Medical School Training











D.
“How to Know a Person: The Art of Seeing Others
PUBLISHED
Traveling Blender, LLC. 10036 Saxet Boerne, TX 78006
PUBLISHER
Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com
ADVERTISING SALES: AUSTIN: Sandy Weatherford sandy@travelingblender.com
SAN ANTONIO: Gerry Lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE: Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2024 SmithPrint, Inc. PRINTED IN THE USA

Ezequiel “Zeke” Silva, III, MD, President
Lyssa Ochoa, MD, Vice President
John Shepherd, MD, President-elect
Jennifer R. Rushton, MD, Treasurer
Lubna Naeem, MD, Secretary
John Joseph Nava, MD, Immediate Past President
Woodson “Scott” Jones, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Ana Rodriguez, MD, Member
Raul Santoscoy, DO, Member
Lauren Tarbox, MD, Member
Nancy Vacca, MD, Member
Col. Elisa D. O’Hern, MD, MC, FS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School
Representative
Cynthia Cantu, DO, Medical School Representative
Lori Kels, MD, Medical School Representative
Ronald Rodriguez, MD, Medical School Representative
Victoria Kohler-Webb, BCMS Alliance Representative
Carolina Arias, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
Melody Newsom, CEO/Executive Director
Monica Jones, Chief Operating Officer
Yvonne Nino, Controller
Al Ortiz, Chief Information Officer
Brissa Vela, Director of Membership & Corporate Partnerships
Phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
Monica Jacqueline Salas, MD, Co-chair
Jennifer C. Seger, MD, Co-chair
Lokesh Bathla, MD, Member
Elizabeth Clanton, MD, Member
Erika Gabriela Gonzalez-Reyes, MD, Member
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. K. Jyothula, MD, Member
Kristy Yvonne Kosub, MD, Member
Jaime Pankowsky, MD, Member
George-Thomas Martin Pugh, MD, Member
Rajam S. Ramamurthy, MD, Member
Adam V. Ratner, MD, Member
John Joseph Seidenfeld, MD, Member
Boulos Toursarkissian, MD, Member
Francis Vu Tran, MD, Member
Faraz Yousefian, DO, Member
Louis Doucette, Consultant
Brissa Vela, Consultant
Monica Jones, Staff Liaison
Trisha Doucette, Editor
Deepthi S. Akella, Student
Moses Alfaro, Student
Victoria Ayodele, Student
Tue Felix Nguyen, Student
Andrew Ta, Student
Alixandria Fiore Pfeiffer, DO, Resident
Elizabeth Allen, Volunteer
Adelita G. Cantu, PhD, Volunteer
Rita Espinoza, DrPH, Volunteer
Natalie Reyna Nyren, PA-C, Volunteer
David Schulz, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer


As a physician, this scene is all too familiar. Late, after your rounds are through or your last patient has left your office, you are still working into the evening. Updating patient records, taking care of paperwork, or just pausing for 10 minutes to close your eyes and think about what you accomplished today and consider what tomorrow will bring – and the dinner kept warm for when you get home.

Your hard work, long hours and sacrifice shows your commitment to the practice of medicine. We sincerely thank you for your dedication. It shows you put your patients first.
Now, it’s time to put your family first with life insurance. As the provider and protector of your loved ones, you can provide the ultimate measure of protection for them. Life insurance helps secure the hopes and dreams you have for them. And it will give you peace of mind knowing that your family will be able to stay in your home, bills will be paid, and your children will be able to afford a higher education.
Make this a family priority. For over 65 years, TMA Insurance Trust has helped physicians protect their family’s future and we would welcome the opportunity to give you the same peace of mind.
For a consultation call (800) 880-8181, Monday to Friday, 8:00 AM to 5:00 PM CST, or visit us online at tmait.org. It will be our privilege to serve you.


In early 1853, 95-year-old Eliza Hamilton, widow of Alexander Hamilton, dined at the White House. President Millard Fillmore “fussed over her, and the first lady gave up her chair to her. Everybody was eager to touch a living piece of American history.”1
Earlier this year, BCMS celebrated its own living piece of San Antonio’s medical history. On February 19, despite her lengthy battle with breast cancer, Mary Nava attended the BCMS February Board of Directors meeting. This meeting marked her last official duty for BCMS, as she passed away six weeks later, on April 2.
Her BCMS Journey
During her 24-year tenure at BCMS, Mary primarily focused on legislative affairs and public policy. She influenced policy at local, state and federal levels. Her profound understanding of San Antonio’s political landscape greatly benefited the medical community.
Reflect on the evolution of medicine since 2000. Mary played an important role informing BCMS’ actions around those policy changes, supporting physicians, patients and public health. Among her numerous contributions, several stand out:
Fluoridation of San Antonio Water: For 15 years, the addition of fluoride to San Antonio’s water supply sparked controversy until voters approved it in 2000. The Centers for Disease Control and Prevention hailed fluoridation as a top public health achievement of the 20th century.2 Mary’s efforts as our new Director of Communications were important in garnering physician support, which influenced voter approval.
Tort Reform: The passage of meaningful tort reform in Texas occurred in 2003. This required a coordinated effort, and BCMS played a pivotal role locally. By then, Mary had become the Director of Marketing and Membership, where her communication skills were invaluable. The 2003 law caps non-economic damages at $250K per physician, per case, marking a significant policy achievement leading to improved access to care and lower liability insurance premiums for physicians.3

Tobacco 21: Mary’s dedication to public health was evident in her support for a San Antonio city ordinance passed in October 2018, which prohibited the sale of tobacco products to individuals under 21. This ordinance influenced Texas Senate Bill 21, passed in 2019, raising the tobacco purchase age to 21 statewide. Mary’s leadership was instrumental in these developments.

Mary’s impact was felt on a personal level by the physicians of BCMS. She staffed several BCMS committees such as Legislative & Socioeconomics, Public Health & Patient Advocacy and our delegation to the TMA. She mentored many physicians, helping them translate their challenges and aspirations into significant policy changes and improved clinical care. Many of these physicians advanced to leadership roles in BCMS, TMA and AMA.
BCMS and its members have long benefited from Mary’s expertise, relationships and understanding of the legislative process. She was adept at drafting laws, resolutions and testimonies, and recognized the importance of fostering relationships with policymakers and community leaders. She knew when to compromise and when to stand firm on critical issues, always approaching her role with energy, charm and a kind smile.
Mary’s legacy is profound. Echoing the musical Hamilton — “Legacy, what is a legacy? It’s planting seeds in a garden you never get to see.” In Mary’s case, that garden is the countless patients who continue to benefit from her efforts.
Our community is forever grateful to Mary for her enduring legacy of advocacy.


1. Chernow, R. Alexander Hamilton. Penguin Books. Mar. 29, 2005
2. Centers for Disease Control and Prevention. USA Department of Health and Human Services. Available from: http://www.cdc.gov
3. Texas Medicine, September 2013
Ezequiel “Zeke” Silva III, MD, is the 2024 President of the Bexar County Medical Society. Dr. Silva is a radiologist with the South Texas Radiology Group, Adjunct Professor of Radiology at the UT Health, Long School of Medicine, and Vice-Chief of Staff at Methodist Hospital Texsan. He is Chair of the TMA Council on Legislation and is a TMA Delegate to the AMA. He chairs the AMA RVS Update Committee (RUC).
Bexar County Medical Society Alliance (BCMSA) has emerged as a beacon of exemplary leadership and unwavering dedication to our community and Texas medicine. Nowhere was this more evident than the recent TexMed/ALLMED conference in Dallas where local Alliance members were installed to serve at the state level and the county received statewide recognition for their work.
Jenny Shepherd stepped into the spotlight as she was inaugurated as the 107th president of the Texas Medical Association Alliance (TMAA). In her address to the TMA House of Delegates, she emphasized the immense impact that each individual can have, shining a light on the tremendous power of one. She considers herself exceptionally privileged to lead during a legislative year, as advocacy is her true passion. She is determined to convey to every member of the family of medicine the importance of active involvement and having a relationship with your legislator. “Physicians can no longer sit on the sidelines if they want to control how they practice medicine. If legislators aren’t hearing our voices, they are listening to someone else. One voice and one vote can make the difference.” The success of her leadership in this area resulted in Bexar County winning the Mary Ann Homer Legislative Award from TMAA this year.
Jenny is not the only Bexar County Alliance member to be chosen to lead at the state level over the next year. Julia Halvorsen, married to ER physician Jake, will serve as secretary. She spent the last year as a statewide Resource Liaison helping guide the direction of the Alliance overall. Julia has strong convictions about why the Alliance matters “I believe there is nothing more important than family; connecting and supporting physician families is at the heart of what the Alliance is about.”




Julia is no stranger to leadership, currently serving as the VP for Community Outreach in Bexar. In addition to traditional TMA Foundation projects such as Hard Hats for Little Heads and BookShare, Julia has spearheaded Bexar’s new signature program, the Period Poverty Project. Combining her heart for service with strategic community partnerships means girls at the Young Women’s Leadership Academy can access what they need, when they need it. The partnership has been so successful that Bexar County was the recipient of not only the TMAA award for Excellence in Community Outreach, but also a $2,000 Alliance Health Education grant to expand the program from the American Medical Association Alliance. Zeke Silva, President of BCMS, is not surprised, “The energy of the Alliance is incredible, powered by the values of medicine and caring for our most needy at their most vulnerable time.”
Julia’s former statewide role as Resource Liaison will be filled by Brittany Garcia-Noche, BCMSA President-elect and spouse of Ramy Noche, sports medicine specialist. BCMSA Past President and advisor Danielle Henkes voices best why Brittany is the kind of leader needed, “A thoughtful and thorough leader, Brittany exudes a quiet energy. Her keen listening and observation skills enable her to forge meaningful connections with other members as well as identify needs and opportunities statewide.”
About the Alliance overall, BCMS President-elect John Shepherd, University Hospital pediatric anesthesiologist, echoes the sentiments of Zeke Silva when he says, “We can never discount the invaluable contributions of this remarkable group. They are the driving force behind so much of our community outreach, demonstrating unwavering passion and tireless dedication as they work towards our shared goals. Their commitment and hard work embody the spirit of service that defines the family of medicine; I am truly grateful for their support both in Bexar County and across the state.”


As for Jenny, she’s not daunted by the vast scope of work that lies ahead. Instead, she is dedicated to focusing on nurturing one legislative relationship, cultivating one new idea and championing one community outreach project at a time because she believes in the power of one, knowing that each one adds up to a huge difference in the end.
For information on the Bexar County Medical Society Alliance, scan the code:



Post graduate medical education has changed radically in the past several decades. Perhaps the most obvious difference is how residents and fellows access information. When I joined the fulltime faculty at the brand-new University of Texas Medical School at San Antonio in 1970, medical knowledge was acquired through lectures, journal articles, conferences and the relatively few textbooks that were available then. For example, in my specialty Orthopaedics there existed a couple of out-of-date fracture books, a single, not very good, volume on general Orthopaedics, a difficult to read pathology text, and a treatise on Pediatric Orthopaedics. Now, every subspeciality in Orthopaedics has several two-or-three volume textbooks. I must confess that San Antonio contributed to this deluge of written texts by publishing “Rockwood and Green’s Fractures in Adults” in 1975 (now in its 9th edition) and seven years later “Green’s Operative Hand Surgery” (now in its 8th edition), plus additional works generated from our department on pediatric injuries, the shoulder and orthopaedic sports medicine. The expansion of medical journals has been even more explosive. In 1975, there was not a single journal devoted to my subspecialty, hand surgery, and now there are more than a half dozen.
Even more remarkable than the proliferation of books is that residents and fellows rarely read the written texts in today’s modern world. Most current textbooks and scientific journals now have online versions on the internet, which have become the primary source of reading for residents and fellows. Whereas my generation spent hours wandering around library stacks looking up articles, young doctors in training today have the entire world of medical information at their fingertips (or thumbs, as it were) on their iPhones.
Another problematic change is the expansion of medical knowledge. Again, to use Orthopaedics as an example, when I was a resident, we had four or five books and a single journal to study in preparation for our specialty board exams. Now, the graduating Orthopaedic resident has a towering stack of books and journals, each of which contains information from which an examiner might generate questions.
It is not surprising then, that the current crop of individuals finishing a residency or fellowship are equipped with far more knowledge than those of my generation. What has NOT changed, however, is the ability to apply that knowledge appropriately, and that is where mentors have a place. Every student at every level needs more experienced teachers and colleagues who do their best to keep the student from making the same mistakes that the mentor did in his or her earlier

years. This exposure to seasoned veterans is perhaps nowhere more critical than in the student’s pursuit of surgical knowledge and techniques. The bottom line of all this is simple. No matter the source of medical knowledge nor how easy it is to access, 90 percent of what any student learns comes from diligent effort and hard work. A teacher will serve as a mentor and guide, but the goal of becoming a proficient, capable and compassionate physician and surgeon is achieved only by the diligence and dedication of the student to learn his or her craft.

