ESCRS CONGRESS PREVIEW



















ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes ISSN 1393-8983










Aglance at our table of contents confirms the incredible research ongoing in every area of clinical ophthalmology, with new treatments for presbyopia, corneal disease, glaucoma, and retina. You will also see reports of the moment on sustainability, battlefield surgery, and telemedicine screening methods born of necessity from the ongoing COVID-19 pandemic.
A year ago, the annual meeting to be held in Amsterdam was in jeopardy, with COVID pandemic travel restrictions an apparent obstacle even to those who wanted to come. Almost miraculously, case numbers dropped, and the conference went forward. A universal feeling among those that attended was it was well worth the effort and that it felt good to be able to meet friends and colleagues in person to learn and grow. This year, we anticipate a return to form at our annual Congress in Milan. (See related articles for a full menu.)
Sustainability has become a priority of the ESCRS and will be a theme at the Congress. Conferences have a major carbon footprint, and ours is no exception. The ESCRS is now working towards making our meetings carbon neutral with a company focused on sustainability and congresses. They are helping us understand what we are doing and how we can reduce our carbon footprint.
The Congress will also see the prize awarded for this year’s John Henahan Essay Contest. Three essay entrants in this issue show the growing awareness of the problems of climate change and sustainability as well as the potential of the medical world to improve its practices. The essays make clear the painful fact of medical waste and provide discussion for the ways to change for the better.
Another step in our recovery from the COVID shutdown will be the return of the in-person Practice Development programme
in Milan. It includes a series of workshops looking at components that will help ophthalmologists improve their skills in marketing, economic management, staff development, retention, and effective leadership. After finishing the programme, ophthalmologists should be able to make the best use of their resources for the benefit of their patients.

Finally, the ESCRS has taken several steps to help our Ukrainian colleagues as part of our ongoing response to the Russian military attack on Ukraine earlier this year. First, all Ukrainians have been offered free registration to Congress—and the number expected to attend in person is around 300. We will give out approximately 23 observerships and some 7 travel grants at the Congress. The travel grants are primarily for older surgeons who have suffered particular losses or been under particular pressure. The observerships— selected by an ESCRS panel—will all be for trainees. Among the observerships, we will send two trainees to Auckland, New Zealand, and one to Utah, United States.
If we cannot find places for most of the observerships this year, we shall offer those trainees 1,000 euro to travel to Milan as a very good secondary option.

We hope to see you in Milan. If you cannot make the trip, please join us for the virtual sessions.
Let’s keep going and look forward to better times.




Noel Alpins (Australia), Bekir Aslan (Turkey), Roberto Bellucci (Italy), Hiroko Bissen-Miyajima (Japan), John Chang (China), Béatrice Cochener-Lamard (France), Oliver Findl (Austria), Nino Hirnschall (Austria), Soosan Jacob (India), Vikentia Katsanevaki (Greece), Daniel Kook (Germany), Boris Malyugin (Russia), Marguerite McDonald (US), Cyres Mehta (India), Sorcha Ní Dhubhghaill (Ireland), Rudy Nuijts (The Netherlands), Leigh Spielberg (The Netherlands), Sathish Srinivasan (UK), Robert Stegmann (South Africa), Ulf Stenevi (Sweden), Marie-José Tassignon (Belgium), Manfred Tetz (Germany), Carlo Enrico Traverso (Italy)
Sustainability has become a priority of the ESCRS and will be a theme at the Congress. Conferences have a major carbon footprint, and ours is no exception.ESCRS PRESIDENT Paul Rosen José Güell

CONGRESS.ESCRS.ORG
The following essays were runners-up in this year’s ESCRS Henahan Prize Essay Competition. Writers were asked to address the question, “What can the field of ophthalmology do to meet the pressing challenges of climate change, sustainability, and social equity?”
Change. The only constant in life, or so the saying goes. As I reflect on what this simple word means, I can’t help but realise that a lot has changed recently. For one, the climate is changing. While the climate crisis and loss of biodiversity affect us all, they have a disproportional impact on marginalised and disadvantaged communities. The current war in Ukraine, rising energy, and food prices further exacerbate these social inequalities.
So, what can our humble specialty really do to address these pressing issues?
Enter the Triple Bottom Line (TBL). Though not without its critics, this framework has been implemented in the business and accounting world for years. Now, the time has come to introduce the concept to ophthalmology. At its core, the TBL urges companies to equally value the 3 Ps: profits, people, and the planet. As ophthalmologists, we need to re-assess our practice to ensure it is not only doing well by our patients and fiscally sound, but similarly appreciates the environment. In order to achieve this goal, a systems change is needed, so that the TBL does not merely become another popular slogan like “carbon neutral” or “zero waste”. Of course, a systems change can be a daunting undertaking—perhaps not dissimilar to the process of first learning cataract surgery. But, just like phacoemulsification, it can become less overwhelming by adopting a systematic approach and breaking it down into individual steps.
First, the Planet: Let’s take a closer look at improving ophthalmology’s ecological footprint.


We should start by getting the basics right. Switching off lights, computers, visual field, and OCT machines, when not in use, are simple, yet often forgotten measures to improve energy efficiency. After reducing our overall energy consumption, the next step is to transition to renewable energy sources. This transition will vary depending on the practice type and location and is certainly not without its challenges. However, we should not forget that healthcare is a large industry with significant collective purchasing power. By working with industry and governments, we can influence a change in practice that may initially seem almost impossible to achieve. Recently, the anaesthetic department at my hospital successfully managed to reduce the use of desflurane, saving about 30,000 kg CO2 per month. It is but one example of a recent paradigm shift in healthcare, showing that collaboration with industry leaders and sustainability experts can make more environmentally friendly alternatives a reality. A comparable problem in ophthalmology is our incessant use of single-use and non-recyclable plastic products. Sterility and convenience are frequently named reasons for our reliance on these items. Yet, alternatives to single-use non-degradable plastic are already used in other sectors with stringent hygiene requirements such as the food industry. Within the field of ophthalmology, examples of more sustainable practice also exist. Aravind’s lifecycle assessments, for instance, show that high-quality, low-carbon, low-waste cataract surgery is not just possible but can become the norm. Now the time has come for the ophthalmic community to not only share best surgical practices but also champion best sustainable practices.
Second, the Profits: Let’s turn our attention to the financial impact of these actions. There is no question that transforming our clinical practice requires an initial financial investment. Our specialty has an established history in investing in new tools and equipment to advance patient care. Buying phaco machines in the ’70s and ’80s seemed like a ludicrous and expensive idea to some. Nowadays, the initial scepticism is hard to comprehend. Challenging the status quo by switching to renewable resources, reducing waste and CO2 emissions will ultimately reduce our bills. Given the current energy prices, we may already regret not having transitioned sooner.
Finally, the People: Let’s consider our social responsibility. As ophthalmologists, we can advocate for disadvantaged communities, and highlight environmental, health, and social injustices where we see them. On social media, American ophthalmologist Dr Will Flanary, better known by his Twitter handle Dr Glaucomflecken, uses humour and unicorn props to shine a light on the idiosyncrasies and inequalities of medical education and the healthcare system. You may ask, what has an ophthalmologist on TikTok to do with tackling environmental and societal issues? Well, he gets people talking (and laughing). Raising awareness is the first step of meaningful change. You can’t change what you don’t acknowledge. As the recent EuroTimes edition on sustainability shows, ophthalmologists have started to talk about these issues. Many have taken practical steps to reduce their environmental footsteps. Yes, more collective action is needed, but it is a start. In the words of American civil rights activist Maya Angelou, “do the best you can until you know better. Then when you know better, do better”. I strongly believe that, as ophthalmologists, we can—and will—do better for the future of our patients and our planet.
The metallic clang echoes in the quiet serenity of the operating theatre as the eyelid speculum slips out of my hand and drops onto the floor.
I glance sheepishly at my scrub nurse colleague and mouth an apology.
“Not to worry,” she smiles back, “we will get you another. Which speculum would you like?”
“One of these disposable ones would be fine, thank you,” I reply.
I put the second speculum in place and continue with my cataract surgery operation—not sparing any further thoughts on the eventual fate of the two disposable speculums that I have used in this case.
Since commencing ophthalmology residency training, I confess that I had not spent much time pondering on the disposal of the surgical equipment (and its packaging) that I use every week. As trainees, we focus on training to become polished ophthalmologists, inadvertently taking for granted the apparent endless supply of surgical stock which we almost nonchalantly discard after use. We keep count of how many ocular surgeries we perform. But what about the number of surgical drapes that we have used? The array of instruments? How many of them are ever used again? How are they disposed of and what are the consequences?
We may be vaguely aware of the potential effects on sustainability and climate change. After all, they do occasionally come up as examination questions, no less. But such notions remain a distant whisper in the recesses of our minds, drowned out by busy clinics, on-calls, post-graduate examinations, research projects, and teaching roles.

Sometimes it is easy to lose sight of the bigger picture.
The emergence of COVID-19 underlined just how complacent we were as a human race to the dangers of a worldwide crisis. In contrast to the immediate effects of infectious diseases, the effects of climate change are more insidious and can take generations to culminate into natural disasters that can affect us all. Hence, as ophthalmologists, it goes without saying we must all act now to make the world a better place for future generations. As a father to a toddler, keeping the dangers of climate change at bay has never been so imperative, and dare I say it, so personal.
It is almost staggering that during an average year as a UK trainee performing cataract surgery, my carbon footprint is about 10 tonnes CO2eq, which is the equivalent of several return flights to the Big Apple from London! Promoting better practices to deliver a sustainable ophthalmology service which minimises negative effects on climate change, as well as catering for all our patient groups is essential. And educating ophthalmology trainees early may be the key for effective progress in the long run. In the UK for example, the GMC guidance for new junior doctors emphasises the importance of sustainability in healthcare. Incorporating compulsory teaching on climate change and healthcare and making participation in “greener ophthalmology” or “sustainable healthcare” projects mandatory, will leave ophthalmology trainees better prepared and more motivated to bring forward positive change. Offering opportunities for research in these fields will
also encourage trainees to take more active roles and make a difference on a larger scale.
We have all encountered patients in the cataract post-op clinic who anxiously seek a date for their second eye surgery. And at times, we have all wondered whether those patients would have made suitable candidates for immediate sequential bilateral cataract surgery (ISBCS). There is growing evidence on the safety and refractive outcomes of ISBCS. Performing more ISBCS cases can reduce patient hospital visits and their subsequent carbon footprint. I was pleased to present the findings of our time and motion study at the winter ESCRS meeting where we found that performing consecutive ISBCS cases under local anaesthesia can potentially lead to a more efficient OR, with more cases performed per list compared to lists with only unilateral eyes. Making more efficient use of the operating room therefore has potential for significant improvements in service provision.
Conferences are one of the yearly highlights for all trainees where we attend lectures from experts, keep up to date with emerging research, meet friends and colleagues, and occasionally treat ourselves to the odd freebies on offer! However, the option of hybrid conferences allows us to tune in virtually and limit our carbon footprint, not to mention leaving us with a healthier bank balance in the process!
Over the past two years, I have learnt to appreciate the role I can play in contributing to a more sustainable ophthalmic healthcare system which can cater to a diverse patient group. Educating myself on the subject matters has been an important turning point. Emphasising the importance of these issues in ophthalmology residency programs for the future generations of trainees can contribute to a better and greener future.
Khayam Naderi MD is a ST5 Ophthalmology Trainee at Western Eye Hospital Imperial College Healthcare Trust, UK. kaynad03@gmail.com
Glaucoma, a chronic, silent, and asymptomatic condition at its onset that becomes symptomatic as it progresses and has an uncertain prognosis when risk factors are not well controlled. Glaucoma, a condition that may lead to irreversible changes in quality of life and loss of vision worldwide.
Does it sound familiar? Now replace the term glaucoma for climate change. It could easily do, right? Could we use, then, our model in the fight against glaucoma to prevent the discouraging results of climate change?
“The eyes are useless when the mind is blind”
—Mark VenturiniEarth’s climate has changed throughout history and has been doing so for hundreds of years and was invisible to the human eye until a few decades ago. Noticeable changes are present nowadays and will not revert to their starting point because, like in glaucoma, what is lost can rarely be recovered.
Therefore, the best we can currently do is to recognise and act on risk factors in order to gain sustainability and equal opportunities in a safe and healthy environment.
“Ophthalmology as a specialty needs to do its part in making a difference”

 —Dr Soosan Jacob MS, FRCS, DNB
—Dr Soosan Jacob MS, FRCS, DNB
According to “Health Care Without Harm Europe”, the health sector is estimated to account for 5% of European carbon emissions.
It is known that one cataract surgery equals driving a car for 500 km, and for each 100 km, two trees are lost. That makes a total of 10 trees depleted per cataract surgery. Imagine the forest destruction caused by nearly 4.5 million of yearly cataract procedures performed worldwide.
Have you ever realised how much sterilised packaging material is being used for one single patient? What about replacing the single packaging of each item with having all of them in a unique “custom pack”? Does eye surgery require covering the patient with multiple plastic layers? And what about the unused surgical supplies, where do they go?
The total carbon footprint of the first eye cataract surgery procedure in a patient equals 181.8 kg CO2eq, where the procedure itself accounts for more than half of the value.
Could we reduce emissions from patient travelling by implementing a telemedicine approach? Decrease the electricity emission by using renewable resources?
Furthermore, if we think about the intraocular lens (IOL) packaging, as described in the study of Morris et al., an IOL weighs less than 1 g, whereas the associated paper and plastic packaging weigh 64 g. This also includes a 70-page booklet in 11 different languages. Truth is, the IOL packaging is ruled by strict legislation, but that does not mean we cannot reach a consensus between governments and pharmaceutical companies, especially with them already being involved in carbon reduction strategies. Maybe the “less is more” rule should be applied here as well.
Coming back to glaucoma, life-long use of eyedrops is required for treatment. In recent years, preservative-free formulations are increasingly used, dispensed by single-dose vials instead of the classic multidose containers. Single-dose vials waste eight times more plastic and use nine times more energy for transporta-
tion than classic containers. A greener solution to this problem advocates moving from eyedrops to safe sustained-release drug delivery systems.
Development is integral to creating sustainability by balancing economic, environmental, and social equity. Environmental health is crucial for obtaining the prosperity of future generations. We should consider integrating the sustainability criteria into ophthalmology departments in order to decrease the emissions arising. By improving standards of care and sharing goals of responsible behaviour, we could contribute to sustainable development and social cohesion.
“There can be no Plan B because there is no planet B”
—Former UN Secretary-General Ban Ki-moon
Nowadays, the world faces some challenging times with both the pandemic and re-emerging of widespread political struggles. The COVID-19 pandemic has taught us among other things that the world’s slowdown had a positive impact on climate change, enriching us with a new perspective about giving rise to innovative sustainability strategies.
Technology has made medicine virtually available, education programmes have never been closer, and ubiquity of a common, invisible threat has never made us more aware of how small of a drop in the ocean we are. Could this experience ignite a new understanding of the common goal of humanity?
We, as ophthalmologists, have already recognised glaucoma as a silent thief of sight. Don’t you think it’s time to look at climate change in a similar way, as a silent thief of life? If so, then find the risk factors, ease the pressure they put on our pretty, blue-coloured ball, and mitigate the inevitable. Be the wind of change.

