UNIVERSITY OF MICHIGAN
W.K. KELLOGG EYE CENTER













47 New Faculty 2
Curbing Drusen Buildup in Dry AMD
Leaders and Best in Education
14 Lipid Droplet Dynamics: A Critical Line of Defense Against AMD?
14 Kellogg Post-Doc Named Michigan Pioneer Fellow
30 Educating Tomorrow’s Educators
31 The Genetic Drivers of Familial Glaucoma
32 Eye-Opening Analyses of the Economics of Ophthalmology
33 Prioritizing Resident Wellness
34 2024-2025 Heed Fellows
36 Otana Jakpor, M.D., M.Sc. Global Ophthalmology Fellow
48 Faculty Honors and Recognition

Honors and Awards
31 Dr. David Zacks Receives the Kreissig Award
41 Victor Elner, M.D., Ph.D., receives the Dortzbach Teaching Award
Philanthropic Support
37 Transformative Gift Enhances and Expands SOURCE Repository
38 The Wadhams' Gift Aims to Save Children’s Sight
39 Gift from Bob and Patti Huiskamp Advances AMD Research
Improving Vision Worldwide
40 The Monaciano Consortium Marks 10 Years
42 Kellogg Returns to Jamaica
Kellogg Updates
4 Shahzad I. Mian, M.D., Named Department Chair, Kellogg Director
23 5 Questions for Kellogg’s New Associate Chair for DEI
44 Alumni Highlights
45 First-year and Graduating Residents
46 Where Are They Now—Departing Clinical Fellows
Front cover clockwise: Emberleigh and Emily Eton, M.D., David Zacks, M.D., Ph.D., Nita Valikodath, M.D., M.S., and Mark Draelos, M.D., Ph.D.


As in years past, this report celebrates the efforts and accomplishments of Kellogg faculty, staff and learners, and all we do to support the patients, families and communities we serve.
I also see it as a chance to celebrate and thank the many individuals and organizations who support us.
Kellogg basic, clinical and translational researchers continue to rank among the nation’s best in securing federal grant support. Highlights include five new R01 grants, a new clinical scholar on our ongoing K12 grant, and the first-ever Kellogg recipient of an F31 predoctoral fellowship to promote diversity in health-related research, all from the National Institutes of Health/National Eye Institute, as well as a grant from the Centers for Disease Control and Prevention.
Just as critical is the support from foundations that fuels our progress. Kellogg investigators received grants from the Foundation Fighting Blindness (two awards), the Retina Research Foundation, Research to Prevent Blindness, the BrightFocus Foundation, the E. Matilda Ziegler Foundation for the Blind, Eversight Eye & Vision Research, and the McKnight Foundation
Philanthropy plays a crucial role in our work this and every year. This report announces game changing gifts from the Eisenshtadt, Huiskamp and Wadhams families.
We are also indebted to our many 2024 collaborators. This year we are participating with another national health system to expand pediatric eye care regionally. We engaged faculty, trainees and alumni in a clinical, educational and research exchange with our counterparts in Jamaica. And we partnered with colleagues within and beyond U-M to expand robot-assisted imaging technology and pursue a next-generation prosthetic retina.
Finally, this report details the transformational work of the Mary Tyler Moore Vision Initiative. We are excited to be part of this consortium to end vision loss from diabetes, and are incredibly grateful for the inspiration, support and leadership of Dr. S. Robert Levine
On behalf of everyone at Kellogg, thanks to you for your interest in and support of our work.

Shahzad I. Mian, M.D.
F.Bruce Fralick Professor of Ophthalmology Chair and Professor, Department of Ophthalmology and Visual Sciences Director, W.K. Kellogg Eye Center
“
THEY TAKE WONDERFUL CARE OF EMBERLEIGH, AND THEY’VE BEEN TREMENDOUSLY PATIENT WITH ME, EXPLAINING HER DIAGNOSIS AND EVERY STEP IN HER TREATMENT AND ANSWERING ALL OF MY QUESTIONS.
“

Jenny Allard
Five-year-old Emberleigh Taggart first visited U-M and Kellogg as an infant. Born with a congenital skull malformation called occipital encephalocele (OE), she requires specialized care to monitor ongoing risks to her vision and has worn glasses since age one.
Emberleigh lives with her guardian, Jenny Allard, in Wells Township, a tiny community near the town of Escanaba in Michigan’s remote upper peninsula. Like most rural areas, there is no local pediatric ophthalmologist. So for her entire young life, family members have been making the 400+ mile trek with Emberleigh to Ann Arbor to meet with the pediatric specialists at Kellogg.
In the summer of 2023, Emberleigh’s exam revealed a worrisome development: her vision had declined to the point of profound nearsightedness.
“Glaucoma was the first thing we considered,” explains pediatric glaucoma specialist Adam Jacobson, M.D. “Elevated pressures in developing eyes can cause them to enlarge, resulting in severe nearsightedness.” But a thorough exam performed under general
anesthesia ruled out glaucoma. Rather, the problem seemed to originate in her retina.
Dr. Jacobson collaborated with pediatric retina specialist Emily Eton, M.D. "We could see evidence of a rare form of nearsightedness caused by a hereditary vitreoretinopathy,” she explains. “It is characterized by a stretching or thinning of the retina, as well as a change in the consistency of the vitreous, causing it to stick to the edge of the retina.”
At first, these signs pointed to an inherited condition called Stickler syndrome. “But we also observed atrophy or thinning in her macula, which is not a feature of the syndrome,” Dr. Eton recalls. “We needed genetic testing to solve the mystery.”
The next steps were closely coordinated with Kellogg’s Multidisciplinary Ocular Genetics Clinic (MOGC), led by Lev Prasov, M.D., Ph.D., and Amanda Pritchard, M.D. Genetic testing was expedited, and the findings were discussed with Jenny Allard before the two headed home.
“Both Emberleigh’s ocular and systemic findings provided clues as to which genes might be involved,” explains Dr. Prasov. “In particular, her history of OE, combined with vitreous and macular abnormalities
and high myopia made me suspect one particularly rare disorder.”
Targeted genetic tests confirmed the diagnosis: Knobloch Syndrome. Since first described in 1971, fewer than 100 cases from about 50 families have been documented.
“Knobloch Syndrome is caused by a mutation in a gene that regulates collagen production,” notes Dr. Prasov. “Disrupted collagen causes the textural changes in her retina, vitreous and macula. It also places her at an increased risk of retinal detachment.”
“That’s why the genetic diagnosis was so helpful in planning Emberleigh’s treatment,” continues Dr. Eton. “We commonly manage that risk with a prophylactic laser procedure—a treatment we wouldn’t automatically recommend for other young children with nearsightedness. With a clearer picture of her long term risk, we were more confident discussing this option with Jenny.”
“Everyone at Kellogg has been terrific,” says Jenny Allard. “They take wonderful care of Emberleigh, and they’ve been tremendously patient with me, explaining her diagnosis and every step in her treatment and answering all of my questions.”
In a subsequent visit, Dr. Eton performed the procedure, called photocoagulation, in both eyes, shoring up the periphery of the retinas to lower the risk of tearing.
While Knobloch Syndrome means Emberleigh’s eye health will always need monitoring, the diagnosis comes with some good news, too. “Compared with
“ “ OUR GOAL IS TO STREAMLINE THE MULTIDISCIPLINARY DIAGNOSIS AND TREATMENT OF PEDIATRIC EYE DISORDERS.
Lev Prasov, M.D., Ph.D.
other children with OE, children with Knobloch Syndrome have a much better prognosis for overall development,” notes Dr. Prasov.
“Emberleigh is thriving,” Jenny reports. “We wondered whether her vision might cause her problems in school, but she started kindergarten and she’s doing just fine.” Jenny also works with Emberleigh at home and makes sure she sees the school district’s vision specialist regularly. As Emberleigh grows, Jenny will continue to make the seven-hour trip to Kellogg as needed, so that she can be monitored for retinal detachments, glaucoma, macular atrophy and central vision changes, and to keep her eyeglass prescription current.
Soon, this process will become easier for children and families living with rare inherited eye disorders. Their care will be coordinated through the new Wadhams Family Center for Children’s Vision. Housed in the Kellogg Pediatric Ophthalmology Clinic, the Center will bring together pediatric specialists in genetics, retina, cornea, glaucoma, oculoplastics, neuro ophthalmology, uveitis, and low vision optometry, and provide access to clinical trials. (see page 38)
“Our goal is to streamline the multidisciplinary diagnosis and treatment of pediatric eye disorders,” says Dr. Prasov, who will direct the Center. “Consolidating and coordinating specialists, testing and support in a ‘one-stop’ destination will be enormously helpful for families, especially those like Emberleigh’s who travel such a great distance.”

“I
AM COMMITTED TO KEEPING KELLOGG ON TOP BY INVESTING
TO ENHANCE CLINICAL
CARE,
RESEARCH
AND
EDUCATION,
AND BY PUTTING INTO ACTION OUR MISSION TO IMPROVE LIVES AROUND THE WORLD BY ENHANCING VISION.
Shahzad I. Mian, M.D.
“Shahzad I. Mian, M.D.,
In April 2024, after serving as interim chair of the Department of Ophthalmology and Visual Sciences at the U-M Medical School since January 2023, Shahzad I. Mian, M.D., began his tenure as the ninth chair of the department, and the third director of the W. K. Kellogg Eye Center.
“It is the honor of a lifetime to lead this amazing organization,” Dr. Mian says. “I am committed to keeping Kellogg on top by investing to enhance clinical care, research and education, and by putting into action our mission to improve lives around the world by enhancing vision.”
Now heading one of the highest volume academic ophthalmology departments in the U.S., Dr. Mian has outlined a number of clinical priorities for Kellogg. “As personalized medicine and targeted treatments continue to revolutionize eye care, we are building our capacity to coordinate and streamline care across multiple specialties, including genetic testing and counseling,” he says. “We are also widening our footprint to bring clinical resources closer to where our patients live.”
Kellogg’s research enterprise also continues to expand under Dr. Mian, with strategic investments in bioinformatics, artificial intelligence and biomechanical engineering, and initiatives in macular degeneration, neuro-ophthalmology and the ophthalmic consequences of neurodegenerative diseases. “Thanks to our close proximity to and even closer partnerships with the Caswell Diabetes Institute and the Brehm Center for Diabetes Research, we are also accelerating the pace of discovery in our search for more effective treatments for diabetic retinal disease.”
“As someone who loves teaching, I am especially excited about our educational initiatives,” he adds. “We continue to launch new programs to keep our curriculum vibrant and attract the top candidates for residency and fellowship, including a dedicated teaching track for those planning careers in academic medicine.”

Dr. Mian earned his medical degree from the Emory University School of Medicine. He completed residency training at the Wills Eye Hospital of Thomas Jefferson University in Philadelphia, and a fellowship in cornea and refractive surgery at Harvard Medical School’s Massachusetts Eye and Ear Infirmary. He joined the U-M faculty in 2002, was promoted to professor in 2016 and was named the F. Bruce Fralick Professor of Ophthalmology in 2024. His research focuses on advanced corneal transplantation techniques, eye banking and medical education.
Widely regarded as an outstanding teacher and mentor, Dr. Mian has repeatedly received the Bergstrom Teaching Award from Kellogg residents and has been recognized with the Straatsma Award for resident education from the Association of University Professors in Ophthalmology. Other honors include Kellogg’s Anthony Adamis Award for Outstanding Research, and the Payton Award from the Eye Bank Association of America. He previously garnered an American Academy of Ophthalmology (AAO) Senior Achievement Award and received an AAO Secretariat award in 2024.
Dr. Mian directs the Association of University Professors of Ophthalmology Surgical Curriculum for Ophthalmology Residents, serves on the board of directors and as senior medical director of Eversight Eye Bank, as the chair of the Eye Bank Association of America medical advisory board, as secretary of the Cornea Society, and president-elect of the Michigan Society of Eye Physicians and Surgeons.
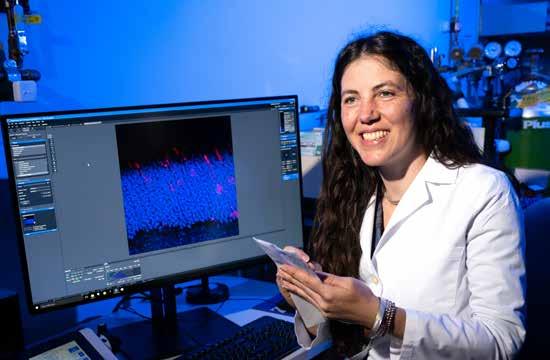
The primary focus in the lab of molecular biologist Jillian Pearring, Ph.D., is studying the light-sensitive photoreceptor cells of the retina, and how defects in their formation, function or trafficking drive blinding inherited retinal diseases (IRDs).
Recently, the Pearring lab identified a new culprit: a disruptive phenomenon occurring in the structure of the retina linked to mutations in the gene Arl3. Two research awards announced in 2024 will fund further studies to better understand this event and its potential relevance as a therapeutic target.
The light-sensing neural tissue of the retina is composed of layers. Neurons communicate across those layers, sending information from the photoreceptor cells that reside in the outermost layer. Dr. Pearring has demonstrated how mutations in the Arl3 gene can cause the Arl3 protein to become hyperactive. This overactivity, which occurs during the development of the retina, results in photoreceptors being stranded in the inner retinal layers, unable to reach their destination in the outer layer.
Dr. Pearring first connected overactive Arl3 with autosomal dominant retinitis pigmentosa and wondered whether the phenomenon might also play a role in other IRDs. To find out, her team zeroed in on another gene, RP2. RP2 is associated with the IRD X-linked retinitis pigmentosa, and has a known connection to Arl3, making it a good target for study.
“ “
WE HOPE TO DESCRIBE HOW MIS-LOCALIZED PHOTORECEPTOR CELLS IMPACT RETINAL HEALTH AND FUNCTION, LEARN MORE ABOUT THE CELLULAR MECHANISMS OF ARL3 AND RP2 MUTATIONS, AND EVENTUALLY IDENTIFY NEW THERAPEUTIC TARGETS FOR INHERITED BLINDNESS.
Jillian Pearring, Ph.D.
“RP2 is known to turn off Arl3 activity,” she explains. “We were able to demonstrate that decreasing RP2 function would pave the way for increased Arl3 activity. Furthermore, in models with mutations in either Arl3 or RP2, we observed the same phenomenon— elevated Arl3 activity combined with photoreceptor misplacement.”
Two aspects of these findings have the potential to change the paradigm for IRDs.
First, they move beyond linking genes to specific IRDs to focus on patterns of cellular activity shared by different IRD genes. Second, the phenomenon of Arl3 hyperactivity occurs early in life, during the fetal stage of retinal development, not later as a consequence of disease.
This new vantage point could change how—and how early—these progressive diseases are identified and treated. Dr. Pearring has been awarded both an NIH R01 grant and a grant from the Foundation Fighting Blindness, to pursue complementary aspects of this pivotal finding.
The Pearring lab will test several techniques for suppressing or corralling Arl3 to determine whether there is an approach that will prevent photoreceptors from being stranded in inner retinal layers. In both neonatal and adult disease models, they will also attempt to determine the available time windows to restore photoreceptors to their proper location in the outer layer.
“We are excited to build on these preliminary findings,” says Dr. Pearring. “We hope to describe how mis-localized photoreceptor cells impact retinal health and function, learn more about the cellular mechanisms of Arl3 and RP2 mutations, and eventually identify new therapeutic targets for inherited blindness.”

Abigail Fahim, M.D., Ph.D.
A key area of focus in inherited retinal disease (IRD) research is dysfunction in the retinal pigment epithelium (RPE), a layer of cells located between photoreceptors (PRs)—the cells that sense vision—and the structure that supplies blood to the retina, called the choroid. Although the RPE is not the source of vision, it nonetheless plays a vital, defensive role, guarding the health and survival of both PRs and the choroid.
Choroideremia is an IRD estimated to strike approximately one in 50,000 patients, predominantly men. Typically diagnosed in childhood, it usually leaves patients legally blind by early adulthood. Like other IRDs, it results in retinal degeneration. But, as its name suggests, the feature that sets it apart is the severity of degeneration sustained by the choroid.
Kellogg clinician-scientist
“
IF
In order to do their job, RPE cells are prolific secreters of various proteins, including a specific type called a protease. Like molecular scissors, proteases are capable of cutting up adjacent cellular structures.
“Our preliminary studies of choroideremia models showed additional secretion and activity of certain proteases,” notes Dr. Fahim. “Others have previously associated RPE proteases with age-related changes like choroidal thinning and macular degeneration. We now hypothesize that increased protease activity could actually be snipping away at the scaffold-like structure of the choroid.”
WE CAN CONNECT RPESECRETED PROTEASES WITH THE SEVERE CHOROIDAL ATROPHY THAT CHARACTERIZES CHOROIDEREMIA, IT MAY PROVE A PROMISING THERAPEUTIC TARGET FOR THIS UNTREATABLE DISEASE.
“
Abigail Fahim, M.D., Ph.D.
Abigail Fahim, M.D., Ph.D., is pursuing a new theory of the role of the RPE in choroidal degeneration. Her work is supported by a 2024 NIH R01 grant.
“We know that genetic mutations can target and destroy RPE cells, leaving the choroid unsupported,” she explains. “We’ve long attributed choroideremia to this ‘passive’ consequence of RPE cell death. But what if something in the RPE is also playing an active, offensive role in injuring the choroid?”
Dr. Fahim employed a number of advanced gene editing and molecular biology tools to arrive at this theory, including CRISPR/Cas-9, Tandem mass tag (TMT) spectrometry, RT-PCR, ELISA, gel zymography, and immunofluorescence. She will employ them again to test it. She also uses stem cells derived from human skin to generate RPE cells with the choroideremia genetic defect. These induced pluripotent stem cells (iPSCs) are a powerful tool to study genetic diseases in a cell culture dish.
“If we can connect RPE-secreted proteases with the severe choroidal atrophy that characterizes choroideremia, it may prove a promising therapeutic target for this untreatable disease,” she says.
More than 20 different conditions fall under the umbrella of Inherited retinal diseases (IRDs), including retinitis pigmentosa, Stargardt disease, macular dystrophy and choroideremia.
While each has a genetic origin, the similarity ends there. Over 300 different genes have been identified as a cause of IRDs. Some IRDs manifest as early as infancy, while others may not be diagnosed until late in life. Vision loss from IRDs ranges from impaired night vision to total blindness.
In the 1940s, Kellogg became the first center in the U.S. to dedicate a clinic to inherited eye diseases. Kellogg is still one of only a few centers in the U.S. offering such a program, serving as a regional referral center for comprehensive, multidisciplinary clinical care, and an international hub for basic, clinical and translational research in IRDs.
The program is directed by K. Thiran Jayasundera, M.D., M.S. Both he and fellow ophthalmic geneticist Abigail Fahim, M.D., Ph.D., provide clinical care and conduct research and clinical trials. Electrophysiology, an essential imaging modality for diagnosing IRDs, is provided by Naheed Khan, Ph.D. Other retina clinician-researchers affiliated with the program include Cagri Besirli, M.D., Ph.D., Emily Eton, M.D., Lev Prasov, M.D., Ph.D., and Thomas Wubben, M.D., Ph.D. Basic research in IRDs is conducted by Drs. Fahim, Prasov and Wubben, along with Rajesh Rao, M.D., Debra Thompson, Ph.D., and David Zacks, M.D., Ph.D.
During an initial clinic appointment, detailed family and medical histories are gathered, and electrophysiology and other advanced imaging and visual field tests are scheduled. The clinic’s genetic counselors, Kari Branham, M.S., CGC, Dana Schlegel, M.S., M.P.H., CGC, and Rachel Sullivan, M.S., guide families through the entire process.
“Prior to genetic testing, we explain the testing process, why we frequently test for mutations in multiple genes, and the importance of arriving at a genetic diagnosis,” explains Branham. “Once a diagnosis is made, we help patients and families understand what to expect next, and over the long term.”
The clinic team also provides treatment and specialty referrals to help manage conditions that commonly accompany IRDs, such as macular edema and cataracts.

