NON PROFIT ORG US POSTAGE PAID SAN ANTONIO, TX PERMIT 1001 SAN ANTONIO


PUBLISHED BY: traveling Blender, llC. 10036 Saxet Boerne, tX 78006

PUBLISHER louis doucette louis@travelingblender.com
BUSINESS MANAGER: vicki Schroder vicki@travelingblender.com
ADVERTISING SALES:
AUSTIN: Sandy Weatherford sandy@travelingblender.com
QUALITY OF LIFE –

San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EditoriAl CorrESpondEnCE: Bexar County Medical Society 4334 n loop 1604 W, Ste. 200 San Antonio, tX 78249
Email: editor@bcms.org
MAGAZinE AddrESS CHAnGES: Call (210) 301-4391 or Email: membership@bcms.org
SuBSCription rAtES: $30 per year or $4 per individual issue
AdvErtiSinG CorrESpondEnCE: louis doucette, president traveling Blender, llC. A publication Management Firm 10036 Saxet, Boerne, tX 78006 www.travelingblender.com
For advertising rates and information
Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national orgin, or an intention to make such preference limitation or discrimination.
SAN ANTONIO: Gerry lair gerrylair@yahoo.com
PROjECT COORDINATOR: denise tapia denise@smithprint.net

For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.

SmithPrint, Inc. is a family owned and operated San Antonio based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2023 Smithprint, inc. prin tE d in tHE u SA
SAN ANTONIO 4 SAN ANTONIO MEDICINE • February 2023
TABLE OF CONTENTS
THE OFFICIAL PUBLICATION OF THE BEXAR COUNTY MEDICAL SOCIETY • WWW.BCMS.ORG • $4.00 • FEBRUARY 2023 • VOLUME 76 NO.2
ENHANCED
Transcervical Carotid Artery Revascularization (TCAR): A New Solution to an Old Problem By Boulos Toursarkissian, MD 12 Cherry Picking and Lemon Dropping By Neal S. Meritz, MD 14 A Wake-Up Call – The Alarming Truth About Snoring and Heart Disease By Monica J. Salas, MD 16 I’m a Physician Battling Long COVID. I Can Assure You It’s Real By Monica Verduzco Gutierrez, MD 18 Post-Thrombotic Syndrome: To Add Insult to Injury By Ashton Lee, MD 20 BCMS President’s Message 8 BCMS Alliance Message 10 Bood Review: Deviate from Denial by Sam Perez, Reviewed by David Alex Schulz, CHP 22 2023 BCMS Installation of Officers and Golden Aesculapius Awards 24 BCMS in the New Millennium: How Have Things Changed? Interview with Vijay N. Koli, MD, By Monica Jones, BCMS COO 26 Welcome Committee Chairs and Co-Chairs 2023 28 2023 Joint Installation of Officers Golden Aesculapius Awards, In Memoriam 29 Disparities in Prenatal Care Among Undocumented Immigrants By Winona Gbedey, Sanjana Ravi and Rozena Shirvani 30 Medicine Achieves Reduction in Medicare Physician Pay Cut Amid Push for Reform By Emma Freer 34 South Texas Blood and Tissue – Sicle Cell Disease Story By South Texas Blood & Tissue 36 BCMS Vendor Directory 40 Auto Review: 2023 Mazda MX-5 By Stephen Schutz, MD 44 Recommended Auto Dealers 46
BY MEDICAL CARE

ELECTED OFFICERS
John Joseph nava, Md, President
Brian t. Boies, Md, Vice President
Ezequiel “Zeke” Silva iii, Md, Treasurer
John Shepherd, Md, Secretary

Brent W. Sanderlin, do, President-elect
rajeev Suri, Md, Immediate Past President
DIRECTORS
Woodson "Scott" Jones, Md, Member
Sumeru “Sam” G. Mehta, Md, Member
priti Mody-Bailey, Md, Member
lubna naeem, Md, Member
lyssa n ochoa, Md, Member
Jennifer r rushton, Md, Member
raul Santoscoy, do, Member
John Shepherd, Md, Member
Amar Sunkari, Md, Member
lauren tarbox, Md, Member
Jenny Case, Alliance Representative
ramon S. Cancino, Md, Medical School
Representative
lori Kels, Md, Medical School Representative
robert leverence, Md, Medical School
Representative
Keiko McManus, Md, Board of Ethics Chair
John pham, do, Medical School Representative
Cheryl pierce-Szender, Alliance Representative
ronald rodriguez, Md, phd, Medical School
Representative
Col. tim Switaj, Md, Military Representative
George F. “rick” Evans, Jr., General Counsel
Jayesh B. Shah, Md, TMA Board of Trustees
Melody newsom, CEO/Executive Director
BCMS SENIOR STAFF
Melody newsom, CEO/Executive Director
Monica Jones, Chief Operating Officer
Yvonne nino, Controller
Mary nava, Chief Government Affairs Officer
Brissa vela, Membership Director
phil Hornbeak, Auto Program Director
August trevino, Development Director
Betty Fernandez, BCVI Director
Al ortiz, Chief Information Officer
PUBLICATIONS COMMITTEE
norys Alexandra Castro-pena, Md, Co-chair
John Joseph Seidenfeld, Md, Co-chair
louis doucette, Consultant
david Schulz, Community Member
Elizabeth Clanton, Md, Member
Kristy Yvonne Kosub, Md, Member
neal Meritz, Md, Member
Jaime pankowsky, Md, Member
Alan preston, phd, Member
rajam S. ramamurthy, Md, Member
Adam v ratner, Md, Member
Faraz Yousefian, do, Member
Moses Alfaro, Student Member
Winona Gbedey, Student Member
tue Felix nguyen, Student Member
niva Shrestha, Student Member
Monica Jones, BCMS Coo, Staff Liason
nancy Salas, Editor
6 SAN ANTONIO MEDICINE • February 2023
BCMS BOARD OF DIRECTORS
Quality of Life
By John J. Nava, MD, 2023 BCMS President
“When I was 5 years old, my mother always told me that happiness was the key to life. When I went to school, they asked me what I wanted to be when I grew up. I wrote down ‘happy’. They told me I didn’t understand the assignment, and I told them they didn’t understand life.” – John Lennon
Up until seven years ago, I had been unfamiliar with this quote attributed to the famous Beatle, content to be swept away by his lyrics and music, which I heard as a young child. I was first exposed to it during a trip to Central Park in New York City with my son, Joshua. He had never been to the Big Apple, and I had visited only once before. My previous visit was for a weeklong National Hispanic Medical Association (NHMA) conference, with a schedule so tightly packed that I had little time for sightseeing. Spring Break seemed the perfect opportunity to return to visit Strawberry Fields. A street vendor provided the quote on a small card, which I snatched up and framed for my office, as a reminder.
Webster’s dictionary provides a few definitions for quality of life (QoL), “overall enjoyment of life, general well-being; specifically: the degree to which a person or group is healthy, comfortable, and able to enjoy the activities of daily living.” This term was first known to be used in 1943. Multiple components impact QoL, those being health, emotional wellbeing, personal safety, social relationships, belonging, work and quality of environment.
Financial wellbeing completes the list, though higher incomes do not always correlate with higher QoL. By definition, the term is nebulous and invites confusion with the standard of living, which is a much more easily quantified concept, typically an assessment of financial resources and other material tools to achieve satisfaction in life.
This is truly significant for patients and physicians. In the case of patients, health related quality of life (HRQoL) is a measurement of the same indices specifically affected by health and health interventions. These are reflected in levels of self-reported satisfaction with their current health plan, clinic site, PCP and associated support staff. Other clinical measures, such as whether they work together with the clinical team to follow evidence-based best practices for prevention, are data driven and typically inform the quality assurance gurus (which we are all encouraged to become).
Of course, patients can always decide to obtain their healthcare services from a different company, clinic or physician if their needs are not met. When it comes down to it, the patient is in control, which is as it should be. Without the cooperation of our patients, we are much less.
QoL for physicians has gotten much recent attention, as healthcare workers are leaving the field in droves. It is truly a challenge for the healers to attend to others when they don’t start with fully charged batteries themselves. For physicians, it is a natural choice to try and pay off student loans, buy a house and start or continue to build a family. Younger newly graduated physicians should carefully examine their future financial plans. All costs should be included, especially the intangible ones. Maybe even mid-career colleagues can do the same.
During the Covid-19 pandemic, increased rates of clinician burnout, symptoms of anxiety and depression, and suicide rates have been noted. In response to these phenomena, physician coaches are leading the medical profession to respond with an emphasis on self-care and prevention of mental health issues. Whether this new awareness is related to the ongoing pandemic or past neglect of the antecedents of symptomatic mental issues, it is an opportune time to address them. I recently came across a post by a physician who was burned out by active clinical primary care, and had developed side employment as a hospice physician, financial advisor and writer. He wrote a book about the perspectives of his hospice patients as they neared the end of life, and was surprised that none of them expressed regrets that they had not worked harder or for more money to leave to their survivors. I suspect they wished they had spent more quality time with their families, nurtured the relationships with people that brought them joy, exercised more to enjoy better health, developed better sleep habits and spent more time experiencing nature. I am looking forward to reading that book.
With regard to preventing mental health issues for physicians, some might ask, they knew the many years of education would be difficult, the hours grueling and the needs endless, right? Perhaps, but under-
8 SAN ANTONIO MEDICINE • February 2023 PRESIDENT’S MESSAGE
neath the armor, we are people too. And despite perhaps being more resilient at the start of our careers, it’s possible we didn’t acquire the requisite skills to meet all the challenges never planned for. I was trained by a number of “iron men”, (both male and female) who inculcated the belief that asking for help was a sign of weakness. The only thing to do when you got stuck in the mud was “pull yourself up by your own bootstraps!” This is Texas, so I could not resist the boot analogy, but hope it is becoming an outdated concept when applied to mental health. Of note, “primary care practices with zero burnout are more often solo practices owned by physicians and practices not involved in transformation initiatives, such as accountable care organizations (ACOs).”1 Quality assurance efforts are wonderful tools, but when added to an already busy day, clinician stress and burnout may spill over to affect patient centered care.
It is never too late. I encourage all my colleagues to question their version of reality, where they have been and where they are going. If they don’t like what they see, they can actively change it. Or, if they do like what they see, share your story with your colleagues. Starting small to create a new work-life balance can lead to widening the vision. Even
the smallest change can be empowering to make a better future for yourselves and your loved ones.
References
1. FamilyPractice News, Vol. 15, No.7, p. 8. July 2021, citing Health Affairs, (2021.doi:101377.hlthaff.2020.02391.
John J. Nava, MD, is the 2023 President of the Bexar County Medical Society. He is interested in Primary Care, Clinical Research and Public Health.

PRESIDENT’S MESSAGE
Visit us at www.bcms.org 9
BCMSA – What does the Alliance do for you?
For over a century physician’s spouses have been a part of the Bexar County Medical Society Alliance. As physicians, you form the foundation of the health care system in our city, and your spouse plays a very important role as well.
Since 1917, the Bexar County Medical Society Alliance has sought to promote fellowship among medical families, while fostering both civic and philanthropic activities that benefit our community. As a member, your spouse will receive our monthly internet newsletter, a member directory and an invitation to social events and community projects.
We have some exceptional programs planned for the year, including outreach programs to benefit the San Antonio community as well as opportunities to be involved in the Texas Medical Association’s political action committee. These activities foster close friendships and support with other family members.
If your spouse has never been a member of the Alliance before, or even if they are busy with work, children or other activities I hope they will consider joining us this year!
We would love for them to become actively involved; however, we appreciate any level of involvement. Your BCMS Alliance dues will support our projects in an important way.
For additional information about the Alliance and membership, please visit www.bcmsalliance.org/
Being a part of BCMSA has been instrumental in meeting friends in the medical life journey. Meeting likeminded people that understand life in medical school, residency, and finally becoming an attending, has been a great way to learn expectations from reality.
Heather Davila, Membership

BCMSA strengthens our community in so many ways. Whether it's by connecting medical families new to the area, helping them get settled, or promoting upcoming blood drives during critical blood shortages. Our members graciously donate their time to service projects that improve wellness for kids and families in need.
Brittany Garcia, VP of Communication
When I think of this organization, I think of three words: family, outreach and fellowship. This organization has brought fellowship during the most difficult years of Covid. We have stood together with the medical community providing masks, and books to children and a sense of unity. As a healthcare professional myself, I’ve seen what this alliance has done for the Bexar community.
We have not only provided helmets for children promoting safety but have provided beds and sheets along with Heavenly Peace for those in need. Our members continue to advocate for our medical spouses to legislators and politicians. As a board member, I can’t wait to see what more we can do for each other and the community!
Stephanie Stewart, VP of Social Programs
By Taylor Frantz, RDN, LD
The medical industry can be overwhelming, especially earlier in careers when everything is new. The BCMSA provides a supportive community and fosters relationships, while also giving opportunities to give back to the communities we all live in and serve.
Tatiana Sweeney, VP of Community Outreach
I have always volunteered my time in school activities as a youth, through clubs and spouses’ groups when my husband was in the USAF, and all through my children’s elementary/high school time. I joined BCMSA because I was soon to become an empty nester. I wanted to meet other people and volunteer to help others.
Virginia Profenna, Treasurer
The friendships I have made over the years through the physician-spouse community are some of the most cherished relationships in my life. It is so nice to have friends who not only understand the triumphs and challenges that come along with being in a physician family, but also share the same familial values centered around the joy that comes from living a life in service to others.
Julia Halvorsen, Secretary
San Antonio has become such a big city! What better way to meet new friends than through BCMSA?! We all already have something in common as part of the medical community. It's a wonderful way to network, give back to the community and make lifelong family friends. BCMSA has been such a blessing in our lives, I look forward to every event!
Victoria Kohler-Webb, President Elect
10 SAN ANTONIO MEDICINE • February 2023 BCMS ALLIANCE
Taylor Frantz, RDN, LD is a registered dietitian and the 2022 President of the BCMS Alliance.

