2023 Texas Legislative Session Wrap-Up





NON PROFIT ORG US POSTAGE PAID SAN ANTONIO, TX PERMIT 1001 SAN ANTONIO

PuBLISHEd BY: traveling Blender, llC. 10036 Saxet Boerne, tX 78006

PuBLISHER louis doucette louis@travelingblender.com
BuSINESS MANAGER: vicki Schroder vicki@travelingblender.com
AdvERTISING SALES:

AuSTIN: Sandy Weatherford sandy@travelingblender.com
2023 TEXAS LEGISLATIVE SESSION WRAP-UP
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EditoriAl CorrESpondEnCE: Bexar County Medical Society 4334 n loop 1604 W, Ste. 200 San Antonio, tX 78249
Email: editor@bcms.org
MAGAZinE AddrESS CHAnGES: Call (210) 301-4391 or Email: membership@bcms.org
SuBSCription rAtES: $30 per year or $4 per individual issue
AdvErtiSinG CorrESpondEnCE: louis doucette, president traveling Blender, llC.
A publication Management Firm 10036 Saxet, Boerne, tX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national orgin, or an intention to make such preference limitation or dis-
SAN ANTONIO: Gerry lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.

SAN ANTONIO 4 SAN ANTONIO MEDICINE • August 2023
TABLE OF CONTENTS
t © 2023 Smithprint, inc. prin tE d in tHE u SA
Copyrigh
THE OFFICIAL PUBLICATION OF THE BEXAR COUNTY MEDICAL SOCIETY • WWW.BCMS.ORG • $4.00 • AUGUST 2023 • VOLUME 76 NO.8
crimination.
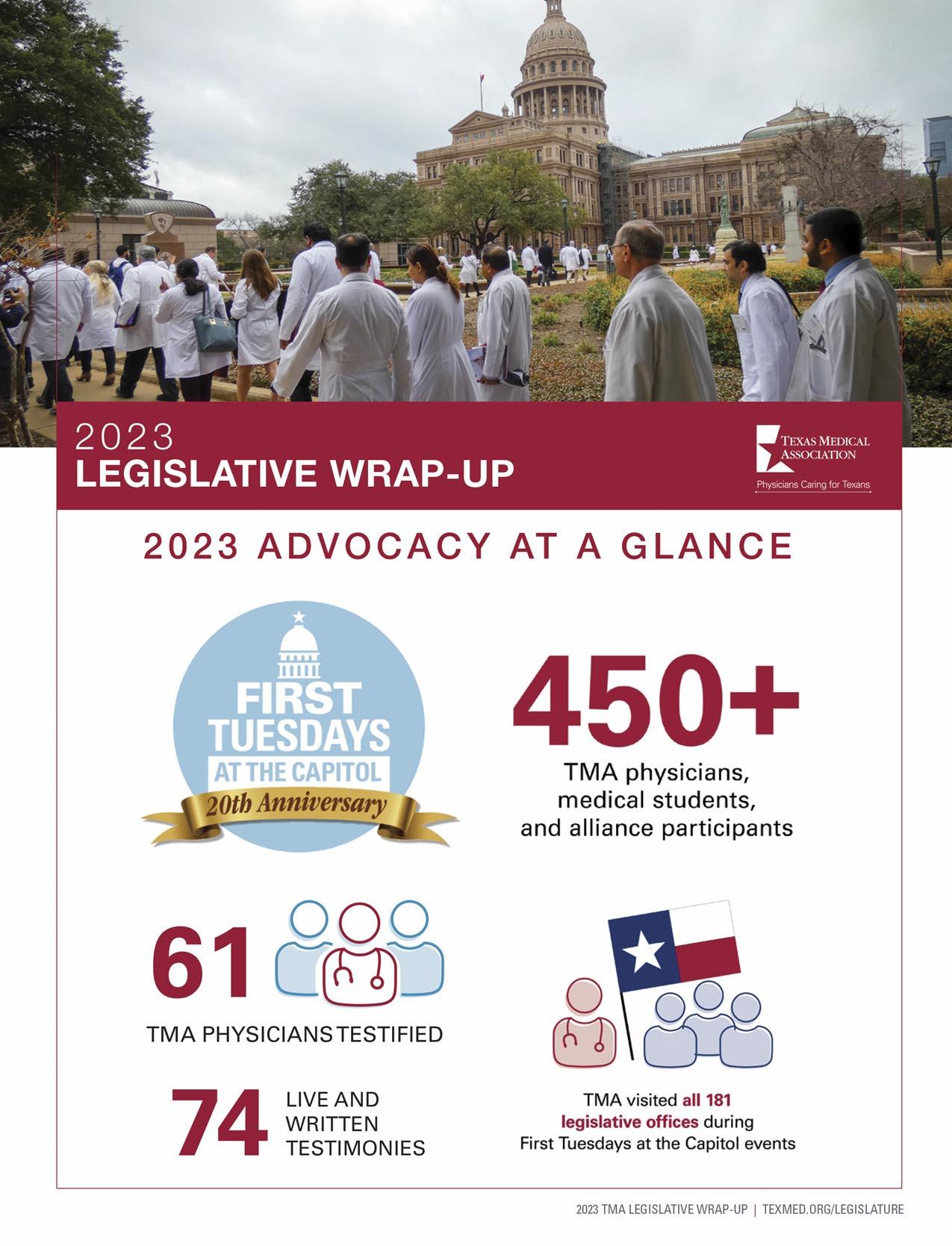
2023 Advocacy At A Glance By The Texas Medical Association 12 The Importance Of Physician Advocacy By John J. Nava, MD 22 TEXPAC – The Party Of Medicine By Adam Bruggeman, MD 24 Medical Student Advocacy Through The American Medical Association (AMA) By Jiwon Park, BA 26 Reforming Medicare Payment By Jayesh Shah, MD 27 Navigating New Health Insurance Laws In Texas: What You Need To Know By Ezequiel “Zeke” Silva III, MD 28 Meeting The Bexar County Health Needs Through Graduate Medical Education By Scott Jones, MD 30 BCMS President’s Message 8 BCMS Alliance Message 10 Leah Hanselka Jacobson, MD Interview By Monica Jones, BCMS, COO 34 Decreasing Barriers To Vaccine-Preventable Diseases In Bexar County By Marina Moreno and Adelita G. Cantu, PhD, RN, FAAN 36 Summer In The City – Cool Down And Wellness Festival 38 BCMS Vendor Directory 40 Auto Review: 2023 Lamborghini Urus SUV By Stephen Schutz, MD 44 Recommended Auto Dealers 46
ELECTEd OFFICERS
John Joseph nava, Md, President
Brian t. Boies, Md, Vice President
Ezequiel “Zeke” Silva iii, Md, President-elect
John Shepherd, Md, Secretary
rajeev Suri, Md, Treasurer and Immediate
Past President
dIRECTORS
Woodson "Scott" Jones, Md, Member
Sumeru “Sam” G. Mehta, Md, Member
M. “Hamed” reza Mizani, Md, Member
priti Mody-Bailey, Md, Member
lubna naeem, Md, Member
lyssa n ochoa, Md, Member
Jennifer r. rushton, Md, Member
raul Santoscoy, do, Member
lauren tarbox, Md, Member
Jenny Case, Alliance Representative
ramon S. Cancino, Md, Medical School
Representative
lori Kels, Md, Medical School Representative
robert leverence, Md, Medical School
Representative
Keiko McManus, Md, Board of Ethics Chair
John pham, do, Medical School Representative
Cheryl pierce-Szender, Alliance Representative
ronald rodriguez, Md, phd, Medical School
Representative
Col. Cecilia Kai Sessions-Carpenter Md, MpH, Military Representative
George F. “rick” Evans, Jr., General Counsel
Jayesh B. Shah, Md, TMA Board of Trustees
Melody newsom, CEO/Executive Director
BCMS SENIOR STAFF
Melody newsom, CEO/Executive Director
Monica Jones, Chief Operating Officer
Yvonne nino, Controller
Mary nava, Chief Government Affairs Officer
Brissa vela, Membership Director phil Hornbeak, Auto Program Director
August trevino, Development Director
Betty Fernandez, BCVI Director
Al ortiz, Chief Information Officer
PuBLICATIONS COMMITTEE
norys Alexandra Castro-pena, Md, Co-chair
John Joseph Seidenfeld, Md, Co-chair
louis doucette, Consultant
david Schulz, Community Member
Elizabeth Clanton, Md, Member
Kristy Yvonne Kosub, Md, Member
neal Meritz, Md, Member
Jaime pankowsky, Md, Member
Alan preston, phd, Member
rajam S. ramamurthy, Md, Member
Adam v ratner, Md, Member
Faraz Yousefian, do, Member
Moses Alfaro, Student Member
victoria Ayodele, Student Member
tue Felix nguyen, Student Member
niva Shrestha, Student Member
Bethanne Bradshaw, Student Member
Andrew ta, Student Member
Monica Jones, BCMS Coo, Staff Liason
trisha doucette, Editor
6 SAN ANTONIO MEDICINE • August 2023
BCMS BOARD OF DIRECTORS

My Own Advocacy Path
By John J. Nava, MD, 2023 BCMS President
“There is a misconception that Buddhism is a religion, and that you worship Buddha. Buddhism is a practice, like yoga. You can be a Christian and practice Buddhism. I met a Catholic priest who lives in a Buddhist monastery in France. He told me that Buddhism makes him a better Christian. I love that.” – Thich
Nhat Hanh
To my contemporaries – does anyone remember back when our boomer generation applied to medical school? We had worked hard on our academic careers, striving to get the best grades. Before we could actually identify what we hoped to become, we knew that education was one key component to achieving future success. How did we know this? The adults in our lives drilled this lesson into our heads. Our transcripts and MCAT scores were ample evidence of our discipline, performance capabilities and determination to become physicians. But what was missing? Since all of the applicants were top-notch, how could we convince the admissions committee that we were more deserving than the next person to be considered for admission to medical school.
The personal statement section of the application would verbally compose a thumbnail sketch, representing our unique motivations to medicine. In one or two pages, we could illustrate how our life experiences had resulted in this inevitable progression to become “healers.” Whether we were the first in our families to attend college, or had been expected to maintain a legacy of a medical heritage, it was necessary to illustrate to this academic panel that the new medical school entering class deserved to have us! We were obliged to show the admission committee that we were not only driven by greed for power, prestige and a fat salary, but actually wanted to help and care for patients.
Despite our glowing self-impressions, we were admitted as unrefined base material to this process. We threw ourselves headlong into the fire, and after a few years, emerged to be further tempered by internship, residency and specialty fellowships. During this time, we had little time to devote to advocacy.
In my own case, I emerged from residency unsure I even wanted to enter into private practice. My initial ideals of providing primary care in a Marcus Welby-esque style seemed unattainable. I don’t recall Dr. Welby actually participating in advocacy activities beyond direct patient care. His patients needed only a supportive word, and followed his instructions without question. In any case, I was busy figuring out my own career path. Apparently, while I had been in school and post graduate training, that ideal had been replaced by a newer, HMO-style of providing medical care.
I initially tried to avoid the conflict by working as a locum tenens
doctor, helping other family practitioners on the southside of San Antonio meet the demands of their own busy practices. I punched a clock, so that when I left their offices, I had no call duty and no administrative hassles. Again, advocacy took a place of lower priority.
I did try solo private practice on my own after a rural hospital recruited me to a small east Texas town. I tried my best to keep my primarily Medicare and Medicaid patients out of the ER and hospital. Unfortunately, this did not help the small, struggling rural hospital that had recruited me. After a year of collaboration, we parted ways. Eventually, I returned to San Antonio as my wife and I were eagerly anticipating the birth of my first son. I became an employed physician in public health. The change from private practice to public health practice moved advocacy to the front burner, with these concerns now a professional expectation. Public health practice was a calling, and I thrived in answering that call.
A few years ago, I was approached to consider becoming an officer in BCMS, and accepted the opportunity on the condition that I would stop short of becoming the president. I then warmed to the idea of providing official leadership as president during the legislative session. Participating in organizational advocacy through BCMS and TMA activities have been personally very rewarding. Resisting scope creep by non-physicians, promoting patient care over corporate concerns, and extending Medicaid coverage to mothers and babies for certain health issues from six to 12 months in the postpartum period are successes we can all be proud of.
I ask all members to contemplate articles in this issue of San Antonio Medicine regarding the vital nature of physician involvement in advocacy. While it may be challenging to do so at certain times in your career, it is never too late to start or resume practicing advocacy alongside medicine. It is possible, and the skills to do so are teachable and practical. If the intent is there, those skills can be applied with minimal effort.
Through our careers, we have likely had many successes and likely a few failures. Maybe through it all, you have been able to maintain that passion for helping others. Imagine that the same sparks of optimism and creativity we had as medical school applicants can be rediscovered. It won’t be fanned into a flame by the untested young people we used to be, but rather developed by the older, wiser and more savvy persons we have become. And your patients will likely appreciate it.
John J. Nava, MD, is the 2023 President of the Bexar County Medical Society. He is interested in Primary Care, Clinical Research and Public Health.
8 SAN ANTONIO MEDICINE • August 2023 PRESIDENT’S MESSAGE

“All You Need To Do Is RSVP”
TMA Alliance leader Jenny Shepherd’s open invitation to medical advocacy is an award-winning approach
By Alisa Pierce
Jenny Shepherd has a story to tell.
“I care about what’s happening in my community, and I want to improve it,” the Texas Medical Association Alliance (TMAA) presidentelect said. “Saying that you don’t care about politics, especially concerning medicine, is the same as saying that you don’t care about your quality of life and the way medicine is practiced in Texas.”
The tireless medical advocate has shared that message through her various roles working with legislators, community members and physicians to strengthen healthcare, raise funds for bodies within organized medicine, and better her community. Her efforts have bolstered medicine’s visibility in the political sphere and, her favorite part, brought people together.
They also earned her this year’s June Bratcher Award for Political Action, making her the first person to win the Texas Medical Association Political Action Committee (TEXPAC) accolade twice.
Named for its first recipient, TMAA leader and political trailblazer June Bratcher of San Antonio, the award honors a member of the TMA Alliance – the association’s advocacy and community service volunteer force – who has shown significant involvement in a political campaign to aid organized medicine.

