TIPS FOR MANAGING UNUSUAL BILLING SITUATIONS P.10
HIGHLIGHTS FROM THE 2024 AOPA POLICY FORUM P.26















FRESH FACES: MEET A CLINICIAN WHO CHAMPIONS PATIENTS AND EDUCATES PAYORS P.32



States of Change

O&P advocates join forces to push for policy and legislative reform at the state level P.16



THIS JUST IN: BUSINESS AND AI EXPERT
CHUCK GALLAGHER NAMED
AOPA NATIONAL ASSEMBLY KEYNOTE SPEAKER P.14















AOPAnet.org With This Issue: 2024 AOPA National Assembly Preliminary Program. View at AOPAAssembly.org MAY 2024 The Magazine for the Orthotics & Prosthetics Profession
SEPTEMBER 12-15, 2024
CHARLOTTE, NC

AOPA National Assembly ignite 24
THE PREMIER MEETING FOR ORTHOTIC, PROSTHETIC, AND PEDORTHIC PROFESSIONALS.
Join us September 12–15, 2024, for an ideal combination of top-notch education and entertainment at the 107th AOPA National Assembly in Charlotte, NC.
FOLLOW US @AmericanOandP
AOPAASSEMBLY.ORG
Exhibits. Education. Networking.

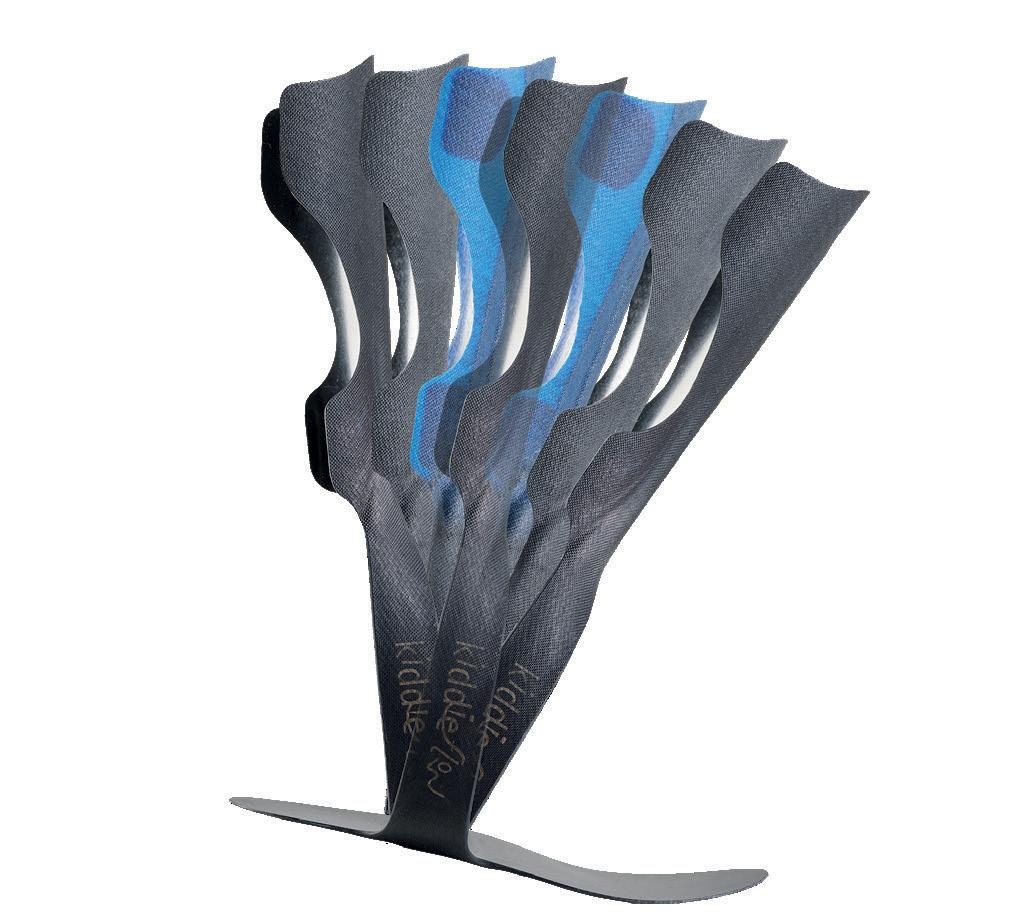
With the same unique features as KiddieGAIT® & KiddieROCKER®!

A more FLEXIBLE SOLUTION
KiddieROCKER®
KiddieGAIT®
Support for Better Life!
KiddieFLOW™
16 STATES OF CHANGE
What’s moving the needle on expanding access to O&P care at the state level and improving outdated reimbursement policies in Medicaid programs? Small but mighty groups of O&P advocates are driving important and much-needed advocacy initiatives, armed with determination, support from AOPA and other O&P-focused organizations, and an occasional “O&P champion” within statehouses.

CHRISTINE UMBRELL
This Just In AI AND THE FUTURE OF O&P
Business and artificial intelligence expert Chuck Gallagher will give the keynote presentation “The AI Revolution: Unlocking the Future of Business” during the 2024 AOPA National Assembly in September. Plan to attend to access can’t-miss information about AI, ethics, and innovation.


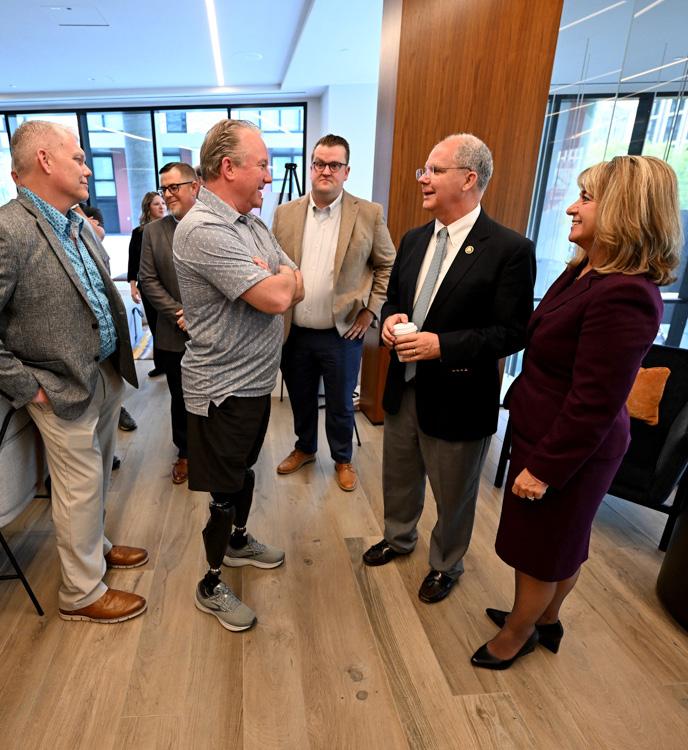
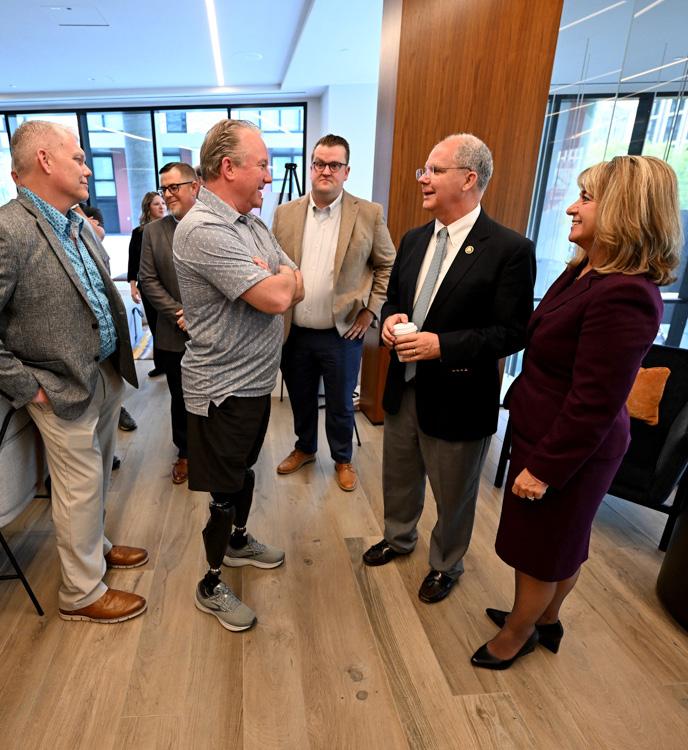
O&P stakeholders from 35 states and territories convened in Washington, DC, in April to take part in the premier O&P advocacy event. View photos from the two-day experience, which culminated in an impressive 138 meetings with legislators and staff.



2 O&P Almanac May 2024 COLUMNS DEPARTMENTS COVER STORY FEATURES CONTENTS May 2024 | Vol. 73, No. 5
26 PRIORITIZING
AT
PATIENT CARE
THE FEDERAL LEVEL
14
4 AOPA Contacts How to reach staff 6 Happenings Research, statistics, and industry news 8 People & Places Transitions in the profession 39 AOPA News AOPA announcements, member benefits, and more 40 Welcome New Members 41 Marketplace 43 Calendar Upcoming meetings and events 43 Ad Index 44 State By State Updates from New Hampshire, Texas, and SEBCM 10 Reimbursement Page RISING TO THE CHALLENGE Tips for billing during atypical patient encounters Opportunity to earn CE credits by taking the online quiz. 32 Fresh Faces GIVING VOICE TO PATIENTS Meet Sheryl Sachs, MSPO, CPO, a clinician at Dankmeyer Prosthetics & Orthotics who makes time to advocate for patients and clinicians in a variety of volunteer roles and activities. 36 Member Spotlight y PHOENIX RISING PROSTHETICS & ORTHOTICS y SUPERFEET RX
IT’S ALL ABOUT FUNCTION. Naked Prosthetics offers four finger prostheses: PIPDriver, MCPDriver, ThumbDriver, and GripLock Finger.


