










LightForce® Therapy Lasers empower you to treat soft tissue with confidence. Harnessing photobiomodulation (PBM)—a powerful form of light therapy—our lasers stimulate cellular metabolism to help treat muscle and joint pain from acute and chronic conditions.
Equipped with smart features like dosing recommendations, real-time visual and haptic feedback, and convenient portability, our range of therapy lasers combines a fusion of power with intelligence to enhance the patient and user experience. With the ability to reach deep tissues, LightForce lasers can cut the time needed by clinicians to treat patients—making light work of pain.
TRUSTED GLOBALLY
More than 250 professional and collegiate sports teams around the world trust LightForce Therapy Lasers to provide rehabilitation and pain management.
Scan the QR code to request a demo, or visit https://learn.chattanoogarehab.com/ijspt-journal-2024.

Turner A Blackburn, APTA Life Member, AT-Ret, AOSSM-Ret President
Mary Wilkinson Executive Director
Michael Voight Executive Editor and Publisher
Joe Black, PT, DPT, SCS, ATC
Eric Fernandez
Jay Greenstein, DC
Skip Hunter, PT, ATC-Ret
Russ Paine, PT, DPT
Tim Tyler, PT, ATC
Sports Legacy Advisory Board
Turner A. Blackburn, PT, ATC
George Davies, PT, DPT, MEd, SCS, ATC, LAT, CSCS, PES, FAPTA
Terry Malone, PT, PhD
Bob Mangine, PT
Barb Sanders, PT, PhD
Tim Tyler, PT, ATC
Kevin Wilk, PT, DPT, FAPTA
Executive Editor/Publisher
Michael L. Voight, PT, DHSc, OCS, SCS, ATC, CSCS
Executive Director/Operations and Marketing
Mary Wilkinson
Editor in Chief
Barbara Hoogenboom, PT, EdD, SCS, ATC
Managing Editor
Ashley Campbell, PT, DPT, SCS, CSCS
Manuscript Coordinator
Casey Lewis, PTA, ATC
AMERICAN SPORTS MEDICINE INSTITUTE
Publisher
Contact Information
International Journal of Sports Physical Therapy 6011 Hillsboro Pike Nashville, TN 37215, US, http://www.ijspt.org
IJSPT is a monthly publication, with release dates on the first of each month.
ISSN 2159-2896
Underwriting Sponsor Genie Health
Founding Sponsors Enovis Exertools Hyperice Trazer Woodway
Platinum Sponsors ATI Elvation
Gold Sponsors Hawkgrips Kayezen Structure + Function Education Winback Partners
Northeast Seminars Academy of Human Movement
American Academy of Sports Physical Therapy
IJSPT is an official journal of the International Federation of Sports Physical Therapy (IFSPT). Countries with access to IJSPT as a member benefit. Reach us at www.ifspt.org.

IJSPT is an official journal of the ICCUS Society for Sports Rehabilitation. www.iccus.org






Stand out in your community with a diversified patient experience. Designed to improve outcomes, attract new patients, and increase revenue through insurance, cash-based services, and retail sales.


Gain access to a robust library of research, clinical education, and marketing tools including:
• On-demand clinical education courses
• Written treatment protocols
• Over 50 research studies specific to Hyperice technology
• Marketing tips and best practices including social media content, videos, and more
• Live trainings

Executive Editor/Publisher
Michael L. Voight, PT, DHSc, OCS, SCS, ATC, CSCS
Belmont University
Nashville, Tennessee – USA
Editor in Chief
Barbara Hoogenboom, PT, EdD, SCS, ATC
Grand Valley State University
Grand Rapids, Michigan - USA
Managing Editor
Ashley Campbell, PT, DPT, SCS, CSCS
Nashville Sports Medicine and Orthopaedic Center
Nashville, Tennessee – USA
Manuscript Coordinator
Casey Lewis, PTA, ATC
Nashville Sports Medicine and Orthopaedic Center
Nashville, Tennessee – USA
Executive Director/Marketing
Mary Wilkinson
Indianapolis, Indiana – USA
Editors
Robert Manske PT, DPT, Med, SCS, ATC, CSCS
University of Wichita Wichita, KS, USA
Terry Grindstaff, PT, PhD, ATC, SCS, CSCS
Creighton University Omaha, NE, USA
Phil Page PT, PhD, ATC, CSCS
Franciscan University DPT Program
Baton Rouge, LA, USA
Kevin Wilk PT, DPT, FAPTA
Clinical Viewpoint Editor Champion Sports Medicine Birmingham, AL, USA
International Editors
Luciana De Michelis Mendonça, PT, PhD UFVJM
Diamantina, Brazil
Colin Paterson PT, MSc PGCert(Ed), MCSP, RISPT, SFHEA
University of Brighton Brighton, England, UK
Chris Napier, PT, PhD
Clinical Assistant Professor
University of British Coumbia, Vancouver, BC, Canada
Nicola Phillips, OBE, PT, PhD, FCSP Professor School of Healthcare Sciences Cardiff University, Cardiff, Wales, UK
Associate Editors
Eva Ageberg, PT, PhD Professor, Lund University Lund, Sweden
Lindsay Becker, PT, DPT, SCS, USAW Buckeye Performance Golf Dublin, Ohio, USA
Keelan Enseki, PT, MS, OCS, SCS, ATC University of Pittsburgh Pittsburgh, PA, USA
John Heick, PT, PhD, DPT, OCS, NCS, SCS
Northern Arizona University Flagstaff, AZ, USA
Julie Sandell Jacobsen, MHSc, PhD
VIA University Aarhus, Denmark
RobRoy L. Martin, PhD, PT, CSCS
Duquesne University Pittsburgh, PA, USA
Andrea Mosler, PhD, FACP, FASMF
La Trobe Sport and Exercise Medicine Research Centre, School of Allied Health, Human Services and Sport, La Trobe University Melbourne, Victoria, Australia
Brandon Schmitt, DPT, ATC
PRO Sports Physical Therapy Scarsdale, NY, USA
Barry Shafer, PT, DPT
Elite Motion Physical Therapy Arcadia, CA, USA
Laurie Stickler, PT, DHSc, OCS
Grand Valley State University
Grand Rapids, MI, USA
Editorial Board
James Andrews, MD
Andrews Institute & Sports Medicine Center
Gulf Breeze, AL, USA
Amelia (Amy) Arundale, PT, PhD, DPT, SCS
Red Bull/Ichan School of Medicine
Salzburg, Austria/New York, NY, USA
Gary Austin, PT PhD
Belmont University Nashville, TN, USA
Roald Bahr, MD
Oslo Sports Trauma Research Center
Oslo, Norway
Lane Bailey, PT, PhD
Memorial Hermann IRONMAN Sports Medicine Institute
Houston, Texas, USA
Gül Baltaci, PT,Ph.D. Professor, CKTI, FACSM
Private Guven Hospital Ankara, Turkey
Asheesh Bedi, MD
University of Michigan
Ann Arbor, MI, USA
David Behm, PhD Memorial University of Newfoundland St. John's, Newfoundland, Canada
Barton N. Bishop, PT, DPT, SCS, CSCS Kaizo Clinical Research Institute Rockville, Maryland, USA
Mario Bizzini, PhD, PT Schulthess Clinic Human Performance Lab Zürich, Switzerland
Joe Black, PT, DPT, SCS, ATC Total Rehabilitation Maryville, Tennesse, USA
Turner A. "Tab" Blackburn, APTA Life Member, ATC-Ret, AOSSM-Ret NASMI Lanett, AL, USA
Lori Bolgla, PT, PhD, MAcc, ATC Augusta University Augusta, Georgia, USA
Matthew Briggs The Ohio State University Columbus, OH, USA
Tony Brosky, PT, DHSc, SCS Bellarmine University Louisville, KY, USA
Brian Busconi, MD UMass Memorial Hospital Boston, MA, USA
Robert J. Butler, PT, PhD St. Louis Cardinals St. Louis, MO, USA
Duane Button, PhD Memorial University St. Johns, Newfoundland, Canada
J. W. Thomas Byrd, MD Nashville Sports Medicine and Orthopaedic Center Nashville, TN, USA
Lyle Cain, MD Andrews Institute & Sports Medicine Center Birmingham, AL, USA
Gary Calabrese, PT, DPT Cleveland Clinic Cleveland, Ohio, USA
Meredith Chaput, PT, DPT, SCS Ohio University Athens, OH, USA
Rita Chorba, PT, DPT, MAT, SCS, ATC, CSCS United States Army Special Operations Command Fort Campbell, KY, USA
John Christoferreti, MD Texas Health Dallas, TX, USA
Richard Clark, PT, PhD Tennessee State University Nashville, TN, USA
Juan Colado, PT, PhD University of Valencia Valencia, Spain
Brian Cole, MD Midwest Orthopaedics at Rush Chicago, IL, USA
Ann Cools, PT, PhD
Ghent University Ghent, Belgium
Andrew Contreras, DPT, SCS Washington, DC, USA
George Davies, PT, DPT, MEd, SCS, ATC, LAT, CSCS, PES, FAPTA
Georgia Southern University Savannah, Georgia, USA
Pete Draovich, PT
Jacksonville Jaguars Footbal Jacksonvile, FL, USA
Jeffrey Dugas, MD Andrews Institute & Sports Medicine Center Birmingham, AL, USA
Jiri Dvorak, MD Schulthess Clinic Zurich, Switzerland
Todd Ellenbecker Rehab Plus Phoenix, AZ, USA
Carolyn Emery, PT, PhD University of Calgary Calgary, Alberta, Canada
Ernest Esteve Caupena, PT, PhD University of Girona Girona, Spain
Sue Falsone, PT, MS, SCS, ATC, CSCS, COMT Structure and Function Education and A.T. Still University Phoenix, Arizona, USA
J. Craig Garrison, PhD, PT, ATC, SCS Texas Health Sports Medicine Fort Worth, Texas, USA
Maggie Gebhardt, PT, DPT, OCS, FAAOMPT Fit Core Physical Therapy/Myopain Seminars Atlanta, GA and Bethesda, MD, USA
Lance Gill, ATC
LG Performance-TPI Oceanside, CA, USA
Phil Glasgow, PhD, MTh, MRes, MCSP Sports Institute of Northern Ireland Belfast, Northern Ireland, UK
Robert S. Gray, MS, AT Cleveland Clinic Sports Health Cleveland, Ohio, USA
Jay Greenstein, DC Kaizo Health Baltimore, MD, USA
Martin Hagglund, PT PhD
Linkoping University Linkoping, Sweden
Allen Hardin, PT, SCS, ATC, CSCS
University of Texas Austin, TX, USA
Richard Hawkins, MD
Professor of surgery, University of South Carolina
Adjunct Professor, Clemson University
Principal, Steadman Hawkins, Greenville and Denver (CU)
John D.Heick, PT, PhD, DPT, OCS, NCS, SCS
Northern Arizona University Flagstaff, AZ, USA
Tim Hewett, PhD
Hewett Consulting Minneapolis, Minnesota, USA
Per Hølmich, MD
Copenhagen University Hospital Copenhagen, Denmark
Kara Mae Hughes, PT, DPT, CSCS
Wolfe PT Nashville, TN, USA
Lasse Ishøi, PT, MSc
Sports Orthopedic Research Center
Copenhagen University Hospital Hvidovre, Denmark
Jon Karlsson, MD Sahlgrenska University Goteborg, Sweden
Brian Kelly, MD Hospital for Special Surgery New York, NY, USA
Benjamin R. Kivlan, PhD, PT, OCS, SCS Duquesne University Pittsburgh, PA, USA
Dave Kohlrieser, PT, DPT, SCS, OCS, CSCS
Ortho One Columbus, OH, USA
Andre Labbe PT, MOPT
Tulane Institute of Sports Medicine New Orleans, LA USA
Henning Langberg, PT, PhD University of Copenhagen Copenhagen, Denmark
Robert LaPrade, MD Twin Cities Orthopedics Edina, MN, USA
Lace Luedke, PT, DPT University of Wisconsin Oshkosh Oshkosh, WI, USA
Phillip Malloy, PT, PhD
Arcadia University/Rush University Medical Center Glenside, PA and Chicago, IL, USA
Terry Malone, PT, EdD, ATC, FAPTA University of Kentucky Lexington, KY, USA
Robert Mangine, PT University of Cincinnati Cincinnati, OH, USA
Eric McCarty, MD University of Colorado Boulder, CO, USA
Ryan P. McGovern, PhD, LAT, ATC Texas Health Sports Medicine Specialists Dallas/Fort Worth, Texas, USA
Mal McHugh, PhD
NISMAT
New York, NY, USA
Joseph Miller, PT, DSc, OCS, SCS, CSCS
Pikes Peak Community College Colorado Springs, CO, USA
Havard Moksnes, PT PhD
Oslo Sports Trauma Research Center Oslo, Norway
Andrew Murray, MD, PhD
European PGA Tour Edinburgh, Scotland, UK
Andrew Naylor, PT, DPT, SCS
Bellin Health
Green Bay, WI, USA
Stephen Nicholas, MD NISMAT New York New York, NY, USA
John O'Donnel, MD
Royal Melbourne Hospital Melbourne, Australia
Russ Paine, PT McGovern Medical School Houston, TX, USA
Snehal Patel, PT, MSPT, SCD
HSS Sports Rehabilitation Institute New York, NY, USA
Marc Philippon, MD
Steadman-Hawkins Clinic Vail, CO, USA
Kevin Plancher, MD, MPH, FAAOS
Plancher Orthopedics and Sports Medicine
New York, NY USA
Marisa Pontillo, PT, PhD, DPT, SCS
University of Pennsylvania Health System Philadelphia, PA, USA
Matthew Provencher, MD
Steadman Hawkins Clinic Vail, CO, USA
Charles E. Rainey, PT, DSc, DPT, MS, OCS, SCS, CSCS, FAAOMPT
United States Public Health Service Springfield, MO, USA
Alexandre Rambaud, PT PhD Saint-Etienne, France
Carlo Ramponi, PT Physiotherapist, Kinè Rehabilitation and Orthopaedic Center Treviso, Italy
Michael Reiman, PT, PhD Duke University Durham, NC, USA
Mark F. Reinking, PT, PhD, SCS, ATC Regis University Denver, CO, USA
Mark Ryan, ATC Steadman-Hawkins Clinic Vail, CO, USA
David Sachse, PT, DPT, OCS, SCS USAF San Antonio, TX, USA
Marc Safran, MD Stanford University Palo Alto, CA, USA
Alanna Salituro, PT, DPT, SCS, CSCS New York Mets Port Saint Lucie, FL, USA
Mina Samukawa, PT, PhD, AT (JSPO) Hokkaido University Sapporo, Japan
Barbara Sanders, PT, PhD, FAPTA, Board Certified Sports Physical Therapy Emeritus Professor and Chair, Department of Physical Therapy Texas State University Round Rock, TX, USA
Felix “Buddy” Savoie, MD, FAAOS Tulane Institute of Sport Medicine New Orleans, LA, USA
Teresa Schuemann, PT, DPT, ATC, CSCS, Board Certified Specialist in Sports Physical Therapy Evidence in Motion Fort Collins, CO, USA
Timothy Sell, PhD, PT, FACSM Atrium Health Musculoskeletal Institute Charlotte, NC, USA
Andreas Serner, PT PhD
Aspetar Orthopedic and Sports Medicine Hospital Doha, Qatar
Ellen Shanley, PT, PhD ATI Spartanburg, SC, USA
Karin Silbernagel, PT, PhD University of Delaware Newark, DE, USA
Holly Silvers, PT, PhD Velocity Physical Therapy Los Angeles, CA, USA
Lynn Snyder-Mackler, PT, ScD, FAPTA STAR University of Delaware Newark, DE, USA
Alston Stubbs, MD Wake Forest University Winston-Salem, NC, USA
Amir Takla, B.Phys, Mast.Physio (Manip), A/Prof
Australian Sports Physiotherapy The University of Melbourne Melbourne, Australia
Charles Thigpen, PhD, PT, ATC ATI
Spartanburg, SC, USA
Steven Tippett, PT, PhD, ATC, SCS Bradley University Peoria, IL, USA
Tim Tyler, PT, ATC NISMAT New York, NY, USA
Timothy Uhl, PT, PhD, ATC University of Kentucky Lexington, KY, USA
Bakare Ummukulthoum, PT University of the Witswatersrand Johannesburg, Gauteng, South Africa
Yuling Leo Wang, PT, PhD Sun Yat-sen University Guangzhou, China
Mark D. Weber, PT, PhD, SCS, ATC Texas Women’s University Dallas, TX, USA
Richard B. Westrick, PT, DPT, DSc, OCS, SCS US Army Research Institute Boston, MA, USA
Chris Wolfe, PT, DPT Belmont University Nashville, TN, USA
Tobias Wörner, PT, MSc Lund University Stockholm, Sweden
VOLUME 19, NUMBER 10
PAGE TITLE
ORIGINAL RESEARCH
1172 Rehabilitation Protocol Variability Following Arthroscopic Bankart Repair and Remplissage for Management of Anterior Shoulder Instability: A Systematic Review.
Villarreal-Espinosa JB, Reinold MM, Khah M, et al.
1188 Implementing the Copenhagen Adductor Exercise and Nordic Hamstring Exercise in West African Academy Football (Soccer) Players: An Intervention Study.
DeLang MD, Ishøi L, Hole MN, et al.
1197 Relationship Between Peak Eccentric Force During the Nordic Hamstring Exercise and the One Repetition Maximum Deadlift Performance.
Nishida S, Ito W, Ohishi T, et al.
1204 Relationship Between Single-Leg Vertical Jump and Drop Jump Performance, and Return to Sports After Primary Anterior Cruciate Ligament Reconstruction Using Hamstring Graft.
Ohji S, Kawasaki T, Koga H, et al.
1216 Relationship of Physical Factors to the Occurrence of Injuries in Young Gymnasts.
Kobayashi Y, Nagano Y, Suzukawa M.
1228 The Clinical Utility of the Seated Wall Angel as a Test with Scoring.
Kofoed C, Palmsten A, Diercks J, et al.
1238 Inferior-Medial Dry Needling at the Thoracolumbar Junction: A Cadaveric Study. Williams CL, Curfman SE, Lindsley SR.
CASE REPORT
1244 Physical and Muscular Performance in a Professional Soccer Player with a Posterior Cruciate Ligament Injury Following an Isokinetic Exercise Program: A Case Report.
Mostagi FQRC, da Silva PAC, Munaro GR, et al.
CLINICAL COMMENTARY/CURRENT CONCEPT REVIEW
1255 Risk Factors for Musculoskeletal Health: A Review of the Literature and Clinical Application. Kiesel K, Matsel K, Bullock G, et al.
1263 Clinical Utility of Qualitative Change of Direction Movement Assessment in ACL Injury Risk Evaluation.
Andreyo E, Unverzagt C, Dos’Santos T, et al.
RESEARCH SYMPOSIUM
1279 2024 IJSPT Orthopedic Summit Research Abstracts International Journal of Sports Physical Therapy..





Tuesday, October 15 6 p.m. - 8 p.m. EST
Represent your PT program and test your board exam knowledge to win Hyperice Prizes and bragging rights.

Scan or click the QR code to register!
Hosted by Tom Denninger, DPT, PTA from ATI Physical Therapy and Jimmy McKay from PT Pintcast.
Questions provided by PT Final Exam.
OCTOBER IS PHYSICAL THERAPY MONTH
Happy PT Month to all clinicians out there who give their all every day to help people get back to their lives.

Most Advanced Electrotherapy Device: Powerful, intuitive and user-friendly
Treat up to three body zones at once on all types of tissues
Effective in less than 10 minutes Enter A New Era of Therapy
TECAR
HIGH FREQUENCY
Metabolic Action at Cell Level
Hi-TENS
LOW FREQUENCY IN PULSED HIGH FREQUENCY
Ultimate Pain Management
Hi-EMS
MEDIUM FREQUENCY
Deep Muscle Contraction














IJSPT thanks these generous sponsors for supporting our Journal and this research competition!

TITLING SPONSOR

AWARD SPONSOR
The IJSPT Research Summit was held Saturday, September 14 at the Fontainebleau Hotel in Las Vegas as part of the 2024 Orthopedic Summit.
First place was given to Kevin Giordano, for Large Sample Normative Data for Throwing Arm Strength and Range of Motion in Baseball Players. He was awarded a $500 cash prize from ATI Physical Therapy and a $1500 Hyperice Legacy Pack. All winnes are shown with publisher Mike Voight and Editor in Chief Barb Hoogenboom.

An Honorable Mention was presented to Phil Page, for Quantifying the Deceleration Index using the 1080 Sprint Device: A Pilot Study. His team was awarded a $250 cash prize from ATI Physical Therapy and a $500 Hyperice Pack.

An Honorable Mention was also given to Ellen Shanley, for Professional Baseball Tichers' Patterns of Use and Results of Weighted Ball Training: An Interim Study

Systematic Review/Meta-Analysis
Villarreal-Espinosa JB, Reinold MM, Khak M, et al. Rehabilitation Protocol Variability
Following Arthroscopic Bankart Repair and Remplissage for Management of Anterior Shoulder Instability: A Systematic Review. IJSPT. Published online October 1, 2024:1172-1187. doi:10.26603/001c.123481
Juan B. Villarreal-Espinosa1 , Michael M. Reinold2 , Mohammad Khak1 , Mohammad J. Shariyate1 , Carol Mita3 , Jeffrey Kay4 , Arun J. Ramappa5a
1 Orthopaedics, Beth Israel Deaconess Medical Center, 2 Champion PT and Performance, 3 Knowledge Services, Harvard University, 4 Orthopaedic Sports Medicine, McMaster University Medical Centre, 5 Orthopaedic Sports Medicine, Beth Israel Deaconess Medical Center
Keywords: anterior shoulder instability, bankart repair, remplissage, rehabilitation protocol https://doi.org/10.26603/001c.123481
International Journal of Sports Physical Therapy
Background
Augmentation of an arthroscopic Bankart repair with the remplissage (ABR) procedure has shown to confer a decrease in recurrence rates, yet, at the expense of potentially compromising shoulder motion.
Purpose/Hypothesis
The purpose was to examine clinical studies that described a post-operative rehabilitation protocol after an arthroscopic Bankart repair and remplissage procedure. It was hypothesized that a review of the literature would find variability among the studies and that, among comparative studies, there would be a limited distinction from protocols for isolated Bankart repairs.
Study design
Systematic Review
Materials and Methods
A search was conducted using three databases (PubMed, EMBASE, and CINAHL) according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines. The following terms were combined while utilizing Boolean operators: (Bankart lesion OR labral tear) AND (remplissage). Studies evaluating patients after arthroscopic stabilization for unidirectional anterior glenohumeral instability with the addition of the remplissage procedure and at least 1 year follow-up were included for analysis.
Results
A total of 41 studies (14 Level IV, 24 Level III, 2 Level II, and 1 Level I) were included with a total of 1,307 patients who underwent ABR. All patients had <30% glenoid bone loss and a range of 10-50% humeral head size Hill-Sachs lesion. Type and position of immobilization were the most reported outcomes (41/41) followed by time of immobilization (40/41). Moreover, 23/41 studies described their initial post-operative shoulder range of motion restrictions, while 17/41 specified any shoulder motion allowed during this restrictive phase. Time to return to sport was also described in 37/41 of the retrieved studies. Finally, only two of the 27 comparative studies tailored their rehabilitation protocol according to the specific procedure performed, underscoring the
a
Corresponding author
Arun J. Ramappa MD
Chief of Sports Medicine and Shoulder Surgery at Beth Israel Deaconess Medical Center, Boston 330 Brookline Avenue, Boston, MA, 02115
Phone: 970.471.1959
Email: aramappa@bidmc.harvard.edu
lack of an individualized approach (i.e. same rehabilitation protocol for different procedures).
The results of the present systematic review expose the variability among rehabilitation protocols following ABR. This variability prompts consideration of the underlying factors influencing these disparities and underscores the need for future research to elucidate optimal rehabilitation. Based on the results of this systematic review and the senior authors´ clinical experience, a rehabilitation approach similar to an isolated Bankart repair appears warranted, with additional precautions being utilized regarding internal rotation range of motion and external rotation strengthening.
Level 3
With an incidence of up to 25 cases per 100,000 personyears, the shoulder is one of the most frequently dislocated joints in the body 1,2 Historically, first time dislocators had been managed conservatively, yet recent authors suggest that high risk patients benefit from early surgical intervention, as they have observed a decrease in recurrence rates and an increase in return to competitive activities.3‑6 The addition of the remplissage procedure, which involves an infraspinatus tenodesis and posterior capsulodesis to an arthroscopic Bankart repair, in patients presenting with a Hill-Sachs defect, further decreases recurrence rates in this patient population.7‑12
Since at least 65-70% and up to 100% of the first time and recurrent anterior shoulder dislocators, respectively, present with a Hill-Sachs defect, arthroscopic Bankart plus remplissage (ABR) has gained popularity in recent years, however, there has been some concern raised regarding potentially compromising shoulder range of motion.2,7,13‑16 Therefore, post-operative rehabilitation plays an important role in both addressing and optimizing range of motion as well as facilitating optimal healing of the of the posterior structures following the addition of the remplissage procedure.17,18
The purpose of this systematic review was to examine clinical studies that described a post-operative rehabilitation protocol after an ABR procedure. It was hypothesized that the present study would find substantial variability among the included studies and that, among the studies, there would be little to no distinct regimen from that used for rehabilitation of isolated Bankart repair
MATERIALS AND METHODS
The present study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.19 Clinical studies discussing outcomes after an arthroscopic Bankart repair augmented by a remplissage procedure for either Bankart or Hill-Sachs lesions of the shoulder were identified by searching Medline / PubMed (National Library of Medicine, NCBI), Embase (El-
sevier, embase.com), and the Cumulative Index to Nursing and Allied Health Literature (CINAHL Complete, EBSCOhost) on July 10, 2023. Controlled vocabulary terms including “Bankart lesion”, “labral tear”, and “remplissage” were utilized and combined via Boolean operators. The search strategies were designed and carried out by a health sciences librarian. No publication date limits were applied. The exact search terms used for each of the databases are provided in the Appendix 1.
Inclusion and exclusion criteria were determined prior to running the searches. Studies that evaluated patients after arthroscopic stabilization for unidirectional anterior glenohumeral instability with the addition of the remplissage procedure, with no other concomitant procedures performed (rotator cuff repair, ALPSA repair, HAGL repair) except for a SLAP/long head of the biceps repair, written in English, and at least one year minimum follow up were included. Review articles, systematic reviews, abstracts, case reports, technical notes, cadaveric or biomechanical studies, and non-English language studies were excluded. Additionally, articles were excluded if minimum follow up was < 1 year, if only revision cases were included, and if overlapping cohorts were found among studies.
Search results were assessed for eligibility by two independent reviewers who performed both abstract screening and full text review Data of included studies was extracted by both reviewers using a pre-designed extraction form on Microsoft Excel spreadsheet (Version 2007, Microsoft, Redmond, WA, USA). Upon discrepancies, the issue was addressed by a third reviewer and resolved by consensus.
Extracted data included title, authors, year of publication, study design, level of evidence, number of subjects per included study, mean age, % of females, mean followup, % glenoid bone loss, size of the Hill-Sachs lesion, and whether the Hill-Sachs lesion was engaging or not. Additionally, the rehabilitation protocols of each included study were assessed, and data grouped and stratified by type and duration of immobilization, exercises allowed in the early post-operative period, early range of motion restriction, start of passive, active assisted, and active exercises, time to achieve full range of motion, start of formal strength training, targeted muscle strengthening plan, return to
sport criteria (including time), and whether the rehabilitation protocol differed between performed procedures.
All non-randomized studies were assessed for quality and risk of bias using the Methodological Index for Non-randomized Studies (MINORS) instrument where comparative studies may reach a global score of 24, whereas non comparative studies may add up to a maximum of 16 points.20 Additionally, comparative/cohort studies were also assessed by the Newcastle-Ottawa Scale for cohort studies.21 Finally, the only clinical randomized controlled trial (RCT) included in the current study was assessed for quality and bias using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool for RCTs.22
Descriptive statistics including means, proportions, and ranges were calculated and presented using Microsoft Excel (Version 2007, Microsoft, Redmond, WA, USA). Due to the highly heterogeneous nature of the reported data, no quantitative analysis was conducted; therefore, the data is presented qualitatively
The search strategy yielded 550 studies across all three databases, after removal of duplicates, 322 were available for screening using Covidence software (Veritas Health Innovation, Melbourne, Australia). The PRISMA Flow Chart Diagram is presented in Figure 1 After screening and full text review, data were retrieved from 41 included studies, including one Level I,11 two Level II,15,23 24 Level III,12, 24‑46 and 14 Level IV7,47‑59 studies. A total of 1,307 patients were included presenting with a mean age of 27.5 years (range 14-72). Among the included patients, 18% were female and all had a minimum follow up of at least 12 months (range 12-180 months) after undergoing an ABR procedure. All patients had <30% glenoid bone loss and a range of 10-50% of the humeral head size, Hill-Sachs defect. Additionally, 37 studies included engaging/off-track lesions7,11, 23‑44,46,48‑59 whereas two studies reported only on non-engaging/on-track lesions12,45 in their cohort with two other studies not reporting on the engagement status of the included population.15,47 A summary of patient demographics can be found in Table 1.
The average MINORS grade for non-comparative studies was 12.6 (range 11-15), whereas for comparative studies, the mean MINORS grade was 20.6 (range 16-24). Additionally, all comparative studies fell under the “Good Quality” category of the Newcastle-Ottawa scale. Finally, the GRADE tool assessment of the only Level 1 study,11 was classified as “High quality ” The quality scores for each individual study can be found in Table 2.
A summary of the rehabilitation protocols of all included studies is shown in Appendix 2. All 41 studies7,11,12,15, 23‑59 reported on the type of immobilization where the most common reported type of immobilization was a simple sling utilized in 34 of the studies11,12,15,23,24,26‑35,37,38, 41‑43,45‑57,59 (83%). Four studies36,39,40,44 (9.7%) reported the usage of either an abduction or neutral rotation brace, in contrast to the rehabilitation protocol of two studies25,58 (4.8%) which used a shoulder or external rotation immobilizer One additional study7 (2.4%) reported the usage of an arm pouch as the type of immobilization used in their rehabilitation protocol. In terms of position of immobilization, a sling in neutral rotation was employed in 20 studies11, 15,29,30,32‑35,37,41,43,45,46,48,51,53,54,56,57,59 (48.7%), and the remaining 21 studies7,12,23‑28,31,36,38‑40,42,44,47,49,50,52,55, 58 (51.3%) included a wide range of 11 different immobilization positions.
Forty studies7,11,12,15,23‑53,55‑59 (97.5%) reported on time of immobilization after surgery which ranged from three to six weeks. Out of the initial 40 studies, eighteen23, 26‑30,32‑35,42,44,45,49‑51,58,59 (43.9%) immobilized the operated shoulder for six weeks, with this time point being the most frequently reported time of immobilization followed by four weeks reported in nine studies12,24,40,41,43,46,48,53,55 (21.9%). Upon stratification by level of evidence, the mean immobilization time was 4, 4.9, and 4.7 weeks for Level I/II, III, and IV studies, respectively
Allowance of post-operative motion, described in 17 studies7,11,12,23,26,34,36,38,42,44,46,48‑50,53,54,58 (41.4%), was also an important extracted data point in the current review Among the included studies, either pendulum or isometric exercises were allowed with the specific time of initiation ranging from post-operative day one to four weeks after surgery Pendular and/or isometric exercises starting on post-operative day one were the most common indication regarding post-operative motion allowance, as it was reported in seven of the 17 included studies11,38,46,48‑50,58 (41.1%).
Twenty-three studies11,12,15,23‑28,30,35,41‑44,49‑54,57,58 (56%) controlled for range of motion restriction in their rehabilitation protocol with four-to-eight-week post-operative ER restriction being the most reported15,25,42,43,49, 50,54,58 (n=8 studies/34.7%). Other studies restricted abduction and external rotation11,23,26,30,52,57 (n=6 studies/ 26%), forward flexion and external rotation12,27,35,44,51,53 (n=6 studies/26%), forward flexion past 90 degrees24,28 (n=2 studies/8.6%), and forward flexion plus external rotation at side and in abduction41 (n=1 study/4.3%). The mean time for range of motion restriction in any plane of motion stratified by level of evidence was 7.2, 5.7, and 5.6 weeks for level I/II, III, and IV, respectively
Thirty-one studies7,11,15,23,25,26,30,31,34,36‑46,48‑52,54‑59 (75%) described at least one of the following in their rehabilitation protocol: start of self, passive or active-assisted motion and the start of formal physical therapy. Initiation of either active-assisted or active motion was the most reported instruction with the initiation time ranging from

two to twelve weeks after surgery Additionally, only four Level III studies12,26,29,41 (9.7%) out of the initial 41, described the goal, in weeks, by when patients must have achieved full range of motion.
Twenty-nine articles7,11,12,23,26‑29,31‑43,46,50,52,53,56‑59 (70.7%) reported on the starting point for shoulder specific strength training initiation with an average starting date of 12, 9.8, and 11.7 weeks for Level I/II, III, and IV, respectively. Moreover, 24 studies7,11,12,23,28,31,34,35,37‑43,45, 46,50,52,53,56‑59 (58.5%) made further suggestions regarding the type of targeted strengthening, yet no detailed targeted strengthening regimen was described in any of the included studies.
Thirty-seven7,11,12,23,24,26‑35,37‑46,48‑59 (90.2%) studies reported on the time to return to sport/play (RTS/RTP) with a mean time of 5.2 months for level I/II, 6.4 months for Level III, and 6.4 months for Level IV studies. Nonetheless, only 11 studies7,12,31,34‑36,41,42,46,53,57 (26.8%) used objective based criteria (strength, ROM, pain, stability) to assess for return to sport/play.
Finally, for comparative studies, 3/3 (100%) of the included Level I/II11,15,23 and 17/19 (89.4%) of the included Level III studies12,24‑26,28‑32,34‑36,39,41,44‑46 (24 total Level III studies, however five were not compared against other type of procedure) reported using the same rehabilitation protocol for their comparative counterpart regardless of the procedure performed. The protocols utilized in these stud-
Table 1. Summary of patient demographics.
Standard deviation reported as mean +/- SD or (SD); Median reported as median (range or IQR).
LOE (Level of Evidence), No. (Number), NA (Not Available)
LOE (Level of Evidence), MINORS (Methodological Index for Non-randomized Studies), GRADE (Grading of Recommendations Assessment, Development and Evaluation), NA (Not Available) *MINORS Score was performed for all comparative and non-comparative studies; Newcastle-Ottawa Scale was additionally utilized solely for comparative/cohort studies as it has not been adapted for non-comparative/case series.
ies did not adopt an individualized approach based on the type of procedure performed.
The variability in reported rehabilitation protocols following ABR for anterior shoulder instability is the most notable finding. Hence, the present review will discuss each aspect of these protocols, encompassing immobilization strategies, early motion exercises, movement restrictions, initiation of formal physical therapy, strength training, and the timeline for returning to sport by delving into the justifications presented in articles, the resultant outcomes reported in these studies, and juxtaposing these findings with our institutional rehabilitation protocol. Through this comprehensive exploration, the authors aim to describe the intricacies surrounding post-operative care, unravel various complex aspects that contribute to the diversity of rehabilitation treatments, identify potential opportunities for refining the management of patients undergoing this combined surgical intervention, and provide the authors’ suggested rehabilitation protocol based on the literature and the clinical expertise of the senior authors.
Among the key findings, it is evident that the type and duration of immobilization exhibit considerable diversity across the included studies. Notably, the majority of studies (83%) favored the utilization of a sling as the primary mode of immobilization. However, intriguingly, a subset of studies (17%) opted for alternatives such as abduction or neutral rotation braces, with a few even employing an arm pouch for immobilization. This observed divergence in immobilization approaches underscores the lack of standardized consensus in the field, possibly influenced by surgeon preference, equipment availability, patient characteristics, or perceived benefits. Moreover, the position for immobilization was discussed at length within the retrieved articles with at least a half reporting immobilization in neutral rotation whereas the other half reported a variety of different positions. Gaunt et al.,60 in the American Society of Shoulder and Elbow Therapists´ (ASSET) rehabilitation guideline for arthroscopic Bankart repair, suggest immobilizing the shoulder with a sling in neutral rotation for patients who have undergone the aforementioned procedure. Yin et al.61 evaluated the position of immobilization after an arthroscopic shoulder stabilization procedure. In their study, they described outcomes after immobilizing the shoulder in external rotation. Although no control group was included in their study, their results showed that immobilization in external rotation (ER) was associated with full range of motion recovery at 3 months, low risk of recurrence in the first 12 months, high functional outcomes scores, and low VAS pain scores. Minkus et al.62 showed no functional or range of motion differences after immobilization in either internal or external rotation after an arthroscopic anterior shoulder stabilization procedure. However, it is not known whether these results could translate after the addition of the remplissage procedure as, to the authors knowledge, no study to date has compared various positions of shoulder immobilization, in aims of enhancing the healing of the posterior structures, after arthroscopic stabilization with the remplissage procedure.
Regarding the duration of immobilization, a range of three to six weeks emerged from the synthesis of the studies. The consensus around a six-week immobilization period is evident, with this timeframe being the most frequently reported among the included studies. However, the mean immobilization time for Level I and II studies averaged four weeks, potentially reflecting a trend toward shorter immobilization periods in higher-quality studies. This discrepancy in immobilization duration raises questions regarding the balance between maintaining shoulder stability through a prolonged immobilization period and the potential benefits of early mobilization in terms of mitigating muscle atrophy and stiffness. Kim et al.,63 reported no differences in terms of recurrence rates after either immediate mobilization or immobilization for at least three weeks. However, their RCT only included patients who had undergone an arthroscopic Bankart repair alone, therefore, no conclusion can be made for cases where the remplissage procedure is added. Longer immobilization times may be warranted upon the addition of the remplissage as tendonbone healing, from reattachment of the infraspinatus tendon into the bone divot, is expected to occur.60 On the other hand, due to concerns regarding loss of motion following the remplissage procedure, there could conceivably be advantages to earlier mobilization as well.
Early post-operative range of motion exercises emerged as another focal point of disparity. While pendulum and isometric exercises were widely incorporated into rehabilitation regimens, the time of their initiation varied significantly, ranging from the immediate post-operative period to four weeks after surgery Among the diverse early motion strategies, the prominence of pendulum exercises initiated as early as postoperative day one highlights the growing acceptance of the benefits of initiating controlled movement earlier in order to potentially speed up the recovery process and reduce complications that may arise from prolonged immobilization. In the only available rehabilitation guideline for arthroscopic Bankart repair,60 only isometrics with the arm adducted to side in neutral rotation are allowed in the first post-operative weeks while MacDonald et al.,11 in the only included RCT, allowed patients from both groups (isolated Bankart repair or ABR) to perform pendular exercises for the first three weeks post-surgery. Substantial variation exists within the rehabilitation protocols after an isolated arthroscopic Bankart repair, as it has been previously reported.64‑66
Notably, restrictions on specific shoulder movements during the early postoperative period demonstrated marked heterogeneity As established by Gaunt et al.,60 controlling for range of motion is of extreme importance as unrestricted movement could stress the repair past the healing stimulatory threshold causing failure. While the majority of studies included in the present systematic review advocated for limitations on external rotation for four to eight weeks, others imposed constraints on abduction and external rotation, or forward flexion beyond 90 degrees. This diversity in movement restrictions can be attributed to the absence of a widely accepted approach to balance the need for protective immobilization against the benefits of graded
early motion. For an isolated Bankart repair, it has been suggested that range of motion not to exceed 30 degrees of external rotation with the arm in adduction would be a safe boundary for the repair, yet whether this remains safe upon the addition of the remplissage is unknown.60
The initiation and progression of formal physical therapy represented an additional realm of variability Although the most commonly reported instructions involved the initiation of active assisted or active motion exercises, the start times ranged widely from two to 12 weeks after surgery. As established in ASSETs rehabilitation guideline, gradually progressing through degrees of range of motion is of utmost importance as reports suggest an inverse correlation between the integrity of the repair and the speed of regaining range of motion.60
Remarkably, the absence of detailed, targeted strengthening regimens in any of the included studies is a noteworthy finding. Despite the emphasis on initiating strength training concomitantly while achieving full motion, the lack of standardized protocols raises concerns about the optimization of muscle recovery and function, which are pivotal for patients seeking to return to sports or daily activities.
Return to sports timeline is a multifaceted parameter
The mean time to return to sport/play ranged from 5.2 to 6.4 months across different study levels. This variation could potentially be attributed to factors such as study design, patient selection, and differing definitions of “return to sport.” Currently, subjective criteria plus time are the most widely used criteria to assess for readiness to return to sport.1 Nonetheless, recent studies have reported on the need of shifting towards an objectively based criteria system, as it has been shown to lower recurrence rates.60,67,68 However, based on the results of this review and from previously published studies, marked heterogeneity exists and the absence of reporting on usage of objectively based and functional criteria to clear a patient to return to their sporting activity is problematic.67 In the present review only 11 studies used previously defined criteria (strength, ROM, pain, stability) to assess for return to sport/play Additionally, in an international consensus statement, the evaluation of psychological readiness to return to sport after anterior shoulder instability reached unanimous consensus.69
The usage of the Shoulder Instability Return to Sport after Injury (SIRSI) scale can be used for assessment of the psychological readiness to return to sport.70 In this review no studies took psychological readiness into account for readiness to return to sport assessment. Moreover, in a survey of shoulder surgeons evaluating the criteria used for clearance to return to sport, 92% of the participants stated that the addition of the remplissage procedure to an arthroscopic Bankart did not influence on the physician’s decision to clear athletes to go back to their activities. In the authors´ experience, patients undergoing an additional remplissage procedure must have an individualized approach which may differ from patients undergoing an isolated arthroscopic Bankart repair as the addition of the infraspinatus tenodesis and capsulodesis has been shown
to potentially result in diminished motion and strength at six months, when compared to its isolated counterpart.16
The trend observed in comparative studies reveals a remarkable homogeneity in the rehabilitation protocols adopted, irrespective of the specific procedure performed. All Level I/II studies (100%) and a substantial majority of Level III studies (89.4%) adhered to identical rehabilitation regimens for their comparative counterparts, regardless of whether arthroscopic Bankart repair was combined with remplissage or if any other procedure was performed (Latarjet, autografts). This notable lack of tailoring rehabilitation protocols based on the distinct surgical interventions raises concerns about the optimization of post-operative care. The emphasis on a uniform rehabilitation strategy could inadvertently limit the potential benefits that tailored protocols might offer, disregarding the varied biomechanical alterations and recovery trajectories introduced by the combined surgical procedures.
A limitation of the present study includes the observed variability in the vocabulary used to describe aspects of the rehabilitation protocols which predisposes the readers to confusion (i.e. whether shoulder immobilizer also refers to sling, strengthening terminology, etc.). Moreover, some of the included studies did not clearly state the physical therapy rehabilitation protocol, with some describing their followed protocol in two or three sentences. Additionally, although three studies were Level of evidence I or II, the remaining 38 were Level of evidence III or IV which reflects the low-quality of some of the included studies. Lastly, specific soft-tissue injury magnitude was not consistently reported within studies, which could have potentially contributed to the decision of early versus delayed range of motion initiation seen across studies.
With the considerable lack of consensus on the most appropriate rehabilitation progression following an ABR, the authors feel it important to provide an example protocol for clinicians to follow (Appendix 3). It is worthy to mention that the proposed approach has not been subjected to rigorous study or scrutiny and is merely a proposed exemplary protocol.
Considering what is known about the surgical technique and healing constraints of the involved tissues, the authors’ approach is to progress patients similar to an isolated Bankart repair with small adjustments to progression of internal rotation range of motion and the initiation of external rotation strengthening. This is designed to protect the remplissage procedure, while also avoiding the loss of motion or persistent loss of function.
Patients are immobilized in a simple sling by their side for the first four weeks, though are allowed to start immediate physical therapy. It is the author´s preference to have a slow and gradual restoration of range of motion, rather than delay for too long and fight hypomobility Range of motion is slowly restored over the first 8-10 weeks, similar to after a Bankart repair While internal rotation is initiated early with gentle pain-free range of motion, caution to not
push through discomfort for the first eight weeks is important. Also, regarding strengthening, avoidance of external rotation isometrics and delaying the initiation of light isotonic exercises is the suggested until week six.
In contrast to the knee, objective functional return to sport tests after shoulder instability procedures have not been commonly standardized. However, functional tests for the upper extremity do exist and should be considered and the authors believe that further research should be performed prior to definitively recommending any particular battery of tests.
The following criteria could help guide the decision in the interim: absence of pain/tenderness, at least six months after the procedure (allows repaired structures to fully heal), achievement of full functional active range of motion, objectively measured injured shoulder strength (at least 90% limb symmetry index [LSI]) including ER and IR at 0º and 90º of abduction, performance of the Closed Kinetic Chain Upper Extremity Stability test (+/- open chain testing for overhead athletes),and psychological readiness to return to sport measured via the SIRSI scale.
Based on the authors´ collective experience and understanding of the basic science and healing of the repair, it is believed that this progression is safe and effective at restoring function without disrupting the natural healing process. Future studies should be conducted to prospectively evaluate this approach and to identify the optimal rehabilitation protocol while incorporating appropriate func-
tional tests for guidance of return to sport. It is the author’s belief that following these strategies after remplissage augmentation could maximize function while limiting stiffness and recurrent instability.
The results of the present systematic review expose the variability among rehabilitation protocols following ABR. This variability prompts consideration of the underlying factors influencing these disparities and underscores the need for future research to elucidate optimal rehabilitation. Based on results and the senior authors´ clinical experience, a suggested rehabilitation approach is provided, similar to an isolated Bankart repair, with additional precautions surrounding internal rotation range of motion and external rotation strengthening.
The authors report no conflicts of interest.
Submitted: January 03, 2024 CDT, Accepted: August 15, 2024 CDT
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Hurley ET, Matache BA, Colasanti CA, et al. Return to play criteria among shoulder surgeons following shoulder stabilization. J Shoulder Elbow Surg. 2021;30(6):e317-e321. doi:10.1016/J.JSE.2021.01.026
2. Rutgers C, Verweij LPE, Priester-Vink S, van Deurzen DFP, Maas M, van den Bekerom MPJ. Recurrence in traumatic anterior shoulder dislocations increases the prevalence of Hill-Sachs and Bankart lesions: a systematic review and metaanalysis. Knee Surg Sports Traumatol Arthrosc 2022;30(6):2130-2140. doi:10.1007/ S00167-021-06847-7
3. Hurley ET, Manjunath AK, Bloom DA, et al. Arthroscopic Bankart repair versus conservative management for first-time traumatic anterior shoulder instability: a systematic review and metaanalysis. Arthroscopy 2020;36(9):2526-2532. doi:10.1016/J.ARTHRO.2020.04.046
4. De Carli A, Vadalà AP, Lanzetti R, et al. Early surgical treatment of first-time anterior glenohumeral dislocation in a young, active population is superior to conservative management at long-term follow-up. Int Orthop 2019;43(12):2799-2805. doi:10.1007/ S00264-019-04382-2
5. Minkus M, Königshausen M, Pauly S, et al. Immobilization in external rotation and abduction versus arthroscopic stabilization after first-time anterior shoulder dislocation: a multicenter randomized controlled trial. Am J Sports Med. 2021;49(4):857-865. doi:10.1177/0363546520987823
6. Hu B, Hong J, Zhu H, Yan S, Wu H. Arthroscopic Bankart repair versus conservative treatment for first-time traumatic anterior shoulder dislocation: a systematic review and meta-analysis. Eur J Med Res 2023;28(1):260. doi:10.1186/S40001-023-01160-0
7 Pathak S, Haidermota MJ, H VKK, Sancheti P Arthroscopic Bankart and remplissage for anteroinferior instability with subcritical bone loss has a low recurrence rate. Arthrosc Sports Med Rehabil 2022;4(2):e695-e703. doi:10.1016/ J.ASMR.2021.12.014
8. Camus D, Domos P, Berard E, Toulemonde J, Mansat P, Bonnevialle N. Isolated arthroscopic Bankart repair vs. Bankart repair with “remplissage” for anterior shoulder instability with engaging HillSachs lesion: a meta-analysis. Orthop Traumatol Surg Res. 2018;104(6):803-809. doi:10.1016/ J.OTSR.2018.05.011
9. Hurley ET, Toale JP, Davey MS, et al. Remplissage for anterior shoulder instability with Hill-Sachs lesions: a systematic review and meta-analysis. J Shoulder Elbow Surg 2020;29(12):2487-2494. doi:10.1016/J.JSE.2020.06.021
10. Liu JN, Gowd AK, Garcia GH, Cvetanovich GL, Cabarcas BC, Verma NN. Recurrence rate of instability after remplissage for treatment of traumatic anterior shoulder instability: a systematic review in treatment of subcritical glenoid bone loss. Arthroscopy 2018;34(10):2894-2907.e2. doi:10.1016/ J.ARTHRO.2018.05.031
11. MacDonald P, McRae S, Old J, et al. Arthroscopic Bankart repair with and without arthroscopic infraspinatus remplissage in anterior shoulder instability with a Hill-Sachs defect: a randomized controlled trial. J Shoulder Elbow Surg 2021;30(6):1288-1298. doi:10.1016/J.JSE.2020.11.013
12. Domos P, Ascione F, Wallace AL. Arthroscopic Bankart repair with remplissage for non-engaging Hill-Sachs lesion in professional collision athletes. Shoulder Elbow 2019;11(1):17-25. doi:10.1177/ 1758573217728414
13. Fox JA, Sanchez A, Zajac TJ, Provencher MT. Understanding the Hill-Sachs lesion in its role in patients with recurrent anterior shoulder instability Curr Rev Musculoskelet Med. 2017;10(4):469-479. doi:10.1007/S12178-017-9437-0
14. Polio W, Brolin TJ. Remplissage for anterior shoulder instability: history, indications, and outcomes. Orthop Clin North Am 2022;53(3):327-338. doi:10.1016/J.OCL.2022.02.005
15. Nourissat G, Kilinc AS, Werther JR, Doursounian L. A prospective, comparative, radiological, and clinical study of the influence of the “remplissage” procedure on shoulder range of motion after stabilization by arthroscopic Bankart repair Am J Sports Med 2011;39(10):2147-2152. doi:10.1177/ 0363546511416315
16. Frantz TL, Everhart JS, Cvetanovich GL, et al. What are the effects of remplissage on 6-month strength and range of motion after arthroscopic Bankart repair? A multicenter cohort study Orthop J Sports Med 2020;8(2). doi:10.1177/ 2325967120903283
17 Shanley E, Peterson SK. Rehabilitation after shoulder instability surgery: keys for optimizing recovery Sports Med Arthrosc Rev 2020;28(4):167-171. doi:10.1097/ JSA.0000000000000284
18. Kelley TD, Clegg S, Rodenhouse P, Hinz J, Busconi BD Functional rehabilitation and return to play after arthroscopic surgical stabilization for anterior shoulder instability Sports Health 2022;14(5):733-739. doi:10.1177/19417381211062852
19. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. PLoS Med 2009;6(7). doi:10.1371/JOURNAL.PMED.1000097
20. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for nonrandomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003;73(9):712-716. doi:10.1046/ J.1445-2197.2003.02748.X
21. Wells G, Wells G, Shea B, et al. The NewcastleOttawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Published online 2020.
22. Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64(4):383-394. doi:10.1016/ J.JCLINEPI.2010.04.026
23. Abouelsoud MM, Abdelrahman AA. Recurrent anterior shoulder dislocation with engaging Hill–Sachs defect: remplissage or Latarjet? Eur Orthop Traumatol 2015;6(3):151-156. doi:10.1007/ S12570-015-0313-3/METRICS
24. Bah A, Lateur GM, Kouevidjin BT, et al. Chronic anterior shoulder instability with significant HillSachs lesion: Arthroscopic Bankart with remplissage versus open Latarjet procedure. Orthop Traumatol Surg Res 2018;104(1):17-22. doi:10.1016/ J.OTSR.2017.11.009
25. Bastard C, Herisson O, Gaillard J, Nourissat G. Impact of remplissage on global shoulder outcome: a long-term comparative study Arthroscopy 2019;35(5):1362-1367. doi:10.1016/ J.ARTHRO.2019.01.013
26. Cho NS, Yoo JH, Juh HS, Rhee YG. Anterior shoulder instability with engaging Hill-Sachs defects: a comparison of arthroscopic Bankart repair with and without posterior capsulodesis. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3801-3808. doi:10.1007/S00167-015-3686-5
27 Ding Z, Cong S, Xie Y, Feng S, Chen S, Chen J. Location of the suture anchor in Hill-Sachs lesion could influence glenohumeral cartilage quality and limit range of motion after arthroscopic Bankart repair and remplissage. Am J Sports Med 2020;48(11):2628-2637 doi:10.1177/ 0363546520945723
28. Feng S, Chen M, Chen J, Li H, Chen J, Chen S. Patient outcomes and fear of returning to sports after arthroscopic Bankart repair with remplissage. Orthop J Sports Med 2021;9(4). doi:10.1177/ 23259671211001775
29. Franceschi F, Papalia R, Rizzello G, et al. Remplissage repair--new frontiers in the prevention of recurrent shoulder instability: a 2-year follow-up comparative study. Am J Sports Med. 2012;40(11):2462-2469. doi:10.1177/ 0363546512458572
30. Garcia GH, Park MJ, Baldwin K, Fowler J, Kelly JD IV, Tjoumakaris FP. Comparison of arthroscopic osteochondral substitute grafting and remplissage for engaging Hill-Sachs lesions. Orthopedics. 2013;36(1). doi:10.3928/01477447-20121217-16
31. Garcia GH, Park MJ, Zhang C, Kelly JD, Huffman GR. Large Hill-Sachs lesion: a comparative study of patients treated with arthroscopic Bankart repair with or without remplissage. HSS J 2015;11(2):98-103. doi:10.1007/S11420-015-9438-8
32. Horinek JL, Menendez ME, Narbona P, Lädermann A, Barth J, Denard PJ. Arthroscopic Bankart repair with remplissage as an alternative to Latarjet for anterior glenohumeral instability with more than 15% glenoid bone loss. Orthop J Sports Med 2022;10(12). doi:10.1177/23259671221142257
33. Horinek JL, Menendez ME, Callegari JJ, et al. Consideration may be given to lowering the threshold for the addition of remplissage in patients with subcritical glenoid bone loss undergoing arthroscopic Bankart repair Arthrosc Sports Med Rehabil 2022;4(4):e1283-e1289. doi:10.1016/ J.ASMR.2022.04.004
34. Hughes JL, Bastrom T, Pennock AT, Edmonds EW Arthroscopic Bankart repairs with and without remplissage in recurrent adolescent anterior shoulder instability with Hill-Sachs deformity Orthop J Sports Med. 2018;6(12). doi:10.1177/2325967118813981
35. Hurley ET, Colasanti CA, Lorentz NA, et al. No difference in outcomes after arthroscopic Bankart repair with remplissage or arthroscopic Latarjet procedure for anterior shoulder instability. Arthrosc Sports Med Rehabil 2022;4(3):e853-e859. doi:10.1016/J.ASMR.2021.12.011
36. Ko SH, Cha JR, Lee CC, Hwang IY, Choe CG, Kim MS. The influence of arthroscopic remplissage for engaging Hill-Sachs lesions combined with Bankart repair on redislocation and shoulder function compared with Bankart repair alone. Clin Orthop Surg 2016;8(4):428-436. doi:10.4055/ CIOS.2016.8.4.428
37. Lee YJ, Kim C, Kim SJ, Yoon TH, Cho JY, Chun YM. Does an “off-track” Hill-Sachs lesion that is misclassified as “non-engaging” affect outcomes from Bankart repair alone compared with Bankart repair combined with remplissage? Arthroscopy 2021;37(2):450-456. doi:10.1016/ J.ARTHRO.2020.09.037
38. Merolla G, Paladini P, di Napoli G, Campi F, Porcellini G. Outcomes of arthroscopic Hill-Sachs remplissage and anterior Bankart repair: a retrospective controlled study including ultrasound evaluation of posterior capsulotenodesis and infraspinatus strength assessment. Am J Sports Med 2015;43(2):407-414. doi:10.1177/0363546514559706
39. Miyamoto R, Yamamoto A, Shitara H, et al. Clinical outcome of arthroscopic Remplissage as augmentation during arthroscopic Bankart repair for recurrent anterior shoulder instability. Open Orthop J. 2017;11(1):1268-1276. doi:10.2174/ 1874325001711011268
40. Park I, Kang JS, Jo YG, Kim SW, Shin SJ. Off-track Hill-Sachs lesions do not increase postoperative recurrent instability after arthroscopic Bankart repair with selective remplissage procedure. Knee Surg Sports Traumatol Arthrosc 2019;27(12):3864-3870. doi:10.1007/S00167-019-05441-2
41. Paul RW, Reddy MP, Sonnier JH, et al. Increased rates of subjective shoulder instability after Bankart repair with remplissage compared to Latarjet surgery J Shoulder Elbow Surg. 2023;32(5):939-946. doi:10.1016/J.JSE.2022.11.001
42. Pulatkan A, Kapicioglu M, Ucan V, et al. Do techniques for Hill-Sachs remplissage matter in terms of functional and radiological outcomes? Orthop J Sports Med 2021;9(6). doi:10.1177/ 23259671211008152
43. Randelli PS, Compagnoni R, Radaelli S, Gallazzi MB, Tassi A, Menon A. Arthroscopic remplissage is safe and effective: clinical and magnetic resonance results at a minimum 3 years of follow-up. J Orthop Traumatol 2022;23(1):5. doi:10.1186/ S10195-021-00624-5
44. Wu D, Zhou Z, Song W, et al. Arthroscopic autologous iliac crest grafting results in similar outcomes and low recurrence compared to remplissage plus Bankart repair for anterior shoulder instability with bipolar bone defects. Arthroscopy 2023;39(7):1600-1607 doi:10.1016/ J.ARTHRO.2022.12.039
45. Yu W, Kim H, Seo JH, Jeon IH, Koh KH. Remplissage in addition to arthroscopic Bankart repair for shoulder instability with on-track HillSachs lesions reduces residual apprehension without external rotation limitation. Arthroscopy 2023;39(3):692-702. doi:10.1016/ J.ARTHRO.2022.10.013
46. Pandey V, Gangadharaiah L, Madi S, et al. A retrospective cohort analysis of arthroscopic Bankart repair with or without remplissage in patients with off-track Hill-Sachs lesion evaluated for functional outcomes, recurrent instability, and range of motion. J Shoulder Elbow Surg 2020;29(2):273-281. doi:10.1016/J.JSE.2019.06.005
47. Bitar AC, Fabiani MC, Ferrari DG, et al. Clinical and functional outcomes of the remplissage technique to repair anterior shoulder dislocation: average 7 years of follow-up. Musculoskelet Surg. 2021;105(1):61-67 doi:10.1007/S12306-019-00630-1
48. Boileau P, O’Shea K, Vargas P, Pinedo M, Old J, Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am 2012;94(7):618-626. doi:10.2106/JBJS.K.00101
49. Bonnevialle N, Azoulay V, Faraud A, Elia F, Swider P, Mansat P. Results of arthroscopic Bankart repair with Hill-Sachs remplissage for anterior shoulder instability. Int Orthop. 2017;41(12):2573-2580. doi:10.1007/S00264-017-3491-5
50. Brejuin A, Girard M, Barret H, Martinel V, Mansat P, Bonnevialle N. Long-term results of arthroscopic Bankart repair with Hill-Sachs remplissage. JSES Int. 2022;6(5). doi:10.1016/J.JSEINT.2022.06.005
51. Brilakis E, Avramidis G, Malahias MA, et al. Longterm outcome of arthroscopic remplissage in addition to the classic Bankart repair for the management of recurrent anterior shoulder instability with engaging Hill-Sachs lesions. Knee Surg Sports Traumatol Arthrosc 2019;27(1):305-313. doi:10.1007/ S00167-018-5261-3
52. Garcia GH, Wu HH, Liu JN, Huffman GR, Kelly JD. Outcomes of the remplissage procedure and its effects on return to sports: average 5-year follow-up. Am J Sports Med. 2016;44(5):1124-1130. doi:10.1177/ 0363546515626199
53. Haviv B, Mayo L, Biggs D Outcomes of arthroscopic “remplissage”: capsulotenodesis of the engaging large Hill-Sachs lesion. J Orthop Surg Res 2011;6(1). doi:10.1186/1749-799X-6-29
54. Martinez-Catalan N, Kazum E, Zampeli F, Cartaya M, Cerlier A, Valenti P Long-term outcomes of arthroscopic Bankart repair and Hill-Sachs remplissage for bipolar bone defects. Eur J Orthop Surg Traumatol 2023;33(4):947-953. doi:10.1007/ S00590-022-03237-8
55. McCabe MP, Weinberg D, Field LD, O’Brien MJ, Hobgood ER, Savoie FH. Primary versus revision arthroscopic reconstruction with remplissage for shoulder instability with moderate bone loss. Arthroscopy 2014;30(4):444-450. doi:10.1016/ J.ARTHRO.2013.12.015
56. Morsy MG. Arthroscopic remplissage: Is it still an option? EFORT Open Rev 2017;2(12):478-483. doi:10.1302/2058-5241.2.160070
57. Park MJ, Tjoumakaris FP, Garcia G, Patel A, Kelly JD IV Arthroscopic remplissage with Bankart repair for the treatment of glenohumeral instability with Hill-Sachs defects. Arthroscopy. 2011;27(9):1187-1194. doi:10.1016/ J.ARTHRO.2011.05.010
58. Scanaliato JP, Dunn JC, Fitzpatrick KV, Czajkowski H, Parnes N. Double-pulley remplissage in activeduty military population with off-track anterior shoulder instability results in improved outcomes and low recurrence at minimum 4-year follow-up. Arthroscopy 2022;38(3):743-749. doi:10.1016/ J.ARTHRO.2021.09.003
59. Zhu YM, Lu Y, Zhang J, Shen JW, Jiang CY Arthroscopic Bankart repair combined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: a report of 49 cases with a minimum 2-year followup. Am J Sports Med. 2011;39(8):1640-1647. doi:10.1177/0363546511400018
60. Gaunt BW, Shaffer MA, Sauers EL, Michener LA, Mccluskey GM, Thigpen CA. The American Society of Shoulder and Elbow Therapists’ consensus rehabilitation guideline for arthroscopic anterior capsulolabral repair of the shoulder. J Orthop Sports Phys Ther 2010;40(3):155-168. doi:10.2519/ JOSPT.2010.3186
61. Yin B, Levy D, Meadows M, et al. How does external rotation bracing influence motion and functional scores after arthroscopic shoulder stabilization? Clin Orthop Relat Res. 2014;472(8):2389-2396. doi:10.1007/ S11999-013-3343-6
62. Minkus M, Wolke J, Akgün D, Scheibel M. Mid- to long-term results of postoperative immobilization in internal vs. external rotation after arthroscopic anterior shoulder stabilization. JSES Int. 2021;5(6):960-966. doi:10.1016/J.JSEINT.2021.07.004
63. Kim SH, Ha KI, Jung MW, Lim MS, Kim YM, Park JH. Accelerated rehabilitation after arthroscopic Bankart repair for selected cases: A prospective randomized clinical study Arthroscopy - J Arthroscopic Rel Surg. 2003;19(7):722-731. doi:10.1016/S0749-8063(03)00397-9
64. McIsaac W, Lalani A, Silveira A, Chepeha J, Luciak-Corea C, Beaupre L. Rehabilitation after arthroscopic Bankart repair: a systematic scoping review identifying important evidence gaps. Physiotherapy. 2022;114:68-76. doi:10.1016/ J.PHYSIO.2021.03.014
65. Kim K, Saper MG. Postoperative management following arthroscopic Bankart repair in adolescents and young adults: a systematic review. Arthrosc Sports Med Rehabil 2020;2(6):e839-e845. doi:10.1016/J.ASMR.2020.05.016
66. DeFroda SF, Mehta N, Owens BD. Physical therapy protocols for arthroscopic Bankart repair Sports Health 2018;10(3):250. doi:10.1177/ 1941738117750553
67 Rossi LA, Pasqualini I, Tanoira I, Ranalletta M. Factors that influence the return to sport after arthroscopic Bankart repair for glenohumeral instability Open Access J Sports Med 2022;13:35-40. doi:10.2147/OAJSM.S340699
68. Drummond Junior M, Popchak A, Wilson K, Kane G, Lin A. Criteria-based return-to-sport testing is associated with lower recurrence rates following arthroscopic Bankart repair. J Shoulder Elbow Surg. 2021;30(7S):S14-S20. doi:10.1016/J.JSE.2021.03.141
69. Matache BA, Hurley ET, Wong I, et al. Anterior shoulder instability part III-revision surgery, rehabilitation and return to play, and clinical followup-an international consensus statement. Arthroscopy. 2022;38(2):234-242.e6. doi:10.1016/ J.ARTHRO.2021.07.019
70. Gerometta A, Klouche S, Herman S, Lefevre N, Bohu Y. The Shoulder Instability-Return to Sport after Injury (SIRSI): a valid and reproducible scale to quantify psychological readiness to return to sport after traumatic shoulder instability. Knee Surg Sports Traumatol Arthrosc 2018;26(1):203-211. doi:10.1007/ S00167-017-4645-0
Download: https://ijspt.scholasticahq.com/article/123481-rehabilitation-protocol-variability-following-arthroscopicbankart-repair-and-remplissage-for-management-of-anterior-shoulder-instability-a-systemati/attachment/ 245141.docx?auth_token=lotvaLft9uB43fpQ3q5t
Download: https://ijspt.scholasticahq.com/article/123481-rehabilitation-protocol-variability-following-arthroscopicbankart-repair-and-remplissage-for-management-of-anterior-shoulder-instability-a-systemati/attachment/ 245142.docx?auth_token=lotvaLft9uB43fpQ3q5t
Download: https://ijspt.scholasticahq.com/article/123481-rehabilitation-protocol-variability-following-arthroscopicbankart-repair-and-remplissage-for-management-of-anterior-shoulder-instability-a-systemati/attachment/ 245140.docx?auth_token=lotvaLft9uB43fpQ3q5t