That’s a typical day for Ms. Shepherd.
Like Ms. Bratcher, who launched grassroots campaigns in the mid1970s to encourage physicians and other health professionals in San Antonio to vote for medically minded candidates, Ms. Shepherd successfully campaigned and raised funds for local lawmakers who had expressed support for Texas medicine.
“June Bratcher was told that ‘nice wives’ don’t get involved in politics. But even though she was told that politics was not for her, she kept going and changed the landscape of how women and physician spouses are involved in the political medical environment,” Ms. Shepherd said. “I knew to make real change, I had to channel my ‘inner June’ to get these candidates (state Rep. Leo Pacheco and state Sen. Jose Menendez, both Democrats from San Antonio) elected. I had to speak one-onone to voters and share the real impact of our cause.”
By sharing personal anecdotes on the importance of electing medicine’s supporters and connecting with voters on an emotional level, Ms. Shepherd built support for both candidates. Her storytelling approach played a vital role in their eventual elections. “This is what I love to do. I’m a cheerleader. I’m an inviter. I’m an advocate,” she told Texas Medicine.
Medicine’s Cheerleader
Initially, Ms. Shepherd believed she wasn’t “qualified” to be an advocate for medicine and was hesitant to showcase her passion for healthcare and its most staunch defenders – physicians and their families.
As the spouse of pediatric anesthesiologist John Shepherd, MD, however, she understood the demands placed upon physicians and what it would take politically to keep their community healthy.
“I’m not an attorney, I’m not a legislator, and I’m not a physician," she said. “But I realized that I already had all the skills I needed. Advo -
10 SAN ANTONIO MEDICINE • August 2023 BCMS ALLIANCE
“The statistics may get the issue noticed, but the real-life stories we share get the vote.”
Photo by Phil Kline
cacy is talking with legislators about what’s going on in the medical community, how doctors are struggling, and how their patients are struggling. It’s about telling a story to help the ones you love.”
Ms. Shepherd’s passion grew after attending TMA's award-winning advocacy program, First Tuesdays at the Capitol, in 2018, the year she became president of the Bexar County Medical Society Alliance (BCMSA). She participated every year thereafter to educate Bexar County legislators on meaningful Medicaid reform, scope-of-practice creep, and improving healthcare coverage and access for mothers and their babies.
Eventually, Ms. Shepherd became the First Tuesdays chair for the TMA Alliance, and continued her work in several leadership roles within BCMSA, including as scholarship chair and legislative chair. She attended every First Tuesdays event this year and spoke to its impact on its 20th anniversary in May.
“First Tuesdays is an award-winning program. It gets results; it gets us seen; it is what we have to do to get the business of medicine done and practice medicine the way you want to practice medicine. … Nothing looks more impressive than the sea of white coats,” Ms. Shepherd said during the inaugural TMA event of 2023 in February. She now serves as the TMA Alliance membership chair for TEXPAC and the vice president of membership for TMAA, using her story to encourage physicians and their families to join their ranks as medical activists.
“The work doesn't get done without those who show up to First Tuesdays and meet with their legislators,” Ms. Shepherd told Texas Medicine. “I’m sending the invitation. … All you need to do is RSVP.”
Party of Medicine
In fact, she created her own Party of Medicine events to encourage physicians and their families to connect and become involved in advocacy – and, of course, to have fun.
The parties connected members of the medical community and showcased Ms. Shepherd’s hospitality skills. Each event included signage designed to educate and encourage conversation among medical professionals, and information on TEXPAC and other organizations each attendee could join after the party.
“We threw a party for those uninvolved in advocacy to learn about what we do,” she said. “At the end of the night, almost all attendees joined TEXPAC, their county medical society or county alliance. This event helped them to become more involved … and have a great time.”
In June 2020, Ms. Shepherd was honored with the American Medical Association Alliance’s Legislative Education and Awareness Promotion Award for the parties she hosted in her home in San Antonio and across the state.
Ms. Shepherd’s desire to help others, coupled with what her friends call a “love for fun,” has enabled her to become a force of support for the medical community.
“Jenny puts so much work into whatever she does. Every event she holds comes out so beautifully,” Pam Udall, TMA’s vice president of communications and marketing said. “More importantly, her real talent is building relationships between legislators and their physician constituents. She's a natural fundraiser, educator, connector and leader. She is just brilliant.”
The events, which Ms. Shepherd planned and advertised herself, boosted TEXPAC membership and successfully raised funds for TEXPAC-endorsed candidates. “We have to be examples of advocacy if we expect others to help,” Ms. Shepherd said. “Having more people join bodies like TMA and the alliance creates better medicine in Texas.”
She has since hosted fundraisers where physicians and their spouses can meet TEXPAC-endorsed candidates running for office and contribute to their campaigns. These fundraisers are an “excellent way to build long-lasting relationships that are key to medicine’s success during the legislative session,” said TEXPAC Director Christine Mojezati. “I know I can always count on Jenny and Dr. Shepherd to host an amazing event and get results. In the short time I’ve known Jenny, she has proved her 100% commitment to medicine and its successes,” Ms. Mojezati added.
Ms. Shepherd also has raised funds and volunteered for TMA’s Vaccines Defend What Matters (formerly Be Wise – Immunize) and Hard Hats for Little Heads campaigns; coordinated a toy donation for the neonatal department of University Hospital; and worked with BCMSA to award scholarships to medical students and future healthcare professionals such as physical therapists and audiologists.
“It makes such a difference in students' lives and is directly impactful in Bexar County,” she said. “Nothing makes me happier than serving as a mentor for the next generation and recognizing potential leaders to nurture.”
Ms. Shepherd’s efforts serve as a reminder that effective advocacy requires more than just facts and figures. To truly make an impact, she says, the only required skill advocates need is that of caring.
“It’s my job to tell people who think they don't have the skills for advocacy that they do,” Ms. Shepherd said. “To be an advocate, you just have to care about your community.”
Alisa Pierce is a reporter for Texas Medicine. You can reach her at 800-880-1300, ext. 1469; 512-370-1469; or alisa.pierce@texmed.org.

BCMS ALLIANCE
Visit us at www.bcms.org 11
“We have to be examples of advocacy if we expect others to help.”
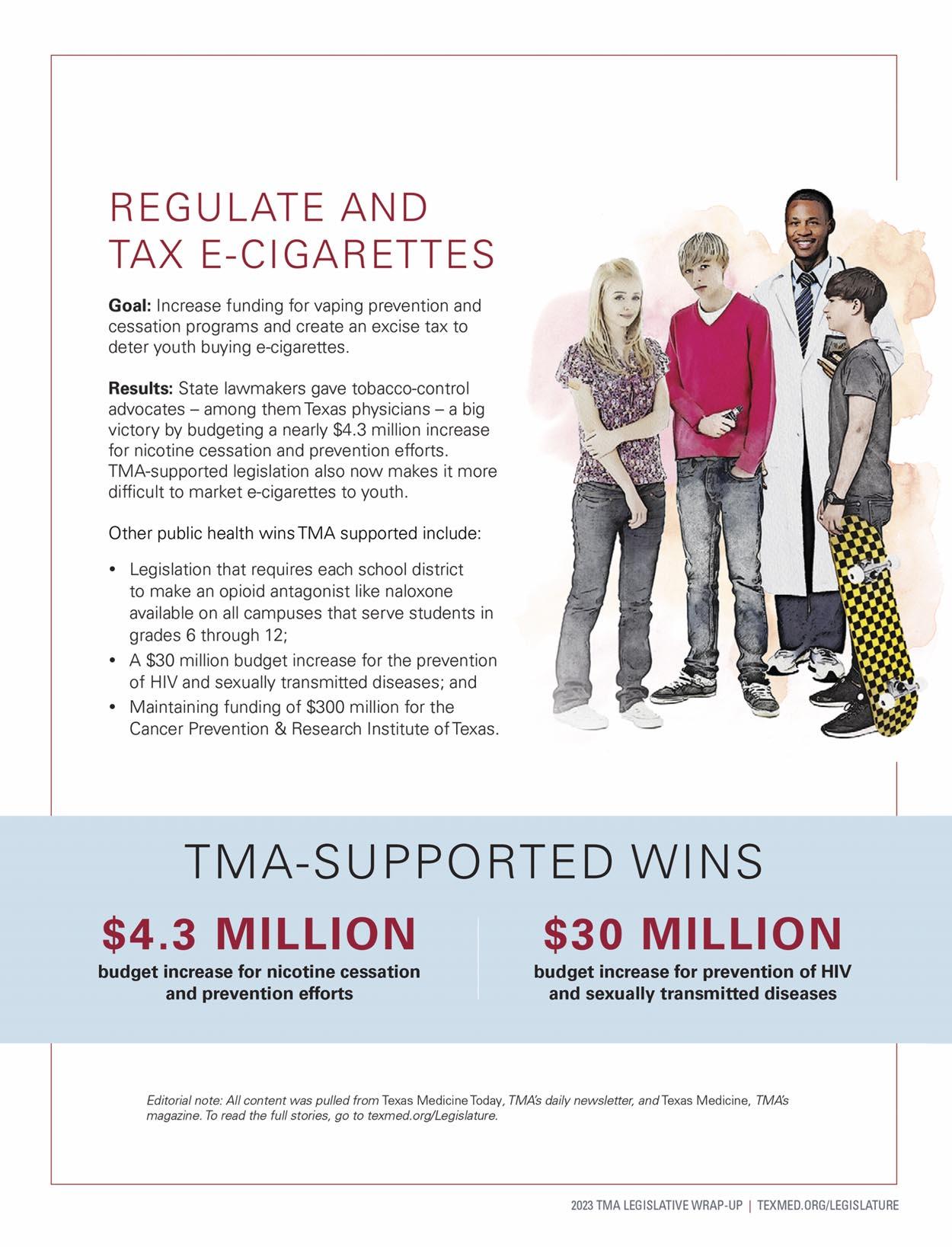
PATIENT CARE PROTECTED
PATIENT CARE PROTECTED
12 SAN ANTONIO MEDICINE • August 2023
Visit us at www.bcms.org 13
The Importance Of Physician Advocacy
By John J. Nava, MD
Do not live half a life
and do not die a half death
If you choose silence, then be silent
When you speak, do so until you are finished
If you accept, then express it bluntly
Do not mask it
If you refuse then be clear about it for an ambiguous refusal is but a weak acceptance
Do not accept half a solution
Do not believe half truths
Do not dream half a dream
Do not fantasize about half hopes
Half the way will get you no where
You are a whole that exists to live a life not half a life.
Khalil Gibran
Book: The Prophet
Definitions:
advocacy: any action that speaks in favor of, recommends, argues for a cause, supports or defends, or pleads on behalf of others - Webster’s Dictionary
advocacy: the act of pleading for, supporting, or recommending on behalf of person or cause
- Random House Dictionary
Ibegin this article with the writing of Khalil Gibran, a Lebanese American writer, whose work was introduced to me in high school. I never relished much poetry or prose earlier in life, perhaps due to a narrow set of pre-med curricular interests. In any case, I recently came across this work, and it seemed appropriate for the current state of political advocacy by physicians. If we can recall a few years ago when the pandemic began, a novel coronavirus had been introduced to the unprepared world. I observed a frantic public health response, which surprisingly was led by politicians rather than medical experts. Thankfully, between natural immunity from infection and a robust immunization drive, most of the U.S. population has developed antibodies that have provided some protection against infection and reinfection. The pandemic has been downgraded to an endemic state, and the world is adjusting to this as best we can.
I was alarmed that policy rather than science guided the response. Different people have opinions on who deserves the blame for the disorganization that characterized some of the public health response. I know other colleagues that were frustrated with a system that seemed to dismiss the input of healthcare leaders. Keeping this in mind, I think the situation represented a call for more involvement by medical practitioners to shape future healthcare responses to emerging infectious agents and other public health threats.
Risk communication and coordination of a response to public health emergencies should be managed by trained and competent, qualified emergency response leaders, not just the first or loudest person who grabs the microphone. In my mind, this is a boundary that needs to be strengthened and respected. As we observe the closure of the most recent U.S. Supreme Court decision, it is alarming that their decisions are being guided by policy preferences rather than strict interpretation of the law. Failure of the medical profession to take this opportunity to speak up now will likely lead to further instances where science takes a back seat to politicized ideology. When I was taught about the three branches of the U.S. government, the Judicial branch did not create law, only interpreted it. The actual laws themselves were created by the Legislative branch and administered by the Executive branch. I suppose it is naïve to continue to cling to that ideal, especially since it seems the boundaries are no longer strictly observed. Perhaps I cannot understand the blurred lines that used to be so clear.
22 SAN ANTONIO MEDICINE • August 2023 2023 TEXAS LEGISLATIVE SESSION WRAP-UP
In a 2006 JAMA® issue, Gruen, et al. wrote about the community participation, political involvement and collective advocacy roles of physicians. In this article, they “reviewed physician responses to the Institute on Medicine as a Profession’s (IMAP) survey to assess physicians’ feelings toward advocacy and their participation in public advocacy activities.”1 These activities were grouped into three types of activity: community participation, individual political activity and collective (organizational) advocacy.1
In 2010, Earnest, et al. wrote an article in Academic Medicine asking “what is physician advocacy and how do we do it?” These thought leaders have attempted to provide a more robust operational definition in the specific contacts of physician advocacy, as “action by a physician to promote the social, economic, educational and political changes that ameliorate the suffering and threats to human health and well-being that he or she identifies through his or her professional work and expertise.”2 Certain obligations are linked to membership in various communities. Fundamental moral and ethical obligations are linked to the basic nature of the profession. They also discuss actual and perceived barriers to advocacy activities by physicians.
In 2011, the president of the Missouri State Medical Association was Gary Pettett, MD. His article was entitled “Obligation or Option? The Physician’s Role in Advocacy.” The entire November-December issue of that group was dedicated to the physician’s role in advocacy. It was admitted that physician political advocacy has not been clearly defined. He continued to attempt to provide background on the issues and controversies surrounding physician advocacy, and discussed barriers to activity. He asked whether advocacy was part of professionalism, or should it be relegated to civics, and cited an article by TS Huddle, MD. In the name of fair and balanced writing, I mention his opinion.
Dr. Huddle has a different take on physician advocacy, and he wrote of this in 2011 in Academic Medicine. While I can appreciate his perspective, with the recent changes in the makeup of the U.S. Supreme Court and their willingness to reverse laws passed by Congress, it is incumbent on the family of medicine to defend itself against the erosion of its well-deserved authority in medical matters. He does not agree that political advocacy is a core professional responsibility for physicians. He argues that “(1) civic virtues are outside the professional realm, (2) even if civic virtues were professionally obligatory it is unclear that civic participation is necessary for such virtue, and (3) the profession of medicine ought not to require any particular political stance of its members.” 3 He also believes that academic centers should not be “systematically involved with fostering advocacy.” 3 He holds that advocacy “seeks change rather than knowledge,” so has no claim on curricula including advocacy skills as an academic concern. He thinks these efforts “will
undermine university aspirations to objectivity and neutrality.” While I can appreciate his perspective, and respectfully leave the option up to the individual physician, recent developments have made the imperative to action much more timely. For those physicians who have considered political advocacy and have declined, we must respect their decision. But for those that have never been politically active, they should realize the opportunity that exists before them. The intent of those individuals in deciding how to practice medicine is of the utmost importance, even after their clinical duties have been completed. Maybe it is just me, but as cost goes up and quality goes down in American healthcare delivery, especially for the most vulnerable, I can no longer support the status quo.
We each need to determine for ourselves how we define the art of medicine. It can represent an opportunity to emphasize beneficence and speak for those without a voice as a professional ethical standard.
I’ve heard politically savvy persons say, “If you don’t have a seat at the table, it is likely that you are lunch.” Is that just an unfortunate, dirty, secret fact about politics? If so, I interpret that as only more reason to become involved to better practice self-care for physicians and healers, and to influence how medicine is practiced in Texas and the United States by learning and sharing the teachable advocacy skills that have been developed. We should encourage students to become involved early and help guide them to better balance this additional duty according to their capabilities.
Especially as we concentrate on physician self-care in this post-pandemic period, let’s make sure we don’t become lunch!
References:
1. Gruen RL, Campbell EG, Blumenthal D. Public Roles of US Physician. Community Participation, Political Involvement and Collective Advocacy. JAMA. 2006;296(20):2467–2475
2. Earnest MA, Wong SL, Federico SG. Physician Advocacy: What Is It and How Do We Do It? Acad Med. 2010;85(1):63–67
3. Huddle TS. Medical Professionalism and Medical Education Should Not Involve Commitments to Political Advocacy. Acad Med. 2011;86(3):378–383
John J. Nava, MD, is the 2023 President of Bexar County Medical Society. He is interested in Primary Care, Clinical Research and Public Health.