Transcervical Carotid Artery Revascularization (TCAR): A New Solution to an Old Problem
By Boulos Toursarkissian, MD
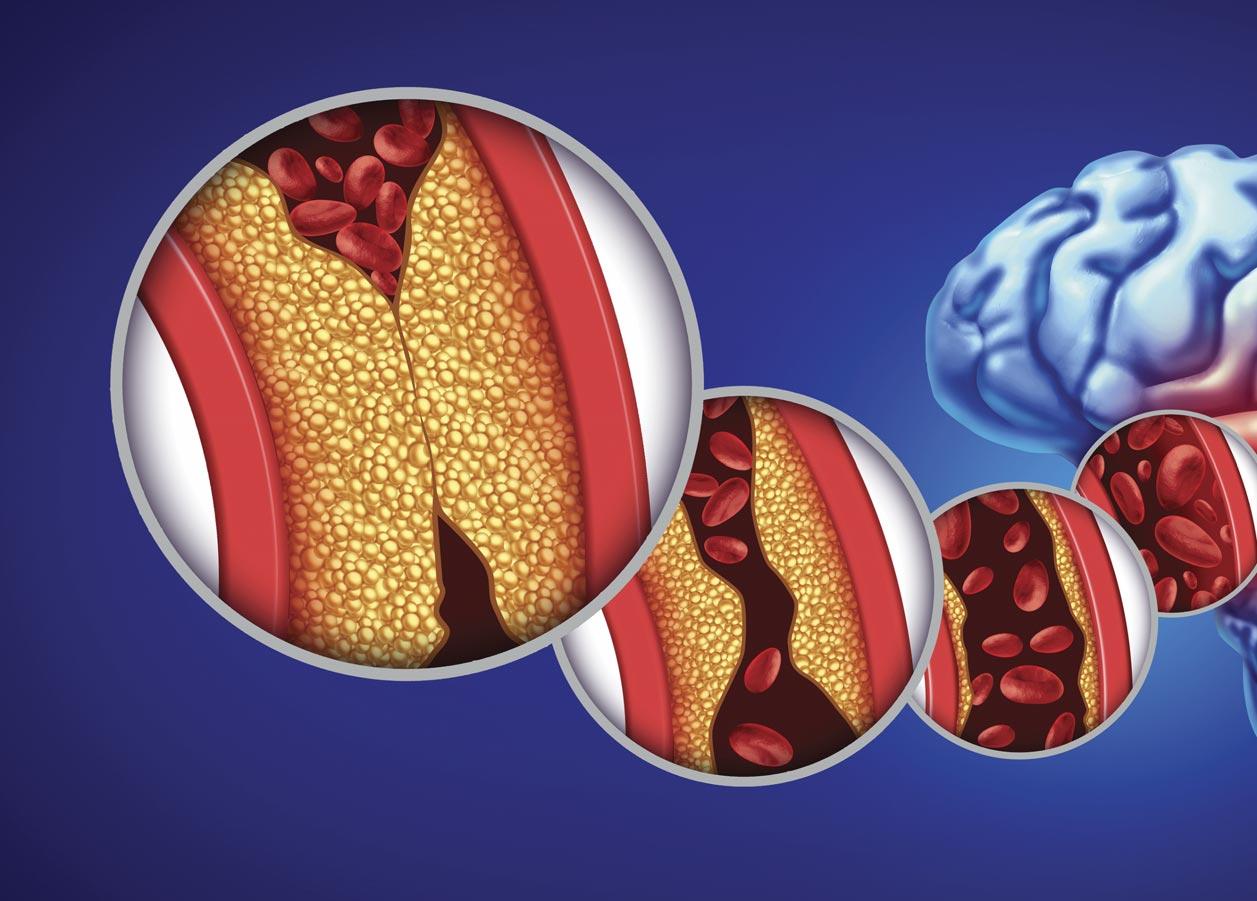
Approximately every 40 seconds, someone in the United States has a stroke. Carotid artery atherosclerotic disease is a major cause of stroke and disability, causing up to a third of cerebrovascular accidents. Studies have irrevocably shown that, in addition to medical management, the direct treatment by an expert of a significant cervical carotid artery stenosis reduces a patient’s future risk of stroke. This is most beneficial for symptomatic stenoses greater than 50%, but is also of benefit for asymptomatic stenoses greater than 60 to 70%.
Physicians can detect if a patient may be at risk for carotid artery disease by determining if they have risk factors, which include diabetes, history of smoking, obesity, hypertension, family history, associated coronary or peripheral arterial disease and hyperlipidemia, among oth-
ers. If carotid disease is suspected, the patient should be referred to a board-certified vascular surgeon who can offer the entire spectrum of endovascular and open surgical options. My team at Peripheral Vascular Associates, for example, includes several physicians who are fully versed in the various and latest diagnostic and therapeutic modalities for carotid disease.
Carotid endarterectomy (CEA), a surgical procedure whereby the blockage is physically removed, has been for years the gold standard treatment for significant carotid stenosis with a low perioperative risk in experienced hands. Nearly 20 years ago, transfemoral carotid stenting came to the forefront of treatment options, offering a less invasive alternative. Over the subsequent two decades, numerous studies have shown that carotid artery stenting (CAS) can afford a significant long
12 SAN ANTONIO MEDICINE • February 2023 QUALITY OF LIFEENHANCED BY MEDICAL CARE
term stroke reduction benefit, similar to CEA. However, transfemoral carotid stenting comes at the cost of a significant perioperative stroke risk, much higher than the risk associated with CEA. This perioperative CAS associated risk is particularly elevated in those who would benefit the most from a less invasive approach, namely the elderly patients. The risk is such that transfemoral CAS never gained much traction
after the initial hype, despite the advent of embolic protection filters destined to catch embolic debris during the stenting procedure.
The reasons for the procedural risks associated with transfemoral CAS lay in the need to cross an often-calcified atherosclerotic aortic arch from a femoral or brachial approach, and the need to traverse the cervical carotid lesion in order to allow the deployment of an embolic protection filter, prior to angioplasty and stenting. To reduce these risks, a new procedure was developed several years ago, referred to as TCAR: transcervical carotid artery revascularization.
TCAR uses an innovative direct cervical approach to the carotid artery at the base of the neck, accessing the common carotid artery via a small cervical cutdown. Therefore, there is no need to traverse any calcified atheromatous aortic arch. A sheath is inserted at the base of the patient’s neck in the artery, through which the stent will be delivered. Furthermore, instead of a filter that requires crossing the carotid lesion for embolic protection, TCAR relies on flow reversal in the internal carotid artery before any wire traverses the lesion. For that purpose, a separate sheath is inserted percutaneously in the patient’s femoral vein. The higher-pressure cervical carotid arterial sheath then is connected
to the low pressure femoral venous sheath, thereby establishing flow reversal in the carotid system. Any debris released during the angioplasty/stenting procedure are thus flushed in the venous system, instead of heading upstream in the intracranial arterial bed. The TCAR procedure reverses the direction of blood flow in the carotid, significantly reducing the patient’s risk of stroke during the procedure.
Since its inception, TCAR has been shown to have a perioperative stroke risk remarkably close to that of CEA, while affording a similar long-term stroke risk protection. Advantages of TCAR include a shorter procedure time and a smaller, less painful, and cosmetically more acceptable incision at the base of the neck, which lessens recovery time. It is particularly useful for high-risk patients, such as those with radiated necks, recurrent stenoses after prior CEA, patients with prior neck surgeries, and those with lesions extending high up in the neck, where the risks of cranial nerve injuries with CEA is elevated. Of course, TCAR cannot be applied to all cases. Calcified lesions in particular should be avoided, since these do not usually respond well to angioplasty and stenting. Thrombus laden lesions should also be avoided. Finally, not every patient is a candidate for this type of procedure. Patients must meet certain criteria, and candidacy should be determined by a vascular surgery expert.

In summary, the advent of TCAR has added an additional tool in our armamentarium for dealing with carotid artery occlusive disease, while offering patients a safer way of using the carotid stenting alternative. Innovations like this allow us to better serve our patients and our South Texas community, which sees an increasing need for such care. In fact, San Antonio recently celebrated a milestone in its medical community when Peripheral Vascular Associates and Methodist Hospital | Specialty and Transplant successfully completed the 100th Transcarotid Artery Revascularization procedure (TCAR).
Carotid artery disease affects many in our community. Learn more about this condition with dozens of educational articles and videos provided by the board-certified, highly specialized surgeons who make up our team at Peripheral Vascular Associates (PVA). We offer these resources on our website at PVAsatx.com as a way of raising awareness within our community.
Boulos Toursarkissian, MD is a vascular surgeon and endovascular specialist at Peripheral Vascular Associates (PVA). He is a member of the Bexar County Medical Society (BCMS) and adjunct Professor of Surgery at the UT Health Science Center.

Visit us at www.bcms.org 13
QUALITY OF LIFEENHANCED BY MEDICAL CARE
Cherry Picking and Lemon Dropping
By Neal S. Meritz, MD
Medicare Advantage companies and other Health Insurers usually try their best to accommodate their insured clients but they also know that time is of the essence when approving requests for medical treatments. They understand that to avoid paying a policyholder’s valid claim is a means to bolster their own profits. Medicare Advantage plans are now adept at enrolling healthy patients while shunting away sick ones. Insurers are able to utilize Health Risk Assessments and leveraged chart reviews to maximize payments to the insurance company, and these maneuvers result in little or no value to the beneficiary.
Health Insurers commonly exclude high risk patients who are more likely to suffer expensive medical catastrophes. Cherry Picking is a
popular term for the practice of Medicare Advantage plans to sell policies to those who don’t need them. Another term, Lemon Dropping describes the custom of canceling those who are insured when they do need the policy. The Insurance Company obtains a favorable and less costly set of patients while shunting away the sick, poorly reimbursed ones.
Sicker, more costly patients withdraw from Medicare Advantage plans at a higher rate than healthier ones. As a group they have medical expenses 28% higher than their Medicare risk factors predict. Medicare Advantage plans utilize selective marketing to design and advertise particular benefits to attract a healthier subset of the Medicare population. They may also emphasize benefits that appeal

14 SAN ANTONIO MEDICINE • February 2023 QUALITY OF LIFEENHANCED BY MEDICAL CARE
to healthier persons, such as sports medicine clinics and dental coverage. There are many more prior authorizations required for sicker patients with complex medical problems, and insurers only minimally advertise prescription drug benefits that appeal to those with more serious chronic conditions. Insurance coverage for memberships to fitness clubs, undoubtedly a valuable benefit, attracts physically active elderly persons, most of whom are less likely to be expensive to the insurance company.
Health Insurance companies perform an honorable and extremely important function in our lives, but the purchase of data about prospective patients allows them to Cherry Pick more easily. A patient with multiple prior hospitalizations for a chronic condition is very likely to require multiple future hospitalizations, a significant expense. Having a company representative as part of the enrollment process, allows selective redirecting of expensive patients from Medicare Advantage plans to traditional Medicare plans. Avoiding the sicker patient allows the plan to be more profitable.
Medicare Advantage plans have become extremely eager to send a doctor or nurse to visit patients at home. These free “house calls” are touted as a major health benefit. In home Health Risk Assessments are often conducted by vendors hired by the Medicare Advantage company, not by the beneficiary’s primary care provider. The quality of care coordination and the validity of diagnoses reported are problematic at best. According to CMS (Centers for Medicare and Medicaid), there is a paucity of evidence showing that home visits make people healthier, improve their care, or do much beyond driving up Medicare’s costs.
Medicare Advantage companies are able to utilize their beneficiaries’ diagnoses to obtain higher capitation payments from CMS, Medicare Advantage companies are thus financially incentivized to make their insureds appear as sick as possible. CMS then risk adjusts payments to companies whose medical costs are expected to be higher than anticipated. Medicare Advantage companies routinely leverage both chart reviews and Health-Risk Assessments in order to maximize these payments. Unsupported risk adjusted payments have resulted in billions of dollars of questionably legitimate income for these plans.
The government has begun litigating multiple lawsuits alleging that insurers fraudulently added diagnosis codes without medical justification in violation of Medicare rules. Illegitimate behaviors include chart reviews to pressure physicians to add diagnoses to the patient’s record, establishing benchmarks to “improve” diagnosis capture and tracking physician performance in adding these diagnoses. The Office of the Inspector General (OIG) of the Department of HHS has issued multiple revelatory reports detailing alleged abuses of the Risk Adjustment Process for improper financial gain, resulting in billions in over-payments.
Most Health Insurance companies agree with and usually strictly follow the implied covenant of good faith and fair dealing in an insurance contract. But Medicare Advantage plans now are very capable of manipulating the Risk Scoring to provide an appearance of more severe illness in order to increase payments to the plan from Medicare. Perhaps the only conceivable entity capable of preventing insurance companies from defrauding consumers is the Government. The survival of our current healthcare system depends upon aggressive oversight of insurance companies.
References
Reed Abelson and Margot Sanger-Katz, The Cash Monster Was Insatiable: How Insurers Exploited Medicare For Billions, The New York Times Oct 8, 2022
Fred Shulte, David Donald, and Erin Durkin, Why Medicare Advantage costs taxpayers billions more than it should, The Center for Public Integrity 910 17th St NW Suite 1030 Washington DC 20006
June 4, 2014
Fred Shute, Health Insurers have their way with regulators, The Center for Public Integrity. June 9, 2014
Fred Shulte, Home is where the money is for Medicare Advantage plans, The Center for Public Integrity June 10, 2014
Brenda Gazzar, Cherry Picking? Lemon Dropping? How Health Insurers weed out sick people, Code Wack Podcast July 26, 2021
Jonathan H. Ferry and Ocasha O. Musah, The National Law Review, Volume XII Number 327 November 21,2022
Eric Roehm MD, FACC, Medicare Advantage Plans Cherry Pick Patients, www.NutritionHeart.com/Medicare-at-Risk
Alicia L. Cooper MPH and Amal N. Trivedi MD MPH, Fitness Membership and Favorable Selection in Medicare Advantage Plans, N Eng J Med 2012; 366: 150-157 January 12, 2012
Jeanmarie Loria, Founder and CEO Advize Health, OIG Files: Health Plans, Cherry Picking, and Lemon Dropping, September 24, 2021
Neal S. Meritz is a retired Family Practice Physician, Graduated from the University of Texas Medical School at San Antonio in 1972. He is a member of the Bexar County Medical Society and an active member of the BCMS Publications Committee.

