





































































For more than a year the media has been trying to uncover in Ontario. But the Ford government did everything it could
This was yet another example of Doug Ford choosing secrecy over transparency. But through a Freedom of Information request, the facts have come out anyway, and they are devastating.
than everyone imagined. Rather than face up to the problem and take action the Ford government attempted to hide, while continuing to push for privatization.
The new numbers show Ontario will need more than 33,200 new nurses and 58,530 PSWs by 2032.
This is the truth Doug Ford has been trying to hide — the truth that nurses have been talking about for years.













































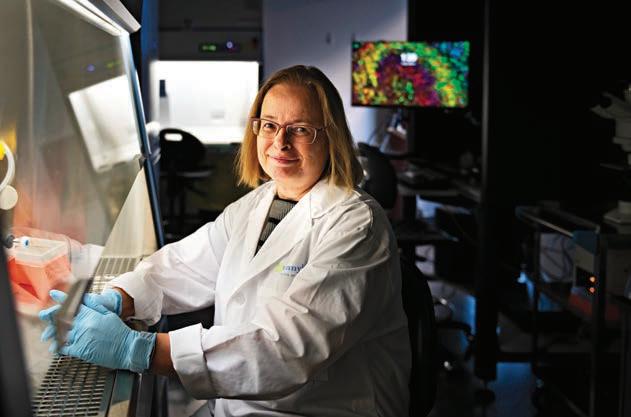
enetic testing is now the standard of care for common diseases such as cancer and heart disease, predicting risk and enabling earlier and more effective patient care. It’s an exciting revolution in patient care that has far-reaching potential and continues to grow and expand. But in Canada, we are not using all of our health human resources to take advantage of this important transformation in healthcare.
Nurses are consistently rated the most trusted health profession and are the largest health care workforce in Canada, providing care to the most vulnerable and remote patients.
At the beginning of the revolution in genetics, nurses were educated to offer genetic care to patients. But the educational opportunities have not kept pace. Genomics services have become siloed, and Canadians are now unnecessarily waiting for care and answers to their common genetics questions.
Nurses are ideally positioned to ensure that patients have access to accurate genetic information about their disease conditions and care options – but they no longer
JULY 2024 ISSUE
EDITORIAL: June 7
ADVERTISING:
Display – June 21 | Material – June 25
Monthly Focus:
Cardiovascular Care/Respirology/Diabetes/ Complementar y Health: Developments in the prevention and treatment of vascular disease, including cardiac surgery, diagnostic and interventional procedures. Advances in treatment for various respiratory disorders, including asthma and allergies. Prevention, treatment and long-term management of diabetes and other endocrine disorders. Examination of complementary treatment approaches to various illnesses.
Patient Rooms Focus
receive adequate training. Our governments, professional societies and post-secondary institutions need to work together and find resources to address this significant gap.
According to the Canadian Nursing and Genomics Initiative (CNGI), Canadian nurses lack crucial supports in their basic and continuing education about genomics when compared to nurses in other countries, such as the U.S. and the UK, where nurses are expected to provide information on condition, inheritance and treatment options for patients using relevant genetic counselling skills.
A recent survey of more than 1000 Canadian nurses revealed that while many patients seek nurses’ knowledge about genomics, nurses report wanting to learn more to better help their patients. Canadian nurses and their patients are missing out.
Basic nursing education should ensure new nurses are prepared to help patients understand their genomic test results and offer strategies for talking about results with family members. Basic nursing education should also prepare nurses to identify people who might benefit from genomic services, answer questions on genetic testing, and help people make lifestyle changes to lower risks.
Continued on page 6
AUGUST 2024 ISSUE
EDITORIAL: July 5
ADVERTISING: Display – July 26 | Material – July 30
Monthly Focus:
Paediatrics/Ambulatory Care/Neurology/ Hospital-based Social Work: Paediatric programs and developments in the treatment of paediatric disorders including autism. Specialized programs offered on an outpatient basis. Developments in the treatment of neurodegenerative disorders (Alzheimer’s, Parkinson’s etc.), traumatic brain injury and tumours. Social work programs helping patients and families address the impact of illness.
Annual Paediatric Supplement
THANKS TO OUR ADVERTISERS Hospital News is provided at no cost in hospitals. When you visit our advertisers, please mention you saw their ads in Hospital News.
610 Applewood Crescent, Suite 103 Vaughan Ontario L4K 0E3 TEL. 905.532.2600|FAX 1.888.546.6189 www.hospitalnews.com
Editor Kristie Jones editor@hospitalnews.com
Advertising Representatives
Denise Hodgson denise@hospitalnews.com
Publisher Stefan Dreesen stefan@hospitalnews.com
Accounting Inquiries
accountingteam@mediaclassified.ca
Circulation Inquiries info@hospitalnews.com
Director of Print Media
Lauren Reid-Sachs
Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications
Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
ASSOCIATE PARTNERS:
Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario.
The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
Canadian Publications mail sales product agreement number 42578518.

nity Health Toronto has received $18.9 million in federal funding to create a national pandemic preparedness system that will improve Canada’s capacity to identify and track new pathogens, monitor disease spread and speed up research and development of diagnostic tests, vaccines and therapeutics.
The PREPARED network will enlist up to 50 primary care clinics and emergency departments across Canada, plus research institutions and industry partners to build a coordinated ecosystem that can swiftly respond to new viruses or pathogens. The PREPARED grant is one of the largest operating grants Unity Health Toronto has received.
The goal is to prepare Canada for the next pandemic – which is only a matter of time, says Dr. Andrew Pinto, project lead and scientist and family physician at St. Michael’s Hospital, a site of Unity Health Toronto.
“I was in medical school during SARS and joined meetings that tried to tackle the rapid spread of a novel virus. Even with learnings from other flu pandemics, Canada still faced the same challenges when COVID arrived,” said Pinto, who is also the director of the Upstream Lab. “We didn’t have an early warning system. We didn’t have a coordinated system to rapidly enroll patients in critical research studies.”
The funding from the Canada Biomedical Research Fund (CBRF) was announced on May 6 in Montreal. PREPARED is one of four research programs endorsed by the Canadian Hub for Health Intelligence and Innovation in Infectious Diseases (HI3) that was funded by CBRF in 2023 with a mandate to bolster Canada’s biomanufacturing capacity and readiness to respond to emerging health threats.
The goal of the PREPARED network is to build an ecosystem that can be activated from the moment

there is news of a novel pathogen emerging, says Norman Umali, Upstream Lab, St. Michael’s Hospital research pharmacist and project team member.
In the new ecosystem, primary care clinics and emergency departments across Canada would be on alert for any signs of the new pathogen. When a patient goes to their family physician or local emergency department showing symptoms, the patient would be assessed and given a diagnostic test that would confirm within minutes whether the patient has the virus.
Swabs from the positive patient would be taken to help identify and sequence the exact pathogens circulating in the community. These samples could also be used to help build the next diagnostic test or vaccine.
Data from patients’ electronic records could be rapidly and securely accessed to support clinicians in decision making, while also contributing to national disease surveillance efforts. As well, patients who test positive would be invited to participate in research studies and trials to gain access to the latest therapies and to help determine which therapies are beneficial.
The ecosystem builds on a Canadian network of primary care clinics and emergency departments. The project team includes leaders of 16 primary care research networks that collectively serve more than 2.5 million Canadians, from British Columbia, Alberta, Manitoba, Ontario, Quebec and Newfoundland and Labrador.
The team has also consulted and will collaborate with 11 industry partners with expertise in specimen collection, diagnostics, genomics, surveillance and data management, therapeutics, gene therapies and vaccine development.
Beyond tracking acute respiratory infections, the team sees other future applications for this model, says Dr. Benita Hosseini, Upstream Lab research scientist and project co-lead.
“We would like to adapt the ecosystem to track other infectious diseases, such as mpox, or other chronic conditions. It could also be adapted to perform surveillance during other public health emergencies, such as those driven by climate change,” she