Visit us at www.bcms.org 23 2023 TEXAS LEGISLATIVE SESSION WRAP-UP
TEXPAC – The Party Of Medicine
By Adam Bruggeman, MD
Every other year, the beginning of summer marks the end of the legislative session in Texas. This year’s session will perhaps best be remembered for the bills that didn’t pass over the ones that did when it comes to healthcare. A flurry of bills that would have significantly impacted the scope of practice, physician compensation and the administration of healthcare were ultimately defeated through the efforts of the Texas Medical Association and TEXPAC. While many physicians are aware of the work of the Texas Medical Association, TEXPAC is not always as well understood. There are 5,000 physicians who contribute to TEXPAC, while there are over 50,000 members of the Texas Medical Association.
TEXPAC is one of the oldest political action committees in the state of Texas with a founding in the 1960s. Political action committees are organizations that take donations from individuals and then utilize that money to influence the election or defeat of political candidates in addition to advocating for or against legislative initiatives. TEXPAC mostly focuses on state issues at this time, including election of physician-friendly legislators and education surrounding healthcare-related legislation. Combined, the TEXPAC and the Texas Medical Association are a very powerful voice throughout the state for physicians and their patients.
In today’s polarized politics, many physicians worry that larger organizations like TEXPAC don’t truly represent their views. The reality is that healthcare is bipartisan and TEXPAC is able to support candi-

dates on both sides of the aisle. While physicians who contribute may not always agree with all of the opinions of legislators supported by TEXPAC, they will find comfort in knowing that those legislators will be strong advocates of physicians’ critical medical issues.

While TEXPAC has been very successful to date, the future is always uncertain. Only 10% of TMA members support TEXPAC, leaving significant room for improvement. As healthcare continues to increase in costs, more companies and legislators will be looking for ways to reduce spending while maintaining or improving quality. If physicians are not at the table, they will see worsening cuts and unfavorable laws written impacting patient-physician relationships and autonomy of practice.
The effectiveness of TEXPAC now and in the future depends on two things: the continued support from current donors, and engaging physicians who aren’t currently giving to the PAC. If you would like to learn more about TEXPAC, you can visit their website at www.texpac.org or email them at texpac@texmed.org.
2023 TEXAS LEGISLATIVE SESSION WRAP-UP
24 SAN ANTONIO MEDICINE • August 2023
Adam Bruggeman, MD, is an orthopedic spine surgeon in San Antonio, Texas. He currently serves as the Chair of the Council on Advocacy for the American Academy of Orthopaedic Surgeons, providing oversight to their national regulatory, legislative and PAC efforts.
Visit us at www.bcms.org 25
Medical Student Advocacy Through the American Medical Association (AMA)
By Jiwon Park, BA
Riding the metro in Houston, I nervously arrived at Westheimer. Serving women in substance use disorder (SUD) recovery, my experience at The Women’s Home catalyzed my passion for advocacy. Orchestrating a health-musicking organization called “Tunes for Life,” I hoped to promote healing by reflecting on themes embedded in music. While the participants and I came from different backgrounds, sharing memories intertwined with the music connected us. During one particular lesson on Adele, the conversations inspired me to take a step beyond volunteer service.
Reflecting on Adele’s “Hello,” one participant shared that the lyric’s depiction of a one-sided phone call reminded her of her estranged relationship with her daughter whom she lost custody of. Another shared that the criminal justice system severed her relationship with her late father. These stories are not isolated. In fact, soon I realized that many women with SUDs were involved in the criminal justice system. Drug use and possession played an important role in contributing to female mass incarceration, with almost a quarter being non-violent, drug-related offenses.1 Yet, despite the system’s failure to facilitate recovery, the justice system remains the largest institution in the U.S. to provide mental healthcare for these patients.2 By working with fellows at the Baker Institute of Policy and co-leading a year-long Alternative Spring Break Program “Women Beyond Bars,” I learned that lasting, impactful advances for patients must start with changes to drug policies, policing and healthcare accessibility. Thus, in medical school, I wanted to continue advocacy by joining the American Medical Association (AMA). While my passion came from advocating for women with SUDs, I want to encourage all fellow physician trainees to channel their unique trajectories to advance the practice of medicine.
Healthcare does not exist as an island. Rather, it is intricately connected to healthcare policy on the state and federal level with various interests involved in how healthcare is delivered and accessed. Thus, the AMA provides a powerful platform for medical students to catalyze change in organized medicine. In particular, AMA’s Medical Student Section (MSS) shares the opportunity for medical students to build experiences with advocacy. Through the annual and interim policy cycle, medical students can author resolutions that address gaps in AMA policy.3 Adopted resolutions that pass the House of Delegates (HOD) become AMA policy that guides AMA’s stance on key issues that impact physicians, patients and the healthcare environment.3 Public health efforts such as opposing smoking on airplanes,4 defending Federal Child Nutrition Programs,5 and considering feminine hygiene products as medical necessities all involved medical student advocacy.6
The AMA also hosts the 2024 National Advocacy Conference to advocate for healthcare reforms on Capitol Hill, which will be held in Washington, DC in February.7 The conference provides opportunities for medical students to talk directly to members of Congress and political insiders about key advocacy issues.7 Interested medical students can learn more about AMA advocacy by joining their local chapter. My conversations at “Tunes for Life” led my journey to the AMA. Similarly, I strongly urge fellow medical students to advocate for issues dear to their hearts and ultimately use advocacy to be at the forefront of shaping healthcare policy for both physicians and patients.
References:
1. Bronson, J & Carson, EA. (2019, April). Prisoners in 2020 – statistical tables - bureau of justice statistics. https://bjs.ojp.gov/content/pub/pdf/p20st.pdf
2. Al-Rousan, T, Rubenstein, L, Sieleni, B, Deol, H & Wallace, RB. (2017). Inside the nation's largest mental health institution: a prevalence study in a state prison system. BMC public health, 17(1), 342. https://doi.org/10.1186/s12889-017-4257-0
3. Medical student section (MSS) Guide to writing a resolution. American Medical Association. (2023, June 22). https://www.amaassn.org/member-groups-sections/medical-students/medical-stude nt-section-mss-guide-writing-resolution
4. Holm, AL & Davis, RM. (2004). Clearing the airways: advocacy and regulation for smoke-free airlines. Tobacco control, 13 Suppl 1(Suppl 1), i30–i36. https://doi.org/10.1136/tc.2003.005686
5. Quality of School Lunch Program H-150.962. American Medical Association Policy Finder. (n.d.-b). https://policysearch.amaassn.org/policyfinder/detail/Quality%20of%20School%20Lunch% 20Programs?uri=%2FAMADoc%2FHOD.xml-0-636.xml
6. Considering Feminine Hygiene Products as Medical Necessities H525.974. American Medical Association Policy Finder. (n.d.). https://policysearch.ama-assn.org/policyfinder/detail/Considering%20Feminine%20Hygiene%20Products%20as%20Medical%20 Necessities%20H-525.974?uri=%2FAMADoc%2FHOD.xml-H525.974.xml
7. American Medical Association. (n.d.). 2024 National Advocacy Conference. American Medical Association. https://www.amaassn.org/about/events/national-advocacy-conference
Jiwon Park is a medical student at the UT Health San Antonio Long School of Medicine, and she is serving as the AMA Chapter Delegate.

2023 TEXAS LEGISLATIVE SESSION WRAP-UP
26 SAN ANTONIO MEDICINE • August 2023
Reforming Medicare Payment
By Jayesh Shah, MD
The Medicare payment system in the United States is in urgent need of an overhaul. Over the years, Medicare physician payments have effectively declined by 26% when adjusted for inflation from 2001 to 2023. This decline has put a financial strain on private practitioners, making it difficult for them to sustain their practices. As a result, many of these private practices are being acquired by hospital corporations or private equity funds, leading to increased costs within the healthcare system.
The shift towards employed physicians is also a continuing trend. According to data from the American Medical Association (AMA), approximately 47.4% of patient care physicians in the U.S. were employed directly by hospitals or medical groups in 2020, and this figure has been gradually increasing over the years. While Texas has seen relatively lower percentages of employed physicians compared to the national average, the state is still experiencing this trend.
The Texas Medical Association (TMA) has been engaged in legislative and regulatory advocacy efforts directed at sustaining private practices.
In June 2023, during the Annual Meeting of the AMA, the TMAled resolution on Medicare payment reform was adopted with overwhelming support. The resolution calls for the declaration of Medicare physician payment reform as an urgent advocacy and legislative priority for the AMA. It also emphasizes the need for increased funding for federal and state advocacy budgets to achieve Medicare physician payment reform and ensure that Medicare physician payments are annually updated at least equal to the annual percentage increase in the Medicare Economic Index. The resolution further requires the AMA's Board of Trustees to report progress in achieving Medicare payment reform at each Annual and Interim Meetings until a predictable, sustainable and fair physician payment system is achieved.
The previous flawed payment system, known as the Sustainable Growth Rate (SGR), was successfully removed in 2013, but it was replaced by the Medicare Access and CHIP Reauthorization Act (MACRA) rule. MACRA aimed to shift the healthcare system away from the fee-for-service model towards a value-based payment system. While the Centers for Medicare and Medicaid Services (CMS) has made efforts to promote value-based care, many physicians working in the field remain skeptical about its ability to increase value and decrease costs. Some solo practitioners and rural physicians have been particularly impacted, leading to the closure of their practices and a risk to patient access to care.
To address these issues, the TMA-led Resolution to the AMA suggests advocacy linking Medicare payment updates for physicians to the Medicare Economic Index. Additionally, there is a bill referred to the subcommittee on Health, called the "Strengthening Medicare for Patients and Providers Act" (HR 2474), which proposes automatic updates to physician Medicare payment rates linked to inflation. The bill was introduced by California Democratic Reps. Raul Ruiz and Ami Bera, along with Republicans Larry Bucshon of Indiana and Mariannette Miller-Meeks of Iowa.
Another issue with the Medicare payment system is the Omnibus Budget Reconciliation Act of 1989, which mandates that estimated increases of $20 million or more to the Medicare physician payment schedule must be offset by cuts elsewhere. Organized medicine aims to increase this budget threshold from $20 million to $100 million, providing more flexibility for adjustments and additions to the payment schedule.
Physicians need to engage in advocacy efforts to address the hardships faced by the physician community. Lawmakers need to hear directly from physicians and their patients about the importance of building stability into the Medicare physician payment system to ensure the survival of private practices. By preserving private practices, overall healthcare costs can decrease, and patient access to care can improve.
Within the AMA, each state has delegates based on the number of AMA members from that state. For every 1,000 members, a state is allocated one delegate in the AMA House of Delegates. I have had the honor of representing Bexar County and Texas as an AMA delegate since 2008, alongside other members of the delegation such as Dr. David Henkes, who currently serves as the chair of the delegation, Dr. Zeke Silva and Dr. Jennifer Rushton.
References:
• AMA: Physicians unite to back cornerstone Medicare pay overhaul
• A new era of physician employment
Jayesh Shah, MD, is an undersea and hyperbaric medicine specialist in practice 29 years. Dr. Shah is President of the South Texas Wound Associates, a re-elected AMA delegate, and member of the BCMS Board of Directors and TMA’s Board of Trustees.

2023 TEXAS LEGISLATIVE SESSION WRAP-UP
Visit us at www.bcms.org 27
Navigating New Health Insurance Laws In Texas: What You Need To Know
By Ezequiel “Zeke” Silva III, MD
Key Points
• The 88th Texas legislative regular session brought both some wins and some draws for the healthcare sector regarding insurance.
• Wins for patients and physicians related to health insurance included: (1) strengthening network adequacy requirements through legislation; and (2) the non-passage of numerous unfavorable insurance bills (including insurance steerage legislation and legislation that would have enabled carriers to offer health plans that carved out numerous critical patient and physician statutory protections, such as prompt pay law and network adequacy requirements).
• An insurance-related draw was the non-passage of favorable legislation aiming to enhance limits on prior authorization, following Texas’ gold carding law (HB 3459) from the previous session.
What you need to know:
• Network Adequacy (HB 3359): A newly passed law that bolsters existing network adequacy requirements. It holds health plans ac-
countable to physicians, employers and patients by: (1) restricting network adequacy waivers to those with valid reasons; (2) ensuring robust networks through specific time, distance and physician specialty criteria; and (3) limiting unfavorable changes during the contract period.

