


PUBLISHED
Traveling Blender, LLC. 10036 Saxet Boerne, TX 78006
PUBLISHER Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com
ADVERTISING SALES: AUSTIN: Sandy Weatherford sandy@travelingblender.com
SAN ANTONIO: Gerry Lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE:
Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2024 SmithPrint, Inc. PRINTED IN THE USA

Ezequiel “Zeke” Silva, III, MD, President
Lyssa Ochoa, MD, Vice President
John Shepherd, MD, President-elect
Jennifer R. Rushton, MD, Treasurer
Lubna Naeem, MD, Secretary
John Joseph Nava, MD, Immediate Past President
Woodson “Scott” Jones, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Ana Rodriguez, MD, Member
Raul Santoscoy, DO, Member
Lauren Tarbox, MD, Member
Nancy Vacca, MD, Member
Col. Elisa D. O’Hern, MD, MC, FS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School
Representative
Cynthia Cantu, DO, Medical School Representative
Lori Kels, MD, Medical School Representative
Ronald Rodriguez, MD, Medical School Representative
Victoria Kohler-Webb, BCMS Alliance Representative
Carolina Arias, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
Melody Newsom, CEO/Executive Director
Yvonne Nino, Controller
Al Ortiz, Chief Information Officer
Brissa Vela, Chief Membership and Development Officer
Phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
Monica Jacqueline Salas, MD, Co-chair
Jennifer C. Seger, MD, Co-chair
Lokesh Bathla, MD, Member
Elizabeth Clanton, MD, Member
Erika Gabriela Gonzalez-Reyes, MD, Member
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. K. Jyothula, MD, Member
Kristy Yvonne Kosub, MD, Member
Jaime Pankowsky, MD, Member
George-Thomas Martin Pugh, MD, Member
Rajam S. Ramamurthy, MD, Member
Adam V. Ratner, MD, Member
John Joseph Seidenfeld, MD, Member
Boulos Toursarkissian, MD, Member
Francis Vu Tran, MD, Member
Faraz Yousefian, DO, Member
Louis Doucette, Consultant
Brissa Vela, Consultant
Gabriella Bradberry, Staff Liaison
Trisha Doucette, Editor
Deepthi S. Akella, Student
Moses Alfaro, Student
Victoria Ayodele, Student
Tue Felix Nguyen, Student
Andrew Ta, Student
Alixandria Fiore Pfeiffer, DO, Resident
Elizabeth Allen, Volunteer
Adelita G. Cantu, PhD, Volunteer
Rita Espinoza, DrPH, Volunteer
Natalie Reyna Nyren, PA-C, Volunteer
David Schulz, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer

Have you thought about what would happen if you could not practice due to a serious illness or injury?
When was the last time you talked with an advisor about how you can protect your income?
It may be time to have that conversation.
Our advisors have been helping Texas physicians protect their incomes for generations.
And their guidance is provided at no cost. They receive no salesbased commissions so you can be assured that their advice and recommendations are provided without bias or obligation.
Start a conversation by calling tollfree 800-880-8181 Monday to Friday, 8:00 AM to 5:00 PM
It will be our privilege to serve you.
By Ezequiel "Zeke" Silva III, President, Bexar County Medical Society (BCMS)
Effective physician advocacy operates across a spectrum of local to national activities. Successful associations like BCMS empower motivated physicians to address their challenges and opportunities throughout this range. Locally, Bexar County physicians also have the chance to meet and learn from peers nationwide, strengthening our collective voice.
BCMS serves as the local voice for San Antonio physicians. Last month, I described how BCMS made an impact at TexMed 2024, the annual meeting of the Texas Medical Association (TMA). This month, I’ll discuss BCMS’ presence at the American Medical Association (AMA) Annual Meeting in Chicago.
The TMA Delegation to the AMA
Similar to BCMS’ delegation to the TMA, the TMA sends a delegation to the AMA. This group includes elected delegates and alternate delegates from the TMA House of Delegates. The TMA has 20 delegates, with approximately the same number of alternate delegates. The broader “Texas Delegation” comprises about 40 other physicians and medical students representing various medical specialty societies within the AMA. The following Bexar County physicians are part of the TMA Delegation to the AMA: Drs. David Henkes, Jennifer Rushton, Jayesh Shah and me.
An essential role of the Texas delegation is to present and review resolutions at the AMA House of Delegates. The delegation concentrates on issues affecting Texas physicians and aligns with the strategic focus of both the TMA and AMA to empower physicians everywhere. Some AMA resolutions originate in Bexar County. For instance, BCMS initially sponsored Resolution 514 on safety with devices producing carbon monoxide at TexMed, which was also adopted by the AMA.
AMA
Like at TexMed, the AMA holds elections during its annual meeting. This includes voting for AMA officers, Board of Trustee members and Council members. The Councils at AMA provide information and recommend policies to the AMA BOT and HOD (Reference:

https://www.ama-assn.org/councils). With support from TMA and BCMS, I was elected to a position on the Council on Medical Service, which examines socioeconomic factors affecting medical practice.
The AMA Alliance (AMAA), a national network of physician families, meets at the AMA Annual Meeting. This group, like the TMA Alliance, focuses on advocacy, community relationships and mutual support. San Antonio’s Jenny Shepherd, spouse of our President-Elect John Shepherd, MD, and current TMA Alliance President, represents BCMS and the TMA. She serves on the AMAA’s Advocacy and Legislation Committee.
As BCMS contributes to the AMA, we bring back the knowledge and successes of physicians across the country. Insights from the AMA inform our local initiatives and educate our members. For example, thanks to the Texas Delegation, the AMA focuses on Medicare payment reform. Although much advocacy occurs in Washington, D.C., BCMS uses our local congressional relationships to advance this and other significant goals.
I am incredibly proud of the physician community in Bexar and surrounding counties. The quality of our care and our local achievements are exemplary and set a standard for the rest of the state and country. With our success comes the responsibility to extend our achievements to state and national levels, thereby amplifying our experience to empower our colleagues beyond Texas
Ezequiel “Zeke” Silva III, MD, is the 2024 President of the Bexar County Medical Society. Dr. Silva is a radiologist with the South Texas Radiology Group, Adjunct Professor of Radiology at the UT Health, Long School of Medicine, and Vice-Chief of Staff at Methodist Hospital Texsan. He is Chair of the TMA Council on Legislation and is a TMA Delegate to the AMA. He serves on the AMA Council on Medical Service, and chairs the AMA RVS Update Committee (RUC).
By Amy Samples, JD
I have often heard, “It takes a village to raise a child.” As a mom to two young toddlers, I wholeheartedly agree. However, I also think it takes a village for anyone to thrive. When my husband and I moved to San Antonio, I was badly in need of a village. The six months prior and the year to come brought many exciting but intimidating changes. I was about nine weeks pregnant with our first baby when we decided to move to San Antonio. I left my job to prepare for our move and baby. I gave birth in the middle of the Delta wave of Covid. Six months later, we closed on our house here and went to our first prenatal appointment for (surprise!) baby number two.
For an introvert, moving away from an established community is especially challenging. Additionally, I was processing a change in identity from a working professional to a stay-at-home-mom of (surprise!) two under 2. And, like everyone else who had a pandemic baby, I had to learn how to move past the pandemic bubble. Luckily for me, my neighbor introduced me to the Bexar County Medical Society Alliance (BCMSA). She invited me to join the Book Club, which was virtual and easy for me even with two small babies. Plus, book-loving people are my people. Later, she also recommended me for the position of Secretary.
BCMSA is full of warm, caring, supportive women who understand what it means to be married to and raise children with a doctor. Most days, their hours are long and stressful. This group of women understands without being told that a 10-hour day for my husband is a day of near solo parenting for me. I went to law school and practiced for seven and a half years in a demanding job. This mom job is harder. This is a community of moms who will look at your stressed face as you tell them, “My baby cries when I put solids in his mouth and I don’t know what to do,” and respond compassionately, “He’ll learn. He won’t be a teenager going out with his friends with his pouches and jarred baby food.” It’s the mom of grown children recounting days when her husband walked in and she was ready to throw (metaphorically, of course) the children at him. It’s powerful to hear anecdotally, “You are not Alone. You are not Alone in your feelings, in your struggles, in your joys. I have been there. I went through the struggles. The joys. The challenges and the wonder. You will be okay.” It’s powerful to look to more experienced moms and see that what they lived through, what I am now living through, has made them compassionate, wise, strong people.
I brought my children to a board meeting recently where my oldest and another board member’s child enthusiastically (loudly) discussed whether they have a “mama and a dada” or a “mommy and a daddy.” No one minded. My neighbor made one of my kids his own (emphasis his) sandwich. No one minded that they ran around the room or the 1,500 times I said, “No, that does not go in your mouth,” or, “No, that’s not a toy.” No one minded when my youngest got overtired and cried as I did the “please stop crying” sway at one end of the room. This meant the world to me.
As much support as I have received for my mom role, BCMSA has also been a badly needed opportunity to have a life outside of my stay-at-home-mom role. I love staying home and I am grateful every day that my husband’s hard work makes that possible. But it can be so easy to let the identity of “mom” consume you. It can be easy for others to reduce your identity to “stay-at-home-mom.” I now have an area where I can be myself separate and apart from my mom identity. It has been invigorating to have adult conversations again and to help make plans for the year. In February of this year, we had a highly successful event assembling period kits for girls in need of period supplies. It’s so fulfilling to have the opportunity to give back to my community again. I’m excited to contribute to BCMSA’s other philanthropic initiatives. I can’t wait for opportunities to deepen the friendships I’ve made. I’m so happy to have found my village.


For information on the Bexar County Medical Society Alliance, scan the code:

By Andrew Ta
Dr. Dianna Burns-Banks’ journey in medicine is a testament to resilience, dedication and the transformative power of leadership in a field often resistant to change. Her story, from a pediatrician in private practice to a pivotal figure in organized medicine, illustrates the impact one individual can have on an entire profession.
After graduating from medical school and pediatrics residency at the University of Louisville School of Medicine, Dr. Burns-Banks founded the South Texas Center for Pediatric Care in the mid-1980s with the goal of supporting families on San Antonio’s East Side, where there was a marked lack of pediatricians.
In her private practice, Dr. Burns-Banks saw the economic disadvantages faced by many of her patients. Her engagement in organized medicine allowed her to advocate for public policies that supported these populations, influencing Medicaid funding and managed care practices. Her work in the 1980s significantly altered the landscape of medicine in San Antonio, demonstrating the power of policy in shaping healthcare delivery.
Dr. Burns-Banks attributes much of her success to the mentors who encouraged her active participation in organized medicine. Early in her career, she joined the Bexar County Medical Society (BCMS), which, at the time, was a conservative, male-dominated group. Her ascent within the organization, culminating in her becoming its second-ever woman president, highlighted the importance of having a unified voice in advocating for the medical profession’s interests, and her mentors within the organization were instrumental in shaping her perspective on the necessity of involvement in such organizations to effect meaningful change. Through her work with BCMS, she became acutely aware of the issues facing the medical community, particularly in relation to insurance policy.
Managed care, as Dr. Burns-Banks explains, deviates from the traditional fee-for-service model by implementing a gatekeeper system where primary care physicians manage patients’ initial consultations. This model allows for better population health management and reduces unnecessary costs. She acknowledges the challenges, such as the lack of provider involvement in clinical applications, but emphasizes the benefits, particularly for chronic conditions like diabetes, where structured care protocols lead to better patient outcomes and lower costs. By screening for and managing these diseases before they progress, the patient potentially will not have to undergo a much more expensive procedure or surgery later on. Her advocacy for managed care, despite its complexities, stemmed from a belief in its potential to provide more efficient and cost-effective healthcare, especially to historically marginalized or underserved communities.
As a Black, female physician in the BCMS, Dr. Burns-Banks faced unique challenges. During her medical training, women were often not seen as doctors, and she was frequently mistaken for a nurse. Furthermore, there were not yet separate locker rooms for male and female physicians, so she often found herself changing in the nurse’s room. Despite these obstacles, however, she was supported by a group of male doctors who encouraged her to pursue leadership roles, such as Chief of Staff at CHRISTUS Santa Rosa. Her dedication to community service and her ability to mobilize others were key to her success.

Dr. Burns-Banks later found, however, that it was challenging to ask physicians to hold positions within BCMS and advocacy groups. Despite her own commitment to community service and outreach, it was not reasonable to expect the physicians around her to feel the same. Nonetheless, Dr. Burns-Banks held steadfast in her commitment to outreach projects. She believed that physicians know what their patients need more than anybody, so these are the people whose voices carried the most weight in advocacy.
Towards the end of our interview, I asked Dr. Burns-Banks if she had any messages or advice she wanted to offer to future generations of physicians. She responded, “[Medical students] have chosen a great career; make sure you have made that career choice based on what you want to do for the patients you see and what you want to do for yourself, not just for finances.” She emphasized that pursuing medicine for financial gain is a fool’s errand that will never result in happiness. True satisfaction, she believes, comes from making a difference in patients’ lives; carrying the weight of their well-being with every decision. “As a physician, you carry people’s lives in your hand with the decisions you make, and they will follow you for years,” she concluded.
Dr. Dianna Burns-Banks’ legacy is one of pioneering leadership, unwavering advocacy and a deep commitment to the betterment of both her patients and the medical community. Her story inspires future generations to lead with compassion, integrity and a steadfast dedication to the art and science of medicine.

Andrew Ta is a medical student at the Long School of Medicine, Class of 2026. He serves on the BCMS Publications Committee.

