TEXAS DENTAL





course concludes, so you will receive immediate CE credit for attendance 4. With the webcast, you can enjoy real-time interaction with the course instructor, utilizing a question and answer format


OUR MISSION STATEMENT: To provide affordable, quality anesthesia education with knowledgeable and experienced instructors, both in a clinical and academic manner while being a valuable resource to the practitioner after the programs. Courses are designed to meet the needs of the dental profession at all levels. Our continuing education programs fulfill the TSBDE Rule 110 practitioner requirement in the process to obtain selected Sedat ion permits. AGD Codes for all programs: 341 Anesthesia & Pain Control; 342 Conscious Sedation; 343 Oral Sedation This is only a partial listing of sedation courses. Please consult our www.sedationce.com for updates and new programs. Two ways to Register: e-mail us at sedationce@aol.com or call us at 214-384-0796

Lynne S. Gerlach,
H.
Priyanshi Ritwik,
Jacqueline M. Plemons, DDS, MS, Editor
Paras B. Patel, DDS, Associate Editor
Nicole Scott, Managing Editor
Barbara Donovan, Art Director
Lee Ann Johnson, CAE, Director of Member Services
Ronald C. Auvenshine, DDS, PhD
Barry K. Bartee, DDS, MD
Patricia L. Blanton, DDS, PhD
William C. Bone, DDS
Phillip M. Campbell, DDS, MSD
Michaell A. Huber, DDS
Arthur H. Jeske, DMD, PhD
Larry D. Jones, DDS
Paul A. Kennedy Jr, DDS, MS
Scott R. Makins, DDS, MS
Daniel Perez, DDS
William F. Wathen, DMD
Robert C. White, DDS
Leighton A. Wier, DDS
Douglas B. Willingham, DDS
PRESIDENT Duc “Duke” M. Ho, DDS 281-395-2112, ducmho@sbcglobal.net
PRESIDENT-ELECT Cody C. Graves, DDS 325-648-2251, drc@centex.net
PAST PRESIDENT Debrah J. Worsham, DDS 936-598-2626, worshamdds@sbcglobal.net
VICE PRESIDENT, SOUTHEAST Glenda G. Owen, DDS 713-622-2248, Dr.owen@owendds.com
VICE PRESIDENT, SOUTHWEST Carlos Cruz, DDS 956-627-3556, ccruzdds@hotmail.com
VICE PRESIDENT, NORTHWEST Teri B. Lovelace, DDS 325-695-1131, lovelace27@icloud.com
VICE PRESIDENT, NORTHEAST Elizabeth S. Goldman, DDS 214-585-0268, texasredbuddental@gmail.com
SENIOR DIRECTOR, SOUTHEAST Shailee J. Gupta, DDS 512-879-6225, sgupta@stdavidsfoundation.org
SENIOR DIRECTOR, SOUTHWEST Richard M. Potter, DDS 210-673-9051, rnpotter@att.net
The Texas Dental Journal is a peer-reviewed publication. Established February 1883 • Vol 139 | No. 8
Texas Dental Association 1946 S IH-35 Ste 400, Austin, TX 78704-3698 Phone: 512-443-3675 • FAX: 512-443-3031 Email: tda@tda.org • Website: www.tda.org
Texas Dental Journal (ISSN 0040-4284) is published monthly (one issue will be a directory issue), by the Texas Dental Association, 1946 S IH-35, Austin, TX, 78704-3698, 512-443-3675. Periodicals Postage Paid at Austin, Texas and at additional mailing offices. POSTMASTER: Send address changes to TEXAS DENTAL JOURNAL, 1946 S IH 35, Austin, TX 78704. Copyright 2022 Texas Dental Association. All rights reserved.
Annual subscriptions: Texas Dental Association members $17. Instate ADA Affiliated $49.50 + tax, Out-of-state ADA Affiliated $49.50. In-state Non-ADA Affiliated $82.50 + tax, Out-of-state Non-ADA Affiliated $82.50. Single issue price: $6 ADA Affiliated, $17 Non-ADA Affiliated, September issue $17 ADA Affiliated, $65 Non-ADA Affili ated. For in-state orders, add 8.25% sales tax.
Contributions: Manuscripts and news items of interest to the membership of the society are solicited. Electronic submissions are required. Manuscripts should be typewritten, double spaced, and the original copy should be submitted. For more information, please refer to the Instructions for Contributors statement printed in the September Annual Membership Directory or on the TDA website: tda. org. All statements of opinion and of supposed facts are published on authority of the writer under whose name they appear and are not to be regarded as the views of the Texas Dental Association, unless such statements have been adopted by the Association. Articles are accepted with the understanding that they have not been published previously. Authors must disclose any financial or other interests they may have in products or services described in their articles.
Advertisements: Publication of advertisements in this journal does not constitute a guarantee or endorsement by the Association of the quality of value of such product or of the claims made of it by its manufacturer.
SENIOR DIRECTOR, NORTHWEST Summer Ketron Roark, DDS 806-793-3556, summerketron@gmail.com
SENIOR DIRECTOR, NORTHEAST Jodi D. Danna, DDS 972-377-7800, jodidds1@gmail.com
DIRECTOR, SOUTHEAST Laji J. James, DDS 281-870-9270, lajijames@yahoo.com
DIRECTOR, SOUTHWEST Krystelle Anaya, DDS 915-855-1000, krystelle.barrera@gmail.com
DIRECTOR, NORTHWEST Stephen A. Sperry, DDS 806-794-8124, stephenasperry@gmail.com
DIRECTOR, NORTHEAST Mark A. Camp, DDS 903-757-8890, macamp1970@yahoo.com
SECRETARY-TREASURER*
Carmen P. Smith, DDS 214-503-6776, drprincele@gmail.com
SPEAKER OF THE HOUSE*
John W. Baucum III, DDS 361-855-3900, jbaucum3@gmail.com
PARLIAMENTARIAN**
Glen D. Hall, DDS 325-698-7560, abdent78@gmail.com
EDITOR** Jacqueline M. Plemons, DDS, MS 214-369-8585, drplemons@yahoo.com
LEGAL COUNSEL
Carl R. Galant
*Non-voting member **Non-voting
As you have seen, this issue includes an article about Dr Jacqueline Plemons, who was awarded TDA’s Gold Medal. She is a leader, a successful periodontist, professor, partner, and mother. She is also our editor, a woman of many hats, if you will, so she hung one up this month and took a break from writing her monthly letter. As her right-hand woman, I’m on deck.

The winds of change are blowing through TDA. Now more than ever, TDA is a diverse group of young and mature dentists, general and specialists from a variety of backgrounds, and doctors who treat patients from all walks of life. I have worked for the Association for more than 10 years, and I am excited for a particular change coming up next month.
Per resolution, a task force was formed to evaluate the Journal, specifically its format, delivery, and content. This group met via Zoom 4 times and discussed the Journal’s future amid a changing print media landscape and the best way to move it forward in a digital world. Not only did the dentists suggest to the Board to publish 10 issues instead of 12, but they also want to see a new look and feel to the publication. The Journal has looked the same for a long time, decades.
With the help of a membership survey conducted in June 2022, some feedback we received included the need for more articles on practice management, trends in technology, personal stories, and more! So, armed with that information, we plan to unveil the Journal’s new design next month (December 2022). We hope that you will like its clean, modern approach and articles that each of you find interesting.
It’s a labor of love for all of us behind the scenes, and we’re excited to show it to you. Stay tuned! Change is coming!


Are you a Dentist who is becoming tired of working chairside, near the end of your career, or merely looking for supplemental income? Dental Expert Witness work could be the answer for you!
Until now there have been no lectures and no instruction available on what it is, what it takes, and how to market yourself as an Expert Witness. Our exclusive workshop is the first ever of its kind!
Using their 30 years of experience, Dr. Boeke DDS & Dr. Krueger DDS/JD have created a 2 day workshop on the beautiful Texas A&M-Commerce campus, that will teach you the ins and outs of becoming an Expert Witness in a way that is informative, effective, and fun.

- what it is to BE a Dental Expert Witness - how it helps serve your peers and community - how it generates additional income outside of the chair

-how to market yourself as an Expert Witness.
- Dr. Krueger’s firsthand records and depositions of trials past
- mock testimonies based on those trials, complete with testimony from a witness stand - end your day with a Texas BBQ experience on Dr. Boeke's Ranch
For an exclusive experience, our program is limited to 10 seats per month!
FOR NOVEMBER & DECEMBER 2022
For more information, and to reserve your seat, please visit www.dentalexpertwitnesstraining.com
RELATIONSHIP. MENTORSHIP. COMMUNICATION.
At every opportunity afforded to me, whether at component visits or at the most recent American Dental Association meeting in Houston, I often give the “elevator speech” to both members and nonmembers on why membership in our Association is so important. It’s a conversation that I never take for granted, even when among friends who have been members for a while, because sharing our story will strengthen our Association and profession.
In the spirit of never missing an opportunity, I will share why it’s important to be a member, how you can join (or renew), and what’s currently happening at the Texas Dental Association.
1. Personalized Help with dental insurance and even compliance issues (including with the TSBDE, DEA, EPA, or DSHS).
2. Information Resources in all our publications and social platforms will keep you informed of any changes in rules or regulations that might affect you.
3. Continuing Education discounts on CE courses on the TDA Dental Concierge App (including Pankey Courses), as well as the TDA Meeting and local component meetings.
4. Advocacy through promoting bills and laws that protect both dentists and patients, while also opposing any intrusion (from third party payors, outside organizations, etc.) that look to interfere with the dentist-patient relationship.
1. Monthly installments for the course of a year.
2. One full payment for the entire year.
• On October 3, 2022, your TDA team participated in the American Dental Association’s (ADA) webinar on “Dental Workforce Shortages: Data to Navigate Today’s Labor Market” (the PowerPoint can be found in the link below).
• We continue to meet with legislators, affiliate associations and even staffing companies to discuss this ongoing problem and look for new, creative opportunities to help members during this difficult time.

• Written testimony was submitted to the House Select Committee on Health Care Reform explaining the need for increased funding to Medicaid Dental so that reimbursement rates match in today’s dollars what they were in 2007 (strengthening the network and helping more patients).
• Prepping for the upcoming legislative session to push for insurance legislation opposing network leasing and disallowables, while also supporting reasonable time limits on retractive denials
“Duke” M. Ho, DDS, FAGD TDA President• TDA Perks’ endorsed vendor ERC Specialists now has more than $11,341,000 in scheduled refunds to TDA members. I encourage those who have not checked your eligibility yet, to do so and apply at https://tdaperks.com/specialtypayroll-company-erc-tax-credit if you haven’t yet.
• Pankey courses added to the TDA Concierge App Library
• Continued preparation of speakers and social events for the 2023 TDA Meeting in San Antonio.
Of course, so much more is happening behind the scenes: more advocacy, more educational programs, more changes to our publications, and more support to local components. So, if you’re not sure how the Association works for you, know that I am always happy to share the “elevator pitch.”
ADA PowerPoint Link: https://www.ada. org/-/media/project/ada-organization/ ada/ada-org/files/resources/research/ hpi/dental_workforce_shortages_labor_ market.pdf?rev=e6025d77df184e6c95dc7 cefde4adee3&hash=225FCBBCCB67174AA FC760FE2287322D
“Our lives are defined by opportunities, even the ones we miss.”
Benjamin Button
Since 1968
We




Jeremiah R. Taylor, D.D.S. Donald D. Landry, D.D.S.