Visit us at www.bcms.org 15 QUALITY OF LIFEENHANCED BY MEDICAL CARE
A Wake-Up Call –The Alarming Truth About Snoring and Heart Disease
 By Monica J. Salas, MD
By Monica J. Salas, MD
Introduction
An old Irish proverb states “A good laugh and a long sleep are the best cures in the doctor's book” and few would disagree. However, unfortunately, long and good quality sleep is becoming more and more elusive in modern society. This is due to a variety of factors, one of the more common ones is Obstructive Sleep Apnea (OSA), which is a chronic disorder characterized by obstructive apneas, hypopneas, and/or respiratory effort-related arousals caused by repetitive collapse of the upper airway during sleep. OSA often goes undetected by the individual experiencing it, but frequently is identified by the presence of snoring. As the most common sleep-related disorder in the world, it is estimated that approximately 1 billion people worldwide suffer from the condition.1 Driven by the global obesity epidemic, (obesity being the most common risk factor for OSA), there is ever-increasing morbidity related to the condition. One of the most serious outcomes of OSA is heart disease, which may include arrhythmias, congestive heart failure, sudden cardiac death and more. In other words, unbeknownst to many, snoring just may be the canary in the coal mine for your heart.
Pathophysiology
How does a seemingly benign event like snoring have such serious consequences? The repetitive episodes of apnea and/or hypopnea that patients with OSA experience due to upper airway obstruction lead to intermittent hypoxemia, hypercapnia, endothelial dysfunction from oxidative stress, alterations in cardiac output and venous return to the heart, and recurrent sleep arousals (which may or may not be recognized by the patient). Although the arousal causes restoration of upper airway patency and normal breathing patterns, the result of these repetitive events is chronic hemodynamic, autonomic, metabolic and inflammatory effects on the body.
A common finding is the increased heart rate and blood pressure that come with increased sympathetic activity associated with OSA events. This hemodynamic aberrance, in conjunction with the other aforementioned changes caused by OSA, is strongly associated with heart disease of different varieties.2
Cardiovascular Diseases Associated with OSA
There is a well-known association between hypertension and OSA, approximately 50% of those with OSA have coexisting hypertension.
16 SAN ANTONIO MEDICINE • February 2023 QUALITY OF LIFEENHANCED BY MEDICAL CARE
Astute clinicians will screen for OSA once a diagnosis of hypertension has been established. Patients with elevated morning blood pressure and resistant hypertension are often found to have OSA once polysomnography is performed. There is a consistent correlation between the two conditions even after controlling for potential confounding factors such as age and obesity.3
Atrial fibrillation (AF) has been found in multiple studies, independent of confounding factors such as obesity, to also have a strong association with OSA (up to fourfold higher odds). A large cross-sectional study showed by polysomnography that there was an increased prevalence of AF in patients with and without sleep-disordered breathing (5 vs 1 %), independent of age, sex, BMI and other types of heart disease (odds ratio 4.0, 95% CI 1.0-15.7).4 OSA is also associated with other nocturnal cardiac arrhythmias. Although it is not clear whether the relationship is causal, it does seem to be temporal in nature with arrhythmias occurring more frequently after a hypoxic event.5 This can lead to, in certain cases (such as QT prolongation in those predisposed), sudden cardiac death.
Patients with Congestive Heart Failure (CHF) are also frequently found to have comorbid OSA. Unfortunately, OSA may often be underdiagnosed in this population due to overlapping signs and symptoms between the two conditions, such as nocturnal dyspnea and nocturia (related to diuretics in CHF). It is of utmost importance to identify the presence of OSA in these patients, as it is a negative prognostic factor for CHF and its treatment can improve heart failure related outcomes such as ejection fraction and exercise tolerance.6
Pulmonary hypertension, while typically mild in those without coexisting lung disease, has been found to be present in approximately 20% of patients with moderate to severe OSA and may be associated with decreased long term survival rates.7
There is also increasing evidence that severe OSA is associated with an increased risk for coronary artery disease related cardiovascular events, independent of other risk factors. Comorbid OSA is also a risk factor for worse outcomes in patients with established coronary artery disease.
The Role of the Primary Care Physician

Primary Care Physicians (PCP) play a vital role in reducing the burden of OSA associated heart disease. Rather than simply treating a patient with a prescription anti-hypertensive for their newly diagnosed hypertension or referring them to cardiology for their atrial fibrillation, it is of utmost importance that we ask, “Why?”. Although there may be multiple contributing factors to a patient’s cardiovascular disease and a specialty referral may be indicated in many cases, OSA screening (such as with the STOP-BANG8 questionnaire or the Epworth Sleepiness Scale) and diagnostic evaluation (polysomnography) should always be part of the picture. In most cases, this can easily be facilitated by the patient’s PCP. When OSA is appropriately identified, diagnosed and treated (whether through weight loss, positive airway pressure, oral
appliances or surgery) through a team effort, this can lead to a significant reduction in cardiovascular morbidity and mortality worldwide.
References
1. Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pepin JL et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir. Med. 2019; 7: 687–98.
2. Bradley TD, Floras JS. Obstructive sleep apnoea and its cardiovascular consequences. Lancet. 2009 Jan; 373(9567):82-93.
3. Lavie P, Herer P, Hoffstein V. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ. 2000; 320(7233):479.
4. Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL, Sahadevan J, Redline S. Association of nocturnal arrhythmias with sleep-disorded breathing: Sleep Heart Health Study. Am J Respir Crit Care Med. 2006;173(8):910.
5. Monahan K, Storfer-Isser A, Mehra R, Shahar E, Mittleman M, Rottman J, Punjabi N, Sanders M, Quan SF, Resnick H, Redline S. Triggering of nocturnal arrhythmias by sleep-disordered breathing events. J Am Coll Cardiol. 2009;54(19):1797.
6. Bradley TD, Logan AG, Kimoff RJ, Sériès F, Morrison D, Ferguson K, Belenkie I, Pfeifer M, Fleetham J, Hanly P, Smilovitch M, Tomlinson G, Floras JS, CANPAP Investigators. Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med. 2005;353(19):2025.
7. Chaouat A, Weitzenblum E, Krieger J, Oswald M, Kessler R. Pulmonary hemodynamics in the obstructive sleep apnea syndrome. Results in 220 consecutive patients. Chest.1996 Feb;109(2):380-6.
8. Pavarangkul T, Jungtrakul T, Chaobangprom P, Nitiwatthana L, Jongkumchok W, Morrakotkhiew W, Kachenchart S, Chindaprasirt J, Limpawattana P, Srisaenpang S, Pinitsoontorn S, Sawanyawisuth K. The Stop-Bang Questionnaire as a Screening Tool for Obstructive Sleep Apnea-Induced Hypertension in Asian Population. Neurol Int. 2016 Apr 1;8(1):6104. doi: 10.4081/ni.2016.6104. PMID: 27127598; PMCID: PMC4830364.
Monica J. Salas, MD is a Board-Certified Family Medicine and Lifestyle Medicine Physician with over a decade of experience. She is co-owner and COO of Salveo Direct Care, a Direct Primary Care and Lifestyle Medicine practice in San Antonio, Texas. She enjoys working with her patients on their wellness journey to achieve their optimal health through prescribing therapeutic lifestyle change strategies. She is also a member of the Bexar County Medical Society (BCMS).
Visit us at www.bcms.org 17 QUALITY OF LIFEENHANCED BY MEDICAL CARE
I'm a Physician Battling Long COVID. I Can Assure You It's Real
By Monica Verduzco Gutierrez, MD
One in 5. It almost seems unimaginable that this is the real number of people who are struggling with long COVID, especially considering how many people in the US have had COVID-19 at this point (more than 100 million). Yet I continue to hear of people who are struggling, and we continue to see a flood of people in the long COVID clinic. It isn't over, and these post COVID conditions are the new pandemic.
Even more unimaginable at this time is that it happened to me. I've experienced not only the disabling effects of long COVID, but I've also seen, firsthand, the frustration of navigating diagnosis and treatment. It's given me a taste of what millions of other patients are going through.
Vaxxed, Masked and (Too) Relaxed
I caught COVID-19 (probably Omicron BA.5) that presented as sniffles, making me think it was probably just allergies. As an avid runner, I noticed my resting heart rate was up on my Garmin watch, so of course I got tested and was positive.
With my symptoms virtually nonexistent, it seemed, at the time, merely an inconvenience because I was forced to isolate away from family and friends, who all stayed negative.
But two weeks later, I began to have urticaria after physical exertion. Did that mean my mast cells were angry? There's some evidence these immune cells become overactivated in some patients with COVID-19. Next, I began to experience lightheadedness, dizziness and tachycardia. The tachycardia was especially bad any time I exerted myself physically, even on a simple walk. Imagine me, a lover of all bargain shopping, cutting short a trip to the outlet mall on a day when my heart rate was 140 after taking just a few steps.
Then came the severe worsening of my migraines, which are often vestibular, making me nauseated and dizzy on top of the throbbing pain.
I was of course familiar with these symptoms. In my role as professor and chair of the Department of Rehabilitation Medicine at UT Health San Antonio, I developed a post-COVID recovery clinic to help patients.
I knew about post-exertional malaise (PEM) and post-exertional symptom exacerbation (PESE), but I was now experiencing these distressing symptoms firsthand.
Clinicians really need to look for this cardinal sign of long COVID as well as any evidence of myalgic encephalomyelitis/chronic fatigue
syndrome (ME/CFS). ME/CFS is marked by exacerbation of fatigue or symptoms after an activity that could previously be done without these after effects. In my case, as an All-American Masters miler with several marathons under my belt, running five miles is a walk in the park. But now, I pay for those five miles for the rest of the day on the couch or with palpitations, dizziness and fatigue the following day. Busy clinic day full of procedures? I would have to be sitting by the end of it or have a terrible migraine. Bed by 9:00 p.m. was not always early enough.
Becoming a Statistic
Here I am, one of the leading experts in the country on caring for people with long COVID, featured in the national news and having testified in front of Congress, and now I am part of that lived experience. Me, a healthy athlete, with no comorbidities, a normal BMI, vaccinated and boosted, and after an almost asymptomatic bout of COVID-19, a victim to long COVID.
You just never know how your body is going to react. Neuroinflammation, immune dysregulation, viral persistence, and dysbiosis has been shown in study after study, and could be happening to me. I do not want a chronic immune-mediated endothelial dysfunction.
18 SAN ANTONIO MEDICINE • February 2023 QUALITY OF LIFEENHANCED BY MEDICAL CARE
So, I did what any other hyperaware physician-researcher would do. I enrolled in the RECOVER trial (a study at UT Health San Antonio and one that that I recommend to my own patients).
I also decided that I should not self-treat, but actually see my primary care provider (PCP).
My PCP recognized she had a limited knowledge of long COVID, and hesitated to order some of the tests and treatments that I recommended, because they were not yet considered “standard of care.” I can understand the hesitation. It is engrained in our medical education to follow evidence based on the highest-quality randomized control research studies. We are slowly learning more about long COVID; but acknowledging the learning curve offers little to patients who need help now.

This has made me realize that we cannot wait decades for an evidence-based approach while people are suffering. It’s imperative that everyone on the front line learn about some of the manifestations and disease management of manifestations of long COVID.
Being hard-headed and driven, I decided to try to push through but I quickly realized, was not the right thing to do.
So again, after a couple of significant crashes and days of severe migraines, I phoned a friend: Ratna Bhavaraju-Sanka, MD, the amazing neurologist who treats patients with long COVID alongside me. She squeezed me in on a non-clinic day. Again, I had the privilege to see a specialist most people wait months to a year to see. I was diagnosed with both autonomic dysfunction and intractable migraine.
She ordered some intravenous (IV) fluids and IV magnesium that
would probably help both and medications to trial for the autonomic dysfunction.
Thanks to my access, knowledge, and other privileges, I got expedited care, enrolled in a research trial and received medications. I knew to pace myself. I knew how to adjust my lifestyle. The vast majority of others with long COVID lack these advantages.

To Help the Patient with Long COVID
Things I have learned that others can learn, too:
• Acknowledge and recognize that long COVID is a disease that is affecting 1 in 5 Americans who catch COVID. Many look completely "normal on the outside." Please listen to your patients.
• Autonomic dysfunction is a common manifestation of long COVID. These patients see their PCPs or end up in the ER. A 10-minute stand test goes a long way in diagnosing this condition, according to a consensus statement from the American Academy of Physical Medicine and Rehabilitation. Please do not assume it is just anxiety.
• "That's only in research" is dismissive and harmful. Think outside the box. Follow consensus guidelines which are available now. Consider encouraging patients to sign up for trials like the RECOVER trial.
• Screen for PEM/PESE and teach your patients to pace themselves because pushing through it or doing traditional graded exercises will be harmful.
• We need to train more physicians to treat post-acute sequelae of SARS-CoV-2 infection (PASC) and other postinfectious conditions, such as ME/CFS.
I am thankful to be on the road to recovery now and am excited to start treatment with Enhanced External Counterpulsation (EECP) next. If long COVID is hard for physicians to understand and deal with, imagine how difficult it is for patients with no expertise in this area.
It is exponentially harder for those with fewer resources, time and health literacy. My lived experience with mild long COVID has shown me that being a patient is never easy. You put your body and fate into the hands of trusted professionals and expect validation and assistance, not gaslighting or gatekeeping.
Along with millions of others, I am ready for relief.
Monica Verduzco Gutierrez, MD. She is a PM&R Physician and Distinguished Chair of the Department of Rehabilitation Medicine at UT Health San Antonio. During the COVID-19 pandemic, she has developed a Post-COVID Recovery Clinic to aid in the rehabilitative recovery of patients with functional, mobility and cognitive deficits after infection with coronavirus. She is also a member of Bexar County Medical Society (BCMS).
Visit us at www.bcms.org 19 QUALITY OF LIFEENHANCED BY MEDICAL CARE
Post-Thrombotic Syndrome: To Add Insult to Injury
By Ashton Lee, MD
D
eep vein thrombosis (DVT) requires prompt treatment to prevent its most feared complications. Physicians have numerous guidelines and a wide armamentarium to address this condition acutely. However, long after patients have been discharged and completed their anticoagulation course, some will continue to have symptoms that interfere with their quality of life. It is estimated that 20-50% of patients will develop post-thrombotic syndrome (PTS) in the first two years after DVT,1,2 and this can result in debilitation and increased healthcare cost, to the tune of $7000 over their lifetime.3
Post-thrombotic syndrome is a direct result of the acute thrombus from DVT. Local inflammation caused by the thrombus damages the venous valves and causes fibrous scarring within the vein, leading to both reflux and obstruction, respectively. Over time, collaterals form around the obstruction and venous hypertension occurs in the affected limb.
As a result, PTS can present itself in a wide variety of symptoms similar to other forms of chronic venous insufficiency. Extremity edema and pain are common and tend to be worse at the end of the day or after prolonged standing. Patients describe the sensation as an achiness or heaviness in their leg, which can be severe enough to limit activity. This can be associated with telangiectasia, varicose veins and lower leg hyperpigmentation. Approximately 5-10% of patients will develop venous ulceration.1

