AEEDC 2021
Bioflavonoid Spray
Efficacy against Respiratory Viruses
Restorative Esthetics at the Gingiva Pioneers in Dentistry































AEEDC 2021
Bioflavonoid Spray
Efficacy against Respiratory Viruses
Restorative Esthetics at the Gingiva Pioneers in Dentistry





























• Unbeatably durable: Fully withstands masticatory forces, excellent physical properties1
• Unbeatably simple: Universal shade with chameleon effect, 4 mm bulk fill
• Unbeatably quick: Exposure time of only 10 seconds (x-tra fil), applied in one layer – only 35 seconds total working time (Futurabond M+)
1 Tiba A et al., Journal of American Dental Association, 144(10), 1182-1183,2013.
2 based on sales figures
More than 13 million restorations worldwide!2

























Based on the close and fruitful cooperation with dental institutes and practicing dentists since the 1940s, we have a uniquely broad portfolio of specially developed, innovative toothpastes, gels, sprays, mouthwashes and mouth baths. These products, which are marketed under the brands Tebodont®, Emofluor®, Emoform®, Depurdent® and Emofresh® are sold exclusively in pharmacies in Switzerland and in more than 40 other countries outside Switzerland, their various innovative formulations and compositions offer excellent solutions for daily dental care, addressing specific needs and problems (e.g. caries prevention, sensitive teeth, gum problems) and general oral health.
With the REDESIGN we have clarified the positioning of the oral care products: every toothpaste and every mouthwash now has a clear application area. At the same time, our new packaging is "digitalized": each product has a QR code that allows detailed information to be downloaded directly to the mobile phone. The redesign of the products should make the Wild brand tangible and perceptible.
• WILD will be used as umbrella brand on all products, which results in an easier promotion among the whole product range
• Same design for all brands leads to recognition and synergy effects across product range
• Clear unique main indication on the packaging avoids confusion among dental profession, pharmacists and end consumers due to overlapping benefits
• New design underscores clinical benefits and professionalism of the products which leads to cross-brand and cross-portfolio products awareness and helps to create trust among the dental profession, pharmacists and end consumers
• Unifying of the packaging system - all toothpastes in the same size and shape of tubes, all mouthwashes in the same size and packaging - leads to a uniform, eye-catching and space-saving shelf-impact
• Product portfolio becomes fresh, easy to recommend and attractive for the POS
Volume XXVIII, Number III, 2021
EDITORIAL TEAM
Alfred Naaman, Nada Naaman, Khalil Aleisa, Jihad Fakhoury, Dona Raad, Antoine Saadé, Lina Chamseddine, Tarek Kotob, Mohammed Rifai, Bilal Koleilat, Mohammad H. Al-Jammaz

COORDINATOR
ART DEPARTMENT
SUBSCRIPTION
ADVERTISING
PHOTOGRAPHY
TRANSLATION
DIRECTOR ISSN
Suha Nader
Marc Salloum
Micheline Assaf, Nariman Nehmeh
Josiane Younes
Albert Saykali
Gisèle Wakim
Tony Dib 1026-261X
DENTAL NEWS IS A QUARTERLY MAGAZINE DISTRIBUTED MAINLY IN THE MIDDLE EAST & NORTH AFRICA IN COLLABORATION WITH THE COUNCIL OF DENTAL SOCIETIES FOR THE GCC.
Statements and opinions expressed in the articles and communications herein are those of the author(s) and not necessarily those of the Editor(s) or publisher. No part of this magazine may be reproduced in any form, either electronic or mechanical, without the express written permission of the publisher.
DENTAL NEWS – Sami Solh Ave., G. Younis Bldg.
POB: 116-5515 Beirut, Lebanon.
Tel: 961-3-30 30 48
Fax: 961-1-38 46 57
Email: info@dentalnews.com
Website: www.dentalnews.com www.instagram.com/dentalnews

September 9 - 11, 2021 Rimini, ITALY www.expodental.it





Congrès International ADF 2021
September 22 - 25, 2021 Cologne, GERMANY www.english.ids-cologne.de

Greater New York Dental Meeting 2021

September 26 - 29, 2021 Sydney, AUSTRALIA www.world-dental-congress.org
October 14 - 16, 2021 Almaty, KAZAKHSTAN www.cadex.kz/en
November 23 - 26, 2021 Paris, FRANCE www.adfcongres.com/en
November 26 - December 1, 2021 New York, USA www.gnydm.com Saudi International Dental Conference 2022
January 20 - 22, 2022 Riyadh, KSA www.sidc.org.sa FDI World Dental Congress Sydney 2021
February 1 - 3, 2022 Dubai, UAE www.aeedc.com
Restorative Esthetics at the Gingiva
George Freedman, Paiman Lalla

Bioflavonoid Spray Efficacy against Respiratory Viruses
George Freedman, Zeeshan Sheikh Dip, Henriette Lerner 26. Fluoride Content in Asian Produced Green Teas

Melissa E. Ing, Britta E. Magnuson, David L. Frantz

40. Oral Cavity and Oropharyngeal Cancer Surveillance and Control in Alberta: A Scoping Review
Parvaneh Badri, Seema Ganatra, Vickie Baracos, Hollis Lai, Maryam Amin,

56. Pioneers in Dentistry Annual Symposium
June 16, 2021 Beirut, Lebanon

60. AEEDC 2021 25th International Dental Conference & Arab Dental Exhibition
June 29 - July 1, 2021 Dubai, United Arab Emirates

3SHAPE 19
A-DEC 33
ACE SURGICAL 29
BA INTERNATIONAL 57
BELMONT 21
BISCO 9, 11
COLD & FLU GUARD 23
COLTENE 45
DENTAURUM 16
DENTSPLY SIRONA C3
DMP 1
DXP 49
DURR 35
EDGE ENDO 39
FKG 53
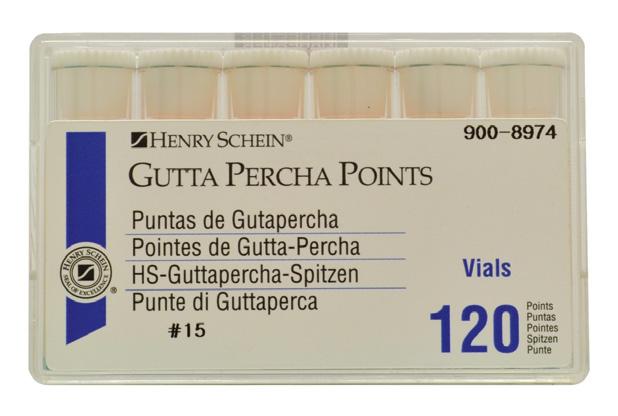
HENRY SCHEIN 37
NSK C1
PROMEDICA 38
ROLENCE 12
SCHEU 30, 34
SEPTODONT 80
TRIDENT C4
ULTRADENT USA 24
VOCO 2, 41
WATERPIK 17
W&H 31, 37
WILD 3, 4, 5

George Freedman DDS, DiplABAD, FIADFE, FAACD, FASDA Adjunct Professor, Western University of Dental Medicine, Pomona CA
Paiman Lalla DDS, FIOCI, FIADFE, FAAIP, FICD freedman@epdot.com
The data is clear; porcelain and composite resin are both biocompatible at the gingival margin and well tolerated.1-3 The caveat is that composite tends to cause tissue irritation if it intimate directly impinges on the gingiva.4-6 This ultimately causes unesthetic gingival recession.
Porcelain is less problematic, but marginal plaque build-up, activated by the thin layer of resin cement, leads to a similar free gingival irritation and, eventually, recession.7, 8
Even skillful subgingival margin placement will typically, within 3-5 years, due to aging, gingival irritation, or lack of home maintenance on the patient’s part, lead to unesthetic recession and full visible exposure of the darker dentinal tissue.9, 10
Thus, the restorative conclusion is to locate composite margins supragingivally,3, 11 with the resin material reasonably away (0.250.50mm) from soft periodontal structures and thereby unlikely to cause tissue irritation.
Today’s adhesives and restoratives make this a rather straightforward task.12-19 Later generation adhesives bond equally well, and predictably, to both enamel and dentin.14, 15 Significantly, 7th and 8th generation adhesives have similar bonding strengths to both enamel and dentin, eliminating the potential stresses caused by unequal polymerization contraction.17-19 It is clinically possible to create a continuous restoration through the dentino-enamel junction (DEJ), covering as much of the enamel and the dentin as necessitated by decay or abfraction (or both).
A significant esthetic predicament quickly presents, however. Dental restorative materials are designed to match the shade of the enamel position of the tooth. While some manufacturers offer “dentin” shades, these hues typically do not closely match the darker coloration of exposed dentin, particularly those observed in endodontically treated teeth. A typical central incisor measures approximately 10.5mm cervico-incisally (CI).20
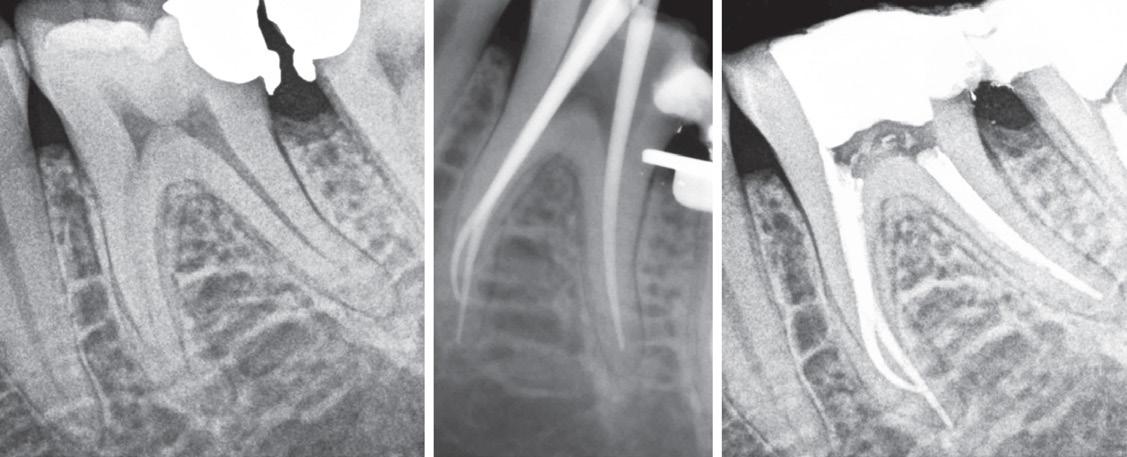
A substantial increase in the apparent length of a tooth, specifically in the anterior labial region, detracts from the esthetic smile. When restoring a Class V decay or abfraction, or perhaps a small gingival recession, an enamel-colored resin is commonly placed at the labial DEJ. Increasing the maxillary central incisor’s vertical aspect (Fig. 1) by a mere 3mm adds 30% to the apparent vertical dimension, significantly altering the cervico-incisal to

mesio-distal (CI:MD) ratio, totally upsetting the esthetic parameters of the smile. (Fig. 2) In situations where there is moderate recession, the visual imbalance is even further impaired. The CI:MD ratio impact is even greater on maxillary laterals and mandibular incisors (average 9.0mm CI). Maxillary and mandibular cuspids (average 10-11mm CI) are often the teeth most affected by gingival recession, and are also highly visible both anteriorly and laterally.

1: Normal length maxillary central incisors – expected appearance
Individuals who have gingival recession, abfraction and/ or decay tend to look older than they really are (long in the tooth). Covering the darker root dentin with an enamel-like resin simply makes their teeth more visible, seemingly longer, and correspondingly less esthetic.

Figure 2: Maxillary incisors apparent length increased by 30%very unnatural and unesthetic
The practitioner must solve this problem practically, esthetically, and with minimum invasiveness. The restoration must be functional, replacing missing dental
structures to natural dimensions and contours. The restoration should restore lost enamel with enamelshaded composite resin, and receded gingiva with gingival-shaded composite resin. By creating an artificial enamel-gingival junction in composite restorative material, the patient’s esthetics and smile can be restored.
Beautifil II Gingiva (Shofu USA, San Marcos CA) has been specifically designed for the re-balancing of pink aesthetics in the cervical areas of the dentition. (Fig. 3) Beautifil II Gingiva is indicated for wedge-shaped defects, cervical decay, the esthetic rectification of gingival recession, shielding exposed cervical areas and splinting of mobile teeth.

The resin material is available in 5 tones (dark pink, light pink, brown, orange and violet) (Fig. 4) which can be layered and/or blended to achieve custom shades that allow the treatment of patients with various hues of gingival pigmentation, according to their clinical needs. (Fig. 5)
Beautifil II is a highly esthetic, fluoride-releasing composite resin material indicated for all classes of restorations.

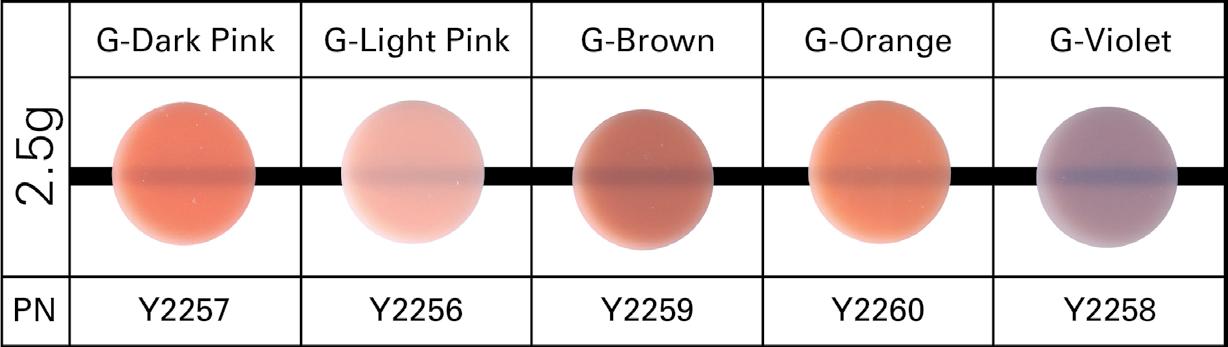
4:
Numerous studies over the past 20 years have shown no secondary caries, no failures, no post-operative sensitivity and a high retention of both color match and surface luster. The material is based on Shofu’s proprietary Giomer technology. (Fig. 6) The significant advantage of the Giomer class of resins is that they not only release fluoride to
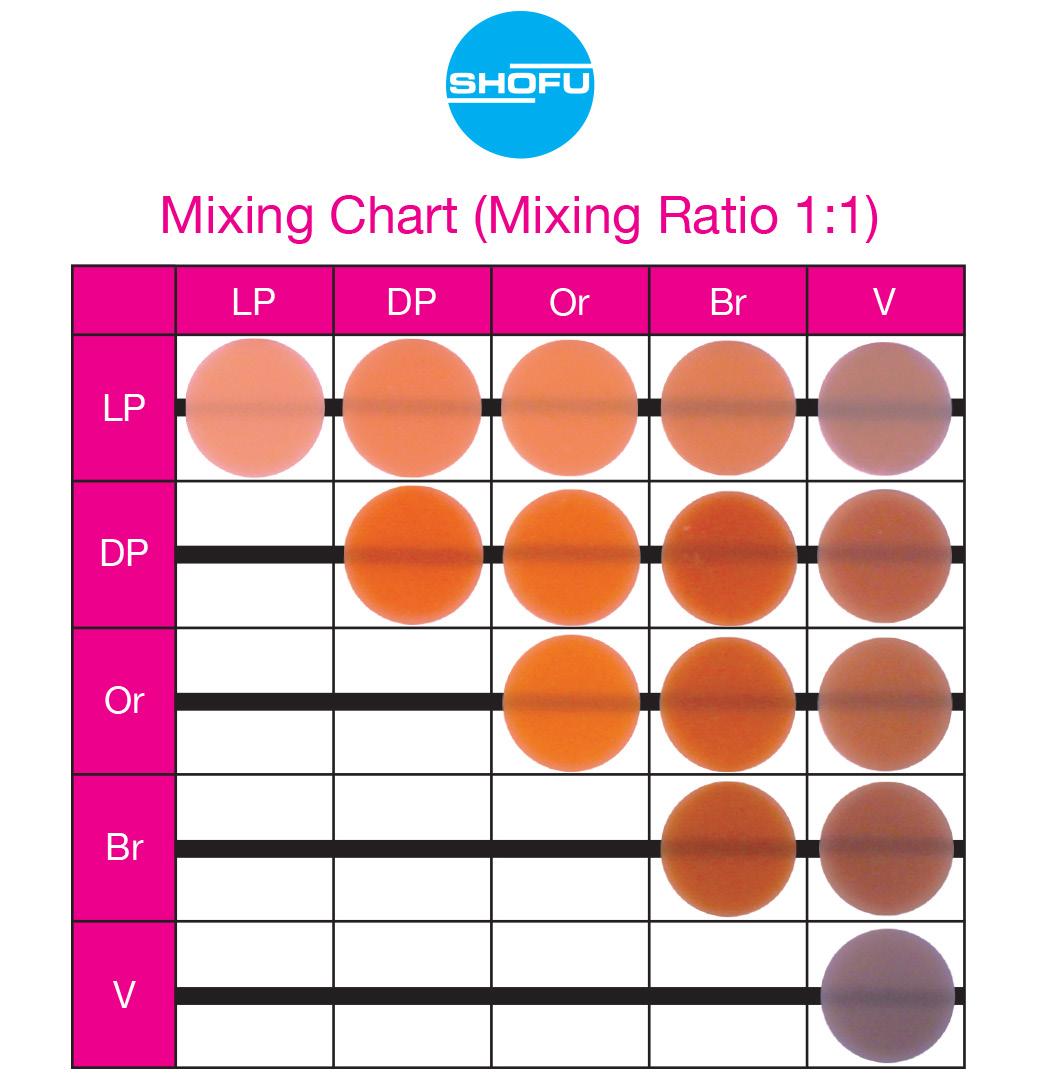
Figure 5: Resins layered and/or blended to achieve custom gingival shades


Huge Panasonic ba�ery capacity 2900mAh. Up to 1500 exposures a�er fully charge. Latest Canon X-Ray D-045 tube. Extremely low dose under the double sca�er shield.


