TABLE OF CONTENTS











PUBLISHED BY: traveling Blender, llC. 10036 Saxet Boerne, tX 78006
PUBLISHER louis doucette louis@travelingblender.com
BUSINESS MANAGER: vicki Schroder vicki@travelingblender.com
ADvERTISING SALES:
AUSTIN: Sandy Weatherford sandy@travelingblender.com
SAN ANTONIO: Gerry lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EditoriAl CorrESpondEnCE:
Bexar County Medical Society
4334 n loop 1604 W, Ste. 200
San Antonio, tX 78249
Email: editor@bcms.org
MAGAZinE AddrESS CHAnGES:
Call (210) 301-4391 or
Email: membership@bcms.org
SuBSCription rAtES:
$30 per year or $4 per individual issue
AdvErtiSinG CorrESpondEnCE:
louis doucette, president traveling Blender, llC.
A publication Management Firm 10036 Saxet, Boerne, tX 78006
www.travelingblender.com
For advertising rates and information
Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national orgin, or an intention to make such preference limitation or
crimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2024 Smithprint, inc. prin tE d in tHE u SA

Ezequiel “Zeke” Silva, iii, Md, President
lyssa ochoa, Md, Vice President
John Shepherd, Md, President-elect
Jennifer r. rushton, Md, Treasurer
lubna naeem, Md, Secretary
John Joseph nava, Md, Immediate Past President
Woodson “Scott” Jones, Md, Member
Sumeru “Sam” G. Mehta, Md, Member
M. “Hamed” reza Mizani, Md, Member
priti Mody-Bailey, Md, Member
dan powell, Md, Member
Ana rodriguez, Md, Member
raul Santoscoy, do, Member
lauren tarbox, Md, Member
nancy vacca, Md, Member
Col. Elisa d o’Hern, Md, MC, FS, Military Representative
Jayesh Shah, Md, tMA Board of Trustees Representative
John pham, do, UIW Medical School Representative
robert leverence, Md, UT Health Medical School Representative
ramon S. Cancino, Md, Medical School Representative
lori Kels, Md, Medical School Representative
ronald rodriguez, Md, Medical School Representative
victoria Kohler-Webb, BCMS Alliance Representative
Carolina Arias, Md, Board of Ethics Representative
Melody newsom, BCMS CEO/Executive Director
George F. “rick” Evans, Jr., General Counsel
Melody newsom, CEO/Executive Director
Monica Jones, Chief Operating Officer
Yvonne nino, Controller
Al ortiz, Chief Information Officer
Brissa vela, Director of Membership & Corporate Partnerships
phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
Monica Jacqueline Salas, Md, Co-chair
Jennifer C. Seger, Md, Co-chair
lokesh Bathla, Md, Member
Elizabeth Clanton, Md, Member
Erika Gabriela Gonzalez-reyes, Md, Member
timothy C. Hlavinka, Md, Member
John robert Holcomb, Md, Member
Soma S. S. K. Jyothula, Md, Member
Kristy Yvonne Kosub, Md, Member
Jaime pankowsky, Md, Member
George-thomas Martin pugh, Md, Member
rajam S. ramamurthy, Md, Member
Adam v ratner, Md, Member
John Joseph Seidenfeld, Md, Member
Boulos toursarkissian, Md, Member
Francis vu tran, Md, Member
Faraz Yousefian, do, Member
louis doucette, Consultant
Brissa vela, Consultant
Monica Jones, Staff Liaison
trisha doucette, Editor
deepthi S. Akella, Student
Moses Alfaro, Student
victoria Ayodele, Student
tue Felix nguyen, Student
Andrew ta, Student
Alixandria Fiore pfeiffer, do, Resident
Elizabeth Allen, Volunteer
Adelita G. Cantu, phd, Volunteer
rita Espinoza, drpH, Volunteer
natalie reyna nyren, pA-C, Volunteer
david Schulz, Volunteer
I am honored to share my installation speech:
By Ezequiel "Zeke" Silva III, President, Bexar County Medical Society (BCMS)Last fall, Bexar County Medical Society celebrated 170 years. This society was founded in 1853. To put that history in perspective, when you leave this evening, notice the Alamo across the street. The Alamo fell just 17 years before our society was founded. I'm especially mindful and cognizant of that history, but one point that I'm especially proud of is that we were the first component medical society for what is today the Texas Medical Association. It was us.
I am especially glad to be here in the Menger Hotel. Our BCMS Alliance was founded in 1917, in this hotel. To show you how forward-thinking the women that founded the Alliance were: A year later, the TMA started their Alliance and a year after that, the AMA started theirs. We were the egg that grew into the TMA, the TMA Alliance and beyond. It started here.
were experiencing. Melody could have said, “Let's study it, let's think about it, let's ponder it.” Instead, she said, “Docs, just so you know, on January 13, we're having a vaccine fair in our building. We're sponsoring it. I've already reached out to H-E-B and they are going to bring the vaccines. Metro Health is on board. I need all of you there.” From there, we accomplished what we needed to accomplish.
... One point that I'm especially proud of is that we were the first component medical society for what is today the Texas Medical Association.
It was us ...
Being mindful of our history, I'd like to share a bit of our more recent history. I want to take you back to early 2021. We were about a year into a crippling, challenging pandemic and we were doing what a medical society does. We were there for our doctors, educating and responding where we could. But we were also listening, and we were hearing that if you were a physician not affiliated with a healthcare system, or you were one of their staff, you did not have access to lifesaving COVID vaccines. In early 2021, we led the effort to vaccinate 2,400 physicians and their medical staff, doing so at a time of great urgency.
Our BCMS Alliance was founded in 1917 ... A year later, the TMA started their Alliance and a year after that, the AMA started theirs. We were the egg that grew into the TMA, the TMA Alliance and beyond.
Now fast forward to 2024. The challenges that physicians face are different, thankfully less urgent, but nonetheless relevant. BCMS is well positioned to help address challenges our physicians are experiencing. Our physicians are contending with different employment models, growing corporate and private equity influence, and increasing vertical integration. Our physicians are asking: What do I need to do to thrive in this environment, to continue providing the best care possible? At the same time, we are seeing non-physicians come into our space and try, with considerably less training, to do what we do. Scope of practice is important and scope creep problematic. We will continue to work to make sure that physicians lead care teams and patients receive what they expect: Care provided by physicians. I wish payment were not always a consideration, but our members are not only facing challenges regarding payment from government payers (Medicare and Medicaid) but also the private payers in our community. The time for Medicare Reform is now.
What did it take for us to accomplish this? We certainly had to have a strong organizational structure, staff and physician volunteers. We had a beautiful building to hold the event. But what really made the difference was that we had the trust and credibility of the physicians in our community, and they knew we had their backs. Equally important, we had leadership. I remember the Zoom leadership call where our CEO, Melody Newsom, described the challenge our physicians
There is so much opportunity as well. There is so much excitement that's coming into our specialties and our profession. In Austin, we are discussing value-based care at the legislative level. This could lead to a time where physicians no longer focus on their volume of services, but we can focus on the quality and the value of care we provide. We are seeing an exciting growth and rapid expansion of digital health technologies. This includes telemedicine and telehealth, but also remote

physiologic monitoring, digital therapeutics and large language models. We are seeing augmented intelligence (AI) come into our space and help us to do better what we can do. An important opportunity around AI is the physician’s ability to guide how technology comes into our exam room and our procedure rooms. We must share with the innovators and regulators how technology can be rolled out responsibly to enable the best care possible.
Another important opportunity, and one which is going to be a focus of mine this year, is strengthening our relationship with our partner, the Texas Medical Association. I mentioned that we were the first component medical society of the TMA. With that comes considerable responsibility and considerable opportunity. I'm so grateful to Dr. Rick Snyder II (TMA President) and Michael Darrouzet (TMA Executive Vice President) for being here tonight and showing their commitment to us, and we will do the same back to them. We will strengthen our delegation to the TMA House of Delegates. We will work to nurture young leaders to serve on TMA councils, committees and caucuses.
Perhaps the greatest opportunity we have relates to an important change in our state: The opening of new medical schools. We are fortunate here in San Antonio to have one at the University of the Incarnate Word. There is also Austin, Sam Houston State, TCU, North Texas and the Rio Grande Valley. We have more students and new physicians being trained in our state than ever. As leaders, we have the opportunity to meaningfully bring these new doctors into BCMS and enable their success.
To further emphasize our important partnership with the TMA. I
will close with a recent story. Last year, during the 88th Texas Legislative Session, we passed a law to strengthen insurance networks. For those of you that don't think about insurance daily, basically, your network includes beneficiaries and the doctors that care for them. For physicians, this is where we want to be, but we want the terms of our contracts to support our practices. Above all, we want those networks to provide what our citizens and our community expect: Access to high-quality care. Late last year, the regulatory language dropped regarding this new law. Regrettably, the proposed language was unfairly tilted more towards the health plans and less towards physicians. Yesterday, I received a call from our TMA lobbying team. I am fortunate that the TMA lobbyists believe in me and trust me to testify on behalf of physicians. It is a job which I never take lightly. I know when I go to the Capitol or a regulatory body like the Texas Department of Insurance, I know who and what I am representing. This Wednesday in Austin, I may be the only physician testifying. Someone will testify on behalf of the health plans or some business group and say: We can't guarantee that patients can have an appointment within three weeks. We can't guarantee that patients will have the ability to see a specialist within a 30-minute commute of where they live. We can't guarantee that the entire spectrum of specialists will be available. And you know what? I'm going to go to that microphone and say: I'm a physician, I care for patients, and I speak for my physician community. The answer is ‘Yes, we can’ do all that this law requires. Because it is the right thing to do. And it is what we, as physicians, have always done. It is what we do in San Antonio and what we did during COVID.
It is what BCMS has done for 170 years. This organization has a remarkable history of success and accomplishment. As your President, I will do everything I can to maintain that legacy.

Ezequiel “Zeke” Silva III, MD, is the 2024 President of the Bexar County Medical Society. Dr. Silva is a radiologist with the South Texas Radiology Group, Adjunct Professor of Radiology at the UT Health, Long School of Medicine, and Vice-Chief of Staff at Methodist Hospital Texsan. He serves on the TMA Council on Legislation and is a TMA Delegate to the AMA. He chairs the AMA RVS Update Committee (RUC).
Every spring our immediate BCMS Alliance Past President contacts Bexar County Medical and Allied Health professions schools to seek out applicants for our scholarships. Scholarship funds are typically disbursed in late July/early August to the winners’ 4-year, Bexar County school, and traditionally BCMSA holds a fall event to recognize the winners. Thank you to our past and current members for keeping these scholarships going!




Our Medical Student Recipients were:
Denise Nemeth: Awarded $3,000 for the Hispanic Medical Student Scholarship. Denise is a student at UIW.
Daniel Derrick: Awarded $1,500. Daniel is a student at the UT Health Long School of Medicine.
Nina Nguyen: Awarded $1,500. Nina is a student at the UT Health Long School of Medicine.
The Allied Health Awards went to:
Emilio Cassaretto: Awarded $500. Emilio is a student at the UIW School of Physical Therapy. Hailey Lechuga: Awarded $1,000 for The Sandra Vela Memorial Scholarship. Hailey is a Pre-Pharmacy Student at St. Mary's University. Morgan Kingsbury: Awarded $1,000 for The Rebecca Christopherson Scholarship. Morgan is studying at the UT Health-Occupational Therapy Program.
The application deadlines for the Allied Health Professions Scholarship is March 15, and the Medical School Scholarship application is due April 15.
If you know of an exceptional student or employee in your practice who is interested in applying, please email bcmsalliance@bcms-alliance.org for information.

Brittany Garcia, BS, MHA, is the 2024 President-Elect for the BCMS Alliance.