DeLang MD,
L,
MN,
P,
M,
K. Implementing the Copenhagen Adductor Exercise and Nordic Hamstring Exercise in West African Academy Soccer Players: An Intervention Study. IJSPT. Published online October 2, 2024:1188-1196. doi:10.26603/001c.123510
Matthew D DeLang1a , Lasse Ishøi1 , Maren Nielsen Hole1 , Prince Wilson1 , Michael Segbefia2 , Kristian Thorborg3 1 Human Performance Group, Right to Dream Academy, 2 Department of Surgery, Orthopedics Unit, Korle Bu Teaching Hospital, University of Ghana Medical School, 3 Arthroscopic Center, Department of Orthopedic Surgery, Hvidovre Hospital, Copenhagen University Hospital, Sports Orthopaedic Research Center- Copenhagen
Keywords: Copenhagen Adductor, Nordic Hamstring, Football, Strength, Soccer https://doi.org/10.26603/001c.123510
International Journal of Sports Physical Therapy
This study implemented the Copenhagen Adductor Exercise (CAE) and Nordic Hamstring Exercise (NHE) to examine 1) whether CAE and NHE interventions are associated with adductor and hamstring strength gains in youth African male soccer players and 2) whether strength changes after a rest period and secondary intervention.
STUDY DESIGN
Pre-post intervention study
METHODS
Forty-four African elite male academy players (age 14.7±1.5 [12-18] years) participated in twice weekly CAE and NHE interventions for 8- and 10-week periods separated by a 4-week rest. Long lever adductor squeeze strength and prone isometric hamstring strength were measured with mixed-effects linear regression models to observe strength changes over time.
Ninety-six and 95% of CAE and NHE sessions were completed in each intervention, with no adverse events related to the execution of the exercises. Adductor squeeze strength increased during the first intervention (baseline 3.23 [2.99-3.47] N/kg, post-intervention 3.53 [3.30-3.76] N/kg, p=0.911) and was maintained following the rest period (3.52 [3.27-3.76] N/kg, p=0.999) and second intervention (3.60 [3.35-3.84] N/kg, p=0.002). Hamstring strength improved during the first intervention (baseline 4.95 [4.42-5.49] N/ kg, post-intervention 5.48 [4.95-6.02] N/kg, p<0.001), decreased to baseline during the rest period (4.98 [4.44-5.53] N/kg, p=0.996), and did not improve during the second intervention (5.01 [4.46-5.55] N/kg, p=0.978).
CAE and NHE interventions can be implemented at an elite African academy with high compliance. Adductor and hamstring strength improved in the first intervention, with no further improvements in the second intervention. Secondary interventions therefore should include higher exercise volume or load to improve longitudinal adductor and hamstring strength.
a
Corresponding Author: Matthew D. DeLang, PT, DPT, SCS, CSCS Farum Park 2, 3520 Farum, Denmark +45 42 37 39 86 mdel@fcn.dk
III (Cohort Study)
In African soccer (football) players, general injury risk reduction strategies have been successful with interventions such as the FIFA 11+.1,2 Although general injury risk was reduced by 41% and 55-71% in these studies, a significant reduction to injuries in the thigh1 and thigh/groin2 were not observed. Despite lacking injury prevalence studies in African players, it is known from other regions that groin and hamstring injuries are common in soccer players.3,4
To target the groin and hamstrings more specifically, injury risk reduction strategies have been recommended in soccer players outside West Africa. The Copenhagen Adductor Exercise (CAE) and Nordic Hamstring Exercise (NHE) have been studied, with randomized controlled trials in European soccer players showing a significant reduction in groin and hamstring injuries, respectively 5,6 Adding the CAE to the FIFA 11+ improves adductor strength,7 and has also been promoted as an addition to the FIFA 11+ by Football Australia’s Perform+ initiative.8 One study in Japanese soccer players even suggests combining the CAE and NHE is more effective at reducing adductor injuries than implementing the CAE alone.9 The only African NHE intervention study shows a 70% reduction in hamstring injuries compared to the previous season in Egyptian players, showing promise for other interventions on the continent.10
Injury risk reduction using the CAE and NHE may be attributed to increases in adductor and hamstring strength, respectively 5,6 Following CAE intervention, under-19 soccer players improved eccentric hip adduction strength by 36%.11 In the adductors, every unit (Nm/kg) of increased long lever adductor squeeze strength reduced injury risk by 35% in Spanish soccer players.12 In amateur male soccer players, a ten-week in-season NHE intervention improved peak eccentric hamstring strength by 19%,13 and lower than 2.4 Nm/kg eccentric hamstring peak torque has been associated with higher injury risk.14
No studies have examined adductor and hamstring strength longitudinally in West African soccer players. First examining whether the CAE and NHE can elicit strength gains in this population is necessary before recommending the interventions for injury risk reduction in West African soccer players. Further, strength booster periods have been suggested to counteract potential strength decay during the season,15 but no studies have explored this yet. Therefore, the authors also examined what happens to adductor and hamstring strength following a rest period and second intervention period to see if the CAE and NHE may have further beneficial and longitudinal effects on strength.
This study aims to implement the Copenhagen Adductor Exercise (CAE) and Nordic Hamstring Exercise (NHE) to examine 1) whether CAE and NHE interventions are associated with adductor and hamstring strength gains in youth West African male soccer players and 2) whether strength changes after a rest period and second intervention.
All male players from the U14, U16, and U18 squads from one elite West African soccer academy were included. Players were excluded if a time-loss injury was present during a testing date. Data were collected in the summer and fall of 2021 on-site at the academy. This study was approved by the University of Ghana College of Health Sciences Ethical and Protocol Review Committee and all participants had a parent/guardian sign consent. The study was conducted in accordance with the ethical standards in the Declaration of Helsinki. This population was chosen to further broaden the scope of sport and exercise medicine research in understudied geographical regions.
The primary intervention period was eight weeks, followed by a four-week rest period, and a secondary ten-week intervention period. The rest period included no formal strength program or soccer training. The intervention periods included twice weekly exposures of the CAE and NHE in addition to normal soccer participation. A linear periodization program was followed with increasing weekly volume every two weeks: CAE (2x6, 2x8, 2x10, 2x12) and NHE (2x6, 3x5, 3x6, 3x8) (Figure 1). Harøy et al.7 demonstrated 470 repetitions over eight weeks leads to injury risk reduction and approximately 10% adductor strength gain. The present study employed a similar dosage in the first intervention, with 576 CAE repetitions over eight weeks. The CAE was performed with a concentric:eccentric ratio of 1:1, with each phase of the exercise spanning 2-3 seconds. The NHE was performed as slowly as possible while maintaining forward movement. The work: rest ratio was approximately 1:1, as the players rested while assisting their partner in the exercise.
The CAE was performed as previously described.5 Players partnered with a teammate of similar body mass to stabilize the static limb, and repetitions were counted aloud by the group. The NHE intervention was also performed as previously described, with the resting partner holding the ankles of the exercising player 6,16 For all intervention sessions, at least one physiotherapist was present (MDD, MNH, PW) who instructed the exercise and tracked adherence. All interventions occurred prior to training, either in association with the warmup on the pitch or in a gym session. Adverse events were defined as time-loss injury related to the adductor and/or hamstring during the study period.
Soccer exposures were tracked for each team during the intervention periods. The U14 squad trained four days per week, and the U16 and U18 squads trained five days per week. The first two weeks of each intervention period were “preseason” with a gradually increasing volume of soccer

Figure 1. Participant flow (n=44).
Two intervention sessions per week (sets x repetitions). NHE, Nordic hamstring exercise. CAE, Copenhagen adductor exercise. Total per first intervention period: CAE 288 repetitions each side, NHE 276 repetitions. Total per second intervention period: CAE 384 repetitions each side, NHE 372 repetitions. *Players who entered the second intervention period after being promoted to the U14 squad. **Players who exited after the first intervention period (graduated from academy n=12, unrelated injury n=1).
participation (three sessions in week one, four sessions in week two). A training deload week occurred in week six, with all squads participating in three training sessions and no matches. All other training weeks included training sessions and one match.
Outcome measures were performed prior to and after each intervention period (four total). To minimize post-soccer fatigue, all testing sessions were performed in lieu of soccer training on that day The day prior to testing was always an off-day to mitigate the effects of fatigue from soccer participation, although the end-of-intervention testing dates occurred on a matchday plus two. All players had previous exposure to the CAE and NHE prior to the study period. Long lever adductor squeeze strength and prone isometric hamstring strength were captured using the microFET2 digital handheld dynamometer (Hoggan Scientific LLC, Salt Lake City, Utah, USA). The long lever adductor squeeze strength test has good reliability (intra-class coefficient 0.95 [0.87-0.98], standard error of measurement 3.2% [1.9-5.1%], minimal detectable change 6.6%.17 Long lever adductor squeeze strength was measured as an iteration of the fivesecond squeeze test by adding a handheld dynamometer component.18,19 The squeeze width was the tester’s forearm (MDD) plus the handheld dynamometer placed in the tester’s palm. Each player was instructed to squeeze isometrically for five seconds with maximal effort using the verbal cue “ready-go-1-2-3-4-5-and relax” Three five-second isometric repetitions were collected with sixty seconds of rest between each. The highest squeeze score was used for data analysis.
Prone isometric hamstring strength was measured isometrically with a rigid, external belt attached to the handheld dynamometer, using the protocol established by Ishøi et al.13 The testing leg was placed in approximately 15 degrees knee flexion, with the dynamometer placed on the posterior shank 5 cm proximal to the lateral malleolus. The standardized verbal cue used was “ready-3-2-1-go-pushpush-push-and relax” Each player performed three trials with 60 seconds of rest between repetitions, and the highest output from the three trials was used for data analysis. Hamstring strength was collected one limb at a time, and an average of the maximal efforts from the left and right limbs were used for analysis.
Isometric hamstring strength and adductor squeeze strength were used as two separate outcome variables. All statistical analyses were performed using R.20 Two mixedeffects linear regression models (one for hamstring, one for adductor) were developed with time and mass as fixed factors and player and team as random factors (random intercepts). Time was included in the models at four points: start of first intervention, end of first intervention, start of second intervention, and end of second intervention. The lm4e package was used:
lmer (Strength Measure ~ time + mass + (1|participant) + (1|team), data = data)
Assumptions were checked for each model using the performance package with the check_model function. None of the models violated any assumptions.
Table 1. Participant descriptive data (n=44).
Sixty-seven players participated in at least one intervention period. Twelve players were not eligible for the first intervention because they had not yet been promoted to the U14 squad. Thirteen players missed the second intervention period due to graduation from the academy (n=12) or injury unrelated to the adductors or hamstrings (n=1). In total, 44 players (age 14.7±1.5 [12-18] years) completed the two intervention periods and were included in the present study (Table 1). Age, height, and body mass increased in the group over the course of the entire 22-week study period. The players’ countries of origin were Ghana (n=28) and Ivory Coast (n=16).
Players were consistently compliant with performing the interventions under the direct supervision of a physiotherapist. Ninety-six percent of all sessions were completed in the first intervention, and 95% in the second intervention period. No adverse events related to the execution of the interventions occurred, but eight groin injuries with minimal time-loss (1-3 days) and two with moderate time-loss (8-28 days) occurred during the study period. There were no hamstring injuries recorded during the intervention period.
Mean and 95% confidence intervals at each timepoint are provided in Table 2, including comparisons between each timepoint. Adductor squeeze strength increased during the first intervention period (mean difference: 0.30 N/kg; p=0.011) and was maintained during the four-week break period (mean difference compared to end of first intervention: -0.01; p=0.999). At the start of the second intervention period, adductor squeeze strength was higher than at the start of the first intervention period (mean difference: 0.29 N/kg; p=0.022). Adductor squeeze strength did not increase during the second intervention period (mean difference 0.08 N/kg; p=0.818). From the start of the first intervention to the end of the second intervention, adductor squeeze strength improved (mean difference: 0.37 N/kg; p=0.002). The increase in adductor squeeze strength during the first intervention period (8.9%) and from the start of the first intervention to the end of the second intervention (10.8%) exceed the minimal detectable change for long lever adductor squeeze strength.
Mean and 95% confidence intervals are included in Table 2, including comparisons between each timepoint. Hamstring strength improved during the first intervention period (mean difference 0.528 N/kg; p<0.001) and decreased during the four-week break period (mean difference -0.501 N/kg; p=0.001). At the start of the second intervention period, there was no difference from the start of the first intervention period (mean difference -0.028 N/kg; p=0.996). Hamstring strength did not improve during the second intervention period (mean difference 0.023 N/kg; p=0.997). From the start of the first intervention to the end of the second intervention, no significant improvement in strength was observed (mean difference 0.051 N/kg; p=0.978).
This study examined the implementation of the CAE and NHE in a West African soccer academy and looked upon whether CAE and NHE interventions are associated with adductor and hamstring strength gains in youth West African male soccer players during the season. Under supervision, players were compliant (96% and 95% in each intervention period), and no adverse events related to the execution of the exercises occurred. Overall, adductor squeeze strength improved in the first intervention period, was maintained during the rest period, and was unchanged in the second intervention, whereas hamstring strength increased in the first intervention, decreased to baseline during the rest period, and was unchanged in the second intervention.
Adductor squeeze strength improved 10.8% from baseline to the end of the study period. Isometric hamstring strength increased in the first intervention, decreased to baseline during the rest period, and was unchanged in the second intervention (+1.2% change from start to end of study period). Although studies have considered injury risk reduction in African soccer players,1,2,10 no studies have observed possible strength changes following CAE and NHE interventions. During the first intervention period, adductor squeeze strength and isometric prone hamstring strength each improved. This aligns with studies of the CAE and NHE in other regions, where strength improvements have also been observed.5,11 Improving strength in the adductors and hamstrings may benefit soccer perfor-
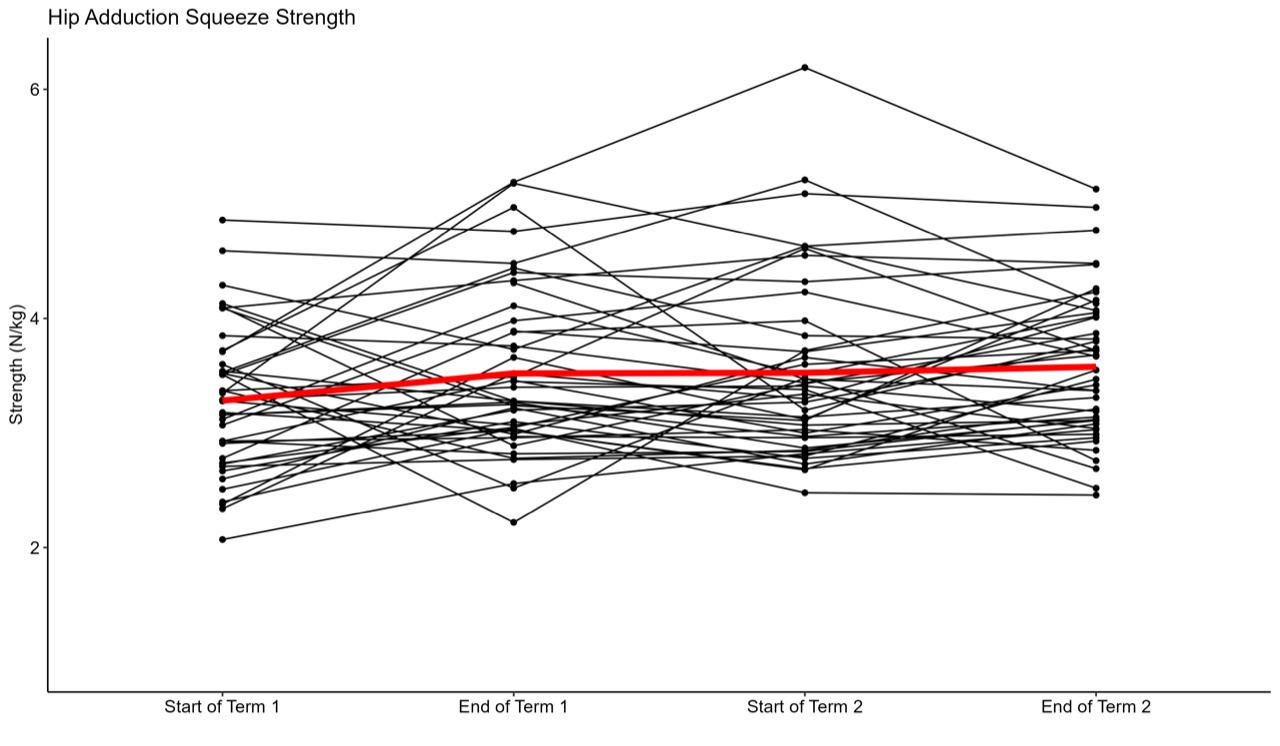
Figure 2. Adductor squeeze strength (N/kg) throughout the study period. Individual players represented by black lines and group average indicated by the red line.
A significant increase occurred from Start of Term 1 to End of Term 1 (p=0.01, 9.3% increase).
Table 2. Changes in adductor squeeze strength and hamstring strength between timepoints statistically significant at p<0.05 in bold; data presented as mean [95% confidence interval].
Adductor squeeze strength
Hamstring strength
mance and also be an underlying mechanism for injury risk reduction in the adductors and hamstrings.12,14 Therefore, primary interventions of the CAE and NHE to improve ad-
ductor and hamstring strength in West African soccer players may be beneficial.
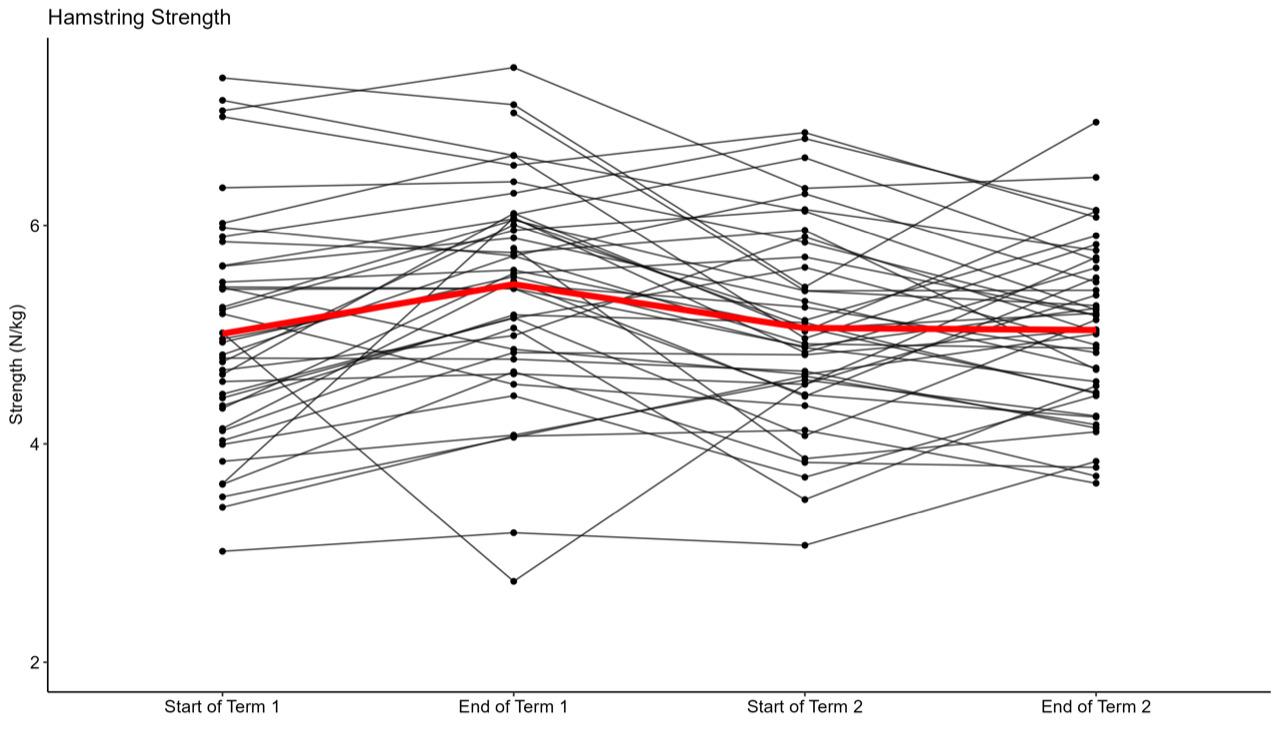
Figure 3. Isometric hamstring strength (N/kg) throughout the study period. Individual players represented by black lines and group average indicated by the red line. Significant increase from Start of Term 1 to End of Term 1 (p<0.001, 10.7%), and decrease from End of Term 1 to Start of Term 2 (p<0.001, -9.2%).
During four weeks of rest from soccer and strength interventions, adductor squeeze strength was maintained but hamstring strength reduced to baseline. Strength reductions with detraining can be expected. With the NHE, decreases in strength following detraining have been reported,21 even with a detraining period of one week.22 With the CAE, detraining periods have reduced adductor longus muscle thickness in sub-elite soccer players and other recreational athletes.23 However, the present study did not demonstrate strength declines during the detraining period for the adductors. Previous studies found that adductor strength was weakest at start of preseason and after a midseason break,24,25 suggesting adductor strength may improve with soccer exposure. Therefore, it is unclear why the adductor strength in the present study did not decrease during a detraining period without soccer participation or the CAE intervention. Perhaps the high training load of the players (5-6 days per week) coupled with CAE elicited an overloading of the adductors. Adductor strength can be decreased for up to 72 hours following a match,26 and a period of match congestion led to nearly three-quarters of Australian youth players demonstrating reduced adductor squeeze strength.27 If the players in the present study were overloaded during the first intervention period, it is possible that the rest during the detraining period was advantageous for strength.
During the second intervention, neither adductor squeeze strength nor isometric hamstring strength improved. The secondary intervention may have lacked novelty to induce neuroplastic changes and/or sufficient progressive overload to induce hypertrophic changes. The linear periodization from the first intervention was re-
peated in the second intervention, and it is possible that this repeated stimulus was not novel enough to elicit strength gains. It is also possible that adductor strength had plateaued at this stage, and the interventions provided maintenance of strength. Strength maintenance may be beneficial during a competitive season when the physical demand is high. For hamstring strength, however, no improvements from baseline to the end of the second intervention period may indicate an insufficient longitudinal stimulus of the NHE. In one NHE study where high-volume and low-volume interventions were compared, no strength gains are observed from mid-intervention to post-intervention; however, this study has only two weeks rest between intervention periods and no stoppage in soccer participation.28 To overcome a plateau in strength, adjusting the periodization in a secondary intervention may provide a boost.15
Compliance is often a barrier to effective interventions. In one survey study, more than 80% of UEFA Champions League and Norwegian Tippeligaen teams failed to adopt the NHE as an injury risk reduction tool.29 Despite 85% of Dutch amateur male soccer players having knowledge of the NHE and 93% of the club medical staffs believing the NHE is effective, 69% of players reported never performing the exercise.30 The present study, supported by supervision of all intervention sessions, shows that high adherence can be achieved in youth soccer players. In the long-term, placing emphasis and promoting adherence to these exercise programs may aid future first team players and staff to understand their importance. Staff who invest in CAE and NHE interventions should supervise sessions to improve compliance.
When a new intervention is introduced to a population, it is important to consider whether any adverse events may occur In this study no adverse events related to the execution of the intervention occurred. During the intervention period eight minimal time-loss (1-3 days) and two moderate time-loss (8-28 days) adductor injuries occurred which is lower or within what is to be expected at this level. It was very positive that there were no cases of long-standing or severe time-loss adductor cases, and no hamstring injuries, as these injuries both may pose a high burden on young soccer players.31 The CAE and NHE exercises, thus seems to be safe interventions to implement in West African academy soccer players.
Although previous studies have shown lacking compliance for the CAE and NHE, these interventions can be effectively implemented under supervision in West African academy soccer players. Developing stronger adductors and hamstrings may be advantageous for soccer players, as these muscle groups experience high demands during soccer actions such as high-speed running, kicking, and cutting.32 Although a direct link to injury risk reduction cannot be made with the current study design, the CAE and NHE can increase adductor and hamstring strength, which has been shown to mitigate both adductor and hamstring injuries.5,6, 14,33
Adductor squeeze strength improved 8.9% during the first intervention and 10.8% from the start to end of the study period, indicating that meaningful detectable change (>6.6%)17 occurred. Maintained improvements in adductor squeeze strength throughout the study period are evident, although strength did not further increase during the second intervention period. CAE interventions should be implemented in academy soccer populations. If additional longitudinal strength gains are desired, perhaps a novel stimulus could be added to the CAE such as increasing the exercise volume, adding external load, or increase the time under tension during the eccentric phase (3:1 eccentric-toconcentric ratio).
Hamstring strength initially improved (+10.2% in the first intervention), suggesting the dosage of the NHE was sufficient to create strength changes. However, hamstring strength returned to baseline during the rest period and did not increase in the second intervention period. Perhaps ongoing hamstring strength exercises during breaks from soccer training seems important to maintain strength. To pro-
mote more longitudinal hamstring strength gains, a novel stimulus should be introduced. This may be achieved by altering the periodization of the programming, adding bandassistance to increase time under tension,34 or include other hamstring-related demands such as a linear sprinting program.35
Because the study was conducted in an applied soccer setting, no control group was included to consider whether injury risk reduction may have occurred. Additionally, no non-soccer control group was included to differentiate between strength changes attributed to the intervention compared to soccer exposure itself. Soccer participation seems to influence adductor strength independent of the CAE, as adductor strength differed 27% between U13 and U15 Danish soccer players even when normalized to body mass.36 The present study controlled for maturation using only values relative to body mass and did not capture leg length to examine torque. A future multifactorial approach should examine CAE and NHE interventions in conjunction with soccer training load and maturation status to better understand the interplay between these factors.
CAE and NHE interventions can be implemented at a West African soccer academy with high compliance and no adverse events. These exercises improve adductor and hamstring strength the after an eight–week intervention period, with no further improvements in adductors and a decrease in hamstring after second intervention period. Secondary interventions during the season therefore may need higher exercise volume or load if the goal is to improve longitudinal adductor and hamstring strength gains in academy players throughout the season.
The authors have no competing interests to report for this study
Submitted: February 26, 2024 CDT, Accepted: August 28, 2024 CDT
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Owoeye OB, Akinbo SR, Tella BA, Olawale OA. Efficacy of the FIFA 11+ warm-up programme in male youth football: A cluster randomised controlled trial. J Sports Sci Med 2014;13(2):321-328.
2. Nuhu A, Jelsma J, Dunleavy K, Burgess T Effect of the FIFA 11+ soccer specific warm up programme on the incidence of injuries: a cluster-randomised controlled trial. PLoS One 2021;16(5):e0251839. doi:10.1371/journal.pone.0251839
3. Werner J, Hägglund M, Waldén M, Ekstrand J. UEFA injury study: a prospective study of hip and groin injuries in professional football over seven consecutive seasons. Br J Sports Med 2009;43(13):1036-1040. doi:10.1136/ bjsm.2009.066944
4. Ekstrand J, Bengtsson H, Waldén M, Davison M, Khan KM, Hägglund M. Hamstring injury rates have increased during recent seasons and now constitute 24% of all injuries in men’s professional football: the UEFA Elite Club Injury Study from 2001/02 to 2021/ 22. Br J Sports Med. 2022;57(5):292-298. doi:10.1136/ bjsports-2021-105407
5. Harøy J, Clarsen B, Wiger EG, et al. The Adductor Strengthening Programme prevents groin problems among male football players: a cluster-randomised controlled trial. Br J Sports Med 2019;53(3):150-157 doi:10.1136/bjsports-2017-098937
6. van der Horst N, Smits DW, Petersen J, Goedhart EA, Backx FJ. The preventive effect of the nordic hamstring exercise on hamstring injuries in amateur soccer players: a randomized controlled trial. Am J Sports Med 2015;43(6):1316-1323. doi:10.1177/ 0363546515574057
7. Harøy J, Thorborg K, Serner A, et al. Including the Copenhagen Adduction Exercise in the FIFA 11+ provides missing eccentric hip adduction strength effect in male soccer players: a randomized controlled trial. Am J Sports Med 2017;45(13):3052-3059. doi:10.1177/ 0363546517720194
8. Whalan M, Lovell R, Thorborg K, Sampson JA. The 11+ of the future: a primary injury prevention framework for sub-elite football. Br J Sports Med 2020;2020. doi:10.1136/bjsports-2020-102788
9. Fujisaki K, Akasaka K, Otsudo T, Hattori H, Hasebe Y, Hall T. Effects of a groin pain prevention program in male high school soccer players: a clusterrandomized controlled trial. Int J Sports Phys Ther. 2022;17(5):841-850. doi:10.26603/001c.36631
10. Elerian AE, El-Sayyad MM, Dorgham HAA. Effect of pre-training and post-training Nordic exercise on hamstring injury prevention, recurrence, and severity in soccer players. Ann Rehabil Med 2019;43(4):465-473. doi:10.5535/arm.2019.43.4.465
11. Ishøi L, Sørensen CN, Kaae NM, Jørgensen LB, Hölmich P, Serner A. Large eccentric strength increase using the Copenhagen Adduction exercise in football: a randomized controlled trial. Scand J Med Sci Sports 2016;26(11):1334-1342. doi:10.1111/ sms.12585
12. Esteve E, Casals M, Saez M, et al. Past-season, pre-season and in-season risk assessment of groin problems in male football players: a prospective fullseason study. Br J Sports Med. 2022;56(9):484-489. doi:10.1136/bjsports-2020-102606
13. Ishøi L, Aagaard P, Nielsen MF, et al. The influence of hamstring muscle peak torque and rate of torque development for sprinting performance in football players: A cross-sectional study Int J Sports Physiol Perform. Published online 2018. doi:10.1123/ ijspp.2018-0464
14. Lee JWY, Mok KM, Chan HCK, Yung PSH, Chan KM. Eccentric hamstring strength deficit and poor hamstring-to-quadriceps ratio are risk factors for hamstring strain injury in football: a prospective study of 146 professional players. J Sci Med Sport. 2018;21(8):789-793. doi:10.1016/j.jsams.2017.11.017
15. Ishøi L, Thorborg K. Copenhagen adduction exercise can increase eccentric strength and mitigate the risk of groin problems: but how much is enough! Br J Sports Med 2021;55(19):1066-1067 doi:10.1136/ bjsports-2020-103564
16. Mjølsnes R, Arnason A, Osthagen T, Raastad T, Bahr R. A 10-week randomized trial comparing eccentric vs concentric hamstring strength training in well-trained soccer players. Scand J Med Sci Sports 2004;14:311-317 doi:10.1046/j.1600-0838.2003.367.x
17. Light N, Thorborg K. The precision and torque production of common hip adductor squeeze tests used in elite football. J Sci Med Sport 2016;19(11):888-892. doi:10.1016/ j.jsams.2015.12.009
18. Thorborg K, Branci S, Nielsen MP, et al. Copenhagen five-second squeeze: a valid indicator of sports-related hip and groin function. Br J Sports Med 2017;51:594-599. doi:10.1136/ bjsports-2016-096675
19. Nielsen MF, Thorborg K, Krommes K, et al. Hip adduction strength and provoked groin pain: A comparison of long-lever squeeze testing using the ForceFrame and the Copenhagen 5-second squeeze test. Phys Ther Sport 2022;55:28-36. doi:10.1016/ j.ptsp.2022.02.002
20. R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2023. https://www.R-project.org/
21. Siddle J, Greig M, Weaver K, Page RM, Harper D, Brogden CM. Acute adaptations and subsequent preservation of strength and speed measures following a Nordic hamstring curl intervention: a randomised controlled trial. J Sports Sci. 2019;37(8):911-920. doi:10.1080/ 02640414.2018.1535786
22. Pollard CW, Opar DA, Williams MD, Bourne MN, Timmins RG. Razor hamstring curl and Nordic hamstring exercise architectural adaptations: impact of exercise selection and intensity. Scand J Med Sci Sports 2019;29(5):706-715. doi:10.1111/sms.13381
23. Alonso-Fernández D, Fernández-Rodríguez R, Taboada-Iglesias Y, Gutiérrez-Sánchez Á. Effects of Copenhagen Adduction Exercise on muscle architecture and adductor flexibility Int J Environ Res Public Health. 2022;19(11):6563. doi:10.3390/ ijerph19116563
24. Jensen J, Hölmich P, Bandholm T, Zebis MK, Andersen LL, Thorborg K. Eccentric strengthening effect of hip-adductor training with elastic bands in soccer players: a randomised controlled trial. Br J Sports Med. 2014;48(4):332-338. doi:10.1136/ bjsports-2012-091095
25. Wollin M, Thorborg K, Welvaert M, Pizzari T Inseason monitoring of hip and groin strength, health and function in elite youth soccer: implementing an early detection and management strategy over two consecutive seasons. J Sci Med Sport. 2018;21(10):988-993. doi:10.1016/ j.jsams.2018.03.004
26. Khaitin V, Bezuglov E, Lazarev A, et al. Markers of muscle damage and strength performance in professional football (soccer) players during the competitive period. Ann Transl Med. 2021;9(2):113. doi:10.21037/atm-20-2923
27 Wollin M, Pizzari T, Spagnolo K, Welvaert M, Thorborg K. The effects of football match congestion in an international tournament on hip adductor squeeze strength and pain in elite youth players. J Sports Sci. 2018;36(10):1167-1172. doi:10.1080/ 02640414.2017.1363452
28. Lacome M, Avrillon S, Cholley Y, Simpson BM, Guilhem G, Buchheit M. Hamstring eccentric strengthening program: does training volume matter? Int J Sports Physiol Perform. 2019;2019:1-27. doi:10.1123/ijspp.2018-0947
29. Bahr R, Thorborg K, Ekstrand J. Evidence-based hamstring injury prevention is not adopted by the majority of Champions League or Norwegian Premier League football teams: the Nordic Hamstring survey Br J Sports Med. 2015;49(22):1466-1471. doi:10.1136/ bjsports-2015-094826
30. van der Horst N, Hoef SV, Otterloo PV, Klein M, Brink M, Backx F. Effective but not adhered to: how can we improve adherence to evidence-based hamstring injury prevention in amateur football? Clin J Sport Med. 2021;31(1):42-48. doi:10.1097/ JSM.0000000000000710
31. Bisciotti GN, Auci A, Bona S, et al. A multidisciplinary assessment of 320 athletes with long-standing groin pain syndrome in keeping with the Italian consensus agreement: the high incidence and the multiple causes of inguinal and hip pathologies and pubic osteopathy J Sports Med Phys Fitness 2021;61(7):960-970. doi:10.23736/ S0022-4707.20.11575-5
32. Dupré T, Tryba J, Potthast W. Muscle activity of cutting manoeuvres and soccer inside passing suggests an increased groin injury risk during these movements. Scientific reports 2021;11(1):7223. doi:10.1038/s41598-021-86666-5
33. Mosler AB, Agricola R, Weir A, Hölmich P, Crossley KM. Which factors differentiate athletes with hip/groin pain from those without? A systematic review with meta-analysis. Br J Sports Med. 2015;49(12):810. doi:10.1136/bjsports-2015-094602
34. Alt T, Knicker AJ, Nodler YT, Strüder HK. Assisted or unassisted Nordic Hamstring Exercise?Resistance exercise determinants at a glance. Sports Biomech 2021;16:1-15. doi:10.1080/ 14763141.2021.1893376
35. Freeman BW, Young WB, Talpey SW, Smyth AM, Pane CL, Carlon TA. The effects of sprint training and the Nordic hamstring exercise on eccentric hamstring strength and sprint performance in adolescent athletes. J Sports Med Phys Fit 2019;59(7):1119-1125. doi:10.23736/S0022-4707.18.08703-0
36. Light N, Thorborg K, Krommes K, et al. Rapid spike in hip adduction strength in early adolescent footballers: a study of 125 elite male players from youth to senior. Int J Sports Physiol Perform. 2022;17(9):1407-1414. doi:10.1123/ijspp.2022-0025