Extremely durable cable passed 70,000 + bending test.
Exchangeable cable easy replaced. Up to 50,000 shots with no quality loss.
High quality from the biggest iphone Taiwanese supplier.
protect the tooth at the restorative margin, but that their fluoride content can be recharged by toothpastes, fluoride rinses and varnishes. Thus, the Giomer’s fluoride releasing capacity does not decrease over time.
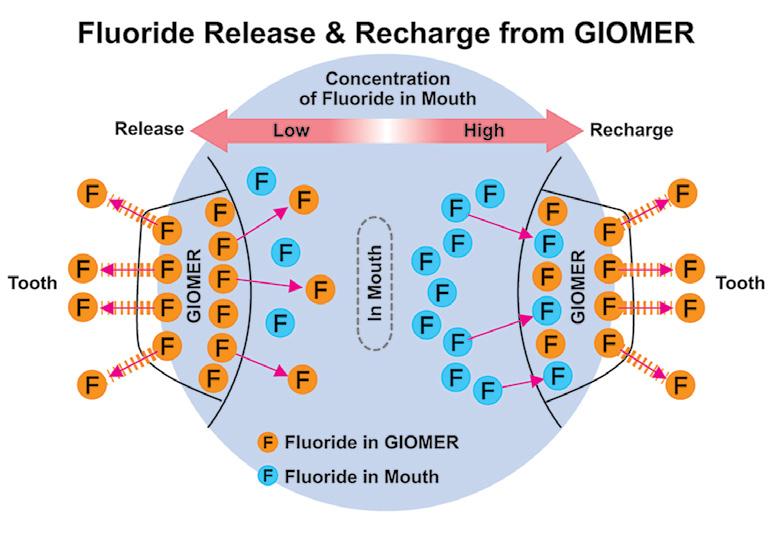
Figure 6: Giomers continue to release fluoride because their fluoride content can be recharged with fluoride toothpastes, rinses and varnishes
Another important consideration is that the gingival margin of the restorative material (whether pink or enamel in color) must be kept supragingival and slightly away from the free gingival margin.3, 4, 6
While a very narrow band of darker root structure may be visible towards the apex, the restoration’s enamel (coronal) and pink gingival (radicular) coloration will focus attention away from this area. With gingivally blended restorations, the professional can

deliver both esthetic and supragingival margins within the same restoration. A supragingival margin facilitates ready access and effective home maintenance for the patient.
It is imperative that a restoration that is so close to the free gingival margin be placed under conditions controlled for moisture and bleeding. Rubber dam placement is impractical (target area is positioned apically) and retraction cord may physically or chemically compromise the working area. Ideally, the patient’s oral hygiene creates a healthy gingival microenvironment, with minimal pocketing and no bleeding on probing.

In most cases, however, the practitioner must modify the actual situation to increase the likelihood of clinical success. The easiest and best technique for predictable tissue sculpting is the use of the diode laser.21-23 Utilizing low power (1.0-1.5 watts), the dentist can produce an ideal, dry, clean, and blood-free working area in less than a minute.
Remarkably, the patient’s chief concern was the gingival recession on the left maxillary lateral, not the mesial caries. (Fig. 8) Fortunately, the patient’s oral hygiene was relatively good, and restoring the MLB decay was
straightforward (BeautiBond (Fig. 7) and Beautifil Flow Plus X, both from Shofu USA, San Marcos CA). The steps for the esthetic rectification of the buccal recession are:
1. Gently micro-abrade the receded area and the apical enamel to remove food debris and plaque. The nozzle of the abrader should be angled incisally to prevent gingival irritation and bleeding. Rinse thoroughly and lightly air dry, leaving the surface slightly moist (although the degree of moistness is not critical).
2. Apply BeautiBond, a 7th generation dental adhesive, and leave for 10 seconds. Thoroughly air dry the adhesive (very critical). Light cure with the Fusion 5 Curing Light (Dentlight, Plano TX), offering deep cure of composite resins within 3 seconds with a uniform 4000 mW/cm2 output. (Fig, 7A)

 Figure 7: BeautiBond 7th generation dental adhesive
Figure 7A: Fusion5 Curing Light (Dentlight, Plano TX)
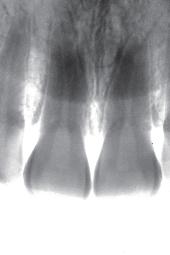
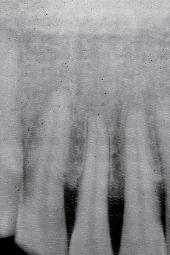
Figure 8: Maxillary left lateral with decay and recession
Figure 7: BeautiBond 7th generation dental adhesive
Figure 7A: Fusion5 Curing Light (Dentlight, Plano TX)
Figure 8: Maxillary left lateral with decay and recession

3. Select the appropriate Beautifil II Gingiva shade (Light Pink and Violet for this patient) and apply to the receded area to restore the buccal dimension and contour of the original soft tissue. Light cure. It is important to leave a small (0.25-0.50mm) gap between the apical margin of the restorative and the free gingival margin. (Fig. 9) This space prevents gingival irritation, is easily maintainable by the patient, and is generally not visible even with closeup photographs. (All photography done with the Shofu EyeSpecial camera, (Fig. 10) Shofu USA, San Marcos CA.)

This is the most commonly encountered recession in the oral cavity. The mandibular anteriors are small, close together, and not effectively cleaned by the tongue and
the lower lip. (Fig. 11) Due to gravity, food debris and plaque tend to accumulate labially and interproximally. (Fig. 12) In this case, the major culprit for the recession is the frenum that pulls the attached gingiva apically. The preliminary process is a diode laser frenectomy to eliminate the muscular forces.21-23

The steps for the esthetic rectification of the buccal recession are:
1. Gently micro-abrade, in an incisal direction, the receded areas and the enamel nearest to the DEJ to remove food debris and plaque. Rinse thoroughly and lightly air dry, leaving the surface slightly moist.
2. Apply BeautiBond and leave for 10 seconds. Thoroughly air dry the adhesive. Light cure.

3. Select the appropriate
and apply to the
the buccal dimension and contour of the original soft tissue. Light cure. Leave a small (0.25-0.50mm) gap between the apical margin of the restorative and the free gingival margin. (Fig. 13) This procedure restores the expected gingival height, and contributes to making the patient’s smile look younger.

Long-term at-home maintenance is best accomplished with procedures that are familiar to the patient and easy to implement. Regular toothbrushing is effective and practiced by most dental patients. Interdental string flossing less so.

Though well-documented, patient resistance to the process and irregular application limit its benefits. Water flossing (Water Pik Inc., Fort Collins CO) not only facilitates in the interdental cleaning process but has been shown to improve the results.24
While there are several models available, the Sonic Fusion offers a simultaneous water flossing and sonic brushing. (Figs. 14 and 15)

Beautifil II Gingiva enables the practitioner to overcome the gingival esthetic dilemma. The gingival rectification technique is predictable and can typically be accomplished without the need for local anesthetic or discomfort to the patient. These restorations are totally functional and replace both hard and soft missing dental structures to natural dimensions and contours with minimum invasiveness.
The restoration of the coronal anatomy with toothcolored composite resins is well established; the development of an artificial enamel-gingival junction and the reconfiguration of missing gingival structures with composite resins is a novel solution that restores the patient’s smile and facial esthetics.
Figure 13: Mandibular anteriors with gingival restorative rectification Figure 15: Combined sonic brushing and pulsating interproximal water flossing Figure 14: Sonic Fusion (Water Pik Inc, Fort Collins, CO)
















1. Freedman G: Ultraconservative Porcelain Veneers, Esthet Dent Update 2:224-228, 1997.
2. Freedman G: Ultraconservative Rehabilitation, Esthet Dent Update 5:80-85, 1991.




























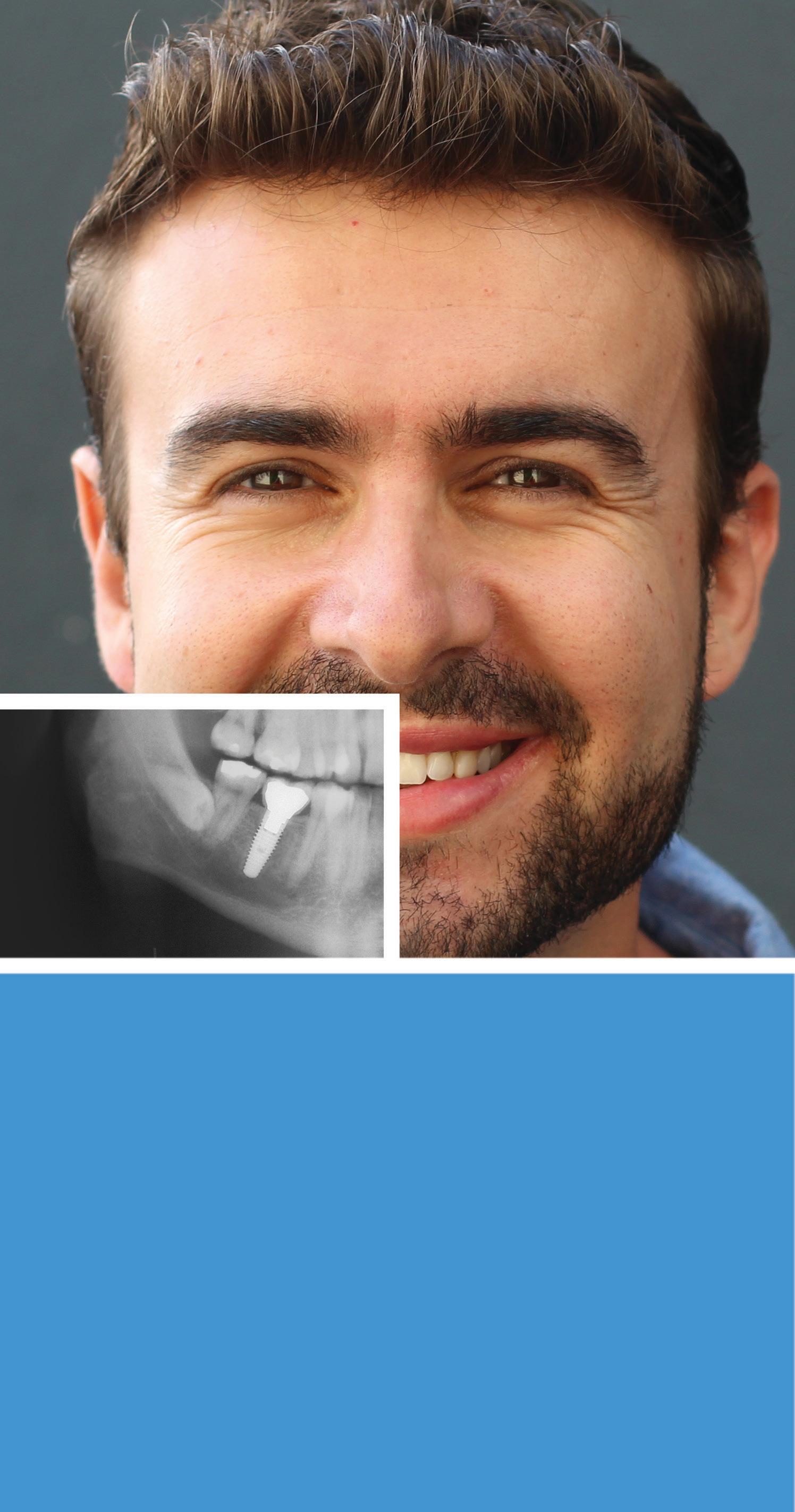
The decision on which abutment is best for your patient – conical or platform – is yours.
3. Freedman G, Fugazzotto PA, Greggs TR: Aesthetic Supragingival Margins, Pract Periodontics Aesthet Dent 2:35-38, 1990.
4. Newcomb GM: The Relationship Between the Location of Subgingival Crown Margins and Gingival Inflammation, J Periodontol 45:151, 1974.
5. Renggli H, Regolati B: Gingival Inflammation and Plaque Accumulation by Well Adapted Supragingival and Subgingival Proximal Restorations, Helv Odont Acta L6:99, 1972.
6. Waerhau SJ: Histologic Considerations which Govern where the Margins of Restorations Should be Located in Relation to the Gingiva, Dent Clin North Am 4:161, 1960.
7. Berman M: The Complete Coverage Restoration and the Gingival Sulcus, J Prosthet Dent 29:1301, 1973.
8. Marcum O: The Effect of Crown Margin Depth upon Gingival Tissues, J Prosthet Dent 17:479, 1967.
9. Freedman GA, McLaughlin G: The Color Atlas of Porcelain Laminate Veneers, St Louis, Ishiyaku EuroAmerica, 1990.
10. Freedman G: Contemporary Esthetic Dentistry, Elsevier Publishing, 2011 Chap 23; 551
11. Freedman G, Klaiman HF, Serota KT, et al: EndoEsthetics: Part II. Castable Ceramic Post and Core Restorations. Ont Dent 70:21-24, 1993.
12. Albers HF: Dentin-resin bonding. Adept Report 1990; 1:33-34.
13. Munksgaard EC, Asmussen E. Dentin-polymer Bond promoted by Gluma and various resins. J Dent Res 1985; 64:1409-1411.
14. Barkmeier WW, Erickson RL: Shear bond strength of composite to enamel and dentin using Scotchbond multi-purpose. Am J Dent 1994; 7:175-179.
15. Swift EJ, Triolo PT: Bond strengths of Scotchbond multi-purpose to moist dentin and enamel. Am J Dent 1992; 5:318-320.
16. Gwinnett AJ: Moist versus dry dentin; its effect on shear bond strength. Am J Dent 1992; 5:127129.
17. Freedman G, Leinfelder K: Seventh Generation Adhesive Systems. Dentistry 2003; January:15–18
18. Freedman G: 7th generation Adhesive Systems. Dental Asia (English) 2019; March-April:50-53
19. Freedman G: Adhesion: Past, Present, and Future. Oral Health 2019: July 109:7 8-14,82
20. Wheeler RC: A Textbook of Dental Anatomy and Physiology. W.B. Saunders 1965: 6:126
21. Goldstep F: Soft Tissue Diode Laser: Where Have You Been All My Life?. Oral Health 2009: 99:7;34-38
22. Goldstep F: Diode Lasers for Periodontal Treatment: The Story So Far. Oral Health 2009: 99:12;44-46
23. Goldstep F: Diode Lasers: The Soft Tissue Handpiece. Dental Asia 2011: Jan-Feb; 28-32
24. Rosema NAM et al. The effect of different interdental cleaning devices on gingival bleeding. J Int Acad Periodontol 2011; 13(1):2-10