• Insurance Steerage (HB 2414): This bill, which failed to pass, aimed to grant health plans the ability to direct and incentivize patients to see specific physicians, providers, pharmacies and hospitals. The Texas Medical Association's (TMA) grassroots efforts played a crucial role in preventing its passage.
• Physician Ranking and Tiering (HB 3351): This bill, which failed to pass, would have undone landmark physician and patient protections when it comes to health plans’ physician ranking programs.
• Consumer Choice of Benefit Plan Carveouts (HB 1001): This bill, which failed to pass, would have allowed consumer choice of benefit plans to be offered that were exempt from the application of numerous non-benefit-related patient and provider Texas law
2023 TEXAS LEGISLATIVE SESSION WRAP-UP
28 SAN ANTONIO MEDICINE • August 2023
protections, such as network adequacy protections, prompt pay and claims administration procedures.
• Prior Authorization/Gold Carding (HB 4343): Unfortunately, this favorable bill also failed to advance, despite its objective to strengthen Texas’ gold carding law and mitigate excessive prior authorization. Political reasons, rather than the content of the bill, hindered its progress. This issue remains a continuous battle for BCMS and the TMA.
Want to take a deeper dive?
General Comments about the process:
The Texas Legislature convenes only once every two years for a 140day period. Thus, time sensitivity is crucial in advancing legislation due to the numerous steps involved, such as bill submission, hearings, votes, conference committees and the Governor's approval. At any point in this process, a bill can stall. The TMA possesses a robust lobbying team, a dedicated Council on Legislation and widespread physician engagement across the state. BCMS physicians actively participate in various ways, including Capitol visits on First Tuesdays, sharing patient care experiences with the TMA, and providing online and live testimony. It's important to note that state laws primarily affect state-regulated health plans, excluding federally administered ones like self-funded ERISA plans. Nevertheless, achievements at the state level often influence policies in other states and at the federal level.
Network Adequacy:
Despite Texas already having robust network adequacy requirements, only 3% of health plans in the state meet these standards. The remaining 97% receive waivers. This situation has multiple consequences, including unfair negotiation practices by health plans during contract negotiations with physicians, leading to challenges in sustaining practices and providing high-quality care. Additionally, patients are unaware that their plans may not meet their primary care and specialty needs (limiting patient choice of in-network physicians and providers and reducing the value of the health plan product purchased). HB 3359 addresses this issue by holding health plans accountable for their networks. The bill ensures greater oversight and transparency in the waiver process, requires valid reasons for exemptions, and establishes clearer network standards based on federal Medicare Advantage guidelines, including factors like time, distance, appointment wait times and required physician specialties.
Insurance Steerage:
The healthcare marketplace is experiencing increased vertical and horizontal integration, leading to a greater likelihood of health plans directing patients towards entities in which they have a financial stake. HB 2414, which failed to pass, aimed to allow health plans to selectively steer patients covered by their insurance. Enabling further con-
solidation would have increased costs and compromised healthcare quality, while the bill also lacked adequate patient protections.
Gold Carding:
A significant victory in the 2021 legislative session was Texas’ gold carding law (HB 3459). This act allows physicians who achieve a 90% prior authorization approval rate for specific healthcare services to earn Gold Card status, granting them exemption from prior authorization requirements for those healthcare services such as drugs, procedures, pathology and diagnostic imaging.
The law has been implemented for only a short period of time. However, it is disappointing to note that according to the Texas Department of Insurance (TDI), only 3% of Texas physicians have attained Gold Card status. This may, in part, stem from TDI rules that imposed a minimum number of eligible services to qualify for Gold Card status. HB 4343 aimed to strengthen Texas’ gold carding law by reducing the minimum number of eligible services, enhancing health plan accountability regarding initial denials through stronger enforcement and physician appeals, and increasing the Texas Medical Board's oversight of medical decisions made by health plans during utilization review.
Unfortunately, HB 4343 failed to advance, primarily due to political reasons rather than shortcomings in the bill's content. Although regrettable, both BCMS and the TMA understand the burdens of prior authorization and the resulting harm to patients. This issue will continue to be an ongoing battle.
Going forward:
Drafting and passing meaningful legislation is crucial for supporting physicians, but it represents just the first step. Once laws are enacted, the regulatory phase commences, where various state agencies, typically the Texas Department of Insurance for health insurance, must implement these laws. Implementation typically involves a rule-making process that includes soliciting comments from medical societies such as BCMS and the TMA. This process may also involve hearings before state agencies or interim hearings before legislative committees. Therefore, the vital role of physicians in the legislative process remains continuous and ever-important.
Ezequiel “Zeke” Silva III, MD, FACR, FSIR, FRBMA, RCC, is the Medical Director of Radiology at the Methodist Texsan Hospital and an adjunct professor at the UT HealthSan Antonio. He is a member of the TMA Delegation to the American Medical Association and TMA Council on Legislation as well as Chair of the AMA/Specialty Society RVS Update Committee and immediate past Co-Chair of the AMA Digital Medicine Payment Advisory Group. Dr. Silva is the President-Elect of the Bexar County Medical Society, Past President of the Texas Radiological Society and currently serves on the board of directors for the South Texas Radiology Group.

2023 TEXAS LEGISLATIVE SESSION WRAP-UP
Visit us at www.bcms.org 29
Meeting The Bexar County Health Needs Through Graduate Medical Education
By Scott Jones, MD
The healthcare community of Bexar County is responsible for identifying and collaborating with other entities, including patients, to improve the health of all our communities. As a fundamental role of physicians, it is paramount that our next generation of physicians are appropriately introduced to these needs, educated, and engaged in our community interventions. So, what are those needs, and how is Graduate Medical Education (GME) currently engaged?
I decided to ask the open-access artificial intelligence platform, ChatGPT, about the most significant healthcare needs for Bexar County. ChatGPT provided seven categories of greatest needs with brief descriptions. While this list is not exhaustive, it was a reasonable starting point. I then sent this list to some GME program leaders in the county, asking for examples of engagement. This article will highlight GME efforts in Access to Healthcare, Health Insurance Coverage, Chronic Disease Management, Behavioral Health Services, Maternal Child Health, Health Disparities, and Aging Population and Geriatric Care. ChatGPT responses are bolded throughout.
Bexar County, Texas, which includes the city of San Antonio, has several notable healthcare needs. Here are some of the greatest healthcare needs in Bexar County:
1. Access to Healthcare: Ensuring equitable access to healthcare services is a significant need in Bexar County. While there are healthcare facilities in the area, disparities in access exist, particularly for underserved populations, low-income individuals and those without health insurance. Improving access to primary care, specialty care, mental health services and preventive care is essential. Given the projections of growing physician shortages in our region, GME is critical to closing these gaps.1 The University of Texas Health Science Center San Antonio Long School of Medicine (LSOM) has trained physicians in Bexar County for over 50 years in every major healthcare system. Other enterprises currently training in the county include Christus Santa Rosa, Baylor College of Medicine and, more recently, Texas Graduate Medical Education Research (TIGMER), the GME branch of the University of Incarnate Word. The Texas Higher Education Coordinating Board GME Expansion Grants have played a significant role in financially supporting Baylor's programs at Children's Hospital of San Antonio and TIGMER, and to a lesser extent, LSOM GME Programs. Soon, Methodist Healthcare System will also
begin to sponsor some core residency programs with HCA. San Antonio has over 100 GME programs with more than 1,000 physicians. Multiple entities have recognized the value of investing in training for the future to meet our regional and county needs.
GME supports underserved communities, with the University Health Robert B. Green Campus downtown serving as the largest ambulatory site for the LSOM GME programs. The TIGMER Family Medicine (FM) residents train at the Communicare West clinic, an FQHC serving the inner westside. University Hospital (UH) is the safety net hospital for San Antonio and the primary inpatient location for LSOM GME and, more recently, TIGMER Internal Medicine (IM) Residents. The LSOM IM residency has an Ambulatory Track, a program that encourages internal medicine residents to enter Primary Care. Many graduates work in clinics throughout San Antonio. Unfortunately, the underprivileged often primarily access care through emergency rooms. The LSOM started an Emergency Medicine (EM) residency program in 2013, and these residents are often the first to see these patients, along with the many GME consulting services. The General Surgery residents and faculty are the first on hand in the trauma bay for the only one of two Level 1 trauma centers serving this region. The LSOM Psychiatry residents provide telepsychiatry services to the underserved communities of Del Rio, Hondo and Uvalde. The programs and services listed are but a small representative sample of how the 100+ GME programs are improving access.
2. Health Insurance Coverage: The uninsured rate in Bexar County remains a concern. Many residents lack health insurance, limiting their access to necessary healthcare services and increasing the burden on safety-net providers. Expanding access to affordable health insurance options and Medicaid eligibility could help address this need.
This generation of new physicians is very engaged in advocacy, including advocacy for patients gaining access to healthcare. LSOM has several residents in different programs engaged with the Texas Medical Association’s First Tuesdays up in Austin. Others advocate through their national or State specialty associations, such as the LSOM FM residents. They attend the Family Medicine Advocacy Summit, where they are given training on advocating with lawmakers and their staff. Expanding Medicaid coverage is recognized as a significant healthcare issue in Texas and even more so in our region.
The residents and fellows in all our County GME Programs see
2023 TEXAS LEGISLATIVE SESSION WRAP-UP
30 SAN ANTONIO MEDICINE • August 2023
the impact on patients they serve who are uninsured or under-insured. They see the challenges of working with hospital care navigators and social workers to get these patients the care they need at times. TIGMER and LSOM trainees have the privilege of caring for patients supported by University Health's CareLink financial assistance program. Further, they see the positive impact of the Texas Health and Human Services Healthy Texas Women program. The TIGMER and LSOM IM residents experience WellMed's Accountable Care Organization approach to delivery. Residents are on the tip of the spear, seeing the challenges for the un- and underinsured patients navigating the healthcare system. We foresee even greater engagement of this generation on this issue.
3. Chronic Disease Management: Bexar County faces a high prevalence of chronic diseases such as diabetes, obesity and cardiovascular diseases. Improving chronic disease management and prevention efforts, including increased access to healthcare, regular screenings, health education and lifestyle interventions, can significantly impact the health outcomes of residents.
Managing patients with chronic diseases is embedded within each of the other six categories as are efforts in GME. Continuity Care Clinics are required for all primary care and some specialty residencies and fellowships. These patients with chronic conditions are followed lon-

