C O VID
Ongoing research seeks possible ocular connections

Ongoing research seeks possible ocular connections
ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

Publisher
Carol Fitzpatrick
Executive Editor
Colin Kerr
Editors
Sean Henahan
Paul McGinn
Managing Editor
Caroline Brick
Content Editor
Aidan Hanratty
Senior Designer
Lara Fitzgibbon
Designer
Ria Pollock
Circulation Manager
Angela Morrissey
Contributing Editors
Howard Larkin
Dermot McGrath
Roibeard Ó hÉineacháin
Contributors
Maryalicia Post
Leigh Spielberg
Gearóid Tuohy
Priscilla Lynch
Soosan Jacob
Colour and Print
W&G Baird Printers
Advertising Sales
Amy Bartlett ESCRS
Tel: 353 1 209 1100
email: amy.bartlett@escrs.org
Published by the European Society of Cataract and Refractive Surgeons, Temple House, Temple Road, Blackrock, Co Dublin, Ireland. No part of this publication may be reproduced without the permission of the managing editor.
Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983
18 Performing bilateral cataract procedures appears to be safe and effective
19 Ophthalmic biomarkers to become routine part of practice in the future
20 EUREQUO finds cataract severity and patient age declining, outcomes improving
21 JCRS highlights
CORNEA
22 Simultaneous and separate approaches can both work in treatment of keratoconus
23 Biologics are an effective option for cases of severe disease
24 Femtosecond laser can aid with improving vision in keratoconus
25 Is tissue engineering the answer to donor shortages?

RETINA
26 Augmented reality device offers visual rehabilitation for AMD patients
27 Ophthalmologica highlights
28
30 Decision to implant IOLs in children must be made on a case-by-case basis 31 An iris-claw lens is safe for the treatment of paediatric aphakia

This year marks the 25th anniversary of the first issue of EuroTimes, published in January 1996.
Enormous advances have been made in that time in the armamentarium we have available to us to diagnose and treat our patients.

And yet 2021 finds us paralysed by a pandemic that has revolutionised our relationships with our patients and our colleagues.
As Dr Malvina Eydelman MD, officer of Health Technology at the FDA, pointed out in her 2020 Peter Barry Memorial Lecture this November, the COVID-19 pandemic has forced doctors to rapidly adopt new ways to take care of their patients. I recommend that you read the report of her presentation in this issue of EuroTimes as it succinctly spells out some of the key challenges we will face in the future.
As ophthalmologists, we will embrace new technologies, artificial intelligence, telemedicine and digital health applications to improve communications between both patients and doctors.
Most of all, I look forward to the time when we can meet friends and colleagues outside of our virtual bubble.
The success of our first virtual meeting, the 38th Congress of the ESCRS, has shown us that it is possible to interact remotely with a first-class scientific programme.
We will convene the 39th Congress of the ESCRS from 27-30 August in the RAI Amsterdam, the Netherlands. As multiple vaccines are rolled out across Europe, our hope is that this will be a hybrid Congress with delegates and industry partners convening onsite in the RAI and at the same time communicating virtually with our colleagues across the world who are unable to travel. As events unfold over the next few months, we will keep you updated on our plans.
Noel Alpins (Australia), Bekir Aslan (Turkey), Roberto Bellucci (Italy), Hiroko Bissen-Miyajima (Japan), John Chang (China), Béatrice Cochener-Lamard (France), Oliver Findl (Austria), Nino Hirnschall (Austria), Soosan Jacob (India), Vikentia Katsanevaki (Greece), Daniel Kook (Germany), Boris Malyugin (Russia), Marguerite McDonald (USA), Cyres Mehta (India), Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands), Leigh Spielberg (The Netherlands), Sathish Srinivasan (UK), Robert Stegmann (South Africa), Ulf Stenevi (Sweden), Marie-José Tassignon (Belgium), Manfred Tetz (Germany), Carlo Enrico Traverso (Italy)
Very best wishes to you for a New Year where we will be free to meet face to face, in the meantime, I urge you, your families and your loved ones to stay safe and stay well.
Rudy MMA Nuijts, ESCRS President




The success of our first virtual meeting, the 38th Congress of the ESCRS, has shown us that it is possible to interact remotely with a first-class scientific programme

Since Li Wenliang MD first warned colleagues of a cluster of SARS-like pneumonia cases in late December 2019, ophthalmologists have been involved with COVID-19. Perhaps most urgently, Dr Li’s subsequent death from the disease, which he contracted from an asymptomatic glaucoma patient, dramatically illustrated the need for universal precautions to combat COVID19 in clinical practice.
In the months since, ocular manifestations of SARS-CoV-2 infection and COVID-19 have been the subject of much study. One recent review estimated the pooled prevalence of ocular manifestations at 7%, with SARS-CoV-2 confirmed present on conjunctival swabs by PCR tests at about 1% (Taiwan J Ophthalmol. 2020 Jul-Sep; 10(3): 153–166.).
However, other research suggests ocular involvement may be more common depending in part on how it is defined. For example, a standardised questionnaire of daily COVID-19 symptoms administered to patients served by hospitals in Strasbourg, Dijon, Nice,
Brest and Colmar in France found that 36.7% reported ocular symptoms, and these were statistically associated with all major systemic manifestations, including flu-like illness, respiratory, neurological and digestive, said Tristan Bourcier MD, PhD, professor of ophthalmology at Strasbourg University Hospital.
“The symptoms reported by the patients resembled to a non-specific mild conjunctivitis confirming the possibility that SARS-CoV-2 targets ocular surface cells creating a potential entry portal. Moreover, SARS-CoV-2 has also been detected in the tears of COVID-19 patients suffering from conjunctivitis during illness,” said Dr Bourcier, who has been supporting patients with COVID19 acute diseases along with ICU and infectious diseases colleagues since the pandemic entered France early last year.
But while COVID-19 anterior infections could theoretically trigger corneal graft rejections, uveitis or neuritis episodes, the reality is different, Dr Bourcier said. “Most of the COVID-19 patients suffer red eye and eyelid swelling with or without discharge. In the very majority
of cases there is no visual impairment neither anatomical sequels.”
This observation coincides with the clinical experience of José Güell PhD, Professor of Ophthalmology at Autonoma University of Barcelona, Spain, and Director of Cornea and Refractive Surgery at IMO Barcelona. But while he has seen many cases of diffuse conjunctivitis in COVID-19 patients, and these cases are often referred to him, he has yet to see a conjunctival swab positive for the virus.
Because these patients also are exposed to other eye-drying circumstances, such as spending much more time looking at computer and smart phone screens, and staying indoors, “it is really difficult to assign the cause to COVID”, he said. Generally, these cases resemble a mild viral conjunctivitis and respond well to low-dose topical corticosteroids. He is much more concerned with the risk of contagion for the staff in treating patients.
Still, SARS-CoV-2 virus may be in the eye that cannot be detected by a conjunctival swab, said Ashok Kumar PhD, associate
professor in the Department of Ophthalmology, Visual and Anatomical Sciences at Wayne State University School of Medicine, Detroit, USA. Research in his laboratory on post-mortem ocular tissues of patients who died of COVID-19 found SARS-CoV-2 RNA on the posterior corneas (endothelial layer) of four patients and in the vitreous of one who was negative for the virus in the conjunctiva (Sawant OB et al. The Ocular Surface in press, online 8 November 2020).
Dr Kumar noted that no live virus has yet been isolated from ocular tissues, and suggested that conjunctival swabs taken later in the course of disease may be negative because the viral load drops off quickly. Indeed, four of the patients his laboratory examined who died of COVID-19 had no detectable viral RNA in their nasopharyngeal swabs. Virus was also detected in small numbers of patients who tested positive within two weeks of death who died of other causes. He emphasised the need to test tissues intended for transplant.
While both the conjunctiva and the cornea express the ACE2 receptors and Furin protease required for SARS-CoV-2 to enter cells, it remains uncertain whether the ocular surface could be another entry route, Dr Kumar said. One of the unique aspects of his study is the presence of SARS-CoV-2 viral antigens (i.e., Spike and Envelope proteins) in the corneal epithelium of COVID-19 donor eyes. This provides a stronger evidence than viral RNA detection and suggest potential susceptibility of ocular surface cells to SARS-CoV-2 infection. With colleagues at the University of California – Los Angeles, USA, he is conducting a study involving mice that express human ACE2 on the cornea to see if they can contract systemic SARS-CoV-2 infections through the eye, establishing a theoretical animal model for this transmission route. They are also examining the virus’ effect on cultured human corneal epithelial cells, particularly the induction of antiviral

and inflammatory responses. These experiments are needed to conclusively prove or refute whether eye is a gateway for SARS-CoV-2 entry – he further added. Sezen Karakus MD and colleagues at the Johns Hopkins Wilmer Eye Institute, Baltimore, Maryland, USA, are taking another approach to detecting whether COVID-19 can manifest solely or initially as an ocular infection. They are testing patients who present with viral conjunctivitis to determine how many are associated with the SARS-CoV-2 virus. Following these patients may also shed light on whether such infections remain isolated in the eye, or can develop into systemic disease. “If SARS-CoV-2 associated conjunctivitis is more common than we thought, patients presenting with conjunctivitis might need to be tested and isolated,” said Dr Karakus, who is an assistant professor of ophthalmology at the Johns Hopkins University School of Medicine.
While the involvement, if any, of SARSCoV-2 in the front of the eye mostly seem asymptomatic, however, the infection at the posterior segment of the eye may be a different matter, Dr Kumar said. In addition to his research with the cornea, he and his UCLA colleagues are examining how the virus affects retina and retinal cells using cell culture and animal models of SARS-CoV-2 infection, again looking for inflammation and antiviral responses.
While there is no current evidence of visual impairment resulting from retinal involvement in COVID-19, longer-term inflammation of retinal blood vessels “could lead to complications down the line”, Dr Kumar said.
Retinal blood vessel dilation associated with COVID-19 might also play a role in assessing the severity and stage of the disease, said Alessandro Invernizzi MD, assistant professor and head of the Uveitis and Ocular Infectious Diseases Service at the Eye Clinic – Department of Biomedical and Clinical Science
“Luigi Sacco”, University of Milan, Italy. Research he conducted with other colleagues from the Eye Clinic, infectious diseases and emergency medicine departments found that both retinal veins and arteries were dilated in 54 COVID-19 patients compared with 133 SARS-CoV-2 negative subjects, and the degree of vein dilation significantly correlated positively with disease severity, and negatively with time from symptom onset. “If our data will be confirmed, retinal veins diameter could represent a useful parameter to monitor the inflammatory response and/ or the endothelial damage in COVID19,” the article said. (Invernizzi et al. EClinicalMedicine published by The Lancet, 20 September 2020.)
The group’s current research is focused on converting these preliminary findings into a clinical process that may be useful in predicting which patients will progress to severe disease, Dr Invernizzi added. “Just by taking a single picture of the fundus we can get a lot of information about the impact of COVID-19 on the vascular system. It’s quite early to say whether this will change the way we manage patients but there is a lot of potential.”
Dr Invernizzi’s study also found a higher than expected incidence of other retinal abnormalities in the COVID19 patients compared to SARS-CoV-2 negative subjects, including haemorrhages in 9.25%, cotton wool spots in 7.4% and tortuous vessels in 12.9%. While these findings were not disease specific and did not appear to compromise vision, they suggest an avenue for further research on the possible effects of SARS-CoV-2 on the retinal microvasculature. Further research is also needed to determine whether the blood vessel dilation observed was directly due to the virus or the product of a massive systemic inflammatory response, he said.
One thing his findings do suggest is COVID-19 patients should have a fundus examination, Dr Invernizzi said. “Most of these patients were not complaining of ocular symptoms. We cannot really rely on patient complaints to tell whether it is worth screening their fundus.”
The newly described viral pathogen SARS-CoV-2 has changed the world as we know it. Belonging to the group of coronaviruses that are known to easily hop between species, SARS-CoV-2 is believed to have hopped from bats to humans.
Presenting with constitutional symptoms such as fever (88%), fatigue (38%), headache, nasal congestion, sore throat, dry (68%) or productive cough (33%) in many cases, SARSCoV-2 can in some patients go on to a severe pulmonary phase (Stage 2) and sometimes onwards to a hyperinflammatory phase (Stage 3). Systemic factors such as inflammation, homeostatic changes, endothelial dysfunction and coagulopathy can cause a progressive thrombotic cascade leading on to microvascular and large vessel thrombosis and multi-organ involvement that can be fatal.
The SARS-CoV-2 pandemic brought a change to the way we practise. At the beginning of the pandemic, all elective eye surgeries as well as routine nonemergent visits to the ophthalmologist were suspended for fear of transmission of infection as well as to conserve personal protective equipment (PPE) for those who needed it more. However, currently in many countries, patients are coming for routine evaluations and elective surgeries. Unfortunately, in many patients, new disease has presented or existing disease has progressed, sometimes irreversibly. Lack of access to care and/or medications as well as fear of going to the hospital despite having serious disease has taken its toll on many patients.
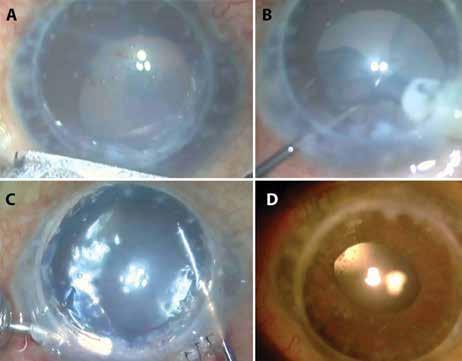
There is a huge backlog of cataract that has built up. Cataract progression has

caused a decrease in uncorrected and best-corrected visual acuity (BCVA). More patients are presenting with mature cataracts and severely limited vision. Patients with progressive nuclear sclerosis where a change in spectacles might have improved BCVA continue to wear old glasses, which no longer adequately correct.
Cataract-related complications are seen in higher numbers such as phacomorphic or phacolytic glaucoma, leaking Morgagnian cataract, progressive zonulopathy with subluxation etc. Bilateral cataracts as well as loss of depth perception from unilateral cataracts can be problematic and may even be the cause for increased risk of falls or road traffic accidents, thereby increasing systemic morbidity and demands on an already strained health system.
In many patients, even if the cataract is mild it may interfere with the patient’s ability to work and in such cases, cataract surgery is indicated without delay.
Other ocular co-morbidities may affect patients with cataract such as progression of glaucoma, relapse of uveitis or even rejection of a previously well-functioning corneal graft. Patients with advanced cataract may not notice worsening of underlying disease such as diabetic retinopathy, age-related macular degeneration etc, resulting in continuing damage.
COVID-positive patients may present to the ophthalmologist in many ways
including non-specific symptoms such as watering, conjunctivitis, pink eye, chemosis, dry eye etc, symptoms that were noticed in one-third of patients with COVID-19. Some of these symptoms were reported to be more common in those with more severe disease.
Retinitis, vasculitis, uveitis and optic neuritis from coronaviruses are reported in animals; however, ocular manifestations in humans were initially considered rare and not very severe.
Recently though, more severe ocular disease has been associated with COVID-19. This includes non-specific retinopathy due to microangiopathy, retinal vascular occlusions including central retinal artery occlusion, vein occlusions, non-arteritic ischaemic optic neuropathy, maculopathy, Miller Fisher syndrome, oculomotor nerve palsies, panuveitis, optic neuritis etc. There are also reports of severe orbital mucormycosis, which may become life threatening.
If found to be positive for SARS-CoV-2, surgery may need to be postponed until about two weeks after symptom onset, though there are various other criteria proposed by professional bodies.