Slow or halt progressive keratoconus and help preserve your patients’ vision.

The iLink™ V corneal cross-linking platform comprises of proprietary VibeX® Rapid riboflavin and the ultra-violet A (UVA) light from the KXL® System used for the treatment of keratoconus.
The iLink™ V corneal cross-linking platform comprises of proprietary VibeX Rapid™ riboflavin and the ultra-violet A (UVA) light from the KXL™ system used for the treatment of progressive keratoconus.
Sunday 18 September | 08.30–18.00
Shareef Mahdavi, US
In this highly interactive and didactic workshop, Shareef Mahdavi will explain the importance of redefining the doctor-patient relationship by describing what patients really want and how ophthalmologists and their staff in public and private practice can lead their teams to create innovative and patient-centred practices.

Contributing panel: Paul Rosen, Sheraz Daya, Arthur Cummings, Daniel Kook, Pavel Stodulka, Kris Morrill, Julien Buratto, Amanda Carones
Monday 19 September | 08.30–18.00
TOPICS INCLUDE:
● The Art of Negotiation
● Building and Developing Your Private Practice

● Managing and Developing a Public Ophthalmology Department
● Who Owns Ophthalmology?
● Using Automation and Artificial Intelligence to Grow Your Practice
● Maximising the Patient Journey
● Why Young Ophthalmologists Need to Learn Business and Management Skills
● Sustainability in Ophthalmology— What Does It Mean for You?
● Ask the Experts
FOR THE FULL PROGRAMME, VISIT: https://congress.escrs.org/programme/

The ESCRS annual Congress returns to full strength in Milan, 16–20 September. After a yearlong diet of Zoom calls and virtual symposia, those attending the conference will now have a full menu of enticing in-person educational and social opportunities. You will find the main courses of the main symposia and clinical research symposia, along with a smorgasbord of educational courses and an abundance of videos, free papers, posters, and workshops.
The conference gets underway on Friday, 16 September, with several interesting offerings. At the top of the list would be the premier of iNovation, an ESCRS interactive symposium that looks to the future of ophthalmology. Sessions throughout the day will focus on the most urgent clinical needs and barriers to success in anterior segment care. The format includes expert panel discussions on key clinical and regulatory issues as well as presentations from many emerging companies, giving attendees a chance to see what’s in the pipeline and network directly with leaders in their fields.
Friday also includes three specialty-day sessions dedicated to Cornea, Paediatrics, and Glaucoma.
On Saturday, the opening ceremony for the Congress will highlight the ESCRS’s efforts to create a sustainable future for ophthalmology. This will include a thought-provoking talk on sustainability in cataract surgery by Dutch ophthalmologist Sjoerd Elferink, with some sobering facts but also some positive suggestions for addressing the global climate situation.
For the first time, the opener will also bring together the winners of the prizes for best poster, best video, and the Henahan Essay Contest. Béatrice Cochener-Lamard MD, PhD will then deliver the annual Ridley Medal Lecture, “How the digital world is entering our practice”.
The topics of subsequent main symposia during the conference will include “Demystifying IOL Optics”; “Fast track Cataract”; and “How Not to Be Surprised by Refractive Surprise”.
The clinical research symposia are always a must-see at the conference. Four sessions throughout the day on Saturday will take a closer look: “Digital Medicine—6 steps for a better future”; “Ocular tissue engineering, artificial Cornea”; “Advancement of IOL optics—how far can we go?”; and finally, “Gene Therapy”. The latter will cover gene therapy throughout the field of ophthalmology, including Stargardt disease, Fuchs’ and other corneal dystrophies, Leber Congenital Amaurosis-RPE65, and AMD.
Young ophthalmologists will also find plenty to keep them busy. The YO Programme has become an essential part of the conference. This year will look at the many challenges of learning phaco surgery. Each step in phaco surgery will be discussed by a leading clinician and accompanied by video cases submitted by young ophthalmologists—a format that has proven very popular at past meetings.
The associated YO session will closely examine the intersection between cataract surgery and other eye diseases, including ocular surface and eyelid disease, corneal ectasia, and endothelial dystrophy. Additionally, it will look between cataract surgery and other eye diseases following corneal transplantation and following refractive surgery.
The Practice Management & Development Masterclass takes place on Sunday. This will be a full day of presentations and discussions covering everything from business and management skills to AI and sustainability. A series of related workshops will occur the following day.
If you are unable to attend in person, you can attend many of the sessions virtually.
Amulti-segmented diffractive intraocular lens (IOL) produced very good visual acuity at all distances from far to near six months after implantation for cataract or clear lens exchange patients. The Precizon IOL (Ophtec, Netherlands) also did not produce bothersome glare or halos in most patients, reports Mike P Holzer MD, FEBO.
Unlike conventional multifocal IOLs that use concentric power rings, the Precizon IOL’s 11 overlapping segments, 6 for near and 5 for far, create a continuous transitional focus, Dr Holzer explained. In addition to reducing photic phenomena, it produces a wide range of vision that is not pupil size dependent and should be decentration resistant.i
In a prospective, multicentre, open-label study involving 118 eyes of 59 patients, of whom 90% had cataracts before surgery, mean uncorrected binocular distance visual acuity was -0.0043 logMAR, and uncorrected near VA 0.1954 six months after surgery. Mean uncorrected binocular intermediate VA was 0.1429 logMAR three months after surgery, Dr Holzer reported.
Looking at refractive outcomes six months after surgery, mean monocular spherical equivalent was 0.29±0.45 D ranging from -0.50 D to 1.50 D; mean cylinder -0.29±0.39 D ranging from -1.25 D to 0.00 D; and mean spherical equivalent 0.14±0.39 D. Achieved spherical equivalent was within 0.5 D of target for 84% of patients. A slight hyperopic shift led the surgeons to optimise the lens A-constant, Dr Holzer said.



The usable defocus curve was also wide, with mean binocular bestcorrected visual acuity -0.04 logMAR at distance, 0.15 logMAR at 1.5 D defocus, and 0.27 logMAR at -3.0 D defocus. All lenses implanted were non-toric. Preoperative mean cylinder was -0.66 D.
Patient-reported quality of vision also was good, Dr Holzer said. For glare, 90% of patients said they never or occasionally experienced it, and 86% said it was never or occasionally bothersome. For halos, 78% said they never or occasionally experienced them, and 84% said the halos were never or occasionally bothersome.
“All surgeries and postoperative outcomes were uneventful. The multi-segmented IOL provided good visual acuities at all
0,6 mm segments
1,4/2,6 mm zone

a good quality of vision,” Dr Holzer concluded.
i Clinical Opthalmology. 2021; 15: 2117–2126.
This research was presented at the 2022 ASCRS Annual Meeting in Washington, DC, US.
Mike P Holzer MD, FEBO owns and operates

Augenzentrum Prof Dr Holzer & Prof Dr Rabsilber in Weinheim and Mannheim, Germany, and is an adjunct professor at the Ruprecht-Karls-University Heidelberg, Germany. info@augenzentrum-holzer.de
40th Congress of the ESCRS congress.escrs.org
2022
MiCo, Milano Convention Centre, Milan, Italy
Alternating segments generate a wide range of foci with minimal glare and halos.
Anew extended depth of focus (EDOF) intraocular lens delivers excellent quantity and quality of vision, with reduced dysphotopsias and a high level of patient satisfaction, according to Gilles Lesieur MD.

“The new lens performed very well and compares favourably with other EDOF lenses we have implanted in recent years. Patient satisfaction is very high, with many patients achieving total spectacle independence and no visual symptoms at the three-month follow-up mark,” he said. Near vision correction for long reading activities is nevertheless often prescribed.
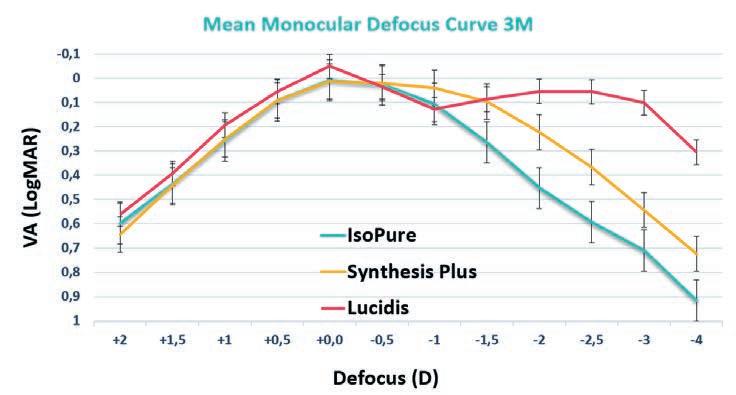
Dr Lesieur reviewed the refractive and visual results of the LUCIDIS IOL (Swiss Advanced Vision) lens and compared the outcomes with those of two other EDOF lenses—Synthesis Plus (Cutting Edge) and ISOPURE (BVI Medical)—implanted between 2018 and 2020.
“The LUCIDIS achieved the best results for near and far vision compared to the other EDOF lenses, with the Synthesis Plus performing best for intermediate vision,” he said.
Discussing the lens properties in more detail, Dr Lesieur said the LUCIDIS is a hydrophilic acrylic lens with a central aspheric element surrounded by an outer refractive ring. It has a closedloop haptic design, with a 6.0-mm optical diameter and a total diameter of either 10.8 mm or 12.4 mm, depending on the IOL model selected. A toric version is also available.
distance-corrected near visual acuity, 94% of patients implanted with LUCIDIS attained 20/32 or better compared to 47% for Synthesis Plus and 14% for ISOPURE. The results for light scatter were also statistically significant in favour of LUCIDIS and showed less light dispersion than with the other two EDOF models.
In terms of side effects and complications, Dr Lesieur said the safety profile of the lens, with around 1,000 lenses implanted to date, has been very positive overall.
“We did have a few instances of capsular folds and a very small number of patients who experienced disturbances in photopic far vision. While we initially thought the issue was related to pupil diameter, we now think it is caused by postoperative inflammation and it is usually resolved within a few months,” he said.
Correct sizing is another issue to be aware of with these lenses, Dr Lesieur advised.
The patented Instant Focus technology of the lens extends depth of focus characterised by a constant resolution and peak of light intensity. This peak of light is obtained through a constructive light wave interference concept generated by an aspheric surface in the centre of the lens. The resulting beam of light is called Pseudo-Nondiffracting Beam (PNDB), which maintains a constant resolution and light intensity on the retina.
Dr Lesieur’s study included 23 patients bilaterally implanted with LUCIDIS through an incision of 1.8–1.9 mm, with follow-up visits scheduled at one day, one month, and three months after surgery.

Defocus curve results showed LUCIDIS performed better than the other EDOF lenses in earlier studies, although the Synthesis Plus came top for intermediate vision. For corrected distance visual acuity, 100% of patients obtained 20/20 with LUCIDIS compared to 82% for ISOPURE and 79% for Synthesis Plus. For
“We had some capsular phimosis for the 124M model in smaller eyes with an axial length less than 21.5 mm and/or a white-to-white of less than 11.5 mm. We now try to avoid these particular implants for these smaller eyes. We also had a few isolated cases of lens rotation with the smaller diameter 108MT model, but unfortunately, it is difficult to screen these patients preoperatively to avoid such issues. The larger diameter IOL, combined with its non-polishing surface, shows excellent stability in the capsular bag, and patients are very happy with their outcomes overall,” he said.
LUCIDIS EDOF enters the field. Dermot McGrath reports
“The LUCIDIS achieved the best results for near and far vision compared to the other EDOF lenses...”
The IIIC (International Intraocular Implant Club) session moderated by Thomas Kohnen MD and Eric Donnenfeld MD at the annual ASCRS Congress in Washington, DC, featured a unique format-case presentation by a well-known speaker with corresponding tips and pearls from a second, interspersed with panel discussion by accomplished surgeons and thought leaders in the field.
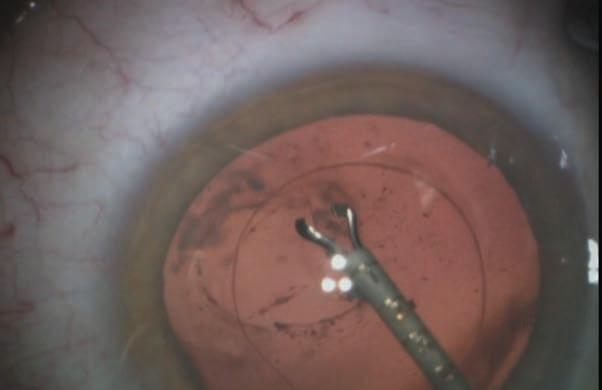
Abhay Vasavada MD began the session discussing posterior polar cataracts. He gave many important tips, such as the need for closed chamber techniques, preventing hydraulic pressure build-up, avoiding cortical cleaving hydrodissection, and maintaining an epinuclear cushion. He also discussed Vasavada’s inside-out hydrodelineation, femtosecond laser-created epinuclear cushions, avoiding forward movement of capsulozonular diaphragm, and bimanual I/A for a better valvular seal.
He noted difficult epinuclear shell removal is assisted by detaching it at multiple areas to create zones of communication between capsular space and anterior chamber, thus preventing hydraulic pressure build-up by allowing any trapped fluid to easily escape. It is important to inform the patient about the different nature of this cataract that may result in multiple interventions, second interventions, and possibly alternate techniques of IOL fixation, he emphasised.
Extreme care up to speculum removal is advisable as posterior capsular rent (PCR) may occur even at the end during stromal hydration, he added.
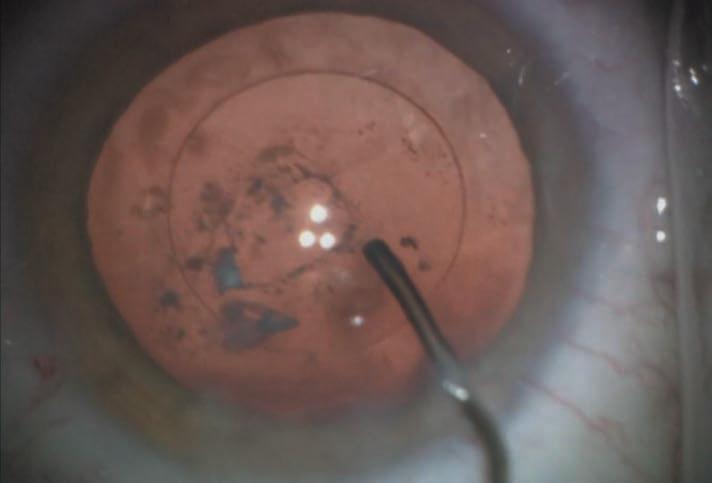
David F Chang MD presented a posterior polar cataract case with planned toric IOL that had a posterior capsule rupture (PCR). Insights offered by the panel included the advantages of early surgery while nucleus is soft, use of intraoperative-OCT or preoperative UBM to evaluate posterior capsule, and the use of the femtosecond laser to decrease nuclear manipulation. Other suggestions included Zepto-capsulorhexis for round and correctly sized rhexis in the eventuality of optic capture and careful surgery treating every eye as though there was a PCR. The panel also advised avoiding chamber fluctuations, desisting from nuclear rotation (which stresses the plaque’s connections with nucleus and epinucleus), using cross-chop and groove and split, viscoelastic to lift pieces, and flipping the epinucleus.
Epinuclear management is difficult in absence of hydrodissection. Instilling subcapsular viscoelastic just sufficient to define an epinuclear plane without going posteriorly can help. In Dr
the 2022 ASCRS Cataract Symposium
Chang’s case, the small PCR was converted to a posterior capsulorhexis to allow in-the-bag toric implantation and IOL rotation to desired axis.
To perform a posterior capsulorhexis, the capsular bag must be filled with enough OVD for the posterior capsule to be reasonably taut. Injecting a small amount of OVD through the posterior capsular defect can displace the hyaloid face further away from the rent. An advantage of the MST-Seibel capsulorhexis forceps is it can be inserted through a paracentesis site. This avoids chamber shallowing caused by placing forceps through the main incision.
IOL exchange was another topic of interest. Eric Donnenfeld showed his case of an unhappy diffractive multifocal IOL patient posted for explantation. The patient had undergone cataract surgery and YAG capsulotomy five and three years back, respectively. He stressed that early explantation (four to six weeks postoperative) is preferred to avoid severe anterior capsular fibrosis and haptic-bag adhesions. However, ascertain the IOL as the cause for visual problems prior to explantation and avoid YAG capsulotomy if the role of capsular opacification on visual complaints is doubtful.
IOL exchange alternatives, such as laser vision correction, glasses, or contact lenses, should be discussed if a refractive surprise is the indication for exchange, he advised.
Capsular fibrosis complicates delayed explantation. Pearls shared by the panel included using the femtosecond laser
to enlarge small rhexes; injecting viscoelastic into the AC, around the haptics, and behind the IOL to dissect and prevent vitreous loss; using a bevel-down 30-gauge needle to dissect fibrosis while injecting viscodispersive viscoelastic; bimanual removal of adhesion complexes; bisecting the IOL and manipulating out pieces; and amputating haptics caught in fibrosis.
The endbulb of the Alcon AcrySof® IOL’s haptics and notched edges on certain haptics make such IOLs more difficult to explant and, often, haptic amputation is safer. Vitreous loss can be expected in up to 90% of cases. Gain preoperative consent regarding possible need for vitrectomy and alternate techniques of IOL fixation, co-management with a retinal
surgeon, and greater risk of postoperative complications such as macular oedema, retinal detachment, glaucoma, and uveitis.
A preplaced trocar can act as a safety valve. The optic can be removed by folding the IOL within the eye, cutting it in half or 75% (Pacman technique) or by first preplacing a threepiece IOL as a scaffold. Bag stabilisation is required in case of zonulodialysis. If the entire bag is weak, it may be preferable to remove it completely.
Douglas Koch MD presented a case of myopic refractive surprise (-2.12 D spherical equivalent) in a +3.25 D hyperope (axial length 21.41 mm, shallow AC depth of 2.39 mm, lens thickness 5.19 mm, corneal diameter 11.49 mm). The Barrett Universal II, Holladay 2, and Hill-RBF 3 formulae all suggested a 28.0 D IOL.
An IOL exchange with 25.5 D IOL predicted by simple mathematical calculation [28 D–(2.12 x 1.2) = 25.5 D] and the Barrett RX formula improved uncorrected vision to 20/20. Postoperative ultrasound showed slightly anterior effective lens position (ELP) of 3.5 mm as cause for myopic error. The anatomically similar contralateral eye needed surgery, which raised the question of how best to adjust IOL power based on the outcome of the first eye.
Dr Koch followed the old rule of adjusting for half the refractive error—but an even greater refractive surprise of -2.6 D appeared in the second eye, resulting in a postoperative refractive error of -1.62 D. As with the first eye, a shallow AC (3.46 mm) was seen. The patient, fortunately, loved her monovision, he noted. The panel agreed that intraoperative aberrometry would not help in this case, though a light adjustable IOL would be of help.