David P. Green, MD, is a founder of The Hand and Upper Extremity Center of San Antonio, with an international reputation in hand surgery, and the first surgeon in San Antonio to devote his practice entirely to hand and upper extremity surgery. Dr. Green is a member of the Bexar County Medical Society, and a recipient of the BCMS Golden Aesculapius Award for Lifetime of Distinguished Service.

Numerous studies show that the development of burnout in physicians begins in Medical School with some studies placing the rate of burnout at 50 percent among all medical students during training.1,2 Matriculating medical students report lower burnout, less depression and higher quality of life compared to college graduates pursuing other fields, however, that pattern looks to be reversed by the second year of medical school.3 To reverse this trend, the Office of Undergraduate Medical Education (OUME) developed interventions, which give students agency to develop effective selfcare strategies and strengthen their resilience. Changing the USMLE Step 1 exam to pass/fail in 2022, moving some curriculum to virtual or asynchronous learning, and limiting overnight call experiences have been some of the methods employed. In addition, students have access to wellness and professional identity coaching, and programs in stress-management. Comparable program adjustments have shown some improvement in reducing rates of stress and burnout.4 There have been some consequences for incoming residents, with program directors across the country concerned their incoming PGY-1 residents may be less prepared for the rigors of internship. In our Graduate Medical Education (GME) programs, the rates of residents accessing mental health services has continued to increase each year since the 20182019 academic year. Clearly the transition from medical student to resident is a critical waypoint on the path to becoming a practicing physician, and a significant focus here provides the greatest opportunity to impact the resident’s well-being throughout training and beyond. Wellness Programs within UME and GME at the University of Texas Health in San Antonio have worked together to create a multi-tiered approach to assisting medical students and residents during this adjustment period.
Headspace for UT Health: Complimentary annual HeadspaceTM memberships are offered to students. Headspace is a mobile application that guides users through the essentials of mindfulness using a library of guided meditations, resources and videos. Users have reported improved productivity, better sleep and reduced stress.
Wellness Matters: Founded in 2018 by a medical student, this organization promotes the eight dimensions of wellness among medical students. The group works closely with OUME, serving as an advisory board for student well-being and assisting with events and programs. Members promote a culture of wellness using the LSOM wellness pledge, encouraging use of wellness spaces on campus, and hosting the annual Wellness event ReDiscover.
Self-Reflection Guide for Medical Students (SRG): The SRG encourages reflection to enhance professional identity formation. It can be used at all stages of training to construct meaning, promote individual and professional well-being, and internalize learning in cognitive and affective domains. In exploring personal values, acknowledging human limitations, and understanding their authentic purpose, students become self-reflective practitioners.
Transition Information Session: For the past four years, the OUME has offered an information session for all graduating medical students. The focus of this session offered jointly by both UME and GME representatives involves a brief presentation followed by a Q&A session. Presentations focus on challenging mindsets like Imposter Syndrome, perfectionism and ways to avoid burnout. Pre-
paring for inpatient services, overnight calls and graded responsibility are also areas of focus.
Interventions on or Around Orientation
Financial Literacy: A majority of medical students enter residency with a large amount of debt. Most recent figures place the average medical school debt between $200-250,000 dollars, resulting in a large degree of initial stress that arises over financial concerns. Beginning shortly after residency MATCH, the OGME sends out detailed information about the resident’s salary, withholdings, budgeting, typical living expenses, apartment lease by size and location, and average loan repayment amounts. We also provide information about student loan forgiveness programs like the Public Service Loan Forgiveness or Income-Driven Repayment Forgiveness. Resources are included.
Transition Screening: Starting a new residency program is challenging. For some residents, however, a disappointing match into a lower ranked program, an alternate specialty or leaving an established support network can add to the stress. If you are someone with an underlying mental health disorder, a physical disability or a major outside stressor like a recent divorce, the transition to residency can be unbearable. The Transition to Residency Risk Index (TRRI) is a questionnaire developed in our institution and now used nationally by programs to assess incoming residents for predictors of a difficult transition.5 Participation is voluntary. Those who score themselves as moderate or high-risk range have a heightened degree of check-ins by program leadership, early faculty and peer mentorship, and an offer of mental health resources. Early community building events are also recommended. In our program, greater than 90 percent of those who score themselves as high-risk ultimately come into a counseling relationship with our Behavioral Health Providers (BHP).
The second tier of our transition screening is the scheduling of OptOut visits with our BHP within the first three months of training for all PGY-1 residents. These 15–20-minute sessions allow for an introduction to counseling, coaching and other resources, a chance to see how well the resident is settling into the city and program, and to screen for other needs. Over the past two years, over 45 percent of all attendees have an essential need like medication refills, counseling, presenting in crisis or information on accessing medical or dental services.
Many residency programs now use “Boot Camps” as a mechanism to prepare incoming residents for the challenges they will face during service time and during overnight call duties. The structure of these Boot Camps is determined by specialty. Common areas of focus for these Boot Camps revolve around team building, working in interprofessional teams, or dealing with urgent or emergency patient care issues. Simulation Centers have been developed to increase the reality of the experiences. Introduction to the Electronic Health Record with time to practice on simulated patient records is critical, along with tips and tools to improve efficiency. Basic procedural competencies like placing IVs, obtaining arterial blood gases, sewing lacerations, and practicing specialty specific procedures like lumbar punctures or speculum examinations may also happen here. A relatively new introduction in Boot Camps in a focus on identifying patient safety issues. Patient Safety Rooms allow new residents to enter a simulated patient
room and see how many patient safety concerns they can identify. Inappropriate fluids, unattached oxygen tubing or inappropriate medications are some examples. Mechanisms to report these safety issues are also taught. Senior resident panels and rotation “tip sheets” provide important lessons, practices or tools for various rotations.
Interactive Screening Program and Mental Health Resources: The Interactive Screening Program (ISP) is a voluntary and anonymous screening tool produced by the American Foundation for Suicide Prevention and licensed to colleges, medical schools and residency programs to provide a mechanism for ongoing screening of individuals for burnout, depression, anxiety, eating disorders, substance abuse and suicidal ideation. Residents who complete the survey are classified into risk categories and the BHPs are sent the results with a unique identifier but no identifying resident information. Counselors can respond directly through the system with a personalized email and resources.
1. IsHak W, Nikravest R, Lederer, S, et al. Burnout in Medical Students, a systematic review. Clin Teacher. 2013; 10 (4): 242-245
2. Morcos, G, Awan, 0. Burnout in Medical School: A Medical Student’s Perspective. Acad Radiol. 2023; 30 (6): 1223-1225
3. Brazeau CM, Shanafelt T, Durning SJ, Massie FS, Eacker A, Moutier C, Satele DV, Sloan JA, Dyrbye LN. Distress among matriculating medical students relative to the general population. Acad Med. 2014 Nov;89(11):1520-5
4. Dyrbye L, Thomas M … Shanafelt T. The Learning Environment and Medical Student Burnout: A Multicenter Study. Medical Education 2009; 43 (3) 274-282
5. Slavin, S, Yaghmour, N, Courand, J. Support for Mental Health and Well-Being in the Transitions to Residency. JGME. 2024 16(2): 241-244

Jon Courand, MD, FAAP, served as Pediatric Residency Director for the UT Pediatric Residency Program and now serves as Vice Chair for Graduate Medical Education. He divides his time between Pediatrics and the Office of Graduate Medical Education where he oversees all resident and fellow Wellness Programs for the Institution. He is actively involved with physician wellness on a local, state and national level, and with the Healer’s Art Program in the Medical School. Dr. Courand is a member of the Bexar County Medical Society.

Paulina Mazurek, EdD, is the founding Director of Wellness and Professional Formation at UT Health Long School of Medicine, Office for Undergraduate Medical Education. With 15 years of experience working in higher education, the majority of which have been in medical education, she has a key role in the strategic planning and execution of programs within Student Affairs. Working collaboratively with partners at the local, state and national levels, she is helping advance initiatives to improve wellness among medical trainees. Paulina has been recognized internationally as a thought leader in the field, named as Headspace’s inaugural Mindful Leader of the Year in 2022.

After training for years, you have a job and you’re going to be paid a living wage. One last thing though. The employer emails you an employment contract with the instruction, “Just sign this contract. It’s our standard contract.” Before you sign it, here’s what you look for.
Duties: Does the contract allow the employer to assign you to different locations? If so, ask that a primary location be specified. Are you expected to provide call coverage? Ask that the contract state that call coverage will be assigned equitably among the physician providers.
Money: The contract should specify how much you are going to be paid. Usually, it’s a fixed monthly amount, i.e., a salary. How do you know if the offered salary is market? The best solution is to tap the annual surveys conducted by the Medical Group Managers Association (MGMA). For a modest fee, MGMA will share survey results for your specialty. Institutional employers, such as hospitals, rely on the surveys to guide their starting salaries. They peg starting salaries at a number that is below the median. You should ask for a salary that is at the median or higher.
In addition to a salary, the contract should contain an opportunity to earn a bonus. This bonus opportunity is tied to additional productivity. It might be a percentage of the employer’s collections above a threshold amount or a dollar amount for wRVUs produced above a minimum number. On a related note, your contract should allow you to retain call coverage stipends and payments for outside work, such
as chart reviews, honoraria for speaking or writing, medical director fees and expert witness testimony. On the other hand, the contract will prohibit moonlighting without the employer’s prior permission.
After the first year or two of employment, the salary might be replaced with a strictly production-based compensation formula. These formulas can track the formula used for a bonus, as described above, or it might shift to a percentage of your profit. The latter is a more complicated formula. The formula credits your compensation with your collections and subtracts the costs associated directly with you, such as salary and benefits, and a share of overhead, such as rent and staff compensation. The resulting number is your profit. As a non-owner, you would be paid a percentage of that profit and the balance is retained by the employer. If you see your compensation shifting to a production-based formula, it is imperative that you establish a reliable referral network while you enjoy the comfort of a salary.
Upfront Money: It is acceptable to ask for a signing bonus. The usual sign on bonus is $10,000 but more is possible if your specialty is in demand. The bonus may be paid when you sign the contract or with your first paycheck. Similarly, it is standard for the employer to reimburse your moving expenses, up to $10,000.
In fairness, the employer will expect you to repay these amounts if you don’t remain employed some minimum time, such as one or two years. In other words, if you leave early, you must repay the employer. Ask that the repayment be amortized monthly. If you leave halfway through a two-year commitment, you only owe half the upfront pay-
ment. Make sure you don’t have to pay anything if the employer chooses to end your employment without cause, which is discussed below.
Hospital Assistance: Hospitals will loan money to a practice adding a newly-trained physician. These arrangements are documented by a separate, complex recruiting agreement and a promissory note. The loan will cover the physician’s salary for the first year and perhaps other added costs. The loan must be repaid with interest, but if the recruited physician remains in the hospital’s service area for a minimum period, such as three or four years, the loan will be forgiven. If you are receiving this type of assistance, it is important to coordinate the hospital’s recruiting agreement with the employment agreement, to clearly establish who is responsible for repaying the hospital if the loan isn’t forgiven.
Benefits: Most employers provide group health insurance coverage of you at no cost. You can add coverage of your spouse and dependents at your cost. Employers also regularly offer the opportunity to participate in retirement plans and may contribute a percentage on your behalf. Ask for a copy of the SPD, summary plan description, which is an excellent source of information about the insurance and retirement plan. For the protection of your family, arrange personal disability insurance if the employer doesn’t offer it as a benefit.
Professional Expenses: To maintain your medical license and specialty board certification, you must undertake continuing medical education (CME). Employers will pay for or reimburse CME. The usual allowance, including travel and lodging, is $2,500 annually. The employer should also pay for your professional expenses. These include your Texas medical license renewal, your DEA registration, Texas Medical Association dues and dues for specialty organizations. Consider asking for reimbursement of the costs of specialty boards and ask for additional paid time off to prepare for the exam. The usual allowance for professional expenses on top of the CME allowance is $2,500 annually.
Paid Time Off: The contract should include paid time off (PTO). PTO ranges from two to three weeks per year of employment, and more for in demand specialties. PTO is on a “use it or lose it” basis. Unused PTO is not paid and does not carry over to a subsequent year. Always confirm how PTO is distributed among the physicians, especially for spring break and summer vacations.
Termination: Your contract will be for a term of years, with automatic extensions after the end of the initial term. However, it will have provisions permitting an earlier end to your employment.
Termination for Cause: The employer may end your employment upon the occurrence of listed, for cause events. The list begins with the objective and winds down to the subjective. The loss of your medical license is an objective event. Disruptive behavior or less than the standard of care is a subjective event. Failure to follow policies is in between. For events that are not clearly objective, the employer should give you a warning and a reasonable opportunity, 10 days, to remedy the problem. This protection is known as “notice and opportunity to cure.”
Termination Without Cause: This provision allows the employer or you to end your employment by giving minimum notice. No reason need be given. It is merely for convenience. The minimum notice should be the same for the employer and you. The typical minimum notice is 60 to 90 days. Keep in mind that if you give the notice, you must work all the days you have been scheduled to work or the employer could ask you to reimburse it for added costs to cover your absence. Along that line, many employers insist in the contract that you pay for unworked days during the notice period, such as $500 per day.
Effect of Termination: If your pay depends on collections, you will want to make sure that the collections the employer receives after the end of your employment will be credited. Usually, this arrangement credits collections that arrive during the 90 days following the end of employment.
Noncompete: Employers do not want former physician employees to compete after the end of employment. Consequently, your employment contract will contain a noncompete. Until recently, it could be said with confidence that physician noncompetes are enforceable in Texas and employers will enforce them. However, a Federal Trade Commission rule has turned that predictability on its head. Favorable to employed physicians, the FTC’s rule outlaws physician noncompetes beginning September 4, 2024. In response, the Chamber of Commerce of the United States of America, among others, has sued to invalidate the rule. It will take years before the issue is resolved. In the meantime, it is possible that the courts will suspend the rule until a final decision is made on its validity. If suspended, physician noncompetes will be enforceable.
Indemnity: Indemnity is a legal description for the obligation to reimburse. Your contract will contain an indemnity obligation whereby you agree to reimburse the employer for any monetary loss it has that you might have caused. Sometimes, the indemnity is conjoined with a statement making the employee responsible for reimbursing the employer for any chargebacks by insurance companies or government programs, e.g., Medicare, for miscoded claims. When presented with this obligation, make sure that it applies only if the loss isn’t covered by insurance. Thus, a malpractice claim will be most likely covered by insurance and not become an issue. In addition, feel free to ask the employer to add a mirror provision indemnifying you against loss the employer might cause you.
Final Word: Consider asking an experienced contract attorney to review your contract and advise you about it. You can easily identify a qualified attorney from an Internet search.