gitudinally throughout the residency. Since most trainees simultaneously do inpatient services, they see the impact of less optimally managed patients. Further, our social determinants of health SDoH efforts are aimed at opening residents' eyes to how much other issues than their care in the clinic or the hospital impacts their patients' health.
Diabetes and obesity, and their se condary comorbidities, are significant issues for our county. Our LSOM Endocrinology fellows are involved in research studying the mechanisms of SGLT2 inhibitors and the effects of ketone elevation in several groups, including in diabetes, heart failure and the elderly. Further, they engage in quality improvement projects, trying to improve all our quality measures in patients with diabetes, including microalbuminuria, lipids and screening for NASH to prevent it and decrease the progression of micro- and macrovascular complications. The LSOM Pediatric Endocrinology Fellowship was actively engaged in enrolling patients into the bionic pancreas trial, an artificial intelligence-powered system recently cleared by the U.S. Food and Drug Administration. 2 Both fellowships are serving the underserved at the Texas Diabetes Institute, making a substantive impact through patient care, quality improvement endeavors and research.
4. Behavioral Health Services: Access to mental health and substance abuse services is a critical need in Bexar County. The area
2023 TEXAS LEGISLATIVE SESSION WRAP-UP
Visit us at www.bcms.org 31
continued on page 32
faces shortages of mental health professionals and limited resources for treating substance abuse disorders. Expanding the availability of mental health services, integrating mental health into primary care, and increasing funding for substance abuse treatment programs are crucial steps to address this need.
The LSOM Child and Adolescent Psychiatry Fellowship (CAP) has increased the number of trainees due to support from the 86th Texas Legislature, creating the Texas Child Mental Health Care Consortium (TCMHCC).3 Texas Child Psychiatry Access Network (CPAN) is an initiative of the TCMHSCC to support family medicine and pediatricians across the State.4 LSOM GME programs capitalize on their services and professional development offerings to provide more complex psychiatric care in primary care. The LSOM Pediatric Residents are trained to screen for mental health issues, including ADHD, Anxiety, Depression (both youth and post-partum) and Suicide ideation. They can evaluate screening tools and apply the most current guidelines for all of these disorders, refer to therapy (even introducing CBT for anxiety and depression for those patients unable to find a therapist), and treat with medication when indicated. Because of screening, they can start to intervene earlier. Furthermore, the Texas Higher Education Coordinating Board (THECB) GME Expansion Grant prioritization of mental health specialties allowed the TIGMER Psychiatry Program to get substantive grant funding for their residency and expand access in locations noted in the first section. Finally, the LSOM Psychiatry residents provide 24/7 inpatient support for Bexar County's two Level 1 trauma centers and the South Texas Veterans Healthcare System (STVHCS).
The LSOM, in partnership with the STVHCS, started its first fellow in the new Addiction Medicine Fellowship this July. Individuals with primary training in the following specialties can enter this oneyear training program: anesthesiology; emergency medicine; family medicine; internal medicine; obstetrics and gynecology; pediatrics; preventive medicine; or psychiatry. Beyond service to veterans, the fellows will work in clinical academic settings with Dr. Jennifer Potter (Vice Dean for Research, Professor in the Department of Psychiatry), the Principal Investigator of the Big South/West Node of the National Institute on Drug Abuse Clinical Trials Network and Director of the Texas Medication for Opioid Use Disorder Initiative. Further, LSOM Pediatrics and OBGyn residents and fellows engage with patients enrolled in the Center of Health Care Services (CHCS) Mommies Program providing prenatal and postnatal care to patients with substance abuse disorders.
5. Maternal and Child Health: Bexar County has specific healthcare needs related to maternal and child health. Reducing infant mortality rates, improving access to prenatal care, promoting
breastfeeding, and addressing social determinants of health that impact maternal and child health outcomes are essential priorities.
The GME Programs within the LSOM Obstetrics and Gynecology (OBGyn) Department and Pediatrics Department are involved in multiple efforts within the county, state and nation. The OBGyn residents, Maternal Fetal Medicine (MFM) and Gynecology Oncology (GYNOnc) Fellows and faculty are the physicians caring for some of the most complicated patients at UH, the only U.S. News and World Report Top Maternity Hospital in the region and a “Breast Feeding Friendly" center. This includes supporting UH's Stork One, the dedicated maternal transport team bringing patients to higher levels of care. The MFM and GYNOnc fellows and residents provide care through the “Placenta Accreta Spectrum Disorder" program to women from all over south central Texas with abnormal placentation and at high risk for maternal hemorrhage, transfusion and death. The GYNOnc Fellows are engaged in research protocols advancing therapies for women's cancers. In the community, they engage in the UT Teen Health Program, involved in education and reducing teen pregnancy.
The LSOM Pediatric Residency implemented the evidenced-based SDoH screening and referral tool, WE CARE. Those with positive screens are offered information on resources in food, housing, parental education, employment, utility assistance and childcare when requested. The LSOM Neonatology Fellows are involved in outreach educational efforts to primary care physicians and research projects to improve child and maternal nutrition. With the opening of the UH Women and Children's Hospital comes a potential for expansion in training opportunities. Baylor Pediatric residents at the Children's Hospital of San Antonio and the Family Medicine residents at the LSOM and TIGMER are undoubtedly involved in newborn and childhood initiatives. The future of pediatric care continues to look better for the county and region.
6. Health Disparities: Like many other areas, Bexar County experiences health disparities, particularly affecting marginalized communities, including Hispanic/Latino populations. Addressing health disparities requires targeted efforts to improve access to care, health education and preventive services, as well as addressing social determinants of health, such as poverty, education and housing.
The LSOM GME changed its mission statement several years ago to move beyond improving healthcare through GME to impacting health. As much as 80% of health happens outside of healthcare. Instead, much of health is affected by structural and social determinants of health. San Antonians in the zip codes on the inner west side have an 18-year lower life expectancy than the San Antonians living 18 miles out Bandera Road beyond loop 1604. Therefore, three years ago, we began orienting all incoming residents to SDoH in the context of San
2023 TEXAS LEGISLATIVE SESSION WRAP-UP
32 SAN ANTONIO MEDICINE • August 2023
from page 31
continued
Antonio. They are introduced to our history, our underserved communities and the disparities in health outcomes across the city. They are introduced to outstanding efforts in these communities, including the work of Promotores and community health workers who live and work in their neighborhoods. This year we added a community health fair so the new physicians will be more familiar with the resources available to patients in the community. This orientation of all incoming at the institutional level is unique among academic medical centers.
This last year, the LSOM IM residency started a Health Equity Track. The IM residents in this Track work with Street Medicine San Antonio, the Refugee Clinic, the Alpha House and the LGBTQ+ Clinic, to name a few. The goal is to grow this Track as an offering across many LSOM GME programs over the next few years. All TIGMER residencies work in the Center of Healthcare Services and Haven for Hope. The LSOM Family Medicine residents work within the South Central Area Health Education Center, where they are involved in community education efforts. Further, they do home visits with the Promotores noted above. The WE CARE screening in Pediatrics stated above is a significant advancement. While there is growing engagement by the GME community in health disparities, there is much more needed.
7. Aging Population and Geriatric Care: Bexar County has a growing aging population, leading to increased healthcare needs related to geriatric care. Expanding geriatric services, promoting healthy aging, addressing the unique healthcare needs of older adults, and enhancing long-term care options are crucial for meeting the needs of this population.
The Medical Center is exploding in the neurosciences with the Biggs Institute for Alzheimer's & Neurogenerative Diseases, Barshop Institute for Longevity and Aging Studies, and the recent groundbreaking for the Center for Brain Health, all of UT Health San Antonio. These expert neuroscientists drawn to San Antonio have started new fellowships: Neuromuscular, Neuroimmunology, Movement Disorders, Behavioral Health & Neuropsychiatry, and CNS Endovascular joining our four existing neurology fellowships and residency. The research and cutting-edge healthcare these centers, research and training programs bring to our region will have a long-term impact for many years. The Neurology residency has also grown with support from the UH and THECB GME Expansion grant funding.
Both LSOM and TIGMER benefit from training arrangements with the STVHCS, the fastest-growing VA in the country. The VA supports close to one-quarter of the LSOM residents and fellows. The partnership with WellMed has also provided an opportunity to work with an ACO primarily serving the elderly. The LSOM also has specialty fellowships in Geriatric Medicine and Hospice and Palliative Care, generating more providers in this area of demand. HCA will soon start an
IM residency, which will help diminish the substantive shortage of internists in the county and region.
Per ChatGPT, "Addressing these healthcare needs in Bexar County requires a comprehensive approach, involving collaboration among healthcare providers, community organizations, policymakers and stakeholders. By focusing on improving access to care, addressing health disparities, promoting prevention and wellness, and enhancing healthcare infrastructure and resources, the overall health and wellbeing of the residents in Bexar County can be improved." This small sample of how GME Programs are engaged in each of these domains will encourage our healthcare community to continue advocating for GME expansion in the county. The recent closure of Texas Vista Medical Center posed a substantive threat to some TIGMER training programs' future. Fortunately, several health systems, including UH, have stepped in to help with talks ongoing with others. The prioritization for funding of existing and new GME positions is a constant challenge and crucial to the continued growth of the pipeline of physicians.1 As noted, the state has embraced GME expansion in multiple ways. Collaboration as well among policymakers and health system leaders at the local level for GME support will remain important in this rapidly growing region. Stakeholders can be assured that the next generation of GME graduates will be better prepared to meet Bexar County's healthcare and health needs due to more collaborative engagement within the community in these seven ChatGPT identified categories.
References:
1. Jones WS. Graduated Medical Education: The Physician Pipeline for Bexar County and South Texas. San Antonio Medicine. The Official Publication of the Bexar County Medical Society. July 2022, Vol 77, No. 7, p. 12 - 14
2. Sansom, Will. FDA green-lights bionic pancreas studied at UT Health Science Center, University Health. University of Texas Health San Antonio Newsroom. https://news.uthscsa.edu/fdagreen-lights-bionic-pancreas-studied-at-ut-health-science-centeruniversity-health/

3. Texas Child Mental Health Care Consortium https://tcmhcc.utsystem.edu/workforce-expansion/
4. The University of Texas System TCMHCC Child Psychiatry Access Network. https://www.texmed.org/CPAN2021/
Woodson “Scott” Jones, MD, is the Vice Dean for GME at UT Health San Antonio. Before moving to UT five years ago, he served as Dean of the San Antonio Uniformed Services Health Education Consortium. Dr. Jones also Chairs the BCMS Joint Academic Collaborative Committee and serves on the TMA Education Council.
2023 TEXAS LEGISLATIVE SESSION WRAP-UP
Visit us at www.bcms.org 33
Leah Hanselka Jacobson, MD Interview
Interviewed by Monica Jones, BCMS COO
This month’s magazine, “Legislative Wrap-up,” is the perfect time to interview Dr. Leah H. Jacobson. Dr. Jacobson was the BCMS President in 2017, and is one of only three women BCMS Presidents in the history of BCMS.

Dr. Jacobson has been a member of BCMS since 1990. She completed her undergrad at Texas A&M University and her Medical Degree at the University of Texas Health Science Center, San Antonio. She continues to support BCMS in the following roles: Delegate to the TMA, BCMS Legislative Committee Member, BCMS Women in Medicine Committee, and is Co-Chair of the BCMS Public Health & Patient Advocacy Committee.
The Texas State Legislature was in Special Session in 2017, during Dr. Jacobson’s term, because the Legislature failed to reauthorize the Texas Medical Board (TMB) and the Texas Medical Practice Act. At the time, she pondered in her President’s message of her concern, “Could we, as physicians, be without a governing board?”1 While the Sunset Bill(s) remained top priority during the Regular and Special Sessions, many bills were passed that influenced the practice of medicine for physicians and patients.
Dr. Jacobson is a strong advocate for getting involved in the process. “Policy-making is not a spectator sport,” she offers. “You cannot sit on the sidelines and say somebody else will do it. You’ve got to be involved and you’ve got to be interested.”
Highlights of 2017 Texas legislative bills included the following:
• HB 10: Established a state mental health parity work group, as well as designated an ombudsman as an advocacy source and clarified benefits for mental health and substance abuse.
• SB 507: Expanded the billing mediation process for out-of-network facilities and providers.
• SB 680: Empowered the physicians to override health plans’ step therapy protocols.
• SB 1066: Required new medical schools to offer new GME positions to keep pace with their medical graduates.
• SB 1107: Established a statutory definition for telemedicine and clarified standard of care.
• SB 1148: Prohibited the state from using maintenance of certifica-
tion (MOC) as a requirement for state licensure, hospital privileges or insurance participation.
• HB 1600: Allowed Medicaid to pay physicians for mental health screenings during annual well-child exams, just to discuss a few.
There were many important events that occurred during Dr. Jacobson’s BCMS Presidency. Tobacco-21 (“T-21”) was approved by the City of San Antonio, after a long, coordinated city effort; the #MeToo Movement emerged; the U.S. declared the opioid epidemic a national emergency; and gun violence was prominent after mass shooting events in Las Vegas (Mandalay Bay Resort) and Sutherland Springs, Texas.
That same year, Hurricane Harvey was one of the worst storms to hit Texas in more than 20 years, with an estimated damage of $75 billion. The storm dropped a record 51 inches of rain on the Houston area over a five-day period. More than 72,000 people had to be rescued during the storm and another 30,000 needed temporary shelter. During Dr. Jacobson’s term, BCMS recruited 207 physician members and 370 other medical personnel volunteers to provide medical services for the benefit of displaced Hurricane Harvey evacuees.2 Working with San Antonio Metro Health and the City of San Antonio Emergency Operations Center “EOC,” BCMS volunteers provided 24-hour medical coverage beginning at a number of shelters set up in San Antonio. Dr. Jacobson gives credit for this community response to the BCMS Emergency Preparedness Committee and the volunteers who worked tirelessly assisting evacuees with medical care and transports.
Dr. Jacobson remains a strong advocate for women physicians, which represent only one-third of practicing physicians in the United States. BCMS’s Women in Medicine Committee has been promoting women
34 SAN ANTONIO MEDICINE • August 2023
“If we do not work to manage medical legislation, it will be managed for us.”
2017 BCMS President, Leah Hanselka Jacobson, MD
SAN ANTONIO MEDICINE
leaders in medicine, recruiting and retaining women members in the Bexar County Medical Society and the TMA for over 31 years. Its goal is to address special needs and issues for women physicians.3 The annual “Women in Medicine Appreciation Dinner” recognizes a large cross-section of the healthcare industry, including may of the large healthcare systems, academic institutions and private groups.
“I have been fortunate to be a part of this committee for most of its existence, starting as a medical student member, over 26 years ago,” notes Dr. Jacobson. It is a part of the Medical Society that holds a special place in my heart.”4 The Women Leaders in Medicine event will be held September 20 of this year.


On medicine and politics, Dr. Jacobson reflects that “as physicians, we take the Hippocratic Oath, which includes the words ‘Do No Harm.’ I would like for us all to continue to hold true to that oath and add to it, ‘Do MORE Good’ for our members, our patients and the San Antonio Community.”
References
1. The Medical News, Bexar County Medical Society, Volume 70 , Number 9, September 2017, page 8.
2. The Medical News, Bexar County Medical Society, Volume 70, Number 10, October 2017, page 33.
3. The Medical News, Bexar County Medical Society, Volume 70, Number 11, November 2017, page 8.
4. The Medical News, Bexar County Medical Society, Volume 70, Number 11, November 2017, page 8.
Monica Jones is the Chief Operating Officer for the Bexar County Medical Society.