Nishida S, Ito W, Ohishi T, Yoshida R, Sato S, Nakamura M. Relationship between Peak Eccentric Force during the Nordic Hamstring Exercise and One Repetition Maximum Deadlift Performance. IJSPT. Published online October 1, 2024:1197-1203. doi:10.26603/001c.123473
Satoru Nishida1a , Wataru Ito2 , Taisuke Ohishi3 , Riku Yoshida4 , Shigeru Sato5 , Masatoshi Nakamura6
1 Faculty of Sport and Health Sciences, Ryutsu Keizai University, 2 Niigata University of Rehabilitation, 3 Niigata Rehabilitation Hospital, 4 Department of Rehabilitation, Maniwa Orthopedic Clinic, 5 Department of Rehabilitation, Matsumura General Hospital, 6 Faculty of Rehabilitation Sciences, Nishi Kyushu University
Keywords: Nordic hamstring, deadlift, hip extensor, trunk extensor, hamstring strain injury https://doi.org/10.26603/001c.123473
International Journal of Sports Physical Therapy
Background
The Nordic hamstring exercise (NHE) is useful for preventing hamstring strain injuries. However, its adoption rates in the sports field are currently low, necessitating a safe and efficient introduction.
Hypothesis/Purpose
The purpose was to examine the relationship between the eccentric force during the NHE and the one repetition maximum of deadlift. It was hypothesized that the eccentric force during the NHE would be correlated with the one repetition maximum (1RM) of the deadlift.
Study design
Cross-sectional study.
Methods
Healthy student rugby players with no history of hamstring tears were recruited to participate. The peak eccentric forces during the NHE, which is the vertical peak force on the part holding the leg, were measured in both legs, while gradually leaning forward to a prone position over three seconds. The 1RM of deadlift was calculated from the weight that could be raised three times during a deadlift (x kg) using the estimated formula (x kg / 0.93). The correlation between the left and right peak eccentric forces during the NHE, the total left and right forces, and the 1RM of the deadlift was examined using Spearman’s rank correlation coefficient, with all values corrected for body mass.
Results
During the NHE, the peak eccentric force of the right and left legs and the total peak eccentric force of both legs were 3.8 ± 1.1 N/BM, 3.8 ± 1.2 N/BM, and 7.6 ± 2.1 N/BM, respectively. The 1RM of deadlift was 1.9 ± 0.3 kg/BM. Weak correlations (r = 0.34–0.37) were found between the 1RM of the deadlift and the peak eccentric force in the right and left legs and the total peak eccentric force of both legs.
Conclusion
The present study revealed a weak correlation between the peak eccentric force during the NHE and 1RM of deadlift
Corresponding Author:
Satoru Nishida, PhD, JSPO-AT
E-mail: satoru.nishida5521@gmail.com a
Faculty of Sport and Health Sciences, Ryutsu Keizai University, Ryugasaki, Ibaraki, Japan 120, Hirahata, Ryugasaki, Ibaraki 301-8555, Japan
Tel.: +81-297-64-0011 (757)
Hamstring strain injury (HSI) is a common injury in sports involving sprinting.1‑3 For the prevention of HSI, sufficient muscle strength (especially eccentric muscle strength) is considered important to control the powerful external load on the hamstring that occurs from the end of the swing phase to ground contact during the sprinting.4,5 Recently, many studies have suggested a relationship between eccentric hamstring strength and HSI,6‑8 and it is generally accepted that hamstring eccentric exercises are important for HSI prevention and rehabilitation in sports.
The Nordic Hamstring Exercise (NHE) is a typical hamstring eccentric exercise, and NHE training provides benefits such as increased eccentric hamstring strength and lengthening of muscle fascicle length that can reduce the risk of hamstring strain injury 9‑11 In their systematic review, Van Dyk et al. concluded that the programs that include the NHE reduce hamstring injuries by up to 51%.12 However, the NHE as a HSI prevention exercise has a low adoption rate, with only approximately 13% in men’s professional football teams in Europe adopting this exercise.13 Low compliance may be related to athletes’ experience of muscle stiffness and soreness after NHE training. To eliminate these potential barriers to adopting NHE as a preventive exercise for HSI, it is important to develop appropriate exercise strategies in order to implement the NHE safely and efficiently
NHE performance is generally evaluated by the eccentric force during NHE, which is the vertical force on the part holding the leg,14,15 and eccentric force during NHE is considered useful for predicting HSI risk.16,17 Previous authors have reported a small or no correlation between eccentric force during NHE and eccentric knee flexor torque measured by an isokinetic dynamometer,18,19 suggesting that some factors other than eccentric knee flexor strength contribute to NHE performance. Interestingly, during NHE, not only knee joint torque but also hip joint torque occurs, and muscle activity of the hip and trunk extensors, such as the erector spinae and gluteus maximus, is also observed,20‑22 indicating the importance of hip and trunk extensor strength during NHE performance. The deadlift is a classic strength training used to strengthen the hip and trunk extensors,23‑25 and similarities to NHE in hamstring muscle activity during exercise have also been reported26; however, the similarity of peak force between the two exercises has not yet been determined. Clarifying the relationship between eccentric force generated during the NHE and the one repetition maximum (1RM) of deadlift, which reflects the hip and trunk extensor strength, will provide new insights into the importance of hip and trunk extensor strength during the NHE, and may also help demonstrate the usefulness of deadlift as an appropriate exercise to perform before progressing to NHE.
Therefore, in the present study, the relationship between the eccentric force during the NHE and the 1RM of deadlift
was examined. It was hypothesized that the eccentric force during the NHE would be correlated with the 1RM of deadlift.
Forty-nine healthy young rugby players, who were the top players in their region, were recruited for the present study Participants habitually performed resistance training, including of the knee flexors two to three times a week for at least one year, and had sufficient experience with NHE. None of the participants had experienced hamstring strain or knee-joint injury A sample size calculation was performed using G*Power 3.1.9.6. Assuming a two-tailed test for the population correlation coefficient with an expected correlation coefficient of 0.4, a significance level of 5%, and a power of 80%, the required sample size was calculated to be 44 cases. This study was approved by the institutional ethics committee and was conducted in accordance with the principles of the Declaration of Helsinki. The study procedures and potential risks were explained to the participants, and each provided written informed consent before participating in the study.
This cross-sectional study was conducted over a single day. After the warm-up, the participants performed the NHE and 1RM deadlift, as explained below The two tests were performed in random order with adequate rest between the two.
For eccentric force evaluation, each participant was placed in a kneeling position on a custom-made NHE device (4Assist Inc, Tokyo, Japan) with each ankle secured above the lateral malleolus with an ankle brace attached to a load cell sensor (Figure 1). The force acting on the ankle brace in the vertical direction was quantified using a load-cell sensor Force data were synchronized and transferred at 1,000 Hz from a PowerLab16/35 data acquisition and analysis system (AD Instruments, Bella Vista, NSW, Australia) to a personal computer (VersaPro; NEC Corporation, Tokyo, Japan). Each participant was instructed by the examiner to gradually lean forward from the initial kneeling position at 90° knee flexion to a prone position over three seconds, with the arms crossed at the chest and hip joints fully extended, and the ankle was passively secured in the dorsiflexed position. Before testing, the participants practiced the NHE two to three times. To standardize the velocity of movement, the participants were instructed to lean forward at a constant angular velocity, as indicated by a metronome. Eccentric force data was corrected for body mass (N/BM), and the
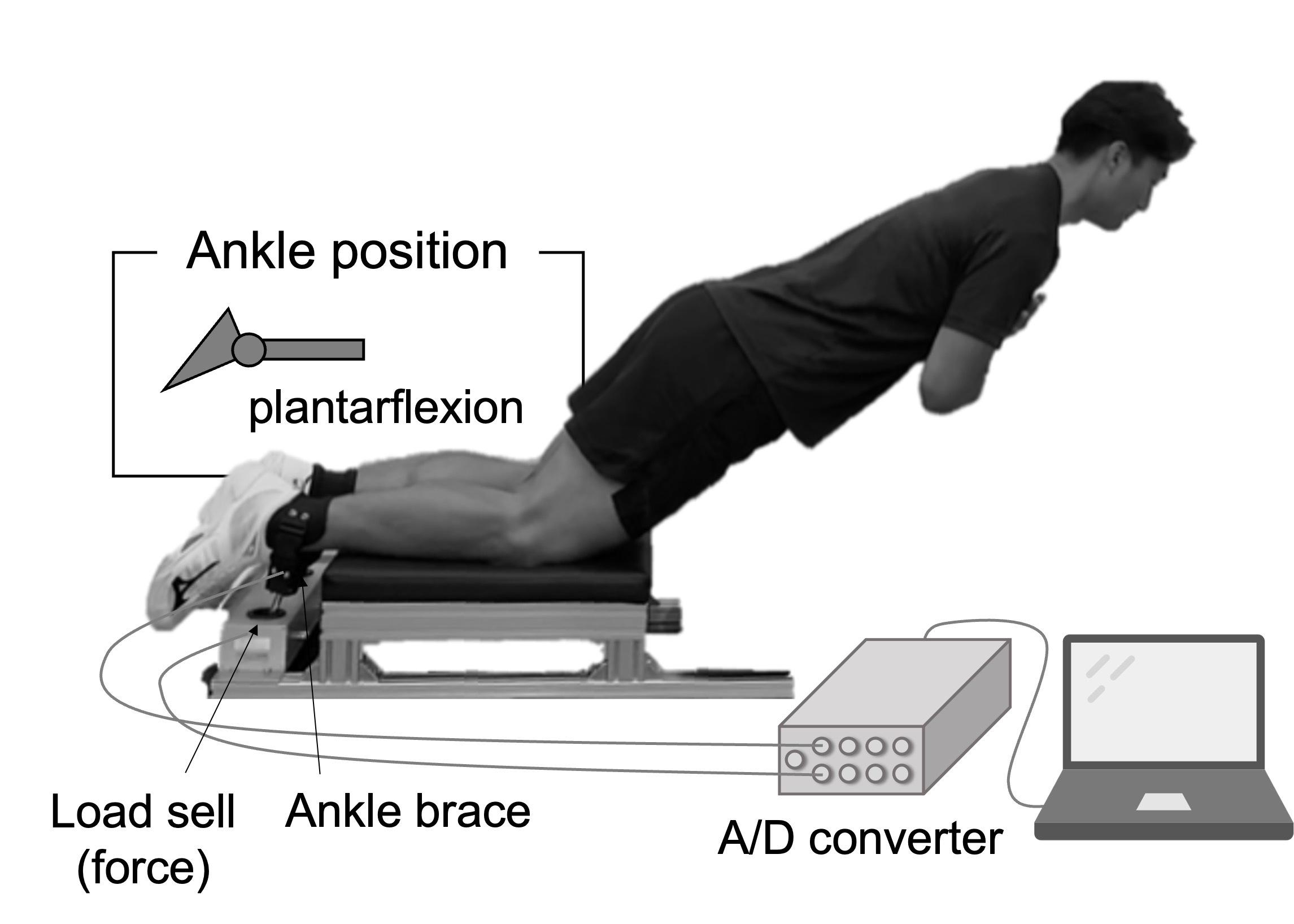
Figure 1. Measurement setup for eccentric force during the Nordic hamstring exercise.
peak eccentric force of both legs and the total peak eccentric force of both legs were used for further analyses.
Before testing, the participants performed three rounds of warm-up trials with submaximal effort. The 1RM of the deadlift was calculated from the weight that could be raised three times (x kg) using the estimation formula (x kg / 0.93) and corrected for body mass (kg/BM)
STATISTICAL ANALYSES
The Shapiro–Wilk test was used to assess the normality of the measures. Since some parameters were not normally distributed, Spearman’s rank correlation coefficients were used to examine the relationships between the peak eccentric force during the NHE and the 1RM deadlift performance. The following correlation criteria were adopted: 0, none; r < 0.4, weak, r < 0.7, moderate; r < 0.9, strong; 1, perfect.27 Statistical significance was set at p < 0.05. Statistical analyses were performed using the SPSS software version 27 (SPSS Inc., Chicago, IL, USA).
Participant’s physical characteristics are shown in Table 1. Table 2 presents the variables in peak eccentric force during NHE and 1RM of deadlift. Figure 2 shows the correlations between the peak eccentric force during the NHE and the 1RM of the deadlift. Notably, a weak but significant correlation was found between the 1RM of the deadlift and the peak eccentric force in the right (r = 0.34, p = 0.02) and left legs (r = 0.37, p = 0.01) and the total peak eccentric force of both legs (r = 0.36, p = 0.01).
Table 1. Participant’s physical characteristics.
Mean ± SD (MIN − MAX) Age (years)
MIN= minimum, MAX= maximum
Table 2. Characteristics of all variables of interest
Mean ± SD (MIN−MAX)
Peak NH-force (N/BM)
Right leg 3.8 ± 1.1 (2.1−6.5)
Left leg 3.8 ± 1.2 (1.8−6.7)
Total of both legs
1 RM of dead lift (kg/BM) 1.9 ± 0.3 (1.0−2.6)
MIN= minimum, MAX= maximum, N= Nordic hamstring, RM= repetition maximum, SD= standard deviation, BM= body mass
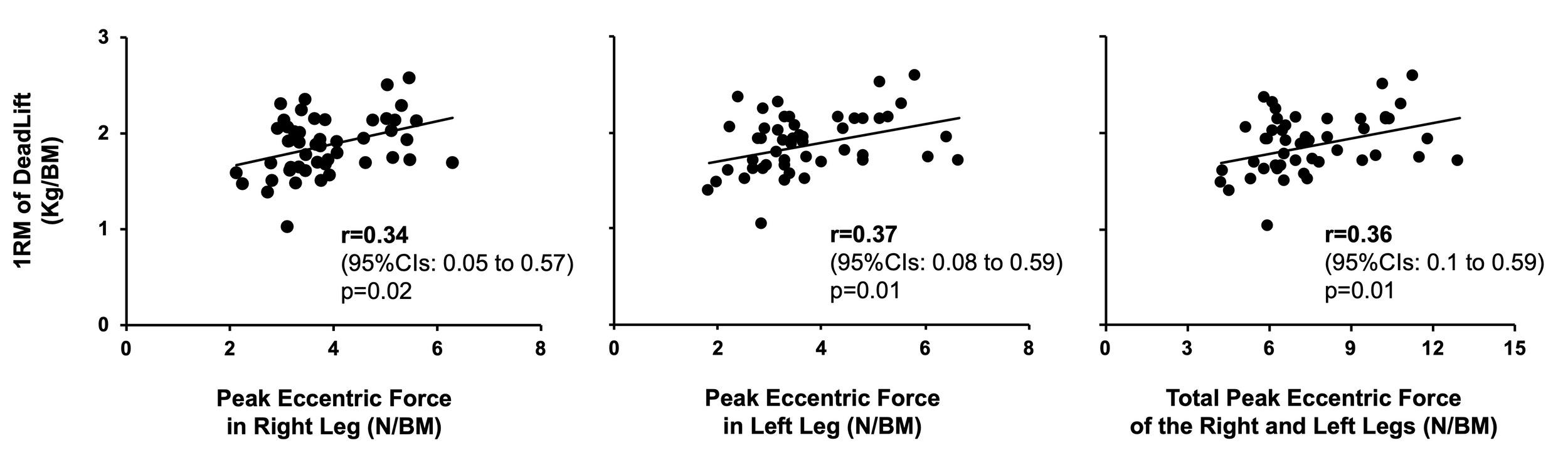
Figure 2. Correlations between the one repetition maximum of deadlift and peak eccentric force during Nordic hamstring exercise among the 49 study participants; r (95% confidence intervals) and p-values of Spearman’s rank correlation coefficient are shown in each figure.
The present study found weak correlations between the peak eccentric forces during NHE and the 1RM of a deadlift (r = 0.34–0.37). These results support the hypothesis. Previous authors have reported a limited correlation between the eccentric force during NHE and eccentric knee flexor strength measured using an isokinetic dynamometer 18,19 van Dyk et al. found a weak correlation (r = 0.35) between eccentric force during NHE and eccentric knee flexion torque at 60 ̊/s, and the authors previously reported no correlations between the peak eccentric torque during NHE and peak eccentric knee flexion torque (r = 0.24).18 Taken together, this would indicate that NHE performance is not expected to reflect only knee flexor strength. Previous authors have indicated that hip joint torque was about half the knee joint torque,22 and muscle activity of the both the hip and trunk extensors20‑22 occurred during the NHE. In addition, exercises emphasizing hip extension improve eccentric force during the NHE,10,28 suggesting an association between eccentric force during NHE and hip and
trunk extensor strength. However, to the best of the authors’ knowledge, no previous study has considered the relationship between the eccentric force during NHE and hip and trunk extensor strength. This was the first study to examine the relationship between eccentric force of the hamstrings during NHE and the 1RM of deadlift, which both reflect hip and trunk extensor strength, and may provide new insights into the importance of hip and trunk extensor strength in NHE.
In the present study, the correlation between eccentric force during NHE and the 1RM of deadlift was weak (r = 0.34–0.37). The eccentric force during the NHE reflects the exerted muscle force during an eccentric muscle contraction, whereas the 1RM of deadlift reflects the exerted muscle force during a concentric muscle contraction. This difference in contraction mode may be reflected in the weak correlation. The degree of correlation between the eccentric force during the NHE and 1RM of deadlift was similar to that reported in a previous study between the eccentric force during the NHE and eccentric knee flexor torque measured using an isokinetic dynamometer (r = 0.35).19 Thus, lower-extremity muscle strength may not be a crucial factor in determining NHE performance. Previously, it was shown that individuals who were able to lean their bodies forward closer to the floor during NHE were able to exert greater eccentric force during NHE,18 suggesting the importance of ability to control NHE movements. Trunk extensor muscle activity has been observed during NHE21,22 and is thought to play an important role in controlling NHE movements. In the future, it will be necessary to examine not only the magnitude of lower limb muscle strength but also the magnitude of muscle activity in the trunk muscles during the NHE and whether the muscle activity patterns of the hamstring, trunk muscle group, and hip extensor muscle group during NHE affect the eccentric force produced during NHE. The effectiveness of NHE for the prevention of HSI has been made clear in previous studies12; however, even in soccer, which has a very high incidence of NHE, the adoption rate of NHE for prevention is remarkably low (13%).13 As transient muscle damage to the hamstrings has been reported after the NHE,29 there are potential barriers, such as post-training muscle stiffness and soreness, which may contribute to a lower adoption rate. As it is difficult to control the NHE intensity and load on the muscles, the safe and efficient implementation of NHE in a phased training program requires exploring the exercises that may be performed before progressing to the NHE. Previous authors have suggested that the deadlift may be an appropriate exercise to consider for progressing to the NHE. The deadlift is typically considered for hip extensor muscle strength training. The electromyographic (EMG) activity of the hamstring during a deadlift is reported to be approximately 20–30% less than that observed during the NHE,26,30 and EMG activity above 60% of maximal voluntary isometric contraction was observed in the erector spine and lumbar multifidus during a deadlift, which are also active during in NHE.23,24 Moreover, Boyer et al., examined the muscle activation ratios of semimembranosus (SM/Hamstring), semitendinosus (ST/Hamstring), biceps femoris (BF/Hamstring)
in total hamstring muscle activation as an index of the contribution of each muscle to the global activation of the hamstrings, and reported that the SM/Hamstring (r = 0.66; p = 0.005), ST/Hamstring (r = 0.42; p = 0.05), and BF/Hamstring (r = 0.60; p = 0.01) activation ratios were moderately correlated between NHE and stiff-leg deadlift.26 These results indicate that the muscle activation patterns during the two exercises are similar within participants and support the idea that the deadlift may be an appropriate exercise for progressing to the NHE. However, the present study showed only a weak correlation between peak eccentric force during the NHE and 1RM of the deadlift. Therefore, the similarity between the two exercises in peak force may play only a limited role in supporting the idea that the deadlift is an appropriate exercise to perform before progressing to the NHE. Considering the difficulty of the exercise and the load on the hamstring, the deadlift is often considered safer than NHE, but further studies are required to clarify its usefulness as an appropriate exercise to perform before progressing to NHE due to the differences in muscular action.
Some limitations of this study must be addressed. Although the 1RM of deadlift was measured in this study, variations in exercise form between individuals may have affected the contribution of each joint. To reduce form variation, it was necessary to select an exercise that is easier to standardize, such as the stiff-leg deadlift, which emphasizes hip extension. As the relationship between the exerted muscle force and deadlift is based on the force exerted during different contraction modes, it may be necessary to examine the relationship when the contraction mode is the same. In addition, the 1RM of deadlift is not a measure of pure trunk and hip extensor strength; therefore, it will be necessary to examine the relationship between hip extensor strength and trunk extensor strength in singlejoint movement, and the eccentric force occurring during the NHE to clarify the contributions of trunk and hip extensor strength during the NHE.
The results of the present study indicate that weak correlations exist between the peak eccentric force during the NHE and the 1RM of deadlift (r = 0.34–0.37). These results may play only a limited role in supporting the idea that the deadlift is an appropriate exercise to perform before progressing to the NHE.
There are no conflicts of interest to declare.
We would like to thank all the participants who volunteered as research subjects.
Submitted: April 01, 2024 CDT, Accepted: August 07, 2024 CDT
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information. Relationship
1. Woods C, Hawkins RD, Maltby S, Hulse M, Thomas A, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football--analysis of hamstring injuries. Br J Sports Med 2004;38(1):36-41. doi:10.1136/ bjsm.2002.002352
2. Brooks JHM, Fuller CW, Kemp SPT, Reddin DB. A prospective study of injuries and training amongst the England 2003 Rugby World Cup squad. Br J Sports Med 2005;39(5):288-293. doi:10.1136/ bjsm.2004.013391
3. Askling CM, Tengvar M, Thorstensson A. Acute hamstring injuries in Swedish elite football: A prospective randomised controlled clinical trial comparing two rehabilitation protocols. Br J Sports Med 2013;47(15):953-959. doi:10.1136/ bjsports-2013-092165
4. Chumanov ES, Schache AG, Heiderscheit BC, Thelen DG. Hamstrings are most susceptible to injury during the late swing phase of sprinting. Br J Sports Med. 2012;46(2):90-90. doi:10.1136/ bjsports-2011-090176
5. Schache AG, Dorn TW, Blanch PD, Brown NAT, Pandy MG. Mechanics of the human hamstring muscles during sprinting. Med Sci Sports Exerc 2012;44(4):647-658. doi:10.1249/ MSS.0b013e318236a3d2
6. Sugiura Y, Saito T, Sakuraba K, Sakuma K, Suzuki E. Strength deficits identified with concentric action of the hip extensors and eccentric action of the hamstrings predispose to hamstring injury in elite sprinters. J Orthop Sports Phys Ther 2008;38(8):457-464. doi:10.2519/jospt.2008.2575
7. Lee MJC, Reid SL, Elliott BC, Lloyd DG. Running biomechanics and lower limb strength associated with prior hamstring injury. Med Sci Sports Exerc. 2009;41(10):1942-1951. doi:10.1249/ MSS.0b013e3181a55200
8. van Dyk N, Bahr R, Whiteley R, et al. Hamstring and quadriceps isokinetic strength deficits are weak risk factors for hamstring strain injuries. Am J Sports Med. 2016;44(7):1789-1795. doi:10.1177/ 0363546516632526
9. Mjølsnes R, Arnason A, Østhagen T, Raastad T, Bahr R. A 10-week randomized trial comparing eccentric vs. concentric hamstring strength training in well-trained soccer players. Scand J Med Sci Sports 2004;14(5):311-317. doi:10.1046/ j.1600-0838.2003.00367.x
10. Bourne MN, Duhig SJ, Timmins RG, et al. Impact of the Nordic hamstring and hip extension exercises on hamstring architecture and morphology: implications for injury prevention. Br J Sports Med 2017;51(5):469-477 doi:10.1136/ bjsports-2016-096130
11. Presland JD, Timmins RG, Bourne MN, Williams MD, Opar DA. The effect of Nordic hamstring exercise training volume on biceps femoris long head architectural adaptation. Scand J Med Sci Sports 2018;28(7):1775-1783. doi:10.1111/sms.13085
12. Van Dyk N, Behan FP, Whiteley R. Including the Nordic hamstring exercise in injury prevention programmes halves the rate of hamstring injuries: A systematic review and meta-analysis of 8459 athletes. Br J Sports Med 2019;53(21):1362-1370. doi:10.1136/ bjsports-2018-100045
13. Ekstrand J, Bengtsson H, Walden M, Davison M, Hagglund M. Still poorly adopted in male professional football: but teams that used the Nordic Hamstring Exercise in team training had fewer hamstring injuries – a retrospective survey of 17 teams of the UEFA Elite Club Injury Study during the 2020–2021 season. BMJ Open Sport Exerc Med. 2022;8(3):e001368. doi:10.1136/ BMJSEM-2022-001368
14. Opar DA, Piatkowski T, Williams MD, Shield AJ. A novel device using the Nordic hamstring exercise to assess eccentric knee flexor strength: A reliability and retrospective injury study. J Orthop Sports Phys Ther. 2013;43(9):636-640. doi:10.2519/jospt.2013.4837
15. Timmins RG, Bourne MN, Shield AJ, Williams MD, Lorenzen C, Opar DA. Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): a prospective cohort study. Br J Sports Med. 2016;50(24):1524-1535. doi:10.1136/ bjsports-2015-095362
16. Bourne MN, Opar DA, Williams MD, Shield AJ. Eccentric knee flexor strength and risk of hamstring injuries in rugby union. Am J Sports Med 2015;43(11):2663-2670. doi:10.1177/ 0363546515599633
17 Opar DA, Williams MD, Timmins RG, Hickey J, Duhig SJ, Shield AJ. Eccentric hamstring strength and hamstring injury risk in Australian footballers. Med Sci Sports Exerc 2015;47(4):857-865. doi:10.1249/ MSS.0000000000000465
18. Nishida S, Nakamura M, Kiyono R, et al. Relationship between Nordic hamstring strength and maximal voluntary eccentric, concentric and isometric knee flexion torque. PLoS One. 2022;17(2). doi:10.1371/JOURNAL.PONE.0264465
19. van Dyk N, Witvrouw E, Bahr R. Interseason variability in isokinetic strength and poor correlation with Nordic hamstring eccentric strength in football players. Scand J Med Sci Sports 2018;28(8):1878-1887 doi:10.1111/sms.13201
20. Murakami Y, Nishida S, Kasahara K, Yoshida R, Hayakawa R, Nakamura M. Eccentric force and electromyogram comparison between the eccentric phase of the Nordic hamstring exercise and the razor hamstring curl. PLoS One 2023;18(12):e0293938. doi:10.1371/JOURNAL.PONE.0293938
21. Narouei S, Imai A, Akuzawa H, et al. Hip and trunk muscles activity during Nordic hamstring exercise. J Exerc Rehabil 2018;14(2):231-238. doi:10.12965//jer.1835200.600
22. Šarabon N, Marušič J, Marković G, Kozinc Ž. Kinematic and electromyographic analysis of variations in Nordic hamstring exercise. Mirkov D, ed. PLoS One 2019;14(10):e0223437 doi:10.1371/ journal.pone.0223437
23. Martuscello JM, Nuzzo JL, Ashley CD, Campbell BI, Orriola JJ, Mayer JM. Systematic review of core muscle activity during physical fitness exercises. J Strength Cond Res. 2013;27(6):1684-1698. doi:10.1519/JSC.0B013E318291B8DA
24. Oliva-Lozano JM, Muyor JM. Core muscle activity during physical fitness exercises: A systematic review Int J Environ Res Public Health 2020;17(12):4306. doi:10.3390/IJERPH17124306
25. Choe KH, Coburn JW, Costa PB, Pamukoff DN. Hip and knee kinetics during a back squat and deadlift. J Strength Cond Res 2021;35(5):1364-1371. doi:10.1519/JSC.0000000000002908
26. Boyer A, Hug F, Avrillon S, Lacourpaille L. Individual differences in the distribution of activation among the hamstring muscle heads during stiff-leg deadlift and Nordic hamstring exercises. J Sports Sci Published online March 7, 2021:1-8. doi:10.1080/ 02640414.2021.1899405
27 Dancey CP Statistics without Maths for Psychology Prentice Hall; 2007
28. Timmins RG, Filopoulos D, Nguyen V, et al. Sprinting, strength, and architectural adaptations following hamstring training in Australian Footballers. Scand J Med Sci Sports. 2021;31(6):1276-1289. doi:10.1111/sms.13941
29. Bourne MN, Williams MD, Opar DA, Al Najjar A, Kerr GK, Shield AJ. Impact of exercise selection on hamstring muscle activation. Br J Sports Med 2017;51(13):1021-1028. doi:10.1136/ bjsports-2015-095739
30. Llurda-Almuzara L, Labata-Lezaun N, López-Decelis C, et al. Biceps femoris activation during hamstring strength exercises: A systematic review. Int J Environ Res Public Health 2021;18(16). doi:10.3390/IJERPH18168733/S1

