






Surgical guidance with AI Page 10 Inside: Ethics | Safe Medication | Long-term Care | Special Focus: Infection Control www.hospitalnews.com March 2024 Edition Are You Protected From An Unexpected Loss of Income? Our Signature package (Life, LTD and ADD&D) is tailor-made for those who already 1-866-768-1477 | www.healthcareproviders.ca FEATURED







Nurses talk truth.



“The government has proven time and time again that they have to be forced to do the right thing.”
Rights upheld.


On February 12, Doug Ford’s Bill 124 was ruled unconstitutional, the second time the Ontario courts have rejected this legislation. The decision is a ringing victory for the nurses and other public sector workers whose wages were punitively suppressed for three years.
Bill 124 was misguided and mean-spirited from the beginning and is a direct cause of the nursing shortage that continues to devastate our public health-care system.

back down from wrongful actions. When a government repeatedly fails to hold itself accountable…others have to do it for them.



NursesTalkTruth.ca





















Surgical guidance with AI Page 10 Inside: Ethics | Safe Medication | Long-term Care | Special Focus: Infection Control www.hospitalnews.com March 2024 Edition Are You Protected From An Unexpected Loss of Income? Our Signature package (Life, LTD and ADD&D) is tailor-made for those who already 1-866-768-1477 | www.healthcareproviders.ca FEATURED 2024 4 Infection Control MARCH 2024 HOSPITAL NEWS 23 www.hospitalnews.com Contents COLUMNS Guest editorial ................4 In brief .............................6 Ethics .............................22 Long-Term care ..............36 Safe medication ............38 March 2024 Edition IN THIS ISSUE: ▲ Special Focus: 2024 Infection Control 23 ▲ Cover story: Surgical guidance with AI 10 ▲ Yukon Home Care embraces e-bikes for service delivery 16 ▲ Viagra to treat oxygen-deprived newborns 8 ▲ Protecting patients and the planet from unnecessary tests 12 Expanding access to cardiac care 5 MARCH 2024 HOSPITAL NEWS 3 www.hospitalnews.com
We need health system solutions now: CMA, CFPC
Medical organizations call on governments to reimagine primary care to help stabilize, rebuild health systems
By Dr. Kathleen Ross
Land Dr. Michael Green
ast February 7, the federal government announced the most significant investment in health care in more than two decades. This investment followed years of health systems struggling to provide timely, equitable care, a crisis exacerbated by the COVID-19 pandemic that ravaged health care in Canada.
One year later, our health systems continue to struggle to provide the care that Canadians need, where and when they need it. More than six million Canadians do not have a family physician. Lengthy wait times for surgeries and diagnostic and life-saving treatments remain. Physicians, nurses, and other providers continue burning out, faced with insufficient system supports, overwhelming administrative burden, and inadequate remuneration. Emergency departments across the country routinely operate well beyond capacity. This cannot continue.
action plans and setting targets to strengthen their respective health systems, with accountability measures in place to monitor progress. To date, only four provinces have reached agreements with the federal government. Meanwhile, Canadians continue to suffer, and they are rapidly losing faith that positive change is coming.
The Canadian Medical Association (CMA) and the College of Family Physicians of Canada (CFPC), speaking on behalf of physicians and medical learners across the country, are calling on governments to act urgently to address Canadians’ concerns. Health care providers can no longer be called upon to prop up systems that are on the verge of collapse.
TO DATE, ONLY FOUR PROVINCES HAVE REACHED AGREEMENTS WITH THE FEDERAL GOVERNMENT. MEANWHILE, CANADIANS CONTINUE TO SUFFER, AND THEY ARE RAPIDLY LOSING FAITH THAT POSITIVE CHANGE IS COMING.
We need action. We need it now.
A significant portion of the federal government’s investment depends on provinces and territories creating
UPCOMING DEADLINES
APRIL 2024 ISSUE
EDITORIAL: March 8
ADVERTISING:
Display – March 22 | Material – March 26
Monthly Focus:
Healthcare Transformation/eHealth and EHR/ Mobile Health: Programs and initiatives that are transforming care and contributing to an effective, accountable and sustainable system including virtual care. Innovations in electronic/digital healthcare, including mHealth and the Electronic Health Record (EHR).
Annual E-Health Supplement & Special Focus
Anesthesiologists
Critical to stabilizing and rebuilding health care is fixing its front door: primary care. Family physicians, working with other primary care providers, offer comprehensive, continuous care while helping patients navigate complex health systems. Having a dedicated family doctor significantly improves patient health outcomes and system efficiency, keeping costs low and emergency departments available to treat emergencies.
Continued on page 6
MAY 2024 ISSUE
EDITORIAL: April 5
ADVERTISING:
Display – April 26 | Material – April 30
Monthly Focus:
Surgical Procedures/Pain Management/ Palliative Care/Oncology: Non-invasive surgery, plastic surgery, orthopedic surgery and new surgical techniques including organ donation and transplantation procedures. New approaches to pain management and palliative care delivery. Approaches to cancer diagnosis and treatment.
Nursing Heroes Supplement
THANKS TO OUR ADVERTISERS Hospital News is provided at no cost in hospitals. When you visit our advertisers, please mention you saw their ads in Hospital News.
610 Applewood Crescent, Suite 103 Vaughan Ontario L4K 0E3 TEL. 905.532.2600|FAX 1.888.546.6189 www.hospitalnews.com
Editor
Kristie Jones editor@hospitalnews.com
Advertising Representatives
Denise Hodgson denise@hospitalnews.com
Publisher
Stefan Dreesen stefan@hospitalnews.com
Accounting Inquiries accountingteam@mediaclassified.ca
Circulation Inquiries info@hospitalnews.com
Director of Print Media
Lauren Reid-Sachs
ADVISORY BOARD
Barb Mildon, RN, PHD, CHE
VP Professional Practice & Research & CNE, Ontario Shores Centre for Mental Health Sciences
Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications
Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
ASSOCIATE PARTNERS:
Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario.
The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
Canadian Publications mail sales product agreement number 42578518.

4 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com
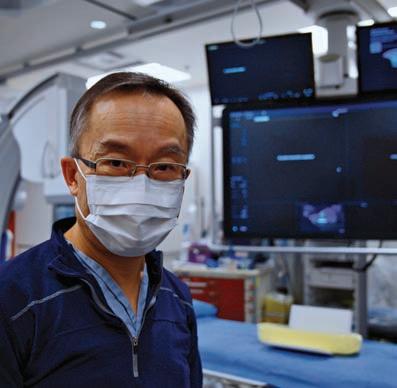
Expanding access to cardiac care
More than 6,000 people are admitted to Fraser Health hospitals for cardiac failure every year. As part of a regional strategy to expand cardiac care, a new cardiac multipurpose interventional suite at Royal Columbian Hospital is now open to provide better access to specialized cardiac procedures. Additionally, a governance structure is in place and project plans are being developed for two new cardiac catheterization (cath) labs at Surrey Memorial Hospital to further enhance access to this important service. The cath labs at Surrey Memorial Hospital will be co-located with a new interventional radiology suite.
The new cardiac multipurpose interventional suite at Royal Columbian Hospital enables health teams to perform specialized procedures, including minimally invasive procedures which improve and save lives. Early diagnosis and timely treatment of cardiac disease, including coronary, valve and electrical disturbances can prevent serious complications including stroke and cardiac arrest.
“With an aging population, we are seeing more patients who require cardiac procedures who may not be suitable for conventional surgery,” says Dr. Albert Chan, director, Cardiac Catheterization Lab. “Being able to provide even more minimally invasive procedures in a third procedure room is a huge benefit to our community. It allows our patients to have a shorter recovery and return to their normal activities much quicker.”
”The new multi-use space give us more flexibility to meet the needs of patients,” says Samina Patel, clinical nurse educator. “It is incredibly rewarding to improve people’s lives by being able to diagnose and treat their cardiac issues.”
Among other things, the multipurpose interventional suite will be used for mapping the circuits of the heart (electrophysiology), and implanting devices such as pacemakers and defibrillators. Demand for these services is growing.
A relatively new procedure, Transcatheter Edge-to-Edge-Repair (TEER),
is designed for patients with valve problems and congestive heart failure for whom open heart surgery is not an option. TEER involves inserting a clip through a plastic tube from the femoral vein in the groin up to the left side of the heart. The clip holds the edges of the mitral valve together, allowing the valve to open and close properly, preventing blood from flowing back into the left side of the heart.
The demand for Electrophysiology (EP) procedures also continues to grow. An estimated 1,015 EP procedures will be completed in 2024/2025, including atrial fibrillation (AF) ablation procedures. When the electrical impulses that coordinate contractions of the heart are out of sync, atrial fibrillation results. AF ablation can correct this problem with significant improvement in outcomes and quality of life.
“Often, the need for medication goes away completely,” says Shawn Muirhead, electrophysiology clinical coordinator. “We see people get back to riding bikes and walking because they received care that literally adds years onto their lives.”
Heart disease remains a primary cause of death among people 65 and older. We know that in the coming years, our communities will continue to grow, resulting in an increased demand for cardiac services, including general cardiology, diagnostics and interventions, surgery and inpatient capacity, outpatient clinics and outreach services.
“Expanding our services and physical spaces and infrastructure when patients are present and receiving life-saving procedures is a challenge and an honour,” says Sharat Chandra, Vice President, Strategic Capital Investments and Facilities. “The Facilities project planning, design, construction and maintenance teams had to be nimble in order to respond to the challenges posed by COVID-19 while creating the new space, equipment and functionality as quickly as possible. The new suite is a testament to the collaboration between clinical and Facilities Management providing physical spaces that are vital to patient care.”

In recognition of the importance of heart health, Royal Columbian Hospital Foundation funded more than $1.6 million of the $12.6 million renovation to the cardiac catheterization lab.
“Royal Columbian Hospital Foundation is incredibly grateful for the support of our generous donors who have helped to make this possible.
Their contributions enable us to provide patients across B.C. with the highest quality of care,” says Jeff Norris, President and CEO. “We are committed to continuing our mission of supporting Royal Columbian Hospital and improving health care outcomes for all those in need across our province.” ■ H


