SEMI-SPLIT
Bulk Placement Technique

THE PREVENTIVE EFFECT of glass ionomer restorations on new caries formation
DENTSPLY SIRONA
Equips Qatar’s first dental school BIDM 2022







































SEMI-SPLIT
Bulk Placement Technique

THE PREVENTIVE EFFECT of glass ionomer restorations on new caries formation
DENTSPLY SIRONA
Equips Qatar’s first dental school BIDM 2022





























































Based on the close and fruitful cooperation with dental institutes and practicing dentists since the 1940s, we have a uniquely broad portfolio of specially developed, innovative toothpastes, gels, sprays, mouthwashes and mouth baths. These products, which are marketed under the brands Tebodont®, Emofluor®, Emoform®, Depurdent® and Emofresh® are sold exclusively in pharmacies in Switzerland and in more than 40 other countries outside Switzerland, their various innovative formulations and compositions offer excellent solutions for daily dental care, addressing specific needs and problems (e.g. caries prevention, sensitive teeth, gum problems) and general oral health.
With the REDESIGN we have clarified the positioning of the oral care products: every toothpaste and every mouthwash now has a clear application area. At the same time, our new packaging is "digitalized": each product has a QR code that allows detailed information to be downloaded directly to the mobile phone. The redesign of the products should make the Wild brand tangible and perceptible.
• WILD will be used as umbrella brand on all products, which results in an easier promotion among the whole product range
• Same design for all brands leads to recognition and synergy effects across product range
• Clear unique main indication on the packaging avoids confusion among dental profession, pharmacists and end consumers due to overlapping benefits
• New design underscores clinical benefits and professionalism of the products which leads to cross-brand and cross-portfolio products awareness and helps to create trust among the dental profession, pharmacists and end consumers
• Unifying of the packaging system - all toothpastes in the same size and shape of tubes, all mouthwashes in the same size and packaging - leads to a uniform, eye-catching and space-saving shelf-impact
• Product portfolio becomes fresh, easy to recommend and attractive for the POS
Volume XXIX, Number IV, 2022
Volume XXIX, Number III, 2022
Alfred Naaman, Nada Naaman, Khalil Aleisa, Jihad Fakhoury, Dona Raad, Antoine Saadé, Lina Chamseddine, Tarek Kotob, Mohammed Rifai, Bilal Koleilat, Mohammad H. Al-Jammaz
Suha Nader
Marc Salloum
Micheline Assaf, Nariman Nehmeh
Josiane Younes
Albert Saykali
Gisèle Wakim
DIRECTOR ISSN
Tony Dib 1026-261X
DENTAL NEWS IS A QUARTERLY MAGAZINE DISTRIBUTED MAINLY IN THE MIDDLE EAST & NORTH AFRICA IN COLLABORATION WITH THE COUNCIL OF DENTAL SOCIETIES FOR THE GCC.
Statements and opinions expressed in the articles and communications herein are those of the author(s) and not necessarily those of the Editor(s) or publisher. No part of this magazine may be reproduced in any form, either electronic or mechanical, without the express written permission of the publisher.
AIDC 2022
Alexandria
International Dental Conference
Kuwait Dental Association Conference
7th Pan Arab Endodontic Conference 2022
November 16-18 2022
Hilton Green Plaza, EGYPT www.aidconline.ney
November 17-19 2022 Jumeirah Hotel, KUWAIT and
DENTAL NEWS – Sami Solh Ave., G. Younis Bldg. POB: 116-5515 Beirut, Lebanon.
Tel: 961-3-30 30 48
Fax: 961-1-38 46 57
Email: info@dentalnews.com
Website: www.dentalnews.com www.instagram.com/dentalnews
ADF 2022
18 – 20 November, 2022 MBRU, Dubai, U.A.E. zzk321@gmail.com
November 22 _ 26, 2022 Palais des Congrès de Paris, FRANCE www.adfcongres.com
Greater NY Dental Meeting
27 – 30 November, 2022 Jacob Javits, New York, USA www.gnydm.com
This magazine is printed on FSC – certified paper. WWW.DENTALNEWS.COM
SIDC 2023
January 19 _ 21, 2023
The Saudi International Dental Conference Hilton Riyadh Hotel, KSA www.sds.org.sa
AEEDC 2023
February 7 _ 9, 2023
Dubai World Trade Center, UAE www.aeedc.com
IDS 2023
March 14 _ 18, 2023 Cologne, GERMANY www.english.ids-cologne.de
7TH PAN ARAB 63
A-DEC 25
AIDC 59
AEEDC 71
BIDM 64
BELMONT 9
DMP 1
DURR 23
Semi-Split Bulk Placement Technique For Overcoming The Loss of Adaptation At The Pulpal Floor of Large Occlusal Bulk-Fill Resin Composite Restorations

The preventive effect of glass ionomer restorations on new caries formation: A systematic review and meta-analysis

Dentsply Sirona equips Qatar’s first dental school with cutting-edge training tools to prepare the next generation of dental professionals

DIRECTA 27-29
DENTSPLY SIRONA 72
EDGE FILE 21
FKG 31
GNYDM 67
HS BA024 17
HENRY SCHEIN 33
ORTHO 15 PROMEDICA 39
ROLENCE 35
SHINING 3D 43
SDI 33
SIDC 55
ULTRADENT HALO 19
48 The Lebanese Orthodontic Society
JULY 15, 2022 - GEFINOR ROTANA, BEIRUT

The Lebanese Dental Association congress AIO 56 68
OCTOBER 13-14, 2022

JUNE 9-11, 2022
CAGLIARI - SARDINIA - ITALY
MANI-JIZAI 37
IDS 71
MANI-JIZAI 37
VOCO 2, 13
WILD 3, 4, 5


Khamis A Hassan*, BDS, MSD, Doctorate, FADI *1, Professor of Operative Dentistry & Senior Clinical Consultant, Global Dental Centre, Vancouver, Canada
Salwa E Khier, BDS, MSD, MSc, PhD, FADM 2
Professor of Dental Biomaterials & Senior Research Consultant, Global Dental Centre, Vancouver, Canada
*Corresponding author
Dr. Khamis A Hassan, Professor of Operative Dentistry & Senior Clinical Consultant, Global Dental Centre, Vancouver, Canada. E-mail: globaldental@ shaw.ca
Keywords
Bulk placement, bulk-fill resin composite, debonding, diagonal gap, displacement, polymerization shrinkage, postoperative sensitivity, pulpal floor gap, semi-split bulk, stress reduction.
Abstract
When composite resin hardens by light curing, it shrinks and undergoes deformation which occurs in one region more than other regions within the composite bulk. This behavior is mainly related to variations in bonding to enamel and dentin of surrounding cavity walls. Bonding to surrounding cavity walls creates restrained shrinkage which develops tensile stresses within the composite bulk. The developed tensile stresses act against the tensile strength of the composite resin, and may cause cracks in enamel or composite, as well as residual strain at the adhesive interface, forming marginal and internal gaps.
Using the bulk filling technique, a bulk of 4mm increment of bulk-fill resin composite is placed in a deep Class I cavity. Within the composite bulk, shrinkage displacement occurs axially in the top region more than in the bottom region, resulting in debonding and gap formation at the pulpal floor. This gap is associated with persistent postoperative
sensitivity and consequent pain. The semi-split bulk filling technique is a modification of the bulk filling technique used for placing bulk-fill resin composites in large occlusal cavities. It aims at diminishing the shrinkage stresses within the composite bulk and minimizing the incidence of pulpal floor gap formation and the consequent postoperative sensitivity and pain.
Introduction
In the past decade, bulk-fill resin composites have been introduced in the dental market as a new concept for restoring posterior teeth. 1-3 They became popular among dentists who prefer simpler clinical procedures with reduced working time. 4,5
Bulk-fill resin composites were claimed by manufacturers to have a depth of cure of up to 4- 5mm. The increased depth of cure is achieved by using more efficient photoinitiators 6 , or by using fillers and monomers with similar refractive index. 7
Another group of bulk-fill resin composite was claimed by manufacturers to have a reduced shrinkage stress, as compared to that of the conventional composites placed incrementally. The stress reduction is achieved by additions in the organic matrix of low-shrink monomers, higher molecular weight monomers, or stress-relieving additives. 1








Polymerization shrinkage is an undesired property of dental composites which causes a discrepancy in dimensions when the restoration hardens. This affects the interface and results in residual strains at the adhesive interface, or marginal/internal gap formation. 5,6
The polymerization shrinkage stress is a complex phenomenon as it depends on several factors. Among which are the boundary conditions, the amount of material, and the polymerization reaction. They all play essential roles in stress development and/or transmission to tooth structures. 8,9
Within a large occlusal composite restoration placed as in bulk of 4mm increment using the bulk filling technique, a greater shrinkage strain or displacement takes place in the top composite region, where it undergoes more axial displacement than the bottom composite. 7,10 Additionally, the top composite displacement exerts an upward pull on the bottom composite region resulting in its debonding from the pulpal floor, and formation of pulpal floor gap beneath the composite restoration. 5,6,11
Several studies found that bulk-fill resin insertion technique resulted in higher rates of postoperative sensitivity compared to conventional resins. This sensitivity was attributed to the formation of pulpal floor gap in bulk-fill resin composite occlusal restorations. The dentinal fluid in the gap undergoes contraction or expansion with cold or hot stimuli, resulting in sudden movement of the fluid in dentinal tubules and causes pain. 1,12-14
The objective of this paper is to present the semisplit bulk filling technique, as a modification of the bulk filling technique which is used for placing bulk-fill resin composites in large occlusal cavities. This technique aims to reduce the shrinkage stresses generated due to the polymerization of bulk-fill resin composites, as well as to minimize the incidence of gap formation at pulpal floor, and consequent postoperative sensitivity and pain.
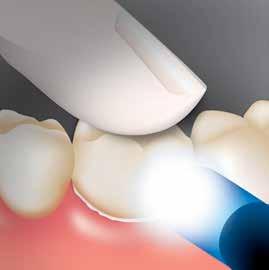
In the semi-split bulk filling technique, a diagonal gap (1.5mm wide) is created vertically into the 4mm composite bulk inserted in a large occlusal bonded cavity. This gap extends for a depth of 2mm, prior to light polymerization, using a Tefloncoated plastic filling instrument in push stroke.
This gap splits the top composite 2mm region into two equal segments. The segmented composite bulk is then light cured. The diagonal gap is then filled with the same bulk-fill resin composite and light cured.
The shrinkage stresses generated in bulk-fill resin composites exert tension on the bonding adhesive and surrounding tooth structure during the polymerization process. If this tension exceeds the adhesive bond, or the strength of either the composite or tooth, it can cause interfacial debonding, resulting in internal/marginal gaps. Comparing the incremental vs. the bulk filling techniques, the bulk filling technique was reported to produce more interfacial debonding. 15-17 In the bulk filling technique, the shrinkage stress occurs during light polymerization within a bulk of 4mm increment of bulk-fill resin composite inserted into a large occlusal cavity. (Fig. 1- A) The magnitude and direction of shrinkage stress varies between the top and bottom composite regions. 7,10 The polymerizing bulk-fill resin composites undergo shrinkage displacement in both axial and lateral dimensions, with less displacement occurring laterally than axially. The axial displacement in the top 2mm composite region occurs in downward direction, whereas it takes place in upward direction in the bottom 2mm composite region. 18,19 Additionally, the top composite displacement exerts an upward pull on the bottom composite region strong enough to result in its debonding from the pulpal floor, and formation of pulpal floor gap beneath the composite restoration. 2022 (Fig. 1-B) The strength of the upward pulling is augmented by bonding the composite in the top region to enamel and dentin of surrounding cavity walls, as compared to bonding to dentin only in the bottom region. Moreover, the upward pull is boosted by the position of the light tip closer to the occlusal outer area of the cavity, leading to its faster polymerization than that at the cavity floor, 22,23 and subsequently resulting in immobilization of the resin matrix in the top composite sooner than in the bottom composite. 24-26 It is noteworthy to mention that scattered areas of bonding and gaps could coexist within the same restoration. 27
It is well understood that bulk-fill resin composites

were introduced in the dental market for their easy placement in cavity preparations as one piece using the bulk filling technique which saves much of the chairside time. However, this technique is reported to cause more axial than lateral shrinkage displacement in the top composite region and to generate more axial stresses which result in debonding at the pulpal floor and gap formation, leading to persistent postoperative sensitivity and pain. 1,5-7,10-14
As a solution, the semi-split bulk filling technique is presented for modifying the bulk filling technique by using an additional step which needs a little extra chairside time. This technique is based on creating a diagonal gap into a bulk of 4mm increment of bulk-fill resin composite, prior to light curing. This gap is 1.5mm wide and extends for a depth of 2mm in the top composite region splitting it into two equal segments. (Fig.2-A) The rationale for the presented technique is that the created diagonal gap would enable, through its adhesion-free surfaces, each composite segment to undergo more lateral than axial shrinkage displacement, in contrast to the more axial than lateral shrinkage displacement which occurs in composite bulk when using bulk fill technique. The outward displacement is expected to exert a lateral pull on each composite segment in opposite direction away from the gap center and towards the bonded cavity walls. The outward displacement of each segment in opposite direction is anticipated to greatly relieve the polymerization shrinkage stress and preserve the marginal and internal gap formation in cavity walls, resulting in volume reduction of each segment and diagonal gap widening. (Fig.2-B) Furthermore, the created diagonal gap is expected to disable the less occurring axial displacement from gaining strength through bonding to enamel and dentin in the top composite region and exerting upward pull on the bottom composite region, preventing/ minimizing its debonding away from the pulpal wall and forming a pulpal gap, in contrast to that which occurs in composite bulk when using bulk fill technique. (Fig.3-A)
Following the light curing of the segmented composite bulk, the diagonal gap is filled with the same bulk-fill resin composite and light cured, (Fig. 3-B). Considering the small composite volume used for filling the diagonal gap, the generating shrinkage stress is judged to be unable to cause
deleterious effects on tooth enamel, composite resin, and/or adhesive interfaces.
There are variations in the number of diagonal gaps and depth between the presented technique and the original split-increment technique. In the presented technique, the gap extends halfway for a depth of 2mm into the 4mm thick composite bulk, whereas in the original split-increment technique 28, it extends into the full thickness of each of the 2mm increments.
(Fig. 4) In the presented technique, the reason for not extending the gap into the full depth of 4mm thick increment is that the diagonal splitting created in the top composite minimizes its axial displacement and greatly decreases the likelihood of exerting an upward pull on the bottom composite. As for the number of diagonal gaps, only one diagonal gap is created into the single composite bulk in the presented technique, whereas two gaps are created in the original technique (Fig. 4). The creation of two diagonal gaps in the presented technique is considered unnecessary because of the generation of lower polymerization shrinkage stress in most bulkfill composites, according to manufacturers, as compared to that developed in the conventional resin composites used in the original technique. Several studies 15,29,30 reported that bulkfill resin composites resulted in higher rates of postoperative sensitivity as compared to conventional composite resins and was attributed to pulpal gap formation beneath the composite restoration. The pulpal gap formation is attributed to postoperative sensitivity which fills with dentinal fluid. This fluid undergoes contraction or expansion by cold or hot stimuli, resulting in its sudden movement in the dentinal tubules which makes postoperative sensitivity persistent and causes pain. 29 It has also been reported that bulk-fill flowable composites also resulted in gap formation over the internal walls of the restored cavities. 30
The restorative techniques, along with some other factors were reported to affect the shrinkage stress generation, debonding, and postoperative tooth sensitivity, as well as microleakage, and secondary caries. 1 The original split-increment technique, as compared to the oblique layering technique, significantly minimized microleakage in Class V silorane-based resin composite restorations. 31 Also, it had the least microleakage




