


















Ontario
a














More than one in three Canadians report serious mental health concerns, and one in four report problematic substance use, according to the most recent data from the Mental Health Commission of Canada and the Canadian Centre on Substance Use and Addiction. These are staggering numbers.
The impacts of the global pandemic on the mental health and substance use of the Canadian population are proving to be complex -- and persistent. The mental health and substance use health workforce is the backbone of the critical response but is at risk of being overshadowed by the crisis in the broader health workforce.
Regulation of this field would help provide Canadians with more equitable access and enable needed critical workforce planning. The federal government has an important role streamlining this process in partnership with the provinces and territories -- and in creating a new national health workforce registry, which would help the health system as a whole.
Mental health and substance use health counselling in some parts of Canada right now is a bit of a wild west.
If you go to a regulated psychotherapist or counselling therapist in Nova Scotia, New Brunswick, Quebec, Ontario or PEI, you will know what kind of service to expect, who is providing it and what kind of accreditation
they’ve received. You are also more likely to get these regulated services paid for by the province, or at least partially covered by your workplace benefits program if you are fortunate enough to have one.
But if you live elsewhere in Canada, many provinces and territories have yet to move forward with psychotherapy regulation. This means you won’t know what you’ve signed up for.
Some protections are in place through the voluntary certification and competency frameworks of provincial associations, but services from these providers may not qualify for public and private funding. And from a health planning perspective, understanding the supply of these mental health and substance use providers is more difficult.
In this way, the fragmented regulatory landscape for mental health and substance use health providers across Canada is undermining equitable access to services and inhibiting our capacity to undertake workforce planning.
Our current research, led by Athabasca University in collaboration with the University of Ottawa and the Mental Health Commission of Canada, is zeroing in on both key barriers and facilitators to these critical regulatory reforms.
For example, progress in New Brunswick was helped by a unique approach.
EDITORIAL:
ADVERTISING:
Monthly
THANKS
610 Applewood Crescent, Suite 401 Vaughan Ontario L4K 0E3
TEL. 905.532.2600|FAX 1.888.546.6189
www.hospitalnews.com
Kristie
editor@hospitalnews.com
Denise
denise@hospitalnews.com
Stefan
stefan@hospitalnews.com
accountingteam@mediaclassified.ca
info@hospitalnews.com
Lauren Reid-Sachs
Johannah
Barb Mildon, RN, PHD, CHE
VP Professional Practice & Research & CNE, Ontario Shores Centre for Mental Health Sciences

Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario.
The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
Canadian Publications mail sales product agreement number 42578518.
Published in Molecular Medicine, researchers at Lawson Health Research Institute have found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition.
Long COVID occurs when someone experiences symptoms like fatigue, cognitive issues, shortness of breath and gastrointestinal issues after an initial COVID-19 diagnosis. It can sometimes take up to 12 months for the condition to occur.
“It’s estimated that 30 to 40 per cent of patients with COVID-19 will develop long COVID,” says Dr. Douglas Fraser, Lawson Scientist and Critical Care Physician at London Health Sciences Centre (LHSC). “Physicians currently rely on symptoms alone to diagnose the condition, but our research offers a unique profile of blood biomarkers that could be used in a clinical test.”
The researchers studied 140 blood samples from participants at LHSC and St. Joseph’s Health Care London, including St. Joseph’s PostAcute COVID-19 Program. Participants were those with presumed long COVID, hospital inpatients with acute COVID-19 infection and healthy control subjects.
“We chose to study blood vessels that link all the body systems together to look for changes after an acute infection,” explains Dr. Fraser, who is also a Professor at Western University’s Schulich School of Medicine & Dentistry.
The team found that blood vessels of those with presumed long COVID were changing rapidly after a confirmed COVID-19 infection. They also found that patients with long COVID had 14 elevated blood biomarkers associate with blood vessels.
With the help of machine learning, they discovered that two biomarkers called ANG-1 and P-SEL could be used to classify long COVID with 96 per cent accuracy.
“Long COVID is a relatively new condition and we have much to learn about it,” says Dr. Michael Nicholson, Associate Scientist at Lawson, Respirologist at St. Joseph’s and Associate

Professor at Schulich Medicine & Dentistry. “This research advances our understanding of long COVID with the potential to improve diagnosis and patient care.”
The advantage of biomarkers is that they not only help diagnose a disease but also provide insight into potential treatments. The team is now focused on using their findings to create a clinical diagnostic test with a goal of also exploring therapeutics.
“With a point-of-care diagnostic test, we could confidently diagnose long COVID and eventually develop targeted therapeutics against these blood vessel changes that we have
discovered,” says Dr. Fraser. “The ultimate goal is to improve patient outcomes following a long COVID diagnosis.”


This research was supported by funding from London Health Sciences Foundation, London Community Foundation and the AMOSO Innovation Fund. It builds on a growing body of COVID-19 research from scientists at Lawson Health Research Institute.

The study’s first author Maitray Patel, is a PhD student from Western’s Schulich School of Medicine & Dentistry. Patel worked on blood analysis under the supervision of Drs. Doug Fraser and Mark Daley. ■ H
Celine Zadorsky is a Communications Consultant at Lawson Health Research Institute.
Dr. Douglas Fraser, Lawson Scientist and Critical Care Physician at London Health Sciences Centre.
Dr. Michael Nicholson, Associate Scientist at Lawson, Respirologist at St. Joseph’s and Associate Professor at Schulich Medicine & Dentistry.
With the provincial legislature returning tomorrow, Ontario’s doctors reiterate their commitment to work with the government to solve the pressing issues facing health care.
from
The Ontario Medical Association has proposed “three solutions” that could be implemented in the short term that would both improve patient care and relieve pressure on the health-care system:
Since 1950, regulation for each new health profession in the province has been introduced through a private member’s bill rather than through the more complex public legislation used in other provinces.
In Alberta, proposed legislation to regulate the mental health and substance use workforce has been stalled since 2018 due to concerns about the impact on addiction counsellors and Indigenous practitioners, whose training and competencies draw more on lived experience and cultural knowledge.
We hear similar concerns from our partners in the peer support and addiction sectors, who have developed robust competency and certification frameworks but are wary of regulatory frameworks that privilege graduate-level professional education above other forms of lived knowledge and training.
In 2021, we held a virtual policy dialogue with diverse provider groups, frontline workers, and policy makers. Sixty participants from across the country met and identified a number of other key priorities that need immediate attention in this critical landscape. Firstly, they recommended better mental health and substance use workforce data collection. They also recommend coordinated workforce planning that includes employment-based benefit programs and publicly-funded services. They also stressed the need for
increased diversity and cultural competence and access to regulation that recognizes lived experience and cultural knowledge.
So, what’s the solution?
Regulatory reform is needed urgently on two tracks. First, psychotherapy and counselling therapy should be regulated across the country as soon as possible.
Second, policy makers need to listen to the full range of providers to develop modern, flexible approaches to regulation and certification that work for the workforce as a whole.
A modern regulatory framework will be key for implementing federal commitments to develop mental health and substance use healthcare standards and ensure equitable access to high-quality services for all.
Each province and territory could continue their own approach to workforce regulation. But there is also an opportunity for the federal government to spearhead a less fragmented approach by fully integrating flexible, modern workforce regulation into a new national health workforce registry. This registry would facilitate robust workforce planning to help ensure the future workforce can meet the population’s needs.
Regulation is a key priority for strengthening the capacity of the mental health and substance use health workforce. Next up, we need a broader health workforce strategy for Canada. ■ H
Mary Bartram is the Director of Policy at the Mental Health Commission of Canada. Kathleen Leslie is an Assistant Professor at Athabasca University.
1. Licensing more foreign-trained physicians, through increased residency spots and a government assessment program to assess who is ready to practice now. We also need more nurses to keep operating rooms and emergency departments open.
2. Creating standalone centres to perform less complicated outpatient surgeries and procedures covered by OHIP. These publicly funded Integrated Ambulatory Centres would ease the burden on hospital and reduce wait times. The OMA is also ready to work with the government to create a centralized referral system so that patients most in need of high-demand surgeries and procedures, regardless of where they live, are distributed among all available doctors
3. Creating more hospice beds and palliative care services to improve the patient experience, support caregivers and reduce pressures on emergency departments.
“Our three solutions come from the experience doctors have of going to
work every day and night with the goal of providing high-quality, compassionate patient care,” said OMA President Dr. Rose Zacharias. “We see the problems first-hand and are committed to working with the government to fix them.”
While these “three solutions” could be implemented in the short term, comprehensive repairs are also needed to address issues such as long-term funding and the needs of an ageing population.
The Ontario Medical Association has a detailed roadmap for what needs to be done over the next four years, Prescription for Ontario: Doctors’ 5-Point Plan for Better Health Care.
“Ontario’s doctors have a plan to help more patients get care faster,” said OMA CEO Allan O’Dette. “Solutions like licensing foreign-trained physicians, opening more centres for outpatient procedures, and creating more hospice and palliative care beds will help address the challenges we are facing in Ontario’s health-care system.” ■ H
The Canadian Academy of Health Sciences (CAHS) announced the recipients of a newly created honour designed to celebrate Canadians who have made an exceptional contribution to Canada’s health care system.
The recipients of the award were chosen by the 2021-2022 Presidents: Dr. Sioban Nelson (President), Dr. Jay Cross (President-Elect) and Dr. Chris Simpson (Past President).
CAHS chose five Canadians whose outstanding contributions to Canada’s health care system merited recognition:
• The Right Honourable Paul Martin, PC
• Camille Orridge
• Sharon Sholzberg-Gray
• Michèle Stanton-Jean
• Siila Watt-Cloutier
“We are pleased to recognize these five outstanding individuals,” said Dr. Chris Simpson, Chair of the Presidents’ Award Committee. “It was important for CAHS to recognize their life-long contribution and dedication to public life, the healthcare system and social justice.”
Dr. Jay Cross, CAHS President (2022-2023) thanked the recipients.
“On a daily basis our work as health scientists is impacted by the efforts, commitment, and passion of individuals like them. The five recipients of the Presidents’ Award were selected to celebrate their exceptional contribution to our health care system.” ■ H
The release of a new dataset sheds light on biological and clinical risk factors for children living with cerebral palsy (CP).
The Cerebral Palsy Integrated Neuroscience Discovery Network (CPNET), an Integrated Discovery Program carried out in partnership with the Ontario Brain Institute (OBI), has just released critical data on childhood hemiplegic CP, a condition characterized by a weakness on one side of the body. In Canada, three in every 1,000 children are diagnosed with CP each year. Currently, there are about 47,500 people living with CP and hemiplegic CP affects 38 per cent of people with the disorder.
The Hemi-NET Clinical Database, which focuses on children and youth aged 2-18 with a confirmed diagnosis of hemiplegic CP, contains data on more than 300 young people from across Ontario. Clinician scientists from nine study sites across the province, along with the children and patients, contributed clinical assessments and test results stemming from CPNET research projects to the database.
“Research and innovation alongside collaboration are vital to the success of Ontario’s healthcare sector,” said Jill Dunlop, Minister of Colleges and Universities. “OBI’s release of this new data set reaffirms its role as a scientific leader. With clinicians and patient partners working together across the province, Ontario is transforming the way in which we study, diagnose, and treat neurological conditions.”
The data are organized around the following platforms:
• Clinical Risk Factors: clinically relevant neonatal and obstetric risk factors from obstetrical and neonatal health charts,
• Genomics: saliva samples acquired from the index child and biological parent(s) with DNA extracted,
• Neuroimaging: standardized coding of clinically acquired neuroimaging, and
• Neurodevelopmental: standardized assessments of gross motor, fine mo-
tor, language, cognitive, behavioural function, and self-reported quality of life.
The standardized, cleaned, and curated data, now shareable on Brain-CODE, OBI’s state-of-theart neuroinformatics platform, allow maximum utility for analysis across disease and across platform – all while protecting the identity of participating individuals.
As an Integrated Discovery Program carried out in partnership with OBI, CP-NET works with researchers, clinicians, and people impacted by cerebral palsy to accelerate the development of neuroscience discoveries. Dr. Darcy Fehlings, senior clinician scientist at Holland Bloor-
view Kids Rehabilitation Hospital and principal investigator at CPNET, who led the OBI-funded research that contributed to improved understanding of the genetic basis of hemiplegic CP, said that these newly released data provides an opportunity for researchers from around the world to further explore new and better ways to prevent, treat, and manage symptoms in children with hemiplegic CP.
“This data set shows that when we embed common data elements, such as health care markers in the care delivery process, standardized assessments of cognitive and behavioural function, and self-reported quality of life, scientists and clinicians working in com-
pletely separate labs and hospitals can come together to improve care and drive change for individuals with CP and their families.”
“In fact,” Dr. Fehlings continued, “members of the CP-NET clinical team – located in different parts of Ontario – are already using these data to improve early care of children with CP such as promoting pediatric CP hip surveillance.”
Dr. Tom Mikkelsen, President and Scientific Director of the Ontario Brain Institute, said: “The creation and release of this data set, OBI’s sixth clinical release in an 18-month period, demonstrates clear progress in better understanding treatment options for conditions like cerebral palsy and underscores the benefits of the team science approach, which champions collective success over the success of any one individual.”
OBI and CP-NET invite all interested researchers to use this dataset in their own research to advance our collective understanding of CP and enhance care for those impacted by it. ■ H
Equitable cancer care for Black patients, medical schools’ responses to anti-Black racism, mental health of Black youth and gaslighting in academic medicine are some of the topics in two anti-Black racism in health care issues of CMAJ (Canadian Medical Association Journal) published October 24 and October 31, 2022.
Anti-Black racism is a threat to public and population health in Canada. Scholars and researchers in social and health sciences have studied and documented the effects of anti-Black racism and its impact on health inequities in Canada for decades, yet systemic racism has undermined the publication of this work. As a result of years of advocacy by the Black Health Education Collaborative (BHEC), CMAJ
is publishing two special issues on the health of Black people in Canada and anti-Black racism in health care, to focus attention on this important topic and to provide a foundation for future content.
“It is incumbent upon health care practitioners to engage in anti-racist practices to improve the health experiences and outcomes for Black people. I believe the articles in the two-part special issue will provide guidance, direction and insights on the steps to take to create better health outcomes for Black people in Canada,” says Dr. OmiSoore Dryden, co-lead of the national Black Health Education Collaborative and associate professor, James R. Johnston Endowed Chair, Black Canadian Studies, Faculty of Medicine, Dalhousie University.
The articles in the special issues follow 2 broad themes: anti-Black racism and patient health, and anti-Black racism in the health system that affects trainees and medical professionals.
“For the last few decades, the Black health community has been involved in advocacy to shed light on the effects of anti-Black racism and systemic inequities that have underpinned poorer health outcomes for Black communities,” says Dr. Mojola Omole, a surgical oncologist in Ontario and journalist who also co-hosts CMAJ Podcast. “The inaugural BHEC and CMAJ special issue is the first step for all health professionals to move beyond treating the disease and treat the whole person. After all, health is not the only goal, but our patients’ well-being.”
H
THE HEMI-NET CLINICAL DATABASE, WHICH FOCUSES ON CHILDREN AND YOUTH AGED 2-18 WITH A CONFIRMED DIAGNOSIS OF HEMIPLEGIC CP, CONTAINS DATA ON MORE THAN 300 YOUNG PEOPLE FROM ACROSS ONTARIO.
Transformative technology developed by Vancouver Coastal Health Research Institute (VCHRI) researcher Dr. Mads Daugaard at the Vancouver Prostate Centre (VPC) is putting cell analytics into the hands of scientists around the globe. The artificial intelligence (AI)-driven smartphone app SnapCyte produces data used in cell growth medical research at a fraction of the cost and in a more timely manner than current technology.
“We developed SnapCyte based on a need for affordable, basic cell analytics that can be accessed by any scientist working in a cell culture or biotechnology laboratory,” says Daugaard. “This app makes commercially available affordable, high-performance laboratory technology that can be conveniently accessed on a smartphone.”
Used in the analysis of cancer cells and other diseases at a microscopic scale, the first-of-its-kind SnapCyte app could supercharge the development of novel, personalized medical treatments.
“The app returns precision data results within five minutes,” he says. “With the former technology, this process would normally take 45 minutes to an hour with the most high-end live-cell imaging and analysis platforms, or 24 hours with colorimetric assays.”
SnapCyte also simplifies workflows without compromising accuracy. Unlike current technology that uses duplicate samples of a cell culture with a medium/serum solution, SnapCyte can be used on experiments in the plates where the cell culture is grown. It also collects and displays cumulative cell data in growth curves to aid with monitoring cell development over time, which can be easily shared among researchers.
“All you have to do is take the plate with the cell culture out of an incubator for a minute and put it under a
microscope where you can then snap a picture of it with your smartphone,” says Daugaard.
Scientists can also monitor cell growth in the same well or stack of plates continuously, and add nucleic acids or other substances – in a process called transfection – when optimal.
“This platform can be very helpful in drug screening,” says Daugaard. “When comparing multiple drug candidates, SnapCyte can very accurately and quickly assess how each drug acts on cancer or other cells to identify the most effective treatment.”
At a few hundred dollars per year, the app’s affordability makes the platform an accessible option for laboratories that are unable to buy costly cell analytics equipment.