Thanks to the streamlined measurement workflow and application-oriented overview screens you further improve your time efficiency. Plus, with tons of studies and a huge user community to support data validity, you are always on the safe side. Optimized workflows, satisfied patients and best possible clinical results are all achieved quickly and reliably and without long training periods.
No risk, just fun – the Pentacam® AXL Wave
www.pentacam.com/axl-wave
Don‘t miss the Satellite Symposium at ESCRS!
Saturday, 17th September 16:00 h, room Brown 2
Gerd U. Auffarth and Michael W. Belin
An interesting twist in the session was Warren Hill MD sharing his prediction for the second eye. The literature recommends different methods for handling the second eye in case of a refractive surprise: including adjusting IOL power by 50% based on deviation from target SE (as done in this case), measuring postoperative IOL position to improve ELP estimation, and finally doing a patient-specific lens constant adjustment or formulaspecific adjustment.
Dr Hill preferred the third option, when the lens constant is treated a surrogate for ELP. Theoretical formulae are forced to estimate the ELP, and their assumptions may not match the anatomy of a specific eye. This is especially common for high axial hyperopes where a small error in the ELP estimation may produce a discorporate refractive error.
Since the power of an implanted IOL is relative and not absolute—and in a two-lens system, the distance between the two lenses determines the total vergence—a formula ELP misestimation of only 0.5 mm in this case will produce an error at the plane of the capsular bag of 1.4 D.
Dr Hill explained the answer for the second eye, especially for high axial hyperopes with similar measurements between two eyes, was to adjust the original lens constant to allow the formula to be more accurate for the second eye. This technique seems to work best when the biometry for both eyes is symmetrical, he added.
To do this, the lens constant is adjusted on the biometer to duplicate the postoperative spherical equivalent of the first eye. A myopic refractive surprise will require a lower lens constant and therefore lesser IOL power. The IOL power for the second eye is then estimated using this new custom lens constant. Using this custom lens constant instead of a standard one would have correctly suggested an IOL exchange power of 25.5 D for the first eye and a 26.0 D IOL for the second eye instead of 28.5 D by the standard lens constant. Compared to the real-life outcome, a 26.0 D IOL would have still resulted in -0.84 D spherical equivalent error, but the patient would have benefitted from mini monovision.
This case nicely illustrated how the typical lens constant used by the ophthalmic community represents an average value based on pooled data—while for the individual case, such a lens constant may not be exact or even close. Yet there are limitations to this technique: It may still not be completely perfect (as in the example) due to an inability to correctly estimate postoperative ELP as well as a decrease in accuracy with greater amount of anisometropia and greater power of the IOL.
Dr Hill ended by reminding the audience to always remember to change the custom lens constant back to its original value on the biometer to avoid an unpleasant refractive surprise for future patients!
Eric Donnenfeld MD and Roberto Zaldivar MD presented the final topic of the Phakic Implantable Collamer Lens (ICL). A great pearl offered by Dr Zaldivar—who has vast experience with the EVO Visian ICL™—was that the CentraFLOW® has decreased the minimum AC depth required for implantation from 3.0 to 2.8 mm and possibly even lower by adjustment of vault. The central hole decreased the risk of anterior subcapsular cataract from hypovault, though risks associated with hypervault still remain. Another great tip shared was rotating the ICL (only in spheric IOls, not in toric IOLs) in case of excess vault from horizontal to vertical or oblique positions to obtain a reduction in vault by an average of 450 and 250 microns, respectively.
Soosan Jacob MD is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.
Eric D Donnenfeld MD is a Clinical Professor of Ophthalmology, New York University Medicine, US. ericdonnenfeld@gmail.com

Abhay Vasavada MD is Director of Raghudeep Eye Clinic and Iladevi Cataract & IOL Research Centre, Ahmedabad, Gujarat, India. icirc@abhayvasavada.com
David F Chang MD is a Clinical Professor at the University of California San Francisco, US. dceye@earthlink.net
Douglas Koch MD is Chair, department of ophthalmology, Baylor College of Medicine, Houston, Texas, US. dkoch@bcm.edu
Warren Hill MD is in private practice, Mesa, Arizona, US. hill@doctor-hill.COM
Roberto Zaldivar MD is President and Scientific Director, Instituto Zaldivar, Mendoza and Buenos Aires, Argentina. zaldivar@zaldivar.com
Small Incision Lenticule Extraction (SMILE) is an effective, stable, and safe procedure for treating myopia and myopic astigmatism, according to the results of a large-scale French study.

“Our study of a large cohort of eyes operated with SMILE confirmed it is an effective and safe refractive corneal procedure and provided a predictable and stable correction of myopia and myopic astigmatism with rapid recovery of vision quality postoperatively,” said David Donate MD.
While the results presented were slightly inferior to previous studies Dr Donate conducted, he said that was due to the inclusion of some initial patients treated with higher laser energy.
“The reduced energy settings of SMILE have definitely improved the outcomes and speed of postoperative visual recovery. We have also adapted our nomograms over time, which has improved the refractive results,” he added.
Dr Donate’s study presented the postoperative visual and optical results of 869 eyes treated at his clinic in Lyon, France.
“We had 2,744 eyes in total treated using SMILE. However, we removed 1,836 eyes lost to follow-up after one year and the first 5 eyes from the analysis because this represented the initial learning curve with SMILE. We also excluded 40 eyes with corrected distance visual acuity less than 20/20 and 20 eyes where the refractive target was different than the treatment plan. Another 4 eyes treated with a combination of corneal cross-linking (SMILE Xtra) were omitted,” he said.
The SMILE treatment parameters using the VisuMax® femtosecond laser (Carl Zeiss Meditec) included a lenticule diameter of 6.50 mm to 7.0 mm, cap thickness of 125 to 140 microns, spot distance of 4.0 to 4.50 microns, laser energy of 100 to 140 nanojoules, and a repetition rate of 500 kHz, Dr Donate said.
The analysis included visual and refractive outcomes, keratometry, pachymetry, topography, ocular surface, and contrast sensitivity testing. At one year follow-up, the mean uncorrected distance visual acuity was -0.06 logMAR with an efficiency index of 1.2. In terms of safety, 11% of eyes lost one line of vision at one year, and 97.5% of eyes attained 20/20 corrected distance visual acuity or better with a safety index of 1.6.
“The stability was also very good over time. We did see a slight tendency towards hyperopic shift because we deliberately chose this strategy based on the age of the patient,” Dr Donate explained.
In terms of astigmatism, 84.2% of eyes had less than 0.50 D of corneal astigmatism and 99.2% less than 1.0 D at one year. The mean contrast sensitivity showed rapid recovery one month after surgery to preoperative levels. Ocular surface index scores and higher-order aberrations also showed very little alteration from preoperative values to more than one year after surgery. Intraoperative adverse events included 0.65% suction loss, compared to 4.68% in the FDA study for SMILE.
“Broken down, the figures were 0.11% for loss of suction in cases where the eye was eventually treated later by another modality such as PRK, LASIK, or ICL; 0.32% for loss of suction and immediate switch to another procedure; and 0.22% [for] loss of suction, but the treatment was successfully completed,” Dr Donate said.
Complications included one abscess, ectasia in 0.14%, and retreatments in 1.55% of cases.
Dr Donate noted that a comparison of the one-month results for those patients lost to follow-up after one year and those who were evaluated at one year found no statistically significant difference between the groups.
“This leads us to suppose that their eventual inclusion would not have had a significant influence on the overall results at one year,” he said.
Corneal refractive surgery is set for a bright future thanks to expanded indications and ongoing advances in technology for minimally invasive intrastromal procedures, according to Liem Trinh MD.
In a keynote address, Dr Trinh said the next few years would see an enhanced choice in lenticular extraction procedures for the correction of myopia, hyperopia, and myopic astigmatism.
“We will soon have the arrival of three new femtosecond laser platforms for lenticular refractive surgery, all of which offer cyclotorsion correction, automatic centration, and rapid treatments. Additive surgery using lenticules to correct hyperopia and for corneal repair surgery in trauma cases and keratoconus will also become more widely available in the near future,” Dr Trinh said.
Lenticular procedures for the correction of myopia and myopic astigmatism have been available since 2010 using SMILE® (Carl Zeiss Meditec). Hyperopic corrections, however, have been absent from the market due to the inherent difficulties of sculpting the requisite shape of lenticule for such treatments.
“The problem lies in the complexity of creating a lenticule that is thicker in the periphery and thinner in the centre and can then be easily extracted after dissection,” Dr Trinh said.
This problem now seems to have been resolved, with very good refractive and safety outcomes reported in initial clinical trials of SMILE for hyperopia. Market approval for hyperopic SMILE is expected in 2023, Dr Trinh added.
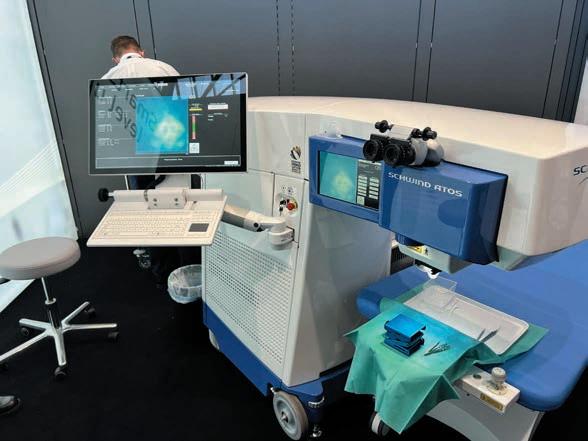
Surgeons will also soon have the option to choose from a variety of laser platforms capable of performing corneal lenticular surgery: the VisuMax 600 and 800 for SMILE; the SCHWIND ATOS® (Schwind eye-tech-solutions) for SmartSight; and the Femto LDV Z8® laser (Ziemer Ophthalmic Systems) for CLEAR procedures.

The VisuMax 800 incorporates new ergonomic features and delivers a lenticule cut in 10 seconds compared to the current 25 seconds. It can treat myopia, myopic astigmatism, and hyperopia (pending approval) and features integrated cyclotorsion control and automatic centration. The SCHWIND ATOS and Femto LDV Z8 platforms also include full eye tracking, pupil recognition, and cyclotorsion compensation.
“The basic concept of lenticule removal is the same, but there are slightly different features available for each platform. With the Z8 laser, for instance, the surgeon can choose to centre the treatment on the pupil or the vertex, and there are two incisions for dissection compared to just one for SMILE procedures,” Dr Trinh said.
Another potentially promising treatment for hyperopia on the horizon is the use of SMILE combined with allogenic corneal intrastromal lenticule inlay, Dr Trinh said. The technique
involves using a donor lenticule from a myopic SMILE procedure, then implanting the same lenticule in a hyperopic eye to correct the refractive error.



“There is no loss of tissue with this approach, and it has been shown to be safe and efficient with no rejection issues and very good refractive outcomes and stability in multiple publications,” he said.

