






























































































Based on the close and fruitful cooperation with dental institutes and practicing dentists since the 1940s, we have a uniquely broad portfolio of specially developed, innovative toothpastes, gels, sprays, mouthwashes and mouth baths. These products, which are marketed under the brands Tebodont®, Emofluor®, Emoform®, Depurdent® and Emofresh® are sold exclusively in pharmacies in Switzerland and in more than 40 other countries outside Switzerland, their various innovative formulations and compositions offer excellent solutions for daily dental care, addressing specific needs and problems (e.g. caries prevention, sensitive teeth, gum problems) and general oral health.


With the REDESIGN we have clarified the positioning of the oral care products: every toothpaste and every mouthwash now has a clear application area. At the same time, our new packaging is "digitalized": each product has a QR code that allows detailed information to be downloaded directly to the mobile phone. The redesign of the products should make the Wild brand tangible and perceptible.
• WILD will be used as umbrella brand on all products, which results in an easier promotion among the whole product range




• Same design for all brands leads to recognition and synergy effects across product range
• Clear unique main indication on the packaging avoids confusion among dental profession, pharmacists and end consumers due to overlapping benefits


• New design underscores clinical benefits and professionalism of the products which leads to cross-brand and cross-portfolio products awareness and helps to create trust among the dental profession, pharmacists and end consumers
• Unifying of the packaging system - all toothpastes in the same size and shape of tubes, all mouthwashes in the same size and packaging - leads to a uniform, eye-catching and space-saving shelf-impact

• Product portfolio becomes fresh, easy to recommend and attractive for the POS
Alfred Naaman, Nada Naaman, Khalil Aleisa, Jihad Fakhoury, Dona Raad, Antoine Saadé, Lina Chamseddine, Tarek Kotob, Mohammed Rifai, Bilal Koleilat, Mohammad H. Al-Jammaz Suha Nader Marc Salloum Micheline Assaf, Nariman Nehmeh Josiane Younes Albert Saykali Gisèle Wakim Tony Dib 1026-261X
February 7 - 9, 2023 Dubai, UAE www.aeedc.com
February 16 – 19, 2023
Hyatt Regency Hotel, Casablanca, MOROCCO www.colfmdc.com
Statements and opinions expressed in the articles and communications herein are those of the author(s) and not necessarily those of the Editor(s) or publisher. No part of this magazine may be reproduced in any form, either electronic or mechanical, without the express written permission of the publisher.
DENTAL NEWS – Sami Solh Ave., G. Younis Bldg. POB: 116-5515 Beirut, Lebanon. Tel: 961-3-30 30 48 Fax: 961-1-38 46 57 Email: info@dentalnews.com Website: www.dentalnews.com www.instagram.com/dentalnews
March 14 – 18, 2023 Koelnmesse, Cologne, GERMANY www.english.ids-cologne.de
May 11 – 14, 2023
Ritz Carlton Hotel, JBR, Dubai, UAE www.totalcoreacademy.ae
May 31, June 1 – 3, 2023 USJ, Beirut, LEBANON www.usj.edu.lb/fmd/
June 8 - 10, 2023
Chia Laguna, Sardinia, ITALY www.congressaio.it
September 6 – 8, 2023 Cairo, EGYPT www.edsic.org
October 6 – 8, 2023
Seaside Arena, Beirut, LEBANON www.lda.org.lb
October 27 – 28, 2023
Madinat Jumeirah, Dubai, UAE www.cappmea.com
on the objectification of sensory perceptions, was very aware of the topic and quickly became fascinated with this new technique.
2. Dr. Wenzler, what brought you to the Vector method?
Dr. Johannes-Simon Wenzler: During my time studying in Marburg, I had learned about conventional scaling and root planing, and I asked myself which
options could be readily translated into a systematic treatment concept. This matter is particularly important for patients who are more sensitive to pain, as – based on my experience – they are are not really well cared for either with manual curettage or with machine instruments, regardless of whether we are talking about acoustic scalers, magnetorestrictive ultrasonic scalers, piezoelectric ultrasonic scalers or jet powder devices. After consulting with
Prof. Braun, I started treating patients who are more sensitive to pain with the Vector system. Coincidentally, this fitted in really well with my scientific endeavours at the time in the project area TransMIT, which was all about in applications in dentistry involving energy transfer.





3. How did you start using the Vector method, and how do you use the system today?
Prof. Dr. Andreas Braun: Well, I started out pretty much as a pilot user, so I embarked on using the new system without any real prior knowledge. I quickly realised that I could use it very effectively, and that the process of using the instrument in the periodontal pockets involved noticeably less pain for the patient than with the other



“Quite a few periodontal surgical interventions could be avoided”

Authors Barry P. Levin, DMD 1
Sergio Rubinstein DDS
Hal Rosenthaler DMD FAGD
Toshi Fujiki RDT
Peter Tawil DDS MS
Email: tawilpeter@gmail.com
1. Private practice Elkins Park, Pennsylvania, USA; Clinical Associate Professor, University of Pennsylvania; Dept. of Periodontology, Philadelphia, Pennsylvania, USA
KEY WORDS: Bone graft, growth factors, prosthetics, dental implants

This case report demonstrates 3-dimensional restoration of a severely-damaged alveolar ridge. Prior extraction, surgical trauma and infection resulted in total loss of facial and palatal cortices in an esthetically-critical area of the dentition. The compromised restorative and endodontic status of the adjacent canine precluded a conventional fixed bridge. Cytokine-enhanced stimulation
of mesenchymal stem cells, combined with a resorbable rigid scaffold reconstructed the alveolar ridge, facilitating implant placement. Additional grafting and implant placement provided the restorative dentist with two osseointegrated fixtures. The residual soft tissue deficiency was compensated for with ceramics combined with CAD/CAM technology to provide an esthetic fixed restoration.









Tooth loss will predictably result in 3-dimentional loss of hard and soft tissue volume.1,2 Not only does this complicate the placement of implants according to the restorative treatment plan, but long-term hygienic complications can result from less than ideal fixture-positioning. When possible, many clinicians choose to place implants either at the time of extraction or shortly thereafter, attempting to minimize these complications.3 The literature contains numerous studies, case series and animal studies supporting this modality.4,5 Often, extraction sockets are augmented to prevent much of this localized atrophy.6,7 When teeth are previously removed, these opportunities for earlier placement are lost, and often favorable hard and soft tissue volume has been lost as well. Reconstructive procedures exist to restore lost bone and soft tissue, providing the surgeon with an opportunity to place implants in restorable positions.8,9 Procedures including autogenous, allogeneic or xenogeneic block grafts, guided bone regeneration (GBR) with and without particulate bone grafts, rigid meshes and biologic mediators such as PRP, recombinant proteins, etc. have been presented by surgeons.10,11 All of these modalities have the potential to regenerate alveolar bone capable of osseointegration. A complication rarely reported in the literature, is what occurs when one of the above-mentioned procedures completely fails, and the resultant defect is more severe than the original one being treated. This case report describes the treatment of a 45 year-old female, who unsuccessfully underwent a regenerative procedure, which became infected and led to the loss of significant alveolar bone and an additional tooth.
A 45-year-old female patient, with a history of smoking, presented to a private periodontal practice after experiencing an unsuccessful ridge-augmentation procedure at a university periodontal clinic. Originally, tooth #7 was surgically extracted and the socket was augmented. This procedure was not successful due to soft tissue complications and possibly smoking. She subsequently underwent a surgical procedure involving the use of a titanium mesh, combined with a bone allograft hydrated with rhPDGF-BB. Early exposure of the mesh and local site infection resulted in the removal of the mesh and debridement of non-incorporated bone graft materials. This resulted in a significant ridge-defect (Fig. 1).
One of the titanium fixation tacks was left in place at this time. The patient was provisionalized from tooth #6 through #11 with a fixed restoration. Her general dentist determined tooth #8 to be nonrestorable due to caries. She was referred to a private periodontal office for extraction of the carious central incisor and ridge-augmentation in the #7 and #8 locations. Previous endodontic therapy and guarded crown-to-root ratio of #6 was determined to be a questionable distal bridge abutment for a long-span fixed partial denture (FPD), and implant therapy was requested by the restorative dentist and patient. The first surgery was geared towards extraction of the carious root of tooth #8, the removal of the fixation tack left behind by the previous surgeon and bone augmenation. The plan was to combine an




osteoconductive, resorbable bone graft of FDBA (Life Net; Virginia Beach) with an osteoinductive graft of rhBMP-2/ACS (Infuse; Medtronic). One of the challenges presented was the lack of facial and palatal bone for vasuclarity and graft containment. After reflection of a full-thickness mucoperiosteal flap, tooth #8 was carefully extracted, attempting to preserve the thin walls of the socket, the tack was easily removed and all loose graft particles were debrided from the defect (Fig. 2).
3:
Figure 2: Following flap-reflection, extraction of the #8 root tip and removal of the retained tack, the loose, non-incorporated DBBM graft particles were debrided until a firm, bleeding osseous surface was identified.



a PLGA resorbable mesh (RapidSorb; Synthes) was warmed in a sterile water bath of 70 degrees Celsius and fixed with two resorbable screws consisting of the same PLGA material (Fig. 4).
The rhBMP-2/ACS was prepared according to the manufacturer’s specifications regarding soakloading the absorbable collagen sponge (ACS) for at least 15 minutes prior to its application. Strips of various sizes were cut of the sponge and mixed homogenously as possible with FDBA particles. This composite graft allowed uniform distribution of osteoinductive (rhBMP-2) and osteo- conductive (FDBA) elements throughout the graft. After molding of this cohesive graft into the alveolus of #8 and the #7 defect (Fig. 3)
Figure 4: A resorbable PLGA mesh was thermoplastically- shaped based on a metal template extra-orally. It was then secured apically with two PLGA screws, providing graftcontainment and stable 3-dimensional spacemaintenance.
Advanced Surgical and Restorative Therapies Aimed at Rehabilitation of a Severe Dentoalveolar Defect in the Esthetic Zone Figure The 2-walled defect in the lateral incisor position, and the extraction socket of tooth #8 was obturated with a composite graft consisting of rhBMP-2/ACS and FDBA.









A connective tissue graft from the palatal flap was utilized to provide crestal coverage of the mesh and a facial periosteal releasing incision was performed to provide nearly-complete closure (Fig. 5).
At about 8 weeks following soft tissue augmentation and 6 months after bone grafting, dental implant surgery was performed. Prior to surgery, a CBCT revealed significant hard tissue regeneration in the lateral and central incisor positions (Figs. 7A & 7B).

Figure 5: The thick palatal mucosa was thinned apically, maintaining blood-supply coronally and sutured to the facial flap, providing primary closure of the grafted site.
Approximately four months after bone augmentation surgery, a subepithelial connective tissue graft was performed to increase the width and thickness of keratinized mucosa in the anticipated implant-placement sites (Fig. 6).

Figure 6: Approximately 4 months after hard tissue grafting, a soft tissue graft was secured from the palatal mucosa of the premolar region. This was done to increase the zone of keratinized mucosa and increase mucosal thickness.

Figurse 7A & 7B : Cross-sectional images of the proposed #7 and #8 implant sites from the CBCT taken approximately 6 months after bone grafting. Planning software is utilized to select implant sizes and positions.



Together we’ll find a way.
For better, easier, and more reliable dentistry. For more information scan the QR code. Visit
The regenerated height of the ridge measured between 8mm-9mm (Fig. 8).
Figure 8: Re-entry demonstrates significant 3-dimensional regeneration of the severe alveolar defect.


