The gender of your doctor may play a part in your prognosis:
New research shows that hospitalized patients are less likely to die if they're treated by a female physician.
About 10.15% of men and 8.2% of women died while under the care of a female doctor, versus 10.23% and 8.4% when treated by a male doctor, according to results published April 22 in the Annals of Internal Medicine. This is a troubling discrepancy, given that patient outcomes
shouldn't differ if men and women practice medicine in the same way, said senior study author, physician Yusuke Tsugawa. He's an associate professor-in-residence of medicine in the division of general internal medicine and health services research at the David Geffen School of Medicine at UCLA in Los Angeles.
“What our findings indicate is that female and male physicians practice medicine differently, and these differences have a meaningful

RPH is hosting a FREE educational speaker series for people impacted by memory impairment. Join us to learn strategies for successful living!


Financial Considerations When Someone you Love has Memory Impairment
Thursday, June 20 from 6:30-7:30PM
Presented By: Ethan Wade, The Wade Group at Brighton Securities
Scams 101 – Signs that your Loved One is a Target
Thursday, July 25 from 6:30-7:30PM
Presented By: Daniel Lyon, Lifespan of Greater Rochester
impact on patients' health outcomes,” Tsugawa said in an UCLA news release.
For the study, researchers analyzed Medicare claims data from 2016 to 2019 for about 458,100 female and nearly 319,800 male patients. Of those, roughly 31% were treated by female doctors.
Not only were patients less likely to die with a female doctor, but they also were less likely to land back in the hospital within a month of dis-
charge, researchers found.
They had several theories why male doctors might not be as effective as female doctors in treating women.
Male doctors might underestimate the severity of a female patient's illness, researchers said. Prior studies have found that male doctors tend to misjudge women's pain levels, heart and GI symptoms and stroke risk.
It also might be that women communicate better and are more comfortable with female doctors, making it likelier they disclose important information leading to better diagnosis and treatment.
More research is needed into how and why male physicians practice medicine differently, as well as the impact this difference has on patient care, Tsugawa said.
“Further research on the underlying mechanisms linking physician gender with patient outcomes, and why the benefit of receiving the treatment from female physicians is larger for female patients, has the potential to improve patient outcomes across the board,” Tsugawa said.
Tsugawa added that these results show gender gaps in physician pay must be eliminated.
“It is important to note that female physicians provide high-quality care, and therefore, having more female physicians benefits patients from a societal point of view,” Tsugawa said.
A 2021 analysis published in the journal Health Affairs found that female physicians earn an estimated $2 million less than male doctors during a 40-year medical career.





Adult Day Health Care is a medical model day program that serves adults with physical, psychosocial and medical needs. Services include medication assistance, cultural arts and lunch or dinner. Transportation available within Monroe County. Ask about our new afternoon program from 2:00 – 7:00 p.m. Call (585) 784-6570 or visit JSLAdultDayHealthCare.org for more information.

Q: What’s different about the osteopathic approach to sports medicine?
up. I never had anyone look at the mechanics of why I was developing injuries.
Q: Do you keep your sports medicine practice separate from family practice or do they blend together?
A: It’s all merged together. People come in with a variety of concerns and I try to address the ones I can. They might come in for a tension headache but if I find it’s related to musculoskeletal issues, I’ll treat those. It can be difficult with the time constraints of medicine these days, but if there’s something I can do like an adjustment I’ll schedule them for it.
Q: Have you found your knowledge useful in avoiding injuries yourself?









A: Our approach involves a mechanical aspect. We try to identify the mechanism of injury, especially for chronic conditions, and then alter or improve those mechanics. So there’s a preventive approach within the treatment. Some sports medicine doctors who are MDs have that approach as well, but it’s part of our holistic approach. We try to understand why a condition is developing instead of just treating it, because that’s usually how it gets better and stays better.
Q: What does this look like in practice? Let’s say I came to you with a minor AC joint separation, how would you go about identifying causes and treatments?
A: We would usually discuss whether or not the patient would be comfortable doing osteopathic manipulation in the office. Depending on how they did it, if it was traumatic, there might be some myofascial restrictions we could address that could promote healing. I’d also give them some stretches to work on that might help them avoid physical therapy depending on the severity. Obviously if they need surgery they’re still going to end up at orthopedics, but if it’s mild we can see how it happened and try to be preventive with our approach. We’ll try to help with the alignment. Usually there’s some compensating going on, so we’ll try to address and prevent compensatory injuries and pain by doing an adjustment. It can alleviate some stress.
Q: How do compensatory move ments make matters worse?
A: It depends on the injury, but you see it a lot in shoul ders. If people have shoulder injuries especially, like you said an AC strain, if they’ve injured their dominant side they’re probably compensat ing with their non dominant side. If they’re still involved in sports they may be devel oping other issues because of that. So if they’re com pensating with their trapezius, they’re going to get trigger points and knots that might cause them neck strain and tension headaches. So we try to make them aware of that. They may not be using diaphragmic breathing because of their injury; they’re using their accessory mus-
cles. And they might be developing tension in muscles they wouldn’t be using normally for that.
Q: Do we learn to misuse our musculoskeletal system? Or did many of us just not learn how to use it efficiently in the first place?
A: I think it’s combination. I think it’s partially learned. Like with breathing, we don’t really learn to breathe. It’s mostly unconscious. But a lot of people, because we’re always trying to have better posture, to stand upright or are self-conscious about our weight and trying to suck out belly in, it can make it difficult to use the diaphragm for respiration, which means using compensatory muscles in their upper back and neck. And it’s compounded by environment, because a lot of people have ergonomic stressors. Like their work position may not be the most optimal. A lot of people sit for a long time. They may not be looking straight in front of them; they’re looking off to the side. So they might develop a tight unilateral side. So recognizing that that’s what they’re presenting with and what might be causing it. That helps more than just giving them an ibuprofen and telling them to ice it and hope that it gets better on its own.
Q: What got you interested in working sports medicine into your family prac-

A: Oh yeah, I could see the benefits, which is why I wanted to go into osteopathic medicine. So I could help other people.
Q: What activities and movements are responsible for the most injuries among your patients?
A: There’s a wide variety around here. It’s not just sports-related injuries. Around Lima I see a lot of overuse injuries. I see a lot of skiing injuries. Everyone plays so many different sports these days.
Q: How do you deal with an overuse injury without just stopping the activity?
A: That’s why it’s important to figure out causes. What activities are causing the strain, which movements, and trying to modify it. Instead of saying you can’t do this anymore we try to figure out how you can do it without hurting yourself.
Q: How do osteopathic manipulations differ from chiropractic?
A: The main difference is that osteopathic manipulations are more likely to be covered as medical procedures since osteopathic doctors are physicians. As far as specific techniques there’s some overlap, but not every DO or chiropractor does things the same, so it can be hard to generalize. We look at ergonomics and the lymphatic system a bit more than most chiropractors. From patient feedback I hear that the procedures we do tend to be more gentle with more facilitated stretching than cracking and popping, but we do use those techniques as well sometimes.
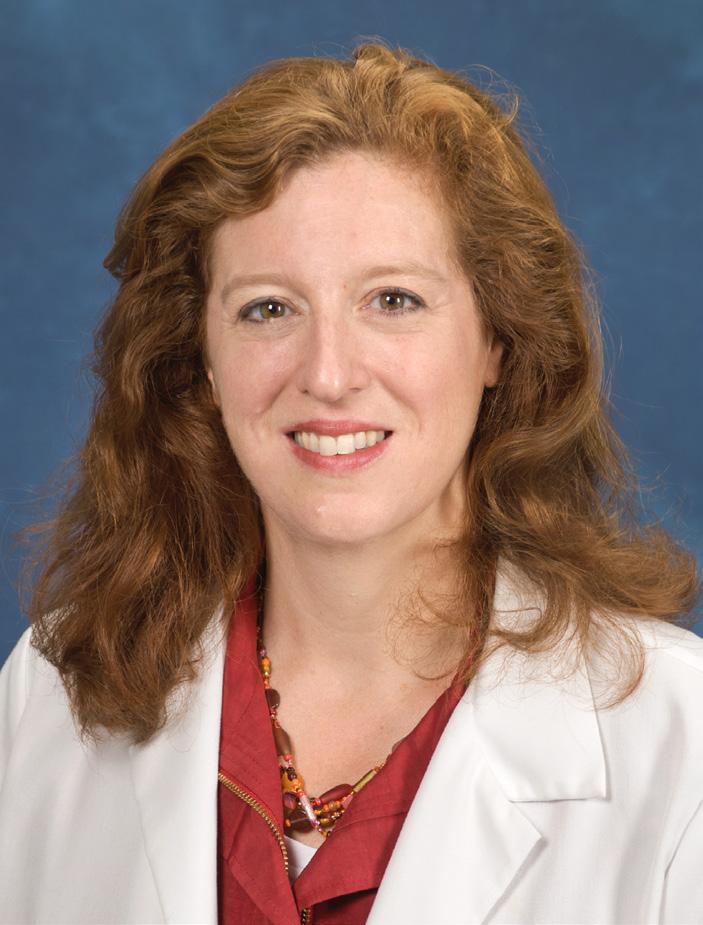
Name: Jennifer Albrecht, DO
Position: Family medicine and sports medicine physician at Thompson Health Lima Family Practice
Hometown: Canandaigua
Education: Midwestern University
Chicago College of Osteopathic Medicine
Affiliations: FF Thompson Hospital, URMC system
Organizations: American Academy of Physicians, American Board of Family Medicine, American Medical Society for Sports Medicine, American Osteopathic Association of Sports Medicine, American Osteopathic Board of Family Medicine
Family: Married
Hobbies: Volleyball,

Want to live longer? Choose the stairs over the elevator, a new review suggests.
Folks who regularly climb stairs have a 24% reduced risk of dying from any cause, and a 39% reduced risk of dying from heart disease, compared to those who always take the elevator, researchers found.
Stair climbing also is associated with a lower risk of developing heart disease or suffering a heart attack, heart failure or stroke, results show.
“If you have the choice of taking the stairs or the lift, go for the stairs as it will help your heart,” said researcher Sophie Paddock, of the University of East Anglia and Norfolk and Norwich University Hospital Foundation Trust in Norwich, U.K..
Stair climbing is a practical, easily accessible form of physical activity, Paddock said. Despite this, it's often overlooked by folks rushing to get to a higher floor.
“Even brief bursts of physical activity have beneficial health impacts,
and short bouts of stair climbing should be an achievable target to integrate into daily routines,” Paddock said.
For the study, researchers pooled data from nine studies involving more than 480,000 people. Studies were included regardless of the number of flights people climbed or the speed at which they took them.
“Based on these results, we would encourage people to incorporate stair climbing into their day-today lives,” Paddock said in a news release. “Our study suggested that the more stairs climbed, the greater the benefits — but this needs to be confirmed. So, whether at work, home or elsewhere, take the stairs.”
Researchers presented the findings recently at ESC Preventive Cardiology 2024, a scientific congress of the European Society of Cardiology. Findings presented at medical meetings should be considered preliminary until published in a peer-reviewed journal.
A monthly newspaper published by Local News, Inc. Distribution: 33,500 copies throughout more than 1,500 high-traffic locations.
In Good Health is published 12 times a year by Local News, Inc. © 2024 by Local News, Inc. All rights reserved. P.O. Box 525, Victor NY 14564. Phone: 585-421-8109 • Email: Editor@GVhealthnews.com
Editor & Publisher: Wagner Dotto
Writers: Deborah J. Sergeant, Chris Motola, George Chapman, Gwenn Voelcker, Anne Palumbo, Jim Miller
Advertising: Anne Westcott (585-421-8109) • Linda Covington (585-750-7051)
Layout & Design: Angel Campos–Toro • Office Secretary Allison Lockwood
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen.