Obstructive sleep apnea (OSA) is a common and serious sleep disorder that repeatedly causes abnormal breathing patterns or pauses in breathing during sleep. It is estimated that OSA affects nearly 30 million adults in the U.S.1 The current prevalence rate of OSA is about 10-20 percent of middle-aged adults, with at least 4-8 percent of men and 2-4 percent of women.2 In the general adult population, 80-90 percent of OSA is untreated and undiagnosed. OSA is secondary to complete or partial airway obstruction caused by recurrent pharyngeal collapse during sleep manifesting as loud snoring or choking with frequent sleep awakenings. Individuals suffering from OSA will experience a wide array of complaints to include loud snoring, witnessed pauses in breathing, nonrestorative sleep, morning headaches, morning dry mouth and excessive daytime fatigue. The consequences of untreated OSA are wide ranging and are thought to result from intermittent hypoxia/hypercapnia, intrathoracic pressure variations, fragmented sleep and increased sympathetic nervous activity. Untreated OSA patients are at an increased risk of developing cardiovascular disease, metabolic dysregulation and increased healthcare utilization.
The American Academy of Sleep Medicine has recently released updated quality measures for the care of adult patients with obstructive sleep apnea focusing on improvement of detection and categorization of OSA symptoms and severity to promote assessment and diagnosis of the disorder.3 There are several OSA screening measurements to include the Berlin questionnaire, Epworth sleepiness scale and STOP-Bang. The Epworth sleepiness scale, first developed by Dr. Johns, is an 8 categorical scale evaluating subjective sleepiness. It is suggestive that a score of 8 or more has a 76 percent sensitivity for the presence of OSA.4 The STOP-Bang questionnaire was developed as an OSA screening tool consisting of four self-reportable traits (snoring, tiredness, observed apnea and high blood pressure) and four demographic criteria to include body mass index, age,

neck circumference and gender). In the initial validation study, a score of at least 3 demonstrated a sensitivity of 84 percent to detect OSA.5
The diagnosis of OSA is accomplished either by a home sleep study (HST) or an in-laboratory diagnostic polysomnography (PSG). The American Academy of Sleep Medicine (AASM) has published recent guidance regarding sleep apnea diagnostic testing.6 A technically adequate home sleep apnea testing device is appropriate for most uncomplicated adult patients for the diagnosis of OSA. HST is less sensitive than PSG in the detection of OSA and a false negative test could result in harm to the patient due to denial of a beneficial therapy. In the event of a single negative, inconclusive or technically inadequate HST result,
performance of a PSG is recommended. The severity of OSA is based upon the Apnea-Hypopnea Index (AHI). Mild OSA is defined by an AHI of 5-14, moderate OSA by an AHI 15-29, and severe OSA by an AHI equal/greater than 30. However, the AHI may not be the most important measure of OSA and outcomes. For example, it was found that the amount of total sleep time with SpO2 less than 90 percent (TST90) to be a better predictor of all-cause mortality in an OSA patient with heart failure.7 In the future, we will see improved diagnostic metrics that improve diagnostic accuracy and treatment outcomes.
The treatment of OSA involves patient education and treatment modalities that result in optimal patient adherence and symptomatic improvement. Patients should be educated about the goals of OSA treatment and should have close clinical follow-up to assess treatment adherence. Kuna et al highlighted the importance of weight management for treatment of OSA.8 Treatment of OSA with CPAP is currently the recommended treatment and has the greatest evidence of efficacy on AHI, symptoms and comorbidities. Symptomatic patients with moderate-severe OSA generally have good adherence to CPAP therapy, while those with mild OSA, female, young and generally paucisymptomatic, have lower CPAP adherence, especially in the medium and long term. The use of CPAP treatment offers that advantage of non-invasive, adjusted therapy with the ability for the provider to monitor treatment adherence and therapeutic response. Common patient complaints include challenges with mask comfort and leak, excessive dry mouth and equipment upkeep. Other treatment options include Mandibular advancement devices (MAD), positional therapy (PT) and hypoglossal nerve stimulation (HSN). The MAD is an attractive treatment option for most patients with mild to moderate OSA. The MAD developed for treatment of sleep-disordered breathing are devices used in the oral cavity during sleep with the purpose of preventing the collapse between oropharyngeal tissues and the base of the tongue.9 Common short term side effects include discomfort in the temporomandibular joint and in the masticatory muscles. Finally, the hypoglossal nerve stimulator is a novel therapeutic device for patients with moderate to severe OSA who are intolerant to traditional treatment.10 A hypoglossal nerve stimulator is a device that generates electrical impulses through a generator that is implanted in the upper right chest. The impulse is transmitted via a tunneled lead that ends up with a cuff that surrounds the hypoglossal nerve, which allows stimulation of the upper airway muscles.
OSA is a common medical condition that requires a high index of suspicion. Untreated, it is associated with significant cardiovascular disease states. Having a strong baseline understanding the evaluation and pre-identification of an OSA patient is critical. After obtaining an appropriate confirmatory diagnostic test, there are several treatment options for OSA.
References:
1. Sleepeducation.org
2. Mannarino MR, De Filippo F, Pirro M. Obstructive sleep apnea syndrome. Eur JF Intern Med 2021; 23: 586-593
3. Lloyd R, Morgenthaler TI, Donald R, et al. Quality measures for the care of adult patients with obstructive sleep apnea: 2022 update after measure maintenance. J Clin Sleep Med. 2022;18(11):2673–2680
4. Rosenthal LD, Dolan DC. The Epworth sleepiness scale in the identification of obstructive sleep apnea. J Nerv Ment Dis. 2008 May;196(5):429-31
5. Pivetta B, Chen L, Nagappa M, et al. Use and Performance of the STOP-Bang Questionnaire for Obstructive Sleep Apnea Screening Across Geographic Regions: A Systematic Review and Meta-Analysis. JAMA Netw Open. 2021;4(3):e211009
6. Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504
7. Won CHJ. When will we ditch the AHI? J Clin Sleep Med. 2020;16(7):1001–1003
8. St-Onge MP, Tasali E. Weight Loss Is Integral to Obstructive Sleep Apnea Management. Ten-Year Follow-up in Sleep AHEAD. Am J Respir Crit Care Med. 2021 Jan 15;203(2):161-162
9. Manetta IP, Ettlin D, Sanz PM, Rocha I, Meira E Cruz M. Mandibular advancement devices in obstructive sleep apnea: an updated review. Sleep Sci. 2022 Apr-Jun;15(Spec 2):398-405
10. Mashaqi S, Patel SI, Combs D, Estep L, Helmick S, Machamer J, Parthasarathy S. The Hypoglossal Nerve Stimulation as a Novel Therapy for Treating Obstructive Sleep Apnea-A Literature Review. Int J Environ Res Public Health. 2021 Feb 9;18(4):1642

David A. Marks, MD, is Board Certified in Pulmonary, Critical Care and Sleep Medicine with 18 years of experience. Dr. Marks’ professional interests include COPD, pulmonary hypertension, sleep disorders and critical care medicine. He graduated from the University Of Texas Health Sciences Center At San Antonio Long School Of Medicine in 1997 and completed a residency at University Of Texas Health Sciences Center/U Hospital. Dr. Marks is a Wellness provider for the San Antonio Fire Department and Senior Aviation Medical Examiner for the FAA, and a member of the Bexar County Medical Society.


Clearly, the primary entry point to care for patients with sleep dis orders is their Primary Care physician. Due to wider recognition of the ubiquitous nature of sleep disorders, decreased reimbursement for sleep specialty procedures, and the marked impact many disorders have on preventive and population health, an explosion of awareness and increased requirements for evaluation and treatment has occurred over the past 15 years.
When a patient presents to clinic with complaints about sleep, they usually fall into one of three categories: I’m sleepy when I don’t want to be; I can’t sleep when or as long as I want to; or my partner, friend or I realize my sleep has abnormal movements or sounds.
Any sleep evaluation must begin with a thorough understanding of the patient’s sleep schedule (including variation on and off work, weekdays and weekends) as the most common sleep disorder is insufficient
of sleep each day. Widely varying sleep schedules and lengths will cause symptoms that mimic or complicate organic sleep disorders. Furthermore, significant sleep schedule variation affects cognitive function, emotions, temperature regulation, GI function, urination schedules and many other hormonally derived functions resulting in discomfort and fatigue.
One scale that is available and helpful in assessing sleep quality is the PSQI – Pittsburgh Sleep Quality Index. The first step to treating patients with excessive fatigue or daytime sleepiness is to have them ensure they are getting sufficient sleep for a minimum of seven days, preferably 14 days, while on a stable sleep schedule. It is only after several days of stable sleep that a realistic assessment of many sleep disorders becomes possible. This principle of assessing sleep periods also applies to those who report insomnia; usually care starts with a 2-week sleep diary doc-
umenting bedtimes, sleep time, awakening times, variations in sleep periods, nap times, and use of sleep effecting substances such as caffeine, tobacco, stimulants, alcohol, opioids as well as environmental factors that can affect the sleep period.
Clearly, sleep disordered breathing (Obstructive Sleep Apnea, Central Sleep Apnea, Nocturnal Hypoventilation) has become the poster child of sleep disorders over the past 15 years, with a population prevalence between 2-26 percent, depending on subgroup definition. Increased community recognition, better understanding of the interplay with heart disease, as well as the general increase in obesity prevalence has brought this to the fore. It is difficult to watch TV for longer than an hour or two and not see an advertisement for some form of OSA treatment. The progressive effects of OSA over time on heart disease patients has resulted in greater efforts to diagnose and treat OSA. The high prevalence of OSA has now pushed diagnosis and treatment for these patients into the Primary Care office. Patients typically present for evaluation with snoring, excessive sleepiness or insomnia, sore throats, morning headaches, night sweats and witnessed apnea. The simple STOP-BANG questionnaire has great sensitivity with scores > 3 (snoring, tiredness, observed apnea, pressure high, BMI>35, Age >50, neck circumference > 40 cm, gender = male), and indicate a need for objective testing. In patients without co-morbidities, or only mild concomitant illnesses, home sleep studies are effective in diagnosing OSA. Several local and national services offer these studies with the option of continuing to manage these patients in the Primary Care setting or referring them to the Sleep Specialist. Reports from these services frequently return with treatment recommendations, particularly for Auto-titrating CPAP, which can be easily prescribed and serves to adjust each night to patient environmental and physiological variation. Patients with poorly controlled heart or lung disease, neurological deficits, or those at significant risk for central apnea or hypoventilation, need to be referred for in-lab monitored testing due to their increased risks of dysrhythmia and gas exchange abnormalities. Patients who are diagnosed with complex sleep disorders or are poorly responsive to first level treatment should likely be followed by a Sleep Specialist.
Those patients who do report unusual sounds or movements at night (parasomnias) have a broad diagnostic differential, several of which are neurological in nature. Often, unusual seizure disorders must be considered and ruled out. Parasomnias may also be associated with nutritional deficiencies, anemia and hypothyroidism. Some of these disorders such as Sleepwalking or Night Terrors are often treated in Primary Care, many times jointly with a Sleep Specialist. The most common parasomnia that is cared for in Primary Care is Restless Legs Syndrome, which has a strong correlation with anemia but may also be
a primary disorder and is also linked with many other conditions, such as Parkinson’s disease. Any concern for neurological disease should be referred to a Sleep Specialist or Neurologist for further evaluation.
In summary, all of us want to feel rested and refreshed from our sleep. All of our patients know that we can’t survive without sleep, but often sacrifice sleep because of different priorities. However, there is a growing reawakening to the importance of sleep as witnessed by the new revolution in multiple commercial sleep monitors and their increasing use. We have the opportunity to encourage our patients to improve their sleep health, and to be aware of potential sleep disorders that may interfere with health. The Primary Care physician is the key link in our system in improving health and preventing disease. With that in mind, perhaps we should start with ourselves, improving our own sleep habits and ensuring that we are treated for any sleep disorders we may have. Getting the best sleep of our lives will enable us to provide the best care to those who come to us for assistance.
References:
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10416725/
2. Buysse DJ, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research 1989:28(2);193-213
3. https://www.sleepprimarycareresources.org.au/insomnia/assessment-questionnaires
4. Lettieri CJ, Eliasson AH, Andrada T, Khramtsov A, Raphaelson M, Kristo DA. Obstructive sleep apnea syndrome: are we missing an atrisk population? J Clin Sleep Med. 2005;1:381–5.
5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9373878/
6. https://www.bjanaesthesia.org/article/S0007-0912(17)322250/fulltext
7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6402728/
8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6402728/
9. https://aasm.org/one-in-three-americans-have-used-electronicsleep-trackers-leading-to-changed-behavior-for-many/

James H. Henderson II, MD, FCCP, FAASM, is a Board-Certified Pulmonology/Critical Care/Sleep Medicine physician with over 30 years of experience in executive leadership, clinical, academic and military medicine, residency program directorship and medical administration. He is a former Clinical Director and Sleep Fellowship Director of the largest sleep medicine facility in the Department of Defense and former Chairman of the largest pulmonary and respiratory department in the U.S. Air Force. Dr. Henderson is a member of the Bexar County Medical Society.