• Excellent adhesion
• Precise marginal fit
• Secure and quick bonding (self-adhesive)
• Almost





Source: Prof. Dr. Jürgen Manhart, Munich / Germany
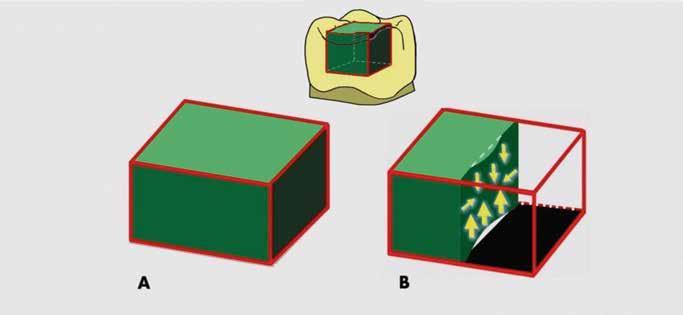
Figure 1: The bulk filling technique for placing a single composite bulk. (a) A large occlusal bulk fill resin composite restoration. (b) A sectional view, illustrating more axial than lateral shrinkage displacement and more upward axial displacement along with gap formation at pulpal floor.
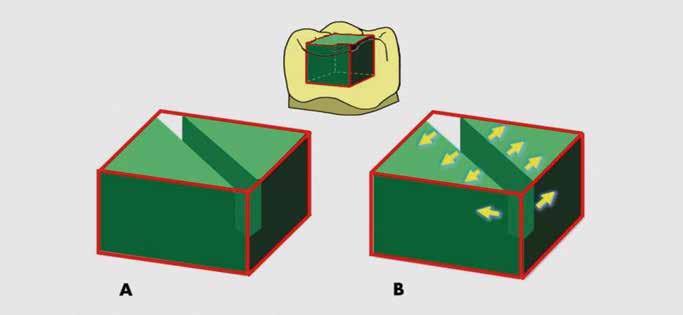
Figure 2: The semi-split bulk filling technique using a single composite bulk; (a) Prior to light curing, a 2 mm deep diagonal gap created in composite bulk; (b) Upon light curing, each composite segment undergoes lateral shrinkage displacement from the gap center outwards, resulting in volume reduction of each segment and diagonal gap widening.
Standardize and simplify your SLX® Clear Aligner cases, reducing total treatment time and the number of aligners required
The Carriere® Motion 3D™ Appliance is used at the beginning of treatment for rapid A/P correction prior to braces or aligners when there are no competing forces operating, and patient compliance is at its highest. By resolving the most difficult part of treatment first, you can achieve an ideal Class I platform in 3 to 6 months, which can then shorten overall treatment time by up to 6 months with SL X 3D Brackets or SLX Clear Aligners.

Employing SAGITTAL FIRST ™ also means many fewer trays and simple, ��-minute bonding is perfect for same-day starts. 3 — 6 MONTHS*

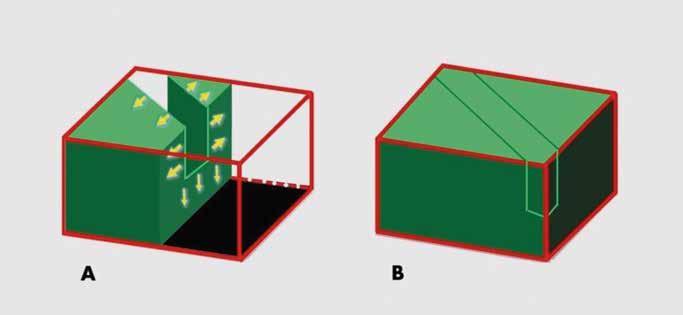
Figure 3: The semi-split bulk filling technique; (a) A sectional view, illustrating more lateral than axial shrinkage displacement of the top composite, resulting in no gap formation at pulpal floor; (b) Diagonal gap filled with the same composite, and light cured.
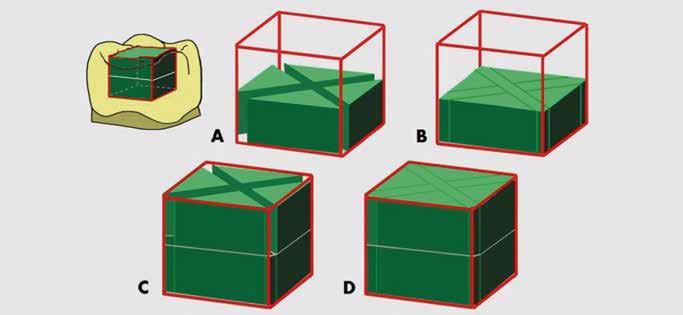
Figure 4: The original split-increment technique using two increments of conventional composite resin; (a) Prior to light curing, two diagonal gaps are created in first composite increment, and light cured; (b) Diagonal gaps filled using the same composite resin, and light cured; (c and d) Diagonal gaps in the second increment created and filled, as in the first increment.



• Plug and play micromotor, easy to install
• Connects to your chair’s air supply
• Cost-efficient conversion to electric
• Perfect for speed increasing handpieces
• Internal spray and LED
• Brushless endo motor with inbuilt apex locator
• 6:1, 360° rotatable contra-angle head.
• Presets for many file types incl. EdgeEndo.
• Small head diameter (8mm) and height (9.7mm): more visibility during operation
• Speed range: 100-2500rpm
• Torque range: 0.4Ncm-5.0Ncm


• 1:5 red band contra-angle
• Anti-retraction valve
• Less aerosol generation
• Ceramic bearings
• Fibre-optics and quadruple spray
• Titanium body with PVD coating

at occlusal and gingival margins in Class II composite restorations, followed by centripetal and oblique techniques. 32 Moreover, the original technique exhibited lower degrees of microleakage at the occlusal and gingival margins of Class V, as compared to the oblique and occlusogingival incremental techniques. 33 Furthermore, the split-increment technique and the group with fiber inserts in gingival increment technique showed significantly lower microleakage at gingival margins in Class II restored with a nanocomposite resin when compared to bulk insertion, oblique, centripetal, and flowable composite techniques. 34
Based on the results of the research studies conducted on the original split-increment technique, it is expected that the presented semi-split bulk filling technique would be able to minimize the shrinkage stress and decrease the incidence of pulpal gap formation beneath the large occlusal bulk-fill resin composite restorations.
A research study is currently underway to investigate the effect the presented technique on reducing shrinkage stresses and pulpal gap formation in large occlusal bulk-fill resin composite restorations.
Summary
The use of the presented semi-split bulk filling technique for restoring large occlusal bulk-fill resin composite restorations can minimize shrinkage stress and prevent or decrease the incidence of pulpal gap formation beneath the restoration. This would consequently result in less occurrence of persistent postoperative sensitivity and pain.
References
1. Al Sunbul H, Silikas N, Watts DC. (2016) Polymerization shrinkage kinetics and shrinkagestress in dental resin-composites. Dent Mater. 32(8): 998-1006.
2. Engelhardt F, Hahnel S, Preis V, et al. (2016) Comparison of flowable bulk-fill and flowable resin-based composites: an in vitro analysis. Clin Oral Invest. 20(8): 2123–2130.
3. Ilie N, Schoner C, Bucher K, et al. (2014)
An in-vitro assessment of the shear bond strength of bulk-fill resin composites to permanent and deciduous teeth. J Dent.
42(7): 850–855.
4. Tauböck TT, Jäger F, Attin T. (2019) Polymerization shrinkage and shrinkage force kinetics of high- and low-viscosity dimethacrylate- and ormocer based bulk-fill resin composites. Odontology. 107(1): 103-110
5. Gonçalves F, Campos LM, RodriguesJúnior EC, et al. (2018) A comparative study of bulk- fill composites: degree of conversion, post-gel shrinkage and cytotoxicity. Braz Oral Res. 32: e17-e26.
6. Menees TS, Lin CP, Kojic DD, et al. (2015) Depth of cure of bulk fill composites with monowave and polywave curing lights. Am J Dent. 28(6): 357-361.
7. Boaro LCC, Lopes DP, de Souza ASC, et al. (2019) Clinical performance and chemicalphysical properties of bulk fill composites resin —a systematic review and metaanalysis. Dent Mater. 35(10): e249–e264.
8. Stansbury JW, Trujillo-Lemon M, Lu H, Ding X, et al. (2005) Conversion-dependent shrinkage stress and strain in dental resins and composites. Dent Mater. 21(1): 56–67.
9. Watts DC. (2005) Reaction kinetics and mechanics in photo-polymerised networks. Dent Mater. 21(1): 27–35
10. Kim HJ, Park SH. (2014) Measurement of the internal adaptation of resin composites using micro-CT and its correlation with polymerization shrinkage. Oper Dent. 39(2): e57– e70.
11. Souza-Junior EJ, de Souza-Regis MR, Alonso RC, et al. (2011) Effect of the curing method and composite volume on marginal and internal adaptation of composite restoratives. Oper Dent. 36: 231–238.
12. Manhart J., Chen H.-Y., Hickel R. (2010) Clinical evaluation of the posterior composite Quixfil in class I and II cavities: 4-year followup of a randomized controlled trial. J Adhes Dent. 12(3):237-243.
13. Correia A., Jurema A., Andrade M.R., et al. (2020) Clinical evaluation of noncarious cervical lesions of different extensions restored with bulk-fill or conventional resin composite: preliminary results of a randomized clinical



The easy-to-use HALO sectional matrix system allows you to create beautiful, anatomically contoured composite restorations in less time.


trial. Oper Dent. 45(1): E11–20.
14. Canali G.D., Ignácio S.A., Rached R.N., et al. (2019) One-year clinical evaluation of bulk- fill flowable vs. regular nanofilled composite in non-carious cervical lesions. Clin Oral Investig. 23(2):889–897.
15. Park J, Chang J, Ferracane J, et al. (2008) How should composite be layered to reduce shrinkage stress: Incremental or bulk filling? Dent Mater. 24(11):1501–1505.
16. AbbasG, Fleming G, Harrington E, et al. (2003) Cuspal movement and microleakage in premolar teeth restored with a packable composite cured in bulk or in increments. J Dent Res. 31(6): 437-444.
17. Li H, Li J, Yun X, Liu X, et al. (2011) Non-destructive examination of interfacial debonding using acoustic emission. Dent Mater. 27(10):964-971.
18. Novaes JB Jr, Talma E, Las Casas EB, et al. (2018) Can pulpal floor debonding be detected from occlusal surface displacement in composite restorations? Dent Mater. 34(1): 161- 169.
19. Sun J, Eidelman N, Lin-Gibson S. (2009) 3D mapping of polymerization shrinkage using X- ray micro-computed tomography to predict microleakage. Dent Mater. 25(3): 314-320.
20. Chiang YC, Rosch P, Dabanoglu A, et al. (2010) Polymerization composite shrinkage evaluation with 3D deformation analysis from microCT images. Dent Mater. 26(3): 223-c231.
21. Cho E, Sadr A, Inai N, et al. (2011) Evaluation of resin composite polymerization by three- dimensional micro-CT imaging and nanoindentation. Dent Mater. 27(11): 10701078.
22. Papadogiannis D, Kakaboura A, Palaghias G, et al (2009). Setting characteristics and cavity adaptation of low-shrinking resin composites. Dent Mater. 25(12): 1509-1516.
23. Sato T, Miyazaki M, Rikuta A, et al. (2004) Application of the laser speckle-correlation method for determining the shrinkage vector of a light-cured resin. Dent Mater J. 23(3): 284-290.
24. Shortall AC, Palin WM, Burtscher P. (2008) Refractive index mismatch and monomer
reactivity influence composite curing depth. J Dent Res. 87(1): 84-88.
25. Van Ende A, Van de Casteele E, Depypere M, et al. (2015) 3D volumetric displacement and strain analysis of composite polymerization. Dent Mater. 31(4): 453-461.
26. Van Meerbeek B, Peumans M, Poitevin A, et al. (2010) Relationship between bondstrength tests and clinical outcomes. Dent Mater. 26(2): e100-e121.
27. Bortolotto T, Bahillo J, Olivier Richoz O, et al. (2015) Failure analysis of adhesive restorations with SEM and OCT: from marginal gaps to restoration loss. Clin Oral Invest. 19(8):1881-1890.
28. Hassan K, Khier S. (2005) Splitincrement horizontal layering: A simplified placement technique for direct posterior resin restorations. Gen Dent. 53(6): 406409.
29. Brännström M. (1984) Communication between the oral cavity and the dental pulp associated with restorative treatment. Oper Dent. 9(2): 57-68.
30. Furness A, Tadros MY, Looney SW, et al. (2014) Effect of bulk/incremental fill on internal gap formation of bulk-fill composites. J Dent. 42(4): 439-449.
31. Usha HL, Kumari A, Mehta D, et al. (2011) Comparing microleakage and layering methods of silorane-based resin composite in Class V cavities using confocal microscopy: An in vitro study. J Conserv Dent. 14(2): 164168.
32. Nadig RR, Bugalia A, Usha G, et al. (2011) Effect of four different placement techniques on marginal microleakage in class ii restorations: an in vitro study. World J Dent. 2(2): 111-116.
33. Khier S, Hassan K. (2011) Efficacy of composite restorative techniques in marginal sealing of extended class v cavities. International Scholarly Research Network. (ISRN) Dentistry. 2011:80197.
34. Bugalia A, Yujvender, Bramta N, et al. (2015) Effect of placement techniques, flowable composite, liner and fibre inserts on marginal microleakage of Class II composite restorations. J Evidence Based Med & Healthcare. 2(11): 4779-4787.