Michael L. Kreager, JD, LLM, is the founder of Kreager Mitchell PLLC, a San Antonio law firm serving the needs of physicians. He has authored several books on physician employment contracts for the Texas Medical Association. In addition, he authored the popular guide, “The Physician Employment Contract,” which is in its fourth edition. It is a free publication.
Excerpts from www.news.uthscsa.edu. Originally posted on March 18, 2024
More than 200 senior students from the Joe R. and Teresa Lozano Long School of Medicine stood on stage in front of their classmates, family, friends and mentors on March 15 to open an envelope revealing their future. It’s a dramatic but festive occasion for the students, who are wrapping up a rigorous four years of medical education.
This year’s ceremony, while celebratory, held extra space for reflection and grief after the unexpected passing of UT Health San Antonio president, William Henrich, MD, MACP, who died the day before.
“Dr. Henrich was a leader, a mentor, a friend, an exceptional physician and teacher, and he was really the best of all of us. We know that Dr. Henrich is here today with us in spirit as he was so many times over the years in body and heart,” said Deb Conway, MD, vice dean for undergraduate medical education, before leading a moment of silence.
Match Day is a geographic rite of passage when graduating medical students throughout the U.S. find out where their residency training will take them — and perhaps where their medical careers will be launched. During their fourth year of medical school, medical students typically interview with several graduate medical education programs and healthcare institutions to compete for residency slots in various specialties and have ranked their top choices. The healthcare institutions and programs also have ranked their top choices of residents.
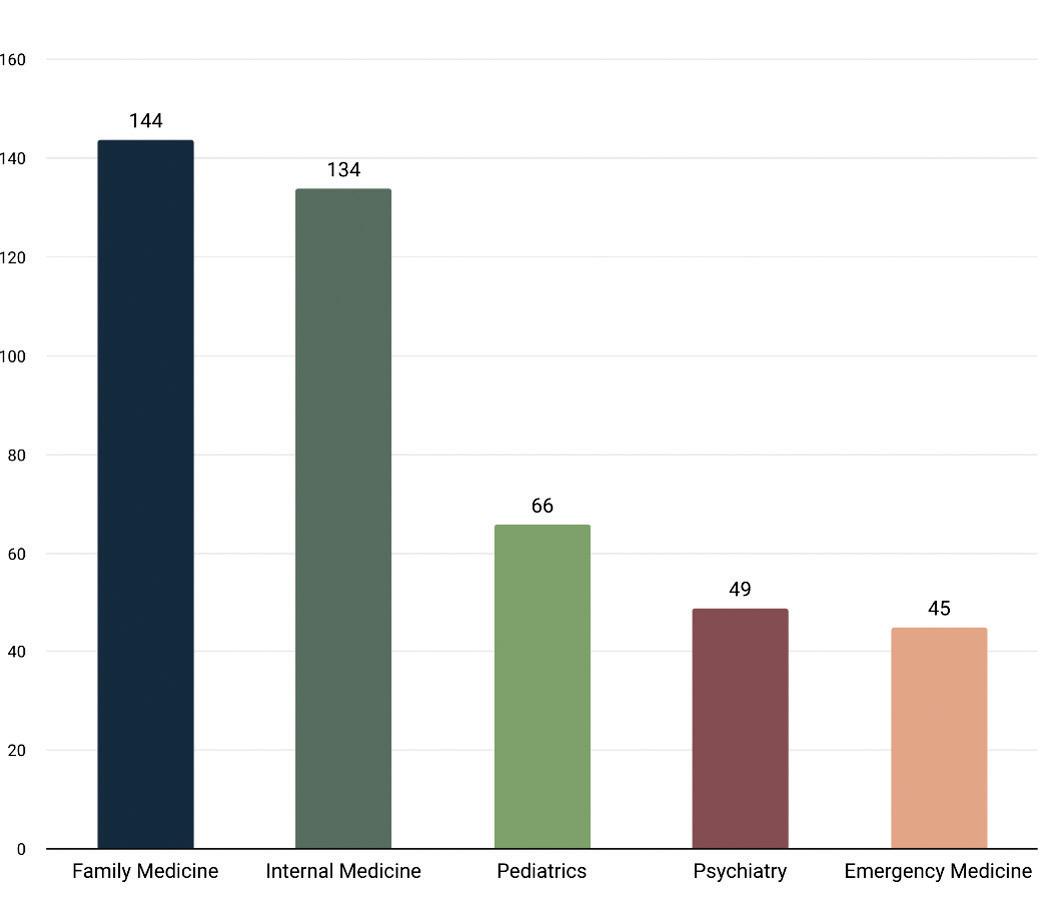
The class of 2024 saw a 99 percent overall match rate to residency programs of their choice. San Antonio will keep 22 percent of those matched graduates, who matched to local programs, bolstering the healthcare workforce in Bexar County and the region.
Of the matched students, 60 percent matched to Texas programs, helping to meet the state’s critical need for quality physicians, and 40 percent matched to primary care specialties including internal medicine,

pediatrics and family medicine. After primary care, other top specialties included psychiatry and anesthesiology.
In his remarks to the crowd, Robert Hromas, MD, Dean of the Long School of Medicine, urged students to never stop learning. “This is not the end, but merely the beginning for you. Medical science saves lives, and in the 40 of 50 years of your career, you’re going to see advances that astound you. Never stop learning, because the minute you stop learning, you stop growing.”
He also advised to expect the unexpected and expect disappoint. “You are going to lose patients because that’s the nature of life,” he said. “Celebrate the births, celebrate the victories, make memories, because they help you get through the hard times. Don’t let disappointment stop you.”
To get through the hard times, Hromas emphasized the importance of the support of colleagues and loved ones and working as a team. “Medicine is football, not golf. You are part of a team,” he said. “And the single most important member on that team is sitting here today with you. It’s your family. You must have your family, they’re the center, they hike the ball. Caring for your family is the same as caring for your patient.”
In his final point of imparted wisdom, Hromas spoke of the importance of mentorship. “We all stand on the shoulders of someone who taught us. Each of you is here because some faculty said I believe in you. They taught you not only their knowledge, but their values and how they care for patients,” he said. “For me, that mentor was Bill Henrich. He believed I could be a dean when no one else did. I stand on his shoulders, just like all of you stand on someone’s shoulders. Never get so big or so smart or so wealthy that you forget that you are there as a gift from someone else.”
With that, the matching commenced, and the class of 2024 began the next step of their journey in medicine.









The University of the Incarnate Word School of Osteopathic Medicine (UIWSOM) stands as a beacon of medical education excellence, having swiftly established a strong reputation since welcoming its inaugural class in 2017. This institution, despite its relatively short history, has made remarkable strides in shaping the next generation of osteopathic physicians. These physicians are recognized not just for their clinical acumen but also for their holistic approach to patient care, embodying the values of compassion, empathy and lifelong learning. Their journey from medical students to residents in training across the United States is a testament to UIWSOM's commitment to excellence and its effective curriculum.
UIWSOM's roots are deeply embedded in the traditions of the University of the Incarnate Word (UIW), a private Catholic university in San Antonio, Texas, founded in 1881 by the Sisters of Charity of the Incarnate Word. This historical backdrop is significant, as it reflects a long-standing commitment to not only academic excellence but also to the service of the community and the holistic development of students. These foundational values have been seamlessly integrated into UIWSOM's mission, shaping its approach to medical education and patient care.
The establishment of UIWSOM was driven by the recognition of a growing need for physicians who are not only clinically adept but


also deeply attuned to the holistic aspects of patient care. Osteopathic medicine, with its emphasis on treating the whole person, offers a unique perspective in healthcare. It considers lifestyle, environmental and mental health factors as integral parts of patient care, alongside physical health. UIWSOM's curriculum is meticulously designed to imbue these principles in its students, fostering a culture of empathy, collaboration and an unwavering commitment to lifelong learning.
John T. Pham, DO, FACOFP, was appointed as Dean of UIWSOM in 2022. Reflecting on UIWSOM’s match history, he said, "As Dean of the University of the Incarnate Word School of Osteopathic Medicine, I take immense pride in four remarkable years of successful matches from 2021 to 2024. Our journey together, underscored by commitment and excellence, has led to outstanding outcomes for our students as they transition into their respective medical careers. Our students have achieved remarkable success, a testament to their hard work, the faculty's guidance, and our school's emphasis on medical knowledge and compassionate care. Each match confirms that UIWSOM not only prepares future osteopathic physicians but also molds leaders prepared to enhance the health and well-being of communities in Texas and throughout the United States. As we look to the future, we are filled with pride for the paths our students have forged and excited for the contributions they will make to the medical field."

The graduation of its inaugural class in May 2021 marked a significant milestone for UIWSOM. This event not only celebrated the transition of its first cohort of students into professional medical practice but also set a precedent for the success of future graduates. Nearly 600 UIWSOM graduates are currently undergoing residency training in various programs nationwide, with Texas hosting the largest number of these residents. This reflects the school's growing influence in the healthcare field and its ability to prepare students for the rigors of residency.
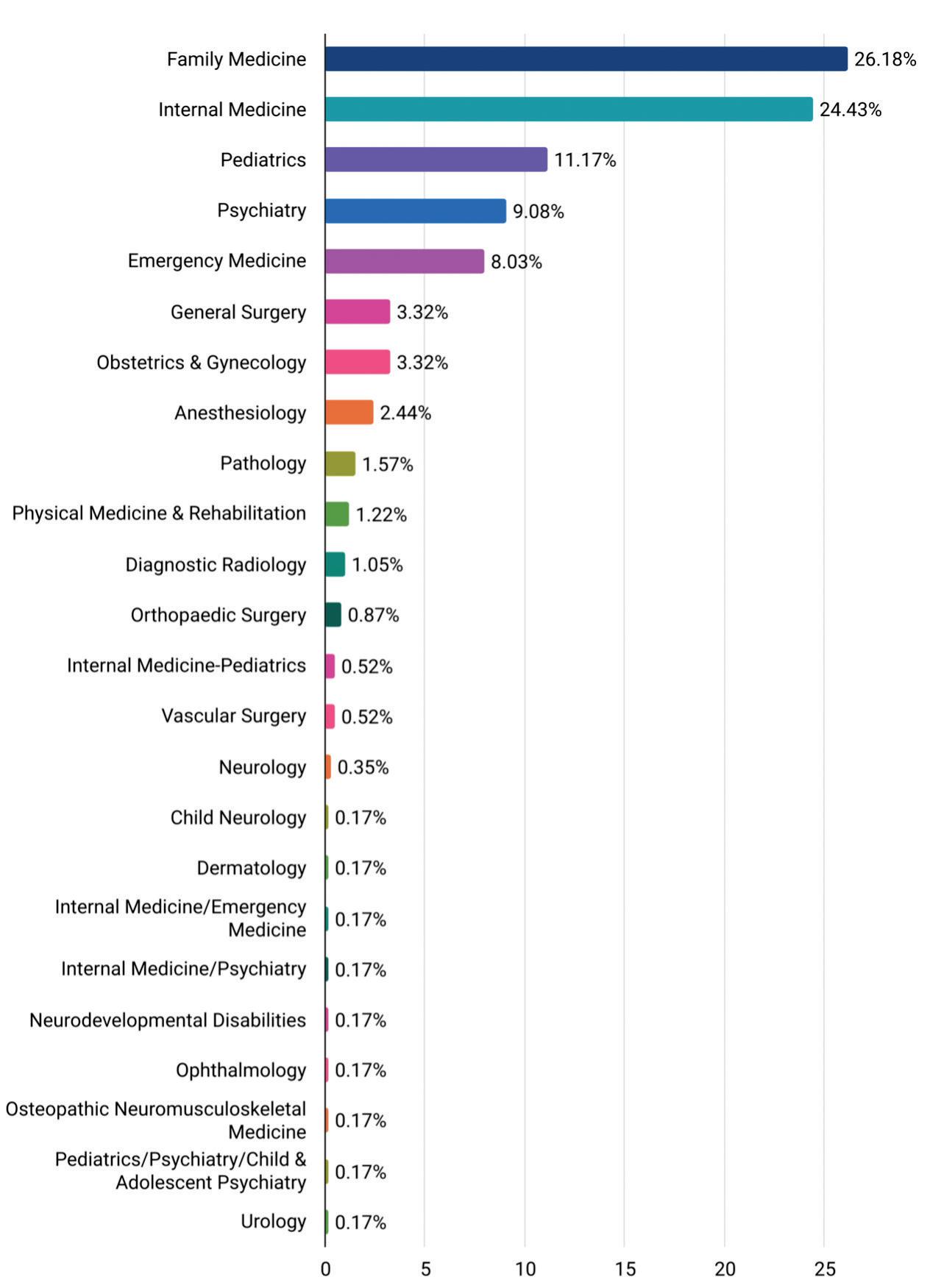
The school's success is further evidenced by the diverse range of specialties its graduates have pursued. Over the past four years, UIWSOM graduates have matched into 22 different specialties, with a notable majority in primary care fields such as Family Medicine, Internal Medicine and Pediatrics. However, their expertise is not limited to these areas. Emergency Medicine and Psychiatry are also popular choices, showcasing the school's broad impact on healthcare.
Surgical specialties, though representing a smaller fraction of the matches, highlight the comprehensive training provided by UIWSOM, preparing students for success in various medical disciplines, including General Surgery, Orthopaedic Surgery, Vascular Surgery, Urology and Ophthalmology.
At the heart of UIWSOM's mission is the dedication to producing physicians who are not only competent in their clinical skills but also compassionate in their patient interactions. The school's rigorous curriculum and emphasis on a holistic approach to medicine encourage students to consider the wider context of their patients' lives, fostering a deep sense of empathy and a collaborative spirit. This approach not only benefits the patients but also enriches the professional and personal growth of the physicians themselves.
The University of the Incarnate Word School of Osteopathic Medicine has rapidly emerged as a distinguished institution for medical education. Its unique blend of academic rigor, commitment to holistic patient care and strong ethical foundation positions UIWSOM as a leader in training the next generation of osteopathic physicians. With a diverse array of specialties represented among its graduates and a significant impact on residency training programs across the country, UIWSOM is poised to continue its trajectory of excellence, shaping the future of healthcare and improving the well-being of communities in Texas and throughout the United States.

