POSTOPERATIVE COMPLICATIONS OF PAEDIATRIC CATARACT SURGERY



ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

Publisher
Carol Fitzpatrick
Executive Editor
Colin Kerr
Editors
Sean Henahan
Paul McGinn
Managing Editor
Caroline Brick
Content Editor
Aidan Hanratty
Senior Designer
Lara Fitzgibbon
Designer
Ria Pollock
Circulation Manager
Angela Morrissey
Contributing Editors
Howard Larkin
Dermot McGrath
Roibeard Ó hÉineacháin
Contributors
Maryalicia Post
Leigh Spielberg
Gearóid Tuohy
Priscilla Lynch
Soosan Jacob
Colour and Print
W&G Baird Printers
Advertising Sales
Amy Bartlett
ESCRS
Tel: 353 1 209 1100
email: amy.bartlett@escrs.org
Published by the European Society of Cataract and Refractive Surgeons, Temple House, Temple Road, Blackrock, Co Dublin, Ireland. No part of this publication may be reproduced without the permission of the managing editor.
Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983 As

25
26
27
The COVID-19 pandemic has transformed completely the way we live our lives and the way we practise as ophthalmologists.
We will continue to rely on our surgical skills but in this new era of uncertainty, we must also start learning new skills.
In a special webinar organised by WSPOS earlier this year, I discussed the importance of telemedicine.
As I pointed out during the webinar, with tele-ophthalmology already gaining traction in recent years as an effective eyecare delivery modality worldwide, the COVID-19 pandemic has served to further amplify this trend.
I do not think that tele-ophthalmology is going to go away and we would be well advised to become familiar with it as we seek to make the best use of the resources we have available to us in caring for our patients in the current crisis.
As we are also obliged to observe new rules on social distancing, we have also been restricted in our personal movements and we have not been able to interact with colleagues in the way we have done in the past.
That is why we were not able to meet in Amsterdam this year for our fifth World Congress of Paediatric Ophthalmology and Strabismus (WCPOS).

Noel Alpins (Australia), Bekir Aslan (Turkey), Roberto Bellucci (Italy), Hiroko Bissen-Miyajima (Japan), John Chang (China), Béatrice Cochener-Lamard (France), Oliver Findl (Austria), Nino Hirnschall (Austria), Soosan Jacob (India), Vikentia Katsanevaki (Greece), Daniel Kook (Germany), Boris Malyugin (Russia), Marguerite McDonald (USA), Cyres Mehta (India), Sorcha Ní Dhubhghaill (Ireland) Rudy Nuijts (The Netherlands), Leigh Spielberg (The Netherlands), Sathish Srinivasan (UK), Robert Stegmann (South Africa), Ulf Stenevi (Sweden), Marie-José Tassignon (Belgium), Manfred Tetz (Germany), Carlo Enrico Traverso (Italy)
In its place, we came together virtually for the WSPOS World Wide Connect meeting on September 26, which allowed delegates from all over the globe connect with the WSPOS online congress. Connect did what we had hoped. It connected the world for 24 hours, promoted education and ideas exchange and established every part of the world as equally important. It allowed friendship and camaraderie to shine through, changed what could be, to what is and created a platform for nurturing. It shifted the paradigm.
We can only hope that there are better times ahead. I wish all readers of EuroTimes my very best for the future. Stay safe and stay well.
Dr Ken Nischal is Chief of the Division of Paediatric Ophthalmology, Strabismus, and Adult Motility at the UPMC Children’s Hospital of Pittsburgh, United States and founding member of WSPOS





As we are also obliged to observe new rules on social distancing, we have also been restricted in our personal movements and we have not been able to interact with colleagues in the way we have done in the past
Using chandelier illumination provides a true bimanual manipulation during vitreoretinal surgery. Our trocar based solution facilitates global intraocular visualization. With our flexible chandelier the surgeon can perform manipulations bimanually and efficiently while maintaining perfect flexibility.
Features and Benefits
→ Global visibility of the fundus for all surgical maneuvers
→ High flexibility in illumination through flexible loop of fiber
→ One-step access with quick trocar based snap lock connection
→ Extrawide and homogeneous illumination
→ Postoperative tight sclerotomy
Make the difference – with the flexible chandelier: www.oertli-instruments.com

Cataract surgery in the younger population is not without risk.
Soosan Jacob, MS, FRCS, DNB reports


Paediatric cataract surgery (PCS) is challenging and needs experience and team effort to manage postoperatively. To maximise results, one should be aware of complications, age-wise distribution, difference from adults and their management.

RISK FACTORS
Complications of PCS depend on aetio-pathogenesis, age at surgery and type of surgery. Generally, dense unilateral cataract is
operated on between six and eight weeks of corrected gestational age and dense bilateral cataract between six and 10 weeks. Performing surgery after eight weeks in these cases causes form vision deprivation amblyopia more resistant to treatment, resulting in poorer visual outcome. Noteworthily, early surgery increases life-long risk for secondary glaucoma. Non-visual axis opacities and eyes with irreversible retinal involvement do not need surgery. A smaller sized eye; low ocular rigidity; increased inflammation; growth changes; difficulty in examination, estimating vision,
intraocular pressure (IOP), refraction, fundus evaluation and visual rehabilitation; difficulty in applying medications, maintaining hygiene and preventing unintentional trauma, all add up and increase challenges while decreasing potential for unqualified success.
Paediatric eyes also have more vascular irides, small pupils, immature trabecular meshwork, shallow anterior chamber and small palpebral aperture with poor ocular exposure
Systemic examination, metabolic and TORCHS screening, genetic analysis and next-generation sequencing are done when indicated.
Postoperative inflammation is stronger in children and more so in infants and in uveitic cataracts. Pupillary membrane formation, iris bombe, posterior synechiae, peripheral anterior synechiae, glaucoma, IOL pigments, pupillary capture and decentration of IOL can all occur. Steroids used to control inflammatory response can increase IOP.
Cushing’s syndrome secondary to topical steroids has been reported and is avoided by punctal occlusion following topical medications.
Cycloplegics applied to prevent posterior synechiae and a constricted tied down pupil have sometimes been associated with an increased incidence of glaucoma.
Excessive prostaglandin release from inflammation can cause darker iris pigmentation and heterochromia.
Glaucoma is variably reported to have an incidence between 2 and 58%, with many studies reporting a 10-to-25% risk. Exact aetiology is unknown; however, IOL implantation does not give protection. Incidence increases with longer follow-up and younger age at surgery, with greatest risk in infants with bilateral cataracts who have undergone cataract surgery at less than 1 month of age. Regular follow-up for life is needed as it may present very late.
Incidence also increases with shorter axial length, use of trypan blue, complex pathology, persistent foetal vasculature, complex surgery, occurrence of intra- or postoperative complications, residual cortex, aphakia and reinterventions.
Glaucoma in children results in optic nerve cupping, visual field defects, enlargement of cornea and globe, Haab’s striae etc. Rebound tonometry may underestimate IOP. Glaucoma is managed medically and if not responsive, with surgery, often requiring a shunt.
Posterior Capsular Opacification (PCO) is common after IOL implantation under 2 years of age because of increased tendency to inflammation and scaffold effect of anterior vitreous face and IOL. Posterior capsulectomy with anterior vitrectomy should be done up to 5-to-7 years age and for older children with developmental delays and nystagmus.
Visual axis opacification (VAO) may occur even after posterior capsulectomy due to membrane formation from increased inflammation. VAO due to lens proliferation is especially common in the first year of life. Fibrin and pigment deposition on IOL secondary to iris inflammation, if confluent, may decrease vision.
PMMA IOLs are more at risk than hydrophobic acrylic IOLs. In-the-bag IOL implantation with optic capture through a posterior capsulorhexis has been proposed to decrease this.
Anterior vitrectomy may be done prior to placement of IOL or after, through a limbal ‘under-the-IOL’ or a pars plana route. Bag-inthe-lens technique may also confer protection from VAO.
Dense amblyopia may occur secondary to stimulus deprivation preoperatively and from VAO, refractive errors, loss of accommodation, strabismus or other ocular pathology, all of which should be attempted to be treated where possible. Anisometropic amblyopia can occur with ≥1.01.5D anisohyperopia, ≥2.0D anisoastigmatism and ≥3.0-4.0D anisomyopia. Isoametropic amblyopia can occur with ≥5.0-6.0D myopia, ≥4.0-5.0D hyperopia or ≥2.0-3.0D astigmatism.
Early visual rehabilitation is needed for high hyperopic errors, even after IOL implantation, because of residual hyperopia usually intentionally left in anticipation of the myopic shift with age.
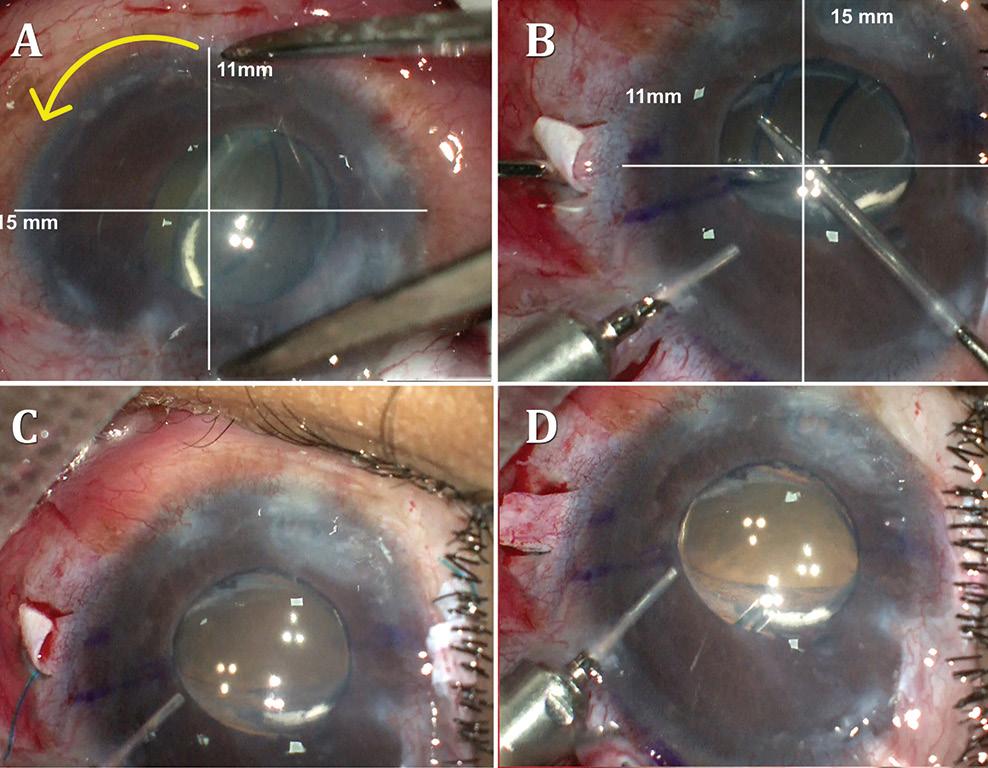
Post-paediatric cataract surgery Glaucoma: A: 3.5 years old child with cataract surgery done in infancy. Glaucoma with enlarged corneal diameter and a dislocated IOL are seen. One previous Ahmed glaucoma valve (AGV) in supero-temporal quadrant has failed to control IOP adequately; B: A second AGV plate is sutured in the infero-temporal quadrant. A closed chamber vertical translocation of haptics to glued IOL is then done sitting temporally, taking advantage of smaller vertical diameter of cornea; C: Adequate length of the externalised haptics of the IOL is seen; D: Haptics are tucked in. A well-centred IOL is seen. The AGV tube tip is positioned posterior to the iris in front of the IOL. Adequate vitrectomy is performed during IOL translocation as well as after inserting the tube tip
Suture-induced astigmatism can occur and suture management should be good.
Myopic shift with growth of eye should be treated with contact lenses, glasses, IOL exchange, piggyback IOLs or corneal refractive surgery.
Paediatric spectacles with small frames are available and preferred. Contact lenses have advantages of avoiding edge effects and loss of peripheral fields that occur with thick hyperopic spectacles as well as the aniseikonia occurring with spectacles after unilateral cataract surgery.
Occlusion therapy plays a major role in case of asymmetric visual acuity or fixation preference and is continued till around 7 years of age. Up to 6 months of age, one hour per month occlusion and till 5 years of age, six hours per day is advisable. Extensive occlusion in infancy disrupts binocularity. Prolonged occlusion resulting in reverse amblyopia in normal eye should be looked for and avoided. Strabismus and nystagmus may develop and should be treated.
Certain eyes, for example, with traumatic cataract, subluxated lens, Stickler syndrome, Marfan’s syndrome, homocystinuria, long axial length, persistent foetal vasculature, complicated or multiple surgeries etc. are at a higher risk of developing retinal detachment. As such, an overall 3% risk of retinal detachment in developmentally normal children with cataract and a 7% 20-year risk of retinal detachment has been reported. This risk increases further to 16% if associated with other ocular or systemic anomalies and even further to 23% in children with mental retardation.
Poor hygiene, posterior capsular rent, vitreous loss, unidentified vitreous wick, wound leak, poor wound closure, iris prolapse etc. are all risk factors for endophthalmitis. Other complications such as toxic anterior segment syndrome, corneal oedema, shallow AC, uveitis, hyphema, capsular block syndrome, corectopia, IOL decentration or dislocation, IOL opacification etc. can all occur in paediatric cataract surgery as well. Self-limited and self-resolving haemorrhagic retinopathy and vitreous haemorrhage has been reported in up to one-third of infants in one study. Chronic hypotony and phthisis may occur as late complications.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com