$778K EAST TEXAS - NEAR LOUISIANA BORDER: 4,400+ sq. ft. facility with 6 fully equipped ops and 2 additional plumbed. All digital with digital Pan (Sirona Galileos CBCT) and paperless with Eaglesoft. The practice has 1,250 active 100% FFS patients with an average of 50 new patients per month. The collections are over $778K on a 4-day work week. The seller would also like to sell the real estate, but is open to leasing to start. Opportunity ID: TX-7432
$850K 15 MINUTES SOUTH OF HOUSTON: 65% Medicaid and 35% PPO with a healthy hygiene program. Operates on 4 doctor days and 9 hygiene days collecting over $850K per year. The facility is 1,950 sq. ft. and has 5 equipped ops with another op plumbed that could be an expanded operatory. If you want a practice where you work with kids and enjoy the diversity of providing more complex dentistry for adults, this practice is the right practice for you! Opportunity ID: TX-7373



Sateesh K. Ummareddy, D.D.S. Niosha Edalat, D.M.D. has acquired the practice of



has acquired the practice of Kilgore, Texas Arlington, Texas We are please to have represented all parties in these transitions.
$600K PRIME AUSTIN OPPORTUNITY: This practice collected $600K pre-Covid on a 4 doctor and 4 hygiene day workweek. Located in a busy retail center, with 5 ops in 1,700 sq. ft. the office is in excellent condition and has digital x-ray and pan. With over 1,350 active FFS 20%, PPO 80%, patients and an average of 25 new patients per month; this practice is primed for growth. Opportunity ID: TX-7183
$890K NEAR GALVESTON BAY: Exceptional 2000, 24-month count PPO/FFS patient base, 30 minutes south of downtown Houston. This 4 op, 2000 sq. ft. facility is located in a free-standing building on a major thoroughfare. It is currently a bread and butter practice focusing on restorations, crown & bridge and hygiene services. Tremendous opportunity for growth for the doctor with implant skills, who enjoys oral surgery, endo and perio, in addition to producing fine restorative dentistry. Opportunity ID: TX-7153 Go to our website or call to request information on other available practice opportunities! 800.232.3826 Practice Sales & Purchases Over $3.2 Billion www.AFTCO.net
 Katie E. Stuchlik, DDS, FAGD
Katie E. Stuchlik, DDS, FAGD
While attending a recent dental conference in Austin, I was asked by a more seasoned dentist why New Dentists are avoiding practice ownership more often than not. Unable to give him a straight answer, I responded, “Maybe they’re not ready yet.” The conversation continued with a few more dentists who cited their beliefs on why new dentists are avoiding practice ownership.
All valid reasons, I came to the realization I have placed myself in a bubble where every few months another friend from dental school is opening or buying a practice. In my eyes, New Dentists are starting and buying practices. In my eyes, New Dentists want to be their own boss. In my bubble of overachievers, we (New Dentists) all want to be practice owners.
Since the large majority of New Dentists are actually not practice owners, I hope to share my experience through this column to help any dentist on the fence about practice ownership. I hope to empower you to take a leap of faith, or to solidify your reasoning otherwise.

It’s only fitting to start by sharing my Why.
During dental school, I never saw myself as a practice owner. I worked hard in school just to become a dentist. I hoped to find an associateship where mentorship would open more opportunity for growth. In the early summer of 2017, my life was turned upside down with my father’s declining health due to pancreatic cancer. As the only child out of 4 still living in Houston, a great responsibility was placed on my husband and me to be available as often as we could for my parents. I’d leave work drained from being “on” all day with my patients and drive 35 minutes straight to M.D. Anderson in the Houston Medical Center to check on my dad as frequently as needed. My associateship was nothing but supportive of any days I needed to leave early or arrive late, but oftentimes I chose not to ask for this time as I felt guilty for burdening the other dentists and staff.
My mental health was suffering during this time (did I mention I was a newlywed, too?). My dad would hear me cry every day that I was a terrible dentist and didn’t belong in this profession. Even on his worst days, he assured me that bad days are always learning experiences to prepare you for the future. His advice, along with that of a good friend and classmate Dr Lindsey Wendt, led me to believe I would be happiest in a setting where I had more control. I’ve never fully aligned with a Type A personality, though I firmly believe it’s impossible to be a dentist without some of those personality traits. Having control of my schedule, my team, and the long-term goals of my dentistry would set me up for success in dentistry.
And just like that, my path to practice ownership began. As a practice owner, I can shape my life and career in a way to be a great dentist, spouse, friend, mother, and dedicated member of organized dentistry. As an associate, I struggled to fit all of the puzzle pieces together. My Why is the need to be a better person all around.
In the end, buying into an existing practice still seemed to prevent me from being the best version of myself. I took a leap of faith with Dr Lindsey Wendt in October 2018 and started Dentistry of the Oaks from scratch. In the coming months, I’ll share my tips, challenges, and insight into starting a practice, working with a partner, and everything in between. My wisdom for this month is to simply discover what brings you joy, and to realize your path in dentistry can fully align with your life goals.
“Too much effort.”
“Too much stress.”
“They like to leave their work at the office.”
“Too many loans.”

When Jacqueline Plemons was 7 years old, her mother had a toothache. She was a single mother working as a telephone operator and funds were lean.
A kind oral surgeon stepped in and offered treatment, alleviating her mother’s pain. His compassion that day extended to Jacque. He gave her a tour of the office, showing her how the foot pump moved the dental chair up and down.
“From that moment on, I wanted to be just like him, a kind and generous dentist who helped people who can’t help themselves,” Dr Plemons recalls. “I never really considered any other profession!”
Born in Princeton, West Virginia, Jacque’s birth father’s last name was Gleason. “Funny story—my official name was ‘Jackie Gleason’ for the first 8 years of my life! It was the early 1960s when The Honeymooners were on prime-time television.”
Her childhood was spent in Miami, Florida, with her mother’s family and a Cuban immigrant family. “They took care of my younger sister and me much of the time,” she says. “I still remember the language that was spoken, the smell of the food, and the sound of the music while in the loving home of Marina and Faustino Fernandez.”
Dr Plemons’ stepfather was in the military, and the family moved many times, in and out of the United States. “In all, I went to 14 different schools from kindergarten through dental school. I played saxophone in the band, which gave me a group to fit in wherever we lived. My first job was at Taco Bell when I was 15 years old. My strangest job was ‘catching chickens’ while living with my aunt and uncle in Arkansas.”
In school, her achievement tests suggested a career in science, and so it began. She graduated from Temple High School and then attended Texas A&M University. She completed her predoctoral program and residency in periodontics at Baylor College of Dentistry (now Texas A&M School of Dentistry).

“When I finished my residency, I really wanted to settle down and put down some roots. I was offered a job teaching at the dental school, and I joined my mentor Dr Hilton Israelson (2016 Gold Medal winner) as an associate. I am very grateful for his support through the years.”
And so, over those years, she made a name for herself. Dr Plemons is a periodontist in Dallas and a clinical professor at Texas A&M School of Dentistry. She has devoted her professional life of almost 4 decades to organized dentistry and the profession, and this year, the TDA awarded her with its well-deserved highest honor, the Gold Medal for Distinguished Service.

Actually, I was born “a coal-miner’s daughter” in Princeton, West Virginia.TDA President Dr Debrah J. Worsham presents the Gold Medal for Distinguished Service to Dr Jacqueline Plemons at the House of Delegates in May 2022.
The 26th recipient of the Gold Medal, she is honored by the distinction. “I was incredibly surprised and extremely proud to receive the Gold Medal,” Dr Plemons says. “I am grateful for the opportunities that have been made available to me through the years and for those who surrounded me and shared their knowledge, support, and friendship. I am in awe of the previous awardees, and I am ever mindful that it is their efforts that have made the dental profession what it is today.”
Dr Plemons credits organized dentistry with her ability to impact the profession. “It was through service in organized dentistry that I saw how members could make a real difference in the way dentistry was practiced on the local, state, and national levels.”
Dr Plemons served as president of the Dallas County Dental Society and chair of the Southwest Dental Conference. She later asked (rather, begged, as she recalls) to join the TDA Council on Dental Education, Trade and Ancillaries. Dr Plemons was named president
of the TDA in 2020 and chair of the ADA Council on Dental Education and Licensure in 2020. “I saw first-hand how the TDA’s efforts made a difference in how we practice dentistry in Texas.”

Describing herself as a naturally shy person, Dr Plemons says she is fortunate to serve with others who mentored and supported her through various stages of her career. “I have never felt alone, and I believe it is now my time to give that support back to others.”


When she is not at her practice or at the dental school, Dr Plemons is at home with her family. Her partner Elain was a certified tobacco treatment specialist at Texas A&M School of Dentistry Department of Public Health Services until retiring in December 2021. Their family was formed through adoption—19-year-old Marin was born in Guatemala and 13-year-old Jayden was born in Dallas.
She says scheduling her daughters’ busy activities of sports and band is more difficult than scheduling her patients in her practice. “Rin is studying architecture and is totally in love with her 2-year-old golden doodle named Brandie. Jayden is in the eighth grade— she is a good 4 inches taller than all of us! She plays trombone in the school band and sings in a chorus.”
Dr Plemons enjoys traveling, reading, gardening, and bird watching, but especially the water. “From swimming to fishing, I feel most at peace near the water.”
MARin is studying architecture and is totally in love with her twoyear-old golden doodle named Brandie.
Dr Plemons is pictured with her partner Elain.



A life at peace can come when one’s profession becomes an avocation, a calling, said the late virologist Jonas Saik, and Dr Plemons relates.


“Having a broader awareness of the issues affecting dentists and the patients they serve has made me be better at positioning myself in a manner that I can make the greatest difference. I view time spent out of my office in service as well worth the effort. Knowledge is power and change begins with awareness. It’s been a real privilege to serve organized dentistry and the dental profession.”
Jayden is in the eighth grade— she is a good 4 inches taller than all of us! She plays volleyball, basketball, tennis, and track.
The Gold Medal for Distinguished Service is the highest honor one can achieve in the Texas Dental Association. Nominations are submitted to the Awards Committee by the Board of Directors, component society presidents, and component executive staff.