Performing cataract surgery safely needs certain changes in protocols. Patient questionnaires about possible exposure to COVID-19, hand hygiene, masking and social distancing should be strictly employed. Telephonic and online consultations should be used where possible to cut down actual visit time to the minimum.
Teleophthalmology may be used where photo documentation together with measurement of physical parameters by
Ophthalmologists should be wary of the impact of COVID-19.
Soosan Jacob MS, FRCS, DNB reports
Unfortunately, in many patients, new disease has presented or existing disease has progressed, sometimes irreversibly
allied health personnel are evaluated by the surgeon to further investigate or order a direct examination or treatment. Electronic records make streamlining easier and e-consenting to surgery may also be done.
Though the virus has been detected in tear samples by RT-PCR, the risk of viral transmission through ocular secretions is possibly low. This has however not been proven conclusively. Precautions such as using cotton-tipped applicators to lift eyelids/ apply eyedrops and proper disinfection techniques for contact surfaces, tonometers, trial frames, B-scan probes, applanation heads and contact lenses should be employed.
Use of appropriate PPE such as N95 masks, gloves, eye protection and/ or a face shield are important. Direct ophthalmoscopy should be avoided. Two teams and staggered schedules may be considered for health care workers.
Preference for surgery may be given to those with advanced cataract, bilateral disease, one-eyed patients, those with ocular co-morbidities that affect decisionmaking and situations such as the second eye in bilateral high myopes with one eye operated to avoid postoperative aniseikonia. Surgeries should be scheduled according to complexity, with more demanding surgeries allotted to senior surgeons so that theatre time can be kept to a minimum.
Immediate sequential bilateral cataract surgery may be considered in some cases to decrease risks associated with presenting for surgery twice. Patients requiring general anaesthesia need special care and protocols to be followed with surgeons and staff not entering the room for 15 minutes after intubation or extubation.
Pre-surgical COVID testing may be decided on a case-to-case basis as well as depending on individual country/ hospital guidelines.
Surgery is ideally done wearing an N-95 mask or a filtering facepiece respirator. Topical anaesthesia is preferred. The patient may be given a mask that is taped along the upper edge to the nose to avoid air leak. Unnecessary talking should be discouraged during surgery.
Infectivity and aerosolisation can be decreased by proper draping, avoiding leak of exhaled air from under the drape, instillation of 5% povidone iodine drops into the conjunctival sac, replacing aqueous with viscoelastic before initiating
ultrasound, switching on irrigation only after entering the anterior chamber and applying viscoelastic (HPMC) over the incision while emulsifying.
Post-surgical counselling time should be kept to a minimum and may be done telephonically.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
The COVID-19 pandemic has exposed the shortcomings of excessive subspecialisation. Priscilla Lynch reports
Excessive subspecialisation in medicine is not a sustainable model for healthcare going forward, as has been shown by the learnings to date from the COVID-19 pandemic, according to Prof Marcel Levi MD, Chief Executive of University College London Hospitals, UK.

Giving the Keynote Lecture entitled ‘Tackling the COVID-19 crisis: professionals in the lead’ during the opening session of the 38th Congress of the ESCRS, Prof Levi said it was important to learn from what had happened during the first wave of the pandemic, not just in relation to how to deal with the virus going forward, but also its lessons for healthcare in general.
He noted that there was massive redeployment of medical staff during the first wave of the pandemic in many countries, in order to deal with patients who contracted the virus and to protect other patients and staff. This situation proved very challenging for many healthcare workers not used to being out of their comfort zone.
“We are now extremely subspecialised. We know fantastically well how to do our jobs but it is still very difficult to do someone else’s job,” he said.
In older patients presenting with many medical comorbidities this is a real issue for clinicians, Prof Levi said, questioning if it is feasible to have a doctor for every individual ailment in one patient.
Giving a hypothetical example, he said if an ophthalmologist only deals with one part of the eye and their patient has an issue with another part of the eye, that is not much use to the patient.
“In the highly specialised medical model of the 21st Century there is a different doctor for every disease,” he said. While acknowledging that this is positive in many ways such as ensuring expert care, “hyper specialisation” can lead to “forgetting that a patient is more than a collection of organs or parts of organs and that there is actually a bigger
picture to address”, Prof Levi maintained.
“So many people, including myself, believe we need to rethink our model of subspecialisation. Of course we need specialists in the highly advanced medicine of the 21st Century, but the need also remains to have a broad base of better understanding of medicine in general, of your specialty and maybe across more than one speciality/ subspecialty, to properly address these implications.”
Prof Levi suggested that clinicians should move away from over-focusing on one small disease area, and aim to instead be “super specialists, who are a little more capable of doing a bit more than their highly specialised area”.
He also spoke about the key role of clinicians in leadership and the need for managers and clinicians to work better together, collaboratively, as has happened during the pandemic.
During the first wave of COVID19 cases, doctors, nurses and other healthcare workers had to step up and lead the response to COVID-19, Prof Levi pointed out. “We asked the professionals to take the lead, we just told them what we needed and they had plenty of ideas about how to do it. We said ‘you do not need permission, just get on with it’. Of course there were managers but in a much more supportive role. Effort was not enough; it was all about results, and it was actually quite effective. And I think it should teach us that this leadership model in hospitals should be adopted much more frequently and could offer an answer to many of the problems we face in healthcare in general.”
Prof Levi said that managers speak a different language, which “doctors and nurses do not really understand or want to understand”, but they really should become more involved in leadership.
“It is not about power, it is about influence,” he commented, comparing
hospital medicine to a symphony orchestra with many talented musicians who have a conductor with influence over them who is responsible for the end result.
He acknowledged that sometimes healthcare workers are reluctant to take a leadership role: “but from my personal experience I can tell you that actually having a leadership role in the hospital, being a professional, is really very, very gratifying. It is not about observing what is happening but actually making things happen yourself.”
Looking at the continuing challenge of COVID -19, Prof Levi said there had been significant learning from the first wave of the pandemic, including how to reconfigure services at short notice as well as the increased use of telemedicine.
Summarising his lessons from the pandemic, Prof Levi said: “‘I think what we’ve learned from this pandemic is that we need to bring together these two worlds; put professionals in the lead, put managers in a supportive role and then we can achieve the most fantastic things much to the benefit of our patients and also to ourselves.”
Marcel Levi: marcel.levi@nhs.net...but from my personal experience I can tell you that actually having a leadership role in the hospital, being a professional, is really very, very gratifying
Prof Marcel Levi MDProf Marcel Levi MD
Technology solutions spurred by the need to contain the spread of SARS-CoV-2, the virus causing COVID19, could permanently change the way ophthalmology is practiced, Bahram Bodaghi MD, PhD, FEBO, told the 38th Congress of the ESCRS Virtual. Ophthalmologists have a particular interest in the virus because the conjunctiva is a potential entry point, and eye exams can expose clinicians to patients’ faces for extended periods.
As a result, online services, artificial intelligence and even robots have begun changing everything from how patients check in to how and where visits are conducted, said Dr Bodaghi, who is chair and professor of Ophthalmology & Visual Sciences at Sorbonne University, Paris, France. “Modern technologies are game changers and diagnostic processes may be decentralised.”
The potential stakes for ophthalmologists are as high as they can be. Dr Bodaghi began his presentation on COVID19 lessons learned with a tribute to Li Wenliang MD, the heroic Chinese ophthalmologist known for blowing the whistle on the novel coronavirus in December 2019. He succumbed to COVID-19 on 7 February 2020.
“He gave his life in the front line of the viral war,” said Dr Bodaghi, who encouraged young physicians to follow Dr Li’s example of fearless public service. He also honoured Prof Yuri Astakhov MD and Dmitry Yarovoy MD, both of Russia, who have died battling the coronavirus.
“I’m sure you all know friends and colleagues who contracted the virus and got ill or died.”
Looking back on previous disease outbreaks for guidance,
Dr Bodaghi noted the response to Creutzfeldt-Jakob variant prions, which caused the field to adopt many measures to avoid its transmission through the eye that brought other benefits.
“I don’t know how successful we were with Creutzfeldt-Jakob, but at that time we made a lot of progress in preventing adenoviral infections and transmission either to patients or ophthalmologists.”
Similarly, Dr Bodaghi observed that slit-lamp shields that are now ubiquitous because of coronavirus serve more than one purpose.
“They are really important tools to protect us not only against COVID, but against other types or infections, especially during fall and winter.”
Previous outbreaks, including SARS and the 1918 flu pandemic, teach us the importance of understanding waves. Using World Health Organization data, Dr Bodaghi suggested that the first wave has not yet ended in the Americas while in Europe a second wave is under way, with significant new outbreaks in Spain, France and elsewhere on the continent. Continued vigilance will be necessary, he added.
From the earliest research on COVID-19, the eye has been identified as a potential port of entry into the body, Dr Bodaghi said. Conjunctivitis is present in about 1% of cases (Guan W et al. N Engl J Med 2020; 382:1708-1720).
“What is also interesting is … eye protection may prevent person-toperson transmission,” with reduced odds of infection for people wearing eye protection (Chu D et al. Lancet June 2020;395: 1973-1987. Zeng W et al.) or wearing glasses for eight or more hours daily ( JAMA Ophthalmol. Published online September 16, 2020).
Regarding potential ocular mechanisms of transmission, there are essentially two,
Dr Bodaghi said. One is the conjunctiva itself, which has several receptors on its surface to which the virus can bind. The second is the canaliculus, which leads to the nose and the upper respiratory tract (Barnett B et al. Vision. 2020;4(3):40).
Some evidence suggests COVID-19 may affect the retina, though there is controversy about interpretation of the data. Shutdowns related to the pandemic also significantly reduced hospital revenues from elective surgeries as well as opportunities for training, Dr Bodaghi said.
Looking to the future, “we have to prepare ourselves to live with the virus for a while”, Dr Bodaghi said. Technology solutions, some already in use, will play a major role.
Telemedicine has taken off with many routine registrations, screening and follow-up visits now carried out remotely.
“It was of course present before but for sure it has more developed in asynchronous, synchronous and hybrid applications for seeing our patients. This is a real opportunity to permanently increase our capabilities,” Dr Bodaghi said.
He expects these applications to expand with remote diagnostic and AI applications powered by 5G mobile networks enabling more remote visits. Such technologies should be useful for addressing a second, third or fourth wave and any future coronavirus variants that may evolve. Robots that meet patients and help them through the measures they must take before being seen are another possibility.
“Overall, the first objective is to prevent transmission of viral infection, and then to adapt to the dynamic of the infection and prepare ourselves for the management of our non-COVID-19 patients,” Dr Bodaghi said.
“We must learn to live with the virus waiting for a spontaneous resolution or a vaccine.”
Modern technologies are game changers and diagnostic processes may be decentralised
Bahram Bodaghi MD, PhD, FEBO
They are really important tools to protect us not only against COVID, but against other types or infections, especially during fall and winter
Bahram Bodaghi MD, PhD, FEBO
Unless you’re in some particularly lone-wolf line of work (ski jumping maybe?) working with colleagues is an essential skill in any professional workplace. For us doctors, there’s even more to it as working with/for/under others is an integral part of our training.
It might seem almost predatory, but I think it’s common for young doctors to see their colleagues through trainingtinted glasses: “What do I get out of this relationship?” for them means: “what can I learn from this person?”
As we get further along in our careers, that balance shifts as we more and more start to hand down what we’ve learned to more junior colleagues, and learn to relish the occasions we can work with colleagues who we are junior to. Everything is relative after all.
Recently I’ve been thinking that when we think about ‘what can I learn here?’ we’re perhaps a bit too focused on the
medical side of things, when there are plenty of extra-curricular activities that our colleagues are engaged in and that can be thought-provoking too.

That thought came to me when working with one of my clinical fellows who, apart from an excellent doctor and colleague, is also — for lack of a better word — a bit of a tree hugger.
When she is not befriending the chickens that roam the hospital grounds (some of the lesser-mentioned benefits of a campus on the outskirts of the city), she reminds me that we should be doing more to look after our planet.
And she’s right, we should be. We all know this, but not all of us have this so ingrained that it’s front and centre in our attention span.
Cataract surgery is the most commonly performed surgery world-wide. Or at least it was until the pandemic led most of us to substantially cut down our clinical
activities. In the face of an uncertain global pandemic, cataract surgery was not a high priority but at the world begins to adjust and heal we can look forward to getting back on track. One thing that we have noticed during the pandemic is how quickly the waste accumulates and while PPE is undoubtedly necessary, we can see the mountains of nonbiodegradable trash that it generates. Our impact on the environment as a profession is already higher than you might think — the healthcare sector was responsible for 10% of total greenhouse gases and 9% of air pollutants in the US before the pandemic hit.
In the early phase of the COVID19 pandemic, the lockdowns led to a reduction in the emissions from transportation. Air quality improved in China, India and Italy and the US Energy Information Administration predicted a reduction of 11.5% in emissions. We even saw images in the media of “nature healing”, as animals were seen wandering empty city streets. The chickens near our hospital had the run of the place.
One lesson to be learned from the COVID-19 pandemic is that ophthalmologists should be doing more to look after our planet, reports Sorcha Ní Dhubhghaill
Unfortunately, these changes are almost certainly going to be temporary and the massive amounts of medical and hazardous waste generated by the healthcare industry will mitigate these environmental benefits.
This year David Chang, in his keynote address at the ESCRS virtual meeting, said that one of the five lessons he wanted to share was about sustainability in cataract surgery and how we should look to India as a model. In 2017 Thiel and colleagues compared the waste and emissions generated by cataract surgery in two clinical centres in India to that produced in the United Kingdom and found that they generated only 5% of their carbon footprint but had similar clinical results.
So as European ophthalmologists, where can we make improvements? In the Aravind Eye Care System (AECS), great care is taken to resterilise and reuse as much material as possible. Many of use reuse surgical instruments but they reused gowns and gloves (after disinfecting of course), phacoemulsification tips, tubing and even blades. This sounds a bit bizarre to us but after data from more than two million cataract patients they could see that postoperative infections were even less common than in the United States.
I can’t really see reusing my surgical blades being received very well. I recently asked if I could use a bottle of balanced salt solution, that I had used less than a third of it, for a second patient. This was the irrigating fluid, connected to flow one-way to the
safer their reusable counterparts. As we start to get back to work, most of us will likely have quite a backlog of patients to treat. Maybe we can start looking more critically at each piece of plastic that ends up in the bin and see if perhaps we can be a bit more like the AECS. I don’t see my hospital approving reusing blades any time soon but I will keep fighting to stem the tide of disposable instruments taking over my surgical table. And I won’t be lazy and use the disposable plastic cups in the coffee room any more either – there are plenty of cups and a dishwasher. It’s only a small effort, and if nothing else, it keeps my fellow happy.
phaco machine that had not had any direct contact with the patient. The first response I received was a questioning – why? We have plenty of fluid. This was followed by a comment that our hospital infection control would surely disimprove. In fact, when surveyed most cataract surgeons and nurses reported that much of the surgical waste was due to rigid regulation imposed by administrations as well as fear of product liability. This is a form of “defensive” medicine that can lead us to adopting disposable instruments when the evidence does not show that they are any
El Hamichi, S., Gold, A., Murray, T.G. et al. Pandemics, climate change, and the eye. Graefes Arch Clin Exp Ophthalmol (2020) Chang DF. Needless waste and the sustainability of cataract surgery. Ophthalmology (2020)
Thiel, Cassandra et al Cataract surgery and environmental sustainability: Waste and lifecycle assessment of phacoemulsification at a private healthcare facility, Journal of Cataract & Refractive Surgery (2017)
Sorcha Ní Dhubhghaill is Professor of Anterior Segment Surgery at Antwerp University Hospital (UZA) and a Consultant Surgeon at the Netherlands Institute for Innovative Ocular Surgery (NIIOS)
The newly integrated post-CXL function and database allow for evaluation of the cornea after crosslinking, based on the full complement of parameters including posterior corneal surface and corneal thickness at its thinnest spot. Monitor your keratoconus treatment with ease and improve your surgery outcomes!