By Cristina Sarro, DNP, APRN, FNP-BC, and Liudmyla Ingle, MSN, APRN, FNP-C, AOCNP
Palliative and hospice services, existing since the Middle Ages, are tailored holistic care provided to patients diagnosed with varying diseases requiring support in the management of spiritual, emotional and physical needs.
Currently known as the hospice care model, homes were historically provided for wounded and dying pilgrims and travelers. The newest hospice model was established in 1967 by Dr. Cicely Saunders at St. Christopher’s Hospice in London. Dr. Saunders’ team included nurses, social workers and physicians who customized patients’ symptom management, specifically taking care of pain and providing end-of-life comfort for patients and families. The pioneer of hospice care in the United States was the dean of Yale School of Nursing, Florence Wlad, who started her first hospice in 1975. In the same year, palliative care that was separate from hospice was launched by Dr. Balfour Mount, a surgical oncologist from McGill University, Canada.1
Palliative care grew out of the hospice care model. Now, palliative care is a wide umbrella that includes hospice and non-hospice systems. Consequently, patients do not always understand the differences and are reluctant to accept these services. It is important to explain to patients that while both provide interchangeable care, non-hospice palliative care should be initiated during the early stages of an illness, acute or chronic, regardless of life expectancy. It supports recovery from the disease or helps to maintain quality of life for chronic conditions. On the other hand, hospice is initiated when a patient is diagnosed with a terminal illness with a prognosis or life expectancy of six months or less if the disease runs its normal course.2 Advance care planning should be introduced when the disease is incurable, resistant to treatment and the patient begins to experience symptoms that affect quality of life. Chang et al., 2022, explains how a recent study indicated that over 56 percent of the elderly are not prepared for end-of-life events, or have not completed advance care planning.
The importance of palliative and hospice care in modern medicine, especially oncology, is hard to underestimate. Patients with chronic illness, especially if terminal, suffer from multiple symptoms that range from mild to severe. Palliative care can help with physical pain, decreased mobility, breathing problems, lack of appetite, weight loss and inability to perform basic daily life activities. A multidisciplinary approach can relieve emotional distress and bring control over the disease process. Even though modern therapies can prolong a patient’s life, they do not always guarantee quality of life. It is nearly impossible to manage multiple symptoms with one medical specialist, and the majority of patients cannot address all the symptoms during one visit with the clinician. For example, oncologists refer patients to pain management to address complex pain management needs. The palliative care service can be provided at patients’ homes and be available 24 hours a day, saving money on transportation and avoiding multiple emergency hospital visits. Patient caregivers also need help, as they express feeling overwhelmed and exhausted. With proper resources and guidance, caregivers benefit from early end-of-life planning, as it reduces trauma and improves decision-making.3
The role of clinicians is to have honest conversations about treatment goals and develop realistic expectations with each patient on every follow-up visit. Unrealistic care goals can delay access to palliative or hospice care.3 This occurs too often because these are multifactorial reasons (spiritual and cultural beliefs, age, family, unrealistic expectations, fear of death) that change over time. The delay in introducing palliative and hospice care results in services being introduced too late, oftentimes causing end-of-life care planning to begin only when someone is hospitalized just days away from death. Teoli et al., 2023, explains that palliative care initiated early, preferably at the time of diagnosis, improves survival in patients diagnosed with metastatic cancer, increases quality of care, and reduces cost. Sheridan et al., 2021, describes how billions of dollars are spent on patients with advanced cancer, and approximately 30 percent is spent on patients in their last year of life. Sharma et al., 2023, explains that intensive care non-hospice hospitalizations in the last 30 days of life averaged $19,000 in costs, versus hospice inpatient care, which averaged $9,000. Further, a cohort study by Sheridan et al., 2021, amongst Medicare patients examined early and late palliative care consultations. The study shows that initiation of palliative care early, more than 28 days before death, had a decrease in cost of approximately $4,643, while late initiation of services, within seven days of death, had a reduction in healthcare cost of only $471.
Unless clinicians start referring patients to palliative/hospice care earlier, the overall cost is likely to triple in the near future, especially with the surge of patients seeking end-of-life care in emergency rooms. Chang et al., 2022, reports that 75 percent of patients visit the emergency department in their last six months of life. The majority of patients were diagnosed with advanced cancer, uncontrolled symptoms and complex needs, and nearly half are admitted to the hospital; 68 percent of admissions result in death. The data shows early referrals could have provided better symptom management for the patient, support for caregivers, time for grieving and a peaceful death at home surrounded by a loving family.
References:
1. Sheikh, M., Sekaran, S., Kochhar, H., Khan, A.T., Gupta, I., Mago, A., Maskey, U., & Marzban, S. (2022). Hospice vs palliative care: A comprehensive review for primary care physician. Journal of Family Medicine and Primary Care, 11(8), 4168–4173. https://doi.org/10.4103/jfmpc.jfmpc_2262_21
2. Centers for Medicare & Medicaid Services (2023). Hospice coverage. https://www.cms.gov/medicare/payment/fee-for-service-providers/hospice
3. Chang, A., Espinosa, J., Lucerna, A., & Parikh, N. (2022). Palliative and end-of-life care in the emergency department. Clinical and Experimental Emergency Medicine, 9(3), 253–256. https:// doi.org/10.15441/ceem.22.341
4. Teoli, D., Schoo, C., & Kalish, V.B. Palliative care. (2023). StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/ NBK537113/
5. Sheridan, P.E., LeBrett, W.G., Triplett, D.P., Roeland, E.J., Bruggeman, A.R., Yeung, H.N., & Murphy, J.D. (2021). Cost savings associated with palliative care among older adults with advanced cancer. The American Journal of Hospice and Palliative Medicine, 38(10), 1250–1257. https://doi. org/10.1177/1049909120986800
6. Sharma, G., Deepak, D., Neeb, J., Garey, J.S., Thomas, H.I., Mills, L., Payne-De Bock, J., Wilfong, L.S., & Indurlal, P. (2023). The impact of hospice on end-of-life expenditures and total cost of care in episodic value-based care models at a community oncology network. JCO Oncology Practice, 19(11), 228–228. https:// meetings.asco.org/abstracts-presentations/228127

Cristina Sarro, DNP, APRN, FNP-BC, is a board-certified family nurse practitioner. She has a Doctor of Nursing Practice from the University of the Incarnate Word. She has experience serving oncology, hospice and palliative patients, as well as their families.

Liudmyla Ingle, MSN, FNP-C, AOCNP, is a nurse practitioner experienced in medical oncology, cancer genetics and hematology disorders. She received her bachelor’s and master’s degrees at University of Texas Health Science Center at San Antonio. Her primary role as a nurse practitioner is to serve oncology patients and help them in their cancer treatment journey.

“There
By Erin Menchaca, LMSW
For many, these words from their physician can make their stomach sink with fear. Understandably so. However, for those of us that have found our calling in hospice, these same words come with the understanding of help that lies ahead.
For years, the word hospice has had a negative connotation to people who have not experienced the care and benefits that come with hospice. Patients and families often hold a preconceived myth that hospice and the medications prescribed through hospice will hasten death. Will hospice give medicine? Of course. Will the purpose of this medicine be solely to sedate the patient or to speed up death? Absolutely not. The purpose of hospice is comfort. The goal of hospice is to provide patients with the medications and support that they need to
be comfortable enough to live the rest of their life the way they want to live it. For some this includes bucket list items such as a last trip to the beach with their family, one more fishing trip with their friends, going to a military service reunion, attending a live sporting event, or even gambling at the casino for one last thrill, among other things. By enrolling in hospice services earlier rather than later, patients are able to maximize their comfort with hospice in order to truly enjoy what life they have left. Hospice is about living, not dying. When that is the focus from the start, then patients and families can truly experience the benefits of hospice and be able to enjoy life.
Many people often want to know, “How long does he/she have left?” There is no perfect answer to this question. However, with hos-
pice in place, there is the ability to ensure that the patient is comfortable and supported, and that the family has the education, resources and support they need to navigate what comes at the end of life. No mortal being knows how much sand is left in their hourglass, but by starting hospice sooner rather than later, there is more time for hospice to maximize the benefits of service and care for patients and families until that last grain of sand falls to the bottom of the hourglass. The hospice mantra has long been “quality over quantity.” Often times, when hospice is started earlier in the patient’s decline, they are able to see how comfortable they truly can be. Patients are able to conserve their energy by not going back and forth to doctors or hospitals, patients and families have assistance with tasks that have proved troubling, and patients and families are able to find some enjoyment and peace in their lives. When the emphasis is placed on quality at this stage of life, many find that quantity is also lengthened. By helping patients and families understand that merely lengthening the patient’s time is not the end-all solution, rather switching their focus to ensuring that there is quality of life along with quantity of life, then they are able to see how beneficial it can be to have hospice with them as the last chapter in their book of their life.
Hospice includes many individuals that provide care for not only the patient but also for the family. These individuals include the hospice nurse, the hospice aide, the hospice chaplain, the hospice social worker and hospice volunteers, to name a few. While examples of the care that these hospice team members provide for the patient is more obvious, the care aspects that are provided to the family are more obscure. Hospice nurse case managers provide clinical assessments and communication with the hospice medical director for treatment plans and adjustments in order to keep the patient comfortable. When it comes to the hospice nurse’s assistance for the family, he or she is able to provide education on the disease/end-of-life process, provide insight into what may be next in the decline progression, provide education on medications and when they should be used, provide the family with reassurance that they are caring for the patient effectively, and provide the family with emotional support. Hospice aides tend to bathing and hygiene needs for patients, which provides an unmatched level of quality for patients. This translates to families as the aide’s assistance with hygiene takes some of the load of patient care off of the family. The hospice chaplain is available for prayerful support, companionship, emotional support and connection to churches for patients and families. This is especially beneficial to family members as oftentimes patients are unable to leave the home, which means that they (and their family) may not be able to attend church services. Hospice chaplains can assist families by coordinating with churches for patients and families to receive religious rites as well as to plan funeral services. Hospice social workers are present with patients for emotional support/processing, companionship and connection to multiple resources. Hospice patients oftentimes do not possess the strength or ability to pursue resources as needed so this often falls on their family. The hospice social worker is able to assist families with connection to federal, state and local governmental support such as food assistance,
electricity resources, state provider services, VA care, Medicaid, Medicare, Social Security and FMLA or disability paperwork. Additionally, the social worker can assist with immigration letters for border crossing for final goodbyes, prison calls or video chats for closure, Advance Directives (POA and DNR) to ensure that family has knowledge of patient’s wishes regarding care and representation at the end of life, and assistance with funeral planning. Hospice volunteers are able to sit with patients for companionship and offer some assistance around the house. With the hospice volunteer present with patients for companionship, caregivers are allowed time to step back and relax as they know that their loved one is in the presence of the hospice volunteer. Some hospice benefits for caregivers that may not be tied to a specific individual of the hospice team are legacy projects and hospice respite. During legacy projects, hospice staff assist patients and families in memory making through art work, writings and other forms for families to cherish for years to come. Hospice respite is when hospice pays for a patient to go to a skilled nursing facility for five nights to provide family with a care-giving break to care for themselves and rest as needed. Hospice support for families continues even after a patient’s passing in the form of bereavement support and grief processing for up to 13 months.
Hospice is patient-centered care but the benefits are so much more than just direct patient care. Hospice care is not only for the patient, but also extends to the family. This allows spouses to be spouses, children to be children, and family to be family as hospice presence removes some of the care-giving tasks from family and allows them more quality time with their loved one. Additionally, this allows family with more time to focus on their own grieving and processing as they prepare to move forward without their loved one.
“There are no more treatments. I am going to refer you to hospice.” These words will always hold a certain amount of fear. However, when those hearing these words are able to understand that hospice not only supports the patient but also supports the family, and that the benefits of hospice are greater when starting hospice earlier rather than later, then these very same words can bring an unmatched level of comfort and reassurance to patients and families at a time when it is needed most.

Erin Menchaca, LMSW, is a hospice social worker for Methodist Hospice and Family Care. Erin has worked in hospice for nine years and although hospice work comes with a certain amount of emotional heaviness, Erin feels that there is a certain beauty in helping patients and families reach a place of peace and acceptance.