Only one person per year may receive the award, and that is only if the Awards Committee believes one of the nominees successfully meets the criteria. The criteria involve service in TDA leadership positions, ADA service, local society contributions that affected state concerns, commitment to organized dentistry through other organizations including teaching, and service to the community.
Owing to its stature, the TDA president presents the award before the House of Delegates. The name of the recipient is not revealed to anyone, including the
recipient, until the actual presentation takes place. The Awards Committee works behind the scenes with the recipient’s family members to make sure they are in attendance without alerting the recipient.
In 2006 the TDA commissioned nationallyrenowned Texas artist Ronadró to design a unique award piece to represent the Association. The result is a beautiful, bronze relief depicting a dentist caring for a patient. This sculpture was adopted for the Gold Medal award in 2008. Inset into the shadowbox are 2 custom designed medallions: the TDA seal and the gold medal.

To date, there have been 25 previous recipients of the Gold Medal: Drs John D. Wilbanks, Michael D. Vaclav, O.V. Cartwright, H.M. “Mit” Sorrels, Jack H. Harris, James E. Bauerle, Robert V. Walker, Frank K. Eggleston, Robert M. Anderton, Rene M. Rosas, Richard M. Smith, Sam W. Rogers Jr, Stephen F. Schwartz, John S. Findley, S. Jerry Long, Patricia
L. Blanton, Paul E. Stubbs, Richard C. Black, Michael L. Stuart, Hilton Israelson, Thomas Harrison, J. Preston Coleman, Larry W. Spradley, Rita M. Cammarata, and John Purdy. By the judgment of their colleagues, they represent the best of the TDA; dentists who have dedicated their lives to the Association and profession, and have advanced both through their commitment, strength, and vision.




There will come a day when most practice owners decide to transition their practice. While some will walk away from their life’s work by simply closing their doors, the overwhelming majority sell to either an individual, small group, or Private Equity (PE). The differences are significant, and these differences determine if you finish well. The seller must first identify their practice transition’s goals, the results of which will lead to the style of buyer which makes the most sense.
First, and prior to deciding the type of buyer, let us evaluate the usual internal issues which dentists should consider: culture, control, and cash. Sage practitioners look to continue the culture of that which they have built, including the clinical quality, patient relationships and their team’s loyalty and employment. Another may look at maintaining important management and clinical control. Others may wish to maximize sales price above all other considerations. There is no right or wrong in these 3 macro categories. You, as the selling doctor, identify and determine the importance of these priorities.
Culture-driven practices include large or small, solo or group. These practices spend significant effort on creating the right team who represents the doctor’s goal of clinical excellence, high ethics, and relationship importance. These practices
tend to focus on one or limited aspects of specialization, and they often refer to local specialists with positive patient outcomes and experiences being of utmost importance.
We refer to this practice as a Legacy Practice. The right buyer could be one groomed to someday take the reins, such as an associate, or simply a doctor who shares the senior doctor’s values and philosophy.
Most dental practice owners have been in charge their entire professional life. They lead their daily activities, manage their clinical and emotional future, and direct the practice’s reputation. Often, these practices are also a culture-first practice. A partnership may make the most sense, allowing the senior doctor to remain in a position of managerial control and influence. Once comfortable with their new partner(s) as well as ready to discontinue practicing, they then sell their remaining equity interest.
Partnerships are often legacy practices as well.
These dental practices operate as pure businesses and are financially driven. They may have multiple locations and multiple doctors, may have non-dentist management, or may
be a selling dentist who seeks the highest bidder above all other considerations. This style practice routinely accepts multiple PPO insurance products. Relationship issues with patients range widely, from important to non-essential. Daily volume is often moderate to high, multiple specialty procedures (restorative, endo, perio, ortho, surgery etc.) are performed routinely in office, and financial expectations are injected into the daily routine.
Dentists who practice with high ethics and standards can fit into any of these 3 categories. As mentioned earlier, there is no right or wrong style. However, as the seller, you must know which of these styles best describes your practice. An honest self-assessment will guide how one proceeds with the conclusion of their career, allowing the doctor to select the right buyer and best method of transition.

A small or medium size practice, where culture is the driving philosophy, will search for a solo buyer or merge with another practice. This traditional transition model can work beautifully by matching the buyer’s and seller’s practice philosophy. Proper matching of goals, clinical expertise and business objectives yields a successful transition. The seller achieves their goal of cultural continuation, meaning their patients will be well-cared for and staff retention is likely. For the buyer, they achieve their goal of becoming a small business owner caring for people. This win-win result is a dream transition, finds the retiring doctor concluding well, and it finds the buyer finally realizing their dream of practice ownership. Life is good!
Conversely, if philosophies of buyer and seller are incongruent, a nightmare can result. Please remember this—you are selling your life’s work, not a car. A qualified and caring transition specialist is an expert guiding you in this process and is instrumental in recruiting and vetting a potential buyer that matches the seller’s objectives.
Secondly, if you seek to maintain control of your work environment, slow down a bit, share the workload, but not ready to conclude clinical dentistry, a partnership may be for you. You may elevate an associate, approach a younger dentist (if your practice is large enough to accommodate 2 dentists), join a small group, or have a transition specialist search for your new partner. Selling a portion of your practice, known as an incremental buy-in, allows the seller to achieve their goals while monetizing a portion
of their asset. The same formula as above would apply—matching styles, expertise and philosophy is imperative!
These first 2 scenarios are the traditional model. However, dentistry is shifting from solo practice dominance towards a private equity model. Historically, dentists would argue this is the bane of dentistry, yet ‘corporatization’ has led many competing practices to improve their oversight and tighten their processes. Solo dentists have adapted by understanding business aspects. They adapt to remain relevant and successfully grow in a more competitive marketplace. Oddly, and despite innumerable headlines and articles, only 10.4% of dentists per the ADA’s Health Policy Institute were associated with DSOs in 2019. Although that percentage continues to increase, DSO practices are still clearly the minority.
The large, insurance-driven GP practices tend towards DSOs. Furthermore, the trend of luring large specialty offices and groups with substantial top line offers continues. Consolidation through private equity acquisitions is real and has altered the dental industry’s landscape. This has been well-received by some, yet others continue to experience far-reaching negative effects.
A transition specialist will guide you towards your best solution, whether a solo buyer, partnership, or private equity. The overriding aim is that the seller achieves their goals with the proper transition style.
The dental industry is changing, and so is the DSO industry. Increasingly, we are seeing DSO firms as offering work/life balance, attractive pay, and competitive benefits. The industry is evolving to offer quality options while the DSO firms who are stuck in the punitive, take-advantage-of-the-dentist is struggling or have exited the DSO space. While the early DSO landscape was replete with DSOs “fighting for the bottom,” those seeking the lowest prices, the most slimmed down service, and high volumes of patient loads, a growing number of quality driven firms are emerging allowing dentists to remain in control.
Supported with private equity funds, the DSO is frequently motivated by its own exit, meaning when they sell their book of practices to another PE firm, they receive an EBITDA multiple. Most DSOs strategically design their business around their own exit, and this is an important criterion in your decision of to whom you sell. So how does a seller know?
Aside from vetting reputation and talking to previous sellers, dealing with a DSO requires an experienced transition specialist to negotiate the terms and conditions, and you will need an experienced lawyer to navigate the contractual language. The contract will live throughout its term, including if/when the PE firm sells to another. This recap event (recapitalization) is how they realize their windfall for their investors. You may have invested in their PE firm when you sold to them, so a recap event can help you, too. Your asset purchase agreement’s (APA) terms and conditions will continue following a recap event so as to not disrupt your office’s workflow.
dentistry is shifting from solo practice dominance towards a Private Equity model. Historically, dentists would argue this is the bane of dentistry, yet ‘corporatization’ has led many competing practices to improve their oversight and tighten their processes.
We frequently see buyers so enthralled with the tasty financial carrot dangling from the PE firm’s stick, that they gloss over the APA’s details. And that is where the vital information lies. We have worked with honest PE backed DSOs with legitimate businesspeople and practices, and we have met others who are unscrupulous sharks. The good ones can facilitate life-changing wealth accumulation. The others can initiate a nightmare.
Every industry has their bad eggs, and the DSO landscape is no different. At last count, the Association of Dental Support Organizations estimates there are 600 corporate firms purchasing practices, and they cannot be painted with the same brush. While positives are abundant, other DSOs are sweat shops where dentists, especially new dentists, may find employment. These DSOs use your talents and your license to their full advantage, tend to not support you if a liability issue occurs, push you into procedures to which you may be uncomfortable treating, and offer hollow promises with limited upside to the dentist. Also, they may have a history of abusive and/or illegal Medicaid practices. Not only do we recommend you not engage these businesses, but all of dentistry should reject them outright, including those that are dentist-owned. No ethics are no ethics, regardless of ownership.
Your transition should lead to a joyous outcome. Understanding your practice style will lead to the right style of buyer. A transition specialist should walk you through the process, negotiate on your behalf, and assure that your dreams come true. You have worked so hard—now it is time to finish well!
Dr Lynne Spencer Gerlach was a successful restorative dentist and businesswoman in her 26+ year career practicing in Plano. From startups to partnerships and solo private practices, her experience in transforming lives through business is a passion. Dr Gerlach’s entrepreneurial experiences in multiple businesses have shaped her desire to assist others with business strategy and growth. She has assisted doctors in their transition and exit planning needs since 2013 with Phase II Dental Transitions. Dr Gerlach often lectures on Practice Transition topics and writes for dental publications.
Dr Gerlach graduated from Austin College and Baylor College of Dentistry. She completed her Certification in the ADA Kellogg Executive Management Program at Northwestern University in 2014. Dr Gerlach has served as visiting faculty and a L.D. Pankey Foundation Advisor since 2008 and served on the Board of Directors as well as secretary. Dr Gerlach is a fellow in the American College of Dentists, International College of Dentists, and a member of ADA, TDA, and Dallas County Dental Society. She has served in numerous positions with Dallas County Dental Society and the Texas Dental Association.
She and her husband, Dr Bill Gerlach enjoy sharing their time off together on the golf course, involved in church activities, or at the lake with their grown children and their spouses. Her hobbies include sports, music, travel, bridge, and cooking.
Dr Bill Gerlach served as president of the Texas Dental Association from 2018-2019 and currently serves as president of the TDA’s Perks Program. In addition to his work with Phase Two Dental Transitions, he works with dentists (especially new practitioners) as a dental coach. He completed the ADA Kellogg Executive Management Program at Northwestern University in 2014, and he practices restorative dentistry as co-owner of Prosper Dental Health, PLLC, in Prosper, Texas. He attended Northwestern University and Baylor College of Dentistry.
The dental industry is changing, and so is the DSO industry Increasingly, we are seeing DSO firms as offering work/ life balance, attractive pay, and competitive benefits.

