Health Literacy













Saxet Boerne,
78006 PUBLISHER Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com ADVERTISING
Sandy Weatherford sandy@travelingblender.com
ANTONIO: Gerry Lair gerrylair@yahoo.com
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE:
Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2024 SmithPrint, Inc. PRINTED IN THE USA

Ezequiel “Zeke” Silva, III, MD, President
Lyssa Ochoa, MD, Vice President
John Shepherd, MD, President-elect
Jennifer R. Rushton, MD, Treasurer
Lubna Naeem, MD, Secretary
John Joseph Nava, MD, Immediate Past President
Woodson “Scott” Jones, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Ana Rodriguez, MD, Member
Raul Santoscoy, DO, Member
Lauren Tarbox, MD, Member
Nancy Vacca, MD, Member
Col. Elisa D. O’Hern, MD, MC, FS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School
Representative
Cynthia Cantu, DO, Medical School Representative
Lori Kels, MD, Medical School Representative
Ronald Rodriguez, MD, Medical School Representative
Victoria Kohler-Webb, BCMS Alliance Representative
Carolina Arias, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
Melody Newsom, CEO/Executive Director
Yvonne Nino, Controller
Al Ortiz, Chief Information Officer
Brissa Vela, Chief Membership and Development Officer
Phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
Monica Jacqueline Salas, MD, Co-chair
Jennifer C. Seger, MD, Co-chair
Lokesh Bathla, MD, Member
Elizabeth Clanton, MD, Member
Erika Gabriela Gonzalez-Reyes, MD, Member
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. K. Jyothula, MD, Member
Kristy Yvonne Kosub, MD, Member
Jaime Pankowsky, MD, Member
George-Thomas Martin Pugh, MD, Member
Rajam S. Ramamurthy, MD, Member
Adam V. Ratner, MD, Member
John Joseph Seidenfeld, MD, Member
Boulos Toursarkissian, MD, Member
Francis Vu Tran, MD, Member
Faraz Yousefian, DO, Member
Louis Doucette, Consultant
Brissa Vela, Consultant
Gabriella Bradberry, Staff Liaison
Trisha Doucette, Editor
Deepthi S. Akella, Student
Moses Alfaro, Student
Victoria Ayodele, Student
Tue Felix Nguyen, Student
Andrew Ta, Student
Alixandria Fiore Pfeiffer, DO, Resident
Elizabeth Allen, Volunteer
Adelita G. Cantu, PhD, Volunteer
Rita Espinoza, DrPH, Volunteer
Natalie Reyna Nyren, PA-C, Volunteer
David Schulz, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer

By Ezequiel "Zeke" Silva III, President, Bexar County Medical Society (BCMS)
Key Point:
The Bexar County Medical Society (BCMS) has a longstanding commitment to healthcare along the Texas-Mexico border.
What This Means:
BCMS collaborates with physicians and medical students from San Antonio to the border, primarily through the Texas Medical Association (TMA) Border Health Caucus. In August, our leadership joined the TMA Border Health Caucus in Laredo, Texas to discuss the mutual challenges and prospects at the border.
Zoom Out:
Established in 1853 as the Western Texas Medical Association, BCMS has deep roots in border health. Initially, our physicians served at the United States Frontier — effectively, the border. This early engagement has fostered a culture deeply committed to supporting both physicians and patients in border areas.
Highlights from the Border Health Conference:
• Senator Judith Zaffirini was honored with the Border Health Caucus’ Champion of Medicine Award.
• U.S. Congressman Henry Cuellar discussed his achievements and future goals for border improvements.
• Keynote speaker Alexander Eastman, MD, the Chief Medical Officer of the Department of Homeland Security, elucidated the U.S. Customs and Border Protection’s medical screening processes designed to aid those in need.
The Key Issues:
Several challenges and opportunities at the border stand out, including:
• Migrant Health.
• Supporting physicians, medical students and institutions along the border.
• Advocating for substantial state and federal support for border areas, including necessary legislative and fiscal measures.
As a constituent county medical society of the TMA, BCMS adheres to policies set by the TMA House of Delegates. Notably:
• 260.005: Community and Migrant Health Centers: TMA reaffirms the importance of funding for comprehensive primary care, access and public health partnership through community and migrant health center programs.

• 260.128: Educating Physicians on the Rights of Immigrant Patients: TMA promotes policies that protect the rights of immigrants seeking medical care and opposes any that would limit healthcare access for immigrants and their dependents, such as collecting patient immigration status information.
TMA and BCMS have a rich history of supporting physicians and their patients on the border. Our network is pivotal, particularly in small, independent practices, notably in primary care where the need is significant. We also back educational institutions along the border like UT-Health Rio Grande Valley School of Medicine in Brownsville, Texas Tech El Paso Foster School of Medicine, and residency programs in Laredo.
San Antonio’s connection to the border extends beyond shared history to include practical realities. Interstate Highway 35, linking Laredo to San Antonio, stands as one of the busiest trucking and commercial routes in the U.S. This dynamic is accompanied by frequent movement between the border and San Antonio for many physicians and patients.
At the heart of our border efforts is the protection of the physician-patient relationship, which hinges on physicians having the resources to deliver high-quality care and maintaining the trust and confidence of our patients.
Ezequiel “Zeke” Silva III, MD, is the 2024 President of the Bexar County Medical Society. Dr. Silva is a radiologist with the South Texas Radiology Group, Adjunct Professor of Radiology at the UT Health, Long School of Medicine, and Vice-Chief of Staff at Methodist Hospital Texsan. He is Chair of the TMA Council on Legislation and is a TMA Delegate to the AMA. He serves on the AMA Council on Medical Service, and chairs the AMA RVS Update Committee (RUC).

By Cheryl Pierce-Szender
2024 marks the 107th year of BCMSA as well as their scholarship fund! This spring, the BCMSA Scholarship Committee, led by Mrs. Cheryl Pierce-Szender, immediate Past President, and eight other distinguished Past Presidents and board members, convened to award scholarships to deserving Medical and Allied Health Professions students that reside in Bexar County. Students from the UT Health Long School of Medicine, the University of Texas Health Science Center San Antonio, the University of the Incarnate Word Osteopathic School of Medicine and St. Mary’s University were recommended by their professors and advisors to apply. Upon review and vetting by the board, we are proud to award scholarships to the following outstanding students:
• Neriah Sosa, a student at UIW-SOM - Hispanic Medical Student Scholarship
• Laureen Raelly Muze, a student at UT-Long SOM - Medical Student Scholarship
• Amber Lewand, a student at UT-Occupational Therapy School - Rebecca Christopherson Memorial Scholarship
• Izabele Reyes, a student at UIW School of Rehabilitation Sciences - Sandra Vela Memorial Scholarship
• Kathya Almanza, a student at St. Mary’s University - Allied Health Professions Scholarship
Congratulations to all of our 2024 BCMSA Scholarship Recipients! BCMSA will be recognizing them at their annual fall luncheon on October 23rd to celebrate. If you would like to attend this event and learn more about BCMSA and their latest community project combating Period Poverty, you are more than welcome to attend. Please RSVP to bcmsalliance@bcms-alliance.org.
Pierce-Szender is the 2023 BCMSA Past President.







For information on the Bexar County Medical Society Alliance, scan the code.


By Michael Arambula, MD, PharmD
When I interviewed for a fellowship position in Forensic Psychiatry at The University of Rochester Medical Center many years ago, I walked the halls of the Department to familiarize myself with where my appointments were the following day. Along the way, I passed by the memorial office of George Engel, an Internist and Psychiatrist who was the author of the Biopsychosocial Model, and postulated that health and illness were due to the interplay of biological, psychological and social factors. Since, there has been a plethora of models involving health and illness, and how physicians and healthcare systems can promote a lifestyle of improved health and disease management for our patients. I am sure that everyone has heard of Health Literacy, but from the small sampling of professionals that I asked for their feedback (re: what it meant) in preparation for this brief article, there were an array of descriptions surrounding this common theme of education. Indeed, a recent publication found over 250 different definitions of Health Literacy in academic literature. Just to let you know, I will not be adding another one to the list of definitions. Generally speaking, I learned that Health Literacy involves patients being able to obtain, process and apply information about their health to their lives, while we as physicians roll up our sleeves and find creative ways to connect with our patients about the promotion of their health, which includes management of their disease. Just to make things a bit more challenging, let me throw in that each of our patients step into the exam room with their unique psychosocial history. I believe this is where the science of medicine takes a backseat to the art of medicine. Everyone is different, and learning about their stories they bring with them to the medical encounter can be very rewarding and shoo away the lurking shadows of burnout. Indeed, making personal connections with our patients fosters Health Literacy.
Owing to my psychiatric training, I will even throw in that those positive moments of interpersonal connections will foster the formation of transitional objects, which will facilitate our patient’s motivation to process and apply the medical information we share with them in the clinical setting. For most of my non-psychiatric medical colleagues, Donald Winnicott introduced the term “transitional object” to describe an object, like a blanket or soft toy, which a child substitutes for the mother-child attachment, to provide a sense of security and comfort when she is away. I am, of course, using this term loosely when speaking about physician-patient encounters, but then again, the psychiatric literature has also shown that treatment non-compliance is more likely to occur when patients have an ambivalent/negative interaction with their physician, and treatment recommendations are conceptualized as an extension or transitional object representation of the ambivalent physician-patient encounter. Of course, this makes sense. Would you be more likely to stick to your exercise program if you have
a positive interpersonal interaction/experience with your trainer or a negative interpersonal interaction/experience?
These kinds of individualized dynamic interpersonal experiences (factors) are hard to measure in a scientific study. No wonder there is so much variance in the Health Literacy literature. At the same time, these dynamic interactions create wide avenues for us to explore ways to connect with our patients in a meaningful way, as we lay the groundwork for them to learn more about health and disease management in such a way that when they leave our office, they will carry that positive clinical experience to their home, and be more motivated to understand, use and apply the transitional object, i.e., our treatment recommendations, to their lives. I know that was a bit shrinky, so common sensically speaking, here are some basic tenets that I find useful in my efforts in Health Literacy:
1. Look at your patient. Simply said, eye contact can open almost any door.
2. Listen to your patient. Remember that old adage, when in doubt ask your patient? Take it from me, a psychiatrist, listening is the most important variable in communication, and that includes non-verbal behavior as well.
3. Break up your diagnosis and treatment recommendations with patients into small chapters and ask for their feedback and questions about your chapter discussions. Remember that repetition fosters learning.
4. Admit what you/the literature doesn’t know; look up drug interactions just to be sure. Doing so humanizes us.
5. Share reliable ways that your patients can have ongoing contact with you prn any concerns that emerge about their health; remember that transitional objects create comfort and security.
References:
1. Urstad et al, Definitions and measurement of health literacy in health and medicine research: a systemic review. BMJ Open.2022; 12.
2. Liu et al, What is the meaning of health Literacy? A systemic review and qualitative synthesis, Family Medicine and Community Health, 2020; 8.

Michael Arambula, MD, PharmD, a San Antonio native, is a General and Forensic Psychiatrist, and past President of the Texas Medical Board and Texas Society of Psychiatric Physicians. Dr. Arambula is a member of the Bexar County Medical Society.