For many patients, living with an IRD also means living with the functional and emotional consequences of vision loss. “We’re here to help patients access the specific support services they need, like low vision re-habilitation, mental health counseling and social work, whether at Kellogg or in their community,” adds Dr. Fahim.
The clinic provides hope to those who live with diseases that do not yet have a cure. “That’s because there is currently only one FDA-approved treatment, a gene therapy, for one IRD,” notes Dr. Jayasundera. “Kellogg is one of only 16 centers in the U.S. to offer this treatment. Until more therapies are available, we look for opportunities to connect patients with experimental treatments available in clinical trials.”
The program is home to significant federally and industry funded research in IRDs.
For example, Dr. Jayasundera is Principal Investigator of a two-part project funded by an NIH R01 grant, focused on the mental health of IRD patients. The first phase studied the interplay between vision disabilities, anxiety and depression in IRD patients. He is now enrolling patients in the second phase—a trial of an intervention combining low vision rehabilitation and a psychotherapy technique called emotion regulation therapy.
“We hypothesize that by tailoring a combination of low vision rehabilitation and psychotherapy, the two components will reinforce each other to help the patient achieve the best possible results.” A number of clinical trials for IRDs are available at Kellogg.

Pediatric retinal diseases, while rare, can lead to permanent blindness if not addressed promptly. Several factors can delay their diagnosis. An infant or toddler may not notice or be able to express a vision concern, especially if it impacts sight in only one eye. Young patients are also most likely to be taken first to a pediatrician’s office or emergency department, locations with limited eye screening tools.
Another obstacle: the limited use of optical coherence tomography (OCT) in pediatric ophthalmology. One of the most valuable imaging advances of the last two decades, OCT is superior to ophthalmoscopy or fundus photography in capturing subtle aspects of retinal pathology. But OCT requires the patient to remain absolutely still and focused on a fixed visual target, constraints not usually achievable with the youngest patients.
“
Dr. Valikodath says, “I became convinced that a similar system could be modified for pediatric patients and revolutionize pediatric eye care. I’m delighted to have Mark as a collaborator as I pursue this project at Michigan. We share the same passion for developing innovative medical devices to improve clinical care, and it has been exciting to build our robotic OCT team.”
The device she is developing combines several key features of RAOCT, including a robotic arm and face and pupil tracking telemetry to compensate for unintended motions of the head and eye, and the ability to adapt to different patient positions (sitting, lying down) and head orientations. It will include a larger field of view of the retina, a less intimidating and more child-friendly exterior appearance, and fixation targets like colored lights or attention-grabbing images. Rigorous pilot and proof-of-concept studies will be conducted to evaluate various measures of performance, accuracy and patient acceptance.
I’M THRILLED TO HAVE THIS OPPORTUNITY TO LEARN FROM THE BEST AND GROW AS AN INDEPENDENT CLINICIAN-SCIENTIST.
Nita Valikodath, M.D., M.S., is committed to extending the benefits of OCT to this vulnerable population. A retinal surgeon who treats patients of all ages, Dr. Valikodath is working with experts at Kellogg and Michigan Robotics to develop and test a robot-assisted OCT device that is both user- and child-friendly.
“
Nita Valikodath, M.D., M.S.
Throughout her training, Dr. Valikodath has been inspired and mentored by several pioneers in applying advancements in telemedicine, artificial intelligence, and OCT to pediatric retina. Her most pivotal mentors have been Cynthia Toth, M.D., at Duke University, and R.V. Paul Chan, M.D., M.Sc., M.B.A., of the University of Illinois at Chicago, as well as Cagri Besirli, M.D., Ph.D., and Maria Woodward, M.D., M.S. at Kellogg.
Her work builds on a contactless robotically aligned OCT (RAOCT) developed at Duke University by her Kellogg colleague Mark Draelos, M.D., Ph.D. She is funded by Kellogg’s NIH Mentored Clinical Scientist Training Grant, or K12, which supports two clinical scholars annually.
“I was first introduced to Mark’s innovations in robot-assisted OCT when we were both at Duke,”
“I’m thrilled to have this opportunity to learn from the best and grow as an independent clinicianscientist,” says Dr. Valikodath. “But I’m even more excited about how these technologies can transform ophthalmic care for kids and other vulnerable populations, guiding diagnosis and treatment in primary care and emergency settings, and bedside in inpatient and neonatal intensive care units to prevent blindness.”

Thanh Hoang, Ph.D.
“
A BETTER UNDERSTANDING OF HOW CNS NEURONS ARE FORMED DURING NORMAL DEVELOPMENT IS CRITICAL TO CONTINUING TO HONE OUR APPROACH TO REGENERATING THEM FROM MATURE CELLS.
“
Thanh Hoang, Ph.D.
Many subtypes of neurons and glial cells make up the central nervous system (CNS), responsible for sight, cognition and movement. These cells are highly vulnerable to damage and disease, including blinding diseases of the retina like macular degeneration, retinitis pigmentosa and glaucoma, and debilitating brain and spinal cord illnesses like multiple sclerosis and Parkinson’s disease.
The novel research of Thanh Hoang, Ph.D., is a driving force behind efforts to move beyond treating the consequences of these devastating neurodegenerative disorders, to defeating them at the cellular level.
“
“We hypothesize that the transcription factor insulinoma-associated protein, Insm1, plays a role in retinal cell generation and regeneration,” he explains. “With this grant we will examine the impact of both increasing and decreasing the function of Insm1 in order to capture a snapshot of cell generation in retinal development and regeneration and test our theory.”
WE HOPE TO DEVELOP MORE CONTROLLED AND UNIVERSALLY APPLICABLE METHODS, AND EVENTUALLY TRANSLATE WHAT WE ACHIEVE INTO HUMAN THERAPEUTICS.
Dr. Hoang joined the U-M faculty in 2023 with a dual appointment in Ophthalmology and Cell & Developmental Biology and is an affiliate of the Michigan Neuroscience Institute. He has developed a highly efficient method of reprogramming mature retinal glial cells into multiple types of neurons. The therapeutic potential of repurposing cells to replace those lost to neurodegeneration is receiving national attention and grant support.
A grant from the Retina Research Foundation will support the next phase of this work in retinal dystrophies: gaining a deeper understanding of the molecular mechanisms driving the generation of different cell types during retinal development and regeneration.
“Thanh Hoang, Ph.D.
With a second grant, the McKnight Foundation Neurobiology of Brain Disorders (NBD) award, Dr. Hoang will apply his cell reprogramming method to other glial cells in the CNS that share characteristics with retinal glial cells. Here too, the long-term goal is to inform future cell-based therapies, but this project addresses neurons damaged in Parkinson’s disease.
“A better understanding of how CNS neurons are formed during normal development is critical to continuing to hone our approach to regenerating them from mature cells,” notes Dr. Hoang. “We hope to develop more controlled and universally applicable methods, and eventually translate what we achieve into human therapeutics.”
The publication of a commentary by Dr. Hoang in the journal Nature illustrates his impact on this emerging field of study. The article has begun an important dialog on the development of more stringent, standardized criteria to guide this pivotal new frontier in neurobiology.

Keratoconus. Cataracts. Mixed mechanism glaucoma. Cystoid macular edema. Any one of these diagnoses is tough to take, at any age. At 36, Roxanne ‘Roxy’ Riggio is familiar with them all, having endured countless exams, medical and surgical treatments over the years to address numerous threats to her vision.
As a young child, Roxy developed keratoconus, a condition that causes the clear front part of the eye, called the cornea, to bulge out into a cone shape, causing improper focusing of light onto the back of the eye leading to blurred vision. Eventually, she required corneal transplants in both eyes. She also developed high eye pressure (glaucoma), clouding of the lens of the eye (cataracts), and swelling in the back of the eye (macular edema).
“
“It seems crazy to have so many doctors,” Roxy says. “At first it was overwhelming. But now they’re like family to me.”
In the fall of 2023, Team Roxy put their heads together to solve the puzzle of a dramatic vision decline in her right eye. Her vision worsened to a level characterized as CF, or ‘count fingers,’ meaning she could barely make out hand gestures directly in front of her.
“In countless conversations and over a very long email chain, we all debated possible causes,” Dr. Wu recalls. “Was her glaucoma well controlled, or was increased pressure damaging the eye? Was it residual retinal swelling from past surgeries? Could there be a problem with her cornea transplant graft, or was there scar tissue on the artificial lens implanted during cataract surgery?”
“ IT SEEMS CRAZY TO HAVE SO MANY DOCTORS, AT FIRST IT WAS OVERWHELMING. BUT NOW THEY’RE LIKE FAMILY TO ME.
Roxanne ‘Roxy’ Riggio
For more than 20 years, these conditions were managed by an ophthalmologist near the family home in Livonia, MI, where Roxy lives with her parents Patty and Ron Riggio. Eventually, Roxy’s cascade of eye issues led her doctor to refer the Riggios to Kellogg for multidisciplinary care.
Her Kellogg care team includes glaucoma specialists Annie Wu, M.D., and Amanda Bicket, M.D., retina specialist Jason Miller, M.D., Ph.D., and cataract and cornea specialist Shahzad Mian, M.D.
Complicating their deliberations were difficulties examining and imaging Roxy’s eyes. “Opaqueness in her cornea and clouding on her artificial lens made it difficult to see what was happening in the back layers of the eye,” notes Dr. Mian. Because of her extreme light sensitivity, Roxy had trouble tolerating the typical imaging tools available in the clinic or even opening her eye.
The team determined that the best approach was to conduct a comprehensive exam under anesthesia. Since this approach is used to image the eyes of infants and small children, they coordinated with pediatric retina specialist Emily Eton, M.D., to conduct the exam

“WE’RE THRILLED
AT ROXY’S PROGRESS IN THE RIGHT EYE. WE ARE NOW WORKING ON REHABILITATING THE LEFT EYE, WHICH REQUIRES A SIMILAR DEGREE OF COMPLEX STEPS AND COORDINATION.
“
Jason Miller, M.D., Ph.D.
in a specially equipped operating room in U-M C.S. Mott Children’s Hospital.
“With Dr. Eton’s assistance, Dr. Wu and I conducted the exam, then met with Roxy’s mom and dad right after to discuss what we saw and plan our next move.” says Dr. Miller.
“That was one of so many ‘above and beyond’ days at Kellogg,” recalls Patty Riggio. “Again and again, we’ve been impressed by the lengths this team goes to, all to help Roxy.”
The exam indicated that scar tissue on the lens was the likely culprit, requiring a procedure to remove it. Steroid injections were planned to reduce retinal swelling, but because they tend to raise eye pressure, Dr. Miller could not resume them until her glaucoma improved. Action was also needed to address haziness in her cornea transplant graft. To make things as easy as possible for Roxy, Drs. Wu and Mian operated in tandem, replacing the cloudy cornea graft and inserting a glaucoma drainage device (GDD) to reduce eye pressure in one session.
The team then debated the best approach to removing the scar tissue on Roxy’s lens. Typically, a tool called a YAG laser is used in the clinic. But this requires a patient to sit very still and look into a bright light—an uncomfortable proposition for Roxy.
“After her previous procedure, Roxy was able to sit at the slit lamp for removal of some of the sutures on her corneal transplant,” Dr. Mian says. “She therefore
bravely agreed to let us try the laser treatment, and she did really well. We are all so proud of her.”
Roxy also needed a GDD in her other eye which was performed by another member of the team, Amanda Bicket, M.D. Recognizing another opportunity to simplify Roxy’s care, Dr. Miller recommended a steroid injection at the same time as the surgery to keep the retinal swelling down.
“Thanks to the GDDs, I no longer need the glaucoma medications that caused me so many problems,” Roxy says. “I feel so much more like myself now.”
With the new corneal transplant, Roxy’s vision improved from “CF” to being able to see fairly small letters on the eye chart (20/50-20/100). And since the removal of the film on her artificial lens implant, Dr. Miller can now see well enough into the back of the eye to manage her retinal swelling without any need for an exam under anesthesia.
“We’re so encouraged by Roxy’s progress in the right eye,” Patty Riggio says. “In the hands of this remarkable team and by the grace of God, she has gone from virtually blind in that eye, to seeing again.”
“We’re thrilled at Roxy’s progress in the right eye,” says Dr. Miller. “We are now working on rehabilitating the left eye, which requires a similar degree of complex steps and coordination. During this whole process, we’ve asked a lot of Roxy and her family. Their grace, patience and humor continue to impress and inspire us at every turn.”

Microbial keratitis (MK) is a painful and potentially blinding infection of the cornea which must be treated as soon as symptoms emerge to save vision. Data suggests that the number of MK cases worldwide may exceed two million annually, and that the disease is reaching epidemic levels in lesser developed regions of the world.
“
One major driver of vision loss in MK is the lack of methods to rapidly and reliably identify the specific microbial organism driving a patient’s infection. Currently, the test results that identify the organism causing MK do not come back for days, leaving most clinicians—especially those in underserved areas—unsure of how best to treat their MK patients.
Deep learning involves aggregating large amounts of data—in this case, patient data and low-cost images acquired from geographically diverse regions—and using that information to train an algorithm capable of rapidly processing and ‘learning’ from it. Dr. Woodward’s collaborators at Duke University, including ophthalmic bioengineer Sina Farsiu, Ph.D., do not just use publicly available algorithms; they employ novel methodologies to create their own.
THE NEI’S STRATEGIC PLAN
HIGHLIGHTS THE CRITICAL NEED TO DEVELOP PRACTICAL, AFFORDABLE, WIDELY AVAILABLE POINT-OF-CARE
“In effect, an eye clinicians anywhere in the world could use an algorithm like this if it became available online,” she explains, “by inputting their patient’s clinical information and photos, they could reach a diagnosis informed by thousands of MK cases,” she explains.
TOOLS TO QUICKLY DIAGNOSE MK AND GUIDE TREATMENT.
Maria Woodward, M.D., M.S.
“Clinician-scientist Maria Woodward, M.D., M.S. is a cornea specialist whose research focuses on improving the quality and affordability of eye care in underserved communities. Her latest initiative, funded by an R01 grant from the National Institutes of Health/National Eye Institute (NEI), harnesses the power of artificial intelligence (AI) to improve MK diagnosis and treatment.
“The NEI’s strategic plan highlights the critical need to develop practical, affordable, widely available point-of-care tools to quickly diagnose MK and guide treatment,” Dr. Woodward says. “We believe that one potential tool could use AI deep learning strategies.”
To ensure that the algorithm reflects the needs of patients and providers in a range of low resource settings, the collaboration is drawing on the expertise of a diverse group of clinicians, notably N. Venkatesh Prajna, M.D., D.O., D.N.B., a cornea expert at India’s Aravind Eye Hospitals, one of the largest eye care providers in the world and many renowned USAbased cornea specialists.
The long-term goal is to create a tool that is easy to use and freely accessible on an open-source, webbased platform. “We’re excited about the potential of this approach to democratize clinical decision making— and patient outcomes—in MK,” she says.
Dr. Woodward discussed the project at the 2024 meeting of the American Academy of Ophthalmology (AAO), where she was invited to give the annual Whitney G. Sampson Lecture. She is also a recipient of a 2024 Secretariat Award from the AAO.
Among the 25+ laboratories conducting basic science research at Kellogg, it might seem surprising to find one focused on neurodegenerative diseases like Multiple Sclerosis (MS). But that’s just one of the unexpected things about the Werneburg lab.
Neurobiologist Sebastian Werneburg, Ph.D., joined the University of Michigan in 2022 as a faculty member in the Departments of Ophthalmology & Visual Sciences and Molecular & Integrative Physiology, and as an affiliate of the Michigan Neuroscience Institute. His laboratory studies how disruptions of synapses in the brain and retina, the connections between nerve cells that allow networks of neurons to communicate and facilitate proper brain function, contribute to disease progression and severity in neurodegenerative conditions like MS.
Despite decades of research into MS, degeneration of neurons and the breakdown of connections between those neurons (neural circuits) continue to cause permanent disability, representing an urgent unmet clinical need. MS is characterized by pronounced inflammation, the destruction of myelin (the protective sheath around nerves), and damage to nerve fibers. Current therapies primarily focus on the immune system’s attacks on these central nervous system components. However, they fall short in addressing the deterioration, or degeneration, of neural circuits that lead to the disabling consequences of MS.
“Dr. Werneburg’s team uses the visual system, a neural circuit frequently affected in MS, to unravel these complexities. They discovered that microglia, the brain's immune cells, cause a loss of connections, or synapses, between nerve cells in the visual system by eating synaptic connections. They further describe that synapse loss, which causes the entire system to dysfunction, can occur even before the loss of neural fibers and myelin damage. While this work highlights the role of synapse disruption in MS-related dysfunctions, much about how these synaptic circuits break down remains unclear.