MARCH 2024 HOSPITAL NEWS 5 www.hospitalnews.com NEWS
Dr. Albert Chan is the director of the Cardiac Catheterization Lab.
Many older adults receiving home care do not receive palliative care before death
Many older adults receiving home care do not receive any palliative home care before death, suggesting we need better methods to identify people who need this support, according to new research in CMAJ (Canadian Medical Association Journal).
“Palliative care is an essential component of a holistic, comprehensive and patient-centred approach to care for all people with a life-limiting illness from the time of diagnosis with the disease,” said Dr. Amy Hsu, investigator at the Bruyère Research Institute and faculty in the Department of Family Medicine at the University of Ottawa, senior author of the study.
Starting palliative care in the months before death is linked to a more positive end-of-life experience, including improved quality of life, less anxiety, better pain and symptom management, and potentially less aggressive care at the end of life. However, Canadian estimates indicate that only 15 per cent of people receive palliative care at home in the last year of life.
The study, conducted by Ottawa researchers, looked at data on almost a quarter million community-dwelling older adults with at least one interRAI Home Care assessment between August 2018 and September 2019. Using a tool called RESPECT, which was developed to help identify frail older
Continued from page 4
adults’ need for palliative care, the research team predicted the risk of dying within 6 months of an assessment and looked at what health services people received.
They found that only about half of the individuals who had an estimated life expectancy of less than three months had received formal palliative home care. Those who had received palliative home care were people who had been flagged by physicians as having a terminal prognosis.
“Prediction algorithms, like RESPECT, can improve how we provide care to frail individuals. They can help clinicians recognize who needs care and when,” said Dr. Doug Manuel,
a family medicine physician and senior scientist at the Ottawa Hospital Research Institute, one of the study’s coauthors.
“These tools and data can also support earlier conversations about patients’ preferences, goals, and wishes as they approach the end of life, and inform advance care planning,” adds Dr. Hsu.
“A substantial proportion of clients likely in their last few months to years of life do not receive any palliative care and continue to be admitted to hospitals and long-term care homes. Most Canadians want to die at home or in a home-like environment, surrounded by their loved ones. When individuals are not supported to die
in the community, their end-of-life care experiences may be misaligned with their preferences,” said Ms. Maya Murmann, research associate at the Bruyère Research Institute, who is supporting the integration of RESPECT in various health settings.
The RESPECT calculator is available at ProjectBigLife.ca. The researchers are working with partners in home, community care, and long-term care to implement RESPECT in their settings.
“Estimated mortality risk and use of palliative care services among home care clients during the last 6 months of life: a retrospective cohort study” was published February 26, 2024. ■ H
P Shorter lifespans for Inuit from Nunavik, Quebec, with lung cancer
eople living in the Inuit region of Nunavik in northern Quebec die earlier after a diagnosis of lung cancer than Montreal residents receiving treatment at the same cancer centre, according to new research published in CMAJ (Canadian Medical Association Journal)
All inhabitants of Nunavik are investigated and treated for cancer at the McGill University Health Centre (MUHC) in Montreal, more than
Health system solutions
The demands placed on primary care providers – from managing growing administrative demands to caring for patients in a system in need of more support – have never been greater. We need leadership and collaboration between jurisdictions to reimagine family medicine and move to interdisciplinary team-based care.
While the CFPC and CMA urge action, we are also providing solutions including the Health Human Resource Policy Recommendations; the CMA’s
Improving Accountability in Health Care for Canadians; and the CFPC’s Prescription for Primary Care and Family Practice Reform Policy Proposal Package.
The CFPC and the CMA are urging the public and health care professionals to join us in demanding action from their local elected officials by using the CFPC’s letter writing tool and participate in the conversation on social media using the hashtag #stopwaiting.
We need action. We need it now. ■ H Dr. Kathleen Ross is CMA President and Dr. Michael Green is CFPC President.
1400 km away from Nunavik hospitals, due to limited resources in the region.
Researchers compared lung cancer survival between 95 Nunavik and 185 Montreal residents being treated at MUHC. They found that Nunavik residents with similar stages of lung cancer had shorter survival than Montreal residents, even after accounting for other differences between the groups.
Analyzing results with community representatives pointed to chronic health care under-resourcing as a possible root cause of these survival differences.
“We underscore that our results should not be interpreted to conclude that Inuit have a genetic predisposition to worse lung cancer outcomes. Rather, our study observations contextualized with other knowledge about health services and access in Nunavik point to chronic underfunding and under-resourcing of Nunavik’s health care services, as well as the lack of Inuit representation in health care provision, as likely upstream determinants of the disparity observed in our study,” writes Dr. Faiz Ahmad Khan, a respirologist and associate professor, MUHC, Montreal, Quebec, with coauthors.
The authors recommend several actions to improve lung cancer survival for Nunavik Inuit, including:
• Deploying Inuit-specific smoking cessation and prevention services
• Making lung cancer screening available immediately, in an accessible, acceptable and culturally safe format, to facilitate earlier detection of lung cancer
• Improving lung health services by, for example, creating x-ray capacity in villages
• Supporting a Nunavik Inuit-specific lung cancer care plan
• Providing training and employment for Inuit health navigators to support patients and families in Montreal
• Increasing funding and human resourcing to strengthen Nunavik health care services
“In the bigger picture, observations such as ours should support Nunavik Inuit efforts toward greater self-governance, as increased Inuit decision-making over health care policy and funding will help ensure health services are aligned with the population’s needs.”
“Nunavimmi puvakkut kaggutimik aanniaqarniq: Qanuilirqitaa? Lung cancer in Nunavik: How are we doing? A retrospective matched cohort study” was published February 20, 2024. ■ H
6 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com IN BRIEF
Anorexia nervosa can be life threatening in males
Anorexia nervosa affects males as well as females, and affected males have a sixfold higher mortality rate than males in the general population. A new article published in CMAJ (Canadian Medical Association Journal) aims to raise awareness of this life-threatening eating disorder.
“Early identification and prompt treatment are essential,” writes Dr. Basil Kadoura, a specialist in adolescent health, British Columbia Children’s Hospital and University of British Columbia, Vancouver, BC, with coauthors.
Five things to know about anorexia nervosa in males:
1. Up to 0.3% of males will be diagnosed with anorexia nervosa. Stigma, poor mental health literacy and gendered
UP TO 0.3% OF MALES WILL BE DIAGNOSED WITH ANOREXIA NERVOSA.
stereotypes reduce help-seeking behaviours and lead to delayed treatment and worse outcomes.
2. Certain adolescent males are at higher risk. Athletes involved in body- and strength-focused sports like cycling, running, and wrestling, are a higher risk of developing the disorder, as are racially and ethnically diverse males and gay, bisexual, trans, and queer people.
Winning together for wellness
After a successful pilot campaign this fall, Split The Pot Lottery is back in support of hospitals across Ontario. This collaborative fundraising effort returns bigger and better than before. From February 8 to March 21, this lottery supports an additional 30 hospital partners and offers players 13 more chances to win early bird prizes. The number and breakdown of the grand prize draws remains the same.
Split the Pot Lottery gives players the chance to win big while contributing to vital healthcare initiatives in their communities. With a total of 51 hospital partners and a guaranteed minimum $500,000 jackpot, it also presents the unique opportunity to participate in the largest partnered fundraising initiative in Ontario.
“As lead sponsor of the Split the Pot Lottery initiative, we’re very excited to see so many hospital foundations come together. The initial lottery exceeded expectations, and we can’t wait to see the impacts of Split the Pot on our local health care. Our portion of the proceeds will support critical projects and infrastructure that improve patient experience across Grand River Hospital,”
says Paul McIntyre Royston, President & CEO, Grand River Hospital Foundation. “By participating in Split the Pot, you help to ensure Care Never Stops in our communities and that patients receive access to the technology and services they need to have the best possible outcomes. Thank you for your rallying support and showing our patients that you care!”
To give players more chances to win, the Split the Pot Lottery jackpot will be divided among 13 grand prize winners, and there will be 26 chances to win a total of $76,000 in early bird prizes. And, of course, Ontario patients win big too, with a portion of proceeds from every ticket purchased going directly to support partnering hospitals through their foundations.
Tickets are on sale now and can be purchased by visiting the Split the Pot website: splitthepot.ca. All tickets purchased before midnight, Thursday, February 15 will be eligible for all 26 early bird prizes, plus the grand prize draws.
Learn all about Split the Pot Lottery, including ticket prices, prizes, draws, important dates, and contest rules by going to splitthepot.ca. ■ H
3. Screening for muscle-enhancing goals and behaviours is important to assess for anorexia nervosa. Diet changes, vomiting, over-exercising, and supplement and anabolic steroid use are potential red flags. The Muscularity Oriented Eating Test is a tool used to assess for these eating behaviours.
4. Complications can be life threatening. These include vital sign instability, slower than normal heart rate, electrolyte abnormalities and other conditions. A detailed history, physical examination and bloodwork will help identify serious medical issues and guide treatment.
5. Family-based treatment is recommended for outpatients. In this guideline-recommended approach, parents are considered experts in their adolescent and lead in re-nourishing their child.
“Most adolescent males with anorexia nervosa can be treated as outpatients with family-based treatment and ongoing medical monitoring. However, some adolescents may require treatment in hospital,” write the authors.
“Anorexia nervosa in adolescent males” was published February 20, 2024. ■ H
Prolonged cough? In most cases, patience is the treatment
Coughing after a respiratory infection is common and, in most cases, will resolve with time, according to an article in CMAJ (Canadian Medical Association Journal).
With the recent bout of respiratory infections across Canada, many people are suffering from a postinfectious cough, or a cough that lasts for weeks after the initial infection has resolved.
“Reassuring patients that postinfectious cough is time limited and self resolving is important and can reduce unnecessary and costly prescriptions, such as asthma puffers or antibiotics,” said Dr. Kevin Liang, a family physician and clinical instructor in the Department of Family Practice at the University of British Columbia, Vancouver, BC. “Most postinfectious cough symptoms will improve without medication.”
Key points about postinfectious cough:
1. Postinfectious coughs are common, affecting about 11 per cent to 25 per cent of adults after a respiratory infection and can last up to 8 weeks.
2. Diagnosis requires an earlier respiratory infection and exclusion of other postinfectious cough mimics, such as asthma and chronic obstructive pulmonary disease.
3. Check for red flags and cough duration. Symptoms such as swallowing difficulty, excessive shortness of breath, and coughing up blood may require investigation. Red flags include a history of recurrent pneumonia or an extended history of smoking, and coughs lasting longer than 8 weeks need further assessment.
4. There is no good evidence for a medication that works to stop postinfectious cough. Evidence shows little benefit with inhalers or oral medications to treat a cough. These medications can be quite costly and cause unwanted side effects as well.
5. Patient reassurance and education are critical. Clinicians should advise patients to arrange a follow-up appointment for further investigation if their cough has not resolved within 8 weeks or if new symptoms appear.
“Postinfectious cough in adults” was published February 12, 2024. ■ H
MARCH 2024 HOSPITAL NEWS 7 www.hospitalnews.com IN BRIEF
Viagra to treat oxygen-deprived newborns
Treatments to help babies who run out of oxygen during pregnancy or at birth (neonatal encephalopathy) are limited. Therapeutic hypothermia is the only option used to prevent brain damage in such cases, but 29 per cent of babies who receive it still develop significant neurological sequelae. The first phase of a new clinical study conducted at the Montreal Children’s Hospital (MCH) shows that the administration of sildenafil, marketed under the brand name Viagra, could be a possible solution.
This is the first proof-of-concept study to attempt to repair the brain damage caused by neonatal encephalopathy. In general, research focuses on how to prevent it. The results indicate that the use of sildenafil in babies who have developed such sequelae despite therapeutic hypothermia is feasible and safe. This first phase also shows encouraging signs of efficacy, and research will be continuing in this area.
“Currently, when a baby has brain damage, there is little we can offer other than supportive care such as physiotherapy, occupational therapy or specialized care. If we had a drug that could repair the brain, it could change the future of these babies. It would be a victory for them, for their family and for society in general,” explains Dr. Pia Wintermark, senior author of the study, a neonatologist at the MCH and scientist with the Child Health and Human Development Program of the Research Institute of the McGill University Health Centre (RI-MUHC)
. STUDIED FOR ADULTS
Research in rat models has shown that sildenafil can have neurorestorative properties in adult stroke patients. It was therefore important to know whether this drug could have similar effects on the brains of newborn babies.
The idea came while Dr. Wintermark was doing her residency in Switzerland. She continued her training on how to work with animal models in

Boston. Upon her arrival in Montreal, she began her laboratory experiments in 2010.
Between 2016 and 2019, Dr. Wintermark and her team were finally able to proceed with the first phase of the clinical study involving 24 babies born at 36 weeks of gestation or more, with moderate to severe neonatal encephalopathy, who had been placed on therapeutic hypothermia and had brain damage despite treatment. Of the group, eight received sildenafil starting on the second or third day of life, twice a day for seven days (total of 14 doses). A placebo was administered to three other babies.
During the first ten days of the children’s lives, the researchers assessed the safety of the treatment by recording the occurrence of adverse events such as hypotension, worsening liver function, persistent pulmonary hypertension, death, etc.
Blood pressure slightly decreased in two of the eight babies after the first dose of sildenafil, but this did not recur thereafter. One newborn who received the drug died after his family decided to transition to palliative care, a
choice parents sometimes make when their child has important brain damage. This event is not considered to be related to the administration of sildenafil. No child in the placebo group died.The study therefore concludes that sildenafil is safe and well absorbed by babies who have developed brain damage due to neonatal encephalopathy and in whom therapeutic hypothermia has proved ineffective.
SIGNS OF RECOVERY
The efficacy of sildenafil was also assessed as an exploratory analysis. At 30 days of age, five newborns treated with sildenafil showed partial healing of injury, fewer signs of brain volume loss and an increase in deep gray matter. Nothing of the kind was noted in the placebo group.
Nine out of 10 patients were also seen at 18 months for neurodevelopmental evaluation. In the sildenafil group, one baby in six developed cerebral palsy, compared to three babies in three in the placebo group. Global developmental and fine motor delays were noted in two out of six children given the drug, while all children in
the placebo group (3/3) suffered from them.
“All neonates enrolled in this study had significant brain damage at baseline. As such, it was expected that they would develop poorer neurodevelopmental outcome compared with a general population of neonates with neonatal encephalopathy treated with therapeutic hypothermia,” says Dr. Wintermark.
The first phase of this study was not designed to establish the efficacy of sildenafil in such cases. However, assessments at 30 days and 18 months ruled out any long-term adverse events and showed encouraging results for the future. Further studies will be carried out on larger cohorts of neonates to confirm the phase I findings, define the optimal dose of sildenafil and establish its neuroprotective and neurorestorative potential.
“Sildenafil is inexpensive and easy to administer. If it holds its promise in the next phases of the study, it could change the lives of babies suffering from neonatal encephalopathy all over the world,” concludes the researcher. ■ H






8 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com NEWS
The study Feasibility and safety of sildenafil to repair brain injury secondary to birth asphyxia: A randomized, double-blind, placebo-controlled phase Ib clinical trial was conducted by Pia Wintermark, Anie Lapointe, Robin Steinhorn, Emmanouil Rampakakis, Jürgen Burhenne, Andreas D. Meid, Gzona Bajraktari-Sylejmani, May Khairy, Gabriel Altit, Marie-Therese Adamo, Alishia Poccia, Guillaume Gilbert, Christine Saint-Martin, Daniela Toffoli, Julie Vachon, Elizabeth Hailu, Patrick Colin and Walter E. Haefeli.





































Respiratory syncytial virus (RSV) is a common respiratory virus that usually causes mild symptoms (cold-like illness) but can cause severe illness, including bronchiolitis (inflammation of the small airways in the lung) and pneumonia (infection of the lungs) that may lead to hospitalization or even death.
While most RSV cases are mild, it is not possible to predict which healthy infants could get seriously ill and end up in hospital. *



















It may also be given to children less than 2 years of age who are vulnerable to severe RSV disease in their second RSV season. Available this Fall! protects your baby from getting RSV in their first season.* get them ready Sanofi & AstraZeneca are collaborating on the development and commercialization of Beyfortus® © 2023 Sanofi Pasteur Limited. All rights reserved.MAT-CA-2301156E-v1.0-11/2023 Ask your doctor about protecting your baby from RSV with Beyfortus® Ask your healthcare professional if Beyfortus® is right for your child. 100% protection cannot be guaranteed. Uncommon side effects (may affect up to 1 in 100 children) can include rash, injection site reaction and fever. Full product information can be found on Sanofi.ca. To report an adverse event, please call 1-866-234-2345.
Surgical guidance with AI
Researchers at UHN’s Toronto General Hospital Research Institute (TGHRI) have utilized artificial intelligence (AI) to identify safe and dangerous zones for deploying a stent graft – a tube made of a metal with a fabric covering that protects the aorta – during surgery to repair an abdominal aortic aneurysm, a condition where the aorta in the abdomen becomes enlarged and weak.
The aorta is the main artery that carries blood from the heart to the rest of the body. An abdominal aortic aneurysm (AAA) can rupture, which is a life-threatening complication.
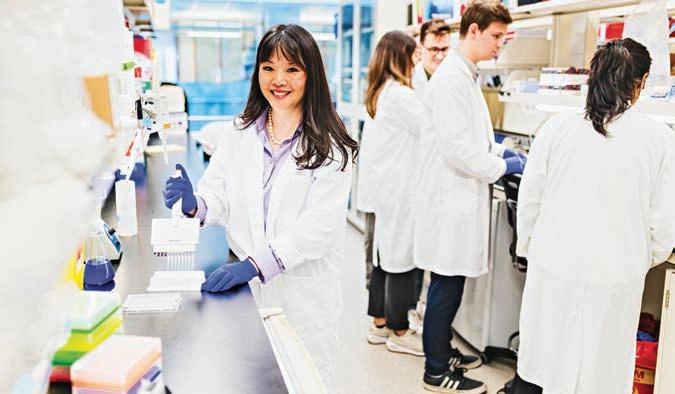
“Endovascular aneurysm repair (EVAR) is a common method of treatment for AAAs where a stent graft is inserted to act as a lining for the aorta and lower the risk of a rupture,” says Dr. Thomas Forbes, UHN’s Surgeon-in-Chief, a clinician investi-

gator at TGHRI and senior author of the study.
“Current practice for this procedure involves manually identifying the correct area of the aorta using fluoroscopy – videos of movement inside the body through the use of X-rays.”
A dangerous complication of this surgery is the partial or complete blockage of blood flow in the renal artery by the deployed stent graft. This
Axe the fax to help Ontario’s family doctors
By Gabriel Tick
In the face of a looming crisis in primary healthcare, Ontario’s government has exhibited a noticeable lack of leadership and action. The Ontario College of Family Physicians (OCFP) raised a red flag, warning that by 2026, one in four Ontarians will be deprived of basic primary care. This isn’t just a forecast; it’s a direct consequence of apathy.
Retirement isn’t the only factor driving family doctors away; an archaic administrative system, drowning in paperwork, is a significant culprit. Astonishingly, 94% of family doctors report that they spend nearly half their week on administrative tasks, much of it uncompensated. It’s a glaring inefficiency that the government has negligently overlooked.
The persistence of outdated technologies like fax machines in medical practices is a clear example of this inefficiency. Despite the government’s 2021 promise to phase out faxes in public service, the healthcare sector remains bogged down by an estimated 152 million faxes a year. This an-

can occur in part due to errors in visual perception and judgement when positioning the stent.
To try and prevent this complication, TGHRI researchers developed a deep learning model trained to identify “no-go’ landing zones – areas where insertion of the stent graft would cause a blockage – during EVAR surgery.
“We used 369 fluoroscopic images from 110 different patients/videos to train our AI model,” says Allen Li, medical student at the University of Ottawa and first author of the study.
“These images were obtained from previous EVAR procedures performed at a single institution (UHN) and from open-access sources.”

