




EDITORS-IN-CHIEF: Jason Lo Hog Tian Mikaeel Valli
EXECUTIVE DIRECTORS:
Stacey J. Butler
Dorsa Derakhshan Elizabeth Karvasarski
DESIGN EDITORS:

Amy Zhang (Director)
Sherry An Amy Assabgui
Yuejun (Mimi) Guo Abeeshan Selvabaskaran Michie (Xingyu) Wu
SOCIAL MEDIA TEAM: Sandy Lee Elizabeth Karvasarski
PHOTOGRAPHER:
Dorsa Derakhshan (Director)
JOURNALISTS & EDITORS:
Archita Srinath
Bahar Golbon
Beatrix Wang
Dorsa Derakhshan
Dorsa Rafiei
Elizabeth Karvasarski
Iciar Iturmendi Sabater
Kate Maksyutynska
Kyla Trkulja
Lindsey Thurston
Madhumitha Rabindranath
Nayaab Punjani
Paras Kapoor
S. Hussain Ather
Shu’ayb Simmons
Stacey J. Butler
Sonja Elsaid
Vaidhehi Veena Sanmugananthan
Yuejun (Mimi)Wehope you all have had a restful and rejuvenating summer break and are ready for the start of the new school year. With the beginning of a new chapter, we would like to reflect on the hard work of the IMS Magazine team this past year. Our biggest goal since taking over as Editors-in-Chief was to restore and maintain quarterly releases of the magazine. We are proud to have accomplished this goal, releasing four insightful magazine issues this year covering diverse topics including the GI Tract and Gut Microbiome, Men’s Health, Patient Engagement in Research, and Novel Laboratory Methods. This could not have been achieved without the hard work and dedication of our team of journalists, copy editors, executive editors, designers, social media team, and distribution team. We thank all the team members who are graduating and moving on from the magazine and we look forward to working with many who are staying with us for the upcoming year.
I would also like to acknowledge the outgoing co-Editor-in-Chief Mikaeel Valli for his many years of service and dedication to the magazine. It has been a great pleasure to work with and learn from him and we look forward to seeing what the future holds for him. This being his last magazine issue, Mikaeel has left us with a few parting words:

When I reflect on my involvement with the IMS Magazine over the years, I can certainly attest that I have grown as a person and learnt a lot along the way. I vividly remember sitting in one of the lecture halls in the Medical Science Building back in September of 2016 where I was attending my first MSC1010-1011Y
class. The executive team from IMS Magazine at the time made a guest appearance showcasing the accomplishments of the magazine. I was excited when they said they were recruiting photographers. I felt this would be a perfect way to get involved with the IMS community and apply my photography skills while embarking on a rigorous research program at IMS. I am grateful that the team welcomed me with open arms and allowed me to experiment with different composition and lighting techniques to communicate with readers.
Little did I realize that my role as a photographer would expand within the organization to include other positions. I soon became a journalist for feature articles—which gave me the privilege to be at the pulse of what was happening at IMS by interviewing faculty and writing about their cutting-edge research. By 2019, I was promoted to feature executive editor and by 2021, I became co-Editor-in-Chief. Not only have I learnt a wide range of life science topics through writing and editing articles, I also have come to realize how important it is to make our content understandable and relevant to readers with diverse backgrounds within and outside the IMS community. This needs effective science communication, which is an art that requires content to spark an interest in readers while at the same time, accurately inform them the advances of scientific research. I cannot be prouder of all the journalists’ and editors’ work over the years that were able to make a deep connection with readers, allowing them to have a firm grasp on complex topics—which is not an easy feat!
While I am sad to leave the magazine, I must say it was a truly enjoyable six years that I will forever cherish. I want to acknowledge that it was an absolute pleasure partnering with co-Editor-in-Chief Jason Lo Hog Tian for the past year in producing four exciting issues together. These issues were made possible with support of the brilliant executive team—Stacey Butler, Elizabeth Karvasarski, Dorsa Derakhshan, and Sandy Che-Eun Lee. The future is bright, and I cannot wait to read the upcoming issues of the IMS Magazine

Lastly, we are thrilled to welcome Stacey Butler who is the incoming co-Editor-inChief that will be working with Jason going forward. She also had a few words to share as she transitions into her new role for the upcoming year:


Since joining the IMS Magazine in 2019, I have learned a great deal about science communication from Mikaeel and I am truly grateful for his support and mentorship. I feel very fortunate to be stepping into Mikaeel’s shoes and joining Jason as co-Editor-in-Chief of the IMS Magazine. I am looking forward to working with our team of talented graduate students to showcase the cutting-edge scientific discoveries and celebrate the diversity of our IMS community.

On behalf of the entire IMS Magazine team, we would like to thank you for your readership, we hope you enjoy reading this issue, and we look forward to producing more magazine issues in the upcoming academic year!
Jason is a fourth year PhD student examining the mechanisms linking HIV stigma and health under the supervision of Dr. Sean Rourke.

Mikaeel is a fifth year PhD student. He works with Dr. Antonio Strafella’s lab that uses neuroimaging techniques to understand the underlying mechanisms in Parkinson’s disease with non-motor complications.
linkedin.com/in/mikaeel-valli/
Stacey is a third year PhD student. Under the supervision of Dr. Andrea Gershon, she is evaluating the quality of care for patients with respiratory disease using a population-based approach.
Summeris a time when academia tends to slow down but the IMS Magazine team has been hard at work preparing the Fall 2022 Issue. In this issue, the team explores how biology and technology intersect in the laboratory. With creativity, innovation and outstanding collaboration, IMS is paving the road for new approaches to studying and treating human diseases.
Researchers in the IMS have embraced new technology, allowing them to overcome unique challenges in their fields. Read about how Dr. Mamatha Bhat is using nanotechnology and targeted therapy to improve outcomes after liver transplantation. Dr. Anurag Tandon is taking an innovative approach to enhance drug delivery across the blood-brain barrier and find effective treatments for Parkinson’s disease using nano- and ultrasound technology. Dr. Katherine Siminovitch’s lab has created new mouse models that better replicate the development and complexity of human autoimmune disease.
Two prominent leaders in the IMS community are also featured in this issue. Our new IMS Coordinator Dr. John Vincent and the outgoing IMSSA Co-President, Kayvan Aflaki share their perspectives on the importance of achieving work-life balance.
After a two-year hiatus, we were finally able to gather in-person as a community for the IMS Scientific Day 2022. Following an invigorating keynote address by Dr. Gelareh Zadeh, we celebrated the exceptional work and perseverance of our graduate students. Much like the faculty featured in this issue, we also embraced technology this year by hosting an eco-friendly, electronic poster presentation session. Members of our community also gathered for IMS Connects, an important career panel and networking event designed to help prepare our graduates for careers in academia or industry. In this issue our students reflect on how in-person events are essential networking opportunities and can renew their sense of community and enthusiasm for research.
I would like to extend a sincere thank you to Mikaeel Valli for his unparalleled dedication to the IMS Magazine. Since joining our department in 2016, Mikaeel contributed to an astounding 18 issues of the IMS Magazine. On behalf of the IMS, we thank you for your commitment and wish you continued success in your future endeavours. I look forward to continuing to work with Jason, and welcome Stacey in her new role as Co-Editor in Chief. Once again, I applaud the journalists, editors, photographers, and design team for their contributions to the Fall 2022 Issue. I hope you enjoy learning about the exciting innovation happening in our laboratories!
Sincerely,
Dr. Mingyao Liu Director, Institute of Medical ScienceDirector, Institute of Medical Science Professor, Department of Surgery Senior Scientist, Toronto General Hospital Research Institute, University Health Network

S. Hussain Ather is a second year PhD student working under John Griffiths at the Centre for Addiction and Mental Health (CAMH). He uses and develops computational modeling techniques to investigate the brain connectivity structures underlying neuropsychiatric disorders. He also likes cosplaying.

Dorsa Derakhshan is a MSc student at IMS investigating the cognitive effects of repetitive transcranial magnetic stimulation in treatment resistant depression under the supervision of Dr. Peter Giacobbe. She enjoys photography, painting and working on creative projects in her leisure time.


Elizabeth Karvasarski is a PhD IMS student studying pulmonary hypertension at Mount Sinai Catheterization Laboratory under the supervision of Dr. Susanna Mak. Her research involves exploring whether the temporality of pulmonary vascular loading differ with exercise in pre-capillary vs. post-capillary pulmonary hypertension. Outside of research, Elizabeth practices martial arts and is a 4th degree black belt.

Stacey J. Butler is a third year PhD student at IMS, specializing in respiratory medicine and epidemiology, under the supervision of Dr. Andrea Gershon. Outside of academia, Stacey enjoys creative activities, board games and cooking hearty vegetarian meals.


Sonja Elsaid is a PhD student investigating brain function and cannabis use in individuals with social anxiety. Prior to going back to school, Sonja was a clinical research and medical communications professional with nearly 20 years of experience.
Kateryna Maksyutynska is a MSc student investigating whether brain insulin resistance is a feature of the biology of depression under the supervision of Dr. Mahavir Agarwal and Dr. Margaret Hahn at CAMH. Outside of the lab, she can be found enjoying a good book, painting, or biking along the water.
Nayaab Punjani is a MSc student at IMS working with Dr. Michael G. Fehlings. Her research is examining a preclinical drug treatment that aims to provide a multifaceted approach targeting neural regeneration and recovery following cervical spinal cord injury. She enjoys watching action and mystery genre movies and TV shows, as well loves sketching in her free time.
Dorsa Rafiei is an MSc student under the supervision of Dr. Nathan Kolla at CAMH. Her research investigates the endocannabinoid system in major depression using PET imaging. Outside of the lab, she enjoys tweeting about science and making pottery.


Sanmugananthan is a PhD student under the supervision of Dr. Karen Davis at the Krembil Brain Institute, Toronto Western Hospital. Her research focuses on examining pain and attention interactions in people that suffer chronic pain. Outside of the lab, Veena loves to run, play squash, sketch, and challenge herself to learn new art mediums!
Kyla Trkulja is a second year MSc student at IMS studying under the supervision of Dr. Armand Keating, Dr. John Kuruvilla, and Dr. Rob Laister at Princess Margaret Hospital. Her work focuses on better understanding the mechanism of action of a novel cancer therapy for lymphoma so it can be better utilized in the clinic. Outside of academia, Kyla enjoys reading, writing, video games, and going for walks in nature.

Madhumitha (Madhu) Rabindranath is a MSc student at IMS who is supervised by Dr. Mamatha Bhat. Her research focuses on leveraging AI to non-invasively diagnose liver graft fibrosis in post-transplant patients. Outside the lab, Madhu likes reading a good book and exploring the city.


Iciar Iturmendi Sabater is a first year PhD student working with Dr. Meng-Chuan Lai and Dr. Hsiang-Yuan Lin at the Center for Addiction and Mental Health. She researches social abilities and adaptation across neurodevelopmental conditions (autism, ADHD, learning disabilities, etc). Iciar likes writing, exploring new places and meeting new people.
Shu’ayb Simmons is a first year IMS MSc Candidate working with Dr. Tripathy at the CAMH Krembil Centre for Neuroinformatics. They research the transcriptomic basis of Black disparities using robust bioinformatics. Shu’ayb enjoys volunteering, advocacy, fashion, and writing songs in their free time.


Beatrix Wang is a third year PhD student who, under the supervision of Drs. Freda Miller and David Kaplan, is trying to better understand the functional transitions undergone by neural stem cells during brain development. In her spare time, she’s passionate about reading, writing, and learning martial arts.



Sandy Che-Eun Lee is a fifth year PhD student under the supervision of Dr. Marianne Koritzinsky at the Princess Margaret Cancer Research Center. Her research focuses on characterizing a novel oxygen sensitive enzyme in the hypoxic tumour microenvironment. Outside of the lab, Sandy enjoys running and exploring new activities like rock climbing!












