Reflecting changing times and legislation, Americans are now more apt to light up a joint or pop a weed gummy on a daily basis than they are to raise a glass of wine or beer, new research shows.
Among folks who said they used either marijuana or alcohol each day, marijuana became the preferred choice as of 2022, according to study author Jonathan Caulkins.
In terms of the sheer number of people who drink or use pot or alcohol at least occasionally, alcohol remains in the lead.
However, "a good 40% of current cannabis users are using it daily or near daily, a pattern that is more

associated with tobacco use than typical alcohol use,” Caulkins told the Associated Press. He's a cannabis policy researcher at Carnegie Mellon University in Pittsburgh.
The new study, published May 22 in the journal Addiction, was based on an analysis of the National Survey on Drug Use and Health which, among other behaviors, tracks tobacco, alcohol and drug use in the United States.
For years, alcohol topped marijuana as the substance of choice among "daily users." But in 2022, 17.7 million people told the survey they ingested marijuana on a daily or near-daily basis, compared to 14.7
million who did so with alcohol.
That's not overly surprising, since rates of daily or near-daily marijuana use rose 15-fold among Americans between 1992 and 2022, Caulkins noted.
It also reflects big changes in public policy, with most states relaxing laws against the use of marijuana, although it's still illegal at the federal level.
The federal government announced earlier this month that it has moved to reclassify marijuana as a less hazardous drug.
Still, having more Americans using marijuana each day isn't necessarily a good thing, one expert said.
Speaking to the AP, Dr. David Gorelick, a psychiatry professor at the University of Maryland School of Medicine, believes far too many people are now reaching problematic levels of weed use.
"High frequency use also increases the risk of developing cannabis-associated psychosis,” a severe condition where a person loses touch with reality, he added.
One study published earlier this week in the journal Psychological Medicine, found that teens are at especially high risk for psychosis, with risks rising 11-fold if they regularly use marijuana.




By Chris Motola
‘I’ve been in recovery for my own addiction issues for over 21 years. Having been through treatment and getting boarded in addiction medicine, I really know the disease inside and out.’
Q: How did you overcome your addiction?
A: There’s a state organization that’s part of the New York State Medical Society. It’s called the Committee for Physician Health. I signed a five-year contract with them that I would participate in whatever treatment they recommended. I did that and it was very helpful. I haven’t, knock on wood, returned to using substances ever since.
Q: Do the treatments you offer have a psychiatric component?
A: I’m not a psychiatrist, but with my background in family medicine I will occasionally prescribe psychotropic medications like anti depressants and anti anxiety drugs. But usually when somebody is still getting sober it takes time for whatever substances they’ve been using to work out of their system and to determine if there’s any underlying psychiatric issue. I might feel comfortable dealing with some of them, some of them not, in which case I’d refer them. Being boarded in addiction medicine also means that I can prescribe a number of medications that are useful in decreasing cravings for opioids, cocaine, alcohol. They’re helpful, but they’re not cures. Recovery requires a lot more than just a pill.
Q: For patients who are interested in your services what’s your intake process?
A: I have a website, winsbergmd. com. They can call or email me from the site. If I don’t answer immediately, they can leave a message and I’ll get back them, usually within 24 hours.
Q: How does pricing work?
career after decades long career with local hospitals, talks about own addiction and how he got hooked
Q: You’ve recently started your own practice. What made you want to go solo? The trend seems to be running in the other direction?
A: I officially opened it in January. I was working for Rochester Regional Health and my particular PCP was a group of doctors who have since left and gone into concierge medicine because of the excessive demands of the hospital system. So I think there’s a trend of more and more doctors doing this. For me, I’m 68 and could retire, but I like doing this work and hope I’m going to like doing it without the trappings of the hospital system.
Q: Are you offering concierge services now?
A: It’s self-pay. I’m not taking insurance. That’s another way I’m getting away from the system. Being involved with the insurers is complicated and since I’m doing this entirely by myself with no administrative person it’s just easier for me to do it this way.
Q: Have you found patients are able to work with a self-pay model?
A: Yeah, I mean, I’m new in the sense that I’m not sure there are that many addiction medicine board-certified physicians doing this in the
community on a solo basis. A number of colleagues in different parts of the state and country have told me that this type of practice is usually well-received.
Q: How would a patient find you or be referred to you?
A: My goal is to help people who are just realizing that they have substance use issues — either alcohol or other drugs — to learn how to approach it, because denial is a big part of having an addiction. Getting through that and addressing the problem can sometimes be pretty difficult. In my advertisement I say that I’ve been in recovery for my own addiction issues for over 21 years. Having been through treatment and getting boarded in addiction medicine, I really know the disease inside and out. So the type of patients I hope to attract are medical, legal and other professionals who are notorious for trying to avoid any possibility of anybody finding out. This just allows the disease to continue to get worse.
Q: Interesting that you say that. Talking to physicians over the years, and you definitely get the sense that there’s a culture of stoicism with regard to the
number of hours being put in and overall demands. Do you think that may contribute to unhealthy coping mechanisms?
A: Absolutely. If you go through the signs of physician burnout, one of them is turning to substance use. In retrospect that was likely what happened to me. I was an emergency room doctor for 12 years and the usual burnout time for an ER doc is 10 years. I didn’t realize what was happening to me. A new drug came on the market in the mid-'90s called Tramadol. At the time it was marketed as a non addictive pain reliever. The drug company representatives would bring samples to the ER, doctors’ offices. I tried it at some point. It wasn’t a good pain reliever, at least not for me, but it did seem to make my 12- to 14-hour ER shifts go better. It was like turning on a switch. I’d never been addicted to any substances, but it took off: one was good, two was better. In retrospect it could have very well been the stress of the job for as long as I was in it. Even after getting treatment, I stayed in emergency medicine for three or four more years before I realized I needed to find something else to do.
A: It’s a set rate. $400 for an evaluation, which usually takes an hour, hour and a half. Follow-up visits are $200 and usually around half an hour. How often someone needs to follow up is based entirely on their own needs and how they’re coming to acceptance of their disease. I have a patient who I’ve seen maybe three or four times. They seem to be doing well, so I’m spacing out the appointments. It starts at once a week, then every two weeks, then every four, then as needed after that.
Name: Mark Winsberg, MD
Position: Addiction medicine physician, solo practice
Hometown: Delray Beach, Florida
Education: University of Miami School of Medicine, Stanford University School of Medicine, Highland Hospital family medicine residency program
Career: Addiction medicine specialist clinician, Rochester Regional Health; medical director, Chemical Dependency Services, Rochester Regional Health; clinical director, Chemical Dependency Services, Unity Hospital; medical director at Clifton Springs Hospital and Clinic
Membership: American Academy of Family Physicians; American Society of Addiction Medicine; American Board of Family Medicine; American Board of Addiction Medicine; Monroe County Opioid Task Force Family: Wife, two daughters Hobbies: Racquetball, drums, biking, hiking
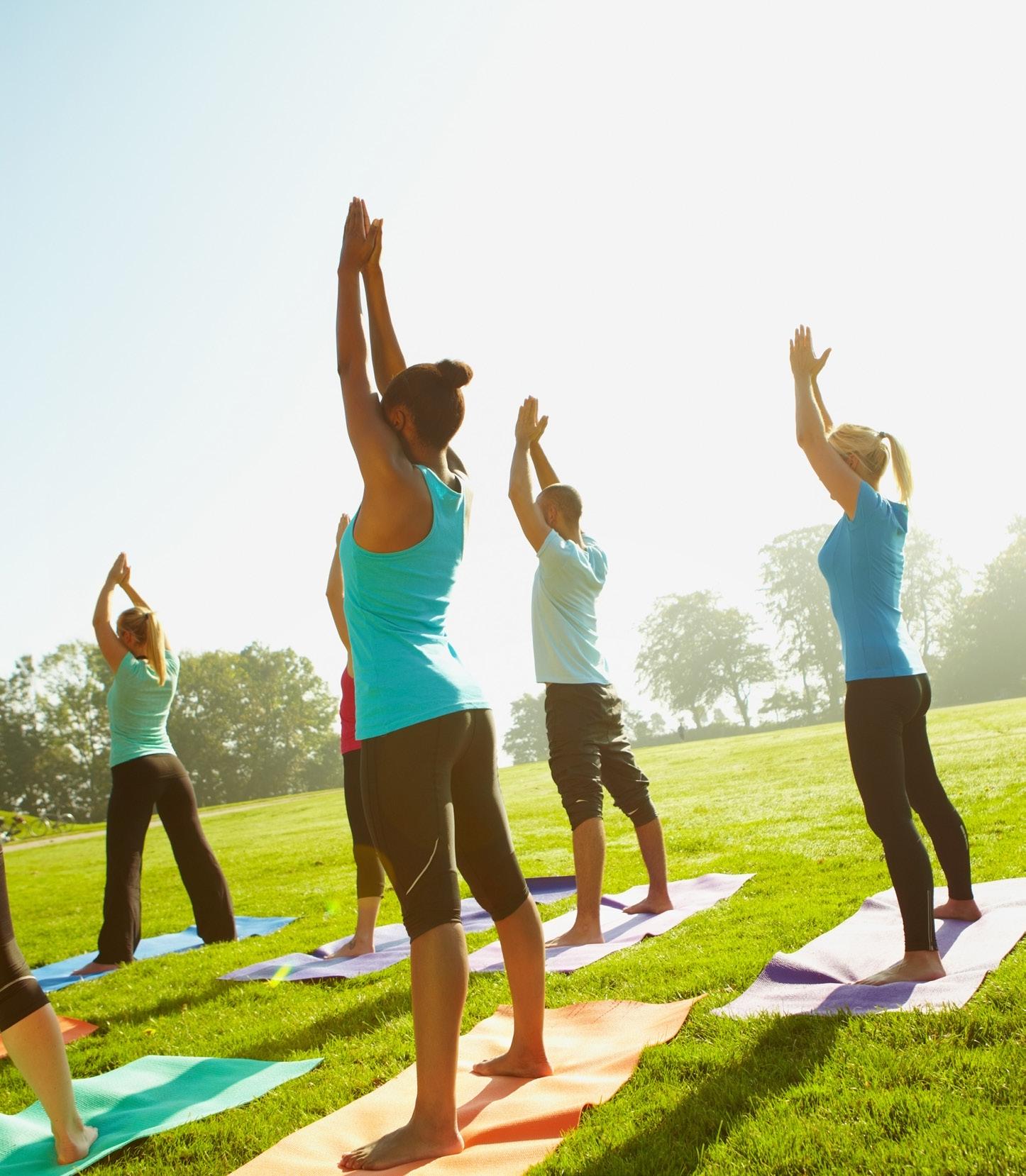
Nearly one in every six U.S. adults have engaged in the ancient practice of yoga over the past year, new government data shows.
In fact, as Americans increasingly turn to alternative or complementary health approaches, "the largest increases [have been] in the practice of yoga," noted researchers Nazik Elgaddal and Julie Weeks. They're with the National Center for Health Statistics (NCHS), which is part of the U.S. Centers for Disease Control and Prevention.
Their new report is based on 2022 data from the ongoing National Health Interview Survey.
According to the data, yoga remains more popular among women (23.3% reporting past-year use) than men (10.3%).
It's also more popular among the young (ages 18 to 44), with 21.3% in that age group saying they practiced yoga, than the middle-aged (14.1%) or those aged 65 or older (8%).
The well-off are also more likely to engage in yoga than less affluent folks. Overall, 23% of people in the
survey's highest income bracket said they practiced yoga versus 10.4% of those at the lowest income level.
As to why Americans are engag ing in the ages-old Indian practice, about 80% of yoga practitioners cited "restoring overall health," the CDC team found. That was especially true for folks aged 45 to 64.
Meditation is often being per formed in conjunction with yoga: Just over 57% of all practitioners said they meditated as part of yoga prac tice. Lower-income people were more likely to engage in meditation and yoga together compared to better-off folks, the data showed.
Pain relief was another reason cited by many who practiced yoga: About 29% said they engaged in yoga to help "treat or manage pain," the survey found.
Again, lower-income people who engaged in yoga were more likely to say that they used the practice to ease pain compared to higher-income people.
The findings were published June 12 as an NCHS Data Brief.
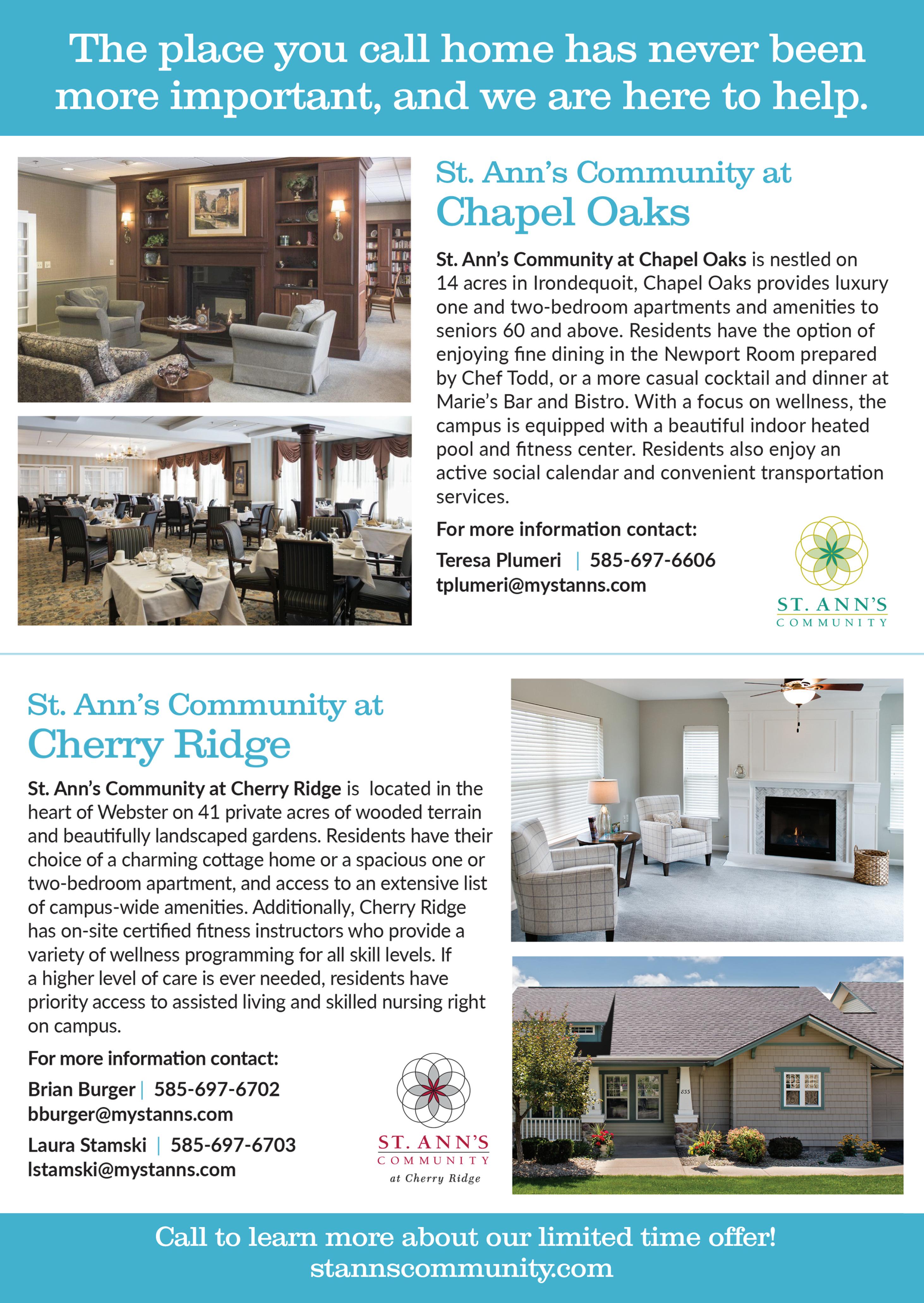
A monthly newspaper published by Local News, Inc. Distribution: 33,500 copies throughout more than 1,500 high-traffic locations.
In Good Health is published 12 times a year by Local News, Inc. © 2024 by Local News, Inc. All rights reserved. P.O. Box 525, Victor NY 14564. Phone: 585-421-8109 • Email: Editor@GVhealthnews.com
Editor & Publisher: Wagner Dotto
Writers: Deborah J. Sergeant, Chris Motola, George Chapman, Gwenn Voelcker, Anne Palumbo, Jim Miller
Advertising: Anne Westcott (585-421-8109) • Linda Covington (585-750-7051)
Layout & Design: Angel Campos–Toro • Office Secretary Allison Lockwood
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen.








