




NON PROFIT ORG US POSTAGE PAID SAN ANTONIO, TX PERMIT 1001 SAN ANTONIO

PUBlISHED By: traveling Blender, llC. 10036 Saxet Boerne, tX 78006

PUBlISHER louis doucette louis@travelingblender.com
BUSInESS MAnAGER: vicki Schroder vicki@travelingblender.com
ADVERTISInG SAlES:
AUSTIn: Sandy Weatherford sandy@travelingblender.com
HEALTHCARE ON THE MOVE –

San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EditoriAl CorrESpondEnCE: Bexar County Medical Society 4334 n loop 1604 W, Ste. 200 San Antonio, tX 78249
Email: editor@bcms.org
MAGAZinE AddrESS CHAnGES: Call (210) 301-4391 or Email: membership@bcms.org
SuBSCription rAtES: $30 per year or $4 per individual issue
AdvErtiSinG CorrESpondEnCE: louis doucette, president traveling Blender, llC.
A publication Management Firm 10036 Saxet, Boerne, tX 78006 www.travelingblender.com
For advertising rates and information
Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national orgin, or an intention to make such preference limitation or discrimination.
SAn AnTOnIO: Gerry lair gerrylair@yahoo.com
PROjECT COORDInATOR: denise tapia denise@smithprint.net


For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2023 Smithprint, inc. prin tE d in tHE u SA
SAN ANTONIO 4 SAN ANTONIO MEDICINE • April 2023
TABLE OF CONTENTS
THE OFFICIAL PUBLICATION OF THE BEXAR COUNTY MEDICAL SOCIETY • WWW.BCMS.ORG • $4.00 • APRIL 2023 • VOLUME 76 NO.4
MOBILE MEDICINE Mobile Medicine is the Future By Erika Gonzales, MD 14 Mobile Medic – Medicine on the Move By Gary Legault, MD, Steven Parks and Mike Kile 16 Building Community ‘Confianza’ (Trust and Confidence) in Collaboration with the San Antonio Independent School District By Jason Rosenfeld, DrPH, MPH 18 The House Call is Effective and Should Be Protected By David Cavazos, MAA and Ramon Cancino, MD, MBA, MS, FAAFP 20 Walking to Promote Health By Richel Avery, MD, FAAFP and Ramon Cancino, MD, MBA, MS, FAAFP 22 Moving Medicine South: Our Duty to the Community By Lyssa Ochoa, MD, Board-Certified Vascular Surgeon and Founder of The SAVE Clinic 24 Community-Wide Mobile Vision Screenings and Their Role in Protecting and Preserving Eyesight By Sahar Z. Ali 28 Frontera de Salud at UT Health San Antonio By Moses Alfaro 29 BCMS President’s Message .................................................................................................................................................8 Doctor Testimonial to the System By John J. Seidenfeld, MD 10 BCMS Alliance Message 12 Leadership in Crisis: Interview with Gerardo Ortega, MD, FACS By Monica Jones, BCMS COO 30 Autism Awareness: A Role for Every Medical Practitioner By Melissa Svoboda, MD and Cynthia Hamilton, MBA 32 Staff Retention in an Era of Wage Inflation By Alan D. Winkler, MHSA, Executive Director of Urology San Antonio, PA 34 88th Texas Legislative Session Almost at Mid-Point By Mary E. Nava, MBA, Chief Government Affairs Officer 36 Artistic Expression in Medicine By Oliver Johnson, Jr, MD 38 BCMS Vendor Directory .....................................................................................................................................................40 Auto Review: Porsche Taycan GTS By Stephen Schutz, MD 44 Recommended Auto Dealers 46

ElECTED OFFICERS
John Joseph nava, Md, President
Brian t. Boies, Md, Vice President
Ezequiel “Zeke” Silva iii, Md, Treasurer
John Shepherd, Md, Secretary

Brent W. Sanderlin, do, President-elect
rajeev Suri, Md, Immediate Past President
DIRECTORS
Woodson "Scott" Jones, Md, Member
Sumeru “Sam” G. Mehta, Md, Member
priti Mody-Bailey, Md, Member
lubna naeem, Md, Member
lyssa n ochoa, Md, Member
Jennifer r rushton, Md, Member
raul Santoscoy, do, Member
Amar Sunkari, Md, Member
lauren tarbox, Md, Member
Jenny Case, Alliance Representative
ramon S. Cancino, Md, Medical School
Representative
lori Kels, Md, Medical School Representative
robert leverence, Md, Medical School
Representative
Keiko McManus, Md, Board of Ethics Chair
John pham, do, Medical School Representative
Cheryl pierce-Szender, Alliance Representative
ronald rodriguez, Md, phd, Medical School
Representative
Col. Cecilia Kai Sessions-Carpenter Md, MpH, Military Representative
George F. “rick” Evans, Jr., General Counsel
Jayesh B. Shah, Md, TMA Board of Trustees
Melody newsom, CEO/Executive Director
BCMS SEnIOR STAFF
Melody newsom, CEO/Executive Director
Monica Jones, Chief Operating Officer
Yvonne nino, Controller
Mary nava, Chief Government Affairs Officer
Brissa vela, Membership Director
phil Hornbeak, Auto Program Director
August trevino, Development Director
Betty Fernandez, BCVI Director
Al ortiz, Chief Information Officer
PUBlICATIOnS COMMITTEE
norys Alexandra Castro-pena, Md, Co-chair
John Joseph Seidenfeld, Md, Co-chair
louis doucette, Consultant
david Schulz, Community Member
Elizabeth Clanton, Md, Member
Kristy Yvonne Kosub, Md, Member
neal Meritz, Md, Member
Jaime pankowsky, Md, Member
Alan preston, phd, Member
rajam S. ramamurthy, Md, Member
Adam v ratner, Md, Member
Faraz Yousefian, do, Member
Moses Alfaro, Student Member
Winona Gbedey, Student Member
tue Felix nguyen, Student Member
niva Shrestha, Student Member
Bethanne Bradshaw, Student Member
Monica Jones, BCMS Coo, Staff Liason
trisha doucette, Editor
6 SAN ANTONIO MEDICINE • April 2023
BCMS BOARD OF DIRECTORS
Healing the Inner Child in Everyone –Health Care Needs Snapshot
By John J. Nava, MD, 2023 BCMS President
Last month, I described in a rudimentary manner the idea of the social determinants of health (SDoH). Every three years, the Bexar County Health Collaborative commissions a Health Care Needs Assessment (HCNA). This report is published to guide the community and policy makers who contribute to planning for the future. The report does not specifically follow the exact format of the SDoHs, but it does give a useful snapshot of the community healthcare needs. It informs the development of the Community Health Plan, which typically is published the next year. I am trying to briefly summarize the results of the 2022 report. The report admits limitations of the data, but I am waiting with great anticipation for the next Healthy Bexar Plan 2023, and I hope many other citizens are patiently doing the same.
The above quote from the HCNA is a bit humbling, noting the small effect our cumulative practices have upon directly improving community health. Not to discourage, but to encourage, and keeping this in perspective, we can as a profession become better versed in other ways to impact and elevate the health status of our patients.
The following topics are typically included in the social determinants of health (SDoH).
1) Economic stability, including food insecurity
“Fundamental root causes of poor health outcomes, health behaviors, and even other social and economic determinants of health, low income and poverty were among the most highly prioritized issues in this assessment.” (p. 142)
“Food insecurity rose in 2018 and 2019. The cause for this increase is not known, as this period falls between the Great Recession and the Covid-19 pandemic. Food insecurity almost certainly further increased during the pandemic.” (p. 23)
“Conversely, Feeding America’s Map the Meal Gap data indicates a small but continuing decrease in food insecurity among children (Figure 1.18). Again, this data predates the Covid-19 pandemic, so 2020 and 2021 are likely to show a higher percentage when that data becomes available.” (p. 24)
“Median family income grew by 15% between 2015 and 2019 (Figure 1.32), a slightly faster rate than median household income. Again, this data predates the Covid-19 pandemic.” The trend may not have continued. (p. 33)
2) Education Access and Quality
“A large proportion of Bexar County’s adult population has low educational attainment (Figure 1.10). One in six residents 25 and older did not finish high school, and another three in six have no college education.” (p. 13)
“The estimated percent of population with an associate’s degree or higher rose very slightly between 2015 and 2019 (Figure 1.11), hovering between an estimated 34% and 37%.” (p. 14)
“While the percent of households with a computer and broadband internet subscription was at a low of 73% in 2015, it has increased every year, reaching 84% in 2019.” (p. 18)
3) Healthcare Access and Quality
“Many forms of preventive and primary care, including cancer screening, prenatal care, dental care, and chronic disease management emerged as priorities. Most of these services show racial/ethnic disparities in access and utilization, as well as in the health outcomes that preventive and primary care are intended to prevent or manage. Although the full impact of the pandemic on preventive and primary care utilization and subsequent health outcomes is not yet known, it is certain that utilization declined.” (p. 141)
“Despite the Affordable Care Act and active local enrollment efforts, the percent of civilian non-institutionalized population that has health insurance remained fairly flat between 2015 and 2019 at an estimated 83% to 85% (Figure 2.1).” (p. 47)
“Health insurance coverage is highest in the Medicare-eligible older population, and next highest among young children eligible for Medicaid (Figure 2.2). Coverage rates are lowest among working-age adults, particularly younger adults aged 19 to 34.” (p. 48)
8 SAN ANTONIO MEDICINE • April 2023 PRESIDENT’S MESSAGE Part 2
“The relative contribution of medical care to health and well-being is only 10% to 20%.”
Bexar County Health Collaborative, Health Care Needs Assessment, 2022
“While young adults may feel social media is a great tool for de-stigmatizing mental health, other residents feel it can be a hindrance when it is the only option for accessing services.” (p. 56)
4) Neighborhood and Built Environment
“Bexar County is experiencing an increasingly acute shortage of affordable housing, especially but not only for low- and moderate-income residents. The available data shows that renters and People of Color are especially likely to experience housing cost burden, and these disparities are likely to have widened during the Covid-19 pandemic.” (p. 140)
“While investment in lower-income communities can help access and availability of housing, it can also make it worse depending on the type of investment. The People Over 65 explained how the only investment they are seeing in their neighborhoods is from gentrification, which is pricing them out of places they have lived their whole lives.” (p. 43, p. 150)
“The percentage of days with air pollution at a healthy level decreased in 2020 and 2021 after an increase in 2018 and 2019 (Figure 1.48), perhaps because of reduced driving during the pandemic.” (p. 46)
“The percent of population considered to have walkable park access has risen significantly since 2017 but is still below half as of 2021 (Figure 1.49). The Trust for Public Land considers park access walkable if the park is within a 10-minute walk, roughly half a mile at a moderate to brisk pace.” (p. 46)
5) Social and Community Context
One clear preference stated by public comment was from young citizens who embraced the option of app-based social media tools to address mental health issues without the stigma that may accompany that type of health-seeking behavior. (p. 56)
Social support needs were also mentioned by the Over 65 focus group, citing a preference for assistance from neighborhood representatives that were more like them when addressing digital literacy skills.
The CDC Preventive Medicine Grand Rounds presented by Didi Ebert, DO, MPH, MSEd, FAAFP, CDC PH-TIPP Class 2021-2022 on 07/06/2022 was titled Addressing Social Determinants of Health in Clinical Care: Learner Integrated Approaches to Align Primary Care and Public Health. This presentation described how clinical care can address SDoHs and how medical student and resident physician learners can be trained to incorporate this activity seamlessly into patient flow. Since this happens in a teaching clinic affiliated with a family medicine department at The University of North Texas Health Science Center at Fort Worth/TCOM (Texas College of Osteopathic Medicine), the learners are a captive audience. Using specific Z codes to upgrade 99213 visits to 99214 visits due to increased complexity is a way for any physician to justify this more complex approach. This does offer increased compensation for specialized team-based clinical care directed at a different clinical performance measure, so practicing
physicians could be motivated to learn voluntarily and develop their own practices.
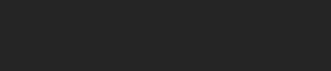
Recently, a Southside San Antonio hospital announced its closure in May 2023. Though there was some hope that other hospital systems could prevent the closure of Texas Vista, formerly known as Southwest General, the help did not materialize. This is not an intentional event, but nonetheless rather typical of healthcare inequities affecting communities of color. A new University Health System facility is planned for the Southside, but will not be in operation until 2027. Sometimes, things have to get worse before they get better. Perhaps this represents another opportunity for innovation and unconventional public-private partnerships as a temporary remedy until that publicly funded hospital is built.
“Latinos and the Nation’s Future” is a book published in 2009, edited by Henry Cisneros, and is a collection of essays from thought leaders on the past, present and future of Latino people in the United States. I would like to close this part of my monthly message with a quote from a colleague and mentor, Elena V. Rios, MD, President of the National Hispanic Medical Association, who contributed a chapter on improving the health of the Nation’s Latinos.
“To improve the health of Latinos in the United States over the next twenty years, the first requirement is to end disparities in the healthcare system. Medical treatments received by Latinos are less attentive, less timely, and less comprehensive than those afforded to other Americans. Good health may be seen as a right, but the preservation and advancement of rights are driven by economics and politics. Given the magnitude of the expected growth in the Hispanic population in coming decades, we should be able to ensure that policymakers in government and the private sector devise strategies for raising Hispanic healthcare standards to the level experienced by other Americans, but only if we develop and exercise the necessary leadership.
At the same time, we must acknowledge that Latino’s own attitudes and behavior contribute to bad health. If we fail to improve on disease prevention in Hispanic communities through healthy living, good diet, and weight control, we are unlikely to improve our own wellness no matter what changes are made in the healthcare system.”
For more information, please access the full report through the Bexar County Health Collaborative website.
John J. Nava is the 2023 President of the Bexar County Medical Society. He is interested in Primary Care, Clinical Research and Public Health.
PRESIDENT’S MESSAGE
Visit us at www.bcms.org 9
Doctor Testimonial to the System: My Gratitude to the Doctors and Staff at St Luke's Baptist Hospital
January 31, 2023
To: BCMS Publications Committee and SAM Readers
From:
John J Seidenfeld, MD