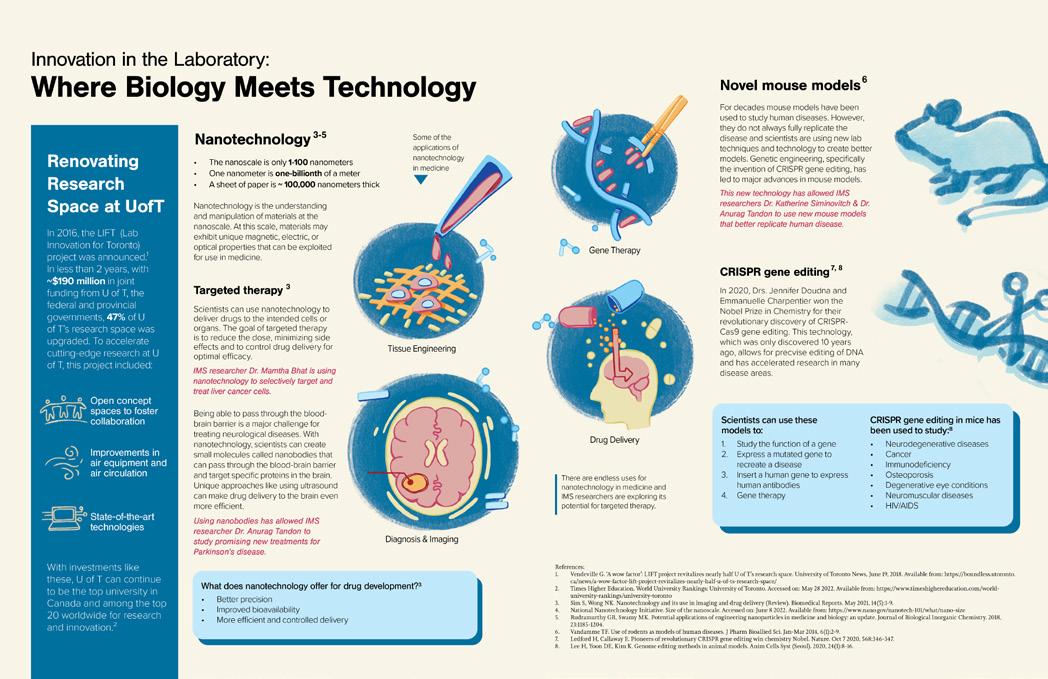
In 2016, the LIFT (Lab Innovation for Toronto) project was announced.¹ In less than 2 years, with ~$190 million in joint funding from U of T, the federal and provincial governments, 47% of U of T’s research space was upgraded. To accelerate cutting-edge research at U of T, this project included:
Open concept spaces to foster collaboration
Improvements in air equipment and air circulation
• The nanoscale is only 1-100 nanometers
• One nanometer is one-billionth of a meter
• A sheet of paper is ~ 100,000 nanometers thick
Nanotechnology is the understanding and manipulation of materials at the nanoscale. At this scale, materials may exhibit unique magnetic, electric, or optical properties that can be exploited for use in medicine.
Scientists can use nanotechnology to deliver drugs to the intended cells or organs. The goal of targeted therapy is to reduce the dose, minimizing side effects and to control drug delivery for optimal efficacy.
IMS researcher Dr. Mamatha Bhat is using nanotechnology to selectively target and treat liver cancer cells.
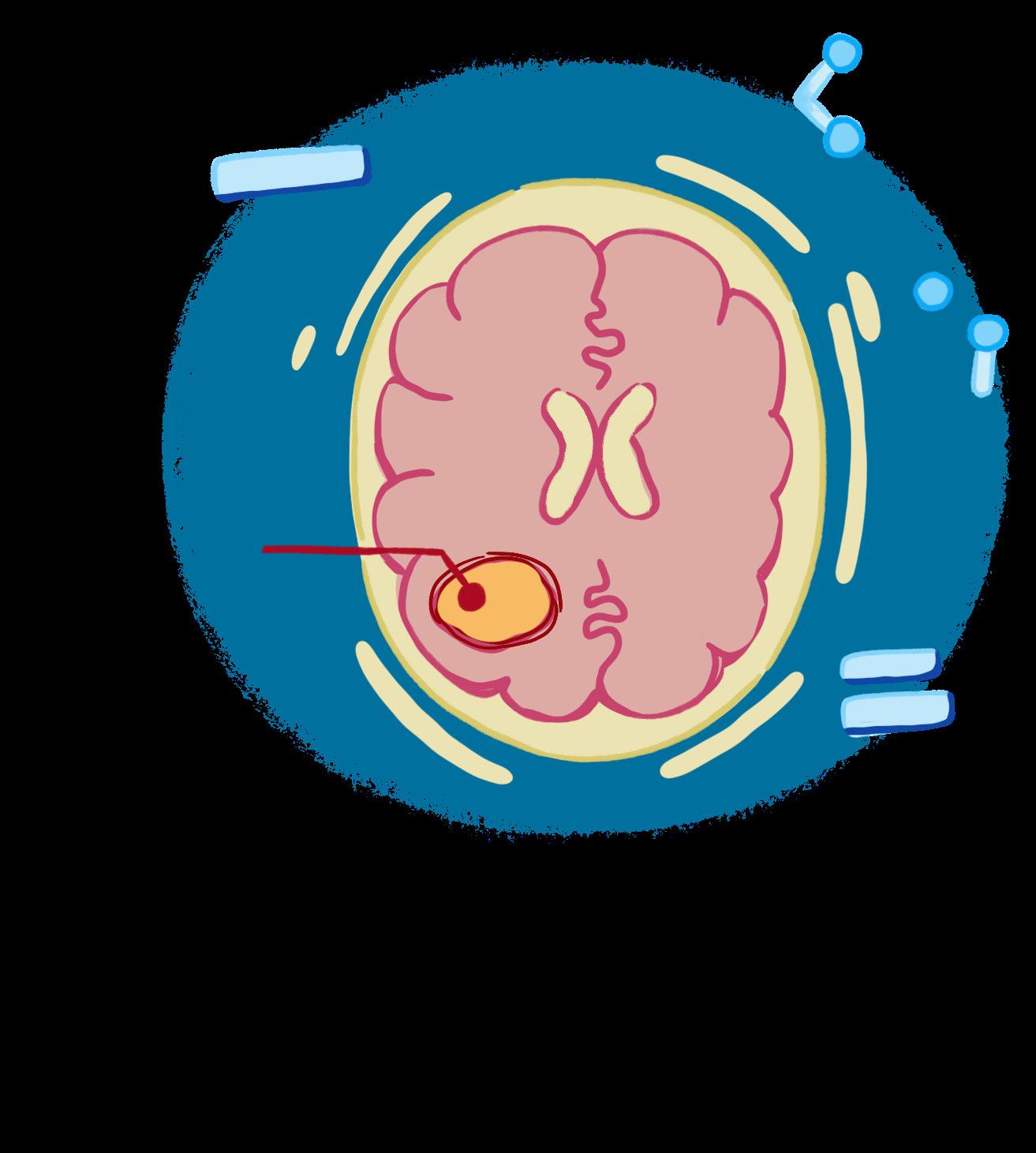
Being able to pass through the bloodbrain barrier is a major challenge for treating neurological diseases. With nanotechnology, scientists can create small molecules called nanobodies that can pass through the blood-brain barrier and target specific proteins in the brain. Unique approaches like using ultrasound can make drug delivery to the brain even more efficient.
State-of-the-art technologies
With investments like these, U of T can continue to be the top university in Canada and among the top 20 worldwide for research and innovation.²
Using nanobodies has allowed IMS researcher Dr. Anurag Tandon to study promising new treatments for Parkinson’s disease.
What
• Better precision
• Improved bioavailability
• More efficient and controlled delivery
There are endless uses for nanotechnology in medicine and IMS researchers are exploring its potential for targeted therapy.
For decades mouse models have been used to study human diseases. However, they do not always fully replicate the disease and scientists are using new lab techniques and technology to create better models. Genetic engineering, specifically the invention of CRISPR gene editing, has led to major advances in mouse models.

This new technology has allowed IMS researchers Dr. Katherine Siminovitch & Dr. Anurag Tandon to use new mouse models that better replicate human disease.

In 2020, Drs. Jennifer Doudna and Emmanuelle Charpentier won the Nobel Prize in Chemistry for their revolutionary discovery of CRISPRCas9 gene editing. This technology, which was only discovered 10 years ago, allows for precvise editing of DNA and has accelerated research in many disease areas.
Study the function of a gene
Express a mutated gene to recreate a disease
Insert a human gene to express human antibodies
Gene therapy
Cancer
Immunodeficiency
Osteoporosis
Neurodegenerative diseases

Degenerative eye conditions
Neuromuscular diseases
HIV/AIDS
Liver cancer is one of the most difficult types of cancer to treat, making it the third most common cause of cancer death around the world. 1 The prognosis for patients diagnosed with the disease is poor, with only 35% of patients with early-stage disease surviving 5 years after diagnosis—and a mere 3-12% of patients surviving this long if the cancer spreads. 1 It is difficult to treat because many of these patients often also have liver disease, making them unable to tolerate chemotherapy or surgery.
Dr. Mamatha Bhat, a hepatologist and clinician-scientist at Toronto General Hospital, is using creative and innovative approaches to try to improve these grim statistics and the lives of patients with liver disease. After completing her medical education and residency in internal medicine and gastroenterology at McGill University, she pursued a research fellowship and obtained her PhD in medical biophysics from the University of Toronto. She currently runs a translational research program using an interdisciplinary approach that aims to improve the outcomes of patients after liver transplantation—of which 35-40% are cancer patients.
Dr. Bhat describes the ability to perform a transplant for those with liver cancer as a “unique paradigm,” as transplantation is not a method of treatment for other types of cancer, with the exception of cancers originating in
the blood. Clinically, she looks after 350 patients who are referred for a liver transplant before, during, and after their surgery. On the research side, she aims to uncover ways to improve patient outcomes post-transplant—specifically by using nanoparticles to prevent and treat recurrence of liver cancer.
Nanoparticles to treat liver disease and cancer were developed in collaboration with Dr. Gang Zheng at the Princess Margaret Cancer Centre. Put simply, these types of nanoparticles contain proteins and drugs that can treat the liver disease and cancer a patient may have. They bind to receptors that are specifically expressed on the liver and its cancer cells, such as the receptors used to take up cholesterol. This new and innovative approach allows the treatment to be targeted and delivered to the specific cells in need.
“With this approach, we can very selectively target the liver cancer cells,” Dr. Bhat explains. “Beyond that, we might be able to target specific molecular profiles, and also [optimize] the dose, depending on the degree of liver dysfunction that the patient has,
so this is a very unique consideration in cancer where people have underlying liver disease.”
Dr. Bhat has demonstrated the efficacy of this treatment in animal models through her collaboration with Dr. Zheng, which has been supported by the Terry Fox Research Institute and the Canadian Liver Foundation. Dr. Zheng’s nanoparticle technology will soon be studied in a clinical trial with oncologists at the Princess Margaret Cancer Center to test this therapy in a variety of cancer types. If the trial is safe and effective, it could be brought to the clinic as a way to treat those with liver cancer and hopefully improve their disease outcomes.
The use of nanoparticles to target and treat liver cancer is a way of overcoming one of the biggest challenges in oncology, which Dr. Bhat describes as treating cancer with a “one-sizefits-all” approach. “Everyone has their own background, their own clinical characteristics, their own disease manifestation,” she explains.

“Each person is unique … but we still go based on clinical guidelines, and

MD, PhD; Hepatologist and Clinician Scientist, UHN Multi Organ Transplant Program, Toronto General Hospital Research Institute; Assistant Professor, Division of Gastroenterology, Department of Medicine at the University of Toronto
challenge is being addressed to make cancer treatments both safer and more effective while considering the patients’ underlying conditions such as chronic liver disease and cirrhosis.
Dr. Bhat stressed the importance of collaboration in making this research possible, both between researchers and between research sites. “The world has become much more complicated, and it isn’t possible for one single person to have the whole skill set to address a specific problem,” she said. “It used to be that you could be one lab doing your own thing. But I think things evolved and changed over time.” She is now utilizing tools she has learned from other disciplines, such as bioinformatics and machine learning, to aid her research in personalizing treatment.
This openness to new approaches and collaborations is described by Dr. Bhat as one of the most important characteristics to have as a researcher, as “the world has become much more interdisciplinary.” This has been exceptionally important in her role as a clinician-scientist, where broad and creative thinking are necessary to tackle an issue seen in the clinical setting. “It’s not just hard work,” she says. “It’s also working smarter.”

clinical guidelines may be good for the population as a whole, but they may not be good for individuals within that population.” By tailoring both the dose and type of treatment inside the liver-specific nanoparticle, this



Using her clinical experience to inform on her research projects is an exceptionally rewarding part of her career, despite the challenges that go along with managing the dual roles. She
explains that a positive attitude, interest and passion for the work being done, and motivation to dedicate extra years to acquiring the skills necessary for both roles are essential to succeeding as a clinician-scientist. If you have the passion and openness, the role is an excellent way to tackle the gaps in healthcare since you can inform projects from your own clinical experiences.
Using these skills, Dr. Bhat is aiming to play a role in the future of liver disease and cancer research and care, which she envisions as moving away from the one-size-fits-all approach to treatment and embracing the potential for new and innovative targeted therapies. She believes that these are key to improving outcomes for patients with liver cancer and reducing fatalities, similar to what has been done for other types of common cancer such as breast and colorectal. Nanoparticle-based therapies are one example of how this may be done, so she looks forward to bringing these from bench to bedside in the coming years.
Werely on our immune system to fight off pathogenic microbes and guard against the growth of malignant cells.1 In recent decades, much progress has been made in mapping out the body’s strategy to defend against infection and immune disease, but fundamental questions remain within the field. How exactly are immune responses regulated? And, just as importantly, what are the mechanisms that lead to immune dysfunction and consequent disease?
“Everything,” Dr. Katherine Siminovitch says, “is about balance.” A healthy and functional immune system exists in a state of homeostasis wherein tightly regulated pathways are able to respond to invading pathogens appropriately.2 This response involves a fine-tuned combination of immune activation and deactivation to ensure that the system neither over- nor under-reacts to stimuli. When this balance is disrupted, immune cells may begin attacking the body—a phenomenon known as autoimmunity—or lose their ability to respond to external (antigenic) stimuli, both of which can lead to debilitating health issues.
Dr. Siminovitch, a Professor of Medicine and Immunology at the University of Toronto and Senior Investigator at the Lunenfeld-Tanenbaum Research Institute, has made it the goal of her research career to identify the cellular and molecular pathways modulating immune function and involved in immune dysfunction, with a particular focus on autoimmune disorders.
“Major gaps still exist in our understanding of how autoimmune diseases develop and persist,” Dr. Siminovitch says. For some conditions, such as systemic sclerosis or vasculitis, the precise mechanisms underlying pathogenesis remain almost entirely unknown. Furthermore, even for extensively studied disorders such as lupus, there is a lack of therapies that go beyond symptom management and immunosuppression.
Identifying drivers of disease and discovering potential therapeutics have been complicated by the extensive heterogeneity that exists within individual immunologic conditions. “Different molecular pathways can lead to the same clinical phenotype,” Dr. Siminovitch says. “Clinical heterogeneity is very obvious, for example, in lupus. It becomes very challenging to find effective treatments when lupus patients are grouped into a study without initial sub-classification or sub-categorization, ignoring the likelihood the disease-causal pathways may differ among these patients and, as such, may need to be managed differently.”
Enormous efforts are continuing to elucidate the mechanisms by which different genes and molecules lead to the immune dysfunction underpinning disease. Dr. Siminovitch has played a vital role in this research. During her postdoctoral training, she became interested in an oftenfatal immune deficiency disorder known as Wiskott-Aldrich syndrome (WAS). During this time, she contributed significantly
to identifying the genetic cause of the illness, mapping the gene responsible, and characterizing various gene mutations that lead to WAS.3 The gene in question turned out to encode Wiskott-Aldrich syndrome protein (WASp), a large adaptor protein that mediates signal transduction, directs immune cell cytoskeletal activity, and is an essential immune regulator.4 Furthermore, these findings allowed for the development of genetic tests to diagnose WAS and identify carriers of the mutant gene.
Dr. Siminovitch subsequently became interested in other adaptor proteins within the WASp family, including WAVE2, another actin cytoskeletal regulator with the potential to play a role in immune function. “Not many people have been working on WAVE2,” Dr. Siminovitch says, “but my group was very interested in this protein’s functions because it is expressed at high levels in immune cells and because of our ongoing interest in cytoskeletal regulatory protein roles in immunity.”
It wasn’t until relatively recently that Dr. Siminovitch and her team had an opportunity to study this protein’s function in immune cells, her group having generated a conditional knockout mouse in which WAVE2 expression is specifically deleted in T lymphocytes. The results were striking. “The mice have an obvious phenotype of very severe autoimmune disease,” Dr. Siminovitch says. “And paradoxically, along with autoimmune disease, they also exhibit profound immune deficiency. So, the lack of WAVE2 in T cells


there is much to learn about how WAVE2 functions in other immune cell types and is particularly interested in exploring an unexpected link between WAVE2 and neurodegenerative disease. Furthermore, the link between TOR hyperactivity and immune dysfunction suggests that drugs that inhibit the TOR pathway may have relevance to the treatment of autoimmune and other immune-mediated disease.