Facial-palatal width was determined to be adequate for implant placement of 3.0mm and 3.5mm implant diameters for the lateral and central incisors, respectively. The plan was to place the implants to the cortical base of the nasal floor and utilize the fixtures and healing abutments as “tent poles” to support the same composite bone graft used in the first procedure (Fig. 9).
Figure 9: Implant insertion prior to additional bone grafting. Implants were purposely not over-seated, to facilitate restorative treatment and avoid hygienic challenges after restoration.

Figure 10: Additional bone grafting, utilizing the same composite graft of rhBMP-2/ACS & FDBA was performed to cover the supracrestal threads of both implants. Short (2.0mm) healing abutments, rather than cover screws, were utilized to support the overlying flaps and achieve maximum vertical regeneration

A large portion of the osteoinductive ACS was applied over the graft and 2.0mm tall healing abutments (Fig. 10), then an amnion- chorion membrane (BioXclude; Snoasis) was applied crestally to aid in soft tissue maturation (Fig. 11)
Figure 11: Application of an amnion-chorion membrane over the grafted site.
Advanced Surgical and Restorative Therapies Aimed at Rehabilitation of a Severe Dentoalveolar Defect in the Esthetic Zone















and the site was closed with monofilament sutures (PTFE; Gore) (Fig. 12).

Figure 12: Closure. Note that primary closure was intentionally not achieved. This was the reason for the application of the amnion chorion membrane.
After approximately 2 months healing, both healing abutments are partially-exposed. When the healing abutment on the #7 position implant was loosened, there was detectable movement of the implant fixture. The healing abutment was re-tightened. The #8 healing abutment was easily removed and a fixture level impression was taken. A screw-retained provisional restoration, supported by the single, central incisor implant was indirectly fabricated. An additional healing period of 8 weeks preceded utilization of this implant for fixation of the temporary restoration. During this time, a restorative post and core and new temporary crown was fabricated to improve retention of a single-unit provisional crown on tooth #6. The provisional FPD was sectioned between #6 and #7 and the patient presented for implant temporization. A minor mucoplasty around the #8 implant was done to facilitate access to the healing abutment and its removal. Prior to seating the cantilevered provisional restoration, the healing abutment on the #7 implant was painlessly removed and re-tightened without any tactile movement of the implant or discomfort. The provisional restoration, which incorporated pink and tooth-colored composite resin was adjusted and tightened to 15 ncm (Figs. 13-15).
Figure 13: Four months after implant placement, a screw- retained provisional restoration was placed, supported by the implant in the #8 position. This was done following post and core placement in tooth #6 and fabrication of a single, temporary crown on the canine.





The patient was referred back to the restorative dentist to begin definitive restorative therapy in the maxillary anterior sextant. Restorative therapy entailed conventional crown preparation on the natural teeth, combined with a transfer impression of the two implant fixtures Fig. 16).
(Atlantis; Dentsply) were fabricated for the two implants (Fig. 18).

A wax-up was performed of the anticipated restorative outcome (Fig. 17), and computerassisted abutments
Figure 18: Two CAD/CAM (Atlantis, Dentsply) abutments were digitally-fabricated and seated on two implant replicas. GC resin copings on the adjacent natural teeth are also fabricated
Splinted porcelain fused-to-metal crowns were created for teeth #9-#11, a single PFM crown was fabricated for tooth #6 and splinted, cementretained crowns, incorporating pink ceramics were designed for the two implants (Figs 19,

Figure 17: Diagnostic wax-up. Anticipated volume of soft tissue necessary to be compensated for with pink ceramics. Symmetrical tooth contours right and left also planned at the waxing stage of treatment.

Figure 19: Conventional, PFM crowns are fabricated for the 4 natural teeth in the premaxilla. Soft tissue colored ceramics are used on the right canine, as well as the implantretained restoration to compensate for vertical discrepancies between the right and left sides of the esthetic zone.
 Figure 16: Maxillary polyvinylsiloxane impression
Figure 16: Maxillary polyvinylsiloxane impression

20A, 20B). A periapical radiograph demonstrated crestal bone present at the level of the implant platforms, suggesting successful regeneration and osseointegration (Fig. 21).
Figure 20A: Final restorations in place
Figure 21: Periapical radiograph taken approximately 2 weeks after delivery of the final restorations. Excellent bone regeneration associated with the two implants, #7 in particular, is appreciated




 Advanced Surgical and Restorative Therapies Aimed at Rehabilitation of a Severe Dentoalveolar Defect in the Esthetic Zone
Figure 20B: Patient’s natural lip position at full smile
Advanced Surgical and Restorative Therapies Aimed at Rehabilitation of a Severe Dentoalveolar Defect in the Esthetic Zone
Figure 20B: Patient’s natural lip position at full smile

Severe ridge defects, whether associated with tooth loss and/or failed surgical procedures, can present unique and difficult challenges for the implant team. Often, a combined surgical and restorative approach accomplishes greater achievement than a single entity. Pertaining to management of extraction sites, most clinicians prefer either immediate or early implant placement to better position fixture-insertion prior to the inevitable ridge resorption.12-14 When this is not possible, augmentation of the alveolus can prevent significant bone loss.15-17 The site of tooth #8 was managed with site preservation in this case report. This was the more predictable component of the case presented in this paper. The challenge was regenerating horizontal and vertical height of viable bone in the lateral incisor location, capable of osseointegration. The lack of osseous walls capable of graft containment and providing a source for vascularity to an inert bone graft was the primary obstacle to overcome. Therefore, a graft with osteoinductive properties, capable of chemotaxis of mesenchymal stem cells from the defect’s periphery, as well as differentiation was a requirement for success in the author’s opinion. The production of vascular endothelial growth factor (VEGF) from invading cells was also critical for the revascularization of the bone graft an eventual modeling and bone remodeling necessary for the regeneration of vital bone in the defect area. BMP-2 has been shown to increase the osteoinductivity of allograft bone in the animal model.18 This material has been successful in the regeneration of bone human extraction sockets, capable of osseointegration with titanium implants.19,20 The only FDA- approved carrier for rhBMP-2 is an absorbable collagen sponge. The manufacturer guidelines provide the sponge be “soak-loaded” with the reconstituted protein for at least 15 minutes prior to its insertion in situ. The claim is that the rhBMP-2 is released from the ACS over an approximately 14 day period. The biggest disadvantage to this delivery method is the near-total lack of space-maintenance of the ACS. Clinicians have reported on incorporating space-providing modalities with rhBMP-2 to compensate for this disadvantage.21-23 The addition of particulate bone grafts increases graft volume, but not necessarily stability in situ. A rigid mesh is capable of containing the graft without obstruction of nutrients from the surrounding tissues associated with membranes. The
authors have combined mineralized allograft bone with rhBMP-2/ACS to add an osteoconductive component to the inductive rhBMP-2/ ACS graft. For purposes of graft containment and more importantly, space-maintenance, a resorbable mesh was implemented to provide long-lasting support for the underlying regenerative process. The virtue of the resorbable mesh is mainly the biodegradation, facilitating less-invasive flap reflection for implant placement since the mesh and fixation screws/tacks do not require removal. A porous PLGA material, similar to that used in this case, was shown to facilitate bone regeneration in experimental sites in dogs.24 Numerous reports of titanium mesh being used as space-maintenance have been published. The incidence of premature exposures and compromised outcomes have also been reported.25 The resorbable mesh utilized in this case report has demonstrated easier management of early mesh exposures compared to titanium scaffolds in the author’s experience.
Meeting the patient’s esthetic expectations are at least as challenging as the clinical procedures often faced surgically and prosthetically. In order to provide a result, the patient will be satisfied with, even when heroic surgical treatment has been accomplished, we must depend on the prosthetic team to make up for any deficiencies surgery did not accomplish. These scenarios could be for example due to the type of defect, loss of adjacent periodontal ligament and existing blood supply, thus resulting in some instances in different bone height and corresponding soft tissues. Among the prosthetic objectives for the final restoration are: duplication of color, shape, translucency and texture. Even when these previous concepts are accomplished, patient’s expectations may still not be met, especially when the resulting crown will have a long gingival-incisal anatomy. Therefore, to overcome this problem, and with the attempt to have a correct proportion between the final restoration and adjacent teeth, pink porcelain or composite is often utilized, thus enabling us to have the appearance of a normal size tooth with the correct proportion as it relates to adjacent teeth and just as important to be pleasing to the patient’s smile.26-30
References available on www.dentalnews.com
Advanced Surgical and Restorative Therapies Aimed at Rehabilitation of a Severe Dentoalveolar Defect in the Esthetic Zone1. Reich KM, Huber CD, Lippnig WR, Ulm C,Watzek G, Tangl S. Atrophy of the residual alveolar ridge following tooth loss in an historical population. Oral Diseases 2011;17:33-44.
2. Atwood DA. Postextraction changes in the adult mandible as illustrated by microradiographs of midsagittal sections and cephalometric roentgenograms. J Prosthet Dent1963;13:810-824.
3. Paoloantonio M, Doci M, Scarano A, e’ArchivioD, di Placido G, Tumini V, Piattelli A. Immediate implantation in fresh extraction sockets. Acontrolled clinical and histological study in man.J. Periodontol. 2001;72:15601571.
4. Botticelli D, Berglundh T, Lindhe L. Hardtissue alterations following immediate implant placement in extraction sites. J Clin Periodontol2004;31:820-828.
5. Sanz M, Cecchinato D, Ferrus J, PjeturssonEB, Lang NP, Lindhe J. A prospective,randomized-controlled clinical trial to evaluatebone preservation using implants with different geometry placed into extraction sockets in themaxilla. Clin Oral Impl Res. 2010;21:13-21.
6. Araujo MG, Liljenberg B, Lindhe J. B-tricalciumphosphate in the early phase of socket healing:an experimental study in the dog. Clin Oral ImplRes. 2010;21:445-454.
7. Iasella JM, Greenwell H, Miller RL, Hill M, DriskoC, Bohra AA, Scheetz JP. Ridge preservation with freezed-dried bone allograft and a collagen membrane compared to extraction alone for implantsite development: A clinical and histologic study in humans. J Periodontol. 2003;74:990-999.
8. Von Arx T, Buser D. Horizontal ridgeaugmentation using autogenous block grafts andthe guided bone regeneration technique withcollagen membranes: a clinical study with 42patients. Clin Oral Impl Res. 2006;17:359-366.
9. Misch CM, Misch CE. The repair of localizedsevere ridge defects for implant placementusing mandibular bone grafts. Implant Dent.1995;4:261-267.
10. Nevins M, Al Hezaimi K, Schupbach P, KarimbuxN, Kim DM. Vertical ridge augmentation usingan equine bone and collagen block infusedwith recombinant human platelet-derived growth factor-BB: A randomized single-maskedhistologic study in non-human primates. JPeriodontol 2012;83:878-884.
11. Bianchini MA, Buttendorf AR, Benfatti CAM,Bez LV, Ferreira CF, de Andrade RF. The use of freeze-dried bone allograft as an alternative toautogenous bone graft in the atrophic maxilla:A 3-year clinical follow-up. Int J PeriodonticsRestorative Dent 2009;29:643-647.
12. Evans CDJ, Chen ST. Esthetic outcomes of immediate implant placemens. Clin Oral ImplRes 2008;19:73-80
13. Meltzer AM. Immediate implant placement and restoration in infected sites. Int J PeriodonticsRestorative Dent 2012;32:e169-e173.
14. Levin BP. Immediate temporization of immediate implants in the esthetic zone: Case reports evaluating survival and bone maintenance. Compend Contin. Ed Dent 2011;32:52-62.
15. Barone A, Ricci M, Toneli P, Santini S, CovaniU. Tissue changes of extraction sockets inhumans: a comparison of spontaneous healingvs. ridge preservation with secondary soft tissuehealing. Clin Oral Impl Res 2012;0:17.
16. Perelman-Karmon M, Kozlovsky A, Lilov R.Socket site preservation using bovine bonemineral with and without a bioresorbablecollagen membrane. Int J PeriodonticsRestorative Dent 2012;32:459-465.
17. Scheyer ET, Schupbach P, McGuire MK.A histologic and clinical evaluation ofridge-preservation following grafting withdemineralized bone matrix, cancellous bonechips, and resorbable extracellular matrixmembrane. Int J Periodontics Restorative Dent2012;32:543-552.
Advanced Surgical and Restorative Therapies Aimed at Rehabilitation of a Severe Dentoalveolar Defect in the Esthetic Zone18. Boyan BD, Ranly DM, Schwartz Z. Use ofgrowth factors to modify osteoinductivity ofdemineralized bone allografts: Lessons fortissue engineering of bone. Dent Clinics NAmerica 2006;50:217-228.
19. Cochran DL, Jones AA, Lilly LC, FiorelliniJP, Howell H. Evaluation of recombinanthuman bone morphogenetic protein-2 in oralapplications including the use of endosseousimplants: 3-year results of a pilot study inhumans. J Periodontol 2000;71:1241-1257.
20. Fiorellini JP, Howell TH, Cochran D, MalmquistJ, Lilly LC, Spagnoli D, Toljanic J, Jones A,Nevins M. Randomized study evaluatingrecombinant human bone morphogeneticprotein-2 for extraction socket augmentation. JPeriodontol 2005;76:605-613.
21. Tarnow DP, Wallace SS, Froum SJ, Motroni A,Prasad HS, Testori T. Maxillary sinus augmentationusing recombinant bone morphogenetic protein-2/acellular collagen sponge in combination with amineralized bone replacement graft: A report ofthree cases. Int J Periodontics Restorative Dent2010;30:139-149.
22. Misch CM. Bone augmentation of the atrophicposterior mandible for dental implants usingrhBMP-2 and titanium mesh: clinical techniqueand early results. Int J Periodontics RestorativeDent 2011;31:581-589.
23. Levin BP. Horizontal alveolar ridgeaugmentation: the importance of spacemaintenance. Compend Contin Ed Dent2011;32:12-22.
24. Matsumoto G, Hoshino J, Kinoshita Y, SugitaY, Kubo K, Maeda H, Arimura H, Matsuda S,Ikada S. Evaluation of guided bone regenerationwith poly(lactic acid-coglycolic acid-co-e-caprolactone) porous membrane in lateralbone defects of the canine mandible. Int J OralMaxillofac Implants 2012;27:587-594.
25 Miyamoto I, Funaki K, Yamauchi K, Kodama T,Takahashi T. Alveolar ridge reconstruction withtitanium mesh and autogenous particulate bonegraft: Computed tomography-based evaluationsof augmented bone quality and quantity. ClinImpl Dent Rel Res 2012;14:304-311.
26. Coachman C, Calamita M. The reconstruction of pink
and white esthetics. Int Dent SA, 2010;12(3):88-93.
27. Coachman C, Salama M, Garber DA, CalamitaM, Salama H, Cabral G. Prosthetic gingivalreconstruction in a fixed partial restoration. Part 1: Introduction to artificial gingival as an alternative therapy. Int. J. Periodontics & Restor.Dent. 2009;29:471-477.
28. Salama M, Coachman C, Garber DA, CalamitaM, Salama H, Cabral G. Prosthetic gingivalreconstruction in a fixed partial restoration. Part2: Diagnosis and treatment planning. Int. J.Periodontics & Restor. Dent. 2009;29:573581.
29. Coachman C, Salama M, Garber DA, CalamitaM, Salama H, Cabral G. Prosthetic gingival reconstruction in a fixed partial restoration. Part3: Laboratory procedures and maintenance. Int.J. Periodontics & Restor. Dent. 2010;30:19-29.
30. Priest GF, Lindke L. Gingival-colored porcelain for implant-supported prosthese sin the aesthetic zone. Practical Periodontic &Aesthetic Dentistry 1998;10:12311240.
Advanced Surgical and Restorative Therapies Aimed at Rehabilitation of a Severe Dentoalveolar Defect in the Esthetic ZoneEXPERIENCE SUPERIOR CARE. Precision hydraulic motion allows quiet, gentle stops and starts. Coupled with the virtual pivot, which synchronises movement with the natural motion of the patient imperceptibly raising the toeboard for a cradling effect, the only thing your patient feels is relaxed.