By George W. Chapman
The mental health crisis within a crisis is the impact of a family member undergoing a mental health issue on their family.
A 2022 study conducted jointly by the Kaiser Family Foundation and CNN found 90% of respondents believe we are in a mental health crisis in our country. Access and cost are the two largest barriers facing patients and their families. A family in crisis could involve a family member living on the streets, a family mem-
As the election looms ever closer, once again the Affordable Care Act is a political football. Ignorantly proclaiming “the ACA is terrible healthcare,” some political leaders denigrate all the insurance companies, physicians, nurses and hospitals that pay for or provide the care to more than 45 million patients. Since the genesis of the ACA in 2010, the number of uninsured has been cut in half from 15% to just more than 7%. Most of those covered by the ACA qualified via expanded Medicaid coverage in their state. (For example, the threshold to qualify for Medicaid was raised from earning less than $12,000 a year to earning less than $15,000 a year.) For those that earn more than the threshold, up to 400%, they can purchase a commercial plan online at discounted rates based on their income. The federal government reimburses the participating insurance plans for the balance of the full premium. The subsidy runs around $1 billion annually. There is now record commercial insurance company participation, averaging six companies per ACA market. The ACA did not just impact the under or uninsured. For ALL of us, you cannot

ber institutionalized because a threat to self or others, a family member overdosed or attempted suicide. The support available to families is just as lacking as the support for the family member in need of treatment. The survey of families in crisis revealed 28% had a family member institutionalized; 21% had a member in an emergency department for an overdose; 14% had a member living on the street; 16% said a member was homeless; 8% had a member
be denied coverage by any carrier for a preexisting condition. Plans cannot charge higher premiums if you had what was once considered a preexisting condition. Plans cannot impose lifetime limits for an illness. The ACA limited out-of-pocket costs and required carriers to offer preventive care without any out-of-pocket costs to the member. Families can keep their children on their plans up to age 26. The ACA made it far easier for consumers and businesses to compare plans. Bronze, silver and platinum levels of insurance must meet basic coverage requirements. (Most covered by employer-sponsored insurance are in silver plan.) Insurers cannot discriminate against small businesses. Finally, insurers must spend at least 85% of their premiums collected on claims. If they spend less than 85%, it must be rebated to the employer. This prevents price gouging by the carriers.
In 2022, 48,000 of us were killed by guns, half by suicide. That’s about 132 gun deaths a day. The leading cause of death among children and teens is guns. To develop an effective prevention and
with an eating disorder; 20% reported a family member with cutting or self-harm behavior; 16% reported a member had attempted suicide; 50% of the families reported one or more of the above; 40% said the member crisis had a major negative impact of family relations; 57% of the families surveyed had incomes less than $40,000 while 43% had incomes more than $90,000.
counseling program, the government needs better data from hospitals, emergency rooms and physicians regarding gun related injuries and deaths. Hospitals will receive extra funding for compiling and reporting the data which has yet to be determined. (The data collection will not reveal names.) Even funding for just studying gun violence is a political football in Congress. A scant $25 million had been earmarked for the study. By comparison, three times that amount is earmarked to study teenage drinking.
The impact and harm of that record-breaking breach a couple of months ago at United Health’s claims clearinghouse, “Change Health,” is still being felt. It disrupted almost HALF of all claims filed by physicians, hospitals and pharmacies. Consequently, the DHHS office of civil rights is allowing affected providers to require United Health to notify their patients of their data that was stolen.

MA plans are offered by commercial carriers as an alternative
to traditional Medicare. Seniors are enticed to enroll by expanded benefits (preventive services, dental, vision and even free gym membership) without an increase in their premiums or what is deducted from their monthly social security check. The concept makes a lot of sense. By offering these extra benefits, MA plans expect that their seniors will be healthier, which reduces future claims. So, the investment in the extra benefits offered to seniors by MA plans will be recouped down the road. More than half of all seniors, about 33 million, have opted for MA plan. Initially, MA plans were covering “younger” or “less risky” seniors (65-70) who still didn’t require a lot of medical services. Commercial profits were good and they couldn’t enroll savvy seniors fast enough. However, those “younger” seniors are now in their 70s and 80s and here come the claims. According to some MA plans, profits are declining. Consequently, they are increasing denials and slowing the approval process. Providers and health systems aren’t standing for this, so many are threatening to refuse participation and accept only traditional Medicare. This could in turn force many MA members back to traditional Medicare, especially if their favorite providers drop their MA plan. MA plans are paid for each member enrolled by CMS, which also runs traditional Medicare. To entice commercial plans, CMS offered an enhanced premium to cover startup costs. So initially, things were running well for these plans. These enhanced MA plans cost CMS about $5,700 year per enrollee versus about $5,000 per traditional Medicare enrollee. Industry experts believe that, despite the kvetching, most MA plans will hang in despite lower profits and will adjust.
The national association that represents skilled nursing facilities is suing CMS over unreasonable staffing requirements that will be harmful to patients and financially untenable. The association argues the staffing requirements are a knee jerk reaction to the nursing home deaths during the pandemic. While a quarter of COVID-19 related deaths occurred in SNFs, the frail elderly were generally acknowledged to be most at risk, no matter if at home or in an SNF. The mandated staffing requirements are NOT supported financially via enhanced reimbursement from either Medicare or Medicaid. Hundreds of financially strapped SNFs could close unless there is some sort of compromise.



George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.