Another potential application is using the lenticules for therapeutic corneal surgery in trauma cases or keratoconus, Dr Trinh added.
“The basic idea is to use lenticules implanted intrastromally to improve the geometrical quality of a pathological cornea affected by keratoconus. We already performed this procedure on a young patient with advanced keratoconus, which enabled him to avert hydrops and the need for a corneal graft,” he said.
Dr Trinh presented at the French Implant and Refractive Surgery Association (SAFIR) Annual Meeting.









Artificial intelligence is showing increasing efficacy in diagnosing pathologies of the anterior segment of the eye and can outperform modern intraocular lens (IOL) power calculation formulae, according to Damien Gatinel MD, PhD.

“Artificial intelligence represents a fundamental change across society. It cannot be treated as a trend that will pass us by in a couple of years. Visual health is an area in which AI has some of the most promising applications due to its foundations in evidencebased, data-driven processes,” Professor Gatinel noted.
Although most of the initial research in deep learning technology in ophthalmology has focused on retinal diseases because of the widespread use of medical imaging in those conditions, recent research has revealed many potential applications in assessing the anterior segment.
Generally, AI refers to a system that uses data processing and pattern recognition to simulate cognitive functions. Machine-learning techniques can be either supervised or unsupervised. Supervised learning in ophthalmology requires experts to label individual features in clinical images to develop the AI solutions. Unsupervised learning involves using entire images without explicit labelling, and the AI itself can discover hidden patterns that may help uncover the predictive features of the pathologies under consideration.
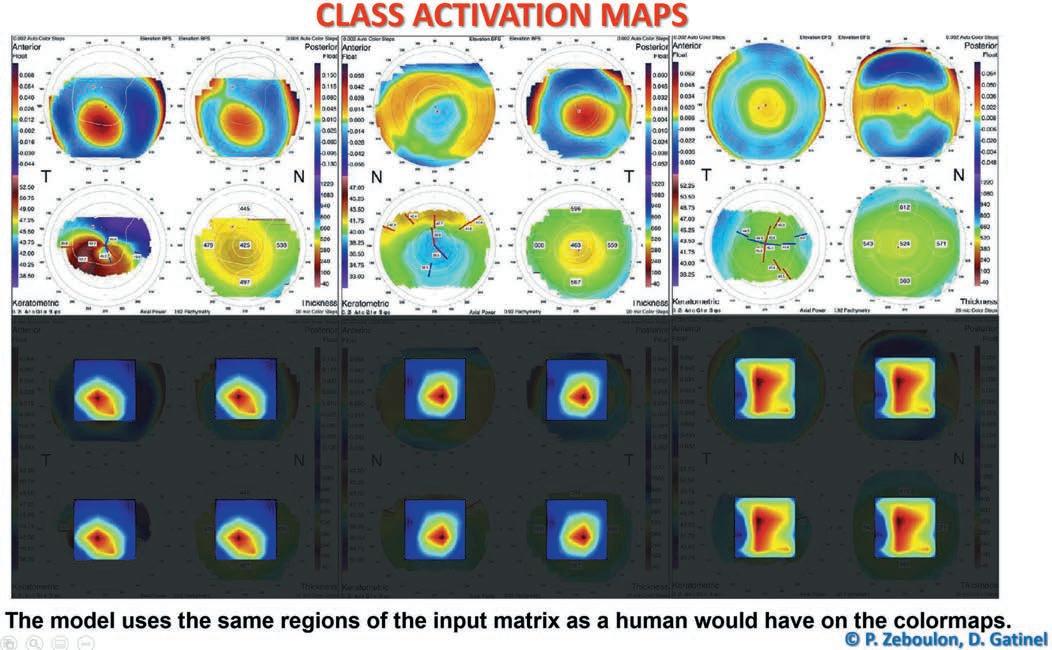
As an illustration of supervised learning, Prof Gatinel described results from a study in which he and his associates used a convolutional neural network to develop an algorithm to distinguish between computerised corneal topography images of normal eyes from those of eyes with keratoconus and eyes that underwent previous refractive surgery. Convolutional neural networks are the current state-of-theart technology for image recognition. Inspired by biological processes, their interconnectivity patterns resemble the visual cortex.
In their study, Prof Gatinel and his team trained the network using 3,000 examinations in total—a thousand for each category. However, instead of using the coloured images, they used the actual raw numerical value constituting these maps to avoid a loss of information.
The network used the region combining the steepest curvature, the thinnest point, and the highest elevations of the anterior and posterior surface to predict keratoconus. For refractive surgery examination, the network used the region combining the flattest curvature, the thinnest point, and the highest and lowest elevations of the anterior and posterior surfaces.
In a test set of 300 Orbscans, the overall accuracy of the clustering algorithm was 99.3%. Only two examinations of the 300test set were misclassified, both of which were refractive surgery examinations. Sensitivity and specificity were 100% for KC, 100% and 99% for normal examinations, and 98% and 100% for RS examinations.i
“Artificial intelligence represents a fundamental change across society. It cannot be treated as a trend that will pass us by in a couple of years.”
Researchers performed class activation mapping to visualise which part of the input matrix predicted each class and present graphic examples. The results are presented as a colour heatmap in which hotter colours represent the matrix elements that were the most useful to the model for making the prediction. The use of class activation mapping helps understand how the network makes its prediction. It showed that their model classified keratoconus (KC) and refractive surgery (RS) examinations by using the same regions of the input matrix as a human would on the colourmaps. The region the network used to predict the KC class combined the steepest curvature, the thinnest point, and the highest elevations of the anterior and the posterior surface. For RS examinations, the network used the region combining the flattest curvature, the thinnest point, and, respectively, the lowest and highest elevations of the anterior and posterior surface.
In another study, Prof Gatinel and his team tested the efficiency of unsupervised algorithms to extract and sort computerised corneal topography images into the same three diagnostic clusters based on data similarity with little human intervention, data cleaning, or feature selection.
The clustering algorithm analysed 7,019 usable examinations extracted from 13,705 Orbscan maps and used 248 manually labelled Orbscan maps to serve as “tracers” to help in designing the algorithm. The researchers found this method had an overall accuracy of 96.5%. The sensitivity and specificity for the three diagnostic categories were, respectively, 99.8% and 85.9% for normal eyes, 88.0% and 99.9% for keratoconus, and 93.1% for eyes that underwent corneal refractive surgery.ii
Prof Gatinel and his associates have also used an unsupervised learning AI approach to develop their Pearl-DGS IOL power calculation formula. The formula is a hybrid that relies on an optical, computational core but uses AI to determine the anatomical position of the IOL (effective lens position in a thick lens model).iii
He noted the actual physical measurement of the IOL position with OCT or other technology is not available in most data sets. Therefore, they created a formula to enable the back-calculation of the effective lens position of the principal object plane of the thick lens IOL in an operated eye, provided they had all the preoperative biometric parameters, the postoperative refraction, and the IOL’s power, geometry, and refractive index.
The results of a recently published meta-analysis, including 1,476 eyes from 14 studies, placed the Pearl-DGS first among all recent formulas in the accuracy of IOL power calculation for short eyes.iv
This reflects the prediction’s precision of the IOL position because, for these short eyes that receive high-power IOLs, the deviation from the predicted position induces a greater predictive error.
Prof Gatinel and his associates have published an open-source overview of all the details and key steps in IOL power computation with the Pearl-DGS formula.v
i P Zébulon et al. American Journal of Ophthalmology, 2020; 219: 33–39.
ii P Zéboulon et al. Scientific Reports, no. 16973, https://doi.org/10.1038/ s41598-020-73902-7.
iii Debellemanière G, Dubois M, Gauvin M, Wallerstein A, Brenner LF, Rampat R, Saad A, Gatinel D. “The PEARL-DGS Formula: The Development of an Open-source Machine Learning-based Thick IOL Calculation Formula”. American Journal of Ophthalmology, 2021 Dec; 232: 58–69.
iv Y Luo et al. International Ophthalmology, 2022, 42(6): 1939–1956.
v Gatinel et al. Translational Vision Science & Technology, 2021, 10(4): 27. doi: https://doi.org/10.1167/tvst.10.4.27.
Prof Gatinel presented his research at the Artificial Intelligence in Ophthalmology 2022 virtual meeting.
Damien Gatinel MD, PhD is head of the Anterior Segment and Refractive Surgery Department of Ophthalmology, Rothschild Foundation Hospital, Paris, France, CEROV (Centre of Expertise and Research in Optics and Vision), Paris, France.
gatinel@gmail.com

AI-enabled patient follow-up screening and at-home visual acuity tests show promise. Howard Larkin reports
“Do you have any redness in your eye?”
“Just in the corner.”
“Is the rest of the eye completely white?”
“Yes, it is.”
“It’s normal for your eye to be a bit red after cataract surgery, and it should get less red with time.”
They are the same screening questions your teleconsultation staff would ask patients in the days after cataract surgery. Except they’re being asked and followed up by an artificial intelligence-enabled autonomous telemedicine programme called Dora.
Dora also asks about pain, vision, flashing lights, and floaters. The program assesses natural language responses and asks follow-up questions about symptoms according to an algorithm. It then flags responses suggesting a problem for immediate review by staff, who may call in patients for in-person visits.
Developed by the UK firm Ufonia, a Dutch language Dora prototype has already been tested, optimised, and its questionnaire validated among healthy individuals at Maastricht University Medical Centre+, said Rudy MMA Nuijts MD, PhD. It will soon undergo a pilot study comparing it with regular care among postoperative cataract patients. If successful, the medical centre will implement the programme.
“Do patients like it? These are older patients after all,” Prof Nuijts said. On average, patients scored Dora 8.6 on a 10-point scale, which is a pretty good outcome, he noted.
The programme is an outgrowth of a shift to telemedicine responding to the COVID-19 pandemic. Before, bilateral cataract surgery involved six in-person visits for two separate surgery dates—with a refraction required by national practice guidelines before implanting the second eye. For many cases, this became three in-person visits, including an immediate sequential bilateral cataract surgery, with the day one followup screening visit conducted by telephone. This is a much more efficient use of residents and staff that Dora could take a step further by relieving them of routine screening calls, Prof Nuijts added.
“I think that visual acuity eHealth tools can function as a reliable screening method.”











A second telemedicine study Prof Nuijts is conducting is evaluating an at-home tool for assessing patients’ visual acuity after cataract surgery. It is based on a CE-marked web-based tool that measures distance and near VA, sphere, cylinder, and axis—and can even issue a prescription for visual aids.

The tool has been validated against in-person ETDRS manifest refractions. One study found an insignificant mean difference in uncorrected distance visual acuity measurements and in refraction of only 0.02 D in healthy patients with -3.0 D or less myopia. This makes it suitable for screening, though refractive accuracy is still an issue, Prof Nuijts noted. “In terms of visual acuity, it is quite, quite accurate.”i


The tool pairs a computer and a smartphone as a remote control and monitors the environment and user behaviour with a webcam. An AI-powered assistant gives instructions and guides the user to three metres from the screen to conduct the tests.
In a pilot study that screened 46 post-surgery cataract patients, Prof Nuijts compared the web-based tool’s results against Snellen and ETDRS manifest refractions. The in-person tests had slightly more consistent test-retest results by about one-third of a Snellen line. However, about 85% of the webbased tool’s measurements for both corrected and uncorrected VA fell within 0.15 logMAR of the ETDRS results, which was the threshold of clinical significance. The tool tended to underestimate VA slightly, which may be related to the lower accuracy of refractive error measurement.
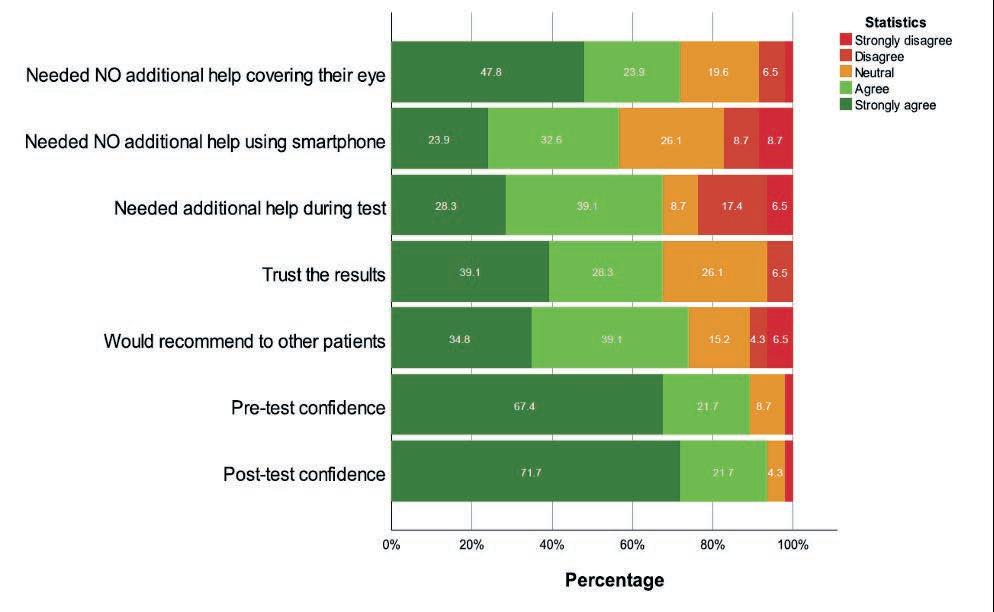
Patient experience was also positive. About 65% said they trusted the results and about 70% said they would recommend the web-based test to other patients. About 15% to 20% might need additional help using the smartphone during the test, Prof Nuijts said.
Now underway is a multicentre, randomised test of the webbased VA and refractive error tool for monitoring patients after cataract surgery. It involves 188 eyes of 94 patients in three countries. In addition to validity, it will assess the safety and cost-effectiveness of remote monitoring, Prof Nuijts said. “We hope to inform you on this topic in Milan in September” at the ESCRS Congress.


“I think that visual acuity eHealth tools can function as a reliable screening method. The patients’ attitudes are quite positive toward it. It will improve the efficiency of our care in the future,” Prof Nuijts said.
Autonomous telemedicine also will help free up clinical staff and could make care more accessible, he said. “If you can do this automatically and save, say, 90% of the consultations, that is quite an efficiency improvement.”

i Wisse R et al. Journal of Medical Internet Research, 2019; 21(11): e14808.
Prof Nuijts’ presentation was part of a symposium featuring an international panel of expert speakers representing each of the Cataract and Refractive Surgery Societies (ASCRS, APACRS, ESCRS, and LASCRS) at the 2022 ASCRS Annual Meeting in Washington, DC.
Rudy MMA Nuijts MD, PhD is past president of the ESCRS, professor of ophthalmology, vice-chairman, and director of the Cornea Clinic and the Centre for Refractive Surgery at the University Eye Clinic Maastricht, Maastricht Medical University, the Netherlands. rudy.nuijts@mumc.nl
Asteady increase in the number of female ophthalmologists and a dramatic rise in the popularity of extended depth of focus (EDOF) IOLs were some of the more pertinent findings of the latest survey of French ophthalmologists conducted by Raphaël Barugel MD and Dominique Monnet MD.
“The increasing preference for EDOF lenses is one of the more notable features of this year’s survey, with 44% of surgeons saying they would select an EDOF lens for their own cataract surgery,” Dr Barugel said.
The latest study of French practice habits carries on the work by Richard Gold MD for the past 25 years—which provided an important gauge for surgeons to see how their own techniques and choices compared to their peers, Dr Barugel explained.
“It was also useful to be able to compare to practices in other countries and innovative in that it also surveyed the choices surgeons would make for their own eyes as well as those of their patients,” he said.
While Dr Gold’s annual survey covered a broad spectrum of practice habits, Drs Barugel and Monnet opted to limit the questions to a particular aspect of cataract and refractive surgery each year, with the 2022 survey focusing on intraocular lenses.
The mean age of the 155 respondents to the 2022 survey was 49 years, with 69% male and 31% female, with over half (61%) working in private practice and 14% within a hospital setting.