George Freedman DDS, DiplABAD, FIADFE, FAACD, FASDA
Adjunct Professor, Western University of Dental Medicine, Pomona CA
COVID-19 has raised new concerns about respiratory viral infections (RVI). This virus can reproduce within the cells that line the human respiratory tract and the resulting infections cause respiratory issues and may infect multiple other sites.
and human rhinovirus. Other viruses of interest include parainfluenza viruses, metapneumovirus, adenovirus, respiratory syncytial virus (RSV) and human enteroviruses (HEV).1
Zeeshan Sheikh Dip.Dh, BDS, MSc, PhD
Henriette Lerner DMD, DICOI freedman@epdot.com
At this time, there are more than 200 known viral strains that cause respiratory infection, including the coronavirus, influenza virus,
• A/B cause seasonal epidemics (flu)
• A is also implicated with seasonal pandemics
Coronavirus can cause symptoms ranging from the common cold to worldwide pandemics. Influenza viruses are categorized into types:
• C/D are generally mild and do not affect humans
Each category has multiple subtypes. Rhinovirus has 3 main species including A/B/C with more than 160 viral types causing the common cold.2-4
Key Respiratory Viruses are transmitted via aerosols, respiratory droplets, and fomites. Factors known to increase the risk of infection include: proximity, ventilation, surface contact, and time of exposure. Thus, gathering areas without adequate ventilation, where distancing is not possible, increase infection risk. These include workplaces, grocery stores, shopping malls, restaurants, indoor gyms, schools, and airplanes. Indoor activities with significant aerosolization increase risk, and while outdoor activities offer ventilation, physical distancing is not always possible.
In the event of an exposure, the respiratory viruses must come in contact with oral or nasal mucosa of a new host to pose a risk of infection. While the mucosal epithelium offers a partial physical and innate immune barrier against viral infection, the virus can still attach and infect the individual.5 It is extremely important to emphasize that for an infection to

occur, the respiratory viruses must gain access to the mucosa, attach, internalize, and replicate within the host.
A novel protection strategy is to break the chain of infection by neutralizing the virus prior to adhesion and penetration of the host cell, either by a virus-encapsulating barrier, and/or via direct neutralization. Both ultimately prevent infection and disease.
The current challenge is two-fold: to reduce risk for COVID-19 and to develop multiple strategies that reduce the risk associated with new viruses with the potential to cause another pandemic crisis. COVID-19 occurred a full 100 years after the Spanish Flu (H1N1), but the next worldwide pandemic may present sooner. Current approaches for minimizing transmission are based on three common strategies:
• Routine and widespread use of personal protection equipment (PPE), including masks, to create a physical barrier to transmission.6
• Frequent and thorough disinfection of hands, surfaces and fomites to mechanically remove and chemically inactivate shed virus particles and prevent their translocation to new hosts.7
• Delivery of aerosolized therapeutics to the mucosal microenvironment to dampen an aggressive immune response in respiratory infections, thereby improving clinical outcomes.8
It is very desirable to prevent viruses that have entered the human body via the nasal and oral passages from gaining access to the mucosal layers, adhering, and causing infection. One practical approach is an oral spray that targets the mucosa in the mouth and throat to create an additional barrier that protects the host from viruses. The ideal spray must be safe and use Generally Recognized as Safe ingredients (GRAS) and have a pleasant taste and sensation.
Additionally, it must be easy to use, acceptable for all ages, and must provide rapid onset to target specific situations. Further desirable properties include: vegetarian compatibility, sustainability, non-GMO sourcing, and no banned substance ingredients.
Flavobac is a plant-based, patented combination of specific water-soluble bioflavonoid molecules with known anti-microbial and anti-viral activity.9 The pharmacological effects of Flavonoids are linked to their antioxidant and free-radical scavenging activity in addition to their interaction with enzymes, adenosine receptors and bio-membranes.10 Flavonoids have also been shown to possess anti-viral activity against influenza viruses HSV-1, HSV-2 and the rotavirus.9
There are several products designed to assist in preventing the onset of infection caused by rhinovirus/coronavirus/ influenza virus by creating a physical barrier to viral and bacterial adhesion at the nasal and throat mucosal membranes. Oral Science International (Brossard, QC) has a unique formulation, Cold & Flu GuardTM, (Fig. 1) that unites bioflavonoids with the mucosal barrier.








Glycerin and hyaluronic acid components form a barrier/ film over the mucous membrane, and act as a delivery method for the bioflavonoids and menthol.
In vitro efficacy studies of Flavobac aqueous solutions have demonstrated concentration-dependent activity against a range of bacterial, fungal and protozoal pathogens.11 Antiviral studies have confirmed activity against various viruses.12-14
Retroscreen Virology Laboratories (now hVIVO, London, United Kingdom) and Biobest Laboratories (Edinburgh, United Kingdom) have independently demonstrated that Flavobac formulations are efficacious in the inactivation of two different subtypes of Influenza A: H5N1 (Bird Flu) and H1N1 (Swine Flu).13, 15
In 2004, Retroscreen Virology Ltd., Barts and The London Queen Mary’s School of Medicine and Dentistry, evaluated the viricidal activity of Flavobac against Urbani SARS virus, Influenza A virus, Human Rhinovirus and HIV. The results demonstrated significant viricidal activity against all the viruses at all concentrations and timepoints.14
The first anti-SARS-CoV-2 evaluation of an oral spray formulation containing Flavobac as the sole active ingredient (developed specifically for routine intranasal or intraoral use) was Reported in March 2021 by the Institute for Antiviral Research (IAR) at Utah State University (Logan, UT) [*data pending publication].

Figure 2: Nasal antiseptic spray solutions and oral antiseptic spray solutions.
The IAR employs recognized scientists to identify antiviral agents and vaccines against a wide range of human pathogenic viruses and has participated in the pre-clinical development of numerous FDA-approved antiviral compounds.
Nasal antiseptic solutions and oral rinse antiseptic solutions (Fig. 2) consisting of aqueous Flavobac BCL concentrate as the sole active ingredient and OSI2021003 oropharyngeal spray solution and other natural ingredients were supplied by Oral Science International (Brossard, Canada).
Flavobac aqueous solution reduced SARS-CoV-2 titer below the limits of detection at all concentrations tested (Table 1). These results generate dose optimization and guide product dosage and concentrations.
a Cytotoxicity indicates the highest dilution of the endpoint titer where full (80-100%) cytotoxicity was observed
b Neutralization control indicates the highest dilution of the endpoint titer where compound inhibited virus CPE in the wells after neutralization (ignored for calculation of virus titer and LRV)
c Virus titer of test sample or virus control (VC) in log10 CCID50 of virus per 0.1 mL
d LRV (log reduction value) is the reduction of virus in test sample compared to the virus control

After incubation with Flavobac commercial solutions OSI-20210203A and OSI-20210203B, SARS-CoV-2 virus titers and LRV were reduced below the limits of detection (LRV>3.0) (Table 2). Each Flavobac containing
solution evaluated was effective at reducing >3 log10 CCID50 infectious virus, from 4.7 log10 CCID50/0.1 mL to 1.7 log10 CCID50/0.1 mL or less (Table 2). This represents a >99.9% efficacy of viral reduction.
a CytotoxIcity indicates the highest dilution of the endpoint titer where full (80-100%) cytotoxicity was observed
b Neutralization control indicates the highest dilution of the endpoint titer where compound inhibited virus CPE in the wells after neutralization (ignored for calculation of virus titer and LRV)
c Virus titer of test sample or virus control (VC) in log10 CCID50 of virus per 0.1 mL
d LRV (log reduction value) is the reduction of virus in test sample compared to the virus control



























The challenge in developing oral and nasal sprays is to create effective topical preparations that are safe and have the required efficacy against respiratory viruses. Ethanol >70%, for example, is known to be an effective viricidal agent but cannot be used safely in the nose. Flavobac solutions and formulations have been shown to be effective against a variety of viral strains and are nontoxic (GRAS status in the USA via the FDA).
Given their efficacy and safety profile, Flavobac oral and nasal spray products such as Cold & Flu GuardTM and Flavobac Health GuardTM, can be considered as a supplementary layer of protection in addition to face masks in combatting respiratory viruses. (Fig. 3) This is particularly beneficial and important for:
• High aerosolization situations
• Individuals at higher risk of respiratory viral complications
• Those not yet vaccinated
• Children
• Everyone gathering where appropriate distancing is not possible
https://www.cdc.gov/coronavirus/types.html https://www.cdc.gov/flu/about/viruses/types.htm https://www.lung.org/
*Pending publication: Efficacy of FLAVOBAC Nasal and Oral Preparations Against Severe Acute Respiratory SyndromeCoronavirus 2 (SARS-CoV-2), A. Barbour, M. Mendenhall, G. Darlington MD, M. Glogauer (Pending Publication in medRxiv).
1. Mäkelä, M.J., et al., Viruses and bacteria in the etiology of the common cold. 1998. 36(2): 539-542.
2. Couch, R.B.J.e.L., Rhinoviruses. 2001.
3. Peiris, J.J.M.m., Coronaviruses. 2012: 587.
4. Zhang, Y., et al., New understanding of the damage of SARSCoV-2 infection outside the respiratory system. 2020: 110195.
5. Gwaltney Jr, J.M.J.T.A.j.o.m., Clinical significance and pathogenesis of viral respiratory infections. 2002. 112(6): 13-18.
6. Organization, W.H., Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19): interim guidance, 19 March 2020. 2020, World Health Organization.
7. Cohen, M.S. and L. Corey, Combination prevention for COVID-19. 2020, American Association for the Advancement of Science.
8. Oslund, K.L. and N.J.F.v. Baumgarth, Influenza-induced innate immunity: regulators of viral replication, respiratory tract pathology & adaptive immunity. 2011. 6(8): 951-962.
9. Bylka, W., I. Matlawska, and N.J.J. Pilewski, Natural flavonoids as antimicrobial agents. 2004. 7(2): 24-31.
10. Harborne, J.B. and C.A.J.P. Williams, Advances in flavonoid research since 1992. 2000. 55(6): 481-504.
11. Hooper, S.J., et al., Antimicrobial activity of Citrox® bioflavonoid preparations against oral microorganisms. 2011. 210(1): E22-E22.
12. Lalani, S. and C.L.J.V. Poh, Flavonoids as antiviral agents for Enterovirus A71 (EV-A71). 2020. 12(2): 184.


Figure 3: Nasal and oral sprays function as supplementary layers of protection (in addition to face masks) to short circuit cold and flu viruses.
13. Reis, A.C.C., et al., Anti-Zika virus activity and chemical characterization by ultra-high performance liquid chromatography (UPLC-DAD-UV-MS) of ethanol extracts in Tecoma species. 2020. 20(1): 1-15.
14. Zou, M., et al., Structure-activity relationship of flavonoid bifunctional inhibitors against Zika virus infection. 2020. 177: 113962.
15. Carrouel, F., et al., Antiviral Activity of Reagents in Mouth Rinses against SARS-CoV-2. 2020: 0022034520967933.

Community Dentistry
Abstract
Melissa E. Ing, DMD, Associate professor, Tufts University School of Dental Medicine, Boston, Massachusetts
melissa.ing@tufts.edu
Britta E. Magnuson, DMD, Assistant professor, Tufts University School of Dental Medicine, Boston, Massachusetts
Background
This study determined the fluoride content of green tea from various parts of Asia, where green tea originates.
Methods
We brewed 2.5 g each of 4 types of green tea (from China, South Korea, Japan and Sri Lanka) using deionized water heated to boiling. Water was cooled to 71°C, then tea was steeped for 2 minutes.
contained. The Chinese sample contained the most fluoride, while the Japanese sample contained the least. Means and interquartile ranges of fluoride concentration were calculated for each sample: Sri Lanka 3.58 ppm (0.1425), Chinese 6.83 ppm (0.140), South Korean 5.36 ppm (0.0975), Japanese 1.88 ppm (0.1375) and control 0.33 ppm (0.0078).
David L. Frantz, DMD, Private practice, Murfreesboro, Tennessee
This process was repeated 20 times, thus providing 20 samples for each tea type. In addition, 20 control samples of deionized water were brewed to the same specifications. Samples were analyzed using a fluoride probe, and statistical power was calculated.
Results
The tea samples from different countries varied in the amount of fluoride they
The origin of tea and environmental factors, such as pollution, groundwater, air and the soil in which it was grown appear to directly affect the amount of fluoride that accumulates in the plants.
Considering the fluoride content revealed by this study, green tea consumption habits should be taken into account when prescribing adjunct fluoride therapy as part of a preventative program for patient care.
Next to water, tea is the world’s most commonly consumed beverage.1 Among the varieties of tea, green tea is the second most popular choice in the world.1 In Canada, green tea ranks as the third most popular type of tea, after herbal and black tea, according to a study by Ipsos-Reid for the Tea Association of Canada.2

While 56% of Canadians drink tea for pure enjoyment and relaxation, 41% of those polled felt that tea’s purported health benefits were a good reason to drink tea. Green tea is a recognized source of antioxidants, being an excellent source of catechins, especially the polyphenol ephigallocatechin-3-gallate (EGCG).3 Catechins in green tea have been

demonstrated to help lower cholesterol3 as well as to reduce the risks of ischemic related diseases4 and glaucoma.5 In addition, research shows that green tea catechins may be effective in preventing various neoplasms, including gastrointestinal, breast, liver, lung and prostate cancer.6-8
Systematic reviews have shown that consumption of large amounts of green tea (> 4 cups/day) might be protective against early-stage breast cancer7 and liver cancer.8,9 However, green tea consumption was not beneficial in the later stages of breast cancer.7 Meta-analyses have indicated that greater consumption of green tea can reduce the risk of liver cancer.8,9 This association was most significant when participants were drinking 4 cups of green tea a day.9
All teas, regardless of whether they are classified as black, green or white, originate from the same tea plant, Camellia sinensis.1,10 The method of bruising or manipulating the leaves, which leads to varying degrees of oxidation, is the primary determinant of whether teas become black, green or white.10 Black tea is made by allowing the leaves to fully oxidize by drying and, thus, turning black, after which they are roasted.10 In making green tea, the oxidation process is bypassed, allowing the leaves to remain green; the leaves are heat treated rapidly by pan frying, baking or steaming, then dried. Tea that is the least oxidized and the least processed becomes white tea.10
There are two major varietals of Camellia sinensis. Camellia sinensis sinensis is grown mainly to produce white and green teas, while Camellia sinensis assamica is grown to make the stronger black teas. Environmental factors, such as weather, harvest time and the soil that the plants grow in can also affect the flavour of tea.
Green tea is packed with nutrients.1,10 In addition, it contains important antioxidants called catechin polyphenols, which contribute to its many health benefits. There are several derivatives of catechins in green tea: epicatechin, epigallocatechin, epicatechin gallate and EGCG. Of these, EGCG is the most potent and is believed to improve health in multiple ways, including lowering cardiovascular and cancer risks.10 Green tea has a very high EGCG content, as well as vitamins B and C.
Despite the benefits of green tea, there are concerns that it might contain toxic amounts of harmful elements, such as
aluminum, lead and fluoride.11 The presence of such toxins is a result of their potential uptake from contaminated soil and subsequent deposition and concentration in the stems, flowers and leaves of Camellia sinensis. Camellia sinensis is a natural “bio-accumulator” of fluoride, which is released when tea is brewed.
Fluoride is the negatively charged ion of fluorine and, in some contexts, it can be quite reactive.12 In terms of its charge and size, fluoride resembles a hydroxide ion, but is less basic13 and has a distinct reactivity that is solvent dependent.14 The highly electronegative nature of fluoride allows it to integrate into bone and tooth hydroxyapatite crystals, converting them into stronger fluorapatite crystals. Fluorapatite crystals are larger, form quicker than hydroxyapatite and render tooth enamel more resistant to acid dissolution.
Naturally occurring fluoride is found in the earth’s surface, where it exists in soil, water and air in the form of calcium fluoride. In some parts of the world, the level of naturally occurring fluoride is high, while in other areas fluoride is deemed to be deficient.
Where water supplies and diets are fluoride deficient, synthetic fluoride may be added systemically, for example in community water fluoridation. Fluoridation of water is considered by the Centers for Disease Control and Prevention to be “one of the 10 great public health achievements of the 20th century” and has been credited with an overall 18–40% reduction in cariogenesis.15
Ontario, Canada, was among the first jurisdictions in the world to introduce community water fluoridation as a public health initiative to reduce dental caries,16 with the city of Brantford taking the lead in 1945.
We now know that there are multiple unanticipated sources of fluoride intake, including topical dentifrices, oral rinses, gels and varnishes. In addition, almost all foods and beverages contain certain amounts of fluoride. In 2007, a Canadian expert panel recommended that the amount of systemic fluoride added to water should not exceed 0.7 ppm to prevent deleterious effects on the human body.17 For perspective, 1 mg of fluoride in 1 L of water is approximately equivalent to 1 ppm.
In April 2015, the United States Department of Health and Human Services also lowered the recommended water fluoridation level to 0.7 mg of fluoride per litre of water.
Solid solutions for maintaining and promoting healthy bone. Backed by years of documented and proven success, our products have been engineered to meet your specific surgical needs.
Innovative double shell construction.