Ohji S, Aizawa J, Hirohata K, et al. Relationship Between Single-Leg Vertical Jump and Drop Jump Performance, and Return to Sports After Primary Anterior Cruciate Ligament Reconstruction Using Hamstring Graft. IJSPT. Published online October 1, 2024:1204-1215. doi:10.26603/001c.123479
Shunsuke Ohji1a , Junya Aizawa2 , Kenji Hirohata1 , Takehiro Ohmi1 , Tomoko Kawasaki1 , Hideyuki Koga3 , Kazuyoshi Yagishita1
1 Clinical Center for Sports Medicine and Sports Dentistry, Tokyo Medical and Dental University, 2 Department of Physical Therapy, Juntendo University, 3 Department of Joint Surgery and Sports Medicine, Tokyo Medical and Dental University
Keywords: anterior cruciate ligament reconstruction, return to sports, single-leg drop jump, vertical hop, single leg vertical jump https://doi.org/10.26603/001c.123479
International Journal of Sports Physical Therapy
Background
After anterior cruciate ligament reconstruction (ACLR), asymmetry is likely to persist in single-leg (SL) vertical jump and drop jump performance than in SL hop distance. However, its relationship with the return to sport (RTS) remains unclear.
Hypothesis/Purpose
This study aimed to determine the association between vertical jump performance after primary ACLR using hamstring tendon autograft and RTS at a pre-injury competitive level.
Study design
Cross-sectional study
Methods
Patients who underwent primary ACLR using hamstring tendon autograft were recruited for this study Participants who returned to pre-injury competition after ACLR were recruited at least eight months postoperatively. Knee condition was assessed, including joint laxity, range of motion, muscle strength, and knee pain intensity during sports activities. Performance variables were also assessed, including SL hop distance, jump height in SL vertical jump, and reactive strength index (RSI; jump height/contact time) in SL drop jump. Participants were asked to subjectively report whether they had returned to the same level of competition as pre-injury and their perceived sport performance intensity Those who answered “Yes” to the dichotomous question and had a postoperative subjective athletic performance of > 80% were categorized into the Yes-RTS group. The primary outcome was the ability to achieve RTS at the preinjury level.
Results
Sixty-five patients (female, 35; male, 30) at 13.0 (13.0) [median (interquartile)] months after ACLR participated in this study Thirty-nine (60%) were assigned to the Yes-RTS group. Regarding knee conditions, the No-RTS group had a significantly higher knee pain intensity, as assessed using a numerical rating scale (p<0.001, effect size -0.45). In the performance tests, the No-RTS group exhibited a significantly lower limb symmetry index
Corresponding author: Shunsuke Ohji
E-mail address: ohji.spt@tmd.ac.jp a
Affiliation: Clinical Center for Sports Medicine and Sports Dentistry, Tokyo Medical and Dental University, Tokyo, Japan
Address: 1-5-45 Yushima, Bunkyo-ku, Tokyo 113-8519, JAPAN
Phone number: +81-3-5803-4721
Fax number: +81-3-5803-4720
of RSI during the SL drop jump compared to the Yes-RTS group (p=0.002, effect size 0.81).
Patients unable to achieve RTS after primary ACLR using hamstring grafts are more likely to exhibit asymmetric performance during the SL drop jump test, suggesting the significance of assessing jump symmetry when evaluating post-ACLR rehabilitation success.
Level of Evidence 3c
Anterior cruciate ligament (ACL) injuries are the most common knee ligament injuries among athletes.1 The annual incidence rate is 68.6 per 100,000 person-years,2 and ACL injuries are estimated to increase further in the future.3 Following injury, many athletes undergo reconstructive surgery in the hope of return to sport (RTS) “at their preinjury competitive level” 4 However, a significant portion of patients—approximately 40%—fail to RTS at their preinjury competitive level after ACL reconstruction (ACLR).5 Hence, it becomes imperative to identify factors that hinder successful RTS at the pre-injury competitive level after ACLR.
One of the key physical functional characteristics associated with RTS after ACLR is asymmetry in the singleleg hop (SL hop) distance. The horizontal SL hop serves as a standard test to gauge physical readiness for RTS.6 However, previous studies examining the relationship between horizontal SL hop and RTS at pre-injury competition level have presented conflicting outcomes. Some studies demonstrated a statistical association,7‑10 while others did not,11‑13 resulting in an absence of consensus. Therefore, recent research highlights the necessity to reevaluate the use of SL hop asymmetry as a criterion for safe RTS.14
In recent years, vertical jumps (specifically, single-leg vertical jump [SL vertical jump] and single-leg drop jump [SL drop jump]) have gained prominence as crucial performance tests post-ACLR.14 Kinematically, vertical jumps exhibit higher knee joint power than horizontal jumps and, therefore, more accurately detect functional asymmetries after ACLR compared to SL hops.15,16 The SL drop jump is a commonly used plyometric exercise or test that relies on the adequate development of critical motor abilities such as explosive strength and stretch-shortening cycle capacity 17 Performance variables in SL drop jump include jump height, ground contact time, and the reactive strength index (RSI), calculated from their ratio. Previous authors have described significant group differences in SL vertical jump height and RSI in SL drop jump post-ACLR, despite the absence of significant differences in SL hop.17‑19
Moreover, earlier studies investigating the risk of re-injury post-ACLR demonstrated that the contralateral injury group had a lower RSI during the SL drop jump compared to the non-contralateral injury group.20 However, to date, no study has established an association between those who do not successfully RTS (No-RTS) and vertical jumps post-ACL.
Clarification of the association between No-RTS and vertical jumps post-ACLR would offer valuable insights into safe postoperative RTS.
Force plates and 3-dimensional analysis systems are necessary to accurately measure RSI. Although these evaluations are the gold standard, their use is limited due to cost and difficulty of use.21 In recent years, technology has improved, and RSI can be evaluated using infrared sensors and smartphone applications; their reproducibility is high and their validity has been demonstrated to be comparable with that of force plate measurements.22,23 Therefore, RSI measurement has become clinically friendly, and evaluation of RSI during a vertical jump after ACLR can provide objective data on recovery for professionals involved in postoperative care.
This study aimed to determine the association between vertical jump performance after primary ACLR using hamstring tendon autograft and RTS at a pre-injury competitive level. The study hypothesis was that participants who returned to pre-injury competition after ACLR who perceived that they had not achieved RTS at their pre-injury competition level would exhibit an excess asymmetry in performance variables during vertical jump compared to those who perceived that they had achieved it.
Participants who underwent primary ACLR using hamstring tendon autograft between April 2012 and December 2020 were included if they met the following criteria: (1) aged between 16 and 45 years at the time of study participation, (2) engaged in sports with a modified Tegner activity scale score24 ≥ 5 before their ACL injury, (3) elapsed time of more than eight months since ACLR, (4) participated in sports after surgery, with physician’s permission, (5) failed to measure SL hop or vertical jump, and (6) expressed intention for RTS before surgery. Participants were excluded if they met the following criteria: (1) underwent surgery other than ACLR six months before reconstruction, (2) underwent multiple ligament reconstruction and lateral extra-articular tenodesis, (3) had a cartilage injury requiring surgery, (4) underwent ACLR previously, (5) had difficulty visiting the clinic due to distance or social reasons, or (6) had missing questionnaire data. Given the distinct characteristics of muscle strength and SL hop asymmetry after
ACLR depending on the graft type, this study opted to unify the graft type as hamstring.25
A priori sample size estimation was performed using the G*Power software package (version 3.1.9.4, Kiel University).26 The input parameters were as follows: statistical test = means (difference between two independent means [two groups]), tail = 2, effect size = 0.8, α error probability = 0.05, power = 0.8, and allocation ratio = 0.6. The allocation ratio was determined based on the observed rate of return to sports after ACLR (approximately 60%).5,27 The target sample size was set at 56 participants (Yes-RTS group = 35, No-RTS group = 21). Ethical approval was obtained from the Ethics Committee (approval number: M2016-197). All participants provided written informed consent before participation in the study
This cross-sectional study was conducted at a single center. Demographic and surgical data were obtained from medical records and questionnaires. Demographic data included age, sex, activity level (modified Tegner activity scale24), participation level, and injury mechanisms. Participation levels were categorized as recreational, competitive, or elite.28 Surgical data included graft type, presence of meniscal repair, number of months since surgery, date from ACL injury to surgery, and number of months from surgery to measurement. Knee condition, SL hop, and SL vertical jump and SL drop jump were measured on the same day In addition, participants completed a questionnaire regarding their RTS status at the time of study participation. The measurement procedure is shown in Figure 1 The order of hops and jump batteries was randomized to reduce the effects of fatigue over time, and the rest periods between hop trials were not standardized, rather were determined by patient readiness.29 Each test was initiated on the non-operated side. Before commencing the test session, participants performed stationary cycling (5 min), light jogging indoors (30 s), movement preparation (calf raise, squatting, lunging), squat jump, countermovement jump, ankle hop, and box landing in accordance with previous study methods.23 Participants performed movement preparation, jump, hop and landing, 5–10 repetitions each.
SURGICAL TECHNIQUE AND POSTOPERATIVE REHABILITATION
The autograft source was the hamstring (semitendinosus). Hamstring surgery involved anatomical double-bundle reconstruction. In cases where the semitendinosus alone proved insufficient as a graft tendon, the gracilis was added. All surgeries were performed by orthopedic surgeons specializing in knee joints. The surgical technique and postoperative rehabilitation protocol were based on previous research.30 Exercises for range of motion (ROM) and isometric muscle contraction commenced three days postsurgery. Initially, a straight-position knee-joint immobilizer (knee brace; ALCARE Co., Ltd., Tokyo, Japan) and crutches were used and then gradually phased out over four weeks post-ACLR. Jogging commenced three months post-
ACLR, with a gradual increase in running speed. RTS was permitted upon meeting specific criteria: a minimum of six months post-ACLR, a limb symmetry index (LSI) of SL hop distance > 90%, and achieving sufficient knee strength recovery (i.e., isokinetic extension and flexion torque LSI > 85%, measured using an isokinetic dynamometer [BIODEX System 4, BIODEX Medical Inc., Shirley, NY] at 60°/s and 180°/s). Participants who underwent repair of the middleposterior segment lesions of the meniscus were advised against deep squatting beyond 90° until three months postACLR.31
In this study, knee conditions were evaluated, encompassing anterior knee laxity, ROM, strength, and knee pain intensity during sports activities. These assessment methods are considered standard with proven reproducibility 32‑35
Anterior knee joint laxity was measured using a KT-1000 instrument (MEDmetric Corp., San Diego, CA, USA). The amount of forward tibial translation at maximum pull was measured twice, and the maximum value was recorded.36 The difference between the non-operated and operated leg values was then calculated.
Passive knee flexion and extension ROM were measured in increments of 1° using a goniometer.37 The assessment of knee extension was conducted with the patient’s heel elevated with a support, allowing for hyperextension when present.38 Normal extension of the knee was considered in the 0° position. A positive ROM score for extension was used for hyperextension. A negative ROM score for extension meant that the patient was unable to reach the 0° position.39 For flexion ROM, the cue was to flex the knee to maximum flexion with the heel on the support surface, using the assistance of hands rather than only the participant’s own muscle strength. The examiner verified that the participant’s hip internal/external rotation and knee valgus/varus were in the intermediate position before measuring the ROM. ROM deficit was defined as the angle obtained by subtracting the value on the operated side from that on the non-operated side.
Strength assessment was conducted using the Biodex isokinetic dynamometer Extensor and flexor peak torques were evaluated at angular velocities of 60°/s and 180°/s. Peak torque was expressed as Nm divided by body weight (Nm/ kg). Additionally, the LSI was calculated as follows: LSI= ([operated value]/[non-operated value])×100 %.
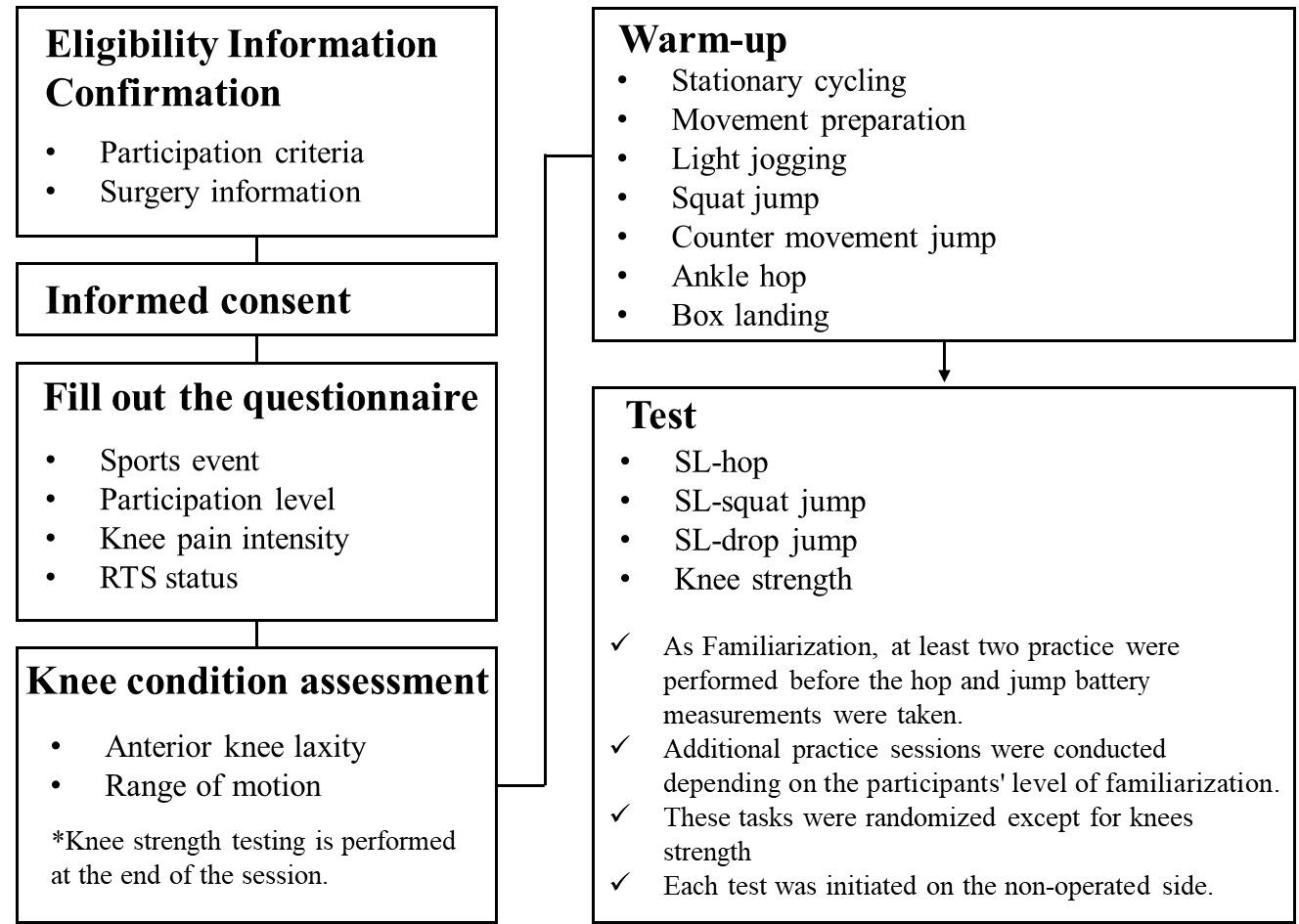
Figure 1. Experimental and Measurement Procedures.
RTS= return to sport, SL= single leg.
Participants were instructed to rate the intensity of their knee pain during sports activities on a numerical rating scale (NRS) of 0–10.40
The SL hop measurement method employed in this study was based on previous research.33 Participants stood on one leg behind a marked line (starting point), hopped forward as far as possible, and landed on the same leg. Arm swing/movement was not restricted in this study based on the results of a previous study41 that showed that work by the knee was not significantly altered by the presence or absence of an arm swing during a hop. Each participant completed three practice hops, followed by two successful trials. An unsuccessful hop was characterized by an additional hop on landing, early touchdown of the contralateral limb, and/or loss of balance. A successful trial was defined as one in which the failure criteria were not met, and the participant could maintain the posture for 3 seconds after landing. The distance from the starting line to the point where the back of the participant’s heel made contact with the ground after a single hop was recorded. The average distance between two trials was recorded. In addition, the LSI was calculated. Previous studies have reported high testretest reliability (intraclass correlation coefficient [ICC]= 0.91, 95% confidence interval 0.87–0.94) and interrater reliability (ICC= 1.00, 95% confidence interval 1.00–1.00).42
SL vertical jump was measured using a force plate (260AA6; Kistler Instrument AG, Winterthur, Switzerland) with a sampling rate of 1000 Hz. The vertical ground reaction force (VGRF) data were filtered through a fourth-order Butterworth low-pass digital filter at a cut-off frequency of 50 Hz and normalized to body weight using software (IFS-4J/3 J, DKH). Participants stood on one leg of the force plate with the opposite hip and knee bent at 45° and 90°, respectively. The arm swing of the vertical jump was restricted in this study considering the results of a previous study that showed smaller work by the knee during vertical jumps with arm swing compared to vertical jumps without arm swing.43 To control for arm movements, participants crossed their arms, placing each hand in the opposite axilla. Additionally, counter-movements during jumping were restricted to eliminate the effects of the SSC and focus on concentric muscle contraction.44 The participant performed a vertical jump from a single-leg squat position and landed on the ipsilateral leg.44 A trial was deemed unacceptable if the sole of the opposite foot touched the force plate or floor, part of the sole of the foot fell outside the force plate during single-leg landing, the foot moved or slid after single-leg landing, or the arms were removed from the chest. Participants were instructed not to intentionally prolong their flight time upon landing. Each participant performed three practice jumps followed by two successful trials. The flight time during single-leg SJ was calculated. (Table 1).45
The average jump height (cm) was recorded, and the LSI of jump height was calculated. Moderate-to-excellent reliability was established using the flight time method.46, 47 The ICCs (1, 2) for SLVJ on the operated and non-op-
Table 1. Vertical jump variables description and calculation method
Variable Measurement unit
Ground contact start time
Ground contact end time
Contact time
Description
s VGRF > 10N
s VGRF < 10N
s
Ground contact start time-ground contact end time
Flight start time s VGRF < 10N
Flight end time
s VGRF > 10N
Flight time s Flight end time-flight start time
Jump height m
RSI m/s
Flight time2×9.81/8
Jump height/contact time
S- seconds’ m/s= meters per second, N=newtons; VGRF=vertical ground reaction force; RSI=reactive strength index
erated sides ranged between 0.96–0.99 and 0.92–0.98, respectively, demonstrated nearly perfect reproducibility in the previous study 19,48
SINGLE-LEG DROP JUMP TEST
SL drop jump assessment methodology was based on previous studies.17,49 A 15-cm-high box was positioned in front of the force plate. Participants stood on the step using their designated leg, with the opposite hip at 45° and the opposite knee at 90°, maintaining neutral hip rotation. For the same reasons as for the SL vertical jump, the participants’ arm swing during the task was restricted. To control for arm movement effects, participants were instructed to cross their arms. After they stepped off the box, they completed a vertical jump as fast (with short ground contact times) and as high as possible. A successful landing was defined as maintaining stability for 3 seconds. Unacceptable trials included instances where the arms left the chest, the foot landed outside the force plate area, post-landing foot movement or sliding occurred, or the sole of the opposite foot contacted the force plate or floor Each participant completed a minimum of three practice jumps followed by a single successful trial for the formal test. Notably, appropriate familiarization and the implementation of standardized warm-up and testing protocols required only one trial when evaluating RSI or jump height during the SL drop jump (ICCs [single measures] value > 0.90).50
The SL drop jump was measured using the force plate. Contact time, flight time, jump height, and RSI during the task were calculated based on a previous study (Table 1).17 Additionally, the LSI was calculated.
Participants return to the same competitive level as before the injury was defined using two questions.11 The first question asked, “Have you returned to the same level of competition as before your ACL injury?” with participants providing a Yes or No response. This question has been used most frequently in prior studies.10,51‑54 The second question was, “What is the subjective performance intensity of the sport you are currently participating in (assuming 100% of your pre-injury performance intensity)?” with participants indicating their response on a scale of
0–100%.30 This question is called the Postoperative Subjective Athletic Performance (PoSAP), in which participants were asked about their performance intensity when playing a specific sport. Ohji et al.30 reported that most post-ACLR patients with a PoSAP of 80% responded “Yes” to the dichotomous question. They noted that relying solely on this question tended to overestimate their RTS status. Therefore, in this study, participants who answered “Yes” to the dichotomous question and had a PoSAP of > 80% were categorized into the Yes-RTS group. The No-RTS group included patients who met none or one of these criteria.11
The normality of each variable’s distribution was determined using a histogram and the Shapiro–Wilk normality test.55 Means and standard deviations were calculated for normally distributed variables, whereas medians (interquartile range) were calculated for non-normally distributed variables.
Differences in demographic data, knee strength, SL-vertical jump, and SL drop jump variables between the YesRTS and No-RTS groups were analyzed using a range of statistical tests: chi-square test, Fisher’s exact test, multiple comparison test (The Bonferroni method), unpaired t-test, or Mann–Whitney U test. Effect sizes (chi-square test = phi coefficient, Fisher’s exact test = Cramer’s V, t-test = Cohen’s d, Mann–Whitney U test = r) were calculated for each variable. Phi coefficient and Cramer’s V defined >0.5 as large effect.56 Cohen’s d defined 0.2 as small, 0.5 as medium, and 0.8 as large.57 The Mann-Whitney U test r was defined as 0.1 for small effect, 0.3 for medium effect, and 0.5 for large effect.57 The significance level for knee condition and performance tests (SL hop, SL vertical jump, and SL drop jump) was adjusted to less than 0.5% using the Bonferroni method to mitigate the risk of type I errors. This adjustment was made to account for multiple comparisons. Statistical analyses were conducted using SPSS version 28.0 (IBM Corp., Armonk, NY, USA).
The study included 65 patients who underwent primary ACLR, with a mean age of 21.0 (5.0) years, of which 29
Table 2. Distribution of demographic variables in participants after ACL reconstruction.
Sports participation level (elite, competitive, recreation), n
†median (interquartile range)
* P < 0.005
RTS, return to sports; Yes-RTS, yes-return to sports; No-RTS, no-return to sports; BMI, body mass index; ACL, anterior cruciate ligament
Table 3. Knee condition variables and return to sport
†median (interquartile range)
* p < 0.005
ACL, anterior cruciate ligament; RTS, return to sports; Yes-RTS, yes-return to sports; No-RTS, no-return to sports; LSI, limb symmetry index.
were female. The median postoperative duration was 13.5 months (interquartile range: 13.0 months), with 39 patients (60%) assigned to the Yes-RTS group (Table 2).
No statistically significant differences were observed in demographic or surgical data between the groups (Table 2). Group differences in knee conditions are shown in Table 3
The No-RTS group exhibited higher knee pain NRS scores during sports activities (p < 0.001, r = -0.45) compared to the Yes-RTS group. However, no significant differences were observed between the groups in terms of anterior knee laxity, ROM, or strength. Descriptive statistics for the operated and non-operated sides are shown in Table 4.
Regarding the performance tests (Table 5), no significant differences were observed in the LSI for SL hop and SL vertical jump. However, in the SL drop jump, the No-RTS group displayed lower LSI in RSI compared to the Yes-RTS group (p = 0.002, d = 0.81). Descriptive statistics for the operated and non-operated sides are shown in Table 6
In this study, the relationship between No-RTS and vertical jump performance asymmetry after primary ACLR using hamstring tendon autograft was examined. As hypothesized, the No-RTS group had lower value in RSI symmetry during the SL drop jump compared to the Yes-RTS group. However, no statistical association was found between LSI in SL hop distance, SL vertical jump height, and RTS. Findings from this study partially supported the authors’ hypothesis.
The RTS rate among the study participants stood at 60% (39/65), consistent with a meta-analysis exploring RTS rates post-ACL (61.8%).5 The self-reported RTS rate for current study participants was 72% (47/65) when only answered whether or not they RTS (dichotomous question). In the present study, PoSAP were aggregated to prevent an overestimation of RTS at pre-injury competition levels. Notably, 40% of patients meeting standard sports participa-
Table 4. Descriptive statistics for operative and nonoperative knee conditions
† median (interquartile range)
ROM, range of motion; LSI, limb symmetry index; NRS, numerical rating scale. Ext 60 and Flex 60 represent the isokinetic knee extension and flexion torque at 60°/s respectively
Table 5. Performance test variables and return to sports
†median (interquartile range)
* P < 0.005
ACL, anterior cruciate ligament; RTS, return to sports; Yes-RTS, yes-return to sports; No-RTS, no-return to sports; SL, single-leg; RSI, reactive strength index; LSI, limb symmetry index.
Table 6. Descriptive statistics for operative and nonoperative performance testing.
hop distance, cm
SL vertical jump height, cm
† median (interquartile range)
SL, single-leg; RSI, reactive strength index.
tion criteria and resuming sports activities failed to reach their preinjury athletic status.
No significant differences were observed between the two groups in terms of LSI in SL hop distance and SL vertical jump heights. Previous studies indicate that vertical jumps have a more substantial impact on the knee joint compared to horizontal hops.58,59 Consequently, the initial hypothesis suggested tha a lower LSI in SL vertical jump height woud be seen in the No-RTS group compared to the Yes-RTS group. However, the study’s findings did not support this hypothesis. Among patients engaged in sports after ACLR, many exhibited significant symmetry improvement with a SL vertical jump height. SL hop in this study was 127.9 cm on the operative side and 129.6 cm on the non-operative side, and SL vertical jump was 12.6 cm on the operative side and 13.9 cm on the non-operative side. These results were consistent with those of similar previous studies.11,19 However, the values of these test batteries varied widely depending on the demographics of the participants and the method of measurement (arm swing or countermovement). Therefore, caution should be taken when interpreting the values.60‑63
In the SL drop jump, the No-RTS group demonstrated a lower LSI in RSI compared to the Yes-RTS group. RSI serves as a valid measure of explosive strength and stretchshortening cycle capacity, crucial for most sports.64 Therefore, achieving balanced RSI improvements is a critical factor for successful RTS post-ACLR. The RSI for the study participants’ was 0.33 on the operated side and 0.38 on the non-operated side, which falls within the range of data from previous studies measured at the same height (operated side: 0.28-0.34, non-operated side: 0.37-0.44).49,65‑67 Although the sex and postoperative follow-up time differ from these previous studies, the data from this study can be used as a reference value.
The explanation for the lack of group differences in the LSI of SL vertical jump and the significant group differences in the LSI of SL drop jump is presumably due to differences in jumping characteristics. In the present study, to evaluate concentric muscle force capacity in SL vertical jump, counter movements during jumping were restricted to a minimum.19,44 On the other hand, the SL drop jump task was set to jump higher with a shorter ground contact time to evaluate the ability to exert explosive muscular force. The results of the present study suggest that explosive
muscle exertion is more important for competitive performance in the post-ACLR.
When assessing knee conditions, the No-RTS group reported higher NPRS scores for knee pain than the Yes-RTS group. Persistent knee pain post-ACLR has been reported as a negative factor for RTS, and the findings from the present study align with those from previous studies.53,54 In previous studies, the presence of knee pain symptoms one year after ACLR was linked to a lack of physical or psychological readiness.68 Incorporating findings from previous studies, controlling persistent knee pain emerges as a challenge in postoperative RTS. The detailed etiology of pain in this study remains unknown, indicating the need for further evaluation. The values of ROM deficit in this study were very small in both groups. However, in a previous study, the standard error of measurement of ROM using a goniometer (flexion/extension: 3.41/1.62 degrees) was greater than that using a smartphone app (flexion/extension: 2.72/1.18 degrees).69 Future studies should consider measuring with tools with better accuracy.
When aiming for RTS after ACLR, it is important to progress gradually through criterion-based or task-based rehabilitation and ultimately pass the RTS test.70‑72 Generally, the RTS test primarily encompasses knee strength and SL hop, with only a small percentage dedicated to vertical jump tasks.6,73 Based on these results, the functional aspects of the RTS criteria can be enhanced by adding the RSI of the SL drop jump as well as the distance data of the SL hop.
This study has some limitations. First, it only included patients who had undergone reconstruction using hamstring tendon autograft to control for specific characteristics,25 potentially overlooking differences that may be seen with other graft types such as bone-patellar tendon-bone or quadriceps tendon. The study’s recruitment process might also have introduced selection bias, as only respondents were included. Additionally, the previously utilized RTS criteria did not incorporate vertical jump tasks, which might have led to significant group differences in unassessed parameters. A detailed biomechanical analysis of vertical jump tasks, crucial for understanding lower extremity joint biomechanics, was not conducted.74 In this study, arm swing was not standardized for each motor task. Since hop
distance and jump height differ with and without arm swing, caution should be considered when interpreting the results.41,43 This study did not include patient-reported outcomes related to RTS at a pre-injury competitive level, such as the International Knee Documentation Committee Subjective Knee Form. Therefore, the subjective knee function status of the study subjects was undetermined.54 Furthermore, the study’s conservative data correction using the Bonferroni method might have implications for type II errors. Future multivariate analyses with larger sample sizes are necessary to address these limitations. However, this is the first study to characterize asymmetry in vertical jump performance in RTS at their preinjury competitive level after ACLR. The strength of this study is that it demonstrates the importance of vertical jump performance assessment, which has been the focus of much attention in recent years. In addition, another strength of this study is the inclusion of potentially confounding knee condition variables in the analysis.
Patients unable to report achieving RTS after primary ACLR using hamstring tendon autograft are more likely to exhibit asymmetric performance, especially for explosive characteristics (e.g., RSI), suggesting the significance of assessing jump symmetry in evaluating post-ACLR rehabilitation success.
The authors certify that there are no conflicts of interest with any financial organization regarding the material discussed in the manuscript.
Submitted: December 24, 2023 CDT, Accepted: August 15, 2024 CDT
©
The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: A 10-year study Knee 2006;13(3):184-188. doi:10.1016/j.knee.2006.01.005
2. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based Study. Am J Sports Med 2016;44(6):1502-1507 doi:10.1177/ 0363546516629944
3. Maniar N, Verhagen E, Bryant AL, Opar DA. Trends in Australian knee injury rates: An epidemiological analysis of 228,344 knee injuries over 20 years. Lancet Reg Health West Pac. 2022;21:100409. doi:10.1016/ j.lanwpc.2022.100409
4. Feucht MJ, Cotic M, Saier T, et al. Patient expectations of primary and revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2016;24(1):201-207 doi:10.1007/ s00167-014-3364-z
5. Xiao M, van Niekerk M, Trivedi NN, et al. Patients who return to sport after primary anterior cruciate ligament reconstruction have significantly higher psychological readiness: A systematic review and meta-analysis of 3744 patients. Am J Sports Med 2023;51(10):2774-2783. doi:10.1177/ 03635465221102420
6. Greenberg EM, Greenberg ET, Albaugh J, Storey E, Ganley TJ. Rehabilitation practice patterns following anterior cruciate ligament reconstruction: A survey of physical therapists. J Orthop Sports Phys Ther 2018;48(10):801-811. doi:10.2519/jospt.2018.8264
7. Kitaguchi T, Tanaka Y, Takeshita S, et al. Preoperative quadriceps strength as a predictor of return to sports after anterior cruciate ligament reconstruction in competitive athletes. Phys Ther Sport 2020;45:7-13. doi:10.1016/j.ptsp.2020.06.001
8. Kitaguchi T, Tanaka Y, Takeshita S, et al. Importance of functional performance and psychological readiness for return to preinjury level of sports 1 year after ACL reconstruction in competitive athletes. Knee Surg Sports Traumatol Arthrosc 2020;28(7):2203-2212. doi:10.1007/ s00167-019-05774-y
9. Webster KE, McPherson AL, Hewett TE, Feller JA. Factors associated with a return to preinjury level of sport performance after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2019;47(11):2557-2562. doi:10.1177/ 0363546519865537
10. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery Am J Sports Med 2011;39(3):538-543. doi:10.1177/0363546510384798
11. Ohji S, Aizawa J, Hirohata K, et al. Single-leg hop distance normalized to body height is associated with the return to sports after anterior cruciate ligament reconstruction. J Exp Orthop 2021;8(1):26. doi:10.1186/s40634-021-00344-z
12. Ohji S, Aizawa J, Hirohata K, et al. Characteristics of landing impact in athletes who have not returned to sports at the pre-injury competition level after anterior cruciate ligament reconstruction. Asia Pac J Sports Med Arthrosc Rehabil Technol 2021;25:47-52. doi:10.1016/j.asmart.2021.05.001
13. Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43(5):377-381. doi:10.1136/bjsm.2007.044818
14. Kotsifaki A, Whiteley R, Van Rossom S, et al. Single leg hop for distance symmetry masks lower limb biomechanics: time to discuss hop distance as decision criterion for return to sport after ACL reconstruction? Br J Sports Med. 2022;56(5):249-256. doi:10.1136/bjsports-2020-103677
15. Wang L, Xia Q, Li T, Wang Z, Li J. Limb symmetry index of single-leg vertical jump vs. single-leghop for distance after ACL reconstruction: A systematic review and meta-analysis. Sports Health Published online November 15, 2023:19417381231205268. doi:10.1177/19417381231205267
16. Zarro MJ, Stitzlein MG, Lee JS, et al. Single-leg vertical hop test detects greater limb asymmetries than horizontal hop tests after anterior cruciate ligament reconstruction in NCAA Division 1 collegiate athletes. Int J Sports Phys Ther. 2021;16(6):1405-1414. doi:10.26603/001c.29595
17 Lem HW, Cheng SC, Chang HY, Hung MH, Yeh WL. Single leg drop jump performance identifies functional deficit in collegiate athletes who have returned to sports after ACL reconstruction: A casecontrol study. Medicine. 2022;101(49):e31790. doi:10.1097/MD.0000000000031790
18. King E, Richter C, Franklyn-Miller A, Wadey R, Moran R, Strike S. Back to normal symmetry? Biomechanical variables remain more asymmetrical than normal during jump and change-of-direction testing 9 months after anterior cruciate ligament reconstruction. Am J Sports Med 2019;47(5):1175-1185. doi:10.1177/ 0363546519830656
19. Ohji S, Aizawa J, Hirohata K, et al. Single-leg hop can result in higher limb symmetry index than isokinetic strength and single-leg vertical jump following anterior cruciate ligament reconstruction. Knee. 2021;29:160-166. doi:10.1016/ j.knee.2021.01.030
20. King E, Richter C, Daniels KAJ, et al. Can biomechanical testing after anterior cruciate ligament reconstruction identify athletes at risk for subsequent ACL injury to the contralateral uninjured limb? Am J Sports Med. 2021;49(3):609-619. doi:10.1177/0363546520985283
21. Bosquet L, Berryman N, Dupuy O A comparison of 2 optical timing systems designed to measure flight time and contact time during jumping and hopping. J Strength Cond Res 2009;23(9):2660-2665. doi:10.1519/JSC.0b013e3181b1f4ff
22. Haynes T, Bishop C, Antrobus M, Brazier J. The validity and reliability of the My Jump 2 app for measuring the reactive strength index and drop jump performance. J Sports Med Phys Fitness 2019;59(2):253-258. doi:10.23736/ S0022-4707.18.08195-1
23. Montalvo S, Gonzalez MP, Dietze-Hermosa MS, Eggleston JD, Dorgo S. Common vertical jump and reactive strength index measuring devices: A validity and reliability analysis. J Strength Cond Res 2021;35(5):1234-1243. doi:10.1519/ JSC.0000000000003988
24. Fältström A, Hägglund M, Kvist J. Patientreported knee function, quality of life, and activity level after bilateral anterior cruciate ligament injuries. Am J Sports Med 2013;41(12):2805-2813. doi:10.1177/0363546513502309
25. Cristiani R, Mikkelsen C, Wange P, Olsson D, Stålman A, Engström B. Autograft type affects muscle strength and hop performance after ACL reconstruction. A randomised controlled trial comparing patellar tendon and hamstring tendon autografts with standard or accelerated rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2021;29(9):3025-3036. doi:10.1007/ s00167-020-06334-5
26. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-191. doi:10.3758/ BF03193146
27 Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play Br J Sports Med 2011;45(7):596-606. doi:10.1136/bjsm.2010.076364
28. Christino MA, Fantry AJ, Vopat BG. Psychological aspects of recovery following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg 2015;23(8):501-509. doi:10.5435/JAAOS-D-14-00173
29. Ebert JR, Du Preez L, Furzer B, Edwards P, Joss B. Which hop tests can best identify functional limb asymmetry in patients 9-12 months after anterior cruciate ligament reconstruction employing a hamstrings tendon autograft? Int J Sports Phys Ther 2021;16(2):393-403. doi:10.26603/001c.21140
30. Ohji S, Aizawa J, Hirohata K, et al. The gap between subjective return to sports and subjective athletic performance intensity after anterior cruciate ligament reconstruction. Orthop J Sports Med 2020;8(9):2325967120947402. doi:10.1177/ 2325967120947402
31. Koga H, Muneta T, Watanabe T, et al. Two-year outcomes after arthroscopic lateral meniscus centralization. Arthroscopy. 2016;32(10):2000-2008. doi:10.1016/j.arthro.2016.01.052
32. Brosseau L, Balmer S, Tousignant M, et al. Intraand intertester reliability and criterion validity of the parallelogram and universal goniometers for measuring maximum active knee flexion and extension of patients with knee restrictions. Arch Phys Med Rehabil 2001;82(3):396-402. doi:10.1053/ apmr.2001.19250
33. Brosky JA Jr, Nitz AJ, Malone TR, Caborn DN, Rayens MK. Intrarater reliability of selected clinical outcome measures following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29(1):39-48. doi:10.2519/jospt.1999.29.1.39
34. Robnett NJ, Riddle DL, Kues JM. Intertester reliability of measurements obtained with the KT-1000 on patients with reconstructed anterior cruciate ligaments. J Orthop Sports Phys Ther 1995;21(2):113-119. doi:10.2519/jospt.1995.21.2.113
35. Alghadir AH, Anwer S, Iqbal A, Iqbal ZA. Testretest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J Pain Res 2018;11:851-856. doi:10.2147/ JPR.S158847
36. Muneta T, Koga H, Ju YJ, Yagishita K, Sekiya I. Effects of different initial bundle tensioning strategies on the outcome of double-bundle ACL reconstruction: a cohort study. Sports Med Arthrosc Rehabil Ther Technol 2011;3:15. doi:10.1186/ 1758-2555-3-15
37 Norkin CC, Joyce White D Measurement Of Joint Motion: A Guide To Goniometry. F.A. Davis; 2016.
38. Shelbourne KD, Benner R, Gray T, Bauman S. Range of motion, strength, and function after ACL reconstruction using a contralateral patellar tendon graft. Orthop J Sports Med 2022;10(11):23259671221138104. doi:10.1177/ 23259671221138103
39. Al-Mahmood MR, Uddin MT, Islam MT, Fuad SM, Rahman Shah T Correlation between goniometric measurements of range of motion and radiographic scores in osteoarthritis knee: An observational study among females. Medicine 2022;101(32):e29995. doi:10.1097/MD.0000000000029995
40. Ohji S, Aizawa J, Hirohata K, et al. Association between landing biomechanics, knee pain, and kinesiophobia in athletes following anterior cruciate ligament reconstruction: A cross-sectional study PM R 2023;15(5):552-562. doi:10.1002/pmrj.12827
41. Hara M, Shibayama A, Arakawa H, Fukashiro S. Effect of arm swing direction on forward and backward jump performance. J Biomech 2008;41(13):2806-2815. doi:10.1016/ j.jbiomech.2008.07.002
42. Haitz K, Shultz R, Hodgins M, Matheson GO Testretest and interrater reliability of the functional lower extremity evaluation. J Orthop Sports Phys Ther 2014;44(12):947-954. doi:10.2519/jospt.2014.4809
43. Hara M, Shibayama A, Takeshita D, Fukashiro S. The effect of arm swing on lower extremities in vertical jumping. J Biomech 2006;39(13):2503-2511. doi:10.1016/j.jbiomech.2005.07.030
44. de Fontenay BP, Argaud S, Blache Y, Monteil K. Motion alterations after anterior cruciate ligament reconstruction: comparison of the injured and uninjured lower limbs during a single-legged jump. J Athl Train 2014;49(3):311-316. doi:10.4085/ 1062-6050-49.3.11
45. Bosco C, Luhtanen P, Komi PV. A simple method for measurement of mechanical power in jumping. Eur J Appl Physiol Occup Physiol. 1983;50(2):273-282. doi:10.1007/BF00422166
46. Caruso JF, Daily JS, McLagan JR, et al. Data reliability from an instrumented vertical jump platform. J Strength Cond Res 2010;24(10):2799-2808. doi:10.1519/JSC.0b013e3181b66679
47. Yingling VR, Castro DA, Duong JT, Malpartida FJ, Usher JR, J O The reliability of vertical jump tests between the Vertec and My Jump phone application. PeerJ. 2018;6:e4669. doi:10.7717/peerj.4669
48. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33(1):159-174. doi:10.2307/2529310
49. Read PJ, Davies WT, Bishop C, Mc Auliffe S, Wilson MG, Turner AN. Residual deficits in reactive strength indicate incomplete restoration of athletic qualities following anterior cruciate ligament reconstruction in professional soccer players. J Athl Train. Published online November 5, 2020. doi:10.4085/169-20
50. Markwick WJ, Bird SP, Tufano JJ, Seitz LB, Haff GG. The intraday reliability of the Reactive Strength Index calculated from a drop jump in professional men’s basketball. Int J Sports Physiol Perform 2015;10(4):482-488. doi:10.1123/ijspp.2014-0265
51. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med. 2015;43(4):848-856. doi:10.1177/0363546514563282
52. Kvist J, Ek A, Sporrstedt K, Good L. Fear of reinjury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2005;13(5):393-397 doi:10.1007/s00167-004-0591-8
53. Lentz TA, Zeppieri G Jr, Tillman SM, et al. Return to preinjury sports participation following anterior cruciate ligament reconstruction: contributions of demographic, knee impairment, and self-report measures. J Orthop Sports Phys Ther 2012;42(11):893-901. doi:10.2519/jospt.2012.4077
54. Lentz TA, Zeppieri G Jr, George SZ, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med 2015;43(2):345-353. doi:10.1177/0363546514559707
55. Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples). Biometrika 1965;52(3-4):591-611. doi:10.1093/biomet/52.3-4.591
56. Montgomery C, Blackburn J, Withers D, Tierney G, Moran C, Simms C. Mechanisms of ACL injury in professional rugby union: A systematic video analysis of 36 cases. Br J Sports Med. 2018;52(15):994-1001. doi:10.1136/bjsports-2016-096425
57 Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):2-18. doi:10.1037/a0024338
58. Meylan CMP, Nosaka K, Green J, Cronin JB. Temporal and kinetic analysis of unilateral jumping in the vertical, horizontal, and lateral directions. J Sports Sci 2010;28(5):545-554. doi:10.1080/ 02640411003628048
59. Fukashiro S, Besier TF, Barrett R, Cochrane J, Nagano A, Lloyd DG. Direction control in standing horizontal and vertical jumps. Int J Sport Health Sci. 2005;3(Special__2005):272-279. doi:10.5432/ ijshs.3.272
60. Chaput M, Onate JA, Simon JE, et al. Visual cognition associated with knee proprioception, time to stability, and sensory integration neural activity after ACL reconstruction. J Orthop Res. 2022;40(1):95-104. doi:10.1002/jor.25014
61. Lee DW, Yang SJ, Cho SI, Lee JH, Kim JG. Singleleg vertical jump test as a functional test after anterior cruciate ligament reconstruction. Knee 2018;25(6):1016-1026. doi:10.1016/ j.knee.2018.07.014
62. Taylor JB, Westbrook AE, Head PL, Glover KM, Paquette MR, Ford KR. The single-leg vertical hop provides unique asymmetry information in individuals after anterior cruciate ligament reconstruction. Clin Biomech 2020;80:105107 doi:10.1016/j.clinbiomech.2020.105107
63. Petschnig R, Baron R, Albrecht M. The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 1998;28(1):23-31. doi:10.2519/jospt.1998.28.1.23
64. Ebben WP, Petushek EJ. Using the reactive strength index modified to evaluate plyometric performance. J Strength Cond Res. 2010;24(8):1983-1987 doi:10.1519/ JSC.0b013e3181e72466
65. Read PJ, Pedley JS, Eirug I, Sideris V, Oliver JL. Impaired stretch-shortening cycle function persists despite improvements in reactive strength after anterior cruciate ligament reconstruction. J Strength Cond Res 2022;36(5):1238-1244. doi:10.1519/ JSC.0000000000004208
66. Maestroni L, Turner A, Papadopoulos K, Pedley J, Sideris V, Read P. Single leg drop jump is affected by physical capacities in male soccer players following ACL reconstruction. Sci Med Footb. 2024;8(3):201-211. doi:10.1080/ 24733938.2023.2225481
67 Kotsifaki A, Van Rossom S, Whiteley R, et al. Single leg vertical jump performance identifies knee function deficits at return to sport after ACL reconstruction in male athletes. Br J Sports Med. 2022;56(9):490-498. doi:10.1136/ bjsports-2021-104692
68. Betsch M, Hoit G, Dwyer T, et al. Postoperative pain is associated with psychological and physical readiness to return to sports one-year after anterior cruciate ligament reconstruction. Sports Med Arthrosc Rehabil Ther Technol 2021;3(6):e1737-e1743. doi:10.1016/j.asmr.2021.08.001
69. Mehta SP, Barker K, Bowman B, Galloway H, Oliashirazi N, Oliashirazi A. Reliability, concurrent validity, and minimal detectable change for iPhone goniometer app in assessing knee range of motion. J Knee Surg 2017;30(6):577-584. doi:10.1055/ s-0036-1593877
70. Joreitz R, Lynch A, Popchak A, Irrgang J. Criterion-based rehabilitaiton program with return to sport testing following ACL reconstruction: A case series. Int J Sports Phys Ther. 2020;15(6):1151-1173. doi:10.26603/ijspt20201151
71. Buckthorpe M, Tamisari A, della Villa F. A ten task-based progression in rehabilitaion after ACL reconstruction: From post-surgery to return to playA clinicial commentary Int J Sports Phys Ther 2020;15(4):611-623. doi:10.26603/ijspt20200611
72. Welling W, Benjaminse A, Lemmink K, Gokeler A. Passing return to sports tests after ACL reconstruction is associated with greater likelihood for return to sport but fail to identify second injury risk. Knee 2020;27(3):949-957 doi:10.1016/ j.knee.2020.03.007
73. Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):192-199. doi:10.1007/s00167-016-4246-3
74. Chen P, Wang L, Dong S, Ding Y, Jia S, Zheng C. Can symmetry of single-leg vertical jump height represent normal lower limb biomechanics of athletes after anterior cruciate ligament reconstruction? Sports Health. 2024;16(4):596-605. doi:10.1177/19417381231190119

Kobayashi Y, Nagano Y, Suzukawa M. Relationship of Physical Factors to the Occurrence of Injuries in Young Gymnasts. IJSPT. Published online
Yuria Kobayashi1a , Yasuharu Nagano2,3 , Makoto Suzukawa3
1 Yokohama Sports Medical Center, 2 Japan Women's College of Physical Education, 3 Yokohama Sports Medical Center
Keywords: gymnastics, joint range of motion, injury, flexibility https://doi.org/10.26603/001c.123475
International Journal of Sports Physical Therapy
Background
There is a large population of young athletes who participate in gymnastics, and the prevention of injury in junior athletes is considered important. However, few studies have prospectively investigated the relationship between physical factors and the occurrence of injury
Purpose
To investigate the physical characteristics that are factors in the injury occurrence in elementary and junior high school gymnasts.
Study Design
Prospective observational study.
Methods
A total of 36 healthy young gymnasts (at national competition level) were enrolled in the study Once a week for 23 weeks, injuries were prospectively investigated using self-report questionnaires under the supervision of a research staff. Joint range of motion (hip, ankle, shoulder, and wrist), tightness (Thomas test, Ely test, straight leg raise [SLR], triceps surae, combined abduction test [CAT], horizontal flexion test [HFT]), and muscle elasticity (multifidus) were assessed to compare differences in physical function between injured and non-injured participants.
Results
Injuries occurred most commonly in the wrist (42.1%), lower back (30.2%), and foot (9.5%) among males, whereas heel (22.2%), knee (16.0%), and lower back (12.8%) were the most common injury sites among females. Wrist injuries in male athletes showed decreased shoulder joint range of motion, and lower back injuries showed decreased hip and shoulder joint range of motion. Lower back injuries in female athletes showed decreased hip extension mobility Heel and knee joint injuries in females also showed increased range of motion and decreased tightness.
Conclusions
The results of this study indicate that the factors related to flexibility differ according to injury location. Further studies are required to clarify the physical factors that influence injury occurrence by examining the effects of the gymnasts’ muscle strength, age, individual factors, and left–right differences.
a
Corresponding Author:
Yuria Kobayashi
3302-5, Kozukue Town, Kohoku Ward, Yokohama City, Kanagawa (inside Nissan Stadium) 222-0036, Japan
Email: xxannu.gymno.1xx@gmail.com Phone: 045-477-5050
Female and male elite gymnasts begin competing at approximately six and nine years of age, respectively 1 The peak performance age for female and male gymnasts is 16–18 years and early 20s, respectively 2 Gymnastics includes a large population of young athletes, and many injuries occur in gymnasts in elementary and junior high school. Previous studies on gymnastics injuries have covered various ages, and few studies have focused on male gymnasts.3 Furthermore, most previous studies used lost practice and competition time as a reflection of injury severity However, because gymnasts tend to modify their events and practice content to be able to continue practicing despite having injuries,1 conventional survey methods may not accurately identify chronic disabilities that are not severe enough to cause them to miss the practice sessions.
Height, weight, body fat, age, rapid growth spurts, life stress, and high levels of practice and competition have been cited as risk factors for injury in gymnasts.1 Among female gymnasts aged 10–20 years, those with greater age, weight, and body mass index, smaller shoulder flexion angles, and greater lower back extension were reported to have a higher risk of injury than their counterparts.4 History and hypermobility have also been shown to potentially contribute to injury risk estimates. In contrast, Wright et al.5 identified age, weight gain, greater height, and lack of flexibility as injury risks in female athletes aged 8–18 years. Flexibility is particularly difficult to define, and its association with injury remains speculative.1
Previous studies have not prospectively investigated injury occurrence and physical factors in gymnasts, and only a few have examined physical assessment. Flexibility, an essential element for gymnasts, has also not been associated with injury In addition, the relationship between physical function and injury occurrence among male and female elementary and junior high school gymnasts was not investigated. Therefore, the purpose of this study was to investigate the physical characteristics that are factors in the injury occurrence in elementary and junior high school gymnasts.
The study enrolled healthy young gymnasts (at the level of national competition) from one gymnastics club. The inclusion criteria required that participants were healthy and free from injuries that would prevent them from completing the measurements. Exclusion criteria were refusal to cooperate in the study and inability to continue the questionnaire. Questionnaires regarding the participant height, weight, age, and medical history were distributed at the beginning of the study. Prior to the start of the study, the purpose, methods, risks associated with participation in the study, and handling of personal information were explained
in writing to the subjects and their guardians, and consent was obtained. In addition, consideration was given to anonymizing the data so that the subjects could not be identified. This study was conducted with the approval of the Research Ethics Committee of the author’s institution.
The incidence of injury was investigated using the Oslo Sports Trauma Research Center questionnaire,6 which was modified and translated into Japanese.7 Because the questionnaire was designed for adult athletes, a modified version for elementary and junior high school gymnasts was used. Responses were made once a week for 23 weeks that began in September 2021, and participants completed the questionnaire under the supervision of the researcher The presence or absence of injury and its severity (0: no injury; 100: injury with maximum severity) were recorded from the responses. When a new injury occurred, the research staff (one identified physical therapist) directly checked the patient’s condition and recorded the distinction between acute trauma and chronic disability, the location, and the name of the diagnosis (if a medical facility was consulted). Acute trauma was defined as an injury that occurred suddenly and had an injury mechanism, whereas chronic disability was defined as an injury in which pain gradually increased or continued without any associated incident.
Baseline assessments for range of motion (hip flexion and extension, ankle plantar flexion, shoulder flexion, external rotation [upper extremity raising position], and internal rotation [upper extremity raising position], wrist active–passive palmar flexion and dorsiflexion), tightness (Thomas test [iliopsoas muscle], Ely test [quadriceps], straight leg raise (SLR) [hamstrings], triceps surae, combined abduction test (CAT) [latissimus dorsi muscle], horizontal flexion test (HFT) [deltoid muscle and teres minor muscles]), and muscle elasticity [multifidus] were performed. Joint range of motion testing was performed using a goniometer in accordance with the method prescribed by the Japanese Society of Rehabilitation Medicine.8 Only passive range of motion of the joints were measured, except wrist joints. Tightness tests were performed using a ruler (Raymay–Fujii Corporation, APJ188W) to measure the distance at the knee for the Thomas test and the heel-buttock distance for the Ely test.9 A goniometer was used to measure the SLR. The triceps surae were measured using an angle meter (Digi-Pas ® Pocket Digital Leveler DWL-80Pro) to measure the maximum dorsiflexion angle of the ankle joint under a load in the standing position; the CAT10 assessed the shoulder joint abduction angle in the back supine, scapular fixation position (Figure 1); the HFT11 measured the shoulder joint horizontal flexion angle while lying on the back in supine, with scapular fixation, using an angle meter

Figure 1. Combined abduction test (CAT) measures the shoulder joint abduction angle. The examiner is holding the scapula and restricting scapular movement.
Muscle elasticity testing of the multifidus muscle at rest was performed using an ultrasound device with shear wave elastography (SuperSonic Imagine, Aixplorer, France) and a linear probe (50 mm, 4–15 MHz). The intraclass correlation coefficient (ICC) for intra- and interobserver reliability has been shown to be excellent for muscle elasticity testing of the multifidus muscle at rest by ultrasound elastography [ICC = 0.99 and ICC = 0.95, respectively].12 In this study, the authors used the method of Koppenhaver et al.13 Measurements were performed at the 4th–5th intervertebral positions with the probe placed over the muscle belly of the bilaterally multifidus muscle. The probe was rotated counterclockwise approximately 10° from the front and tilted approximately 10° from the sagittal plane to ensure that it was parallel to the muscle fibers of the multifidus muscle. The shear modulus (kPa) was calculated by dividing the Young modulus obtained from the measurement by three. Three pictures were taken on each side, and the average was calculated since the average of the three measurements was considered better with respect to test–retest reliability 13 Three images were taken from each side, and the average was calculated.
Injury was defined as a severity of ≥1 on the questionnaire. The injury retention rate was calculated as the 23-week average of the ratio of the number of injured participants divided by the number of respondents per week. The injury retention rate (%) and injury retention rate by location (%) were calculated using the collected data, and 95% confi-
Table 1. Demographic characteristics of the participants
*Abbreviations: SD, standard deviation
dence intervals (CI) were obtained. Next, the relationships between the top three most frequently injured locations and physical function were examined according to sex. Participants with injuries at each location (wrist, lower back, and foot for males; heel, knee, and lower back for females) were defined as the injury group, and those without injuries were defined as the noninjury group. Differences in physical assessment according to injury location were examined using unpaired t-tests. The significance level was set at 5%. SPSS ver. 22 (IBM Corporation, Chicago, USA) was used for statistical processing.
Thirty-six gymnasts (19 males and 17 females, mean age 12.0 ± 1.8 years) consented to participate. Participant details are presented in Table 1. Of the 19 males, 18 participated in six events (floor exercise, pommel horse, rings, vault, parallel bars, and high bars) and one participated in three events (floor exercise, vault, and high bars). In the female competition, 15 of 17 athletes competed in four events (vault, uneven bars, balance beam, and floor exercise), and two competed in three events (vault, floor exercise, and balance beam).
The average overall injury incidence was 65.9% (95% CI: 62.3–69.5), with averages of 70.0% (65.3–74.8) and 61.7% (57.8–65.6) for males and females, respectively Overall, 21.2% (19.8–22.7) of the injuries occurred in the lower back, 21.2% (19.2–23.1) in the wrist, and 13.8% (12.4–15.2) in the heel. Among males, common injury locations were the wrist (42.1% [38.1–46.1]), lower back (30.2% [26.9–33.5]), and foot (9.5% [6.5–12.5], whereas for females, injuries occurred most often in the heel (22.2% [19.8–24.6]), knee (16.0% [14.0–18.0]), and lower back (12.8% [10.9–14.7]).
Among male participants, the wrist injury group showed a significantly decreased range of motion in the internal rotation of the left and right shoulder joints (Table 2).
Among male participants, the lower back injury group had significantly lower values for left hip flexion, right hip extension, right and left shoulder external rotation, right and left wrist active palmar flexion, and right and left wrist
Table 2. Wrist injuries and physical assessments in male athletes
*Measurements with significant differences.
†Abbreviations: SD, standard deviation; SLR, straight leg raise; CAT, combined abduction test; HFT, horizontal flexion test
passive palmar flexion range of motion (Table 3). There was no significant difference in the shear modulus of the multifidus muscle between males with and without lower back injury. No significant differences in physical function were observed between males with and without foot injuries.
Regarding physical function in females with injury, the heel injury group had a significantly higher left SLR and a significantly lower left CAT than the noninjury group (Table 4).
Table 3. Lower back injuries and physical assessments in male athletes
*Measurements with significant differences.
†Abbreviations: SD, standard deviation; SLR, straight leg raise; CAT, combined abduction test; HFT, horizontal flexion test
The knee injury group had significantly lower values for left hip flexion and left wrist passive dorsiflexion range of motion, significantly higher values for left shoulder flexion range of motion, and significantly lower values for the right
iliopsoas test than the females without knee injury (Table 5).
Although the lower back injury group had significantly higher values for the right Thomas test than the noninjury group (Table 6), there was no significant difference in the
Table 4. Heel injuries and physical assessments in female athletes
*Measurements with significant differences.
†Abbreviations: SD, standard deviation; SLR, straight leg raise; CAT, combined abduction test; HFT, horizontal flexion test
shear modulus of the multifidus muscle between the two groups.
The assessment of incidence of injury in male and female young gymnasts indicates that wrist injuries in males were
Table 5. Knee injuries and physical assessments in female athletes
*Measurements with significant differences.
†Abbreviations: SD, standard deviation; SLR, straight leg raise; CAT, combined abduction test; HFT, horizontal flexion test
associated with decreased shoulder joint internal rotation range of motion, and lower back injuries were associated with decreased hip flexion and extension range of motion, shoulder joint external rotation range of motion, and wrist joint palmar flexion range of motion. Male gymnasts often
support themselves with their upper extremities; the wrist joints in particular are subjected to excessive physical loading, including compression, rotation, and traction, which have been reported to be twice their body weight and up to 16 times their weight by different authors.14,15 DiFiori et
Table 6. Lower back injuries and physical assessments in female athletes
*Measurements with significant differences.
†Abbreviations: SD, standard deviation; SLR, straight leg raise; CAT, combined abduction test; HFT, horizontal flexion test
al.14 reported that wrist joint injuries were the most common injury among gymnasts aged 10–14 years, with high weekly practice volume and high skill level as risk factors, but no association with physical function was shown. It is likely that reduced shoulder joint mobility and high lev-
els of support during upper extremity loading places more stress on the wrist joint, and the demonstrated association between reduced shoulder joint range of motion and wrist joint injury may help in intervention for wrist joint injury prevention. The results also suggested that a lack of
overall range of motion was associated with the development of lower back injuries in male gymnasts. In this study, the results indicated that lower back injury was associated with decreased hip flexion and extension range of motion, shoulder joint external rotation range of motion. Males have more upper limb supportive techniques and well-developed upper limb muscles, which may be related to the lack of shoulder joint range of motion, which therefore may be relevant. When swinging on the rings and high bar, in order to extend the trunk in during the swinging motion or during shoulder return (from forced shoulder joint flexion to shoulder joint extension), decreased range of motion of the scapulohumeral joint may compensate for the decreased range of motion caused by extension of the thoracolumbar spine. The internal rotation alignment of the humerus characteristic seen in gymnasts may lead to injury,16 and the results of the current study suggest that a decrease in the external rotation range of motion of the shoulder joint during upper limb elevation position may lead to excessive extension of the lumbar spine as a compensation, which may lead to lower back injuries. (Figure 2) Additionally, since hip extension is required during the swinging motion,17 inadequate hip extension range of motion may cause excessive extension stress on the lower back, leading to the onset of the injury.
Heel injuries in female gymnasts were associated with decreased hamstring tightness, knee injuries were associated with increased shoulder joint range of motion and decreased iliopsoas tightness. These findings indicate that the lack of joint range of motion and mobility may not be the only problems contributing to injury In this study, heel injuries were more common in gymnasts diagnosed with Sever’s disease and were more common in elementary school gymnasts. Mackie et al.18 reported that Sever’s disease was the most common overuse disorder in female gymnasts aged 7–18 years. The primary risk factors include obesity and high-intensity physical activity, with high-impact sports being the primary cause.19 It is necessary to consider age-related characteristics, including muscle strength, due to the age of predilection and athleticism in developing athletes.
Furthermore, lower back injuries were associated with reduced hip extension mobility among female gymnasts. Desai et al.20 reported that a general anterior pelvic tilt in gymnasts influences the development of chronic low back pain and requires improvements in hip flexor group, quadriceps flexibility, trunk muscle strength, and hamstring muscle strength. The results of the current study support the findings of Desai et al.20 that flexibility of the hip flexor group is necessary. Sweeney et al.21 reported decreased iliotibial ligament tightness as a risk factor for lower back pain in female gymnasts, indicating that limited joint flexibility was not associated with lower back pain. However, Sweeney et al.21 also included high school gymnasts, whereas the current study only included elementary and middle school gymnasts. The results of the current study also included participants who reported a history of lower back pain, suggesting that decreased hip extension mobility, which was also associated with a history of lower

Figure 2. Swinging motion of the men’s high bars requires a large extension of the trunk, which affects the shoulder and hip joint ranges of motion, and the thoracic spine. A lack of these ranges of motion may lead to excessive extension of the lumbar spine, increasing the risk of injury.
back pain, may be also related to the occurrence of lower back injuries (Figures 3 and 4).
There was no association between lower back injury and multifidus muscle elasticity in either sex. Masaki et al.22 showed that adults with lower back pain had significantly greater muscle stiffness in the multifidus muscle (L4 level) at rest in the supine position compared to those without the same. These results differed because the age group of the participants in the current study was prone to maturity, and the results may have reflected a variation in muscle elasticity. In addition, Murillo et al.23 found a lower increase of muscular stiffness with contraction of the multifidus muscle in the group with lower back pain than in the group without, suggesting a deficit in multifidus activation. Therefore, there may be a relationship between muscle elasticity during multifidus contraction and lower back injuries in elementary and junior high school athletes, and future studies are warranted.
It is difficult to identify physical factors that influence the occurrence of injury based on joint range of motion, tightness, and muscle elasticity alone. Regression analysis should be used to consider the effects of muscle strength, age, individual factors, and left–right differences as well. In this study, there were some items in which left–right differences occurred; the characteristics of gymnasts that tend to cause left–right differences, such as the kicking and pivot leg, as well as the direction of twisting, should be examined in the future.
Moreover, the results of this study were limited by its duration, which did not cover the entire competitive season,

Figure 3. Hip and thoracic extensions should be performed during trunk extension.
and scope, as the injury incidence survey and intervention were conducted in only one club.
The results of this study indicate that the factors related to range of motion and flexibility differ according to injury location and between males and females. Further studies are required to clarify the physical factors that influence injury occurrence by examining the effects of the gymnasts’ muscle strength, age, individual factors, and left–right differences.

Figure 4. Lack of hip extension during trunk extension increases lumbar kyphosis and may increase injury risk.
The authors report no conflicts of interest
Submitted: February 19, 2024 CDT, Accepted: August 07, 2024 CDT
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Caine DJ, Nassar L. Gymnastics injuries. Med Sport Sci 2005;48:18-58. doi:10.1159/000084282
2. Westermann RW, Giblin M, Vaske A, Grosso K, Wolf BR. Evaluation of men’s and women’s gymnastics injuries: A 10-year observational study Sports Health 2015;7:161-165. doi:10.1177/1941738114559705
3. Campbell RA, Bradshaw EJ, Ball NB, Pease DL, Spratford W Injury epidemiology and risk factors in competitive artistic gymnasts: A systematic review. Br J Sports Med 2019;53:1056-1069. doi:10.1136/ bjsports-2018-099547
4. Steele VA, White JA. Injury prediction in female gymnasts. Br J Sports Med. 1986;20:31-33. doi:10.1136/bjsm.20.1.31
5. Wright KJ, Crée CD The influence of somatotype, strength and flexibility on injury occurrence among female competitive Olympic style gymnasts—A pilot study J Phys Ther Sci 1998;10:87-92. doi:10.1589/ jpts.10.87
6. Clarsen B, Myklebust G, Bahr R. Development and validation of a new method for the registration of overuse injuries in sports injury epidemiology: The oslo sports trauma research centre (OSTRC) overuse injury questionnaire. Br J Sports Med 2013;47:495-502. doi:10.1136/bjsports-2012-091524
7 Nagano Y, Kobayashi-Yamakawa K, Higashihara A, Yako-Suketomo H. Japanese translation and modification of the Oslo Sports Trauma Research Centre overuse injury questionnaire to evaluate overuse injuries in female college swimmers. PLoS One. 2019;14:e0215352. doi:10.1371/ journal.pone.0215352
8. Yonemoto K, Ishigami J, Kondo T Measurement method for range of joint motion. Jap J Rehab Med. 1995;32:207-217 doi:10.2490/jjrm1963.32.207
9. Azuma N, Someya F. Injury prevention effects of stretching exercise intervention by male high school soccer players. Scand J Med Sci Sports 2020;30:2178-2192. doi:10.1111/sms.13777
10. Kotoshiba S, Maeda N, Urabe Y, et al. Effect of short-term intervention on infraspinatus muscle activity during throwing motion and physical examination in baseball players with throwing disorder Isokinet Exerc Sci 2020;28:91-99. doi:10.3233/IES-193192
11. Laudner KL, Stanek JM, Meister K. Assessing posterior shoulder contracture: The reliability and validity of measuring glenohumeral joint horizontal adduction. J Athl Train 2006;41:375-380.
12. Moreau B, Vergari C, Gad H, et al. Non-invasive assessment of human multifidus muscle stiffness using ultrasound shear wave elastography: A feasibility study Proc Inst Mech Eng H 2016;230:809-814. doi:10.1177/0954411916656022
13. Koppenhaver S, Kniss J, Lilley D, et al. Reliability of ultrasound shear-wave elastography in assessing low back musculature elasticity in asymptomatic individuals. J Electromyogr Kinesiol 2018;39:49-57 doi:10.1016/j.jelekin.2018.01.010
14. DiFiori JP, Puffer JC, Mandelbaum BR, Mar S. Factors associated with wrist pain in the young gymnast. Am J Sports Med 1996;24:9-14. doi:10.1177/ 036354659602400103
15. DiFiori JP, Caine DJ, Malina RM. Wrist pain, distal radial physeal injury, and ulnar variance in the young gymnast. Am J Sports Med. 2006;34:840-849. doi:10.1177/0363546505284848
16. Beyranvand R, Mirnasouri R, Mollahoseini S, Mostofi S. The functional stability of the upper limbs in healthy and rounded shoulder gymnasts. Sci Gymnastics J 2017;3:279-290.
17 Williams G, Irwin G, Kerwin DG, Newell KM. Kinematic changes during learning the longswing on high bar Sports Biomech 2012;11:20-33. doi:10.1080/ 14763141.2011.637120
18. Mackie SJ, Taunton JE. Injuries in female gymnasts. Phys Sportsmed 1994;22:40-45. doi:10.1080/00913847.1994.11947679
19. Ramponi DR, Baker C. Sever’s disease (calcaneal apophysitis). Adv Emerg Nurs J. 2019;41:10-14. doi:10.1097/TME.0000000000000219
20. Desai N, Vance DD, Rosenwasser MP, Ahmad CS. Artistic gymnastics injuries; epidemiology, evaluation, and treatment. J Am Acad Orthop Surg 2019;27:459-467. doi:10.5435/JAAOS-D-18-00147
21. Sweeney EA, Daoud AK, Potter MN, Ritchie L, Howell DR. Association between flexibility and low back pain in female adolescent gymnasts. Clin J Sport Med. 2019;29:379-383. doi:10.1097/ JSM.0000000000000660
22. Masaki M, Aoyama T, Murakami T, et al. Association of low back pain with muscle stiffness and muscle mass of the lumber back muscles, and sagittal spinal alignment in young and middle-aged medical workers. Clin Biomech 2017;49:128-133. doi:10.1016/j.clinbiomech.2017.09.008
23. Murillo C, Falla D, Rushton A, Sanderson A, Heneghan NR. Shear wave elastography investigation of multifidus stiffness in individuals with low back pain. J Electromyogr Kinesiol. 2019;47:19-24. doi:10.1016/j.jelekin.2019.05.004

