













KNOW THE FACTS:
NursesTalkTruth.ca
PRIVATIZATION:















KNOW THE FACTS:
NursesTalkTruth.ca
PRIVATIZATION:







A critical staffing shortage. ER closures. Longer wait times. And a gamble on privatization. Under Doug Ford’s watch, public health-care isn’t getting better –it’s bleeding out.










The federal government often talks about fostering an ‘innovation economy’ – and for good reason. The application of technological innovations and entrepreneurship have been at the forefront of economic growth in the globalized economy for some time already, and that only promises to accelerate in the coming years.
Canada, of course, should not be left at the sidelines cheering on critical innovations but pioneering them. And it’s a balanced research environment that will get us there.
History shows it’s not so easy to back research ‘winners’ over ‘losers.’ It’s better instead to create a healthy research environment where basic foundational research thrives and leads to multiple commercialization opportunities. The innovations which then best meet societal demands are the ones which go on to be successful and adopted.
It’s a robust ecosystem, not a horse race, in other words. And every stage of the research cycle should be bolstered and encouraged.
Our governments at every level should be embracing a ‘patient investor’ approach to create a healthy pipeline from rich foundational research toward commercialization. Such a balanced approach requires robust funding
EDITORIAL: Sept. 7
ADVERTISING:
Display – Sept. 22 | Material – Sept. 26
Monthly Focus:
Mental Health and Addiction/Patient Safety/ Research/Infection control: New treatment approaches to mental health and addiction. Developments in patient-safety practices. An overview of current research initiatives. Developments in the prevention and treatment of drug-resistant bacteria and control of infectious (rare) diseases. Programs implemented to reduce hospital acquired infections (HAIs).
+ANNUAL INFECTION CONTROL SUPPLEMENT
for post-secondary research, like the recent announcement through the Canada First Research Excellence Fund. Investments like this will create the essential foundation for the ‘innovation economy’ -- keeping Canada competitive both now and into the future.
This is why we need sustained investment in aging research.
Canada is rapidly approaching the status of a ‘super-aged’ society; by 2035, one in four Canadians will be older than 65 years of age. Overwhelmingly, most Canadians want to age in place, in their own homes. When surveyed, more than 92 per cent of Canadians reported that they support government investments in programs that enable healthy aging (Nanos, 2021).
Unfortunately, this contrasts greatly with the reality that we have not adequately invested in healthy aging in Canada, and our approach has been to rely on acute care institutions and residential facilities to take care of Canadians as they age and require assistance.
Already we can’t keep up with demand for long-term care facilities or homecare need and this will only get worse as our society ages. So, what needs to happen?
We clearly need to embrace new ways of healthy aging, and we need new government funding and policies to achieve it. This is part of the innovation economy too.
Continued on page 6
EDITORIAL: Oct. 5
ADVERTISING:
Display – Oct. 22 | Material – Oct. 26
Monthly Focus: Technology and Innovation in Healthcare / Artificial Intelligence (AI) /Patient Experience/ Health Promotion: New treatment approaches to mental health and addiction. An overview of current research initiatives Programs and initiatives focused on enhancing the patient experience and family centred care. Programs designed to promote wellness and prevent disease including public health initiatives, screening and hospital initiatives.
+ SPECIAL MEDTECH SUPPLEMENT
THANKS TO OUR ADVERTISERS Hospital News is provided at no cost in hospitals. When you visit our advertisers, please mention you saw their ads in Hospital News.
610 Applewood Crescent, Suite 401 Vaughan Ontario L4K 0E3 TEL. 905.532.2600|FAX 1.888.546.6189 www.hospitalnews.com
Editor Kristie Jones editor@hospitalnews.com
Advertising Representatives
Denise Hodgson denise@hospitalnews.com
Publisher
Stefan Dreesen stefan@hospitalnews.com
Accounting Inquiries accountingteam@mediaclassified.ca Circulation Inquiries info@hospitalnews.com
Director of Print Media
Lauren Reid-Sachs
Barb Mildon, RN, PHD, CHE
VP Professional Practice & Research & CNE, Ontario Shores Centre for Mental Health Sciences

Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications
Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
ASSOCIATE PARTNERS:
Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario.
The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
Canadian Publications mail sales product agreement number 42578518.
We need a balanced research environment to foster a real ‘innovation economy’
Time is now to invest
For most people who die from major trauma incidents, like car accidents and gunshot wounds, death occurs before they even make it to the hospital. That troubling fact led a team of St. Michael’s physicians and scientists to ask: what if we could bring aspects of the hospital to them?
Drs. Johannes von Vopelius-Feldt and Brodie Nolan, emergency physicians and trauma team leaders at St. Michael’s, are leading a chart review study to examine the feasibility of stationing prehospital critical care teams (CCTs) in Toronto to respond to major traumas. These teams, which successfully operate in several European cities, would bring elements of hospital care like blood transfusions, general anesthesia, and focused surgical procedures directly to patients in the field.
“The idea isn’t to replace pre-existing paramedic care, but to augment it for the small percentage of critically ill or injured patients,” said Nolan.
The study will use Emergency Medical Services (EMS) data, coroner’s reports, and geospatial analysis to identify where major traumas occur in Toronto and evaluate the best way for CCTs to reach sick and injured patients.
The study, a collaboration between St. Michael’s, Sunnybrook and the

University of Toronto, recently won two small seed grants, including the Trauma Association of Canada (TAC) Learners Research Grant and the University of Toronto’s EMH Seed Grant.
The care teams would include physicians and paramedics, and pre-existing dispatch systems would alert them to major trauma incidents. Nolan and von Vopelius-Feldt are studying the efficacy of using both ambulances and helicopters.

“Patients who arrive at a trauma centre early do better,” said Dr. Nolan,


adding that having a continuum of care from the field straight to the hospital or operating room can be vital.
The team says St. Michael’s is well positioned to support CCT research because of its location, patient population, and strong research and trauma background. St. Michaels’ is one of only two adult level 1 trauma centres in Toronto.
“It’s an urban trauma centre. Trauma tends to effect regions with marginalization more heavily. These populations have challenges in access
to healthcare. There’s an element of equity here,” said von Vopelius-Feldt.