Dr. Mark Winsberg, MD, a seasoned Addiction Medicine Specialist with over 15 years of experience and dual board certification in Addiction Medicine and Family Medicine, is dedicated to supporting you through every stage. In recovery for over 21 years from his own bout with addiction, Dr. Winsberg empathizes with the challenges you may be facing.
Dr. Winsberg provides discrete, nonjudgmental, personalized care and is available for individual consultations or speaking engagements addressing the myriad complexities of this disease. Let’s take the first step towards a brighter future together.
Let your journey to recovery start today!

Our programs help people make small changes they can maintain for life. Offered both virtually and in person, programs help you:
Rochester Diabetes Prevention Program
An evidence-based, CDC-recognized program designed to help people who have been diagnosed with prediabetes prevent the development of type 2 diabetes.
Cancer Services Program of the Finger Lakes Region
A New York State grant-funded program that provides free breast, cervical and colorectal cancer prevention education and ageappropriate screenings for uninsured men and women throughout Monroe, Yates, Seneca, Livingston, Wayne and Ontario Counties.
Prostate Cancer Education
A New York State grant-funded program focused on prostate cancer education and shared decision making in prostate cancer screening for Black men ages 45 - 69 living in Monroe County. Program outreach addresses the risks of prostate cancer, the benefits of and guidelines regarding screening and support to engage participants in shared decision making about screening.

New dean at Roberts Wesleyan University School of Nursing discusses her new role and why she chose to move to Rochester to lead the school
By Mike CostanzaOn April 2, Annemarie Dowling-Castronovo, Ph.D., registered nurse, became the new dean of the Roberts Wesleyan University School of Nursing. Located on 188 rolling acres in North Chili, Roberts Wesleyan University offers its students “a supportive Christian academic environment,” according to the release that announced the hiring of its new dean. The school of nursing offers a variety of undergraduate and graduate programs that are intended
and health studies at Monmouth University in New Jersey, where she chaired the nursing department, was the chief academic nursing officer and taught courses as a professor of nursing. She is board-certified in palliative and gerontological care and has extensively researched the clinical care of the elderly. The school of nursing has five staff, 15 faculty and 275 students.
In Good Health spoke to Dowling-Castronovo about her aims for the school of nursing, its challenges and the way she intends to overcome them.
Q: You were considering going to other educational institutions when you decided to apply to become the dean of the school of nursing. What led you to uproot from your home in the New York metropolitan area and come to Roberts?
A: It was the faith-based nature that really drew me. I was very impressed about Roberts’ commitment to a Christ-centered mission, and specifically to prepare thoughtful, spiritually mature, service-oriented people who will help transform society.
Q: How did your own faith affect your decision?
A. I identify as a catholic, a practicing catholic. Having an opportunity to kind of come back home, if you will, to be able to practice my beloved profession through the Christ-centered lens, the timing’s right. And yes, there was a calling indeed, in addition to me clicking around looking at a job.
Q: Can you point out one unique feature of Roberts’ nursing program that you found attractive?
A: The direct-admit option for nurses is appealing to me because we’re getting people from high school. I think that affords a university with their mission and values to inspire those young nursing students. Also, I think the instructional focus is a little bit better.
Q: Were there other features that drew you to the school of nursing?
A: Faculty support for faculty development and also our staff support. I think there is a great effort here at Roberts, where we have staff that adds support to students and faculty. They are an essential piece to the organizational flow for students as they navigate the different aspects of university life.
Q: What challenges does the school of nursing face these days?
supportive role, because simulation requires various layers in order to operate caregiving scenarios across the patient lifespan.
Q: Can you give us examples of the external changes?
A: We rely heavily on our health care partners to be able to place our students. We go to hospital systems; we go to nursing home facilities. When you have built relationships with people and you have transitions, you then forge and build new relationships. It’s a challenge, but I like to flip it and say it’s also an opportunity.
Q: How do you plan to help the school of nursing overcome such challenges?
A: Internally and externally making collaborations, all while focusing on the mission and the pillars that are part of our Vision 2030 [Strategic] Plan at the university. That collaboration is key. I work with the faculty and the staff within the School of Nursing to focus on the university-wide strategic plan.
Q: How might you increase the school of nursing’s level of collaboration with other local institutions?
A: You can’t do it without engaging who your community or stakeholders are. I have already gone to an area meeting known as RASON, Rochester Area Schools of Nursing. They have these regular meetings where they have all their nursing leaders come from the various schools to learn what are the issues that we’re all sharing together and how do we collaborate to be able to meet the needs of all of our individual institutions and agencies. One of the things I heard at that meeting, [and] what I’ve been seeing and hearing throughout my practice and scholarship area, is that there’s a need for nursing to get back to the basics.
Q: What do you mean by “get back to the basics?”
A: In a technology-driven world, it’s becoming increasingly challenging for health care professionals to make sure that we’re addressing the fundamental needs of people. As an educator and as a nurse leader, I want to make sure that I develop a very clear vision that faculty, staff and students…are poised here at Roberts to contribute to a growing body of knowledge about how we improve, how we teach those fundamental care basics.
Q: What are some simple examples of basic care?
to train students to care for patients, take leadership positions in the field of nursing and teach others how to give care and function as leaders. Students can also obtain the Master of Science degree needed to become a family nurse practitioner.
Dowling-Castronovo has spent more than 35 years caring for patients, teaching others how to care for them and administrating nursing education programs. She came to Roberts Wesleyan from the Marjorie K. Unterberg School of Nursing
A: There are transitions happening within the university and then there’s transitions happening outside. Within the university, people just changing jobs and new people coming in and such. Some are retirements. I think the fact that all of this is happening in the context of a very dehumanized world challenges what we do here in the school of nursing.
Q: Can you give us some examples of those internal changes?
A: At this point in time, we have one faculty position that’s being posted today. We typically have openings for adjunct faculty and those are looking like we’re getting good applicants. And, we currently have a position open for a simulation technician. We have a very impressive simulation center with its own director. That position for a tech is a
A: Toileting a patient, making sure they have oral care, making sure their nutritional needs are met.
Q: As the population ages, the need to care for the elderly is growing more acute. Will you make use of your background in gerontology when shaping instruction at the school of nursing?
A: It can naturally happen just because of the skill set that I bring. Rather than reading about some of the work that I do, [students are] realizing “Oh my gosh, she’s here.” That’s been a wonderful kind of “lightbulb” moment when somebody found one of my pieces of work and they came down holding it in their hand. It naturally stimulates discussion, and then allows me to connect them to other nurse leaders in the care of older adults.
As the dust settles on the finalization of the New York state budget, it has become abundantly clear that Gov. Hochul does not prioritize older adults. The recently approved Medicaid budget falls woefully short of aiding our most frail and vulnerable.
While I applaud the efforts of our local members of the Legislature who championed the fight for adequate funding for older adults, the governor’s failure to prioritize nursing home residents and long-term care is shameful.
Inadequate Medicaid rates make it impossible for nursing homes to recruit and retain staff, keep beds open and invest in the quality of life and care that residents deserve. New York’s neglect has created a health care crisis that’s on fire and poses serious threats to everyone who needs access to care.
In addition, the budget serves as a reflection of NYS priorities. Gov. Hochul’s budget has made it obvious that the state’s fast-growing population of older adults is not a priority.
Despite a nominal Medicaid increase approved this year, the inadequacy of the overall Medicaid rate is devastating—especially when coupled with additional significant rate cuts to nursing homes within this budget.
1. The NYS budget has enacted a 10% cut to nursing home capital rates. These capital dollars are reinvested in facilities to cover care-related infrastructure expenses, such as new buildings, new beds, HVAC systems, etc. These capital expenses are either preauthorized or required by New York with the understanding and agreement that the state will reimburse facilities in their capital rates. With this retrospective 10%
capital cut, investments have already been made and purchases completed, effectively breaking the agreement. To illustrate, imagine buying a home seven years ago with a fixed mortgage from your bank at a 3% interest rate, only to receive a letter today informing you that your bank decided to raise your fixed mortgage interest rate to 7%.
2. During the intense pandemic years of 2020-23, numerous regulations were waived or adjusted to accommodate the challenges brought about by the crisis. However, nursing homes in New York faced a unique predicament. The state began enforcing a decades-old regulation stipulating that if a nursing home's occupancy dropped below 90%, the facility would be "imputed" up to that 90% threshold. Essentially, this means that even if the occupancy falls below the mandated level, the facility is penalized. Consequently, nursing homes are now facing thousands of dollars in financial penalties in the form of rate cuts, as the state has not extended a waiver for this regulation. This regulatory enforcement exacerbates the financial strain on nursing homes, which already struggled with low occupancy rates during the