tiquated method isn’t just slow; it’s a productivity sinkhole.
Digital solutions are readily available, offering rapid processing and greater efficiency. Yet the government’s inertia in incentivising the adoption of these technologies directly undermines the already strained healthcare system. As more doctors retire or leave, the value of remaining practitioners’ time skyrockets. The government’s failure to modernise is not just a technological oversight; it’s a dereliction of duty.
Some defend the status quo, arguing against the cost and time of adopting new systems. This short-sightedness misses the bigger picture: the long-term ramifications of a doctor shortage far exceed the temporary inconvenience of technological transition. By stubbornly clinging to the fax machine, the healthcare system in Ontario is compromising patient care.
Moreover, the security risks posed by fax machines, with sensitive information vulnerable to interception, are unacceptable. Misdirected faxes are the leading cause of unauthorized disclosure of personal health infor-
mation in Ontario, according to the province’s Information and Privacy Commissioner. Nearly 5,000 privacy breaches related to misdirected faxes were reported to the commissioner’s office in 2021. Modern, secure digital platforms offer a clear solution.
The Ontario Ministry of Health’s five-year plan to phase out fax machines is a step, but it’s too little, too late. The OCFP’s alarming projections demand immediate, decisive action. Modern medical administration systems, designed for rapid implementation and ease of use, are not futuristic dreams but present-day necessities.
The overall reluctance to update healthcare’s administrative infrastructure is akin to ignoring the evolution of medical equipment. It’s not just about convenience; it’s about enabling efficient, effective patient care. With each day that passes without action, Ontario’s families bear the burden of this inertia. Efficient healthcare for all Ontarians is imperative. The time for half-measures and delays is over. Ontario’s families deserve better, and they deserve it now. ■ H
Dr. Amin Madani, co-author of the study, endocrine surgeon at UHN and Director of the Surgical AI Research Academy (SARA) says: “Our results showed that AI was able to successfully identify the area of the abdominal aorta during surgery where insertion of the stent graft would cause renal blockage – the ‘no-go’ zone.
“However, more work is needed to optimize the AI model’s performance when using datasets from more than one institution.”
Dr. Forbes, who is also a professor and Vice-Chair in the Department of Surgery at U of T, adds: “This study shows that AI can be used as an intraoperative tool and methods from this study may be useful for other types of endovascular surgeries.
“These results provide further insight into the use of AI in surgery applications as it becomes an increasingly important part of the operating room.” ■ H
This work was supported by UHN Foundation and the University of Toronto Temerty Centre for Artificial Intelligence Research and Education in Medicine.


10 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com COVER










Protecting patients and the planet from unnecessary tests
By Sarah Ripplinger
Climate change is a universal problem that impacts both environmental and human health. In response, Vancouver Coastal Health Research Institute researcher Dr. Andrea MacNeill and Dr. Karina Spoyalo are looking at how sustainable health care can contribute to reducing greenhouse gas emissions and mitigate the harms associated with climate change.
“One of the biggest takeaways in the emerging field of sustainable health care is that what is good for the environment is good for patients,” states Spoyalo. “The sum of the parts becomes greater in the end.”
In her 2021 research paper, MacNeill defines a framework for constructing the emerging field of environmentally sustainable health systems. She describes it as reducing the demand for health services through preventive measures; avoiding unnecessary investigations and treatments; and decarbonizing processes of care.
“The health sector is uniquely positioned to lead global climate action,” states MacNeill. “Rethinking health care through a holistic lens of sustainability will help realise the Canadian federal government’s goals of achiev-

ing net zero emissions by 2050 and developing low-carbon, sustainable and resilient health systems.”
A CALL FOR REDUCING UNNECESSARY BLOOD WORK
MacNeill and Spoyalo’s recent study, published in BMJ Open Quality, applies a triple bottom line framework that estimates the burden of unnecessary blood work on acute care surgical patients. The triple bottom line approach is used to assess treatment outcomes in terms of impacts to patient health, health care expenditures and the environment.
The research team looked at the hospital records of 304 patients admitted to hospital with a handful of acute yet uncomplicated conditions. Of these, 83 patients were randomly selected for an in-depth chart review.
The team compared the blood work requested in the studied cohort against recommendations for appropriate investigations that were agreed upon by 17 general surgeons at VGH. They found that 76 per cent of the patients reviewed in-depth underwent unnecessary blood work.
Researchers found that the unnecessary blood work ordered con-
tributed to a mean 1.84 additional requisitioned blood draws, 16.5 blood tests – individual tests that pathologists conduct on blood draws – and 18 millilitres of blood per patient. This resulted in $5,235 of additional costs from the health care system and an extra 61 kilograms of greenhouse gas emissions known to contribute to climate change.
“Ordering tests reflexively can result in false positive or negative results that can lead to unnecessary care that drains health care resources, taking them away from other patients in critical need,” states Spoyalo. “It can also lead to avoidable anxiety and potential negative side effects for patients.”
However, getting to the stage of promoting smarter testing first requires a body of evidence to back up triple bottom line recommendations, adds Spoyalo. “You cannot fix or improve something that you do not fully understand.”
“What we need now is thoughtful ordering of laboratory investigations,” says Spoyalo. “This could include unbundling blood tests to avoid wastage, as well as educating physicians and patients about the costs and human and environmental harms associated with unnecessary lab work.” ■ H
Funding to take LHSC developed technology global
By Roxanne Beaubien
On average it takes five to seven years to diagnose a rare disease. But, for growing numbers of rare diseases, that is all about to change with new artificial intelligence-led technology developed by researchers at London Health Sciences Centre (LHSC) and Lawson Health Research Institute that will be going global. With funding of $7,551,693 that includes a Genome Canada Genom-
ic Applications Partnership Program (GAPP) grant and support from Illumina Inc., a leading developer of tools for analysis of genetic variation, research led by Dr. Bekim Sadikovic will change what has been years of trial and error in the search for a diagnosis into a simple blood test that could ultimately be available in any lab around the world.
“Despite advances in genome sequencing, it is estimated that nearly 70 per cent of people with a rare genetic
disease are not diagnosed,” says Dr. Sadikovic, Research Chair in Clinical Genomics and Epigenomics with the Archie and Irene Verspeeten Clinical Genome Centre at LHSC, and Scientist at Lawson.
“To receive specialized care, you need a specific genetic diagnosis. Without one, you can’t access therapy and, unlike other types of diseases, genetic diseases don’t only affect the patient, they affect whole family because they can be inherited,” he says.
Using machine learning, Dr. Sadikovic has developed EpiSign™, the first technology that uses a patient’s epigenome to diagnose genetic disorders. At its most basic level this means that artificial intelligence is used to detect the pattern of chemical signals, called epigenetics, that turn genes within a person’s DNA on or off. The position of this on-off switch for any specific gene could mean someone has blue eyes versus brown eyes, or it could mean they have a rare genetic disease.
Continued on page 18
Sarah Ripplinger is a senior writer for Vancouver Coastal Health Research Institute.
12 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com NEWS
A new era in heart failure management: The promise of digital therapeutics
By Dr. François Bernard Tournoux
Heart failure is one of the fastest growing cardiovascular conditions in the world that places significant strain on patients, families, and healthcare systems worldwide. It is a chronic condition caused by the heart not functioning properly or having structural issues1, often accompanied by other serious chronic diseases such as diabetes, hypertension, atrial fibrillation, kidney problems, and chronic obstructive pulmonary disease.
Patients experience a wide range of symptoms, including unexpected weight gain, swelling of lower extremities, fatigue, shortness of breath, loss of energy, or extreme fatigue. Additionally, many experience depression, anxiety, and reduced quality of life. The emotional weight of heart failure impacts both patients and caregivers, who must manage medication, appointments, and frequent trips to the emergency room.2
In Canada, there are currently over 750,000 people living with heart failure, with an additional 100,000 new diagnoses each year. Heart failure is one of the top reasons for hospitalization across the country, and by 2030, associated healthcare costs are expected to reach $2.8 billion per year.3 While early diagnosis, lifestyle changes, innovative medicines, and medical devices can make a big impact, more tools are needed to help patients manage and track their symptoms to avoid a visit at the emergency room or a hospitalization.
CONTINUUM is a remote patient monitoring and digital therapeutics program working to help heart failure outpatients improve their overall wellbeing and reduce the number of emergency room visits and/or
hospitalizations. The technology was recently piloted at the Centre Hospitalier de l’Université de Montréal (CHUM).
In a three-month pre-post pilot study for heart failure outpatients at risk of hospitalization, the CONTINUUM program was evaluated against the standard of care alone.
THE CONTINUUM PROGRAM INCLUDES:
• a smartphone/tablet application that patients use to enter vital signs, weight, and symptoms and then their data is monitored by clinical nurses from their home,
• heart failure education modules tailored to each patient relating to their condition and keeping them informed of treatment practices, lifestyle suggestions or other pertinent information,
• a dashboard for healthcare professionals that displays alerts,
• a digital therapeutics module that aids the medical team by providing suggestions to optimize care based on guideline-based treatment algorithms.
Preliminary results, presented at the American Heart Association Conference in 2023, demonstrated when patients use this application there is a direct link to significant reduction in emergency room visits and/or hospitalizations among the intervention group . Moreover, the total cost of healthcare consumption in the intervention group was $134,088 CAD, twenty-three per cent less than the $174,924 CAD in the control group.4
The success of the program is the result of a collaborative effort between the CHUM, the CHUM Research Centre, MEDTEQ+, Greybox
Solutions Inc., and Boehringer Ingelheim (Canada) Ltd./ Ltée. With healthcare budgets and hospital staff under increased strain, this public-private partnership supported and helped fund this innovative healthcare solution. The program was recently awarded the MEDTEQ+ RSI prize by the Québec government at the ADRIQ innovation gala in
recognition of its ability to transform health outcomes.
CONTINUUM is looking to expand throughout Québec and reach patients of other chronic diseases. It is my hope we see CONTINUUM and other innovative solutions stretch across the country to enable more medical professionals the ability to offer new possibilities to our heart failure patients. H

1, 2, 3Heart and Stroke Foundation. Heart failure in Canada: complex, incurable and on the rise. Available at: https://www.heartandstroke.ca/what-we-do/media-centre/news-releases/ heart-failure-in-canada-complex-incurable-and-on-the-rise
4AHA Journals. Abstract 12585: The Impact of Remote Patient Monitoring and Digital Therapeutics on Major Clinical Events and Costs in Heart Failure Patients: Early Experience in the Quebec Public Healthcare System. Available at: https://www.ahajournals.org/doi/10.1161/circ.148.suppl_1.12585
Dr. François Bernard Tournoux is a Cardiologist at the CHUM, Associate Professor, University of Montréal, FRQS Clinical Researcher at the CHUM Research Centre and principal investigator of the CONTINUUM trial.
SPONSORED CONTENT
MARCH 2024 HOSPITAL NEWS 13 www.hospitalnews.com
Dr. François Bernard Tournoux
Finding innovative solutions to reduce substance use costs on health care
By Chandni Sondagar Aisha Giwa and Siri Chunduri
Substance use is quietly adding significant stress to the currently strained health-care system in Canada.
Health-care costs related to substance use account for nearly 30 per cent ($13.4 billion) of the overall costs of substance use. Over two hundred people in Canada die every day because of issues related to substance use.
Our health-care system is already grappling with significant workforce shortages and the lasting impacts of the COVID-19 pandemic. Issues related to substance use health add strain to an already strained system. Continued monitoring of the costs and harms of substance use and implementing more diverse and innovative strategies is critical to addressing the impact of substance use on the health-
care system and reducing the financial costs.
MAJOR COSTS ASSOCIATED WITH SUBSTANCE USE IN HEALTH CARE
Since 2016, the Canadian Substance Use Cost and Harms (CSUCH) project has studied crucial insights into substance use trends and estimated direct and indirect costs of substance use, including the cost to the healthcare system. The Canadian Centre on Substance Use and Addiction (CCSA) and the University of Victoria’s Canadian Institute for Substance Use Research (CISUR) collaborate on the CSUCH project to better understand the overall cost and harms of substance use in Canada. The project determined that substance use cost the Canadian economy $49.1 billion in 2020.