Visit us at www.bcms.org 35
SAN ANTONIO MEDICINE
Decreasing Barriers to VaccinePreventable Diseases in Bexar County
 By Marina Moreno and Adelita G. Cantu, PhD, RN, FAAN
By Marina Moreno and Adelita G. Cantu, PhD, RN, FAAN
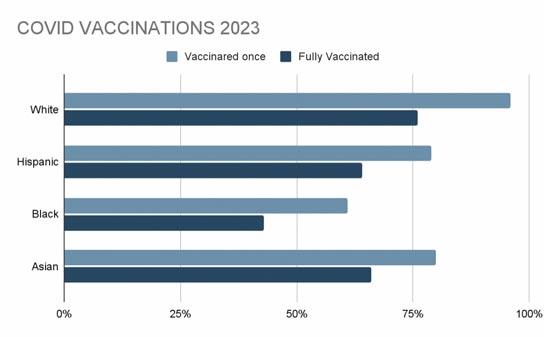
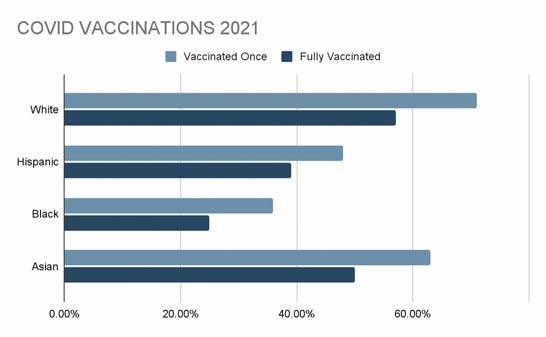
Background: Vaccination disparities continue in Texas’ five most populous counties, including Bexar County. According to the City of San Antonio, Sean Cummings has estimated that 296,019 out of 417,222 non-Hispanic white people were vaccinated at least once against COVID in 2021. The percentage of those people who were vaccinated is roughly 71%. On the other hand, 437,807 out of 906,742 Hispanics in San Antonio were vaccinated at least once. The percentage of Hispanics vaccinated was roughly 48% in 2021.1
The Centers for Disease Control and Prevention (CDC) states that, “Immunization information systems (IIS) are confidential, populationbased, computerized databases that record all immunization doses administered by participating providers to persons residing within a given geopolitical area.”2 In clinical practice, these information systems assist healthcare providers and public health agencies by authorizing access to an individual’s vaccination record to determine appropriate vaccination interventions. In the United States, many states use an IIS to collect “aggregate data on vaccinations for use in surveillance and program operations,” but the overall goal is to guide public health action by “improving vaccination rates and reducing vaccine-preventable disease.”2
ImmTrac (Immunization Registry of Texas) is an online IIS database that tracks immunization records in the state of Texas. It was enacted by Texas HB 1921, which was first passed in 2003 by the 78th state legislature. ImmTrac2 replaced the original ImmTrac in April 2017.
The bill was initially passed to increase the use of authorized consent and transition from paper forms to online forms. The registry was designed to keep patient information secure and private while allowing access to authorized healthcare providers, schools and public health departments. “The registry is secure and confidential, and safely consolidates and stores immunization records from multiple sources in one centralized system.”3
Certain vaccinations are mandatory for childcare, school, military enlistment, travel, employment, and may be necessary in other fields. Records of those vaccinations last a lifetime. However, tracking records from various sources can be time-consuming, and may lead to over or under use of vaccinations. “Reducing the hassle of record-keeping prevents children from being either under- or overimmunized.”4 In addition, ImmTrac2 stores individual information on antiviral immunizations and medications that are associated with disaster events.4 Thus, keeping a centralized database of immunization records prevents user error and confusion.
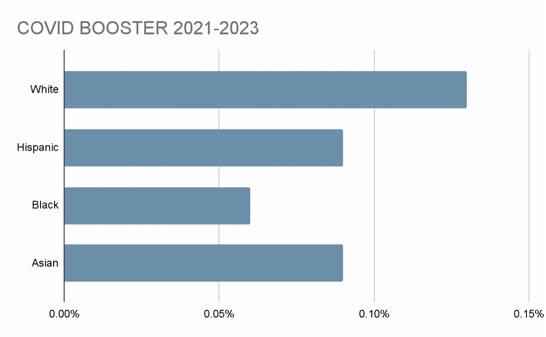 Figure 1 Comparison of ethnicities in Bexar County vaccinated in 2021 https://cosacovid-cosagis.hub.arcgis.com/datasets/CoSAGIS::vaccinations-weekly-totalspublic-share-1/about
Figure 2 Comparison of ethnicities in Bexar County vaccinated in 2023 https://cosacovid-cosagis.hub.arcgis.com/datasets/CoSAGIS::vaccinations-weekly-totals-public-share-1/about
Figure 1 Comparison of ethnicities in Bexar County vaccinated in 2021 https://cosacovid-cosagis.hub.arcgis.com/datasets/CoSAGIS::vaccinations-weekly-totalspublic-share-1/about
Figure 2 Comparison of ethnicities in Bexar County vaccinated in 2023 https://cosacovid-cosagis.hub.arcgis.com/datasets/CoSAGIS::vaccinations-weekly-totals-public-share-1/about
36 SAN ANTONIO MEDICINE • August 2023 SAN ANTONIO MEDICINE
Figure 3 Comparison of boosters by ethnicity in Bexar County 2021-2023 https://cosacovid-cosagis.hub.arcgis.com/datasets/CoSAGIS::vaccinations-weekly-totalspublic-share-1/about
Storing patient information regarding adverse reactions to immunizations and other medications helps prevent future adverse responses; this could be the difference between life and death in emergency events. For example, people with egg allergies have been advised to avoid certain flu vaccines due to the potential for an allergic reaction. When a healthcare provider knows that a severe egg allergy is present, alternative vaccines that are not produced in eggs, such as recombinant flu vaccines, may then be considered.
Enrollment to ImmTrac2 is not automatic when a person in Texas receives a vaccine. Healthcare providers are required by the state of Texas to report all immunization records for persons under the age of 18. When a child is born, parents are asked to give consent for their child to be enrolled in ImmTrac2. The DSHS implemented HB 1921 in 2005 to confirm that parents give consent to participate in the registry at the time they register a birth certificate. If a minor (under the age of 18) was born before 2005, a parent can submit the child's immunization history to ImmTrac2 for inclusion in the registry.
Once a person turns 18, they “would have to sign a new consent or their records will be deleted when they turn 26.”5 The new consent must also be signed by one parent/legal guardian to participate in ImmTrac2. Once an adult grants individual consent to participate in ImmTrac2, the consent is then valid unless revoked by the same individual.
Obtaining consent may differ depending on the healthcare setting, such as hospitals, clinics or private practices. “Electronic or digital consent forms must contain all the same text and content as the most current official state registry consent forms, and all of the same client information must be filled out to be valid. Alterations to the text and content are not allowed. Digitized consent forms are subject to the same retention, production and disposal requirements as written consents.”6 The signed consent form is then kept and sent to the State of Texas, and the state encrypts the information.
It is important for healthcare providers, retail pharmacies and other healthcare professionals to stay updated with the latest CMS regulations (The Centers for Medicare and Medicaid Services) and Texas requirements to ensure compliance. Additionally, healthcare providers and other vaccine providers can play a part in assuring accurate vaccine data by educating patients about the purpose and benefits of ImmTrac2.
Widespread utilization of ImmTrac2 will increase the ability to identify low-income individuals, minority populations and individuals with limited access to healthcare and vaccinations. We can foster trust in the healthcare system and promote equal and equitable access to healthcare. Improved equity results in higher rates of herd immunity and prevents the spread of vaccine-preventable diseases.
For the most recent versions of the official state registry consent forms, visit the Texas Department of State Health Services – Immunization Registry website at: https://www.dshs.texas.gov/immunizationunit/immtrac2-texas-immunization-registry/immtrac2-forms-documents
The registry consent forms are:
• Immunization Registry – Minor Consent Form is identified as C-7 https://www.dshs.texas.gov/sites/default/files/immunize/immtrac/do cs/C-7.pdf
• Immunization Registry – Adult Consent Form is identified as F1113366 https://www.dshs.texas.gov/sites/default/files/immunize/ immtrac/docs/F11-13366.pdf
For more state information and support, contact the Texas Immunization Registry.
Email: ImmTrac2@dshs.texas.gov, Phone: 800-348-9158
Website: https://www.dshs.texas.gov/immunize/immtrac
For more local information and support, contact:
Adelita Cantu, Chair of Immunization Coalition of San Antonio
Email: cantua2@uthscsa.edu, Phone number: 210-567-7623
References:
1. Vaccinations weekly totals - public share. (COSA) City of San Antonio GIS COVID HUB. (n.d.). https://cosacovid-cosagis.hub.arcgis.com/ datasets/CoSAGIS::vaccinations-weekly-totals-public-share-1/about
2. Centers for Disease Control and Prevention. (2019, June 7). About immunization information system (IIS). Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/programs/iis/ about.html
3. Organizations, A. (n.d.). Immtrac2 Texas Immunization Registry. ImmTrac2 Texas Immunization Registry | Texas DSHS. https://www.dshs.texas.gov/immunization-unit/immtrac2-texas-immunization-registry
4. Talk to patients about: What is IMMTRAC2? by Sean Price. Texas Medicine August 2020. Texmed. (n.d.). https://www.texmed.org/ Template.aspx?id=54305
5. Price, Sean. Texas Medical Association. (2021, March 1). Texas Medicine March 2021 page 28. Texas Medicine March 2021 Page 28. https://www.qgdigitalpublishing.com/publication/?m=55178&i=69 3653&p=30&ver=html5
6. The Texas Immunization Registry: Consent Overview. (n.d.). https://www.dshs.texas.gov/sites/default/files/immunize/immtrac/d ocs/11-15702.pdf
Marina Moreno is a Nursing Student at UT Health San Antonio, School of Nursing.

Adelita G. Cantu, PhD, RN, is an Associate Professor at UT Health San Antonio, School of Nursing and the Chair of Immunization Coalition of San Antonio (IZSA).

Visit us at www.bcms.org 37 SAN ANTONIO MEDICINE
Summer in the City –Cool Down & Wellness Festival

BCMS participated in the “Summer in the City – Cool Down & Wellness Festival” presented by the Health Confianza on June 9th at the UTSA Downtown Campus. The BCMS “Ask A Doctor” table assisted with questions on vaccination hesitancy and health screenings, which were given by UT Health. A special thank you goes to Dr. John Carter, Dr. Wendy Wu, Dr. Justin Williams and Dr. Bellur Ramanath for staffing our “Ask a Doctor” table.

To see all the pictures from the event, go to www.bcms.org/photos/photogallery.php.

38 SAN ANTONIO MEDICINE • August 2023
SAN
ANTONIO MEDICINE




Visit us at www.bcms.org 39 SAN ANTONIO MEDICINE
Shop Vendors Who Support BCMS

BCMS Vendor Directory
We encourage you to use our supporting vendors whenever you or your practice needs supplies or services.
ACCOUNTING FIRMS
Sol Schwartz & Associates P.C. (HHH Gold Sponsor)

Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Jim Rice, CPA 210-384-8000, ext. 112 jprice@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”
ACCOUNTING SOFTWARE
ASSET WEALTH MANAGEMENT
Aspect Wealth Management (★★★ Gold Sponsor)

We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President
210-268-1520
mclark@aspectwealth.com
www.aspectwealth.com
“Get what you deserve … maximize your Social Security benefit!”
BANKING
Express Information Systems (HHH Gold Sponsor)

With over 29 years’ experience, we understand that real-time visibility into your financial data is critical. Our browser-based healthcare accounting solutions provide accurate, multi-dimensional reporting that helps you accommodate further growth and drive your practice forward.
Rana Camargo
Senior Account Manager
210-771-7903
ranac@expressinfo.com www.expressinfo.com
“Leaders in Healthcare Software & Consulting”
ATTORNEYS
Kreager Mitchell (HHH Gold Sponsor)
At Kreager Mitchell, our healthcare practice works with physicians to offer the best representation possible in providing industry specific solutions. From business transactions to physician contracts, our team can help you in making the right decision for your practice.
Michael L. Kreager
210-283-6227
mkreager@kreagermitchell.com
Bruce M. Mitchell
210-283-6228
bmitchell@kreagermitchell.com
www.kreagermitchell.com
“Client-centered legal counsel with integrity and inspired solutions”

Broadway Bank (HHH Gold Sponsor)

Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@Broadway.Bank www.broadwaybank.com
“We’re here for good.”
Denise Smith
Vice President | Private Banking
210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales Assistant Vice President | Private Banking
210-343-4494
Scott.Gonzales@amegybank.com
www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help Physicians get the banking services they need.
Synergy FCU Member Services
210-750-8333 info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”
CLINICAL DIAGNOSTICS
always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison
(210) 503-0003
yulia@genicslabs.com
Kevin Setanyan
Managing Partner
(210) 503-0003
kevin@genicslabs.com
Artyom Vardapetyan
Managing Partner
(210) 503-0003
www.genicslabs.com
“Accurate results in record time.”
CREDENTIALS VERIFICATION ORGANIZATION
Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for health care entities.

Betty Fernandez
Director of Operations
210-582-6355
The Bank of San Antonio (HHH Gold Sponsor)

We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Brandi Vitier
210-807-5581
brandi.vitier@thebankofsa.com
www.thebankofsa.com
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead
210-343-4526
Robert.Lindley@amegybank.com
Livingston Med Lab (HHHH 10K Platinum Sponsor) High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease & Genetics. Robert Castaneda (CEO)

210-316-1792
Robert@livingstonmedlab.com
Joey Martinez (Director of Operations) 210-204-7072
Joey@livingstonmedlab.com
Dwight Chapman (Account Manager)
210-591-2649
Dwight@livingstonmedlab.com
www.livingstonmedlab.com/home
“Trusted Innovative, Accurate, and STAT Medical Diagnostics”
Betty.Fernandez@bexarcv.com
www.BexarCV.com
“Proudly serving the medical community since 1998”
FINANCIAL ADVISORS
Oakwell Private Wealth Management (HHHH 10K Platinum Sponsor)

Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA
Senior Private Wealth Advisor
512-649-8113
SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
Genics Laboratories (HHH Gold Sponsor)

Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are
“More Than Just Your Advisor, We're Your Wealth Management Partner”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals.
40 SAN ANTONIO MEDICINE • August 2023
Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney
Financial Advisor
210-858-5880
Elizabeth.olney@edwardjones.com www.edwardjones.com/elizabeth-olney
"Making Sense of Investing"
FINANCIAL SERVICES
jsanderson@nhsltd.com
Nexus Neurorecovery Center 227 Lewis St, San Antonio, TX 78212
https://nexushealthsystems.com
“To return patients to lives of productivity and meaning”
sional reporting that helps you accommodate further growth and drive your practice forward.
Rana Camargo
Senior Account Manager
210-771-7903
ranac@expressinfo.com
www.expressinfo.com
“Leaders in Healthcare Software & Consulting”
INSURANCE
Aspect Wealth Management (HHH Gold Sponsor)

We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520 mclark@aspectwealth.com www.aspectwealth.com
“Get what you deserve … maximize your Social Security benefit!”
GERIATRICS/PRIMARY CARE
Provider's Choice Scribe Services (HHH Gold Sponsor)

Our accurate and complete documentation helps our customers focus on what’s most important, their patients. Let us take on the task of documenting your patient encounters, it’s what we do.
Yoceline Aguilar COO
yaguilar@pcscribes.com
915-691-9178
Luis Chapa
MD/CEO
210-796-4547
lchapa@pcscribes.com
www.providerschoicess.com/
“An Unparalleled Scribe Experience”
TMA Insurance Trust
(HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.

Wendell England Director of Member Benefits
512-370-1776
wendell.england@tmait.org
800-880-8181
www.tmait.org
“We offer BCMS members a free insurance portfolio review.”
The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)

We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
katy.brooks@bosainsurance.com
www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze 512-658-0262
Kirsten.Baze@medpro.com www.medpro.com
INVESTMENT ADVISORY REAL ESTATE
Conviva Care Center (HHH Gold Sponsor)

Conviva’s value-based care model allows physicians to deliver high quality, personalized care and achieve better outcomes, while feeling free to focus on health equity and patient outcomes.
Kim Gary Senior Physician Recruiter (812) 272-9838
KGary4@humana.com www.ConvivaCareers.com
“Fuel Your Passion & Find Your Purpose”
HOSPITALS/ HEALTHCARE FACILITIES
UT Health San Antonio MD Anderson Cancer Center (HHH Gold Sponsor)

UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado
Business Development Manager (210) 450-3713
delgador4@uthscsa.edu
UT Health San Antonio MD
Anderson Mays Cancer Center
Laura Kouba
Business Development Manager (210) 265-7662
norriskouba@uthscsa.edu
https://uthscsa.edu/
Appointments: 210-450-1000
UT Health San Antonio
Humana
(HHH Gold Sponsor)
Humana is a leading health and well-being company focused on making it easy for people to achieve their best health with clinical excellence through coordinated care.
Jon Buss: 512-338-6167
Jbuss1@humana.com
Shamayne Kotfas: 512-338-6103 skotfas@humana.com
www.humana.com
INSURANCE/MEDICAL MALPRACTICE
Nexus Neurorecovery Center (HHH Gold Sponsor)

A post-acute rehabilitation facility focusing on brain injuries. Programming provides individual and group physical, occupational, cognitive and speech therapy. We help residents return to lives of productivity and meaning.
Sydney Kerr, Liaison 346-339-2654
skerr@nhsltd.com
Caitlyn Tewksbury ctewksbury@nhsltd.com
Justin Sanderson, CEO
210-854-4732
7979 Wurzbach Road San Antonio, TX 78229
INFORMATION AND TECHNOLOGIES
Express Information Systems (HHH Gold Sponsor)

With over 29 years’ experience, we understand that real-time visibility into your financial data is critical. Our browser-based healthcare accounting solutions provide accurate, multi-dimen-
Texas Medical Liability Trust
(HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting, and defending physicians.