As we start to get back to work, most of us will likely have quite a backlog of patients to treat
In an editorial reprinted from the Journal of Cataract and Refractive Surgery (JCRS), Associate Editor Sathish Srinivasan reports on the impact of COVID-19 pandemic on ophthalmology service provisions and training
Although the world is full of suffering, it is also full of the overcoming of it. —Helen Keller
In the realm of infectious diseases, pandemic is the worst-case scenario. When an epidemic spreads beyond a country’s international border, then it snowballs into a pandemic. Communicable diseases existed during humankind’s hunter-gatherer days, but the shift to agrarian life 10, 000 years ago created communities that made epidemics possible. Diseases such as malaria, tuberculosis, leprosy, influenza, smallpox and others first appeared during this period. The more civilised the humans became, building cities and forging trade routes to connect with other cities and waging wars with them, the more likely the pandemics became.
The plague of Justinian struck in the Sixth Century and killed as many as 50 million people, perhaps half the global population at the time. The Black Death of the 14th Century, likely caused by the same pathogen, might have killed up to 200 million people. Three influenza pandemics occurred at intervals of several decades during the 20th Century, the most severe of which was the so-called “Spanish flu” (caused by A/H1N1 virus), estimated to have caused 20-to-50 million deaths in 1918 to 1919. Milder pandemics occurred subsequently in 1957 to 1958 (the “Asian Flu” caused by an A/H2N2 virus) and in 1968 (the “Hong Kong Flu” caused by an A/H3N2 virus), which were estimated to have caused 1-to-4 million deaths each. (1)
On December 31, 2019, the World Health Organization’s (WHO) China office became aware of first reports of a previously unknown virus behind several cases of pneumonia in Wuhan, a city in Eastern China with a population of over 11 million. What started as an epidemic that was mainly limited to China has now become a truly global pandemic. The International
Committee on Taxonomy of Viruses coined the term “severe acute respiratory syndrome coronavirus 2,” or SARS-CoV-2, because this respiratory illness caused by coronavirus was related to the virus that caused the SARS outbreak in 2003. On February 11, 2020, the WHO announced the official name, COVID-19, a shortened version of coronavirus disease 2019. On March 11, 2020, WHO declared COVID-19 infection as a global pandemic.
The pandemic that started in China rapidly spread to West. The outbreak of COVID-19 in Europe started in northern Italy in mid-February 2020, when the local government issued shutdowns that brought routine eyecare to a standstill(2). As this infectious wave continued across Europe, it swept almost every country into lockdown, bringing countries to a standstill, pushing hospital systems to the brink and dragging the global economy into recession. Most healthcare systems stopped elective outpatient eyecare and surgery because their resources were stretched beyond capacity to dealing with the pandemic. Slow resumption of routine eyecare services across Europe began in May and June 2020 based on local scenarios and public health guidelines. However, this has caused considerable backlog of routine surgical procedures such as cataract surgery and has had a significant impact on residency training.
A recent survey among ophthalmology trainees in the United Kingdom to access the impact of COVID on training showed that lack of cataract surgery training was the single mostoften concern raised (3). The pandemic has necessitated triage to prioritise urgent cases requiring an examination and
possible intervention. Although waiting rooms are not crowded and in-person chronic disease management is less regular, this assessment process might provide a unique learning experience for involved trainees. Effective use of surgical simulators and online surgical videos can be helpful and might augment the trainees’ learning curve.
The pandemic has also resulted in adjustments to national board examinations, with varied adoption of virtual methods. The American Academy of Ophthalmology is exploring at-home testing with its Ophthalmic Knowledge Assessment Program, and the American Board of Ophthalmology is transitioning to a virtual format for its oral examination (4). The UK Royal College of Ophthalmologists for the first time has replaced in-person clinical examination of patients with video clips of clinical examinations as part of their fellowship examinations (5)
With the advent of physical distancing norms, face-toface interactions in large numbers are no longer feasible. As such, departmental Grand Rounds, seminars and other didactic sessions have been cancelled or are now held virtually through online platforms. Major international ophthalmology organisations such as ESCRS, ASCRS and the American Academy of Ophthalmology had to cancel their face-to-face meetings and switch over to virtual meetings. These societies have always served as powerhouses, providing a platform for presenting scientific information, learning cutting-edge new advances in our field and networking and building friendships with our colleagues and peers across the globe.
Overall, however, in the midst of this global crisis, clinical activity within eyecare has significantly diminished. Cataract surgery is probably the most cost-effective, quality of life improving procedure performed by the National Health Service (NHS) in the United Kingdom. Prior to the pandemic, it was the most common operation in the NHS: approximately 500,000 NHS cataract procedures were performed in the 12
months preceding April 2019. At the start of the pandemic, routine cataract surgery was suspended to protect patients. It is likely that COVID-19 will continue to affect NHS activity for at least another 18 months. Recently, the Royal College of Ophthalmologists published a white paper on restarting and redesigning of cataract pathways in response to the COVID-19 pandemic, detailing the issues and ways to address the cataract backlog in the United Kingdom.(6)
We all live in unprecedented times. This pandemic has required rapid adaptation to continue to educate our medical students, provide surgical training for our residents and fellows and, most importantly, provide adequate and much needed care to our patients. Although most education has gone virtual, we must also be vigilant that the best of being human — highquality human engagement with our patients, colleagues, peers and students — is not diminished permanently.
1. Past pandemics. World Health Organization. Available at: https://www.euro.who.int/en/health-topics/communicablediseases/influenza/pandemic-influenza/past-pandemics. Accessed September 22, 2020.
2. Ophthalmology and the Cornavirus. Eurotimes 2020;25:8
3. Hussain R, Singh B, Shah N, Jain S. Impact of COVID-19 on ophthalmic specialist training in the United Kingdom–the trainees prespective. Eye 2020. doi: 10.1038/s41433-020-1034-6
4. COVID-19 Information Center. American Board of Ophthalmology. Available at: https://abop.org/covid19#. Accessed September 22, 2020
5. Examinations. The Royal College of Opththalmologists. Available at: https://www.rcophth.ac.uk/examinations. Accessed September 22, 2020
6. Ophthalmic Services Guidance. Restarting and Redesigning of Cataract Pathways in Response to the COVID 19 Pandemic. 2020. The Royal College of Opththalmologists. https://www. rcophth.ac.uk/wp-content/uploads/2020/08/Resumptionof-Cataract-Services-COVID-August-2020-2.pdf. Accessed September 22, 2020
Journal of Cataract & Refractive Surgery: November 2020Volume 46 - Issue 11 - p 1455-1456

This pandemic has required rapid adaptation to continue to educate our medical students

Given appropriate precautions, corneal transplantation and eye banking are safe in the COVID-19 era, Diego Ponzin MD told the 38th Congress of the ESCRS Virtual. New methods of extending the shelf life of corneal tissues are also making progress, said Dr Ponzin, who is medical director of Veneto Eye Bank, Venice, Italy.
“Current eye banking practices allow for continuation of provision of safe corneal tissues,” Dr Ponzin said. These practices include protocols Veneto developed to ensure a COVID-19-free route to corneal transplantation that affect donors, recipients and staff.
Donors are deferred if they have a positive post-mortem nasopharyngeal swab or had active COVID-19 symptoms or risk factors. Donors with close contacts with infected individuals are acceptable if those contacts were at least four weeks past and they have a negative nasopharyngeal test.
Cornea recipients receive an outpatient nasopharyngeal swab on day one. Procedures are performed as day surgery