Martin Timoney, EdD, MS, MA, LPC, NCC, is a native of Ireland. He attended the Pontifical University at Saint Patrick’s College, Maynooth, for undergraduate studies. He holds a Master of Arts in Theology, a Master of Science in Clinical Mental Health Counseling, and a Doctor of Education in Community Care and Counseling. He is a licensed counselor in Texas and Washington.
At the University of the Incarnate Word School of Osteopathic Medicine (UIWSOM), it’s not uncommon to see first-year students deliver babies by themselves and then perform the newborn’s APGAR assessments. Occasionally, students also treat patients suffering from acute heart attacks. These lifesaving measures are routinely performed in the safety of the medical school’s SIM Lab, a specialized space dedicated for students to learn clinical skills before they must use them in the real world
UIWSOM is an osteopathic medical school located in the southside of San Antonio where the U.S. Air Force School of Aerospace Medicine formerly stood. The campus boasts four state-of-the-art facilities in the Brooks City Base, including its high-fidelity SIM Lab. The SIM Lab is an instructional facility aimed at giving medical students realistic training opportunities for their future careers, regardless of what specialty they go into. Utilization of the SIM lab takes place during all phases of the curriculum and is integrated as a part of learning and partaking in a low-stakes environment where students can learn from their mistakes and strive to become great physicians.
The lab consists of four rooms, two of which perfectly emulate full surgical suites, complete with everything you would see in an operating room in any hospital. When you walk into the operating room, you’ll see your patient — a mannequin that has a heartbeat, lungs and can even talk — in an adjustable electronic surgical bed. Behind the bed is a fully functioning headwall with medical gas and electrical outlets
that can connect to a machine that administers anesthesia. On the other side of the room is a one-way mirror where professors can control the mannequin to replicate real-life scenarios, and monitor the students via audio and video and provide suggestions for improvement without getting in the way.
Not too long ago, medical schools relied on actual patients with real presentations to volunteer at schools for students to learn from them via incessant poking and prodding. “Mannequins don’t complain,” remarked Dr. Robert Allen, the Medical Director of CIELO (Center for Interprofessional Experiential Learning & Observation) at UIWSOM. The SIM Lab boasts a variety of mannequins with different purposes. Along with the mannequin that can simulate a live birth, there are mannequins you can perform surgery on, listen for various heart and lung diseases, use ultrasound to view various pathologies in 3D, insert IVs and central lines, as well as authentic trainers on which students can learn how to perform more sensitive but imperative exams, like breast and rectal exams, physical exams and pap smears.
Once students enter their clinical years, the more practice they have before having to perform clinical skills on real patients, the better. Alicia Cortez, the Clinical Outreach and Standardized Patient Manager of CIELO, emphasized, “Once student doctors go out into clinics and hospitals, they become part of the rapid response teams. Students need to know these skills now so they become more used to it, and are ready to go when the time comes.” When the mannequin actively complains

UIWSOM’s state-of-the-art simulation lab, featuring interactive mannequins capable of simulating critical patients and allowing medical students to simulate patient care.


of crushing chest pain and you can hear their shortness of breath, there’s much less pretending and much more focused assessment — it becomes so much more real. The experience breeds familiarity and allows students to handle the situation in a more professional and efficient manner. Graduates of UIWSOM find the simulations relevant and applicable to their experiences working as doctors in the field, and feel as if the simulated encounters strengthened their confidence for when the time came. If anything, Mark Zuniga, the Simulations Operations Specialist, claims that “learners don’t get enough.” With so many possible outcomes doctors come across, there is no such thing as too much practice.
As medical technology advances, so will the SIM Lab. As artificial intelligence becomes more prevalent in the field, the CIELO team hopes to incorporate the technology into the simulations. Right now, sights are on incorporating virtual reality so that student doctors can see through the birthing mannequin as the baby proceeds through the
UIWSOM’s simulation lab features high-fidelity pediatric mannequins capable of providing medical students with an opportunity to practice their pediatrics.
The simulation lab also contains 12 functional clinic rooms where medical students practice important clinical skills such as taking a history, performing a physical exam, and performing osteopathic manipulative medicine (OMM) as well as osteopathic manipulative treatment (OMT).
birthing canal so that they can better understand the mechanics of the birthing process. CIELO also is working on expanding the SIM Lab to its own building so that all of UIW’s health professional schools can use them and collaborate to simulate interdisciplinary teams that doctors rely on during their clinical practice. As the years pass, it will be exciting to see what vital skills medical students graduate with. After all, the mannequin is the limit.

Fatima Ali is a San Antonio resident and is currently a second-year medical student at UIWSOM.

Patryk Tomaszkiewicz is from Houston, Texas. He is a second-year medical student at UIWSOM interested in pursuing Radiology or Internal Medicine.

Dr. Ronald Rodriguez, a practicing urologist at UTHSCSA, was responsible for designing a partnership agreement with UTSA to help create a dual-degree program that allowed UTHSCSA medical students to enroll at UTSA to learn about artificial intelligence and earn a master's degree. After their third year of medical school, students are required to take a gap year to take master’s level courses at UTSA. After the gap year, students return to UTHSCSA to complete their fourth year of medical school as well as a capstone project for their master’s to then graduate with MD and MS in AI degrees.
This program was approved by both administrative offices and made official to UTHSCSA students in the spring of 2024. However, two students deserve credit for forging their own path back in the spring of 2023, when they helped work with Dr. Rodriguez and UTSA to begin the process of organizing the program. Those two students are Eri Osta and Aaron Fanous, and they have just graduated with both MD and MS in AI degrees.
What has the experience been like so far?
I struggled at first because I lacked experience in computer science and coding at the start of the program. I tried learning some python functions on my own and participated in a boot camp that taught me some of the basics about different machine learning models. On a conceptual level, I seemed to grasp most of the information well, but implementing these concepts into actual python code has definitely been the most challenging aspect of the program so far. Thanks to many resources that are available to me, including my classmates, friends, professors, the internet and chatbots like ChatGPT, I have been able to overcome my coding limitations so that I can do well in my courses.
What will this program look like in the future?
By the summer of 2025, three students will have graduated from UTHSCSA with dual-degree MD and MS in AI degrees. Many individuals agree that having any experience in AI will be beneficial
towards advancing their careers and their respective impacts that they can make on their field, but there are some reasons why students at UTHSCSA may shy away from enrolling in this program: It adds one extra year of classwork to the four-year medical school track; and students without a computer science background and prior coding experience may feel out of their depth, despite my experiences as evidence that it is still possible.
Nevertheless, I believe there will be a greater effort to accommodate students like myself who lack a computer science background and therefore would benefit from more dedicated time working with python and data analytics applications. This would likely help attract more students without prior coding experience to this dual-degree program so that it will continue to grow and provide more AI-capable professionals to the field of medicine.
What do you believe to be the value of this program?
Artificial intelligence is a powerful tool that will likely have a major impact on many career fields over the next 10 to 20 years. I personally feel that medicine, like many career fields, has its issues with providing equitable care to individuals of lower socio-economic status. This has been studied by many research groups around the world, with results showing some of the most disproportionate health outcomes to those of lower socio-economic background, which usually included ethnic minorities. Despite modern technological innovations and medicines that have given rise to many advanced healthcare methods, this issue of inequitable healthcare has remained.
That being said, I believe that AI can help us make a lot of progress towards addressing this serious issue. Inherently, the way machine learning models work is by analyzing data, studying the inherent patterns within the data, and arriving at a conclusion while trying to minimize any biases as much as possible. In healthcare, there is simply an abundance of data that is collected every day, and even every hour, about patients that guide healthcare providers to form plans of care. AI would help augment the capabilities of healthcare providers to evaluate a patient and determine what the next steps of care should be more effectively. Doing so would ideally help providers deliver more standardized care to individuals of any background and improve health outcomes in individuals of lower socio-economic status. There have been issues raised in the medical community about AI replacing jobs in healthcare, and I believe this to be a valid concern. I cannot say for sure what the extent of AI’s impact would be on the job availability within healthcare, but I still stand by my belief that its impact towards improving overall health outcomes while improving the efficiency of providers would be of much greater benefit than harm.
Once I enrolled in this program, I became particularly interested in the field of Interventional Radiology, a subspecialty within Radiology. Many experts would agree that computer vision models have already been developed and had a great impact on the field of Radiology
because many models have been accurate at diagnosing certain conditions like pneumonia and other diseases from plain-film chest X-rays and even CT-scans. The masking capabilities of computer vision models have helped oncologists to accurately outline tumors in the body to improve the precision with which we can surgically remove cancer without harming healthy tissue. I would like to further advance computer vision models by training them on different data that has not been used before. Particularly, my capstone project will focus on using CT angiograms to map out arteries in different parts of the body. This would have future applications for trauma teams that need to address arterial injuries or oncology teams that are studying blood flow to tumors in the body. As a practicing physician, I hope that my experience with AI and medicine will allow me to help develop more AI applications and technologies that hospitals can use to provide more standardized and equitable care for their patients.
How will you transition back to medical school?
I will be finishing my coursework and resume medical school in July. I will be completing my fourth-year responsibilities such as applying for residency and interviewing whilst I complete my capstone project, which is a master's degree graduation requirement.
I think taking time away from medical school can be challenging because I feel like I was in a good rhythm with regards to understanding my medical responsibilities as I began transitioning from thinking like a medical student to thinking like a resident physician. However, I am confident that once I put in some time and effort to re-familiarize myself with the medical knowledge, I should be able to match the level of competence of the other fourth-year students. The learning curve exists, but I do not expect it to be too challenging.

Ronald Rodriguez, MD, PhD, is the Henry B. and Edna Smith Dielmann Memorial Professor of Urologic Science at the UTHSCSA. Dr. Rodriguez is a highly experienced urologic surgeon with expertise in urologic oncology, particularly focusing on prostate and kidney cancer, and a world expert in the use of cryoablative technologies for kidney and recurrent prostate cancer. Dr. Rodriguez is a member of the Bexar County Medical Society.