By Hema Navaneethan Seaworth, MD
For many, pregnancies are a joyous time. However, some are faced with learning the difficult information that their fetus has a life-threatening or life-limiting condition. Despite advances in modern medicine, the perinatal period has the highest rate of morbidity and mortality of all pediatric patients. In 2022 alone, there were over 20,000 infant deaths in the U.S., with the majority of those deaths occurring due to congenital abnormalities. At the same time, these advances have allowed for earlier detection of congenital anomalies and, ultimately, earlier diagnosis of potentially life-limiting fetal conditions. While certain conditions may not be confirmed until a baby is born, this early diagnosis facilitates discussions between providers and families about potential outcomes. It often allows families time to process and think about the goals of care for their child. A perinatal palliative care team can be beneficial in helping families navigate the many tough decisions that may arise during the perinatal end-of-life process.
A joint statement between the American Academy of Pediatrics and the American College of Obstetrics and Gynecology describes perinatal palliative care as a “coordinated care strategy that comprises options for obstetric and newborn care that include a focus on maximizing quality of life and comfort for newborns with a variety of conditions considered to be life-limiting in early infancy.” A perinatal palliative care team may consist of various interdisciplinary team members, including a hospice and palliative care physician, neonatologist, maternal-fetal medicine physician, chaplain, nurses, child life specialists, social workers and many other interdisciplinary team members.
Parents who received news of a life-limiting fetal diagnosis describe “grieving multiple losses,” including the loss of their healthy baby, the loss of a normal pregnancy, and the loss of future parenting. Amid processing this grief, parents are often forced to make difficult and often time-sensitive decisions regarding multiple aspects of care for the fetus. Crucial discussions include plans for ongoing prenatal maternal and fetal care, including potential interventions and fetal monitoring. Some families choose to deliver within their community to be closer to their support systems and home, while some plan for delivery in a tertiary care center with more access to neonatology and potential life-sustaining supports for their neonate. The family’s wishes and hopes may be documented in a birth plan to ensure that the wishes are communicated to the medical care team. A birth plan should include basic information, such as the baby’s name and family members to be present during delivery, and more complicated decisions, such as the family’s wishes for medical care for their baby following delivery. This may include plans for invasive interventions versus focusing on comfort measures. A birth plan may also include information regarding the family’s wishes for memory-making and legacy creation.
Whether a family has received a prenatal diagnosis or a family faces another challenging diagnosis, such as extreme prematurity or other post-natal life-limiting or life-threatening conditions, there are additional discussions and options to support families through the end-oflife process after the birth of their child. This may include the location for end of life. End-of-life care may occur in a variety of locations; however, it most commonly occurs within the neonatal intensive care unit. If the child’s clinical status allows, a family may choose to bring their baby home for end-of-life care. If available in their region, a pediatric or perinatal hospice team may aid with this transition to home and
continue to provide comprehensive end-of-life care in the home setting. A shift to end-of-life-focused care does not mean “giving up” or “withdrawing care.” Instead, it refers to a shift in medical care focused on promoting comfort, treating symptoms, and alleviating suffering. Important comfort care management includes relieving symptoms such as pain, respiratory distress, secretions and agitation, along with any other distressing symptoms that may arise. Psychosocial care for the family unit is also a key part of the provision of perinatal end-of-life care. This includes helping prepare families for what to expect during the end-of-life process, facilitating spiritual support and rituals that may be helpful for family processing and closure, and assisting with memory-making activities and the gathering of legacy items. Hospice differs from palliative care, as hospice is a specific philosophy and form of palliative care provided at the end-of-life period.
Longitudinal bereavement and grief support is another important component of providing comprehensive perinatal end-of-life care. The impact of the loss of an infant is described as profound and prolonged, with parents never “getting over” the loss of their child but instead integrating memories of their child and adjusting to a “new normal.” The loss of an infant affects the entire family and community. It often has a deep impact on the medical care team and community as well. Families should be given resources for community bereavement support, including counseling and support groups.
References:
1. Centers for Disease Control and Prevention. (2023). Child health. National Center for Health Statistics: FastStats. http:// www.cdc. gov/nchs/fastats/child-health.htm. Updated July, 25.
2. Perinatal palliative care: ACOG COMMITTEE OPINION, number 786. Obstet Gynecol. (2019) 134(3):e84–9. 10.1097/ AOG.0000000000003425
3. Côté-Arsenault, D., Denney-Koelsch E., “My baby is a person”: parents’ experiences with life-threatening fetal diagnosis. J Palliat Med. 2011 Dec;14(12):1302-8. doi: 10.1089/jpm.2011.0165. Epub 2011 Nov 11. PMID: 22077542
4. Linebarger, J.S., Johnson, V., Boss, R.D.; Section on Hospice and Palliative Medicine; Linebarger, J.S., Collura, C.A., Humphrey, L.M., Miller, E.G., Williams, C.S.P., Rholl, E., Ajayi, T., Lord, B., McCarty, C.L. Guidance for Pediatric End-of-Life Care. Pediatrics. 2022 May 1;149(5):e2022057011. doi: 10.1542/peds.2022057011. PMID: 35490287
5. Cortezzo, D.E., Ellis, K., Schlegel, A. Perinatal Palliative Care Birth Planning as Advance Care Planning. Front Pediatr. 2020 Sep 8;8:556. doi: 10.3389/fped.2020.00556. PMID: 33014940; PMCID: PMC7505922
6. Currie, E.R., Navaneethan, H., & Weaver, M. (n.d.). Chapter 91 - Palliative Care Family Support in Neonatology. In Principles of Neonatology (pp. 783–789), essay, Elsevier

Hema Navaneethan Seaworth, MD, is an Assistant Professor of Pediatrics at UTHSCSA, Medical Director for Pediatric and Perinatal Supportive Care Services - University Health, and a Pediatric Palliative Care Fellowship Director. She is a member of the Bexar County Medical Society.

Interview with Wisdeen Wu, DO, Clinical Associate Professor, Division of Complex and Palliative Care, Department of Pediatrics at UT Health San Antonio; conducted by Rajam Ramamurthy, MD, Professor Emeritus, Department of Pediatrics/Neonatology at UT Health San Antonio
Dr. Wisdeen Wu is a pediatrician in the Department of Pediatrics, Division of Complex and Palliative Care at UT Health San Antonio. Dr. Wu serves those patients and families with complex medical problems. These children may be technology-dependent, born with genetic or metabolic disorders, or premature babies with multiple medical problems that need comprehensive care.
How long has Pediatric Palliative Care been in practice as a specialty? Is there board certification?
Typically, complex care and palliative care training happen in large medical centers where different specialties are available. Usually, a team of physicians care for these children. Complex care has more of an outpatient focus, whereas palliative care is more focused on symptom relief and end-of-life care, and hospice provides care for patients with terminal illnesses, which by definition is six months of life expectancy. These are the definitions of these three distinct areas. Complex care does not have board certification. In 2000, the American Academy of Pediatrics (AAP) formalized end-of-life and palliative care principles. In 2010, AAP established a section on End-of-Life and Palliative Care. There is a one-year fellowship that you can do after
general pediatrics in these specialties. We get fellows who come after a sub-specialty training to the one-year palliative care track under the Hospice umbrella fellowship.
What patients are typically referred to the specialty?
A large number of cancer patients are referred to palliative care. In complex care, we see patients with chromosomal abnormalities like Trisomy 13, 18. We also see patients with metabolic disorders, mitochondrial disease and brain anomalies. They may not be at the end of life, may live for a long time, and need long-term care.
What are conversations like with families and children who need this type of care?
Conversations with families and children in need of this type of care are inclusive. It is important to include the children in the conversation at an age-appropriate level. Often, the children have insights about their bodies, and parents also benefit from knowing what their child wants. Siblings could also be involved based on the age of the sibling. The sibling may also need care and counseling. Their inclusion in the care process fosters a sense of consideration and inclusivity within the family.
What role do religion and faith play in the ability of families to cope with complex medical problems in their child?
Some families request their priest or faith leader to be present at these conversations. For example, in the case of a Jehovah’s Witness, a child who needs a transfusion may seek the advice of the faith leader. Sometimes they request that the faith leader be present at the care conference to help them with some decisions. Almost all religions have beliefs about what happens at the end of life on this side. It is a good thing to ask them about their belief and understanding. It is important to support their values and beliefs that are meaningful to them.
Stress and burnout are so common for the medical team that care forthesepatients.Letustalkaboutthetollittakesonteammemberscaringforcomplexcarepatientsandpalliativecarepatients.
This is an important question. I feel it is a privilege for me to care for these patients and help them and their families. I am not there day after day with the child and I empathize with the families who are there constantly. I also have a different perspective. I see these patients in the hospital, very sick, and go home with multiple problems. I see them in the clinic. They will come back and tell me that they went to the park, and something as simple as that tells me that the family is coping in ways acceptable to them. I get to see the whole spectrum. Not all of them will go home. When a child is very ill in a NICU for example, and never goes home, the care team that sees them at that point in time may think that all the things they are doing are futile, and why do a procedure when the overall outcome will not be good. I remember this patient who had a portion of the brain and skull missing. There was a gaping hole. Neurosurgery decided not to do surgery. The child went home and lived for two years, at which point we requested neurosurgery to fix the defect so that it was easier to handle the child. Team debriefing is very helpful. The physician may have a different perspective, as they see the whole picture of the child’s illness. A respiratory therapist or the nurse may see only that piece of the care. So, it is important to have debriefing meetings periodically, so all the team members are on the same page. When the child dies, some families will invite us to the viewing or memorial service. We try to attend; it helps to put a closure to that patient’s chapter and think of the happy memories of the child.
I would like your takeaway message to other physicians who may not have pediatric training but do take care of children — for example, a neurosurgeon, ear, nose and throat specialist or orthopedic surgeon — about complex and continuing care and end-of-life care.
I believe that every life has value. These families already feel isolated. Their child does not walk or talk, but they do things that bring happiness to these families. The siblings learn so much compassion. There is a lot of value that the family is receiving. We can think that we are taking care of them, and they are just there, but they have a lot of value and joy that they bring if you are willing to see it. It teaches me humility; I know that I am not there to fix all their problems. I feel that it is a privilege to walk with these families in their difficult medical journey. I am inspired by the families I work with; I have learned from their example. It has helped me to become a better person.
Suggested Readings:
• Palliative Care for Children, American Academy of Pediatrics, Committee on Bioethics and Committee on Hospital Care, Pediatrics Vol. 106 No. 2 August 2000 351
• Response to Suffering of the Seriously Ill Child: A History of Palliative Care for Children, Sisk, B.A., Feudtner, C., Bluebond-Langner, M., et al., Pediatrics. 2020;145(1):e20191741
• Palliative Care Across the Continuum of Childhood, Rachel J. Vandermeer, MD; Victoria J. Kain, RN, MN, NICC, PhD; and K. Sarah Hoehn, MD. MBe. Pediatr Ann. 2022;51(1):e40-e46.

Wisdeen Wu, DO, is a Clinical Associate Professor in the Division of Complex and Palliative Care in the Department of Pediatrics at UT Health San Antonio. She cares for patients and families with complex and chronic medical conditions as their primary care pediatrician. She also teaches medical students and pediatric residents in the outpatient pediatric clinics as a clinical faculty member. She believes building meaningful connections with patients and families is at the heart of pediatric care.

Rajam Ramamurthy, MD, is the Professor Emeritus in the Department of Pediatrics/Neonatology at UT Health San Antonio. Dr. Ramamurthy is a Past President of the Bexar County Medical Society and serves on the BCMS Publications Committee.