said. The goal is to build an adaptable, patient-centered healthcare system, to improve our readiness for current and future health challenges and for transforming healthcare efficiency and effectiveness.
Part of the project is to train the next generation of researchers through the PREPARED Talent Development Program, Hosseini adds. In this program, trainees can choose a learning stream to focus on surveillance, data science, Implementation Science or Community-Based Participatory Research.
Pinto notes that in the United Kingdom, clinicians were able to quickly enroll patients into clinical trials within weeks of the first COVID cases being detected. As a result, the U.K. led the world in understanding what therapies worked in treating COVID, he said. One of the goals of PREPARED is to facilitate linkages to research trials by integrating recruitment efforts within primary care clinics and emergency departments, he said.
“We are excited about the opportunity to create a coast-to-coast shield that will help protect Canada and Canadians in the future,” said Pinto. ■ H
Marlene Leung works in communications at Unity Health. Dr. Andrew Pinto, Dr. Benita Hosseini and Norm Umali.Homelessness doesn’t only happen to young people but also affects older adults in growing numbers, write authors in an analysis in CMAJ (Canadian Medical Association Journal) that describes this emerging crisis.
People experiencing homelessness are considered older adults at age 50, as visible aging is often evident at younger ages in individuals experiencing homelessness compared with individuals who have secure housing.
Individuals experiencing homelessness often develop chronic medical conditions earlier, as well as age-related conditions like cognitive impairment.
Continued from page 4
As well, the risk of premature death for older people experiencing homelessness is 3.5 times higher than for those who are housed, and the risk is especially high for people experiencing homelessness for the first time late in life.
In 2021, 32 per cent of people in Canadian shelters were aged 50 and older. There are also many older people living outdoors or living temporarily with friends or family.
“Older adults experiencing homelessness deserve shelter policies and government strategies that consider their care needs, and age-friendly shelters that have adequate physical en-
To deliver this education, nurse educators need programs, supports and incentives to develop their own competency in genomics.
A health care system that expects nurses to provide genomics-informed care must provide proper training. Canadian health systems are ripe for re-design to better utilize nurses to meet the needs of patients, families and communities affected by genetic conditions and risks.
Nurses in the workforce need to be equipped with genomic knowledge about their patients through continuing education courses, toolkits and clinical decision support aids. These resources are available to nurses in other countries, and they are making a difference to the quality, accuracy and safety of patient care.
Armed with genomics knowledge, nurses could work more effectively with genetic counsellors, physicians and pharmacists to provide care to thousands of people requiring genomics services.
Imagine the impact of Canada’s nearly half a million nurses, once armed with genetics knowledge. Genetic testing can only improve health when health care professionals can employ the results.
Knowledge about genetic testing, risks, and therapies needs to be better integrated into nurses’ basic and continuing education programs, to get into the “DNA” of the nursing profession.
Nurses are poised to deliver the worldclass health care Canadians expect –employing their knowledge of genetics to provide the best patient care. ■ H
Nicole Letourneau PhD RN FRSC is a Professor and University of Calgary Research Excellence Chair in Parent and Child Health.
Jacqueline Limoges PhD RN is an Associate Professor at Athabasca University and co-lead of the Canadian Nursing and Genomics Initiative.
THE RISK OF PREMATURE DEATH FOR OLDER PEOPLE EXPERIENCING HOMELESSNESS IS 3.5 TIMES HIGHER THAN FOR THOSE WHO ARE HOUSED.
vironments, appropriate staffing, and access to required medical services,” writes Dr. Jillian Alston, a geriatrician at St. Michael’s Hospital, Unity Health Toronto, with coauthors.
“Older adults experiencing homelessness may have faced substantial marginalization, dehumanization, and structural violence, and care models should prioritize trust, rapport building, and ensuring personal safety.
To support older adults at risk of and experiencing homelessness, adequate housing that supports individual needs is essential. Conditions that become more common with aging, like cognitive impairment and mobility concerns, can make maintaining housing more difficult for some older adults. Some solutions to prevent homelessness include tenancy monitoring programs, individualized in-home supports, and community programs that address isolation. In-shelter health care programs, such as primary care and geriatric outreach programs can help support older adults living in shelters. Innovative permanent supportive housing such as The Oaks in Ottawa, and other housing models that support aging in the right place can help provide appropriate homes for older people experiencing homelessness to relocate to. For some, the most appropriate environment to support their needs will be long-term care homes.
Addressing this growing problem requires collaboration between health, long-term care, public health, and housing and other community supports. As well, trauma-informed approaches are important for those who have experienced adversity and trauma earlier in their lives.
“Without urgent action, older adults experiencing homelessness will remain marginalized, undergo early aging, and continue to be at risk for deterioration and death in shelters and other temporary accommodations that are neither equipped nor designed to meet their needs,” conclude the authors.
“The human toll of homelessness is immense,” writes Dr. Andrew Boozary, a primary care physician and executive director of the UHN Gattuso Centre for Social Medicine, Toronto, with coauthors Dr. Catherine Varner, CMAJ deputy editor and emergency medicine physician, and CMAJ editor Dr. Andreas Laupacis in an editorial. “People who are chronically unhoused live half as long as those who are housed, experience accelerated aging, have many more comorbidities, and develop health conditions at a much younger age than those who are housed. Homelessness disproportionately affects Indigenous, Black, refugee and newcomer, and 2SLGBTQ+ people.”
To help address this chronic problem, some health networks are building affordable housing for unhoused people – a novel approach that the authors say speaks to the magnitude of the homelessness crisis.
“The fact that hospitals are dedicating scarce resources to provide housing is a testament to how undeniable the homelessness crisis has become and how ineffective and costly conventional approaches, such as lengthy hospital admissions, have been,” they write.
“Tackling late-life homelessness in Canada” and “Homelessness is a health crisis: why hospitals are resorting to building housing” were published May 21, 2024. ■ H
More than one-in-five adults in Canada did not have access to primary care, with large regional gaps in access, found new research in CMAJ (Canadian Medical Association Journal)
“Translated to the population of Canada, our survey estimates that more than 6.5 million adults across the country don’t have access to a family doctor or nurse practitioner they can see regularly,” says Dr. Tara Kiran, a family physician and researcher at the MAP Centre for Urban Health Solutions at St. Michael’s Hospital, Unity Health Toronto and the University of Toronto. “And even those lucky enough to have a family doctor are struggling to get timely care for urgent concerns or care on evenings and weekends.”
As part of an 18-month, across-Canada initiative to develop a vision with patients and the public for primary care called OurCare, researchers conducted a survey to understand people’s values and experiences with primary care. They analyzed data from more than 9200 people via survey, with 73 per cent of surveys in English and 27 per cent in French to provide a national overview.
“What is most surprising is the provincial variation in access to primary care,” says Dr. Kiran. “Primary care is the front door to the health care system – the first point of access for acute concerns, managing chronic disease, preventing illness, and helping people access other supports. It is simply unconscionable that in some parts of the country, this door is now closed for almost one-third of the population.”
In Quebec and the Atlantic provinces, almost 1 in 3 people reported they did not have a primary care clinician, even after the authors adjusted for differences in age, gender, education, and other demographic characteristics of survey respondents. People in Ontario were most likely to report having a primary care clinician. Men, people younger than 65 years, and those with poor health
“OUR SURVEY ESTIMATES THAT MORE THAN 6.5 MILLION ADULTS ACROSS THE COUNTRY DON’T HAVE ACCESS TO A FAMILY DOCTOR OR NURSE PRACTITIONER THEY CAN SEE REGULARLY.”
were less likely to have a primary care clinician.
People with primary care clinicians also reported challenges in accessing care, as most practices did not offer appointments outside of usual weekday 9–5 hours, and more than half of respondents said they could not get an urgent appointment within three days of attempting to book. Many
turn to walk-in clinics, which do not provide continuity of care, something that patients indicated was important.
The research team notes that 90 per cent of survey respondents would be comfortable with getting care from another member of a primary care health team, suggested internationally as one solution to address the pri-
mary care crisis. Yet less than 15 per cent of respondents reported that their primary care clinician worked with a social worker or pharmacist or dietitian. There was substantial provincial variation, with the odds of working with any health professional lower for people living outside Ontario and Quebec.
“The crisis in access to primary care is in stark contrast to the values that people in Canada hold dear – that everyone should have access to health care regardless of where they live and who they are,” says Dr. Kiran.
“Public experiences and perspectives of primary care in Canada: results from a cross-sectional survey” was published May 21, 2024. ■ H
The prevalence of Carbapenemase-producing organisms (CPO) is increasing in B.C. with new cases reported in both long-term care homes and hospitals.
To better protect long-term care residents from a common superbug that can cause serious illness, we are proactively screening for CPO in owned and operated care communities.
“We know that long-term care residents often have weakened immune systems which put them at risk for multi-drug resistant organisms,” says Dr. Kevin Afra, executive medical director, Infection and Prevention Control and Antimicrobial Stewardship Programs. “Being able to identify CPO early will provide more opportunities for quicker intervention and reduced transmission within the long-term care community, and possibly, acute settings, as there can be transfer back and forth between both.”
The screening project aims to achieve several objectives:
• Determine the prevalence of CPO among residents.
• Identify risk factors associated with CPO positivity.
• Inform surveillance strategies.
• Provide recommendations for enhanced infection prevention and control practices.
During the screening process, longterm care staff collect stool samples or rectal swabs, which are then tested for CPO.
“Our residents’ comfort and dignity remain a priority,” says Dr. Akber Mithani, regional medical director, Integrated Long-Term Care and Assisted Living. “We’re collaborating with residents, family members and care providers across communities to facilitate testing and create a safe and healthy environment for everyone.”
If a resident is found to be carrying or colonizing CPO, they can still fully participate in daily and social activities. Care teams will monitor for early
signs of illness and implement enhanced environmental hygiene measures to ensure the safety and well-being of all residents.
It’s essential to recognize that everyone carries germs. For most people, having CPO bacteria in the gut is no more dangerous than encountering other germs. However, vulnerable individuals, especially those in long-term care, face a higher risk of developing serious infections that are challenging to treat.
The World Health Organization (WHO) has declared antimicrobial resistance a significant public health threat. The WHO and the European Centre for Disease Prevention recommend surveillance of longterm care residents to understand the prevalence of CPO and other multi-drug-resistant organisms within this population. ■ H

The human brain is the most complex organ in our body and unlike any other structure, the brain is what makes humans, human. The brain has many important functions such as storing memories, sending signals about feelings and emotions, enabling speech and movement and so much more.
The unique and intricate structure of the human brain enables us to do many tasks, however, its complexity poses a challenge towards understanding, diagnosing and treating different brain disorders. Conditions that affect the brain such as ALS, Alzheimer’s disease and some cancers, can have devasting impacts on an individual, and given the complexity of the brain, are very difficult to treat.
In order to better understand the organization of the brain and disease progression, scientists depend on models that accurately represent the human brain. Currently, much of our scientific understanding of the brain is based on animal biology and while those models continue to play a valuable role in brain research, they remain limited because the human brain is dramatically different and unique from those of other animals.
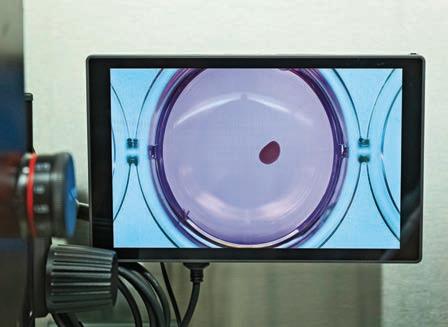
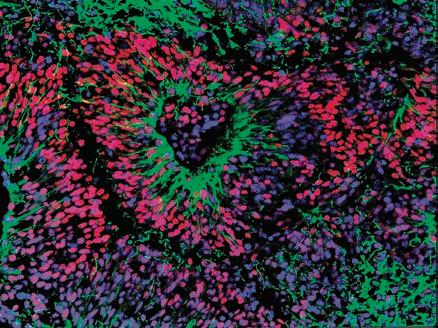
Scientists at Sunnybrook Research Institute (SRI) are advancing the understanding of the human brain by developing models with more precision than ever before. Dr. Carol Schuurmans, senior scientist in the Hurvitz Brain Sciences Research Program and Dixon Family Chair in Ophthalmology Research, leads Sunnybrook’s stem cell and organoid facility, which is managed by Dr. Dawn Zinyk. Dr. Schuurmans’ lab specializes in growing cerebral organoids, which are miniature and simplified versions of brain tissue, to better understand the cellular and molecular features of the human brain.







“We can use cerebral organoids to study many different things including developmental principles and disease mechanisms,” says Dr. Schuurmans. “Currently, these organoids are helping us understand which genes contribute to human brain development, with hopes of applying this tool to disease models to better recognize disease pathology and mechanisms.”
Organoids are grown in vitro using pluripotent stem cells. Scientists isolate human blood or skin cells and convert them into pluripotent stem cells, which are cells that can give rise to and act as any one of the body’s
more than 200 cell types. These stem cells are then mixed with a variety of molecules, which direct them to grow into different types of tissue, including brain tissue (i.e., cerebral organoids).
At SRI, scientists are currently growing organoids that resemble the neocortex, the front part of the brain that’s responsible for sensation and cognition. It can take three to four months to develop an organoid to a stage that models the cell composition of a human brain. At SRI, organoids have been grown for up to 10 months, where they become larger, more mature and increasingly complex.
“The hope for these models is to support personalized medicine and treatments,” explains Dr. Schuurmans. “Using organoids, scientists and clinicians can observe disease progression in specific individuals, and with this knowledge, clinicians can determine the most effective course of treatment for that patient.”
Right now, scientists at SRI are growing cerebral organoids to study their potential to create personalized treatments for neurogenerative diseases like dementia. Possessing models that more accurately represent the unique and complex human brain will provide scientists with more effective tools to aid in advancing the future of brain health. ■ H
Anna McClellan is a Communications Specialist, Sunnybrook Health Sciences Centre. Left: A 100-day old cerebral organoid at Sunnybrook, visible to the human eye (enlarged to show detail). Middle: A 18-day old organoid at Sunnybrook, under the microscope. Photos: Kevin Van Paassen













