We




















We

















It’s been a while since I sat down to write our magazine’s opening gambit, and to be honest, it has been a struggle. What’s changed in men’s health over those 11 and a half years when I began?
When I look back at editions past of this annual men’s issue, subjects such as PSA reliability, men’s tardiness to deal with health issues, concussion, domestic violence, work-life balance are perennial favourites.
So, yes, it’s definitely a Back to the Future moment with some of these important issues returning yet again in Men’s health 2023. However, we are blessed that technology and collective knowledge has created more precision diagnosis and treatment of prostate cancer – read on, it is a ray of sunshine (p41, p42) and new guidelines (p20) will hopefully make it easier for GPs to guide their patients more securely on this confronting path.
Round x – so many rounds – of the concussion story (p24) sees CTE come out of the shadows and clinicians able to make some educated ‘premortum’ assumptions of who has it and how they developed it. There is still enormous work to be done here in sporting codes which may be too influenced by the rewards of putting on a gladiatorial spectacle than a fair and safe game, but the docs and researchers are on their tails.
There are a lot of health issues to lay men low, not the least of them around issues that challenge their mental health and wellbeing. Is this changing?
I’d like to think so, if based on nothing but the evidence within my own large, male-heavy family. Watching as this circus ages, a remarkably different tone is being struck by the younger generation, particularly around work and wellbeing.
Perhaps watching their elders completely at a loss in their retirement, or delaying health red flags, and relying on the Emu to lift flagging spirits, these younger men are taking a new road. They have life-affirming experiences beyond a job in which they have negotiated adequate flexibility to accommodate being an integral part of their young families’ lives, and have time left over to care for their own health and wellbeing.
This should be celebrated and encouraged but still somehow their endeavours are often judged unreasonably.
Mutual respect – recognising the importance of everyone’s contribution to the working whole as well accepting individual needs – is essential and it will pay out in spades for future generations. What a world that could be!

SYNDICATION AND REPRODUCTION
Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
There are a lot of health issues to lay men low, not the least of them around issues that challenge their mental health and wellbeing. Is this changing?
12 Surgery time tug of war
16 Close-up: Dr Lachlan Henderson

20 Prostate guidelines review

24 Concussion update

LIFESTYLE
54 One Medicine by Dr Matt Morgan
55 Minnie Hodgson – a nurse at war
56 Opera: Otello
57 Wine review: Nikola Estate – Dr Martin Buck
1 Editorial: Celebrating X and Y
– Jan Hallam
4 News & views
8 In brief
28 Helping refugees access WA care

39 Different gaps
– Dr Joe Kosterich
Our cover: Dr Lachlan Henderson
GP Dr Smitha Pillay, from the Balcatta Family Practice, will be able to enjoy the magnificent selection of wines from Singlefile over the winter as the lucky wine winner for May.
This month, Dr Martin Buck tastes some of Nikola Estates’ efforts coming from the beautifully aged vines of the former Houghton vineyard in the Swan Valley. Check out his review on page 57.
To win this month’s wine selection, use the QE code on this page or go to www.mforum.com.au and hit the competitions tab.

PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au


Journalist Eric Martin 08 9203 5222 eric@mforum.com.au
Clinical Editor Dr Joe Kosterich 0417 998 697 joe@mforum.com.au











Marketing Rhiannon Arnold rhiannon@mforum.com.au

Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager

Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory
Andrew Bowyer 08 9203 5222 andrew@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222
Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au OUR
Professor Khattak presented at the 2023 American Society of Clinical Oncology congress in early June, which attracted more than 45,000 attendees. He outlined how survival and disease recurrence rates among people who had high-risk skin cancers (melanomas) removed, improved significantly when an mRNA vaccine tailored to suit an individual’s tumour genetics was added to common immunotherapy treatment.
After 18 months, cancer-free survival among patients who received the vaccine and the immunotherapy treatment was 78.6%, compared to 62.2% of those who only received immunotherapy.
Two years after treatment, 22.4% of patients who had received the vaccine/immunotherapy combination had either died or seen a recurrence of the disease, which rose to 40% for the immunotherapy-only group.
Overall, after an average of two years, those who received the vaccine saw a 44% lower risk of death or melanoma returning to the same area of the body, and a 65% reduction in the risk of death or the cancer returning in a different area of the body.
Changes to working conditions at North Metropolitan Health Service sites have been given the thumbs up by the junior doctors the service hopes to attract and retain.
The Junior Doctor Manifesto, devised by Dr George Eskander and his team, has seen 33 part-time positions created, which as has led to a drop in vacancy rates from 42 positions to nil in February 2023. It has been a remarkable turnaround from a previously stressed junior doctor cohort that saw increasing absenteeism, to a workforce that is enjoying part-time flexibility.

“These part-time opportunities – enshrining a culture of psychological safety, creating a streamlined overtime approval process, embedded leave-taking and implementing a medical workforce on-call, along with a below the line pathway for reporting – have really challenged previous behaviours and traditions within the group,” Dr Eskander said.
“Our doctors are [now] reporting
There was no significant increase in rates of adverse side effects.
The global trial, with the biggest recruitment taking place at Hollywood Private Hospital, may be a herald of things to come in cancer care.
“This is the biggest trial to show treatment improves with an individualised approach — and I think research into personal cancer vaccines is going to increase dramatically after this positive study,” Professor Khattak said.
much greater satisfaction. We increased our retention rate and approved 75% of requests for annual leave within five days and 94% of our interns have renewed their contracts to further their medical careers and, for us, that has had a profound impact on our overall workforce.”
RACGP is calling on changes to referral protocols saying they waste too much of GPs’ precious time.
Too many GP hours are wasted on non-standardised templates, unnecessary naming of specific specialists in referrals, and outdated data-sharing, it says in its submission to the National Health Reform Agreement (NHRA) Addendum 2020-2025 Mid-term Review.
To achieve this, the RACGP said the NHRA review should:
• put an end to hospital named referral requirements, which require GPs to name a specific
specialist for a referral
• support hospitals and other health services to use standardised, secure, interoperable digital systems for data sharing, referral, and discharge between general practices and hospitals
• pilot data-sharing between hospitals and primary care to better identify at-risk patients, reduce low-value care and meet community needs
• set an objective to reduce demand for hospital services through Commonwealth- and state-funded preventative healthcare by GPs, with a future objective to add GP services in hospitals to coordinate care for patients with complex needs and identify and manage preventable admissions.
“These changes would streamline the whole system,” RACGP president Dr Nicole Higgins she said.
continued on Page 8
An mRNA vaccine trial run by leading melanoma expert ECU Professor and Director of the Medical Oncology Clinical Trials unit at FSH Adnan Khattak is showing promising findings.
COVID-19 and diabetes can interact at multiple levels. We know that in patients with existing diabetes the risk of developing COVID-19 is higher, as is the risk of a more severe illness. Also, similar to other viral infections, diabetes may be more difficult to control and require medication changes during an acute COVID-19 infection.
Several recent studies have also shown that some people can also develop type 2 diabetes after COVID-19 infection.
One such study is from Germany and was published in 2022.1 The subjects were from a primary care setting who mostly had mild COVID-19 disease.
The incidence of new diabetes was compared with a control group who had non-COVID-19 acute upper respiratory tract infections. The two groups were matched on a range of factors including sex, age, health insurance coverage, month of disease and comorbidity factors including obesity, hypertension, hyperlipidaemia, myocardial infarction and stroke. Patients with a prior history of diabetes or steroid use were excluded. Each group had a total of almost 36,000 participants.
The COVID-19 group had a 28% higher rate of developing type 2 diabetes compared with the control group. (15.8 vs 12.3 per 1000 personyears). There was no increased rate for other forms of diabetes.
This study is from the US and utilised the databases of the US Department of Veterans Affairs for patient data.
Researchers also compared postacute phase COVID-19 patients (181,000) with a control group who had not contracted SARS-CoV-2 (4.1 million), as well as a historical control group (4.3 million) from a prepandemic era. All members of these groups were free of diabetes before the study and were followed up for a median of 352 days.
By Dr David Deam MBBS, MAACB, FRCPA
Lab: Clayton Speciality: Chemical Pathology
Areas Of Interest: Endocrine Function Testing, Protein Abnormalities, Laboratory Automation
Measures of incident diabetes and antihyperglycaemic use, and a composite of the two outcomes were used to assess the development of diabetes post COVID-19. They reported the results as a hazard ratio and burden per 1000 people at 12 months.
People with COVID-19 exhibited an increased risk (40% higher) than the control group and excess burden (13.46 per 1000 people) of incident diabetes. This was also seen in antihyperglycaemic use with an increased risk (85% higher) than the control group and excess burden (12.35 per 1000 people).
The composite endpoint gave an increased risk (46% higher) than the control group and an excess burden of 18.03 per 1000 people at 12 months. The hazard ratios and burdens increased according to the severity of the acute phase of COVID-19 (whether patients were non-hospitalised, hospitalised or admitted to intensive care).
All the results were consistent in analyses using the historical control as well as the reference category. These are just two of several studies that have shown the link between diabetes and COVID-19. Most of the studies associate COVID-19 with type 2 diabetes and a Scottish study found no increase in type 1 diabetes post COVID-19.3
There are several possible mechanisms by which COVID-19 could increase the incidence of type 2 diabetes. One is by altering the metabolic and hormonal status of post COVID-19 patients which results
in higher blood glucose levels and diabetes, especially in people who are predisposed to the condition. It is also possible that the virus may affect the beta cells of the pancreatic islets and cause disruption of normal insulin production and release. The virus could also result in crossreacting antibodies which could affect the beta cells.
Other factors which also should be considered include any drugs, such as steroids, that may have been used by COVID-19 infected patients, as well as the diet, weight and exercise level of people post COVID-19. We also should not discount the effect of post COVID-19 patients having more medical contact which may increase the pick-up rate of diabetes.
Discussion
As the COVID-19 patients in the above studies were only followed for a relatively short time, further follow-up is needed to determine if the diabetes is just temporary and may resolve or whether it becomes a chronic condition.
Although type 2 diabetes is not likely to be a problem for the vast majority of people who have mild COVID-19 and there are no specific guidelines yet to screen post COVID-19 patients for diabetes, it may be wise to have a high index of suspicion and check for diabetes if there are any features suggestive of diabetes in post COVID-19 patients, especially if they already have risk factors or prediabetes.
References on request



June has been honours month. Here’s roundup of the health professionals who have been honoured: King’s Birthday Honours
Emeritus Professor Carol Bower has been made Companion of the Order of Australia for her eminent service to medical research as a paediatric epidemiologist, particularly in birth defects and early childhood development, to health and welfare through public health initiatives, and to medical education.


Officer of the Order of Australia: Former WA doctor now Deputy CMO Professor Michael Kidd

Member of the Order of Australia: Dr David Blacker for his service to medicine and to neurological research; Assoc. Prof. Rosanna Capolingua for her service to patient care, to medicine, and as a role model to women; Adj. Prof. Dale Fisher, CEO of Silverchain for service to medicine, health care management and nursing; Dr George Galvin for service to military history, to governance in sport and to emergency medicine; Dr Kenneth Whiting for service to paediatric medicine and to neurodevelopmental disorder organisations.
Medal of the Order of Australia: Dr Andrew Davies, the lead of Homeless Healthcare has been recognised for service to medicine and to the community.
The Western Australian of the Year awards has recognised Telethon Kids Institute autism researcher Professor Andrew Whitehouse in the HBF Professions category, and Professor Marcus Atlas, founder of the Ear Science Institute, in the Alcoa Community Award.
Murdoch University’s Professor Elaine Holmes has been elected as fellow to the Australian Academy of Science. She is the director of the Centre for Computational and Systems Medicine at Murdoch’s Health Futures Institute.
Professor Beth Armstrong is the Bunbury-based director of the new Edith Cowan University Department of Rural Health (UDRH) in the South West, which has $17 million federal funding to encourage more graduating health professionals to practise in the region.
continued from Page 4
“GPs should be spending time with their patients, not on navigating long forms and frustrating processes that can be unique to each hospital. It’s not facilitating quality health care, it’s just exporting hospital bureaucracy into general practice.”
WA procedural GP Olga Ward said hospital-specific templates can be clunky, full of boxes to tick, and wasteful of GPs’ time.
“I’m starting to want the Danish system where all the health software across all systems has to, by law, be compatible, communicate and contain all the information and be readily available,” she said. “Imagine how many tests would not have to be endlessly repeated if you could see it all there at once and look up what has gone before.”
Two Perth Children’s Hospital clinicians – oncologist Dr Neha Jain and Dr Fran Gehrmann, a clinical fellow in endocrinology –have been selected to undertake a new PhD pathway program supported by Child and Adolescent Health Service, University of WA, PCH Foundation and Telethon Kids Institute.

Dr Jain will be researching an RNA-based treatment for children with solid tumours, which will aim to target the tumour microenvironment to stop the cancer cells from returning after surgery. Dr Gehrmann will investigate new models of care for children with type 1 diabetes using changes in a child’s Continuous Glucose Monitoring (CGM) data to target personalised treatment.
Both doctors will begin their degree preparation this year, with formal studies to commence in 2024.
A national survey of primary health care (PHC) nurses has shown that their skills are not being used to their full potential often or most of the time. The 2022 survey was conducted by the Australian Primary Health Care Nurse Association (APNA) to the nearly 100,000 nurses.
Other findings include more than half (53%) of underutilised nurses had requested to use more skills or experience; less than 39% successfully negotiated a change; 26% were denied the request with 43% of that group being told it was because there was no financial benefit to their employer.
APNA says with the growing nurse shortage and the exponential rise in chronic disease, it is critical that nurses be empowered to do more to meet the healthcare needs of the nation.
“Nurses are prevented from working independently to their full scope of practice by outdated Medicare billing protocols. Many patients are managed by nurses
continued on Page 8
Refer your public patients to St John of God Mt Lawley Hospital's Restorative Unit to help them regain movement and independence in daily living activities, retain function and reduce deterioration.


Patient admission criteria*:
(Indigenous people with chronic disease and/or complications can be <65 years old)
Low risk of requiring after hours intervention
Recent change in functional status
Be able to benefit from and participate in multidisciplinary therapy
Clear diagnosis and rehabilitation treatment goals, with expectation they will make improvements
Willingness and ability to participate in rehabilitation program and be motivated to achieve goals
*Terms, conditions and exclusion criteria applies
Public admission steps:
Send patient information and history to:
Referral accepted via discussion with rehabilitation assessment nurse, nurse unit manager and consultant
Rehabilitation assessment nurse arranges admission
Admission accepted within office hours
Proud Yamatji Naaguja woman Jenna Greaves – the much-loved Clinical Coordinator & Child-Health Nurse at Aboriginal health service South Coastal Babingurr Mia in Rockingham – as won the 2023 NAIDOC Nursing and Midwifery Award.
Jenna, who is committed to supporting self-empowerment of young Indigenous women and their families at a time that can be particularly challenging, was first motivated to pursue her nursing career as a young patient of the clinic 16 years ago.
“I attended South Coastal Babbingur Mia (BBM) as a young pregnant mum 16 years ago and now here I am as the clinical coordinator and child-health nurse, it really is a full circle.
“Helping my community as a nurse is the most amazing reward in life. I love to be able to help young Aboriginal mums and families be the best possible parents they can be,” she said.
BBM CEO Dr Gill Walker said she
was extremely proud to see Jenna honoured in the NAIDOC Awards 2023 – and was touched that the community of their not-for-profit organisation put Jenna forward for the honour.