Treating a patient with an immobile eye due to thyroid disease requires a multidisciplinary approach that takes into account the entire spectrum of the disease and its impact on the eye, reports David B Granet MD, MHCM, FACS, FAAP, FAAO, Shiley Eye Centre, University of California, San Diego, US.
“Thyroid disease may be difficult, but with careful planning and understanding and working with your colleagues in oculoplastics you can change these patients’ lives and make them smile again,” Dr Granet told the 2020 WSPOS Virtual Meeting.
The physician needs to understand the condition from the patient’s point of view. Often they will experience frustration because they don’t understand that they have to wait for the disease to get better and stabilised. Also confusing is the fact that the systemic effects of thyroid disease sometimes don’t become manifest until after they have developed the associated eye problems.
“Perhaps the first and foremost is the psychological impact of the disease; the disfigurement that we have is more impactful than the double vision, which is astonishing to people. So, if you don’t take care of the psychological burden then you are not helping your patients,” Dr Granet explained.
He noted that thyroid eye disease has two stages of development. There is the active inflammatory phase, which is characterised by sore, red eyes and cosmetic problems. It usually resolves within three years (many much sooner). However, 10% develop serious long-term ocular complications. Then there is the quiescent stage where a much less inflamed
orbit and motility defect may be present. Severity at this stage may range from being a nuisance to blindness from exposure keratopathy or optic neuropathy.
There are also two different clinical spectrums of disease. Type I, where there is largely fat infiltration and associated proptosis and type II, where there is extraocular muscle involvement.
In 1997, Dr Granet and Don Kikkawa MD established the Thyroid Eye Center at UCSD, and they have developed a five-step approach to treating thyroid eye disease. The first step is medical treatment, the second is Botox, the third is orbital decompression, the fourth is strabismus repair and the fifth is lid repair.
He noted that research conducted by Dr Kikkawa at their centre has shown that it is possible to grade the amount of orbital decompression required based on the degree of proptosis present. In addition, they have shown that if you inject Botox at the time of decompression you can affect the strabismus and sometimes actually prevent strabismus.
Moreover, their research also shows that in correctly selected patients, outpatient administration of Botox chosen can correct small strabismus deviations, completely eliminating the need for strabismus surgery in up to onethird of cases, Dr Granet pointed out.
The goal in strabismus surgery is to get the patient to primary position and, if possible, reading position. It is possible to accomplish both by aiming just below the primary and allowing the patient to obtain a small chin-up position. Under-correcting the vertical alignment will help compensate for late changes and asymmetric surgery is needed in asymmetric problems.
“While most have inferior rectus contraction/over-action problems, many have superior rectus inferior oblique or even superior oblique type patterns. Look carefully, before you start,” he cautioned.
“Our group uses delayed adjustable sutures. Delaying the suture adjustment by five-to-seven days decreases risk of infection, decreases splinting and provides the patient with a better chance for binocular recovery.”
The introduction and FDA approval of the monoclonal antibody teprotumumab (Tepezza, Horizon Therapeutics) heralds a new era in the treatment of thyroid eye disease, Dr Granet noted.
“Don Kikkawa and I used to say that in the future thyroid eye disease will be stopped with medication and not the scalpel. The future has arrived,” he announced.
The human monoclonal antibody was approved for use in the United States in January 2020. It binds to the insulin-like growth factor 1 receptor (IGF-1R) and by doing so also inhibits thyroid stimulating hormone (TSH). In this way it inhibits the inflammatory cascade thereby reducing oedema and glycosaminoglycan production. It is administered intravenously at a dosage of 20mg/kg in eight cycles over 24 weeks, Dr Granet noted.
The FDA approved teprotumumab based on two randomised controlled studies showing meaningful reduction in proptosis in 71% and 83% of patients receiving the monoclonal antibody, compared to 20% and 10% of control patients.
Dr Granet presented two case studies from the UCSD oculoplastics team, Dr Kikkawa and Dr Bobby Korn, one with active disease and the other with chronic disease. In both cases, patients returned to their normal state after completing eight cycles of treatment.
“This is a game changer; however, there are side-effects and of course we have to pay attention to the teratogenicity of this in someone who might be pregnant. There may be relapses as well and it is expensive,” Dr Granet added.
David Granet: dgranet@gmail.com
Perhaps the first and foremost is the psychological impact of the disease; the disfigurement that we have is more impactful than the double vision
David B Granet MD, MHCM, FACS, FAAP, FAAO
There are many new treatments under investigation for the treatment of amblyopia that may provide useful alternatives to patients who are not amenable or unresponsive to traditional patching, reports Shira L Robbins MD, Professor of Ophthalmology at the Shiley Eye Institute, University of California, San Diego, California, US.
“The best treatment is whatever treatment the family can do. And every family unit is different and we as paediatric ophthalmologists know that almost better than anyone else,” Dr Robbins told the 2020 WSPOS Virtual Meeting.
She noted that occlusion therapy for amblyopia has a long history, dating back to 800 AD, when Thābit ibn Qurrah al-Harrānī first described occlusion of the better eye to improve vision of the strabismic eye.
In more modern times, David Hubel and Torsten Wiesel were able to explain why occlusion therapy works on a histologic level and subsequently received the Nobel Prize for their work, the first to be awarded for ophthalmic disease.
She pointed out that amblyopia affects many different aspects of visual function, including colour and contrast perception, peripheral vision. Moreover, amblyopic patients have a three times greater likelihood of losing vison in their fellow eye during the course of their life, making the search for new treatments all the more urgent.
Pharmacotherapy with various agents is among the new lines of research in the treatment of amblyopia, Dr Robbins noted. Prominent among the agents under investigation is levodopa, a precursor of the neurotransmitter dopamine, which is found in the brain and the retina. The theory behind its use is that will increase neuroplasticity.
Research where levodopa has been combined with patching has been confined to small studies, yielding
mixed results. On the other hand, some functional MRI studies have shown increased activation of the occipital lobe following levodopa therapy. However, other studies have yielded contradictory results. Moreover, the agents may also have only a temporary effect. And as with any neurotransmitter there are potential concerns regarding long-term side-effects, she said.
Another medication that has been investigated is citicoline, which is an intermediate in the creation of phospholipid cell membranes and which may blunt nerve cell damage. However, like levodopa it has had mixed results when used to augment occlusion therapy. In addition, the studies have only had short term follow-up.
A new approach to occlusion therapy is the use of electronically controlled liquid crystal glasses. Through a shuttering effect they occlude the amblyopic eye at intervals of 30 seconds throughout the day. In a small study they were noninferior to patching at three months follow-up. However, the expected increased compliance with this treatment was only at 50%.
“I can tell you from my own experience that these glasses can be very well accepted even among the children who are most adamantly resistant to patching. I have had cases where other treatments failed miserably and these have done the trick,” Dr Robbins said when measured with temperature monitors.
Perceptual learning is an approach that has been researched for over 40 years. It is designed to induce changes in visual perception through repetitive practice of specific controlled visual tasks. There have been studies involving a small number of patients that have shown an improvement in orientation discrimination stereoacuity and contrast sensitivity. However, the studies lacked long-term follow-up.
Transcranial magnetic stimulation, a technology that is now used in neurology and psychiatry, is also being investigated as a treatment for amblyopia. The magnetic field is applied to the visual cortex, which induces a weak electrical current that stimulates the cortical areas transiently.
A study conducted in Canada showed that adult amblyopic patients undergoing this treatment had improvements in their contrast sensitivity. In another study, conducted in Portugal, the treatment appeared to produce transient improvements in both visual acuity and stereoacuity when applied to the right occipital lobe.
Acupuncture is currently the subject of fairly intensive investigation as a treatment of amblyopia with 14 randomised controlled trials involving over more than 2,000 patients.
“This a well-studied modality and it should not be overlooked,” Dr Robbins said.
Another means of potentially stimulating visual rehabilitation is to place the patient in total darkness for three-to-10 days. The theory is that darkness can biochemically prime the brain for reactivation of synaptic plasticity, thereby encouraging synaptic modifications and promoting visual recovery. Animal studies have shown it to be very effective. However, it would probably be an unattractive option for paediatric amblyopes.
Exercise may be another useful tool in the treatment of amblyopia. In a recent clinical trial out of Italy involving 10 adult amblyopes, interval cycling combined with patching resulted in a mean visual acuity improvement of 0.15 logMAR, and six of the patients also recovered stereopsis.
“We have come a long way since 800AD, but sometimes simple can still be good – patching is still powerful,” Dr Robbins concluded.
Shira L Robbins: srobbins@ucsd.edu
A range of new therapies may offer hope to treatment-resistant amblyopes. Roibeard Ó hÉineacháin reports
Spectacles, patching and atropine have strong evidence as effective treatments for amblyopia, whereas many other treatments must be regarded with a degree of scepticism until they have been studied in rigorous randomised controlled trials asserts Jonathan M. Holmes MD, Professor and Chair of Ophthalmology and Vision Science, University of Arizona-Tucson, USA.
“Clearly, initial pilot studies are very useful to show potential proof of concept, but we need randomised clinical trials so that we don’t all jump on the latest bandwagon and start treating amblyopia without appropriate evidence,” Prof Holmes told the told the 2020 WSPOS Virtual Meeting.
He noted that in many small case series, amblyopic patients appear to improve in response to treatment, but closer scrutiny shows the response was in fact illusory because of poor study design. Often the studies lack controls or are not randomised and suffer from other design flaws.
In uncontrolled case series, observer bias can influence results, simply because the clinicians naturally want their patients to improve and will be inclined to look for evidence confirming that hope. In addition, in many case series, data are influenced by regression to the mean, resulting from test-retest variability. A patient’s visual acuity will vary somewhat from day to day, and they tend to be enrolled into a study when the visual acuity is worse than a specific threshold, i.e. on day when the vision is poor. On a subsequent day their visual acuity may appear to have improved, when, in reality, it is just an artefact of test-retest variability.
Furthermore, a study’s design may fail to take into account such factors as the natural history of the disease; some patients will improve without treatment. Study data may also be influenced by other treatments patients may be simultaneously receiving, he pointed out.
“To avoid the problems of apparent improvement due to natural history and regression to the mean we should have simultaneous controls. To avoid observer bias we should have masked examiners and to avoid the problems of other treatments we should have a defined protocol,” Prof Holmes said.
However, even with controls, allocation bias – consciously or unconsciously choosing patients for the control or treatment group – must also be avoided, he stressed. That can be
achieved with randomisation, which will result in known and unknown confounding factors being equally distributed between treatment and control groups.
“We need to move rapidly from a case series to a randomised clinical trial, with masking of outcome assessment, before we can conclude definitively that a new treatment is effective,” he added.
Trial duration can also influence the interpretation of study results, Prof Holmes said. As an example, he cited a randomised study conducted by the Paediatric Investigator Group (PEDIG) that compared occlusion for at least six hours a day with an atropine eye drop each day in a cohort of amblyopic patients.
The six-month assessment showed similar mean visual acuity gains of 3.16 logMAR lines in the patching group and 2.84 logMAR in the atropine group, concluding that the treatment effect was similar. However, if the trial had only lasted five weeks it would have shown that the patching group had a significantly greater improvement; a mean improvement of 2.22 logMAR lines in the patching group, compared with a mean improvement of 1.37 logMAR lines in the atropine group.
“If we had stopped the trial at five weeks, we would have had an entirely different conclusion, that patching was superior to atropine,” he added.
In order to minimise the potential bias of study duration it is important to have some pilot data on the time course of treatment effect and advocates for each treatment should be involved during the study planning process.
There is strong evidence based on well-designed studies that spectacles alone are a profoundly effective treatment for strabismic, anisometropic and combined amblyopia, Prof Holmes said. He cited a randomised controlled trial, led by Michael Clarke in the UK, comparing no treatment to spectacles alone in amblyopes, with either straight eyes or a microtropia, aged three-to-five years with a visual acuity of 6/9 to 6/36 in their worst eye and 6/6 in their better eye. Masked assessment of best-corrected VA at 54 weeks found modest improvement with no treatment, but mean improvement with spectacles alone was 0.85 logMAR lines greater than those with no treatment. (Clarke et al BMJ 2003;327;1251).
However, “spectacles alone” result in resolution of amblyopia in only around a quarter to a third of patients, and in patients who do not fully respond, part-time patching should be considered as the next step with the strongest evidence, he said. He cited a randomised PEDIG study that compared two hours a day of prescribed patching to patching prescribed six hours a day in children three-to-seven years of age. Masked assessment at four months showed that visual acuity in both groups had improved from a baseline mean value of 20/63 to 20/32. (PEDIG, Arch Ophthalmol 2003;121:603).
Prof Holmes noted that, based on these studies, he now starts his patients with anisometropic, strabismic or combined amblyopia, on spectacles alone. If that does not result in resolution of the condition, he then moves patients on to low-dose patching (two hours/day) or weekend atropine (1%) drops.
Jonathan M. Holmes: JHolmes@eyes.arizona.eduThe best amblyopia treatments are those based on strongest evidence. Roibeard Ó hÉineacháin reports
To avoid the problems of apparent improvement due to natural history and regression to the mean, we should have simultaneous controls
Jonathan M. Holmes MD
Penetrating keratoplasty is extremely challenging in a paediatric patient population, but favourable outcomes may still be obtained with careful case selection, rigorous surgical technique and meticulous postoperative care, according to Nikolas Ziakas MD, PhD.
Speaking at the World Ophthalmology Congress 2020 Virtual, Dr Ziakas, Professor of Ophthalmology at the Aristotle University of Thessaloniki Medical School, Greece, said that a number of factors needed to be considered before embarking on penetrating keratoplasty (PK) surgery in children,
“We need to bear in mind the technical difficulty of the procedure, problems with postoperative care and the likelihood that amblyopia will limit visual rehabilitation. Even if the operation is successful and we have a clear graft and meticulous follow-up care, the reality is that the final visual outcomes are often disappointing in infants,” he said.
Nevertheless, the positive news is that there is often a noticeable postoperative improvement in children’s behaviour, communication and quality of life after PK surgery, even in the presence of cloudy grafts or a measured visual acuity of 20/200 or less, Dr Ziakas added.
The majority of indications for paediatric keratoplasty are congenital, such as Peter’s anomaly, sclerocornea, endothelial dystrophy and congenital glaucoma, with trauma the second single biggest indication.

PK in children requires a different approach than when performed in adult patients, said Dr Ziakas.
“Unique to children is the crucial need for timely optical correction and amblyopia therapy after PK. That is why we need a team approach that includes physicians, parents and optometrists to obtain the best possible outcome,” he said.
Preoperative challenges include dealing with an uncooperative patient, poor visual acuity evaluation and imprecise examination, as well as deciding on the optimal timing for the surgery.
“This is often a balancing act between earlier intervention with the risk of graft failure or rejection and a later intervention with the increased risk of amblyopia,” he said.
Among the multiple intraoperative challenges facing the surgeon in paediatric PK, Dr Ziakas highlighted low scleral rigidity, thinner and more pliable corneas, smaller donor size, smaller anterior segment dimensions, higher posterior vitreous pressure, increased fibrin release and difficult wound closure with the risk of extrusion and suprachoroidal haemorrhage.
Postoperative challenges include the difficulty of conducting routine follow-up examinations, eye rubbing, broken sutures and the risk of infection and wound dehiscence.
“We need constant vigilance and frequent examinations to prevent graft failure,” he said.
Dr Ziakas recommended oversizing the graft by 0.5-to-1.0mm because of the increased elasticity of the infant cornea and sclera, and also using the Price graft-overhost technique to manage positive pressure. This involves suturing the graft across the trephinated host cornea, maintaining a formed anterior chamber.
You’ll gain access to our wide library of videos, including our “Masters in Surgery” archive and also get the chance to collaborate on our global case report quiz.
Surgeons should remain open to the possibility of trying alternative techniques to penetrating keratoplasty for select cases of congenital corneal opacities in paediatric patients, according to Ken Nischal MD, FRCOphth.
“Our goal should not necessarily be to perform a penetrating keratoplasty at all costs. Rather we should focus on the goals of visual rehabilitation and developmental vision, which is more important the younger the child is. We also want to achieve a clear visual axis, which does not necessarily have to be perfectly centred as children can use eccentric fixation very well,” he said at the World Ophthalmology Congress 2020 Virtual.

Dr Nischal, Professor of Ophthalmology at the University of Pittsburgh School of Medicine, noted that the possible alternatives to PK such as iridectomy and selective endothelial removal depend on a number of