Annual mean wage for a genetic counselor in New York is $93,050
By Deborah Jeanne SergeantMany people think of genetic counseling as only discussing prenatal tests with parents. However, there’s much more to the career than that. Mysti Geiger, genetic counselor with the Hereditary Cancer Screening program at URMC, helps patients understand their test results relating to cancer.
“It’s a very rewarding career,” Geiger said. “Everyone I talk with about this says it’s very rewarding career and I’ve yet to come across someone who’s a genetic counselor who doesn’t love it.”
Geiger earned her bachelor’s
degree at North Carolina State University and her master’s in genetic counseling at Long Island University.
Geiger said that while taking a genetics course in college, she heard a guest speaker discuss her career as a genetic counselor. Among all the healthcare careers she checked out, nothing stood out to her as much as genetic counseling.
The career relies on both soft and technical skills.
“Most of our coursework is in psycho-social, empathetic in how to be a good counselor and the other coursework is learning about genetic
pandemic due to various factors, including staffing and infection control mandates.
I want to thank all the residents, families, staff and legislators who advocated tirelessly for adequate funding for long-term care. Unfortunately, we hit a stone wall with the governor and her staff.
Now more nursing homes will close, families will travel farther to visit loved ones and our health care system will continue to burn.
New York is shortchanging its most vulnerable residents.


disorders and all these very scientific things,” Geiger said. “That’s one of the things I loved about it: the mix.”
Most of the time, she has good news to relate to patients, that their tests are negative. But sometimes, it’s not good news; it’s the worst day of the patient’s life. For these cases, the genetic counselor’s sense of empathy and caring nature make a big difference.
Geiger sees about 16 patients a week. When not in clinic, she’s writing notes or contacting patients about their results.
“We want to catch cancer early in those who are high risk of certain cancer types,” Geiger said. “I love that we can be preventive. Unfortunately, it’s too common that people who are at high risk don’t get checked.”
The demand for genetic counselors is huge. Geiger is booked through September and she knows genetic counselors who are booked a year or two in advance (although that’s not the case with prenatal genetic counselors).
Genetic counselors need to maintain 12.5 continuing education units every five years to maintain
their credential. These credits may be obtained in person and online. The credential is valid nationwide.
“Don’t give up if you want to do it,” Geiger said. “I know a number of people who didn’t get into school the first time around but did the second or third time. Anyone who puts their mind to it can do it. The average number in the school is eight and the number of applicants is in the hundreds. It’s definitely very competitive, comparable to physician assistant school and medical school as there are not enough slots. Each student who comes in has to have rotation. You need more genetic counselors to do rotations.”
Geiger feels grateful that she was able to get into her dream career.
“Being able to help patients when they need it is one of the biggest rewards and struggles,” Geiger said.
According to the Bureau of Labor Statistics, the annual mean wage for a genetic counselor in New York is $93,050. Local information was not available.
Editor’s Note: We recently featured Gwenn’s travel adventures in the MayJune issue of “55Plus” — www.roc55. com. Her article included tips for solo travel, which we also wanted to share with readers of “In Good Health.”
“Oh, I could never do that!”
exclaimed an old friend of mine
I bumped into recently. She was reacting to my enthusiastic account of traveling by myself to Paris this past September.
And, she was right of course — she will never experience the fun and fulfillment of traveling solo, as long as she holds onto that attitude.
Traveling alone, just like living alone, requires the right frame of mind for it to be successful and enjoyable.
But why travel solo in the first place, you might ask.
Why go to Paris alone?
Why not grab a friend or two and make it a shared experience?
And to that I answer, because the potential for self-discovery and savoir-faire that comes with solo travel is absolutely priceless.
While I’m not suggesting an exclusive diet of solo travel, I am encouraging those who live alone (and even those who don’t) to consider this occasional mode of travel for two really good reasons: you’ll gain confidence and you’ll gain wisdom from your experiences.
For me, solo travel is a journey of growth and empowerment, much
like the adventures depicted in “Eat, Pray, Love.”
Below are 10 tips to make your solo experience safe, enjoyable, and memorable:
1. Adopt the right attitude: It starts here. You can do this, even if a spouse or partner took care of travel plans in the past. Solo travel can evoke powerful insights about yourself and your life.
Many discover that they are more capable, wiser, and self-reliant than they thought.
2. Start small and close to home: Ease into solo travel by taking short overnight or weekend trips to nearby destinations to build your confidence.
3. Follow your heart when choosing a destination: Let love be your guide. Do you love the beach? Cities? Food and wine? Outdoor adventures? Select a destination that aligns with your interests and desires.
And ask yourself: What do I want to get out of my trip? Relaxation, physical activity, cultural immersion, personal growth? Design your trip accordingly.
4. Plan, plan, and plan (and budget!): I started planning for my Paris trip two years prior to take-off. I opened a Paris savings account into which I weekly (and automatically) transferred money from my checking account.
Then, the research began — the fun part! I scoured the internet, purchased travel guides, talked with
friends, and delved into everything Parisian. Voila! My itinerary took shape and I booked my flight.
5. Carefully select accommodations: While rentals can offer a more local experience, I recommend hotels for solo travelers.
Take a close look at hotels with onsite cafés or courtyards where you can connect with other travelers. I’ve met wonderful people that way and picked up excellent tips for what to see and do.
Hotels also provide added security, convenience and helpful services for solo travelers. I always let the front-desk staff know I’m traveling alone and welcome their recommendations for dining, excursions, and transportation.
6. Keep safety a priority. Just as I do at home, I steer clear of unsafe areas, trust my instincts, and walk with confidence. In Paris, I dress to blend it and avoid looking like a tourist.
I know I’m doing something right, when other travelers mistake me for a local Parisian and ask for directions. There are safety tips galore on the web. Check ‘em out!
7. Stay connected: Sharing your experiences by phone or social media with friends and family can enhance your solo adventure.
It allows you to capture special moments and share your excitement. It also adds a layer of safety and peace of mind when others know of your whereabouts.
8. Pack light and smart: I learned this lesson early on. Waiting at a baggage carousel or hauling a heavy bag through crowded streets was not how I wanted to spend my time in Paris.
I bring a very small carry-on roller bag and a day tote for when I’m out and about. Rick Steves is my trusted travel guru. Find his packing tips on Ricksteves.com
9. Explore and immerse yourself: Embrace the freedom of solo travel by trying new things. Immerse
yourself in the local culture, try new foods, and engage with locals. Join guided tours and activities to meet like-minded travelers.
I’ll never forget the midnight “rain or shine” bike tour I booked in Paris. As soon as the group assembled, the skies opened up. Disposable rain ponchos were quickly distributed and off we went in the pouring rain.
It’s one of my fondest and wettest memories!
10. And finally, importantly . . . pace yourself. Trying to see and do too much can be exhausting and unfulfilling. A more relaxed itinerary – focused on what matters most to you – enables you to appreciate your chosen activities and sites more deeply.
It will also leave room for spontaneity and personal reflection on your solo journey. This way, you’ll be able to savor each moment, create meaningful memories, and return home feeling refreshed and inspired.
Are you on board? Ready to take off?
Whether it’s a one-day, a weekend or weeklong adventure, I encourage you to go it alone and embrace the joie de vivre that traveling solo can inspire.

Gwenn Voelckers is the author of “Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own.” She welcomes your thoughts on this column as well as topic suggestion for future essays at gvoelckers@rochester. rr.com.
Acheap cavity-fighting liquid typically used to treat sensitive teeth appears to work as well as dental sealants in preventing tooth decay, a new study finds.
A single treatment of either silver diamine fluoride (SDF) or a typical dental sealant prevented 80% of cavities for four years among thousands of New York City elementary schoolchildren, researchers report March 4 in the journal JAMA Pediatrics.
The treatments also kept 50% of existing cavities from worsening during the same period of time.
The study “reaffirms that both sealants and SDF are effective against cavities,” said lead researcher Ryan Richard Ruff, an assistant professor of epidemiology and health promo-
tion at the NYU School of Dentistry.
SDF's advantage is that it can be applied by school nurses as well as dental hygienists, potentially expanding the number of kids who could receive such protective care while in class, Ruff said.
“Nurses may be an untapped resource for addressing oral health inequities,” Ruff added in a university news release. “Our results suggest that nurses can effectively provide this preventive care, which could dramatically improve access, given the role of school nurses and the size of the nursing workforce.”
The U.S. Centers for Disease Control and Prevention promotes and funds school-based sealant programs, in which dental professionals

visit kids at elementary schools to apply a thin, protective coating that hardens teeth and protects them against decay, researchers said in background notes.
The CDC estimates that each tooth sealed saves more than $11 in dental treatment costs. Applying sealants at school to the nearly 7 million low-income children who lack such dental care could prevent more than 3 million cavities and save up to $300 million in dental costs.
Unfortunately, these programs can only succeed in preventing cavities if there are enough health professionals available to apply the cavity-fighting substances.
For the study, 4,100 New York City kids received either SDF or a sealant at their elementary school twice a year. More than a quarter of
the kids had untreated cavities at the start of the study.
Sealants were applied by dental hygienists, while SDF was applied by either a dental hygienist or a registered nurse. All operated under the supervision of a dentist.
“Most research shows that SDF can stop a cavity from progressing further. Our study demonstrated that SDF can prevent cavities from happening in the first place,” said researcher Tamarinda Barry Godín, a research scientist at NYU College of Dentistry.
What's more, kids who had SDF applied by either a dental hygienist or a registered nurse did just as well, suggesting that school nurses could play a crucial role in cavity prevention programs.