Sebastian Werneburg, Ph.D.
cognitive impairment in another neurodegenerative disorder, Alzheimer’s disease,” he adds.
SYNAPTIC CIRCUITRY IS A VASTLY UNDERSTUDIED ASPECT OF MS, IN PART BECAUSE IT IS NOT AS EASILY NOTICEABLE AS OTHER FACTORS. BUT OUR WORK HIGHLIGHTS THAT DISRUPTIONS IN SYNAPSES, INCLUDING THE VISUAL SYSTEM, ARE VERY LIKELY KEY DRIVERS OF DISEASE PROGRESSION AND SEVERITY IN MS.
“Sebastian Werneburg, Ph.D.
To test this novel theory, the Werneburg lab aims to investigate key biological processes such as alterations in neuronal activity and microglial reactivity to better understand how the nervous and immune systems interact to drive neural circuit disruption. Another project focuses on the potential to repair synaptic circuits damaged in MS. “Most patients are first diagnosed with the relapsing/remitting form of MS, which alternates between phases of degeneration (relapse) and regeneration (remission),” he explains. “That potential for regeneration—however tenuous it may be—may represent another key target for therapeutic interventions by enhancing synaptic repair.”
His team also conducts research specific to retinal dysfunction in MS, recently identifying degeneration of synapses in the retina as a potential diagnostic target to predict and track the progression of MS.
Dr. Werneburg explains, “Synaptic circuitry is a vastly understudied aspect of MS, in part because it is not as easily noticeable as other factors. But our work highlights that disruptions in synapses, including the visual system, are very likely key drivers of disease progression and severity in MS.”
“One reason to suspect this is that similar disturbances in brain circuitry are the strongest link to
These innovative research directions have significant clinical relevance. Establishing a clear link between synaptic circuitry disruptions and neural degeneration could pave the way for groundbreaking treatments to halt or even reverse functional decline seen in MS and other related neurodegenerative diseases. Thus, Dr. Werneburg’s novel research focus holds the promise of filling critical gaps in our understanding and treatment of these debilitating conditions.
The retina is home to light-sensitive photoreceptor cells, which are supported by a cell layer in the back of the eye called the retinal pigment epithelium (RPE). The RPE gets its energy from lipids (fat), through a dynamic process of temporarily storing fat in spheres called lipid droplets (LDs) prior to using them for energy, then discarding unused lipids outside of the RPE.
This buildup of lipid “leftovers” is a hallmark of age-related macular degeneration (AMD). The processes of lipid handling and dysregulation have been linked to other syndromes as well, such as fatty liver disease. And research in other disease models has shown that enzymes involved in those processes are sensitive to existing therapies.
Yet more research is needed to better understand the lipid dynamics specific to the RPE.
John Han, Ph.D., is addressing this knowledge gap. A second-year post-doctoral fellow in the lab of Kellogg retina specialist Jason Miller, M.D., Ph.D., Dr. Han has received the BrightFocus Foundation Postdoctoral Fellowship in Macular Degeneration Research, as well as the foundation’s 2024 Helen Juanita Reed Award
“We have so much to learn about how lipids are metabolized in the RPE,” he says. “Moreover, if we can manipulate lipid dynamics so that less toxic fat ends up pooling outside the RPE, that could lead to promising new therapies for AMD.”

“SO GRATEFUL FOR THIS OPPORTUNITY, AND FOR DR. MILLER’S SUPPORT AND MENTORSHIP. I HOPE TO SOMEDAY PAY IT FORWARD TO OTHERS WHO DREAM OF A CAREER IN SCIENCE.
“ I’M
John Han, Ph.D.
John Han, Ph.D., was one of twelve postdoctoral investigators to receive the 2023-2024 Michigan Pioneer Fellowship.
Awarded by a partnership of U-M’s Medical School Endowment for the Basic Sciences, Life Sciences Institute and College of Literature, Science and the Arts, this highly competitive award provides mentoring support to basic science researchers of extraordinary promise to help them prepare for independent, research-intensive careers.
A self-described ‘academic late bloomer,’ Dr. Han showed little motivation or aptitude until a freshman biology class at Pennsylvania’s Shippensburg University. “Suddenly, biology wasn’t just facts to memorize. It was an elegant process of molecules evolving into entire ecosystems,” he recalls. “I was hooked.”
Catapulted from C-student to the honors society, Dr. Han went on to earn a Ph.D. in cell biology at Thomas Jefferson University in Philadelphia, PA, where he was mentored by world-renowned eye researcher Nancy Philp, Ph.D. “In her lab, the metabolic ecosystem came to life again,” he says. “Where one cell’s byproducts become another’s building blocks.”
“John combines insatiable curiosity with an unending enthusiasm for experimentation, and takes genuine joy in helping others succeed,” says Dr. Han’s research mentor Jason Miller, M.D., Ph.D. “He has all the characteristics of a truly great collaborative scientist.”
“I’m so grateful for this opportunity, and for Dr. Miller’s support and mentorship,” Dr. Han says. “I hope to someday pay it forward to others who dream of a career in science.”

Lindsey De Lott, M.D., M.S.
At some point in their lives, between five and 15 percent of Americans will experience chronic ocular surface pain (COSP). Sometimes occurring in combination with dry eyes, COSP symptoms, including burning, aching and irritation, can compromise daily function and quality of life.
Understandably, the first stop for patients experiencing eye pain is an ophthalmologist. But for more than half of COSP patients, conventional treatments targeting the surface of the eye—the perceived source of the pain—are not effective.
Kellogg neuro-ophthalmologist Lindsey De Lott, M.D., M.S., is exploring the possibility that for those patients, the pain in their eyes may actually originate in their brains.
“
As Principal Investigator on an NIH R01 grant, Dr. De Lott will lead the most comprehensive study to date of the clinical, neurobiological and treatment response features of pain in a group of COSP sufferers. “A study of this magnitude could only be possible in collaboration with pain experts like my colleagues in the U-M Chronic Pain and Fatigue Research Center,” she notes.
“ WE HOPE TO LAY THE FOUNDATION FOR THE DEVELOPMENT AND CLINICAL TESTING OF TAILORED TREATMENTS TO BRING RELIEF TO PATIENTS EXPERIENCING CHRONIC EYE PAIN.
Research in other chronic pain conditions like fibromyalgia has shown that some patients experience pain in one or more areas far from the primary site, as well as non-pain symptoms such as fatigue, sleep disturbance and mood disorders.
Lindsey De Lott, M.D.,
M.S.
The project begins with a survey conducted with about 200 patients. Validated patient-reported outcome measures will capture their perceptions and experiences living with pain and other non-pain symptoms such as fatigue and mood changes. Surveys will be followed by comprehensive ocular exams to assess eye health and identify any relevant conditions. This data will be used to identify a subset of patients to undergo more intensive examinations, including multimodal sensory testing of the eyes and sites remote from the eyes, and functional brain magnetic resonance imaging (MRI) of regions implicated in their pain.
“The theory is that when certain pathways in the brain are amplified or become dysfunctional, they can cause pain in seemingly unrelated areas,” Dr. De Lott explains. “We refer to this as ‘nociplastic pain,’ and we see anecdotal evidence that this may be the case for some COSP patients in our clinic.”
“This study has the potential to fundamentally change how ocular pain syndromes are diagnosed and treated,” says Dr. De Lott. “We hope to lay the foundation for the development and clinical testing of tailored treatments to bring relief to patients experiencing chronic eye pain.”

Roughly 18 million Americans are living with agerelated macular degeneration (AMD), the most common cause of irreversible vision loss in the U.S. Unfortunately, for too many patients, the handful of available therapies are not effective.
AMD is, at least in part, driven by genetics. People can inherit genetic mutations that increase their risk of AMD. Yet for reasons science has yet to describe, not everyone who inherits a mutation—or risk allele—goes on to develop AMD. The key to solving this mystery is mapping the mechanism by which AMD risk alleles cause disease.
Kellogg physician-scientist and vitreoretinal surgeon Rajesh Rao, M.D., believes that map goes through unexpected and largely uncharted territory. Research to Prevent Blindness has awarded Dr. Rao a Catalyst Award for Innovative Research Approaches for AMD to explore it.
“Most genetic research looks for defects in the coding part of a gene’s DNA—the area containing instructions that turn DNA into protein,” explains Dr. Rao. “But mutations can also occur in non-coding part of a gene— the DNA tasked with regulatory housework.”
Dr. Rao is zeroing in on the non-coding genetic variant rs11200638, which, through mechanisms he hopes to help explain, is associated with a tenfold increase in a person’s risk of developing AMD.
“It’s the location of non-coding variants like rs11200638 that has thrown researchers off their trail,” he says. “rs11200638 is located in a non-coding, regulatory region known as a promoter. Classically, it is
“
“ THE BODY HAS TRILLIONS OF CELLS AND EACH CONTAINS PERHAPS SIX FEET OF DNA. THE ONLY WAY TO CONTAIN ALL OF THAT IS TO FOLD THE STRANDS OF DNA. WHEN PICTURING THE GENOME FOLDED, ONE CAN IMAGINE HOW VARIANTS LIKE RS11200638 MIGHT ‘CONTACT’ FARAWAY GENES WHEN FOLDED IN 3D SPACE.
Rajesh Rao, M.D.
thought that variants in promoter regions influence their closest neighbor genes. But variants in promoters—and promoters themselves—are known to regulate genes thousands or millions of DNA bases away.”
“That leads us to hypothesize that rs11200638 could be regulating distant genes in AMD,” he continues. Located in the promoter of the gene HTRA1, rs11200638 can regulate previously unknown genes far away from its location, interacting with them through the phenomenon of genome folding.
“The body has trillions of cells and each contains perhaps six feet of DNA,” he explains. “The only way to contain all of that is to fold the strands of DNA. When picturing the genome folded, one can imagine how variants like rs11200638 might ‘contact’ faraway genes when folded in 3D space.”
Using retinal stem cell organoids, or living models of the retina, derived from patients carrying the high risk rs11200638 allele, Dr. Rao will attempt to correct the mutation, altering it to resemble the corresponding low risk allele common in people without AMD. Then, he will use 3D genome mapping tools such as MicroCapture C technology to see if long range contacts across the genome differ in retinal organoids derived from patients with the high risk rs11200638 variant compared to those of organoids in which the high-risk allele has been corrected to the low-risk allele, using gene editing techniques such as CRISPR-Cas9.
“This is one of the first studies, if not the first, to explore 3D genome folding as an AMD risk factor,” says Dr. Rao. “We hope it will help shed more light on the process by which a mutation in a non-coding region contributes to the disease, and ultimately yield new insights with therapeutic applications for AMD.”

Kellogg researcher James Weiland, Ph.D., is Principal Investigator on a new NIH R01 grant with a very am bitious long-term goal: restoring sight to those left blind by degenerative diseases such as retinitis pigmentosa and age-related macular degeneration.
Dr. Weiland, who holds a dual faculty appointment in the Medical School’s Department of Ophthalmology and Visual Science and the Department of Biomedical Engineering, leads a multidisciplinary U-M team that will design and test a next generation implantable retinal prosthesis.
The idea of an artificial retina is not new. Efforts to develop devices to stimulate retinal activity date back more than 30 years. About 500 people received the first commercially available implants, generating plenty of excitement. But while these early prostheses demonstrated that implantation and electrical stimulation in the retina is safe, the vision provided was limited to detecting large objects and recognizing simple shapes. Letter recognition was possible in some implant patients, but not at the speed of natural reading.
“The first-gen prostheses rested on top of or beneath the retina, too far away from the retinal cells to deliver high precision stimulation,” explains Dr. Weiland. “With advances in biomaterials and brain-machine interfaces, we believe we can develop an implant that overcomes this and other past shortcomings.”
One potential game-changer is the application of carbon fiber microelectrode arrays, a technology
“IN TERMS OF IMPROVING VISION, WE’RE SETTING THE BAR VERY HIGH. THE BEST VISUAL ACUITY REPORTED FOR ANY CLINICAL DEVICE IS 20/438. OUR LONG TERM GOAL IS 20/80—TRULY FUNCTIONAL ARTIFICIAL VISION ACHIEVED THROUGH RETINAL STIMULATION.
“
advanced by co-investigator Cynthia Chestek, Ph.D. Dr. Chestek is a Professor of Biomedical Engineering and Associate Chair for Research in Biomedical Engineering.
These new cellular-scale carbon fibers—just six microns in diameter—are tipped with platinum-iridium for superior conduction. Arranged in an array like the bristles of a toothbrush, they can be positioned to penetrate the retina. In theory, establishing more intimate contact with retinal bipolar cells will make it possible to deliver more—and more precise—electrical stimulation, while minimizing tissue damage.
Other co-investigators include Kellogg retinal neurobiologist Kwoon Wong, Ph.D., who will measure the response of retinal cells to intraretinal stimulation; Kellogg vitreoretinal surgeons and researchers Nita Valikodath, M.D., M.S., and David Zacks, M.D., Ph.D., who will determine the optimal strategy for implanting the device; and Parag Patil, M.D., Ph.D., an expert in restorative neuro-engineering in the U-M Department of Neurosurgery, who will implant brain electrodes in animal models to record responses elicited by retinal stimulation.
The objective of this initial research is to establish the feasibility of the team’s intraretinal array. Established animal models of photoreceptor degeneration will be used to evaluate parameters for effective stimulation and safety of long-term implantation.
“In terms of improving vision, we’re setting the bar very high,” says Dr. Weiland. “The best visual acuity reported for any clinical device is 20/438. That’s significantly worse than 20/200, the threshold of legal blindness. Our long term goal is 20/80—truly functional artificial vision achieved through retinal stimulation.”
Age-related macular degeneration (AMD) is the leading cause of irreversible blindness in the developed world. There are effective treatments for the ‘wet’ stage of the disease. But treatments targeting the more prevalent, slower progressing, and ultimately more threatening ‘dry’ form of the disease have so far had minimal impact.
Dry AMD is the primary research focus of Kellogg clinician-scientist Jason Miller, M.D., Ph.D. His lab aims to better describe and ultimately disrupt a primary pathway of the disease—lipid (fat) deposits called drusen that build up outside of the retinal pigment epithelium (RPE).
The RPE is a vital cell layer at the back of the eye that supports the photoreceptor cells (PRs) that convert light to sight. In dry AMD, drusen accumulation ultimately destroys the RPE. Left unprotected,PRs subsequently die, leading to vision loss.
“We know that lipids are one source of energy for the RPE,” Dr. Miller explains. “And there is good evidence that the toxic drusen buildup we see in dry AMD is largely a by-product of the RPE casting off lipids it doesn’t use, like trash piling up in an alley.”
In consultation with lipidomics expert Subramaniam Pennathur, M.D., Chief of Michigan Medicine’s Division of Nephrology, the Miller lab will conduct studies to understand how those piles build up and explore ways to reduce their size. Three new grants will fund this work:
The E. Matilda Ziegler Foundation for the Blind and Eversight Eye & Vision Research will support complementary projects to better describe the processes by which the RPE secretes lipids and deposits discarded lipids as drusen outside the RPE. A Foundation Fighting Blindness grant will explore strategies to minimize the amount of drusen buildup.
Dr. Miller’s lab also continues to receive instrumental support from the James Grosfeld Initiative for Dry AMD, whose funding led to the preliminary data necessary to successfully compete for these external grants. Additional support comes from the Discovering Hope Foundation.
The Miller lab previously confirmed what logic would suggest: that if the RPE consumes more fat, that will leave less to discard. “We will now focus on encouraging the RPE to maximize its consumption of available lipids,” says Dr. Miller, “We’ll also attempt to identify obstacles that might keep that from happening.”

“AND THERE IS GOOD EVIDENCE THAT THE TOXIC DRUSEN BUILDUP WE SEE IN DRY AMD IS LARGELY A BY-PRODUCT OF THE RPE CASTING OFF LIPIDS IT DOESN’T USE, LIKE TRASH PILING UP IN AN ALLEY.
Jason Miller, M.D., Ph.D.
“One project will attempt to persuade the RPE to make lipids its sole energy source. Unlike PRs, which survive only on glucose (sugar), the RPE may choose to consume either, a choice influenced by certain amino acids. “We hope we can manipulate those amino acids to encourage them to prefer fats over glucose,” says Dr. Miller. “This should have two benefits: increasing lipid consumption in the RPE and making more glucose available to the PRs.”
Another project will deactivate an enzyme critical to degrading (consuming) lipids, to test the theory that hindering the RPE’s lipid degradation will cause it to ‘spit out’ (secrete) what it can’t use. “When turning off that enzyme, we should see a corresponding increase in drusen deposits outside the RPE,” he explains. “The ultimate goal is to create a new model for testing future dry AMD therapeutics.”

Communities and health systems across the U.S. are grappling with a shortage of physicians practicing in pediatric specialties, including pediatric ophthalmology. With fewer specialists to go around, families must wait longer and travel farther for appointments.
In 2022, a partnership between Trinity Health Michigan and University of Michigan Health’s Mott Children’s Hospital was formed to address the problem in Southeast Michigan. The program paved the way for Mott pediatric specialists to provide care at Trinity Health’s location in the northern Oakland County community of Pontiac.
“
I’VE
For Kathleen St. Germaine, who lives in nearby Oxford, the new location means not only convenience, but peace of mind. Diagnosed as a child with a congenital glaucoma, St. Germaine has received surgical care and medical management at Kellogg ever since. She gave birth to her first child, daughter Riley, in Spring 2024.
BEEN A PATIENT FOR MORE THAN 20 YEARS, AND I LOVE AND TRUST MY KELLOGG DOCTORS,” KAUFFMAN SAYS. “IT’S WONDERFUL TO KNOW RILEY CAN GET THE SAME EXCELLENT CARE, MUCH CLOSER TO HOME.
Beginning with cardiology, the available pediatric specialties expanded to include urology, orthopedics and surgery. In May 2024, Kellogg added pediatric ophthalmology to the list.
“Kathleen St. Germaine
“With a new clinical ‘home’ in Pontiac, we’re able to offer a full range of medical and surgical care to infants and children in the area with eye diseases, injuries and vision problems,” says the clinic’s medical director, Christopher Gappy, M.D. When more complex care is needed, the team can facilitate referrals to Kellogg.
“One of my first concerns was Riley’s risk of developing glaucoma,” she says. “My disease was caught early, so I was anxious to begin having her monitored right away.”
Riley made her first trip to the Pontiac clinic at just two weeks old. Though her exams to date have been normal, Dr. Gappy suggested that both mom and daughter undergo genetic testing at the Multidisciplinary Ophthalmic Genetics Clinic at Kellogg. “If they find a shared genetic mutation linked to glaucoma, that could give us an important head start to assess her risk.”
“I’ve been a patient for more than 20 years, and I love and trust my Kellogg doctors,” Kathleen says. “It’s wonderful to know Riley can get the same excellent care, much closer to home.”