factors including the location of the opacity, the state of the endothelium, the social circumstances of the child, the state of the limbal stem cells and the condition of the ocular surface, in particular the lids.
Classifying opacities in terms of primary and secondary corneal disease is a helpful approach in trying to determine the best option for a particular case, he said.
“Indications such as corneal dystrophies, corneal structural deficits due to dermoids and rarer conditions such as CYP1B1 cytopathy tend to do well with transplants, as do iridocorneal adhesions only. However, development anomalies of the anterior segment where the lens fails to form or where the lens fails to separate from the cornea, or where the lens separates but fails to form thereafter, are possible candidates for some of the alternative procedures,” he said.
Dr Nischal cited the example of a paediatric patient with keratolenticular adhesion who obtained a good outcome
without resorting to full-blown keratoplasty.
“The technique I used was enter the capsular bag, evacuate the lens and then cut the stalk of the lens to the cornea without tearing it off the endothelium. I was able to do optic capture on the posterior capsule and increase the area of the pupil. The child achieved a good red reflex in both eyes and developmental vision without the need for a corneal transplant,” he said.
A case report by Jodhbir Mehta et al in Singapore has also shown the use of selective endothelial removal in a patient in which a central opacity was present, and a posterior stroma was missing, said Dr Nischal.
“It was interesting in that the endothelium around the diseased area seemed to grow in once the tissue was removed, and in select cases you actually get clearing of the cornea. It underlines the point that while corneal transplantation is very important, it is not always the only or best option for every case,” he concluded.
Analysis of astigmatism values using double-angle plots is highly informative and easily accessible to cataract surgeons through an online tool, reported Douglas D Koch, MD, at the 2020 ASCRS Virtual Annual Meeting.
“Analysing astigmatism outcomes can be complicated because it involves two variables, power (magnitude) and meridian (axis), and their values cannot be simply added or subtracted. Instead, the analysis requires doubling the angle to convert the data into a true Euclidean vector, performing vector algebra and then halving the angles to return them to standard format that we are accustomed to using,” said Dr Koch, Allen, Mosbacher, and Law Chair in Ophthalmology, Baylor College of Medicine, Houston, TX, USA.
“Single-angle or double-angle plots can be used to display astigmatism data combining both power and meridian. I believe that the double-angle plots are optimal because they are clearer visually and numerically.”
Dr Koch explained that a single-angle plot of astigmatism data is attractive because it resembles phoropters in that eyes having withthe-rule (WTR) astigmatism are oriented vertically and eyes that have against-the-rule (ATR) astigmatism lie to the right or the left.
“With this display, however, it can be harder to know what the data show,” he said.
A single-angle plot is converted into a double-angle plot by doubling the angle for each datapoint. As a result, the datapoints for all WTR eyes are grouped together on the left of the double-angle plot, and the datapoints for all ATR eyes are clustered to the right.
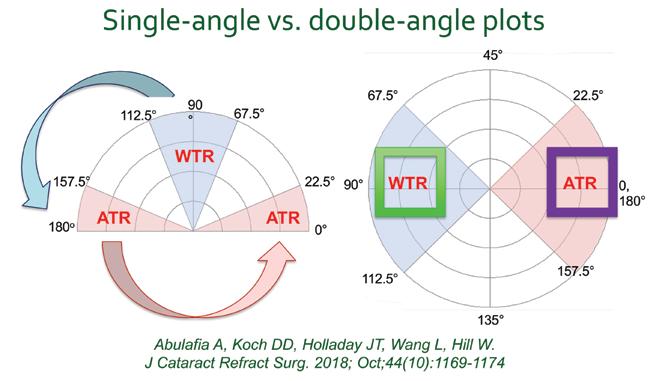
Dr Koch and colleagues reviewed the advantages of displaying astigmatism data using double-angle plots in a guest editorial that was published in the October 2018 issue of the Journal of Cataract and Refractive Surgery (JCRS). The article also proposes simple terminology to use for astigmatism analysis in toric IOL surgery and describes a set of figures, including various double-angle plots, that best display astigmatic outcomes of toric IOL surgery. In addition, the journal article introduces a downloadable Excel spreadsheet that allows surgeons to generate the latter figures using their personal data. The spreadsheet is available on the JCRS, ESCRS, and ASCRS websites.
The figures for depicting toric IOL surgery outcomes include a cumulative histogram of the magnitude of the preoperative corneal astigmatism and postoperative refractive astigmatism data that shows the percentages of eyes falling within different dioptric ranges before and after surgery. Vector analysis is presented on double-angle plots that include text and graphical information on the data means and spread.
The centroid in each plot represents the vectoral centre of the data, with its standard deviation. The data spread is appreciated graphically with an ellipse that surrounds 95% of the values in the dataset, and statistical analysis can readily be performed on these data, Dr Koch explained.
The third type of figure generated from the spreadsheet is a double-angle plot of the postoperative refractive astigmatism prediction error for eyes in the dataset. This outcome provides insight into the accuracy of toric IOL calculation formulas.
Dr Koch illustrated the latter point by comparing a figure created from a set of eyes having toric IOL power calculations done using anterior keratometry (K) data alone versus with the Abulafia-Koch formula that takes into account posterior corneal astigmatism. The
This illustrates what occurs in double-angle plots. The with-the-rule eyes are grouped on the left, and the against-the-rule eyes, which are split apart in single-angle plots, now are grouped together to the right, allowing appropriate display of centroids and confidence ellipses
centroid values for the two datasets were 0.55D @ 180° ±0.47D and 0.05D @ 174°±0.44D, respectively, showing superiority of the method that incorporates posterior corneal astigmatism. Its benefit was also seen clearly on the double-angle plots.
“On the plot for the calculations done using anterior K only, the centroid is located to the right of the vertical meridian, indicating an ATR prediction error,” Dr Koch said. “In contrast, the centroid for the prediction error using the Abulafia-Koch formula is almost at the 0 point, which indicates there is no particular bias in the results for WTR astigmatism, ATR astigmatism, or along any oblique meridian.”
Although the online tool facilitates analysis of toric IOL surgery outcomes, hopefully the task will become even easier in the future with introduction of a method that will automatically populate data into the spreadsheet.
“Currently, the data need to be input manually, but I am looking forward to the development of a system that will allow for electronic data entry,” Dr Koch said.
He noted that he is currently using both the IOLMaster 700 (Carl Zeiss Meditec) and Lenstar LS 900 (Haag-Streit) for measuring keratometry and is analysing the data from each device separately.
“I find that results are excellent with both of these devices. However, I would remind surgeons that different devices can give different measurements, and any one device can give an erroneous measurement in a given patient. Therefore, it is important to use more than one device for measuring the cornea, or, if only one device is available, consider getting two sets of measurements with that device,” Dr Koch said.
Douglas D Koch: dkoch@bcm.edu
Reference:
Abulafia A, Koch DD, Holladay JT, Wang L, Hill W. Pursuing perfection in IOL calculations. IV. Rethinking astigmatism analysis for intraocular lens-based surgery: Suggested Terminology, analysis, and standards for outcome reports. J Cataract Refract Surg. 2018; Oct;44(10):1169-1174
Use of double-angle plots for displaying astigmatism data permits optimal understanding. Cheryl Guttman Krader reportsCourtesy of Douglas D Koch, MD
As clinical studies and basic research that were put on hold around the world begin to resume, researchers are finding something of a silver lining in the COVID-19 cloud. Reduced clinic hours allowed many to finish analysing, writing, editing and submitting studies, papers and letters, resulting in a marked increase in literature volume. The need to use internet platforms to communicate during lockdowns has also resulted in unexpected opportunities for new collaboration.
From March through early May, submissions to the Journal of Cataract and Refractive Surgery increased by about 40%, said Editor Thomas Kohnen MD, PhD, of Goethe University, Frankfurt, Germany.


“I personally was very productive, too.”
With his surgery schedule down to three or four cases daily from 10-to-15, Dr Kohnen estimates he completed 10-to-15 studies and letters to the editor over the period and had time to develop new ideas.
“It was like a little COVID sabbatical for three months.”
As the pandemic took hold in March and April, every ongoing clinical study at Goethe was shut down for eight weeks, Dr Kohnen said. Elective cataract surgeries were cancelled as well, leaving only emergencies such as corneal perforations, retinal detachments and acute glaucoma, with a few patients receiving regular doses of anti-VEGF.
With COVID-19 cases stabilising in the German state of Hessen, and protocols in place to prevent infection, Goethe University began reopening in early May, Dr Kohnen said. Patient volume has since built toward normal, and with it, clinical research has resumed, with all postponed studies restarted.
However, effects of the pandemic are being felt, Dr Kohnen added. “Patient recruitment is slower; some may not come because they are afraid they can get the virus.” A few patients also may be lost to follow-up for this reason.
Study protocols were disrupted in some cases as well. For example, three-month follow-up was missed for some patients in a study for FDA approval of an IOL for presbyopia. “Because of the COVID, we saw them at 100 days instead of 90 days,” Dr Kohnen said. These deviations will be reported, and adjustments made. Sponsors and regulators are supportive of the effort.
Overall, the impact on research was minor, Dr Kohnen said. “It was just a hole for eight weeks,” he said.
Both basic research and clinical studies were shut down at the S Fyodorov Eye Microsurgery State Institution based in Moscow, Russia, said Boris Malyugin MD, PhD. Overall, the system has about 35 studies in progress at the Moscow clinic with three-tofive studies at each of the 10 locations around Russia.
As the clinics reopened, bench studies resumed as researchers returned to work. Clinical studies are beginning to resume as patient volume grows – though as of early July it had reached about 35% of previous capacity with full capacity unlikely to be reached until year’s end, Dr Malyugin added.
The lockdown and restrictions on travel for older persons both resulted in disruptions to several ongoing trials, causing missed follow-up appointments. Even in an ongoing anti-VEGF study that was continued, protocol deviations occurred, and some patients may have to be excluded from the study analysis because of it, Dr Malyugin said.
However, the study sponsors are well aware of the problem and are extending study timelines to accommodate the need for additional patient recruitment. Because inclusion criteria are so tight, recruitment will also be slower due to reduced patient volume, Dr Malyugin said.
“It is more or less good news for us. However, the development of some drugs and other products will be delayed.”
Dr Malyugin also found his time off from clinic productive.
“It was a good time to sit at home and work reading and writing papers and editing papers. It was a productive time away from actual research.”
It also created an opportunity to collaborate with colleagues all over the world using internet platforms, Dr Malyugin added. “We discussed ways to be more effective under the epidemic circumstances and did some nice brainstorming.”
The result was several articles on coping with the pandemic for publication, including two in the EuroTimes COVID-19 e-newsletter.
“It will change collaborative research. We are seeing a surge in communication among doctors on different internet platforms in a way we have never seen before.
Still, the pandemic is taking its toll. Dr Malyugin said it has not affected him or his family directly but noted that a lot of colleagues have been affected.
“We even had some casualties in the ophthalmic community and that is very sad to mention,” he said.
shutdown had some unexpected benefits including more research articles submitted. Howard Larkin reports
It is more or less good news for us. However, the development of some drugs and other products will be delayed
Boris Malyugin MD, PhD
Patient recruitment is slower; some may not come because they are afraid they can get the virus
Thomas Kohnen MD, PhD
Unilateral implantation of the IC-8 (Acufocus) small-aperture IOL seems to be a safe and effective option for providing spectacle independence in cataract patients who have undergone previous laser vision correction, reports Josh Cuthbertson MB ChB, University Hospital Ayr, Ayr, Scotland UK.
Speaking at the 24th ESCRS Winter Meeting in Marrakech, Morocco, Dr Cuthbertson presented the results of a prospective interventional case series in which 11 cataract patients with a history of corneal laser refractive surgery underwent implantation of the IC-8 small aperture lens. The mean uncorrected visual acuity at six months follow-up in the eye with the implant was 0.01 logMAR for distance, -0.16 logMAR for intermediate and N5 (0.2 logMAR) for near vision. Some 90% of patients achieved spectacle independence. In addition, there were no intraoperative or postoperative complications.
He noted that all patients in the study underwent optical biometry, Placido-based topography and dual Scheimpflug tomography (GALILEI). The ASCRS post-refractive surgery online calculator was used for IOL power calculation and aimed for a mild myopia of -0.75D. The mean absolute error (MAE) was 0.7D.
The IC-8 lens is based on the same pinhole lens optical principle as the Kamra (Acufocus) corneal inlay and is designed to provide an increased depth of focus compared to a standard spherical IOL. Initial studies and case reports relating to corneal pinhole inlays for the correction of presbyopia in patients with previous LASIK are promising. However, studies investigating unilateral small aperture IOL implantation in LASIK-treated eyes for treatment are limited, Dr Cuthbertson said.

“Unilateral implantation of a small aperture IOL in eyes with prior laser vision correction is safe and will achieve spectacle independence postoperatively in most patients. Aiming for a mild myopia in the non-dominant eye enhances the uncorrected intermediate and near vision without compromising on the distance visual acuity,” he added.
In the discussion that followed Dr Cuthbertson’s presentation, session co-chair Béatrice Cochener-Lamard MD, PhD, asked what implant the fellow eye should receive.
In reply, Dr Cuthbertson’s co-author Sathish Srinivasan FRCSEd, FRCOphth, FACS, also at University Hospital Ayr, noted that similar results to those of the present study have been achieved with bilateral implantation of the IC-8 small aperture lens.
Josh
Cuthbertson: cuthbertsonjosh@gmail.com
IOL data from all over the world collected by leading cataract surgeons is the foundation for the Hill-RBF. This big data is analyzed by pattern recognition based on artificial intelligence leading to highly accurate IOL predictions and providing confidence thanks to a unique reliability check.
Hill-RBF 3.0 is based on an enlarged dataset, particularly for long and short eyes, leading to more reliable predictions in extreme cases (i.e. less out of bounds calculations). For even more refined outcomes, it optionally considers additional patient parameters: lens thickness, white-to-white distance, central corneal thickness and gender.
www.haag-streit.com
Josh
A library of symposia, interviews, video discussions, supplements, articles and presentations









Spotlight on:
Toric IOLs and Presbyopia



Glaucoma
Ocular Surface Disease
Corneal Therapeutics

















forum.escrs.org
Decompressing the anterior chamber at this point, by letting some of the OVD come out, Angela

Trifocal intraocular lenses (IOLs) are a good choice for many cataract patients because they provide good vision at far, intermediate and near distances. However, a good tear film and ocular surface, careful biometry and accurate toric alignment are critical for preserving vision quality, said Matteo Piovella MD, of Monza – Milan, Italy, at the 2020 ASCRS Virtual Annual Meeting.
Dr Piovella stressed that getting toric lenses properly aligned is essential to preserve the integrity of the image transmitted to the retina. To ensure proper axis alignment, he uses the microscope mounted Callisto marker-less digital system and the IOLMaster 700 TK (Carl Zeiss Meditec), which measures both the anterior and posterior corneal surfaces. This combination is the best for avoiding alignment errors due to cyclotorsion, he said, noting that it is not possible to do this manually.
Accurately measuring the corneal surface and other biometric parameters requires a stable corneal tear film, Dr Piovella emphasised. To ensure functional Meibomian glands and tear film quality, he provides BlephEx (BlephEx) to remove debris on the lid margin and LipiFlow (Johnson & Johnson Vision) thermal treatment to liquify and remove impacted lipid build-up in the Meibomian glands to all patients receiving multifocal IOLs.
Dr Piovella has used the AT Lisa Trifocal since it became available in 2012. He noted that early bifocal IOLs lacked intermediate vision needed for computers, mobile phones and tablet devices. For this reason, trifocal lenses have largely replaced bifocals in countries where they are available.

Dr Piovella’s experience bears out the promise of trifocal technology. He reported on 491 eyes in 269 patients implanted with the AT Lisa Trifocal followed for a mean of five years. Of these, 222 had bilateral implants, with 77 both trifocal IOLs, 108 both trifocal toric IOLs and 37 with one of each.
In the entire bilateral implant group, 95% reached a spherical equivalent within 0.5D of target, with 80% reaching it in both eyes. In the bilateral trifocal group, 94% had one eye within 0.5D and 84% had both eyes, while the bilateral toric group had 96% and 83% respectively. Sphere equivalent and uncorrected distance visual acuity remained excellent and stable for five years.
Overall, just 2% of patients reported using spectacles sometimes for near vision. Dr Piovella had them implanted in his own eyes in 2014.
Matteo Piovella: piovella@piovella.com
“For many years I have worked on optimising a lens for
I collaborated with Rayner on bringing this
Stable tear film, and accurate biometry and toric alignment improve outcomes. Howard Larkin reports
Accurately measuring the corneal surface and other biometric parameters requires a stable corneal tear film
• ESCRS Research Study Portals (ESCRS-funded research projects)
• ESCRS Podcasts
• EyeJC (The ESCRS Journal Club)
• Case Studies
• EBO – ESCRS Examination
• ESCRS Media Player
• ESCRS On Demand
• ESCRS iLearn
• Astigmatism Double Angle Plot Tool and more...
Apaired multifocal intraocular lens combination, with one lens favouring near vision and the other intermediate, intended to binocularly complement each other across a wide range of focal distances while achieving the intended goal of continuous vision, demonstrated little difference between the lenses at intermediate vision. Sheraz Daya MD said at the 2020 ASCRS Virtual Annual Meeting.
In a prospective study designed to test the patented “continuous phase” technology and the complementarity of the Artis Symbiose (Cristalens) lens system, Dr Daya implanted the intermediate, or Mid, lens into the dominant eye and the near, or Plus, lens into the non-dominant eye of 50 patients. The continuous phase technology is designed to smooth the defocus curve of diffractive lenses by correcting for phase inversions that can blur images.
All lenses were implanted through a 1.8mm scleral incision using a Victus (Bausch + Lomb) femtosecond laser. Astigmatism greater than 0.75D or more was managed with limbal-relaxing incisions, said Dr Daya, of the Centre for Sight, London, UK.
At six weeks after surgery, monocular and binocular defocus were evaluated along with contrast sensitivity. In Mid eyes, 92% were within 0.5D of target and 94% within 1.00D. In Plus eyes, 91% were within 0.5D and 98% within 1.00D. Two percent lost two lines due to cystoid macular oedema in bilaterally and this recovered with resolution. Forty-five percent of Plus eyes and 21% of mid eyes gained one or more lines vision. Predictability was good in both cohorts, Dr Daya reported. Uncorrected distance vision was good in both eyes, and better with both eyes open. The Plus lens performed better visually at near and intermediate range, with 52% v 45% at 20/20 near monocularly, and 62% v 57% 20/20 at intermediate. For contrast sensitivity, the Mid performed slightly better at most frequencies, Dr Daya said. However, this might be a result of better neuroadaptation due to implanting the Mid lens in the dominant eye.
In 14 patients able to participate, defocus curves showed slightly better vision at all distances for the Plus lens. The defocus curves of both lenses were stable with no dips. No patient complained about reduced intermediate vision, though two complained of lack of near vision with the Mid lens. Patients adapted rapidly to the lenses, Dr Daya said.
“Performance of both Mid and Plus lenses was good, there was no comparable loss of intermediate between the Mid and Plus lenses. There is no clear evidence the lenses complement each other and perhaps patients will do better with Plus lenses in both eyes. We have now commenced a study of bilateral Plus lenses and shall compare outcomes to this cohort,” Dr Daya concluded.
Sheraz Daya: sdaya@CentreforSight.com
Full and continuous depth of focus achieved with complementary lens system. Howard Larkin reports
We have now commenced a study of bilateral Plus lenses and shall compare outcomes to this cohort
Sheraz Daya MDTHOMAS KOHNEN European Editor of JCRS


VOL: 46 ISSUE: 9 MONTH: SEPTEMBER 2020
AEROSOL AND PHACO SAFETY
There is surprisingly little data on aerosols generated during phacoemulsification cataract surgery. Researchers in the UK have performed an ex vivo study looking at the size and number of particles generated by phacoemulsification. Using a TROTEC PC200 optical particle counter, they measured particles generated during continuous power mode: 80% longitudinal setting, 100% torsional setting, and 80% longitudinal setting. The study found no aerosol generation of particles ≤10μm during phacoemulsification for any of the three settings evaluated. The copious use of hydroxypropyl methylcellulose did not have an effect on aerosol generation. They conclude that phacoemulsification does not appear to be a small-particle aerosol-generating procedure. However, they note further in vivo and ex vivo studies using different aerosol counting methods are needed. H Lee et al., JCRS, “Aerosol generation through phacoemulsification”, Vol. 46, #9, 1290-96.