“The study showed an increase in the number of female ophthalmologists: the figure was 36% for those younger than 50 compared to 24% for those over 50 years of age,” Dr Barugel said.
The vast majority of respondents (96%) said they practiced at least one other type of surgery in addition to cataract, with refractive (68%) and glaucoma (44%) the most common surgeries. About one-third (34%) performed less than 300 surgeries a year, while 37% performed more than 500 operations annually.
In terms of the type of IOL implanted, most respondents used hydrophobic lenses (71%), with 70% saying refractive
predictability was the most important criteria in their lens choice, followed by capsular bag stability (50%), and having a pre-loaded implant (39%).
For IOL power calculation formulae, 87% of respondents said they used the SRK/T formula, followed by Barrett (43%), Hoffer Q (33%), and Haigis (28%). Some 61% of respondents said they routinely use at least two different formulae, with Haigis, ASCRS calculator, and Barrett the most used formulas for post-refractive surgery patients.
The threshold for implantation of a toric lens was astigmatism of less than 1.25 D for 80% of those surgeons who implanted toric IOLs when it was possible to do so versus 32% who said they implant these lenses only occasionally.
The main barriers to implantation for those who never implant toric lenses were uncertainty about the outcome (68%), the extra cost to the patient (43%), and increased consultation time (57%). The three most important criteria in the choice of a toric implant were postoperative rotational stability (80%), ease of IOL rotation into position when implanting the lens (54%), and the absence of or minimal extra cost to the patient (46%).
When surgeons were asked about their choices if undergoing cataract surgery themselves, 86% said they would pick their own implants, with 44% preferring an EDOF lens, 40% a monofocal, and 16% a multifocal IOL. The key criteria orienting their choice of IOL were quality of vision and the risk of side effects (92%), spectacle independence (67%), and IOL material (49%).
Waste produced by phacoemulsification cataract surgery can be significant and underestimated, according to a new study presented by Dr Emilie Mahon at the annual Irish College of Ophthalmologists (ICO) conference.

Dr Mahon conducted a study in her department on perceptions of the eye theatre staff on waste generated by cataract surgery. She also assessed the weight of waste produced from a single straightforward phacoemulsification cataract surgery. The staff was found to significantly underestimate the waste generated by surgery in equivalent carbon dioxide emission and equivalent petrol consumption. The mean waste produced by a standard, uncomplicated surgery was four kilograms.
Dr Mahon also identified a potential appetite for change: most staff (77%) reported they regularly think about the environmental impact of cataract surgery, and most felt that waste produced by surgery is not environmentally sustainable.
Waste production due to cataract surgery is a hot topic, with David F Chang MD speaking on the environmental impact of the surgery and drawing comparisons between standard phacoemulsification in the West with the much smaller waste production—and thereby carbon footprint—of manual small incision cataract surgery in India in his Ridley Medal Lecture at the ESCRS Congress in 2020. In the UK, the President’s session in the Royal College of Ophthalmologists 2022 Congress, chaired by Professor Bernie Chang, centred around sustainability in ophthalmology. This focus ties in with the UK’s National Health Service net-zero emission goal. Sustainability is also a theme of the ESCRS Annual Congress in Milan.
What approaches are possible to reduce the carbon footprint of our cataract surgeries? That classic triad of principles—reduce, reuse, recycle—is a good starting point. In particular, reducing and reusing may have a large impact.
Reducing the carbon footprint can be achieved by streamlining the usage of equipment and materials in surgery. Single-use equipment opened during surgery should not include instruments or materials not routinely used. Within surgery, another important source of emissions can be anaesthesia. Cutting down requests for sedation and general anaesthesia, which utilise gases
such as nitrous oxide that have a much worse environmental impact than carbon dioxide, will cut emissions further.
The streamlining efforts can extend on from cutting down on physical waste to reducing wasted time and energy by looking at the patient pathway and the efficiency of the operating theatre. In Ireland, Mr Paul Mullaney has pioneered these efforts. Mullaney, Consultant Ophthalmic Surgeon in Sligo University Hospital, developed a high-volume cataract surgery service, including a postoperative care pathway where patients follow up with community optometrists rather than hospital-based ophthalmologists.
In the global effort to reduce the environmental impact of our profession, every little bit helps, including efforts to examine our carbon footprints in our own ophthalmology departments.
“Ophthalmologists must now contribute to the transition of reducing carbon footprint by including ecologic and economic pillars of sustainability in choosing the components of their cataract surgery trays, thereby playing their part in ‘keeping an eye’ on the planet,” she emphasised.


An ESCRS Heritage Lecture delivered by Patrick Condon MCh, FRCS, FRCOphth at last year’s annual ESCRS Congress in Amsterdam—and now viewable on YouTube—takes viewers through the earliest 19th-century experiments in refractive surgery up to the present day, outlining the successes and failures of the pioneering innovators of this continually evolving specialty. In an interview with EuroTimes Contributing Editor Roibeárd O’hÉineacháin, Dr Condon shared his recollections of his experiences during this revolutionary era of ophthalmology.
I first became involved with the European Intraocular Implant Club in the 1980s when Cornelius Binkhorst invited me to be the Irish representative on the board. During the subsequent 10 years, I became extremely friendly with role models Harold Ridley, Peter Choyce, and many others in lens implant surgery and watched the many top surgeons participate in surgery.
My first interest in refractive surgery began while treating advanced cases of keratoconus. In the early days, it could only be treated with a specialised type of contact lenses—many of which were extremely difficult for patients to wear and produced vectorisation of the cornea. For these cases, epikeratoplasty—originally pioneered by José Barraquer in Bogota and subsequently Herbert Kaufman and Marguerite McDonald in the US—seemed to be the answer. The failure of this technique for these patients stimulated Jörg Krumeich—who I would consider another role model—to use his guided trephine system (GTS) for nonfrozen donor corneas. It initially worked well for epikeratoplasty and corneal transplant work, which we were doing a lot of in Waterford at the time.
Because of the difficulties of using the Barraquer microkeratome for the refractive procedures for myopia, Lucio Buratto used the Summit laser in 1989 to perform the refractive cut on the posterior surface of the excised corneal button. That same year, Ioannis Pallikaris introduced the technique of using a hinged corneal flap and applying the laser to the stromal bed. Lucio Buratto spent three months in Dublin with Michael O’Keefe and myself, discussing these developments, as well as with Pallikaris—who also visited us regarding the development of his aberrometer for measuring corneal topography.
By 1990, although stromal bed ablation technique was acceptable practice, there was still the problem with the Barraquer microkeratome. This was where Luis Ruiz in Bogota came into the picture with the development of his automatic corneal shaper (ACS) and the automatic lamellar keratoplasty technique. Having met Ruiz personally at courses in the US organised by Charles Casebier, I paid a visit to Dr Ruiz’s clinic in Bogota, where I watched him operate and examine his patients postoperatively. I subsequently purchased a microkeratome from a company in Florida, US. At my hospital in Waterford, Ireland, the manager at the time allowed me to set up a wet laboratory to practice using the microkeratome on pig eyes to perfect the technique.
This then led to combining the use of the ACS with the Summit laser Michael O’Keefe was using for PRK at the Mater
Hospital. And in Dublin, at the end of 1993, we performed the first LASIK procedure in the UK and Ireland on a patient with high myopia. With my deep involvement with the ESCRS at the time, Lucio Buratto and I started the European lamellar keratoplasty group in Gothenburg in 1994. Our aim was to train doctors beginning to use the microkeratome to get involved in refractive surgery.
Where refractive surgery goes from now on is a good question. There is no doubt the changes brought about by femtosecond laser technology has changed the pattern of intracorneal surgery. My video illustrates the therapeutic uses as well as its use in refractive surgery (particularly small incision lenticule extraction, or SMILE)—an indication of the success of these changes.
The parallel development and perfection of the implantable collamer lens (ICL) has been a major advance in refractive surgery, especially when looking back at Svyatoslav Fyodorov’s original design. The amazing improvements in the ICL technology provide a real alternative to corneal laser refractive surgery.
One of the main challenges for refractive surgeons is to avoid becoming too casual about these procedures, as many of them are irreversible and may result in further problems. For the future, the ESCRS will continue to highlight advances in refractive surgery, encourage further research, and maintain standards of practice with wet labs and courses—as they are already doing very successfully.
Dr Condon’s heritage lecture may be viewed at https://www.youtube.com/watch?v=cKOSSfwm_hg
Patrick Condon MCh, FRCS, FRCOphth lives in Waterford, Ireland. During his long career, Dr Condon acquired Fellowships from the Royal Colleges of Surgeons of Ireland, England, and Scotland and a Mastership in Surgery (National University of Ireland). He is currently a life fellow of the Royal Society of Medicine (London), an emeritus member of the International Intraocular Implant Club, and an active member of the Royal Academy of Medicine in Ireland and the Irish College of Ophthalmologists. pcondon251@eircom.net
Anew screening system that simultaneously evaluates multiple biomarkers could help target therapy for dry eye disease and help identify refractive surgery candidates, according to its developers from Narayana Nethralaya Eye Hospital, Bangalore, India.

“Currently available clinical biomarkers for dry eye disease (DED) do not necessarily correlate with patient symptoms. Furthermore, due to overlapping findings in patients with DED and other ocular surface conditions (such as allergic disease or infection), [the biomarkers] may not help clinicians with accurate differentiation, which can lead to selecting a treatment that can be ineffective or even exacerbate the patient’s condition,” Sailie U Shirodkar MD, MS told ARVO delegates.
“In addition, a molecular biomarker test could help guide therapeutic selection for OSDs using targeted therapies that are on the market or in clinical trials; provide quantitative information for following treatment response; and identify patients planning to have refractive surgery who have subclinical inflammation so that they could be properly managed preoperatively to mitigate the risk of postoperative complications.”
The system detected the biomarkers in all cases and showed good reproducibility, high sensitivity, and high specificity. As expected from previous information, it showed significantly elevated MMP-9 in the keratoconus group and significantly elevated levels of all inflammatory biomarkers in the DED group.
In addition to MMP-9, levels of other pro-inflammatory markers increased progressively across the three “control groups”, were significantly greater in the subclinical inflammation I and II groups compared to controls with no inflammation, and were almost identical in the subclinical inflammation II and DED cohorts.
The testing, sample preparation, and platform processing take 90 minutes. In addition to MMP-9, the test measures levels of four pro-inflammatory cytokines (interleukin [IL]-1β, IL-6, IL-17A, TNF-α), VEGF, soluble ICAM-1, and IL-10, an antiinflammatory cytokine included to help understand the balance between pro- and anti-inflammatory factors, Dr Shirodkar said.
None of the study groups had elevated levels of IL-10 or VEGF, Dr Shirodkar reported.
The system uses a customised ELISA platform (Bio-M Pathfinder) to measure eight soluble factors in tear fluid extracted from Schirmer’s strips. The developers conducted a study that included 107 patients with DED diagnosed per TFOS DEWS II guidelines, 125 patients with keratoconus, and 389 controls scheduled for refractive surgery who had no overt signs of DED. The controls were further stratified into three groups based on matrix metalloproteinase-9 (MMP-9) level: no inflammation <50,000 pg/mL (n=214); subclinical inflammation I 50,000 to 162,000 pg/mL (n=95); and subclinical inflammation II >162,000 pg/mL (n=80).
Currently, the researchers are generating additional data sets to improve the robustness of the analysis and are adding to the keratoconus cohort to hopefully identify grade-specific differences and progression-related changes.
“We hope to popularise our concept of targeted therapy for DED that uses a biomarker-based algorithm to rationalise the manner in which we deliver care to these patients,” Dr Shirodkar said.
“We hope to popularise our concept of targeted therapy for DED that uses a biomarker-based algorithm to rationalise the manner in which we deliver care to these patients.”
Comorbid glaucoma is associated with an increased likelihood of refractive surprise after uncomplicated cataract surgery, according to a retrospective cohort study conducted by researchers at the University of Washington, Seattle, US.
The analysis included 483 controls without glaucoma and 194 glaucomatous eyes and found significantly higher proportions of controls compared to glaucoma patients achieved a refractive outcome within 1.0 D of target (96% vs. 92%) and within 0.5 D of target (72% vs. 66%).
“A prior study described worse refractive outcomes in glaucoma patients undergoing cataract surgery, but no study has evaluated refractive outcomes of standalone cataract surgery in glaucoma patients without visually significant comorbidities,” said Johnson Huang BS, explaining the motivation for the research project.

“Our study excluded those with ocular comorbidities and potential confounding factors. We are continuing to investigate the issue, including trying to identify specific differences in eyes with glaucoma that might underly refractive errors. Nevertheless, we think our findings could provide important information for preoperative patient counselling as well as represent a risk-to-benefit ratio consideration for any cataract surgeon.”
The single-centre study identified the first qualifying eye of patients with uncomplicated phacoemulsification cataract surgery without any other concurrent eye surgery from 2007 to 2020. The glaucoma group included only eyes with a definite glaucoma diagnosis. Glaucoma suspects and eyes with ocular hypertension were excluded, as were eyes with any vision-limiting systemic disease, retinal or corneal disease, or prior ocular surgery. The study used the Barrett Universal II calculator to calculate the estimated refractive outcome based on the preoperative ocular biometry and the intraocular lens implanted at the time of surgery. Researchers then compared postoperative month-one refractions to the estimated refractions.
The percentage of eyes with preoperative CDVA of 20/40 or better was not significantly different in the glaucoma and nonglaucoma groups (95% vs. 97%). Corresponding with the difference found in the refractive outcomes, mean postoperative CDVA was worse in the glaucoma group compared to controls (0.06 vs. 0.02 logMAR), and the difference was statistically significant.
Further analysis of the refractive outcomes showed the glaucoma patients had significantly higher rates of myopic surprises than the controls looking both at subgroups of eyes >1.0 D off-target (5% vs. 1%) and >0.5 D off-target (19% vs. 9%). The proportion of eyes with a hyperopic surprise >0.5 D was significantly higher in the control group compared to the glaucoma group (20% vs. 16%). However, a hyperopic surprise >1.0 D occurred
significantly more often within the glaucoma group compared to controls (4% vs. 3%).
The glaucoma cohort included 94 eyes with primary openangle glaucoma, 47 eyes with normal-tension glaucoma, 27 eyes with chronic angle-closure glaucoma (CACG), and 18 eyes with pseudoexfoliation glaucoma. Analyses of refractive outcomes for the different glaucoma subtypes showed refractive surprises were most common for eyes with CACG—38% of eyes with this diagnosis had a myopic surprise >0.5 D.
The investigators postulated that some biometric factor could explain their findings.
“Comparing regression lines for plots of the ratio of anterior chamber depth to axial length against the magnitude of refractive surprise, we see a statistically significant difference between the glaucoma and control groups, suggesting the refractive outcome differences may be based on biometric factors,” Mr Huang said. However, biometric values in and of themselves did not correlate with refractive surprises. This is an area of further investigation.
Mr Huang presented these findings at ARVO 2022 in Denver, Colorado, US.
Johnson Huang BS is a medical student at the University of Washington, US. huangc85@uw.edu
Andrew Chen MD is an assistant professor in the Department of Ophthalmology at the University of Washington, US. achen20@uw.edu
Philip P Chen is the Grace E Hill Chair professor in the Department of Ophthalmology at the University of Washington, US. pchen@uw.edu
Astem cell-based approach for restoring trabecular meshwork (TM) function and IOP control in eyes with primary open-angle glaucoma (POAG) appears promising in preclinical studies.