The benefits of physical fitness for kids spill over into their mental health, new research shows.
Getting plenty of exercise may guard against depressive symptoms, anxiety and attention-deficit hyperactivity disorder (ADHD), a new study
published April 29 in the journal JAMA Pediatrics found.
And the more exercise, the better: Higher performance in cardiovascular activities, strength and muscular endurance were each associated with even greater protection against mental health issues.
The cost to American families of caring for a child with a mental health condition rose by almost a third between 2017 and 2021, a new report finds, to an average $4,361 per year.
Overall, American families spent an estimated $31 billion in 2021 on child mental health services, which now make up nearly half (about 47%) of all child medical spending, the report found.
The findings “underscore the large financial burden associated with pediatric mental health conditions on the U.S. health care system,” said a team led by Theoren Loo. He works for Brightline, a California company focused on virtual mental health care for kids.
The findings were published March 11 in the peer-reviewed journal JAMA Network Open.
As the study authors noted, “the prevalence of pediatric mental health conditions and the demand for behavioral health services is growing in the U.S.”
In 2021, U.S. Surgeon General Dr. Vivek Murthy issued a report outlining “alarming increases in the prevalence of certain mental health challenges” among kids.
In the study, Loo's group tracked 2017-2021 federal data on medical spending from a representative sampling of American households.
They found that diagnoses for mental health conditions in kids
The findings arrive as America continues to grapple with a surge in mental health diagnoses among children and adolescents.
The new study, conducted by researchers in Taiwan, compared data from the Taiwan National Student Fitness Tests and the National Insurance Research Database, which records medical claims, diagnoses, prescriptions and other medical information. The researchers used the anonymous data to compare students' physical fitness against their mental health.
The risk of mental health disorder was weighted against cardio fitness, as measured by a student's time in an 800-meter run; muscle endurance, indicated by the number of sit-ups performed; and muscle power, measured by the standing broad jump.
What did they discover? Higher performance in each activity was linked with a lower risk of a mental health disorder. For instance, a 30-second decrease in the 800-meter time was associated with a lower risk of anxiety, depression and ADHD in girls. In boys, it was associated with lower anxiety and a lower risk of ADHD.
Meanwhile, an increase of five sit-ups per minute was associat-
ed with lower anxiety and risk of ADHD in boys, and it was linked to a decreased risk of depression and anxiety in girls.
“These findings suggest the potential of cardiorespiratory and muscular fitness as protective factors in mitigating the onset of mental health disorders among children and adolescents,” the researchers wrote in the study.
U.S. Surgeon General Vivek Murthy has called mental health a national crisis and has focused heavily on adolescent mental health. In 2021, he issued a rare public advisory on the topic. Statistics at the time revealed alarming trends: From 2001 to 2019, the suicide rate for Americans aged 10 to 19 rose 40%, while emergency visits related to self-harm rose 88%.
Experts suggest that heavy screen use has replaced sleep, exercise and in-person activity, all of which are considered key to healthy development.
“The [new] finding underscores the need for further research into targeted physical fitness programs,” the researchers concluded. Meanwhile, exercise programs “hold significant potential as primary preventive interventions against mental disorders in children and adolescents,” they wrote.
aged 5 to 17 rose by almost 22% over those five years.
By 2021, about one in every four (25.9%) American children was diagnosed with a mental health issuethat's over 9 million children in total, the researchers estimated.
Household spending on child mental health services also rose by about 31%, to an average of $4,361 per year, Loo's group reported.
A rise in spending on the mental health of a child was also linked to a concurrent $2,337 average rise in medical expenses for other family members, the researchers noted. That makes sense, they said, since “poor mental health among caregivers is associated with child mental health disorders.”
“Overall, pediatric mental health conditions were associated with $31 billion in child spending” by 2021, the team concluded, and $59 billion in overall household medical spending.
As to what types of mental health services are being provided, Loo's team said that money spent on psychiatric drugs and doctor's office visits may be warranted “if the care is high quality and evidence-based.”
However, in many cases kids aren't being treated until they receive expensive care in hospital emergency departments. That points to “the need for improved care” for children before crises arise, Loo's team said.

U.S. births declined in 2023, marking end to post-pandemic rise
The short post-pandemic uptick in U.S. births may be over, with 2023 numbers showing a decline in births.
According to provisional data from the U.S. Centers for Disease Control and Prevention, just under 3.6 million babies were born in America in 2023, about 76,000 fewer than the year before.
It's also the lowest number of births recorded in the United States since 1979.
Demographers weren't surprised, since the U.S. birth rate had been falling for more than a decade before the pandemic.
Births did chart a slight rise in the two years after the pandemic (2021 and 2022), perhaps because some couples had put off pregnancies until the crisis eased.
However, the 2023 numbers "seem to indicate that bump is over and we're back to the trends we were in before,” Nicholas Mark told
the Associated Press. He's a University of Wisconsin researcher focused on social factors influencing health and fertility.
For American women generally, the decision to have a child seems to have shifted to later in the lifespan, as more women focus on education and careers prior to childrearing.
Birth rates have steadily fallen for women in their teens and 20s, but have risen among women in their 30s and 40s over time, the statistics show.
However, in 2023 birth rates fell across the board — they declined among women younger than 40 and were largely unchanged for women in their 40s, the CDC stats showed.
Declines in births were also observed across all races and ethnicities.
The new data was published online April 25 as a National Vital Statistics Services Rapid Release.
Have you wondered if a sleep lab could benefit your slumber?
Jazeela Fayyaz, doctor of osteopathic medicine, specializing in pulmonary and sleep medicine at Rochester Regional Health, offered an inside glimpse of what happens inside the walls of a sleep lab and how patients can benefit.
First comes a referral from a
physician. Discussing symptoms like daytime sleepiness, or suspected sleep apnea or restless leg syndrome can help the primary care provider determine if a referral is in order.
“If we’re concerned about sleep apnea, we’ll set up a sleep study where they’d go to the lab,” Fayyaz said. “These studies can be set up at home sometimes.”
Patients undergoing a sleep
study in the lab stay there overnight in a room set up like a hotel room to encourage good rest. They wear electrodes and leads head to toe so that the provider can take readings to study later.
“Most people fall asleep pretty easily,” Fayyaz said. “We have a first night effect where some might find it difficult to fall asleep away from home, but most people get a couple hours’ sleep. We also have patients who say it’s nice to get away because they sleep better away from home.”
In a couple of weeks, the results are compiled and the provider can meet with the patient to go over the results and as needed, pursue treatment. They may receive a CPAP machine to help with breathing if sleep apnea is diagnosed. The CPAP machine works by pushing air into the back of the throat via a breathing mask.
CPAP is 90% successful for improving sleep in people to whom it is prescribed.
“Sometimes, they have other treatment options like dental devices that adjust the jaw or tongue while sleeping or if it’s mild, we don’t treat pts as no other therapy is needed,” Fayyaz said. “It may be hypoglossal nerve stimulation, which involves a few more tests.”
This therapy is for patients who struggle with CPAP. A newer treatment, hypoglossal nerve stimulation involves implanting a device under the skin on the right side of the upper chest to stimulate a nerve to push the tongue forward while sleeping. That prevents sleep apnea.
Providers may also recommend losing weight, exercising and better sleep positions. Sleeping on the back promotes sleep apnea, but pillows can help encourage side sleeping. Fayyaz also said that elevating the head of the bed helps with apnea.
With any patients struggling with sleep, sleep hygiene can improve the quality and quantity of rest.
People should have a bedroom that is dark, cool and comfortable and wear comfortable night clothing. The bedroom should free of stressors like clutter, bills and unfolded laundry. This area should be used only for sleep and intimacy. Fayyaz also recommends limiting caffeine and electronics before bedtime, as both are stimulants.
“Maintain a regular bedtime and wake time,” Fayyaz said. Exercising earlier in the day can and limiting napping can also promote better sleep.
Ambien, Lunesta, Sonata: Millions of bleary-eyed Americans turn to this class of so-called "Z-drugs" to get restful sleep.
But how do these drugs work, and do they come with risks?
Experts at the U.S. Food and Drug Administration have issued an advisory to boost awareness about the meds.
All of these medications — generically known as zolpidem (Ambien, Ambien CR, Edluar and Zolpimist), eszopiclone (Lunesta) and zaleplon (Sonata) — work by putting the brakes on brain activity, allowing you to drift off to sleep.
But the FDA warns that Z drugs also come with risks, most notably upping your odds for "complex sleep behaviors" — things like sleepwalking, sleep driving, sleep cooking or even taking other medicines.
"The FDA has received reports of people taking these insomnia medicines and accidentally overdosing, falling, being burned, shooting themselves and wandering outside in extremely cold weather, among other incidents," the agency noted.
You might not even recall any of these behaviors occurring once you reawaken, according to the FDA.
The onset of complex sleep
While more than half of Americans say they would feel better with more sleep, only 42% say they are getting as much shut-eye as they need, a new poll finds.
"This is nearly a reversal of the figures last measured in 2013, when 56% of Americans got the sleep they needed and 43% did not," the poll authors wrote.
Women under the age of 50 are particularly tired, the Gallup poll released in April showed. The latest tally finds only 36% of women say they get enough sleep, compared to 48% of men.
Exactly how much sleep are folks getting?
Only 26% said they got eight or more hours, while just over half (53%) reported getting six to seven hours. Twenty percent said they got five hours or less, a jump from the 14% who reported getting the least amount of sleep during the 2013 poll.
The poll doesn't delve into why
so many Americans are coming up short on sleep.
But what's notable, according to Gallup senior researcher Sarah Fioroni, is the shift toward more Americans thinking they would benefit from more sleep and also the jump in the number of those saying they get five hours of sleep or less a night.
“That five hours or less category ... was almost not really heard of in 1942,” Fioroni told the Associated Press. “There's almost nobody that said they slept five hours or less.”
In recent years, there also has been “this pervasive belief about how sleep was unnecessary — that it was this period of inactivity where little to nothing was actually happening and that took up time that could have been better used,” Joseph Dzierzewski, vice president for research and scientific affairs at the National Sleep Foundation, told the AP.
It's only relatively recently that the importance of sleep to physical, mental and emotional health has
behaviors tied to Z drug use is also unpredictable. For some, the behavior can begin after the first dose, while for others it might begin much later into use.
Many sleep medicines can also cause daytime drowsiness, so avoid driving and other hazardous tasks under those circumstances.
Some other tips for safe use of Z drugs:
Always discuss the risks and benefits of these medicines with your doctor, and read the Patient Medication Guide before you start taking the drug
Always take the medicine at the recommended dose, and don't use a Z drug in combination with other sleep medications (including OTC meds)
If you discover that you've been engaging in any complex sleep behavior, stop taking the drug immediately and contact your doctor Don't drink alcohol while using a Z drug because this will make side effects more likely