Despite the prevalence of DVT, there are no strong guidelines for PTS treatment. Compression therapy and leg elevation are the main strategies for reducing symptoms from not only PTS, but all forms of chronic venous insufficiency. In cases of patients who lack the dexterity or grip strength to apply compression stockings, there are alternatives including Velcro and zippered stockings, as well as application assistants which can be purchased at pharmacies or through large retailers. Certain advanced centers provide endovascular recanalization of chronic venous lesions for select patients, although this is still a relatively new therapy. Similarly, prevention of PTS remains an area of uncertainty. Research suggests patients with proximal (iliac and femoral) DVT, obesity, subtherapeutic anticoagulation, and persistent leg symptoms one month after DVT are at higher risk for developing PTS.2 Multiple studies have shown that there is benefit to use of elastic compression stockings after proximal DVT, although the duration of treatment and
full extent of benefits are unknown. Notably, catheterdirected thrombolysis of acute DVT has been shown to have some benefit in reducing PTS.4 However, this therapy is only applicable for certain patients, given the increase in bleeding risk compared to anticoagulation alone. The likely candidate for this procedure is a young, otherwise healthy person who ambulates without difficulty.
The priority when treating DVT is managing the acute phase and reducing the risk of immediate complications. During follow-up, it is important to reassess the patient’s symptoms to detect and treat PTS as it develops. The ultimate goal is reducing the impact of PTS on both patient’s quality of life and economics.
References
1. Kahn, S.R. The Post-thrombotic Syndrome: The Forgotten Morbidity of Deep Venous Thrombosis. J Thromb Thrombolysis 21, 41–48 (2006). https://doi.org/10.1007/s11239-006-5574-9
2. Anat Rabinovich, Susan R. Kahn; How I treat the postthrombotic syndrome. Blood 2018; 131 (20): 2215–2222. doi: https://doi.org/10.1182/blood-2018-01-785956
3. Caprini JA, Botteman MF, Stephens JM, Nadipelli V, Ewing MM, Brandt S, Pashos CL, Cohen AT. Economic burden of long-term complications of deep vein thrombosis after total hip replacement surgery in the United States. Value Health. 2003 Jan-Feb;6(1):5974. doi: 10.1046/j.1524-4733.2003.00204.x. PMID: 12535239.
4. Broderick C, Watson L, Armon MP. Thrombolytic strategies versus standard anticoagulation for acute deep vein thrombosis of the lower limb. Cochrane Database of Systematic Reviews 2021, Issue 1. Art. No.: CD002783. DOI: 10.1002/14651858.CD002783.pub5
Ashton Lee, MD is a vascular surgeon with special interests in dialysis access, limb salvage and preoperative risk assessment. She is also a member of Bexar County Medical Society (BCMS)

20 SAN ANTONIO MEDICINE • February 2023 QUALITY OF LIFEENHANCED BY MEDICAL CARE
Visit us at www.bcms.org 21
A Fresh Look at an Age-old Problem –Book Review
By David Alex Schulz, CHP
Addiction to painkillers is a perpetual problem: even a war between Britain and China over opium caused barely a hiccup in its usage. But anyone whose understanding of the issue was formed before the current opioid crisis … indeed, before the COVID pandemic … needs to reassess from a new perspective, and that’s precisely what journalist Sam Perez offers in her book, “Deviate from Denial: Erasing the Stigma of Addiction and Recovery Through Inspirational Stories.”
The author’s family story provides authority to serve as a guide to the world of use, abuse, hopelessness and hopefulness of today’s drug addict.
“At the beginning of my senior year of high school, my parents made a decision that changed my family’s life forever. They opened DV8 Kitchen, a bakery that is more than just a restaurant. It is also a second chance employment opportunity, which means that 100 percent of the people working there are in recovery from substance use disorder. Before DV8, my parents had been restaurant owners for more than a decade, and over ten years they lost thirteen employees … They were dead—all thirteen from drug and alcohol overdoses.”
“My parents saw this massive problem within the industry which breeds partying. They were deeply affected by the deaths they’d experienced and knew they wanted to find a way to address the pattern of fatal addiction so common among their employees. They knew they wanted to try to fix it, but they weren’t sure how.”
The book’s entry point is not that of the recovering DV8 employees but of its owners – the authors’ parents – and the incipient alcohol abuse prevalent in Food and Beverage Industry.
“My mom helped my dad realize he had a problem. Before long, he enrolled in a rehabilitation program for his alcoholism. This disease affected both my parents. It transformed the early part of their marriage and was responsible for many deep-rooted problems in their relationship.”
No quick solutions is the author’s refrain from experience. Rehab programs experience recidivism as often as success, but after bouncing around the country from Los Angeles and New Orleans to Orlando and Dallas, the restauranteur brought his family to Lexington, Kentucky and spiritual epiphany.
The epiphany? That all behavior they defined as making themselves “good Christians” were transactional activities, comprising a quality of quid pro quo
“You need to be more relational,” she pleaded. “It would benefit you, our family, our community, our business, and your faith if you focused
on building relation ships, not just turning profit! I promise.”
It triggered devo tion to exploring solutions to substance abuse. No easy answers: losing employees to addiction meant a job alone wasn’t sufficient for rehab; and recovery without a job leads directly to recidivism. Both are necessary, neither are sufficient. Thus, “DV8,” a restaurant that balances the two, devoted to the recovery of its employees.
The restaurant serves as springboard for a deep, up-to-date dive into the storied lives of abusers, how they were introduced to addiction, and routes out of the wilderness what worked and what didn’t.
“Stories of Strength and Hope,” the core of the book, pulls no punches. “Addiction doesn’t discriminate” is relentlessly driven home. No economic class, race, religion, or educational attainment precludes addiction. A college student whose tooth-extractions led to reliance on prescribed Percocet frames the first story.
“I was not doing them every single day.” She paused, taking time to recount the details to me with precision and accuracy. “And then all of a sudden I was.”

Percocet turned into $160-a-day black-market OxyContin. Before long, pharmaceuticals led to heroin. But not before the addict attempted cold-turkey recovery. “At three in the morning I woke up totally drenched in sweat and feeling like I was going to vomit and like my skin was just crawling off.”
While it's no surprise to our readership that today a sizable number of addicts are initiated through prescribed medicine, the excesses of the 20th Century have left significant hangovers in new generations, for whom drug abuse is all they’ve ever known. Ecstasy led to crack led to
22 SAN ANTONIO MEDICINE • February 2023 SAN ANTONIO MEDICINE
speed and eventually all roads lead to heroin; broken homes lead to more broken homes, and violence is often an aspect of abuse. “Breaking the cycle of addiction can be hard when it’s all you’ve ever known, it isn’t impossible but it’s what they grew up around,” says Perez. “It’s all they’ve seen. It should be met with an attempt to understand and help, not an automatic judgment.”
The need to refrain from judgmentalism is another recurring lesson, corollary to the maxim that addiction doesn’t discriminate. Following Perez detailing, in very personal terms, the life experiences of successful recoveries, unresolved cases, or terminal addictions. She offers her observations on how the pandemic and associated lock-down exacerbated prescription painkiller reliance and the links between mental health and substance abuse issues.
She reviews today’s programs for recovery (including Alcoholics Anonymous, residential programs, outpatient clinics and drug courts) leading to a discussion of harm reduction methods for those addicts nearing turning points – but not quite there yet.
Perez closes with the observation, “Drug use and abuse shouldn’t be taboo. We’ve swept it under the rug for far too long. It’s time we start talking about the complexities of substance use disorder, not trivialize the simple yes or no choice the “Say No to Drugs” campaign might
make it appear to be. Approaching the topic of drug addiction with full transparency and focusing on recovery without judgment is the quickest way to work toward a solution.”
I grew up five blocks from Manhattan’s notorious Needle Park, and thought I had a handle on the situation. I was wrong. For the freshest look at drug abuse in today’s society, with both anecdotal and well sourced scientific research, check out Sam Perez’s “Deviate from Denial: Erasing the Stigma of Addiction and Recovery Through Inspirational Stories” (New Degree Press).

Visit us at www.bcms.org 23 SAN ANTONIO MEDICINE
David Alex Schulz, CHP is a community member of the BCMS Publications Committee.
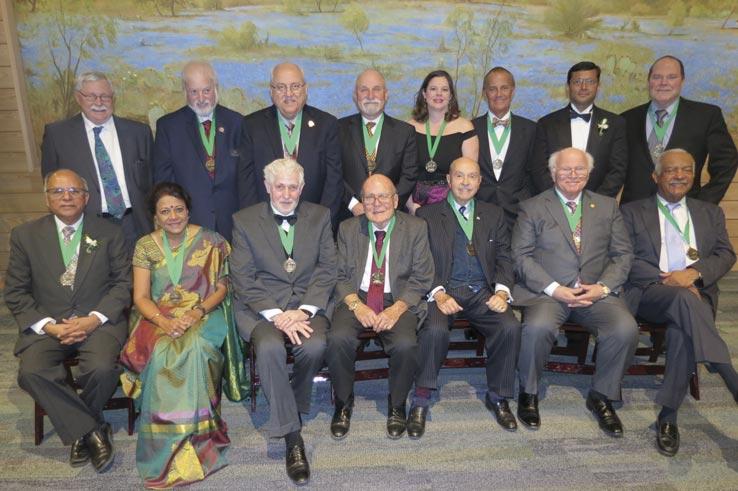
2023 BCMS Installation of Officers and Golden Aesculapius Awards




24 SAN ANTONIO MEDICINE • February 2023 SAN ANTONIO MEDICINE
Above: Immediate Past President Dr. Rajeev Suri swears in 2023 BCMS Board Officers. From left to Right: Secretary John Shepherd, MD, Treasurer Ezequiel “Zeke” Silva, III, MD, Vice President Brian T. Boies, MD, President John Joseph Nava, MD, President-Elect Brent W. Sanderlin, DO
BCMS Alliance Immediate Past President Taylor Frantz, RDN, LD swears in Co-President Jenny Case, MSN, MBA, RN
Thank you to our Event Sponsors of the 2023 Joint Installation of Officers






Dr. and Mrs. Piotr Kuklinski
Dr. and Mrs. Rajeev Suri
SAN ANTONIO MEDICINE Visit us at www.bcms.org 25
BCMS in the New Millennium: How have things changed?
Interview with Vijay N. Koli, MD
By Monica Jones, BCMS COO
It was January of 2000, Dr. Vijay N. Koli gave his first Board of Directors President’s message by quoting Edward Everett Hale, “Coming together is a beginning; keeping together is progress; working together is success”. It was the dawn of the new millennium states Dr. Koli. Our profession was facing challenges, some old some new. Loss of physician income, barriers to medical care, and the impact of managed care, to name a few. Our challenges were lack of communication between physicians, hospitals, and the public; the emergence of unions; keeping pace with advancing technology; recruitment of new members, especially physicians in large groups, in academics, and the military and attracting new physicians in the workforce. We were preparing for the upcoming election year, pushing advocacy for our patients and activism from physicians, students and others within the medical community.1 Our goal in 2000 was to provide members of the medical community with a political voice and with opportunities for effective political and public-affairs participation. In preparation for the 2000 elections, we searched for even more avenues to involve members of the medical community while simultaneously providing quality healthcare for our patients.
Dr. Koli was born in Mumbai, India. In 1965 he left for Moscow, Russia, to study medicine on a scholarship from the government of India and the Soviet Union (Russia). His postgraduate training was in England and Scotland. In 1978 he came to Texas for four years and worked in a small town called Goldthwaite. He moved to San Antonio in 1982 when he joined the Bexar County Medical Society (BCMS). After 18 years of mem-

bership, he was elected President of BCMS in 2000. Dr. Koli has received several outstanding community service awards, including the Golden Aesculapius Award from BCMS for a lifetime of distinguished service in 2016. Dr. Koli is now retired after practicing for more than 40 years.
Dr. Koli discussed how medicine has changed throughout the years. “It’s undeniable that the quality of medical care has never been better.” Robotic surgical systems win U.S. Food and Drug Administration approval. With the emergence of web-based software in the early 2000s, the need for electronic medical record (EMR) systems developed through remotely hosted systems. Accessing information remotely or storing made the method of keeping medical records more appealing and ultimately more affordable for physicians to implement into their practice. However, some things never change. Dr. Koli recalls how pa-
tients yearned to spend more time with their doctors. This became obvious when BCMS held a live Doctor’s Day phone bank on KSAT-12 TV on March 30, 2000. Thirty physicians from various specialties volunteered their time. According to Southwestern Bell 10,000 callers tried to get through. We answered only 1,305. It only showed how eagerly patients want to talk to their doctors. The calls were from a simple viral throat infection to a liver transplant.2 Patients want to feel that their doctors are accessible and care about their well-being. Patients also seek convenience which we are seeing today in younger patients and online access. Patients want to schedule an appointment, communicate with their doctors, see test results and health information as well as pay their bills all from their computer or phone. Convenience is key.
There were many notable events in 2000, but one that stood out was when the BCMS
26 SAN ANTONIO MEDICINE • February 2023 SAN ANTONIO MEDICINE
Past BCMS Board Presidents
International Health Committee (IHC) embraced the responsibility to portray the high level of medical diversity that exists in San Antonio to ignite interest in medicine among the different ethnic/cultural groups, as well as to strengthen the communication with other countries.3 The BCMS IHC adopted the policy of “Mi casa es su casa” and went global. The committee organized international learning excursions, like going to Peru in June during “The fiesta del sol” festivities in Cuzco and another to India in February of 2001. The purpose was to broaden our understanding of medical systems in other countries.
Challenges in 2000: There was a relative shortage of primary care physicians, the implementation of EMR gave additional burdens, productivity was down, and expenses were up. There was less time spent interacting with the patient. Managed care or HMOs reduced healthcare costs by significantly controlling payments to physicians. Pre-authorization prolonged patient care.
Today in Texas, new medical schools are focusing on increasing primary care specialties. Medical students and physicians are now fa-

miliar with and more comfortable using the EMR. Physician burnout is not new but has become more evident and gaining attention at the local, state and national levels. Women physicians are getting more involved despite their professional and personal commitments. The advent of telemedicine has increased efficiency, and patient satisfaction is improved.
Dr. Koli said in May of 2000 “Today’s physician groups are diverse; specialist, super-specialties, from different backgrounds and practice settings. Therefore, cooperative behavior is essential for working together. We need to learn methods to recognize and acknowledge the difference between us. Let us focus on bonds that unite us rather than divide us.”4 His message is still the same today for future generations. Advocacy: Get involved in organized medicine; with your local (BCMS), state organization (TMA), national organization (AMA) and/or specialty organizations.