like Dr. Siminovitch are poised to address fundamental questions about the immune response and how it becomes dysregulated in disease. The ultimate hope is that this research will illuminate the complex combinations of factors that can trigger autoimmunity and can then be clinically translated to allow improved detection, more effective treatment, and prevention of immune disorders.
leads to a disease representing both ends of the immunologic spectrum.” Using this mouse model, Dr. Siminovitch and her team identified WAVE2 as a suppressor of the TOR protein, a key regulator of cell metabolism, proliferation, apoptosis, and multiple other functions.5,6 They found that in the absence of WAVE2, TOR is hyperactivated, leading to spontaneous T cell activation, with loss of immune homeostasis and diminished responsiveness to antigenic stimuli. These abnormalities, in turn, cause the severe immune disease observed in the mice.5
This work has served as an exciting starting point for Dr. Siminovitch and her team. Moving forward, Dr. Siminovitch believes
Notably, Dr. Siminovitch’s findings also demonstrate how much more there is to learn about proteins and pathways even after they have been assigned specific functions. For both WASp and WAVE2, regulation of the cytoskeleton is only the beginning of the story. “These proteins have been primarily studied as cytoskeletal regulators because they contain domains that allow them to promote actin polymerization,” Dr. Siminovitch says.
“But they have additional functions and I believe our current understanding of their functions represents only the tip of the iceberg of their biological contributions.”
Dr. Siminovitch has no doubt that the coming years will bring a wealth of answers to many complex questions about immune disease. “This is an incredible time to be involved in biomedical research,” she says. “I thought the same thing when I first set up my lab, but now the research tools available to scientists— technical and computational—are truly unprecedented in terms of the types of questions you can ask and reasonably hope to answer.” In this context, immunologists
1. Chaplin DD. Overview of the Immune Response. J Allergy Clin Immunol. 2010 Feb;125(2 Suppl 2):S3-23.
2. da Gama Duarte J, Woods K, Andrews MC, et al. The good, the (not so) bad and the ugly of immune homeostasis in melanoma. Immunology & Cell Biology. 2018;96(5):497–506.
3. Kolluri R, Shehabeldin A, Peacocke M, et al. Identification of WASP mutations in patients with Wiskott-Aldrich syndrome and isolated thrombocytopenia reveals allelic heterogeneity at the WAS locus. Hum Mol Genet. 1995 Jul;4(7):1119–26.
4. Ngoenkam J, Paensuwan P, Wipa P, et al. Wiskott-Aldrich Syndrome
Protein: Roles in Signal Transduction in T Cells. Frontiers in Cell and Developmental Biology [Internet]. 2021 [cited 2022 Jun 5];9. Available from: https://www.frontiersin.org/article/10.3389/ fcell.2021.674572
5. Liu M, Zhang J, Pinder BD, et al. WAVE2 suppresses mTOR acti vation to maintain T cell homeostasis and prevent autoimmunity. Science. 2021 Mar 26;371(6536):eaaz4544.
6. Zou Z, Tao T, Li H, et al. mTOR signaling pathway and mTOR inhibitors in cancer: progress and challenges. Cell & Bioscience. 2020 Mar 10;10(1):31.
Parkinson’s Disease (PD) is a neurodegenerative disorder that affects more than 100,000 Canadians.1 This condition is often characterized through motor symptoms such as tremors and non-motor symptoms including constipation and sleep disturbances.2 PD pathology involves the build-up of a protein (alpha synuclein or α-Syn) in the brain, along with the loss of dopaminergic neurons.3 Trying to find a way to reduce the expression of α-Syn, and stopping early PD progression is key to improving the patients’ quality of life. Dr. Anurag Tandon, Scientist at the Tanz Centre for Research in Neurodegenerative Diseases and Associate Professor in the Department of Medicine, Division of Neurology, uses unique approaches to address this pervasive disease.
As a cell biologist, Dr. Tandon began to understand PD through studying the role of α-Syn in vesicular trafficking and neurotransmission. Understanding of PD pathology has evolved and we now recognize the prion-like spread of α-Syn pathology between neurons. Novel therapies for PD aim to reduce α-Syn expression through either targeting its gene expression by studying viral gene knockdown vectors,4 or to decrease the concentration of the protein to reduce aggregation.
When developing immune therapies for PD, Dr. Tandon discusses the challenges of targeted delivery to the brain. Antibodies are often composed of long polypeptide chains, thus when delivered intravenously, only 0.5% pass the blood-brain-barrier (BBB) and enter the cerebrospinal fluid. However, these large proteins are very specific to the target protein. Therefore, being able to take the gene sequence for
Neurons in culture (shown in red) expressing the anti-α-Syn nanobody developed less pathology (green) than neurons expressing a non-specific control nanobody.
 Photo Credit: Dr. Anurag Tandon
Photo Credit: Dr. Anurag Tandon
these antibodies, bridging immunotherapy with gene therapy, and express them in the brain, is a promising therapeutic avenue.
Dr. Tandon employs the use of small molecules called nanobodies. These molecules were developed through research conducted by his collaborators, Dr. David Butler and Dr. Anne Messer.5 The process of creating nanobodies involves isolating the variable domain, which recognizes α-Syn, on the heavy chain of a single chain polypeptide antibody from a human blood cell library. Human cells normally do not express single chain antibodies, however, through isolating this sequence and placing it in an expression vector, the nanobody can now bind to α-Syn, allowing it to be degraded and reduce the accumulation of this protein. In order to further improve delivery of the nanobodies using viral vectors across the BBB in PD relevant brain regions, Dr. Tandon is also exploring the use of focused ultrasound, a technique which helps large molecules
to cross the BBB and can be used multiple times, to reduce α-Syn levels.

The in vitro cell work, done by graduate student Sabrina Armstrong, demonstrates the benefit of this therapy to help reduce intracellular pathology induced by the presence of α-Syn fibrils, so his current research has shifted to examine this in animal models. Dr. Tandon explains, “The other incredible aspect of this is once there is proof of principle that it works in one model, any neurodegenerative disease could be targeted, and I do not think this is a single treatment approach, it may work in combination with other treatments as well but having a brain cell produce the therapeutic factor continuously has a certain appeal to it.” This research also opens many pathways to consider targeting α-Syn misfolding and pathological spread between cells.
While developing therapeutics for PD, it is important to use the appropriate
by adapting animal models of enteric pathology developed by other labs, which include overexpression of α-Syn fibrils in the GI tract. Dr. Tandon aims to explore the pathology transfer from these enteric neurons to higher cortical regions of the brain, which results in dementia-like pathology of late-stage PD. Optimization of this research is ongoing and various factors will need to be considered to enhance delivery of the nanobody gene therapy vectors to peripheral neurons.

Scientist, Tanz Centre for Research in Neurodegenerative Diseases, University of Toronto; Associate Professor, Department of Medicine, Division of Neurology; Full Member, Institute of Medical Science
animal models which can be challenging. “We have models that replicate aspects of the disease but we do not have an allencompassing model”. Furthermore, “We do not fully appreciate where the disease begins in humans. There is quite a bit of research suggesting that it begins in the peripheral nervous system particularly in the gastrointestinal (GI) tract. So enteric neurons certainly show pathological changes very early on, but that may not be the case for all patients. Some patients may have a disease that starts in the brain, others may be peripheral”.
Patients generally present with PD when it has progressed to neuron loss in the brain, while the early peripheral symptoms are often missed. Thus, it is important to target this primary origin of the disease to stop progression and preserve function. Dr. Tandon is also investigating this approach
Through targeting the early underlying PD pathology in the peripheral nervous system, Dr. Tandon mentions, “Now you might have the ability to first block the spread of the pathology and then the second approach would be to see if we can rescue the existing neurons that are on the verge. We may or may not be able to rescue cells that have died completely, the distances in the brain are very challenging because to have a neuron project from the substantia nigra to the striatum, these are many centimeters, which is not a minor thing in either an animal model or humans where all the neurons are already beautifully laid out, so re-establishing connections may be a challenge, but we might be able to strengthen the existing ones”.
If your family has been impacted by Parkinson’s Disease, Dr. Tandon highlights many avenues where you can seek more information. One, is by reading magazine articles that provide updates on the current state of science in the field. Second, the Parkinson Society of Canada is a great resource to support you and assist in understanding the condition, while also connecting you with researchers. Finally, he indicates the importance of funding agencies, both government-based
(Canadian Institutes of Health Research or CIHR) and private philanthropy operations like the Weston Brain Institute, which support cutting-edge research.
Dr. Tandon encourages graduate students to read about the research areas they are interested in and also examine crossdisciplinary applications. He highlights how essential collaboration is to advance scientific discoveries. Despite not having a strong virology or immunology background, through collaboration he is able to incorporate these fields into his work. He recalls, “I do not need to know how to make these things, I just need to know how I could reach the person who made them and ask them to collaborate with us on a project.” Dr. Tandon stresses the importance of humility and being open to sharing your knowledge and collaborating with scientists in other fields.
There is a lot that is yet to be explored in this field, particularly if we consider personalized medicine and assessing individual progression of PD pathology. Cross-disciplinary collaboration will be key to advancing therapies for PD and other neurodegenerative disorders.
1. Parkinson’s Disease [Internet]. Parkinson Canada. [cited 2022 Jun
Available from: https://www.parkinson.ca/about-parkinsons/
2. Symptoms
Parkinson’s [Internet]. Parkinson Canada.
https://www.parkinson.ca/about-parkinsons/
M., Granado, N., García-Sanz, P., et al. Modeling
Disease
the Alpha-Synuclein Protein.

Nabbouh F, Xhima K, Al-Fahoum Y, Lang man T, et al. Viral alpha-synuclein knockdown prevents spreading synucleinopathy. Brain Communications.
Oct 1;3(4):fcab247.
intracellular antibodies (intra bodies/nanobodies) to treat neurodegenerative disorders. Neurobiol Dis.
A, Butler DC.
Feb;134:104619.
Every year, The Vesalius Trust for Visual Communication in the Health Sciences awards grant funding to students enrolled in medical illustration programs. These competitive grants are intended to help fund student research projects and masters’ theses.

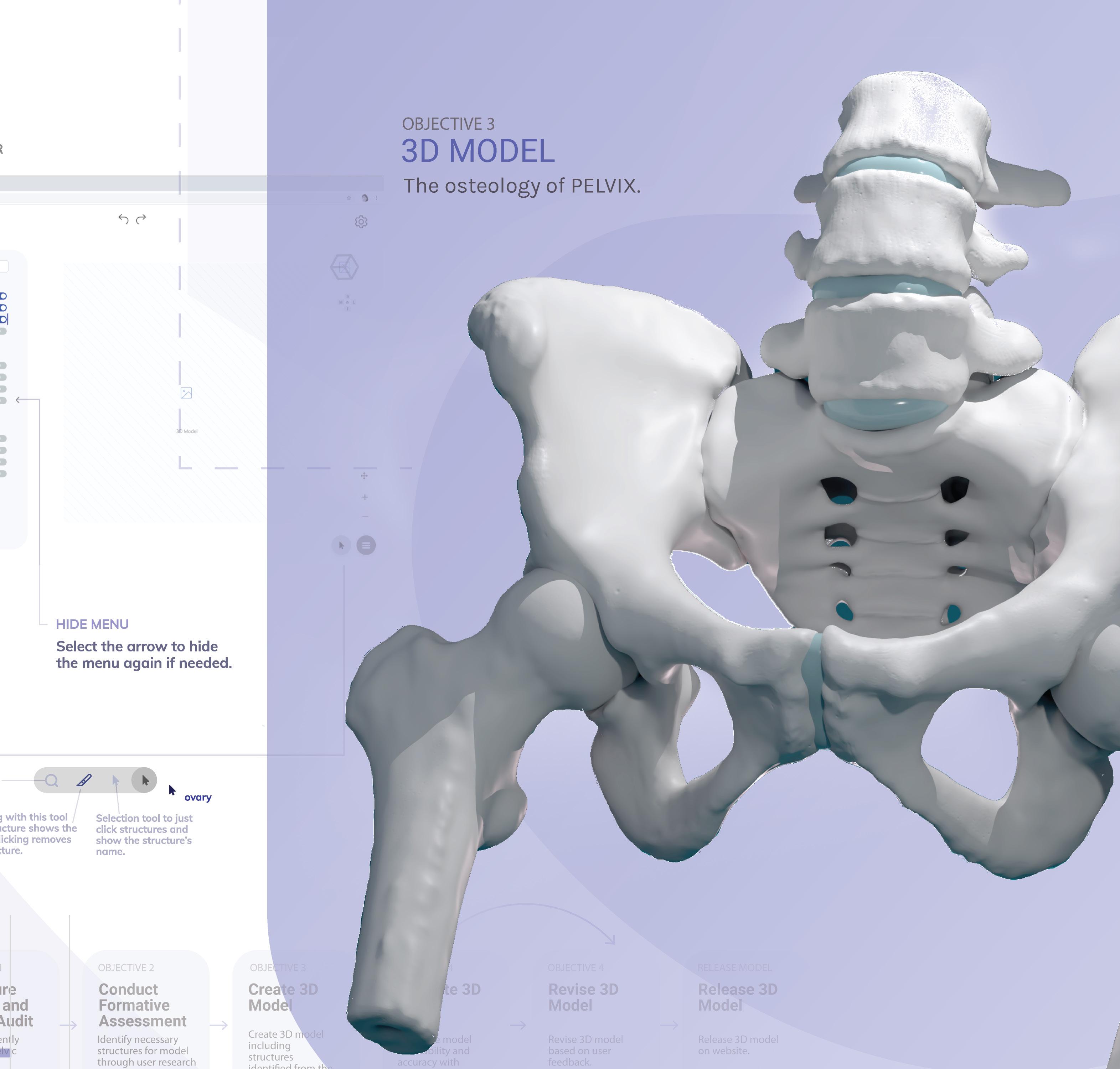
A User-Informed, Interactive, Digital Three-Dimensional Pelvic Anatomy Model for Pelvic Healthcare Professionals
Pelvic anatomy understanding is critical in treatment and can be facilitated through digital 3D models. Evaluations of such models developed academically and commercially concluded that very few are curated to meet the needs of pelvic healthcare professionals. This project involved creating one of the first user-informed and expert-validated digital 3D representations of female pelvic anatomy for physiotherapists. A Vesalius Trust Research Grant was awarded for this interactive media project. Naomi was also awarded the Inez Demonet Scholarship, given to the medical illustration student with the highest academic and personal achievements in the field of visual communications in the health sciences.