“The number of cells residing within the TM declines with age, and it is particularly low in eyes with POAG. The concept that it might be possible to restore IOP control in glaucomatous eyes by restoring TM cellularity has been around for some time, and with the development of induced pluripotent stem cells (iPSCs), the possibility emerged that we might be able to do that using autologous material,” said
Markus H Kuehn PhD.Dr Kuehn’s group used human skin samples to create iPSCs that could be differentiated into a cell type resembling primary TM cells. The group investigated the effects of injecting the iPSCderived TM-like cells (“iPSC-TMs”) in two genetically engineered mouse models of glaucoma chosen because they exhibit loss of TM cells without gross alteration of TM structure.
The studies included wild-type animals as one control arm and groups of transgenic mice receiving anterior chamber injections of labelled iPSC-TMs or phosphate-buffered saline (PBS).
The study results showed that iPSC-TM transplantation was associated with a rapid increase in TM cell density and prevented the reduction in aqueous humour outflow facility and increase in IOP observed in the PBS-treated transgenic control group.
Surprisingly, the injected labelled iPSC-TMs represented only a small fraction of the increased TM cellularity, Dr Kuehn said.
“Gene expression analysis of the TM post-transplantation indicated the increase was secondary to cell proliferation,” he said. Advancing into experiments performed in perfusioncultured human eyes, the researchers similarly found that the
injected iPSC-TMs integrated into the TM and resulted in increased TM cellularity mainly accounted for by inducing proliferation of endogenous cells.
“The fact we are inducing division of endogenous cells has advantages and disadvantages. One advantage is that, as opposed to exogenous material, the endogenous cells do not trigger an inflammatory reaction, so host immune rejection may not present a significant problem for this approach. In addition, it suggests that long-term survival of transplanted material may not be necessary, and that in turn suggests the possibility of creating an iPSC line that could be used for all donors and avoiding the need for a patient-specific iPSC line,” Dr Kuehn said.
Moving ahead, there are challenges and questions to address. From a technical perspective, the researchers hope to increase the efficiency and targeting specificity of the delivered iPSC-TM cells.
Noting the human eye experiments were done using eyes from older adults without frank glaucoma, Dr Kuehn said it remains to be seen whether TM cells in eyes with POAG are irreversibly damaged or modified in ways that prevent rescue and if the approach can work in secondary types of glaucoma. Further research is also needed to determine how long the functional rescue benefit persists after iPSC-TM injection.
Dr Kuehn presented these findings at ARVO 2022 in Denver, Colorado, US.
Markus H Kuehn PhD is a professor of ophthalmology and visual sciences in the Department of Ophthalmology and Visual Sciences, University of Iowa, Iowa City, US. markus-kuehn@uiowa.edu
Belong
to something inspiring. Join us.
Intravitreal treatment with the complement C3 inhibitor pegcetacoplan (Apellis Pharmaceuticals) administered monthly or every other month is well-tolerated and slows geographic atrophy (GA) growth secondary to age-related macular degeneration (AMD), new findings from phase 3 registration studies indicate.
The phase 3 study program includes two identically designed trials—OAKS and DERBY. Across the two studies, 1,258 patients were randomised to receive pegcetacoplan 15 mg/0.1 mL monthly or every other month (EOM) or sham monthly or EOM.
As previously reported, only the OAKS trial met the primary endpoint assessing change from baseline to month 12 in total GA lesion area (measured by fundus autofluorescence). Roger A Goldberg MD, MBA presented 18-month results that showed continued reductions in GA lesion growth from month 12 to month 18 for both pegcetacoplan regimens versus sham in both DERBY and OAKS, with widening of the differences between the pegcetacoplan and sham groups. Pegcetacoplan slowed the growth in both foveal and extrafoveal lesions.
Pegcetacoplanreduced
Sunir J Garg MD presented a post-hoc subgroup analysis adjusting for baseline imbalances between treatment arms in covariates affecting GA lesion growth. This led to convergence of the treatment effect of pegcetacoplan at 12 months across OAKS, DERBY, and the 12-month phase 2 FILLY study and at 18 months between OAKS and DERBY, including in the subgroups of patients with foveal and extrafoveal GA.
At 18 months, the monthly and EOM pegcetacoplan groups in OAKS showed reductions in GA growth compared to sham of 16% and 22%, respectively, and 12% and 13%, respectively, in DERBY.
“The 18-month percentage results are similar to the 12-month results, but visually, the GA lesion growth curves continue to separate over time, and that separation represents in absolute terms an increased amount of retinal tissue preserved with pegcetacoplan,” Dr Goldberg said.
He also presented an analysis looking at GA growth over 6-month intervals that showed the relative underperformance of pegcetacoplan in DERBY during the first 6 months with an increasing benefit between months 6 and 12 and 12 and 18.
Analyses of data from subgroups of patients with foveal and extrafoveal lesions showed both pegcetacoplan regimens were associated with a continuous and clinically meaningful reduction
Longer term follow-up and post-hoc analyses support efficacy and safety of treatment.
Cheryl Guttman Krader reports
in the growth rate of lesions, regardless of location. A robust effect on extrafoveal lesions observed at 12 months was maintained, and there was an improved effect on foveal lesions with ongoing pegcetacoplan treatment, he said.
The adverse event review identified no new safety signals with a lengthened treatment duration.
“Importantly, no cases of retinitis or vasculitis have been reported,” Dr Goldberg said.
Converging treatment effect of pegcetacoplan in OAKS and DERBY in covariate - adjusted post- hoc analysis continues at Month 18
Pooled analyses of data from DERBY and OAKS showed rates of exudative AMD development (identified by the investigator) in the pegcetacoplan monthly, EOM, and sham groups were 9.5%, 6.2%, and 2.9%, respectively. Rates of exudative AMD per 100 patient-years were similar at months 12 and 18 for both pegcetacoplan regimens. Per injection rates of endophthalmitis and intraocular inflammation at month 18 in the pooled pegcetacoplan groups were 0.04% and 0.23%, respectively.
“One of the goals of randomisation is to balance risk factors between treatment groups, but chance imbalances can occur that can lead to differing estimates of the treatment effect. A covariate
TOMEY has been supplying ophthalmologists worldwide with instruments for high-tech ophthalmic diagnostics for more than 50 years.

apEye is revolutionising eye prostheses. At ESCRS we will be presenting a world first: A 3D-printed artificial eye prosthesis, which owes its unique true colour and the natural appearance of the iris to high-resolution scans from the TOMEY ASOCT CASIA2.

Learn all about the ground-breaking Light Source Technology in CASIA2 and apEye –products which will revolutionize the market.

analysis is one way to compensate for that effect. The reason for doing this work is that the results of OAKS mirrored those of the phase 2 FILLY study, whereas DERBY missed its primary endpoint in both treatment arms. Since the design of the studies, we have a better understanding of many variables that affect GA growth,” Dr Garg explained.
The post-hoc covariate analyses identified imbalances in the DERBY trial in proportions of study eyes with unifocal lesions and with extensive intermediate/large drusen that favour sham treatment. Identified imbalances in the OAKS trial were in the proportion of eyes with extrafoveal lesions that may have attenuated the effect of pegcetacoplan and in the FILLY trial in proportions of eyes with low-luminance deficit and extensive
intermediate/large drusen favouring pegcetacoplan.
After adjusting for the covariates, the magnitude of pegcetacoplan effect at month 12 in OAKS was the same or slightly greater than observed in the primary analysis. The covariate adjustments in DERBY and FILLY led to results that more closely mirrored the results in OAKS.
A covariate-adjusted analysis of lesion growth at month 18 in patients with extrafoveal lesions showed that all pegcetacoplan treatment arms in DERBY and OAKS had a nominally significant effect as was observed in the primary analysis but with somewhat better convergence between studies. Data from the subgroup with foveal lesions showed the treatment effect of pegcetacoplan was similar in the covariateadjusted and primary analysis for OAKS but improved in the covariate-adjusted analysis in DERBY, Dr Garg said.
He reiterated that the covariate analysis does not fully explain treatment group imbalances nor replace the primary analysis.
Dr Goldberg and Dr Garg presented at the annual ARVO conference in Denver, Colorado, US.
Roger A Goldberg MD, MBA is a partner at Bay Area Retina Associates, Walnut Creek, California, US, and a Volunteer Professor at the CPMC Ophthalmology Residency program, San Francisco, California, US. rgoldberg.eyemd@gmail.com
Sunir J Garg MD is a partner with MidAtlantic Retina and a Professor of Ophthalmology on the Retina Service of Wills Eye Hospital, Philadelphia, Pennsylvania, US. sgarg@midatlanticretina.com


The 2022/2023 ESCRS Systematic Review Award (“SRA”) is a new initiative sponsored by the ESCRS to produce a high quality body of research aimed to prepare, collate, analyse, synthesise and report medical research.

Preliminary results from the phase I/ II FOCUS study suggest subretinally delivered GT005—a recombinant adenoassociated viral (AAV2) vector encoding Complement Factor I (CFI)—could offer a onetime gene therapy for geographic atrophy (GA) secondary to age-related macular degeneration (AMD), said Jared S Nielsen MD, MBA.



“Although injection of agents that inhibit C3 or C5 has shown to slow GA progression, these treatments demand burdensome ongoing injections and display sawtooth pharmacodynamics, which may not be the best way to interact with the complement system,” said Dr Nielsen.
“GT005 is designed to induce expression of CFI, which acts as a key downregulator of complement. Instead of inhibiting the complement pathway, the rationale for GT005 is to modulate some of the key regulatory proteins in the complement cascade to restore a homeostatic balance with a one-time intervention that will have a continuous and durable effect to hopefully prevent the development or progression of AMD.”
FOCUS is an open-label multicentre study, evaluating subretinal delivery via two different approaches—a transvitreal approach and a suprachoroidal cannulation approach using the Orbit Subretinal Delivery System. It includes dose-escalation and dose-expansion cohorts for both delivery approaches.
Eligible patients have bilateral GA. The study is evaluating safety data at 48 weeks for the primary outcome. Secondary efficacy endpoints for analysis include anatomic and functional measures as well as changes in vitreous biomarkers for complement expression.
Dr Nielsen presented safety data for the first 31 enrolled patients and biomarker data from 13 patients. The patients were all treated with the transvitreal delivery and represented 11 patients enrolled in the dose-escalation phase and 20 in the doseexpansion cohort. Dr Nielsen reported the treatment was welltolerated so far. No serious adverse events or laboratory safety signals have been seen.
There were 31 treatment-emergent adverse events in the study eye, of which 20 were mild. Changes in the RPE (5

mild, 1 moderate) that were restricted to the bleb area and not accompanied by significant visual changes were noted in some patients who received the highest dose of GT005.


Encouragingly, GT005 has so far demonstrated a benign immunogenicity profile. There were no signs of GT005-related inflammation, no antibodies to CFI detected, and the vector shedding profile aligns with other recombinant AAV ocular therapies, Dr Nielsen said.
Analyses of intraocular fluid samples showed increased CFI in the vitreous that was mirrored by increased aqueous levels of the protein along with downstream modulation of complement biomarkers consistent with reduced complement activity.
“The increase in CFI in the aqueous is something we would expect in vitrectomised eyes and suggests the possibility of monitoring intraocular CFI by sampling the aqueous,” said Dr Nielsen.
“The observed changes in biomarkers of the complement system suggest that GT005 is not only inhibiting the downstream effects of the complement pathway, but it is also affecting the amplification or upregulation and decreasing parental C3, and that is exciting.”
Dr Nielsen presented these findings at ARVO 2022 in Denver, Colorado, US.
Jared S Nielsen MD, MBA is Director of Retina Clinical Research, Director of the Retina Fellowship Training Program, and based at the Wolfe Eye Clinic, West Des Moines, Iowa, US. jnielsen@wolfeclinic.com
Post-hoc analyses of data from a phase 2/3 study investigating avacincaptad pegol (“ACP”, Zimura, IVERIC bio) as a treatment for geographic atrophy (GA)—a chronic progressive degeneration of the macula and form of late-stage, age-related macular degeneration—should provide insights about the complement 5 inhibitor’s effect on earlier stages of GA and disease progression.
Carl J Danzig MD presented the findings from the primary endpoint and post-hoc analyses in the GATHER1 study. The international trial enrolled patients with non-centre pointinvolving GA and excluded those with evidence of choroidal neovascularisation in either eye or any sign of diabetic retinopathy.
GATHER1 consisted of two parts, each with a duration of 18 months. Part 1 randomised 77 patients 1:1:1 to monthly injections with sham, ACP 1 mg, or ACP 2 mg. Part 2 started after part 1 was completed and randomised 209 patients 2:1:2 to sham, ACP 2 mg, or ACP 4 mg.
Describing results from the primary endpoint of the trial, Dr Danzig reported the mean rate of GA area growth—as measured by square root transformation—was significantly reduced in the ACP 2 mg and 4 mg groups compared with sham (27% and 28%, respectively). Extrapolation to 18 months showed reductions in GA growth rate of 28% and 30%, respectively.
Results of a post-hoc analysis of patient subgroups defined by baseline characteristics showed the mean rate of GA growth from baseline was consistently lower in the ACP groups than in the sham group for subgroups stratified by baseline GA area (<4 DA and ≥4 DA) and by part 1 and part 2 of the study.
“There were too few patients to allow for proper analysis and meaningful conclusions of the treatment effect for subgroups of patients categorised by baseline VA or pattern of fundus autofluorescence at the junctional zone of GA,” Dr Danzig noted. Another post-hoc analysis examined how ACP might affect the evolving atrophic process. Masked readers at the Doheny Image Reading and Research Lab received OCT images to grade for the presence of drusen, incomplete RPE and outer retinal atrophy (iRORA), and complete retinal pigment epithelium and outer retinal atrophy (cRORA) by applying
Classification of Atrophy Meeting criteria.
Characteristics of the patients with drusen at baseline and the patients with iRORA at baseline were well balanced between the ACP and sham groups. At 18 months, ACP 2 mg was associated with a reduction compared to sham in the rate of progression from drusen to iRORA or cRORA and progression from iRORA to cRORA. The treatment effect was evident by 6 months and increased over time. By month 18, investigators observed a reduction in the progression rate of approximately 50% with avacincaptad pegol compared with sham in the progression from iRORA to cRORA.
Dr Danzig noted GATHER2, a phase 3 trial investigating ACP for treating GA, was fully enrolled in July 2021. GATHER2 randomised 448 patients to monthly treatment for 12 months with ACP 2 mg or sham. At 12 months, the patients in the ACP group will be re-randomised to receive the treatment monthly or every other month. Primary efficacy endpoint 12-month assessment results are expected in the third quarter of 2022.
The new OS 4 marks the beginning of the next generation of retina, glaucoma and cataract surgery. The all-in-one platform has received numerous exciting features that provide even more comfort, precision and safety.
Laser integration: More safety, fully automated user protection filter
Light: 45% more power*, maximum visibility