IOL calculation in patients who have previously undergone LAISK continues to challenge cataract surgeons. Newer formulas have improved visual results, but outcomes are often inferior compared with untreated eyes. German researchers evaluated IOL calculation formulas provided by the ASCRS online tool for an extended depth-of-focus (EDOF) IOL after previous myopic LASIK. The retrospective study included 25 eyes, all of which received the Tecnis Symfony IOL during femtosecond laser-assisted cataract surgery. Formulas evaluated included Shammas, Haigis-L, average, Barrett True-K, modified Masket, Barrett No History and Masket. Of these, the Shammas and Haigis-L formulas had the most eyes within ±0.5D of target refraction with 52% and 48% respectively.
C Lwowski et al., JCRS, “Prediction accuracy of IOL calculation formulas using the ASCRS online calculator for a diffractive extended depth-of-focus IOL after myopic laser in situ keratomileusis”, Vol. 46, #9, 1240-6.

Anterior segment OCT can help define posterior opacity-capsular morphology preoperatively, which should help to reduce complications associated with posterior polar cataracts, report researchers. A team in New Delhi used the newer-generation AS-OCT, CASIA-2 (Tomey Corp.) system to evaluate 101 eyes diagnosed with posterior polar cataracts. They observed that deficient capsular morphology in posterior polar cataracts is likely to show different patterns depending on the type and extent of capsule loss with opacity localisation. They report that specific capsular morphologies could be categorised into conical, moth-eaten and ectatic types. They suggest that these findings could result in better case management. A Pujari et al., JCRS, “Study 1: Evaluation of the signs of deficient posterior capsule in posterior polar cataracts using anterior segment optical coherence tomography”, Vol. 46, #9, 1260-65.
JCRS is the official journal of ESCRS and ASCRS








Small-Incision Lenticule Extraction with accelerated corneal cross-linking (SMILE® Xtra) is a viable option for refractive correction in eyes at moderate risk for ectasia after corneal refractive surgery, according to a study presented by Sung Min Kim MD at the 2020 ASCRS Virtual Annual Meeting.


The investigation included 130 eyes of 65 patients operated on at the NUNEMISO Eye Centre, Seoul, Republic of Korea. All eyes had a cumulative score of 3 on the Randleman Ectasia Risk Score System and completed two years of follow-up. Eyes with keratoconus or that were keratoconus suspects were excluded.
The treatment protocol involved application of 0.25% riboflavin solution with a 90-second soak time followed by 60 seconds of UVA irradiation 30 mW/cm2 (total energy 1.8 J/cm2).
Compared with a group of eyes that underwent SMILE at the same centre, the SMILE Xtra cohort had poorer UCVA on the first postoperative day (mean decimal, 0.80 vs. 0.94). However, visual outcomes were similar in the two groups from one week to two years, and safety outcomes were comparable as well.
“Our study shows that the safety and predictability of SMILE are not affected by combined cross-linking and indicates that SMILE Xtra may be an effective and safe strategy for refractive surgery in moderaterisk patients,” said Dr Kim.
Preoperatively, the 130 eyes treated with SMILE Xtra had a mean sphere of -6.22D, mean cylinder of -1.59D and mean SEQ of -7.01D. At two years, 97.7% of eyes were within ±0.5D error range of SEQ. Other two-year SMILE Xtra results showed mean UCVA was 1.08 (vs 1.12 for SMILE), and the efficacy index was 1.13 (vs 1.16 for SMILE Xtra). At two years after SMILE Xtra, BCVA was the same or improved in 99.2% of eyes and decreased by one line in 0.8% of eyes. The safety index was 1.16 and endothelial cell count had not changed significantly from baseline.
Outcomes of SMILE Xtra were also analysed for four subgroups representing eyes with abnormal topography (n=36), low residual bed thickness (<300 microns; n=44), high refractive error (spherical equivalent >-9.5D or lenticule thickness >130µm; n=21) and thin preoperative central corneal thickness (<510µm; n=29).
There were no statistically significant differences between the subgroups in visual recovery or refractive change over two years, although there was a tendency towards poorer outcomes in the eyes with high refractive error. Endothelial cell count was also stable after SMILE Xtra in all subgroups.
Sung Min Kim: pkim82@naver.com
SMILE with CXL safe, effective and predictable for eyes at risk of ectasia.
Cheryl Guttman Krader reports
Our study shows that the safety and predictability of SMILE are not affected by combined crosslinking
Sung Min Kim MD

Poor hygienic practices like showering and sleeping while wearing contact lenses can increase the risk of microbial keratitis by up to seven-fold, according to a study led by Professor Parwez Hossain PhD, FRCOphth, FRCS (Ed), FHEA, recently published online in the in the British Medical Journal-Ophthalmology.
The case-control study involved 37 contact lens wearers with microbial keratitis and 41 control contact lens wearers without infection attending University Hospital Southampton Eye Casualty between October 2015 and December 2015. Participants underwent face-to-face interviews to identify lens wear practices, including lens type, hours of wear, personal hygiene and sleeping and showering in lenses.

This is the first study of its kind to identify and grade the different personal hygiene practices, using face-to-face interviews with a validated approach on contact lens wearers who present to hospital and have clinically proven contact lens infection, Dr Hossain told EuroTimes.
In a univariate analysis, the greatest risk factor the study’s authors identified was showering in contact lenses (p=0.03), with showering daily in lenses compared with never, increasing the risk of microbial keratitis by over seven times (p=0.002). Other risk factors included sleeping in lenses (p=0.026), and being aged 25-to-39 years (p=0.010) and 40-to-54 years (p=0.056).
Showering while wearing contact lenses has the potential to introduce pathogens like acanthamoeba into the contact lens-cornea interface, the authors said. Sleeping while wearing contact lenses can impair oxygen diffusion on the corneal surface. Studies have shown that corneal hypoxia when a contact lens is present can lead to increased binding of pseudomonas bacteria, the most common cause of microbial keratitis.
Non-compliance with annual after-care appointments did not appear to be a risk factor for microbial keratitis. Compliance in attending annual follow-up appointments was high among both the case group (83.7%) and the control group (78%). However, nearly half of both the case group and the control group said they had not been informed or were not sure if they had been informed of the risks of infections when first prescribed contact lenses.
The study’s authors noted that despite advances in contact lens technology, the incidence of contact lens microbial keratitis has remained consistent at around four per 10, 000 daily contact lens wearers per annum. Previous research suggest that two-thirds of complications observed in contact lens wearers are attributable to poor hygiene practices.
“Focusing attention on improving education of infection and

retention of information may help improve compliance with lens wear practices, which may help reduce incidence of CLMK and associated sight loss,” they concluded.

The full article is available at http://bmjophth.bmj.com/cgi/ content/full/bmjophth-2020-000476.
Parwez Hossain: P.N.Hossain@soton.ac.uk
Showering and sleeping while wearing contact lenses are the most important risk factors for microbial keratitis. Roibeard Ó hÉineacháin reports
Focusing attention on improving education of infection and retention of information may help improve compliance with lens wear practices

Using a 3D-capable digital ophthalmic microscope (Artevo 800, Carl Zeiss Meditec) offers a number of advantages for ocular surgery including improved visualisation, flexibility, comfort and workflow benefits, according to Natarajan. S., MD, FRCS (Glasgow), DSc, FICO, FELAS, FAICO (Retina Vitreous).
“There was no steep learning curve in adapting to this new device in the OR. It was very comfortable to use with no strain on the eyes and with a very relaxed head and neck posture for the surgeon. To avoid back problems, I advise ophthalmic surgeons to do regular exercise for back and neck. It gives excellent views of the various tissue layers and renders high-resolution images with natural colours,” Dr Natarajan said at the World Ophthalmology Congress 2020 Virtual.
Explaining the principal features of the Artevo 800 system, Dr Natarajan, Aditya Jyot Eye Hospital, Mumbai, India, said that it produces a stereoscopic 3D image that is viewed using passive polarised glasses on a 55-inch 4K monitor. The monitor can be positioned anywhere in the operating room, providing the surgeon with a comfortable position and the rest of the operating team with a clear view of the ocular anatomy.
The device transmits 25% percent more light than conventional optics so surgery can be performed at a reduced light intensity, exposing least light to retina.
“It delivers very crisp resolution with improved visualisation of the surgical field. The depth of focus enables a smooth
transition to different stages of the surgery without the need to refocus the microscope. It’s all automatic and the lag in transmission is much less than what we used to experience with previous 3D systems. The contrast and colour of tissue are unaltered from the real image which is very useful benefit during surgery,” he said. The experience of using ARTEVO 800 is watching all the retinal structures in a big screen, which enhances depth perception and helps to differentiate various planes like ILM, ERM, etc.
The ARTEVO 800 incorporates a hybrid mode in which the surgeon can use the oculars while the OR staff can continue to use the 3D screen, so that the operating room layout need not be altered for every surgeon, said Dr Natarajan.
“The ARTEVO offers a lot of
advantages. For cataract surgery, the depth of the trench is notable and posterior capsule tension and wrinkling can be seen very well. For vitreoretinal surgery, the best view is obtained by combining with chandelier illumination. There is clear distinction of membranes when dissecting and better visualisation of stained vitreous,” he said.

The digital microscope can also overlay data such as preoperative biometry, phaco vitrectomy values, patient information, surgical tracking and intraoperative OCT in real time without blocking the surgical field.
Dr Natarajan added that the combined features of the ARTEVO 800 make it very useful for teaching residents and fellows in the OR room.
Natarajan. S: prof.drsn@gmail.com
The 38th Congress of the ESCRS was a congress like no other congress, in a year like no other year.
Over three days, the ESCRS convened virtually on a digital platform that allowed delegates who were prevented from travelling to Amsterdam for a live congress to enjoy a first-class educational programme.
In his address to delegates at the Opening Ceremony of the Congress, the society’s President Rudy MMA Nuijts reflected that delegates should have been in Amsterdam enjoying scientific contributions from all over the world at the RAI congress centre, exchanging ideas and enjoying social interaction.

“However,” he said, “in March the ESCRS took the difficult decision to move to a hybrid virtual meeting, with speakers and moderators presenting live in Amsterdam to an online audience. Unfortunately, with the number of COVID cases rising rapidly again in many countries, we took another difficult decision to convert to a fully virtual format,” he said.
“Certainly, this is not the ESCRS Congress we have become accustomed to, but many of the elements that always make this meeting so special still remain.”
On the final day of the Congress, in his closing remarks to delegates, the Dr Nuijts paid tribute to all the participants that had made the virtual event such a resounding success.
“The ESCRS is only as strong as the world class speakers and audience that we attract, and this strength was on display in every session these past few days,” he said.
Dr Nuijts said that a huge amount of effort had gone into organising the virtual congress and he hoped that all the delegates had found it a worthwhile experience.
“We hope that you have enjoyed your time and will take the knowledge you have gained over the past few days back to your hospitals and clinics to ultimately benefit your patients,” he said.
Dr Nuijts expressed gratitude to the many industry partners who had supported the move to a virtual platform and to all the speakers, moderators and chairpersons who provided the backbone of the scientific programme.
Dr Nuijts reminded delegates that all the main sessions, presentations and posters of the past weekend would be available on the online platform for viewing until the end of the year.
“You can log in any time and review everything you might have missed the
first time around or watch any session again that you found particularly enjoyable,” he said.
Dr Nuijts ended by expressing his fervent wish that next year’s Congress will be able to return to the usual format of an in-person event.
“We will meet again next year and this time hopefully in person. Although this meeting was, I think, a tremendous success as a virtual meeting, this can never replace the charm of a physical meeting. So please stay safe, stay healthy, and thank you very much for your support,” he concluded.
The ESCRS is only as strong as the world class speakers and audience that we attract, and this strength was on display in every session these past few days
Rudy MMA Nuijts MD, PhD
first ESCRS Virtual Congress, the 38th Congress of the ESCRS, was broadcast from Friday 2 October to Sunday 4 October 2020
The scientific programme of the 38th Congress of the ESCRS was centred on four rooms streaming sessions across a wide range of topics with lively discussion interspersed throughout the programme.
At the Opening Ceremony, the President of the ESCRS, Prof Rudy MMA Nuijts, welcomed delegates to the Congress before he invited David F. Chang, USA, to deliver the Ridley Medal Lecture.
“I have long felt that our single greatest challenge in ocular surgery was not the invention of an accommodating IOL but rather the rapidly increasing backlog of cataract blindness in the developing world, which accounts for half of all global blindness,” said Dr Chang.
Dr Chang’s lecture focused on the Aravind Eye Care System in southern India, which has grown into the largest eye care provider in the world.
Reflecting on his own association with Aravind, which dates back to 2003, Dr Chang, Clinical Professor at the University of California, San Francisco, said that there are many lessons to be learnt from the Aravind model of providing large-volume, high-quality and affordable care through its network of 13 eye hospitals and 75 primary eye care facilities.
Aravind’s unique assembly-line approach, with rates often exceeding 14-to16 cases per hour per surgeon, increases productivity but without compromising on safety or quality, said Dr Chang. Every patient receives the same high-quality care and service, regardless of their economic status, he said.
“When I first saw this, I marvelled at how well choreographed it all was. Around 40% of private paying patients subsidise eye care for the other 60%, who receive services either free of cost or at a steeply subsidised rate, yet the organisation remains financially self-sustainable. The message is that we can use this type of cost-recovery model
to reduce and eventually eliminate global cataract blindness,” said Dr Chang.

On the opening day of the programme delegates also heard a presentation from Prof Marcel Levi MD, Chief Executive of University College London. Hospitals, UK, on “Tackling the COVID-19 crisis: professionals in the lead”.
Prof Levi noted that there was massive redeployment of medical staff during the first wave of the pandemic in many countries, to deal with patients who contracted the virus and to protect other patients and staff, which proved very challenging for many healthcare workers.
“We are now extremely subspecialised. We know very well how to do our jobs but it is very difficult to do someone else’s job,” he said, adding that in older patients presenting with many comorbidities this is a real challenge.
One of the highlights of the second day of the programme was the Clinical Research Symposium on “Artificial Intelligence”.
Béatrice Cochener-Lamard MD, PhD, outlined the development of AI in ophthalmology and the role of deep learning to assist in diagnosis, citing its successful use in diabetic retinopathy.
Looking at the latest developments, she said we are now well on the road to automatic image classification and that the use of AI will become a widespread tool in all imaging modalities (2D and 3D and beyond). Thanks to the creation of more refined algorithms, the use of ‘big data’ is not
always necessary now and there are “multiple additional applications” that are on the way. These include using AI as an integrated part of “screening, diagnosis, decision support and maybe even surgical help”.
“So, the future looks very exciting to help ophthalmologists for sure, but never to replace us,” Prof CochenerLamard concluded.
The ESCRS and EURETINA held a combined online symposium entitled “Cataract Surgery in Patients with AMD”, chaired by Nic Reus MD, PhD, and Carel Hoyng MD.
The symposium covered crucial topics intended to help the surgeon’s decisionmaking process before, during and after cataract surgery in patients with agerelated macular degeneration (AMD).
Dr Hoyng opened the symposium with an overview of the differential diagnosis of AMD. His presentation zoomed in on five important macular diseases that can closely mimic AMD. These monogenetic diseases, such as late-onset Stargardt disease and pattern dystrophy, might represent up to 10% of cases diagnosed as AMD.
“You should suspect a retinal dystrophy in patients with an early age of onset, a positive family history, marked lesion symmetry and foveal sparing,” said Dr Hoyng.
In the Main Symposium “What To Do When The Unexpected Happens”, delegates were told that “Expect The Unexpected” should be the guiding mantra of every cataract surgeon who presumes that each procedure will inevitably proceed in a smooth and controlled manner.
“The only surgeon who doesn’t encounter complications is one who doesn’t operate at all. The overall message is not to panic when things go wrong and to realise that there are possible solutions,” said David Spalton, MD, FRCS.
Despite all the advances in technology and surgical techniques, post-cataract surgery visual issues persist in some

...the rapidly increasing backlog of cataract blindness in the developing world, accounts for half of all global blindness
David F. Chang
We are now extremely subspecialised. We know very well how to do our jobs but it is very difficult to do someone else’s job
Prof Marcel Levi MD
patients and must be dealt with honestly and practically while continuously striving to improve outcomes.