Seven million people live with visual impairment in the U.S., and glaucoma is a leading cause. Though glaucoma is treatable, half of all people with the disease are never diagnosed. Black, Hispanic, and Native American people, people living with low incomes, and people living in medically underserved communities all bear a disproportionate share of the burden of glaucoma and vision impairment.
There is a critical need to expand screening for these at-risk populations, and to help people who test positive access appropriate eye care. Glaucoma specialist and health services researcher Paula Anne Newman-Casey, M.D., M.S., is developing and testing innovative strategies to achieve those goals as successfully and costeffectively as possible.
“
Her latest initiative, funded by a grant from the U.S. Centers for Disease Control and Prevention (CDC), aims to identify best practices for screening, triage and follow-up care that can be structured and scaled to implement in lowresource settings nationwide. It builds on key learnings from a previous study led by Dr. Newman-Casey, the Michigan Screening and Intervention for Glaucoma and Eye Health Through Telemedicine (MISIGHT) program.
ted via electronic health records to ophthalmologists at Kellogg, whose screening results and recommendations were returned to the technician to review with the patient. MISIGHT’s technology-based protocol was shown to identify significantly higher rates of glaucoma and other eye diseases than national averages.
But while successful, the MISIGHT protocol was administered through an academic medical center and supported by grant funding, which is neither geographically scalable nor economically sustainable.
WE HOPE THIS WORK WILL INFORM FUTURE POLICIES TO IMPROVE ACCESS TO QUALITY SCREENING AND CARE TO ADDRESS THE STRIKING AND PERSISTENT INEQUITIES IN EYE HEALTH OUTCOMES.
“
Paula Anne Newman-Casey, M.D., M.S.
In the MISIGHT protocol, eye care technicians were placed in two different community clinic settings to conduct comprehensive screenings and imaging beyond the traditional eye examination. Findings were transmit-
“In this project, we’re evaluating a more pragmatic approach,” Dr. Newman-Casey says. “We hope to determine how best to achieve a comprehensive screening intervention using infrastructure already in place in underserved communities.”
The clinical infrastructure targeted for this test intervention is the Federally Qualified Health Center, or FQHC. The approximately 1,400 FQHCs in the U.S. provide primary care for people who live in poverty. Their patients are disproportionately of minority race and ethnicity and are therefore at higher risk of both having glaucoma and not receiving adequate treatment for it. Yet, only about a quarter of FQHCs currently offer eye care of any kind, and only two percent of patients receive eyecare through FQHCs.
“Despite the significant challenges faced by FQHCs—chronic underfunding, and insufficient resources and expertise in specialties like ophthalmology—they
have the best available foundation on which to build,” notes Dr. Newman-Casey. “They are organized and staffed to meet the specific needs of the communities they serve. Many employ social workers and staff with expertise navigating insurance, assistance programs and transportation resources, as well as interpreters.”
One of the two MISIGHT test sites, the Hamilton Community Health Center, an FQHC in Flint MI, is the site of this trial.
Hamilton patients will be randomized into two groups. One group will receive traditional eye examinations, checking vision and eye pressure and examining the eyes with a slit lamp. In the other group, an FQHC
eye doctor will review digital, objective ophthalmic data captured by FQHC ophthalmic technicians, triaging patients to receive appropriate in-person care. Technicians will help patients navigate access to follow up medical treatment and low-cost glasses.
Dr. Newman-Casey’s team will evaluate which approach detects more eye disease and shows greater improvement in vision-related outcomes. They will also identify best practices, conduct resource cost/ value analyses, and develop a ‘toolkit’ for implementing evidence-based eye care in the FQHC setting.
“We hope this work will inform future policies that leverage FQHCs to improve access to quality screening and care to address the striking and persistent inequities in eye health outcomes,” says Dr. Newman-Casey.
The Kellogg Clinical Research Center (KCRC) continues to flourish, supporting a portfolio of clinical trials that is expanding in both volume and variety.
Active Sponsored Clinical Research Studies and Clinical Trials
In the last five years, the KCRC has seen an increase of more than 50 percent in the number of sponsored clinical research studies and trials it supports. At the same time, the volume of clinical studies initiated by Kellogg investigators has increased by more than 40 percent.
The KCRC team works hard to manage that growth while ensuring that the process is as easy as possible for the patients who so generously participate in clinical research.


Modern biomedical research requires analysis of complicated datasets in which thousands to millions of datapoints are obtained with cutting edge technology. These are called “omic” datasets—for example, proteomic and genomic analysis of an eye biopsy sample would give a researcher the relative levels of every single gene and protein in the sample—likely representing more than ten thousand datapoints.
The discipline of analyzing such massive “omic” datasets falls to the mighty bioinformatics analyst. Such a person, trained in computer science and statistics, will take this overwhelming number of datapoints and attempt to determine trends and meaning in the complicated dataset.
Before now, Kellogg lacked such a formally trained bioinformatics analyst. Instead, Kellogg basic science researchers have relied on general bioinformatic specialists available to all of Michigan Medicine. While their expertise is vast, these general bioinformatics specialists lack specific knowledge of vision science and the novel features of ophthalmic genes.
Hannum, Ph.D., who joined the team in August.
There are several aspects to Dr. Hannum’s new role. He supports multiple principal investigators on a range of ongoing studies, building the specific data sets and tools they need. He is also helping Kellogg researchers navigate and interpret the exponentially growing body of external data and published omics studies.
“It’s exciting to have this unique vantage point,” he says. “With a view of both the Kellogg research portfolio and the larger ophthalmology research landscape, I can look for patterns, common data sets, and opportunities to consolidate, collaborate and learn from each other’s analyses.”
“ “
WITH THE EXPERTISE TO SORT THROUGH THE MOUNTAIN OF DATA AVAILABLE TO US, WE CAN UNCOVER THINGS WE DIDN’T EVEN KNOW WE WERE LOOKING FOR. IT’S TRULY A GAME-CHANGER FOR KELLOGG.
Jason Miller, M.D., Ph.D.
Recognizing the clear advantage of a bioinformatics specialist who knows all the quirks and peculiarities of the eye, Kellogg leadership approved the launch of a bioinformatics core in 2024, modeled after similar operations in the U-M Department of Cell and Developmental Biology and the National Eye Institute. Kellogg is now one of the few academic eye centers with this dedicated resource. The core is overseen by Lev Prasov, M.D., Ph.D., Jason Miller, M.D., Ph.D., and Thanh Hoang, Ph.D., and managed by bioinformatician D. Ford
This core also makes Kellogg even more competitive in the grant space. “More and more submissions require an explanation of how data will be handled,” notes Dr. Prasov. “Adding a bioinformatician to our grant applications answers that question.”
Finally, Dr. Hannum will be Kellogg’s go-to bioinformatics educator. “Increasingly, the scientific questions we ask are addressed using bioinformatics,” Dr. Hoang explains. “We now have an expert to provide bioinformatic support and train our faculty, post docs and graduates to gain the knowledge and skills to perform these analyses themselves.”
“We are thrilled to add this discipline to our research arsenal, and to have Dr. Hannum on our team,” says Dr. Miller. “With the expertise to sort through the mountain of data available to us, we can uncover things we didn’t even know we were looking for. It’s truly a game-changer for Kellogg.”

Brittany Simmons, M.D.
In July 2024, Brittany Simmons, M.D., was named Associate Chair of Diversity, Equity and Inclusion (DEI) at Kellogg. To learn more about her vision for DEI, the Annual Report posed five questions to Dr. Simmons.
How would you describe the current state of DEI initiatives at Kellogg?
We have been fortunate over the years to have so many Kellogg stakeholders committed to the principles of diversity, equity and inclusion, especially Dr. Lee, Dr. Mian, and my wonderful predecessor, Dr. Angela Elam. We’ve also benefitted from resources, support and ideas from across U-M, Michigan Medicine, and the field we all love – ophthalmology. All that is to say that I’ve inherited a strong foundation on which to build.
What kind of structure do you have to work with?
DEI initiatives are envisioned, planned and executed by a committee made up of faculty, staff and learners from across Kellogg. We coordinate closely with the University’s Office of Diversity, Equity, and Inclusion and take inspiration from Michigan Medicine’s DEI 2.0 strategic plan. In addition, I meet monthly to share successes and problem solve with my fellow U-M DEI associate chairs and our DEI drivers group at Kellogg. Ophthalmology is also a DEI leader among medical specialties, and we’re plugged into the initiatives of top organizations like AAO, AUPO and (my favorite as an oculoplastics specialist) ASOPRS.
You kicked off your tenure with a survey of staff, faculty and trainees – can you share a few takeaways?
Sure, I’ll share three.
First, there was a strong emphasis across the board to support our patients and improve their care in thoughtful, inclusive ways. It was heartening to see so much emphasis on making the Kellogg environment and experience better for patients, and to see our teams embrace the same theme: patients come first.
Second, there was a lot of interest in broadening our shared cultural education about different identities and communities; suggestions included guest lecturers and shadowing opportunities, some of which we have already started to implement with great support from our Kellogg leadership.
Third, the survey provided baseline metrics for datadriven programs we can enact. If they prove useful, we’ll publish and share our experiences with other institutions.
What do you see as your biggest challenge?
I think the most immediate hurdle to conquer is the bad rap DEI gets in the current public discourse. We have to work hard to counteract negative characterizations of DEI efforts.
What’s your ‘elevator pitch’ to discourage that characterization and encourage skeptics to embrace DEI?
Simply put, DEI is here to benefit everyone. It’s not about putting one group above another; it’s about taking everyone as they come, and appreciating the unique contributions each individual can make to the fabric of Kellogg and our patient care. The better we get at understanding and valuing everyone, the more we’ll accomplish together.
IT’S SO IMPORTANT THAT PATIENTS KNOW THAT, DESPITE THEIR HEALTH CONDITION OR WHAT’S HAPPENING WITH THEIR VISION, THERE ARE STRATEGIES AVAILABLE TO HELP THEM MAXIMIZE THEIR INDEPENDENCE AND QUALITY OF LIFE.
Erin Klukas, O.D.

Erin Klukas, O.D., is passionate about helping people with vision challenges make the most of the sight they have and continue to pursue the activities they love.
An optometrist in Kellogg’s Low Vision and Visual Rehabilitation Service, she’s the program’s unofficial ambassador, taking every opportunity to educate individuals with all levels of vision loss on the benefits of consulting with a low vision specialist.
“It’s so important that patients know that, despite their health condition or what’s happening with their vision, there are strategies available to help them maximize their independence and quality of life,” she says. “A low vision exam is a critical first step.”
“Most people—even many providers—don’t know what’s involved in a low vision examination,” she continues. “It’s more comprehensive and individualized than a standard ocular health exam, because it’s designed to lead to a personalized vision rehabilitation plan.”
Diagnostic procedures and a detailed health history are conducted to assess patients’ remaining functional vision, close up and distance vision, and contrast sensitivity, and to understand their daily activities, interests and priorities. In Kellogg’s low vision clinic, a technician and an occupational therapist are available to demonstrate applicable vision assist devices, guide patients through training and practice applying tools and techniques to their specific activities and hobbies.
Dr. Klukas and her colleagues maintain an active schedule of presentations and events to carry their message throughout the community:
• In 2024 she was a featured speaker at the low vision support group at one of Ann Arbor’s largest senior living communities and at Michigan Medicine’s Geriatric Center. She provided an overview of common eye conditions, described the low vision exam, encouraged people to discuss referrals with primary care providers, and conducted a hands-on review of assistive devices.
• The Low Vision Service was represented at the annual Visions event at the Ann Arbor District Library. The event promotes local and state programs, support organizations, devices and library resources for the visually impaired.
• She has forged an ongoing partnership with the senior adult outreach coordinator at the Ypsilanti District Library to advise on the library’s low vision device loan program, which allows library patrons to ‘check out’ devices as they would library books.
To get the word out about low vision rehab, provider education may be just as important as patient education. “Every day, primary care providers and specialists of all kinds see patients who struggle with reduced vision,” says Dr. Klukas. “My message to them is that, even for those at the earliest stages of vision loss, referrals are always appropriate. We can partner with them to enhance their patients’ function, outlook and quality of life.

PHASE II CLINICAL TRIAL UNDERWAY
Rhegmatogenous retinal detachment (RRD), the most common form of retinal detachment, is an acute, visionthreatening condition in which the retina separates from the wall of the eye. While RRD can result from trauma or severe nearsightedness, it is most often a due to agerelated changes in the vitreous (the gel-like substance between the lens and the retina). These changes can create a tear in the retina, allowing the vitreous to seep under the light-sensitive photoreceptor (PR) layer of the retina. This separates it from its chief source of nutrition, the retinal pigment epithelium.
“RRD initiates a complex set of events within the PRs, which, if the detachment is left untreated, eventually leads to cell death and vision loss. But the RRD does not send a pain signal to indicate an emergency. Instead, the first symptoms are more subtle, like seeing floaters or flashes of light, followed by a loss of sight that begins in the side, or peripheral, vision, and spreads to the center.
diagnosis, and between diagnosis and surgery,” he explains. “We need proven tools to minimize the damage that occurs before surgery.”
As co-founder and Chief Scientific Officer of ONL Therapeutics, Dr. Zacks has developed such a tool— ONL1204. Used in conjunction with surgery, ONL1204 is solution that is injected into the vitreous to block the molecular pathways responsible for cell death in RRD.
IN EACH OF THESE TRIALS, WE’VE SEEN STRONG EVIDENCE THAT ONL1204 CAN PREVENT CELL DEATH IN THE RETINA. IT’S AN EXCITING ADVANCE WITH GREAT POTENTIAL AS A THERAPEUTIC PLATFORM FOR RETINAL NEUROPROTECTION.
David Zacks, M.D., Ph.D.
Timely diagnosis and surgical repair (the standard of care) provide the best chance to preserve vision.
Kellogg retinal surgeon and clinical researcher David Zacks, M.D., Ph.D., has performed countless RRD repair procedures. “In too many cases, precious time is lost between noticing symptoms and confirming a
Following a Phase IB clinical trial that confirmed its safety, a Phase II clinical trial of ONL1204 was undertaken. “This trial evaluated two alternative dosages, and determined the optimal timing for administering the treatment,” he explains.
“In addition to testing ONL1204 in RRD, Phase I trials have also been completed using the drug to prevent retinal cell death in two other blinding diseases—open-angle glaucoma and geographic atrophy secondary to macular degeneration, for which a Phase II trial will soon begin.
“In each of these trials, we’ve seen strong evidence that ONL1204 can prevent cell death in the retina,” Dr. Zacks says. “It’s an exciting advance with great potential as a therapeutic platform for retinal neuroprotection.”

New and more effective injectable medications have come to market in recent years to treat retinal conditions like macular degeneration and diabetic retinopathy. To keep pace with the increasing number of patients who can benefit from these therapies, Kellogg is pursuing new clinical strategies to maintain the highest safety standards for these injections.
“Injections are now the most common in-office procedure in ophthalmology,” says Jennifer Weizer, M.D.
“Yet it’s not a one-size-fits-all process. Patients may require multiple injections, in different formulations and dosages, in one or both eyes, delivered on varying schedules.”
When managing all of those variables in a growing volume of patients, improving efficiency must go handin-hand with the priority of ensuring patient safety. As head of the Kellogg Patient Safety Committee, Dr. Weizer is spearheading efforts to increase dedicated injection capacity and fine-tune the injection protocol in Kellogg’s retina clinics, while prioritizing safety above all else.
In 2024, Dr. Weizer and the committee, including continuous improvement specialist Beth Hansemann, B.A., C.O.T., plus Anjali Shah, M.D., and the Kellogg retina faculty, re-examined every step in the injection process to develop one common, streamlined protocol.
“THE GOAL IS TO MINIMIZE OPPORTUNITIES FOR CONFUSION AND AVOID POTENTIAL SAFETY EVENTS, ENSURING THAT, AS OUR VITREORETINAL INJECTION VOLUME GROWS, WE CONTINUE TO DELIVER THE SAFEST POSSIBLE PATIENT EXPERIENCE.
Jennifer Weizer, M.D.
“
“For example, we’ve analyzed the procedure for preparing injections, putting steps in place to verify that every patient receives the correct medication, delivered into the correct eye,” says Hansemann.
Patient flow within the clinic is also being reimagined to address bottlenecks in the workflow. “The usual process calls for a patient to be seen by a technician in an exam room, then be transferred to an injection room,” Dr. Weizer explains. “If we were equipped to perform exams and injections in the same room, we would streamline each visit for physicians and staff and make it easier for patients, with fewer steps in the flow process.”
Another approach the team is exploring is revamping patient and provider scheduling to cluster injection appointments in a common block of a physician’s clinic time.
Changes like these require adding the specialized injection equipment found in dedicated injection rooms to more exam rooms. “These are costly upgrades, so we are rolling them out in stages,” notes Dr. Weizer. To date five exam rooms are being retrofitted, and the goal is to complete the remaining rooms in the months ahead.
“The goal is to minimize opportunities for confusion and avoid potential safety events,” she continues, “ensuring that, as our vitreoretinal injection volume grows, Kellogg continues to deliver the safest possible patient experience.”

Vision-threatening diabetic retinal disease (DRD) leaves no aspect of life untouched—from basic daily activities, to treasured hobbies, to regulating emotions, making decisions and interacting with others. Patients and their care teams need tools to help them speak the same language about the many functional, cognitive and emotional aspects of living with DRD, in order to inform and monitor treatment plans. Standardized qualitative and quantitative snapshots are equally essential for researchers developing and testing new interventions in clinical trials.
Kellogg retina specialist K. Thiran Jayasundera, M.D., M.S., is at the forefront of developing and validating patient-reported outcome measurement (PRO) tools for patients afflicted with retinal diseases. His customized PROs for patients with inherited retinal diseases (IRDs) have been translated into more than ten languages and are currently in use in clinical trials involving 50 centers worldwide.
The need for comprehensive, easy-to use PROs is just as great in the DRD community. Now, with startup support from the Mary Tyler Moore Vision Initiative’s Founder and CEO S. Robert Levine, M.D., (see page 28) a team led by Dr. Jayasundera is tailoring a PRO questionnaire specifically for DRD patients.
“This is not the first PRO for DRD, but it’s by far the most thorough one,” says Dr. Jayasundera. “Measures of central, color, photopic peripheral and mesopic peripheral vision, contrast sensitivity, scotopic function and photosensitivity are organized in domains corresponding to specific pathways of vision physiology. And unlike previous tools, we take a deep dive into
“
MTM VISION EXISTS TO ADDRESS RESOURCE GAPS THAT IMPEDE PROGRESS TOWARD ENDING VISION LOSS FROM DIABETES. WE ARE THRILLED TO TAP INTO DR. JAYASUNDERA’S EXPERTISE TO EXPEDITE THIS CRUCIAL PROJECT.
“
S. Robert Levine, M.D.
the emotional, psychological and psychosocial aspects of living with DRD.”
“From the very start, this has been a top priority of patients, advocates, researchers and pharma leaders in our consortium,” Dr. Levine says. “MTM Vision exists to address resource gaps that impede progress toward ending vision loss from diabetes. We are thrilled to tap into Dr. Jayasundera’s expertise to expedite this crucial project.”
Assisting Dr. Jayasundera on this project are research fellows Rafid Farjo, Timothy Mayotte and Alex Zmejkoski. They are coordinating the additional support provided by specialists in ophthalmology, endocrinology, psychology and pharmaceutical development.
“Beyond measuring and trending many of the same variables we follow in IRD patients, we need to capture how worsening vision impacts the many steps patients take to manage their diabetes, like monitoring blood glucose and insulin use, and mustering the motivation to eat right, exercise and lose weight,” Farjo explains.
Following the IRD PRO model, the process of creating the DRD questionnaire began with focus groups of clinical experts, followed by a series of in-depth patient interviews. “At every step, we’ve continued to refine the topics and questions included, as more and more associations and challenges are raised,” says Mayotte.
An evaluation with 300 DRD patients is planned for fall 2024, with an ambitious goal of completing the PRO by May, 2025.
“This project is only possible thanks to the leadership of Dr. Levine and MTM Vision,” adds Dr. Jayasundera. “His involvement sparked additional support from the Macula Society, the Retina Society, and two pharmaceutical leaders. Together, we’re bringing this tool to market for use by stakeholders across the DRD community.”