Pedal: Multifunctional with over 100 setting options

Phaco: Speedier readiness, greater controllability
User comfort: Even more userfriendly and communicative Visit
Early results promising from first in-human trial of a CRISPR-Cas9 gene editing therapy.
Cheryl Guttman Krader reportsInitial results from a phase 1/2 clinical trial using CRISPRCas9 gene editing to treat patients with Leber congenital amaurosis type 10 show some signs of efficacy for the novel strategy without any dose-limiting toxicities or serious adverse events, said Mark Pennesi MD, PhD.
Known as BRILLIANCE, the study is investigating EDIT-101 (Editas Medicine), which represents the first clinically researched in vivo CRISPRCas9 gene editing therapy. It is evaluating the safety, tolerability, and efficacy of escalating doses of EDIT101 and enrolling adults and paediatric patients (ages 3 to 17) with Leber congenital amaurosis 10 caused by a homozygous or compound heterozygous mutation involving c.2991+1655A>G in intron 26 of the CEP290 gene.
The adult cohort includes low, middle, and high dose groups, and the paediatric cohort uses the middle and high doses. The treatment is delivered as a single subretinal injection into the worse-seeing eye’s parafoveal region.
Dr Pennesi reported full enrolment for the three dose groups for adults and the first paediatric patient treated. He presented results from the first five adult patients in the study.
“The findings thus far suggest positive biological activity and potential clinical benefits for EDIT-101, but they are anecdotal, and the data are very early. We are continuing to enrol participants in the paediatric cohort and hope to report additional data from BRILLIANCE later in 2022,” Dr Pennesi said.
Currently, there are no approved treatments for CEP290-related retinal degenerations. Gene augmentation using a vector to deliver a normal copy of CEP290 is not viable because the CEP290 coding sequence exceeds the packaging capacity of available vectors, Dr Pennesi explained.
EDIT-101 is designed to remove the aberrant splice donor created by the mutation in the CEP290 gene and thereby restore normal CEP290 expression. It uses a photoreceptor-tropic AAV5 vector to deliver guide RNAs highly specific to the CEP290 target sequence and incorporates a photoreceptor-specific promoter for targeted expression of the CRISPR-Cas9 system.
Investigators conduct BRILLIANCE research at five clinical sites across the United States. The first patients enrolled had very severe vision loss (light perception to 1.6 logMAR [20/800 Snellen equivalent]), but subsequent patients were allowed to have vision up to 0.4 logMAR (20/50 Snellen equivalent).

All participants receive a low-dose oral prednisone regimen for approximately six weeks after surgery as immune response prophylaxis. So far, there are reports of only mild treatment-related inflammation, and no detection of a Cas9specific antibody.
The most frequently reported adverse event is eye pain related to the surgical procedure. There have been no cases of treatmentrelated cataracts, oedema, or retinal thinning.
Various functional tests are being used in BRILLIANCE to assess the potential efficacy of EDIT-101, including age- and vision-level-appropriate tests of best-corrected visual acuity (BCVA). Other evaluations include the full-field light sensitivity threshold test (FST) to measure retinal sensitivity and using different chromatic stimuli to differentiate whether function is coming from rods or cones. In addition, participants are undergoing mobility testing using four separate navigation courses with varying difficulty levels that can each occur under different illumination conditions.
patient demonstrated improvement in BCVA at month three with some subjective improvements. The BCVA gain, however, was not sustained during longer follow-up. And although the patient’s performance in the mobility test also improved, a positive change was seen when the testing as performed with the patient using only his untreated eye.
Results were more promising in the middle dose cohort. The first patient treated showed a 0.7 improvement in logMAR BCVA by six weeks that was sustained at six months and accompanied by improvement in FST and mobility test performance. The patient also described multiple subjective improvements in vision.
“Most striking to me was the patient said that when they looked out at their porch before the study, they would see what looked like a single piece of wood. After the treatment, they see the porch’s individual boards,” Dr Pennesi said.

A second patient treated in the mid-dose cohort had been followed for three months and had improvement in the FST and mobility tests without any improvement from baseline BCVA (logMAR 1.4). The final patient in the mid-dose cohort had baseline BCVA of logMAR 0.5 OD/0.6 OS with no improvement in any of the functional tests at last available follow-up after three months.
Dr Pennesi reported the first enrolled patient had baseline BCVA of logMAR 3.5 OU and showed a BCVA gain of 0.3 logMAR at month six. The patient, however, showed no improvement based on the FST or the mobility test and was lost to follow-up after six months due to the COVID-19 pandemic.
The second enrolled patient—also treated with the lowest dose of EDIT-101—had baseline BCVA of logMAR 3.9 OU. The

“Most striking to me was the patient said that when they looked out at their porch before the study, they would see what looked like a single piece of wood. After the treatment, they see the porch’s individual boards.”Dr Pennesi presented these findings at ARVO 2022 in Denver, Colorado, US. Mark Pennesi MD, PhD is Chief, Paul H Casey Ophthalmic Genetics Division, Casey Eye Institute, OHSU, Portland, Oregon, US. pennesim@ohsu.edu
Daniel Briscoe MD, Consultant Oculoplastic and Orbital surgeon and Head of the Department of Ophthalmology at the Emek Medical Center, Afula, Israel, gave a timely talk on orbital trauma as part of the Oculoplastics Specialty day at the Royal College of Ophthalmologists annual congress.
His talk was titled “Approach to orbital trauma: inspection, detection, decisions, and management”.
“Orbital trauma is head trauma and not just of the eye, so you need to search for undetected injuries of the brain, maxillofacial structures, sinuses, and neck, including blood vessels and vertebrae,” Dr Briscoe said.
He emphasised thinking carefully and focusing attention to detect the most important injuries. “Search for the undetected injury,” he advised.
“Good communication with the neuroradiologist will help you make decisions. Look out for a tight orbit, globe injuries, eyelid injuries, and CSF leaks, and check for abnormal mouth closure,” Dr Briscoe said.
Preservation of vision may require orbital surgery. Urgent orbitotomy to release retro bulbar bleeding or perform optic nerve decompression may be needed in a few cases, but this is not common, he said.
He emphasised the importance of prioritising ocular injuries appropriately.
“In the presence of globe injuries, it is better to delay orbital fracture repair until the eye is deemed stable. Eyelid injuries should be treated urgently. Multidisciplinary teams are often needed, so initial surgical repairs should be coordinated and maximised between the teams. Remember that this is only the beginning of a patient’s journey, which can be longer or shorter depending on our decisions.”
Dr Briscoe has had direct experience treating suicide bomb victims and presented cases with horrific injuries from the war in Syria treated by colleagues in Nahariya hospital, Israel.
“War and explosion injuries are a different trauma. Terrorist bombs are built to cause maximal bodily injury to people in their vicinity. They are packed with metal objects which penetrate the whole body, including the eyes. They also cause burn injuries and large shock wave injuries in enclosed spaces such as buses, trains, or buildings.”
The ophthalmologist is usually one of a team of surgeons who operate on these patients. Multidisciplinary team involvement and careful surgical planning are essential without delay in these cases, he stressed.
“War injuries often involve neurosurgical procedures, reconstructing large areas of missing bone and tissue. Eyes are often repairable, so no effort should be spared to save them.”

He reflected on the personal effect on surgeons who treat the severely injured.
“Terrorist bombs and war injuries can have a great emotional toll on the treating surgical team. I was involved in treating patients in several bomb attacks. I found it a very traumatic experience particularly dealing with the parents of injured or dying children—and later on, with recovering children themselves. I don’t have any particular advice on how to deal with it, and I would not wish it on anyone. However, I think talking to colleagues involved in treating victims helped each of us cope in his own way and carry on.”
Daniel Briscoe MD is a Consultant Oculoplastic and Orbital Surgeon, Head of the Department of Ophthalmology at the Emek Medical Center, Afula, Israel, and graduate of the Royal College of Surgeons, Ireland. dr.danielbriscoe@gmail.com
“In the presence of globe injuries, it is better to delay orbital fracture repair until the eye is deemed stable.”
Watch the latest video content from the ESCRS and EuroTimes, FREE on the ESCRS
• EyeJC (ESCRS Journal Club)
• ESCRS CONNECT Academy
• Webinar with HSIOIRS
• Eye Contact Interviews
• Video of the Month
• Video Journal of Cataract, Refractive & Glaucoma Surgery
• Young Ophthalmologists Videos: “My Early Surgeries”
Player.ESCRS.org

Dr Paul Rosen, Chairman of the ESCRS Practice Management & Development committee, says YOs need to understand the business of ophthalmology if they want to provide the best service to their patients.

The ESCRS has always made the education of young ophthalmologists in training one of its major priorities.
This applies not only to clinical training but also an understanding and training in business through the ESCRS Practice Management & Development Programme.
While our programme has focused primarily on business skills for ophthalmologists who have completed their training, we have become increasingly conscious in recent years of the need to expand the programme’s scope to address the specific needs of YOs.
We have updated the programme to reflect this at the 40th ESCRS Congress in Milan, Italy, when there will be a one-hour presentation called “Why Young Ophthalmologists Need to Learn Business and Management Skills”.
The session—held during the ESCRS Practice Management & Development Programme Workshops on Monday, 18 September, 2022—is aimed at YOs intending to either remain in public practice in a hospital or clinic setting or set up their own private practice.

While medical training focuses primarily on acquiring specialist clinical knowledge and practical skills, career success is based on several capabilities rarely, if ever, taught or addressed in medical school and residency.
Negotiation is one of these skills.
The first presentation, “Negotiating Your Way to Success” by Dr Daniel Kook, Germany, will explore how YOs can get a competitive advantage in their career by learning how to negotiate successfully in the various stages of its development. As Dr Kook will explain, it is not always the smartest YOs who get the best jobs, but those who can successfully negotiate their way to better training positions during their residencies and then to more senior positions once completing those residencies.
For YOs who plan to go into private practice, negotiating skills are also essential to agree on their starting salaries with the practice owners and a path to sharing the practice profits in the long term. Contract negotiations can be complex, and Dr Kook’s discussion can develop skills in YOs that will allow them to successfully negotiate when joining a private practice for the first time.
However, negotiation is important for all ophthalmologists daily—especially in competition for clinical resources such as operating theatre time or equipment.
Dr Nic Reus, the Netherlands, the chairperson of the ESCRS
Young Ophthalmologists Committee, will present “What Makes a Good Leader”.
As Green (et al.) points out in a recent article in the Annals of Eye Science, young ophthalmologists must learn how to lead themselves when learning the technical content and skills required in their specialty. In the early stages of their training, YOs may also receive minor leadership roles, and as they progress, they may start to run clinics and operate without direct supervision.i
Dr Reus will give practical examples of how YOs can become good leaders and explain the important differences between leadership and management.
The session will conclude with a presentation from Dr Artemis Matsou, Greece, “What They Don’t Teach You at Medical School”.
Dr Matsou will make suggestions on how the existing training curriculum could expand and give her perspective on how she has progressed on her career path. Clinical training can be very stressful, but if YOs are prepared to think outside the box and take a more holistic view of their training, they will become better doctors.
I realise YOs will have a busy schedule at this year’s Congress, but I would urge them to take the time to attend the Practice Management & Development Masterclass and Workshops, which will be held on Sunday, 18 September, and Monday, 19 September. Further information is available at congress.escrs.org/programme/
i Green C, Atik A, Hay M. “Developing leadership skills in young ophthalmologists,” Ann Eye Sci, 2019; 4:37.

Heidelberg Engineering reported the latest software upgrade allows existing ANTERION customers to add epithelial thickness measurements, intuitive visualisation for assessing corneal ectasia, and automatic anterior chamber measurements to their devices. New customers will find the clinical tools already integrated into the comprehensive platform.
The optional Epithelial Thickness Module allows clinicians reproducible evaluation of corneal epithelial thickness. The parameters and colour maps are intended to assist in refractive surgery planning and treatment control, ocular surface evaluation, screening for corneal ectasia, and other diagnostic areas. The new module for the ANTERION Cornea App also generates thickness maps and measurements for the residual stroma, providing further insights into patients’ corneal health.
Another addition, the ANTERION Ectasia View, is a new comprehensive toolset aiding the assessment of ectatic changes in the cornea. The diagnostic dashboard combines all relevant information in one place. Clinicians can evaluate the most important tomographic maps and parameters at a glance and track progression details with intuitive visualisation tools.
The dashboard also includes the SCORE (Screening Corneal Objective Risk of Ectasia) Analyzer, a unique analysis tool for keratoconus and other ectatic diseases. SCORE, developed by French surgeons Dr Damien Gatinel and Dr Alain Saad, combines multiple corneal indices that describe the magnitude of corneal steepening, thinning, and asymmetry, helping eyecare specialists assess the probability of ectatic changes in their patients’ eyes.
First introduced in 2018, the ANTERION system combines biometry, IOL calculations, cornea diagnostics, and anterior chamber metrics based on high-resolution, swept-source OCT images.

www.anterion.com
www.heidelbergengineering.com/int/company
Schwind announced the initiation of a research project to develop an ophthalmic refractive laser system that uses ultra-short laser pulses. The project will evaluate the feasibility of the Laser-Induced Refractive Index Change (LIRIC) procedure for treating ametropia. This non-invasive approach does not remove tissue to change the refractive power of the cornea—rather, LIRIC corrects refractive errors using local modification of optical qualities of the cornea.
The company believes LIRIC has the potential to correct not only common refractive errors such as myopia, hyperopia, and astigmatism but also high order aberrations as well as presbyopia. This might include ametropic patients who could not previously undergo laser correction—for example, those whose corneas are too thin or too curved.
The company is planning initial investment in basic research of more than 1.6 million euro, of which 52% is funding from the German Federal Ministry of Education and Research (BMBF). Through its “KMUInnovativ” initiative, the BMBF is supporting Schwind and its project partner—the Ruhr Universität Bochum (RUB) University Eye Hospital, Bochum, Germany—in their efforts to give many more people the opportunity of laser vision correction.
Prof. Dr. med. Stephanie Joachim of the University Eye Hospital at RUB is designing and conducting a tailored preclinical study with hydrogel and ex vivo animal eyes to analyse and validate the efficacy and safety of the LIRIC procedure. www.eye-tech-solutions.com
Lensar reported it had received US FDA 510(k) clearance for its ALLY Adaptive Cataract Treatment System. The company says this will be its first platform to integrate its proprietary imaging with an optimised femtosecond laser in a compact system. The integrated system is said to allow the surgeon to perform the entire cataract procedure in an operating room or in-office surgical suite, increasing efficiency and decreasing costs. ALLY includes the company’s proprietary Streamline® software technology. The system uses advanced astigmatic management tools improve accuracy and precision.
lensar.com/technology/ally-adaptive-cataract-treatment-system
The ESCRS is happy to include the Video Journal of Cataract, Refractive, and Glaucoma Surgery among our education resources. I encourage all of our members to visit the site and take advantage of the nearendless educational opportunities in cataract, refractive, and glaucoma surgery,” said Oliver Findl MD, current president of the ESCRS.
The VJCRGS was the first video journal in medicine, founded back in the day of videotape—before the internet existed. Now online at vjcrgs.com, the resource offers at least an hour of the highest quality education for the anterior segment surgeon four times each year. The journal is free to all practicing ophthalmologists and teaching institutions.
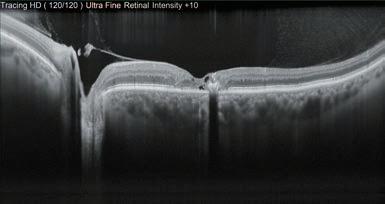
Current visitors will find a series of video presentations from the ESCRS 2021 Video Symposium “Pumping Adrenaline”. Topics include preoperative challenges such as posterior lenticonus; intraoperative complications such as a mature cataract with an anterior capsule tear; and postoperative surprises, including decentration of premium IOLs.