Ashley wears one MCPDriver. © 2023 Naked Prosthetics All Rights Reserved.
™ ™ ™ ™
AOPA Contacts
A world where orthotic and prosthetic care transforms lives.
Board of Directors OFFICERS
President
Mitchell Dobson, CPO, FAAOP Hanger Clinic, Austin, TX
President-Elect
Rick Riley
O&P Boost, Bakersfield, CA
Vice President
Kimberly Hanson, CPRH Ottobock, Austin, TX
Treasurer
Chris Nolan
Össur, Foothills Ranch, CA
Immediate Past President
Teri Kuffel, JD
Arise Orthotics & Prosthetics, Spring Lake Park, MN
Executive Director/Secretary Eve Lee, MBA, CAE AOPA, Alexandria, VA
DIRECTORS
Arlene Gillis, MEd, CP, LPO International Institute of Orthotics and Prosthetics, Tampa, FL
Adrienne Hill, MHA, CPO(L), FAAOP Kennesaw State University, Kennesaw, GA
John “Mo” Kenney, CPO, LPO, FAAOP Kenney Orthopedics, Lexington, KY
James Kingsley
Hanger Clinic, Oakbrook Terrace, IL
Lesleigh Sisson, CFo, CFm Prosthetic Center of Excellence, Las Vegas, NV
Matt Swiggum Proteor, Tempe, AZ
Linda Wise
Fillauer Companies, Chattanooga, TN
Shane Wurdeman, PhD, CP, FAAOP(D) Research Chair
Hanger Clinic, Houston Medical Center, Houston, TX
AMERICAN ORTHOTIC & PROSTHETIC ASSOCIATION (AOPA)
330 John Carlyle St., Ste. 200 Alexandria, VA 22314
Office: 571-431-0876
Fax: 571-431-0899
AOPAnet.org
AOPA Staff
EXECUTIVE OFFICES
Eve Lee, MBA, CAE, executive director, 571-431-0807, elee@AOPAnet.org
Akilah Williams, MBA, SHRM-CP, director of finance and strategic operations, 571-431-0819, awilliams@AOPAnet.org
HEALTH POLICY AND ADVOCACY
Joe McTernan, director of health policy and advocacy, 571-431-0811, jmcternan@AOPAnet.org
Devon Bernard, assistant director of coding and reimbursement services, education, and programming, 571-431-0854, dbernard@AOPAnet.org
Sam Miller, manager, state and federal advocacy, 571-431-0814, smiller@AOPAnet.org
MEETINGS & EDUCATION
Tina Carlson, CMP, senior director, education and meetings, 571-431-0808, tcarlson@AOPAnet.org
Ashley Vande Bunte, CMP, director, meetings and education, 571/431-0860, avandebunte@AOPAnet.org
Kelly O’Neill, CEM, assistant director, meetings and exhibitions, 571-431-0852, kelly.oneill@AOPAnet.org
MEMBERSHIP & COMMUNICATIONS
Joy Burwell, director of communications and membership, 571-431-0817, jburwell@AOPAnet.org
Betty Leppin, senior manager of member services, 571-431-0810, bleppin@AOPAnet.org
Nicole Ver Kuilen, manager of public engagement, 571-431-0836, nverkuilen@AOPAnet.org
Madison McTernan, coordinator of membership and communications, 571-431-0852, mmcternan@AOPAnet.org
AOPA Bookstore: 571-431-0876
Reimbursement/Coding: 571-431-0833, LCodeSearch.com
O&P ALMANAC
Eve Lee, MBA, CAE, executive director/publisher, 571-431-0807, elee@AOPAnet.org
Josephine Rossi, editor, 703-662-5828, jrossi@contentcommunicators.com
Catherine Marinoff, art director, 786-252-1667, catherine@marinoffdesign.com
Bob Heiman, director of sales, 856-520-9632, bob.rhmedia@comcast.net
Christine Umbrell, editorial/production associate and contributing writer, 703-662-5828, cumbrell@contentcommunicators.com
PUBLISHER EVE LEE, MBA, CAE
EDITORIAL MANAGEMENT CONTENT
COMMUNICATORS LLC
ADVERTISING SALES RH MEDIA LLC
DESIGN & PRODUCTION MARINOFF DESIGN LLC
PRINTING SHERIDAN
SUBSCRIBE
O&P Almanac (ISSN: 1061-4621) is published monthly, except for combined issues in June/July and November/ December, by the American Orthotic & Prosthetic Association, 330 John Carlyle St., Ste. 200, Alexandria, VA 22314. To subscribe, contact 571-431-0876, fax 571-431-0899, or email info@aopanet.org. Yearly subscription rates: $59 domestic, $99 foreign. All foreign subscriptions must be prepaid in U.S. currency, and payment should come from a U.S. affiliate bank. A $35 processing fee must be added for non-affiliate bank checks. O&P Almanac does not issue refunds. Periodical postage paid at Alexandria, VA, and additional mailing offices.
ADDRESS CHANGES
Postmaster: Send address changes to: O&P Almanac, 330 John Carlyle St., Ste. 200, Alexandria, VA 22314.
Copyright © 2024 American Orthotic and Prosthetic Association. All rights reserved. This publication may not be copied in part or in whole without written permission from the publisher. The opinions expressed by authors do not necessarily reflect the official views of AOPA, nor does the association necessarily endorse products shown in the O&P Almanac. The O&P Almanac is not responsible for returning any unsolicited materials. All letters, press releases, announcements, and articles submitted to the O&P Almanac may be edited for space and content. The magazine is meant to provide accurate, authoritative information about the subject matter covered. It is provided and disseminated with the understanding that the publisher is not engaged in rendering legal or other professional services. If legal advice and/or expert assistance is required, a competent professional should be consulted.
ADVERTISE WITH US
Share your message with AOPA membership— approximately 9,000 orthotic and prosthetic professionals, facility owners, and industry personnel. Contact Bob Heiman at 856-520-9632 or email bob.rhmedia@comcast.net. Learn more at bit.ly/24AlmanacMediaKit
4 O&P Almanac May 2024

Happenings
PARALYMPIC PREVIEW
RECORD MEDIA COVERAGE EXPECTED
The 2024 Paralympic Games, which begin Aug. 28, will feature more than 140 hours of TV coverage on USA Network, CNBC, and NBC. NBC Universal will air a Paralympic record 1,500-plus hours of TV and streaming programming of the Paris Games.
FAST FACT ORTHOSES
COMMON FOR CHILDREN WITH CP
RESEARCH ROUNDUP
Virtual Rehab Tested Among Transtibial Prosthesis Users

Researchers in Turkey conducted a randomized controlled study to evaluate the effectiveness of a telerehabilitation-based structured exercise program for individuals with unilateral transtibial amputation.
The research team studied rehab outcomes among two groups: 24 individuals who received telerehabilitation combined with home exercise
Nighttime Bracing May Benefit Some Scoliosis Patients
For adolescents with moderate-grade idiopathic scoliosis, nighttime bracing may be an effective alternative intervention for some patients, according to a team of researchers in Sweden studying the Conservative Treatment for Adolescent Idiopathic Scoliosis (CONTRAIS).
and 24 individuals who received home exercise alone. Outcomes were assessed using the TimedUp-and-Go test, the 30-second chair-stand test, the Activities-Specific Balance Confidence Scale, the Trinity Amputation and Prosthesis Experience Scales, the Amputee Body Image Scale, and the Nottingham Health Profile.
Results indicate that “telerehabilitation combined with home exercise can offer greater benefits in improving gait, muscle strength, balance confidence, activity restriction, prosthesis satisfaction, and quality of life compared to home exercise alone for individuals with transtibial amputation,” according to the researchers. They noted that telerehabilitation has “great potential to facilitate access to physiotherapy for individuals with amputation and reduce resource utilization.” The study was published in February in Disability and Rehabilitation
Brazilian researchers found that 85% of children with cerebral palsy (CP) have had at least one orthotic device. The most commonly used lowerlimb orthoses among CP patients are anklefoot orthoses that provide direct control of the ankle and foot to improve gait.
SOURCE: “RESULTS
The researchers conducted a randomized clinical trial of 135 patients with adolescent idiopathic scoliosis, ages 9 to 17, with skeletal immaturity and primary curve Cobb angles between 25 and 40 degrees. Patients were categorized into three groups: those with nighttime bracing, who wore orthoses for approximately 8 hours each night and were encouraged to perform physical activity for 60 minutes each day; those who engaged in scoliosis-specific exercise (SSE) plus performed 60 minutes of physical activity each day; and a control group, who were asked to perform physical activity for 60 minutes each day.
“Treatment success” was seen in 76% of the nighttime bracing group, 58% of the SSE group, and 53% in the physical activity-alone group. “Treatment with

nighttime bracing prevented curve progression of more than 6 degrees to a significantly higher extent than did physical activity, while SSE did not,” reported the researchers.
“The findings of the present study have direct clinical implications, as we provided evidence on the effectiveness of nighttime bracing to reduce the risk of curve progression in patients with moderate-grade adolescent idiopathic scoliosis,” concluded the researchers. “Nighttime bracing may be an effective alternative intervention in patients rejecting full-time bracing.” Results were published in January in JAMA Network Open
6 O&P Almanac May 2024
PHOTOS: ADOBE STOCK
OF ORTHOSES USED ON AMBULATORY PATIENTS WITH BILATERAL CP,” ACTA ORTOP BRAS.
Ultrasound Useful in Monitoring Bone Movement Within Sockets
Ultrasound images can be used to successfully monitor in vivo residual bone movement within a transtibial prosthetic socket during stepping tasks, according to an international team of researchers.
Noting that transtibial prosthesis users may struggle to achieve optimal prosthetic fit and subsequently experience residual limb pain or stump/socket instability, researchers sought to leverage ultrasound technology to assist prosthetists in objectively assessing the impact of prosthetic adjustments on residual limb loading.
The researchers worked with three transtibial prosthesis users, capturing ultrasound images during five dynamic conditions and quantifying bone movement relative to the socket by tracking the bone contour. The researchers found that participants exhibited consistent range of motion, and the research team analyzed the signal-to-noise ratios as well as medial-lateral and anteriorposterior absolute range of motion.
“This study demonstrated that it is feasible to use B-mode ultrasound to monitor in vivo residual bone movement inside an intact prosthetic socket during stepping tasks,” noted the researchers. “The proposed method has the potential to enhance the understanding of the causes and effects of residual bone movement within the prosthetic socket.” The study was published in April in Scientific Reports
By the Numbers
LLPR OPPORTUNITY O&P Foundation Launches LLPR Subscription Award Program

The O&P Foundation has launched a national Limb Loss & Preservation Registry (LLPR) Subscription Award program Through contributions from and in partnership with Brandt Ventures, the O&P Foundation will accept applications from O&P patient-care organizations from June 10 to July 10, 2024, to receive a one-year sponsored subscription to the LLPR.
LLPR was originally funded by the National Institutes of Health and the Department of Defense but is now privatized. LLPR connects hospitals, O&P providers, and patient-reported outcomes data together in one centralized database, allowing for improved predictive analytics with a goal of improving patient care and outcomes.
The new program will support three LLPR subscriptions in 2024 and three more in 2025. To apply, visit the Subscription Award Program Page on the LLPR website: oandpfoundation. org/professional-awards/llpr-subscription-award. Email info@ oandpfoundation.org with questions.
ABC Certifications and Accreditations
The American Board for Certification in Orthotics, Prosthetics, and Pedorthics (ABC) has published updates on credentialing and accrediting activities
12,174
3,726
7 May 2024 O&P Almanac TOTAL ACTIVE ABC CERTIFICATIONS
ABC-ACCREDITED FACILITIES
ABC CERTIFICATIONS AWARDED IN 2023 TYPES OF ABC-ACCREDITED FACILITIES
Happenings
SOURCE: “ABC 2023 REPORT TO THE PROFESSION,” ABC
Practitioners Assistants Technicians Pedorthists Orthotic Fitters Mastectomy Fitters Therapeutic Fitters 461 42 22 20 168 51 64 Comprehensive O&P Pharmacy Pedorthics Mastectomy Central Fabrication Ocular 2,854 542 114 193 17 6
DIABETES DOWNLOAD GLOBAL NUMBERS ON THE RISE
The worldwide prevalence of diabetes mellitus is anticipated to increase to 643 million (11.3%) by 2030 and 783 million (12.2%) by 2045.
SOURCE: “DIABETES
O&P FACILITY SURVEY
Participate in the AOPA 2024 Compensation, Benefit, & Operations Survey
All O&P facilities are invited to participate in AOPA’s 2024 O&P Compensation, Benefit, & Operating Performance Survey, which will collect, analyze, and compare the relative compensation/benefits and financial performance of the profession. Participants will receive a customized report that compares the performance of an individual practice to other participants in the region of similar size with easy, at-a-glance evaluation, including infographics of the results.
Participating companies will receive a report with measurable data that will aid in retaining employees; making informed, strategic decisions; and running
People & Places
PEOPLE IN THE NEWS
Taylor Haines has been selected as the 2024 George and Dena Breece Fellow by the National Association for the Advancement of Orthotics & Prosthetics. Haines, a community care coordinator for Hanger Clinic in Portland, Oregon, grew up in Alaska using belowknee prostheses from a young age. Today, she focuses on patient relations, helping new prosthesis users.
During the 10-week Breece Fellowship Program, scheduled to take place May 20-July 26 in Washington, DC, Haines will focus on O&P policy and advocacy in the context of the broader rehabilitation and disability policy agenda.
Tim Misuraca, based in Atlanta, has been hired as Allard USA’s new Southeast district manager, servicing customer needs in Florida and Georgia. Misuraca earned a bachelor’s degree in exercise and sport sciences from the University of Florida and has spent several years as a sales professional. He has experience in sales within hospital, surgical, physician, and rehab facilities, specializing in orthopedics, neurology, spine, and wound care. Misuraca has received annual sales achievement awards 13 times, including Presidents Club and national and regional awards.