The purpose of this 2D animation is to educate PTSD patients and help them make informed decisions about substance use. Using non-triggering and non-stigmatizing visual graphics, the story follows the journey of a PTSD patient recovering from substance use. It is intended to serve as an educational tool in clinics and possibly online for the Public Health Agency of Canada.


A Vesalius Trust Research Grant was awarded for this animation project.
This Master’s Research Project is a patient education 2D/3D animation aimed to increase awareness of modern options to restore peripheral nerve injury deficits and encourage patients to consult a nerve surgeon early. A friendly, non-triggering visual style with simple language, patient-centered content, and visual metaphors is integrated to create an engaging online resource. A Vesalian Scholar Grant was awarded for this animation project.
Whatif a picture of your brain could tell you the exact state of your mental health? While some scientists and psychiatrists argue that neuroimaging has the power to do just that, other professionals, including the American Psychiatric Association (APA), disagree.1
The dawn of neuroimaging techniques that allow for the assessment of the structural anatomy and functional activity of the brain has lent a significant helping hand in the study and detection of brain disorders. For example, computed tomography scans can identify various neurological disorders, such as cancerous tumours, brain haemorrhages, and head injuries.2 In Alzheimer’s disease, magnetic resonance imaging and positron emission tomography can be used in the diagnostic process to assess brain atrophy and betaamyloid plaque formation, respectively.3 However, while there have been significant advances in the use of neuroimaging for diagnostic purposes, there remain a number of limitations to applying this approach within psychiatry.

In medicine, it is typical to look at the organ of concern during the diagnostic process. For instance, x-rays are used to visualize broken bones, ultrasounds are used to visualize abdominal organs, and so on. Psychiatry is the one medical field where the organ of concern, the brain, is rarely ever looked at prior to treatment. There are significant gaps in medical literature with regards to psychiatric
disorders in general. In fact, medications are often prescribed without knowing the true cause of the psychiatric illness.
The current gold standard for making a clinical diagnosis is using the Diagnostic and Statistical Manual for Mental Disorders, 5th edition (DSM-5), which relies on behavioural presentation to make psychiatric diagnoses.4 However, the DSM-5 comes with its own limitations, namely low thresholds for diagnosis that may lead to inappropriately classifying certain behaviours as disorders and thereby overdiagnosis (or even misdiagnosis) and overtreatment.5,6,7
There are currently no laboratory tests for psychiatric disorders in the same way that a blood test or biopsy could determine the presence of thyroid dysfunction or cancerous cells, respectively. The aim of using neuroimaging as a diagnostic tool is to objectively identify psychiatric disorders via biomarkers. The idea is that, once a biomarker is established for a certain illness, neuroimaging can be used to detect said biomarker to aid in the diagnosis of the illness.
At the forefront of the movement to use neuroimaging as a diagnostic tool in psychiatry is Dr. Daniel Amen, MD, who has become well-known for his forwardthinking approach to diagnosing psychiatric disorders using single photon emission computed tomography (SPECT), which measures blood flow in various parts of
the brain and is conventionally used for neurological disorders. Amen claims to be able to use SPECT to diagnose distinct subtypes of attention deficit hyperactivity disorder and to even identify Alzheimer’s in the brain years before symptom onset.8,9 He also performs SPECT scans before and after treatment to assess its effectiveness. The International Society of Applied Neuroimaging, who believe that functional neuroimaging provides valuable insights into patient diagnosis, support Amen’s work.10
However, Amen’s approach has been deemed controversial, unethical, and lacking scientific validity by his academic peers. In fact, his work has been compared to modern-day phrenology.11
Research studies have found reproducible neural differences between diagnostic groups; for example, hippocampal atrophy has been commonly observed in depression and enlarged ventricles have been commonly observed in schizophrenia.12,13 However, these studies may still not be enough to conclude that neuroimaging can diagnose psychiatric illness. Why? Because these research studies depict deviations between groups of patients, not deviations between individual patients.
This raises the issue of generalizability because of individual differences in age, sex, medication, comorbid psychiatric disorders, and stage of illness. Therefore, what may be true for most individuals with a disorder may not be true for all individuals with a disorder. Psychiatric
disorders are heterogeneous in nature, which makes diagnosis and treatment all the more difficult. In the context of neuroimaging for diagnosis, mental illness can present differently at the neural level between individuals with the same illness.
There are several other factors to consider when asking the question of whether neuroimaging is capable of diagnosing psychiatric disorders. First, it is important to note that existing studies demonstrate correlational, not causal, relationships. That is, an abnormality in a certain brain region does not cause the psychiatric disorder per se, but rather the brain abnormality and the psychiatric disorder co-occur. Second, several disorders may show similar brain abnormalities. Third, psychiatric disorders are not solely caused by observable brain abnormalities; rather, psychiatric disorders are best viewed through the lens of the biopsychosocial model that takes into account biological, psychological, and sociocultural factors.


All of the factors discussed above limit the validity of neuroimaging as a diagnostic tool. In fact, the APA has maintained that “neuroimaging has yet to have a significant impact on the diagnosis or treatment of individual patients in clinical settings” and that “at this time, the majority of neuroimaging’s utility remains as a research tool only.”
Even though it is said that a picture is worth a thousand words, this logic may not apply to brain scans in psychiatry—
at this point in time. Neuroimaging techniques have contributed a great deal to our understanding of the brain and its related disorders. While these contributions have promise, current neuroimaging technology lacks the sensitivity and specificity to reliably diagnose psychiatric disorders. Much advancement in neuroimaging technology is needed in order to confidently rely on its ability to single handedly diagnose such disorders.
1. Botteron K, Carter C, Castellanos FX, et al. Consensus Report of the APA Work Group on Neuroimaging Markers of Psychiatric Disor ders. Arlington, VA: American Psychiatric Association; 2012.
2. Computed Tomography (CT) SCAN [Internet]. Johns Hopkins Medicine. 2021 [cited 2022May21]. Available from: https://www. hopkinsmedicine.org/health/treatment-tests-and-therapies/ computed-tomography-ct-scan#:~:text=CT%20scans%20may%20 be%20performed,a%20tissue%20or%20fluid%20biopsy.
3. Gazzaniga M, Irvy RB, Mangun GR. Cognitive Neuroscience: The Biology of the Mind, Fifth Edition. W. W. Norton & Company; 2019.
4. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Arlington, VA: American Psychiatric Association; 2013.
5. Wakefield JC. Diagnostic issues and controversies in DSM-5: Return of the false positives problem. Annual Review of Clinical Psychol ogy. 2016;12(1):105–32. https://doi.org/10.1146/annurev-clinp sy-032814-112800
6. Thombs B, Turner KA, Shrier I. Defining and evaluating overdi agnosis in Mental Health: A Meta-Research Review. Psycho therapy and Psychosomatics. 2019;88(4):193–202. https://doi. org/10.1159/000501647
7. Raskin JD, Gayle MC. DSM-5: Do psychologists really want an alternative? Journal of Humanistic Psychology. 2016;56(5):439–56. https://doi.org/10.1177/0022167815577897
8. Attention deficit disorder (ADD/ADHD) [Internet]. ADD & ADHD Treatment | Attention Deficit Disorder Therapy | Dr. Amen. [cited 2022May15]. Available from: https://www.amenclinics.com/ conditions/adhd-add/
9. Burton R. Brain scam [Internet]. Salon. Salon.com; 2011 [cited 2022May15]. Available from: https://www.salon.com/2008/05/12/ daniel_amen/
10. Henderson TA, van Lierop MJ, McLean M, et al. Functional neuro imaging in psychiatry—aiding in diagnosis and guiding treatment. What the American Psychiatric Association Does Not Know. Frontiers in Psychiatry. 2020;11.
11. Tucker N. Daniel Amen is the most popular psychiatrist in
America. to most researchers and scientists, that's a very bad thing. [Internet]. The Washington Post. WP Company; 2012 [cited 2022May15]. Available from: https://www.washingtonpost.com/ lifestyle/magazine/daniel-amen-is-the-most-popular-psychiatristin-america-to-most-researchers-and-scientists-thats-a-very-badthing/2012/08/07/467ed52c-c540-11e1-8c16-5080b717c13e_story. html