Nolan, who is a scientist at the Li Ka Shing Knowledge Institute, and von Vopelius-Feldt both work as transport medicine physicians for Ornge, the provincial critical care transport service that treats and transports critically ill or injured patients to St. Michael’s. They say that conducting these early stages of research before potentially launching a CCT service in Toronto will allow future decision making to be data-driven.
“We’ll be able to match what we provide to the needs of our communities,” said von Vopelius-Feldt.
The team plans to use the grants to hire a student to review coroners’ reports and embed graduate students in both the feasibility and equity analyses, including geospatial analysis.
Nolan and von Vopelius-Feldt, along with Program Manager Melissa McGowan, are part of a newly established research collective at Unity Health focusing on pre-hospital, trauma and resuscitation sciences. They say this study is part of the early stages of their goal to become a world-leading group.
“It’s the first step,” said von Vopelius-Feldt. “Every journey starts with the first step.” ■ H
Olivia Lavery is a Communications Advisor at Unity Health.New guidance aimed at helping standardize community overdose response and take-home naloxone kits across Canada is published in CMAJ (Canadian Medical Association Journal). The guidance is an important document to optimize the effectiveness of take-home naloxone to save lives.
The guidance was developed by a panel of experts, including people with lived experience of drug use and overdose response, front-line and harm-reduction workers, public health professionals, clinicians and academics with expertise in harm reduction across Canada. It is targeted toward policy-makers who develop and fund take-home naloxone programs, as well as distribution sites, harm-reduction organizations and workers, community overdose responders, clinicians and public health professionals.
Continued from page 4
As published evidence on takehome naloxone is of low quality, clinical and community expertise was especially important.
“The development of Canadian take-home naloxone program guidance was led by BC Centre for Disease Control in a truly collaborative process with diverse stakeholders from across the country,” said Dr. Jane Buxton, with the BC Centre for Disease Control, Vancouver, BC and nominated principal investigator.
“We found the quality of published data was low, so the insights of the
How can we modernize Canada’s approach to aging? We need both basic research and commercialization opportunities to get there.
We speak from experience. Our organizations, AGE-WELL and the Canadian Frailty Network, have created Healthy Aging Canada as a new research collaboration to leverage the expertise and infrastructure of our organizations to lead evidence-based social, health care and technology research that will improve the healthy aging experience of older Canadians and their care partners.
We are combining our research gleaned from clinical practice and behaviour change research from across the community with develop-
ing and validating technology-based solutions for daily living and caregiving across settings. It’s a marriage of basic research and application possibilities.
While government funding has kept pace with commercialization, we need to ensure that healthy-aging research is given similar priority. Funding research is a crucial piece of a successful innovation pipeline to modernize Canada’s approach to aging. It’s going to be how Canada tackles our ‘super-aged’ society ‘problem’ and makes it a benefit.
A lack of sustained funding that supports healthy aging puts at risk Canada’s ability to address the indisputable and urgent needs of our aging population and related infrastructure.■ H
Dr. John Muscedere is CEO of Canadian Frailty Network and Professor of Critical Care Medicine, Queen’s University. Dr. Alex Mihailidis is CEO of AGE-WELL and the Barbara G. Stymiest Research Chair in Rehabilitation Technology, University of Toronto and KITE Research Institute at University Health Network. The two organizations work in partnership on Healthy Aging Canada.
affected community (with many years of experience of overdose response with naloxone) was invaluable in developing guidance.”
The guidance makes three key recommendations:
• Take-home naloxone programs should, where possible, offer both intramuscular and intranasal formulations of naloxone.
• Kits should include a recognizable carrying case, breathing mask,
non-latex gloves, instructions on how to administer naloxone, naloxone and supplies to administer naloxone.
• Trained responders should provide rescue breathing as part of the response in addition to verbal and physical stimulation, calling emergency medical services, administering naloxone and providing cardiopulmonary resuscitation if required.
“The most important considerations in overdose response are the preservation of life and mitigation of harms,” write the authors.
“Guidance on take-home naloxone distribution and use by community overdose responders in Canada” was published August 28, 2023. ■ H
Indigenous females living “off reserve” face many disparities in health care access, use and unmet needs, found new research in CMAJ (Canadian Medical Association Journal).
The study included 2902 First Nations, 2345 Métis, 742 Inuit and 74 760 non-Indigenous females of reproductive age (aged 15–55 years) obtained from the Canadian Community Health Survey from 2015 to 2020, including 4 months during the COVID-19 pandemic.
“We found that ‘off-reserve’ First Nations, Métis and Inuit females reported higher morbidity and continue to face various disparities in health care access, use and unmet needs,” writes Sebastian Srugo, a researcher with the Public Health Agency of Canada. “Specifically, fewer Indigenous females reported having access to a regular health care provider, especially in the territories and Prairies; more waited longer for an appointment; and more used hospital services for nonurgent care.”
The authors, who include patients and members of community organizations on the Indigenous Advisory Committee, note that racism and lack of equity are widespread and contribute to disparities in health access and higher rates of illness among Indigenous females. A key issue is having access to a consistent primary care provider for continuity of care.
“To alleviate these disparities, our Indigenous advisors recommend that Canada leverage more accessible and culturally competent health care providers and that survey developers try to fill outsized gaps in Indigenous health data,” the authors conclude. “Future work should monitor these disparities over time and fill large gaps in our findings, such as by ascertaining data on ‘reserves.’”
“Disparities in primary and emergency health care among “off-reserve” Indigenous females compared with non-Indigenous females aged 15–55 years in Canada” was published August 28, 2023. ■ H
“THE MOST IMPORTANT CONSIDERATIONS IN OVERDOSE RESPONSE ARE THE PRESERVATION OF LIFE AND MITIGATION OF HARMS,”
Global rates of hospital readmission and mortality are high for heart failure (HF) patients. According to a new study from the Ted Rogers Centre for Heart Research at the Peter Munk Cardiac Centre at UHN, variability in readmission rates for this population cannot be explained by health care spending, risk of mortality, or comorbidities.
HF is a global pandemic affecting approximately 64 million people worldwide. It is the leading cause of hospitalization in the United States and Europe. The global cost of HF is about US$346 billion per year.
“Our goal was to better understand the factors associated with readmission for HF patients on a global scale,” says Dr. Farid Foroutan, study lead and associate scientist, Ted Rogers Centre Computational Program at Peter Munk Cardiac Centre, UHN. “Our study is the first to provide a global comparison of HF readmission rates.”
Based on a comprehensive analysis of 1.5 million HF patients, researchers found that on average, 13.2 per cent of HF patients were readmitted to hospital within 30 days of hospitalization, and 35.7 per cent were readmitted within one year.
The mortality rate was 7.6 per cent within 30 days of hospitalization, and 23.3 per cent within one year. The research was published in the Journal of the American College of Cardiology. Read more about the study.
“We found substantial global variability in readmission rates for hospitalized HF patients,” says Dr. Foroutan. “We also found significant variability across countries that may not be simply explained by a country’s health care spending, mortality rates, or HF comorbidities.”
Dr. Foroutan highlights the need for further studies that evaluate differences in the structure and processes of care delivery for HF interventions.
Such studies are crucial in reducing the global burden of HF.
In the meantime, the comparative regional and national data presented by the research team holds the potential to inspire more immediate action.
“This comparison can assist policymakers in understanding the potential effects of interventions at a population level,” explains Dr. Douglas Lee, senior author of the study, Ted Rogers Chair in Heart Function Outcomes,
and cardiologist, Peter Munk Cardiac Centre, UHN.
“The data may guide countries performing below global benchmarks, emphasizing the urgency of adopting new HF treatment strategies.”
The findings of this study carry significant implications for improving HF patient care worldwide. They have the potential to inform health care policies, shape clinical practices, and contribute to reducing the burden of heart failure on a global scale. ■ H
Most people in Canada now have hybrid immunity against SARS-CoV-2 through a mix of infection and vaccination, new research in CMAJ (Canadian Medical Association Journal) shows.
Nitrous oxide is a popular recreational drug, especially among young people, that can cause serious and sometimes permanent neurological defects. A new review in CMAJ (Canadian Medical Association Journal) aims to help clinicians recognize signs of nitrous oxide toxicity.
Also known as “laughing gas,” nitrous oxide is an anesthetic sometimes used in pediatric and dental procedures. Inexpensive and easily obtainable online, it is increasingly used for a quick high. In the 2021 Global Drug Survey, 10 per cent of all respondents, and 15 per cent of Canadian respondents, indicated having used the drug in the previous year.
“The low cost of and ease of access to nitrous oxide make it a popular recreational drug, especially among younger people,” writes Dr. Cyrille De Halleux, a specialist in internal medicine, critical care and resident at The Hospital for Sick Children (SickKids)
and chief fellow in the Division of Clinical Pharmacology and Toxicology at the University of Toronto, Toronto, Ontario.
Chronic use of nitrous oxide can cause functional vitamin B12 deficiency, which can result in long-term health effects, especially neurological consequences. The three most common presentations of toxicity are damage to the spinal cord (myelopathy), nerve damage affecting strength and sensation (neuropathy) and behavioural abnormalities (encephalopathy). Treatment includes stopping use of the substance, vitamin B12 supplementation and methionine.
“Clinicians should enquire about nitrous oxide use in patients with unexplained findings suggestive of vitamin B12 deficiency or other compatible neurologic symptoms,” the authors conclude.
“Diagnosis and management of toxicity associated with the recreational use of nitrous oxide” was published August 21, 2023. ■ H
Using pan-Canadian blood sample data from a subset of studies backed by the COVID-19 Immunity Task Force (CITF), researchers from the CITF, in collaboration with those from supported studies, estimated changing levels of seroprevalence – from infection or vaccination, or both – over 3 time periods: prevaccination (March to November 2020), vaccine roll-out (December 2020 to November 2021) and the Omicron waves (December 2021 to March 2023). In the first 2 phases, seroprevalence from infection was low, with less than 0.3 per cent of the Canadian population showing exposure to the virus in July 2020, reaching 9 per cent in November 2021. With the circulation of the Omicron variant, infection-acquired seroprevalence rates changed dramatically.
“Despite high vaccine coverage in Canada, all previous increases in seroprevalence due to infection were dwarfed by the increase caused by the Omicron variant. After 6 months of the Omicron variant circulating in Canada, infection-acquired seroprevalence had risen to 47 per cent by midJune 2022, with an average monthly increase of 6.4 per cent per month
between December 15, 2021, and July 2022. That seroprevalence ultimately reached over 75 per cent by March 2023,” explains Dr. Bruce Mazer, Associate Scientific Director, Strategy at the CITF, one of the study leads, and Senior Scientist at the Research Institute of the McGill University Health Centre, Montréal, Quebec.
“During Omicron, rates of infection-acquired immunity increased faster in younger age groups, with close to 80 per cent seroprevalence in adults under age 25, approximately 75 per cent in ages 25–39 years, 70 per cent in ages 40–59 years, and 60 per cent in those 60 and over by spring 2023,” adds study colead Dr. David Buckeridge, Scientific Lead, Data Management & Analysis at the CITF and Professor, School of Population and Global Health, McGill University.
The low infection rates in Canada before Omicron were also evident in other high-income countries in Europe and North America.
“[M]any people in Canada have hybrid immunity against SARS-CoV-2, but variations by age and geography and the potential for waning antibody levels suggest that public health policy and clinical decisions will need to be tailored to local patterns of population immunity,” the authors conclude.
“The evolution of SARS-CoV-2 seroprevalence in Canada: a time-series study, 2020-2023” was published August 14, 2023. ■ H
Recreational nitrous oxide use is no laughing matter
ommon examples of opioids include morphine, hydromorphone, and fentanyl, etc. When taken as instructed for pain, opioids are deemed safe. However, the potential risk of dependence and withdrawal, particularly with prolonged use of opioids, will always be present. Tolerance, which is a sign of physical dependence, occurs when the body requires more of the drug to create the same desired effect, for example, for pain relief. In this case, a patient experiencing opioid dependence will require higher doses for pain control which may then increase the risk of an overdose. High doses of opioids can lead to slowed breathing, low heart rate, low blood pressure, drowsiness, etc. On the other hand, when opioid use is suddenly stopped, the patient may experience withdrawal symptoms (which is also a sign of physical dependence), such as muscle pain, nausea, diarrhea, sweating and chills, and cravings for the drug. Patients experiencing withdrawal may continue to use opioids to avoid the undesirable symptoms. (Readers can learn more about Safe Use of Opioids at the https://myhealth.alberta.ca/ website where Patient Care Handouts are available with Care Instructions for opioid overdose, opioid withdrawal, reducing or stopping opioid medications, etc.) In general, it is important for patients to understand the risks and benefits of opioids, follow prescription instructions, and consult their pharmacists and healthcare providers accordingly regarding any concerns with opioid use.
OTC medications are a great alternative to opioids for pain control. These medications are available without a prescription and do not present the same risks of dependence or withdrawal symptoms.
Popular NSAIDs include ibuprofen, naproxen, and acetylsalicylic acid (ASA). A major caution of NSAID use is the risk of stomach bleeds. However, this can be prevented by taking the medication at the prescribed dose with food to prevent stomach upset. Stomach-acid reducing medications can also be incorporated with NSAID drug regimens to protect the stomach and avoid NSAID-associated gastrointestinal bleeds.
Another OTC medication commonly used for pain is acetaminophen. Besides being a pain reliever, Acetaminophen is also a common fever reducer that can be given, sometimes, with NSAIDs and opioids to provide additional fever or pain relief. Acetaminophen is usually well tolerated by patients, but at high doses, it could lead to liver damage. Therefore, it is essential to ensure that the dose/ strength of Acetaminophen, whether in single-entity products or in combination OTC/prescription medications, is verified with your pharmacist or healthcare provider.
While NSAIDs, acetaminophen, and opioids are all pain relievers, opioids are the most potent and are often not required for the management of moderate pain. After exhausting OTC options, the rule of thumb is to take the lowest effective dose of an opioid
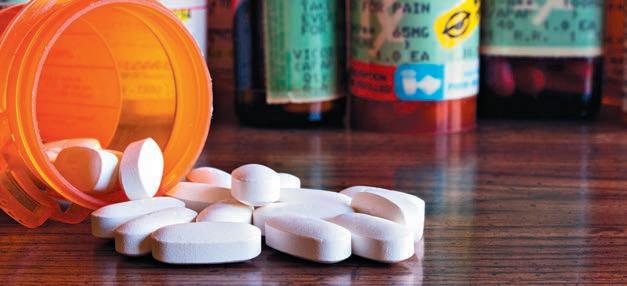
medication for the shortest amount of time possible.
According to the Public Health Agency of Canada (https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/), in 2022, our country grappled with a staggering toll of over 7000 opioid-related deaths. As healthcare providers with the ability to assess prescriptions, monitor drug effectiveness, and communicate with patients, pharmacists play a key role in preventing opioid overdoses and related patient safety events. Opioid stewardship refers to coordinated efforts and interventions to improve, monitor, and evaluate the use of opioids to support/protect public health and prevent harm. Pharmacists, healthcare providers, and patients/caregivers all have a role in opioid stewardship. Below are some selected strategies that everyone can be engaged in supporting safe opioid use.
When patients fill a prescription at a pharmacy, a medication information pamphlet detailing the benefits (or the use) and risks (or side effects) of the medication is usually provided. Similarly, when an opioid prescription is dispensed, in addition to the pamphlet, pharmacists can ensure that proper use of opioids, how to manage or prevent an overdose, and potential risks of opioids, etc., are addressed/
discussed with the patient/caregiver during counseling and provide additional follow-up support/monitoring. When dispensing opioid medications to children, the Hospital for Sick Children Safe Opioid Checklist for Kids (https://assets.aboutkidshealth.ca/ AKHAssets/OpioidSafetyChecklist. pdf) can be used for family/caregiver education.
Any unused medications, opioids or not, should be brought back to the pharmacy and not be disposed of through regular household garbage.
Warning and auxiliary labels, particularly for opioids, should be applied on prescription vials/bottles to alert patient/caregivers to prevent medication safety incidents. Any medication or liquid vials/bottles containing controlled substances (e.g., opioids) should also have a child-safety cap.
Naloxone is a life-saving medication that can be administered intranasally or intramuscularly during an opioid overdose incident. It is fast-acting and will temporarily reverse the effects of opioid overdoses. Pharmacists can educate patients on the use of Naloxone and provide them with a takehome Naloxone kit when an opioid medication is dispensed. Take-home naloxone kits are available at most pharmacies in Canada, and they do not require a prescription. Readers are encouraged to read more about Naloxone at https://www.canada.ca/en/ health-canada/services/opioids/naloxone.html.)
The Institute for Safe Medication Practices Canada (ISMP Canada) developed an online resource on Opioid Stewardship (https://ismpcanada.ca/ resource/opioid-stewardship/) to inform the public and healthcare providers about safe opioid use. ■ H
Replacing nutrients and rehydrating the body after sport is an important way to promote muscle repair and replenish energy, and athletes are always looking for an edge. Many rely on optimal nutrition to help fuel their sport and post-exercise recovery. Milk is a go-to recovery beverage for athletes because of its unique mix of nutrients, including fluid, protein, carbohydrates and electrolytes.
Milk naturally contains a mixture of high-quality protein (with all essential amino acids), carbohydrates, water and sodium, which are all nutrients that are required after sport. Plus, milk is considered to be isotonic (osmolality of 280–290 mosmol/kg). All of these have been shown to independently enhance rehydration after sport.
Studies show that drinking milk after exercise can support both acute recovery and chronic training adaptation. Milk is also known to reduce post-exercise muscle soreness, reduce muscle loss, and reduce symptoms of stress after sport, even more than carb-based sport recovery drinks.

1. Protein and muscle synthesis
Protein helps the body repair the muscles that were used during exercise. Milk contains whey and casein proteins, which enhance post-exercise muscle protein synthesis rates. Milk also has a high concentration of branched-chain amino acids (such as leucine) to support muscle protein synthesis.
Plus, the protein in milk adds to post-exercise muscle protein synthesis and rehydration.
2. Carbohydrates and glycogen synthesis
Milk contains carbohydrates in the form of lactose, which can act as a fuel source before and during exercise. Lactose may also play a role in a post-exercise recovery by optimizing muscle and liver glycogen, which is the storage form of carbohydrates in the body. Lactose may also act as a prebiotic, which can promote beneficial changes to gut microbiota. Chocolate milk, which contains added sugars in addition to the natural occurring lactose sugar, may be more advantageous when additional carbohydrate is needed, such as training for a triathlon or being in a sports tournament.