taken hold, he noted.
So why are Americans staying awake too long? One likely reason is cultural, as millions in this country place a premium on industriousness and productivity, experts said.
“It has been a core part of American culture for centuries,” Claude Fischer, a professor of sociology at the graduate school of the University of California Berkeley, told the AP. “You could make the argument that it ... in the secularized form over the centuries becomes just a general principle that the morally correct person is somebody who doesn't waste their time.”
In her research in rural American communities over the years,
Washington State sociology professor Jennifer Sherman says a common theme among people she interviewed was the importance of having a solid work ethic.
A key component of American cultural mythology is the idea of being “individually responsible for creating our own destinies,” she told the AP. “And that does suggest that if you're wasting too much of your time ... that you are responsible for your own failure.”
While the poll shows a broad shift in sleep patterns over the past decade, living through the pandemic seems to have also significantly shifted people's sleep patterns, the National Sleep Foundation says.
Agood night's sleep can make you feel years younger, while crummy sleep leaves you doddering around like an oldster, a new study shows.
Sleeping well enough to feel extremely sharp when you wake is associated with feeling four years younger than one's actual age, researchers found.
On the other hand, extreme sleepiness makes a person feel six years older than they really are, results show.
“This means that going from feeling alert to sleepy added a striking 10 years to how old one felt,” said researcher Leonie Balter, with Stockholm University's Department of Psychology.
For this study, researchers first surveyed 429 people aged 18 to 70 about how old they felt, how much sleep they get and how sleepy they felt.
The survey results showed that for each night a person had insufficient sleep, they felt about three months older than they actually were, on average.
Based on this, the researchers designed an experiment to test whether good sleep could make someone feel young and vibrant.
Previous research has shown that feeling younger than one's actual age is associated with living a longer and healthier life, and there's even evidence that people who feel young have younger brains, researchers said.
“Given that sleep is essential for brain function and overall well-being, we decided to test whether sleep holds any secrets to preserving a youthful sense of age,” Balter said.
The experiment involved 186 people aged 18 to 46. Participants were asked to restrict their sleep to just four hours in bed for two nights, and at another time asked to sleep nine hours in bed for two nights.
After a couple four-hour nights, participants felt 4.4 years older, on average, than they did when they got sufficient sleep, researchers report.
The new study was published March 27 in the journal Proceedings of the Royal Society B Biological Sciences.
“Safeguarding our sleep is crucial for maintaining a youthful feeling,” Balter concluded. “This, in turn, may promote a more active lifestyle and encourage behaviors that promote health, as both feeling young and alert are important for our motivation to be active.”









Now that peak hot dog season is in full swing—with Americans consuming 7 billion hot dogs from Memorial Day to Labor Day—it’s the perfect time to think outside the hot dog bun and give plant-based hot dogs a try.
Let’s start with the good.
Most vegetarian hot dogs are an excellent source of quality protein, ranging anywhere from 6 to 20 grams. An essential nutrient with benefits above and beyond building muscles and bones and repairing tissues, protein helps with weight loss and maintenance by suppressing hunger signals, boosting metabolism and taking longer to digest. What’s more, protein’s essential role in collagen production promotes healthy skin, stronger bones and joint integrity. A final shout-out: Most plantbased hot dogs have no cholesterol, while others boast some fiber and iron.
Now, the (semi) bad.
Unfortunately, many, but not all, plant-based hot dogs are just as processed as other heavily processed foods. Translation? They may contain ingredients that could be harmful if consumed in excess, such as saturated fats, added salt and sugar and unrecognizable additives. Research indicates that eating highly processed foods can lead to weight gain and an increase in the risk of cancer, heart disease, diabetes and overall mortality. However, in contrast to some ultra-processed foods, like sodas and cookies, that are calorie-rich and nu-
trient-poor, veggie dogs balance the processing with several nutritional benefits, including fewer calories.
Finally, the beautiful.
When it comes to protein sources, the environmental benefits are clear. Pound for pound, meat has a much higher water footprint than vegetables, grains, beans or legumes. For example, 4 ounces of hamburger takes 600 gallons of water to produce while 4 ounces of tofu takes only 60 gallons. In addition, researchers estimate that 15% of global greenhouse gas emissions come from raising meat. Producing approximately 1 pound of protein from beef, for example, sends the same carbon emissions into the atmosphere as driving 30 miles, whereas making the same amount of tofu amounts to less than a mile. Worried about global warming? Adopt a more plant-based diet!

Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
People who eat large amounts of ultra-processed foods have a slightly higher risk of premature death than those who mostly shun the industrially produced eats, a new 30-year study says.
Those who ate the most ultra-processed foods — an average of seven servings a day — had a 4% higher risk of death overall, and a 9% higher risk of death from causes other than cancer or heart disease.
These higher risks of death “were mainly driven by meat, poultry, seafood-based ready-to-eat products, sugar and artificially sweetened beverages, dairy based desserts, and ultra-processed breakfast foods,” wrote the team led by senior researcher Mingyang Song, an associate professor of epidemiology and nutrition at

1 tablespoon cumin 2 teaspoons paprika 1 teaspoon allspice 1 teaspoon cinnamon
1. In a large saucepan or soup pot, sauté onions in cooking oil over medium heat till golden. Add tofu crumbles, stir in 3 tablespoons water, cover, and cook for 5 minutes over medium-low heat. Break up any large tofu crumbles, then stir in remaining ingredients, including water, and simmer, covered, for 2 hours.
For this study, researchers tracked the long-term health of nearly 75,000 female registered nurses and nearly 40,000 male health professionals.
Ultra-processed foods are made mostly from substances extracted from whole foods, like saturated fats, starches and added sugars. They also contain a wide variety of additives to make them more tasty, attractive and shelf-stable, including colors, emulsifiers, flavors and stabilizers.
Examples include packaged baked goods, sugary cereals, readyto-eat or ready-to-heat products, and deli cold cuts, researchers said.
Mounting evidence has linked these foods to higher risks of obesity, heart disease, diabetes and bowel cancer, researchers said. However, few long-term studies have examined these products' links to a person's overall risk of death.
Read labels carefully. Calories, sodium, fat (especially saturated fat), protein, fiber and ingredients vary widely among plant-based hot dogs. So it pays to know what you are consuming. I chose Lightlife hot dogs because they had no saturated fat, less sodium than most, and a decent amount of protein.
3 tablespoons tomato paste 1 tablespoon Worcestershire sauce Plant-based hot dogs
2. Let cool for 10 minutes, then puree with a hand or traditional blender to desired consistency. Adjust seasonings; add more water if sauce seems too thick or simmer uncovered if sauce seems too thin. Serve with plant-based hot dog of choice. Note: Sauce thickens with refrigeration, so add water as needed.

Both groups took part in separate health studies that ran from the mid-1980s to 2018. Every two years, participants provided information on their health and lifestyle habits, and every four years they completed a detailed food questionnaire.
During an average 34-year follow-up period, researchers identified more than 48,000 deaths.
Although increased consumption of ultra-processed foods was linked to a higher risk of death, researchers noted that the association became less pronounced after they took a person's overall dietary quality into account.
The study found that dietary
quality had a greater influence on risk of early death than did consumption of ultra-processed foods. That could mean that eating lots of healthy whole foods might offset the detrimental effects of ultra-processed chow, researchers said.
“The findings provide support for limiting consumption of certain types of ultra-processed food for long term health,” the team concluded, adding that “future studies are warranted to improve the classification of ultra-processed foods and confirm our findings in other populations.”
In an editorial accompanying the study, experts pointed out that recommendations to avoid ultra-processed foods might give the idea that certain whole but unhealthy foods like red meat are fine to eat often.

Integrative health modalities work alongside of medical care to help patients mitigate the effects of pain.
Heather Sovocool, a Reiki practitioner at Rose Fire Energy Healing in Rochester, uses this modality to ignite the parasympathetic nervous
system to help reduce stress, help with grounding and emotional balance and to support any treatment patients receive.
“It’s an excellent form of preventive help and it can be integrated into your current plan,” she said.
A form of energy work, Reiki involves the practitioner’s hands lightly touching or hovering over the client’s body.



•
•
•
•
•


2.
“These keep our immune system very strong,” said Arunie Malwatta, a physician at Unity Health who also holds a master of science in human nutrition and a master of science in lifestyle medicine.
Although many herbal preparations and natural products are designated to address certain issues, many people also take them preventively, as they help reduce inflammation, which has been associated with many diseases.
Malwatta also said that engaging the parasympathetic nervous system through deep breathing can help combat anxiety.
“The other thing with deep breathing is that your lung capacity and residual capacity of the lung is really getting reduced when you get a big volume of air,” Malwatta added. “You make sure that your oxygenation of your lung is better. It’s good for muscle activity in the lung and oxygen exchange.”
Massage therapy, chiropractic care, osteopathic manipulation and other “hands-on” modalities can


help people reduce pain and reclaim function.
“I expect more doctors to prescribe it like a prescription,” Malwatta said. “It has come a long way in gaining their acceptance as it has helped so many people with back pain and joint issues.
“Mindfulness grounds us in the moment through breath awareness,” said Natasha Sodhi, lifestyle medicine physician at Rochester Regional Hospital. “We always have our breath to turn to and even a few deep breaths can bring clarity to the mind and body.”
Mindfulness helps people bring their attention to the present moment to be aware of sensations in their surroundings, pay attention to their breath and tune in to their senses. This helps mitigate stress and bring a sense of well-being.
“There’s been an increase in this over time. For certain indications this modality can help with pain alongside conventional care,” said physician Alissa Huston, at Pluta Integrative Oncology & Wellness Center. “We’re seeing greater evidence that acupuncture is supported for chronic back pain. It’s covered by certain payors and it’s a recognized oncology modality.”
“There’s a whole movement in culinary medicine, so you’re teaching how and why those foods are important,” Huston said. “People are learning how to prepare foods and why that impacts health.
“We have to teach basic skills in making dietary changes. It’s always good to make sure you talk with your own physician so they’re aware and can weigh in and guide or connect you with someone else, especially for exercise and nutrition support. You can have a comprehensive, integrative approach to your overall care.”