12. Cole J, Costafreda SG, McGuffin P, et al. Hippocampal atrophy in first episode depression: a meta-analysis of magnetic resonance imaging studies. Journal of affective disorders. 2011 Nov 1;134(13):483-7.
13. Weinberger DR, Torrey EF, Neophytides AN, et al. Lateral cerebral ventricular enlargement in chronic schizophrenia. Archives of General Psychiatry. 1979 Jul 1;36(7):735-9.
Onceupon a time, doctors were called ‘magnetizers’. They were thought to heal through ‘magnetic hypnotism’ - a hypnotic method that used magnets to re-orient living creatures’ drive towards life. This is not fiction, but the medical reality of the 18th century. As unscientific as it may sound today, German doctor Franz Mesmer, the father of this theory called “mesmerism”, may have been onto something about the usefulness of measuring magnetic forces to understand biological processes.
In 1990, Japanese biophysicist Seiji Ogawa discovered that functional magnetic resonance imaging (fMRI) could be used to detect brain activation by measuring magnetic field changes driven by the brain’s blood oxygenation levels, which increase with brain activity. For over 30 years, this finding has enabled scientists to link changes in brain function to psychological phenomena, such as memory, perception, or emotions.
Yet, my undergraduate advisor warned me against conducting fMRI research in my MSc or PhD thesis, as if fMRI were as fallacious as mesmerism. Perhaps he did not want me to be ‘fooled by the brain’. He sensed my naïve excitement about producing colourful brain figures one finds in highly cited neuroimaging publications, which research suggests actually bias scientific judgement.1
My advisor mostly wanted to make me aware of the false positive risks of fMRI
research. He showed me the Dead Salmon Study: brain activation was found in a dead Atlantic salmon that looked at pictures of emotional faces during an fMRI scan.2
The Atlantic salmon paper did not imply dead fish can feel or think about humans’ emotions, but rather warned: “fMRI research is at a high risk of false positives”.
If fMRI can find activation where there is certainly none, so it can in living human brains. Then how would you deal with such a false positive risk?
the standards for publication have changed since then, I’m in awe of students who manage to publish multiple neuroimaging papers before completing their PhD”
Increasing sample sizes entails greater analytical load, costs, and recruitment efforts. These are limited resources to graduate students, more so after the pandemic, since non-essential in-person experimenting has been restricted or moved online. It is already challenging for students conducting MRI research to reach sample sizes of even 30 participants. Are we expected then to avert false positives by testing thousands?
In March 2022, Nature published two papers insisting on the importance of increasing sample sizes to reduce the risk of false positives and inflated effect sizes, and to improve the replicability of neuroimaging research.3, 4 The first found that false positives risk in MRI studies only begins falling when sample sizes surpass the thousand. Yet the median sample size in neuroimaging studies is currently 25.3
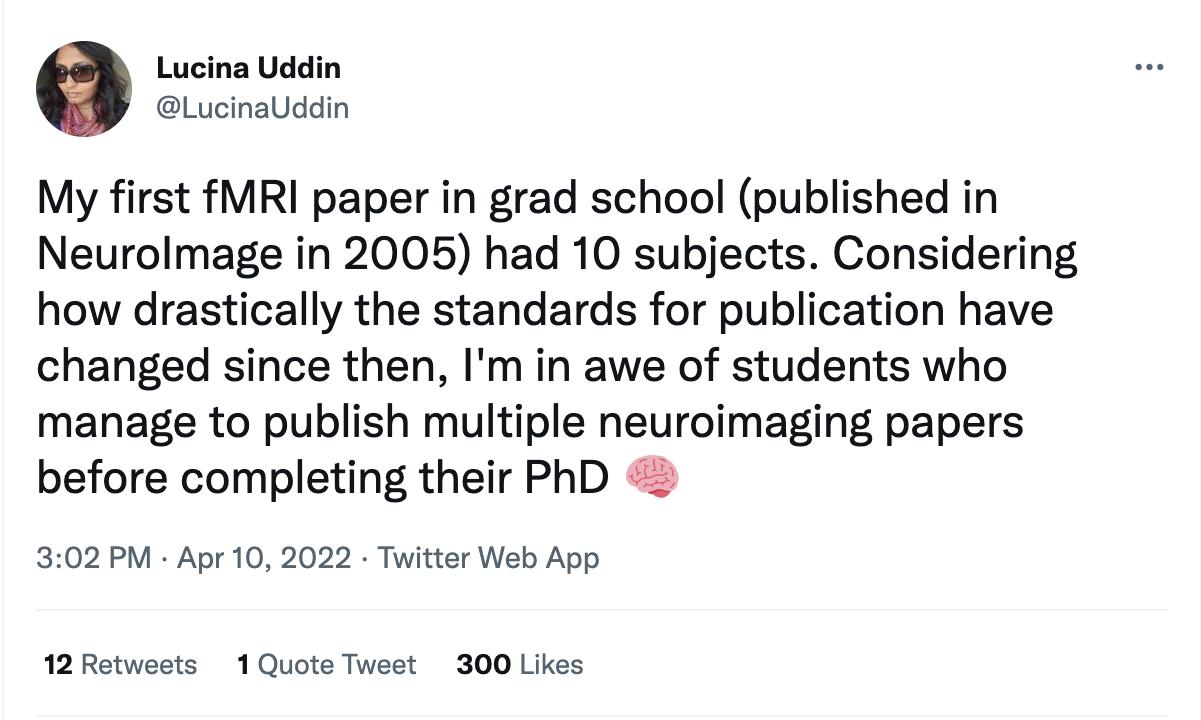
Since Ogawa’s fMRI discovery in 1990 up until 2018, sample sizes in fMRI studies have increased yearly at a rate of approximately 0.74 participants.4 Dr. Lucina Uddin, a professor at the Center for Cognitive Neuroscience Analysis Core at the University of California, Los Angeles, recently tweeted:
“My first fMRI paper in grad school had 10 subjects. Considering how drastically
Big data could be a solution for graduate students conducting fMRI research. The Adolescent Brain Development Study (ABCD, N = 11,874), the Human Connectome Project (HBN, N = 1200), and the UK Biobank (N = 35,735) are examples of big fMRI datasets accessible worldwide.
In a collaborative effort by neuroimaging researchers all over the globe, the second March 2022 Nature paper brought hope to neuroimaging by aggregating more than 100,000 structural MRI brain scans collected throughout over 100 studies (including ABCD, HBN and UK Biobank) from participants between 155-days postconception and 100-years-old.4 The study
Big Data for Big Problems
“Sample size, sample size, sample size”
found that just like height and weight can be measured along the decimal scale and compared across persons, the integration of brain scans could soon generate a scaling system along which individual MRI scans can be compared across population standards.5 Findings from individual studies with small sample sizes could in the near future be evaluated against these ‘brain charts’ to test if they are coherent with big data trajectories.
Tweet by Dr. Lucina Uddin, posted on April 10th 2022.
datasets is that the researcher conducting (secondary) analysis does not design the study themselves. As such, researchers are not bound to pre-established hypotheses and are free to “torture” the data until they find interesting results which could be claimed as hypothesized from the beginning. This takes us back to the beginning: data torturing increases false positives. As the number of statistical tests rises so does the probability of finding an effect that does not exist.
or accessing data. This can be done through platforms such us Open Science Framework and ensures findings are not selectively chosen.
fMRI findings can be mesmerizing and cloud scientific judgment. But despite the scepticism looming over fMRI research, we may avoid being ‘fooled by the brain’ by increasing sample sizes and responsible open-science practices.
1. Schweitzer NJ, Baker DA, Risko EF. Fooled by the brain: Re-ex amining the influence of neuroimages. Cognition. 2013 Dec 1;129(3):501–11.
2. Bennett CM, Baird AA, Miller MB, Woldford GL. Neural correlates of interspecies perspective taking in the post-mortem Atlantic Salmon: An argument for multiple comparisons correction. J Seren dipitous Unexpected Results. 2009 Nov 7;1(1):1–5.
3. Marek S, Tervo-Clemmens B, Calabro FJ, et al. Reproducible brainwide association studies require thousands of individuals. Nat 2022. 603(7902):654–60.
4. Bethlehem RAI, Seidlitz J, White SR, et al. Brain charts for the human lifespan. Nat 2022;1–11.
5. Szucs D, Ioannidis JP. Sample size evolution in neuroimaging research: An evaluation of highly-cited studies (1990-2012) and of latest practices (2017-2018) in high-impact journals. Neuroimage. 2020 Nov 1;221.
In the meantime, PhD students may dive into already existing datasets (ABCD, HBN, UK Biobank, etc) to conduct research. A danger of resorting to big
The counterpart to the “sample size” mantra could be: “pre-registration, preregistration, pre-registration.” If you are using big data to test your hypothesis overcoming sample size limitations, share your hypotheses with the scientific community prior to running analyses
“Pre-registration, preregistration, pre-registration”
 By Syed Hussain Ather
By Syed Hussain Ather
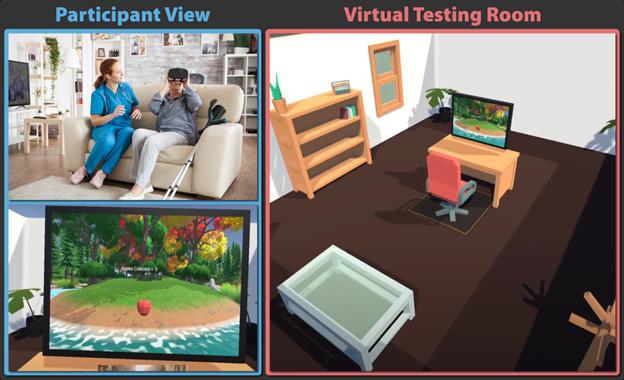
Virtual reality (VR) and augmented reality (AR) continue to surge in popularity among the general public, with students and employees embracing virtual classrooms and workplaces, and scientists taking advantage of the ability to conduct experiments in simulated learning environments. While these technologies revolutionize the way we interact with the world and study our behaviour, many researchers lack the technical resources to use them to their fullest potential. A new initiative aims to change that.
SilicoLabs, a new startup created by Benjamin Alsbury-Nealy, a Ph.D. candidate in Cognitive Neuroscience at the University of Toronto, offers an experimental design platform to let researchers (primarily scientists, as well as discipline and industry professionals) deploy surveys and experiments in immersive environments without the need for programming.
Using their no-code software, ‘Experimenter’, scientists can create and manage tasks using behavioural and biosensor data, including that from electroencephalogram (EEG), electromyography (EMG), and electrocardiogram (ECG). Experimenter provides a flexible no-code experiment design framework that allows researchers to create a wide range of 2D and 3D tasks that can be administered across various devices, including desktop computers, virtual and augmented reality headsets, and mobile devices.
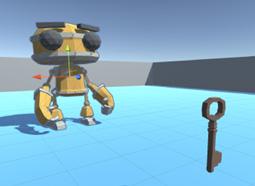
Top: Participants at Cambridge University interact with virtual objects, like this cat, while wearing an AR headset and mobile EEG cap. Bottom: Researchers at Mila are training AI models in 3D environments like this one with the robot and key.

Photo Credit: Kyla Alsbury-Nealy
“Virtual reality, augmented reality, and artificial intelligence are revolutionizing the way we interact with the world around us and provide exciting new ways to study human behaviour,” Alsbury-Nealy said. This would increase researchers’ abilities to collect data from participants in more varied and lifelike settings compared
to the traditional desktop computers in psychology laboratories – though the software is built to make any kind of experiment or survey easy to create.
Researchers are already using Experimenter internationally to create a wide range of tasks in both 2D and 3D environments for desktop computers, mobile devices, and headsets from virtual and artificial reality. At the University of Toronto, Experimenter is being used to run full 3D environment experiments remotely, which has allowed data collection to continue during the COVID19 pandemic. Researchers at Cambridge University in the United Kingdom have used Experimenter to create one of the world’s first augmented reality and mobile EEG studies, where participants navigate the campus to locate virtual objects placed in real-world locations (see photo).
But Experimenter is not just for human participants. In fact, any task created in Experimenter can also be performed by artificial intelligence (AI) models. This allows human behaviour to be modelled with “unprecedented comparative accuracy.” Using this feature has allowed researchers at the Mila Quebec Artificial Intelligence Institute to test models of human cognition.
The startup also hopes, that in making scientific research more accessible, they can address greater issues of mistrust and misinformation in science. As it is the responsibility of the scientific community

SilicoLabs Founder/CEO Benjamin AlsburyNealy poses with the Oculus Quest 2 headset for simulating environments with VR technology. The use of VR/AR technology offered by startups like these lets researchers do more with less.

to find better ways of communicating research to the general public, this can be accomplished, in part, by sharing research, discovery, and technology tools with the general public. Making these technologies more accessible, approachable, and shareable would allow for greater transparency in the research process. In addition, conducting experiments under more immersive and lifelike conditions will improve the applicability of scientific findings to real-world problems.
VR technology has already shown compatibility with non-invasive imaging
technologies alongside invasive cell recording techniques.1 Its uses have included testing spatial cognition and navigation in experiments like the Morris water maze, in which animals must swim and remember where different platforms are located underwater. Virtualizing this classic experiment makes it easy to test human subjects (without needing a swimming pool) and adds critical layers of experimental control and reproducibility. In the virtual world, experiments in which subjects must integrate information and experiences across different senses, such as using disparate inputs like sight, sound, and touch into a greater perceptual experience can also be performed in ways to modify or change inputs more accordingly. For the “rubber hand” experiment, in which the subject feels the “touch” of a rubber hand as though it were their own, the “imposter limb” syndrome can be easily recreated. This experiment has been conducted in VR, demonstrating that body ownership, or the feeling that your body is your own, can be altered by interacting with a virtual body.
Going virtual also provides more opportunities for improving the accuracy and efficiency of the research process itself. Experimenter allows users to independently iterate experiments faster and with fewer resources, so they can answer more questions, make discoveries, and improve transparency. More research means more discoveries that can lead to timely and accurate diagnoses, as well as effective treatment options for the many
Mobile testing rooms using virtual reality headsets, mimicking traditional lab environments.

mental, cognitive, and behavioural health conditions that people are living with today.
Moving forward, Alsbury-Nealy’s group predicts a bright future for virtual reality and neuroscience. He sees his startup’s work having the potential in advancing virtual technologies beyond the lab setting, providing access to populations that may be difficult to reach such as senior residents of long-term care homes. Examples of these farreaching applications include transforming standalone VR headsets into mobile testing rooms for use in a variety of contexts as well as AR for human behaviour in real-world settings. By making research more accessible to scientists and subjects alike, these new VR startups can then revolutionize the way scientific research is performed.
References
1. Bohil CJ, Alicea B, Biocca FA. Virtual reality in neuroscience research and therapy. Nature reviews neuroscience. 2011 Dec;12(12):752-62.
Duringmy undergraduate degree, I only took two statistics-related courses out of over 40 pre-requisites and electives. As an individual interested in scientific research, it is concerning that I may not have sufficient statistical understanding. But I am not alone. By graduate school, most research-stream students have little to no statistical training prior to their enrolment and may not be required to take research methods or statistics courses during their degree.1 This lack of statistical comprehension could span entire research careers and is predominantly due to the fear of the discipline that comes from decreased exposure. This apprehension can prevent scientists from seeking appropriate training. A scientific field without statistical expertise can be limited in its exploration and progress. Notably, the current reproducibility crisis in scientific literature, where many papers are published but their results cannot be reproduced by other research groups, significantly floods the literature with irrelevant results that can hinder scientific progress. To combat this issue, we must consider prioritizing the integration of statistics in scientific training.
Science is predominantly an exploratory field: we observe a specific phenomenon
and describe what we see. This essentially indicates that the experimental design and analyses are data-driven and subject to change. For example, if there are three ways to quantify a biomarker in blood samples, I would conduct three different experiments and pick the method that most accurately determines the biomarker’s concentration as reported by previous research groups. Subsequent statistical inferences in a study are not compatible with an exploratory research design.2 Any valid statistical modeling to predict certain outcomes requires a pre-planned study design and analyses to confirm our findings. Many studies are far from a confirmatory stage and are essentially documenting observations.2 For example, when screening novel biomarkers for diagnosing cancer, the aim should be to identify as many potential candidates and understand the potential role of each biomarker for diagnostic purposes before testing their performance and clinical applications. Ultimately, we cannot use our own study to claim specific associations but statistical analyses at this stage of our research can help design further studies to confirm our findings.
The accurate use of statistics is also dependent on understanding that statistics is not equivalent to calculations.
A statistical framework is an integral part of the entire scientific process.3 Contrary to popular belief, the bulk of statistical thinking does not occur at the end of a study (i.e., statistical inferencing) but in study design and execution.4 It is at this early stage where methodological biases can be introduced and must be appropriately accounted for. Sampling and measurement bias could include admission rate, non-response, recall, and family information biases which can affect odds ratio calculations depending on the type of study (e.g., case-control versus cohort studies).4 Without any foresight into the study design methodology, bias can plague the results of the study, leading to misrepresentation of research findings.
Inadequate interpretation of results is also affected by one statistical concept: the p-value. Despite being one of the most misused and misunderstood parts of statistics, the p-value has dominated scientific interpretation. Results that are “statistically insignificant” are deemed as having no effect while “statistically significant” results show a strong association.5 Having a dichotomous view on p-values invites misuse such as manipulating analyses to identify statistically significant associations (i.e., p-hacking). A recent commentary
in Nature calls for scientists to retire statistical significance in all contexts and use other metrics such as point estimates.5 While this approach may not be well-received, it does highlight the importance of statistical training in science as continued misuse has dire effects. Statistical misinterpretations flood the literature with inaccurate studies which can affect scientific progress and clinical translation.5 The scientific community has to contend with the continued misuse of statistics and meaningfully consider potential solutions.
The most important step to address the misuse of statistics in science is to better integrate statistical courses into research training. This involves requiring graduate students to take field-relevant statistics courses as part of their degrees to ensure that they have a foundation for applying statistical principles to their projects.1 Institutions may need to change their curricula in the sciences and emphasize a statistical framework. For example, there is a statistics course offered in Seattle for undergraduate and graduate students in the sciences that focuses on overarching statistical concepts rather than calculations, ensuring students can confidently navigate statistics.3 Addressing apprehension towards statistical methods
through education is an effective way to ensure that as students progress in their careers, they are capable of making accurate interpretations.