By Rebecca S. Charlton, MS, CCLS
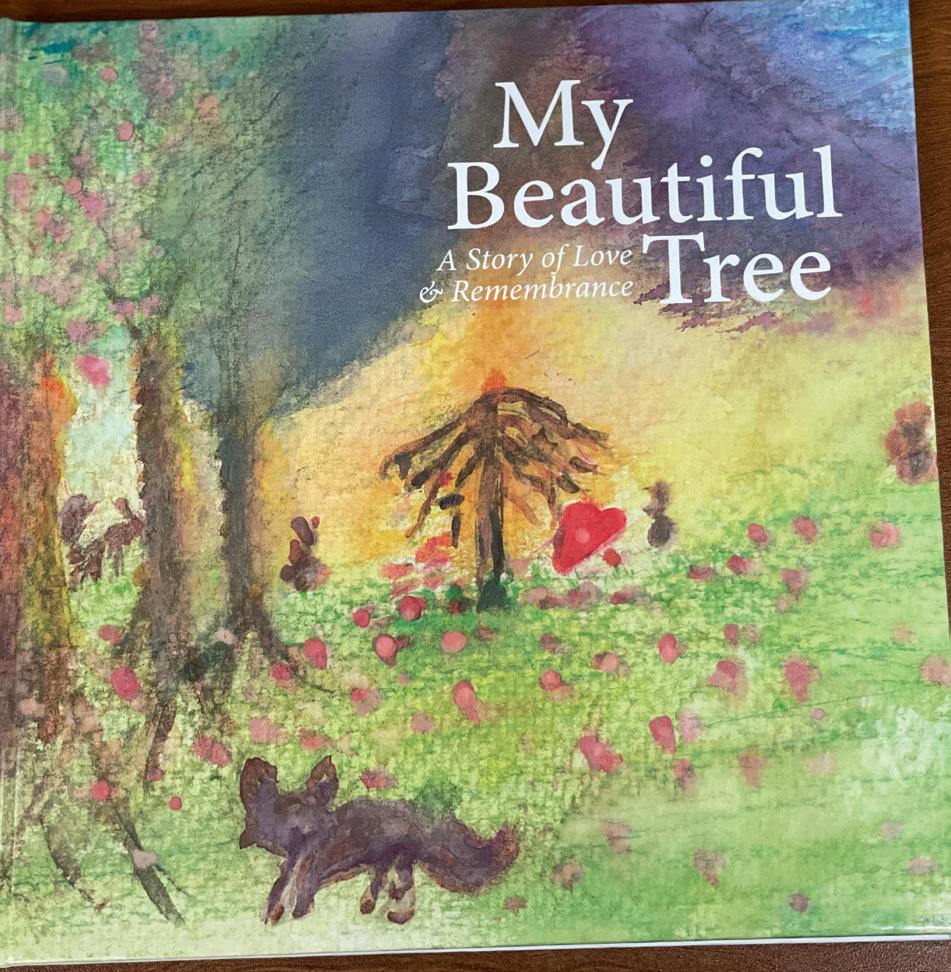
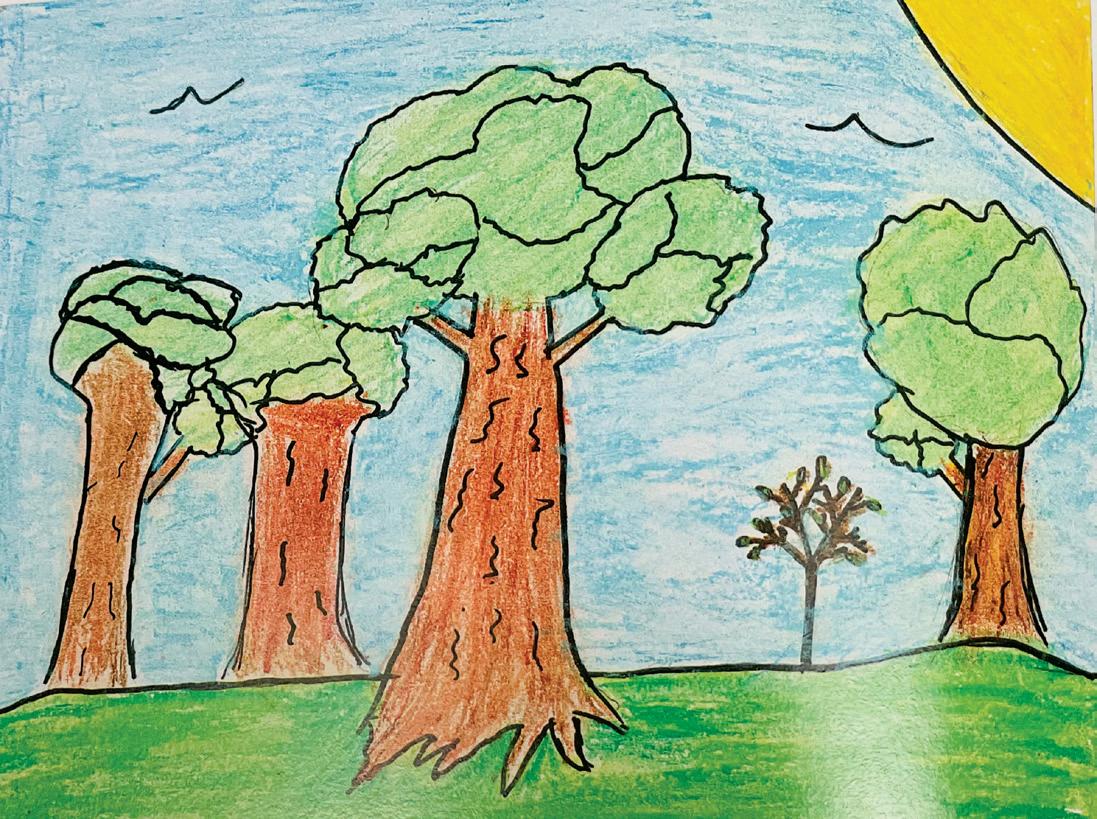
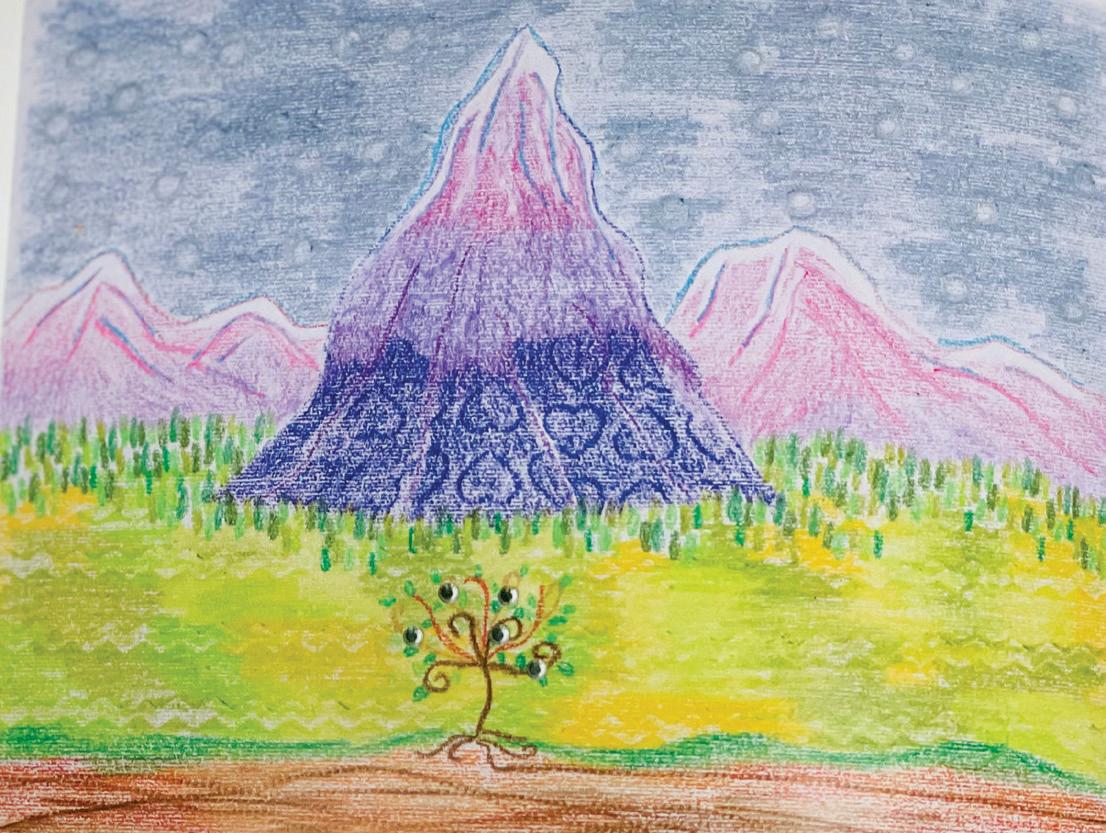
Illustrations from My Beautiful Tree: A Story of Love & Remembrance, courtesy of Rebecca S. Charlton, MS, CCLS
The two words, children and grief, should not be in context of each other. Death is a subject that most adults avoid addressing and dread talking about. However, helping a child with grief is a whole other ballgame. Our society does not like to bring up the subject of death and one may ask how often children experience grief. According to the 2024 Childhood Bereavement Estimation Model, an estimated 6.3 million children, or one in 12 children, in the United States will experience the death of a parent or sibling by the age of 18.1 This report stressed that comprehensive, grief-focused and trauma-informed care could assist in avoiding disrupted development for these at-risk children. In the state of Texas, one in 13 children will lose a parent or sibling by the age of 18. That equates to 559,000 children or 7.5 percent of children in the state who are bereaved.
These astonishing numbers bade the question of how pediatric professionals address these at-risk children. Let us look at the definition of grief. The American Psychological Association (APA) defines grief as the anguish experienced after a significant loss, usually the death of a beloved person.2
From 37 years of working with pediatric hospitalized children and pediatric palliative patients, I have found these strategies to be helpful.
1. Be honest.
When a death of a parent, sibling or family member occurs, do not use words that may confuse a child, i.e., they are sleeping, they are in a better place or we have lost your sister. When these are used, a child may be afraid to fall asleep, may want to go visit their loved one in the “better place,” or will want to find their “lost” sister. Honesty builds trust with the child.
2. Use age-appropriate language.
Be mindful of their age and developmental level. Younger children do not need the specific details of how a person died. As children grow older, they may request more information. The best description to use to let a child know a loved one has died is to say their body has stopped working. This is an honest statement and one that children can relate to, i.e., their toy may have stopped working.
3. Children grieve differently than adults.
Children may express their emotions with a family member for a brief time, but then will go off to play. They grieve in spurts and this dance may repeat itself frequently. It may be that they can only “be with the emotion” for so long until they go to something that they are more comfortable with.
4. There is no wrong or right amount of time for a child to grieve.
Each child’s grief journey is individual. Many factors can affect their grief. What was their relationship with their loved one? Did they live close to their loved one or would the child only see them once or twice a year? There can be religious or cultural influences on how the family views and observes death. These influences are of utmost importance to family and should be respected by all professionals. I share with parents that if they notice big fluctuations in the child’s eating and sleeping behaviors, that may indicate the child is having difficulty coping with the death, i.e., sleeping too much or not eating.
5. Suggestions for expressing emotions:
Younger children are often not able to verbalize feelings, so providing art materials allows the child to make a card for their loved one. Using art may also open the door for children to express feelings through colors and images. Older children may want to write a letter to their loved one. This gives the older child the ability to say things safely in a letter instead of saying it face-to-face to their relative.
6. Methods to help children process grief:
I like to ask children who are grieving to share things their loved one liked to do. With the answer given, I propose a project that the family could do to honor that loved one. For example, if their loved one enjoyed gardening, maybe the children could have a special place in their yard where they could plant flowers and tend to those flowers. If a loved one liked sports, the family could possibly donate sports equipment to a school or youth facility.
An effective tool to use with grieving children is bibliotherapy. Bibliotherapy is incorporating books to help children learn and process their feelings through a story. These stories can be about a child or a story shared through a child’s viewpoint. The Perinatal Supportive Care team at University Hospital has a book that addresses the tragedy of a family losing their baby. My Beautiful Tree: A Story of Love and Remembrance describes the story of a family of trees who experience the death of their youngest “child.” Despite everything in its surroundings, this tree did not grow as big nor as strong. When the tree dies, the tree parents explain to everyone around them the reason for the death. They also ensure that everyone knows the beauty of its love and that their memory will remain with them forever. The depiction helps parents who have to share this type of news with their children. This book was created with this in mind and it has been very well received by the families who are gifted the book.
A bereaved parent shared their family’s experience with reading the book.
“We read the book as a family last night. We had all the grandparents there with us, too. We didn’t get any pictures but I want you to know that it was a Holy moment that will live on forever in our family legacy. It was very meaningful. Thank you so much for your loving and caring and tender support through this process. I will never forget you.”
Addressing the grief of children and their families is always difficult, but with intention and care, adults can help their children grieve in healthy ways.
References:
1. Judi’s House/JAG Institute/ & New York Life Foundation, 2024 CBEM National & State reports, Childhood Bereavement Estimation Model, 2024
2. American Psychological Association, https://www.apa.org/topics/grief/ APA definition of grief, April 19, 2018

Rebecca S. Charlton, MS, CCLS, is a Family Support Specialist in Pediatric Palliative Care at University Hospital.


By Steven Pliszka, MD, and Kristina Martinez Fields, LMFT
“ My patients were already waiting months to be seen by Psychiatry. As a PNP in primary care, my hands were tied with not being able to provide a solution. With CPAN (the Child Psychiatry Access Network) I was able to create a behavioral health program at our office and utilize the psychiatry team to start treatment for our patients.
- Samantha Reeh, CPNP-PC, APRN “
Long wait lists and difficulty locating in-network mental health providers are a common concern we hear at UT Health San Antonio, CPAN. Pediatric providers are struggling to manage the increasing demands of mental and emotional health for their patients. Yet we know, timely engagement and treatment is of the utmost importance for young developing minds.
During the past decade, there has been a significant transformation in children’s mental health. Generations Z and Alpha are navigating a distinct set of challenges that directly contribute to their mental and emotional wellbeing. With the rise of smart phones, social media, the COVID-19 pandemic, lockdowns, the rise of political polarization and mass violence, these young generations endorse the highest levels of depression, anxiety, substance use and academic challenges.
Mental health has become a focal point among the pediatric community, as many recognize its critical role in child development. Somatic symptoms and behavioral concerns must be considered through a broader and more critical lens. Physicians manage physical health while simultaneously assessing environmental factors, family structure dynamics and patient safety. Given early and routine well-visit interactions with children, pediatric physicians can play a pivotal role in the early detection and treatment of mental health concerns, as well as intervention support. Providers are being asked to serve as our front-line mental health screeners. At the same time, they are limited by high caseloads, minimal training in psychopharmacology, and are up against waitlists for patient referrals to mental healthcare experts. This increasing demand for physicians to navigate mental health underscores the necessity for a support care framework within medicine.
UT Health San Antonio is part of a state funded program, The Texas Child Mental Health Care Consortium (TCMHCC), an initiative created by the 86th Texas Legislature in 2019. The TCMHCC was developed to address urgent mental health challenges in Texas and improve the mental healthcare system for children and adolescents. One of the initiatives of TCMHCC is the Child Psychiatric Access Network (CPAN), which serves as a direct consultation hotline for pediatric providers. Physicians and advanced practice providers can call 888-901-2726 to speak with a board-certified child psychiatrist within five minutes of calling. They can engage in case consultations or ask diagnosis and medication questions. CPAN staff can help locate mental health support and therapy referrals, specific to patient’s needs and insurance. Additionally, CPAN offers monthly continuing edu-
cation credits for medical providers to expand their knowledge and confidence in managing the mental health concerns of their pediatric patients.
The Perinatal Psychiatric Access Network (PeriPAN), a sister program to CPAN, is connecting OBGYN’s and family providers to a perinatal psychiatrist. Continuing education is offered to providers to advance their knowledge and skills, while also offering resources and referrals for their patients. Early intervention is effective. Providing supportive care to mothers in the perinatal period is vital to the family, and ultimately, the emotional and mental health of their children.
Through proactive involvement of physicians and their dedication to both physical and mental wellbeing, positive health outcomes are being achieved. CPAN/PeriPAN is available to work collaboratively with our medical partners in the hope of fostering healthier and more resilient future generations.
We look forward to supporting you and your patients.

Steven Pliszka, MD, is a Dielmann Distinguished Professor and former Chair of the Department of Psychiatry of the University of Texas Health Science Center at San Antonio until 2023. He has been a faculty member at UT Health San Antonio since 1986, joining the Department of Psychiatry after completing his general and child adolescent psychiatry residencies at UT Health San Antonio. Dr. Pliszka is a member of the Bexar County Medical Society.

Kristina Martinez Fields, LMFT, serves as Faculty Specialist with the School of Medicine at UT Health San Antonio and is a Licensed Marriage and Family Therapist in the state of Texas. Kristina joined the Department Psychiatry and Behavioral Health in 2013 and has since served in clinical, research and administrative roles.
CPAN is such a fantastic program that gives us pediatricians the support and guidance needed to help our children. I am comfortable with straight forward cases, but many are complex and having CPAN readily available is really life changing for me and my patients ...They also go the extra mile to send me therapists for my patients in their zip code and insurance plan!
- Linda Parsi, MD

By Saquib Anjum, MD
The topic of death and dying is often avoided due to its inherent difficulty or the differing definitions across cultures, tribes and religions. As an inpatient palliative care physician, discussing death with patients and their families during acute illness and active medical management is one of the most challenging conversations.
For many, death is perceived as a peaceful passing, akin to sleeping. Interestingly, in the age of modern medicine, deaths occurring during sleep only account for approximately 10 percent of all deaths nationwide. The majority of deaths take place away from home and family, typically within hospitals or other healthcare institutions.
Historically, death was defined as occurring when breathing and heartbeat ceased — a concept known as “last breath” or clinical death. This definition, resonant in many cultures and religions that believe in an afterlife, marks the soul’s departure from the body. The advent of mechanical ventilation, spurred by events like the polio epidemic in the 1940s and innovations like the Iron Lung, significantly altered perceptions and definitions of death in healthcare.
Subsequently, “brain death,” or legal death, emerged with advancements in cardiopulmonary resuscitation. Unlike reversible events like pulmonary and cardiac arrest, brain death signifies irreversible and complete loss of all brain functions. However, this definition poses operational challenges due to varying degrees of brain activity observed in conditions like persistent vegetative states, coma or lockedin syndrome. This complexity has sparked ongoing ethical debates, particularly in countries where organ donation hinges on the classification of death.
Presently, new medical technologies like Extracorporeal Membrane Oxygenation (ECMO) further complicate the definition of death. ECMO provides extended cardiac and respiratory support during cardiac and pulmonary arrest scenarios, potentially preventing brain death. Yet, the mortality rate on ECMO exceeds 50 percent after one month, prompting critical discussions around the boundaries of life and death.
Despite these medical and ethical discussions within the medical community, they often remain disconnected from broader societal, religious and legal frameworks. Traditional definitions of death are evolving, yet unfamiliar to many patients facing acute healthcare challenges.
In conclusion, the understanding and definition of death continue to evolve alongside medical advancements and ethical considerations. Bridging these discussions with broader communities is essential for navigating the complexities of end-of-life care and medical ethics.