Special Happenings & Facts throughout the 2000 BCMS BoD Presidency
• Y2K - The year 2000 is the last year of the century, but because the calendar changes
to 2000, it is considered the beginning of the 21st century.
• Change of BCMS executive directors, Kay E. Peck replaced Dennis E. Dawson.
• San Antonio Mayor Howard Peak
• Texas Governor George W. Bush (Election night win for George W. Bush took on Dewey-Esque proportions as newspapers across the country scrambled to yank banner headlines declaring Bush the presidential victor)
• President of the United States Bill Clinton
References:
1. San Antonio Medicine, January 2000 page 4
2. San Antonio Medicine, May 2000 page 4
3. San Antonio Medicine, March 2000 page 16
4. San Antonio Medicine, May 2000 page 4
Monica Jones, BCMS Chief Operating Officer
SAN ANTONIO MEDICINE Visit us at www.bcms.org 27
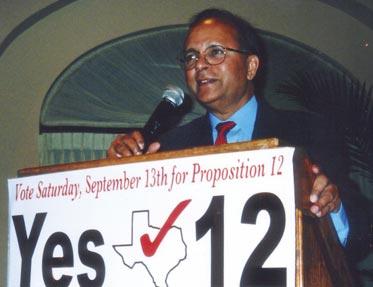
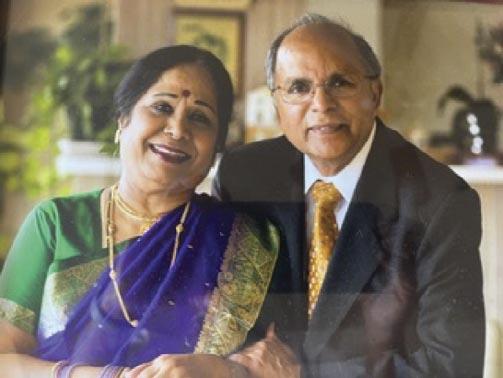
Clockwise from Left: TMA Board of Trustees Dr. Jayesh Shah with Dr. Vijay Koli; Dr. Koli speaking on proposition 12 and below, Dr. Koli and wife Malathi Koli.
Welcome Committee Chairs and Co-chairs 2023
Board of Ethics
Keiko McManus, MD, Chair
Publications
John Seidenfeld, MD, Co-Chair
Norys Alexandra Castro-Pena, MD, Co-Chair
Delegation to TMA
Jesse Moss, MD, Chair
Jayesh Shah, MD, Vice Chair
Emergency Preparedness
David Marks, MD, Chair
David Cohen, MD, Vice Chair
International Committee
James “Jim” Humphreys, MD, Chair
Leadership Development
David N. Henkes, MD
Legislative Socioeconomics
Ezequiel “Zeke” Silva III, MD, Chair
Jennifer Rushton, MD, Vice Chair
Joint Academic Collaboration
Woodson “Scott” Jones, MD
Medical Student Collaboration

Adam Ratner, MD
Medical-Legal Liaison
David Siegel, MD
Nominating/Constitution and Bylaws
Rodolfo Molina, MD, Chair
Rajeev Suri, MD, Vice Chair
Physician Health and Rehabilitation Advocacy
Priti Mody-Bailey, MD, Chair
Leah Jacobson, MD, Co-Chair
28 SAN ANTONIO MEDICINE • February 2023 SAN
ANTONIO MEDICINE
service
leadership
the Bexar County Medical Society
2023
Thank you for your
and
as you represent
in
2023 Joint Installation of Officers Golden Aesculapius Award Honorees






Oliver H. Johnson Jr., MD.
Jesse Moss Jr., MD, FACS, PA
Lloyd Pierce Van Winkle, MD
James Charles Martin, MD
Bernard T. Swift Jr., DO, MPH
Richard Samuel Wayne, MD
SAN ANTONIO MEDICINE Visit us at www.bcms.org 29
Dr. Molina, Dr. Johnson and Dr. Sertich
Dr. Martin with Dr. Molina
Dr. Molina with Dr. Van Winkle
Dr. Moss, Melody Newsom, Dr. Rudy Molina
Dr. Swift, Melody Newsom and Dr. Rudy Molina
Dr. Molina with Dr. Wayne
Disparities in Prenatal Care Among Undocumented Immigrants
By Winona Gbedey, Sanjana Ravi and Rozena Shirvani
Despite representing 6% of Texas’s population (1.8 million individuals), undocumented residents face substantial barriers to healthcare, both in Texas and across the nation.1-2 In addition to being ineligible for Medicaid, CHIP and the ACA Marketplace, undocumented immigrants utilize the services they are eligible for at much lower rates than their United States born counterparts. Furthermore, private insurance coverage is only accessible to those that can afford to pay full price without a subsidy. As a result, many undocumented residents depend on federally qualified health centers, charity clinics, and safety net hospitals for all aspects of their healthcare.3 These factors combined with lack of language interpretation services, unreliable
transportation, limited knowledge of available resources, and cost to make the U.S. healthcare system incredibly complex and inaccessible to many immigrants. Consequently, immigrants with conditions that require constant management are left to struggle for care.
Pregnant women, in particular, are a special demographic because both them and their unborn child have unique particular/special healthcare needs. This problem is particularly pronounced in Texas, which is home to the second-largest population of undocumented residents in the country. Historically, undocumented women are more likely to miss prenatal visits and experience complications during delivery. When compared to their counterparts, babies born to these women are

more likely to be premature and underweight, both of which contribute to the high rates of infant morbidity and mortality in this population.4 These poor outcomes have been linked to the aforementioned barriers to healthcare, which lead to underutilization of preventive health services.
Healthcare inaccessibility is not unique to undocumented immigrants. Of the over 14.6 million women living in the state of Texas, almost 30% are uninsured.5 To combat the innate health disparities that accompany these numbers, Texas created free and low-cost safety net programs, including Healthy Texas Women and Healthy Texas Women Plus, the Texas Family Planning Program and the Breast and Cervical Cancer Services.6-8 Unfor-
30 SAN ANTONIO MEDICINE • February 2023 SAN ANTONIO MEDICINE
tunately, even though these programs have helped so many U.S. born residents, they fail to address the complex needs of undocumented residents, allowing many to fall through the cracks.

Currently, undocumented pregnant women can qualify for the Texas CHIP Perinatal program, which covers up to 20 prenatal visits, delivery-related charges and two postpartum visits. 9-12 In 2002, the Centers for Medicare and Medicaid Services permitted state governments to set aside funds for unborn children. Some states, like Texas, have used this money to support pregnant mothers, regardless of immigration status. In order words, pregnancy qualifies undocumented women for essential prenatal and preventative medical care. However, once her child is born, these services are no longer available to her.
Undocumented residents who meet requirements for Medicaid but who cannot use it due to their immigration status may also be eligible for Emergency Medicaid, which has special provisions for labor and delivery. Ad-
ditionally, if a patient’s condition is a medical emergency, emergency departments must treat them under the Emergency Medical Treatment and Labor Act (EMTALA). In fact, the EMTALA was specifically designed to serve the medical needs of the country’s uninsured and undocumented.13
Finally, undocumented women can seek services from clinics funded by Title V and Title X. Patients can locate these clinics through the Texas Health and Human Services (HHS) site and the national HHS online directory. The Title V Maternal and Child Health Fee-for-Service Program provides funding to support women, children, and families providing care to over 60 million individuals annually. With Title V funding, clinics are able to provide preventive and wellness visits, supply prenatal, delivery, postpartum care and much more.14 Likewise, the Title X Family Planning Program is the only federal program solely dedicated to providing family planning services to low-income families. Through Title X, over four million men and
women receive wellness exams, cancer screenings, reproductive and education care, STI testing and treatment annually.15
In addition to gaps in services, mistrust of governmental and government-adjacent agencies (including healthcare and social welfare agencies) remains a significant barrier to care for undocumented individuals.16 Despite living in the margins of society, many immigrant families are wary of government assistance due to fear of potential repercussions, such as detainment by U.S. Immigration and Customs Enforcement (ICE) agents or deportation. Legislation such as the now-repealed Public Charge rule, which prohibited those who used public benefits for more than 12 months from becoming lawful permanent residents, has resulted in disenrollment and foregoment of public benefits despite eligibility for these services.17-18
In conjunction with advocating for increased coverage and access to social welfare programs, we must also focus on building trust among communities that have repeatedly been discriminated against by government
Visit us at www.bcms.org 31 SAN ANTONIO MEDICINE
agencies.19-22 We can start by educating ourselves and our patients on available resources, while also working upstream to create inclusive and equitable policies that defend the health of our most vulnerable communities.
To find more information and/or resources visit the following websites: National HHS Directory for Title X clinics https://opa-fpclinicdb.hhs.gov/
National Directory of State Hotlines for Title V Clinics https://mchb.tvisdata.hrsa.gov/Home/StateHotlines
Texas Medicaid & Chip FAQs https://www.hhs.texas.gov/services/health/m edicaid-chip
References
1. Immigrants in Texas. American Immigration Council. https://www.americanimmigrationcouncil.org/research/immigrants-in-texas. Published August 7, 2020.
2. Profile of the unauthorized population - TX. Migration Policy Institute. https://www.migrationpolicy.org/data/unauthorized-immigrantpopulation/ state/TX. Published May 1, 2022.
3. Dunkelberg A. Immigrants’ Access to Health Care in Texas: An Updated Landscape. Center for Public Policy Priorities. 2016. https://everytexan.org/images /HW_2016_ ImmigrantsAccess_FullReport.pdf. Accessed May 19, 2022.
4. Health Care for Unauthorized Immigrants. American College of Obstetricians and Gynecologists. https://www.acog.org /clinical/clinical-guidance/committee-opinion/articles/2015 /03/health-care-for-unauthorized-immigrants. Published 2019. Accessed May 19, 2022.
5. State Summaries Texas | 2016 Health Of Women And Children Report. America's Health Rankings. https://www.americashealthrankings.org/learn/reports/2016health-of-women-and-children-report/state-su mmaries-texas. Published 2022. Accessed May 19, 2022.
6. Take charge of your health. Home | Healthy Texas Women. https://www. healthytexaswomen.org/. Published 2022. Accessed May 17, 2022.
7. Family Planning Program. Family Planning Program | Healthy Texas Women. https://www.healthytexaswomen.org/healthcare-programs/family-planning-program. Published 2022. Accessed May 17, 2022.
8. Breast & Cervical Cancer Services | Texas Health and Human Services. https://www.hhstexas.gov/providers/health-servicesproviders/ womens-health-services/breast-cervical-cancer-services. Published 2022. Accessed May 17, 2022.
9. Dunkelberg A. Immigrants’ access to health care in Texas. https://everytexan. org/images/HW_2016_ImmigrantsAccess_FullReport.pdf. Published 2016.
10. Medical assistance programs for immigrants in various states. https://www.nilc. org/wp-content/uploads/2015/11/med-services-forimms-in-states.pdf. Published July 2021.
11. Immigrant women's access to sexual and reproductive health coverage and care in the United States. Immigrant Women's Access to Sexual & Reproductive Coverage & Care. https://www. commonwealthfund.org/publications/issue-briefs/2018/nov/immigrantwomens-access-sexual-reproductive-health-cov erage. Published November 20, 2018.
12. CHIP Perinatal FAQs . https://www.hhs. texas.gov/services/health/medicaidchip/provider-information /texas-medicaidchip-chip-perinatal-coverage/chip-perinatal-fa qs. Published 2022. Accessed May 17, 2022.
13. Health Care for Unauthorized Immigrants. https://www.acog.org/clinical/ clinical-guidance/committee-opinion/articles/2015/03/ health-care-for-unauthorized-immigrants. Published 2015. Accessed January 29, 2022.
14. Title V Maternal and Child Health Services Block Grant Program. U.S Department of Health and Human Services. https://www.hhs.gov/guidance/document/titl e-v-maternal-and-child-health-services-blockgrant-states-program-guidance-and-forms-2. Published 2021. Accessed May 19, 2022.
15. What is Title X?. Every Body Texas. https://www.everybodytexas.org/everybody/what-is-title- x?gclid=Cj0KCQiA6 NOPBhCPARIsAHAy2zD5qBUS46q3L5dj2 _z3s2pb-xOiqcC0W2yJKRB Ec65H8IsUApxEEagaAsbnEALw_wcB. Published 2020. Accessed May 19, 2022.
16. Kerani RP, Kwakwa HA. Scaring Undocumented Immigrants Is Detrimental to Public Health. Am J Public Health. 2018;108(9):1165-1166. doi:10.2105/A JPH.2018.304596
17. Bernstein H, Gonzalez D, Karpman M, Zuckerman S. Adults in Immigrant Families Report Avoiding Routine Activities Because of Immigration Concerns. Urban Institute. https://www.urban.org/research/publica -
tion/adults-immigrant-families-report-avoiding-routine-activities-because-immigrationconcerns. Published 2019. Accessed May 19, 2022.
18. Public Charge. U.S. Citizen and Immigration Services. https://www.uscis.gov/public-charge. Published 2022. Accessed May 19, 2022.
19. Family Separation and Detention. Americanbar.org. https://www.americanbar. org/advocacy/governmental_legislative_work/priorities _policy/immigration/familyseparation/. Published 2022. Accessed May 19, 2022.
20. Tau B, Hackman M. Federal Agencies Use Cellphone Location Data for Immigration Enforcement. The Wallstreet Journal. https://www.wsj.com/articles/federal-agencies-use-cellphone-location-data-for-immigration-enforcement-11581078600. Published 2020. Accessed May 19, 2022.
21. FOIA Request - DHS, CBP, and ICE Purchase and Use of Cell Phone Location Data. American Civil Liberties Union. https://www.aclu.org/foia-document/ foia-request-dhs-cbp-ice-cell-phone-location-data. Published 2020. Accessed May 19, 2022.
22. Wessler N. The U.S. Government Is Secretly Using Cell Phone Location Data to Track Us. We’re Suing. | News & Commentary | American Civil Liberties Union. American Civil Liberties Union. https://www.aclu.org/news/immigrantsrights/the-u-s-government-is-secretly-usingcell-phone-location-data-to-track-us-were-suin g. Published 2020. Accessed May 19, 2022.
Winona Gbedey is a fourth-year medical student at UT Health San Antonio Long School of Medicine. She is a member of the BCMS Publications Committee and the Texas Medical Association (TMA).