3. Fluid, electrolytes and hydration
Milk contains a high concentration of electrolytes, including calcium, sodium and potassium, which facilitate fluid recovery, rehydration, and electrolyte replenishment following exercise (when fluid is lost through sweat). They also help improve the recovery of skeletal muscle. One study showed that gradually drinking milk restored fluid balance better than water or carbohydrate electrolyte drinks, due to how these beverages are digested. Milk is released more slowly from the stomach compared to water or sports drinks, and dairy proteins contribute to this beneficial effect.
Studies show that resistance training can be paired with 20 grams of high-quality milk-based protein to provide anabolic stimulus for muscle protein synthesis. Each cup of milk contains 9 g protein, so you need about 2 cups for post-workout muscle recovery. Milk can be used in smoothies or enjoyed as-is. The other benefit to milk is that it’s readily available, making it a convenient and easy option to facilitate post-exercise recovery.
Whether it’s a weekday hockey game, a weekend run or a week-long volleyball tournament, milk is an excellent beverage to promote glycogen storage, muscle synthesis and rehydration. H
THE FLUID, PROTEIN, CARBOHYDRATES, AND ELECTROLYTES IN MILK MAKE IT IDEAL FOR POST-EXERCISE REHYDRATION AND PROTEIN SYNTHESIS.
Imagine there’s been a blast at Pearson Airport with reports of multiple people injured and deaths. St. Michael’s Hospital, one of a few Level 1 trauma centres in Ontario, has received word that 24 patients are headed to its busy Emergency Department (ED). The ED team springs into action, initiating a Code Orange – the hospital-wide alert for an external emergency. Frontline ED staff prepare and decant the unit, making space for a surge of new patients. As the injured arrive, triage staff allocate spaces based on the severity of their injuries.
This simulated scenario was the basis for a recent Code Orange tabletop exercise at St. Michael’s Hospital. These exercises, which involve ED staff, physicians, hospital administrators and stakeholders from other departments, are designed to assess and improve the hospital’s preparedness for when real-life external emergencies take place.
“Mass casualty events are one of the most challenging situations an ED will face,” says Emergency Physician and Trauma Team Leader Dr. Rachel Poley. “It is important that we test and practice our protocols, so we can continue to improve and be ready to care for the patients who need us. We must

practice these exercises regularly to stay on top of our game.”
St. Michael’s Hospital played an important role in caring for the injured in the 2019 Raptors Championship parade and the 2018 Danforth shooting. As one of only two Level 1 adult trauma centres in Toronto and one of nine in the province, the hospital has a responsibility to make sure it’s prepared for when the next incident happens, Poley said.
“These exercises are integral to us feeling a sense of control when a mass casualty event occurs,” she said. “Among the chaos there is power in knowing what you are supposed to do. This serves our patients well,
and makes us proud to work at St. Michael’s.”
Poley and her team spent more than three months planning all aspects of the tabletop exercise, from creating the scenario, writing simulated patient profiles, and mapping out hospital bed occupancy levels and resources. They used data from the ED to make sure the scenario mirrored typical conditions in the hospital.
“We try to make these scenarios as realistic as possible,” Poley said, noting that the inspiration for the exercise was a recent evacuation at Billy Bish-
op Airport due to a possible explosive device that turned out to be a false alarm. “We played off that event. An explosion also creates unique injuries that involve both penetrating and blunt injuries, and allows us to run through a breadth of clinical scenarios that require specific resources.”
During the exercise, Trauma Program Manager of Registry Amanda McFarlan stands in line to be registered as a patient. “Hello, I’m patient 49,” she tells registration staff as she reads off a card containing her patient profile. “I have shrapnel in my abdomen, I’m awake and alert and I’m on a stretcher.”
McFarlan says that every time the team conducts a Code Orange simulation they discover something about their processes that could be improved.
“It could be something as simple as, ‘Oh, that box we need is under a big pile of heavy stuff, so it should be moved,’” she said. “Or it could be figuring out how to quickly register a whole bunch of people with similar injuries without mixing them up.”
The last time the ED held a Code Orange exercise, the team saw that there were inefficiencies during the registration process and refined them afterward as a result, she said.


“This time around, one of the great takeaways was that registration was a strength and we had greatly improved efficiencies to reduce registration time,” McFarlan said. ■ H
 Photos: Eduardo Lima
Marlene Leung is a communications advisor at Unity Health.
Photos: Eduardo Lima
Marlene Leung is a communications advisor at Unity Health.

What an incredible year it’s been since I became President and CEO of Waypoint Centre for Mental Health Care in June 2022. I’m more inspired, energized (and yes, challenged) than ever. As a 315 bed specialized hospital serving central Ontario and the province, Waypoint provides mental health, addictions and specialized geriatric services. This past year I have been deeply moved by the care and compassion the Waypoint team has shown our patients, families, and each other. I appreciate everyone’s commitment, ingenuity and servant leadership in the important work we do at the hospital and in the system. I’m humbled to be at Waypoint’s helm, and grateful for our amazing staff, physicians, leaders, and volunteers. In particular, our board members and Chair have been generous with their wisdom, support and energy to help me and our whole organization learn, grow, and thrive.
It’s been a year of remarkable accomplishments and tremendous effort to move the needle on our priorities to Serve, Discover and Lead. The most recent is the June achievement of Accreditation with Exemplary Standing from Accreditation Canada. This is the highest possible rating an organization can achieve and it is due to the collective commitment to excellence, teamwork and perseverance of our staff, physicians and volunteers.
In February, we launched five ambitious and energizing Enabling Plans. These integrated plans are inspiring us and ensuring our efforts are focused and impactful. The plans also commit us to take action on four cross cutting themes: partnerships and servant leadership, Waypoint without walls, becoming a learning health system, and equity, diversity and inclusion.
One of the major projects embedded in the Enabling Plans is a multiyear model of care transformation we embarked last year. With participation from across the hospital including patients and families, this new model of care will ensure we continue to foster and sustain a therapeutic environment, actively engage and include
patients and families in care, and support staff to provide the safest and best possible care, achieving the intended outcomes for and with patients.
With acute mental health-related hospitalizations in Simcoe Muskoka rapidly growing, a 21 per cent increase from 2017 to 2021, Waypoint continues to support the broader health care system as a regional centre. Waypoint has temporarily operated an additional 14-25 acute mental health beds in addition to our permanent 20 beds. We have proposed to the Ministry of Health to make 20 of these additional beds permanent, including five psychiatric ICU beds, which would be the first of their kind in the region leveraging Waypoint’s unique expertise.
We also expanded the neurostimulation electroconvulsive therapy (ECT) program to five days a week, launched an urgent psychiatric consultation service to support rapid outpatient follow-up after emergen-

cy department visits, supported new LOFT supportive housing, and helped to launch 16 beds at County of Simcoe long-term care homes and through the North Simcoe Muskoka Specialized Geriatric Services.
The Central Ontario Specialized Health (COSH) Network launched 1door.ca, providing convenient online appointment booking for several free, no/low barrier counseling and other mental health services. COSH aims to improve access to excellent care for people with complex needs, through delivering regional specialized services and building capacity throughout our region. Working with partners and primary care providers, we are transforming how the system is organized so that care is more integrated and connected. In addition to 1door.ca, we are collaboratively developing integrated care pathways for children, youth, adults and seniors with depression and anxiety, to ensure people receive
high quality care no matter where they are and to smooth out the bumps and gaps people otherwise experience with a more coordinated and timely care experience. The launch of the myDAWN pathway for children and youth with the South Georgian Bay OHT is a great example of what we have accomplished together.
With these and many other clinical innovations underway, it is more important than ever that we engage clinicians in research and evaluation. Waypoint’s new research and scholarship award program for health professionals is increasing the integration of research across the hospital. The impactful research underway sees us co-designing and launching a youth resiliency program, collaborating with patients to conduct research in the forensic mental health context, guiding law enforcement in assessing and responding to intimate partner violence, leveraging artificial intelligence to make inpatient mental healthcare safer, and engaging people who use opioids in advising on the impacts of COVID and how public policy can support better care. We have been thrilled to see significant growth in major competitive grants to support these projects.
With a strengthened focus on equity, diversity and inclusion, we are participating in the Institute for Healthcare Improvement’s Pursuing Equity Learning Network. This is a learning collaborative with teams from across North America who are coming together to learn, build and practice skills, and develop a deep understanding of equity and racial justice. It’s been inspiring to see frontline staff across Waypoint raise their hands to play a leadership role in advancing EDI across our organization, and I personally look forward to learning from and walking alongside them in this critically important work.
In this vein, the Ontario Structured Psychotherapy Program received an Award of Excellence in Mental Health and Addictions Quality Improvement from the Canadian College of Health Leaders for their efforts to increase the cultural sensitivity, accessibility and effectiveness of services for people from priority populations that are underserved.
Continued on page 33
IT’S BEEN A YEAR OF REMARKABLE ACCOMPLISHMENTS AND TREMENDOUS EFFORT TO MOVE THE NEEDLE ON OUR PRIORITIES TO SERVE, DISCOVER AND LEAD.
 By Victoria Schramm
By Victoria Schramm
ver two million people worldwide depend on dialysis or a kidney transplant, according to the National Kidney Foundation. In Canada, the number of individuals facing kidney failure has climbed 35 per cent since 2009 and nearly half (46 per cent) of new kidney disease patients are under age 65, according to The Kidney Foundation of Canada.
Using the Canadian Light Source (CLS) at the University of Saskatchewan (USask), researchers have developed a better membrane for dialysis machines that could lead to safer treatment and improved quality of life for patients with kidney failure.
Video: Improved treatment for patients with kidney failure
A dialysis machine is used to filter toxins, waste products, salts, and excess fluid from a patient’s blood when their kidneys can no longer perform this function well. However, negative reactions between dialysis membranes and the patient’s blood can lead to serious complications like blood clots, heart conditions, anemia, blood poisoning, infections, and more.
Dr. Amira Abdelrasoul, an associate professor with USask’s College of Engineering, is an expert on membranes and is determined to help patients on dialysis. “I lost a close family member due to dialysis,” she said. “I saw all the complications he experienced and how he suffered. So, I put all my efforts, knowledge, and background into this research area because I would like to support patients and avoid anyone having to lose a loved one from this treatment.”
The new dialysis membrane developed by her team is a significant improvement over those used in hospitals today, according to Abdelrasoul. Some of the commercial membranes currently in use contain heparin, a medicine that reduces blood clots; however, they also have an intense negative charge on their surface that causes serious side effects.
In a paper recently published in the journal Membranes, Abdelrasoul and her team describe how their new membrane not only maintains a reduction in blood clotting but also has a neutral surface that is biocompatible and should lead to improved outcomes for patients.
“This will lead to less cell destruction and means that we could regulate inflammation to prevent any tissue
damage,” she said. “It has a more stable hydration layer that is ten times better than commercial ones. This is the best we have ever achieved.”
The team used the CLS’s BMIT beamline to analyze and develop their membrane.
“Working at CLS was always an amazing experience for me because with advanced-control imaging we could see human serum proteins inside
membrane channels during the flow like never before. Other techniques would only show us the top of the membrane and at the end of the filtration process,” she added.
The BMIT beamline enabled the team to monitor – in real time -- the flow in each layer of their membrane.
“It helped us to understand why and how proteins accumulate and block membranes under different conditions,” she shared. “I believe that the quantitative and qualitative data that we achieved at CLS will lead to a real change for dialysis patients, and of course it’ll make the University of Saskatchewan and Canada leaders in dialysis membrane technology.”
Her research group recently filed a provisional patent for one of the top-performing membrane materials they developed, and they are continuing to test and develop their membrane to ensure it is safe for a variety of patients. They are hopeful that their membrane could have long-term benefits for patients on dialysis.
“This achievement could lead to a reduction in physical and psychological symptoms that patients experience and improve their quality of life,” said Abdelrasoul. ■ H
Anew study from the Peter Munk Cardiac Centre at UHN finds individuals who recovered from mild COVID-19 reported more cardiac symptoms than individuals who had not contracted the disease, furthering our understanding of the long-term effects on the heart of mild COVID-19.
Researchers invited participants who had undergone COVID-19 testing between August 2020 and January 2022 to take part in the study, includ-
ing a group with mild COVID-19 disease and a control group who tested negative for it.
The participants underwent cardiac MRI, echocardiography, a blood test, and assessment of cardiac symptoms and quality of life three to six months after COVID-19 testing, with follow-up evaluations between 12 and 18 months.
This is one of the most comprehensive imaging studies that has been performed after COVID-19 illness.
“At three to six months after COVID-19 testing, we found that the percentage of participants with abnormalities on echocardiography and cardiac MRI was similar between those who tested positive and negative,” says Dr. Dinesh Thavendiranathan, senior author of the study and a cardiologist and clinical scientist at the Peter Munk Cardiac Centre, and Director, Ted Rogers Program in Cardiotoxicity Prevention.
Continued on page 14
ooking to find an alternative medical imaging option that can be easily implemented and provide extra clinical information for the ICU population at the bedside, KA Imaging and Grand River Hospital (GRH) have partnered on an innovative commercialization project supported by the Coordinated Accessible National (CAN) Health Network. Aiming to transform existing hospital workflow
for intensive care unit (ICU) imaging, GRH has added KA Imaging’s Reveal 35C, a device that is designed to simultaneously produce both conventional chest X-ray at low dose and higher-contrast spectral radiographic images for improved patient monitoring and faster, more accurate bedside imaging in its ICU.