• EdgeEndo®’s #1 selling file system - globally
• Leading file used by Endodontists
• Proprietary heat treatment process
- FireWire™ NiTi Alloy improves strength and flexibility
• Available in .04 and .06 Constant Taper
- Variable Pitch
• Maximum flute diameter 1mm allows for minimally invasive preparation
• Parabolic Cross Section non-cutting tip
- Maximizes file cutting efficiency
• Reduced handle length for increased posterior access
• ISO tip size 17-45
• Available lengths: 21, 25 & 29 mm


The preventive effect of glass ionomer restorations on new caries formation: A systematic review and meta-analysis


PrevalenceandRiskofDentalErosioninPatientswith ,SvetlanaV.Lyamina , MoscowStateUniversityofMedicineandDentistryNamedafterA.I.Evdokimov,127473Moscow,Russia; mail@msmsu.ru(O.O.Y.);igormaev@rambler.ru(I.V.M.);nataly0088@mail.ru(N.I.K.);svlvs@mail.ru(S.V.L.); phlppsokolov@gmail.com(F.S.S.);estetstom.fpdo@gmail.com(M.N.B.);p.bely@ncpharm.ru(P.A.B.); Aim:Thepresentpaperaimstosystematizedataconcerningtheprevalenceandriskof dentalerosion(DE)inadultpatientswithgastroesophagealrefluxdisease(GERD)comparedto controls.Materialsandmethods:Coreelectronicdatabases,i.e.,MEDLINE/PubMed,EMBASE, Cochrane,GoogleScholar,andtheRussianScienceCitationIndex(RSCI),weresearchedforstudies assessingtheprevalenceandriskofDEinadultGERDpatientswithpublicationdatesrangingfrom 1January1985to20January2022.Publicationswithdetaileddescriptivestatistics(thetotalsample sizeofpatientswithGERD,thetotalsamplesizeofcontrols(ifavailable),thenumberofpatients withDEinthesampleofGERDpatients,thenumberofpatientswithDEinthecontrols(ifavailable)) wereselectedforthefinalanalysis.Results:Thefinalanalysisincluded28studiesinvolving4379 people(2309GERDpatientsand2070controlsubjects).ThepooledprevalenceofDEwas51.524% (95CI:39.742–63.221)inGERDpatientsand21.351%(95CI:9.234–36.807)incontrols.Anassociation wasfoundbetweenthepresenceofDEandGERDusingtherandom-effectsmodel(OR5.000,95%CI: =79.78%)comparedwithcontrols.Whenanalyzingstudiesthatonlyusedvalidated instrumentalmethodsfordiagnosingGERD,alongsidevalidatedDEcriteria(studiesthatdidnot specifythemethodologiesusedwereexcluded),asignificantassociationbetweenthepresenceofDE =85.14%).Conclusion:Themeta-analysis demonstratedthatDEisquiteoftenassociatedwithGERDandisobservedinabouthalfofpatients
Kelsey XingyunGe,
Faculty of Dentistry, The University of Hong Kong, 34 Hospital Road, Hong Kong SAR, China
RyanQuock,
,SvetlanaV.Lyamina , MoscowStateUniversityofMedicineandDentistryNamedafterA.I.Evdokimov,127473Moscow,Russia; mail@msmsu.ru(O.O.Y.);igormaev@rambler.ru(I.V.M.);nataly0088@mail.ru(N.I.K.);svlvs@mail.ru(S.V.L.); phlppsokolov@gmail.com(F.S.S.);estetstom.fpdo@gmail.com(M.N.B.);p.bely@ncpharm.ru(P.A.B.); Aim:Thepresentpaperaimstosystematizedataconcerningtheprevalenceandriskof dentalerosion(DE)inadultpatientswithgastroesophagealrefluxdisease(GERD)comparedto controls.Materialsandmethods:Coreelectronicdatabases,i.e.,MEDLINE/PubMed,EMBASE, Cochrane,GoogleScholar,andtheRussianScienceCitationIndex(RSCI),weresearchedforstudies assessingtheprevalenceandriskofDEinadultGERDpatientswithpublicationdatesrangingfrom 1January1985to20January2022.Publicationswithdetaileddescriptivestatistics(thetotalsample sizeofpatientswithGERD,thetotalsamplesizeofcontrols(ifavailable),thenumberofpatients withDEinthesampleofGERDpatients,thenumberofpatientswithDEinthecontrols(ifavailable)) wereselectedforthefinalanalysis.Results:Thefinalanalysisincluded28studiesinvolving4379 people(2309GERDpatientsand2070controlsubjects).ThepooledprevalenceofDEwas51.524% (95CI:39.742–63.221)inGERDpatientsand21.351%(95CI:9.234–36.807)incontrols.Anassociation wasfoundbetweenthepresenceofDEandGERDusingtherandom-effectsmodel(OR5.000,95%CI: =79.78%)comparedwithcontrols.Whenanalyzingstudiesthatonlyusedvalidated instrumentalmethodsfordiagnosingGERD,alongsidevalidatedDEcriteria(studiesthatdidnot specifythemethodologiesusedwereexcluded),asignificantassociationbetweenthepresenceofDE =85.14%).Conclusion:Themeta-analysis demonstratedthatDEisquiteoftenassociatedwithGERDandisobservedinabouthalfofpatients
- Faculty of Dentistry, The University of Hong Kong, 34 Hospital Road, Hong Kong SAR, China
- Department of Restorative Dentistry and Prosthodontics, School of Dentistry, The University of Texas Health Science Center at Houston, TX, United States
Chun-HungChu, Faculty of Dentistry, The University of Hong Kong, 34 Hospital Road, Hong Kong SAR, China
Ollie YiruYu
Faculty of Dentistry, The University of Hong Kong, 34 Hospital Road, Hong Kong SAR, China
Abstract
Objective
To investigate the effectiveness of glass ionomer cement (GIC) restorations on preventing new caries in primary or permanent dentitions compared with other types of restorations.
Data
Randomized controlled clinical trials evaluating caries experience increment or caries incidence in patients with GIC restorations, including conventional GIC (CGIC) and resin-modified GIC (RMGIC) restorations, were included.
Sources
A systematic search of publications in English was conducted in PubMed/ Medline, Web of Science, Cochrane, and Scopus databases.
Study selection/results
This review included 10 studies reporting caries preventive effect of GIC restorations and selected 5 studies for meta-analysis. Patients with GIC restorations showed lower caries incidence compared with other restorations in primary and permanent dentition [RR=0.67, 95% CI:0.55–0.82, p < 0.0001]. Patients with CGIC restorations showed lower caries incidence compared with amalgam restorations [RR=0.57, 95% CI:0.43–0.76, p = 0.0001] and RMGIC restorations [RR=0.70, 95% CI:0.56–
0.87, p = 0.002], but no statistical difference with composite resin restorations [RR=0.73, 95% CI:0.51–1.04, p = 0.08] in primary dentition. Patients with RMGIC restorations showed no statistical differences of caries incidence compared with composite resin restorations in primary and permanent dentition [RR=0.83, 95% CI:0.56–1.22, p = 0.33].
GIC restorations presented a better preventive effect on new caries than other restorations did in primary and permanent dentitions. CGIC restorations presented a better caries preventive effect on new caries than RMGIC and amalgam restorations in primary dentitions did. RMGIC restorations showed similar preventing effect on new caries with composite resin restorations in primary and permanent dentitions.
This review affirmed the potential of GIC in preventing new caries development in the dentition.
Glass ionomer cement, Resinmodified glass ionomer cement, Caries prevention, Fluoride, Systematic review


Dental caries, or tooth decay, is one of the most common chronic diseases worldwide [1] . According to the World Health Organization’s (WHO) report, dental caries affects 60–90% of schoolchildren globally and almost all adults [2]. Dental caries can occur throughout life in both primary and permanent dentitions. It can damage the tooth crown and expose the root surfaces in a later lifetime [3]. Untreated caries can cause pain, develop into apical periodontitis, form abscesses and even infection [4]. A survey reported that pain and discomfort due to untreated dental caries were found in 18% of 5–6-year-olds and 64% in older adults [5] Different types of direct restorative materials are used to restore teeth affected by dental caries. Glass ionomer cement (GIC), including conventional glass ionomer cement (CGIC) and resin-modified glass ionomer cement (RMGIC), are commonly used as dental restorative materials [6]. The Government Chemist Laboratory (London, UK) developed CGIC in 1969. They are used as restorative materials, liners and bases, fissure sealants and bonding agents [7]. CGIC has several advantages, including adhesion to tooth structures, biocompatibility, long-lasting fluoride release and simple clinical operation [6,8]. However, CGIC also has disadvantages, such as moisture sensitivity, low mechanical strength and compromised aesthetics [9]. To overcome the problems traditionally associated with the CGIC materials [10], Mitra introduced RMGIC as evolution of CGIC in 1989 [11]. RMGIC are used for numerous specific applications in clinical dentistry, notably as liners/bases, luting agents and restorative materials [12]. The RMGIC maintain the clinical advantages of the CGIC, such as the fluoride release and simplicity in clinical operation. They are more aesthetic than CGIC [13]
Based on laboratory data regarding sustained fluoride release, CGIC and RMGIC have been associated with caries prevention. An in vitro study showed that CGIC or RMGIC restorations increased the fluoride uptake in adjacent tooth structure [14]. Previous in vitro studies also showed that interproximal caries-like lesions adjacent to CGIC restorations presented a higher degree of remineralisation compared with those
of resin-based restorations [15]. Because the fluoride can diffuse through the saliva in the oral cavity, CGIC or RMGIC restorations may promote the remineralisation in the other teeth in the dentition [16]. Therefore, CGIC and RMGIC may prevent new caries formation in the dentition.
Although in vitro studies have demonstrated the potential effect of GIC restorations on caries prevention, clinical evidence of the effect of GIC restorations, including CGIC or RMGIC restorations, in preventing new caries formation is limited. A systematic quantitative evaluation of the available evidence on the preventive effect of GIC restorations, including CGIC or RMGIC, on new caries formation has never been undertaken. Therefore, this review aimed to evaluate the preventive effect of GIC restorations, including CGIC or RMGIC restorations, on new caries compared with other types of dental restorations.
2.1.
This review answered the research question of, ‘What is the effectiveness of glass ionomer cement (GIC), including conventional glass ionomer cement (CGIC) restorations and resin-modified glass ionomer cement (RMGIC) restorations, on preventing new caries formation in permanent and primary dentitions compared with other types of dental restorations?’. This systematic review was written following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Statement [17]. This systematic review and meta-analysis was registered with the International Prospective Register of Systematic Reviews (PROSPERO Registration ID: 302,578).
2.2.
A comprehensive literature search was conducted on May 15, 2022, to identify the available studies evaluating the prevention of caries lesions in GIC restorations, with no limits of publication year. The literature search was conducted in four databases, including PubMed/ Medline, Web of Science, Cochrane and Scopus. The search strategy was developed as follows. 1 “demineralization” OR “tooth demineralization” “teeth demineralization” OR “caries” “carious”

OR “tooth decay” OR “teeth decay” OR “dental caries” OR “caries susceptibility”
2 “glass ionomer cement” OR “glass ionomer” OR “GIC” “glass polyalkenoate cement” OR “glass-ionomer cement” OR “ART” OR “atraumatic restorative procedure”.
3 “#1″ AND “#2″
Two independent reviewers (KXG & OYY) conducted the study selection. Both authors independently screened titles, compared findings and included full texts after deduplication. The third author (CHC) was consulted when there was disagreement. Studies with consensus being reached through discussion were included.
This review used participants, intervention, comparison, outcome and type of study (PICOT) to formulate questions in evidencebased practice. The inclusion criteria were developed based on PICOT strategy. The PICOT strategy for the inclusion criteria is summarized in Table 1.
Table 1. The PICOT (participants, intervention, comparison, outcome and type of study) strategy used for selection of publications in the review.
The inclusion criteria of the studies were:
Participants Studies with participants of all ages were included
Intervention GIC restorations including CGIC or RMGIC restorations for caries treatment
Comparison CGIC restorations compared with other types of dental restorations
RMGIC restorations compared with other types of dental restorations
Outcome
Type of study
1 To be the randomized controlled clinical trials.
2 To investigate GIC for restorations application in patients.
3 To evaluate the caries incidence or caries experience increment. Caries incidence refers to the rate of new caries development in the adjacent teeth after the restoration. The development of secondary caries was not
Caries incidence Caries experience increment
Randomized controlled clinical trial (RCT)
included. Caries experience increment refers to DMFT/DMFS (decayed, missing, and filled teeth/surfaces in permanent teeth) increment or dmft/dmfs (decayed, missing, and filled teeth/surfaces in primary teeth) increment.
The exclusion criteria of the studies were:
1 To be the in vitro studies, animal studies, reviews, letters to the editor, case report/series and observational studies.
No need for forceps.
The foil is pre-mounted in a sturdy plastic frame.
No ink on your fingers. The foil is covered on both sides at the grip.
Super thin foil.
The foil is only 8 micron thick and inked on both sides. Available in blue or red.