By Monica Salas, MD
Imagine your home’s electrical system with faulty wiring. At first, the issues might be minor — flickering lights or occasional short circuits. However, if left unchecked, these seemingly small problems can escalate into a devastating house fire, endangering your home and everyone in it. Not unlike the firefighter who extinguishes the flames of a burning home that caught fire due to faulty electrical wiring, many patients receive treatment for medical conditions once symptoms become severe, which can lead to more complex and costly treatments. Unfortunately, in today’s fast-paced world, healthcare is typically a reactive rather than a proactive experience.
As a Family Doctor in a Direct Primary Care (DPC) model, one of my key roles is to educate and help change this mindset by encouraging proactive health management. A prime example of this approach is in the realm of pre-diabetes — a condition that, when addressed early, can significantly alter a patient's health trajectory and empower them to take control of their well-being. This condition is a warning sign that lifestyle changes are necessary to prevent the progression to type 2 diabetes. It affects millions of people worldwide, yet many are unaware they have it until more severe symptoms arise. As a primary care physician, my goal is to identify individuals at risk before the condition progresses and to provide them with the tools and knowledge they need to make impactful changes. In other words, help them address the flickering lights before the house goes down in flames.
The foundation of proactive healthcare is early detection. For pre-diabetes, this means regular screening, particularly for those with risk factors such as obesity, insulin resistance, a sedentary lifestyle or a family history of diabetes. By incorporating routine blood tests and evaluating risk factors, we can identify pre-diabetes early. This approach allows us to intervene before the condition becomes more serious, thereby reducing the risk of complications such as heart disease, stroke and kidney damage.
Once pre-diabetes is detected, education is crucial. Many patients are unaware of what pre-diabetes means or the steps they can take to prevent its progression. As a Family Doctor, I strive to demystify the condition by explaining the connection between blood sugar levels, lifestyle choices and long-term health. Empowering patients with knowledge about how healthy nutrition, regular physical activity, restful and adequate sleep, and stress and weight management affect their blood sugar levels helps them feel more in control of their health. For instance, discussing the role of whole foods and processed versus unprocessed carbohydrates in blood sugar management, explaining how physical activity improves insulin sensitivity, and outlining the benefits of maintaining a healthy weight can make a significant difference. This educational approach helps patients understand that their actions have a direct impact on their own health outcomes.
Empowerment also comes from setting and achieving realistic health goals. When working with pre-diabetic patients, I emphasize the importance of setting small, manageable goals that build upon each
other over time, rather than overwhelming them with broad lifestyle changes all at once. For example, starting with a goal of incorporating 10 minutes of moderate exercise into their daily routine can be more manageable than an immediate overhaul of their entire lifestyle.
Furthermore, I encourage patients to track their progress (to a reasonable degree) and celebrate their successes, no matter how small. This positive reinforcement can boost their motivation and commitment to their health journey. Regular follow-up appointments provide an opportunity to reassess goals, address challenges, and adjust plans as needed, fostering a sense of partnership in the patient-doctor relationship.
In the digital age, technology can be a powerful ally in proactive healthcare. Tools such as mobile apps for tracking nutrition, exercise and sleep, online educational resources and telemedicine consultations can enhance patient engagement and provide continuous support. For patients with pre-diabetes, these technologies can offer real-time feedback and personalized recommendations, making it easier to stay on track with their health goals.
Lastly, creating a supportive environment both in the clinic and at home is essential for empowering patients and helping them to be informed healthcare consumers. In the clinical setting, this means providing a non-judgmental space where patients feel comfortable discussing their health challenges and triumphs. At home, patients benefit from having a support network that includes family and friends who encourage and participate in healthy lifestyle changes. Involving family members in dietary changes or exercise routines can create a shared sense of commitment and accountability, making it easier for patients to adhere to their health plans.
Being proactive in healthcare, particularly with conditions like pre-diabetes, involves more than just treating symptoms as they arise. It requires early detection, patient education, realistic goal-setting, leveraging technology, and creating a supportive environment. By embracing these proactive strategies, we can increase health literacy and thereby empower patients to take charge of their health, prevent the progression of conditions like pre-diabetes, and improve their overall quality of life. In this world, I work hand in hand with my patients as an electrician, and not solely a firefighter.

Monica Salas, MD, is a board-certified Family Medicine and Lifestyle Medicine physician with over a decade of experience. She is co-owner and COO of Salveo Direct Care, a Direct Primary Care and Lifestyle Medicine practice in San Antonio. She enjoys working with her patients on their wellness journey to achieve their optimal health through prescribing therapeutic lifestyle change strategies. Dr. Salas is a member of the Bexar County Medical Society and co-chair of the BCMS Publications Committee.

By Claudia Aguero, MD
This past spring, I had the opportunity to attend the American College of Lifestyle Medicine conference. It was unlike any other conference I had been to before. The quote that comes to mind is, “Physician, heal thyself.” It is easy to give people advice regarding their healthcare; however, it is another thing to live that out. It is important to practice what we preach. In today’s fast-paced world, the decisions we make every day — often unconsciously — can significantly impact our mental and physical health. As healthcare providers, it’s crucial to empower our patients with the knowledge and tools they need to make informed choices that promote long-term well-being. This is where lifestyle medicine comes into play. By focusing on six key areas — healthful eating, physical activity, stress management, maintaining relationships, improving sleep, and avoiding risky substances — we can guide our patients toward healthier, more fulfilling lives.
The foundation of good health starts with what we eat. A balanced diet rich in fruits, vegetables, whole grains and lean and plant-based proteins provides the necessary nutrients our bodies need to function
optimally. There is extensive scientific evidence to support the use of whole-food, plant-strong diets as a treatment for diet-related chronic diseases. Educating patients about the benefits of healthful eating, such as maintaining a healthy weight, reducing the risk of chronic diseases, and improving mental health, is essential. Simple, practical advice — like reading food labels, planning meals, and understanding portion sizes — can empower patients to make better dietary choices daily. We, as physicians, need to be mindful of what foods are available to our patients. Some patients are located in food deserts and may find it more difficult to choose the best nutrition.
Regular physical activity is a cornerstone of a healthy lifestyle. It’s not just about preventing weight gain; it also helps in managing chronic conditions like diabetes, hypertension and depression. Encouraging patients to incorporate at least 150 to 300 minutes of moderate-intensity activity or 75 to 150 minutes of vigorous activity each week, along with two or more days of weekly strength training, can have profound effects on their overall health. Physical activity can also improve
patients’ balance and decrease the risk of future falls. Whether it’s walking, cycling, swimming or engaging in strength training, the key is to find an activity they enjoy and can stick to.
Chronic stress is a silent killer, contributing to a host of health problems, including heart disease, anxiety and digestive issues. Chronic stress can lead to impaired health and productivity as well as to chronic illnesses such as anxiety, cardiovascular disease, irritable bowel syndrome, immune dysfunction and associated poor health outcomes. Teaching patients about stress management techniques, such as mindfulness, meditation, deep breathing exercises and time management, can significantly reduce their stress levels. It’s important to help patients recognize the sources of their stress and develop personalized strategies to manage it effectively.
Human beings are inherently social creatures, and strong relationships are vital to our mental and emotional well-being. Positive relationships with family, friends and colleagues can provide support during tough times and enhance our sense of belonging. Encouraging patients to nurture these relationships, engage in community activities, and seek out social support can improve their mental health and overall quality of life.
Quality sleep is often underestimated in its importance to health. Poor sleep can lead to a variety of health issues, including obesity, diabetes, cardiovascular disease and cognitive decline. Sleeping less than six to eight hours a night increases the risk of early death by approximately 12 percent. Sleep apnea and other sleep disorders are associated with increased cardiovascular, cardiometabolic and neuropsychiatric risks. Educating patients on the importance of establishing a regular sleep schedule, creating a restful sleep environment, and avoiding stimulants like caffeine before bed can greatly enhance their sleep quality. Good sleep hygiene is a critical component of a healthy lifestyle.
Substance abuse, including smoking, excessive alcohol consumption and drug use, poses significant health risks. More than 40 million Americans meet the clinical criteria for addiction to nicotine, alcohol and other drugs. Addiction or misuse doubles the risk of chronic conditions such as chronic pain, hypertension, heart disease, stroke, diabetes and asthma. Educating patients about the dangers of these behaviors and providing support for those struggling with addiction is crucial. Encouraging patients to avoid risky substances and promoting healthier alternatives, such as physical activity or engaging in hobbies, can help them lead healthier lives.
Incorporating lifestyle medicine into patient education is not just about treating illness; it’s about preventing it. By empowering patients to make better everyday decisions in the areas of diet, exercise, stress management, relationships, sleep and substance use, we can help them achieve a higher quality of life and reduce their risk of chronic diseases.
Physicians would benefit greatly from taking better care of themselves, as lifestyle choices play a significant role in the physician’s well-being. As healthcare providers, our goal is to guide patients on this journey as we too take appropriate steps to improve our quality of life and decrease our risks for chronic future diseases.
References:
• 2018 Physical Activity Guidelines Advisory Committee. (2018). 2018 Physical Activity Guidelines Advisory Committee scientific report. U.S. Department of Health and Human Services.
• American Diabetes Association. (2019). Standards of medical care in diabetes—2019. Diabetes Care, 42(Supplement 1), S46–S60. https://doi.org/10.2337/dc19-S004
• Brummett, B. H., Barefoot, J. C., Siegler, I. C., et al. (2001). Characteristics of socially isolated patients with coronary artery disease who are at elevated risk for mortality. Psychosomatic Medicine, 63(2), 267–272. https://doi.org/10.1097/00006842200103000-00010
• Cappuccio, F.P., D’Elia, L., Strazzullo, P., & Miller, M. A. (2010). Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep, 33(5), 585–592. https://doi.org/10.1093/sleep/33.5.585
• The CASA Columbia National Advisory Committee on Addiction Treatment. (2012). Addiction medicine: Closing the gap between science and practice. CASA Columbia.
• Lambert, G., Schlaich, M., Lambert, E., Dawood, T., & Esler, M. (2010). Stress reactivity and its association with increased cardiovascular risk: A role for the sympathetic nervous system? Hypertension, 55(6), e20–e21. https://doi.org/10.1161/ HYPERTENSIONAHA.109.144050
• National Sleep Foundation. (2021, March 10). How much sleep do adults need? National Sleep Foundation. Accessed October 22, 2021, from https://www.sleepfoundation.org/how-sleepworks/how-much-sleep-do-we-really-need
• Reddy, O. C., & Van der Werf, Y. D. (2020). The sleeping brain: Harnessing the power of the glymphatic system through lifestyle choices. Brain Sciences, 10(11), 868. https://doi.org/10.3390/ brainsci10110868
• U.S. Department of Health and Human Services Office of the Surgeon General. (2016). Facing addiction in America: The Surgeon General’s report on alcohol, drugs, and health. HHS.
• Wright, N., Wilson, L., Smith, M., Duncan, B., & McHugh, P. (2017). The BROAD study: A randomized controlled trial using a whole food plant-based diet and community support for obesity, ischemic heart disease, or diabetes. Nutrition & Diabetes. https://doi.org/10.1038/nutd.2017.3

Claudia Aguero, MD, is board certified in Family Medicine and practices at HealthTexas Medical Group, Val Verde Clinic. Dr. Aguero is a member of the Bexar County Medical Society. HealthTexas Medical Group has 100% membership in BCMS and TMA.
By Amy Cobb, MD, BSPH, BA, FAAP, FACP