The hospital has been measuring success metrics around image quality, impact on work processes, and wheth-
er follow-up imaging was needed after Reveal’s images. Results have been promising in all areas.
Medical imaging plays a critical role in monitoring the condition of ICU patients, commonly to check for conditions like pneumonia or pneumothorax or to rule out other potentially serious pulmonary issues along with verifying the tips of catheters or endotracheal tubes. Imaging in the ICU can be challenging because of reduced patient mobility, the need for imaging outside regular operating hours, and the need for quick imaging turnaround for bedside decision making.
Generally limited on tissue differentiation, portable chest radiography can be ineffective at accurately spotting complex pulmonary issues and sometimes even to localize the tips of lines and tubes. Other modalities like CT are not portable, bring increased radiation exposure, in addition to risks associated with intra-hospital patient transportation. Furthermore, reimbursement for ICU patients is capitated so an unnecessary CT scan increases cost of care and the financial burden for hospitals.
The Reveal™ 35C, created by KA Imaging, is a single-exposure, portable, digital dual-energy subtraction X-ray detector. It’s powered by SpectralDR technology, which produces spectral images that separate materials such as water (ie soft tissue, lung lesions etc) and calcium (i.e bones, retained foreign objects, in dwelling devices or other calcifications) and are higher contrast thus, easier to read for a variety of clinicians of varying ability. It also uses the same ra-
diation dose as a traditional X-ray to create the 3 different images without blurring or streaking due to patient movement.
“Dual energy x-ray technology has been around for years, but it’s the first time we can really see the benefit from it at the bedside” explains Carla Girolametto, Director of Innovation and Research at GRH. According to Girolametto, Director of Innovation and Research at GRH, older versions of the dual energy x-ray technology have their limitations, as they need dedicated rooms, require more radiation than traditional X-ray, and can have image quality issues. The high cost of implementation of older technologies also prevents adoption.
According to KA Imaging, Reveal 35C solves these problems and can be retrofitted onto existing x-ray machines, including portable machines –very used in ICU settings.
KA Imaging’s device has been installed on one of Grand River Hospital’s existing portable x-ray machines and has been piloted to help clinicians validate patient tube and line placements as well as monitor the health of patients to prevent respiratory conditions.
“This is an exciting project and we are pleased to partner with Grand River Hospital to support innovation that will improve patient care and outcomes,” says Amol Karnick, president and CEO of KA Imaging. “This is a great opportunity for Grand River Hospital and KA Imaging to be a showcase for Canadian hospitals, especially the ones that are overburdened and feeling the pressure in their emergency rooms and ICUs” says Karnick.
Canadian manufacturer KA Imaging specializes in developing innovative X-ray imaging technologies and systems. Reveal 35C is currently available for sale as a retrofit solution in Canada. Coming soon, the device will also be available as part of an integrated mobile system. H
Ontarians in need of urgent medical care will soon have a new option to consider thanks in part to the team behind Sunnybrook Health Sciences Centre’s virtual emergency department.

Continued from page 12
“However, those who tested positive for COVID-19 reported experiencing more cardiac symptoms – chest pain, palpitations, shortness of breath –compared to the control group despite only having mild COVID-19 illness.”
Fortunately, at 12 to 18 months follow-up, most patients had improvement in their cardiac symptoms.
‘Reassuring’ symptoms decreased between initial assessment and follow-up
Interestingly, amongst the multitude of cardiac imaging parameters studied, only a single cardiac MRI parameter –native T1 – was associated with higher odds of experiencing cardiac symptoms both at the time of cardiac imaging and at 12 to 18 months follow-up.
T1 mapping is a technique that allows assessment of changes to heart muscle and can indicate increase water (a consequence of inflammation) or scarring.
These findings suggest that although many patients with mild COVID-19 may experience cardiac symptoms months after testing positive, their symptoms don’t seem to be linked to heart structural and functional abnormalities. At 12 to 18 months follow-up, many have resolution
of symptoms, most don’t require hospital admission and none experienced adverse heart events.
“This research helps us better understand the relationship between mild COVID-19 and heart health,” says Dr. Kate Hanneman, a cardiac radiologist and Director of Cardiac Imaging Research at the Joint Department of Medical Imaging and the Peter Munk Cardiac Centre.
“Considering the majority of COVID-19 infections are mild, it’s important we learn all that we can about the long-term effects on the heart particularly in relation to patients who have persistent symptoms even months after COVID-19.
“It is reassuring that symptoms decreased between the initial assessment and longer-term follow-up and that there were no differences in the frequency of abnormalities on imaging between individuals who had recovered from mild COVID-19 and those who had tested negative,” she said. “However, further research is needed to identify risk factors for persistent symptoms and to determine the role of native T1 mapping in guiding management.” ■ H
Sunnybrook’s virtual emergency department launched in December, 2020, as part of a pandemic pilot project involving Unity Health Toronto and University Health Network. Together, the institutions worked to provide Toronto’s Virtual Emergency Department, offering same-day appointments with emergency department physicians from across the city seven days a week.
Amid a decrease in emergency department visits during the first wave of the COVID-19 pandemic, the goal was to reach patients in their homes so they would not have to come to the hospital, service under-served populations, reduce wait times and improve the patient and family experience.
Since it began, Sunnybrook’s virtual emergency department has seen more than 5,500 patients seeking medical attention for health concerns that are not life-threatening.
“Most patients speak positively about it,” says Dr. Justin Hall, an emergency physician and program lead for Sunnybrook’s virtual emergency department. “We often think of virtual care as lesser care but many patients have found it to be a better option.”
Sunnybrook has now received funding from the Ontario Ministry of Health to continue offering this trusted resource in partnership with UHN.
Sunnybrook will also help lead the province’s transition to one regionally coordinated virtual urgent care model.
Under the new model starting this fall, Ontarians will be able to access regional urgent care by contacting
Health811. After speaking with a registered nurse for intake and triage, they will be provided with a link to book an appointment online with a nurse practitioner.

Nurse practitioners are specially trained and authorized to assess, diagnose and treat a wide range of health conditions and can prescribe medications and order some tests. Nurse practitioners offering virtual urgent care will be able to consult with a physician if needed. Patients may also be booked for further testing, a follow-up appointment or a referral to another clinic or specialist.
At a time when emergency departments across Ontario face ongoing pressures, virtual urgent care offers patients with less severe illness another option to consider.
It also represents Sunnybrook’s ongoing commitment to help invent the future of healthcare.
“Technology can help enable urgent care that is timely, compassionate and accessible to all, including under-served patients and those without primary care providers,” says Dr. Hall.
“Ultimately, we hope to see virtual care that is seamlessly integrated with in-person care.”
Sunnybrook President and CEO Andy Smith says he welcomes the move by the Ontario government to extend funding for the virtual emergency department to March 2024.
“As an institution committed to inventing the future of healthcare, we are pleased to be able to offer this leading-edge and trusted resource for Ontarians,” he says.
“We have seen that virtual urgent care aligns with excellent, patient-centered and integrated care delivery and we look forward to continuing to collaborate with our partners in government and across the healthcare system to provide people with this option.” ■ H
A study led by Drs. Dinesh Thavendiranathan, (L), and Kate Hanneman of UHN’s Peter Munk Cardiac Centre is one of the most comprehensive imaging studies that has been performed after COVID-19 illness. Photo: UHN
available (Signature, Supreme & Standard)
extended health plans & two optional dental plans
BONUS
eligible employees under 35
HCP is a voluntary group plan designed for your part-time, casual, contract and temporary employees and retirees. All you have to do is communicate the opportunity to your employees and we handle the rest, including enrollments, premium collection, and claims administration.

It’s really that easy!
To learn more about our plans and HR support programs, reach out today!
1-866-768-1477 x2214 or jatkinson@healthcareproviders.ca

Family physicians who provided more virtual care did not have more patients visit emergency departments (ED) compared to family physicians who saw more patients in-person, according to new research.
The study, led by researchers at Unity Health Toronto and ICES, showed that even after adjusting for patient characteristics like age, medical conditions and income, physicians who provided more virtual care did not have patients who visited the ED more. However, differences in ED visit rates between physician practices largely mimicked patterns seen before the pandemic.
The findings refute speculation that patients were visiting emergency departments more frequently because family physicians were providing too much virtual care. Physician billing codes for virtual care were introduced in Ontario as an emergency measure at the start of the pandemic and became permanent in October 2022.
“The data does not support the allegations that family physicians not
seeing people in-person was driving an increase in ED visits,” said Dr. Tara Kiran, lead author of the study and a scientist at the MAP Centre for Urban Health Solutions at St. Michael’s Hospital and ICES.
“The vast majority of family doctors were seeing people in-person, and those that provided more virtual visits did not have more patients who went to the ED,” said Kiran, who is also a family physician with St. Michael’s Academic Family Health Team.
Researchers analyzed data linked to ICES administrative health records from nearly 14,000 Ontario family physicians from February to October 2021 and their nearly 13 million patients. Physicians were categorized into groups based on the percentage of care they delivered virtually. Most physicians provided between 40 and 80 per cent of care virtually. Over 330 physicians (2.4 per cent) delivered 100 per cent care virtually and over 860 physicians (6.2 per cent) delivered no virtual care.
The mean number of ED visits was highest among patients whose phy-
sicians provided only in-person care (470 visits per 1,000 patients), and was lowest among patients whose physicians provided more than 80 per cent to less than 100 per cent of care virtually (242 visits per 1,000 patients).
The study also found ED visit rates during the first 18 months of the pandemic were lower than pre-pandemic levels. Between 2019 and 2021, there was an overall 13 per cent decrease in the mean number of ED visits in Ontario. Periods in which the ED visit rates were highest did not coincide with periods when family physicians were providing more care virtually.
“This finding is not to say that emergency departments weren’t overcrowded – but it wasn’t because of increased volumes,” said Dr. Rick Glazier, co-author of the study, a senior scientist at ICES, scientist at the MAP Centre for Urban Health Solutions at St. Michael’s Hospital.
“The reasons are likely multifactorial, including patients who put off receiving care due to media reports of high volumes in EDs or fear of getting COVID-19. Staffing shortages
and strained hospital and long-term care capacity also contributed to ED crowding despite lower visit volumes,” said Glazier, who is also a family physician with St. Michael’s Academic Family Health Team.
The findings are in contrast to the authors’ study published earlier this year that found people who attended virtual-only walk-in clinics were more likely to have an ED visit than those who had a virtual visit with any family doctor. The authors say the two papers taken together support virtual care as a tool that supplements in-person care, ideally in the context of an ongoing relationship with a family physician or team. They encourage caution towards virtual-only walk-in clinics where there is no option for in-person care and where the physician has no existing relationship with the patient.
The study was supported by ICES, which is funded by the Ontario Ministry of Health and Ministry of LongTerm Care. The study was also funded by Ontario Health and the Canadian Institutes of Health Research. ■ H
did not lead to more emergency department visits
n initiative aimed at making UHN’s Emergency Department (ED) run more effectively has come up with several methods to increase operational efficiency and decrease wait times at Toronto General and Toronto Western hospitals.

About 60 staff participated in the first phase of the Flow, Access, Safety Throughout in the ED (Fast-ED) Initiative, where frontline health care workers from all disciplines in the ED worked together to improve flow and “time to triage” in two of the busiest sites at UHN.
“Fast-ED is about looking at what’s adding value versus what isn’t,” says Dr. Sam Sabbah, Medical Director of Emergency Medicine at UHN.
Patient flow is a critical component in ensuring the ED operates smoothly and involves a variety of medical care professionals, resources and systems to deliver effective care.
“Improving flow is about applying a critical lens and asking which tasks can be automated, delegated, or eliminated to reduce waste and deliver the most value to our patients and staff,” says Dr. Sabbah.
The first two days of Fast-ED included structured discussions about what was working well and what needed improvement. The rest of the week was spent implementing change ideas developed in these meetings.
To implement change, staff from professions across the ED – including nurses, personal support workers (PSWs), physicians, physician assistants, nurse practitioners and patient care coordinators – participated in brainstorming sessions to find ways to reduce triage process time, improve patient safety, and enhance the patient and provider experience within the ED.
The diversity of the group was crucial for fresh and “outside the box” thinking to come forward.
One idea was cleaning out unnecessary clutter such as printers, paper and other supplies in the photocopy room at TGH – made redundant by the implementation of UHN’s health information system powered by Epic –and transforming the space into a patient exam and treatment room.
“The space was being wasted, so we thought why not turn the room into a patient care area?” says Michael De Wit, ED Manager at TGH.
The team cleaned out the room and transformed the space in just half a day so that it could be used more effectively for blood and specimen collection.
“This new and enhanced space is a functionality that the team plans to keep moving forward,” Michael says.
Another change idea that was implemented was leveraging PSWs to help with triage by delegating tasks previously performed by nurses such as bringing patients into rooms, helping them change into gowns, and checking that they have the appropriate patient identification and allergy bands.
“I’m excited to be able to contribute more to my team and ensure that
our patients remain safe,” says Lourdes Abaday, a PSW at TGH, who was part of the brainstorming group during the workshop and a key member of the team implementing suggested changes within the PSW profession on the frontlines.
“The beauty of this initiative is that it empowers people who do the work to create solutions that will make their work more effective and enjoyable,” says Dr. Sabbah. “People’s voices are being heard, which encourages them to bring forth more suggestions on how to make improvements in the future.”
Triaging patients is a key step in the ED flow process – prioritizing cases based on severity.
The current state of “time to triage” in UHN’s ED is 18 to 20 minutes on average. When a patient comes into the ED, they screen at the front desk, visit the triage nurse, and then register, with additional minutes of waiting added in between each step.
One of the priorities of Fast-ED was to trial combining the screen-

ing and registration processes at the same time, resulting in fewer points of contact between the patients and staff.
“With this change idea, patients no longer need to stand up, sit down, and take their health card out multiple times, all of which increases the average time of a patient’s visit in our Emergency Department,” Michael says.
Taking the process from three steps – screening, triaging and registering – to just two – screening and registering combined – can save a significant amount of time in the ED flow process.
“Shaving a minute off here and minute off there eventually adds up to hundreds of thousands of minutes over time,” says Dr. Sabbah.
At TWH, the team also reorganized unclear signage causing issues with wayfinding at the ED entrance.
“Staff have said that it’s impacted their work in a positive way by simplifying their workflow,” says Anna Nowacki, Emergency physician at TWH. “After implementing new clear, universal signage, patients are experiencing less
uncertainty about navigating their way through entrance to registration.”
Another area that was particularly improved was the role of the triage nurse. They can now start treatment right away, as patients are immediately given a wristband upon registering which allows to do things such bloodwork and electrocardiograms earlier in the process.
“The wristbands also result in a safer process for patients, because staff are able to identify who is being registered right away, rather than confusing two people in the waiting room with the same name,” says Dr. Nowacki.
“It was inspiring to see front-line ED staff motivated and excited to make

changes that were meaningful to them,” says Sabrina Bennett, Clinical Director of UHN General Internal Medicine, ED and the Family Health Team.
“The positive impact of these

changes ensures the success of our future FAST-ED events where we anticipate looking at other time points in an ED patient’s journey throughout the department.”
The second phase of the Fast-ED Initiative is set for September, with goals to decrease time to discharge, as well as time for diagnostic imaging of lower acuity patients. ■ H


Medline helps clinicians deliver advanced wound care with our wide variety of products and programs. Our DIMES system of wound bed preparation and treatment includes Debridement, Infection/Inflammation, Moisture Balance and Edge/Environment.