Sleep is the most conserved physiological activity exhibited by most members in the animal kingdom, and affirms the role it plays in health. As humans, we spend one third of our lives sleeping. The quality and quantity of sleep has an impact on our physical and emotional wellbeing. During my medical education and subsequent training, the uniform theme was sleep is wasted time. There was a pervasive disdain for the concept of rest and rejuvenation. As physicians, we have only embraced the importance of sleep hygiene in the past couple of decades due to some pioneering research done to study effects of sleep deprivation on health and cognitive functions of physicians.1 Beyond the impact on individual physicians' health, sleep-related impairment leads to cognitive impairment and medical errors. ACGME has set duty hour limitations on trainees as a common program requirement for accredited residency programs in the United States, recognizing the importance of adequate sleep for trainee physicians and the deleterious effects of sleep impairment. Unfortunately, unpredictable work hours are the norm for a practicing physician. In addition, personal obligations, family responsibilities and various social activities subtract further time.
I consulted with Dr. Ritwick Agrawal, triple boarded in Pulmonary, Critical Care Medicine and Sleep Medicine. He is an educator and researcher with a focus on the impact of sleep-related issues in practicing
physicians. We discussed this important topic, particularly in times of increased recognition of burnout in physicians.
Dr. Jyothula: Thank you for joining us and sharing your expertise with the physician members in our BCMS family. First thing, why is sleep important for a practicing physician, both personally and professionally?
Dr. Agrawal: Sleep is not just important, it's essential, especially in the high-stress, high-reward field of clinical practice. In our profession, where the stakes are always high, having a mechanism for relaxation is crucial. Sleep is a basic, natural way to relax and rejuvenate. Studies consistently show that good sleep is beneficial for both physical and mental well-being. After a long day of making critical decisions and navigating complex situations, sleep is the body's way of resetting and maintaining optimal well-being. On a personal level, adequate sleep is vital for mental health, emotional resilience and physical well-being, helping to combat the high stress that comes with the medical profession.
Dr. Jyothula: There has been a spurt in recognition of burnout in physicians. Do you think sleep impairment is the cause or effect?
Dr. Agrawal: It's a bit of both. Sleep impairment can lead to burnout
by exacerbating stress, reducing cognitive function, and impacting emotional well-being. However, burnout itself can also lead to sleep problems, creating a vicious cycle. Stress and anxiety associated with burnout can make it harder to fall asleep or maintain restful sleep, further compounding the issue.
I've seen firsthand how sleep impairment can play a significant role in physician burnout. Recently, a colleague of mine, an intensivist, went through a rough stretch both personally and professionally. His sleep suffered quite a bit, and it showed in his work. He started coming to work like a zombie, treating patient care as just a job, with no compassion. Fortunately, he opened up to me, and we focused on improving his sleep quality. It was remarkable to see how better sleep brought back the compassionate doctor we all knew. While sleep isn't the only factor, it can significantly compound burnout issues.
Dr. Jyothula: In my professional role, I take calls from home. What is your advice for professionals like me who take home calls, and some of my colleagues who work shift-based work including night shifts?
Dr. Agrawal: Managing sleep while taking calls from home or working night shifts can be quite challenging . I recall a fellow doctor who frequently took night calls. She realized that her sleep schedule was becoming erratic, impacting her daytime alertness. Her solution? On days she wasn't on call, she adhered strictly to a regular sleep schedule, almost religiously. This regularity helped her maintain a balance. She also believed in 'paying off sleep debt' — if she lost sleep one night, she'd find time later to catch up on rest. While it's not always possible to completely recoup lost sleep, this approach helped her stay on top of her game both personally and professionally. It's a reminder that while our schedules can be unpredictable, making concerted efforts to balance our sleep when we can is crucial.
For those engaged in consistent shift work, like a week of night shifts, there are specific strategies to help them work more efficiently at night and transition back to a day schedule. It involves gradually adjusting their sleep-wake cycle a few days before the night shift starts. This could mean staying up a bit later each night and sleeping in longer in the mornings. Using light exposure strategically is also key; bright light at work during the night can help maintain alertness, while avoiding bright light when it's time to wind down aids in falling asleep. After the night shift cycle ends, it’s important to shift the sleep schedule back to daytime hours. This can be done by gradually moving bedtime earlier, in small increments, to re-sync the body’s internal clock with the day schedule.
Dr. Jyothula: As one of my colleagues used to say, caffeine during the day and night caps at night are the secrets to a productive day. What is your advice regarding food and alcohol intake?
Dr. Agrawal: While caffeine can be a useful tool for alertness, it should be used judiciously. It's best to avoid caffeine close to bedtime as it can significantly disrupt sleep. As for alcohol, while it might seem like it helps with falling asleep, it impairs the quality of sleep and can lead to fragmented rest. So, moderation is key, and avoiding alcohol close to bedtime is advisable.
Dr. Jyothula: The Dalai Lama says, “Sleep is the best medication.” Any interventions you recommend for improving sleep hygiene?
Dr. Agrawal: Good sleep hygiene also involves regular sleep schedules, a comfortable sleep environment and pre-sleep routines that promote relaxation. Limiting screen time before bed, avoiding large meals and caffeine close to bedtime, and engaging in relaxing activities like reading or meditation can greatly improve sleep quality.
I often tell my patients that “your bedroom is your sanctuary.” I've seen patients transform their sleep and, in turn, their lives by making small changes. One patient started a nightly ritual of a warm bath and reading, which helped her transition from the day's chaos to a peaceful night's sleep. Another patient found that simply changing his mattress and pillow made a significant difference. This was a factor we discussed about making the bedroom environment most comfortable. It's about finding what works for you and sticking to it.
Dr. Jyothula: Finally, the trick question: What does Dr. Agrawal practice in regards to his sleep habits?
Dr. Agrawal: I try to be disciplined about my sleep habits, though I'm not perfect. My family knows I'm strict about bedtime and waking up at a consistent time. We've removed the large screen TV from our bedroom and keep cellphones out of reach at night (except when I'm on call). I also use a blue light blocker on my laptop and employ software like f.lux to minimize blue light exposure in the evenings. These small steps help maintain my sleep hygiene, although I do slip up sometimes!
Reference:
1. Trockel MT, Menon NK, Rowe SG, et al. Assessment of Physician Sleep and Wellness, Burnout, and Clinically Significant Medical Errors. JAMA Netw Open. 2020;3(12):e2028111

Soma Jyothula, MD, FCCP, is a practicing pulmonary and critical care physician, and is the Chief of Pulmonary Medicine and Lung Transplantation at Methodist Hospital. Dr. Jyothula is a member of Bexar County Medical Society and serves on the Publications Committee.
He snores, she tosses and turns. She moves her legs all night long, he takes several trips to the John. When it comes to sleep habits, it’s difficult to make a perfect match, isn’t it? Be honest. Is there at least one thing about your partner’s sleep you would change? You’re not alone, as nearly one in four couples choose some form of sleep separation from their partner, consistent with a survey indicating that around one in four people sleep better alone.1 Another study shows sleeping apart can improve communication, and reduce con flict and irritability.
There is a growing tide of openness and honesty regarding our sleep, and coupled with an increased understanding of sleep’s importance to overall health, has an increasing number of couples considering a divorce …. of sorts — a “sleep divorce.” Quite simply, a sleep divorce is sleeping sepa rately — maybe in another bed in the same room, or maybe in different rooms altogether. Not necessarily the most romantic of terms, but the sleep divorce must have some merit, as it is becoming quite common. Let’s figure out why!

Current evidence supports what we as humans have always known: we need ample quality and adequate quantity of sleep to be our best. Sleep deprivation can lead to depression, anxiety and difficulty with executive function. It also increases the risk for untoward health prob -
lems such as obesity, diabetes, heart disease and additional cognitive decline. The data is less instructive on whether co-sleeping or solo sleeping is better. In one survey-based study of over 1,000 adults, sleeping with a partner/spouse was associated with better sleep quality and mental health overall.2 Another study compared 10 couples, over 28 days, sleeping both apart and together, and found that while co-sleeping had negative effects on sleep in women, sleeping alone had negative effects on sleep in men.3 Another concluded that transitions into and out of either co-sleeping or solo sleeping (read into and out of relationships, marriages, etc.) are worse for sleep than is consistency (remaining either co- or solo sleeping).4 It’s not clear that any emerging data will settle the score.5
So,
One needn’t search too long to find both “for” and “against” arguments for sleep divorce. Just ask CNN, the New York Times, Harvard Health, or even movie stars like Cameron Diaz!6-9 They are all happy to openly discuss the pros and cons of breaking away and creating a customized sleep environment for one. But don’t take anyone’s (or maybe any study’s) word for it, as sleep is highly personal — and very difficult to study! As you consider the following, take comfort in knowing there are improvements you can make to your sleeping situation that will be worth it!
The sleep doctor is in
Here are my recommendations: first and foremost, ensure there are no undiagnosed/untreated sleep disorders. The most prevalent of these are Obstructive Sleep Apnea (up to 20 percent of U.S. adults) and Insomnia (up to 30 percent of U.S. adults), but there are over 80 different types of sleep disorders! Some disorders like Restless Leg Syndrome occur before sleep onset but can also negatively impact sleep. Fortunately, research and technology afford both simpler and more convenient diagnostic modalities, as well as newer and less invasive ways to treat many of these debilitating conditions. An example of this is neurostimulation (currently the only FDA-approved device is the Inspire system), which can help those with moderate to severe Obstructive Sleep Apnea who cannot tolerate Positive Airway Pressure or Oral Appliance Therapy. A comprehensive evaluation from a Board-Certified Sleep Physician can lead to accurate diagnoses and treatment plans that significantly improve troubled sleeping conditions — whatever they may be.
If at this point the problem persists and is primarily a predicament of preference, it is best to ap proach the discussion with an open mind and sincere consideration for you and your partner. Much of how we feel about sleep is deeply entrained. It will likely take time, pa tience and clear and honest communication in working together to find a best-fit scenario. Ensure that you arrange for at least some consistent time during the day for touchpoints with your partner. Make both sleeping spaces comfortable and cozy, as one should not feel relegated to a lesser inviting sleep environ ment. Consider ways for intimacy to continue — some couples even schedule it. Lastly, whatever arrangement you’ve decided on, assess it regularly. This can be a fluid situation — remember there are times and seasons for everything.
extolling the health benefits of good sleep — both quantity and quality — continue to mount. You won’t regret your efforts — facing your days with renewed vigor and clarity can be just around the corner!
References:
1. RZ, Do You Need a Sleep Divorce? Prevention July 2023, 26-27
2. BF, et al. Bed Sharing Versus Sleeping Alone Associated with Sleep Health and Mental Health. Sleep 2022. Vol. 45: Supplement 1
3. JD, et al. Sex differences in the reactions to sleeping in pairs versus sleeping alone in humans. Sleep and Biological Rhythms 2007; 5: 271-6
4. KA, Marital Status, Marital Transitions, and Sleep Quality in Mid to Late Life. Research on Aging 2022; Vol. 44(3-4): 301-311
5. MB, et al. Effect of sleeping alone on sleep quality in female bed partners of snorers. Eur Respir J 2009; 34: 1127-1131
6. Tips to navigate a “sleep divorce.” Harvard Health Letter, January 2024
7. How to tell if it's time for a 'sleep divorce.' CNN Wire, Dec. 4, 2021
8. Why Two Beds Are Better Than One. The New York Times, Aug. 4, 2019

9. Cameron Diaz wants to "normalize separate bedrooms." Here's what to know about "sleep divorce." CBS News Healthwatch. December 21, 2023. By Sarah Moniuszko
Rest assured that this work can be hard, but it is worth it! Literature