On the 27th of December 2022, I collapsed unable to speak or move the right side of my body amidst family and friends. The ambulance very promptly arrived from a San Antonio fire station nearby and I was transported to St. Luke’s Baptist Hospital. There I was met by Brandon Larrington DO and the emergency room staff. They promptly recognized the stroke and began diagnostic studies, treatment and referrals to appropriate consultants. Within minutes, Justin Mascitelli MD and his fellow Matthew Webb DO began a procedure to remove the clot from the left middle cerebral artery, which resulted in the return of my speech and use of right-side musculature.
“Time is brain”.
I was then transferred to the neurology intensive care unit for blood pressure control and observation. Gerardo Garza-Gutierrez MD and Stephanie Whitenack NP, and Jose Martinez-Ochoa MD provided intensive and medical care. Fuad-Al Ali MD and Brittney Medders NP, neurology, and Eduardo Pollono MD, cardiology, with support from the laboratory, anesthesia and radiology staff helped diagnose and treat what may have led to the events of the day. The nursing staff gave me excellent care as well in the Emergency Department, Neurology Intensive Care Unit, General neurology unit, Cath Labs and Cardiac procedure labs.
We have all lived through the difficult few years of the COVID pandemic and I can only imagine how hard it has been for you and your staff. Please accept and extend my thanks to your staff and the members mentioned above for their continued dedication and care of their patients. Without their skillful work and thoughtful care, I would not be using my right hand to type this note or speaking to my wife and children about what happened at the end of December at your facility. I have returned to teaching the learners at the University of the Incarnate Word, School of Osteopathic Medicine through the grace of the Lord and the skills of your staff. Thank you to all for doing the excellent work you do each day.
Sincerely and with gratitude,
By John J. Seidenfeld, MD
10 SAN ANTONIO MEDICINE • April 2023 DOCTOR TESTIMONIAL

Bexar County Medical Society Alliance
By Brittany Garcia, BS, MHA, Vice President of Communication

In what seems like a previous life, before marriage and children, 18-year-old me believed healthcare on the move meant studying drugs so physicians could effectively treat patients as quickly as possible. I spent the summers during college in the rat and mouse labs of UT Health, formerly UTHSCSA. I had the incredible opportunity to pick an investigator whose research profile matched my interests, drugs of abuse.
For context, I wasn’t a drug-obsessed child. I was never exposed to drugs at home and I never tried drugs. But I attended a school where I was exposed to gangs, drugs and violence. I remember beginning middle school as a naive girl with glasses. I even entered the school’s science fair and won! However, I didn’t win because I was the brightest, I was just one of the few willing to try in an environment where parents, teachers and students were merely trying to survive. That was abundantly clear when I went on and traveled to the state science fair and lost miserably. My school district was ill equipped, and instead of spending money on lab equipment, books or computers, our school was spending money on portables for childcare to accommodate our growing population of teen parents. Teachers were depleted and a childhood friend of mine even died by suicide, due to rape. With the future looking so bleak, I turned to books and applied to summer camps to escape. My first summer camp away from home was at Texas A&M University School of Medicine in BryanCollege Station. At A&M, I attended my first college classes and I spent the week with medical students who showed me my first heart and knee surgeries. Exposure to the study of medicine was healing. So, as a teenage girl, learning that I’d be able to study the date rape drug, a growing public health concern at the time, was of huge importance to me and a way to move forward.
It isn't any wonder why I continue to acknowledge and give praise to our research community. Without those tireless hours of research, we wouldn’t have continued advancements in medicine. Most memorable as of late, the quick development of the COVID vaccine. Given my background, I also want to encourage those
who are able to continue outreach to disadvantaged and vulnerable communities. Events like Walk with a Doc do have an impact and will quite literally get your patient moving on the path to better health. The Alliance is looking forward to working with the Children’s Bereavement Center and distributing books to children via the Texas BookShare project, to encourage literacy and healthy lifestyles to young readers.
Last of all, 20 years later, healthcare on the move has another meaning to me. Being married to my physician spouse has meant I have moved with him constantly, near and abroad. It takes a tremendous amount of sacrifice to become a physician. People often think of the extended hours studying, but what I will remember most is moving and the financial impact.
Although, I am thankful for so many things: from meeting lifelong friends on this path, to programs that were innovative and gracious enough to offer zoom interviews during the pandemic, and to my husband’s residency program and how they saw fit to allocate funds for resident spouse events during those grueling years.
This profession takes a tremendous amount of sacrifice and impacts both parties in a relationship. So, if your spouse is not a member of the Alliance, consider this an invitation to join. We’d love to meet them and have them with us at events and community projects this year. For more information, please visit: https://www.bcmsalliance.org/
12 SAN ANTONIO MEDICINE • April 2023 BCMS ALLIANCE
Brittany Garcia, BS, MHA is the 2023 Vice President of Communication for the BCMS Alliance.

Mobile Medicine is the Future
By Erika Gonzales, MD
While the pandemic brought light to the need for accessible and innovative healthcare, and taught us that we need and can be flexible to serve those in need, the lack of physical access to medical services isn’t specific to the pandemic.
The medical community quickly pivoted to telemedicine as a primary resource to guarantee continual care during the pandemic. One of the key objectives focused on was ensuring that people's baseline chronic conditions were as controlled as possible, so that we could mitigate any increased risk that they might have if they were infected with SARS-COV-2. Being able to address the concerns of our patients from the safety of our home was invaluable and yet, unfortunately, not equally accessible. The digital divide runs deep, and it's beyond not having access to Wi-Fi or owning a smart device to connect with a healthcare provider. Digital solutions are not inclusive to people with lower digital literacy, which often includes our older patients. Lack of access to technology should not be an obstruction to equitable healthcare, and solely prioritizing digital solutions will further broaden health disparities, leaving behind a large population of those in need. There’s a second alternative that’s on the move: mobile medicine.
Many community organizations have been utilizing mobile health initiatives to expand access to quality healthcare in historically underserved areas. The use of mobile units, which can range from vans to

buses to trailers, allows healthcare workers to provide medical services to those who would otherwise struggle to obtain it. They can travel out into communities where health disparities are the strongest, and are well suited to deploy to areas that might unexpectedly need health support. This resource can help to address transportation inaccessibility and the distance from medical facilities that often deters families in poorer ZIP Codes from seeking care.
Some services offered through mobile clinics include:
• COVID testing
• Direct access to providers administering vaccines and immunizations
• Health screenings
• Primary care visits, mental health and chronic disease management
Mobile health units help disenfranchised communities overcome common barriers to accessing healthcare. While mobile clinics are a nationwide initiative, many rural areas, border towns and impoverished neighborhoods continue to suffer from health disparities that could be lessened by expanding and investing in mobile healthcare. In Bexar County, we are faced with the unique challenge of also providing healthcare to immigrants and refugees within San Antonio and the sur-
14 SAN ANTONIO MEDICINE • April 2023
HEALTHCARE ON THE MOVE – MOBILE MEDICINE
rounding border towns. This is a topic that, although politically charged, is a reality that we cannot pretend doesn’t exist. The overall health of our community is dependent on all people having equal access to healthcare and is the only true way to avoid a public health crisis.
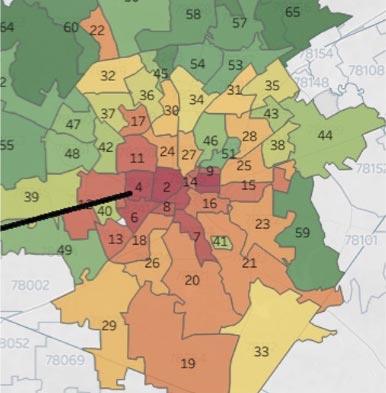
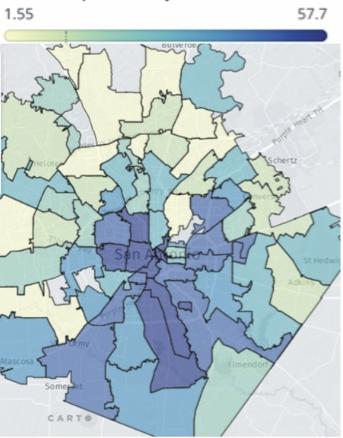
People in Bexar County have been geographically disadvantaged for years depending on the ZIP Code they live in. Hospitals, clinics and other healthcare resources are concentrated in the northern regions of San Antonio. There is only one surgery center south of downtown in San Antonio, and for every eight emergency rooms in wealthy parts of the city, the south side has one. (Garcia, 2022) This means that finding personalized or specialized care in the southern districts in Bexar County is much more challenging, if not impossible. A report published by University of Texas researchers calculated life expectancy by ZIP Code in counties all over Texas, including Bexar County. This report found that in Bexar County, the average lifespan in ZIP Codes with ≤5% below the poverty line was 82.4 years. In contrast, ZIP Codes with ≥20% below the poverty line were likely to live an average of 76.4 years. Further, life expectancy varied almost 22 years across different ZIP Codes, with Bexar County’s lowest life expectancy at 67.6 years in ZIP Code 78208, which encompasses neighborhoods just northeast of Downtown San Antonio, and 89.2 years in ZIP Code 78254, a northwest region. For reference, the average life expectancy in Bexar County is 79.1 years, a large jump from the life expectancy in ZIP Code 78208. (Pruitt,
Sandi L, et al.)
Broadened by not just the physical distance, health inequities are often perpetuated by an unequal access to transportation. Whether this is a family that shares one car or a household that may not have one at all, and accompanied by potentially unreliable public transportation, being able to physically make it to a hospital is often an overlooked hurdle that can reduce a person’s chances of getting the care they need. This barrier can also discourage patients from seeking healthcare, especially when a patient has conditions that require constant management. Beyond economic challenges, reliable transportation is especially crucial for people with chronic illnesses or physical disabilities who may need extra assistance making the trip.
only broaden the digital divide and work against this initiative. The advancement of medicine should include investing in and creating as many opportunities to expand healthcare for all people, regardless of geographical location, socioeconomic standing or historical access to resources.
References:
Ackerman, Todd. Texans’ Life Expectancy Varies Wildly Depending on ZIP Code. San Antonio Express-News, 28 Feb. 2019. https://www.expressnews.com/news/local/article/Texans-life-expectancy-varies-wildly-depending-13652231.php
Garcia, Laura. A Broken System Got Worse: How Covid Ravaged San Antonio's South Side. Center for Health Journalism, USC Anneberg, 20 Apr. 2022. https://centerforhealthjournalism.org/fellowships/projects/broken-system-got-worse-how-covid-ravaged-san-anton io-s-south-side

Garcia, Laura. San Antonio's Wealthy, Healthy Areas Have More Hospitals and Clinics - and There's Little Motivation to Change That. San Antonio Express News, 29 July 2022. https://www.expressnews. com/special-projects/article/san-antonio-southside-health-care17150492.php
“New Interactive Map First to Show Life Expectancy of Texans by ZIP Code, Race, and Gender.” UT Southwestern Medical Center, 27 Feb. 2019, https://www.utsouthwestern.edu/newsroom/articles/year2019/life-expectancy-texas-zipcode.html#:~:text=Within%20Bexar %20County%20(San%20Antonio,to%2089.2%20years%20(78254)
Owens, Remekca. UTSW Scientists Map Life Expectancy of Texans by Area, Race, and Gender. Center Times PLUS, UT Southwestern Medical Center, 19 Apr. 2019. https://www.utsouthwestern.edu/ctplus/stories/2019/life-expectancy-texas.html
Pruitt, Sandi L, et al. Life Expectancy at Birth in Communities Across Texas: 2005-2014.
Mobile clinics are an innovative solution to provide services to populations in need; they can be the bridge between vulnerable, underserved communities and clinical healthcare without compromising accessibility. To advance health equity, we need to turn our efforts towards innovative ideas that expand the traditional healthcare system. Continuing to prioritize and innovate exclusively for patients with high digital literacy will
Dr. Erika Gonzalez is the CEO & President of both South Texas Allergy & Asthma Medical Professionals (STAAMP) and STAAMP Clinical Research. She previously served as the Chief of the Allergy, Immunology & Rheumatology division at the Children’s Hospital of San Antonio and was an Associate Professor of Clinical Pediatrics at Baylor College of Medicine. She is an Advisor to the Dean of Science Engineering & Technology at St. Mary’s University and she is on the Stock Epinephrine Committee with the Texas Department of State Health Services. She was selected as a 2019 Presidential Leadership Scholar and was appointed to serve on the National Medal of Science Committee by President Joe Biden. Most recently, STAAMP was awarded San Antonio Business Journal’s 2022 Diversity and Inclusion Award for their work to promote diversity, equity and inclusion in the workplace. Dr. Gonzalez is a member of Bexar County Medical Society.
Visit us at www.bcms.org 15
To create a more inclusive healthcare system in the future, we need to focus on making these services available to all without boundaries.
HEALTHCARE ON THE MOVE – MOBILE MEDICINE
Mobile Medic –Medicine on the Move
By Gary Legault, MD, Steven Parks and Mike Kile
“MEDIC!!!” is a call from Soldiers when someone is injured; it results in an Army Medic (68W) quickly coming to the rescue even amid danger. Army Medics are trained in basic life support, emergency medical skills, battlefield medicine principles and tactical combat casualty care.1 In the Navy, they are called Corpsman and in the Air Force, Medical Technicians. All military basic medical training now occurs on Joint Base San Antonio (JBSA) at Fort Sam Houston, Texas. After medical job training, Medics are assigned to operational units or medical treatment facilities. Despite their duty assignment(s), they always need to be ready to provide a variety of medical support in a moment’s notice.
Recognizing the need for ensuring Medics maintain their skills and modernize their capabilities, Brigadier General Jeffrey Johnson (previous Brooke Army Medical Center Commander) started the Mobile Medic Program. The mission of the program is to increase utilization and improve primary care skills of the Medic/Corpsman using readily available virtual health capabilities to ensure a ready medical force. The concept was simple, create opportunities for Medics to provide handson care to service members with the benefit of having technology to provide supervision and reach-back capabilities. The Virtual Medical Center at Brooke Army Medical Center was provided with Medics and given the task to implement the program.
In the beginning, the Medics built workflows and protocols, and then became proficient with their electronic equipment. Next, they looked for opportunities to deploy Medics to various areas within JBSA at Fort Sam Houston and Camp Bullis. The initial scenario was embedding a Medic around a unit of troops training in the field, away from the clinic or hospital. The Medic would set up sick call close to the trainees every morning and evaluate any trainees that felt unwell. The Medics would synchronously (real-time) review each patient with a nurse practitioner for guidance through a video-to-video platform and used peripheral equipment to look into the patient’s eyes, ears, nose, mouth and throat. Additionally, they used a magnifier lens for dermis/skin irritations. For disposition, many service members were sent back to training, while more acute patients were evacuated to the clinic or hospital. If the Medics were not present, all the Service Members would have to be sent to clinic where they often waited in long lines for two to three hours.
Once others heard about the Mobile Medics, the San Antonio team began traveling to other military installations to implement the program. Additionally, the team was on standby to deploy to humanitarian missions and was activated for Hurricane Maria Disaster Relief in Puerto Rico. During the COVID-19 pandemic, the Mobile Medics were able to support the JBSA training population by providing health care in the quarantined quarters provided to house Service Members who tested positive for COVID-19. The Mobile Medics are also helping the 5G program located in San Antonio and sponsored by the Office of the Under Secretary of Defense.2
The concept of Mobile Medic is not reliant on any specific technology. The minimum requirements are to secure communications between a Medic and a provider, often a physician assistant or nurse practitioner. Lightweight, portable technology is essential in the field. The Medics typically use a Transportable Exam Station (TES) or TeleHealth In A Bag (THIAB). In many environments, connectivity can be a challenge. The Mobile Medics carry Mobile Broadband Kits (MBKs) in a backpack to ensure connectivity anywhere. Technology is rapidly evolving; therefore, the Mobile Medics stay abreast of the newest platforms that remain portable, secure and reliable in austere environments.
Medics, providers and Service Members can all benefit from the Mobile Medic program. Medics gain the hands-on patient skills and learn how to triage and manage patients. They become proficient in the Algorithm Directed Troop Medical Care (ADTMC) and are better prepared to provide care if all alone. Providers gain the opportunity to train their Medics, evaluate their skills, and support the frontline from afar. Service Members gain access to medical support where they are training at/or deployed, saving training time and decreasing unnecessary patient movement. The Navy recognized the benefits and adopted the program, naming it Connected Corpsman.
In future conflicts, lack of air superiority and limited medical staff will lead to prolonged casualty care requiring Medics to manage patients beyond their skillset. Therefore, to support them and ensure quality patient care, they need the capability to connect to a provider at another location. Future plans include adding this program to military doctrine and requirements, expanding it to all military service branches and operational sites, and training all Medics in the program. Hopefully, soon all Medics will feel comfortable in having the
16 SAN ANTONIO MEDICINE • April 2023 HEALTHCARE ON THE MOVE – MOBILE MEDICINE
capability to use tele-health equipment to reach back and get an expert’s recommendation when they need advice. Thank you to our Medics on the frontlines and all the providers answering the call to support them!
References:
1. Combat Medic Specialist training program. Medical Education and Training Campus. Retrieved February 22, 2023, from https://www.metc.mil/ Academics/Programs/Combat-Medic Specialist-Training-Program/
2. Vincent B. Vendors were recently selected to push forward military telemedicine experiments. Nextgov. Retrieved February 22, 2023, from https://www.nextgov.com/cxo-briefing/2022/01/defense-officials-develop-5g-enabled-medical-applicatio ns-support-future- troops/360786