This was the key message for delegates watching the “20/20 in 2020: The Lens” Main Symposium.
Scott MacRae MD highlighted the success of early studies on novel femtosecond laser-induced refractive index change for IOL touch-ups, which, he explained, is biocompatible, relatively non-invasive and can treat refractive error, presbyopia and high-order aberrations.
“We are very, very excited about this technology and look forward to presenting more information in the future,” said Dr MacRae.
The highlight of Sunday’s programme was the 2020 ESCRS Heritage Lecture delivered by Theo Seiler MD, PhD.
In his talk, Prof Seiler discussed the overlap between LVC and cataract surgery and the difficulty of obtaining consistently predictable refractive outcomes now that the first-generation of LVC patients has reached cataract age.
The early history of laser vision correction (LVC) was a far cry from the high-tech technological precision that refractive surgeons today take for granted, said Prof Seiler.
“The first PRK surgeries that I performed were quite rudimentary by modern standards. The eye tracking and the IOL centration were performed using only my hands and my eyes so you can imagine that safety suffered accordingly,” he said.
Turning to modern cataract surgery, Prof Seiler noted that while significant improvements have been achieved in IOL power calculations due to advances in optical biometry, there is still considerable inaccuracy when it comes to keratometry measurements for post-LVC eyes.
“Studies have shown that despite better preoperative diagnostics that the chance of postoperative refractive surprise is still greater than 20%,” he said.
Another highlight on Sunday was the Young Ophthalmologists Programme. When performing cataract surgery “capsulorhexis should be continuous, curvilinear and it should overlap the optic 360 degrees,” said Nic Reus MD, Netherlands, at the “Starting Phaco” session “This is to reduce incidence of PCO [posterior capsule opacification] and to get a stable lens inside the bag, which is helpful for refraction,” he said.
To ensure a continuous curvilinear capsulorhexis, he said, the surgeon should make a mental note of the size of the circle they want to make, and follow that imaginary line.
During his practical presentation, Dr Reus demonstrated the three different incisions that can be used; single-plane corneal incision, biplanar, and three-step scleral incision.
When entering the anterior chamber, the most stable incisions are square (not too short and not too long), he said.
Regarding hydrodissection, Dr Reus advised looking out for both the anterior wave and the posterior wave.
In his address to delegates at the Opening Ceremony, the President of the ESCRS Professor Rudy MMA Nuijts had stressed the importance of the virtual social programme for delegates.
On Friday night October 2, Lucas & Steve, Europe’s most uplifting DJs, played an exclusive gig for ESCRS 2020 delegates.
The duo hail from Maastricht, home of Prof Nuijts. Tapping into the rich history of dance music in the Netherlands, Lucas & Steve explored glorious melodies and emotive sounds in their music,
On the Saturday night, there was another musical treat for delegates when the world-famous Royal Concertgebouw Orchestra played a special concert featuring the music of the renowned American composer George Gershwin.
The orchestra was founded in 1888 and on the occasion of its 100th anniversary in 1988, the orchestra officially received the appellation ‘Royal’ from Her Majesty the Queen, Beatrix Of the Netherlands.

The orchestra is based in Amsterdam, and has been acclaimed as one of the very best orchestras in the world, as ESCRS delegates will have discovered.
And so, the ESCRS Congress is over for another year. As Prof Nuijts said in his closing remarks:
“We will meet again next year and this time hopefully in person. Although this meeting was, I think, a tremendous success as a virtual meeting, this can never replace the charm of a physical meeting. So please stay safe, stay healthy, and thank you very much for your support,” he said.
So, the future looks very exciting to help ophthalmologists for sure, but never to replace us Béatrice Cochener-Lamard MD, PhD
The first PRK surgeries that I performed were quite rudimentary by modern standards. The eye tracking and the IOL centration were performed using only my hands and my eyes...
Theo Seiler MD, PhD



The only surgeon who doesn’t encounter complications is one who doesn’t operate at all
All
Bruce Allan MD, at a dedicated Clinical Research Symposium on Artificial Intelligence


Chop techniques provide significant advantages in terms of reduction of phaco power and time and result in less strain on the zonula

machine learning data studies require the same thing; high-quality label data, usually collected for routine clinical practiceFilomena Ribeiro MD giving an expert overview of phacoemulsification during the Young Ophthalmologists Starting Phaco session
There is an increased demand in the presbyopia age group for IOL procedures and there is improved staff satisfaction because of improved efficiencies in the patient journey and processes, so not everything about COVID has been negativeArthur Cummings MD, discussing the impact of COVID 19 on his private practice in at the Wellington Eye Clinic, Dublin, Ireland
Our results suggest a role for PACK-CXL as an alternative to antimicrobials as primary treatment for infectious corneal infiltrates and early corneal ulcersEmilio Torres-Netto MD, winner of the award for Best Poster – Refractive, at the 38th Congress of the ESCRS
Many of us are feeling additional stress from change in, or lack of, routine and overall uncertainty around COVID-19. Jotting down my thoughts regularly during this time has helped me to clear my mind and stay groundedJennifer Kim MD, winner of the 2020 John Henahan Prize, the ESCRS writing competition for Young Ophthalmologists
Recent advances in transplantation techniques and tissue engineering have greatly improved outcomes in limbal stem cell deficiency (LSCD) and other indications requiring ocular surface reconstruction, according to Harminder Dua CBE, MD, PhD.

“A lot of progress has been in recent years in the surgical management of these challenging cases. Our goal is to save the eye, regenerate the ocular surface and restore sight and we have a variety of techniques now available to us to help us achieve that,” he said at the World Ophthalmology Congress Virtual 2020.
Reviewing the options for ocular surface reconstruction in LSCD, Prof Dua, Professor of Ophthalmology and Visual Sciences, at the University of Nottingham, United Kingdom, said it was important first of all to establish an accurate diagnosis and then treat accordingly.
“There are several steps to consider. It is vital to determine whether the inflammation is active or not. We need to establish corneal and conjunctival involvement with fluorescein staining and slit lamp examination, impression cytology and in vivo confocal microscopy (IVCM). We need to know if the disease is limited or progressive. We then need to evaluate the extent of stem cell deficiency; is it partial or total, unilateral or bilateral and is the visual axis involved or not,” he said.
Prof Dua said that the final consideration is to look at every other structure of the eye taking account of eyelids, tear function, cataract, fundus and IOP – and consider their potential to impact on any surgical procedure related to ocular surface reconstruction.
“We really need to ensure there is nothing that needs to be treated first in order to obtain the best possible outcomes from our reconstructive procedure and to establish the visual potential of the eye. The key message is that we should only operate when all inflammation is controlled,” he said.
For partial limbal stem cell deficiency, with conjunctivalised, metaplastic epithelium on the cornea where the visual axis is not involved, Dr Dua said non-intervention might be the wisest approach for such cases.
“However, if the visual axis is involved then the first minor
procedure, I would recommend is sequential sectoral conjunctival epitheliectomy (SSCE),” he said.
He explained that SSCE is a procedure designed to prevent conjunctival epithelial cells migrating on to the corneal surface as this can compromise the healing process of the corneal epithelium and negatively affect vision and corneal transparency. To illustrate the point, he discussed the case of a patient with severe chemical burn.
“In this patient the upper part of the limbus and conjunctiva have survived the chemical burn. As healing progresses the conjunctiva is approaching close to the limbus. If this is allowed to cross on to the limbus, we will get an admixture of corneal and conjunctival epithelium on the cornea and this is not desirable. We therefore scrape that conjunctival epithelium away and it may need to be done more than once to allow the entire corneal surface to heal from limbus-derived epithelium,” he said.
For cases of total limbal stem cell deficiency there are several viable surgical options, said Prof Dua.
“We can either do in vivo expansion techniques such as auto limbal transplant, Simple limbal epithelial transplant (SLET) or an allo limbal transplant for bilateral cases either from a cadaver donor or a living relative or friend. We can also perform ex vivo expansion techniques with limbal, conjunctival, or buccal mucosal cells on amniotic membrane or fibrin, collagen or other substances,” he said.
Although SSCE has proven effective at preventing admixture of corneal and conjunctival epithelium, the technique is onerous in that the patients need to be seen every day or every other day to monitor the spread of conjunctival epithelial cells and perform scraping if necessary, said Prof Dua. Bleeding can also occur, and it can be painful.
To try to overcome these issues, Prof Dua introduced an alternative procedure – amnion-assisted conjunctival epithelial redirection (ACER).
“With ACER, we perform a 360-degree peritomy and we take away all of the fibrovascular pannus. We then take two explants from the other eye and suture them top and bottom. If the substrate is not healthy, we can put a small amniotic membrane graft inside. The key step is to put a large amniotic membrane graft outside covering all the affected area such that the edge of the amniotic membrane goes underneath the edge of the conjunctiva. This forces conjunctival epithelial cells to grow on the amniotic membrane,” he said.
In a recent study of 26 patients undergoing limbal stem cell transplantation with either ACER or SCCE, the former technique was found to reduce multiple patient visits, bleeding and pain compared to those treated with SSCE.
Prof Dua noted that allografts, whether from a cadaver or a living donor, require long-term systemic immunosuppression.
“The outcomes are best for auto limbal grafts and worst for cadaver transplants, with living relative grafts being somewhere in between,” he concluded.
Harminder Dua: profdua@gmail.com
Our goal is to save the eye, regenerate the ocular surface and restore sight and we have a variety of techniques now available to us to help us achieve that
Harminder Dua CBE, MD, PhD
Although the pathogenesis of dry eye disease (DED) is multifactorial, with some aspects still not fully understood, ongoing research into the role that inflammation plays in the development and propagation of DED is opening compelling new avenues for the treatment of this complex disorder, according to Marc Labetoulle MD, PhD.
Speaking at the World Ophthalmology Congress 2020 Virtual, Prof Labetoulle, Hôpital Bicêtre, Paris, France, said that recent progress on the pathophysiology of DED has led to greater appreciation of the central role that inflammation plays in DED and its consequences for the eye.

“There are many consequences of ocular surface inflammation, including the loss of neuronal network in the cornea and infiltration of the lachrymal glands. It also participates in the induction / exacerbation of Meibomian gland disease (MGD) and triggers apoptosis of goblet cells. This inflammatory cascade can lead to aqueous deficient dry eye (ADDE) disease and/or evaporative dry eye (EDE) disease due to either lipidic or mucin instability,” he said.
The most obvious clinical consequence and direct marker of inflammation is epithelial damage on the cornea, noted Prof Labetoulle.
“This is what we have to assess in our everyday clinical practice. Assessing the epithelial damage is mandatory for the follow-up of patients and the efficacy of any anti-inflammatory treatment,” he said.
Corneal fluorescein staining (CFS), which is easy to perform, inexpensive, reproducible and which correlates with visual acuity and disease severity, is one of the most commonly used diagnostic tests for assessing the health of the cornea and DED, said Prof Labetoulle. Disease severity is typically assessed based on the Oxford classification, with a score greater than 3 (out of 5) indicating severe DED.
There is currently no single gold standard biomarker to diagnose and detect ocular surface inflammation, but ophthalmologists can already use different approaches, said Prof Labetoulle.
“In an ideal world, biomarkers could be our allies to defeat inflammation,
not only by permitting us to detect the inflammatory process but also enabling us to determine the scale of severity and to confirm the effectiveness of treatments, when to stop drug use, and to check the absence of relapse after their withdrawal,” he said.
Such biomarkers could ideally also help in the recognition of the pathogenic mechanisms underlying the inflammation, added Prof Labetoulle.
“They could help in distinguishing between ADDE and EDE or a combination of both, or to see if there is an associated allergy or other potential conditions that may participate in dry eye disease,” he said.
The most commonly used biomarker in clinical research is osmolarity, said Prof Labetoulle.
“Following on from the International Dry Eye Workshop (DEWS) reports, we know that hyperosmolarity can be both a cause and a consequence of DED,” he said.
The most frequently used machine to test osmolarity is TearLab (TearLab Corp.), which analyses tear fluid samples in a single test.
“The advantages are that the procedure is painless and quickly performed with less than two minutes for complete results. The quantitative results can be explained to patients and it has been shown that osmolarity provides a good combination of specificity and sensitivity when comparing patients against controls,” he said.
On the downside, Prof Labetoulle said that the reproducibility is not ideal and decreases in relation to ocular surface dryness.
“We typically need several measurements to increase reliability, it is quite expensive to use and, according to some studies, correlation with subjective and objective response to treatment is poor,” he said.
There are other specific devices to measure osmolarity such as the i-Pen
(I-Med Pharma), said Prof Labetoulle, with complementary studies are needed to know if this device is comparable to TearLab.
Matrix metalloproteinase 9 (MMP-9) testing can also be used in clinical practice for assessing the inflammatory component when facing ocular surface dryness, said Prof Labetoulle.
“The test is fast, simple and painless with a positive/negative result, easy to communicate to the patient, and there is no real quantification. A study by Messmer in Ophthalmology 2016 showed that there is a correlation between MMP-9 positive test and subjective symptoms (as assessed by ocular surface disease index, OSDI), tear break-up time, Schirmer test results, conjunctival and corneal staining and number of obstructed Meibomian ducts and pathologic Meibomian gland secretion,” he said.
Other more technical options to assess DED include impression cytology for histological staining, noted Prof Labetoulle.
“The density in goblet cells is another good marker of chronic inflammation. It is also possible to look at the presence of inflammatory cells and it has been shown recently that in vivo confocal microscopy can give similar results. Conjunctival imprints can also be used to make a flow cytometric analysis of inflammatory markers in conjunctival epithelial cells of patients with dry eyes,” he said.
In the future, tear and serum biomarkers will probably play a greater role in the diagnosis and management of DED, concluded Prof Labetoulle.
“We are seeing a lot of interesting research in this area. The final step will probably be the use of microfluidic multipurpose machines, which will allow us to test multiple biomarkers from a very small sample of tears or serum,” he concluded.
Marc Labetoulle: marc.labetoulle@aphp.frIn an ideal world, biomarkers could be our allies to defeat inflammation, not only by permitting us to detect the inflammatory process but also enabling us to determine the scale of severity...
Marc Labetoulle MD, PhD
Eyes implanted with any type of phakic intraocular lenses (IOLs) require follow-up visits to monitor for possible damage to the corneal endothelium, said Roberto Bellucci MD, FEBOS-CR, Verona, Italy.

“Endothelial damage was demonstrated early in the history of phakic IOLs, but the reasons for the damage is still debated,” he told the 34th Winter meeting of the ESCRS in Marrakech, Morocco.
Dr Bellucci noted that corneal endothelial cell loss has been the reason for the withdrawal from the market of all angle-supported phakic IOLs. The Baikoff lens had on average a surgically induced endothelial cell loss of 3%, followed by an annual cell loss of 1-2%. That compares to a normal physiological loss of 0.6% cells per year in adults.