Professor, Department of Periodontology, St Joseph University, Beirut, Lebanon.
Key words: occlusal overload, osseointegration, periimplant bone loss
The purpose of this case report is to demonstrate the relation between occlusal overload and periimplant bone loss and the reversal of the situation after removal of the offending forces. The placement of an unstable removable prosthesis on 3 well-integrated implants that had been stable for 9 years caused noticeable bone loss after 6 months. The elimination of the traumatic occlusion reversed the situation, and a remarkable healing of the peri-implant tissue occurred until the pretrauma condition was nearly restored. The condition has been stable for the past 4 years. Int J Oral Maxillofac 2008;23:153–157
The maintenance of a healthy and stable bone-implant interface is largely dependent on the control of microbial and biomechanical environmental factors. A limited amount of bone loss occurs the first year post loading around wellintegrated implants.1,2 This bone loss has been interpreted as an adaptation to function3 or the result of the surgical procedure.2 It may be related to the presence of a micro gap between the implant and the abutment, microbial contamination,4 the need to re-establish a biologic width,5–7 and/or the hardware
used.8–10 Thereafter, little or no bone loss should be observed.11 The stability of the peri-implant tissues may be understood as a balance between the functional forces and the reaction of the supporting structures, and bone remodeling can be a positive expression in response to mechanical stimulation. The boneimplant interface is maintained by a continuous remodeling process that replaces fatigued bone.12 Increased modeling and remodeling occurs at the loaded interface, as microdamage is followed by repair.13 Bone is a dynamic tissue that remodels remarkably in response to mechanical, nutritional, or hormonal influences. It responds favorably to functional forces by improving the quality of its structure and the bone-implant interface.14 It has been recognized that the increase in the bite-force level (up to 40% over 3 years when changing from full dentures to implant-supported prostheses15) and the absence of periodontal ligament neuroreceptors16 may contribute to over function beyond the threshold of tolerance of the implant- supporting structures. Also, a history of clenching or recorded occlusal wear on the prosthesis has been strongly related to bone loss.17 Increased marginal bone loss as well as a total loss of integration after several
Peri-implant
by Occulusal Overload: Repair of the Peri-implant Defect Following Correction of the Traumatic Occlusion.
No need for forceps. The foil is pre-mounted in a sturdy plastic frame.
Super thin foil. The foil is only 8 micron thick and inked on both sides. Available in blue or red.





No ink on your fingers. The foil is covered on both sides at the grip.
Protective strip Easily removed before use.
Video: TrollFoil
The only articulating foil you will ever need!
TrollFoil takes the guesswork out of occlusal adjustments. TrollFoil can be used under a wide variety of clinical situations including wet or dry teeth, limited opening, limited vestibular space, gaggers, and metal and non-metalic restorations. You are able to verify occlusal contacts for both arches from one tooth to an entire quadrant using the mini or the original quadrant size. The double-sided foil is only 8 microns thick, and it has no problem marking wet surfaces, dry surfaces or highly polished surfaces such as cast gold or BruxZir.

For further information please contact your local dealer or Annelie Johansson, Area Sales Manager – Product specialist TrollDental x-ray, Finland, Baltic, East Europe, Greece, Turkey, MENA annelie.johansson@directadental.com www.directadental.com


years of functional loading may be the result of occlusal overload.18 Although it is difficult to precisely determine the load threshold that can result in bone destruction, intensity, point of application, direction, duration, and frequency of the applied forces are among the variables that can influence the magnitude of the transferred load. These forces can be differently resisted by the implant-supporting structures. The quality of the bone-implant interface encompasses multiple factors, including bone quality and the length, diameter, surface properties, shape, and design of the implant. Implant properties are a major determinant in this biomechanical interaction. Controversy exists regarding the relationship between occlusal overload and peri-implant osseous destruction. Clinical and experimental published studies have produced conflicting results. Based on these results, it is difficult to determine the precise circumstances under which occlusal overload may be implicated in the pathogenesis of peri-implant bone loss. In the present case report, functional overload was directly related to peri-implant marginal bone loss. The condition was reversed following the control of the offending forces.
A 57-year-old female patient reported to the author’s office and complained about the unesthetic appearance of her recently made maxillary fixed partial prosthesis, discomfort during mastication, and difficulties with her speech. She mentioned that the prosthesis had had to be redone twice because of fracture of the ceramic veneers and cement failure. The clinical and radiographic examination revealed generalized gingival inflammation due to poor oral hygiene and the poor fit of the prosthesis, marginal bone loss, and missing teeth (both maxillary right premolars and a right second molar). There was bone loss around and furcation involvement of the maxillary right first molar, which served as a distal abutment, and overclosure of the occlusal vertical dimension. The diagnosis was generalized chronic periodontitis with posterior occlusal collapse, a history of clenching, and ill-fitting fixed partial prostheses. Periodontal treatment included scaling, root planing, and prophylaxis. Surgery was carried out to eliminate pockets and re-establish biologic width. The maxillary right first molar had
a D-B root amputation. It served temporarily as a distal abutment for the partial prosthesis following restoration of the occlusal vertical dimension. The patient was advised of the necessity of implant therapy for a more stable rehabilitation of the maxillary right quadrant. Three 16-mm-long machined-surface Screw-Vent implants (CoreVent System, Encino, CA) were placed to replace the maxillary right premolars and first molar. In November 1991, the abutments were connected, and an implant-supported fixed partial prosthesis with a distal cantilever was placed. The patient was seen every 6 months for maintenance. Periapical radiographs were obtained annually of the patient’s right side (Figs 1 and 2).


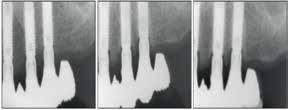
Fig 1 - Peri-implant bone level 1 year post-loading. Minimal bone loss on the intermediate implant. Stability of the bone level on the 2 adjacent implants, which were placed in the maxillary right first premolar and first molar sites.
Fig 2 - Bone level 5 years postloading. Stability of the periimplant bone level can be observed
Ultimate Interproximal Solution - ContacEZ dental strips for restorative, orthodontic, and laboratory needs. The innovative, single-handed design of ContacEZ Dental Strips offers optimal tactile control and grants easy access to tight anterior and posterior spaces. Flexible strips curve and conform to the natural contours of the teeth, while the central opening offers better visual perception and access for tools. This user and patient-friendly design eliminates gagging and prevents soft tissue irritation.
ContacEZ Restorative Strips System are designed to achieve ideal proximal contacts and complete marginal sealing as well as removing subgingival overhangs and more.