From the occasional sneeze to life-threatening reactions, allergies come in all shapes and sizes.
Allergies aren't just about pollen in the spring as the summer can cause just as much havoc on the sinuses. They can be triggered by foods, medications, insect stings and more.
Allergies occur when a person’s immune system reacts to a substance in the environment. These substances are known as allergens and can be dust mites, pets, pollen, insects, ticks, molds, foods and medications.
“Allergies are a very common problem. We have more than 80 million people in the United States that have allergic rhinitis,” said physician Emily Weis, department of allergy, immunology and rheumatology at UR Medicine.
Weis offers five pieces of information for chronic allergy sufferers.
Pollen from grasses and weeds, mold spores and air pollution
When a person comes into contact with a particular allergen, the body reacts through constant sneezing, runny nose, watery eyes, breaking out in hives, eczema and trouble breathing.
Around 31.8% of adults in the United States had a seasonal allergy, eczema or food allergy, according to the Centers for Disease and Prevention. This includes 25.7% with a seasonal allergy, 7.3% with eczema and 6.2% with a food allergy. There are multiple remedies for seasonal allergies than for any other type of allergy.
In the spring, many flower buds and trees are blooming, which affect millions of people who have seasonal allergies which can result in
sneezing, congestion, a runny nose and other bothersome symptoms. In the summer, pollen from grasses and weeds, mold spores and air pollution cause issues.
“For seasonal and perennial allergic rhinitis, symptoms can be nasal congestion, itchy and watery eyes, post nasal drips and a cough,” said Weis.
2.Rain is your friend
Having allergies doesn’t mean you have no choices. Although allergies can be a pain, you can deal with them in various ways that offer relief.
Experts suggest reducing your exposure to allergy triggers, which means staying indoors on dry and windy days. Figure out the best times to venture outside with rain being your friend because it helps clear the pollen from the air. Also try avoiding lawn mowing, weed pulling and other gardening chores that can stir up allergens. In addition, get in the habit of removing clothes worn outside and shower to rinse any pollen from your skin and hair.

tients have also taken allergy shots and Food and Drug Administration approved tablets in consultation with an allergist.”
3.Young and old: Allergies can develop at any age

Whether it’s home remedies or misinformation, experts say they hear common misconceptions. For those who believe allergies are not serious, while some instances may seem mild, others can be severe or even life-threatening. Anaphylaxis, a severe allergic reaction, can be fatal if not treated promptly. In addition, not all allergies are the same. Allergies vary widely in their symptoms, triggers and severity. Some people may have seasonal allergies to pollen, while others may be allergic to specific foods, medications or insect stings.
“I have also heard people say you are too old to develop allergies, but allergies can be developed at any age,” she added. “Another myth is people who say ‘my dog doesn’t shed so I can’t be allergic to it.’”
essential to check how much pollen exists in the air and adjust your behavior from there. If the pollen counts forecasted are high, start taking allergy medications before symptoms hit you. Closing doors and windows during the day becomes another step when pollen problems occur and especially avoid outdoor activity in the early morning when the counts are at their peak.
“Pollen is more prominent in the morning hours, so patients may feel more symptoms at that time than during the afternoon hours,” said Weis.
Several types of nonprescription medications help ease allergy symptoms. This includes oral antihistamines which aids and relieves sneezing, itching, stuffy and runny nose and watery eyes. Examples of antihistamines include Zyrtec Allergy, Allegra Allergy, Claritin and Alavert. Nasal sprays medications improve nasal symptoms such as Flonase Allergy Relief, Rhinocort Allergy and Nasacort Allergy 25 hours. Although these can help stop nasal symptoms for a short term, talk to your health provider for longer-term relief options. Experts still say that if you have chronic allergies, you should see a professional.
“I tell patients that they should avoid many outdoor allergens, especially on days when the pollen count may be high. There are plenty of over-the-counter allergy medications such as nasal sprays and non-sedating antihistamines,” said Weis. “Pa-

Allergic reactions are found in pet dander, saliva and urine, which can be carried by a pet’s hair.
4.Pollen is more prominent in the morning hours
Seasonal allergy symptoms flare up when pollen exists in the air. It’s
“As a board-certified allergist, we do skin testing and under certain circumstances blood work,” said Weiss. “If there are any questions if you are suffering from allergies, talk with your primary care physician and consider seeing a board-certified allergist.”


Historically, erectile dysfunction represents a health issue that most men older than 45 face to an extent.
But in recent years, the number of cases of ED in younger men has increased.
According to the multinational Men's Attitudes to Life Events and Sexuality (MALES) study published by the National Institutes of Health, about 8% of men aged 20-29 and 11% of men 30-39 have ED.
“The Massachusetts Male Ageing Study determined that at approximately 20 years of age, 20% of men will complain of some form of ED — but this covers mild, moderate and severe [cases]. At 30 years of age, it is 30%, and so on.”
Compared with previous cohorts, more young men are contacting a healthcare provider to treat their ED, according to several studies.
But does this mean that more have ED or that they feel more comfortable presenting with ED at their doctor’s office than the previous generation?
Physician Pebble Kranz, sexual medicine specialist with Rochester
Center for Sexual Wellness, thinks that both could be factors, but a higher comfort level is likely the primary reason for the uptick.
“I see a lot of people, a lot of young men with ED,” Kranz said. “There are a lot of factors that can contribute.”
She listed performance anxiety as a major factor, as this can raise adrenaline which can restrict blood flow to the penis.
“It is impossible to have an erection in that state,” Kranz said.
Before taking other approaches, she encourages patients to address performance anxiety and general stress first. Unfortunately, stress is commonplace among young men.
Kranz said that certain medications can also contribute to ED such as some of those affecting mood. Since 2020, there’s been an increase in use of these drugs among young adults — as high as a 63.3% jump, according to the American Academy of Pediatrics, which looked at youth aged 12-25. The young men in that cohort are trying to pay off college debt, launch a career and find affordable housing (or staying with Mom
and Dad).
“There’s extra stress compared with how it’s been in the past,” Kranz said. “I also have to wonder about cardiovascular risk factors in younger people because ED is an important marker of cardiovascular disease, particularly when it occurs in a younger person. If there’s a greater prevalence of things that are causing cardiovascular risk, that may be a contributor as well.”
She explained that the blood vessels in the penis are one to two millimeters in diameter, compared with coronary arteries, which are three to four millimeters and carotid arteries, which are five to seven millimeters. This means that ED in young men can indicate heart disease is present also. Numerous studies report that cardiovascular disease is increasing among young adults because of poor diet, unmanaged stress and lack of exercise.
Physician Ryan Sidebottom, urologist with Auburn Community Hospital, also views ED as a multifaceted issue. In addition to greater reporting and the psychological components affecting young men,
Sidebottom noted that “we’re seeing more early onset diabetes, metabolic syndrome and obesity. It can affect vascular health and hormonal health and that can affect erections.”
He said that essential to any exam involved ED is a general medical history, medication review, lab work and addressing any metabolic issues. For example, men who are diabetic need to address weight and control their blood sugar levels. Those with low testosterone may seek replacement therapy. Smoking cessation can help increase blood flow throughout the body.
For many men, using medication can help achieve better erections. Sidebottom noted that phosphodiesterase inhibitors (PDE 5) help by stimulating the nerve going to the penis to increase blood flow and with dilation of the penis.
“If this fails, there are further options for ED,” Sidebottom said. “There are injections that can go into the blood vessels to the penis. There are tablets that can be placed in the urethra that can cause dilation into the penis. And vacuum pumps. They can help draw venous blood into the penis. And surgical interventions with penile prostheses. It replaces the chambers that fill with blood with chambers attached to a pump to fill the balloons to fill with water as desired. There is a very high satisfaction rates. It’s a big step and a last step in the process. But it does work very well.”


Heart disease is the leading cause of death among men, according to the American Heart Association, and half of the time, no symptoms indicate a problem.
Fortunately, men have several strategies for reducing risk of heart disease.
It’s vital to recognize that age correlates with higher risk.
“As you reach 40, your risk jumps,” said physician Scott Feitell, director of heart failure at RGH Sands Constellation Heart Institute. “Patients as young as 20 need to recognize those risk will climb as you get older.”
Instead of reacting to a problem, he encourages patients to talk with their providers early to prevent heart trouble, especially if they have a family health history of heart attack.
Talk about family health history so you know if heart disease or other diseases run in your family.
Feitell said that in one’s 40s, it’s even more vital to talk with a primary care provider about lab work to monitor cholesterol, blood pressure and particularly for those who are obese, diabetes screening.
He also encourages patients to
check out the 10-year risk calculator on the website of the American College of Cardiology (www.acc.org).
Physician Andrew Mathias, cardiologist with URMC, reminds patients that although not all heart disease is preventable, “in any one individual there’s a lot in your control to reduce your overall risk.”
He noted that the Centers for Disease Control and Prevention states that 60% to 80% of risk is governed by factors within the patient’s control.
The top factor Mathias listed is smoking, as it raises risk of heart attack and stroke, among other effects deleterious to good health.
“Even someone smoking a few cigarettes a day increases the risk two to four times compared with someone who doesn’t smoke,” Mathias said.
He also advocates for regular exercise, a minimum of 30 minutes of moderate exercise five times a week. “Moderate exercise” could be a brisk walk. But Mathias said finding an activity you like is important to maintain consistency.
“A lot of people say they don’t have time or are too busy,” Mathias said. “You don’t have to do a two-

times daily gym session for two hours. Take 10 minutes a few times a day to do something active. That’s something people can commit to: bite-sized pieces of exercise.”
For heart health, what you eat matters a lot.
“There are a lot of data on diet and its association with heart disease,” Mathias said. “Heart disease has to do with deposition of cholesterol plaque on the artery. When a plaque ruptures, it blocks blood flow to the heart. That’s a heart attack. That heart tissue not getting oxygen will die.”
Shifting to an eating plan such as DASH or the Mediterranean diet reduces intake of saturated fat, trans fat, processed carbohydrates, high-sugar foods and red meat.
“A balanced eating pattern rich in fiber, whole plant foods and lean proteins helps to prevent heart disease through a myriad of pathways,” said April Ho, registered dietician certified personal trainer at the Center for Community Health & Prevention at URMC. “This type of eating pattern helps to decrease inflammation, lower blood pressure and reduce cholesterol and triglycerides in the blood.”
She encourages clients to think of nutrition in terms of “complete meals” instead of “healthful foods.”
A balanced meal includes equal portions of fruit, vegetables, pro-