Patty Spann
512-425-5932
patty-spann@tmlt.org
www.tmlt.org
Recommended partner of the Bexar County Medical Society
Alamo Capital Advisors LLC

(★★★★ 10K Platinum Sponsor)
Alamo Capital Advisors is focused on Sourcing, Capitalizing, and Executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current projects include new development acquisitions and sales, lease representation and financial (RE)-structuring for existing investments.
Jon Wiegand, Principal 210-241-2036
jw@alamocapitaladvisors.com
www.alamocapitaladvisors.com
MEDICAL BILLING AND COLLECTIONS SERVICES
Wave Online (★★★ Gold Sponsor)

Our team of professionals will act as your extended AR office enhancing your revenue through our proprietary metrics and claim management systems. In addition, you keep 100% control of your RCM. Contact us today for a no cost evaluation.
Visit us
continued on page 42
at
41
www.bcms.org
BCMS Vendor
Saranraj (Raj) Venkatesh
Vice President – RCM | Sales and Client Relations
726-228-1097
saranraj@wavemt.com
https://rcmwave.com/ “Innovation towards Solutions”
Commercial & Medical Credit Services (HH Silver Sponsor)
A bonded and fully insured San Antonio-based collection agency.
Henry Miranda 210-340-9515
hcmiranda@sbcglobal.net www.cmcs-sa.com
“Make us the solution for your account receivables.”
MEDICAL SUPPLIES AND EQUIPMENT
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol 210-413-8079
tom.rosol@henryschein.com www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
MILITARY
San Antonio Army Medical Recruiting office (★★Silver Sponsor)
Mission: Recruit highly qualified and motivated healthcare professionals for service in the Army Reserves or Active Duty Army, in support of Soldiers and their families.
1LT Thomas Alexandria 210-328-9022
Alexandria.n.thomas12.mil@army. mil
https://recruiting.army.mil/mrb/ “Service to Country, Army Medicine, Experientia et Progressus”
PRACTICE MANAGEMENT
best performance. Contact us today for a no cost evaluation.
Saranraj (Raj) Venkatesh Vice President – RCM | Sales and Client Relations
726-228-1097
saranraj@wavemt.com
https://rcmwave.com/ “Innovation towards Solutions”
PROFESSIONAL ORGANIZATIONS
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber President
210-308-7907 (Direct) kbarber@bdo.com
Valerie Rogler Program Coordinator
210-904-5404
Valerie@thehealthcell.org
www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Lindsey Herman Nolan, MHR, CMPE President
info4@samgma.org
www.samgma.org
REAL ESTATE SERVICES COMMERCIAL
RETIREMENT PLANNING
Oakwell Private Wealth Management

(HHHH 10K Platinum Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA
Senior Private Wealth Advisor 512-649-8113 SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
STAFFING SERVICES
Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)

Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
Cindy M. Vidrine Director of Operations- Texas 210-918-8737
cvidrine@favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”
TRANSCRIPTION SERVICES
Provider's Choice Scribe Services (★★★ Gold Sponsor)

Our accurate and complete documentation helps our customers focus on what’s most important, their patients. Let us take on the task of documenting your patient encounters, it’s what we do.
Yoceline Aguilar COO
yaguilar@pcscribes.com
915-691-9178
Luis Chapa MD/CEO
210-796-4547
lchapa@pcscribes.com
www.providerschoicess.com/ “An Unparalleled Scribe Experience”
Wave Online (★★★ Gold Sponsor)

Professional Analysis focusing on Low Collections, High Denials Rates. Our Business Intelligence tools will identify Cash Pockets and Cash Leakages. With a 360degree view on your practices’ financials, we can tune your AR for
Alamo Capital Advisors LLC (

★★★★ 10K Platinum Sponsor)
Alamo Capital Advisors is focused on Sourcing, Capitalizing, and Executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current projects include new development acquisitions and sales, lease representation and financial (RE)-structuring for existing investments.
Jon Wiegand Principal 210-241-2036
jw@alamocapitaladvisors.com
www.alamocapitaladvisors.com
42 SAN ANTONIO MEDICINE • August 2023
Directory continued from page 41

Visit us at www.bcms.org 43
2023 Lamborghini Urus SUV




 By Stephen Schutz, MD
By Stephen Schutz, MD
AUTO REVIEW 44 SAN ANTONIO MEDICINE • August 2023
The recent movie, “Lamborghini: The Man Behind The Legend,” tells the story of Italian industrialist Feruccio Lamborghini’s attempts to get Enzo Ferrari to “fix” what Mr. Lamborghini believed were problems with Ferrari clutches. After being told dismissively to go back to making tractors, Lamborghini famously started his own sports car company, which today, more than 60 years after that (possibly apocryphal) exchange, constitutes Ferrari’s most potent competitor.
So, after its founding, Lamborghini Inc. grew steadily over the decades, is still Italian owned, and now sells over 9,000 vehicles per year at an average price of almost $300,000, right?
Um, no. The 9,000/$300,000 part is correct, but in 1973, 10 years after founding the company, Mr. Lamborghini was forced to sell it, and Automobili Lamborghini SPA bounced around from marginal owner to marginal owner until it was finally rescued in 1998 by Volkswagen AG, which owns it to this day.
What Volkswagen brought to the table, in addition to financial stability, was access to Porsche and Audi parts, components and platforms, which have enabled Lamborghini to produce vehicles cheaper and more reliably than they could have if they were a stand-alone company.
Which brings us to the 2023 Lamborghini Urus SUV, a triumph of platform sharing if there ever was one. Based on the Porsche Cayenne and Audi Q8 platform, the Urus shares its engine, transmission and many other bits with the top-of-the-line Cayenne Turbo S and Audi RS Q8. That’s good because those SUVs are great performers, but it’s bad because the Urus is more German than it is Italian.
That doesn’t mean that the Urus as a vehicle is bad, nor does it mean that it’s not Italian (the Urus is manufactured in Italy). But it does mean that the Urus is quite different from its competitor Ferrari, the Purosangue, which is smaller and sportier than the Urus. The Purosangue is also more “Ferrari” because it sports a true Ferrari V12 engine and transmission.
Keep in mind though, that the car gods giveth, and the car gods taketh away: MSRP for a new Urus starts at around $235,000, while a base Purosangue will set you back more than $400,000. Using Porsche/Audi parts allowed Lamborghini to keep Urus pricing relatively low.
For the record, the Urus is fast. Zero-to-sixty MPH takes just 3.1 seconds thanks to a 657HP twin-turbo 4.0L V8 engine, and its top speed is 190MPH. Naturally, fuel economy suffers: EPA estimates are 14MPG City, 19MPG Highway. I doubt customers will give that a thought.
Thanks to a design with many sharp edges and lots of angularity, the Urus definitely looks like a Lamborghini. In fact, with all of the “Lambo boi” design elements and a lower profile than its platform mates the Cayenne and Q8, this Lamborghini could never be confused with any other brand, even by non-enthusiasts.
Driving the Urus is a pleasure, mostly because you get lots of “Lambo-ness” without too much of it. Other reviewers have criticized the Ferrari Purosangue (which I haven’t yet driven) because it drives
too much like a Ferrari sports car when SUV owners, even exotic SUV owners, want an SUV driving experience when they get into their SUVs, and that makes sense to me. If I owned a Lamborghini Aventador and bought a Urus SUV, I would want a less intense driving experience when I drove the Urus. Yes, I would value the “Lambo-ness” of the Urus’ design and interior, but I would appreciate its higher seating position, extra elbow room and softer ride.
Speaking of the Urus’ interior, it is very Lamborghini. To start the engine, you have to lift a “protective” cover over the red Start button— as if the Urus were asking, “are you *sure* you’re ready for this?” My test car was black over (very) red leather, which is classic Italian and quite fetching. In any other car, the bright red interior in my Urus would be too much, but in this SUV it works. In fact, a subtle exterior color over a bright interior is the best way to go in a Urus in my opinion.
Not surprisingly, the UI/screens/etc. are very Volkswagen AG, and Porsche in particular. Yes, there are many Lamborghini-specific fonts and graphics, but if you own a modern Audi or Porsche, you’ll be able to find your way around the Urus’ tech easily.
Of course, because of its slinky styling the Urus is less roomy than the aforementioned Porsche Cayenne or Audi Q8. Is it good for taking four adults to dinner in Boerne? Yes, but don’t volunteer to drive those same friends to Denver. It won’t be a good trip for anyone in the rear seats.
The fact that the Lamborghini Urus SUV isn’t really a Lamborghini is a feature not a bug. In fact, its Audi-based engine and transmission make it a better SUV, which may explain the Urus’ popularity. I approve.

As always, call Phil Hornbeak, the Auto Program Manager at BCMS (210-301-4367) for your best deal on any new car or truck brand. Phil can also connect you to preferred financing and lease rates.
Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.

AUTO REVIEW Visit us at www.bcms.org 45
11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-581-0512
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Charles Williams 210-912-5087
Chuck Nash Chevrolet Buick GMC 3209 North Interstate 35 San Marcos, TX
William Boyd 210-859-2719
Kahlig Auto Group
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Kahlig Auto Group
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
Kahlig Auto Group
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
Kahlig Auto Group
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Kahlig Auto Group
14610 IH 10 West San Antonio, TX 78249
Mark Hennigan 832-428-9507
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
Kahlig Auto Group
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Al Cavazos Jr. 210-366-9600
Kahlig Auto Group
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211

Justin Boone 210-635-5000
9455 IH 10 West San Antonio, TX 78230
Douglas Cox 210-764-6945
Kahlig Auto Group
Audi North Park 15670 IH-35 North Selma, TX 78254
Camden Steele 325-374-9897
Call Phil Hornbeak 210-301-4367 or email phil@bcms.org
As of June 1, 2023, our loan rate will be 5.0% for 60 months with approved credit.