High elasticity and break resistance thanks to the double shell construction with flexible elastomer core. CA® Pro
constant force level less initial force continuous force transmisson high wearing comfort
A common question is, how much fluoride is too much? Fluoride toxicity is rare. For an acute fluoride overdose to cause death in a 70-kg man, a 1-time ingestion of 5–10 g of sodium fluoride is required.18 Smaller acute exposures can cause mild to serious symptoms, most of which are related to gastrointestinal discomfort. These include vomiting, abdominal pain, diarrhea and nausea.19
Chronic toxicity can also develop after ≥ 10 years of ingesting large amounts of fluoride.18 Skeletal fluorosis, a health condition associated with long-term high fluoride exposure, can lead to brittle and painful bones.18 The severity and extent of development of skeletal fluorosis depend on the amount and duration of fluoride intake. The mild form of skeletal fluorosis is called osteosclerosis. Advanced skeletal fluorosis can be crippling; however, this is considered a rare condition in Canada and the United States.
Dental fluorosis is more common and is caused by ingesting fluoride during enamel formation. Children, ≤ 8 years of age, can develop fluorosis while their permanent teeth are still forming. The mildest form of dental fluorosis can appear as random white flecks or lacy white patterns across the enamel surface. According to the Canada Health Measures Survey, 16% of children may have very mild or mild fluorosis.20 Surveyed cases of severe dental fluorosis were too minimal to report.20
More severe dental fluorosis cases include brownish discolouration and pitting of the enamel. Severity depends on how much, how long and when fluoride was consumed.19 Studies have shown that as the extent of water fluoridation increases, dental caries levels in children decline; but as fluoridation increases, dental fluorosis also rises.21
Previous studies have investigated the amount of fluoride released during the brewing of black tea. In 2013, Chan et al.22 found that just 1 L of economy-range, bagged black tea provided a significantly greater amount of fluoride than the recommended adult intake of 4 mg/day. They also found that the amount of fluoride released by tea varied significantly by type (loose leaf tea vs. economy bagged tea), with bagged tea releasing the most fluoride. Furthermore, different steeping and brewing methods and times will affect the amount of fluoride released.
Green tea is sourced from a number of countries with different environmental standards. Although research









shows the amount of fluoride released from black tea, similar studies have not been conducted for green tea. Because of the popularity of green tea, we sought to quantify fluoride release from whole loose-leaf organic green tea from various parts of Asia, where green tea is mainly produced. We aimed to compare teas from China, Japan, South Korea and Sri Lanka to determine which contained lower fluoride content for safer consumption.
A convenience sample size of 4 types of green tea (Chinese, Japanese, South Korean and Sri Lankan) was chosen and brewed according to the following protocol. Deionized water was used to ensure a purified water source.
For each tea sample, 2.5 g of loose tea was measured into a stainless-steel mesh tea ball. Deionized water was boiled and 80 mL was poured into a fresh disposable paper coffee cup, as Asian green tea is traditionally served in small portions. Water temperature was monitored with a digital thermometer and when it reached 71°C, the tea ball was placed in the cup and steeping was allowed to begin. Steeping time was measured using a chronograph with a digital readout. Each sample was steeped for 2 minutes. Harney and Sons Master Tea Growers (harney. com/pages/green-teas), an award-winning company internationally known for quality teas and education of
how to handle tea, recommends a brewing time of 1–3 minutes for green tea; thus, a standard of 2 minutes was chosen for all the teas. After 2 minutes, the tea ball was removed from the cup, and the brewed tea was analyzed using a fluoride probe (Thermo Scientific Orion DualStar, Thermo Fisher Scientific, Waltham, Mass., USA). Each tea type was brewed 20 times, resulting in a total of 80 samples. As a control, the same process was carried out using a clean, empty tea ball of the same type as the experimental tea ball. All reusable articles (thermometer, tea ball) were cleaned with deionized water between experimental runs.
Statistical power was calculated using nQuery Advisor (v. 7.0, GraphPad Software, San Diego, Calif., USA).
The Kolmogorov-Smirnov test was used to assess the statistical assumption of normality.
Because of the presence of non-normally distributed data, the Kruskal-Wallis test was used to compare the groups in terms of their fluoride concentrations. Medians and interquartile ranges (IQRs) were reported as descriptive statistics. IQR is the difference between the 75th percentile and the 25th percentile, with a higher IQR indicating greater variability.
Following a significant Kruskal-Wallis test, Mann-Whitney U tests with the Bonferroni correction were employed as pairwise comparisons to determine which sample pairs exhibited statistically significant differences. SPSS v. 22 was used in the analysis.
Table 1: Differences in median fluoride concentration and interquartile range among 4 types of green tea, measured in 20 samples of each.
The following tea types were significantly different at the p < 0.001 level: control versus Sri Lanka, control versus China, control versus South Korea, Sri Lanka versus China, China versus Japan, and South Korea versus Japan.The following types were significantly different at the p = 0.029 level: control versus Japan, Sri Lanka versus South Korea, Sri Lanka versus Japan and China versus South Korea.






Top pressure moulding performance for unlimited applications in practice and laboratory.
leading technology for more than 50 years heater reaches working temperature in 1 second scan function for immediate programming great variety of pressure moulding material for any kind of application 3 years warranty, 10 years on availability of spare parts
SCHEU-DENTAL GmbH
Dubai Office www.scheu-dental.com phone +971 50 6255046 a.hbous@scheu-dental.com
We calculated median fluoride concentration and IQR for each tea type (Table 1): Sri Lanka 3.58 ppm (0.1425), Chinese 6.83 ppm (0.140), South Korean 5.36 ppm (0.0975), Japanese 1.88 ppm (0.1375) and Control 0.33 ppm (0.0078).
Based on a Kruskal-Wallis test, we found a significant difference in fluoride concentration between tea types (H = 95.06, df = 4, p < 0.001). The Chinese samples contained the highest concentration, while the Japanese samples had the lowest. A Mann-Whitney U test with the Bonferroni correction revealed significant differences between the Chinese samples and both the Sri Lankan and Japanese samples, and a significant difference between the South Korean and Japanese samples. All tea types differed significantly from the control (Table 1).

The amount of time taken to brew green tea affects the amount of fluoride released, but different types of green tea require slightly different brewing times to fully release their flavours. We consulted the recommendations of Harney and Sons Master Tea Growers (harney.com/ pages/green-teas) for brewing and steeping directions. They recommend that to fully experience the complex sweet, fragrance and flavour of green tea, the water boiling point should be ~160 °F, which equates to the ~ 71 °C used in this study. According to Harney and Sons, different green teas have varying steeping times, but the average steeping time is two (2) minutes. If brewing temperature is above 71°C and tea is steeped longer than the recommended time, the tea may taste bitter. Increased steeping time will also result in a tea infusion that has increased fluoride content.22




The VistaPano S Ceph is the efficient X-ray solution for jaw orthopaedics and more. It supplies fast Ceph shots (4.1 seconds) with outstanding image quality and low exposure to radiation. At the same time, thanks to S-Pan technology, its 2-D panorama shots provide excellent definition. More at www.duerrdental.com



Tea quality will also influence fluoride content. The highest grades of tea consist of the bud and the youngest leaves of the tea plant, usually those closest to the bud.23 Thus, loose leaf and younger leaf teas are higher in quality and more expensive. Less expensive teas include older leaves, woody stems and branches. The least expensive teas are often made up of leftover bits of tea leaves and stems, called “tea dust,” packaged in teabags. Studies have demonstrated that inexpensive, lower quality teas contain much more fluoride than higher quality looseleaf teas.22
Bagged teas were not considered in this research, on the understanding that these could contain lower quality tea parts, which might affect fluoride levels. Instead, we sought pure (non-blended) loose-leaf organic tea samples. Organic cultivation methods do not use synthetic pesticides, some of which contain fluoride and would affect the collection results.
Nevertheless, the organic Chinese tea samples revealed high levels of fluoride. Organic South Korean tea samples contained the second highest level of fluoride, followed by Sri Lankan tea samples. The Japanese organic tea samples contained the least amount of fluoride.
Geographic and environmental factors may account for the results in this study. As mentioned in the introduction, natural fluoride exists at various concentrations in different parts of the world. Fluoride is found in soil and in fresh, salt and rainwater. The concentration of fluoride in rainwater is influenced by fluoride-containing particulates that may be released into the atmosphere from various pollutant sources.24
As a natural bio-accumulator, tea plants take up fluoride from the soil, water and air. Plants transport fluoride via the xylematic system resulting in much of the fluoride ending up in the tea leaves.25
In China, the concentration of fluoride in groundwater is naturally high, with levels up to 8 mg/L in some parts of the country.26 In South Korea, 1 study demonstrated fluoride concentrations of 4.4mg/L in bedrock groundwater.27 In Sri Lanka, there is a significant difference in fluoride levels between wet and dry areas28: fluoride concentrations of > 8.0 mg/L were found in dry zones, while wet zones were found to contain < 0.8mg/L of fluoride. Sri Lankan tea is produced in many parts of the wet zone.29 According to the World Health Organization, the fluoride content of
groundwater in Japan varies from 0.01 mg/L to 7.8 mg/L, but fluoride was not found in a quantifiable amount in soil.26 Fluoride levels in Canada’s natural groundwater are low compared to those of China, South Korea, Sri Lanka and Japan; most are < 0.05 mg/L.26
Environmental factors may also affect fluoride concentrations. China is the world’s largest producer and consumer of coal, which is used to drive electrical power plants. Coal has a high fluoride content; when burned, it releases high fluoride-containing particulates into the air.30 These pollutants float in the atmosphere and eventually leach into the soil or fall into bodies of water.30 This leaching can impact farming environments, even the 28% of China’s cultivatable land that is “certified organic.”31 In China, coal is also used in household heating, cooking and food drying. Indoor airborne fluoride emissions are inhaled; or are ingested once the fluoride particulates land on food and beverages, accounting for unanticipated and potentially harmful ambient sources of fluoride.30
South Korea is also largely dependent on fossil fuels for energy; coal accounts for 40% of electricity generation and is also a main pollutant.32 Meanwhile, Japan relies on coal for a fourth of its electricity and is particularly dependent on fossil fuels after the Fukushima nuclear disaster of 2011.33
Cai et al.34 demonstrated that the harvesting season affects fluoride content in a variety of teas made from the Camellia sinesis plant. There are typically 3 harvesting seasons for tea: spring, summer and late summer/fall. Leaves picked in early spring contained the least amount of fluoride, whereas those harvested in the last summer season contained the most.34
Finally, just as the cuisines of China and Japan differ, so too do the methods used to cultivate, harvest, oxidize and process green tea. This might also account for differences in fluoride content. Chinese teas are grown on more spreading bushes and the tea leaves are picked by hand, then quickly pan fried or lightly roasted. In contrast, because Japan’s arable land is minuscule compared with China’s, Japanese tea bushes are cultivated in compact rows and leaves are harvested by machine. Leaves are then quickly steam processed, allowing Japanese green tea to retain its vibrant green colour.
We used deionized water in this study. Most people









brew tea with tap water, which may already be fluoridated. In addition, some people may live in areas containing much higher natural fluoride in the groundwater than in other areas of the country. Therefore, it is important to note that people may be ingesting much more fluoride while drinking tea than reported in this project.
The origin of tea plants and the environment in which they grow appear to affect the amount of fluoride that accumulates in them. As future research, it would be prudent to study environmental factors in different parts of the arable land in the 4 Asian countries chosen as tea sources in this research, including the soil in which the tea plants are grown, the water used to irrigate them and the surrounding air.
Consideration might also be given to studying how fermentation and processing methods (pan frying vs. steaming) affect the fluoride content of green tea. Although we chose green teas that were labeled “organic,” fluoride was found in the samples. This is quite possibly because the tea plants were irrigated with fluoridated water or the plants were subjected to atmospheric pollutants that contain fluoride.30
When deciding on adjunct fluoride therapy as part of a preventative program for patient care, the dental professional must consider the fluoride concentrations in fluoridecontaining toothpastes, oral rinses, gels, varnishes and fluoride-releasing restorative

Dentists must also think about their patients’ habits in terms of drinking fluoridated water as well as the fluoride content of foods and beverages. Although virtually all foods crustaceans, fish, grapes and tea contain the highest levels.35,36
In addition, conventionally grown fruits and vegetables will possibly contain more fluoride than organically sourced produce, and conventionally grown tea plants will possibly contain more fluoride than organically sourced ones. Fruit and vegetables grown in chemically laden soil can also be irrigated as well as sprayed with fluoride-containing pesticides and Different crops tend to absorb fluoride through their root system at various
Light-curing Glass Ionomer Filling Material
• Excellent working time and the setting time is individually adjustable by light-curing
• Immediately packable after placement in the cavity
• No varnish required- fill, polymerise and finish
• No need to condition the dental hard tissue
• Does not stick to the instrument and is easy to model
• Suitable for large cavities
Are you interested in our entire product range and detailed product information? Visit our website or contact us directly!

When a dental professional considers a person’s daily fluoride intake, green tea consumption should be taken into account. This is especially prudent for habitual tea drinkers who drink multiple cups a day on
1. Gold C, Stern L. Culinary tea. Philadelphia: Running Press; 2010. 2. Canadians and tea. Toronto: Ipsos-Reid; 2004. Available from: https:// www.ipsos.com/en-ca/canadians-and-tea
3. Ahmad RS, Butt MS, Sultan MT, Mushtaq Z, Ahmad S, Dewanjee S, et al. Preventive role of green tea catechins from obesity and related disorders especially hypercholesterolemia and hyperglycemia. J Transl Med. 2015;13:79.
4. Pang J, Zhang Z, Zheng TZ, Bassig BA, Mao C, Liu X, Zhu Y, et al. Green tea consumption and risk of cardiovascular and ischemic related diseases: a meta-analysis. Int J Cardiol. 2016;202:967-74.
5. Patel S, Mathan JJ, Vaghefi E, Braakhuis AJ. The effect of flavonoids on visual function in patients with glaucoma or ocular hypertension: a systematic review and meta-analysis. Graefes Arch Clin Exp Opthalmol. 2015;253(11):1841-50
6. Liu J, Xing J, Fei Y. Green tea (Camellia sinensis) and cancer prevention: a systematic review of randomized trials and epidemiological studies. Chin Med. 2008;3:12.
7. Seely D, Mills EJ, Wu P, Verma S, Guyatt GH. The effects of green tea consumption on incidence of breast cancer and recurrence of breast cancer: a systematic review and meta-analysis. Integr Cancer Ther. 2005;4(2):144-55.
8. Huang YQ, Lu X, Min H, Wu QQ, Shi XT, Bian KQ, et al. Green tea and liver cancer risk: a meta-analysis of prospective cohort studies in Asian populations. Nutrition. 2016; 32(1):3-8.
9. Ni CX, Gong H, Liu Y, Qi Y, Jiang CL, Zhang JP. Green tea consumption and the risk of liver cancer: a meta-analysis. Nutr Cancer. 2017;69(2):211-20.
10. Carloni P, Tiano L, Padella L, Bacchetti T, Customu C, Kay A, et al. Antioxidant activity of white, green and black tea obtained from the same tea cultivar. Food Res Int. 2013;53(2):900-8.
11. Li L, Fu QL, Achal V, Liu Y. A comparison of the potential health risk of aluminum and heavy metals in tea leaves and tea infusion of commercially available green tea in Jiangxi, China. Environ Monit Assess. 2015;187(5):228.
12. Wiberg N, Holleman AF (editors). Inorganic chemistry. San Diego, Calif.: Academic Press; 2001.
13. Fluoride ion. Canada: DrugBank Online. [updated 2020 June 12; cited 2020 Sept. 9]. Available from https://www.drugbank.ca/drugs/DB11257
14. Sun H, DiMagno SG. Anhydrous tetrabutylammonium fluoride. J Am Chem Soc. 2005;127(7):2050-1.
15. Centers for Disease Control and Prevention. Ten great public health achievements — United States, 1900–1999. MMWR Morb Mortal Wkly Rep. 1999;48(12):241-3.
16. Mullen J. History of water fluoridation. Br Dent J. 2005;199(7 Suppl 1):1-4.
17. Findings and recommendations of the Fluoride Expert Panel (January 2007). Ottawa: Government of Canada; 2008. Available from: https://www. canada.ca/en/health-canada/services/environmental-workplace-health/ reports-publications/water-quality/findings-recommendations-fluorideexpert-panel-january-2007.html
18. LuiG, Ye QF, Chen W, Zhao ZJ, Li L, Lin P. Study of the relationship between the lifestyle of residents residing in fluorosis endemic areas and adult skeletal fluorosis. Environ Toxicol Pharmacol. 2015;40(1):326-32.
19. Committee on Fluoride in Drinking Water. Effects on the gastrointestinal, renal, hepatic, and immune systems. In: Fluoride in drinking water: a scientific review of EPA’s standards. Washington, DC: National Academies Press;
2006:268-303. Available from: https://www.nap.edu/read/11571/chapter/11
20. Fluoride and oral health. Ottawa: Government of Canada; 2017. Available from: https://www.canada.ca/en/health-canada/services/healthy-living/ your-health/environment/fluorides-human-health.html
21. Heller KE, Eklund SA, Burt BA. Dental caries and dental fluorosis at varying water fluoride concentrations. J Public Health Dent. 1997;57(3):136-43.
22. Chan L, Mehra A, Saikat S, Lynch PT. Human exposure assessment of fluoride from tea (Camellia sinensis L.): a UK based issue? Food Res Int. 2013;51(2):564-70.
23. Fluoride. Corvallis, Ore.: Linus Pauling Institute; 2015. Available from: https://lpi.oregonstate.edu/mic/minerals/fluoride
24. Agency for Toxic Substances and Disease Registry. Public health statement for fluorides, hydrogen fluoride, and fluorine. Atlanta, Ga.: Department of Health and Human Services, Public Health Service; 2003. Available: https:// www.atsdr.cdc.gov/phs/phs.asp?id=210&tid=38
25. Bhattacharya P, Samal AC. Fluoride contamination in groundwater, soil and cultivated foodstuffs of India and its associated health risks: a review. Res J Recent Sci. 2018;7(4):36-47.
26. Fawell J, Bailey K, Chilton J, Dahi E, Fewtrell L, Magara Y. Fluoride in drinking-water. Geneva: World Health Organization; 2006.
27. Chae GT, Yun ST, Mayer B, Kim KH, Kim SY, Kwon JS, et al. Fluorine geochemistry in bedrock groundwater of South Korea. Sci Total Environ. 2007;385(1-3):272-83.
28. Jayawardana D, Pitawala HMTG, Ishiga H. Groundwater quality in different climatic zones of Sri Lanka: focus on the occurrence of fluoride. Int J Environment Sci Dev. 2010;1(3):244-50.
29. Peiris GH, Arasaratnam S. Sri Lanka. In: Encyclopeadia Britannica. Chicago: Britannica Group; 2020. Available from: https://www.britannica.com/place/ Sri-Lanka
30. Ando M, Tadano M, Asanuma S, Tamura K, Matsushima S, Watanabe T, et al. Health effects of indoor fluoride pollution from coal burning in China. Environ Health Perspect. 1998;106(5):239-44.
31. Taylor DA. Recovering the good earth: China’s growing organic market. Environ Health Perspect. 2008;116(8):A346-9.
32. Overview. In: South Korea: analysis. Washington, DC: Independent Statistics & Analysis, U.S. Energy Information Administration; updated 6 Nov. 2020. [cited 2020 Sep 09]. Available from: https://www.eia.gov/international/ analysis/country/KOR
33. Japan’s electricity prices rising or stable despite recent fuel cost changes. Washington, DC: Independent Statistics & Analysis, U.S. Energy Information Administration; 2016 Sept. 9 [cited 2020 Sept. 9]. Available from: https:// www.eia.gov/todayinenergy/detail.php?id=27872
34. Cai H, Zhu X, Peng C, Xu W, Li D, Wang Y, et al. Critical factors determining fluoride concentration in tea leaves produced from Anhui province, China. Ecotoxicol Environ Saf. 2016;131:14-21.
35. Whitebread D. Top 10 foods and drinks highest in fluoride. My Food Data; updated 2021. [cited 2020 Sept. 9]. Available from: https://www.myfooddata. com/articles/high-fluoride-foods-and-drinks.php
36. Kanduti D, Sterbenk P, Artnik B. Fluoride: a review of use and effects on health. Mater Sociomed. 2016;28(2):133-7.