 The Fast-ED Team at Toronto General Hospital involved staff from all professions across the ED, including nurses, personal support workers, physicians and patient care coordinators.
The Fast-ED Team at Toronto General Hospital involved staff from all professions across the ED, including nurses, personal support workers, physicians and patient care coordinators.
Two residents practice a procedure called a bougieassisted cricothyrotomy. Jamie Riggs, a fourth-year resident, said, “Skills day is, in my opinion, the best and most useful academic activity we do all year. My only complaint is that we don’t get to do something similar more often.”
Inside St. Michael’s Hospital a tense scene is unfolding.
“The patient is a 32-year-old pregnant female,” Dr. Emily Austin, an emergency physician and trauma team leader, announces to the room. “Five minutes out.”
A group of medical residents, emergency nurses and respiratory therapists close ranks around a hospital bed, huddling together to split up duties.
“I’ll lead,” says one. The others nod. The patient arrives and the clinicians begin to move. One steps onto a bedside foot stool and starts chest compressions, another picks up a scalpel. They call out information to each other, listing steps aloud and ordering more intravenous medication. Some-

one verbally marks each tense minute as it passes.
The procedure they’re conducting is called a resuscitative hysterotomy, a rare event when an emergency C-section must be performed on a patient in cardiac arrest. Everything about the scene seems real – the intensity, the sounds, the whirring machines – and that’s exactly how Unity Health Toronto’s simulation program wants it to be.
The patients – both mother and baby – are simulation “manikins”, and the scenario has been set up by highly trained instructors, simulation educators and specialists who are guiding a group of interprofessional clinicians through real-time training for emergencies they could encounter in their
careers. It’s all part of a specially designed critical care skills training day.
Every year St. Michael’s hosts this day for senior University of Toronto emergency medicine residents, nurses and respiratory therapists in its stateof-the-art simulation centre. More than 300 participants have completed the training. They practice a variety of skills like inserting chest tubes, handling difficult or obstructed airways, and even run through complicated emergency scenarios like the resuscitative hysterotomy and emergency thoracotomy.
“These procedures are known as high acuity, low occurrence – or HALO – events,” says Dr. Andrew Petrosoniak, an emergency physician at St. Michael’s and the co-director
of skills day alongside Dr. Sara Gray, emergency physician and intensivist. HALO procedures are hard to prepare for because they happen so infrequently, meaning medical professionals often don’t get a chance to see what they look like in real life before having to respond to one.
“When I was training we didn’t have such comprehensive simulation sessions like this,” says Petrosoniak. “Of course there were ways to practice skills, but your first time really experiencing or performing that procedure would be when it was actually happening.”
Critical care skills day, now in its ninth year, is a huge draw for residents across Toronto, as well as nurses and respiratory therapists from St.


Michael’s, to hone their abilities. The Simulation Program team goes to great lengths to make it as educational and realistic as possible. Simulation Specialist Sue Zelko, who played a key role in the design and flow of the day, said the team spent almost 40 hours putting together props for the simulated scenarios – using materials like yoga mats, water balloons and outdoor furniture cushions to create realistic models.
Participants get a chance to learn from emergency medicine, critical care and trauma surgery experts, and get hands-on practice that will prepare them for difficult cases down the line.


Dr. Evelyn Dell, now an emergency physician and trauma team leader at St. Michael’s, attended skills day as a resident. That year trainees practiced a procedure called a cricothyrotomy, when a doctor has to make an incision in a patients’ throat to open up the airway. Dell found herself having to perform one in an emergency situa-
tion within a year of the training. As a staff physician, she also performed the procedure once more with a positive outcome for the patient. She says skills day gave her the confidence and comfort to handle both cases.
“The training helped me develop an element of muscle memory for procedure performance,” says Dell. “I believe it also reduces error and streamlines decision making.”
The St. Michael’s emergency department is one of only two Level I trauma centres in Toronto. The program is working towards being accredited as a Level I centre by the American College of Surgeons, a designation that has only been achieved by one other hospital outside of the United States. Events like skills day are part of the culture that makes St. Michael’s such an excellent place to be treated for emergencies and trauma.
Back in the simulation centre, the resuscitative hysterotomy ends. The baby sits safely on a small delivery table,
swaddled in a white blanket and the manikin mother lies supine on the bed.

Dr. Austin applauds the group.
“That was really, really great,” she says, met with smiles from the train-

Resident Hanna Jalali practices a procedure called ultrasound guided central venous catheter insertion.
Interested in a provincial certificate through Emergency Management Ontario (EMO)?
You can receive both a record of completion from George Brown College and an EMO certificate with the following courses:
BEM: Basic Emergency Management
Basic Incident Management System 200
Intermediate Incident Management System 300
ees who exchange high-fives and pat each other on the back. Then she’s back to teaching mode. “Now let’s talk about physiological changes in pregnancy.” ■ H
Explore
Our programs are geared to health and security professionals and can be conveniently completed at your own pace on a course-by-course basis. You can pursue these programs fully online or by taking a mix of online and on-campus delivery methods. We also offer courses through compressed delivery and provide corporate training opportunities, such as in emergency exercise design.
Emergency Management Program
Public Health Emergency Management Program
For more information, contact us at 416-415-5000, ext. 6651, or kmelo@georgebrown.ca
Olivia Lavery is a Communications Advisor at Unity Health.
ffective communication is crucial in the medical profession, but how do internal medicine residents develop their communication skills?
A recent study led by Dr. Shiphra Ginsburg, a clinician-scientist at The Institute for Education Research (TIER) at UHN and the Wilson Centre for Research in Education at UHN, found that while formal communication training was valuable, it was limited in scope.
Instead, residents found working independently with patients to be the most instructive for developing their skills.

The study was conducted between November 2020 and January 2021, and involved 15 virtual, one-on-one interviews with internal medicine residents. The interviews explored how the residents developed their communication skills and the role of formal training in this development.


“Participants consistently stated that interacting directly with patients contributed most to the development of their communication skills,” says Dr. Gabriel Burke, a resident in respirology at Mount Sinai Hospital and the lead author of the study. “Through these interactions, residents were able to identify communication techniques that they found effective, enabling them to gradually develop their own unique, natural and authentic style.”
“Residents learned strategies for communication through observing staff physicians, rather than from staff observing their interactions with patients and receiving feedback,” adds Dr. Lindsay Melvin, a clinician-investigator at TIER and co-author of the study. “Any direct feedback that they did receive was often positive, generic and not very actionable.
“Moreover, when staff were directly observing communication interactions, residents often felt the need to




deviate from their authentic practice,” adds Dr. Melvin, who is also an assistant professor in the Department of Medicine at the University of Toronto (U of T).
Many participants also described the pressure to become faster with communication due to workload demands.
The study’s findings suggest that in the inpatient setting, residents developed their communication skills primarily through self-reflection on unobserved interactions with patients, with smaller contributions from formal training and feedback from staff physicians.

“Effective communication in medicine is crucial for building trust with





patients, as well as ensuring that patients have a clear understanding of their health and the treatments available to them,” says Dr. Ginsburg, who is also a staff physician at Sinai Health and a professor in the Department of Medicine at U of T. “Medical educators should consider incorporating patient feedback when working with residents, as well as providing more specific and actionable feedback on communication skills.
“By doing so, medical educators can help ensure that future physicians are better equipped to communicate effectively with their patients – and ultimately, improve the quality of care.” ■ H

As the complexity of chronic diseases evolve and rates rise in Canada, St. Joseph’s Health Care London hopes to help create a new generation of pharmacists with expertise in outpatient care of a rapidly growing patient population.
St. Joseph’s has launched a residency program for pharmacists focused on outpatient chronic disease management and the critical role of pharmacists in providing wholistic care to patients. The intensive, one-year program for new pharmacy graduates is one of few in Canada providing handson training in team-based, outpatient hospital care for chronic diseases and conditions. With placements at all five
St. Joseph’s sites and in a variety of clinical settings, the pharmacy resident will complete training within the Pain Management Program, Rheumatology Centre, Palliative Care Unit, Rehabilitation Program, Mental Health Care Program, and the organization’s outpatient community pharmacy, with electives available in forensic mental health care and other specialties.
Particularly unique is what the pharmacy resident will learn about the connection between chronic disease, mental health and rehabilitation, establishing trusting relationships with patients, and the integral role of pharmacists as a member of a broad team of health care professionals, explains Denise Kreutzwiser, who led the de-
Our curriculum is designed to provide internationally educated health professionals with enhanced skills and knowledge, and to bridge the gap between their existing education and experience with their career goals in Canada.
The Bridging Medical Laboratory Science program caters to internationally educated medical laboratory technologists who are seeking to integrate into the Canadian healthcare system. This program equips students with the necessary knowledge and competencies to write the CSMLS National Certification Exam with the goal of practicing in their field of medical laboratory science in Canada.
The Bridging Radiological Technology program is aimed at internationally educated medical radiological technologists. Participants enhance their proficiency in imaging technology, patient care, and professional communication, aligning with Canadian standards. This program helps students prepare to write the CAMRT national certification exam and ultimately gain entry to practice in Canada.
The Bridging Ultrasound course is designed for internationally credentialled Sonographers with prior education and experience in ultrasound. It offers specialized in-class training, honing advanced skills in ultrasound techniques and technologies, crucial for effective clinical practice, with the goal of preparing students to write Sonography Canada’s Canadian Clinical Skills Assessment (CCSA) Exam. For more information, visit https://michener.ca/academic-programs/bridging-programs-2
THERE ARE ONLY 130 RESIDENCY SPOTS
ACROSS CANADA FOR YEAR ONE PHARMACY RESIDENTS – PREDOMINANTLY IN HOSPITAL ACUTE CARE PHARMACY.
velopment of St. Joseph’s pharmacy residency program.
“No other Canadian pharmacy residency program offers an intensive focus in interdisciplinary chronic pain management or rheumatology, addressing a critical need identified by the national bodies of those specialties to better understand and serve those living with chronic pain or rheumatic and musculoskeletal diseases,” says Denise.
With applicants applying from as far as Qatar and Australia, the successful inaugural pharmacy resident is Sumani Vij, a graduate of University of Waterloo’s School of Pharmacy. Drawn to the ambulatory care focus at St. Joseph’s, Sumani says the training opportunity is the ideal middle ground between acute care and community pharmacy work.
“You’re able to create pharmacist-patient relationships, which I really like, but also to collaborate with many allied health professionals – social workers, occupational therapists, nurses, physiotherapists and others,” says Sumani. “You get the best of both worlds.”
While pharmacy rotations during the four years of pharmacy school are compulsory, a residency after graduating and passing the certification exams is voluntary, explains Denise. A residency is additional training that provides pharmacists with proficiency in a particular area. There are only 130 residency spots across Canada for year one pharmacy residents – predominantly in hospital acute care pharmacy.
“Our program is so unique because it’s not an acute care hospital residency program,” says Denise, a pharmacist
with St. Joseph’s Pain Management Program. “There are just a handful of ambulatory or chronic disease-based residency programs in the country.”
The program, she adds, embraces the continuity of care concept. An inpatient rehabilitation rotation provides the pharmacy resident with insight into how patients with chronic conditions travel through the health care system and how pharmacists support patients during transitions in care.
Not only does the pharmacy resident emerge from St. Joseph’s with proficiency in chronic disease management but also in helping patients make important changes to improve their health. It’s the only Canadian residency program providing 30 hours of specialized training aimed at helping health care providers support patients in making lasting behaviour changes for overall wellness.
“These elements, along with the unique culture at St. Joseph’s, having patients and caregivers help shape the program to ensure their perspective and lived experience is featured, and the provision of care through the lens of equity, diversity, inclusion and belonging creates a learning experience like no other,” says Denise.
For Sumani, it was the opportunity she was seeking. Particularly intriguing, says the driven 25-year-old, “is the focus on chronic pain and mental health, how complex and intermingled they can be, and the pharmacist’s role in supporting patients and making sure they are being treated wholistically – from all angles and by multiple disciplines.”
She also looks forward to an elective in forensic mental health care – a rare
learning opportunity in Canada – and a rotation in palliative care, which she describes as another unique role for pharmacists because “it’s about looking less at what you can prescribe and more at what you can take away to ensure the patient’s comfort.”