a more efficient practice. This year, the survey has been revamped and is digital, shorter, and easier to complete.
New in 2024, the survey is open to nonmembers The survey will be conducted independently by Kai Analytics, a market research firm that compiles the results and ensures the confidentiality of data provided by each facility participant.
The survey will close June 30, with final tabulated results available in September. Be on the lookout for your access code. Contact info@ AOPAnet.org with questions.
BUSINESSES IN THE NEWS
Allard USA Inc., through its Dralla Foundation, has awarded several grants for 2024 to help fund adaptive recreational events. Grant awards will go toward the following entities:
• Catalyst Sports will use Dralla funding to host the Southeast Adaptive Climbing Competition.
• Enhancing Skills for Life will use Dralla funds to provide two scholarships to enable individuals living without arms to learn how to bowl at events that include bowlers with similar disabilities.
• Rochester Accessible Adventures will take a group of 40 individuals to Letchworth State Park for a day of whitewater rafting on the Genesee River.
• Spina Bifida Association of Greater New England will give members an opportunity to experience the open ocean on the Impossible Dream, a universally accessible catamaran.
• STRIDE Adaptive Sports will host the Third Annual Upstate New York Sled Hockey Invitational.
The Hanger Institute for Clinical Research and Education published its 2023-2024 Annual Report. The report focuses on the Institute’s mission of advancing clinical practice through research in the O&P field and reflects the efforts made to improve clinical outcomes and provide evidence-based care.
The report highlights a broad range of work, from analyses of real-world clinical outcomes data such as the CASTLE 1 and SAFE-AMP series, to translating knowledge to the broader rehabilitation community. Access the Annual Report at hangerclinic. com/wp-content/uploads/2023-hanger-institute-annual-report.pdf
8 O&P Almanac May 2024 Happenings
Tim Misuraca
MELLITUS, THE FASTEST GROWING GLOBAL PUBLIC HEALTH CONCERN,” HEALTH SCIENCE REPORTS, MARCH 2024
Hip-knee-ankle triple flexion with 125° knee flexion and 42° ankle ROM STABILITY
92% greater flat-foot time for greater stability
LIFE
Greater confidence with more shoe options, longer battery life, and ease while walking

855.450.7300 shop.proteorusa.com
MICROPROCESSOR FULL-LEG SYSTEM AN ENTIRELY NEW ANGLE ON:
MOTION
BY JOE MCTERNAN
Rising to the Challenge
Tips for navigating unusual billing situations


O&P billing should be simple: A patient comes to your office; you provide appropriate clinical care; you collect applicable co-insurance and deductible amounts; you submit a claim to the patient’s insurance company; and you receive payment.
As we all know, this is rarely how it works. Even straightforward claims often require that you jump through several administrative hoops. Whether it’s pursuing prior authorization, chasing down documentation, or making sure you are using current versions of required forms, even simple claims can become difficult to manage.
If the challenges ended there, most administrators would gladly accept them and go about their business of submitting claims and booking accounts receivable collections. Unfortunately, everyday challenges represent only a small percentage of the frustrations that O&P administrators face. This month’s Reimbursement Page examines some of the more unusual billing situations and offers suggestions to make them more manageable.
Inpatient Billing
Some of the most common inquiries AOPA receives originate from O&P facilities seeking guidance regarding billing for O&P


services that are provided to patients in an inpatient setting.
While there are limited exceptions, if an orthosis or prosthesis is provided to a patient during an inpatient stay, the inpatient facility is generally responsible for paying for that service out of the global or prospective payment that it receives from either Medicare or another payor. If a global payment does not include all services provided during the inpatient stay, you may be able to bill the insurance company directly for your services—but this is the first thing you should determine before preparing and submitting any claims.
10 O&P Almanac May 2024
Take advantage of the opportunity to earn .75 CE credits. Quiz me! Scan the QR code or visit bit.ly/aopaversityquiz CE credits accepted by certifying boards: Reimbursement Page
Board of Certification/Accreditation
When Medicare is the primary payor, the rules are clear. For Medicare Part A-covered inpatient hospital stays, Medicare will make a single prospective payment to the hospital that covers all medically necessary services that a patient receives while in the facility. This applies to both acute hospital stays and rehabilitation hospital stays, and, in most cases, the O&P provider will have to negotiate payment terms with the facility prior to providing care.
An often misunderstood exception to inpatient hospital billing rules—the two-day rule—allows O&P providers to bill Medicare directly for care provided to a hospital inpatient, but it is very limited in scope and should be used only when truly appropriate. The two-day rule states that if a service is provided to a Medicare beneficiary during the last two days of a Medicare Part A-covered stay solely for the sake of
facilitating discharge, it may be billed as a Medicare Part B service using the date of discharge as the date of service on the claim. There must be no medical need for the patient to use the device during any part of the Part A stay, and the patient may not wear or use the device until after discharge except for basic fitting and education on how to wear it after discharge. Medicare has explicitly stated that inpatient facilities may not rely on the two-day rule to avoid responsibility for payment of medically necessary services to their inpatients.
Inpatient billing rules in a skilled nursing facility (SNF) are very similar to those in the hospital setting—with one major difference. Most prosthetic services are excluded from the SNF prospective payment system, meaning that even when a patient is in a Medicare Part A-covered SNF stay, they may be billed directly to
Medicare as Part B claims. This exemption does not apply to immediate postsurgical prostheses, partial hands and feet, supply items, or L5987, which describes a prosthetic foot that integrates shock absorption in its design. These limited prosthetic codes and all orthotic codes remain subject to inpatient billing rules, and payment must be negotiated directly with the SNF.
Custom Devices That Cannot Be Delivered
In most cases, once you begin fabrication of a custom prosthesis or orthosis, you deliver a clinically appropriate and complete device to the patient. However, there are times where circumstances prevent the completion of the service, and no prosthesis or orthosis is ultimately provided.


Identify areas for improvement.
Compare your company’s financial performance with industry leaders and others in similar markets.
Help inform business decisions.
Retain valuable employees.
11 May 2024 O&P Almanac Reimbursement Page
AOPA 2024 O&P Compensation, Benefit & Operations Survey www.AOPAnet.org ●
●
●
●
New and Improved Virtual Format Easier and Faster to Complete $ $ $ NOW AVAILABLE COMPLETE THE SURVEY FOR A CHANCE TO WIN 1 of 10 $500 GIFT CARDS To request access to the survey, scan the QR Code to complete this short form. Be on the lookout for YOUR unique access code to participate in this year’s survey. NEW! OPEN TO MEMBERS AND NONMEMBERS
If you are providing a prefabricated device, this usually results in the return of the item to the manufacturer or your inventory for future use.
A custom-fabricated or permanently modified prosthesis or orthosis cannot simply be returned to inventory because it can no longer be used for any patient other than the individual for whom it was made. Medicare has addressed this scenario in its Internet-Only Manual as “Custom Items Furnished But Not Delivered.” Under this provision, Medicare allows you to submit a claim for the completed prosthesis or orthosis, minus the value of any re-usable components, when one of the following three conditions has been met: patient death, a change in condition that no longer supports medical necessity of the item, or cancellation of the order by the beneficiary. Your date of service on your claim will either coincide with the date of the patient’s death or the date that you learned of either the change in condition or cancellation of the order by the beneficiary. Regardless of the qualifying event, your documentation should support the specific reason why you were unable to facilitate delivery of the completed prosthesis or orthosis.
Advanced Beneficiary Notices
Advanced Beneficiary Notices (ABNs) are used exclusively for Medicare fee-forservice claims and allow the patient to accept financial responsibility for a service that you believe will be considered not medically necessary. Medicare rules do not expect patients to inherently know what services are considered medically necessary and what services are not. Providers, on the other hand, are expected to be fully versed in medical policies and therefore know if a service is typically considered medically necessary.
As a result of this expectation, patients may not be held financially liable for not medically necessary services unless they have been informed in advance of receiving the service. Medicare requires the use of an ABN form to accomplish this notification.
For an ABN to be considered valid, it must be signed and dated by the patient, and the

specific reason why the provider believes the service will be deemed not medically necessary must be listed on the form. In addition, the current version of the ABN form—which includes an Office of Management and Budget expiration date of Jan. 31, 2026—must be used. ABN forms without this date in their lower left corner will be automatically invalidated.
ABNs can be a very useful tool when executed properly but can also lead to a false sense of security when they are not. Understanding the specific requirements necessary to use them properly is tremendously important.
Miscellaneous Codes
The use of miscellaneous codes is a perpetual source of debate and discussion in O&P circles. Some believe that these codes never get paid and are therefore not worth using. Others believe they are an invaluable tool when providing services that don’t fall within the traditional O&P universe of services.
The truth is that miscellaneous codes can be a very valuable billing tool—but only when used correctly and supported by appropriate documentation.
Miscellaneous codes are designed to be used to describe services that simply cannot be described with an existing Healthcare Common Procedure Coding System
(HCPCS) code. They are not to be used when you are dissatisfied with the reimbursement for an otherwise appropriate code, and they should not be used if your documentation does not support the medical necessity of the service you are providing. When used properly, they can facilitate appropriate communication with payors and create a pathway toward reimbursement for the service you are providing.
Miscellaneous codes, when used properly, often lead to consideration for creation of new HCPCS codes and can be very beneficial to patients, providers, and payors.
Prepared for Challenge
While the examples above only represent a small sample of the unique billing challenges that O&P practices face every day, these are some of the more common scenarios for which AOPA staff members regularly offer advice.
While these scenarios can be challenging, learning how to successfully navigate such situations can provide you with a competitive advantage in a complex marketplace.

Joe McTernan is director of health policy and advocacy at AOPA. Reach him at jmcternan@AOPAnet.org
12 O&P Almanac May 2024
Reimbursement Page


A step up for foot drop
Turbomed’s premium foot drop or thosis sits on the outside of the shoe to facilitate maximized ankle movement while reducing the risk of injury .
Stepinto 2024

PDAC validated (L1951)
Simplified assembly
18% more dorsi-flexion power
35% more media-lateral strength
US website
SEPTEMBER
12-15, 2024 | CHARLOTTE, NC
AI and the Future of O&P
Business expert Chuck Gallagher will present an AI-themed keynote address at the 2024 AOPA National Assembly
How will artificial intelligence (AI) impact your business in the months and years to come? This hot topic is the subject of the keynote presentation at the upcoming AOPA National Assembly in Charlotte, North Carolina, Sept. 12-15. Business and AI expert Chuck Gallagher will share his vast knowledge of “The AI Revolution: Unlocking the Future of Business” during the Opening Remarks and Keynote Presentation beginning at 8 a.m. on Friday, Sept. 13. Gallagher will explain what it takes to harness the boundless power of AI to the benefit of your O&P company. He will provide live demonstrations of AI applications and other cutting-edge technologies—offering a sample of the realm of possibilities to come. Be sure to attend this important presentation to stay at the forefront of AI advancements and acquire the insights necessary to fuel innovation and expansion at your O&P organization.
Hear From a High-Profile Expert
Gallagher is well-positioned to discuss the topic of AI. An author and frequent contributor to business programming on CNN, CBS, and NPR, Gallagher has spoken at length on the topics of ethics, ethical leadership, and business success. Described as creative, insightful, captivating, and a person that “connects the dots” between behavior, choices, and success, Gallagher currently serves as chief operating officer of a national company and formerly served as vice president of sales for a public company—but he came from humble beginnings selling potholders door to door.
Gallagher will offer practical, tested, and time-proven methods that can enhance personal and professional performance and will explore what motivates behavior—a relevant topic in the age of AI. Read more about Gallagher and his insights in his books, Every Choice Has a Consequence and Second Chances: Transforming Adversity Into Opportunity
Explore O&P Ethics
In addition to headlining the keynote presentation, Gallagher will lead a second session, “Every Choice Has a Consequence—Ethics, Integrity, and the Power of Choices in Life and Business” at 10:30 a.m. on Friday, Sept. 13. He will delve into his personal history— explaining how the choices you and your employees make shape your personal and professional lives.

Ethics has become an important topic to Gallagher: In the middle of a rising career, he lost everything because he made some bad decisions. He has since rebuilt his career and his life. During his Assembly presentation, Gallagher will share his life journey, the consequences of his unethical choices, and how life gives you second chances when you make the right decisions. Take part in this session to learn how to leverage ethics and integrity to drive success and motivate your employees and colleagues to make positive choices.
The AOPA National Assembly will take place at the Charlotte Convention Center in downtown Charlotte. Access the 2024 AOPA National Assembly Preliminary Program in print—mailed with this issue of O&P Almanac —or online at AOPAAssembly.org
14 O&P Almanac May 2024 This Just In
MADE WITH OPTIGEL, GRAY FABRIC, AND AN ADDED LAYER OF INTERNAL FABRIC, THE REINFORCED FLEX SLEEVE (RFX) PROVIDES A HIGH DEGREE OF FUNCTIONALITY AND USER COMFORT, WHILE WITHSTANDING WEAR AND TEAR TO ENSURE LONG LASTING USAGE.


