fragment, root tip, foreign object, or thickened pus or mucus.52 Maxillary antroliths are uncommon and generally do not produce symptoms. They are frequently detected as incidental findings during routine radiographic exams.53 It is important to understand the clinical significance of incidental antroliths in order to provide appropriate treatment and avoid unnecessary interventions.53 Radiographic evidence of sinusitis, including sinus lining thickening, polyps, and fluid levels, is often observed in conjunction with antroliths.52 In contrast, if a comparable calcification forms in the nasal cavity, it is termed a rhinolith. Antroliths are visualized as radiopaque masses of different sizes and shapes on radiographs. These conditions often coincide with inflammation in the maxillary sinus, which is characterized by thickening of the sinus lining and the presence of fluid. However, periapical, panoramic, and other standard radiographs have limited efficacy in detecting antroliths. Small antroliths can be overlooked on two-dimensional radiographs due to projection effects and the overlapping of anatomical structures.53 However, computed tomography (CT) and conebeam computed tomography (CBCT) offer detailed visualization of antroliths, including their location, characteristics, and associated inflammation. These imaging techniques provide clearer results without subjecting the patient to excessive radiation exposure (Figure 13).54
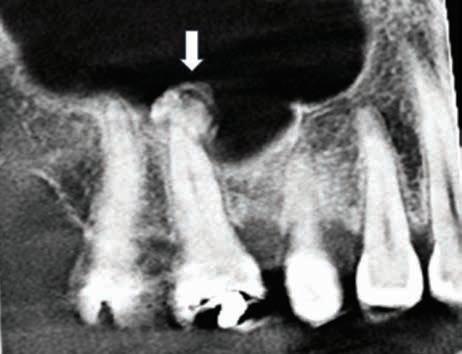
Histopathology of soft tissue calcification
Most of the soft tissue calcifications have varying degrees of calcified zones, usually globular lamellar structures that display alternating areas of basophilic and eosinophilic concentric layers. The size may also vary based on the time of formation and mineral content. Sometimes calcificationsmay be coated with a layer of bacteria, more likely in the context of a sialolith and may or may not fill the lumen of the duct where it is formed (Figure 13).