“This is the second consecutive NAIDOC Awards honour for our staff here at South Coastal Babbingur Mia” said Dr Walker. “Babbingur Mia came Runner-Up in last year’s Program of the Year.” Babbingur Mia’s Midwife and Aboriginal Health Services offer support during and after pregnancy, by providing in-home and clinic care before the birth, in-home and clinic care after the birth, doctor and hospital appointments, transport and emotional wellbeing.
Preterm babies in WA will benefit from new research findings that show the benefits of different probiotics on infant nutrition.
The work by consultant neonatologist Dr Gayatri Jape will be used to help the most premature babies in the Child and Adolescent Health Service’s neonatal intensive care units at King Edward Memorial Hospital and Perth Children’s Hospital.

Dr Jape completed a randomised controlled trial known as SiMPro as part of her recent PhD award from the University of WA. Her trial looked at the effect of single or three-strain probiotic supplements in extremely premature babies, born at less than 28 weeks gestation.
The trial also examined prevention of necrotising enterocolitis, a disease that contributes to significant death and disability in premature babies, and the impact on timing for the baby to achieve full milk feeds.
“My research compared the use of different probiotics given to our premature babies to maximise their prospects of surviving and thriving through new and improved nutritional options,” Dr Jape said. The three-strain probiotic proved superior with
continued from Page 4
for chronic disease management, lifestyle and self-care support visits, immunisation, dressings, and care coordination catch-ups,” APNA President Karen Booth said.
“The 2023 Federal Budget announced Medicare reforms around a multidisciplinary model of care, which lays the groundwork for structural change, but there is more work to be done. Adequately funded bundled payments for individuals with chronic and complex health issues would allow flexible use of nurses within a multidisciplinary team. Such models free up GP time to focus on the higher level and acute needs of their patients, while the nurse provides support through planned care activities.”
A Monash IVF commissioned poll of more than 500 Australian women aged 28-42 has revealed that many have poor knowledge about men’s fertility. Almost one quarter believed men never experience a decline in fertility, while nearly one in five were unsure at what age male fertility declined (for the record it starts from about the age of 40).
decreased rates of NEC. The babies also achieved better oral nutrition and they moved onto full milk feeds faster.
Following the SiMPro study and strong evidence supporting the use of multi-strain probiotics from other parts of the world, the new probiotic has recently been introduced for routine supplementation in the NICU units at KEMH and PCH for babies born at less than 35 weeks, who are the most vulnerable for developing feed intolerance and NEC.
“My advice to women and men is not to ignore the male biological clock – it does exist, and it too can affect your chances of conceiving a baby. Don’t simply assume the issue lies with the female partner,” said Monash IVF fertility specialist Professor Beverley Vollenhoven.
Monash Professor Rob McLachlan added that while age is a major cause of fertility issues for both men and women, fertility struggles also happen at any age.
“About 30% of problems can be attributed to what we refer to as male factor, which can include blockages in the sperm tubes or poor semen quality of known –especially genetic problems - or unknown cause.”
The promotional campaign to get bowel screening rates up has started as a response to the participation rate dropping to 40.9% of the eligible population down from 43.8%. The latest participation rate (2020-21) is the same as it was in 2015-16 despite almost $20 million invested by the Australian Government in raising awareness of the National Bowel Cancer Screening Program (NBCSP) since 2019. In WA, participation rate was 41.5%
The latest NBCSP report also reveals that colonoscopy wait times exceed the recommended 30 days in every state and territory, with WA recording the lowest of 119 days and Tasmania the highest (235 days), results that negate the benefits of early detection.
Only 15.6% participants were recorded as receiving a colonoscopy within the recommended 30-day time frame following a positive screening result.
According to the report, 6.1 million people aged 50-74 were invited to participate in the NBCSP in 2020-21 and 2.49 million tests were returned. Of those who participated, 76,880 received a positive result.”
Prolific author Helen Milroy – who has many other roles to her name including commissioner with the National Mental Health Commission – has added a new children’s picture book to the bookshelf.
The child and adolescent psychiatrist and proud descendant of the Palyku people of the Pilbara region is the author of the bestselling Backyard series which has been reprinted several times.

Her latest book – Bush Birds – aims to help young readers better observe local birds such as blue wrens, lorikeets and eagles when out for a walk in the bush. It features Helen’s familiar bold illustrations, and marks her sixth book to be published by Fremantle Press.
There were 300 delegates from around the state at Perth Urology Clinic’s sixth urology masterclass, which has been accredited by the RACGP for CPD hours.



The day started with a moving Welcome to Country by Dr Robert Isaacs OAM, and was followed by 18 separate presentations, quizzes, and Q&A sessions. The program included presentations on a wide spectrum of urological conditions from PUC consultants, regular associates Ms Melissa Hadley-Barrett and Dr Ahmed Kazmi, and invited guest speakers Dr Donald Latchem and Dr Duncan McLellan.
Perth Urology Clinic acknowledge the ongoing support of sponsors Ramsay Health Care, St John of God Health, Genesis Care and Icon Cancer Care among others, many of whom have supported the conference since its inception.
A lack of theatre time to do complex surgery is frustrating some Western Australian plastic surgeons, who claim pricing agreements have de-incentivised longer operations.
 By Cathy O’Leary
By Cathy O’Leary
A stoush is developing between surgeons, private hospitals and health insurers over lengthy cosmetic surgery which is increasingly struggling to get theatre time.

Plastic and reconstructive surgeons in some specialties argue their access to theatre space in private hospitals is being reduced because their lengthy procedures are not generating sufficient returns from private insurers.
As a result, privately insured patients, many with painful and progressive medical conditions, are facing tougher hurdles to obtain essential treatment in private hospitals, with waiting lists for protracted surgeries growing every week.
That includes patients needing treatment for invasive skin cancers, the removal of painful breast implants, abdominoplasty, 360-degree body lifts after major weight loss, breast reconstruction after a mastectomy, and surgeries to prevent the progression of lipoedema.
Their concerns have been echoed by several leading professional bodies, including the Australian Society of Aesthetic Plastic Surgeons and the Australian Society of Plastic Surgeons.
Doctors blame the reduced profitability of these surgeries partly on the ranking system which some private health funds use to determine the remuneration hospitals receive from insurers for each procedure.
Banding categories were decided by a National Procedure Banding Committee, consisting of private insurers and hospital representatives.
Doctors cite knee replacements, which are usually a 45- to 60-minute procedure and attract a higher banding and therefore greater remuneration to the hospital than surgery after weight loss, or a breast reconstruction (six to eight hours for a bilateral reconstruction) after a mastectomy.
Australian Society of Aesthetic Plastic Surgeons vice president Dr Amira Sanki said the current system for determining remuneration to hospitals meant their


agreements with private insurers for some procedures – usually involving long hours in a theatre and several days in-hospital after care – were not beneficial enough to them.
Some areas of plastic and reconstructive surgery were increasingly pushed out of the safe settings of private hospitals, she said.
Gastric sleeve operations, which often took 45 minutes and required a relatively short hospital stay, returned $10,500 to hospitals and were generally relatively easy for privately insured patients to access.
On the other hand, the more time-consuming belt lipectomy (also known as a lower body lift) returned $3500 to a hospital and was becoming increasingly difficult for patients to access.
“Hospitals are saying their agreements with private insurers for some procedures are simply not beneficial enough, Dr Sanki said.
“It’s understandable that the hospital has to make these tough measures because hospitals must remain financially viable.
“However, it seems really unfair that patients who have paid their private insurance premiums for years cannot access treatment with a surgeon of their choice in the safe setting of a private hospital.”
Dr Sanki said that in some cases a hospital might only agree to allow
theatre space for some of the lengthy procedures if a patient was admitted as uninsured and paid for all costs out of their own pocket.
She argued that a fairer system would be for all insurer agreements to remunerate hospitals on the basis of time in theatre and hospital after care.
“We currently have a situation whereby a privately insured patient can have gastric sleeve surgery in a private hospital, they then go on to lose a massive amount of weight and need a follow up procedure to remove extensive excess skin but cannot access it,” Dr Sanki said.
“These patients, who have done all they can to improve their health, cannot be expected to live with all that loose skin which creates considerable problems for them.”
Along with blown-out waiting lists, more patients were finding that the surgery they had waited over a year or more for was cancelled at short notice.
In one case – a woman who was booked into a private hospital for a 360-degree body lift, liposuction and multiple hernia repair – was told the day before that her scheduled surgery could not go ahead.
The surgery did go ahead after her surgeon advocated for her, but not without considerable trauma to the South West grandmother who had organised time off work for herself and a family member to support her recovery.
West Perth-based plastic and reconstructive surgeon Dr Adrian Brooks said some essential procedures were at risk of becoming almost extinct.
Up until 2020, he did up to three body lift surgeries a week, whereas now he did one a month in the only hospital that permitted it. And whereas a body lift was generally one procedure, most hospitals now required it to be split into two. This shortened each operation and in-patient stay, but meant two operations for the patient.
continued on Page 14
continued from Page 13
Some abdominoplasty cases were being declined by private hospitals.
“I used to be able to book these patients into any of four private hospitals, now I’m down to one and even then, most patients are declined,” Dr Brooks said.
Australian Society of Plastic Surgeons president

Dr Nicola Dean said reduced equity of access to essential surgical treatment in public and private hospitals was a growing concern.
She said there was inequity in terms of medical rebated procedures in private hospitals, which was partly due to bureaucratic processes.
As an example, many breast cancer patients who have had mastectomies could not access reconstructions as a consequence of private hospital operating lists.
She said a national uniform pricing regulation system for hospitals led by the Commonwealth Health Department could help, as current funding models were not transparent and varied widely.
Several private hospitals in Perth were contacted for comment but they declined or referred Medical Forum to the Australian Private Hospitals Association.
In a statement, the APHA said the National Procedure Banding Committee (NPBC) did not determine the remuneration hospitals received from insurers – only relativities between MBS procedures based on factors including labour, time in theatre, anaesthetics, consumables and specific high cost equipment. Each MBS procedure was placed in a theatre band based on these relativities.
The APHA said the NPBC only made non-binding recommendations which were often ignored by health insurance companies.
“The amount paid to a hospital
for any procedure is ultimately determined by each health insurer. One hospital will receive different payments from different insurers for the same procedure and one insurer will pay different hospitals different amounts for the same procedure,” it said.
HBF’s Executive General Manager Insurance and Health Services

Dr Daniel Heredia told Medical Forum that the bulk of the fund’s contracting was done on a case basis, using the DRG system.
(The Independent Health and Aged Care Pricing Authority publishes the Australian Refined Diagnosis Related Groups (AR-DRG) to calculate public hospital funding on an activity basis, and this is also used in funding agreements between private hospitals and insurers).
Dr Heredia said that while the codes themselves did not change, the weighting did change, based on detailed data from all public and private hospitals, including consumables used for a particular procedure, how long it took, and how long patients stayed in hospital.
“For example, with joint replacements, length of stay keeps dropping, so unsurprisingly, the weight that gets applied to those
procedures is slowly reducing over time,” he said.
“We think that it is a fair system because it’s independent of both the hospitals and the insurer, so as a matter of principle we don’t mess with that.
“Every two or three years when we go to the hospitals, we say that what is non-negotiable for us is that the new contract is on the most recent version of the DRG, because that should represent contemporary practice, recognising that there is a lag of a year or two.
“But that tends to be a point of contention in the negotiations because hospitals like to pick the DRG version that suits their particular cases.
“What is happening, over time, is that with plastic surgery, the newer versions of the DRG system are starting to recognise that these cosmetic procedures do take longer and have more input costs, so what we’re finding is that the cost weight that is attached to a lot of these procedures is higher.
“If hospitals agree to the most recent DRG version, they’ll see an increase in their reimbursement for those procedures, but some hospitals are using very old versions – some 20 years old.”

Dr Heredia said he believed that hospitals should commit to being on the most recent DRG, because that meant they were being paid fairly and for contemporary practice.
“The other thing we would say as a matter of principle is that as a hospital you can’t pick the most profitable procedures, you need to provide a comprehensive service,” he said.
“Breast cancer is a perfect example of that. You can’t just say we want to do the chemotherapy and take out the lesion, but we don’t want to do the reconstructive work because it doesn’t pay as well.
“There are swings and roundabouts in all of this. There are some procedures where we’re paying way more than it actually costs, and there’s others where we might be paying less.
“And what the plastic surgeons are finding is that when you have situations where theatre time is scarce and there’s more demand than supply, hospitals are looking at it and saying ‘we have to make tough decisions and might cut out
things that are not as profitable as others’.
“But you have to look at it as an end-to-end thing – some things make a lot of profit, others don’t.
“And while we try very hard not to mess with the DRG weightings, if there are particular pressure points, hospital operators should raise them with the funders during their contract process. We’re not hearing grumbles from the hospitals – it’s not being raised with us.”
Dr Heredia said it also had to be recognised that because a lot of the procedures in question were cosmetic, when there were scarce resources and limited theatre time, hospitals had to make decisions on urgent versus cosmetic surgery. He predicted some of the cosmetic work would increasingly move into day surgery, or doctor-run type, facilities.
“We’re already seeing that – but I think we’ll see more of them
GenesisCare at Hollywood offers access to radiation oncology consultations, treatment, and access to allied health support services. We offer modern evidence-based techniques and technology combined with compassionate care – aiming to deliver the best possible patient experience and outcomes.
We offer patients:

• Personalised treatment plans, striving for minimal wait times
• Tattoo-free technology
• Access to a wide range of allied health services (including exercise physiology), accommodation, and transportation packages
• For patients who are eligible for Medicare, approximately 80 to 90% of radiation therapy treatment costs are often covered by Medicare rebates

• Private health insurance is not required for radiation therapy
• A multidisciplinary team of supportive clinical professionals
*For radiation treatment patients. Based on patient survey results Oct 2021–2022.
CSAT score 100%
genesiscare.com
done in purely cosmetic surgery facilities to manage that supply and demand,” he said.
Mount Lawley-based plastic and reconstructive surgeon Dr Paul Quinn warned Australia might find itself mimicking situations in other parts of the world, with a proliferation of mini operating theatres attached to a surgeon’s office, or complex surgical procedures being performed in under-resourced small peripheral hospitals or day surgeries.
“Patients who have paid their private health insurance premiums for many years deserve to be treated in a private hospital by surgeons with the appropriate additional 12 years of medical and specialist training,” Dr Quinn said. “A hospital is the most appropriate place for patients to be having surgery of this nature.”