under local anaesthesia with no ICU personnel to minimise the risk of in-hospital contagion or spread. Patients then receive a COVID-19 serology test 30 days after surgery to ensure no transmission has occurred.
Eye bank staff follow strict social distancing, personal protective equipment and disinfection guidelines, and are thoroughly trained in infection control procedures. The staff has been divided into two groups that work on alternate days, Dr Ponzin said.
The approach enabled Veneto to continue recovering and distributing corneal tissue throughout the COVID-19 crisis, Dr Ponzin said. Donations during 100 days studied fell 25% to 1,233 and distributions 44% to 735 compared with 2019.
Maintaining operations was easier and better met patient needs than shutting down and trying to restart the programme, he added. This was especially important because Veneto is one of Europe’s largest eye banks, providing 51% of corneal tissues in Italy and exporting internationally.
Following these protocols, Veneto deferred 5% of donors for symptoms and 0.6% had positive post-mortem swabs. A study of 588 donors found three patients with positive swabs, and SARS-CoV-2 was detected in two corneas of two patients for a positivity rate of 0.3%.
Dr Ponzin believes that even infected corneas may not transmit the virus to recipients.
“In my opinion the chances of transmission are negligible. Even when we found virus RNA in the donor cornea we could not isolate an infective form of the virus.”
Anticipating longer times from donation to distribution, Veneto began research into extending storage time from 35 to 75 days by dehydrating some tissues. Validation is ongoing, though the studies appear to have succeeded, Dr Ponzin said.
But the crisis is not yet over, Dr Ponzin said. “We must keep very vigilant and monitor the pandemic indicators on a daily basis.”
Diego Ponzin: diego.ponzin@fbov.it
The COVID-19 pandemic has had a profound impact on the delivery of ophthalmic care over the past year, accelerating the use of telemedicine, artificial intelligence and digital health applications as ophthalmologists try to adjust to the new normal, said Malvina Eydelman MD in her 2020 Peter Barry Memorial Lecture.
Dr Eydelman MD, Director of the Office for Ophthalmic, ENT, Anesthesia, Respiratory and Dental Devices, Food and Drug Administration in the United States, told her online audience that there would be no return to the status quo before COVID-19.
“Shortly after the start of pandemic, it became clear that we were not returning to pre-COVID norms and that we would now have to develop the process of providing patient care in a new normal. Of great concern was U.S. Centers for Disease Control and prevention’s (CDC) finding that an estimated 41% of adults in the United States had delayed or avoided medical care, including urgent or emergency care, due to COVID concerns. It was becoming rapidly clear that healthcare systems and regulatory bodies around the world had to rapidly adopt new ways to take care of our patients,” she said.
In April 2020, an American Academy of Ophthalmology Survey found that 81% of ophthalmologists were at just 0-10% of pre-COVID clinical volumes and 96% were at 0-10% of pre-COVID surgical volumes. Furthermore, most ophthalmologists said that telemedicine was not a significant help at this stage of the pandemic and nearly 90% applied for federal grants and loans to cushion the financial impact of the reduced patient volumes, said Dr Eydelman.
To respond to the crisis, the FDA’s Center for Devices and Radiological Health (CDRH) took unprecedented measures in terms of volume, speed and agility, spanning multiple areas such as regulatory flexibility, Emergency Use Authorizations (EUAs) for devices, shortage mitigation activities, Public Health Service Corps deployments and extensive engagement with numerous stakeholders.
One example of CDRH policy to help expedite access to devices, was the guidance for remote ophthalmic assessment. In this guidance, FDA stated that it does not intend to object to the marketing of visual acuity charts, visual field devices, and generaluse ophthalmic cameras without prior submission of a premarket notification where such submission is otherwise required, as long as the device does not create an undue risk in light of the public health emergency.
“The increased regulatory flexibility enabled ophthalmologists to monitor and assess patients remotely during the pandemic.” she said.
Dr Eydelman noted that governments around the world have also taken steps to facilitate the rapid upscaling of telehealth. As a result, there has been a surge in the number of beneficiaries getting telemedicine services. A recent study from Johns Hopkins University found that while telemedicine adoption in ophthalmology was disproportionately lower than other surgical departments, the COVID-19 crisis accelerated the ophthalmic move to digital health applications.
“In some ways we were very fortunate that the pandemic waited to hit us in 2020, as the past decade has allowed the development of a magnitude of digital tools that can be used to remediate the COVID-19 outbreak,” she said.
These digital health technologies include wearable devices, software solutions and healthcare analytics, among others, which have enabled a shift in healthcare from the clinic to the patient, said Dr Eydelman.
Consistent regulatory strategies and policies are needed to expedite access to all aspects of digital technologies, especially given the unique features of software as a medical device (SaMD) that extend beyond traditional medical devices or hardware and include artificial intelligence and machine learning applications, said Dr Eydelman.
In this respect, she highlighted the important role played by the International Medical Device Regulators Forum (IMDRF), a voluntary group of medical device regulators from around the world, who have come together to accelerate international medical device and regulatory harmonisation and convergence.
FDA adopted IMDRF’s recommendations for SaMD and have added these to a number of guidance that FDA has issued in the last 7 years to provide clarity on the FDA’s regulation of digital health products.
To address the unique challenges presented by digital health and ophthalmology, FDA in partnership with five ophthalmic professional organisations and Stanford University, held Ophthalmic Digital Health Workshop in 2017. Soon after, the FDA approved IDx-DR as the first artificial intelligence device to perform diagnosis of diabetic retinopathy without physician input.
Since 2018, ophthalmic AI has become mainstream. The pandemic has turned into a gateway for AI adoption in health care. However, it brings both opportunity and risk. Dr Eydelman stressed the importance of protecting public health and avoiding any unintended consequences to patients from the accelerated uptake of digital health applications. To that end, she said that collaborative communities such as the recently formed Collaborative Community on Ophthalmic Imaging (CCOI) can help to clarify challenges, best practices, strategies and standards while advancing responsible innovation worldwide.
Summing up, Dr Eydelman said that the COVID-19 pandemic represents a unique opportunity for ophthalmology to embrace the digital health revolution.
“The American Medical Association predicts a $250 billion per year utilisation of digital health going forward. This would mean 20% of all emergency room visits could be avoided, 24% of healthcare office visits and outpatient volume could be delivered virtually and 35% of regular home health attendant services could be virtualised. It also opens the door beyond telehealth to drive growth in new markets and populations and scale other applications,” she said.
Hosted every year by the Royal Victoria Eye and Ear Hospital, Dublin, the Peter Barry Memorial Lecture was established to honour the memory of Dr Barry, a founding member and past president of the ESCRS, who passed away in 2016.
Malvina Eydelman: malvina.eydelman@fda.hhs.gov
An overview of the exciting potential of hydrogen to revolutionise treatment of a range of ocular diseases, tips for small pupil management and a new artificial implant for corneal transplantation were among some of the topics discussed in an ESCRS online review session of the best videos from the 38th Congress of the ESCRS.
Co-chaired by Oliver Findl MD and Boris Malyugin MD, the session brought together a panel of international experts – Bruce Allan MD from the United Kingdom, Guy Kleinmann MD from Israel and Gabor Scharioth MD, PhD, from Germany.
The session commenced with a video from Hisaharu Suzuki MD of Japan entitled “Hydrogen will change the world of ophthalmology” which was awarded the best overall video award at the 38th Congress. Dr Suzuki highlighted hydrogen’s ability to selectively scavenge free radicals – and in particular cytotoxic hydroxyl – and thereby potentially improve outcomes in the treatment of retinal ischaemia as well as in cataract surgery. The video outlined the beneficial effect of using hydrogen in an irrigation solution in protecting the corneal endothelium in phacoemulsification in a randomised clinical trial in 32 patients.
In the panel discussion, Dr Kleinmann said that the research was very interesting and that anything that could help to have better and safer surgery represented a welcome development. However, he said that it was not clear how hydrogen-infused BSS would be commercially produced for surgical use. He also stressed the importance of ensuring that the action of hydrogen to scavenge free radicals did not lessen the efficacy of the phaco tip during surgery.
Dr Malyugin added that free radicals are just one of many factors, including mechanical and chemical trauma, affecting intraocular structures during phaco. He also questioned how the hydrogen solution would perform alongside the use of dispersive OVDs that protectively coat the corneal endothelium. Dr Scharioth suggested that hydrogen might also have potential applications in posterior segment surgery in helping to control inflammatory response and combating cystoid macular oedema.
The next video, by Milan Izák MD, PhD, from Slovakia, featured lessons learned from the cataract surgery of a 66-yearold patient who had undergone radial keratotomy (RK) 30 years previously. Both eyes had extensive corneal scarring and the endothelial cell density was particularly low in the left eye. Dr Izák’s take-home message was to go through the scleral tunnel in order to perform cataract surgery as safely and gently as possible and to avoid touching the RK scars to promote swifter healing.
Dr Malyugin said that while the video was strong on some technical aspects of the surgery, it did not really address one of
the key challenges of such cases, namely the issue of IOL power calculation. Dr Allan said that he typically used the Haigis-L formula but that it is never easy to ensure accurate postoperative refraction for such complex eyes. Dr Kleinmann said it was very important to remain patient after the surgery as he had often witnessed significant improvement of the postoperative refraction over time in such post-RK eyes.
Small pupil cataract surgery was the topic of the subsequent video by Jiří Cendelín MD of the Czech Republic. Dr Cendelín weighed the pros and cons of various iris hooks and pupil expanders and the multiple options now available to surgeons to provide capsular support during small pupil cataract surgery. Dr Scharioth said that he rarely uses any mechanical device for pupil expansion. “For the past 10 or 15 years I have usually been able to manage small pupils with cohesive viscoelastic devices such as Healon 5 or DisCoVisc and it works well in my hands,” he said. Dr Allan remarked, meanwhile, that iris hooks are the modality of choice at Moorfields Eye Hospital. Dr Malyugin added that the surgical community is currently divided into two more or less equal parts – the first one is using iris hooks, the second one, pupil-expansion rings for small pupil cataract surgery. However, there is a growing body of evidences that pupil-expansion rings are more friendly to the iris tissue, require less operative time and decreases the chance of atonic, fixed pupils postoperatively.
The next video up for discussion was Jung Yeol Choi MD from South Korea, which looked at the effect on corneal endothelial cell loss during phacoemulsification using novel thermosensitive hydrogels (Poloxamer) versus sodium hyaluronate. Dr Scharioth remarked that while the research was very interesting he felt that endothelial cell loss was not as critical an issue as in times past thanks to advances in phacoemulsification and fluidics technology. He also wondered how IOLs would potentially react to these new hydrogel materials and said that there were a few unresolved issues which merited further investigation in the future.
The final video of the session featured research at CSI Heidelberg from Gerd Auffarth MD and colleagues who have been looking into the possibility of performing Descemet’s Membrane Endothelial Keratoplasy (DMEK) using an artificial implant instead of human tissue.
“The proof of concept presented in the video is certainly exciting,” said Dr Allan. “Anything that can help us to deal with the problem of the shortage of expensive donor tissue may have a massive impact. If this continues to perform well in future trials it could be a complete game-changer,” he added.
Panel of international experts discusses best videos from the 38th Congress of the ESCRS. Dermot McGrath reports
...the surgical community is currently divided into two parts – the first one is using iris hooks, the second one, pupilexpansion rings for small pupil cataract surgery
Boris Malyugin MD
He also stressed the importance of ensuring that the action of hydrogen to scavenge free radicals did not lessen the efficacy of the phaco tip during surgery
Guy Kleinmann MD
Adequate preparation and a clear strategy can help surgeons to deal successfully with posterior capsule rupture (PCR) when it occurs during cataract surgery, according to Richard Packard MD, FRCS, FRCOphth.
“It is important to have a strategy in place and not to panic. Denial at its most basic is saying something hasn’t happened, which means denying a painful reality. We need to be able to recognise trouble early and get over the denial that the posterior capsule is really gone. We generally do not lose vitreous and we usually know where it has gone but just don’t like to admit it,” he said at the 38th Congress of the ESCRS.
Mr Packard, Senior Consultant at Arnott Eye Associates, London, United Kingdom, said it was important to remember that a broken capsule during phacoemulsification does not necessarily equate to vitreous loss. “We need to check the edge of the break for vitreous prolapse. If it is sharp, it means that the anterior hyaloid has not been breached. However, if there is a scalloped edge there is vitreous prolapsing and we need to plan accordingly,” he said.
Once a rupture has been identified, it is critical not to allow the eye to decompress, as this will allow vitreous to prolapse, advised Mr Packard.
“Fill the eye with a dispersive ophthalmic viscosurgical device (OVD) before removing the phaco probe. It is important to maintain irrigation while the dispersive viscoelastic is being injected to tamponade the break. At this point, the anterior hyaloid has not been breached so it is perfectly feasible to fill the eye and get things stable so that you can make a plan to rescue the situation,” he said.
In 2000 it was shown that
triamcinalone could allow vitreous to be made visible. This has transformed the way that it is dealt with.
Should an anterior vitrectomy be required, it is advisable to have an emergency kit available that contains all the required tools for the task in hand, said Mr Packard.
The kit should include a vitrector set up for bimanual use with a trocar, dispersive OVD, triamcinolone for intracameral use, Miochol for pupil constriction, a Sheets glide, a vectis, and 10/0 nylon suture and needle holder. An appropriate lens for the post-vitrectomy eye should also be available. As already stated, injecting triamcinolone will help the surgeon to uncloak the vitreous and facilitate vitreous clean-up in cases of PCR.
The next step is to decide if the vitrectomy will be performed through corneal or pars plana incisions, said Mr Packard.

“Whether you go through the pars plana or not will to some extent depend on the size of your vitrectomy cutter: 25-gauge will be pars plana, 23-gauge could be either corneal or pars plana, and 20-gauge will be the corneal route,” he said.
Although pars plana is more efficient, Mr Packard said the surgeon should proceed with this technique only if they are prepared to check for and able to deal with peripheral retinal breaks. “Otherwise, use the corneal entry point. In any event, postoperatively a check for peripheral retinal breaks should be carried out,” he said.
Once the eye has been filled with dispersive OVD, the surgeon needs to ensure a second paracentesis for bimanual
vitrectomy. “Do not use the main wound or coaxial vitrectomy as it will just bring more vitreous forward and it’s very inefficient. It will also put stress on the vitreous base,” he said.
For trocar insertion, Mr Packard advised advancing the trocar about 1.5 mm obliquely, then changing the direction of the trocar to 90 degrees towards the posterior pole before pushing inwards.
“Then with a pair of forceps, withdraw the trocar and leave the opening in place. It is important to see that it deviates at an angle because this means you have created a tunnel which is less likely to leak when you remove the trocar,” he said.
Options to remove any nuclear fragments include using dispersive OVD or a Sheets glide to prevent pieces dislocating into the vitreous cavity, or an IOL scaffold approach using a three-piece IOL as a barrier to compartmentalise the anterior and posterior chambers and enable phacoemulsification of the remaining fragments.
Mr Packard recommended clearing central vitreous first using cut/irrigationaspiration settings and injecting triamcinolone as required to check for residual vitreous.
“A key word of advice here is not to use a sponge to pull on the vitreous wick because that will put stress on the vitreous base and is more likely to lead to breaks in the retina. It is important to clear the wound so that the vitrector can then cut away the vitreous,” he said.
The choice of IOL will depend on the status of the capsule, said Mr Packard.
“In the event of a small capsular tear with a continuous edge, a one-piece lens may be placed in the capsular bag. If you have got a good rhexis edge with a large posterior capsule tear, then sulcus fixation and optic capture is the best approach. If capsular support is inadequate, then consider an Artisan IOL or the Yamane technique. One can even use a suitably sized anterior chamber IOL in older patients as it can give a reasonable result,” he said.
Fill the eye with a dispersive ophthalmic viscosurgical device (OVD) before removing the phaco probe
Richard Packard MD, FRCS, FRCOphth
Performing bilateral cataract procedures in one surgical session appears to be as safe and effective as performing the procedures in two separate sessions on different days, provided that there is good patient selection and appropriate standardised precautions are taken, according to Rudy MMA Nuijts MD, Maastricht University Medical Centre.
“In today’s COVID-19 world, patients should be given an informed option between immediate and delayed-sequence bilateral cataract surgery,” Dr Nuijts told the 38th Congress of the ESCRS.
Proponents of immediate sequential bilateral cataract surgery (ISBCS) argue that it is less expensive for the health providers, is more efficient and provides patients with a faster visual recovery compared to delayed-sequence bilateral cataract surgery (DSBCS), he noted. Additional benefits it offers to patients include less costs for travel, less home care and decreased absence from work. However, there are also those who caution that bilateral cataract surgery could pose medico-legal risks in the event of serious, potentially blinding complications in both eyes.
The bulk of available data indicate that ISBCS poses no additional risk in terms of complications and is as effective in terms of visual outcome for both the first and second eye, Dr Nuijts said. However, he noted that in their responses to the 2019 ESCRS practice survey, 70% of respondents said they never perform ISCBCS, while 19% said they only do it when there are extenuating circumstances such as when general anaesthesia is required or in cases of mental retardation.
A similar survey of cataract surgeons in the Netherlands in 2020, during the COVID period, showed again that 70% of cataract surgeons do not perform ISBCS, and of the 26% who do perform ISBCS, 90% only do so in one-to-five cases per month. On the other hand, 45.6% said that they would consider performing ISBCS in the near future, Dr Nuijts noted.
Dr Nuijts noted that current guidelines in the Netherlands do not allow ISBCS to be performed and for that reason he and his associates, including Lindsay S. Spekreijse MD, have initiated the Bilateral Cataract Study in the Netherlands (BICAT-NL). The multi-centre randomised controlled trial will be conducted in 10 hospitals in the Netherlands and will include 858 patients who will undergo ISBCS or delayed sequence bilateral surgery (DSBCS).
The protocol in the ISBCS arm of the study will follow the 2009 General Principles for Excellence of the International Society of Bilateral Cataract surgeons. That is, in all cases there will be strict separation of instruments, and intraocular medication for the right and left eye. In addition, all eyes will receive standard administration of intracameral antibiotics and the routine in all cases will be to perform the surgery in the right eye first and the left eye second. Furthermore, all reusable surgical instruments will be sterilised using different autoclaves.
The exclusion criteria for the study include eyes with axial lengths less than 21mm or more than 27mm, eyes with previous ocular surgery and eyes with significant comorbidity. Based on these criteria, around 40% of cataract patients would be eligible for ISBCS, as would 25-to-35% of cataract patients at tertiary care centres such as the Maastricht University Hospital, Dr Nuijts noted.
Preliminary results in the 630 patients who have so far been included in the BICAT-NL study show that, when corrected for axial length and baseline visual acuity, there were no significant differences between the outcomes in the second eye in the two treatment groups in terms of subjective refraction and corrected or uncorrected visual acuity.
The proportion of eyes with a postoperative refraction within less than 1.0D of target in the ISBCS group and the DSBCS group was 96.2 % and 96.8%, respectively (p=0.689), and the proportion with a postoperative refraction within less than 0.5D of target refraction was 78.9% and 75.5% respectively (p=0.339).
The mean logMAR visual acuity of the second eye were also very similar in the two groups both for uncorrected (p=858) and best-corrected (p=0.913) visual acuity, the latter value being roughly zero in both groups. Moreover, the proportion with postoperative visual acuity of 0.1 logMAR or better in the ISBCS and DSCBS groups was 49.0% and 48.1%, respectively (p=0.820), without correction and 87.4% and 89.0%, respectively, with best correction.
Adverse events in the ISBCS group included one case of bilateral uveitis (0.0015%) developed at 10.5 weeks postoperatively Adverse events in the DSBCS group included one case of bilateral corneal decompensation (0.0015%) which developed at six weeks postoperatively, and one case of bilateral macular oedema (0.0015%) which developed at 4.5 weeks postoperatively. There were no cases of endophthalmitis in either group. The two treatment groups had a comparable incidence of mild adverse events such as dry eye and dysphotopsias.
“The preliminary results of our study showed comparable safety and effectiveness for ISBCS and DSBCS. Potential hurdles include product availability, reimbursement issues for surgeons and training young ophthalmologists to perform the procedures,” Dr Nuijts concluded.
The preliminary results of our study showed comparable safety and effectiveness for ISBCS and DSBCS
Rudy MMA Nuijts MD
The role of diagnostic biomarkers in ophthalmology is continuing to evolve and they will soon become a routine part of clinical practice, with many more exciting potential developments on the way, said speakers during a dedicated session on ‘Biomarkers: from inflammation to genetic disease,’ held during the 38th Congress of the ESCRS.
Biomarker tests are increasingly being used in diagnosis of disease, but also have significant potential for disease monitoring, predicting disease progression and assessing therapy success, thus facilitating more personalised treatment, noted session co-chair José Benítez-delCastillo MD, PhD, Spain.
However, key challenges include knowing when and how exactly to use such tests, specificity, costs, and the need to identify many more useful biomarkers.
A number of expert speakers during this session emphasised the role of inflammation as the key pathway in many ocular surface disorders, noting the emergence of useful inflammatory biomarkers in recent years.
Rohit Shetty MD, India, spoke about his research on identifying biomarkers in a range of eye conditions, eg, tear fluid diagnostic tests for inflammatory markers in keratoconus such as LOX enzyme and collagen levels. While these tests are easy to use, point of care and translation kits are needed to fully realise their potential, he said.
The future of successful biomarker use is going to include combining imaging, demography, molecular markers and predictive modelling with “artificial intelligence to ensure we have a very, very robust point of care kit”, Dr Shetty concluded.
Elisabeth Messmer MD, Germany, speaking about detection of inflammation in dry eye, noting that while inflammation is a significant pathogenetic factor, it can often be subclinical, thus making diagnosis a challenge: “So we need to test for inflammatory markers in the tear film (eg, MMP-9) as direct evidence of inflammation, or hyperosmolarity of the tear film as indirect evidence of inflammation.”
However, inflammation is also the key pathway in allergy, and differentiating dry eye disease from allergy remains a diagnostic challenge, she acknowledged.
A number of ‘bed-side’ tear film tests are currently available, which are helpful to identify patients with significant ocular surface inflammation and autoimmune disease, which may facilitate clinicians to commence ani-inflammatory treatment, Dr Messmer said. None of the currently available tests are perfect, however, and more work needs to be done on improving accuracy and refining the use of such tests, she said.
Also speaking during this session was Marlies Gijs PhD, the Netherlands, who gave a fascinating overview of ongoing research on the potential for diagnosis of neurodegenerative diseases through the eye.
Given the close relationship between the brain and the eyes, ocular symptoms and changes in functional vision can be among the first early signs of many neurogenerative diseases like Alzheimer’s and Parkinson’s disease. Thus there is increasing interest in the potential of noninvasive eye-based scans and tear fluid analysis to help diagnose these serious diseases earlier, and allow a better chance at successful treatment, she explained. There have been some useful early lab findings to date, but a lot of work remains to be done before such diagnostics will become commercially available.
Meanwhile, Marc Labetoulle MD, France, discussed optimising detection of ocular viral infections, in particular the creation of biomarkers for adenovirus and herpes simplex keratitis.