The
Mary Tyler Moore was an entertainment pioneer whose body of work set the gold standard performers strive for to this day. She first charmed audiences in the 1960s sitcom classic The Dick Van Dyke Show, but it was her groundbreaking role in the 1970s hit The Mary Tyler Moore Show that reshaped how women were portrayed on TV. Embracing for the first time the possibilities of life as a single career woman, she epitomized independence, optimism and loyalty, and turned the world on with her smile.
Diagnosed with type I diabetes (T1D) at age 33, Mary stepped into another defining role in the 1980s. Named the first International Chairman of the Juvenile Diabetes Research Foundation (JDRF, now Breakthrough T1D) she was arguably the original celebrity health activist. In partnership with her husband of 33 years, S. Robert Levine, M.D., Mary continued to advocate tirelessly for diabetes awareness, patient support, and research funding until her death in 2017.
“Of all the complications of diabetes Mary endured, vision loss was the most devastating,” Dr. Levine says. “Diabetic retinal disease (DRD) robbed Mary of her sight, and with it, her independence and her joy.”
To realize Mary’s dream of a world without vision loss from diabetes, Dr. Levine founded the Mary Tyler Moore Vision Initiative (MTM Vision) in 2018, bringing together stakeholders from academia, industry, government, non-profits, and entertainment, as well
“
OF ALL THE COMPLICATIONS OF DIABETES MARY ENDURED, VISION LOSS WAS THE MOST DEVASTATING. DIABETIC RETINAL DISEASE (DRD) ROBBED MARY OF HER SIGHT, AND WITH IT, HER INDEPENDENCE AND HER JOY.
“
S. Robert Levine, M.D.
as technology innovators, patients and families. The initiative is a hub for workshops, symposia, scholarly publications, public awareness campaigns, the fostering of cross-sector collaborations and data sharing, and the development of critical path research resources and tools. Through these efforts, MTM Vision is accelerating the pace of discovery and translating scientific advances into new ways to preserve and restore vision in people with DRD.
Michigan Medicine has played a pivotal role in MTM Vision from the start. Both the Elizabeth Weiser Caswell Diabetes Institute (CDI) and the Kellogg Eye Center are MTM Vision partners, along with the Beetham Eye Institute, Joslin Diabetes Center at Harvard Medical School, Breakthrough T1D, and the Entertainment Industry Foundation. Dorene Markel, M.S., M.H.S.A., who recently retired from leadership at the CDI and the Brehm Center for Diabetes Research at U-M, serves as managing director and senior advisor. Kellogg’s Thomas Gardner, M.D., M.S., serves as co-scientific director, along with Joslin’s Jennifer Sun, M.D., M.P.H. Patrice Fort, Ph.D., M.S., directs the MTM Vision Ocular Biorepository and Resource Center, housed at Kellogg.
An ambitious, multiphase roadmap guides MTM Vision. Significant progress has been made on the first phase: a DRD cure platform to address three fundamental gaps in the DRD research pipeline:
#1: Staging based only on vascular damage tells only part of the story.
“DRD is not just a microvascular complication of diabetes, it involves the entire neurovascular unit, and vascular changes don’t appear until the disease has advanced,” explains Dr. Levine. “We need a more wholistic DRD staging system and severity scale so DRD can be tackled early, and from every angle.”



Between August 2023 and April 2024, each of MTM Vision’s six working groups of global experts published recommendations for modernizing DRD staging. Together, they form the basis for a staging system that considers not only vascular, but neuronal, cellular, systemic, functional and quality of life measures.
#2: You can’t expect to cure a human disease without studying it in humans. Unlike other tissues in the body, the retina cannot be biopsied. Researchers need access to reliably preserved and cataloged postmortem eye tissue and fluids for study. The Mary Tyler Moore Vision Initiative’s Ocular Biorepository and Resource Center was launched at Kellogg in 2022 to fill that need.
“In 2024 we began the process of characterizing the initial samples collected, which include eyes from donors with and without diabetes, and with and without DRD in its different stages,” says Dr. Fort. “Our approach also evolved this year based on feedback from our different stakeholders and partners, including expanding the type of samples collected (blood samples along with tissue and eye fluid) as well as modification of the process, further increasing value.”
stabilize or reverse over time – informs the identification of both biomarkers for targeted treatments and end points for evaluating the effectiveness of those treatments. In DRD research, that means arriving at consistent ways to gauge how patients feel, how well they see, and what’s happening in their retinas.
For example, some researchers hypothesize that changes in visual function might precede retinal damage in DRD visible on retinal photographs or by ophthalmoscopic exam. That would make visual function a relevant therapeutic end point. MTM Vision led the design and is co-sponsoring, in partnership with the DRCR Retina Network, a federally funded clinical research organization, two upcoming observational clinical studies to evaluate a range of advanced technologies that objectively measure visual function.
“ “
WITH MARY AS ITS NORTH STAR, MTM VISION IS TRULY MEETING THE MOMENT, ROBERT IS PROVIDING INSPIRATION, FOCUS AND LEADERSHIP TO ACCELERATE DRD DISCOVERY WHERE IT’S NEEDED MOST–AT THE INTERSECTION OF ENDOCRINOLOGY AND OPHTHALMOLOGY.
Thomas Gardner, M.D., M.S.
In addition to the roadmap, MTM Vision’s other imperative is raising awareness and funding for DRD research. 2024 marked the debut of a public service announcement narrated by Mary’s longtime friend Kevin Kline and featuring three women whose lives and careers were inspired by Mary: Julia Louis-Dreyfus, Oprah Winfrey and Reese Witherspoon.
#3: We need new ways to measure the trajectory of DRD.
How the evolution of a disease is characterized— measures of its severity, and how it may progress,
“With Mary as its north star, MTM Vision is truly meeting the moment,” says Dr. Gardner. “Robert is providing inspiration, focus and leadership to accelerate DRD discovery where it’s needed most–at the intersection of endocrinology and ophthalmology.”
The Kellogg Eye Center is consistently ranked in the top tier nationally in both clinical care and research grant funding. The same is true when it comes to the third pillar of our mission: medical education. Two national rankings of residency programs—the Doximity Residency Navigator and Ophthalmology Times’ Best Residency Program listing—rank the U-M Department of Ophthalmology and Visual Sciences in the top ten.
One way to stay on top is to continually innovate. In the academic year ahead, Kellogg will launch a supplementary curriculum designed for ophthalmology residents aspiring to careers as not only clinicians and researchers, but medical educators as well.
The program— Pathway for Residents Interested in Medical Education, or PRIME, is the brainchild of Kellogg’s Co-directors of Medical Student Education, Ariane Kaplan, M.D., and Anjali Shah, M.D.
“We see an opportunity to enhance the bestin-class residency education we already provide by offering the instruction and hands-on practice needed to become effective teachers and mentors in ophthalmology,” Dr. Kaplan explains.
A two-year PRIME curriculum is being designed to run parallel to the ACGME-accredited ophthalmology curriculum, beginning during residents’ PGY-2 or PGY-3 years. The objective is to allow residents interested in a career in medical education the opportunity to build a portfolio of exposure and experience, in areas including:
• curriculum design
• medical student mentorship
• facilitating small group sessions
• designing lectures and wet labs
• participating in educational research
Each year, Kellogg offers an informative series of continuing medical education (CME) programs designed to share new approaches to the diagnosis and management of eye disease across subspecialties. For more information, visit: www.umkelloggeye.org

“This is the core skillset of a medical educator,” Dr. Shah says. “We think PRIME will make Kellogg a more attractive residency destination for an aspiring ophthalmologist who imagines a career in academic medicine.”
A 2024 survey of Kellogg applicants and current residents affirms this. More than 90 percent indicated they would be more likely to consider a program if specialized tracks like this were offered.
“Participants will receive a certificate of completion at graduation,” adds Dr. Kaplan. “That acknowledgement will be important currency when interviewing for fellowships or faculty positions.”
“Supplementing the traditional curriculum with additional complementary training is a trending topic in medical education,” notes Dr. Shah. “For example, Kellogg offers targeted training to prepare residents interested in global ophthalmology. We’re now poised to be one of the first—if not the first—academic eye centers to offer a parallel learning track for aspiring medical educators.”
For questions: contact Jennifer Burkheiser, CME Coordinator, at (734) 763-2357 or kelloggCME@umich.edu.

Unlocking the secrets of eye diseases with genetic origins is a top research priority at Kellogg. Among the rising stars in this field is William Presley, whose work garnered accolades and major grant support in 2024.
A Ph.D. candidate in human genetics, Presley works in the lab of Lev Prasov, M.D., Ph.D. One of his current projects focuses on understanding the genetic basis of treatment-resistant normal-tension glaucoma (NTG).
Presley has received the National Eye Institute’s 2024 Ruth L. Kirschstein National Research Service Award / Individual Predoctoral Fellowship to Promote Diversity in Health-Related Research. This is the first time this grant, known as the F31, has been awarded to a Kellogg candidate. His work was also recognized with the Members-in-Training Outstanding Poster Award in genetics at the 2024 meeting of the Association for Research in Vision and Ophthalmology (ARVO).
“This project began several years ago, when our lab learned of a large family suffering from a dominant form of early-onset NTG. They were experiencing very aggressive disease progression that was unresponsive to traditional glaucoma therapies,” he says.
Isolating the culprit gene proved a complex puzzle. A variant in RPAP3 was associated with NTG in all but two family members, whose optic atrophy may be secondary to a separate condition.

“Preliminary data suggest that the RPAP3 variant is inhibiting production of the proteins that make up a key optic nerve supporting structure called the lamina cribrosa,” Presley explains. “Understanding the pathways involved may eventually point toward new screening and treatment options for this family, as well as other patients with comparable disease presentations.”
Recently, a second NTG family carrying a similar RPAP3 mutation was identified, further strengthening the disease-gene association.
Presley was also recognized in 2024 with an award at the annual Kellogg Research Day conference for a project identifying a genetic variant in a family with plateau iris and angle closure glaucoma.

The Association for Research in Vision and Ophthalmology (ARVO) Foundation recognized David Zacks, M.D., Ph.D., with the 2023 Kreissig Award for Excellence in Retinal Surgery.
The Edna H. Perkiss Research Professor of Ophthalmology and Visual Sciences at Kellogg, Dr. Zacks’ research focuses on understanding the molecular pathways responsible for cell death and developing novel strategies for thwarting the damage they cause in retinal diseases such as macular degeneration, glaucoma, and inherited retinal degenerations.
“I’m honored to receive this recognition from the ARVO Foundation,” says Dr. Zacks. “It’s a career highlight, and validation for 20-plus years of teamwork seeking solutions for patients with retinal diseases. It’s also testament to an environment at Kellogg that encourages collaboration and celebrates the pursuit of big ideas.”
“ “ IT’S EXCITING TO BE PART OF AN INSTITUTION WITH UNPARALLELED DATA RESOURCES AND THE FORESIGHT TO PUT THEM TO WORK.
David Portney, M.D.

David Portney, M.D.
Kellogg PGY-4 David Portney, M.D., combines a passion for ophthalmology with a keen interest in healthcare economics. He is part of a team tapping into Michigan Medicine’s wealth of health services data to study some of the most challenging aspects of delivering ophthalmic care in an academic medical setting.
For one group of studies, an accounting tool called time-driven activity-based costing was used to analyze Kellogg data on the costs and insurance reimbursements associated with complex cataract and retinal procedures.
“We compared the incremental costs and Medicare reimbursement for standard to complex cataract surgery and vitrectomy,” Dr. Portney explains.
The team found that a complex cataract procedure costs $877 more to perform than a standard procedure. But Medicare reimburses only $231 more. The gap is even more pronounced for retinal detachment repair. A complex pars plana vitrectomy costs about $2,700 more than a standard procedure, while the incremental reimbursement is only about $430.
“The numbers help explain what Kellogg surgeons are observing anecdotally—why more and more complex cases are being referred to academic medical centers like ours,” he says. “Surgeons in private practice are finding the incremental cost of more difficult cases is just too high. There is greater financial incentive in seeing more patients with less complicated conditions.”
The consequences for access to care are significant. With fewer options, patients needing complex care may wait longer and travel farther. The stakes are especially high in retinal detachment, where timely intervention is
critical to rescuing vision.
A similar cost/value analysis was conducted on corneal transplantation. In 2017, Kellogg began using preloaded corneal grafts for Descemet membrane endothelial keratoplasty (DMEK), which adds about $500 to the tissue costs associated with the transplant. The analysis showed a reduction of about 14 minutes in surgical time, saving about $450 after covering the additional cost of the grafts.
“This example is a win-win,” Dr. Portney notes. “Surgeons have further justification to use preloaded grafts, and patients spend less time in the operating room.”
Another topic analyzed: ophthalmology resident call volume.
Several years of data show a significant increase in call volume, both in the Adult Emergency Department and systemwide. In 2019, Michigan Medicine emergency room physicians consulted with on-call ophthalmologists 1,255 times. By 2023, that number doubled. Over the same period, systemwide ophthalmology consult volume increased from 2,730 to 4,385.
“The burden on residents is especially pronounced when you consider that, in the same time frame, there was no corresponding increase in the number of ophthalmologists in the on-call pool,” he notes.
“These analyses have the potential to inform policies that improve quality and access to ophthalmic care at Michigan Medicine and other academic medical centers,” says Dr. Portney. “It’s exciting to be part of an institution with unparalleled data resources and the foresight to put them to work.”

Amid the countless commitments of residency, PGY4 Delaram Mirzania, M.D., has found time and energy to devote to the wellness of her fellow residents. The initiative she spearheads is fostering a more enjoyable work culture, prioritizing personal growth, work-life balance and interpersonal connections.
Resident wellness is not a new concept at Kellogg, but until recently, individual events were suggested, funded and promoted on an ad hoc basis. Dr. Mirzania approached fellow residents Rachana Haliyur, M.D., Ph.D., and Alexander Valentine, M.D., to collaborate and create an organized approach to wellness for residents. “We felt that wellness needed to be integrated into the curriculum,” Dr. Mirzania says. “For that, we needed organization, a specific proposal, and a budget.”
The first step was forming a resident-run wellness committee, led by two Kellogg residents and overseen by Kellogg Wellness Director Amy Zhang, M.D. Their efforts led to a comprehensive program with four primary components:
• Recognition and Socialization Opportunities— staging events outside of work to mark milestones, such as welcoming new residents, marking the completion of the Ophthalmic Knowledge Assessment Program exam, match day and graduation. Recent events included bowling, kayaking, and a
game night in Ann Arbor. “Our goal is to celebrate our community and residents’ achievements,” says Dr. Mirzania.
• Professional Development and Coping Strategies— partnering with the Michigan Medicine Office of Counseling and Workplace Resilience to host regular seminars and speakers, and facilitator-guided “reflection rounds” to discuss the residency experience, improve group connections and communication, and learn about coping resources to mitigate residency-related stressors.
• A Wellness Visiting Professor—in 2024, the wellness committee hosted Duke University Associate Professor William Bynum, M.D., for a dinner and workshop with residents. He shared his research on the experiences and emotions—both positive and negative— of medical learners progressing through training.
• General health initiatives to enhance wellness— including making improvements to the resident lounge and offering healthy snack options.
Initial metrics from a resident survey confirmed that the initiative is already having a positive impact. Eighty six percent of respondents reported that the programming was relevant to their wellness.
“I can’t overstate the level of support we’ve received from leadership and faculty,” says Dr. Mirzania. “Their engagement shows Kellogg’s commitment to helping residents thrive despite the rigors of our training.”
FIVE KELLOGG TRAINEES WERE APPOINTED TO THE CURRENT CLASS OF THE PRESTIGIOUS SOCIETY OF HEED FELLOWS, RECEIVING MERIT AWARDS FOR POSTGRADUATE STUDIES IN OPHTHALMOLOGY.

During his residency at Kellogg, Warren Pan, M.D., M.Phil., Ph.D., worked in the lab of Thomas Wubben, M.D., Ph.D., and Cagri Besirli, M.D., Ph.D., two experts in the molecular pathways that drive blinding retinal diseases.
Now furthering his training with a vitreoretinal fellowship at Kellogg, Dr. Pan continues to study under these influential mentors and to pursue research in photoreceptor metabolism in inherited retinal diseases (IRDs).
“Consider that to date, just one FDA-approved treatment has been shown to be effective against just one of the more than 300 mutations implicated in the development of IRDs,” says Dr. Pan. “Many of those 300+ mutations are known to involve genes linked to cellular metabolism. Clearly, there is a pressing unmet need for more targeted therapies, especially those aimed at pathways, like PR metabolism, that are common to different IRDs.”
PR metabolism is a promising and largely unexplored area of IRD research. PRs require a great deal of energy to function. Yet unlike other cells that metabolize multiple energy sources, PRs metabolize only glucose. The process of breaking down glucose in PRs is driven by the enzyme pyruvate kinase muscle isozyme 2 (PKM2).
Dr. Pan is utilizing the small molecule MCTI-566, which activates PKM2. With funding from the Heed Foundation, he will test the ability of MCTI-566 to enhance the energy production and ultimate survival of PR cells.
“MCTI-566 may hold the key to novel, gene-agnostic treatments for IRDs,” says Dr. Pan. “It’s an exciting project with real translational potential.”