Oral pathology

Parvaneh Badri, DDS, MSc, PhD candidate
Seema Ganatra, DDS, MSD, FRCD(C), Clinical professor division of oral medicine, pathology & radiology
Vickie Baracos, PhD, Professor, department of oncology, Cross Cancer Institute
Hollis Lai, PhD, Associate professor, assistant dean of education quality and accreditation
Maryam Amin, DMD, MSc, PhD, Professor, associate chair of research, dentistry graduate program director
Faculty of medicine and dentistry, University of Alberta, Edmonton, Alberta maryam.amin@ualberta.ca
Republished from the Journal of

Abstract
Objectives
This scoping review provides a comprehensive overview of oral cavity cancer (OCC) and oropharyngeal cancer (OPC) in Alberta.
Methods
A database search was conducted up to 2018 using Web of Science, Scopus, Medline, PubMed and Embase, along with a manual search of gray literature. Data from the Alberta Cancer Foundation’s dedicated fund for research, Cancer Surveillance and Reporting and Alberta Cancer Registry were also collected.
Results
Our review included 8 published papers and 14 other sources, including data on 3448 OCC and OPC patients from Surveillance and Reporting and Alberta Cancer
Registry. Cancer registry data (2005–2017) showed that most OCC and OPC lesions were diagnosed at an advanced clinical stage, with a significantly large number of advanced OPC lesions in stage IV (OCC 45.2%, OPC 82.4%); 47.9% of these patients died. Survival rates were lowest in rural and First Nations areas. In Alberta, 35% of HPV-associated cancers were linked to OPCs, which were more prevalent in men and younger age groups. No routine public oral cancer screening program currently exists in Alberta. General practitioners and dentists refer patients to specialists, often with long waiting times.
OCC and OPC patients in Alberta continue to be diagnosed in stage IV and experience high mortality rates.
Oral and pharyngeal cancer remains a significant global public health issue, with about 657 000 new cases reported each year and more than 330 000 deaths.1 In 2019, 53 000 North Americans were diagnosed with oral and oropharyngeal cancer (OPC), resulting in over 9750 deaths. 2 The 2019 Canadian Cancer Statistics report estimated that 5300 Canadians will be diagnosed with oral cancer (3700 men and 1600 women), of which 1480 died (1050 men and 430 women).3
Oral cancer is 3 times more common than cervical cancer and almost twice as common as liver cancer.4 Despite existing evidence indicating that early detection of precancerous and early-stage lesions can significantly improve the survival rate and quality of life of oral cancer patients,5 3 people die from oral cancer every day in Canada.
Excellent material properties and terrific handling characteristics!
• High filler degree (> 83 % w/w), minimal shrinkage (< 1,8 %)
• Outstanding abrasion resistance
Developed to make the day-to-day running easier
• Universal application
• Easy handling, won’t stick to instrument

Alberta is 4th, after Ontario, Quebec and British Columbia, in terms of oral cancer incidence and related death prevalence among Canada’s provinces and territories.3 This ranking is expected to rise, given the fast growth of the South Asian community in Alberta as the province’s second largest immigrant group. The literature has shown a high prevalence of oral cancer in this population.5,6
Oral cancer represents almost 30% of malignancies of the head and neck (H&N). The development of cancer in the oral mucosa is classified by the World Health Organization7 as a 2-step process. Oral cancer is thought to arise in premalignant lesions that undergo malignant transformation. Precancerous lesions of the mouth include leukoplakia (white patch) and erythroplakia (red patch), which are considered clinical terms. Oral cancer is more likely to occur in people with precancerous lesions than in their apparently normal counterparts.8
Unfortunately, oral cancer continues to be diagnosed mainly in advanced stages, giving patients less chance of survival.9 For decades, the survival rate for oral cancer has remained steady at 50–60%, despite several advances in cancer management.10 In India, which is wellknown for its high rate of oral cancer, a study showed that prevention and early detection through visual screening of precancerous lesions dramatically decreased oral cancer mortality rates and improved quality of life in high-risk populations.5
Late detection of oral cancer can result in poor quality of life, profound psychosocial consequences and complications in the H&N area after conventional treatments, such as radical surgery, radiation therapy and chemotherapy.10 The poor prognosis is because many vital functions, including speaking, smelling, swallowing, hearing and mastication, can be seriously affected.10
Evidence has shown a strong correlation between late detection of oral cancer and poor quality of life compared with patients diagnosed in early stages.10 Moreover, early detection of oral cancer leads to treatment that is less costly for families and the health care system compared with cases diagnosed in advanced stages.11
Recent evidence has shown significant shifts in etiological factors and age groups at risk for oral cancer.12 Oral cancers have been primarily associated with tobacco and alcohol use and have been more prevalent in older age groups.13 However, increasing numbers of cases
associated with human papillomavirus (HPV) occur in younger individuals.9 Analysis of social, clinical and demographic characteristics and p16 protein status of patients diagnosed with OPC at 5 Canadian cancer centres, including 2 in Alberta, showed a steady increase in HPV-associated OPCs, rising from 47.3% in 2000 to 73.7% in 2012. 14 In Alberta between 1975 and 2009, the age-standardized incidence of OPCs increased for each 5-year period by 3.4% annually among men (p < 0.001) and 1.5% among women (p = 0.009). 15
A meta-analysis of 17 studies16 showed the strongest association between HPV and tonsillar cancer, an intermediate association with OPC and the weakest link with oral cancer. Oropharyngeal cancer as an additional entity, can be screened by dentists/dental hygienists where possible, through a careful examination of the soft palate, tonsils and neck.
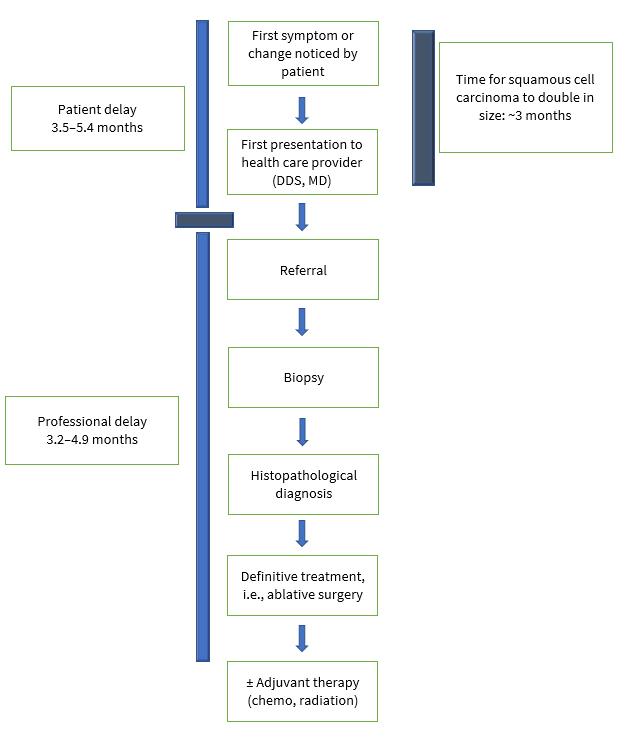
Figure 1: Two categories of delay in diagnosis of oral cancers: patient and professional.18
Oral cavity cancer (OCC) and OPC are deadly diseases, particularly in stages III and IV. However, the survival rate is more than 80% for patients diagnosed in stages I or II.17 Both diseases continue to be diagnosed at advanced stages even though, in most cases, they could easily be detected visually by health professionals, especially dentists and family physicians.
The literature describes 2 distinct categories of delays: “patient delay” or time from the patient’s awareness of changes to her/his presentation to health professionals and “professional delay” or time from patient’s presentation to a heath care provider to definitive diagnosis and treatment (Fig. 1). 18
If left untreated, 5% of leukoplakia and 50% of erythroplakia can develop into oral cancer.19 Early clinical detection of oral lesions and confirmation of premalignant status (thus facilitating timely treatment) could prevent the development of aggressive malignancies. A comprehensive investigation is required to unfold how and where suspicious lesions are ignored. The sooner a patient with oral cancer is identified, diagnosed and given initial treatment, the better their chance of survival.
The statistical evidence regarding OCC and OPC incidence and related projected death rates in Alberta is alarming: an increase of 76.1% in new cases of OCC and OPC is expected between 2003–07 and 2028–32.20
Few peer-reviewed studies show the status of OCC and OPC in the province, and the most important related data are scattered across a number of governmental and nongovernmental institutions and organizations. Therefore, the objectives of this scoping review were to investigate:
• The prevalence of OCC and OPC in Alberta according to patients’ demographics and tumour characteristics
• The usual route from detection of OCC and OPC to treatment
• Existing OCC and OPC prevention initiatives
• Funding of OCC and OPC prevention
• Where and by whom patients with OCC and OPC are initially diagnosed
A preliminary search for scoping reviews on this topic was conducted at Web of Science, Scopus, Medline, PubMed, Embase, the Joanna Briggs Institute Database of Systematic and Implementation Reports and the Cochrane Database of Systematic Reviews, but no related review was found.
Our protocol was developed based on the methodological framework for scoping studies proposed by Arksey and O’Malley.21 It consists of 5 stages: identifying research questions and objectives; identifying relevant studies based on inclusion criteria; selecting studies; charting the data; and collating, summarizing and reporting the results. Ethics approval for data extraction from the Alberta Cancer Registry was obtained from the Health Research Ethics Board of Alberta’s Cancer Committee.
Research question: What is the prevalence, demographics, initial diagnosis, prevention, management and research funding allocated for early detection of OCC and OPC in Alberta?
This scoping review included adults aged 18 years and older living in Alberta.
Provincial OCC and OPC data are reported in diverse media, and our search strategy aimed to gather data from as many resources as possible. These included peerreviewed, published, unpublished and hand-searched gray literature (e.g., primary research studies, systematic reviews, letters, guidelines, Google and Google Scholar). In addition, the search included governmental and nongovernmental institutions and organizations.
A 3-step search strategy22 was performed for the timeframe 1990–2018. We used all key terms to crosssearch all databases, including Web of Science, Scopus, Medline, PubMed and Embase.
We also conducted a search of the Joanna Briggs Institute Database of Systematic Reviews and Implementation Reports and the Cochrane Database of Systematic Reviews to retrieve potential similar published reviews.
Keywords were ((mouth or oral or gingiv* or lip or lips or palat* or tonsil or parotid or sublingual or lingual or tongue or cheek*) and (cancer or neoplasm* or tumor* or tumour* or malignan* or carcinoma*)) AND TOPIC: (alberta or calgary or edmonton). We also conducted a hand-search of gray literature and used Google and Google Scholar search engines to find relevant articles. Finally, we emailed and telephoned Alberta Cancer Foundation Surveillance and Reporting, Alberta Prevents Cancer, Alberta Health Services and Alberta Cancer Registry to gather relevant information uncovered by the search engines.
Published literature
The search strategy resulted in identification of studies from Medline (n = 48), Embase (n = 74), Pubmed (n = 33), Scopus (n = 74) and Web of Science (n = 55) for a total of 284. Of these, 153 were eliminated because of duplication. Two reviewers excluded 96 irrelevant studies based on title and abstract. After reviewing the full text, 25 more studies were screened and excluded as they did not meet the inclusion criteria of the study. A final set of 8 studies23-30 were included in this review (Fig. 2).31

Relevant thesis monographs (n = 2)32,33 and clinical guidelines for H&N cancer delivery and management in Alberta (n = 2)34,35 were identified and included in the study. Other sources were Canadian Cancer Statistics for 2015–2017,20,36,37 the Alberta Cancer Foundation,38 data on 3448 patients from the Surveillance and Reporting–Alberta Cancer Registry, Alberta Health Services,39-41
Alberta Innovates,42 Canadian Cancer Society and Alberta Cancer Prevention Legacy Fund (ACPLF)43 and Canadian Institutes of Health Research.44
The information that was relevant to our study objectives, including descriptive and numeric data, reports and chart information on patients, was extracted and charted according to Joanna Briggs Institute guidelines.22 For the published studies, extracted data included: author(s)/ year/country of origin; aims; population/characteristics/ size; study design; concepts relevant to our study objectives; context relevant to our study objectives; and outcome relevant to our study objectives.
Of the 8 published studies, 7 were quantitative,23-29 and 1 was qualitative.30 All were conducted in Alberta and published between 2004 and 2016. They focused on care plans and quality management of OCC and OPC,30 factors influencing survival,23-25 comorbidity and risk management26,27 and the epidemiological evolution of HPV associated with OCC and OPC.28,29 Detailed characteristics of these studies are presented in Table 1.
The 2 master’s theses reported on quality of life, especially for young patients diagnosed with OCC and OPC in Alberta,32 and referral patterns of patients to the University of Alberta oral medicine clinic, a specialty clinic where dentists refer patients with suspicious oral lesions to be evaluated by certified specialists in oral medicine and pathology in Edmonton.33 Detailed data from gray resources are presented in Tables 2–6 and Figure 3.

Figure 3: Trends in the incidence of oral cavity cancer (OCC) and oropharyngeal cancer (OPC), based on data from the Alberta Cancer Registry, 2005–2017.

´ Safer use
´ Preparation following the anatomy
´ Regeneration for reuse
1: Summary of data extracted from 8 published papers.
Note: H&N = head and neck, HPV = human papillomavirus, NA = not applicable, OCSCC = oral cavity squamous cell carcinoma, OPC = oropharyngeal cancer, OPSCC = oropharyngeal squamous cell carcinoma.
Table 2: Summary of data extracted from 8 published papers.
Note: H&N = head and neck, HPV = human papillomavirus, NA = not applicable, OCSCC = oral cavity squamous cell carcinoma, OPC = oropharyngeal cancer, OPSCC = oropharyngeal squamous cell carcinoma.
Collating, Summarizing and Reporting the Results
In Tables 1–6, information is classified according to the objectives of the study and it provides an overview of factors associated with OCC and OPC in Alberta.
Tumour location/site was categorized according to the topographical codes in the International Classification of Diseases for Oncology, 3rd edition, ICD-0 3. OCC sites included lip (C00.3-C00.9), oral tongue (C2.0-C2.3, C2.8 and C2.9), gum (C3.0-C3.0), floor of mouth (C4.0-C4.9), palate (C5.0-C5.9) and other and unspecified parts of the mouth (C6.0-C6.9). OPC sites included base of tongue (C01), lingual tonsil (C2.4), tonsil (C9.0-C9.9), oropharynx (C10.0-C10.9), pharynx not otherwise specified (C14.0) and Waldeyer ring (C14.2). External upper and lower lip (C00.0-C00.1), parotid gland (C07.9) and other and unspecified major salivary gland tumours (C08.0-C08.9) were excluded.
According to 2005–2017 Alberta Cancer Registry data, 45.2% of OCC patients and 82.4% of OPC patients were diagnosed at stage IV, of which 47.9% died (OCC 27.41%, OPC 20.05%). The tonsils, tongue and base of tongue were the main locations of these cancers. The increased incidence of HPV-associated OPC is most striking in males < 45 years of age.36 Although most mouth and throat cancers were primarily associated with tobacco and alcohol use, about 25–35% of OCCs and OPCs were attributed to high-risk HPV types.37
Referrals and access to clinical specialists for patients with suspicious oral lesions were evaluated and reported.33 The waiting time between receiving a referral and seeing a specialist was 105.5 days on average, with a maximum of 905 days. The reported travel distance was 55.44 km on average, with a maximum of 2028 km. In this study,33 general dentists (74.5%) were found to be the main source of referrals to oral pathologists, oral surgeons and
Table 3: Characteristics of patients diagnosed with oral cavity cancer (OCC) and oropharyngeal cancer (OPC), based on data from the Alberta Cancer Registry, 2005–2017.
* Based on household income of patients at diagnosis.