“Many laboratories do not have the funding to purchase new $25,000 to $30,000 machines, or the budget to support the ongoing investment of thousands of dollars per month required to use the equipment,” says Daugaard.
SnapCyte’s cloud-based platform allows users to not only accurately measure their collective cell culture data in minutes – the big data it gathers could also provide important insights to further advance scientific research.
SnapCyte’s AI algorithm is continuously learning from the data received from its users, says Daugaard. While the data is protected, the app’s efficacy will improve over time as it learns from and shares insights with the research community.
“It is time to democratize research, and that is what we are doing here,” says Daugaard. “We are putting something on the market for a fraction of the cost that will perform at least as
good as – or even better than – many other devices currently available.”
The SnapCyte App is currently undergoing final beta testing and is expected to launch worldwide beginning of 2023.
Vancouver Coastal Health Research Institute (VCHRI) is one of the top funded research institutes in Canada, translating health research into practice. The breadth and scope of research at VCHRI have long-lasting impacts on patient care and health care systems in British Columbia and around the world. With more than 2,400 personnel engaged in research across 15 world renowned research centres and programs, VCHRI’s research activities range from laboratory-based research to gain understanding about the human body and health
conditions, to clinical research focused on evaluating new ways to provide patient care. Across all of its centres, VCHRI is creating healthier lives through discovery. www.vchri.ca
The Vancouver Prostate Centre (VPC) has a track record of success that has earned it a reputation as one of the world’s most respected cancer facilities. It is a National Centre of Excellence and a designated Centre of Excellence for Commercialization and Research. The combination of a large patient clinic and clinical trials facility, together with a world-class translational research program under the same roof, make the VPC the largest program of its kind in Canada. VPC is hosted by Vancouver Coastal Health Research Institute and the University of British Columbia. www.prostatecentre.com
ACanadian startup that has created a digital assessment tool for monitoring Parkinson’s disease symptoms has won the 2022 AGE-WELL National Impact Challenge.
In making the winning pitch, Bronwyn Bridges, Co-Founder and CEO of PragmaClin, said the ultimate goal is for people living with Parkinson’s to get help faster with more accurate results.
The idea came when Bridges was a master’s student, working with Gord Genge, who lives with Parkinson’s. “He came to me with a brilliant idea to help others, and that progressed into a full software which we’ve developed called PRIMS.”
The PRIMS system monitors motor and non-motor symptoms of Parkinson’s. How it works: First, the person living with Parkinson’s completes an at-home survey to determine their daily living skills. Next, at the doctor’s office, the individual stands in front of a computer equipped with body-tracking cameras, and completes a series of tasks. The PRIMS software then assigns a score, based on real-time data, on an internationally recognized Parkinson’s scale.
“Data from the software will help clinicians assess and monitor a patient’s condition and adjust their medications or physical therapy, if needed,” Bridges said. For people living with Parkinson’s, PRIMS “helps them keep track of those symptoms they are having, from their own personal portal.”
Bridges said the $20,000 cash prize from winning the AGE-WELL National Impact Challenge will go towards the next phase of validation trials, patent filing, team expansion and more. The hope is to fully commercialize and enter the market by 2024.


Five finalists took part in yesterday’s pitch event, describing how their technology-based solution could positively impact older Canadians or their caregivers.
The runner-up prize went to Singular Hearing, which uses artificial intelligence to create new kinds of hearing assistance that help people stay connected. The company makes HeardThat, a smartphone app for those who have trouble hearing speech in background noise, such as restaurants. Singular Hearing won a cash prize of $5,000.
Care2Talk Technologies received the People’s Choice Award for its accessible and intuitive communication and health platform designed to revolutionize the way seniors connect with their healthcare providers and loved ones.
One of the most exciting startup competitions in Canada, the AGEWELL National Impact Challenge recognizes and supports top startups in the country’s growing AgeTech sector. This year’s competition was held as part of the AGE-WELL Annual Conference in Regina, Saskatchewan.
AGE-WELL thanks the generous sponsors of the 2022 AGE-WELL National Impact Challenge: key sponsor, the Ontario Brain Institute (OBI), and Bereskin & Parr.
Dr. Chika Stacy Oriuwa Physician and Time
Dr. Alika Lafontaine President, Canadian Medical Association
Next-level patient empowerment: that’s how Dr. Andrea Tricco describes an initiative that encourages Canadians to submit questions that will guide scientific research.
Dr. Tricco, the director of the Knowledge Synthesis Team in the Knowledge Translation Program at Unity Health Toronto, leads a federal initiative called the Strategy for Patient-Oriented Research (SPOR) Evidence Alliance. The team recently received a $2.6-million top-up from the Canadian Institutes for Health Research (CIHR) for this work, which promotes evidence-informed health policy and practice changes.
Now, they’re reaching out across Canada to gather ideas for research that will generate health practice and policy impact. The 20 people whose projects are selected will become embedded in their research and lead from their lived experience, alongside researcher co-leads. We asked Dr. Tricco more about this initiative, the unique model it offers for patient-oriented research, and its impact.
What is the importance of patient-oriented and patient-engaged research?
Dr. Andrea Tricco: Patient and public partners have lived experience, and they are the ones who are interacting with our health system every day. They have a lot of knowledge about the barriers and challenges of our health system, sometimes even more than providers and other decision makers working in the system. They play an all-important role in our research. They provide us with the health-care consumer perspective, provide opportunities to work with the community, help shape our research questions, make sure our research is relevant and impactful, and they ensure our findings are useful for important health system decisions. Patient
and public partners make our research better.
We have a recent example where there was a question from a public health body. When we discussed it with the patient and public partners, they felt that the question wasn’t quite right. They suggested a completely different approach. This is a good example of where the policy decision maker didn’t have the lived experience expertise required to understand the underlying issues. This also shows us why it’s so important to get feedback from patients and the public early on in the research process.
What is the main focus of the SPOR Evidence Alliance?
Dr . Tricco : Different health decision makers, such as policy decision makers, health-care providers, as well as patient and public partners submit research questions that will help inform a decision they’re trying to make. The SPOR Evidence Alliance works alongside these decision-makers to co-create research projects that will answer their research questions. We are mandated by CIHR to answer their questions using knowledge synthesis, knowledge translation or clinical practice guideline methods.
Over the last six years we’ve completed more than 125 projects and we’ve worked with 45 different decision-making organizations across Canada and abroad. That includes the mechanism where patients can submit topics and we conduct patient co-led queries for the topics that patient and public partners suggest. More information on our initiative can be found in our recent series of papers published in the Facets Journal.
The SPOR Evidence Alliance has investigators across the country, led out of the Knowledge Translation Program at Unity Health. Why is Unity Health well positioned to be the centre of this work?
Ana Gajic is a senior communications advisor at Unity Health Toronto.

Dr. Tricco: We have a long history working with patient and public partners and also with policy decision makers, health-care providers, and other decision makers in the health system. It takes years to build these relationships. Having them in place prior to beginning this initiative was a facilitator to our success. We also have experience leading Canadian initiatives so we have been able to take learnings from other initiatives and apply them to this.
In the first round of this funding, your team ran three patient and public partner co-led pilot projects. How were the three projects that were prompted by patient questions selected?
Dr. Tricco: Over one year, patients submitted 11 topics. These topics were prioritized by a panel of 25 individuals with diverse experience as policy-makers, health-care providers, trainees, researchers, and patient and public partners.
From the 11, we selected three topics that were deemed in scope of our initiative, unique in order to reduce research waste, and highly impactful. The projects were then co-led by research teams alongside the person with lived experience who submitted the topic. We are now scaling this up. Since July, we have received almost 50 topics that
will be prioritized and result in 20 additional projects.
Why is this approach unique?
Dr. Tricco: Patient and public partners are truly involved at every level. They are involved in the governance of our initiative through various committees, and then we have patients and the public engaged in every project. At the highest level of empowerment, patient and public partners are submitting the topics and they co-lead projects from start to finish.
What has the impact of patient-created and co-led projects been so far and what do you hope the impact will be for the next set of projects?
Dr. Tricco: We’re getting to very relevant questions to inform health systems change.
Patient partners co-lead with their lived experience. They provide unique content expertise as those frequently using and navigating our health system that a researcher doesn’t necessarily have. The impact of this is to reduce research waste, answer the most impactful and important questions, and develop evidence that can be used for everyone in the health system.
The SPOR Evidence Alliance is currently collecting research questions from the public and patient partners. To submit a question, please visit this page on the SPOR Evidence Alliance website. ■ H
PATIENT PARTNERS CO-LEAD WITH THEIR LIVED EXPERIENCE. THEY PROVIDE UNIQUE CONTENT EXPERTISE AS THOSE FREQUENTLY USING AND NAVIGATING OUR HEALTH SYSTEM THAT A RESEARCHER DOESN’T NECESSARILY HAVE.Dr. Andrea Tricco
Without truth, there can be no reconciliation.
That’s one of the messages Dionne Nolan is hoping to spread this National Day of Truth and Reconciliation.
Nolan is the Indigenous navigator and works with cancer patients and their families. The main focus of her role includes supporting Indigenous patients and families by going to appointments, explaining medical information, making home visits, finding spiritual care and advocating on their behalf.
“Mino-pimatisiwin means ‘the good life’ in Anishinaabemowin. It is holistic and balanced in the four realms of human experience. Physical, emotional/social, spiritual and intellectual/mental,” Nolan explains. “We are whole health practitioners. We offer what mainstream health care cannot.”
Nolan is Anishinaabe and says her love for her culture is one of the reasons why she wanted to help her community.
“I’ve always been a bridge builder, a good communicator, an empathic listener and I strive to develop healthy relationships. Following my heart lead me to be a helper. My love for my culture and my community keeps me going, even on hard days.”
For many Sept. 30 will be a hard day. While National Day for Truth and Reconciliation aims to honour the children who never returned home and survivors of residential schools, Nolan feels healing will only occur once Indigenous Peoples can share their whole truth.
“Every single Indigenous person alive today is a survivor or related to a survivor of these so called schools, or the Sixties Scoop or the Millennium Scoop. Every single Indigenous person alive today carries that trauma within their blood. That pain is burned into our hearts. The truth is anger is pain and grief is pain.”
That’s why she says it’s so important for Indigenous Peoples to get the opportunity to speak up in an honest way, without judgement or fear, and for Canadians from coast to coast to listen.
“Truth will free those more than 10,000, and the number keeps growing, children buried at residential schools. Truth telling will free us to move forward, and to move forward we need to tell the whole truth about what is going on. This isn’t in the past, mind you, this is right now. We are a whole group of people whose language, culture and identity the church and government tried to erase.”
To help make Kingston Health Sciences Centre (KHSC) a more welcom-
ing and inclusive place, an Inclusion Steering Council was formed in 2021.
Nolan is a member of the council which aims to improve diversity, equity, access to opportunities, recognition and celebration of all people, regardless of who they are or where they’re coming from.
KHSC also has a goal to identify and address gaps in health care, to make sure everyone who turns to the organization for care will be treated with compassion, respect and dignity.
Nolan has high hopes her role as a navigator will one day turn into an Indigenous wellness department. Not only at KHSC, but also at health-care organizations across the country.
“We need spiritual care practitioners who are Indigenous. We need an entire department that focusses on relationships with Indigenous communities, especially the urban Indigenous community of Katarokwi. We need a department to oversee all things Indigenous. That is my dream.”