Priyanshi Ritwik, BDS, MS
Professor, University of Texas Health Science Center at Houston, School of Dentistry, Department of Pediatric Dentistry
The role of Dr Ritwik was to prepare the manuscript.
Elsa Alfonso-Echeverri,
Clinical Associate Professor, University of Texas Health Science Center at Houston, School of Dentistry, Department of Pediatric Dentistry
The role of Dr alfonso-Echeverri was to provide the treatment to the patient.
Professor, University of Texas Health Science Center at Houston, School of Dentistry, Department of Pediatric Dentistry
The role of Dr Cardenas was to help prepare the manuscript.
This case report documents a 15year follow-up of severe intrusive luxation in a 7-year old boy. The patient sustained 6-7mm intrusive injury to his maxillary left permanent central incisor at school. The patient was brought to his pediatric dentist within 30 minutes of the injury. The treating pediatric dentist elected to perform surgical repositioning due to the severity of intrusion and the advanced stage of root development. A physiologic splint was bonded to all the maxillary permanent incisors to secure the repositioned tooth. The patient was prescribed systemic amoxicillin suspension and advised to maintain a soft diet. The splint was removed in 13 days. The patient was followed up for 15 years, during which he also received orthodontic treatment. The maxillary left permanent incisor exhibited root maturogenesis and did not develop any pulpal or periodontal complications during the 15 years. This case report exemplifies that prompt treatment can lead to long term favorable outcomes in intrusive dental injuries.
Intrusive luxation, surgical repositioning
Intrusive luxation is the axial displacement of a tooth in an apical direction into the alveolar bone subsequent to a traumatic impact. A tooth which has suffered intrusive injury is usually immobile, exhibits a high metallic (ankylotic) sound on percussion and is unlikely to respond to pulp vitality testing.1
Radiographically, the periodontal ligament (PDL) space may be absent from all or part of the root and the cemento-enamel junction appears (CEJ) located more apically in the intruded tooth than in adjacent non-injured teeth. Depending on the severity of intrusion, the CEJ is often apical to the marginal bone level.1
The current guidelines by the International Association of Dental Traumatology recommend that an immature permanent tooth with intrusion be monitored for spontaneous eruption for 4 weeks.1 If no occlusal movement of the tooth is noted over a 4-week period, then orthodontic extrusion should be initiated.1 The management of a permanent tooth with mature root and closed apex is slightly different due to the reduced potential for spontaneous eruption. The management of an intruded permanent tooth depends on the degree of intrusion. Teeth with less than 3mm intrusion should be monitored for spontaneous eruption for 8 weeks.1 Should re-eruption not occur within 8 weeks, surgical repositioning and placement of a passive flexible splint is recommended for 4 weeks.1 Mature teeth with 3-7mm of intrusion can be repositioned either surgically or orthodontically.1 Mature teeth with greater than 7mm intrusion ought to be surgically repositioned.1 In all intrusive luxation injuries, pulp vitality should be monitored. Endodontic treatment should be initiated for mature teeth within 2 weeks after the injury, or as soon as endodontic access is feasible.1
Intrusive injuries result in severe damage to the neurovscular bundle as well as the PDL. The alveolar socket sustains comminuted fracture(s). Timely management of intrusive luxation injuries is important to prevent untoward sequelae such as inflammatory root resorption or replacement resorption. Other possible complications of intrusive luxations include pulp canal obliteration, pulp non-vitality, arrested root development and periodontal defects arising from discrepancy in bone and gingival levels.
The authors present the management and 15-year follow-up of a young patient who sustained intrusive luxation of his maxillary permanent central incisor.
A seven-year-old boy fell on his school playground and sustained dental trauma. His parents brought him to his pediatric dentist within 30 minutes of the injury. The patient was healthy and did not have underlying health problems. He had received all scheduled immunizations, including tetanus vaccination. The pediatric dentist performed a rapid neurological assessment. The patient did not exhibit any neurological deficits, loss of consciousness or memory lapse, and he was oriented to time and place. Extraoral assessment of the head, neck, jaws, and the temporomandibular joint were within normal limits.
Intraoral assessment revealed that the maxillary left permanent central incisor was intruded 6-7mm along with buccal displacement. No other extraoral, intraoral or dental injuries were noted. Intraoral radiographs taken confirmed the intrusive luxation injury. The permanent lateral incisors had erupted and the primary canines were not mobile. The initial clinical presentation of the child and associated radiograph are shown in Figure 1. Informed consent was obtained from the patient’s parents to initiate treatment.

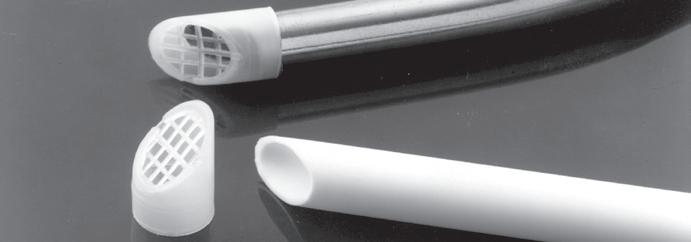
Due to the severity of intrusion, the treating dentist decided to perform surgical repositioning and stabilize with a physiologic splint. Local anesthesia was achieved with the use of 20% topical benzocaine gel and infiltration with 25mg of 2% lidocaine with 1:100,000 epinephrine. Surgical repositioning of the maxillary left permanent central incisor was achieved with the use of gentle force with straight maxillary forceps (#99C). Figure 2 shows the position of the tooth after surgical repositioning.

A 0.016” Nitinol wire with bonded composite resin was used to secure the repositioned tooth. The physiologic splint engaged all the four maxillary permanent incisors. The radiograph in Figure 3 shows the repositioned tooth with splint in place. The patient was very anxious about feeling pain and about how much it would hurt. However, the pediatric dentist was able to use basic behavior guidance techniques such as tell-showdo, verbal reassurance and positive reinforcement to complete the treatment.
The patient was prescribed 250mg/5 cc amoxicillin suspension to be taken three times a day for 10 days. The parents were advised to administer 100mg/5cc of ibuprofen as needed for pain management and to maintain a soft diet.
The long-term prognosis of the intruded tooth was discussed with parents. The scope of potential future complications was identified as pulp necrosis, need for endodontic treatment and ankylosis. However, due to the short time elapsed since the injury and level of root maturity, the anticipated prognosis was favorable.
The patient returned for follow-up care in 13 days. The patient was comfortable and in good spirits at the follow-up

appointment. There were no dental or soft tissue pathologies noted at this appointment. A radiograph taken confirmed that the traumatized tooth and supporting bone did not exhibit any pathology. Figure 4 shows the radiograph taken at this appointment. The splint was removed after confirming that the maxillary left permanent central incisor did not exhibit pathologic mobility.
The patient returned for his routine preventive visit after 2 months. At this visit, the traumatized tooth was free of pain or discomfort, maintained a favorable position and did not exhibit any discoloration. Thermal testing was performed and all the maxillary permanent incisors responded comparably without any lingering sensitivity. The clinical picture and radiograph at this 2-month mark is shown in Figure 5.
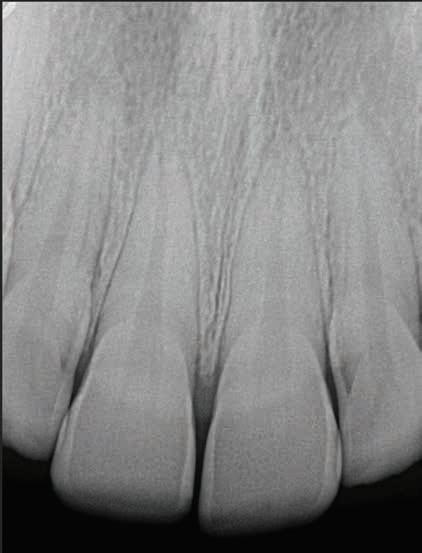
The patient continued to return to his pediatric dentist for routine dental check-ups and preventive visits. Figure 6 shows the clinical and radiographic appearance at 5 years


after the traumatic intrusion. Root maturogenesis and apical closure of the maxillary left permanent central incisor is notable. The patient received orthodontic treatment when he was
14 years old, which was 7 years after sustaining dental trauma. Orthodontic treatment spanned 1.5 years, during the course of which the pediatric dentist monitored the maxillary left permanent
central incisor for any root and/ or pulpal pathosis. Figure 7 shows the radiographic presentation of the tooth during and after orthodontic treatment.