Rachana Haliyur, M.D., Ph.D., completed her residency at Kellogg in 2024, serving as co-chief resident in her final year. Prior to U-M, Dr. Haliyur earned a Ph.D. in molecular physiology and biophysics at Vanderbilt University, where she collaborated on groundbreaking research in diabetes, describing for the first time important connections between clinical data and functional testing in pancreatic tissue.
Dr. Haliyur credits her experiences as an ophthalmology resident with giving new focus to her diabetes research. “In my clinical training, I witnessed the devastating effects of vision loss driven by diabetes, which fueled my passion for translational research in this area,” she says. “I’m passionate about developing therapeutic targets and strategies to intervene early in the disease process, when vision can still be preserved.”
Vision loss in DR is believed to be driven at least in part by inflammation in the vitreous and retina. In collaborations with her two research mentors at Kellogg, Patrice Fort, Ph.D., and Rajesh C. Rao, M.D., Dr. Haliyur has developed a body of research suggesting that the inflammation that occurs in early stages of DR is different from that associated with the later, proliferative stage (PDR).
“My hypothesis is that in early-stage DR, inflammation arises from the body’s innate immunity, the protective system we are born with,” she explains. “Conversely, the adaptive immune system plays an important role in later stages of disease such as PDR.”
The Heed award will be applied to continue these studies. To identify early disease-driving immune events, Dr. Haliyur will study human tissue samples of DR and PDR. She hopes to better characterize immune responses in terms of specific gene expression and protein levels.
“Understanding the changing character of inflammation over the course of disease is a vital step in identifying molecular pathways unique to early-stage DR—pathways that can be targeted therapeutically,” she says. “I am grateful to the Heed Society for the opportunity to advance this work and continue to develop as a clinician-scientist. And I am excited about the potential of translational research like this to directly impact patients whose sight is threatened by diabetic retinal disease.”

As a resident at Kellogg, Daniel Balikov, M.D., Ph.D., worked with Rajesh Rao, M.D., and Noah Brown, M.D., investigating the genomic underpinnings of vitreoretinal lymphoma (VRL) and testing a new strategy of sampling ocular fluids to detect cell-free DNA (cfDNA) associated with VRL cells.
Surgically-obtained vitreous samples are usually examined with conventional pathology methods to make a diagnosis of VRL, but this often misses the mark. DNA from lymphocytes that cause VRL circulates in eye fluids. Drs. Rao, Brown, and Balikov have demonstrated the success of a new molecular diagnostic test targeting cfDNA from these fluids for VRL, improving the ability to diagnose it relative to conventional methods.
Now a vitreoretinal surgery fellow at the University of Miami’s Bascom Palmer Eye Institute in Florida, Dr. Balikov is applying the principles he practiced in cfDNA analysis to study endophthalmitis. A severe infection inside of the eye, endophthalmitis can result in catastrophic vision loss if not diagnosed and treated expeditiously.
“Early in my fellowship, I treated several patients with endophthalmitis and noticed that some displayed significantly more inflammation and toxic microbial activity than others,” he explains. “Those patients tended to have worse outcomes. If we could predict these responses earlier, we could do a much better job of triaging higher risk eyes for more aggressive treatment.”
Dr. Balikov hypothesizes that these more serious responses arise from microbial toxins and their possible mutations. Under the mentorship of Bascom Palmer retinal specialists Harry Flynn, M.D., Luis Haddock, M.D., and Darlene Miller, DHSc, he will develop a protocol to conduct whole genome sequencing on cfDNA obtained from patient samples.
“Our goal is to expand our understanding of the mechanism of endophthalmitis and identify new molecular targets for improved testing,” says Dr. Balikov. “I’m so grateful to the Heed Foundation for their support of this project and my continued development as a physician scientist.”

For Angela Gupta, M.D., Ph.D., receiving the Heed award coincides with arriving at Kellogg to begin a one-year fellowship in Cornea and External Disease.
Though her main focus in the year ahead is growing as a clinician and surgeon, Dr. Gupta is equally committed to continuing to build her research skillset, and to pursuing opportunities to improve the eye health of the medically underserved.
Dr. Gupta has already laid the foundation for a diverse research portfolio. While pursuing both an M.D. and Ph.D., her focus was basic research in glial cell biology. She expanded into clinical research as a resident. That work focuses on improving treatments for inflammatory corneal conditions and dry eye disease.
One of her projects involves an off-label ophthalmic application of Losartan which is used to treat high blood pressure and reduce stroke risk, but has also been shown to impact the transforming growth factor beta signaling pathway, which plays a key role in tissue health and repair.
“This has led to a proposed use of Losartan in eye drop form to treat corneal scarring,” she explains. “I am now analyzing data to determine its effectiveness.”
In 2023, Dr. Gupta co-authored a study of the expanded use of another medication—the nasal spray varenicline, which is FDA-approved to treat dry eye disease—for patients with Sjogren’s syndrome, an inflammatory condition that leads to dry eye disease.
“While the study sample was small, we saw a statistically significant improvement in tear production in these patients,” she reports.
Dr. Gupta also plans to continue her involvement in community interventions to address healthcare disparities in ophthalmology. As a resident, she organized diabetic retinopathy screenings for uninsured patients and investigated the socioeconomic factors influencing which patients received corneal crosslinking.
In recognition of her accomplishments, Dr. Gupta was one of ten 2024 recipients of the Resident Excellence Award from the American Society of Cataract and Refractive Surgery (ASCRS).
“I’m so grateful to be writing my next career chapter at Kellogg,” says Dr. Gupta, “and to receive this valuable support from the Heed Foundation.”

Now a vitreoretinal surgery fellow at Wills Eye Hospital in Philadelphia, P.A., Nikhil Bommakanti, M.D., completed his residency in 2023. He worked on several big data projects, most notably with Joshua Stein, M.D., during his residency at Kellogg.
He will apply his Heed fellowship to conduct two big data analyses of the safety and efficacy of biosimilar ranibizumab in eyes previously treated with branded ranibizumab for neovascular age-related macular degeneration (nAMD), diabetic macular edema, or macular edema following retinal vein occlusion, and in eyes which were not previously treated with any medication.
Ranibizumab and other anti-VEGF medications are biological products (biologics) used to treat retinal diseases such as nAMD. Biologics can be expensive, so there is an abbreviated Food and Drug Administration (FDA) approval pathway to encourage the development of biosimilar products (biosimilars).
The condensed approval pathway largely depends on analytical studies, resulting in comparatively smaller human clinical trials. Vision-threatening events have also been identified with other (non-biosimilar) medications after they were already approved by the FDA and were being used in clinic.
“This may be why surveys show that some retina specialists have concerns about the safety and efficacy of biosimilars,” notes Dr. Bommakanti.
Some biosimilars are also designated as ‘interchangeable biosimilars.’ The initial FDA guidance recommended a clinical study be performed, where medications are switched back and forth, before this designation being given. Interestingly, the biosimilar ranibizumab-eqrn (marketed as Cimerli®) was deemed interchangeable with the reference drug, Lucentis®, without a switching study.
“The dataset for these studies has more than ten times as many eyes as were included in the clinical trial for Cimerli®,” he says. “I’m excited to use big data to answer this practical and timely question.”

Otana Jakpor, M.D., M.Sc., a Global Ophthalmology Fellow at Kellogg, was accepted into the Community of Medical Educators in Training (CoMET) Program for the 2024-2025 academic year.
Sponsored by the Graduate Medical Education Office of the U-M Medical School, CoMET brings together trainees from across Michigan Medicine looking to sharpen their teaching skills and network for future collaborations in medical education, scholarship and innovation.
In addition to training and practicing education skills in the classroom, at the bedside, and during procedures, each participant completes a project of their own design. Dr. Jakpor’s project involves curating the many diverse international resources available at Kellogg into a global ophthalmology curriculum for residents. She is also creating an optional honors program for residents in the specialty, the Global Ophthalmology Academic Track (GOAT), encompassing mentorship, self-directed learning, didactic sessions and a capstone project.
“I’m thrilled to represent ophthalmology in CoMET this year,” says Dr. Jakpor. “Kellogg has a strong track record for encouraging future medical educators in ophthalmology. This is an opportunity to reimagine our wealth of global ophthalmology and health equity resources as an intentional curriculum that is more attractive and accessible to prospective applicants, and easier to navigate for faculty and trainees.”
Dr. Jakpor will be joining the Kellogg faculty next year after completing both a Global Ophthalmology fellowship as well as a fellowship in Pediatric Ophthalmology.

Wendy and Jeffrey Eisenshtadt (LSA ’89) want to make a difference. The Bloomfield Hills couple are known for their commitment to helping others in their community and beyond through their thoughtful philanthropy. Longtime supporters of the University of Michigan and Michigan Medicine, their recent gift to the W.K. Kellogg Eye Center marks their second gift to the SOURCE (Sight Outcomes Research Collaborative) project.
The SOURCE repository at the Kellogg Eye Center links clinical data from electronic health records, ocular diagnostic tests, environmental and community-level factors, and more to help clinician-scientists better understand risk factors and improve outcomes for patients with ocular diseases. The Eisenshtadts’s $500,000 gift makes an important difference for the repository.
“Our hope for this project is for SOURCE to expand collaboration in data aggregation and analysis for ophthalmology professionals worldwide, to exponentially improve eye care and outcomes for patients everywhere,” said the Eisenshtadts.
Joshua D. Stein, M.D., M.S., Frederick G. L. Huetwell Professor of Ophthalmology and Visual Sciences, assistant chair of data analytics in the Medical School, and associate professor of Health Management and Policy, is thrilled by the Eisenshtadt’s latest gift. “Their incredible generosity will enhance and allow us to build on our data collection while also helping us utilize this data in
“OUR HOPE FOR THIS PROJECT IS FOR SOURCE TO EXPAND COLLABORATION IN DATA AGGREGATION AND ANALYSIS FOR OPHTHALMOLOGY PROFESSIONALS WORLDWIDE, TO EXPONENTIALLY IMPROVE EYE CARE AND OUTCOMES FOR PATIENTS EVERYWHERE.
The Eisenshtadts
new and exciting ways,” said Dr. Stein. “By collaborating with the world’s leading ophthalmic researchers in the collection and assessment of this data, we believe we can answer some of ophthalmology’s most challenging questions, which is especially meaningful for rare diseases of the eye.”
“Since our first gift to the SOURCE project in 2021, advancements in big data analytics, and more recently the promise of artificial intelligence, are leading the improvement of disease identification and therapies,” said the Eisenshtadts. “The expanding collaboration among participating universities in SOURCE and the increasing speed in which electronic health records are analyzed have inspired us to provide a second gift. We’re also incredibly inspired by Dr. Stein’s passion for conceptualizing and advocating the idea for SOURCE into a collaborative, functioning platform that uses data analytics to enhance medical science.”
Their support of SOURCE is personally significant to the Eisenshtadts. “Our family has experience with a rare, potentially life changing visual condition. Our hope is that through shared information, treatments for even the rarest conditions can be identified and applied to expedite patients’ medical journeys. We are grateful to be in a position to be able to support communities and causes meaningful to us.”
The Eisenshtadts are firm believers in the importance of supporting medical research, especially for critical disorders that historically lack broad support.
“Our personal experience supporting medical research has yielded some incredible advancements in immunotherapy and neurology, as well as ophthalmology. We are equally amazed by the brilliant researchers and faculty we have met and look forward to their future accomplishments.”
THE W.K KELLOGG EYE CENTER IS ONE OF THE NATION’S FEW ACADEMIC INSTITUTIONS THAT PROVIDES CHILDREN WITH WORLD-CLASS CARE ACROSS ALL SUBSPECIALTIES, WHICH MEANS WE CAN TREAT AND ADVANCE RESEARCH FOR EVEN THE MOST RARE AND COMPLEX DISEASES.
Shahzad I. Mian, M.D.

Congenital eye disorders are the leading cause of childhood blindness worldwide. Saving vision requires a prompt diagnosis and complex treatment. But without access to care, too many kids lose their sight.
W.K. Kellogg Eye Center donors Timothy and Laurie Wadhams wanted to help save kids’ vision. “I experienced challenges with my eyesight at an early age, and with successful treatment, was able to overcome them,” says Mr. Wadhams. “Laurie and I want to help ensure that treatments exist for all of the diseases that threaten vision.”
The Wadhams’ recent $5 million gift to the Kellogg Eye Center is poised to transform children’s eye care. By establishing the Wadhams Family Center for Children’s Vision—a programmatic center housed in the pediatric ophthalmology clinic—the Wadhams hope to save and restore children’s sight through leading-edge, multidisciplinary care.
Lev Prasov, M.D., Ph.D., assistant professor of ophthalmology and visual sciences and of human genetics, will lead the center. His expertise in pediatric eye disease genetics is improving outcomes. “Not only has the Wadhams’ generosity supported cutting-edge research like mine, but their latest gift will help kids with congenital eye disorders get the care needed to save their sight.”
“The W.K Kellogg Eye Center is one of the nation’s few academic institutions that provides children with world-class care across all subspecialties, which means we can treat and advance research for even the most
rare and complex diseases,” says Shahzad I. Mian, M.D., F. Bruce Fralick Professor of Ophthalmology and chair of the Department of Ophthalmology and Visual Sciences.
The Wadhams previously endowed the Wadhams Family Foundation Children’s Vision Fund, part of the Paul R. Lichter, M.D., M.S. Vision Research Discovery Fund. Dr. Lichter, past department chair of ophthalmology and visual sciences, founding director of the Kellogg Eye Center, and currently professor emeritus (active) said, “The Wadhams’ visionary investments have already contributed to scientific discovery. Their latest gift will make a life-changing difference for children facing vision loss.”
Paul Lee, M.D., J.D., executive director, U-M Medical Group, senior associate dean, Clinical Affairs, and professor of ophthalmology and visual sciences, agrees, saying, “This investment by the Wadhams toward our shared goal of eliminating childhood vision loss will accelerate remarkable collaborations in research and care. Our fantastic faculty and teams at the Kellogg Eye Center work side-by-side with colleagues from across the University of Michigan campus and around the world.”
The Wadhams’ latest gift brings their giving to the Kellogg Eye Center to over $6.5 million, or nearly $17 million when combined with their giving across Michigan Medicine and the University of Michigan. Former Masco Chief Executive Officer Timothy Wadhams and his wife, Laurie, reside in Ann Arbor. Masco is the one of the world’s largest manufacturers of home improvement and building products.
To support our efforts, visit Wadhams Family Children’s Vision Fund to make your gift! https://giving.umich.edu/basket/fund/702966

Bob and Patti Huiskamp are known for their dedication to helping others as generous philanthropists and active community volunteers. Recently, the couple made a gift of $250,000 to the Taubman Emerging Scholars Program at the University of Michigan to support the research of Thomas Wubben, M.D., Ph.D., assistant professor in the W.K. Kellogg Eye Center.
Dr. Wubben specializes in vitreoretinal surgery and his research is identifying new ways to prevent vision loss from retinal degenerative diseases. His work on wet age-related macular degeneration (AMD) has identified how a protein activated in the cells of the eye can alter glycolysis—the process cells use to change sugar into energy. Glycolysis contributes to the formation of blood vessels characteristic of wet AMD, which can lead to irreversible vision loss. Dr. Wubben’s work is vitally important as the Centers for Disease Control and Prevention estimate that nearly 20 million Americans aged 40 and over are affected by AMD. Current AMD treatment requires frequent injections into the eye with varying results.
“
Patricia Huiskamp Emerging Scholar, and it is a great recognition of the impactful work being done by all members of the laboratory,” said Dr. Wubben.
The Taubman Institute and the Taubman Emerging Scholars Program were established by the late A. Alfred Taubman who believed supporting the research of early-career scientists is critical to advancing biomedicine. Director of the program, Charles F. Burant, M.D., Ph.D., said, “Generous donors such as the Huiskamp family underwrite the Emerging Scholar grants, and we are extremely grateful for their forward-thinking philanthropy and interest in our researchers and their projects.”
WE ARE EXCITED TO SUPPORT DR. WUBBEN’S SKILLS AND INNOVATIVE RESEARCH THROUGH THE EMERGING SCHOLAR PROGRAM.
The Huiskamps
“We are excited to support Dr. Wubben’s skills and innovative research through the emerging scholar program,” said the Huiskamps. In addition to five years of research funding, as the Robert and Patricia Huiskamp Emerging Scholar, Dr. Wubben will also benefit from many opportunities for collaboration and mentoring within the Taubman Institute community. “I am truly honored and grateful to be appointed the Robert and
Bob and Patti Huiskamp moved from Asheville, N.C. to Kalamazoo, Michigan, where Bob became operations manager of the KVP Paper Mill for the James River Corporation. In 1993, Bob founded his own registered investment advisory business, N.V.N.G. Investments. Bob is an active volunteer and has served on the boards of the Kalamazoo Rotary, Family and Children Services, and the Kalamazoo Institute of Arts. Like Bob, Patti has been involved in many community organizations including Junior League, Ministry with Community, the Kalamazoo Institute of Arts, and the Gilmore Piano Festival. For the past 17 years, she has been director of the Kids Hope USA mentoring program at El Sol Elementary, a dual language school in Kalamazoo. The Huiskamps have two children and four grandchildren.
“

In January 2024, three dozen physicians and scientists from around the world, including ten representatives from Kellogg, joined forces in Italy to accelerate the progress of research in blinding inherited retinal dystrophies (IRDs).
The symposium was not the first, but the third convening of the Monaciano Consortium, an influential gathering designed to foster collaboration and develop shared policy and research agendas. Previous meetings were held in 2013 and 2018. “When we first gathered more than ten years ago, we could hardly believe we were being given this once-in-a-lifetime opportunity,” says Kellogg investigator Debra Thompson, Ph.D., one of the event’s organizers. “We never dreamed the meeting would be so successful that we would experience it three times.”
“treatment advances here and around the world. Continually looking for opportunities to make a difference, the Pipernos did just that in 2013: opening the doors of Tenuta de Monaciano, the family villa and vineyards in the Tuscan countryside, for an international scientific meeting focused on IRDs. They hosted the group again at the same location in 2018 and moved the symposium to Rome in 2024.
PAST POSITION PAPERS HAVE GARNERED MORE THAN 14,000 VIEWS AND 3,700 DOWNLOADS, AND WE LOOK FORWARD TO PUBLISHING OUR LATEST CONSENSUS OPINIONS.
“Debra Thompson, Ph.D.
For hosts Celeste Pavoncello and Bruno Piperno, the symposia are the realization of a dream. Steadfast advocates for IRD patients in their home country, the couple has a longstanding connection to the University of Michigan. Bruno earned a graduate degree in business at U-M, and several of the Piperno children have also studied here.
Diagnosed with an IRD as a young man, Bruno was treated at Kellogg and has long followed research and
Monaciano I: Siena, Italy, 2013
At the first symposium, participants discussed the characterization of disease progression, the latest therapeutic advances in gene and cell therapy and RPE and photoreceptor transplantation, and the challenges of measuring clinical outcomes. Consensus goals for advancing treatments and actions that could be taken together to achieve them were outlined in a position paper published in the February 2015 issue of the journal Investigative Ophthalmology & Visual Science.
Monaciano II: Siena, Italy, 2018
The treatment landscape changed markedly in five years. With advances like the first FDA-approved gene therapy for Leber Congenital Amaurosis, IRDs took center stage
in the emerging field of precision medicine. Again, attendees identified and prioritized strategies to move the field forward, and again, their consensus opinions were published in the June 2020 issue of Translational Vision Science & Technology (TVST). Recommendations included prioritizing natural history studies to guide clinical trial design, developing and validating standardized, patient-friendly outcome measures, curbing gene therapy-associated inflammation, developing a pediatric action plan, and improving advice to patients and overall transparency, accountability and accessibility.
This year, three generations of the Piperno family hosted the symposium in Rome. Recent developments have again sharpened the group’s focus, now aimed at identifying barriers limiting progress and proposing options to improve the process of developing and testing novel therapies.
“Past position papers have garnered more than 14,000 views and 3,700 downloads, and we look forward to publishing our latest consensus opinions,” Dr. Thompson says. “We’re incredibly grateful to the Piperno family for their generosity. These symposia have ignited fresh ideas and fostered enduring collaborations that are changing the future for patients and families impacted by IRDs.”