When an adult teaches a child to ride a bicycle, most people follow a similar series of steps that help the child achieve mastery and independence. My husband and I started our children on a balance bike to teach equilibrium, advanced to a stationary bike to teach pedal stroke, then they rode a standard bike on the sidewalk while we ran alongside. Even after they were confident riders, we still coached them on street safety before they were allowed to ride around the neighborhood independently. Unfortunately, when it comes to helping our teens make the transition to the adult model of care at age 18, they rarely have been coached on the skills and rules of the road they will need to successfully navigate the healthcare system. As a med/peds physician, I have witnessed many youth struggle to find healthcare funding in early adulthood, to provide their own medical history, and to keep up with health-related to-dos, like scheduling appointments and refilling medications.
Data from the 2020 National Survey of Children’s Health suggested that 81 percent of adolescents do not receive adequate preparation for transition to adult care. The composite measure of transition readiness looked at whether the following four statements were true:
1. The healthcare provider talked to the caregiver about having the adolescent transition to a provider who treats adults.
2. The provider actively worked with the adolescent to help them gain skills to manage their own healthcare.
3. The provider coached the adolescent on the changes that happen in healthcare at age 18.
4. The provider spoke to the adolescent alone during their last preventive checkup.
The American Academy of Pediatrics (AAP), American Academy of Family Physicians (AAFP) and American College of Physicians (ACP) recommend transition planning in early adolescence and continuing into young adulthood for all youth, regardless of whether they have special healthcare needs. I want to emphasize that transition is much more than simply transferring care between providers. In fact, transition is necessary even if the healthcare provider can see the patient into adulthood. Transition is the process of building self-management skills, teaching health literacy and preparing youth to go from a child/family-focused model of care to a patient/adult-focused model of care.
A multidisciplinary clinical work group at University Health has developed a structured process that will be used to support both adolescents and caregivers, and that is aligned with the recommendations of the AAP, AAFP and the ACP. The process will include the following steps from the Got Transition program by The National Alliance to Advance Adolescent Health:
• At 12 years old, we will conduct the SSHADESS screening questions, typically with the guardian in the room, to prepare both the pre-teen and their guardian for the transition to more child-directed questions and coaching. We will also introduce the concept that we may treat items discussed in the SSHADESS interview confidentially starting at age 13.
• At 13 years old, we will encourage teens to sign up for their own unique access to our electronic patient portal, MyChart, with
parental consent. This allows them to start learning about their health information, as well as to send secure messages to their healthcare team. We will privately conduct one-on-one interviews during the annual preventative health visit and more often, if indicated.
• At 16 years old, we will perform a teen transition readiness evaluation and document the result in our electronic health record. We will provide coaching and resources related to areas where the adolescent or the family require additional support.
• At 17 years old, we will send a letter to the guardian and teen about the need to select a new healthcare provider by the 18th birthday. We will also provide education on considerations for health insurance after age 18 and how to change their primary care doctor with their insurance carrier.
• At 18 years old, the goal is for the youth to establish care with their adult care provider, unless they have a condition that may be better served by extended time within the pediatric-model of care. The established provider assists in scheduling the first visit with the adult provider and will provide a warm handoff whenever possible.
Just as with teaching a child to ride a bike, implementing a transition plan for adolescents and young adults can be a rewarding experience that combines highs and lows, but culminates in a youth who is confident and prepared to navigate the road ahead.
References:
1. Mulkey M, Baggett AB, Tumin D. Readiness for transition to adult health care among US adolescents, 2016-2020. Child Care Health Dev. 2023 Mar;49(2):321-331. doi: 10.1111/ cch.13047. Epub 2022 Aug 26. PMID: 35993998; PMCID: PMC10087515.
2. Patience H. White, W. Carl Cooley, TRANSITIONS CLINICAL REPORT AUTHORING GROUP, AMERICAN ACADEMY OF PEDIATRICS, AMERICAN ACADEMY OF FAMILY PHYSICIANS, AMERICAN COLLEGE OF PHYSICIANS; Supporting the Health Care Transition From Adolescence to Adulthood in the Medical Home. Pediatrics November 2018; 142 (5): e20182587. 10.1542/peds.2018-2587. March 9, 2018
3. White P, Schmidt A, Ilango S, Shorr J, Beck D, McManus M. How to Implement the Six Core Elements of Health Care Transition™ 3.0. Washington, DC: Got Transition, The National Alliance to Advance Adolescent Health, July 2020.

Amy Cobb, MD, BSPH, BA, FAAP, FACP, is a board-certified internist and pediatrician. She is a National Health Service Corps Scholar and has worked at University Health since 2017. She is an Adjunct Assistant Professor with the Long School of Medicine at UT Health San Antonio and Texas A&M University School of Medicine. Dr. Cobb has served as Pediatric Service Line Medical Director within Ambulatory Services at University Health since 2022. Dr. Cobb is a member of the Bexar County Medical Society.

By Arianne Felicitas, DO
Istepped outside my host family’s house and looked to my right. Unfortunately, it was yet another overcast day that blocked my view of the Chimborazo mountain that would otherwise tower in the sky. In May, I sought to improve my medical Spanish by spending one month in Riobamba, Ecuador as part of the Cacha Medical Spanish Institute

(Cachamsi) program, a nonprofit organization that offers medical Spanish lessons, international clinical rotations and volunteer opportunities among a unique indigenous population. In the mornings, I went to my clinical assignment at a rural primary care clinic or the local teaching hospital. I spent my afternoons in tailored medical Spanish classes.
Cacha is a rural town adjacent to Riobamba, and its population is composed primarily of indigenous citizens. I spent my first week at its primary care clinics. The scene was idyllic, and we often traversed along the hills, listening to the sound of sheep and cattle as we made house calls. The team at the clinic sites in Cacha included recent medical graduates completing their year of public health service, nurses, technicians and a dentist. While Quechua is the first language of many patients, visits were conducted in Spanish. Medical staff were often familiar with basic Quechua phrases, however. One family expressed their gratitude not only with words but also by sharing boiled eggs from their chickens.
Public health campaigns were an integral part of the job. One morning, we walked uphill to administer vaccinations to students in the local school. I spent the second week of my rotation in Calpi, another rural community adjacent to Riobamba. On Tuesdays and Thursdays, the family physician hosted bailoterapia (dance therapy) with older patients. These sessions allowed us to promote healthy lifestyles by physically engaging in a fun activity with patients.
Like in the United States, cost was a significant barrier to providing patients with more treatment options. During my time at the Riobamba teaching hospital, sertraline was the only SSRI on the formulary by the end of the month since the fluoxetine supply was depleted. Patients who had been stabilized on fluoxetine needed to be transitioned to sertraline, unless they had sufficient funds to purchase their own supply as opposed to using the hospital formulary. We needed to counsel patients on how to safely cross-taper to sertraline with clear and straightforward instructions.
It was humbling having to rely on my intermediate-level Spanish skills to navigate the country for the month. Under the supervision of the attending physician, I conducted a new psychiatric evaluation in Spanish. I sometimes asked the patient to reword their responses when I could not understand what they initially said. I thought about how difficult it can be to navigate our American healthcare system and how the challenge is compounded for individuals who do not speak English. Fortunately, translation services through iPads or our phones can bridge the gap in translation. Yet, it is worth the extra effort of learning phrases in our patients’ language to establish some rapport at the start.
Spending a month in Ecuador allowed me to embrace its beauty, from the green pastures in Cacha to the occasional clear skies showcasing the peak of Chimborazo, while furthering my medical Spanish skills. Although parts of my Ecuador experience were unique (for example, leading patients through dance therapy), I also noticed parallels to medicine in the United States. For instance, I saw several cases of schizophrenia, depression and borderline personality disorder during the psychiatry portion of the rotation. The limitations of the hospital formulary reiterated the importance of balancing evidence-based treatment with what is most accessible for our patients. Lastly, despite the inability to directly control which resources or lack thereof were available, medical staff sought to provide the best care possible for patients.

Arianne Felicitas, DO, is a second-year psychiatry resident at The Texas Institute for Graduate Medical Education and Research. Her interests include child psychiatry, asylum medicine, and taking care of Rudy, her chihuahua mix.



By Cleo Garcia, City of San Antonio Metropolitan Health District
During the 2024 annual National Association of County and City Health Officials (NACCHO) 360 Conference, the City of San Antonio Metro Health and UT Health San Antonio’s Health Confianza were honored with the Promising Practice Award for their work to improve health literacy in underserved areas in San Antonio.
Health Confianza began as a partnership between the University of Texas Health Science Center at San Antonio (UT Health San Antonio), Metro Health and the University of Texas at San Antonio in 2020 as a direct response to the Covid-19 pandemic. Health Confianza has set out to address the health disparities experienced by our mostly Hispanic and Black neighbors living in 22 zip codes in San Antonio (Westside, Southside and Eastside neighborhoods). In 2024, Health Confianza transitioned to UT Health San Antonio.
Health Confianza — Spanish for Trust or Confidence — is a county-wide health literacy non-profit that provides education, workforce training, health information and resources to the greater San Antonio area. It is rooted in the belief that health literacy, which is the ability to find, understand and use health information so that you and your family can be as healthy as possible, is a valuable tool in transforming health and achieving health equity for all.
About 90 percent of Americans struggle with health literacy challenges, resulting in worse health outcomes, less use of preventive health services, more emergency room visits, fewer cancer screenings and fewer immunizations, and leading to billions of dollars in avoidable healthcare expenses.
“People with low health literacy may not be able to follow instructions on a prescription label, navigate the jargon on health insurance paperwork or know how to make diet changes to prevent diabetes — one of our community’s biggest health challenges,” said Melanie Stone, DrPH, MEd, Assistant Professor of Family and Community Medicine at UT Health San Antonio and Co-Director of Health Confianza. “We know health literacy can improve people’s confidence in their ability to make good health decisions for themselves and their families. We hope this award raises awareness of the importance of health literacy and encourages greater community involvement in our efforts.”
“This U.S. Department of Health and Human Services’ Office of Minority Health grant allowed Metro Health, UT Health San Antonio and partners to launch a health literacy initiative in our community’s under-resourced neighborhoods,” said Claude A. Jacob, DrPH, MPH, Metro Health Director and Past President of NACCHO.
“These milestones showcase the new ways Metro Health and overall partners have grown and positioned themselves to impact our community’s well-being. I would like to congratulate Drs. Jason Rosenfeld and Melanie Stone (of Health Confianza) for the collaboration, and I am very proud of this national recognition.”
“We are honored to be recognized for Health Confianza’s innovative approaches to public health and health equity,” said Jason Rosenfeld, DrPH, MPH, Associate Professor at UT Health San Antonio and Co-Director of Health Confianza. “To sustainably address health inequities, we must address health literacy at the community, workforce and organizational levels — it shouldn’t be the sole responsibility of already marginalized communities to change. It’s incumbent upon all of us to design more responsive systems to deliver culturally and linguistically appropriate services and information.”
Health Confianza provides in-person and webinar training to educate professionals and organizations on health literacy strategies, enabling them to better serve their patients and clients. Additionally, workshops can be tailored to the needs of small business owners, high school/college student leaders, faith leaders, neighborhood associations, small media outlets and others so that local leaders can navigate and understand health information in order to engage in meaningful discussions and problem solve with community members. Through this education, Health Confianza empowers our community to advocate for their health.