Sanjana is a third-year dual degree MD/MPAff student at Dell Medical School and LBJ School of Public Affairs. She is an active member of the Texas Medical Association (TMA) and the American Medical Association (AMA).

Rozena Shirvani is a second-year medical student at the UT Rio Grande Valley School of Medicine. She is a student member of the Texas Medical Association (TMA).

32 SAN ANTONIO MEDICINE • February 2023 SAN ANTONIO MEDICINE

Medicine Achieves Reduction in Medicare Physician Pay Cut Amid Push for Reform
By Emma Freer
After a concerted advocacy campaign by the Texas Medical Association and others in organized medicine, Congress lessened a Medicare physician pay cut that took effect Jan. 1. Despite this intervention, physicians still face declining Medicare payments in 2023 and in 2024, underscoring the need for comprehensive reform.
Meanwhile, TMA experts continue to analyze other potentially positive provisions of the extensive spending law that averted the cuts and its specific implications for Texas.
The Centers for Medicare & Medicaid Services’ (CMS’) 2023 Medicare physician fee schedule final rule lowered the conversion factor that determines Medicare physician payments by 4.5% compared with the 2022 conversion factor. The cut mostly stems from an expiring physician pay increase funded by Congress through 2022 as well as from a much-maligned federal budget neutrality provision that requires any physician pay increase or decrease to be offsetting.
In response, Texas physicians sent nearly 2,000 messages to their federal representatives, raising concerns about how the cut would impact practice viability and access to care among Medicare patients. This advocacy led to some relief when President Joe Biden signed into law the Consolidated Appropriations Act on Dec. 29. The $1.7 trillion spending legislation updated the 2023 conversion factor, reducing the scheduled physician pay cut from 4.5% to 2%. But it also requires CMS to cut Medicare physician payments by 1.25% in 2024.
The omnibus law has other positive implications for Medicare and Medicaid coverage, which include:
• Extending pandemic-era telehealth waivers and alternative payment model incentive payments (albeit at 3.5% instead of 5%);
• Making permanent an option for states to provide 12 months of continuous Medicaid coverage to children and postpartum women;
• Authorizing 200 additional graduate medical education residency positions, half of which will be dedicated to psychiatry;
• Incentivizing domestic drug manufacturers to address supply shortages; and
• Funding more mental health, maternal health, and substance use disorder services.
In the final weeks of 2022, TMA, the American Medical Association, and others in organized medicine pushed Congress to eliminate the pay cut altogether, including in a December 8 letter to congressional leadership.
“Put simply, the cost of congressional inaction is an across-the-board cut that will further amplify the financial hardship physician prac-
tices are already facing while inhibiting Medicare from delivering on its promises to seniors and future generations,” the signatories wrote.
To rescue physicians from the semi-annual rigmarole of asking Congress to address Medicare physician payments, TMA has endorsed a set of AMA principles to guide Medicare physician payment reform.
The Characteristics of a Rational Medicare Physician Payment System call on Congress to:
• Provide a baseline annual physician pay raise to keep up with inflation;
• Eliminate, replace, or revise budget neutrality requirements;
• Incentivize value-based care that suits various practice settings; and
• Support physician efforts to reduce health disparities.
For a deep dive into this year’s Medicare Physician Fee Schedule, check out TMA’s ondemand CME webinar, “2023 Medicare Update,” available in the Education Center at no cost to members, compliments of TMA Insurance Trust. Earn 1 AMA PRA Category 1 Credit (enduring) and 1 ethics credit.
Emma Freer is a reporter for Texas Medicine. She previously worked in local news, covering city politics, economic development, and public health.

34 SAN ANTONIO MEDICINE • February 2023 SAN ANTONIO MEDICINE
Reprinted with permission from
Copyright Texas Medical Association.
Texas Medicine Today.

Visit us at www.bcms.org 35
South Texas Blood & Tissue –A Story of Sickle Cell Disease
By South Texas Blood & Tissue
About South Texas Blood & Tissue
South Texas Blood & Tissue (STB&T) is a nonprofit community blood center that provides blood, plasma, platelets and other blood components to 100 hospitals in 48 South Texas counties. It is the largest blood supplier in our region. In addition, STB&T supports the development of advanced therapies, including those derived from donated human cells and tissues used in research and in new therapies and cures for cancers and degenerative diseases.
Breanna Morgan, who was born with sickle cell anemia, heard from an early age she could not do things healthy people can do. She has spent the last two decades proving her doctors wrong. At 27, she has found her passion in life. She is taking a new medication to help with her symptoms and she passionately wants to give hope to kids with this vicious disease.

“I just want to be a good example,” Breanna said.
Sickle cell disease affects the shape of the red blood cells, making them crescent-shaped in-
stead of round. The misshapen cells can get stuck in the veins and block blood flow, causing excruciating pain, among other symptoms. The inherited disease is most commonly found in African Americans. This disease has caused Breanna to spend many months of her life in hospitals, receiving treatment (including more than a dozen blood transfusions that were given to replenish her low blood cell counts). She started advocating for blood donation with South Texas Blood & Tissue as a teenager.
“Usually when I get blood transfusions it’s
36 SAN ANTONIO MEDICINE • February 2023 SAN ANTONIO MEDICINE
a positive experience. You feel recharged, like your body’s getting better,” Breanna said.
While Breanna may look healthy, sickle cell anemia is an invisible disease that has affected every aspect of her life.
“It feels like we’re about to race with healthy humans, but for those of us with sickle cell, we have an anchor attached to our legs,” Breanna said. “Society looks especially at us with sickle cell and says, ‘You don’t look sick.’”
Breanna will always need treatment for sickle cell disease, but she hasn’t let it ruin her dreams. After looking up to medical professionals for her whole life (because of being in and out of hospitals), Breanna graduated from college planning to go into a health career.
However, one day she had the epiphany that she wanted to try out acting.
“I started having a lot of dreams about just being on set, being on stage and a lot of acting just kept coming to my mind. I didn't understand it because I don't come from that background,” Breanna said.
She took the leap and started going to acting classes and auditions. A few years later, Breanna is a part-time professional actor and has appeared in three movies.
Breanna wishes she could thank all her lifesaving blood donors and emphasize the importance of giving blood.
“One thing I think about when getting transfusions is, 'Whose blood is this?’ I want to get to know them and send a thank you card,” Breanna said. “There are a lot of people in the world who could really use that blood and I’ve been in situations before where the shortage affected me.”
Breanna has encountered situations in recent years where doctors had to make the decision of which patient should get a blood transfusion because of the low blood supply, she said. Because of her severe pain crises, Breanna has thankfully always gotten the blood she needs.

Visit us at www.bcms.org 37 SAN ANTONIO MEDICINE
Copyright & Printed Permission from South Texas Blood & Tissue.
38 SAN ANTONIO MEDICINE • February 2023
Shop Vendors Who Support BCMS

BCMS Vendor Directory
We encourage you to use our supporting vendors whenever you or your practice needs supplies or services.
ACCOUNTING FIRMS
Sol Schwartz & Associates P.C. (HHH Gold Sponsor)

Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Jim Rice, CPA
210-384-8000, ext. 112 jprice@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”
ACCOUNTING SOFTWARE
Express Information Systems (HHH Gold Sponsor)

With over 29 years’ experience, we understand that real-time visibility into your financial data is critical. Our browser-based healthcare accounting solutions provide accurate, multi-dimensional reporting that helps you accommodate further growth and drive your practice forward.
Rana Camargo
Senior Account Manager
210-771-7903
ranac@expressinfo.com www.expressinfo.com
“Leaders in Healthcare Software & Consulting”
ATTORNEYS
Kreager Mitchell (HHH Gold Sponsor)
At Kreager Mitchell, our healthcare practice works with physicians to offer the best representation possible in providing industry specific solutions. From business transactions to physician contracts, our team can help you in making the right decision for your practice.
Michael L. Kreager
210-283-6227
mkreager@kreagermitchell.com
Bruce M. Mitchell
210-283-6228
bmitchell@kreagermitchell.com www.kreagermitchell.com
“Client-centered legal counsel with integrity and inspired solutions”
ASSETT WEALTH MANAGEMENT
Synergy Federal Credit Union (HH Silver Sponsor)
Managing Partner (210) 503-0003

Bertuzzi-Torres-Fernandez Wealth Management Group (HHH Gold Sponsor)

We specialize in simplifying your personal and professional life. We are dedicated wealth managers who offer diverse financial solutions for discerning healthcare professionals, including asset protection, lending and estate planning.
Mike Bertuzzi
First Vice President Senior Financial Advisor
210-278-3828
Michael_bertuzzi@ml.com
Ruth Torres Financial Advisor 210-278-3828
Ruth.torres@ml.com
http://fa.ml.com/bertuzzi-torres
Will C. Fernandez, CEPA
Senior Portfolio Advisor Financial Advisor
210-278-3812 wfernandez@ml.com
https://fa.ml.com/texas/san-antonio/bertuzzi-torres-fernandez
BANKING Broadway Bank (HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@Broadway.Bank
www.broadwaybank.com

“We’re here for good.”
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help Physicians get the banking services they need.
Synergy FCU Member Services
210-750-8333
info@synergyfcu.org
www.synergyfcu.org
“Once a member, always a member. Join today!”
CLINICAL DIAGNOSTICS
www.genicslabs.com
“Accurate results in record time.”
CREDENTIALS VERIFICATION ORGANIZATION
Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for health care entities.

Betty Fernandez Director of Operations
The Bank of San Antonio (HHH Gold Sponsor)

We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Brandi Vitier
210-807-5581
brandi.vitier@thebankofsa.com
www.thebankofsa.com
Livingston Med Lab (HHHH 10K Platinum Sponsor)

High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease, & Genetics.
Robert Castaneda (CEO)
210-316-1792
Robert@livingstonmedlab.com
Joey Martinez (Director of Operations)
210-204-7072
Joey@livingstonmedlab.com
Dwight Chapman (Account Manager)
210-591-2649
Dwight@livingstonmedlab.com
www.livingstonmedlab.com/home
“Trusted Innovative, Accurate, and STAT Medical Diagnostics”
210-582-6355
Betty.Fernandez@bexarcv.com www.BexarCV.com
“Proudly serving the medical community since 1998”
FINANCIAL ADVISORS
Oakwell Private Wealth Management (HHHH 10K Platinum Sponsor) Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.

Brian T. Boswell, CFP®, QKA Senior Private Wealth Advisor 512-649-8113
SERVICE@OAKWELLPWM.COM www.oakwellpwm.com
Genics Laboratories (HHH Gold Sponsor)

Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison
(210) 503-0003 (Phone)
yulia@genicslabs.com (Email)
Kevin Setanyan
Managing Partner
(210) 503-0003
kevin@genicslabs.com
Artyom Vardapetyan
“More Than Just Your Advisor, We're Your Wealth Management Partner”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney, Financial Advisor
210-858-5880
Elizabeth.olney@edwardjones.com
www.edwardjones.com/elizabeth-olney "Making Sense of Investing"
40 SAN ANTONIO MEDICINE • February 2023
FINANCIAL SERVICES
HEALTHCARE BANKING
Amegy Bank of Texas (HH Silver Sponsor)
Regina Delgado
Business Development Manager (210) 450-3713
delgador4@uthscsa.edu
Jon Buss: 512-338-6167
Jbuss1@humana.com
Bertuzzi-Torres-Fernandez Wealth Management Group ( Gold Sponsor)
We specialize in simplifying your personal and professional life. We are dedicated wealth managers who offer diverse financial solutions for discerning healthcare professionals, including asset protection, lending & estate planning.
Mike Bertuzzi
First Vice President Senior Financial Advisor
210-278-3828
Michael_bertuzzi@ml.com
Ruth Torres Financial Advisor
210-278-3828
Ruth.torres@ml.com
Will C. Fernandez, CEPA Senior Portfolio Advisor Financial Advisor
210-278-3812 wfernandez@ml.com
https://fa.ml.com/texas/san-antonio/bertuzzi-torres-fernandez
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Jeanne Bennett
EVP | Private Banking Manager
210-343-4556
Jeanne.bennett@amegybank.com
Karen Leckie
Senior Vice President | Private Banking
210-343-4558
karen.leckie@amegybank.com
Robert Lindley
Senior Vice President | Private Banking

210-343-4526
robert.lindley@amegybank.com
Denise C. Smith
Vice President | Private Banking
210-343-4502
Denise.C.Smith@amegybank.com www.amegybank.com
“Community banking partnership”
HOSPITALS/ HEALTHCARE FACILITIES
UT Health San Antonio MD
Anderson Mays Cancer Center
Laura Kouba
Business Development Manager (210) 265-7662
norriskouba@uthscsa.edu
https://uthscsa.edu/ Appointments: 210-450-1000
UT Health San Antonio
7979 Wurzbach Road
San Antonio, TX 78229
INFORMATION AND TECHNOLOGIES
Express Information Systems (HHH Gold Sponsor)

With over 29 years’ experience, we understand that real-time visibility into your financial data is critical. Our browser-based healthcare accounting solutions provide accurate, multi-dimensional reporting that helps you accommodate further growth and drive your practice forward.
Rana Camargo
Shamayne Kotfas: 512-338-6103
skotfas@humana.com
www.humana.com
INSURANCE/MEDICAL MALPRACTICE
Texas Medical Liability Trust
(HHHH 10K Platinum Sponsor)
With more than 20,000 health care professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of health care for patients by educating, protecting, and defending physicians.