Drs. Marcelo Cypel, (L), and Shaf
Keshavjee invented the Toronto Ex-Vivo Lung Perfusion (EVLP) System in 2008. In March 2024, UHN celebrated its 1,000th EVLP procedure, a milestone for the homegrown invention that has been commercialized around the world.
By Catherine Dankohaf Keshavjee and Marcelo Cypel continue to see the future for the Ex-Vivo Lung Perfusion (EVLP) System they invented.
Having reached the 1,000th procedure of the EVLP – a milestone occurring more than a decade after its inception – they see nothing but monumental outcomes for lung transplantations at UHN and around the world.
“I saw the 1,000th coming, and I see the 10,000th coming,” Dr. Keshavjee, Chief of Innovation at UHN and co-creator of the homegrown EVLP, says of the system, which was invented in 2008, became a fully approved and funded clinical therapy in 2011, and marked its 1,000th procedure just last month.
The EVLP maintains donor lungs outside the body by mimicking body temperature and providing nutrients prior to transplantation, resulting in increased lung health and lower rates of rejection following the surgery.
The milestone transplantation surgery for the EVLP was performed in
March on one of about 1,400 patients in Ontario currently awaiting an organ transplant. The patient’s information cannot be disclosed to protect privacy, but the number itself speaks volumes to the utility of the procedure.
“This is significant because it really shows how much this technique has matured, and that it has a strong track record of benefiting those needing a lung transplant,” says Dr. Cypel, Surgical Director of UHN’s Ajmera Transplant Centre and staff thoracic surgeon at UHN, and a professor in the Department of Surgery at the University of Toronto.
“I don’t think we’d get to 1,000 procedures in any surgical procedure without seeing the striking benefits it’s bringing to patients,” he says.
The EVLP System was developed at UHN but has since been recognized and implemented internationally.
It’s now used across five continents, including leading transplant centres in the United States such as Duke University Hospital, Cleveland Clinic,
Mayo Clinic, as well as Europe, South America, Asia, Israel and Australia, with the highest volume of transplants occurring in the U.S.
“UHN has invented a new solution, and just as important has assisted in its development into a commercial product that can now be applied and implemented at transplantation sites around the world,” says Dr. Brad Wouters, Executive Vice President of Science and Research at UHN.
“It’s a good example of translation of research to benefit patients here at UHN and around the world, identifying unmet patient needs, which is what our physicians here are experts at doing,” he says.
The Toronto General Hospital Research Institute (TGHRI) – the research arm of Toronto General Hospital – is one of top medical research programs worldwide, supporting the medical programs of the hospital with multidisciplinary experts in the fields of organ transplantation, regenerative medicine, cardiol-
ogy, diabetes and infectious diseases, among others.
TGHRI is home to more than 150 scientists and clinicians who work together to bring innovative research findings from the lab directly to patients, with notable findings including the first clinical use of insulin and the first cardiac pacemaker, among many other novel approaches, including EVLP.
The EVLP System can be used to make the donor lungs look more like the recipient’s, resulting in increased lung health prior to transplantation, higher chances of donor matches and lower rates of rejection following the surgery.
Prior to this system, 80 per cent of donated organs went unused because the lungs did not meet standard acceptance criteria.
“People sign up to become organ donors assuming they’re going to donate their organs, when in reality, the majority of lungs around the world are not used because [medi-
cal professionals] can’t be sure that they’re safe for transplantation,” says Dr. Keshavjee.
Dr. Keshavjee and Dr. Cypel’s development poses a monumental change for patients waiting for an organ transplant and has more than doubled the number of clinically acceptable lung donations at UHN.
“[EVLP] allows people who choose to be organ donors to be sure that their lungs are going to be successfully donated,” says Dr. Keshavjee.
“Over 40 per cent of donated lungs in Toronto are now able to be used for transplantation, whereas before only 20 per cent were utilized,” he says.
The Toronto Lung Transplant Program in UHN’s Ajmera Transplant Centre at Toronto General Hospital is the largest and most successful lung transplant program worldwide. It was the first centre in the world to perform both a single (1983) and double lung (1986) transplant and in 2008, conducted the first human EVLP surgery to repair and recondition donor lungs prior to transplantation.
UHN’s Sprott Department of Surgery is the largest surgical program in Canada, spanning 13 surgical divisions – from cardiovascular to neurosurgery to thoracic – across three UHN hospitals: Toronto General Hospital, Toronto Western Hospital and Princess Margaret Cancer Centre.
In 2020, a UHN team of transplant surgeons, led by Dr. Keshavjee, were awarded a $24-million New Frontiers in Research Fund (NFRF) grant from the CIHR and the federal government to further advance ex-vivo transplant technology, including repairing and rebuilding other organs outside the body. This team also received support from UHN Foundation, whose donors have been supporting the development and evolution of EVLP since its very early days.
Both Drs. Keshavjee and Cypel continue to work towards advancing the future and clinical potential of ex-vivo perfusion. Recently, Dr. Cypel and his team used EVLP to modify organ blood type to universal type O blood organs (universal blood type) for transplantation.
Catherine Danko works in communications at UHN.
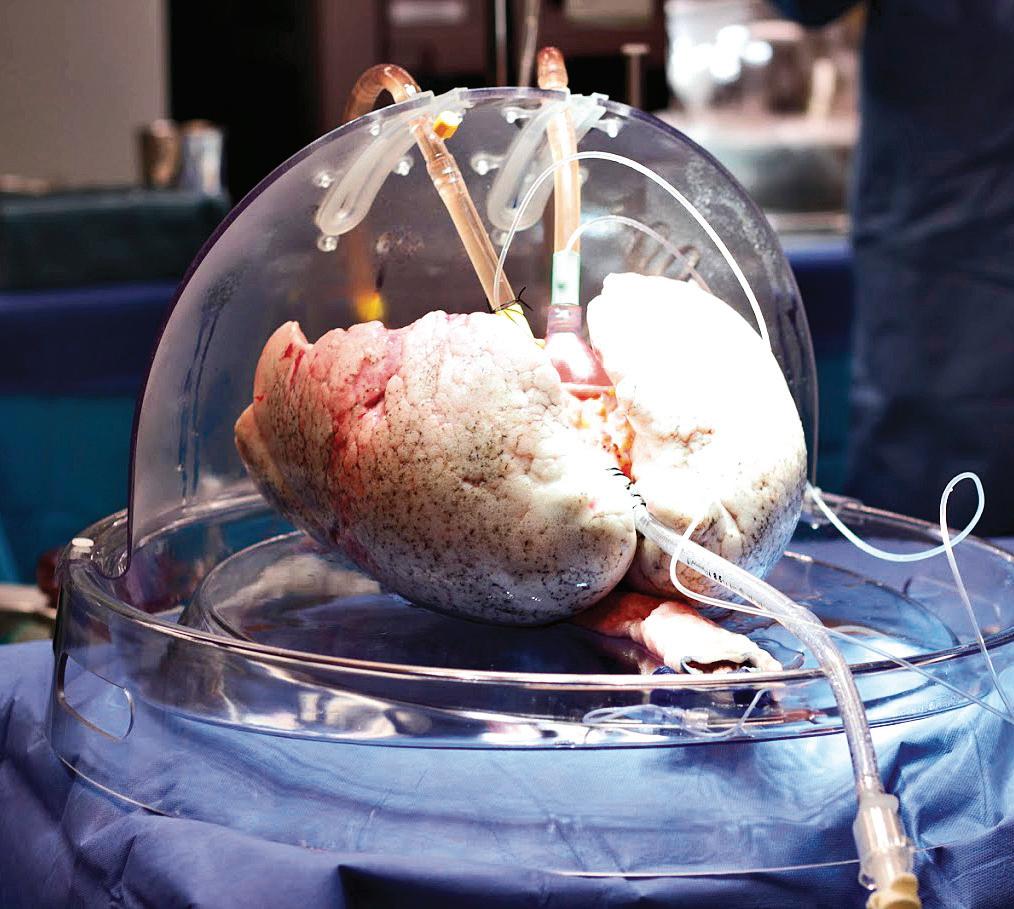

The EVLP System maintains donor lungs outside the body by mimicking body temperature and providing nutrients prior to transplantation, resulting in increased lung health and lower rates of rejection following the surgery.
“This could have a dramatic change in how we currently allocate organs for transplant,” says Dr. Cypel.
“EVLP is ultimately a platform that allows us to do more sophisticated
things,” says Dr. Keshavjee, who believes it’s just the beginning for ex-vivo perfusion – and will be the future of all organ transplantation, whether it’s the kidney, pancreas, lungs or the heart. ■ H





UHN-created tool that supports Emergency Department (ED) physicians in deciding whether to admit or discharge a heart failure patient is now available in Epic, UHN’s electronic patient record system.
The Emergency Heart Failure Mortality Risk Grade (EHMRG) calculator estimates the risk of a heart failure patient dying within one week, and over the course 30 days, based on 13 key metrics calculated in the ED.
Based on the score, different courses of action are recommended depending on a patient’s risk category.
The Epic integration at UHN is the first in Canada for this decision-support tool.
The EHMRG calculator, which was created by Dr. Douglas Lee, a cardiologist at UHN’s Peter Munk Cardiac Centre where he is Ted Rogers Chair in Heart Failure Outcomes, was validated in a clinical trial –“Comparison of Outcomes and Access to Care for Heart Failure (COACH)” – at 10 hospitals across Ontario. The results were in a study published in the New England Journal of Medicine in 2023.
“UHN Emergency Department clinicians enrolled patients into the COACH trial and contributed to the development and validation of the score,” says Dr. Sam Sabbah, Chief of Emergency Medicine at UHN.
“Fast forward, and it’s now becoming a best practice and is integrated into our workflow in Epic – let’s take a moment to celebrate that.”
The EMHRG calculator provides a low-risk, intermediate-risk, or highrisk score based on the patient’s presenting metrics at the ED, such as age, blood pressure, creatinine and potassium levels, and whether they arrived by ambulance.
Low-risk patients can be safely discharged from the hospital and given a follow-up appointment with a heart function clinic within two weeks. High-risk individuals should be admitted from the ED for immediate care and ongoing monitoring.
Dr. Douglas Lee, (L), a cardiologist at UHN’s Peter Munk Cardiac Centre and founder of the Emergency Heart Failure Mortality Risk Grade (EHMRG) calculator, discusses use of the tool with Dr. Erin O’Connor, a UHN Emergency physician and Division Director of Emergency Medicine at the University of Toronto.


An intermediate-risk score prompts further consultations with hospital specialists to determine if the patient can be discharged with a follow-up appointment within a few days, or should be admitted for monitoring.
The EHMRG calculator’s benefits extend beyond individual patients, however.
It supports clinical decision-making with an objective and evidence-based score – generated automatically and quickly – to help ensure the safety of patients and efficiency of the workflow in a busy ED. This improves patient quality of life, ensures allocation of hospital resources to those in most critical need and reduces health care expenses.
“In the fast-paced environment of Emergency Departments, where decisions can mean the difference between life and death, the Emergency Heart Failure Mortality Risk Grade (EHMRG) score provides timely insights to help make the right decision,” says Dr. Lee, whose work on the project was funded by the Ted Rogers Centre for Heart Research and Institute for Clinical and Evaluative Sciences (ICES).
“Heart failure is complex, and objective measures like the EHM-
RG score can complement physician clinical judgment.”
Before receiving the greenlight for integration into Epic, the EHMRG calculator was first validated in the COACH trial.
The trial at 10 Ontario hospitals saw more than 5,000 patients who came into the ED with acute heart failure divided into two groups. One received usual care, and the other received a special hospital-based strategy using the EHMRG calculator to help physicians determine which patients were able to be safely discharged with follow-up.
The results showed that within 30 days of receiving treatment, the group using the EHMRG calculator had a lower rate of either dying from any cause or being hospitalized again for heart problems compared to the group that received usual care. Over 20 months, the difference in health outcomes between the two groups continued to be better for the EHMRG care group.
Specifically, only the patients in the EHMRG calculator group experienced a statistically significant reduction in death or repeat hospitalization for cardiovascular reasons compared to the control group.
The study concluded that for patients with acute heart failure, receiving care informed by their individual risk level determined with the EHMRG calculator score in tandem with rapid follow-up at a heart function clinic resulted in a lower risk of mortality or re-hospitalization.
It was this promising result that led the Epic and UHN teams to design an integrated care pathway for the ED that incorporated the EHMRG calculator score and integrated it into Epic at multiple UHN sites.
This is the latest tool from the Ted Rogers Centre for Heart Research to be integrated for widescale use across Ontario hospitals, showcasing the incredible impact of both the research and translational work being done by its scientists and clinicians.
“By integrating this calculator into the Epic system at UHN, we’re not just enhancing the decision-making process, we’re helping to transform the way heart failure is managed in the Emergency Department,” says Dr. Lee. “It’s a step forward in our mission to improve the quality of care for heart failure patients across the province.” ■ H
new approach for early cancer treatment was shown to significantly reduce the risk of advanced neuroendocrine tumour progression and death by 72 per cent in otherwise challenging areas to treat.
“This is a game changer in the practice of not only the treatment of higher Grade 2 and 3 neuroendocrine tumours of the gastrointestinal tract, but for cancer treatment broadly,” says Dr. Simron Singh, global principal investigator of the trial, and medical oncologist, affiliate scientist at Sunnybrook Research Institute (SRI) and cofounder of the Susan Leslie Clinic for Neuroendocrine Tumours at Sunnybrook’s Odette Cancer Centre.
Presented at the 2024 American Society of Clinical Oncology (ASCO) Gastrointestinal (GI) Cancers Symposium, an overview of the results from the NETTER-2 Phase III multi-centre international clinical trial provided evidence for the first time that radioligland therapy (RLT) – when applied in the early stages after a patient’s diagnosis – significantly and safely slowed down the progression of neuroendocrine tumour growth, extending the average time of “progression-free survival” from approximately 8.5 months to 22.8 months. This is the first trial to show efficacy of first-line RLT in any cancer.
RLT – a more precise form of radiation therapy being used and researched in the treatment of some cancers – involves injecting radioactive isotopes through an IV (in this case, with the



drug known as Lutathera) in order to target cancer cell receptors, and deliver more targeted and precise radiation to kill cancer cells.
This study evaluated the use of RLT earlier as a first-line (or “up front”) treatment for patients newly diagnosed with grade 2 or 3 advanced gastrointestinal neuroendocrine tumours. Although neuroendocrine cancer is uncommon, its incidence is rising rapidly and few treatments exist for these patients as this kind of cancer is resistant to most treatments; making it challenging to treat.
“The results confirm the clinical benefit of earlier use of RLT for newly-diagnosed patients with these
types of aggressive and life-threatening tumours,” says Dr. Singh, also an associate professor of medicine at the Temerty Faculty of Medicine at the University of Toronto. “This is the next step in personalized targeted cancer therapy for patients, focused on more effectively killing cancer cells, while limiting the damage to surrounding healthy tissues.”
Further investigations of RLT as a therapeutic option are ongoing to evaluate overall survival and longterm safety, which will better define next steps for this change to practice in cancer treatment world-wide.
The multi-site trial included investigators and participants from Canada,


France, Germany, Italy, Netherlands, South Korea, Spain, UK and USA. World leaders in the care of neuroendocrine tumours and research, the multidisciplinary Susan Leslie Clinic for Neuroendocrine Tumours at Sunnybrook’s Odette Cancer Centre is the only one of its kind in Canada. With a team of surgical oncologists, medical oncologists, radiation oncologists, nuclear medicine physicians, interventional radiologists, dedicated pathologists, and geneticists under one roof, their integrated care model is improving outcomes for patients with neuroendocrine tumours, as it studies care delivery, trials new therapies, and leads expert consensus. ■ H
In my over 20 years as an Otolaryngologist-Head and Neck Surgeon at North York General (NYGH) I have witnessed firsthand the evolving landscape of health care. From local communities to remote regions in Northern Canada and across the globe, these experiences have shaped my approach to leadership in this critical moment for our healthcare system.
Since becoming North York General’s President and CEO in December 2023, I frequently hear: “This must be a fascinating time to lead North York General,” or, “With so many big challenges, where do you start?”
This period will be remembered as a defining moment for health care. It is impossible to overstate the significant challenges healthcare providers are facing today. We are in a period of rapid change and must keep pace with very limited resources. It is both the best and one of the most challenging times to be a hospital CEO. Within the multiple challenges lie opportunities for us to facilitate change for the better. Achieving change is not easy and requires a shared passion, shared purpose, and a shared vision.
Our health system in on the brink of a demographic crisis, driven by a rapidly aging population with an increasing life expectancy and a higher prevalence of complex medical conditions. Today, Canada has the largest seniors population in our nation’s history. The fastest-growing group in our catchment area is people over the age of 65. We expect that in 15 years, the number of people who are 65 years and older will double. Estimates indicate that there will be a 200 percent increase in those living with dementia in Canada within the next 20 years. To add fuel to the fire, demographic shifts have contributed to our current undersupply of physicians, nurses, and other health professionals, exacerbated by the COVID-19 pandemic.