By Rishi Goswamy, Hunter Buescher, Garret Williford and Ramaswamy Sharma, MS, PhD
The national inflation rate, which measures the rate of increase in price for products or services, spiked to 7 percent in 2021 from 1.4 percent in 2020. It remained at 6.5 percent in 2022 but has slowly declined to 2.5 percent as of August 2024. A high inflation rate reduces purchasing power, which invariably makes food and medicine expensive, leading to the exacerbation of a myriad of healthcare-related issues. Unabated inflation also affects the viability of physician practices in the context of Centers for Medicare and Medicaid Services (CMS)-related payment models. Policies to reduce inflation rates, however, can lead to economic recession and unemployment, which will also negatively affect health outcomes. Understanding the broad impact of inflation on healthcare is, therefore, critical, as it affects both patients and physicians.
From a patient perspective, research shows that inflation negatively affects wellbeing and can lead to increased suicidal behavior, especially in males who are unemployed and are older than 40 years of age. In females, inflation appears to positively correlate with postpartum depression and negatively correlate with fertility. The American Psychiatric Association Healthy Minds Poll estimated that 90 percent of Americans felt anxious about inflation in 2022. In conjunction with rising healthcare costs due to inflationary pressures, premiums associated with health insurance also ascended at an alarming rate. At the height of inflation in 2022, health insurance prices rose by 28 percent as compared to 2021, resulting in higher premiums, deductibles and out-of-pocket expenses. A survey showed that 72 million adults in the United States in 2022 were less prepared for unexpected medical costs that may have come their way, as compared to their preparedness in 2021; this was particularly true in lower income households already reeling from high food costs.
Inflation can also induce healthcare behavioral changes. These include changing healthcare plans to reduce expenses or purchasing those that include use of virtual visits with their physicians to save time and money. Virtual visits or telehealth may be the only choice for those who cannot afford to purchase or maintain a personal vehicle or use public transportation due to increased costs. However, telehealth depends on reliable internet access, which may not be feasible for
everyone, further accentuating the “digital divide” that separates those with essential resources from those that lack them. Inflation can, therefore, enhance existing health disparities. Health inequities increase the risk of syndemics that can raise overall healthcare costs.
Drug costs also increase during inflation; while the Inflation Reduction Act, signed into law in 2022, helped reduce prices of several drugs including insulin for older adults supported by Medicare, non-Medicare patients suffering from chronic diseases had to seek alternate resources. From 2017 to 2022, the inflation-adjusted cost of insulin rose by 24 percent. Approximately 1.2 million Americans reported spending 40 percent of their available income on insulin. The National Bureau of Economic Research determined that an increase of $10 on prescription drugs for chronic ailments such as hypertension or diabetes correlated with a 33 percent increase in mortality rates. Given these data, it is not surprising that inflation positively correlates with mortality and thereby with decreased life expectancy.
From a physician perspective, a high inflation rate significantly increases the cost of physician services. Measured as the Medicare Economic Index, physician cost of services grew to 4.7 percent in 2022 and 3.8 percent in 2023, as compared to the historical average of 1-2 percent every year. However, payments to physicians have continued to decline, which may lead to detrimental effects on patient care and access to quality healthcare. Upward inflationary pressures also have far-reaching and consequential effects on Medicare Fee-For-Service (FFS) and Value Based Care (VBC) payment reform models. The process behind Medicare payment and payment reform is complex; both, however, revolve around the Medicare Physician Fee Schedule (MPFS), the American Medical Association’s Relative Value Update Committee (RUC), and the national inflation rate. Although there are several other factors that contribute to the CMS-associated fee schedule, these three are among the most significant. The Medicare Physician Fee Schedule (MPFS) directly determines payment rates for services rendered by physicians via CMS. Updates to the MPFS occur via the RUC. Physicians on the RUC review and refine the conversion factor used to generate payments to their colleagues for the over 8,000 service codes that exist within the CMS data registry.
Three components determine the relative value unit (RVU) of the codes: physician work, which includes the time and intensity required to furnish the service, practice expenses associated with the service; and the attributed malpractice costs. It is important to note that the MPFS has remained largely stagnant for almost two decades. The conversion factor for 2024 decreased by approximately 3.37 percent, further reducing Medicare payment to physicians who have seen a dip of 22 percent from 2001 to 2021 after adjustment for inflation. These estimates could be higher as this is largely dependent on practice and specialty. Surgery has been one of the most affected specialties, with MPFS payments per patient visit decreasing by 22.8 percent for surgical procedures from 2013 to 2023 (after adjustment for inflation), even as the Consumer Price Index (CPI), which measures the average change in prices over time for goods and services, increased by 29.3 percent. Therefore, it is imperative that physician payments keep up with inflation and the cost of practice.
In summary, inflation aggravates barriers to health in many ways. It is up to the individual or household to proactively plan for rising health-related costs by proper budgeting, becoming aware of their employer-provided health benefits packages, educating themselves on nutrition, consuming healthy foods and exercising as preventative measures, and forming a social support system. Studies have shown that the return on investments (ROI) by governments on health equity and social determinants of health may help mitigate these barriers and improve their gross domestic product (GDP) as they retain their human capital, making it a win-win situation.
References:
1. Bosch R. The compounding effects of inflation on health and health outcomes. MedCity News. (2022, August 30). https:// medcitynews.com/2022/08/the-compounding-effects-of-inflation-on-health-and-health-outcomes/
2. Citroner G. Nearly 90% of Americans report Inflation-Related anxiety. Healthline. (2022, July 15). https://www.healthline. com/health-news/nearly-90-percent-of-americans-report-inflation-related-anxiety
3. Dhar A., Korenda L., Bhatt J., & Gerhardt W. Inflation signals unrest ahead for health care. Deloitte Insights. (2023, June 6). https://www2.deloitte.com/us/en/insights/industry/healthcare/health-care-affordability-inflation.html
4. Duffy S. When inflation rises, health outcomes fall. Harvard Business Review. (2023, January 10). https://hbr.org/2022/11/ when-inflation-rises-health-outcomes-fall
5. Endocrine Society. CY 2024 Medicare Physician Fee Schedule Final Rule Summary. https://www.endocrine.org/-/media/endocrine/files/advocacy/pdfs/mpfs-final-rule-summary.pdf
6. Ginsburg P.B., Lieberman S.M. Multi-Year Medicare physician fee freeze threatens access: Pair relief with reforms. (2022). Health Affairs Forefront. https://doi.org/10.1377/forefront.20221020.322922
7. Krishna A. and Singhal S. (2022, September 19). The gathering storm: The transformative impact of inflation on the healthcare sector. McKinsey & Company Healthcare. https://www.mckinsey. com/industries/healthcare/our-insights/the-gathering-storm-thetransformative-impact-of-inflation-on-the-healthcare-sector
8. Mallatt J., Dunn A,, Fernando L. Consumer Out-Of-Pocket Drug Prices Grew Faster Than Prices Faced By Insurers After Accounting For Rebates, 2007-20. Health Aff (Millwood). 2024 Sep;43(9):1284-1289. doi: 10.1377/hlthaff.2023.01344
9. Movsisyan A., Wendel F., Bethel A., Coenen M., Krajewska J., Littlecott H., Stöckl H., Voss S., Wollmershäuser T., Rehfuess E. Inflation and health: a global scoping review. Lancet Glob Health. 2024 Jun;12(6):e1038-e1048. doi: 10.1016/S2214-109X(24)00133-5
10. Resneck Jr, J. Medicare physician is long overdue. (2022, October 3). American Medical Association. https://www. ama-assn.org/about/leadership/medicare-physician-payment-reform-long-overdue
11. Romaniuk P., Poznańska A., Brukało K. and Holecki T. (2020) Health System Outcomes in BRICS Countries and Their Association With the Economic Context. Front. Public Health 8:80. doi: 10.3389/fpubh.2020.00080
12. Sibia U.S., Millen J.C., Klune J.R., Bilchik A., Foshag L.J. Analysis of 10-year trends in Medicare Physician Fee Schedule payments in surgery. Surgery. 2024 Apr;175(4):920-926. doi: 10.1016/j. surg.2023.12.012.
13. Srinivasan, H. (2024, July 31). Historical U.S. inflation rate by year: 1929 to 2024. Investopedia. https://www.investopedia. com/inflation-rate-by-year-7253832
14. Srinivasan H. Historical U.S. inflation rate by year: 1929 to 2024. Investopedia. (2024, July 31). https://www.investopedia.com/ inflation-rate-by-year-7253832
15. US Inflation Calculator. US inflation rates: 2000-2024. (2024, August 14). Current US Inflation Calculator | Easily Calculate How the Buying Power of the U.S. Dollar Has Changed From 1913 to 2023. Get Inflation Rates and U.S. Inflation News. https:// www.usinflationcalculator.com/inflation/current-inflation-rates/




Rishi Goswamy is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. In addition to medicine, he has an interest in healthcare strategy and economics.
Hunter Buescher is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. His interests include preventative medicine and community health.
Garret Williford is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. He is interested in researching the positive impacts of preventive and lifestyle medicine.
Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life.