156 Texas Dental Journal | Vol 141 | No. 3
Figure 13. Maxillary antrolith (Sagittal section)
Figure 13. Histopathology showing a globular basophilic calcified material deposited in a concentric lamellated pattern within a ductal lumen (Courtesy of Dr Victoria Woo).
Conclusion
Soft tissue calcifications in the oral and maxillofacial region are relatively common, and while some may be benign, others require treatment or further investigation. They are often discovered incidentally during routine radiographic examinations. The location, number, distribution, and pattern of the calcifications are important factors to consider when interpreting radiographic images of soft tissue opacities. The presence of incidental findings increases the responsibility of the general dental practitioner and oral radiologist in providing valuable information for diagnosis and planning patient care.
References
1 Carter L, Farman AG, Geist J, Scarfe WC, Angelopoulos C, Nair MK, Hildebolt CF, Tyndall D, Shrout M; American Academy of Oral and Maxillofacial Radiology. American Academy of Oral and Maxillofacial Radiology executive opinion statement on performing and interpreting diagnostic cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008 Oct;106(4):561-2. doi: 10.1016/j.tripleo.2008.07.007. PMID: 18928899.
2. Barghan S, Tahmasbi Arashlow M, Nair MK. Incidental Findings on Cone Beam Computed Tomography Studies outside of the Maxillofacial Skeleton. Int J Dent. 2016;2016:9196503. doi: 10.1155/2016/9196503. Epub 2016 Jul 4. PMID: 27462350; PMCID: PMC4947649.
3. Çağlayan F, Sümbüllü MA, Miloğlu Ö, Akgül HM. Are all soft tissue calcifications detected by cone-beam computed tomography in the submandibular region sialoliths? J Oral Maxillofac Surg. 2014 Aug;72(8):1531.e1-6. doi: 10.1016/j. joms.2014.04.005. Epub 2014 Apr 13. PMID: 25037186.
4. Yeşilova E, Bayrakdar İŞ. Radiological evaluation of maxillofacial soft tissue calcifications with cone beam computed tomography and panoramic radiography. Int J Clin Pract. 2021 May;75(5):e14086. doi: 10.1111/ijcp.14086. Epub 2021 Mar 1. PMID: 33576139.
5. Missias EM, Nascimento E, Pontual
M, Pontual AA, Freitas DQ, Perez D, Ramos-Perez F. Prevalence of soft tissue calcifications in the maxillofacial region detected by cone beam CT. Oral Dis. 2018 May;24(4):628-637. doi: 10.1111/odi.12815. Epub 2018 Mar 13. PMID: 29224195.
6. Yalcin ED, Ararat E. Prevalence of soft tissue calcifications in the head and neck region: A cone-beam computed tomography study. Niger J Clin Pract. 2020 Jun;23(6):759-763. doi: 10.4103/njcp. njcp_269_19. PMID: 32525108.
7. Takeshita WM, Vessoni Iwaki LC, Da Silva MC, Tonin RH. Evaluation of diagnostic accuracy of conventional and digital periapical radiography, panoramic radiography, and cone-beam computed tomography in the assessment of alveolar bone loss. Contemp Clin Dent. 2014 Jul;5(3):318-23. doi: 10.4103/0976237X.137930. PMID: 25191066; PMCID: PMC4147806.
8. Price JB, Thaw KL, Tyndall DA, Ludlow JB, Padilla RJ. Incidental findings from cone beam computed tomography of the maxillofacial region: a descriptive retrospective study. Clin. Oral Impl. Res. 23 2012, 1261–1268.
9. Lopes IA, Tucunduva RM, Handem RH, Capelozza AL. Study of the frequency and location of incidental findings of the maxillofacial region in different fields of view in CBCT scans. Dentomaxillofac Radiol. 2017 Jan;46(1):20160215. doi: 10.1259/dmfr.20160215. Epub 2016 Oct 5. PMID: 27604390; PMCID: PMC5595051.
10. Ilgüy D, Ilgüy M, Fişekçioğlu E, Dölekoğlu S. Assessment of the stylohyoid complex with cone beam computed tomography. Iran J Radiol. 2012 Dec;10(1):21-6. doi: 10.5812/ iranjradiol.4891. Epub 2012 Dec 27. PMID: 23599709; PMCID: PMC3618901.
11. Al-Amad SH, Al Bayatti S, Alshamsi HA. Stylohyoid Ligament Calcification and Its Association With Dental Diseases. Int Dent J. 2023 Feb;73(1):151-156. doi: 10.1016/j. identj.2022.06.021. Epub 2022 Jul 26. PMID: 35902309; PMCID: PMC9875230.
12. Green BN, Browske LK, Rosenthal CM. Elongated styloid processes and calcified stylohyoid ligaments in a patient with neck pain: implications for manual therapy practice. J Chiropr Med. 2014 Jun;13(2):12833. doi: 10.1016/j.jcm.2014.06.006. PMID: 25685122; PMCID: PMC4322018.
13. MacDonald D, Chan A, Harris A, Vertinsky T, Farman AG, Scarfe WC. Diagnosis and management of calcified carotid artery atheroma: dental perspectives. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012 Oct;114(4):533-47. doi: 10.1016/j. oooo.2012.06.020. PMID: 22986250.
14. Friedlander AH, August M. The role of panoramic radiography in determining an increased risk of cervical atheromas in patients treated with therapeutic irradiation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Mar;85(3):33944. doi: 10.1016/s1079-2104(98)90020-8. PMID: 9540095.
15. Scarfe WC, Angelopoulos C. Maxillofacial Cone Beam Computed Tomography: Principles, Techniques and Clinical Applications. (Springer International Publishing, 2018). doi:10.1007/978-3-31962061-9.
16. Carter LC. Discrimination between calcified triticeous cartilage and calcified carotid atheroma on panoramic radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000 Jul;90(1):108-10. doi: 10.1067/ moe.2000.106297. PMID: 10884645.
17. Ahmad M, Madden R, Perez L. Triticeous cartilage: prevalence on panoramic radiographs and diagnostic criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005 Feb;99(2):225-30. doi: 10.1016/j.tripleo.2004.06.069. PMID: 15660097.
18. Barut O, Ahlqvist J, Garoff M, Johansson E, Johansson M, Wester P, Levring Jäghagen E. Calcifications in the neck region of patients with carotid artery stenosis: a computed tomography angiography study of topographic anatomy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020 May;129(5):523-530. doi: 10.1016/j. oooo.2019.09.018. Epub 2019 Oct 15. PMID: 31932251.
19. Wenaas AE, Tran B, Ongkasuwan J. The progression of thyroid cartilage calcification as it relates to the utilization of laryngeal ultrasound. Laryngoscope. 2016 Apr;126(4):913-7. doi: 10.1002/ lary.25582. Epub 2015 Sep 15. PMID: 26371447.
20. Rabinov K, Kell T Jr, Gordon PH. CT of the salivary glands. Radiol Clin North Am. 1984 Mar;22(1):145-59. PMID: 6709866.
21. DelBalso A. SALIVARY IMAGING. Oral Maxillofac. Surg. Clin. N. Am. 7, 387–422 (1995). https://doi.org/10.1016/S10423699(20)30838-4.
22. Jensen JL, Howell FV, Rick GM, Correll RW. Minor salivary gland calculi. A clinicopathologic study of forty-seven new cases. Oral Surg Oral Med Oral Pathol. 1979 Jan;47(1):44-50. doi: 10.1016/00304220(79)90100-2. PMID: 282564.
23. Dreiseidler T, Ritter L, Rothamel D, Neugebauer J, Scheer M, Mischkowski RA. Salivary calculus diagnosis with 3-dimensional cone-beam computed tomography. Oral Surg Oral Med
www.tda.org | April 2024 157
Oral Pathol Oral Radiol Endod. 2010 Jul;110(1):94-100. doi: 10.1016/j. tripleo.2010.03.013. PMID: 20610300.
24. Kumar G A, Deora SS. Dystrophic Calcification in the Oral Cavity Resulting in Mechanical Dysphagia: A Case Report and Review of Calcification in the Head and Neck Region. Cureus. 2020 Mar 30;12(3):e7469. doi: 10.7759/cureus.7469. PMID: 32328392; PMCID: PMC7174858.
25. Wells, Adam B. 1977-, “Incidence of soft tissue calcifications of the head and neck region on maxillofacial cone beam computed tomography.” (2011). Electronic Theses and Dissertations. Paper 1545. https://doi.org/10.18297/etd/1545.
26. Babu B B, Tejasvi M L A, Avinash CK, B C. Tonsillolith: a panoramic radiograph presentation. J Clin Diagn Res. 2013 Oct;7(10):2378-9. doi: 10.7860/ JCDR/2013/5613.3530. Epub 2013 Oct 5. PMID: 24298535; PMCID: PMC3843407.
27. Silvestre-Donat FJ, Pla-Mocholi A, EstellesFerriol E, Martinez-Mihi V. Giant tonsillolith: report of a case. Med Oral Patol Oral Cir Bucal. 2005 May-Jul;10(3):239-42. English, Spanish. PMID: 15876967.
28. Cerný R, Bekárek V. Tonsillolith. Acta Univ Palacki Olomuc Fac Med. 1990;126:267-73. PMID: 2151095.
29. Pruet CW, Duplan DA. Tonsil concretions and tonsilloliths. Otolaryngol Clin North Am. 1987 May;20(2):305-9. PMID: 3601388.
30. Capote, Ticiana S O, Marcela de AlmeidaGonçalves, Andréa Gonçalves and Marcelo Gonçalves. “Panoramic Radiography — Diagnosis of Relevant Structures That Might Compromise Oral and General Health of the Patient.” (2015).
31. Hubert V, Chauveau F, Dumot C, Ong E, Berner LP, Canet-Soulas E, Ghersi-Egea JF, Wiart M. Clinical Imaging of Choroid Plexus in Health and in Brain Disorders: A Mini-Review. Front Mol Neurosci. 2019 Feb 12;12:34. doi: 10.3389/fnmol.2019.00034. PMID: 30809124; PMCID: PMC6379459.
32. Gonzalez SM. Interpretation Basics of Cone Beam Computed Tomography. 2nd edition. John Wiley & Sons, 2021
33. Booth FM. The human pineal gland: a review of the “third eye” and the effect of light. Aust N Z J Ophthalmol. 1987 Nov;15(4):329-36. doi: 10.1111/j.14429071.1987.tb00092.x. PMID: 3435677.
34. Gheban BA, Rosca IA, Crisan M. The morphological and functional characteristics of the pineal gland. Med Pharm Rep. 2019 Jul;92(3):226-234. doi: 10.15386/mpr-1235. Epub 2019 Jul 31. PMID: 31460502; PMCID: PMC6709953.
35. Mutalik S, Tadinada A. Prevalence of pineal gland calcification as an incidental
finding in patients referred for implant dental therapy. Imaging Sci Dent. 2017 Sep;47(3):175-180. doi: 10.5624/ isd.2017.47.3.175. Epub 2017 Sep 21. PMID: 28989900; PMCID: PMC5620462.
36. Belay DG, Worku MG. Prevalence of pineal gland calcification: systematic review and meta-analysis. Syst Rev. 2023 Mar 6;12(1):32. doi: 10.1186/s13643023-02205-5. PMID: 36879256; PMCID: PMC9987140.
37. Whitehead MT, Oh C, Raju A, Choudhri AF. Physiologic pineal region, choroid plexus, and dural calcifications in the first decade of life. AJNR Am J Neuroradiol. 2015 Mar;36(3):575-80. doi: 10.3174/ajnr.A4153. Epub 2014 Oct 29. PMID: 25355815; PMCID: PMC8013049.
38. Grech R, Grech S, Mizzi A. Intracranial calcifications. A pictorial review. Neuroradiol J. 2012 Sep;25(4):427-51. doi: 10.1177/197140091202500406. Epub 2012 Sep 6. PMID: 24029036.
39. Kıroğlu Y, Callı C, Karabulut N, Oncel C. Intracranial calcifications on CT. Diagn Interv Radiol. 2010 Dec;16(4):263-9. doi: 10.4261/1305-3825.DIR.2626-09.1. Epub 2009 Dec 18. PMID: 20027545.
40. Tepe RD, Cakir Karabas H, Erturk AF, Ozcan I. Physiologic intracranial calcifications incidentally detected on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022 Nov;134(5):e281-e286. doi: 10.1016/j. oooo.2022.04.050. Epub 2022 May 1. PMID: 35701294.
41. Tsitouridis I, Natsis K, Goutsaridou F, Tsitouridis K, Tarazi L, Chondromatidou S, Papapostolou P, Papastergiou C, Emmanouilidou M. Falx Cerebri Ossification: CT and MRI Evaluation. Neuroradiol J. 2006 Nov 30;19(5):621-8. doi: 10.1177/197140090601900511. Epub 2006 Nov 30. PMID: 24351265.
42. Archana R, Anita R, Jyoti C, Punita M, Rakesh D. Incidence of osseous interclinoid bars in Indian population. Surg Radiol Anat. 2010 Apr;32(4):383-7. doi: 10.1007/s00276-009-0582-z. Epub 2009 Oct 28. PMID: 19862467.
43. Touska P, Hasso S, Oztek A, Chinaka F, Connor SEJ. Skull base ligamentous mineralisation: evaluation using computed tomography and a review of the clinical relevance. Insights Imaging. 2019 May 21;10(1):55. doi: 10.1186/s13244019-0740-8. PMID: 31115710; PMCID: PMC6529485.
44. Gupta V, Khandelwal N, Mathuria SN, Das Palash J. Calcified interclinoid ligament: an unusual cause of misinterpretation on cerebral CT angiography. Clin Radiol.
2013 Jul;68(7):e426-8. doi: 10.1016/j. crad.2013.03.019. Epub 2013 Apr 25. PMID: 23622793.
45. Cederberg RA, Benson BW, Nunn M, English JD. Calcification of the interclinoid and petroclinoid ligaments of sella turcica: a radiographic study of the prevalence. Orthod Craniofac Res. 2003 Nov;6(4):22732. doi: 10.1034/j.1600-0544.2003.00243.x. PMID: 14606526.
46. Tay KY, U-King-Im JM, Trivedi RA, Higgins NJ, Cross JJ, Davies JR, Weissberg PL, Antoun NM, Gillard JH. Imaging the vertebral artery. Eur Radiol. 2005 Jul;15(7):1329-43. doi: 10.1007/s00330-005-2679-z. Epub 2005 Jan 27. PMID: 15968519.
47. Burle VS, Panjwani A, Mandalaneni K, Kollu S, Gorantla VR. Vertebral Artery Stenosis: A Narrative Review. Cureus. 2022 Aug 16;14(8):e28068. doi: 10.7759/ cureus.28068. PMID: 36127977; PMCID: PMC9477552.
48. Ahmed MA, Parwani D, Mahawar A, Gorantla VR. Subclavian Artery
Calcification: A Narrative Review. Cureus. 2022 Mar 19;14(3):e23312. doi: 10.7759/ cureus.23312. PMID: 35464515; PMCID: PMC9015066.
49. Wu XH, Chen XY, Wang LJ, Wong KS. Intracranial Artery Calcification and Its Clinical Significance. J Clin Neurol. 2016 Jul;12(3):253-61. doi: 10.3988/ jcn.2016.12.3.253. Epub 2016 May 10. PMID: 27165425; PMCID: PMC4960208.
50. Mokin M, Dumont TM, Kass-Hout T, Levy EI. Carotid and vertebral artery disease. Prim Care. 2013 Mar;40(1):135-51. doi: 10.1016/j.pop.2012.11.006. Epub 2012 Dec 8. PMID: 23402465.
51. Singer, Steven Richard; Mupparapu, Mel1,. Cone Beam Computed Tomography Detection of Extracranial Vertebral Artery (EVA) Calcification and Ectasia. Journal of Orofacial Sciences 11(1):p 65-70, Jan–Jun 2019. | DOI: 10.4103/jofs.jofs_130_18.
52. Omami G. Soft Tissue Calcification in Oral and Maxillofacial Imaging: A Pictorial Review. Int. J. Dent. Oral Sci. 219–224 (2016) doi:10.19070/2377-8075-1600046.
53. Cho BH, Jung YH, Hwang JJ. Maxillary antroliths detected by cone-beam computed tomography in an adult dental population. Imaging Sci Dent. 2019 Mar;49(1):59-63. doi: 10.5624/ isd.2019.49.1.59. Epub 2019 Mar 25. PMID: 30941289; PMCID: PMC6444011.
54. Choi J. Dental radiology reporting status and recording frequency of reporting items in Korea. Imaging Sci Dent. 2023 Mar;53(1):35-42. doi: 10.5624/ isd.20220152. Epub 2022 Dec 8. PMID: 37006784; PMCID: PMC10060759.
158 Texas Dental Journal | Vol 141 | No. 3

Recruit for Rewards Caring • Connections
• Create • Commitment
You know first-hand the value you receive from your ADA membership. Through the community and resources you’ve come to count on, the ADA provides the support you need to help achieve your goals. You can help colleagues and friends thrive by inviting them to join the ADA.

For every 5 new members
you recruit, you’ll receive a chance to win a 7-day interisland Hawaiian cruise* for you and a guest.
Eligibility
Who can recruit? Any ADA member dentist (including graduate student, resident, active licensed, active life, retired and retired life) is eligible to participate as a recruiter
Who can be recruited? Any degreed dentist who was not an ADA member in 2023 (including graduate students, residents)
Who is not eligible to be recruited for this program?
• A renewing member (someone who was a member in 2023)
• Dental students
• Retired dentists
How to Participate
• Newly recruited members are required to indicate the recruiter’s name and contact information as a referral on the membership application.
• ADA member recruiters will receive an email notification after the dentist referred has been accepted into membership.
• A raffle entry for quarterly drawings will be awarded for each new, active member recruited who pays national dues (as applicable) in the current year. Recruiters will receive a chance to win a 7-day Hawaiian cruise* for every five new recruited members who pay national dues (as applicable).
Recognition
• All recruiters will be recognized at SmileCon 2024. Top recruiters will receive additional recognition.
• Quarterly winners and top recruiters will be announced in ADA Morning Huddle.