OUR
North York General is at the coalface of this demographic crisis. The area we serve has the highest concentration of seniors in Toronto and some of the city’s fastest growing and most ethnoculturally diverse neighbourhoods. Today’s seniors have different needs and expectations about how they want to live as they age than generations past.
Despite these incredible challenges, I am optimistic. The confluence of medical and digital technological advances offers unprecedented opportunities to create a stronger, safer and more equitable healthcare system.
One of the most pressing issues we face is ensuring that we can meet the needs of our rapidly growing population of older adults. At North York General, we are reimagining seniors’ care. Our transformation plan includes expanding our facilities, strengthening community partnerships, and innovating how and where we provide care. The result will be a more integrated system where more care is delivered in the community and in people’s homes. Doing so is not an option, but a necessity if we are to meet the needs of future generations.
The cornerstone of our transformation is the development of a new
528-bed long-term care (LTC) home poised to become one of Ontario’s largest and most advanced homes for seniors. The LTC home will redefine a new global standard of excellence in seniors’ care, demonstrated not only in its advanced design, but also in the best-in-class personalized care provided to the residents. The home will form a hub of excellence for seniors-focused care for the broader community.
Our seniors built the Canada we know today. We have a duty to ensure that the system they worked so hard to build will be there for them when they need it most.
This is an incredible time to lead an organization like NYGH. We have a once-in-a-generation opportunity to improve the lives of our older citizens right now and into the future. Doing so will change the trajectory for ourselves, our loved ones, and all those who will follow. ■ H
Dr. Everton Gooden is President and CEO of North York General.
 By Samantha Sexton
By Samantha Sexton
very hospital pharmacy faces issues regarding drug stability (how long a drug can be stored once prepared to remain safe and effective) and compatibility (how two or more drugs react when combined), but few hospital pharmacies are positioned to conduct studies to address these gaps and translate results to practice.
Sunnybrook Health Sciences Centre is home to the only hospital pharmacy quality control lab in Ontario. Led by pharmacist Nathan Ma and supported by Shirley Law, the lab works to reduce drug wastage, support clinical trials and navigate drug shortages.
Together with pharmacy experts in formulation, quality assurance and front-line clinical staff, the Pharmacy Quality Control Lab works to design studies to answer questions that are clinically focused on improved patient care and/or financially focused on drug cost savings.
“These types of studies need to be conducted whenever there is no published research supporting compatibility, extended stability once a drug is reconstituted and for each brand of a drug to ensure patient safety due to different formulations for each product,” says Danette Beechinor, Director of Pharmacy at Sunnybrook. “Sunnybrook Pharmacy is a national
leader in creating and providing innovative, high-quality, personalized and precise medication therapy by working to optimize the delivery of specific medications on a local and national level. These initiatives allow us to lead in environmental and financial stewardship and quality and patient safety.”
Since its inception in the 1980s, the Pharmacy Quality Control Lab at Sunnybrook has conducted nearly 100 studies which has saved healthcare systems across the world millions of dollars.
One recent example is a drug compatibility study performed by the lab that helped Sunnybrook achieve annual cost savings of $277,000.
“The drugs leucovorin and oxaliplatin are usually administered via y-site IV infusion, as part of a standard treatment for colorectal cancer, to reduce chair time for patients in most cancer programs,” says Nathan Ma, lead of the Pharmacy Quality Lab. “Recently a new brand of the drug leucovorin came onto the market, which was less expensive but also contained the excipient trometamol”
The oxaliplatin monograph indicates it can’t be mixed with or co-administered with drugs containing trometamol, but the pharmacy team noted there were no published studies to demonstrate the incompatibility.
“We decided to conduct a stability study to determine the compatibility of oxaliplatin and the new leucovorin,” says Ma. “The results were impactful.”
The Pharmacy Quality Control Lab demonstrated that the new brand of leucovorin is compatible with oxaliplatin. The use of this brand will save the Odette Cancer Centre $277,000 annually and the findings have been disseminated nationally to impact practice recommendations.
Nathan Ma presented the results of the study at the 2023 Canadian Association of Pharmacy in Oncology Annual Conference.
“A speaker at the conference from the UK tweeted that my leucovorin study poster alone made his trip worthwhile,” says Ma. “It’s satisfying to see that our work at the Pharmacy Quality Control Lab doesn’t just benefit Sunnybrook or Toronto or Canada, but also colleagues around the world.” ■ H
 Samantha Sexton works in communications at Sunnybrook Health Sciences Centre.
Samantha Sexton works in communications at Sunnybrook Health Sciences Centre.
Life has its way to open paths you would not suspect on your journey.
There are enlightening moments that set a cornerstone and its rippled effect might only amplified to become apparent later in time. This happened to me in 2014 after having a transformational experience at the International Space University (ISU) Summer Program in Montréal. During this two-month intensive program, I had the opportunity to meet with inspiring people from various professional backgrounds, countries, and personal experience, who all shared the same passion: aerospace!
Now, you might be wondering why I started sharing my story with aerospace when the topic of this article is sustainability! Well, I had an “Aha!” moment during my time at ISU while listening to astronauts tell us about their life-changing experiences in Space and what stuck with me the most was what they called the “overview effect.” The overview effect was described back in 1987 by author and space philosopher Frank White, as the intense emotions astronauts go through when seeing our home planet against the blackness of space and the thin line atmosphere that protects life on our planet, raising awareness about the fragility of Earth and a deep connection to humanity. This learning in mind, I led then my first collaborative interdisciplinary and international project in aerospace, healthcare, and planetary health within the ISU community: “Space4Health: Exploring innovative ways to utilize space for disaster relief.”
Fast-forward to summer 2021, when I joined the Children’s Hospital of Eastern Ontario – Ottawa Children’s Treatment Center (CHEO) as Director of Pharmacy. I was excited to learn that the organization has included a sustainability pillar in its strategic

THE PATH TOWARDS SUSTAINABLE HOSPITAL PHARMACY PRACTICE IS BEING PAVED. I ENCOURAGE EVERYONE TO JOIN THE MOVEMENT AND TAKE CARE OF OUR PLANET.
planning called “Kick the Carbon.”
This pillar has an inspiring goal of reducing its carbon emissions by five percent each year, totaling 30 percent by 2025. That’s the equivalent of driving nine million kms in agas-powered car! To reach that goal, CHEO has put in place a Sustainability Steering Committee and a Sustainability Working Group, uniting passionate healthcare leaders who wanted to do more for our planet, our pediatric patients, youth, and their families. This was an important opportunity to translate our organizational strategy into our Hospital Pharmacy departmental strategy.
With those futures to fight for I had the why, but I was missing where to start, what to tackle first, who to involve and how to make it happen. In parallel, one of my colleagues shared with me that the University of Ottawa Telfer School of Management offers consulting projects led by their MBA students. A former MBA student myself, I thought it would be a wonderful opportunity for teaming up and building a hospital pharmacy sustainability strategy with the business lens. This collaboration led to our interdisciplinary project which, in turn, earned us the 2023 CSHP Excellence in Pharmacy Practice
– Leadership Award. Our winning project, “Eco-Friendly Pharmacy Practices to Support a Sustainable Green Transition in Hospital Pharmacy,” included internal and external surveys to gain knowledge on hospital pharmacy sustainability practices.
From there we realized that there were gaps in this field and a need for a roadmap for sustainability practices. As a result, we launched a national survey, to learn more about Canadian hospital pharmacy and pharmacy professionals’ knowledge on eco-initiatives. Then, the results were presented as a poster at CSHP Professional Practice Conference and an article is currently under review for publication in the Canadian Journal of Hospital Pharmacy. An important takeaway from our survey was that hospital pharmacy staff and leaders want to do more to reduce carbon footprint in their professional environment, but they are perceiving challenges to start or im-
Tplement eco-initiatives. At that time, the top three perceived challenges by pharmacy leaders were cost, time and added complexity. Since then, however, multiple sustainability-based quality improvement projects have bloomed in hospital pharmacy. The publication of their projects’ successes offers timely knowledge translation, which supports pharmacy staff and leaders, looking to implement greener strategies in their professional environment.
The green wave is also gaining momentum, propagating throughout associations and the academic communities. For example, in January 2023, CSHP launched its Sustainability Task Force. As a participating member, I can testify to the positive and engaging energy it is bringing to the hospital pharmacy eco-movement. In March 2024, Caitlin Roy and Shellyza Sajwani, clinical pharmacists at the Saskatchewan Health Authority and the Ottawa hospital, respectively, founders of the Canadian Association of Pharmacy for the Environment (CAPhE), inaugurated the strategic plan. Robert Pammett, a co-lead at CAPhE, and Dr. Karen Dahri, both pharmacists and associate professors at the Faculty of Pharmaceutical Sciences of University of British Columbia, have also shared their visionary and collaborative initiative to promote and integrate planetary health in pharmacy curricula in Canada.
The path towards sustainable hospital pharmacy practice is being paved. I encourage everyone to join the movement and take care of our planet. Building a healthy and thriving environment for the future generations starts by implementing and sharing green actions, however small they might feel, makes a difference! ■ H
Ariane Blanc is Director
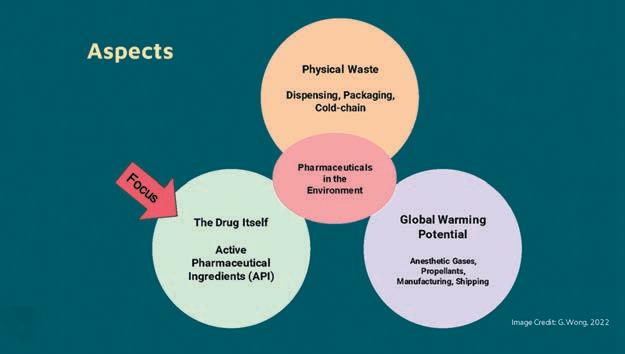
of Pharmacy, Chief Clinical Pharmacistypically, there are three main aspects brought up when considering pharmacy’s impact on planetary health: greenhouse gas emissions, physical waste, and pharmaceuticals impact as chemical contaminants that pose harm to wildlife. This article will specifically focus on the latter of the three.
There are three main aspects of pharmaceuticals in the environment.
The main pathway for drugs entering the environment is through human consumption, with excretions in urine and feces accounting for 88 percent. As these drugs containing the active pharmaceutical ingredient (API) pass through the body, they may or may not be metabolized, and their metabolites can also have active effects. As these excretions make their way to wastewater treatment plants (WWTP), they are not always able to effectively remove pharmaceuticals, leading to their entry into our shared environment through water leaving the WWTP. As drug consumption increases, so do excretion rates, leading to more profound impacts. Remaining routes of entry into the environment include the disposal of expired, damaged, or unwanted medication making up ten per cent, and the remaining two per cent comes from manufacturing.
Drugs pose unique and concerning chemical risks as they are, by design, intended to cause a desired biological effect on the human body. As humans share a common physiology with other living things, some mechanisms of drug action effective in humans may also affect wildlife. This makes sense when considering the drug development process. In initial stages drugs are tested on mice, later cats and dogs, then non-human primates. Where a drug shows promise, it progresses to testing in humans. This is so logical yet is oddly and quietly alarming.
The first example of wildlife impacts is a story about birds - of three species of vultures in Southeast Asia. A staggering 99.9 percent of the population
were dead in the devastating speed of 15 years. The culprit drugs? Diclofenac, a drug commonly used for both livestock and humans alike throughout Southeast Asia. As vultures are natural scavengers that feed on the carcasses of livestock, some of whom have been given this medication. This example may surprise readers, as diclofenac is widely used in Canada for pain, fever, and inflammation, available in various forms with or without prescription and belongs to a class of medication called non-steroidal anti-inflammatory drugs, or NSAIDs.
A couple interesting things in this vulture story. First, is regarding the type of adverse effect. A well-known side effect of NSAIDs in humans is kidney failure (one to five percent). The vultures died from kidney failure too, with uric acid build-up leading to gout in the body cavities. Second relates to dose-response curves. You may be wondering what type of dose killed the birds? This might surprise you: when adjusted for weight in mg/ kg, what is a five to ten percent of a therapeutic human dose is the 100 percent lethal dose in vultures. Indeed, a limitation and the point of this calculation is that diclofenac is processed differently in humans and vultures. This comparison is impactful as it illuminates how little is known about the dose-response curves of drugs in non-target organisms.
The second example of wildlife impacts focuses on flat-headed min-
nows. in freshwater lakes in Ontario. Researchers explored the effects of synthetic estrogen, common in birth control pills. Using concentrations that mimic those found in the environment in parts per trillion, they found that male fish became intersex and started producing eggs, there was a reduced ability of fertilized eggs to progress into offspring, and at the end of the seven year whole-lake experiment, the fish population was on the brink of extinction.
Perhaps this article will inspire action. Each of us can start today. A good starting point is to begin within your sphere of influence. Clinicians can use tools such as the climate-conscious Choosing Wisely Canada Recommendations on 20+ clinical specialties, weaving this together with a quality improvement for sustainable healthcare. Hospital pharmacies can explore ways to minimize preventable drug waste in its processes - an opportunity may be in medication returns being discarded instead of sorting for recirculation or exploring ways to better manage drug inventory with short dates. Supply chain leads can use our hospital procurement power in selection criteria of products and vendors. Executives and directors could embed this into their organization’s strategic plan, like Fraser Health Authority in Metro Vancouver, BC. Health-system leaders can also shape requirements for drug life cycle assessments to support more informed decisions. ■ H
at the Children’s Hospital of Eastern Ontario Gigi Wong is a Clinical Pharmacy Specialist for the Fraser Health Authority as part of the Lower Mainland Pharmacy Services in Vancouver, BC.
The World Health Organization identified climate change as a major threat to human health and wellness. As healthcare professionals, we, as so aptly put by our peer Dr. Celia Culley, “have a duty to provide high-quality patient care today without compromising our ability to care for your patients tomorrow.”
Keeping this in perspective, the Canadian Society of Hospital Pharmacists (CSHP) is pleased to showcase the efforts undertaken by hospital pharmacy professionals to tackle climate change and the environmental footprint of pharmaceuticals in this dedicated section for Hospital News.
Internally, CSHP recognized the need to be leaders in this area and acted. One such initiative involved forming the Sustainability Task Force
at the beginning of 2023, comprised of individuals actively involved in sustainable pharmacy advocacy, including some members of the Canadian Association of Pharmacy for the Environment (CAPhE). Immediately the Task Force identified four pillars for the organization to focus on: Advocacy and Partnership, Education, Policy and Procedure Development, and Research and Quality Improvement.
The Task Force crafted detailed recommendations within each pillar, which were subsequently improved through stakeholder input. These specific objectives establish CSHP’s strategic focus on sustainability in pharmacy and are as follows:
Advocacy and Partnership. On behalf of CSHP, Professional Practice Specialist Kiet-Nghi Cao, in partnership with the Canadian Pharmacists