The $13.4 billion in health-care costs attributed to substance use in 2020 include day surgeries, emergency department visits, inpatient hospitalizations, paramedic services, prescription drugs, physician time and specialized treatment for substance use disorders.
These three areas account for the highest costs:
• Physician time: $4.48 billion
• Prescription drugs: $4.24 billion
• Inpatient hospitalizations: $3.29 billion
These costs and the implications for the health-care system cannot continue to go unaddressed, especially since we know they can be reduced.
The Government of Canada is starting to act. The new Canadian Drugs and Substances Strategy calls for equitable access to the “full continuum of care, including treatment, harm
reduction and recovery options as well as other social services and supports to help people reduce their substance use and related harms.” This means putting evidence-based practice into place in both specialized treatments and broader health and social services and through establishing a foundation of compassionate care.
TAKING NEW APPROACHES TO SUBSTANCE USE CARE
Several bold and innovative ideas have recently been put in place by member organizations of HealthCareCAN, the national voice of hospitals and health-care and health research organizations across Canada, to help tackle the stresses of substance use issues on the health-care system.
Health Sciences North hospital in Sudbury opened the Addictions Medi-












14 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com NEWS
cine Unit in 2021 for patients in a state of crisis due to alcohol use disorder or other substance use disorders. Uniquely, this unit operates with the understanding that the patients may continue to use substances while in care and supports them with safe injection kits, including clean needles and cookers, where needed.
The Addictions Medicine Unit employs a diverse team of addiction workers, social workers, peer consultants, registered nurses and psychiatrists. While the unit is not a treatment centre, the nonjudgmental and stigma-free environment helps providers build trust with patients and connects them to community programs such as getting on a waiting list for subsidized housing. Not only has the program helped patients, but it has also inspired providers to learn and, in turn, teach nursing students about substance use disorder, which is an aspect of health care not usually included in their curriculum. Accreditation Canada has called it a “novel and leading practice in addiction medicine.”
Several of HealthCareCAN’s member organizations offer Rapid Access Addiction Medicine (RAAM) clinics. While most substance use treatment centres require appointments or a formal referral, RAAM clinics are easy to access and offer walk-in consultations for targeted treatments in a timely manner. The clinics also offer counselling and referrals to community services. A 2020 report by CCSA found that hospital-based RAAM clinics were engaging and retaining patients in ongoing substance use treatment, thereby reducing emergency department visits, repeat visits and inpatient care, all while being cost-effective.
Additionally, the University Health Network in partnership with the City of Toronto, United Way Greater Toronto and community partners are implementing a new social medicine supportive housing project. A first of its kind in Canada, this initiative will offer 51 units in a four-storey building for people who use substances. The project will address the social determinants of health, including housing,
food and financial security, all while offering a range of onsite services related to mental health, career development, income, and food security. The project will also provide connections to primary care and health services, which sets this project apart from other subsidized social housing initiatives.
MOVING FORWARD
Initiatives like these illustrate that meaningful investment in research and innovation are foundational to reducing the costs and harms of substance use.
Accurate and timely research and data are vital in supporting evidence-based decision making and informing innovative approaches. Projects like CSUCH build the capacity to understand the impact of harms related to substance use, but further investment is needed to support the targeted data collection required to understand trends and impacts among diverse and vulnerable populations across Canada.
Investment and innovation in substance use must not stop here. It means rethinking initiatives on prevention,
education and harm reduction that go beyond those that are typically associated with heavy or risky substance use. It means focusing on strategies that address risk factors (e.g., adverse child events, trauma, mental health, chronic pain) and promote protective factors (e.g., coping skills, social inclusion, safe environments) related to substance use and its harms. Incorporating substance use education in health-care training and standardizing requirements for substance epidemiology monitoring and reporting will also advance and promote the health and well-being of people living in Canada. With a daily death toll of over two hundred people, there is no time for incremental change. Investments to rapidly identify, spread and scale innovative and effective approaches like the Addictions Medicine Units, Rapid Access Addiction Medicine clinics, and social medicine supportive housing will help advance the system transformation needed to better serve people at risk and the health-care providers that care for them. ■ H




Discover the Power of AI — Transforming Colorectal Care and Decreasing Colorectal Cancer Risks.1
Chandni Sondagar and Aisha Giwa, Canadian Centre on Substance Use and Addiction. Siri Chunduri, HealthCareCAN
Corley
AR JR,
New
of Medicine. 2014; 370: 2539–2541.
1.
DA, Jenson CD, Marks
et al. Adenoma detection rate and risk of colorectal cancer and death. The
England Journal
2020;
colonoscopies help physicians identify more abnormalities, patients’ risk of undetected polyps.3 82%2 faster polyp endoscopist (RT) <1%2 false activations 99.7%2 sensitivity Performance March is Colorectal Cancer Awareness MARCH 2024 HOSPITAL NEWS 15 www.hospitalnews.com NEWS
2. validation study versus experienced endoscopists for colorectal polyp detection. Gut. 2020;69:799–800. detection of colorectal neoplasia in a randomized trial. Gastroenterology.
159:512–520.e7.

























Continued from page 16
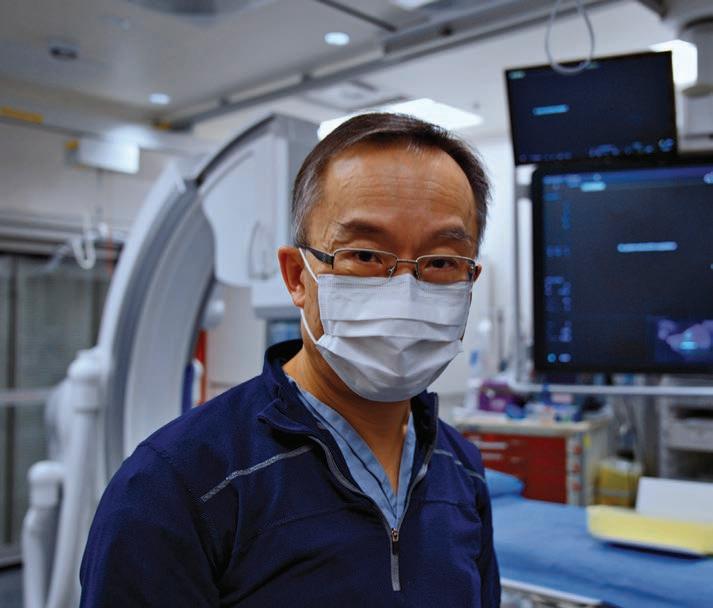
E-bikes for service delivery
Prior to project approval, the YHCP team had to submit a formal proposal to management and clearly articulate how the bikes would deliver benefits for the community, for the health care system and for individuals. Determined benefits include reduced reliance on fossil fuels to deliver YHCP programming and a concomitant reduction in GHG emissions, improved health of users, and an increase in the fun quotient for participating staff.
With the increased levels of burnout in the last few years, Drennan say he in particular has been able to maintain positive mental health, increased productivity and a stronger commitment to remain working for YHCP.
On a very positive note, Drennan says “Even staff who were not riding the bikes gave a tremendous amount of positive feedback on the initiative.”
The bike naming contest helped engage staff and served to increase the number of conversations around alternative forms of transportation and biking activities, which promoted health aspects of the e-bikes.
Perhaps the biggest concern was determining how a staff member was going to pack up all their equipment, do a home treatment, and return safely within an efficient timeframe.
The planning stage of the initiative also included determining how to make the jump from theory to practice; answering questions about how things would work on the ground and how the practice of home visits would actually play out.
The advocates researched studies that looked at speed, traffic conditions, and parking opportunities at client homes. From here they determined the optimal service distance was in the 1015 km ranges and that an e-bike would be as fast if not faster than a motor vehicle. In fact, the e-bike proved faster in under five km commutes. These results helped support advocates in their claim they could get the job done faster than with a staff motor vehicle.
Health care organisations considering the adoption of a similar e-bike program are encouraged to closely look at individual, environmental and facility benefits. Team members should look at e-bike adoption from
several perspectives and at the myriad of ways the initiative might bring benefits.
Encouraging both like-minded and closed-minded people to engage in the process may help in revealing some previously unthought of factors that might just win over a few new supporters. Further, open communications and promotion can help build capacity for the initiative. “Be prepared for things to start slowly,” says Drennan who adds, “Remember, you are initiating a culture shift. It is going to take time.”
He further reminds us that the more micro-mobility devices there are on the road, the more bike lanes/trails will
be built, and the safer these alternative modes of transportation will become. Advocacy will help make future initiatives easier and will make our communities safer, healthier and will reduce our overall carbon footprint.
DOING THE MATH –INITIATIVE LOGISTICS
The manufacturer’s suggested list price for the first e-bike was $6,000. A cost reduction resulted from participation in the Yukon government‘s rebate program and an additional discount was attributed to territorial health funding leaving a balance that was covered by the YHCP budget. “We pulled in all
possible incentives to make the program a reality,” says Drennan who further reports, “Given the initial success of the initiative, we have begun budgeting to allow for the purchase of additional e-bikes.” Drennan claims that if just one out of ten home visits were conducted by e-bike, the savings would outweigh the cost of the initiative.
His last words of advice: Be persistent, respectful and above all, make the process clear for senior leaders who may not have the time to heavily engage in the minute details of the proposed initiative. And most importantly, have fun!
To learn more about the Coalition’s work in battery-powered micro-mobility, visit: https://greenhealthcare.ca/micro-mobility/ ■ H
Continued from page 12
Funding
Over the last ten years, Dr. Sadikovic has been researching epigenetics and has created a database that contains the epigenetics of hundreds of genetic diseases, and diseases caused by toxic environmental exposures, the largest database of its kind in the world.
This decade of research has culminated in an ongoing national trial of this diagnostic technology called EpiSign-CAN. Funded by Genome Canada, the trial involves testing of thousands of patients across 14 Canadian academic hospitals.
Dr. Bekim Sadikovic and Jen Kerkhof, Senior Laboratory Technologist, Molecular Genetics, in the lab where samples are analyzed.
“It is these episignatures that allow us to diagnose patients that otherwise cannot be diagnosed with standard genetic techniques,” Dr. Sadikovic explains. “So, we can now interpret this genetic data that we couldn’t understand before, and provide critical answers for patients and families affected by hundreds of rare diseases.”
This $7.44 million grant funding from the Government of Canada through Genome Canada will enable the next phase of the project in which EpiSign™ technology will be imple-




mented in labs at academic institutions in 15 countries around the world.
“This research is a great example of LHSC’s commitment to supporting the world-leading advances in diagnosis of patients with rare diseases,” says Brad Campbell, Corporate Hospital Administrative Executive at LHSC.
Along with Dr. Sadikovic’s laboratory at LHSC, two industry partners will be involved in this project. Illumina Inc. will be developing custom microchip hardware to facilitate streamlined sample collection, and EpiSign Inc., a Canadian startup biotechnology company which is a partnered venture between
LHSC and Dr. Sadikovic, will develop end-user software for automated data analysis in labs around the world.
“The support provided by Genome Canada and Illumina will enable adoption of EpiSign technology and place it at the forefront of patient care globally,” Campbell says.
Dr. Sadikovic’s work has also been supported with funding through LHSC’s Academic Realignment Initiative Awards and generous donor support through London Health Sciences Foundation, including through the Archie and Irene Verspeeten Clinical Genome Centre. ■ H
Roxanne Beaubien is a Senior Media Relations Consultant at London Health Sciences Centre

 Kent Waddington is the Communications Coordinator, Canadian Coalition for Green Health Care.
Dr. Bekim Sadikovic and Jen Kerkhof, Senior Laboratory Technologist, Molecular Genetics, in the lab where samples are analyzed.
Kent Waddington is the Communications Coordinator, Canadian Coalition for Green Health Care.
Dr. Bekim Sadikovic and Jen Kerkhof, Senior Laboratory Technologist, Molecular Genetics, in the lab where samples are analyzed.
18 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com NEWS
Tackling the issue of unused medication waste
By Gurleen Dhessi
When patients and programs don’t use all the medication that is prescribed, it is often incinerated, creating pharmaceutical waste.
“Within our pharmacy teams, we often discuss the different approaches our hospitals take with recycling oral solid medications, and we are concerned about the impact when recycling doesn’t occur,” says Aaron Tejani, pharmacist, Medical Use Evaluation, Lower Mainland Pharmacy Services. “We wanted to find the best way to improve medication recycling, to prevent waste and reduce our environmental impact.”
“Evaluations done previously at specific hospitals showed that recycling medications was cost-effective,” says Tejani. “But we wanted to see a bigger picture. What would be the total financial impact on all of our sites in the

lower mainland, and how much waste could we prevent?”
Tejani and Drummond, along with their pharmacy students, decided to see what they could do to recycle more medication and help the planet. First, they sent a survey to hospital pharmacies in the lower mainland.
“We wanted initial insights to understand who returned medications,

how often and why only some unused medications were being returned,” says Tejani.
After collecting the survey, Surrey Memorial Hospital was one of three sites selected for the research study.
“We picked three sites that already had workflows for recycling unused medication and represented the diversity in medication distribution systems,” adds Tejani.
Next, two research students tracked the time it took to separate, sort and credit unused medication in the electronic pharmacy system and return it to the dispensing bins at the selected sites.
The team calculated how much money sites could save by recycling unused medication. They subtracted labour costs from the return value of recycled medication and used a formula to estimate yearly savings.