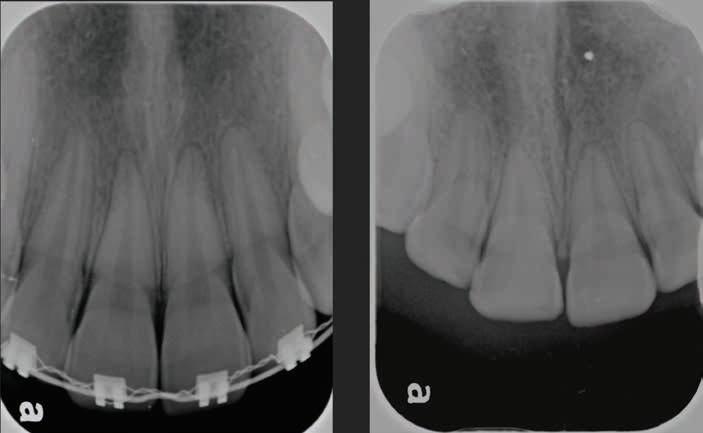
Figure 8. Radiograph at fifteen years after intrusion injury.
The patient continued to return to his pediatric dentist for routine preventive care till he turned 22 years old. His maxillary left permanent central incisor remained free of pulpal and periodontal pathoses for 15 years since the initial trauma. Figure 8 shows the radiograph at 15 years after the traumatic injury.
Intrusion is a complex dental injury due to the concomitant disruption of marginal gingival seal, PDL, alveolar bone and neurovascular supply to the tooth.2 Long term sequelae due to intrusion include pulp necrosis, pulp calcification, inflammatory root resorption, replacement resorption (ankylosis), and loss of marginal bone support.3 Pulp necrosis is the most common complication after intrusion in mature intruded teeth.3 External root resorption can occur in 54.8% of dental intrusion injuries.2 The objective of prompt management of intrusive dental injuries is two-fold: 1) to bring the intruded tooth to the appropriate clinical position and 2) prevent or minimize pulpal and periodontal complications.
The dental age of our patient was advanced, compared to his chronologic age. The stage of root maturity of the intruded central incisor was estimated to be at Cvek stage 4, with nearly complete root length but with an open apex. The degree of intrusion was assessed to be severe, with 6-7 mm of displacement.4 The treatment options were 1) allow spontaneous repositioning 2) orthodontic repositioning and 3) surgical repositioning. The treating pediatric dentist elected to utilize surgical repositioning out of concerns for pulp vitality (based on the severity of intrusion and stage of root development). This child was treated in the year 2002, and it should be kept in mind that regenerative endodontic treatment was not a mainstream modality of management at the time.5 This was also a time when the
guidelines for management of traumatic dental injuries set forth by the American Academy of Pediatric Dentistry recommended surgical or orthodontic repositioning of intruded permanent teeth if the root exhibited greater than two-thirds development.6
The most effective treatment modality for intrusive dental injuries remains debatable and the quality of evidence for any of the treatment recommendations is poor.7,8 Spontaneous re-eruption is recommended for immature permanent teeth with intrusion injuries.1 However, the term “spontaneous eruption” is falsely optimistic as tooth movement after intrusion is unpredictable.9 A meta-analysis comparing surgical repositioning versus spontaneous re-eruption found no significant differences in outcomes.10 Further, pulp non-vitality in these immature teeth poses endodontic complications, which may necessitate regenerative procedures in the future.9 In cases of mature teeth with severe intrusion, endodontic management may need to be deferred till adequate pulpal access can be achieved.
Surgical repositioning for the current case with a 15-year follow-up resulted in long-term retention of a vital permanent central incisor without any periodontal complications. The patient also underwent orthodontic treatment without complications. The authors attribute this success to prompt treatment which alleviated sustained trauma to the neurovascular supply and PDL. It has been shown that teeth which are repositioned within 90 minutes of the displacement injury exhibit lower frequency of root resorption.11 Clinicians who treat intrusive traumatic dental injuries should assess pulp and
PDL prognosis, and not just the clinical positioning and esthetics when making treatment decisions.
This case report with the 14-year followup shows that prompt treatment of intrusive luxation can lead to long-term favorable outcomes with retention of the tooth without pulpal and periodontal complications.
1. Bourguignon C, Cohenca N, Lauridsen E, et al. International association of dental traumatology guidelines for the management of traumatic dental injuries: 1. fractures and luxations. Dent Traumatol. 2020;36(4):314-330.
2. Ghafoor R. Conservative management of progressive external inflammatory root resorption after traumatic tooth intrusion. J Conserv Dent. 2013;16(3):265-268.
3. de Alencar AH, Lustosa-Pereira A, de Sousa HA, Figueiredo JH. Intrusive luxation: A case report. Dent Traumatol. 2007;23(5):307312.
4. Cvek M. Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha. A retrospective clinical study. Endod Dent Traumatol. 1992;8(2):45-55.
5. Tzanetakis GN. Management of intruded immature maxillary central incisor with pulp necrosis and severe external resorption by regenerative approach. J Endod. 2018;44(2):245-249.
6. American Academy of Pediatric Dentistry Reference Manual. Guideline on management of acute dental trauma. American Academy of Pediatric Dentistry Reference Manual of Pediatric Dentistry Chicago, Ill. 2001;32(6):202-12.
7. Costa LA, Ribeiro CC, Cantanhede LM, Santiago Junior JF, de Mendonca MR, Pereira AL. Treatments for intrusive luxation in permanent teeth: A systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2017;46(2):214229.
8. Kirzioglu Z, Karayilmaz H. Repositioning of a completely intruded permanent incisor with surgical extrusion: A 4-year follow-up case. Pediatr Dent. 2009;31(3):253-256.
9. Gungor HC, Cengiz SB, Altay N. Immediate surgical repositioning following intrusive luxation: A case report and review of the literature. Dent Traumatol. 2006;22(6):340344.
10. Elkhadem A, Kotb A. Spontaneous re-eruption, surgical or orthodontic extrusion: What is the choice for intrusive luxation in permanent teeth? Evid Based Dent. 2017;18(3):74.
11. Andreasen JO. Luxation of permanent teeth due to trauma. A clinical and radiographic follow-up study of 189 injured teeth. Scand J Dent Res. 1970;78(3):273-286.












It is my pleasure to announce that, “We’re baaack!” While COVID caused the Founda�on to cancel and postpone our clinical care programs scheduled for 2020, we were able to come back strong in 2021 with 3 Texas Missions of Mercy, 6 SMART Smiles clinics, and 4 successful fundraising events.
All in all, the Founda�on, having met the challenges of the new Infec�on Control requirements, fulfilled its mission, and provided many deserving Texans with much needed care and improved oral health.
Financially, the Founda�on ended 2021 in good health and with a posi�ve cash flow, thanks to our generous supporters and the government’s Paycheck Protec�on Program.
We look forward to more good news and more smiles for Texans in 2022.
There is no greater joy than serving others, and our Associa�on, through its charitable arms–the Texas Dental Associa�on Smiles Founda�on (TDASF) and the Texas Missions of Mercy, Inc. (TMOM Inc.)–exemplify the very best of such: service to the underserved.
Throughout the year, the staff and volunteers of both organiza�ons (Missions of Mercy and Smart Smiles) partner with communi�es, churches, and local component socie�es to fundraise, find facili�es, prescreen pa�ents, transfer mobile dental equipment, and provide quality dental care to those who may not be able to afford it. Perhaps most impressive is that they do this successfully several �mes a year, a feat few other states can claim.
Watching den�sts, caregivers, and volunteers from throughout the state mobilize in one area to provide tens of thousands of dollars’ worth of donated care is almost as sa�sfying as the smile and gra�tude each pa�ent gives in return. Each of us has an opportunity to feel the joy of giving and an obliga�on to serve. Whether it’s mailing a check (or a monthly auto-debit), dona�ng �me to volunteer at an event, or simply suppor�ng an event in your community, remember that it’s as important to you as to those you may serve.
So, if able, consider dona�ng �me or money to the most noble of causes. Appreciate and be thankful for an amazing staff and volunteer leaders who work quietly behind the scenes to help provide care to those most in need. And always remember there is no greater joy than that of serving others.
Dr Don Lutes Benbrook
Dr Kent Macaulay Round Rock
Paula Owens Burleson
Dr Michael Rainwater Dallas


Carol Woods Georgetown
Dr Delton Yarbrough Bryan
TDA Board of Directors Liaison
TDA President-elect Dr Duc “Duke” M. Ho Houston
Atlanta
Dr Susan Jolliff Brady
Beth Voorhees Austin
Dr J Michael Wedin Sweetwater
TDA Alliance Liaison Janet Crow Spicewood
PLATINUM ($50,000-$100,000)
Texas Dental Associa�on
GOLD ($25,000-$49,999)
Delta Dental
San Antonio District Dental Society
SILVER ($10,000-$24,999)
First United Methodist Church of San Angelo Methodist Health Ministries Texas Smile Riders Mr & Mrs William Wya�
BRONZE ($5,000-$9,999)
Alliance of the Texas Dental Associa�on DentaQuest
SUPPORTERS ($1,000-$4,999)
Brady Clergy Associa�on
City of Luling
Commercial Na�onal Bank–Brady Dr Brian Dunagan
Heart of Texas Healthcare System
Highland Lakes Service League Becky Long Real Estate
The Dental Specialists Southland Bap�st–San Angelo Dr Paul Stubbs
Victory Chris�an Center–San Angelo Aus�n Oral Surgery
Dr Jay Adkins Dr Craig Armstrong Dr Wade Barker Dr John Baucum III Dr & Mrs Doug Bogan Drs Ron & Dath Collins Dr Kenneth Crossland Dr B.J. Currey Dr Rocco DeSan�s Mrs Jane Evans Dr Stanley Fry Dr Corbin Gatlin Dr William Gerlach Dr Michael Giesler Dr Tommy Harrison Dr Duc “Duke” Ho Dr Susan Jolliff Dr Paul Kooi Dr Ronald Lee Dr Teri Lovelace Dr Kurt Loveless Dr Don Lutes Dr Kent Macaulay Dr Rise’ Mar�n Dr Dan McCauley Dr Ben Melton Dr Keith Metzger Dr Sco� Morse Dr Lee Oneacre Dr Russell Owens Dr Jacqueline Plemons Dr Richard Po�er Dr Michael Rainwater Dr Ronald Rhea Dr Jerry Roach Dr Richard Smith Dr Larry Spradley Dr Mary Swi� Dr Ben Taylor Dr Carolyn Walker Dr J. Michael Wedin Dr David Wilbanks Dr John Wise Dr David Woodburn Mrs Carol Woods Dr Delton Yarbrough II




In 2021, Texas Mission of Mercy treated a total of 789 pa�ents and delivered $891,021 worth of donated care.





I've never been treated so well by other people, in my en�re life. You guys are angels. Thank you from the bo�om of my heart.”
-Marshall, San Angelo TMOM pa�ent who received care, understanding, and compassion from Dr Susan Jolliff of Brady

I had to come back today to thank this fine lady. She helped me get out of pain quickly and safely. I would like to shake her hand.”
-Alan, TMOM Brady pa�ent who came back to the event to see Dr Stephanie Ganter of Dallas







Thank you so much for helping me smile again!”
-Juanita, TMOM San Antonio pa�ent whose par�al dentures were created by Dr Michael Rainwater of Dallas and delivered by Dr Richard Po�er of San Antonio