Still worse endothelial damage occurred with the foldable Icare anterior chamber phakic IOL lens, which induced 7-14% annual endothelial cell loss. More recently, Alcon withdrew the Cachet anterior chamber phakic IOL because of abnormally high endothelial cell loss in a small number of patients.
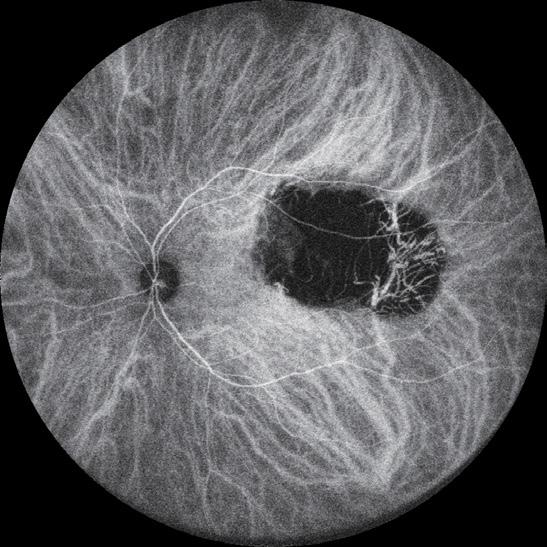
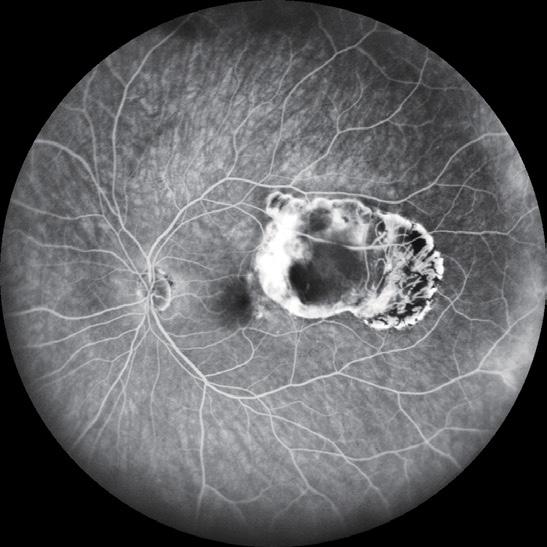
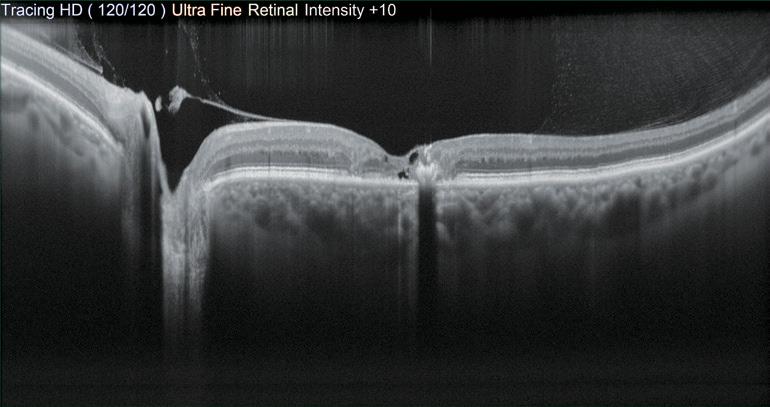
The iris-fixated and posterior chamber phakic IOLs can also induce endothelial cell loss. In the case of iris-fixated IOLs, the reported annual endothelial cell loss has ranged from 0.6-2%, with generally somewhat worse results with the Artiflex than with the Artisan lens. The reported annual endothelial cell loss following implantation ICL and iPCL posterior chamber phakic IOLs ranges from 1% to 1.5%.
Research shows a correlation between postoperative endothelial cell loss and proximity of phakic IOLs to the endothelium. A study conducted in 2010 showed that in eyes where the distance between the lens to the endothelium was 1.2mm the annual rate of cell loss was 1.7% That compared to 0.2% annual loss when the distance was 1.66mm.


There is also a growing body of evidence suggesting that aqueous humour stream is impaired by phakic IOLs, especially during non-REM sleep, depriving in the endothelium of glucose.
Several papers from Spain and from other countries have been published on this topic. These models might explain why the largest AC IOL – the Icare from France – proved to be the worst as for corneal endothelium preservation.

The AAO currently recommends that phakic IOLs should be explanted when there is 25% cell loss after three years. Research suggests that 1-to-3% of eyes with the Artisan/ Verisyse lens implanted and 3% of eyes with the Artiflex fit into this category.

In eyes where the cornea is no longer transparent, endothelial grafts are necessary. Although good results can be achieved leaving the phakic lens in place, Dr Bellucci said that he prefers to remove the lens and perform a triple procedure with crystalline lens extraction and IOL implantation.
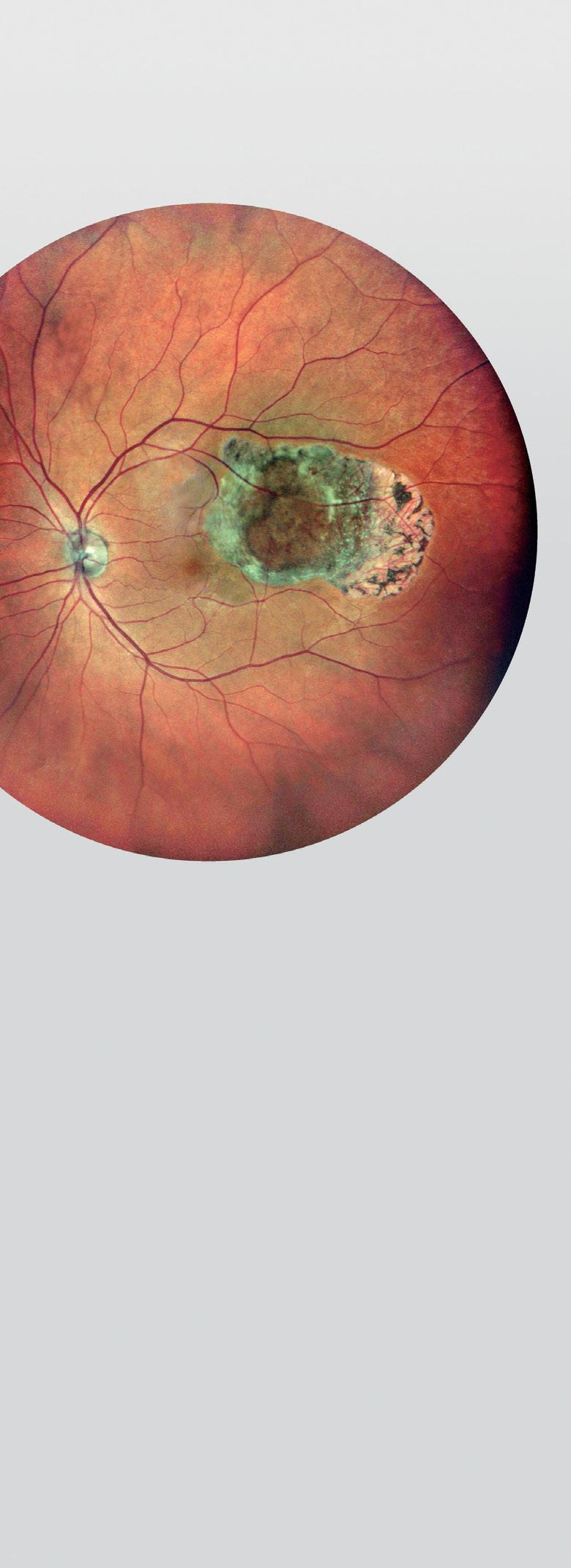
All phakic IOLs increase corneal endothelial cell loss. Roibeard Ó hÉineacháin reports
The aim of the project is to build a common assessment methodology and establish an EU web-based registry and network for academics, health professionals and authorities to assess and verify the safety quality and efficacy of corneal transplantation.
Clinicians now have multiple options at their disposal in the treatment of dry eye disease (DED), including topical over-the-counter medications and a growing range of devices that target Meibomian gland dysfunction, according to Jose M. Benitez-del-Castillo MD, PhD.
“We have more treatment options for DED than ever before and there are many more in the pipeline. However, the success of any treatment depends on the correct diagnosis and appreciation of the underlying aetiology,” Dr Benitez-del-Castillo said at the World Ophthalmology Congress 2020 Virtual.
In a broad overview of current treatments for DED, Dr Benitez-del-Castillo, Professor and Chairman of Ophthalmology at Hospital Clinico San Carlos and Clínica Rementería, Madrid, Spain, said it was important to appreciate dry eye in the context of the revised TFO Dews II definition.
“We need to understand dry eye as a multifactorial disease of the ocular surface characterised by a loss of homeostasis of the tear film and accompanied by ocular symptoms in which tear film instability and hyperosmolarity, ocular surface inflammation and damage and neurosensory abnormalities play aetiological roles,” he said.
Over the counter (OTC) artificial tears have traditionally been the first line of treatment for dry eye syndrome and dry eye‐related conditions, and more are coming on the market every year, said Dr Benitez-del-Castillo.
the ECCTR Registry
www.ecctr.org
ECCTR is a project funded by the ESCRS with initial support from the EU
“We tend to use treatments today combining different viscosity-enhancing agents such as hyaluronic acid (HA), carboxymethyl cellulose (CMC), hydroxypropyl-guar (HP-guar) and trehalose for optimal effect,” he said.
A wide range of biological tear substitutes are now available, said Dr Benitez-del-Castillo, including autologous serum, adult allogenic serum, umbilical cord serum, platelet preparations, mucolytic agents and TRPV1 receptor antagonists.
Tear preservation strategies to treat DED may include punctal plugs, surgical punctal occlusion and moisture chamber spectacles and humidifiers.
Other options include secretagogues, in oral or topical formulations, designed to stimulate aqueous and/or mucin secretion, and nasal neurostimulation, which aims to induce normal tear production via stimulation of the nasolacrimal reflex, he said.
Fostering good lid hygiene and treating lid abnormalities where appropriate is a key part of DED management in many patients, noted Dr Benitez-del-Castillo.
As well as specific treatments for Demodex mite lid infestation, a wide range of warming/massage devices are now available to try to regulate and improve Meibomian gland function, including LipiFlow (Johnson & Johnson Vision), iLux (Alcon), IPL (Lumenis) and others, he said.
Dietary modifications as part of a holistic approach to DED may also be helpful, and it is important to consider patient education encompassing environmental, health, lifestyle and psychological factors that may all play a role in managing the condition, he concluded.
Jose M. Benitez-del-Castillo: benitezcastillo@gmail.comWide range of treatment options in ever-changing dry eye treatment landscape. Dermot McGrath reports
Descemet’s membrane endothelial keratoplasty (DMEK) appears to offer the best option today for long-term graft survival for the management of endothelial dysfunction, but remains a challenging procedure, Donald Tan FRCS told delegates in his EuCornea Medal Lecture delivered at the 11th EuCornea Congress.

In a wide-ranging lecture, Dr Tan spoke about the paradigm shift in corneal transplantation techniques in recent years away from penetrating keratoplasty (PK) towards lamellar and endothelial keratoplasty approaches.
“Over the last 10-to-15 years we have seen a trend away from PK towards selective lamellar transplantation, where we do not replace the whole cornea in one stage, using techniques such as deep anterior lamellar keratoplasty (DALK), Descemet stripping automated endothelial keratoplasty (DSAEK) and DMEK. The main reason why we are transplanting less tissue is that physiologically there are less complications and reduced rejection rates with these lamellar approaches compared to PK,” he said.
National and international corneal transplant registries are useful in determining the real-world success rates of different techniques, said Dr Tan. For instance, data from the Australian Corneal Graft Registry showed that DMEK fared worse compared to PK in terms of graft survival.
“This might have something to do with the learning curve. The data showed that surgeons who performed more than 100 transplants got better results in terms of graft survival,” he said. Similar findings were also reported by studies based on the United Kingdom Transplant Registry.
“I think these unexpected results from the major registries show that selective lamellar keratoplasty results vary a lot. In the best-case scenario of a singlecase series with an experienced surgeon who has mastered the technique, EK has major advantages over PK. However, in the real world the results may not be as good and there are many possible reasons for this including the learning curve with lamellar keratoplasty, variable surgical techniques and patient selection, among others,” he said.
The Singapore Corneal Transplant Registry (SCTR) provides prospective
tracking on more than 5,000 transplants performed since 1991 and covers about 85% of all transplants in Singapore, said Dr Tan. Unlike other registries, the SCTR unified surgical protocols for each lamellar keratoplasty procedure with ongoing training of corneal surgeons to adopt new techniques and protocols and included a constant review of surgical results and long-term registry data.
“The upshot is that similar PK, DALK and DSEK, clinical protocols have evolved over time for our Asian phenotype. When we look at the graft survival rate out to 10 years both endothelial keratoplasty and anterior lamellar keratoplasty have significantly better graft survival compared to PK,” said Dr Tan.
Based on the SCTR, a recent study of patients who underwent DMEK, DSAEK and PK for Fuchs’ endothelial corneal dystrophy (FECD) and bullous keratopathy (BK), showed that for both conditions, PK showed poorer fiveyear graft survival compared to EK. Interestingly, while DSAEK and DMEK showed very similar good five-year outcomes for FECD, for BK cases, DMEK was found to be superior to DSAEK.
The complications profile was also better in DMEK compared to DSAEK and PK, with less graft rejection and less risk of elevated IOP, said Dr Tan.
“The rate of secondary glaucoma was around 23% for both PK and DSAEK compared to 11% for DMEK. With less rejection for DMEK we were able to halve the amount of topical steroids being administered,” he said.
However, despite its advantages DMEK remains challenging surgery and not all cases of endothelial dysfunction are created equally, said Dr Tan.
“For instance, pseudophakic bullous keratopathy with co-morbidities such as peripheral anterior synechiae, dilated or distorted pupils, unstable IOLs,
glaucoma blebs or tubes, open capsules or vitreous and abnormal anterior chambers make DMEK a much more challenging procedure,” he said.
To overcome some of these issues, Dr Tan said he has modified his DMEK technique over time to enhance surgical control and improve outcomes.
One such adaptation is the ‘pullthrough endo-in’ DMEK technique, which involves the use of specialised forceps to hold on to a donor graft that has been precoiled endothelium-in, and pulling it into the anterior chamber for enhanced control and less risk of tissue eversion. The evolution of this technique involves redevelopment of the EndoGlide inserter device (Network Medical Products) originally designed for DSAEK, into a new model for DMEK, the DMEK EndoGlide device – in this approach, the DMEK graft is trifolded endothelium-in, into a narrower cartridge that enters a 2.6mm incision, and is pulled into the AC using EndoGlide forceps.
This approach enables better control of the donor tissue and results in reduced endothelial cell loss, enabling more complex cases to be treated using DMEK, he said.
The latest innovation is to restore and reconstruct the anterior chamber, by performing synechiolysis of abnormal iris and scar tissue, and replacing the abnormal iris with the Humanoptics CustomFlex Artificial Iris.
“This all helps to restore a stable anterior chamber environment, essentially clearing the decks for DMEK to be performed more easily. With better surgical control, we can now perform more complex cases where anterior segment and chamber abnormalities may make conventional DMEK a real challenge,” he concluded.
Donald Tan: donald.tan.t.h@ singhealth.com.sg
The data showed that surgeons who performed more than 100 transplants got better results in terms of graft survival
Donald Tan FRCS
The past decade has seen an acceleration in the discovery of new disease genes and pathogenetic mechanisms underlying inherited retinal dystrophies (IRDs), thereby paving the way to a new era of targeted gene therapy to treat these degenerative diseases, according to Birgit Lorenz MD, PhD, FEBO, FARVO.
“IRDs are a large and heterogeneous group of neurodegenerative disorders that are associated with progressive visual dysfunction and are caused by mutations in any one of more than 220 different genes with a lot of genotypic and phenotypic variability. The last decade has seen a rapid increase in identifying genes enabled by next-generation sequencing (NGS) technology. At the same time, we have learned a lot about the pathophysiology of the retina as most of the genes are involved in formation, maintenance and functioning of the photoreceptors, both rods and cones,” said Prof Lorenz speaking at the World Ophthalmology Congress 2020 Virtual.
IRDs can be classified based on aetiology and describing pathophysiology: localised versus generalised disease, autosomal dominant or autosomal recessive, isolated or syndromic, rod versus cone loss, regional or longitudinal, she said.
“It is important to remember that the distribution of cones and rods are different throughout the retina and this distribution also influences the phenotype that we see. We therefore have to measure not only cone function for visual acuity but also rod function by dark adapted visual field and other specific tests,” she said.
Diagnostic tools for IRDs include imaging modalities such as fundus photography, fundus autofluorescence imaging (FAF) and optical coherence tomography (OCT).
Electrophysiology is also commonly used for diagnostics in conjunction with psychophysical testing for visual acuity, contrast sensitivity, kinetic and static perimetry, colour vision, and full-field stimulus threshold. In more advanced degenerative stages of IRDs ERG is often below detection level.
The fact that IRDs are highly heterogeneous with inter-individual variability makes them particularly challenging to diagnose and treat, noted Prof Lorenz.
“There is a need for more natural history studies of rare inherited retinal
degenerations to understand more about disease and stage specific inter-ocular differences. While long-term prospective longitudinal studies are required, we usually have only retrospective crosssectional data available. Furthermore, the value of short-term prospective studies often used by companies nowadays is questionable in slow, progressive diseases such as most IRDs,” she said.
Reviewing the progress of gene-based therapies in recent years, Prof Lorenz said that a major breakthrough was achieved in 2017 with the first-ever FDA approval of a gene therapy, Luxturna (Spark Therapeutics), for individuals with an inherited retinal disease due to mutations in both copies of the RPE65 gene.
Luxturna uses an adeno-associated virus vehicle to deliver normal copies of the RPE65 gene directly to the retinal pigment epithelial cells underlying the neuroretina via a subretinal injection.
The phase III trial that led to its approval showed significant improvements in navigation in dim light, full-field light sensitivity threshold, and visual field in the treated group, said Prof Lorenz.
“It was the results of the multiple luminance mobility testing (MLMT) that convinced the FDA and European authorities EMA to finally approve Luxturna as a gene therapy. However, we have got to remember that at least one paper has elaborated on the fact that the human retinal gene therapy for Leber congenital amaurosis shows advancing retinal degeneration despite enduring visual improvement. So we have to really collect more data to determine when and if gene therapy can actually prevent progression of
retinal degeneration,” she said.
The picture for choroideremia gene therapy is more mixed, with initial trials showing only modest improvements in visual acuity in a minority of patients.
“One of the challenges with choroideremia is that we are treating the fovea and injecting into the subretinal space with all the complexities that entails. There is debate about the preservation of the retina after the therapy with conflicting data: some groups say that there is continuous degeneration similar to the untreated eye while others claim there is better preservation in the treated eye,” she said.
Other clinical trials are also under way for Stargardt’s disease, achromatopsia, Usher syndrome and X-linked retinitis pigmentosa due to mutations in the RPGR gene.
Going forward, Prof Lorenz stressed the importance of obtaining objective, measurable data to show real clinical benefit from any gene therapy treatment.
“We are dealing with progressive disorders, with all that entails in terms of documenting natural course and treatment effect. We have new read-out parameters that are not all recognised at the moment by the health authorities, which have to be shown to be patient relevant. One of the critical questions right now is how early should we treat for optimal benefit. While early treatment in principle appears to be an advantage, there are specific surgical challenges especially for subretinal application at a very young age, so we need more data to improve our therapeutic strategies,” she said.
Birgit Lorenz: birgit.lorenz@ augen.med.uni-giessen.deGene therapy offers transformative potential to greatly reduce treatment burden and potentially improve patient outcomes with a single intravitreal injection in patients with age-related macular degeneration, according to Szilard Kiss MD.
“The future is bright for intraocular gene therapy especially after the efficacy that was noted with voretigene neparvovec-rzyl (Luxturna, Spark Therapeutics) resulting in FDA approval of the first ocular gene therapy in the United States for patients with inherited retinal disease due to mutations in the RPE65 gene. There is every reason to hope that similar success may be obtained with gene therapy for non-inherited ocular disorders such as wet AMD, diabetic retinopathy (DR), diabetic macular oedema (DME) and retinal vein occlusion (RVO),” Dr Kiss said at the World Ophthalmology Congress 2020 Virtual.
In a broad overview of the progress made to date in gene therapy for non-inherited retinal diseases (IRD), Dr Kiss, Director of Clinical Research and Associate Professor at Weill Cornell Medical College, New York, said that initial trials of therapies such as RGX-314 (RegenexBio) and ADVM022 (Adverum) have shown promise for the treatment of exudative AMD.
RGX-314, which uses an adeno-associated virus serotype 8 (AAV8) as a vector, contains a gene encoding for a monoclonal antibody fragment that binds to and neutralises VEGF. It is administered as a one-off subretinal injection in the operating room, said Dr Kiss.
In the phase I/IIa trial, 42 wet AMD patients in five different dosing cohorts received a subretinal injection of RGX-314.
“The mean age was around 80 and patients received an average of nine anti-VEGF injections a year, so these are heavily treated macular degeneration patients. RGX was shown to be well tolerated in all dosing cohorts, with most adverse events rated mild in severity,” he said.
The best-corrected visual acuity remained stable and mean central retinal thickness improved over the course of the follow-up for patients in the fourth and fifth dose cohort. Five (42%) patients were injection-free over the follow-up in the fourth cohort, while nine of the patients (75%) remained injection-free in the fifth cohort.
Positive data also emerged from the OPTIC phase 1 doseranging study of ADVM-022, which aims to treat neovascular AMD by delivering long-term expression of therapeutic levels of anti-VEGF aflibercept protein. ADVM-022 is delivered via an in-office intravitreal injection similar to what is being done with the current anti-VEGF treatment regimens.
ADVM-022 was found to be safe and well tolerated and showed consistent and sustained anatomic improvements in OCT and stable to improved best-corrected visual acuity, noted Dr Kiss. No rescue injections were required an any of the first cohort patients, with one patient out past 84 weeks of followup. Some cases of intraocular inflammation associated with ADVM-022 were successfully controlled with topical steroids.
Going forward, Dr Kiss said that dry AMD, for which no treatment is currently available, may also be amendable to gene therapy, with a number of promising therapeutic agents currently undergoing clinical trials.
The patient-reported outcome is linked to clinical data in EUREQUO. This enables better knowledge of indications for surgery and o ers a tool for clinical improvement work based on the patients’ outcome.
Gene therapy as a drug delivery platform for non-inherited retinal issues. Dermot McGrath reports
Anovel minimally invasive conjunctival surgical (MICS) technique may provide a safe, efficient and effective approach to the problem of leaking blebs after trabeculectomy surgery in glaucoma patients, according to Neeru Gupta MD, PhD, MBA.