Added layer of internal fabric to offer increased durability around the trim line of the user's socket
30° pre-flexion to ease bending and reduce bunching behind the knee
Gel adheres to the patient's skin, preventing the sleeve from rolling down the amputee's limb and eliminating the need for additional support
Gray fabric's differential stretch provides maximum comfort and stability, enabling users to move around with ease and confidence
LEARN MORE T: 727.528.8566 | 800.574.5426 | F: 727.528.8862 www.easyliner.com | info@easyliner.com MAKING LIVES BETTER™ THE ULTIMATE SLEEVE FOR PERFORMANCE.
CHRISTINE UMBRELL






















STATES OF CHANGE
O&P advocates lead groundbreaking efforts to improve care for individuals with limb loss, limb difference, and mobility impairment














16 O&P Almanac May 2024
Cover Story COVER STORY BY
Across the United States, small but mighty groups of O&P stakeholders are uniting to promote positive change for patients and practitioners in their home states.
From New York to California and in many states in between, teams of O&P advocates are pushing state legislators to adopt proposed policies that would improve access to care and expand insurance coverage of orthotic and prosthetic devices. Armed with determination, the knowledge that they’re doing the right thing, support from AOPA and other O&P-focused organizations, and an occasional “O&P champion” within a statehouse, these advocates are driving change for the good.
With the recent rise of the So Every BODY Can Move (SEBCM) initiative seeking coverage of activity-specific devices in “28x28”—passing bills in 28 states before the 2028 Paralympic Games in the United States—state-level advocacy is flourishing. Through a partnership between AOPA, the National Association for the Advancement of Orthotics and Prosthetics, the American Academy of Orthotists and Prosthetists, and the Amputee Coalition, SEBCM is driving engagement and increasing awareness of the need to ensure access to medically necessary O&P care for physical activity.
NEED TO KNOW:
f O&P professionals in several states are spearheading efforts to improve access to care and expand insurance coverage of O&P devices via legislation and policy proposals.
f In addition to embracing the increasingly popular So Every BODY Can Move initiative—which aims to ensure coverage of activity-specific devices—advocates are drafting bills to improve reimbursement within state Medicaid programs, implement insurance fairness, and more.
But expanded advocacy at the state level goes far beyond the SEBCM movement. Advocates in several states are forging important and much-needed efforts to improve reimbursement within state Medicaid programs, implement insurance fairness legislation, ensure coverage of showering or bathing devices, and much more. As these initiatives gain steam and legislation is considered or passed, the effects reverberate across the country— spurring others to action in similar endeavors.
NEW YORK: Bills To Update Medicaid MCO Rates
In several states, O&P stakeholders are ramping up pressure to garner more favorable reimbursement rates for Medicaid patients. O&P business owners in states where Medicaid rates are exceptionally low find it challenging to make a profit, and O&P consumers experience reduced options and choices.
In New York, Medicaid managed-care organizations (MCOs) reimburse at 50%-70% of the Medicaid fee-for-service rates set in 1987, a situation that has made providing care to Medicaid patients increasingly less viable. “O&P businesses are going out of business” on a frequent basis, says Michael Caputo, CPO, owner and general manager of JK Prosthetics & Orthotics, who
f Advocates in New York, California, and New Hampshire are leading efforts to revamp Medicaid-focused policies and legislation to expand access to O&P care for local limb loss and limb difference patients and prevent attrition of O&P providers.
f O&P professionals in some states are seeking to improve access for specific patient populations—for example, patients in need of cranial remolding orthoses in North Carolina and Texas, and individuals with limb loss or difference who would benefit from showering and bathing devices in Arkansas and Minnesota.
f Oregon and Nebraska volunteers are working to introduce insurance fairness legislation, with a goal of ensuring adequate coverage for prosthetic and custom orthotic care.
f Those individuals pursuing statelevel efforts are hopeful that advances in their regions will provide foundational information and set examples for other states to follow in pursuing similar initiatives across the country.
17 May 2024 O&P Almanac
Cover Story



Currently, S 3468 is scheduled for a floor vote of the full Senate, but A 3408 appears stalled. “A 3408 has been referred to the Health Committee as of Jan. 4, 2024, and has not been brought up on the agenda by committee leadership to discuss and vote,” Johnson says. He and Caputo are hopeful that passage of the Senate bill would draw movement in the Assembly.
was forced to shut down his facility for one week last summer when no payments were coming in. Such low Medicaid MCO reimbursement rates mean that patients may receive components made of subpar materials, lose access to nearby care when facilities shut down, or experience longer wait times for appointments and device delivery, explains Caputo.
“We have been successful at increasing awareness of the O&P profession and access to care issues that exist related to the Medicaid/Medicaid MCO population by targeting specific legislative leaders, being professionally persistent in coordinating meetings, and involving patient advocates to communicate the impact the legislation would have on their lives,” notes Johnson. He plans to continue “to establish relationships and awareness of the O&P profession within the New York Department of Health,” he says. “This work is very important for continuing to improve care for Medicaid/Medicaid MCO recipients and avoid further attrition of providers/services in the state.”

In an effort to boost Medicaid MCO reimbursement rates, Caputo is working with other state advocates, including Matthew Johnson, MPT, CEAA, a project manager at Hanger Clinic, in introducing bills in the state legislature. Assembly Bill (A) 3408 and Senate Bill (S) 3468 would “provide parity to durable medical equipment (DME) providers [including O&P] by requiring Medicaid MCOs to reimburse providers at no less than 100% of the medical assistance DME and complex rehabilitation technology fee schedule for the same service or term,” according to the bills’ language.
Johnson notes this legislation would have significant impact: “It would improve access to the latest O&P technology/services available that are currently not available to recipients of Medicaid MCOs and would also impact access to DME services,” he says. “It will slow/reverse the attrition of provider locations in the state, which is impacting access to care for all New Yorkers regardless of insurance.”
The push to advance A 3408 and S 3468 has been bolstered by a flurry of activities beginning last summer. Caputo held two rallies at his facility, and Caputo and Johnson organized a rally in Albany where three members of the Assembly spoke out in support of the legislation. One of Caputo’s patients, Latavia Sturdivant, has served as a patient advocate, assisting with social media as well as podcast and radio appearances to highlight the initiative. Patient advocacy groups, including the Amputee Coalition, have helped drive the movement forward, and “AOPA has been awesome with setting up call-to-action letters and emails,” Caputo says.
CALIFORNIA: Proposal To Boost Medicaid Reimbursement Structure
Medicaid is a hot topic in California, where advocates at the California Orthotic and Prosthetic Association (COPA) are looking to increase Medicaid access to O&P via budgetary update.
“Medi-Cal reimbursement for O&P devices has been stagnant for decades,” explains Spencer Greene, MS, CPO, president of COPA and regional vice president at Hanger Clinic. “As a result of extremely low reimbursement for O&P devices by the Medi-Cal program, many providers in California have made the difficult decision not to participate with Medi-Cal. As a result, Medi-Cal beneficiaries experience reduced access to O&P care,” he explains. “Updating the Medi-Cal reimbursement structure to reasonable levels will encourage more providers to participate in the Medi-Cal program and will open more options for care to Californians in need.”
AOPA and Sam Miller, AOPA’s manager of state and federal advocacy, are assisting in gathering support for the budgetary change via a letter-writing campaign.

18 O&P Almanac May 2024
Michael Caputo, CPO, addressed the crowd at a rally in Albany.
New York advocates: Caputo (second from left) and Johnson (far right), with Hanger Clinic’s Paul Selph and Maggie Baumer, JD
Matthew Johnson, MPT, CEAA
Cover Story
Spencer Greene, MS, CPO, spoke to the crowd during a COPA rally at the State Capitol.
PHOTO: HANGER CLINIC
PHOTO: HANGER CLINIC

Naked Prosthetics now offers four finger prostheses: PIPDriver, MCPDriver, ThumbDriver, and GripLock Finger. IT’S ALL ABOUT FUNCTION.

To drive support among lawmakers, COPA has conducted several tours for key legislators through O&P facilities and hosted a rally on the steps of the State Capitol. COPA recently participated in a panel discussion with the Senate Budget Subcommittee on Health #3, regarding targeted rate increases for providers. “We described the importance of the rate increase on improving access to care for patients but also illustrated that the investment in improved rates would be outweighed by savings elsewhere in the healthcare system,” Greene explains. “In mid-May, our legislators will receive the revised budget from California’s governor. The legislators will have until mid-June to finalize the budget. COPA is hopeful that the O&P field will be included in the targeted rate increases from the MCO tax included in the budget.”
California tends to be a leader with progressive policies, according to Greene, so “if we are successful, we are hopeful that other states will follow California’s lead to ensure that O&P device users have equitable access to high-quality care close to their homes.”
NEW HAMPSHIRE:
Push for Medicaid Parity
New Hampshire O&P stakeholders are fighting for Medicaid parity via Senate Bill (SB) 455, legislation that would set Medicaid reimbursement at 90% of Medicare rates. Samantha Case Torrice, an AOPA state rep and practice manager at New Hampshire Prosthetics/dba Seacoast Prosthetics, provided testimony in support of the bill at a hearing in mid-April.

Torrice got involved in the New Hampshire movement after a Medicaid recoupment effort spurred her to investigate “how, exactly, our Medicaid and MCOs worked,” she says. She studied the contracts between the state and the MCOs, and began contacting local officials with concerns about low reimbursements. Initially, state officials were unsympathetic—but then Torrice and other advocates connected with New Hampshire Sen. Sue Prentiss. Prentiss “brought forward SB 455 based off data I compiled showing the disparity in reimbursements for our industry,” says Torrice.
The data Torrice collected proved instrumental to demonstrating inequity in reimbursements: “I created a spreadsheet that detailed


the costs of our devices and compared that with reimbursements,” she explains. “As the O&P industry is paid in a bundled payment system, this amount is supposed to cover the cost of the device and office visits. Our New Hampshire Medicaid rates have not increased since 2021, and they are inadequate in covering the cost of the device, which means our office costs were not covered.” She contacted various state officials with her concerns and attempted to work with the MCOs directly to raise rates, with little response.
Things began looking up when Prentiss joined the cause: “In January, myself and Chris Phillips, CPO, [co-owner of New Hampshire Prosthetics] testified in front of the Senate Committee regarding this bill, which ultimately passed the Senate” in early April, she says. In mid-April, they testified in front of the House Committee and are awaiting the outcome. “Our testimony was a combination of relaying data and reimbursement information to show the inadequacies but educating those on each committee of the importance of our industry in our community.”
If passed, SB 455 will increase access to quality care for community members with limb loss, limb difference, and mobility issues, according to Torrice. “We know of other companies like ours who have begun to drop their contracts with Medicaid, causing patients to have to travel far distances for care, or forgo treatment due to lack of access,” she says.


20 O&P Almanac May 2024
Samantha Case Torrice
Greene and Baumer in front of the Capitol after COPA’s rally
Greene and California State Sen. Caroline Menjivar
Cover Story
Greene and California State Assembly Member Mia Bonta
PHOTO: HANGER CLINIC
PHOTO: HANGER CLINIC
PHOTO: HANGER CLINIC
PHOTO: HANGER CLINIC
Audience gathering at COPA’s “Mobility Saves” rally on the State Capitol

Unsurpassed smoothness + stability.
Searching for a lightweight hydraulic foot that provides confidence and control? The Motion Foot SLX supports each phase of foot function from heel strike to toe-off resulting in a foot that adapts well to sloped conditions.
© 2024 Fillauer LLC
Minnesota Poised to Enact “Power-Packed” O&P Law
After 14 years of pushing for legislation to provide greater access to care and devices for individuals with limb loss or limb difference living in Minnesota, advocates in the state are expecting O&P provisions to become law within the next few weeks.
House File (HF) 3339 and Senate File (SF) 3351, identical companion bills, would implement insurance fairness for state commercial plans; cover activity-specific and showering/bathing devices for state commercial health plans and Minnesota Medicaid; remove reasonable useful lifetime restrictions; and require that insurance companies follow nondiscrimination standards related to the coverage of O&P care. After passing various committees, the bills have been included in House and Senate supplemental budget bills.
The bills, which are being combined, are expected to be included in the final Omnibus Bill to be presented to Gov. Tim Walz for his signature at the end of May. If the legislation passes, Walz has promised to sign it into law, marking a great achievement for the O&P advocates who have been working on the issue for years.
“Minnesota’s bill is one of the most comprehensive O&P bills in the country,” says Teri Kuffel, JD, AOPA past president, vice president at Arise O&P, and an AOPA state rep. Kuffel and her team began working with a lobbyist in 2010 to pass various forms of O&P legislation, beginning with a bill focused on insurance fairness legislation. While the initial bill failed to pass, Minnesota advocates refused to let up and have relied on “grit, perseverance, and persistence” in continuing to fight on behalf of patients and clinicians.