Kofoed C, Palmsten A, Diercks J, Obermeier M, Tompkins M, Chmielewski TL. The Clinical Utility of the Seated Wall Angel as a Test with Scoring. IJSPT. Published online October 2, 2024:1228-1237. doi:10.26603/001c.123512
Chad Kofoed1a , Allison Palmsten1 , Jonathon Diercks1 , Michael Obermeier, Marc Tompkins2 , Terese L Chmielewski1
1 Physical Therapy, TRIA Orthopedic Center, 2 Orthopedic Surgery, TRIA Orthopedic Center
Keywords: functional outcomes, shoulder, shoulder stretch, shoulder instability, testing battery https://doi.org/10.26603/001c.123512
International Journal of Sports Physical Therapy
Background
The seated wall angel (SWA) is an intervention to improve upper quarter mobility but has not been described as a clinical test with scoring.
Hypothesis/ Purpose
To explore the clinical utility of the SWA as a test with scoring. The authors hypothesized that SWA test scores would be lower on the injured than uninjured side, improve over time, and show stronger association with patient-reported shoulder function than shoulder mobility tests.
Study Design
Prospective cohort.
Methods
Patients diagnosed with anterior shoulder instability and referred to physical therapy participated. Testing occurred after physical therapy examination (initial) and six weeks later (follow-up). Rehabilitation was not controlled. Testing included clinical tests (SWA, passive shoulder external rotation range of motion, total arc of motion) and patient-reported outcomes including the American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, (ASES) and the Western Ontario Shoulder Instability Index (WOSI). The SWA test was scored 0 to 3 points bilaterally based on number of body contacts with the wall (i.e., elbows and fingertips, posterior fingers, posterior forearm). Passive range of motion was measured with a standard goniometer. SWA scores were compared between sides at initial testing and compared between testing timepoints on the injured side. Associations among injured side clinical test values and patient-reported outcome scores were examined.
Results
Mean (SD) SWA score on the injured side was significantly lower than the uninjured side at initial testing [1.6 (1.0) vs 2.2 (1.1), p = 0.045] and significantly increased at follow-up testing [2.4 (1.0), p = 0.041]. Only SWA test score was significantly correlated with ASES (r=0.597) and WOSI (r=-0.648) scores at initial testing, and SWA test score was significantly correlated with WOSI score at follow-up testing (r=-0.611).
The clinical utility of the SWA test is supported by distinguishing the injured and uninjured sides and having stronger associations with patient-reported shoulder function than shoulder mobility tests.
Fax: 952-806-5510 a
Corresponding Author: Chad Kofoed, PT, DPT chad.kofoed@tria.com
Phone: 952-806-5705
Upper extremity function requires adequate mobility in the upper quarter, including the extremity joints, the scapulothoracic articulation, and the thoracic spine.1‑3 For patients with shoulder conditions, clinical testing typically focuses on mobility of the shoulder, and specifically glenohumeral active and passive range of motion (ROM).4,5 Additionally, assessing glenohumeral active and passive external rotation ROM is important during return to sport decision making.6 Total arc of motion is the sum of shoulder internal and external ROM measured at 90 degrees of shoulder abduction7 and has been studied extensively in overhead athletes.5,7‑12 A side-to-side difference greater than 5 degrees in total arc of motion has been associated with shoulder and elbow pain and risk for shoulder injury in overhead athletes.7,8,13,14 While shoulder ROM and total arc of motion identify impairments in glenohumeral mobility, they do not integrate scapulothoracic and thoracic spine mobility that might give a more comprehensive indication of upper extremity function.
The seated wall angel (SWA), sometimes referred to as the W-stretch, has been described on the internet and on social media sites as an exercise to improve upper quarter mobility.15‑17 The goal of the SWA is to get the entire posterior upper extremity in contact with the wall and some recommend arm elevation (movement) in this position.15, 18 Because the SWA requires scapular retraction and thoracic extension, it may give additional information about shoulder complex function compared to glenohumeral mobility testing. In addition, the SWA may be more functional than other glenohumeral mobility tests for overhead athletes and could be used as a screen of upper extremity function in athletes prior to returning to an overhead sport after an injury or as part of a comprehensive upper extremity mobility assessment. The SWA has not been described as a clinical test with a mechanism for scoring.
The purpose of this study was to explore the clinical utility of the SWA as a test with scoring. The authors hypothesized that SWA test scores would be lower on the injured than uninjured side, improve over time, and show stronger association with patient-reported shoulder function compared to other clinical tests of shoulder mobility. Knowledge generated by this study can help clinicians discern the potential for utilizing the SWA test during clinical examination and clinical decision-making.
STUDY OVERVIEW
This study is a secondary analysis of data acquired for a study focused on developing an upper extremity testing battery Clinical tests and patient-reported outcomes were collected soon after the physical therapy examination (initial testing) and six weeks later (follow-up testing).
Between April 2017 and March 2020, patients with anterior shoulder instability undergoing physical therapy were recruited for this study (Figure 1). Inclusion criteria for the study were age 16 to 30 years, physician-diagnosed anterior shoulder instability determined by recent traumatic dislocation or subluxation, and participation in at least 50 hours of exercise in the year prior to injury. Patients were excluded from participation if they had resting shoulder pain greater than 5 on the 0 (no pain) to 10 (worst pain imaginable) point Numeric Pain Rating Scale (NPRS),19 an additional episode of shoulder instability before completing the study; or history of another physician-diagnosed shoulder, elbow, or wrist injury to either upper extremity All patients provided written informed consent to participate in the study on a form approved by the Institutional Review Board.
Patients participated in initial testing soon after their physical therapy examination and follow-up testing six weeks later. The interval between test sessions was selected to allow time for improvement in shoulder function and near the anticipated end of the physical therapy episode of care. Testing consisted of collection of demographic information, performance of clinical tests (SWA test, external rotation passive ROM, and total arc of motion), and completion of patient-reported outcomes focused on shoulder function.
Demographic information was collected by self-report including age, sex, height, weight, the number of prior shoulder instability events, the date of the most recent shoulder instability event, the side of injury, and the arm used to throw a ball (dominant extremity). The NPRS was used to determine the intensity of shoulder pain (0= No pain, 10=Worst pain imaginable).19 Patients rated their current, usual, best, and worst levels of pain, which were averaged to create a composite of shoulder pain intensity. Height and weight were used to compute body mass index (BMI). The time from the most recent shoulder instability event to initial testing and from the physical therapy evaluation to initial testing were computed. The number of physical therapy visits attended was determined from the electronic medical record.
Testing was administered by a physical therapist or athletic trainer, each with more than 10 years of clinical experience treating patients with upper extremity conditions. The same clinician administered initial and follow-up testing for a given subject. Before the study was initiated, the clinicians reviewed and practiced the standardized testing and scoring procedures.
Pre-testing warm-up consisted of five minutes of light upper body ergometry, 30 small forward and backward arm
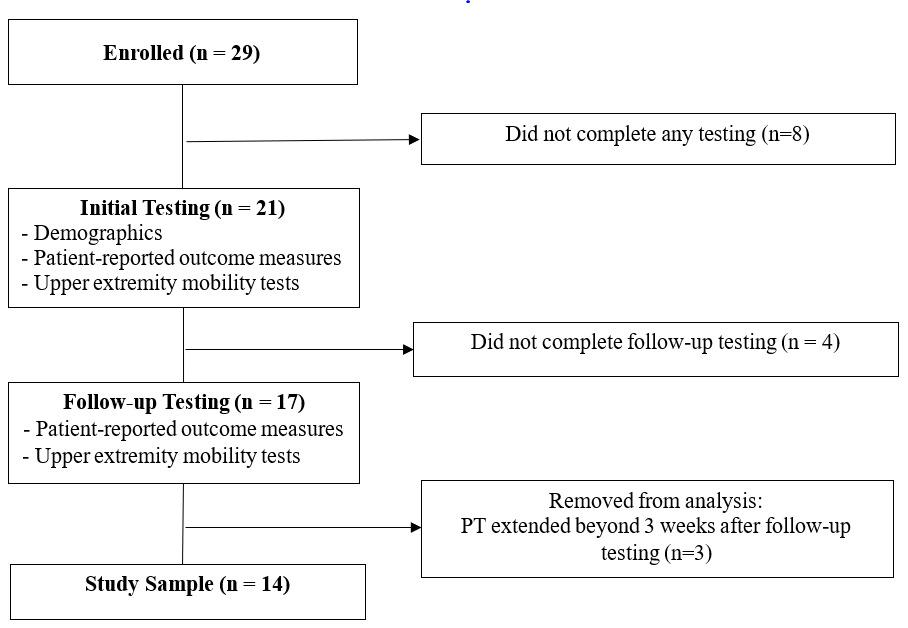
Figure 1. Study Flow Diagram.
circles, and self-stretching as desired by the patient. For all tests, patients were given standardized instructions and a practice trial.
The test was performed with the patient seated on the floor with knees bent, feet flat on the floor, and the lumbar spine and head in contact with the wall (Figure 2). From this position, the patient was instructed to elevate elbows to shoulder height, and externally rotate the shoulders as much as possible. The patient held the position for scoring, which differs from the SWA as an intervention during which the arms are elevated overhead while maintaining contact with the wall. Scoring was based upon the number of contact points with the wall (elbow and fingertips, posterior fingers, posterior forearm). 0: < 2 points of contact, 1: elbow and fingertip contact, 2: elbow and posterior finger contact, 3: elbow, posterior forearm, and posterior hand contact. The injured and uninjured sides were scored separately.
Reliability of the SWA test was assessed during the study with a sample of convenience. Inter-rater reliability of the scoring method was assessed for the right and left sides of two patient study participants and 10 uninjured controls. One rater performed scoring in real-time, and one rater performed scoring from video. Intraclass correlation coefficients [95% confidence interval] were 0.894 [0.681, 0.968] for the right side and 0.867 [0.618, 0.959] for the left side. Additionally, intra-rater reliability of scoring was assessed for the right and left sides of 11 study participants and 11 uninjured controls. Scoring was completed from video on two occasions, 10 days apart. Intraclass correlation coefficients [95% confidence interval] were 0.891 [0.758, 0.953] for the right side and 0.891 [0.751, 0.954] for the left side.
SHOULDER EXTERNAL ROTATION RANGE OF MOTION AND TOTAL ARC OF MOTION
Total arc of motion is the sum of passive shoulder internal and external rotation ROM (Figure 3).7 Testing was performed with the subject in supine and the arm abducted to 90 degrees in the scapular plane with manual stabilization of the scapula at the coracoid process.7 A small towel roll was placed under the humerus to ensure motion occurred in the correct plane. External rotation ROM was measured with a standard goniometer when the end point was perceived by the tester or if a patient had apprehension. Internal rotation was measured in the same position with a standard goniometer when the end point was perceived by the tester Total arc of motion was determined by summing external rotation and internal rotation ROM.
The American Shoulder and Elbow Surgeons Shoulder Assessment Form (ASES) is a standardized questionnaire for measuring shoulder pain, instability, and activities of daily living.20,21 Scores range from 0 to 100 points, and higher scores represent better shoulder function. The ASES is responsive to change, and the minimal clinically important difference (MCID) is 6.4 points.20
The Western Ontario Shoulder Instability Index (WOSI) is a disease-specific quality of life questionnaire for patients with shoulder instability.22 Scores range from 0 to 2100 points, with lower scores representing better function. The WOSI is responsive to change, and the MCID is 220 points.22
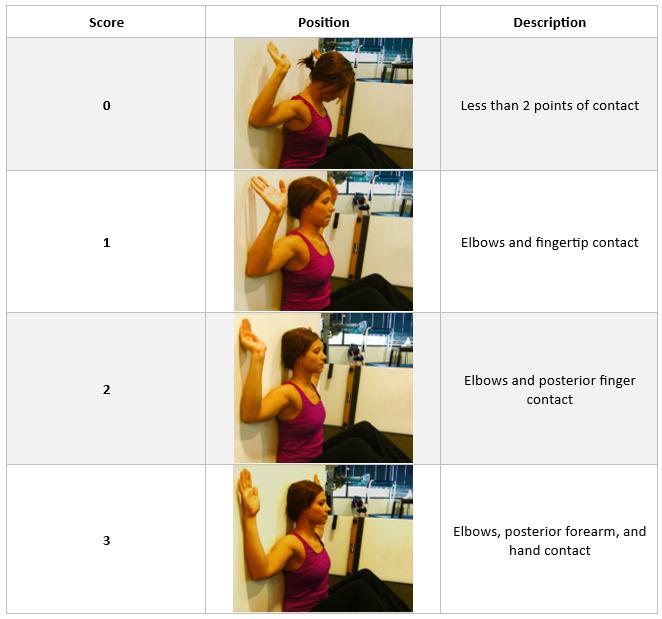

No a priori power calculations were performed for this study because it is a secondary analysis. All analyses were performed with commercial software (IBM SPSS Statistics version 28). Descriptive statistics were generated for demographic information variables, clinical test variables, and patient-reported outcome scores. Statistical significance was set at alpha less than 0.05.
Paired t-tests were used to compare SWA test scores between sides at initial testing and to compare injured side SWA test scores at initial and follow-up testing. Effect sizes (Cohens d) were calculated for the difference in clinical test values and patient-reported outcome scores from initial testing to follow-up testing using the standard deviation of the difference. An effect size of 0.2 is considered a small effect size, 0.5 is considered moderate, and > 0.8 is considered large.23
Associations among the clinical test values on the injured side (SWA test, external rotation ROM, and total arc of motion) and patient-reported outcome scores were examined at initial testing and follow-up testing with Pearson correlation coefficients. Correlation coefficients less than 0.4 were considered weak correlations, between 0.4 and 0.69 considered moderate correlations, and 0.7 and higher considered strong correlations.24 If more than one clinical test showed significant correlation with a patient-reported outcome score, stepwise linear regression analysis was performed with the clinical tests as independent variables and patient-reported outcome score as the dependent variable to understand the relative contribution of the clinical tests to patient-reported shoulder function. The criteria for removal from the model was p> 0.05.
Demographic information for the patients is found in Table 1 Males comprised 71% of the sample. Initial testing occurred on average about four weeks after the most recent instability event, and approximately a week after the physical therapy evaluation. The number of instability events ranged from one to 20. Patients attended between one and 13 physical therapy visits in the six weeks from initial to follow-up testing. Only two patients had additional physical therapy visits after follow-up testing: one visit and two visits, respectively.
SWA test scores, values for shoulder external rotation ROM, total arc of motion, and patient-reported outcome scores are found in Table 2 Shoulder external rotation ROM was unavailable for two patients at both testing dates and three additional patients at follow-up testing because only total arc of motion was recorded. Thus, analyses involving shoulder external rotation ROM include data from 12 patients at initial testing and nine patients at follow-up testing. At initial testing, the mean injured side SWA test score was significantly lower than the score on the uninjured side (p = 0.045). Also, the injured side SWA test score significantly increased from initial testing to follow-up testing (p = 0.041). The distribution of SWA test scores is found in
Figure 4 Only 21% of patients achieved the highest score (i.e., “3”) on the injured side at initial testing, whereas 64% achieved the highest score on the injured side at follow-up testing. Effect sizes for the change from initial to follow-up testing did not cross 0 for injured side SWA test score, injured side total arc of motion value, and patient-reported outcome scores. The magnitude of the effect sizes in descending order was ASES score, WOSI score, injured side SWA test score, and injured side total arc of motion value (Table 2).
SWA test was the only clinical test to show significant correlation with ASES and WOSI scores at initial testing (r=0.597 and r=-0.648, respectively; Table 3). The magnitude of the correlations is moderate, and the direction of association is positive for ASES and negative for WOSI, indicating that a higher injured side SWA test score is associated with better patient-reported shoulder function. SWA test score and total arc of motion on the injured side were both associated with WOSI score at follow-up testing (r=-0.611 and r=-0.574, respectively; Table 4). The magnitude of the correlations is moderate, and the direction of associations is negative, indicating that higher values for the injured side SWA test and total arc of motion on are associated with better patient-reported shoulder function. The linear regression model with these clinical tests retained only the injured side SWA test score, and the correlation to WOSI score as indicated in Table 4. In addition, significant positive correlations of a moderate to high magnitude were found among clinical tests at initial testing and follow-up testing.
This study explored the clinical utility of the SWA as a test with a proposed scoring mechanism. This is novel because the SWA has previously been described as an intervention, not as a clinical test. The hypotheses for the study were supported. First, the injured side SWA test score was lower than the uninjured side at initial testing and improved at follow-up testing. Moreover, the injured side SWA test score demonstrated significant associations with ASES score and WOSI score at initial testing and WOSI score at follow-up testing. Injured side values for the other clinical tests (i.e. total arc of motion and external rotation ROM) were not significantly correlated with ASES and WOSI scores at initial testing and total arc of motion was removed from the regression model in favor of the SWA test score for association with WOSI score at follow-up testing. The clinical utility of the SWA test is supported by distinguishing the injured side from the uninjured side and by having stronger associations with patient-reported shoulder function than shoulder mobility tests.
The patient population and the timing of initial and follow-up testing may contribute to the findings of this study. The population for this study was patients with anterior shoulder instability As opposed to passive shoulder range of motion testing that took place in the scapular plane, the SWA test position of combined shoulder abduction and external rotation in the frontal plane could make patients ap-
Table 1. Demographic Information.
Table 2. Values for Clinical Tests and Patient-Reported Outcome Measures.
Rotation ROM (degrees)†
Total Arc of Motion (degrees)
ROM: range of motion
ASES: American Shoulder and Elbow Surgeons Shoulder Assessment Form
WOSI: Western Ontario Shoulder Instability Index
*Value is significantly lower than uninjured side at initial testing (p<0.05)
**Value is significantly higher than initial testing (p<0.05)
†Data available for 12 patients at initial testing and 9 patients at follow-up testing

prehensive of experiencing instability25‑27 and may explain the lower test score on the injured side than the uninjured side at initial testing. Further testing in patient populations with other shoulder conditions is necessary to confirm whether the SWA test discriminates the injured side from the uninjured side. Significant improvement in the SWA test score on the injured side at follow-up testing indicates more body contacts with the wall. It cannot be determined how much of the improvement was the result of increased shoulder external rotation ROM, decreased apprehension, changes in scapular movement and thoracic spine ROM, or improved scapular and rotator cuff muscle strength. At follow-up testing, which was near the end of rehabilitation for the patients, 64% achieved the highest score on the SWA test. The six-week interval between testing time points was intended to allow time for a change in shoulder function and not to coincide with return-to-sport testing. Recovery
Table 3. Correlations Coefficients Among Clinical Tests and Patient-Reported Outcome Measures at Initial Testing.
ROM: range of motion
ASES: American Shoulder and Elbow Surgeons Shoulder Assessment Form
WOSI: Western Ontario Shoulder Instability Index
†Data available for 12 out of 14 patients.
*p<0.05
n.s.=not significant
Table 4. Correlations Coefficients Among Clinical Tests and Patient-Reported Outcome Measures at Follow-up Testing.
ROM: range of motion
ASES: American Shoulder and Elbow Surgeons Shoulder Assessment Form
WOSI: Western Ontario Shoulder Instability Index
†Data available for 9 out of 14 patients.
*p<0.05
n.s.=not significant
time after a shoulder anterior instability event varies in the literature but many athletes return to sport within two to three weeks after injury 28‑30 If testing took place at returnto-sport, it is unknown if the SWA test would show a ceiling effect. Regardless, experts recommend including ROM as a part of upper extremity return-to-sport testing.6
The glenohumeral joint, thoracic spine and scapula make contributions to maximal external rotation of the upper quarter.1 To achieve the highest score on the SWA test, a patient must have the necessary shoulder external rotation ROM, scapular movement, and thoracic extension to contact the entire posterior upper extremity with the wall. At initial testing, five patients achieved 90 degrees or more of external rotation ROM on the injured side, however, none of these patients received the highest possible score on the SWA test, suggesting apprehension or possible limitations at the thoracic spine or with scapular movement. The SWA test may guide the clinician to examine both the thoracic spine and scapular movement to determine limitations in these areas if the patient has 90 degrees or more of shoulder external rotation ROM.
Change in ASES and WOSI scores exceeded thresholds for MCID, demonstrating clinical improvement over the sixweek interval from initial to follow-up testing. The SWA test score demonstrated moderate associations with ASES and WOSI scores at initial testing and WOSI score at follow-
up testing. These findings support the validity of the SWA test as being related to patient-reported shoulder function. It is possible that the SWA test was not associated with ASES score at follow-up testing because ASES score approximated the maximum score (ceiling effect). Additionally, the WOSI has been shown to be more responsive than the ASES in patients with shoulder instability.31‑33 Interestingly, the shoulder mobility tests (total arc of motion and external rotation ROM) did not show association with the patient-reported outcome scores at initial testing, and the association between total arc of motion and WOSI score at follow-up testing was not retained in multivariate analysis. The authors are unaware of any other studies that have examined the association between total arc of motion and patient-reported shoulder function.
The strength of this study is the exploration of the SWA maneuver, commonly used as an intervention, to a novel clinical test with proposed scoring. The SWA test can be performed quickly in the clinic without special equipment and is less burdensome to the clinician than performing individual measurements of shoulder rotational ROM, thoracic posture and mobility, and scapular function. However, this study has limitations that must be acknowledged. First, the sample size is small and was further reduced for the analyses of shoulder external ROM due to missing data. Second, the patient population is limited to those with an-
terior shoulder instability and may not be generalizable to other patient groups with shoulder pain. Third, rehabilitation during the six-week study period was not monitored nor was scapulothoracic function, thoracic spine mobility, or scapular or rotator cuff muscle strength tested. Thus, the changes in the SWA test score cannot be interpreted to have occurred with respect to any clinical intervention or changes at the scapulothoracic joint, thoracic spine, or scapular and rotator cuff muscle strength. Future studies of the SWA test should include assessment of scapular stabilizer and rotator cuff muscle strength. Fourth, follow-up was based on time, not clinical milestones, and return to sport status was not recorded, so extrapolation of the study findings to return-to-sport decision-making is not appropriate. Finally, the position of the head was not standardized during testing. Adding criteria for head position may improve the reproducibility of testing.
The results of this study indicate that the SWA test distinguishes the injured side from the uninjured side, demonstrates a relationship with patient-reported outcome scores, and could augment clinical assessment of shoulder function alongside other shoulder mobility tests. These data provide initial evidence to support further examination of the psychometric properties of the SWA as a clinic test for future inclusion in functional testing batteries.
The authors report no conflicts of interest.
Submitted: February 27, 2024 CDT, Accepted: August 15, 2024 CDT
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Miyashita K, Kobayashi H, Koshida S, Urabe Y Glenohumeral, scapular, and thoracic angles at maximum shoulder external rotation in throwing. Am J Sports Med 2010;38(2):363-368. doi:10.1177/ 0363546509347542
2. Lugo R, Kung P, Ma CB. Shoulder biomechanics. Eur J Radiol 2008;68(1):16-24. doi:10.1016/ j.ejrad.2008.02.051
3. Barrett E, O’Keeffe M, O’Sullivan K, Lewis J, McCreesh K. Is thoracic spine posture associated with shoulder pain, range of motion and function? A systematic review. Man Ther. 2016;26:38-46. doi:10.1016/j.math.2016.07.008
4. Stamm MA, Brahmbhatt PS, Brown SM, Miskimin LC, Mulcahey MK. Evaluating risk factors for biceps tendon injuries in softball players: A systematic review Clin J Sport Med 2023;33(6):623-630. doi:10.1097/JSM.0000000000001153
5. Ellenbecker TS, Roetert EP, Bailie DS, Davies GJ, Brown SW Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc 2002;34(12):2052-2056. doi:10.1097/00005768-200212000-00028
6. Barber P, Pontillo M, Bellm E, Davies G. Objective and subjective measures to guide upper extremity return to sport testing: A modified Delphi survey Phys Ther Sport. 2023;62:17-24. doi:10.1016/ j.ptsp.2023.05.009
7 Wilk KE, Macrina LC, Fleisig GS, et al. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med 2011;39(2):329-335. doi:10.1177/0363546510384223
8. Manske R, Wilk KE, Davies G, Ellenbecker T, Reinold M. Glenohumeral motion deficits: friend or foe? Int J Sports Phys Ther 2013;8(5):537-553.
9. Torres RR, Gomes JL. Measurement of glenohumeral internal rotation in asymptomatic tennis players and swimmers. Am J Sports Med 2009;37(5):1017-1023. doi:10.1177/ 0363546508329544
10. Garrison JC, Cole MA, Conway JE, Macko MJ, Thigpen C, Shanley E. Shoulder range of motion deficits in baseball players with an ulnar collateral ligament tear Am J Sports Med 2012;40(11):2597-2603. doi:10.1177/ 0363546512459175
11. Keller RA, De Giacomo AF, Neumann JA, Limpisvasti O, Tibone JE. Glenohumeral internal rotation deficit and risk of upper extremity injury in overhead athletes: A meta-analysis and systematic review Sports Health 2018;10(2):125-132. doi:10.1177/1941738118756577
12. Gouveia K, Kay J, Memon M, Simunovic N, Ayeni OR. Glenohumeral internal rotation deficit in the adolescent overhead athlete: A systematic review and meta-analysis. Clin J Sport Med 2022;32(5):546-554. doi:10.1097/JSM.0000000000000945
13. Ruotolo C, Price E, Panchal A. Loss of total arc of motion in collegiate baseball players. J Shoulder Elbow Surg 2006;15(1):67-71. doi:10.1016/ j.jse.2005.05.006
14. Rosen M, Meijer K, Tucker S, et al. Shoulder range of motion deficits in youth throwers presenting with elbow pain. Sports Health. 2022;14(4):478-482. doi:10.1177/19417381211036387
15. Galic B. How to do wall angels for strong, painfree shoulders. Livestrong.com. Accessed January 20, 2024. https://www.livestrong.com/article/ 13769150-wall-angels/
16. Patient RM. January 21. https:// www.youtube.com/watch?v=vhFxQbTi9AM
17 [P]rehab. November 24, 2023. https:// www youtube.com/watch?v=mlstZw2dTHU
18. Intelligence B. November 15. https:// www.youtube.com/watch?v=_dweNZfF24s
19. Jensen MP, Turner JA, Romano JM, Fisher LD Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83(2):157-162. doi:10.1016/s0304-3959(99)00101-3
20. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594. doi:10.1067/ mse.2002.127096
21. Goldhahn J, Angst F, Drerup S, Pap G, Simmen BR, Mannion AF. Lessons learned during the crosscultural adaptation of the American Shoulder and Elbow Surgeons shoulder form into German. J Shoulder Elbow Surg. 2008;17(2):248-254. doi:10.1016/j.jse.2007.06.027
22. Kirkley A, Griffin S, McLintock H, Ng L. The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability. The Western Ontario Shoulder Instability Index (WOSI). Am J Sports Med 1998;26(6):764-772. doi:10.1177/03635465980260060501
23. Sullivan GM, Feinn R. Using effect size-or why the P value is not enough. J Grad Med Educ. 2012;4(3):279-282. doi:10.4300/JGME-D-12-00156.1
24. Schober P, Boer C, Schwarte LA. Correlation coefficients: Appropriate use and interpretation. Anesth Analg 2018;126(5):1763-1768. doi:10.1213/ ANE.0000000000002864
25. Olds MK, Ellis R, Parmar P, Kersten P. Who will redislocate his/her shoulder? Predicting recurrent instability following a first traumatic anterior shoulder dislocation. BMJ Open Sport Exerc Med. 2019;5(1):e000447 doi:10.1136/bmjsem-2018-000447
26. Eshoj H, Rasmussen S, Frich LH, Jensen SL, Sogaard K, Juul-Kristensen B. Patients with nonoperated traumatic primary or recurrent anterior shoulder dislocation have equally poor self-reported and measured shoulder function: a cross-sectional study BMC Musculoskelet Disord 2019;20(1):59. doi:10.1186/s12891-019-2444-0
27. Olds M, Ellis R, Parmar P, Kersten P. The immediate and subsequent impact of a first-time traumatic anterior shoulder dislocation in people aged 16-40: Results from a national cohort study. Shoulder Elbow 2021;13(2):223-232. doi:10.1177/ 1758573220921484
28. Buss DD, Lynch GP, Meyer CP, Huber SM, Freehill MQ. Nonoperative management for in-season athletes with anterior shoulder instability Am J Sports Med. 2004;32(6):1430-1433. doi:10.1177/ 0363546503262069
29. Watson S, Allen B, Grant JA. A clinical review of return-to-play considerations after anterior shoulder dislocation. Sports Health. 2016;8(4):336-341. doi:10.1177/1941738116651956
30. Hasebroock AW, Brinkman J, Foster L, Bowens JP Management of primary anterior shoulder dislocations: a narrative review Sports Med Open 2019;5(1):31. doi:10.1186/s40798-019-0203-2
31. Hajewski CJ, Glass NA, Westermann RW, Bollier M, Wolf BR, Hettrich C. Performance of the PROMIS after operative interventions for shoulder instability Orthop J Sports Med. 2019;7(5):2325967119846920. doi:10.1177/2325967119846920
32. Kemp KA, Sheps DM, Beaupre LA, Styles-Tripp F, Luciak-Corea C, Balyk R. An evaluation of the responsiveness and discriminant validity of shoulder questionnaires among patients receiving surgical correction of shoulder instability. Sci World J. 2012;2012:410125. doi:10.1100/2012/410125
33. Kirkley A, Griffin S, Dainty K. Scoring systems for the functional assessment of the shoulder. Arthroscopy 2003;19(10):1109-1120. doi:10.1016/ j.arthro.2003.10.030

Williams CL, Curfman SE, Lindsley SR, Falyar CR, McConnell RC. Inferior-Medial Dry
at the Thoracolumbar Junction: A Cadaveric Study. IJSPT. Published online October 1, 2024:1238-1243. doi:10.26603/001c.123477
Christi L. Williams1a , Sue E. Curfman1 , Stacey R. Lindsley1 , Christian R. Falyar2 , Ryan C. McConnell1
1 Physical Therapy, Belmont University, 2 Nurse Anesthesia, Middle Tennessee School of Anesthesia
Keywords: cadaver, dry needling, multifidus, safety considerations, ultrasound https://doi.org/10.26603/001c.123477
Background
Dry needling (DN) has emerged as a popular therapeutic intervention for managing musculoskeletal pain. While major adverse events are generally rare, those that have been reported in vulnerable areas such as the spine and thorax can be serious and warrant further investigation regarding safe techniques in and around these areas.
Purpose
The purpose of this study was to reproduce the methods employed by Williams et al. but with an inferior-medial multifidus DN technique to determine if a dry needle can penetrate the ligamentum flavum (LF) and breach the spinal canal at the thoracolumbar junction.
Study Design
Descriptive Cadaveric study
Methods
The procedure was performed on a cadaver in the prone position. The needle was advanced under ultrasound guidance to determine if a 0.30 x 40 mm dry needle inserted lateral to the spinous process of T12 and directed inferior-medially could penetrate the LF and enter the spinal canal.
Results
A 0.30 x 40 mm dry needle inserted 1.9 cm lateral to the spinous process of T12 was able to traverse the space between the vertebral laminae of T12 and L1, penetrate the LF, and enter the spinal canal with an inferior-medial needle angulation of 33-degrees medial and 18-degrees inferior
Conclusion
The results of this study demonstrate the feasibility of a dry needle entering the spinal canal at the thoracolumbar junction using an inferior-medial technique. These findings support the potential role of ultrasound guidance in the training and clinical practice of DN, especially in regions where safety issues have been documented.
Level of Evidence
Level IV
Corresponding Author:
Christi L. Williams
School of Physical Therapy, Belmont University Nashville 37212, USA 615-260-0940 christi.williams@belmont.edu a
Dry needling (DN) has emerged as a popular therapeutic intervention for managing musculoskeletal pain, with more than half of physical therapists surveyed using DN in the treatment of their patients.1 Numerous authors have reported DN as an effective tool when used in conjunction with other interventions to manage back pain.2‑6 While major adverse events due to DN are reported to be rare,7 those that have been reported to occur from DN around the spine and thorax can be serious, and include pneumothorax, quadriparesis related to acute cervical epidural damage, and hemiplegia related to subdural or epidural hematomas.8‑12 In addition, the lack of a standardized method for reporting adverse events likely leads to underreporting, which suggests there may be more adverse events occurring than those currently documented in the literature.1,13
Dry needling of the multifidi is a common intervention for the treatment of back pain and is one that has generally been regarded as a safe technique given that the bony backdrop of the lamina is considered to be protective. While using a bony backdrop, such as the lamina, is thought to decrease the risk of inadvertently entering other unintended structures, this DN strategy for the multifidi presumes the needle tip will not land between adjacent vertebral lamina, where it could potentially pierce through the ligamentum flavum (LF) and enter the spinal canal. Despite this presumption, there is no specific DN technique that has been universally accepted as being the safest approach to ensure the needle successfully reaches the protective bony backdrop of the lamina.
Reported techniques for DN the multifidi suggest that needles should be placed 1-2 cm lateral to the lumbar spinous process and directed medially or inferior-medially until the needle reaches the lamina.14‑20 Both the inferior and the medial needle orientation documented among the inferior-medial techniques vary considerably, ranging between 15° and 45°.14,15,17‑21 Williams et al. demonstrated that a 0.30 x 50 mm needle can penetrate the LF and enter the spinal canal at the thoracolumbar junction with a needle inserted approximately 1.0 cm lateral to the spinous process, directed in a posterior-anterior orientation, and inclined medially at a 22-degree angle from vertical.22 The purpose of this study was to reproduce the methods employed by Williams et al. but with an inferior-medial multifidus DN technique to determine if a dry needle can penetrate the LF and breach the spinal canal at the thoracolumbar junction.
The study was performed on a 77-year-old female, freshfrozen, lightly-fixed cadaver at Middle Tennessee School of Anesthesia. Ultrasound scans were performed by a certified registered nurse anesthetist with over 20 years of diagnostic ultrasound imaging experience and 15 years of experience performing and teaching regional anesthesia, including ultrasound-guided spinal anesthesia procedures.
The fresh/lightly embalmed cadaver was received through the Willed Body Program at The University of North Texas Health Science Center Exemption from Institutional Review Board approval was granted by Advarra IRB (Pro00070509).
The cadaver was placed in the prone position with the lumbar spine in a relatively neutral position. A Sonosite Edge II ultrasound system with an rC60xi 5-2 MHz curvilinear array transducer (Bothell, WA) was placed in a parasagittal orientation with the orientation indicator facing cephalad. The sacrum, L5-S1 interspace, and L5 spinous process were identified. The transducer was moved cephalad until the interspace between T12 and L1 was identified. A DBCTM ProMaxx 0.30 x 40 mm dry needle was inserted approximately one finger-breadth lateral to the spinous process of T12 and directed in an inferior-medial angulation toward midline while being visualized by ultrasound. If the needle reached the lamina, it was left in place, and another needle was placed in very close proximity The process was repeated until a needle breached the LF and entered the spinal canal. After the final attempt, measurements were taken to determine the distance along the skin between the needle and the spinous processes and the medial and inferior needle angulations for the needle which entered the spinal canal.
A range of needle lengths between 40 mm and 100 mm have been described when studying DN techniques in the thoracic and lumbar regions, with 50 mm and 60 mm being the most commonly utilized in clinical practice, depending on the spinal location.14,16‑21,23 Dry needle length is selected based on the size of the patient’s soft tissue and musculature.14,24 In the previous study by Williams et al., a 50mm needle was used,22 whereas this study utilized a shorter needle (40 mm).
A 0.30 x 40 mm dry needle was able to traverse the space between the vertebral laminae of T12 and L1, penetrate the LF, and enter the spinal canal on the fourth attempt. The needle that entered the spinal canal was located 1.9 cm lateral to the spinous process of T12. More specifically, the insertion point was approximately 4.3 mm inferior to the center of the spinous process of T12, the medial angulation of the needle was 33-degrees from vertical (Figure 1), and the inferior angulation of the needle was 18-degrees (Figure 2).
The purpose of this study was to reproduce the methods employed by Williams et al. but with an inferior-medial multifidus DN technique to determine if a dry needle could penetrate the LF and breach the spinal canal at the thoracolumbar junction. The results of this study corroborate a previous finding that a dry needle can enter the spinal canal at the thoracolumbar junction using a medial technique, and also when using an inferior-medial technique.22 The thoracolumbar junction is an area of complex anatomy and an area of presumed increased risk and therefore, it may


be important for physical therapists to consider the overall safety of DN techniques when treating this area of the spine.
This study is the second to use ultrasound guidance to document dry needles entering the spinal canal at the thoracolumbar junction when using techniques outlined in the literature for targeting the multifidi. While other healthcare professions utilize ultrasound guidance as a standard tool for training and practicing needle techniques, ultrasound guided DN during training courses for physical therapists is not common practice, nor is ultrasound guided DN routinely used in clinical physical therapist practice in the United States.25 Using ultrasound guidance during DN training may prove valuable, especially in light of the poor reliability and validity of palpation-based methods seen as cornerstone in DN training.26,27 Ultrasound guidance of-
fers a potential solution by providing enhanced visualization and accuracy. Additionally, using ultrasound during DN training may promote trainee’s tactile sensation and spatial awareness by allowing trainees to visualize anatomical structures in real-time to correlate tactile sensations as different tissue layers and structures are engaged. Given the fact that some physical therapists are now being trained in ultrasound imaging techniques in entry-level physical therapy programs,28 as well as dry needling,29 it stands to reason that ultrasound guided DN, especially in areas of increased risk, may be an important consideration in future training and clinical use to improve patient safety
There are a number of procedural considerations and limitations in this study First, it is important to recognize that this study did not attempt to determine the likelihood of penetrating the spinal canal during the clinical use of DN, but merely explored the possibility of a dry needle entering the spinal canal when using a technique commonly described in the literature for the multifidi. Therefore, specific needle locations relative to the spinous process and needle angulations are intended to help with replication in future studies, not to be extrapolated as safe/unsafe zones for DN to be performed. Given that the determination of the center of the spinous process was based on palpation and neither imaging nor dissection were used to confirm a true center of the spinous process, generalization of unsafe zones relative to the spinous process would be speculative and inappropriate.
Second, this study was a feasibility study using a 77-year-old, fresh-frozen, lightly-fixed, female cadaver It is plausible that differences in tissue turgor in cadavers versus living subjects, as well as the age of the donor may have impacted the outcomes. Several authors have documented that the thickness and stiffness of the LF increase linearly with the degree of disc degeneration30 and age31 and can also differ between various lumbar segments.32 The donor in this study was 77-years-old and thus, similar to 90% of individuals 65 years and older, very likely had disc degeneration.33 The age-related changes in the donor used in this study may have actually been protective; however, the dry needle was still able breach the spinal canal. Studies using a larger sample size may have resulted in different outcomes if performed in vivo and with more variability in subjects.
The results of this study demonstrate the feasibility of a dry needle entering the spinal canal at the thoracolumbar junction using an inferior-medial technique for the multifidi. These findings support the potential role of ultrasound guidance in the training and clinical practice of DN, especially in regions where safety issues have been documented. Evaluating the safety profiles of DN techniques currently being used, exploring the feasibility and potential impact of ultrasound guidance during training and clinical practice, and examining the clinical outcomes associated with ultrasound-guided dry needling are important next steps.
Submitted: May 15, 2024 CDT, Accepted: August 12, 2024 CDT
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Gattie E, Cleland JA, Snodgrass S. A survey of American physical therapists’ current practice of dry needling: Practice patterns and adverse events. Musculoskelet Sci Pract 2020;50:102255. doi:10.1016/ j.msksp.2020.102255
2. Liu L, Huang QM, Liu QG, et al. Evidence for dry needling in the management of myofascial trigger points associated with low back pain: A systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99(1):144-152.e2. doi:10.1016/ j.apmr.2017.06.008
3. Rajfur J, Rajfur K, Kosowski Ł, et al. The effectiveness of dry needling in patients with chronic low back pain: a prospective, randomized, singleblinded study. Sci Rep. 2022;12(1):15803. doi:10.1038/s41598-022-19980-1
4. Hu HT, Gao H, Ma RJ, Zhao XF, Tian HF, Li L. Is dry needling effective for low back pain?: A systematic review and PRISMA-compliant meta-analysis. Medicine 2018;97(26):e11225. doi:10.1097/ MD.0000000000011225
5. Lara-Palomo C, Gil-Martínez I, Lopez-Fernandez D, Gonzalez G, De Los Ángeles Querol-Zaldívar LM, Castro-Sanchez M. Efficacy of dry needling for chronic low back pain: A systematic review and metaanalysis of randomized controlled trials. Altern Ther Health Med. 2023;29(8).
6. Sánchez-Infante J, Navarro-Santana MJ, BravoSánchez A, Jiménez-Diaz F, Abián-Vicén J. Is dry needling applied by physical therapists effective for pain in musculoskeletal conditions? A systematic review and meta-analysis. Phys Ther 2021;101(3). doi:10.1093/ptj/pzab070
7. Boyce D, Wempe H, Campbell C, et al. Adverse events associated with therapeutic dry needling. Int J Sports Phys Ther. 2020;15(1):103-113. doi:10.26603/ ijspt20200103
8. Patel N, Patel M, Poustinchian B. Dry needlinginduced pneumothorax. J Am Osteopath Assoc. 2019;119(1):59-62. doi:10.7556/jaoa.2019.009
9. Lee JH, Lee H, Jo DJ. An acute cervical epidural hematoma as a complication of dry needling. Spine 2011;36(13):E891-E893. doi:10.1097/ BRS.0b013e3181fc1e38
10. Berrigan WA, Whitehair CL, Zorowitz RD Acute spinal epidural hematoma as a complication of dry needling: A case report. PM R 2019;11(3):313-316. doi:10.1016/j.pmrj.2018.07.009
11. Uzar T, Turkmen I, Menekse EB, Dirican A, Ekaterina P, Ozkaya S. A case with iatrogenic pneumothorax due to deep dry needling. Radiol Case Rep 2018;13(6):1246-1248. doi:10.1016/ j.radcr.2018.08.019
12. Ji GY, Oh CH, Choi WS, Lee JB. Three cases of hemiplegia after cervical paraspinal muscle needling. Spine J 2015;15(3):e9-13. doi:10.1016/ j.spinee.2014.11.007
13. Kearns GA, Brismée JM, Riley SP, Wang-Price S, Denninger T, Vugrin M. Lack of standardization in dry needling dosage and adverse event documentation limits outcome and safety reports: a scoping review of randomized clinical trials. J Man Manip Ther. 2023;31(2):72-83. doi:10.1080/ 10669817.2022.2077516
14. Loizidis T, Nikodelis T, Bakas E, Kollias I. The effects of dry needling on pain relief and functional balance in patients with sub-chronic low back pain. J Back Musculoskelet Rehabil 2020;33(6):953-959. doi:10.3233/BMR-181265
15. Hannah MC, Cope J, Palermo A, Smith W, Wacker V Comparison of two angles of approach for trigger point dry needling of the lumbar multifidus in human donors (cadavers). Man Ther 2016;26:160-164. doi:10.1016/j.math.2016.08.008
16. Clark NG, Hill CJ, Koppenhaver SL, Massie T, Cleland JA. The effects of dry needling to the thoracolumbar junction multifidi on measures of regional and remote flexibility and pain sensitivity: A randomized controlled trial. Musculoskel Sci Pract 2021;53:102366. doi:10.1016/j.msksp.2021.102366
17. Koppenhaver SL, Walker MJ, Su J, et al. Changes in lumbar multifidus muscle function and nociceptive sensitivity in low back pain patient responders versus non-responders after dry needling treatment. Man Ther 2015;20(6):769-776. doi:10.1016/ j.math.2015.03.003
18. Puentedura EJ, Buckingham SJ, Morton D, Montoya C, Fernandez de Las Penas C. Immediate changes in resting and contracted thickness of transversus abdominis after dry needling of lumbar multifidus in healthy participants: A randomized controlled crossover trial. J Manip Physiol Ther 2017;40(8):615-623. doi:10.1016/j.jmpt.2017.06.013
19. Wang-Price SS, Etibo KN, Short AP, Brizzolara KJ, Zafereo JA. Validity and reliability of dry needle placement in the deep lumbar multifidus muscle using ultrasound imaging: an in-vivo study. J Man Manip Ther 2022;30(5):284-291. doi:10.1080/ 10669817.2022.2051239
20. Koppenhaver SL, Walker MJ, Smith RW, et al. Baseline examination factors associated with clinical improvement after dry needling in individuals with low back pain. J Orthop Sports Phys Ther. 2015;45(8):604-612. doi:10.2519/jospt.2015.5801
21. Wang-Price S, Zafereo J, Couch Z, Brizzolara K, Heins T, Smith L. Short-term effects of two deep dry needling techniques on pressure pain thresholds and electromyographic amplitude of the lumbosacral multifidus in patients with low back pain - a randomized clinical trial. J Man Manip Ther 2020;28(5):254-265. doi:10.1080/ 10669817.2020.1714165
22. Williams CL, Falyar CR, McConnell RC, Lindsley S. Safety considerations when dry needling the multifidi in the thoracolumbar region: A cadaveric study Int J Sports Phys Ther 2023;18(6). doi:10.26603/001c.89663
23. Rainey CE. The use of trigger point dry needling and intramuscular electrical stimulation for a subject with chronic low back pain: A case report. Int J Sports Phys Ther. 2013;8(2):145-161.
24. Fernanfernández-De-Las-Peñas C, Layton M, Dommerholt J. Dry needling for the management of thoracic spine pain. J Man Manip Ther 2015;23(3):147-153. doi:10.1179/ 2042618615Y.0000000001
25. Yildizgoren MT, Bagcier F. Obtaining local twitch response with ultrasound-guided dry needling. Med Ultrason 2023;25(3):362-363. doi:10.11152/mu-4199
26. Nolet PS, Yu H, Côté P, et al. Reliability and validity of manual palpation for the assessment of patients with low back pain: a systematic and critical review. Chiropr Man Ther. 2021;29(1):33. doi:10.1186/ s12998-021-00384-3
27 Alexander N, Rastelli A, Webb T, Rajendran D The validity of lumbo-pelvic landmark palpation by manual practitioners: A systematic review. Int J Osteopath Med 2021;39:10-20. doi:10.1016/ j.ijosm.2020.10.008
28. Whittaker JL, Ellis R, Hodges PW, et al. Imaging with ultrasound in physical therapy: What is the PT’s scope of practice? A competency-based educational model and training recommendations. Br J Sports Med 2019;53(23):1447-1453. doi:10.1136/ bjsports-2018-100193
29. Matthews L, Ford G, Schenk R, Ross M, Donnelly J. Dry needling curricula in entry-level education programs in the United States for physical therapists. J Man Manip Ther. 2021;29(2):83-91. doi:10.1080/ 10669817.2020.1813471
30. Yabe Y, Hagiwara Y, Tsuchiya M, et al. Factors associated with thickening of the ligamentum flavum on magnetic resonance imaging in patients with lumbar spinal canal stenosis. Spine 2022;47(14):1036-1041. doi:10.1097/ BRS.0000000000004341
31. Mihara A, Nishida N, Jiang F, et al. Tensile test of human lumbar ligamentum flavum: Age-related changes of stiffness. Appl Sci 2021;11(8):3337 doi:10.3390/app11083337
32. Safak AA, Is M, Sevinc O, et al. The thickness of the ligamentum flavum in relation to age and gender Clin Anat 2010;23(1):79-83. doi:10.1002/ca.20883
33. Hicks GE, Morone N, Weiner DK. Degenerative lumbar disc and facet disease in older adults: prevalence and clinical correlates. Spine 2009;34(12):1301-1306. doi:10.1097/ BRS.0b013e3181a18263