Alex McKinlay, MD, is dual Board Certified in Otolaryngology and Sleep Medicine and is retiring from the U.S. Army after 24 years this summer. He is excited to bring comprehensive ENT and Sleep Care to San Antonio by starting Gold Standard Sleep & ENT, with a formal opening on May 3, 2024. Dr. McKinlay is a member of the Bexar County Medical Society.
The Lufthansa flight landed in Mumbai, India at 1:00 a.m. The passengers were wide awake after traveling from San Antonio via Chicago and Frankfurt for 21 hours halfway around the world. You can think that the Indian Standard Time (ISD) is exactly 12 hours ahead of our central time plus-minus 30 minutes to an hour and a half based on our daylight savings time. Yes, according to my San Antonio time, I was wide awake in the middle of the afternoon. After clearing the customs and immigration formalities, I boarded the flight to Bengaluru (formerly Bangalore), which I reached at 6:00 a.m. ISD. At 9:00 a.m., I spoke at the Indian Academy of Pediatrics National Conference. I was satisfied with my presentation and enjoyed the delicious lunch, the local cuisine, which is my hometown, and meeting so many friends, colleagues and medical students. In the afternoon, I was on a panel. Uncontrollable fatigue overtook me, and I woke up with a jolt when my head dropped on my shoulder; it was past my usual bedtime in San Antonio, 1:00 a.m. Jet lag, I thought. I did manage the rest of the day tired, with low energy and a royal headache, all symptoms of jet lag. At about the same time, my spouse had a scrumptious breakfast prepared by his sister, with whom we stayed. He slept from 9:00 a.m. till 5:00 p.m. ISD, which coincided with his San Antonio sleep time and was bright and cheerful at dinner. However, I was completely adjusted to the ISD the following day, and he could not sleep at night for the next few days. I was in bright daylight, and he was still in the U.S. zone. People often marveled at my ability to jump into a working mode. Yes, the pressure of work, not to minimize my compulsive shopping spree when I was in India, kept me awake. The same disruption happens upon returning home to San Antonio; however, it is not so pronounced. This may be partially due to the necessity of work and other chores. It is also known that jet lag is worse with travel to the east.
What is jet lag? Jet lag, or flight fatigue, is a temporary disruption of the body's internal biological clock caused by rapid travel across multiple time zones. Our circadian rhythm (the body’s internal clock), which regulates the sleep-wake cycles, becomes misaligned with the external environment, the presence of darkness and light.
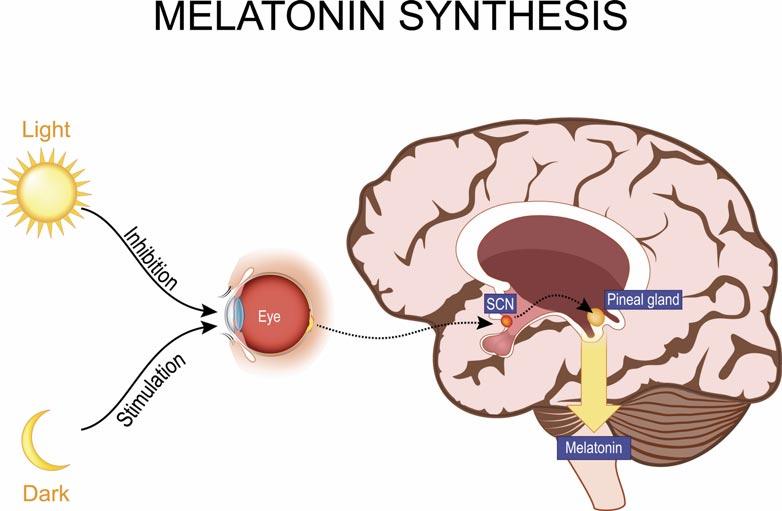
Delving a little into physiology, the circadian rhythm is a natural physiological process that repeats
every 24 hours and controls our sleep-wake cycle. The anterior hypothalamus is an area in our brain where the suprachiasmatic nucleus (SCN), a pair of distinct neuronal clusters, is located. This tiny area reacts to external cues like light and darkness, and synchronizes the body’s internal clock with the external environment in peripheral tissues and other brain regions. The scientific name for jet lag is “Desynchronosis.” Light is sensed by the ganglion cells in the retina that convert the photon energy into an electrical signal. This is directly projected onto the SCN regions of the brain, which will influence the secretion of melatonin. These signals maintain a consistent rhythmic order of the biological processes.
Experimental, bilateral ablation of the hypothalamus in rodents, pituitary tumors and human vascular disease could disrupt the circadian control of behavior, and metabolic and endocrine functions. The misalignment causes a disturbance in the secretion of the hormone melatonin, which regulates sleep — thus, there is interest in melatonin as a treatment modality. Sleep deprivation, as happens in night shift workers, late-night eating for the same reason, and chronic jet lag, with frequent international travels, has led to a public health crisis. Mood disorders, obesity, diabetes and cancer are found to be associated with

chronic jet lag. Studies in animal models have shown that melatonin regulates the circadian expression of what are called clock genes.
Symptoms of jet lag include fatigue, irritability, difficulty concentrating, digestive disorders, insomnia, memory loss, anxiety, dizziness and headache. The duration of jet lag is based on the number of time zones crossed. There is a 7-hour time difference between Amsterdam and San Antonio. I was traveling alone and stayed overnight in Amsterdam, which I reached very early in the morning. The hotel room wasn’t available until 3:00 p.m. So, I took a city tour. One of the stops was a diamond factory that Amsterdam was known for. Diamonds as big as marbles were displayed. The store manager jokingly said we could try any of them on. All the women were grabbing the rings and trying to push them onto their fingers. I fell asleep sitting in front of a tray of diamonds. The lack of concentration and fatigue is overwhelming with jet lag; no diamond could keep me awake. A day per zone traveled is needed to overcome jet lag. Traveling from San Antonio, I crossed one time zone to New York, two more to Frankfurt, and one more to Mumbai. It would take four days to get over jet lag.

Steps one could take to mitigate jet lag:
• Gradually adjusting sleep schedules before the travel.
• Proper hydration.
• Exposing oneself to natural daylight at the destination.
• Use of medications like melatonin.
Melatonin, a hormone synthesized from tryptophan, is a neuro-hormone produced by the pineal body and acts on the MT1 and MT2 receptors. It is secreted at night and signaled by daylight. It is most beneficial when taken a few days before and after the travel. The dosage varies, and there are fewer side effects. Different dosing is recommended for westward and eastward travel.
Several melatonin dietary supplements are on the market. These are not FDA-regulated. Therefore, at the present time, it is essential to know that the dosage, duration of therapy and purity of supplements need further study. High melatonin-containing foods are eggs, fish, nuts (almond and pistachio), gogi berry, cherries, germinated legumes and cereals.
A 2022 study found that melatonin use increased in the U.S. by 150 percent between 2016 and 2020. This availability in homes has increased accidental ingestions by younger children and intentional ingestion by teens. The U.S. Poison Control Center reports that from the year 2012 to 2021, ingestion by children under 19 years increased from 8,337 to 52,563. Common symptoms are drowsiness, increased bedwetting, headache, dizziness and agitation. There is some concern that melatonin could interfere with hormones and delay puberty.
Reading the published reports in preparation for writing this article gave me an understanding of the universe I least expected. Circadian (Circa-about, Diem-Day) is an autonomous timing system that has a 24-hour cycle that is programmed by natural light and darkness. It exists in the most primitive organisms like the drosophila, fungi, bacteria and plants. It even affects seasonal variations in hot and cold, ocean waves, feelings and mood. The universe's interconnectedness forces us to respect everything we are with.

Rajam Ramamurthy, MD, is the Professor Emeritus in the Department of Pediatrics/Neonatology at UT Health San Antonio. She is a Past President of the Bexar County Medical Society and serves on the Publications Committee.

Sleep plays an important role in various aspects of health and wellbeing. Considering we spend almost a third of our life sleeping, we have a tendency to dismiss the profound impact of sleep deprivation. When it comes to our children, we emphasize studying and tutoring for academic success rather than focusing on sufficient sleep. We underestimate the role sleep plays in our children’s neurocognitive development, academic performance and mood. Instead of talking about medical conditions related to pediatric sleep, I will focus on the importance of a good night of sleep.
Age group
Recommended amount of sleep
3 to 5 years 10 to 13 hours per 24 hours, including naps
6 to 12 years 9 to 12 hours per 24 hours
13 to 18 years 8 to 10 hours per 24 hours
Adults 7 or more hours a night
Sleep has an important role in our physiologic well-being. Insufficient or poor-quality sleep has shown to affect every organ system in our body.
One of the primary functions of sleep is memory consolidation. During the different stages of sleep, the brain processes and consolidates newly acquired information. The hippocampus works in conjunction
with the neocortex during sleep to solidify memories.
Having enough time in the different stages of sleep — Rapid Eye Movement (REM) and Non-Rapid Eye Movement (NREM) — is important in memory processing. REM sleep is associated with emotional memory consolidation, while NREM sleep, especially slow-wave sleep (SWS), is crucial for declarative memory, which involves facts and events. REM sleep also has been associated with creativity and insight. Slow-wave sleep is associated with enhanced synaptic plasticity. Synaptic plasticity, the ability of synapses to strengthen or weaken over time, is a key mechanism associated with learning and memory. This process is thought to contribute to the optimization of neural connections associated with learning.
Sleep is intricately linked to neurocognitive development, particularly in children and adolescents. During sleep, the brain undergoes critical processes essential for learning, memory consolidation and overall cognitive function. Inadequate sleep has been associated with impaired attention, memory deficits and reduced executive functioning in both school-aged and college-aged individuals.
The transition from high school to college often brings changes in sleep patterns, with many students experiencing disruptions due to academic, social and lifestyle factors. Sleep quality and quantity are closely tied to academic performance in college. Students who prioritize reg -
ular and sufficient sleep tend to demonstrate improved concentration, problem-solving skills and enhanced memory recall, contributing to better grades and academic success. Conversely, chronic sleep deprivation can lead to decreased cognitive performance, increased susceptibility to stress and difficulty managing the demands of a rigorous academic environment. A study performed by J. David Creswell, et al. reinforces the effects of sleep in college. It found that on average, every additional hour of nightly sleep gained was associated with a 0.07 increase in end-of-term GPA. Sleep less than six hours each night shifted to a harmful end-of-term GPA.
Sleep and mental health are intertwined, and disruptions in sleep patterns can significantly impact mood, contributing to the development or exacerbation of depression and anxiety. For school-aged and college-aged individuals, the pressures of academic performance, social interactions and personal growth can contribute to stress and emotional challenges. Adequate sleep serves as a protective factor against mood disorders and can enhance emotional resilience. Sleep deprivation, on the other hand, has been linked to increased irritability, heightened stress levels, and an elevated risk of developing or worsening symptoms of depression and anxiety.
As medical professionals, it is imperative to recognize the profound impact of sleep on neurocognitive development, academic performance
in college, and mental well-being in school-aged and college-aged individuals. Promoting healthy sleep habits, educating students and their families about the importance of sufficient sleep, and addressing sleeprelated issues can contribute to better overall health outcomes and pave the way for academic success and emotional well-being. Integrating sleep education and support into healthcare practices can empower the next generation to achieve their full potential both academically and emotionally.
Reference:
Nightly Sleep Duration Predicts Grade Point Average in the First Year of College, J. David Creswell, Michael J. Tumminia, Stephen Price and Marsh C Lovett. Feb 13,2023. 120(8). Proceedings of the National Academy of Sciences of the United States of America

Tarak Patel, MD, is Board Certified in Pediatric Pulmonology, Pediatrics and Sleep Medicine. He is an Assistant Professor of Pediatrics at Baylor College of Medicine/San Antonio, Medical Director at Academy Diagnostics Sleep/EEG Center and Christus Children’s Sleep Center, and practices at Texas Pediatric Specialties and Family Sleep Medicine and Christus Children’s Pulmonary, Sleep and Cystic Fibrosis Clinic. Dr. Patel is a member of the Bexar County Medical Society.


We have all heard the question, in many different variations from many different patients and family members. "Hey doc, you got anything for insomnia, my sleep is terrible?" After we run through the litany of established diagnostics and therapeutics, including the latest "state-of-the-art" medications or treatments, the eye rolls and shoulder shrugs we experience coming from our patients are almost palpable. And with reason. Sleep is critical — the understatement of the year. How we feel and function on a given day is defined by the quantity and quality of our sleep.
Broadly speaking, there are many alternatives for that index patient ... for whom everything has been studied and tried and they are still zombie-like in our offices. For simplicity, I will cover those therapies that are delivered by a healthcare provider. There are many self-help and self-administered therapies, but literature is scarce regarding outcomes. I will cover a functional medicine approach, psychological interventions and acupuncture and related practices.
An intriguing approach, fostered by functional medicine providers, is to recognize the critical times of the day and activities that produce
sleep pathology and counter them. Good sleep hygiene is a given for these patients. They have read every book under the moon, because they were still awake! Good sleep begins on arising, and what is done in the first hour of awakening begins to set the circadian rhythms that are disturbed in sleep disorders. Early morning sunshine and movement are critical in resetting these rhythms. Since a sleep disorder almost never has a single cause, evaluating for sleep "disturbers" is critical. Caffeine tolerance is variable, but its contribution to sleep disturbances is easily identified by an historical query ... if you have ever had caffeine withdrawal, your sleep is sensitive to caffeine. Alcohol, a diet high in refined sugars and late-night eating that will disturb glucose levels are also contributing factors. Combined, they affect sleep stages and impair sleep quality by sedation and spikes and drops in blood glucose that may provoke awakening. Indeed, critical information from a CGM may be the most important clue in evaluating these patients. Comorbidities like thyroid dysfunction, menopause, andropause and obesity must be addressed. Sleep disturbances are common symptoms of endocrine deficiency or excess. Therapies may be the only intervention necessary to
improve sleep — low hanging fruit for the frustrated provider.
CBT-I (Cognitive Behavioral Therapy for Insomnia) is a well-recognized intervention, with ample evidence-based research documenting positive outcomes. Typically requiring on average six sessions for efficacy, it is especially beneficial for those whose sleep disturbances are due to anxiety. It is divided into chronic vs circumstantial, as the therapeutic approach and goals are distinct. Acute CBT-I, when sleep is disrupted by a major life stressor, must deal with the grief and trauma simultaneously with the sleep disorder. If the condition becomes chronic, the approach is different. Counterproductive thoughts are explored by a series of probing questions, which attempt to address the emotional content behind the troubling thoughts. The goal is to counter catastrophizing thoughts like, "I'll never fall asleep," or "Tomorrow is going to be a terrible day if I don't get some sleep," with a more positive outcome from a given thought process. The intent is to reframe the cognitive scenario to distance the psyche from fixed expectations of failure to affect a different outcome. "You have to change the thinking to change the results.” CBT-I can also be useful for those attempting to discontinue benzodiazepines and other pharmacologic interventions. This is best accomplished by a proactive approach with several sessions before attempting the tapering process to familiarize the patient with CBT-I to promote a successful outcome upon withdrawal.
It is ironic that medications for sleep fall under the broad category of "hypnotics." Since the days of Franz Mesmer, the utility of inducing trance-like states for therapeutic interventions has been known, long before modern pharmacology made contributions. Far evolved from the "swinging pocket watch" techniques of hucksters and frauds, modern hypnotherapy uses a variety of techniques to induce a trance-like
state to allow the subconscious mind to surface and take charge. The theory is that if you relax the body enough, the conscious mind will relax as well and allow the subconscious to emerge. The goal is to allow access to the source of traumas and troubling thoughts, and to implant new ideas that are more likely to take root. This process takes practice and the clients develop variable skil ls, but it can be quite useful for sleep issues. The key is to train the subconscious to respond to a simple, but specific cue, called an anchor, that can be called on in the midst of the crisis. This may be as simple as placing the tips of one's index finger and thumb together in an "OK" sign. Patients are always able to control and remember the experience; they are able to follow only the suggestions of the hypnotherapist that they see compatible with their goals of therapy.
Neurofeedback (NF), a subcategory of biofeedback, involves training our brain waves to respond appropriately to a given auditory or visual stimulus. The stimulus, a video or music, is used as positive reinforcement when EEG activity corresponds to the training goal. The withdrawal of the positive stimulus is used as negative reinforcement for divergent brainwave function. Typically, between one and 10 EEG electrodes are placed (you do not get your head shaved!) depending upon the therapist's training. Slow waves (11-15 Hz) are the desired level of brain activity. Using hypnotherapy as an enhancement to NF – using the hypnotic suggestions as the stimulus for appropriate brain wave activity – has led to enhanced outcomes over either therapy alone.
Acupuncture or acupressure and related techniques have been used for millennia for sleep disorders. The literature is mixed, as many of the studies involve concomitant therapies with Traditional Chinese Medicine (TCM) or continuance of pharmacologic interventions. For a troubled patient, when all else has failed, it may be an avenue that proves valuable to explore. Commentary on patient outcome studies indicates that as many "swear at it" as those that "swear by it."
Goodnight. I'll see you in the morning!
I interviewed Margaret Erben, MA LPC and licensed hypnotherapist, and Charlotte Widdick, NP of Root Causes Functional Medicine, for this article whose contributions were invaluable and essential. I cannot repay the debt of gratitude I owe them.