Dr Lachlan Henderson’s time as a GP ha informed his work in medical management, which extends to his recent appointment as CEO of WA-based health insurer HBF.
 By Ara Jansen
By Ara Jansen
A young Lachlan Henderson would have preferred to be an international sports star out on the cricket pitch. But during his much-loved career as a doctor and now medical administrator he has still managed to stay connected to the sport.
Back in Perth after six years in Melbourne, Lachlan has been reacquainting himself with seeing our big blue sky more often.
“I’m home and it’s familiar,” says Lachlan. “I like that I know where I am going in the car. Most of my family and friends live here.”
For the first time in his career, Lachlan is working in the CBD. He’s seeking out his favourite local coffee haunts and sushi bars. One of the first orders of business was putting his toes back in the Indian Ocean. He’s also enjoying having his office out of Tigers territory and being able to barrack for the Eagles in their home state.
Lachlan returned home at the start of the year and took up the position of CEO of one of the largest notfor-profit health funds in Australia – HBF, with $2 billion in revenue. His previous position was Group Chief Executive of Epworth HealthCare, the largest private, not-for-profit hospital group in Victoria with revenue in excess of $900 million, employing more than 7,000 staff across 10 sites. It was also where he saw the group through a pandemic in the most locked down city in the world.

Hailing from a family of school teachers, Lachlan did medicine at UWA, the usual hospital rounds and his first year of residency at Sir Charles Gairdner Hospital and PMH. He worked south of the river as a GP in the 1990s and had no aspirations to move into a management role, though it unexpectedly provided solid grounding for the future.
“GPs get a very broad knowledge across the health system and I was dealing with patients and families for 10 years. That helped me become very aware of how things worked in later roles.
“I had an interest in science and health when I started my degree and it also proved a good introduction to science and people. Over that time, the rise of digital technology has changed things and that has been a transition for those of us who studied in the Eighties and Nineties. The rise of technology in health and what it is going to do for diagnosis and care is changing the role of doctors and hospitals.”
In the mid-90s, Lachlan says WA was one of the first states to take on the corporate GP model and around 1997 he was one of the first GPs to work under a corporate umbrella. While he didn’t know it at the time, the experience of working in a group practice and learning the ropes of its administration gave him a new skills base. It also showed him examples of how to stay in the medical field but move away from being a GP.
This corporate model allowed nondoctor owners into medicine and paved the way for salaried doctors who didn’t run the practice and for related specialties to create onestop shops.
“It was a different model and some GPs might have lost a bit of their autonomy, particularly older GPs.
Just like the corner deli which turned into a shopping centre, there are not many doctors in a house at the end of the street anymore.”
As one of the first GPs working in a corporate practice in the country, those 10 years fostered Lachlan’s interest in the business of health and how organisations run.

The first role he stepped into was as GP Liaison Doctor at St John of God Murdoch, with a little bit of surgical assisting on the side. He was still assuming he would be a GP for part of the time.
“Being a GP was one of the toughest jobs I have done. I admire GPs who continue to work solely in that space. For my sanity I started to do some different things.”
It was with a twinge of regret, but with an eye on the future, Lachlan saw his last patient in April 2007 as he set a course for a career in the business of health. In order to move forward, he needed to supplement his medical qualifications with business knowledge and did a Master of Health Services Management at Monash University – basically a medical MBA. This “gave me more of the language of the business of health”.
“I was a bit of an anomaly going in to running a hospital in my early 40s as people with medical business backgrounds usually do it earlier.”
Subsequent roles included being Executive Director Perth Northern Hospitals at St John of God Health Care and General Manager at the Mount Hospital. He’s also held a variety of university and board appointments, including President of the Australian Private Hospitals Association (APHA) and was a board member for SwanCare.
Lachlan says having been a doctor helped moving into hospital management because “having been a doctor now in these roles, you have knowledge about how it is to be a patient navigating a hospital and how to co-ordinate their care.
“Plus, I think working in a hospital with a medical background gives you more credibility in the role. You understand the language and can talk to people in their language.
“I think it has allowed me to use some of the medical and tech skills I
continued on Page 19
•
•


continued from Page 17
have learnt, along with a reasonable aptitude with people I needed as a GP, to translate that to solve bigger problems in more complex organisations.”
Having worked for a number of not-for-profits, of which HBF is one, Lachlan says he’s found his niche.
“Doctors are big on making decisions based on evidence and my mantra is making decisions based on evidence. I think I’m relatively consistent with that. In some of the roles I have taken on, where big decisions have to be made and a lot of people impacted, hopefully I have brought a calmness in dealing with people and an empathetic attitude.”
Lachlan describes himself as “pretty competitive” and a man who likes to achieve things. In the organisations he runs, he wants to do right by people, while making the business grow. Equally his jobs require that ever delicate balance of people with a financial imperative to grow or expand.
“Working in hospitals is all about the patients. If I was in a business conversation, I was always thinking what is the impact on the person who is going to receive the care. That’s always the natural tension –how do you provide care and how does that assist the business.”
Lachlan and his wife Cathy have three children in their 20s – Anna, Ollie and Laura. The pair were in the same year of medical school and she went on to become a child psychiatrist. They married soon after completing their studies.
“We chose medical careers that work pretty well with family. I grew up with a lot of people who had medical parents and they were often the absent seat at the table. Cathy sacrificed more of her career in having children at the same time as getting specialist qualifications.”
A lover of many sports, cricket and AFL are his favourites. Lachlan played cricket growing up – the “main sporting interest which kept me going” – which included University Cricket Club and A Grade district cricket in his 20s, until family became a priority. He’ll

also tell you a lack of ability halted any further progression.
At one point in his studies, Lachlan thought about aligning cricket and medicine but found in general practice he was doing plenty of sports medicine anyway. He holds a Certificate in Sports Medicine.
While not getting to play much while he was raising his family and back studying, he kept close to cricket in roles such as being Chairman and board member of the WACA for just over three years before heading to Melbourne. He was then appointed to the board of Cricket Australia, becoming Chair of the Board of Directors in February 2022 before retiring from the position on starting at HBF.
“It was a fun 12 months and a busy role. I got to see a good amount of cricket and travelled to the UK and India as well. I encourage people
in executive positions to have roles outside what they do. It gives you a lens on people and another organisation as well as a different perspective on leadership.”
He likes to run and pool swim for health and fitness and is a “very average” golfer. Working in health helps you keep an eye on your own wellbeing, he says. He has always kept fit and uses sport as a way to unwind after a busy work day. While living in Melbourne he was also a member of a book club of blokes and joins remotely when he can.
A traveller, reader and music lover, Lachlan also enjoys a variety of styles from pop to classical and has kept an ear on current hits and trends through his kids, this year seeing Harry Styles and Ed Sheeran live.
The next 20 years will see an estimated 600,000 men be treated for prostate cancer. The current review of national guidelines aims make their outcomes more favourable and the journey less confusing.
Eric Martin reportsA diagnosis of prostate cancer was a life-altering discovery for more than 24,000 men last year, one which set off a chain of events involving rounds of testing, treatment, and what could have been significant side effects for the patient and their family.
Potentially, just as concerning for the diagnosing clinician, was the question of whether to launch the patient on that journey, especially if they were an older person, as well as wondering if they might have found the lump earlier with a digital rectal examination (DRE), which was dropped from the Australian screening guidelines at the end of 2015, causing uncertainty for GPs and patients in the process.
The other issue raised by specialists was that the reliance on PSA testing was resulting in overdiagnosis and overtreatment, which according to the Australian Institute of Health and Welfare (AIHW) peaked during the mid to late 2000s – after the 2002 decision to reduce the PSA threshold for a prostate biopsy referral.
In addition, false-positive test results were common with PSA screening and US research suggested that only 25% of people who had a prostate biopsy due to an elevated PSA level were found to have prostate cancer.
While the 2016 guidelines helped address these concerns, reducing the potential risk of misdiagnosis or over-treating prostate cancers that posed minimal risk, further confusion was added that year with the emergence of a large, Australian-led, international study that called the whole screening process into question.
Screening for prostate cancer, an international, a systemic review of best practice, led by Monash University’s Department of Epidemiology & Preventive Medicine, examined the entire data set generated by the UK’s randomised controlled trials (RCTs) and found that prostate cancer screening did not significantly decrease prostate cancer-specific mortality.
“Only one study reported a 21% significant reduction of prostate cancer-specific mortality in a pre-specified subgroup of men aged 55 to 69 years, and pooled data currently demonstrates no significant reduction in prostate cancer-specific and overall mortality,” the authors reported.
“Any reduction in prostate cancerspecific mortality may take up to 10 years to accrue; therefore, men who have a life expectancy less than 10 to 15 years should be informed that screening for prostate cancer is unlikely to be beneficial.
“Men should be informed of this and the demonstrated adverse effects when they are deciding whether to undertake screening for prostate cancer,” – a recommendation echoed in the Australian guidelines. However, the risk of missing or delaying the diagnosis could be worse.
According to one recent UK study, prostate cancer was found to have a missed or delayed diagnosis (despite red-flag symptoms) in 2.4% to 13.8% of cases, with a severity-weighted serious harm rate per diagnostic error of 52.2%.
With these things in mind, the Federal Government commissioned the Prostate Cancer Foundation of Australia (PCFA) to review the national guidelines at the end of 2022, a process being co-Chaired by Professor Jeff Dunn – PCFA’s
Chief of Mission Head of Research and President of the Union for International Cancer Control – and Adjunct Professor Peter Heathcote, a past president of the Urological Society of Australia and New Zealand.


Medical Forum spoke with both men as well as the PCFA’s CEO, Ms Anne Savage, to discuss the progression of the two-year review, some of the issues revealed by the process, and examine the advances in research and treatment that will inform the new guidelines.
“Chief among our aims is to harmonise testing protocols, ensuring full alignment between GP practice and relevant areas of implementation, such as MBS item numbers and a uniform model for measuring and reporting pathology thresholds for PSA levels,” she said.
“Currently, the guidelines recommend PSA testing every two years for men over the ages of 40/45 with a strong family history of the disease and/or symptoms, and asymptomatic men between the ages of 50 and 69, with no PSA testing for men over the age of 70 on the basis that the ‘harms may outweigh the benefits.’
“However, the risks of overdiagnosis have almost entirely been mitigated and the 2016 guidelines are now out of step with current evidence and practice and require review: data supporting PSA testing has matured, reinforcing long-term significant survival advantages with appropriately utilised PSA testing.
“In addition, there have been substantial changes in practice with a paradigm shift in prostate cancer diagnosis and treatment pathways which have reduced the risks associated with PSA testing, as well as significant advances in prostate cancer diagnosis, staging and management, which must be incorporated in a revised set of guidelines.”
Several of the previous concerns regarding the harm of
PSA testing are now mitigated with “risk stratified” PSA testing strategies, whereby the shortcomings of ineffectively performed PSA testing programs have been identified.
For example, the Chinese Prostate Cancer Consortium published research in 2021 which showed that by adjusting the prostate-specific antigen density (PSAD) they were able to detect nearly 89% of prostate cancers, avoiding the need for biopsies in 20.2% of patients.
Likewise, the introduction of multiparametric Prostate Magnetic Resonance Imaging (mpMRI) has reduced unnecessary prostate biopsies and the detection of clinically insignificant prostate cancers, and advances in biopsy techniques (including transperineal biopsies and MRI fusion) have increased clinically significant prostate cancer detection.
These techniques have also reduced the morbidity associated with biopsy.
“Australia has among the highest rates of prostate cancer in the world yet the prospects for survivorship are excellent, with five-year relative survival increasing from 63% in the late 1980s to 95.5% today - which is why we should be making the case even more strongly for testing,” Professor Heathcote said.
“The guideline review is Australia’s opportunity to become a world leader. Most importantly, it is a chance to save men’s lives, and to save thousands of families from the pain of a prostate cancer diagnosis.”
There are just over 89,000 men currently living in Australia who were diagnosed with prostate cancer in the past five years, and while detailed national data on the impact of treatment is unavailable, the Life After Prostate Cancer Diagnosis (LAPCD) study, part of the UK’s Prostate Cancer Outcomes program, investigated the quality of survival of more than 35,000 men from the UK dealing with the same situation – living 18-42 months after diagnosis of prostate cancer –between October 2015 and January 2018.
continued on Page 23
Enabling eligible HBF members* access to fully covered rehabilitation treatment at home following surgery for a joint replacement or fracture.
About Rehab in the Home:
Fully covered for eligible HBF members*
Eligible HBF members* can access the service at no additional cost when delivered by Life Ready Mobile.
Comfortable, private and convenient for patients
This service enables patients to recover in the privacy and familiarity of their own home with a personal and medical support network, instead of staying in a clinical setting. Exercises are practical and tailored to the member’s home environment.