Patty Spann
512-425-5932
patty-spann@tmlt.org
www.tmlt.org
Recommended partner of the Bexar County Medical Society
Aspect Wealth Management (HHH Gold Sponsor)

We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520 mclark@aspectwealth.com www.aspectwealth.com
“Get what you deserve … maximize your Social Security benefit!”
GERIATRICS/PRIMARY
CARE Conviva Care Center (HHH Gold Sponsor)

Conviva’s value-based care model allows physicians to deliver high quality, personalized care and achieve better outcomes, while feeling free to focus on health equity and patient outcomes.
Kim Gary Senior Physician Recruiter
(812) 272-9838
KGary4@humana.com www.ConvivaCareers.com
“Fuel Your Passion & Find Your Purpose”
Nexus Neurorecovery Center (HHH Gold Sponsor)

A post-acute rehabilitation facility focusing on brain injuries. Programming provides individual and group physical, occupational, cognitive, and speech therapy. We help residents return to lives of productivity and meaning.
Sydney Kerr Liaison 346-339-2654
skerr@nhsltd.com
Caitlyn Tewksbury
ctewksbury@nhsltd.com
Justin Sanderson CEO 210-854-4732
jsanderson@nhsltd.com
Nexus Neurorecovery Center
227 Lewis St, San Antonio, TX 78212
https://nexushealthsystems.com
“To return patients to lives of productivity and meaning”
Senior Account Manager
210-771-7903
ranac@expressinfo.com
www.expressinfo.com
“Leaders in Healthcare Software & Consulting”
INSURANCE
The Bank of San Antonio Insurance Group, Inc.

(HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
TMA Insurance Trust (HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.

Wendell England Director of Member Benefits
512-370-1776
wendell.england@tmait.org
800-880-8181
www.tmait.org
“We offer BCMS members a free insurance portfolio review.”
katy.brooks@bosainsurance.com
www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze
512-658-0262
Kirsten.Baze@medpro.com www.medpro.com
ProAssurance (HH Silver Sponsor)
UT Health San Antonio MD Anderson Cancer Center (HHH Gold Sponsor)

UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
Humana (HHH Gold Sponsor)
Humana is a leading health and well-being company focused on making it easy for people to achieve their best health with clinical excellence through coordinated care.
ProAssurance professional liability insurance defends healthcare providers facing malpractice claims and provides fair treatment for our insureds. ProAssurance Group’s rating is AM Best A (Excellent).
Mike Rosenthal
Senior Vice President, Business Development 800-282-6242
Visit us at www.bcms.org
continued on page 42
41
BCMS Vendor
MikeRosenthal@ProAssurance.com
www.ProAssurance.com
INVESTMENT ADVISORY REAL ESTATE
Alamo Capital Advisors LLC (★★★★ 10K Platinum Sponsor)


Focused on sourcing, capitalizing, and executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current projects include new developments, acquisitions & sales, lease representation and financial restructuring (equity, debt, and partnership updates).
Jon Wiegand, Principal 210-241-2036
jw@alamocapitaladvisors.com www.alamocapitaladvisors.com
MEDICAL BILLING AND COLLECTIONS SERVICES
one of the world’s most ethical companies by Ethisphere.
Tom Rosol
210-413-8079
tom.rosol@henryschein.com
www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
MILITARY
San Antonio Army Medical Recruiting office (★★Silver Sponsor)
Mission: Recruit highly qualified and motivated healthcare professionals for service in the Army Reserves or Active Duty Army, in support of Soldiers and their families.
1LT Thomas Alexandria 210-328-9022
Alexandria.n.thomas12.mil@army. mil
https://recruiting.army.mil/mrb/ “Service to Country, Army Medicine, Experientia et Progressus”
MOLECULAR DIAGNOSTICS LABORATORY
Wave Online (★★★ Gold Sponsor)
Our team of professionals will act as your extended AR office enhancing your revenue through our proprietary metrics and claim management systems. In addition, you keep 100% control of your RCM. Contact us today for a no cost evaluation.
Saranraj (Raj) Venkatesh
Vice President – RCM | Sales and Client Relations
726-228-1097
saranraj@wavemt.com
https://rcmwave.com/ “Innovation towards Solutions”
Commercial & Medical Credit Services (HH Silver Sponsor)
A bonded and fully insured San Antonio-based collection agency. Henry Miranda 210-340-9515 hcmiranda@sbcglobal.net www.cmcs-sa.com
“Make us the solution for your account receivables.”
MEDICAL SUPPLIES AND EQUIPMENT
Henry Schein Medical (HH Silver Sponsor)

From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as
iGenomeDx ( Gold Sponsor)

Most trusted molecular testing laboratory in San Antonio providing FAST, ACCURATE and COMPREHENSIVE precision diagnostics for Genetics and Infectious Diseases.
Dr. Niti Vanee Co-founder & CEO 210-257-6973
nvanee@iGenomeDx.com
Dr. Pramod Mishra Co-founder, COO & CSO 210-381-3829
pmishra@iGenomeDx.com
www.iGenomeDx.com
“My DNA My Medicine, Pharmacogenomics”
PRACTICE MANAGEMENT
https://rcmwave.com/ “Innovation towards Solutions”
PROFESSIONAL ORGANIZATIONS
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber, President 210-308-7907 (Direct) kbarber@bdo.com
Valerie Rogler, Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Lindsey Herman Nolan, MHR, CMPE, President info4@samgma.org www.samgma.org
REAL ESTATE SERVICES COMMERCIAL
ment services to those within the medical community.
Brian T. Boswell, CFP®, QKA
Senior Private Wealth Advisor 512-649-8113 SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
STAFFING SERVICES
Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
Cindy M. Vidrine Director of Operations- Texas 210-918-8737
cvidrine@favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”
Wave Online (★★★ Gold Sponsor)


Our team of professionals will act as your extended AR office enhancing your revenue through our proprietary metrics and claim management systems. In addition, you keep 100% control of your RCM. Contact us today for a no cost evaluation.
Saranraj (Raj) Venkatesh
Vice President – RCM | Sales and Client Relations
726-228-1097
saranraj@wavemt.com
Alamo Capital Advisors LLC
(★★★★ 10K Platinum Sponsor)
Focused on sourcing, capitalizing, and executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current projects include new developments, acquisitions & sales, lease representation and financial restructuring (equity, debt, and partnership updates).
Jon Wiegand, Principal 210-241-2036 jw@alamocapitaladvisors.com www.alamocapitaladvisors.com
RETIREMENT PLANNING
Oakwell Private Wealth Management (HHHH 10K Platinum Sponsor) Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth manage-

continued from page 41 42 SAN ANTONIO MEDICINE • February 2023
Directory

Visit us at www.bcms.org 43
2023 Mazda MX-5




 By Stephen Schutz, MD
By Stephen Schutz, MD
AUTO REVIEW
44 SAN ANTONIO MEDICINE • February 2023
The fourth generation of the Mazda MX-5, better known as the Miata, is notable for being very dedicated to its roots. Most cars, especially sports cars, become as overweight and bloated over time as their owners (I’m looking at you Nissan 400Z). Not so the Miata, which has entered its 33rd year of production weighing just 300lbs more than it did when it debuted way back in 1989.
It’s worth mentioning what a big deal the Miata was back in 1989. All of the “great” British roadsters of old like the MGB, Triumph TR6, and Jaguar E-type had died out mostly because of reliability concerns and it seemed at the time that they wouldn't be missed. But Mazda thought that a similar car that offered a devil-may-care top-down experience might succeed in the US in the 1990s, so they created the Miata, a sorta Lotus Elan with reliable Japanese hardware. And boy did it succeed.
Supported by wonderful print ads with exhortations like, “There’s something you should do before life hits you in the knees with ten bags of groceries and the need for a garden hose,” the Miata became a home run for Mazda, creating goodwill galore that boosted sales of their otherwise fairly ordinary cars like the Protege, 626 and 929. The Miata made Mazda cool.
Anyway, according to Mazda it’s now the MX-5 so that’s what I’ll call it. Sigh...
Driving the MX-5 is a joy. The combination of light weight (2345lbs), good power (181HP from a 2.0L normally aspirated in-line four-cylinder engine), and a honed suspension results in a terrific driving experience. Naturally, the MX-5 mostly relishes twisty back roads, where its close-ratio six-speed manual transmission keeps the engine in its happy place, while the magical steering allows the driver to hit every apex. I don’t want to slobber here, but driving an MX-5 on quiet back roads is as good as it gets in a car. Like, there’s nothing better.
Of course, it should be noted that taking an MX-5 on a long trip on the interstate will get old fast thanks to a droning engine and not much sound deadening, running errands in town can get frustrating because you can’t see over any other vehicles, and it's just a two-seater.
Despite the passage of more than three decades of time, the newest MX-5 looks remarkably like the original. The proportions are about
the same, as are the size and weight. Gone are the pop-up headlights from the original, regrettably, but nobody will mistake an MX-5 for any other car.
It’s worth pointing out that, while the MX-5 hasn’t gotten chubby since 1989, almost every other vehicle on the road has, so safety is an issue. The MX-5 passes every applicable crash test, of course, but I wouldn’t want to be sitting in one that gets t-boned by a Ford F-150 pickup truck.
The interior of the MX-5 is nice but not luxurious. The plastics and other materials look and feel g ood, but they do remind you to focus on driving (and that Mazda did what was necessary to keep the price low).
Naturally the MX-5’s interior is small. Tall drivers will feel cramped—I’m 6’2” and wished for more headroom—and there’s not much space for luggage or what-have-you. And as noted above, it’s a two-seater so the kids will have to Uber home.
For the record, the MX-5 starts at just over $29,000 for the Sport version, and even a loaded Club RF, the most expensive MX-5, has an MSRP under $41,000. Fuel economy is an impressive 26MPG City/34MPG Highway.
A personal note: while an automatic transmission is available in the MX-5, the glorious 6-speed manual is absolutely the way to go.
In 2021 and through most of 2022 MX-5s—and many other desirable vehicles—commanded premium pricing thanks to global supply chain SNAFUs etc, but those headaches are subsiding, thankfully. As always, a call to BCMS’ own Phil Hornbeak should be your first step whenever you’re starting to consider buying a new vehicle.
The MX-5 RF, by the way, is a hard-top with a removable roof something like a Porsche Targa. Until this the fourth generation of Mazda’s iconic roadster, all you could get was a convertible. Now the RF version is available, which is nice for cold climates or club racing. I would imagine that this option will not be popular in South Texas.
All hail the Mazda MX-5, a two-seat sports car that’s been remarkably true to its roots in order to deliver a driving experience that can’t be beat. Get one before somebody hits you in the knees with 10 bags of groceries. You won’t regret it.

As always, call Phil Hornbeak, the Auto Program Manager at BCMS (210-301-4367), for your best deal on any new car or truck brand. Phil can also connect you to preferred financing and lease rates.
Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the US Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.

AUTO REVIEW Visit us at www.bcms.org 45
11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Rick Cavender 210-681-3399
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Charles Williams 210-912-5087
Chuck Nash Chevrolet Buick GMC 3209 North Interstate 35 San Marcos, TX
William Boyd 210-859-2719
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Kahlig Auto Group
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
Kahlig Auto Group
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
9455 IH 10 West San Antonio, TX 78230
Douglas Cox 210-764-6945
Kahlig Auto Group
Audi North Park 15670 IH-35 North Selma, TX 78254
Camden Steele 325-374-9897
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Paul Hopkins 210-988-9644
Kahlig Auto Group
14610 IH 10 West San Marcos, TX 78249
Mark Hennigan 832-428-9507
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
North Park Mazda 9333 San Pedro San Antonio, TX 78216
John Kahlig 210-253-3300
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Gary Holdgraf 210-862-9769
North Park Lexus 611 Lockhill Selma San Antonio, TX
Tripp Bridges 210-308-8900
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Al Cavazos Jr. 210-366-9600
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000
 Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group


