Tim Hlavinka, MD, is the Medical Director of Vidamor Medical and has been a member of the Bexar County Medical Society for three decades. The father of five and grandfather of four, he firmly believes that the power of collegiality among physicians as great potential to bring us lasting and effective changes in healthcare. Dr. Tim is anxious to hear your stories.


Maybe you have heard this from a family member or friend:
“I don’t sleep at all. I just lie awake the whole night.” Though this is typically a vast exaggeration, we’ve all encountered this patient before. In a sleep medicine clinic, it seems to occur daily. The bottom line is, most people know when they’re not getting adequate sleep, and they feel the effects. Whether the cause is psychological, mental illness, behavioral health, pain or something else entirely, it’s up to us to help the patient find relief.
Various medications have been used offlabel for decades to help induce or maintain sleep, sometimes with very undesirable side effects. There are also a handful of FDA-approved sleep medications — mostly benzodiazepine hypnotics — but they also have risks of side effects, dependence and tolerance. However, the newest class of medications available, dual orexin antagonists (DORAs), seem to be showing more promise. Cognitive behavioral therapy for insomnia (CBT-I) has also been recommended as a first-line treatment for chronic insomnia, though there are many barriers to treatment. There is new data showing that an abbreviated form of CBT-I can be an effective treatment, as well.
DORAs include lemborexant (Dayvigo), suvorexant (Belsomra) and the newest addition: daridorexant (Quviviq). These medications prevent wake-promotion by blocking the binding of neuropeptides, orexin A and orexin B. These medications had excellent efficacy compared against placebo and zolpidem in clinical trials, but are more appealing since they appear to have fewer side effects. They are effective at improving sleep onset, duration and quality, with studies showing sustained effects at 12 months. There has been no evidence of respiratory depression with DORAs, and users experienced fewer falls while using DORAs compared to BZRAs. That makes them an ideal choice for geriatric patients or those with underlying sleep apnea or other respiratory conditions. These medications also had no evidence of physical dependency and low abuse potential. There were also no reports of complex sleep behaviors such as sleep walking/talking/eating or memory disturbance, which are sometimes seen with BZRAs. However, they do carry the same risk of next-day somnolence as with other sleep medications, but to a lesser degree. Additionally, concomitant use with strong CYP3A inhibitors is not recommended. Thus far, the biggest obstacle we’ve experienced with prescribing DORAs has been poor insurance coverage. Few insurances include DORAs on their formulary and prior authorizations are frequently denied.1
In addition to pharmacotherapy options, CBT-I is still recommended as a first line therapy for treatment of chronic insomnia. However, treatment is not always attainable. It typically consists of about six sessions of provider-directed therapy, making it time-consuming for the patient. It also requires immense self-discipline and commitment from the patient. Finding a provider who is educated in CBT-I can also be difficult. Lastly, it is not always covered by insurance, so six sessions can become cost prohibitive. However, a recent study utilizing nurses to direct sleep restriction therapy over four sessions showed improvement in insomnia compared to providing education on sleep hygiene alone.2
Though insomnia continues to be a common problem for patients, the newer treatment options all appear to be an improvement. Traditional insomnia medications and even off-label medications certainly still have their place. They are still used frequently in our sleep medicine practice at University Health, which includes our Sleep Lab where specialists use technology to monitor you while you sleep. We anticipate increased use of DORAs and the various forms of CBT-I as insurance coverage improves.
1. Neubauer, David N. “Pharmacotherapy For Insomnia in Adults.” UpToDate, 29 Jan. 2024. www.uptodate.com/contents/pharmacotherapy-for-insomnia-in-adults?sectionName=Special+populations&to picRef=107235&anchor=H1357008358&source=see_link#H337 9101117
2. Kyle SD, Siriwardena AN, Espie CA, et al. Clinical and cost-effectiveness of nurse-delivered sleep restriction therapy for insomnia in primary care (HABIT): A pragmatic, superiority, open-label, randomized controlled trial. Lancet 2023; 402:975

Elise Vader is a physician assistant who received an undergraduate degree in biology from Texas A&M University, College Station and a master’s degree in Physician Assistant Studies from University of Texas Medical Branch, Galveston. She has been in practice at University Health for nine years, providing care to patients in both primary care and sleep medicine and has been certified to provide cognitive behavioral therapy for insomnia.
Sleep is an essential component of human life. The average adult requires seven to nine hours of sleep per day to promote optimal function and health.1 Despite the fact that many people place a high importance on sleep, many struggle to maintain a healthy sleep schedule. Medical professionals have long been concerned about sleep deprivation, particularly as it relates to medical residents who put in long, demanding hours. In a survey performed by Baldwin and colleagues, 66 percent of medical residents reported getting less than six hours of sleep per night.2 Lack of sleep can have an impact on patient care, but it is also necessary to understand how it might affect health. The purpose of this article is to highlight potential short- and longterm health risks associated with sleep deprivation.
The importance of sleep on various biological systems is not commonly known to the general public. Our respiratory system, circulation system and endocrine system, to mention a few, all require sleep to function properly.3 When adequate sleep is not maintained, organ systems such as the ones listed above are susceptible to impairment, consequently increasing the risk of disease. Sleep lowers heart rate and blood pressure. This is a result of the body being in non-REM (NREM) sleep during most of the sleep cycle. Since the body and brain are at rest during this period, the heart does not need to pump as much blood as it would while one is conscious. NREM sleep is controlled by the parasympathetic nervous system. During REM sleep and waking, the sympathetic nervous system takes over, which causes an increase in heart rate and blood pressure. Sleep deprivation can lead to sympathetic nervous system hyperactivity.4 Increased heart rate, salt retention and vasoconstriction due to elevated sympathetic nervous system activity may increase one's risk of developing cardiovascular disease.5 One study reported that individuals who sleep less than six hours per night had a 20 percent increased chance of heart attack.6 As mentioned previously, sleep is also important for metabolic function. Lack of sleep has been associated with Type 2 diabetes mellitus.3 In one study, participants who slept for fewer than six hours a night were more likely than those who slept for seven to nine hours to have an impaired glucose tolerance.7 Furthermore, inadequate sleep
increases the risk of uncontrolled disease in people with Type 2 Diabetes. While the pathophysiology of this association is still being investigated, changes in the hypothalamo-pituitary-adrenal (HPA) axis as well as sympathetic nervous system activity are believed to play a role.8
The most commonly recognized benefit of sleep is its ability to preserve cognitive function. Sleep is necessary for a number of processes, including language, coordination, memory consolidation and decisionmaking. Chronic sleep deprivation can affect cognitive function in several ways, including reduced alertness, slowed processing speed and short-term memory loss.9 Although the exact mechanisms underlying this hypothesis are still being studied, neuroimaging studies have demonstrated reduced activity following sleep deprivation in a number of brain regions, particularly the frontal and prefrontal cortex.10 Multiple studies have examined how chronic sleep deprivation affects cognitive performance, which has become a topic in research regarding patient outcomes.11 Barger and colleagues found that first-year residents who worked prolonged shifts had a higher risk of adverse events, attentional problems and serious medical errors compared to those who did not work any extended shifts.12 In another study, videotapes of surgical residents performing surgery were observed. Surgical residents with inadequate sleep took longer to finish their procedures than those

with adequate sleep.13 The study also found that the sleep-deprived surgeons were more likely to perform ill-executed surgical maneuvers. Additionally, chronic sleep deprivation affects cognitive function in ways that go beyond diminished work performance. Those who suffer from chronic sleep deprivation are also more at risk of falls, motor vehicle accidents and injuries.14
Sleep deprivation comes at a cost, not just to patients, but to medical residents. It is important for medical residents to maintain proper sleep hygiene during these years of training to prevent negative health outcomes in the future. The demands and difficulties of residency may make this hard to maintain. There are certain measures that residents and residency programs can use to prevent sleep deprivation and its associated health risks. Some helpful measures include limiting caffeinated drinks, avoiding electronics before bed, and exercising regularly as much as one’s schedule allows.15 These techniques can lessen disruptions and increase the duration of sleep.
Effective sleep education should also be prioritized in programs. By providing education on sleep hygiene, residents can feel supported by their program and acquire knowledge on how to optimize their sleep. However, sleep education by itself is unlikely to significantly influence residents' well-being; it is also important to make sure that initiatives are implemented to foster such wellbeing. For example, offering free transportation to residents after a long shift may have a greater impact on their sleep hygiene than a short presentation on the topic.
The prevention of sleep deprivation during medical training is a complex issue that will necessitate collaboration between multiple institutions in order to be effectively addressed. Until then, it is necessary for us all to promote an environment that encourages sleep in the world of medicine.
References:
1. Centers for Disease Control and Prevention. (2022, September 14). How Much Sleep Do I Need? Centers for Disease Control and Prevention. https://www.cdc.gov/sleep/about_sleep/how_much_sleep.html
2. Baldwin, DC and Daugherty, SR (2004). Sleep deprivation and fatigue in residency training: Results of a national survey of first- and second-year residents. Sleep, 27(2), 217–223. https://doi.org/ 10.1093/sleep/27.2.217
3. U.S. Department of Health and Human Services. (n.d.). Why is sleep important? National Heart Lung and Blood Institute. https://www.nhlbi.nih.gov/health/sleep/why-sleep-important
4. Gangwisch, JE, Heymsfield, SB, Boden-Albala, B, Buijs, RM, Kreier, F, Pickering, TG, Rundle, AG, Zammit, GK and Malaspina, D. (2006). Short sleep duration as a risk factor for hypertension. Hypertension, 47(5), 833–839 https://doi.org/10.1161/01.hyp.0000217362.34748.e0
5. Nagai, M, Hoshide, S and Kario, K. (2010). Sleep duration as a risk factor for cardiovascular disease-a review of the recent literature. Current cardiology reviews, 6(1), 54–61. https://doi.org/10.2174/ 157340310790231635
6. Suni, E and Callender, E. (2023, October 30). How sleep deprivation affects your heart. Sleep Foundation. https://www.sleepfoundation.org/sleep-deprivation/how-sleep-deprivation-affects-yourheart
7. Gottlieb, DJ, Punjabi, NM, Newman, AB, Resnick, HE, Redline, S, Baldwin, CM and Nieto, FJ. (2005). Association of Sleep Time with diabetes mellitus and impaired glucose tolerance. Archives of Internal Medicine, 165(8), 863–867. https://doi.org/ 10.1001/archinte. 165.8.863
8. Hirotsu, C, Tufik, S and Andersen, ML. (2015). Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep science (Sao Paulo, Brazil), 8(3), 143–152. https://doi.org/10.1016/j.slsci.2015.09.002
9. Diekelmann, S. (2014). Sleep for cognitive enhancement. Frontiers in Systems Neuroscience, 8. https://doi.org/10.3389/fnsys. 2014.00046
10. Verweij, IM, Romeijn, N, Smit, DJ, Piantoni, G, Van Someren, EJ and van der Werf, YD. (2014). Sleep deprivation leads to a loss of functional connectivity in frontal brain regions. BMC Neuroscience, 15(1). https://doi.org/10.1186/1471-2202-15-88
11. Veasey, S, Rosen, R, Barzansky, B, Rosen, I and Owens, J. (2002). Sleep loss and fatigue in residency training. JAMA, 288(9), 1116–1124. https://doi.org/10.1001/jama.288.9.1116
12. Barger, LK, Ayas, NT, Cade, BE, Cronin, JW, Rosner, B, Speizer, FE and Czeisler, CA. (2006). Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Medicine, 3(12). https://doi.org/10.1371/journal.pmed.0030487
13. Goldman, LI, McDonough, MT and Rosemond, GP. (1972). Stresses affecting surgical performance and learning. Journal of Surgical Research, 12(2), 83–86. https://doi.org/10.1016/00224804(72)90125-4
14. Institute of Medicine. 2006. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington, DC: The National Academies Press. https://doi.org/10.17226/11617
15. Suni, E and Vyas, N. (2023, December 8). Mastering sleep hygiene: Your path to quality sleep. Sleep Foundation. https://www.sleepfoundation.org/sleep-hygiene

Victoria Ayodele is a medical student at the Long School of Medicine, Class of 2026. She is a member of the BCMS Publications Committee.