“This is the fourth time we’ve gone to the Minnesota state capital with an access-to-care bill. Two of the three times prior, we were successful in passing legislation,” explains Kuffel. Over the years, Kuffel and her team have made inroads by educating legislators and explaining the importance of O&P intervention. The latest version is “power-packed and bipartisan,” with several provisions to benefit the O&P community, and “the majority of legislators we have approached wanted to sign on,” she says.
The bills were introduced last spring, and Minnesota advocates spent the past year raising awareness by highlighting the legislation on the website of the Minnesota Society of Orthotists, Prosthetists, and Pedorthists (msopp-mn.com), posting on social media, launching letter-writing campaigns with the assistance of AOPA, and holding a “Rally in the Rotunda” at the state capital in April. Approximately 125 O&P advocates took part in the rally, where Walz joined in “to show his support and present us with his proclamation declaring April Limb Loss and Limb Difference Awareness Month.”
Once approved, the legislation “will improve life exponentially” for people with limb loss and difference in Minnesota, says Kuffel.
“Right now, we are waiting for a vote from the House Health, Human Services, and Elderly Affairs Committee, and if passed, it will go to the New Hampshire House of Representatives for a large vote,” Torrice says. “So it’s an uphill battle, and I really don’t know which way this will swing. I’m hoping for a positive outcome but will not be deterred if it’s not.” She is grateful for the assistance AOPA has provided along the way, including hosting the annual Policy Forum, “as it inspired me to get more involved.”
NORTH CAROLINA: Seeking Increased Access to CROs
North Carolina advocates are pulling together to improve access for cranial remolding orthoses (CROs). AOPA’s CRO Workgroup was approached by North Carolina’s Medicaid program, NC Medicaid, to assist with updating its CRO policy to align with the most up-to-date clinical standards.
In a collaborative effort, NC Medicaid and the AOPA Workgroup “were able to quickly polarize key vested stakeholders that included cranial manufacturers, leading O&P teaching institutions, and orthotists who specialize in cranial care programs,” says Bill Gustavson, vice president of business development for Orthomerica and co-chair of the CRO Workgroup. “It was a great collaborative effort working with NC Medicaid medical directors, consultants, and other allied healthcare professionals.”

The collaboration culminated in a policy that has been approved by NC Medicaid’s Physician Advisory Group and underwent an ensuing public comment period, which recently concluded. Advocates are optimistic the policy will be officially adopted soon. If and when that
22 O&P Almanac May 2024
Teri Kuffel, JD
Minnesota advocates
Cover Story
Bill Gustavson
PHOTO: MARGIE O’LOUGHLIN

occurs, “infants with moderate to severe cranial deformities will be eligible to receive orthotic care during key periods of growth when optimal clinical outcomes are obtained,” explains Gustavson. The policy “provides greater access to care based upon a sound medical policy that minimizes confusion and possible claim denials.”
Gustavson believes the multidisciplinary approach to policy change was instrumental in a positive outcome. “Historically, most Medicaid programs make medical policy changes without collaborating with providers, physicians, and advocacy groups,” he says. “Going forward, our goal is to be more proactive in working with other Medicaid and commercial payors regarding medical policy and reimbursement for CROs.”
He hopes that North Carolina’s CRO policy will trigger significant change beyond the state’s borders. “These initial efforts have resulted in a draft CRO policy that can be shared with other groups making changes to various CRO coverage policies,” Gustavson notes. “This draft document provides foundational information about the patient population and medical criteria considered prior to orthotic treatment. Having been developed and approved by a multidisciplinary group of interested parties increases the applicability to other states and payor policy review efforts.”
TEXAS: Early Efforts To Introduce Legislation
In Texas, a group of advocates is in the early stages of tackling several O&P issues. “Texas desperately needs to improve its coverage for O&P,” explains Kimberly Hanson, director of reimbursement, North America, for Ottobock. She is working with Rob Burcham; Bruce “Mac” McClellan, CPO, LPO; Mark Kirchner, CPO; Justin Pfaff,
CPO, LPO; Lisa Abernethy, CPO, LPO; Catherine Mize, CPO; and others to help patients in Texas access “life-changing” and medically necessary O&P care.
This team is tackling three major challenges: O&P coverage for Medicaid enrollees ages 21 and older; CRO coverage for infants with nonsynostotic plagiocephaly; and coverage of activity-specific devices as per the SEBCM initiative.

“Cranial helmets for babies are not a convenience or cosmetic item; they are a necessity to help the shape of the head,” Hanson explains. “Individuals with limb loss or limb difference deserve to have access to orthotics and prosthetics that are medically necessary. Texas is the only state in the United States that does not cover O&P for Medicaid adults.”
The Texas advocates are partnering with several Texas-based patient-care and O&P manufacturing companies. They have recently hired a lobbyist and will seek assistance from AOPA and the Academy in launching a letter-writing campaign to encourage Texans to contact their legislators for support.
The Texas group is hopeful that the movement will eventually lead to the adoption of all three provisions, “but we also are realistic knowing the budget constraints for the state and that these products would be additive to the budget,” Hanson says. “We are working to understand what that spend will be and may have to make some tough decisions later in order to get one, two, or all three priorities through.” The advocates plan to introduce the legislation in November 2024 for the 2025 session.
23 May 2024 O&P Almanac
In Nebraska, where advocates are pushing for insurance fairness, advocates—including Vincent Lau, CPO (second from left) —met with Gov. Jim Pillen, where he showed support for Limb Loss and Limb Difference Awareness Month.
Cover Story
Kimberly Hanson
PHOTO: VINCENT LAU, CPO
The Texas team is “passionate and driven to make a difference”— key ingredients to a successful advocacy movement, says Hanson. “It takes money to support such an effort, and this will be a new experience for many of us,” she adds. “It also takes time. Fortunately, we have experts in this field who are willing to dedicate the necessary time to this cause, and I am excited to see how many volunteers we can get involved once we kick off our campaign to contact the representatives.”
OREGON AND NEBRASKA: Advocating for Insurance Fairness
Insurance fairness legislation is accelerating in some states, including Oregon and Nebraska, with a goal of ensuring adequate coverage for prosthetic and custom orthotic care. Implementing insurance fairness laws can serve as a foundation for introducing SEBCM laws requiring coverage for activity-specific devices.

In Oregon, insurance fairness was on the books until 2017, when it was sunset due to a statute that requires certain health mandates to be renewed. Last year, a group of advocates, led by Nicole Ver Kuilen, AOPA’s manager of public engagement, successfully advocated for re-enactment of the bill, SB 797. After passing in the legislature, the bill was signed into law by Gov. Tina Kotek and took effect Jan. 1, 2024.
In Nebraska, Vincent Lau, CPO, market leader in the Omaha branch of Limb Lab, leads the push for insurance fairness legislation. He has built connections with Erin Fox, JD, a local workers’ compensation attorney; The Blade 5K, a charitable organization that raises money for activity-specific devices; and AOPA’s Miller, who educated Lau on the basics of O&P-related legislation in the states.
Last year, Fox introduced Lau to State Sen. John Cavanaugh, who joined the insurance fairness cause after meeting with Lau and visiting his O&P facility. Legislative Bill 1274 was introduced in January, and Lau provided testimony during a committee meeting in February. Although the legislature adjourned before the bill could pass, introduction of the bill in 2024 paves the way for a re-introduction in the future.
ARKANSAS:
Coverage for Showering & Bathing Devices
Momentum is growing for coverage of waterproof devices that allow users to shower or bathe. Arkansas advocates put forth a law last year mandating coverage of showering or bathing devices—and the law passed within a matter of months, taking effect July 2023. Francois Van Der Watt, CPO, LPO, owner of Van Der Watt
HB 1252, which requires payors to cover activity-specific devices as well as showering/bathing devices, gained traction in Arkansas after Van Der Watt noticed Maine had passed a law mandating activity-specific prostheses for children. Van Der Watt approached Johnson—who has a background as an emergency room physician— requesting equivalent legislation in his home state. Johnson “took the ball and ran with it,” recalls Van Der Watt. Arkansas is a smaller state with fewer legislators, and Johnson presented a case for safe waterresistant showering devices that was “hard to argue with,” Van Der Watt says. The legislation was introduced in January 2023, signed into law April 2023, and took effect as Act 805—an amendment to an existing Health Consumer Act—last July.
Van Der Watt notes that while coverage of activity-specific devices is important, coverage of showering devices also impacts many individuals with limb loss. “Everyone needs to shower or bathe,” he says. “It’s so much safer” and less of a mental strain for patients to know that transferring into the shower stall or tub will be safer. The new law is “making a big impact,” Van Der Watt adds— one that other states are hoping to emulate.
For example, Minnesota’s new bill that is expected to be passed soon includes a mandate for coverage of showering or bathing legs, according to Teri Kuffel, JD, AOPA past president and a state rep for Minnesota. “People feel most in fear of falling in a wet environment,” she explains. (See sidebar on page 22 for details of the proposed Minnesota legislation.)
Join the Cause in Your Home State
These recent state-focused activities from across the country demonstrate the power of determination and collaboration. O&P professionals at any level of their career can get involved and make an impact to drive efforts to boost access to better O&P care and more equitable O&P reimbursement. AOPA offers assistance in many forms to help O&P professionals get started or support ongoing advocacy efforts.
Anyone interested in more information on advocacy in their states or advice on how to get involved should contact Sam Miller, AOPA’s manager of state and federal advocacy, at smiller@AOPAnet.org.
Christine Umbrell is a contributing writer to O&P Almanac Reach her at cumbrell@contentcommunicators.com

Francois Van Der Watt, CPO, LPO
Prosthetics and Orthotics and an advocate in Arkansas, attributes the success of the bill, originally called House Bill (HB) 1252, to securing a “champion” in the form of State Rep. Lee Johnson, MD.
Keep Current With State-Level Advocacy Activity
To view the latest legislative, regulatory, and policy-focused advocacy initiatives in the states, read the State By State column in each issue of the O&P Almanac (see page 44 for this month’s update).
Also, be on the lookout for AOPA’s popular “State Policy Forecast” videos, presented each month by Sam Miller, AOPA’s manager, state and federal advocacy, in an entertaining and informative format.

24 O&P Almanac May 2024
AOPAVOTES.ORG Cover Story
Vincent Lau, CPO


ADVANCED POLYMER FORMULA EPOXY RESIN
ONGER TER TER
RESTECH+ advanced laminating epoxy is the strongest and easiest, crystal clear resin system on the market!
▶ Fast Curing Time
▶ Easy 2:1 Mixing By Volume
▶ Superior Toughened Resin Matrix
▶ Crystal Clear High Luster Finish
▶ Thin High Flow Viscosity

▶ Vacuum Socket Certified & Tested
▶ Imperceptible Shrinkage
▶ 2 Year Shelf Life
▶
▶ Sold In Gallons, Each Or Kit Ships Non-Hazmat

RECOMMENDED ACCESSORIES
RESIN EPOXY METER MIXER
2:1 ratio mixer offers a fast, clean and accurate way for you to meter your epoxy resin ratio. The Epoxy Meter Mixer prevents errors in mixing by removing the need to use the gram to scale system and keeps your work area clean.

RAPID CURE HEAT BAG
The Fabtech Rapid Cure Heat Bag is a inexpensive mobile oven that gets pulled over your prosthetic and orthotic epoxy laminated devices to speed up the curing process. Easily reducing the cure time in

CARBON & GLASS MATERIALS
Fabtech Ultra-lite fiberglass tapes are specifically designed for use when additional reinforcement layers are needed in prosthetic and orthotic device designs and the shear strength of fiberglass is required. Technician TOUGHENED BAGS

DESIGNED FOR O&P
Our PVA bags are incredibly consistent, have a far greater breaking tolerance and stretch more than any other PVA bag on the market.