Table 4: Sites of oral cavity cancer and oropharyngeal cancer, based on data from the Alberta Cancer Registry, 2005–2017.
Table 5: Stage of oral cavity cancer (OCC) and oropharyngeal cancer (OPC) at diagnosis, based on data from the Alberta Cancer Registry, 2005–2017.*
*Total Missing Data: 20
Table 6: Summary of data extracted from gray literature.
Note: HPV = human papillomavirus, OCC = oral cavity cancer, OPC = oropharyngeal cancer.
*based on data from the Alberta Cancer Registry, 2005–2017.
otolaryngologists, followed by family physicians (15.8%).
Of all referrals, 38% were diagnosed with malignant and premalignant lesions, which represents the highest
percentage among all conditions requiring the care of a specialist.33 However, according to Alberta Cancer Registry data, otolaryngologists were the most common
clinicians referring OCC and OPC patients to oncologists (cancer care) followed by surgeons (general, oral, and thoracic) and general practitioners with dentists being in 8th place.
In general, management was guided by 2 sources.34,35 The recommended guidelines for H&N cancer in Alberta were adapted by the executive of the Alberta Provincial Head and Neck Tumour Team using “The Management of Head and Neck Cancer in Ontario: Section 1, Organizational and Clinical Practice Guideline Recommendations.”45
The guideline considers H&N cancer a complex chronic disease that should be managed by a qualified team with particular recommendations for: health care team components; minimum cancer centre and team member volumes; infrastructure; and waiting time. The practice guideline will be updated at least annually with any new evidence or contextual information. The latest guidelines for OCC (2014) and OPC (2019) are presented in Table 6.
Oral cancer survival was explored in 4 recent studies.23-25,30 They found that geographic location,24 ethnicity,25 quality of management30 and disparities in clinical versus pathological staging diagnosis23 could affect survival outcomes.
Pre- and post-operative risk assessments and quality of life were investigated in 3 studies.26-28 Although the findings of 1 study26 indicated that the risk of stroke in patients undergoing neck dissection surgery is low and there is no need for pre-operative screening, another study28 showed that there was a higher risk for hypothyroidism after radiation therapy in OCC and OPC patients. Thus, patient screening was recommended to achieve a higher quality of care. In addition, severity of depression was identified as a predictor of post-operative functional performance, quality of life and adherence to treatment.28
We did not identify any H&N cancer screening programs in Alberta. However, preventive HPV vaccination was approved for females aged 9–26 in 2006 and males aged 9–26 in 2012 to prevent 95% of cervical cancers and 25% of OPC.36 Furthermore, multiple websites offer intraoral cancer information and list risk factors for developing oral cancer and preventive recommendations for the public.38-41 The resources of multiple health funding agencies37,41-43 are dedicated mostly to OCC and OPC treatment studies and research investigations that target
better post-treatment quality of life for OCC and OPC cancer patients rather than studies aimed at identifying effective preventive strategies for those cancers in Alberta.
According to the Alberta Cancer Registry data from 2005 to 2017, although the incidence of OCC increased somewhat, the number of OPC cases increased significantly. In our study, the numbers of OCC and OPC cases included were almost equal (51% and 49%, respectively). Although male predominance was found for both OCC and OPC, the gender difference was larger for OPC (82.7% males among OPC cases vs. 58.2% for OCC).
This scoping review provides an overview of OCC and OPC in Alberta based on various data sources distributed across multiple bodies. Our finding is in agreement with the recent literature that HPV- associated OPCs occur in younger people compared to those diagnosed with oral cancers associated with smoking and alcohol consumption.
Although we found no published studies on strategies for preventing OCC, we did note that the upward trend in HPV-associated OPC has received significant attention. Canadian Cancer Statistics 2016, which was dedicated to HPV-associated cancers, stated that the annual number of OPC cases (for both sexes combined) is already rivaling cervical cancer in Canada.36
That report predicted that the age-standardized incidence of OPC in males may surpass that of cervical cancer in females in the near future, which is alarming. A study conducted by Shack and colleagues28 confirmed this trend in Alberta.
Following the lead of Prince Edward Island, Alberta has introduced a public health policy46 to vaccinate young people of both sexes, 9 -26 years old, to prevent HPVassociated cervical cancer. However, effective preventive strategies for non-HPV-associated OCC and OPC — e.g., regular oral/H&N cancer screening — are still lacking in Alberta, even for populations with higher vulnerability, such as those who are socioeconomically disadvantaged and/or exposed to tobacco, alcohol and recreational drugs.
The findings of this study indicate that, as in Ontario (2003–2013),47 men in Alberta are at higher risk for OCC and OPC. However, a retrospective study conducted in British Columbia analyzing OCC and OPC in 1981–2020 shows that OCC incidence is decreasing in men and increasing in women, while rates for OPC are increasing in both men and women.48
In contrast, new evidence points to an increasing incidence of OCC among Caucasian women in the United States (1973–2012), rising to the same level as men.49 This might be explained by recent changes in lifestyle. The trend also accords with the findings of a study that investigated recent OCC and OPC data globally.50
Our study shows that, as of 2017, Alberta is 4th in terms of new cases of OCC and OPC (430) behind Ontario (1950), Quebec (1070) and British Columbia (600).37 Compared with earlier data, these numbers are rising, except for a slight decrease in British Columbia.48 The large number of South Asian and Chinese ethnic minorities, known for their high incidence of OCC (South Asians)6 and OPC (Chinese),48 could explain the high rates and increases in the disease in Ontario, British Columbia and Alberta. This shows that ethnic-associated practices, such as particular smoking habits, are risk factors for OCC and OPC, despite current geographic location.48,51 Further investigation is needed to identify potential risk factors in Quebec.
Our findings for Alberta are in accord with worldwide reports and confirm the lack of improvement in terms of delays in diagnosis and survival of OCC and OPC patients, as found in the literature. This continues to be a tremendous concern for health care providers and health authorities. From 2005 to 2017, more than half the accumulated cases of OCC and OPC were diagnosed in stage IV, and 47.9% of all patients died.
This finding is striking and deserves attention. There is a lack of data on prevalence of stage IV OCC and OPC cancers in the general population in Canada. Analysis of various datasets suggests that the assessment section of Alberta’s guidelines needs further investigation of the gaps identified in this scoping review regarding late access to initial clinical assessment32 and late diagnosis of OCC34 and OPC.35
This study found that the treatment and management of OCC (2014)34 and OPC (2019)35 in Alberta is guided
by the Alberta Health Services H&N cancer guidelines. However, there is a lack of emphasis on the efficacy of the practice algorithm for patients, including the required waiting time for each step.
Suspected premalignant white and red oral lesions are the most common reason for referral of patient to specialists, and our findings highlight a long wait time for these patients.32 This deserves further attention as these lesions have a high potential of becoming cancerous in an interval of 1–30 year time period (leukoplakia 0.1%–36% and erythroplakia 14%–50% chance of malignant transformation).19
Reducing wait times and facilitating access for patients in remote areas to competent oral health care professionals, including oral medicine specialists, oral pathologists, oral surgeons and otolaryngologists/ear, nose and throat specialists, could improve the detection of these lesions at an earlier stage. Earlier access can have a tremendous impact on care and regular follow-ups, which, in turn, would lead to a much better treatment outcome. Friesen’s study33 also indicates the need to enhance dentists’ and physicians’ skills in the initial assessment of oral precancerous lesions. This finding has been confirmed by other studies worldwide.52,53
Multiple governmental and nongovernmental organizations and websites provide information to raise awareness about OCC and OPC and preventive instructions. Although this information could contribute to better public knowledge, no studies have evaluated their effectiveness in preventing OCC and OPC in Alberta.
This study included every category of data source to answer comprehensive objectives. However, in a scoping review, no quality assessment is provided, mainly because of the diversity of sources.22
In Alberta, the high prevalence of stage IV OCC and OPC and the associated mortality rate indicate an urgent need to investigate strategies that may improve the detection, diagnosis and management of these diseases across the province. Some suggestions include public awareness about signs and symptoms of OCC and OPC and when to approach a physician or dentist.

Barriers, such as long waiting lists for first visits and long travel distances to specialized health care centres, should also be addressed. Also, implementing routine oral/H&N cancer screening in public settings, especially in at-risk communities, may lead to early detection and, consequently, better outcomes in the management of OCC and OPC in Alberta.
1. Oral cancer. Geneva: World Health Organization; n.d. Available: https://www.who.int/cancer/prevention/diagnosis-screening/oralcancer/en/ (accessed 2020 May 23). 2. Oral and oropharyngeal incidence rates for 2019. Newport Beach, Calif.: Oral Cancer Foundation; 2017. Available: https:// oralcancerfoundation.org/oraloropharyngeal-incidence-rates-2017/ (accessed 2019 Jan. 24).
3. Canadian Cancer Statistics Advisory Committee. Canadian cancer statistics 2019. Toronto: Canadian Cancer Society; 2019. Available: http://cancer.ca/Canadian-Cancer-Statistics-2019-EN (accessed 2020 Jan. 29).
4. Oral cancer. Ottawa: Government of Canada; rev. 2019. Available: https://www.canada.ca/en/public-health/services/oraldiseases- conditions/oral-cancer.html (accessed 2018 Jan. 28). 5. Sankaranarayanan R, Ramadas K, Thomas G, Muwonge R, Thara S, Mathew B, et al. Effect of screening on oral cancer mortality in Kerala, India: a cluster-randomised controlled trial. Lancet. 2005;365(9475):1927-33.
6. Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45(4-5):309-16. 7. A digital manual for the early diagnosis of oral neoplasia. Geneva: World Health Organization. 2021. Available: https://screening. iarc.fr/atlasoral_list.php?cat=A&lang=1 (accessed 23 Feb 2021)
8. Napier SS, Speight PM. Natural history of potentially malignant oral lesions and conditions : an overview of the literature. J Oral Pathol Med. 2008;37(1):1-10. 9. Epstein JB, Huber MA. The benefit and risk of screening for oral potentially malignant epithelial lesions and squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(5):537-40. 10. LeHew CW, Epstein JB, Kaste LM, Choi Y-K. Assessing oral cancer early detection: clarifying dentists’ practices. J Public Health Dent. 2010;70(2):93-100. 11. Laronde DM, Hislop TG, Elwood JM, Rosin MP. Oral cancer: just the facts. J Can Dent Assoc. 2008;74(3):269-72.
12. Isayeva T, Li Y, Maswahu D, Brandwein-Gensler M. Human papillomavirus in non-oropharyngeal head and neck cancers: a systematic literature review. Head Neck Pathol. 2012;6(suppl 1):S104-S20. 13. Denson L, Janitz AE, Brame LS, Campbell JE. Oral
cavity and oropharyngeal cancer: changing trends in incidence in the United States and Oklahoma. J Okla State Med Assoc. 2016;109(7-8):339-45.
14. Habbous S, Chu KP, Lau H, Schorr M, Belayneh M, Ha MN, et al. Human papillomavirus in oropharyngeal cancer in Canada: analysis of 5 comprehensive cancer centres using multiple imputation. CMAJ. 2017;189(32):E1030-40.
15. Shack L, Lau HY, Huang L, Doll C, Hao D. Trends in the incidence of human papillomavirus–related noncervical and cervical cancers in Alberta, Canada: a population-based study. CMAJ Open. 2014;2(3):E127-32.
16. Hobbs CGL, Sterne JAC, Bailey M, Heyderman RS, Birchall MA, Thomas SJ. Human papillomavirus and head and neck cancer: a systematic review and meta-analysis. Clin Otolaryngol. 2006;31(4):259-66. 17. Ribeiro IP, Barroso L, Marques F, Melo JB, Carreira IM. Early detection and personalized treatment in oral cancer: the impact of omics approaches. Mol Cytogenet. 2016;9:85.
18. Stefanuto P, Doucet JC, Robertson C. Delays in treatment of oral cancer: a review of the current literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(4):424-9.
19. Queiroz SIML, Costa de Medeiros AM, Pereira da Silva JS, Dantas da Silveira ÉJ. Clinical and histopathological evaluation and habits associated with the onset of oral leukoplakia and erythroplakia. J Bras Patol Med Lab. 2014;50(2):144-9. 20. Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian cancer statistics 2015: special topic: predictions of the future burden of cancer in Canada. Toronto: Canadian Cancer Society; 2015. Available: https://www.cancer.ca/~/media/cancer. ca/CW/ cancer%20information/cancer%20101/Canadian%20cancer%20 statistics/Canadian-Cancer-Statistics-2015-EN.pdf?la=en (accessed 2021 Feb. 11).
21. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method. 2005;8(1):19-32. 22. Peters MDJ, Godfrey CM, McInerney P, Baldini Soares C, Khalil H, Parker D. The Joanna Briggs Institute reviewers’ manual 2015: methodology for JBI scoping reviews. Adelaide, Australia: Joanna Briggs Institute; 2015. 23. Biron VL, O’Connell DA, Seikaly H. The impact of clinical versus pathological staging in oral cavity carcinoma — a multi- institutional analysis of survival. Otolaryngol Head Neck Surg. 2013;42(1):28. 24. Zhang H, Dziegielewski PT, Jean Nguyen TT, Jeffery CC, O’Connell DA, Harris JR, et al. The effects of geography on survival in patients with oral cavity squamous cell carcinoma. Oral Oncol. 2015;51(6):578-85. 25. Erickson B, Biron VL, Han Z, Seikaly H, Côté DWJ. Survival outcomes of First Nations patients with oral cavity squamous cell carcinoma (Poliquin 2014). Otolaryngol Head Neck Surg. 2015;44(1):1-5. 26. Thompson SK, Southern DA, McKinnon JG, Dort JC, Ghali WA. Incidence of perioperative stroke after neck dissection for head and neck cancer: a regional outcome analysis. Ann Surg. 2004(3):428-31. 27. Barber B, Dergousoff J, Nesbitt M, Mitchell N, Harris J, O’Connell D, et al. Depression as a predictor of
postoperative functional performance status (PFPS) and treatment adherence in head and neck cancer patients: a prospective study. Otolaryngol Head Neck Surg. 2015;44:38. 28. Shack L, Lau HY, Longlong H, Doll C, Hao D. Trends in the incidence of human papillomavirus-related noncervical and cervical cancers in Alberta, Canada: a population-based study. CMAJ Open. 2014;2(3):E12732. 29. Marzouki HZ, Biron VL, Harris J, O’Connell D, Seikaly H. Human papillomavirus-associated oropharyngeal squamous cell carcinoma and anogenital cancers in men: epidemiologic evaluation of association. Head Neck. 2016;38(suppl. 1):E2100-2. 30. Collie K, McCormick J, Waller A, Railton C, Shirt L, Chobanuk J, et al. Qualitative evaluation of care plans for Canadian breast and headand-neck cancer survivors. Curr Oncol. 2014;21(1):e18-28. 31. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-9. 32. Grattan KS. The experiences of the younger head and neck cancer client. Master’s thesis. Edmonton: University of Alberta; 2013. 33. Friesen R. A retrospective analysis of referral patterns to a university oral medicine clinic. Master’s thesis. Edmonton: University of Alberta; 2018. 34. Team APHaNT. Clinical practice guideline: HN-002 version 1. Edmonton: Alberta Health Services; 2014. Available: https:// pdfslide.net/ documents/oral-cavity-cancer-alberta-health-201606-23developing-oral-cavity-cancer-oral.html (accessed 2018 Feb. 20). 35. Oropharyngeal cancer treatment: clinical practice guideline HN-004 version 1. Edmonton: Alberta Health Services; 2019. Available: https://www.albertahealthservices.ca/assets/info/hp/ cancer/if-hp-cancer-guide-hn004-oropharyngeal.pdf (accessed 2020 February 10). 36. Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian cancer statistics 2016 — special topic: HPV-associated cancers. Toronto: Canadian Cancer Society; 2016. Available: http://www.cancer.ca/~/media/cancer. ca/CW/cancer%20information/ cancer%20101/Canadian%20 cancer%20statistics/Canadian-Cancer-Statistics-2016-EN. pdf?la=en (accessed 2018 February 27). 37. Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian cancer statistics 2017 — special topic: pancreatic cancer. Toronto: Canadian Cancer Society; 2017. Available: http://www.cancer. ca/~/media/cancer.ca/CW/cancer%20information/cancer%20101/ Canadian%20cancer%20statistics/Canadian-Cancer-Statistics2017-EN.pdf (accessed 2018 February 27).
38. Our investment. Edmonton: Alberta Cancer Foundation; 2018. Available: https://www.albertacancer.ca/our-investments (accessed 2018 Feb. 27).
39. Cancer patient education, symptom management, mouth and dental care. Edmonton: Alberta Health Services; 2016. Available:https://www.albertahealthservices.ca/cancer/ cancer.aspx (accessed 2018 Feb. 30). 40. Cancer care Alberta. Edmonton: Alberta Health Services; 2018. Available: https://www. albertahealthservices.ca/cancer/cancer.aspx (accessed 2018 Feb.
30). 41. Human papillomavirus (HPV-9) vaccine. Edmonton: Alberta Health Services; 2018. Available: https://www.albertahealthservices. ca/assets/info/hp/cdc/If-hp-cdc-hpv-info-sht-07-240-r01.pdf (accessed 2018 Feb. 30).
42. Annual impact report: health 2015–16. Edmonton: Alberta Innovates; 2015-16. Available: https://albertainnovates.ca/wpcontent/uploads/2018/02/Alberta-Innovates-Health-ImpactReport.pdf (accessed 2018 Feb. 30). 43. About the ACPLF: Alberta Cancer Prevention Legacy Fund. Edmonton: Alberta Health Services; 2018. Available from: https:// www.healthiertogether.ca/ about/about-us/about-the-acplf/ (accessed 2018 Feb. 30).
44. Project grant: fall 2018 results. Ottawa: Canadian Institutes of Health Research; rev. 2019. Available: https://cihr-irsc.gc.ca/e/51312. html (accessed 2019 Feb. 30).
45. Gilbert R, Devries-Aboud M, Winquist E, Waldron J, McQuestion M, Head and Neck Cancer Disease Site Group. The management of head and neck cancer in Ontario.organizational and clinical practice guideline recommendations. Toronto: Cancer Care Ontario; 2013. Available: https://hncrehab.ca/wp-content/ uploads/2015/06/Cancer-Care-Ontario-The-Management-ofhead-and-neck-cancer- in-ontario.pdf (accessed 2021 Feb. 16). 46. Human papillomavirus (hpv-9) vaccine. Government of Alberta. 2020. Available: https://myhealth.alberta.ca/Alberta/Pages/ immunization-human-papillomavirus.aspx (accessed 23 Feb 2021)
47. Ontario cancer facts: new cases of intra-oral cancers increasing after decades of decline. Toronto: Cancer Care Ontario; 2019. Available: https://www.cancercareontario.ca/en/cancer-facts/ new-cases-intra-oral-cancers-increasing-after-decades-decline (accessed 2019 Feb. 30). 48. Auluck A, Hislop G, Bajdik C, Poh C, Zhang L, Rosin M. Trends in oropharyngeal and oral cavity cancer incidence of human papillomavirus (HPV)-related and HPVunrelated sites in a multicultural population: the British Columbia experience. Cancer. 2010;116(11):2635-44. 49. Tota JE, Anderson WF, Coffey C, Califano J, Cozen W, Ferris RL, et al. Rising incidence of oral tongue cancer among white men and women in the United States, 1973–2012. Oral Oncol. 2017;67:146-52. 50. Sankaranarayanan R, Ramadas K, Amarasinghe H, Subramanian S, Johnson N. Chapter 5: oral cancer: prevention, early detection, and treatment. In: Gelband H, Jha P, Sankaranarayanan R, Horton S, editors. Cancer: disease control priorities, 3rd ed., volume 3. Washington, DC: World Bank; 2015. Available: https://www.ncbi.nlm.nih.gov/books/NBK343649/ (accessed 2021 Feb. 16). 51. Gupta N, Gupta R, Acharya AK, Patthi B, Goud V, Reddy S, et al. Changing trends in oral cancer — a global scenario Nepal J Epidemiol. 2016;6(4):613-9. 52. Jaber MA. Dental practitioner’s knowledge, opinions and methods of management of oral premalignancy and malignancy. Saudi Dent J. 2011;23(1):29-36. 53. Psoter WJ, Morse DE, Sánchez-Ayendez M, Vega CMV, Aguilar ML, Buxó-Martinez CJ, et al. Increasing opportunistic oral cancer screening examinations: findings from focus groups with general dentists in Puerto Rico. J Cancer Educ. 2015;30(2):277-83.
Wednesday June 16th, 2021 - Issam Fares Hall, American University of Beirut