For each new member
you recruit, you’ll be entered into a quarterly drawing for a chance to win $1,000 in prizes from ADA-endorsed providers or products from the ADA Store.
Program Rules
• This program will run January 1 – August 31, 2024.
• For each new, active member who joins in that timeframe, the referring member’s name will be entered into quarterly drawings for a chance to win $1,000 in prizes from ADAendorsed providers or products from the ADA Store. Referring members will also receive a chance to win a 7-day interisland Hawaiian cruise* for every five new, eligible members they recruit.
• Referring members will receive a qualifying entry each time their name is listed as the “referring member” on the new member’s application (one entry for quarterly drawings for every one member recruited, one entry for the grand prize drawing for every five members recruited). There is no limit to the number of new members who can be recruited or entries in the drawing.
• Referring members will automatically win a quarterly prize (up to $1,000 value) when they recruit 25 eligible new members. Quarterly prize winners are also eligible to win the grand prize should they recruit at least five new members.
• The grand prize drawing will take place at SmileCon® 2024 in New Orleans. SmileCon attendance is not required to win.
* The grand prize winner will receive a 7-day interisland Hawaiian cruise with a balcony room and airfare for two to be redeemed in 2025, an estimated value of $7,500. If winners do not wish to claim the Hawaiian cruise package, they are able to select another trip from AHI’s catalog at equal or lesser value, or take a cash prize option of $3,500. Learn more about the available cruises provided by ADA Member Advantage endorsed partner, AHI Travel.
The ADA Member Recruitment Initiative is subject to all applicable federal, state and local laws and regulations, and is void where prohibited by law. Visit ADA.org/R4R for more details.
www.tda.org | April 2024 159
© 2023 American Dental Association All rights reserved. Updated: 12/11/2023
 By Phil Nieto; President, Best Card
By Phil Nieto; President, Best Card

160 Texas Dental Journal | Vol 141 | No. 3 Provided by: PERKS P R O G R A M value for your profession Accepting Credit Card Payments is Getting Increasingly Expensive. Here’s What You Want to Know—and How to Find Out What It’s Costing You.
Dentistry can be an isolating profession, and it can be difficult to know how your practice’s volume and profitability compares with those of your peers.
In this article, Best Card—the endorsed payment processor of TDA Perks Program and ADA Member Advantage— used data from thousands of dental offices it’s worked with over the past 15 years to provide insight into what the average dental practice experienced.
• How much does the average dental office collect in credit card payments?
• Have dentists raised their prices to keep up with inflation?
• What are other dentists paying to accept credit card payments?
• How much SHOULD you be paying?
You may find drastic changes have slipped under your radar—even as they significantly affect you.
How much does the average dental office collect in
credit cards?
In 2023, the average dental office ran $44,925 in credit card payments per month. That figure represents a:
• 45.5% increase over the 2019 average ($30,876).
• 195% increase over the 2009 average ($15,221).
Today the average practice runs almost 3 times as much in credit cards as it did in 2009!
Dental offices saw a large increase in the total amount of credit card payments collected over the past 10+ years. But Covid accelerated that trend considerably, as patients moved towards payment methods that were more convenient and involved less physical contact. Furthermore, many
insurance providers started issuing virtual credit cards as payment for their remittances, which also increased the amount of card payments accepted.
Have practices raised their costs to keep up with inflation?
Every dentist knows Covid and the resulting supply chain and inflation issues increased the costs of many items used regularly in the practice. In response, many dentists had to raise their prices over the last several years.
We can clearly see this trend across all practices by looking at the size of the average payment.
Average Card-Payment Amount
The average credit card payment accepted by dental offices increased by 11.87% from 2019–2023, a four-year period. It was $306 in 2023 and $273 in 2019.
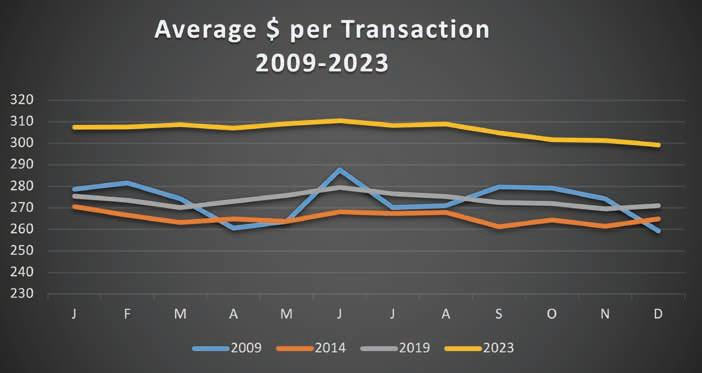
www.tda.org | April 2024 161
value for your profession continued
The average payment only increased by 0.12% from 2009–2019, a 10-year period. 2023 saw a slight decrease in the average payment compared with 2022—from $307 to $306, indicating increases due to inflation may be slowing.
The Consumer Price Index shows inflation in the U.S. from 2019–2023 was 19.2%.
This means the 11.87% increase (in the average dental transaction amount) during the same time period didn’t keep up with the economy-wide price hike, though the increase was substantial compared to 2009-2019.
What does the average practice pay to run cards?
With more patients and insurance providers choosing to pay with cards, accepting cards ensures offices can quickly and easily collect payments. But accepting cards is also a much more substantial factor in a practice’s profitability than in the past.
While the average dental office’s payment volume increased, the costs to run those payments has also increased—and processing fees can be hard to understand. However, it’s easy to discern their impact on your bottom line.
With more patients and insurance providers choosing to pay with cards, accepting cards ensures offices can quickly and easily collect payments.
But accepting cards is also a much more substantial factor in a practice’s profitability than in the past.

162 Texas Dental Journal | Vol 141 | No. 3
To do this, you need to calculate your effective rate with simple math:
• Total Fees Paid (for the month) ÷ Total Amount Run in Card Sales (for the month) = Your Effective Rate
In 2023, the average dental office in the U.S. paid 3.53%, compared to 3.06% in 2019. These rates are already too high; but to put it in perspective, in 2014, the average dental office paid 2.84%.
What this means is, the average practice pays more per payment (as a percentage) while accepting 45% more card payments than it did before the pandemic. This is significant, as you’ll see in the following.
The average office ran the following in card payments:
• $30,876 at 3.06% for a total of $944/month in fees in 2019.
• $45,000 at 3.45% for a total of $1,585/month in fees in 2023.
That’s a cost increase of $7,692/year in 4 years.
What can you do?
It’s easy to overlook small increases in the costs of services you’re using, but those small increases are frequently enough to have a big impact. Any part of your business that increases substantially over time should be analyzed periodically so you know how it’s affecting your bottom line.
With credit card processing, the first step you can take is to calculate the effective rate you’re paying, as mentioned above. The average office paid more than 3.53% in 2023; however, TDA members working with Best Card paid 2.22% in 2023 for an average savings of $6,496 per year.
If you see you’re paying more to accept credit cards, it might be time to look for a better option.
Best Card is the endorsed credit card processor of TDA Perks Program and ADA Member Advantage. You can send Best Card a recent monthly statement via email to Compare@bestcardteam.com or you can fax it to (866) 717-7247 to receive a complimentary cost analysis and learn exactly what your practice could be saving. Best Card offers exclusive rates to TDA members. Learn more about Best Card at tdaperks.com (Financial & Real Estate) or call (877) 739-3952.