“I have found this new approach extremely useful in my own practice. The outcomes have been very good, all of the leaks using this MICS approach were sealed almost immediately and patients were able to return to their regular activities very soon after surgery,” she said at the World Ophthalmology Congress 2020 Virtual.
Dr Gupta, professor and Dorothy Pitts Chair at the University of Toronto, Canada, explained that leaking filtration blebs are a common complication of trabeculectomy that can occur days, months or years after the initial surgery.
“A leaking bleb can lead to devastating problems such as blebitis and endophthalmitis. With a bleb leak there is also a reduction in IOP, leading to significant structural changes with shallowing of the anterior chamber, fluid build-up through the choroidals and the risk of hypotony maculopathy,” she said.
A wide variety of different approaches have been employed to try to manage bleb leaks after trabeculectomy surgery, said Dr Gupta.
“Conservative treatment is usually first-line treatment with antibiotics, reducing the frequency of topical steroids, or administering an aqueous suppressant. We can use a pressure patch to try to seal the leak. Other treatments such as bandage contact lens, collagen shields or cyanoacrylate tissue glue, which can lead to foreign body sensation and can be difficult to apply, have also been tried with limited success,” she said.
Other strategies to deal with a leaking bleb include argon or Nd:Yag laser treatment to try to seal the leak, or autologous blood patch injection into the bleb to stimulate fibrosis and promote scarring and healing.
Microsurgical techniques have also been tried with varying degrees of success, said Dr Gupta.
These approaches include re-suturing of the bleb for early postoperative period leaks, with excision of the bleb and conjunctival advancement followed by creation of a conjunctival pedicle flap that is sutured to the area and is typically used in cases of late-onset leakage. Other microsurgical techniques that have been tried include fascia lata grafts, corneal patch grafts, amniotic membrane, conjunctival graft, scleral patch graft and buccal mucosa transplant.

“All of these various techniques have had limited success, which explains why we continued to search for a more effective solution to the problem of a leaking bleb,” she said.
Dr Gupta’s solution was to come up with a minimally invasive conjunctival surgical procedure without tissue incision or excision which she said has proven very effective in patients with late-onset bleb leaks.
After injection of topical anaesthesia, a lid speculum is inserted to bring the superior avascular leaking bleb into view. The eye is then rotated downward to expose the superior bulbar conjunctiva behind the bleb and injected with subconjunctival lidocaine 2% with epinephrine. The superior bulbar conjunctiva behind the bleb is injected to balloon the conjunctival tissue which is then advanced over the thin bleb toward the limbus and
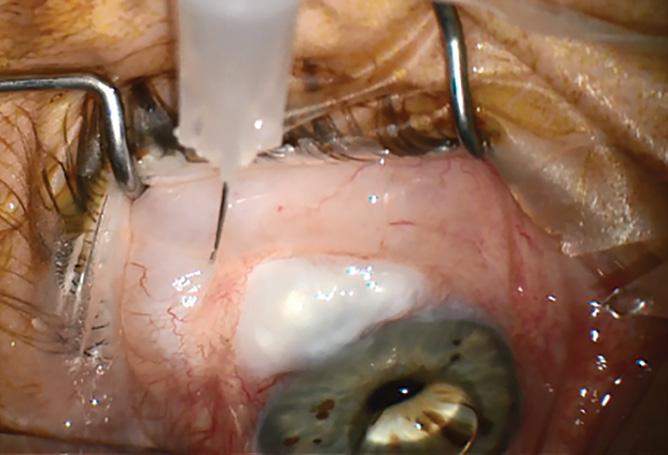
Conservative treatment is usually first-line treatment with antibiotics...
Neeru Gupta MD, PhD, MBASubconjunctival anesthetic is injected behind the leaking bleb to balloon conjunctival tissue to the outer edge of the bleb
sutured in place. The procedure is repeated in order to cover the entire area of the leak, with two-to-four sutures typically used to cover the leaking bleb.
Once the procedure has been completed, the conjunctival integrity and IOP are re-assessed at the slit lamp to check for bleb leak and prednisolone and antibiotics are administered for approximately one week, she said.

Dr Gupta has published her results in 14 eyes of 13 patients, 12 of whom had open-angle glaucoma and one iridocorneal endothelial syndrome (Am J Ophthalmol. 2019;207 https://www. ajo.com/article/S0002-9394(19)30213-2/fulltext). The mean age of presentation was 70.2 years (± 14.8 years), and all patients had a history of mitomycin use at the time of glaucoma surgery. The onset of bleb leak following trabeculectomy ranged from seven months to 16.3 years. In all cases, the initially repaired filtering blebs remained functional at last follow-up, and no additional medications were required.
“The outcomes of this technique have been very good in this consecutive series of patients with all of the leaks sealed tight away and patients being able to return to their regular activities without any problem,” she said.
Dr Gupta said that the MICS procedure is particularly suited to dealing with classic focal avascular bleb close to the limbus that requires little tissue coverage from the conjunctiva above. However, it is not a viable option in patients with severe conjunctival scarring or in whom conjunctival mobilisation is impractical.
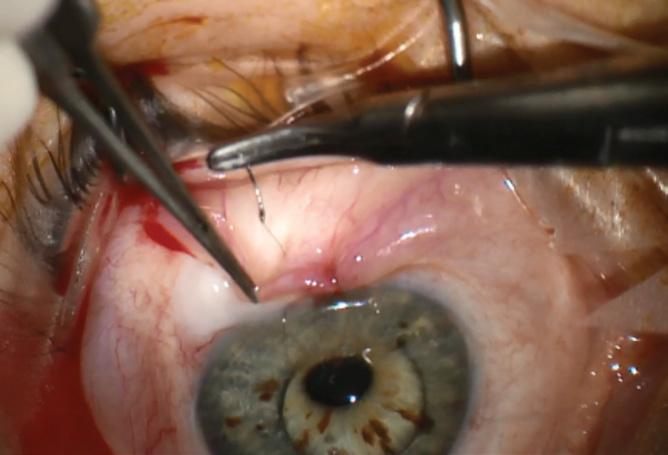
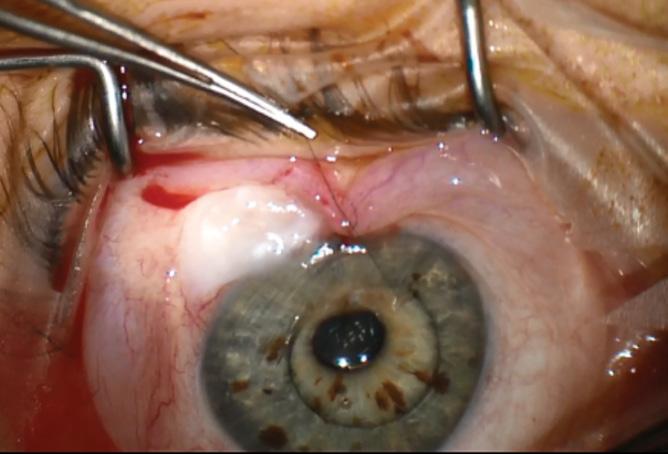
Summing up, Dr Gupta said that the MICS approach offers a relatively simple, economical and effective option for treating lateonset leaking blebs without cutting or excising conjunctival tissue.
“It is incision free with a good success rate. It is relatively simple, inexpensive and efficient and can be performed in a minor OR room, and the patient is able to resume their normal activities with minimal inconvenience,” she said.

Although topical prostaglandins remain the first-line medical treatment of choice for glaucoma with proven safety and efficacy over many years, there remains a compelling unmet need for effective alternatives that have a longer duration of action and address issues of adherence, according to Paul Rafuse MD, PhD.
“In the near future we are going to have to start with new routes of administration of known compounds which do not rely on patient adherence and which have longer durations of action,” he said at the World Ophthalmology Congress 2020 Virtual.
In a wide-ranging talk on the future of the medical management of glaucoma, Dr Rafuse, Associate Professor at the Department of Ophthalmology & Visual Sciences at Dalhousie University, Halifax, Canada, said that although there have been improvements in formulations and fixed combination therapies over recent years, no novel class of drugs for the treatment of glaucoma has been approved since latanoprost in 1996. The progress has been evolutionary rather than revolutionary, he said.
“We have seen the introduction of some other prostaglandin analogues such as bimatoprost and travoprost, as well as combinations of existing hypotensive lipids with beta blockers such as timolol. We have also seen an increase in benzalkonium chloride (BAC) avoidance strategies because of the known negative impact of preservatives on the ocular surface,” he said.
In the past two years, two promising drugs that represent entirely new classes of glaucoma medication have also come on the market, said Dr Rafuse: Vyzulta (latanoprostene bunod ophthalmic solution 0.024%, Bausch & Lomb) and Rhopressa (netarsudil ophthalmic solution 0.02%, Aerie Pharmaceuticals).
Both of these drugs have mechanisms of action different from previous glaucoma medications.
“Vyzulta is a monotherapy consisting of two active moieties: latanoprost acid, a prostaglandin analogue, works primarily
within the uveoscleral pathway and butanediol mononitrate releases nitric oxide, which is thought to relax the trabecular meshwork. Some initial studies suggest that it is more efficacious than timolol and perhaps even more effective than latanoprost,” he said.
The rho kinase (ROCK) inhibitor Rhopressa lowers IOP by enhancing trabecular meshwork outflow and seems to work well combined with latanoprost, said Dr Rafuse.
“One of the concerns with this drug, however, is that corneal deposits may form in some patients. If the deposits are centrally located they can blur vision. Some patients have developed red eye problems and even conjunctival haemorrhage in certain cases, so we need more safety data on this going forward,” he said.
There are many known issues with topical drugs for glaucoma that limit their potential usefulness, noted Dr Rafuse. This includes problems of adherence, local and systemic side-effects, cost and the question of whether they really do slow visual field progression.
“Getting the drop in the eye for an elderly patient with arthritis can be a major obstacle and we have seen many devices and approaches to this over the years to try to address the problem. Local side-effects include redness, foreign body sensation, itch, burning, tearing and blurred vision. Eye drops also make a subsequent trabeculectomy more difficult,” he said.
Systemic side-effects of beta-blockers are also problematic and renders them contraindicated in patients with pulmonary disease and some cardiac conditions, he added.
The prohibitive cost of some glaucoma medications is another formidable barrier to their widespread adoption, noted Dr
Rafuse. He cited a study by Zhao et al. in 2018 that looked at median annual household income (MA-HHI) and how much of it was used up by medications compared to laser trabeculoplasty, and trabeculectomy surgery.
“It was a cross-sectional observational study with the prices of drugs, laser and surgery obtained for 38 countries, 17 developed and 21 developing. There was a threshold where if a drug cost less than 2.5% of MA-HHI it was deemed affordable,” he said.
The authors found that timolol was the most affordable medication in all countries studied and was 2.5% or more of MA-HHI in only two countries (5%). The annual cost of latanoprost, however, was 2.5% or more of MA-HHI in 15 countries (41%) (15 developing countries [75%] and no developed countries). In 18 countries (53%), laser trabeculoplasty cost less than a three-year latanoprost supply.
There is strong evidence from the scientific literature that less than half of patients actually take their glaucoma medication.
“The most vexing aspect is that we don’t know which half is non-compliant,” said Dr Rafuse.
Despite the obstacles, topical medications are effective when used properly, he said, citing Garway-Heath’s study in 2015 that showed that topical latanoprost is effective at slowing the rate of visual field progression in open-angle glaucoma.
“This is why we need sustained release strategies in the future, which may come in the form of contact lenses, scleral plugs, punctal plugs, cul-de-sac rings or slowrelease reservoirs that can be implanted. We need to circumvent the ocular surface so that the drug gets to the site of action inside the eye,” he concluded.
Paul Rafuse: prafuse@dal.ca
There remains an unmet need for effective alternatives with longer duration of action that address issues of adherence. Dermot McGrath reports
One of the concerns with this drug, however, is that corneal deposits may form in some patients
Paul Rafuse MD, PhD
Surgeons can expect to find higher rates of zonulopathy in patients with various forms of angle closure pathologies and should plan lens extraction surgery with this possibility in mind, according to Paul Harasymowcyz MD.
“We looked at this in a recent study and found that the rates of zonulopathy in primary angle-closure suspect (PACS), primary angle closure (PAC) and primary angle-closure glaucoma (PACG) patients undergoing lens extraction was significantly higher than reported in the general population. Secondary pigment dispersion is also associated with a higher rate of zonulopathy. Ophthalmologists should be aware of the risks and be prepared to manage the zonulopathy intraoperatively,” he said at the World Ophthalmology Congress 2020 Virtual.
“Our hypothesis was that because angle closure glaucoma is in part caused by weak or loose or absent zonules that the rate of vitreous loss or zonulopathy would be much higher in the PACS, PAC or PACG population. A secondary hypothesis was that the rate of secondary pigment dispersion and rubbing of the lens and iris pigment epithelium would also be more frequent in this population,” said Dr Harasymowcyz, University of Montreal, Canada.
Dr Harasymowcyz’s retrospective cohort study included 1,013 consecutive eyes that underwent lens extraction by a single surgeon (PACS 266, PAC 366, PACG 381). The primary outcome was the rate of intraoperative zonulopathy as indicated by floppy capsule, phacodenesis, capsular tension ring use, anterior vitrectomy, or lens particles in the anterior vitreous. Secondary outcome was the presence of secondary pigment dispersion. Patients with a history of trauma, exfoliation syndrome or hereditary diseases were excluded.
“We found a 3.5% incidence of zonulopathy versus 0.5% in the general population. Three-quarters of patients (75%) required CTRs and the rate of secondary pigment dispersion was 15.3%. We feel that it is probably underestimated as a cause of angle closure glaucoma. Ophthalmologists should be aware of the intraoperative risks of cataract surgery in patients with angle closure, discuss this with their patients prior to surgery and prepare accordingly,” he said.
In the future, ophthalmologists will be able to draw on advances in imaging technologies such as ultrasound biomicroscopy (UBM) in order to better assess the condition of the zonules prior to surgery in patients with angle closure.
“There is definitely an unmet need for direct imaging of the zonules as many of the signs we currently use to detect zonulopathy are indirect ones. With UBM, we can show the presence or absence of zonules, but we need improved modalities in the future to determine the length and strength of the zonules,” he concluded.