Protective strip Easily removed before use.

TrollFoil takes the guesswork out of occlusal adjustments.
The only articulating foil you will ever need!
TrollFoil can be used under a wide variety of clinical situations including wet or dry teeth, limited opening, limited vestibular space, gaggers, and metal and non-metalic restorations. You are able to verify occlusal contacts for both arches from one tooth to an entire quadrant using the mini or the original quadrant size. The double-sided foil is only 8 microns thick, and it has no problem marking wet surfaces, dry surfaces or highly polished surfaces such as cast gold or BruxZir.


For further information please contact your local dealer or Annelie Johansson, Area Sales Manager – Product specialist TrollDental x-ray, Finland, Baltic, East Europe, Greece, Turkey, MENA annelie.johansson@directadental.com www.directadental.com


2 To investigate other types of restorations but did not include the GIC.
3 To investigate GIC for nonrestorative application in clinic (i.e., fissure and sealant, liners/bases or cement).
4 To output data that did not contain the caries incidence or caries experience increment.
The reviewers collected the required information of the eligible studies. For each included study, the following data were systematically extracted from each paper:
• Publication details: authors name, publication year and duration
•Tooth characteristics: type of dentition and number of restorations for each material
•Outcome information: assessment, outcome measure, and main findings
All the data obtained from patients with GIC restorations were extracted to Group CGIC or RMGIC in this review, regardless of the original study design.
The assessment of risk of bias to longitudinal trials assessment was performed according to bias assessment forms (Cochrane Handbook for Systematic Reviews of Interventions 5.4.1).
The Cochrane ‘risk of bias’ instrument was used to assess the risk of bias. Three independent reviewers performed this evaluation. Disagreements between estimators were resolved through discussion until consensus was reached. The risk of bias was classified into three categories:
(a) Low risk of bias: all domains were marked as ‘low risk’.
(b) Moderate risk of bias: no domain was marked as ‘high risk’; one or more domains were coded as ‘unclear risk’.
(c) High risk of bias: one or more domains were marked as ‘high risk’.
The participants’ caries experience increment in DMFT/DMFS and dmft/dmfs was based only on the first and last measurements. The DMFT/DMFS and dmft/dmfs increments were calculated by subtracting the results at baseline from the results at follow-up.
Meta-analysis of the caries incidence after GIC restorations, including CGIC or RMGIC restorations, was carried out. The Review Manager 5.4.1 was used for conducting the meta-analysis. Heterogeneity was assessed via the I2 statistic on the level of α=0.10. If there was considerable or substantial heterogeneity (I2>50%), a random-effects mode was adopted; otherwise, a fixed-effects model was used. The results of the intervention effect were presented as risk ratio (RR) utilizing 95% confidence intervals (CI). All tests were 2-tailed, and p ≤ 0.05 was considered statistically significant.
A total of 5456 studies was retrieved from the four databases. After subtracting 2486 duplicated studies, 2970 potential studies were identified and screened for inclusion. After screening the titles and abstracts, 2616 studies were excluded. 354 studies were considered potentially relevant and were read for the full text. With the reviewers’ consensus, 10 studies that reported the new caries preventive effect of the GIC restorations were included for this review. Seven of the studies were on CGIC restorations while three were on RMGIC restorations. The details of search procedure are presented in a flowchart (Fig. 1).

Ultimate Interproximal Solution - ContacEZ dental strips for restorative, orthodontic, and laboratory needs. The innovative, single-handed design of ContacEZ Dental Strips offers optimal tactile control and grants easy access to tight anterior and posterior spaces. Flexible strips curve and conform to the natural contours of the teeth, while the central opening offers better visual perception and access for tools. This user and patient-friendly design eliminates gagging and prevents soft tissue irritation.
ContacEZ Restorative Strips System are designed to achieve ideal proximal contacts and complete marginal sealing as well as removing subgingival overhangs and more.
The ContacEZ IPR strips makes it easy to perform safe and stress-free interproximal reduction in connection with orthodontic treatment.
5 Reasons – to switch to ContacEZ Strips
• Optimal tactile control – prevent cutting lips and gums
• Built-in flexibility conforms to natural contours
• Ergonomic design eliminates hand fatigue
• Better visibility with central opening
• Autoclavable


5,456 studies were retrieved in four databases
• PubMed (Medline): 1,745
• Scopus: 1,599
• Cochrane: 994
• Web of Science: 1,118
2,486 duplicate studies were excluded
2,970 potential studies identi ed and screened for inclusion
Step 1 - Titles and abstracts were reviewed
2,616 studies were excluded, including
• studies not relevant (n=2,118)
• reviews, case report or laboratory studies (n=273)
• studies did not investigate GIC restorations (n=225)
354 studies were retrieved for full text evaluation
Step 2 - Full-lenght articles were retrieved
344 studies were excluded, including
• studies did not investigate caries preventinve effect (n=58)
• studies on GIC sealants, liner, base or cement (n=62)
• studies on preventive effect on secondary caries (n=224)
10 studies reported the new curies preventive e ect of the GIC restorations
7 studies reported the new caries preventive e ect of the CGIC restorations
3 studies reported the new caries preventive e ect of the RMGIC restorations
3 studies were eligible for CGIC meta-analysis
2 studies were eligible for RMGIC meta-analysis
4 studies in GIC were eligible for meta-analysis
Fig. 1. Flow diagram of the systematic review. GIC: glass ionomer cement (including CGIC and RMGIC); CGIC: conventional glass ionomer cement; RMGIC: resin-modified glass ionomer cement.





3.2.1.
Seven included studies published between 1997 and 2020 investigated the preventive effect of the CGIC restorations on new caries. The included studies involved 2655 CGIC restorations, 2182 participants, aged from 2 to 74 years old. The average follow-up period of the included studies was 3.3 years. One study was performed in permanent dentition, published in 2003. The study involved 417 CGIC restorations in 81 participants [18]. Six studies were performed in primary dentition, published between 1997 and 2020. These studies involved 2238 CGIC restorations in 2101 participants, aged from 2 to 13 years [19], [20], [21], [22], [23], [24].
3.2.2.
Three studies were included for the RMGIC restorations, published between 2000 and 2004 [25], [26], [27]. These studies investigated 328 RMGIC restorations in 271 participants, aged from 4 to 53 years. The average follow-up period of the included studies was 1.7 years. One study, published in 2000, had the outcome assessment in permanent dentition [27]. This study involved 114 RMGIC restorations and 106 composite resin restorations in 118 participants, aged from 4 to 53 years. Two studies, published in 2004, had the outcome assessment in primary dentition [25,26]. These studies investigated on 214 RMGIC restorations and 41 composite resin
et al. 2000 (Meta-analysis)
Kotsanos et al. 2004 (Meta-analysis)
Qvist et al. 1997
ysis)
Foley et al. 2004
(Meta-analysis)
Qvist et al. 2004 (Meta-analysis)
restorations on 153 participants, aged from 4 to 15 years. The main characteristics of the studies included in the study are presented in Table 2.
Table 2. Characteristics of included randomized controlled clinical trials studies. CGIC: conventional glass ionomer cement; RMGIC: resin-modified glass ionomer cement. Main findings showed the results of the outcome measure for each study.
















Among the 10 included RCTs, 7 studies had one or more ‘high’ ratings due to the method about the blinding of participants and outcome
Faley et al.(2004)
Kotsanos et al.(2004)
Moura et al.(2020)
Arrow et al.(2015)
Bolgul et al.(2004)
Qvist et al.(2004)
Arrow et al.(2016)
Qvist et al.(1997)
Vilkinis et al.(2000)
Zanata et al.(2003) Random sequence generation (selection bias) Allocation concealment (selection bias) Blinding of participants and personnel (performance bias) Blinding of outcome assessment (detection bias) Incomplete outcome data (attrition bias) Selective reporting (reporting bias) Other bias
Fig. 2. Risk of bias summary: review authors’ judgements about each risk of bias item for each included study.
assessment. The statement of the method of allocation concealment was not reported in 4 studies. Four studies had ‘unclear’ ratings due to lack of information. The risk of bias assessment ratings for each study are shown in Fig. 2, Fig. 3 .
(Random sequence generation (selection bias (Allocation concealment (seleciton bias (Blinding of participants and personnel (performance bias (Blinding of outcome assessment (detection bias (Incomplete outcome data (attrition bias (Selective reporting (reporting bias Other bias
Fig. 3. Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies.
Zanata et al. assessed the caries experience increment by analysing DMFS score in the dentition with CGIC restorations compared with that of zinc oxide-eugenol (ZOE) and composite resin restorations. The results showed that permanent dentitions with CGIC restorations showed a lower increase of the DMFS compared with dentitions with ZOE or composite resin restorations [18]
Three studies assessed the caries incidence by bitewing radiographs in the primary dentition with CGIC restorations and compared with dentitions with amalgam [24], RMGIC [22] or composite resin restorations [23]. These studies showed that primary dentitions with CGIC restorations showed a lower caries incidence compared with amalgam, RMGIC and composite resin restorations.
Three separate studies investigated the caries experience increment by analysing dmft/ dmfs score in the primary dentitions with CGIC restorations. No other types of restoration were included. These studies investigated the dmft/ dmfs increment after CGIC restorations with different clinical protocols, such as the atraumatic


restorative treatment (ART), standard care approach and minimum intervention dentistry (MID-ART) [19], [20], [21]. The results suggested the use of the CGIC by ART technical may be an effective option for managing caries in preschool-aged children.
Vilkinis et al. investigated the caries incidence in the permanent dentitions with RMGIC restorations compared with composite resin restorations. Main findings showed that RMGIC and composite resin had a 15.9% and 10.0% caries incidence respectively. The results showed that no statistical significant differences between the RMGIC restorations and composite resin restorations were observed with respect to the caries incidence [27].
Bolgul et al. investigated caries experience increment by dmft score in the primary dentition with RMGIC restorations and reported the dmft differences between different controlled levels of the insulin-dependant diabetes mellitus (IDDM) patients [26]. The results showed that the dmft
Study or Subgroup
1.1.1 Amalgam
Qvist et al. (1997)
Subtotal (95% CI)
Heterogeneity: Not applicable
Test for overall effect: Z= 3.83 (P= 0.0001)
1.1.2 Composite resin
Foley et al. (2004)
Kotsanos et al. (2004)
Vilkinis et al. (2000)
Subtotal (95% CI)
score decreased in all the IDDM patients’ primary dentition with RMGIC restorations. Kotsanos and Arizos evaluated the caries incidence by radiographs in the primary dentitions with RMGIC restorations compared with composite resin restorations. The results showed no statistically significant differences between the RMGIC and composite resin restorations with respect to the caries incidence [25].
Five studies were included for the meta-analysis. Three studies were on CGIC restorations and two were on RMGIC restorations. We also pooled the data of CGIC and RMGIC restorations to analyse the caries preventive effect of GIC restorations. Four out of the five studies were included the meta-analysis on GIC restorations. One study was not included in the meta-analysis of GIC restorations, because this study compared the caries preventive effect of CGIC restorations with that of RMGIC restorations, not with other types of restorations [22]. The main results of the metaanalysis are presented in Fig. 4, Fig. 5, Fig. 6, Fig. 7, Fig. 8, Fig. 9.
[0.43,
[0.43, 0.76]
-0.3198 0.1833 29.0% 0.73 [0.51, 1,04]
0.2114
0.87 [0.57, 1.32]
0.5539 3.2% 0.58 [0.20, 1.72] 53.9% 0.77 [0.59, 1.00]
Heterogeneity: Chi2 - 0.69, df - 2 (P = 0.71): 12 - 0%
Test for overall effect: Z = 1.94 (P = 0.05)
Total (95% CI)
Heterogeneity: Chi2 - 2.93, df - 3 (P = 0.40): 12 - 0%
Test for overall effect: Z = 4.02 (P < 0.0001)
Test for subgroup differences: Chi2 - 2.24, df - 1 (P = 0.13): 12 - 55.3% 100.0% 0.67 [0.55, 0.82]

Fig. 4. Meta-analysis of caries incidence in all dentitions with all GIC restorations vs amalgam or composite restorations. GIC: glass ionomer cement.
The preventive effect of glass ionomer restorations on new caries formation: A systematic review and meta-analysis