• Optimal tactile control – prevent cutting lips and gums
• Built-in flexibility conforms to natural contours
• Ergonomic design eliminates hand fatigue
• Better visibility with central opening

The peri-implant bone level was found to be stable at the level of the first thread after 9 years of loading (Fig 3).
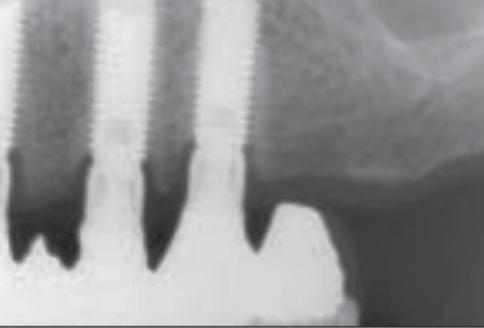

Prosthetic failure of the maxillary left premolars and first molar occurred in October 1999. The fixed partial prosthesis became loose due to recurrent decay and poor crown-to-root ratio. It was decided to extract the remaining teeth and convert to an implant-supported fixed restoration. Three Brånemark implants (Nobel Biocare, Göteborg, Sweden) were placed in the maxillary left quadrant, and the patient was referred to her dentist for the placement of a temporary removable prosthesis to restore esthetics and function while implant osseointegration was achieved. The dentist removed the maxillary right implant-supported partial prosthesis and placed an overdenture. The patient was seen in May 2000 for abutment connection on the maxillary left implants. Periapical radiographs were obtained to assess the osseointegration. Severe bone loss was observed on the implants in the maxillary right first premolar site and the maxillary right first molar site (Figs 4 to 6).

5-6
The removable prosthesis was found to be very unstable; it was rocking around the maxillary right implants and had been doing so for 6 months, according to the patient. In collaboration with the dentist, all 6 implants were splinted, and a properly fitted removable prosthesis was fabricated. Oral hygiene was reinforced to improve the patient’s home care. The peri-implant condition was re-evaluated radiographically every 3 months. The bone lesions started to heal within 3 months after elimination of the traumatic condition. At 6
 Fig 3 - Bone level 9 years postloading.Bone positioned at the level of the first thread. Minimal bone loss occurred over 9 years of functional loading.
Fig 4 - Six months after placement of the unstable removable overdenture. Note the severe bone loss on the implant in the maxillary right first premolar site (down to the sixth thread) and the maxillary right first molar site (down to the third thread). However, no bone loss was observed on the intermediate implant.
Fig 3 - Bone level 9 years postloading.Bone positioned at the level of the first thread. Minimal bone loss occurred over 9 years of functional loading.
Fig 4 - Six months after placement of the unstable removable overdenture. Note the severe bone loss on the implant in the maxillary right first premolar site (down to the sixth thread) and the maxillary right first molar site (down to the third thread). However, no bone loss was observed on the intermediate implant.





months, 1.5 mm of vertical bone gain could be observed on a periapical radiograph obtained with the same angulator but without standardization (Fig 7).




At 1 year, the healing was remarkable (Fig 8).
Eighteen months later, the bone defects were nearly completely healed. Two implants were then added in the anterior maxilla, and the patient was rehabilitated 4 months later with a full maxillary implant supported fixed restoration. Periapical radiographs obtained 4 years later (Fig 9) confirmed the stability of the situation.
Fig 7 - Six months after the elimination of the traumatic occlusion. Bone is at the level of the third thread of the implant placed in the maxillary right first premolar site. Bone level is near the pretraumatic level for the implant in the maxillary right first molar site
Fig 8 - One year after elimination of the traumatic occlusion. Bone is near the level of the first thread on the 2 implants that experienced bone loss.
Fig 9 - Four years after control of the traumatic occlusion and the placement of an implant-supported full maxillary fixed prosthesis. Note the stability of the bone level


DiscussionMechanical overload can cause damage beyond the capacity of repair of the tissues involved, which can induce marginal bone resorption19 or total loss of integration,20 depending on the intensity and duration of the load and the levels of stress and strain concentration. Bone remodeling can compensate for excessive forces that are within the limits of tolerance.21 Early signs of unfavorable reaction, histologically expressed by the presence of osteoclasts in selective sites, indicate that the threshold of resistance is being passed.22
In the present case, the exact dynamics of the tissue response to overload cannot be precisely determined in terms of the time sequence of bone resorption and initiation of bone formation. The intensity, frequency, and duration of the occlusal overload could not be measured.23–26 The instability of the complete denture, the severe malocclusion, and the clenching habits of the patient dramatically increased the bending moments and the stress and strain on the marginal bone surrounding the 16-mm-long well-integrated machined-surface implants, which had functioned well for 9 years. It has been determined that cortical bone is the least resistant to shear stress, which is seriously increased by bending overload.27 The marginal bone loss observed radiologically 6 months after the placement of an unstable removable denture could only have been related to occlusal overload, considering the well-documented longterm stability of the bone level and the absence of pathological changes in the marginal soft tissues. In the present case, radiographs were obtained with the same angulator but without standardization. This method may be insufficient for an exact interpretation of the healing events. However, despite this lack of standardization, the bone healing that compensated for the initial bone loss was remarkable on the radiographs
obtained over the observation period. The reversibility of traumatically induced bone loss has not been clearly reported in the literature. Based on clinical observations and experimental studies, it is not possible to determine the exact circumstances of the reversal process. One can only speculate that the process of repair remains possible if the microbial contamination has been kept under control during the period of overload application and if the duration and the intensity of the applied load has not overwhelmed the repair potential of the bone. In the sequence of events that occurs during bone loss, the first phase is the dissolution of the hydroxyapatite crystals by the acid-producing osteoclast, which lowers the pH in the immediate vicinity of its ruffled border. The organic matrix left behind is later degraded by proteolytic enzymes. Finally, bone degradation products are removed from the resorption lacuna, and the osteoclast disappears, most likely by apoptosis. One may speculate that acute trauma in the absence of concurrent microbial infection may allow the organic matrix to remineralize and bone to regain its structure and function. This hypothesis needs to be confirmed under careful experimental conditions. It has been shown that occlusal overload may cause marginal bone loss, but in the absence of plaquerelated infection, the marginal soft tissues remain unaffected,28 much like what happens around the natural teeth.29 Plaque accumulation has been shown to cause marginal bone loss around the implants.30–32 However, when microbial infection is superimposed on traumatic occlusion, more severe and rapid peri-implant destruction can be observed. Control of the applied occlusal load therefore seems important for the longterm stability of the peri-implant tissues and the prevention of biomechanical complications.
References available on www.dentalnews.com
1. Adell R, Lekholm U, Rockler B, Brånemark P-I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981;10:387–416.
2. Bragger U, Hafeli U, Huber B, Hämmerle CH, Lang NP. Evaluation of post surgical bone levels adjacent to non-submerged dental implants. Clin Oral Implants Res 1998;9:218–224.
3. Misch CE. Dental evaluation: Factors of stress. In: Misch CE (ed). Contemporary Implant Dentistry, ed 2. St Louis: Mosby, 1999.
4. Quirynen M, van Steenberghe D. Bacterial colonization of the internal part of two-stage implants. An in vivo study. Clin Oral Implants Res 1993;4:158–161.
5. Hermann JS, Buser D, Schenk RK, Cochran DL. Crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged and submerged implants in the canine mandible. J Periodontol 2000;71:1412–1424.
6. Cochran DL, Hermann JS, Schenk RK, Higginbottom FL, Buser D. Biologic width around titanium implants. A histometric analysis of the implant-gingival junction around unloaded and loaded non-submerged implants in the canine mandible. J Periodontol 1997;68:186–198.
7. Berglundh T, Lindhe J. Dimension of the periimplant mucosa. Biologic width revisited. J Clin Periodontol 1996;23:971–973.
8. Vaillancourt H, Pilliar RM, McCammond D. Factors affecting crestal bone loss with dental implants partially covered with a porous coating: A finite element analysis. Int J Oral Maxillofac Implants 1996;11:351–359.
9. Jung YC, Han CH, Lee KW. A 1 year radiographic evaluation of marginal bone around dental implants Int J Oral Maxillofac Implants 1996;11:811–818.
10. Norton MR. Marginal bone levels at single tooth implants with a conical fixture design. The influence of surface macro and micro structure. Clin Oral Implants Res 1998;9:91–99.
11. Goodacre CJ, Kan JWK, Rungcharassaeng K. Clinical complications of osseointegrated implants. J Prosthet Dent 1999;81:537–552.
12. Roberts WE, Garetto LP, De Castro RA. Remodeling of devitalized bone threatens periosteal margin integrity of endosseous titanium implants with threaded or smooth surfaces. Indications for provisional loading and axially directed occlusion. J Indiana Dent Assoc 1989;68:19–24.
13. Hoshow SJ ,Brunski JB, Cochran GVB. Mechanical loading of Brånemark implants affects interfacial bone modeling and remodeling. Int J Oral Maxillofac Implants 1994;9:345–360.
14. Schenk R, Buser D. Osseointegration: A reality. Periodontology 2000 1998;17:22–35.
15. Haraldson T, Carlsson GE, Ingervall G. Functionnal state, bite force and postural muscle activity in patients with osseointegrated oral implant bridges. Acta Odonotol Scand 1979;37:195–206.
16. Hämmerle CH, Wagner D, Bragger U, et al. Threshold of tactile sensitivity perceived with dental endosseous implants and natural teeth. Clin Oral Implants Res 1995;6:83–90.
17. Lindquist LW, Rockler B, Carlsson GE. Bone resorption around fixtures in edentulous patients treated with mandibular fixed tissue-integrated prostheses. J Prosthet Dent 1988;59:59–63.
18. Quirynen M, Naert I, van Steenberghe D. Fixture design and overload influence marginal bone loss and fixture success in the Brånemark system. Clin Oral Implants Res 1992;3:104–111.
19. Duyck J, Ronold HJ, Van Oosterwyck H, Naert I, Vander Sloten J, Ellingsen JE. The influence of static and dynamic loading on marginal bone reactions around osseointegrated implants: An animal experimental study. Clin Oral Implants Res 2001;12: 207–218.
20. Isidor F. Loss of osseointegration caused by occlusal load of oral implants. A clinical and radiographic study in monkeys. Clin Oral Implants Res 1996;7:143–152.
21. Frost H. Wolff’s law and bone’s structural adaptations to mechanical usage: An overview for clinicians. Angle Orthod 1994;64:175–188.
22. Barbier L, Schepers E. Adaptive bone remodeling around oral implants under axial and non axial loading conditions in the dog mandibule. Int J Oral Maxillofac Implants 1997;12: 215–223.
23. Heitz-Mayfield LJ, Schmid B, Weigel C, et al. Does excessive occlusal load affect osseointegration? An experimental study in the dog. Clin Oral Implants Res 2004;15:259–258.
24. Ogiso M, Tabata T, Kuo PT, Borgese D. A histologic comparison of the functional loading capacity of an occluded dense apatite implant and the natural dentition. J Prosthet Dent 1994;71:581–588.
25. Miyata T, Kobayashi Y, Araki H, Motomura Y, Shin K. The influence of controlled occlusal overload on peri-implant tissue: A histologic study in monkeys. Int J Oral Maxillofac Implants 1998;13:677–683.
26. Miyata T, Kobayashi Y, Araki H, Takaichi O, Shin K. The influence of controlled occlusal overload on peri-implant tissue. Part 3. A histologic study on monkeys. Int J Oral Maxillofac Implants 2000;15:425–431.
27. Oh Tae-ju,Yoon J, Misch CE, Wang HL. The causes of early implant bone loss: Myth or science. J Periodontol 2002;73: 322–333.
28. Sanz M, Alandez J, Lazarro P, Calvo JL, Quirynen M, van Steenberghe D. Histopathologic characteristics of peri-implant soft tissues in Brånemark implants with two distinct clinical and radiological patterns. Clin Oral Implants Res 1991;2:128–134.
29. Polson AM. The relative importance of plaque and occlusion in periodontal disease. J Clin Periodontol 1986;13:923–930.
30. Isidor F. Histological evaluation of periimplant bone at implants subjected to occlusal overload and plaque accumulation. Clin Oral Implants Res 1997;8:1–9.
31. Lindhe J, Berglundh T, Ericsson I, Liljenberg B, Marinello C. Experimental breakdown of peri-implant and periodontal tis- sues. Clin Oral Implants Res 1992;3:9–16.
32. Lang NP, Bragger U, Walther D, Beamer B, Kornman KS. Ligature induced peri-implant infection in the cynomolgus monkeys. I. Clinical and radiographic findings. Clin Oral Implants Res 1993;4:2–11 [erratum 1993;4:111].
33. Miyata T, Kobayashi Y, Araki H, Shin K, Motomura Y. An experimental study of occlusal trauma to osseointegrated implants. Part 2. J Jpn Soc Periodont 1997;39:234–241.















