

Discounts
for WA GPs








for WA GPs










It’s why more than 50% of GPs trust our local medico-legal and risk expertise, backed by our national strength
Local support from Avant Law nationwide Our on-the-ground solicitors are experienced in your state’slaws.
Medico-legal experts and resources
Access
advisers, 24/7








The perpetrators are not always male, but mostly they are, raising questions about what is creating so many angry, disturbed men.
Men’s mental health has been in the news for all the wrong reasons lately, with distressing headlines about family and domestic violence incidents.
At the start of last month, 35 Australian women had lost their lives in only 22 weeks.
The perpetrators are not always male, but mostly they are, raising questions about what is creating so many angry, disturbed men who are driven to horrific acts of violence or emotional abuse, often towards people they claim to love.
The vast majority of men find this violence abhorrent, so where are things coming undone?
A finger of blame has been levelled at a lack of support for women needing help, with the number of domestic violence workers labelled a national shame.
In October 2022, the Federal Government allocated $169 million to recruit 500 frontline service and community workers to support people experiencing family violence, but it was recently revealed that only 63 workers had been hired.
In our cover story this month, we unpack the extent of the national epidemic, and the ways experts believe we need to be alert to the early signs.
That includes the role of GPs in picking up subtle signs of abuse, such as the nervous patient continually texting her partner during a consult.
And yes, it does add another layer of work for our overstretched primary care health professionals, who continue to provide a wider range of care, without the wider financial recognition.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.




12 Identifying DV and extending the hand 16 Close-up: Dr Mariam Bahemia
20 A heavy weight for popular meds 28 From benchtop to market
46 Celebrating life in short – micro-memoirs

Positive results for sarcoma
The winner of our May doctors dozen, featuring wine from West Cape Howe, is Dr Dorothy Graham, pictured here collecting her prize.
This month we have extended the chance to win another great selection of wines, from Below and Above, with the winner announced next month.
We continue to have a bounty of free movie tickets to give away, with five double passes to the 2024 Scandinavian Film Festival, and 10 double tickets to It Ends With Us, the first film adaptation from a Colleen Hoover novel. See more details on page 47.
To win the wine or movie tickets, use the QR code on this page or go to mforum.com.au and hit the competitions tab.
PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor Cathy O'Leary 08 9203 5222 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au
Journalist Eric Martin 08 9203 5222 eric@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager Ross Bulman 0428 759 076 ross@mforum.com.au
Clinical Services Directory Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au















By Cathy O’Leary
A complex surgical service set up in Perth last year to treat connective tissue disease (CTD) has already saved lives and avoided emergency travel interstate for treatment.
A group of medical specialists set up the open thoracoabdominal service at Fiona Stanley Hospital to treat CTD, which causes weakening or splitting of the aorta.
It is coordinated by a specialist surgical team, including vascular surgeons
Dr Jens Carsten Ritter (top right), Dr Rick Bond and Dr Anwar Choudhary, cardiothoracic surgeon
Dr James Edelman and cardiothoracic anaesthetist Dr Warren Pavey