www.tda.org | April 2024 163
classifieds
Opportunities Online at TDA.org and Printed in the Texas Dental Journal
CLASSIFIEDS INFORMATION
DEADLINE
Copy text is due the 20th of the month, 2 months prior to publication (ie, January issue has a due date of November 20.)
MONTHLY RATES
PRINT: First 30 words—$60 for ADA/TDA members and $100 for non-members. $0.10 each additional word.
ONLINE: $40 per month (no word limit). Online ads are circulated on the 1st business day of each month, however an ad can be placed within 24 business hours for an additional fee of $60.
SUBMISSION
Ads must be submitted, and are only accepted, via www.tda.org/Member-Resources/TDAClassified-Ads-Terms. By official TDA resolution, ads may not quote specific incomes or revenues and must be stated in generic terms (ie “$315,000” should be “low-to-mid-6 figures”). Journal editors reserve the right to edit and/or deny copy.
PRACTICE OPPORTUNITIES
ALL TEXAS LISTINGS FOR MCLERRAN & ASSOCIATES. AUSTIN-NORTH
(ID #604): Legacy FFS practice with an impeccable reputation located in a budding community north of Austin. The office has relied solely on word-of-mouth referrals with very little marketing/advertising and refers out many specialty procedures leading to upside potential for an incoming buyer. The real estate is also available for purchase. AUSTIN (ID #636): Rare opportunity to purchase a turnkey, FFS/PPO general dentistry practice and real estate in Austin. This spacious 2,500 sq ft office features 4 operatories, digital radiography, iTero, and paperless charts. The practice is situated in a highly desirable Austin community. AUSTIN (ID #649): PPO/FFS general dentistry practice in Austin. Located in a retail center off a busy street, the office features 3 computerized operatories, digital x-ray sensors, digital pano, Itero scanner, and paperless charts. With 1,800+ active patients and 50+ new patients per month, this office is set up for immediate and future success. AUSTIN (ID #662): Large, general dentistry practice (with a recent focus on implants) located in a free-standing building with great visibility in north Austin. Large facility with 8 fully equipped operatories, digital radiography, an iTero digital scanner, and a 3D
164 Texas Dental Journal | Vol 141 | No.3
CBCT unit. FFS/PPO patient base, over 2,000 active patients, and has a stellar reputation. The owner invested heavily in growing the implant side of the business.
DALLAS (ID #650): Beautiful, state-of-the-art, general dentistry practice located in a budding suburb just north of the DFW metroplex. The large, freestanding building is ideally located with access to a major thoroughfare and provides ample space for future growth in the 7 well-appointed operatories featuring digital radiography, computers throughout, digital scanner, and a milling unit. The office treats a large PPO/FFS patient base with approximately 20 new patient visits per month, robust hygiene recall, and over 2,200 active patients.
FORT WORTH (ID #664): Established, fee-for-service general dentistry practice in Fort Worth with computerized operatories, digital x-ray sensors, CBCT, and paperless charts. There is plenty of room to continue growing by adding several specialty procedures currently being referred out.
HOUSTON-SOUTHWEST (ID #625): Modern GD practice in a high-visibility retail location in a desirable suburb in southwest Houston. Large, 2,800 sq. ft. office that features 6 fully equipped operatories, computers in operatories, intra oral cameras, a digital scanner, and CBCT. The practice is on track to collect over 7 figures in 2023 with strong historical year over year
growth. The office serves a primarily FFS patient base with a limited number of patients innetwork, has over 1,450 active patients, and has added 25+ new patients per month over the last 12 months. HOUSTON-SOUTHEAST (ID #644): 100% FFS, legacy practice in SE Houston. The 2,500+ sq ft office features 7 ops, computers throughout, digital pano, digital x-rays, digital scanner, intraoral cameras, and paperless charts. If you’re looking for a centrally located, profitable practice with a dedicated patient base and room to grow, call us now for more details. NORTHEAST TEXAS (ID #584): 100% FFS general dentistry practice in a desirable town in northeast Texas with 7 figures in revenue and strong net income. The turn-key practice features 4 fully equipped operatories with digital radiography, intra oral cameras, paperless charts, CBCT, and a digital scanner.
SAN ANTONIO (ID #639): Legacy, general dentistry practice with a stellar reputation in North San Antonio. The practice serves a large, majority Fee-For-Service patient base with over 1,900 active patients and sees approximately 20 new patients per month. The fully digital office has 5 equipped operatories with computers in all ops, digital radiography, intra oral cameras, paperless charts, and a digital pano. SAN ANTONIO (ID #654): PPO/FFS general dentistry practice in San Antonio. The 3,000+ sq ft office
www.tda.org | April 2024 165
classifieds
is prominently located on a busy street and features 6 computerized operatories, digital x-ray sensors, digital pano, digital scanner, intraoral cameras, and paperless charts. With 2,000+ active patients, 25+ new patients a month, and a stellar reputation, this practice is poised for continued success. TEXAS
HILL COUNTRY,
ORTHO (ID #616): Rare opportunity to purchase an orthodontic practice located in a serene, rapidly growing community in the Texas hill country (Austin, San Antonio, and the Texas wine country all available within a short drive). State-of-the-art facility with extensive, modern upgrades and top-of-the-line digital technology. The buyer will have the option of purchasing or leasing the real estate. The current owner will be retiring but is available to provide a transition period to the incoming buyer. SOUTH TEXAS (ID #651): General dentistry practice located in south Texas. This state-of-the-art office occupies 3,500 sq ft with room for 10 total operatories, is fully digital with CBCT, a digital scanner, handheld X-ray units, and a 3-D printer. The practice serves a large PPO/ Medicaid patient base with over 3,000 active patients seen over the last 24 months with a strong monthly new patient flow. WEST TEXAS (ID #661): FFS, legacy practice in a growing west Texas community. Located in a free-standing building, the office features 4 equipped
operatories (5 total plumbed), computers throughout, digital x-rays, 3D CBCT, CAD/ CAM, intraoral cameras, and paperless charts. This turn-key practice has a solid foundation, and the current trends indicate it poised for substantial growth in the future. The real estate is also available for purchase. TO REQUEST
MORE
INFORMATION ON MCLERRAN & ASSOCIATES’ LISTINGS: Please register at www.dentaltransitions.com or contact us at 512-900-7989 or info@dentaltransitions. com.
BEAUMONT: GENERAL (REFERENCE
“BEAUMONT”). Small town practice near a main thoroughfare. 80 miles east of Houston. Collections in 7 figures. Country living, close enough to Houston for small commute. Practice in a stand-alone building built in 1970. The office is 1,675 sq ft with 4 total operatories, 2 operatories for hygiene and 2 operatories for dentistry. Contains reception area, dentist office, sterilization area, lab area. Majority of patients are 30 to 65 years old. Practice has operated at this location for over 38 years. Practice sees patients about 16 days a month. Collection ratio of 100%. The practice is a fee-for-service practice. Building is owned by dentist and is available for sale. Contact Christopher Dunn at 800-930-8017
166 Texas Dental Journal | Vol 141 | No.3
(SHARPSTOWN AREA): GENERAL (REFERENCE “SHARPSTOWN GENERAL”). Motivated seller. Well-established general dentist with high6 figure gross production. Comprehensive general dentistry in the southwest Houston area focused on children (Medicaid). Very, very high profitability. 1,300 sq ft, 4 operatories in single building. 95% collection ratio. Over 1,200 active patients. 20% Medicaid, 45% PPO, and 35% fee-for-service. 30% of patients younger than 30. Office open 6 days a week and accepts Medicaid. Contact Christopher Dunn at 800-930-8017 or christopher@ddrdental. com. HOUSTON (BAYTOWN AREA): GENERAL (REFERENCE “BAYTOWN GENERAL”). Motivated seller. Well-established general practice with mid-6 figure gross production. Comprehensive general dentistry in Baytown on the east side of Houston. Great opportunity for growth! 1,400 sq ft, 4 operatories in single story building. 100% collection ratio. 100% fee-for-service. Practice focuses on restorative, cosmetic and implant dental procedures. Office open 3.5 days a week. Practice area is owned by dentist and is available for sale. Contact Christopher Dunn at 800-930-8017 or christopher@ddrdental. com. WEST OF AUSTIN: ORTHODONTIC (REFERENCE “HILL COUNTRY ORTHO”) Located in a rapidly growing small town, this practice
is in the heart of the Texas hill country. This practice serves the youth of the area. There are 4 operatories in the practice. The practice is 100% fee-for-service. Orthodontic care is the only service provided at this office. 1,300 sq ft Open 4 days per week. Digital X-rays and pano and Cloud9Ortho software. The practice has excellent visibility and is located near a hospital. Contact Christopher Dunn at 800-930-8017 or christopher@ddrdental.com.
McLerran & Associates is the largest dental practice brokerage firm in Texas. When it’s time to buy or sell a practice, we’ve got you covered.
C S PRACTICE SALES
Austin 512-900-7989
DFW 214-960-4451
Houston 281-362-1707
San Antonio 210-737-0100
South Texas 361-221-1990 or christopher@ddrdental.com. HOUSTON
Email: texas@dentaltransitions.com PRACTICE
www.dentaltransitions.com
www.tda.org | April 2024 167
DSO
APPRAISALS
classifieds
HOUSTON, COLLEGE STATION, AND LUFKIN (DDR DENTAL Listings). (See also AUSTIN for other DDR Dental listings and visit www. DDRDental.com for full details. LUFKIN: General practice on a high visibility outer loop highway near mall, hospital and mature neighborhoods. Located within a beautiful single-story, freestanding building, built in 1996 and is ALSO available for purchase. Natural light from large windows within 2,300 sq ft with 4 operatories (2 hygiene and 2 dental). Includes a reception area, dentist office, a sterilization area, lab area, and break room. All operatories fully equipped. Does not have a pano but does have digital X-ray. Production is 50% FFS and 50% PPO (no Medicaid), with collection ratio above 95%. Providing general dental and cosmetic procedures, producing mid-6 figure gross collections. Contact Christopher Dunn at 800-930-8017 or Christopher@DDRDental. com and reference “Lufkin General or TX#540”. HOUSTON: GENERAL (SHARPSTOWN). Well established general dentist with high-6 figure gross production. Comprehensive general dentistry in the southwest Houston area focused on children (Medicaid). Very, very high profitability. 1,300 sq ft, 4 operatories in single building. 95% collection ratio. Over 1,200 active patients. 20% Medicaid, 45% PPO, and 35% fee-for-service. 30% of patients
younger than 30. Office open 6 days a week and accepts Medicaid. Contact Chrissy Dunn at 800-930-8017 or chrissy@ddrdental. com and reference “Sharpstown General or TX#548”. HOUSTON: GENERAL (PEARLAND AREA). General located in southeast Houston near Beltway 8. It is in a freestanding building. Dentist has ownership in the building and would like to sell the ownership in the building with the practice. One office currently in use by seller. 60% of patients age 31 to 80 and 20% 80 and above. Four operatories in use, plumbed for 5 operatories. Digital pano and digital X-ray. Contact Christopher Dunn at 800-930-8017 or christopher@ddrdental.com and reference “Pearland General or TX#538”.
HOUSTON: PEDIATRIC (NORTH HOUSTON). This practice is located in a highly soughtafter upscale neighborhood. It is on a major thoroughfare with high visibility in a strip shopping center. The practice has 3 operatories for hygiene and 2 for dentistry. Nitrous is plumbed for all operatories. The practice has digital X-rays and is fully computerized. The practice was completely renovated in 2018. The practice is only open 3.5 days per week. Contact Christopher Dunn at 800-930-8017 or christopher@ddrdental.com and reference “North Houston or TX#562”. WEST HOUSTON: MOTIVATED SELLER. Medicaid practice with
168 Texas Dental Journal | Vol 141 | No.3
production over 6 figures. Three operatories in 1,200 sq ft in a strip shopping center. Equipment is within 10 years of age. Has a pano and digital X-ray. Great location. If interested contact chrissy@ddrdental.com. Reference “West Houston General or TX#559”.
LAKE JACKSON: Located 40 minutes outside Houston. Are you seeking a dental practice that is fee-for-service, located in a great community with a robust economy (Dow Chemical, BASF, and Freeport LNG), and strongly rooted in the community with an exceptional reputation? Would you like to work with well trained and tenured staff? If yes, this is a great opportunity for you, we are seeking a dentist committed to excellence and providing the best possible dentistry available. The practice has blended a strong cosmetic and implant practice with family dentistry. Seeking associate for a busy and ever expanding practice. Great compensation, sign on bonus, and benefit package. AGD or GPR preferred or 2 years experience. To inquire about this opportunity contact Dr Brian Bell at bkbellgolf@hotmail. com; office phone: 979-297-1201; 102 Flag Lake Dr, Ste C, Lake Jackson, TX 77566.
ROCKPORT: Practice for sale in Rockport. Two chairs, plumbed for 3. Currently being worked 3 days a week producing near mid6 figures. Fee-for-service, no DMO, HMO or PPO contracts. Hygienist 3 days a week and will stay, been with practice since 2019. Digital X-rays, paperless, Newtom 3D/Panorex, 3 X-ray sensors. Practice is in older house, which can be leased or purchased. Great starter practice or for someone slowing down and wants to live on the coast. Send inquires to jim@jlongdds.com or call: 281-726-1812, leave message.
WATSON BROWN PRACTICES FOR SALE: Practices for sale in Texas and surrounding states. For more information and current listings please visit our website at www. adstexas.com or call us at 469-222-3200 to speak with Frank or Jeremy.
INTERIM SERVICES
HAVE MIRROR AND EXPLORER, WILL TRAVEL: Sick leave, maternity leave, vacation, or death, I will cover your general or pediatric practice. Call Robert Zoch, DDS, MAGD, at 512-517-2826 or drzoch@yahoo.com.
www.tda.org | April 2024 169
170 Texas Dental Journal | Vol 141 | No. 3 YOUR PATIENTS TRUST YOU. WHOM CAN YOU TRUST? If you or a dental colleague experiences impairment due to substance use or mental illness, the Professional Recovery Network is here to provide support and an opportunity for confidential recovery. PRN Helpline (800) 727-5152 Visit us online www.txprn.com AFTCO 121 Anesthesia Education & Safety Foundation, Inc... 115 Choice Transitions ........................... Inside Back Cover DentaQuest 119 E-Vac, Inc .................................................................... 146 Henry Schein Financial Services ............................. 126 JKJ Pathology 118 Law Offices of Mark J. Hanna .................................. 146 McLerran & Associates............................................. 167 MCNA Dental 148 Proconsult Group...................................................... 140 Texas Pharmacy Association/Professional Recovery Network ................................................ 170 Professional Services Technologies ........................ 118 TDA Perks Inside Front Cover Texas A&M School of Dentistry ............................... 117 Texas Dental Sleep Services .................................... 126 Texas Health Steps 127 UTSD Houston ........................................................... 147 Watson Brown ........................................................... 141 ADVERTISERS