Until then, she will continue to help the patients and families she serves at KHSC find their mino-pimatisiwin.
“Every day I go home knowing I made someone’s day a little better and every day I learn to be better than I was the day before. I am grateful for each new day that I get to be a helper. It is through giving that I feel we can truly receive.”
H
KHSC sits on the ancestral lands of the Anishinaabe and Haudenosaunee and serves the community of Tyendinaga and the local Katarokwi community, as well as several northern Indigenous communities along the coast of James Bay such as Moose Factory, Attawapiskat and Kashechewan through our long-standing partnership with the Weeneebayko Area Health Authority.
Every test, vital sign measurement and medication prescribed is a data point on a patient’s care journey in the hospital. But how can we use that data to measure and improve the quality of patient care within and across different institutions, when hospitals don’t use the same data systems to generate and store information?
More than seven years ago, two General Internal Medicine physicians and researchers at St. Michael’s Hospital, Dr. Fahad Razak and Dr. Amol Verma, set out to answer this question and bridge the gaps that exist in hospital data collection. They wanted to understand the care provided on medical wards and use data to improve it.
Their goals set into motion GEMINI, a program that collects, formats, standardizes and analyzes clinical data from hospitals to improve how health care is delivered. Since its inception, GEMINI has grown from a pilot project anchored at Unity Health Toronto and just a few other Toronto area hospitals to the largest network of its kind in Canada, covering 33 hospitals and 60 per cent of the province.
During the pandemic, GEMINI continued to lead the way in hospital data collection and analysis, helping quickly bring to light information about Canadian hospital care that no one else in the country had access to. We spoke to the Dr. Razak to learn about GEMINI’s recent work and what’s on the horizon.
How has GEMINI progressed since its inception?
The main barrier we faced when we started this program was that the huge trove of data that’s generated as part of clinical care was not available to be used to understand the kind of care that we’re providing. The lab tests we order, the medications we prescribe, the vital signs that are measured are all data points that are collected, but where in the hospital are they, and how do you get access to them and extract them?
The core mission of GEMINI was to get all of that information out of complex hospital systems, and to bring it into a central dataset that can be used for analysis for reporting for quality improvement.
In Canada and Ontario, there is no single way that data is stored in hospitals or across hospitals and so every hospital has its own complex backend to store information. Imagine decades upon decades of layered on systems with often incomplete documentation. It has taken a lot of elbow grease to figure out how to transfer data from more than 1 million patient admissions (and counting) containing billions of data points worth of information out and ensure their accuracy. We have accuracy from 97 to 100 per cent now which means this data is ready to use to improve quality of care and for research.
How have the last two years enhanced GEMINI’s purpose?
The evidence we saw from other parts of the world early in the pandemic was that hospitals were one of the highest risk parts of the health system for collapse – places like Italy and New York City come to mind. The question we focused on was what can we do to understand our hospital care capacity and how can we help address similar collapse from occurring here? In Canada, there was no single dataset to look at the hospitals – until GEMINI. With the enhanced concern about hospitals being vulnerable, GEMINI’s role became more important.
A lot of pivotal papers about the Canadian response to the pandemic were produced by GEMINI and that was a really important opportunity for us to use our data rapidly and demonstrate
to hospitals why rapid data turnaround was important.
For example, the first and largest study of patients hospitalized with COVID in Canada was a GEMINI paper. The first paper in Canada to look at hospitalized patients with disabilities was also GEMINI-led. As was the first paper to look at Canadian shortages in one of the few life sustaining therapies for COVID-19 Tocilizumab, which also proposed an ethical allocation framework.
Quality improvement is one of the pillars of GEMINI’s work. How does the data collection and analysis lead to improvements in care?
GEMINI has worked towards a learning health system, which is the idea that there is a continuous circle of feedback that happens between those who are providing care, the data that’s generated as part of providing care and researchers and quality improvement experts who are very quickly analyzing and feeding the information back to the providers so that you get this circle of improvement happening.
It’s about having insight on everything that we do. Prior to GEMINI, if you were a physician who worked in hospitals, there was a reasonable chance that in your entire career you may have never received any data about the care you provide. This is a very complex environment that we practice in. We can’t expect anyone to improve what they’re doing without having any information about it. A circle of improvement is impossible without data.
How does Artificial Intelligence (AI) integrate with the work that GEMINI does?
We have really started to move the needle with patient safety. Some of the most important things that happen with patient safety in hospital are things that are preventable or addressable if you were able to identify them, and identify where they’re occurring more frequently.
One example is blood clots: Patients in hospital have a higher risk of clots because when they’re sick and in bed, as the blood is not circulating as much and is more inflamed in some ways. A blood clot in the leg (a deep vein thrombosis) can break off and move to the lungs – causing a life threatening pulmonary embolism. This is an important patient safety event we can prevent but we have very little information about the frequency that it occurs in hospital. GEMINI developed an algorithm that reads the text of radiology reports for patients across the province to identify when these clots occur and we can now see where and when there are higher rates of clotting and physicians can intervene.
What are some of challenges that exist in the space GEMINI occupies?
One challenge is cultural: There aren’t a lot of incentives for hospitals to share resources or data with one another. Before GEMINI there wasn’t any example in the country of large network of hospitals coming together to share such enormous data repositories – that requires a lot of trust.
It wasn’t a coincidence that Unity Health took the lead on this as the site to do it. We are known to be a team player as an institution. We are known to be world class with our data and analytics. We recognized as a group that we would not try to make all of the leadership and value add anchored to Unity because we wanted people to share this across the system. This is a win for the people of Ontario. That’s been critical to our growth because if hospitals try and compete with each other, there’s never going to be an incentive for them to share. We’ve demonstrated that by sharing we can collectively do more.
IN CANADA AND ONTARIO, THERE IS NO SINGLE WAY THAT DATA IS STORED IN HOSPITALS OR ACROSS HOSPITALS AND SO EVERY HOSPITAL HAS ITS OWN COMPLEX BACKEND TO STORE INFORMATION.
How does equity and inclusion play a role in the work GEMINI is doing?
We want to demonstrate that even though electronic data has some limitations, we can take the existing information we have, and still show important gradients across equity parameters, whether it’s the neighborhood you live in, whether it’s your age, whether it’s disability status. We’re trying to use every advanced analytic method we have to pull out as much as we can around the equity characteristics and demographic characteristics of patients.
We also think we’re an important group to demonstrate that even at the very cutting edge of what you can do with electronic data, there’s certain things you cannot recreate without directly asking people. You cannot understand their home situation, whether they have trouble getting groceries, whether they’re on the verge of being evicted.
We want to show you can do a lot, but we also want to show where the real gaps are to help make the case
that we should gather this information systematically for patients because it’s important to health.
A major thrust is going to be helping physicians to understand how to use this information, make concrete targets for improving quality of care and then helping them track over time whether they achieve those targets by using GEMINI data.

These kinds of deep clinical holdings are valuable in delivering improved patient care. We have a major partnership with the Vector Institute and a lot of our work over the next few years will be taking the best AI scientists in the world, giving them access to GEMINI and seeing what they can predict, analyze and provide for hospitals.

GEMINI has also become one of the most widely used data sets for students to learn how to analyze health data.
In the next few years, we will become probably one of the largest groups in the country supporting the next gen-
eration of scientists and clinicians to understand the role of health data and learn how to use it.
What would you like people to know about the work you do?
We are we are holders of deeply sensitive information about patients. That information can be used with the highest standards of privacy protection to improve the care of individuals,
and to ensure the sustainability of our health system.
This is a partnership with the public and with the health system to use individuals’ data – which is deeply sacred – to help improve their care but also in a shared way to improve the system. We want people to understand that that can be done in a very safe way and that all of us in Ontario and people in Canada can benefit greatly from it. ■ H
New data just released by the Canadian Institute of Health Information (CIHI) show unintended hospital harm is up across Canada for the second year in a row. With healthcare systems across the country under ongoing strain, it is more important than ever to focus on safety. Renewed efforts to encourage effective “safety conversations” aimed at identifying and reducing potential risks can help to turn this trend around.
We know everyone across Canada wants – and deserves – safe, high-quality healthcare. Everyone providing care should also be safe in the workplace. But we also recognize that even before the pandemic began, neither were a reality for all. Given ongoing challenges, Healthcare Excellence Canada wants to equip everyone with tools we all can use to realize shared safety objecctives. While most people cared for in Canadian hospitals receive safe care, unintended harms do happen. According to CIHI, during 1 in 17 acute hospital visits in 2021-22, patients experienced unintended harm. That equates to about 140,000 out of 2.4 million hospital stays.
While not all instances of unintended hospital harm could be prevented, of course, we know adoption of evidence-informed practices could have helped prevent many of them. The overall Hospital Harm Measure, at 6 per 100 hspitalizations in 2021-22, is up from a pre-pandemic rate of 5.4 per 100 hospitalizations in 2019-20 – a rate that had been stable since it was first reported in 2014-15. Harm rates were mainly driven by healthcare- and medication-associated conditions and healthcare-associated infections.
The Hospital Harm Measure is intended to monitor variations in patient safety in inpatient, acute-care settings at the national level (with the exception of Quebec, which was not included for methodological reasons). The measure captures unintended harm across facilities over time and
is designed to help identify safey improvement opportunities.
Of the unintended hospital harms reported by CIHI:
• 47 per cent involved healthcare and medications, such as bedsores or getting the wrong medication
• 31 per cent involved infections, including those related to surgical sites
• 18 pecent were procedure-related, such as bleeding after surgery
• 4 per cent involved patient accidents, such as falls
The theme of this year’s Canadian Patient Safety Week, from Oct. 24 to Oct. 28, was “Press Play on Safety Conversations.” This call to action highlighted the importance of having ongoing safety discussions – and acting on them. Safety conversations
Jennifer Zelmer is President and CEO, Healthcare Excellence Canada
ly and honestly about the factors that influence their ability to deliver safe care and to be safe at work themselves. Care recipients and their essential care partners also need to feel comfortable speaking up about their care, asking questions, and articulating what they need to feel safe. It’s about learning from past experiences, understanding the reliability of clinical systems and processes, reflecting continuously on whether care is safe today, anticipating and preparing for safer care in the future, and systematically responding and improving.
To support opportunities to reflect, be inquisitive, think ahead, plan, and respond appropriately to safety needs, Healthcare Excellence Canada has assembled an array of evidence-informed online resources – including easy-touse tip sheets and other knowledge products – available at SafetyConversations.ca. These resources are designed to help everyone, whether care providers or recipients, to ask, listen and act to help reduce risks, as well as to deliver and get safer care, each and every day.
We invite those delivering and receiving care to:
• Dig deeper into safety conversations at the Now is the Time to Press Play on Safety Conversations recorded webinar
are respectful discussions about safety between two or more individuals involved in organizing, delivering, seeking, and/or receiving care. They can fundamentally change the way we think about safety.
Together, we have opportunities to help shift our perspectives on safety collectively. It is not simply the absence of harm but a sustained, proactive effort involving everyone in the care journey. This includes physicians, clinicians, and other care providers, as well as patients and those who support them, such as family members and other caregivers. It’s all about creating space that invites impactful dialogue and empowers effective responses.
Healthcare providers, managers and leaders need to be able to talk open-
• Use quality and safety tools and resources to make care safer, especially for older adults, who experience higher rates of unintended hospital harm
The latest patient safety data offer a timely reminder of the importance – and the challenges – of making care safer. Everyone has an important role to play in reversing unintended hospital harm and Healthcare Excellence Canada encourages you to take the time to access our online tools and resources to help.
Now, more than ever, let’s strengthen Canada’s healthcare safety culture by creating environments that invite safety conversations, empower effective responses and drive ongoing, positive change. ■ H
London Health Sciences Centre (LHSC) is the first in the region to introduce a non-invasive advanced aneurysm repair method that reduces a patient’s hospital stay by 80 per cent, improving recovery time by 11 months.
Like all health care organizations across the province, LHSC strives to find innovative solutions to improving access and flow within the hospital, while delivering on its commitment to patient-centered care. Recently, the vascular surgery team at LHSC adopted a new approach to managing life-threatening aortic aneurysms, which not only decreases a patient’s hospital stay from four weeks to three days but decreases overall recovery time from a year to just one month.
“This is a game changer for us,” said Dr. John Landau, a vascular surgeon at
LHSC. “We frequently perform endovascular repairs; however, this new approach is so personalized through a patient’s anatomy, allowing us to remove the aneurysm quickly and effectively, resulting in a speedy recovery. The normal procedure would require the patient to stay up to several weeks in hospital, but we’ve seen patients leave
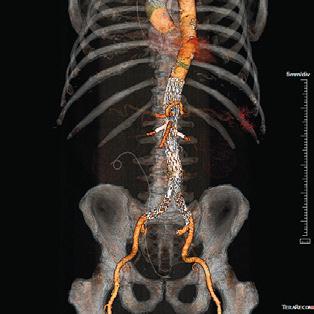
as soon as three days returning to the comfort of their own home shortly after the procedure.”
Endovascular aneurysm repair (EVAR) is a minimally invasive procedure used to manage abdominal aortic aneurysms. This advanced life-saving method uses a custom-made endovascular stent-graft, placed in the aorta which is the largest artery that carries blood from your heart to other parts of the body to prevent it from rupturing. This is completed using x-ray guidance through a tiny incision in the groin no larger than a drinking straw. The procedure prevents the abdominal aortic aneurysm from bursting which is a life-threatening event, significantly decreasing the risk of death or major complications compared to a large open surgery.
For 75-year-old Mr. Thomas Barker, this advanced aneurysm repair saved his life. In 2017 underwent an
aortic valve and coronary bypass, later discovering he had an aneurysm and was referred to LHSC to be considered for advanced endovascular repairs.
“I am beyond grateful for Dr. Landau and his team,” said Thomas Barker. “Not only did they save my life, but they gave me the gift of being home with my family sooner. No one wants to stay at a hospital longer than they have too, so being able to check-out in three days was a blessing. It’s been two and a half months since I had the procedure and I am back to my normal self, thoroughly enjoying doing yard work and golfing with friends and family.”
Due to the success of this minimally invasive procedure, there are plans to do several of them in the fall at LHSC while ongoing research for advanced endovascular outcomes continues. LHSC has several similar surgeries scheduled for the fall of 2022. ■ H