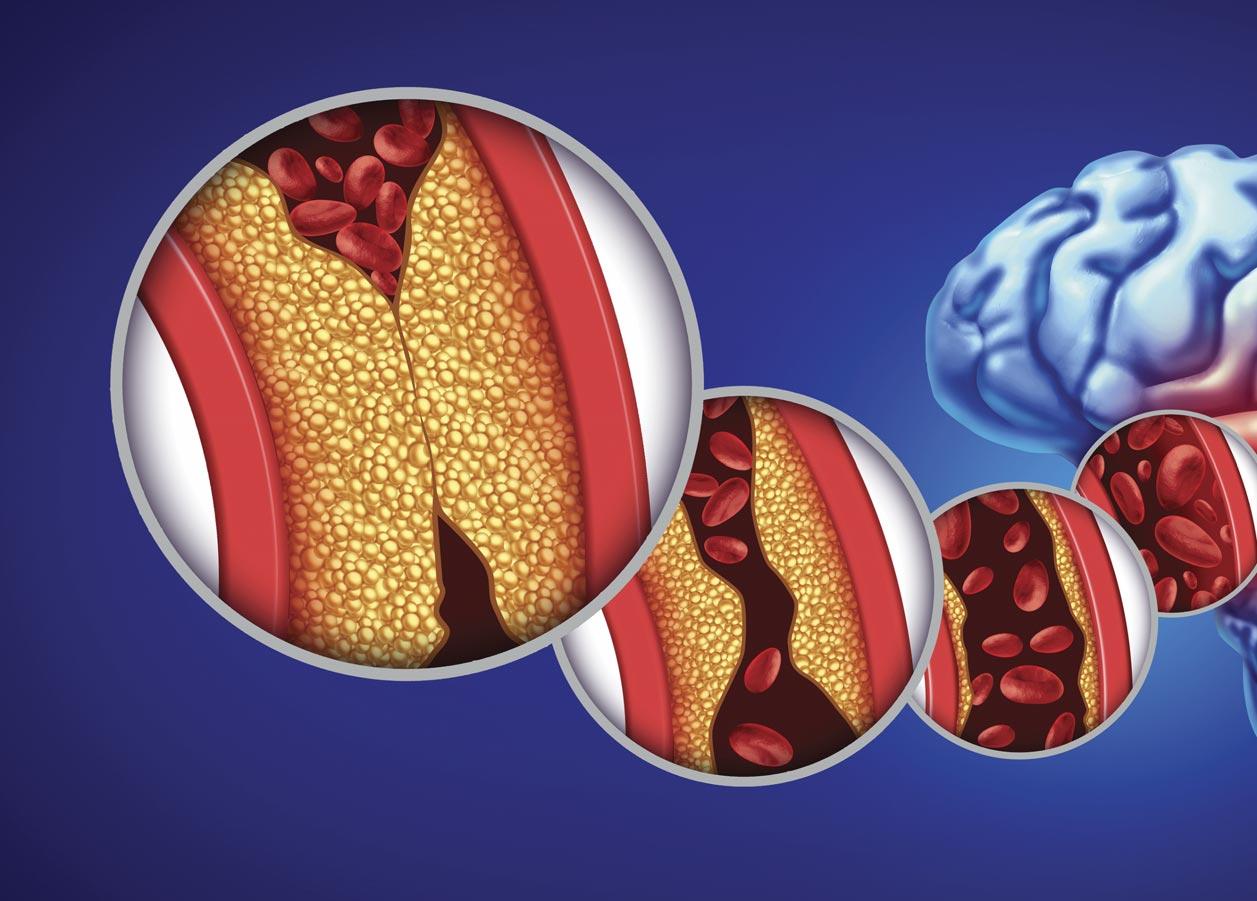




 By Monica J. Salas, MD
By Monica J. Salas, MD

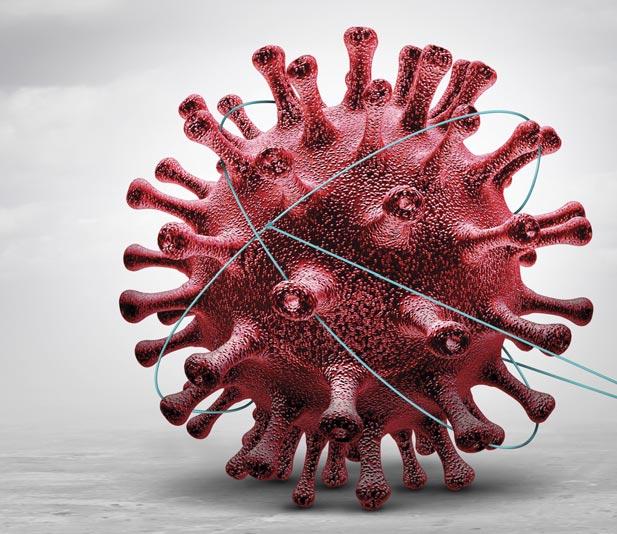




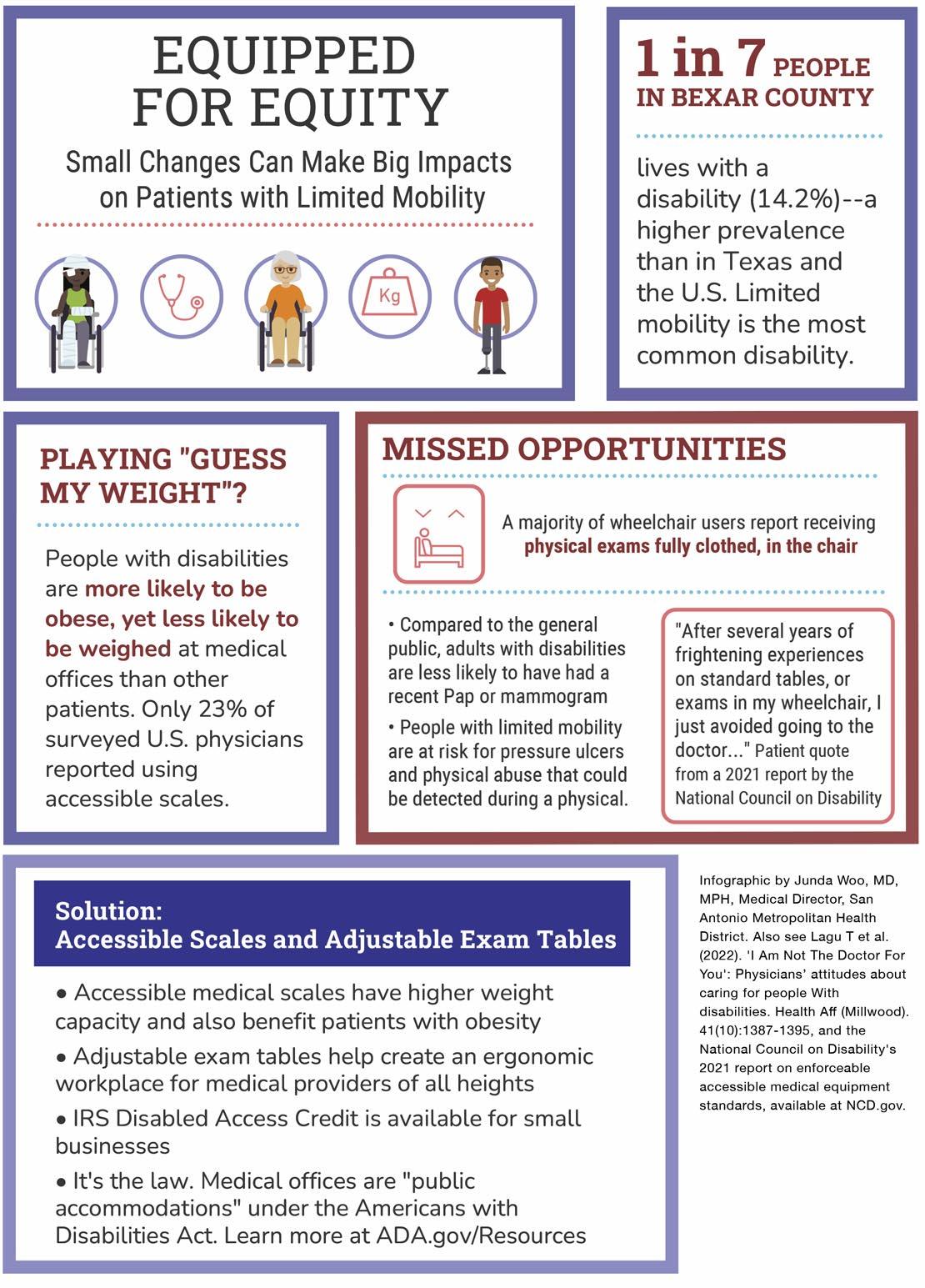












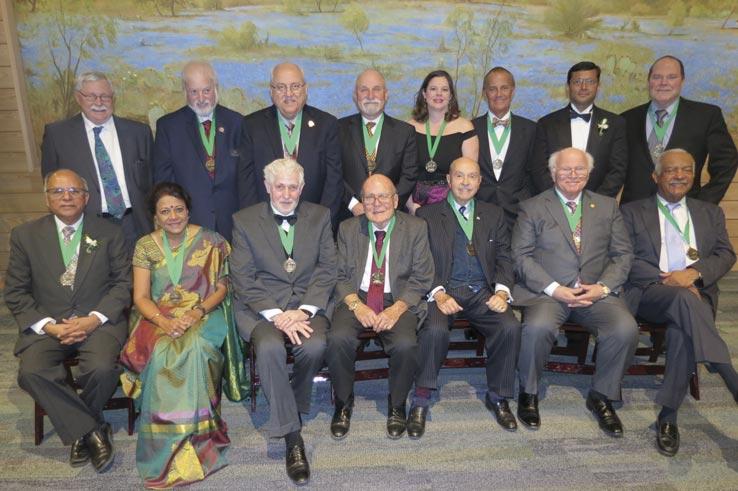

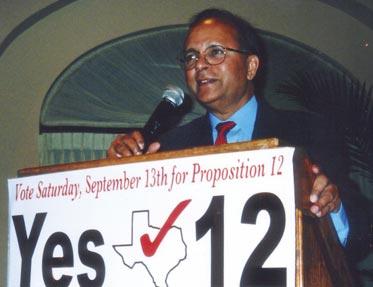

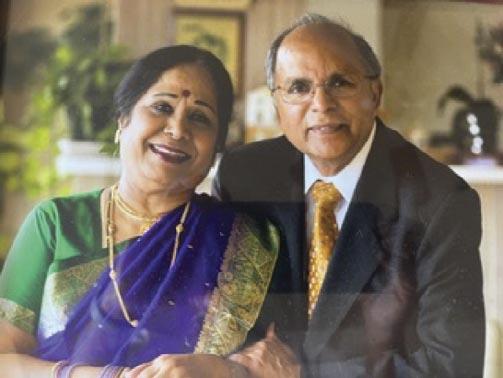

















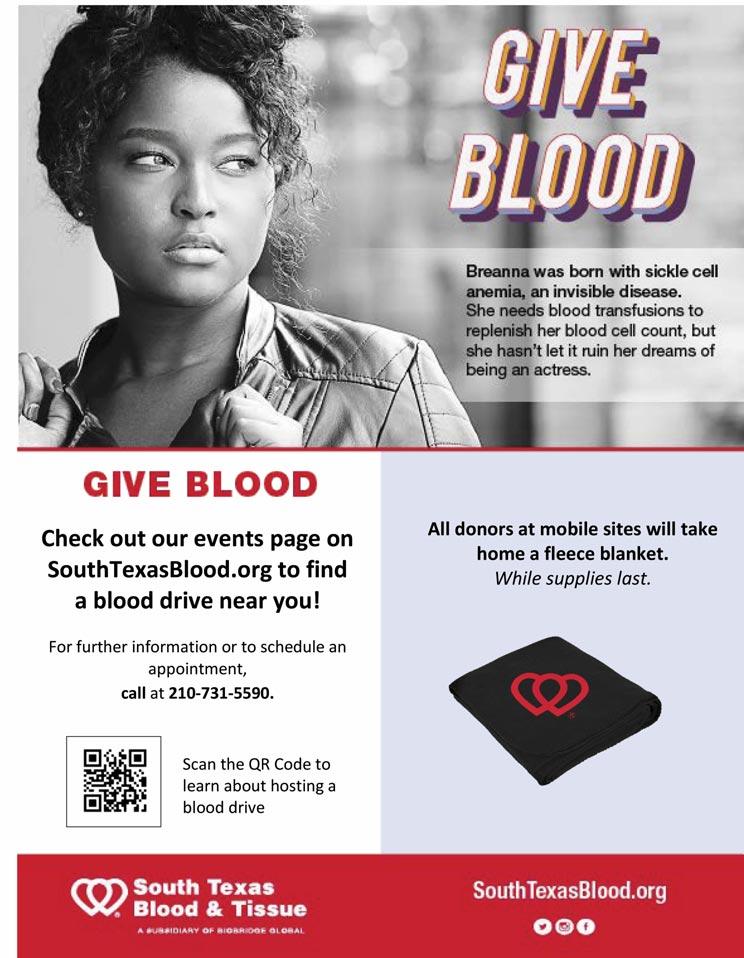























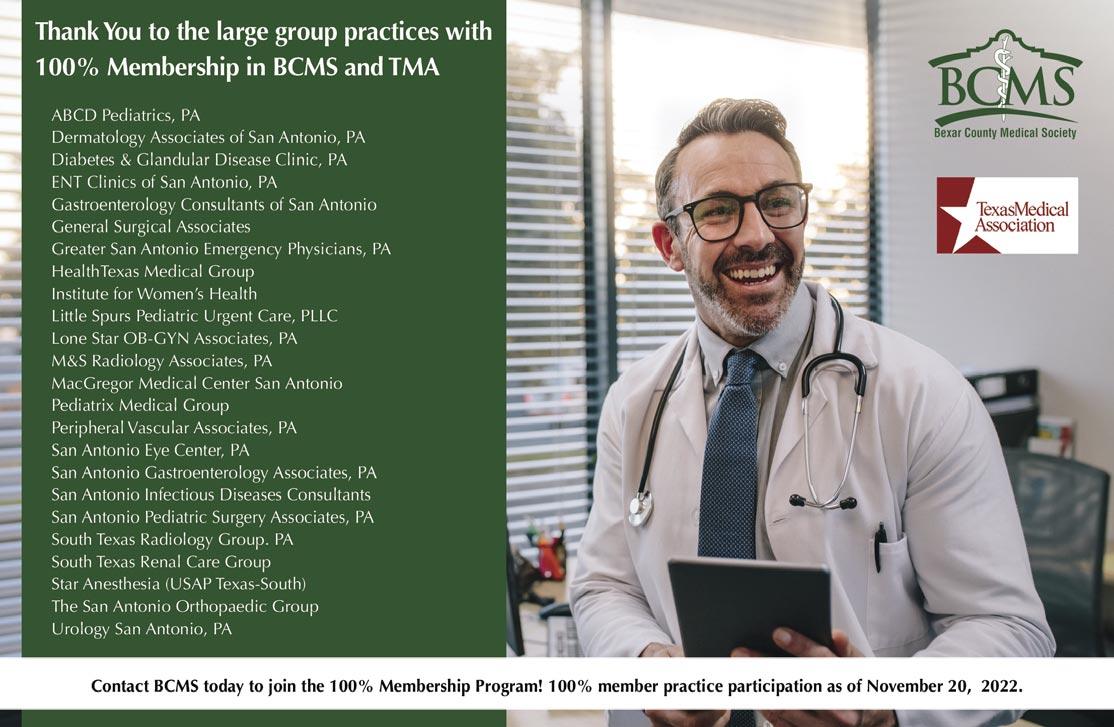




 By Stephen Schutz, MD
By Stephen Schutz, MD


 Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group