By Jessica Treviño Jones, MD
Exciting news everyone — cancer treatment and cancer care are nothing like it used to be! We are perfecting our recipes of treatment based on a patient’s personal gene mutations and tumor DNA. We are entering an era of personalized precision cancer care and curing more advanced cancers with enhanced drug delivery. It is an exciting time to be an oncologist, and between October-December 2023 alone, the FDA featured 45 oncology drug approvals, including 17 for drugs new to the market.1 Though we have much to be grateful for, as a breast cancer medical oncologist, I found myself looking at the woman in front of me and wondering: “Could this have been avoided for you?” It isn’t a far-fetched thought. After all, the FDA first approved the use of breast cancer prevention therapy in 19982, then again in 2007.3 We just have to ask a cancer patient for them to share that their greatest wish would have been to prevent the cancer in the first place, rather than face a diagnosis and undergo treatment.
So, while I am proud to be an oncologist in these exciting times, knowing no one should suffer from cancer is how I found myself in the space of breast cancer prevention. I am honored to share that I am the director for May’s Cancer Center Cancer Risk Reduction and Education (CaRE) clinic. How does this care model differ from our current care model for prevention and screening? The CaRE clinic utilizes a unique approach with a multidisciplinary program that includes primary care, medical oncology, genetics and surgeons, and reinforces screening strategies but brings in precision prevention. The better question one should ask is, “If primary care and gynecology are ordering screening tests for women, why should we bring in these other disciplines?”
I think now is the right time to stand up from our seats and salute our primary care physicians. In 2022, we learned that primary care doctors need 26.7 hours per day to do the necessary preventative, chronic and acute care in this age of documentation and inbox management.4 There are multiple challenges our primary care physicians
are up against right now, including a shortage of primary care physicians, reimbursement system-issues and fragmented communication in an evolving EMR world. The United States Preventive Services Task Force (USPTF) has lowered the age on mammogram screening, already increasing a workload across our medical system.5 The Prostate Cancer Foundation has also updated guidelines on prostate cancer, with a younger age of 40 and including all Black men.6 There are other consortiums such as the International Cancer of the Pancreas Screening Consortium who met in 2018 and released recommendations for the management of individuals with increased risk of pancreatic cancer based on family history or genetic mutations like BRCA.7 Why are we seeing such a rise in recommendations for screening? A recent study reviewed 23 million patients and found that 17 of 34 cancers are increasing in Generation X and Millennials (those born between 1981 and 1996) compared to older generations.8
There is a tremendous amount of value in having a medical oncologist reenforce the call to prevention, so instead of having survivors — we can have pre-vivors. Since our risks are going up without a clear correlation, the CaRE clinic model has been very intentional in stepping away from the word “prevention” and instead using “risk reduction.” A patient can have their own personalized risk assessment performed to gauge what cancers they are at a higher risk for, and then discuss what additional screening beyond the USPTF that they qualify for. This includes discussing risk reducing medications like tamoxifen, a drug managed with ease by an oncologist given our expertise in navigating side effects and extensive training in risk benefit analysis regarding uterine cancer or clots. Research conducted by Dr. Megan Whisenant and I validated a survey to objectively measure the patient-reported outcomes for patients at higher risk of breast cancer, since there was no standard metric among trials to compare to former breast cancer survivors.9
The risk and benefit of potential overdiagnosis is a tough discussion, which is still riddled with grey areas and shadowed with social determinants of health. Factors such as financial impact and mental burden should be addressed alongside overdiagnosis. Multiple studies, including our own research, confirmed higher levels of anxiety for pre-vivors than survivors of breast cancer. Knowing that the language “high-risk” is anxiety provoking, this model addresses this ageold concern by moving away from the old rhetoric and uses a more friendly verbiage. CaRE clinic sounds much more lovely than HighRisk Screening clinic, don’t you agree? A patient is more likely to show up to an appointment if they are less scared, and more likely to be adherent.10 Having an oncologist help carry the load for what primary care now has less time to carry, with potentially more options, brings value to the entire healthcare system. With an oncologist coordinating breast MRI screening in addition to mammogram screening for those who qualify, if a biopsy does confirm cancer, the patient will have two important advantages. One, she will have her breast cancer found at the earliest, most curable stage, allowing her to have the best opportunity to avoid chemotherapy. Second, she has early integration into oncologic care, which is an increasing challenge during this rise of cancer and fall in number of oncologists.11
Cancer-adjacent diseases, like obesity, tobacco use and alcohol use, are reversible risk factors addressed in each appointment.12 The CaRE clinic was meant to support the community, so any referring physician is consulted for any internal initiatives such as weight loss programs. In this way, the CaRE clinic will reinforce adherence to their primary care doctor’s internal initiatives. If a referring provider does not have an internal weight loss program, alcohol cessation program or tobacco cessation program, then opportunities are found for the patient based on location. It is a happy coincidence that downstream impact for heart disease, diabetes and stroke prevention also come from the CaRE clinic.
Every day, I remind myself that if asked, a cancer patient will share that their greatest wish would have been to prevent the cancer in the first place, rather than face a diagnosis and undergo treatment. We have always had the tools to do this, and the CaRE clinic model takes into consideration all the barriers with intentional methods to overcome those historic challenges. It is a team that is meant to cure cancer, and I’m honored to see this model grow in Texas. Cancer doesn’t stand a chance, because we CaRE!
References:
• AACR. (2024) “FDA Approvals in Oncology October-December 2023”, The American Association for Cancer Research, https://www.aacr.org/blog/2024/01/03/fda-approvals-in-oncology-october-december-2023/
• Fisher B., Costantino J.P., Wickerham D.L., Redmond C.K, Kavanah M., Crothenin W.M., et al. Tamoxifen for prevention of breast cancer: report of National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst 1998;90:1371-88
• Vogel, V.G. et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA 295, 2727–2741 (2006)
• Porter, J., Boyd, C., Skandari, M.R. et al. Revisiting the Time Needed to Provide Adult Primary Care. J GEN INTERN
MED 38, 147–155 (2023). https://doi.org/10.1007/s11606022-07707-x
• USPTF. (2024). “Screening for Breast Cancer: US Preventive Services Task Force Recommendation Statement.” JAMA
• Garraway I.P., Carlsson S.V., Nyame Y.A., Vassy J.L., Chilov M., Fleming M., Frencher S.K., George D.J., Kibel A.S., King S.A., Kittles R., Mahal B.A., Pettaway C.A., Rebbeck T., Rose B., Vince R., Winn R.A., Yamoah K., Oh W.K.. Prostate Cancer Foundation Screening Guidelines for Black Men in the United States. NEJM Evid. 2024 May;3(5):EVIDoa2300289. doi: 10.1056/EVIDoa2300289. Epub 2024 Apr 23. PMID: 38815168
• Goggins M., Overbeek K.A., Brand R., Syngal S., Del Chiaro M., Bartsch D.K., Bassi C., Carrato A., Farrell J., Fishman E.K., Fockens P., Gress T.M., van Hooft J.E., Hruban R.H., Kastrinos F., Klein A., Lennon A.M., Lucas A., Park W., Rustgi A., Simeone D., Stoffel E., Vasen H.F.A., Cahen D.L., Canto M.I., Bruno M.; International Cancer of the Pancreas Screening (CAPS) consortium. Management of patients with increased risk for familial pancreatic cancer: updated recommendations from the International Cancer of the Pancreas Screening (CAPS) Consortium. Gut. 2020 Jan;69(1):7-17. doi: 10.1136/gutjnl-2019-319352. Epub 2019 Oct 31. Erratum in: Gut. 2020 Jun;69(6):e3. doi: 10.1136/gutjnl-2019-319352corr1. PMID: 31672839; PMCID: PMC7295005
• Sung H., Jiang C., Bandi P., Minihan A., Fidler-Benaoudia M., Islami F., Siegel R.L., Jemal A. Differences in cancer rates among adults born between 1920 and 1990 in the USA: an analysis of population-based cancer registry data. Lancet Public Health. 2024 Aug;9(8):e583-e593. doi: 10.1016/S2468-2667(24)001567. PMID: 39095135
• Whisenant, M.S., et al. (2023). “The symptom burden of women with a known risk of breast cancer receiving risk reducing medication.” Cancer Treatment and Research Communications
• Atreja A., Bellam N., Levy S.R. Strategies to enhance patient adherence: making it simple. MedGenMed. 2005 Mar 16;7(1):4. PMID: 16369309; PMCID: PMC1681370
• Key Trends in Tracking Supply of and Demand for Oncologists. American Society of Clinical Oncology. May 2018. Accessed May 24, 2021. https://bit.ly/3yKYwzo
• Avgerinos K.I., Spyrou N., Mantzoros C.S., Dalamaga M. Obesity and cancer risk: Emerging biological mechanisms and perspectives. Metabolism. 2019 Mar;92:121-135. doi: 10.1016/j. metabol.2018.11.001. Epub 2018 Nov 13. PMID: 30445141

Jessica Treviño Jones, MD, is an associate professor at Long School of Medicine, and practices at Mays Cancer Center, UT Health San Antonio MD Anderson Cancer Center. She is a firstgeneration Latina physician, clinical researcher and educator for trainees across the state of Texas. Her work and publications over the last decade reflect her dedication to overcoming healthcare disparities, improving adherence through understanding symptom burdens, empowering patients with culturally sensitive informed decision making, and education for all utilizing novel methodologies.

By Shreya Vakil and Ramaswamy Sharma, MS, PhD
With modern technology and advances in medical science, our life expectancy has increased, averaging 77.5 years in the United States. Unfortunately, our brains have not been able to keep up. Approximately 6 million Americans over the age of 65 are affected by Alzheimer’s disease, a condition in which our brain function deteriorates, thereby clouding our memory, understanding, language, attention, reasoning and judgement.2 The Center for Disease Control and Prevention (CDC) has ranked Alzheimer’s as the seventh leading cause of death in the U.S., killing more people than breast and prostate cancer combined.5 As there is no known cure for Alzheimer’s disease or other similar brain-related disorders, prevention by identifying and alleviating risk factors is key for preserving the quality of life with aging.
“You are what you eat,” is a loosely adapted quote from Jean Anthelme Brillat-Savarin’s “Dis-moi ce que tu manges, je te dirai ce que tu es.”13 Recent research suggests that our brain health, identity, decision-making, mood, behavior and even cravings for sugar are regulated by chemicals that emanate from our gut, specifically produced by the microbiota. A microbiota is defined as an ecological community of microorganisms that live in our body and play a vital role in physical and mental health and in disease.6 Our gut is rapidly colonized by microbiota at birth and, as we reach adulthood, each of us have a distinct composition of several different types of microorganisms composed of Actinobacteria, Bacteroidetes, Firmicutes, Fusobacteria, Proteobacteria and Verrucomicrobia. The composition of our gut microbiome is influenced by our environment, lifestyle, diet, hor-
mones and genetics. This microbiome plays a crucial role in regulating food intake, feeling full, producing glucose and fats, maintaining insulin sensitivity, and preventing harmful microorganisms from entering our gut. An unhealthy diet can disrupt this balance or alter the diverse composition of the gut microbiome, a condition known as dysbiosis, which can result in unwanted signals affecting our brain.
Our nervous system controls gut movement and digestion, but how does the gut microbiota communicate with our brain? Gut bacteria can activate nerves and release chemicals that affect our brain and immune cells. For example, 4-ethylphenol (4EP) is produced by gut bacteria when we consume foods rich in the amino acid tyrosine.8 This compound is converted to 4-ethylphenyl sulfate (4EPS), which can cross the blood-brain barrier, a protective shield that blocks harmful substances from reaching the brain via blood. In the brain, 4EPS hinders the formation of oligodendrocytes, cells that insulate neurons. Low levels of these cells can impair brain function, and children with autism have seven times more 4EPS than normal.8 Notably, mice treated with substances that absorb 4EPS showed reduced anxiety and irritability. This bidirectional, or two-way, communication between the gut and brain, known as the brain-gut axis, is under extensive study.3
Recurrent chronic gastrointestinal disorders such as Irritable Bowel Syndrome (IBS) are now seen as disorders of gut-brain interaction (DGCI), as they are often associated with psychological symptoms including anxiety and depression. A common link among these disorders, Alzheimer’s disease and aging is inflammation. While inflammation is a protective mechanism that allows our immune cells
to deal with foreign substances entering our bodies, it can, however, become excessive and repetitive (called chronic inflammation) in some people, wherein our immune cells can attack our own cells. Aging is associated with an increase in inflammation. Studies have shown that in Alzheimer’s patients, dysbiosis can result in fewer anti-inflammatory bacteria and more pro-inflammatory bacteria.10 Dysbiosis can, therefore, cause inflammation in the gut, making it more permeable to inflammatory chemicals that pass through the blood-brain barrier and trigger inflammation in the brain, resulting in the formation of protein aggregates called amyloid plaques and tau proteins, and consequently, Alzheimer’s disease.6,12 Some studies have also reported the presence of harmful bacteria in the brains of Alzheimer’s patients.
So, how can we ensure that our brain-gut axis is healthy and functioning well? How do we maintain “good” microbiota (eubiosis)? A step in the right direction for a healthy brain-gut axis would be to consume sufficient probiotics and prebiotics.4,11 Probiotics are live microorganisms that promote gut health and may regulate the immune system’s balance between inflammatory and anti-inflammatory responses. Prebiotics, on the other hand, are food for those microorganisms. Together, these maintain the gut microbiome balance. The most well-known probiotics are Bifidobacterium and Lactobacillus strains, which are found in dairy products such as yoghurt and cheese, vegetables and many dietary supplements.1 Consumption of Bifidobacterium and Lactobacillus for at least 12 weeks has been shown to improve cognitive function in patients in the early stages of Alzheimer’s.10 Along with other preventative strategies, probiotics may help slow the progression of Alzheimer’s.7,9 Probiotics can also enhance mental flexibility and relieve stress.
Alcohol and tobacco can cause dysbiosis and their consumption should be reduced. Antibiotics are absolutely essential for getting rid of many harmful microorganisms that attack our bodies. However, many studies have noted an association with behavioral and chemical changes in the brain with the use of antibiotics1; it must be noted that contrasting results have also been reported. Thus, the role of antibiotics in modulating the brain-gut axis needs to be further evaluated. Nevertheless, consuming probiotics following antibiotic therapy may help in the recovery of eubiosis.
It is becoming increasingly clear that fostering a healthy brain-gut axis holds significant potential for enhancing our quality of life as we age and for combating neurodegenerative diseases such as Alzheimer’s. Hippocrates, considered to be the father of modern medicine, may not have been fully correct when he quoted, “All diseases begin in the gut;” however, his emphasis on taking care of the gut to reduce the risks for serious health conditions still holds true!
References:
1. Angelucci, F., Cechova, K., Amlerova, J., & Hort, J. (2019). Antibiotics, gut microbiota, and Alzheimer’s disease. Journal of Neuroinflammation, 16(1), 108. https://doi.org/10.1186/ s12974-019-1494-4
2. Coradduzza, D., Sedda, S., Cruciani, S., De Miglio, M. R., Ventura, C., Nivoli, A., & Maioli, M. (2023). Age-Related Cognitive Decline, Focus on Microbiome: A Systematic Review and Meta-Analysis. International Journal of Molecular Sciences, 24(18), 13680. https://doi.org/10.3390/ijms241813680
3. Kraimi, N., Ross, T., Pujo, J., & De Palma, G. (2024). The gut microbiome in disorders of gut–brain interaction. Gut Microbes, 16(1), 2360233. https://doi.org/10.1080/19490976.2024.2360 233
4. Krüger, J.F., Hillesheim, E., Pereira, A.C.S.N., Camargo, C.Q., & Rabito, E.I. (2021). Probiotics for dementia: A systematic review and meta-analysis of randomized controlled trials. Nutrition Reviews, 79(2), 160–170. https://doi.org/10.1093/nutrit/ nuaa037
5. Kumar, A., Sidhu, J., Lui, F., & Tsao, J. W. (2024). Alzheimer Disease. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm. nih.gov/books/NBK499922/
6. Megur, A., Baltriukienė, D., Bukelskienė, V., & Burokas, A. (2020). The Microbiota–Gut–Brain Axis and Alzheimer’s Disease: Neuroinflammation Is to Blame? Nutrients, 13(1), 37. https://doi.org/10.3390/nu13010037
7. Naomi, R., Embong, H., Othman, F., Ghazi, H. F., Maruthey, N., & Bahari, H. (2021). Probiotics for Alzheimer’s Disease: A Systematic Review. Nutrients, 14(1), 20. https://doi.org/10.3390/ nu14010020
8. Needham, B. (2024). Exposed wires: A microbial metabolite influences myelination in the brain. Science (New York, N.Y.), 385(6704), 37. https://doi.org/10.1126/science.adq2344
9. Pluta, R., Ułamek-Kozioł, M., Januszewski, S., & Czuczwar, S.J. (2020). Gut microbiota and pro/prebiotics in Alzheimer’s disease. Aging, 12(6), 5539–5550. https://doi.org/10.18632/ aging.102930
10. Sánchez-de-Lara-Sánchez, S., & Sánchez-Pérez, A.M. (2022). Probiotics Treatment Can Improve Cognition in Patients with Mild Cognitive Impairment: A Systematic Review. Journal of Alzheimer’s Disease: JAD, 89(4), 1173–1191. https://doi. org/10.3233/JAD-220615
11. Shahrokhi, M., & Nagalli, S. (2024). Probiotics. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/ NBK553134/
12. Varesi, A., Pierella, E., Romeo, M., Piccini, G. B., Alfano, C., Bjørklund, G., Oppong, A., Ricevuti, G., Esposito, C., Chirumbolo, S., & Pascale, A. (2022). The Potential Role of Gut Microbiota in Alzheimer’s Disease: From Diagnosis to Treatment. Nutrients, 14(3), 668. https://doi.org/10.3390/nu14030668
13. You Are What You Eat. (2022, April 28). Kennedy Center. https://kennedy.byu.edu/alumni/bridges/features/you-are-whatyou-eat