‘I
felt wonderful the next day … I called and signed up for three months of sessions’
By Joe Sarnicola
Ican no longer call myself a young man. But I exercise regularly and I am a certified yoga instructor.
When I signed up for an introductory session at StretchLab in Victor, I wondered if I might end up like the 1980s toy, Stretch Armstrong, only I might not snap back into my original position. I am not as flexible as I used to be.
But what was my experience at StretchLab really like?
After I told the receptionist I was there for my appointment with Jason, I was asked if I had skid-resistant socks, which are required for safety. I did, but if I didn’t, I could have borrowed or purchased a pair there. I was also wearing the recommend comfortable clothing. I wore what I typically wear to the YMCA. Then I sat and waited for my turn.
Waiting for an appointment can be boring or even uncomfortable if the chairs are hard, but that was not the case at StretchLab. The regular chairs were comfortable and massage chairs were available, too. The studio itself is well-lit and spacious with therapy tables arranged in rows to allow the flexologists to work.
The whats?
The treatment at StretchLab is called flexology (not to be confused with reflexology, which involves pressure points on the feet and hands), so the therapists are called
flexologists. On a simpler level, the practice is also called one-on-one assisted stretching.
Jason and Jodi, another flexologist, were working with their clients while I was waiting. I noticed they were having friendly conversations with their clients, which helped to put them at ease, to establish a personal connection and, most importantly, to listen to them in order to give a customized treatment within their limits.
I had a similar experience with Jason. He would always ask me how I was feeling during treatment and he listened. It was never the case where he tried to impose a treatment on me. He proceeded based on the feedback I gave him and I am sure that is case with all of the flexologists there.
According to one of their brochures, “Increasing your range of motion and maintaining your flexibility is an integral part of your overall health and wellness. An assisted stretch helps you get a deeper, more concentrated stretch than you could on your own, allowing you to improve your mobility and flexibility.”
Although my session was considered introductory, the flexologists usually design a path to wellness, working with the clients over a given period of time.
StretchLab offers a variety of
session packages to help their clients reach their goals. The sessions themselves are either 25 or 50 minutes in length. The standard 50-minute is a full body stretch that focuses on all major muscle groups and extremities, which helps to loosen tight muscles and ease stiff joints. The 25-minute is a maintenance session that works on just the major muscle groups. This is recommended for those who may not have the time for a full body stretch or just want some muscle relief.
Maria is the lead flexologist at the Victor studio, so she manages the staff, coordinates their regular continuing education and training and provides customer service to the clients. “Much of what we do here is forward flexion and strengthening and working muscles to correct imbalances. The first stretch is a discovery,” she said.
As part of developing a plan for each client, StretchLab offers a tool called MAPS, which stands for mobility, activation, posture and symmetry. This full body, 3D infrared scan evaluates how well the clients can move and calculates a score that helps the flexologists create the plan.
“Our therapists follow the plans for their clients,” Maria said. “We only hire people who are compassionate and knowledgeable. Yes, this is a commitment. It takes repetition. Every plan is personalized. The more
often you come here, the better. It takes about three months to experience real results.”
The flexologists at StretchLab have a wide range of fitness backgrounds, including yoga, occupational therapy, sports medicine, personal training and martial arts. The practice itself is based on commitments to freedom, energy, growth, community and caring. The staff I met at Victor was welcoming, friendly and understanding.
Remember my Stretch Armstrong analogy? Jason assured me we would never go past my physical limits and we never did. Notice I said “we” and not “he?” I was not so much receiving therapy as I was participating in it with Jason.
You may be wondering the same thing I did: How was I going to feel the next day?
I worked at a job that was physically demanding, so I have had my share of strained muscles and overstressed joints plus a torn rotator cuff and a whiplash injury to my neck. But I felt wonderful the next day. I had more movement in my neck than I have had in a long time. I called and signed up for three months of sessions.
For me it is worth the drive from Auburn, where I live, to Victor, just off Thruway exit 45 to receive this wonderful treatment.
There are two StrechLab locations in Rochester. One at 3349 Monroe Ave., Pittsford; the other at 237 High Street Extension in Victor (behind the Fleet Feet near East view Mall). The phone for both is 585-5128100. For more information, visit www.stretchlab.com.
By Gwenn Voelckers
When the challenges of living alone and the troubles of the world overwhelm you, the quote below by Mother Teresa may give you hope and a renewed focus on living a life of love, service and charity.
“Not all of us can do great things. But we can do small things with great love.”
Mother Teresa
In Mother Teresa’s long life, she touched millions through her presence and acts of charity. My interest in her was piqued in 1979 when she won the Nobel Peace Prize for her dedication to the poor and work to promote peace.
I was 25 at the time. She donated her entire cash prize to the poor in India.
In her words and especially in her actions, she helped me see that a life of generosity and everyday kindness — however big or small, anonymous or acknowledged — is meaningful and powerful.
As we navigate life’s later stages as older adults, it’s helpful to remember that our actions, no matter how small, can profoundly impact others as well as our own sense of well-being.
Below are 10 examples of simple yet meaningful gestures that can bring joy, peace, laughter and a deeper understanding to those around us:
1. Express your love
In her twilight years, my mother wrote beautiful, heartfelt letters to each of her children: to me and my three siblings. Unbeknownst to us, she tucked the letters away for safe keeping.
After her passing in 2014, we discovered her letters — personalized and crafted to celebrate each of our unique attributes.
I cherish her letter and keep it close at hand in my bedside stand.
In my mother’s eyes, these letters might have been a small token of her
affection, but her words held immeasurable worth to each one of us.
2. Offer a helping hand
I recently witnessed neighbors helping neighbors after high winds sent our trash bins sprawling in all directions.
I joined “the party” and as we were raking up the bits and pieces, our local trash collector showed up with a big box of doughnuts.
Many hands, many smiles and lots of cream-filled delights!
3. Do good on top of good (including baked goods!)
My sister volunteers at Tool Thrift Shop in Fairport, whose proceeds benefit the elderly.
But she does more than staff the cash register; she brings in goodies for her co-workers and treats them to healthy black-bean brownies — a small, but welcome (and tasty!) gesture.
Here’s an example of a small act that gathered momentum during COVID: the act of leaving uplifting notes in public spaces.
On my morning walks I often happen upon painted stones with inspirational messages created by children. I take photos of my favorites and text them to my friends, creating a ripple effect.
Some of my fondest expressions are “Look for the beauty around you.” “Good things take time.” “Just breathe.”
While it was my full intention to attend the funeral service, I was tempted to skip it.
I know that sounds terrible, but I had gardens to plant. And it turned out to be a gorgeous day. There was so much to do.
But then, I re-read the obituary, noted the time and place of the service and powdered my nose.
I’m so glad I made the right decision. I went to the service.
I’ll never again underestimate the value of showing up. What I initially rationalized to be inconsequential was very consequential.
I felt the warm embrace of those grieving for their mother and was so grateful to be a source of strength and solace during a difficult time. Show up. It matters.
Have you read the book titled, Miss Rumphius about the real-life “Lupine Lady” who scattered lupine seeds everywhere she went?
The plentiful and colorful lupines that adorn the coast of Maine are her legacy.
We can all be “Lupine Ladies.”
Anonymously leave a bouquet of flowers on your neighbor’s doorstep. Plant a garden on the perimeter of your property for passersby to enjoy, even if you can’t see the garden from your house. Or create a charming container mini-garden for your friend in their apartment.
Small seeds can produce an abundant harvest on so many levels!
Don’t you just love it when people freely share their favorite books, brands, recipes, movies, music and restaurants, not to mention their knowledge and expertise.
This simple and generous act of helping others by exchanging “trade secrets” can save everyone time, trouble, and money.
I have a dear friend who, like me, is an avid reader. We trust each other’s book recommendations and reap the rewards.
Next up? A Gentleman in Moscow.
Openly sharing information can foster connections, promote conversation, self-reflection, and understanding.
Literally, in this case, making monetary donations — no matter the size — can help support people in need and global causes that make a positive difference in our world.
Whether you contribute pennies to the Salvation Army’s Holiday Kettle campaign, make donations to
your favorite charity, or contribute outright to a struggling family, you empower yourself to be a part of a solution, promoting change and funding a better future.
Every little bit counts.
9. Vote
Yes, voting — a small (but huge) act and privilege. Easy to do. And so impactful.
Ultimately, voting is not just about individual preferences, but about expressing our love and concern for the greater good, making it a powerful and compassionate singular step with profound effects.
Perhaps one of the smallest, quietest and most loving thing we can do is to listen to each other with intention and open hearts.
Many consider “active” listening to be one of the highest forms of respect. And it costs nothing.
Offering a listening ear to someone in need, whether a family member, friend or stranger, can help relieve suffering, brighten a mood, deepen an understanding, and enable someone to feel “heard.”
I know my readers hear me.
For those living alone and who may be grappling with feelings of loneliness or questioning their purpose, embracing these small acts can help restore a sense of self-worth and connection.
When we contribute to the happiness, safety, and health of others, we rediscover our value and recognize that our lives matter.
By focusing on doing small things with great love, we can not only enhance the lives of others, but also enrich our own lives with a deep sense of purpose and fulfillment.

Gwenn Voelckers is the author of “Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own.” She welcomes your thoughts on this column as well as topic suggestion for future essays at gvoelckers@rochester. rr.com.
I
f your child is among the youngest in their school grade, it's more likely they'll be mistakenly identi-
fied by teachers as having ADHD or autism, a new study confirms. "Adults involved in identifying
or raising concerns over a child's behavior — such as parents and teachers — may be inadvertently misattributing relative immaturity as symptoms of ADHD," explained senior study author Kapil Sayal, a professor of child and adolescent psychiatry at the University of Nottingham, in England.
"The child's age in relation to their classmates [their 'relative' age] needs to considered when making this kind of diagnosis," he said in a university news release.
It's a phenomenon that's been picked up on in prior studies. This time, Sayal's team conducted what's known as a "meta-analysis," combining the collected data on the issue from 32 studies conducted worldwide.
They found that "children who are younger relative to their peers within the same school year are 38% more likely to receive an ADHD diagnosis and 28% more likely to be prescribed ADHD medications," compared to older kids in the same class.
When it came to autism spectrum disorders (ASDs), similar trends emerged. In two "high-quality" studies conducted in Taiwan, "children who were the youngest in their school year were more likely to be diagnosed with ASD than those who were the eldest," Sayal and colleagues found.
The meta-analysis was published recently in the journal European Child & Adolescent Psychiatry.
By Deborah Jeanne Sergeant
Afew local providers offered ideas of what’s on the forefront of women’s healthcare.
1. Healthcare Equity
Numerous studies indicate that women’s health concerns are considered less important to their healthcare providers than men’s concerns.
One example is a study published by the Journal of Women’s Health that said women presenting with chest pain are twice as likely as men to be diagnosed with mental health issues instead of possible cardiac issues.
Women are also “substantially underrepresented” in medical research than men for issues that affect both genders, according to a study published by Harvard in 2022.
“I ask each and every woman to join me in advocating in more equitable healthcare and increase awareness, education and support for the fight of women in heart disease,” said physician Nelly Kazzaz, a board member representing the American Heart Association Western and Central New York Chapter.
2. Mental healthcare
According to the AJPM Focus — the journal of the American College of Preventive Medicine and the Association for Prevention Teaching and Research — a study of women in 2022 showed that “compared with reports before the pandemic, partic-


ipants reported increased frustration or boredom (69.1%), loneliness (51.6%), anxiety (64.3%), depression (52.4%) and changed sleep patterns (68.3%).”
In addition to providing most of the home’s housekeeping duties and care giving to children and elders, women found themselves juggling, working at home and while schools closed, providing more caregiving and overseeing education at home. Although some of these issues have abated, others such as inflation persist.
“Since the pandemic, women have been under increased pressure at home and work,” Kazzaz said. “Instead of prioritizing mental healthcare, we reduced the priority of preventive healthcare. We are still seeing the consequences of it and we aren’t at the pre-pandemic status of mental health.”
3. Dearth of healthcare providers
It is estimated that about 20% of the healthcare workforce left medicine during the pandemic. This affects women twofold: both in securing providers for their own healthcare needs and for those of their family, as women tend to act as the guardians of their family’s health.
“It’s very concerning and there’s no end in sight,” Kazzaz said. “Most physicians who left healthcare during the pandemic didn’t retire. The pandemic increased a load that



led to early retirements and a lot of people leaving the healthcare professions. We still struggle fully staffing our office and the hospitals are struggling as well.”
According to Johns Hopkins Medicine, the decades after age 50 is the riskiest time for women’s bones, when half of them experience osteoporosis-related breaks, compared with only 20% of men.
Brittle bones can lead to significant downturns in women’s health.
A study in Acta Orthopaedica, a peer reviewed journal that publishes basic and clinical research in the field of orthopedics and related subdisciplines, sates that 21% of people who receive surgical repair for a broken hip die within a year.
Kerri Howell, online personal trainer and nutrition coach and owner of The Hourglass Mom, LLC in Rochester, recommends that women strength-train.
“Women can turn around osteoporosis if they start lifting weights,” she said.
Lifting weights works to build bones in two ways. The strain of muscles working helps build more bone where they’re connected. Plus,
women are engaging in weight-bearing exercise.
Although it’s laudable that many women want to work on losing weight, Howell said that it’s commonplace to go about it in the wrong way.
“They lack muscle,” Howell said. “For years, women have been marketed to do endless cardio and eat less and eat low-fat food when in reality, they should be lifting weights. So many women don’t lift weights. They think they’ll be bulky or it will be hard. We don’t have an obesity problem we have an under-muscled problem.”
She also warned that reliance on drugs like Ozempic alone for weight loss is not enough, as women aren’t eating enough and lose muscle tone. This effect can kick off a “starvation mode” in the body, which causes the body to hoard calories as stored fat, particularly in women who aren’t exercising enough.
“They really need a trainer and nutrition coach to avoid losing muscle and when they go off it, make sure they have the habits they need,” Howell said.