www.tda.org | April 2024 171

Financial Report of the Texas Dental Association A Glance into Financial Stability
 Dr Carmen Smith Secretary-Treasurer, TDA
Dr Carmen Smith Secretary-Treasurer, TDA
As the custodians of fiscal oversight within our organization, it is both a privilege and a responsibility to present a comprehensive Treasurer’s Report on behalf of the Texas Dental Association Board. This report not only reflects our commitment to transparency but also serves as a testament to our dedication to sound financial management.
Overview of Financial Performance 2023
Over the past fiscal period, our organization has demonstrated commendable financial stability despite the challenges posed by economic fluctuations and unforeseen circumstances. Here is a brief synopsis of our financial performance:
1. Revenue Generation: Our revenue streams have remained robust, with income from membership dues, investment earnings from our sweep account, miscellaneous revenue (includes but not limited to sponsorships, grants from ADA, and income from Member Benefits Limited (MBL)). This revenue generation has fortified our financial position and provided a reliable source of income. In 2023, TDA also received an ERC credit, and a signing bonus from TXDOT for the right of way (ROW) access to the TDA property.
2. Expense Management: While the TDA Board strives to provide prudent financial planning and rigorous expense management, our expenses in 2023 outpaced income in two key areas, continuing education and publication. First, 2023 saw the development of two new continuing education programs—the Regional Meeting held in Lubbock, TX and the Dental Symposium held in Austin. Positive feedback was received from both events, however, attendance fell short of expectations, thereby creating a shortfall in revenue. Second, increased printing and postage costs raised expenses for the publications of the TDA Today and the Texas Dental Journal
3. Budget Adherence: Adhering to our established budgetary framework has been instrumental in maintaining financial discipline and accountability. At the end of 2023, the TDA Board was able to show a net positive position of $53,367 for operating activities. (reference 2023 Unaudited Actual results in attached 2025 Proposed Budget report).
4. Reserve Fund Maintenance: Upholding our commitment to fiscal prudence, we have diligently maintained a healthy reserve fund to safeguard against unforeseen contingencies and mitigate financial risks. This reserve fund serves as a vital buffer, providing us with the flexibility to navigate economic uncertainties with confidence. As of December 31, 2023, TDA had reserves at a fair market value (FMV) of $5,237,636. The TDA Relief Fund had reserves at a fair market value (FMV) of $558,049.
Texas Dental Association Budget | www.tda.org | April 2024 1
Navigating Financial Waters: Budget Allocation 2025
As stewards of fiscal responsibility, it is imperative to review our financial journey through a comprehensive Budget Report. This report is intended to shed light on our path forward towards sustainable growth.
Overview
The cornerstone of effective financial management lies in the intentional allocation of resources to support our organizational goals and initiatives. Our budget is meticulously aligned with our strategic priorities, reflecting our commitment to advancing our mission and vision. Resources are directed towards key areas such as program development, operational efficiency, reserve fund allocation, and other key expenses.
1. Operational Expenditures: A significant portion of our budget is dedicated to covering essential operational expenses, including personnel costs, office space cost and other administrative overhead. These expenditures are essential for sustaining day-today operations and maintaining the infrastructure necessary for organizational functionality. While we will likely not have a Texas Dental Association building in 2025, we must account for expenses that will be accrued from temporary housing and storage for the staff, as well as meeting space for the TDA Board, Councils, and Committees.
2. Programmatic Investments:
Investing in our programs and initiatives lies at the heart of our budgetary strategy. The budget allocates funds for the TDA Meeting, as well as, 1 regional meeting (location to be determined). In an effort to control expenses, the TDA Today will become an online publication only. The Texas Dental Journal will also be reduced from 10 to 8 issues, which will bring a savings of over $70,000. The TDA Leadership Conference will be hosted online. This allows for maximum participation, as well as the ability to review the recordings afterward, if someone is not able to attend. The budget anticipates revenue from the newly developed CE Concierge LLC., developed and managed by FSI, in conjunction with Eleventh and Gather. TDA remains contracted with MCI as our source for sponsorship acquisitions that support our programs.
3. Reserve Fund: Austin Assets will continue to advise on our portfolio strategy, in line with the TDA investment policy, with a financial overview and updates to be presented to the TDA Board of Directors twice yearly.
4. Other Expenses: The ADA House of Delegates will be held in Washington, D. C. in 2025 and the budget accounts for delegate and alternate delegate travel related expenses. The Board voted on a cap of $3,500/person for 2025. The TDA Board voted to not budget a Texas Reception at the 2025 ADA House of Delegates.
The TDA Board of Directors voted to submit a budget of $5,446,180 to be approved by the Texas Dental Association House of Delegates. While this is a deficit budget, the Board felt that a method of finance adjustment (reserve funds will be used to cover the operating expenses if there is a shortfall) was the prudent manner to handle the 2025 budget for two main reasons: 1) The Association is in negotiations with the Texas Department of Transportation (TxDOT) to potentially acquire our largest asset, and 2) the deficit of $128,768 is less than 1% of the total budget. At the time of writing this article, the sale of the TDA Building is not complete, and therefore, with full transparency, the Board may need to take further action at a later date to update the 2025 budget. The Board is granted this authority via the TDA Bylaws, Chapter IV, House of Delegates, Section 40, Transfer of Powers of the House of Delegates. If the TDA Board of Directors approves a revised budget, the House of Delegates will be notified via the online version of the Texas Dental Journal and/or the email distribution group.
Looking ahead, we remain steadfast in our commitment to fiscal responsibility, prudent financial management, and transparency. We will continue to prioritize investments that promote long-term sustainability and facilitate organizational growth. This includes expanding revenue streams and exploring strategic partnerships to enhance our financial resilience.
I wish to thank Ms. Linda Brady, Ms. Kelly Doolittle, The Budget, Assets, and Finance Committee, as well as The TDA Board of Directors for their diligence in the preparation of our 2025 budget.
2 Texas Dental Association Budget | www.tda.org | April 2024
2025 Proposed Budget Texas Dental Association
Texas Dental Association Budget | www.tda.org | April 2024 3 1. TDA Meeting 583,910 1,139,043 1,329,968 1,385,443 1,378,000 2. Continuing Education Programs 150,000 193,846 664,699 431,889 200,125 3. Journal 326,151 228,002 358,806 197,856 203,288 4. TDA Today 40,970 39,470 38,384 36,587 40,610 5. TDA Website 37,000 22,150 45,000 13,200 22,000 Total Publications/Website 404,121 289,622 442,191 247,643 265,898 6. Building 313,562 309,505 304,713 314,557 17,916 7. Operating a. Dues 2,549,468 2,688,058 2,571,971 2,754,350 2,756,108 b. Investment Earnings-Sweep 40,000 136,373 10,000 30,000 150,000 c. Miscellaneous 168,640 354,520 75,000 95,000 105,000 d. ADA Tx Reception Sponsorships 0 0 0 75,000 0 e. Affiliates Administration 96,908 97,044 96,446 97,049 104,366 f. MBL Partnership 275,000 315,093 275,000 300,000 310,000 g. CE Concierge 0 0 0 0 30,000 Total Operating 3,130,016 3,591,088 3,028,417 3,351,399 3,455,474 TOTAL REVENUES 4,581,609 5,523,105 5,769,988 5,730,930 5,317,413 8. TDA Meeting 76,083 902,790 1,043,700 979,165 1,036,335 9. Continuing Education Programs 30,000 214,546 354,110 171,954 78,625 10. Journal 230,050 299,344 305,220 279,200 242,853 11. TDA Today 110,500 101,715 98,750 85,834 35,000 12. TDA Website 55,800 20,999 53,750 38,564 6,315 Total Publications/Website 396,350 422,058 457,720 403,598 284,168 13. Building 325,141 292,322 295,235 272,650 102,000 14. Capital Improvements 10,000 0 0 22,100 0 15. Non Budgeted Contingency 29,000 0 5,000 0 0 16. Central Office Departments 2,866,450 3,026,097 2,971,172 3,187,619 3,275,047 17. Board of Directors 204,665 146,142 181,895 181,250 172,750 18. Committees 21,220 14,293 18,070 16,000 16,000 19. Councils 164,895 145,815 164,230 137,149 167,620 20. ADA /National Organizations 165,815 138,928 135,180 217,730 198,310 21. House of Delegates 45,350 84,423 80,675 58,715 60,325 22. Other expense 196,640 57,326 38,000 58,000 30,000 23. TDA Smiles Foundation 50,000 25,000 25,000 25,000 25,000 TOTAL EXPENSES 4,581,609 5,469,739 5,769,988 5,730,930 5,446,180 REVENUE OVER EXPENSE 0 53,367 0 0 (128,768) 24. Method of Finance Adjustment 128,768 25. TDA Financial Services, Inc. Cash Dividend ADJUSTED REVENUE OVER EXPENSE 0 53,367 0 0 0 Revenues ANNUAL SESSION PUBLICATIONS/ WEBSITE BUILDING OPERATIONS Expenses ANNUAL SESSION PUBLICATIONS/ WEBSITE BUILDING CAPITAL IMPROVEMENTS CONTINGENCY CENTRAL OFFICE BOARD OF DIRECTORS COMMITTEES COUNCILS ADA/NATIONAL ORGANIZATIONS HOUSE OF DELEGATES OTHER EXPENSE CONTRIBUTIONS
UNAUDITED 2022 2023 2023 2024 2025 Budget Actual Budget Budget PROPOSED
2025 Proposed Budget Texas Dental Association
Central Office Departments
16. Central Office Departments
4 Texas Dental Association Budget | www.tda.org | April 2024
Personnel: a. Regular Salaries 1,655,619 1,777,189 1,753,146 1,948,128 2,021,817 b. Payroll Taxes 125,395 131,850 133,662 148,577 154,669 c. Health Insurance 173,634 171,939 206,053 209,014 218,801 d. Retirement 157,868 158,112 163,400 187,602 202,182 Total Personnel 2,112,516 2,239,090 2,256,261 2,493,321 2,597,469
e. Insurance—Directors/Officers 59,733 57,006 57,681 65,097 66,775 f. Leases—Equipment 42,447 23,437 34,526 23,520 8,940 g. Maintenance 15,800 29,564 16,550 17,752 17,752 h. Postage and Couriers 10,975 4,950 7,975 6,250 6,250 i. Printing 12,300 7,220 12,300 8,350 8,350 j. Supplies—Office 13,112 7,673 8,112 9,562 9,562 k. Taxes—State and Local 3,539 2,632 4,500 4,000 2,289 l. Information Technology 10,728 20,780 10,672 16,538 16,538 Total Office Operations 168,634 153,262 152,316 151,069 136,456 Services: m. Accounting Services—Payroll 4,800 5,064 4,800 10,356 5,500 n. Accounting and Auditing Services 35,000 36,500 36,450 37,250 37,850 o. Bank Charges 19,000 9,285 19,000 16,000 3,600 p. Consultants 31,200 38,775 31,200 40,168 40,168 q. Legal Services 159,000 163,903 159,000 159,000 162,000 r. Lobbying 190,500 221,500 201,500 190,500 201,500 s. Gifts and Memorials 1,950 1,736 1,450 1,450 1,500 Total Services 441,450 476,763 453,400 454,724 452,118 Other Expenses: t. Dues Processing 100,000 90,636 75,000 50,000 50,000 u. Education and Organizational Development 10,000 5,176 7,500 5,750 4,750 v. Marketing 0 5,430 0 10,000 10,000 w. Meetings 4,000 4,253 2,000 1,300 2,300 x. Professional Dues and Memberships 3,430 3,743 2,800 3,800 4,750 y. Subscriptions 6,800 1,350 5,850 4,555 4,355 z. Recruiting 1,000 19,133 500 750 500 aa. Travel 18,620 27,262 15,545 12,350 12,350 Total Other Expenses 143,850 156,982 109,195 88,505 89,005 Total Central Office 2,866,450 3,026,097 2,971,172 3,187,619 3,275,047