The “Pioneers in Dentistry” at the American University of Beirut is a program of recognition dedicated to honor in a scientific setting one or more dentists or associated professionals for their seminal contributions to the science, education and/or practice of dentistry. The Pioneers Committee has decided to honor in the year 2021 dentists in Lebanon who have contributed in 2 major themes: foundation and sustained contribution to clinical science and community service. They have selected 4 colleagues to this honor:

DR. JEAN-MARIE MEGARBANE WHOSE SELECTION WAS FOR: “ESTABLISHING THE DEpARTMENT OF pERIODONTICS AT THE LEBANESE UNIvERSITY, AND MAINTAINING A SUSTAINED RECORD OF CONTRIBUTION TO THE SCIENCE OF pERIODONTICS THROUGH pUBLICATIONS AND INvITED LECTURES WORLDWIDE, AND SERvICE TO THE LEBANESE AND REGIONAL DENTAL COMMUNITY INCLUDING THE pRESIDENCY OF THE INTERNATIONAL COLLEGE OF DENTISTS/MIDDLE EAST SECTION.”

DR. ELIE MAALOUF WHOSE SELECTION WAS FOR “ESTABLISHING THE DEpARTMENT OF ENDODONTICS AT THE UNIvERSITé SAINT JOSEpH, MAINTAINING A SUSTAINED RECORD OF ACADEMIC TEACHING, AND DISTINGUISHED SERvICE TO THE LEBANESE DENTAL COMMUNITY IF ONLY DEMONSTRATED BY HIS ELECTION TWICE TO THE pRESIDENCY OF THE LEBANESE DENTAL ASSOCIATION.”

DR. ROY SABRI WHOSE SELECTION WAS FOR: “ESTABLISHING THE DEpARTMENT OF ORTHODONTICS AT THE LEBANESE UNIvERSITY, AND MAINTAINING A SUSTAINED RECORD OF ACADEMIC TEACHING, pUBLICATIONS IN INTERNATIONAL JOURNALS, INvITED LECTURES WORLDWIDE, AND SERvICE TO THE LEBANESE AND REGIONAL DENTAL COMMUNITY INCLUDING THE pRESIDENCY OF THE INTERNATIONAL COLLEGE OF DENTISTS/MIDDLE EAST SECTION.”
DR. GEORGES TAWIL WHOSE SELECTION WAS FOR: “ESTABLISHING THE FIRST pOSTDOCTORAL pROGRAM IN pERIODONTICS IN LEBANON AT THE UNIvERSITé SAINT JOSEpH, AND MAINTAINING A SUSTAINED RECORD OF ACADEMIC TEACHING, INvITED LECTURES WORLDWIDE, pUBLICATIONS, AND SERvICE TO THE LEBANESE AND REGIONAL DENTAL COMMUNITY INCLUDING THE pRESIDENCY OF THE INTERNATIONAL COLLEGE OF DENTISTS/MIDDLE EAST SECTION.”



• Plug and play micromotor, easy to install
• Connects to your chair’s air supply
• Cost-efficient conversion to electric
• Perfect for speed increasing handpieces
• Internal spray and LED
Optima
• Handpiece kit incl. BA45E, BA520FM and BA604E
• BA45E: 1:1 push button contra-angle
• BA520FM: Midwest fixed up to 19W power

• BA604E: Midwest air motor, external spray

1:5 red band contra-angle
Anti-retraction valve
Less aerosol generation
Durable DLC coated bearings
Fibre-optics and quadruple
Titanium body

• Anti-retraction valve.
• Hygienic head
Fibre-optic and quadruple spray
• Titanium body
• Made in Japan Made in Germany
• Quick stop function
Fittings available for most common coupling types on the market



The Italian industry is present in Arabia and the Middle East. What is the major focus of the Italian industry in this part of the world?
The Italian dental industry is today one of the leading industries in the world, manufacturing equipment and material. The Italian companies exhibiting here in this edition of AEEDC are covering almost all types of equipment and material. In the last years of course there has been a huge development in digital technologies, and we also have a lot of new companies that are introducing digital equipment, hardware and software. So this is one of the new branches in which many Italian companies are investing to develop new products.
What we know about the Italian industry before, the strong point were radiology, sterilization and dental units. What is the position of the Italian industry in these traditional manufacturing lines?
In these traditional manufacturing fields, Italy is consolidating its position. Regarding dental units for example, we have one of the biggest groups for manufacturing dental equipment called Cefla, which is reuniting different brands like Anthos, Castellini and many others. We also have a lot of smaller manufacturers that are still developing new products in this field. Hence, the activity of our industry is developing and is setting as one of the leading manufacturers worldwide, not only in this region but everywhere in the world.
And what about the chemical industry, like polymer and impression materials?
Same as for the equipment, we have quite a good number of companies that are developing and selling products from the traditional materials, like acrylics and composites, but we have also many companies that are developing a more advanced line of products related to the digital dentistry like 3D printers.
Actually, the dental industry in Italy is very active after many years when the situation was static. The digital revolution in the last years has created a lot of development, so now many companies are introducing many products and new technologies, and many companies have entered the market, maybe they were in the mechanical sector and now they are entering the dental sector through dental printing equipment and this is therefore revitalizing the sector.
We know that dental implants now are in the core business of dentistry, where is Italy positioned in the business of implants and accessories?
Similarly to the other types of equipment and materials, also in implants we are in the leading position, specially that in Italy the percentage of implant use is huge, and we can say that Italy is one of main clusters in manufacturing implants. We are very well positioned and a lot of companies that are exhibiting in the Italian Pavilion here in Dubai are showing their implant products, and all the products have the EU certification as well as other international certifications and they are producing very high quality equipment for implants.
350 exposants internationaux
100 séances de formation
450 conférenciers

June 29 - July 1, 2021
Dubai, United Arab Emirates

AHMED BIN MOHAMMED INAUGURATES THE 25TH EDITION OF THE UAE INTERNATIONAL DENTAL CONFERENCE AND ARAB DENTAL ExHIBITION
His Highness Sheikh Ahmed bin Mohammed bin Rashid Al Maktoum, Chairman of the Mohammed bin Rashid Al Maktoum Knowledge Foundation, inaugurated the 25th edition of the UAE International Dental Conference and Arab Dental Exhibition (AEEDC Dubai) being held at the Dubai World Trade Centre (DWTC) on June 29, 2021.
Dr. Nasser Al Malik, Scientific Chairman, AEEDC Dubai, said: “This year’s edition marks a major milestone in the journey of AEEDC Dubai, with the event completing a quarter of a century as the global dental industry’s most anticipated meeting. This year’s scientific programme was carefully put together to tackle key topics, highlight recent advancements in oral healthcare during the COVID-19 pandemic and provide a platform for specialists to discuss the latest findings and developments of the year 2021 in all areas of dental care, including surgery, restorative dentistry, dental hygiene and dental assistance.”

This year, the event’s rich scientific programme included 173 scientific sessions, six workshops and over 160 poster presentations. Attendees had the opportunity to explore the latest in dental technology and delve into the field’s most recent innovations, which was showcased in the exhibition featuring over 4,000 international brands from more than 3,000 companies. A total of 18 country pavilions participated this year, the largest of which are the






HIS HIGHNESS WITH DR. AMRO ADEL, GENERAL MANAGER DENTSpLY SIRONA DENTAL SYSTEMS DURING THE INAUGURATION

THE NEW LISA STERILIZER ON THE W&H BOOTH


DR. GERHARD SEEBERGER, pRESIDENT OF THE FDI WITH DR. ABDULSALAM ALMADANI

Exhibition Floor

DURR DENTAL CELEBRATING 80 YEARS ANNIvERSARY

DR. WILD ExHIBITING THEIR NEW LINE OF ORAL CARE pRODUCTS

DR. AND MRS. JOHN YOUNG AT THE GNYDM BOOTH WITH THE ORGANISERS

DR. kHALIL ALEISA, pRESIDENT OF THE SAUDI DENTAL SOCIETY

pR. ANTOINE CHOUFANI, DR. TONY DIB, pR. MONA GHOSSOUB

Dubai, UAE
June 29 - July 1


DR. AL NASRY FROM SUDAN

DR. TONY DIB, MAJOR GENERAL DR. AHMED AMIN, DR. NAHAWAND THABET, MAJOR GENERAL pROF. RAAFAT RIAD


DR. ABDULRAHMAN AL AZRI, pRESIDENT OF THE OMANI DENTAL SOCIETY


pROF. EDMOND kOYESS LECTURING ABOUT NITI FILES IN SHApING CURvED AND NARROW CANALS

pROF. DALIA EL-BOkLE ExpLAINING HOW “GOING DIGITAL” CAN BE A GAME CHANGER

Speakers
DR. DIMITAR FILTCHEv TALkING ABOUT TISSUE DEvELOpMENT pREpARATION TECHNIQUES


DR. ADNAN ISHGI LECTURING ON ETHICAL AND pROFITABLE ESTHETIC DENTISTRY
pROF. IBRAHIM ALSHAHRANI LECTURING ABOUT THE SUCCESSES AND CHALLENGES IN ONLINE TEACHING


DR. HAMAD ALRUMAIH CONFERENCE ABOUT THE AppLICATIONS OF INTRAORAL SCANNERS IN pROSTHODONTICS
DR. JOHN J. YOUNG JR FROM NEW YORk LECTURING ON REGENERATIvE ENDODONTICS

DR. FILIppO CARDINALI LECTURE ON INFECTION CONTROL IN ENDODONTICS
DR. RANDA ZEIN LECTURE ON LASER-ASSISTED ORAL SOFT TISSUE MANAGEMENT


Dubai, UAE
June 29 - July 1


DR. TARIQ ROWAIHY AND DR. SAMI FARSI LECTURE ON CERAMIC LAMINATE vENEERS

DR. HANAA ASHkAR LECTURE ABOUT pSYCHOLOGICAL AppROACH TO pATIENTS COMING FROM ESTHETIC TREATMENT

DR. EMAN ABDULBASET
AHANSHAL CONFERENCE ON MILE DESIGN
DR. MOHAMED kOLEILAT LECTURE ON ERROR IN TREATMENT pLANNING MANAGEMENT

DR DINA DEBAYBO, pRESIDENT EMIRATES pEDIATRIC DENTISTRY CLUB (EMA)

The new 3D/2D X-ray system for cutting-edge imaging in a wide range of indications
Axeos, the versatile 3D/2D extraoral imaging solution from Dentsply Sirona, recently received the international iF Design Award.
The 98-member international jury recognized the device primarily for its form and functionality – in these categories the product achieved the best ratings.
Axeos provides general practitioners and specialists with a hybrid system that
covers a wide range of dental indications and meets modern imaging requirements: sharp images with the lowest possible dose, various selectable volumes and intuitive operability.
The new extraoral imaging system from Dentsply Sirona, Axeos, has been awarded another prestigious design prize. In 2020, the imaging device received the esteemed Red Dot Award for product design.
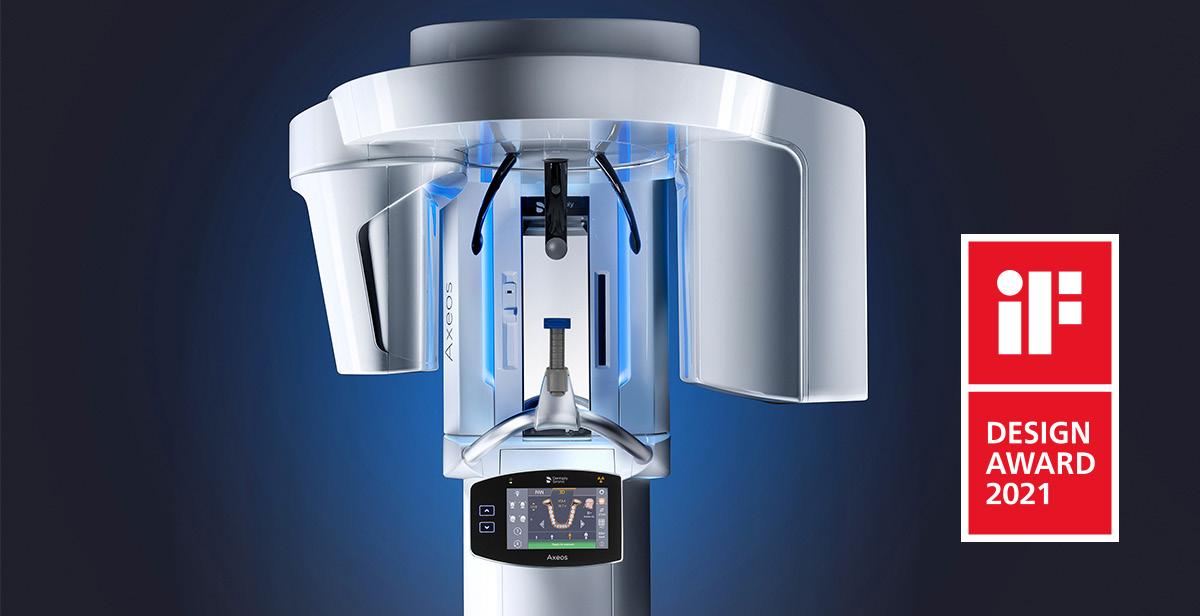
In 2021, Axeos has received another award by the international iF Design Award. In their evaluation, the 98-member international jury awarded points for the product idea, form, function, distinctiveness and utility.
Axeos received superior marks in all areas. The jury members were particularly impressed by its form and functionality, which leads to an increased quality in performance and treatment comfort.
«We are very delighted to receive this award,» said Niels Plate, Group Vice President, Digital Devices & Solutions at Dentsply Sirona.
«It confirms our goal of offering our customers solutions that stand for high clinical safety, patient comfort and efficient treatment processes. A successful form and functionality of the device contribute to this.»
As a modern imaging solution, Axeos offers excellent image quality in 2D and 3D, flexible volumes, seamless connection to Sidexis 4 software as well as to numerous treatment programs. In addition, several features focus on maximum patient comfort: positioning aids (e.g. unique auto-positioner with patented occlusal bite block, automatic temple width measurement, smart height adjustment) support in rapidly achieving the optimum alignment for the image. Lastly, lighting concepts like ambient light create a more pleasant, calming atmosphere for patients.
With Axeos, both classic standard panoramic exposures – which is especially good for children – and extraoral bite wing exposures can be taken. If desired, Axeos can be equipped with a cephalometric arm (left or right) that can be retrofitted at any time. This versatility also convinces users. Dr. Neal Patel, dentist and owner of the Infinite Smiles clinic in Powell, Ohio, says: «Axeos gives us all the X-ray diagnostic options we need.
Both temporomandibular joints can be displayed in one image, we receive information about the airways, and we can take HD images when it comes to special endodontic aspects. The low-dose mode further expands the range of indications.» This makes Axeos an imaging solution particularly beneficial to clinicians in various disciplines.