By Deborah Jeanne Sergeant
Up to 75% of menstruating women experience premenstrual syndrome, according to Healthywomen.org, a site dedicated to educating women aged 35 to 64 so they can make informed health decisions.
But only 20% to 40% encounter disruptions in their daily activities because of PMS.
The term “premenstrual syndrome” or “PMS” refers to a group of symptoms related to starting a month’s menstruation, including mood swings, anxiety, depression, change in appetite, bloating, breast sensitivity and feeling tired. This isn’t an exhaustive list; some number as many as 150 distinct symptoms. Since nearly all women menstruating have cramps while bleeding, that is not considered a PMS symptom.








Of course, over-the-counter preparations like Midol can reduce cramps and bloating. Healthywomen.org offered a few suggestions that may help, such as taking a calcium supplement of 600 mg. twice daily, although it’s unclear as to why this can make a difference. Other studies show that supplementing with vitamin E, vitamin B-6 and magnesium help.
Some women report anecdotally that the supplement chasteberry helps relieve PMS symptoms.

Before taking any supplements, always discuss it with your primary care provider.
Other lifestyle modifications can also ease PMS.
“What you need to do is build more muscle, which helps with the menstrual cycle,” said George Barnes Jr. weight loss specialist and certified personal trainer at Que Fitness World in Rochester. “You won’t get bulky and boxy — you’d have to take hormones to do that. Just challenge the muscle.”
Try exercise bands, moderate free
weights or body weight exercise. This may not be a good time to engage in lifting really heavy weights.
Some cardiovascular exercise can also help out, as the body releases the “feel good” hormones — endorphin and serotonin — during exercise. This helps improve mood and alleviate depression. But if you’re not feeling up to it, try a light workout such as brisk walking, gentle yoga, Pilates or cycling.
Overall, maintaining a healthful lifestyle can help reduce PMS symptoms, including eating a balanced diet low in refined foods such as snack cakes, pastries and boxed mixes and simple carbohydrates like white flour-based foods and sugar. A good diet is also rich in whole produce and grains, complex carbohydrates and lean protein sources.
Ironically, many women experience PMS-related food cravings for foods that aggravate their symptoms, such as chocolate or other sweets and caffeine, but it’s better to reduce these. Herbal tea may help ease symptoms. Most is caffeine-free. Look for preparations billed to reduce PMS.
Reduce sodium and increase water intake to prevent bloating. Avoid nicotine.
As stated above, regular exercise is important. Aim for 150 minutes of moderate exercise weekly.
Women who experience severe depressive symptoms — not just a bout of low mood for a day — should seek help from a healthcare provider. This could signal premenstrual dysphoric disorder (PMDD), a rare disorder that causes more significant mood symptoms and more pronounced PMS symptoms. Care providers may prescribe antidepressants or, for those seeking contraception, certain oral contraceptives that help regulate PMDD symptoms.
By Deborah Jeanne Sergeant

Although the pink ribbon campaigns to raise funds and awareness for breast cancer are important, heart disease represents the disease that kills more women annually than any other disease.
One reason for heart disease death prevalence among women is that even healthcare policy influencers tended to focus more on men’s heart health to the neglect of women’s heart health.
“Even in not-very-distant history, even the American Heart Association addressed women as to how to help their husbands’ hearts,” said physician Nelly Kazzaz, a board member representing the Western and Central New York chapter of the American Health Association.
The medical community has focused so much on women’s health such as lowering childbirth-related deaths and other reproductive issues that heart disease has not been as studied and researched.
When women were included in heart disease research, “the research did not have enough women to apply it. Now we know the differences and have more women involved in the research and can apply the different treatments and diagnostics,” said Kazzaz.
One reason that women weren’t historically as studied in medical research is that fluctuating hormones from monthly cycles, childbearing and menopause were viewed as effects skewing studies’ results. But
recent attention on heart disease among women has pushed for more study in this area.
In addition, “there’s lack of awareness among patients themselves,” Kazzaz said.
Women haven’t asked about heart health, perhaps in part because men’s heart health has received so much attention.
That awareness extends to providers as well, Kazzaz added, since women can present with atypical symptoms.
“Women tend to talk about all other issues and not on the symptoms,” Kazzaz said. “They describe it differently to their providers than men. They say, ‘I was attending a wedding, wearing this dress, and they had these flowers, and then was short of breath.’ That might affect how healthcare providers pay attention to their symptoms.”
She added that providers may skip over the pertinent parts of the narrative when discussing health crises with women. Or miss the importance of symptoms that differ from men’s symptoms.
“Many of my patients walk in and say, ‘It’s probably anxiety’ which it might be, but give us the chance to rule it out,” Kazzaz said. “They don’t want to be judged. I’m not saying it’s not a real health issue that needs to be addressed, but they think that if it is anxiety, they’ve wasted my time.”
She assures patients that “false alarms” waste no one’s time. Providers can also use these moments for


patent education on topics such as how heart attack presents in women.
“We classically think of chest pain and shortness of breath as the hallmarks of heart attacks, but women can present differently,” said physician Amanda Congiglio, who works at Rochester Regional Health. “If someone doesn’t feel normal, they should be assessed.”
She noted that because so many people rely on women, such as their spouses, children, senior parents and employers, women may feel stoic to push through symptoms like dizziness, flu-like symptoms, and jaw pain.
“Up to 80% of cardiovascular disease is preventable, said Nelly Kazzaz, MD. To reduce their risk of heart disease, women should follow these steps from Kazzaz:
“Be aware of your risk and know your numbers: blood pressure, cholesterol, blood sugar, and ideal, healthy weight.
see indicators. The patient may need referral to a cardiologist.”
Physician Amanda Congiglio, who practices at Rochester Regional Health, also offered steps for reducing heart disease risk:
“Don’t smoke. That’s the biggest thing.
“Weight, blood pressure, blood sugar, cholesterol, activity level, smoking and sleeping we can change to reduce the risk.
“In some people, we can start with ‘and if we can’t achieve that, we can look at medication.’ We are trying very hard to catch these patients as young as possible in their child bearing age. Maternal healthcare is a big concern in healthcare with hypertension, diabetes, preeclampsia or eclampsia during pregnancy. OBGYNs may
“Get 150 minutes of aerobic exercise a week. Walking is a great way to exercise, and some weightlifting, which is also good for preventing osteoporosis.
“Eat a healthful diet.
“People struggling with obesity should reach out to their primary care provider to get started on medicines that help with weight loss.
“If you have high cholesterol or have diabetes, keep it well-managed.”



By Shaina Zazzaro
Let’s start eating healthy. Today is the day to make a change. Let’s do this together.
First thing is first. You will need to figure out what you eat on a regular basis.
What do you eat? Start a food log, whether it is with a pen and paper or using an app like My Fitness Pal.
For the first week, don’t even worry about calories or macronutrients. Just jot down what you eat in your normal diet.
A week later, give it a review and ask yourself simple questions. Did you eat out a lot? When you ate out did you have appetizers, an entrée and dessert? How many days a week do you drink alcohol, if any? Do you eat fried foods often? How many days do you eat whole foods?
Take a step back and evaluate your current habits and see what areas you can improve on.
After you have evaluated a week of your regular eating, create goals for yourself. Remember, everyone is different, but at the end of the day we all have one thing in common: if we want to live long, we have to eat healthy.

Losing weight isn’t easy, but these mistakes make it much harder
By Deborah Jeanne Sergeant
Trying to lose weight? Make it easier by avoiding these common pitfalls.
• “Thinking exercise alone is the only answer.
• “Thinking changing the way you eat is the only answer.
• “Expecting instant results.” Jean Sica, certified tai chi instructor and owner of Kokoro Fitness in Rochester.
• “They don’t eat enough. I see this a lot with women. They cut, cut,
cut, cut. They’re down to 1,000 or 1,200 calories a day. Most food pyramids are based on 2,000. What that does is slow the metabolism and it tells the body to hold onto fat. It has the opposite effect.
• “They exercise too much. The body gets so stressed that it tries to hold onto that fat. I describe this as if you’re running all the time. Think of the people who run the Boston Marathon who are tall and lean. Their body is built for running. But if you want to have muscle and curves, you need to exercise and eat right.
Yes, eating healthy extends your life. Eating healthy is a primary preventive measure that you can control to avoid illness in the future. Medical News Today states that “following a healthy diet has many benefits, including building strong bones, protecting the heart, preventing disease and boosting mood.”
I will say one thing I have learned is meal prepping is super helpful for a sustainable healthy lifestyle. It takes the guessing game out of eating and prepares you for a healthy day. If you know what you are going to eat the day before, or even the morning for the day, you are less likely to fall off your healthy habits and more likely to stay on. Preparation is key. Create a healthy habit and stick to it. You can do this. If I can do it, you can do it.
Shaina Zazzaro is a devoted wife and mother of two, blending her roles with a passion for health and wellness. She is the owner of local meal delivery service, Effortlessly Healthy. For more information, visit www.ehmeals.com.

food and you don’t know about it. If you can’t pronounce it, why are you eating it?
• “You don’t know how much you’re eating. If you go to a financial planner and you have debt and no money and they ask what you spend your money on, and you say you have no idea they will want you to track what you’re spending. Two to three weeks of tracking your diet will be very eye opening. You may see you’re eating too little protein and 3,000 calories. Weighing food on a food scale helps people see where they are today.”
Kerri Howell online personal trainer and nutrition coach and owner of The Hourglass Mom, LLC in Rochester.
• “Ninety percent of my clients are women from their mid 20s to 70s. More than half I have a hard time convincing to weight train to lose weight. Most say I don’t want to look like a man; I don’t want to look bulky.
• “One of the biggest issues is
• “I tell classes that to lose weight, they have to eat more fat.
• "One of the things I find with clients is they want to go with dietitians and nutritionists, but that is one thing that we’ll feed the body—great. Those are all great people, but the one thing you have to do is apply a load to the human body and you have to get it to move. It doesn’t matter if you’re only eating healthy but you’re sedentary. You have atrophy.
• “There’s a psychology piece that goes into this. I always put into my client plans about who else is in their household. I design the meals for the person but if he or she has a family, the meal is one they can all eat. It’s tasty and the whole family can get behind them. We have to know what their output is in the gym and their basal metabolic rate and daily energy expenditure.”
By Anne Palumbo
Even though Americans eat more potatoes than any other vegetable, a good many of us don’t.
Worried about carbs and calories, we shun this tasty tuber.
Assuming we’re not missing anything anyway, we sail by these perceived starch bombs in the grocery store.