ABU DHABI HOSTED THE 12TH WORLD CONGRESS OF ESTHETIC DENTISTRY – IFED 2022 , A UNIQUE DENTAL MEETING THAT WAS jOINTLY ORGANIZED BY THE INTERNATIONAL FEDERATION OF ESTHETIC DENTISTRY AND INDEx. IFED 2022 BROUGHT TOGETHER LEADING DENTISTS AND SpECIALISTS FROM AROUND THE WORLD WHO DISCUSSED kEY TOpICS IN vARIOUS BRANCHES OF DENTISTRY AND HIGHLIGHTED THE LATEST TECHNOLOGY ADvANCEMENTS. THE EvENT TOOk pLACE AT THE CONRAD ABU DHABI ETIHAD TOWERS - ABU DHABI, UNITED ARAB EMIRATES FROM THE 27TH TO THE 29TH OF OCTOBER 2022.













 DentAl neWs booth Dr. AishA sultAn soueiDi, mrs. josiAne younes, Dr mAimounA qAzi, Dr reem AbDulrehmAn
Dr nouf AlmArzouqi, mrs josiAne younes, Dr. jAmAl kAChouh
Drs.; tony Dib, robert sADer, jAime jil, ghAssAn merhi, fADi DAou
DentAl neWs booth Dr. AishA sultAn soueiDi, mrs. josiAne younes, Dr mAimounA qAzi, Dr reem AbDulrehmAn
Dr nouf AlmArzouqi, mrs josiAne younes, Dr. jAmAl kAChouh
Drs.; tony Dib, robert sADer, jAime jil, ghAssAn merhi, fADi DAou







 DRS.; HAIFA HANNAWI, AISHA SULTAN SOUEIDI, NABIL HMOUD, MAIMOUNA QAZI, REEM ABDULREHMAN
DRS.; HAIFA HANNAWI, AISHA SULTAN SOUEIDI, NABIL HMOUD, MAIMOUNA QAZI, REEM ABDULREHMAN
 Interview
Interview
Over 20 years of the Vector method: since 1999, this technique has been used to treat periodontal diseases with the aid of ultrasound – using a low-pain therapy that focuses on the cause of the disease. In our interview, Univ.-Prof. Dr. Andreas Braun and Dr. JohannesSimon Wenzler from the Clinic of Restorative Dentistry, Periodontology and Preventive Dentistry at RWTH Aachen University tell us about their experiences and offer advice for application of the techniques in practice.

Prof. Dr. Andreas Braun: To start with, it was Prof. Nolden from the University of Bonn who drew my attention to it. That was around 2000, just after market launch. Prof. Nolden told me in particular about how the Vector can be used for low-pain periodontal treatment. Because I had written my thesis on the objectification of sensory perceptions, I was very aware of the topic and quickly became fascinated with this new technique.
options could be readily translated into a systematic treatment concept. This matter is particularly important for patients who are more sensitive to pain, as – based on my experience – they are are not really well cared for either with manual curettage or with machine instruments, regardless of whether we are talking about acoustic scalers, magnetorestrictive ultrasonic scalers, piezoelectric ultrasonic scalers or jet powder devices. After consulting with Prof. Braun, I started treating patients who are more sensitive to pain with the Vector system. Coincidentally, this fitted in really well with my scientific endeavours at the time in the project area TransMIT, which was all about in applications in dentistry involving energy transfer.
3. How did you start using the Vector method, and how do you use the system today?
Dr. Johannes-Simon Wenzler: During my time studying in Marburg, I had learned about conventional scaling and root planing, and I asked myself which

Prof. Dr. Andreas Braun: Well, I started out pretty much as a pilot user, so I embarked on using the new system without any real prior knowledge. I quickly realised that I could use it very effectively, and that the process of using the instrument in the periodontal pockets involved noticeably less pain for the patient than with the other

1. Professor Braun, when did you first become aware of the Vector method?
2. Dr. Wenzler, what brought you to the Vector method?
“Quite a few periodontal surgical interventions could be avoided”

pain and discomfort during treatment. Prof. Braun has also confirmed this in studies.

alternatives that were available. However, some of my practising colleagues were irritated because they had hoped for a faster procedure. This is why I also felt it was my duty to promote correct understanding of the Vector method among dental practitioners – that it was primarily not about speed, but about a low-pain and gentle alternative to conventional therapies. The manufacturer, Dürr Dental, subsequently developed and refined the system to the point where we now use a combination of two different piezoelectric handpieces to achieve much faster results than we did back in the early days.
Prof. Dr. Andreas Braun: Yes, together with Priv.-Doz. Dr. Krause I was able to document this early on already. Initially, we asked the patients to gauge their pain sensitivity on a visual scale after treatment. Because, empirically speaking, the most recent perception tends to dominate, we also asked them to assess their sensitivity during the overall procedure. We gave the patients a pressure recorder they could hold in their hand and asked them to squeeze it according to the level of
Dr. Johannes-Simon Wenzler: I was impressed right away. With the Scaler handpiece and the slim Scaler instruments, my supragingival cleaning work is much faster. For subgingival instrument work, I then switch to the Vector Paro and apply the Vector Fluid polish suspension directly from the handpiece for treatment that is as effective as it is gentle in the removal of biofilm. I was first introduced to the system in 2015 and basically grew up with this combined approach.
4. What exactly is it about the Vector system that makes it so successful for you personally?
pain they were experiencing so that we could measure it – the more pressure they exerted, the stronger the pain. This allowed us to record updated pain sensations once a second. In the process, the Vector method achieved significantly better results than both manual scaling and root planing and one other ultrasonic method. SRP and the second ultrasonic technique performed equally well as each other during this investigation.
6. Which practising colleagues would you recommend Vector to, and how should they approach the system?
Prof. Dr. Andreas Braun: Based on my assessment, actually I think the method is suitable for any practice that offers periodontology treatments. A vast store of knowledge has now been built up, so for anyone who is new to the technique I can recommend that they get training on the Vector method from an experienced colleague.
In terms of patients with the highest sensitivity to pain, I would also perhaps recommend use of a topical anaesthetic, which can often help. Patients often welcome the fact that they are not being given an injection. However, if a “Vector session” does ever need to be stopped, then I think it is acceptable for the patient to come back in one to two weeks’ time so that the
quadrants that have not yet been treated can then be worked on with the instruments.
Dr. Johannes-Simon Wenzler: I examine the classic periodontological parameters such as BOP, changes to the gingiva involving inflammation, periodontal attachment gain. Normally, initial success starts to show after just a few days. In addition, I always ask my patients to what extent they felt pain sensations during treatment with the instrument or afterwards.
7. Where are we at with the Vector method today, and how do you think things might evolve over the next twenty years?

Prof. Dr. Andreas Braun: The Vector method is currently a cost- effective, low-pain method for periodontal therapy. It is not particularly fast, but it is very gentle on the surfaces of the tooth. Particularly in the root areas, I can use this method for selective removal of concrement without excessive abrasion of hard tooth substance and without leaving unwanted traces of my work. The fact that the process is slightly slower actually turns out to be an advantage. But, in particular, the Vector method can help to prevent quite a few periodontal surgical interventions. I believe that this particular aspect is not yet adequately recognised by the German health insurance providers in their assessments.


Prof. Dr. Andreas Braun: Changes to the individual bacterial spectrum are generally not a sole indication of success. I will only perform special microbiological investigations if I suspect the presence of a specific pathogenic bacterial spectrum that I would need to tackle with targeted antimicrobial therapy. However, it is generally much more likely that a bacterial spectrum will shift in response to systematic periodontological treatment. When it comes to regular checks, it is primarily the clinically verifiable parameters that we look at.
5. Question: What is your assessment of the scientific evidence?
Dr. Johannes-Simon Wenzler: Based on my experience, the Vector method is almost always superior to other ultrasonic and powder jet treatments in terms of reduced
Dr. Johannes-Simon Wenzler: In the future, in addition to periodontal therapy, peri-implantitis treatments will also be increasingly in demand. I could imagine that the Vector system will also be able to demonstrate its strengths in this area as well – perhaps even with dedicated new working approaches specially developed for this application.
Prof. Dr. Andreas Braun: As part of the research work we have carried out, we have also looked at first experiments in endodontic applications. Subject to targeted further development in this direction, I believe that – under certain conditions – in the future it will be possible to establish the Vector method alongside periodontal therapy and peri- implantatis treatments in the field of endodontics as well.
pain and discomfort during treatment. Prof. Braun has also confirmed this in studies.
Prof. Dr. Andreas Braun: Yes, together with Priv.-Doz. Dr. Krause I was able to document this early on already. Initially, we asked the patients to gauge their pain sensitivity on a visual scale after treatment. Because, empirically speaking, the most recent perception tends to dominate, we also asked them to assess their sensitivity during the overall procedure. We gave the patients a pressure recorder they could hold in their hand and asked them to squeeze it according to the level of
quadrants that have not yet been treated can then be worked on with the instruments.
7. Where are we at with the Vector method today, and how do you think things might evolve over the next twenty years?
Prof. Dr. Andreas Braun: The Vector method is currently a cost- effective, low-pain method for periodontal therapy. It is not particularly fast, but it is very gentle on the surfaces of the tooth. Particularly in the root areas, I can use this method for selective removal of concrement without excessive abrasion of hard tooth substance and without leaving unwanted traces of my work. The fact that the process is slightly slower actually turns out to be an advantage. But, in particular, the Vector method can help to prevent quite a few periodontal surgical interventions. I believe that this particular aspect is not yet adequately recognised by the German health insurance providers in their assessments.


pain they were experiencing so that we could measure it – the more pressure they exerted, the stronger the pain. This allowed us to record updated pain sensations once a second. In the process, the Vector method achieved significantly better results than both manual scaling and root planing and one other ultrasonic method. SRP and the second ultrasonic technique performed equally well as each other during this investigation.
Dr. Johannes-Simon Wenzler: In the future, in addition to periodontal therapy, peri-implantitis treatments will also be increasingly in demand. I could imagine that the Vector system will also be able to demonstrate its strengths in this area as well – perhaps even with dedicated new working approaches specially developed for this application.
Prof. Dr. Andreas Braun: As part of the research work we have carried out, we have also looked at first experiments in endodontic applications. Subject to targeted further development in this direction, I believe that – under certain conditions – in the future it will be possible to establish the Vector method alongside periodontal therapy and peri- implantatis treatments in the field of endodontics as well.
Prof. Dr. Andreas Braun: Based on my assessment, actually I think the method is suitable for any practice that offers periodontology treatments. A vast store of knowledge has now been built up, so for anyone who is new to the technique I can recommend that they get training on the Vector method from an experienced colleague.
In terms of patients with the highest sensitivity to pain, I would also perhaps recommend use of a topical anaesthetic, which can often help. Patients often welcome the fact that they are not being given an injection. However, if a “Vector session” does ever need to be stopped, then I think it is acceptable for the patient to come back in one to two weeks’ time so that the
6. Which practising colleagues would you recommend Vector to, and how should they approach the system?