The result: Recycling medication in 21 hospitals could divert 461,000 individual doses of capsules or tablets from incineration, saving an estimated $415,000 annually and reducing negative environmental impacts.
“Recycling unused medication will help the environment and make the health care system eco-friendlier and more cost-effective,” says Tejani. “It’s within our reach to work collaboratively to reduce pharmaceutical waste, and the environmental impacts should motivate us.”
The findings of the study were so impressive that a pilot project is planned for two more hospitals in the coming months. Pharmacy students will act as environmental stewards, recycling medication wherever possible and educating staff about how their recycling efforts can help to improve the planet. ■ H


Spaces are limited. Apply today. Learn more at begin.werpn.com
Bridging Educational Grant in Nursing
reimbursements
New enrollees also now have the opportunity to gain experience in one of four priority sectors: Hospitals, Primary Care, Long-Term Care or Home and Community Care. NEWS
Gurleen Dhessi is a consultant in Public Affairs at Fraser Health.
The
(BEGIN) program provides eligible PSWs and RPNs with up to $10,000 per year in tuition
to grow their careers.
How global nursing talent is driving healthcare system transformation
By Tina Novotny
The current nursing shortage, which the Canadian Nurses Association predicted in 2009 would be at 60,000 by 2022, has peaked well beyond that number in 2024. In 2022, two years into the COVID-19 pandemic, the Canadian Federation of Nurses Unions quoted a study that puts the nursing shortage at 117,600 nurses in Canada by 2030. In Ontario alone, the province’s fiscal watchdog projects a shortage of 33,000 nurses by 2028.
Nurses have long been called the backbone of the healthcare system, and they are the largest group of regulated health professionals in Canada, representing 48.2 per cent of that workforce. That is almost half of all healthcare workers. Governments may announce funding and plans for new healthcare facilities, additional beds in both hospitals and long-term care, but if there are not enough nurses to provide bedside care, beds may sit empty with the quality of care in potential jeopardy. For patients needing community or home care, they may have to wait much longer for the care they urgently need.
The systemic shortfalls in addressing the current nursing shortage had been on the radar for many years: demographics warned there would be a wave of retirements, the patient population was living longer with more complex conditions, and nursing schools were not bolstering enrollment sufficiently to address the looming crisis with cuts to higher education along with diminished healthcare spending. The COVID-19 pandemic upended the healthcare system with unprecedented demand, and many nurses left the profession to preserve their own health. Surveys continually report that nurses are stressed, unhappy and making plans to quit their current jobs. A 2023 survey by the Registered Practical Nurses Association of Ontario (WeRPN) found that 6 in 10


nurses were considering or will leave nursing.
Another pressure on the healthcare system are hundreds of thousands of immigrants welcomed to this country in the last number of years to meet Canadian labour demands. It is among those newcomers that a solution to the nurse staffing crisis is at hand. Internationally Educated Nurses (IENs) come to Canada with years of experience and global perspectives, eager to return to the profession they love. For many years obtaining registration with regulators across the country has been an arduous journey, especially in provinces with high immigration levels.
CARE Centre for Internationally Educated Nurses was founded in 2001 to support IENs on their journey to registration and employment, funded by the Ontario government. A pre-arrival supports and services (PASS) program with funding from Immigration, Refugees and Citizenship Canada since 2016, assists IENs headed any-
where in Canada to jump-start their nursing careers. Now CARE Centre has launched a Workplace Integration Program to help employers recruit and keep nurses on staff, satisfied and growing in their nursing careers.
“Retention is key to solving the nursing shortage,” says CARE Centre’s Professional Practice Lead, Ruth Wojtiuk. “Recruitment and successful on-boarding are the first steps in IEN integration, but our program also gives employers the tools to fully utilize and deploy IENs so that they stay on the job and contribute to healthcare transformation.”
If there was any positive aspect to the tragedy of the pandemic, CARE Centre has witnessed IENs finally being recognized for the valuable health human resource that is needed. Regulatory bodies across the country have modified their registration processes by removing barriers to facilitate earlier completion. Employers have stepped up to hire IENs in non-regulated positions, to support them in their reg-
istration process and have them well oriented when nursing registration is achieved.
“Our Workplace Integration Program enables employers to facilitate a smooth transition and successful integration of IENs into their workforce and empower them to succeed and excel in the workplace,” says Wojtiuk. “We can offer Cross Cultural Customized Recruitment, Workplace Diversity, Cultural Competence and Early Transitional Issues training, facilitation in Orientation Planning, Self-Assessment and Quality Assurance, promotion of Client-Centered Care, and a module on Language and Communication: Real and Perceived Barriers. Employers can choose from this menu of offerings to address their particular workplace needs, and we are constantly reviewing additional areas where we can share more of our knowledge.”
For more information about CARE Centre’s Workplace Integration Program, visit https://care4nurses.org/ workplace-integration-program. ■ H
20 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com NEWS
Tina Novotny is Case Manager and Communications Lead, CARE Centre for Internationally Educated Nurses.

Enhancing Patient Care Through Caregiver Inclusion




















Different from visitors, family caregivers or essential care partners play an active role in providing physical, psychological and emotional support to a family member, partner or friend. Evidence shows that including essential care partners as part of the care team leads to improved quality of care and patient outcomes, improved working conditions for health professionals and less pressure and reduced cost on the health system.
Contact the Essential Care Partner Support Hub at ontariocaregiver.ca/essentialcarepartner for free expert guidance and evidence-informed resources to build or enhance an Essential Care Partner program.

Navigating the fallout:
23andMe’s data breach and the ethics of consumer genetic testing
By Keithan Vigna
By unlocking secrets encrypted within our DNA, genetic testing has become a powerful tool, offering valuable insights about our health, ancestry, and fertility. It unveils not only our physical characteristics but also tells a unique biological story, shedding light on our potential health and life outcomes. Despite our incomplete understanding of the human genome, which continues to grow, millions of people have turned to genetic testing to provide a glimpse of the distinct factors that make us who we are.
However, as the allure to unravel the complexities behind the genetic code rises, so do the ethical implications, specifically when it comes to protecting some of our most valuable personal information. The tension that exists between protecting individuals’ privacy while at the same time making genetic testing increasingly available took centre stage during a major data breach at 23andMe, a renowned American genetic testing and biotechnology company.
In October 2023, 23andMe experienced a significant data breach. In order to obtain personal data stored within the 23andMe database, hackers used a technique known as credential stuffing, where they exploited the compromised login details reused by 23andMe customers from other services. Through this method, hackers gained access to about 14,000 profiles, or 0.1% of 23andMe’s user accounts. The breach further affected an additional 5.5 million customers who were using 23andMe to connect with genetically similar individuals via the DNA Relatives feature. Moreover, an additional 1.4 million profiles’ family tree information were also compromised. In total, approximately 6.9 million people, making up almost half of 23andMe’s customers, were impacted by the data breach.
In many cases, hackers obtained the names, relationship labels, birth years, self-reported locations, family trees, and
various other profile information from users. They soon began selling each account for between $1 and $10. Subsequently, they publicly released the information of 4 million 23andMe customers.
In response to the mass breach, 23andMe implemented reactive measures to enhance user protection. They required all of its users to change their passwords, ensuring that every customer gained new credentials, thereby reducing the risk of another credential stuffing attack. They also implemented two-factor authentication (2FA) for their customers, enhancing the overall security of user accounts. Notably, other consumer genetic services like myHeritage and Ancestry adopted similar policies.
CONSUMER GENETIC TESTING, GENETIC TESTING COMPANIES MUST EMBRACE A STRONGER ETHICAL OBLIGATION TO PROTECT THEIR CUSTOMERS AND PRIORITIZE DATA SECURITY.
The major privacy breach experienced by 23andMe shed light on the lucrative nature of genetic data for hackers, particularly given our society’s widespread interest in DNA and genetic code. Police agencies, for instance, may seek out genetic databases to track down criminals; researchers may use genetic information to further medical knowledge; and insurance companies may use it to assess an individual’s health risks and determine insurance premiums.
In the 23andMe breach, hackers revealed the interpreted genetic information of millions of consumers, showcasing some of the most practically useful data stored on genetic testing sites for both hackers and their clients.
In contrast to interpreted genetic information, the raw genetic code is made of 4 nucleotides (AGCT) and requires genetic literacy for comprehension. Consequently, the interpreted genetic information, which includes someone’s health depositions, ancestry, and fertility, holds greater significance when made publicly available.
The release of genetic data from 23andMe holds substantial implications now that it is in the public domain. The information may be used to create genetic discrimination in places without relevant legislation, leading to increased insurance costs for people genetically predisposed to diseases or even mortgage denials for those deemed unlikely to settle their debt before they die. While law enforcement agencies and most companies will unlikely seek out information acquired through data breaches intentionally, the origin of data available on the internet is often unclear. Ultimately, assuming that information resulting from a hack will remain untouched is unrealistic, which adds an increased layer of uncertainty to the use of exposed genetic data.
In conventional data breaches involving financial and personal information, an individual can change their information to reduce the risk associated with the breach; however, genetic information is unalterable. This unchanging nature intensifies privacy concerns, especially when considering the fact that genetic information can be involuntarily shared. For example, if someone’s relative uses 23andMe, they become genetically searchable because they are genetically related. In cases with identical twins, the genetic data of one individual will directly reveal information about the other. In short, the immutable and indirect nature of sharing genetic information complicates the challenges associated with protecting personal information.
In addition to the significance of protecting consumers’ genetic data, there exist other ethically relevant
considerations associated with consumer-led genetic testing. One of these considerations involves the lack of accuracy associated with test results. Genetic health reports are prone to false positives and are often unregulated. Moreover, it is crucial to recognize that these tests compare a person’s genotype to a limited number of genetic variants, and most diseases are influenced by not only genetic factors but also environmental factors. As a result, genetic testing does not necessarily provide conclusive results in determining if a customer will develop the genetic disease. The uncertainty associated with genetic test results may lead some consumers to experience unanticipated confusion and/or distress, particularly if their genetic report indicates that they may develop a disease with no known cure and insofar as no genetic counsellor is readily available (due to the genetic test being done at a consumer-level). Although access to one’s genetic information may be desired and empowering for some individuals, the potential uncertainty and/or undesired consequences should be contemplated during one’s decision-making process.
To address many of the ethically relevant challenges associated with consumer genetic testing, genetic testing companies must embrace a stronger ethical obligation to protect their customers and prioritize data security. This commitment should extend beyond the minimal legal requirements. Companies ought to be transparent about their data sampling, usage, and storage practices, take proactive steps to reduce the risk of breaches, and implement rigorous encryption measures. Additionally, if stronger consumer genetic testing regulations are implemented, then this would help to ensure that consumer genetic information has the same level of protection as other personal health information. Such steps will not only improve the security of genetic information but also the trust between consumers and genetic testing companies. ■ H
Keithan Vigna is currently completing his BHSc in Honours Biochemistry at McMaster University. Keithan has a particular interest in biomedical ethics, with a specific focus on the responsible utilisation of sensitive health information, data privacy, and the ethical considerations surrounding artificial intelligence in healthcare. The author would like to acknowledge Andria Bianchi for her editorial support.
22 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com ETHICS





Infection Control



2024
MARCH 2024 HOSPITAL NEWS 23 www.hospitalnews.com
®
“My symptoms seemed endless”
By Dr. Jennifer Hulme
In April 2022, another COVID wave was sweeping Toronto. It was the sixth since the March 2020 declaration of a pandemic due to the spread of the coronavirus.
Restrictions and mask mandates in schools had been lifted after a decidedly unpopular delay in return to school during the previous COVID wave in January. Children under five had yet to have access to COVID vaccines and classrooms remained poorly ventilated in older schools.
At the time, I was working on the frontline of potential COVID exposure – in the UHN Emergency Department (ED) and at the COVID recovery site for people experiencing homelessness, where every single resident at the hotel was isolated with the disease.
But like many, I didn’t get COVID at work. I got it from my junior kindergarten-aged son after kissing him goodnight in between the stairway banisters.
My son and I dutifully isolated together upstairs, away from my husband, who was working long hours every day at the hospital caring for COVID patients. We had the usual flu-like symptoms of alternating fever, chills, congestion and severe fatigue; the only alarming symptom for me was migrating joint pain, which traveled around my body for several days before fading into the background.
It wasn’t long before I realized how lucky we were that my husband escaped infection, because soon he would have to do absolutely everything.
At the time, I remember feeling lucky to be fully vaccinated, and anticipated a full recovery. I returned to work on day 11 after testing positive for COVID, fatigued, but otherwise fine. I was training for a 10-kilometre run, and on day 16 tried to go for a jog. I couldn’t get down the street. I walked home.
“That’s odd.” I thought, believing it was just a premature return to sport. I worked two overnight shifts in the ED that weekend. By day 21, I was sud-

“At the time, I remember feeling lucky to be fully vaccinated, and anticipated a full recovery,” Dr. Jennifer Hulme, an Emergency physician at UHN, writes of the immediate aftermath of her diagnosis with COVID-19 in April 2022. Soon after, the symptoms of long COVID began.
denly, terrifyingly, sick with something that felt altogether very new. That’s when my life changed forever.
After that, long COVID took over my life. My symptoms seemed endless.
I was mostly bed bound with relentless post exertional malaise, fatigue, cognitive impairment, memory loss, headaches, pulsatile tinnitus – which is a constant whooshing in the ear, and a disturbing sensitivity to sound called hyperacusis. I lost hearing in one ear and developed constant ringing in it.
I was breathless at rest. I couldn’t remember my address. I went off work and onto disability. I secretly dreamed of losing a limb – at least then someone could tell me what was wrong and try to help me. Instead, I looked pale but “fine” while barely being able to walk.
The symptoms encroached on every aspect of my identity – mother,
active and social person, a physician, researcher. I embarked on a desperate quest for answers; submerged in a sea of Reddit anecdotes and scientific papers, I explored every hypothesis, and every medication and supplement on the market out of pure desperation.
Early on, I squeezed my way into the long COVID clinic at UHN, led by Dr. Angela Cheung. Just having some validation and a diagnosis was helpful. I learned that I had a combination of long COVID phenotypes, or groupings.
The first is the brutal cocktail of severe fatigue, brain fog and post-exertional malaise – which is the worsening of symptoms after physical, mental or emotional effort. This is known as myalgic encephalomyelitis, or the misnomer chronic fatigue syndrome, termed “ME/CFS” for short.
It’s a disruption in the energy metabolism at a cellular level that’s akin to a smartphone running out of battery much faster than the latest model. Staying within my “energy envelope” became the centre of my being.
The second phenotype is related to autonomic dysfunction, with increased heart rate, lightheadedness, dizziness when standing, shortness of breath, headaches, nausea and other gastrointestinal symptoms. The Canadian postural orthostatic tachycardia syndrome (POTS) guidelines are helpful, and trialing medications can be a game changer. I wish I had started ivabradine sooner.
The third phenotype is dominated by allergic-type symptoms, including rashes, headaches, worsening asthma, joint pain, or abdominal pain, nausea or diarrhea made worse with specific types of foods. This grouping is thought to be related to mast cell activation.
Observational data suggest that antihistamines can be helpful for most COVID long haulers, likely as they can modulate T-cells which are very abnormal in long COVID. Neurological symptoms and depression are also caused in part by brain inflammation and glial cell damage, particularly in the areas of the brain responsible for pleasure.
Microglia are the immune cells of the brain, and would be constantly activated by persistent COVID virus, driving neuroinflammation and brain fog. Antidepressant medication can help reduce neuroinflammation, and I know of some long haulers who got some relief with SSRIs.
Slowly there emerged small victories. I felt very lucky to get access to hyperbaric oxygen therapy (HBOT). Because I suffered from sudden hearing loss, I qualified for HBOT funded by provincial health insurance.
Within five sessions, my hearing came back in my left ear, tinnitus and pulsatile tinnitus – extremely distressing symptoms – completely resolved. And there is early evidence that HBOT could help long haulers with fatigue, cognition and brain functioning.
An ER doctor’s experience with long COVID
24 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com INFECTION CONTROL 2024
Photo credit: Dawn Lim
I’ve also been lucky to participate in Dr. Cheung’s UHN-led Reclaim Trial, where I benefited from the medication offered.
After a long and difficult road, I’m now grateful to be able to work again and for the good hours and good days, which are more frequent.
Many people ask me what I want the public and physicians to know about long COVID. I think the first is that “the tests are not normal” – we are just not ordering the right tests. Every study of long haulers shows unbelievable pathology: immune dysregulation, mitochondrial dysfunction, neuroinflammation, brain damage, vascular damage, gut dysbiosis, poor perfusion of the brain, lungs and other organs. We just don’t have an easily accessible biomarker yet.
The second thing is that while there are no approved treatments for long COVID yet, there IS hope, and there are treatments that help! Antihistamines, antidepressants for neuroinflammation, aggressive treatment
of autonomic dysfunction, or POTS, resting and pacing for post-exertional malaise – these things can help.
The third is that the best way to prevent long COVID is to avoid getting COVID. I use Can95 masks, nasal sprays and HEPA filters. And, if you do get COVID, have a plan to enroll in CanTreatCOVID to contribute to the science on long COVID secondary prevention.
And finally, we need a rapid acceleration of double-blinded, placebo-controlled, randomized clinical trials. Of the trials that are ongoing right now, only 12 of them are looking at pharmaceutical treatment of long COVID. This is in part because we don’t fully understand the root cause of post-viral illness – whether this is persistent virus, viral debris, reactivation of latent viruses, gut dysbiosis – and what is driving all of the downstream effects of end organ, vascular damage and microclotting.
Until then, I hope everyone with long COVID is seen, supported and heard. ■ H