Saquib Anjum, MD, is a board-certified physician specializing in hospice-palliative care, geriatric and internal medicine. With over nine years of experience in medical education, Dr. Anjum has taught medical students and residents in inpatient and outpatient settings. His most recent role was as Program Director in Internal Medicine at an Internal Medicine residency program in Chicago. Dr. Anjum is a member of the Bexar County Medical Society.

By David Alex Schulz, CIPP
Hospital chaplains cater to diverse faiths, handling requests that church ministers, priests, rabbis and imams might never encounter, for instance, providing a shaman to facilitate a peyote ritual for a Native American patient in palliative care.
Austin Frederick, MDIV, BCC, Vice President for Pastoral Services at Methodist Healthcare Systems, shared such an instance: “We began with a mobility assessment: Can this person leave the grounds or go to a safe and secluded place on the grounds and feel comfortable enough to express their faith tradition, which did happen, very briefly. It was our duty to affirm their faith tradition and practice.”
Nourishing a patient’s spiritual health regardless of their faith is a cornerstone of chaplaincy, especially at end of life. Methodist Healthcare Systems Pastoral Services boast representatives from 10 different faith traditions, and connections with local religious leaders provide comprehensive support. “If a Sikh guru, Wiccan priest or Native American shaman is needed, we can reach out to our community contacts,” Frederick explained.
Unlike autonomous church pastors, hospital chaplains work as members of an interdisciplinary team. “A hospital or hospice chap -
lain is one authority among many,” said Joseph Perez, MDIV, BCC, Chief Mission & Ministry Officer for the Baptist Health System in San Antonio. “Regular team meetings with doctors, nurses, social workers and chaplains ensure holistic patient care. The interdisciplinary team discusses overall prognoses, physical aspects, social needs and spiritual coping mechanisms for patients facing end of life,” Perez concluded.
Spiritual support is so integral to patient well-being that Methodist Healthcare Ministries’ contractual partnerships highlight its importance. “Our commitment is based on total beds, not the changing numbers of patients,” Frederick noted. “The contract requires one FTE chaplain for every seventy-five beds.”
Chaplains also support patients’ families. “Even if the patient isn’t anxious, family members often are,” Perez said. “In hospice care, the patient is never just the patient; they are always part of a family and community. Chaplains accompany families as they navigate the emotional journey of losing a loved one, visiting homes and hospital rooms where patients may be too ill to communicate. But the family is going through it with them. And so, we’re journeying with families as they walk this path.”
This emphasis on family relations distinguishes the chaplain’s role from most of the medical team. In many ways, the chaplain’s role is to serve as the connective tissue between a palliative patient and their faith, their community and their family.
Perez recounted, “The wife of an uncommunicative patient with his hospital bed in the living room, one day said to me, ‘You guys are angels!’ I said, ‘No, we’re not, why would you say that?’ It was simply because we treated her husband’s dying process as a typical, universal part of life. It was a perspective she hadn’t considered, and it provided comfort and normalcy in a difficult time.”
Pastoral support’s crucial role in healthcare, fostering a sense of peace and dignity for patients and their families, extends to medical colleagues as well when crisis breaks. COVID-19 had such a swift and relentless impact on hospitals that, like their colleagues in scrubs, the chaplaincy was pushed to its limits.
“COVID was Hell,” said Perez, a significant metaphor for a Baptist Minister. Safety protocols required patients to be cared for in isolation. Family members could not be with their loved ones when they were dying.
“We had to find ways to bring the community back safely, recognizing the toll loneliness had on patients and staff alike. Caregivers were distressed. They were doing everything they could to give patients’ bodies a chance to get through it. Despite every effort, many weren’t getting through it; they were dying,” recalled Perez.
“We had over half a million visits within hospitals and throughout the system during COVID,” said Methodist’s Franklin. “The loneliness of isolation exacerbated terribly. When the lockdown ended and small normalcies returned, we urged our managers to treat their chaplains to kindnesses like lunch at their favorite reopened restaurant, to see and feel the community returning.”
Of course, in the end, we are alone in approaching the final curtain. Dr. Elisabeth Kübler-Ross’s seminal work, On Death and Dying, points out that after passing through phases of anger, depression, denial and bargaining, one comes to acceptance. In reaching acceptance, the world surrounding the patient loses more and more relevance. “We have seen the majority of our patients die in the stage of acceptance, an existence without fear and despair,” said Kübler-Ross. The patient becomes increasingly uncommunicative, not out of diminished capacity, but recognizing that their connections with the world are fraying.
This is when the chaplain’s efforts culminate, for after community and family lose relevance, their spirituality is the bridge to the next phase of their existence as the chaplain accompanies them as they transition.

David Alex Schulz is certified in HIPAA privacy and security compliance, serves on the BCMS Publications Committee and is a contributing writer to San Antonio Medicine magazine.
By Hank Dunn, published May 4, 2020
— Giving up implies a struggle…
Letting go implies a partnership…
Letting be implies, in reality, there is nothing that separates.
— Giving up says there is something to lose…
Letting go says there is something to gain…
Letting be says it doesn’t matter.
— Giving up dreads the future…
Letting go looks forward to the future…
Letting be accepts the present as the only moment I ever have.
— Giving up lives out of fear…
Letting go lives out of grace and trust…
Letting be just lives.
— Giving up is defeat at the hands of suffering…
Letting go is victory over suffering…
Letting be knows suffering is often in my own mind in the first place.
— Giving up is unwillingly yielding control to forces beyond myself…
Letting go is choosing to yield to forces beyond myself…
Letting be acknowledges that control and choices can be illusions.
— Giving up believes that God is to be feared…
Letting go trusts in God to care for me…
Letting be never asks the question.
By Jim Baggett, MD, JD

Caregivers who deal with end-of-life issues understand the importance of documentation, which expresses the wishes of the patient. Nevertheless, it is not uncommon for confusion to exist due to the number of different possible advance directives. This confusion can be most easily dispelled by an understanding of the specific purpose of each document and the manner in which each contributes to the well-being of the patient and his or her loved ones, as well as to the ability of the caregiver to provide appropriate care.
The primary documents involving end of life care include Directive to Physicians, also known as a Living Will, Medical Power of Attorney and Durable Power of Attorney.
This document allows a competent patient to express preferences regarding their care should they be, at some future time and in the judgment of their physician, suffering from a “terminal condition” with an expectation of death within six months, or an “irreversible condition” causing them to be unable to make decisions or to care for themselves. There is no six months of life expectancy requirement in the case of an irreversible condition. A patient may begin in an irreversible condition and progress to one that is terminal. This form is most often employed to express a desire for comfort care only or alternatively for the use of any life sustaining treatment regardless of the patient’s condition. If the patient enters hospice care, the preference for the use of any life sustaining treatment no longer applies. In addition, the statutory form provides a section for additional wishes on the part of a patient, for example, artificial nutrition and hydration, as well as pertinent definitions of important terms for the patient and the caregiver. Beyond its obvious importance, this directive can be used by the caregiver in discussions with the patient’s loved ones should there be discord among them when decisions need to be made, as is often the case. The express wishes of the patient in this type of directive override a decision by an agent holding a Medical Power of Attorney.
The statutory form may be downloaded from the Texas Health and Human Services website. The form is self-explanatory and does not require an attorney. https://www.hhs.texas.gov/regulations/
forms/advance-directives/directve-physicians-family-or-surrogates-living-will
What happens though when an unexpected circumstance arises, which is not easily answered by a Living Will (or if there is no Living Will)? This is the situation in which a Medical Power of Attorney comes into play. This document allows a competent patient to designate an agent to make medical decisions, (and only medical decisions), should the patient become unable to do so. There are statutory limitations as to who can be named as an agent so as to avoid conflicts of interest between the patient and caregivers. However, even if there is a Medical Power of Attorney, remember that the agent may face disagreement among family members and so the existence of a Living Will is still useful as evidence of the patient’s wishes. It is not legally required to have both, but it is advantageous to do so.
The statutory form may be downloaded from the Texas Medical Association website. It is self-explanatory and does not require an attorney. https://www.texmed.org/template.aspx?id=65
This is not a medical form but should ideally be mentioned to the patient. It allows the patient to designate an agent to handle their financial and property affairs should they become unable to do so. Absent this designation, the family may have no way of accessing assets to pay for the patient’s care other than what is sometimes a time consuming and expensive guardianship proceeding. While not medical in nature, it can be crucial in cases of dementia, for example, which require expensive memory care facilities.
The statutory form may be downloaded from the Texas Health and Human Services website. An attorney is not strictly required but is recommended. https://www.hhs.texas.gov/regulations/forms/advance-directives/statutory-durable-power-attorney-sdpoa
The information in this article does not, and is not intended to, constitute legal advice. Instead, all content is for general information purposes only.
Jim Baggett, MD, JD, received his JD from UT School of Law, and graduated from the UTHSCSA Long School of Medicine in 1999. He did his Family Medicine Residency at Spohn Memorial Hospital in Corpus Christi, and his Palliative Care Fellowship at Audie L. Murphy Memorial Veteran’s Hospital. Dr. Baggett specializes in family medicine and is a member of the Bexar County Medical Society.
The following is reprinted in part with permission from the National Institute on Aging
You might want to prepare documents to express your wishes about a single medical issue or something else not already covered in your advance directives, such as an emergency. For these types of situations, you can talk with a doctor about establishing the following orders:
• Do not resuscitate (DNR) order: A DNR becomes part of your medical chart to inform medical staff in a hospital or nursing facility that you do not want CPR or other life-support measures to be attempted if your heartbeat and breathing stop. Sometimes this document is referred to as a do not attempt resuscitation (DNR) order or an allow natural death (AND) order. Even though a living will might state that CPR is not wanted, it is helpful to have a DNR order as part of your medical file if you go to a hospital. Posting a DNR next to your hospital bed might avoid confusion in an emergency. Without a DNR order, medical staff will attempt every effort to restore your breathing and the normal rhythm of your heart.
• Do not intubate (DNI) order: A similar document, generally incorporated into a DNR, a DNI informs medical staff in a hospital or nursing facility that you do not want to be on a ventilator.
• Out-of-hospital DNR order: An out-of-hospital DNR alerts emergency medical personnel to your wishes regarding measures to restore your heartbeat or breathing if you are not in a hospital. Statutorily sanctioned bracelets can be ordered through the Texas Medical Association.
• Physician orders for life-sustaining treatment (POLST) and medical orders for life-sustaining treatment (MOLST) forms: POLST and MOLST are not statutory in Texas though they can be used, ideally in conjunction with an Advance Directive. These forms provide guidance about your medical care that healthcare professionals can act on immediately in an emergency. They serve as a medical order in addition to your advance directive. Typically, you create a POLST or MOLST when you are near the end-of-life or critically ill and understand the specific decisions that might need to be made on your behalf. These forms may also be called portable medical orders or physician orders for scope of treatment (POST). Their usefulness lies in the fact that they direct desired care while the patient is still able to make decisions whereas an Advance Directive comes into play only once the patient cannot make decisions for him or herself.
Getting your affairs in order can also mean making decisions about organ donation and funeral arrangements, or what you want to happen to your body after you die.
• Organ donation and brain donation. You can register to be an organ donor when you renew your driver’s license or state ID at your local department of motor vehicles. You can also register online. Some people also choose to donate their brain to advance scientific research. It may be possible to donate organs for transplant as well as the brain for scientific research.
• Funeral arrangements. You can decide ahead of time what kind of funeral or memorial service you would like and where it will be held. You can also decide whether you would like to be buried or
cremated and whether you want your body’s ashes kept by loved ones or scattered in a favorite place. Be sure and specify certain religious, spiritual or cultural traditions that you would like to have during your visitation, funeral or memorial service. Put your preferences in writing and give copies to your loved ones and, if you have one, your lawyer.
Everyone approaches the process differently. Remember to be flexible and take it one step at a time. Start small. For example, try simply talking with your loved ones about what you appreciate and enjoy most about life. Your values, treatment preferences and even the people you involve in your plan may change over time. The most important part is to start the conversation.
• Reflect on your values and wishes. This can help you think through what matters most at the end of life and guide your decisions about future care and medical treatment.
• Talk with your doctor about advance directives. Advance care planning is covered by Medicare as part of your annual wellness visit. If you have private health insurance, check with your insurance provider. Talking to a healthcare provider can help you learn about your current health and the kinds of decisions that are likely to come up. For example, you might ask about the decisions you may face if your high blood pressure leads to a stroke.
• Choose someone you trust to make medical decisions for you. Whether it’s a family member, a loved one or your lawyer, it’s important to choose someone you trust as your healthcare proxy. Once you’ve decided, discuss your values and preferences with them. If you’re not ready to discuss specific treatments or care decisions yet, try talking about your general preferences.
• Complete your advance directive forms. To make your care and treatment decisions official, you can complete a living will. Similarly, once you decide on your healthcare proxy, you can make it official by completing a durable power of attorney for healthcare.
• Share your forms with your healthcare proxy, doctors and loved ones. After you’ve completed your advance directives, make copies and store them in a safe place. Give copies to your healthcare proxy, healthcare providers and lawyer. Some states have registries that can store your advance directive for quick access by healthcare providers and your proxy.
• Keep the conversation going. Continue to talk about your wishes and update your forms at least once each year or after major life changes. If you update your forms, file and keep your previous versions. Note the date the older copy was replaced by a new one. If you use a registry, make sure the latest version is on record.
This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
• https://www.nia.nih.gov/health/advance-care-planning/ advance-care-planning-advance-directives-health-care#find
• https://www.nia.nih.gov/health/advance-care-planning/getting-your-affairs-order-checklist-documents-prepare-future
By M&S Radiology Associates
M&S Radiology Associates stands as an independent physician group with a storied legacy of innovation in imaging services spanning over 60 years in San Antonio. Unlike corporate-run physician groups focused on shareholder profits, M&S offers a distinct alternative.
The physicians of M&S have deep roots in San Antonio’s medical imaging history, dating back to their involvement with the Baptist Health System’s predecessor facility in the 1920s. They were foundational in the development of what became Baptist Memorial Hospital, later evolving into the flagship Baptist Medical Center.