At William Osler Health System (Osler), a quality excellence mindset guides the organization, driving it to continuously pursue quality improvements that minimize risk and contribute to positive outcomes. Throughout the COVID-19 pandemic, this mindset never wavered. Instead, a heightened focus on quality, safety, communication and collaboration emboldened its teams to accelerate a number of key strategic initiatives, including the implementation of iHuddle Boards.
“Osler’s iHuddle Boards are the manifestation of a visionary and purposeful approach to quality and patient safety that is used to visually translate our strategic plan so that it is as meaningful to our frontline teams as it is to the Executive and the Board,” said Tiziana Rivera, Vice President, Quality and Chief Nursing Executive, William Osler Health System. “iHuddle Boards enable senior leaders to share strategic, operational, and quality metrics with clinical units in real time so that we’re all working with the same data to support timely decision-making locally and organization-wide.”
Recently recognized as a global leading practice by the Health Standards Organization (HSO) and Accreditation Canada, Osler’s digitally-driven iHuddle Boards are a standardized visual management tool available to clinical teams via accessible 55-inch touchscreen monitors in each emergency department and inpatient and outpatient unit. Unit managers are encouraged to invite patients and families to join unit huddles in front of the iHuddle Boards to discuss patient safety with the team, ask questions and offer solutions.
“This initiative has transformed how our teams manage quality and safety, review unit/program performance, and collaborate on key organizational initiatives,” said Tony Raso, Associate Vice-President, Clinical Practice and Quality, William Osler Health System. “Staff and physicians are quickly able to see and understand what is happening on their unit and across the organization through easy access to real-time
data and a process that facilitates input, engagement and feedback.”
Supported by an iHuddle App developed in-house by Osler’s Business Innovation team, each digital board features both standardized and unit-specific performance metrics that align to clinical unit goals and Osler’s four corporate strategic directions, all in an easy-to-read visual format.
There are also sections that provide opportunities for staff engagement and recognition, quality improvement, organizational announcements and campaigns relevant to teams at the point of patient care, and staff feedback and improvement ideas. Managers at Osler are also able to customize sections of the board specific to their team’s needs.
“It’s great to be able to access unit-specific metrics and link them to the organization’s broader strategy during team huddles,” said Shailesh Nadkarni, Clinical Services Manager, Mental Health and Addictions, William Osler Health System. “This way, staff are able to see how their daily activities at the point-of-care influence and connect to the strategic directions of the organization.”
Prior to the implementation of the iHuddle Boards, Shailesh had to access multiple screens or databases to deliver relevant information to his team for discussion in team huddles. Now that he and his teams have access to real-time data at their fingertips, they are able to maximize their 15-minute huddles, and include more meaningful discussions.
“The iHuddle Board gives us decision points for improvement, providing immediate line-of-sight as to whether or not the actions we are taking as a team are moving the needle on a performance indicator we are seeking to improve. It’s this type of dialogue that leads to innovation,” said Shailesh.
Earlier this year, Osler’s Quality Team leveraged the digital solution to help prepare clinical teams for Accreditation by conveying learning materials regarding required organizational practices (ROPs) directly on the iHuddle Boards for discussion in team huddles. This included short videos, quizzes and one-page communiques.
“Because the iHuddle Boards standardized our approach to huddles across Osler’s sites, we were able to focus clinical team discussions on the same quality-related topics each week, with managers drilling down the relevance of each ROP to the team’s dayto-day activities on the unit,” noted Tony. “The use of the iHuddle Boards to reinforce the integration of ROPs into practice was among the organizational strengths noted by visiting Accreditation Canada surveyors, who ultimately awarded Osler the Accredited with Exemplary Standing designation, the highest rating granted by the accreditation body.”
At a time when hospitals are facing unprecedented challenges moving patients through the system due to high patient volumes, patient complexity and staffing shortages, the real-time data available on the iHuddle Boards is proving crucial to supporting improved patient flow across Osler sites.

“The metrics for admissions to the emergency department and the inpatient bed census across the organization is live on the board,” said Gresham Kimm, Interim Clinical Services Manager, Stroke Unit, William Osler Health System. “Seeing live data helps our team members better understand why decisions are made that may direct-
ly impact the unit, because they can see first-hand where the challenges are.”
Another aspect of the iHuddle Board experience that Gresham likes is the opportunity to devote time to new improvement ideas from the team that are then reflected on the board.
“Typically, we’ll come up with a quality improvement initiative every couple of weeks that we want to work on as a team, based on a challenge we’re experiencing on the unit,” said Gresham. “Whether it’s something that needs to be addressed by myself, the resource nurse or by the team in their day-to-day work, we’re able to post the solution to the iHuddle Board and track its development from idea to ‘in progress’ to implementation. This really promotes problem-solving as a team, while allowing individuals to see the positive impact their ideas can have on the unit and ultimately for the patient.”
Roll-out of Osler’s iHuddle Boards began in late 2020 and was accompanied by robust resources and onboarding including scripts, training and technical videos for directors and managers. Materials were also posted on the hospital’s intranet site where they were accessible to staff and physicians.
For more information on Osler’s iHuddle Boards, visit the HSO Leading Practices Library. ■ H






 By Hana Irving
By Hana Irving
Hospitals are complex ecosystems of people – patients, families, caregivers, staff, physicians, and volunteers – all experiencing a range of emotions and witnessing those of others: joy, sadness, relief, fear, grief. The fast-paced nature of work and care can make it challenging to find time to pause, reflect, connect and process, especially since the pandemic.


Dr. Paula Chidwick, William Osler Hospital System’s (Osler) Director of Ethics and Spiritual Care, believes that finding innovative ways to support the mental health and well-being of patients, families, caregivers, staff, physicians, and volunteers across the continuum of care is critical to building a more resilient health care system. She has been a key supporter of bringing the Reflection Room project to Osler’s Brampton Civic Hospital, Peel Memorial Centre for Integrated Health and Wellness and Etobicoke General Hospital sites. The Reflection Rooms opened on September 6 and everyone who is being cared for, visiting or working in the hospital is welcome to visit and reflect.
The Reflection Room project is led by the SE Research Centre as part of SE Health’s commitment, as a social enterprise, to action-oriented research. Reflection Rooms are evidence-based, participatory art installations that offer an immersive physical space for people to write stories about their experiences and read the stories shared by others.
In a research study from 2016-2020, 62 Reflection Rooms were installed across Canada, with over a thousand visitors’ reflections collected and uploaded to www.thereflectionroom.ca. The study confirmed that storytelling can be an important part of witnessing loss and processing emotions such as grief, and that Reflection Rooms create space for remembering, cele-


brating, teaching, learning, and connecting. “Part of the success of the project,” said Dr. Paul Holyoke, SE Research Centre Executive Director and study co-principal investigator, “is that it is rooted in evidence, which allows the Reflection Room to adapt, grow and expand to fit needs, spaces and contexts.”
During the pandemic, the Reflection Room project evolved to address pandemic-related grief and loss in residential long-term care (LTC) homes. Supported by the Saint Elizabeth Foundation and others, Reflection Rooms have been installed in a variety of LTC homes across Ontario.
Emerging research findings suggest that the Reflection Rooms helped LTC residents, caregivers, and staff to look inwards in a helpful way, find moments of calm and peace, and feel a sense of connection and compassion. Feedback from LTC home administrators indicates that a Reflection Room is a good support for those who are grieving and it has the potential to aid holistic well-being for individuals and communities. These findings affirm key principles of resiliency: maximizing social cohesion, collaboration, empowerment, participation, and consideration of local characteristics and issues.
Karen Sedore, Director of Organizational Development at Osler, believes the Reflection Room project aligns with Osler’s other Healthy Workplace initiatives. “At Osler, we have prioritized our commitment to supporting the health and wellness of our Osler team members,” she said. “To do so, we’ve enhanced programming focused on both the physical and emotional well-being of our entire Osler team. Among our many initiatives, the Reflection Room project provides another opportunity to further focus on hope, resiliency, and personal welfare.”
The Reflection Room project is not designed to take away emotional pain. Instead, it offers patients, families, caregivers, staff, physicians, and volunteers an opportunity to slow down and start – or continue – to work through the feelings that they carry. The Reflection Rooms can be explored and used by everyone in any way they see fit – to write and read reflections, pray, or simply have a quiet moment away from hustle and bustle.
Augustus Oku, Spiritual Care Coordinator at Osler, believes in the power of storytelling to support one another during difficult times. “For me, the Reflection Room is a spiritual environment that may help us understand that we can only heal and grow when we take some time to reflect about our challenges,” he said.
For information about the Reflection Room project, contact research@ sehc.com. ■ H