“Causes of keratitis can include contamination, funghi or bacteria, and it is very difficult in just the clinical setting to differentiate between the causes… biomarkers are needed to improve the reliability of our diagnosis.”
PCR testing on tear samples has
emerged as a more accurate diagnostic test in HSV keratitis, though it has some practical limitations, he noted. “Probably in the future we will combine the presence of antibodies in the tears with PCR in the tears as we will have two clues for the diagnosis. This combination has a very high positive predictive value; 90.9% in a study from Shoji (2016), and confirmed by another study by Qiu (2017).”
Dr Labetoulle predicted that within five-to-10 years, all ophthalmic practices could have their own mini diagnostic “labon-a-chip machines”. “These would be a combination of microfluidic technologies and in-home portable PCR machines, which could help us in the future with one tear to test many biomarkers, and to finally search for several infectious agents.”
The final speaker in this session, Jesús Merayo-Lloves MD, Spain, spoke about moving biomarkers from the laboratory to clinical practice, and the challenges therein. It is a long, demanding process to bring potential biomarkers to market, and promising study results and clinical validation does not always translate into successful creation of a commercial product. Finding interested companies willing to produce and market potential products is a particular challenge, he said, discussing his own research attempts to develop biologicals and biophysical biomarkers for keratoconus, dry eye disease and corneal innervation and sensitivity.
However, there is a lot of work ongoing in the ophthalmic biomarker field, with new products coming on stream that will be very useful in aiding accurate diagnosis.
Jesus Merayo-Lloves: merayo@fio.as
Marc Labetoulle: marc.labetoulle@aphp.fr
Marlies Gijs: marlies.gijs@mumc.nl
Rohit Shetty: drrohitshetty@yahoo.com
Causes of keratitis can include contamination, funghi or bacteria, and it is very difficult in just the clinical setting to differentiate between the causes… biomarkers are needed to improve the reliability of our diagnosis
Marc Labetoulle MD
Applications are open for the Peter Barry Fellowship 2021. This Fellowship commemorates the immense contribution made by the late Peter Barry to ophthalmology and to the ESCRS.
The Fellowship of €60,000 is to allow a trainee to work abroad at a centre of excellence for clinical experience or research in the field of cataract and refractive surgery, anywhere in the world, for 1 year.
Applicants must be a European trainee ophthalmologist, 40 years of age or under on the closing date for applications and have been an ESCRS trainee member for 3 years by the time of starting the Fellowship.
The Fellowship will be awarded at the ESCRS Annual Congress in 2021, to start in 2022.
To apply, please submit the following:
A detailed up-to-date CV
A letter of intent of 1-2 pages, outlining which centre you wish to attend and why
A letter of recommendation from your current Head of Department
A letter from your potential host institution, indicating that they will accept you if successful
Closing date for applications is 1 May 2021
Applications and queries should be sent to programme@escrs.org
Cataract patients are being treated earlier, while surgical complications have dropped and visual outcomes have improved in the past decade, Mats Lundström MD, PhD, Karlskrona, Sweden, told the 38th Congress of the ESCRS. These findings reflect surgical trends across Europe drawn from more than 3.1 million cases reported to EUREQUO, the European Registry of Quality Outcomes for Cataract and Refractive Surgery, since its founding in 2007. Data in 2019 came from 330,202 cases reported from 16 countries.
Demographically, more men are now having cataract surgery, with women making up 56.7% of all patients in 2019, down from 60.6% in 2008. Mean age is dropping as well, to 73.4 years from 74.5 years 11 years earlier. Ocular comorbidities were reported in 27.9% of cases and a surgical difficulty in 9.8%.
Patient severity at the time of surgery trended down over the period, with mean CDVA falling to a mean value of 0.41 LogMAR from 0.46. Visual outcomes improved as well, to a mean CDVA of 0.04 LogMAR, with 78.4% at 0 LogMAR, or 6/6, and 96% at 0.3 LogMAR, or 6/12. Biometry prediction error stood at a mean of 0.39D and median of 0.28D with 74.4% within ±0.5D of target, Dr Lundström reported.
In terms of surgery, phacoemulsification made up 98-to-99% of procedures during the entire period with topical anaesthesia gaining ground to 77.9% of procedures in 2019. Hydrophobic acrylic lenses are also gaining favour, making up 78.5% of implants.
Surgical complications also continue to decline over time, Dr Lundström said. In 2019, intraoperative complications and postoperative complications both stood at 1.2%.
“Altogether it is a very bright picture of improving quality of cataract surgery.”
Based on 12,192 cases reported from 65 sites, mean age of refractive surgery patients in 2019 was 42.0 years with 48.7% female, Dr Lundström reported. Mean preoperative manifest refraction was -3.1D (-0.12D to – 16.75D) for myopia, and +1.75D (+0.10 to +11.75D) for hyperopia.
In this sample, refractive lens exchange dominated, accounting for 46.6%, including 38% receiving trifocal IOLs; followed by LASIK at 33.9%, including 32% with laser-cut flaps; LASEK at 7.5% and PRK at 6.0%.
EUREQUO allows surgeons to monitor their own results and compare them anonymously with other colleagues, clinics and countries, Dr Lundström said. A new feature supports audit reports based on surgeons’ own data.
For more information, please visit https://www.eurequo.org
Mats Lundström: mats.lundstrom@karlskrona.mail.telia.com
EUREQUO finds cataract severity and
VOL: 47 ISSUE: 1 MONTH: JANUARY 2021

Photorefractive keratectomy has been a controversial procedure for treating keratoconus patients because the surgery removes tissue from an already thinning cornea. However, combining the latest PRK approach with epithelium-off cross-linking appears to offer a safe and an effective option, a new study suggests. A prospective case series included 19 patients (35 eyes) who all underwent topography/ wavefront-guided (TWFG) PRK using the VISX STAR S4 IR excimer laser and the new iDesign 2.0 system, followed by accelerated epithelium-off CXL. All the assessed parameters showed statistically significant changes six months postoperatively. In particular, 80% of eyes achieved a postoperative UDVA of 20/25 or better, and 46% reaching 20/20. At the six-month follow-up mark, 57% were within ±0.50D and 86% had a postoperative spherical equivalent of ±1.00D. 71% achieved a six-month postoperative amount of cylinder within ±0.50D, vs only 14% preoperatively. The mean time for refractive and visual acuity stabilisation was 16.7 ± 3.9 weeks. A Russo et al., “Topography/wavefront-guided photorefractive keratectomy combined with crosslinking for the treatment of keratoconus: preliminary results”, Vol. 47, #1, 11-17.





An artificial intelligence study aimed at improving the discrepancy between target and actual IOL power in an African cataract campaign proved quite successful, a special report suggests. Research utilised a machine learning model to evaluate patients from 29 cataract outreaches in Ethiopia between 2017 and 2018. This algorithm computes the optimal IOL supply distribution that would minimise the difference between actual implanted IOL power and targeted IOL power using a large set of biometry data. In the original data, only 45.6% of patients received their target IOL power and 23.6% received under-powered IOLs with current inventory with a 50% surplus. The AI-generated IOL inventory ensured that more than 99.5% of patients received their target IOL when using only 39% IOL surplus. AR Brant et al., “Artificial intelligence in global ophthalmology: using machine learning to improve cataract surgery outcomes at Ethiopian outreaches”, Vol. 47, #1, 47(1):6-10.












One of the main barriers to higher adoption rates of SMILE has been a slower visual recovery than LASIK postoperatively. A retrospective study of 147 eyes of 106 patients compared outcomes in FS-LASIK and low-energy SMILE. SMILE with lower energy settings (125-130nJ and 4. μm spot spacing) achieved postoperative day-one vision comparable with that of FS-LASIK. In addition, lower-energy SMILE caused less induced spherical aberration compared with that by FS-LASIK. RD Hamilton et al. “Comparison of early visual outcomes after low-energy SMILE, high-energy SMILE, and LASIK for myopia and myopic astigmatism in the United States”, Vol. 47, #1,18-26.





Corneal cross-linking (CXL) combined with topographyguided photorefractive keratectomy (partial in refraction PRK) to help normalise the corneal surface is a safe and effective treatment for keratoconus. But should they be performed simultaneously, or CXL first followed by PRK later? Both approaches can be successful according to debaters at the JCRS Symposium at the 38th Congress of the ESCRS, held virtually for the first time.
Arguing for combining the two procedures in the approach known as the Athens Protocol, A John Kanellopoulos MD noted that the simultaneous procedure can flatten the corneal ectasia several times more than either procedure can do alone collectively. “We started performing CXL first and a normalising surface ablation later back in 2003-2005. Then the idea of combining the two ensued,” said Dr Kanellopoulos.
“You cannot achieve this with crosslinking alone; you cannot achieve this with laser alone with the specific ablation depths used. It is the combination of the two that has a synergistic effect.”
Indeed, in a study involving 358 cases comparing almost in half CXL followed by topo-guided PRK six months later vs the Athens protocol (simultaneous combined procedure) in the other half of cases, Dr Kanellopoulos found the greater flattening of the mean keratometry by 3.2D in the Athens protocol cases versus 2.5D for the procedures performed six months separate, and improved uncorrected and corrected vision and central corneal thickness significantly better than in the separate procedure group (Kanellopoulos AJ. J Refract Surg. 2009;25:S812-8).
This greater flattening often is needed to normalise keratoconic corneas enough so that patients can achieve acceptable vision with spectacles or soft contacts rather than gas-permeable hard contacts.
“In our part of southern Europe, having a lot of sand and particles in the air, hard contact lenses have proven in clinical practice almost impossible to tolerate on a daily basis,” said Dr Kanellopoulos, of the Laservision Clinical & Research Eye Institute, Athens, Greece, and New York University Medical School, New York City, USA.
The Athens Protocol, developed by Dr Kanellopoulos, is a four-step procedure designed not to correct refractive error per
se but to normalise the corneal surface to correct asymmetric astigmatism. It involves a partial in refraction PRK, followed by PTK to account for epithelial removal, followed by mitomycin C, followed by accelerated CXL at 6mW/cm2 for 15 minutes. He has followed more than 3,000 eyes for topography changes after the combined procedure, the last three years even cases performed in his New York City practice, over 1,000 of those published in detail in dozens of peerreviewed articles already. Outside the US, a customised partial in refraction surface ablation combined with accelerated CXL has become the treatment of choice by most clinicians for progressive keratoconus.
Besides treating each patient, Dr Kanellopoulos evaluates carefully any available family members, as his team’s experience in Greece is that there is almost 100% chance at least one of the two parents will have at least tomographic signs of keratoconus. Important considerations include whether there is enough residual stroma to allow the surface ablation, how well the patient functions with his or her current refractive error and if there is documented progression. He makes sure patients understand that the goal may not be emmetropia and they may still need spectacles or contacts afterward. Careful ocular surface management is required after the procedure, he added, as healing issues may persist for one-to-two weeks. In regard to the refractive outcome with the Athens protocol: “The result is not completely predictable, Dr Kanellopoulos said. “You may get a 6.0D flattening or you may end up with an impressive 15.0D flattening over the tip of the cone.”
Dr Kanellopoulos noted that separating the procedures may have significant downsides.
“It may prove counterintuitive to go back and remove some of the best biomechanical part of the cornea you have strengthened when performing the surface ablation months after the CXL strengthening.”
In a 10-year follow study published recently he found less than 1% overflattening, and this can be corrected with a hyperopic laser treatment, he added. In general, results are stable after one year with the Athens Protocol, though longer follow-up studies are needed.
This unpredictability of corneal flattening after CXL – along with its effect on both stromal and epithelial corneal remodelling, residual corneal thickness and any adverse events – is a major reason why it makes more sense to wait for the cornea to stabilise after CXL before proceeding with PRK, argued Alanna Nattis DO, FAAO, of SightMD, Babylon, New York, USA. This typically takes 12-to-18 months, but helps ensure a safer and perhaps better refractive outcome, she reasoned.
“When you are planning refractive surgery for these patients you want to make sure you are not working on a moving target.”
The wide and changing range of CXL procedures, including epi-on, epioff and various strengths and lengths of UV exposure, further complicates predictability, Dr Nattis said. How CXL affects corneal remodelling remains a significant uncertainty, she noted.
“We should be able to see the refractive result of this remodelling before we move on to topography-guided PRK.”
Corneal thinning can vary by technique, Dr Nattis added. In a study she conducted involving 62 eyes in 56 patients, 45% of eyes were limited to treatment for topographic irregularities only due to insufficient corneal thickness to support refractive PRK after CXL. Mean time between CXL and PRK was 30.5 months, and 82% overall achieved 20/40 or better corrected vision one year after PRK with no adverse events (Nattis et al. JCRS 2020;46:507-516).
In the end, Dr Nattis acknowledged Dr Kanellopoulos’ success with the simultaneous procedures. Techniques vary by the equipment available as well as surgeon preferences and surgeon comfort. She also noted that individualised treatment planning is essential, and advocated more research to better understand the biomechanics of corneal remodelling.
“We can reshape the cornea; it is just a matter of how.”
Dr Kanellopoulos agreed that both the simultaneous combined and separate procedures are effective for treating keratoconus. He sees no problem going with a separate approach for those uncomfortable with the Athens Protocol. Studying carefully “suspicious” young myopic astigmats, teaching to avoid eye rubbing, evaluating family members and early intervention before the cornea thins under 400 microns is far more important.