Initially based at the M&S Clinic and later the Baptist hospitals, M&S Radiologists have grown alongside Baptist Health, now providing radiology services to all six (and soon to be seven) Baptist Hospitals. They were pioneers in outpatient imaging in San Antonio and were the first in the city to recognize and invest in PET imaging for oncology.

In 2004, M&S formed a joint venture partnership with Baptist Health, creating the Baptist M&S Imaging centers, which have become synonymous with high-quality, accessible outpatient imaging across the city. This partnership also facilitated M&S’s expansion into teleradiology, significantly amplifying their capacity to deliver imaging services beyond San Antonio, covering medical facilities across Texas.
Dale Skrnich, M&S’s Chief Operating Officer, emphasized how their origins in hospital and imaging center-based imaging enabled their growth into a leading independent teleradiology service provider. This expansion underscores their commitment to providing stable, high-quality teleradiology services across a broad geographical area.
Dr. Phillip Fortenberry, President of M&S Radiology Associates, underscored their commitment to patient-centered care and innovation in imaging. He highlighted their culture of empowering physicians and ensuring consistent, high-quality care across all services, from advanced diagnostic testing to specialized interventional services.
With a mission rooted in over six decades of experience, M&S Radiology Associates continues to lead with advanced technology and specialized care, delivering precise diagnostic interpretations and supporting excellence in patient care across Texas and beyond. Their comprehensive services include subspecialized diagnostic and interventional radiology such as body imaging, breast imaging, musculoskeletal radiology, neuroradiology, pediatric radiology, and vascular and interventional radiology. They continuously invest in cutting-edge technology and AI algorithms to stay at the forefront of advanced patient care.

Phillip Fortenberry, MD President, M&S Radiology Associates
By TMA Insurance Trust
Have you ever considered how well-protected your income is in the event of an unexpected illness or injury? As a physician, you’re skilled at managing your finances, from savings and investments to retirement plans. However, one crucial aspect that many overlook is protecting your income with disability insurance. Discovering that your coverage falls short when you need it most is a situation best avoided. TMA Insurance Trust urges you to consider three essential factors that contribute to effectively safeguarding your income.
Verify that your coverage helps protect your income in case of a disability.
• There are several factors that could lead to your benefits not being enough to adequately protect your income. Perhaps you bought a policy years ago, only to discover that your benefit did not grow with your income. If you’re a practice owner, you might assume your long-term disability insurance is sufficient to cover your personal expenses, but then realize it is not enough to also cover your practice expenses and retain your staff. Another factor that could lead to reduced benefits, potentially subjecting you to taxation, is if your premiums are being paid as an expense of your practice instead of being paid out of your personal income.
• Change is inevitable throughout your career as a physician. TMA Insurance Trust recognizes this and offers support to ensure your disability insurance coverage remains relevant by aligning it with your current needs and circumstances. By being proactive, you can adapt to your changing circumstances without leaving yourself financially vulnerable.
Uncover any hidden limitations in your employer-provided coverage.
• TMA Insurance Trust’s disability insurance can effectively help protect your income and bridge any coverage gaps. For employed physicians, your employer’s disability coverage may only cover 60-65 percent of your salary. Additionally, your employer might set a cap on the monthly benefit amount, typically around $10,000, or $120,000 annually.
• For example, if you earn $250,000 per year and become disabled, your total benefits would be limited to $120,000 before taxes. This leaves $130,000, or 52 percent of your total salary, uncovered. It’s important to address this gap if your salary exceeds these limits.
Have your disability insurance stay with you.
• Typically, coverage is not portable, meaning you will lose your coverage if you were to leave your employer. This could pose a problem if your health declines and you need to seek a new policy. At that juncture, you may face higher premiums to replace the lost coverage or even denial of coverage altogether. TMA Insurance Trust can assist you in obtaining coverage that follows you wherever you go, thus helping you navigate many potential pitfalls.
Don’t wait until it’s too late to help secure your financial future. Whether you’re an independent or employed physician, our experienced advisors can assist you in exploring disability insurance options tailored to your specific needs. TMA Insurance Trust is a full-service insurance agency dedicated to helping all physicians in Texas. We work with leading disability insurers, offering discounts of up to 40 percent for the life of the policy. Additionally, members can save with a 25 percent statement credit¹, saving thousands of dollars over the life of your coverage.
Protecting your income is crucial for your financial security, and disability insurance plays a key role in this protection. Our licensed advisors have decades of experience in helping physicians protect their income. Speak directly to an advisor to help protect yours today, call 800-880-8181 weekdays from 8:00 a.m. to 5:00 p.m., CST.

By David P. Green, MD
To bring a medical school to the city, the San Antonio Medical Foundation was established in 1947. After more than 20 difficult years, the medical school and teaching hospital were dedicated on July 12, 1968. The only other building on the 200 acres donated to create the Medical Center in then far northwestern San Antonio was Southwest Texas Methodist Hospital, which had opened in 1963. With two exceptions, streets in the South Texas Medical Center are named to honor individuals who helped create the complex.
Audie L. Murphy (1924–1971) was born in Kingston, Texas and joined the Army around his 18th birthday. Having received every medal that the United States gives for valor — two of them twice — as well as decorations from several foreign governments, he is the most decorated combat soldier in U.S. history. David Hackworth and Ernest Edgar Hume were awarded more medals, but Murphy had more citations for heroism in the face of enemy fire. His Medal of Honor was for valor in France, where he was credited with killing or wounding 50 German soldiers and stopping an attack by enemy tanks. After the war, he became a movie star, appearing in 45 motion pictures. Not so well known were the lyrics he wrote for 14 songs. He died in a plane crash at the age of 47.
Roger
After success as an insurance salesman, in 1958 he started Columbia 300 Industries, which became the largest bowling ball manufacturing company in the world, turning out 5,000 balls a day. During their 55 years of marriage, the Zellers made numerous charitable contributions in San Antonio.
Before the CTRC moved to its present location, it was housed on Medical Drive in the Charles F. Urschel Pavilion, named in honor of the father of its major donor, Charles F. Urschel, Jr. (1917-1981) and his wife, Betty (1917-1988). This newer building in the relocated CTRC is named the Charles and Betty Urschel Tower in honor of those original donors, and given by the family foundation. Charles Jr. was the first cousin and stepbrother of Tom Slick, Jr., with whom he shared many interests, including oil and gas exploration, ranching, airplanes and automobiles. At one time he was one of only two Mercedes distributors in the entire United States, and for several years he sponsored cars in the Indy 500 race with his other stepbrother, Earl Slick. Betty (nee Mary Elizabeth Hails), whom Charles met at Stanford University and married in 1939, was a well-known founder, officer and patron of many San Antonio arts organizations.

This CTRC wing is named for a self-made millionaire and another of San Antonio’s quiet philanthropists. After a six-week courtship during his pilot training in San Antonio in 1942, Second Lt. Roger Zeller (1917–1997) proposed to Laura “Cherry” Dietzel. Shortly thereafter they were married, but within a few months he was based in North Africa as a B-26 pilot. On his 19th combat mission — over Sardinia — he was shot down, captured and sent to a prisoner-of-war camp in Italy. He and a comrade escaped, and after 24 days made it back to Allied lines. After the war, he rose to the rank of brigadier general in the Reserves and at the age of 39, he became the youngest officer elected president of the National Reserve Officers Association of the United States.
The son of a prominent and politically powerful rancher father from Uvalde, Dolph Briscoe, Jr. was Texas governor from 1973 to 1979. His wife, Janey Slaughter Briscoe (1923–2000), had more direct involvement with the UT Health Science Center; the children’s wing at University Hospital is named in her honor. She served six years on the University of Texas Board of Regents. The decision to name the library for the former governor was made at her last board meeting.

The Ewing Halsell Foundation has made significant contributions to the South Texas Medical Center.
The father of Ewing Halsell (1877–1965) owned part of the famous XIT Ranch. In 1942, Ewing Halsell bought the 90,000-acre Farias Ranch in Maverick County and moved his ranching headquarters to San Antonio. For many years he lived in the St. Anthony Hotel with his wife and “unadopted daughter,” ranch secretary Helen Campbell. In 1957, the Halsells established the Ewing Halsell Foundation, which made substantial contributions to the Medical Center, though Halsell was never involved directly with the work of the San Antonio Medical Foundation or the Medical Center. Instrumental in the distribution of funds from the Ewing Halsell Foundation was its board chairman, Gilbert Denman, who died in 2004.

Robert Floyd Curl (1897–1971) was a Methodist clergyman for nearly 55 years, serving as pastor, district superintendent, administrator and professor at Perkins School of Theology. As executive secretary of the Southwest Texas Conference, Dr. Curl, on January 24, 1955, presided over the first meeting of trustees for Methodist Hospital. When one of the first streets in the Medical Center was named for him, the only building on the street was Methodist Hospital. When his son, Robert F. Curl, Jr. was 9 years old, his father gave him a chemistry set. The younger Dr. Curl went on to win the Nobel Prize in chemistry.
William E. “Bill” Greehey has been one of San Antonio’s most generous philanthropists. Born In Iowa, he came to San Antonio to serve a tour of active duty at Lackland AFB and later studied accounting at St. Mary’s University. Beginning as an internal auditor for Coastal States Gas Corporation in Houston, at age 37 he was named president and later CEO of a subsidiary that evolved into Valero Oil Company. In addition to funding the Children’s Cancer Research Institute, Greehey was also the founder of San Antonio’s Haven for Hope, matching his own $50 million donation with other contributions, and then continuing to provide funds for its ongoing operating expenses. He also raised the money to fund a basketball facility at St. Mary’s that also bears his name.

The 12th floor “private wing” of the old University Hospital was named in honor of a highly respected local surgeon, Dr. Albert Hartman, Jr. (1907-1983). Long before San Antonio had a medical school or university-based teaching program, there was a surgical training program at the old Robert B. Green Hospital. The hospital was closed in the late 1940s because of financial and staffing problems, and Dr. Hartman played a leading role in reopening “the Green” in 1950 and establishing a surgical residency program there. A strong supporter of medical research, he was a driving force behind the Southwest Foundation for Research and Education, and served as chairman of its board for nine years. Later, he worked hard to help bring a medical school to this city, but he was on the losing side of those who favored locating it downtown near the Robert B. Green Hospital.
Jim Hollers Drive
This street does not exist yet — but it should. James P. Hollers, DDS (1899–1976), a past president of the American Dental Association, was a key force behind the creation of the Medical Center. In 1956, while president of the San Antonio Chamber of Commerce, he was elected to
replace one of two Medical Foundation directors who had resigned because of disagreement over the proposed site. Taking over as chairman in 1957, he served until 1970, when he was given a five-year contract as executive director. He was instrumental in securing creation of the Audie Murphy VA Hospital adjacent to the new medical school. In 1983, the San Antonio Medical Foundation board discussed appropriate memorials to Hollers; among the recommendations was that a street in the Medical Center be named for him. This has not happened yet, so Jim Hollers is the only name listed in this book before a street is named for him.

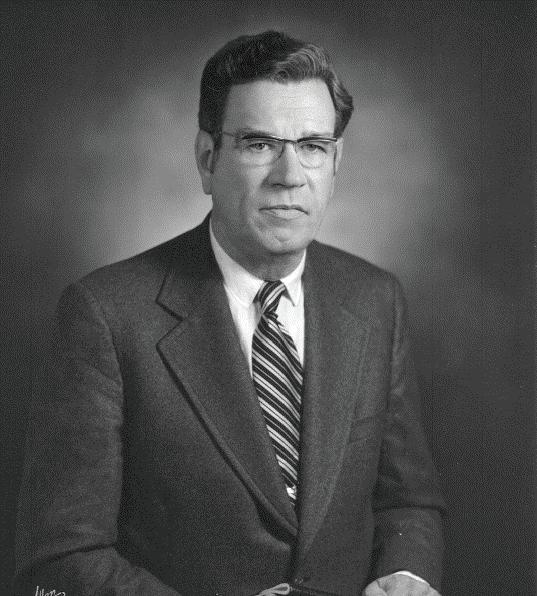
As spokesman for the Bexar County Medical Society in 1955, John M. Smith, Jr., MD (1914–2003), presented a plan to the bishop of the Methodist Church’s Southwest Conference asking the conference to administer a new hospital in San Antonio. Having set in motion creation of the first occupant of the South Texas Medical Center, Smith’s efforts in securing and co-coordinating support from the Texas legislature, UT Board of Regents and other bodies were pivotal in developing the new Medical Center. As a Texas Department of Health board member, Smith was also instrumental in obtaining Hill-Burton matching funds to make up the shortfall in construction costs for the Teaching Hospital that had been approved by the voters of Bexar County. Smith was active in medical politics for his entire career, serving as president of both the Bexar County Medical Society and Texas Medical Association. His son, Dr. J. Marvin Smith, a cardiovascular surgeon, later became president of the Bexar County Medical Society, the only father and son pair to fill that chair.
Lewis E. Fite worked closely with Sid Katz and Melrose Holmgreen in acquiring an additional 400 acres for the Medical Center. A modest man, he resisted efforts to name a street for him during his lifetime. After his death, however, the San Antonio Medical Foundation put his name on the short street between what is now St. Luke’s Baptist Hospital and Methodist Plaza, connecting Ewing Halsell and Floyd Curl Drives.
In 1878, George Holmgreen bought a struggling foundry and built it into one of San Antonio’s longest lasting businesses, Alamo Iron Works. As company president, descendant Melrose Holmgreen (1890–1975) was one of the original seven trustees of the San Antonio Medical Foundation, in addition to serving for 30 years as a Chamber of Commerce director and helping establish the San Antonio River Authority and the United Way. In the 1960s, he was on the land acquisition committee that gradually purchased 400 acres of adjacent land. A nephew, John C. Holmgreen, later was foundation president.
Merton Melrose Minter, MD (1903–1977), a key supporter in establishing a medical school in San Antonio, opened the Minter Clinic in San Antonio in 1932 and was a Texas Medical Association trustee (1951–1952), chairman of the University of Texas regents (1959–1961), and San Antonio Medical Foundation chairman (1971–1976).
As a recent graduate of Jefferson High School and an 18-year-old Marine on Okinawa, Blair “Bruzzie” Reeves (1925–1997) took a Japanese sniper’s bullet in his spine. It left him paraplegic for the next 50 years. Unable to fulfill his dream of becoming a coach, he went to law school and continued to live a very active life. In 1966, he was elected Bexar County judge. The following year, he cast a tie-breaking vote to double the hospital tax rate to build and maintain the teaching hospital, overriding the wishes of voters who had rejected such a proposal in a previous election. This act of political courage is considered to have saved the teaching hospital and Medical Center. Reeves later was Fourth Court of Appeals Chief Justice, and the new Justice Center was named in his honor.