Humber River Hospital (Humber) has launched the use of the Acessa ProVu® system – a new way to treat uterine fibroids. Uterine fibroids are the most common benign tumour in women, affecting up to 70 per cent of women during their reproductive years. Although most patients with fibroids are asymptomatic, approximately 30 per cent become symptomatic. These symptoms can include abnormal menstrual bleeding, pelvic pain and pressure, urinary problems, difficulty getting pregnant or issues during pregnancy, among others.
Typically, women do not need to proceed with treatment for fibroids if they have mild symptoms or are near menopause, when fibroids typically shrink on their own. But for patients experiencing severe symptoms, procedures are available to shrink or remove fibroids. In the past, the most common approaches to treatment has been surgical removal of the uterus, referred to as a hysterectomy, or myomectomy, removal of the fibroids.
The Acessa ProVu® procedure allows for a thorough and minimally invasive method of treating fibroids, and Humber is one of two centres in Canada offering this approach. “The Acessa ProVu® system is a novel, unique, revolutionary system that utilizes radiofrequency ablation (LapRFA), laparoscopic ultrasound and monopolar cautery,” says Dr. Bruce B. Lee, the inventor of the Acessa ProVu®. “It is the first and only system that allows physicians to treat fibroids of varying sizes and locations, relieve fibroid symptoms and shrink the fibroids without incision or cutting of the uterus.”
Acessa ProVu® was designed to preserve healthy uterine tissue by delivering heat (radiofrequency) directly into a fibroid to destroy the proteins of the fibroid tissue. Once broken down into
small fragments through coagulative necrosis, it is reabsorbed by the surrounding normal tissue, and the treated tissue softens and shrinks over time. As the procedure is minimally invasive and recovery pain is typically mild, narcotics are rarely used post-operatively and patients are able to return to normal function quickly. In addition, the procedure is cosmetically advantageous, as only two to three small incisions are required for the laparoscope and laparoscopic ultrasound probe for a full view of the pelvic anatomy.
Humber’s Chief of Obstetrics and Gynecology, Dr. Andre LaRoche, performed the first procedure in Ontario. “The Acessa ProVu® is part of the technology that helps guide us and make sure we are able to view, identify and specifically target uterine fibroids

in a safe manner,” explains Dr. LaRoche. “The Hospital is always looking to deliver innovative healthcare and be the frontrunner in advancing technology and services for our patients. When the Acessa ProVu® system became available in Canada, Humber was quick to jump at the opportunity of being one of the first to offer this in the country.”
The first few cases in Canada were performed in Regina, Saskatchewan then executed at Humber a couple of days later on September 15 and 16, 2022. This is the first time this innovation has been used in Toronto and Eastern Canada as a whole. During the first two days of cases, Dr. Lee joined Dr. LaRoche through a partnership between Humber, its administration and Hologic, a medical technology
company that acquired the Acessa ProVu® system. “The first couple of cases went very well. Dr. Lee is an amazing mentor; it was perfect having him there to ensure that we were on track. He pushed me to find every fibroid we could,” notes Dr. LaRoche.
The Acessa ProVu® system presents tremendous benefits for Humber’s patients, particularly for the demographic in the community. “Many individuals in our community cannot afford to take six to eight weeks off work and need to get back to work more quickly. They may have young families or need symptom relief, and too often are not paid to be off, so they need to get back to work as soon as possible,” says Dr. LaRoche. “This is an amazing way to introduce the technology to Canadians that need it, but also to promote the Hospital as a centre for opportunity. Eventually, the goal is to become a training centre for other hospitals to learn the technology and spread this knowledge to other facilities.”
In 2023, Dr. LaRoche will begin to train other surgeons at Humber to perform the Acessa ProVu® procedure. “Once we have more cases under our belt, I will start to train other surgeons so that they can become experts. Also, making sure that the quality of the cases we are doing is high. It’s not just about volume.”
Dr. Lee adds, “With physicians like Dr. LaRoche spearheading the program with Acessa ProVu®, I have no doubts that it will succeed. I think we are going to find that this procedure will be sought after by many patients, and there will be many other centres and physicians wanting to learn it and promote it.”
With the Acessa ProVu® system, women have a new, favourable option for fibroid treatment that has not existed before. It furthers Humber’s mission is to deliver innovative, safe and compassionate healthcare in the community.
H
ACESSA PROVU® WAS DESIGNED TO PRESERVE HEALTHY UTERINE TISSUE BY DELIVERING HEAT (RADIOFREQUENCY) DIRECTLY INTO A FIBROID TO DESTROY THE PROTEINS OF THE FIBROID TISSUE.



ecently-published research suggests that the Canadian healthcare system is making steady progress toward broader implementation of Value-Based Procurement (VBP), though more work needs to be done.

In August, the Conference Board of Canada published a briefing document, Setting the Stage: The Status of Value-Based Procurement in Canada, followed in October by a more in-depth paper titled Different Is Necessary: Approaches to Advance Value-Based Procurement in Canada. October also saw the publication of Improving Health Care Through Pro-competitive Procurement Policy, the second of three reports published as part of the Competition Bureau’s digital health care market study.
These studies highlight the important role that procurement plays in Value-Based Healthcare (VBHC), where value is measured as “the best patient-centred clinical and operational outcomes at the lowest total cost over the full care cycle.” In this context, Value-Based Procurement (VBP) supports VBHC by assessing the overall value of a product or solution in terms of its ability to improve patient outcomes and experiences. VBP interacts with VBHC, and is foundational to it.
“It would be interesting to look at the interplay between VBHC and VBP,” Dov Klein, Vice-President of Value-Based Care, Ontario Health, told the Conference Board. “They are distinct things.”
Klein’s comments speak to the central and unique roll played by VBP. Often, VBP can be what initiates a larger shift to VBCH, because at times the requirements for VBP, though challenging, can be more easily defined. The numerous practical changes required by VBP can support a cultural shift to VBHC, wherein an organization actively sees the benefit in moving the emphasis away from price, or volume, to the long-term value for patients and healthcare systems.
In its research, the Conference Board provided four methodologies where VBP brought considerable financial and non-financial value to the contracting authority. Benefits were also realized for key stakeholder groups including patients, providers, hospitals, healthcare systems, and our broader society.
In the first, the MEAT (Most Economically Advantageous Tendering) VBP framework was applied to the procurement of bloodstream infection prevention solutions in an intensive care unit (ICU), with potential savings in the millions of dollars, as well as improved outcomes.
The second example came from the Southlake Regional Health Centre Cardiac Program, which saw program costs reduced by 35% in 2017 compared with the base year (2014–15). This is equivalent to approximately $10.5 million in 2021 dollars. Importantly, these savings can then be reinvested to improve both patient access and quality of care.
In the third, Eastern Health – Newfoundland’s largest health authority – implemented a VPB model that now has about 20 ongoing initiatives. These range from patient-focussed, evidence-based targets for diabetes mitigation, to addressing issues re-
lated to staff scheduling and patient flow. Here, fixed bundle payments, risk sharing, and competitive dialogue have generated positive results.
The final example is well-known to industry observers. In 2018, a collaboration among Ontario’s Ministry of Health and Long-Term Care, CorHealth Ontario, Plexxus, and the province’s 12 ICD-implanting centres, resulted in the first provincial value-based procurement of implantable cardioverter defibrillator (ICD) and cardiac resynchronization therapy (CRT). The VPB process analyzed the total cost of care over a patient’s lifetime, resulting in financial and non-financial value for patients, providers and hospitals, the healthcare system, and the supplier community.
The Competition Bureau’s digital health care market study placed specific attention on several initiatives that are modernizing healthcare procurement.
At the national level, these include CAN Health Network’s “Edges,” which are groups of hospitals, home care organizations, health authorities, and private clinics that collaborate to procure innovative solutions. There is
also the Canadian Collaborative Procurement Initiative (CCPI), which is led by Public Services and Procurement Canada. The CCPI brings together groups of buyers across Canada, making it easier for vendors to sell to multiple organizations, and thus avoid duplicative procurement processes.
There are also many compelling examples from coast-to-coast at the provincial level.
In Newfoundland and Labrador, the 2018 Public Procurement Act promotes increased transparency, consistency, and flexibility within procurement practices, thus helping the province move toward VBP in healthcare.
In Quebec, the provincial Ministry of Health and Social Services and the Treasury Board secretariat have laid the groundwork for innovation procurement in the province through the Quebec Life Sciences Strategy and the Public Markets Strategy. These strategies, once fully deployed, will help facilitate the integration and adoption of innovative medical technologies into the health care system.
Ontario is also showing progress. The provincial government has launched its Innovation Procurement framework, which focuses on an outcome-based procurement model. As well, with the launch of Supply Ontario, which is expected to be fully operational by the end of 2023, Canada’s most populous province is moving toward a centralized, whole-of-government procurement approach. The Ontario government also has its BPS Primer on Innovation Procurement, an impressive document that can help with the planning and implementation of VBP.
There are examples in western Canada, too. Alberta has been learning from its well-integrated senior leadership structure, which supports effective decision making to operationalize VBP approaches and practices, and to generate value for patients and other stakeholders across the province. As well, British Columbia’s Procurement Concierge Program promotes innovative procurement approaches, ensuring that all suppliers can participate.
In the Competition Bureau’s digital health care market study, six barriers were identified that can stop the best solutions from taking hold in Canada. These are: fragmentation; restrictive contracting requirements; emphasis on price; risk-averse contracting; lengthy procurement cycles; and prescriptive polices.
All of these, in their way, can act as barriers to VBP, but the focus on price rather than value is the most pertinent. As the report notes, exclusive emphasis on the short-term cost of a solution does not result on effective competition. Instead, the entire range of benefits must be taken into consideration, including both lower long-term costs and better patient outcomes.
In its research, The Conference Board also arrived at six barriers –though these are specific to VBP. They include health and hospital system finance models; provincial funding models; data and measurement; policy and legislation; and professional capacity.
For its part, the Competition Bureau’s study came up with three recommendations to address the barriers. First among these was to establish a national innovation procurement centre of expertise, followed by the removal of barriers to competition, and policies that support innovation-friendly procurement processes. These policies would promote innovation via demand-side policies that reward those who solve problems. This is, in effect, the government acting to “buy” innovation, with public procurement harnessed to achieve demand-side solutions.
This is an exciting time for VBP, but more work needs to be done. Initiatives that renew how funding is structured, and that encourage competition, are long overdue. The good news is that with timely, affordable access to actionable data – supported by the right policies – VBP will be playing an increasingly important role within VBHC. The result will be a more competitive and innovative healthcare system, with better outcomes for all Canadians. ■ H
Tim Wilson is a freelance writer.
We’re very pleased to once again be a part of this year’s Hospital News Medtech supplement.
For those who aren’t familiar with Medtech Canada, our association represents the medical technology industry (medtech companies) in Canada. Our membership consists of nearly 120 member companies that range from small, emerging companies to large multinationals serving the Canadian health care system – collectively employing over 35,000 Canadians in a variety of highly skilled professions, many of whom work directly with their healthcare partners, ensuring the supply of necessary products and supporting the delivery of care across the country. We also have another sixty Allied and Associate members of Medtech Canada which represent organizations and stakeholders in the medtech ecosystem that we collaborate with on a regular basis.
Medtech Canada works closely with the federal and provincial-territorial governments, health professionals, patients, and other stakeholders to deliver a patient-centred, safe, accessible, innovative, and sustainable, universal healthcare system supported by the use of medical technology.
I have worked for the association for several years, first as the Vice-President of Ontario, and last year I had the privilege of assuming the role of President and CEO. While the challenges facing our Canadian healthcare system and our industry are significant, I believe there are also tremendous opportunities and I’m excited about leading our association at this critical moment in time.
Throughout the pandemic the medtech industry became recognized more than ever before given the necessity of so many medical technologies that were required to keep Canadians safe and healthy. We also saw during the pandemic that there was increased ability by governments and healthcare systems Canada to adopt innovations, as highlighted by many digital health technologies that were adopted for the first time.
We must maintain this momentum, as our industry has so much more to offer to help address current challenges such as addressing health system backlogs and making work more efficient for a strained health system workforce. Our industry is solutions oriented and I think that’s reflected in the partnerships we’ve forged across the country.
Barriers exist to the adoption of innovative technologies in Canada, including siloed funding models, lack of appropriate billing codes or an absence of dedicated funding for technologies. We advocate to address these challenges – working with governments, medical associations, and many others – offering tangible solutions to break down these barriers (implementing value-based procurement is one such solution). Recently we have also worked collaboratively to advocate for federal and provincial investments to address wait times and backlogs, as we all know how detrimental these waits have been to the health and well being of Canadians.
Addressing these challenges are of the utmost importance at this critical juncture in Canadian healthcare. We know that Canada’s healthcare workforce has given so much and is strained after years of tirelessly working through waves of the pandemic and the current healthcare worker shortages.
Medical technology companies have solutions that can help address these challenges by creating efficien-
cies in our hospitals, reducing healthcare workloads, and enabling care to be provided in the community (which can free up hospital beds for those that truly need them). These are just a few of the areas where our industry can provide solutions to health system challenges. We have created a microsite to highlight some of the technologies and solutions available at: medtechinnovation.ca/medtech-solutions.
We also know that clinicians want to have access technology that will enable them to provide the best possible care to their patients and access to innovative technologies can be an important recruitment tool during this time of global competition for health care talent.
As Medtech Canada, we are very proud to work on behalf of what we like to call a “win win” industry in Canada – helping make our health care system better and helping Canadian clinicians save and improve the lives of patients better every day.
Our association takes a great deal of pride in being highly collaborative solutions oriented – this was evident during our recent Medtech Conference where our industry engaged with health system stakeholders, and government and political officials on collaborations, partnerships, and continuing to find ways to come together for the betterment of Canadians. The conference left me invigorated and it reaffirmed my belief that we can find solutions together. I’m very excited to see our industry, government and healthcare partners continue to come together in the days ahead – working together to improve patient care, enhance health system efficiency, and reduce the workload placed on our overburdened healthcare system.
To our healthcare partners: thank you so much for all you do to provide exceptional care to patients every day. Our industry will continue to support you and your unwavering commitment to Canadians. ■ H
Nicole Decort, President and CEO, Medtech CanadaA




















VIRTUES



comprehensive digital health

































































that provides equity of care to meet the needs of all
regardless of geographical, cultural, or systemic barriers.
to
at
in patients’ community.
VIRTUES is a digital health
and
the


























for cardiac patients. It is always there to answer their questions,
to
CANet is making a difference, helping to save cardiac patients’ lives while encouraging more organizations to join the movement of patientdriven healthcare.
With support across Canada, CANet has developed the VIRTUES digital health platform.