Gary Legault, MD, is Director of the Military Health Systems Virtual Medical Center (VMC).

He is an active duty, board certified ophthalmologist stationed at Brooke Army Medical Center specializing in cornea and refractive surgery. He is an Associate Professor at the Uniformed Services University. Dr. Legault is a member of Bexar County Medical Society.
Mike Kile is the VMC Operational Virtual Health Program Manager.
Steven Parks, MHA, is the VMC Operational Virtual Health Program Administrator.
The views expressed herein are those of the author(s) and do not necessarily reflect the official policy or position of the Defense Health Agency, Brooke Army Medical Center, the Department of Defense, nor any agencies under the U.S. Government.
Visit us at www.bcms.org 17 HEALTHCARE ON THE MOVE – MOBILE MEDICINE
Mobile Medic reaching back to a provider to present a patient.
Building Community ‘Confianza’ (Trust and Confidence) in Collaboration with the San Antonio Independent School District
By Jason Rosenfeld, DrPH, MPH

San Antonio
As people began exiting the Lanier High School auditorium last fall, the small group of vaccine protestors sought out members of our Health Confianza team to thank them. Their original intent, which was to disrupt the community conversation and vaccine event, was forgotten. Our team had listened to, did not look down upon, and acknowledged these individuals’ perspectives using inclusive and culturally appropriate language. These two health literacy strategies—active listening and acknowledging perspectives—are at the core of Health Confianza, which collaborated with the San Antonio Independent School District (SAISD) to host a community conversation at Lanier on San Antonio’s westside. The town hall-style event was a conclusion of a sequential community engagement strategy designed to raise awareness about COVID-19 vaccines, address their campus community’s fears and concerns about the vaccines, and reduce barriers to vaccination.
Building Confidence
Health Confianza is a Bexar County project led by UT Health San Antonio (UT Health SA) and the San Antonio Metropolitan Health District (Metro Health), with evaluation support provided by University of Texas at San Antonio faculty. Launched in August 2021 with funding from the U.S. Department of Health and Human Services’ Office of Minority Health, Health Confianza was established to address health disparities experienced by our mostly Hispanic and Black neighbors living in 22 ZIP Codes in San Antonio (Westside, Southside and Eastside neighborhoods). Health Confianza aims to increase the availability, accessibility and utilization of vital health information and services, with the goal of building trust in the health and social service systems and increasing people’s confidence in making the best decisions for themselves and their families. Our partnership with San Antonio Independent School District (SAISD), one of the top 10 largest employers in the city with at least 11,000 employees and almost 46,000 students, was a valued opportunity to scale up our efforts and test the strength of health literacy as a tool for health equity.
A Sequential Strategy
To empower the SAISD community, the Health Confianza team designed a sequential community engagement strategy that increased health
literacy while fostering connection and a sense of community. The goal was to amplify the voices and creativity of natural campus leaders, known as Confianza Ambassadors. These Ambassadors encouraged participation at town hall-style events (Confianza Conversations), with vaccines available, where the community could ask questions and participate in a safe, judgement free learning environment. This strategy began with Confianza Ambassador training. First, campus principals identified up to 25 student and campus leaders (e.g., teachers, social workers, counselors). Then Ambassadors participated in a two-hour workshop to equip them with COVID-19 and vaccine knowledge, and build self-efficacy using core health literacy and communication skills including active listening, acknowledging different perspectives and respectful bridging. Ambassadors were tasked to design innovative health-promoting messages (e.g., adapting Queen’s song Bohemian Rhapsody into a COVID-19 vaccine song) and engage in respectful dialogue with friends, family and neighbors to encourage attendance at a Confianza Conversation and vaccine clinic.
Two weeks after the Ambassador training, SAISD leadership co-organized town hall-style evening events marketed as Confianza Conversations. For our part, Health Confianza organized panels of three to four public health experts and Community Health Workers (CHWs), at least two of whom were bilingual, from Metro Health, UT Health SA Physicians (infectious diseases and pediatrics) and local organizations. SAISD provided simultaneous translation and live streamed the events. After a brief entertainment by the campus mariachi or marching band, each session opened with an introduction to COVID-19, the COVID-19 vaccines and the known risks of vaccination versus remaining unvaccinated.
18 SAN ANTONIO MEDICINE • April 2023 HEALTHCARE ON THE MOVE – MOBILE MEDICINE
The audience was then invited to ask questions and raise any concerns with our panelists. Note cards and pencils were handed out for those that felt uncomfortable speaking in public. Each session concluded with a testimonial from a Confianza Ambassador.
Simultaneous to the Confianza Conversation, our partners at the University of Incarnate Word (UIW) School of Nursing and the Health Collaborative set up pop-up clinics in the cafeterias and other appropriate on-campus spaces. A second pop-up clinic was provided the following day. All three types of COVID-19 vaccines were provided, along with influenza, Tdap, meningitis, HPV and other vaccines promoted by the Vaccine for Children (VFC) program. Other social service agencies like the San Antonio Food Bank were invited to participate and provide related services.
A+ Achievements
Across three high school campuses, we:
• Trained 92 Confianza Ambassadors
• Facilitated three town halls attended by 247 people
• Provided 291 vaccines, including 258 COVID-19 vaccines.
Most notably, the sequential community engagement strategy (Ambassador training, Confianza conversation and pop-up clinic) resulted in an average of 86 vaccinations per clinic, as compared to 16 vaccinations per traditional pop-up clinic, proving that consistent education, vaccine convenience and community building are key to changing health behaviors and engendering trust.
Even after the initial strategy concluded, the Health Confianza outreach team maintained a collaboration with two of the three campus Ambassadors, meeting monthly to form Community Health Clubs. Community Health Clubs are neighborhood or school-based peer groups formed to facilitate learning about priority health topics and advocate for health in their communities. Through this collaboration, Health Confianza’s trained CHWs facilitated monthly meetings using engaging learning techniques to share important health information and listen to the priorities of these high school leaders. One group named their Club the CHAMOY (Community Health and Mental Organization for Youth) Club as the members prioritized discussing and maintaining their mental wellness.
Impactful Lessons Learned
Schools have a convening power based upon trusting relationships and are rife with natural leaders who have the ability to facilitate conversations about health and social issues that others may find difficult. Our teachers, nurses, social workers, students and parents are essential public health partners who have powerful voices to help others around them make informed decisions. Through this sequential community engagement strategy with SAISD, Health Confianza learned that to
effectively build trust and community confidence in health messages and services, we must adhere to the following core principles:
1. Respect and acknowledgement. Even if you do not agree with someone, show respect for their opinions and acknowledge their lived experience. This is the foundation of a trusting relationship and an essential starting point for engaging in meaningful conversation.
2. Partnerships. Public health is a team sport—we will only increase trust and achieve health equity through effective and respectful collaborations between the institutions and organizations that serve our community and with the community itself.
3. Natural leaders. Trusted and respected community members are essential members of the public health team who know the culture and context of the communities where they live. They are ambassadors in the truest sense, helping open doors to deeper conversations and generate messages that are culturally and linguistically appropriate.
4. Meeting people where they are. We can no longer expect the communities we serve to come to us; we must meet people where they live, socialize and congregate. When vital health services like vaccinations are brought closer to the people who have already been activated by natural leaders, we can overcome some of the most common barriers.
The act of learning is continuous and the public health priorities of our communities change over time, and so Health Confianza is planning additional Confianza Ambassador trainings for school nurses, social workers and counselors, along with new Community Health Clubs for both students and parents, across all SAISD high schools and middle schools. We hope that this work at one of San Antonio’s largest employers and community-facing organizations can signal to both public health partners with regards to alternative ways to engage in community-based health promotion and service delivery, as well as other employers that there are innovative and efficient programs available that can contribute to the health of their employees and promote health equity.
Dr. Jason Rosenfeld is a public health professional with almost 20 years of experience designing, implementing and evaluating international and domestic community health education and behavior change programs. Jason obtained his Masters in Public Health from the Rollins School of Public Health at Emory University and completed an Executive DrPH in Public Health Leadership through the University of North Carolina’s Gilling’s School of Global Public Health. At UT Health San Antonio, Dr. Rosenfeld is the Assistant Director for Global Health at the Center for Medical Humanities & Ethics, the Assistant Professor in the Department of Medicine and the Principal Investigator of Implementation for Bexar County’s Health Confianza health literacy project funded by the Department of Health and Human Services and the South Texas Community Health Worker Workforce Preparedness Collaborative funded by the Health Resources and Services Administration.

Visit us at www.bcms.org 19 HEALTHCARE ON THE MOVE – MOBILE MEDICINE
The House Call is Effective and Should be Protected
By David Cavazos, MAA and Ramon Cancino, MD, MBA, MS, FAAFP
Given the changing patient population, new models of care continue to emerge. Patients 85 years and older are the most rapidly growing patient population in the United States. This group is projected to quadruple by 20501. At the same time, there is an increase in value-based care investment. In fact, funding of models quadrupled during the pandemic2. As a result of this confluence of related components, models of home-based care have been demonstrated to improve the lives of high-cost, frail, homebound patients and their caregivers while reducing costs by keeping patients at home and reducing the use of hospitals and nursing homes3. Physicians in San Antonio have leveraged the home visit model in several ways. One example is Doctor At Your Service (DAYS), a model, once considered a unique model, now is hitting its stride.

Dr. Antonio Cavazos founded DAYS in 2010. Dr. Cavazos spent his early career as an OBGYN. As an OBGYN, he was accustomed to deal-
ing with babies and the beginning of life. As fate would have it, after retiring as an OBGYN, he was asked by VITAS Hospice to work part time as a hospice physician and help those nearing the end of life. Dr. Cavazos’s job at VITAS was to decide whether or not a patient was eligible to be on hospice. He soon began realizing that there was an enormous segment of the population who was chronically ill (five or more chronic conditions) and struggled to get to the doctor’s office but were not eligible for Hospice services. This population, those over the age of 65, became the target pop ulation for DAYS. These patients (10% of the Medicare population)
drive more than half of Medicare cost.