Shreya Vakil is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. She is interested in exploring the multi-factorial process of aging and associated disorders, and intends to pursue a career in internal medicine or neurology.

Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life.
By David Alex Schulz, CIPP

In the last quarter-century, the landscape of medicine has been reshaped. While advances in minimally invasive surgery, imaging and telemedicine have transformed care — and often dominate the spotlight — the true revolution lies in changing attitudes toward patients themselves. Where patients once were passive recipients of care, they are now increasingly viewed as active partners, encouraged, and often expected to take the reins of their own health management. Nowhere is this shift more evident, or more profound, than in the realm of end-of-life care.
Dr. Jenny Seger’s personal journey through the passing of both her parents — her mother in 1996 and her father in 2023 — vividly illustrates how far palliative care has come. Her experiences highlight the evolution of patient-physician relationships and underscore the additional responsibilities both parties now bear in ensuring dignified, compassionate care.
Dr. Seger, a physician dedicated to patient advocacy and wellness, recalls the stark contrast between the end-of-life care her mother received in 1996 and the care her father received nearly three decades later. Her medical education had just begun when she learned that her mother, an outwardly healthy, active woman of 54, was diagnosed with Stage IV Small Cell Lung Cancer. The battle with cancer would end just nine months later, weeks after her mother’s 55th birthday.
“In 1996, as a brand-new medical student, I was taken aback by how cold and impersonal the experience played out with my mom,” Dr. Seger reflected. She described the moment when an oncologist covering for her mother’s oncologist who was out of town, coldly informed Dr. Seger and her stepfather that her mother was dying. “The doctor asked — right in front of my mom — to speak to my stepfather and me outside. Then, outside the room, she told us that since she didn’t really know my mother and I was a medical student, I should probably be the one to tell my mother that this was it … that she was dying and needed to be admitted to a nearby inpatient hospice facility,” Dr. Seger recounted. “Seriously?”
The family was not even offered the option of in-home hospice care. Instead, they were directed to an inpatient facility, where the atmosphere felt sterile and impersonal. Dr. Seger recalls having to chase down nurses for help with pain control. “It felt at the time as though we had checked into a sterile, budget hotel to watch our mother die.”
The experience of losing her father, Ron Cobb, in 2023 could not have been more different. At 81, Mr. Cobb suffered a massive stroke and never regained consciousness. When it became clear that he would not recover, hospice was swiftly consulted. “It was truly such a completely different experience from that which we lived earlier,” Dr. Seger said.
From the moment she arrived at the ER to her father’s final breaths, taken in the comfort of his own home, Dr. Seger describes the experience as one that could not have gone better. The hospice team’s responsiveness and empathy were worlds apart from what her family had encountered years earlier. “Early on, we asked about moving him back to his home of 40 years, which he so deeply loved, and much to our surprise, the hospice team immediately said, ‘no problem.’”
Within 24 hours, her father was transported home, a hospital bed and IV equipment were set up, and pain management was initiated — all without burdening the family. “The hospice staff was attentive and responsive, frequently checking in to see if we needed anything. They even arranged for a chaplain to visit,” Dr. Seger noted.
What stood out most to her was the hospice team’s focus on understanding her father’s life rather than just his death. “It felt like they truly cared and that the consult was not simply another checkbox on their list of things to do,” she said.
Reflecting on the changes over the past 25 years, Dr. Seger believes that the most important lesson is this: “Advocate for the patient but also for yourselves. It is the family members who will have to live with the memory of that experience.”
The evolution of end-of-life care from a cold, detached process to one centered around the patient’s and family’s wishes represents the most meaningful advancement in medicine — one that respects and empowers the human experience.

David Alex Schulz is certified in HIPAA privacy and security compliance, serves on the BCMS Publications Committee and is a contributing writer to San Antonio Medicine magazine.

Courtesy of Insperity
For many of us, our occupations play a central role in our lives, providing much more than financial resources. The workplace can give us a sense of purpose and offer valuable social connections, where coworkers frequently become lifelong friends. Our jobs can also impact our physical and mental health. Because this is the case, leading employers are increasingly launching initiatives aimed at supporting healthy lifestyles. So how can an employer get started? Here are a few ideas.
As we all know, one powerful strategy for improving our overall health is via preventative healthcare, where your doctor proactively addresses wellness concerns. And, of course, the best way to make this happen is by offering health insurance coverage within your workplace. That said, even if employees have access to preventative care, they need to use it. One proposal is hosting workshops where staff are instructed on how their benefits work. You might also consider sending out occasional email reminders or newsletter articles, encouraging employees to schedule their annual physicals, along with details about time-off policies to ensure these visits occur.
Let’s face it: most office workers are relatively sedentary throughout the workday. Even moderate amounts of physical activity can make a big difference. For instance, managers in offices with nearby green spaces could encourage employees to take short walks over their lunch break or even turn a meeting into a walk. Standing desks (desks that allow employees to stand or sit) can also help employees limit sedentary positions.
An important key to an effective wellness program is support from within. The results are typically more positive whenever company leadership sets an example for any given initiative, including participation in healthy workplace initiatives. If managers are seen taking power walks or the CEO mentions using the stairs instead of the elevator, employees will often take notice and respond.
A monthly wellness stipend can help team members pay for a gym membership or fitness classes. Some organizations even set up a gym in the building where employees can easily exercise before or after work. Another option is implementing flex scheduling so employees can adjust their daily commutes to fit in their exercise.
The benefits of healthy workplace initiatives are widespread and noteworthy. In addition to being the right thing to do, these programs can improve morale, increase quality of life, bolster retention and even reduce illness in the workplace.
Insperity is a leading provider of human resources and business performance solutions.
Insperity is a Silver Member of the BCMS Circle of Friends program.
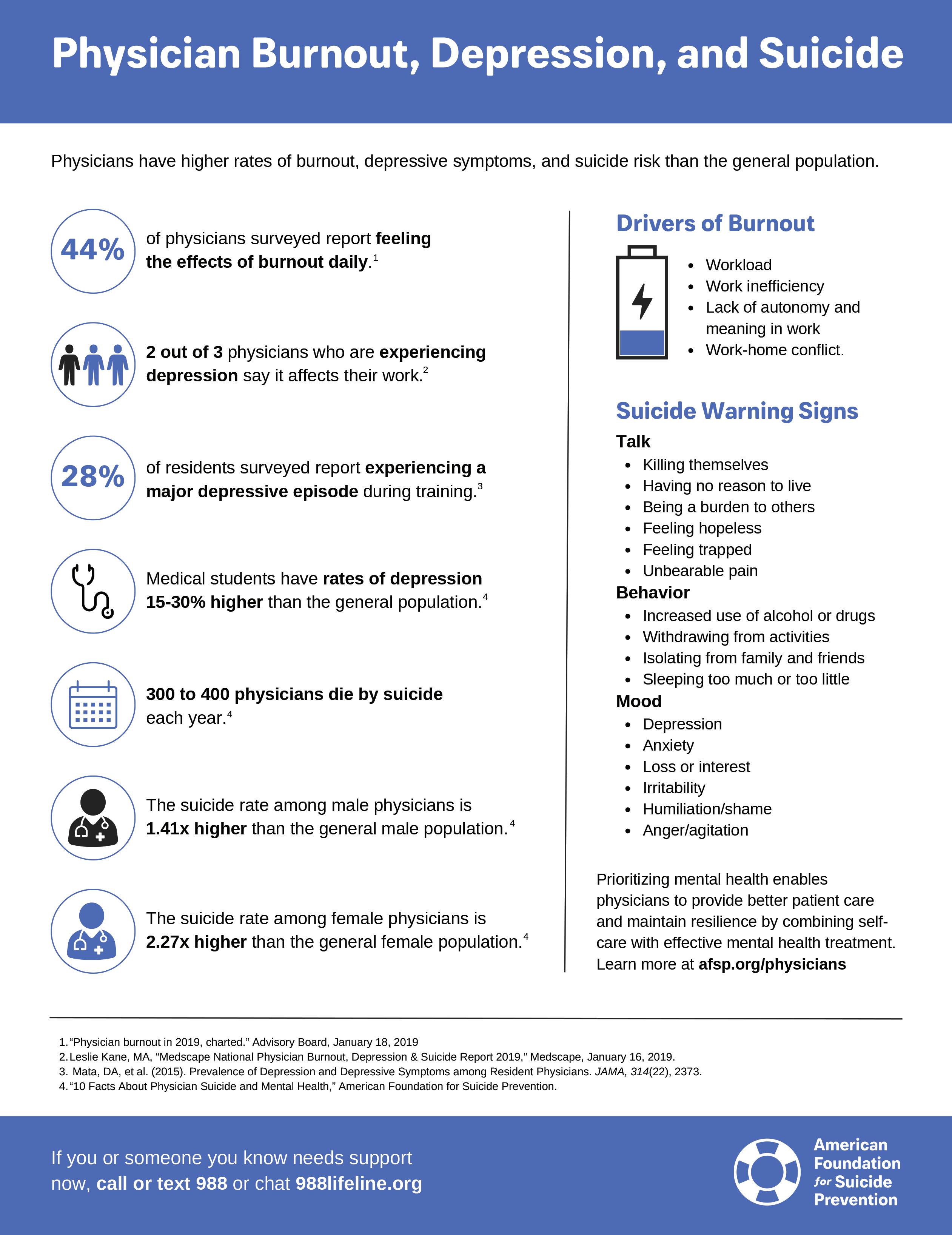