A platform designed to provide patients with the most relevant medical information, facilitate access to effective care options and connect them with physicians who understand their medical and personal care requirements.
“Our VIRTUES digital health platform utilizes state-of-the-art biosensor-driven diagnostics and health informatics—augmented with advanced analytics and wireless connectivity—to provide cardiac patients access to on-demand virtual care,” says Dr. Anthony Tang, CEO
VIRTUES is a digital health companion for cardiac patients, always there to answer their questions, support them, and offer the best treatment options and access to relevant caregivers. The platform’s database consists of comprehensive health data, input by patients from multiple sources; analyzed and interpreted for patients and their caregivers.
Patients can access the platform from the comfort of their homes for guideline-recommended treatment options and personalized support resources at any time. Healthcare providers of choice can also access patients’ information, no matter their location.
VIRTUES can integrate with any device, including those implanted in the heart, to constantly monitor the device status, as well as the health of the for patients. With the VIRTUES platform at their side, patients can rest assured that they are always prepared to tackle any unexpected event.
Developed in alignment with the Personal Health Information Protection Act (PHIPA) and other Canadian healthcare privacy laws, patient information is always secure in the VIRTUES platform. VIRTUES and replication capabilities.
VIRTUES is not owned by hospitals, businesses, insurance companies, or physicians; it is in the hands of CANet’s patients.
health platforms, where patients are involved only at the end of the development process. However, VIRTUES was co-designed by patients, for was designed to be a patient-controlled digital health system from the
CANet is a comprehensive network of healthcare professionals, ground-breaking cardiac research to deliver practical solutions for personal, healthcare, and business applications; while facilitating an equal level of access to care for every patient across the country.
CANet ensures its digital health services are always aligned with evolving patient requirements. It conducts regular virtual health-related studies, spearheaded by a patient working group, to ensure its digital health tools and medical content are always aligned with the unique needs of the patient population. CANet’s patient partners take an active part in enhancing the delivery of educational material to patients.
By bringing advanced virtual communication technologies to the forefront, CANet enables heart patients to get the appropriate care they need no matter

patient insights and helps them in their care journey. The organization, in this regard, is researching new approaches of leveraging sensors, voice recognition, cloud computing, and data analytics to facilitate remote diagnoses and disease tracking from the comfort of the patient’s home.
Federally funded, CANet is housed in the Schulich School of Medicine & Dentistry at Western University.
collaboration and data sharing among clinician-scientists, basic scientists, engineers, and social scientists across the country,”







contribution to developing novel digital health technologies will allow patients to receive vital and potentially life-saving medical care no matter where they live in the world.”

CANet’s patient-driven research perfectly aligns with Western University’s goal of enhancing targeted treatments for patients in Canada and globally.
CANet will take the competencies of its network beyond cardiac diseases and enhance healthcare accessibility for patients suffering from other chronic conditions, including diabetes, hypertension, and lipid disorder. CANet aims to help patients manage their diseases, especially when they need to make crucial lifestyle changes.
As patients seek to take control of their health, CANet is helping them do it effectively.


With the sound described only as that of a buzzing swarm of bees, an innovative drone delivery pilot project has literally taken flight. Dubbed Care by Air – Halton Healthcare and partners DSV Air & Sea Inc. Canada, Drone Delivery Canada (DDC), McMaster University and Air Canada Cargo, have launched a six-month pilot project with the hopes of clearing the path for drone deliveries of medical supplies – a project that is among the first of its kind in Canada.
“Advancing how we deliver care, includes finding new and efficient ways to use technology. Being at the forefront of an innovative drone delivery system is the ideal way to contribute to the advancement of healthcare so we can be more responsive to the care needs of our patients, families and communities,” says Hilary Rodrigues, Senior Vice President, Corporate Services, Performance & Chief Financial Officer, Halton Healthcare.
Halton Healthcare is located in a growing community covering both urban and rural populations. The organization has three hospitals that stretch a nearly 34km distance between Georgetown and Oakville Trafalgar Memorial Hospitals, with its Milton District Hospital sitting almost at the mid-way point. With specialized specimen testing occurring at the Oakville Trafalgar Memorial Hospital (OTMH) site, transporting samples from hospital to hospital over that distance means that time is always of the essence.
“As a hospital organization, we are sensitive to many of the same issues that impact other service providersrising fuel costs, supply chain issues and a responsibility to support our natural environment,” continues Rodrigues. “And because we’re re-
sponsible for delivering care – even small disruptions can make a critical difference.”


So when an internal innovation grant was submitted by a team of staff covering diagnostics, lab and pharma-
cy at Halton Healthcare, encouraging the organization to consider options for advancing the delivery of care using drones, the organization was ready to help the idea liftoff.
“We log multiple courier trips from our Milton and Georgetown Hospitals to OTMH each day and it is only going up as we see a higher volume of patients,” relates Shairoz Kherani, Director, Diagnostic Imaging & Laboratory Services, Halton Healthcare.

“ADVANCING HOW WE DELIVER CARE, INCLUDES FINDING NEW AND EFFICIENT WAYS TO USE TECHNOLOGY. BEING AT THE FOREFRONT OF AN INNOVATIVE DRONE DELIVERY SYSTEM IS THE IDEAL WAY TO CONTRIBUTE TO THE ADVANCEMENT OF HEALTHCARE SO WE CAN BE MORE RESPONSIVE TO THE CARE NEEDS OF OUR PATIENTS, FAMILIES AND COMMUNITIES.”



Accelerating innovation with minimally invasive therapies, like Micra™ - the world’s smallest leadless pacing system.






“The financial and environmental costs of that are significant, but what’s even more critical are the potential for delays in clinical results, and therefore care for our patients,” continues Kherani.
Officially launched on October 13, 2022. The Care by Air pilot project will initially define flight routes from DSV’s Milton, Ontario headquarters to Halton Healthcare’s Oakville Trafalgar Memorial Hospital using DDC’s Sparrow drone, its DroneSpot® takeoff and landing zones and the company’s proprietary FLYTE software.
“This project aims to demonstrate the benefit and value of a drone delivery system in healthcare, especially compared to more traditional transportation methods. With their speed, agility and efficiency this innovative
delivery system can easily respond to urgent calls,” adds Steve Magirias, CEO of Drone Delivery of Canada.
“We envision creating a web of flight routes to service Georgetown, Milton District and Oakville Trafalgar Memorial hospitals to interconnect all three
hospitals with a reliable, cost-effective, emission-free solution.”


The test will involve transport of goods starting with a neutral substance like water, progressing to medical isotopes – which are some of the most time-critical medical supplies. Depending on the type of isotope, timelines for expiry can be under two hours. The current path of medical isotopes sees them travelling the congested 400 series highways through the Greater Toronto and Hamilton Area.
“The post pandemic era has highlighted the need to find innovations in healthcare, enabling safe, secure, and reliable ways to deliver vital or urgent medical supplies to facilitate patient care,” explains Martin Roos, Managing Director of DSV Air & Sea Inc. Canada. “The Care by Air project represents a critical step toward optimizing these supply chains. We are excited to take this next step in drone logistics by partnering as the hub for deliveries to Oakville Trafalgar Memorial Hospital and to play an
integral role in developing drone delivery routes in Halton. This will benefit both Halton Healthcare’s hospitals and the patients they serve.”
Care by Air will see daily cargo drone test flights tracked for support and regulatory approval for the eventual transport of a wide range of healthcare supplies and products, including specimens such as blood or human tissue and medical isotopes (supplied by McMaster University). These items fall under a “dangerous goods” classification and require demonstration to aviation regulators for approval.

“Once we meet the regulators’ requirement to deliver dangerous goods, it really opens up a lot of possibilities for hospitals throughout the system,” says Rodrigues. “That designation will open a whole host of things that we can deliver.”
“The benefits of what we can move with these machines in the years to come is profound,” concludes Kherani, “Drones are where and how the future is moving.”
■ H
Laura Zilke is Manager, Communications & Public Affairs, Halton Healthcare.

“THIS PROJECT AIMS TO DEMONSTRATE THE BENEFIT AND VALUE OF A DRONE DELIVERY SYSTEM IN HEALTHCARE, ESPECIALLY COMPARED TO MORE TRADITIONAL TRANSPORTATION METHODS.”
overned by a mandate to provide universal access to high-quality, value-based care, Canada’s healthcare system faces ongoing challenges and opportunities for improving cost- and time-efficiencies across departments and facilities.
Achieving these efficiencies is especially critical for operating rooms focused on cataract and retina surgeries, which have long wait lists that have become even longer because of COVID-19. According to the Canadian Institute for Health Information, in 2020 around half of Canadians did not undergo their cataract surgeries within recommended time frames, compared with roughly one-third in 2019.1
Yet by making just one change –in particular, switching from generic to comprehensive surgical packs – in their operating rooms, Canadian hospitals can realize numerous benefits for patients, doctors and for the healthcare system. Before a cataract procedure can be performed, each item required for surgery must be ordered, received, stored, and brought to the operating room storage space. The circulating nurse pulls each required item from inventory, and then unwraps each element for the scrub nurse prior to every surgery. Each step has a hidden cost of labour hours.
A recent budget impact model study by Alcon found a community hospital performing 2,500 cataract procedures per year can save up to 287 labour hours for materials management by using one system of pre-assembled instrument trays (Custom Pak®) customized for each practice, surgeon and case, and that include both pure disposable supplies, such as syringes, and sterile equipment-specific surgical supplies, such as surgical handpieces. Surgery preparation time is also reduced by making this change. This
in turn allows for potential additional procedures totalling almost 200 a year.2 From a financial perspective, the OR realizes more than $37,000 in cost savings.2
At an aggregate level, a province that does 50,000 cataract surgeries per year realizes savings of more than 5,600 hours and frees up room and time for more than 3,900 additional procedures. The total potential hidden costs would be reduced by close to $737,000.2
The results are similarly positive for retina procedures. At a facility with 1,000 retina surgeries annually, switching from a generic pack to a complete custom surgical pack saves about $10,270 each year in potential hidden costs.2 This one solution could allow for 127 additional retina procedures.2
“As a user who switched to a complete custom surgical pack system, our quality, efficiency and value were taken to a much more elevated level,” says Donna Punch, past Clinical Director, Kensington Eye Institute. “The custom pack system hit all the buttons, streamlining operations while at the same time adding superior quality and significant savings.”
The time- and cost-savings from complete surgical packs can be attributed in part to efficiencies in supply chain and materials management procedures. Instead of sourcing instruments from multiple vendors, materials management departments deal with one service. There are also time savings in the OR, resulting from reduced handling of surgical supply material for surgical preparation and from streamlined storing and pulling of supplies.

The benefits of switching to complete custom surgical packs go beyond ophthalmological procedures. In a study of custom surgical splint packs for orthopedic surgeries, pre-surgery preparation went from 209 seconds using a bulk supply pack to 86 seconds using a custom splint pack, while materials retrieval time decreased from 68 seconds to 33 seconds. Total splinting time shrank from 526 seconds to about 350 seconds.3
For doctors and patients, the benefits of upgrading to complete custom surgical pack systems mean smoother, more seamless OR experiences and higher-quality care delivered within recommended timelines. Ultimately, these benefits translate into greater opportunities to ensure the sustainability of the healthcare system, today and in the future.
Virtual care is quickly transforming the Canadian health care system. Virtual care can be defined as any interaction between patients and care providers that occurs remotely, using any form of communication or information technology, and that aims to facilitate or improve patient care. Even before the COVID-19 pandemic, Canada’s experience and interest in virtual care had been growing, but the pandemic accelerated the adoption of its use.
For most of us, our first experiences with virtual care happened during the pandemic when health care providers needed to quickly come up with alternative solutions to in-person care. According to an early analysis of Canada’s pandemic response by Health Canada however, “while change was forced upon us by the pandemic it was, in many cases, long overdue.” Virtual care has the potential to improve health care by increasing access to health care and by making health care more convenient for patients.
Now that some health care decision makers have had a few (albeit very brief) moments to catch their breath, they have asked CADTH – an independent agency that finds, assesses, and summarizes the research on drugs, medical devices, tests, and procedures – what the evidence says on virtual care. With in-person care resuming, health care providers want to know which services they should continue to offer virtually, and which services are best offered in person.
CADTH has published many reports on various virtual care topics. In one recent report, CADTH searched for and summarized recent evidence-based guidelines on the appropriate use of virtual care. CADTH found 5 guidelines, 3 of which were developed in the context of COVID-19 after the demand for and use of virtual

care had increased. The guidelines developed before the pandemic include 1 guideline on the use of remote telecommunications in stroke care and 1 guideline, from the World Health Organization (WHO), on digital interventions for all areas of health.
The guidelines developed during the pandemic include 2 on virtual care in rheumatology and 1 on telehealth for oncology.
A recurring theme among all the guidelines is that virtual care should be a complement to, not a substitute for, in-person care. Further, they recommend that virtual care should be considered only when adequate resources and personnel are available and patient privacy can be pro-
tected. Multiple guidelines note that it’s not a one-size-fits all approach when using virtual health care with patients.
The guidelines developed during the pandemic reflect the new experiences and insights gained during that time –such as the recommendation that teleconsultation be used for rheumatology patients who must adhere to social distancing restrictions, or the guidance that rheumatologists use telemedicine for patient consultations during medication changes when normal health services are disrupted. One of these guidelines suggests virtual modes as a way to bring medical care to people who are home-bound or those who live in remote areas or underserved com-
munities, which could benefit patient care outside of a pandemic.
For various reasons, some patients prefer not to use virtual care. There may barriers or factors that pose challenges to its use, such as issues with internet access, technical support, and infrastructure.