20 SAN ANTONIO MEDICINE • April 2023
HEALTHCARE ON THE MOVE – MOBILE MEDICINE
Early on, federal, state and private payers did not reimburse well enough for this concierge-like care. Another unique issue was that the fluctuating price of gas was not properly considered in reimbursement models thus impacting model sustainability. The DAYS teams found themselves traveling hundreds of miles a week to care for San Antonio’s most frail patients but were struggling to make ends meet.
The DAYS team had to develop unique processes to become sustainable. For example, efficient scheduling practices to keep down total mileage was necessary. This was done by implementing processes that took advantage of evolving service payments. The DAYS team also implemented a Chronic Care Management (CCM) program. CCM uses risk profiles, care coordination teams and technology to identify needs. DAYS utilizes data to close quality gaps and to target proactive clinical interventions to improve outcomes. Real-time data comes in the form of monthly multi-modal engagement with the patient capturing evidence-based data, social determinants of health, behavioral health indicators and physiological data. In-between visit care management support is performed using care plans developed with evidence-based risk assessments and scales standardized across the patient population yet personalized to each patient’s individual needs. Some of the outcomes of CCM are that the program increases connectivity between patients and their DAYS practitioners, matches patients with appropriate resources and encourages patient self management of chronic medical and behavioral conditions. Assessments include: Activities of Daily Living (ADLs), Advanced Care Planning, Availability of Care Assistance, Care Coordination and Goals of Care. Additional modules include Acute Care History, Falls History, Gagne Mortality Index, John Hopkins Fall Risk Assessment, Medication Review, PHQ9 Depression Screening, Risk of Hospitalization, Social Needs Screening Tool, specialist’s follow-up, cardiology module, COVID-19 screenings, diabetes module, etc. CCM allowed DAYS to bill Medicare for patient outreach, oversight, communication and collaboration between provider appointments. In addition, the team implemented telemonitoring workflows for patient vitals. Telemonitoring was employed for blood pressure monitoring, blood glucose tracking and weight management. Telemonitoring and CCM allowed DAYS to improve its management of patients while cutting down on miles traveled by vehicle.
The DAYS team began a partnership with UT Health San Antonio Regional Physician Network in 2019. Having gained experience with a successful home visit model with one of its internal practices, the Regional Physician Network ACO had interest in expanding its knowledge of home-based care models for its attributed patients. The DAYS team believed that their goals aligned. In addition to being able to continue its home-visit model for its complex patient population, DAYS was supported virtually by the Regional Physician Network’s care management team who outreached to complex patients, especially those who
utilized emergency rooms or local hospitals. Approximately 65-70% of DAYS Medicare patients are on CCM and about 50% are also on telemonitoring. As a result of this partnership, among its attributed CMS Medicare Shared Savings Programs (MSSP) patients, inpatient admissions improved from 1.2 admissions per patient per year (1,200 per 1,000 patients) in 2020 to 0.6 admissions per patient per year in 2022 (600 per 1,000 patients). This improvement was the result of integration of complex care management protocols and constant communication between the DAYS team and the Regional Physician Network ACO.
Home-visit models will continue to thrive. There are more than 4 million patients who could benefit from home-based primary care but only 12% are receiving it. These numbers are expected to double over the next two decades. Approximately 10,000 baby boomers turn 65 every day and beneficiaries with five or more chronic conditions represent the fastest-growing segment of the Medicare population.
The Home-Based Primary Care model brings value and cost savings to society. Clinicians working this model often find themselves driving across a city and climbing multiple flights of stairs of an apartment complex with equipment to spend 30-60 minutes with an extremely complex and frail patient who would not have been able to travel to the physician’s office. This visit currently is reimbursed about $100 (sometimes less), which is more or less the same as what a provider receives seeing a patient in an office. The model has proven to be effective and a high value. It should be protected and reimbursed appropriately.
For more information about Doctor At Your Service, please visit www.doctoratyourservice.com or call 210-479-3297.

References:
1. West L, Cole S, Goodkind D, He W. Current Population Reports: 65+ in the United States: 2010. United States Census Bureau. Published online June 30, 2014. https://www.census.gov/content/dam/ Census/library/publications/2014/demo/p23-212.pdf

2. Investing in the new era of value-based care | McKinsey. Accessed February 18, 2023. https://www.mckinsey.com/industries/healthcare/our-insights/investing-in-the-new-era-of-value-based-care
3. Cornwell T. House Calls Are Reaching the Tipping Point — Now We Need the Workforce. J Patient Cent Res Rev. 2019;6(3):188191. doi:10.17294/2330-0698.1719
Visit us at www.bcms.org 21
David Cavazos, MAA is the CEO of Doctor At Your Service (DAYS).
HEALTHCARE ON THE MOVE – MOBILE MEDICINE
Ramon S. Cancino, MD, MBA, MS, FAAFP is Executive Director of UT Health San Antonio Primary Care Center, and Senior Medical Director of Medical Management at UT Health Physicians. Dr. Cancino is a member of Bexar County Medical Society.
Walking to Promote Health
By Richel Avery, MD, FAAFP & Ramon Cancino, MD, MBA, MS, FAAFP
Mr. Anderson is a 74-year-old male who has struggled with weight all his life, including while he was in the military. After his service, he became less active and he developed chronic medical problems, which included high cholesterol, high blood pressure and prediabetes. His UT Health San Antonio (UTHSA) primary care physician referred him to the UTHSA Primary Care Center Weight Management program where he began a plan and became a regular walker with the Walk with a Doc (WWAD) monthly walking events.
There is strong evidence that physical activity prevents multiple chronic diseases. A cohort study suggested that even moderate exercise was associated with a 60% lower risk of death among breast cancer survivors1. Another study found higher daily step volume was associated with a lower risk of premature all-cause mortality among Black and White middle-aged women and men2. Further, being overweight and having obesity are linked with a higher risk of getting 13 kinds of cancer, including breast, colon, rectum, uterus, liver and thyroid3. In 2015, Dr. Vivek Murthy, U. S. Surgeon General, promoted walking as an easy, readily available way to increase physical activity, and improve health and mental well-being4
As a result, the UTHSA Primary Care Center partnered with the Texas Medical Association (TMA) to become a WWAD member. WWAD was started in 2005 by Dr. David Sabgir5 and is a physicianled community engagement program, which is free and open to the public, and occurs outdoors, in community gyms or recreational areas.
Since joining WWAD in 2022, Dr. Richel Avery, medical director at UT Health Verde Hills and a diplomate in obesity medicine, says it has been a positive experience for both patients and physicians. On the second Saturday of every month, patients, physicians, students and staff meet at OP Schnabel Park. A doctor gives a short talk about a health topic such as healthy eating, diabetes prevention and mental health, then the group goes for a 1.7-mile walk.
The TMA partnership has been essential to the program’s success. Membership in WWAD includes ongoing support, liability insurance (if needed), marketing materials, webpage development and merchandise like t-shirts. The WWAD events are publicized through UT Health San Antonio marketing outlets and via the TMA website. In 2018, a review of the WWAD gatherings showed that walkers felt the program helped improve physical activity and created connections with others as well as improved well-being among the physicians6.
Mr. Anderson’s story is not uncommon. The many people who struggle with chronic medical problems and the effect of inactivity mirror his struggles. Mr. Long is a 77-year-old man who suffers from weight-
related medical problems. He walks regularly with the WWAD group and hopes to be able to bring his wife to the gatherings.
Health care professionals have a role in promoting healthy behaviors. Not only will the Primary Care Center be expanding its weight management program, but programs such as Walk with a Doc provide a starting point for all community members to begin their own journey of health improvement.
References
1. Chen LH, Irwin MR, Olmstead R, Haque R. Association of Physical Activity With Risk of Mortality Among Breast Cancer Survivors. JAMA Network Open. 2022;5(11):e2242660. doi:10.1001/jamanetworkopen.2022.42660
2. Paluch AE, Gabriel KP, Fulton JE, Lewis CE, Schreiner PJ, Sternfeld B, Sidney S, Siddique J, Whitaker KM, Carnethon MR. Steps per Day and All-Cause Mortality in Middle-aged Adults in the Coronary Artery Risk Development in Young Adults Study. JAMA Network Open. 2021;4(9):e2124516. doi:10.1001/jamanetworkopen. 2021.24516
3. Obesity and Cancer | CDC. Published July 13, 2022. Accessed February 17, 2023. https://www.cdc.gov/cancer/obesity/index.htm
4. Office of the Surgeon General (US). Step It Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities. US Department of Health and Human Services; 2015. Accessed February 20, 2023. http://www.ncbi.nlm.nih.gov/books/ NBK538433/
5. Who We Are – Our Story. Accessed February 17, 2023. https://walkwithadoc.org/who-we-are/our-story/
6. Sabgir D, Dorn J. Walk with a Doc-a Call to Action for PhysicianLed Walking Programs. Curr Cardiol Rep. 2020;22(7):44. doi:10.1007/s11886-020-01297-y

Richel Z. Avery, MD, DABOM, FAAFP is Medical Director of UT Health Verde Hills Primary Care and leads the Primary Care Center Medical Weight Management program at UT Health Physicians San Antonio.
Ramon S. Cancino, MD, MBA, MS, FAAFP is Executive Director of UT Health San Antonio Primary Care Center, and Senior Medical Director of Medical Management at UT Health Physicians. Dr. Cancino is a member of Bexar County Medical Society.

22 SAN ANTONIO MEDICINE • April 2023
HEALTHCARE ON THE MOVE – MOBILE MEDICINE

Visit us at www.bcms.org 23
Moving Medicine South: Our Duty to the Community
By Lyssa Ochoa, MD, Board-Certified Vascular Surgeon and Founder of The SAVE Clinic
Introduction
As readers of this magazine are certainly aware, San Antonio continues to face challenging disparities in health outcomes based on minority status and geography, down to the ZIP code level of geographic specificity. Much has been written about these circumstances in this publication by many thoughtful authors, and many physicians undoubtedly incorporate a health-disparities perspective in their practices.
A recent development, however, is creating even greater urgency to move more medicine south.
Some Background
For those who don’t practice in a hospital setting or have narrow hospital exposure in their practices, the hospital landscape in Bexar County is largely dominated by four systems: Baptist Health System, Methodist Health System, Christus Santa Rosa Health System, and University Health System. Between them, there are no less than 16 full-service hospitals in San Antonio.
Only one is south of downtown: Mission Trail Baptist Hospital, which represents a downsizing of the Southeast Baptist Hospital it replaced in 2011.
For over 40 years there has been one other full-service hospital south of downtown: Southwest General Hospital (renamed to Texas Vista Medical Center circa 2019). On March 1, 2023, Texas Vista announced it would be closing no later than May 1, 2023, citing overwhelming financial distress.