Additional statistical training cannot replace the value of consulting statisticians.1 As trainees and scientists, we have limited resources and time to thoroughly understand statistical concepts. Including a statistician as part of the research team can help mitigate any statistical errors by providing novel perspectives and guidance, especially in the study design. Faculty and students should consult the available resources at their institutions to enable collaborations with statistics experts. Institutions should also encourage and facilitate interdisciplinary collaborations or provide appropriate assistance to improve their research output.
Although statistics is widely used in the sciences, there persists an underappreciation and continued misuse of statistical analyses. This has severe consequences for the scientific community as incorrect interpretations of the data can hinder scientific progress and potential applications. Research trainees, scientists, and institutions have an obligation to upgrade their statistical training and to
seek collaborations with their statistics departments to change the current scientific literature landscape.

1. Weissgerber TL, Garovic VD, Milin-Lazovic JS, Winham SJ, Obra dovic Z, Trzeciakowski JP, et al. Reinventing Biostatistics Education for Basic Scientists. PLoS Biol. 2016;14:e1002430.
2. Tong C. Statistical Inference Enables Bad Science; Statistical Think ing Enables Good Science. Am Stat. 2019;73:246–61.
3. Steel EA, Liermann M, Guttorp P. Beyond Calculations: A Course in Statistical Thinking. Am Stat. 2019;73:392–401.
4. Sackett DL. Bias in analytic research. J Chronic Dis. 1979;32:51–63.
5. Amrhein V, Greenland S, McShane B. Scientists rise up against statistical significance. Nature. 2019;567:305–7.

Dr. Howe is a Vascular Surgeon-Scientist at the UHN and TGHRI. She is an Assistant Professor in the Department of Surgery. Her laboratory is focused on endothelial communication within vulnerable carotid plaques to find new targets to prevent stroke.
 Dr. Clement Zai
Dr. Clement Zai

Dr. Zai completed his PhD in schizophrenia genetics and pharmacogenetics, and his MPH in Epidemiology. His research interests include genomics and pharmacogenomics in psychiatric disorders, suicidal ideation, and behaviours.
Dr. Matthew Sloan
Dr. Sloan specializes in the treatment of substance use disorders and their psychiatric comorbidities. His research is in developing new treatments for substance use disorders & exploring determinants of psychopharmacological response to drugs.
Dr. Jin is a full member of the School of Graduate Studies, IMS. Her research interests include evaluation of vision health policy, access to healthcare, health services delivery, health insurance, and epidemiology of eye diseases.

Dr. Minian’s research focuses on increasing the accessibility, efficiency, and effectiveness of interventions, with particular focus on smoking cessation. She is dedicated to promoting health equity by working with communities, researchers, and policy makers.
 Dr. Furqan Shaikh
Dr. Furqan Shaikh
Dr. Shaikh is a pediatric oncologist at SickKids, with a research interest in the management of children with rare solid tumors (germ cell tumors, retinoblastoma, liver tumors), and the Chair of the Germ Cell Tumor Committee at the Children’s Oncology Group.
 Dr. Andrew Lim
Dr. Andrew Lim
Dr. Lim is a neurologist at Sunnybrook and an associate professor of medicine at UofT. His lab, sleepandbrainhealth.ca, is dedicated to unraveling the biological links between sleep and circadian rhythms and neurological diseases in older adults.


Dr. Chintoh applies an interdisciplinary lens to improve outcomes in treatment resistant schizophrenia. A psychiatrist and former elite national athlete, she also provides technical, scientific, and clinical expertise to international sporting organizations.


Dr. Kumar is a Clinician Investigator in the Allogeneic Blood and Marrow Transplant (BMT) program with research interest in clinical outcomes of BMT. His primary focus is on frailty, aplastic anemia, and sickle cell disease.
Dr. Gill is a Clinician Investigator, Assistant Professor with the Department of Obstetrics and Gynecology. Her research interests intersect digital health, sexual and reproductive health, and global women’s health.


 Dr. Justyna Bartoszko
Dr. Justyna Bartoszko
Dr. Bartoszko’s clinical area of focus is cardiovascular anesthesia, with research in blood management, treatment of coagulopathy in perioperative settings, and the association of preoperative risk factors/ anesthesia interventions with outcomes.
Dr. Upton’s clinical and research interests are food allergy treatments including desensitization therapies, allergy diagnostics, and advancing the recognition and treatment of immunodeficiencies.

Dr. Lau is a palliative care physician and Medical Director of the acute palliative care unit in Princess Margaret Cancer Centre. Her clinical and research interests are focused on the intersection of palliative care and addictions.

 By Sonja Elsaid
By Sonja Elsaid
has recently welcomed the new graduate coordinator, Dr. John Vincent. To get better acquainted with Dr. Vincent, IMS Magazine has interviewed him about his research interests and motivations for helping graduate students achieve their optimal educational performance at the University of Toronto.
After completing his B.Sc. in Biochemistry at Manchester University, Dr. John Vincent moved to London to work as a Laboratory Technician at the Charing Cross Hospital, which is one of the hospitals affiliated with the University of London. In his technician role, he focused on the genetic basis of atherosclerosis, which sparked his interest in pursuing genetics as a Ph.D. student at the Molecular Psychiatry laboratory of Dr. Hugh Gurling, at the Middlesex Hospital, University College London. “I decided to pursue academia because I was interested in genetics, and at that time, there were not many opportunities working in the industry in the genetics field. Only after the human genome was completely mapped did the pharmaceutical industry become interested in genetics. By this time, I was already a post-doctoral fellow pursuing academia”.
“I finished my Ph.D. in England and then traveled around central Asia for a couple of months, after which it seemed too unexciting to return to a mundane job in England. My decision to come to Toronto was facilitated by a friend working with Dr. Peter St. George Hislop, who suggested
I apply for a post-doctoral position with Dr. Jim Kennedy at the Centre for Addiction and Mental Health (CAMH). During my Ph.D., I worked on the genetic basis of autism spectrum disorders (ASD), specifically the fragile X syndrome, caused by DNA mutation of the FMR1 gene. Within the FMR1 gene, genetic segments called CGG triplet repeats are multiplied more than 200 times in those with fragile X syndrome. Given that Dr. Kennedy was interested in the possibility of trinucleotide repeat expansions in individuals with Schizophrenia and Bipolar Affective Disorder—a genetic phenomenon similar to the one in fragile X syndrome—I decided to join his lab. My second postdoctoral position was with Dr. Steve Scherer at the Hospital for Sick Children. In this role, I was able to resume my work on the genetics of ASD. A few years later, in 2002, I started my lab at CAMH.”
Dr. Vincent’s research currently provides a better understanding of genetic predispositions for neurodevelopmental disabilities, including ASD and Rett syndrome. Rett syndrome is a type of ASD characterized by defects in the X chromosomal gene MECP2, and as such, it affects girls almost exclusively. During development, individuals affected by Rett syndrome experience a loss of their communication skills and motor coordination, including purposeful hand movements. “We identified an alternative isoform of the Rett syndrome gene, MECP2, and evidence points to this being the disease-relevant isoform”.
In addition, Dr. Vincent’s group attempted to identify autosomal recessive genes for neurodevelopmental disorders. “The most significant findings include the identification of many new genes causing intellectual disability disorders. The work was done by mapping genes from hundreds of families in Pakistan where multiple family members were affected. It led to the discovery of at least 40 new genes, including one for Joubert syndrome—a rare autosomal recessive disorder that affects regions of the brain such as the cerebellum, as well as eyes, and kidneys, and leads to poor muscle control, vision problems, and developmental delay.”
Go to the Athletic Centre! Play frisbee in the King’s College Circle! Go for coffee with your colleagues! Your graduate training is NOT incompatible with your life. For me, having a balance was important.
“ “
The clinical significance of Dr. Vincent’s work is mainly its utility for diagnosis in affected families. Dr. Vincent explained: “By identifying probable disease-causing mutations, we can provide clinicians and genetic counselors valuable information for the diagnosis and treatment of children with these rare neurodevelopmental disorders. This way, the parents and clinicians will better understand the disorder and what to expect as it progresses.”
Before becoming an IMS Graduate Coordinator, Dr. Vincent was the Director of Research Training and Mentorship at CAMH. He was instrumental in helping graduate students and post-doctoral trainees navigate their fellowships at CAMH while helping to ensure that they are assigned to tasks that are appropriate and within the scope of their mandated training. Dr. Vincent was instrumental in raising the awareness that trainees are often pushed to assume various roles outside the

scope of their training. As a result of Dr. Vincent’s efforts, his successor is currently working on implementing policies that will help ensure that the education of postdoctoral fellows stays on course.

Dr. Vincent accepted the role of the IMS Coordinator because of his previous dedication to helping students complete their post-graduate training at CAMH. “The IMS Coordinator’s role fits very nicely with my previous role,” he explained. “My role at IMS involves both administrative duties and student counseling. On the administrative side, I work on finetuning IMS policies and procedures, checking the course enrollment forms, and ensuring that students follow through with their thesis submissions. On the counseling side, I provide support and guidance to students related to their academic and interpersonal challenges, such as conflicts that may occur between them and their supervisors. I try to step in to resolve the issues.”
Dr. Vincent also offered a word of advice on succeeding in graduate school: “Spending time in the lab is all well and good, but not the best for your mental health and development. Go to the Athletic Centre! Play frisbee in the King’s College Circle! Go for coffee with your colleagues! Your graduate training is NOT incompatible with your life! For me, having a balance was important. I spent lots of time playing soccer and squash during my post-graduate training. You need a good balance between work and life to burn the candles on both ends. So, enjoy life! It will help you recharge your system.”
To ensure a balance in his life, in the past 15 years, Dr. Vincent has been running an indoor soccer group at CAMH. Before the COVID-19 outbreak, the league was meeting weekly. “We had terrific players, some of whom had played soccer professionally or semi-professionally, so it was fantastic being able to play with such a skilled group of people.” Dr. Vincent hopes to restart the league once COVID-19 hospital measures are permanently lifted.
When asked how he encourages and motivates his students to do their best in graduate school, Dr. Vincent replied: “I listen to my students, first, when they join my lab, but also as their graduate studies progress. I try to find out what they hope to achieve through their graduate training and which career path they wish to follow, for instance, the academic route or industry. I then try to enhance their graduate experience by creating a path to ensure that they achieve their ultimate goal.”
 By Elizabeth Karvasarski
By Elizabeth Karvasarski
mortality can be defined as a death of a woman during pregnancy, delivery, or after pregnancy. Although Canada is far from being a dangerous place to give birth, there are still mothers who unfortunately pass away before, during, and after childbirth. It is important to understand the reason as to why these deaths occur. Kayvan Aflaki, a second-year MSc student from the Institute of Medical Science (IMS) program, focuses on studying this population under the supervision of Dr. Joel Ray to identify and determine why women in Canada die during, shortly after, or a year after pregnancy. With the opportunity to partner with the Ontario Coroner, who is responsible for death investigations, Kayvan is able to conduct one of the largest studies done in Canada on this typically understudied population. Furthermore, as a new uncle, Kayvan hopes his research can help prevent these deaths from arising in the future as he believes, “giving birth to life should never have to come at the expense of losing your own life.”
Kayvan’s research journey began during his undergraduate degree at the University of Toronto. He had the opportunity to study Chagas disease, a tropical

disease transmitted by insect vectors predominantly in South America. This lab experience allowed Kayvan to develop skills to perform different techniques such as polymerase chain reaction. However, Kayvan found that conducting basic science research was not the best fit. Always having a strong interest in the healthcare sphere, he decided to continue his research journey, but adjust the approach of his research and perhaps have an opportunity to work more directly with patients. After spending time investigating potential research interests, Kayvan landed a spot working with Dr. Ray.
With over 600 faculty members at the IMS, there are many potential supervisors with countless publications, prestigious awards, and great laboratories. However, when it comes to the supervisor-student relationship, Kayvan emphasizes that it is important to seek out a supervisor, “who can double as a mentor in more ways than just your research.” Kayvan describes that in a lot of ways his supervisor has been a fantastic mentor and support system. Not only does Dr. Ray provide honest feedback and asks thoughtful questions to help Kayvan understand his research, but Dr. Ray also helps guide Kayvan through important decisions regarding his ultimate
career path and life goals. Furthermore, Kayvan’s experience with his research has taught him important professional skills such as independent thinking. As well, in our graduate experience it is very common to be met with hurdles, thus being able to digest and interpret constructive criticism in a positive and helpful manner allows one to realize the potential gaps in


our work. Learning how to process the criticism was an important skill Kayvan developed in order to push his research forward and make it stronger.
From being one half of the IMS Student Association presidency, to being a show host on the Raw Talk Podcast, Kayvan is quite active in the IMS community. Kayvan’s goal with his involvement is to help bring students together to build connections and a community and also to make people’s lives more engaging and stimulating, especially after two years of the pandemic. He has also achieved this through his collaborative efforts with his peer Serena Peck in the creation of the Health Care Innovation Challenge. Their idea was awarded the Jay Keystone Memorial Award. The challenge took place for the first time this summer and involved the opportunity for students to work together to solve real world healthcare issues and pitch their idea in written form or verbally to potential investors and clinicians. Through this experience, students had the chance to network professionally with one another and be creatively stimulated.
Imagine having the opportunity to travel back in time and meet yourself right
before you began your graduate studies. What would you say to your younger self? Kayvan mentioned that the years go by much faster than one realizes, “so it helps to stop and smell the roses.” As deadlines for grants and abstracts pass by and PAC meetings and conferences quickly approach, you may get caught up in just preparing and anxiously awaiting the next event. This may cause one to miss out on the opportunity to be present and appreciate where you are in life. “I would tell myself to be more present in the day, exercise gratefulness and mindfulness,” Kayvan adds. Kayvan also mentions to, “appreciate your accomplishments.” He discusses that when publishing a manuscript or completing a PAC meeting, one should take a minute to celebrate as these are major milestones in graduate school. He adds, “do not let the idea of doing things for a CV or an application cloud that appreciation.” It is important to ground yourself in things that make you happy so you can appreciate your accomplishments and life itself.