Congratulations to Apotex Inc. on entering into its 50th Year of business! Apotex has undergone a remarkable journey of growth and development, establishing a solid foundation focused on enhancing access to affordable medicines. Driven by this commitment, the company has led – and continues to lead – the Canadian generics market with products that can be found in virtually every Canadian pharmacy and healthcare facility. As a champion for strengthening healthcare systems, Apotex consistently advocates for improved access to affordable medicines by bringing new products to market each year. Apotex’s leadership position in generics is enhanced by its important role in advocating for biosimilars and supporting cost-effective alternatives to biologic products, especially in critical areas like oncology. We applaud the organization’s unwavering commitment to patient access and look forward to the next phase of growth for Apotex.
Association (CPhA), spearheaded the creation of our latest hospital pharmacy-specific recommendations for Choosing Wisely Canada with a focus on climate consciousness. Readers will be able to see these recommendations later in this section.
Furthermore, CSHP has collaborated with CASCADES’ “Climate Resilient, Low Carbon Sustainable Pharmacy Playbook,” advocating for change in our practices and outlining tools and strategies to achieve this needed change. Plus, CSHP is leading the creation of a second playbook with CASCADES that will address ways in which the operational side of hospital pharmacy can implement more sustainable practices.
Education. Another task force recommendation was to include more sustainability topics in the organization’s educational programming. As such, at this year’s Professional Practice Conference, delegates could attend multiple sessions related to environmental sustainability. Genevieve Ouellet from Ste-Justine Hospital described the various environmental initiatives that have been implemented at her site, to inspire others to make changes at their own practice sites. Dr. Celia Culley from Island Health addressed the strategies that can be used to reduce the climate impact of inhalers. Other CSHP conferences from this year also included topics on environmental sustainability, including Dr. Valeria Stoynova presenting on the pivotal role of pharmacy professionals in climate change at the Banff Seminar and one of this article’s authors, Dr. Karen Dahri, presented on the work that CSHP has done in this area and the ways in which hospital pharmacies can begin to act at the Harrison Seminar. Policy and Procedure Development. Guidelines for sustainable conference practices are currently under development. These guidelines will include information for conference hosts, sponsors, and attendees to help reduce
the carbon footprint of conferences through multiple strategies.
Research and Quality Improvement. This past year, the annual CSHP membership survey was updated to contain questions on sustainability. Results revealed that 86 per cent of respondents identified climate change and sustainability as a pressing issue that required action within the next five years. Survey findings also indicated that while 37 per cent of respondents have engaged in sustainability initiatives, most respondents (63 per cent) felt unknowledgeable on the topic. CSHP responded to these insights by bolstering support for members, notably through the efforts of the Sustainability Task Force and by spotlighting individuals within the CSHP community involved in sustainability research. For instance, projects addressing climate change receive special attention in the Excellence in Pharmacy Practice awards.
CSHP further backed sustainability efforts through their #PharmacyDoesMore Pharmacy Appreciation Month campaign, specifically highlighting the critical role pharmacy professionals play in promoting climate resilient, low carbon, and sustainable care. Lastly, a section of the CSHP website is being developed to house sustainability related information and continue to promote task force recommendation. Pharmacy professionals play a key role in addressing climate change adaptation and mitigation. With CSHP and its Sustainability Task Force taking proactive steps to enhance planetary health, we can collectively enhance the well-being and health outcomes of our patients across generations.
To discover how healthcare professionals can incorporate environmental sustainability into their practice, we invite you to continue reading this section and stay updated on CSHP. ca for the latest information on its sustainability initiatives. ■ H
Dr. Karen Dahri, BSc, BSc (Pharm), ACPR, PharmD, FCSHP, and Kirsten Tangedal, BSP, ACPR – Co-chairs for the Canadian Society of Hospital Pharmacists’ Sustainability in Pharmacy Task Force
Introducing Pr PACLITAXEL Powder for Injectable Suspension NANOPARTICLE, ALBUMIN-BOUND PACLITAXEL












The urgency to address climate change is undeniable, and every sector, including the healthcare sector, must play its part.
Our work is responsible for five per cent of greenhouse gas emissions, with pharmaceuticals alone contributing another five percent to that total. Our sector’s environmental impact from medications can stem from the chemical composition of Active Pharmaceutical Ingredients (APIs), which directly affect environmental health, the manufacturing and distribution methods contributing to a sizable carbon footprint, or the pharmaceutical waste challenges. These statistics serve not only as a wake-up call to us all, but they can also be motivators. Pharmacy profes-
sionals possess a unique opportunity to drive change. Consider the life cycle of a medicine – from its inception to disposal. At each stage, from design to prescription, we have the power to implement sustainable practices and reduce our environmental impact.
It’s with this in mind that CSHP has committed itself to supporting and advocating on behalf of the profession to make pharmacy’s voice heard and stimulate action in areas that require multi-agency or systemic change, which includes climate change in health care. One of our partners in this includes Choosing Wisely Canada, who have embarked on the development of climate-conscious recommendations through leadership and collaboration with national society and association partners, inviting CSHP along to help given the two


organization’s alignment, specifically relating to environmental sustainability in healthcare and especially in the context of medication management.
CSHP, in collaboration with the Canadian Pharmacist Association (CPhA), represent pharmacy professionals in a range of practice settings. Both organizations shared Climate Action recommendations relevant to their memberships. Consequently, CSHP worked alongside CPhA to develop five joint recommendations, alongside crafting an additional five climate-focused recommendations tailored to hospital pharmacy based on current research.
• CSHP and CPhA joint climate action recommendations:
– Don’t prescribe greenhouse gas-intensive metered-dose inhalers (MDIs) for asthma and/or COPD where an alternative inhaler with a lower carbon footprint (e.g. dry powder inhaler (DPI), soft-mist inhaler, or MDI with a low greenhouse gas potential propellant) containing medications with comparable efficacy is available, and where the patient has demonstrated adequate technique and patient preference has been considered.
– Don’t start or continue medications without an indication or where the risks outweigh the benefits.
– Don’t pour any pharmaceuticals or chemicals down sinks, toilets, drains or dispose of in the trash.
– Don’t print prescription or educational materials when providers and patients have access to digital communication.
– Don’t use disposable gloves when standard hand hygiene disinfection practices are safe and sufficient.
• CSHP climate action recommendations:
– Don’t continue an intravenous medication when and if clinically appropriate to step down to oral therapy.
– Don’t use desflurane when other anesthetic drugs and techniques are equally effective and less harmful to the environment.
– Don’t discard medications that are appropriate for re-dispense.
– Don’t continue medications upon hospital transitions (admission, transfers, and discharge) unless there is a clinical indication.
– Don’t make formulary decisions without consideration of environmental impact.
As of May 15, 2024, Choosing Wisely Canada unveiled over 40 groundbreaking recommendations spanning over 20 clinical specialties, shedding light on tests, treatments, and procedures detrimental to the environment. These directives serve as a rallying call, urging clinicians to cease or curtail low-value practices and champion the health of both patients and the planet. CSHP had the privilege of contributing to the program launch through a webinar spotlighting Climate Action recommendations alongside its peers at the Canadian Critical Care Society. With hopeful hearts, CSHP believes that our recommendations, alongside those of fellow societies, will herald positive transformations in patient health and foster a brighter, healthier future for our planet. Together, let’s forge ahead on this journey of healing and sustainability! ■ H