While just getting underway, St. Joseph’s pharmacy residency program has already drawn attention with numerous applicants for the first year and other organizations reaching out for advice on setting up their own residency programs, says Andrey Andriets, Director of Pharmacy Services. The plan is to grow the program and offer more than one spot in subsequent years.
“Pharmacy Services is pleased to contribute to the extensive teaching role of St. Joseph’s and advance pharmacy learner opportunities with a focus on ambulatory care of tomorrow,” say Andrey.
Sumani chose pharmacy as a profession because of its growth and


evolution in recent years related to prescribing powers, opportunities to forge relationships with patients, and the diverse workplace options. As she begins her learning journey at St. Joseph’s, she looks forward to
gaining experience, confidence and knowledge that will shape her future career, and all the possibilities that loom.

“Within pharmacy there’s a whole world to explore and I want to see
where I fit best,” says Sumani. “St. Joseph’s residency program is super well rounded and offers really unique electives. I’m excited by everything it offers. I want to learn and create a better version of myself.” ■ H
To learn more, visit our website at michener.ca/ce and dive deeper into our offerings with the 2023 Continuing Education brochure

Elevate your career through our expert-led, cutting-edge programs, courses, workshops and micro credentials – designed to fuel your success in the healthcare industry. Your journey starts here.
Astudy of ChatGPT found the artificial intelligence tool answered less than half of the test questions correctly from a study resource commonly used by physicians when preparing for board certification in ophthalmology.
The study, published in JAMA Ophthalmology and led by St. Michael’s Hospital, a site of Unity Health Toronto, found ChatGPT correctly answered 46 per cent of questions when initially conducted in Jan. 2023. When researchers conducted the same test one month later, ChatGPT scored more than 10 per cent higher.
The potential of AI in medicine and exam preparation has garnered excitement since ChatGPT became publicly available in Nov. 2022. It’s also raising concern for the potential of incorrect information and cheating in academia. ChatGPT is free, available to anyone with an internet connection, and works in a conversational manner.

“ChatGPT may have an increasing role in medical education and clinical practice over time, however it is important to stress the responsible use of such AI systems,” said Dr. Rajeev H. Muni, principal investigator of the study and a researcher at the Li Ka Shing Knowledge Institute at St. Michael’s.
“ChatGPT as used in this investigation did not answer sufficient multiple choice questions correctly for it to provide substantial assistance in preparing for board certification at this time.”
Researchers used a dataset of practice multiple choice questions from the free trial of OphthoQuestions, a common resource for board certification exam preparation. To ensure ChatGPT’s responses were not influenced by concurrent conversations, entries or conversations with ChatGPT were cleared prior to inputting each question and a new ChatGPT account was used. Questions that used images and videos
Anna Tersigni, Director of Quality & Risk, Chief Privacywere not included because ChatGPT only accepts text input.
Of 125 text-based multiple-choice questions, ChatGPT answered 58 (46 per cent) questions correctly when the study was first conducted in Jan. 2023. Researchers repeated the analysis on ChatGPT in Feb. 2023, and the performance improved to 58 per cent.
programs. Given her vast professional experience, she has also participated as faculty on a few programs.

If you truly want to be an informed quality/risk/health information management/privacy professional, the OsgoodePD curriculum will not only help you in your role in any healthcare organization – it will lead to much better outcomes for the vulnerable people we support...
programs have advanced Anna Tersigni’s career and kept her inspired: osgoodepd.ca/blog-hn
“ChatGPT is an artificial intelligence system that has tremendous promise in medical education. Though it provided incorrect answers to board certification questions in ophthalmology about half the time, we anticipate that ChatGPT’s body of knowledge will rapidly evolve,” said Dr. Marko Popovic, a co-author of the study and a resident physician in the Department of Ophthalmology and Vision Sciences at the University of Toronto.
ChatGPT closely matched how trainees answer questions, and selected the same multiple-choice response
as the most common answer provided by ophthalmology trainees 44 per cent of the time. ChatGPT selected the multiple-choice response that was least popular among ophthalmology trainees 11 per cent of the time, second least popular 18 per cent of the time, and second most popular 22 per cent of the time.
“ChatGPT performed most accurately on general medicine questions, answering 79 per cent of them correctly. On the other hand, its accuracy was considerably lower on questions for ophthalmology subspecialties. For instance, the chatbot answered 20 per cent of questions correctly on oculoplastics and zero per cent correctly from the subspecialty of retina. The accuracy of ChatGPT will likely improve most in niche subspecialties in the future,” said Andrew Mihalache, lead author of the study and undergraduate student at Western University. ■ H
“CHATGPT MAY HAVE AN INCREASING ROLE IN MEDICAL EDUCATION AND CLINICAL PRACTICE OVER TIME, HOWEVER IT IS IMPORTANT TO STRESS THE RESPONSIBLE USE OF SUCH AI SYSTEMS.”
designed
for a rapidly-changing healthcare landscape.

Open to all learners, an Osgoode Certificate is a micro-credential that gives you the opportunity to learn from industry leaders with expertise and experience.



• Expand your practical legal knowledge and skills in a targeted area
• Designed by and for working professionals your schedule
• Build your network with an influential, professional network
To preview program content, visit: osgoodepd.ca/health-hn

Starts September 27, 2023
Discipline in the Ontario Health Care Sector
Starts November 8, 2023
Starts December 5, 2023
Starts January 16, 2024
Starts March 5, 2024
Obstetrical emergencies are rare, but when they happen nothing is more important than a team of highly trained and skilled nurses and physicians.
On Wednesday, July 26, Niagara Health (NH) hosted an emergency simulation kick-off event in the Women and Babies Unit. The St. Catharines hospital recently purchased a SimMom so that staff can practise mock codes and intense childbirth emergency situations in a safe learning environment. The SimMom is a high-tech, interactive mannequin that can be used in high-risk delivery and post-delivery simulation events to assist with the gap between theory and practice.
“Interprofessional simulations provide an excellent learning opportunity for healthcare teams in the closest


thing to real life,” says Debbie Audet, Advance Practice Nurse with Niagara Health. “So, when an emergency does happen, our staff will approach it with a sense of confidence, knowledge, skill, teamwork and interprofessional collaboration.”
SimMom has the ability to talk, breathe, bleed, have seizures, and push as if she is actually giving birth.
NH nurses and physicians participated in two obstetrical emergencies during Wednesday’s simulation, including a post-partum hemorrhage and seizure that required quick action from the team. The SimMom was given the name Mary, an 18-year-old patient complaining about feeling dizzy after giving birth about one hour earlier.
During one of the simulations, the initial nurse noticed excessive bleeding and called for four more registered nurses, followed by obstetrician Dr.
The Joint Health and Safety Committee (JHSC) – Foundational in creating a safer and healthier workplace, the JHSC certification helps to achieve compliance and excellence in occupational health and safety. PSHSA understands the importance of prioritizing employee safety and well-being, offering flexibility in the mode of delivery through in class, online and self-paced eLearning with the option of having training held at your workplace for ten or more learners needing certification.
With a learner-centred approach to training, participants learn about workplace-specific hazards through guided instruction. This approach helps enhance the knowledge and skills required to meet the learning objectives and the requirements of the JHSC Training Program Standard.
Our Health and Safety Consultants facilitate using their sectorspecific expertise in public sector workplaces, including healthcare. The hazard-specific modules designed for part 2 certification were selected based on input from employers and labour stakeholders. These modules address the greatest risks faced by workers in workplaces like yours.
Visit our website today to register!
Emily Baker, who diagnosed the teen with postpartum hemorrhaging. A flurry of activity ensued as the team worked to stabilize the patient before the simulation concluded.
“By simulating these emergencies with the SimMom, it can increase confidence levels, identify areas for improvement, and improve teamwork and communication,” Audet says. “All of which improve patient safety and outcomes.”
The Laerdal Medical team was at the St. Catharines Hospital to facilitate Wednesday’s event. “Niagara Health was chosen to pilot our Accelerate OB program in Canada because they are passionate about safety and investing in their people,” says Russell Smith, Business Development Sales and Program Manager with Laerdal Medical, which created SimMom.
SimMom has the ability to talk, breathe, bleed, have seizures, and push as if she is actually giving birth.
“As a nurse, I can say finding an employer who values their staff and invests in their success is really important to providing safe care and developing as a professional,” he says.
The SimMom is an investment in staff training at the St. Catharines’ Women and Babies program and will be built into the orientation process for new hires. It will also be integrated into the everyday culture of practice and emergency preparedness.
In addition to the SimMom, Niagara Health’s Pediatrics department has also purchased a SimBaby that will be integrated into that program’s training. The goal is to eventually create simulations that start with a SimMom birth and transition into caring for a SimBaby.
“I’m super excited to see what the future is going to bring,” Audet says. ■ H
Diane Moore is a Communications Specialist at Niagara Health.“BY SIMULATING THESE EMERGENCIES WITH THE SIMMOM, IT CAN INCREASE CONFIDENCE LEVELS, IDENTIFY AREAS FOR IMPROVEMENT, AND IMPROVE TEAMWORK AND COMMUNICATION.”
 By Marlene Leung
By Marlene Leung
Anew pilot program at St. Michael’s Hospital provides mentorship to high school students from communities that are under-represented in the field of cardiac surgery, in the hopes of developing more diversity in the profession.
The Next Surgeon program, launched earlier this year by Unity Health Toronto and Toronto Community Housing, brought about 25 high school students into St. Michael’s to study cardiac surgery over the winter.

Dr. Bobby Yanagawa, head of the Division of Cardiovascular Surgery, founded the program with medical school students Akachukwu Nwakoby
and Lina Elfaki as a way to tackle the lack of diversity in the field.
“If you look at the cardiac surgeons across the country, only about 10 per cent are female, and we don’t have much ethnic diversity. Never in the history of this country have we had a Black heart surgeon, and we’ve only had one Indigenous heart surgeon,” said Yanagawa.
“We want the best and brightest to become heart surgeons, and it’s my belief that talent is equally distributed in all people. If we’re only getting talent from one group of people, then we’re missing out on some brilliant future surgeons.”


At first, the three wanted to develop a program that would encourage more diversity at the residency level. They soon realized that if they wanted to be
impactful, they had to start outreach earlier, said Yanagawa.
Through a contact at Toronto Community Housing, a group of interested high school students signed up to complete the program, which included men-
toring, Q&A’s with prominent Black cardiologists and anesthesiologists, and a skills training, where students completed an online suturing course.
Continued on page 30

hat contributes to an enriched learner experience at UHN?

When Lisa McQueen, a speech-language pathologist (SLP) in Toronto Rehab’s Brain Rehab Program, posed that question to SLP students in a pre-placement survey she developed and has been sharing with incoming students since 2007, the number-one response was: “I want to feel safe” – to ask questions, when caring for patients and even to make mistakes.
To meet this expressed need, the program embraces paired placements, or, buddy systems, where two or more students work collaboratively, under the supervision of one clinical educator.
“We are starting to see more and more enthusiasm around collaborative learning models within the Allied Health group,” says Lisa, who is also the Site Coordinator for SLP placements across Toronto Rehab.
“There are obvious benefits to learners as well as patients – but we’re also recognizing how this approach can impact clinical educators as well.”
Former SLP learners Paige Saltsman and Melanie Lamarca say their paired placement helped them feel more comfortable in their roles – especially in their early days – since they were able to plan, practice and implement assessments and treatments together.
“The alternative may have made me feel more confused and alone, with nobody to work through my questions with,” reflects Melanie.
Paige agrees, adding that, knowing Melanie had her back, she felt safer taking risks and bouncing around questions about newer, more complex concepts.
“I remember feeling unsure about the type of aphasia one of our patients was experiencing,” Paige says. “It felt good to be able to talk it out with one-another in a safe space.”
As their learning advanced, and they transitioned from shared to independent practice, the habits they formed approaching care as a duo increased their sense of confidence and made for a smoother switch.
“Even during independent practice, we still supported each other’s clinical growth,” says Melanie.
When faced with treating a patient with non-fluent aphasia, it had been Paige’s experience with a similar patient that helped guide Melanie’s assessment. They even brainstormed treatment plans together, making Melanie feel more confident when sharing her ideas with her educator.
“Sharing my insights helped solidify my own learning, too,” says Paige. “It was a win-win.”


And the benefits of a paired placement impact educators, as well, making their involvement with learners more meaningful and efficient.
“I make a point of ensuring my learners know I’m here, every step of the way, to support their clinical experience,” Lisa says. “But instead of coming to me first with questions, they appreciate collaborating with their peers.
“This also allows me more time to focus on my own work, whether that be catching up on essential administrative tasks or caring for patients.”
But in the end, it’s patients who benefit most from paired placements.
“Imagine a world where a patient is being treated by not one but three clinicians, passionate about their shared discipline,” says Lisa.
“By intensifying rehab – since more learners can result in more therapy –and bringing multiple perspectives to treatment plans, we’re enhancing care for patients.”
Through 250 responses and over 560 comments, the desire to feel safe











OntarioMD (OMD) is excited to announce that our OMD Educates: Digital Health Conference 2023 will be back in person on September 28 at the Beanfield Centre in Toronto. Join us for a full day of interactive discussions, networking, and learning focused on optimizing the use of EMRs and digital health tools to be benefits, not burdens, to your practice.