Range of rehabilitation services offered
Physio, nursing, occupational therapy with consultation of a rehab physician.
As soon as the patient is admitted to hospital, the Life Ready Mobile team can carry out an eligibility check.
continued from Page 21
Men were asked to rate their overall health on a scale of 0-100 and while the average self-assessed health score was 76.6, participants commonly reported problems with pain and discomfort (42%), usual activities (37.7%), mobility (36.1%), anxiety/depression (33.6%), and self-care (14.3%), with 62% of men reporting at least one of these issues.
While high functional outcome scores indicated positive results for bowel function (89%), urinary irritation (86%) and urinary incontinence (82.7%), sexual function scores averaged just 25.2% and nearly half of respondents (45.3%) experienced moderate to severe problems.
Most prostate cancer treatments carry the risk of infertility, but erection problems are a common side effect of surgery, radiation and hormone therapy and many men “may not be able to have or maintain an erection firm enough for sexual penetration.
“In those men experiencing psychological distress following diagnosis and treatment, contributing factors centred around a theme of loss: loss of self (identity, masculinity, selfconfidence); loss of function (sexual, urinary, bowel); loss of connection (partner, family and friends) and loss of control (over lives and future),” the study noted.
“Follow up interviews found that little changed for most men over 12 months with regards to the problems they faced, and while some became increasingly resigned to them, or found co-morbidities became more important, for others the physical and psychological impact of unresolved problems remained undiminished.”
The UK study also found that men's experiences of decision-making about possible treatment pathways with their doctor differed greatly.
“Where clinicians promoted a shared approach to decisionmaking, men generally reported feeling comfortable with their treatment decisions,” the authors said.
“However, respondents often undertook greater responsibility for deciding their treatment pathway than they desired, often reporting that no clinical recommendations were offered or that they received conflicting recommendations.”
Professor Heathcote (right) urged better tools for clinicians so they could confidently discuss PSA testing with their patients.
“Managing how we communicate with patients about screening and the discovery of low-risk cancers where active surveillance may be the best option,” he said.
He explained that the benefits of testing have been further strengthened by a recently published long-term data follow-up from the European Randomised study of Screening for Prostate Cancer (ERSPC) trial, which revealed a significant population survival advantage from appropriately performed PSA testing programs.
Similarly, the LAPCD study found that while most men (58.0%) still received a diagnosis of prostate cancer after attending their GP with symptoms, a third of men (33.9%) were now diagnosed without symptoms after receiving a PSA test.
“Taking what we have learned from large-scale studies in Europe showing the benefit of using the PSA test to screen selected asymptomatic men, we can reduce the burden of prostate cancer on Australian men, their families and the healthcare system,” Professor Heathcote said.
Cancer Australia found that only
36% of prostate cancers are detected at Stage I in Australia, most (46%) are detected at Stage II, 11% are detected at Stage III, and 4% are detected at Stage IV.
“Yet research has found that 98% of Australians support the introduction of reminders for eligible men to get tested,” Professor Dunn said.
“In terms of the potential harms of treatment itself, improved staging (such as with PSMA Positron Emission Tomographic scans) has ensured optimised treatment plans and improvements in surgical and radiation techniques have resulted in lower treatment-related sideeffects and morbidity.
“Estimates suggest that over 600,000 Australian men will be diagnosed with prostate cancer between 2020 and 2044, and 116,385 men will die from the disease. We can save many lives if we simply detect the disease earlier and new guidelines will help us do that.”
“Consumers will be involved at all stages of the review and their voices will be reflected in a refreshed set of recommendations for clinicians and consumers,” Ms Savage said.
“Following publication of our findings, our highest priority will be awareness and education, to ensure the guidelines are observed, and in the interim, PCFA has endorsed the USANZ Position Statement on PSA Testing.”
ED: See our clinical section for prostate updates

How can GPs play a better role in the management of concussion and information regarding CTE?
 Suzanne Harrison reports
Suzanne Harrison reports
When Barry Beecroft first started playing professional football for South Melbourne in the early 1970s, he and his teammates were regularly concussed on the oval – and simply kept on playing.
At the time there was “zero” concern about concussion, Beecroft now says from his North Fremantle home.
“I could get knocked out cold about three or four times, a game,” he says of his early days with South Melbourne, later Claremont Football Club (prior to the Eagles) and also with the Sydney Swans.
“Someone might say, ‘you OK, Barry?’ You’d feel a bit strange for half an hour or so, and then feel fine. But you’d keep on playing. I recollect one time being knocked out early in my career and a trainer came out with smelling salts and they got me going again. You didn’t want to lose your position in the team.”
In those days of elite AFL, there were no cameras and only two umpires (now there are four) meaning players had a greater likelihood of getting away with dangerous tackles or deliberate violence. And if you stopped playing due to injury, you either didn’t get paid or your salary was reduced.
“We never stopped playing or missed a week after being knocked out,” he says.
However, Beecroft – who still works out daily and remains fit – feels he is one of the lucky ones. After retiring from football in the late 1980s, he enjoyed a successful career as a senior corporate executive and has not suffered from any of the common symptoms associated with head trauma, nor have his former teammates.
But for many others, it’s a different story. In recent years, awareness of chronic traumatic encephalopathy (CTE) has become much more widespread, partly due to the deaths of high-profile sporting personalities around the world, alongside dogged research, initially from the US.
A degenerative brain disease, CTE is caused by the kind of repetitive brain trauma seen in contact sports. It can only be diagnosed postmortem, yet for many, symptoms such as poor impulse control, depression, anxiety, insomnia, aggression and severe headaches, have led to dire consequences.
Danny Frawley, for example, played 240 senior AFL matches for St Kilda between 1984 and 1995. The former Richmond senior coach died in 2019 aged 56. A post-mortem examination of his brain found he was suffering from CTE.

In 2022, it was reported that a post-mortem following the death at aged just 49 of former NRL player and coach, Paul Green, showed he suffered from one of most “severe forms” of pure CTE the neurologist had seen, a disease that would have affected his decision-making and impulse control.
In February last year, the Medical Journal of Australia announced findings that twelve of 21 brains donated by sports players prone to repetitive head injury and assessed by the Australian Sports Brain Bank, were found to have CTE. All but one brain showed some form of neurodegeneration.
The problem is widespread in the US. According to the Boston University CTE Research Centre, the repeated brain trauma (within some sports) triggers progressive degeneration of the brain tissue, including the build-up of a protein called tau in a unique pattern. The pattern of tau seen in the brains of those with CTE is distinct from other neurodegenerative diseases such as Alzheimer’s disease.
“These changes in the brain can begin months, years, or even decades after the last brain trauma or end of active athletic involvement,” the Boston centre states.
The centre’s researchers reported in February this year that they have now diagnosed CTE in the brains of 345 of 376 (91.7%) of NFL players studied.
In Australia, Dr Sarah Hellewell, senior research fellow in neurotrauma at Curtin University, says that at present, CTE is a terminal diagnosis, meaning it can only be definitively diagnosed post-mortem by the presence of hyperphosphorylated tau, deep in the sulci of the brain. It’s the symptoms that need to be more widely understood.

These symptoms may be cognitive, including memory and attention difficulties and poor impulse control. They can be somatic, including headaches, dizziness, sensitivity to light and noise; moodrelated, including depression, anxiety and irritability; or related to sleep, including fatigue, insomnia or sleeping too much.
“There are many symptoms of CTE in the living, and this is part of the difficulty with a living diagnosis,
because symptoms may be different for different people, and aren’t static from one day to the next. This means that diagnostic criteria have been hard to agree on,” Dr Hellewell said.
Earlier this year, the Royal Australian College of GPs (RACGP) submitted to a 2023 Senate inquiry into concussions and repeated head trauma in contact sports.
“This submission, among other things, urged for adaptation of rules to prevent concussions from occurring, highlighted the need for consistency in player safety and decisions regarding return to play, and reiterated the need for funding into research on long-term consequences of head injury,” Dr Hellewell said.
Attitudes to concussion have improved substantially, but while sporting, medical and community groups now take it much more seriously than in Beecroft’s playing days – indeed the overall wellbeing of players –there is still a way to go when it comes to CTE.
It’s no news to players such as Beecroft, but Dr Hellwell says that even as recently as a decade or two ago, concussion was seen almost as a badge of honour, par for the course when playing tough and being strong and fearless, “and the symptoms and consequences were ignored or minimised for fear of seeming weak”.
Researchers, she says, didn’t focus much attention on concussion because the traditional thinking was that everyone recovered well in a matter of days or weeks. Similarly, GPs sent concussed patients home with instructions to rest, and rarely followed them up. Part of the difficulty was the long time between head injuries and the onset of neurodegenerative symptoms – often decades – which made it difficult to link a history of sports concussion to symptoms later in life.
“Now we know better. We have evidence of long-term pathology in the brains of former contact sports players, and we know concussion is a risk factor for several neurodegenerative diseases,” Dr Hellewell adds.
continued on Page 26
continued from Page 25
“High profile sportspeople and their families have brought community attention to these issues, and we have reached a certain point that it has now become too difficult to ignore. Governments and sporting bodies are beginning to listen to calls for change in the prevention, diagnosis and long-term management of concussion.”
As for how GPs can deal with the ongoing problem, Dr Hellewell says there are a number of things that can be done to improve the care of people presenting with concussion.
“The most important thing is to ensure their knowledge is up-todate on concussion management and recovery,” she says. “While we used to tell people to sit in a darkened room until they were no longer symptomatic, evidence now suggests that light exercise can speed up recovery and help to mitigate symptoms for many people with concussion.
GPs could also consider information provided to patients about recovery: reassuring them that it is common to be symptomatic for several days or weeks, and that recovery can be different for everyone, she adds. Consider providing this information in written form, as patients may be confused and have difficulty remembering instructions. In future consultations with a patient with a history of concussion, Dr Hellewell suggests GPs should be alert for symptoms which may have persisted or developed since the injury, particularly those relating to mental ill health, headaches and cognitive decline.
At the time of the submission to the Senate inquiry earlier this year, RACGP president Dr Nicole Higgins called for stronger action.

“More can and should be done to prevent the damage caused by concussions
and head trauma,” she said. “We are learning more and more about the management of prolonged concussion symptoms, such as post-concussion syndrome and suspected CTE, which many people may recognise from an increasing number of concerning media reports following the deaths of sports stars.
“CTE must be taken extremely seriously. It isn’t just something that we need to worry about in adult sport, damage to the brain can happen at an early age, whenever there are repeated knocks to the head.”
GPs, Dr Higgins stresses, play a vital role, and with greater support, can do even more to help patients.
“We are the ones often required to assess and provide clearance for patients to return to play following a concussion, such as a local footy player or netballer who has received a knock to the head. This includes
balance, memory and cognitive testing and ensuring the patient does not experience recurring symptoms when exercising.”
Improvements to the current model could be longer GP consults, providing an opportunity for GPs to take the time to assess and address any issues. She said that GPs needed to know what they were dealing with.
“There is insufficient evidence to fully understand and determine the long-term impacts of concussion and repeated head trauma, and we also need to clarify and standardise the definition of concussion,” she said.
“In addition, the development of an Australian-wide concussion registry will provide a valuable source of data to determine the longterm impacts of concussion and repeated head trauma. First aiders at sporting venues should have access to specific training about head injury and concussion too, particularly in amateur and social leagues where a qualified health-

care worker is less likely to be there to help.”
Many ask about the efficacy of helmets in sports such as rugby. When asked about these as a form of prevention, Dr Hellewell concurs with other global research.
“An increasing body of evidence suggests that helmets don’t protect the brain from concussion,” she said. “This is because concussion, and particularly sports concussion, usually has an element of head rotation during the fall or hit to the head or body. This rapid rotation, while the head accelerates downwards, is likely to account for much of the pathology and symptoms of concussion, and head gear won’t prevent that.”
There is even evidence, she says, from American gridiron that the sport adapted with the introduction of helmets, with the helmets being used as ramming weapons in the misguided belief that the head would be protected.
It may come as no surprise that such measures are in their early stages. The history of concussion’s longterm effects and CTE is very new.
According to the US-based group Concussion Legacy (CLF), CTE was first described in 1928 when Dr Harrison Martland characterised a group of boxers as having ‘punch drunk syndrome.’
CLF explains on its site that over the next 75 years, several researchers reported similar findings in boxers and other victims of brain trauma, but fewer than 50 cases were confirmed. Then in 2005, pathologist Bennet Omalu published the first evidence of CTE in an American football player: former Pittsburgh Steeler Mike Webster.

“The publication caught the attention of CLF co-founder Dr Chris Nowinski, who envisioned the world’s first athlete brain bank. Nowinski began reaching out to the families of former NFL players and other athletes who had recently died to arrange brain donations.”
CLF goes on to say that he and Dr Robert Cantu soon founded the CLF and partnered with Boston University and the US Department of Veterans Affairs to form the UNITE Brain Bank, which has now
studied the brains of more than 1,300 athletes and veterans.
As for Beecroft, he believes football has come a long way and is supportive for his nine-yearold grandson to play the game, a sport which – coincidentally – his grandson has shown signs of being pretty good at.
“They really look after them now,” Beecroft says, “These days, there’s protocols with concussion. It’s 3000% better than when I was playing. I have no problem with my grandson playing.”
That said, there are still improvements to be made when it comes to how GPs engage with patients about ongoing care following from a concussion, and how parents can monitor their children. Dr Hellwell recommends a number of free resources and training courses for GPs and the community online, such as Connectivity Traumatic Brain Injury Australia.
For more information about CTE, visit https://www.brainbank.org.au/ cte-research/
For the thousands of refugees and humanitarian entrants who enter Australia each year, there are many health issues they may be experiencing, ranging from physical to psychological and emotional.
Recent statistics show that up until this year, 950,000 refugee and humanitarian entrants have arrived in Australia since World War II and most recently they have come from war-torn or poverty-stricken communities in countries including Afghanistan, Iran, Syria, Myanmar, Ukraine, South Sudan, Venezuela and Guatemala.
Many refugees have experienced the trauma of war, conflict, poverty, economic crisis, food insecurity, family or community separation or isolation, political unrest, persecution or torture. As a result, refugees are likely to be at higher risk of psychological disorders including depression, anxiety and post-traumatic stress disorder (PTSD).
There is also higher prevalence of unmanaged chronic health conditions, noncommunicable diseases, infectious diseases, under-immunisation, poor dental
and optical health and higher rates of nutritional deficiencies among refugees.
According to the RACGP, culturally sensitive and accessible health care that’s conscious of refugee and migrant challenges is critical for their wellbeing and safety.
Health literacy can be low among refugees, who may have had limited access to stable health care or education. Given their circumstances and diverse cultural backgrounds, refugees may have

GPs play a critical role in ensuring refugees have access to patient-centred and culturally receptive health care.
Kathy Skantzos reports
altered perceptions of abuse, trauma, nutrition, reproductive health, sexual health, chronic disease and immunisation.
Research indicates that refugees may be reluctant to share mental or physical health concerns with medical professionals for cultural or personal reasons or associated stigma.
RACGP WA chair Dr Ramya Raman says care and sensitivity is required when assessing the health of refugees, particularly with trauma-related health concerns such as domestic violence, sexual violence and PTSD.