Study or Subgroup
2.1.1 2 years
Kotsanos et al. (2004)
Vilkinis et al. (2000)
Subtotal (95% CI)
-0.1398 0.2114 40.4% 0.87 [0.57, 1.32] -0.5428 0.5539 5.9% 0.58 [0.20, 1.72] 46.3% 0.83 [0.56, 1.22]
Heterogeneity Chi2 = 0.46, df = 1 (P = 0.50); I2 = 0%
Test for overall effect: Z = 1.97 (P = 0.33)
2.1.2 7 years
Foley et al. (2004)
Subtotal (95% CI) -0.3198 0.1833 53.7% 0.73 [0.51, 1,04] 53.7% 0.73 [0.51, 1.04]
Heterogeneity: Not applicable
Test for overall effect: Z = 1.74 (P = 0.08)
Total (95% CI)
Heterogeneity: Chi2 - 0.69, df = 2 (P = 0.71): I2 = 0%
Test for overall effect: Z = 1.94 (P = 0.05)
Test for subgroup differences: Chi2 = 0.23, df = 1 (P = 0.63), I2 = 0% 100.0% 0.77 [0.59, 1.00]
Fig. 5. Meta-analysis of caries incidence in all dentitions with GIC restorations vs composite resin restorations, with defined follow up period. GIC: glass ionomer cement.
Risk Ratio Risk Ratio
Study or Subgroup
log(Risk Ratio)
3.1.1 Amalgam - primary dentition
Qvist et al. (1997)
Subtotal (95% CI)
Heterogeneity : Not applicable
Test for overall effect: Z = 3.83 (P= 0.0001)
3.1.1 Amalgam - permanent dentition
Subtotal (95% CI)
Heterogeneity : Not applicable
Test for overall effect: Not applicable
3.1.3 Composite resin - primary dentition
Foley et al. (2004)
Kotsanos et al. (2004)
Subtotal (95% CI)
SE Weigh IV, Fixed, 95 % CI IV, Fixed, 95 % CI
0.1453
0.57 [0.43, 0.76]
0.57 [0.43, 0.76]
Heterogeneity Chi2 = 0.41, df = 1 (P = 0.52); I2 = 0%
Test for overall effect: Z = 1.75 (P = 0.08)
3.1.3 Composite resin - permanent dentition
Vilkinis et al. (2000)
Subtotal (95% CI)
Heterogeneity : Not applicable Test for overall effect: Z = 0.98 (P = 0.33)
Total (95% CI)
Heterogeneity: Chi2 = 2.93, df = 3 (P = 0.40): I2 = 0%
Test for overall effect: Z = 4.02 (P < 0.0001)
0.67 [0.55, 0.82]
Test for subgroup differences: Chi2 = 2.51, df = 2 (P = 0.28), I2 = 20.4%
Fig. 6. Meta-analysis of caries incidence in dentitions with GIC restorations. Not estimable: no studies were eligible for meta-analysis. CGIC: conventional glass ionomer cement; RMGIC: resinmodified glass ionomer cement; GIC: glass ionomer cement (including CGIC and RMGIC).
• Excellent working time and the setting time is individually adjustable by light-curing
• Immediately packable after placement in the cavity
• No varnish required- fill, polymerise and finish
• No need to condition the dental hard tissue
• Does not stick to the instrument and is easy to model
• Suitable for large cavities
Are you interested in our entire product range and detailed product information? Visit our website or contact us directly!
Material GmbH

Study or Subgroup
4.1.1 RMGIC
Qvist et al. (2004)
Subtotal (95% CI)
Heterogeneity : Not applicable
Test for overall effect: Z = 3.15 (P= 0.002)
4.1.2 Amalgam
Qvist et al. (1997)
Subtotal (95% CI)
Heterogeneity : Not applicable
Test for overall effect: Z = 3.83 (P= 0.0001)
4.1.3 Composite resin
Foley et al. (2004)
Subtotal (95% CI)
Heterogeneity : Not applicable
Test for overall effect: Z = 1.74 (P= 0.08) -0.3542 0.1123 50.7% 0.70 [0.56, 0.87] 50.7% 0.70 [0.56, 0.87] -0.5561 0.1453 30.3%
(95% CI)
Heterogeneity: Chi2 = 1.50, df = 2 (P = 0.47): I2 = 0%
Test for overall effect: Z = 5.11 (P < 0.00001)
1.04]
0.66 [0.57, 0.78]
Test for subgroup differences: Chi2 = 1.50, df = 2 (P = 0.478), I2 = 0%
Fig. 7. Meta-analysis of caries incidence in primary and permanent dentitions with CGIC restorations vs RMGIC, amalgam or composite resin restorations. CGIC: conventional glass ionomer cement; RMGIC: resin-modified glass ionomer cement.
5.1.1 RMGIC - primary dentition
Qvist et al. (2004)
Subtotal (95% CI)
Heterogeneity : Not applicable
Test for overall effect: Z = 3.15 (P= 0.002)
5.1.2 RMGIC - permanent dentition
Subtotal (95% CI)
Heterogeneity : Not applicable
Test for overall effect: Not applicable
5.1.3 RMGIC - primary dentition
Qvist et al. (1997)
Subtotal (95% CI)
Heterogeneity : Not applicable Test for overall effect: Z = 3.83 (P= 0.0001)
5.1.4 RMGIC - permanent dentition
Subtotal (95% CI)
Heterogeneity : Not applicable
Test for overall effect: Not applicable
5.1.5 Composite resin - primary dentition
Foley et al. (2004)
Subtotal (95% CI)
Heterogeneity : Not applicable
Test for overall effect: Z = 1.74 (P= 0.08)
5.1.6 Composite resin - permanent dentition
Subtotal (95% CI)
Heterogeneity : Not applicable
Test for overall effect: Not applicable
0.66 [0.57, 0.78] Total (95% CI)
Heterogeneity: Chi2 = 1.50, df = 2 (P = 0.47): I2 = 0%
Test for overall effect: Z = 5.11 (P < 0.00001)
Test for subgroup differences: Chi2 = 1.50, df = 2 (P = 0.47), I2 = 0%
Fig. 8. Meta-analysis of caries incidence in primary or permanent dentitions with CGIC restorations vs RMGIC, amalgam or composite resin restorations. Not estimable: no studies were eligible for meta-analysis. CGIC: conventional glass ionomer cement; RMGIC: resinmodified glass ionomer cement.
6.1.1 Composite resin-primary dentition
Kotsanos et al. (2004
Substotal (95% CI)
Heterogeneity: Not applicable
-0.1398 0.2114 87.3% 0.87 [0.57, 1.32] 87.3% 0.87 [0.57, 0.32]
Test for overall effect: Z= 0.66 (P= 0.51)
6.1.2 Composite resin-primary dentition
Vilkinis et al. (2000)
Substotal (95% CI)
Heterogeneity: Not applicable
-0.1398 0.2114 12.7% 0.58 [0.20, 1.72] 12.7% 0.58 [0.20, 1.72]
Test for overall effect: Z= 0.98 (P= 0.33)
Heterogeneity: Chi2 - 0.46, df = 1 (P = 0.50): 12 - 0%
Test for overall effect: Z = 0.97 (P = 0.33)
Test for subgroup differences: Chi2 - 0.46, df - 1 (P = 0.50): 12 - 0% 100.0% 0.87 [0.56, 1.22] Total (95% CI)
Fig. 9. Meta-analysis of caries incidence in primary or permanent dentitions with RMGIC restorations vs composite resin restorations. RMGIC: resin-modified glass ionomer cement.
Meta-analysis showed that patients with GIC restorations showed a lower caries incidence compared with other restoration types [RR=0.67, 95% CI: 0.55–0.82, p<0.00001] (Fig. 4, Fig. 5, Fig. 6). The heterogeneity of this meta-analysis was 2.93 (I2=0%). Patients with CGIC restorations showed a lower caries incidence compared with other restoration types [RR=0.66, 95% CI: 0.57–0.78, p < 0.00001] (Figs. 7 and 8). The heterogeneity of this meta-analysis was 1.50 (I2=0%). Patients with RMGIC restorations showed no significant differences in the caries incidence compared with composite resin restorations [RR=0.83, 95% CII:0.56–1.22, p = 0.33] (Fig. 9). The heterogeneity of this metaanalysis was 0.46 (I2=0%).
3.5.1. Preventive effect of GIC on new caries in primary and permanent dentition
The results of meta-analysis showed that patients with GIC restorations (either CGIC or RMGIC restorations) exhibited a lower caries incidence compared with amalgam restorations [RR=0.57, 95% CI:0.43–0.76, p = 0.0001]. Patients with GIC restorations exhibited a lower caries incidence compared with composite resin restorations [RR=0.77, 95% CI:0.59–1.00, p = 0.05] (Fig. 4).
Data from the studies with different follow-up periods showed that patients with GIC restorations
exhibited no significant differences in the caries incidence compared with composite resin restorations in 2 years [RR=0.83, 95% CI:0.56–1.22, p = 0.33] and 7 years [RR=0.73, 95% CI:0.51–1.04, p = 0.08] (Fig. 5).
Preventive effect of GIC on new caries in primary dentition
The results of meta-analysis showed that primary dentition with GIC restorations exhibited a lower caries incidence compared with amalgam restorations [RR=0.57, 95% CI:0.43–0.76, p = 0.0001]. Patients with GIC restorations showed no significant differences in the caries incidence compared with composite resin restorations in primary dentition [RR=0.78, 95% CI:0.60–1.03, p = 0.08] (Fig. 6).
Preventive effect of GIC on new caries in permanent dentition
Patients with GIC restorations showed no significant differences in the caries incidence compared with composite resin restorations in permanent dentition [RR=0.58, 95% CI:0.20–1.72, p = 0.33] (Fig. 6).
3.5.2. Preventive effect of CGIC on new caries in primary and permanent dentition
The results of meta-analysis showed that patients with CGIC restorations exhibited a lower caries
incidence compared with RMGIC restorations [RR=0.70, 95% CI:0.56–0.87, p = 0.002] and amalgam restorations [RR=0.57, 95% CI:0.43–0.76, p = 0.0001], but no statistical difference with composite resin restorations [RR=0.73, 95% CI:0.51–1.04, p = 0.08] (Fig. 7).
Preventive effect of CGIC on new caries in primary dentition
The results of meta-analysis showed that primary dentition with CGIC restorations exhibited a lower caries incidence compared with amalgam restorations [RR=0.57, 95% CI:0.43–0.76, p = 0.0001] and RMGIC restorations [RR=0.70, 95% CI:0.56–0.87, p = 0.002]. Primary dentition with CGIC restorations exhibited a lower caries incidence compared with composite resin restorations, but the difference had no statistical significance [RR=0.73, 95% CI:0.51–1.04, p = 0.08] (Fig. 8).
Preventive effect of CGIC on new caries in permanent dentition
No study that investigated the preventive effect of CGIC on new caries in permanent dentition was eligible for meta-analysis. The results of the preventive effect of CGIC on new caries in permanent dentition are listed as ‘not estimable’ in Fig. 8.
3.5.3. Preventive effect of RMGIC on new caries in primary and permanent dentition
Patients with RMGIC restorations showed no significant differences in the caries incidence compared with composite resin restorations [RR=0.83, 95% CI:0.56–1.22, p = 0.33] (Fig. 9).
Preventive effect of RMGIC on new caries in primary dentition
Primary dentition with RMGIC restorations showed no significant differences in the caries incidence compared with composite resin restorations [RR=0.87, 95% CI:0.57–1.32, p = 0.51] (Fig. 9).
Preventive effect of RMGIC on new caries in permanent dentition
Permanent dentition with RMGIC restorations showed no significant differences in the caries incidence compared with composite resin restorations [RR=0.58, 95% CI:0.20–1.72, p = 0.33] (Fig. 9).
This review’s results showed that patients with GIC restorations, had a lower caries incidence compared with other types of restorations, demonstrating that GIC restorations obtain a better caries preventive effect. Since the RMGIC restorations did not present a better preventive effects than other restorations, this result may be due to the effect of CGIC in the pool of the collected data. This result is consistent with previous studies that claimed that GIC restorations can be used as a tool in caries prevention28 This may be due to the fluoride-releasing and recharging ability of GIC. Fluoride delivered by dentifrices or topical fluoride treatments can be taken up into GIC and released again [29]. In addition, fluoride can inhibit biofilm formation by S. mutans and other bacterial species. Caries treatment of GIC may offer enhanced protection for the surrounding tooth structure [30]
We found that GIC restorations were more effective in preventing new caries compared to amalgam restorations. Amalgam contains silver compounds, which have antimicrobial effects on the Streptococcus mutans and Actinomyces viscosus [31]. GIC obtains the cariostatic effect, which is partially due the antibacterial effect of GIC. Meanwhile, the fluoride release of GIC might contribute to the inhibition of bacterial acid production [32]. The hypothesis that the preventive effect of GIC restorations on new caries was related to the sustained fluoridereleasing property instead of the antibacterial property was supported with the result [33] .
This review’s results suggested that GIC restorations might result in a lower caries incidence effect compared to composite resin with a statistical significance (p = 0.05), though CGIC (p = 0.08) and RMGIC (p = 0.33) had no significant differences in the reducing the caries incidence compared with composite resin restorations. The composite resin system has a hydrophobic medium, and the ion exchange from the fluoride component is reduced [34]. A previous study reported that GIC materials showed better cariostatic effects compared to composite resin [35], which is consistent with our results. Note that the CGIC meta-analysis only included one study. Further high-quality randomized control trials are needed to support the results.
The study included in our review showed that CGIC restorations presented a better cariostatic effect of than RMGIC restorations did [22]. We analysed