Years ago, I too was a spud-shunner. But then I did some digging and, much to my surprise, discovered multiple studies that linked potatoes and their nutrients to a variety of desirable perks.
Let’s begin with starch. Although potatoes don’t contain as much starch as flours, baked goods or cereals, they do contain more starch than other vegetables. However, unlike the refined starch in processed goods that causes blood sugar to spike and then drop, a potato’s “resistant starch” is not broken down and fully absorbed by the body. Instead, it feeds the “good” bacteria in your gut. Research has linked resistant starch to numerous health benefits, including better blood sugar control and improved gut health.
Red, white or purple, this popular vegetable is surprisingly rich in nutrients.
One serving provides decent amounts of brain-boosting vitamin B6, constipation-preventing fiber, and bone-strengthening manganese. The biggest surprise of all? Potatoes are an excellent source of vitamin C and potassium. A powerful antioxidant that protects cells from disease-forming free radicals, vitamin C supports
the immune system and helps form collagen. Potassium, on the other hand, is a mineral that’s essential for heart health and plays a role in every heartbeat.
Potatoes are packed with antioxidants, compounds that neutralize potentially harmful molecules known as free radicals. When free radicals accumulate, they can increase the risk of chronic diseases like diabetes, heart disease, and cancer. Since the skin of colorful varieties like red and purple potatoes can have up to 12 times more antioxidants than the flesh, I gravitate to those.
Potatoes are quite filling, which means they may help you regulate or lose weight by curbing hunger pangs. Undoctored and simply boiled or roasted, potatoes are not that caloric: 110 calories per average serving. Deep-fry them in oil or smother them with the works, however, and this healthy spud quickly becomes a nutritional dud.

Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.

2 tablespoons spicy mustard
1. Make potatoes: Preheat oven to 400 F. Cut the potatoes in half (quarters if large) and place in a bowl. Toss with a little oil, salt, and pepper and then arrange, cut-side down, on a rimmed baking sheet. Roast in the oven for 45 to 50 minutes until tender when pierced with a fork and golden brown. Transfer to a large bowl.
2. Prep pepper and beans: While potatoes are cooking, cook beans until tender-crisp by steaming or microwaving. When cool, slice into 1½-inch pieces and add to the potatoes. Cut the pepper into sticks
Select firm potatoes, minus sprouts and cuts. Remove any green spots in skin or eyes. If your potato is green in more than a few spots, it’s better to toss as cooking doesn’t get rid of the toxins. Properly stored in a cool, dark place— away from onions which expedite spoiling—most potatoes last about a month.
about the same width and length as the beans and place in the bowl, along with the slivered red onion.
3. Make dressing: Stir together mustard, vinegar, garlic, salt, and pepper in a small bowl. Drizzle in the oil, whisking constantly to make a creamy dressing. Add a few dashes of Tabasco to boost flavor.
4. Mix it all up: Add dressing (some or all) to vegetables, give it a good stir, and serve. Note: leftover dressing tastes great on meat and meat alternatives.




By Deborah Jeanne Sergeant
If you were raised in the ‘80s and ‘90s, you probably experienced a few sunburns — and now have the freckles, age spots and lines to prove it. Beyond the pain of sunburn and the subsequent premature aging, it can raise your risk of skin cancer. But before you slather sunscreen on your children this summer, take a few tips.
Dermatologist MaryBeth Parisi prefers cream or lotion sunscreens over sticks and sprays.
Sticks can be challenging to apply to her four kids and the risk of
inhaling aerosol sunscreen makes her shy away from it.
“There are no long-term studies on aerosol sunscreen and if you’re spraying it, kids are breathing it,” she said. “A lot of times, it doesn’t get on the skin. It’s hard to get even application.”
Schweiger Dermatology Group operates offices in Brighton, Rochester, East Syracuse and Utica among its several Upstate locations. Parisi wrote the children’s book “Into My Beach Bag Goes…” to help children understand the importance of using
By Deborah Jeanne Sergeant
Seeking summer refreshment?
Sugary lemonade and soda are packed with calories. And the artificially sweetened alternatives? They’re not much better.
Numerous studies have discovered a correlation between regularly using artificial sweeteners resulting in weight gain, not weight loss as anticipated.
Jean Sica, certified tai chi instructor and owner of Kokoro Fitness in Rochester, said that she likes “coconut water mixed with plain water and iced tea with added peppermint leaves.”
It may seem like a soda here and a sweet tea there won’t really matter much, but it’s all about the cumulative total.
“Calories from beverages can be sneaky and substantial,” said Kimberly Higgins, registered dietitian and owner of Kimberly Higgins Food & Nutrition in Syracuse. “Some frozen coffee drinks can contain more than 800 calories and more than 150 grams of sugar, the equivalent of 38 teaspoons of sugar. Even fruit smoothies and fruit drinks from fast food and fast casual restaurants

Gian Vinelli, a skin cancer surgeon and dermatologist with Rochester Regional. sunscreen.
She advises parents to wait until children are older than 6 months to begin using sunscreen on them and to choose a mineral-based product containing titanium or zinc oxide as active ingredients instead of chemical-based sunscreens. But “if they’re not going to apply the creams or lotions, then go with the spray over nothing at all,” Parisi said.
She added that lip balm containing SPF 15-30 is helpful as well. Just as with sunscreen, it should be applied every two hours or after swimming or excessive sweating. Some sunscreen is designated as water-resistant and very water-resistant. Parisi said that these last 40 minutes or 80 minutes, respectively.
The sunscreen SPF should be 30 to 50.
“Once you’re over 50, there’s not much change in how much it will protect you as long as you apply enough,” she said.
A higher SPF won’t buy you
water, which offers the fizz of soda without sugar and water flavored with fresh fruits.
“Cut strawberries steeped in water make a delicious drink,” Higgins said. “Or lemon slices with a few slices of fresh ginger. Try watermelon with fresh mint.”
more time. She advises applying enough to fill a shot glass to cover the head, neck, arms and legs.
Some people don’t like the white tint of mineral-based sunscreen. However, Parisi said that the formulas with nanoparticles are just as effective as the “white chalk” type.
“Teen girls really like tinted sunscreen as they’re interested in makeup,” Parisi added.
Many companies offer makeup primer and foundation with SPF. However, they need reapplication after two hours just like sunscreen.
Parisi also mentioned the merit of wide-brimmed hats and other sun protective clothing. That’s a favorite strategy of Rochester Regional Health’s physician Gian Vinelli, a skin cancer surgeon and dermatologist.
“There’s nothing perfect for sun protection. However, when it comes to children, start with clothing options,” he said.
He said that white cotton T-shirts and loose weave material isn’t as protective as tighter woven fabric. Look for garments with a UV rating.
A dad to a 3-year-old and 2-yearold, Vinelli said that he started his kids out with wide-brimmed hats as early as possible so that they become accustomed to wearing them. He does the same with zinc- and titanium-based sunscreen. He feels most comfortable with these as “they have the longest safety data,” he said.
While at the beach, he sets up an umbrella for shade. However, shade near the water can still allow indirect sun exposure as the light reflects on the water.
Many people believe that sun protection is not needed on cool, cloudy days. However, Vinelli said that even on cloudy days, 80% of UV rays pass through and temperature does not affect UV risk.
Wegmans brand) contain kombucha and sparkling water to create a lighter, less tangy version of traditional kombucha. They are a good option for folks who are new to kombucha, as it can be an acquired taste.”
contain hundreds of calories and as much as 80 grams of sugar, much of it from added sugars rather than natural fruit sugar.”
Added sugars cause the blood sugar to spike and crash and lead to overeating — not ideal for people who want to lose weight.
“For weight control, it is important to choose beverages that are low in calories and added sugars, checking the nutrition facts before you order can help you make better choices, so you don’t unknowingly derail your weight loss progress,” Higgins said.

Instead of hitting the drivethrough for McExcessive Calories in a cup, Higgins whips up homemade fruit smoothies made with fresh or frozen fruit. She includes yogurt, nut butters or protein powder to add protein, if she’s drinking it for a meal.
Keep that blender handy for Higgins’ agua frescas.
“They are light, fruity drinks made by whizzing up fresh fruit, water, ice, and a squeeze of lime juice,” she said. “You can blend a delicious one with watermelon, pineapple or honeydew melon.”
Skip sweet tea — it’s loaded with added sugar. Instead, Higgins brews tea: black, green, herbal or fruit teas may all be made into iced tea.
“Hibiscus tea is particularly delicious as a cold tea and has been shown to help manage high blood pressure,” she added.
Imbibing an adult beverage without blowing too many calories can be tricky. Kerri Howell, online personal trainer and nutrition and owner of The Hourglass Mom, LLC in Rochester, said that marketing phrases like “skinny, light beer and low - calorie” implies that they’re weight loss-friendly, but “they still have calories and will fill you up. Make sure you offset your beverage with a full glass of water first. You can have a glass of wine, but don’t have the whole bottle. Have a smaller dinner or smaller piece of cake.”
Cooling off with these beverages is more interesting than plain water, yet brings no calories to the glass. Higgins suggested sparkling
She’s also a fan of kombucha and new kombucha spritzers. A fermented drink, kombucha tastes “both tart and lightly sweet and mildly effervescent. It contains probiotics that support a healthy GI system. Kombucha spritzers (like the
She added that in general, alcohol isn’t good for the body, but as it’s a social beverage for many people, she doesn’t want to tell clients they shouldn’t have a beer if that’s what they want at the ballgame or barbecue.
“If it’s one day, it won’t ruin your goals,” she said. “Don’t give up your socialization; that’s part of health too.”
Why it’s important to stay hydrated most of your body is water, after all
By Deborah Jeanne Sergeant
About 60% of the average person’s body is water. That makes it pretty important for health to stay hydrated.
“Hydration is important for our bodies to function,” said Kerri Howell online personal trainer, nutrition coach and owner of The Hourglass Mom, LLC in Rochester. “When you drink enough, it helps with circulation and digestion. You think more clearly. Otherwise, you get tired and have brain fog.”
She also attributed healthier looking skin and healthy joints in part to staying sufficiently hydrated.
Howell tells her clients to aim for drinking half their weight in ounce daily and more if they’re sweating or taking certain medications that
require more fluid intake.
“Honestly, it’s hard to even get there for most people,” Howell said. “If the average woman weights 140 pounds, that’s a little over half a gallon.”
She recommends downloading an app to remind you to drink enough. Or programming a phone alarm as a reminder. It may also help to measure the goal amount as a certain number of refills of the travel mug. Howell did the Two Stanley Challenge on her social media platform as the large Stanley mugs hold 32 to 40 ounces and drinking two of those provided plenty of hydration for her.
Using the most appropriate vessel can make a difference. A flip-top