“Dealing with health issues with these patients requires very careful inquiry and it needs to be culturally sensitive,” Dr Raman tells Medical Forum
“It’s about understanding their cultural background, and Eastern cultural values will be very different to Western. As a treating doctor or GP, what we may recognise as a potential concern may not be a concern for the patient and we have to find a common ground.”
While GPs can reach out to the refugee health unit at their local hospital, or units within the tertiary hospitals, as well as at Perth Children’s Hospital for paediatric care, there are resources and support services at arm’s length to guide doctors through patient assessments.
HealthPathways WA is a comprehensive resource providing guidance for clinicians to assess and manage refugee patient health through a range of primary, community and acute health assessment pathways.
Refugees and humanitarian entrants who have arrived in Australia within the past 12 months are eligible for an MBS refugee health assessment for their physical, psychological and social functioning, and whether preventive health care and education should be offered to improve their health.
RACGP’s refugee health assessment template is a useful tool to help GPs complete the MBS refugee health assessment,
while also being a helpful general resource to assess the health of refugee children, adolescents and adults.
Translation and interpreting services are also available.
“Doctors should not hesitate to use an interpreter, whether face-toface or over the phone to ensure the consultations are robust,” Dr Raman says.
While it may be convenient for a patient’s family or children to interpret for them, it is advised to use an interpreter where possible due to confidentiality in medical assessments and to take the responsibility off family members.
Refugee children, teenagers and their primary carers can be referred to CAHS’ refugee health service (RHS), while the Humanitarian Entrant Health Service (HEHS) can link patients with community GPs. It also provides a holistic health assessment service for refugees and humanitarian entrants who are resettled in WA under the Australian Government’s Humanitarian Program and Special Humanitarian Program.
CAHS RHS is based with WA’s community Refugee Health Team, working alongside a multidisciplinary team of medical specialists, nurses, dietitians, social workers, clinical psychologists, dentists and special needs educators at PCH, assisted by professional interpreters.
The Refugee Health Team helps young refugees and their families, who have limited English language skills, transition to mainstream health services. Patients are assessed using a family-centred, evidence-based, culturally appropriate and trauma-informed approach, incorporating a review of medical, neurodevelopmental, educational, psychological and socio-economic domains.
Preventative health for both women and men should be prioritised to prevent risk factors, such as cardiovascular disease and diabetes, while undermanaged chronic health conditions should be screened for.
GPs should also screen for cancers, such as bowel and breast cancers, and consider the patient’s family history of any other conditions and chronic diseases.
“Certain ethnic populations are at a higher risk of developing diabetes and cardiovascular risk factors and heart disease, so it needs to be addressed,” Dr Raman says.
“Also, nutritional concerns and dietary deficiencies can be present, depending on where the patients are from. In certain populations we see conditions like rickets and poor bone health in kids.”
It is common to see nutritional deficiencies such as vitamin B, vitamin D, calcium and iron. Gastrointestinal symptoms can often be present as well.
“We often check for helicobacter pylori. Certain groups of patients are at a higher risk because it is endemic in some regions, so it’s important to test and look out for symptoms,” she says.
“A lot of children and some older patients tend to complain about abdominal discomfort, so we need to think about constipation and the underlying cause of that.”
Infectious diseases, such as STIs, hepatitis B and C, HIV, syphilis, and tuberculosis, are also common.
“It’s important to think through considerations for tuberculosis and taking sexual health history and screening, of course with consent,” Dr Raman says.
Testing for parasitic infections such as malaria should also be considered, depending on the patient’s geographical risk.
Dental care, eye health, and foot care are all important to monitor as well, to ensure healthy teeth, eyes and feet, and reduce associated risks, since visual, dental and audiological issues are common and undertreated in refugee populations.
Mental health and psychological distress can often be present as Dr Raman says they have most likely gone through a very traumatic time. However, there is often stigma and altered perceptions about mental health within refugee communities.
continued on Page 31



At Perth Radiological Clinic your prostate MRI investigations are reported locally by Perth Radiological Clinic’s team of fellowship trained prostate MRI experts.
• Always available to discuss imaging requirements for your prostate patients.
• Teaching hospital consultant radiologist appointments.




• Involved in public and private multidisciplinary team meetings including Fiona Stanley Hospital, Royal Perth Hospital, Joondalup Health Campus and Midland Health Campus.
Visit our new website perthradclinic.com.au
Please contact your customer relations team for more information or email assist@perthradclinic.com.au

continued from Page 29
“The incidence of PTSD of survivors of torture and trauma is quite high, so it is important to think through the implications of stigma around mental illness in certain cultural communities. It’s important that it is addressed and in a sensitive matter,” Dr Raman says.
Psychological and mental health screening spans all the way from the paediatric population to the geriatric population, no matter where they are in their stage of life.
GPs can refer patients to Association for Services to Torture and Trauma Survivors (ASeTTS), a specialised service providing holistic care and counselling for survivors of torture and trauma.
A key area for GPs to be aware of and screen for with a high degree of sensitivity is domestic violence.
“Patients from migrant and refugee backgrounds can be hesitant to disclose some of the experiences of family abuse and violence,” Dr Raman says. “That could be due to cultural reasons, and it also depends on who’s at home with them, and whether they consider what is happening to be a type of family domestic violence.
“Because of their level of health literacy, they may not even realise that is what’s going on.”
Dr Raman points to the RACGP White Book 5th edition chapter on ‘Working with migrants and refugee communities’ to help guide clinicians to provide a safe pathway for migrants and refugees who are experiencing family or domestic violence in the home.
“It provides important and practical information for GPs and specialists in terms of managing patients from culturally and diverse backgrounds, specifically screening for possibility of domestic violence,” Dr Raman says.
“It’s been shown that it’s mostly women who have been affected from domestic violence. When we think about family domestic violence there’s physical abuse, sexual abuse, emotional abuse, and financial abuse, and there are concerns around children,” she says.
“Some people of migrant and refugee backgrounds may be quite hesitant to disclose their experiences of family abuse and domestic violence due to cultural differences or potentially language or level of health literacy.”
GPs should also consult women on their sexual and reproductive health and give them options for contraception, while being culturally sensitive of their choices.
Gynaecological issues are typically underreported in women, and female genital cutting/mutilation (FGC/M) is still prevalent in many countries of origin. The HealthPathways WA Female Genital Cutting / Mutilation (FGC/M) Pathway is available for clinical guidance.
ECU Professor Loretta Baldassar, lead researcher of BEFRIENDING with GENIE, a governmentfunded research project to increase social support and service access for people living with dementia and caregivers from culturally and linguistically diverse communities, says dementia is a key issue for migrant Australians, with one in three people currently living with dementia in Australia born overseas.

“People from migrant backgrounds living with dementia, and their caregivers, often have less knowledge about, access to, and uptake of medical and health services, including prevention activities that support their social interaction,” Professor Baldassar says.
“This can put them at increased risk of significantly reduced social connection and isolation, which in turn increases their risk of disease and mortality.
“Family caregivers from migrant backgrounds often have the additional care burden of managing English language and other cultural barriers to service access for themselves and their loved ones,” she adds.
Dr Raman points to the 'Multiculturalism in aged care'
chapter in the RACGP aged care clinical guide, also known as the Silver Book, which explains that many older people from refugee backgrounds have had poor or no prior access to health care before arriving in Australia. Undiagnosed and undertreated chronic illnesses are common, such as diabetes, hypertension, osteoarthritis, chronic obstructive pulmonary disease.
High rates of PTSD are seen in those who have experienced war, imprisonment, torture and dislocation, including older refugees. However, stigma surrounding mental illness in many refugee communities may strongly affect an elderly person’s engagement with assessment and treatment, according to the Silver Book.
Health professionals should also consider social isolation among older migrants with the transition from rural, village life with close-knit communities and large families often living under one roof where elders played a central role, to a drastic social change when living in Australia.
Dr Raman says that taking time with people is key.
“The benefits of being a GP is you don’t just see that patient that single time for a single issue, you get to learn about that patient over time, whether it’s physical, mental health, their social circumstances and helping them through that, and in addition we end up seeing their family members as well,” Dr Raman says.
“It’s important to keep in mind that cultural, religion and settlement experiences influence perceptions of health care, and working together with an open mind and knowing about the services that you can call on for help if you need it.”


The benefits of regular exercise are well established. It can prevent or improve all the major risk factors that contribute to cardiovascular disease (CVD), including hypertension, diabetes, central adiposity and dyslipidaemia. Exercise also has significant benefits for mental health disorders, which are common but often ignored contributors to CVD.
Atherosclerotic coronary disease is the predominant cause of exerciserelated cardiac events in people aged 35 years and over. Although relatively rare, exercise may trigger sudden cardiac arrest and death in individuals with underlying coronary artery disease (either clinically known or not), particularly those who were previously sedentary, or have advanced disease.
For patients with known coronary disease, a cardiac event can occur on average once in every 62,000 hours of exercise. Importantly, the risk of a cardiac event is significantly lower among regular exercisers. Individuals who exercise regularly are much less likely to experience a problem during exercise.
The three major causes of sudden cardiac death during exercise include exercise-induced plaque rupture – more than 50% will not have pre-existing symptoms or a known history of coronary artery disease; myocardial scarrelated ventricular arrythmias –silent or known coronary disease with previous MI and associated myocardial fibrosis; and demand ischaemia – an imbalance between coronary blood supply and demand resulting from stable coronary disease with a fixed stenosis. Ultimately, knowing the coronary plaque burden of the active
weekend warrior can help direct investigations to stratify this risk. Given we are now in the era of coronary artery calcium scores being compared by cyclists at the local coffee shop, should all exercising patients over the age of 45 years be screened for underlying coronary artery disease, and if so, how?
The evidence base for cardiovascular screening in middleaged athletes is limited. Screening, if performed, needs to target the higher prevalence of coronary artery plaque associated with age.
The 2020 European Guidelines on Sports Cardiology provide a pragmatic approach to the evaluation of the asymptomatic middle-aged athlete. Initial evaluation should always begin with assessment of cardiac risk and consideration of characteristics of the intended exercise program. Characteristics of exercise include the frequency, intensity, time and type of exercise undertaken.
The Australian absolute CVD risk calculator is easily accessible and provides an excellent starting point for assessment. If the CVD risk score is low and the individual is already physically active, then no further investigations are suggested.
However, it is not unreasonable to offer plaque burden assessment in low-risk middle-aged individuals who wish to undertake high or very-high intensity endurance events. A coronary artery calcium score (CAC) can be useful in the over 45 age group for initial plaque burden assessment, with the need for further anatomical or functional imaging dependent on the result.
Intermediate or high-risk CVD scores can be managed depending on the intensity level of intended
physical activity. If an individual is undertaking low intensity exercise, then no further investigations are generally required, with the ongoing focus aimed at risk factor surveillance and modification.
At-risk individuals who wish to undertake high or very high intensity activities, should have further assessment, including a measure of plaque burden (CAC or CT coronary angiogram) in addition to a maximal exercise test, preferably with imaging. If there are high risk features identified, then invasive coronary angiography is indicated, and the risk of the coronary lesions assessed and managed.
Exercise is good!
Everyone should be encouraged to exercise. However, particular attention and caution should be given to the previously sedentary middle-aged athlete beginning to exercise, with an increased cardiovascular risk profile, or those middle-aged athletes wanting to exercise at high or very-high levels. Referral to a cardiologist with a special interest in sports cardiology should be considered.
Shared decision-making following diagnosis and risk stratification is essential for exercise prescription in the middle-aged exercising individual.
Physical activity counselling needs to strike a balance between the multiple proven benefits of exercise, the small risk of adverse cardiovascular outcomes, including sudden death, and the patients’ goals for fitness and ongoing participation in relatively strenuous exercise.



With eight out of 10 men visiting their GP regularly, and with the focus for Men’s Health Week this year on Healthy Habits, general practice is well placed to support men focus on their wellbeing.
When we think about men’s health, one aspect that often gets overlooked is the close link between work and wellbeing. While family dynamics continue to change, it is still common to see men not just expected to earn an income, but a substantial income as the main wage earner in the family.
Many men give up aspects of their family life for their career, and the impact of this on their wellbeing can be huge.
I hear of women compromising their career to have a family and I’m eternally grateful to my mum and so many women in my life for their support. But I’m realising more within my own life, and the lives of men I meet that many men are making sacrifices in other areas of their life for their career.
A career provides many things beside an income, but when it comes to male-dominated roles, they can typically be task-focused, discourage empathy, and lack recognition and praise.
There’s always the next task to focus on and get started. I realise now that my task-brain was highly developed and typically focused on what was achieved (the past) and what needs to be achieved next (the future).
So, at knockoff and on the weekend my task brain was supercharged and was unfamiliar with the requirement to be in the present and to recognise and engage in the subtleties of human expression and human interaction.
My work included little to chat about or generate interest around a dinner table. Take into consideration that the job often becomes a large part of a man’s
identity, and even more alarmingly his refuge, and it explains how difficult it can be for many when retirement looms.
It’s no wonder that with mounting workplace pressures, increased hours spent away from their family, and workplace cultures that don’t embrace the depth of the human experience, men can struggle with their mental and physical wellbeing.

It appears there is a turning point – typically when a man gets to around 50 years of age, they embark on searching for something more, or there’s the opportunity to unhook themselves from having to generate a high-income stream.
Where social connection has typically been considered to be the least valuable, more men are coming to understand that it is, and always has been, the most valuable.
There is great value in acknowledging the contributions men make, but there’s also an opportunity to recognise the impact that focusing on career or job can have on their health, and to make changes when change needs to be made.
It’s important to embrace sensitivity and fragility and communication as the ONLY way forward for all – they are our greatest strength.
However, only one in five men over 45 speak to their GP about their emotional and psychological health. The Ten to Men study published in 2021 reports that “men who conformed to traditional masculine norms of stoicism, self-reliance and avoidance of negative emotions, were less socially connected” and noted that “Limited social connectedness – which the report says is more common among Australian males than females – is associated with a variety of poorer mental and physical outcomes and risk behaviours, including depression, substance use, sleep problems and cardiovascular disease”.
Under the theme of Healthy Habits this year, Men’s Health Week is a chance to focus on encouraging men and boys to build healthy habits by identifying small changes they can make that benefit their health and wellbeing. GPs are wellplaced to take the opportunity of a standard consultation to check in with men and encourage them to consider making small changes that can impact on their health.
ED: John Rich is Chairperson of Men’s Health and Wellbeing WA, which is the peak independent not-for-profit charity organisation dedicated to representing and promoting the health and wellbeing of boys and men in Western Australia.



Understanding how your sleep changes across the night and throughout our lives, enables us to have realistic expectations around sleep. The most common myths around sleep are that we spend most of the night in deep sleep; waking is abnormal; and dream sleep is deep sleep.
However, these statements are inaccurate. Most of our deep sleep occurs in the first third of the night. The brain tends to take what it needs first. When we have been sleep-deprived, deep sleep is increased. We generally only spend 20% of the night in deep sleep. The brain and in particular the cortex rests with reduced electrical activity.
Most of our sleep is spent in relatively light sleep (45-55%), or Non-Rapid Eye Movement (NREM2 or N2). This is probably an evolutionary response. This light sleep allows for changing our body position and to be aware of any altered environmental factors.
We wake 2-3 times per night which can increase between 5-9 times per night with age – we do not usually remember these wake times. Waking during the night is normal as is the need to change our body positions and check our environment.
Movement sleep (REM) is the opposite to deep sleep being similar to an awake state. The cortex is active but the body is atonic (semi-paralysed) so we do not get up and act out our dreams. We generally need to be awake for several seconds in order to remember dreams.
Understanding normal sleep reduces the pressure of inaccurate sleep expectations.
We cycle through all the stages of sleep every 90 minutes (with a range of 70-100 minutes).
We start the night in very light sleep called NREM1. We generally spend around 5% of the night in transitional sleep, which can be described as half-awake/halfasleep.
Next is our dominant sleep NREM 2 or N2.
After about 25-30 minutes of sleep, we descend into Slow Wave Sleep (SWS), Deep Sleep or Delta Sleep, known as Non-Rapid Eye Movement 3 (NREM 3 or N3). Only 20% of the night is spent in Deep Sleep. Children secrete Growth Hormone (GH) during N3 while adults have reduced GH secretion to repair damaged cells.
SWS is followed by NREM 2 sleep and then we go into Rapid Eye Movement sleep (REM) – Dream Sleep. In REM sleep, we have rolling eye movements, hence the name.
A young healthy person may have 2-3 wakes a night but may not be aware of them. As we age, our sleep changes as does everything else. With increasing age, our sleep is characterised by an increase in the number of wakes. Very light sleep increases dramatically with age, and there is more rapid cycling between N1 & N2. Deep Sleep is reduced.