A sniper’s bullet on Okinawa confined Blair Reeves to a lifetime in a wheelchair, but his courage in overriding the voters of Bexar County made possible what is now University Hospital.
Born of Jewish immigrant parents from Lithuania, Sid Katz (1893–1968) was a well-known South Texas oilman, but he spent his earliest years in Clinton, Kentucky. There was no synagogue in which the family could worship, so they attended the local Methodist church — which presumably explains why Katz was a dedicated fundraiser for planning and construction of the Southwest Texas Methodist Hospital. He was also chairman of the San Antonio Medical Foundation’s land acquisition committee. His son, Charles, succeeded him as a trustee.
Thomas Baker Slick, Jr. (1916–1962), best known as founder of the Southwest Research Institute and the Southwest Foundation for Biomedical Research, was also a millionaire oilman, rancher, philanthropist, adventurer, author, art collector and inventor. With New York architect Philip Youtz in the 1970s, he developed the Youtz-Slick construction method, which used hydraulic jacks to lift precast concrete slabs into place. Many buildings at Trinity University, as well as the Tower of the Americas, were built with this technique. Slick was an original San Antonio Medical Foundation board member but died at the age of 46 in a private plane crash just as the Medical Center was beginning to develop. He was the cousin and stepbrother of Charles F. Urschel, Jr.
In the late 1950s and early 1960s, a bitter fight was waged over whether to put the medical school downtown or at the edge of the city. Edgar Von Scheele was one of four investors who owned the 200 acres of Oak Hills land in northwest San Antonio that they donated to the San Antonio Medical Foundation and Methodist Hospital once the remote site was selected.

David P. Green, MD, is a founder of The Hand and Upper Extremity Center of San Antonio, with an international reputation in hand surgery, and the first surgeon in San Antonio to devote his practice entirely to hand and upper extremity surgery. Dr. Green is a member of the Bexar County Medical Society, and a recipient of the BCMS Golden Aesculapius Award for Lifetime of Distinguished Service.
The Bexar County Medical Society strives to keep physicians connected, involved and informed even after retirement! The 1853 Club Luncheons are opportunities to reconnect with former colleagues and forever friends while enjoying lunch and learning
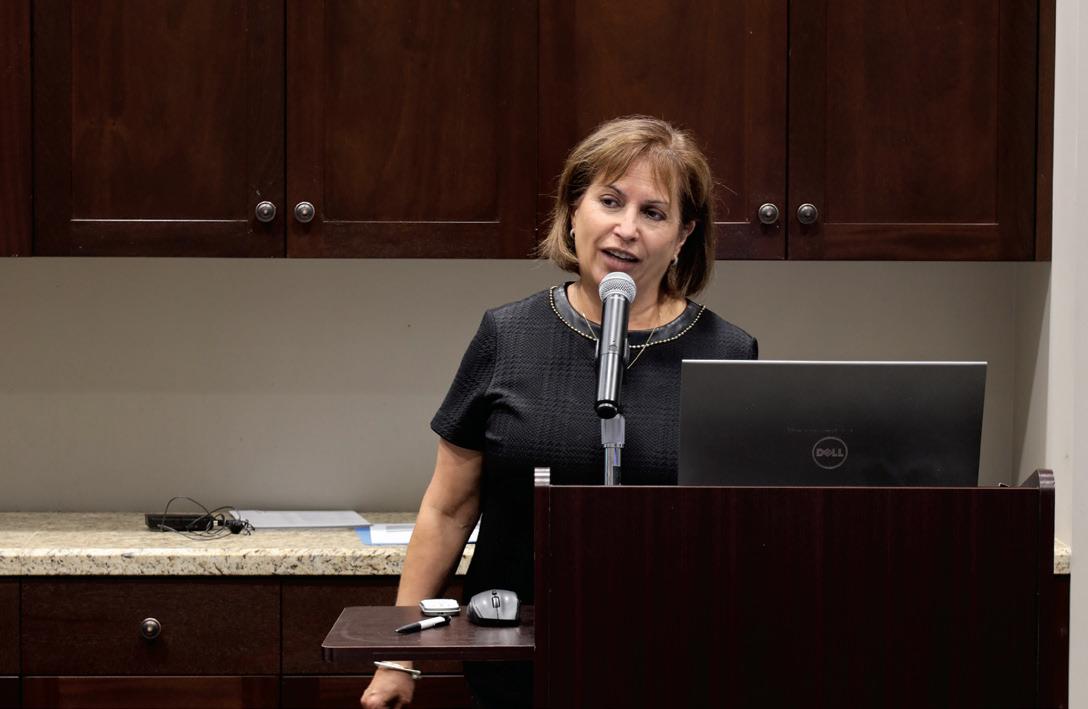


from a guest speaker. At this month’s luncheon, we were joined by Broadway Bank’s Senior VP, Tom Duran, and their Estate Settlement Specialist, Monica Bonilla. Bonilla shared a presentation on “Safe Banking for Seniors.”



Earlier this month, Bexar County Medical Society hosted a Summer Networking Mixer event with Hancock Whitney Bank, a BCMS Gold Level Circle of Friends Sponsor.



The evening was filled with great networking opportunities. We hope to see you at our next event!



We encourage you to use our friends of medicine businesses whenever you or your practice need supplies or services.

Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 CDavis@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”

Aspect Wealth Management (★★★ Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark
President
210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”

Broadway Bank
(HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@Broadway.Bank www.broadwaybank.com
“We’re here for good.”

The Bank of San Antonio (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the
few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Brandi Vitier 210-807-5581
Brandi.Vitier@thebankofsa.com www.thebankofsa.com
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking 210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking 210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help physicians get the banking services they need.
Synergy FCU Member Services 210-750-8333
info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”

Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison
210-503-0003
Yulia@genicslabs.com
Kevin Setanyan Managing Partner
210-503-0003
Kevin@genicslabs.com
Artyom Vardapetyan
Managing Partner
210-503-0003
www.genicslabs.com
“Accurate results in record time.”
Livingston Med Lab (HH Silver Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease and Genetics.
Robert Castaneda CEO 210-316-1792
Robert@livingstonmedlab.com
www.livingstonmedlab.com/home
“Trusted Innovative, Accurate and STAT Medical Diagnostics”

American Health Imaging (★★★ Gold Sponsor)
American Health Imaging (AHI) has 5 state-of-the-art imaging centers in San Antonio, TX with industry- boardcertified subspecialized radiologists delivering precise, reliable results. Easy scheduling and prompt report turnaround times, serving both physicians and their patients. Imaging at AHI is priced up to 60% less than hospitals and in-network with 99% of health plans with competitive rates to save patients money. AHI has an additional 37 best-in-class diagnostic imaging facilities in Alabama, Florida, Georgia, Texas and South Carolina. US Radiology Physician Number 210-572-1211
Casey Allen
Regional Sales Director | San Antonio US Radiology Specialists 210-846-0606
Casey.Allen@usradiology.com
Jasmine Mendoza
Jasmine.Mendoza@usradiology.com
Jaime Zamora
Jaime.Zamora@usradiology.com
Sydnie Caradec
Sydnie.Caradec@usradiology.com
Sarah McMindes
Sarah.Mcmindes@usradiology.com
Scott Roberson
Scott.Roberson@usradiology.com
Ryan Denman
Ryan.Denman@usradiology.com www.americanhealthimaging.com (main site) www.americanhealthimaging.com/ physician-resources/ (Physician Resources to refer to American Health Imaging)


Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for healthcare entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com www.bexarcv.com
“Proudly serving the medical community since 1998”

Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA Senior Private Wealth Advisor 512-649-8113 Service@oakwellpwm.com www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney Financial Advisor
210-858-5880
Elizabeth.Olney@edwardjones.com www.edwardjones.com/elizabeth-olney "Making Sense of Investing"

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com
www.aspectwealth.com
“Your wealth. . .All aspects”

Hancock Whitney (HHH Gold Sponsor)
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services.
www.hancockwhitney.com
John Riquelme San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Larry Anthis Corporate Banking, Relationship Manager 210-507-9646
Larry.Anthis@hancockwhitney.com
Serina Perez San Antonio Business Banking 210-507-9636
Serina.Perez@hancockwhitney.com
Erik Carrington Texas Regional Wealth Management Manager 713-543-4517
Erik.Carrington@hancockwhitney.com

Conviva Care Center (HHH Gold Sponsor)
Conviva’s value-based care model allows physicians to deliver high quality, personalized care and achieve better
outcomes, while feeling free to focus on health equity and patient outcomes.
Kim Gary
Senior Physician Recruiter 812-272-9838
KGary4@humana.com www.convivacareers.com
“Fuel Your Passion & Find Your Purpose”

UT Health San Antonio
MD Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado
Business Development Manager 210-450-3713
DelgadoR4@uthscsa.edu
UT Health San Antonio
MD Anderson Mays Cancer Center
Laura Kouba Business Development Manager 210-265-7662
NorrisKouba@uthscsa.edu
https://uthscsa.edu/ Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229
Healthcare Administration Consultants (HH Silver Sponsor)
Our mission is to help healthcare organizations small or large to achieve sustainable growth and success by providing them with expert healthcare administration consulting services. We focus on key factors such as: revenue, supply chain visibility, and aligning operations to save time so that your team can focus on improving the patient’s health and well-being. We transform patient care outcomes and employee working experiences while driving brand and revenue growth.
Dr. Reshma Beherry, DHA
Doctor of Healthcare Administration
210-602-6905
RB@administrative-consultants.com
https://administrative-consultants.com/
SERVICES

Equality Health
(HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com “Reimagining the New Frontier of Value-Based Care.”
(H Bronze Sponsor)
We were founded to meet a need: helping business owners succeed by giving them simple, quality, affordable U.S.-based contact solutions. In only a few years, our focus on nurturing client relations and building trust not only helped our customers grow their businesses, but helped us stake our claim in the highly competitive TAS industry as one of the most well-regarded and referred. Our 50 years of collective experience are the driving force behind our clients’ satisfaction.
Rachel Caero Managing Partner 844-554-3473 Rachel@dialops.net
Insperity
(HH Silver Sponsor)
Insperity’s HR solutions offer premium service and technology to facilitate growth by streamlining processes related to payroll, benefits, talent management and HR compliance. We provide the tools to help you lighten your administrative load, maximize productivity and manage risks – so you can focus on growth.
Fran Yacovone
Business Performance Advisor 210-558-2507
Fran.Yacovone@insperity.com
Dayton Parker Business Performance Advisor 210-558-2517
Dayton.Parker@insperity.com www.insperity.com
“Insperity’s mission is to help businesses succeed so communities prosper”

TMA Insurance Trust
(HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England Director of Member Benefits 512-370-1746
Wendell.England@tmait.org 800-880-8181 www.tmait.org
“We offer BCMS members a free insurance portfolio review.”