“Just having some validation and a diagnosis was helpful,” Dr. Jennifer Hulme writes of learning she had a combination of long COVID phenotypes, or groupings. She is seen here trying on a mask for the Hi-OxSR study to find out if increasing arterial PC02 – carbon dioxide levels – with sequential rebreathing can be safely used as a treatment of post-COVID
dysfunction.
Dr. Jennifer Hulme is an Emergency physician at UHN and a clinician investigator at the Toronto General Hospital Research Institute. She cochairs the Health Equity Committee of the Global Health Emergency Medicine group, which brings together health professionals seeking solutions to improve outcomes for marginalized communities.
 cognitive
cognitive
MARCH 2024 HOSPITAL NEWS 25 www.hospitalnews.com INFECTION CONTROL 2024
Photo credit: Dawn Lim
COVID-19 rapid tests: How good are they?
A new study indicates that COVID-19 self-tests effectively identify non-infected individuals as well people with high viral loads and high infectiousness
The COVID-19 pandemic marked the first time in the history of pandemics where self-testing was used as an essential component of a widespread public infection control and prevention strategy. Nearly four years into the pandemic, a study sheds a light on the diagnostic accuracy and impact of the SARS-CoV-2 antigen-detection rapid diagnostic tests used for COVID-19 self-testing. The study, led by Dr. Nitika Pant Pai at the Research Institute of the McGill University Health Centre (RI-MUHC) and published this week in the journal PLOS Global Public Health, suggests that the value of self-testing lies in the
rapid identification and isolation of highly contagious individuals and that some aspects of the self-testing strategy can improve self-test performance, like clear instructions for use and result interpretation, and adequate pretest training.
“Overall, the results of our study are impressive. Evidence shows that self-testing is an effective tool to prevent transmission of SARS-COV-2 and suggests that it helped control outbreaks and limit transmission, and allowed work to continue during the pandemic. In the future, public health agencies and governments should not hesitate to invest in accurate, rapid, portable and perhaps digitally en-




hanced self-testing strategies, like apps, websites and video-based instructions, not only for respiratory viruses but also for non-respiratory pathogens,” says Dr. Pant Pai, senior author of the study, Scientist in the Infectious Diseases and Immunity in Global Health Program at the Centre for Outcomes Research and Evaluation of the RIMUHC and Associate Professor of Medicine at McGill University.
The study consists of a living systematic review, i.e., it will be updated in one year, and a meta-analysis of 70 studies – with pooled data from 25 countries – that have evaluated the diagnostic accuracy of rapid tests for COVID-19. The authors analyzed the data according to a number of different variables, such as sampling site, symptomatic status, supervised/unsupervised self-testing method and the presence/absence of digital support. The researchers also examined the feasibility, acceptability and impact of self-testing, as well as people’s preferences and motivations, and key facilitators and barriers to the adoption of the self-testing strategy.
AN EFFECTIVE, FEASIBLE AND ACCEPTABLE PREVENTIVE STRATEGY
According to the study findings, rapid tests for COVID-19 have a very high specificity (the capacity to de-
tect negative cases/healthy individuals), with a true negative proportion consistently above 98 per cent. Most false negative test results reported in the study occurred when the person was less contagious and outside the transmissibility window.
Test sensitivity (the ability to detect positive cases/infected individuals) differed from subgroup to subgroup, depending on the variable studied, and was consistently low in asymptomatic individuals (the test missed picking infection in them) but high in symptomatic (the test did not miss picking up infection).
Highest sensitivities, or highest true positive proportions, were observed within groups of people who:
• conducted their test in supervised settings (86.7%),
• were symptomatic (73.9%)
• used mid-turbinate nasal specimens, i.e., sample taken just from further up the nostrils inside the nose (77.8%)
• used digital support strategies like apps, websites and video-based instructions to improve test conduct (70.%).
Further, the researchers found that users had a strong preference for COVID self-tests and were willing to use them, but their interest in repeated or daily use was low.
Continued on page 28

Try it first on your unit. Visit www.scjp.com/en-ca/poc-trial to register for a free trial.
26 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com INFECTION CONTROL 2024

EFFECTIVE AGAINST





























VIRUSES* (norovirus/rotavirus), butnot all non-enveloped viruses.
BACTERIA FUNGI CERTAIN
*
Report outlines public health response to COVID-19 outbreaks at mink farms
A
report co-authored by Fraser Health Medical Health Officer Dr. Emily Newhouse and published by the Public Health Agency of Canada sheds light on the public health response to COVID-19 outbreaks at mink farms.
When workers at mink farms in the Fraser Valley first tested positive for COVID-19 in late 2020, public health teams already knew that mink were a potential reservoir for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Earlier outbreaks in the Netherlands and Denmark revealed the virus could spread rapidly within mink farms.
An epidemiological investigation of mink farm outbreaks in Fraser Health found SARS-CoV-2 was likely transmitted from humans to mink (anthropogenic transmission) and from mink to humans (zoonotic transmission).


In two outbreaks where both human and mink infections were detected, mink farm staff were symptomatic before detection in the minks, and the viral makeup from mink and human-derived samples were closely related.
“We found that SARS-CoV-2 was most likely introduced into farmed mink by farm staff, where it then evolved in the mink before being re-
STERIS is a leading global provider of products and services that support patient care with an emphasis on infection prevention. WE HELP OUR CUSTOMERS CREATE A HEALTHIER AND SAFER WORLD by providing innovative healthcare, life sciences and dental products and services.
STERIS Healthcare’s complete focus is in the peri-operative environment. We partner to understand where you are today, create a plan together, and provide full solution sets to support the Operating Room (OR), GI / Endoscopy Suites and Medical Device Reprocessing Area (MRDA) environment. Our commitment is to help Customers solve their biggest challenges, leverage opportunities for growth, and advance the care of patients. We put the full power of our market leading solutions and our people to work every day in order to help Customers elevate patient care.
To learn more about how STERIS can help you, call STERIS Canada Sales ULC at 800-661-3937 or visit www.steris.com/healthcare-canada.
introduced into humans,” says Dr. Newhouse.
The evidence gathered from the mink farm outbreaks – the first such outbreaks documented in Canada –suggested the risk of humans acquiring COVID-19 from mink can last for months during longer outbreaks in mink herds.
According to the report, quarantine of infected farms, isolation of infected workers and their close contacts, and enhanced infection control practices helped to break the chains of transmission. While vaccination of farmworkers and enhanced biosecurity practices reduced the risk of transmission on farms, those measures did not fully eliminate mink-to-human transmission from the established “mink reservoir.”
Continued from page 26
“What this means is that conditions in the environment enabled the virus to persist in the mink herd and potentially spread to humans,” says Dr. Newhouse. “The information we gathered during the course of the public health response to the COVID-19 outbreaks at mink farms will help to inform our response to zoonotic diseases in the future.”
The public health response to the mink farm outbreaks took a “One Health” approach, with multiple agencies all contributing expertise to help minimize the impact. A working group which included a Fraser Health medical health officer, environmental health officer, communicable disease nurse coordinator, cluster investigator, and analyst helped guide the outbreak response. ■ H
COVID-19 rapid tests
Most importantly, impact outcomes were many: self-testing strategies not only led to fewer school closures and workday savings for essential workers, they also prevented further transmission of infection amongst healthcare workers, facilitated the continuation of work at health laboratory sites and allowed social activities to continue with a lower risk of infection. These findings highlight their significant public health impact.
Finally, the authors highlight that pre-training sessions, detailed self-test instructions in layman language and special testing kits designed for low-literacy, rural, peri-urban and senior populations could further improve selftest performance and uptake by such populations.
“Equitable access to COVID-19 self-testing will empower individuals and dismantle barriers, paving the way to a healthier and more inclusive society. The high impact of rapid, point-
of-care, digitally supported self-tests in the COVID-19 pandemic highlights the need for increased research in such innovative diagnostic approaches,” says Apoorva Anand, first author of the study and trainee of Dr. Pant Pai at the RI-MUHC.
“COVID self-tests have helped democratize the access to self-testing and normalize the conversation about their use in homes, workplaces, offices and gatherings. Self-testing strategy is now here to stay, not just during pandemics, but as a strategy to control other infectious and non-infectious diseases and conditions. We must provide high-quality self-tests to maintain public confidence in the self-testing process and encourage individuals and communities to use them proactively for their own benefit,” adds Dr. Pant Pai, who is recognized as a global diagnostic expert on self-tests and point-of-care testing technologies. ■ H
The study Self-tests for COVID-19: What is the evidence? A living systematic review and meta-analysis (2020–2023) was co-authored by Apoorva Anand, Fiorella Vialard, Aliasgar Esmail, Faiz Ahmad Khan, Patrick O’Byrne, Jean-Pierre Routy, Keertan Dheda and Nitika Pant Pai.

STERISCanadaSalesULC_QuarterVertical.indd 1 2023-10-20 12:37 PM
Dr. Emily Newhouse
28 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com INFECTION CONTROL 2024

BUILD AN OPTIMAL ENVIRONMENT OF CARE TO LEARN MORE: Call STERIS Canada Sales ULC at 800-661-3937 | Or email us at Canada_Resource@steris.com However simple or complex your goals are, STERIS can help you create an optimal perioperative environment of care. Through technology and healthcare design services, let’s improve patient EQUIPMENT & REPAIR SERVICES OR & ENDOSCOPY ENVIRONMENT SURGICAL TABLES & LIGHTING HEALTHCARE DESIGN SERVICES EQUIPMENT MANAGEMENT OR & ENDOSCOPY INTEGRATION SYSTEMS
Pressure injury education offering potentially life-saving approach to skin health
When Jay De Alwis was admitted to Toronto Rehab, Lyndhurst Centre following spinal hematoma surgery that led to paralysis from the chest down, nurses noticed something amiss with his skin health. They took immediate action.
What they discovered during their standard intake skin assessment, was Jay had stage three pressure wound injuries (PIs) on his left and right buttocks. A PI progresses in four stages, with each stage leading to deeper layers of skin cell breakdown. Each subsequent stage is also harder to recover from.
If left untreated, PIs have the potential of leading to a life-threatening condition.
PIs are caused by long periods of pressure placed on an area of the skin, which leads to a loss of blood flow and eventually cell breakdown. This
FEATURED PRODUCT
is mostly seen in patients who spend extended periods of time seated in a wheelchair or laying down.
Due to his paralysis, Jay couldn’t feel the pain of his growing PIs which had been undiagnosed for weeks before he arrived at Lyndhurst Centre, where multidisciplinary teams are committed to helping patients regain as much functional independence as possible, following an SCI, before safely transitioning back into the community.
“To learn that I also had these wounds to heal from, on top of learning how to cope with my new life as a paraplegic, was difficult,” recalls Jay, who is 56 and works in the automotive industry.
“It is almost a blessing in disguise that I have no feeling, since the team told me the pain would be excruciating if I had sensation.”
Since some PIs can be prevented, it’s important for health care profes-
Greening Health Care:
PCS Four-Fold Wipes Hypochlorous Acid and Sodium Hypochlorite compatible can be dispensed from the bucket wet or dry. Contains 90 Wipes 10 inches x 12 inches / 25.4 cm x 30.48 cm.
Use to apply NPH 2000 Concentrated Neutral pH Oxidizing Cleaner Disinfectant and No Rinse Sanitizer DIN: 02465582.
Use to apply PCS 1000 Plus Oxidizing Disinfectant Cleaner DIN: 02521431.
Oxidizing Hospital Grade Disinfectant, Oxidizing Broad Spectrum Virucide.
PCS NPH 2000 Neutral pH Concentrated Oxidizing Disinfectant Cleaner is a synergistic blend of Hypochlorous acid and Sodium hypochlorite when diluted to 200 ppm. Is a Health Canada approved
No Rinse Sanitizer for food contact surfaces and an Oxidizing Cleaner and Oxidizing Disinfectant Cleaner. Kills Bacteria, Kills Viruses, Kills Fungi. Add 1100 mls of diluted 200 ppm solution to bucket of PCS Four Sided Wipes. Ideal for one-step cleaning, no rinsing frequently touched surfaces in nonintensive care wards, non-critical medical equipment, washrooms, and public spaces.
PCS 1000 Plus Oxidizing Disinfectant Cleaner - Active ingredients: Hypochlorous acid and Sodium hypochlorite. Oxidizing Cleaner, Oxidizing Hospital Grade Disinfectant, and Broad Spectrum Virucide.
sionals, patients and families to be provided proper education.
Recognizing the opportunity to fill this need, teams at Toronto Rehab have set an exceptional example of how sites across UHN can teach staff, patients and families PI prevention and treatment, and how to maintain skin health.
EMPOWERING TEAMS THROUGH PI EDUCATION
Carol McAnuff, a clinical nurse specialist, who specializes in skin, wound, and ostomy management, is part of a cross-UHN group called the Wound Care Clinical Leadership Team, dedicated to providing wound care education and treatment.
“It is paramount that staff have the knowledge, skills, and education to prevent these injuries, since it is UHN’s philosophy to ensure patients
are being cared for to the highest standard,” says Carol.
To that end, Toronto Rehab’s local Wound Care Clinical Leadership Team regularly presents to staff on different topics concerning pressure injury care.
Last year alone, the team engaged staff in 12 “Let’s Talk Skin Health” presentations, focusing on topics such as wound management and assessment, products, new wound technologies and case reviews. The sessions had an overall turnout of more than 120 attendees.
World Pressure Injury Prevention Day is another important event that runs across TR’s sites each year in November where the interprofessional team hosts sessions on the main concepts of PIs.
“PI prevention is a team effort,” says Carol, who explains that once colleagues receive education, they can teach it to patients, at the bedside.
Continued on page 32

DIN: 02521431. Critical care environments and during outbreaks.