Being passionate about the healthcare world has resulted in Kayvan joining the IMS program. His academic and research experiences continue to fuel that passion and therefore he hopes to continue
working in healthcare. However, how that will manifest itself, Kayvan is still unsure. Kayvan believes in serving people and serving those who are in times of need. Therefore, he is interested in pursuing medicine. As well, he is interested in continuing his research journey by pursuing a PhD. Furthermore, Kayvan is continuously looking for opportunities for soul searching. For example, he went to pilot school to learn how to fly a plane! He is enthusiastic about taking up experiences that really push his boundaries to help him grow as a person. Until you spread your wings, you’ll have no idea how far you can fly!
Challenging. Fun. Nuanced.
Theseare the three words that Krystal Jacques, Institute of Medical Science (IMS) alumna, used to describe her graduate experience. Krystal successfully defended her thesis in December 2021 and graduated with a Master of Science degree. Her project explored the embryonic origin of the pancreatic stem cell—a question she studied under the supervision of Dr. Derek van der Kooy at the Terrence Donnelly Centre for Cellular & Biomedical Research. Krystal sat down with the IMS Magazine to reflect on and share her journey through graduate school, while offering advice to incoming students who are considering pursuing a career in scientific research.
Krystal’s journey involved personal discovery and growth which, just like science, was not always a linear process. Throughout the program, aspirations and inspirations transformed and were met with reinvention of goals and strategies to address these changes.
Prior to starting at IMS, Krystal’s innate interest in science allowed her to develop a strong scientific background and motivated her to consider medicine as a career; continuing her studies in graduate school
was a big part of actualizing this goal. This career goal served as a strong source of motivation during the first two years of Krystal’s graduate work. This drive was reinforced by like-minded individuals that shared similar interests and support from others. Despite this external validation, Krystal continued to reflect on her academic and career path. She shared that although there were aspects of graduate school and her research that she liked, such as the flexible hours, the reward of mastering certain hands-on procedures, and interacting with her peers, Krystal did not enjoy academia as a whole and it often only left her feeling drained and unfulfilled. Through what Krystal described as a long and organic process of self-discovery, she realized that this was no longer what she was drawn to do.
I went on a journey to understand— why did I make these choices? Is there something else I would rather be doing and spending all my time on?
Naturally, exploring alternative career paths was a part of this process as Krystal’s desire to pursue medicine wavered and her interest in a career in the arts grew. Krystal was always very passionate about the arts; however, it was considered a hobby and it was difficult to dedicate significant time and resources during her graduate degree. This changed when Krystal started to explore the possibility of engaging in this hobby as a full-time career.
When I thought of the possibility of becoming a full-time artist, my heart jumped.
and energy into science and academia, she believed the most reward would be gained by continuing in the same path. This was not enough to prevent Krystal from considering all arguments and exploring new avenues.
The introduction of photography to Krystal’s graduate journey was one of the many intersections of art and science in her life. Krystal joined the IMS Magazine as a journalist and photographer in the first year of her studies. Excited about her role as a photographer for the IMS Magazine, Krystal purchased her first DSLR camera and made a critical investment into a new interest that would change her life. By her second year, she expanded the scope of her involvement in the magazine and became the executive photographer, as well as an executive editor, for the team. She took on the role with great curiosity to learn and develop her skills despite having no previous experience with photography.
Krystal realized that this was a field in which she could build a career and could picture herself pursuing—one that would fulfill her desire to express her creativity. However, coming to this realization, and then fully accepting it, was a challenge. It was difficult trying to rationalize such a drastic change mid-way through her studies. Krystal explained the struggle with the decision by alluding to the Sunk Cost Fallacy: since she had already invested so much time
Krystal shared that during her first photography assignment, she was fixated on all elements of the photo such as the setting, composition, and lighting. She recalled being so nervous that it took many tries to capture the shot. Over time, as photography became of greater interest, taking photos got easier and the process was optimized. While progressing with her photography, Krystal kept having recurring doubts about pursuing a PhD. To overcome this, Krystal persevered with her research work but sought opportunities to incorporate more art into her life and encouraged herself to make more time for this hobby. Eventually, through seeking more photography opportunities, Krystal understood that she wanted to be a full-time artist and photographer.
Through her experiences, Krystal realized an important theme such that skills acquired in the arts and sciences are directly transferable and complementary. She noted many parallels between the two fields and credits her artistry to have contributed to a successful completion of her thesis work.

“ “ “
“
As a photographer who struggled to be sure of what I really loved to do, and then struggled to make the leap in that direction— this photo is partly a token to carving out a life path that’s meaningful to you.
Innovation in science requires an artistic approach—it’s not cut and dry and requires you to think outside the box.

Creativity, which is a trait that is encouraged and developed in the arts, can also aid in designing experiments and problem solving. Similarly, resourcefulness and integration of ideas are necessary for achievements in both fields. Krystal’s unique journey which encompassed both domains allowed her to grow in both fields simultaneously. The intersection of these two fields is best showcased by Krystal’s photography work entitled, “When the heart jumps,” that captures the essence of research.
Krystal also highlighted memorable experiences and lessons learned from completing her thesis such as attending the 2019 International Society for Stem Cell Research conference in California.
Presenting her work for the first time to an international audience emphasized the importance of communication and was reflective of the work she put in to develop her presentation skills over the years. Krystal stated that the ability to see growth and development in her skills often outweighed the final output of her work. The process of self-governing and recovering from failures, along with the energy required to persevere, is often overlooked and not captured in the final product. These are common student experiences that contributed to Krystal’s personal growth.
As she reflects on a successful completion of her Master’s degree, Krystal encourages students considering pursuing research or medicine to take the time to understand whether the reasons stem from a personal choice or if they are shaped by expectations from external factors. She stresses that
although exploring all interests and understanding all perspectives is an integral part of making such important decisions, the final decision must be yours, and often takes a lot of courage.
Krystal has many aspirations for her career in the arts and is currently building her business and portfolio specializing in portraiture and wedding/engagement photography. She is also involved in science communication roles such as writing for the Signal’s blog and works to supplement science with media. One of her long-term goals is to expand to new art mediums, such as painting, and displaying her work in a gallery.
From everyone at the IMS Magazine, we would like to thank Krystal for sharing her story and wish her all the best in her journey ahead!

These summary scores are then added as a covariate, helping to mitigate confounding relationships such as race and adverse past health events.8
for a second, you are tasked with assessing the association between A and B across X, but C influences said relationship. This is problematic since the existence of variable C on variables A and B confuses the nature of the association— potentially affecting statistical findings and likely threatening the validity of your study. This issue becomes amplified when considering huge variables such as race, which affects many other variables. This article discusses race-related confounding variables, biomedical research validity, and possible ways to evaluate these confounds.
Confounders—also known as confounding variables—influence the correlation between the predictor (the independent variable) and the outcome (the dependent variable), and are not statistically accounted for.1,2,3 In other words, think of a confounder as a hidden factor distorting the predictor-outcome relationship.
For any variable to be considered a confounder, it must be: 1) associated with the predictor, 2) associated with the outcome, and 3) not be an intermediary between the outcome and predictor.1
For example, let’s say you are trying to establish a relationship between the day (i.e., the predictor) and the number of Toronto Green P bikes rented (i.e., the outcome) but are not accounting for weather changes.
Here, the weather could be a potential confounder since weather and bike rentals are likely correlated. This is problematic as confounding variables can change the directionality of the effect, magnitude, and significance of the results. For this reason, the appropriate consideration of confounders is key to ensuring that your statistical model is measuring its intended metric—a concept known as validity.2
To account for confounders, biomedical researchers add them as covariates in their models. In doing so, they adjust for (or remove) the effect of that variable in the predictor-outcome relationship.
Unfortunately, the addition of covariates is not always linear (if you’ll pardon the pun), as some confounding relationships are not always explicit. In these cases, failing to consider less obvious confounders can lead to false or nonvalid results. Prominent examples of historically poorly accounted confounding variables include race and race-related variables such as socioeconomic status and demographic distribution. The complex nature of race-related confounds is primarily due to the overarching impact of race on lived experience. Race dictates social experiences such as poverty and stress.4, 5 In this manner, belonging to a particular racial group will likely correlate with specific life experiences. For example, Black communities are more likely to experience socioeconomic stress due to systemic prejudice and racism.4 The relationship between race and socioeconomic status in particular has been subject to a great deal of research due to its substantively confounding effect on biomedical health outcomes.2
Given this context, treating race as a covariate to account for race without adjusting for other race-related confounders may not always be statistically valid.6 Generally, adjusting for race has been a common move by researchers as it does not necessitate splitting the data and lowering the sample size. The severe lack of non-white biomedical data, in large part, is a substantial driving force behind this consideration. However, before treating race as a covariate, one should first establish the research question and whether adding covariates is justified. If trying to account for the effect of race, it is essential first to evaluate all potential race-related confounds, then to adjust for them as covariates in the model if this information is available. If you have enough samples, another solution would be to split the data accordingly to remove the confounding relationship—granted, this cleaves the sample size.7 In cases where this is not possible, a prospective solution is to create a new variable summarizing the correlation between the chosen confounding variables, known as a confounder summary score.3
Race-related confounders and correlated variables threaten research validity, rendering them key considerations for racial equity in biomedical research.6 As biomedical scientists, accounting for race-related confounds in our research paradigms is crucial to the robustness of our findings and achieving biomedical health equity. By doing so, we can better the healthcare received by racialized communities while actively demonstrating to subjugated communities’ that biomedicine considers their plights socially and statistically.

1. Greenland, S, Robins, JM (1985). Confounding and misclassifica tion. American journal of epidemiology, 122(3), 495–506. https:// doi.org/10.1093/oxfordjournals.aje.a114131
2. Greenland, S., Morgenstern, H (2001). Confounding in health research. Annual Review of Public Health, 22(1), 189–212. https:// doi.org/10.1146/annurev.publhealth.22.1.189
3. Greenland, S. (2015). Confounder Summary score. Wi ley StatsRef: Statistics Reference Online, 1–3. https://doi. org/10.1002/9781118445112.stat05133.pub2
4. Smedley, B. D. (2012). The lived experience of race and its health consequences. American Journal of Public Health, 102(5), 933–935. https://doi.org/10.2105/ajph.2011.300643
5. Brondolo, E., W-Giscombé, C L, Gianaros, PJ, et al. (2017). Stress and health disparities report. American Psychological Association. https://www.apa.org/pi/health-equity/resources/stress-report
6. Jay S. Kaufman, Richard S. Cooper, Commentary: Considerations for the use of Racial/Ethnic Classification in Etiologic Research, American Journal of Epidemiology, Volume 154, Issue 4, 15 August 2001, Pages 291–298, https://doi.org/10.1093/aje/154.4.291
7. Pourhoseingholi, MA., Baghestani, AR., Vahedi, M. (2012). How to control confounding effects by statistical analysis. Gastroenterology and hepatology from bed to bench. https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC4017459/
8. Cadarette, SM., Gagne, J J., Solomon, DH., et al. (2010). Confounder summary scores when comparing the effects of multiple drug expo sures. Pharmacoepidemiology and drug safety, 19(1), 2–9. https:// doi.org/10.1002/pds.1845
 By Stacey J. Butler
By Stacey J. Butler
Aftera two-year hiatus, in-person conferences finally resumed this spring and I was overjoyed at having the opportunity to travel to beautiful Victoria, British Columbia, for the 2022 Canadian Respiratory Conference (CRC). In-person conferences offer so much more than their virtual counterparts. I was able to reconnect with colleagues, talk candidly about the sessions and our research with peers, and network with experts in my field–all experiences that were missed with virtual meetings. Better yet, I was able to do all of this while embracing the change in scenery and exploring a new city.
The conference opened with a traditional indigenous blanket ceremony to show our respect to the Saanich Nation of Coast Salish Peoples, who welcomed us to their land. Throughout downtown Victoria, you can see totem poles celebrating the island’s Indigenous heritage. Victoria’s Beacon Hill Park is also home to one of the world’s largest totem poles, at an astounding 127 feet high.