s pharmacy students, we are trained to prioritize the safest and most effective medications for patients. However, we are not equally taught to value the importance of providing environmentally sustainable care. I find this troubling, considering that despite the healthcare sector’s move towards more sustainable practices, it remains a major contributor to overall greenhouse gas emissions, with medications being a significant part of the problem. However, hospital pharmacists can significantly impact environmental conservation efforts, and should we learn to support these initiatives at the beginning of our careers, we can continue to do so throughout our professional lives. Personally, I have only come across one or two slides discussing how certain types of inhalers are more environmentally friendly than others. This limited exposure suggests that environmental considerations have not routinely integrated into future pharmacists’ education. I believe it’s just as crucial to incorporate this aspect into every pharmacy program, as safety, effectiveness, cost, and tolerability when choosing medications for patients. It enables us to shift away from the paternalistic model of care, where healthcare decisions are made by the healthcare provider without much input from the patient, towards a more patient-centered approach, where greater emphasis is placed on collaborating with the patient. When patients need a new inhaler to manage their asthma, pharmacists can choose one that’s environmentally friendly. For instance, metered dose inhalers, a common type of inhaler prescribed by physicians, have a carbon footprint equivalent to driving up to 139 km by car. For environmentally conscious patients, this may conflict with their personal values as they seek to minimize their environmental impact. As a result, they may prefer to explore alternative options for manag-
ing their asthma. This also provides an opportunity for pharmacists to educate patients on proper medication disposal methods available at community pharmacies, thereby preventing medication residues from being released into the atmosphere.
In my time working in hospital environments, I’ve seen extensive use of single-use personal protective equipment such as gloves, gowns, and face shields, all discarded after one use for sterility. By exploring sustainable alternatives like biodegradable materials or reusable options, we could significantly reduce waste. To date, re-
usable personal protective equipment options have proven to be effective in infection control while also being environmentally friendly. For instance, a study in the United Kingdom found that switching from disposable PPE to reusable gowns and face shields over a six-month period could have cut total emissions by 20 per cent.
Pharmacists shoulder the dual responsibility of safeguarding patient health and considering the environmental impact of healthcare practices. Environmental sustainability in healthcare aims to provide medical services while minimizing harm to
the planet, benefiting both patients and the environment. Hospital pharmacists can play a pivotal role in this endeavor by prioritizing medications with lower carbon footprints and integrating environmental considerations into patient care decisions. Despite the current lack of emphasis on environmental education in pharmacy programs, advocating for its inclusion is essential to cultivate a holistic approach to patient care. Embracing a patient-centered model and exploring sustainable alternatives can lead to a healthier future for both patients and the planet. ■ H
The pharmacy sector produces a range of environmental effects, encompassing greenhouse gas emissions, ecological ramifications of pharmaceuticals in the environment, and plastic waste from pharmaceutical packaging. Let’s delve into their impact on our climate, our health, and discuss actions we can take to mitigate the harm.
Greenhouse gas emissions. Healthcare contributes just under five per cent of Canada’s total greenhouse gas emissions. A quarter of these emissions stem from the production of pharmaceuticals with 90 per cent of those emissions originating from supply chains and the remaining ten per cent from healthcare facilities. This major contributor to climate change and its adverse impacts on health include an increased frequency of heat-related
illness, exacerbations of asthma and chronic obstructive pulmonary disease due to exposure of wildfire smoke made more due to climate change and worsening of mental disorders.
Ecological effects of pharmaceuticals on the environment. Pharmaceuticals enter the environment through various pathways, including human excretion and improper disposal, leading to contamination of waterways and landfills. This contamination poses ecological risks as pharmaceuticals bioaccumulate in the food chain, potentially affecting humans who consume these organisms. Research has identified pharmaceutical levels in the environment that induce toxicity and provoke worries regarding antimicrobial resistance. This renders infections more challenging to manage and heightens the likelihood of disease spread, severe illness and death.
Plastic waste from pharmaceutical packaging. Plastic waste poses a major concern, constituting 30 per cent of hospital waste. In Canada, 87 per cent of plastics, including healthcare-related ones, find their way into landfills or the environment. Packaging makes up almost half of this waste. Exposure to plastic harms wildlife and releases harmful chemicals such as phthalates and bisphenol A, disrupting hormone levels and reproduction. These chemicals are linked to health issues like metabolic abnormalities, reproductive dysfunction, and cancer in humans. Despite these issues, however, there is still plenty of ways that healthcare professionals can help to make Canada’s drug supply more sustainable. There are many things individual pharmacy professionals, for instance, could be doing to help. One such way could be adding environmental im-
Canada is caught in a vicious cycle when it comes to maintaining respiratory health in the face of climate change.
The cycle commences with an increase in respiratory ailment diagnoses, with 3.8 million Canadians, constituting ten per cent of the population aged one or above, grappling with asthma, alongside an additional two million individuals afflicted by chronic obstructive pulmonary disease (COPD). The diagnoses of these persistent conditions are anticipated to rise even more as Canada’s population ages and air quality worsens.
Because of these conditions, inhalers are often prescribed to help with symptoms.
However, the irony is found in the fact that the most used inhalers, such as pressurized metered dose inhalers (pMDI) or breath-actuated inhalers (BAI), contain hydrofluorocarbon (HFC) propellants which are potent greenhouse gases. The very same greenhouse gases contribute to climate change with something as simple as their usage, on top of the plentiful number of environmental stressors that the production and disposal of these inhalers produce.
PROFESSIONALS CAN AIM TO CUT DOWN ON INHALERS’ IMPACTS ON OUR CLIMATE IS THROUGH PROPER DIAGNOSIS AND DEPRESCRIBING.

pact to the list of considerations one must make when choosing a medication for a patient, alongside efficacy and cost-effectiveness. By considering environmental impact in clinical decision-making, such as promoting eco-friendly inhalers and identifying unnecessary medications to deprescribe, pharmacy professionals can reduce environmental harm while bettering care.
Beyond individual efforts, hospitals can make the active choice to work with suppliers who are committed to green practices and can establish their own sustainability committees to advocate for more eco-friendly procurement. By implementing green inventory procurement and management practices, hospital pharmacies can fur-
ther reduce waste and emissions. Collaboration can also extend further with drug manufacturers and Health Canada to integrate these considerations in their drug approval processes.
The environmental footprint of healthcare is undeniably significant, yet it holds the potential for change. Through a green-minded approach across the entire supply chain, we can diminish its adverse effects on both the planet’s health and the well-being of our patients
For a more in-depth clinical perspective on this topic, I encourage readers to explore my Clinical Pearl and Resource Spotlight on CSHP.ca. ■ H
Toronto.
These factors exacerbate environmental degradation, furthering the effects of climate change. This, in turn, worsens environmental conditions that aggravate respiratory conditions, leading to uncontrolled symptoms, increased inhaler usage, and a heightened risk of asthma and COPD exacerbations. Thus, the cycle continues, perpetuating the rise in respiratory ailments among individuals. But, as pharmacy professionals, we can and must help to put a stop to this cycle. Pharmacy professionals possess a unique opportunity to inform prescribers, colleagues, and patients about environmentally sustainable inhaler practices.
One potential approach could involve discontinuing the prescription of HFC-heavy pMDIs and BAIs, opting instead for dry powdered inhalers (DPI) and soft mist inhalers (SMI), which lack these propellants and therefore have a reduced carbon footprint.
Another is to properly educate prescribers, colleagues, and patients on environmentally sustainable practices including the proper use and disposal of inhalers. Educating patients on correct inhaler use improves medication delivery and reduces environmental impact. Spacer devices and dose counting methods enhance efficiency.
Additionally, education on proper disposal of all inhalers by a pharmacy team remains equally important. For
instance, the aforementioned pMDIs’ high carbon footprint does not end in their use. Shockingly, their disposal phase accounts for approximately 85 per cent of the total pollution they cause. By championing proper disposal, including incineration to destroy HFCs, we can mitigate these effects. There are programs in several provinces that even support medication returns through community pharmacies, promoting environmentally responsible disposal.
Finally, another way pharmacy professionals can aim to cut down on inhalers’ impacts on our climate is through proper diagnosis and deprescribing. Eliminating unnecessary inhalers helps avoid overuse and waste, decreasing the healthcare sector’s carbon footprint. In fact, The Canadian Thoracic Society advocates for this, stating that if inhaler therapies exhibit no clinical improvement or lack confirmatory test results in patients, to stop using them. This strategy aims to mitigate patient risks and reduce healthcare resource strain from misdiagnosis and overprescribing.
Pharmacy professionals, through education, interventions, and advocacy, can lead the charge in promoting eco-friendly inhaler practices. By incorporating these strategies into daily practice, pharmacists can contribute to a healthier planet and better patient outcomes.
To dive deeper into a more clinical perspective on this topic, I invite readers to check out my Clinical Pearl and Resource Spotlight on CSHP.ca! ■ H
Layne Liberty is a former CSHP student and Doctor of Pharmacy graduate from the University of British Columbia.
Huy Pham is a former CSHP student and Doctor of Pharmacy candidate at the Leslie Dan Faculty of Pharmacy at the University ofAs North America’s leading digital hospital, Humber River Health (Humber) believes that exceptional healthcare requires more than just medical expertise – it demands innovation, dedication, and community support. In a world where technology is rapidly advancing, Humber understands the importance of leveraging digital means to drive innovation in healthcare. From cutting-edge medical equipment to pioneering medical community-based solutions, Humber is committed to harnessing the power of digital tools to revolutionize patient care.
In Humber’s pursuit of innovative healthcare, fundraising plays a crucial role. Through numerous fundraising initiatives, Humber utilizes the power of creativity, technology, and collaboration to raise vital funds for the ground-breaking, critical work done at the Hospital.
From pioneering medical community-based initiatives like the AI-Enabled Virtual Queue Management Application, to the state-of-the-art technologies within the Robotics Surgery Program, Humber’s fundraising efforts fuel innovation across all aspects of patient care. By engaging donors, volunteers, and community partners, Humber remains at the forefront of healthcare innovation, delivering excellent care to those who need it most.
Volunteers are the lifeblood of the Hospital, embodying the spirit of compassion, generosity, and community service. Whether they are lending their time, talents, or resources, volunteers play a pivotal role in driving fundraising initiatives forward.
From serving on boards to supporting signature fundraising events like Illuminate: A Diwali Celebration and the Awesome Invitational Golf Tournament, volunteers bring passion, expertise, and a deep commitment to Hum-

ber’s mission of accessible and equitable community healthcare. Their tireless efforts help the organization reach new heights, empowering Humber to make a meaningful impact on the lives of patients and families in the community.
Humber’s innovative programming empowers every member of their community to contribute in their unique way. Staff express their gratitude
Surrey Memorial Hospital is one of 12 hospitals around the globe involved in a clinical trial to help determine optimal treatments for bloodstream infections.
The monkeypox outbreak and COVID-19 pandemic taught us that microbes can spread quickly through continents, countries and communities. Some infections are becoming increasingly difficult to treat because the germs have become more resistant to antibiotics. One form of antibiotic resistance in particular called extended spectrum beta-lactamase (ESBL) is becoming a common threat in Canada. ESBL bacteria, most commonly E. coli, are found in common infections like urinary tract infections. They can also cause infections after surgery and during chemotherapy. The World Health Organization considers ESBL a critical priority for research and drug
development. The big guns of the antibiotic world – carbapenems – are often used to treat ESBL and other serious infections. However, they come with problems of their own, including the possibility of antibiotic resistance, which could render these “last line of defence” drugs useless.
To help improve care for the treatment of ESBL infections, Surrey Memorial Hospital is participating in an international, randomised clinical trial comparing two commonly used antibiotics: piperacillin–tazobactam, a member of the penicillin family, with meropenem, a carbapenem. Both drugs are widely available and the trial will help to determine which medication is best for different patients.
“This is an opportunity for Surrey Memorial Hospital to contribute to important research in a unique way. Our patients are often underrepresented in clinical trials,” says Dr. Kev-
in Afra, executive medical director for antimicrobial stewardship and infection control. “Our clinical teams including physicians, pharmacists, nurses and laboratory staff have embraced this important research, and patients have also been excited to participate.”
The study is being carried out by the Surrey Memorial Hospital Clinical Research Unit team. “Collaborating internationally in clinical research allows us to optimize current care for our patients and help shape future treatments,” says Christopher Condin, Clinical Research Lead. “With global challenges like antibiotic resistance, we need global collaboration to move the dial forward. Fraser Health teams are committed to doing this and we’re really proud of how our hospital is contributing to this effort.”
The PETERPEN study will enrol more than 1,000 patients worldwide. Participation is voluntary and patients are told which drug they are receiving. ■ H
through Humber’s Very Own – an employee-giving program. Patients, families, and colleagues can honour exceptional care through donations to the Gifts of Gratitude program. The Star is Born program gives new parents and families an opportunity to honour their newborns with a twinkling, shining, or shooting star on the Star is Born wall in Humber’s Birthing Unit. With healthcare philanthropy, volunteers offer their time, skills, and resources through programming like Planned Giving, Rising Philanthropic Leaders (RiPL), and Women in Kindness (WINK). Through creative programming, corporate sponsorships, and community-driven initiatives, Humber maximizes fundraising impact and creates lasting change in healthcare. Together with their volunteers and supporters, Humber is building a healthcare system that is not only exceptional, but also accessible and inclusive.
Without the selfless dedication of their volunteers, Humber’s healthcare fundraising would falter in their mission to transform lives and empower patients within the community. As fundraisers, their pivotal role in advancing fundraising innovations ensures that Humber River Health will continue to push boundaries while delivering world-class care. Through the collective efforts of volunteers and fundraisers, healthcare innovation thrives at Humber River Health, promising a brighter and healthier future for all. ■ H
s healthcare professionals, we are acutely aware of the challenges facing Ontario’s healthcare system. Long wait times, primary care provider shortages, and unequal access to care are just a few of the pressing issues we confront daily. Amidst these challenges, nurse practitioners (NPs) have emerged as a crucial component of the solution. With their advanced training and unique scope of practice, NPs offer a vital lifeline to alleviate the strain on our healthcare system and foster a healthier population.
Research published in the Canadian Journal of Nursing Informatics demonstrates the effectiveness of NPs in delivering accessible and timely care, particularly in underserved communities. Patients seen by NPs experience short-
er wait times and report higher satisfaction with care received compared to traditional physician-led practices.
Furthermore, a study by the Commonwealth Fund, a renowned international healthcare research organization, found that countries with a higher proportion of NPs in their healthcare workforce tend to have better health outcomes, including lower infant mortality rates and improved management of chronic diseases. This research underscores the critical role NPs can play in enhancing the quality and equity of care.
NPs bring a holistic approach to healthcare delivery, emphasizing preventive measures and patient education. By empowering individuals and families to take charge of their health, NPs reduce the burden on our healthcare system by decreasing preventable diseases and hospital admissions. Their ability to
fill gaps in primary care, especially in regions facing physician shortages, makes them an invaluable resource.
To fully harness the potential of NPs, we must address the need for fair compensation and explore innovative models of care. Permitting NP-led private-pay clinics to operate, under a time-boxed pilot, could provide valuable insights into the effectiveness of a hybrid model. This approach has been successfully adopted in Australia and many European countries. Alternatively, we could follow Alberta’s lead and enable NP-led clinics to function independently, but with more comprehensive reforms. Or, we could amend the Health Act federally to treat NPs on par with MDs from a billing perspective. Each approach has its pros and cons, but a choice must be made to unlock the full potential of NPs and alleviate the strain on our healthcare system.
With over 100,000 nurses eligible to become NPs, expanding their scope of practice to operate clinics independently could instantly increase our pool of healthcare professionals. This would not only improve access to care but also provide an alternative career path for RNs and RPNs. Ontario’s plan to increase educational seats for NPs from 200 to 350, while a step in the right direction, is insufficient to address the scale of the problem. We must push for a more substantial increase to make a meaningful impact.
In conclusion, NPs hold the key to transforming Ontario’s healthcare landscape. By empowering them to take on a more central role in our healthcare system, we can address the pressing challenges we face. Let us seize this opportunity to revolutionize patient care and drive positive change in our healthcare sector. ■ H
Thomas Jankowski is the CEO of Medimap, a trailblazer in AI-driven healthcare solutions. With a deep passion for the intersection of technology and healthcare, Thomas Jankowski is committed to harnessing AI’s potential to revolutionize patient care and drive positive change in the healthcare sector.