Users of these guidelines should keep in mind that the quality of evidence they are based on, if reported, is generally low, with consensus-based recommendations made when evidence was lacking. In addition, many of the recommendations might not translate well into Canadian clinical practice given that only 1 of the 5 guidelines is Canadian.
Future guidelines on virtual care that are supported by high-quality evidence are needed. As the research on virtual health care is rapidly evolving, living guidelines (guidelines that are updated as soon as new evidence becomes available) may be useful to decision makers seeking continued direction when using this form of care. In fact, the WHO proposed updating its guidelines as a living document.
One thing is for sure – if virtual care continues to be seen as providing increased convenience, flexibility, and time and cost-savings, patients and health care providers will continue to be interested in its use. CADTH will continue to support health care decision makers by summarizing future evidence on virtual care.

The CADTH report on virtual care guidelines is freely available at cadth. ca/virtual-care-use-primary-care-orspecialty-care-settings. To see all of CADTH’s work in this space, or to find additional reports on telehealth and telemedicine, visit cadth.ca/ digital-health. To learn more about CADTH, visit our website, follow us on Twitter @CADTH_ACMTS, or speak to a Liaison Officer in your region.
H
for evidence to help navigate the path forward for virtual care
RECURRING THEME AMONG ALL THE GUIDELINES IS THAT VIRTUAL CARE SHOULD BE A COMPLEMENT TO, NOT A SUBSTITUTE FOR, IN-PERSON CARE.
























Assessing the nutritional needs of critically ill patients is an ongoing challenge for dietitians. To support meeting the caloric needs of these individuals, Halton Healthcare’s Oakville Trafalgar Memorial Hospital (OTMH) is pleased to be the first hospital in Ontario to be home to a Q-NRG+ Indirect Calorimeter machine. The machine uses new technology to measure oxygen and carbon dioxide levels in patients’ breath to determine their resting energy expenditure (REE).
“The Indirect Calorimetry is a new method to assess a critically ill patient’s nutrition needs, and give us the information we need to create individualized nutrition care plans for people in the Intensive Care Unit. The needs of these individuals are very different than of other patients,” says Hilda Seyler, Dietitian, Halton Healthcare.
Before the Indirect Calorimetry (IC) device was introduced at Halton Healthcare, the practice was to use predictive equations based on age, weight, height and gender.
“The Q-NRG+ gives me more confidence that the nutrition I’m recommending is accurate and individualized to the patient, because we’re using real-time measurements,” adds Seyler.
Introducing the world’s first 80-cm patient bore and High-V MRI, MAGNETOM Free.Max redefines MRI accessibility and opens up new clinical opportunities.

High-V MRI – Value beyond barriers

High-V MRI takes the power of digitalization and deliberately applies it to a new field strength of 0.55T with inherent clinical benefits. High-V MRI combines the best of both worlds to offer a new era in MRI that embraces diagnostic confidence in daily routine and new clinical opportunities.



Diagnostic confidence for daily excellence


Powered by our unique innovations in the field of image acquisition and deep learning based reconstruction MAGNETOM Free.Max delivers excellent diagnostic quality for your standard clinical MRI applications.

The world’s first 80 cm patient bore With the world’s very first and only 80 cm patient bore, MAGNETOM Free.Max breaks






























barriers in patient comfort and accessibility –making the experience a realistic option for claustrophobic, anxious, and more corpulent patients.

Infrastructure radically simplified MAGNETOM Free.Max is the world’s most compact whole-body MRI and with DryCool technology it provides a virtually helium-free infrastructure. MAGNETOM Free.Max radically simplifies infrastructure requirements to break down the barriers imposed by siting constraints.

Redefining MRI affordability MAGNETOM Free.Max breaks down financial barriers resulting in new opportunities to offer MRI right at the front line of diagnostic services.
Older models of IC devices are typically big and time consuming, usually taking more than an hour to calculate results. Tina Stewart, Clinical Nutrition Manager, says the major benefit of the Q-NRG+ Indirect Calorimeter is that it’s portable and quick. “It only takes 10 to 15 minutes to collect the necessary data, so it’s quite efficient,” she says. “It’s also just slightly larger than a blood pressure machine, and easily mobile.”
The adoption of the Q-NRG+ device has offered a unique connection across teams within Halton Healthcare. Thanks to the collaborative efforts of Dietitians and Respiratory Therapists (RTs), the machine has been successfully integrated into both their practices. With the RTs calibrating the device and using it to measure a patient’s oxygen intake and Dietitians using the calorimeter’s readings to measure the nutrition needs of the patient.

“The Q-NRG+ is very easy to use, very accurate and doesn’t disrupt the clinicians on either side. We RTs are used to ventilators and this machine uses parts similar to what a ventilator uses to measure flow. It’s been a very easy and valuable tool for everyone to use,” explains Margaret Coburn, Respiratory Therapist, Halton Healthcare.
“For acute care this is a great device to have, especially in light of the pandemic, with some patients being ventilated longer,” says Coburn. “This definitely helps us provide better care to our patients because we can fine tune to their individual needs.”
The Q-NRG+ is currently integrated as a patient care option in the OTMH Intensive Care Unit and can be used on any critically ill patient.
The device was purchased through Halton Healthcare’s Innovation Grant, which is an organizational initiative that supports innovative ideas by staff, physicians and volunteers to advance patient care. Halton Healthcare introduced the Innovation Grant program in 2017 and to date has invested approximately $612,000 in more than 70 staff-led initiatives. ■ H
THE MACHINE USES NEW TECHNOLOGY TO MEASURE OXYGEN AND CARBON DIOXIDE LEVELS IN PATIENTS’ BREATH TO DETERMINE THEIR RESTING ENERGY EXPENDITURE (REE).
MAGNETOM Free.Max breaks barriers to expand the reach of MRI. Where patients have felt discomfort, the world’s first 80 cm bore sets a new paradigm in patient comfort. Where infrastructure was an obstacle to MRI, MAGNETOM Free.Max slots into an existing helium-free




infrastructure. Where access to MRI was not viable, MAGNETOM Free.Max makes access affordable. And where conventions have limited our thinking, MAGNETOM Free.Max breaks out of conventions to explore new clinical opportunities in MRI.
out more – get in touch with us today: customeradvocate.ca@siemens-healthineers.com


Home to the largest Epilepsy Monitoring Unit (EMU) in Canada, London Health Sciences Centre (LHSC) has added new state-of-the-art Electroencephalogram (EEG) machines that will advance epilepsy research and diagnosis. It will provide faster reporting, and clearer, more detailed imagery.
Founded in 1987, the EMU has provided patient-centric care and assessments to more than 10,000 people over three decades. The Centre of excellence has also helped patients with complex epilepsies from around the world, including Holland, Mexico, Spain and Australia. This new static and mobile technology have the functionality to measure electrical activity in the brain. It uses small, metal discs (electrodes) attached to the scalp, which are then communicated through electrical impulses which are active all the time, even during sleep. As the main diagnostic test for epilepsy, an EEG plays a vital role in providing important health care information to patients and their care teams.
“With almost 90 billion neurons, the brain is the most complex human organ in the body, which requires advanced technology and equipment to further ignite research and benefit the patient experience,” said Dr. David Steven, Chair/Chief of Clinical Neurological Sciences. “This new equipment will provide a clearer more accurate picture of what is happening in the brain during a seizure, helping doctors gain crucial information about a patient’s seizures to help guide care options.”
The Centre is a leader in its field and is active in training neurologists and neurosurgeons from around the globe. The department supports world-class research and teaching, with more than 30 neurologists and neurosurgeons coming from various countries.
“Diagnosing and treating epilepsy is a convoluted process,” said Dr. Jorge Burneo, Neurologist Chair/Chief Division of Neurology of the Epilepsy program at LHSC. “With the ability to monitor a larger number of patients, through the implantation of electrodes
Dr. Jorge Burneo and Dr. David Steven.in the part of the brain associated with the spread of seizures, we will be able to diagnose and treat epilepsy faster. The mobile technology can collect data wherever the patient is in the hospital, which provides more consistent data, ultimately allowing our teams to fully understand the scope of the patient’s unique situation.”
Since September, this $2 million investment in 13 new portable machines has increased the level of data collected among patients, resulting in higher-quality images being captured during the day and at night. Committed to advancing research and finding innovative solutions to health care, the new EEG is an investment that will
have lasting impacts on both patients and researchers at LHSC for years to come.

With roots going back a century and a half, London Health Sciences Centre (LHSC), is an award-winning, research-intensive acute tertiary and quaternary teaching hospital, one of only 14 such hospitals in Ontario. LHSC is also home to Children’s Hospital, one of just four acute tertiary care paediatric hospitals in the province. Our unique place in the health system positions us well to inform and advise on provincial, national and international health policy. We are the cornerstone of care for many specialized programs and services in Western
Ontario. And, as a major provider of emergency care and through our community hospital mission, we also care for the more than 400,000 people who call London home as well as many in surrounding communities. With Ontario’s health system continuing its transformation, LHSC has an opportunity to inform it and to place itself at the locus of the regionalized health system by virtue of its size, specialized capabilities, research and education capacity and its current regional footprint. LHSC’s formal relationship and strong bond with Western University provide a mechanism for collaboration to enable the delivery of high-quality care through a process of continuous learning and research. At its core, the affiliation is a reciprocal relationship that leverages the learning, teaching and care environments of both Western University and LHSC. LHSC is a 15,000 person strong team of physicians, staff and volunteers – collaborators, innovators and pioneers, meeting the care needs of those we serve and charting a course for the future.
“WITH ALMOST 90 BILLION NEURONS, THE BRAIN IS THE MOST COMPLEX HUMAN ORGAN IN THE BODY, WHICH REQUIRES ADVANCED TECHNOLOGY AND EQUIPMENT TO FURTHER IGNITE RESEARCH AND BENEFIT THE PATIENT EXPERIENCE.”
Canada’s hospitals are under tremendous pressure. Wave after wave of COVID-19, health staffing shortages and an immense surgical and procedural backlog have dominated headlines for months. Governments and healthcare systems across the country are responding and investing in hospital infrastructure, developing significant recruitment and retention plans and rethinking the best way to cut waiting times.
Behind the scenes though, a new challenge has hit our healthcare system: a shortage of medical supplies and devices. This has caused difficulties for healthcare providers during an already highly demanding time.
Global supply chain issues have affected all sorts of devices. The COVID-19 pandemic and other global events, such as the war in Ukraine, have resulted in increases in the cost of fuel and raw materials. These and many other factors including global staffing shortages are driving up prices.
Consumers are well aware of the increases in food prices and have seen the challenges associated with buying new cars and electronics, but less noticed have been the consequences for the manufacturers and suppliers of medical devices and supplies.