Giving back to the profession he loves is natural to Jayesh “Jay” Shah. Throughout his medical career, he has been known both for his excellence in patient care and as an avid supporter of physicians nationwide.
I have witnessed Dr. Shah’s exceptional talents across a spectrum from our local medical staff to the national stage that is the AMA. At every level, his commitment, confidence and vision inspire others to do great things.
Ezequiel “Zeke” Silva III, MD – President, BCMS; Chair, AMA RVS Update Committee (RUC)
LEADING Medicine in San Antonio, Texas and Nationwide:
• BCMS President, Vice President, Secretary and Treasurer
• Secretary to TMA Board of Trustees, serving six years on the Board
• Chair of the BCMS Delegation to the TMA House of Delegates
• Chair of TMA’s International Medical Graduate Section
• President of the Texas Indo-Physician Society State level
By David N. Henkes, MD• President of the Southwest Chapter of the Texas Indo-Physician Society
• Texas Delegate to the AMA, and has chaired the AMA International Medical Graduate Section and AMA Resolution Committee
• President, VP, Secretary and Treasurer for the American Association of Physicians of Indian Origin
Jay’s strong business acumen and organizational leadership have been assets to TMA Board of Trustees for the past several years. Having an MBA, Jay understands the “business of medicine” as well as the “practice of medicine” and always advocates for quality health care. I think the attributes that I most admire about Jay are his ability to build consensus and his perseverance and persistence while dealing with issues.
David N. Henkes, MD – Past President, BCMS; Past Chair, TMA Board of Trustees; Chair, Texas Delegation to AMA
BUILDING the Future of Texas’ Medical Leaders:
• Chair of TMA’s Educational Scholarship and Loan Committee, which serves the
needs of our medical students and residents in building a strong Texas physician base
• Vice Chair of BCMS Leadership Committee
• Chair of BCMS Nominating Committee
• Adjunct Associate Professor – University of Incarnate Word – School of Osteopathic Medicine for internal medicine preceptorship
• Adjunct Assistant Professor, UT Health –Department of Community Medicine
• Adjunct Clinical Faculty – International ATMO, Hyperbaric Team Training and Wound Course, 2000-current
• Co-chair of WoundCon, a global, multidisciplinary educational conference
Dr. Jayesh Shah is [a] most important person in my success. [The] mini-externship program, initiated by Dr. Shah helped me and many international medical graduates in gaining U.S. clinical experience and helped in getting into residency programs. He is a most insightful, selfless, helping man who can do any work with utmost ease.
Dr. Niranjan Banda – Resident, Maricopa Medical Center

• President of South Texas Wound Associates, PA
• President of TIMEO2 Healing Concepts, LLC
• Medical Director for Northeast Baptist Wound Healing Center
• Co-Medical Director for Mission Trail Baptist Wound Healing Center
• President of American College of Hyperbaric Medicine, 2016-2020
• President of American College of Clinical Wound Specialists, 2013-2015
• Medical Director of Southwest Center for Wound Care, 2000-2012
• Executive Committee for Northeast Baptist Hospital, 2020-Present
• Vice Chief of Staff for Southwest General Hospital, 2009-2011
• Medicine Chair for Southwest General Hospital, 2008-2009
• Chief of Staff for Uvalde Memorial Hospital, 1999
Dr. Shah is a kind, compassionate and caring person in all he does. He is a great listener, inclusive and collaborative in working with others. Dr. Shah has demonstrated excellent leadership in fulfilling key leadership roles at all levels of organized medicine. He has well served patients and clinicians for many years, and I am confident he will continue to do so if elected as a TMA President.
MichaelBattista, MD – Past Board of Directors, BCMS
• Co-chair of TMA Foundation’s 2018 Gala, raising funds for statewide initiatives to improve health and access to care as well as awarding funds to the next generation of doctors and nurses.
• Vice Chair of TexPac District 21
• Board of Directors for American Association of Physicians of Indian Origin Charitable Foundation
• President of India Asia Association of San Antonio
• Vice Chair of BCMS Publications Committee
As TMAA President-Elect, I love working with Jay. He recognizes the diverse contributions the Alliance brings to the family of medicine. His leadership style promotes a cohesive and supportive medical community.
Jenny Shepherd – TMAA President-Elect; TexPac Board Member; Past President,
BCMSAIn all of these organizations, Jay has a reputation not only for performing his job excellently, but also for being an innovator and leader in driving positive change throughout the entire organization and profession. Jay has dedicated six years serving on the Board of the Texas Medical Association, and 16 years as a Texas Delegate to the American Medical Association. His extensive background contributes both vast leadership expertise and cultural diversity. With this wealth of experience, Jay is now poised to assume the role of President and spokesperson for the most prestigious medical organization in the country, the Texas Medical Association. Bexar County physicians are fortunate to have a representative and leader like Jay advocating for our profession.


Dr. Jay Shah has clearly demonstrated his commitment to organized medicine throughout his many years of service to the TMA and as a delegate to the AMA. We, physicians of Texas, can be very proud of Jay’s service and his commitment to the principles of physicians in the practice of medicine, whether it be private practice, academic endeavors, group practice, multispecialty groups, specialty or Internal Medicine. His experience in serving Texas physicians is why we need Dr. Jay Shah as TMA’s President-Elect to continue his excellent service.
Dr. Tom Garcia – Past President, Texas Medical Association

David N. Henkes, MD, is a 2005 Bexar County Medical Society President; Past Chair, TMA Board of Trustees; and Chair, Texas Delegation to AMA. Dr. Henkes is a member of the Bexar County Medical Society.
March 1, 2024 marks the 50th anniversary of the San Antonio Fire Department Emergency Medical Services (EMS), whose Emergency Medical Technicians (EMTs) and modulances answered their first calls on March 1, 1974. Getting EMS rolling in 1974 required the combined efforts of many governments and organizations in our community, including the San Antonio Fire Department, the University of Texas Health Science Center at San Antonio, Southwest Research Institute and the Bexar County Medical Society.
The Medical Society played a key role in organizing this collective effort to launch an EMS system for San Antonio. In May 1972, Bill Center, President of the Medical Society, asked me to chair a new Emergency Medical Services Committee to develop plans for the City of San Antonio and Bexar County to implement an EMS system.1 As an orthopaedist who had been practicing in San Antonio emergency rooms since 1961, I had seen many victims of trauma who arrived at the hospital in terrible condition. The ambulance company who held a contract with the city did not have trained EMTs, and their ambulances, which were similar to the hearses they also operated, lacked the space or equipment to provide effective medical care in transit.2
I knew that San Antonio could offer its citizens better emergency care. At the Texas Medical Association meeting in May 1972 at the HemisFair convention center, I had spoken with members of the Houston Fire Department, who were displaying one of their new “modulances” that had ample room and equipment to care for patients in transit.3 San Antonio needed not only modulances, but also crews of EMTs stationed across the city who could be dispatched quickly to accident
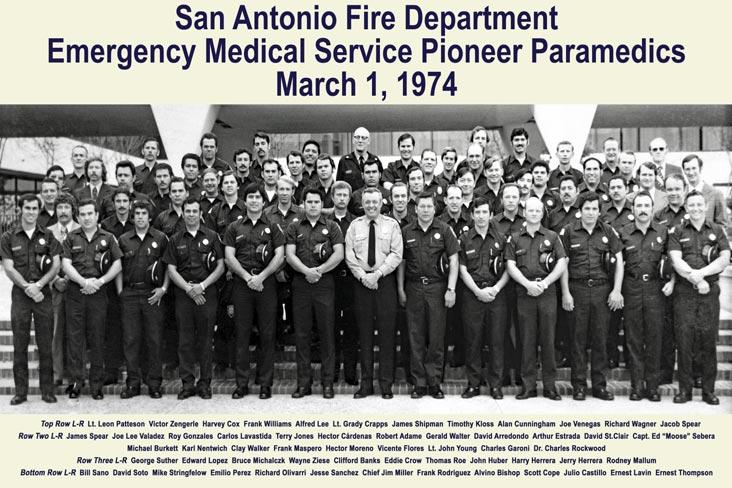

scenes to start trained medical care within minutes.4 Direct two-way radio communications between EMTs and emergency room staff was also required to provide the right care during transport and after delivery.5
In late May 1972, members of the Medical Society EMS Committee attended the first national meeting on emergency medical serv-
ices in Houston and began developing recommendations on how to implement EMS in San Antonio.6 One of the recommendations was to train firefighters as EMTs.7
In the following weeks, the EMS Committee quickly evolved into the San Antonio and Bexar County EMS Council, sponsored jointly by the city, county and Medical Soci-

ety. The EMS Council included dozens of officials from municipalities in Bexar County that would have to pay the expected cost of the systems of approximately $1 per citizen, per year. In July 1972, the EMS Council held its first meeting at the Medical Society, and voted in favor of adopting an EMS system.8 Southwest Research Institute developed a detailed plan to implement the system, which was delivered to the EMS Council in January 1973.9
To implement the various elements of the plan, the EMS Council formed six task forces, four of which were chaired by members of the Medical Society: EMTs (Charlie Rockwood), Communications (Larry Higgins), Transportation (Larry Dotin), Hospital Emergency Facilities (John Knox), Grant Support and Funding, and Inter Government Coordination. Numerous other members of the Medical Society also served on the task forces for Transportation (George Pruett and Curtis Heinrich), Hospital Emergency Facilities (Wayne Crawford, David Root, Warren Harding, Rodney Bobbitt, and my former partner Milton Butler), and Grant Support Funding (Charlie Rockwood and Larry Dotin).10
Charlie Rockwood was the natural choice to chair the EMTs task force because of his recent work on an American Academy of Orthopaedic Surgeons manual to train EMTs.11 Charlie chaired the Orthopaedics Department at what was then called the University of Texas Medical School at San Antonio, and he enlisted its support in the training program, which the University of Texas Health Science
Center’s Emergency Medical Technology Department has continued to provide to this day.12 Charlie became the Medical Director for EMT Training. He trained the first class of 55 EMTs in 1974, and hundreds more in the following 15 years. He was assisted with the cardiovascular module by Dr. Robert Schnitzler, who was a faculty member and director of the Intensive Care facility at the University.
The Chief of the San Antonio Fire Department, Bart Mulhern, was not initially enthusiastic about fire fighters serving as EMTs. I recall him saying, “My men fight fires, they don’t drive ambulances.” However, Captain Jim Miller was an early supporter of training fire fighters as EMTs. In early 1973, he was promoted to District Chief and began leading the Fire Department’s implementation of the plan developed by Southwest Research Institute and ratified by the EMS Council.13
Launching the system also required winning approvals from all participating municipalities as the detailed costs of the system became clearer. The EMS Council and its task forces worked with many city and county officials to build and maintain broad support for a comprehensive EMS system that would serve the entire San Antonio metropolitan area.
In less than two years — from concept to activation — well-equipped modulances staffed with trained EMTs started answering calls from San Antonio citizens at midnight, March 1, 1974. The lasting success of EMS is a tribute to the many citizens and organizations in and around San Antonio who came
together and contributed their time, energy and expertise to establish a vital service that has saved many lives in our community.
1. “President’s Message,” June 1972 Bexar County Medical Society The Medical News, page 4
2. “Emergency Medical Services Division,” Gene Mireles, page 1
3. “Emergency Medical Services Committee Report 1972,” September 1972 Bexar County Medical Society The Medical News, page 6
4. “Emergency Medical Services Committee Working,” Bexar County Medical Society The Medical News July 1972, page 8
5. “Emergency Medical Services Committee Report 1972,” September 1972 Bexar County Medical Society The Medical News, page 6
6. Id
7. “Society Renews Call,” San Antonio Light, June 1, 1972
8. “Med Service System Ratified,” San Antonio Light, July 26, 1972
9. “Emergency Medical Services Plan for San Antonio and Bexar County,” Southwest Research Institute, January 16, 1973, Appendix A
10. Id
11. “Emergency Care and Transportation of the Sick and Injured,” American Academy of Orthopaedic Surgeons, Committee on Injuries, 1971, cited in “History of Emergency Medical Services in the United States,” Charles A. Rockwood, Jr., M.D., Colleen M. Mann, J.D. Farrington, M.D., Oscar P. Hampton, Jr., M.D., and Robert E. Motley, The Journal of Trauma, Vol. 16, No. 4, page 306
12. San Antonio Fire Department Emergency Medical Services (EMS), https://www.sanantonio.gov/SAFD/About/Divisions/EmerencyMedical-Services
13. “Emergency Medical Services Division,” Gene Mireles, pages 1-2

John A. “Jack” Williamson, MD, is a BCMS Life Member and retired orthopaedist who practiced in San Antonio for over 40 years. He was Chair of the San Antonio and Bexar County EMS Council 197277, and Chief of Staff at Southwest Texas Methodist Hospital 1985-1986. Dr. Williamson is a graduate of Alamo Heights High School (1946), Texas A&M University (1950) and Baylor College of Medicine (1954), and served as an officer in the United States Air Force.