Office Operations:
PERSONNEL OFFICE OPERATIONS SERVICES OTHER EXPENSES
UNAUDITED 2022 2023 2023 2024 2025 Budget Actual Budget Budget PROPOSED
Board of Directors, Councils, Committees,
17.
2025 Proposed Budget Texas Dental Association
18.
Texas Dental Association Budget | www.tda.org | April 2024 5
of Directors: a. President 28,705 10,225 20,985 16,000 16,000 b. President—Stipend 36,000 31,600 32,400 32,400 32,400 c. President Elect 8,520 6,781 7,070 7,000 7,000 d. President Elect—Stipend 8,400 6,300 7,200 7,200 7,200 e. Past President 5,230 5,551 4,830 7,000 7,000 f. Secretary Treasurer 5,230 4,464 4,830 5,000 5,000 g. Secretary Treasurer—Stipend 8,400 7,200 7,200 7,200 7,200 h. Editor 3,830 4,935 3,430 5,600 5,600 i. Editor—Stipend 8,400 7,200 7,200 7,200 7,200 j. Vice Presidents 21,280 13,414 19,480 15,000 15,000 k. Senior Directors 21,280 17,677 19,480 14,000 14,000 l. Directors 21,280 16,400 19,480 17,000 17,000 m. Other Officers 8,460 9,300 7,910 8,000 8,000 n. Board Meetings 19,650 5,095 20,400 32,650 24,150 Total Board of Directors 204,665 146,142 181,895 181,250 172,750
Board
Committees: a. Audit 1,615 0 0 0 0 b. Awards 17,095 13,630 17,220 15,250 15,250 c. Budget, Assets and Finance 0 0 0 0 0 d. Community Fluoride 1,300 9 600 500 500 e. Strategic Affairs 1,210 655 250 250 250 Total Committees 21,220 14,293 18,070 16,000 16,000
Councils: a. Annual Meeting & CE Programs 10,850 6,573 7,970 10,311 13,765 b. Legislative and Regulatory Affairs 58,560 83,375 87,995 49,183 78,320 c. DENPAC 40,345 28,116 32,425 34,220 36,300 d. Dental Licensing, Standards and Education 10,155 0 7,475 4,775 275 e. Ethics and Judicial Affairs 2,180 185 1,980 2,100 2,000 f. Governance 7,910 3,501 2,760 5,860 0 g. Membership, New Dentists and Students 18,695 22,287 16,525 23,500 30,590 h. Peer Review 2,600 345 1,500 2,600 2,500 i. Professions and Trends 5,250 651 3,340 3,350 3,620 j. Public Health and Access to Care 8,350 563 2,260 1,250 250 k. TOHPAC 0 220 0 0 0 Total Councils 164,895 145,815 164,230 137,149 167,620 20. ADA /National Organizations: a. ADA Delegates 120,015 135,546 135,180 132,230 187,810 b. ADA 15th Trustee Headquarters 10,000 0 0 10,500 10,500 c. ADA Texas Reception 35,800 3,383 0 75,000 0 Total ADA /National 165,815 138,928 135,180 217,730 198,310
of Delegates: a. HOD 50 Year and Life Luncheon 7,700 0 7,700 0 0 b. HOD Headquarters 35,650 81,090 70,975 56,715 58,325 c. HOD Past President’s Breakfast 2,000 3,332 2,000 2,000 2,000 Total House of Delegates 45,350 84,423 80,675 58,715 60,325
a. Federal Income Tax 35,000 20,396 30,000 30,000 22,000 b. TDA Conferences 10,000 28,930 0 20,000 0 c. Alliance/TDAA Stipends 8,000 8,000 8,000 8,000 8,000 d. Building Loan Interest 143,640 0 0 0 0 Total Other Expense 196,640 57,326 38,000 58,000 30,000
19.
21. House
22. Other Expense
ADA, HOD BOARD
DIRECTORS
ADA/NATIONAL ORGANIZATIONS HOUSE OF DELEGATES OTHER EXPENSE
OF
COMMITTEES COUNCILS
UNAUDITED 2022 2023 2023 2024 2025 Budget Actual Budget Budget PROPOSED
SESSION
2025 Proposed Budget Texas Dental Association
1. TDA Meeting Revenue
8. TDA Meeting Expense
6 Texas Dental Association Budget | www.tda.org | April 2024
a. Advertising 0 7,200 8,000 15,000 12,000 b. Clinics for Continuing Education 0 615,768 690,525 725,000 735,000 c. Exhibits 0 354,475 450,000 450,000 450,000 d. Miscellaneous 583,910 0 0 0 0 e. Other Groups 0 0 17,000 6,000 6,000 f. Registration 0 63,575 74,443 74,443 75,000 g. Sponsorships 0 98,025 90,000 115,000 100,000 Total TDA Meeting Revenue 583,910 1,139,043 1,329,968 1,385,443 1,378,000
Audio-Visual 0 125,533 150,000 150,000 150,000 b. Bank Charges 0 29,538 25,000 25,000 30,000 c. Clinician Honorariums 0 146,150 150,000 165,000 170,000 d. Clinician Support 0 72,721 90,000 90,000 90,000 e. Consultants 50,000 199,840 228,250 129,500 114,500 f. Exhibits 0 90,458 150,000 150,000 165,000 g. Hospitality Suite 0 37,680 15,000 20,000 35,000 h. Insurance 0 5,582 10,425 5,600 5,100 i. Miscellaneous 0 983 1,750 1,750 1,750 j. Onsite Program 0 0 0 0 0 k. Other Groups 0 3,400 16,000 6,000 6,000 l. Postage 0 17,205 6,000 6,000 8,000 m. Promotion 0 4,844 20,000 20,000 20,000 n. Registration 0 107,736 125,000 125,000 130,000 o. Scouting 0 0 0 11,600 17,220 p. Shuttle Services 0 0 10,000 0 0 q. Stipends 15,000 15,000 15,000 15,000 15,000 r. Supplies 0 900 200 200 500 s. TDA Party 0 16,029 0 15,000 35,000 t. Travel 11,083 22,358 31,075 38,515 35,765 u. VIP Reception 0 6,834 0 5,000 7,500 Total TDA Meeting Expense 76,083 902,790 1,043,700 979,165 1,036,335 TDA Meeting Net Revenue (Loss) 507,827 236,253 286,268 406,278 341,665
EXPENSE
a.
ANNUAL
ANNUAL SESSION REVENUE ANNUAL SESSION
UNAUDITED 2022 2023 2023 2024 2025 Budget Actual Budget Budget PROPOSED
2025 Proposed Budget Texas Dental Association
Texas Dental Association Budget | www.tda.org | April 2024 7 Continuing Education REVENUE EXPENSE
Continuing Education Revenue a. Advertising 0 0 6,000 2,000 3,000 b. Clinics for Continuing Education 150,000 134,966 213,738 125,000 150,000 c. Exhibits 0 7,500 11,500 5,000 7,500 d. Miscellaneous 0 0 9,335 0 0 e. Subscriptions 0 14,207 40,446 29,964 17,000 f. Registration 0 25,174 332,640 207,425 15,625 g. Sponsorships 0 12,000 51,040 62,500 7,000 Total Continuing Education Revenue 150,000 193,846 664,699 431,889 200,125
a. Audio-Visual 0 11,987 30,000 15,000 1,000 b. Bank Charges 0 7,770 6,000 5,740 6,850 c. Clinician Honorariums 30,000 25,500 85,000 47,500 16,500 d. Clinician Support 0 525 12,000 7,500 1,500 e. Consultants 0 76,006 102,806 13,000 28,125 f. Exhibits 0 0 1,000 500 500 g. F&B 0 68,209 85,750 60,000 4,500 h. Insurance 0 0 0 0 0 i. Miscellaneous 0 109 900 400 0 j. Postage 0 0 100 100 50 k. Promotion 0 1,741 10,000 3,500 1,250 l. Registration 0 1,881 2,000 2,000 2,000 m. Stipends 0 0 0 0 0 n. Supplies 0 0 1,000 350 150 o. Travel 0 5,969 5,350 4,160 1,200 p. Website Hosting 0 14,848 12,204 12,204 15,000 Total Continuing Education Expense 30,000 214,546 354,110 171,954 78,625 Continuing Education Net Revenue (Loss) 120,000 (20,699) 310,589 259,935 121,500
2.
9. Continuing Education Expense
UNAUDITED 2022 2023 2023 2024 2025 Budget Actual Budget Budget PROPOSED
2025 Proposed Budget Texas Dental Association
8 Texas Dental Association Budget | www.tda.org | April 2024 3. TDA Journal Revenue a. Advertising 222,248 129,802 265,600 99,162 104,814 b. Single Issue Purchases 255 0 100 0 0 c. Subscriptions—Membership Dues 103,648 98,201 93,106 98,694 98,474 Total TDA Journal Revenue 326,151 228,002 358,806 197,856 203,288 10. TDA Journal Expense a. Consultants 49,500 69,668 49,500 65,000 48,000 b. Meetings 200 0 200 0 200 c. Postage and Couriers 50,000 49,668 45,000 43,333 40,926 d. Printing and Production 129,950 149,507 140,500 151,867 128,902 e. Sales Commissions 0 30,501 69,720 18,900 24,800 f. Supplies 200 1 100 100 25 g. Travel 200 0 200 0 0 Total TDA Journal Expense 230,050 299,344 305,220 279,200 242,853 4. TDA Today Revenue a. Advertising 11,000 11,000 11,000 8,000 12,000 b. Subscriptions—Membership Dues 29,970 28,470 27,384 28,587 28,610 Total TDA Today Revenue 40,970 39,470 38,384 36,587 40,610 11. TDA Today Expense a. Consultants 49,500 31,866 35,000 27,500 35,000 b. Postage 31,000 40,971 31,000 31,667 0 c. Printing and Production 30,000 28,878 30,000 26,667 0 d. Sales Commissions 0 0 2,750 0 0 Total TDA Today Expense 110,500 101,715 98,750 85,834 35,000 5. TDA Website Revenue a. Advertising 37,000 22,150 45,000 13,200 22,000 b. TDA Affiliates Advertising 0 0 0 0 0 Total TDA Website Revenue 37,000 22,150 45,000 13,200 22,000 12. TDA Website Expense a. Consultants 50,000 16,998 42,000 32,500 0 b. Sales Commissions 0 0 11,250 3,564 2,565 c. Software and Software Support 300 720 0 0 750 d. Subscriptions—Publications 500 0 100 0 0 e. Website Hosting 5,000 3,282 400 2,500 3,000 Total TDA Website Expense 55,800 20,999 53,750 38,564 6,315 3-5. Total Publications/Web Revenues 404,121 289,622 442,191 247,643 265,898 10-12. Total Publications/Web Expense 396,350 422,058 457,720 403,598 284,168 Communications Net Revenue (Loss) 7,771 (132,436) (15,529) (155,955) (18,270) Publications/ Website JOURNAL REVENUE JOURNAL EXPENSE TDA TODAY REVENUE TDA TODAY EXPENSE WEBSITE REVENUE WEBSITE EXPENSE
UNAUDITED 2022 2023 2023 2024 2025 Budget Actual Budget Budget PROPOSED
2025 Proposed Budget Texas Dental Association
Texas Dental Association Budget | www.tda.org | April 2024 9 6. TDA Building Revenue a. Lease Income 313,562 309,505 304,713 314,557 17,916 Total TDA Building Revenue 313,562 309,505 304,713 314,557 17,916 13. TDA Building Expense a. Building Lease Broker Fees 9,000 0 0 0 0 b. Building Management Fees 23,000 26,417 28,000 25,000 0 c. Insurance—Operating 34,141 25,190 23,235 24,650 7,200 d. Office Rent/Lease 0 0 0 0 24,000 e. Repairs and Maintenance—Equipment 40,000 18,298 30,000 15,000 5,400 f. Service Contracts 85,000 93,373 90,000 84,000 27,300 g. Supplies 5,000 3,156 2,000 2,000 900 h. Taxes—State & Local 82,500 76,964 85,000 85,000 22,800 i. Utilities 46,500 48,924 37,000 37,000 14,400 Total TDA Building Expense 325,141 292,322 295,235 272,650 102,000 Building Net Revenue (Loss) (11,580) 17,183 9,478 41,907 (84,084) Building BUILDING REVENUE BUILDING EXPENSE
UNAUDITED 2022 2023 2023 2024 2025 Budget Actual Budget Budget PROPOSED
Texas Dental Association 2025 Budget Explanation
1a. Income from vendor advertising for the annual TDA meeting programs.
1b. Income from ticketed clinician courses and workshops.
1c. Income from exhibit booth fees.
1d. Other income associated with the annual TDA meeting.
1e. Fees from alumni lunches and other professional groups’ events.
1f. Income from registration fees.
1g. Income from corporate sponsorships.
2a. Income from vendor advertising associated with continuing education programs.
2b. Income from ticketed clinician courses and workshops, separate from the TDA Meeting.
2c. Income from exhibit booth fees, separate from the TDA Meeting.
2d. Other income associated with TDA continuing education programs.
2e. Subscription income from the TDA Dental Concierge app.
2f. Income from registration fees, separate from the TDA Meeting.
2g. Income from corporate sponsorships associated with TDA continuing education programs.
3a. Income from sale of classified and display advertising in Texas Dental Journal
3b. Sale of single issues of the Texas Dental Journal
3c. Member subscriptions allocated from dues for the Texas Dental Journal at $17 per dues-paying member.
4a. Income from advertising in TDA Today
4b. Member subscriptions allocated from dues for the TDA Today at $5 per dues-paying member.
5a. Income from advertising on the TDA website.
5b. Payment from affiliates for website advertising.
6a. Income from leased space in the TDA building.
7a. Dues income available for operations after allocation of $22 per member for Texas Dental Journal and TDA Today.
7b. Earnings from operating sweep account.
7c. Miscellaneous income for new digital sponsorships and ADA grants.