Biologics are an effective therapeutic option worth considering in cases of severe corneal and external eye diseases refractory to systemic steroids and conventional immunosuppressive drugs, according to Omar Elhaddad MB BCh, MSc, MRCS (Ophth), FRCOphth.
“In our experience biologic agents show a very early response to disease activity, usually within two weeks, and particularly with infliximab. They are effective in treating severe cases such as peripheral ulcerative keratitis (PUK) and mucous membrane pemphigoid (MMP) that failed to respond to more conventional treatments such as prednisolone or mycophenolate mofetil,” he said.
Biologic drugs include a wide variety of products derived from human, animal, or microorganisms and are usually administered as a drip infusion or an injection, said Dr Elhaddad. He noted that two broad categories of biologics are used at the Bristol Eye Hospital – anti-TNF alpha agents such as infliximab and adalimumab and non-antiTNF drugs such as rituximab.
Dr Elhaddad presented a selection of case studies to illustrate the utility of biologics in a real-world clinical setting. The first example was two patients, both in their 60s, who presented with no symptoms apart from bilateral corneal thinning and extensive inflammation.
Both had been on long-term oral steroids for at least three months before referral. They were administered prednisolone and mycophenolate mofetil, but showed no improvement over four to six weeks. Methotrexate was also tried in one patient without any positive impact. After they were switched to infliximab, both patients showed rapid improvement, with complete control of disease activity and conjunctivalisation of the ulcerated cornea after two to three weeks.
The second clinical scenario presented by Dr Elhaddad concerned a patient who presented with ocular manifestations of mucous membrane pemphigoid, including fibrosis, limbitis, and diffuse conjunctival hyperaemia in all four quadrants. Again, various drugs such as prednisolone, mycophenolate mofetil and cyclophosphamide were ineffective. He was then treated with a rituximab infusion which resolved the limbitis and calmed the inflammation.
Before starting patients on biologics, it is important to screen patients for malignancies and infectious diseases such as tuberculosis, as well as hepatitis B and C, said Dr Elhaddad. In terms of outcomes, Dr Elhaddad said that all patients treated at Bristol Eye Hospital showed a very early response. Patients were switched to different anti-TNF agents in about 67% of cases and standard immunosuppression drugs were also continued for all patients while on biologics. All patients achieved good preservation of visual acuity. There was one death of unknown cause of a patient on rituximab.
Dr Elhaddad added that the experience of the clinic in Bristol Eye Hospital accorded with the limited studies in the scientific literature concerning the use of biologics in severe cases of corneal disease.
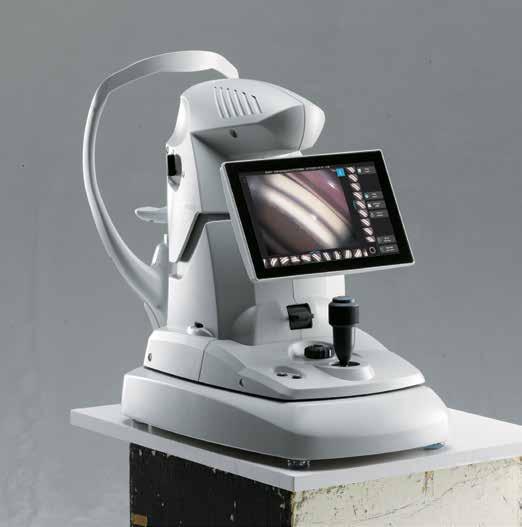 Omar Elhaddad: o.z.elhaddad@gmail.com
Omar Elhaddad: o.z.elhaddad@gmail.com
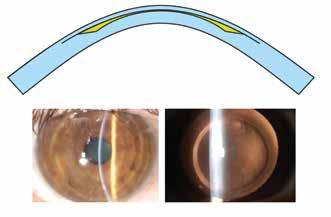
Stromal lenticule addition keratoplasty (SLAK) is a promising new technique that has shown good safety and efficacy in early trials in improving the corneal shape and vision in patients with keratoconus, according to Mario Nubile MD, PhD.
“It is a very promising era in keratoplasty with the introduction of lenticule implantation procedures such as SLAK. The concept is to provide a less invasive surgical technique as compared to standard keratoplasty, with novel approaches to treat keratoconus and corneal ectasia now possible,” he said at the 11th EuCornea Congress.
Explaining the concept in more detail, Dr Nubile, Excellence Eye Research Centre (Directed by Prof. L. Mastropasqua) at the University Gabriele d’ Annunzio of Chieti Pescara, Italy, said that the original idea was to try to make use of extracted stromal lenticules deriving from SMILE® refractive surgery. In theory, the lenticules could be used to insert tissue into a pathological cornea in order to obtain an effect and potentially treat conditions such as keratoconus, ectasia and certain corneal dystrophies. To date tissues from Eye Bank corneas suitable for transplantation, can be used in Europe.
“The concept of SLAK is reliant on implanting a negative meniscus shaped lenticule that is thinner in the centre and thicker in the periphery with the aim to reshape and stabilise the cornea in eyes with progressive keratoconus (Figure). The basic idea is to implant lenticules intrastromally to improve the geometrical quality of pathological corneas affected by keratoconus and ectactic disorders,” he said.
After successful proof-of-concept studies, the technique was then successfully tested in 10 cases of advanced keratoconus. The lenticules were implanted in a pocket created by femtosecond laser at a depth of approximately 150 microns in the anterior stroma.
“The extended follow-up results up to 24 months showed very stable results in terms of keratometry, anterior corneal asphericity in the central 8.0mm zone, and corneal volume. The visual and refractive outcomes were also encouraging with improved uncorrected and best-corrected visual acuity and a reduction in mean spherical equivalent,” said Dr Nubile.
Vector analysis of the refractive astigmatism showed a mean reduction of 45%. More recent optical coherence tomography (OCT) studies have shown the extent of epithelial and stromal remodelling following SLAK, said Dr Nubile.
“We showed that intrastromal lenticules implanted in SLAK promotes corneal reshaping characterised by central flattening and both stromal thickening and epithelial thickness restoration. From a clinical point of view, this is important because the increase of the corneal stromal thickness allows us to perform cross-linking in progressive diseases when the cornea is very thin,” he said.
Likewise, SLAK may also benefit keratoconus patients who are contact lens intolerant and could potentially avoid the need for invasive graft surgery.
Another exciting possibility in the future is to use decellularised lenticules as a transplantable bio-scaffold with native-like stromal architecture and chemistry for specific ocular pathologies, concluded Dr Nubile.
Mario Nubile: m.nubile@unich.itECCTR is a project funded by the ESCRS with initial support from the EU
The aim of the project is to build a common assessment methodology and establish an EU web-based registry and network for academics, health professionals and authorities to assess and verify the safety quality and efficacy of corneal transplantation.
www.ecctr.org

With a worldwide shortage of donor corneas, one of the best hopes for a viable and sustainable solution to the problem may well lie in tissue engineering, specifically the development of a bioengineered corneal stroma, according to Neil Lagali PhD.
Speaking at the 11th EuCornea Congress, Prof Lagali, Linköping University, Sweden, said that there is a strong rationale for replacing corneal stroma alone in cases that normally require transplantation.
“Stromal keratoplasty has emerged in recent years as a new additive or replacement therapy for the cornea. There are cases where the endothelium is still healthy and we can avoid the use of techniques that harm the endothelium or the epithelium and its cells and underlying nerves, so we can preserve both layers. This could be used for example in advanced keratoconus or in cases of stromal scarring or for stromal dystrophies,” he said.
The advantages of using a bioengineered stroma in such circumstances are multiple, said Prof Lagali.
“A bioengineered stroma could be made cell-free or could incorporate stem cells. This would make it immune tolerant and avoid issues of rejection. Furthermore, there would theoretically be a limitless supply of stroma, so there would be no need for donation, eye banking or preservation. We could also provide a customised size, thickness and shape of the implant and perhaps even provide additional functions such as sustained drug release beyond what human tissue can offer,” he said.
Promising results have been achieved by Jorge Alió’s group in Alicante using corneal stromal enhancement based on stem cell therapy in advanced keratoconus patients, while Zheng et al. in China have reported success using acellular porcine corneal stroma in herpes simplex keratitis patients.
While these results have been encouraging, the decellularisation process involved still requires corneal donor tissue, noted Prof Lagali.
A fully tissue-engineered anterior human cornea to treat severe corneal trophic ulcers currently being tested in a phase I/II clinical trial in Andalusia, Spain, has shown good early feasibility and safety results.
Prof Lagali’s own group has been involved in the development of a collagen-based bioengineered stroma.
“It is cell free and made from medical grade porcine collagen that is cross-linked to make it mechanically strong. It is transparent and we can customise the size, thickness, shape and swelling characteristics of the stroma,” he said.
After successful animal feasibility studies, the bioengineered stroma, manufactured by the Swedish company LinkoCare Life Sciences, is currently undergoing trials in patients with advanced keratoconus.
“Initial results are very good with improved curvature of the anterior and posterior surfaces, improved uncorrected visual acuity and no reports of scarring or rejection,” he concluded.
The work described by Prof Lagali has been supported by a grant from the EU Horizon2020 Programme, ARREST BLINDNESS, Grant No. 667400 (www.arrestblindness.eu).
Neil Lagali: neil.lagali@liu.seWhat is augmented reality? Is it the same as virtual reality?
“No,” said Dr Linda A Lam MD, MBA, Associate Professor at the University of Southern California Keck School of Medicine, Los Angeles, California, USA, during her presentation at EURETINA 2020 Virtual.
“Whereas virtual reality replaces the real world by shutting out the physical world and providing a completely immersive experience, augmented reality enhances the real world, providing a digital overlay over real-world surroundings.”
Dr Lam said that augmented reality (AR) might be an ideal modality to help patients with age-related macular degeneration (AMD), and explained how a new glasses-like device, the Oculenz, helps reduce central scotomas’ negative
effects on patients’ vision.
“The Oculenz is revolutionary in that it allows for pixel mapping around the blind spot,” she said.
“Currently available devices for patients with AMD use VR systems, which are generally heavy, tethered and intended for indoor use only. They do not provide peripheral vision and thus do not allow users to walk around with the device,” she explained.
On the other hand, Oculenz, developed by Ocutrx, uses AR technology for patients with central vision loss. How does this work?


“The patient first takes a visual field test while wearing the headset,” she explained. “Based on the results of this test, the device maps the areas that the patient cannot see, creating a scotoma marker.” This scotoma marker shows remarkable correspondence when overlaid by fundus autofluorescence; the scotoma marker fits nearly perfectly on the zones of retinal damage.
Step 2 is called pixel mapping.
“The scotoma marker data is stored in the processing unit. 4K cameras produce videos from the real world, which are processed to move the images outside of the scotoma,” said Dr Lam. These images are then projected on to the inside of the glasses, to be seen by the healthy retina.
In Step 3, infrared lights illuminate eye gaze, allowing eye-tracking cameras to follow eye movement. “This eye-tracking keeps the scotoma marker in line with the augmented image on the glasses lens. This allows Step 4 to occur, in which the image is moved away from the scotoma to areas of healthy retina.
Additionally, the device sends visual field test results to the patient’s physician, alerting the physician if the scotoma changes, indicating possible disease progression.
“The initial pilot trial of five patients showed a mean improvement from 20/200 to 20/63, with an average improvement of 17 to 19 letters.
This new device is anticipated to be available in mid-2021.
Linda A Lam: linda.lam@med.usc.edu
Currently available devices for patients with AMD use VR systems, which are generally heavy, tethered and intended for indoor use only
Linda A Lam MD, MBA



VOL: 243 ISSUE: 6 MONTH: DECEMBER 2020

The onset of nascent geographic atrophy (nGA) detected by optical coherence tomography (OCT) imaging warrants consideration for use in age-related degeneration AMD preventative trials once it has been established that its characteristic features can be reproducibly graded, according authors of a review article. They note that research has identified a number of anatomical signs of nGA detectable on OCT that could act as evidence of photoreceptor loss, including subsidence of the inner nuclear layer (INL) and outer plexiform layer (OPL) and/or, a hypo-reflective wedgeshaped bands within Henle’s fibre layer. Z Wu et al, “Can the Onset of Atrophic Age-Related Macular Degeneration Be an Acceptable Endpoint for Preventative Trials?” Ophthalmologica 2020; 243:399–403
Around one-in-10 patients with macular oedema (ME) secondary to diabetic retinopathy or retinal vein occlusion (RVO) may develop a rebound phenomenon following intravitreal triamcinolone (IVTA) injection, a new study suggests. The retrospective analysis showed that in 268 eyes of 211 consecutive ME patients, 9.7% had a greater than 10% increase in central retinal thickness from baseline at two months after IVTA injection. The incidence of the rebound phenomenon was 9.5% among those with diabetic retinopathy, 5.2% among those with central retinal vein occlusion and 15.4% among those with branch vein retinal occlusion. The mean number of prior injections of vascular endothelial growth factor inhibitor or corticosteroid agent was statistically significantly higher in the rebound group (6.8 vs. 5.3) than in the non-rebound group (p = 0.01). O Diketmas et al “Rebound Phenomenon after Intravitreal Injection of Triamcinolone Acetonide for Macular Edema” Ophthalmologica 2020; 243:420–425
A cross-sectional, case control study involving 240 type 1 diabetes patients showed that serum levels of C-reactive protein were higher among 80 who had proliferative diabetic retinopathy (PDR) than among 160 controls without diabetic retinopathy. The patients were matched for gender and duration of diabetes C-reactive protein was the only inflammatory biomarker that was positively related to PDR (OR 1.96; 95% CI 1.01–3.78, p = 0.0045). The study found no link between PDR and serum levels of VEGF, TNF-α or IL-6 but did find an association between PDR and high glycated haemoglobin levels, the use of angiotensin-converting enzyme inhibitor and low glomerular filtration rate. Melo L.G.N. et al, “Relationship between Proliferative Diabetic Retinopathy and Inflammatory Markers in Patients with Type 1 Diabetes in Brazil: A Nested Case Control Study” Ophthalmologica 2020;243:471–478
The Save Sight Years (SSY) Engine should aid clinicians in their management of patients with glaucoma who are showing an unacceptable rate of perimetric progression. Intended to offer a guide for choosing a new target IOP that will reduce the risk of severe vision loss, the SSY Engine gives an individualised estimation of future disease progression rates in relation to different levels of IOP.
It was created by Anders Heijl MD, PhD, Skåne University Hospital, Malmö, Sweden, and Magnus Brandel, Allergan, with financial support from Allergan. An article in Acta Ophthalmologica co-authored by Dr Heijl and Mr Brandel describes the rationale for the development of the SSY Engine and how it is used.
“Although clinicians have been able to extrapolate Rate of Progression (RoP) regression lines to identify eyes that are progressing at an unsafe rate and need further reduction of IOP, the SSY Engine adds something novel for assisting with the difficult and not always intuitive task of resetting the target IOP. By using the information, it provides in conjunction with other clinical aspects and their expert judgment, clinicians may be better equipped to make decisions on how best to intensify treatment,” Dr Heijl explained.
Dr Heijl told EuroTimes that discussions leading to the development of the SSY Engine began in 2014, and the first version was launched in 2016. The system itself is an outgrowth of the SSY Concept that was introduced by Allergan in the form of an education programme several years earlier.
The SSY Engine is CE-marked and has been available as an app for a few years in a number of countries. Now it is being launched as a web-based version (www. ssyengine.com) in which the analyses can
be performed in the cloud.
“It became clear to us that the iPad and Android tablets were not the optimal platform for our system because these devices are not used that much in ophthalmic outpatient practices,” said Dr Heijl. “With the web-based analyses, there is no need for users to download any software. Furthermore, because the analyses are completely anonymous, there are no concerns about patient confidentiality.”
To use the SSY Engine, clinicians input four items found on the perimetric results form – the patient’s age at the first visual field, current age, the current Visual Field Index (VFI, if using a Humphrey perimeter) or the current Mean Defect (MD, if using the Octopus perimeter) and the measured RoP. As a fifth item, they enter the patient’s mean IOP, which is estimated from the patient records and includes values measured after the patient was started on IOP-lowering treatment and during the period for which the RoP was calculated.
The SSY Engine then generates a graph of the current RoP trendline extrapolated 20 years into the future. Using a mouse,
clinicians can then reduce the slope of the trendline to areas in the age/function diagram with better visual field status, where patients’ vision-related quality of life would be less affected. For each age-based simulation, the SSY Engine will display the new target IOP, the recalculated RoP (% per year) and the number of “Sight Saved Years”.
Dr Heijl said that it is probably best to wait to use the SSY Engine until data are available from five or six visual fields, which would occur about two-to-three years after a patient is diagnosed with glaucoma and the RoP becomes available for the first time.