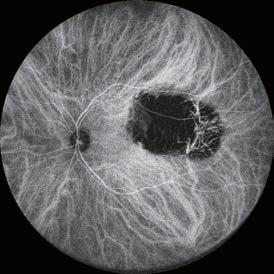
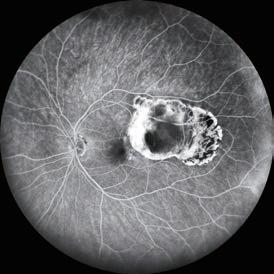
Dr Osher said he watches every video from the ASCRS, ESCRS, AAO, and the other major film festivals around the world to develop content for the VJCRGS. A distinguished editorial board hand-picks surgical videos from ophthalmologists that demonstrate excellent skill and sophisticated technique. The board includes Drs Graham Barrett, Michael Snyder, George Waring IV, and Ike Ahmed.
“We feature an international cast of surgeons who show innovative techniques, challenging cases, complication management, and award-winning videos and named lectures. We avoid any advertising or promotional content interfering with the viewer’s education. For example, the issue I am presently editing will focus on intrascleral haptic fixation and at least a dozen modifications of the Yamane technique,” Dr Osher said.
The VJCRGS began in 1985 as a quarterly subscription serving the needs of cataract and refractive surgeons. In 2018, the Video Journal’s scope expanded to include glaucoma surgery—in line with the evolving trends in anterior segment surgical management.
Robert H Osher MD served his residency at the Bascom Palmer Eye Institute and completed three fellowships in Miami, Florida, US, and at the Wills Eye Hospital in Philadelphia, Pennsylvania, US. Dr Osher is Professor of Ophthalmology at the College of Medicine of the University of Cincinnati and Medical Director Emeritus of the Cincinnati Eye Institute, Ohio, US. His practice has been limited to cataract and implant surgery by referral for thirtyeight years.
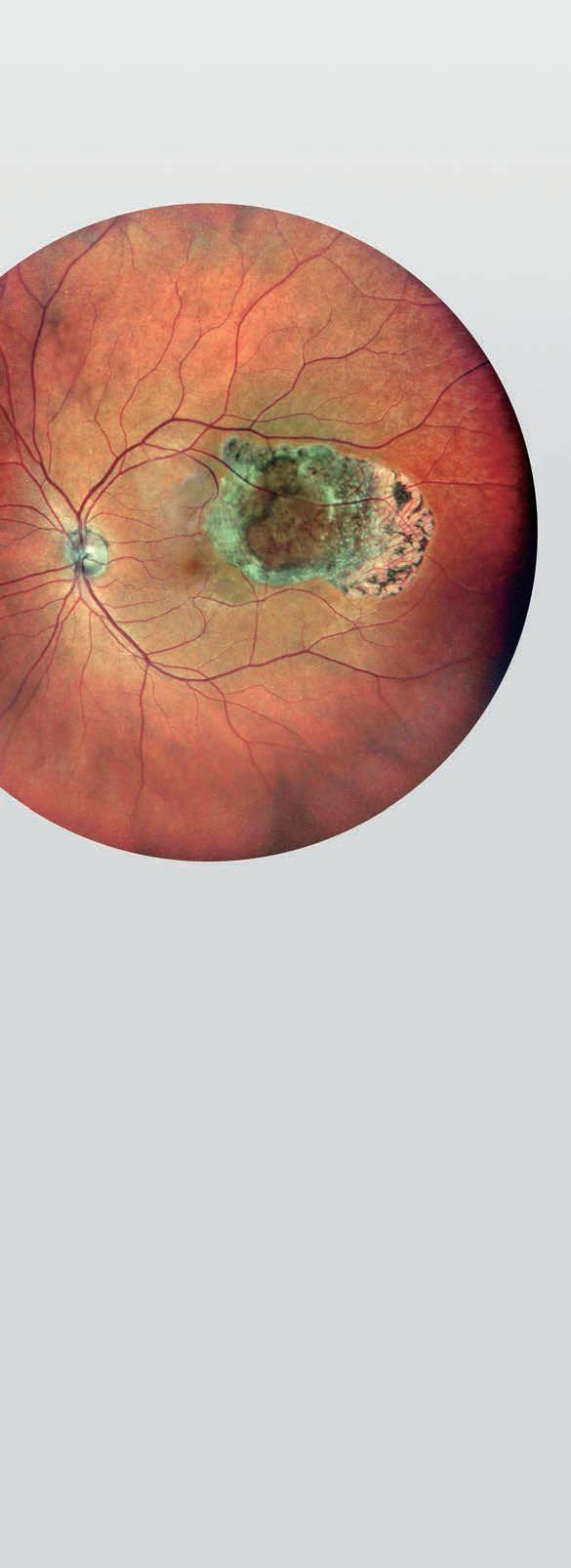
Developed by Dr Robert Osher four decades ago, the Video Journal of Cataract, Refractive, and Glaucoma Surgery (VJCRGS) has become a mainstay for ophthalmic surgeons.
In his brief life, German anatomist and botanist Johann Gottfried Zinn made significant contributions to the anatomical study of the eye. His most well-known work, Descriptio anatomica oculi humani, “gave the first detailed and comprehensive description of the anatomy of the human eye”.i Zinn was born in the village of Schwabach, the son of a counsellor of the regional royal treasury in Ansbach, Bavaria. He attended the medical school of the newly established University of Göttingen under the mentorship of the famous professor of anatomy, physiology, and botany, Albrecht von Haller (1708–1777), and obtained his doctorate in 1749. He left Haller and Göttingen for Berlin. Here he had access to extensive tools and materials with which to pursue his ophthalmological research.
Zinn returned to Göttingen in 1753 to accept a position as extraordinary professor of medicine and director of the town’s botanical gardens.ii He was one of the first to render an accurate description of the eyeball, and he investigated the vessels and nerves of the eye cavity.
His most important publication was his Descriptio anatomica oculi humani, a fundamental work in the history of ophthalmology. This work provides the first description of many ocular structures that bear his name—including the zonule of Zinn, Zinn-Haller’s arterial circle, and the annular tendon of Zinn, which serves as attachment for all
the extraocular muscles of the eye and the optic nerve passes through the centre of the ring.

In his capacity as director of the botanical gardens, he composed his Catalogus Plantarum Horti Academici Et Agri Gottingensis, in which he provided a comprehensive description of the plants in the university’s collection. During this time, he also published the first botanical illustration of flowers grown from seeds he received in an envelope from the German Ambassador to Mexico—describing the plant blossoms in detail. He shared the seeds with other botanists throughout Europe. Carolus Linnæus, who corresponded with Zinn, named the genus of the flower Zinnia in his honour.
The broad scope of his work and the lasting impression he made are even more amazing considering the brevity of his life. He died of tuberculosis in 1759 at the age of 31.
Sources: H Mark, Arch Ophthalmol 2009; 127: 1215–1217.

i Streng, B et al. “Johann Gottfried Zinn—ein fränkischer Anatom und Botaniker” [Johann Gottfried Zinn—a Franconian anatomist and botanist]. Klinische Monatsblatter fur Augenheilkunde, 1991; 199(1): 57–61. doi:10.1055/s-2008-1046048.
ii “Johann Gottfried Zinn.” https://www.whonamedit.com/doctor. cfm/3203.html#:~:text=Biography%20of%20Johann%20Gottfried%20 Zinn&text=He%20left%20Haller%20and%20G%C3%B6ttingen.


A nanoemulsion of difluprednate twice a day proved equal to traditional treatment with prednisolone acetate four times a day, a recent study shows. The prospective, multicentre, double-blind study enrolled 259 patients in a randomised, parallel-group protocol. The primary endpoint was central corneal thickness. There was no difference in endothelial cell loss rates between the treatment groups. Both groups experienced transient IOP elevations. The main advantage of difluprednate nanoemulsion use is the possibility of reducing dosing frequency in the perioperative period, which could improve patients’ compliance, the researchers note. G Valvecchia et al., “Difluprednate 0.05% twice a day vs prednisolone acetate 1% 4 times a day for cataract postsurgical inflammation treatment: noninferiority trial”, 48(7): 753–758.

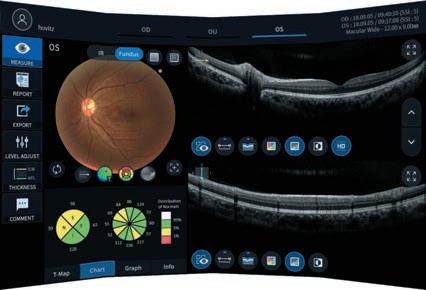
At a time of increasing concern about opioid abuse in communities around the world, the prescription rate for opioids after ophthalmic procedures, including cataract surgery, has been paradoxically increasing. Phenylephrine/ketorolac (P/K) could be a viable nonopioid alternative for managing both intraoperative and early postoperative pain. A study enrolled 112 eyes of 56 patients—mean age, 70 years—undergoing bilateral cataract surgery. Half of the patients received epinephrine for the first eye, followed two weeks later by P/K in the second eye; the other half received P/K in the first eye, followed by epinephrine in the second.

Patients treated with P/K had a statistically significant lower use of the opioid fentanyl intraoperatively while also experiencing significantly less pain than those treated with epinephrine. Pain reduction was significantly greater with P/K administration versus epinephrine at all evaluated timepoints: intraoperatively, immediately postoperatively, and one-day postoperatively. The researchers concluded that this finding could lead to decreased use of intraoperative opioids. E Donnenfeld et al. “Pain control and reduction of opioid use associated with intracameral phenylephrine1.0%–ketorolac 0.3% administered during cataract surgery”, 48(7): 759–764.
Unnecessary waste of perioperative topical ophthalmic medications is an important component of clinical ophthalmology’s carbon footprint. A task force comprised of representatives of several ophthalmic societies released a position paper on this issue. The task force noted that discarded topical eyedrops and ointments from unused or partially used containers account for considerable costs locally and significant additions to global CO2 emissions. Citing clinical studies, the group suggests surgical facilities should be able to use topical drugs in multidose containers on multiple patients until the drugs expire, with proper guidelines. They also propose surgical patients be allowed to bring partially used medication home for postoperative use. DJ Palmer et al. “Reducing Topical Drug Waste in Ophthalmic Surgery: Multi-society Position Paper”, online, jcrs.org, May 2022.
Friday 16 th September 2022
MiCo Milano Convention Centre, Milan, Italy
Learn of the latest innovative technologies, including presentations from several emerging companies, and perspectives on how they will change the future of European ophthalmology over the next several years.

Including leaders from the medical, industry and financial communities
30 Minute Panel Discussions on
• Presbyopia • Cataract extraction • MDR
• Digital health
• Glaucoma • Sustainability
• Industry leadership • Financial future of eyecare
Data from over 1,000 delegates will be reviewed on key clinical opinions and practice patterns impacting the integration of the latest technologies
Participate in onsite attendee survey of prevailing trends and barriers
www.inovation.escrs.org
Participate in this first iNovation meeting in European Ophthalmology
1 – 4 September
Hamburg, Germany
ESCRS iNovation Day
16 September
Milan, Italy
WSPOS Subspecialty Day
16 September
Milan, Italy
40th Congress of the ESCRS
16 – 20 September
Milan, Italy

FRIDAY 16 SEPTEMBER
Emerging Treatment Options for Corneal Endothelial Disease
Main Symposium
17:00 – 19:00 | Auditorium
SATURDAY 17 SEPTEMBER
Opening Ceremony & Ridley Medal Lecture
Opening Ceremony
10:00 – 11:00 | Silver Room
Demystifying IOLs Optics
Main Symposium
11:00 – 13:00 | Silver Room
SUNDAY 18 SEPTEMBER
High Volume Cataract Surgerys
Main Symposium
11:00 – 13:00 | Silver Room
MONDAY 19 SEPTEMBER
Heritage Lecture Main Symposium
10:30 – 11:00 | Silver Room
Where are we in Intracorneal Implantation?
Main Symposium
11:00 – 13:00 | Silver Room
Surgical Video Session Getting Into Trouble?
Main Symposium
14:00 – 16:00 | Silver Room
TUESDAY 20 SEPTEMBER
How Not to be Surprised by Refractive Surprise
Main Symposium
10:30 – 12:30 | Silver Room
Best of the Best
12:45 – 14:45 | Auditorium


Powerful technology for sustained intraocular pressure and medication reduction. Predictable outcomes from a truly tissue-sparing procedure. All on a proven platform with the most clinical evidence of any MIGS device.
Experience the latest evolution of the iStent® legacy of excellence in your practice.
iStent inject® W IMPORTANT SAFETY INFORMATION

INDICATION FOR USE: The iStent inject W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS:
• For prescription use only.
• This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised.
• Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.”
• There are no known compatibility issues with the iStent inject W and other intraoperative devices. (e.g., viscoelastics) or glaucoma medications. • Unused product & packaging may be disposed of in accordance with facility procedures. Implanted medical devices and contaminated products must be disposed of as medical waste. • The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. If intraocular pressure is not adequately maintained after surgery, the surgeon should consider an appropriate treatment regimen to reduce intraocular pressure. • Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. ADVERSE EVENTS: Please refer to Directions For Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events.

Glaukos®, iStent®, and iStent inject ® W are registered trademarks of Glaukos Corporation. All rights reserved. ©2022 PM-EU-0187