Mostagi FQ, Silva PA, Munaro GR, et al. Physical and Muscular Performance in a Professional Soccer Player with a Posterior Cruciate Ligament Injury Following an Isokinetic Exercise Program: A Case Report. IJSPT. Published online October 1, 2024:1244-1254. doi:10.26603/001c.123471
Fernanda QRC Mostagi1 , Pedro AC Silva1 , Giovana R Munaro1 , Raiane G Marcato1 , Daniel B Nampo1 , Gabriel F Santiago1 , Karen Obara1 , Jefferson R Cardoso1a
1 Laboratory of Biomechanics and Clinical Epidemiology, PAIFIT Research Group, Universidade Estadual de Londrina
Keywords: posterior cruciate ligament, dynamometer, knee, muscle strength, torque https://doi.org/10.26603/001c.123471
The comprehensive treatment for an athlete who sustains a complete posterior cruciate ligament (PCL) injury remains unclear. The purpose of this case report is to describe the effects of an isokinetic exercise program on muscle performance and physical function in a professional soccer player with a PCL injury
Study Design
Case Report
Case Description
A 23-year-old male professional soccer player injured his right knee (non-dominant) during a soccer match, with magnetic resonance imaging confirming a complete PCL rupture. The athlete completed 23 sessions of isokinetic treatment over nine weeks to improve physical function and muscle performance. The concentric mode was used to evaluate quadriceps and hamstrings performance isokinetically at angular velocities of 60 °/s, 120 °/s, and 300 °/s. The LEFS questionnaire was used to evaluate physical function. The assessment occurred before starting the treatment and at the end of nine weeks. An athlete with similar anthropometric characteristics was invited to participate and serve as a control, in order to better understand the athlete’s assessment results.
After nine weeks, peak torque normalized to body mass (PT/BM) improved to 4.0 N.m/kg for knee extensors (control: 3.6 Nm/kg) and 2.3 N.m/kg for knee flexors (control: 1.9 Nm/ kg) at 60 °/s. This increase in PT was reflected in the hamstrings-to-quadriceps (H:Q) ratio post-treatment (57 %). At the end of treatment, the athlete returned to sports activities with 98.7 % restored physical function as measured by the LEFS (Score: 79 points).
Discussion
The results demonstrated that the isokinetic treatment improved knee functional capacity, with increased PT/BM for knee extensors and flexors and enhanced torque-holding capacity, indicating improved muscle performance.
Corresponding Author:
Prof. Jefferson Rosa Cardoso, PT, PhD Laboratory of Biomechanics and Clinical Epidemiology, PAIFIT Research Group Universidade Estadual de Londrina Av. Robert Koch, 60 86038-440 – Londrina, PR, Brazil jeffcar@uel.br a
The posterior cruciate ligament (PCL) is one of the main knee stabilizers, primarily resisting posterior translation of the tibia relative to the femur. Additionally, the PCL acts as a stabilizer and prevents excessive tibiofemoral rotation, particularly between 60° and 120° of flexion.1,2 Composed of two bundles (anterolateral and posteromedial), the PCL plays a crucial stability role in knee flexion and extension, especially in movements that require a lot of stability, such as jumping and pivoting. While traditional literature demonstrates that these two bundles function independently, recent research suggests that they act synergistically.2,3
PCL injuries are often severe and have devastating longterm effects, such as degenerative changes in the medial and patellofemoral compartments and impaired lower extremity function. Isolated PCL injuries are rare, with 60–95% of cases involving capsuloligamentous injuries.4‑8 Common mechanisms of PCL injury involve external trauma resulting from a posteriorly directed force on the anterior region of the proximal tibia with the knee flexed, often referred to as a “dashboard injury” resulting from motor vehicle accidents. In sports, isolated PCL injuries may result from a direct blow to the anterior tibia or a fall onto the knee with the foot in a plantar-flexed position. Noncontact mechanisms, such as hyperflexion or hyperextension, are less common.8‑11
Diagnosis of a PCL injury relies on clinical history, physical examination, and imaging tests. After inspection, palpation, range of motion (ROM) assessment, neurovascular examinations, and provocative tests are used to evaluate the PCL integrity or any concomitant injuries. The combination of clinical tests, injury mechanisms, and symptoms such as pain, swelling, and joint instability is crucial for establishing a PCL injury diagnosis.8,11
Several treatment options have been described in the literature, enabling an individualized approach based on lesion patterns (acute or chronic), treatment adherence, and patient demands. The ideal treatment for PCL injuries to restore joint stability, promote joint functionality, and return to activities remains unclear in the scientific literature. Conservative treatment, typically recommended for acute and isolated PCL injuries (Grades I and II), involves using a brace for immobilization, controlling weight-bearing and swelling, restoring ROM, and recovering muscle strength.8,12‑14
Surgical intervention is considered for symptomatic patients with complete injuries (Grade III) who do not obtain satisfactory results in conservative treatment, those with a high degree of joint instability, or those with associated intra-articular and capsuloligamentous injuries.13‑15 Postsurgical complications may occur in up to 53% of patients and can include intra-articular hematoma, infection, reflex sympathetic dystrophy, anterior knee pain, neurovascular
injuries, and graft failure, potentially resulting in pain and instability.15‑17
Low risk of bias studies that investigate the effects of different treatments of PCL injuries are limited. However, whether post-surgery or as part of a conservative protocol, the approach focuses specifically on increasing the quadriceps muscle strength and restoring joint stability. Exercises based on quadriceps strengthening are the focus of treatment to maintain dynamic stabilization of the knee, avoiding tibial posteriorization.13,18
Currently, the isokinetic dynamometer is considered the gold standard resource for assessing muscle performance and could be considered for treating lower-extremity injuries, especially knee injuries.19,20 The isokinetic dynamometer allows the evaluation of parameters, such as muscle power, total work, and peak torque normalized by body mass (PT/BM). Isokinetic exercises are characterized by using a constant velocity that accommodates muscle work throughout the ROM.21,22
Another analysis that can be performed using isokinetic data is to divide the ROM into three phases: acceleration (A), load range (LR), and deceleration (D). LR is the phase with a sustained, set specific velocity. These three phases can provide some information, such as reaction time and ability to maintain velocity. These data can increase the clinical evaluation and implementation of specific protocols to optimize the treatment.23
Currently, no studies have investigated protocols using an isokinetic dynamometer for muscle strengthening as a form of conservative treatment in individuals with PCL injuries. Therefore, the primary purpose of this case report is to describe the effects of isokinetic exercises on the muscle performance and physical function of a soccer player with PCL injury and the second purpose is to observe the results compared to a matched control.
A 23-year-old male professional soccer player with a body mass index (BMI) of 22.1 kg/m², who plays as a left-back defensive specialist, was investigated in this case report. The participant reported spraining his non-dominant right knee while changing direction when running backward. Magnetic resonance imaging detected a Grade III PCL injury, accompanied by a partial rupture of the medial collateral ligament and a medial meniscal injury (Figure 1).
Preoperatively, the subject underwent a course of nonoperative management with a team of physical therapists, which was later deemed unsuccessful, leading to a recommendation for surgical consultation. According to the soccer team physical therapist and medical department, the initial and second phases of treatment (six weeks) were administered satisfactorily. The interventions included passive and active knee mobility exercises, quadriceps reedu-
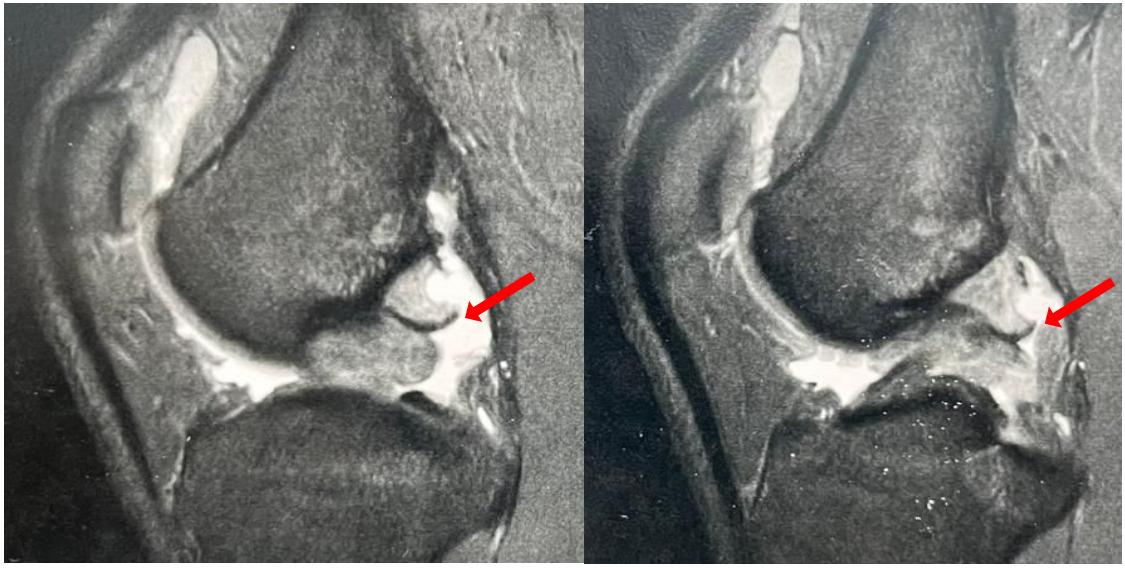
cation exercises (with or without neuromuscular electrical stimulation [NMES]), proximal hip strengthening exercises, bracing, weight-bearing precautions during gait, and cryotherapy However, when progressing to functional exercises, strengthening, endurance, and neuromuscular control activities, the subject reported pain, instability, and a return of swelling, which hindered his treatment progress and return to sports. Consequently, surgical reconstruction and meniscal repair were recommended. Due to the risks associated with surgery and potential for complications, the subject opted for additional conservative treatment. Guided by the medical team, he was referred to the Laboratory of Biomechanics and Clinical Epidemiology at the University Hospital (Health Sciences Center) for a muscle performance assessment and to implement an innovative treatment that focused on increasing muscle strength.
The participants (the subject and a matched control) signed informed consent forms, and the study was approved by the IRB (#00768812.0.5231). Using the unaffected lower limb after ligament injuries as a control may have limitations, since muscle changes are not limited to the injured limb. Given this, another athlete from the same team, with similar anthropometric characteristics, was invited to participate and serve as a control for data analysis.
The initial assessment consisted of a medical history followed by a physical examination, and a patient-reported outcome measure (PROM) to assess physical function. Two assessments were conducted pre- and post-treatment. The pre-treatment assessment occurred five months after the initial injury
The anthropometric characteristics of the subject were as follows: age, 23 years; weight, 70 kg; height, 178 cm; and
BMI, 22.1 kg/m2 , and that of the control athlete were 21 years, 70 kg, 185 cm, and 20.8 kg/m2 , respectively (used exclusively to compare the isokinetic performance).
The physical examination included the ROM, specific orthopedic tests (quadriceps active test, posterior drawer test, and posterior sag sign), and an examination muscle performance.11 The active flexion ROM was 120° and 0° extension. All specific orthopedic tests (quadriceps active test, posterior drawer test, and posterior sag sign) were positive. To assess muscle performance, the Biodex System 4® isokinetic dynamometer (Biodex Medical System Inc., Shirley, NY) was used in the concentric mode at angular velocities of 300°/s, 120°/s, and 60°/s, with a rest time of 90 s between each series. Finally, the Lower Extremity Functional Scale (LEFS) was chosen as a patient reported outcome measure. This instrument was used because of the absence of a specific PROM for PCL injury This questionnaire consists of 20 items with responses from 0 to 4 points, with a maximum score of 80 points. The higher the score obtained, the better the participant’s physical function. The cut-off for clinically meaningful improvement is 11 (area under the receiver-operator curve, 0.96; 95% confidence interval [0.88;0.99].24
Before the isokinetic test, a warm-up was performed on an ergometric bicycle for 10 min at a velocity of 30 km/h.25 The subject was positioned, seated on the dynamometer and stabilized by belts around his trunk, thighs, and ankle ipsilateral to the limb to be tested. The dynamometer axis was aligned with the lateral femoral condyle, and the ankle pad was positioned just above the medial malleolus. All calibration and gravity correction procedures adhered to the manufacturer’s instruction manual.26 The subject per-
formed repetitions at each of the test velocities for familiarization prior to performing the test.
The subject was instructed to use maximum force during all repetitions, and verbal encouragement and visual feedback were provided. A coefficient of variation of < 10% for each series was considered acceptable, and a sampling frequency of 100 Hz was adopted.27 The results were presented compare involved, noninvolved, pre- and post-treatment, and are also compared to results from the control. Variables including peak torque (PT), peak torque normalized to body mass (PT/BM), angle of peak torque, and hamstring/quadriceps (H:Q) ratio were evaluated. The H:Q ratio was calculated by dividing the peak torque of the flexor by the extensor at 60°/s. A Matlab® program was used to analyze the percentage of LR according to the pre-stipulated ROM (0–90°), and the isokinetic variables were calculated during the sustained velocity phase (LR).28‑30
Qualitative data were evaluated using 3D surface maps (Isomaps). The map was created using a Matlab® mathematical algorithm program, compiling the repetitions at each velocity based on the phase duration. The algorithm estimated the intrinsic geometry considering the torque (zaxis), joint angle (x-axis), and angular velocity (y-axis) in the same time interval. The z-axis defined the height of the map in relation to the force intensity, whereas the x- and yaxes formed the surface boundaries. Surface maps allow observation of the interaction between torque, velocity, and ROM. Three-dimensional surface map (3DTAV) analysis can help interpret isokinetic results and can be used to characterize muscle performance.29
Taking into account the history of the injury and data from the physical and functional examination, associated with the fact that the traditional conservative treatment did not achieve the expected result, an innovative treatment, based on isokinetic exercises, was proposed as the subject chose to decline surgical treatment.
The program consisted of 23 sessions over nine weeks. Each session was divided into a warm-up period (initially on an ergometric bicycle and, after the 6th week, on the dynamometer), followed by strengthening exercises in the isokinetic dynamometer, according to the weekly program stipulated based on the evolution of clinical signs presented by the subject, finishing with lower limb stretching exercises (Table 1). The strengthening exercises were performed only on the injured limb.
The percentage of sustained velocity (LR) based on prestipulated ROM, ROM, peak torque values normalized by body mass (PT/BM), and angle of PT (AngPT) are described in Table 2 For knee extension, PT/BM increased from 2.8 to 4 Nm/kg at 60°/s (control: 3.6 Nm/kg), from 2.0 to 3.4 Nm/ kg at 120°/s (control: 2.9 Nm/kg), and from 1.5 to 2.0 Nm/ kg at 300°/s (control: 1.9 Nm/kg). For knee flexion, PT/BM increased from 1.3 to 2.3 Nm/kg at 60°/s (control: 1.9 Nm/
kg), from 1.6 to 2.1 Nm/kg at 120°/s (control:1.0 Nm/kg), and from 1.1 to 1.3 Nm/kg at 300°/s (control:1.2 Nm/kg).
Initially, the H:Q ratio for the affected limb was 69%, compared to 51% for the noninvolved limb. After the treatment program, the H:Q ratios improved to 57% for the affected limb and 46% for the unaffected limbs. The patient scored 71 points on the LEFS questionnaire in the pretreatment assessment, indicating 88.7% lower-limb function. At the end of the treatment program, the score improved to 79 points, reflecting 98.7% of physical function.
Figure 2 shows the 3DTAV of the affected knee extension compared to the control. The 3DTAV shows the patient’s improved ability to generate torque after the treatment program, exceeding that of the control athlete (color intensity is proportional to each surface in the entire ROM, with light gray/blue representing less torque).
Muscle strength measurement is crucial for evaluating and predicting muscle condition, alongside functional capacity Studies support this concept, with isokinetic peak torque assessment being one of the most widely applied methods for evaluating lower extremity muscle strength in soccer players.31‑33
To achieve satisfactory outcomes in both post-surgical and conservative treatments, recovery of quadriceps strength is crucial. Furthermore, knee stability during highperformance activities is vital to prevent posterior displacement of the tibia and mechanical stress on the PCL.13,18,34, 35
This case report evaluated the effects of conservative treatment program, incorporating isokinetic exercises, on muscle performance and physical function in a soccer player with a PCL injury Results indicated that for knee extension, PT/BM increased from 2.6 to 4 Nm/kg at 60°/s (control: 3.6 Nm/kg), from 2.0 to 3.4 Nm/kg at 120°/s (control: 2.9 Nm/kg), and from 1.5 to 2.0 Nm/kg at 300°/s (control: 1.9 Nm/kg). These values indicate a 42% increase in extensor torque generation at 60°/s. For knee flexion, PT/ BM increased from 1.8 to 2.3 Nm/kg at 60°/s, from 1.6 to 2.1 Nm/kg at 120°/s, and from 1.1 to 1.3 Nm/kg at 300°/s. Comparative studies have shown that isokinetic strength performance profiles vary among elite soccer players based on field positions. For example, Śliwowski et al. indicated that the PT/BM of extensors at 60°/s for external defenders was 3.3 Nm/kg, while Delvaux et al. reported an average of 2.93 Nm/kg at 60°/s for quadriceps PT/BM in professional soccer players.31,36
The increased peak torque values can be attributed to the fact that isokinetic exercise is a muscle-strengthening modality that enables the development of maximal muscle tension throughout the ROM at constant velocity, thus recruiting a large number of muscle fibers, potentially requiring greater muscle performance compared to other strengthening modalities.37‑39
The conventional H:Q ratio measured at an angular velocity of 60°/s in elite soccer players has been reported in several studies and has been used as a criterion for mus-
Table 1. Treatment Program.
Week
Week 1 and 2 (sessions 1 - 5)
Cycle ergometer Isokinetic Stretching
Week 3 (sessions 6 - 8)
Week 4 (sessions 9 - 11)
Week 5 (sessions 12 -14)
Week 6 (sessions 15 - 17)
Week 7 (sessions 18 - 19)
Weeks 8 and 9 (sessions 20 - 23)
Cycle ergometer Isokinetic Stretching
Cycle ergometer Isokinetic Stretching
Cycle ergometer Isokinetic Stretching
Isokinetic warm up Isokinetic Stretching
Isokinetic warm up Isokinetic Stretching
Isokinetic warm up Isokinetic Stretching
% percentage; °/s: degree per second; and PT: peak torque.
Velocity of 30 km/h - 10 min.
Isokinetic Protocol
60% of PT at 300°/s - 3 sets x 25 reps
60% of PT at 120°/s - 4 sets x 15 reps
60% of PT at 60°/s - 3 sets x 8 reps
Hamstring, Iliopsoas, and Rectus Femoris stretching - 2 x 30 seconds
Velocity of 30 km/h - 10 min.
70% of PT at 300°/s - 3 sets x 25 reps
70% of PT at 120°/s - 4 sets x 15 reps
70% of PT at 60°/s - 3 sets x 8 reps
Hamstring, Iliopsoas, and Rectus Femoris stretching - 2 x 30 seconds
Velocity of 30 km/h - 10 min.
75% of PT at 300°/s - 3 sets x 25 reps
70% of PT at 120°/s - 4 sets x 15 reps
70% of PT at 60°/s - 3 sets x 8 reps
Hamstring, Iliopsoas, and Rectus Femoris stretching - 2 x 30 seconds
Velocity of 30 km/h - 10 min.
80% of PT at 300°/s - 3 sets x 25 reps
75% of PT at 120°/s - 4 sets x 15 reps
75% of PT at 60°/s - 3 sets x 8 reps
Hamstring, Iliopsoas, and Rectus Femoris stretching - 2 x 30 seconds
300°/s - 3 sets x 25 reps
80% of PT at 120°/s - 3 sets x 15 reps
80% of PT at 60°/s - 3 sets x 8 reps
Hamstring, Iliopsoas, and Rectus Femoris stretching - 2 x 30 seconds
300°/s - 3 sets x 25 reps
80% of PT at 120°/s - 3 sets x 15 reps
85% of PT at 60°/s - 3 sets x 8 reps
Hamstring, Iliopsoas, and Rectus Femoris stretching - 2 x 30 seconds
300°/s - 3 sets x 25 reps
80% of PT at 120°/s - 3 sets x 15 reps
85% of PT at 60°/s - 3 sets x 8 reps
Hamstring, Iliopsoas, and Rectus Femoris stretching - 2 x 30 seconds
cle imbalance and risk of injury in the knee joint.36,40,41 The pre-treatment H:Q ratio (69%) suggests a significant quadriceps weakness. After the isokinetic exercise program, this ratio dropped to 57%, approaching the values suggested by previous studies.41‑43 Although the post-treatment H:Q ratio was slightly below 60%, some literature suggests that H:Q ratio imbalance in professional soccer players may be associated with high quadriceps strength and not low hamstrings muscle strength.40,42
The analysis of the isokinetic variables demonstrates that the affected limb incurred a decrease in the% LR (pretreatment: 93.8%; post-treatment 92.8%). However, the values are higher than expected per the study of Mazuquin et al. Those authors analyzed the decomposition of these same variables in professional and under 17 soccer players and found an LR value of 83.2% for the dominant limb. The authors indicated that professional soccer players sustain the torque in a large ROM, showing greater muscular efficiency Figure 1 shows a deficit in extensor torque generation in the affected limb pre-treatment. Post-treatment, the map demonstrates an improved torque generation capacity, surpassing that of the control.
As for the physical function, the score achieved in the LEFS questionnaire (79 points) post-treatment revealed that the subject returned to sports activities after the treat-
ment program, reflecting 98.7% restoration of his lowerlimb functionality Although the LEFS questionnaire is a PROM, return-to-sports was primarily determined based on isokinetic performance values. Agolley et al. followed 46 athletes for five years after undergoing conservative treatment for Grade II and III PCL injuries. They found that the time to return-to-sports activity was approximately 10.6 weeks and after two years, 42 athletes continued their sports in the same category 44
Conservative management based on functional bracing and exercises is often reasonable for treating some athletes with PCL injuries. Although the PCL has an intrinsic ability to heal, residual posteriorization is a frequently observed disadvantage in conservative treatment. However, Shelbourne et al. reported that, on average, 14 years post-injury, patients had good subjective and objective outcomes not statistically significantly different between grades of PCL laxity Most patients regained the functional ROM (and sufficient quadriceps strength) to return to activities of daily living, with 45% participating in jumping and pivoting activities.45
Recent research by Rasmussen et al. evaluated changes in patient reported outcomes using the International Knee Documentation Committee Subjective Knee Form (IKDCSKF) over a two-year follow-up and muscle strength at an
Table 2. Pre- and post-treatment results of the isokinetic muscle assessment.
°/s: degrees per second; LR: load range; %: percentage of the LR in relation to total range of motion; ROM: range of motion; deg: degrees; PT/BM: peak torque/body mass; N.m/kg: newton meter/kilogram; Ang PT: peak torque angle; Inv: involved member; and Uninv: uninvolved member.

Figure 2. Three-dimensional knee extension surface maps, pre- and post-treatment, as well as one from the control subject.
eight-month follow-up after exercise and support brace interventions for patients with acute PCL injuries. This study concluded that patients with acute isolated and multiligament PCL injuries treated with the physical therapy-led exercise and support brace intervention reported clinically relevant improvements from baseline to the two-year follow-up. Those authors acknowledged several limitations in the study, e.g., the lack of a control group.46
Some limitations of this case report can be described: a) the absence of performance-based functional tests alongside isokinetic variables for return-to-sports decisions; b) the absence of longer term follow-up assessments, c) a lack of evaluation of muscle performance in eccentric contraction/mode and other velocities, such as 180°/s, and d) the results found are unable to be generalized due to the nature of a case report.
The treatment for PCL injuries remains controversial. Surgical treatment can entail complications and conservative treatment has not shown robust results in clinical studies
with a low risk of bias. The use of the isokinetic dynamometer, both for evaluation and treatment, has a high cost, however, professional soccer teams have previously used this type of resource and as there is a scarcity of clinical studies with a low risk of bias. The results of the current case report support an approach for managing a PCL injury in a professional soccer athlete that did not respond to conventional conservative treatment.
The use of an isokinetic exercise protocol with the isokinetic over the course of nine weeks of treatment, had a beneficial effect on maintaining physical function and improving extensor peak torque (42%), in addition to positively affecting the H:Q ratio of a professional soccer player with a posterior cruciate ligament injury, allowing for a successful return to sports.
The authors wish to thank the FINEP (MCT/AÇÃO TRANSVERSAL PRÓ-INFRA #01/2007 / #01/2009) for the funding to obtain the isokinetic dynamometer. KO and FQRC received doctoral financial support from CAPES (Funding Code: 001), PACS and RGM received a Fundação Araucária
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information. Physical
scholarship, and GRM and JRC also thanked the CNPq for their scholarships.
The authors report no conflicts of interest.
Submitted: January 11, 2024 CDT, Accepted: August 07, 2024 CDT
© The Author(s)
1. LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med 2015;43(12):3077-3092. doi:10.1177/0363546515572770
2. Arthur JR, Haglin JM, Makovicka JL, Chhabra A. Anatomy and biomechanics of the posterior cruciate ligament and their surgical implications. Sports Med Arthrosc Rev. 2020;28(1):1-10. doi:10.1097/ JSA.0000000000000267
3. Logterman SL, Wydra FB, Frank RM. Posterior cruciate ligament: anatomy and biomechanics. Curr Rev Musculoskelet Med 2018;11(3):510-514. doi:10.1007/s12178-018-9492-1
4. RF, Wentorf FA, Fritts H, et al. A prospective magnetic resonance imaging study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthroscopy 2007;23:1341-1347 doi:10.1016/ j.arthro.2007.07.024
5. Winkler PW, Zsidai B, Wagala NN, et al. Evolving evidence in the treatment of primary and recurrent posterior cruciate ligament injuries, part 1: Anatomy, biomechanics, and diagnostics. Knee Surg Sports Traumatol Arthrosc 2021;29(3):672-681. doi:10.1007/ s00167-020-06357-y
6. Owesen C, Sandven-Thrane S, Lind M, et al. Epidemiology of surgically treated posterior cruciate ligament injuries in Scandinavia. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2384-2391. doi:10.1007/s00167-015-3786-2
7 Schlumberger M, Schuster P, Eichinger M, et al. Posterior cruciate ligament lesions are mainly present as combined lesions even in sports injuries. Knee Surg Sports Traumatol Arthrosc 2020;28(7):2091-2098. doi:10.1007/ s00167-020-05919-4
8. Pache S, Aman ZS, Kennedy M, et al. Posterior cruciate ligament: current concepts review. Arch Bone Jt Surg. 2018;6(1):8-18.
9. Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186-191. doi:10.1007/s00402-002-0471-y
10. Strickland JP, Fester EW, Noyes FR. Lateral, posterior, and cruciate knee anatomy In: Noyes’ Knee Disorders Surgery, Rehabilitation, Clinical Outcomes. Saunders; 2009. doi:10.1016/ B978-1-4160-5474-0.00002-3
11. Verhulst FV, MacDonald P. Diagnosing PCL Injuries: History, physical examination, imaging studies, arthroscopic evaluation. Sports Med Arthrosc Rev. 2020;28(1):2-7. doi:10.1097/ JSA.0000000000000251
12. Winkler PW, Zsidai B, Wagala NN, et al. Evolving evidence in the treatment of primary and recurrent posterior cruciate ligament injuries, part 2: Surgical techniques, outcomes, and rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2021;29(3):682-693. doi:10.1007/s00167-020-06337-2
13. Rosenthal MD, Rainey CE, Tognoni A, Worms R. Evaluation, and management of posterior cruciate ligament injuries. Phys Ther Sport 2012;13(4):196-208. doi:10.1016/j.ptsp.2012.03.016
14. Montgomery SR, Johnson JS, McAllister DR, Petrigliano FA. Surgical management of PCL injuries: indications, techniques, and outcomes. Curr Rev Musculoskelet Med. 2013;6(2):115-123. doi:10.1007/ s12178-013-9162-2
15. Spiridonov SI, Slinkard NJ, LaPrade RF. Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Joint Surg Am 2011;93(19):1773-1780. doi:10.2106/JBJS.J.01638
16. Marom N, Ruzbarsky JJ, Boyle C, Marx RG. Complications in posterior cruciate ligament injuries and related surgery Sports Med Arthrosc Rev 2020;28(1):30-33. doi:10.1097/ JSA.0000000000000247
17 Chahla J, Moatshe G, Cinque ME, et al. Singlebundle and double-bundle posterior cruciate ligament reconstructions: a systematic review and meta-analysis of 441 patients at a minimum 2 years’ follow-up. Arthroscopy. 2017;33(11):2066-2080. doi:10.1016/j.arthro.2017.06.049
18. Pierce CM, O’Brien L, Griffin LW, Laprade RF. Posterior cruciate ligament tears: Functional and postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc 2013;21(5):1071-1084. doi:10.1007/s00167-012-1970-1
19. Gaines JM, Talbot LA. Isokinetic strength testing in research and practice. Biol Res Nurs. 1999;1(1):57-64. doi:10.1177/109980049900100108
20. Gleeson NP, Mercer TH. The utility of isokinetic dynamometry in the assessment of human muscle function. Sports Med 1996;21(1):18-34. doi:10.2165/ 00007256-199621010-00003
21. Kannus P. Isokinetic evaluation of muscular performance: Implications for muscle testing and rehabilitation. Int J Sports Med 1994;15 Suppl 1:S11-8. doi:10.1055/s-2007-1021104
22. Sapega AA. Muscle performance evaluation in orthopaedic practice. J Bone Joint Surg Am 1990;72(10):1562-1574. doi:10.2106/ 00004623-199072100-00023
23. Brown LE, Whitehurst M, Gilbert R, Buchalter DN. The effect of velocity and gender on load range during knee extension and flexion exercise on an isokinetic device. J Orthop Sports Phys Ther 1995;21(2):107-112. doi:10.2519/jospt.1995.21.2.107
24. Pereira LM, Dias JM, Mazuquin BF, et al. Translation, cross-cultural adaptation and analysis of the psychometric properties of the lower extremity functional scale (LEFS): LEFS- BRAZIL. Braz J Phys Ther 2013;17(3):272-280. doi:10.1590/ S1413-35552012005000091
25. Altamirano KM, Coburn JW, Brown LE, Judelson DA. Effects of warm-up on peak torque, rate of torque development, and electromyographic and mechanomyographic signals. J Strength Cond Res 2012;26:1296-1301. doi:10.1519/ JSC.0b013e31822e7a85
26. Biodex. Biodex Multi-Joint System. Clinical Resource Manual.; 1991.
27 Kaminska E, Piontek T, Wiernicka M, et al. Differences in isokinetic strength of the knee extensors and flexors in men with isolated and combined cruciate-ligament knee injury J Sport Rehabil. 2015;24(3):268-277. doi:10.1123/ jsr.2014-0157
28. Brown LE, Whitehurst M, Gilbert R, Buchalter DN. The effect of velocity and gender on load range during knee extension and flexion exercise on an isokinetic device. J Orthop Sports Phys Ther 1995;21:1071-12. doi:10.2519/jospt.1995.21.2.107
29. Pelegrinelli ARM, Guenka LC, Dias JM, et al. Isokinetic muscle performance after anterior cruciate ligament reconstruction, A case control study. Int J Sports Phys Ther 2018;13(5):882-889. doi:10.26603/ ijspt20180882
30. Mazuquin BF, Bela LFD, Pelegrinelli ARM, et al. Torque-angle-velocity relationships and muscle performance of professional and youth soccer players. Int J Sports Med. 2016;37(12):992-996. doi:10.1055/ s-0042-108199
31. Śliwowski R, Grygorowicz M, Hojszyk R, Jadczak Ł. The isokinetic strength profile of elite soccer players according to playing position. PLoS One. 2017;12(7):e0182177 doi:10.1371/ journal.pone.0182177
32. Daneshjoo A, Rahnama N, Mokhtar AH, Yusof A. Effectiveness of injury prevention programs on developing quadriceps and hamstrings strength of young male professional soccer players. J Hum Kinet. 2013;39:115-125. doi:10.2478/hukin-2013-0074
33. Rahnama N, Lees A, Bambaecichi E. Comparison of muscle strength and flexibility between the preferred and non-preferred leg in English soccer players. Ergonomics 2005;48(11-14):1568-1575. doi:10.1080/00140130500101585
34. Bedi A, Musahl V, Cowan JB. Management of posterior cruciate ligament injuries: an evidencebased review. J Am Acad Orthop Surg. 2016;24(5):277-289. doi:10.5435/JAAOS-D-14-00326
35. Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med 1986;14(1):35-38. doi:10.1177/036354658601400107
36. Delvaux F, Schwartz C, Rodriguez C, Forthomme B, Kaux JF, Croisier JL. Preseason assessment of anaerobic performance in elite soccer players: comparison of isokinetic and functional tests. Sports Biomech 2023;22(5):689-703. doi:10.1080/ 14763141.2020.1750681
37. Obara K, Silva P, Silva M, et al. Isokinetic training program to improve the physical function and muscular performance of an individual with partial injury of the medial meniscus: A case report. Int J Sports Phys Ther 2023;18(3):758-768. doi:10.26603/ 001c.74945
38. Zinke F, Warnke T, Gäbler M, Granacher U. Effects of isokinetic training on trunk muscle fitness and body composition in world-class canoe sprinters. Front Physiol. 2019;10:21. doi:10.3389/ fphys.2019.00021
39. Gomes M, Santos P, Correia P, Pezarat-Correia P, Mendonca GV. Sex differences in muscle fatigue following isokinetic muscle contractions. Sci Rep 2021;11(1):8141. doi:10.1038/s41598-021-87443-0
40. Bogdanis GC, Kalapotharakos VI. Knee extension strength and hamstrings-to-quadriceps imbalances in elite soccer players. Int J Sports Med 2016;37(2):119-124.
41. Ruas CV, Minozzo F, Pinto MD, Brown LE, Pinto RS. Lower-extremity strength ratios of professional soccer players according to field position. J Strength Cond Res. 2015;29(5):1220-1226. doi:10.1519/ JSC.0000000000000766
42. Denadai BS, de Oliveira FB, Camarda SR, Ribeiro L, Greco CC. Hamstrings-to-quadriceps strength and size ratios of male professional soccer players with muscle imbalance. Clin Physiol Funct Imaging 2016;36(2):159-164. doi:10.1111/cpf.12209
43. Yeung SS, Suen AM, Yeung EW A prospective cohort study of hamstring injuries in competitive sprinters: preseason muscle imbalance as a possible risk factor Br J Sports Med 2009;43(8):589-594. doi:10.1136/bjsm.2008.056283
44. Agolley D, Gabr A, Benjamin-Laing H, Haddad FS. Successful return to sports in athletes following nonoperative management of acute isolated posterior cruciate ligament injuries: medium-term follow-up. Bone Joint J 2017;99-B(6):774-778. doi:10.1302/ 0301-620X.99B6.37953
45. Shelbourne KD, Clark M, Gray T Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med. 2013;41(7):1526-1533. doi:10.1177/ 0363546513486771
46. Rasmussen RG, Jacobsen JS, Blaabjerg B, Nielsen TG, Miller LL, Lind M. Patient-reported outcomes and muscle strength after a physiotherapy-led exercise and support brace intervention in patients with acute injury of the posterior cruciate ligament: A two-year follow-up study Int J Sports Phys Ther 2023;18(4):807-819. doi:10.26603/001c.83214

Kyle Kiesel1a , Kyle Matsel1 , Garrett Bullock2 , Todd Arnold3 , Phil Plisky1
1 Physical Therapy, University of Evansville, 2 School of Medicine, Wake Forest University, 3 NA, NA
Keywords: Movement systems, musculoskeletal disorder, prevention, risk factor https://doi.org/10.26603/001c.123485
Musculoskeletal disorders (MSKD) are currently the leading contributor to disability worldwide. Unlike other prevalent and disabling healthcare conditions such as CVD, risk factors associated with MSKD are not commonly discussed or integrated into current medical practice, rehabilitation practice or wellness programs. The primary purpose of this review is to describe the known risk factors most closely associated with MSKD. The secondary purpose is to propose a clinical model to manage MSK health aimed at maximizing the healthy pursuit of a physically active and healthy lifestyle.
In this review the most common MSKD risk factors, with a focus on those that can be easily screened in clinical practice are presented. The importance of understanding the magnitude and number of risk factors present as well as the multidimensional nature of MSKD risk is discussed.
A total of 11 MSKD risk factors were identified. Most of the risk factors are modifiable, and the evidence associated with modifiability for the most prominent risk factors is reviewed.
Researchers have found that often patients are discharged from care with several known MSKD risk factors. In such instances, local pain and dysfunction are managed well, but expanding our rehabilitation care to include comprehensive risk factor management would ultimately benefit the patient and reduce healthcare costs.
Conclusion
The most common MSKD risk factors are discussed and a clinical framework to individualize intervention is proposed. Addressing key risk factors within rehabilitation may be an important step to reduce the enormous and growing burden these disorders are having on society.
Level of Evidence
5
Corresponding Author: Kyle Kiesel, PT, PhD
Professor Emeritus
University of Evansville 515 Bob Jones Way Evansville, IN 47708
Phone: 812 589 5826
Email: kyle@sfma.com
Musculoskeletal disorders (MSKD) include more than 150 diagnoses that affect the locomotor system of individuals. MSKD are initially recognized by musculoskeletal (MSK) pain, and then secondarily, by limitations in mobility, motor control, dexterity, and general function. They range from disorders that arise suddenly, such as fractures, sprains, and strains, to chronic conditions contributing to functional limitations and disability 1 Often the muscle, bone, or joint condition is mechanical in nature as is the case in osteoarthritis. Additionally, disorders affecting the body’s inflammatory process are included, such as rheumatoid arthritis, psoriatic arthritis, gout, and ankylosing spondylitis. World-wide, the most common MSKD reported are low back pain and osteoarthritis.2 MSKD are on the rise around the world.3 The total number of MSK-related disability-adjusted life years have increased by 25% from 2000 to 2015 with MSK diseases being the second cause of years lived with disability worldwide. MSKD are known to contribute to significant mental health decline, cluster around common chronic diseases and increase all-cause mortality 3
MSKD are the highest contributor to the need for rehabilitation across the globe with two-thirds of all adults in need of rehabilitation.4 More than one in two adults in the United States (US), 124 million over the age of 18, report a musculoskeletal medical condition. That exceeds the next two most common health conditions including circulatory conditions (such as heart disease, stroke, and hypertension) and respiratory conditions.5 Across all adult age categories, MSKD are either the most reported medical conditions (among those < 65 years old) or second most reported (among those 65 years and older). In 2015, 36% of the US adult population reported difficulties performing routine activities of daily living (ADLs) due to a medical condition. Of those adults reporting ADL limitations, 64 million had a concomitant musculoskeletal condition. Individuals in the US population with an MSKD are likely to have other associated conditions and comorbidities, affecting health overall and complicating the MSKD diagnosis and treatment process.6
A recent survey conducted in Australia7 focused on the impact of MSKD on the population and described similar results with an estimated seven million adults affected by chronic and painful MSKD. Of those affected, 57% report two or more MSKD, 66% indicated their condition had an adverse effect on their family and personal relationships, 72% report adverse effects on sleep, and 50% report a negative impact on their mental health. Additionally, MSKD can severely disrupt work for adults since 58% affected are in their prime working years between 25-64 years of age. In the United States, low back and neck pain are the most expensive health conditions, estimated at $134.5 billion. As this condition often occurs in the working-age population, the indirect costs, including disability benefits and days of work missed, are estimated to be as high as $624.8 billion.8
Considering millions of people seek rehabilitation currently, aligning rehabilitation professionals to focus on identifying the most prominent MSK risk factors for every-
one under their care through a standardized operating procedure could be helpful. While prevention and physical activity promotion are clearly within the scope of the rehabilitation provider, efforts in these domains are falling short.9 Most patients conclude their rehabilitation program with little knowledge of the value of physical activity, without the awareness of their most prominent risk factors for MSK health and prevention.
Known strategies to prevent and treat MSKD are generally described around increasing physical activity levels. Good MSK health habits, like smart exercise, have an abundance of positive effects from decreased obesity to improved mental health and reduced pain.10 But, simply suggesting an individual with a MSKD become more active may not be an adequate solution. While most individuals are aware of the benefits of physical activity and exercise, many are unable to engage in routine physical activity because of existing MSKD pain. Approximately 76% of adults with an MSKD report that it directly limits their physical activity.7 Although increased physical activity is a proven way to decrease the prevalence of all-cause mortality risk factors and improve overall health, physical inactivity seems to be on the rise,11 and trends suggest MSKD are a contributing factor While efforts focused on behavioral change can be helpful to increase activity level for some individuals12 a concurrent consideration for current MSK health status and risk should be considered as well.
There is a tremendous burden associated with MSKD directly and, because of their attenuating effect on physical activity levels, MSKD are also a silent contributing factor to the well-established chronic diseases that make up metabolic syndrome.13 In 2015, Carlson et al. noted that 11.1% of all health care costs were associated with “inadequate” physical activity and that this is on the rise.14 Theoretically, addressing MSKD by identification and management of common risk factors could result in improved physical activity levels, decreased injury rates, and less overall financial burden. Therefore, the primary purpose of this review is to describe the known risk factors most closely associated with MSKD The secondary purpose is to propose a clinical model to manage MSK health aimed at maximizing the healthy pursuit of a physically active and healthy lifestyle.
A health risk factor is anything that increases a person’s chances of getting a disease or other health-related condition.15 Risk factors are well established for many lifethreatening conditions present in adults such as cardiovascular disease. But there is little public health focus on risk factors associated with MSKD, which is surprising given the massive burden MSKD have on our society.1,2,5 In this commentary the authors discuss risk factors that have been associated with the development of MSKD overall and discuss strategies that may help to manage these risk factors more effectively Perhaps, if risk factors for MSKD are managed more effectively, the burden associated with MSKD will be reduced.
MSKD are multifactorial and a good understanding of the key risk factors and conditions associated with MSKD is important. While most MSK risk factor research has focused on MSK function or a singular injury, researchers now have demonstrated the multifactorial nature of MSKD and the specific risk factors associated with the overall development of MSKD in adults.16 For example, individuals with behavioral health needs are at greater risk for MSKD17,18 as are those who have had a recent MSK injury.16,19,20 A previous injury within the prior 12 months is a known strong risk factor,19 but also the magnitude of that injury16 as well as the self-perception of recovery16,20 from that injury are also independent risk factors that deserve consideration in an individual’s overall risk profile.
Recent research has shown that individuals with multiple risk factors are at increased risk for MSK injury16,21, 22 and have reduced physical performance.21 Not surprisingly, there is a linear relationship between the number of risk factors and injury risk.16 The more risk factors that an individual has, the more likely they are to ultimately develop an MSKD Therefore, it may be important to screen for MSKD risk factors, to consider the presence of multiple risk factors, and the combinations of these factors to establish everyone’s overall risk level. Screening can help to determine the most important domain of MSK health which should be prioritized and provide rationale and guidance for direct intervention for those at greatest risk. For example, it is well known that individuals with higher BMI are at greater risk for OA. But, simply sharing this with a patient and expecting changes in exercise and diet to address high BMI is not likely to be an effective strategy 23 Perhaps employing a screening process that prioritizes risk factors for MSK health, with a focus on the most prominent and modifiable areas could be helpful. When key risk factors are screened for and considered together, an appropriate migration strategy can be developed, in conjunction with the patient’s current rehabilitation program to enhance and promote overall MSK health.
Comprehensive review of the literature has resulted in the summation of the risk factors most closely associated with overall MSK health. These risk factors can be identified through the MSK screening process in clinical practice as routine annual wellness check-ups or throughout the course of rehabilitation. Like cardiovascular risk factors, MSK risk factors are interrelated suggesting that healthcare professionals must systematically evaluate the entire profile of an individual. For example, a previous ankle sprain injury where the ankle dorsiflexion ROM was not fully restored could potentially result in another ankle sprain or possibly an injury to the knee. Furthermore, reduced ankle mobility will have negative effects on functional movement (i.e. squatting, stepping, lunging) and dynamic balance which could limit the individual’s ability to be physically active, resulting in poor cardiovascular fitness, increased BMI, and suboptimal psychological status. Restricted ankle
dorsiflexion does respond favorably to direct intervention and/or education when appropriately identified and administered. The following are key MSK risk factors, presented alphabetically.
Asymmetrical ankle dorsiflexion of at least 4 degrees has been identified as a significant risk factor for time loss injury in military and sport populations. Asymmetrical ankle dorsiflexion has been identified as a risk factor for future falls in elderly populations.16,24,25
High body mass index has been associated with increased risk of sustaining an injury in military and sport populations. High body mass index has also been identified as a significant risk factor in future osteoarthritis and total joint replacement.26‑30
Decreased cardiovascular fitness has been identified as an independent risk factor for future time loss injury in military, sport populations, and elderly populations.16,30
Impaired dynamic balance has been identified as a significant risk factor in future time loss injury for military and sport populations.16,24,31
Impaired functional movement (measured by the Functional Movement Screen and the Selective Functional Movement Assessment) has been identified as a significant risk factor in future time loss injury for military and sport populations.30,32‑36
Decreased muscle strength has been identified as an independent risk factor to sustain a future injury in sport and elderly populations.10
Pain with movement was identified in three separate military populations as a significant risk factor in future time loss injury.16,24,30
Perceived recovery as measured by the Single Assessment Numeric Evaluation (SANE) score following an injury was identified as an independent prospective risk factor for future injury Individuals who report their SANE score following an injury at <92% were shown to be more likely to sustain a future time loss injury 16
Low physical activity has been identified as a significant risk factor for the development of osteoarthritis and sustaining a fall in elderly populations.27
The presence of a previous time loss injury has been identified in multiple studies as an independent and robust risk factor. Additionally, the magnitude of the injury, as measured by the number of days missed, has also been identified as a risk factor for future injury.16,19,24,37
Diagnosis of anxiety and/or depression has been identified as an independent significant risk factor in musculoskeletal pain or injury.17,18,38
There is a need for a modern and innovative model to approach MSKD. The MSKD health problem is extremely complex requiring management with more than one tactic. However, the first step in addressing this large-scale problem is identifying known risk factors and providing individuals with awareness of the biggest limiting factors impacting their own MSK health.
Consideration of the number of risk factors present and the magnitude of each factor is contemplated in the overall care of the patient. With a good understanding of a patient’s current risk, a comprehensive rehabilitation plan can be executed to mitigate the impact that risk factors have on overall physical activity and function. This approach is a more systematic and comprehensive model to evaluate MSK health, rather than a purely pathoanatomical approach where treatment is dictated simply by current symptoms or medical diagnoses. In a recent study conducted in 18–45 year-old adults, the researchers captured multiple physical performance measures and known MSKD risk factors at time of discharge from rehabilitation for lower extremity or spine dysfunction.39 This entire sample of 469 subjects had been cleared to return to full activity by their healthcare professional. The researchers found that over 70% of the sample had at least five known MSKD risk factors at time of discharge and 44% had pain with global movements. This does not include the obvious previous injury that was an inclusion criterion for the study. In this case, local pain was managed well, but these data demonstrate the need to expand conventional rehabilitative care to include comprehensive risk factor management.39 There are a variety of evidence-based approaches that are utilized by rehabilitation providers to directly address the pain and disability associated with a given MSK condition. It may seem overwhelming to add MSKD risk factor management to current models, but a commonsense approach that optimizes a standardized process is the key to establishing MSKD risk factor management into current rehabilitation practice. When the most prominent and modi-
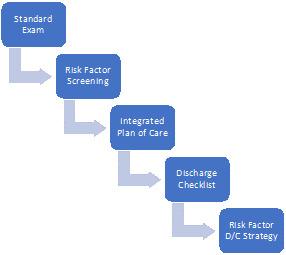
fiable risk factors are considered rather than each one individually, the process becomes attainable. It can be as simple as screening for functional movement40,41 (including presence of pain), ankle mobility42,43 and balance44,45 which is approximately a 15-minute investment. Risk factor screening can occur as part of the standard physical therapy examination or can be executed in the early phases of the rehab process. The timing of screening will be somewhat dependent on the acuity and nature of the primary condition the patient is being seen for. Ultimately, the plan of care should include intervention targeted at the most prominent risk factors as well as a discharge plan that addresses ongoing risk factor management. (Figure 1).
Evidence-based interventions, prescribed to address identified risk factors, can be integrated into the locally focused rehabilitation program, and built into the program progression. In a study by Schwarzkoph-Phifer et al46 that measured risk factor management during rehabilitation, it was demonstrated that with traditional interventions focused on manual therapy and therapeutic exercise, the number of risk factors present following the intervention period was significantly reduced with an average reduction of three risk factors. In another study by Huebner et. al. it was demonstrated that overall MSK risk category can change significantly from higher risk to lower risk with individualized interventions.47 A combination of manual therapies and therapeutic exercise has been shown to improved ROM and dynamic balance in subject with ankle dorsi-flexion restrictions.48‑50 Individualized therapeutic exercise programs have been shown to significantly improve functional movement abilities when compared to control subjects,51,52 and dynamic and static balance has been shown to improve in multiple studies with a variety of interventions across different age groups.53,54
Awareness of the number of risk factors is also considered. Some individual factors are in and of themselves non-
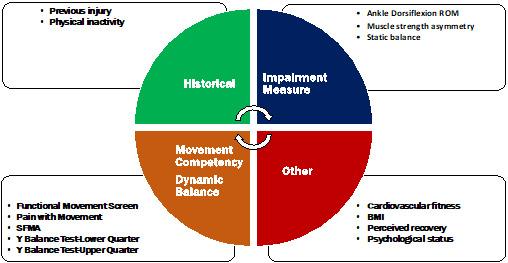
Figure 2. Musculoskeletal Risk Factors by Category.
modifiable, making it even more important to address the factors that are amenable to intervention, to reduce overall risk. Additionally, some patients may benefit from referral for professional help with areas such as behavioral health or to a training specialist for help with cardiovascular fitness and/or strength training. Organizing risk factors by category can help the clinician clarify which risk factors to intervene on and provides a risk factor profile to help understand each patient’s prognosis. (Figure 2).
A thorough understanding of each patient’s individual risk profile at discharge time can help to instill confidence in the therapeutic relationship and serve to provide clear guidance to the patient of what they should be working on to maximize their MSK health and benefits gained from a physically active lifestyle. As clinicians become more comfortable with this full body, risk factor approach, it simply becomes how they practice rather than a disconnected portion of the program that is added on near the end.
MSKD are the leading contributors to disability worldwide and present a substantial burden to healthcare systems. Unlike other prevalent and disabling healthcare conditions,
risk factors associated with MSKD are not commonly discussed or integrated into current medical practice or wellness programs. In this review the authors describe the most common MSKD risk factors, and it is suggested that addressing known risk factors for MSKD in rehabilitation may be an important factor moving forward to reduce the enormous and growing burden these disorders are having on society.
Dr. Kiesel and Dr. Plisky report a relationship with Functional Movement Systems where they own stock. Dr Arnold is a compensated instructor for Functional Movement Systems. The other authors report no potential conflicts of interest.
Submitted: February 22, 2024 CDT, Accepted: August 28, 2024 CDT
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Murray CJ, Vos T, Lozano R, et al. Disabilityadjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2197-2223. doi:10.1016/ S0140-6736(12)61689-4
2. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391:2356-2367. doi:10.1016/ S0140-6736(18)30480-X
3. Briggs AM, Cross MJ, Hoy DG, et al. Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 world health organization world report on ageing and health. Gerontologist. 2016;56 Suppl 2:S243-55. doi:10.1093/geront/gnw002
4. Cieza A, Causey K, Kamenov K, et al. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease. Lancet 2021;396:2006-2017. doi:10.1016/ S0140-6736(20)32340-0
5. United states bone and joint initiative. The Burden of Musculoskeletal Diseases in the United States (BMUS) 4th ed. Rosemont, IL; 2020.
6. Yelin E, Weinstein S, King T The burden of musculoskeletal diseases in the United States. Sem Arthritis Rheumatism. 2016;46:259-260. doi:10.1016/ j.semarthrit.2016.07.013
7 Musculoskeletal Australia. Making the Invisible Visible; Australians Share the Impact of Musculoskeletal Conditions on Their Lives Baseline survey report; 2021.
8. Dagenais S, Caro J, Haldeman SA. Systematic review of low back pain cost of illness studies in the United States and internationally Spine J 2008;8:8-20. doi:10.1016/j.spinee.2007.10.005
9. Lowe A, Littlewood C, McLean S. Understanding physical activity promotion in physiotherapy practice: A qualitative study. Musculoskel Sci Pract. 2018;35:1-7 doi:10.1016/j.msksp.2018.01.009
10. Bull FC, Al-Ansari SS, Biddle S, et al. World health organization 2020 guidelines on physical activity and sedentary behavior Br J Sports Med 2020;54:1451-1462. doi:10.1136/ bjsports-2020-102955
11. Booth FW, Roberts CK, Thyfault JP, et al. Role of inactivity in chronic diseases: evolutionary insight and pathophysiological mechanisms. Physiol Rev. 2017;97:1351-1402.
12. Rethorn ZD, Covington JK, Cook CE, et al. Physical activity promotion: moving from talking the talk to walking the walk. J Orthop Sports Phys Ther 2022;52:236-242. doi:10.2519/jospt.2022.10859
13. Samson SL, Garber AJ. Metabolic syndrome. Endocrinol Metab Clin North Am 2014;43:1-23. doi:10.1016/j.ecl.2013.09.009
14. Carlson SA, Fulton JE, Pratt M, et al. Inadequate physical activity and health care expenditures in the United States. Prog Cardiovasc Dis 2015;57:315-323. doi:10.1016/j.pcad.2014.08.002
15. Burton WN, Conti DJ, Chen CY, et al. The role of health risk factors and disease on worker productivity J Occup Environ Med 1999;41:863-877 doi:10.1097/00043764-199910000-00007
16. Teyhen DS, Shaffer SW, Butler RJ, et al. identification of risk factors prospectively associated with musculoskeletal injury in a warrior athlete population. Sports Health 2020;12:564-572. doi:10.1177/1941738120902991
17. Bair MJ, Wu J, Damush TM, et al. Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med. 2008;70:890-897. doi:10.1097/PSY.0b013e318185c510
18. Kroenke K, Wu J, Bair MJ, et al. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain 2011;12:964-973. doi:10.1016/ j.jpain.2011.03.003
19. Toohey LA, Drew MK, Cook JL, et al. Is subsequent lower limb injury associated with previous injury? A systematic review and metaanalysis. Br J Sports Med 2017;51:1670-1678. doi:10.1136/bjsports-2017-097500
20. Does HT, van der D, Brink MS, et al. injury risk is increased by changes in perceived recovery of team sport players. Clin J Sport Med 2017;27:46-51. doi:10.1097/JSM.0000000000000306
21. Teyhen DS, Shaffer SW, Butler RJ, et al. Association of physical inactivity, weight, smoking, and prior injury on physical performance in a military setting. J Athl Train. 2016;51:866-875. doi:10.4085/ 1062-6050-51.6.02
22. Lehr ME, Plisky PJ, Butler RJ, et al. Fieldexpedient screening and injury risk algorithm categories as predictors of noncontact lower extremity injury Scand J Med Sci Sports 2013;23:e225-232. doi:10.1111/sms.12062
23. Burgess E, Hassmén P, Pumpa K. Determinants of adherence to lifestyle intervention in adults with obesity: a systematic review Clin Obes 2017;7:123-135. doi:10.1111/cob.12183
24. Teyhen DS, Shaffer SW, Butler RJ, et al. What risk factors are associated with musculoskeletal injury in us army rangers? a prospective prognostic study. Clin Ortho Relat Res 2015;473:2948-2958. doi:10.1007/ s11999-015-4342-6
25. Kemoun G, Thoumie P, Boisson D, et al. Ankle dorsiflexion delay can predict falls in the elderly J Rehabil Med 2002;34:278-283. doi:10.1080/ 165019702760390374
26. Bastick AN, Runhaar J, Belo JN, et al. Prognostic factors for progression of clinical osteoarthritis of the knee: a systematic review of observational studies. Arthritis Res Ther 2015;17:152. doi:10.1186/ s13075-015-0670-x
27. Chapple CM, Nicholson H, Baxter GD, et al. Patient characteristics that predict progression of knee osteoarthritis: a systematic review of prognostic studies. Arthritis Care Res. 2011;63:1115-1125. doi:10.1002/acr.20492
28. Nicholls AS, Kiran A, Javaid MK, et al. Change in body mass index during middle age affects risk of total knee arthoplasty due to osteoarthritis: a 19-year prospective study of 1003 women. Knee 2012;19:316-319. doi:10.1016/j.knee.2011.06.008
29. Reyes C, Leyland KM, Peat G, et al. Association between overweight and obesity and risk of clinically diagnosed knee, hip, and hand osteoarthritis: a population-based cohort study Arthritis 2016;68:1869-1875.
30. Rhon DI, Molloy JM, Monnier A, et al. Much work remains to reach consensus on musculoskeletal injury risk in military service members: A systematic review with meta-analysis. Eur J Sport Sci. 2022;1:16-34. doi:10.1080/17461391.2021.1931464
31. Plisky PJ, Rauh MJ, Kaminski TW, et al. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36:911-919. doi:10.2519/jospt.2006.2244
32. Busch AM, Clifton DR, Onate JA. Relationship of movement screens with past shoulder or elbow surgeries in collegiate baseball players. Int J Sports Phys Ther 2018;13:1008-1014. doi:10.26603/ ijspt20181008
33. Kiesel KB, Butler RJ, Plisky PJ. Prediction of injury by limited and asymmetrical fundamental movement patterns in american football players. J Sport Rehabil 2014;23:88-94. doi:10.1123/JSR.2012-0130
34. Bunn P, Rodrigues AI, da Silva EB. The association between the functional movement screen outcome and the incidence of musculoskeletal injuries: A systematic review with meta-analysis. Phys Ther Sport 2019;35:146-158. doi:10.1016/ j.ptsp.2018.11.011
35. Wainner RS, Whitman JM, Cleland JA, et al. Regional interdependence: a musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther 2007;37:658-660. doi:10.2519/ jospt.2007.0110
36. Sueki DG, Cleland JA, Wainner RS. A regional interdependence model of musculoskeletal dysfunction: research, mechanisms, and clinical implications. J Man Manip Ther. 2013;21:90-102. doi:10.1179/2042618612Y.0000000027
37 van Meer BL, Meuffels DE, van Eijsden WA, et al. Which determinants predict tibiofemoral and patellofemoral osteoarthritis after anterior cruciate ligament injury? A systematic review Br J Sports Med 2015;49:975-983. doi:10.1136/bjsports-2013-093258
38. Wride J, Bannigan K. Investigating the prevalence of anxiety and depression in people living with patellofemoral pain in the UK: the Dep-Pf Study. Scand J Pain 2019;19:375-382. doi:10.1515/ sjpain-2018-0347
39. Rhon DI, Teyhen DS, Kiesel KB, et al. Recovery, rehabilitation, and return to full duty in a military population after a recent injury: differences between lower-extremity and spine injuries. Arthrosc Sports Med Rehabil 2022;4:e17-e27 doi:10.1016/ j.asmr.2021.09.028
40. Glaws KR, Juneau CM, Becker LC, et al. Intra- and inter-rater reliability of the Selective Functional Movement Assessment (SFMA). Int J Sports Phys Ther 2014;9:195-207.
41. Rhon DI, Plisky PJ, Kiesel KB, et al. Predicting subsequent injury after being cleared to return to work from initial lumbar or lower extremity injury Med Sci Sports Exerc. 2023;55:2115-2122. doi:10.1249/MSS.0000000000003257
42. Gourlay J, Bullock G, Weaver A, et al. The reliability and criterion validity of a novel dorsiflexion range of motion screen. Athl Train Sports Health Care 2020;12:40-44. doi:10.3928/ 19425864-20190214-02
43. Plisky PJ, Bulluck G, Garner MB, et al. The dorsiflexion range of motion screen: a validation study Int J Sports Phys Ther 2021;16:306-311. doi:10.26603/001c.21253
44. Matsel K, Kirsch J, Netelbeek T, et al. Selfmovement screening using the symmio application is reliable and valid for identifying musculoskeletal risk factors. Int J Sports Phys Ther 2023;18:439-449. doi:10.26603/001c.73319
45. Plisky PJ, Schwartkopf-Phifer K, Huebner B, et al. Systematic review and meta-analysis of the y-balance test lower quarter: reliability, discriminant validity, and predictive validity. Int J Sports Phys Ther. 2021;16:1190-1209. doi:10.26603/001c.27634
46. Schwartzkopf-Phifer K, English RA, Mattacola CG, et al. The effect of one-on-one intervention in athletes with multiple risk factors for injury Int J Sports Phys Ther 2019;14:384-402. doi:10.26603/ ijspt20190384
47 Huebner BJ, Plisky PJ, Kiesel KB, et al. Can injury risk category be changed in athletes? an analysis of an injury prevention system. Int J Sports Phys Ther. 2019;14:127-134. doi:10.26603/ijspt20190127
48. Basnett CR, Hanish MJ, Wheeler TJ, et al. Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability Int J Sports Phys Ther. 2013;8:121-128.
49. Stanek J, Sullivan T, Davis S. Comparison of compressive myofascial release and the graston technique for improving ankle-dorsiflexion range of motion. J Athl Train. 2018;53:160-167. doi:10.4085/ 1062-6050-386-16
50. Cruz-Díaz D, Vega LR, Osuna-Pérez MC, et al. Effects of joint mobilization on chronic ankle instability: a randomized controlled trial. Disabil Rehabil 2015;37:601-610. doi:10.3109/ 09638288.2014.935877
51. Kiesel KB, Plisky PJ, Butler RJ. Functional movement test scores improve following a standardized off-season intervention program in professional football players. Scand J Med Sci Sports 2011;21:287-292. doi:10.1111/ j.1600-0838.2009.01038.x
52. Bodden JG, Needham RA, Chockalingam N. The effect of an intervention program on functional movement screen test scores in mixed martial arts athletes. J Strength Cond Res 2015;29:219-225. doi:10.1519/JSC.0b013e3182a480bf
53. Liu-Ambrose T, Nagamatsu LS, Graf P, et al. Resistance training and executive functions: a 12-month randomized controlled trial. Arch Intern Med. 2010;170:170-178. doi:10.1001/ archinternmed.2009.494
54. Gribble PA, Hertel J, Plisky PJ. Using the star excursion balance test to assess dynamic posturalcontrol deficits and outcomes in lower extremity injury: a literature and systematic review J Athl Train. 2012;47:339-357. doi:10.4085/ 1062-6050-47.3.08