End of Year Giving: November 1December 31, 2022
TMOM Marble Falls: February 24-25, 2023
TMOM Bonham: April 14-15, 2023
TMOM Abilene: July 14-15, 2023
TMOM McAllen: September 15-16, 2023 or September 22-23, 2023 (TBD by venue)
Due to COVID-19, please check each meeting’s website for up-to-date information related to cancellations or rescheduling.
THE TEXAS DENTAL JOURNAL’S CALENDAR will include only meetings, symposia, etc., of statewide, national, and international interest to Texas dentists. Because of space limitations, individual continuing education courses will not be listed. Readers are directed to the monthly advertisements of courses that appear elsewhere in the Journal
Mark Burchard
Austin 11/30/56–9/21/22
Good Fellow: 2009 • Life: 2021
Howard Powers Cassada Jackson, TN 5/18/34–8/10/22
Good Fellow: 1987 • Life: 2000
Clifford John Hackett Sugar Land 4/2/35–10/19/22
Good Fellow: 1986 • Life: 2000
Fifty Year: 2011
Larry Bishop Hancock Nacogdoches 10/5/44–10/15/22
Good Fellow: 1997
Michelle R Lindsay Arlington 2/10/64–10/23/22
Billy Noel Lovett
Round Rock 5/18/31–9/12/22
Life: 1996 • Fifty Year: 2012
Wimberley 6/10/35–6/4/22
Good Fellow: 1984 • Life: 2001
Fifty Year: 2008
Ricardo Marquez
El Paso 12/16/47–9/28/22
Good Fellow: 2009 • Life: 2014
Robert Michael Morrow
Osceola, MO 2/22/31–7/26/22
Good Fellow: 1997 • Life: 1996
Fifty Year: 2005
Russell G Owens
Burleson 8/18/32–10/1/22
Life: 1997 • Fifty Year: 2008
David Oliver Rathke
Huntsville 1/18/54–9/22/22
Good Fellow: 2005 • Life: 2019
Chester E Spencer Grand Prairie 5/23/34–10/13/22
Good Fellow: 1996 • Life: 2000
Fifty Year: 2019
Harry L Sugg Dallas 6/29/40–8/3/22
Good Fellow: 1997 • Life: 2005
Fifty Year: 2020
Colbert Wayne Trawhon
League City 8/27/41–8/20/22
Good Fellow: 1996 • Life: 2006
Fifty Year: 2017
An 82-year-old Hispanic female was referred to the Oral Medicine clinic at UT Health San Antonio for evaluation of an asymptomatic 1 cm nodule on the lower lip mucosa. She presented with a chief complaint of, “I have been diagnosed with amyloidosis and I am afraid the lumps on my lips are connected to it”. The patient reported frequent biting of the nodule and an increase in size since it was discovered 2 months prior. Her medical history was positive for amyloidosis affecting the tongue, hypothyroidism, hyperlipidemia, pericardial effusion, and history of breast cancer. Medications included lenalidomide, levothyroxine, atorvastatin, clopidogrel and torsemide. Social history was positive for moderate alcohol use. Her family history was non-contributory. The review of systems was unremarkable. She denied any history of cosmetic procedures in the area and expressed concern that her amyloidosis was progressing, now affecting the lips.
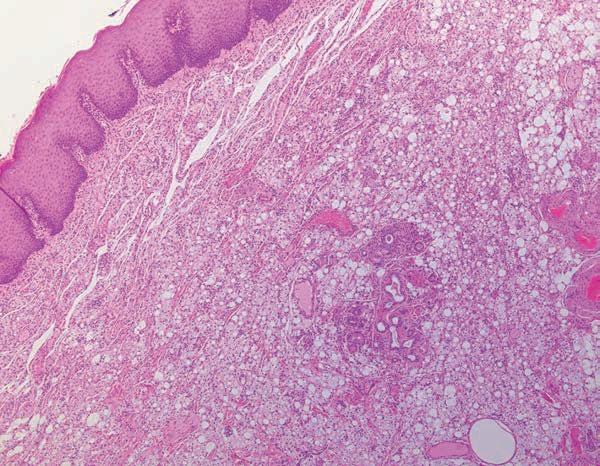
Extraoral examination revealed bilateral pre-auricular scar tissue post rhytidectomy, telangiectasia on the periorbital region and zygomatic area, and diffuse black pigmentation on the scalp consistent with exogenous pigmentations to conceal alopecia. Stiffness and enlargement of the neck and the entirety of the submandibular region were also observed. Intraoral examination revealed an enlarged tongue and the entire lower lip with diffuse swelling and firm consistency. In addition, a painless solitary, rubbery, 1 cm in diameter nodule presented on the right lower lip mucosa (Figure 1 and Figure 2). The patient underwent an excisional biopsy of the nodular lesion, which was then submitted for histopathologic examination.
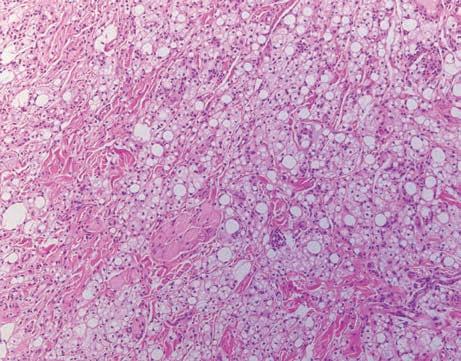
Histopathologic examination demonstrates sheets of lipid-laden macrophages dissecting through the collagen fibers, striated muscle bundles, and associated multinucleated giant cells at the periphery of empty vacuoles (Figures 3 and 4). In one area, macrophages proliferate into the minor salivary gland tissue (Figure 5). No polarizable foreign material is noted.
What was the most likely diagnosis?
See page 701 for the answer and discussion.
Rachel Marie Boice, BS
Fourth-year dental student, School of Dentistry UT Health San Antonio
Clinical Assistant Professor Board Certified Oral Medicine Specialist, UT Health Oral Medicine—Clinic Director, School of Medicine, Department of Pathology and Laboratory Medicine, UT Health San Antonio, San Antonio, Texas
Juliana Robledo, DDS

Assistant Professor, School of Medicine, Department of Pathology and Laboratory Medicine, UT Health San Antonio, San Antonio, Texas


Anne Cale Jones, DDS Distinguished Teaching Professor, School of Medicine, Department of Pathology and Laboratory Medicine, UT Health San Antonio, San Antonio, Texas

Figure 2.


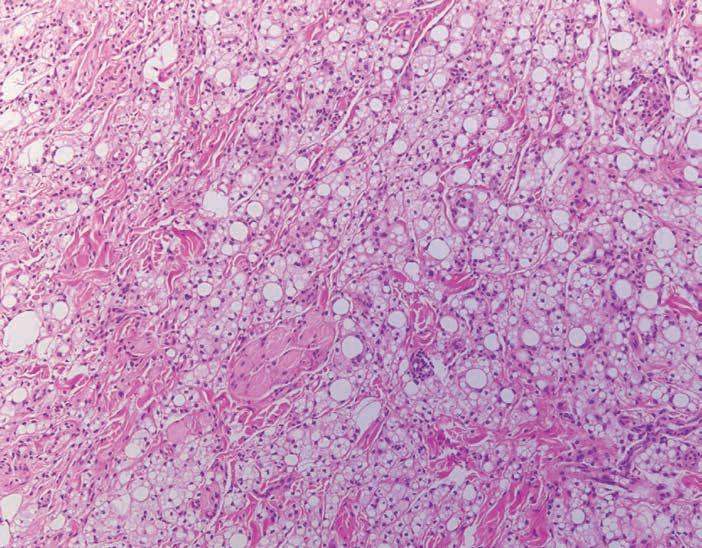
Figure 5. Sheets of macrophages proliferate and replace the minor salivary gland tissue.
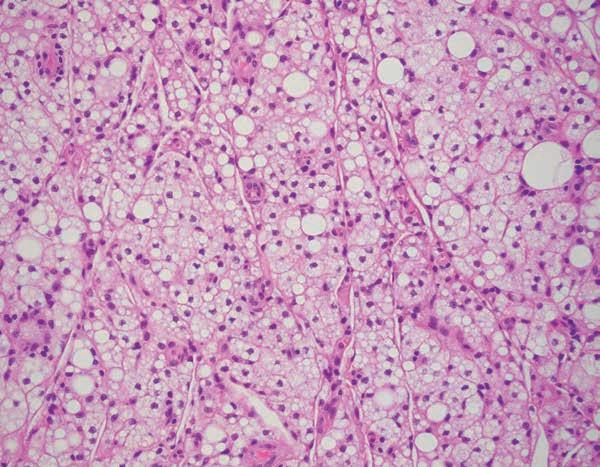
Figure 4. High power section of lipid-laden macrophages.


If you’re a practice associate, seeing your patients and going home at night without the responsibility of being an owner can feel comfortable.
But if you have the dream of owning your own practice, deciding to act on it can improve your career and provide the opportunity for growth, financial freedom, and security for you and your family for years. It’s a decision that will create a valuable asset for your future. And success as an entrepreneur can lead to immense satisfaction as you build your practice, create jobs, and contribute to your community as business owner.
It can also be intimidating. Feeling apprehensive is normal when you take a big step in your career. After years of working with dentists who decided to open their own practice, we understand well the most common fears associated with the process.
In this article, we’ll talk about the most common fears and why you shouldn’t allow them to hold you back from pursuing your professional goals. You’ll understand you’re not alone in the startup process—or afterward. We’ll also talk about planning. That cliché, “failure to plan is planning to fail,” is true. As you explore launching a practice or buying an existing one, the plan is step one and will be the foundation of your success.