Add 1100 ml of PCS 1000 Plus to the bucket of PCS Four Sided Wipes. Apply to surfaces following the institution’s procedures. To remove residual organic soils and dry biofilm matrix, wipe surfaces dry with a PCS Hygienic microfibre cloth.
Process Cleaning Solutions | processcleaningsolutions.com | 877.745.7277
Cleaning and Disinfecting
30 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com INFECTION CONTROL 2024
According to the National Institutes of Health (NIH), up to 80% of human bacterial infections are caused by bacterial biofilms, which are difficult to cure.
PCS 1000 Plus Oxidizing Disinfectant Cleaner
Active Ingredient
Sodium hypochlorite - 0.13%
Hypochlorous acid - 0.01%
Oxidizing Cleaner
Oxidizing Hospital Grade Disinfectant
Oxidizing broad spectrum virucide
DIN: 02521431
PCS 1000 Plus Oxidizing Cleaning Process for removal of Dry Surface Biofilm Matrix.
(1) Apply PCS 1000 Plus Oxidizing Disinfectant Cleaner to surface with PCS Four fold Wiper.
(2)Wipe dry with PCS Hygienic Microfibre cloth.




PCS 1000 Plus Oxidizing Disinfectant/Cleaner
5906-4 • 4 x 3.78 litre
Now Available
PROCESS CLEANING SOLUTIONS PROUDLY CANADIAN.
be a biofilm buster

PCS 1000 Plus Oxidizing Cleaning Process for removal of Dry Surface Biofilm Matrix
• Apply PCS 1000 Plus undiluted to surface, wipe dry with PCS microfibre cloth.
• Single use wipes do not provide the friction needed to remove dry surface biofilms.
How biofilm changes our understanding of cleaning and disinfection Maillard
PCS 1000 Plus process, provides Oxidation and FRICTION, KEY TO REMOVING DRY SURFACE BIOFILMS.
PCS 1000 Plus efficacy on bacteria removed from 12-day old dry surface biofilm.
CONCLUSION: Under the test conditions specified in the protocol, the test substance PCS 1000 PLUS, Lot #3108L004 met the acceptance criterion against the dry biofilm-isolated S. aureus and P. aeruginosa. This shows the performance of the test substance against both planktonic and biofilm-related forms of the bacteria remain the same.
Scan QR Code to Learn More

www.processcleaningsolutions.com • 1.877.745.7277
Think globally but buy local.
®
THINK GLOBALLY BUT BUY LOCAL. PROCESS CLEANING SOLUTIONS PROUDLY CANADIAN.
Continued from page 30
Pressure injury education
Another way UHN is supporting staff in optimizing skin PI care is by leveraging Epic, UHN’s new health information system, which provides a single source of truth to TeamUHN. By offering a standardized platform to document and share information, staff are harnessing the power of technology, to help ensure no information is missed while also staying up to date on a patient’s health.
EVERYONE PLAYS A ROLE IN PI PREVENTION
The best way to prevent PIs, which can form in a matter of hours, is for a patient to switch positions as often as possible, to relieve the pressure. However, patients at the most risk of developing these injuries often can’t reposition themselves and require assistance from others.
That’s where families can play a vital role, says Joshua Moralejo, a clinical nurse specialist at Toronto Rehab, Bickle Centre, where teams care for
Does your organization have 20 or more regular employees?
patients experiencing one or more complex medical conditions.
“We want families to be aware that they are a part of the care, so that if a nurse is unavailable for a few hours or when the patient is discharged from the hospital, everyone will have the necessary knowledge to prevent these injuries,” says Joshua, who also specializes in wound and ostomy Care.
Patients are also involved in PI education. Wound specialists such as Carol and Joshua provide them with resources such as UHN’s Spinal Cord Essentials website, which has a dedicated section dedicated to pressure injuries. They also keep patients informed about their skin health during their assessments at the bedside.
Joshua and Carol are a part of a group of more than 20 skin and wound care experts that work across UHN to provide patients with care at all stages of their healing journey.
The Interprofessional Skin Health Steering Committee is another way
You are required to have a Joint Health and Safety Committee (JHSC) in place.
From training workers on their rights and responsibilities to performing regular workplace inspections, having a Joint Health and Safety Committee (JHSC) in place is an integral step to creating and managing a safer and healthier environment for all workers.
Public Services Health and Safety Association (PSHSA) approaches training using personalized workplace experience scenarios. Attendees learn about hazards specific to their actual workplaces in a guided and individual approach. JHSC course facilitators provide the instruction and framework but each participant can learn based on what’s most relevant to their work environment. This approach enhances the knowledge and skills needed to meet learning objectives and requirements of the JHSC Training Program Standard.
Whether it’s for you or on behalf of your organization, there is flexibility on where, when, and how you complete your training with PSHSA.
Learn more about our flexible training options at pshsa.ca/flexiblelearning.

that UHN has provided experts like Josh and Carol the opportunity to collaborate on clinical care, research, education, strategic leadership and decision-making around skin health with other clinical nurse specialists, physiotherapists, occupational therapists, dietitians and patient partners.
UHN is committed to continuing to find the best ways to optimize skin health for all patients by supporting experts that are leading contributors to the field.
‘PREVENTION IS BETTER THAN A CURE’
To treat Jay’s pressure wounds, he was repositioned every two hours. The wounds were also redressed each day and special wound care products are applied to promote healing.
Carol, who was Jay’s wound specialist, also ensured the wounds are kept to the standard protocol approved by UHN professional practice leads, to avoid infection.
“The patient is part of this learning so that when they leave the door, we know we have set them up for a better transition back into their community,” says Carol. “Everyone, from staff to patients and their families, deserve the best education on how to prevent PIs and we are honoured to be a part of that process.”
For patients such as Jay, who has been discharged from Lyndhurst since June, explains how education to support his PI healing journey has made all the difference.
“To me, prevention is better than a cure,” Jay says. “If I knew this information from the beginning, I would’ve made the conscious effort to get myself repositioned every couple of hours.”
“This education is so valuable, and Lyndhurst did an amazing job right from the first inspection. I look forward to using this education to continue healing and getting back to my life.” ■ H
 Jay De Alwis, (R), an inpatient at Toronto Rehab’s Lyndhurst Centre for the Spinal Cord Rehabilitation program, with Carol McAnuff, a clinical nurse specialist, discussing Jay’s pressure wound treatment.
Photo credit:UHN
Jay De Alwis, (R), an inpatient at Toronto Rehab’s Lyndhurst Centre for the Spinal Cord Rehabilitation program, with Carol McAnuff, a clinical nurse specialist, discussing Jay’s pressure wound treatment.
Photo credit:UHN
32 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com INFECTION CONTROL 2024














Researching a new treatment for sepsis
For people who are in the intensive care unit (ICU) with a serious health condition, injury or recent major surgery, infections are a concern. Sometimes an infection is even what brought them into the hospital in the first place, like COVID-19. But any infection could lead to a life-threatening condition called sepsis.
“When it comes to sepsis, the ultimate goal is to select the right treatment, at the right time, for the right patient,” says Dr. Patricia Liaw, a scientist at the Thrombosis & Atherosclerosis Research Institute (TaARI) of Hamilton Health Sciences (HHS) and McMaster University. “There is no one-size-fits all treatment so it’s important to find alternative options that are effective for different types of sepsis patients.”
Liaw focuses her research on immunothrombosis, which is the process by which immune cells contribute to blood clotting in the presence of a severe infection. She is exploring a new
treatment for patients with sepsis and is working closely with Dr. Alison Fox-Robichaud, an HHS critical care physician and national expert in sepsis, to ensure her work in the lab can translate well into a clinical setting.
Sepsis is caused when the body has an improper and aggressive response to an infection and is the leading cause of death worldwide. A type of immune cells called neutrophils respond to severe infections by releasing DNA into the blood stream which form sticky web-like structures. These structures can help trap and kill microorganisms, but they can also attach to blood cells and form blood clots. Since blood clots limit or block blood flow, this affects the supply of oxygen and nutrients that are delivered throughout the body. This can result in tissue damage, organ failure and death.
BREAKING DOWN THE BLOOD CLOTS
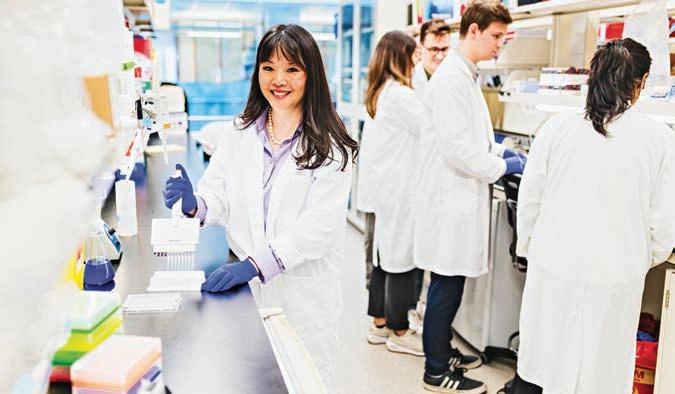
“IF THE








PATIENTS ARE LIKELY TO HAVE THE MOST BLOOD CLOTS, AND BLOOD THINNERS AREN’T WORKING AT THIS STAGE, THE DRUG WE’RE TESTING MIGHT BE THE ANSWER.”
Research from Liaw and her team have shown that some patients with severe sepsis have very high levels of circulating DNA in their blood, presumably released when the neutrophis encounter the infection. So, they conducted a multi-center study of 400 patients in the ICU with sepsis and found that patients with high levels of DNA in their blood have the poorest outcomes.
Liaw wondered if stopping the DNA from creating blood clots could be a solution. So, she’s found a drug that can do just that.


“We’re working on a Phase I clinical trial with a drug that breaks the connection between the sticky DNA structures and the blood cells, which essentially breaks down the blood clots,” says Liaw.
weeks. This is a safety and feasibility study which will recruit a small number of sepsis patients at HHS and Maisonneuve-Rosemont Hospital in Montreal. This study is funded by the Canadian Institutes of Health Research.
“In this first phase we’ll also determine the appropriate dose and duration of treatment and ensure that the process to administer the drug is realistic for the clinical staff,” says Liaw.
If this Phase 1 study has a successful outcome, the team will move on to a larger scale study to determine if the drug is effective.




















In early testing, Liaw and her team found the DNA-digesting drug to be most effective when sepsis is in advanced stages. Liaw says these preliminary findings are what make her clinical trial promising. “If the sickest patients are likely to have the most blood clots, and blood thinners aren’t working at this stage, the drug we’re testing might be the answer.”
LAUNCHING A CLINICAL TRIAL
Liaw and her team will begin the first phase of the trial in a few
Liaw strongly believes in ensuring there is a two-way bridge that connects lab-based research with applications that benefit patients. Her collaborations over the years with clinical colleagues such as Fox-Robichaud have helped to accelerate the translation of basic science discoveries to applications that improve human health. If this drug proves to be effective, she and her research team will continue to work to make it available to clinical teams at HHS. She’s hopeful that this treatment can help patients with life-threatening cases of sepsis not just in our community, but around the world. ■ H
SICKEST
YOU don’t have to wait! Get your digital copy of Hospital News emailed to you, the minute it comes out. Sign me up! Sign me up! Just send email to subscriptions@hospitalnews.com (please include full name to personalize) or scan QR code. Hospital News does not share subscription email addresses 34 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com INFECTION CONTROL 2024
Researcher Dr. Patricia Liaw (left) and her team are are working closely with clinical teams at Hamilton Health Sciences on a treatment for sepsis that breaks down the blood clots that form when there’s a severe infection in the body.