In October 2023, Kellogg oculoplastic surgeon Victor Elner, M.D. Ph.D., was awarded the Richard K. Dortzbach Teaching Award from the American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS).
As the highest teaching honor in the specialty, the award recognizes the significant teaching contributions and scholarly achievements Dr. Elner has made throughout his career. This is the fifth ASOPRS award Dr. Elner has received. He has previously been recognized with four awards: the 1989 Research Award, the 2000 Merrill Reeh Pathology Award, the 2008 Lester T. Jones Surgical Anatomy Award, and the 2016 Merrill Reeh Pathology Award.

“THESE SYMPOSIA HAVE IGNITED FRESH IDEAS AND FOSTERED ENDURING COLLABORATIONS THAT ARE CHANGING THE FUTURE FOR PATIENTS AND FAMILIES IMPACTED BY IRDs.
“
Debra
Thompson, Ph.D.
“This recognition is particularly meaningful to me because Drs. Richard Dortzbach, Bradley Lemke, and Russell Gonnering were my mentors in oculoplastic surgery at the University of Wisconsin,” says Dr. Elner. “Their philosophical approach applies anatomic, surgical, and medical principles to devise treatments to obtain optimal results. This philosophy, together with that of my mentors in pathology, Drs. Robert Wissler, Seymour Glagov, and Werner Kirsten at the University of Chicago and Drs. Lorenz Zimmerman, Ian McLean, and Ahmad Hidayat at the Armed Forces Institute of Pathology, who stressed the importance of basic principles, was formative for me.
“During my career, their teaching permitted me to combine oculoplastic and pathologic principles to further optimize the understanding of disease and enhance treatment,” he continues. “These inspiring educators set excellent examples for the teaching of residents and fellows. This award validates years of work by my colleagues and me to advance oculoplastic surgery.”

Michigan’s Jamaican connection dates back to 1996, when a U-M Health Service optometrist of Jamaican ancestry organized a mission trip to provide vision screenings and eyeglasses to underserved residents of the island nation. Kellogg faculty and trainees first provided diagnostic and surgical support in 2015.
Fast forward to 2024, when Kellogg contingents returned twice to Jamaica. Again they provided ophthalmic care, but this time they also offered education to faculty, residents and trainees at two locations in the capital city of Kingston, and collaborated on research.
“One of the lessons we’ve learned over many years and many exchanges is to be flexible in the assistance we offer,” says Christine Nelson, M.D., Co-director of the Jerome Jacobson Program for International Ophthalmology, who led both 2024 trips. “Each country and community is unique, and their needs evolve over time.”
built long before the trips, to identify the challenges on which to focus, and exchange ideas about the kinds of clinical and research support and education Kellogg could provide.
In February, Sangeeta Khanna, M.D., lectured and provided diagnostic skill transfer sessions in her specialty, neuro-ophthalmology. “It was so rewarding to meet students in person after interacting with them in a number of Zoom sessions before the trip,” she says. “Neuro-op is not part of their curriculum, and they were so enthusiastic and eager to learn.”
“ “
THIS STUDY FEATURED A FRUITFUL COLLABORATION BETWEEN RESIDENTS FROM BOTH INSTITUTIONS. OUR GOAL WAS TO HAVE A CULTURALLY COMPETENT, EQUITABLE EDUCATIONAL EXCHANGE BETWEEN ALL COLLABORATORS.
—Kirsten Simmons, M.D., M.H.Sc.
In this case, Kellogg faculty, residents, medical students and even alumni participated on the ground and remotely, navigating the separate and shared objectives of the University of the West Indies (UWI) and neighboring Kingston Public Hospital (KPH). Relationships were
Dr. Khanna also oversaw a research project conducted by faculty and trainees from both U-M and UWI. The Kellogg team included glaucoma specialist Amy Zhang, M.D., PGY-4 resident Alex Valentine, M.D., and medical student Karolina Leziak. The project involved surveying individuals in the KPH eye clinic waiting room about their awareness and knowledge of glaucoma.
In April, the focus was on Dr. Nelson’s specialty, oculoplastics, and she was accompanied by fellow James Zhao, M.D., PGY-4 resident Kirsten Simmons, M.D., M.H.Sc., and medical students Andrea Orji and

Mikaelah Johnson-Griggs. Dr. Nelson and Dr Zhao operated daily and taught faculty and residents. Dr. Simmons assisted in lectures on urgent oculoplastic bedside procedures and radiographic imaging. She was also the principal investigator for an epidemiological study of ocular and orbital traumas presenting at KPH.
As one of the few public hospitals in Jamaica with a dedicated eye center, the KPH emergency department handles a large volume of orbital traumas, including injuries and burns from industrial, construction and farming accidents and domestic violence.
“This study featured a fruitful collaboration between residents from both institutions. Our goal was to have a culturally competent, equitable educational

“
I’M
HOPEFUL THAT THE WORK WE’VE DONE AND THE RELATIONSHIPS WE’VE BUILT WILL LAY THE FOUNDATION FOR FUTURE OPPORTUNITIES TO TEACH, LEARN AND MAKE A DIFFERENCE IN JAMAICA.
“
exchange between all collaborators,” Dr. Simmons explains. Together, they analyzed one month of data, revealing several supply-chain and infrastructure challenges to maintaining their target standard of care. “For example, patients face a range of social and economic barriers that can cause them to delay seeking care for traumas that require immediate intervention. KPH residents also face equipment and training limitations with providing long-term care in subspecialities such as retina and cornea.”
The Jerome Jacobson program also provides opportunities for alumni to get involved, even if international travel isn’t possible. Amjad Ahmad, M.D., is a U-M Medical School graduate who completed his residency and fellowship at Kellogg. Despite leading one of the busiest oculofacial surgery practices in the Chicago area, Dr. Ahmad still found time to instruct faculty and trainees in Jamaica via a series of lectures over Zoom.
“Dr. Nelson was my fellowship director 25 years ago, and remains a valued colleague and mentor,” he says. “I wanted to be part of her international efforts, but was unable to leave my practice unattended. Zoom lectures proved the ideal solution. To me, being a Michigan grad means always pursuing excellence. When I give these talks, I am planting seeds from the Kellogg Eye Center that will bloom to improve the quality of eye care in the West Indies.”
“Like Dr. Khanna, Dr. Ahmad has been a wonderful resource for remote instruction in Jamaica, where subspecialty education is in high demand,” adds Dr. Nelson. “We encourage anyone in our Kellogg family interested in international ophthalmology to connect with us to explore ways to get involved.”
“MOST IMPORTANT ARE THE PRINCIPLES OF ETHICAL, COMPASSIONATE, PATIENT-CENTERED CARE INSTILLED IN ME BY MY KELLOGG INSTRUCTORS AND MENTORS.
“Odette Houghton, M.D.

In January 2024, Odette Houghton, M.D., was named Chair of the Department of Ophthalmology at the Mayo Clinic in Scottsdale, AZ.
A vitreoretinal surgeon, Dr. Houghton completed her ophthalmology residency at Kellogg in 2004. “I believe the first retinal surgery I observed was a procedure performed by Dr. Mark Johnson,” she recalls. “Inspired by that, I knew the specialty I wanted to pursue.”
Prior to joining the faculty at Mayo in 2017, Dr. Houghton was an Assistant Professor at the University of North Carolina Chapel Hill, where she served as a senior retina specialist and the retina fellowship director. She was also President of the North Carolina Society of Eye Physicians and Surgeons
Dr. Houghton is one of the youngest physicians to be inducted into the Retina Hall of Fame. She also serves on the board of the American Society of Retina Specialists, where she serves as the chair of the Federal Affairs Committee.
She brings that leadership experience to her current role at Mayo Clinic Arizona, where she has launched both a retina service and an ocular oncology service.
“Every day, I rely on the outstanding diagnostic, clinical, surgical and research training I received during residency,” Dr. Houghton says. “But most important are the principles of ethical, compassionate, patientcentered care instilled in me by my Kellogg instructors and mentors.”
“Those values are foundational to the Kellogg culture, and here at Mayo I strive to place them front and center in every patient encounter, teaching opportunity, and leadership challenge.”

César Briceño, M.D., was named Division Chief of Oculoplastics at the University of Pennsylvania Scheie Eye Institute in July 2024.
A specialist in ophthalmic plastic and reconstructive surgery, Dr. Briceño, who also serves as co-director of the institute’s Thyroid Eye Disease Program, completed a fellowship in the specialty at Kellogg. As a faculty member, he participated in the U-M Medical School’s Medical Education Scholars Program and was active in the Office for Health Equity and Inclusion.
Among his ever-expanding responsibilities, Dr. Briceño serves as Assistant Dean for Diversity and Cultural Affairs at Penn’s Perelman School of Medicine. He has lectured widely on implicit bias and health disparities affecting groups underrepresented in medicine (UIM), including LGBTQ+ persons.
Dr. Briceño cites his involvement in building the American Association of Ophthalmology (AAO)’s Minority Ophthalmology Mentoring program (MOM) among his proudest accomplishments.
“Historically, ophthalmology is among the least diverse medical specialties,” he notes. “MOM outreach is changing that. For two years running, UIM candidates’ match rates in ophthalmology have exceeded those of the general pool of U.S. applicants. We’re also seeing great success in our efforts to encourage LGBTQ+ young people to pursue careers in the ophthalmic specialties.”
“My years at Kellogg had an enormous impact on the trajectory of my career, as a surgeon, a researcher, an educator and an advocate for greater diversity in ophthalmology,” says Dr. Briceño. “In particular, my fellowship director, Dr. Christine Nelson, was, and still is, an inspiration. Beyond modeling surgical excellence, she showed me how to navigate the university setting, and how to approach medical education in more holistic, scholastic and compassionate ways. I continue to aspire to follow her lead.”
“ “
MY YEARS AT KELLOGG HAD AN ENORMOUS IMPACT ON THE TRAJECTORY OF MY CAREER, AS A SURGEON, A RESEARCHER, AN EDUCATOR AND AN ADVOCATE FOR GREATER DIVERSITY IN OPHTHALMOLOGY.
César Briceño, M.D.

Iman Barre, M.D., M.P.H.
B.S. – University of California
M.P.H. – Johns Hopkins
Bloomberg School of Public Health
M.D. – Meharry Medical College

George Lin, M.D.
B.S. – Princeton University
M.D. – Vanderbilt University School of Medicine

Jovany Franco, M.D.
B.S. – Rice University M.D. – Harvard Medical School

Marium Sohail, M.D.
B.A. – Columbia University
M.D. – Columbia University Medical School

Emily Lawrence, M.D.
B.A. – University of Virginia
M.D. – University of Pennsylvania Medical School

Chanon Thanitcul, M.D.
B.S. – Johns Hopkins
M.D. – Johns Hopkins School of Medicine

Sarah Garnai, M.D.
Comprehensive Ophthalmology
Kellogg Eye Center Ann Arbor, MI

Matthew Johnson, M.D.
Vitreoretinal Surgery Fellowship
Keck School of Medicine of USC Los Angeles, CA

Jessica Waninger, M.D., Ph.D.
B.A. – St. Mary’s University
M.D. – University of Michigan
Ph.D. – University of Michigan

Joseph Giacalone, M.D., Ph.D.
Vitreoretinal Surgery Fellowship Mayo Clinic Rochester, MN

Alejandra Maiz, M.D.
Vitreoretinal Surgery Fellowship
The Johns Hopkins Wilmer Eye Institute Baltimore, MD

Rachana Haliyur, M.D., Ph.D.
Vitreoretinal Surgery Fellowship
Kellogg Eye Center Ann Arbor, MI

Warren Pan, M.D.
Vitreoretinal Surgery Fellowship
Kellogg Eye Center Ann Arbor, MI

Breanna Tracey, M.D.
Pediatric Ophthalmology Fellowship
Kellogg Eye Center Ann Arbor, MI

Kaushik Annam, M.D. Glaucoma
Eye Specialists of Illinois Park Ridge, IL

Richard Helms, M.D., Ph.D.
Pediatric Ophthalmology and Adult Strabismus
Children’s Mercy Hospital Kansas City, MO

Letita Pirau, M.D.
Neuro-Ophthalmology
Kellogg Eye Center Ann Arbor MI

Sina Rezaei, M.D.
Cornea, External Disease and Refractive Surgery
Kelsey Seybold Clinic Houston, TX

Emily Cole, M.D., M.P.H.
Adult and Pediatric
Vitreoretinal Surgery
University of Colorado Aurora, CO

Otana Jakpor, M.D., M.Sc.
Global Ophthalmology Fellowship
Kellogg Eye Center Ann Arbor, MI

Boonkit Purt, M.D.
Vitreoretinal Surgery
Madigan Army Medical Center Tacoma, WA

David Skanchy, M.D.
Pediatric Ophthalmology and Adult Strabismus
Pediatric Eye Specialists Fort Worth, TX

Tania Padilla Conde, M.D.
Cornea, External Disease and Refractive Surgery
Omaha Eye and Laser Institute Omaha , NE

Sarinee Juntipwong, M.D.
Ocular Oncology and Pathology
Emory Eye Center
Emory School of Medicine Atlanta, GA

Rithambara Ramachandran, M.D., M.S. Glaucoma
University of Pennsylvania Philadelphia, PA

Michelle Sun, M.D., M.P.H.
Comprehensive Ophthalmology
University of Pennsylvania Philadelphia, PA

Zhengyang Zhao, M.D. Oculoplastics
Emory Eye Center Atlanta, GA



Sarah Garnai, M.D., attended Harvard Medical School through the Harvard-MIT Division of Health Sciences and Technology. She then completed her ophthalmology residency training at the University of Michigan Kellogg Eye Center. She provides comprehensive ophthalmology care to patients at Kellogg’s Ann Arbor and Chelsea clinics as well as the VA.
Joshua Grant, M.D., earned his medical degree from Wayne State University. He then completed his residency at University of South Florida and went on to complete his fellowship in medical retina at the University of Michigan Kellogg Eye Center. He provides retinal care at Kellogg’s Grand Blanc clinic.
Andrew Kocab, Ph.D., received his degree in immunology from the University of Michigan. He focuses on understanding the underlying biology of retinal diseases in collaboration with David Zacks, M.D., Ph.D. He also serves as Vice President of Research at ONL Therapeutics.


Letitia Pirau, M.D., attended medical school at California Northstate University. She then completed her neurology residency followed by a neuro-ophthalmology fellowship at the University of Michigan. She sees patients both in Ann Arbor and Brighton.
Nicholas Silvestros, O.D., received his optometric degree from Ferris State University, where he also completed his residency. He was a staff optometrist at VisionFirst Pediatric Eye Center in Louisville, Kentucky before joining the faculty at the Kellogg Eye Center. He provides ophthalmic care for pediatric and adult patients at Kellogg-Wall Street and our new Trinity Oakland location in Pontiac, Michigan.

Annie Wu, M.D., attended medical school at Brown University. She then completed an ophthalmology residency at the University of Michigan Kellogg Eye Center, followed by glaucoma fellowship at Massachusetts Eye and Ear Infirmary. She provides comprehensive and glaucoma care at Kellogg’s Ann Arbor and Brighton clinics as well as the VA.