As we observe National Nutrition Month in March, it's crucial for health professionals to think about their role in fostering a culture of nutritious food choices and health in the community. Nutrition is essential for overall wellbeing and the City of San Antonio Metropolitan Health District (Metro Health) is committed to collaborating with medical professionals to encourage healthy living and prevent longterm illnesses by providing guidance, education and increasing awareness of available resources.
National Nutrition Month®, initiated in 1973 by the Academy of Nutrition and Dietetics, is an annual campaign that encourages community members to explore the realm of informed food choices and the cultivation of healthful eating and physical activity habits throughout the month of March.
The theme for the 2024 annual campaign is "Beyond the Table," emphasizing the holistic journey of nutrition, from food production, distribution, navigating grocery stores and farmers markets, and best practices for storage and safety. The theme also highlights how we can eat healthier when we are on-the-go and keeping sustainability in mind, whether it is at schools, offices, restaurants or events.
A balanced diet that includes a diverse variety of nutritious foods is one of the best defenses against chronic diseases such as heart disease and diabetes. Yet, these conditions are very common in San Antonio, especially in the most disinvested areas, and are usually the top causes of mortality. Food insecurity, defined as a lack of consistent access to sufficient, safe and nutritious food, which meets dietary needs and food preferences for an active, healthy life, affects approximately 14 percent of Bexar County residents and nearly 20 percent of children under the age of 18.
In response, Metro Health launched its SA Forward Plan in 2022. This five-year blueprint is Metro Health’s strategic roadmap to address
health disparities in the community. A key area in the plan is Nutrition and Food Insecurity, which envisions more equitable, sustainable and diverse food systems, and making nutritious foods more accessible across the entire county. Metro Health’s Policy and Civic Engagement Office (PaCE) and Community Nutrition program have partnered to build partnerships with community organizations to promote equitable health outcomes by building strong cross-sector and community partnerships, and coordinating policy and systems change initiatives.
Metro Health also continues to educate the community on the importance of switching to healthier food options and engaging in regular physical activity. It provides resources such as workshops aimed at preventing and managing chronic diseases, like diabetes, and a range of tools including nutrition tips, informative sheets, educational materials, games and more to support families maintaining a healthy diet and well-being. Its ¡Por Vida! program acknowledges local restaurants that promote healthy eating environments through good nutrition, cleanliness, sustainability and community involvement.
National Nutrition Month is an opportunity to commemorate the dedication of public health workers, registered dietitians (RDs), healthcare professionals and community organizations who play a crucial role in ensuring the community has access to fresh, nutritious foods and a more equitable, diverse and sustainable food system. Metro Health continues to uphold its vision of “healthy people thriving in a healthy community” by fostering collaborations and community engagement to increase food security and encourage healthy living.
Making healthy food choices is about looking Beyond the Table and Metro Health encourages individuals to spend more time making better decisions on what they eat and drink. To learn more about Metro Health’s programs, nutrition guides and other resources, visit www.sa.gov/health.
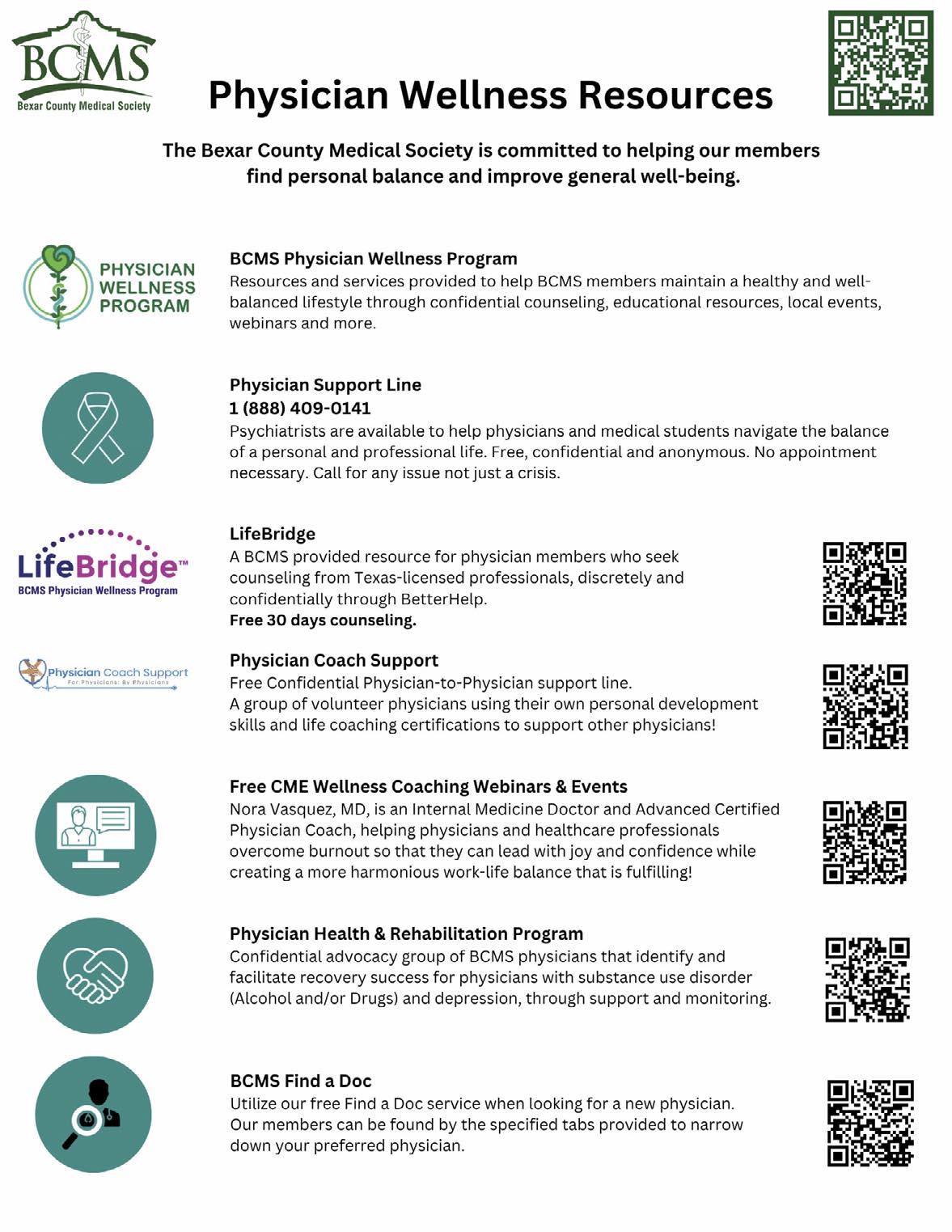

Fraud and Cybercrime: It's not a matter of ‘if,’ it's a matter of ‘when’
Businesses of every size and every industry will, at some point, experience cybercrime attempts. How companies execute their cyber protection strategy can be the difference between a mere bump in the road and an economic disaster. A solid cyber protection strategy includes many fraud prevention tools to safeguard your accounts and practice. Consider putting together a fraud protection team comprising not only your banker but also a treasury solutions expert who collaborates with you and your banker to recommend customized cash management solutions and cyber protection tools. This collaborative approach leverages the insights of experts so that you have a critical advantage in keeping your patients protected and your business financially healthy and growing.
Fraud protection tools are necessary now more than ever
Fraud is a $7 billion "industry," and Texas businesses are the third-hardest hit in the United States. The attacks on healthcare operations nationwide are at an all-time high, doubling since 2016. Thieves no longer need to come to your front door to steal money or data. Someone sitting on their couch two
states away or across the globe can steal millions from a business with the click of a mouse.
"You will have a cyber incident if you own a business. It will happen. It is probably happening today."
– Andrew Moore, COO, IronEdge Group.
A robust cybersecurity game plan includes protection on two fronts: your internal data and your financial assets within your bank. IronEdge Group executives and cybersecurity experts, Andrew Moore and Patrick Maese, implore business owners to take fraud prevention seriously. "As a business owner, the biggest lie you can tell yourself is that if you haven't been attacked yet by cybercrime, you won't be," said Patrick Maese, Vice President, San Antonio Client Experience, IronEdge Group. "For healthcare practices, implementing fraud protection tools is a matter of patient and practice safety."
Adequate cybersecurity requires time and resources, so it pays to collaborate with the right team of experts and enact ongoing, third-party assessments of your plan. As the owner of a healthcare practice, knowing where your data is and which of it needs protection is essential. For example, protect internal practice data by keeping a copy of data off-site and testing backups regularly. Most important, however, is employee
training. Your employees are your first line of defense, and no one should be exempt from participating in frequent exercises to keep your practice safe in the ongoing fight to protect your practice from experiencing cybercrime.
Cybercrime protection strategies are rarely at the forefront of business strategies; however, the increasing sophistication of cybercrime attempts forces increased urgency for business owners to remain tirelessly vigilant. Leveraging the expertise of your banker and treasury management thought partners to ensure you have the right tools in place to protect your growing practice is vitally important.

Maria Breen, Executive Vice President, Private Banking Manager at The Bank of San Antonio is a San Antonio native and financial expert with a heart for serving her clients and community. As the head of Private Banking at The Bank of San Antonio, Maria uses her over 30 years of financial services experience to help her clients build the lives and legacies they envision. maria.breen@thebankofsa.com
Beyond her work at the Bank, Maria is also the Board chair for AVANCE San Antonio and Committee Co-chair for Impact SA. With a deep-rooted love for serving others, Maria sees private banking as an extension of her passion for taking care of people in her community.
The annual Bexar County Medical Society General Membership Meeting took place on February 7, 2024, at the Bariatric Counseling Center of San Antonio. Guest speaker Rick W. Snyder II, MD, TMA President, presented a summarization on the 2023 Legislative Session.









Rick W. Snyder II, MD, TMA President
John Nava, MD, BCMS Immediate Past President;
Hinchey, MD;
Shah, MD;
Guests listen to the legislative wins and challenges, while earning CME at the General Membership meeting.
We encourage you to use our friends of medicine businesses whenever you or your practice need supplies or services.
Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 jprice@ssacpa.com
www.ssacpa.com
“Dedicated to working with physicians and physician groups.”

Aspect Wealth Management (★★★ Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520
mclark@aspectwealth.com
www.aspectwealth.com
“Your wealth. . .All aspects”

Broadway Bank (HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@Broadway.Bank
www.broadwaybank.com
“We’re here for good.”

The Bank of San Antonio (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the
state who specialize in medical malpractice and all lines of insurance for the medical community. Brandi Vitier
210-807-5581
brandi.vitier@thebankofsa.com
www.thebankofsa.com
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking
210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking
210-343-4494
Scott.Gonzales@amegybank.com
www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help Physicians get the banking services they need.
Synergy FCU Member Services 210-750-8333
info@synergyfcu.org
www.synergyfcu.org
“Once a member, always a member. Join today!”

Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison
210-503-0003
yulia@genicslabs.com
Kevin Setanyan
Managing Partner
210-503-0003
kevin@genicslabs.com
Artyom Vardapetyan
Managing Partner
210-503-0003
www.genicslabs.com
“Accurate results in record time.”
Livingston Med Lab (HH Silver Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease, & Genetics. Robert Castaneda, CEO
210-316-1792
Robert@livingstonmedlab.com
www.livingstonmedlab.com/home
“Trusted Innovative, Accurate, and STAT Medical Diagnostics”

Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor) Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for health care entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com
www.BexarCV.com
“Proudly serving the medical community since 1998”
Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA Senior Private Wealth Advisor
512-649-8113
SERVICE@OAKWELLPWM.COM

www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney Financial Advisor
210-858-5880
Elizabeth.olney@edwardjones.com
www.edwardjones.com/elizabeth-olney "Making Sense of Investing"

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520
mclark@aspectwealth.com
www.aspectwealth.com
“Your wealth. . .All aspects”

Hancock Whitney (HHH Gold Sponsor)
www.hancockwhitney.com
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork, and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana, and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services.
John Riquelme
San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Larry Anthis
Corporate Banking, Relationship Manager
210-507-9646
Larry.Anthis@hancockwhitney.com
Serina Perez
San Antonio Business Banking
210-507-9636
Serina.Perez@hancockwhitney.com
Erik Carrington
Texas Regional Wealth Management Manager 713-543-4517
Erik.Carrington@hancockwhitney.com

Conviva Care Center (HHH Gold Sponsor)
Conviva’s value-based care model allows physicians to deliver high quality, personalized care and achieve better outcomes, while feeling free to focus on health equity and patient outcomes.
Kim Gary
Senior Physician Recruiter 812-272-9838
KGary4@humana.com
www.ConvivaCareers.com
“Fuel Your Passion & Find Your Purpose”

UT Health San Antonio MD
Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado
Business Development Manager
210-450-3713
delgador4@uthscsa.edu
UT Health San Antonio MD
Anderson Mays Cancer Center
Laura Kouba
Business Development Manager
210-265-7662
norriskouba@uthscsa.edu
https://uthscsa.edu/
Appointments: 210-450-1000
UT Health San Antonio
7979 Wurzbach Road
San Antonio, TX 78229
SERVICES

Equality Health (HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination, and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager
210-608-4205
cleos@equalityhealth.com
www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting, and defending physicians.
Patty Spann
Director of Sales and Business Development
512-425-5932
patty-spann@tmlt.org
www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

representation projects include new development acquisitions and sales, lease representation and financial (RE)-structuring for existing investments.
Jon Wiegand
Principal
210-241-2036
jw@alamocapitaladvisors.com
www.alamocapitaladvisors.com

Henry Schein Medical (HH Silver Sponsor)
Insperity (
★★Silver Sponsor)
Insperity’s HR solutions offer premium service and technology to facilitate growth by streamlining processes related to payroll, benefits, talent management and HR compliance. We provide the tools to help you lighten your administrative load, maximize productivity and manage risks – so you can focus on growth.
Cynthia Marshall
Business Performance Advisor 210-558-2520
cynthia.marshall@insperity.com
Dayton Parker Business Performance Advisor
210-558-2517
dayton.parker@insperity.com
www.insperity.com
“Insperity’s mission is to help businesses succeed so communities prosper”

TMA Insurance Trust (HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England
Director of Member Benefits
512-370-1776
wendell.england@tmait.org
800-880-8181
www.tmait.org
“We offer BCMS members a free insurance portfolio review.”
The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
katy.brooks@bosainsurance.com
www.thebankofsa.com
“Serving the medical community.”
MedPro Group
(HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com
www.medpro.com
REAL ESTATE

Alamo Capital Advisors LLC (★★★★ 10K Platinum Sponsor)
Alamo Capital Advisors is focused on Sourcing, Capitalizing, and Executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current and
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol
210-413-8079
tom.rosol@henryschein.com
www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”

Provider's Choice Scribe Services (★★★ Gold Sponsor)
Our accurate and complete documentation helps our customers focus on what’s most important, their patients. Let us take on the task of documenting your patient encounters, it’s what we do.
Yoceline Aguilar
COO
915-691-9178
yaguilar@pcscribes.com
Luis Chapa MD/CEO
210-796-4547
lchapa@pcscribes.com
www.providerschoicess.com/ “An Unparalleled Scribe Experience”
Equality Health (★★★ Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination, and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager
210-608-4205
cleos@equalityhealth.com
www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President
210-797-8412
healthcareleaderssa@gmail.com
Gary Meyn, LFACHE Vice President 210-912-0120
gmeyn@vestedbb.com
https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber
President
210-308-7907 (Direct)
kbarber@bdo.com
Valerie Rogler Program Coordinator
210-904-5404
Valerie@thehealthcell.org
www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Jeannine Ruffner President info4@samgma.org
www.samgma.org

Alamo Capital Advisors LLC (★★★★ 10K Platinum Sponsor)
Alamo Capital Advisors is focused on Sourcing, Capitalizing, and Executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current and representation projects include new development acquisitions and sales, lease representation and financial (RE)-structuring for existing investments.
Jon Wiegand
Principal
210-241-2036
jw@alamocapitaladvisors.com
www.alamocapitaladvisors.com
Oakwell Private Wealth Management
(
★★★ Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA
Senior Private Wealth Advisor
512-649-8113
SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”

Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and
continued from page 41
protect their revenue cycle. Mike DeQuattro
Director of Operations - Texas & New Mexico
210-918-8737
Mike.DeQuattro@ favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout. Join us in transforming healthcare delivery, prioritizing your wellbeing and patient care. Pedro Caretto, VP of Business Development 786-437-4009
pcaretto@eleosvhs.com www.eleosvhs.com

Provider's Choice Scribe Services (★★★ Gold Sponsor)
Our accurate and complete documentation helps our customers focus on what’s most important, their patients. Let us take on the task of documenting your patient encounters, it’s what we do. Yoceline Aguilar COO
yaguilar@pcscribes.com
915-691-9178
Luis Chapa MD/CEO 210-796-4547
lchapa@pcscribes.com www.providerschoicess.com/ “An Unparalleled Scribe Experience”


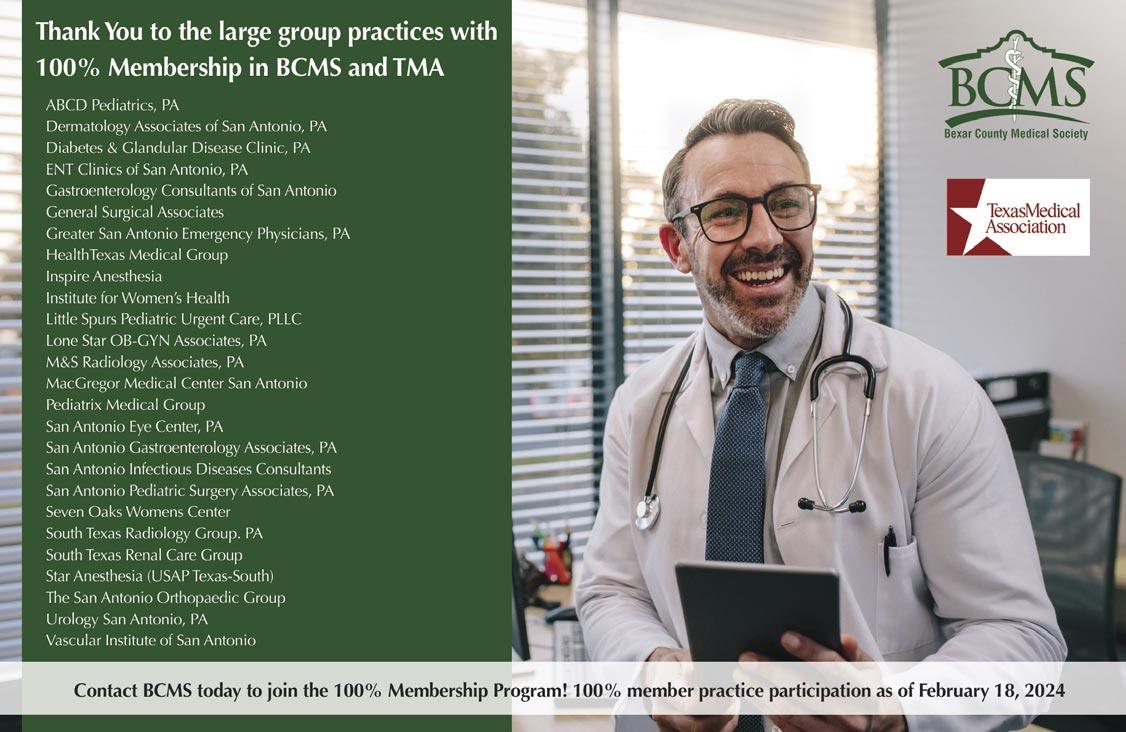





Anyone with even a rudimentary knowledge of the auto industry is aware that Porsche, a sports car maker that only about 20 years ago began producing non-sports cars, is a money-making machine. What most observers probably don’t appreciate is that, despite the presence of some very exclusive and expensive sports cars like the GT3, GT4 and 911 turbo in their lineup, it’s the non-sports cars that make most of Porsche’s profits.
This month I’m going to focus on the original Porsche non-sports car, the Cayenne SUV. First introduced in 2002, the OG Cayenne was derided by most Porsche aficionados, including me, as a sacrilege. Once it became clear that the Cayenne, and later the Panamera and Macan, would produce the profits that would allow the company to continue manufacturing special sports cars like the 2016 911R, 2018 GT2 RS and 2024 911 S/T, all was forgiven.
I was able to drive a 2024 Porsche Cayenne Coupe recently, and it was impressive.
For the record, I’m aware that the Cayenne Coupe is neither a coupe nor a SUV, and that SUVs turned into sedans — think BMW X6 and the like — are generally unloved in the enthusiast community.
I’m willing to bet, however, that most of the haters haven’t actually driven one of these vehicles. I say that because I criticized the original X6 as just an X5 with less utility until I reviewed one and learned that their suspensions, powertrains and software are modified to make them sportier than their more utilitarian siblings. Plus, these sedanized SUVs sit higher than “normal” sedans, which helps you see around and through the pickups and Suburbans that clog our streets and highways.
So, the Cayenne Coupe, which shares almost everything with the Cayenne SUV, drives better than the SUV. An enthusiastic jaunt on a twisty back road was a pleasure thanks to taut suspension, which enables confident steering with little body roll. And the powertrain has been tweaked for quicker throttle response and gear changes, which make the car feel quicker, even though it really isn’t.
Still, the 5,000lbs Cayenne Coupe is most comfortable driving into town to run errands or cruising on the interstate, maybe especially the latter.
A quick aside: it is something to realize that a sedan-ified SUV like this one can outperform a BMW M5 from 20 years ago, all while providing more passenger and luggage space.
My test car was the $80,850 base model, which comes with a 348 HP V6 engine that pulls enthusiastically but sounds just OK. Slotting above the base model is the 463 HP plug-in hybrid turbo V-6 Cayenne E-Hybrid that starts at $93,350, and just above that in the range is the 468 HP Cayenne S that will set you back $109,850. At the top of the lineup is the 650 HP Turbo GT that goes for almost $200,000. Gulp. The Turbo GT is only available in the coupe body style, by the way.
While only a few subtle exterior design changes differentiate the
facelifted 2024 Cayenne line from prior models, the interior has been improved significantly. A new 12.6-inch curved digital instrument display sits behind the steering wheel alongside the 12.3inch central touchscreen that controls the updated PCM 6.0 infotainment system. Porsche has decided to go all-in with Apple CarPlay and Android Auto, which I think is a better choice than forcing their own system on customers who are quite happy with their phones and don’t want to learn another user interface.

The previous gear-selector lever located on the central console has been replaced by a smaller toggle switch that now sits just to the left of the central touchscreen on the dash. The center console now houses a new haptically controlled HVAC panel, which I like a lot.
The Cayenne also offers an optional 10.9-inch touchscreen for the front passenger, which allows the front passenger to enjoy their own streaming entertainment, control several vehicle features, and even “help” with navigation. The display's polarized filter makes it invisible to the driver for safety reasons.
I find it interesting that in 1998 after the first large luxury SUV, the Lincoln Navigator, was introduced, most automotive journalists, including the venerable David E. Davis of Automobile magazine, predicted that upscale buyers wouldn’t be interested. Those experts were proven wrong as every luxury brand eventually introduced a SUV, and now we’re seeing more SUVs from sports car brands, most notably Lamborghini and Ferrari.
Anyway, the Cayenne Coupe is a car that I believe many BCMS members will find appealing. It combines luxury with performance in a vehicle that provides more space and better visibility than a sedan. Call Phil Hornbeak and ask for a test drive!
As always, call Phil Hornbeak, the Auto Program Manager at BCMS (210-301-4367) for your best deal on any new car or truck brand. Phil can also connect you to preferred financing and lease rates.

Stephen Schutz, MD, is Board-Certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.
Kahlig Auto Group
11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Chuck Nash Chevrolet Buick GMC 3209 North Interstate 35 San Marcos, TX
William Boyd 210-859-2719
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Chris Martinez 210-366-9600
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Kahlig Auto Group
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000
As of November 1, 2023, our loan rate will be 5.5% for 60 months with approved credit.Kahlig Auto Group Kahlig Auto Group Kahlig Auto Group Kahlig Auto Group Kahlig Auto Group