 DRS.: FELIPE AGUIRRE, TONY DIB, RODRIGO SALAZAR, YEHIA ABOUSHADY
DR. TONY DIB, DR. ZAHY HAWAS، PROF. MONA GHONEIM CHAIRWOMAN SCIENTIFIC COMMITTEE
DR. ZAHY HAWAS THE CONGRESS GUEST OF HONOUR DURING THE OPENING CEREMONY REVEALING THE SECRETS OF THE PHARAOS
THE SIGNING OF A COOPERATION AGREEMENT BETWEEN THE UNIVERSITIES OF ALEXANDRIA AND MANCHESTER UK
FRONT ROW; PROF. IHAB HAMMAD, PROF. YEHIA ASHOUR, DR. TONY DIB WITH THE ORGANINZING COMMITTE MEMBERS
DRS.: FELIPE AGUIRRE, TONY DIB, RODRIGO SALAZAR, YEHIA ABOUSHADY
DR. TONY DIB, DR. ZAHY HAWAS، PROF. MONA GHONEIM CHAIRWOMAN SCIENTIFIC COMMITTEE
DR. ZAHY HAWAS THE CONGRESS GUEST OF HONOUR DURING THE OPENING CEREMONY REVEALING THE SECRETS OF THE PHARAOS
THE SIGNING OF A COOPERATION AGREEMENT BETWEEN THE UNIVERSITIES OF ALEXANDRIA AND MANCHESTER UK
FRONT ROW; PROF. IHAB HAMMAD, PROF. YEHIA ASHOUR, DR. TONY DIB WITH THE ORGANINZING COMMITTE MEMBERS


Dear colleagues,
It gives me great pleasure to welcome you to the 5th International Pediatric Dentistry Congress of EPDA which hosts this year the 10th International Congress of Mediterranean Societies of Pediatric Dentistry and the 13th International Congress of the Arab Society of Pediatric Dentistry.



For the 2nd time these two organizations meet together under one roof making it a great chance for communication and exchanging views and experiences for the benefit of our children. This year, the congress theme is “Facing new challenges” which reflects the importance of acknowledging the changing patterns of life that will be reflected on our professional practice in the near future.
Once again I welcome you to Alexandria, bride of the Mediterranean
has always been the cradle and crossing point of all human civilizations.
that Prof. Aly Sharaf EPDA president and Congress president




 The egypTian SocieTy of pediaTric denTiSTry Board , aly Sharaf preSidenT, amr aBdel aziz Vice preSidenT , faTma aBdel moneim SecreTary wiTh The american academy of pediaTric denTiSTry delegaTionprof amr morSi preSidenT and paST preSidenTS JeSSica lee and Jeannie Beauchamp and The coming nexT preSidenT ScoTT caShion
wiTh The leBaneSe delegaTion of pediaTric denTiSTry; marlene Khoury, Bechar alaSmar, naThalie aBouSamra, aly Sharaf (preSidenT egypTian SocieTy of pediaTric denTiSTry), Sandra dagher (preSidenT leBaneSe SocieTy of pediaTric denTiSTry), amr aBdelaziz
wiTh prof amr morSi preSidenT of american academy of pediaTric denTiSTry
wiTh The SudaneSe aSSociaTion of pediaTric denTiSTry
The egypTian SocieTy of pediaTric denTiSTry Board , aly Sharaf preSidenT, amr aBdel aziz Vice preSidenT , faTma aBdel moneim SecreTary wiTh The american academy of pediaTric denTiSTry delegaTionprof amr morSi preSidenT and paST preSidenTS JeSSica lee and Jeannie Beauchamp and The coming nexT preSidenT ScoTT caShion
wiTh The leBaneSe delegaTion of pediaTric denTiSTry; marlene Khoury, Bechar alaSmar, naThalie aBouSamra, aly Sharaf (preSidenT egypTian SocieTy of pediaTric denTiSTry), Sandra dagher (preSidenT leBaneSe SocieTy of pediaTric denTiSTry), amr aBdelaziz
wiTh prof amr morSi preSidenT of american academy of pediaTric denTiSTry
wiTh The SudaneSe aSSociaTion of pediaTric denTiSTry














 troPhy Presentation to dr. meshal alKandari
troPhy Presentation to dr. ehab heiKal, President of the egyPtian dental assoCiation
dr. hussein ghadanfari, dr. mohamed Kamal, Prof. JaWad behbehani, dr. mohamed dashti, dr. meshal alKandari, dr. eyad al muqait, dr. abdulaziz alJazzaf
troPhy Presentation to dr. meshal alKandari
troPhy Presentation to dr. ehab heiKal, President of the egyPtian dental assoCiation
dr. hussein ghadanfari, dr. mohamed Kamal, Prof. JaWad behbehani, dr. mohamed dashti, dr. meshal alKandari, dr. eyad al muqait, dr. abdulaziz alJazzaf






 dr. JosePh Kan talKing about biologiC anterior imPlant esthetiCs
dr. Chimène Chelala leCture on the interaCtion betWeen orthodontiCs, PeriodontiCs and restorative dentistry
dr. Carlos falCao reCeiving the CertifiCate of aPPreCiation for his leCturing about imPlant ProsthodontiCs
dr. mauro fradeani leCture on full mouth rehabilitation
dr angelo Cardarelli leCture on imPlant PlaCement in atroPhiC JaW
dr. JosePh Kan talKing about biologiC anterior imPlant esthetiCs
dr. Chimène Chelala leCture on the interaCtion betWeen orthodontiCs, PeriodontiCs and restorative dentistry
dr. Carlos falCao reCeiving the CertifiCate of aPPreCiation for his leCturing about imPlant ProsthodontiCs
dr. mauro fradeani leCture on full mouth rehabilitation
dr angelo Cardarelli leCture on imPlant PlaCement in atroPhiC JaW




 dr. mohamed dashti, President of the Kda, dr. abdelrahman azri, President of the oman dental assoCiation, dr. tony dib
dr tony dib, dr meshari alotaibi from the saudi dental assoCiation, dr. nazem haffar, President lda-triPoli
PiCture of attendees of the 22nd KuWait dental ConferenCe
drs: Karim Kabbara, nazem haffar, President lda-triPoli, meshari alotaibi, tony dib, aJay JuneJa
dr. mohamed dashti, President of the Kda, dr. abdelrahman azri, President of the oman dental assoCiation, dr. tony dib
dr tony dib, dr meshari alotaibi from the saudi dental assoCiation, dr. nazem haffar, President lda-triPoli
PiCture of attendees of the 22nd KuWait dental ConferenCe
drs: Karim Kabbara, nazem haffar, President lda-triPoli, meshari alotaibi, tony dib, aJay JuneJa
Tune in with our case presentations and live surgeries.
Share your case in our forum and interact with other members.
Read our published articles in international peer review journals.




















www.borea-dental.com
The Rayplicker Cobra during the AEEDC 2023 exhibition in Dubaï
After the release in 2018 of its first digital shade scanner, the Rayplicker Handy, the company BOREA presents its new spectrophotometer, the Rayplicker Cobra. A device intended for cosmetic dentistry professionals and which revolutionizes shade taking as well as communication between the dental office and the laboratory.
The aim of the Rayplicker Cobra is to offers an objective, reliable and reproducible color analysis of teeth based on a technology that today has been validated and approved by the scientific community, the spectrophotometry. The tooth shade is analysed according to the CIE L*a*b* / L*C*h standards and is also indicated under different shade mappings (Overall shade, 3 parts, 9 parts and a detailed mapping). This new version of the Rayplicker is made in France and offers innovative ergonomic features. The device is equipped with a miniaturized measuring head and the remote LEDs at the end of the measuring head allow easy access to all patient teeth. The autoclavable calibration tips allow the self-calibration of the device and protect against cross-contaminations. In addition, its Oled screen guides the user for color taking as well as the wifi transmission of the live video on the computer screen. This device offers a truly didactic experience with the patient.

The spectrophotometer along with the free Rayplicker Vision software allows to
carry out colorimetric and the translucency analysis of the tooth. This software provides optimized patient data management as well as numerous applications, such as the evaluation of bleaching treatments, the edition of shade reports, etc.

In order to optimize the transmission of information, users both dental practices and dental laboratories benefit from a free access to the Borea connect platform. The Borea Connect is the essential tool for optimizing the management and real-time monitoring of orders while ensuring easy and fast sending of the data necessary for the proper production of the prosthesis (shades, patient photos, digital impressions). This platform is accessible from a simple web browser (computer, smartphone, tablet).
This new shade scanner developed by Borea provides a complete and innovative solution in dentist and prosthetist communication. It allows a reduction of scrap related to shade problems, it brings real comfort and time savings in his work while improving communication with its patients.



www.ultradent.com
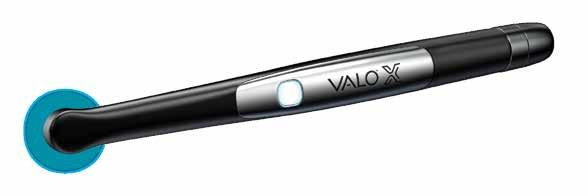
Ultradent Products, Inc., a leading developer and manufacturer of hightech dental materials and equipment, launched the newest edition of its multiaward-winning VALOTM curing light— the completely redesigned VALOTM X broadband LED curing light.
As Ultradent’s most innovative curing light yet, the VALO X curing light offers the ultimate in engineering and design when it comes to every aspect of the light— including durability, power, accessibility, and versatility.
Thanks to its larger 12.5 mm lens and new powerful custom LED chip, the VALO X curing light offers a more complete cure than ever before. Its superior features allow clinicians to cure with confidence, and not have to question the capabilities of their light. This includes improved curing depth, beam collimation, and thermal management. The VALO X curing light comes equipped with two power modes (Standard Power and Xtra Power), two diagnostic light modes (black light and white light), as well as the ability to work corded or cordless.
The light’s one-button activation also sports a user interface with an accelerometer, so users can cycle between the light’s power and diagnostic modes with just the wave of the wand, a light drum tap, or the push of a button. This helps reduce mid-procedure fumbling
and the likelihood of dropping the light. The VALO X light also comes with five accessory lenses, which further enhance its capabilities. A simplified, low-profile design enables the light’s head to reach posterior restorations with ease.
“We simplified the VALO X curing light even more by making it the only light that allows you to change modes without pushing buttons, thanks to its new accelerometer,” says Ultradent VP of Research and Development Neil Jessop. “In fact, it’s engineered so well that it won't change modes by accident, providing the experience and performance you expect from a VALO curing light.”