High temperatures across the Northern Hemisphere last summer were scorching and frequent enough to make it the hottest summer in two millennia, new research shows.
Weather records based on scientific instruments only goes back as far as 1850, noted researchers at Cambridge University in England. That data already had confirmed the summer of 2023 as the hottest ever recorded.
However, the Cambridge crew turned to tree ring data to reach back 2,000 years and last summer was still the hottest over that entire period of time.
“When you look at the long sweep of history, you can see just how dramatic recent global warming is,” said study co-author Ulf Büntgen, a professor of geography at Cambridge. “2023 was an exceptionally hot year, and this trend will continue unless we reduce greenhouse gas emissions dramatically.”
His team published its findings May 14 in the journal Nature.
As Büntgen's group explained, it can be easy for climate change skeptics to criticize "hottest year ever" claims if records don't go further back than 1850.
“Many of the conversations we have around global warming are tied to a baseline temperature from
insulated travel mug can help keep beverages cold longer while on the go. Some people prefer a lidded mug with a straw or a coffee mug with a fun logo. The key is choosing what will keep a beverage with you at all times.
It’s easy to become bored with water. For this problem, Howell suggested adding a splash of fruit juice, cucumber slices, mint or other produce to add flavor. Infuser pitchers can help make this easier, as they keep the items from floating in the pitcher while still adding flavor.
Howell said that sparkling water that has no sweetener added can help hydrate. But she is willing to compromise for people who truly struggle to hydrate as drinking something sweetened is better than dehydrating.
Caregivers can sneak in hydration to their elder’s diet through moisture-rich foods such as produce. Grapes, watermelon, oranges, celery, lettuce, cucumbers and melons are good examples. Smoothies, soups and stews can also increase hydration.
is additionally amplified by El Niño conditions, so we end up with longer and more severe heat waves and extended periods of drought,” said study lead author Jan Esper, of Johannes Gutenberg University Mainz in Germany. “When you look at the big picture, it shows just how urgent it is that we reduce greenhouse gas emissions immediately.”
One easy way to tell if you’re getting enough to drink is to pay attention to urine color.
“Unless you are on medication that affects the color, your urine should ideally be clear or almost clear,” said Jean Sica, certified tai chi instructor and owner of Kokoro Fitness in Rochester.
Since the amount of water needed can vary by age, size and medical conditions, Sica likes this handy visual cue regarding hydration.
“One very important thing to remember is that once you feel thirsty, you've already gone past the time that you should have hydrated yourself,” Sica said. “That said, studies have found that as we age our ability to recognize being thirsty decreases.”
That is why it’s vital for caregivers to offer reminders to drink and to ensure their loved ones have a readily accessible beverage. Fortunately, thirst recognition can increase.
“Once we get into the habit of keeping hydrated, our ability to recognize our thirst improves,” Sica said.
The study also found that in the Northern Hemisphere, the 2015 Paris Agreement to limit warming to 1.5 degrees Celsius above pre-industrial levels has already been surpassed. Because the current El Niño period isn't expected to subside until well into this summer, the summer of 2024 could also be a record-breaker, the researchers said.
the mid-19th century, but why is this the baseline? What is normal, in the context of a constantly changing climate, when we've only got 150 years of meteorological measurements?”
Büntgen noted in a Cambridge news release.
“Only when we look at climate reconstructions [from much deeper into the past] can we better account for natural variability and put recent anthropogenic climate change into context," he said.
To help reach farther back into the past, Büntgen's group compared known instrumental data on weather against tree ring growth patterns for the same years.
They found that reading tree rings was accurate in spotting weather trends.
For example, tree ring changes accurately reflected the "Little Antique Ice Age" cooling period of the 6th century, as well as the Little Ice Age of the early 19th century. These cooling periods typically follow large volcanic eruptions, which spew ash and other contaminants into the atmosphere, cooling the Earth down.
In contrast, the Northern Hemisphere heats up during El Niño weather changes, which was also recorded on tree rings.
“It's true that the climate is always changing, but the warming in 2023, caused by greenhouse gases,

By Deborah Jeanne Sergeant
If you’re never heard of pelvic floor physical therapy for improving urinary continence, you’re not alone.
“It’s an area that not a lot of people know about,” said Liz Loycano physical therapist with Finger Lakes Health.
She explained that muscles control continence and these are muscles below the pelvic area that can become weak because of age, surgery or being sedentary. Physical therapy can strengthen and retrain those muscles to coordinate better.
After taking a patient’s medical history, a physical therapist can better understand how and why the patient is experiencing incontinence. Loycano said she looks at posture and breathing and if any specific action causes leakage, such as rising from a chair, lifting objects, coughing, sneezing, laughing or squatting.
Her exam also includes assessing muscle strength and if the patient assents, an internal exam of the pelvic muscles, which can help her better understand what’s going on.
Sometimes, patients achieve results in as few as four visits, along with daily homework between visits.

Sometimes it takes longer, as it depends upon the nature of the problem and how long it’s been going on.
Loycano also counsels patients on bladder irritants, such as caffeine, processed foods and cigarettes.
The results of pelvic floor physical therapy last, especially if the patient performs any exercises prescribed a few times a week to maintain their progress.
Amy Shurtliff, doctor of physical therapy at Lattimore Physical Therapy in South Greece, said that pelvic floor physical therapy can also aid in bowel and sexual function, in addition to continence.
Some people believe that performing Kegel exercises is the answer. However, “doing Kegels too much or incorrectly can make the problem worse,” Shurtliff said. “Sometimes learning how to relax is what you need, which is more difficult than you would imagine.”
Shurtliff said that many believe that pelvic floor physical therapy is only for women. However, since everyone has a pelvic floor, the therapy can help men also. Some male patients have experienced surgery and receive benefit from the therapy.

Some people have urge incontinence, where they feel the need to urinate frequently and instantly. Others have stress incontinence, where straining to do something else like picking up a heavy box or sneezing can cause leaks. Still others experience both types.
Shurtliff said that she hears many people say, “Of course you pee when you sneeze; you’ve had three kids,” as if urinary incontinence is a normal part of being a mother. However, she views incontinence as very treatable.
“It’s not something you have to suffer with in silence,” she said.
Instead of assuming surgery is the first way to treat incontinence, Priya Akbari, master’s in physical therapy at Limitless Physical Therapy Specialists in Rochester, wants
more people to try physical therapy, as it’s conservative management.
“Medication and surgery can be helpful, but if we can have results without those, it’s great for our patients,” Akbari said. “They can get more active and stronger. It reduces the burden on the healthcare system. It is highly effective. The men and women I see receive a lot of benefit from this type of treatment.”
She added that even people who have had surgical interventions or plan to schedule surgery can benefit from pelvic floor PT.
New York is an open-access state for physical therapy, meaning that most health insurance that covers physical therapy will not require a physician’s referral to cover a limited number of visits.
Frank Guido couldn’t be happier he had a choice for treating his prostate cancer!

To hear more of Frank’s story and learn if CyberKnife is right for you, visit hoacny.com

Frank chose non-surgical CyberKnife® at HOA –offering 5 treatments instead of 35!
“The original diagnosis was to treat my prostate cancer with seven weeks of radiation, five days a week. I was kind of upset that I was never given the option of CyberKnife,” said Frank. “The precise radiation achieved by CyberKnife, far fewer treatments, and the personalized care I received from Dr. Chin and his team made my decision an easy one. Better, the treatment was a real success!”

By Deborah Jeanne Sergeant
You may associate art therapy with children using crayons in a therapeutic setting. But art therapy can include different media and all ages.
At Spotted Rabbit Studio in Rochester, Kit Shulman, licensed art therapist, works with all media, including oils, pastel, clay, drawing — "anything and everything,” he said. He primarily works with clients aged 16-plus. Creating art may not seem like therapy. However, Shulman uses art as a tool to help clients express themselves.
“They wonder why they’re repeating this story over and over,” he said. “It’s a different way to access pieces they didn’t think about during the art-making process.”
Art therapy also functions as an
effective buffer. His clients have experienced traumatic events that can be very difficult to speak about.
“You realize you’re talking about big, scary things but there’s a distraction,” Shulman said.
The artwork can divert the client’s gaze and focus while still allowing for conversation, as creating art is not that absorbing.
Which media they use varies.
“When it comes the therapeutic drawing, we have the expressive therapies continuum,” Shulman said. “On one end, there are restrictive materials like pen and colored pencils. You have more control over it. It can help you access different parts of the brain than when you’re talking with someone. Paint, clay helps you get into emotions. You can stay more

•
•


Ellen Horovitz, Ph.D., is a boardcertified creative art therapist and owner of At Creative Arts Therapy Practice, PLLC
grounded with materials like colored pencils.”
Art therapists are often called “art teachers” and their sessions are sometimes called “art class.” However, Shulman’s education includes an undergraduate degree in fine arts, master of fine arts and master of arts therapy.
Those in the profession must have the same requirements as a licensed, professional counselor and education as to how to incorporate

Although Shulman expressed disappointment that recent legislation signed by Gov. Kathy Hochul eliminated Medicaid coverage for licensed art therapy, he hopes that patients who could benefit from art therapy continue to seek it.
At Creative Arts Therapy Practice, PLLC in Canandaigua, owner Ellen Horovitz, Ph.D., board-certified creative art therapist, uses multiple media and yoga to help clients. Her media include ceramics, paint, pastels, glass and fabric.
“You have to be an artist, teacher and therapist all at once,” Horovitz said. “You have to know your materials. You have to be a skilled artist. If you have someone who wants to work with a medium you’re not familiar with, you have to get familiar with it.”
Part of the reason that art therapy helps people is that it enables them to relax once they’re into the project, what Horovitz calls a “flow state” which can also occur with music, dance and exercise.
“Then your stress and cortisol tamp down and is replaced with feelgood hormones,” she said. “That’s one way in which it works.”
She has also found that movement works well as a means to help clients regain skills in speech, language and movement. Horovitz works with individuals of all ages, although some therapists work with groups. When clients feel frustrated with a medium, she offers a different one.
perfectly. She recalled a young child -
“It turned out he was not, but he was dyslexic,” she said. “I taught him to read by making clay shapes of the alphabet. He ended up being a model maker for George Lucas. He probably the psychologist in the school system hadn’t selected him for art therapy.”













In the realm of healthcare, men often find themselves lagging behind in prioritizing their well-being.
Whether it's societal expectations, cultural norms or simply a reluctance to address health concerns, many men tend to neglect their physical and mental health until a problem becomes unavoidable. However, from the perspective of a urologist, this approach is not just impractical but potentially dangerous.
“Men often are not interested or proactive in asking questions about their health,” said Jean Joseph, urologist at UR Medicine. “They often come in when the problem has already arisen. People put their heads in the sand and don’t want to hear about health symptoms until it is too late.”
Joseph also serves as W.W. Scott professor and chairman of the department of urology at UR Medicine. He specializes in robotic surgery for urologic diseases, particularly prostate cancer.
He recently discussed five issues involving men’s health.
One of the biggest concerns for men as they age is prostate health. The prostate gland, while small, plays a crucial role in reproductive function. Unfortunately, conditions like prostate cancer can develop without noticeable symptoms until the disease has progressed significantly. Regular check ups and
By Ernst Lamothe Jr
screenings with a urologist can detect prostate cancer early when treatment is most effective, potentially saving lives in the process. The initial symptoms can be detected by a blood test.
“Prostate cancer is one of the most preventable diseases that we can cure. The earlier patients come in, the earlier we can identify causes and prevent medical conditions,” said Joseph. “If they are informed and empowered to get checkups with their doctors, we can maximize the chances of problems and create a chance to return to normalcy.”
2.Erectile Dysfunction: There Are Remedies
Erectile dysfunction is not just an inconvenience. It can be a red flag indicating broader health issues. Diabetes, heart disease, hypertension and psychological factors can all contribute to ED. By addressing these underlying health concerns, men not only improve their sexual function but also mitigate the risk of more severe complications down the line.
“People don’t understand how common it is,” said Joseph. “There are things that can be done.”
3.Frequent Urination: Sign Something is Wrong
Urologists are experts in diagnosing and treating a wide range of urinary tract issues, from urinary tract infections to kidney stones and prostate enlargement. Ignoring symptoms like frequent urination, pain during urination or blood in the urine can lead to more severe compli-
Don’t miss the August issue of In Good Health. For advertising information, please email editor@GVhealthnews.com
cations. Seeking prompt medical attention from a urologist can prevent these conditions from worsening and impacting overall health and quality of life.
“The more we drink liquid, the more it comes out and the bladder fills up. When a man’s bladder is not acting appropriately, it can back up. That means urine can back up to the kidneys and stop the kidney from functioning correctly,” said Joseph. “People say they are just used to getting up at night to use the bathroom three or four times, but that could be an indication that something is wrong. For most men over 40, there is no such thing as a normal prostate.”
4.Reproductive Health: Men Are Half the Battle
For men desiring to start a family, fertility concerns can be a significant source of stress. Urologists play a crucial role in assessing and addressing male infertility issues, offering solutions and treatments that can improve the chances of conception. Additionally, sexual health encompasses more than just fertility; it's about overall well-being and satisfaction, something that a urologist can help optimize.
“With pregnancy, we sometimes don’t realize that men are half the battle. It can be stressful for men to accept that fertility problems could be on them and not their wife,” said Joseph. “If you have tried for a year or two, sometimes the question remains what is causing abnormal
sperm production or delivery.”
Joseph said the first step is a semen analysis for both volume and mobility.
Prevention is always better than cure, and this holds especially true in urology. Many urological conditions can be prevented or managed through lifestyle changes such as maintaining a healthy weight, regular exercise and avoiding harmful habits like smoking and excessive alcohol consumption. By adopting a proactive approach to health, men can reduce their risk of developing urological issues in the first place. Urologists understand that physical health and mental well-being are intricately linked. Conditions like ED or infertility can take a significant toll on a man's mental health, leading to stress and anxiety. By addressing these concerns holistically, urologists not only improve physical health but also enhance overall quality of life.
“Men tend to let a problem keep festering. Many don’t know key health numbers like their cholesterol, blood pressure or PSA,” said Joseph. “You have to know the facts and part of your lifestyle has to be proactive to seek information about your health. Men should be involved in getting the appropriate physicals so their doctors can put together a plan.”