the caries preventive effect of CGIC and RMGIC separately. The differences of the cariostatic effect between CGIC and RMGIC could be due to replacing part of the water in the GIC by the resin, which might affect the fluoride release kinetics of RMGIC [36]. In addition, the fluoride content of restorative resins is limited by the need for the restorative cements’ translucency. The enhanced translucency of the RMGIC had improved aesthetic effects but was accompanied by a reduction in fluoride content [37,38]. Meanwhile, the resin matrix might firmly encapsulate the fluoride ions in RMGIC. Consequently, the fluoride release rate of RMGIC into an aqueous environment might be smaller and slower compared to that of CGIC [39]. The lower fluoride release of RMGIC might attribute to the reduced preventive effect of RMGIC on new caries than CGIC.
This study’s results showed that no statistically significant differences were observed with respect to the caries incidence between RMGIC and composite resin restorations in permanent dentition. Similarly, Yengopal et al. compared the preventive effect of RMGIC on recurrent caries to the composite resin and found no evidence to indicate that RMGIC had a superior cariostatic preventive effect in primary dentition [40]. The possible explanations might be that the high level of fluoride ions released initially from RMGIC might plateau within the first weeks of setting and that its composition behaves similarly to the composite resin thus leading to a lower fluoride release rate than CGIC [38,41]
Only 1 out of 7 studies investigating the preventive effect of CGIC on new caries were performed on permanent dentition. None of these studies were eligible for the meta-analysis, and thus were listed as not estimable in the results of metaanalysis (Fig. 8). The limited investigation on CGIC in permanent dentition might be due to its poor mechanical strength [42]. Further randomized control trials about CGIC on permanent dentition are needed.
In the results of meta-analysis on the preventive effect of RMGIC on new caries, we only obtained the RR of RMGIC restorations compared to composite resin restorations (Fig. 9). The data from one study assessing the caries incidence in primary dentition with RMGIC vs CGIC restorations were pooled and presented in the meta-analysis of caries progression of CGIC [43]. One of the included studies assessing the caries incidence in primary dentition contained data of both CGIC and RMGIC restorations. The
data from this study were pooled and presented in the meta-analysis of caries incidence in dentitions with CGIC restorations with RMGIC restorations as comparison [22]. Therefore, it was not appropriate to present the data again in the results of meta-analysis of caries incidence of dentition with RMGIC restoration. In this case, the caries incidence in dentitions with RMGIC restorations were not compared with CGIC again in Fig. 9. Other studies on RMGIC included for meta-analysis only compared the caries incidence between RMGIC and composite resin restorations. Therefore, this review only presented the results of the comparison between RMGIC and composite resin restorations regarding the caries preventive effect of RMGIC.
The follow-up periods of the included studies ranged from 1 year to 8 years. The average followup period of the included studies with CGIC restorations was 3.3 years, while on the RMGIC restorations, it was 1.7 years. Seven studies had the follow-up period of less than 3 years. The included studies had relatively short follow-up periods, which could be another limitation of the study. The follow-up periods were relatively short. This may be because most of the GIC were used in the primary dentition, which have a limit on follow up time due to natural exfoliation. In addition, CGIC is brittle and easily to fracture. Previous studies showed a CGIC restoration fracture rate of 10% after two years, which prevented follow up6. Studies also reported that GIC restorations showed an overall 18% cumulative loss rate during the 6-year follow-up [44]. This may be the reason why the most included GIC studies had shorter follow-up years.
The follow-up periods of the included studies in the meta-analysis varied. To minimize the effect of the follow-up period on the review’s results, we compared the new caries preventive effect of GIC with composite resin in 2 years and 7 years, respectively (Fig. 5). Regarding the meta-analysis of the new caries preventive effect of RMGIC compared with other restorations, we did not separate them into different follow-up groups because they had similar follow-up periods.
We included three studies on CGIC and two studies on RMGIC reporting the caries incidence for the meta-analysis. The other included studies with the outcome measure of caries experience increment were not eligible for the meta-analysis and were included only in qualitative analysis. The reason was because three studies assessed the caries experience increment in the dentition
after CGIC restorations without a negative control group [19], [20], [21],[45]. Meanwhile, some included studies did not perform the blinding of participants or examiners due to the obvious visual differences of CGIC and other types of restoration [46]. The failure of blinding might cause detection/performance bias, which led to the ‘high’ ratings for risk of bias. The results of the included studies might have been affected [47]. Further high-quality randomized control trials are needed to verify the results.
The number of the included studies were limited due to the insufficiency of previous publications on clinical studies, which was a limitation of this review. Since the included studies did not provide enough data (Fig. 6), comparing the caries preventive effect of GIC restorations on permanent dentition with primary dentition was not achievable in this review. Meanwhile, the number and size of restorations received by the patients, caries risk of the patients and the fluoridated factors might have influences on the caries incidence. Due to the limited data and information collection, these factors were not considered in the current review.
The preventive effect of GIC restorations on secondary caries, i.e., caries developed beneath the restoration, was not the aim of the review. Previous studies on secondary caries were always evaluated by United States Public Health Service (USPHS) criteria [48]. The outcome measures of these study were very different from the studies on new caries. Therefore, it was not appropriate to pool the data and perform the meta-analysis.
GIC is a favourable restorative material class with unique and advantageous properties, especially with a better preventive effect on new caries compared to other restorative materials. However, brittleness may limit their use in the load-bearing posterior regions. Several attempts to improve their mechanical strength and caries preventive effect might expand their clinical application.
Based on the limited evidence, GIC restorations have a better preventive effect on new caries compared to other restoration types in primary and permanent dentition. CGIC present a better preventive effect on new caries compared to RMGIC and amalgam restorations, but no statistical differences with composite resin restorations in primary dentition. RMGIC restorations showed no statistical differences in
preventive effect on new caries compared with composite resin restorations in both primary and permanent dentitions.
1- R.H. Selwitz, A.I. Ismail, N.B. Pitts
Dental caries
Lancet, 369 (2007), pp. 51-59, 10.1016/S01406736(07)60031-2
2-P.E. Petersen, D. Bourgeois, H. Ogawa, S. Estupinan-Day, C. Ndiaye
The global burden of oral diseases and risks to oral health
Bull. World Health Organ., 83 (2005), pp. 661-669
3- R.A. Bagramian, F. Garcia-Godoy, A.R. Volpe
The global increase in dental caries. A pending public health crisis
Am. J. Dent., 22 (2009), pp. 3-8
View Record in ScopusGoogle Scholar
4- C.H. Chu, S.S.S. Wong, R.P.C. Suen, E.C.M. Lo
Oral health and dental care in Hong Kong
Surgeon, 11 (2013), pp. 153-157, 10.1016/j. surge.2012.12.010
5- L. Prasai Dixit, A. Shakya, M. Shrestha, A. Shrestha
Dental caries prevalence, oral health knowledge and practice among indigenous Chepang school children of Nepal BMC. Oral. Health, 13 (2013), 10.1186/1472-6831-13-2020-20
6- U. Lohbauer
Dental glass ionomer cements as permanent filling materials? – Properties, limitations future trends
Mater, 3 (2009), pp. 76-96, 10.3390/ma3010076
-7 S.K. Sidhu, J.W. Nicholson
A review of glass-ionomer cements for clinical dentistry
J. Funct. Biomater., 7 (2016), pp. 16-31, 10.3390/ jfb7030016
8- S. Hoshika, S. Ting, Z. Ahmed, F. Chen, Y. Toida, N. Sakaguchi, B. Van Meerbeek, H. Sano, S.K. Sidhu
Effect of conditioning and 1 year aging on the bond strength and interfacial morphology of glass-ionomer cement bonded to dentin
Dent. Mater., 37 (2021), pp. 106-112, 10.1016/j. dental.2020.10.016
9- R. Nantanee, B. Santiwong, C. Trairatvorakul, H. Hamba, J. Tagami
Silver diamine fluoride and glass ionomer differentially remineralize early caries lesions, in situ Clin. Oral Investig., 20 (2016), pp. 1151-1157, 10.1007/s00784-015-1603-4
10- J. Zhao, D. Xie
A novel hyperbranched poly (acrylic acid) for improved resin-modified glass-ionomer
restoratives
Dent. Mater., 27 (2011), pp. 478-486, 10.1016/j. dental.2011.02.005
11- A. Agha, S. Parker, M.P. Patel
Development of experimental resin modified glass ionomer cements (RMGICs) with reduced water uptake and dimensional change
Dent. Mater., 32 (2016), pp. 713-722, 10.1016/j. dental.2016.03.004
12- S.K. Sidhu
Clinical evaluations of resin-modified glassionomer restorations
Dent. Mater., 26 (2010), pp. 7-12, 10.1016/j. dental.2009.08.015
13- J. Vaikuntam
Resin-modified glass ionomer cements (RM GICs) implications for use in pediatric dentistry
ASDC. J. Dent. Child., 64 (1997), pp. 131-134
14- C.F.C. Salas, C.A.B. Guglielmi, D.P. Raggio, F.M. Mendes
Mineral loss on adjacent enamel glass ionomer cements restorations after cariogenic and erosive challenges
Arch. Oral Biol., 56 (2011), pp. 1014-1019, 10.1016/j. archoralbio.2011.03.005
15- H.S. Lee, J.H. Berg, F. García-Godoy, K.T. Jang
Long-term evaluation of the remineralization of interproximal caries-like lesions adjacent to glassionomer restorations: a micro-CT study
Am. J. Dent., 21 (2008), pp. 129-132
16- L.S. Bueno, A.F.S. Borges, M.F.L. Navarro, J.W. Nicholson, R.G. Hill, S.K. Sidhu
Determination of chemical species of fluoride during uptake mechanism of glass-ionomer cements with NMR spectroscopy
Dent. Mater., 37 (2021), pp. 1176-1182, 10.1016/j. dental.2021.04.011
17- D. Moher, A. Liberati, J. Tetzlaff, D.G. Altman, P. Group
Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement
Br. Med. J., 339 (2009), pp. 25-35, 10.1016/bmj. b2535
18- R.L. Zanata, M.F. Navarro, S.H. Barbosa, J.R. Lauris, E.B. Franco
Clinical evaluation of three restorative materials applied in a minimal intervention caries treatment approach
J. Public. Health Dent., 63 (2003), pp. 221-226, 10.1111/j.1752-7325.2003.tb03503.x
19- M.S. Moura, G.P. Sousa, M. Brito, M.C.C. Silva, M.D.M. Lima, L. Moura, C.C.B. Lima
Does low-cost GIC have the same survival rate as high-viscosity GIC in atraumatic restorative treatments? A RCT
Braz. Oral. Res., 33 (2020), pp. 125-135, 10.1590/1807-3107bor-2019.vol33.0125
20- P. Arrow
Restorative outcomes of a minimally invasive restorative approach based on atraumatic restorative treatment to manage early childhood caries: a randomised controlled trial
Caries. Res., 50 (2016), pp. 1-8, 10.1159/000442093
21- P. Arrow, E. Klobas
Minimum intervention dentistry approach to managing early childhood caries: a randomized control trial
Commun. Dent. Oral Epidemiol., 43 (2015), pp. 511520, 10.1111/cdoe.12176
22- V. Qvist, E. Manscher, P.T. Teglers
Resin-modified and conventional glass ionomer restorations in primary teeth: 8-year results
J. Dent., 32 (2004), pp. 285-294, 10.1016/j. jdent.2004.01.001
23- J. Foley, D. Evans, A. Blackwell
Partial caries removal and cariostatic materials in carious primary molar teeth: a randomised controlled clinical trial
Br. Dent. J., 197 (2004), pp. 697-701, 10.1038/ sj.bdj.4811865
24- V. Qvist, L. Laurberg, A. Poulsen, P.T. Teglers
Longevity and cariostatic effects of everyday conventional glass-ionomer and amalgam restorations in primary teeth: three year results
J. Dent. Res., 76 (1997), pp. 1387-1396, 10.1177/00220345970760070901
25- N. Kotsanos, S. Arizos
Evaluation of a resin modified glass ionomer serving both as indirect pulp therapy and as restorative material for primary molars
Eur. Arch. Paediatr. Dent., 12 (2011), pp. 170-175, 10.1007/bf03262801
26- B.S. Bolgül, S. Celenk, B.E. Ayna, F. Atakul, E. Uysal
Evaluation of caries risk factors and effects of a fluoride-releasing adhesive material in children with insulin-dependent diabetes mellitus (IDDM): initial first-year results
Acta Odontol. Scand., 62 (2004), pp. 289-292, 10.1080/00016350410001766
27- V. Vilkinis, P. Hörsted-Bindslev, V. Baelum
Two-year evaluation of class II resin-modified glass ionomer cement/composite open sandwich and composite restorations
Clin. Oral Investig., 4 (2000), pp. 133-139, 10.1007/ s007840000075
28- S. Mickenautsch, V. Yengopal, S.C. Leal, L.B. Oliveira, A.C. Bezerra, M. Bönecker
Absence of carious lesions at margins of glassionomer and amalgam restorations: a metaanalysis
Eur. J. Paediatr. Dent., 10 (2009), pp. 41-46, 10.1186/1756-0500-4-58
29- C. Trairatvorakul, S. Itsaraviriyakul, W.
Wiboonchan
Effect of glass-ionomer cement on the progression of proximal caries
J. Dent. Res., 90 (2011), pp. 99-103, 10.1177/0022034510381265
30- G.M. Knight, J.M. McIntyre, G.G. Craig, P.S.Zilm Mulyani, N.J. Gully
An in vitro investigation of marginal dentine caries abutting composite resin and glass ionomer cement restorations
Aust. Dent. J., 52 (2007), pp. 187-192, 10.1111/j.18347819.2007.tb00487.x
31- I. Nedeljkovic, J. De Munck, V. Slomka, B. Van Meerbeek, W. Teughels, K.L. Van Landuyt
Lack of buffering by composites promotes shift to more cariogenic bacteria
J. Dent. Res., 95 (2016), pp. 875-881, 10.1177/0022034516647677
32- A.M. Bynum, K.J. Donly
Enamel de/remineralization on teeth adjacent to fluoride releasing materials without dentifrice exposure
ASDC J. Dent. Child., 66 (1999), pp. 89-92
33- A. Wiegand, W. Buchalla, T. Attin
Review on fluoride-releasing restorative materialsfluoride release and uptake characteristics, antibacterial activity and influence on caries formation
Dent. Mater., 23 (2007), pp. 343-362, 10.1016/j. dental.2006.01.022
34- P. Weidlich, L.A. Miranda, M. Maltz, S. Samuel
Fluoride release and uptake from glass ionomer cements and composite resins
Braz. Dent. J., 11 (2000), pp. 89-96
35- S. Schlafer, T. Bornmann, S. Paris, G. Göstemeyer
The impact of glass ionomer cement and composite resin on microscale pH in cariogenic biofilms and demineralization of dental tissues
Dent. Mater., 37 (2021), pp. 1576-1583, 10.1016/j. dental.2021.08.007
36- M. Lezaja Zebic, N. Jakovljevic, V. Miletic
Fluoride release from conventional, resin-modified and hybrid glass ionomer cements
Serb. Dent. J., 65 (2018), pp. 187-194, 10.2478/sdj2018-0018
37- P. Karantakis, M. Helvatjoglou-Antoniades, S. Theodoridou-Pahini, Y. Papadogiannis
Fluoride release from three glass ionomers, a compomer, and a composite resin in water, artificial saliva, and lactic acid
Oper. Dent., 25 (2000), pp. 20-25
38- G. Vermeersch, G. Leloup, J. Vreven
Fluoride release from glass-ionomer cements, compomers and resin composites
J. Oral. Rehabil., 28 (2001), pp. 26-32, 10.1046/j.13652842.2001.00635.x
39- Y. Momoi, J. McCabe
Fluoride release from light-activated glass ionomer restorative cements
Dent. Mater., 9 (1993), pp. 151-154, 10.1016/01095641(93)90112-4
40- V. Yengopal, S. Mickenautsch
Caries-preventive effect of resin-modified glassionomer cement (RM-GIC) versus composite resin: a quantitative systematic review
Eur. Arch. Paediatr. Dent., 12 (2011), pp. 5-14, 10.1007/BF03262772
41- P. Hörsted-Bindslev
Fluoride release from alternative restorative materials
J. Dent., 22 (1994), pp. 17-20, 10.1016/03005712(94)90166-x
42- G.J. Mount
An Atlas of Glass-Ionomer cements: a Clinician’s Guide
CRC Press (2001), 10.3109/9780203215456
43- V. Qvist, L. Laurberg, A. Poulsen, P.T. Teglers
Eight-year study on conventional glass ionomer and amalgam restorations in primary teeth
Acta. Odontol. Scand., 62 (2004), pp. 37-45, 10.1080/00016350310008689
44- J.W. van Dijken
Retention of a resin-modified glass ionomer adhesive in non-carious cervical lesions. A 6-year follow-up
J. Dent., 33 (2005), pp. 541-547, 10.1016/j. jdent.2004.11.015
45- C.M. Da Silva, M.C. Figueiredo, L. Casagrande, T.L. Lenzi
Survival and associated risk factors of atraumatic restorative treatment restorations in children with early childhood caries
J. Dent. Child., 87 (2020), pp. 12-17
46- V. Qvist, L. Laurberg, A. Poulsen, P.T. Teglers
Longevity and cariostatic effects of everyday conventional glass-ionomer and amalgam restorations in primary teeth: three-year results
J. Dent. Res., 76 (1997), pp. 1387-1396, 10.1177/00220345970760070901
47- P.J. Karanicolas, F. Farrokhyar, M. Bhandari
Practical tips for surgical research: blinding: who, what, when, why, how?
Can. J. Surg., 53 (2010), pp. 345-348
48- J.F. Cvar, G. Ryge
Criteria for the clinical evaluation of dental restorative materials, US department of health, education, and welfare
Public Health Serv. (1971)