VALO X curing light even more by making it the only light that allows you to change modes without pushing buttons, thanks to its new accelerometer,” says Ultradent VP of Research and Development Neil Jessop. “In fact, it’s engineered so well that it won't change modes by accident, providing the experience and performance you expect from a VALO curing light.”
Like Ultradent’s other award-winning VALO curing lights, the VALO X curing light is milled from a single bar of aerospacegrade aluminum—a material that improves thermal management, LED longevity, and provides unmatched durability.
For more information please contact sophia.yadi@ultradent.com

As starlynr® celebrates its first-year anniversary, they unveil their new CEO Dr. Amro Adel at Westin Katameya in Cairo under the slogan “The Journey to Egypt.” As a result of starlynr®, traditional metallic braces are gradually being replaced by transparent aligners in Egypt. Despite the use of aligners as an alternative in the past, starlynr® offers a new revolution in aligners based on personalized and customized approach.


The starlynr® system creates a fully customized treatment plan using the most reliable AI-driven and trusted softwares for anatomically correct and more predictable tooth movement.
The starlynr® journey enables a holistic lifestyle and approach to oral health in today’s world for both patients and doctors. starlynr® reduces the oneto-one time of direct patient contact and enables faster and more precise fabrications by introducing artificial intelligence and delivering aligners with variable trimlines using FDA approved essix® plastic for maximum patient comfort for predictable tooth movement. The main services offered by starlynr® are satellite clinics, an online doctor data portal and around-the-clock customer support.
As Per Dr. Fady Yaacoub Founder and chairman, the starlynr® mission is to optimize the setup of the cases, and help doctors to reduce total treatment time, the number of refinements and introduce clear aligner cases over metallic braces.
starlynr® provides doctors and patients with an accurate and predictable 3D viewer of the treatment plan simulation before the actual treatment has taken place. This method has proven to keep the patient’s excitement & enthusiasm present throughout their starlynr® journey.
starlynr® international pioneers, doctors, and specialists from Europe and the MENA hope to
continue to create breakthroughs in orthodontics through the starlynr® community. Up to one million aligners are produced annually by starlynr®.
In their community, all-star smiles are people who travel this journey together from satellite clinics to final patient results. starlynr® believes “everyone deserves to have a beautiful smile and we want to contribute to smiles across our orbit” – Fady Yaacoub.
STARLYNR® THE CUSTOMIZED SOLUTION IN ALIGNERS Dr. Amro ADel the Ceo of StArlYNr




 Dr fADY YAACoub fouNDer AND ChAirmAN of StArlYNr
Dr mohAmeD AllAm, Prof. Atef ShAker, Dr Amro ADel
DrS: fADY YACoub, Amro ADel, mohAmmeD hASSANeiN, mohAmeD AllAm, AliCe rAmSiS
Dr Amro ADel, Dr. ehAb heikAl-PreSiDeNt of the eDA, Dr fADY YAACoub, mohAmeD AllAm
Dr fADY YAACoub AND Dr Amro ADel
Dr fADY YAACoub fouNDer AND ChAirmAN of StArlYNr
Dr mohAmeD AllAm, Prof. Atef ShAker, Dr Amro ADel
DrS: fADY YACoub, Amro ADel, mohAmmeD hASSANeiN, mohAmeD AllAm, AliCe rAmSiS
Dr Amro ADel, Dr. ehAb heikAl-PreSiDeNt of the eDA, Dr fADY YAACoub, mohAmeD AllAm
Dr fADY YAACoub AND Dr Amro ADel




























Company name: Takara Belmont Corporation
Country of origin: Japan
Website: dental.takarabelmont.co.jp/
Takara Belmont has been contributing to people's wish to stay healthy and beautiful through a century of our history. Founded in Japan in 1921, and we drew on our hydraulic technology and began manufacturing dental chairs in 1960s. Committing to the healthy life not only for patients, but also for dentists & staff, our products are designed and developed to support dentist, forging a bond of trust with their patients. Based on the spirit of Japanese manufacturing, each belmont chair is the result of more than 50 years of product research and development, meticulous engineering expertise and innovative production methods. Through our worldwide network of offices and subsidiaries,
BAHRAIN
MEDICAL & PHARMACEUTICAL SERVICES CO. W.L.L. Road 13, Block 711 Building 111 Phone: +973 17715785 bashirco@bashirco.com.sa
SAFWAN EGYPT
41 Lebanon St., Mohandessen, Giza Phone: +20 2 33 03 17 96 +20 2 33 04 02 08 info@safwanegypt .com
IRAN
ARDIN CO.
2nd Floor, No 86 Darya Blvd, Saadat Abad, Tehran Phone: +98 21 88 73 004 ardincommercial2020@gmail.com
IRAQ
TECHNICAL MEDICAL CORNER
Bab Al-Moatham St Erbil-40st Near Aya Moll, Baghdad Phone: +964 7708386000 +964 770175573 info@tmc-iraq.com
JORDAN
KHOURY DENTAL
P.O. Box 306 Amman Phone: +962 6 582 7015
KENYA
Belmont continually monitors current industry and market needs as we strive to design and introduce high quality, creative products that help increase work efficiency and productivity.

DENTMED KENYA LTD.


Woodvale Grove, Westlands, P.O. Box 43873, Nairobi Phone: +254 2 04 44 53 07 info@dentmedkenya.com
AL-SAYAFE MEDICAL & PHARMACEUTICAL SUPPLIES CO. W.L.L Al-Arabia Tower, 18th Floor Ahmed Al-Jaber Street, Kuwait Phone: +965 69028580 alsayafe@alsayafemedical.com
FIMALCO DENTAL
Mar Elias Street, Hariri Center 1st Floor, Beirut Phone: +961 1 30 24 32 fimalco@hotmail.com
OMAN
MEDICAL& PHARMACEUTICAL SERVICES CO. L.L.C 209 Postal Code 116 Muscat Phone: + 968 24567561 info@bashirco.com.sa
SAUDI ARABIA
MEDICAL & PHARMACEUTICAL SERVICES BASHIR SHAKIB AL JABRI & CO. LTD P.O. Box 9584 - Jeddah 21423 Phone: +966 l 26 70 04 30 bashirco@bashirco.com.sa
SUDAN
RASD PHARMA MULTI ACTIVITIES CO. LTD. No.761, Block 22, Altaif, Khartoum Phone: +249 155 141414
The hydraulic mechanism of the chair ensures smooth and quiet movement of the joints and provides a comfortable feeling for patients. One of the characteristics, touch screen interface has been designed to improve efficiency and reduce stress during treatment. When a handpiece is chosen and picked up, the screen displays only necessary information, helping the dentist concentrate on the treatment.



EURUS is shown in AEEDC Dubai 2023, so we welcome your visit at our Belmont booth.
• Easy changeover to right/left handed use

• Base-mount doctor table can be moved lightly and smoothly
• Making comfortable operating space


• Providing a variety of operating styles and preparation zones as you like

Company name: BISCO, INC.

Country of origin: United States of America Website: www.bisco.com
BISCO, a global leader in aesthetic dentistry continues to develop innovative products for contemporary dentistry. At BISCO “Adhesion is our passion” and we dedicate our lives to understanding and improving the bond. We understand the importance of the supporting layer of the restoration. Whether you are working with implants, zirconium, ceramics/lithium disilicate, or porcelain fused to metal we focus on dentistry from the bottom up so your patients can enjoy top down esthetics.
GLOBAL MEDICAL ESTABLISHMENT
Block 644, road 4433 Building 627, flat 3, Nuwaidrat
Contact: dr. Abdullah nasser Phone: 973- 172 17093 Email: admin@gme-bh.Com
ALEX DENT
31 El Rashidi St., Kasr EL Ainy Shaheen Medical Mall, Cairo Phone & Fax: (20100) 140-6378 heshamelsheikh79@yahoo.com
DONYAYE KALAYE SINA (DKS) CO. #1, No.9 Vernous St. Keshavarz Blvd. Tehran 1415953131 Phone: 98-21-88998248 farazbehzadi@gmail.com
MZK DENTAL PRODUCTS
Bloomfield Township, MI. 48302
Contact: Dr. Nizar Mansour Phone: (248) 423-4644
JORDAN
BASAMAT MEDICAL SUPPLIES
125 Al-Razi Street Jabal Al-Hussein, Abdali Area, Amman Phone: 962-6-5605395 ziad@basamat.com
ALPHA MEDICAL
BISCO proudly manufactures its materials in the United States and markets its products through highly trained, focused distributors outside the United States. At BISCO, we understand that product quality, consistency and freshness are of great importance. BISCO Dental Products are available worldwide with award winning brand names such as ALL-BOND UNIVERSAL®, AELITE ™, DUO-LINK UNIVERSAL™, TheraCal LC®, TheraCem® and Z-PRIME ™ Plus.
Shareq, Ahmed Al Jaber St. Dasman Complex, Block 1 9th Floor, Office 22 Code: 35153, Dasmah Phone: 965-2-2478611 georgesaba@alphamedicale.com
DENTAL MEDICAL SUPPLIES - DMS Lebanon - Sed el Bouchreih Imad el Hachem Center, 2nd Floor, Beirut Phone: (961) 124-0444 dms@dms-leb.com
AL RADWAN GROUP
Dat Elmad complex, tower NO 5, H7 first floor, Tripoli Phone: (21891) 900-1106 muataz@alradwangroup.org
DENTAL EXPERT
Rue Ibnou Katir Lot 7, Maarif Extension, Casablanca Phone: (21262) 350-5758 dentalexpert1@gmail.com
DELTA NEW VISION
S.I. Building No. 93, 2nd Floor Preah Sihanouk Blvd Muscat, Sultanate of Oman Contact: Mr. SAMI KANAAN sami@odontoprimegroup.com
NASSER TRADING & CONTRACTING Salwa Rd, Midmac Roundabout, Nawar Building, Doha Phone: (9744) 466-5409 ntc@qatar.net.qa
CIGALAH BIO MEDICAL 5th. Floor, Al-Ma’moun Tower, Ali Bin Abi Taleb Street, Al-Sharafiyah District, Jeddah Phone: (96612) 231-6194 ifarra@cigalah.com.sa
L’EXCELLENCE MEDICALE Avenue des Martyres, IMB Palmaruim 4 B71, Sfax 3000, Tunisia Phone: (2163) 153-8072 import@excellencemedicale.tn
BIO LINK MEDICAL AND SURGICAL TRADING
Office 301& 302, 3rd Floor Jumeirah Terrace Building, 2nd December St., Jumeirah 1, Dubai Phone: 971-4-3596242 info@biolinkdubai.com
EZ DENTAL MATERIALS
Mujahid St. Sana’a Phone: (96777) 022-2319 ezzaden.m@gmail.com
TheraCal PT is a biocompatible, dual-cured, resinmodified calcium silicate designed for pulpotomy treatment. TheraCal PT maintains tooth vitality by performing as a barrier and protectant of the dental pulpal complex.