Can I secure financing?
Are you worried you can’t secure a loan or afford it? Are you concerned about the expenses associated with owning a practice? How expensive is insurance? Does anything make us more fearful than money issues? Luckily, the solution to facing fear is straight-forward. It’s knowledge.
Those are the right questions to ask; but don’t force yourself to shoulder the burden alone. Any dentist seeking to purchase or open a practice of their own should seek advice from a skilled financial advisor—preferably one that specializes in financing for healthcare professionals.
Consult with your lender; ask them if they have experience with loans for dentists. Reach out to insurance professionals that tailor coverage for dentists and doctors. Many dentists worry their school debt will keep them from borrowing the money needed to purchase or open a practice. Not true. Historically, dentists default on a practice loan about 1% of the time, which means lenders are often eager to secure financing for a dentist who wants to open a new practice. According to Xite’s research, banks are typically willing to loan a dentist $350,000–$500,000 (or more) for a first practice.
Often, a dentist will say “I can’t open my own practice; there are already too many dentists in my town.” Surprisingly, the number of dentists who can make a go of it in a narrow geographical region is much higher than you might think. No matter where you live, there are people; and all of them need a skilled dentist.
However, the most crucial factor to the success of a dental practice is its location within the region. Using a data-driven analysis, professional dental consultants can
assess patient demographics of an area that are conducive to your practice’s success. (Xite Realty provides a free initial demographic analysis to TDA members.)
Additionally, there’s never been a better time to open a practice. Many dentists are retiring, and not enough younger dentistry professionals are stepping in to replace them.
If you’re planning to open a practice, start the process of locating a property a year or more in advance. Only that way can you ensure you have enough time for planning, paperwork, construction, and customization of your office.
I don’t know how to run a business
You’ve been elbow-deep in molars and crowns making a living. Who has time to keep up with the business aspect of dentistry?
It’s okay if you’re a little fuzzy on all the details of running a business; if you have a strong financial and administrative team, you won’t be on your own; you’ll have help. Your team should include a realtor, attorney, CPA, financial advisor, insurance agent, and management consultant.
Here’s an expert tip: Don’t do back-ofthe-napkin planning. Plan very carefully, always thinking about growth. Build your practice for success now and in the future.
Thinking about the following questions will help guide you and your team through the process:
• What are my practice goals?
• Where do I see myself and the practice in five years? In ten years?
• Do I plan to add associate dentists?
• Have I secured enough space to accommodate the goals of my practice?
It’s too much responsibility
It’s natural to feel overwhelmed by the prospect of starting your own practice. But think about your life; has anything worthwhile come easily? As you entered dental school, didn’t it seem daunting? But here you are, ready to meet other challenges.
Again, how do you strip away the fear of being overwhelmed? Learn as much as you can. Once you understand the process of running your own practice, it will become second nature. You’ll feel a sense of accomplishment and experience a completely different workload as a dentist and owner. Here’s another expert tip: Let others help you! Don’t try to do it all by yourself. This isn’t you alone in a chair with your hands in a patient’s mouth.
You need to allow members of your support team to help you launch your practice. That means trusting your lawyer, your CPA, realtor, the contractor, and so on to alleviate your worries and responsibilities.
I can’t handle the debt
How will you pay off the debt associated with opening your practice? Will you still be able to afford life’s expenses? You will pay off the debt—and you will be
able to afford your expenses. Most owners of new dental practices tighten the financial belt the first year or two as they build their business. But with proper planning, your lender will provide enough working capital to cover living expenses. That means you breathe easier in the early stages of being a business owner.
A good loan for a dental practice will include funds for the construction project, equipment and furniture, marketing, working capital, and survival expenses.
You are taking on large responsibilities when you launch your own office, so it’s expected you may feel worried. But keep in mind that based on historical data, the probability of success is very high; and that with responsibility comes great rewards that can be long-term.
TDA Perks Program partner Xite Healthcare Real Estate finds the best location for a practice to increase a dentist’s probability of success. Xite identifies a target patient base using key demographic criteria; and uses the most comprehensive dentalpractitioner real estate database to provide a comprehensive assessment of competition in an area.
Xite can negotiate your lease, help with the purchase of a practice, and assist you with having it built to your specifications.
TDA members receive a free initial demographic analysis. Learn more at https://tdaperks.com/programs/dentalstartup-project-management; or contact Xite to discuss your goals at 214-3064555.
The lips are the barrier between the external environment and the oral cavity. Many diseases that occur in the oral mucosa can manifest exclusively or preferably on them. Since the lips are constantly exposed to UV radiation, trauma, food, oral hygiene, and cosmetic products, they are susceptible to developing a broad spectrum of diagnostic categories ranging from reactive inflammation to malignancies making the diagnosis more challenging. Therefore, obtaining an accurate medical history remains the cornerstone of the diagnostic process. The ability of a clinician to conduct an effective patient interview is imperative since it has been demonstrated that by harboring effective communication, a clinician may gather 60-70% of the information relevant for a diagnosis with the medical history alone.1
Upon consideration of the patient’s clinical findings and review of systems, differential diagnoses included amyloidosis, lipoma, and fibroma. Also, a foreign body reaction to a cosmetic material was considered; however, the patient vehemently denied any cosmetic procedure. Amyloidosis is characterized by deposition of extracellular proteinaceous material termed amyloid.2 Although several classifications of amyloidosis have been noted, two major forms have been identified clinically: organ-limited amyloidosis and systemic amyloidosis.
page 697
Oral manifestations of amyloidosis include oral nodules and xerostomia. Macroglossia may also occur in 10-40% of individuals with amyloidosis due to deposition of amyloid between the muscle fibers of the tongue, leading to bulk lesion. Muscle fibers can atrophy and cause the tongue to become hypomobile.2
A lipoma is a benign tumor of fat. Although lipomas represent a common mesenchymal neoplasm occurring on the trunk and proximal portions of the extremities, approximately 1-4% occur in the oral and maxillofacial region.2 Most individuals with lipomas are 40 years or older. The most common location intraorally for a lipoma to arise is the buccal mucosa or buccal vestibule. Less common intraoral sites include the lips, tongue, and floor of the mouth. Intraoral lipomas appear as smooth-surfaced nodular masses that are soft upon palpation. Lipomas are generally asymptomatic, with most lesions appearing less than 3 cm in size.2
Fibromas are defined as a reactive hyperplasia of fibrous connective tissue due to local irritation or trauma. They are considered the most common “tumor” in the oral cavity but are not true neoplasms. Fibromas appear most often in the fourth to sixth decades of life, with a female predominance.2 The most common location is the buccal mucosa, near the occlusal plane where cheek biting may occur. Other common
sites include the gingiva, tongue, and labial mucosa. The lesion will generally appear as a smooth-surfaced nodule, similar in color to the surrounding mucosa. However, some lesions may present with a white surface due to continued irritation stimulating hyperkeratosis. Fibromas can range anywhere from millimeters to several centimeters in size, although most are 1.5 cm or less in diameter.2
Histopathologic examination displayed sheets of lipid-laden macrophages and scattered multinucleated giant cells around empty vacuoles (Figure 3). There was no evidence of extracellular eosinophilic material, mature fat cells or mass of fibrous tissue; findings expected to be seen in amyloidosis, lipoma, or fibroma, respectively. However, these findings were suggestive of lipogranuloma associated with cosmetic lip fillers.
Lipogranuloma is a granulomatous inflammatory soft tissue reaction which consists of lipid deposition and/ or a material which contains an oil-like substance.4 Although uncommon in the head and neck, lipogranulomas have been found to develop in the region in one of 2 ways. The first is a foreign body reaction to an exogenous lipid/oil-like substance such as paraffin or silicone, while the second is a granulomatous reaction caused by endogenous degeneration of lipids secondary to infection, trauma, extremes of temperature, or allergic reaction.5
students: A systematic review. BMC medical education, 15(1). https.// doi.org/10.1186/s12909-0150443-x.
2. Neville BW, Damm DD, Allen CM, Chi AC. Oral and Maxillofacial Pathology, 4th Ed. Elsevier, 2016, 374-389,462-464, 555-558, 614618.
3. Walker, L., & Cetto, R. (2021). Lip Augmentation Using Hyaluronic Acid Filler and a 4-mm Needle: A Safer, More Natural and Predictable Approach. Journal of Clinical and Anesthetic Dermatology, 14(1).
4. Zhang, F., & Chen, Y. (2017). Lipogranuloma after facial cosmetic procedures. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 123(4). https://doi. org/10.1016/j.oooo.2016.11.003.
Typically, this reaction will manifest as palpable lymphadenopathy and subcutaneous nodules.4 The majority of lipogranulomas found in the head and neck have coincided predominantly with foreign body reactions, developing months to years after a facial cosmetic procedure.4,5 Polymers used in cosmetic procedures can incite an unexpected foreign body granuloma formation that clinically presents as a painless nodule up to 2-4 cm away from the area of the initial injection.6 Since a variety of conditions such as a mucocele, fibroma, and low-grade mucoepidermoid carcinoma can resemble a lipogranuloma, an honest and thorough medical history is crucial to achieve an accurate differential diagnosis list that would help the clinician to define the diagnostic process.4 The treatment
of choice is surgical excision with a good prognosis.6 Patient reluctance in admitting cosmetic procedures generates a diagnostic challenge to the clinician.5 Therefore, as cosmetic facial fillers continue to gain popularity, establishing a favorable patient-doctor relationship with movement through appropriate systematic questioning is essential to generating an honest, accurate medical history.
This case was presented to attendees at the AAOM Annual Conference 2022.
1. Keifenheim, K. E., Teufel, M., Ip, J., Speiser, N., Leehr, E. J., Zipfel, S., & Herrmann-Werner, A. (2015). Teaching history taking to medical
5. Fundakowski, C., Chapman, J., & Sargi, Z. (2012). Lipogranuloma of the Head and Neck. International Journal of Case Reports in Medicine, 1-4. https://doi. org/10.5171/2013.410335.
6. Eversole, R., Tran, K., Hansen, D., & Campbell, J. (2013). Lip Augmentation dermal filler reactions, histopathologic features. Head and neck pathology, 7(3), 241-249. https://doi.org/10.1007/ s12105-013-0436-1.
ALL TEXAS LISTINGS FOR MCLERRAN & ASSOCIATES. TO REQUEST MORE INFORMATION ON OUR LISTINGS: Please register at www.dentaltransitions.com or contact us at 512-900-7989 or info@
DEADLINE
Copy text is due the 20th of the month, 2 months prior to publication (ie, January issue has a due date of November 20.)
PRINT: First 30 words—$60 for ADA/TDA members & $100 for non-members. $0.10 each additional word.
ONLINE: $40 per month (no word limit). Online ads are circulated on the 1st business day of each month, however an ad can be placed within 24 business hours for an additional fee of $60.
Ads must be submitted, and are only accepted, via www.tda.org/Member-Resources/TDAClassified-Ads-Terms. By official TDA resolution, ads may not quote specific incomes or revenues and must be stated in generic terms (ie “$315,000” should be “low-to-mid-6 figures”). Journal editors reserve the right to edit and/or deny copy.