Vinay Aakalu, M.D., M.P.H., FACS
• Castle Connolly Top Doctors
• Editorial Board Member, Translational Vision Science and Technology
• Editorial Board Member, Orbit
• Senior Associate Editor, The Ocular Surface
• Alternate Chair, Ad Hoc Reviewer; Study Section: Special Emphasis Panel (SEP): Neurotechnology and Eye Diseases NV-S (02); Center for Scientific Review, National Institutes of Health (NIH-CSR)
• Ad Hoc Reviewer, Study Section: Special Emphasis Panel (SEP): ZEY1 VSN (11) NEI Clinical Applications; National Eye Institute, National Institutes of Health (NIH-NEI)
• Ad Hoc Reviewer, Study Section: ZEY1 VSN (06); NEI Translational Research Program for Therapeutics; National Eye Institute, National Institutes of Health (NIH-NEI)
• Chair, Written Qualifying Exam Working Group, ASOPRS
• Award Committee, Membership Committee, ASOPRS
• Publications Committee, ARVO
• Methodologist: Ophthalmic Technology Assessment Committee (Oculoplastic)
• Patient Safety Article Based Question Committee Member, American Board of Ophthalmology (ABO)
• “Method for treating lysosomal storage diseases with histatin peptides”; Israel (IL) Pat. 298323
Steven Abcouwer, Ph.D.
• Chief Editor, Journal of Ophthalmology (Wiley Online Library)
• Associate Editor, Frontiers in Ophthalmology, Retina Section
• Associate Editor, Frontiers in Immunology, Multiple Sclerosis and Neuroimmunology Section
• Editorial Board Member, Investigative Ophthalmology and Vision Science (IOVS)
• Editorial Board Member, Translational Vision Science & Technology (TVST)
• Editorial Board Member, International Journal of Molecular Sciences (IJMS)
• Editorial Board Member, American Journal of Physiology: Endocrinology and Metabolism
• Scientific Review Editor, Molecular Vision Journal
• Chair, National Institutes of Health (NIH) Neurotechnology and Vision (NV) Study Section ZRG1 NV-Q 91 (02)
• Study Section Member, NIH National Eye Institute Special Emphasis Panel ZEY1 VSN (03), NEI Individual Training Grant Applications (Ks)
• Grant Review Board Member, Pennsylvania Lions Sight Conservation and Eye Research Foundation
• Grant Reviewer, United States-Israel Binational Science Foundation, Jerusalem, Israel
Kari E. Branham, M.S., CGC
• Chair, Genetics Review Committee, Foundation Fighting Blindness Clinical Consortium
• Member, Steering Committee for the National Ophthalmic Disease Genotyping and Phenotyping Network (eyeGENE®), National Eye Institute
• Expert Review Panel Member, Early Onset Retinal Degeneration Variant Curation, ClinGen
• Expert Review Panel Member, Retinal Disease Gene Curation, ClinGen
• Scientific Advisory Board, Foundation Fighting Blindness
• Evidence Based-Guideline for Retinal Dystrophies Workgroup, American College of Medical Genetics
• Editorial Board Member, Investigative Ophthalmology & Visual Science
• Leadership Award, National Society of Genetic Counselors (NSGC)
Theresa Cooney, M.D.
• US News and World Report Best Doctors in America
• Castle Connolly Top Doctors
• Board of Directors, Michigan Society of Eye Physicians and Surgeons (MiSEPS)
Sherry Day, O.D., FAAO
• Board Member, American Academy of Optometry Foundation
• Board Member, Vision Rehabilitation Committee, American Optometric Association
Karen DeLoss, O.D., FAAO, FSLS
• Vice Chair, Education Committee, Global Specialty Lens Symposium
• Vice Chair, American Optometric Association, Cornea and Contact Lens Section
• Education Chair, Global Ophthalmic Women
Joshua Ehrlich, M.D., M.P.H.
• Associate Editor, special issue, Journal of Gerontology: Medical Sciences
• Reviewing Editor, Ophthalmic Epidemiology
• Grant Reviewer, NIH Special Emphasis review panel (ZEY1 VSN (01) 1), National Eye Institute Clinical Applications, National Institutes of Health, (Ad Hoc)
• Lecturer, The Lefeber Hughes Winter Series on Aging, Sealy Center on Aging, University of Texas Medical Branch, 02/2024, Galveston, TX
• Co-Chair, Center for Vision and Population Health, Prevent Blindness
• Secretary, International Society of Geographic and Epidemiologic Ophthalmology
• Member, Committee on Aging, American Academy of Ophthalmology (AAO)
Angela Elam, M.D., M.P.H.
• Invited Inaugural Academic Leadership Program, The National Medical Association (NMA)/Association of University Professors of Ophthalmology (AUPO)
Susan Elner, M.D.
• US News and World Report Best Doctors in America
• Castle Connolly Top Doctors
• Member, The American Ophthalmological Society
Victor Elner, M.D.
• ASOPRS Dortzbach Teaching Award
Abigail Fahim, M.D., Ph.D.
• Council of Vision Editors Fellow Program – Investigative Ophthalmology & Visual Science
Thomas Gardner, M.D., M.S.
• Associate Editor, JCI Insight
• Chair-Elect, ADA Eye Health Interest Group Leadership Team
• External Advisory Board, Mass Eye and Ear Infirmary K12 Program
• Grant Reviewer, Yale University Diabetes Research Center Pilot & Feasibility
• National Advisory Eye Council
• Reviewer, ADA Standards of Medical Care in Diabetes
• Scientific Advisory Board, EviRed (France)
• Castle Connolly Top Doctors
Thanh Hoang, Ph.D.
• McKnight Neurobiology of Brain Disorders Award
• Alcon Research Institute Young Investigator Award
Mark Johnson, M.D.
• Associate Editor, American Journal of Ophthalmology
• Alex R. Irvine Lecture, Pacific Retina Club, Los Angeles
• US News and World Report Best Doctors in America
• Castle Connolly Top Doctors
• Chair, Awards Committee, The Macula Society
• Chandler Lecture, Massachusetts Eye & Ear
• Editorial Board, Retina: The Journal of Retinal and Vitreous Diseases
• Gass Founder’s Lecture and Visiting Professor, Bascom Palmer Eye Institute
• Senior Honor Award, American Society of Retina Specialists
Ariane Kaplan, M.D.
• Vice President, Association of University Professors of Ophthalmology (AUPO) Directors of Medical Student Education
• Selected Participant, Association of University Professors of Ophthalmology (AUPO) Academic Leadership Development Program
• Achievement Award, American Academy of Ophthalmology (AAO)
JULY 1, 2023 — SEPTEMBER 30, 2024
Shilpa Kodati, M.D.
• AEVR Emerging Vision Scientist Program
Shahzad I. Mian, M.D.
• US News and World Report Best Doctors in America
• Board of Directors, Membership Director, Secretary, Michigan Society of Eye Physicians and Surgeons (MiSEPS)
• Big Data Task Force, Board of Directors, Governance Committee, Eye Bank Association of America (EBAA)
• Examination Content Writer, American Board of Ophthalmology (ABO)
• Host, Lions Club International, Ann Arbor Lions Club
• Leadership Development Program, Association of University Professors in Ophthalmology and Visual Sciences (AUPO)
• Secretariat Award, American Academy of Ophthalmology (AAO)
• Subspecialty Day Advisory Committee, AAO
Jason Miller, M.D., Ph.D.
• Ryan Initiative for Macular Research (RIMR) Task Group Leader
• Guest Editor, Journal of Visualized Experiments
• Invited Lectures: Calico Life Sciences (an Alphabet company); KU Leuven (Belgium); Foundation Fighting Blindness Visions Conference
David Musch, Ph.D., M.P.H.
• Grant Reviewer: Health and Medical Research Fund, Government of Hong Kong SAR
• Member, Editorial Boards: JAMA Ophthalmology, Retina, & Eye and Vision
• Advisory Board, Cochrane Eyes and Vision U.S. Satellite
• Chair, Data and Safety Monitoring Committees for numerous NEI/NIH and company-sponsored multicenter randomized clinical trials
Jacqueline Nguyen, O.D., M.S.
• Fellowship Admittance Committee, American Academy of Optometry (AAO)
Christine Nelson, M.D., FACS
• Board of Directors, ASOPRS Foundation Committee
• Board of Directors, World Association of Eye Hospitals
• Senior Advisor, ASOPRS International Opportunities Committee
Donald Puro, M.D.
• Castle Connolly Top Doctors
Rajesh Rao, M.D.
• Awarded U.S. Patent Application No.: 16/251,740: Compositions And Methods To Derive Mesodermal Lineage Cells And Mixed Tissue Organoids From Embryonic Stem Cells
• Catalyst Award for Innovative Research Approaches for Age-related Macular Degeneration, Research to Prevent Blindness
• Achievement Award, American Academy of Ophthalmology (AAO)
• Study Section Reviewer, Neurobiology-F VA Merit Grant Review Program
• Study Section Member, The Aging and Development, Auditory, Vision and Low Vision Small Business Study Section (ETTN 12/SBIR/STTR), Center for Scientific Review, National Institutes of Health (NIH)
• Retina Social Media Editor, American Academy of Ophthalmology (AAO) Journals
Elise Savier, Ph.D.
• Council of Vision Editors Fellow Program – Ophthalmology and Vision Science
Nita Valikodath, M.D.
• Membership Committee, Vit-Buckle Society
Sara Weidmayer, O.D., FAAO, FORS
• Editorial Review Board, Journal of Medical Optometry
• Secretary, Michigan Foundation for Vision Awareness (MFVA)
• Council Member, National Board of Examiners in Optometry (NBEO): Part I Applied Basic Science: Subject Matter Expert, Standard Setting; Part III Patient Encounters and Performance Skills Exam: Subject Matter Expert
James Weiland, Ph.D.
• Permanent Member, Bioengineering and Tissue Engineering for Neuroscience Study Section, National Institute of Health (NIH)
Marguerite Weinert, M.D.
• Young Ophthalmologist Liaison, American Academy of Pediatrics Section on Ophthalmology Executive Committee
Sebastian Werneburg, Ph.D.
• Grant Reviewer, Study Section Member, National Multiple Sclerosis Society, 2024 Remyelination and Neuroprotection Request for Applications
• Grant Reviewer, Study Section Member, US Department of Defense, 2023 Multiple Sclerosis Research Program of the Congressionally Directed Medical Research Programs (CDMRP)
• Grant Reviewer, United Kingdom Multiple Sclerosis Society, UK, Early Career Fellowships
• Grant Reviewer, Action for Ataxia Telangiectasia (A-T), A-T research project grant program, UK
JULY 1, 2023 — SEPTEMBER 30, 2024
Sebastian Werneburg, Ph.D. (cont.)
• Grant Reviewer, Alzheimer's Association Research Fellowship (AARF/AARF-D) Program
• Grant Reviewer, 2023 United Kingdom Multiple Sclerosis Society, Early Career Fellowships
Sarah Wood, O.D., M.S., FAAO
• Secretary, Membership Committee, Optometric Glaucoma Society
• Awards Committee, Women in Ophthalmology (WIO)
• Fellowship Curriculum Project Committee, International Council of Ophthalmology
• NASAOS Membership Committee
• Membership Committee, Optometric Glaucoma Society
• Glaucoma Diplomate Executive Committee, American Academy of Ophthalmology (AAO)
• Guest Reviewer, American Academy of Optometry Journal (AAO)
Kwoon Wong, Ph.D.
• Associate Editor, Frontiers in Cellular Neuroscience
• Grant Proposal Evaluation Committee, Swiss National Science Foundation
• Grant Reviewer, Hong Kong Research Grants Council
Maria A. Woodward, M.D., M.S.
• Whitney G. Sampson Lecture, American Academy of Ophthalmology (AAO)
• Chair, Cornea Society Advocacy Committee
• Council-Appointed Representative, AAO Awards Committee
• Secretariat Award, AAO
• Deputy Section Lead, AAO
• Senior Editor, Cornea
• Board Member, Cornea Society
• Dermatologic and Ophthalmic Drugs Advisory Committee, Food and Drug Administration
• Member, JAMA Ophthalmology Advisory Committee
• Member, World Cornea Congress IX Program Committee
David Zacks, M.D., Ph.D.
• Kreissig Award for Excellence in Retinal Surgery, The Association for Research in Vision and Ophthalmology (ARVO)
Amy D. Zhang, M.D.
• Invited Section Editor, Advances in Ophthalmology and Optometry
• Patient Engagement Subcommittee, Patient Care Committee, American Glaucoma Society (AGS)
• Abstract Review Committee, American Society of Cataract and Refractive Surgery (ASCRS)
• Abstract Review Committee, Women in Ophthalmology (WIO)
• Recipient of the Health Care Policy Leadership Development Program Fellowship, American Glaucoma Society (AGS)














































































































































Vinay Aakalu, M.D., M.P.H.
Fernanda Abalem M.D., Ms.C., Ph.D.
Steven Abcouwer, Ph.D.
Robin Ali, Ph.D.
David Antonetti, Ph.D.
Steven Archer, M.D.
Bernadete Ayres, M.D.
Audree Bass, O.D.
Cagri Besirli, Ph.D.
Amanda Bicket, M.D.
Jill Bixler, M.D.
Brittany Boland, O.D.
Kari Branham, M.S., CGC
Roland Chen, Ph.D.
Grant Comer, M.D.
Theresa Cooney, M.D.
Wayne Cornblath, M.D.
Julia Dalia, M.D.
Sherry Day, O.D., FAAO
Lindsey De Lott, M.D., M.S.
Karen Deloss, O.D., FAAO
Monte Del Monte, M.D.
Hakan Demirci, M.D.
Tatiana Deveney, M.D.
Courtney Dewey, O.D.
Elaine Downie, M.D.
Mark Draelos, Ph.D.
Joshua Ehrlich M.D., M.P.H.
Angela Elam, M.D., M.P.H.
Samantha Elliott-Gagnon, O.D.
Susan Elner, M.D.
Victor Elner, M.D.
Emily Eton, M.D.
Abigai Fahim, M.D., Ph.D.
Cherie Farkash, O.D.
Charles Frank, M.D.
Patrice Fort Ph.D., M.S.
Carlton Foster, O.D.
Bruce Furr CO, Ph..D
Philip Gage, Ph.D.
Christopher Gappy, M.D.
Thomas Gardner, M.D.
Sarah Garnai, M.D.
Andriea Goncalves, Ph.D.
Joshua Grant, M.D.
Paul Grenier, O.D.
Farida Hakim, M.D.
Sean Hansen, M.D.
Peter Hitchcock, Ph.D.
Thanh Hoang, Ph.D.
Christopher Hood, M.D.
Bret Hughes, Ph.D.
Michael Huvard, M.D.
Adam Jacobson, M.D.
K. Thiran Jayasundera, M.D., M.S.
Vanitha Jeyaraj, M.D.
Denise John, M.D.
Mark Johnson, M.D.
Ariane Kaplan, M.D.
Harjeet Kaur, M.D.
Naheed Khan, Ph.D.
Sangeeta Khanna, M.D.
Denise Kim, M.D.
Erin Klukas, M.D.
Shilpa Kodati, M.B.B.S.
Andrew Kocab, Ph.D.
Zvi Kresch, M.D.
Amy Lagina, O.D., FAAO
Paul Lee, M.D., J.D.
Helios Leung, O.D.
Qiang Li, Ph.D.
Paul Lichter, M.D., M.S.
Executive Officers of Michigan Medicine
Marschall S. Runge, M.D., Ph.D.
Executive Vice President for Medical Affairs, Dean, University of Michigan Medical School, C.E.O., Michigan Medicine
David C Miller, M.D., M.P.H
President, University of Michigan Health System, Executive Vice Dean for Clinical Affairs, Medical School
Debra F. Weinstein, M.D.
Executive Vice Dean for Academic Affairs, Medical School
Chief Academic Officer for Michigan Medicine
Steven L. Kunkel, Ph.D.
Executive Vice Dean for Research, Medical School
Chief Scientific Officer, Michigan Medicine
The Regents of the University of Michigan
Jordan B. Acker, Michael J. Behm, Mark J. Bernstein, Paul W. Brown, Sarah Hubbard, Denise Ilitch, Ron Weiser, Katherine E. White, Santa J. Ono (ex officio)
© 2024 Regents of the University of Michigan
A Non-discriminatory, Affirmative Action Employer
Nathan Liles, M.D.
Cheng-Mao Lin, Ph.D.
Xuwen Liu, Ph.D.
April Maa, Ph.D.
Matthew McKee, M.D.
Shahzad Mian, M.D.
Jason Miller, M.D., Ph.D.
Sayoko Moroi, Ph.D.
Kevin Mundy, M.D.
David Musch, Ph.D., M.P.H.
Mikiko Nagashima, Ph.D.
Nambi Nallasamy, M.D.
Christine Nelson, M.D.
Paula Newman-Casey, M.D., M.S.
Jacqueline Nguyen, O.D.
Santa Ono, Ph.D.
Gale Oren, M.I.L.S.
Jillian Pearring, Ph.D.
Howard Petty, Ph.D.
Letita Pirau, M.D.
Colleen Podd, O.D.
Lev Prasov, M.D., Ph.D.
Donald Puro, M.D., Ph.D.
Rajesh Rao, M.D.
Julia Richards, Ph.D.
Alan Robin, M.D.
Julie Rosenthal, M.D., M.S.
Maria-Dolors Sans-Gili, Ph.D.
Elisa Savier, Ph.D.
Dana Schlegel, M.S., M.P.H., CGC
Thielen Seng, O.D., FAAO
Anjali Shah, M.D.
Roni Shtein, M.D., M.S.
Brittany Simmons, M.D.
Nicholas Silvestros, M.D.
Annual Report Team
Terry Smith, Ph.D.
Kyung No Son, Ph.D.
H. Kaz Soong, M.D.
William Sray, M.D.
Joshua Stein, M.D., M.S.
Alan Sugar, M.D.
Jeffrey Sundstrom, Ph.D.
Bradford Tannen, M.D., J.D.
Sally Temple, Ph.D.
Debra Thompson, Ph.D.
Jonathan Trobe, M.D.
Meagan Tucker, O.D.
Nita Valikodath, M.D., M.S.
Angela Verkade, M.D.
Grace Wang, M.D., Ph.D.
Eric Weh, Ph.D.
Sara Weidmayer, O.D., FAAO
James Weiland, Ph.D.
Marguerite Weinert, M.D.
Jennifer Weizer, M.D.
Sebastian Werneburg, Ph.D.
Adrienne West, M.D.
Donna Wicker, O.D., FAAO
Pamela Williams, M.D.
Kwoon Wong, Ph.D.
Sarah Wood, O.D., M.S., FAAO
Maria Woodward, M.D., M.S.
Rebecca Wu, M.D.
Annie Wu, M.D.
Thomas Wubben, M.D., Ph.D.
Guan Xu, Ph.D.
David Zacks, M.D., Ph.D.,
Amy Zhang, M.D.
Jason Zhang, M.D.
Qitao Zhang, Ph.D.
Editor-in-Chief: Julie Rosenthal, M.D., M.S.
Design and Art Direction: David Murrel
Head Writer: Shelley Zalewski
Contributing Writer: Kristy Demas
Editorial Assistant: Christy Ford, Jo Kristine Scott
Photographers: Erin Kirkland, Daryl Marshke, Andrew Mascharka, Christina Merrill, Scott Soderberg, Leisa Thompson
FOR PATIENT APPOINTMENTS, PLEASE CALL 734.763.8122
For additional copies, please contact: University of Michigan
Department of Ophthalmology and Visual Sciences
W.K. Kellogg Eye Center
1000 Wall Street Ann Arbor, Michigan 48105 www.umkelloggeye.org
Department of Ophthalmology and Visual Sciences
1000 Wall Street
Ann Arbor, MI 48105

The University of Michigan Kellogg Eye Center is proud to be ranked in the top 10 in the country by U.S. News & World Report—recognizing our outstanding care for patients with complex eye conditions.
Kellogg has seen extraordinary growth in all aspects of patient care, research and education since the department was established over 150 years ago, in 1872. Every day, our clinicians, scientists, trainees and staff work together to shape the future of eye care and vision science. We are proud to be part of Michigan Medicine.
~ Our Purpose ~ To improve lives through curing, preventing and treating eye disease