By Victoria (Tori) Vargas
Every child deserves the chance to shine. By creating opportunities for those with diverse special needs, Kinetic Kids leads the way in advocacy and inclusion for our youth with disabilities. This outstanding organization is committed to enhancing the lives of children with varying disabilities, offering them the opportunity to engage in sports, fine arts and other recreational activities adapted to their needs. Kinetic Kids harmonizes physical fitness, mental health and creative expression, ensuring that every child, regardless of ability, can experience the joys and developmental benefits of an active and enriched life.
At the core of Kinetic Kids’ purpose is the belief that every child deserves access to comprehensive health literacy, especially in physical education and health. Founded by practicing physical therapists in the early 2000s, the program was created in response to a recognized need for increased opportunities for physical activity among children with special needs. Many of these children are unable to participate in typical summer sports camps due to inadequate accommodations and insufficient safety measures. With Kinetic Kids, children with special needs can enjoy the same activities as any other child.
While Kinetic Kids’ mission began with simply finding ways for children with various disabilities to be active, it has expanded to include a broad selection of sports, from well-known soccer and tennis to snow skiing and skateboarding. Understanding the need for more programs that accommodate children with special needs, Kinetic Kids expanded their services to include fine arts. Children can sign up for musical activities, dance and various crafting workshops. All programs include skilled faculty who are educated to meet each child’s individual needs.
Kinetic Kids recognizes the importance of involving parents and the broader community in promoting health literacy. During sports activities, children learn the rules of the game along with how exercise
benefits their bodies, helping them understand the connection between physical activity and health. The program also offers resources and workshops for parents and children, equipping them with the knowledge to support their children’s health education at home. Their annual free resource fair, EXPO, gives faculty the chance to reach families and advocate for children with various disabilities in the community, offering free equipment, resources, services and teachings on the benefits of physical activity in children’s lives. By educating parents about healthy practices and how to incorporate them into daily routines, Kinetic Kids ensures that the benefits of its programs extend beyond the activities themselves.
Community events and outreach programs further extend the impact of Kinetic Kids, raising awareness and fostering a supportive environment for all children. Kinetic Kids enhances understanding, acceptance and integration through Discovering Disabilities Day. Recognizing the challenges many children with special needs encounter in being accepted from their peers, this initiative seeks to foster empathy

and inclusion by educating all children about the experiences of those with special needs. The day features interactive stations where children can experience various disabilities firsthand, such as learning to navigate a wheelchair or button a shirt with one arm.
The positive effects of physical activity on overall wellness are wellknown, but observing this change in children with various disabilities highlights its even greater importance. For physically disabled children, finding ways to enjoy the same sports that fully able-bodied children do can be especially challenging. The scarcity of suitable sports options for children with special needs contributes to a higher rate of sedentary lifestyles, which is often accompanied by increased mental health issues like depression and anxiety. Children with special needs may already face greater mental health challenges, and the lack of accessible sports and recreational activities exacerbates these difficulties.
While improvements in overall well-being through physical activity are significant, it’s the additional elements of Kinetic Kids that truly make a difference. For example, ending each session with affirmations like “I am strong, I am courageous, I am a Kinetic Kid” instill a sense of capability in each child. The small competitions at the end of programs, where kids showcase what they’ve learned and compete with others, provide motivating goals like those in any typical summer camp. These aspects enhance the overall well-being of the children, addressing health disparities and making a meaningful impact.
I feel honored to have had the opportunity to volunteer and work with Kinetic Kids over the past year and understand the extent of its impact on these children. My time volunteering with Kinetic Kids was with the CrossFit program, known as AgilityFit. This program met once a week for six weeks, focusing on teaching children how to use the weight room and introducing them to beginner CrossFit techniques. This hands-on experience was incredibly rewarding. While I have always believed in the overall health benefits of physical fitness, witnessing the boost in each child’s confidence by the end of the six-week program was particularly gratifying. To understand the overall benefits of CrossFit and physical activity on the lives of these children, I partnered with Kinetic Kids through UT Health Science Center to administer surveys assessing changes in mood and behavior before and after the six-week program. We noted significant decreases in anxiety-related behaviors like fidgeting or restlessness after the AgilityFit program. We aim to continue this project and extend it to the rest of Kinetic Kids’ programs to truly understand and showcase the benefits for these children.
Kinetic Kids stands as a beacon of health literacy, demonstrating that with the right accommodations and support, every child can learn to lead a healthy, active life. By integrating health education into enjoyable and inclusive activities, Kinetic Kids not only enriches the lives of children with disabilities but also empowers them and their families with the knowledge to make informed health decisions. As the program continues to grow and evolve, its positive impact will undoubtedly inspire and benefit countless more children and communities.
Photography courtesy of Kinetic Kids.




By Rosalie Cisneros, City of San Antonio Metropolitan Health District
Domestic violence involves the misuse of power and control by one partner over another, manifesting as physical, emotional or psychological abuse. This issue is critical to address as it has significant repercussions on the health and well-being of individuals and families. October is recognized as Domestic Violence Awareness Month, a time to focus on education and awareness.
The City of San Antonio Metropolitan Health District (Metro Health) is launching a new initiative to address domestic violence in our community. In October 2023, the City of San Antonio passed the Domestic Violence Signage Ordinance, which takes effect October 1, 2024. The ordinance requires all public facilities to display resource signs inside all restrooms. The signs will provide essential resources and access to domestic violence services. This initiative reflects Metro Health’s ongoing commitment to fostering a safer and supportive environment for everyone.
San Antonio has one of the highest rates of domestic violence in Texas, highlighting the urgency of this measure. The ordinance is designed so that individuals in distress can access support in a private setting, potentially removing the barriers to seeking help.
For medical professionals, understanding the link between domestic violence and public health is important. Domestic violence significantly impacts physical and mental health, often resulting in chronic conditions, injuries and psychological trauma. By supporting
initiatives like the Domestic Violence Signage Ordinance, healthcare providers can contribute to a broader public health strategy aimed at reducing domestic violence in our community.
Understanding and addressing domestic violence is crucial for our community. Here are ways you can make a difference.
• Support the Domestic Violence Signage Ordinance by ensuring public places comply with the new law.
• Share information about support services with those who might be affected.
• Encourage your community to raise awareness and support local initiatives.
By taking these actions, we can help those in need and contribute to a safer, more supportive community.



Artist’s Note: This digital art piece illustrates the impact of environmental pollution on human health, focusing on San Antonio’s unique challenges. Inspired by a passion for advocacy, it explores how air quality and urban heat disproportionately affect vulnerable populations. Promoting wellness — rather than merely treating diseases — is at the heart of this work. I hope to raise awareness, promote health literacy, and inspire action toward a healthier, more equitable San Antonio.

Class of 2025
Long School of Medicine UT Health San Antonio


Artist’s Note: Diptych, oil paint on wood panels. In my household, the default lunch was a peanut butter and jelly sandwich. It had protein, fruit (products), grain, and of course plenty of sugar, which made it the perfect balanced meal for picky children.
Lily Lindstrom
Class of 2024
Long School of Medicine
UT Health San Antonio
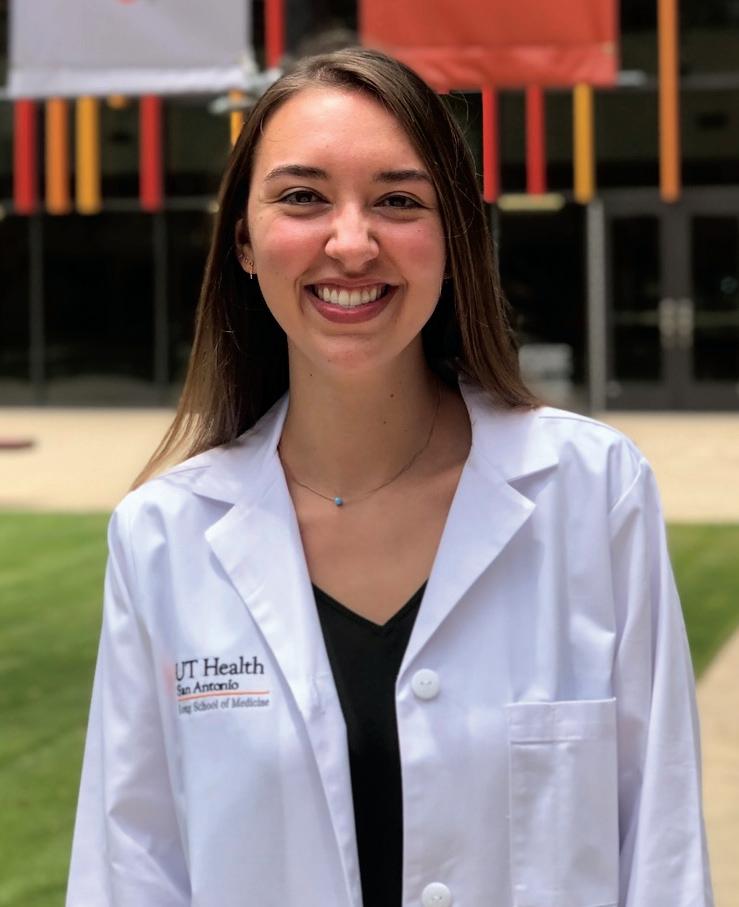
We encourage you to use our friends of medicine businesses whenever you or your practice need supplies or services.

Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 CDavis@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”

Aspect Wealth Management (★★★ Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President
210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”

Broadway Bank
(HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@Broadway.Bank www.broadwaybank.com
“We’re here for good.”

Texas Partners Banks (HHH Gold Sponsor)
Our private banking team specializes in healthcare banking and will work with you to craft and seamlessly integrate financial solutions for you and your practice, including practice loans, lines
of credit and custom local lockbox solutions headquartered in San Antonio. Maria Breen 210-807-5562
Maria.Breen@texaspartners.bank www.texaspartners.bank

Lone Star National Bank (HHH Gold Sponsor)
Established in 1983, Lone Star National Bank has provided banking services to communities in South Texas for the past 41 years. LSNB is an independent and locally owned bank subsidiary of Lone Star National Bancshares-Texas, Inc with consolidated assets of $3 billion (12/31/23) and 36 full-service banking centers throughout Starr, Hidalgo, Cameron and Bexar counties. Aside from personal and business banking, LSNB offers investments, wealth management & trust along with property and casualty insurance, health insurance and supplemental coverage.
Summer L. Reyes Banking Officer 210-479-4716
ReyesS@lonestartnationalbank.com
Ivan Corona Molina
Assistant VP 210-479-4713
MolinaI@lonestartnationalbank.com www.lonestarnationalbank.com
“We do what the Little Banks can’t, and the Big Banks won’t!”
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking 210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking 210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help physicians get the banking services they need.
Synergy FCU Member Services 210-750-8333
info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”

Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison 210-503-0003
Yulia@genicslabs.com
Kevin Setanyan Managing Partner 210-503-0003
Kevin@genicslabs.com
Artyom Vardapetyan Managing Partner 210-503-0003
www.genicslabs.com
“Accurate results in record time.”
Livingston Med Lab (HH Silver Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease and Genetics.
Robert Castaneda CEO 210-316-1792
Robert@livingstonmedlab.com www.livingstonmedlab.com/home
“Trusted Innovative, Accurate and STAT Medical Diagnostics”

American Health Imaging (★★★ Gold Sponsor)
American Health Imaging (AHI) has 5 state-of-the-art imaging centers in San Antonio, TX with industry- boardcertified subspecialized radiologists delivering precise, reliable results. Easy scheduling and prompt report turnaround times, serving both physicians and their patients. Imaging at AHI is priced up to 60% less than hospitals and in-network with 99% of health plans with competitive rates to save patients money. AHI has an additional 37 best-in-class diagnostic imaging facilities in Alabama, Florida, Georgia, Texas and South Carolina.