tein and starch. A meal commonly thought of as healthful, such as a salad with chicken strips or a breakfast omelet is not nutritionally complete.
“When we combine all of the food groups together in one meal, we create a synergy in which the whole is greater than the sum of its parts,” Ho said. “Fiber that we get from whole starches, fruits and vegetables bind with the cholesterol found in animal products and prevents its absorption into the bloodstream. That means that a meal of eggs, bacon and white toast (high in cholesterol, low in fiber) will raise your cholesterol to a far greater extent than a veggie omelet paired with whole wheat toast and an apple (high in cholesterol, high in fiber).”
She encourages patients to stock up on grab-and-go foods from each food group and start reading nutritional panels for fiber and added sugar.
“The good news is that when thinking about fiber and added sugar you only need to remember one number,” Ho said. “For women that number is 25, and for men that number is 38. Women should aim for at least 25 grams fiber daily and no more than 25 grams added sugar daily. Men should aim for at least 38 grams fiber daily and no more than 38 grams added sugar daily.”
When prostate cancer strikes, one question is paramount: Is it aggressive and requiring immediate treatment or slow-growing and worthy of monitoring only?
Right now, an invasive biopsy is the only way to answer that query, but researchers say they've developed a urine test that could do the job instead.
The test, called MyProstateScore2.0 (MPS2), was developed by researchers at the University of Michigan, who reported their findings April 18 in the journal JAMA Oncology.
“If you're negative on this test,
it's almost certain that you don't have aggressive prostate cancer,” said physician Arul Chinnaiyan, a professor of pathology and urology at Michigan Medicine.
The approach to prostate cancer care has changed radically over the past few decades, noted study co-senior author, physician John Wei.
“Twenty years ago, we were looking for any kind of [prostate] cancer," said Wei, a professor of urology at the university. "Now, we realize that slow-growing cancer doesn't need to be treated. All of a sudden, the game changed. We went from having to find any cancer to finding only significant cancer."
In decades past, the prostate-specific antigen (PSA) blood test was used routinely to help spot cancers. But its inefficiency in differentiating between aggressive and slow-growing tumors led to over-treatment, and the test is now used much less frequently.
Almost 10 years ago, University of Michigan researchers developed the first generation MyProstateScore test. It tracked two genes, TMPRSS2::ERG, that fuse together to cause prostate cancer, along with another cancer marker called PCA3.
That test was good, but maybe not quite good enough, Chinnaiyan said.
“There was still an unmet need with the MyProstateScore test and other commercial tests currently available," he explained. "They were detecting prostate cancer, but in general they were not doing as good a job in detecting high-grade, or clinically significant, prostate cancer. The impetus for this new test is to address this unmet need."
In the latest-generation test, the Ann Arbor team added analyses of 54 more genes — all linked to aggressive prostate tumors - into the mix. Further testing narrowed that list of genes down to 16, which are now included into MyProstateScore2.0.
Traditionally, women tend to outlive men by an average of seven years. However, emerging data from United Nations Population Division tracking longevity worldwide from 1990 to 2020 indicate that that longevity gap is shrinking and will continue to narrow. By 2030, the average life expectancy for women will be 86.54 and for men 83.13.
One of the reasons that age gap is narrowing has to do with men’s health improving, according to Natasha Sodhi, lifestyle medicine physician at Rochester Regional Hospital.
“The disparity between men and women and lifespan partly has to do with the instance of chronic disease,” Sodhi said.
More men embracing healthy living such as eating right, eschewing tobacco products and exercising, is making a difference. For most people, this begins with patient education in the doctor’s office.
Generally speaking, women have been the family’s health champion. During their childbearing years, women become accustomed to regular doctor’s visits and are typically the parent who takes the children to pediatrician visits. This segues into healthcare can aid in keeping women on track with health. Stereotypically, men are not as proactive about pro-


connected with each other on a deeper emotional level with their friends and loved ones than the stereotypical man who relies only on himself. As men have begun to take more time to socialize and build strong relationships and connections than in the past, this factor may be helping with longevity.
In the past, women have been more concerned about maintaining a slim build through exercise and dieting than men. Although many “diets” are not healthful, the awareness of food choices and the role of the family chef has helped women understand more about how food affects health. But in more recent years, men have begun educating themselves on nutrition — and not only in athletic circles.
Sodhi said that the plant-based diet favored in Blue Zones promotes good health, along with a lifestyle of
physical activity.
“We know 80% of all chronic diseases are due to lifestyle,” Sodhi said. “When we meet with patients, we take time to hear their story and understand aspects of their lives that impact their health. There’s opportunity to prevent and even reverse disease through lifestyle. We collaborate with patients.”
Engaging in risky behavior is another area which has in the past disproportionately involved men, whether the male-dominated dangerous occupations like commercial fishing, forestry, farming and construction; engagement in hobbies like motorcycling or base jumping; performing ill-advised stunts; or substance abuse.
Safety education and equipment are helping save lives, such as rollover protection structures on tractors that keep farmers safer. More
men than women use tobacco (13.1% compared with 10.1% of women as of 2021, says the National Institute on Drug Abuse and between the two, men who smoke use more tobacco than women who smoke); however, fewer people overall use it currently. In addition, more women are engaging in dangerous occupations and activities, which statistically narrows the gender gap.
Sodhi said that discussing risky substances is one of the aspects of patient education her office covers, along with physical activity, restorative sleep, stress management and social connection.
“My experience is by explaining all of these areas and the intersection between them, a patient can identify areas in which they can make lifestyle changes and significantly impact their overall health mentally and physically,” Sodhi said. She added that the right support from friends and family along with guidance from healthcare providers can help people stay healthy.
Although COVID-19 deaths and drug overdoses in the past few years have statistically widened the gender longevity gap according to a report in JAMA Internal Medicine, it’s likely that this anomaly will not affect the gap long-term and it’s likely women will on average outlive men.
Researchers have indicated that men’s Y chromosomes in cells linked to age-related disease and death may be why they tend to die younger than women. That’s why it’s especially important for men to make the necessary lifestyle changes to support good health.

It’s not uncommon for men to marry younger women. But an age gap of 16 or so years may offer surprising benefits.
A study by German demographer Sven Drefahl indicates that a man who’s 50 and marries a woman 16 years younger is 4% less likely to die by the end of the year than those who marry a contemporary. By contrast, women who are 16 years older than their husbands are 40% more likely to die by the end of the year.
Drefahl’s study doesn’t indicate why older wives die sooner. Perhaps women who marry younger men don’t mind defying societal norms (since women typically don’t marry younger men) and also are more likely to engage in risky behavior. They may face isolation as their “unusual” age difference cuts them off from other people who judge them for their decision. The benefits afforded the older party don’t seem to apply when it’s the woman who is older.
It makes sense that a younger wife can mean for the older husband a longer life. The matter may lie in the positive changes she brings to his life. If this is a second wife, she may put some wind in his sails after the death or divorce of a previous wife. Change can be stimulating. He may become more social by meeting her young, dynamic friends—people who think differently than his contemporaries. Engaging in socialization with new people helps foster greater longevity.
A younger wife can bring fresh new ideas to someone who is becoming a little stuck in his ways. This could include trying new, healthful foods instead of sticking with unhealthful processed foods. Many younger people are well-educated about healthful eating. Kale smoothie, anyone? But this effect will only work if he’s willing to make positive
It’s not uncommon for men to marry younger women. But an age gap of 16 or so years may offer surprising benefits, according to a German study.
dietary changes.
The same holds true for physical activity. Instead of maintaining a sedentary lifestyle, many younger people like to–and are healthy and fit enough—to stay physically active. If she can get him out of the recliner and into the gym or on the walking trail, that extra movement could add years to his life. A wife his age may be less motivating when it comes to exercise as she is experiencing similar age-related aches and pains. The same holds true for intimacy. A same-age wife may lack the libido of a younger wife.
In general, younger people are more internet-savvy and likely to turn to reputable, up-to-date sources online to find sound health information. This can help the older husband to become more proactive about his health with preventive screenings (did you know that the onset of colonoscopies is now 45?).
Of course, establishing a marriage should be based upon love, trust and mutual respect. But gaining a few extra healthy years represents a nice perk. But that only holds true if the younger wife promotes good health and if her older husband adopts new, healthful habits.

 By Jim Miller
By Jim Miller

Dear Savvy Senior,
Can you recommend some good resources to help me locate some quality doctors in my area? I’m looking for an orthopedic doctor for my 77-year-old mother and a new internist for me, since my doctor retired last year.
Searching Susan
Dear Susan,
Finding and researching doctors is a lot easier than it used to be. Today, there are variety of websites you can turn to that provide databases of U.S. doctors, their professional medical histories, and ratings and reviews from past patients on a number of criteria. Here are some good sites to help you get started, along with a few additional tips that can help you find the right doctors.
To help you locate some good doctors in your area, a good first step is to get referrals from trusted friends, along with any doctors, nurses or other healthcare professionals you know.
You also need to check your insurance provider. Call your insurer for a list of approved doctors or ask whether the doctor you’re considering is in-network.

If your mother is enrolled in original Medicare, you can use the care compare tool at “Medicare.gov/ care-compare” — click on “Doctors & Clinicians.” This will let you find doctors by name, medical specialty or by geographic location that accept original Medicare. If she’s enrolled in a Medicare Advantage plan, call or visit the plan website to get a list of approved candidates.
Once you find a few doctors, you need to call their office to verify that they still accept your insurance, and if they are accepting new patients.
You should also consider hospital affiliation. Your choice of doctor can determine which hospital you go to, if needed, so find out where the doctor has admitting privileges. Then use some hospital ratings services like “Medicare.gov/care-compare” (click on “Hospitals”) to see how it
compares with other hospitals in the area.
After you find a few doctors you’re interested in, there are various websites you can consult, to help you evaluate them.
For example, the Federation of State Medical Boards offers a tool at DocInfo.org that will let you find out doctor’s board certifications, education, states with active licenses, and whether or not a physician has been disciplined by a state medical board.
The Centers for Medicare & Medicaid Services (CMS Data) is also a good source for researching doctors. For example, it will help you find out how many times a doctor did a particular procedure and what they charge for it — go to “Data. CMS.gov/tools” and click on “Medicare Physician & Other Practitioner Look-up Tool.” And to learn about the financial relationship that doctors have with drug and medical device companies, visit “OpenPaymentsData.CMS.gov.”
Some other good sites for finding and researching healthcare professionals include Healthgrades (healthgrades.com) and Vitals (vitals.com).
Both sites provide substantial doctor’s information on education and training, hospital affiliations, board certification, awards and recognitions, professional misconduct, disciplinary action, office locations and accepted insurance plans.
They also offer five-star ratings scales from past patients on issues such as communication and listening skills, wait time, time spent with the patient, office friendliness and more. But be aware that while physician rating websites can be helpful, they can also be misleading and unreliable.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.