All of these changes are a normal part of the ageing process. It is so important to be active mentally and physically with increasing age. When older adults keep
their fitness up, the prevalence of insomnia is the same as the general population. Exploring diet and exercise regimen and making relevant changes is another component of healthy sleep.
It is useful to remember that we learn how not to sleep well therefore we can learn to sleep better again.
• Have a constant waking time as much as possible. This behaviour anchors sleep to the environment and sets a sleep/wake pattern for the brain. Going to bed at a certain time does not guarantee sleep onset unless you are feeling sleepy.
• Outside exercise and morning light is a great way to suppress your sleep hormone melatonin and to help you feel more alert –even 20 minutes is useful.
• Reduce exposure to bright light and electronic devices (blue/ green light) at night make space for some much needed “slow down time.”
• Deal with the necessities and then figuratively put them into the background. Holding onto concerns, worries, plans will only keep you awake.
• If in bed and feeling wide awake and wired – don’t stay there, get up, have a gentle stretch, release those tight body muscles – breathe. You could sit on the edge of the bed in the dark and put the effort into staying awake. Sounds weird but it works, as trying too hard to sleep often sends a message to your brain there is danger. This strategy does the opposite. Sit up for 5-10 mins and then lie down and see what happens. You may need to repeat this strategy.
ED: Clinical Associate Professor Delwyn Bartlett is from The Woolcock Institute of Medical Research. For more information on sleep strategies or clinic services go to www.woolcock.org.au
Dr Shane La Bianca
Dr Andrew Tan
Dr Jeff Thavaseelan
Dr Trent Barrett
Dr Matt Brown
Dr Akhil Hamid
Dr Manmeet Saluja
Dr Alarick Picardo
Dr Steve McCombie
Dr Sarah O’Neill
With the largest partnership of Urologists in Western Australia, Perth Urology Clinic can manage all urological conditions, offering a wide range of treatment options.

For urgent referrals or queries, use our GP Hotline on 1800 487 656 (Press 9). refer@perthurologyclinic.com.au
Healthlink: puclinic
Hollywood Clinic | Wexford Clinic

There is a gender gap that does not attract much attention and that is the one where males do worse on just about any health measurement. Life expectancy for a male born today is about two year less than that of a female. Cardiovascular disease, diabetes and various cancers including lung are more prevalent in males. Workplace injury and trauma are also far more common in males.
Some may say that this is in part related to choices men make and the tendency of men to present later and be less engaged with measures and advice to improve health. This has validity. However, men are far more likely to work in manual jobs where the risk of injury is greater. There is no one solution to this issue and the life expectancy gap has narrowed slightly over the last decade. Generation Z males appear to be more focused on the importance of their physical and mental health than their forebears so perhaps we will see natural improvement over time. However, in the main, we are ignoring the current problem.
Step one may be to actually recognise that male health could do with improvement and that as doctors we are part of the solution.
Speaking of gaps AIHW data shows that people living in very remote areas used 8.5 services per person in 2022, with a subsidy rate of 85%, while people in major cities used 18.3 services with a subsidy rate of 76%. Nationally in April 2023 85.1% of GP fees (down from 95.2% at the Covid peak) and 53.5% of specialist fees were paid by Medicare. The latter down from a high of 88% in October 1984.
Obstetric services were the “most expensive” with Medicare funding 38.3% (anaesthetics 38.6% surgery 49.1%) whilst pathology at 94.3% was the most covered (diagnostic imaging 85.6% GP 85.1%). Drill deeper and aside rural/metro divides there are significant differences across states with 69.4% cover in the ACT, 78.8% in Tasmania and 87.8% in NSW.
What does this data tell us? The overarching trend is a steady decline in the percentage of total medical costs covered by Medicare since its introduction. In my opinion this reflects that costs have gone up (e.g. inflation, new technologies) and government capacity to be the sole funder has declined.
Realistically, government cannot afford to pay all the health wants and needs of all. There will be gaps. The challenge is to be honest about it.
Step one may be to actually recognise that male health could do with improvement and that as doctors we are part of the solution.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
 By Dr Suki Gill, Radiation Oncologist, SCGH
By Dr Suki Gill, Radiation Oncologist, SCGH
Prostate cancer treatment with radiotherapy has witnessed remarkable progress due to technological advancements. These developments have resulted in improved side effect profiles, particularly in terms of urinary continence and erectile function, when compared to surgery.
In the context of screening-detected early prostate cancer, the ProtecT trial, which randomised 1643 patients to active monitoring, surgery or radiotherapy, confirmed that radiotherapy and active monitoring yield similar rates of normal erectile function after seven years. Notably, upfront radiotherapy demonstrated fewer cases of urinary incontinence requiring pads compared to active monitoring. Additionally, at the 15-year mark, both prostatectomy and radiotherapy groups exhibited only 5% rates of metastasis development, confirming their equivalence.
Recent advancements in the treatment of radio-curable prostate cancer, exemplified by technologies like the CyberKnife, MRI linac, and Varian TrueBeam, have significantly enhanced treatment precision. These innovations have allowed for a reduction in the irradiation of normal tissue during radiotherapy, resulting in a significant decrease in rectal side effects over the past 15 years.
Modern radiotherapy is equivalent to surgery for early prostate cancer with 15 years of follow-up in a large, randomised trial CyberKnife is comparable to 20 days of modern radiotherapy in a randomised trial with up to two years follow-up
The PACE-A study randomised patients with prostate cancer to CyberKnife or surgery, with surgical patients primarily treated with the Da Vinci robot.
Modern radiotherapy now enables most patients to complete their treatment in just 20 days through a concept known as "hypofractionation". Building on this concept, stereotactic radiotherapy has emerged, enabling the administration of even larger doses per session in a technique referred to as "extreme hypofractionation", thereby shortening the overall treatment duration to a mere five days.
Evaluating extreme hypofractionation with stereotactic radiotherapy
Assessing the outcomes of extreme hypofractionation in a biological system is a complex endeavour because there is an organ at risk, the urethra, inside the target.
The Lancet Oncology published the PACE-B randomised study in September 2022, which compared stereotactic radiotherapy using a linac or CyberKnife versus conventional radiotherapy for early prostate cancer (T1,2 G3+4, PSA<20). The study revealed that at the two-year mark, grade 2 or higher urinary toxicity was more frequent with the five-day treatment. However, a subgroup analysis of patients treated with the CyberKnife platform demonstrated equivalent toxicity levels to those treated with 20 days of modern radiotherapy at two years. It is worth noting that shorter
treatment durations, similar to the five-day approach, have been utilised since the 1960s at St. Thomas' Hospital in London. Notably, Sir Laurence Olivier, a renowned actor, underwent a 6-fraction protocol for prostate cancer at St Thomas' in 1967, reporting no major side effects and living a further 22 years until 1989 when he passed away due to an unrelated condition.
The PACE-A study, recently reported, was a randomised trial comparing surgery (primarily utilising the Da Vinci robot) with CyberKnife. The study enrolled 123 men with a median follow-up of 50 months. Stereotactic radiotherapy patients reported fewer instances of urinary pad use and sexual dysfunction, while a higher number reported moderate bowel symptoms.
Presently, patients with intermediate-risk prostate cancer have the option of receiving a gel inserted between the rectum and prostate before radiotherapy to mitigate rectal side effects, although Medicare funding is not available for this yet.
Stereotactic radiotherapy holds promise in the treatment of early prostate cancer. While it may not necessarily reduce toxicity when compared to modern radiotherapy, it provides an alternative for patients who face challenges in attending frequent appointments. Further research is necessary to refine patient selection criteria and determine the long-term efficacy of stereotactic radiotherapy in treating prostate cancer, especially in comparison to robotic surgery or modern radiotherapy.
ED: Dr Gill is director of research in the radiation therapy department of Sir Charles Gairdner Hospital.

– References on request
Author competing interests: Dr Gill is one of the few providers of CyberKnife in the public sector in WA.

Prostate MRI is a vital tool in the diagnosis, staging and management of prostate cancer, and is part of established diagnostic and management guidelines.
The detection of prostate cancer through screening is complicated by a significant occurrence of cancer diagnoses that may not require immediate treatment. Prior to prostate MRI, diagnostic processes inclusive of PSA levels, digital rectal examination (DRE) and transrectal ultrasound guided (TRUS) biopsies had problems with under as well as over-diagnoses of prostate cancer.
In addition to PSA and clinical assessment, multiparametric MRI (mpMRI) has emerged as an important risk stratification tool to better detect significant prostate cancer early, and guide biopsy. It is also advantageous that MRI generally does not pick up indolent disease, and in turn avoids overdiagnosis and potentially unnecessary treatments.



When performed, a prostate MRI is reported according to PI-RADS (Prostate Imaging Reporting and Data System), which is a standardised assessment tool to evaluate and report findings related to the likelihood of clinically significant prostate cancer.
A PI-RADS report categorises lesions or areas of concern on a scale from one to five, with higher scores indicating a higher probability of clinically significant cancer. The report provides information about the location, size and locoregional staging and characteristics of the identified lesions and assists in treatment decision-making and guiding further diagnostic procedures including prostate biopsy.
In addition, if a lesion has been detected on MRI, the report should include a standardised diagram showing the target(s) with their location and PI-RADS suspicion score.
The NICE prostate cancer diagnosis and management guideline recommends multiparametric MRI be offered as the first-line investigation for people with suspected clinically localised prostate cancer. This facilitates improved biopsies, earlier detection of higher-grade tumours and decreases under-staging and over-detection.
Studies show a low PSA density (PSAd) of less than 0.15ng/ml/ml in combination with a non-suspicious MRI has a negative predictive value between 84% and 100%. By comparison, TRUS biopsy has an approximate negative predictive value of 74%.
The NPV of MRI in low-risk

patients assists in shared decision making for clinicians and patients who choose to omit biopsy after discussion of the risks and benefits. Using multi-parametric MRI to triage men may allow 27% of patients to avoid a primary biopsy. In high-risk patients with clinical suspicion for prostate cancer, MRI is not accurate enough to replace prostate biopsy. A meta-analysis of published data suggests 7-10% of men with an elevated PSA and a negative MRI will miss a diagnosis of clinically significant prostate cancer if biopsy is not performed. The scenario of a rising PSA after one or more negative biopsies is the best established role of MRI, which localises a suspicious prostate lesion in over 30% of such patients. These tumours are typically found in the anterior prostate. Conversely, if MRI is negative after a negative biopsy, studies suggest the NPV ranges between 88% and 96%.
The NICE guideline also recommends MRI be offered to patients having active surveillance who have not had an MRI previously. Up to one-third of men commenced on active surveillance have upgrading of disease (e.g. from Gleason 3+3 = 6 to 3+4 = 7 or higher) on serial biopsy. In some men, this may represent true progression of cancer; however,
The PIRADS MRI report is a risk stratification assessment categorising prostatic lesions' likelihood of being malignant on a scale from 1 to 5
Using MP-MRI as a first line investigation to triage men may allow 27% of patients to avoid a primary biopsy. It significantly reduces overdiagnosis of indolent/insignificant cancer
Prostate mpMRI is essential in initial diagnosis, staging, assessing suitability for active surveillance and management of prostate cancer.
in some cases it may reflect incomplete sampling during the initial biopsy.
MRI is often repeated on followup for patients during active surveillance, although further data is required before it can replace regular biopsies in active surveillance protocols. Accurately locating extracapsular extension on MRI may aid in determining surgical suitability of patients for nerve
sparing radical prostatectomy without compromising surgical margin status.
A multi-parametric prostate MRI utilises several sequences to provide information about the prostate gland. The main sequences used are:
1. T2 weighted sequences: T2 weighted imaging provides the high-resolution images of the prostate gland and surrounding structures. T2-weighted images alone can often detect tumours or other abnormalities by highlighting differences in tissue characteristics. T2 allows for description of prostate and tumour size, PSA density calculation, and locoregional staging.
2. Diffusion-weighted imaging (DWI): DWI measures the movement of water molecules within tissues and helps assess tissue cellularity and the diffusion of water. In prostates, DWI is the key sequence as cancers most often present as areas of restricted diffusion.
3. Dynamic contrast-enhanced
imaging (DCE): DCE imaging requires injection of an intravenous gadolinium-based contrast agent. DCE imaging shows the vascularity and blood flow within the prostate and helps identify regions of increased blood supply which can be indicative of prostate cancer.
At times, difficulty will be encountered with imaging artefact if there is metal work in the pelvis –total hip replacements are the most commonly encountered artefact in prostate MRI. If patients have poor renal function, the MRI may be performed without the gadoliniumbased contrast agent.
To be eligible for a Medicare rebate for prostate MRI, the referring clinician must be a urologist, medical oncologist or radiation oncologist. The patient must meet defined PSA and/or digital rectal examination (DRE) criteria; or be already diagnosed with prostate cancer and on active surveillance.
Author competing interests – nil





Adora Fertility provides affordable IVF without compromising on quality. By referring your patient to one of our highly qualified specialists, they will receive a tailored approach to their fertility treatment plans with medications sensitive to their needs. Out-of-pocket costs are typically less than $2,000 for a fully stimulated IVF cycle. Give your patients the best chance of conception without the financial sacrifice.
Our range of fertility treatment options has expanded to include our newly launched, Known Donor Program. As part of this program, patients can access affordable fertility treatment with donated sperm, eggs or embryos from a donor known to the patient. By facilitating sperm, egg and embryo donation in this way, we know that we can help more people grow their families in more ways.