n international team of researchers led by The Hospital for Sick Children (SickKids) have, for the first time, developed strategies to diagnose and treat an aggressive syndrome that leads to cancer in almost all cases.
Constitutional mismatch repair deficiency (CMMRD) syndrome is a rare genetic condition. Children who inherit the syndrome are considered “predisposed” to cancer, meaning they have a high likelihood of developing many different types of cancer – most commonly in the brain, digestive system and blood. In the past, these patients rarely survived to adulthood.
Research into CMMRD published in The Lancet Oncology studied more than 330 malignant tumours from 201 patients with the syndrome from the International Replication Repair Deficiency Consortium (IRRDC). The research team, including PhD student Ayse Ercan, observed that patients with CMMRD develop a new tumour every two years, suggesting the condition is the most aggressive human cancer predisposition syndrome.
The researchers also discovered that the type and severity of CMMRD is dependent on the specific inherited gene variation. Currently, there are four major genes associated with CMMRD: MLH1, MSH2, MSH6 and PMS2.
“All patients with CMMRD are not the same, and how we approach their care is dependent on many factors. Developing targeted therapies based on gene-specific cases could help patients with CMMRD have better health outcomes,” said Dr. Anirban Das, co-lead author of the paper, Staff Physician in the Division of Haematology/Oncology and Project Investigator in the Genetics & Genome Biology program at SickKids.
All day, cells in the human body are dividing and multiplying – it’s a process essential to life. Occasionally, a
change during cell division can cause a slight variation in genetic material. A process called the DNA mismatch repair system clears these errors to maintain regular function in cells. In patients with CMMRD, the DNA mismatch repair system is unable to clear errors. As a result, genetic variations can accumulate and can lead to cancer.
In order to identify cancers as early as possible, many individuals with CMMRD undergo regular screening to stay on top of cancers that might be developing. The research team found that 90 per cent of patients with CMMRD will develop at least one cancer by the age of 18 and if they survive to the age of 40, all will develop multiple cancers. Preventative monitoring can be very successful, but new findings suggest that this screening protocol has the highest impact among patients with variations in the MLH1 or MSH2 genes. In addition, patients with variations in MSH6 and PMS2 received the
greatest benefit from treatment with immunotherapy.
“Until now, it was not known that the type and severity of CMMRD was predictable based on the specific gene affected,” says Dr. Uri Tabori, co-lead author of the paper, Section Head of the Neuro-Oncology and a Senior Scientist in the Genetics and Genome Biology program.
“We show how the different links between affected genes and variant types determine the type of cancer, onset and outcome for each patient. Knowing these variations will help inform the future individualization of patient care through Precision Child Health,” Tabori says.
The IRRDC, a collaborative network of physicians, scientists, policy makers, patients and families from
more than 50 countries, was established in 2007 by Tabori and other SickKids physicians including Dr. Eric Bouffet, Director, Paediatric Neuro-Oncology Program and Dr. Carol Durno.
Now run by Das and Tabori, the IRRDC hosts weekly rounds to discuss global patient cases and manage more than 150 patients participating in active immunotherapy under the expertise of a SickKids-led team.
“Global collaboration is an essential part of learning more about CMMRD and developing future care. The consortium allows us to help patients in real time from diagnosis to treatment,” says Das.
By sharing data and patient stories, the international team has worked together to see patients with CMMRD live past university age for the first time. Future research on the syndrome may further improve the diagnosis, management and prognosis for those with CMMRD. ■ H
rtificial Intelligence (AI) has generated significant excitement globally. One notable AI system is ChatGPT (https://chatgpt.com/), which has become widely used for information seeking and ideas generation, etc. It has significantly simplified the lives of many by providing rapid access to information and various resources, influencing not only individuals, but also the health care system. However, convenience and efficiency may also come with the potential of uncertainty regarding the accuracy of the information generated by AI.
The increasing utilization and accessibility of AI presents potential risks to patients and clinical practice. Online tools, such as symptom checkers, have been publicly available. Users may share experiences where these tools are “trained” to generate a list of possible diagnoses based on the symptoms presented or entered by the patient. A user presenting with stomach pain may end up with diagnoses ranging from constipation to colon cancer. With such a wide range of “possible diagnosis” outputs, these tools often lack the nuanced clinical context that healthcare providers would consider in their patient assessments. It is possible that patients might self-diagnose and self-treat, potentially worsening their condition or exposing themselves to the risks of side effects due to inappropriate medication use. In addition, with increasing access to online drug-drug interaction checkers, patients may identify a potential interaction, self-assess and decide to stop taking their medication(s) without consulting their healthcare providers, thereby compromising their health outcomes.
The advancement of technology facilitates information access – information seeking (by patients and healthcare practitioners) and information generating (e.g., by various online tools and AI systems). However, the subsequent use and application of the information obtained would require clinical reasoning and critical appraisal skills in addition to the consideration of clinical contexts that are unique to individual patients. In health profession education, students and trainees go through clinical training to develop their critical thinking skills and apply their clinical knowledge to diverse patient scenarios. No single patient is alike. It is the role and responsibility of a healthcare professional to contextualize patient health information and make appropriate recommendations accordingly.
Despite undergoing rigorous training, missing essential clinical contexts is still possible among healthcare providers. The introduction of prescribing algorithms can assist healthcare providers in performing patient assessments to some extent, but they should not be solely relied upon. This caution arises from the recognition that a patient’s health is influenced by a complex array of factors, particularly, the social determinants of health. It is important to acknowledge the potential biases in these AI generated algorithms based on their development process, the developers involved, the specific patient populations studied and used, etc. Clinical reasoning may be lacking in these algorithms. Clinical contexts and social determinants of health may not be fully considered either. The need for critical thinking is crucial particularly when considering red-flag symptoms to make differential

diagnoses, for instance. Should redflag symptoms within the context of a patient’s characteristics be missed, it can have a profoundly negative impact on their health.
Over-reliance on AI tools may have adverse effects on the health outcomes of marginalized populations, as these algorithms might not account for the unique circumstances of individuals in such groups. Patients may often fall into a grey area not precisely covered by the AI generated algorithm’s criteria. In such cases, healthcare providers must exercise their clinical judgment to make the best possible recommendations for patients, underscoring the importance of clinicians possessing a thorough understanding and clinical reasoning of the conditions they are assessing.
The use of AI should be embraced responsibly, both by healthcare providers and by patients. Healthcare professionals have greater accountability than ever to contextualize and discern information as AI technology becomes smarter and simpler to use for patients and clinicians. Doing so will help mitigate potential biases in AI tools that may impact patient health outcomes.
Recently, a 2024 Journal of the American Pharmacists Association (JAPhA) publication (https://www.japha. org/article/S1544-3191(24)001390/abstract) identified that medication-related patient education materials generated by ChatGPT presented variable accuracy of information. Therefore, with respect to medication safety, patient should always consider the following five questions to ask about their medications (https://www.ismp-canada.org/medrec/5questions.htm) during a clinical encounter with their healthcare providers:
• Are there any changes in my medications?
• What medications do I need to keep taking?
• How should I use this medication correctly?
• What should be monitored while taking this medication?
• Is there any follow-up required after starting this medication? The use of AI to answer medical/ medication related questions may seem like a reasonable approach; however, be mindful that patients’ health is influenced by a complex set of factors that AI is not well equipped enough to answer for the time being. ■ H
Samir Kanji is a PharmD Student at the Leslie Dan Faculty of Pharmacy, University of Toronto; Neil Patel is a 2023 PharmD gradu ate at the Leslie Dan Faculty of Pharmacy, University of Toronto; and Certina Ho is an Assistant Professor at the Department of Psychiatry and Leslie Dan Faculty of Pharmacy, University of Toronto.

anada Health Infoway (Infoway) recently launched the Infoway Centre for Clinical Innovation in Digital Health (CIDH). Aligned to the strategic goals of the Shared Pan-Canadian Interoperability Roadmap, the CIDH aims to drive meaningful engagement with clinical leaders; and by doing so, accelerate the adoption of interoperability.
By advancing interoperability – the ability for different digital health systems to communicate, exchange, and use personal health data seamlessly and securely – we enable healthcare providers to access comprehensive patient information when and where it’s needed. This leads to more informed decision-making, reduced administrative burden, and ultimately, supports better health outcomes for Canadians. With a focus on interoperability, the CIDH looks to play a crucial role in transforming Canada’s healthcare system.
The CIDH will encompass several activities launching in 2024, with the most immediate including:
• Connected Care Innovation Grant for Clinical Leaders
• Connected Care Innovation Scholarship for Clinical Learners
The Centre aims to foster a culture of innovation and collaboration among clinical leaders, with the objective of driving innovation and continuous improvement in healthcare delivery. This will not only benefit patients and providers, but also seeks to position Canada as a global leader in digital health innovation and interoperability.
“By harnessing the expertise and insights of clinical leaders, the CIDH will help to ensure that digital health solutions are tailored to meet the needs of frontline healthcare providers and ultimately improve patient care for years to come,” said Dr. Rashaad Bhyat, Senior Clinical Leader in Connected Care at Canada Health Infoway.
Alongside the launch of the CIDH, we are pleased to announce the Centre’s first initiative: The Connected Care Innovation Grant.
Infoway is investing in clinical leaders across Canada to advance
grassroots clinical initiatives that focus on progressing innovative digital health interoperability-related efforts and improving connected care for patients and providers. Successful applicants can receive up to $50,000 per project.
“A well-supported and skilled healthcare workforce contributes to the overall sustainability and resilience of the healthcare system. By investing in our clinical leaders, we strengthen the backbone of our healthcare infrastructure, ensuring that it can effectively adapt to evolving healthcare needs,” said Abhi Kalra, EVP of Connected Care at Canada Health Infoway.
Eligible clinical leaders interested in applying to the Connected Care Innovation Grant can visit Infoway’s website to learn more. Applications will be accepted from May 22 to July 5, 2024.
At the end of summer, the CIDH will also launch the Connected Care Innovation Scholarship, targeted to clinical learners who are driving inventive digital health interoperability endeavors aligned with the strategic goals of the Roadmap.
To learn more about the CIDH and upcoming initiatives, visit www.infoway-inforoute.ca.
At Canada Health Infoway (Infoway) we believe a more connected and collaborative system is a healthier system, and one that leads to better health outcomes for all Canadians. By leveraging digital technologies and innovations, we’re working with governments, healthcare organizations, clinicians, and patients to advance connected care across the country. This improves care coordination, empowers patients to have a more active role in managing their health, and equips care providers with information and insights to support better care both at the point of care and throughout their patients’ health journey. Most importantly, it modernizes our health care system towards a future with patient-centered care at its heart. Infoway is a not-for-profit organization funded by the federal government and accountable to our Board of Directors and Members of the Corporation (Canada’s 14 federal, provincial and territorial deputy ministers of health). Infoway is led by a team of seasoned professionals who are specialists in their respective fields, including health care, administration, information technology and privacy.
For more info: infoway-inforoute.ca.
Infoway has conducted the fourth national survey of Canadian nurses on the use of digital health technologies in practice. This survey constitutes a series of surveys on the use and the impact of digital health technologies on nursing practice conducted in partnership with the Canadian Nurses Association (CNA) and the Canadian Nursing Informatics Association (CNIA). Three iterations of the national survey of Canadian nurses have been conducted in 2014, 2017, and 2020.
Nine in ten nurses (91%) providing direct patient care surveyed use electronic record / clinical information systems (an increase from 86% in 2020), with 38% saying they use electronic records only – up from 27% in 2020. Compared to 2020, there has been an increase in reported use of various electronic record/clinical information system functionalities to
support patient care, including: communication to other health professionals within their organization, list of all medications and discharge summaries, medication reconciliation, access to provincial/territorial patient electronic health record systems, clinical decision support tools, and transfer of patients’ health information securely to other health professionals. Improved interoperability is perceived to be beneficial to nursing practice, with about nine in ten nurses surveyed agreeing that the ability to electronically access/seamlessly exchange structured patient information will improve their access to complete patient information, enable better coordination of patient care with other providers, and enhance communication with HCPs outside their practice.
Nurses report that they needed to access health information that was collected outside of their practice setting