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting and defending physicians.
Patty Spann Director of Sales and Business Development 512-425-5932
Patty-Spann@tmlt.org www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
Katy.Brooks@bosainsurance.com www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM
AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com

LASO Health Telemedicine and Rx App (HHH Silver Sponsor)
LASO Health is the industry’s only solution that makes healthcare services accessible, cost-transparent and convenient. Its mission is to reinvent “healthcare” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care.
LASO combines an intuitive, mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, onestop-shop, comprehensive health solution.
Ruby Garza, MBA 210-212-2622
RGarza@texaskidneycare.com www.lasohealth.com

Parvis Medical Suites
(HHHH 10K Platinum Sponsor)
Parvus Medical Suites offers a new way to start your own private clinical practice, either full-time or part-time, at a much lower cost than a traditional clinic. We take care of providing well-qualified employees, so that you can focus solely on delivering high-quality patient care. Our turn-key practice spaces in San Antonio and New Braunfels are available for short- and long-term lease options, and come complete with all amenities. Micropractice medicine is revolutionizing independent clinical care.
John Rodriguez, MD Chief Medical Officer
210-632-3411
DrJohn@parvussuites.com www.parvussuites.com
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol Field Sales Consultant 210-413-8079
Tom.Rosol@henryschein.com www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”

Equality Health (HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination, and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President 210-797-8412
HealthcareLeadersSA@gmail.com
Gary Meyn, LFACHE Vice President 210-912-0120
GMeyn@vestedbb.com https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber President 210-308-7907 (Direct)
KBarber@bdo.com
Valerie Rogler Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor) SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Jeannine Ruffner President info4@samgma.org www.samgma.org

Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP® QKA Senior Private Wealth Advisor 512-649-8113
Service@oakwellpwm.com www.oakwellpwm.com
“More Than Just Your Advisor, We’re Your Wealth Management Partner”

Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
Mike DeQuattro
Director of Operations - Texas & New Mexico 210-918-8737
Mike.DeQuattro@favoritestaffing.com “Favorite Healthcare Staffing offers preferred pricing for BCMS members.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout. Join us in transforming healthcare delivery, prioritizing your wellbeing and patient care.
Chris Stansbury SVP Growth 816-309-9991
CStansbury@eleosvhs.com www.eleosvhs.com


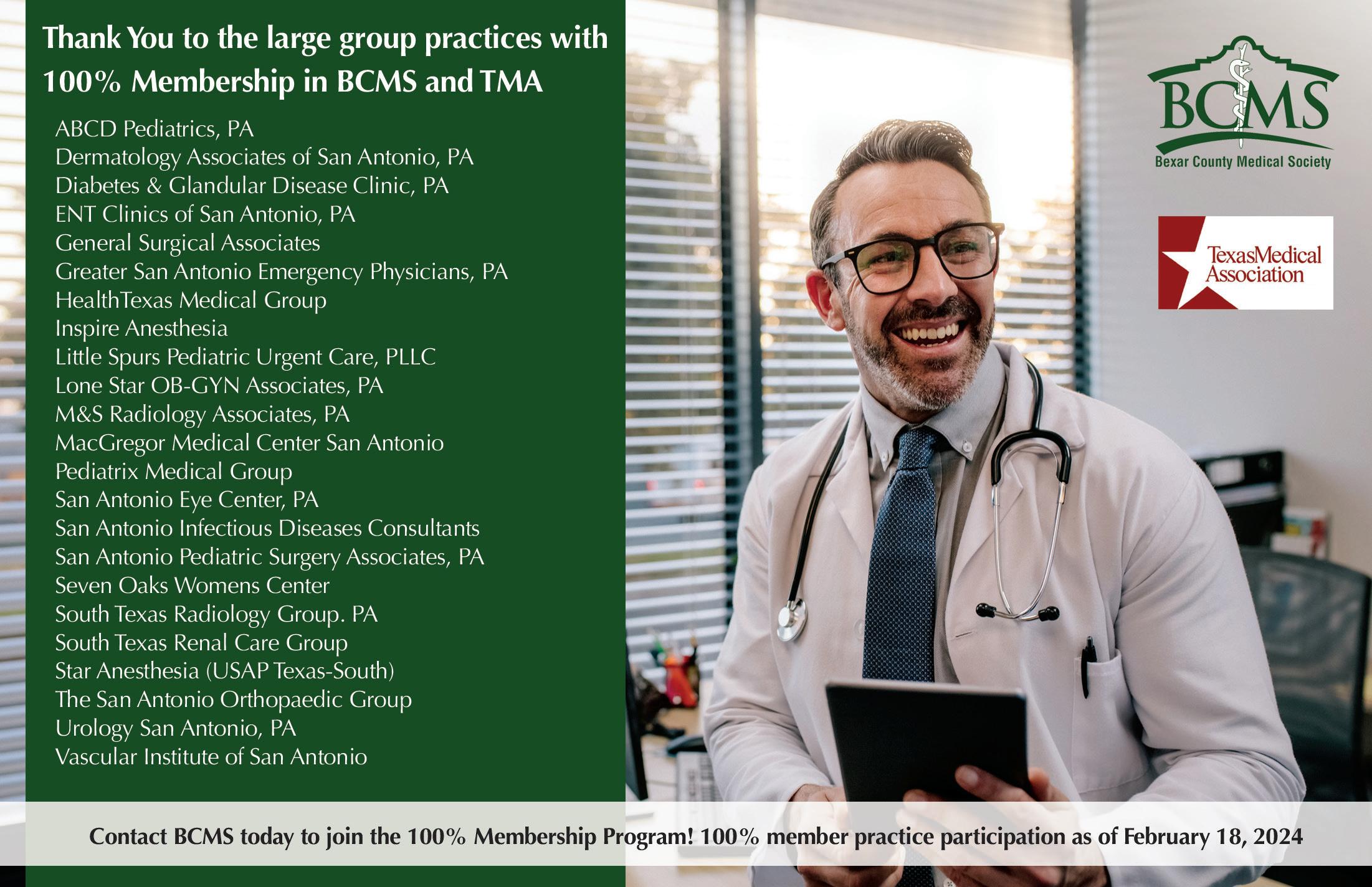
By Stephen Schutz, MD
In the post-World War II era, Americans thought cars were great. They improved every year, and by the time we hit the 1960s, we had it all: muscle cars — think Pontiac GTO, Hemi Cuda and Boss Mustang — luxury cars like the Buick Riviera, Chrysler Imperial and Cadillac Eldorado, and lots of other cars and trucks that we loved. People were happy.
Then around 1974, times changed (obviously, I don’t mean 1974 exactly. I mean the early ‘70s, but I think it’s useful to pick a specific year).
The influential 1962 Rachel Carson book, SilentSpring, and obvious pollution almost everywhere in the 1960s led to a push to decrease automobile exhaust emissions (remember the ubiquitous bumper sticker, “Give a hoot! Don’t pollute!”?)
In addition, the Vietnam War claimed the lives of 50,000 teenage and 20-something soldiers, and Americans became averse to more deaths among young people. Yet in the mid- to late-1960s, many youths were dying or being injured in powerful muscle cars, so a push for less powerful and safer cars developed.
Then, the 1974 OPEC oil embargo led to increasing gas prices, which in turn sparked a desire for more fuel-efficient cars.
All of that led to what I would call a decade of chaos: 1974 to 1984 is best described as America saying, in essence, “We don’t know what we want, but we know what we don’t want: cars that pollute, are unsafe and get lousy fuel economy.”
During that 10-year period of Americans deciding what they didn’t want, we saw the death of the muscle car, the decline of the large American luxury car, the rise of fuel-efficient imported cars like the Volkswa-


gen Rabbit and Honda Civic, and the introduction of lots of weird cars, like the AMC Pacer, Ford Pinto, Chevy Vega, Subaru Brat and the DeLorean.
Then right around 1984, fuel economy became less crucial thanks to increased availability of oil from non-OPEC sources, catalytic inverters and other advances had dramatically reduced tailpipe emissions, and anti-lock brakes and airbags had improved safety significantly.
Once we got all of that, U.S. car buyers finally figured out what we wanted: Japanese quality and German driving feel.
As a result, the 1980s saw the Mercedes E-class, S-class and SL, as well as BMWs like the 3-series and 5-series from that era basically sell out, and it was the same for the Honda Accord, Civic, Toyota Corolla and other Japanese models. The birth of Acura, Lexus and Infiniti in the late ‘80s and early ‘90s was the capstone of that movement.
The automotive era of “Japanese quality, German driving feel, and ever-improving fuel economy and emissions” extended from roughly 1984 to probably five or so years ago, which means we enjoyed around 40 years of being relatively happy with our cars, just like we were from the end of World War II until 1973.
Interestingly, during the period from 1984 to 2024, we experienced a second muscle car era, although this time it included Mercedes AMG models, BMW M-models and Audi RS-cars in addition to American classics like the Ford Mustang GT, Dodge Challenger Scat Pack and Chevrolet Camaro SS.

We also saw the rise of new market segments such as luxury SUVs, like the Cadillac Escalade, Mercedes GLS, Porsche Cayenne and others, which mirrored the popularity of American luxury sedans in the post-WW II period. And we also observed the rise of uber-luxury cars like Bentley, Rolls-Royce, Range Rover and Aston Martin. During this period, those brands all grew and set sales records.
Again, people, until maybe just a few years ago, were generally happy with their vehicles. However, as was the case in the years leading up to 1974, times have been changing.
For starters, we live increasingly virtual lives. Since the iPhone was introduced in 2007, and especially since the advent of social media, we have increased the time we spend with virtual friends as well as people that we don’t know but follow online. Think of your high school friends, for example. It used to be that we would write an occasional letter or phone call, but really, we would lose touch. Now we have regular contact with some of them, or at least we follow those friends on apps like Facebook, Instagram or TikTok.
Not only that, but we are now increasingly broadcasting our lives and thoughts as we consume more content produced by people we either know or want to know (or don’t know and don’t want to know). That desire to consume and produce more online content is an important reason why so many people are less interested in driving. They’d rather be on TikTok than behind the wheel.
There is also a general desire to put less CO2 into the air. The environmental movement is front and center now, just like it was in the 1970s, and people are increasingly uncomfortable with vehicles like the Ford F150, Mercedes GLS or Cadillac Escalade, which produce and emit lots of CO2.
There is a creeping weariness with the relentless reality of 40,000 or so Americans dying on our roadways every year. Despite herculean


efforts by automotive manufacturers, government regulators and worried parents, that figure remains stubbornly high year after year.
For all those reasons, I believe that the 2024 to 2034 era will be a period of chaos just like the years 1974 to 1984 were. Just like then, we don’t know what we want, but we know what we don’t want: vehicles that keep us away from our phones, emit CO2 and aren’t safe.
Going forward, I think that we’ll see the rise of cars and trucks that produce less CO2, as well as the rise of self-driving vehicles, which will allow us to spend more time either consuming or producing content on social media, and will be safer. I believe that performance internal combustion cars will die off completely — that’s already happening with the discontinuation of the Challenger, Camaro and some V8 German performance cars. Similarly, I think that large internal combustion luxury SUVs and personal use pickup trucks that emit copious CO2 will fade away over the next five to 10 years.
Amusingly, just like 1974 to 1984, we’ve already seen some weird vehicles. The weirdest, of course, is the Tesla Cybertruck, but the Cadillac Celestiq, Hummer pickup truck, Jaguar I-Pace (used by Waymo in their self-driving fleet, ironically), and others are also weird, and presumably more will be coming in the years ahead. I can’t wait.
So, I think that right now is a lot like 1974. We are not happy with our current automotive choices, we know what we don’t want but not really what we want, and we’re seeing some weird vehicles for sale. Where will the automotive world be in 10 years? Who knows, but wherever that is, I think it’ll be a helluva decade.

Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.


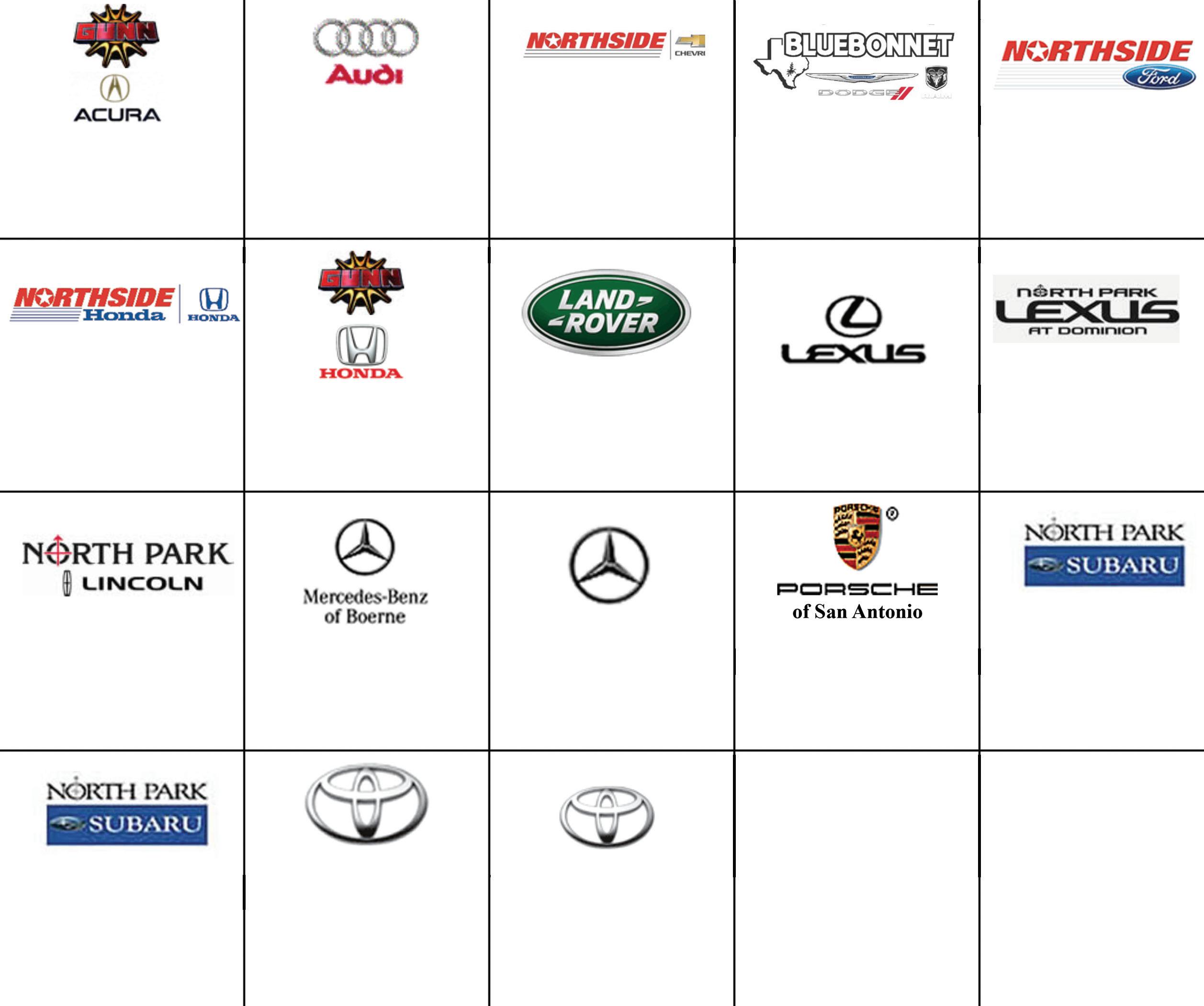
11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Northside Honda
9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Kahlig Auto Group
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson
877-356-0476
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Chris Martinez 210-366-9600
Auto Group
Bluebonnet Chrysler
Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000