Located in the southwest quadrant of San Antonio near I-35 and Military Drive, Southwest General Hospital was originally physicianowned. It has since changed hands among corporate entities in multiple transactions until most recently being acquired by Steward Health Care System in 2017. There are no other Steward hospitals in the San Antonio area.
The systems mentioned above collectively represent well over 2,000 hospital beds north of downtown. After the closure of Southwest General, there will only be 110 hospital beds south of downtown.
Using Maps to Identify the Need
Of course, none of this happened overnight. As my career has pro -
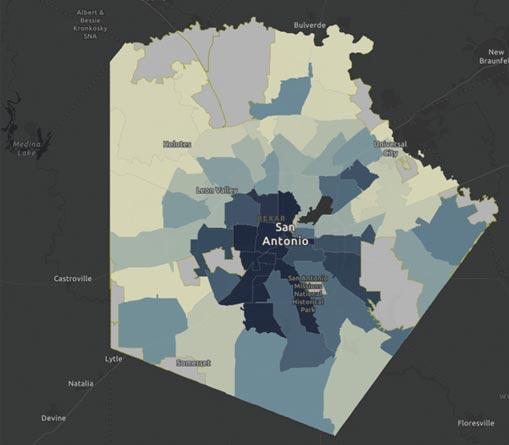
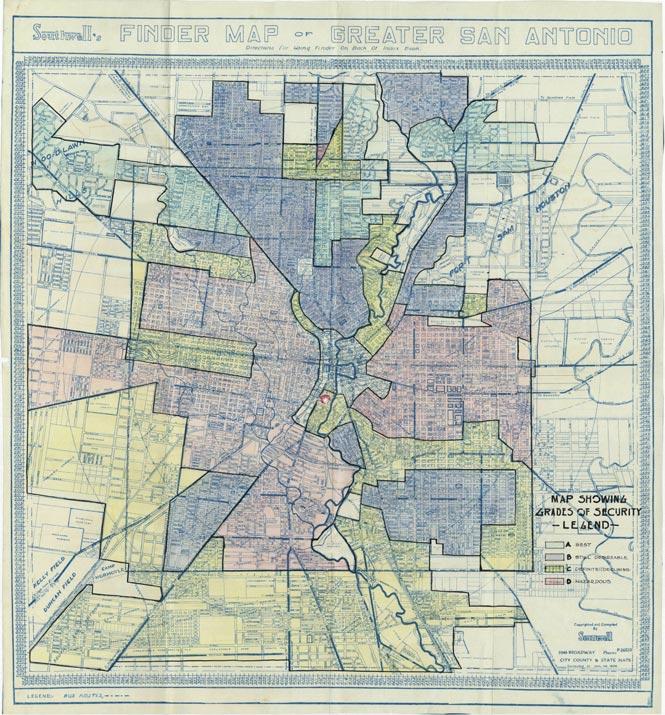
gressed, I have found the use of maps to illustrate and communicate spatial relationships in healthcare to be especially powerful. The first such map that changed how I look at healthcare was a contemporaneous map of diabetic amputation rates in Bexar County by ZIP Code. The next layer that allows one to seemingly peer back in time at some of the root causes of geographic disparities was the set of maps known as “redlining.” Back in the 1930s, these maps were drawn in a context of unabashed racism to exclude predominantly black and brown neighborhoods from the economic stimulus that the state and federal governments were providing to help relieve the Great Depression. The resulting lack of infrastructure funding and loss of personal, family wealth due to this process has a clear multigenerational impact.
Layering in a map of asthma-related hospitalization, COVID deaths, and “pick-your-adverse-healthcare-outcome” alongside maps of poverty, generational dependency, and “pick-your-Social-Determinantof-Health-metric” and the correlations only continue to build.
Thankfully, the maps don’t only illustrate the problems. They also illustrate the solution:
If we want to reverse decades, even centuries of healthcare disparities, we need to go where the disparities are and make the requisite investments of time, energy and resources until our goals are met.
24 SAN ANTONIO MEDICINE • April 2023
HEALTHCARE ON THE MOVE – MOBILE MEDICINE
Source:SouthwestTexas RegionalAdivsory Council;Texas Association ofFreestanding Emergency Centers
Amputations by ZIP Code, 2015
It’s Impossible. How Can the Status Quo be Corrected?
In the year 1546, English playwright John Heywood coined a phrase that continues to reverberate around the world as groups of people take on challenging tasks: “Rome wasn’t built in a day…”
As with many quips, we’ve cut it short as we’ve repeated it over the years. The original quote continues: “… but they were laying bricks every hour.” They, in this metaphor, are us. Our version of “laying bricks” can be to extend our clinical reach into the areas where the people need our care. In the case of the SAVE Clinic, we accomplish this by renting offices in specific ZIP codes on a “timeshare” basis, meaning, we have an agreement to pay rent only for the days we utilize the clinic. This prevents our small practice from absorbing the burden of a long-term, full-time lease, yet we are able to go into our patients’ neighborhoods in lieu of asking them to find their way to us.
Brookings Institute Hardship Index
By ZIP Code, Sept. 19, 2017 continued
Timeshare opportunities can typically be found in partnering with other small practices. For example, we have a clinic on alternating Thursdays in an orthopedic surgeon’s office. We rent his space on the day he routinely spends in the operating room. The rent we pay offsets some of his full-time-rent expense. We are able to see a full day’s clinic of patients. The patients are able to be seen closer to home. Everyone wins, especially the patient. We also have timeshare arrangements with larger offices that have extra exam rooms. One busy primary and specialty care clinic with over 20 exam rooms has a gap in their schedule where five rooms are free on Friday mornings. We rent only those rooms on only those days. Again, our cost is low, but it’s still rent revenue for the clinic that would have had empty rooms, and our access has been expanded for patients towards even more patients’ homes.
Every practice will have its unique challenges in making a model like this work efficiently. As a full-service vascular surgery practice, we need to be able to perform diagnostic ultrasound exams to fully evaluate patients during their visit with the doctor. To accomplish this, we purchased only mobile ultrasound equipment. Each of our ultrasound techs has two carry-on size suitcases: one with an imaging device and one with a physiological device. They can easily pack, unpack and repack the equipment in minutes.
Our medical assistants pack rolling-storage containers with gloves, gauze, forms, a laptop and everything they need to conduct a visit with the patient and the doctor. In some of our timeshare locations, we’re able to designate a small storage area to leave some supplies behind and reduce our travel load, but this is more of a luxury than an absolute necessity.
The same goes for our front desk, check-in, check-out personnel. They are able to pack a lightweight, travel-size printer, scanner, laptop, clipboards and all the supplies they need to effectively process patients, collect any patient payments, and perform all of their other job duties.
While this may sound like a massive endeavor, it pales in comparison to putting ourselves in our patients’ shoes: is it harder for our team to pack supplies provided by the clinic and travel to a satellite during normal
Visit us at www.bcms.org 25 HEALTHCARE ON THE MOVE – MOBILE MEDICINE
page 26
on
scheduled work hours, versus each of our 25 patients dealing with their individual mix of barriers, restraints and scarcity just to get to the doctors’ office?
Let’s Get Medicine on the Move… to the Southside!
We at The SAVE Clinic have seven timeshare clinics, and five of our locations, including our only fulltime location, are south of downtown. So many organizations are already laying their bricks in their respective ways. The Metropolitan Health District, dozens of nonprofit organizations, healthcare institutions of all sizes, and elected officials of all stripes have health equity initiatives that they are pursuing. Physicians are uniquely positioned to be able to go where the patients need us, and if we all lay those bricks together, we’ll build our road to health equity right through the Southside of San Antonio!
Dr. Lyssa Ochoa is a board-certified vascular surgeon and founder of the San Antonio Vascular and Endovascular Clinic (The SAVE Clinic) in South San Antonio. The mission of The SAVE Clinic is to reduce the number of diabetesrelated amputations in San Antonio, which occur in rates up to three times the statewide rate in some of the city’s most underserved and socioeconomically challenged ZIP codes. Dr. Ochoa fulfills this mission by forming deep partnerships throughout the community with any and all stakeholders that share a goal of reducing health disparities in San Antonio. The SAVE Clinic strives to address patients’ Social Determinants of Health barriers to help patients achieve better outcomes. Dr. Ochoa was born and raised in Mission, TX, along the Texas-Mexico border and attended medical school, general surgery residency and vascular surgery residency at Baylor College of Medicine in Houston, TX. She has been practicing vascular surgery in San Antonio since 2011 and is a current member of the Bexar County Medical Society Board of Directors.

26 SAN ANTONIO MEDICINE • April 2023 HEALTHCARE ON THE MOVE – MOBILE MEDICINE
COVID Death Rate As of June 29, 2021
25
Redlined Neighborhood Map – Jan. 1, 1934
continued from page



Visit us at www.bcms.org 27
Community-Wide Mobile Vision Screenings and Their Role in Protecting and Preserving Eyesight
 By Sahar Z. Ali
By Sahar Z. Ali
ision screenings can serve as the first step towards helping identify individuals at risk from various eye diseases and directing them to seek care from a physician. The free eye screenings conducted out of the Mobile Eye Screening Unit (MESU) bus allow volunteers to perform visual acuity, visual field and eye pressure tests for individuals young and old. Thanks to the portable nature of the mobile unit, volunteers perform these screenings at locations across the community from grocery store parking lots to communitywide health fairs, and even sporting events. The unit is sponsored by the Lions Sight Research Foundation and operates thanks to the Lions Club members of District 2-A2.
Eye diseases are extremely common and can by asymptomatic and unnoticed for long periods of time before they manifest in a noticeable way. San Antonio has higher than average rates of chronic diseases like diabetes that have eye manifestations with potentially devastating consequences. In fact, 14% of residents of Bexar County have diabetes, which is higher than the Texas state average of 11.4% and national average of 10.5%.1 People diagnosed with diabetes can be affected by diabetic retinopathy, cataracts, glaucoma and more. Diabetic retinopathy itself is the leading cause of blindness in adults.2 As these are all conditions that can lead to vision loss, early diagnosis plays a critical role in preserving eyesight.
ing point. The MESU has been providing eye screenings since 1996 and has screened 70,000 community members to date.3
Aside from providing an essential service to populations that need it most, the MESU also allows volunteers to engage with community members. Medical students from the University of Texas Health Science Center at San Antonio volunteer at screening events with the MESU regularly. “It’s incredible to think that spending 15 minutes after a grocery trip could save someone’s vision! I am so grateful to be a part of the mobile eye screening unit team,” said first-year student Jared Tuttle. It is often the community interaction aspect that inspires these students to volunteer their time at the MESU. “It has allowed me to engage with Bexar County in a way that I never had before. The friendly interactions and conversations I’ve had with everyone bring me back to the MESU each month,” said first-year Kannan Freyaldenhoven. Volunteers get exposure to a field they hope to enter one day and hear about what future patients want and need out of their health care team. These interactions actively prepare students to provide empathetic and informed care that will best suit the needs of the community.
Overall, the MESU takes essential vision screenings to diverse locations across the community. Its mobile nature allows it to reach and encourage many who may not otherwise be prompted to seek comprehensive eye care. It also provides an avenue for volunteers to build deeper connections with the community at large, making it a valuable tool and experience for all parties involved.
References:
1. Diabetes Care & Education: San Antonio. University Health System. Accessed February 10, 2022. https://www.universityhealth.com /services/diabetes-endocrinology/care-education
Vision screenings are not comprehensive eye exams that one might receive at an optometrist or ophthalmologist’s office. Rather, an eye screening performed by trained volunteers aims to quickly test for symptoms of diseases like diabetes and recommends high-risk and symptomatic individuals to schedule an exam. Through free vision screenings, countless community members have been advised to seek care earlier rather than later. These individuals can approach physicians with more targeted issues and receive care from a more informed start-
2. Diabetes and Vision Loss. Centers for Disease Control and Prevention. Published December 19, 2022. Accessed February 10, 2022. https://www.cdc.gov/diabetes/managing/diabetes-visionloss.html#:~:text=Eye%20diseases%20that%20can%20affect,way %20toward%20protecting%20your%20eyesight
3. Lions Sight Research Foundation: About. Lions Sight Research. Accessed February 10, 2022. https://lionssightresearch.org/ about.html
Sahar Z. Ali is a medical student at the Long School of Medicine at UT Health San Antonio, Class of 2025. She is also the student president of Mobile Eye Screening Unit (MESU) volunteering.

HEALTHCARE ON THE MOVE – MOBILE MEDICINE
V 28 SAN ANTONIO MEDICINE • April 2023
Frontera de Salud at UT Health San Antonio
By Moses Alfaro
At the University of Texas Health Science Center San Antonio, an organization called “Frontera de Salud” (Border Health) is heavily involved in delivering healthcare to underserved border cities and populations in San Antonio. Frontera de Salud was founded in 1998 by Dr. Kirk Smith, MD, PhD and other medical students at the University of Texas Medical Branch (UTMB). Since its founding, Frontera has expanded to UT Houston, UT Health San Antonio and UT Southwestern. At UT Health San Antonio (UTHSA), Frontera serves over 1,000 patients each year in the cities of Laredo, Del Rio, Eagle Pass, Rio Grande City and San Antonio.
With the support of the Center for Medical Humanities and Ethics (CMHE) and other partners, Frontera de Salud is able to provide sport physicals, immunizations and health screenings, such as blood glucose levels, blood pressure, cholesterol levels and more. Volunteers at these events include physicians, physician associates, nurse practitioners and health profession students from medicine, physician associate and nursing programs. In this past year of 2022, volunteers have accumulated over 1,000 hours from planning and putting on these healthcare events for patients.
Students at UTHSA love volunteering their time to participate in these events because it gives them unique opportunities to provide free healthcare to these patient populations and expand on their clinical skills at the same time. Many times, patients will only speak Spanish and a large number of students are fluent in Spanish, so they’re able to break through these barriers and communicate effectively with patients. At the same time, having healthcare providers who speak the same lan-

guage as the patient makes patients comfortable in sometimes vulnerable clinical situations. Additionally, our medical student chapter of the Latino Medical Student Association (LMSA) offers students the opportunity to learn clinical Spanish. This helps students hone in on their Spanish speaking skills so they can adequately convey healthcare information when attending these events.
One memorable experience from my time working with Frontera de Salud was putting together a vaccination clinic for the Windcrest community here in San Antonio. In October of 2022, Frontera partnered with Methodist Healthcare Ministries and we administered influenza and COVID-19 vaccines to their constituents at their church. At the vaccine clinic, there were numerous families who did not have insurance or were unable to travel far from their home to a physician's office or pharmacy, so having this vaccine clinic nearby was incredibly beneficial to them in receiving this type of healthcare. Personally, this was a formative
experience in my journey to becoming a physician because I was able to directly observe how socioeconomic barriers can impede these populations from receiving basic and necessary healthcare. I realized the impact that we, as future healthcare professionals, can have on these residents by providing these healthcare opportunities.
Funding and local support tremendously helps Frontera de Salud reach our mission and goals to deliver healthcare to these patients. For the future of the organization, we hope to expand our impact into other underserved communities along the border and within our community of San Antonio.
Moses Alfaro is a medical student at the Long School of Medicine at UT Health San Antonio. He was the 2022 Vice President of Public Relations and Vaccine Training for Frontera de Salud. Moses is also a member of the BCMS Publications Committee.

Visit us at www.bcms.org 29 HEALTHCARE ON THE MOVE – MOBILE MEDICINE
Leadership in a Crisis Interview with Gerardo Ortega, MD, FACS
By Monica Jones, BCMS COO
The COVID-19 pandemic has forced leaders to find new ways to thrive amidst developing chaos. COVID-19 was not the first catastrophe of this generation to force meaningful change. Almost 22 years ago, the shocking terrorist attack on the World Trade Center left behind painful recollections and influential instructions about how leaders must learn and acclimate.
In 2001, Dr. Gerardo Ortega started his Presidents message with “The events of September 11 have changed our world forever.” After the shock settled in, Dr. Ortega remembers how the Bexar County Medical Society responded rapidly and assertively. BCMS responded with the tools and training available to participate in a communitywide response effort. BCMS mobilized physicians, communicated with members, and worked with city and county officials at the Emergency Command Center, the National Disaster Medical System “NDMS” response system, military and private hospital administrators, trauma units and regional blood banks several times a day in order to plan our response to the 911 events. BCMS and city leaders formed a group to prepare for the possibility of casualties being transferred to San Antonio, as well as prepare for the possibility of another terrorist attack, one maybe in our great city.1 Within six hours of the 911 attacks, BCMS provided a conference on biological terrorism. Dr. Ortega thanked the late Dr. Charles Bauer who was chair of the Emergency Preparedness Committee of BCMS for his leadership and determination to keep BCMS informed and involved. The Emergency Preparedness Committee took the proactive approach in communication, education, seeking funding and preparing our members over the months after 911. BCMS held educational courses, added links to the BCMS website and disseminated information to all members on bioterrorism issues.2 We were extremely fortunate to have such dedicated doctors in our membership. Dr. Ortega believes strongly that organized medicine is the only way physicians can impact healthcare issues.
BCMS was the first county medical society in the State of Texas, founded on September 22, 1853. Founders included Drs. George Cupples, J.H. Lyons, Ferdinand Herff and F.M. Giddings. BCMS is one of the largest county medical societies in the United Sates. Our mission is to support activities that result in the best medical care to patients served by Bexar County physicians operating in the optimal physician practice environment. BCMS acts on behalf of medicine in general,
acting in the best interest of physicians, patients and the public.3
Dr. Ortega was born in Monterrey, Mexico, went to medical school at the Universidad Autonoma de Nuevo Leon, and specializes in vascular surgery. He has been a member of BCMS since 1981 and was the 100th BCMS President in 2001. He has served as President of Baptist Health System Medical Staff, member of Baptist Health System Board of Trustees and was on the Baptist Health System Medical Executive Board. He has held multiple leadership positions over the years including that of the Hispanic Medical Society President, San Antonio Vascular Surgery Society President, founding President of the University of Nuevo Leon Medical School Foundation and past Chair of the Philanthropic Committee of the BCMS Library Association.
In the mid-1990s, Baptist Medical Center was going to replace a hospital incinerator. Dr. Ortega negotiated a donation of the older incinerator to the University Hospital Medical School in Monterrey, Mexico, his alma mater, and raised $50,000 for transportation of this large incinerator to Monterrey, Mexico. The incinerator still continues to work and provides income to the University Hospital Medical School in Monterrey, Mexico. As the founding President of the University of Nuevo Leon Medical School Foundation, Dr. Ortega has identified 80 physicians that graduated from the medical school who were practicing in San Antonio; 500 physicians were identified at that time practicing in the U.S.
Dr. Ortega received the Golden Aesculapius Award in 2020. The award reminds him that it takes a community of colleagues, friends and family to achieve accomplishments: “From my fifth-grade teacher (who told me I’d never be a doctor) classmates, friends, professors, family and my wife, they have all been critical to each and every accomplishment. Someone helped me take each step in each journey. It is all about how many doors you can open for other physicians, just as doors have been opened for you.
“I will always be grateful for the opportunity to serve the Bexar County Medical Society. 2001 was dominated by the September 11 attacks against the United States, but BCMS, through inspiration, sought opportunities of leadership by reestablishing the Socioeconomic committee. We met with hospital CEOs, medical directors and healthcare plan providers to tackle the healthcare crisis in the United States. Topics included medical record privacy, children’s health insur-
SAN ANTONIO MEDICINE 30 SAN ANTONIO MEDICINE • April 2023
ance, tobacco settlement funds distribution, managed care scope of practice, the impact of professional liability on patients and medical practice, and clean claims. We looked at the nursing shortage and the changes precipitated by Y2K. A group of our physicians met with the editorial board of the Express News to discuss the causes and problems that physicians are having in the practice of medicine. Governor Rick Perry’s veto of physician-related legislation and the number of IPAs that had recently filed for bankruptcy were hot topics. Even though the 911 attack was still fresh in our minds, it didn’t stop BCMS from hosting Kumamoto Medical Association from Kumamoto Japan, as planned and promised. Our sister city relationships provide excellent opportunities to improve our understanding of other cultures and helps us to explore alternative methods of medical practice. The BCMS relationship with Kumamoto Medical Society continues today, next trip planned this year.”