JULY FOCUS: Cardiovascular Care/ Respirology/Diabetes/Complementary Health: Developments in the prevention and treatment of vascular disease, including cardiac surgery, diagnostic and interventional procedures. Advances in treatment for various respiratory disorders, including asthma and allergies. Prevention, treatment and long-term management of diabetes and other endocrine disorders. Examination of complementary treatment approaches to various illnesses.
Advertising Booking Deadline June 21st
Material Deadline June 25th
For more info email advertising@hospitalnews.com
for nearly half (44%) of the patients they saw in the past 12 months on average. A majority (60%) say they are confident they have access to all the health information needed to plan and provide the best patient care. In addition, nurses estimate they spend about an hour more than they should during a shift, looking for patient information outside of their own organization. Only a third (34%) are satisfied with their time spent on non-patient-facing tasks, such as data entry, clinical notes, and searching for patient information.
Only six per cent of nurses surveyed report AI being used in any of their care settings. A majority (70%) of nurses surveyed do not feel knowledgeable about what AI is; however, nearly two in five (37%) say they are comfortable with its use in healthcare. A majority believe AI will have a significant impact on healthcare in the future, and roughly half feel it will
reduce time spent on administrative tasks, improve care planning, reduce medical errors/provide safer care, improve clinical decision making, and improve workflows. However, many are unsure of AI’s impact on these aspects of nursing.
Appropriate training/education related to use of AI, appropriate regulatory/ accreditation system, and policies/ guidelines from government/clinical bodies are seen as priorities to support AI in nursing, among three quarters of nurses. 5 Key Findings (3/3) Barriers/ Challenges with Digital Health Technologies Nurses report various barriers preventing them from accessing, using, or getting full value from digital health technologies. Challenges related to time constraints/logistics are most often reported, followed by barriers associated with equipment/technology and lack of education, training, and skills related to digital health technologies. Compared to 2020, there has been an increase in proportion of nurses reporting several barriers to use of digital health technologies. ■ H

AUGUST FOCUS: Paediatrics/Ambulatory Care/ Neurology/Hospital-based Social Work: Paediatric programs and developments in the treatment of paediatric disorders including autism. Specialized programs offered on an outpatient basis. Developments in the treatment of neurodegenerative disorders (Alzheimer’s, Parkins on’s etc.), traumatic brain injury and tumours. Social work programs helping patients and families address the impact of illness.
Annual Paediatric Supplement and Added Distribution to CHC Members (+8,200)

Advertising Booking Deadline July 26th
Material Deadline July 30th For more info email advertising@hospitalnews.com



SEPTEMBER FOCUS: Technology and Innovation in Healthcare/Artificial Intelligence (AI)/ Patient Experience/Health Promotion Online Education:
New treatment approaches to mental health and addiction. An overview of current research initiatives Programs and initiatives focused on enhancing the patient experience and family centered care. Programs designed to promote wellness and prevent disease including public health initiatives, screening and hospital initiatives.
Annual Medtech Technology Supplement & Distribution To Conference Attendees
Advertising Booking Deadline August 23rd
Material Deadline August 27th For more info email advertising@hospitalnews.com
olunteers are highly valued members of the health care team at KHSC, and they play a vital role in helping to improve the patient experience and complement the high standard of patient care provided by staff and physicians.
During National Volunteer Week, April 14 to 20, Kingston Health Sciences Centre (KHSC) recognized and celebrated the importance of each and every volunteer’s impact.
“Every Moment Matters, the theme for National Volunteer Week highlights the importance of every volunteer and each contribution they make,” says Alan Archer, Director, Workforce Planning and Labour Relations at KHSC. “The sharing of time, skills, empathy, and creativity is vital to the inclusivity, strength, and well-being of our communities.”
“KHSC volunteers support patients and family members throughout their health care journey. From calling to remind them of an appointment through walking them to meet their ride after a procedure, our volunteers can enhance each step of the patient experience,” says Archer. “Before the pandemic, KHSC had more than 800 volunteers and we are currently seeking people in the community who may be interested in joining our volunteers who make KHSC a warmer, more positive place for everyone who enters our sites to receive care.”
Volunteers who directly support patients generally have hobbies or interests they would like to share such as playing music, cards, reading together, doing puzzles, crafts, or simply going for a walk. These volunteers are guided by a genuine desire to adapt to best meet the needs of the individuals they are engaging with in that moment. Sometimes they simply provide a warm blanket or sit quietly with an individual while their family takes a break.
Gananoque resident Penny Huntley, says her volunteer role at KHSC has been a fulfilling way to help make a difference in the lives of others.
“When I retired, I needed to find a sense of purpose that my previous career as a teacher had once provided, and it was initially decided that volun-

teering on the pediatric floor would be a great fit for me. Sometimes I would read stories and play games with children, other times I’d go for walks or do crafts. I was just there to offer some extra interaction with the children and a break to parents who might need it.
“Recently I have returned to working as a part-time supply teacher and my volunteer role has shifted to making appointment reminder calls to patients. The people in the Dermatology department that I work with have been so incredibly understanding and flexible with my volunteering schedule and have been very accommodating in allowing me to work around my supply teaching days. This has helped make volunteering at KHSC a very rewarding experience that has allowed me to give back to our community in a very satisfying way.”
Liaison and information volunteers alleviate fear, anxiety, confusion by playing a crucial role helping people get where they need to be! Their objective is to be accessible to anyone who is lost, overwhelmed, or confused at KHSC. They initiate contact offering to be of assistance by providing directions, walking with someone to where they need to be, or calling
for information or assistance on their behalf.
Individuals who volunteer in the tuck shop, gift shop or lottery booth contribute to creating a warm and welcoming atmosphere and make a tangible difference in people’s hospital experiences. If you enjoy meeting new people, helping them find the perfect gift or product, making small talk and providing a listening ear in addition to a cup of coffee or lotto ticket, this is the role for you. Not only will you feel great about providing this highly appreciated service, but the profits raised from these businesses are donated back to the hospital to enhance the care patients receive.
“Volunteer roles are determined based on the volunteer’s skills, experience, talents and availability,” says Archer. “We appreciate that people have busy lives, and we offer flexible scheduling including weekday, evening and weekend options that can vary anywhere from one to four hours weekly depending on the needs of the program.”
As a volunteer, Penny appreciates the scheduling flexibility. “Over recent years, my volunteer role has been making reminder calls to patients,
and I have returned to working as a part-time supply teacher. The people in the Dermatology department that I work with have been so incredibly understanding and flexible with my volunteering schedule and have been very accommodating in allowing me to work around my supply teaching days. This has helped to make volunteering at KHSC a very rewarding experience that has allowed me to give back to our community in a very satisfying way.”
KHSC recently refined its application and orientation processes which results in a streamlined experience for volunteers. Virtual volunteer information sessions are offered that include an overview of the patients and families we serve, and the roles in which volunteers support our patients, families, staff and visitors.
Applicants receive an invitation to attend the information session as soon as they apply, or people can sign up to attend if they would like more information before they decide whether they would like to apply.
To learn more about KHSC volunteer opportunities or to sign up for an information session, visit the Working and Volunteering page at www.kingstonhsc.ca. ■ H
ew research led by Unity Health Toronto that examines how fibroblast cells in the body are activated to cause fibrosis and organ scarring has been published in the prestigious scientific journal Nature Reviews Molecular Cell Biology. Fibrosis and organ scarring are leading causes of death, with data suggesting they are responsible for up to 45 per cent of deaths in the developed world.
Fibrosis is a process by which fibroblast cells in our body produce an excess amount of a protein mixture called extracellular matrix (ECM). ECM contains proteins including collagen, elastin and fibronectin and can be thought of as a sort of “glue” at the organism level that connects the different organs of our body while respecting their boundaries.
Typically, fibroblasts produce ECM to help support tissue structures and to help repair tissue that has been injured or wounded. For example, under normal circumstances, when you cut yourself, fibroblasts will travel to the site of the cut or wound, proliferate and produce ECM to help heal the cut. With fibrosis, however, fibroblasts receive certain signals which activate them to overproduce ECM. This excess ECM, in particular the excess collagen, can result in the formation of scar tissue which can impair organ function. Fibrosis can occur in any tissue or organ in the body, including the lungs, liver, kidney and heart, and is associated with many common diseases – often as an endstage condition.
The new research review summarizes some of the signals and molecular mechanisms that play a role in activating fibroblasts to produce excess ECM. The researchers also discuss the heterogeneous nature of fibroblasts, and how their vast heterogeneity can impact the healing process.
“This review tries to untangle some of our knowledge and understanding – or misunderstanding of fibroblasts and fibroblast activation,” said Dr. Boris Hinz, corresponding study author, St. Michael’s Hospital scientist and Keenan Chair in Fibrosis.
“We generally talk about activation of fibroblasts from a dormant state in normal healing and fibrosis. But the cells activated to make new ECM were neither really dormant, nor are they all fibroblasts,” said Hinz. “We wanted to understand which cells in particular are activated. What types of activations take place – for example, ‘What are the key signals that activate these fibroblasts and how?’”
PhD student Fereshteh Sadat Younesi helped lead the review. Younesi is a member of Hinz’s lab and is a student at the Research Training Centre at St. Michael’s Hospital.
“One key signal arises from the mechanical cues present in the stiffened environment of fibrotic regions. When tissues undergo fibrosis, they become way stiffer than normal because of these fibroblasts going into overproduction and rearranging the ECM,” Younesi said.
“Those fibroblasts can feel the stiffness around them, which keeps them switched on, even after the initial injury has healed. These mechanically induced fibroblasts exacerbate the fibrotic area with their persistent activity.”
Hinz said once researchers have a better understanding of the signals and mechanisms involved in fibroblast activation, they can develop therapies and interventions to interrupt the process and stop the overproduction of ECM, thus halting fibrosis.
“We need a cure for fibrosis. Scientists have known about fibrosis
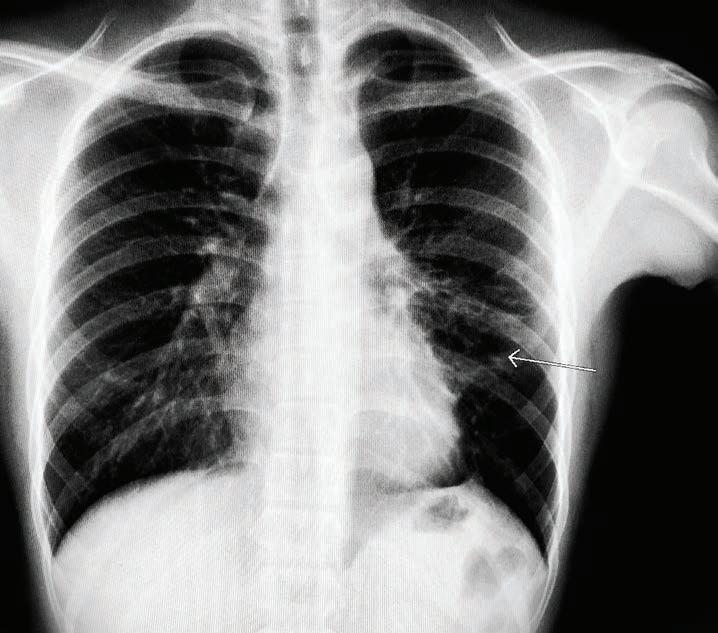
for roughly a century and there still is no cure,” Hinz said. “With only two currently approved drugs, we can only stop fibrosis in some organs – at best. An end goal would
be to instruct the scar-making cells to remove excess ECM with pharmaceutical guidance. This is where the science is going and this is the ultimate dream.” ■ H
Leung works in communications at Unity Health.