“However, the SSY Engine can be potentially valuable for assisting with management decisions at any time when the rate of disease progression seems unacceptable or threatening,” he said.
The web-based SSY Engine is currently available in about a dozen European countries along with Australia, Brazil, and India, and it will be launched in more countries in 2021. Dr Heijl acknowledges that the SSY Engine calculates IOP based on the “best current knowledge”, which comes from four multi-centre randomised glaucoma/ocular hypertension treatment trials. Studies validating the performance of the SSY Engine would be valuable, he said.
“We are looking seriously at conducting a validation study and believe that it would be feasible using patients who were implanted with the XEN Gel Stent. We also invite other researchers to apply the SSY Engine on their data,” Dr Heijl said.
...the SSY Engine adds something novel for assisting with the difficult and not always intuitive task of resetting the target IOP
Anders Heijl MD, PhDSSY Engine analysis of a glaucomatous eye of a 65-year-old patient who has been followed for three years with a mean IOP of 19mmHg. The measured rate of progression of 2.5%/year is not safe (the extrapolated solid line). The engine suggests that if a new target IOP of 15mmHg is achieved, the rate of progression might be reduced to approximately 1.2%/year; a much improved outcome (dotted line) Courtesy of Anders Heijl MD, PhD
Despite a re-evaluation of its utility in recent years, laser peripheral iridotomy (LPI) remains standard first-line treatment in patients with narrow angles, narrow angle glaucoma and acute closed angle glaucoma and eyes at risk for this condition, according to Beatrice Des Marchais MD, PhD.
“Glaucoma management continues to change and evolve in our daily practices and the indications for LPI have been revised accordingly in recent years. However, some fundamentals have not changed, and I still offer LPI to selected patients, informing them of the risk of complications and photopsia in particular,” she said at the World Ophthalmology Congress 2020 Virtual.
Dr Des Marchais said that LPI has been used since the 1980s both as treatment and prevention of angle closure glaucoma.
“This has been the case even though the natural history of untreated shallow angle is not known and the efficiency of LPI is not obvious based on the evidence in the scientific literature,” she said.
One of the few controlled studies to look at the efficacy of prophylactic LPI in bilateral angle-closure suspects, the Zhongshan Angle Closure Prevention (ZAP) trial, suggested that perhaps laser iridotomy is not required in all angleclosure suspects, she said.
The study included 889 patients at different centres in China who were randomised to receive laser iridotomy in one eye, while the other eye remained an untreated control. The risk of converting from suspect angle closure to confirmed angle closure was low during this six-year study.
“The ZAP trial came out against the widespread practice of LPI in suspect cases because of the limited cost-benefit ratio. Laser iridotomy decreases the risk of this conversion, although the incidence of primary angle closure is remarkably low,” she said.
Based on a literature review carried out in conjunction with Jean-Philippe Rozon, Dr Des Marchais said it was important to check IOP after LPI for all patients with more than one risk factor.
“We need to watch for bleeding in the anterior chamber, pigment dispersion, high IOP pre-treatment, Asian ethnicity, patients with thick iris or those with pre-existing optic nerve damage,” she said.
Dr De Marchais also carried out a separate study to determine the rate of gonioscopy after LPI treatment.
“We were surprised that despite recommendations only 28% of patients received gonioscopy exams as part of their standard follow-up,” she said.
To address the situation, an interventional plan was implemented to educate surgeons and staff on the necessity to perform gonioscopy as part of the follow-up to LPI.
“It was successful, and our results one year later showed an increased rate of gonioscopy post iridotomy from the documented 28% to 64%, proving the value of an interventional plan to improve patient safety and quality of care,” she concluded.
Glaucoma management continues to change but some fundamentals have not changed. Dermot McGrath reports
The landmark infant aphakia treatment study (IATS) showed that aphakia is safe in very young infants. However, the decision to perform the surgery must be based on a range of considerations and equivalent or better results can be achieved by implanting an IOL in infants, notes Ramesh Kekunnaya MD, FRCS, LV Prasad Eye Institute, Hyderabad, India.
“IOL implantation can be considered even in selected babies who are less than six months of age. But the decision must be decided on case-by-case basis, not purely based on age. One must acquire adequate skills. If IOL implantation is not feasible, aphakia can be an effective alternative,” Dr Kekunnaya told the ESCRS/WSPOS symposium at the 38th Congress of the ESCRS.
He noted that based on current evidence, most paediatric ophthalmic surgeons are comfortable performing IOL implantation in infants between seven months and one year and age. Beyond 12 months there is little controversy regarding the safety and efficacy of IOL implantation. However, between zero and six months some doubt remains owing to the considerable changes that occur in axial length and keratometry that occur in that stage of an infant’s eye development.
The IATS study is a randomised, multicentre clinical trial involving 114 infants ranging in age from four weeks to seven months with unilateral congenital cataract who underwent cataract surgery either with IOL implantation or with contact lenses.
The IATS study has generated several peer-reviewed reports regarding its short-term and long-term outcomes complications in the two study groups. Most recently, a publication in JAMA Ophthalmology showed that after a followup of 10 years implanting an IOL was neither beneficial nor detrimental in terms of visual outcomes (Lambert et al, JAMA Ophthalmol 2020; 138: 365-372).
The most common complications at five years were glaucoma suspect (19%) and
contact lens related (18%) complications in the aphakia group and lens cell proliferation in the visual axis (40%), pupillary membrane (28%) and corectopia (28%) in the IOL group. There was also a 19% incidence of glaucoma in the IOL group, Dr Kekunnaya said.
In addition, 72% of patients in the IOL group required additional surgeries during five years of follow-up. That compared to only 16% of patients in the aphakia group. The most common follow-up surgery in the IOL group was clearance of visual axis opacities (68%). 14% of patients in the contact lens group required the same procedure.
However, most of the secondary surgeries in the IOL group were carried out in the first year after their cataract procedure and the number of surgeries required during second-to-third postoperative year were identical in the two groups.
Moreover, during postoperative years six through 10, half of those in the contact lens group underwent secondary IOL implantation, and four underwent glaucoma surgery. In the IOL group there were only four patients who required IOL exchange, one required glaucoma surgery and one underwent repair of a retinal detachment.
Overall there were more complications and more parental stress in the IOL group and greater expense during the first year than in the contact lens group. However, costs were greater after the first year in the contact lens group.
The IATS study had a number of limitations that make translation of the findings to clinical decision making
difficult, Dr Kekunnaya observed. Those limitations include the random allocation of patients to each patient group and the range of corneal diameters the groups. Furthermore, intraoperative findings were not included in the analysis. There were also variable dosages of steroids administered postoperatively.
“Basically, we need to take preoperative, intraoperative and postoperative factors into consideration. Also, we need to take socioeconomic factors into consideration. IATS was a study where insurance was available, it was not really representing the real world. IATS had a perfect situation, its results cannot be extrapolated to every patient,” he said.
Another factor to take into consideration is the compliance with follow-up visits. A study he and his associates conducted in India showed that attendance at followup visits fell of dramatically after the first six months among both paying and nonpaying patients.
In addition, most congenital cataracts occur in Asia and Africa where most cases are bilateral. In the IATS study all were unilateral. Furthermore, in many parts of the developing world contact lenses are not as easily available. Moreover, the surgeon treating the patient must have adequate experience to perform the complex surgery involved in implanting the IOLs in infant eyes.
“We cannot say with the toss of a coin whether this patient will get an intraocular lens and that patient will get a contact lens, we need to look into the eye factors, the age factor and other factors before making the decision which surgery to perform,” Dr Kekunnaya added.
Ramesh Kekunnaya: drrk123@gmail.com
implantation in infants with congenital cataracts is safe, but decision must still be made on a case-by-case basis. Roibeard Ó hÉineacháin reports
IOL implantation can be considered even in selected babies who are less than six months of age
Ramesh Kekunnaya MD, FRCS, LV

The Artisan (Ophtec) iris-fixated intraocular lens appears to be a safe and effective option for the refractive correction of aphakia in children with insufficient capsular support, reported Marije L Sminia MD, PhD, at the ESCRS/WSPOS joint symposium during the 38th Congress of the ESCRS.

Dr Sminia, Noordwest Ziekenhuisgroep/ Amsterdam University Medical Center, noted that a primary concern with the anterior chamber IOL is its potential to induce endothelial cell loss, especially in children because of their long-life expectancy. However, research suggests that endothelial cell loss remains within acceptable limits over time in paediatric patients who undergo implantation of the lens as children, she said.
She and her associates conducted a retrospective study with a follow-up of 8.9-to-12.7 years involving 33 eyes of 25 children who underwent implantation of the Artisan lens. The study showed that in 20 bilateral cases there was a normal mean endothelial cell count at four-to-11 years of follow-up. But there was also a large range in endothelial cell loss and two eyes were outliers, one of which had two traumatic IOL dislocations, the other of which had no predisposing factors.
Dr Sminia noted that over 10-to15 years of follow-up there was no difference between the endothelial cell loss in four eyes of Marfan syndrome patients and that of 29 control eyes from Marfan syndrome patients without IOLs. However, the eyes with Artisan IOLs had an abnormal morphology of the endothelial cells, higher coefficient of cell size variation and lower number of six-sided cells.
Among patients that underwent unilateral implantation of the Artisan lens, there was no difference in endothelial cell loss between fellow eyes and eyes with the IOL in six nontraumatic cataract cases. However, among three eyes with traumatic cataracts, endothelial cell density decreased by 41%.
A recent prospective cohort study supported the findings of her centre’s study, she said. It showed that over a mean follow-up period of 39.3 months, there was a mean total endothelial cell loss of 18 % and a mean annual endothelial cell loss of 5.04% in 21 eyes of 12 children who underwent implantation of the Artisan lens for ectopia (Catala-Mora et al. 2017 Acta Ophthalmologica).
She added that some studies suggest that retropupillary fixation of the Artisan may have advantages in terms of endothelial cell loss. However, there have been no comparative studies in paediatric patients, and studies in adults have yielded contradictory results.
Marije L Sminia: m.l.sminia@nwz.nl...over 10-to-15 years of followup there was no difference between the endothelial cell loss in four eyes of Marfan syndrome patients
Marije L Sminia MD, PhD
Computer games and other treatments employing a binocular approach may provide better outcomes than patching in terms of visual acuity of the affected eye, while also mildly enhancing stereoacuity and reducing interocular suppression in amblyopia patients, Krista Kelly PhD told the 2020 WSPOS Virtual Meeting.
“Normal visual development requires equal input from the two eyes so connections can be formed that combine this information in the brain; the key is that both eyes must work together during development,” said Dr Kelly, Retina Foundation of the Southwest, Dallas, Texas.
She noted that amblyopia has traditionally been treated as a monocular disorder. She pointed out, however, that while patching is effective, 40% of patients who undergo the treatment fail to achieve normal visual acuity and 19-to-50% of those who do will regress. Normal binocularity and stereoacuity is rarely restored.
Research has shown that decreasing felloweye contrast vision reduces suppression of the amblyopic eye, suggesting that amblyopic patients have a structurally intact binocular visual system. Based on that research, Dr Kelly and her associates have been investigating amblyopia treatments that rebalances the contrast between the two eyes. She highlighted a randomised study her team conducted that compared outcomes between patching and the use of a videogame called Dig Rush, wherein anaglyph glasses provide high-contrast video to the amblyopic eye and lowcontrast video to the fellow eye. It showed that at two weeks, children in the Dig Rush group had 1.5 lines improvement in their amblyopic eye, which was double that seen with patching at 0.7 lines. In fact, after four weeks, almost 40% in the Dig Rush group achieved normal vision.
More recently, studies using his approach have also shown mild improvements in
stereoacuity and reductions in interocular suppression, showing that contrast rebalancing can improve binocularity typically impaired in amblyopia.
Multiple randomised clinical trials have also shown significant improvements in visual acuity from baseline using this kind of treatment. However, unlike the Retina Foundation’s study, the studies did not show superiority of binocular treatment over patching. The failure to show a superior outcome in those studies may have been due to the older age of patients, intractable amblyopia after years of patching treatment and a higher proportion of patients with strabismus.
Meanwhile, research into binocular approaches in treating amblyopia is continuing at centres around the world, using virtual reality, iPads and other tablets with games and movies that manipulate contrast and also use perceptual learning and three-dimensional imaging to address stereoacuity deficits.
 Krista Kelly: kkelly@rfsw.org
Krista Kelly: kkelly@rfsw.org
Delaying intraocular lens (IOL) implantation in children with congenital cataracts until refraction has stabilised can provide a better refractive outcome than primary surgery, according to a 10-year follow-up study of patients in in the Infant Aphakia Treatment study (IATS), said Scott R Lambert MD, Stanford University School of Medicine, Palo Alto, California, US.
“Fewer than half of children randomised to aphakia in the IATS underwent secondary IOL implantation. Delaying 1OL implantation to an age of five or more years was associated with lower refractive error at age 10.5 years,” Dr Lambert told the ESCRS/WSPOS symposium during the 38th Congress of the ESCRS.
The IATS study is a 12-centre clinical trial involving 114 infants with unilateral congenital cataract who were randomised to undergo cataract surgery either with or without IOL implantation at ages ranging from four weeks to seven months. Secondary IOL implantation was only allowed in children below 4.5 years of age if they were contact lens intolerant, Dr Lambert said.
He noted that at 10.5 years, 30 of the 57 children in the aphakia group remained aphakic and 24 had undergone secondary IOL implantation. The median age at second IOL surgery was 5.4 years (range 1.7 to 10.3 years). A further two patients were lost to follow-up, and one had phthisis bulbi.
Dr Lambert noted that there was no significant difference in median best-corrected logMAR visual acuity between those who remained aphakic (0.8, range 0.1 to 2.9) and those who underwent secondary IOL implantation (0.9, range 0.2 to 1.7). However, for eyes undergoing IOL implantation after the 4.5-year study visit, the mean refraction at age 10.5 years was significantly better, at -3.2D (range -9.9 to 1.1D), than in eyes that underwent primary IOL implantation at -5.5D (range -26.5 to 3.0D) (p=0.03).
To illustrate the good results that can be achieved with aphakia, Dr Lambert presented a case study of a congenital cataract patient who underwent lensectomy at six weeks of age. The infant was first fit with +29.0D Silsoft contact lens and switched to a silicone hydrogel lens at five years of age. At age 16 years, the patient had a best-corrected visual acuity of 20/20 in both eyes. She had a refraction of +14D in her aphakic eye, in which she wore a +18D contact lens. In addition, she was orthotropic and had high-grade stereopsis of 40 seconds of arc, he said.
Scott R Lambert: lambert7@stanford.eduThe patient-reported outcome is linked to clinical data in EUREQUO. This enables better knowledge of indications for surgery and o ers a tool for clinical improvement work based on the patients’ outcome.
Delaying IOL implantation provides a better refractive outcome.
Fewer than half of children randomised to aphakia in the IATS underwent secondary IOL implantation
Scott R Lambert MD
Around half of the world’s blind population could have their vision restored if the necessary training and resources were made available for the elimination of blindness due to cataract, asserts Prof Serge Resnikoff MD, PhD, President and Chair of Organisation pour la Prévention de la Cécité (OPC), Paris, France.
“Keeping in mind that cataract accounts for between 40-to-50% of all causes of world blindness and the vast majority of preventable blindness, the priority is to do much more cataract surgery. That is where the fight has to take place,” Prof Resnikoff told the 38th Congress of the ESCRS.
He noted that if using a visual acuity of 3/60 as the threshold of clinical blindness, there are roughly 17 million people that are in urgent need of benefiting from cataract surgery. Lowering the threshold of visual disability to 3/18 raises that number to roughly 100 million. At present, only 20-to-25 million surgeries are performed worldwide.
The vast majority of people who are blind from cataract live in Asia, particularly in China, India, Southeast Asia and Oceania. These are places where most people live and where the ageing of the population is progressing at a very high rate.
South Asia (India)