While PTSD is typically associated with a single traumatic event, Complex Post-Traumatic Stress Disorder (C-PTSD) is characterised by exposure to multiple and ongoing traumatic experiences, including “traumas of omission”. Trauma of omission refers to trauma resulting from experiences of significant neglect, lack of support or emotional unavailability occurring during development. This lack of responsive co-regulation, insufficient protection, and lack of overall support for an individual’s needs is often co-occurring in the face of “traumas of commission” (where an individual is subjected to intentional or deliberate actions that cause physical, emotional, or sexual harm), exacerbating the impacts of these experiences.
C-PTSD has additional features related to prolonged or repeated traumas, which can be grouped into four main clusters:
• Re-experiencing: Intrusive memories, flashbacks, or nightmares related to the traumatic experiences.
• Avoidance: Efforts to avoid reminders of the trauma. People may also withdraw from relationships.
• Negative self-concept: Experience feelings of shame, guilt or worthlessness and feelings of inadequacy.
• Dysregulation of emotions and relationships: significant difficulties in forming and maintaining stable relationships (particularly if the trauma has interpersonal origins).
Other symptoms commonly associated with C-PTSD include changes in self-perception, disturbances in concentration and memory, difficulties with trust and intimacy, a sense of detachment from others, and physical symptoms such as headaches or gastrointestinal problems. Individuals with C-PTSD may also have co-occurring mental health conditions such as depression, anxiety disorders, substance abuse or borderline personality disorder.
C-PTSD can affect both men and women. However, the experiences and expressions of trauma may vary between genders due to societal expectations, cultural factors and individual differences. It is important to understand that trauma is a deeply personal experience, and the impacts can be unique to everyone. When considering complex trauma in men, there are several important factors to keep in mind.
Societal expectations: Traditional notions of masculinity often discourage men from openly discussing their emotions or seeking help for mental health concerns. The perceived pressure to conform to ideas of traditional masculinity can create barriers to seeking support and expressing vulnerability, leading to a reluctance to express emotions or seek support (exacerbating the effects of trauma).
Shame and stigma: Men may face significant internal and social stigma and stereotypes around mental health. This may tie into issues with traditional masculinity or may be related to more specific cultural understandings and expectations of mental health, or around the types of trauma experienced by an individual. Stigma can perpetuate a culture of silence and shame. For men who have experienced trauma this may translate into further difficulties with disclosing their trauma and seeking support.
Expression of symptoms: Men may have different communication styles and patterns than women, and can be more inclined to express emotional distress through anger, irritability or risk-taking. Consider this when planning individual supports and thinking with individuals about alternative outlets for self-expression, social engagement and physical regulation. This may include planning activities such as art, sports or other hobbies and interests.
Help-seeking challenges: Men are more likely to complete suicide, which may be influenced by factors
such as an overall under-reporting of mental health symptoms, reluctance to seek help, and the use of more lethal methods of self-injury at times of significant distress.
Optimal trauma informed care for engaging with men with C-PTSD involve establishing a therapeutic relationship with an early focus on trust and rapport and fostering a sense of empowerment and agency by involving individuals in the decision-making process regarding care.
Encourage active participation in setting goals and determining best suited strategies and interventions, as this can help restore a sense of control and autonomy, which has often been compromised by the experiences of trauma. Importantly, encourage men to explore and express their emotions, providing validation and helping them understand that emotional expression is a strength rather than a weakness.
Further, using a strength-based approach means building on coping mechanisms and skills that have helped them navigate through their trauma. Highlighting strengths can boost self-esteem and foster a sense of hope and empowerment. As every individual’s experience with trauma is unique, it is important to approach trauma-informed care with flexibility, empathy and a personcentred focus.
Lastly, promoting mental health awareness and education can help reduce stigma and encourage early intervention. Providing resources, information, and screenings that are accessible and relevant to men can support early identification and treatment of mental health concerns.
Author competing interests – nil
GUARANTEED ACCESS TO A SURGEON ALL YEAR ROUND








Bladder outlet obstruction, which is most commonly caused by benign prostate enlargement in men over the age of 40 years, is widely recognised as a cause for symptoms, but its impact on longterm bladder function deserves further attention.
There is now evidence that in a similar way high blood pressure damages the heart, high urinary pressures lead to morphological and functional changes in bladder, which can be irreversible.
Optimal bladder functioning occurs when low pressure is maintained throughout the storage (bladder filling) and voiding (bladder emptying) phases. An increase in outlet resistance leads to hypertrophy of smooth muscle of the bladder wall, coupled with some extracellular matrix deposition. This has been named the "compensatory" response of the bladder, an attempt to increase contractility to maintain emptying despite the increase in outlet resistance.
Prolonged and/or more severe obstruction can give rise to a "decompensation" phase in which further increases in pressure and hypoxia lead to excessive collagen deposition and degeneration of smooth muscle cells and neurons.
Bladder health is frequently overlooked in men
Prolonged increased pressure is damaging to the bladder
Early identification and management can prevent bladder damage.
Chronic conditions such as diabetes, hypertension and dyslipidaemia can contribute to more rapid deterioration of the bladder. This phase can manifest functionally as a decrease in bladder contractility, decrease in bladder compliance, and/or overactivity. These changes are irreversible, making timely recognition and management of the primary issue important.

There are several pitfalls in the recognition and management of bladder outlet obstruction in men.
1. Patients under report symptoms
Many men think that Lower Urinary Tract Symptoms (LUTS) are a normal part of ageing and it is not something that needs to be addressed. It is still common to see patients whose first presentation is in acute retention to emergency department after neglecting symptoms for a long time.
2. Presenting symptom may not represent the primary pathology
The initial symptoms of bladder outlet obstruction can be purely irritative (storage) – urinary frequency, urgency and nocturia. This is due to the compensatory changes described above. It is important to recognise that in men over 40 years it is more likely that irritative symptoms are a secondary manifestation of obstruction than the primary pathology. By addressing the primary issue, the bladder outlet obstruction, further changes and bladder decompensation can be mitigated.
3. A "normal" prostate size on renal tract ultrasound does not exclude bladder outlet obstruction
Prostate size does not correlate well with degree of bladder outlet obstruction and having a normal prostate size on ultrasound does not exclude bladder outlet obstruction. Even if the total volume of the prostate is normal, its anatomy can cause obstruction, for example, if a middle lobe is present. Moreover, transabdominal ultrasound measurements of the prostate can be inaccurate due to its location deep inside the pelvis.
Early identification and management of bladder outlet obstruction can prevent bladder damage. The management of bladder outlet obstruction in men starts with medical therapy and there are several procedural options to help achieve not only symptom resolution but also prevent long-term bladder damage. Let's protect the bladder!
– References available on Request Author competing interests – nil


Endometriosis is an oestrogen dependant, chronic inflammatory disorder characterised by the presence of ectopic endometrial tissue. There are three histologically distinct types: peritoneal, ovarian and deeply infiltrating endometriosis (DIE). Australian data indicate that approximately 11% of reproductive aged women are affected, with higher prevalence among those presenting with subfertility or pelvic pain.
Endometriosis can be a debilitating condition which represents a significant health burden in Australia. The cost of treating it is estimated at $9.7 billion a year, when direct and indirect costs are considered.
Historically endometriosis has been under-recognised. This is changing partly due to the introduction of the National Action Plan for Endometriosis.
Early detection and treatment are crucial for effective management. Unfortunately, the average delay in diagnosis is 6.5 years, given its nonspecific symptoms and surgical diagnosis. Patients may visit their general practitioner six times or more before gynaecological referral.
The exact cause of endometriosis remains unclear. Sampson's theory is widely accepted and proposes that retrograde menstruation, via the fallopian tubes, leads to implantation of endometrial cells onto peritoneal surfaces. Retrograde menstruation, however, occurs in 80% of women, indicating involvement of other factors.

Underlying immune dysregulation may explain why implants progress. The theory of coelomic metaplasia postulates that endometriosis arises from the metaplasia of specialised peritoneal cells. Other hypotheses suggest that micro-embolisation or metastasis of endometrial cells can occur via blood vessels
and lymphatics. Hormonal, environmental and genetic factors may contribute, with a sevenfold greater risk in patients with a positive family history.
The symptoms of endometriosis vary widely from asymptomatic, to severe and debilitating pain. Common symptoms include cyclic and non-cyclic pelvic pain including dysmenorrhoea, dyspareunia, dyschezia and dysuria. Patients may also present with fatigue or bloating and subfertility. Symptom severity often correlates poorly with the extent or surgical stage of endometriosis. Impact on fertility, however, directly correlates.
Careful history taking is essential for diagnosis. Physical examination can be negative in patients with superficial endometriosis and may not be possible in some due to pain. Where DIE is present, uterosacral nodules and immobility of the pelvic organs may be noted.
Transvaginal ultrasound scan (TUS) is first-line imaging to investigate pelvic pain and, whilst unreliable for the diagnosis of superficial endometriosis, is highly sensitive and specific in identifying DIE or endometrioma. MRI is equally effective but cost and access may be prohibitive.
In working up patients with DIE for surgery, a combination of
USS and MRI is recommended for preoperative planning and recognition of deeply infiltrating lesions. Laparoscopy remains the gold standard for formal diagnosis, allowing direct visualisation and excision of lesions for histopathological confirmation.
Potential biomarkers allowing for easier, cheaper, readily accessible and less invasive diagnosis are a current hot topic. These include unique glycoproteins specific to endometriosis potentially detectable in blood, urine, menstrual fluid and hair. Numerous biomarkers have been proposed and investigated. Their use is limited by the lack of evidence and the high false positive rate for most.
NSAIDs are effective in relieving pain and are suited to patients who desire conception.
Where fertility is not desired, level 1 evidence indicates that hormonal treatments are equally effective in reducing pain associated with endometriosis compared to placebo, though differ in cost and tolerability. These therapies establish a hypo-oestrogenic or hyper-progestogenic milieu, induce decidualisation and atrophy of endometriotic implants, and prevent or delay recurrence. For patients with symptoms presumed due to endometriosis, empirical therapy with the combined oral contraceptive pill (COCP), or oral drospirenone is recommended. Oral dienogest (fourth-generation progestogen with highly selective progesterone activity) is effective in reducing pain and lesion size. Older generation oral progestogens are generally avoided due to their undesirable side effects.
All long-acting reversible contraceptives are effective. Of these, the Mirena IUS is preferred due to the greater body of supporting evidence and lower
Historically, endometriosis has been overlooked and under-recognised
There is now a growing movement towards greater awareness, education, diagnosis, treatment, and research
Future advances will hopefully see earlier and more accurate diagnosis, superior treatments and improved quality of life for those living with endometriosis.
side effect profile. Implanon and Depo Provera are sometimes avoided due to risk of irregular bleeding with the former, and risk of reduction of bone density with the latter.
Gonadotropin-releasing hormone (GnRH) agonists may be considered where severe or refractory symptoms are encountered. Newer GnRH antagonists are superior in that they are orally active and do not cause an initial flare or exacerbation of symptoms. Add-back HRT should be initiated with GnRH analogues for maintenance of bone mineral density. Aromatase inhibitors (AI) are also an approved medical option. Following discontinuation of hormonal treatment. Symptom recurrence reliably occurs.
Surgery is recommended for patients with severe or refractory symptoms of endometriosis, known endometrioma >4cm and in selected patients who desire fertility.
The goal of surgery is to restore normal anatomy, remove all visible endometriotic tissue and preserve ovarian function. Laparoscopic excision (or ablation) of endometriotic lesions has been shown to be better than placebo in reducing pain and improving quality of life. Excision is preferable to ablation as recurrence risk is decreased and histological confirmation is possible. Despite optimal surgery, 20-50% of patients experience recurrence of endometriosis at five years. Postoperatively, hormonal suppression is advised until menopause.

Where possible, laparoscopic surgery for endometriosis should be carried out by a suitably trained gynaecologist. Where DIE involves the urinary tract or bowel, a multidisciplinary approach is important with pre-operative imaging review, and intra-operative colorectal or urological input. The goal of treatment is to improve symptoms, improve fertility and to limit the lifetime number of surgeries.
Endometriosis is strongly associated with chronic pelvic pain; the exact mechanisms are not fully understood. Effective management requires a multidisciplinary approach addressing both physical and psychological aspects of pain, and typically involves a trained women’s health physiotherapist, pain specialist and psychologist. Evidence suggests that following an antiinflammatory diet and avoidance of sugar, dairy, gluten and lactose may be of benefit.
Author competing interests- nil
By Mr Peter Ammon Foot Ankle & Knee Surgery






 By Prof. Robert U. Newton and Prof. Daniel A. Galvão, Edith Cowan University
By Prof. Robert U. Newton and Prof. Daniel A. Galvão, Edith Cowan University
Our team at the Exercise Medicine Research Institute at Edith Cowan University has been researching men’s health for two decades through an intentionally targeted men’s health initiative. Much of this work has centred on the application of exercise as medicine in the management of men with prostate cancer, which is the most common cancer in men.

Treatments for prostate cancer are generally highly effective at slowing progression of the disease but the side-effects are concerning for both patients and clinicians. Many years ago, while presenting our work on ameliorating muscle and bone loss, fat gain and the increased risk of cardiovascular disease, several men and their partners congratulated us on our work but pointed out we were not addressing the most significant side-effects of prostate cancer treatment.
Poor sexual health was stated as a major concern which was severely impacting quality of life, mental health and their relationships. Several of the men had considerable decision regret, wishing they had not undergone their prostate cancer treatment, such was the magnitude of impact of sexual health issues on their life.
In the main, men who develop prostate cancer are older with average age at time of diagnosis about 66 years. Unfortunately, there is an unjustified perception that sexual activity is not important for older men, but this is not the case and greater research and clinical effort must be directed towards supporting the sexual health of men at all ages.

Based on this feedback, our team embarked on a series of research trials to examine if exercise medicine could prevent declines in sexual health or even produce improvement. While our work has
Sexual health is important to men regardless of age
Several diseases and the medical treatments negatively impact erectile function and sexual health including libido
Exercise, in particular resistance training, increases feelings of masculinity, virility and vitality, improves body composition, mental health, enhances erectile function and libido.
been exclusively in men being treated for prostate cancer the findings really apply to all men at any age.
In our initial research trials, we found that a combination of resistance (strength) training and cardiorespiratory (aerobic) training improved sexual activity frequency and satisfaction and reduced the number of participants that reported little to no interest in sex. These findings were deemed so impactful that in 2013 our team was awarded a large research grant from the National Health
and Medical Research Council so that we could more thoroughly investigate the impact of targeted exercise medicine on sexual health in older men.
We can report that erectile function and intercourse satisfaction increase significantly in the exercise group compared to those receiving usual care. Interestingly, a group that received additional self-managed psychosexual therapy experienced no additional improvement.
The mechanisms by which exercise medicine improves sexual health span both physiological and psychological (Figure 1). The men in the exercise group increased their physical strength and muscle size while also reducing body fat. This gave them a feeling of greater vitality and virility and they reported improvement in their feelings of masculinity.
Exercise, specifically resistance training, increases the circulating levels of several hormones, in particular testosterone, which have
continued on Page 52
Congenital cyctomegalovirus (CMV) is one of the most common congenital infections, affecting approximately 0.5% of births equating to over 200 infants annually in WA.
While postnatal CMV typically causes mild, cold-like symptoms, congenital CMV (cCMV) represents one of the most significant threats to the developing foetus. Although cCMV causes no symptoms in most infected babies, its high frequency results in being one of the most significant congenital viruses.
Sensorineural hearing-loss (SNHL) is the most common permanent effect of cCMV along with neurodevelopmental disability such as cerebral palsy, blindness and intellectual disability.
Despite the frequency of cCMV and the potential for the virus to have devastating effects on neurodevelopment, awareness levels are low among expectant families and health providers alike.
Avoiding CMV infection during pregnancy is the key strategy to prevent cCMV. Other health messages such as avoiding sharing spoons, glasses, bottles and other saliva containing items especially with toddlers and washing hands after changing nappies are also key. All health care providers can promote knowledge of this devastating infection and the strategies to avoid CMV acquisition during pregnancy.
If CMV is acquired during pregnancy, testing for the virus in newborns is rapid (48 hours to a PCR result), highly sensitive and specific (>90%), non-invasive (saliva swab or urine sample) and low cost (approximately $40). Testing prior to 21 days of life is necessary to distinguish congenital from postnatally acquired CMV. Along with a narrow testing window, early treatment with antiviral medication, if indicated, needs to be started by day 30 of life.
Despite the widespread availability of safe and cost-effective testing, diagnostic rates across Australia are low so it is likely that over 90% of cases go undiagnosed. Guthriecard testing for CMV is possible up to age two. However, the sensitivity of this test is limited. It performs much better for infants with hearing loss and neurodisability than infants who are asymptomatic as it relies upon the infant being CMV viraemic when tested. Many infants will have acquired the virus but may not be viraemic.