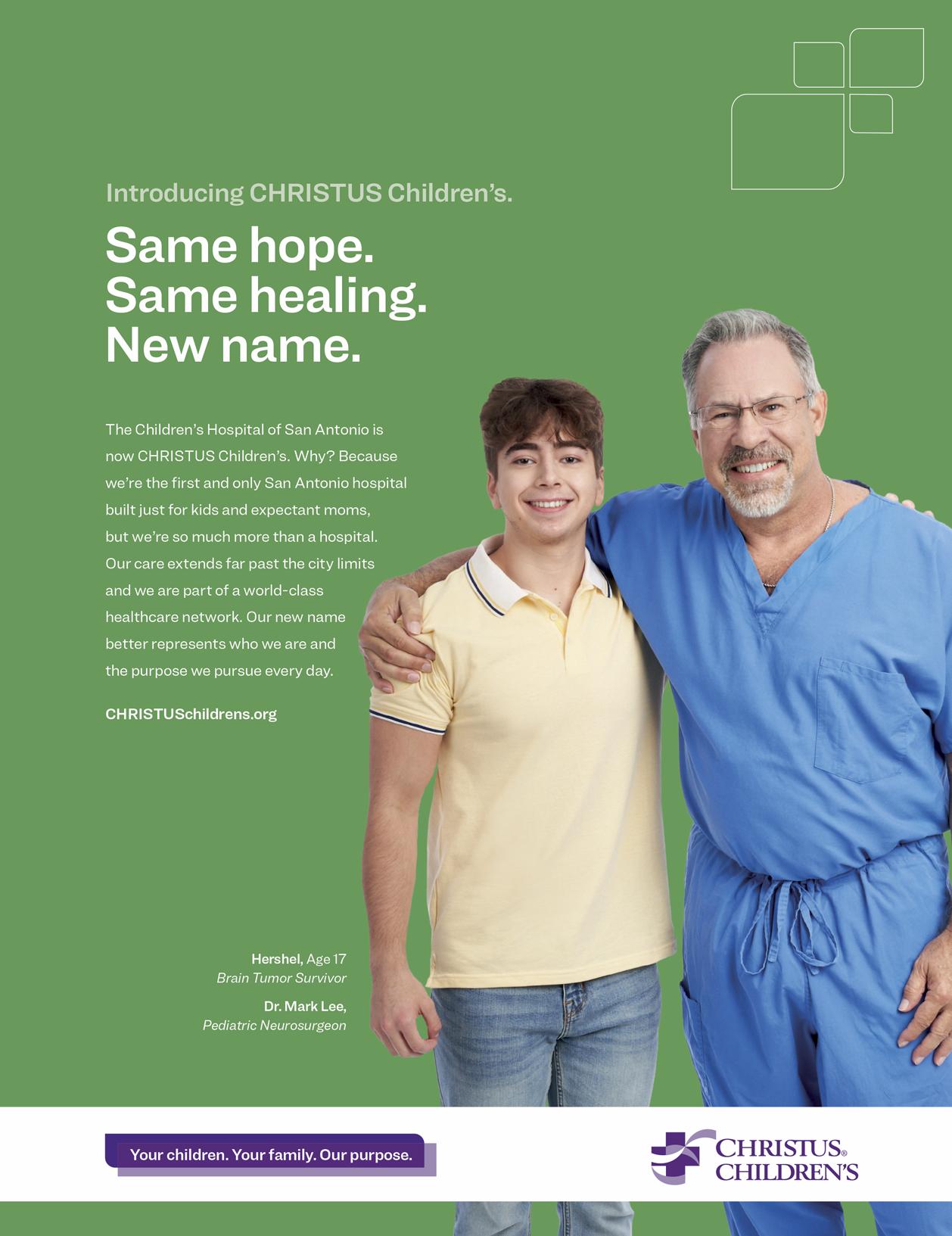




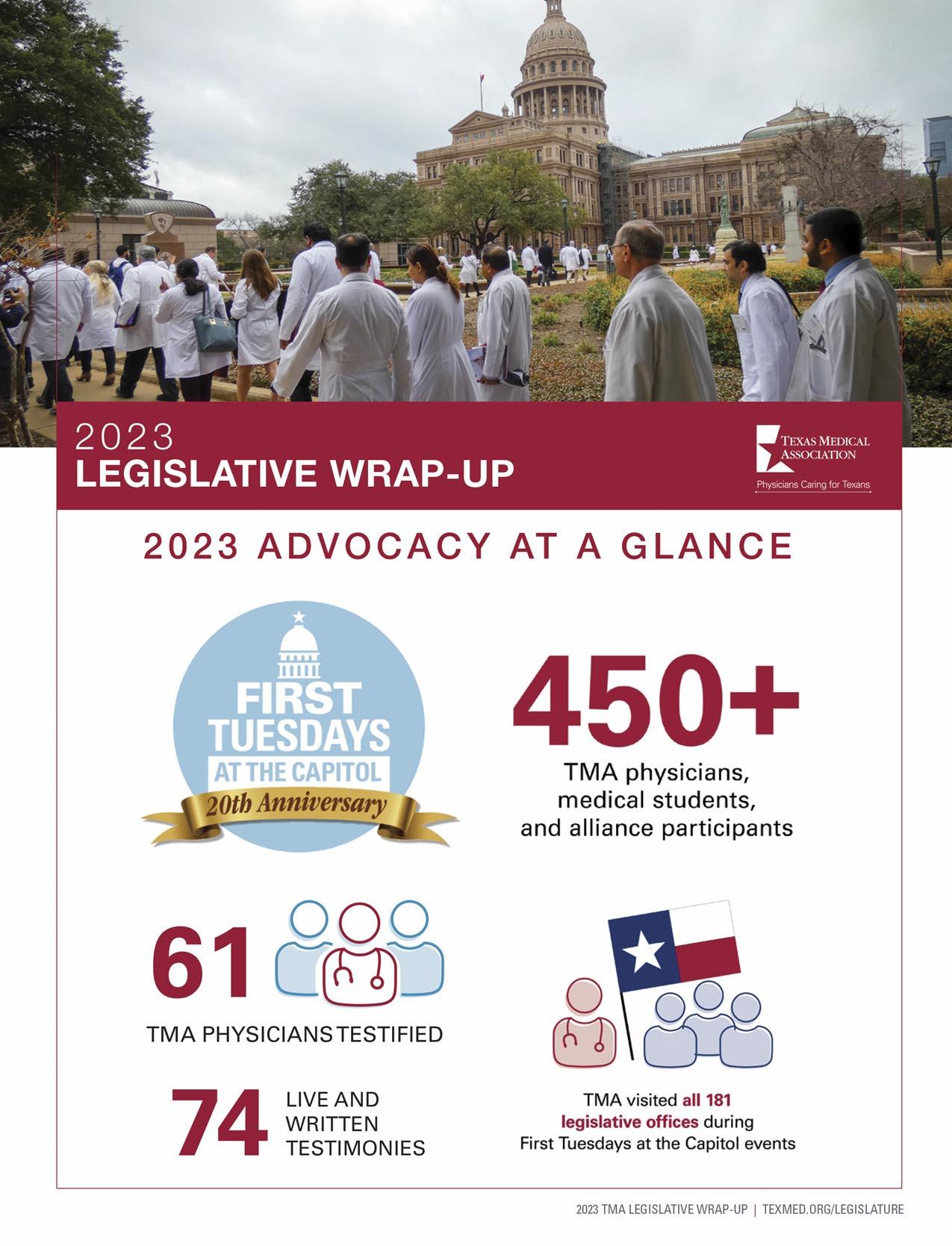
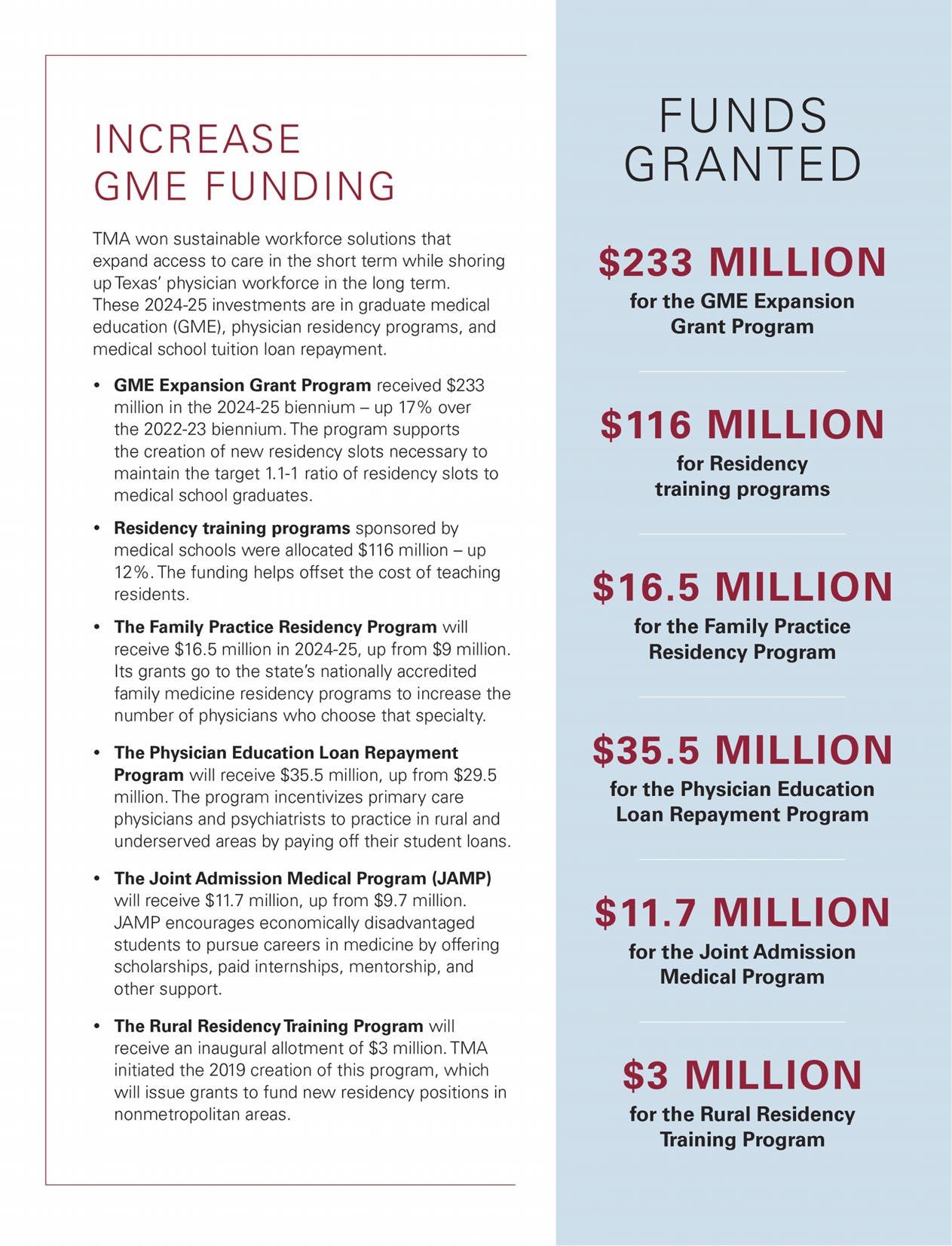
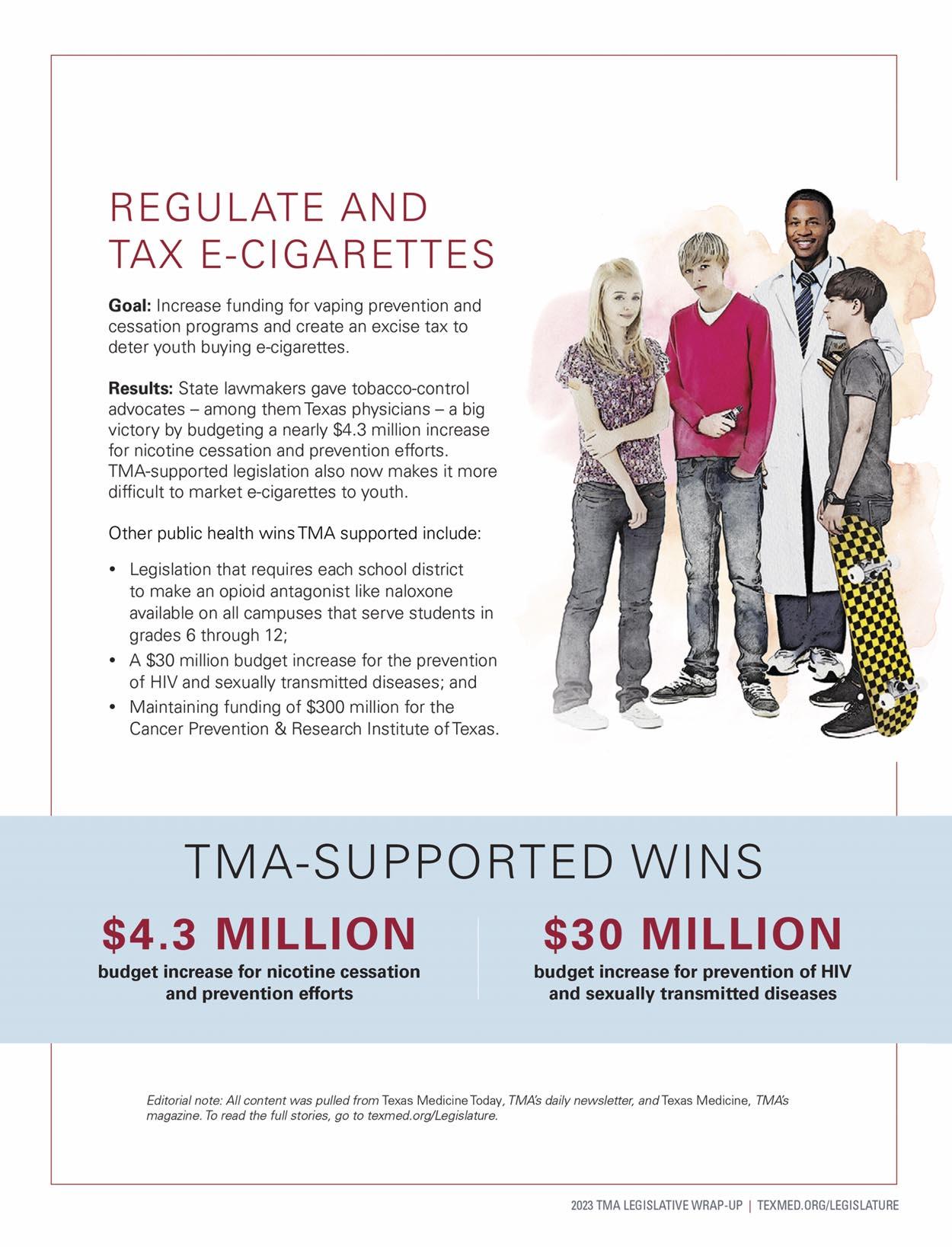















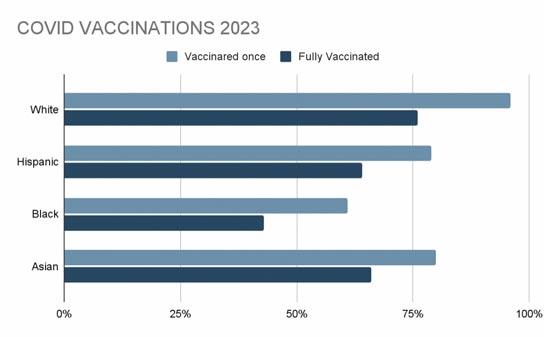 By Marina Moreno and Adelita G. Cantu, PhD, RN, FAAN
By Marina Moreno and Adelita G. Cantu, PhD, RN, FAAN
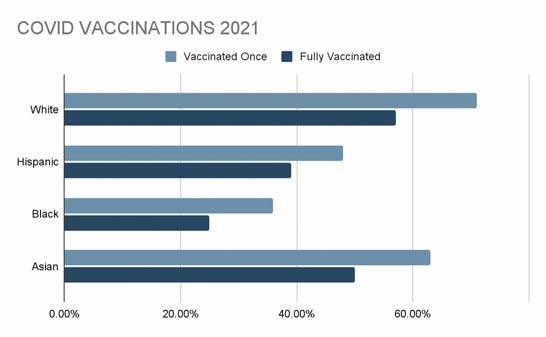
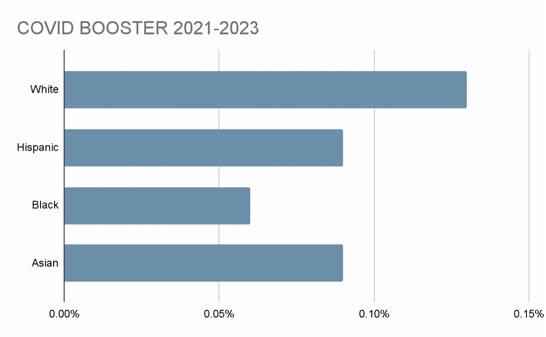 Figure 1 Comparison of ethnicities in Bexar County vaccinated in 2021 https://cosacovid-cosagis.hub.arcgis.com/datasets/CoSAGIS::vaccinations-weekly-totalspublic-share-1/about
Figure 2 Comparison of ethnicities in Bexar County vaccinated in 2023 https://cosacovid-cosagis.hub.arcgis.com/datasets/CoSAGIS::vaccinations-weekly-totals-public-share-1/about
Figure 1 Comparison of ethnicities in Bexar County vaccinated in 2021 https://cosacovid-cosagis.hub.arcgis.com/datasets/CoSAGIS::vaccinations-weekly-totalspublic-share-1/about
Figure 2 Comparison of ethnicities in Bexar County vaccinated in 2023 https://cosacovid-cosagis.hub.arcgis.com/datasets/CoSAGIS::vaccinations-weekly-totals-public-share-1/about

































 By Stephen Schutz, MD
By Stephen Schutz, MD