According to the CD Howe Institute, prices for plastics and resin, which are critical components of broadly used medical supplies including needles and syringes have doubled, transportation costs have tripled and the prices of other raw materials such as metal have increased by more than 30 per cent. The result is skyrocketing costs to produce and supply medically necessary devices ranging from IV bags and gauze, to stents, hip and knee replacements and pacemakers.
Medical supply contracts in Canada are far less flexible than their global counterparts. Manufacturers and suppliers are locked into contracts for five to seven years at fixed prices, which means, unlike in other sectors, manufacturers and suppliers are often unable to simply adjust their prices in real time to reflect the impact of these macroeconomic and geopolitical market forces.
Our industry is working hard every day to ensure that our healthcare partners have the necessary devices and supplies to continue to provide high-quality care to Canadians.
But, unless governments and purchasing organizations work with suppliers on solutions to reflect this current supply chain crisis, manufacturers and suppliers are looking at continuing to supply these devices at significant losses. This is simply unsustainable.
In March 2022, Medtech Canada released our position paper outlining four key recommendations for governments to tackle the effects of the global shipping and supply chain crisis, and its potentially detrimental impacts on patient care.
In the case of scarce supply, governments need to work with manufacturers to ensure that the Canadian health care system has access to the devices and supplies we need to support patients.
One of the latest examples of this is epidural catheters used to manage pain during labour and c-sections. Product shortages can contribute to even longer wait times – a problem when we are already dealing with record surgical backlogs – and dramatically poorer health outcomes for Canadians.
To help address supply chain challenges jurisdictions across Canada, we
Nicole DeKort is President and CEO, Medtech Canadaneed to be more flexible in contracting systems for medical devices and supplies. We can and should provide greater clarity to suppliers around product need forecasting, improve contingency planning for future geopolitical events, as well as consider incentives to promote greater domestic manufacturing. However, these solutions will not be put in place overnight, and the problem is immediate and urgent.
Just as it would be beneficial to industry to have data on health system demand forecasting, we also understand that our industry needs to do its part to ensure that our healthcare and government partners are informed about foreseeable product shortages. Medical device companies provide information with Health Canada when shortages occur, and the regulator posts these shortages publicly on its website. We’ve also been engaging with government purchasing departments and group purchasing/shared service organizations to share information. We were pleased to learn at our recent annual conference that Health Canada would soon be convening a Medical Device Shortage Multi-Stake-
holder Committee, which should also be beneficial to foster communication nationally and ensure efforts aren’t being duplicated.
While that work is being done to communicate about shortages, government investments are needed to help ensure that they don’t occur in the first place. Just as we have seen investments in other areas to stabilize the health system, we need investment in medical devices and supplies to help ensure that our healthcare partners can deliver the quality and timeliness of care that Canadians expect.
With the health system backlog resulting from the pandemic, Canadian patients have suffered enough from long wait times and limited access to the critical medical services they need. Medical devices and supplies are critically important to providing the quality of care we rightly expect in Canada.
We can’t ignore these supply chain issues and we urge governments to come together with the sector to ensure that our health care system not only has the capacity – but also the necessary supplies – to support Canadian patients.
It’s no secret that pointof-care staff and caregivers are aware of the wide range of challenges that older adults face – from loss of independence due to cognitive decline to the inability to do basic everyday tasks. As the country’s population ages, there’s a growing need for innovative ideas to improve the quality of life and care for an aging demographic. Who better to develop these innovative ideas than clinical staff, managers, researchers, and caregivers who hold extensive knowledge and key insights into what can be transformed in this sector?
Last month, the Centre for Aging + Brain Health Innovation (CABHI), powered by Baycrest, announced the return of the Spark program, CABHI’s funding program
supporting the development of grassroots solutions solving real-world healthcare challenges. Project applications are now open to point-of-care staff (workers, managers, researchers) working at Canadian healthcare delivery organizations and informal caregivers. Successful applicants will receive up to $50,000 (CAD) in funding over 12 months to help develop, refine, and implement these innovations.
This year, the Spark program is accepting applications aimed at addressing one or more of the following innovation themes:
• Caregiver Support: Solutions that support caregivers (formal and informal) in their care for older adults living with dementia
• Aging in Place: Solutions that enable older adults with dementia to maximize their independence so they can age in their desired setting
• Care Coordination & Navigation: Solutions that help older adults, caregivers, and healthcare providers to better coordinate and navigate care for older adults with dementia

• Cognitive & Mental Health: Solutions that improve brain/cognitive
health for aging adults and/or support the identification and assessment of adults at risk for dementia/ cognitive impairment
• Financial Health & Wellness: Helping older adults remain financially independent, stay safe in the workforce longer, seek later-life employment, prepare for retirement, and prevent financial exploitation
Beyond financial support, the Spark program offers CABHI’s Acceleration Services including tailored coaching, mentorship, networking, and end-user validation through CABHI’s Leap community for older adults and caregivers.
Past Spark innovations include:
• Advancing Reminiscence Therapy through Virtual Reality Application to Promote the Social Connectedness of Persons with Dementia – An innovative frame-
AS THE COUNTRY’S POPULATION AGES, THERE’S A GROWING NEED FOR INNOVATIVE IDEAS TO IMPROVE THE QUALITY OF LIFE AND CARE FOR AN AGING DEMOGRAPHIC.
ly
in a
of
evidence-based,
mind
•
tialed
to teach
of geriatric
to un-
the benefits and educational outcomes of a virtual 12-week certificate program. The course is delivered through an established virtual learning platform (ALPHA/LIPHA),



uses a simulated educational environment to foster effective, interactive, and motivated learning.



Do you have an idea to improve seniors’ care? Take advantage of this opportunity to move your innovation for-


ward! Submit your application by Friday, December 2, 2022. To learn more and to apply, visit www.cabhi.com/spark.
H

Dan Levitt is the CEO of KinVillage, a Fraser Health affiliate partner and non-profit society in Tsawassen. He and his team provide a combination of housing (long-term care, assisted living and independent living), health services and programs for older adults in the community.
“We work closely with Fraser Health and its leadership,” says Dan. “Together, we want to set a new narrative on what long-term care is, which includes creative and innovative new ways of doing great things for seniors.”
Part of this innovation includes the promotion of food equity – so that no matter a resident’s age, health or ability, they feel valued and seen when it comes to their nutrition and meals.
“Food is all about dignity,” says Dan. “We want to make sure that anyone sitting down to eat in our dining room feels equal to their fellow diners.”
To support this goal, KinVillage has implemented an initiative for individuals with dysphasia – a condition that causes swallowing difficulties, which can lead to coughing or choking when eating or drinking.
“It’s something that we see in individuals who have neurological conditions, such as dementia or Parkinson’s disease, or who maybe have suffered a stroke,” says Dan.
For these residents, food must be served liquefied or as purees, which makes it safe for consumption, but can also make it less palatable or visually appealing.

“We wanted to make pureed food more appetizing. So we’re now shaping and re-forming textured food into solid forms, so they resemble the different pieces the dish. Effectively, the steak looks like steak, carrots look like carrots, and potatoes look like potatoes.”
Dan and his team have seen immediate positive impacts.
“One staff member actually returned a plate saying ‘This is not for the person I’m feeding – they can’t eat solid food.’ That’s how good it looks like. Another person who couldn’t feed themselves, can now feed themselves. And others who
used to struggle to eat, are clearing their plates.”
Janice Sorensen registered dietitian, PhD, is the clinical research leader with Fraser Health’s Integrated Long-Term Care and Assisted Living team and stresses the positive impact work like this has, especially on resident populations at higher risk of malnutrition.
“Evidence shows that individuals on a modified consistency diet typically experience reduced food intake and undernutrition, which can result in functional decline and poorer health status,” she says. “Allowing individuals to participate during mealtime in ways they were accustomed to can increase one’s motivation to eat, improve mealtime experience and impact quality of life in a big way. It brings back the joy of food.”
Janice encouraged and provided advice for Dan and the KinVillage team to apply for seed grant funds through the Healthcare Excellence Canada LTC+ program, to support their project.
The success of their application made the program possible, and they are now currently working on securing permanent funding.
“We want this to become the standard,” says Dan.
He believes that the momentum from projects like this one carry on into new, creative ways of delivering excellent seniors care.
“Our focus is, if we can change one thing in long-term care, it puts the spotlight on the next thing we can work on. It’s all part of re-thinking the long-term care home all together.” ■ H
With more than half a million Canadians living with Alzheimer’s disease or other forms of dementia and no cure on the horizon, research and care is focused on prevention and protective interventions to help slow cognitive decline. In a recent study published in the Lancet, hearing loss was reported as being the leading potentially modifiable risk factor, accounting for up to 8 per cent of new dementia cases. Baycrest has launched a new online screening tool to help detect hearing loss. The tool is available to the public at no cost and takes approximately 10 minutes to complete.
Supported by Baycrest’s Audiology Department and the Baycrest Innovation Office, the online tool asks questions to identify individual hearing concerns, such as difficulty with conversations over the phone or in noisy environments, as well as other questions which can help guide Baycrest’s Hearing Services to assess one’s
hearing ability and offer individualized solutions for hearing loss. The tool can be accessed on the Baycrest website.
“Baycrest’s new screening tool has the potential to slow cognitive decline and prevent dementia by identifying early risk factors for hearing loss. Most importantly, it can help improve the management of hearing loss, allowing older adults to live a more fulfilling life,” says Deb Galet, Vice President, Long-Term Care, Ambulatory Clinical Services, and Chief Heritage Officer.
Although hearing loss is very common among older adults, affecting two out of three of those over 70 years of age, it remains largely undiagnosed and untreated. Early identification and management of hearing loss helps to improve communication, social participation, and quality of life, and may help slow cognitive decline and the onset of dementia. The World Health Organization (WHO) recommends that all adults aged 50 years and older be screened regularly for hearing loss
to identify those who would benefit from hearing rehabilitation at the earliest possible stage.

Baycrest is a global leader in research, innovation, education and care for older adults, with a special focus on brain health and aging. Baycrest is home to a robust research and innovation network, including one of the world’s top research institutes in cognitive neuroscience, the Rotman Research Institute; the scientific headquarters of the Canadian Consortium on Neurodegeneration in Aging, Canada’s largest national dementia research initiative; and the Baycrest-powered Centre for Aging + Brain Health Innovation, a solution accelerator focused on driving innovation in the aging and brain health sector.
Baycrest helps aging adults assess, monitor, maintain and enhance cognition through an innovative portfolio of evidence-based products and services offered through its brain health company, Cogniciti.

Fully affiliated with the University of Toronto, Baycrest provides excellent care for older adults combined with an extensive clinical training program for the next generation of healthcare professionals.
Through these initiatives, Baycrest has remained at the forefront of the fight to defeat dementia as our organization works to help individuals Fear No AgeTM and create a world where every older adult enjoys a life of purpose, inspiration and fulfilment. ■ H


Home care is about trust. It is feeling comfortable with a provider coming into the home of someone you care for and, possibly, Bayshore’s home care services are extensive, tasks or round-the-clock care, Bayshore’s caregivers can help your loved ones to live

Let’s talk. 1.877.289.3997
bayshore.ca
It’s hard being in lockdown. Having endured multiple of them since March 2020, it’s something pretty much everyone can agree on. Being separated from family and friends, being restricted in our movement and experiencing complete isolation can prompt a wide range of emotions and physical reactions. For people living with dementia and their caregivers, lockdown is even harder.
There’s no doubt that the COVID-19 pandemic was catastrophic for Long-Term Care Homes (LTCH). Between March 1, 2020 and February 15, 2021, more than 2,500 care homes in Canada experienced a COVID-19 outbreak resulting in the deaths of over 14,000 residents and close to 30 staff, according to The Dementia Strategy for Canada 2021 Annual Report. The majority of those LTCH residents are living with dementia. This brutal reality, especially in the early days of the pandemic, underscored the need for some type of tool to help LTCH residents and staff.
Dr. Andrea Iaboni, a geriatric psychiatrist and clinical researcher based at the Toronto Rehabilitation Institute at UHN and the Medical Lead of the Specialized Dementia Unit, quickly put a plan into action to develop a Dementia Isolation Toolkit (DIT). She and a diverse team of both KITE resources and external partners got to work quickly on the first DIT as the pandemic was declared.

Within six weeks they had designed, built and launched DIT version 1.0. Since then, the DIT has been downloaded 9,000 times. When asked how they did it, Dr. Iaboni says, “the structure and support at KITE gives us the confidence to launch and ask people to use it.”

The DIT’s overall purpose is to provide ethical guidance on how to safely and effectively isolate people living with dementia in LTCH while supporting their personhood.
The DIT has two specific goals. The first goal is to support the im-
plementation of compassionate and effective infection control and prevention measures in LTCH, such as isolation and quarantine of LTCH residents.
The second goal is to help caregivers with any moral distress they feel by having to enforce isolation and quarantine of residents. Keeping residents in their rooms is necessary for the good of the whole LTCH, but is also in conflict with person-centred care principles used to guide LTCH settings. This ethical conflict can cause moral distress.
The DIT is a set of three tools: Ethical Decision-making, Person-Centred Isolation Care-Planning, and Isolation Communication tools. The tools can be used together or separately, and each tool can be downloaded from the website dementiaisolationtoolkit.com. Collectively, these three tools achieve the DIT’s purpose and goals.
The Ethical Decision-making tool sets out the principles of public health ethics in the context of LTCH and
provides a structured approach for LTCH staff to discuss and apply these principles. The tool is a worksheet that facilitates discussion and documentation on how to isolate a resident for infection control and prevention. It covers the strategies to be considered, risks and benefits of these strategies, and the chosen plan of action. It includes input from many stakeholders, including the resident and the resident’s family.
The Person-Centred Isolation Care-Planning tool has been the most popular tool so far. This tool is also a worksheet that helps the LTCH staff identify and communicate practical steps that can be taken to support the resident in isolation. It prompts discussion on questions such as: why the person leaves their room and what brings them back, what they like to talk about, what kinds of reminders work for them and whether they understand why they need to stay in their room and can’t visit others?
The Isolation Communication tool. This tool has 13 signs that are remind-

ers for people living with dementia to stay in their room, stay back from others, wear a mask and wash their hands.
Dr. Iaboni and her team have their work cut out for them. Two evaluation studies are currently in progress. First, the team has a research paper currently under peer review which does a deeper dive on moral distress. Second, they’re doing an implementation study at three Ontario LTCH to look at barriers to applying the DIT and find ways around them. This study will inform future research on how to support person-centred care in LTCH.
And, DIT version 2.0 is also in progress. It will reflect where we are now in the pandemic, as vaccinations have significantly reduced the risks in LTCH but those risks remain. It will also reflect feedback from users to be shorter and more geared for use in their huddle settings.
DIT version 2.0 will also be translated into more languages than version 1.0. Short training videos are already available in seven languages.
Keep residents connected to the people and things they love the most. With Managed Wi-Fi, TELUS Business makes it easy to connect residents to their own personal area network. Our property-wide Wi-Fi is secure and reliable, our technology is easy to learn and use, and we offer bilingual 24/7 technical support for residents and employees.