GET A FREE AMPLE!
MIXER
SCAN FOR MORE INFO VISIT FABTECHSYSTEMS.COM FOR MORE INFORMATION OR CALL: 800.FABTECH
PRIORITIZING PATIENT CARE
AT THE FEDERAL LEVEL
O&P stakeholders visit Congress to advocate for patients and the profession



26 O&P Almanac May 2024 AOPA Policy Forum


Optimism was in the air among the more than 120 O&P advocates who took part in the 2024 AOPA Policy Forum. This year’s event followed the exciting announcement March 19 that Sens. Mark Warner (D-Virginia) and Steve Daines (R-Minnesota) introduced the bipartisan Medicare O&P Patient-Centered Care Act in the U.S. Senate. The legislation was introduced in the House of Representatives last summer and now has support in both houses of Congress.
Policy Forum attendees, hailing from 35 states, convened April 15-16 in Washington, DC, with a purpose: educate lawmakers about the Medicare O&P Patient-Centered Care Act. O&P business owners, managers, clinicians, and educators joined forces to discuss advocacy basics, strategize for one-on-one congressional visits, and meet with legislators and their staff. This year, a record 38 students took part in the premier O&P advocacy event.
Day 1 of the Policy Forum featured sessions highlighting key topics, including quantifying and scaling the work of O&P professionals; legislation versus regulation; tips for successful Capitol Hill visits; and a deep dive into the three main provisions of the Medicare O&P Patient Centered Care Act. O&P experts, advocates, and AOPA staff led the discussions and prepared attendees for individual visits with legislators. The day ended with an appearance from Rep. Brett Guthrie (R-Kentucky), a long-time supporter of AOPA’s advocacy efforts.

Participants spent Day 1 hearing from O&P experts, advocates, and community spokespersons about the importance of and nuances involved in advocacy in 2024.

DAY 1


27 May 2024 O&P Almanac
A record 38 students took part in this year’s Policy Forum.
AOPA Policy Forum
Rep. Brett Guthrie
PHOTOS: AOPA


DAY 2

On Day 2, participants went to Capitol Hill to visit their senators and representatives or staff members to share their stories and to ask that the legislators sign on and support the proposed legislation. The Medicare O&P Patient-Centered Care Act would prohibit “drop shipping” of custom orthoses and prostheses to Medicare beneficiaries; ensure Medicare beneficiaries can access the full range of orthotic care from one O&P practitioner rather than requiring patients to visit multiple providers when the treating orthotist or prosthetist does not have a competitive bidding contract; and ensure Medicare beneficiaries can access replacement custom-fitted and custom-fabricated orthoses when a change in their condition or clinical needs occurs. These provisions are designed to ensure beneficiary access to patient-centered clinical O&P care.


Attendees spent Day 2 of the Policy Forum visiting legislators and legislative aides, explaining the O&P profession and the important care provided by qualified prosthetists and orthotists, and discussing the Medicare O&P Patient-Centered Care Act.

28 O&P Almanac May 2024
PHOTOS: AOPA AOPA Policy Forum
MAKING YOUR FOOTPRINT SMALLER

CUSTOM: FOOT ORTHOTICS • AFO’S • RICHIES
At Hersco, our first priority is to fabricate custom orthotics accurately and precisely. We have mastered the art of accepting scans and 3D printing to deliver better orthotics for your patients and the environment. 3D printing is not only environmentally friendly, but allows us to specify modifications that were not possible before.


ORTHO LABS TM BUILT ON TRUST.

30 O&P Almanac May 2024 AOPA Policy Forum

Fresh off the news that the bill had been introduced in both houses of Congress, participants in this year’s Policy Forum connected with legislators in an impressive 138 meetings, equating to meeting with 26% of Congress. The advocates participated in 78 meetings with representatives or their offices and 60 meetings with senators or their offices. Policy Forum attendees appreciated the opportunity to make connections with lawmakers, explain the value of O&P clinicians as care providers, and increase awareness of the Medicare O&P Patient-Centered Care Act.
AOPA and the Policy Forum participants expect the April visits to have an ongoing impact, as some legislators expanded their comprehension of the important work of O&P clinicians and industry professionals— and several are expected to add their names to the Medicare O&P Patient-Centered Care Act.
To continue the momentum, O&P stakeholders are asked to visit AOPAvotes.org for assistance in writing to representatives and senators to ask them to support the legislation.

By the end of the day, Policy Forum attendees had connected with legislators in 138 meetings— 78 meetings with members of the House and 60 meetings with members of the Senate or their aides.





31 May 2024 O&P Almanac
PHOTOS: AOPA AOPA Policy Forum
Giving Voice to Patients
Clinician Sheryl Sachs, MSPO, CPO, prioritizes patient care while driving positive change for O&P
clinicians, consumers, and students


New this year, O&P Almanac features Fresh Faces, where we introduce readers to prominent O&P professionals who are making an impact with their contributions to the orthotics and prosthetics profession. This month, we speak with Sheryl Sachs, MSPO, CPO.
Sheryl Sachs, MSPO, CPO, has worked at Dankmeyer Prosthetics & Orthotics for more than 12 years. After earning a master’s degree in O&P, Sachs completed both her prosthetics and orthotics residencies at Dankmeyer. She was the lead practitioner and ran the North Baltimore office located on the main campus of Sinai Hospital for seven years, and currently works as a senior clinician and a residency mentor.
Sachs is an active member of AOPA and the American Academy of Orthotists and Prosthetists. She serves
O&P Almanac: What brought you to a career in O&P?
Sheryl Sachs, MSPO, CPO: While I was in my junior year at the University of Maryland, College Park, I had the opportunity to spend time in the physical therapy gym at Walter Reed. It was there that I was first
on the Executive Committee for the National Commission for Orthotic and Prosthetic Education (NCOPE) and is the current chair of NCOPE’s Residency Standards Committee. For AOPA, she serves on the Government Relations Committee, is a state representative, and plays an active role at the association’s annual Policy Forum. Sachs leads Maryland’s So Every BODY Can Move (SEBCM) initiative, recently working with legislators to introduce legislation that passed during the 2024 legislative session.
introduced to the world of prosthetics and orthotics, and I felt an immediate connection. I was fortunate enough to spend the next 1.5 years shadowing Art Molnar, CPO, in the prosthetics lab at Walter Reed. When I graduated from college, I enrolled in the O&P master’s program at the Georgia Institute of Technology.
32 O&P Almanac May 2024
Sheryl Sachs, MSPO, CPO, works in the machine room at Dankmeyer Prosthetics & Orthotics.
SHERYL SACHS, MSPO, CPO
PHOTO:
Fresh Faces
O&P Almanac: What are your responsibilities as senior clinician at Dankmeyer?
Sachs: Not including a brief move to New Jersey, I have worked for Dankmeyer since August 2011—first as a resident and now as a senior clinician. My day-to-day consists mostly of clinical care, working with both prosthetic and orthotic patients, with a focus on lower-extremity devices.
The thing I enjoy the most about my clinical role is the ability to provide a sense of hope for my patients. It is always my goal that when my patients leave the office, they feel better off than when they first arrived. We are fortunate enough to change individuals’ lives for the better, and that is a responsibility that I take very seriously.


and weaknesses, there are two items that I prioritize when they are under my direct mentorship.
The first is developing the clinical skills and competencies for lower-extremity orthosis patients, specifically foot orthoses and ankle-foot orthoses. By the end of their three-month rotation, my goal is that they would feel confident and have the skills to evaluate the average lower-extremity orthosis patient and develop a plan of care, even if they still need some clinical decisionmaking support.
technician, and assistant) and residency programs. I also serve as chair of the Residency Standards Committee, which is in the process of overhauling standards for all residency programs. There will be many updates to the standards, but perhaps the most drastic change is a shift away from device-driven competencies to clinical/technical skill-based competencies.
O&P Almanac: What is involved in your role as an NCOPE residency mentor, and what are your priorities in working with clinicians-to-be?
Sachs: Educating and mentoring is very important to me. Under the leadership of Chief Executive Officer Mark Hopkins, PT, CPO, and Chief Operating Officer Angela Bryl, CPO, Dankmeyer has a wonderful residency program that, while tailored to each individual resident, still follows a structured curriculum. After residents spend their first few months in the on-site lab, they typically complete a three-month rotation under my supervision.
While I try to tailor the experience based on the individual resident’s strengths
My second priority is to help residents develop good habits from a paperwork, documentation, and time management standpoint. It is so important for them to develop these good habits early in their careers, as it will help them with their worklife balance as their patient loads grow and they get further into their careers.
O&P Almanac: Tell us about your other responsibilities associated with NCOPE.
Sachs: I have a passion for education, and I have been involved with NCOPE since completing my residencies and earning my certification. I was first a regional residency liaison, and then served on the Residency Review Committee before becoming a board member. I have served on the Executive Committee for NCOPE over the past three years, where our priorities include oversight of education for schools (clinician,
Once our committee develops the new standards and they are approved by the board, they will be sent to the entire O&P group of stakeholders for feedback, after which we can finalize the new standards prior to implementation. NCOPE recognizes that we are a profession that provides healthcare, not simply devices, and we are committed to ensuring that future clinicians have the appropriate baseline competencies to provide safe patient care.
O&P Almanac: Why is advocacy a priority for you?
Sachs: I first became interested in policy in 2015, when Medicare released a draft Local Coverage Determination for LowerLimb Prostheses. The proposal would have had an incredibly negative impact on patient care. The O&P field came together to rally for our patients, and the proposal was ultimately rescinded. Ever since then, I have felt that it is my responsibility to be a voice for my patients, to ensure that they have access to the medically necessary orthotic and prosthetic care that they deserve.
33 May 2024 O&P Almanac
PHOTOS: SHERYL SACHS, MSPO, CPO Fresh Faces
Sachs (fourth from right), Delegate Ashanti Martinez (far left), and So Every BODY Can Move (SEBCM) advocates after attending a Health & Government Operations (HGO) Committee bill hearing
SEBCM advocate and Dankmeyer clinician Rochelle Dumm, CPO; Charles Dankmeyer, CPO (retired); and Sachs prior to the HGO hearing



Up until spring of 2020, I was the lead clinician for one of our satellite offices located near West Baltimore, where I saw patients with a large range of socioeconomical backgrounds. Most of those patients did not have the knowledge or means to advocate for themselves, and I even more so felt it my responsibility to be their voice. I have served on AOPA’s Government Relations Committee since January 2020 and have attended the AOPA Policy Forum eight times, helping to host student representatives from all of the O&P schools.
O&P Almanac: How have you been involved in the SEBCM initiative?
Sachs: Over the past year, I have served as the lead advocate for Maryland’s SEBCM Initiative. There has been so much that has gone into this experience, and I have met so many amazing people throughout this process—both patient advocates and elected officials.
Ensuring that patients have access to medically necessary prostheses and
orthoses should be obvious, but as many of us know, most insurance companies do not provide this coverage. It was a long effort, but Maryland’s So Every BODY Can Move Act (Senate Bill 614/House Bill 865) passed and will be headed to the governor’s desk to be signed into law in May!
O&P
Almanac: Please tell us about
Dankmeyer’s effort to educate payors about O&P.
Sachs: Throughout the legislative process for the SEBCM legislation, it became abundantly clear that the field of prosthetics and orthotics was new to most people.
One of the many things that Dankmeyer prides itself on is education. This includes not just education for our patients, referral sources, the healthcare professionals we work with, and students—but also for the payors.
Many of the payors I met over the legislative session acknowledged that there was a lot that they could learn about O&P, and we are thrilled that they will be visiting the Dankmeyer office in the coming weeks to expand their knowledge. We also learned that education goes beyond those directly affected by O&P care.