“To leave the world a bit better, whether by a healthy child, a garden patch or a redeemed social condition; to know that even one life has breathed easier because you have lived, this is to have succeeded.”
– Ralph Waldo Emerson
Far left: Dr. Ortega wearing a YUCATA (Japanese costume) at his last board meeting as president at the Plaza Club Frost Bank.
Immediate left: Dr. Sheldon Gross, 2018 BCMS President, presents Dr. Ortega with the Golden Aesculapius Award in 2020.
SAN ANTONIO MEDICINE Visit us at www.bcms.org 31
Below: Dr. Gerardo and Catherine Lee Ortega, married for 46 years.
Autism Awareness: A Role for Every Medical Practitioner
 By Melissa Svoboda, MD and Cynthia Hamilton, MBA
By Melissa Svoboda, MD and Cynthia Hamilton, MBA
The prevalence of Autism Spectrum Disorder (ASD) is now one in every 44 children, an increase of 241% since 20001 . The dramatic rise in the number of children affected by autism compounded by a shortage of developmental pediatricians and pediatric psychologists in most cities, including San Antonio, has led to lengthy wait times for an initial diagnosis and delays in critical early interventions. April is Autism Awareness month, and a good time to discuss some of the challenges facing medical professionals in Bexar County and the ways local providers are working together to improve access to care and long-term outcomes for children in our community.
Autism is a problem with the social stream of development. While many children with autism will also have speech delays or language impairments, this isn’t true for all of them. Social problems can manifest differently depending on where a person is on the spectrum. For example, some children struggle with eye contact while others make eye contact just fine. The diversity of symptoms can make autism difficult to diagnose without expert training. On the other hand, some children have more “classic” autism and are easier to diagnose. Old dogma dictated that only experts in autism (typically developmental pediatricians and child psychologists) could diagnose autism and generally needed a multidisciplinary team to do so. Experts now agree
32 SAN ANTONIO MEDICINE • April 2023 SAN ANTONIO MEDICINE
that more classic, easily-diagnosed cases should be given a diagnosis by their primary care physician if the patient meets DSM-5 criteria and appears to have a clear-cut case of autism so they can begin treatment right away. Multidisciplinary teams are often now reserved for more complex cases like the child with good eye contact who also has ADHD but some social skills deficits or the anxious child that refuses to make eye contact. This is when you need a diagnostic team and, on average, four hours of testing and observation to determine if the cause is autism, anxiety or something else.
The most significant delay a child with autism can experience is the lapse in time between diagnosis and therapeutic interventions. The earlier a child can begin receiving treatment, the greater the improvements in their overall development and long-term outcomes. The gold-standard of treatment for autism is Applied Behavior Analysis (ABA), a research-based therapy that uses positive reinforcements to improve communication, social skills and self-help skills. The American Academy of Pediatrics has recommended that treatments for children with autism be based on the principles of ABA. Younger children have typically been prescribed 20-40 hours per week for two years; however, more modern approaches tailor the specific types of ABA therapy and hours to the individual patient. There should never be a one-size-fits-all approach.
To address the current backlog of children waiting for an autism diagnosis in Bexar County and other parts of the country, some ABA therapy companies are now performing diagnostic testing using one part of an autism exam, typically the ADOS 2 test (Autism Diagnostic Observation Schedule, 2nd edition). The ADOS is one of the more sensitive tests and will over diagnose autism if used alone2. ABA therapists are not trained in diagnostics and the ADOS can be misinterpreted if not administered by highly experienced professionals. Pediatricians and primary care physicians are encouraged to use caution if they receive a finding of autism based solely on an ADOS score.
Just as there has been a shortage of diagnostic professionals to meet the needs of children in Bexar County, there has also been a deficit of providers on the treatment side. Board Certified Behavior Analysists (BCBAs) are the masters-level therapists trained to provide ABA, and for many years San Antonio could not retain or recruit enough BCBAs to serve children in our community. The good news is that, thanks to partnerships between The Children’s Hospital of San Antonio, the Autism Treatment Center and the UTSA Department of Educational Psychology, both diagnostics and treatment are becoming more accessible in San Antonio. The Children’s Hospital has expanded the multidisciplinary diagnostic team at their downtown Comprehensive Autism Program and opened a satellite clinic to diagnosis children at the Multi-Assistance Center at Morgan’s
Wonderland. The Autism Treatment Center provides paid internships to students in the BCBA program at UTSA allowing more of these professionals to remain in San Antonio after graduation. Funding from the state’s Children’s Autism Program has also made it possible for the Autism Treatment Center to provide affordable ABA therapy to low and middle-income children who could otherwise not receive this life-changing treatment.
As the number of children diagnosed with autism continues to increase, so does the number of adults living with this life-long disorder. It is important for all medical practitioners, not just pediatricians, to recognize and understand the unique combinations of social, communication and cognitive disorders present in individuals with autism and how these affect their healthcare experiences.
References:
1. CDC 2021. Data & Statistics. https://www.cdc.gov/ ncbddd/autism/data.html
2. Randall M, Egberts KJ, Samtani A, Scholten RJPM, Hooft L, Livingstone N, Sterling-Levis K, Woolfenden S, Williams K. Diagnostic tests for autism spectrum disorder (ASD) in preschool children. Cochrane Database of Systematic Reviews 2018, Issue 7. Art. No.: CD009044. DOI: 10.1002/14651858.CD009044.pub2

Melissa Svoboda, MD is Chief of Pediatric Neurology and an Assistant Professor with Baylor College of Medicine and The Children’s Hospital of San Antonio, where she is Director of the Comprehensive Autism Program. She received her medical degree from the University of Texas Health Science Center at San Antonio, where she also completed her pediatric residency. She completed her Child Neurology/Neurodevelopmental Disabilities fellowship at Oregon Health & Science University, Portland, Oregon. She is involved in clinical research projects as well as advocacy for children with special health care needs and is active in the care of Spinal Muscular Atrophy children in the South Texas region.
Cynthia Hamilton is the Development Director for the Autism Treatment Center (ATC). She has a Master of Business Administration and has been working with nonprofits that serve individuals with developmental disabilities for more than 20 years. The Autism Treatment Center is a 501(c)3 nonprofit that provides education, residential treatment and outpatient Speech, Applied Behavior Analysis and Occupational Therapy for children and adults with autism. The mission of ATC is to assist individuals with autism throughout their lives as they learn, play, work and live in the community. Contact ATC for more information on autism resources in Bexar County at (210) 590-2107 or learn more about our services at www.atcoftexas.org.

Visit us at www.bcms.org 33 SAN ANTONIO MEDICINE
Staff Retention in an Era of Wage Inflation
 By Alan D. Winkler, MHSA, Executive Director of Urology San Antonio, PA
By Alan D. Winkler, MHSA, Executive Director of Urology San Antonio, PA
The pandemic did not cause the staffing crisis. Staff recruitment and retention were issues long before the pandemic began. Shortly after the 2008 recession, healthcare employment experienced month-over-month increases ranging from 24,000 new jobs per month in 2010 to monthly increases as high as 45,000 over the past decade according to the U.S. Bureau of Labor Statistics (BLS).
Staffing demands were exacerbated by the aging of the population, retirement of Baby Boomer healthcare workers, and an expanding economy. The Bureau of Labor Statistics Job Openings and Labor Turnover Survey (JOLTS) shows a gap between openings and new hires consistently widening since 2014.
With a 79% female healthcare workforce, the exodus of workers during the pandemic when schools and daycares closed was a tipping point. The occasional virtual workfrom-home models employed by progressive companies became the norm. It should not be surprising that workers who preferred to work from home became workers who would only work from home. Traditional “in person” work environments, like much of healthcare, became the last resort instead of the first choice.
Even with healthcare’s rapid adoption of telehealth during the pandemic, most medical groups reverted to the comfort of the past and
to the brick-and-mortar model of care delivery shortly after the initial crisis had passed. No one is arguing that telehealth could never replace the communicative nuances of an in-person visit, but even those visits which could be handled through telehealth were eliminated in favor of a return “to normal.”
Normal no longer exists. Each day our practices struggle to deliver much needed care to a growing population. According to AMN Healthcare, “The number of people over 65 will grow from 43 million in 2012 to 84 million in 2050, rising from 14% of the population to 21%.” It is that aging population that also needs more healthcare delivered in varied settings.
The pandemic did not cause the staffing crisis, but it did provide workers an opportunity to reassess their personal and professional priorities. It also provided them with a measure of financial security to take risks they might never have taken otherwise.
34 SAN ANTONIO MEDICINE • April 2023 SAN ANTONIO MEDICINE
So, what is the solution?
• Will wage growth entice workers to leave one employer for another?
• Will wage growth pull workers who disengaged from the workforce to suddenly reengage and create a more stable team of caregivers?
Difficulty recruiting and retaining employees is not isolated to any age-determined groups like the Millennials. It is not a problem created by unrealistic job expectations or a restlessness about the importance of work. Commitment is about establishing a career which is both meaningful and flexible enough to provide an employee with a reasonable workload comprised of tasks that accomplish a purpose delivered in an environment which fosters respect, trust and a sense of belonging. Even if I am working remotely, I still want to be part of a team and doing things which bring value not just to me and my family but also to my community.
Paying a reasonable wage becomes the new baseline. A Medical Group Management Association (MGMA) survey conducted in February 2022 showed 59% of workers left for better pay and benefits, so pay and benefits matter. Being average means your practice will be no different than any other practice. Being “interchangeable” means living in a
constant state of flux with employees coming and going.
At the same time, the same MGMA survey showed 21% of employees left due to burnout with another 7% retiring. If you pay an average wage and offer basic benefits, you just factored out more than 80% of job applicants from even considering your medical practice.

Addressing recruitment and retention requires market-appropriate wages, so “Yes” it will cost more. It also requires engaging the employees in work where they feel a sense of accomplishment or contribution. Make sure your employees understand the importance of their role in the lives of your patients. This is not a job; it’s a mission of enhancing the quality of life for others. If you want them to leave home, you must give them a good reason to do so—even if you don’t like it.
At the same time, we as employers must be enhancing the quality of life for our own employees through on-going positive feedback, tangible evidence that we believe their contribution matters through incentive programs (as simple as a $10 Starbucks gift card in a handwritten note on their work anniversary), or through group activities like picnics or holiday parties. Do your physicians know the names of everyone with whom he or she works? If you don’t know my name, why should I care about your business?
Incorporating flexibility through non-tra -
ditional work models such as job sharing (two employees cover one employee’s work commitment), conducting 30-60-90 day “Stay” interviews to confirm that what was promised during the interview has been delivered by the practice (training, schedule flexibility, ongoing communication about what is happening in the workplace, and their role in respect to accomplishing the practice’s goals). It is equally important to ensure that there are no disincentives in the workplace. Is bad behavior addressed in an open, honest manner to help ensure a safe and fair work environment?
The pandemic did not cause the staffing crisis, but it certainly has provided us with new opportunities to deliver care in non-traditional ways. In the end, we all win … especially the patient.
References:
AMN Healthcare. Future for healthcare jobs: seven charts show intensifying demand for services and workforce. February 13, 2018. https://www.amnhealthcare.com/amn-insights/news/future-for-healthcare-jobs/#jobs MGMA Staff. Mitigating the many costs of turnover by investing in leadership. April 2022. MGMA Connection. https://mgma. com/data/data-stories/as-compensation-competition-continues,-medical-gro
Alan D. Winkler, MHSA is the Executive Director of Urology San Antonio, PA. He has worked in both private and corporate settings, working with physicians in many specialties and has 42 years of healthcare experience. Alan has been a member of MGMA at the state and national level, serving on a variety of committees in Arkansas MGMA including as state president and in Texas as the San Antonio Chapter president (2021-2022). Also, he has been a Fellow in the American College of Medical Practice Executives (MGMA ACMPE) since 1998 and served on the ACMPE board of directors for nine years, concluding as its chair. He also served as co-chair of MGMA.