ExECUTIvE COMMITTEE OF THE LOS; DRS.; ELIE KHOURY, FADI DAHBOUL, RONALD YOUNES, RAMZI HADDAD, SAMER RIFAII, MARIA HAIDAR, BACHAR REDA, ALI FAHS, GIvING THE

JULY 15 , 2022, GEFINOR ROTANA, BEIRUT
On July 19, 2022, the President of the Lebanese Orthodontic Society, Dr. Ramzi Haddad, welcomed the delegates of the 19th Annual meeting at the Gefinor Rotana, on behalf of the LOS executive committee. He presented the lecturers; Dr. Naji Abou Chebel (maxillofacial Surgeon,) Prof. Mona Sayegh Ghossoub, Prof. Lina Medawar, Dr. Roy Sabri, and Prof Stephane Barthelemi from Montpellier, France.
Since 1965, the year of the foundation of the LOS by late Prof. Rizkallah, the LOS members always participated in local, regional and international events as attendees as well as lecturers, and the LOS hosted international Key opinion leaders from around the world to exchange knowledge.
Dr. Haddad highlighted that there are around 500 specialists in Lebanon, for 5,000.000 inhabitants, each registered orthodontist serving around 10.000 population.
During the coffee breaks the delegates had the chance to browse the latest innovations the dental industry has to offer to the orthodontists. It was a nice occasion for colleagues to network after a long time of interruption.
He ended by thanking the LOS committees officers and invited colleagues to check the website http://www.leborthosoc.org/ to keep updated.


PROF. RONALD YOUNES, PRESIDENT OF THE LDA





 LEFT TO RIGHT; DRS. ELIE KHOURY, FADI DAHBOUL, NAZEM HAFFAR (PRESIDENT OF THE LDA-TRIPOLI), RAMZI HADDAD, SAMER RIFAII OFFERING HIM THE TROPHY.
DRS.; ANTHONY MAKARI, MARIA SAADEH HADDAD, RAMZI HADDAD
LEFT TO RIGHT; DRS. ELIE KHOURY, FADI DAHBOUL, NAZEM HAFFAR (PRESIDENT OF THE LDA-TRIPOLI), RAMZI HADDAD, SAMER RIFAII OFFERING HIM THE TROPHY.
DRS.; ANTHONY MAKARI, MARIA SAADEH HADDAD, RAMZI HADDAD

PROF. MONA SAYEGH GHOSSOUB LECTURING
ABOUT THE MANAGEMENT OF ExCESSIvE GINGIvAL DISPLAY

DR. SAMER RIFAII AND DR. JOSEPH GHAFARI CHAIRING THE SESSIONS DURING THE LOS MEETING



PROF. STéPHANE BARTHéLEMI LECTURING ABOUT THE TIMING OF EARLY ExPANSION


DR. ROY SABRI TALKING ABOUT EARLY TREATMENT OF ARCH LENGTH DEFICIENCY
 SAMER RIFAII, MONA GHOSSOUB, JOSEPH GHAFARI
SAMER RIFAII, MONA GHOSSOUB, JOSEPH GHAFARI







 DRS.; MARIA ELKHOURY ABBOUD, AMIN ZOGHBY, ABDULNABI BASSAM, TONY DIB
DRS.; MARIA ELKHOURY ABBOUD, AMIN ZOGHBY, ABDULNABI BASSAM, TONY DIB
Success CD is PROMEDICA’s composite-based, selfcuring paste-paste system for quick and easy chairside production of temporary crowns, bridges, inlays and onlays.
Compressed air is indispensable in dental practices. For instance, it ensures a long-term adhesive bond when dry blowing in restorative therapy and prosthetics. More importantly it can reduce pathogen contamination at the place of treatment and helps avoid infections. But this presupposes that the compressed air itself is completely hygienic. Simple filters alone are not enough. The following article explains the important factors in dental air.
Compressed air is required in many applications in dentistry. It drives a whole range of appliances and components – from turbines in handpieces and pressure moulding machines for the pressure moulding technique up to the control of precision milling cutters in the laboratory. Not least, dental air is used for drying the treatment site directly in the mouth of the patient. But in all these areas of application various factors have to be taken into account and are connected with risks which should not be underestimated.
Compressed air with an excessive water content reduces the adhesive strength of dental adhesive. There is also a risk of corrosion of the driven instruments. In addition, moist air – especially if it is warm too – creates the ideal environment for bacteria, viruses and fungi: Alarm stage red! The dentist must always expect the presence of open wounds in the patient’s mouth.
TheraBase is a dual-cured, calcium and fluoride releasing, self-adhesive base/liner. TheraBase contains MDP, chemically bonds to tooth structure, and utilizes THERA technology.
If the finest particles are also added to this, together with water and oil they can form an emery paste that acts like sand in a gearbox. It impairs the functioning of all bearings in the turbine, disrupts the air circulation in turbine heads and destroys the bearings and shaft. The cooling required for rapidly rotating components is diminished, causing the wear of many components. Even the patient can become aware of this in the form of unpleasant musty odours.
Simple appliances in the industry use triedand-tested oil lubrication. It reduces the wear of piston, bearings and shafts and supports the work with low-pulsation, constant air output. But
this also means potential exposure to residues of oil droplets, oil mist or oil/water emulsions.
High-quality temporary restorations within 5 minutes
After a retention time of 30 to 60 seconds in the oral cavity, the material takes on an elastic consistency, which facilitates removal without risking deformation. The material cures completely within a further 3 minutes and can then be polished. This procedure is timesaving and thus highly economical.
Excellent physical properties and great aesthetic results
This potential contamination also involves several undesirable risks. The viscous lubricating oil can add to the low viscosity oil of dental turbines and, especially after partial oxidation and resin deposits when exposed to heat, the gaskets in turbine heads can stick. This leads to total failure of the turbine. Any oil film in the patient’s mouth will prevent the adhesion of composites. which can result in the failure of the restorative therapy.
As far as the material’s physical properties are concerned, Success CD convinces with its excellent flexural and overall strength as well as its capacity to withstand high functional loads.
Air is used as a propellent medium in industrial compressors. It must achieve certain volume flows and pressures yet does not necessarily satisfy special hygienic requirements. Mainly the task
The product’s minimal polymerisation shrinkage results in precisely fitting temporary restorations. Success CD’s high colour stability and brilliant, enamel-like gloss ensure long-term aesthetic results. Moreover, its natural fluorescence and the choice of available shades promote perfect aesthetic results.
website: www.promedica.de

is only in transportation, assembly, control, etc. Stricter conditions are imposed by the foodstuffs or pharmaceuticals industries – and, naturally, the most restrictive regulations must be observed where air is used as the working medium for treatment in immediate contact with hard and soft tissues directly on the patient.
It is radiopaque allowing for effective identification on radiographs. Its dual-cure ability ensures the material will cure even in deep restorations where light cannot reach!
website: www.bisco.com
Dental compressors typically have an integrated air drying process. Modern membrane drying systems work the most efficiently. Firstly they bring the compressed air to room temperature in a cooler. Next the air flows through thin membrane fibres that further dehumidifies it. Dry purging air on the other side of the membrane fibres absorbs more moisture. This means that three times more water is separated than in conventional systems. Furthermore, compressors
with conventional drying systems can only utilise around 50 percent of their capacity as the drying medium must be regenerated at regular intervals. This is not necessary in the membranedrying unit – the compressor can run non-stop 24 hours a day. A membrane-drying unit provides dependable, high-quality dental air at all times
In the case of conventional air drying, the compressed air is cooled first, e.g. via a cooling coil. The moisture that condenses out is «flung to the edge», as it were, in a cyclone chamber by specifically targeted turbulence and pulled downwards into a separation tank by the force of gravity. Residual moisture is typically eliminated by an adsorption agent. This is regenerated in the shut-off phase of the compressor.
Currently, there is not a single compressed air system working on the basis of oil-lubricated pistons that can guarantee 100 % oil-free air. The dental solution can, therefore, only be an oil-free compressor. In such «self-lubricating» systems, the pistons move in finely machined cylinder bores. The piston rings are made from a special compound that is distinguished by outstanding sliding properties. And where there is no oil, it cannot affect the function of a dental turbine or the adhesive strength of an adhesive.
Oil-free, dry and hygienic – apart from minimised infection risk and greater treatment efficiency, this also leads to lower maintenance. The annual filter change that the dental team easily carries out itself in seconds is normally all that is required. Apart from that, compressors from leading manufacturers (e.g. Dürr Dental, Bietigheim-Bissingen, Germany) are completely maintenance-free. This also saves the practice expensive technician hours and bothersome down times. The team need not be concerned about such a compressor after installation.
Compressors from Dürr Dental are equipped with membrane technology as standard. Existing systems can be retrofitted with a membranedrying unit if necessary. Models that precisely match the respective requirements are available for any size of practice – from «Tornado» for
one treatment room, through the «Duo» and «Trio», right up to the «Quattro» for four to five therapists. In the case of models with the «Tandem» name affix, the performance can be simply doubled with an additional unit for extending the practice.
The «Quattro Tandem» model, that produces its enormous output from two units with a total of eight cylinders, is particularly suitable for larger dental practices and dental laboratories. For clinics, Dürr Dental offers equipment with compressed air stations for 30 to 50 treatment places and beyond that if necessary. Such systems are running, for instance, at the universities of Prague, Toulouse, Santiago de Chile, Madrid and Valencia – to name but a few.
Not only do compressed air supply systems simplify the treatment of the patient, they also play an important role in practice hygiene. Systems with membrane drying units run extremely reliably for prolonged periods entirely free of maintenance and offer maximum security. It saves the practice unnecessary work and costs due to premature wear and ensures the success of the treatment through durable fillings. Also with regard to the increased mobility of people, growing tourism and continually emerging new illnesses, high-quality and robust compressed air systems for minimising infections are a solid investment for every dental practice to ensure therapeutic and hygienic security for many years to come.