We were fortunate that since January, we had five new stories to share [via videos and TV spots] about the SEBCM initiative and Limb Loss/Limb Difference Awareness Month (LLLDAM). The Baltimore Orioles recognized two young boys in Maryland living with limb difference in honor of LLLDAM, and they are even throwing out the first pitch at an Orioles’ baseball game.
O&P Almanac: What are the biggest challenges
and opportunities for the future of O&P?
Sachs: There are a handful of challenges and opportunities for O&P. A lot of these start at the education level. This was the theme of the Education Summit NCOPE hosted in August 2023, with a focus on sustainability of O&P education. I also was honored to co-author an article published in the Journal of Prosthetics and Orthotics that identifies recurring themes in O&P education since the 1970s.
We also face challenges as a field— perhaps one of the largest being reimbursement challenges. We need to keep up with, if not establish and lead, when it comes to reimbursement to ensure that we continue to provide quality care to our patients, and to do it in a manner that is sustainable from both a business practice standpoint, as well as a clinical standpoint— preparing new clinicians to succeed in the current healthcare environment.
We have an opportunity to work collaboratively across organizations and states to really amplify our voices on behalf of the patients we care for each and every day.
For those younger clinicians, or even those who have been in the field for years, there are so many ways to give back and help shape our field for generations to come. All of the O&P professional organizations have volunteer committees, so don’t be afraid to get involved.
34 O&P Almanac May 2024
PHOTOS: SHERYL SACHS, MSPO, CPO
Sachs (right) testifying at the Senate Finance Committee bill hearing for SEBCM
Sachs (right), Heath (middle), and reporter Elizabeth Worthington during WMAR-TV’s visit to Dankmeyer P&O
Sachs (right) and patient-advocate John-Edward Heath at the 2024 AOPA Policy Forum
Sachs (right) and SEBCM patient-advocate Colin Potts on the set of “Good Morning Washington”
PHOTO: RON SACHS/CNP


Savings That Count! Save on UPS shipping and services with your AOPA membership. •50% off Domestic Next Day/Deferred •30% off Ground Commercial/Residents • Free UPS Smart Pickup® Service. • UP to 50% off International Imports/Exports Start saving today at savewithups.com/aopa
FACILITY:
Phoenix Rising Prosthetics & Orthotics



Why Am I an AOPA Member?
“I joined AOPA because it helps a lot with the business end— reimbursement, the documentation chase, coding— as well as for the educational offerings.”
—Sandra Schechner, CPO
OWNER: Sandra Schechner, CPO
LOCATION: Palatine, Illinois HISTORY: Four years
Meeting Patients Where They Are
Sole practitioner specializes in O&P care for older adults
Sandra Schechner, CPO, picked up the business license for her new O&P facility in March 2020— the day before the country closed down for the COVID-19 pandemic. Despite that inauspicious beginning, Phoenix Rising Prosthetics & Orthotics has survived, and thrived, in part because Schechner was willing to meet patients where they were—in that case, in their homes. Until COVID-19 restrictions lifted enough to open her office space, Schechner worked entirely through house calls to provide care and assess, fit, and deliver orthoses and prostheses.
Schechner’s commitment to meeting people where they are goes beyond their physical location. Several years ago, “I was working for another provider, but I wanted to go out on my own and figure out how to make people of all backgrounds welcome,” she says. “O&P has lots of Caucasian imagery, but we serve everyone—all races, all income levels, and those who are homebound or find it difficult to obtain care elsewhere.”
Phoenix Rising, a name connoting new life after devastation, offers the full range of orthotic and prosthetic services to patients. Although the facility serves all ages, Schechner specializes in caring for older adults. “I was a child of older adults, and I feel I have an understanding of that population,” she explains. While most O&P clinicians encounter some patients with comorbidities or mental and physical disabilities, “some of us deal with those issues more than others,” she says. “I strive to be compassionate and address what I can without going beyond my scope of practice.”
Because she is a sole practitioner, office visits are more efficient, but she continues to see some patients in their homes, assisted living and skilled nursing facilities, physical therapy and rehab centers, and senior living centers. “I try to limit house calls,” she says, “but if you’re an amputee and you have nothing to walk on, you may initially have to have someone come to you.”
Her facility features a fabrication lab, where Schechner builds nearly all devices using primarily traditional fabrication methods. “We’re small and
we started during the pandemic, so we’ve had to keep overhead low,” she says. “But I expect to try digital scanning and more advanced technologies as we grow.”
Schechner takes a personal approach to every patient. “Many folks who come in are not well on multiple levels. I try to listen to them, to bond with them, and to back off as needed,” she says. Being aware of and managing patients’ expectations is essential to a good outcome, and Schechner is modifying her intake package to better identify patients’ goals and expectations.
“If something hasn’t worked for a patient in the past, you need to know why and not repeat it, so they don’t take their device home and put it in the closet,” she says. “When we take the time to figure out the patient’s preconceptions and expectations, and then try different approaches, we can” more easily return that patient to mobility. Schechner also leverages several outcome measurement tools, including the Timed-Up-and-Go test and the Amputee Mobility Predictor.
One of Schechner’s favorite patient stories is that of a 90-year-old woman with bilateral 45-degree equinovarus. “She is an example of someone I would not digitally scan,” says Schechner, “because of the severe contortion of her feet. She had a disorder that caused her hands to contort as well, but she kept trying and wouldn’t give up. She had tried other clinicians and came to me through a former instructor of mine at Northwestern University. We worked with her to find the right solution—and now she is walking again.”
Schechner describes herself as extremely detail oriented, but she has learned to distinguish between patients who want to know everything and those who prefer a summary during consultations. “That doesn’t eliminate the fact that I incorporate a million details, “she says. “That’s how I make things work for folks.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net
BY DEBORAH CONN Member Spotlight
PHOTOS: PHOENIX RISING PROSTHETICS & ORTHOTICS
Phoenix Rising P&O features a fabrication lab, where Schechner builds nearly all of the devices she provides.
36 O&P Almanac May 2024
Sandra Schechner, CPO


































































































































Ready to start?
100+ TOP-QUALITY ORTHOTIC, PROSTHETIC, AND PEDORTHIC EDUCATION COURSES. EARN SCIENTIFIC, BUSINESS, AND PEDORTHIC CE CREDITS BY STUDYING THE COURSE MATERIAL AND PASSING THE QUIZ. ACCESS YOUR PERSONAL ACCOUNT, VIEW VIDEOS, PRINT CERTIFICATES, OR REVIEW CE CREDIT HISTORY 24/7. Visit www.AOPAnet.org/education. It’s as easy as 1-2-3! Set up your free personal online account Choose your education and study Take the quiz and print your certificate EARN CE CREDITS AT YOUR OWN PACE www.AOPAnetonline.org/aopaversity LEARN
& EARN
in at www.AOPAnet.org/education. Your username is the email used to create your profile.
not currently have an AOPAversity account,
your
member
1 2 3 Top quality orthotic, prosthetic and pedorthic education and CE credits from the organization that knows O&P.
Log
If you do
visit www.AOPAnet.org/education to create a profile. Use
AOPA
ID and the zip code a liated with your membership when you create your profile to access the free o ering.
BY DEBORAH CONN
OWNER: Privately Held


Superfeet Rx leverages a 3D foot scanning app to create orthotic inserts.
Why Am I an AOPA Member?
“Superfeet Rx is excited about our new AOPA membership, which provides us with a valuable platform to engage with a diverse audience of healthcare professionals and showcase our innovative orthotic solutions. We hope this collaboration fosters meaningful connections and the opportunity to exchange knowledge within this community.”
—Chris Patten
LOCATION: Ferndale, Washington; Canada; and the United Kingdom
HISTORY: One year
Digital Designs
Company helps clinicians create customized orthotic inserts
Superfeet Rx is a new division of Superfeet, an orthotic insole company founded in 1977 as the Sports Medicine Division of Northwest Podiatric Laboratory. Superfeet launched its first over-the-counter insole in 1980 and reached a global market by 1995. The company began a partnership with the 3D-printing firm Materialise and in 2023 launched Superfeet Rx.
Chris Patten came on board as director of the new group, which works with clinicians—including orthotists, podiatrists, sports medicine doctors, and chiropractic providers—to help them create customized orthotic inserts for their patients.
“We provide hardware and software that allow practitioners to perform 3D volumetric scanning as well as 2D gait analysis pressure scanning,” says Patten. “Our technology lets clinicians obtain static and dynamic analysis, 3D visualizations, force graphs, and sideby-side comparisons.” As a result, he notes, patients can better understand what is happening to their feet by seeing the results on screen and hearing the clinician’s assessment.
Once scans are completed, they are combined with proprietary software, the Materialise Phits Suite, that defines appropriate treatment plans, creates customized 3D-printed orthotic inserts, and tracks patients’ progress. “The entire process is digital,” says Patten. “We 3D print the devices using high-end commercial HP printers and then ship them to practitioners to dispense to their patients.”

This results in practitioners achieving more successful patient outcomes and lower orthotic adjustment rates.”
Phits 3D-printed custom orthoses are thinner and lighter than other custom inserts, Patten says, which means they will fit into a wider choice of footwear. The technology allows modifications for zone-specific flexibility and stiffness to make corrections without increasing bulk, according to Patten.
Superfeet Rx offers several variations on the devices, including a ski version to fit in Alpine or Nordic ski boots, a comfort version for semiorthopedic and everyday shoes, safety workwear, and versions tailored to runners, golfers, cyclists, and soccer players.
The company markets its services via attendance at trade shows directed at a variety of healthcare providers, as well as print advertising and an informative website that includes opportunities to arrange demonstrations and speak with representatives.
Superfeet Rx’s stated mission is to make a positive difference in people’s lives by shaping a strong foundation. The company has adopted three core values: putting people first, being responsible global citizens, and focusing on innovation. In alignment with its commitment to corporate responsibility, Superfeet donates 1% of sales and more than 1,000 volunteer hours to nonprofit organizations each year, and every employee can make an annual donation of $1,000 to a cause of their choice. “We support access to clean air and water with corporate memberships to organizations like the Conservation Alliance and Protect Our Winters,” adds Patten, “and Superfeet has pledged to be carbon neutral by 2025.”
The digital process allows for much faster turnaround time and improved customization, and, says Patten, it improves the experience for patients. Because the workflow is entirely digital—from data capture to assessment to design to manufacturing— the process is more reliable and efficient compared to traditional orthoses, he says. “The improved customization is achieved by a data-driven orthotic design combined with automated 3D-printing manufacturing.
As technology continues to evolve, Patten expects to see more advanced bespoke data-driven devices. “I think we’ll see the share of 3D-printed devices grow, while the proportion of mass-produced products will shrink,” he says. “Materials will evolve, data-point and data-driven design will evolve, and Superfeet … will capitalize on those improvements as they occur. We will continue to invest to meet the demand of future consumers and patients.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net
COMPANY: Superfeet Rx 38 O&P Almanac May 2024
PHOTOS: SUPERFEET RX
Spotlight
Member
Chris Patten
Foot scans are a key aspect of the digital design process.
Don’t Miss AOPA’s Next Coding & Billing Seminar
Take part in the virtual event Aug. 19-20
Sign up for the next AOPA Virtual Coding & Billing Seminar, slated for Aug. 19-20. You’ll learn how to get claims paid, survive audits, collect interest from Medicare, and file successful appeals. Earn CEs!
Visit AOPAversity online at bitly.aopaversity for details and to register. For questions regarding seminar content, email Devon Bernard at dbernard@aopanet.org

Visit the SEBCM Website
So Every BODY Can Move (SEBCM) is at the forefront of the national disability rights movement, focusing on creating equitable and life-changing access to prosthetic and orthotic care for physical activity in 28 states by the 2028 Paralympic Games.
SEPTEMBER 12-15, 2024 | CHARLOTTE, NC
Register Now!
Mark your calendar for the AOPA National Assembly in September
The 2024 AOPA National Assembly, with a theme of “Ignite 24,” takes place Sept. 12-15 in Charlotte, North Carolina. Plan now to attend this year’s Assembly. Why attend?
• Earn continuing education credits
• Hear from physicians, researchers, and top-notch practitioners
• Participate in hands-on learning and demonstrations
• Network with an elite and influential group of professionals
• Explore the largest O&P exhibit hall in the western hemisphere, featuring devices, products, services, tools, and the latest technology from exhibitors around the world.
Registration is now open! Register and learn more at AOPAAssembly.org