VANCOUVER • CALGARY • WINNIPEG • TORONTO • MONTREAL • HALIFAX VANCOUVER • CALGARY • WINNIPEG • TORONTO • MONTREAL • HALIFAX THANK YOU
How to achieve accountability in long-term care
By Michael Wolfson
Memories of the tragedy in Canada’s long-term care (LTC) homes from the pandemic are fading all too fast. However, this tragedy was not an accident; it was the result of a series of deeper problems with the ways LTC is funded, managed and understood. Without concerted action, these problems will continue to fester, and indeed grow with Canada’s aging population.
Addressing these problems requires actions on a number of fronts, from operating standards to staffing, to assuring the human rights of LTC home residents. The most important actions form the core recommendations of a just-released report from the Royal Society of Canada (RSC).
One reason for the failures in Canada’s LTC homes is their general invisibility. It has only been the unnecessary spike in residents’ deaths from the pandemic that brought these to light. With this tragic visibility, there has been a flurry of government actions. But as myriad experiences have taught us, as soon as the light fades, actions weaken.
One of the core recommendations of the recent RSC report is the creation of a robust “accountability framework,” in turn, based on strong data reporting. This is not a new idea; the 2003 First Ministers Health Accord also spoke repeatedly about accountability. However, governments’ support for the underlying data waned over only two or three years, as did support for the short-lived Health Council of Canada a few years later.
In order to avoid yet another failure, we must understand what an accountability framework involves, and why it has failed in the past.
One fundamental reason for failures is the constitutional division of powers. The provinces and territories, with primary jurisdiction for healthcare, do not want to be “accountable” to the
federal government, even though the federal government channels billions of Canadian taxpayer dollars to them. However, they should be accountable to their own populations.
The only way Canadians can learn what works and what doesn’t from each region, no matter their differences, is if the data are comparable –this is a legitimate role for the federal government.
Here we come to the reason for past failures: no provincial/territorial government wants to be shown to have poor performance in any area of its jurisdiction, certainly including healthcare. In a phrase, “why shoot the messenger if instead you can prevent there ever being a messenger?”
In the face of such self-interested resistance, an obvious response is for the federal government to incent the needed standardized data generation across jurisdictions, and then assure these data flow in ways that can populate a well-designed accountability framework.
Such a framework should include key indicators, such as the levels of direct care staffing per resident on LTC homes, and the frequencies of falls leading to fractures and hospitalizations. But the data flows must be much more than a handful of indicators. Analysts need to be able to drill down in the data to see, for example, what kinds of staffing levels and mixes are associated with the lowest rates of hospitalizations for falls, and other factors, including language and broader social determinants of health.
The federal government has ample constitutional powers to give effect to the needed data, not least from its spending powers and its power for “peace, order, and good government.”
The federal government does appear to be going through the right motions here. The major cash transfers announced in 2023 to the provinces

and territories include $500 million for data and assign the Canadian Institute for Health Information (CIHI) a central role.
Yet in the 2017 First Ministers Health Accord, where billions of dollars were transferred from the federal government focusing on LTC and mental health and addiction, all governments agreed that CIHI should be given the mandate to develop relevant indicators. Three years after the Accord, CIHI had published only one indicator relating to LTC, and it was based on hospital rather than LTC data.
CIHI does the best it can, but it is seriously limited by the data provided to it by the provinces and territories. For example, data about LTC resi-
dents are not connected to staffing levels, hospitalizations and other kinds of healthcare utilization, nor to surveys of all those waiting to access homecare or LTC homes.
It is impossible for provincial/territorial residents to hold their governments accountable for their responsibilities in LTC if the data available are biased, and the most important kinds of data are completely absent.
We take for granted in other areas, such as GDP, unemployment and inflation, that there are ample underlying data enabling a dissection of the observed trends. We deserve the same for LTC.
It’s long past time the federal government used all its constitutional powers. ■ H

36 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com LONG-TERM CARE NEWS
Michael Wolfson, PhD, is a former assistant chief statistician at Statistics Canada and co-author of the Royal Society of Canada report, Repair and Recovery in Long-term Care.

Restoring trust in long-term care after COVID-19 requires federal and provincial action and leadership
The Royal Society of Canada (RSC) has released its latest report, Repair and Recovery in Long-Term Care: Restoring Trust in the Aftermath of COVID-19 (2020-2023) under the guidance of an expert Working Group and as part of the RSC Task Force on COVID-19.
Three and a half years after the World Health Organization (WHO) first declared COVID-19 a global pandemic and the disease first appeared in a Canadian long-term care (LTC) home, older adults in LTC still die every week from COVID-19. The LTC workforce emergency continues, and remaining staff work short-handed, some without benefits.
Despite new cash injections, LTC homes remain deeply under-resourced; newly crafted major and robust LTC standards remain voluntary; and the promised Safe Long-term Care Act has yet to be tabled in Parliament.
The report states that the need for federal and provincial action and leadership on long-term care (LTC) is urgent and provides eight concrete recommendations that could be implemented now, based on a comprehensive deliberation and review of the most recent evidence.
“Long term care homes and the systems that support them were unprepared for a global pandemic, having suffered decades-long under-resourcing and inaction. Repair and recovery, while they may take near Herculean effort and a grit akin to dust-bowl determination, is possible,” says Dr. Carole Estabrooks, Chair of the Working Group, and Scientific Director of the pan-Canadian Translating Research in Elder Care (TREC) and Professor & Canada Research Chair, Faculty of Nursing at the University of Alberta.
“Our long-term care sector could be a highly resilient system equipped to
meet the challenges ahead with longterm care homes that older adults do not fear but understand as places where life and the end-of-life are lived with dignity, choice and enough joyful moments to make a good life.
It is going to take consequential action,” says Dr. Estabrooks.
During the pandemic, Canada and the provinces made mistakes, as the first in this series of RSC reports on LTC, Restoring Trust, noted. This new follow-up report highlights the many improvements in infection control and other measures that have been implemented in LTC since the beginning of the COVID-19 crisis, the innovative programs that were created and the policy gaps that have been tackled.
But now we need immediate and concrete action to strike at the heart of the many challenges that remain for a genuine transformation of LTC. This action must tackle the LTC workforce
crisis, including adequate recruitment and effective retention policies and practices; the accountability structure in LTC; federal transfer payments conditional on transparent outcomes and performance metrics, according to the report.
Recommendations also include building enhanced and integrated data systems; embracing consideration of the social and moral determinants of health for both LTC residents and staff; and enacting human rights reform in the governance laws and practices of LTC, as well as in education and training for LTC staff – among others.
“Living well is what matters most” for our older adults in LTC, the report authors state – and that is the vision that must be embraced by our governments and community leaders. We can get there with action: “It is as much a human rights mission as a mission of care,” the report concludes. ■ H

















LONG-TERM CARE NEWS
Polypharmacy: Impact on patient and medication safety
By Jasmina Jovanovic and Certina Ho
Anna (68-year-old female) was hospitalized after a fall, bringing along 14 medications she routinely takes at home. During the medication history review, it was revealed that she is taking seven vitamins and minerals based on friends’ advice. Upon examining her blood pressure medications, a concerning issue was identified –duplication of hydrochlorothiazide, one in combination with ramipril and another one prescribed by a different doctor. This raises concerns of potential polypharmacy, involving duplicate and/or unnecessary medications.
DEFINING POLYPHARMACY
Polypharmacy is commonly defined as the concurrent use of five or more medications, encompassing both prescribed and over-the-counter products, by a single individual. In 2014, 66 per cent of Canadians over the age of 65 took at least five different prescription medications. Polypharmacy is particularly prevalent among older adults. Multiple medical conditions are likely associated with complex medication regimens.
DEPRESCRIBING EMERGES AS A CORNERSTONE SOLUTION IN MITIGATING POLYPHARMACY.
different prescribers, resulting in drug therapy problems (e.g., duplication of therapy, drug-drug interactions, etc.). Lack of coordination among healthcare providers is particularly problematic during transitions of care, such as, when patients are transferred from hospitals to long-term care facilities or home, and vice versa. Mis- or lack of care coordination/communication between the healthcare team and the patient (and/or family) may also trigger a prescribing cascade and missed opportunities for deprescribing. A prescribing cascade occurs when side effects are misinterpreted as new health conditions, leading to additional prescriptions and a subsequent cycle of escalating treatments. This also highlights the important consideration of deprescribing, a systematic process of reducing or stopping medications that may no longer be necessary or may be causing harm, in mitigating polypharmacy associated risks. Sometimes, the
IN 2014, 66 PER CENT OF CANADIANS OVER THE AGE OF 65 TOOK AT LEAST FIVE DIFFERENT PRESCRIPTION MEDICATIONS.
UNTANGLING POSSIBLE CAUSES OF POLYPHARMACY
With the advancement in healthcare, there is an expanding array of treatment options available for medication therapy management of medical conditions, potentially contributing to polypharmacy. Fragmented communication within the healthcare team may lead to patients with multiple medical conditions receiving prescriptions from
complexities of polypharmacy may be augmented with self-medicating practices without a comprehensive understanding of risks-versus-benefits, side effects, and/or potential interactions among medications (as in Anna’s case above).
EXPLORING CONSEQUENCES OF POLYPHARMACY
Polypharmacy is associated with an elevated risk of adverse drug events
(ADEs) and ADE-related healthcare visits. The susceptibility of the aging population to ADEs is heightened by physiological changes in how their bodies process and respond to medications. The complex interplay of multiple medications also escalates the risk of drug-drug interactions, a frequent cause of preventable ADEs, and medication-related hospitalizations. Non-adherence to medication regimens was often linked to the complexity of drug regimens and the presence of polypharmacy, which may lead to potential disease progression, treatment failure, hospitalization, and life-threatening ADEs. In addition, functional decline, cognitive impairment, falls, and urinary incontinence in older adults have been linked to polypharmacy. Finally, polypharmacy contributes to increased healthcare costs for both patients and the healthcare system due to preventable emergency visits and hospitalizations, while also raising individual out-of-pocket expenses for unnecessary medication use.
ADDRESSING POLYPHARMACY
Embracing patient-centered care is paramount. Actively involving patients in decision-making processes, coupled with systematic medication reviews and patient education, will support tailored prescribing practices. Transparent communication between healthcare providers and patients by fostering interprofessional collaboration will enhance care coordination, prevent therapy duplication, minimize drug interactions, and optimize the overall medication therapy management.
RESOURCES AND SELECTED TOOLS
Deprescribing emerges as a cornerstone solution in mitigating polypharmacy. Regular deprescribing considerations/assessments integrated into patient care will allow healthcare providers to personalize medication regimens, minimizing the risk of potential ADEs and drug interactions. Online platforms, such as Deprescribing.org and DeprescribingNetwork.ca offer valuable resources and guidance with evidence-based information to assist healthcare professionals and patients in the deprescribing process. Choosing Wisely Canada is another valuable resource for clinicians and patients, prompting discussions about the risks, harms, and benefits of tests and treatment options. This initiative is designed to empower patients to make informed and effective care decisions while supporting healthcare providers in delivering personalized and evidence-based care. Furthermore, leveraging specialized tools that were developed based on the Beers Criteria ® and the Screening Tool of Older Persons’ Prescriptions/Screening Tool to Alert to Right Treatment (STOPP/START) criteria can better support prescribing decisions. The Beers Criteria ®, developed by the American Geriatrics Society, provides insights into medications inappropriate for older adults, aiding in risk identification. The STOPP/START criteria offer explicit recommendations for stopping or starting specific medications in older adults, with comprehensive considerations in both inappropriate prescriptions and underprescribing situations. These tools play an active role in safely reducing polypharmacy, fostering deprescribing, and facilitating patients in attaining optimized clinical and financial benefits. ■ H
Jasmina Jovanovic is a PharmD Student at the Leslie Dan Faculty of Pharmacy, University of Toronto; and Certina Ho is an Assistant Professor at the Department of Psychiatry and Leslie Dan Faculty of Pharmacy, University of Toronto.
38 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com SAFE MEDICATION













NURSING HERO AWARDS Celebrating Canada’s Nurses and Their Contributions If you do not recieve confoirmation within 24 hours of emailing your nomination, please follow up at editor@hospitalnews.com or by telephone 905.532.2600 x2234. Have you been inspired, encouraged or empowered by an employee or a colleague? Have you or your loved one been touched by the care and compassion of an outstanding nurse? Do you know a nurse who has gone above and beyond the call of duty? Hospital News will once again salute nursing heroes through our annual National Nursing Week (May 7th to 13th) contest. Nominations can be submitted by patients or patients family members, colleagues or managers. Please submit by April 6 and make sure that your entry contains the following information: • Full name of the nurse • Facility where he/she worked at a time • Your contact information • Your nursing hero story Along with having their story published, the winner also will take home: CASH PRIZES: 1st PRIZE $1,500 2nd PRIZE $1000 3rd PRIZE $500 Please email submissions to editor@hospitalnews.com or mail to: Hospital News, 610 Applewood Crescent, Suite 401, Vaughan, ON, L4K 0E3 19th Annual Hospital News 2024 NOMINATE A NURSING HERO!


40 HOSPITAL NEWS MARCH 2024 www.hospitalnews.com
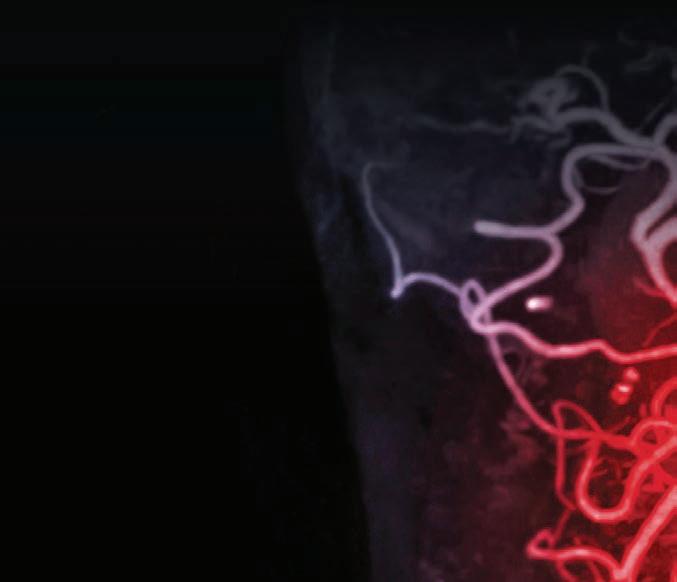



























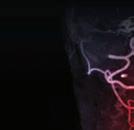









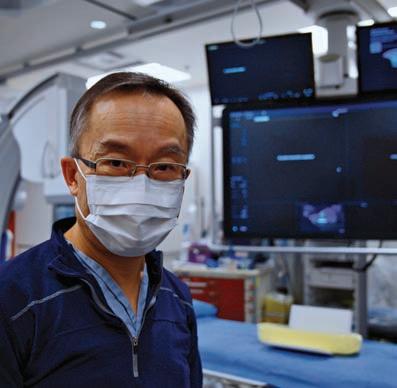




















































































































 Kent Waddington is the Communications Coordinator, Canadian Coalition for Green Health Care.
Dr. Bekim Sadikovic and Jen Kerkhof, Senior Laboratory Technologist, Molecular Genetics, in the lab where samples are analyzed.
Kent Waddington is the Communications Coordinator, Canadian Coalition for Green Health Care.
Dr. Bekim Sadikovic and Jen Kerkhof, Senior Laboratory Technologist, Molecular Genetics, in the lab where samples are analyzed.





































 cognitive
cognitive











































 Jay De Alwis, (R), an inpatient at Toronto Rehab’s Lyndhurst Centre for the Spinal Cord Rehabilitation program, with Carol McAnuff, a clinical nurse specialist, discussing Jay’s pressure wound treatment.
Photo credit:UHN
Jay De Alwis, (R), an inpatient at Toronto Rehab’s Lyndhurst Centre for the Spinal Cord Rehabilitation program, with Carol McAnuff, a clinical nurse specialist, discussing Jay’s pressure wound treatment.
Photo credit:UHN