Andreyo E,
C,
T, Dawes JJ. Clinical Utility of Qualitative Change of Direction Movement Assessment in ACL Injury Risk Evaluation. IJSPT. Published online October 1, 2024:1263-1278. doi:10.26603/001c.123483
Evan Andreyo1a , Casey Unverzagt2 , Thomas Dos'Santos3 , J. Jay Dawes4
1 Health Sciences, Rocky Mountain University of Health Professions, 2 Physical Therapy, Baylor University, 3 Exercise and Sports Science, Manchester Metropolitan University, 4 School of Kinesiology, Oklahoma State University
Keywords: anterior cruciate ligament (ACL), injury prevention, return to sport, change of direction, movement assessment https://doi.org/10.26603/001c.123483
Anterior cruciate ligament (ACL) injuries are complex and influenced by numerous internal and external risk factors that should be considered to effectively mitigate injury and facilitate informed return to sport decision-making. Among these risk factors, movement quality exhibited during sport-specific tasks has been identified as a significant predictor of injury occurrence. Particularly, change of direction (COD) movements, when performed with sub-optimal movement quality, such as knee valgus and lateral trunk flexion, are prominent mechanisms of ACL injury in multidirectional sports. Unfortunately, the formal and objective assessment of COD movement quality is underutilized in clinical and sports practice, with existing methods often confined to expensive, sophisticated laboratory settings impractical for everyday clinicians. The purpose of this clinical commentary is to demonstrate the necessity of integrating COD movement assessments to screen for potential ACL injury risk, particularly among higher-risk populations. The authors will review cost-effective and clinic-friendly objective tests used to qualitatively screen COD movements, such as the Cutting Movement Assessment Score and The Expanded Cutting Alignment Tool. Additionally, this commentary will discuss key considerations when assessing COD movement.
Level of Evidence
5
Anterior cruciate ligament (ACL) injuries are prevalent in athletic populations, with approximately 80,000 to 250,000 ACL injuries occurring annually in the United States alone.1 Approximately 100,000 individuals undergo ACL reconstructions (ACLR) annually, making it the sixth most common orthopedic procedure in the United States.1 The incidence of ACL injuries and ACLR have increased over the last two decades, particularly among young female athletes.2‑4 The consequences of an ACL injury are substantial, with most injuries being season-ending and resulting in the most missed games compared to other injuries across competition levels.5,6 Additionally, only 69-81% of athletes return to sport, with only 55% returning to a competitive level.7‑9 Moreover, there is a particularly high rate of ACL re-injury, reported as high as one out of five, with a six times greater likelihood of ACL injury compared to healthy
controls.10,11 An ACL injury can also result in a significant economic burden, psychological consequences, and an increased likelihood of developing knee osteoarthritis.12‑16 Consequently, further investigation regarding the factors that may predispose an individual to this injury and available strategies to screen and mitigate injury risk are warranted.
Up to 75% of sports ACL injuries occur without physical contact (i.e., non-contact) with another player or object, most often during deceleration and a change of direction (COD) through a planted lower limb.1,17,18 These injuries are most prevalent in multidirectional sports that require frequent COD movements, such as soccer, basketball, lacrosse, and football.19‑22 Females participating in schoolaged sports have a significantly greater risk of experiencing
Corresponding Author: Evan Andreyo, PT, DPT, PhD
Department of Health Sciences, Rocky Mountain University of Health Professions, Provo, UT, 84606, USA
Email Address: evan.andreyo@augie.edu
a non-contact ACL injury when compared to males at the same age and sport.19‑24 Female athletes have been reported to have an ACL injury incidence rate (IR) of 1.88 per 10,000 athletic exposures (AEs) compared to 0.87 per 10,000 AEs among male athletes across sports such as basketball, lacrosse, and soccer.22 The overall injury incidence rate ratio (IRR) for female athletes compared to males is reported to be 1.40 to 3.00.20,22,25,26 IRR is the ratio of injuries per AEs in females compared to males. Considering these findings, clinicians should evaluate why certain populations are at a greater risk of ACL injury than others and what appropriate and actionable mitigation strategies may be.
When considering what factors may be involved in this sex disparity in injury incidence, one must acknowledge that injury risk is multifactorial in nature. A review by Ruddy et al.27 highlights the complexity of team sport injuries and the need to account for multiple variables when assessing injury risk rather than a reductionist approach. This complexity is particularly true for ACL injuries, with intrinsic (non-modifiable) and extrinsic (modifiable) factors influencing injury risk. There are various intrinsic characteristics more common in females that may promote a greater predisposition to an ACL injury, including hormonal influences, intercondylar femoral notch width, anterior knee laxity, and tibial plateau slope.28,29 However, these non-modifiable risk factors offer limited opportunities for strategizing and implementing ACL injury mitigation compared to their modifiable counterparts.
Poor neuromuscular control during landing and COD movements are common modifiable contributors to ACL injury risk.1,17,30‑32 Neuromuscular control is defined by Herrington et al.33 as “the ability to deliver a movement in an ‘optimal’ manner which minimizes loading stresses or maximizes the distribution of loading stresses on the tissues.”
Suboptimal trunk and lower extremity movement quality during COD or landing tasks have been identified as visible characteristics of non-contact ACL injury and are determinants of potentially hazardous knee joint loads that increase ACL loading.34‑39 Specifically, a dynamic knee valgus movement during deceleration or COD can pose a multiplanar load to the ACL and, when it exceeds its load capacity, result in injury.17,34,40,41 A knee abduction moment (KAM) describes the kinetic forces applied to the knee during knee valgus.32,42 Several authors have identified an increased KAM, increased hip adduction, decreased hip and knee flexion, and increased hip internal rotation in females compared to their male counterparts in both cutting and landing tasks common in sports participation, which may partially account for the greater relative ACL injury risk observed in females.35,43‑49
Several studies using video analysis have identified knee valgus as a prominent movement pattern during sport-related ACL injury, with some authors reporting knee valgus during 81-88% of non-contact ACL injuries.34,36,37,50 Additionally, frontal and sagittal plane trunk positioning, lateral foot width placement, knee flexion angle, and penultimate foot contact braking have been demonstrated to significantly influence knee joint loading during COD tasks.51
These findings have also been recognized for second ACL injuries, with Paterno et al.30,31 reporting increased lower extremity neuromuscular control deficits and knee valgus during postural control and landing tasks among those going on to experience a second ACL injury compared to those who did not. Collectively, these findings suggest that specific movement characteristics and quality deficits, particularly with increased KAM, can potentially lead to increased strain on the ACL.
The assessment of tasks associated with ACL injury (i.e., jump landing and changing direction) is crucial for mitigating first and subsequent ACL injuries, especially in female athletes participating in multidirectional sports. While a review by Arundale et al.52 highlights that no test can solely predict ACL injury, the utilization of movement screening may offer insight into the presence or absence of specific movement patterns associated with ACL injury, which, in theory, increases the relative risk of injury Several strategies have been investigated and recommended to identify modifiable movement patterns associated with ACL injury risk.36,44,50,53 With better insight into movement quality, clinicians can implement targeted exercise-based knee and ACL injury prevention strategies to promote better movement control and injury risk reduction, an approach outlined by Dos’Santos et al.42 supported by strong evidence in the Exercise-Based Knee and ACL Injury Prevention Clinical Practice Guidelines.54 Furthermore, an assessment of movement quality can also serve as an important component of a testing battery when making return to sport decisions. While the use of return to sport testing has inconsistent predictive value in determining reinjury after ACLR, this finding should only bolster the need to ensure the use of comprehensive and individualized testing.55,56 Several review publications recommend assessing movement quality as part of a larger testing battery to quantify an athlete’s readiness for return to sport after ACLR.57‑61
Researchers have demonstrated the use of 3-dimensional (3D) movement analysis coupled with force plate technology to assess kinetic and kinematic variables, serving as a reference standard for other measures of movement quality 53,62‑65 A 3D movement analysis can allow for a thorough evaluation of an athlete’s neuromuscular control during sport-related movements, with KAM serving as a significant predictor and surrogate measure for ACL injury 32 While certainly the gold standard, utilizing 3D movement analysis requires extensive time, equipment, trained staff, and costs that are not always practical or realistic for those who are within a clinical setting working with a greater number of athletes, fewer staff, and fewer resources.32 As an alternative to 3D movement analysis, 2-dimensional (2D) video analysis has been proposed as a means of assessing movement quality McLean et al.66 compared 2D and 3D movement assessments to screen for
movements associated with ACL injury risk. Their study demonstrated strong correlations between 2D and 3D assessment of knee valgus during side-step and side-jump maneuvers. Several other authors have proposed clinicfriendly qualitative 2D video or real-time assessment tools to identify movement patterns associated with ACL injuries, including different variations of a single leg squat,67, 68 the Drop Vertical Jump (DVJ),32,69 the Landing Error Scoring System (LESS),62,70 the Tuck Jump Assessment (TJA),71,72 and the Vail Sports Test.73,74
While the various 2D video and real-time assessment tools presented offer clinical utility, they are predominantly limited to assessing vertical landing or squatting mechanics. Indeed, these tasks are important and have application, particularly for screening athletes who participate in jumplanding sports such as basketball, volleyball, and netball. However, none of the included assessments focus on COD movements. This is pertinent as changing direction is biomechanically different from jump-landing, is a common movement in multidirectional sports, and directional changes are a prominent mechanism for ACL injury 17,34, 37,40,41,75 Movement assessment may be task-dependent, with several studies demonstrating differences in movement quality between drop landing and COD tasks.76‑78 An individual who displays sub-optimal mechanics or higher knee joint loads during landing may not necessarily display poor mechanics and higher knee joint loads during COD and vice versa.76‑78 Cowley et al.79 identified that basketball and soccer players had increased knee valgus with a 45-degree COD compared to the drop vertical jump. Additionally, King et al.80 reported that biomechanical differences during sidestep maneuvers were identified nine months after ACLR in a group of 156 subjects. These findings suggest that a qualitative assessment of movement during a COD task is warranted to screen for potential first and second ACL injury risk among athletes who must replicate these movements in their sport.
Despite the evidence favoring the utilization of a qualitative 2D assessment of COD, two literature reviews reported that this is rarely assessed in clinical practice after ACLR.58,81 Burgi et al.58 suggest that assessing movement quality or other performance-based tests may be less commonly used than impairment-based measures (like strength and knee laxity) because of the potential need for equipment, large amounts of space, and lack of testing standardization. However, the authors point out that impairment-based measures may not relate as strongly to sports participation as performance-based measures. The specificity of sport-specific movement testing requires consideration, given the frequency of COD actions in multidirectional sports and the propensity to generate hazardous mechanical loads with poor movement quality
Authors commonly use terms such as COD, agility, quickness, and cutting, often with no consistency in definition and context.82 The Essentials of Strength Training and Conditioning textbook by Haff and Triplett83 defines COD as a situation when an individual must utilize “skills and abilities needed to change movement direction, velocity, or modes.” Dos’Santos et al.84 identified several COD strategies, including a sidestep, crossover cut, split step, pivot, and shuffle step. There are also multiple means of formally assessing COD As previously mentioned, while often the gold standard, 3D movement analysis and force plates are not always realistic in clinical settings.32 By contrast, Welling et al.85 propose various on-field tests to consider after ACLR. However, of the tests identified, only one of the proposed tests formally assesses athletes for movements that may predispose them to an ACL injury.63,64 Furthermore, work conducted by Nimphius et al.86 provides an overview of over 40 tests of non-reactive and reactive COD that can be used to assess an athlete’s performance, typically through time to completion. However, while the authors advocate using qualitative movement assessment in conjunction with quantitative performance, none of the included tests offer a formalized or objective means of doing so.
Several methods of objectively assessing 2D movement quality during a COD task have been proposed, with varying methodologies and populations. The Cutting Movement Assessment Score (CMAS),42,63,64 the Expanded Cutting Alignment Scoring Tool (E-CAST),87,88 and tests proposed by Della Villa et al.,65 Di Paolo et al.,53 and Weir et al.89 all utilize 2D video analysis to assess COD movements.89 Each assessment entails subjects performing between a 45 and 90-degree side step maneuver or a transition to a backward sprint, with movement quality later assessed using frontal and sagittal plane 2D video.
Among these 2D COD assessments, the CMAS and the E-CAST have demonstrated the most promising concurrent validity compared to 3D movement analysis, as well as inter-rater and intra-rater reliability 63,64,87,88,90‑92 Additionally, these assessments can be set up and performed in a way that is feasible for clinical practice, requiring minimal equipment. As for the remaining tests by Weir et al.,89 Della Villa et al.,65 and Di Paolo et al.,53 some considerations may make their clinical utility challenging. For example, the 2D movement analysis by Weir et al.89 has fewer studies investigating its reliability and requires the use of manual measurements and digitization, which can be time-consuming. Tools proposed by Della Villa et al.93 and Di Paolo et al.53 both require more complex use of vectors through force platforms in addition to measuring 2D angles during video analysis. Thus, for the purpose of this commentary, the authors will focus on qualitative movement screening tools that require subjective evaluation of techniques and postures.

Figure 1. Setup for the Cutting Movement Assessment Score (CMAS) as demonstrated in Dos’Santos et al.42
The green arrow and cameras are used for a right foot cut, and the orange arrow and cameras are used for a left foot cut. The blue arrow and camera are used for both.
The CMAS is a validated screening tool that utilizes a 9-item scoring rubric (Appendix 1) to assess an athlete’s movement quality during a 45-90° COD maneuver 42,63,64 A higher score in this assessment represents the presence of a greater number of movements associated with ACL injury Each of the nine items included in the CMAS, operationally defined by Dos’Santos et al.,42 is based on technical determinants of KAM during COD movement and has been demonstrated as having a significant influence on knee joint loading associated with ACL injury 51,63,64
The CMAS can be performed with two high-speed cameras, cones, and the CMAS grading rubric, making it a more clinically practical tool than 3D movement analysis.42 In the testing procedure, subjects sprint 5 meters “ as fast as possible” and perform a 45-90° side step cut at a designated area under video recording (Figure 1).42 Video sampling should be recorded using a minimum of two cameras capable of recording at least 100 frames per second (fps), a feature available for most smartphones and tablets.42 Dos’Santos et al.42 recommend using an additional camera 20° from the frontal plane view to reduce parallax error in subjects who pre-rotate. However, in a more recent study, Jones et al.94 identified excellent reliability for total CMAS scores with only two camera angles, as long as one included the sagittal plane view. Practitioners should evaluate 2-3 trials per limb for each athlete, with video footage ideally viewed in software that enables videos to be played at different speeds and be viewed frame-by-frame.42
Several studies have reported the concurrent validity of the CMAS in identifying movements associated with ACL injury compared to 3D movement analysis.42,63,64 The overall inter-rater and intra-rater reliability of the CMAS has been moderate to excellent, with only one study by Aparicio-Sarmiento et al.95 identifying poor reliability of the CMAS. Their findings may have been confounded by insufficient training regarding the use of the CMAS.95 A study by Jones et al.94 also assessed the reliability of the CMAS using sports scientists and medical practitioners, including physical therapists. They identified good to excellent interrater agreements across all practitioners for total scores (K = 0.63-0.84), offering promising implications for using the CMAS across disciplines. A summary of the CMAS validity and reliability is provided in Table 1. Dos’Santos et al.42 further proposed a stratification of injury risk based on a subject’s total score: low risk is a CMAS ≤3; moderate risk is a CMAS 4-6; and high risk is a CMAS ≥7, with athletes displaying scores ≥ 7 displaying greater knee joint loads and postures associated with ACL loading compared to athletes with lower scores.
The E-CAST is a validated screening tool that uses a 6-item dichotomous scoring rubric (Appendix 2) to assess movement quality during a 45° COD maneuver, with a higher score representing a greater number of movements associated with ACL injury.88,91 A score of “1” is awarded for each item when the movement fault is present and the total score is determined.51,87 The E-CAST is an expansion from
Table 1. A comparison between the CMAS and the E-CAST CMAS42,63,64
Number of Items 9 6
Scoring Items 2 and 6 scored 0, 1, or 2 All remaining items scored 0 or 1
87,91,92,96
All items scored 0 or 1
Number of Cameras 2 or 3 2
Proposed recording quality ≥100fps
Cutting Angle 45 to 90°
Instructions for subject forward sprint effort “as fast as possible”
1080p
maximum effort
Approach distance 5 meters 8.8 meters
Concurrent Validity compared to 3D movement analysis
Reliability
Dos’Santos et al.64
Spearman’s correlation revealed a significant and very large association between CMAS and peak KAMs. (ρ = 0.796, 95% CI = 0.647-0.887, p < 0.001)
Significantly greater cutting multiplanar knee joint loads were demonstrated by subjects with higher CMASs compared to lower, with moderate to very large effect sizes.
Jones et al.63
Spearman’s correlation revealed a significant large association between CMAS and KAMs (ρ = 0.633; p < 0.001).
Jones et al.94
Good to excellent inter-rater reliablity for total score (k=0.63-0.84)
Olivares-Jabalera et al.97
Excellent intra-rater reliability for total score (ICC = 0.70)
Moderate inter-rater reliability for total scores (ICC = 0.58)
Needham and Herrington90
Excellent intra-rater reliability for total score (ICC = 0.98)
Aparicio-Sarmiento et al.95
Poor inter-rater reliability for total score (ICC = 0.11-0.45)
Moderate intra-rater reliability for total score (ICC = 0.71)
Dos’Santos et al.64
Excellent intra-rater reliability for total score (ICC = 0.95)
Moderate inter-rater reliability for total scores (ICC = 0.69)
Jones et al.63
Excellent intra-rater reliability for total scores (ICC = 0.922)
Excellent inter-rater reliability for total scores (ICC = 0.913)
the 4-item Cutting Alignment Scoring Tool (CAST) that originally only included a frontal plane assessment of trunk lean, cut width, and knee valgus.87 The expanded version now includes sagittal plane assessments of knee flexion angle and ankle plantar flexion.88 Butler et al.92 compared the use of the E-CAST qualitative scoring rubric against a quantitative version requiring 2D kinematic measurements and found no significant differences between the two, suggesting that either can serve as a reliable means of assessing movement quality
The E-CAST can be performed in a means similar to that of the CMAS using two high-speed cameras, cones, and the E-CAST grading rubric, making it more practical than 3D movement analysis.92 Subjects sprint 8.8 meters at 80% of their maximum speed towards an “opponent cone” placed
Butler et al.91
Each item demonstrated sensitivity and specificity ranging from 70-85% and 55-89%, respectively Across items, the area under the curve ranged from 0.67 to 0.91.
Butler et al.87
Good intra-rater reliability for total score (ICC=0.78)
Moderate inter-rater reliability for total score (ICC=0.71)
Butler et al.92
Good intra-rater reliability for total scores (ICC=0.821)
Good inter-rater reliability (ICC=0.752)
just beyond the pivoting area (Figure 2). A side step cut is performed at a 45° angle under video recording.87 Previous investigations of the E-CAST recorded video at 60fps with 1080p quality that was later slowed down by 50% for video analysis.87 Subjects completed three trials per direction, with one randomly selected for analysis.87,91
Butler et al.88,92 have demonstrated the concurrent validity of the E-CAST with 3D movement analysis as well as good inter- and intra-rater reliability (ICC=0.752 and ICC=0.821).88,91 The original 4-item CAST demonstrated good inter-rater and intra-rater reliability (ICC=0.808 and ICC=0.753) among medical doctors, physical therapists, and athletic trainers.87 However, the utility of the E-CAST has only been assessed with physical therapists as the adminis-

Figure 2. Setup for the Expanded Cutting Alignment Scoring Tool as demonstrated in Butler et al.96
trators and raters.88,91,92 A summary of the E-CAST validity and reliability is provided in Table 1
The CMAS and the E-CAST can both potentially serve as a practical and insightful standardized assessment of ACL injury risk with COD movements. Given their clinicfriendly utility and objective information about COD movement quality, implementing one of these assessment tools is merited to screen for both first ACL injuries and after injury as part of a return to sport testing battery. While The CMAS and the E-CAST have similar qualities, they also carry noteworthy differences. For example, they each have a different number of items (9 vs. 6), with the CMAS including an assessment of penultimate foot contact and foot rotation, each correlated with knee joint loads.51,63,64,88 Further examples of the differences between the CMAS and the E-CAST are outlined in Table 1. Each clinician must assess the unique needs and movement characteristics of the individual athlete they are working with, their respective sport, and the set up most conducive to the clinician’s setting.
A significant limitation of the presented 2D COD movement analysis tools is that there is currently no prospective evidence showing they can predict injury. While the evidence strongly supports the concurrent validity and reliability of the presented measures, a further direction of research should be determining their predictive validity, particularly for ACL injury Despite mixed validity for the utilization of return to sport testing as a whole, it is still advisable to screen for movements associated with ACL injury in sportspecific movement patterns, as opposed to limiting screening to time from injury and basic clinical examination measures.58,98‑102 Some investigations have suggested that
COD biomechanical issues may still be present longer than strength deficits post-op ACLR and that improved movement quality during return to sport testing is associated with a decreased risk of second ACL injury 80,101 Additional limitations of the provided movement analysis tools are the potential barriers related to space, time, and cost. The CMAS requires an open space that is roughly 8x10 meters, with the E-CAST requiring roughly 13x7 meters. Many clinicians may not have access to an open area this size if they are limited to a small office already filled with treatment tables and equipment. Also, performing all the required practice trials and valid trials does take time, an indispensable resource in clinical practice. However, Dos’Santos et al.42 have reported completing six CMAS trials in groups of athletes as large as twelve in less than 15 minutes. This suggests that, with experience, testing can be completed in a reasonable time. Lastly, clinicians must consider equipment costs. Utilizing timing gates and highend cameras comes at a significant economic cost that may not be attainable for practitioners. Fortunately, the test setup can be completed with cones and with the use of any recording device capable of recording at a higher frame rate, a feature available on all iPad and iPhone devices. When considering these limitations, not all clinics may be capable of conducting these tests. Patients may need to be referred to specific testing sites with the appropriate space and equipment, in line with recommendations by Unverzagt et al.59
Marques et al.103 offer insight into the application of COD movement assessment after ACLR. In their review, they do not emphasize a specific tool such as the CMAS or E-CAST,
but they do identify key variables to consider when utilizing field and laboratory-based COD testing, such as planned vs. unplanned, approach velocity, and cutting angle.
An additional consideration for the assessment of COD movement quality should be whether the COD is planned or unplanned. Sports participation often requires an athlete to process multiple sources of information and stimuli when executing sporting actions. In the context of COD, athletes often need to respond to an external stimulus, such as an opponent or a ball, that requires externally directed attention.104 Several researchers have suggested that this external focus on unplanned stimuli increases neurocognitive loads, presenting a particular after ACL injury given changes in neuroplasticity and neurocognitive compensation.104‑108 Sheppard et al.82 propose that “In order to be considered ‘reactive’ agility, the movement should not only involve a change in speed and direction, but must also be an open skilled task, involving a reaction to a stimulus.”
The performance of COD tasks under reactive conditions has been proposed as a uniquely different task compared to pre-planned COD, entailing different cognitive challenges in response to spatial and temporal stimuli.82,109,110 Unplanned COD may be more representative of sports participation, given the requirements in team sports to respond to an external stimulus, such as an opponent or ball, without pre-planning. Without a reactive element, movement assessment tools only replicate a portion of the conditions and scenarios common in sports and ACL injuries. While most ACL injuries are non-contact, the majority occur with externally directed attention and increased neurocognitive loading, typically with an opponent or ball.36,50 Several authors have described that knee movement mechanics and timed performance differ in unplanned and planned movements.111‑115 Specifically, increased KAM and internal rotation moments have been identified at the knee under unplanned conditions compared to planned conditions, both associated with increased risk of ACL injury.111,113,116 Moreover, the 2016 Consensus on Return to Sport and additional authors have suggested that utilizing unplanned movements may be superior to incorporate over planned tasks alone.57‑60 Separate reviews by Grooms et al.108 and Wilk et al.60 recommend utilizing neurocognitive and reactive testing to assess return to sport readiness after ACLR. The combined recommendations of these authors suggest that the formal assessment of movement quality under unplanned movements is warranted. However, while unplanned COD may hold many benefits, there are challenges with producing a valid, standardized sport-specific stimulus that has good reliability
A study by Needham and Herrington90 investigated differences in CMASs between planned and unplanned sidestep maneuvers for female soccer players. They identified significantly greater total CMASs for unplanned COD maneuvers (5.53±0.71) compared to planned maneuvers (3.55±0.85, p<0.012). The findings of this study match previous results that unplanned movements may reveal a higher number of movement patterns associated with ACL
injury risk.111,113 This study suggests that a 2D COD movement assessment tool can offer utility in assessing both planned and unplanned conditions and that only assessing planned conditions may not wholly represent an athlete’s injury-risk profile.
There are noteworthy challenges with the implementation of unplanned movement assessment. There is often a tradeoff between ecological validity and standardization when selecting a stimulus for unplanned movement. In the study by Needham and Herrington,90 a soccer ball pass was used to cue the subjects in their cutting direction. Their approach may promote greater ecological validity compared to light or sound-based stimuli. However, as acknowledged by Needham and Herrington,90 this approach does carry limitations in its consistency of timing and trajectory, thus potentially influencing subsequent reaction times and movement patterns. By contrast, the utilization of light stimuli is easier to regulate but is lacking in sport specificity Additionally, caution and a stepwise progression must be utilized when integrating unplanned COD maneuvers given the potential for increased knee joint loads, particularly in the context of return to sport testing after injury
One additional variable that is pertinent in the assessment of COD is the velocity at which the individual enters into the COD task (i.e., approach velocity). Reviews by Marques et al.103 and Dos’Santos et al.117 highlight that approach velocity significantly influences COD speed and biomechanics. Kristianslund et al.118 demonstrated that increased KAMs are seen with higher approach velocities compared to lower velocities among female athletes during COD maneuvers. Further studies have found that when subjects performed COD maneuvers with higher approach velocities, they exhibited greater knee joint stiffness and peak knee valgus.119‑121 An investigation on injury mechanisms for ACL injuries in handball by Olsen et al.34 also identified that non-contact ACL injuries commonly occurred at high approach velocities during COD tasks. When considering this in practical application, approach velocity should be considered when assessing movement quality, as those moving at faster speeds may be more likely to exhibit more potentially hazardous movement mechanics.103,117 As a potential means of mitigating injury and improving standardization in movement assessment, Vanrenterghem et al.121 suggest that velocity should be standardized to 4 meters per second.
Both Dos’Santos et al.117 and Marques et al.103 highlight that cutting angle is also a pertinent consideration when assessing COD movement quality. These authors identify that sharper COD angles (90 vs 45°) result in increases in knee joint loading and require lower approach velocities for optimal execution (i.e., COM angle deflection). Dos’Santos et al.117 identifies this as the “angle-velocity tradeoff,” whereby faster approach velocities can compromise
the COD execution. Given the established correlation between approach velocity and COD movement quality, it must be accounted for as a variable for execution performance and should be considered when screening COD movement quality
The clinical assessment of COD movement quality to determine ACL injury risk would be limited in value if there were no opportunities for measurable improvement. Fortunately, COD movement quality has been shown to be modifiable. Clinicians should first utilize a cutting assessment tool to identify movement patterns associated with increased injury risk. While this may have standalone value in making return to sport decisions, clinicians should also use their findings to formulate impairment-based neuromuscular interventions to address underlying movement patterns. For example, testing results may indicate movement deficits related to poor trunk control, increased knee valgus, or a lack of knee flexion. Interventions aimed at improving muscle strength and neuromuscular control can be prescribed to mitigate the identified movement patterns.
Neuromuscular training has been demonstrated to improve proprioception and decrease biomechanical deficits.122,123 These strategies can vary considerably but generally include unilateral and bilateral lower limb and core exercises with visual, verbal, and/or tactile feedback to improve trunk and knee control.122,123 This approach can be integrated through foundational exercises, plyometrics, and cutting maneuvers. A review by Buckthorpe124 provides recommendations for a movement retraining progression after ACLR, beginning with foundational movement training, then progressing to high-load ‘sport-type’ movement retraining, and lastly, integrating sport-specific movement retraining.
Studies by Olivares-Jabalera et al.125 and Dos’Santos et al.126 investigated the effectiveness of separate six-week technique modification programs to improve cutting and jump-landing movement quality among soccer players. Both studies identified significant pre-to-post improvements in CMAS scores after six weeks of COD movement training with individualized feedback from a practitioner. Additionally, a study by Nijmeijer et al.127 identified improvements in CMAS scores when subjects were provided video and verbal feedback, particularly when they were given autonomy to select the timing in which they received it. These findings indicate that COD movement quality can be improved with task-specific training. Additionally, movement assessment can serve as a valuable test-re-test measure to track modifiable risk factors associated with ACL injury risk. Dos’Santos et al.128 describe this process for movement assessment, treatment, and reassessment, depicted in Figure 3. This process can be completed multiple times over the course of an individual’s episode of care

Figure 3. A process for screening movement quality and applying interventions. or season to track patient improvement and reduce injury risk.
ACL injuries are formidable and consequential injuries in athletics that are influenced by considerable intrinsic and extrinsic risk factors.5,6,12‑16 Of these risk factors, an individual’s movement quality has been demonstrated as a significant variable associated with ACL injury risk, particularly among female athletes in multidirectional sports.1, 17,19‑23,26,30‑32 While there are various means of assessing movement quality, an assessment during a COD maneuver provides task-specific insight that is a prevalent mechanism of ACL injury.76‑78 The CMAS and the E-CAST both provide valid, reliable, and objective means of assessing movement quality during COD tasks worth considering when screening for ACL injury and re-injury risk.42,63,64,88,91,92,94 Additionally, variables such as planned and unplanned movement, approach velocity, and cutting angle should all be considered as pertinent influences on task performance and injury risk and must be considered when screening and profiling movement quality 82,103‑110,117
The authors report no conflicts of interest.
Submitted: April 17, 2024 CDT, Accepted: August 28, 2024 CDT
© The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
1. Logerstedt DS, Scalzitti D, Risberg MA, et al. Knee stability and movement coordination impairments: knee ligament sprain revision 2017: clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther 2017;47(11):A1-A47. doi:10.2519/jospt.2017.0303
2. Zbrojkiewicz D, Vertullo C, Grayson JE. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2015. Med J Australia 2018;208(8):354-358. doi:10.5694/mja17.00974
3. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med 2016;44(6):1502-1507 doi:10.1177/ 0363546516629944
4. Maniar N, Verhagen E, Bryant AL, Opar DA. Trends in Australian knee injury rates: An epidemiological analysis of 228,344 knee injuries over 20 years. The Lancet Regional Health - Western Pacific. 2022;21:100409. doi:10.1016/j.lanwpc.2022.100409
5. Agel J, Rockwood T, Klossner D Collegiate ACL injury rates across 15 Sports: National Collegiate Athletic Association injury surveillance system data update (2004-2005 through 2012-2013). Clin J Sport Med. 2016;26(6):6. doi:10.1097/ JSM.0000000000000290
6. Drakos MC, Domb B, Starkey C, Callahan L, Allen AA. Injury in the National Basketball Association: A 17-Year overview Sports Health 2010;2(4):284-290. doi:10.1177/1941738109357303
7. Ardern CL, Taylor NF, Feller JA, Webster KE. Fiftyfive per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 2014;48(21):1543-1552. doi:10.1136/ bjsports-2013-093398
8. Randsborg PH, Cepeda N, Adamec D, Rodeo SA, Ranawat A, Pearle AD. Patient-reported outcome, return to sport, and revision rates 7-9 years after anterior cruciate ligament reconstruction: results from a cohort of 2042 patients. Am J Sports Med. 2022;50(2):423-432. doi:10.1177/03635465211060333
9. Fones L, Kostyun RO, Cohen AD, Pace JL. Patientreported outcomes, return-to-sport status, and reinjury rates after anterior cruciate ligament reconstruction in adolescent athletes: minimum 2-year follow-up. Orthop J Sports Med 2020;8(11):232596712096447. doi:10.1177/ 2325967120964471
10. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med 2014;42(7):1567-1573. doi:10.1177/ 0363546514530088
11. Barber-Westin S, Noyes FR. One in 5 athletes sustain reinjury upon return to high-risk sports after ACL reconstruction: a systematic review in 1239 athletes younger than 20 years. Sports Health 2020;12(6):587-597 doi:10.1177/1941738120912846
12. Hewett TE. Preventive biomechanics: A paradigm shift with a translational approach to biomechanics. J Sci Med Sport 2017;45(11):2654-2664. doi:10.1016/ j.jsams.2017.01.002
13. Baez SE, Hoch MC, Hoch JM. Psychological factors are associated with return to pre-injury levels of sport and physical activity after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2020;28(2):495-501. doi:10.1007/s00167-019-05696-9
14. McPherson AL, Feller JA, Hewett TE, Webster KE. Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sports Med. 2019;47(4):857-862. doi:10.1177/0363546518825258
15. Poulsen E, Goncalves GH, Bricca A, Roos EM, Thorlund JB, Juhl CB. Knee osteoarthritis risk is increased 4-6 fold after knee injury – a systematic review and meta-analysis. Br J Sports Med 2019;53(23):1454-1463. doi:10.1136/ bjsports-2018-100022
16. Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 2007;35(10):1756-1769. doi:10.1177/ 0363546507307396
17. Wetters N, Weber AE, Wuerz TH, Schub DL, Mandelbaum BR. Mechanism of injury and risk factors for anterior cruciate ligament injury. Op Tech Sports Med. 2016;24(1):2-6. doi:10.1053/ j.otsm.2015.09.001
18. Bates NA, Schilaty ND, Nagelli CV, Krych AJ, Hewett TE. Multiplanar loading of the knee and its influence on anterior cruciate ligament and medial collateral ligament strain during simulated landings and noncontact tears. Am J Sports Med 2019;47(8):1844-1853. doi:10.1177/ 0363546519850165
19. Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train 2013;48(6):810-817 doi:10.4085/1062-6050-48.6.03
20. Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and metaanalysis. Am J Sports Med 2016;44(10):2716-2723. doi:10.1177/0363546515617742
21. Beynnon BD, Vacek PM, Newell MK, et al. The effects of level of competition, sport, and sex on the incidence of first-time noncontact anterior cruciate ligament injury. Am J Sports Med. 2014;42(8):1806-1812. doi:10.1177/ 0363546514540862
22. Montalvo AM, Schneider DK, Webster KE, et al. Anterior cruciate ligament injury risk in sport: a systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train. 2019;54(5):472-482. doi:10.4085/1062-6050-407-16
23. Montalvo AM, Schneider DK, Yut L, et al. “What’s my risk of sustaining an ACL injury while playing sports?” A systematic review with meta-analysis. Br J Sports Med 2019;53(16):1003-1012. doi:10.1136/ bjsports-2016-096274
24. Bram JT, Magee LC, Mehta NN, Patel NM, Ganley TJ. Anterior cruciate ligament injury incidence in adolescent athletes: a systematic review and metaanalysis. Am J Sports Med. 2021;49(7):1962-1972. doi:10.1177/0363546520959619
25. Zech A, Hollander K, Junge A, et al. Sex differences in injury rates in team-sport athletes: A systematic review and meta-regression analysis. J Sport Health Sci 2022;11(1):104-114. doi:10.1016/ j.jshs.2021.04.003
26. Bram JT, Magee LC, Mehta NN, Patel NM, Ganley TJ. Anterior cruciate ligament injury incidence in adolescent athletes: a systematic review and metaanalysis. Am J Sports Med 2021;49(7):1962-1972. doi:10.1177/0363546520959619
27 Ruddy JD, Cormack SJ, Whiteley R, Williams MD, Timmins RG, Opar DA. Modeling the risk of team sport injuries: A narrative review of different statistical approaches. Front Physiol. 2019;10:829. doi:10.3389/fphys.2019.00829
28. Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature—part 2: hormonal, genetic, cognitive function, previous injury, and extrinsic risk factors. Sports Health. 2012;4(2):155-161. doi:10.1177/ 1941738111428282
29. Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature part 1: neuromuscular and anatomic risk. Sports Health 2012;4(1):69-78. doi:10.1177/ 1941738111428281
30. Paterno MV, Schmitt LC, Ford KR, et al.
Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 2010;38(10):1968-1978. doi:10.1177/ 0363546510376053
31. Paterno MV, Kiefer AW, Bonnette S, et al. Prospectively identified deficits in sagittal plane hip–ankle coordination in female athletes who sustain a second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Clin Biomech 2015;30(10):1094-1101. doi:10.1016/j.clinbiomech.2015.08.019
32. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study Am J Sports Med 2005;33(4):492-501. doi:10.1177/0363546504269591
33. Herrington L, Munro A, Jones P Assessment of factors associated with injury risk. In: Performance Assessment in Strength and Conditioning 1st ed. Routledge; 2018:53-95. doi:10.4324/ 9781315222813-7
34. Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med 2004;32(4):1002-1012. doi:10.1177/0363546503261724
35. Salci Y, Kentel BB, Heycan C, Akin S, Korkusuz F. Comparison of landing maneuvers between male and female college volleyball players. Clin Biomech 2004;19(6):622-628. doi:10.1016/ j.clinbiomech.2004.03.006
36. Della Villa F, Buckthorpe M, Grassi A, et al. Systematic video analysis of ACL injuries in professional male football (soccer): injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases. Br J Sports Med 2020;54(23):1423-1432. doi:10.1136/ bjsports-2019-101247
37. Johnston JT, Mandelbaum BR, Schub D, et al. Video analysis of anterior cruciate ligament tears in professional american football athletes. Am J Sports Med 2018;46(4):862-868. doi:10.1177/ 0363546518756328
38. Larwa J, Stoy C, Chafetz RS, Boniello M, Franklin C. Stiff Landings, Core Stability, and Dynamic Knee Valgus: A Systematic Review on Documented Anterior Cruciate Ligament Ruptures in Male and Female Athletes. Int J Enivr Res Pub Health 2021;18(7):3826. doi:10.3390/ijerph18073826
39. Saki F, Tahayori B, Bakhtiari Khou S. Female athletes with ligament dominance exhibiting altered hip and ankle muscle co-contraction patterns compared to healthy individuals during single-leg landing. Gait Posture 2022;93:225-229. doi:10.1016/ j.gaitpost.2022.02.011
40. Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. Mechanisms, prediction, and prevention of ACL injuries: Cut risk with three sharpened and validated tools: ACL injury prevention. J Orthop Res 2016;34(11):1843-1855. doi:10.1002/jor.23414
41. Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359-367. doi:10.1177/ 0363546506293899
42. Dos’Santos T, Thomas C, McBurnie A, Donelon T, Herrington L, Jones PA. The cutting movement assessment score (CMAS) qualitative screening tool: application to mitigate anterior cruciate ligament injury risk during cutting. Biomech. 2021;1(1):83-101. doi:10.3390/biomechanics1010007
43. Pollard CD, Davis IM, Hamill J. Influence of gender on hip and knee mechanics during a randomly cued cutting maneuver. Clin Biomech. 2004;19(10):1022-1031. doi:10.1016/ j.clinbiomech.2004.07.007
44. Weir G, Stillman M, van Emmerik R, Wyatt H, Jewell C, Hamill J. Differences in Kinetics, Kinematics and Muscle Activation Strategies in Male and Female Team Sport Athletes During Unanticipated Sidestepping. J Sci Sport Exerc 2019;1(2):159-167 doi:10.1007/s42978-019-0019-2
45. Mclean SG, Lipfert SW, Van Den Bogert AJ. Effect of gender and defensive opponent on the biomechanics of sidestep cutting. Med Sci Sports Exerc. 2004;36(6):1008-1016. doi:10.1249/ 01.MSS.0000128180.51443.83
46. Malinzak RA, Colby SM, Kirkendall DT, Yu B, Garrett WE. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech 2001;16(5):438-445. doi:10.1016/S0268-0033(01)00019-5
47. Ogasawara I, Miyakawa S, Wakitani S. Gender difference in neuromuscular hip and knee joint control during single-leg landing. MJHES 2014;4(1):1-11.
48. Ford KR, Myer GD, Hewett TE. Valgus Knee Motion during Landing in High School Female and Male Basketball Players. Med Sci Sports Exerc. 2003;35(10):1745-1750. doi:10.1249/ 01.MSS.0000089346.85744.D9
49. Russell KA, Palmieri RM, Zinder SM, Ingersoll CD. Sex differences in valgus knee angle during a singleleg drop jump. J Athl Train 2006;41(2):166-171.
50. Lucarno S, Zago M, Buckthorpe M, et al. Systematic video analysis of anterior cruciate ligament injuries in professional female soccer players. Am J Sports Med. 2021;49(7):1794-1802. doi:10.1177/03635465211008169
51. Donelon TA, Dos’Santos T, Pitchers G, Brown M, Jones PA. Biomechanical determinants of knee joint loads associated with increased anterior cruciate ligament loading during cutting: a systematic review and technical framework. Sports Med - Open. 2020;6(1):53. doi:10.1186/s40798-020-00276-5
52. Arundale AJH, Silvers-Granelli HJ, Myklebust G. ACL injury prevention: Where have we come from and where are we going? J Orthop Res 2022;40(1):43-54. doi:10.1002/jor.25058
53. Di Paolo S, Zaffagnini S, Tosarelli F, et al. A 2D qualitative movement assessment of a deceleration task detects football players with high knee joint loading. Knee Surg Sports Traumatol Arthrosc. 2021;29(12):4032-4040. doi:10.1007/ s00167-021-06709-2
54. Arundale AJH, Bizzini M, Dix C, et al. Exercisebased knee and anterior cruciate ligament injury prevention: Clinical Practice Guidelines linked to the International Classification of Functioning, Disability and Health From the Academy of Orthopaedic Physical Therapy and the American Academy of Sports Physical Therapy. J Orthop Sports Phys Ther. 2023;53(1):CPG1-CPG34. doi:10.2519/ jospt.2023.0301
55. Gill VS, Tummala SV, Sullivan G, et al. Functional return-to-sport testing demonstrates inconsistency in predicting short-term outcomes following anterior cruciate ligament reconstruction: A systematic review Arthroscopy Published online January 11, 2024. doi:10.1016/j.arthro.2023.12.032
56. Hurley ET, Mojica ES, Haskel JD, et al. Return to play testing following anterior cruciate reconstruction – A systematic review & metaanalysis. The Knee. 2022;34:134-140. doi:10.1016/ j.knee.2021.11.010
57 Ardern CL, Glasgow P, Schneiders A, et al. 2016 consensus statement on return to sport from the first world congress in sports physical therapy, Bern. Br J Sports Med 2016;50(14):853-864. doi:10.1136/ bjsports-2016-096278
58. Burgi CR, Peters S, Ardern CL, et al. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review Br J Sports Med. 2019;53(18):1154-1161. doi:10.1136/ bjsports-2018-099982
59. Unverzagt C, Andreyo E, Tompkins J. ACL return to sport testing: it’s time to step up our game. Int J Sports Phys Ther 2021;16(4):1169-1177 doi:10.26603/001c.25463
60. Wilk K, Thomas ZM, Arrigo CA, Davies GJ. The need to change return to play testing in athletes following ACL injury: A theoretical model. Int J Sports Phys Ther. 2023;18(1). doi:10.26603/001c.67988
61. Meredith SJ, Rauer T, Chmielewski TL, et al. Return to sport after anterior cruciate ligament injury: Panther Symposium ACL Injury Return to Sport Consensus Group. Journal of ISAKOS 2021;6(3):138-146. doi:10.1136/jisakos-2020-000495
62. Hanzlíková I, Hébert-Losier K. Is the landing error scoring system reliable and valid? A systematic review Sports Health 2020;12(2):181-188. doi:10.1177/1941738119886593
63. Jones P, Donelon T, Dos’Santos T. A preliminary investigation into a qualitative assessment tool to identify athletes with high knee abduction moments during cutting : Cutting Movement Assessment Score (CMAS). Prof Strength Condit Published online 2017:37-42.
64. Dos’Santos T, McBurnie A, Donelon T, Thomas C, Comfort P, Jones PA. A qualitative screening tool to identify athletes with ‘high-risk’ movement mechanics during cutting: The cutting movement assessment score (CMAS). Phys Ther Sport 2019;38:152-161. doi:10.1016/j.ptsp.2019.05.004
65. Della Villa F, Di Paolo S, Santagati D, et al. A 2D video-analysis scoring system of 90° change of direction technique identifies football players with high knee abduction moment. Knee Surg Sports Traumatol Arthrosc 2021;30(11):3616-3625. doi:10.1007/s00167-021-06571-2
66. McLean SG. Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury Br J Sports Med 2005;39(6):355-362. doi:10.1136/bjsm.2005.018598
67. Ressman J, Grooten WJA, Rasmussen Barr E. Visual assessment of movement quality in the single leg squat test: a review and meta-analysis of interrater and intrarater reliability. BMJ Open Sport Exerc Med 2019;5(1):e000541. doi:10.1136/ bmjsem-2019-000541
68. Almangoush A, Herrington L, Jones R. A preliminary reliability study of a qualitative scoring system of limb alignment during single leg squat. Phys Ther Rehabil. 2014;1(1):2. doi:10.7243/ 2055-2386-1-2
69. Numata H, Nakase J, Kitaoka K, et al. Twodimensional motion analysis of dynamic knee valgus identifies female high school athletes at risk of noncontact anterior cruciate ligament injury Knee Surg Sports Traumatol Arthrosc. 2018;26(2):442-447. doi:10.1007/s00167-017-4681-9
70. Padua DA, DiStefano LJ, Beutler AI, de la Motte SJ, DiStefano MJ, Marshall SW. The landing error scoring system as a screening tool for an anterior cruciate ligament injury–prevention program in elite-youth soccer athletes. J Athl Train. 2015;50(6):589-595. doi:10.4085/1062-6050-50.1.10
71. Fort-Vanmeerhaeghe A, Montalvo AM, Lloyd RS, Read P, Myer GD. Intra- and inter-rater reliability of the modified tuck jump assessment. J Sports Sci Med 2017;16:117-124.
72. Myer GD, Ford KR, Hewett TE. Tuck jump assessment for reducing anterior cruciate ligament injury risk. Hubbard TJ, ed. Athl Ther Today 2008;13(5):39-44. doi:10.1123/att.13.5.39
73. Hannon J, Wang-Price S, Swank C, et al. The validity and reliability of the Vail Sport TestTM as a measure of performance following anterior cruciate ligament reconstruction. Phys Ther Sport 2019;38:162-169. doi:10.1016/j.ptsp.2019.05.001
74. Garrison JC, Shanley E, Thigpen C, Geary R, Osler M, DelGiorno J. The reliability of the vail sport test as a measure of physical performance following anterior cruciate ligament reconstruction. Int J Sports Phys Ther 2012;7(1):11.
75. Kimura Y, Ishibashi Y, Tsuda E, Yamamoto Y, Tsukada H, Toh S. Mechanisms for anterior cruciate ligament injuries in badminton. Br J Sports Med 2010;44(15):1124-1127. doi:10.1136/ bjsm.2010.074153
76. Chinnasee C, Weir G, Sasimontonkul S, Alderson J, Donnelly C. A biomechanical comparison of singleleg landing and unplanned sidestepping. Int J Sports Med 2018;39. doi:10.1055/a-0592-7422
77 Jones PA, Herrington LC, Munro AG, GrahamSmith P. Is there a relationship between landing, cutting, and pivoting tasks in terms of the characteristics of dynamic valgus? Am J Sports Med 2014;42(9):2095-2102. doi:10.1177/ 0363546514539446
78. Kristianslund E, Krosshaug T Comparison of drop jumps and sport-specific sidestep cutting: implications for anterior cruciate ligament injury risk screening. Am J Sports Med 2013;41(3):684-688. doi:10.1177/0363546512472043
79. Cowley HR, Ford KR, Myer GD, Kernozek TW, Hewett TE. Differences in neuromuscular strategies between landing and cutting tasks in female basketball and soccer athletes. J Athl Train 2006;41(1):7
80. King E, Richter C, Franklyn-Miller A, et al. Biomechanical but not timed performance asymmetries persist between limbs 9 months after ACL reconstruction during planned and unplanned change of direction. J Biomech 2018;81:93-103. doi:10.1016/j.jbiomech.2018.09.021
81. Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after nterior cruciate ligament reconstruction: A systematic review Orthop J Sports Med. 2014;2(1):232596711351830. doi:10.1177/ 2325967113518305
82. Sheppard J, Dawes J, Jeffreys I, Spiteri T, Nimphius S. Broadening the view of agility: a scientific review of the literature. J Australian Strength Condit 2014;22(3):6-25.
83. Haff G, Triplett T. Essentials of Strength Training and Conditioning 4th Edition. National Strength and Conditioning Association; 2016.
84. Dos’Santos T, McBurnie A, Thomas C, Jones PA, Harper D. Attacking agility actions: match play contextual applications with coaching and technique guidelines. Strength Condit J. 2022;44(5):102-118. doi:10.1519/SSC.0000000000000697
85. Welling W, Frik L. On-field tests for patients after anterior cruciate ligament reconstruction: a scoping review Orthop J Sports Med 2022;10(1):232596712110554. doi:10.1177/ 23259671211055481
86. Nimphius S, Callaghan SJ, Bezodis NE, Lockie RG. Change of direction and agility tests: challenging our current measures of performance. Strength Condit J. 2017;40(1):26-38. doi:10.1519/ SSC.0000000000000309
87. Butler LS, Milian EK, DeVerna A, et al. Reliability of the cutting alignment scoring tool (CAST) to assess trunk and limb alignment during a 45-degree side-step cut. Int J Sports Phys Ther. Published online April 1, 2021. doi:10.26603/001c.21419
88. Butler LS, Martinez AR, Sugimoto D, et al. Reliability of the Expanded Cutting Alignment Scoring Tool (E-CAST) to assess trunk and limb alignment during a 45-degree side-step cut. Int J Sports Phys Ther. 2022;17(3). doi:10.26603/ 001c.33045
89. Weir G, Alderson J, Smailes N, Elliott B, Donnelly C. A reliable video-based ACL injury screening tool for female team sport athletes. Int J Sports Med 2019;40(03):191-199. doi:10.1055/a-0756-9659
90. Needham C, Herrington L. Cutting movement assessment scores during anticipated and unanticipated 90-degree sidestep cutting manoeuvres within female professional footballers. Sports. 2022;10(9):128. doi:10.3390/sports10090128
91. Butler L, Martinez A, Erdman A, et al. Concurrent validity of the expanded cutting alignment scoring tool (E-CAST). Int J Sports Phys Ther 2023;18(5). doi:10.26603/001c.87633
92. Butler L, Wyatt C, Martinez A, et al. No difference in two-dimensional kinematic assessment of a 45-degree sidestep cut compared to qualitative assessment. Int J Sports PhysTher. 2023;18(3). doi:10.26603/001c.74366
93. Della Villa F, Di Paolo S, Santagati D, et al. A 2D video-analysis scoring system of 90° change of direction technique identifies football players with high knee abduction moment. Knee Surg Sports Traumatol Arthrosc. 2021;30(11):3616-3625. doi:10.1007/s00167-021-06571-2
94. Jones PA, Rai A, Dos’Santos T, Herrington LC. Inter-professional and methodological agreement in using the cutting movement assessment score (CMAS). Biomech 2023;3(2):181-192. doi:10.3390/ biomechanics3020016
95. Aparicio-Sarmiento A, Hernández-García R, Cejudo A, Palao JM, Sainz de Baranda P. Reliability of a qualitative instrument to assess high-risk mechanisms during a 90° change of direction in female football players. IJERPH 2022;19(7):4143. doi:10.3390/ijerph19074143
96. Butler LS, Martinez AR, Sugimoto D, et al. Reliability of the expanded cutting alignment scoring tool (E-CAST) to assess trunk and limb alignment during a 45-degree side-step cut. Intl J Sports Phys Ther 2022;17(3). doi:10.26603/001c.33045
97 Olivares-Jabalera J, Fílter-Ruger A, Dos’Santos T, et al. Is there association between cutting and jumplanding movement quality in semi-professional football players? Implications for ACL injury risk screening. Phys Ther Sport. 2022;56:15-23. doi:10.1016/j.ptsp.2022.05.015
98. Webster KE, Hewett TE. What is the Evidence for and Validity of Return-to-Sport Testing after Anterior Cruciate Ligament Reconstruction Surgery? A Systematic Review and Meta-Analysis. Sports Medicine. 2019;49(6):917-929. doi:10.1007/ s40279-019-01093-x
99. Manoj Rajakaruna P, Dempsey AR, Learmonth YC. Reliability, validity, and predictability of screening methods for noncontact anterior cruciate ligament injury- A systematic review J Sci Med Sport 2023;26:S110-S111. doi:10.1016/j.jsams.2023.08.136
100. Fältström A, Hägglund M, Hedevik H, Kvist J. Poor validity of functional performance tests to predict knee injury in female soccer players with or without anterior cruciate ligament reconstruction. Am J Sports Med 2021;49(6):1441-1450. doi:10.1177/ 03635465211002541
101. Van Melick N, Pronk Y, Nijhuis-van Der Sanden M, Rutten S, Van Tienen T, Hoogeboom T Meeting movement quantity or quality return to sport criteria is associated with reduced second ACL injury rate. J Orthop Res 2022;40(1):117-128. doi:10.1002/ jor.25017
102. Capin JJ, Snyder-Mackler L, Risberg MA, Grindem H. Keep calm and carry on testing: A substantive reanalysis and critique of ‘what is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Br J Sports Med 2019;53(23):1444-1446. doi:10.1136/ bjsports-2019-100906
103. Marques JB, Paul DJ, Graham-Smith P, Read PJ. Change of direction assessment following anterior cruciate ligament reconstruction: a review of current practice and considerations to enhance practical application. Sports Med 2020;50(1):55-72. doi:10.1007/s40279-019-01189-4
104. Piskin D, Benjaminse A, Dimitrakis P, Gokeler A. Neurocognitive and neurophysiological functions related to ACL injury: A framework for neurocognitive approaches in rehabilitation and return-to-sports tests. Sports Health Published online July 8, 2021:194173812110292. doi:10.1177/ 19417381211029265
105. Grooms DR, Chaudhari A, Page SJ, NicholsLarsen DS, Onate JA. Visual-motor control of drop landing after anterior cruciate ligament reconstruction. J Athl Train 2018;53(5):486-496. doi:10.4085/1062-6050-178-16
106. Gokeler A, Neuhaus D, Benjaminse A, Grooms DR, Baumeister J. Principles of motor learning to support neuroplasticity after ACL injury: implications for optimizing performance and reducing risk of second ACL injury Sports Med 2019;49(6):853-865. doi:10.1007/s40279-019-01058-0
107 Faltus J, Criss CR, Grooms DR. Shifting focus: A clinician’s guide to understanding neuroplasticity for anterior cruciate ligament rehabilitation. American College of Sports Medicine. 2020;19(2):8. doi:10.1249/ JSR.0000000000000688
108. Grooms DR, Chaput M, Simon JE, Criss CR, Myer GD, Diekfuss JA. Combining neurocognitive and functional tests to improve return to sport decisions following ACL reconstruction. J Orthop Sports Phys Ther. Published online May 15, 2023:1-14. doi:10.2519/jospt.2023.11489
109. Serpell BG, Young WB, Ford M. Are the perceptual and decision-making components of agility trainable? A preliminary investigation. J Strength Condit Res 2011;25(5):1240-1248. doi:10.1519/JSC.0b013e3181d682e6
110. Safaric A, Bird S. Agility drills for basketball: Review and practical applications. J Australian Strength Condit 2011;19:24-32.
111. Brown SR, Brughelli M, Hume PA. Knee mechanics during planned and unplanned sidestepping: a systematic review and meta-analysis. Sports Med. 2014;44(11):1573-1588. doi:10.1007/ s40279-014-0225-3
112. Simonek J, Horicka P, Hianik J. Differences in pre-planned agility and reactive agility performance in sport games. Acta Gymnica 2016;46(2):68-73. doi:10.5507/ag.2016.006
113. Besier TF, Lloyd DG, Ackland TR, Cochrane JL. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med Sci Sports Exerc Published online July 2001:1176-1181. doi:10.1097/ 00005768-200107000-00015
114. Fuerst P, Gollhofer A, Gehring D Preparation time influences ankle and knee joint control during dynamic change of direction movements. J Sports Sci 2017;35(8):762-768. doi:10.1080/ 02640414.2016.1189084
115. Mornieux G, Gehring D, Fürst P, Gollhofer A. Anticipatory postural adjustments during cutting manoeuvres in football and their consequences for knee injury risk. J Sports Sci 2014;32(13):1255-1262. doi:10.1080/02640414.2013.876508
116. Hughes G, Dai B. The influence of decision making and divided attention on lower limb biomechanics associated with anterior cruciate ligament injury: a narrative review. Sports Biomech. 2023;22(1):30-45. doi:10.1080/ 14763141.2021.1898671
117. Dos’Santos T, Thomas C, Comfort P, Jones PA. The effect of angle and velocity on change of direction biomechanics: an angle-velocity trade-off Sports Med. 2018;48(10):2235-2253. doi:10.1007/ s40279-018-0968-3
118. Kristianslund E, Faul O, Bahr R, Myklebust G, Krosshaug T. Sidestep cutting technique and knee abduction loading: implications for ACL prevention exercises. Br J Sports Med 2014;48(9):779-783. doi:10.1136/bjsports-2012-091370
119. Kimura K, Sakurai S. A sidestep cut preparation strategy decreases the external load applied to the knee joint. Int J Sport Health Sci. 2013;11(0):109-117. doi:10.5432/ijshs.201309
120. Nedergaard NJ, Kersting U, Lake M. Using accelerometry to quantify deceleration during a highintensity soccer turning manoeuvre. J Sports Sci 2014;32(20):1897-1905. doi:10.1080/ 02640414.2014.965190
121. Vanrenterghem J, Venables E, Pataky T, Robinson MA. The effect of running speed on knee mechanical loading in females during side cutting. J Biomech 2012;45(14):2444-2449. doi:10.1016/ j.jbiomech.2012.06.029
122. Nagelli CV, Wordeman SC, Di Stasi S, Hoffman J, Marulli T, Hewett TE. Neuromuscular Training Improves Biomechanical Deficits at the Knee in Anterior Cruciate Ligament–Reconstructed Athletes. Clin J Sport Med Published online 2019. doi:10.1097/ JSM.0000000000000723
123. Arumugam A, Björklund M, Mikko S, Häger CK. Effects of neuromuscular training on knee proprioception in individuals with anterior cruciate ligament injury: a systematic review and GRADE evidence synthesis. BMJ Open 2021;11(5):e049226. doi:10.1136/bmjopen-2021-049226
124. Buckthorpe M. Recommendations for movement re-training after ACL reconstruction. Sports Med. 2021;51(8):1601-1618. doi:10.1007/ s40279-021-01454-5
125. Olivares-Jabalera J, Fílter A, Dos´Santos T, Ortega-Domínguez J, Soto Hermoso VM, Requena B. The safe landing warm up technique modification programme: an effective anterior cruciate ligament injury mitigation strategy to improve cutting and jump-movement quality in soccer players. J Sports Sci 2022;40(24):2784-2794. doi:10.1080/ 02640414.2023.2193451
126. Dos’Santos T, McBurnie A, Comfort P, Jones PA. The effects of six-weeks change of direction speed and technique modification training on cutting performance and movement quality in male youth soccer players. Sports 2019;7(9):205. doi:10.3390/ sports7090205
127 Nijmeijer EM, Elferink-Gemser MT, McCrory S, Cortes N, Benjaminse A. How to improve movement execution in sidestep cutting? Involve me and I will learn. Hum Mov Sci. 2023;90:103115. doi:10.1016/ j.humov.2023.103115
128. Dos’Santos T, Thomas C, McBurnie A, Donelon T, Herrington L, Jones PA. The Cutting Movement Assessment Score (CMAS) Qualitative Screening Tool: Application to mitigate anterior cruciate ligament injury risk during cutting. Biomech. 2021;1(1):83-101. doi:10.3390/biomechanics1010007
Download: https://ijspt.scholasticahq.com/article/123483-clinical-utility-of-qualitative-change-of-directionmovement-assessment-in-acl-injury-risk-evaluation/attachment/245157.docx?auth_token=RoTN899fp6DyVILgQGZx
Download: https://ijspt.scholasticahq.com/article/123483-clinical-utility-of-qualitative-change-of-directionmovement-assessment-in-acl-injury-risk-evaluation/attachment/245156.docx?auth_token=RoTN899fp6DyVILgQGZx