University of Toronto’s own Dr. Samir Gupta opened the conference with a discussion of Long COVID, featuring videos from three Canadians living with this condition. We got to hear first-hand how Long COVID has affected their lives and how they have struggled to be taken seriously by healthcare providers. This was the first time I had seen patient perspectives included in a presentation and it really drove home the message Dr. Gupta was trying to convey. In addition to COVID-19, there were many other timely topics such as the impact of air pollution and wildfires on lung health, and early integration of palliative care for people with chronic respiratory diseases.
The absolute highlight of the conference for many was the concluding plenary session by Dr. Timothy Caulfield entitled ‘Infodemic: misinformation in the media’.
Dr. Caulfield is a very dynamic speaker and had the audience in hysterics as he walked us through the different COVID19 conspiracy theories. Dr. Caulfield spoke about how celebrities had both
positive and negative influences and provided insight into how some people could fall victim to these wild ideologies. He also provided us with effective strategies to debunk misinformation. Beginning and ending the conference with sessions on COVID-19 was bittersweet. It is a topic many of us are tired of hearing about, yet it was important to celebrate all of the incredible research that has been done at a truly phenomenal pace.
Travelling for conferences is one of the biggest perks of graduate school. One of my best friends went to law school in Victoria and created a tour guide for me, fully equipped with a table of contents. Thanks to Emily, I indulged in the best food and explored the best places. The sun was shining for my final day in Victoria and I took the opportunity to take a long walk by the ocean and breathe in the salty air. Returning to Ontario I felt invigorated and had renewed motivation to continue my thesis and help the millions of Canadians living with respiratory disease.
TheIMS Scientific Day is the academic highlight of the year for IMS as it has been established with the purpose of showcasing novel and current research by the students in this program.1 Held on May 17, 2022 at Hart House, this event provided students with the opportunity to showcase their research achievements, network with their peers and compete for student awards such as the Laidlaw Manuscript Competition and the Alan Wu Poster Competition.1,2
Kyla Trkulja is a first year MSc. student at the IMS researching novel therapies for lymphoma and a member of this year’s planning committee. For her, the highlight of this event was the outdoor student booths as well as meeting new people after two years of virtual networking and conferences (which are just not the same as in-person!). With regards to the planning process, she mentioned that the greatest challenge the committee faced was the uncertainty around whether the event would be held virtually or in-person - especially in light of the rapid rate with which the pandemic was evolving. She encourages IMS students to join the planning committee as it was an incredible experience to be involved in the decisionmaking process for the keynote speaker presentation, the research panels, and the themes of the event.
Dr. Gelareh Zadeh was the distinguished keynote speaker of this year’s IMS Scientific Day. Through her engaging presentation, she showcased key findings of her current research on clinically relevant molecular data driving surgical management for brain tumours. Importantly, she discussed the significance of this work and its implications for clinical decision-making and current management paradigms. For Dr. Zadeh, one of the most noteworthy aspects of this year’s scientific day was the long-awaited opportunity to network
 design by Abeeshan Selvabaskaran
design by Abeeshan Selvabaskaran
in-person following the easing of pandemic restrictions. She stated that it was immensely refreshing to finally meet with faculty and students in person. Additionally, another highlight of this year’s event for Dr. Zadeh was the novel delivery of poster presentations through an electronic poster format. She graciously provided words of encouragement for future IMS students, emphasizing participation throughout graduate school, as well as the importance of building supportive relationships both within and outside of the lab for future scientific collaborations.
The Great Hall of Hart House featured an enthusiastic crowd of students and faculty who had attended to learn and evaluate student poster presentations. One notable presentation was from Delara Emtyazi, a second year MSc student at IMS who presented her translational research on the behavioural effects of deep brain stimulation (DBS) and focused ultrasound (FUS)-assisted drug delivery on a posttraumatic stress disorder (PTSD) rodent model. Similar to comments provided by Kyla and Dr. Zadeh, Delara also mentioned that the highlight of this event for her was the return of in-person networking with peers and faculty after a prolonged period of working remotely. Moreover, she shed light on her process of preparing for her presentation, noting that it was similar to her preparation for program advisory committee (PAC) meetings. She had initially developed an outline to incorporate key findings into a powerpoint style format, which was ultimately adapted into a poster. For future student presenters, Delara emphasized the creation of visually appealing posters which are not text heavy and feature captivating and digestible figures and images, especially in methods and results sections of the poster.
1. Institute of Medical Science. Scientific Day [Internet]. University of Toronto. [cited 2022 Jun 10]. Available from: https://ims.utoronto. ca/scientific-day
2. Institute of Medical Science. Scientific Day Student Awards [In ternet]. University of Toronto. [cited 2022 Jun 10]. Available from: https://ims.utoronto.ca/scientific-day-student-awards


It doesn’t matter if you don’t have much experience, if you just go with an open mind and you have the right support, then you can make something like this happen.
Take the opportunity to meet new people, participate as you go through graduate school, and build those relationships for future collaborations.
Enjoy the process and savour the milestones throughout your journey as a researcher.
The IMS Scientific Day was one of my greatest academic experiences at IMS.
 By Kyla Trkulja
By Kyla Trkulja
to the combined efforts of the IMS P2P Mentorship Program, and the IMS Student Association, IMS Connects took place on May 2nd, 2022 at the U of T Medical Sciences Building. This career panel and networking event featured professional guests from all facets of medical sciences.

The first panel focused on academic careers, featuring four U of T assistant professors: Dr. Gabriella Chan, Dr. Dmitry Rozenberg, Dr. Golmaz Karoubi, and Dr. Helen Miliotis. Dr. Chan is a lawyer that runs her firm specializing in biomedical patents and intellectual property. In contrast, Dr. Rozenberg is a clinician-scientist focusing on respiratory and skeletal muscle dysfunction, while Dr. Karoubi is a scientist at Toronto General Hospital using stem cells for regenerative medicine. Dr. Miliotis is highly involved in teaching and the Graduate Professional Development (GPD) program for student success.
With Dr. Nana Lee as the moderator, the panel shared their respective professional journeys and answered questions regarding their academic careers, simultaneously navigating parenthood, and how they made their strengths and passions into their dream jobs. Their talks emphasized the importance of not getting discouraged by minor setbacks, making your opportunities, and taking risks – which was encouraging to hear as someone who thought the academic career journey was a linear path.
We then took a break for refreshments and networking among the students and panelists. I talked more to Dr. Miliotis about her background and how she ended up where she was; I was very intrigued that she did not do a postdoc and instead got her Leadership in Higher Education certificate at the Ontario Institute for Studies in Education (OISE). This further showed me how open career options are and how you can create your niche and do what you love with a bit of creativity.
The second session focused on careers in industry, featuring Dr. Bruce Seet, Dr. Molly Shoichet, and Dr. Sam Esfandiari. Dr. Seet is the Director of Medical Affairs at Sanofi Pasteur, Dr. Shoichet is an entrepreneur and Tier 1 Canadian Research Chair, and Dr. Esfandiari is a Medical Science Liaison at Boehringer Ingelheim. With Dr. Pamela Plant as the moderator, they discussed how they
shifted into industry fields, found careers suiting their strengths, and advising us graduate students who did not know how to find a career they loved. My key takeaway from this panel was the importance of networking, both virtual and face-to-face. One can do this by adding people on LinkedIn to find out about job opportunities you will not see on a job board, asking questions during events so you are memorable, and not being afraid to ask people questions. You will learn so much about what is out there and get a foot in the door for your career.
I left the event with seven new LinkedIn connections and abundant information regarding my viable career options. The event made me feel more empowered to create my future and taught me how there is no linear path to success – it truly is what you make it, and there is enough room for anyone who wants to get there.








From our favourite crime shows to chilling murder mystery podcasts, forensic science is often depicted to be very entertaining and glamorous. However, as we learned in episode #106 “Raw Talk Unsolved: Investigating Forensics”, the source of this entertainment comes less from crimefighting or action filled storylines of investigations and more from the exciting contributions of the various specialties within forensic science. In this episode, we took a deep dive into the fascinating intersection between two very different yet complementary fields, law and medicine, and learned more about how these fields intertwine to form different career branches within the field of forensics.

Forensic medicine is an important component of forensic science that involves the application of different medical professions to legal situations and questions.1 Forensic medicine is not limited to only deaths and major crimes, but encompasses the non-discriminatory care given to patients who have been involved in criminal cases. There are multiple different professions within forensics that involve medicine including: coroners, forensic pathologists, forensic nurses, and many more.2 In Raw Talk episode #106, we learn more about the unique and vital roles these professions play in forensics from our guests.
As shared by our first guest Sheila Early, a longstanding forensic nurse, forensic nursing is a new term that has been developing over the years. She shares “…forensic nursing is where health care, the judicial system and law enforcement intersect… all three spheres will coincide. For example, a child is being abused at home, they may see a family doctor, they may go to the emergency department…and there may be a fairly plausible explanation for the injury. If you look at that same child with a forensic lens, [the] nurse has the expertise to say the mechanism of injury does not match what I see. There is a difference between intentional and unintentional injuries. They’re what we call either biomarkers or red flags. So, when a forensic nurse sees that patient, the documentation [and referrals] may be very different.”
According to the International Association of Forensic Nurses, forensic nurses are registered or advanced practice nurses that are specially trained to contribute to forensic related situations. They provide care for victims of trauma, treating their short- or long-term health impacts and ensuring their needs are met.3 They are also often called upon to contribute to testimonies and consultations for civil and criminal proceedings to provide a clinical lens.3
“The other part that’s really important to remember about forensic nursing, it is not about victims. It is about anyone who has
been subjected to some sort of violence or trauma which affects them… [Some people think] forensic nursing is about law enforcement. No, it’s not. It’s about the nursing care of people who have had an unalterable event in their life, which is usually due to trauma and violence.” Indeed, forensic nursing is a unique discipline that focuses on providing care and support to those subjected to harmful situations.
Forensic pathology is a specialization that medical doctors can pursue, requiring additional training in pathology, to become experts in diseases and injuries that cause or are associated with sudden death.4 They can be thought of as “the voice of the deceased” in legal environments. This entails performing autopsies, determining the cause of death, testifying in court and (in some scenarios) acting as coroners for suspicious death cases.4
Dr. Jayantha Herath, the Program Director of Forensic Pathology and associate professor at the University of Toronto, spoke about his role as a forensic pathologist. “The main duty of a forensic pathologist is to [identify]...the deceased and exclude trauma when a body comes. Once you exclude the trauma, then you explore whether any toxicological causes [are] related. Then [you] do a complete body examination…collect samples and do internal examination by medical
process and the pathological processes. [This includes identifying] what kind of force [was], applied whether it’s a blunt force, whether it’s a sharp force, whether it’s a gunshot wound, and then we try to age the injury. We collect evidence of documentation by examining a body and asking for various testing, like toxicology, microbiology, molecular diagnostics. After that we collect all their test results and provide an opinion. We call it [a] postmortem examination report, or autopsy report.”
Within Ontario, the Ontario Forensic Pathology Service (OFPS)5 is in charge of providing forensic pathology services under the Coroners Act.6 This service also collaborates with other organizations to ensure high-quality of death investigations and civilian safety.5 Forensic pathologists are essential to solving criminal cases.
Within each province, one person is appointed as the Chief Coroner. According to the Canadian Society of Forensic Medicine, this person must be within Ontario, but can be lay individuals or come from other professional backgrounds in the other provinces and territories.4 Dr. Herath shares that generally, the coroner’s role is to answer five main questions at the end of the investigation. “... Who is dead? Where did the person die? When did [they] die? And... cause of death? And by
what…[is] the manner of death...whether it is a homicide, whether it’s a suicide, whether it’s an accident, whether it’s a natural, [or] undetermined.”
Dr. Dirk Huyer, the current Chief Coroner of Ontario, shares that the coroner’s job mainly “would entail…working in their general practices most of their time. And then when there’s a sudden or an unexpected death, or a traumatic death, or something unnatural they would get called by our office to attend and work together with the police…to understand the circumstances of what happened…they would then meet with the police officers… and make a plan on what…investigation steps would be taken.” Coroners generally act as one of the representatives for an investigation and are expected to adhere to the coroner’s code of ethics as part of their duty.7 These individuals are essential to the fluid and successful progression of criminal investigations, as they must ensure each criminal case they are appointed to properly addresses all questions and investigation steps needed to solve and close the case.
coroners are unique in their own demands, but play equally important roles in criminal investigations. We encourage you to learn more about the aforementioned professions, forensic medicine, and where you can study forensic science in Canada.
We would like to acknowledge the efforts and ideas of the rest of the episode #106 team. To learn more about the forensic medicine, we invite you to listen to episode #106 of Raw Talk Podcast, titled “Raw Talk Unsolved: Investigating Forensics”. Also, check out our references for more information on the bolded topics, as well as some interesting resources the team has compiled in the episode’s show notes on the Raw Talk Podcast website.

References
1. Forensic medicine [Internet]. Encyclopædia Britannica. Ency clopædia Britannica, inc.; [cited 2022Jul13]. Available from: https:// www.britannica.com/topic/forensic-medicine
2. Careers by Major - Forensic Science [Internet]. Careers by Major - Forensic Science | Career Centre. [cited 2022Jul13]. Available from: https://www.utm.utoronto.ca/careers/careers-by-major-fo rensic-science
3. Forensic nursing [Internet]. IAFN. [cited 2022Jul13]. Available from: https://forensicnurses.org/page/WhatisFN/ .
4. Medical [Internet]. Canadian Society of Forensic Science. [cited 2022Jul13]. Available from: https://www.csfs.ca/what-we-do/disci plines-sections/medical/
5. Ontario Forensic Pathology Service annual report - April 1, 2019March 31, 2020 [Internet]. ontario.ca. [cited 2022Jul13]. Available from: https://www.ontario.ca/document/ontario-forensic-patholo gy-service-annual-report-april-1-2019-march-31-2020/what-we-do
6. Coroners Act, R.S.O. 1990, c. C.37 [Internet]. Ontario.ca. 2018 [cited 2022Jul13]. Available from: https://www.ontario.ca/laws/ statute/90c37/v5
This episode is just a snippet into the vast variety of specialties that exist in the field of forensics. The responsibilities of forensic nurses, forensic pathologists, and chief
7. Office of the chief coroner and the Ontario Forensic Pathology Service [Internet]. ontario.ca. [cited 2022Jul13]. Available from: https://www.ontario.ca/page/office-chief-coroner-and-ontario-fo rensic-pathology-service#:~:text=The%20Office%20of%20the%20 Chief,prevent%20deaths%20in%20similar%20circumstances.
Learn more about professions in forensic medicine and how to get involved