Currently in WA there are no established protocols to test mothers during pregnancy or identify high-risk infants for screening, despite these being recommended by national and international bodies such as The Royal Australian and New Zealand
Other Australian states have implemented cCMV screening programs or are in the process of assessing this. Across the US and Europe, cCMV testing is commonplace and, in some places, universal. Studies conducted interstate and overseas have found early cCMV testing to be costsaving or at least cost-neutral.
Acknowledging the significance of cCMV and frequent association with SNHL, a state-wide study was conducted from November 202022 through PCH. Infants at high-risk of the virus were recruited to the study and saliva/urine tested for the CMV virus.
High-risk infants were identified as those who had failed their newborn hearing screen – a test provided
Congenital CMV is one of the most significant congenital viruses
Sensorineural hearing loss is the commonest effect
Infant screening (done in other jurisdictions) should be considered in WA.
universally (rural and metro) to infants across WA soon after birth.
The study tested over 200 infants identifying five as being CMV positive. These infants were treated and monitored according to established protocols – involving review by an infectious disease physician, serial audiological and ENT review, ophthalmology review and developmental paediatrics input.
Two study infants were identified as eligible for early cochlear
implantation, and one received antiviral treatment. The study successfully showed that early diagnosis of cCMV in WA for infants at high-risk is achievable and makes the case for targeted-cCMV testing in Australia as outlined in our article published in the MJA last year.
Results of our study were positive on all fronts. Firstly, all participants on the study were able to access timely diagnosis and intervention regardless of their location in WA. Secondly the team achieved a successful recruitment rate of 79% and the participation rate (eligible infants who completed testing) was 67%.
Finally, the dedicated testing program combined with early diagnosis facilitated by the study provided gold-standard monitoring and access to early intervention for infants on the trial. Overall, the results present a strong case for reviewing the present approach to cCMV across WA.
Long-term clinical outcomes of affected infants within the study are being monitored and the study team is in the process of applying for funding to continue targeted testing of high-risk infants. A cost-saving analysis of the WA program is underway and feedback from families involved in the study is being collected to inform the implementation of targeted screening for cCMV as a new standard of care within WA.
– References on request
Author competing interests – The authors were involved in the research described. The Garrett-Passe and Rodney Williams Memorial Foundation provided funding for the project. The study team comprised Jafri Kuthubutheen (research lead), Asha Bowen, Christopher BrennanJones, Hayley Herbert, Helen Klingberg, Allison Reid and Shyan Vijayasekaran.
continued from Page 51
highly beneficial effects on sexual health, confidence, and libido. Having low muscle mass and elevated fat mass compromises the sexual health of men and so another mechanism is the improvement in body composition from exercise.
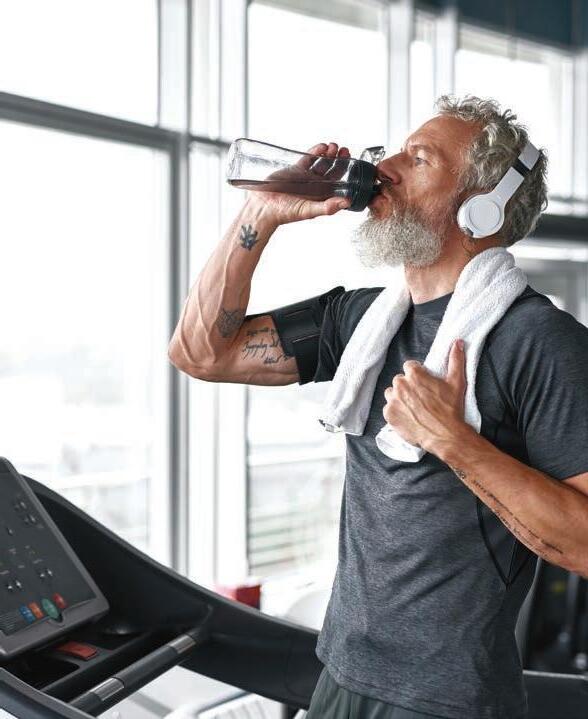
High blood pressure and specifically the medications used to treat hypertension can impact erectile function. Exercise is one of the most effective ways to treat hypertension and reduction of the need for blood pressure lowering medication translates to improved erectile function.
Finally, exercise improves mental health, including anxiety and depression and this also supports better sexual health.
To maintain or improve sexual health it is important to be physically active on most if not every day and this must include at least 2-3 resistance training sessions each week. If you need assistance to get started on an exercise program, we recommend consultation with an accredited exercise physiologist and the professional body provides a search facility at https://www.essa.org.au/find-aep
ED: Both Professors Newton and Galvao are involved in the Exercise Medicine Research Institute at ECU
– References available on request
Authors competing interests – the authors were involved in the research described
Could a kiss from a frog save your life? According to Dr Matt Morgan in his latest book, One Medicine, there’s so much more to learn from animals and how they live.
By Ara JansenGranted, running nude on a Scottish island covered in honey is not regular everyday behaviour. But it is just what the doctor ordered. Well, it’s what Dr Matt Morgan ordered for himself while he was working on his latest book.

Titled One Medicine, it examines animal science and how much more it has to offer human medicine.
Launched recently at the Margaret River Readers & Writers Festival, the book is informative, witty and warm, exploring what human medicine has already discovered in the animal kingdom and suggesting there should be a lot more to come.
Littered with self-experiments – like exploring why a masseuse gives him an erection – music and pop culture references and personal anecdotes, it’s also a highly enjoyable read for the non-medically minded.
The book started with an unusual premise. While the intensive care consultant was examining a patient who had a cardiac arrest because he inhaled some biscuit crumbs, he saw a flock of birds fly past his window. Matt wondered how
these birds survive what they must inadvertently inhale all the time while flying.
“I wanted to be Fox Mulder but I wasn’t allowed to be, so medicine seemed the next best thing,” says the Welshman who has been working at Royal Perth for the last few years. “It’s the perfect combination of gadgets, science and humans, which are probably three of the things I enjoy the most. I loved questions but preferred answers, solving mistakes and questions.”
The son of a nurse and an engineer who built roads, Matt has always been an avid reader, but a terrible speller (bless the spell checker) with atrocious handwriting – maybe he was destined to be a doctor. One Medicine is Matt’s second book. He started writing after attending a medical conference where there were so many interesting ideas flying around but none of the public would ever necessarily hear about them. His debut book Critical, told stories from the frontline of intensive care
medicine. After featuring on UK television, his open letter addressed to patients during COVID has been read by more than half a million people.

Matt now also teaches medical and science types how to write books which will appeal to a more mainstream audience. He offers hacks and tips but also ideas on how to write more personal hospital notes, aimed at patients and their families. He writes a regular column for the British Medical Journal and has been featured in The Guardian, The Times, Esquire and on CNN
Minnie Hodgson was among a contingent of nurses who evacuated Singapore on a naval ship but were later bombed, imprisoned and murdered.
The War Nurses, by Minnie’s greatniece Anthea Hodgson, is an historical fiction based on the story of Minnie, who was aged 33 when she was killed, and her nursing colleagues.

After the fall of Singapore, among the hundreds evacuated on the Red Cross ship SS Vyner Brooke, were the last 65 Australian nurses who stayed behind to tend to the wounded. When the naval ship was bombed, 21 of the nurses, including Minnie, were raped and murdered on Bangka Island after surrendering to Japanese forces.
The full details of the massacre were suppressed by the Australian
government and the truth was only made public in 2019.
The remaining nurses who survived the sinking of the Vyner Brooke were interned as prisoners of war. Before the war was over, eight more nurses died from the inhumane conditions in the camps.
Anthea said she wrote her novel because she did not think the nurses had been recognised for their bravery, loyalty and sacrifice.
“I had grown up with the family story that my aunt Minnie had died in the Bangka Island Massacre, but it was never regarded as a big deal – she was ‘only a nurse’ and not a soldier on the front lines.”
“I wrote The War Nurses for all the girls, because I wanted to bring them to life again.”
Since the book was released, a
One Medicine also tells stories of his patients (with their permission) woven in between stories of how we’ve already used animal knowhow to inform human advances – the needle, an understanding of sonar from bats or how studying female kangaroo’s three vaginas has improved in-vitro fertilisation success rates.
“With more and more zoonotic diseases in the world, One Medicine offers a powerful way to think about these things. Most of the things I am talking about in the book, like biomimicry, is also something you see in animal physiology,” he says.
Matt believes vets and doctors have much to learn from and with each other. He queries why vets swear an oath to animal and human health while doctors only swear to maintain the utmost respect for human life.
One Medicine is published by Simon & Schuster.
community park in West Leederville has been named in Minnie’s honour. The move to rename the park on the corner of Woolwich and McCourt streets was put forward by the Town of Cambridge’s Deputy Mayor Kate Barlow at a council meeting last August.
Born in 1908, Minnie grew up in the area, living in Tate Street, Leederville (as it was then) and attended Presbyterian Ladies College.
A nurse who died in the 1942 Bangka Island Massacre on Radji Beach during World War II has inspired a novel and had a Perth park named in her honour.
When Naomi Johns found out she was going to be playing Desdemona in the opera Otello, she dug into all the source material she could find.
She collected together Shakespeare’s original play Othello, live performances of the Italian opera, Otello’s libretto, musical score and phonetic translation, to name a few and started studying.
“I think it’s essential to have all these sources,” says the soprano about her breakthrough principal role. “Especially with a Shakesperean role where you are translating it to a different language and a new medium. It’s important to understand the context in order to see what parts Verdi chose to keep.”
In this West Australian Opera production, Naomi stars as Desdemona, the wife of lead character Otello (played by Paul O’Neill). Otello’s soldier Iago (Jose Carbo) holds a grudge after being overlooked for promotion. He decides to manipulate Otello into believing his wife is unfaithful and drives the general to a tragic end.
“I love the story, the characters and the drama. It’s written so well that it’s a pleasure to sing but it also gives you some licence and freedom to move within the character’s story.”
By the time rehearsals commence about a month ahead of opening night, performers are expected to have memorised all their parts and have done all of the in-depth background work need to deliver the character authentically.
The born and bred WA soprano says Otello is an exciting challenge and technically a difficult part to perform.

“The music shows you a lot about the character’s temperament. It’s also written in the expression and the dynamic marks Verdi put on his score, like if a line needs to sound like a sob, he’ll write the drama into the music. As a singer you have to decide how to deliver that in a way that has integrity within the whole piece,” she says.
“How I learn and prepare for this role determines and grounds me for how I sing this role for the rest of my life. That’s our job as an artist, to keep that artistic integrity and your personal strength and give the best of what you are capable of. While it will be informed by similar things, how I sing this role this year, won’t be the same as in 10 years.”
An emerging Australian soprano, Naomi attended the Sydney Conservatorium of Music after completing her certificate of Music Theatre at the West Australian
She has been a frequent finalist of many national singing competitions, including being the first female winner of the Bel Canto Award from the Joan Sutherland and Richard Bonynge Opera Foundation in 2013 which enabled her to continue coaching in New York, Cardiff and London.
While now based in Perth, one of her most recent performances was Carlotta in The Phantom of the Opera, outdoors for Opera Australia. She made her WA Opera debut in The Barber of Seville
This is the first time Naomi has performed Desdemona, while it has been almost a decade since WAO staged it.
“I feel fortunate to have come to this point in my life. I feel like I am the right age and vocal skill and temperament to play this part. It doesn’t happen often in your career.
“I have never enjoyed learning a role so much in my life and I’ll also be working with very seasoned singers in Paul O’Neill and Jose Carbo. To be able to make a role debut in their company is special as is being able to do it in my hometown.”
Otello is at His Majesty’s Theatre from July 20.
There’s much more preparation for singing opera than just warming up your voice. Homegrown soprano Naomi Johns talks about how she’s readying to perform in WA Opera’s Otello.
Nikola Estate at Middle Swan has some of the oldest grapevines in Australia, with the original vines dating back to 1836 when the original Houghton’s plantings were made.

The Yukich family have recombined the properties of Houghton estate and embarked on a bold plan to modernise the vineyard and winemaking to produce contemporary Swan Valley wines. There are plenty of reasons to like the Nikola Estate wines and they deliver a new freshness to some of the older varieties.
This wine is showing the flexibility of the chenin blanc variety with a crisp, clean wine with a fine bead. There are soft pear aromas with hints of apple and stone fruit on the palate. A very enjoyable aperitif and good value.

As a dry wine, the 2022 Nikola Chenin Blanc has been made with hand-picked fruit, whole bunch pressing and a wild ferment to extract the best flavours. Hints of citrus aromas and a soft, textural palate with melon and honeysuckle flavours. A very well presented chenin ready to drink now.

The warm Swan Valley climate is perfect for bold red wines and the 2022 Nikola GSM is a vibrant cherry red with aromas of spice and dark fruits with some funky hints. With only six months in oak, the tannins are delicate while the bold fruit flavours have some spice and pepper for complexity. The finish is persistent and a wine perfect for a winter beef casserole.
Fortified wines are making a comeback and the Muscadelle variety is hard to find in the valley. The Rare Topaque is blended using the Solera system dating back to 1976, so is ‘rare’ by virtue of around 35 years of average age. This wine shows its age with amazing fruit cake, toffee and cinnamon flavours that keep you coming back for more. Perfect with your favourite cheese on a winter’s night.
Verdelho and the Swan Valley have been a great combination since the early plantings of the 19th century. Using the 1958 plantings, the 2022 Nikola Estate Verdelho was a great vintage and displays lovely tropical fruit flavours with a soft, creamy palate. This was my favourite wine and would be perfect with spicy Indian food.

We respect your time is precious. Humphrey Homes’ integrated model of architecture, building and interior design ensures you realise your vision with unrivalled efficiency, construction quality and budget control. To learn how our approach makes the process seamless and enjoyable, contact Dean Humphrey for an informal chat