Southeast Asia and Oceania
East Asia (China)
Sub-Saharan Africa
Latin America and Caribbean
Nor th Africa and Middle East
High-income
Central & Eastern Europe and Central Asia
has a relatively small number of people in urgent need of cataract surgery because of its much younger population.
In addition to the need for an increased volume of surgeries is the need in many places for improvements in the quality of cataract surgery, Prof Resnikoff said. A recent review of cataract surgery outcomes in 19 mainly lower- and middle-income countries showed that 20-to-40% of
Asia
in infrastructure, equipment, consumables and human resources, especially welltrained ophthalmic surgeons, he noted.
Prof Resnikoff maintained that conquering cataract blindness is not an over-ambitious goal. He noted that just as surgical techniques have improved, so has surgical training, making it much easier to quickly train surgeons to perform quality cataract surgery.
He also pointed to the example of trachoma, which was for centuries the world’s leading cause of blindness but which through a concerted global effort has
Norlase has been granted the European CE Mark for the LION™ green laser system, which the company says combines the Keeler Vantage Plus diagnostic indirect with Norlase’s groundbreaking compact laser technology into one device.
“We are excited to greet 2021 with this important milestone,” said Oliver Hvidt, Norlase President and CEO. “With CE Mark approval for LION, following the recent establishment of our strategic distribution partnerships, we have expanded our reach and will arm even more ophthalmologists with innovative laser solutions to optimise practice efficiency and workflow,” said Mr Hvidt. www.norlase.com
VSY Biotechnology GmbH has launched Protectalon Duo. “Protectalon DUO Kit demonstrates VSY’s commitment to Ophthalmic Surgery Eye Care Professionals and will help to meet their OVD needs at different stages of cataract surgery with a single kit. It is available now for safe, fast and smooth surgery,” said a company spokesperson.
Protectalon DUO is a dual pack containing high filling volume of one unit cohesive (14mg/mL, 1.1mL) and one unit dispersive (30mg/ml, 1.1ml) NaHA-based OVDs, providing reliable anterior chamber maintenance with exceptional cohesivity and superior endothelial cell protection, according to VSY.

The product has CE and it is now available in Europe, said the spokesperson. “VSY Biotechnology GmbH is an innovation-driven company with its progressive R&D activities in ophthalmology, orthopaedics, aesthetics and biotechnologic drugs. VSY Biotechnology focuses on developing, designing and manufacturing superior, state-ofthe-art products to serve doctors, patients and consumers beyond their expectations,” he said. www.vsybiotechnology.com
NIDEK has announced the launch of the B-scan Denoising Software for the NIDEK OCT series.
“This software converts a B-scan retinal OCT image to a high-definition image by a denoising technique using deep learning,” said a NIDEK spokesperson. “A large data set of images that are each averaged from 120 images are used as teaching data for deep learning to create clear retinal images comparable to images generated by averaging 120 images,” he said. “Different from image averaging, which is an ordinal technique to create clear B-scan images, this unique denoising technique does not require capturing multi-frame images to remove speckle noise. This feature provides better patient flow and increased patient comfort. Providing exquisite image quality, this software is particularly useful when capturing multiple B-scans for wide area screening,” said the spokesperson. www.nidek-intl.com
EVEON and Laboratoires Théa have announced a partnership that will assist both companies in the development of innovative medical devices.
“We are delighted to be able to join forces with EVEON. This partnership is part of our continued commitment in favour of innovative solutions for the care of eye disorders. Connected medical devices are a revolution that must be made available to eyecare professionals for the greater benefit of their patients,” said Jean-Frédéric Chibret, President of Laboratoires Théa.
“This joint endeavour with Théa Open Innovation is a pledge of confidence and commitment. We are proud to contribute together to the development of new-generation devices that respond to the challenges of modern medicine, which seeks to become more personalised, more responsive to each patient’s needs,” said Vincent Tempelaere, CEO of EVEON. www.eveon.eu, www.laboratoires-thea.com
IRIDEX has reported that MicroPulse Transscleral Laser Therapy (TLT), which is performed using the IRIDEX Cyclo G6® Laser System and MicroPulse P3® Delivery Device, has been included in the European Glaucoma Society (EGS) Terminology and Guidelines for Glaucoma. The EGS guidelines represent recommendations on the diagnosis and management of glaucoma to standardise practice within the European Union. The new guidelines, the Society’s 5th edition, were presented at the Annual EGS Meeting on 12-13 December 2020.
“We are very encouraged with the broadening recognition of MicroPulse TLT in the ophthalmic community,” said David Bruce, CEO, IRIDEX. www.iridex.com
Aerie Pharmaceuticals has announced that the European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending approval of the marketing authorisation application (MAA) for Roclanda® (netarsudil and latanoprost ophthalmic solution) 0.02%/0.005%.
“We are delighted that the CHMP has adopted a positive opinion for Roclanda®,” said Vicente Anido, Jr., Ph.D., Chairman and Chief Executive Officer at Aerie. Roclanda is currently marketed as Rocklatan® in the United States and is indicated for the reduction of elevated intraocular pressure in patients with open-angle glaucoma or hypertension. www.aeriepharma.com

Disturbed, I noticed the discomfort one evening after work; numbness, tingling, mild weakness. A little cramping pain. My hand, along the side and down towards my little finger, was not feeling right. What was causing it? Would it progress? I fast-forwarded, seeing myself developing a progressive weakness that limited the function of my hand, affecting my ability to do surgery. Eventually, ending my operating completely. I recalled one of my trainers, Shivona Chetty, had suggested that it was wise to have a nonsurgical area of practice as a backup – just in case something unfortunate happened to stop you from operating. Her specialty is oculoplastics, but she also has a non-surgical area of practice, neuro-ophthalmology. I had felt that the issue was unlikely ever to come up, so I had not given it much thought, as I looked around and saw spry ophthalmologists in their 60s keeping up busy surgical practices. So these new symptoms were a little shock. I slept on it, and the next morning my hand felt back to normal. I forgot about the twinges then...
Dublin had by now entered a higher tier of lockdown, but I was kept busy, on my glaucoma rotation. It was starting to feel like glaucoma could be straightforward.
Dublin had by now entered a higher tier of lockdown, but I was kept busy, on my glaucoma rotation. It was starting to feel like glaucoma could be straightforward. The patients coming in under the glaucoma umbrella were subject to the same basic questions – how far were they from their target intraocular pressure? Was the angle open or closed, and were there signs of progression or not? The answers to these questions guide the management decisions, and narrow down the suite of treatment options to offer the patient. But this, it turned out, was just the routine work, the everyday sorts of problems. More and more, in the tertiary referral service, there were stickier cases coming in. Aqueous misdirection, persisting with pressures in the 40s, even after pars plana vitrectomy. Complex anterior segment dysgenesis in children, when the risk of vision loss, but also the risk of surgery is high. As well as taking in the decision-making principles in the clinic, and learning about more thorny glaucoma problems, I was getting trained in the surgeries too.
Trabeculectomy, I discovered, looks easier than it actually is. Fashioning a scleral flap, not too thin, and certainly not too thick, when you have about 500 microns of tissue to work with is challenging. Scleral flap sutures must be placed at
just the right tension – not so tight that there is no flow, but not so loose that the eye will be too soft. And then when you’re happy with your scleral flap closure, ready to relax, you still have the conjunctiva left to deal with. Prior to this, I had felt that I knew how to suture. I was happy with my skills honed doing squint and oculoplastics. But I quickly discovered that microscopic suturing was different, as I placed stitch after stitch of 10-0 nylon, more slowly, less smoothly than I would like. This was a skill I had better work at.
Alongside the glaucoma in clinic, we also see general patients, including medical retina. One man I met in clinic had a central retinal vein occlusion. I was puzzled about what the aetiology could be. He was a builder in his 40s, and reported being healthy, no medications. He played football and had exercised regularly until recently, when chest pains had stopped him from pushing himself too hard. He said the pains had started in the months after he had been diagnosed with COVID. Investigations had shown signs of myocarditis. Long COVID was something I had vaguely heard about, but my impression had been that it was something like post-traumatic stress disorder. I had never imagined we would be seeing it in the eye clinic.
Meanwhile, after my cycle home one evening, my hand developed the unpleasant weak, numb sensation again. I said it to my husband this time. We decided I should try to figure out what was going on, so I looked it up. Quickly scanning the possible causes of my symptoms, I sighed with relief after a few minutes research. One of the top hits was ‘Cyclist’s Palsy’. I read that gripping handlebars can cause pressure on the ulnar nerve in the wrist, leading to nerve compression. The next morning I paid more attention to my grip on the handlebars, making sure not to over extend my wrists, keeping them in a more neutral position. I realised that the wintry conditions were causing me to grip too tightly as I cycled to and from work in the cold, dark mornings and evenings. My skiing mittens came out of storage. The weakness and tingling have not happened since. I am delighted – you do not realise what you have till it’s gone – or maybe till you fear you might be at risk of losing it.
Unexpected pains can lead to serious reflections. Clare Quigley reports
• Reduced Registration Fees for ESCRS Congresses
• Subscription to Journal of Cataract & Refractive Surgery
• Access to ESCRS Grants, Bursaries and Research Awards
Access to:
• ESCRS iLearn
Online CME accredited interactive courses
• ESCRS On Demand

Online library of presentations from ESCRS Congresses
• EUREQUO
European Registry of Quality Outcomes for Cataract and Refractive Surgery
• ECCTR
European Cornea and Cell Transplantation Registry
Due to the COVID-19 virus, a number of meetings have been cancelled or rescheduled. The information in this calendar is correct at the time of going to print; please check the meeting website or email the conference organisers to confirm all meeting dates.
FEBRUARY 2021
25th ESCRS Winter Meeting
Virtual Meeting
19 – 21 February www.escrs.org
APRIL
6th San Raffaele OCT & Retina Forum
Virtual Meeting
9 April: 17.30 – 20.00
23 April: 17.30 – 20.00
30 April: 17.30 – 20.30
https://www.octforum2021.eu/
American Association for Pediatric Ophthalmology and Strabismus 2021 (AAPOS 2021)
Virtual Meeting
9 – 11 April https://aapos.org/meetings/ meetings-future
MAY
ARVO 2021
Virtual Meeting
1 – 7 May https://www.arvo.org/
12th Annual Congress on Controversies in Ophthalmology: Europe (COPHy EU)
Virtual Meeting
21 – 22 May
http://cophy.comtecmed.com/
JUNE
AECOS 2021
European Symposium
3 – 6 June
Florence, Italy
https://aecosurgery.org/ 2021-european-symposium/
46th Meeting of the European Paediatric Ophthalmological Society (EPOS)
17 –19 June
Copenhagen, Denmark
https://epos2021.dk/

JULY
AECOS 2021 Summer Symposium
15 – 18 July
Utah, USA
https://aecosurgery.org/ 2020-summer-symposium/
33rd APACRS–
SNEC 30th Anniversary Joint Meeting
29 – 31 July
Suntec City, Singapore
https://apacrs-snec2020.org/
ASCRS Annual Meeting 2021
13 – 17 August
San Francisco, USA
https://ascrs.org/news/ ascrs-news/2021-ascrs-annualmeeting-update

39th Congress of the ESCRS
27 – 30 August
Amsterdam, The Netherlands
https://www.escrs.org/
49th European Contact Lens and Ocular Surface Congress (ECLSO)
3 – 4 September
Paris, France
https://www.eclso.eu/
EURETINA 2021 Virtual
10 – 12 September
https://www.euretina.org/
Joint event: 14th National Congress of Bulgarian Society of Ophthalmology and Conference
Innovation in Ophthalmology 2021
14 – 17 October
Borovets, Bulgaria
https://mareamedical.com/en/events/ ophthalmology_oct_2021_english/
AAO 2021
12 – 15 November
New Orleans, USA
https://www.aao.org/ annual-meeting
SOE Congress 2021
2 – 4 December
Prague, Czech Republic
https://soe2021.soevision.org/

20 FEB
Sponsored Symposium
Saturday February 20th | 1.00 - 2.00 PM CET
AcrySof® IQ Vivity® - Novel technology broadens Patient access to Presbyopia Correction
Join us at Alcon Advanced Technology PCIOL Symposium as we discuss the AcrySof® IQ Vivity® with X-WAVE™ technology - the first of its kind non-diffractive presbyopia correction IOL with monofocal simplicity1-7
Listen in as guest moderator Prof. Thomas Kohnen and esteemed KOLs from around the world share their personal Vivity® IOL experiences and discuss the evolution of presbyopia correction technology.
Moderator: Thomas Kohnen (Germany)
Saturday February 20th | 4.45 – 5.45 PM CET
Experts Discuss Latest Innovations from Industry 20 FEB

During this session, short updates will be presented by various companies in the industry. Alcon will present our latest innovation: AcrySof® IQ Vivity® IOL
Speaker: Kieren Darcy (United Kingdom)