We found a 3.5% incidence of zonulopathy versus 0.5% in the general population
Paul Harasymowcyz MD
On 8 May, 2020, AbbVie (North Chicago, Illinois, USA), a research-based global biopharmaceutical company, announced completion of its acquisition of Allergan plc. The $63 billion deal is part of a strategy to strengthen AbbVie’s current and future product portfolio, according to a statement by Richard A Gonzalez, chairman and chief executive officer, AbbVie.
We discuss what the future holds for the new company with both Dr Ignacio Tudurí MD, MBA, Vice President, Specialty, Global Marketing for AbbVie and Mr Charles Holmes, Associate Vice President, Head of Global Eye Care for Allergan an AbbVie company.
“The new AbbVie will be a well-diversified leader in many important therapeutic categories, with both on-market and pipeline assets, and our financial strength will allow us to continue to invest in innovative science and continue to serve unmet medical needs of patients that rely upon us,” Mr Gonzalez said.
Eye care will play an important role, Dr Tudurí told EuroTimes. “Ophthalmology is critical for the new AbbVie. The population is ageing and chronic disorders are rising, such as diabetes provoking diabetic retinopathy, or conditions like macular degeneration, glaucoma, dry eye and other eye diseases. Within the new AbbVie we appreciate Allergan’s history as a leader in ophthalmology for more than 70 years developing and providing innovative treatments for many ophthalmic disease areas.
“Allergan fits very well within AbbVie. We are a company based in R&D; a very patient-centric company aimed at finding solutions for existing unmet needs. We have a special interest on improving eye care
management, facilitating the chance that patients can get the treatment they need.” Dr Tudurí added.
“Ophthalmology is allowing us to diversify into new areas where we had no presence beforehand. AbbVie is very strong in immunology, oncology, neuroscience, virology, and now, we are adding eye care. It gives us critical mass so we can invest in new solutions for patients,” Dr Tudurí said. Adding Allergan will also increase AbbVie’s global footprint, giving greater reach in countries where AbbVie was not present.
Being part of a large, diversified organisation may result in crosspollination across therapeutic areas, benefiting ophthalmology research, added Charles Holmes. “One thing AbbVie brings to the table is a whole bunch of products that AbbVie has developed. We are currently looking at the possibility of using some of these products for ophthalmic purposes. It’s very early days so I can’t give specifics, but we are looking at retina, glaucoma and ocular surface in the cupboard of products that AbbVie has worked with over the years and the assets might not even be on the market today,”
AbbVie has retained the Allergan name, but it is not a separate company. “We will continue to operate as we have but now under the AbbVie umbrella,” Mr Holmes said. “The arrangement brings more resources and opportunities as the firm strives to address unmet ophthalmic need.”
“What we bring to that is we have the Allergan footprint, the Allergan people, the Allergan R&D, the Allergan presence and affiliates, the Allergan distribution
network. Now we add on top of that the AbbVie experts, the AbbVie management, the AbbVie scientists – and some of the AbbVie molecules that we could potentially use in ophthalmology,” Mr Holmes said.
Glaucoma is a case in point. Historically, Allergan had products such as eye drops that address early disease and a drainage implant that addresses late disease but few products that fit in between, Dr Tudurí said. Much of the research will focus on filling in this gap.
Reducing the burden of treatment is another research goal, Mr Holmes added. “I’ve been in the business for a long time and from the early days the biggest challenge has been red, irritated eyes [from eyedrops]. A lot really hasn’t changed; we need new ways to treat glaucoma.”
Similarly, frequent injections of antiVEGF and other treatments for age-related macular degeneration and diabetic macular oedema can put a strain on both patients and clinicians. Reducing the need for them is a major research issue for the new AbbVie, Mr Holmes said. “Less burden for the patient. That is our main focus.”
With COVID-19 pushing both the use of masks and working at home in less-than-optimal conditions, this is exacerbating the already high incidence of dry eye, Mr Holmes noted. Allergan has a wide range of treatments for dry eye and research is under way with the goal of developing more.
The two companies’ history, culture and goals improve the chances that the merger will bring about truly innovative ophthalmology treatments, Mr Holmes said. “Allergan has been in ophthalmology for 70 years. Being part of AbbVie just makes us stronger… Innovation is most important. AbbVie is research-based and has a history of life-changing products. Now we are part of two research-based companies bringing product to market.”
Dr Tudurí concurs. “We are committed to identifying and developing products that may be transformative for people with vision impairment. Not just one more product in a category, but something that makes a remarkable impact on people’s lives.”
Allergan fits very well within AbbVie. We are a company based in R&D; a very patient-centric company aimed at finding solutions for existing unmet needs
Dr Ignacio Tudurí MD, MBA, Vice President, Specialty, Global Marketing for AbbVie
ZIEMER Ophthalmic Systems has received CE mark clearance for its new ablation laser. “AQUARIUZ”, a newly engineered, compact solid-state ablation laser for refractive surgery.

According to Zeimer, the new ablation laser is different from excimer lasers as it operates at wavelengths which are less absorbed by water molecules. This allows the ablation process to be significantly less affected by temperature or humidity in the OR leading to more consistent surgical results.
“With the release of the AQUARIUZ solid-state laser, we can soon offer the complete refractive surgical suite together with our FEMTO LDV Z-models and the GALILEI devices.” said Frank Ziemer, CEO and President of Ziemer Ophthalmic Systems.
The AQUARIUZ is CE marked but not yet FDA cleared for use in the United States. For some countries, availability may be restricted due to regulatory requirements. www.ziemergroup.com
Oertli has announced the release of two trocarbased chandelier solutions that also offer a one-step access for an easy and quick connection.
Oertli say the chandelier illuminators offer a one-step access through a quick trocarbased solution either in three or four port vitrectomy surgeries.
Due to the reliable snaplock connection, an accurate fixation into all Oertli Caliburn trocars is ensured. The surgeon can expect an extrawide and homogeneous illumination, as well as postoperative tight sclerotomies.
www.oertli-instruments.com
At the 38th Congress of the ESCRS, Carl Zeiss Meditec (Jena, Germany) officially launched the IOLMaster 700 with Central Topography (CT), which detects and measures visually relevant central cornea asymmetries at the same time that it takes internal biometry measurements.
The device eliminates the need for a separate step to measure central topography, and is one of a range of solutions designed to improve accuracy and efficiency in cataract, refractive and glaucoma practice. www.zeiss.com
FREE 5 year membership for trainees
• Reduced Registration Fees for ESCRS Congresses

• Subscription to Journal of Cataract & Refractive Surgery
• Access to ESCRS Grants, Bursaries and Research Awards
Access to:
• ESCRS iLearn
Online CME accredited interactive courses
• ESCRS On Demand
Online library of presentations from ESCRS Congresses
• EUREQUO
European Registry of Quality Outcomes for Cataract and Refractive Surgery
• ECCTR
European Cornea and Cell Transplantation Registry
The 1918-1919 influenza epidemic killed more than 50 million people and infected between one-fifth and half of the world’s population. Colin Kerr reports
In Stacking The Coffins – Influenza, War and Revolution in Ireland, 1918-19 (Manchester University Press), Dr Ida Milne, a historian of disease and European history lecturer at Carlow College, Ireland, tells the story of the 1918-1919 influenza pandemic which killed more than 50 million people and infected between one fifth and half of the world’s population.
While Dr Milne’s book focuses on the effect of the epidemic in Ireland, she also gives an overview of the influenza outbreak globally.
The outbreak of the epidemic came at the end of the First World War. Dr Milne, in the opening chapter of the book notes that the newspapers of the day flagged it as a “mysterious disease”, “a mysterious malady”. The pandemic disrupted the Paris Peace Conference, after delegations charged with negotiating a lasting peace, were affected by the mystery flu and in early spring 1918, doctors paid 125 house calls in one day to the American delegation.
Dr Milne quotes a passage from Alfred Crosby’s America’s Forgotten Pandemic
(1976), which states: “The most important and almost incomprehensible fact about the Spanish flu is that it killed millions of people in a year or less. Nothing less – no infection, no war, no famine – has ever killed so many in such a short period. And yet it has never inspired awe, not in 1918 and not since, not among the citizens of the United States”.
The final global death toll was more than 40 million people but as Dr Milne notes death registration was rudimentary in many parts of the world so the final number of mortalities will never be known.
This short article cannot do justice to Dr Milne’s book so I will focus briefly on Chapter 5 which deals with the doctor’s view of the disease. As Dr Milne notes, even today diagnosing influenza poses difficulties. The 1918 ailment could be a mild disease in some people with sore throat, fever and aches. In other cases, it could lead to death within a matter of hours.
“A man could rise from bed, have his breakfast and leave for work. By lunchtime his wife could be informed that he had died,” said Dr Milne.
Dr Milne also notes that some patients
recovered from the influenza attack and resumed normal life but died from post-influenza pneumonia, heart attacks caused by the illness or other complications. The disease damaged the heart and lungs in some cases and could also cause various types of nerve, eye and ear disorders. The cranial nerves could also be affected leading to disturbed or temporary loss of smell. Ophthalmologists will also be interested to note that inflammation or atrophy of the nerves in the eye and ocular palsies occurred among some of those who were treated for the new strain of influenza.
As Dr Milne concludes at the end of this excellent book the 1918-1919 has legacies that still endure. This book is essential reading for ophthalmologists and other health professionals.
Colin Kerr is Executive Editor of EuroTimes
Due to the COVID-19 virus, a number of meetings have been cancelled or rescheduled. The information in this calendar is correct at the time of going to print; please check the meeting website or email the conference organisers to confirm all meeting dates.
BEAVRS 2020
Virtual Meeting
6 November
https://beavrs.org/
AAO 2020
Virtual Meeting
13 – 15 November
https://www.aao.org/annual-meeting
100th SOI National Congress
25 – 28 November
Rome, Italy
https://www.congressisoi.com
XXI International Congress of the Brazilian Society of Ophthalmology
Virtual Meeting
26–28 November
https://sistemacenacon.com.br/site/ sbo2020/mensagem
14th EGS Congress
13 – 15 December
Online & in Brussels, Belgium www.egs2020.org/
JANUARY
NEW
ISOPT Clinical: The International Symposium on Ocular Pharmacology & Therapeutics: Cornea and Glaucoma 2021 (ISOPT 2021)
14 – 16 January
Paris, France
https://www.isoptclinical.com/
NEW
12th International Course on Ophthalmic and Oculoplastic Reconstruction and Trauma Surgery 2021
13 – 15 January
Vienna, Austria
https://ophthalmictrainings.com /workshops/
7th Annual Congress on Controversies in Ophthalmology: Asia-Australia (COPHy AA)
29 – 30 January
Bangkok, Thailand
http://cophyaa.comtecmed.com/
FEBRUARY
25th ESCRS
Winter Meeting Virtual Meeting
19 – 21 February
www.escrs.org
NEW
American-European Congress of Ophthalmic Surgery Winter Symposium 2021

21 – 24 February
Aspen, USA
https://aecosurgery.org/ 2021-winter-symposium/
10th EURETINA
Winter Meeting
26 – 27 February
www.euretina.org
MARCH
6th San Raffaele OCT & Retina Forum
5 – 6 March
Milan, Italy
https://www.octforum2021.eu/
12th Annual Congress on Controversies in Ophthalmology: Europe (COPHy EU)
18 – 20 March
Lisbon, Portugal
http://cophy.comtecmed.com/
APRIL
NEW
American Association for Pediatric Ophthalmology and Strabismus
2021 (AAPOS 2021)
Virtual Meeting
9 – 11 April
https://aapos.org/meetings/ meetings-future
MAY
NEW
ARVO 2021
2 – 6 May
San Francisco, USA
https://www.arvo.org/
NEW
SOE 2021
10 – 12 June
Prague, Czech Republic
https://soe2021.soevision.org/
AECOS 2021
European Symposium
3 – 6 June
Florence, Italy
https://aecosurgery.org/ 2021-european-symposium/
46th Meeting of the European Paediatric Ophthalmological Society (EPOS)
17 –19 June
Copenhagen, Denmark
https://epos2021.dk/
JULY
AECOS 2021 Summer Symposium
15 – 18 July
Utah, USA
https://aecosurgery.org/ 2020-summer-symposium/
33rd APACRS–
SNEC 30th Anniversary
Joint Meeting
29 – 31 July
Suntec City, Singapore
https://apacrs-snec2020.org/
ASCRS Annual Meeting 2021
13 – 17 August
San Francisco, USA
https://ascrs.org/news/ascrs-news/ 2021-ascrs-annual-meeting-update

AUGUST
NEW
2nd World Congress on Ophthalmology and Optometry
23 – 24 August London, UK
https://ophthalmology. ophthalmologyconferences.com/
NEW
21st Global Ophthalmologists
Annual Meeting
23 – 24 August London, UK
https://annualmeeting.conferenceseries.com/ ophthalmologists/
5th International Glaucoma Symposium
3 – 4 September Mainz, Germany
https://glaucoma-mainz.de/
49th ECLSO Conference
3 – 4 September Paris, France https://www.eclso.eu/
NEW World Glaucoma Congress
9 – 12 September Kyoto, Japan https://www.worldglaucoma congress.org/
NEW AAO 2021
13 – 16 November
New Orleans, USA https://www.aao.org/
Watch
EyeJC (ESCRS Journal Club)
Advanced Instructional Courses
Eye Contact Interviews
Video of the Month
Video Journal of Cataract, Refractive & Glaucoma Surgery
Young Ophthalmologists Videos: “My Early Surgeries” player.escrs.org
the latest video content from the ESCRS and EuroTimes, FREE on the ESCRS Player
With the FEMTO LDV Z8 you can perform more:
• New: Cataract now also CE marked for pediatric surgery

• LASIK
• Tunnels for Rings
• Pockets for Inserts
• Keratoplasties
• Lenticules (now CE marked)
be restricted due to regulatory requirements. Please contact Ziemer for details. www.ziemergroup.com
The FEMTO LDV Z8 is CE marked and FDA cleared. For some countries, availability may