International Journal of Sports Physical Therapy
Keywords: OSET, research symposium, ortho rehab, sports rehab https://doi.org/10.26603/001c.123874
The International Journal of Sports Physical Therapy is pleased to publish abstracts from the fourteenth Orthopaedic Summit (OSET) taking place in Las Vegas, September 13-18, 2024. The IJSPT hosted the third annual research forum and reception at OSET, sponsored by ATI Physical Therapy and Hyperice. The abstracts presented in the following pages were selected by the OSET Research Committee and editorial staff of the International Journal of Sports Physical Therapy After careful review, a total of 18 research abstracts were accepted and presented at OSET 2024. Awards for outstanding abstracts were presented on September 14.
The 2024 abstracts include contemporary orthopaedic and rehabilitation topics across various research designs. Each abstract presents only a brief summary of a research project / presentation and does not permit full assessment of the scientific rigor with which the work was conducted. While the abstracts offer only preliminary results that may require further refinement and future validation, they do serve an important role in sharing new research ideas and rehabilitation advancements. This sharing of ideas helps to encourage dialogue among researchers, clinicians, and educators that will ultimately contribute to the orthopaedic and rehabilitation body of knowledge. We strongly encourage authors to continue pursuing the publication of their research as a full manuscript.
Thank you to all submitting abstracts for consideration. We look forward to another outstanding season of submissions for OSET 2025.
Phil Page PhD, PT, ATC
Chuck Thigpen PhD, PT, ATC
OSET Research Committee Co-Chairs
EVIDENCE OF MAIN QUALITIES MEASURING BY UPPER EXTREMITIES FUNCTIONAL PERFORMANCE TESTS: A SYSTEMATIC REVIEW
Tao Shang,1 Ruiqian Zhou,1 Yongni Zhang,1 RobRoy Martin,2,3
1 Duquesne-China Health Institute, Duquesne University, Pittsburgh, PA, USA
2 Department of Physical Therapy, Duquesne University, PA, USA
3 UPMC Center for Sports Medicine, PA, USA
Background: Upper extremities Functional Performance Tests (FPTs) have been used to assess the impact of these shoulder impairment on an individual’s ability to perform their desired activity Studies recommend twenty-five upper extremities FPTs in clinical working. However, few of these upper extremities FPTs have evidence to show what they are supposed to measure.
Purpose: The purpose of this systematic review is to identify the purpose of the FPTs and the factors these tests measures.
Study Design: Systematic review
Methods: Databases (PubMed, Medline, EMBASE) were searched in May 2024. One reviewer rated the methodological quality based on the Consensus-based Standards for the Selection of Health Measurement Instruments (COSMIN) checklist.
Results: Twenty-one studies were included with Twenty-five FPTs. The FPTs analyzed were Closed Kinetic Chain Upper Extremity Stability Test (CKCUEST), Posterior Shoulder Endurance Test, Modified Closed Kinetic Chain Upper Extremity Stability Test (m-CKCUEST), Shoulder Endurance Test, The Athletic Shoulder Test, Upper Quarter YBalance Test, Seated medicine ball throw (SMBT), Ball abduction-external rotation test, Ball taps on wall test, Prone ball drop test, Push up test, Pull up test, One Repetition Maximum Bench Press Test, Unilateral Maximum Chest Press Test, Unilateral Pulling Assessment, Single Arm Pushing Assessment, Single Arm Seated Shot Put Test (SSPT), Upper Extremity Hop Test, Medicine Ball Explosive Power Test, Arm Jump Board Test, Upper Limb Rotation Test, Finger Hang Test, Two Arm Bent Hang Test, Pull Up Shoulder Endurance Test. Most FPTs are not supported by evidence what they suppose to measure. CKCUEST have moderate evidence supporting measuring upper extremities stability and coordination. SMBT and SSPT have moderate
to strong evidence supporting measuring power of upper extremities.
Conclusion: SMBT and SSPT are clinically valid in measuring strength and power of upper extremities. CKCUEST is considered to be a potential tool for accessing upper limb stability and coordination. More evidence is needed to clarify what main qualities are suppose to measure in other upper extremities FPTs.
Presenting author: shangt@duq.edu
Ramos S, Antle K, Byrnes R, Heick JD Northern Arizona University, Department of Physical Therapy and Athletic Training, Flagstaff, Arizona 86011
Background: The Functional Movement Screen (FMS) is used to evaluate seven fundamental movement patterns in athletes. The FMS is not intended to diagnose orthopedic problems but to demonstrate opportunities for improving movement in athletes.
Purpose: The purpose of the current study was to evaluate the effects of a 4-week intervention on FMS total scores and FMS component scores in a subset of 18 Division I football athletes. Study Design: Oxford Centre for EBM Level 3 Non-randomized controlled Cohort study Methods: Eighty-eight Northern Arizona University Division 1 football players were assessed using the FMS in the spring and summer before the athletic season. Eighteen football athletes (mean age, SD; 21.10 ± 1.96 years) received corrective exercise interventions over 4 weeks, considering FMS total and component scores and the Symmio Self-Screen conducted weekly The intervention group was assessed for pain with movement, movement dysfunction, and deficits in dynamic balance in concordance with Matsel et al., 2023. Corrective exercise interventions were implemented by entry-level student physical therapists for 20 minutes per day, 3 times per week for 4 weeks. FMS scores from the corrective exercise group were compared to the control group.
Results: FMS total scores were statistically significant differences compared to the control group (p=.003; 95% CI -4.14, -0.31) and 6 of 7 FMS component scores for Deep Squat, Hurdle Step, Inline Lunge, Shoulder Mobility, Trunk Stability, and Rotary Stability were statistically significant (all p<.05).
Conclusion: The FMS can identify movement limitations, and individualized corrective exercises may improve FMS scores in football athletes. Future studies may consider how corrective exercises may improve performance.
Presenting author: sdr338@nau.edu
Submitting author: John.Heick@nau.edu
Giordano, K.
Louisiana State University Health Science Center, Department of Physical Therapy, New Orleans, LA
Background: Technological advancements have democratized access to objective data in athletes of all ages. Strength and range of motion (ROM) testing are critical in examining a pitcher’s upper extremity However, current sports medicine professionals rely on normative data published from small clinical sample sizes.
Purpose: To predict strength and ROM data in baseball pitchers using anthropometrics and provide normative data from a large population. We hypothesize height, weight, and age will be positive predictors of strength metrics, positive predictors of external rotation (ER) and flexion ROM, and negative predictors of internal rotation (IR) ROM.
Study Design: Original Research.
Methods: Data were collected on 7,654 pitchers between 7-30 years old. Strength variables of interest were IR, ER, scaption, and grip. ROM variables of interest were IR, ER, and flexion. Participants used an inertial measurement unit and dynamometer for self-assessment after viewing educational videos. IR, ER, and scaption strength measurements were taken in supine with the shoulder elevated 90-degrees. Grip strength was measured in half-kneeling with the shoulder in 90-degrees of abduction and ER. ROM tests were performed half-kneeling with the throwing arm fixed on a wall to prevent compensation.
Results: Age, weight, and height were positively associated with all strength measurements; however, height did not add predictability beyond age and weight. Strength variables could be predicted with the following equations: 1) ER=0.64*(age)+0.16(weight)–3.54 (r2=0.53, p<0.001), 2) IR=0.59*(age)+0.18(weight) (r2=0.42, p<0.001), 3) SCAPTION=0.54*(age)+0.12(weight)–2.63 (r2=0.61, p<0.001, 4) GRIP=0.66*(age)+0.12(weight) (r2=0.41, p<0.001). Age weakly predicted ER and IR ROM, using the following equations: 1) ER=104.59+1.03*(age) (r2=0.03, p<0.001), 2) IR=100.38-1.01*(age) (r2=0.02, p<0.001). Flexion ROM could not be predicted with an effect size r2>0.01.
Discussion/Conclusion: IR, ER, scaption, and grip strength can be predicted with anthropometrics. Throwing arm ROM measurements are weakly dependent on anthropometrics and can likely be referenced to provided normative values with minimal regard for anthropometrics.
Presenting Author: KGior1@lsuhsc.edu
Bianco L, Wasik M, Durics B St. Luke’s University Health Network
Introduction: Shoulder dislocations occur during athletic events due to the shallow glenoid and overall laxity of the joint. Shoulder dislocations are the most common dislocation that occur based on joint. It is more common
for the shoulder to dislocate then another other joint in the body. Hill-Sachs deformity can occur when the humerus makes contact with glenoid during the dislocation. Orthopedic surgeons treating patients with this condition commonly choose between arthroscopic bankart repair with remplissage or laterjet produce.
Case Description: The purpose of this case study was to delineate the rehabilitation specialist role in providing care to the patient deciding between bankart with remplissage and laterjet to assist in restoration of function.
Outcomes: This case was documented as part of general patient care. Following the patient’s plan of care, it was determined that the case may be an opportunity to compare two surgical options for patients with recurrent shoulder dislocation competing in wrestling. Outcomes were based on the number of dislocations and patient’s perceived level of stability in his shoulder This is a clinical case study of one patient. The patient in this case had both the bankart with remplissage and laterjet surgery on this ipsilateral shoulder. The return to sport was similar with both surgeries but the number of redislocations was greater with the bankart with remplissage.
Discussion: Following a shoulder dislocation patients may have questions about prognoses and return-to-sport plans. In specific sports or activities the rehabilitative specialist may be more well-versed in the biomechanics than the surgeon or other medical professionals. Providing the patient with previous examples of effect strategies while tailoring a patient centered plan around the chosen intervention can lead to long-term outcome improvements. The rehabilitation specialist can function as a guide to educate with research and practice-based evidence related to the specifics of the patient.
Presenting author: lucasbianco4915@gmail.com
Bianco L, Miles C, Wasik M. St. Luke’s University Health Network
Background: Interventions involving mindfulness have been used to manage pain, stress, anxiety, and general wellness When incorporated into physical rehabilitation these interventions can positively affect outcomes for physical and mental health. Vibrational therapy has emerged as a viable option for orthopedic conditions. Color therapy has many dimensions that harness the power of color to benefit the patient. It is assumed that vibrations of color (presumably different frequencies/wavelengths of visible light) influence one’s body and mind.
Purpose: The purpose of this study was to explore the perceived colors participants felt during a therapeutic vibrational stimulus.
Study Design: Original Research.
Methods: A convenience sample of 30 student-athletes received tactile vibrational therapy from the Hypersphere Go (Hyperice, Irvine, California). All participants received the stimulus on their hamstring in a log sit position. Par-
ticipants were tested post-treatment after each vibrational setting (Low 45Hz, Medium 68Hz, High 92Hz) for their perception of color (red, yellow, or blue). Statistical analysis was completed to compare the perceived color to the vibrational frequencies.
Results: The vibrational frequencies were positively correlated (r=.46) to the hypothesized perceived color The perceived colors of blue and yellow were selected with the hypothesized vibrational frequencies 43% of the time. Red was selected with the hypothesized vibrational frequency 73% of the time.
Discussion/Conclusion: Exploring the vibrational and color connection of tissue mobilization can add to this alternative therapy The frequencies at which light travels to generate (blue, yellow, red) color did not correlate with the intensity of the vibration therapy (low, medium, high). It is more likely that individual beliefs and perceptions of what colors represent to them influence their selections. Blue was the most selected for “feeling the best.” More research is needed on the relationship between color therapy and recovery techniques.
Presenting author: lucasbianco4915@gmail.com
Jianing Wang,1 Yongni Zhang,2 Linxia Gu,1 RobRoy L Martin.3,4
1 Florida Institute of Technology, FL, USA
2 Duquesne-China Health Institute, Duquesne University, PA, USA
3 Department of Physical Therapy, Duquesne University, PA, USA
4 UPMC Center for Sports Medicine, PA, USA
Background: The function of the ligamentum teres (LT) continues to be an area of debate and interest. Cadaver studies found the LT to be a rotational stabilizer in all hip positions. Hip external rotation (ER) may be of particular interest as it relates to microinstability and focal rotational laxity of the iliofemoral ligament.
Purpose: To use finite element analysis (FEA) modeling to support the function of the LT as a structure that stabilizes the hip by limiting ER.
Study Design: Lab study
Methods: Onshape was first used to recreate the hip anatomy. FEA modeling during hip movement simulation was then performed with Ansys. These movements were segregated into two sequential steps: flexion in the first step and ER in the second step. Three flexion angles (0°, 30°, and 60°) were considered, with adduction set at 0°. The simulation captured the maximum von-Mises stress during various degrees of ER.
Results: The von Mises stress on the LT remained low until ER range of motion approached end range. Stress on the LT then increased exponentially as ER range of motion approached a maximum value. The increase in stress varied by the flexion angle, with the stress starting to increase exponentially at approximately 28°, 37°, and 42° of ER when the flexion angle was at 0°, 30°, and 60°, respectively. The
von-mises stress was allied with the LT limiting ER range of motion.
Conclusion: This FEA modeling study supports the function of the LT in restraining hip ER range of motion. It also supports a ball and string model to describe the function of the LT. The results endorse a ball and string model where the LT tightens with ER, increasing stress and presumably pulling the femoral head into the acetabulum to enhance stability at the end range of ER.
Presenting author: martinr280@duq.edu
DEFINING REGION AND DURATION-SPECIFIC SUBSTANTIAL CLINICAL BENEFIT VALUES FOR THE SIMPLIFIED CHINESE LOWER EXTREMITY FUNCTIONAL SCALE
Yongni Zhang,1 RobRoy L Martin.2,3
1 Duquesne-China Health Institute Duquesne University, Pittsburgh, PA, USA
2 Department of Physical Therapy, Duquesne University, PA, USA
3 UPMC Center for Sports Medicine, PA, USA
Background: A single substantial clinical benefit (SCB) value for the Simplified Chinese Lower Extremity Functional Scale (SC-LEFS) that can be applied generally to those with lower extremity musculoskeletal injuries is available. However, unique SCB values defined by specific body region and symptom duration may enhance the precision of the SC-LEFS in clinical assessments.
Purpose: To determine unique SCB change scores values for the SC-LEFS based on symptom duration and body region.
Study Design: Longitudinal retrospective study
Methods: Patients aged 18-50 with knee or ankle/foot injuries completed the SC-LEFS at initial assessment and 4-weeks follow-up. Demographic information and duration of symptoms were obtained. Patients were classified into “improved” and “not improved” groups based on self-report after 4-weeks of physical therapy SCB values were determined to best distinguish between the two groups. Receiver operator characteristic (ROC) curve analysis defined the sensitivity and specificity.
Results: 313 patients with a mean age of 33.7 (SD 9.3) years were included in the knee region and 354 with a mean age of 32.9 (SD 9.4) years in the ankle/foot region. For those with knee region injuries, SCB values of 9.5 and 5.5 were found for patients with symptom duration ≤ 3 months and symptom duration > 3 months, respectively For those with ankle/foot injuries, SCB values 12.5 and 8.5 were found for patients with symptom duration ≤ 3 months and symptom duration > 3 months, respectively. The sensitivity and specificity for these SCB values ranged from 0.67 to 0.72 and from 0.66 to 0.68, respectively, with area under the cures (AUC) being between 0.67 to 0.72.
Conclusion: This study determined specific SCB values for the SC-LEFS after four weeks of physical therapy based on region of injury and symptom duration. These unique values may better allow clinicians to distinguish those “im-
proved” from “not improved” in Chinese-speaking patients with knee, ankle, or foot injuries.
Presenting author: zhzh19920903@163.com
DEFINING SUBSTANTIAL CLINICAL BENEFIT VALUES BASED ON PATIENTS’ AND CLINICIANS’ PERCEPTIONS FOR THE SIMPLIFIED CHINESE LOWER EXTREMITY FUNCTIONAL SCALE
Yongni Zhang,1 RobRoy L Martin,2,3
1 Duquesne-China Health Institute, Duquesne University, Pittsburgh, PA, USA
2 Department of Physical Therapy, Duquesne University, PA, USA
3 UPMC Center for Sports Medicine, PA, USA
Background: Substantial clinical benefit (SCB) values are used to define clinical improvement on patient reported outcome measures. However, it is unclear whether clinicians and patients agree on improvement and how these perceptions may affect Simplified Chinese Lower Extremity Functional Scale (SC-LEFS) SCB.
Purpose: To define agreement in perceived improvement between clinicians and patients as well as define SCB values for the SC-LEFS based on 1) patients’ and 2) clinicians’ rating of improvement.
Study Design: Longitudinal study
Methods: Patients aged 18-50 years with lower extremity injuries completed the SC-LEFS at initial assessment and 4-weeks follow-up. After 4-weeks of physical therapy, patients were classified into “improved” and “not improved” groups based on 1) patient self-report and 2) clinician rating. Quadratic weighted kappa was done to define the agreement between the patients’ and clinicians’ rating of improvement. Separate SC-LEFS SCB values were determined that best distinguished between the 2 groups for the patient and clinician rating. Receiver operator characteristic (ROC) curve analyses were done to define the sensitivity and specificity for these SCB values.
Results: 763 patients were included, with a mean age of 32.9 years (SD 9.4). 494 (64.7%) and 525 (68.8%) were classified as “improved” with 269 (35.2%) and 238 (31.1%) classified as “not improved” based on patient self-report and clinician rating, respectively Agreement between patients’ and clinicians’ rating was substantial (kappa=0.8: 95% CI 0.77-0.84). SCB values of 9.5 were found for both patient report and clinician rating, with sensitivity and specificity ranging between of 0.66 and 0.72. The area under the cures (AUC) were 0.74 (95% CI 0.71-0.78) for both patient report and clinicians rating.
Conclusion: Patient and clinician agreed on improvement ratings after 4-weeks of physical therapy. SC-LEFS SCB values to define improvement were the same for both patients and clinicians.
Presenting author: martinr280@duq.edu
Yongni Zhang,1 Yifan Liu,1 Xinwei Huang,1 Zhichen Pan,1 Hui Gao,2 RobRoy L Martin,3,4
1 Duquesne-China Health Institute, Duquesne University, Pittsburgh, PA, USA
2 University of Kansas Medical Center, KS, USA
3 Department of Physical Therapy, Duquesne University, PA, USA
4 UPMC Center for Sports Medicine, PA, USA
Background: There is evidence for reliability and validity with the single leg squat test (SLST) using a variety of visual rating methods. The optimal number of categories that should be used to visually rate movement quality with the SLST is currently unknown.
Purpose: To determine the number of ordinal scoring categories that would be most informative in describing performance with reliable results for visually rating the SLST.
Study Design: Cross-sectional study
Methods: 29 subjects (11 male 18 female; mean age = 23.1 years) with lower extremity injuries participated in this study Reliability was evaluated by two physical therapists using ordinal scales of four, three, and two categories to assess trunk deviation, hip adduction, and lower extremity internal rotation during the SLST. Interrater reliability between the two raters was assessed by unweighted kappa(κ) value.
Results: The overall inter-rater reliability total score was κ=0.65, 0.5, and 0.26 for the two, three, and four-category scales, respectively When specifically looking at trunk deviation, hip adduction, and lower extremity internal rotation, inter-rater reliability was good to excellent (κ= 0.65-0.86) for two-category, good to excellent (κ= 0.69-0.86) for three-category and fair to excellent (κ= 0.55-0.76) for four-category
Conclusion: This study supports visual assessment of trunk deviation, hip adduction, and lower extremity internal rotation using a three-category ordinal scale with the SLST for patients with lower extremity injuries. Two physical therapists could reliably assess trunk deviation, hip adduction, and lower extremity internal rotation with visual assessment of the SLST When comparing two, three, and four categories, the three-category ordinal rating scale produced the best results effectively balancing detailed evaluation with high inter-rater reliability.
Presenting author: liuy20@duq.edu
STRENGTHENING EXERCISES CAN STABLIZE HIP PERFORMANCE DURING THE SINGLE LEG SQUAT TEST
Yongni Zhang,1 Yifan Liu,1 Xinwei Huang,1 Zhichen Pan,1 Hui Gao,2 RobRoy L Martin.3,4
1 Duquesne-China Health Institute, Duquesne University, Pittsburgh, PA, USA
2 University of Kansas Medical Center, KS, USA
3 Department of Physical Therapy, Duquesne University, PA, USA
4 UPMC Center for Sports Medicine, PA, USA
Background: The single leg squat test (SLST) has been used in movement system assessment to analyze dynamic lower extremity alignment during functional movement. Hip strengthening and neuromuscular control training often aim to improve SLST performance. However, it is unclear whether these exercises can improve performance by reducing the amount of variation in hip frontal plane motion during the SLST
Purpose: To determine whether neuromuscular control and strengthening exercises can reduce variation in hip frontal plane performance during the SLST.
Study Design: Cohort study
Methods: Twenty-five healthy subjects (10 males, 15 females; mean age = 26 years, SD = 5.3) performed three SLST trials on both legs at initial assessment and at a 4-week follow-up. Subjects participated in a neuromuscular control and strengthening exercise program every other day for 4 weeks, including side plank abduction, front plank with hip extension, and single-leg squat exercises. Kinematic data for hip abduction and adduction during the SLST were collected using a 3D-motion analysis system at both time points. The performance was defined by the amount of variation in frontal plane hip movement with standard deviation (SD) of the movements. For each subject, the largest SD (ie poorest performance) across the three SLST trials from either leg was used for analysis. A paired t-test compared the SDs of the kinematic data between the initial assessment and the 4-week follow-up.
Results: The SD of kinematic hip frontal plane data across the three trials significantly decrease (p<0.05) after 4-week neuromuscular control and strengthening exercises. This change represented a large effect with a Cohen’s d of 1.0 (95% CI: 0.52, 1.4) with the SD decreased from 1.6 degrees at the initial assessment to 1.0 degrees at the 4-week follow-up.
Conclusion: A 4-week neuromuscular control and strengthening exercise program can improve SLST performance by reducing the variation in hip frontal plane movement.
Presenting author: liuy20@duq.edu
Smith C, Phillips B.
Medical University of South Carolina College of Health Professions Orthopedic Residency, Charleston, South Carolina
Human Performance & Rehabilitation Centers, Columbus, Georgia
Introduction: Symptoms of whiplash-associated disorder (WAD) transition from acute to chronic at high rates. Physical therapy (PT) literature shows efforts to decrease this prevalence has not been effective. Joint position error (JPE) is reported to occur after a whiplash injury, however, there is limited evidence for the PT management of this impairment. The purpose of this case report is to present the outcomes of managing WAD with the addition of cervical proprioceptive training to improve JPE.
Case Description: A sixteen-year-old, female presented to physical therapy after a whiplash injury with complaints of cervical pain. She demonstrated a Neck Disability Index of 16%, a numeric pain rating scale (NPRS) of 5/10, cervical flexion of 45°, cervical extension of 35°, cervical right rotation of 45°, cervical left rotation of 65°, a right rotation JPE of 6.02°, and a left rotation JPE of 9.02.° She participated in a rehabilitation program for 8 visits (1x/week) with interventions used to address pain, mobility, postural reeducation, and cervical proprioception. In addition, the treatment of JPE included head repositioning accuracy and precision tracing activities.
Outcome: At discharge, the patient demonstrated a Neck Disability Index of 4%, a NPRS of 0/10, cervical flexion of 65º, cervical extension of 60º, cervical right rotation of 70º, cervical left rotation of 70º, a right rotation JPE of 6.47º, and a left rotation JPE of 2.41º. Treatment resulted in significant improvements in disability, pain, range of motion, and JPE in left rotation.
Conclusion: This case demonstrated the use of cervical proprioceptive training as an effective tool to manage WAD symptoms. The assessment and rehabilitation of JPE could be considered in the clinical setting as a treatment option to promote recovery after a whiplash injury and to reduce the risk of transitioning to a chronic state of symptoms.
Presenting author: smitcore@musc.edu
DOPPLER ULTRASOUND COMPARISON OF THE EFFECTIVENSS OF BRACHIAL ARTERY OCCLUSION BETWEEN BLOOD FLOW RESTRICTION DEVICES
OConnor R, Davis L, Page P
DPT Program, Franciscan Missionaries of Our Lady University, Baton Rouge, LA
Background: Commercial blood flow restriction (BFR) devices range in price from $200 to $5000. Despite their
benefits for muscle hypertrophy and strength, the efficacy of commercial BFR devices has not been compared to standard blood pressure cuffs in inducing blood flow restriction.
Purpose: This pilot study assessed 2 BFR devices (SmartCuff, BStrong cuff) and a standard sphygmomanometer for effectiveness in inducing blood flow restriction.
Study Design: Observational cross section.
Methods: Fifteen healthy students (ages 21-26) participated. Parameters including brachial artery diameter, area, peak systolic velocity, end diastolic velocity, and time were measured utilizing Doppler ultrasound (Butterfly IQ). Mean flow velocity of the brachial artery assessed blood flow restriction effectiveness.
Results: A one-way repeated measures ANOVA test revealed a statistically significant difference between the pretest and 3 BFR conditions (p=0.046); however, there was no significant difference between the BFR devices and the sphygmomanometer (p=.16). The sphygmomanometer had a very large effect on BFR (d=1.1) compared to the moderate effect of the commercial devices (d=0.48).
Discussion/Conclusion: The study suggests comparable efficacy between commercial BFR devices and a standard sphygmomanometer in reducing blood flow In essence, the brand of the blood restriction device is unlikely to significantly influence the brachial artery occlusion percentage. Nevertheless, when a sphygmomanometer is inflated to an equivalent pressure as the SmartCuff, it results in a more pronounced brachial artery occlusion compared to the other groups. This research supports the comparable effectiveness of commercial BFR devices and a standard sphygmomanometer in inducing blood flow restriction. BFR outcomes research using sphygmomanometers is warranted.
Presenting author: Phillip.Page@Franu.edu
QUANTIFYING THE DECELERATION INDEX USING THE 1080 SPRINT DEVICE: A PILOT STUDY
Trahan A, Vicknair H, Page P Franciscan Missionaries of Our Lady University DPT Program, Baton Rouge, LA.
Background: The “Deceleration Index” (DI) theory is based on the assumption that deceleration forces and speed should be at least equivalent to acceleration forces and speeds.1 An increased efficiency in the ability of an athlete to decelerate or “break” during a change in direction of movement may be associated with improved performance and lowered risk of injury
Purpose: The purpose of this pilot study is to develop the methods to quantify the DI during change-of-direction (COD) via the “5-10-5” sprint test using the 1080Sprint device (1080Motion, Sweden).
Study Design: Observational Cross Section Research.
Methods: Moderately active, healthy adults were eligible for this pilot study Five trials were completed by each participant. Subjects were attached to the 1080 device cable at the waist and performed a “5-10-5” shuttle run: 5
yard “assisted” sprint, changed direction, and performed a 10 yard “resisted” sprint, and reversed direction for a 5 yard “assisted” sprint. Raw data were exported at a sampling rate of 333 Hz and were averaged across the middle 3 repetitions. The peak velocity of each phase was determined. Points of interest at 50% of peak velocity were identified during the 2 assisted and resisted phases of each COD The DI ratios of velocity and acceleration were determined from points of interest for COD 1 (Assisted-Resisted) and COD 2 (Resisted-Assisted).
Results: 10 subjects participated. The average DI for COD 1 and COD 2 for deceleration/acceleration were 1.43+.44 and 1.66+.95, respectively. The DIs for speed were .86+.09 and .87+.7 at COD 1 and COD 2, respectively The coefficients of variation were generally high for COD 2 in speed and acceleration, and for COD 1 during acceleration (.81, .57, and.31).
Conclusion: Quantifying the DI may help improve athletic performance or identify parameters for return to sport. These methods should be repeated in an athletic population.
Presenting author: Phillip.Page@Franu.edu
Pool T,1 Page P 2
1 Baylor Scott & White Institute for Rehab, Waxahachie, TX
2 DPT Program, Franciscan Missionaries of Our Lady University, Baton Rouge LA
Background: Abnormal scapular movement (“scapular dyskinesis”) has been identified as a possible contributor to shoulder pain. Scapular kinematics are typically quantified through biomechanical analysis using high speed cameras and markers; however, this method can be expensive and inconvenient. Inertial Motion Units (IMUs) are now used to assess kinematics without cameras or markers; however, few researchers have used IMUs to quantify scapular kinematics.
Purpose: The purpose of this study was to assess the reliability of measuring scapular kinematics using Noraxon® Ultium IMUs (Noraxon USA, Scottsdale AZ).
Study Design: Original Research.
Methods: 15 healthy adult subjects participated between 21 and 28 years old. IMUs were placed on the scapular spine, posterolateral acromion, spinous process of T1, and deltoid insertion of the dominant arm. Subjects performed 2 sets of shoulder flexion and scaption (6 reps at 6o/s) while their 3-dimensional scapular kinematics were captured. ICC (3,1) values were calculated for each scapular sensor and direction of motion.
Results: Excellent reliability (>=.90) was noted for upward rotation and anterior tilt from the acromion-based sensor during flexion and scaption. Excellent-to-good reliability (>.75) was noted using the acromion-based sensor for internal rotation. The scapular spine sensor ranged from poor to excellent reliability across all conditions (.36 to .97). The scapular motions at the acromion during averaged 49.5
to 52.2o for upward rotation and 15.2 to15.6o for anterior tilt. The measures for internal rotation were -45.8 to -50.9o.
Discussion/Conclusions: Traditional IMU measurements of scapular motion have used sensors placed on the scapular spine, with researchers often reporting various results. The Noraxon Ultium IMUs demonstrated high reliability in measuring scapular kinematics when placed on the acromion of healthy subjects. More research is needed using larger samples of both healthy and injured populations, as well as validation against gold-standard kinematic assessment.
Presenting author: Phillip.Page@FranU.edu
Lutz A,1,2,3 Thigpen C,1,2,3 Floyd S,3,4 Denninger T,1,2,5 Brooks J3,6
1 ATI Physical Therapy
2 Institute for Musculoskeletal Advancement (i-MSKA)2
3 SC SmartState Center for Effectiveness Research in Orthopaedics (CEROrtho)
4 Clemson University Department of Public Health Sciences
5 South College
6 University of South Carolina Department of Health Services Policy and Management (HSPM)
Background: A musculoskeletal (MSK) pathway was established between a physical therapy (PT) organization and a health system (Med) to promote early PT for patients with MSK conditions. To understand the influence of patient beliefs and preferences on care decisions, investigators established a REDCap protocol that surveyed patients after their first MSK PT or Med visit. The REDCap survey collected outcomes (Modified Oswestry Low Back Pain Disability Questionnaire [MDQ], Neck Disability Index [NDI], Veteran’s RAND 12-Item Health Survey Mental (MCS) and Physical (PCS) Component Scores), and validated beliefs & preference questions.
Purpose: The purpose was to understand factors associated with first provider (PT vs Med) in patients with spine conditions.
Study Design: Prospective Cohort
Materials and Methods: Patients were surveyed via REDCap for patient reported outcomes (PROs), beliefs, and preferences after first MSK visit. REDCap data was combined with that of large PT and orthopedic repositories. The belief question asked if patients believed PT would improve their condition. The preference question asked patients to spread 100 points across pain, mobility, activity, and strength by relative importance. If any preference achieved ≥50 points, it was considered dominant. Logistic regression predicted first provider considering preference, belief in PT, body region, MDQ/NDI score, sex, MCS, and PCS. Odds ratios (OR) were derived from regression coefficients.
Results: Patients (n=482) were mostly female (72%), 49.1±10.8 years, had back pain (89%), and moderate initial
disability (MDQ 38.9±18.2; NDI 36.9±15.5); all were health system beneficiaries. Most (54%) had no preference dominance, pain (38%) was a strong preference; the rest were not (total 8%). Most (66%) had belief in PT. Men (OR 3.2[95% CI 1.6,6.7]), higher disability (1.1[1.0,1.1]), and higher MCS (1.1[1.1,1.1]) were more likely to seek Med care. Belief in PT (0.2[0.1,0.4]) and neck conditions (0.1[0.1,0.2]) were more likely to seek PT first.
Conclusion: Beliefs and preferences should be considered when designing and implementing alternative care models to improve value.
Level of Evidence: Level III
Presenting Author: Adam.Lutz@i-MSKA.org
Additional Authors: Charles.Thigpen@i-MSKA.org; SBF@Clemson.edu; Thomas.Denninger@i-MSKA.org; JBrooks2@Mailbox.SC.edu
Denninger T,1,2,3 Lutz A,1,2,4 Davenport J,1,2 Shanley E,1,2,4 Thigpen C.1,2,4
1 ATI Physical Therapy
2 Institute for Musculoskeletal Advancement (i-MSKA)
3 South College
4 SC SmartState Center for Effectiveness Research in Orthopaedics (CEROrtho)
Background: Continuing education (CE) courses have yielded improved participant knowledge, but few have demonstrated a positive influence on patient reported outcomes (PROs). The Musculoskeletal Certificate (MSK Cert), a self-paced, long-form educational program, was made available to clinicians across a national platform at no cost. Course content centered around clinical practice guidelines and used a treatment-based classification approach.
Purpose: The purpose was to compare PRO change and visit utilization before, during, and after MSK Cert.
Study Design: Retrospective Cohort
Materials and Methods: Therapists that enrolled and completed the MSK Cert program between 2022 and 2023 were included. Patient episodes completed 2021-Q2 2024 and managed by included therapists were considered. Episodes were classified as: pre-, mid-, post- program if 75% of days in an episode were completed within the classification dates. Patient demographics, PROs, and visit counts were derived from the Patient Outcomes Registry.
Analyses of covariance compared visits, final PRO, and PRO change between program periods controlling for age, sex, payer, initial PRO, BMI categorization, body region, and specific PRO utilized. Tukey’s post-hoc tests quantified differences when significance was observed.
Results: Patient episodes (n=193,882) were 58.6% female, 52.1±19.0 years old, and largely insured by commercial (64.5%) and Medicare (15.7%) payers. Significant differences in visits, final PRO, and PRO change between program classification cohorts (p<0.001). Visits were 11.8±0.4, 12.3±0.4, & 11.1±0.04; final PRO was 67.3±0.9, 67.9±0.9, & 68.3±0.9; and PRO change was 13.2±0.9, 13.8±0.9, & 14.2±0.9. This demonstrates a consistent tra-
jectory of improvement during and after the education intervention. Tukey’s post-hoc tests identified that all differences were significant at p<0.001 aside from final PRO midvs. post- program (p=0.001).
Conclusion: Clinicians completing a 30-week CE program demonstrated significant improvements in PROs and doing so more efficiently with post-course episodes on average having one fewer visit. When combined, the improvements in metrics result in a sizable improvement in patient value.
Level of Evidence: Level IV
Presenting Author: Thomas.Denninger@i-MSKA.org
Additional Authors: Adam.Lutz@i-MSKA.org; Jacqueline.Davenport@i-MSKA.org; Ellen.Shanley@i-MSKA.org; Charles.Thigpen@i-MSKA.org
PROFESSIONAL BASEBALL PITCHERS’ PATTERNS OF USE AND RESULTS OF WEIGHTED BALL TRAINING: AN INTERIM STUDY
Shanley E,1,2,3 Bullock G,4 Noonan T,5,6 Kissenberth M,7 Thigpen C.1,2,3
1 ATI Physical Therapy
2 Institute for Musculoskeletal Advancement (i-MSKA)
3 SC SmartState Center for Effectiveness Research in Orthopaedics (CEROrtho)
4 Wake Forest School of Medicine
5 UCHealth Steadman Hawkins Clinic–Denver, Englewood, CO
6 University of Colorado School of Medicine
7 Prisma Health Upstate Steadman Hawkins Clinic of the Carolinas, Greenville, SC
Background: Professional pitchers demonstrate an average fastball velocity of 91-93 miles per hour Based on perceived importance of velocity, development of velocity is a focus for pitchers. Pitchers use traditional (weight training) and non-traditional training methods (weighted ball training [WBT]) to improve velocity Studies have demonstrated that higher velocity increases load on the elbow and upper extremity injury risk in pitchers. Little is known about the benefits and risks associated with WBT use by professional baseball pitchers.
Purpose: To 1) describe WBT and injuries in professional pitchers; 2) compare injury rates between professional pitchers that used WBT during the 2023 pre and regular season with pitchers that used no WBT (NWBT) prior to or during the last three seasons.
Study Design: Prospective Cohort.
Materials and Methods: Pitchers were surveyed on their use of WBT prior to spring training. Throughout spring training and the MiLB season, pitchers were monitored for athletic exposures and injuries. Injury rates per 1000 game exposures (GE) were calculated by WBT cohort and grouped by body part.
Results: Of 88 pitchers included, 52% were in the WBT cohort, and 28 injuries were reported (Upper extremity = 20; Trunk/Core = 8; Lower Extremity = 0). Pitchers that used WBT suffered 8 more injuries at a 1.1 greater injury rate per 1,000 exposure days compared to pitchers in the NWBT co-
hort. WBT pitchers arm injury rate was 11.8 per 1000 GE compared to 7.5 per 1000 GE in the NWBT cohort; and WBT pitcher core injury rate was 5.9 per 1000 GE compared to 2.1 per 1000 GE in NWBT pitchers.
Conclusion: Pitchers presented with similar workload and velocity regardless of WBT cohort. Results of the initial analysis were important because of the number and types of injuries in this WBT cohort. The major limitation of this ongoing study is that it is currently underpowered.
Level of Evidence: Level III
Presenting Author: Ellen.Shanley@i-MSKA.org
Additional Authors: GBullock@WakeHealth.edu; Thomas.Noonan@CUAnschutz.edu; Mike.Kissenberth@HawkinsFoundation.com; Charles.Thigpen@i-MSKA.org.
Authors who provided posters for visual reference can be found in the supplemental file. © The Author(s)
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CCBY-NC-4.0). View this license’s legal deed at https://creativecommons.org/licenses/by-nc/4.0 and legal code at https://creativecommons.org/licenses/by-nc/4.0/legalcode for more information.
Supplemental File 1
Download: https://ijspt.scholasticahq.com/article/123874-2024-ijspt-orthopedic-summit-research-abstracts/ attachment/246694.pdf?auth_token=UCaEgZ1TxIWMUeDPpeRa