TheraCal PT’s chemical formulation consists of synthetic Portland Cement calcium silicate particles in a unique hydrophilic matrix which facilitates calcium release. TheraCal PT is radiopaque allowing for easy identification and differentiation
from recurrent decay and other restorative materials. TheraCal PT’s physical properties resist breakdown and degradation leading to a durable seal. TheraCal PT is also indicated for direct and indirect pulp capping (liner) and as a base.
BISCO’s THERA brand includes TheraCal LC, TheraCem, TheraCal PT and now TheraBase. BISCO believes that better dentistry can be achieved when practicing the THERA way.
TheraBase is a dual-cure, calcium and fluoride releasing, self-adhesive base/liner. Utilizing the THERA technology, TheraBase chemically bonds to tooth structure, and releases and recharges calcium and fluoride ions.1

TheraBase’s calcium release generates an alkaline pH which promotes pulp vitality. 2
It is a dual-cured material that will polymerize even in deep restorations where light cannot reach.
TheraBase is stronger and more durable than other base materials, glass ionomers and resin-modified glass ionomers.* Additionally, it is radiopaque allowing for easy identification on radiographs, providing a quick and effective diagnosis.
TheraBase has the strength, durability, and THERA technology to provide the best foundation for each restoration.
Base and Liner. The THERA way.
*Data on file, BISCO Inc.
1. Gleave CM, Chen L, Suh BI. Calcium & fluoride recharge of resin cements. Dent Mater. 2016 (32S):e26
2. T. Okabe, M. Sakamoto, H. Takeuchi, K. Matsushima. Effects of pH on Mineralization Ability of Human Dental Pulp Cells.Journal of Endodontics. Volume 32, Number 3, March 2006
Company name: DenMat Country of origin: United States of America Website: www.denmat.com
Since 1974, DenMat has been a leader in high-quality dental products for dental professionals in more than 60 countries around the world. DenMat makes and assembles most of its products at its world headquarters on the Central Coast of California. DenMat offers three main product categories: Consumables, Small Equipment, and a full-service Dental Laboratory. DenMat’s consumables include the brands known and trusted: Geristore®, Core Paste®, Tenure®, Ultra-Bond®, Infinity®,Splash®,Precision®,Perfectemp®,andLumiBrite®and infection control.
DenMat’s small equipment includes a broad suite of products, including NVpro3™,, and SOL™ soft-tissue diode lasers, Rotadent® PeriOptix™ magnification loupes and lights, Flashlite™ curing lights, & VizilitePRO for oral lesion screening. DenMat is the home of the world’s #1 patient-requested thin veneer, Lumineers®. Now better than ever and backed by


www.denmat.com
Thinnovation®: DenMat’s fresh multi-disciplinary approach to anterior esthetics using the latest generation of Lumineers, all hand-finished by skilled lab artisans in California. DenMat also features Snap-On Smile®, the ultimate provisional appliance.
Each of DenMat’s more than 400 employees is focused on assuring that you—our dental customers—love our products and love your customer experience.
We’re building one of the world’s great dental companies—one happy dentist at a time!
For all inquiries please contact us: international@denmat.com
Zen CP+® desensitizing gel alleviates discomfort from dentin hypersensitivity by actively mineralizing and occluding the dentin surface and deep inside the dentin tubules. 1
Formulated with innovative microsphere technology (CAPOSAL® ), Zen CP+ features small particles consisting of amorphous calcium magnesium phosphate that penetrate the dentin tubules and rapidly release calcium and phosphate ions for intra-tubular mineralization of a carbonate substituted hydroxyapatite.2,3




• Favorable particle size and form allows for deeper penetration into dentin tubules2,3
• Controlled degradation rate increases pH and promotes effective hydroxyapatite formation4
• Minerals formed deep into tubules unaffected by wear and acid5
• Does not contain any milk-derived proteins – can be used on all patients 18 years and older!
• Low abrasion formula does not harm enamel surface
MENA DISTRIBUTORS www.denmat.com
For all inquiries contact us at: international@denmat.com







Company name: DMP

Country of origin: Greece Website: www.dmpdental.com
With more than 35 years of experience in dental material manufacturing DMP successfully supplies the dental market worldwide. Certified with ISO 9001, 13485 and MDSAP, DMP’s products carry the CE mark and have U.S. FDA clearance. DMP creates bright smiles achieving excellence and reliability through integrity, passion and commitment which are ingrained in DMP’s culture.
DMP specializes in three main groups of dental materials. The largest group of products are the precision silicone impression materials both for the dentist and the dental laboratory. The second major group of products are the composites for aesthetic dentistry, including bonding and etching materials. They are primarily resin-based materials and are available in light, self or dual cure varieties. The last group is the amalgams which were launched with the establishment of DMP and consist of various types for every need.
DMP aims to create BRIGHT smiles and to provide the highest level of satisfaction, by closely cooperating with its customers and maintaining a high degree of flexibility for individual market needs.
AL WARDANY FOR IMPORT & COMMERCIAL AGENCIES
5 Alsraya Street - Fl. No.2 Office 14, Almnyal, Cairo Phone: +20 23654 322 alwardany@link.net
IRAN
PARSEH ETTEKAL Co.
Miremad St, Motahari Ave, Suite 4, Building 12, 13th Alley, Tehran Phone: +98 (21) 88545400 vaheh@parsehettekal.com
DANA AMIN ABDALRAHMAN COMPANY FOR GENERAL TRADING Medicine Street _40m, 44001, Erbil Phone: +964 751 2383432 dana.amin.arch@gmail.com
BADAWNEH MEDICAL SERVICE
Almallab Albalady Str., Irbid, P.O. Box 2873, Jordan
Phone: +96227261901 badawneh@hotmail.com
M&H MEDICAL COMPANY TO IMPORT MEDICINES & MEDICAL SUPPLIES
Salem Al Mubarak St., KIB Bldg, Reem Mall, Flr-2, Office No-8, Block-2, Salmiya Phone: +96551719517 sanjay@mh-kw.com
Principal St, Bld. Botros EL Achkar, Area Maten, Ground Floor – Next To Champville School Main Gate, Deek El Mehdi Phone: +961 78 942 468 khalil.achkar@gmail.com
AL BASMA DENTAL CENTER
310 Mizran St., Tripoli, Libya Phone: +218 213615043 basmacenter.ly@gmail.com
5 Rue Jabal Bouiblane, App1, Agdal, Rabat, Phone: + 212537671145 ihssan.b@amed.ma
GLOBAL GULF ELITE
Nuzha Street 3152 - Flat Number 22, Wadi Kabir, Muscat, Oman Phone: + 96891718373 info@globalgulfelite.com
ABM4 TRADING AND CONTRACTING
Building No:9, Office No: 39, Barwa Village, Al Wakara, Cr No.113157, Doha Phone: +97444365531 drazeem@abm4trades.qa
GHAYDAA HOSPITALITY & BIOMEDICAL TRADE
Building No 06, st. No 873, Zone No 54, Muraick, Doha, Qatar Phone: +97444365531 imthath@ghaydaa.org
SAUDI ARABIA
ASNAN EST. FOR MEDICAL SERVICES
Buraida Street, Building no 40, P.O.Box 26316, Al-Rayyan, Riyadh, Phone: +966(11)4451075 anis@asnan.net.sa
AFIA AL KHALEEJ TRADING EST Batha Quraish, Jabal Thawr Rd, Makkah, 23343, Saudi Arabia Phone: +966 567373720 afiaa.m.s.info@gmail.com
SYRIA
OMAR ALKASHTO FOR DENTAL SUPPLIES Almazzeh - Alalam St. 9/5519, Damascus Phone: + 963992722111 omar.alkashto@dentacham.com
DENTAL ATLAS S.R.L
1st floor- Rouached Medical Center, Sidi Ahmed Zarroug, Gafsa, 2112, Tunisia Phone: +216 76211720 dental.atlas.tn@gmail.com

NEW VISION LE SERVICE
MEDICO–DENTAIRE
12 Rue Jawhara Cite El Mouna, Boumhel, 2097, Tunisia Phone: + 216 71 905065 beji.bennsib@newvision-tn.com
UNITED ARAB EMIRATES
ADVANCED HEALTHCARE MEDICAL EQUIPMENT AND DRUG TRADING LLC
1903 Lake Central Tower, Marasi Drive, Business Bay, P.O. BOX: 234923 Phone: + 97144547730 alaay@advanced-hc.com
DMP expands its BRIGHT Temporary Crown & Bridge family with the 10:1 and 4:1 delivery systems.
Exceptional aesthetic results, combined with optimal mechanical and physical properties, make them ideal products to fabricate provisional restorations.
The unique and highly advanced technology of BRIGHT Temporary C&B also offers:

• Natural tooth-looking aesthetics due to the perfect combination of shade opacity and fluorescence
• Very low temperature during intra-oral setting which protects against damage of the dental pulp

• Very high compressive and flexural strength for long lasting provisionals
• Colour stability
• Easy polishing due to low oxygen inhibition layer
• Optimum elastic properties
• Easy to cut and trim
Leading the BRIGHT range of composites is NANOCERAM-BRIGHT, a strongly radiopaque nanohybrid composite with exceptional aesthetic results. its creamy consistency and ease of sculpting make it the ideal composite for both anterior and posterior restorations.
Moreover, the high filler loading combined with fine particle size distribution, leads to low polymerization shrinkage, yielding high marginal integrity and minimized post-operative sensitivity. Its benefits include:
• Outstanding aesthetic results with chameleon effect
• Excellent handling characteristics with no slumping
• Extremely high polishability
• High resistance to wear
• Universal composite
Company name: MANI, INC.
Country of origin: Japan Website: www.mani.co.jp/en
MANI, INC. is a manufacturer of medical devices and dental instruments. Ever since we started manufacturing surgical needles in 1956, we have contributed to society as a medical device manufacturer supplying surgical and dental instruments. Our products, which are safe and high-quality medical devices that satisfy the needs of doctors and patients, have also passed the strict standards of countries overseas.

GLOBALMED
Manama Phone: +97317896322 dwms.bh@gmail.com
EGYPT
Baghdad Phone : +96407903760781 zuhair@zuhairbureau.iq JORDAN MATEST
Kuwait Phone: +96522431647 ab@globalmedtechnology.org
DIETI PHARM DENTAL PRODUCTS
Beirut Phone: +9611500991 dietipha@inco.com.lb
LIBYA
AL BYAN CENTER Tripoli Phone: +218213333021 albyan_almotagaded@yahoo.com
BEST MADE
Casablanca Phone: +212522834482 best.made@yahoo.fr
SALA MEDICAL COMPLEX
Muscat Phone: +96824485159 salamedical@yahoo.com
AL MANARA Ramallah Phone: +97222953718 kshatara@p-ol.com
SHARQ MEDICAL SUPPLIES Doha Phone: +97444566100 samer@sharq.qa
AL RAZI MEDICAL SUPPLIES Jeddah Phone: +966126520132 alrazimed@yahoo.com
SYRIA
SALLOUM DENTAL CO Damascus Phone: +963112248772 psalloum@scs-net.org
SAWHNEY TRADING LLC

Dubai Phone: +97143597756 sawbros@eim.ae
YEMEN STORES Sana’a Phone: +9671444622 s.radman@yemenstores.com












International Special Clinic Solutions is Dentsply Sirona’s project team. As the global leader in dental education, with over 60 years of experience and more than 1,000 successful projects, we are the right partner for bringing your education to the next level.
We deliver expert consultation and planning, a complete product portfolio, training, and fully responsive aftercare. Together with you, we develop a tailor-made, future-proofed solution to successfully prepare future dentists in pre-clinical and clinical departments of your university or clinic.

Find more details here: www.dentsplysirona.com/clinics For further information please contact: salzburgaut-clinicsolutions@dentsplysirona.com
dentsplysirona.com

