FUN FACT
The Charlotte Convention Center opened in 1995 and attracts more than 500,000 visitors each year. A LEED Gold-certified building, the convention center is situated steps from Uptown’s hotels, attractions, dining, and nightlife, and is located just 7 miles from Charlotte Douglas International Airport.
SEBCM, developed through a partnership between AOPA, the National Association for the Advancement of Orthotics and Prosthetics, the American Academy of Orthotists and Prosthetists, and the Amputee Coalition, advocates for a policy solution rooted in dignity and justice by empowering state-by-state legislative action, expanding access to medically necessary orthotic and prosthetic care for physical activity.
For more information and to get involved, log on to soeverybodycanmove.org, a dynamic platform featuring a user-friendly interface, engaging content, an interactive state map, and much more.
Access AOPA’s 2024 Webinars
Six virtual webinars cover key topics
AOPA will offer six webinars throughout 2024—in February, April, June, August, October, and December.
February’s webinar covered “Changes & Updates to Medicare Policies: Do You Still Know the Rules?” April’s webinar is a must-see “AOPA Ask the Expert” event.
Webinars are $99 for members and $199 for nonmembers. All webinars are live, but everyone who registers will receive access to the recordings.
To purchase the February or April webinar or register for future sessions, access your AOPA Connection account or visit aopanet.org. Questions? Contact Devon Bernard at dbernard@aopanet.org
39 May 2024 O&P Almanac
AOPA News
Welcome New AOPA Members
The officers and directors of the American Orthotic & Prosthetic Association (AOPA) are pleased to present these applicants for membership. Each company will become an official member of AOPA if, within 30 days of publication, no objections are made regarding the company’s ability to meet the qualifications and requirements of membership.
Orthotics & Prosthetics
Solutions LLC
7754 Florida Blvd.
Baton Rouge, LA 70806-4706
225-316-5444
thelegguy.com
D’Andre Mostella, CP Patient-Care Facility





















40 O&P Almanac May 2024 AOPA Members
Visit AOPAnet.org/join for more information. Be Part of the CHANGE Join AOPA SCAN TO FIND YOUR NEXT JOB!
new career opportunities for FREE!
on any websites, emails, and videos to learn more.
the guide to look back on organizations and opportunities that appeal to you. Explore Click AOPA- Program Book Ad.indd 1 8/7/23 9:49 PM
•Explore
•Click
•Download

KiddieFLOW™
KiddieFLOW™, Allard USA’s extension to our pediatric AFO line, was introduced in response to clinician requests for an orthosis with more foot plate flexibility. KiddieFLOW™ allows for better control of foot positioning in late swing, which aids in stability during stance. FLOW models offer increased range of motion in the sagittal plane and a smoother transition (flow) throughout the gait cycle.
For more information, contact customer service at 888-678-6548 or info@allardusa.com and request your free teddy bear tape measure!


NEW 2024 PRICING!
BEST IN O&P



The wait is finally over!
Fillauer’s ProCover is now available for the adult AllPro DM, AllPro PM, AllPro XTS, or Wave Comfort 3. The ProCover is a sleek foot cover with a split design that protects the foot, enhances performance, and is easy to install and remove for cleaning and maintenance. Visit fillauer.com to find out more.

Hersco 3D Printing
Hersco is delighted to offer HP’s advanced 3D-printing technology for custom orthotics. 3D printing has unique design capabilities not possible with other methods—reducing landfill waste by 90%! The accuracy of 3D is unparalleled, specs exceed direct-milled polypro, and manual plaster fabrication. Among the benefits: a 90% reduction in landfill waste, many new design possibilities for posting, and the ability to vary thickness and flexibility across the shell. The PA-11 polymer is a biobased renewable material that has been tested and proven in research and industry. Call today, 800-301-8275, for a free sample.
41 May 2024 O&P Almanac Marketplace HAVE A PRODUCT OR SERVICE FOR MARKETPLACE? Contact Bob Heiman at bob.rhmedia@comcast.net
SAVE WEIGHT! For more information visit www.fabtechsystems.com or call 800.FABTECH SCAN FOR PRICING AND DETAILS
ON OUR ECONOMICAL LINE OF BONDTEK ADHESIVES C M Y CM MY CY CMY K Marketplace-Ad-Bondtek-20240419.pdf 1 4/19/24 1:53 PM



RUSH Feet
You’ve been asking and we have listened! All RUSH feet are now available in sandal toe options including all the RUSH series.

This expansion opens a world of footwear possibilities including sandals or flip flops while enjoying the same exceptional performance and confidence of RUSH feet.
With the full line available in sandal toe, there’s more choices for everyone to explore. More choices for pure satisfaction, step after For information, visit proteor.com

Turbomed Foot Drop AFOs
Turbomed’s leading line of foot drop ankle-foot orthoses sit completely outside the shoe for an invisible, painless support that will follow you as long and as far as you want. Their unique design acts as an exoskeleton to the impaired limb, keeps the foot at 90 degrees, and provides the user with unparalleled levels of function. Each model takes minutes to assemble and is easily transferrable to most shoes, boots, and sandals through an innovative lace clip design.
The Xtern Summit is the lightest model, has the most dorsiflexion power, and features a see-through design. The Xtern Frontier was designed for patients with reduced hand dexterity and requiring front leg support. Visit turbomedusa.com, and think outside the shoe!

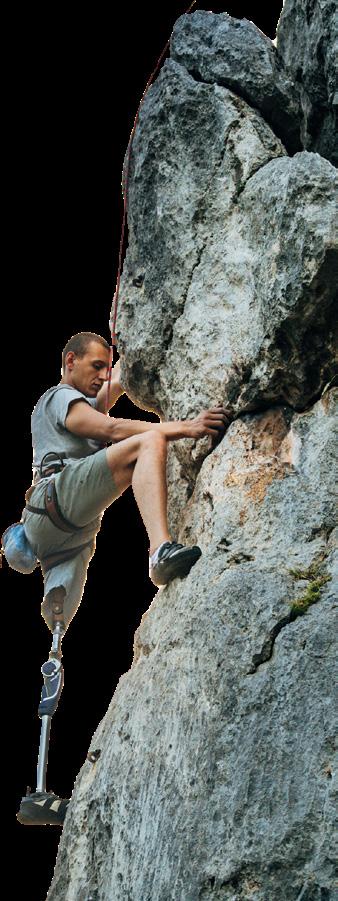
42 O&P Almanac May 2024
AOPAnet.org/education Learn & Earn It’s as easy as 1-2-3: 1. Set up your free personal online account 2. Choose your education and study 3. Take the quiz and print your certificate! Board of Certification/Accreditation
Naked Prosthetics offers four finger prostheses: PIPDriver, MCPDriver, ThumbDriver, and GripLock Finger. IT’S ALL ABOUT FUNCTION. ™ ™ ™ ™
Contact Bob Heiman at bob.rhmedia@comcast.net
May 1–31
ABC: Application Deadlines, Exams Dates, O&P Conferences, and More! Check out ABC’s Calendar of Events at ABCop.org/calendar for the latest dates and event details, so you can plan ahead and be in the know. Questions? Contact us at info@abcop.org; ABCop.org/contact-us
May 13–14
AOPA Virtual Coding & Billing Seminar. To register, visit aopanet.org

June 28–29
PrimeFare East. Sheraton Grand Hotel Downtown Nashville. In-person meeting. For information, contact Cathie Pruitt at 901-359-3936, primecarepruitt@ gmail.com, or visit primecareop.com
June 30
Application Deadline for AOPA 2025 Call for Volunteers. Visit aopanet.org/volunteer or contact info@aopanetorg
August 19–20
AOPA Virtual Coding & Billing Seminar. To register, visit aopanet.org

September 12–15
AOPA National Assembly. Charlotte, NC. For more information, visit aopanet.org
A large number of O&P Almanac readers view the digital issue— If you’re missing out, visit issuu.com/americanoandp to view your trusted source of everything O&P.
Scan the QR to start advertising in the O&P Almanac or visit bit.ly/24AlmanacMediaKit

Live and Online/On Demand CEs
The Pedorthic Footcare Association: Diabetic Wound Prevention, Management, and Healing Program. 10-session online education program series. Approved CEs by ABC and BOC, monthly classes are 1.5 hours each. For more information and to register, visit pedorthics.org/page/. Diabetic_Series_LMS_List

Share Your Calendar Event
Advertise O&P events for maximum exposure with O&P Almanac Contact Bob Heiman at bob.rhmedia@comcast.net or learn more at bit.ly/24AlmanacMediaKit. Announcement and payment may also be sent to O&P Almanac, Calendar, P.O. Box 34711, Alexandria, VA 22334-0711 or emailed to jburwell@AOPAnet.org along with VISA or MasterCard number, cardholder name, and expiration date. Make checks payable in U.S. currency to AOPA. Note: AOPA reserves the right to edit calendar listings for space and style considerations.
Advertisers Index
43 May 2024 O&P Almanac
COMPANY PAGE PHONE WEBSITE Allard USA 1 866-678-6548 www.allardusa.com ALPS South LLC 15 800-574-5426 www.easyliner.com ComfortFit Orthotic Labs 5 888-523-1600 www.comfortfitlabs.com Fabtech Systems 25 800-322-8324 www.fabtechsystems.com Fillauer Companies 21 423-624-0946 https://fillauer.com/products/motion-foot-six/ Hersco 29 800-301-8275 www.hersco.com Naked Prosthetics 3, 19 888-977-6693 www.npdevices.com Ottobock C4 800-328-4058 www.professionals.ottobockus.com PROTEOR USA 9 855-450-7300 www.proteorusa.com TurboMed Orthotics 13 888-778-8726 www.turbomedorthotics.com
2024 SHARE YOUR UPCOMING EVENT WITH O&P PROFESSIONALS
Calendar
If you are interested in participating
O&P Activities
Updates
from
New Hampshire and Texas
New Hampshire
Senate Bill 455, which would set Medicaid reimbursement at 90% of Medicare, has officially passed the Senate and will now move to the House. The bill is sponsored by Sen. Sue Prentiss, a champion of quality, timely O&P care and sponsor of New Hampshire’s So Every BODY Can Move bill.

Texas
The Texas Department of Licensing and Regulation has proposed regulations that would require accredited O&P facilities to provide itemized bills to patients. If adopted, bills to patients at these O&P facilities would be required to include a plain language description of each distinct healthcare service or supply provided. If the facility sought or is seeking reimbursement from a third party, any billing code submitted to the third party; the amounts billed to and paid by that third party; and the amount due from the patient for each service and supply also would be required to be provided to the patient.
The Latest From So Every BODY Can Move
Below are the most recent developments in the So Every BODY Can Move initiative, developed by AOPA in conjunction with the National Association for the Advancement of Orthotics and Prosthetics, the American Academy of Orthotists and Prosthetists, and the Amputee Coalition. The movement advocates for a policy solution rooted in dignity and justice by empowering stateby-state legislative action, ensuring access to medically necessary orthotic and prosthetic care for physical activity.
Maryland
Senate Bill 614, recently renamed the So Every BODY Can Move Act, was approved by the Senate Finance Committee, successfully passed its Senate floor vote with a unanimous 45-0 vote, and then passed the House Government Operations Committee in a flurry of legislative activity. The bill has been amended to address potential budgetary concerns; these include removing orthotic coverage from the bill and placing a cap on
Activity on the Federal Front
House Resolution 4315, the Medicare Orthotics & Prosthetics Patient-Centered Care Act, officially has a Senate companion. Introduced March 19 by Sen. Mark Warner and championed by Sens. Steve Daines, Amy Klobuchar, and John Cornyn, Senate 3977 would ensure access to
Medicaid managed care organization coverage for a year.
Massachusetts
House 4096, which requires that state commercial plans, public employee plans, and Massachusetts Medicaid provide coverage for activity-specific O&P care, has successfully passed the Joint Financial Services Committee and will now move to the Joint Committee on Healthcare Financing.
Minnesota
Senate File 3351, which would implement insurance fairness, cover activity-specific and showering/bathing devices, and require that insurance companies follow nondiscrimination standards related to the coverage of O&P care, has passed its final Senate committee and will now move to the Senate floor for a vote. The bill has the potential to be enacted via inclusion in a larger omnibus spending package currently under consideration by the legislature.
timely, quality O&P care while saving the Medicare program millions of dollars in fraud prevention.
To show your support, visit AOPAvotes. org, where you can fill out a short form to automatically send a message to your representative and senators requesting their support for the bills.
44 O&P Almanac May 2024 State By State BECOME AN AOPA STATE REPRESENTATIVE
in the AOPA State Reps network, email smiller@AOPAnet.org
New Hampshire State House
The Ottobock MyCRO Band.
The MyCRO Band is an innovative, 3D-printed cranial helmet, customized precisely for your littlest patients.
Scan the QR code to learn more today!




04/24 ©2024 Otto Bock HealthCare, LP 21520 · Technical changes and printing errors reserved.