dentaltransitions.com. AUSTIN-WEST (ID #539): 100% fee-for-service practice in the Texas hill country with strong hygiene recall (approximately 30% of total production) and an increasing revenue trend over the past 3 years. The practice is located in a freestanding building that features 3 fully equipped operatories, newly installed computers in each room, digital sensors, hand-held x-ray units, practice management software (Dentrix Ascend), and paperless charts. The real estate is also for sale. DALLAS/FORT WORTH (ID #558): Gorgeous general dentistry practice in a highly desirable and growing suburb of Dallas. Large 3,000 sq ft office that features 4 fully equipped operatories with 4 additional operatories built-out and ready to be equipped. The practice features computers in all operatories, digital radiography, digital sensors, a digital pano, a digital scanner, intra oral cameras and paperless charts. The office serves a FFS/PPO patient base with revenue of over 6 figures annually and strong hygiene recall on 4 doctor days per week. EAST TEXAS (ID #486): Located in a growing east Texas community, this general practice caters to a dedicated multi-generational active patient base. The well-appointed 2,500 sq ft space
contains 5 fully equipped operatories, digital pano, plumbed nitrous, and computers throughout. EAST TEXAS (ID #542): Large practice and real estate in east Texas with over 7 figures in revenue. The recently updated 2,400 sq ft facility features 5 fully equipped operatories with digital radiography, paperless charts, CBCT, digital pano, and an iTero digital scanner. The practice serves a large FFS/PPO, multi-generational patient base with over 3,000 active patients and a stellar online reputation. The seller is open to providing a long-term transition period to the buyer. NORTHEAST TEXAS (ID #554): 100% FFS general dentistry practice in a desirable town in northeast Texas with 7 figures in revenue and strong net income. The turn-key practice features 4 fully equipped operatories with digital radiography, intra oral cameras, paperless charts, CBCT, and a digital scanner. HOUSTON-NORTHEAST (ID #488): FFS/PPO practice plue real estate, growing suburb 45 minutes NE of Houston. 1,800 total patients, steady flow of new patients, solid hygiene recall, and consistent revenue of high-6 figures per year. The office contains 6 fully equipped operatories, plumbed nitrous, digital X-rays, CBCT, and computers throughout. HOUSTON-NORTH (ID #553):
Large, extremely profitable practice and real estate in north Houston (Spring/Woodlands). The 5,600 sq ft standalone building contains 10 fully equipped operatories, computers throughout, digital technology, and room for future expansion. The massive active patient base is comprised of Capitation (40%), PPO (35%), Medicaid (15%), and FFS (10%) with 175+ new patients visiting the office per month. The owner is open to exploring a sale to a DSO, multi-location owner, or a well-qualified private practitioner. The 10,000+ sq ft property is also available for sale which offers additional rental income and the possibility for future development. SAN ANTONIO, ORTHODONTIC (ID #547): Rare opportunity to purchase a primarily FFS orthodontic practice in north central San Antonio. The facility has a modern feel and is equipped with a 3-chair open bay, 2 additional private treatment rooms, and digital radiography. In 2021, revenue was high-6 figures with strong net cash flow. The practice has been a staple in the community with over 40 years at its present location and is located near several highly desirable neighborhoods.
SAN ANTONIO (ID #557): Majority fee-forservice general dentistry practice in northwest San Antonio. The practice is situated in a
high visibility retail center near a bustling intersection and features 4 fully equipped operatories with computers in all ops, a digital scanner, digital radiography, a digital pano, and intraoral cameras. The office has a solid active patient count, a fantastic online reputation, and annual revenue of mid-6 figures year over year. TO REQUEST MORE INFORMATION ON MCLERRAN & ASSOCIATES’ LISTINGS: Please register at www.dentaltransitions. com or contact us at 512-900-7989 or info@ dentaltransitions.com.
“BEAUMONT“): Small town practice near a main thoroughfare. 80 miles east of Houston. Collections in 7 figures. Country living, close enough to Houston for small commute. Practice in a stand-alone building built in 1970. The office is 1,675 sq ft with 4 total operatories, 2 operatories for hygiene and 2 operatories for dentistry. Contains, reception area, dentist office, sterilization area, lab area. Majority of patients are 30 to 65 years old. Practice has operated at this location for over 38 years. Practice sees patients about 16 days a month. Collection ratio of 100%. The Practice is a fee-for-service practice. Building
is owned by dentist and is available for sale. Contact Christopher Dunn at 800-930-8017 or Christopher@DDRDental.com. HOUSTON (SHARPSTOWN AREA)—GENERAL (REFERENCE “SHARPSTOWN GENERAL”). MOTIVATED SELLER. Well established general dentist with high6 figure gross production. Comprehensive general dentistry in the southwest Houston area focused on children (Medicaid). Very, very high profitability. 1,300 sq ft, 4 operatories in single building. 95% collection ratio. Over 1,200 active patients. 20% Medicaid, 45%
McLerran & Associates is the largest dental practice brokerage firm in Texas. When it’s time to buy or sell a practice, we’ve got you covered.
PPO, and 35% fee-for-service. 30% of patients younger than 30. Office open 6 days a week and accepts Medicaid. Contact Christopher Dunn at 800-930-8017 or Christopher@DDRDental. com. HOUSTON (BAYTOWN AREA)—GENERAL (REFERENCE “BAYTOWN GENERAL”). MOTIVATED SELLER. Well established general practice with mid-6 figure gross production. Comprehensive general dentistry in Baytown on the east side of Houston. Great opportunity for growth! 1,400 sq ft, 4 operatories in single story building. 100% collection ratio. 100% fee-for-service. Practice focuses on restorative, cosmetic and implant dental procedures. Office open 3 - 1/2 days a week. Practice area is owned by dentist and is available for sale. Contact Christopher Dunn at 800-930-8017 or Christopher@DDRDental.com.
ready to retire! Upstairs rental spaces income for over 5 years: 5 figures per year. For info call 214-215-2525, Sandy Ward, Adm.
DALLAS: Hageman Family Dentistry, 9,900 sq ft building, on 2/3 acre. Prime location with easy access on and off Highway 67. 9 fully equipped operatories, digital x-rays, new computers in operatories, office and doctor’s offices. Cephalometric, laser, and Panorex machines. Beautiful waiting room seats 20 patients comfortably; practice thriving for 50 years, 40 years in present location. Annual income for past 5 years: 7 figures. Dr David Hageman is
HOUSTON, COLLEGE STATION, AND LUFKIN (DDR DENTAL Listings). (See also AUSTIN for other DDR Dental listings and visit www. DDRDental.com for full details. LUFKIN— GENERAL practice on a high visibility outer loop highway near mall, hospital and mature neighborhoods. Located within a beautiful single-story, free-standing building, built in 1996 and is ALSO available for purchase. Natural light from large windows within 2,300 sq ft with 4 operatories (2 hygiene and 2 dental). Includes a reception area, dentist office, a sterilization area, lab area, and break room. All operatories fully equipped. Does not have a pano but does have digital X-ray. Production is 50% FFS and 50% PPO (no Medicaid), with collection ratio above 95%. Providing general dental and cosmetic procedures, producing mid six figure gross collections. Contact Christopher Dunn at 800930-8017 or Christopher@DDRDental.com and reference “Lufkin General or TX#540”.
HOUSTON—GENERAL (SHARPSTOWN). Well Established general dentist with high-6 figure
gross production. Comprehensive general dentistry in the southwest Houston area focused on children (Medicaid). Very, very high profitability. 1,300 sq ft, 4 operatories in single building. 95% collection ratio. Over 1,200 active patients. 20% Medicaid, 45% PPO, and 35% fee-for-service. 30% of patients younger than 30. Office open 6 days a week and accepts Medicaid. Contact Chrissy Dunn at 800-930-8017 or chrissy@ddrdental.com and reference “Sharpstown General or TX#548”.
HOUSTON —GENERAL (PEARLAND AREA). GENERAL. Located in southeast Houston near Beltway 8. It is in a freestanding building. Dentist has ownership in the building and would like to sell the ownership in the building with the practice. One office currently in use by seller. 60% of patients age 31 to 80 and 20% 80 and above. Four operatories in use, plumbed for 5 operatories. Digital pano and digital X-ray. Contact Christopher Dunn at 800-930-8017 or christopher@ddrdental.com and reference “Pearland General or TX#538”.
HOUSTON— PEDIATRIC (NORTH HOUSTON)
This practice is located in a highly soughtafter upscale neighborhood. It is on a major thoroughfare with high visibility in a strip shopping center. The practice has 3 operatories
for hygiene and 2 for dentistry. Nitrous is plumbed for all operatories. The practice has digital X-rays and is fully computerized. The practice was completely renovated in 2018. The practice is only open 3 - 1/2 days per week. Contact Christopher Dunn at 800-9308017 or christopher@ddrdental.com and reference “North Houston or TX#562”. WEST HOUSTON —MOTIVATED SELLER: Medicaid practice with production over 6 figures. Three operatories in 1200 sq ft in a strip shopping center. Equipment is within 10 years of age. Has a pano and digital X-ray. Great location. If interested contact chrissy@ddrdental.com. Reference “West Houston General or TX#559”.
SAN ANGELO—#TX3082: 5 ops & low O/H. Highly profitable on a 4-day schedule/wk. 100% FFS. Specialties referred. Room to grow. R/E available for purchase or lease. Contact Geremy Haseloff, geremy.haseloff@henryschein. com, 806.777.4732. HOUSTON—#TX3114: Beautiful. Prosthodontic. Uptown/West Oaks area. 3+1 Ops. Digital, Dentrix, digital pan and X-ray, i/o camera. Consistent 7 figures plus annual revenues past 5 years. Contact Josh Griebahn, josh.griebahn@henryschein. com, 713.882.8485. CINCO RANCH/KATY
AREA—#TX3183: A gem startup opportunity! Beautiful 6 op practice in major hotspot. Digital, paperless, CBCT/with Ceph, all ADEC units with integrated electric handpieces, i/o cams. Contact Josh Griebahn, josh.griebahn@ henryschein.com, 713.882.8485. AMARILLO
AREA—#TX3221: Profitable 7 figures GR. 41 yrs goodwill. Beautiful R/E available for purchase. >90% FFS, high patient numbers, great location, best equipment and tech. 12 equipped ops. Room for expansion! Contact Geremy Haseloff, geremy.haseloff@henryschein.com. DALLAS —#TX3258: GP w/3 ops & equipment in nice shape. Great location on busy, main road with low O/H. Reasonable rent, affluent area. Seller to retire. 50+ years of caring for area patients. Contact Geremy Haseloff, geremy.haseloff@ henryschein.com. SAN ANTONIO—#TX3284: Located in rapidly growing area, 4 ops Pediatric, fully digital w/real estate. 52 new patients/ mo. Don’t miss this opportunity! Contact Josh Griebahn, 713-882-8485 to discuss this opportunity! HOUSTON -#TX3297: 4 ops, Montrose area, amazing location. Dentrix, Dexis, CBCT, i/o cams & fantastic team. R/E for sale for tenant income. Net earnings are mid-6 figures on 3 days per week. Details? Contact Josh Griebahn at 713-882-8485.
SAN ANGELO: To those desiring the perfect balance between work and play: Are you interested in taking over a successful readymade practice with a great salary low-to-mid 6 figures? Located in west central Texas, San Angelo is a city of 100,000+ but offers a small town feel and excellent quality of life. The city was named the Visual Arts Capital of Texas in 2021 and is alive with a vibrant mixture of arts and culture for children and adults. It is consistently ranked as one of the best small cities for business and employment. San Angelo is home to award winning Angelo State University, three lakes, the beautiful Concho Riverwalk, an incredible nationally ranked Art Museum, and one of the best preserved forts in the nation, Fort Concho—all with numerous kid-involved programs. As a Texas friendly city, live music is offered almost daily at one of many venues and one-of-a-kind restaurants in town. The community is diverse, with an active young professional group, outstanding medical facilities, ranked sports teams, great hunting and fishing, and a low cost of living. Easy traffic takes you anywhere in the city within 10 minutes. Itís a great place to raise a family and a great place to live, work, and play. The 2,400 sq ft newly remodeled dental office, built
to accommodate 2 dentists, is a free-standing building with natural light in each operatory. An extremely healthy hygiene program is in place with two hygienist. There are 6 operatory rooms—4 equipped. The majority of practice is FFS cash, with over 3,000 active patients. The practice has an excellent reputation in the local community. A bonus package is included for preferred equipment needs. Contact Geremy Haseloff @ 806-777-4732 or geremy.haseloff@ henryschein.com.
Practices for sale in Texas and surrounding states, For more information and current listings please visit our website at www. adstexas.com or call us at 469-222-3200 to speak with Frank or Jeremy.
HAVE MIRROR AND EXPLORER, WILL TRAVEL: Sick leave, maternity leave, vacation, or death, I will cover your general or pediatric practice. Call Robert Zoch, DDS, MAGD, at 512517-2826 or drzoch@yahoo.com.