The conference keynote features André Picard, one of Canada’s top health & public policy observers and commentors. Other conference features include EMR training workshops with OMD Peer Leaders and CME accredited (For Family Physicians and Specialists) sessions on relevant topics to clinicians including cybersecurity, reducing admin burden, AI, quality improvement and optimizing billing. A new addition to the conference this year is our short snappers’ stream which will feature new innovations your colleagues are using to help reduce admin burden and enhance patient care.

Let Bayer support you in your educational journey
during their placement is one of four main themes learners expressed in the pre-placement surveys. Others include: wanting the opportunity to improve skills; feedback on how they’re doing; and, knowing what to expect before and during their placement.
“The goal of these surveys was to get inside students heads, so we could be better supervisors,” says Lisa, who, along with colleague Steve Wilcox, was invited to present her results last fall at the American Speech and Hearing Association – an international conference of 15,000 attendees.
The survey reflects Toronto Rehab’s commitment to developing the next generation of care providers, by ensuring exceptional educational experiences.

And, as UHN, a teaching hospital, welcomes about 5,000 new clinical learners, this year alone, across the organization, spreading this approach couldn’t come at a better time. ■ H



This article was submitted by UHN News.
The students also met with Nwakoby and Elfaki, two Black medical school students, to hear about their journeys to medical school, and get tips and tricks about perfecting their university applications.
“Growing up, I was one of the few Black male students in my science classes in both high school and university. I rarely saw Black medical students and Black doctors, let alone Black cardiac surgeons,” Nwakoby said.
“I wanted the students to see that medicine and surgery is a very possible career path for them, despite being from an under-represented group. I also realize that by virtue of my background, I may share unique experiences with some of the students.”
Nwakoby credits his own mentors and a high school co-op placement he completed at Credit Valley Hospital
with sparking his desire to become a physician. “My supervisor (at Credit Valley) was the only Black male in my department. He went above and beyond to make me feel integrated in the hospital,” he said.
Participating students said they enjoyed the program, and particularly valued the chance to speak with mentors who represented their communities.
“It was just very uplifting to be able to work with mentors who know how I feel and have gone through similar experiences as me,” one Grade 10 student said.
The program, which Yanagawa hopes to grow with the help of sponsors, also allowed participants to form new friendships with like-minded
students who are also interested in science.
And as much as the students gained from the program, it was just as rewarding for the physicians and mentors involved.
“Seeing the students ask thoughtful questions and attempt to sew simulated blood vessels re-kindled the spark I have for teaching and mentorship,” said Nwakoby. “It was also very rewarding to hear that some of them became interested in medicine and got accepted to their top university choices.”
Yanagawa agrees. “The kids always give you a lot of energy – energy that comes from their aspirations and dreams. It’s a wonderful feeling to contribute to that,” he said. “Oftentimes I would say that we adults got more satisfaction and joy from it than the students themselves.” ■ H
ver the past number of years, Canada’s housing crisis has made news headlines. Many of these stories have focused on the fact that the demand for homes exceeds supply. Other news stories have highlighted that aspiring home owners are shut out of purchasing due to record-high housing costs.
Another subject that has been discussed in the news, and one that –from my perspective – deserves even greater attention, is the need for affordable and accessible housing to be developed and maintained. It is presumably the case that having affordable and accessible housing available for residents is valuable in and of itself. However, having this type of housing available is also directly related and relevant to the strength of our health care system for at least two reasons.
First, we know that housing is a social determinant of health. People who are insecurely housed are at increased risk of experiencing food insecurity, chronic illness, infectious disease, as well as so much more.

The second reason that housing is directly related to our health system is because a lack of accessible, affordable, and available housing means that some people who are admitted to hospital may have no suitable discharge destination. In other words, some patients may be medically ready for discharge, but remain admitted for a greater amount of time. To demonstrate this challenge, consider the following case:
Ms. W is a 53-year-old teacher who lives in the east end of Toronto, Ontario. Ms. W has lived in a 3-storey walk-up apartment building for the past 15 years. Ms. W lives alone and immensely values her independence. Three weeks ago, Ms. W was in a bicycle accident. A person walking nearby saw Ms. W lying on the ground next to her bike and called Emergency Medical Services, who brought her to the local acute care hospital. While in acute care, it was discovered that Ms. W had a severe concussion, multiple fractures, and a broken hip. She required surgery and remained in acute care for 3 weeks. Ms. W was motivated to get back
to her “old self” and was transitioned to a nearby rehabilitation hospital with the hope that she could regain her previous cognitive and physical functions. Unfortunately, due to Ms. W’s previous medical comorbidities, as well as some unanticipated consequences associated with her accident, Ms. W plateaued after 2 weeks of rehab, remained reliant on a wheelchair, and was unable to walk up stairs safely.
At this point in time, Ms. W was medically ready to be discharged, but her apartment building is a walk-up (i.e., no elevator or accessible entrance). From the clinical team’s perspective, the only possible discharge options were: (1) discharge Ms. W to her apartment, where she would be carried on a stretcher to her (small) unit, and require a paid service to transport her out of her home when needed, (2) discharge Ms. W to a long-term care home (LTC), (3) discharge Ms. W to a different, accessible building. None of these options were immediately available, affordable, nor desired.
Consequently, Ms. W remained in-hospital for a longer than necessary period of time.
As an ethicist working in a postacute care setting, I can say with confidence that versions of the above scenario arise all too frequently. The lack of available, affordable, and accessible spaces for Canadians means that some medically stable patients may need to remain in-hospital (i.e., use hospital beds and resources) for longer than necessary periods of time.

In relation to the above scenario, each discharge option may seem reasonable upon first glance. However, there exist meaningful and important challenges associated with each.
The challenge with the first option is that Ms. W would be unable to navigate living in her apartment building in a way that contributes to her overall health and well-being. With Ms. W being unable to walk up multiple flights of stairs, she would need to rely
on (and pay for) external providers to carry her outside whenever needed. This may be unfeasible from a financial perspective, nor desired from a quality of life standpoint.
The second option of discharging to LTC is a possibility, but Ms. W may be hesitant to pursue this option because of the setting and population of residents who live in LTC.
As a 53-year-old teacher who values independence, the idea of residing in a communal environment with LTC residents may be undesired, particularly when thinking about quality of life and mental well-being. Furthermore, even if she agreed to LTC, she may have to wait for years to get a place at a desired location.
The third option of discharging to an accessible building may seem most reasonable, but the lack of affordable places make this plan moot. This option, namely, the one that
may be most seemingly reasonable, is the one that requires changes to occur in regard to public priorities and commitments. Building residential spaces that are available, accessible, and affordable (the 3 As) will be of benefit to (a) all individuals’ health and well-being, since housing is a social determinant of health, as well as (b) our health care system given the number of people who are or may be in positions like Ms. W. Ultimately, insofar as housing is a social and systemic determinant of health, this ought to be a priority. ■ H
Andria Bianchi, PhD, is a Clinical Ethicist at Unity Health TorontoCentre for Clinical Ethics, where she offers ethics support to postacute care settings. She is also an Assistant Professor (status-only) at the Dalla Lana School of Public Health – University of Toronto.
Continued from page

Collaborating with people and partners who are Indigenous, Francophone, and members of the2SLGBTQ+ community was paramount to our collective success.
Of course, none of this would be possible without our staff, who are at the heart of everything we do. Their compassion, dedication and expertise inspire and deepen my own commitment to our cause. I am so grateful to our staff and honoured to lead such a remarkable team. This year we prioritized launching (and in some cases relaunching) leadership development programs for emerging, front line leaders, and seasoned leaders as part of our investment in ensuring every Waypoint staff has opportunities to learn and grow within the organization. The combined impacts of demographic shifts and the pandemic have further highlighted the
critical nature of these efforts. Enabling our staff to continuously improve and develop is essential to maintain our commitment to delivering evidence-based, compassionate mental health, addictions, and specialized geriatric care that our patients, clients, and their families expect and deserve.

We were humbled to have achieved a Mental Health at Work® Certificate of Merit from Excellence Canada in recognition of many years of commitment to workplace mental health, psychological safety and wellness. Given our unique role in Ontario Central region, we’ve been pleased to be leading a strategy for organizational health and staff well-being on behalf of hospitals across our region, that is now expanding to the Community Support Services sector.
Looking back at the past year, I am grateful for and inspired by the
unwavering dedication of our team who have been so mission driven and collaborative in providing exemplary care to those in need. We are steadfast in our commitment to continue to overcome obstacles and learn and grow together. With our strategic plan and enabling plans guiding us, we continue to Serve, Discover and Lead in the collaborative #WaypointWay, strengthening partnerships to improve care and shape the transforming healthcare system, engaging in meaningful research and co-design with those we serve, and investing in leaders and efforts to improve the staff and patient experience. The future really is bright at Waypoint.
As I said last summer, these are challenging but exciting times – I can’t wait to see what new adventures year two brings. When I look at those around me, I have full confidence we will rise to the challenges, continue to innovate and grow, and be servant leaders in our communities and in a transforming health system. ■ H
Dr. Nadiya Sunderji became Waypoint President and CEO on June 13, 2022. She is a psychiatrist with nearly 20 years of leadership experience. She is also an Associate Professor in the Division of Adult Psychiatry and Health Systems in the Department of Psychiatry at University of Toronto.
Two senior care facilities in Canada are the first long-term care facilities in North America to adopt technology that uses artificial intelligence (AI) technology to assess pain in residents.


The PainChek® pain assessment solution was recently introduced at two Edmonton-based facilities, St. Michael’s Health Group and Sherwood Care (222 beds). These are the first pilot projects of their kind in North America and are already making a significant impact on the quality of care the facilities can provide for residents.
PainChek® is the world’s first regulatory-cleared medical device for the assessment of pain, enabling best-practice pain management for people living with pain in any environment, from those who cannot reliably self-report their pain, to those who can, and for those whose ability to self-report their pain fluctuates. It uses artificial intelligence (AI) and facial recognition technology to detect and quantify pain in real-time by analyzing microfacial expressions indicative of pain.
James Matthias, Head of Product at PainChek, says: “We are delighted to launch our pilot projects in the Edmonton region, which is a hub for innovation and has a fantastic artificial intelligence ecosystem. Moving into Canada means PainChek can better facilitate best practice pain management for residents who need it most. Sherwood Care and St Michael’s Health Group are leading by example in recognizing the importance of accurate pain assessment, and ensuring their residents have access to gold standard care and support.”
Tatsiana Haidukevich, Director of Care, St Michael’s Health Group, comments: “As an innovative facility, we are constantly looking for advancements in care to improve residents’ quality of life. We consider ourselves lucky that we came across PainChek® through Edmonton Global, as it represents the next level of pain assessment.
PAINCHEK® IS THE WORLD’S FIRST REGULATORY-CLEARED MEDICAL DEVICE FOR THE ASSESSMENT OF PAIN, ENABLING BESTPRACTICE PAIN MANAGEMENT FOR PEOPLE LIVING WITH PAIN IN ANY ENVIRONMENT, FROM THOSE WHO CANNOT RELIABLY SELFREPORT THEIR PAIN, TO THOSE WHO CAN, AND FOR THOSE WHOSE ABILITY TO SELFREPORT THEIR PAIN FLUCTUATES.
“As Director of Care, I consider best practice very important, and PainChek ® has helped us provide best-practice pain assessment technology for our nurses and residents. Nurses now feel more confident in conducting thorough pain assessments, and families are very happy to see improvements in pain assessments and medication management.”
Pain management is one of the top quality indicators Sherwood Care is looking to improve on, according to its CEO Kathy Fortunat: “This was far too intriguing to pass up on and it matched our priorities,” she says. “It will improve the quality of life for our residents, and it will also improve the quality of work life for our staff. It’s not paper driven, it’s easier to trigger the assessment, and it’s easy to do.”
Danielle Buchanan, Clinical Education and RAI Lead at Sherwood Care, adds: “I hope that use of PainChek will give us some real insight into some of our residents. They’re not able to tell us how they’re feeling. We see behaviors like agitation or vocalizations, and often, it’s just the norm to treat the behavior rather than looking into what’s the cause behind it. Our staff are really great at being detectives into what’s going on, and this is another great tool to use.”
PainChek, which started out in Australia and is now the most popular clinical digital tool in Australian aged care, has conducted over 3,000,000 digital pain assessments worldwide, with 70,000 aged care beds contracted internationally across the UK, Europe, Australia, New Zealand, Singapore, and now, Canada.
The PainChek® app is available on smartphones and tablets and com-
 PainChek® is the world’s first regulatory-cleared medical device for the assessment of pain.
PainChek® is the world’s first regulatory-cleared medical device for the assessment of pain.
bines PainChek’s AI pain assessment tool, which intelligently automates the multidimensional pain assessment process, with the Numerical Rating Scale (NRS). This hybrid functionality allows accurate, consistent pain assessment at the point of care, and for care to be considered in PainChek’s detailed reporting suite, PainChek® Analytics.
PainChek® has successfully supported accurate pain assessment and management for thousands of adults worldwide living with dementia, disability, or other conditions impacting their ability to self-report pain. It also has applications within hospitals, hospices, home care, and other care environments, where the PainChek technology is enabling more personalized and targeted care for individuals facing pain-related challenges. ■ H
PainChek® is the world’s first regulatory-cleared medical device for the assessment of pain, enabling best-practice pain management for people living with pain in any environment, from those who cannot reliably selfreport their pain, those who can, and for those whose ability to selfreport their pain fluctuates.
PainChek’s vision is to give a voice to those who cannot reliably verbalize their pain.
The PainChek® app is available on smartphone and tablets and combines PainChek’s AI pain assessment tool, which intelligently automates the multidimensional pain assessment process, with the Numerical Rating Scale (NRS). This hybrid functionality allows accurate, consistent pain assessment at the point of care, and for care to be considered in PainChek’s detailed reporting suite, PainChek® Analytics.
Using PainChek®, facilities can:









● Ensure greater consistency, continuity and diagnostic






certainty in pain assessment and management by decreasing subjectivity and removing unintentional assessor bias



● Streamline the pain assessment process for time-poor carers, with access to the PainChek® tool, the NRS, pain trends, and charting in one solution
● Simplify record-keeping and documentation to demonstrate compliance and support funding claims, with all historical pain assessment data in one place





● Enhance engagement with GPs and allied healthcare professionals

Clinical studies conducted in Australian and UK residential aged care centres have been published in various peer reviewed journals including Journal of Alzheimer’s Disease. An article in BMC Geriatrics indicates that PainChek® is a valid and reliable instrument to assess the presence and severity of pain in people with moderate-tosevere dementia living in aged care in the UK. Further information on clinical studies can be found here.
PainChek® has successfully supported accurate pain assessment and management for thousands of adults worldwide living with dementia, disability, or other conditions impacting their ability to self-report pain. Building on this success of this technology, the clinically validated PainChek® Infant app identifies and detects six facial action units indicative of post-procedural pain in infants aged one month to 12 months.
The PainChek® Infant app has received regulatory clearance in the UK, Australia, Europe, Singapore, Canada and New Zealand, with FDA review in the US currently in progress.