SAN ANTONIO MEDICINE Visit us at www.bcms.org 35
88th Texas Legislative Session Almost at Mid-Point
By Mary E. Nava, MBA, Chief Government Affairs Officer
The 88th Legislative Session is going fast and furious and at the time of this writing is almost at the halfway mark. The ‘First Tuesdays at the Capitol’ program continues and physician and Alliance members from BCMS participated during the second “First Tuesdays” on March 7, 2023. A growing list of topics of importance to medicine were discussed, including: scope of practice; prior authorization; “white-bagging” policies; nonmedical switching; “copay accumulators”; emergency care; patient choice limitations by disincentivizing cash payments; health plan network adequacy; physician workforce; Graduate Medical Education (GME); Texas Medicaid; Medicaid postpartum coverage; Healthy Food is Good Medicine pilot program; the opioid crisis; Texas Medical Board funding; contraception; vaccinations; improving maternal and children’s health; tobacco prevention; and changes to the federal 21st Century Cures Act regarding direct notification to patients of serious and sensitive test results. To read more about these topics, go to texmed.org/advocacy and click on Key Issues.
Many thanks to the attendees who made our visits a success: Dan Deane, MD; Carmen Garza, MD; Sanjiv Kumar, MD; BCMS President John Nava, MD; Ninza Sanchez, MD; Jayesh Shah, MD; John Shepherd, MD; Ezequiel “Zeke” Silva, III, MD; medical student, John Michael Austin; and Alliance members, Neha Shah and Jenny Shepherd.
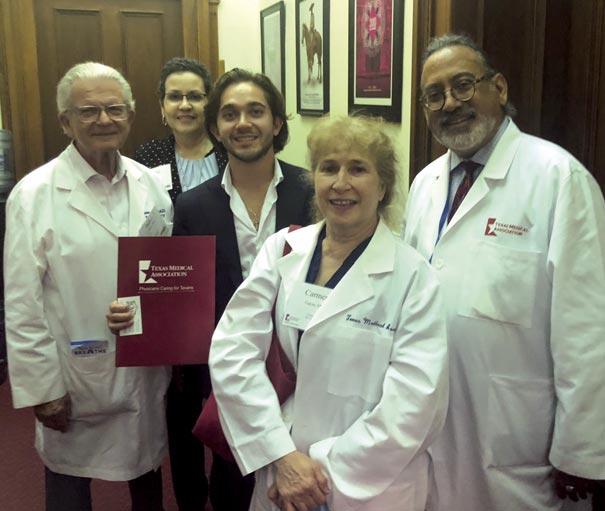

The next First Tuesdays at the Capitol is on April 4. We encourage all BCMS members to get involved and make plans to attend at least one First Tuesdays during this legislative session. All you have to do is plan to travel to Austin during one of the First Tuesdays and BCMS staff does the rest, including scheduling appointments for our visits with legislators and their staff, and gathering handouts pertinent to our visits. To register, please visit texmed.org/firsttuesdays.
For local discussion on these and other legislative advocacy topics, consider joining the BCMS Legislative and Socioeconomics Committee by contacting Mary Nava at mary.nava@bcms.org.
SAN ANTONIO MEDICINE LEGISLATIVE NEWS
BCMS physicians and staff pause for a photo just outside the north entrance to the Texas State Capitol during the March 7 First Tuesdays event.
36 SAN ANTONIO MEDICINE • April 2023
BCMS physicians and staff visit with Miguel Ruiz, (standing, center) legislative aide in the office of Rep. Trey Martinez Fischer (HD 116) during the March 7 First Tuesdays visits. Physicians standing (from l-r) are: Dan Deane, MD; Carmen Garza, MD; and BCMS President, John Nava, MD. Standing in back is Mary Nava, BCMS Chief Government Affairs Officer.



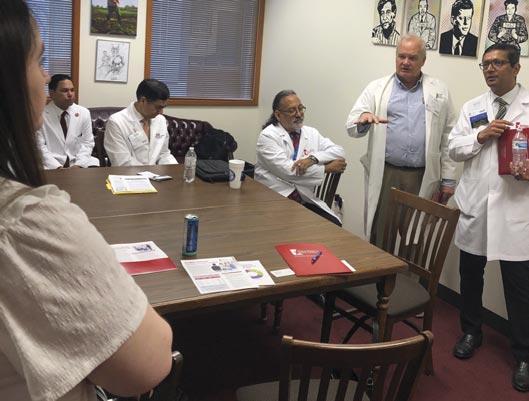


SAN ANTONIO MEDICINE LEGISLATIVE NEWS
On March 7, during the First Tuesdays visits to the Capitol, BCMS physicians discuss key medicine issues with Rep. John Lujan (HD 118) (in white shirt and blue tie).
On March 7, during the First Tuesdays visits to the Capitol, BCMS physicians discuss issues of importance to medicine with Rep. Barbara Gervin-Hawkins (HD 120) (standing, right) and her legislative aide, Garret Buechler (seated, in blue suit).
During the March 7 First Tuesdays visits, BCMS physicians and medical student met with Rep. Josey Garcia (HD 124) to discuss key issues of importance to medicine. Standing (from l-r) are: Ezequiel “Zeke” Silva, III, MD; John Shepherd, MD; Rep. Garcia; medical student, John Michael Austin; Carmen Garza, MD; and Dan Deane, MD.
Ninza Sanchez, MD shares information on medicine’s issues with Rep. Ray Lopez (HD 125) during the March 7 First Tuesdays visits to the Capitol.
BCMS physicians visit with a member of the legislative staff (standing, foreground) in the office of Rep. Diego Bernal (HD 123), during the March 7 First Tuesdays visits to the Capitol.
us at www.bcms.org 37
Sen. Roland Gutierrez (SD 19) (standing, left) visits with BCMS physicians during the March 7 First Tuesdays visits to the Capitol.
Visit
Artistic Expression in Medicine
Photography by Oliver Johnson, Jr, MD
This page, above: Church in Iceland
This church is in Iceland. We got up during the ‘blue hour’ which precedes the sunrise. The church and the surrounding parking lot were empty. Light was perfect. You can see the sea stacks in the background on the left in the ocean. It was 34 degrees, raining heavily, and on the coast, the wind was gusting to 45 mph. You don’t see the rain because the time of day required a longer exposure on a tripod, and the moving raindrops disappear in the image. The major challenge other than the obvious was to not let the wind blow over your tripod and dump your expensive camera on the pavement.

Opposite page: Venice Peaceful
This, my wife titled ‘Venice peaceful.’ The major challenge was to get this very popular bridge in good lighting without the thousands of tourists who are usually there, pushing and waving at you. The answer is to get up really early and get the image. Tourists don’t get up at sunrise.
Oliver Johnson, Jr, MD is a retired Anesthesiologist who dedicated 30 years to the medical field. Since 1995, he has chaired the BCMS Physicians Health and Rehabilitation Program. Dr. Johnson’s passion for photography takes him on photo trips around the world where he is surrounded by professional photographers who teach and advise. He currently shoots with a FUJIFILM X-T4 Mirrorless camera.

38 SAN ANTONIO MEDICINE • April 2023 SAN ANTONIO MEDICINE

SAN ANTONIO MEDICINE Visit us at www.bcms.org 39
“The essential ingredient in good photography, as in good medicine is time.”
Shop Vendors Who Support BCMS
BCMS Vendor Directory
We encourage you to use our supporting vendors whenever you or your practice needs supplies or services.
ACCOUNTING FIRMS
Sol Schwartz & Associates P.C. (HHH Gold Sponsor)

Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Jim Rice, CPA 210-384-8000, ext. 112 jprice@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”
ACCOUNTING SOFTWARE
ASSET WEALTH MANAGEMENT
Aspect Wealth Management (★★★ Gold Sponsor)

We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520
mclark@aspectwealth.com www.aspectwealth.com
“Get what you deserve … maximize your Social Security benefit!”
The Bank of San Antonio (HHH Gold Sponsor)

We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community. Brandi Vitier 210-807-5581
brandi.vitier@thebankofsa.com www.thebankofsa.com
Synergy Federal Credit Union (HH Silver Sponsor)
rate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison (210) 503-0003


yulia@genicslabs.com
Kevin Setanyan Managing Partner (210) 503-0003
kevin@genicslabs.com
Artyom Vardapetyan Managing Partner (210) 503-0003
www.genicslabs.com
“Accurate results in record time.”
Express Information Systems (HHH Gold Sponsor)

With over 29 years’ experience, we understand that real-time visibility into your financial data is critical. Our browser-based healthcare accounting solutions provide accurate, multi-dimensional reporting that helps you accommodate further growth and drive your practice forward.
Rana Camargo
Senior Account Manager
210-771-7903
ranac@expressinfo.com www.expressinfo.com
“Leaders in Healthcare Software & Consulting”
ATTORNEYS
Kreager Mitchell (HHH Gold Sponsor)
At Kreager Mitchell, our healthcare practice works with physicians to offer the best representation possible in providing industry specific solutions. From business transactions to physician contracts, our team can help you in making the right decision for your practice.
Michael L. Kreager
210-283-6227
mkreager@kreagermitchell.com
Bruce M. Mitchell
210-283-6228
bmitchell@kreagermitchell.com www.kreagermitchell.com
“Client-centered legal counsel with integrity and inspired solutions”
Bertuzzi-Torres-Fernandez Wealth Management Group (HHH Gold Sponsor)

We specialize in simplifying your personal and professional life. We are dedicated wealth managers who offer diverse financial solutions for discerning healthcare professionals, including asset protection, lending and estate planning.
Mike Bertuzzi
First Vice President Senior Financial Advisor
210-278-3828
Michael_bertuzzi@ml.com
Ruth Torres Financial Advisor
210-278-3828
Ruth.torres@ml.com
http://fa.ml.com/bertuzzi-torres
Will C. Fernandez, CEPA Senior Portfolio Advisor Financial Advisor
210-278-3812
wfernandez@ml.com
https://fa.ml.com/texas/san-antonio/bertuzzi-torres-fernandez
BANKING
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help Physicians get the banking services they need.
Synergy FCU Member Services
210-750-8333 info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”
CLINICAL DIAGNOSTICS
Livingston Med Lab (HHHH 10K Platinum Sponsor) High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease & Genetics. Robert Castaneda (CEO) 210-316-1792

Robert@livingstonmedlab.com
Joey Martinez (Director of Operations)
210-204-7072
Joey@livingstonmedlab.com
Dwight Chapman (Account Manager)
210-591-2649
Broadway Bank (HHH Gold Sponsor)

Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead
210-283-6640
TDuran@Broadway.Bank
www.broadwaybank.com
“We’re here for good.”
Dwight@livingstonmedlab.com
www.livingstonmedlab.com/home
“Trusted Innovative, Accurate, and STAT Medical Diagnostics”
CREDENTIALS VERIFICATION ORGANIZATION
Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for health care entities.

Betty Fernandez Director of Operations
210-582-6355
Betty.Fernandez@bexarcv.com
www.BexarCV.com
“Proudly serving the medical community since 1998”
FINANCIAL ADVISORS
Oakwell Private Wealth Management (HHHH 10K Platinum Sponsor)

Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA
Senior Private Wealth Advisor
512-649-8113
SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accu-
“More Than Just Your Advisor, We're Your Wealth Management Partner”

40 SAN ANTONIO MEDICINE • April 2023
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney, Financial Advisor
210-858-5880
Elizabeth.olney@edwardjones.com www.edwardjones.com/elizabeth-olney
"Making Sense of Investing"
FINANCIAL SERVICES
Aspect Wealth Management (HHH Gold Sponsor)

We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520 mclark@aspectwealth.com www.aspectwealth.com
“Get what you deserve … maximize your Social Security benefit!”
allows physicians to deliver high quality, personalized care and achieve better outcomes, while feeling free to focus on health equity and patient outcomes.
Kim Gary Senior Physician Recruiter (812) 272-9838
KGary4@humana.com
www.ConvivaCareers.com
“Fuel Your Passion & Find Your Purpose”
HEALTHCARE BANKING
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Jeanne Bennett
EVP | Private Banking Manager
210-343-4556
Jeanne.bennett@amegybank.com
Karen Leckie
Senior Vice President | Private Banking
210-343-4558
karen.leckie@amegybank.com
Robert Lindley
Senior Vice President | Private Banking

210-343-4526
robert.lindley@amegybank.com
UT Health San Antonio MD
Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
Regina Delgado
Business Development Manager (210) 450-3713
delgador4@uthscsa.edu
UT Health San Antonio MD

Anderson Mays Cancer Center
Laura Kouba
Business Development Manager (210) 265-7662
norriskouba@uthscsa.edu
https://uthscsa.edu/ Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229
INFORMATION AND TECHNOLOGIES
“We offer BCMS members a free insurance portfolio review.”
Humana (HHH Gold Sponsor)
Humana is a leading health and well-being company focused on making it easy for people to achieve their best health with clinical excellence through coordinated care.
Jon Buss: 512-338-6167
Jbuss1@humana.com
Shamayne Kotfas: 512-338-6103
skotfas@humana.com www.humana.com
INSURANCE/MEDICAL MALPRACTICE
Bertuzzi-Torres-Fernandez
Wealth Management Group ( Gold Sponsor)
We specialize in simplifying your personal and professional life. We are dedicated wealth managers who offer diverse financial solutions for discerning healthcare professionals, including asset protection lending and estate planning.
Mike Bertuzzi
First Vice President Senior Financial Advisor
210-278-3828
Michael_bertuzzi@ml.com
Ruth Torres Financial Advisor
210-278-3828
Ruth.torres@ml.com
Will C. Fernandez, CEPA Senior Portfolio Advisor Financial Advisor
210-278-3812 wfernandez@ml.com
https://fa.ml.com/texas/san-antonio/bertuzzi-torres-fernandez
GERIATRICS/PRIMARY
CARE
Denise C. Smith Vice President | Private Banking
210-343-4502
Denise.C.Smith@amegybank.com www.amegybank.com
“Community banking partnership”
HOSPITALS/ HEALTHCARE FACILITIES
Nexus Neurorecovery Center (HHH Gold Sponsor)

A post-acute rehabilitation facility focusing on brain injuries. Programming provides individual and group physical, occupational, cognitive and speech therapy. We help residents return to lives of productivity and meaning.
Sydney Kerr Liaison
346-339-2654
skerr@nhsltd.com
Caitlyn Tewksbury
ctewksbury@nhsltd.com
Justin Sanderson CEO 210-854-4732
jsanderson@nhsltd.com
Nexus Neurorecovery Center
227 Lewis St, San Antonio, TX 78212
https://nexushealthsystems.com
Express Information Systems (HHH Gold Sponsor)

With over 29 years’ experience, we understand that real-time visibility into your financial data is critical. Our browser-based healthcare accounting solutions provide accurate, multi-dimensional reporting that helps you accommodate further growth and drive your practice forward.
Rana Camargo Senior Account Manager 210-771-7903
ranac@expressinfo.com www.expressinfo.com
“Leaders in Healthcare Software & Consulting”
INSURANCE
Texas Medical Liability Trust (HHHH 10K Platinum Sponsor) With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting, and defending physicians.