US Radiology Physician Number 210-572-1211
Casey Allen
Regional Sales Director | San Antonio US Radiology Specialists 210-846-0606
Casey.Allen@usradiology.com
Jasmine Mendoza
Jasmine.Mendoza@usradiology.com
Jaime Zamora
Jaime.Zamora@usradiology.com
Sydnie Caradec
Sydnie.Caradec@usradiology.com
Sarah McMindes
Sarah.Mcmindes@usradiology.com
Scott Roberson
Scott.Roberson@usradiology.com
Ryan Denman
Ryan.Denman@usradiology.com
www.americanhealthimaging.com (main site)
www.americanhealthimaging.com/ physician-resources/ (Physician Resources to refer to American Health Imaging)

Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for healthcare entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com www.bexarcv.com
“Proudly serving the medical community since 1998”

Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP® , QKA
Senior Private Wealth Advisor 512-649-8113 Service@oakwellpwm.com www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney Financial Advisor 210-858-5880
Elizabeth.Olney@edwardjones.com www.edwardjones.com/elizabeth-olney "Making Sense of Investing"

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”

Hancock Whitney (HHH Gold Sponsor)
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services. www.hancockwhitney.com
John Riquelme
San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Larry Anthis Corporate Banking, Relationship Manager 210-507-9646
Larry.Anthis@hancockwhitney.com
Serina Perez
San Antonio Business Banking 210-507-9636
Serina.Perez@hancockwhitney.com
Erik Carrington
Texas Regional Wealth Management Manager 713-543-4517
Erik.Carrington@hancockwhitney.com

UT Health San Antonio
MD Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado Business Development Manager 210-450-3713
DelgadoR4@uthscsa.edu
UT Health San Antonio
MD Anderson Mays Cancer Center
Laura Kouba
Business Development Manager 210-265-7662
NorrisKouba@uthscsa.edu https://uthscsa.edu/
Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229
Healthcare Administration Consultants
(HH Silver Sponsor)
Our mission is to help healthcare organizations small or large to achieve sustainable growth and success by providing them with expert healthcare administration consulting services.
We focus on key factors such as: revenue, supply chain visibility, and aligning operations to save time so that your team can focus on improving the patient’s health and well-being. We transform patient care outcomes and employee working experiences while driving brand and revenue growth.
Dr. Reshma Beherry, DHA
Doctor of Healthcare Administration 210-602-6905
RB@administrative-consultants.com https://administrative-consultants.com/
SERVICES

Equality Health
(HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and
deliver value-based care for diverse communities. Our model offers technology, care coordination and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”
(H Bronze Sponsor)
We were founded to meet a need: helping business owners succeed by giving them simple, quality, affordable U.S.-based contact solutions. In only a few years, our focus on nurturing client relations and building trust not only helped our customers grow their businesses, but helped us stake our claim in the highly competitive TAS industry as one of the most well-regarded and referred. Our 50 years of collective experience are the driving force behind our clients’ satisfaction.
Rachel Caero Managing Partner
844-554-3473
Rachel@dialops.net
Insperity
(HH Silver Sponsor)
Insperity’s HR solutions offer premium service and technology to facilitate growth by streamlining processes related to payroll, benefits, talent management and HR compliance. We provide the tools to help you lighten your administrative load, maximize productivity and manage risks – so you can focus on growth.
Fran Yacovone Business Performance Advisor 210-558-2507
Fran.Yacovone@insperity.com
Dayton Parker Business Performance Advisor 210-558-2517
Dayton.Parker@insperity.com www.insperity.com
“Insperity’s mission is to help businesses succeed so communities prosper”

(HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service
insurance agency offering a full line of products – some with exclusive member discounts and staffed by
professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England Director of Member Benefits 512-370-1746
Wendell.England@tmait.org 800-880-8181
www.tmait.org
“We offer BCMS members a free insurance portfolio review.”

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting and defending physicians.
Patty Spann Director of Sales and Business Development 512-425-5932
Patty-Spann@tmlt.org
www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

The Bank of San Antonio Insurance Group, Inc.
(HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
Katy.Brooks@bosainsurance.com www.thebankofsa.com
“Serving the medical community.”
MedPro Group
(HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM
AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com

LASO Health Telemedicine and Rx App (HHH Silver Sponsor)
LASO Health is the industry’s only solution that makes healthcare services accessible, cost-transparent and convenient. Its mission is to reinvent “healthcare” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care. LASO combines an intuitive, mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, onestop-shop, comprehensive health solution.
Ruby Garza, MBA 210-212-2622
RGarza@texaskidneycare.com www.lasohealth.com

Parvis Medical Suites
(HHHH 10K Platinum Sponsor)
Parvus Medical Suites offers a new way to start your own private clinical practice, either full-time or part-time, at a much lower cost than a traditional clinic. We take care of providing well-qualified employees, so that you can focus solely on delivering high-quality patient care. Our turn-key practice spaces in San Antonio and New Braunfels are available for short- and long-term lease options, and come complete with all amenities. Micropractice medicine is revolutionizing independent clinical care.
John Rodriguez, MD Chief Medical Officer 210-632-3411
DrJohn@parvussuites.com www.parvussuites.com
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol
Field Sales Consultant 210-413-8079
Tom.Rosol@henryschein.com www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”

Equality Health (HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination, and hands-on support to optimize practice performance for Medicaid patients in Texas.
Darby Rodriguez Regional Client Executive 281-753-3565
D.Rodriguez@eleosvhs.com www.equalityhealth.com “Reimagining the New Frontier of Value-Based Care.”
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President 210-797-8412
HealthcareLeadersSA@gmail.com
Gary Meyn, LFACHE
Vice President 210-912-0120
GMeyn@vestedbb.com https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor) “Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber President 210-308-7907 (Direct)
KBarber@bdo.com
Valerie Rogler Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Jeannine Ruffner President info4@samgma.org www.samgma.org

Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP® QKA Senior Private Wealth Advisor 512-649-8113 Service@oakwellpwm.com www.oakwellpwm.com
“More Than Just Your Advisor, We’re Your Wealth Management Partner”

Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
Mike DeQuattro
Director of Operations - Texas & New Mexico 210-918-8737
Mike.DeQuattro@favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout. Join us in transforming healthcare delivery, prioritizing your wellbeing and patient care.
Chris Stansbury SVP Growth 816-309-9991
CStansbury@eleosvhs.com www.eleosvhs.com



By Stephen Schutz, MD

The Toyota Tundra is a full-size pickup truck built in America — in San Antonio, actually — and designed to compete with the Chevrolet Silverado and Ford F150. Believe it or not, it has been in continuous production since 1999, and it continues to compete head-to-head with the “big boys.”
It should be noted that, while the Tundra does indeed compete with Ford and Chevy, it has a way to go before it’s, “there.” Here’s what I mean: in 2023, Toyota moved just 125,185 Tundra pickups, while Ford sold over 700,000 F-series trucks and Chevy found buyers for more than 400,000 Silverados, so Toyota has a ways to go before they’re fully competitive with their U.S. competitors. I think that’s because full-size pickup truck buyers are more brand loyal than sedan, SUV or crossover customers, and I’d add that Ford and Chevrolet, along with their dealers, have figured out how to consistently give their pickup buyers what they want.
Interestingly, before Toyota named their large pickup truck the Tundra, it was the T100. Back in the late 1990s they actually planned to name its successor the T150, but Ford objected strenuously, and Toyota switched the name to the Tundra.

Since breaking into the full-size pickup market has historically been difficult for foreign brands — Nissan just discontinued their large Titan after 20 years! — Toyota has been smart and patient.
For starters, they decided to build the Tundra in the United States rather than Japan. And not just the U.S., but Texas. Texas loves fullsize pickup trucks, so manufacturing Tundras in our state was a smart move because many plumbers, home builders, contractors, drywallers, ranchers, farmers, electricians, etc., etc., etc., want to buy a pickup truck that’s built by dudes like them.
It’s worth a minute to give Toyota a tip of the hat here: the popular Toyota Tundra pickup truck is built in San Antonio. How cool is that? They could have picked Dallas or Houston, but they chose our city. Yay!
I’m going to assume that all readers understand that the Tundra is roughly the same size as the aforementioned F150 and Silverado, and has a similar engine and transmission.
The thing about full-size pickups, which is different from most other vehicles, is that they go from similar foundations to almost anything you might want. In other words, once you choose a truck and its


powerplant, each brand will allow you, nee encourage you, to choose among many different options and configurations until you find the truck that’s just right for you. Whether you need something to haul your cattle to market, or a truck that can carry four dudes, lawn mowers, rakes and weed eaters around, or you’re a city slicker who wants a Lexus in the shape of a pickup, Ford, Chevy, Ram and Toyota will sell you what you want, and it’s probably already on the dealer’s lot.
For the record, the Tundra offers three powertrain options, all of which are based on a twin-turbocharged 3.4-liter V-6 engine. In the base SR model, the engine puts out 348HP, higher trim Tundras produce 389HP, and the third option is a 473HP hybrid. All use a nice 10-speed automatic transmission. Tundras equipped with four-wheel drive come with a part-time setup, but there’s no full-time AWD system like those offered in rival trucks.
Driving the Tundra is a pleasant experience because Toyota, like its competitors, focuses on driving comfort, and the long wheelbase and soft-sprung suspension combine to make the Tundra really good on the interstate. So good, in fact, that despite driving for two hours on the highway through a torrential thunderstorm, I felt completely comfortable and safe.
I always think the same thing when I drive a full-size pickup: highway driving is great, tootling around in town is fine and parking sucks.


The Tundra’s interior is nice, and my top-of-the-line press car’s Capstone version featured semi-aniline leather upholstery, walnut interior trim, acoustically laminated side windows and a head-up display. Analog gauges and a small driver-information screen are standard, but higher trim levels like the one I drove include a larger (and better) 12.3-inch digital instrument cluster.
Double Cab Tundras are available with either a 6.5- or 8.1-foot bed while the longer crew cab (CrewMax) can only be had with 5.5- or 6.5foot beds. Opting for the shorter cab won’t affect front-row comfort but reduces rear-seat legroom from 41.6 inches in the CrewMax to just 33.3 in the Double Cab.
The 2024 Toyota Tundra is a really good pickup that, in my opinion, should sell about the same number as Ford and Chevy do. It’s at least as good and adds excellent Toyota quality and resale value to the mix. Plus, it’s made right here in San Antonio, Texas, which is very cool.

Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.



11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Northside Honda
9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Kahlig Auto Group
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson
877-356-0476
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Chris Martinez 210-366-9600
Auto Group
Bluebonnet Chrysler
Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000








Dr. Patrick Ramsey MFM, OB/GYN