The need for PainChek as a bestpractice pain management solution also extends to older people living at home and with access to home care packages that enable long-term home living. PainChek is now expanding into home care by partnering with home care and disability service providers. For more information, visit: https://painchek.com

Rebekah Churchyard’s grandfather was diagnosed with dementia at age 63. A former Christmas tree farmer, he found himself with little to do and increasingly confused in his environment. He’d sit on the stoop of his home, refusing to go to a day program designed for people living with dementia. His granddaughter vowed to find better options for Canadians with dementia, and for their caregivers.
In 2022, Churchyard opened Green Care Farms in Milton, Ontario – the first of its kind in Canada – a half-acre sensory garden with programming created for people living with dementia. Set amid the 165-acre Andrews Farm
Market & Winery, it was the culmination of her education, including a Master of Social Work in Gerontology, work experience (providing specialized geriatric services at home and community care support services), and travelling down a long road to make her dream project a reality.
Green Care Farms couples a therapeutic supportive setting with agricultural activities. “We have two aims,” says Churchyard, CEO and founder. “One, to provide a meaningful and fun engagement for the person with
dementia. It’s their community, their space, their garden. It gives them a sense of community and purpose. So many people have lost those parts of their identity. And two, to provide respite to caregivers.”

The latter hits close to home. Churchyard saw how much her grandma struggled to take care of her grandpa. “She ran herself ragged and couldn’t get the support she needed,” recalls Churchyard.
Her grandfather was also struggling. After moving to a long-term care
home, he was on a locked unit and unable to go outside, where he had spent so much of his life farming. He was unoccupied and spent most of his day in bed. He passed away at age 77.
Green Care Farms was created to meet the needs of people like Churchyard’s grandparents. Caregivers can enroll loved ones in a summer-long, supervised program, where they can do chores – planting, watering and harvesting produce. “Many people from various backgrounds thrive in this program,” she explains. “I love seeing them making jokes, brainstorming ideas and making plans to bring seeds and garden tools on their next visit.”
While there are care farms worldwide, they’re relatively new to Canada. When Churchyard heard about them
at a conference, her journey to create one for those with dementia began. She spent five years with the Toronto Council on Aging, learning how charities work, how to develop programs, access grant funding and, most importantly, what older Canadians needed. Later, when she had a chance to lease some land for her sensory garden, she leapt at the opportunity.
She credits AGE-WELL training and programs for helping her hone her concept and being able to pitch it effectively by focusing on the need it fulfilled and having the research to back it up. From day one, researcher Dr. Arlene Astell, Churchyard’s mentor at AGE-WELL, believed in Green
Care Farms and the vision behind it.





“Having exposure to mentors and to people who are interested in your




ideas and in helping you flesh out and strengthen your ideas was extraordinarily valuable to me,” says Church-
yard. “I wouldn’t have been able to create Green Care Farms without that support.” ■ H
Michele Sponagle is a freelance journalist and editor. AGE-WELL is a federally-funded Network of Centres of Excellence. AGE-WELL brings together researchers, older adults, caregivers, partner organizations and future leaders to accelerate the delivery of technology-based solutions for healthy aging. www.agewell-nce.ca
The goal to advance patient-centered care and optimize operational efficiencies by leveraging digital health solutions is experiencing a rapid uptake.
Sault Area Hospital (SAH) recently shared the results of launching a surgical remote monitoring program by leveraging a Digital Care Journey solution as part of their Digital Health strategy. Keeping up with the rising demands for accessible care, the program is focused on improving engagement and timely communication between patients and care teams. A form of digital patient engagement, the platform enables improved pre-surgical readiness, safer hospital-to-home transitions, and improves patient satisfaction and clinical outcomes, such as lower emergency department visits and readmissions.
Dr. James Chan, Director of Innovation, SAH, sees immense value in leveraging interoperable digital patient engagement tools to deliver high-quality care more efficiently. He shared that at SAH, “Technology has increased our ability to connect with patients and encourage them to become active participants in their healthcare journey. Our patients report feeling more supported because of it.”
Since the initial deployment in 2021 for hip and knee replacement surgery, SAH has expanded the use of Digital Care Journeys to a total of 13 care pathways across General Surgery (Colorectal, Hernia, Urology, and more), Orthopedic Surgery, and Women’s Health (C-section and Hysterectomy).
Using the SaaS-based platform, SAH can engage patients with a mobile and web-enabled, virtual companion – guiding them step-by-step from pre-admission preparation through post-discharge recovery as well as de-

LEVERAGING THESE PLATFORM FEATURES, SAH CARE TEAMS HAVE BEEN ABLE TO INTERVENE SOONER FOR AT-RISK PATIENTS AND PROVIDE PERSONALIZED CARE RECOMMENDATIONS TO IMPROVE THE PATIENT EXPERIENCE AND OUTCOMES, INCLUDING REDUCING ED VISITS BY 72 PER CENT AND READMISSIONS BY 64 PER CENT.
liver multimedia education, reminders, and tasks for patients throughout their care journey. While recovering at home, patients can self-report data such as pain scores, range of motion, symptoms, and share incision photos through the platform with their care team.
“Visuals on exercises, daily reminders, the fact that a healthcare professional is available, list of places to get needed equipment, reminders to look for infection, lists to get you ready for surgery like planning for meals once on your own, what kind of help you will require. Overall - Excellent,” shared a SAH patient on what they valued about the program.
Meanwhile, the SAH care teams can remotely monitor recovery progress and patient compliance, automate patient self-care guidance via smart algorithms and workflows (e.g., education on how to manage low-risk issues
or when to escalate to a provider), receive alerts and monitor dashboards to identify at-risk patients more quickly and intervene sooner.
The program also helped expand accessibility to care and efficiency, serve the rural patient population more effectively, as well as the use of actionable insights from collected data to optimize hospital protocols and procedures.
The implementation has been further enhanced by platform integration with MEDITECH Expanse. It has helped expedite patient enrollment, access remote monitoring dashboards from within the Expanse patient chart and send patients instructions and reminders. This turnkey integration has reduced manual processes, saving SAH care teams and their pa-
tients valuable time and creating a more effortless provider and patient experience.
For instance, when a surgery is booked in Expanse, patients who consent to the program are automatically enrolled into the Digital Care Journey app. If their surgery date changes, that information is automatically updated in the app, along with pre-surgery steps and reminders. Providers can easily monitor patient-reported information in the platform without ever exiting the electronic health record.
“The turnkey integration of SeamlessMD with MEDITECH Expanse streamlines our clinical workflows, reducing manual effort and enabling our providers to save valuable time. Automating care delivery strengthens our ability to easily track and monitor patient compliance and adherence with treatment plans to improve patient outcomes, while at the same time empowering patients to take charge of their health through self-management,” said Dr. Derek Garniss, CMIO, SAH.
Leveraging these platform features, SAH care teams have been able to intervene sooner for at-risk patients and provide personalized care recommendations to improve the patient experience and outcomes, including reducing ED visits by 72 per cent and readmissions by 64 per cent.
SAH patients also found that self-managing their care journey was easy and staying connected to their care team helped reduce surgical anxiety. Of the patients enrolled, 37 per cent reported that the app prevented 1+ calls to the hospital, 94 per cent felt it helped them feel more confident before surgery, and 91 per cent felt it helped them feel more confident at home after surgery.
“Since this was my first surgery of this type, it helped me to know whether or not my recovery was on track, gave me access to helpful tools and to the healthcare team if you needed,” shared a SAH patient. ■ H
Since its launch in May 2022, SCOPE Niagara –Seamless Care Optimizing the Patient Experience –has registered more than 135 family physicians and nurse practitioners.

“The program provides an easy, quick connection between community primary care providers and the hospital,” says Sarah Furnival, SCOPE Nurse Navigator and recipient of this year’s Nursing Excellence Award – Excellence in a Non-Traditional Nursing Role. “By creating pathways, we are able to help identify and improve gaps in care all while reducing unnecessary visits to the ED.”
physicians and primary care providers to the program.”
“I was very impressed with the service that SCOPE offered for my family doctor in coordinating my care with the General Internal Medicine Rapid Assessment Clinic and diagnostic imaging,” says Niagara resident Lukas Gotfryd, who is grateful for the timely care the program provided. “I was not required to have long wait times in the ED for appointments, scans and blood work. All of my appointments have scheduled times, which helps with time management, work and family.”
As of May 2023, there were nearly 500 calls to SCOPE Niagara, which

SCOPE Niagara connects family physicians and nurse practitioners to a dedicated team of specialists from Niagara Health and from Home and Community Care. The primary care providers connect with SCOPE Niagara’s nurse navigator, who directs them to the most appropriate service, providing support for complex and urgent patients in real-time.
The program originated in 2012 to support family physicians in Toronto. The program has since grown and has been effective in streamlining care and averting both ED visits and hospitalizations.
“We are fortunate to be a part of this extension to create a local solution for seamless patient care in Niagara,” says Dr. Darija Vujosevic, Clinical Lead, Niagara Ontario Health Team and SCOPE Niagara Steering Committee Member. “As SCOPE Niagara continues to grow, it will attract more family

varied in nature, such as requests for support with general internal medicine, diagnostic imaging and kidney care. Opportunities to expand the program are currently being explored, including orthopedic services, mental health and addictions.
“I cannot say enough about how grateful I am for this service, especially being a new doctor to this area and still finding my bearings,” says Dr. Victor Ogala from Grantham Medical Clinic in St. Catharines. “SCOPE Niagara has given me confidence with my work, knowing I have somewhere and someone to turn to when help is needed to navigate the system and get the best care for my patients.”
SCOPE Niagara is a partnership between Niagara Health, Niagara Practitioners Healthcare Alliance and Home and Community Care as part of the Niagara Ontario Health Team –Équipe Santé Ontario Niagara.


■ H
A program that connects Niagara Health physicians with community primary care providers diverted an average of 90 per cent of calls each month away from emergency departments in its first yearSarah Furnival, SCOPE Nurse Navigator, connects primary care providers to a dedicated team of specialists from Niagara Health and from Home and Community Care, providing support for complex and urgent patients in real-time.
“THE PROGRAM PROVIDES AN EASY, QUICK CONNECTION BETWEEN COMMUNITY PRIMARY CARE PROVIDERS AND THE HOSPITAL.”

ALLEVYN LIFE dressings help protect at risk individuals from the onset of pressure injuries*.2-4 In fact, ALLEVYN LIFE has been proven to redistribute pressure over a

Cost Effective
Cost savings up to 69% per patient2,6
Breathable
Film layer provides a bacterial barrier
Innovative EXUMASK Change Indicator helps patients and caregivers own the recovery process2 while providing high patient satisfaction through fewer dressing changes7,8,9
Hyper-absorbent
Lock-away core helps minimize leakage of 10
Protective
Hydrocellular foam cushions, with a 71% reduction in incidence of sacral pressure injuries11





Gentleandsecure
Silicone adhesive wound contact layer can be repositioned9 and may reduce trauma to the wound during dressing changes

Download a copy of our comprehensive guide to using ALLEVYN Dressings to prevent pressure injuries in at-risk hospital patients.
Get in touch with a representative.
For detailed product information, including indications for use, contraindications, precautions and warnings, please consult the product’s Instructions for Use (IFU) prior to use.
*when used as part of a comprehensive prevention program and when compared to standard care alone. **leading competitors defined as: Biatain