Niklesh Akula is a third-year medical student at the University of Texas Health Science Center at San Antonio, class of 2025.
The University of Texas Health Science Center at San Antonio’s Military Health Institute (MHI) was created in 2014 to enhance collaboration with the Department of Defense (DoD) and Veterans Administration (VA). As a healthcare leader in San Antonio — also referred to as Military City, USA — the university, also called UT Health San Antonio, understood the need to partner and promote military health. The mission of the Military Health Institute is to enhance the military health research, education and clinical activities of UT Health San Antonio, improving the lives of our military service members, veterans and their families. The university understands the complexity and challenges to the military health system, and the MHI is actively working collaboratively with partners across the U.S. to help address those challenges.
In the 10 years since its inception, MHI has advanced a military health focus across the university. The institute has instilled a heightened interest in DoD and VA research. Since 2014, faculty at UT Health San Antonio have earned over $86 million in DoD health research funding. The institute contributes to many initiatives for the university including a number of leading initiatives.
The Distinguished Lecture Series is a recurring event that hosts senior military leaders and emerging researchers who are making an impact in military health. Historically occurring in both the fall and spring semesters, the Distinguished Lecture Series has provided meaningful networking opportunities for researchers and community leaders interested in collaboration. Retired Air Force Maj. Gen. Byron Hepburn, MD, FAAFP,
the associate vice president and director of the Military Health Institute, describes the lecture as “a special opportunity for anyone wanting to collaborate with innovators and emerging scientists who globally impact military health.” Past lectures have included directors of the Defense Health Agency, such as retired VADM. Raquel Bono and retired LTG. Ron Place, as well as retired Army surgeon general and former secretary of Veterans Affairs, James Peake, MD.
The Joe and Patty Robles Endowed Postdoctoral Fellowship in Military Health offers an opportunity for emerging scholars to participate in research that impacts military health. The past fellows have helped to shape the way we serve the military community. For example, Roxana Delgado, PhD, MS, a tenured professor and scholar of military research in the UT Health Science Center’s School of Nursing, and the current director of the Caring for the Caregiver program, boosted her career at UT Health Science Center San Antonio as the MHI’s first postdoctoral fellow. She has contributed nationally through her scholarship and input to the 2014 RAND Report, Hidden Heroes: America’s Military Caregivers, and the 2023 Caring for Veterans and Their Families: A Guide for Nurses and Healthcare Professionals.
Sponsored by the MHI, The Military Health Interest Group (MHIG) is a student led organization that provides educational opportunities for students interested in military health. These opportunities — events, networking and volunteering — provide insight into the world of military health. MHIG has conducted programs such as a wounded warrior panel discussion, where students, faculty and staff learned about caring for this important population. Most recently, a panel discussion on DoD-funded research showcased student opportunities to conduct research. The current MHIG president, a first-year medical student, Air Force 2nd Lt. Omar Valencia, explains, “MHIG is focused on connecting students to military opportunities to not only increase their understanding of the military, but to also spark their career interest in serving our military, veterans and their families.”

The Trauma Research and Combat Casualty Care Collaborative (TRC4) is a recent research initiative. MHI played an important role in the strategic planning and institutional
development stages of TRC4. This initiative has brought research funding to the university and The University of Texas System, and has broadened faculty and student opportunities to conduct military health research. The executive director of TRC4 stated, “MHI has been an integral part of the success of TRC4 and continues to show great value as a long-term collaborative partner.” MHI assisted the university in obtaining over $20 million to fund these initiatives and continues to work collaboratively to ensure their success and longevity at the university.
The Veteran and Caregiver Health Partnership (VCHP) leverages UT Health San Antonio resources to create health programs for the military-affiliated community. These programs are in partnership with UT Health Science Center San Antonio schools and centers such as the schools of medicine, nursing and dentistry, and the Mays Cancer Center, as well as with the South Texas Veterans Affairs Social Work Services. Program manager, Micah Wright, PhD, explains: “forming partnerships with other schools and community resources that are interested in serving this population is the first step in making a bigger impact for the military affiliated community, especially those who live in areas with less access to health services.” The partnership will pilot two events this summer: The Mays Cancer Center Listening Sessions and the Veteran and Caregiver Health Resource Fair at the Kerrville VA Medical Center. Both events are aimed at not only providing support, but also to find innovative ways of improving healthcare for military-affiliated populations.
Over the last 10 years, the Military Health Institute has significantly enhanced UT Health San Antonio’s focus on military health. In the next 10 years, the MHI will continue to be a catalyst and academic leader, enhancing efforts to revolutionize combat medicine and veteran and caregiver care. The military landscape is continuously changing, and the associated medical threats to our service members, veterans and their families require innovation. MHI will foster that innovation and help conquer the challenges that lie ahead to best serve our active military and veteran communities.



Testosterone Replacement Therapy (TRT) continues to grow in popularity thanks to radio, internet and social media advertisements and testimonials. Its initial popularity in the realm of men’s fitness has expanded to include promises that often are misstated and negative impacts when use escalates without appropriate monitoring and management.
Often physical results drive its use absent informed management. Testosterone’s currently accepted medical use in the United States is focused on testosterone deficiency (hypogonadism), but it must be strictly monitored. Testosterone can be administered via injections, topical gels, oral pills and even subdermal pellets. All therapies can be very effective in bringing patients back to a eugonadal state. Management remains essential.
Testosterone is an essential hormone for males produced primarily in the testicles and is required for differentiation, developmental growth, and maintenance of phenotype; namely.
• Bone density
• Fat distribution
• Muscle strength and mass
• Facial and body hair
• Red blood cell production
• Sex drive
• Sperm production
Testosterone levels generally peak during adolescence and early adulthood. As men age, the testosterone level gradually declines — typically about one percent per year after age 30 or 40. For older men, it is important to determine if a low testosterone level is due to normal aging or if it is due hypogonadism.6
Hypogonadism hampers the ability to produce normal amounts of testosterone due to a problem with the testicles (primary hypogonadism) or with the pituitary gland (secondary hypogonadism). Multiple treatment modalities exist for this condition and can greatly and effectively treat symptoms in these men.
Testosterone use in the United States has tripled from 2001 to 2019, mostly in men without a clear medical indication for its use.1,6 Some studies have estimated that up to 25 percent of men receiving TRT have not even had their initial T level checked prior to initiating therapy, and nearly half of those individuals do not have their levels checked after initiating therapy. It is also estimated that up to a third of these men do not meet the criteria to be diagnosed as testosterone deficient.2,3

Clinicians should make a proper diagnosis of testosterone deficiency (TD) with both a low testosterone level and the presence of select symptoms, such as reduced energy, poor libido, reduced endurance, fatigue, depression, poor concentration or changes in erectile function. The American Urological Association (AUA) defines the presence of TD as a testosterone level consistently lower than the threshold of 300ng/dL on at least two consistent serum levels, obtained early in the morning.3 Men’s T levels are naturally highest in the morning, so most insurance care plans will not cover therapy unless two morning T levels are obtained.
Other patients who could consider screening for TD include patients with a history of unexplained anemia, bone density loss, diabetes, exposure to chemotherapy, exposure to testicular radiation, HIV/AIDS, chronic narcotic use, male infertility, pituitary dysfunction or chronic corticosteroid use. These are targeted patients, and do not necessarily need to have symptoms and signs of TD.3
Unfortunately, it is all too common for some younger men who have been diagnosed with TD, to be placed on improper therapies. Any younger male wishing to maintain his fertility should absolutely not be placed on any form of exogenous TRT, without consulting with a urologist. Patients with TD desiring fertility should initially have their serum FSH (follicle stimulating hormone), LH (luteinizing hormone) and prolactin levels checked. FSH is responsible for intrinsic production of sperm, while LH is responsible for the production of testosterone. By measuring these, it can help the practitioner differentiate between primary and secondary hypogonadism, and therefore provide the proper treatment.
Prolactin levels should be considered in the screening of young male patients as well. Persistently elevated prolactin levels could possibly indicate the presence of pituitary tumors, such as prolactinomas, and the patient should be referred to an endocrinologist for further evaluation. For patients presenting with a Total T level <150ng/dL and a low LH, a pituitary MRI should be done regardless of prolactin levels to properly identify pituitary adenomas.3,4
Lastly, a baseline PSA, hemoglobin and hematocrit should be obtained prior to starting any therapy. TRT commonly stimulates the production of red blood cells (polycythemia). If the patient’s baseline Hct is >50 percent, then TRT should be held until the etiology is formally investigated. Secondary polycythemias caused by TRT can easily
place patients at an increased risk for cardiovascular complications like stroke and heart attack. PSAs should be measured as well, as the initiation of TRT can cause an elevation of the PSA. Elevated PSAs prior to induction of TRT raise concern for the possibility of an occult prostate cancer and need stronger evaluation before proceeding with TRT.
Injectable Testosterone: The most common form of TRT still remains injectables. Testosterone Cypionate and Enanthanate are very commonly prescribed by practitioners. They are affordable and easy to titrate. The AUA recommends starting patients at 100mg of either agent, once a week. It is sometimes given as 200mg every other week, but this should be discouraged, as the risk of polycythemia increases and persists longer when given in larger doses. If administered in this manner, the patient tends to feel great for the first week, then “crashes” the next. It can create a rollercoaster effect on the patient.
Newer studies are showing that T Cypionate and T Enanthanate can be given subcutaneously instead of intramuscular. This tends to be gentler on the body and does not typically cause polycythemia because of the absorption route. T Cypionate is easier to inject SQ vs Enanthate due to its carrier oil. Testosterone Cypionate uses olive oil as its carrier. Olive oil is far more fluid than sesame oil, almost like water, so it is a preferable choice in administering TRT via the subcutaneous route as it is less likely to congeal and is a more effective delivery system.5
Topical Therapies: Topical ointments can also be used. These have been around for quite some time, are easy to apply and tend to work best in the older population. As therapies evolve, the choice of medication treatments often is dictated by the insurance carrier. Most topical testosterone solutions come in a generic formulation, so authorization tends to be easier to obtain. However, these should be avoided in men who come into close contact with grandchildren or children in general, as the risk of contact transference is high.
Oral Options: There are currently three different types of oral testosterone formulations. They are listed as Tlando, Jatenzo and Kyzatrex. These are all newer medications, so a generic is not available. They are a good option for the patient who has needle phobia or just prefers an oral route. Previous oral formulations were found to cause hepatotoxicity and were removed from the market. These new formulations avoid the hepatic first pass system, and are absorbed directly within the small intestine, so they should be taken with food.
Subdermal Testosterone Pellets: Testosterone subdermal pellets are also a great option for the patient who does not like injections and is looking for a long-term simple TRT option. Pellets are inserted under the skin in the buttock area and slowly release testosterone into the body over the course of four or five months. Once in place, they do not need to be removed and absorb over time. Testopel is the only FDA-approved subdermal testosterone replacement therapy. These can be done in the urology office in about five minutes. Patients are usually very satisfied with the results and convenience factor.
It is not uncommon to see young men of childbearing age who have been improperly treated with TRT, placing them at risk for issues with infertility. Exogenous testosterone shuts down the hypothalamic-pituitary-gonadal (HPG) axis, and can shut down natural spermatogenesis.
These patients may be offered the medication Clomid, which is a nonsteroidal stimulant. This acts on the pituitary gland to stimulate more natural production of FSH and LH and causes intrinsic production of testosterone while preserving fertility. A standard dose is 50mg daily PO, but can be increased to 75mg PO daily, based on the patient's weight and lab results.
References:
1. Baillargeon, J, Urban, RJ, Ottenbacher, KJ, Pierson, K & Goodwin, JS. (2013). Trends in androgen prescribing in the United States, 2001 to 2011. JAMA Internal Medicine, 173(15), 1465. https://doi.org/10.1001/jamainternmed.2013.6895
2. Baillargeon, J, Urban, RJ, Kuo, YF, Holmes, HM, Raji, M, Morgentaler, A, Howrey, B, Lin, YL & Ottenbacher, KJ. (2015). Screening and monitoring in men prescribed testosterone therapy in the U.S., 2001–2010. Public Health Reports, 130(2), 143–152. https://doi.org/10.1177/003335491513000207
3. Mulhall, JP, Trost, L, Brannigan, RE, Kurtz, EG, Redmon, JB, Chiles, KA, Lightner, DJ, Miner, M, Murad, MH, Nelson, CJ, Platz, EA, Ramanathan, L & Lewis, RW. (2018). Evaluation and Management of Testosterone Deficiency: AUA Guideline. The Journal of Urology, 200(2), 423–432. https://doi.org/10.1016/j. juro.2018.03.115
4. Citron, JT, Ettinger, B, Rubinoff, H, Ettinger, VM, Minkoff, JR, Hom, F, Kan, PB & Alloo, R. (1996). Prevalence of Hypothalamic-Pituitary Imaging Abnormalities in Impotent Men with Secondary Hypogonadism. The Journal of Urology, 155(2), 529–533. https://doi.org/10.1016/s0022-5347(01)66441-3
5. Choi, E, Xu, P, Barham, DW, El‐Khatib, FM, Yafi, FA & Kavoussi, P. (2022). Comparison of Outcomes for Hypogonadal Men Treated with Intramuscular Testosterone Cypionate versus Subcutaneous Testosterone Enanthate. The Journal of Urology, 207(3), 677–683. https://doi.org/10.1097/ ju.0000000000002301
6. Park, HJ, Ahn, ST & Moon, DG. (2019). Evolution of guidelines for testosterone replacement therapy. Journal of Clinical Medicine, 8(3), 410. https://doi.org/10.3390/jcm8030410

Matthias D. Hofer, MD, PhD, is a board-certified urologist at Urology San Antonio’s Men’s Health and Wellness Clinic. He sees a variety of patients ranging from general urology concerns to reconstruction and trauma. After completing his six-year residency in Urology at Northwestern University in Chicago, Dr. Hofer specialized further in one of the country’s top-ranked fellowships for Urologic Reconstruction, Trauma, and Prosthetics at UT Southwestern in Dallas. He also completed a three-year residency in Pathology at Harvard and earned a PhD. Dr. Hofer is a member of the Bexar County Medical Society.