Fig. 2: Niels Plate, Group Vice President, Digital Devices & Solutions at Dentsply Sirona: “This award confirms our goal of offering our customers solutions that stand for high clinical safety and efficient treatment processes.”
Every year, the iF Design Award recognizes outstanding design, its relevance to business and everyday life, and distinguishes one of the world’s most important seals of excellence. Awarded in Germany since 1953, the iF label is a reliable sign of good design for both consumers and the design community.
Get more information on Axeos here: www.dentsplysirona.com/axeos

 Agnes
Agnes
Hufnagl agnes.hufnagl@wh.com
W&H is redefining freedom in rotary polishing: With the new Proxeo Twist Cordless Polishing System, you now have even more freedom of choice and freedom of movement. Regardless of which cup system you prefer – LatchShort, Screw-in or Disposable Prophy Angles – you have the choice! The new system’s wireless design offers improved ergonomics and greater mobility for your IPC workflow.
Proxeo Twist Cordless is about polishing without any restrictions – in many respects. The lack of cables means that you can enjoy full freedom of movement.
The modular system also allows you to choose your preferred cup system. And with the unique LatchShort system, you also benefit from the significantly reduced working height.
With just one cordless handpiece, you can use several attachments. The new modular system can be used with handpiece and contra-angle heads for Disposable Prophy Angle, Screw-in prophy cups and the LatchShort system – with a shorter shaft and up to 4 mm lower working height.

The Proxeo Twist Cordless Polishing System therefore offers full flexibility for top-class rotary polishing treatment.
Wireless drive and wireless foot control
With the Proxeo Twist Cordless handpiece, you can change your treatment position as required – without having to worry about inconvenient cables. Its low weight and ergonomic design mean it adapts perfectly to your movements. This enables fatiguefree polishing and a back-friendly posture.

Completely flexible and cordless – the perfect tool for rotary polishing!
The wireless foot control also means that you can move around with much more freedom and quickly change your position in relation to the patient.

You have the choice with the new Proxeo Twist Cordless Polishing System!
The speed can be adjusted smoothly from 0 to 3,000 rpm, and it can be constantly adapted to the clinical requirements. The foot control is also compatible with the Proxeo Ultra Piezo Scaler PB-530. This allows users to make use of the full functionality of two devices.

The new Proxeo Twist Cordless Polishing System ensures fatigue-free polishing and a back-friendly posture.
W&H offers the appropriate Disposable Prophy Angle and LatchShort prophy brushes and cups in various hardness for the Proxeo Twist Cordless Polishing System.

The W&H prophy cups impress with their optimal adaptation and gentle cleaning up into the sulcus.
They were designed in consultation with prophy users. Great emphasis was placed on features such as optimal adaptation, simple paste pickup and distribution as well as gentle cleaning up into the sulcus.
In addition to the new modular Proxeo Twist Cordless Polishing System, W&H offers the classic Cordless handpiece with Doriot connection for disposable prophy angles.
Both product offerings are synonymous with maximum freedom of movement and the best polishing results.

www.vhf.de
vhf camfacture has set another milestone for efficient and safe milling and grinding in modern dentistry. In addition to the continuous improvement of milling machines, software, and tools, vhf has also rethought the handling of tools and redesigned the simple standard packaging to a multifunctional tool packaging.
This unique and patented solution further increases the efficiency in the workflow for the production of dental restorations.
The innovative design of the tool packaging offers the decisive added value for dental laboratories, milling centers and dental practices when it comes to storage and handling. Each package consists of a protective casing and a colored socket in which the tool is held.



With seven distinct colors, it is clearly visible which tool is applicable for which material class. The respective article match code is prominently marked on the protective casing. A unique feature is that the individual packages can be coupled, separated and combined as required by means of an innovative sliding mechanism, so that the best possible overview of the tool contingent is available at all times.
The handling of the milling machine tools is not only easier but also safer thanks to the innovative packaging. In addition to protecting the tool from damage, the new packaging offers safe handling because the tool contained in the socket is not touched directly.
This minimizes the risk of injury to the user. Another plus: The socket serves as a holder to directly and easily insert or remove the tool in the tool magazine of the milling machine.
















«It’s my choice»; with this slogan, Dentaurum Implants has developed an implant system that is unique world-wide – tioLogic® TWINFIT. The operator can look forward to a patented system that has much to offer: not only safety and efficiency in handling, but also maximum flexibility during implant insertion, final restoration and in situations that change as the patient grows older.
With the revolutionary Abutment Switch, one and the same implant has two connector geometries for restorations –conical and platform. Moreover, a system of depth stops offers flexibility and safety during surgical preparation.
The tioLogic® TWINFIT implant system covers all indications in the fields of surgery and prosthetics. Using modern FEM analyses, both the design of the implant and its thread geometry were optimized, ensuring that the flow of forces is even and gentle on the bone.
The optimal grading of the implant diameters and lengths means that the appropriate implant can be used for the indication in question. The comprehensive assortment of prosthetics offers maximum flexibility where the restoration is concerned.
The proven S-M-L concept and the integrated Platform Switch mean the assortment for tioLogic® TWINFIT is easy to manage: 5 implant diameters, 5 implant lengths, 3 series of abutments, 2 connector geometries – conical and platform.
Thanks to the revolutionary Abutment Switch, one implant has two connector geometries (conical/platform) for the prosthetic restoration. This is currently a unique selling point on the implant market.
It offers flexibility throughout the entire life cycle of the implant – from insertion to final restoration and in situations that change as the patient grows older.
Operators remain flexible in their decision on which abutment best suits each individual patient – conical or platform –, both from a functional and from an aesthetic point of view.
The depth stop sleeves for single use allow more flexibility and security during surgical preparation. They are included with every delivery.
The sleeves are designed to match the preparation protocol and serve to support the operator during implant insertion. The sleeves are simply pushed onto each of the drills if required.
Color coding indicating the diameter protect against using the wrong instrument. Together with the ADVANCED instruments, it is possible to prepare the implant site in a way that is gentle on the bone. At the same time valuable autologous bone chips can be collected.
The prosthetic assortment is rounded off by the innovative 4Base system for screw-retained superstructures with angulations up to 50°. A uniform interface facilitates prosthetic restoration. This minimizes augmentative measures, thereby reducing treatment time.
The angulated screw aperture is also the best solution for the entire segment that is occlusally screw-retained, both for 4Base and for hybrid constructions. This guarantees prosthetic results that are aesthetic and functional. The screw aperture can be inclined at an angle of 20° to the implant axis, allowing discrete emergence in the palatal area, particularly in the anterior region.
The patented tioLogic® TWINFIT implant system with all of its components is designed to suit a digital workflow. As your digital partner, the Dentaurum Group places value on process sequences that are efficient and easy to follow, using materials that have been validated – from scanning through to manufacture.
tioLogic® TWINFIT sets new standards in the field of implantology. The system offers solutions that are flexible, efficient and tailor-made for the patient. The program is rounded off with a wide offer of services for the user and the patient.



Based on the current state of scientific knowledge, there is uncertainty over the degree to which SARS-CoV-2 viruses can be transmitted via dental aerosols. By contrast, latest research results obtained as part of an in vitro pilot study from Dürr Dental do indeed offer certainty in relation to the suction of aerosols. These results show that, with effective suction in the mouth of the patient at a rate of around 300 l/min, all dental treatments can be carried out and all the normal equipment can be used. These results have now also been confirmed by the S1 guide «Umgang mit zahnmedizinischen Patienten bei Belastung mit Aerosolübertragbaren Erregern (S1) Langfassung 2021». (at the moment only available in german language)
In this study, a team of three people carried out a pilot study on various aspects of suction. Here, the so-called shadow technique was used for the first time in the dental area. This is an industry standard based on state-of-the-art LED technology and digital imaging. The technique can be used to determine the size and speed of particles, in particular of aerosol particles. The team applied this technique to a phantom head in the in vitro model. In this way it was possible to compare the particle emissions of different devices. In the process, it emerged that powder jet handpieces create the most aerosols, followed by turbines operating at 400,000 rpm.
However, with the aid of effective suction it is possible to reduce the number of particles below the detection limit. According to the study results, the key here is the flow rate. It is this – and not e.g. a high vacuum – that represents the single most important physical variable. Ideally, 300 litres of suction volume per minute is needed. This can even compensate for situations where the suction position is less than optimal, for example in treatment areas where access is difficult. Certain loss of suction down to a flow rate of 250 litres per minute can still be compensated for with an optimised suction position. However, below this rate hygiene and infection control both become critical issues.
«The thing that surprised me most was how little impact a saliva ejector has», says Study Leader Dr. Martin Koch. «It would definitely be wrong to assume that the aerosol reduction was sufficient.»
Only with optimised application of a large suction cannula (Dürr Dental universal cannula, 16 mm) or a special aerosol cannula (Dürr Dental) is it possible to push the particle count below the detection
limit. In the case of powder jet devices, we would go a step further and say that use of an aerosol cannula is recommended. Looking at this the other way round, this also means that the powder jet device itself can be operated without increased risk provided high-volume suction is carried out using an aerosol cannula, with the cannula being held at a distance of around one centimetre from the tooth (= guide value). The in vitro pilot study draws clear conclusions about both the underlying theoretical principles (catchphrase: «it’s all about the flow rate») and the implications for dental practices (catchphrase: «high-volume suction at a rate of 300 litres per minute with a large cannula»). Based on this pilot study, clinical follow-up studies are currently being planned in order to obtain further wellfounded results on all aspects of avoiding dental aerosols.
These results have been underlined very recently by the updated S1 guide «Handling dental patients under a burden of aerosoltransmissible pathogens» published in March 2021: Provided the measures recommended in dental medicine for the use of watercooled instruments are met, which include […] and high-volume suction at a rate of around 300 l/minute using a suction canula with a diameter of at least 10 mm, protection for the treatment team and the patient against droplets and aerosols is ensured by a combination of specific prevention measures […]. As long as this is ensured, there is at present no solid evidence in support of additional equipment for suction.





The 2-in-1 model of the X-VIEW family, is a multifunctional and integrated system that puts the advantages of 2D and cephalometric imaging within the reach of the general dentists, periodontists, orthodontics and other specialists working from medium offices to hospitals and clinics.
X-VIEW 2D PAN CEPH incorporates a high-frequency generator and a noise- and imperfection-free acquisition system, providing high quality clinical images.
X-VIEW 2D offers the inherent advantages of CCD (Charge-coupled devices) to capture panoramic images of the skull and jaw with excellent resolution in less time and lower patient exposure: noiseless charge transfer, high signal-to-noise ratio and the unique features of time-delay integration (TDI):
• Capturing clear and bright images with the best possible contrast and uniform density.
• Increased sensitivity for signal detection at lower light levels.
• Larger full-well capacity to provide high dynamic range.
In addition to the CCD-TDI detector for all 2D programs, X-VIEW 2D PAN CEPH is equipped with a dedicated DR flat panel detector for Ceph images acquisition.
The DR (Digital Radiography) version is the highest quality technology available to obtain sharp images:
• Better contrast
• More details and filtering
• No background disturbance
• Exposure time: 200-500ms
• Reading time: immediate
• Detector-PC image transmission: 2sec
• Image store after shot: 200
• Calibration Method: easy intuitive and manageable from remote


Success CD is PROMEDICA’s composite-based, selfcuring paste-paste system for quick and easy chairside production of temporary crowns, bridges, inlays and onlays.

High-quality temporary restorations within 5 minutes
After a retention time of 30 to 60 seconds in the oral cavity, the material takes on an elastic consistency, which facilitates removal without risking deformation. The material cures completely within a further 3 minutes and can then be polished. This procedure is timesaving and thus highly economical.
Excellent physical properties and great aesthetic results
As far as the material’s physical properties are concerned, Success CD convinces with its excellent flexural and overall strength as well as its capacity to withstand high functional loads.
The product’s minimal polymerisation shrinkage results in precisely fitting temporary restorations. Success CD’s high colour stability and brilliant, enamel-like gloss ensure long-term aesthetic results. Moreover, its natural fluorescence and the choice of available shades promote perfect aesthetic results.
website: www.promedica.de

TheraBase is a dual-cured, calcium and fluoride releasing, self-adhesive base/liner. TheraBase contains MDP, chemically bonds to tooth structure, and utilizes THERA technology.

It is radiopaque allowing for effective identification on radiographs. Its dual-cure ability ensures the material will cure even in deep restorations where light cannot reach!
website: www.bisco.com

Material-viscosity as key factor for controlled procedures and effective results
Patient cases requiring medical tooth whitening protocols are frequently challenging. Medical whitening procedures are used to treat obvious intense discoloration inside the tooth, e. g. as a result of diseases, drugs, tooth malformations and bleeding after accidents or trauma. These kinds of discolorations typically do not affect the entire arch, but only one or several teeth.
Studies by Prof. Polydorou (Freiburg/Germany) have shown, that it is appropriate in such cases, to use a higher concentration of peroxide. The studies regarding safety aspects show additionally, that these treatments maybe considered to be absolutely safe, as they are executed under the full supervision of the practice team.
In order to achieve the best results, it is vital to have suitable procedures in place, supported by perfectly matching products, thus enabling the clinician to proceed in a controlled, yet effective way. Talking about effectiveness and the highest level of control, the viscosity of the whitening product used plays an important role: It is key for precise application, for reliable handling and consequently for convincing results.

For many years, OpalescenceTM BoostTM with 40% hydrogen peroxide has been the state-of-the-art power whitening solution for bespoke medical inoffice treatments. The whitening gel is suitable for the treatment of one or more teeth, parts of a tooth or for accelerated chairside-whitening techniques. It can also be used on non-vital teeth, including in-office intracoronal whitening.
As part of Ultradent Products’ continuous commitment to research and development, Opalescence Boost has been reformulated in order to further improve its performance, usability, consistency and viscosity. The updated material with its higher viscosity provides for advanced handling properties and a more precise placement. Consequently, the newly formulated gel reliably stays in place during the entire treatment.
The re-designed mixing syringes incorporating a gold element, deliver fresh chemicals for each application. A short treatment time of 2 x 20 minutes is sufficient to achieve excellent whitening results. Opalescence Boost’s new improved viscosity means that it should no longer be applied with Micro 20ga and MicroTM 20ga FXTM Tips. Ultradent Products’ well-known BlackTM Mini Tips ensure easy expression of the more viscous formula and are therefore perfectly suitable for its accurate placement.
Unlike other in-office whitening products, Opalescence Boost is chemically activated and consequently does not require activation by expensive, hot and uncomfortable lights. Due to its high concentration of 40% hydrogen peroxide, Opalescence Boost is categorized as a medical device product*). Despite its high content of active ingredients, Opalescence Boost is pH neutral. Thus, the tooth structure will not be affected, even when used repeatedly. Opalescence Boost also contains PF (potassium nitrate and fluoride) to strengthen the enamel and to reduce sensitivity. If an activated gel syringe is not completely used, the contents remain active for up to 10 days if stored in a refrigeretor.
Chairside whitening, the fastest, most targeted and controlled method of tooth whitening can be performed effectively, safely and economically with Opalescence Boost in its new formulation. Once the teeth have been whitened, the patients usually show an increased awareness for their general oral health. They demonstrate their appreciation for the treatment by their loyalty to the dental practice and by good oral hygiene. What more could a professional wish for?
website: www.ultradent.com



Enjoy the scan. With the connectivity options of Primescan. Scan and connect digitally. Or treat it in a single visit. Either way, it‘s prime.