By Jim Miller
Dear Savvy Senior,
How can I tell if the health info on a website is trustworthy? I usually do a Google search on a symptom, drug or health condition when I want to research something, but with so much information out there I’m not sure what I can trust.
Skeptical Sal
Dear Sal,
You’re wise to be skeptical! There’s an overwhelming amount of health advice on the internet today and it can be hard to tell what’s credible. To help you sort through the online clutter and locate reliable, trustworthy health information, here are a few tips to follow, along with some top-rated sites you can turn to with confidence.
Savvy Searching
First, know that Google or Bing is not always the best place to start a search. You’ll increase your odds of finding reliable health information if you begin with websites run by government agencies (identified by URLs ending in .gov), medical associations (often .org) or academic institutions (.edu).
Commercial websites (usually ending in .com), such as drug or insurance companies who may be trying to sell you their products, are usually not the most trustworthy options. To find out who’s sponsoring a site and where the information came from, click on the “About Us” tab on the site’s home page.
Also note that good health and medical information changes all the time so check the date that information was published to make sure it’s current.
Some other areas you need be wary of include online symptom checkers and artificial intelligence (AI) tools.
While symptom checkers do offer potential diagnoses that could fit your set of symptoms, they are often inaccurate and tend to err on the side of caution, says physician Ateev Mehrotra, a professor of health care policy at Harvard Medical School. AI tools, like ChatGPT, can also be wrong or generate false but scientific sounding information.
You also need to be cautious about using medical information from social media, online forums or YouTube. Comments in these places may sound authoritative even if the authors have no medical training or expertise.
While there are many excellent

websites that provide reliable health and medical information, one of the best all-purpose sites that’s recommended by Consumer Reports for researching symptoms and conditions is MedlinePlus (medlineplus.gov).
A service of the National Library of Medicine, the world’s largest medical library, and part of the National Institutes of Health, MedlinePlus provides high-quality, trustworthy health and wellness information that’s easy to understand and free of advertising.
Here are a few additional websites, recommended by the Medical Library Association and others, to help you find reliable information on specific diseases, conditions and treatments.
• Cancer: National Cancer Institute (cancer.gov), American Cancer Society (cancer.org) and National Comprehensive Cancer Network (nccn.org).
• Heart disease: American Heart Association (americanheart.org), National Heart, Lung and Blood Institute (nhlbi.nih.gov).
• Diabetes: American Diabetes Association (diabetes.org).
• Alzheimer’s disease: Alzheimer’s Association (alz.org) and Alzheimers. gov.
• Public health and vaccines: Center for Disease Control and Prevention (cdc.gov).
• Alternative medicine: National Center for Complementary and Integrative Health (nccih.nih.gov) and the National Institutes of Health’s Office of Dietary Supplements (ods. od.nih.gov).
Any research you do online before seeing a doctor, be sure to save or print your findings out on paper, including the site you got your information from, so you can review it together.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.

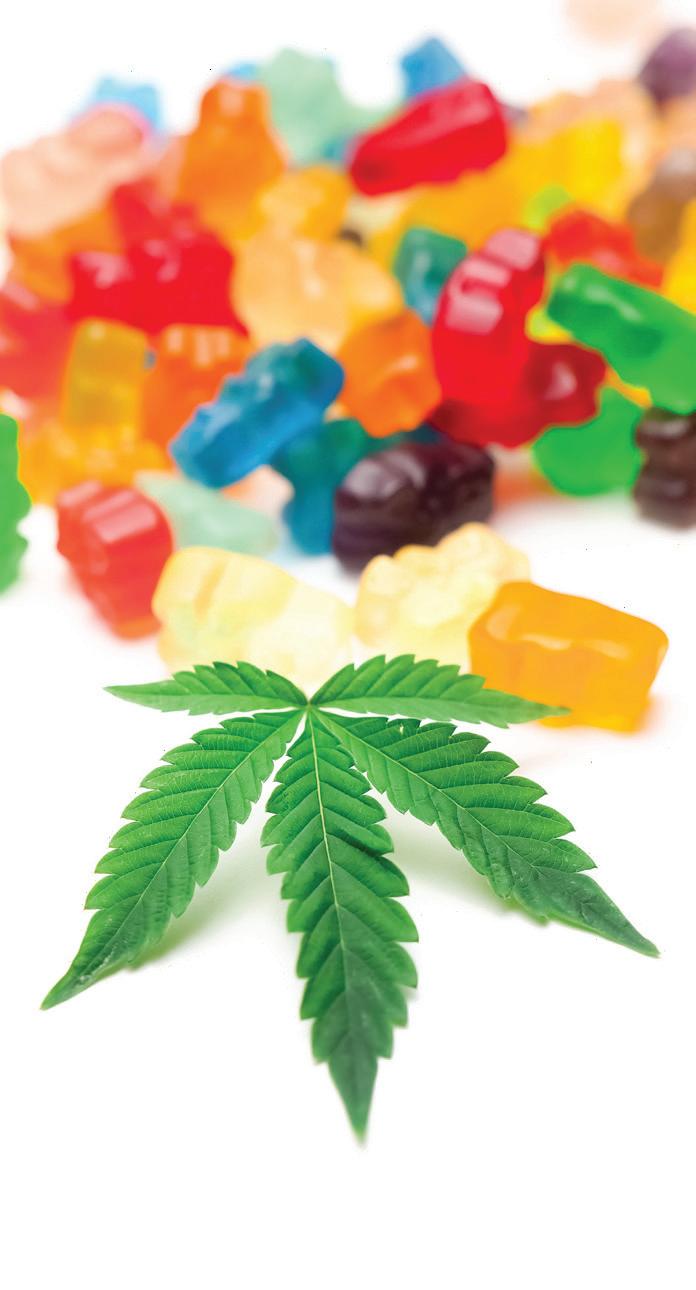



By Brian Burger
What comes to mind when you think of assisted living?
At St. Ann’s Community, we describe assisted living as “private apartments, with helping hands.” Apartments are our residents’ private space, and unless help is scheduled or requested through a predetermined individual care plan, any resident here can enjoy a full expectation of privacy.
Additionally, today’s assisted living communities are vibrant places; they’re full of life and activity! Residents find convenience in onsite restaurants, and a community in gathering places. While some choose to bring their car, most residents enjoy the ease of the provided transportation to their appointments.
There’s a lot more to assisted living than just personal care.
Quality assisted living facilities will work hard to make sure that residents have a wide variety of social events to attend each day. With offerings like exercise classes, a variety of games, support groups and other special interest groups like book clubs or bible study groups, there should be something for everyone.
In many cases, a married couple may find that one of them needs more help than the other. The good news is that in almost every case, both spouses can make the transition to an assisted living apartment together — even if only one person wants to take advantage of the care being offered by the community. Both people can still enjoy the fine-dining style food, the social engagements, and the sense of community.
For many, knowing when the right time is to consider more help is a challenge. There’s no universal life event that indicates that ‘now is the time to think about assisted living’. Much like individual care plans, it
always depends on someone’s personal situation.
Social isolation is another important thing to consider when deciding on next steps.
Oftentimes seniors will forgo the hobbies that make them happy simply because it has become too difficult to get ready on their own. With the help of care staff, residents are able to thrive and find themselves participating in their favorite activities again.
Once you make the leap and move into your new home, settling into the new routines may take some time. That’s completely normal! As the moving process is wrapping up, it’s also not uncommon to feel a surprising sense of relief. Many newly settled residents describe a renewed feeling of security and comfort that they didn’t realize they had been missing for a long time.
If the topic of assisted living has been on your mind, or if it has been a topic of family conversation, the best thing you can do is to prepare a list of any questions on your mind and call a community to chat. A big part of what we do at St. Ann’s is guiding seniors in the community through this whole process, and it’s a very rewarding part of our days. We always look forward to talking to you!