Success CD is PROMEDICA’s composite-based, selfcuring paste-paste system for quick and easy chairside production of temporary crowns, bridges, inlays and onlays.
As technology moves forward, we start to see certain features of equipment as standard, and we start to demand these features from products . You wouldn’t dream of buying a car today without ABS (or equivalent feature), you will probably expect Bluetooth connectivity for your phone and a satellite navigation system. We do the same with dental equipment and generally we chose these features to benefit our patient experience, enhance our capabilities or improve our working conditions. One such feature to become standard over recent years has been an LED treatment light, but does an LED treatment light necessarily improve our working conditions?
There are undoubted benefits in moving towards LED technology in our practice: less heat, no need to change halogen bulbs and a more modern appearance are undeniable benefits we can attribute to most LED light offerings in the market.
High-quality temporary restorations within 5 minutes
TheraBase is a dual-cured, calcium and fluoride releasing, self-adhesive base/liner. TheraBase contains MDP, chemically bonds to tooth structure, and utilizes THERA technology.
But when you are considering a new treatment light, are you also considering the quality of the light generated? In my experience this can often be overlooked. You may assume that as LED lights are a more modern technology, that the quality of light generated will be better than your ageing halogen light. You may be shocked to learn that this may not necessarily be the case. Dental manufacturers had decades to develop and enhance the light quality of their halogen treatment lights, in some cases, the light quality from halogen lights was actually excellent, even if hot to work under, more expensive to run and the bulbs need replacing from time to time. So what should you look for in a dental treatment light? The four top areas I would recommend exploring are:
You want to create a bright working light in the oral cavity to enhance the vision of the whole dental team. This light should be brighter than your ambient lighting but beware that too large of a contrast can cause its own issues such as eye fatigue. You want to ensure that the lighting levels are safe for you to look into day in day out. Illumination of around 25-30,000 LUX will provide brilliant illumination in the oral cavity at a safe level.
CCT defines the colour appearance of a white LED and is defined in degrees Kelvin or ‘K’. The aim for a dental treatment light is 5,000K which emits a neutral, white light. Anything less than 5,000K could be a compromise and provide a slightly warm yellow looking light. Higher than 5,000K and the light may appear a cool blue colour.
After a retention time of 30 to 60 seconds in the oral cavity, the material takes on an elastic consistency, which facilitates removal without risking deformation. The material cures completely within a further 3 minutes and can then be polished. This procedure is timesaving and thus highly economical.
Excellent physical properties and great aesthetic results
As far as the material’s physical properties are concerned, Success CD convinces with its excellent flexural and overall strength as well as its capacity to withstand high functional loads.
Colour Rendering Index (CRI) provides a measure of how well light reproduces the colour of an object it is illuminating in comparison to an ideal or natural light source. On a scale of 0 –100CRI with 100 being perfect natural light you need a high CRI score combined with a CCT at 5,000K to allow accurate colour matching and soft tissue examination.
Composite Curing
The product’s minimal polymerisation shrinkage results in precisely fitting temporary restorations. Success CD’s high colour stability and brilliant, enamel-like gloss ensure long-term aesthetic results. Moreover, its natural fluorescence and the choice of available shades promote perfect aesthetic results.
website: www.promedica.de
How often have you had to work without a treatment light just when you are completing your most technical restorations to avoid composites curing early? Light cure composites are cured using the blue spectrum of light. ‘Cure Safe’ in many cases is simply a dimmer light. This means that you are still curing your composite (allbeit a little slower) and working with a compromised light. For a true ‘cure safe’ mode look for a light which filters out the blue spectrum of light and allows you to work with a bright illuminance without curing your composite.
The author has a passion for dental ergonomics and is certified by The Back School in the USA. Nick offers free dental ergonomics work shops both in person and online.
It is radiopaque allowing for effective identification on radiographs. Its dual-cure ability ensures the material will cure even in deep restorations where light cannot reach!
Nick Olive CEAS
Territory Manager
Middle East & Egypt
A-dec
nick.olive@a-dec.com
+971 (0)585931983




THE PRESIDENT OF THE REPUBLIC MICHEL AOUN, RECEIvING THE PRESIDENTS OF THE INTERNATIONAL DENTAL DELEGATIONS.
THE LEBANESE DENTAL ASSOCIATION CONGRESS OCTOBER 13-15, 2022, SEASIDE PAVILLON, BEIRUT, LEBANON


DR. GEORGES AOUN, PRESIDENT OF THE SCIENTIFIC COMMITTEE IN THE OPENING CEREMONY


DR. ANTOINE CHOUFANI, MASTER OF THE CEREMONY

DR. AZEM QADDOUMI, PRESIDENT OF JORDANIAN DENTAL ASSOCIATION, WITH HIS COLLEAGUES AT THE OPENING CEREMONY

THE PRESIDENT OF THE LEBANESE DENTAL ASSOCIATION, PROF. RONALD YOUNES AND DR. MARIA ABBOUD, OFFERING THE TROPHY TO THE MINISTER HECTOR HAJJAR, REPRESENTING THE PRESIDENT OF THE REPUBLIC.

DR. HOUSSAM JASSAR, GENERAL SECRETARY OF THE LDA

PROF. TAREK ABBAS, DR. AZEM QADDOUMI, DR. TONY DIB




HANINE PERFORMING WITH A vIOLIN SHOW DURING THE OPENING CEREMONY



 DRS: ZAHRA AYOUB, TONY DIB, FADI DAHBOUL, RAMZI HADDAD, MO AMUZIAN, MONA GHOSSOUB, JOSIANE DIB
DRS: MARLENE KHOURY, NAHIDA ASSAF, DEAN NADA MCHAYLEH, JOSIANE DIB, TONY DIB
DRS: ZAHRA AYOUB, TONY DIB, FADI DAHBOUL, RAMZI HADDAD, MO AMUZIAN, MONA GHOSSOUB, JOSIANE DIB
DRS: MARLENE KHOURY, NAHIDA ASSAF, DEAN NADA MCHAYLEH, JOSIANE DIB, TONY DIB






 L TO R: DRS; SAMER RIFAI, TONY DIB, CAMILLE HADDAD, MOHAMED DARWISH, MAGID AMIN, TAREK ABBAS, RONALD YOUNES, COLETTE BOUEIZ, AZEM QADDOUMI, AHMAD RIZK, ABOUBAKR ELIWA, AMIN ZOGHBI
DRS.: JULIEN LAUPIE, AHMAD RIZK, TONY DIB, MARWAN DAAS, PATRICK ROUASS
DRS.:. TONY DIB, NAJIB KHALAF, ROLA KHALAF, RONALD YOUNES, JOSIANE DIB, ANTOINE CHOUFANI
DRS.: HAMADI GTAT, ARBIA TAMIM , TONY DIB
TONY DIB, SAMER RIFAI, DIETMAR GOLDMANN, ISSAM GHAZAL, ZIAD MJAES, ROULA ABIAD, JOSIANE DIB
L TO R: DRS; SAMER RIFAI, TONY DIB, CAMILLE HADDAD, MOHAMED DARWISH, MAGID AMIN, TAREK ABBAS, RONALD YOUNES, COLETTE BOUEIZ, AZEM QADDOUMI, AHMAD RIZK, ABOUBAKR ELIWA, AMIN ZOGHBI
DRS.: JULIEN LAUPIE, AHMAD RIZK, TONY DIB, MARWAN DAAS, PATRICK ROUASS
DRS.:. TONY DIB, NAJIB KHALAF, ROLA KHALAF, RONALD YOUNES, JOSIANE DIB, ANTOINE CHOUFANI
DRS.: HAMADI GTAT, ARBIA TAMIM , TONY DIB
TONY DIB, SAMER RIFAI, DIETMAR GOLDMANN, ISSAM GHAZAL, ZIAD MJAES, ROULA ABIAD, JOSIANE DIB














YEARS OF BIDM


Krystel Winiker Villalobos
Corporate Communications Manager
Sirona Straße 1
5071 wals bei Salzburg, Austria
T: +43 664 60097 612
krystel.winikervillalobos@ dentsplysirona.com
Winiker Villalobos
Marion Par-Weixlberger
Communications Manager
Straße 1
Wals bei Salzburg, Austria
664 60097 612
Vice President Public Relations & Corporate Cimmunications
krystel.winikervillalobos @dentsplysirona.com
Sirona Straße 1
5071 Wals bei Salzburg, Austira
Marie Rautenberg
T +43 (0) 662 2450-588
GmbH Schöneberger Str. 15
Berlin, Germany
221829 058
F +43 (0) 662 2450-540 marion.parweixlberger@ dentsplysirona.com
dentsplysirona@edelman.com www.edelman.com
Par-Weixlberger
President Public Relations & Communications
Straße 1
Wals bei Salzburg, Austria
662 2450-588
662 2450-540
marion.par-
Qatar University, the country’s primary institution for higher education, is partnering with Dentsply Sirona to equip the university’s brand-new preclinical lab at the newly founded College of Dental Medicine. Dentsply Sirona is providing state-of-the-art simulator workstations, instruments, as well as the latest CEREC and inLxab software systems to prepare students for the digital future of dentistry.
Universities and large clinics around the world have entrusted Dentsply Sirona’s International Special Clinic Solutions (ISCS) division and its comprehensive approach to achieve their specific goals. When Qatar University’s College of Dental Medicine in Doha, envisioned their brand-new preclinical laboratory, they worked with Dentsply Sirona’s team to comprehensively equip it with state-of-the- art technology to prepare students for dentistry’s digital future.
32 Sim Intego workstations plus
two additional instructor units now offer the best possible learning environment following the latest technological advancements. Additionally, 15 CEREC AI units and the inLab system will be used to support future dentists in their training for highly specialized procedures.
“The new College of Dental Medicine at Qatar University sees it as part of its core mission to incorporate digital technologies and the latest advancements into its teaching. Thanks to Dentsply Sirona’s innovative products and team of experts we were able to create a future-proof training environment,” said Dr. Hanin Daas, Director of Dental Laboratories at Qatar University.
Preparing for the future of dentistry on cutting-edge equipment
All products installed at the University of Qatar have been designed and produced in Germany using particularly robust and durable materials that are ideal for a
university setting. The state-of-the-art Sim Intego workstations in the preclinic allow students to train in practice-like conditions. Sim Intego includes key components of treatment centers such as the dentist element so that students already familiarize themselves with the actual treatment process in their preclinical semesters. Furthermore, the university also opted for the lightweight T1 line instruments series. These easyto-handle instruments help ensure the College of Dental Medicine is able to deliver the best training of correct instrumentation techniques to deliver optimal results.
The International Special Clinic Solutions team selected the ideal product mix for Qatar University to fulfill their plan to make the most modern learning tools available to their students. During the preclinical training, CEREC and inLab systems will prepare the students for using CAD/ CAM technology in dentistry. Additionally, staff will be supported by a multimedia teaching system designed to enhance communication and to give students the best view of demonstrations at the master workstation. With a one touch button, it is possible to share real-time, highquality images from any device on any screen in the classroom.
Dentsply Sirona is proud to have been selected by Qatar University to help turn their vision of educating world-class dental professionals and the nation’s first graduates of dental medicine into a reality. In consultations for the preclinic area, the International Special Clinic Solutions team discussed the university’s ideas and goals thoroughly and addressed each individual requirement in detail. The engineering team in Germany then developed a custom-made concept that delivers the required portfolio from start to finish.
The College of Dental Medicine’s preclinical lab educates students in the basics of clinical dentistry before they practice on actual patients. The new lab provides a technologically advanced environment to train students in digital dentistry thus ensuring that the next generation of dental practitioners are well prepared to meet the demands of the future.


The newly founded College of Dental Medicine at Qatar University selected Dentsply Sirona to equip its preclinic area.
Dentsply Sirona is the world’s largest manufacturer of professional dental products and technologies, with over a century of innovation and service to the dental industry and patients worldwide. Dentsply Sirona develops, manufactures, and markets a comprehensive solution offering including dental and oral health products as well as other consumable medical devices under a strong portfolio of world class brands.Dentsply Sirona’s products provide innovative, high-quality and effective solutions to advance patient care and deliver better and safer dental care.
Dentsply Sirona’s headquarter is located in Charlotte, North Carolina.
The company’s shares are listed in the United States on NASDAQ under the symbol XRAY. Visit www.dentsplysirona.com for more information about Dentsply Sirona and its products.



JUNE 9-11, 2022
View More Pictures On

Five hundred attendees representing the dental team: dentists, dental students, dental hygienists, dental assistants, dental technicians and office personnel. Almost 200 foreign visitors from all over the world. Seventy speakers. Fifty guests. One hundred operators representing dental companies. These are the final numbers of the 11th AIO/Italian Dental Association International Congress that took place in Chia, a seaside resort town on the spectacular island of Sardegna, last weekend.
Organized by AIO branch of Cagliari/Oristano, the Congress touched on an exciting and evolving topic: equality between men and women in dentistry. Today the number of women practicing dentists is steadily increasing. Just two years ago women made up 40% of graduates from dental school. Now, in many countries, women make up from 50% to 70% of the total number of dental students. Dentistry is well on the way to becoming a female dominated profession!
The AIO International Congress, “Focus on the Gender Shift in Dentistry: A New Perspective or a Future Challenge?” remained true to its theme, exploring this trend on an even playing field equally divided between male and female lectures in their respective specialties.
A panel of top leaders in dentistry gathered to discuss this gender shift during the Inaugural Ceremony that was opened by the President of the FDI World Dental Federation, Imane Ben Yahya with contributions from the founder of the Washington Institute of Dentistry Claudia Cotca and the Canadian endodontist and chairman of the ceremony, Ken Serota.





















































International Special Clinic Solutions is Dentsply Sirona’s project team. As the global leader in dental education, with over 60 years of experience and more than 1,000 successful projects, we are the right partner for bringing your education to the next level.
The realistic visualization of a project makes the construction process more coordinated and precise. Dentsply Sirona thus has a design team specialized in both precise twodimensional floor plans and 3D simulation. In the interactive 3D floor plan, we can guide you through all the rooms and levels of your new clinic or university complex, both from a first-person perspective and as a bird’s-eye view.
Find more details here: www.dentsplysirona.com/clinics
For further information please contact: salzburgaut-clinicsolutions@dentsplysirona.com
dentsplysirona.com