D. Scott Christensen, RN, MSN, ACNP-BC, treats men’s general urologic health concerns at Urology San Antonio’s Men’s Health and Wellness Clinic at the Medical Center location. Scott earned his Acute Care Nurse Practitioner degree from the University of Texas Health Science Center San Antonio in 2013 and has worked exclusively in Men’s Health for Urology San Antonio since that time.
Books come to this page primarily from readers’ suggestions. The recent focus on Artificial Intelligence here and throughout the medical community prompted a member to suggest David Brooks’ “How to Know a Person: The Art of Seeing Others Deeply and Being Deeply Seen” for curative contrast.
Indeed. By page 10, the author writes, “Artificial intelligence is going to do many things for us in the decades ahead, and replace humans at many tasks, but one thing it will never be able to do is to create person-to-person connections. If you want to thrive in the age of AI, you better become exceptionally good at connecting with others” (emphasis added).
Brooks, a New York Times Editorial Page writer, has covered social, economic, arts and political issues for The Wall Street Journal, The Weekly Standard, Newsweek, The Atlantic Monthly, NPR and the PBS NewsHour as well. His thirty-thousand-foot view sees our social fabric fraying under stress and repeated shocks. He also recognizes that, as a writer with significant voice and some agency, he was obligated to analyze it more closely, and suggest ways to ameliorate — to repair the fabric, reweaving where needed.
“The purpose of this book,” writes author David Brooks, “is to help us become more skilled at the art of seeing others and making them feel seen, heard, and understood.”
In his 40 years of journalism, Brooks has interviewed and profiled hundreds of luminaries. “When I started research on this subject,” writes Brooks, “I had no clue what this skill consisted of. But I did know that exceptional people in many fields had taught themselves versions of this skill.”
“The purpose of this book,” writes author David Brooks, “is to help us become more skilled at the art of seeing others and making them feel seen, heard, and understood.” “ “
““Artificial intelligence is going to do many things for us in the decades ahead, and replace humans at many tasks, but one thing it will never be able to do is to create person-to-person connections. If you want to thrive in the age of AI, you better become exceptionally good at connecting with others.”
He goes on to detail his exploration that led to an understanding of the social dynamic of people acting as either Diminishers or Illuminators.
“Diminishers make people feel small and unseen … They stereotype and ignore,” Brooks writes. “Illuminators, on the other hand, have a persistent curiosity about other people … They shine the brightness of their care on people and make them feel bigger, deeper, respected, lit up.” These are the forces that stress and tear at our fabric, the author feels. Rather than overgeneralize, Brooks takes a deep dive into the characteristics that comprise these types:
Distinctive among Diminishers is behavior marked by Egotism (“The number one reason people don’t see others is that they are too self-centered to try); Anxiety (“… too much noise in their own heads, can’t hear what’s going on in others”); Naïve Realism (assuming the way the world appears to you is the same for everyone); The Lesser-Minds Problem (a person’s assumption of being deeper, more interesting, more subtle and more high-minded than others); Objectivism (observing but not participating; judging and measuring but not involving); Essentialism (stereotyping from generalizations); and The Static Mindset (unwillingness to recognize that people change in time).
In defining and understanding Diminisher behaviors, a certain amount of self-reflection — inventorying one’s own behavior — is natural; fortunately, the author is extremely articulate in defining without advising — simply pointing out features that have become too common in public discourse.
Brooks then moves on to define Illuminators and their characteristics, beginning fortuitously with an example just up the road in Waco in a journey to find the kind of people who knit towns and neighborhoods together — people “who drive civic life.” The characteristics of Illuminators require fewer explanatory notes, as qualities to which I believe we each aspire: Tenderness; Receptivity; Active Curiosity; Affection; Generosity; and A Holistic Attitude.
Brooks writes that we deal too much in abstraction and that, “The real act of building a friendship or creating a community involves performing a series of small, concrete social actions well … these are some of the most important skills a human being can possess, and yet we don’t teach them in school. Some days it seems like we have intentionally built a society that gives people little guidance on how to perform the most important activities of life. As a result, a lot of us are lonely and lack deep friendships. … And a life spent on social media is not exactly helping people learn these skills.”
The rest of the book compiles examples of putting these virtues into action, particularly in learning to express authentic compassion for those suffering or hurting; and heartfelt joyfulness for those marking achievement.
But is the read worth your time; moreover, are these tools necessary to those in the medical community?
“Considering that all patients are individual humans with foibles and particular ways of being, knowing and processing information,” said a career nurse I know who had read Brooks’ book enthusiastically, “the better a healthcare professional can listen to the level of articulation and read the nonverbal clues, the better they will communicate medical findings in the most advantageous way.”
This former head of hospice nursing is now navigating How to Know a Person’s companion workbook, designed by Brooks for those wanting “exercises, reflections, and actionable steps designed to enhance your ability to connect authentically.” More than a diagnosis of society’s post-pandemic condition, Brooks provides a manual of therapies and a course of recuperation — the very warp and woof needed for a reweaving.

David Alex Schulz is certified in HIPAA privacy and security compliance, and a contributing writer to San Antonio Medicine magazine.
Phil Hornbeak, Auto Program Director for Bexar County Medical Society (BCMS), recently celebrated his 20th anniversary with the organization. I sat down with Phil to gain some insight into his long-standing service to BCMS along with his professional and personal growth over the last 20 years.
Describe the different offices/buildings you have been in the past 20 years.
When I started, BCMS was at the building on W French Place, which was a little “long of tooth,” needing repair and lacking elbow room. Then we moved to the IH-10 office building while a search for a new location was done, and eventually, our current building was built; it worked well for the time we leased the space. The final move was to our new building at 4334 N Loop 1604 W, which was built from the ground up, is an absolutely beautiful building and a great space. The current building is purpose-built with every space accounted for. It even has lights built into the sides, specifically for the annual BCMS Auto Shows; its unbelievable.
How has BCMS changed in the last 20 years?
As the world has changed to a digital format, so has BCMS. Gone are the expensive mail campaigns. Gone is expensive fax usage. We talk through the internet face-to-face, which is an amazing advancement in a 20-year time period.
Why have you stayed for 20 years?
I had always worked in the automotive and financial industry, but learned about BCMS through my brother, who was the CEO of the Methodist Healthcare System at the time. I had recently moved to Texas and ultimately stayed at BCMS because it is “Home.” I also enjoy the “big city, small town” feel that San Antonio offers.
How has your life changed in the past 20 years?
There have been more life-changing events in 20 years than I had ever expected: loved ones and co-workers passing, massive changes to the city, and new challenges each day. It has been “Life” with a capital “L.”
Tell us about the BCMS Auto Show.
I have managed the BCMS Auto Show for the last 20 years and enjoy the fellowship with our members. The auto dealers that participate in the BCMS Auto Program bring vehicles to display around the BCMS building for the attendees’ viewing pleasure. This year is the 38th annual Auto Show which, as always, will have 100+ new automobiles of all makes and models, live music and food. It truly is a must-attend event, and if you attend, you’ll see our special lighting.
Do you have any favorite projects you’ve worked on during your time here?
My favorite projects have been the Auto Show and adding Travis and Harris counties to the Auto Program. By agreement, both Travis and
Phil Hornbeak, Auto Program Director, BCMS, and Melody Newsom, CEO/Executive Director, BCMS

Harris counties have been installed into the Auto Program. Over the past few months, I’ve worked diligently on revitalizing the program and am really looking forward to seeing it all come together.
What do you like most about BCMS?
Overall, there has been seamless leadership for the entirety of my time here. It is as it should be — honest, fair and balanced. Do your job and help the team to the best of your abilities. There is truly a sense of trust, respect and kindness among the staff.
What are your favorite memories from your time here thus far?
The employees at BCMS. Great friends, lunch buddies and family members!
How would you describe our company’s culture?
The culture is at a professional level that is expected due to the high standards of our physicians. BCMS adjusts to the needs of its members quickly and with the care to uphold standards.

Melody Newsom is the CEO/Executive Director for the Bexar County Medical Society. She has been with the company for 24 years.
“The Masks We Wear”

Watercolor and color pencil.


Her body her worst enemy, a cruel comedy. A fate written in her genes but never justified. Blistering the skin, disfiguring the nails, a pain unbearable. A syndrome of fragile skin not of fragile soul. Each day she chose smile over cynicism, laughter over languish. When it hurts, she laughs when she laughs, she lives.
Class of 2026
Long School of Medicine UT Health San Antonio Aamerah Haque

This poem is dedicated to a patient who suffers from a terrible skin disease. At her worst moments, she laughs through her pain to maintain a positive outlook.
 By Akash Sharma, Class of 2024, Long School of Medicine, UT Health San Antonio
By Akash Sharma, Class of 2024, Long School of Medicine, UT Health San Antonio
A beaming couple watches in awe, As their newborn takes his first breath. A cancer patient receives her weekly infusion, Wondering how much time she has left.
A teenage boy smiles, The doctor declares, “You’re all set to leave!” An elderly man says goodbye to his wife, Unprepared to grieve.
A weary resident sighs, Enters her final note of the shift. Estranged siblings visit their mother, Healing a deep-seated rift.
A young girl weeps, She’s never known this kind of pain. Her father silently asks, “How will I manage this financial strain?”
A wide-eyed medical student, I walk through the trauma bay. What immense privilege and responsibility, Caring for these delicate lives today.
A reminder to all in healthcare of the weight of our daily encounters and why we do what we do. I wrote this as I was stressed about beginning clinical rotations and began to reflect on how many lives are touched at University Hospital each day.

By Charlotte Clark, Class of 2026, Long School of Medicine, UT Health San Antonio.
There’s a saying in Vietnamese: uống nước nhớ nguồn. When drinking water, remember its source. Thanks to you, my water is different –it is no longer a torrent fighting for survival in a new region. Instead, it is healing and calm. But when my patients drink from me, I hope they are reminded of you.
I wrote this story for immigrant parents whose children embody their dreams.
 By Andrew Ta, Class of 2026, Long School of Medicine, UT Health San Antonio. Andrew is a member of BCMS Publications Committee.
By Andrew Ta, Class of 2026, Long School of Medicine, UT Health San Antonio. Andrew is a member of BCMS Publications Committee.
(a haiku on the impact of our first patient)
Teaching through silence. Gift of self, life’s final act to erase disease.
A tribute to the first patients of each medical student - the impact of whom is long withstanding.

By Mujtaba Khandoker, Class of 2027, Long School of Medicine, UT Health San Antonio.
Because it’s all I know, because I want to help, because I love learning, because they told me it’d be too hard, because mom taught me to love, because I want to be like dad, because I already drank 500mg of caffeine, because God asked me to, because the family expects it, because if I stop, I’ll feel guilty, because I want to be better, because they’re depending on me to provide, because I have to pass this class, because I hope to inspire others like me, because I feel like I have to, because I can’t sleep, because my wife believes in me, because I’ve been given an opportunity, because change is overdue, because the future is bright.
Because…
I wanted to write something to describe my values and experiences when it comes to why I study every day and why I chose this career. I often think that, and I think a lot of my classmates do, too. I don’t want anyone to feel like they’re the only one juggling all these different stressors and motivations.
 By Jose C. Gaspar de Alba, Class of 2025, Long School of Medicine, UT Health San Antonio.
By Jose C. Gaspar de Alba, Class of 2025, Long School of Medicine, UT Health San Antonio.

During the TexMed 2024 conference, BCMS representatives met with Cale Perry, a medical student at UT Health San Antonio Long School of Medicine. There, Perry had brought a poster summarizing Project HEART, a health literacy initiative, for TexMed’s annual Poster Session. The TexMed Poster Session is an opportunity for physicians and medical professionals to share their successes and breakthroughs in improving patient care with their peers from around the state.
The team behind Project HEART is a group of first and second-year medical students from both the University of Texas Health Science Center at San Antonio Long School of Medicine and the University of the Incarnate Word School of Osteopathic Medicine. The project was initially started by Karen Liu, a current fourth-year medical student, in the fall of 2022.