Taking a fall is never enjoyable. But if you’re an older adult, it can cause serious health issues and even take years off your life.
T








According to the Centers for Disease Control, falls are the leading cause of injuries (fatal and non fatal) among people over 65. Falls lead to more than 800,000 hospitalizations a year. And 60% of falls occur in the home.
As we age we generally don’t have the same agility and flexibility we did when we were younger. Our bones lose strength and density (osteoporosis), making the consequences of a fall much more serious, including fractures and broken bones. Other health-related issues like vision impairment and low blood pressure (often caused by standing up too quickly) can contribute to a loss of balance, increasing the likelihood of falling.
And it’s not just the fall that causes problems. The resulting lack of mobility as a person recovers can reduce both the quality of life and the number of years of life one has left. It can lead to social isolation, depression and, potentially, the inability to continue living independently.
But falls are preventable and don’t need to be an inevitable part of aging. Here are some simple steps you can take to reduce the risk of falling.

• Keep paths clear of clutter, including electrical cords, shoes and papers.
• Get rid of throw rugs or use double-stick tape to secure them to the floor.
• Install grab bars in the bathtub and consider a shower bench. Place non-slip mats in the tub and on the bathroom floor.
• Make sure there are sturdy handrails on all stairways.
In your daily routine
• Wear sensible footwear. Shoes should fit properly and have a good tread to give you traction. Avoid slippers with no back—they’re not a good idea!
• Don’t let a fear of falling limit your activity. Walk regularly and do gentle exercises (like tai chi) that strengthen your legs and improve balance. Look online or check with your local community center about exercise classes for seniors.
• Consider a medical alert button that can be worn on the wrist or around the neck. These devices allow you to summon help immediately if you fall or suffer an injury.
• Contact the local nonprofit Lifespan, which can connect you with resources to support a healthy lifestyle.
Most importantly, tell your doctor if you’ve fallen or are experiencing dizziness or a lack of balance. He or she can assess the situation, provide appropriate treatment and refer you to a physical or occupational therapist if warranted.
By taking the proper steps you can stay healthy while staying on your feet!

• Use nightlights so you can see where you’re going after dark.


If you’re hurt, seeking care from a chiropractor or physical therapist can help you get back to doing what you want. But knowing which provider to see can make a difference in when you can find pain relief and how long it lasts.
“When someone has an injury, it comes down to how quickly can they get in,” said Erica Gurak, clinical supervisor for Rochester Regional Health Physical Therapy & Rehabilitation in Brockport.
For Rochester Regional Health, a referral from a primary care provider
is necessary. However, many physical therapists provide direct access, meaning most insurance companies will cover a limited number of visits to a physical therapist without a referral. That can expedite treatment.
In general, physical therapists tend to focus more on addressing issues long-term through requiring patients to perform at-home exercises between sessions. These movements can help strengthen the soft and connective tissues and balance complementary muscle groups to fight pain, restore movement and prevent future
injury. Some chiropractors recommend at-home work as well.
Both physical therapists and chiropractors take patient history, perform assessments and as needed, order diagnostic tests. They may refer patients to the other type of provider if that’s better suited to their problem.
Because chiropractors do not require a referral, “patients tend to go to a chiropractor if they had a previous relationship with one and they can’t get into physical therapy,” said Jake Keller, physical therapist
We may not think of loneliness as posing serious health risks, but if feelings of loneliness are not addressed, they can significantly impact our health. There are ways to help prevent loneliness and the resulting health impacts. If you’re feeling lonely, consider the following:
• Seek support: Reach out to friends, family or a therapist. Support groups can also foster a sense of community and understanding.
• Volunteer: Helping others can boost self-esteem and foster meaningful relationships.
• Take up a hobby: Engage in activities that bring you joy. Join a club or group with shared interests to meet new people and build relationships.
• Practice self-care: Maintain a healthy diet, get enough sleep, exercise regularly, and practice mindfulness and self-compassion.
• Try something new: Step outside your comfort zone. It can be intimidating but can also lead to new connections and relationships.
Listen to our episode, “The Loneliness Epidemic” on the Community Check-in to learn more about this issue and who is most at risk.

specializing in spine at University of Rochester.
When treating pain issues, chiropractic care can offer prompt relief when patients present for care soon after the injury. Although chiropractors also offer ongoing care for chronic issues, as with physical therapists, it will require more sessions to get relief.
Rae Smith, doctor of chiropractic and master of human anatomy at East Avenue Chiropractic P.C. in Rochester, said that she helps patients decide whether a chiropractic treatment or physical therapy would better benefit their condition. She makes and receives patient referrals.
“We typically co-manage with other providers, depending on what the patient needs,” Smith said. “It also varies with the provider. If they think active care is more beneficial to the patient or active care.”
She believes that chiropractic care focuses on more passive care, with stretches and movements whereas physical therapy offers patients a regimen of exercises as part of their care.
Many people believe that physical therapy and chiropractic care are only for when a patient experiences an acute or chronic pain or function issue. Smith said that’s not true.
“Daily stressors can bring on patterns that are not 100% optimal for the patient’s daily activities,” she said. “Both chiropractic and physical therapy can address those even if they don’t have outward pain. A lot of people come to us with acute care but stay for functional care longterm. If something new or different comes up, they know where to find us.”

Jewish Senior Life announced it has returned to its former name, Jewish Home, following a year-long endeavor aimed at rejuvenating its identity and making its services easier to recognize and access. Established in 1920 by four pioneering women, Jewish Home stands as a testament to a century of unwavering dedication to providing care and services to older adults from all faiths and backgrounds.
"Our return to the name Jewish Home is a tribute to our rich Jewish heritage, traditions, and values, where families unite to provide care and support,” said President and Chief Executive Officer Michael S.
King. “This rebranding presents an opportunity for us to reimagine the concept of 'home' as we forge ahead with forward-thinking programs and services designed to meet the evolving needs of the Rochester community and the people we serve today and in the future."
A new advertising campaign was launched on television, radio, print, and digital platforms. This campaign underscores the organization’s commitment to empowering older adults to live their best lives while challenging outdated perceptions of aging.
“We remain committed to cultivating a vibrant and inclusive community where every individual is welcome, valued, embraced and celebrated,” said King.
Jewish Home’s new website is www.jewishhomeroc.org and social media handles are @jewishhomeroc.
Representatives from Rochester Regional Health, University of Rochester Medical Center and the Alliance for Senior Care recently hosted legislators at the Greater Rochester Chamber of Commerce.
The purpose of the meeting was to continue the dialogue with elected officials that was established during the New York state budget process. The discussion specifically addressed furthering essential priorities including the distribution of increased rates for nursing homes, capital reimbursements and expeditious federal funding for increased clinical staffing.
“We greatly appreciate our local delegation’s commitment to this community’s older adults and recognition that change is needed,” said Glen Cooper, chair of the Alliance for Senior Care and President and CEO of Friendly Senior Living.
“While our health system re-
mains in crisis in large part due to severe underfunding from New York state to nursing homes, our Rochester delegation has and will continue to work tirelessly to get a fair reimbursement to provide seniors with the care they deserve. We will continue to advocate diligently for necessary legislation and funding to support the older adults that we serve today and will serve in the future,” said Cooper.
The Alliance for Senior Care is a consortium of five nonprofit skilled nursing facilities in Greater Rochester: Episcopal SeniorLife Communities, Friendly Senior Living, Jewish Home, St. Ann’s Community and St. John’s.
The alliance was first formed in May, 1997, to address industry issues, generate cost savings and share best practices.

Excellus BlueCross BlueShield has been recognized by Forbes as one of the best employers in the United States for diversity.
The health plan was honored among 500 organizations, with 1,000 or more employees, on the list of Forbes Best Employers for Diversity 2024.
“Inclusion, diversity, equity and access are core to who we are and what we do every day,” said Jim Reed, president and chief executive officer, Excellus BCBS. “This recognition is evidence of the ways our employees contribute to an environment where each of us can feel seen,
valued and empowered to be our best selves.”
This is the second consecutive year Excellus BCBS made the list. The nonprofit health insurer ranked No. 25 among all employers nationally and No. 5 among employers in the insurance industry.
"I couldn’t be prouder of our employees for the way they show up each and every day,” said Sady Alvarado-Fischer, vice president, diversity, equity and inclusion officer, Excellus BCBS. “Inclusion, diversity, equity and access is everyone's responsibility, and I’m excited that the dedication, passion, and work of so many throughout our organization is having a positive impact."
The Best Employers for Diversity 2024 were identified through an independent survey of 170,000 U.S.-based employees.















Last summer was a record-breaker for heat emergencies, so the U.S. Centers for Disease Control and Prevention in April launched a new online heat forecaster to help folks better prepare as summer nears.
The HeatRisk Forecast Tool is a joint effort between the CDC and the National Oceanic and Atmospheric Administration's National Weather Service to give Americans a weeklong heads-up that broiling temperatures are headed their way.
It's all close at hand at the HeatRisk Dashboard online — just plug in your zip code for the latest forecast and updates.
“Heat can impact our health, but heat-related illness and death are preventable,” CDC Director Mandy Cohen said in a statement. “We are releasing new heat and health tools and guidance to help people take simple steps to stay safe in the heat.”
Climate change is making for more and longer periods of hot, humid weather. ER visits for heat-related illness peaked in many regions of





Welcome to The Village at Unity, where hospitality-based care and resort-style amenities are perfectly blended to deliver next-level senior living. From our signature program, PrimeFit Wellness, to a community calendar filled with activities, there’s never been a better time to come home to The Village at Unity.
Call 585-684-8082 today to schedule your visit!
the country last summer, and working-age folk who were forced to labor outside faced higher risks.
But extreme heat experienced without the help of air conditioning can also be hazardous to people with underlying health issues, the CDC added.
The new HeatRisk tool "identifies health and temperature data to deliver a seven-day outlook for hot weather," the CDC explained. "The tool uses a five-level scale to indicate how risky the heat level is in a specific area."
The tool is calibrated to assess the unique risks from heat to health that might come in specific areas of the United States.
"Pulling in data from the HeatRisk Forecast Tool, in the Dashboard people can enter their zip code and get personalized heat forecast information for their location alongside protective actions to take," the CDC said.
Visit https://ephtracking.cdc. gov/Applications/heatTracker/