Patty Spann
512-425-5932
patty-spann@tmlt.org
www.tmlt.org
Recommended partner of the Bexar County Medical Society
The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)

We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Conviva Care Center (HHH Gold Sponsor)

Conviva’s value-based care model
“To return patients to lives of productivity and meaning”
TMA Insurance Trust (HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.

Wendell England
Director of Member Benefits 512-370-1776
wendell.england@tmait.org
800-880-8181
www.tmait.org
Katy Brooks, CIC 210-807-5593
katy.brooks@bosainsurance.com
www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze 512-658-0262
Kirsten.Baze@medpro.com
www.medpro.com
continued on page 42
Visit us at www.bcms.org 41
BCMS Vendor Directory continued
INVESTMENT ADVISORY REAL ESTATE
Alamo Capital Advisors LLC (★★★★ 10K Platinum Sponsor)
Focused on sourcing, capitalizing and executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current projects include new developments, acquisitions and sales, lease representation and financial restructuring (equity, debt and partnership updates).
Jon Wiegand, Principal 210-241-2036
jw@alamocapitaladvisors.com www.alamocapitaladvisors.com
MEDICAL BILLING AND COLLECTIONS SERVICES
tom.rosol@henryschein.com
www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
MILITARY
San Antonio Army Medical Recruiting office (★★Silver Sponsor)
Mission: Recruit highly qualified and motivated healthcare professionals for service in the Army Reserves or Active Duty Army, in support of Soldiers and their families.
1LT Thomas Alexandria 210-328-9022
Alexandria.n.thomas12.mil@army. mil
https://recruiting.army.mil/mrb/ “Service to Country, Army Medicine, Experientia et Progressus”
MOLECULAR DIAGNOSTICS LABORATORY
from page 41
PROFESSIONAL ORGANIZATIONS
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more! Kevin Barber, President 210-308-7907 (Direct) kbarber@bdo.com
Valerie Rogler, Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
Brian T. Boswell, CFP®, QKA
Senior Private Wealth Advisor
512-649-8113
SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
STAFFING SERVICES
Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Wave Online (★★★ Gold Sponsor)


Our team of professionals will act as your extended AR office enhancing your revenue through our proprietary metrics and claim management systems. In addition, you keep 100% control of your RCM. Contact us today for a no cost evaluation.
Saranraj (Raj) Venkatesh
Vice President – RCM | Sales and Client Relations
726-228-1097
saranraj@wavemt.com
https://rcmwave.com/ “Innovation towards Solutions”
Commercial & Medical Credit Services (HH Silver Sponsor)
A bonded and fully insured San Antonio-based collection agency.
Henry Miranda 210-340-9515
hcmiranda@sbcglobal.net www.cmcs-sa.com
“Make us the solution for your account receivables.”
MEDICAL SUPPLIES AND EQUIPMENT
Henry Schein Medical (HH Silver Sponsor)

From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol
210-413-8079
iGenomeDx ( Gold Sponsor)

Most trusted molecular testing laboratory in San Antonio providing FAST, ACCURATE and COMPREHENSIVE precision diagnostics for Genetics and Infectious Diseases.
Dr. Niti Vanee Co-founder & CEO
210-257-6973
nvanee@iGenomeDx.com
Dr. Pramod Mishra Co-founder, COO & CSO
210-381-3829
pmishra@iGenomeDx.com
www.iGenomeDx.com
“My DNA My Medicine, Pharmacogenomics”
PRACTICE MANAGEMENT
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising. Lindsey Herman Nolan, MHR, CMPE, President info4@samgma.org www.samgma.org
REAL ESTATE SERVICES COMMERCIAL
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
Cindy M. Vidrine
Director of Operations- Texas 210-918-8737
cvidrine@favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”
Wave Online
(★★★ Gold Sponsor)
Our team of professionals will act as your extended AR office enhancing your revenue through our proprietary metrics and claim management systems. In addition, you keep 100% control of your RCM. Contact us today for a no cost evaluation.
Saranraj (Raj) Venkatesh
Vice President – RCM | Sales and Client Relations
726-228-1097
saranraj@wavemt.com
https://rcmwave.com/ “Innovation towards Solutions”
Alamo Capital Advisors LLC (★★★★ 10K Platinum Sponsor)


Focused on sourcing, capitalizing and executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current projects include new developments, acquisitions and sales, lease representation and financial restructuring (equity, debt and partnership updates).
Jon Wiegand, Principal 210-241-2036
jw@alamocapitaladvisors.com www.alamocapitaladvisors.com
RETIREMENT PLANNING
Oakwell Private Wealth Management (HHHH 10K Platinum Sponsor) Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.

42 SAN ANTONIO MEDICINE • April 2023


Visit us at www.bcms.org 43
Porsche Taycan GTS




 By Stephen Schutz, MD
By Stephen Schutz, MD
AUTO REVIEW
44 SAN ANTONIO MEDICINE • April 2023
The Porsche Taycan, which launched in 2020, is Porsche’s first bite of the battery electric vehicle (BEV) apple, and it is different from the market leader Tesla in some important ways. Driver involvement is the major focus, as you’d expect with Porsche, and luxury is much more prominent than it is in a Tesla.
Let’s start with the driving experience, which is quite something. In fact, I can summarize it like this: the Taycan drives like an electric 911. The Taycan is much bigger and heavier than a 911, more on that later, but somehow that’s what it feels like from behind the wheel.
While the Porsche doesn’t feel different from a Tesla model S accelerating in a straight line, handling and braking are clearly better. The steering in particular is very Porsche-like, with quick turn in, neutral cornering and good road feel. I own a current generation (992) 911, and the Taycan feels surprisingly like that car to drive.
How does Porsche do it? In the old days, suspension tuning, weight management and careful tire selection were the keys to good handling. Now it’s mostly software, specifically software that analyzes vehicle speed, available traction and steering input information, and then uses sophisticated torque vectoring—sending just the right amount of power to the wheels that need power while simultaneously braking the wheels that need braking—to get you around the corner you’re trying to negotiate. And to make the car feel like a Porsche. Torque vectoring has been around since the mid-1990s, but modern computing power has taken the technology to another level altogether.
It’s a good thing the software is sophisticated, because the Taycan weighs around 5,000 pounds, roughly the same as a current Cayenne SUV and about 50% more than a 911. Somehow the software and some smart engineers have made it so that the Taycan can dance despite its hefty BMI.
Most of that additional weight comes from the battery pack, which enables the Taycan to travel from 206-246 miles on a charge according to Car and Driver. Those numbers are pretty good for everyday driving but compare poorly with the Tesla Model S, which can go between 396405 miles after charging.
While a Tesla will take you farther than a Taycan, there is much more of a luxury feel inside the premium German automaker’s electric vehicle cabin than there is in any Tesla. The materials and interfaces are much nicer than they are in the BEV market leader, which really shouldn’t be the case since a base Porsche Taycan costs about the same as an equivalent model S. Presumably, the fact that the Model S is an 11-year-old car has something to do with that.
The outside of the Taycan also looks cool and futuristic, which can no longer be said for the Model S. The Taycan’s LED head and tail lights look very sleek, and the aerodynamic design is attractive from all angles.
The base Taycan has 402HP, while the most expensive Turbo S has 750 (yes, I know there’s no turbocharger, no, I don’t like the nomenclature, yes, I can live with it). Other Taycan models in between those bookends are the 4S, GTS and Turbo, and Taycans range in price from $88,150 for the base version to, gulp, $188,850 for the Turbo S. And that’s before options.
Before buying a Porsche Taycan or any other BEV, think about how you’ll use it. If you have a home charger, commuting and running errands in a Taycan are fantastic, but long trips may be problematic. Automotive News and the Wall Street Journal have recently reported that the charging infrastructure isn’t what it should be to support long trips in a BEV, and outages at existing charging stations are an increasing challenge.
During my time with my Taycan GTS press car, I spoke with a 2020 Taycan owner at a charging station. He said, “I love my Taycan and am very happy that I bought it, but I don’t take it on long trips because I don’t trust charging stations yet.” Something to consider.
The Taycan is Porsche’s first crack at making a BEV, and it’s a good one. While the Taycan’s range isn’t what you can get with a Tesla, its driving experience and luxuriousness are what you’d expect from a topshelf German automaker and better than Tesla’s. The BEV world is growing and maturing, and we’ll see how legacy automakers and Tesla grow and mature with it.

As always, call Phil Hornbeak, the Auto Program Manager at BCMS (210-301-4367), for your best deal on any new car or truck brand. Phil can also connect you to preferred financing and lease rates.
Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.

AUTO REVIEW Visit us at www.bcms.org 45
11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Rick Cavender 210-681-3399
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Charles Williams 210-912-5087
Chuck Nash Chevrolet Buick GMC 3209 North Interstate 35 San Marcos, TX
William Boyd 210-859-2719
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Kahlig Auto Group
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
Kahlig Auto Group
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Paul Hopkins 210-988-9644
Kahlig Auto Group
14610 IH 10 West San Marcos, TX 78249
Mark Hennigan 832-428-9507
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
North Park Lexus 611 Lockhill Selma San Antonio, TX
Tripp Bridges 210-308-8900
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
North Park Mazda 9333 San Pedro San Antonio, TX 78216
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
John Kahlig 210-253-3300
James Godkin 830-981-6000
Al Cavazos Jr. 210-366-9600 9455 IH 10 West San Antonio, TX 78230
Douglas Cox 210-764-6945
Kahlig Auto Group
Audi North Park 15670 IH-35 North Selma, TX 78254
Camden Steele 325-374-9897
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Gary Holdgraf 210-862-9769
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000
 Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Call Phil Hornbeak 210-301-4367 or email phil@bcms.org
Kahlig Auto Group
































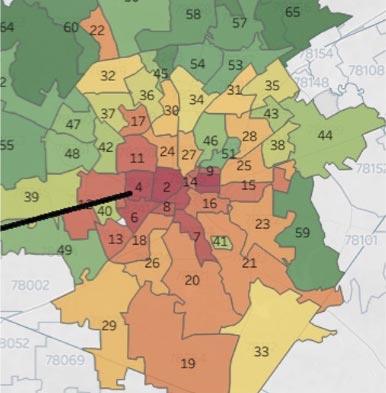
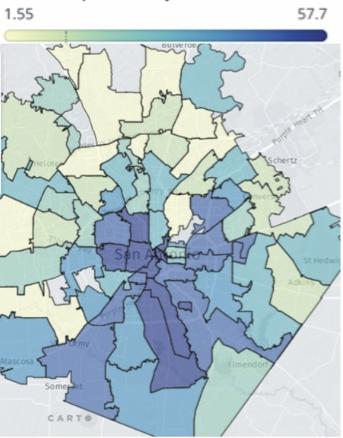
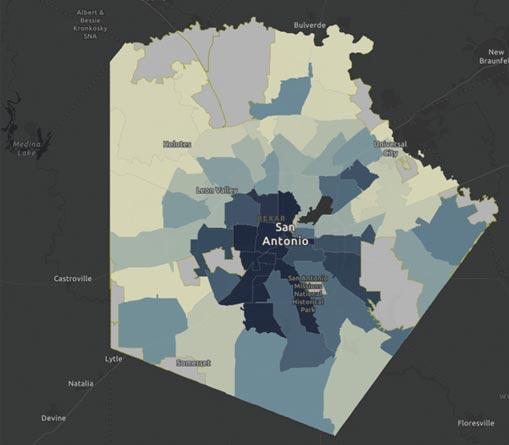
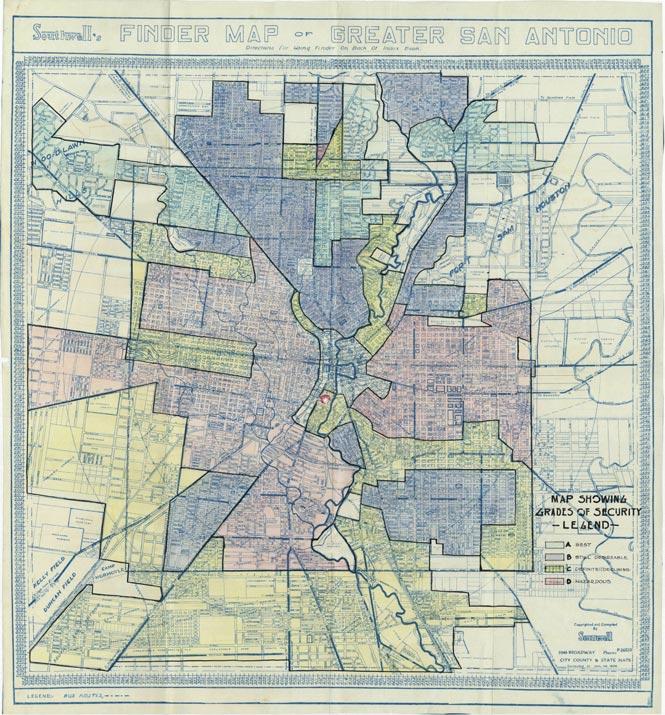




 By Sahar Z. Ali
By Sahar Z. Ali






 By Melissa Svoboda, MD and Cynthia Hamilton, MBA
By Melissa Svoboda, MD and Cynthia Hamilton, MBA


 By Alan D. Winkler, MHSA, Executive Director of Urology San Antonio, PA
By Alan D. Winkler, MHSA, Executive Director of Urology San Antonio, PA






































 By Stephen Schutz, MD
By Stephen Schutz, MD


 Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group