Project HEART was created to educate and improve the health literacy of 3rd graders in San Antonio as an effort to prevent heart disease. More specifically, Karen Liu, the project’s founder, wanted to reach areas of San Antonio that do not typically benefit from our school’s community projects due to their distance from UTHSCSA. Heart disease is very common within the San Antonio population and can develop for many years before patients experience symptoms. While its development and progression are multifactorial, the goal of Project HEART was to address some of these factors by educating children on the importance of healthy dietary and exercise practices. By educating patients at a young age, Project HEART aims to instill life-long habits that reduce their risk of heart disease and make them happier and healthier as a whole.
Project HEART was implemented through a 6-lesson curriculum at Bob Hope Elementary over the period of six weeks, from October through mid-November of 2023. Each lesson was approximately an hour long. The curriculum focused on three primary areas: heart anatomy, dietary choices and exercise, with each subject split into two sections. The medical students also included interactive components to keep the students engaged and make learning fun. These components included having the students color diagrams of the pathways of oxygenated and deoxygenated blood through the “heart house” (a metaphor comparing heart anatomy to the rooms and doors of a home), building stethoscopes out of paper towel rolls and funnels to listen to each other’s hearts, and actively doing exercises, such as jumping jacks and pushups, together as a group.
To record results, the elementary students were surveyed before and after the lessons to evaluate the change in their knowledge of heart health. Project HEART focused on evaluating student knowledge of heart anatomy, nutrition and exercise. In all three subjects, the medical students observed a statistically significant increase in median scores between the pre- and post-lesson survey, indicating that the
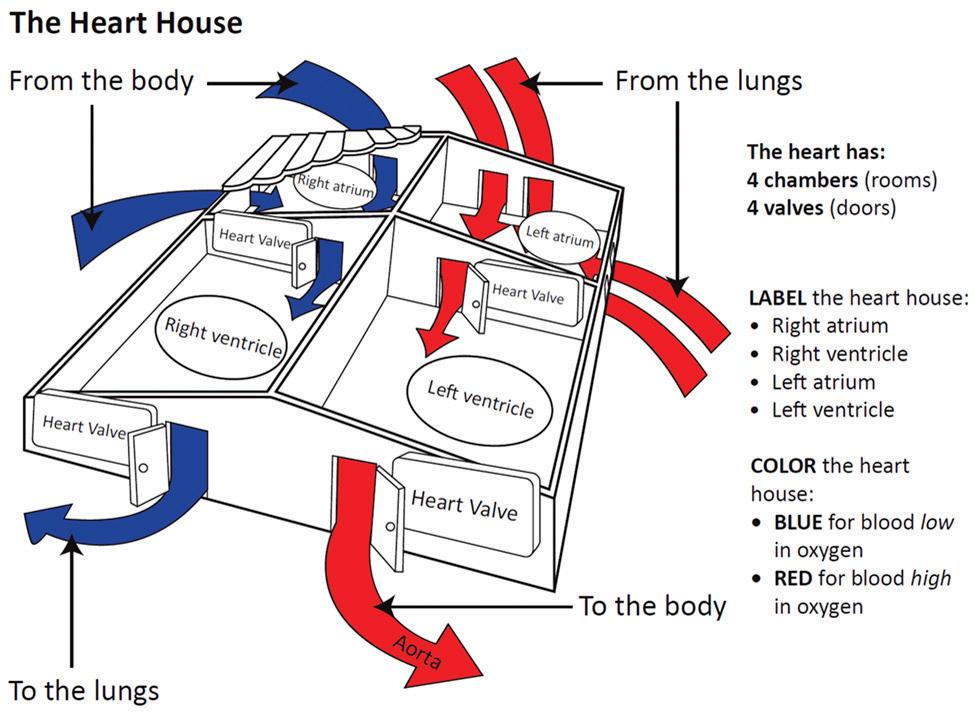
elementary students had learned from the curriculum. Differences in scores between English-speaking and Spanish/Bilingual-speaking students were also evaluated. San Antonio has a significant Spanish/ Bilingual-speaking population; therefore, the Project HEART creators worked to implement a curriculum that was equally accessible and effective for that population. In the pre- and post-surveys of all three subjects, there was not a statistically significant difference in the median scores of English-speaking versus Spanish/Bilingual-speaking students. This suggests the curriculum had equally effective outcomes for both of these student groups.

As for the future of Project HEART, there are plans to continue its implementation at Bob Hope Elementary for next year’s group of 3rd graders. Additionally, as Project HEART works to recruit more volunteers, they hope to expand the program to other schools and educate even more students

Gabriella Bradberry is the Admin/Communication Specialist for the Bexar County Medical Society.
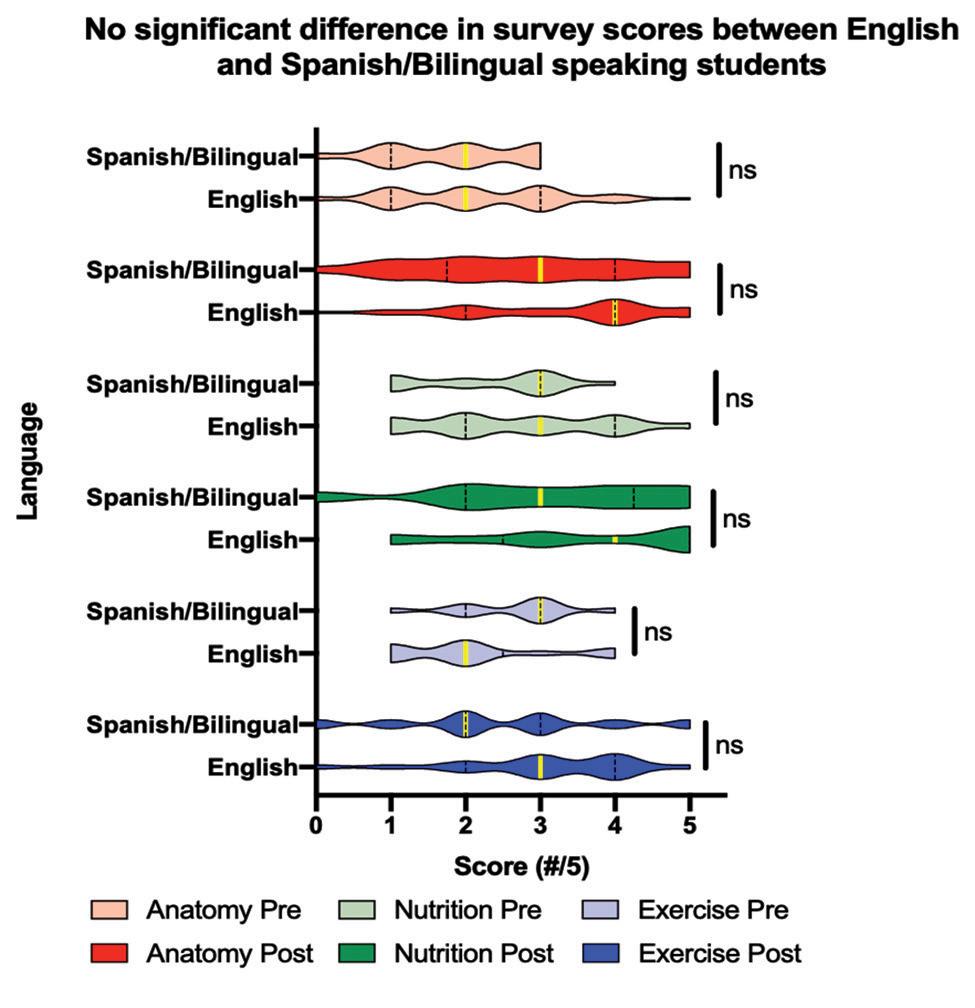
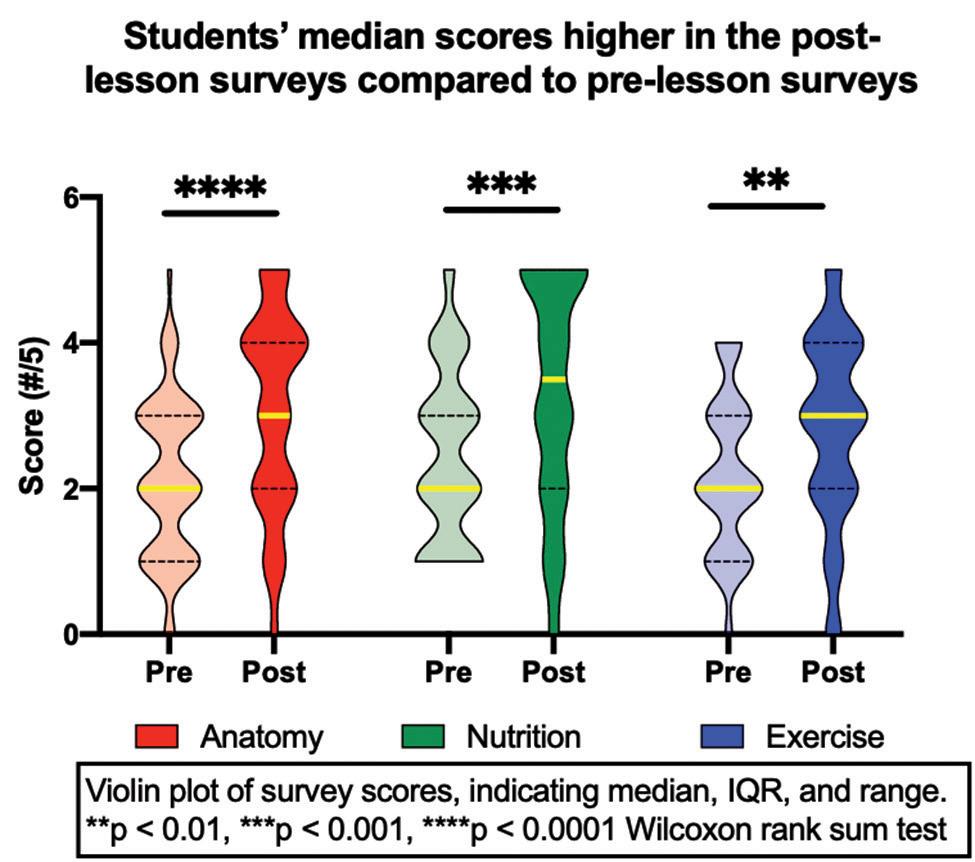
TexMed is TMA’s largest annual conference, and this year’s conference took place in Dallas, Texas on May 2-4. It is an opportunity to network with physician leaders, explore CME tracks, and enjoy two keynote presentations. Attendees can also find an Expo Hall full of the latest technologies, services and product knowledge.
During this year’s TexMed conference, BCMS physicians participated in a wide array of committees that discussed all aspects of health issues and policy affecting the daily honored practice of medicine.
This year’s conference ended with the exciting announcement of TMA’s newest President-elect and TMA Alliance President, who are two of Bexar County’s own. San Antonio internist and hyperbaric medicine specialist, Jayesh “Jay” Shah, MD, was announced as President-elect. Dr. Shah is the first Indian American TMA President-elect and will serve as TMA’s 160th president in 2025. Another representative of Bexar County, Jenny Shepherd, began her presidency of the TMA Alliance during this year’s TexMed. Ms. Shepherd is a long-time advocate of medicine. Bexar County Medical Society is elated to have two of our very own as leaders of the Texas Medical Association.

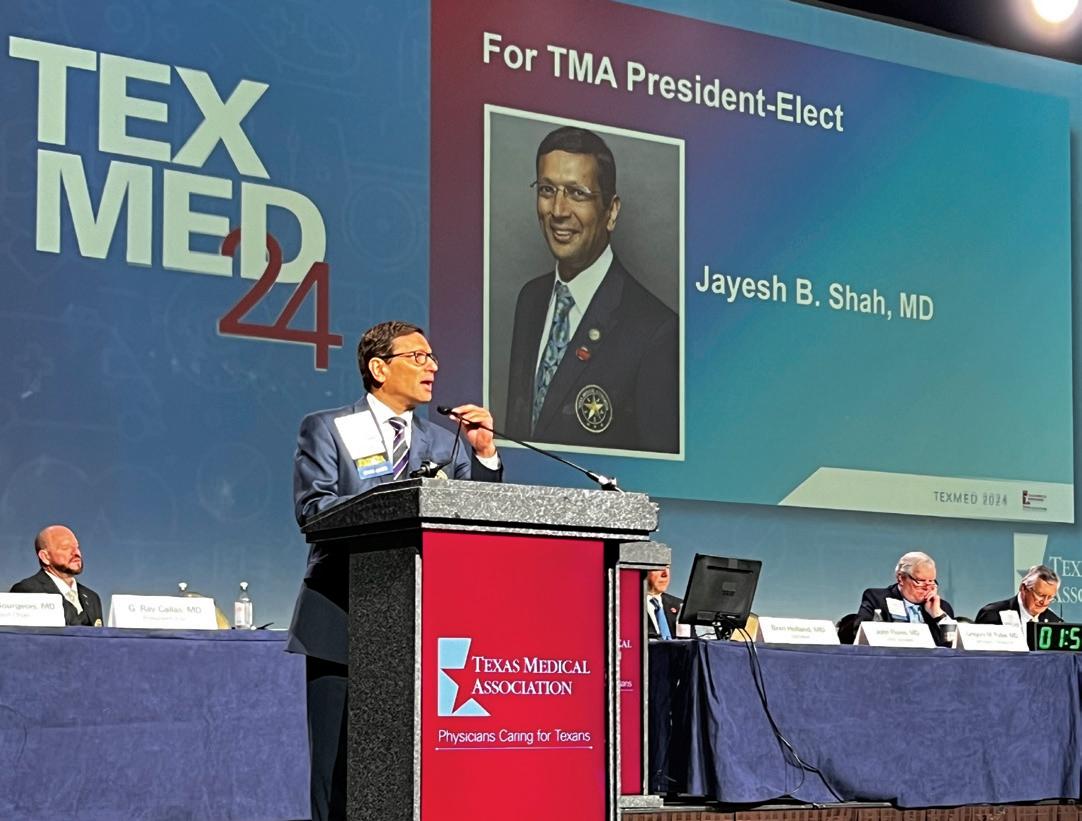



We encourage you to use our friends of medicine businesses whenever you or your practice need supplies or services.

Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 CDavis@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”

Aspect Wealth Management (★★★ Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark
President
210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”

Broadway Bank (HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@Broadway.Bank www.broadwaybank.com
“We’re here for good.”

The Bank of San Antonio (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state
who specialize in medical malpractice and all lines of insurance for the medical community.
Brandi Vitier 210-807-5581
Brandi.Vitier@thebankofsa.com www.thebankofsa.com
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking 210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking 210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help physicians get the banking services they need.
Synergy FCU Member Services 210-750-8333
info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”

Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison
210-503-0003
Yulia@genicslabs.com
Kevin Setanyan Managing Partner
210-503-0003
Kevin@genicslabs.com
Artyom Vardapetyan
Managing Partner
210-503-0003
www.genicslabs.com
“Accurate results in record time.”
Livingston Med Lab (HH Silver Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease and Genetics.
Robert Castaneda CEO 210-316-1792
Robert@livingstonmedlab.com
www.livingstonmedlab.com/home
“Trusted Innovative, Accurate and STAT Medical Diagnostics”

American Health Imaging (★★★ Gold Sponsor)
American Health Imaging (AHI) has 5 state-of-the-art imaging centers in San Antonio, TX with industry- boardcertified subspecialized radiologists delivering precise, reliable results. Easy scheduling and prompt report turnaround times, serving both physicians and their patients. Imaging at AHI is priced up to 60% less than hospitals and in-network with 99% of health plans with competitive rates to save patients money. AHI has an additional 37 best-in-class diagnostic imaging facilities in Alabama, Florida, Georgia, Texas and South Carolina. US Radiology Physician Number 210-572-1211
Casey Allen
Regional Sales Director | San Antonio US Radiology Specialists 210-846-0606
Casey.Allen@usradiology.com
Jasmine Mendoza
Jasmine.Mendoza@usradiology.com
Jaime Zamora
Jaime.Zamora@usradiology.com
Sydnie Caradec
Sydnie.Caradec@usradiology.com
Sarah McMindes
Sarah.Mcmindes@usradiology.com
Scott Roberson
Scott.Roberson@usradiology.com
Ryan Denman
Ryan.Denman@usradiology.com www.americanhealthimaging.com (main site) www.americanhealthimaging.com/ physician-resources/ (Physician Resources to refer to American Health Imaging)


Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for healthcare entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com www.bexarcv.com
“Proudly serving the medical community since 1998”
Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA Senior Private Wealth Advisor 512-649-8113 Service@oakwellpwm.com www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney Financial Advisor
210-858-5880
Elizabeth.Olney@edwardjones.com www.edwardjones.com/elizabeth-olney "Making Sense of Investing"

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com
www.aspectwealth.com
“Your wealth. . .All aspects”

Hancock Whitney (HHH Gold Sponsor)
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services.
www.hancockwhitney.com
John Riquelme
San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Larry Anthis Corporate Banking, Relationship Manager 210-507-9646
Larry.Anthis@hancockwhitney.com
Serina Perez San Antonio Business Banking 210-507-9636
Serina.Perez@hancockwhitney.com
Erik Carrington Texas Regional Wealth Management Manager 713-543-4517
Erik.Carrington@hancockwhitney.com

Conviva Care Center (HHH Gold Sponsor)
Conviva’s value-based care model allows physicians to deliver high quality,
personalized care and achieve better outcomes, while feeling free to focus on health equity and patient outcomes.
Kim Gary
Senior Physician Recruiter 812-272-9838
KGary4@humana.com
www.convivacareers.com
“Fuel Your Passion & Find Your Purpose”

UT Health San Antonio
MD Anderson Cancer Center
(HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado
Business Development Manager 210-450-3713
DelgadoR4@uthscsa.edu
UT Health San Antonio
MD Anderson Mays Cancer Center
Laura Kouba
Business Development Manager 210-265-7662
NorrisKouba@uthscsa.edu
https://uthscsa.edu/
Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229
Healthcare Administration Consultants (HH Silver Sponsor)
Our mission is to help healthcare organizations small or large to achieve sustainable growth and success by providing them with expert healthcare administration consulting services. We focus on key factors such as: revenue, supply chain visibility, and aligning operations to save time so that your team can focus on improving the patient’s health and well-being. We transform patient care outcomes and employee working experiences while driving brand and revenue growth.
Dr. Reshma Beherry, DHA
Doctor of Healthcare Administration 210-602-6905
RB@administrative-consultants.com
https://administrative-consultants.com/

Equality Health (HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com “Reimagining the New Frontier of Value-Based Care.”
(H Bronze Sponsor)
We were founded to meet a need: helping business owners succeed by giving them simple, quality, affordable U.S.-based contact solutions. In only a few years, our focus on nurturing client relations and building trust not only helped our customers grow their businesses, but helped us stake our claim in the highly competitive TAS industry as one of the most well-regarded and referred. Our 50 years of collective experience are the driving force behind our clients’ satisfaction.
Rachel Caero Managing Partner 844-554-3473 Rachel@dialops.net
Insperity
(HH Silver Sponsor)
Insperity’s HR solutions offer premium service and technology to facilitate growth by streamlining processes related to payroll, benefits, talent management and HR compliance. We provide the tools to help you lighten your administrative load, maximize productivity and manage risks – so you can focus on growth.
Fran Yacovone
Business Performance Advisor 210-558-2507
Fran.Yacovone@insperity.com
Dayton Parker Business Performance Advisor 210-558-2517
Dayton.Parker@insperity.com www.insperity.com
“Insperity’s mission is to help businesses succeed so communities prosper”

TMA Insurance Trust
(HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England Director of Member Benefits 512-370-1776
Wendell.England@tmait.org 800-880-8181 www.tmait.org
“We offer BCMS members a free insurance portfolio review.”

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting and defending physicians.
Patty Spann Director of Sales and Business Development 512-425-5932
Patty-Spann@tmlt.org www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
Katy.Brooks@bosainsurance.com www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM
AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com

LASO Health Telemedicine and Rx App (HHH Silver Sponsor)
LASO Health is the industry’s only solution that makes healthcare services accessible, cost-transparent and convenient. Its mission is to reinvent “healthcare” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care.
LASO combines an intuitive, mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, onestop-shop, comprehensive health solution.
Ruby Garza, MBA 210-212-2622
RGarza@texaskidneycare.com www.lasohealth.com
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol Field Sales Consultant 210-413-8079
Tom.Rosol@henryschein.com www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”

Provider's Choice Scribe Services (HHH Gold Sponsor)
Our accurate and complete documentation helps our customers focus on what’s most important, their patients. Let us take on the task of documenting your patient encounters, it’s what we do.
Yoceline Aguilar COO
915-691-9178
YAguilar@pcscribes.com
Luis Chapa MD/CEO 210-796-4547
LChapa@pcscribes.com
www.providerschoicess.com
“An Unparalleled Scribe Experience”

Equality Health (HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination, and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President 210-797-8412
HealthcareLeadersSA@gmail.com
Gary Meyn, LFACHE Vice President 210-912-0120
GMeyn@vestedbb.com https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor) “Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber President 210-308-7907 (Direct)
KBarber@bdo.com
Valerie Rogler Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Jeannine Ruffner President info4@samgma.org www.samgma.org
Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP® QKA Senior Private Wealth Advisor 512-649-8113 Service@oakwellpwm.com www.oakwellpwm.com
“More Than Just Your Advisor, We’re Your Wealth Management Partner”

Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
Mike DeQuattro
Director of Operations - Texas & New Mexico 210-918-8737
Mike.DeQuattro@favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout. Join us in transforming healthcare delivery, prioritizing your wellbeing and patient care.
Pedro Caretto VP of Business Development 786-437-4009 PCaretto@eleosvhs.com www.eleosvhs.com

Provider’s Choice Scribe Services (HHH Gold Sponsor)
Our accurate and complete documentation helps our customers focus on what’s most important, their patients. Let us take on the task of documenting your patient encounters, it’s what we do.
Yoceline Aguilar COO
YAguilar@pcscribes.com 915-691-9178
Luis Chapa MD/CEO 210-796-4547
LChapa@pcscribes.com www.providerschoicess.com/ “An Unparalleled Scribe Experience”












After recently driving a new Chevrolet Tahoe, it occurred to me that this vehicle, along with its sister General Motors (GM) full-size SUVs, the GMC Yukon and Cadillac Escalade, are woefully underappreciated, even by GM.
Here’s what I mean: these big trucks sell well, are loved by their customers, and make GM around $3Bil a year in profits.
Yes, that’s right, three *billion* dollars. A year. In profit. And yet no one except for their happy owners (and Chevrolet dealers) seem to give them any respect.
Who are those happy owners? Parents of young children who need to be shuttled from school to ballet practice or a soccer game or a piano recital or a baseball tournament in OMG Houston. Or police departments or government agencies or grandparents or empty nesters who like to travel. Or busy Bexar County physicians who need to drive all over San Antonio taking care of sick patients and would like to do so comfortably and safely. You get the picture — there’s a reason GM moves 300,000 or so of these year after year after year.
And yet GM hardly acknowledges these vehicular rainmakers while at the same time lavishing praise on their new battery electric vehicles (BEVs) that will be “the Future” soon.
I agree that BEVs will indeed be the future someday, but for now big internal combustion SUVs that are the present are paying the bills at GM and deserve some respect and gratitude.
Ok, rant done. Let’s talk about the 2024 Chevrolet Tahoe. It’s big inside, which is a lot of the reason why it’s so popular. And two major changes that came with the introduction of the current 5th gen Tahoe back in 2021 made the cabin even bigger: the five-inch longer wheelbase added legroom for the second and third rows of seats, and the switch from a solid rear axle to an independent rear suspension system allowed for a lower floor, which increased headroom and luggage space.
When the Tahoe was first launched about 30 years ago, it was much more utilitarian than it is now. Current models, on the other hand, rival luxury vehicles with sumptuous seat surfaces, plenty of soft touch materials and lots of tech.
Of course, Tahoes now are significantly more expensive than they used to be. Twenty years ago, a nice Tahoe would cost around $40,000, and current models can easily run you more than $75,000. Ain’t nothing for free, right?
Driving the Tahoe is a pleasant if not energetic experience. Zipping around town is a breeze — although parking these big trucks is not as easy as it is with a Toyota RAV4 — and on the open road, the Tahoe is a delight. In fact, road tripping in a Tahoe is about as good as it gets.
As you’d expect, a spacious and comfortable full-size SUV will never be a fuel sipper, and that’s the case with the Tahoe. Its standard 355 HP 5.3L V8 engine manages just 16 MPG Highway and 20 MPG City, and that’s a lot better than it used to be thanks to evolutionary improvements over the years and a 10-sp automatic transmission.

For the record, a more fuel efficient 3.0L in-line six-cylinder diesel engine (21 MPG City/28 Highway) and thirstier 6.2L gasoline V8 (14/20 MPG) are available as options.
My two cents? Buy the larger gas-powered V8. The smaller 5.3L engine struggles with the weight of the Tahoe sometimes, and I’m nervous about the availability of Diesel fuel in the future.
In addition to many active safety systems that garner the 2024 Tahoe a 4-star safety rating from NHTSA, the Tahoe has the intrinsic benefit of large crumple zones around all passengers just because it’s a big truck.
Numerous options or option packages are available to make your Tahoe better suit your life, from the Z71 package for off-roading all the way to the loaded High Country version, which comes with the 6.2L V8 by the way.
While a base model Tahoe will get the job done for most owners, I suspect most BCMS members will prefer the more luxurious Premier and High Country versions because of their better audio systems and tech, nicer interior appointments, chrome accents outside and better looking (larger) wheels.
Naturally, if you have lots of kids or for any other reason need a larger vehicle, Chevrolet will happily sell you the larger Suburban.
Electrification is coming for all the cars and trucks we love, and the Tahoe and its corporate siblings won’t be spared. I hope they stay internal combustion for a long time, presumably with hybridization to minimize emissions.
And I hope that everyone who overlooks these wonderful and popular vehicles, which regrettably seems to include GM itself, will give them a little love. They deserve it

Stephen Schutz, MD, is board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.
11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
Auto Group
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
Auto Group
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Kahlig Auto Group
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Chuck Nash Chevrolet Buick GMC 3209 North Interstate 35 San Marcos, TX
William Boyd 210-859-2719
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
Kahlig Auto Group
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Auto Group
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Auto Group
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras
320-308-8900
Chris Martinez 210-366-9600 9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945
Auto Group
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000