Brian Burger is a marketing representative for St. Ann’s Community at Cherry Ridge in Webster. Contact him at bburger@ mystanns.com or 585-697-6702 or visit www.stannscommunity.com.
very July 4, we celebrate our nation’s independence. For nearly 90 years, our programs have helped create financial independence for millions of hardworking people. We have useful online resources like the Social Security Statement (statement) and our benefits estimator tool that helps people not yet receiving benefits. The statement shows the benefits that you and your family may be eligible for and provides personalized fact sheets tailored to your age and earnings situation. The benefits estimator tool allows you to get estimates based on different ages. These online tools can help you better prepare for your retirement.
If you’re not receiving benefits
You can get the most out of your online experience if you have a personal my Social Security account. You can:
• Request a replacement Social Security card.
• Get estimates for spouse’s benefits.
• Get your statement instantly.
• Get proof that you do not receive benefits.
Q.: I haven’t received my Social Security Statement in the mail the last few years. Will I ever get one again?
A.: We currently mail Social aged 60 and over who aren’t receiving Social Security benefits and do not yet have a personal My Social Security account. We mail the statements three months prior to your birthday. Anyone can access their statement online if they have a personal My Social Security account. We encourage you to create your own account at www. ssa.gov/myaccount and check your statement at your convenience.
Q.: I am receiving Social Security retirement benefits and I recently went back to work. Do I have to pay Social Security (FICA) taxes on my income?
A.: Yes. By law, your employer must withhold FICA taxes from your paycheck. Although you are retired, you do receive credit for those new earnings. Each year Social Security automatically credits the new earnings. If your new earnings are higher than in any earlier year used to calculate your current benefit, your monthly benefit could increase. For more information, visit www.ssa. gov or call us at 1-800-772-1213 (TTY 1-800-325-0778).
Q.: My doctor said he thinks I have a
• Check your application status.
If you’re receiving benefits
You can use your personal my Social Security account to:
• Request a replacement Social Security card.
• Get an instant benefit verification letter.
• Start or change your direct deposit. (Social Security beneficiaries only)
• Change your address. (Social Security beneficiaries only)
• Get a replacement SSA-1099 or SSA-1042S instantly for tax season.
• Opt out of mailed notices for those available online.
You can create your personal my Social Security account at www.ssa. gov/myaccount.
Our blog at blog.ssa.gov features news and information about our programs and services. You can subscribe and get notified each time we post a new blog so you can stay informed. From the blog, you can also connect with us on Facebook, X, LinkedIn, Instagram, and YouTube.
With so many services and helpful information available online, we are here for you when you need us. Learn more at www.ssa.gov.
disability. Who decides if I meet the requirements for Social Security disability benefits?
A.: We first will review your application to make sure you meet some basic requirements for Social Security disability benefits, such as whether you worked enough years to be eligible for benefits. Then we will send your application to the disability determination services office in your state, often called the “DDS” or “state agency.” Your state agency completes the disability decision for us. Doctors and disability specialists in the state agency ask your doctors for information about your condition. They consider all the facts in your case. They use the medical evidence from your doctors and hospitals, clinics, or institutions where you have been treated and all other information.
The state agency staff may need more medical information before they can decide if you have a disability. If more information is not available from your current medical sources, the state agency may ask you to go for a special examination. We prefer to ask your own doctor, but sometimes the exam may have to be done by someone else. Social Security will pay for the exam and for some of the related travel costs. Learn more at www.ssa.gov/ disability.
By Jennifer Faringer
It’s clear that we are living in an age of increased anxiety.
Since 1980, anxiety disorders have increased by 80% with nearly 50% of Americans feeling more stress today than they did five years ago. Stress is affecting both our personal and professional lives. Accumulated stress often leads to burnout in the workplace.
In the workplace, a lack of professional well-being can result in burnout, which has been recognized as a diagnosis by the World Health Organization, when it was added to the International Classification of Diseases in 2019.
Defined as a psychological syndrome resulting from unmanaged prolonged stress at work causing “energy depletion, cynicism related to one’s work and reduced professional efficacy,” burnout is “a state of physical, mental, or emotional exhaustion.” It’s important to recognize that burnout can affect anyone in any profession.
What are the signs to recognize burnout?
Physically, one might experience cardiac or respiratory issues, sleep disturbances or extreme fatigue and exhaustion. Emotionally, it may cause anxiety or depression. If the situation is severe and prolonged, one might even show signs of post-traumatic stress disorder (PTSD) due to a toxic work environment.
Employees note that workplace burnout is most often a result of several factors including insufficient knowledge to complete required tasks, inadequate resources to be successful, a lack of autonomy and an unreasonable workload.
How might you improve your well-being in the workplace?
Set realistic goals, request access to resources and tools as well as rele vant training and procedures on how to manage tasks and workload.
Workplaces and businesses can also request Team Awareness Work place Wellness workshops provided by the National Council on Alcohol
Employees note that workplace burnout is most often a result of several factors: insufficient knowledge to complete required tasks, inadequate resources to be successful, a lack of autonomy and an unreasonable workload.
ism and Drug Dependence-Rochester Area and its multi-county team of educators. Available at no cost, available workshops include:
• The Ripple Effect of Well-being: explores the power of positive stress, the costs and benefits of health decisions, the strengths of the team, and connectivity.
• Resilience and Thriving: explores both the effects of stress and healthy coping skills.
• Empowered Health Consciousness: explores how to embrace a wellness-focused lifestyle, reduce substance misuse and increase overall mental well-being.
For more information, contact Jennifer Faringer at jfaringer@depaul. org or visit the NCADD-RA's Team Awareness Workplace Wellness website page at https://ncadd-ra. org/services/team-awareness-workplace-wellness/

Jennifer Faringer, CPP-G (Credentialed Prevention Professional—Gambling), is the director of the National Council on Alcoholism and Drug Dependence — Rochester Area
Excellus BlueCross BlueShield has recently named four community leaders to its Rochester Regional Advisory Board.
The new members are:
• Rufus M. Judson is chief execu

tive officer at Pike Construction Services, a role he has held since 2015. Pike is a fifth-generation business started in 1873 and is headquartered in Rochester, with offices across Upstate New York and Central Florida.
Judson involves himself in numerous community and industry pursuits. He is current board chairman of the United Way of Greater Rochester and the Finger Lakes. He serves as treasurer of the board of directors of the Associated General Contractors New York State (AGC NYC). Judson also has board positions or affiliations with ROC 2025, CenterState CEO, Greater Rochester Enterprise (GRE) and the regional board of KeyBank.
• Efrain Rivera joined Paychex

in June 2011 as senior vice president, chief financial officer and treasurer. During Rivera’s tenure, Paychex has grown from $2 billion in revenue to approximately $5 billion.
Rivera serves on the board of directors of Rochester Regional Health, Franklin Covey and Jones Lange LaSalle, Inc. In 2014 he was named financial executive of the year for a public company by the Rochester, New York Financial Executives International and the Rochester Business Journal. In 2022, he was named a Business Icon by The Rochester Business Journal.
• Jaime Saunders is president and chief executive officer of United Way of Greater Rochester and the Finger Lakes. As CEO, she leads United Way and more than one hundred talented team members in mobilizing resources and relationships to close gaps, create opportunities, and build a stronger, healthier region. Annually United Way raises and leverages $25-$35 million to support the six-county region.
Saunders has provided her
experience and perspective to several

regional and statewide initiatives, including Finger Lakes Regional Economic Development Council (FLREDC), ESL Federal Credit Union board of directors, Gov. Cuomo’s NY Forward, Monroe County Plan Forward, TogetherNow Board, Rochester/Monroe Anti-Poverty Initiative, NYS Office for the Prevention of Domestic Violence (OPDV) Advisory Council, NYS Council on Women and Girls Steering Committee, the NYS OPDV Fatality Review Committee, and a host of local and statewide coalitions.
• Miguel A. Velazquez is the

Miguel A. Velazquez
chief executive officer at The Rochester Genesee Regional Transportation Authority (RGRTA). Since joining RGRTA in 1999, Velazquez has successfully led the organization through significant projects and change that have improved the customers’ experience with the public transit system. He oversaw the transformation of the authority’s information systems, infrastructure, services, and operations. He created the vision for TIDE (Technology Initiatives Driving Excellence), an ambitious $25 million customer-focused technology project, he was the executive sponsor for the construction of the $50 million RTS Transit Center in Downtown Rochester, and for Reimagine RTS a complete redesign of the 40-year-old service profile which is now providing a more equitable and modern transportation system to our community.
Velazquez has raised funds for youth programs in the Rochester community for over a decade. He serves on the board of several community-based organizations as well as public transportation industry associations. He is a member of the Rochester Monroe Anti-Poverty Initiative steering committee, board member of Together Now, a trustee at Nazareth University, and a member of the Partners for Downtown Rochester, among others.
Christine Corbett of Manlius

has been named vice president for development for the Upstate New York Chapters of the Alzheimer’s Association. In this newly created position, Corbett is responsible for the fundraising and development operations of three Upstate New York chapters of the Alzheimer’s Association, including Central New York, Rochester Finger Lakes region and Western New York.
Her primary focus is the Walk to End Alzheimer’s, the world’s largest event to raise awareness and funds for Alzheimer’s care, support and research programs. Fourteen walks are held throughout the Upstate New York Chapters each fall, with a combined 2024 revenue goal of $2.2 million.
In addition, Corbett will supervise development staff in all three chapters, manage corporate sponsorships and partnerships, cultivate major and planned gifts and oversee special events.
“We are so pleased to have Christine on our team,” says Kate Flannery, executive director for Upstate New York Chapters. “Her passion for her work, her knowledge of fundraising and the development process, and her vast network of local individuals and companies make her the perfect individual for this vital role.”
Corbett most recently served as director of philanthropy for David’s Refuge, a nonprofit organization providing respite, resources and support to families of children with special needs or life-threatening medical conditions.
In her six years at David’s Refuge, revenue was nearly tripled through engaging dedicated and hardworking volunteers and philanthropists. During that time, she also successfully managed special events, corporate partnerships, leadership giving and grant funding.
Prior to David’s Refuge, Corbett served as director of development for Make-A- Wish Central New York and in development positions at the Hospice Foundation and United Way of Central New York.
“I’ve been privileged to spend nearly 20 years fundraising in the Central New York community,” Corbett says. “As a local ‘friend-raiser,’ I’m driven by connecting people to missions of impact in order to create positive change, and as a wife and mother of three girls, I embrace philanthropy and giving back in every aspect of my life.”
A graduate of Mount Saint Mary
College, Corbett holds a dual bachelor’s degree in psychology and public relations. She currently serves on the board of directors at the Central New York Association of Fundraising Professionals and Eastwood Rotary.
Highland Hospital has honored

Chin-Lin Ching physician ChinLin Ching as physician of the year and nurse practitioner Rachel A. James as advanced practice provider (APP) of the year. Ching, associate professor of clinical medicine at the University of Rochester Medical Center, serves as medical director of the palliative care division at Highland Hospital. She recently stepped down as the chairwoman of Highland’s ethics committee after five years of growing the committee. She has been a part of Highland since 2010 and has been a champion for palliative care throughout her career.
“It is always an honor to be nominated for this recognition; to be awarded leaves me speechless for once,” said Ching. “A person is only as good as her team, so I would like to recognize my palliative care team for always supporting me and lifting me up. I don’t think that I would be the physician I am today without the constant support and encouragement from the leadership at Highland. I’ve been thriving at Highland for almost 15 years, and it’s because I’ve been lucky enough to find amazing colleagues and inspiring mentors all along the way.”
James, a nurse practitioner in the

Rachel James department of nephrology, practices in inpatient nephrology care and adult health. She has been part of Highland for 10 years and previously served as a charge nurse and preceptor in the intensive care unit. She was previously recognized with the Highland Hospital Nurse of Distinction Award in 2016.
“Since learning I was going to receive the APP of the Year award, I feel surprised, humbled and most of all, embraced by the community of amazing professionals I am privileged to work alongside,” said James. Ching and James were recognized during a reception in May and at a Highland board of directors meeting.


RPH is hosting a FREE educational speaker series for people impacted by memory impairment. Join us to learn strategies for successful living!


Financial Considerations When Someone you Love has Memory Impairment
Presented By: Ethan Wade, The Wade Group at Brighton Securities
Scams 101 – Signs that your Loved One is a Target Thursday, June 20 from 6:30-7:30PM
Thursday, July 25 from 6:30-7:30PM
Presented By: Daniel Lyon, Lifespan of Greater Rochester



SELECT STORIES IN THE NEW ISSUE OF 55 PLUS
• Celebrity —TV legend Don Alhart signs off
• Aging — Healthful aging isn’t just up to chance. A conversation with an URMC expert
• Your Health — Turnng 55? Here are the tests your doctor will ask you to get
• Wellness — Meet the ‘Fantastic Four’ at RIT wellness program
• On the Water — Meet the team at Corn Hill Waterfront Navigation Foundation
• Staycation — No plans for this season? Try these staycation ideas | The ultimate road trip: take Route 5 and 20
to 55Plus, the
• Pickleball — Pickleball at Dinkers, Rochester’s largest pickleball facility
• Grandkids — Recreation and activities you can enjoy with grandkids
• Music — Host of WXXI’s midday classical music program, Julia Figueras reflects on 40-plus-year career
• Profile — Ann Mitchell jazzed about music
• Collecting Social Security at 62 and very happy about it ...and so much more!