7d. Sponsorships specifically in support of the ADA TX reception event.
7e. Payment from the for-profit affiliate, FSI, for administrative support of staff and equipment provided by the TDA.
7f. Cash distribution from TDA Member Benefits, Ltd, in which TDA is the limited partner.
7g. Cash distribution from CE Concierge, LLC, in which TDA is the limited partner.
8a. Audio-visual for courses and workshops at the TDA Meeting.
8b. Charges in connection with the TDA meeting bank accounts and credit card charges.
8c. Cost of clinician honoraria at the TDA meeting.
8d. Cost of clinician hotel, travel, course supplies, electrical, meeting rooms, and signs at the TDA meeting.
8e. Fees for outsourced services and sales commission for the TDA meeting.
8f. Exhibit hall costs, printing of exhibitors’ prospectus, refreshments, electrical/ decorating setup for exhibitors and security.
8g. Cost of catering for speakers, VIPs, staff and Council on Annual Meeting & CE Programs during the TDA meeting.
8h. Insurance premiums paid to cover meeting cancellation.
8i. Charges for other costs associated with the TDA meeting.
8j. Cost of printing the on-site program.
8k. Alumni luncheons and other classes.
8l. Postage used for the TDA meeting.
8m. Marketing, direct mailing, promotional items, and print and digital advertising.
8n. Cost of registration firm for the TDA meeting, as well as onsite setup cost, electrical, and staffing.
8o. Meeting planning and Council on Annual Meeting & CE Programs travel to scout other dental meetings.
8p. Cost of shuttle transportation for remote parking to the convention for attendees.
8q. Stipend paid to the San Antonio District Dental Society.
8r. Supplies purchased for use at the TDA meeting.
8s. Catering, space rental, and other expenses for the TDA Party, open to all TDA meeting attendees.
8t. Meeting planning and Council on Annual Meeting & CE Programs travel to attend the TDA meeting.
8u. Catering, space rental, and other expenses for the VIP Reception.
9a. Audio-visual for continuing education programs.
9b. Charges in connection with the continuing education banking and credit card charges.
9c. Cost of clinician honoraria for courses and workshops.
9d. Cost of clinician hotel, travel, course supplies, electrical, meeting rooms, and signs at TDA continuing education programs.
9e. Fees for outsourced services and sales commission for TDA
10 Texas Dental Association Budget | www.tda.org | April 2024
continuing education programs and 20% revenue sharing fees with partner Eleventh & Gather.
9f. Exhibit hall costs, printing of exhibitors’ prospectus, refreshments, electrical/ decorating setup for exhibitors and security.
9g. Food and beverage costs at TDA continuing education programs.
9h. Insurance premiums paid to cover CE programs cancellation.
9i. Charges for other costs associated with TDA continuing education programs.
9j. Postage used for TDA continuing education programs.
9k. Marketing, direct mailing, promotional items, and print and digital advertising.
9l. Cost of registration hosting for TDA continuing education programs.
9m. Stipends paid to local component societies.
9n. Supplies purchased for use at TDA continuing education programs.
9o. Cost of travel for staff to attend TDA continuing education programs.
9p. Information technology expenses for TDA continuing education programs.
10a. Fees for outsourced graphic design and editing services.
10b. Cost of meetings held in connection with Texas Dental Journal business.
10c. Cost of mailing the Texas Dental Journal to all members.
10d. Cost of printing and artwork for the Texas Dental Journal.
10e. Sales commission paid for selling advertising in the Texas Dental Journal
10f. Supplies used for the Texas Dental Journal
10g. Staff travel in connection with Texas Dental Journal business.
11a. Fees for outsourced graphic design and editing services.
11b. Cost of mailing newsletter, TDA Today
11c. Cost of printing and artwork for the newsletter, TDA Today
11d. Sales commission paid for selling advertising in TDA Today
12a. Fees for outsourced website administration and design services.
12b. Sales commission paid for selling advertising on the TDA website.
12c. Costs associated with software and support for the website.
12d. Professional publications related to the website.
12e. Costs to host website.
13a. Broker leasing commissions for building leasing services.
13b. Management fees associated with managing the building.
13c. Premiums paid for insurance associated with the TDA building.
13d. Costs of leasing short-term office space for the Central Office.
13e. Cost of equipment repair and maintenance for the building.
13f. Service contracts associated with building such as the elevator service, security, HVAC, landscaping, etc.
13g. Supplies used to maintain the building.
13h. Property taxes paid on building.
13i. Gas, water and electricity expenses.
14. Projected estimated costs of capital improvements needed.
15. Contingency for approved expenditures by the Board of Directors.
16a. Full-time and part-time employee compensation. The amount reflects annual salary adjustments, and merit-based bonuses.
16b. Employer’s portion of FICA and Medicare plus state and federal unemployment tax.
16c. Health, vision, and dental insurance for eligible employees.
16d. Payments to retirement plan for all eligible employees.
16e. Liability coverage for TDA Officers and Component Society Officers, and personal property coverage.
16f. Cost of leasing postage meter and copier equipment.
16g. Maintenance costs for office equipment and general office operations.
16h. Postage, UPS, and Federal Express charges.
16i. All printing jobs done outside office such as stationery, business forms, and dues statements.
16j. General office, printing and copy machine supplies.
16k. Personal property taxes of the Central Office furniture and equipment.
16l. Information technology services for Central Office.
16m. Cost of payroll service used by TDA.
16n. CPA firm fees for annual audit, consulting services, and tax return preparation.
16o. Charges for bank transaction fees and returned checks.
16p. Expenses associated with information technology consultants.
16q. Retainer for legal counsel and related legal expenses.
16r. Expenses associated with consulting firms engaged for legislative lobbying services.
16s. Flowers for funerals, special gifts to VIPs, members, and their families.
16t. Credit card processing fees and other bank charges for processing TDA dues payments (excludes ADA and local component society portions).
16u. Continuing education and organizational development costs for TDA employees.
16v. Marketing related expenses associated with membership marketing initiatives.
16w. Meals and supplies not directly related to a specific council, committee, or Board meeting.
16x. Memberships to the Austin Club, TSAE, ASAE, and other organizations for TDA staff.
Texas Dental Association Budget | www.tda.org | April 2024 11
16y. Press clippings and other subscriptions used in the Central Office.
16z. Advertising cost for open staff positions.
16aa. Travel expenses for executive director and TDA staff not related to a council or committee.
17a. Travel reimbursement for the president while on TDA business.
17b. Stipend paid to the president.
17c. Travel and per diem reimbursement for the president-elect while on TDA business.
17d. Stipend paid to the presidentelect.
17e. Travel and per diem reimbursement for the past president while on TDA business.
17f. Travel and per diem reimbursement for the secretarytreasurer while on TDA business.
17g. Stipend paid to the secretarytreasurer.
17h. Travel expenses for the editor while on TDA business.
17i. Stipend paid to the editor.
17j. Travel and per diem reimbursement for the 4 vice presidents while on TDA business.
17k. Travel and per diem reimbursement for the 4 senior directors while on TDA business.
17l. Travel and per diem reimbursement for the 4 directors while on TDA business.
17m. Travel and per diem reimbursement for the speaker of the house and parliamentarian while on TDA business.
17n. Costs associated with conducting Board meetings such as beverages, lunches, Board dinners (the cost of the Board meals are deducted from Board per diem), mailing and printing of Board-approved communications, and remote meetings.
18a. Meeting costs and travel reimbursement for committee
that monitors the TDA audit functions.
18b. Cost of awards presented by the TDA, including meeting and travel reimbursement costs for committee.
18c. Meeting costs and travel reimbursement for committee that formulates initial budget recommendations for the Board of Directors, has oversight of the investment activity and monitors the financial functions.
18d. Meeting costs and travel reimbursement for the Community Fluoride Committee.
18e. Meeting costs and travel reimbursement for the Strategic Affairs Committee.
19a. Reimbursement for travel, meeting costs, and council projects for the Council on Annual Meeting and CE Programs.
19b. Reimbursement for travel, meeting costs, and council projects for the Council on Legislative, Regulatory, and Governmental Affairs.
19c. Administrative support for DENPAC.
19d. Reimbursement for travel, meeting costs, and council projects for the Council on Dental Licensing, Standards and Education.
19e. Reimbursement for travel, meeting costs, and council projects for the Council on Ethics and Judicial Affairs.
19f. Reimbursement for travel, meeting costs, and council projects for the Council on Governance.
19g. Reimbursement for travel, meeting costs, and council projects for the Council on Membership, New Dentists and Students.
19h. Reimbursement for travel, meeting costs, and council projects for the Council on Peer Review plus training sessions for component officers.
19i. Reimbursement for travel, meeting costs and council projects for the Council on Professions and Trends.
19j. Reimbursement for travel, meeting costs and council projects for the Council on Public Health and Access to Care.
19k. Administrative support for TOHPAC.
20a. Reimbursement for travel and hotel for Delegates and Alternates to attend the ADA House of Delegates and precaucus meeting, and related meeting costs.
20b. Printing, supplies, meeting rooms, and general expenses associated with the 15th Trustee District Headquarters at the ADA House of Delegates.
20c. Reception given by the TDA at the ADA House of Delegates.
21a. Costs of luncheon for 60 Year, 50 Year, and Life Members at the annual TDA meeting.
21b. Costs associated with meetings of the TDA House of Delegates, including reference committees.
21c. Costs for breakfast for past presidents and past vice presidents at the annual TDA meeting.
22a. Estimated costs for federal income taxes for non-related business income.
22b. Cost associated with TDA leadership conferences other than the annual TDA meeting.
22c. Stipends paid to the Alliance of the TDA and the Texas Dental Assistants Association.
22d. Cost of building loan interest for building renovation.
23. Funding for the operating costs of the TDA Smiles Foundation.
24. Expenditure reduction subject to funding by cash reserves, if available, as per the Method of Finance Rider.
25. Dividend payment from the for-profit affiliate, TDA Financial Services, Inc.
12 Texas Dental Association Budget | www.tda.org | April 2024

























































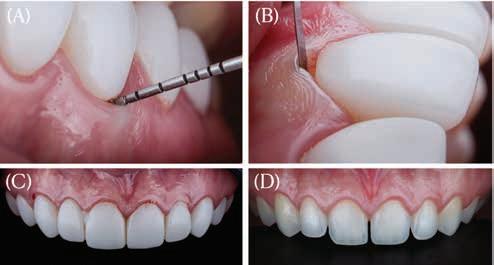



 Former General Counsel, Texas Dental Association
Former General Counsel, Texas Dental Association












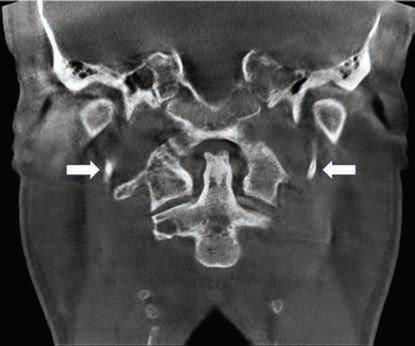
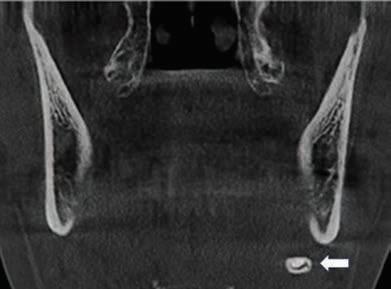

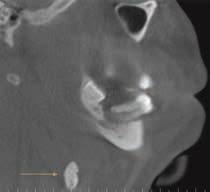








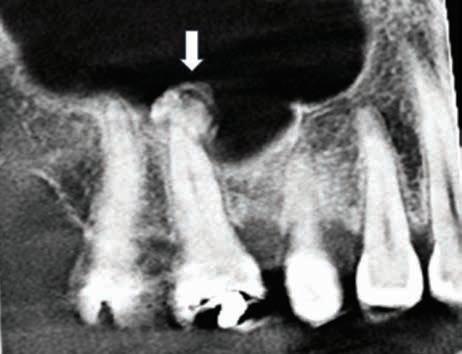




 By Phil Nieto; President, Best Card
By Phil Nieto; President, Best Card

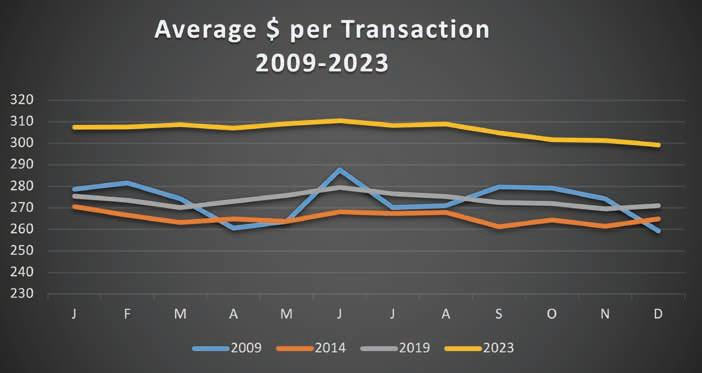




 Dr Carmen Smith Secretary-Treasurer, TDA
Dr Carmen Smith Secretary-Treasurer, TDA