CTD is a relatively rare, but complex disorder that can lead to death. It includes Marfan’s syndrome, which affects one in every 3000-5000 people, Loey’s-Dietz syndrome, Ehlers-Danlos syndrome type 4 (vascular type) and Familial Thoracic Aneurysm and Dissection syndrome.
Before the open thoracoabdominal service was offered at FSH, some patients with CTD had to travel interstate for life-saving treatment.
Dr Pavey, who is also chair of the Heart and Lung Research Institute of WA, said the new service was an example of what could be achieved when research and frontline medicine combined.
“At the HLRI, for example, most researchers are practising medics, so we see the problems that exist for our patients,” Dr Pavey said. “Complications of CTD can affect
relatively young people and the consequences can be catastrophic if left unattended. When we do these types of surgeries, we return people to a full and active life.
“You never know when you may have problems such as heart or lung disease or CTD. It’s not always related to lifestyle, diet or hereditary. Everyone is at risk so it’s important we have the resources to fix these issues.”
Dr Ritter said the new service was supporting CTD patients nationwide.
“The key was to find and form a group of clinicians in WA that had an interest in managing these complex patients, and who were willing to bring the input and expertise required to undertake these long, large, complex and high-risk surgeries,” he said.
A clinic run in conjunction with the new service means patients newly diagnosed with CTD and those with a high suspicion of having the
condition can be closely monitored for vascular complications.
“They will receive genetic counselling as part of the service as well as routine screening for vascular complications, so that they can undergo surgery at the ideal point of time before catastrophic complications arise,” Dr Ritter said. One of the people to benefit from the service since it opened is 69-year-old former Australian national kayak champion Patrick Tullock.
When discomfort in his chest forced him to abandon a morning’s paddling on the Swan River one morning in 2016, he could never have predicted he would undergo multiple surgeries – including a marathon operation to replace his main blood vessel, from neck to pelvis.
While out on the water, Mr Tullock had suffered a life-threatening but relatively silent thoracic aortic dissection – the “freeway” that carries oxygen-rich blood from the heart to the rest of body.



More than 300 delegates from Perth and regional WA attended a GP Urology Masterclass held in Perth last month.
Organised by Perth Urology Clinic, the seventh annual event held at the Westin Hotel on June 8 was designed to provide GPs with gold standard education on all aspects of urology, which is acknowledged as a broad field of practice.
The program covered topics such as men and women’s health, urological cancer, an update on PSA, guest speakers, patient presentations and Q&A sessions.
It also provided educational value, being eligible for selfassessment by the RACGP for accredited CPD hours, with the content featuring 19 educational presentations.
Presenters included Perth Urology Clinic consultants, regular associates Melissa Hadley Barrett and Dr Ahmed Kazmi, and invited guest speakers Dr Eve Tiong, Dr Andrew Barker, Dr Manusha Ratnayake and physiotherapist Irena Nurkic.
Sponsors included Ramsay Health Care, St John of God Health, Genesis Care, Lawley Pharma, GKS and BXTA.
As part of the Chronic Heart Failure pilot project, the WA Primary Health Alliance has partnered with the WA branch of the Pharmaceutical Society of Australia to integrate non-dispensing pharmacists into multidisciplinary teams in two general practices in Geraldton.
GP Dr Shaun Millns-Sizer from Midwest Aero Medical said his team had been reviewing practice data through the Primary Sense system to identify CHF patients who had been recently discharged, diagnosed or previously identified as living with the condition.
It worked with a non-dispensing pharmacist and the Geraldton Health Campus.
“Using the telehealth model, Susan Shipway, the non-dispensing pharmacist, and our GPs have been improving medication optimisation and titration plans to ensure CHF patients receive the best possible treatment,” Dr Millns-Sizer said.
“Susan has also been providing patients with education about CHF, enabling them to manage their condition more effectively to reduce hospital readmissions.”


Although he had a family history of connective tissue disease, he was initially not overly concerned.
“I went home and initially thought I’d have a sleep but just as well I decided to head to the hospital instead, because if I had gone to sleep, the doctors told me I would never have woken up,” Mr Tullock said.
Emergency open heart surgery that morning at FSH saved Mr Tullock’s life and was followed by a second surgery in 2017 that included the reconstruction of the carotid artery, running up the side of his neck to his brain.
Because of the new service at FSH, he was able to have his mammoth third lot of surgery – to replace his aorta – in WA, instead of having to travel interstate.
The specialist team swapped out his aorta altogether, replacing it with a man-made graft with side branches surgically joined to Mr Tullock’s own arteries. Involving an 80cm-long incision from upper
chest to pelvis and cutting through Mr Tullock’s ribs, the complex and high-risk open surgery took about 15 hours.
Before last year, this type of surgery was not performed routinely in WA owing to its complexity, and only offered in select centres in the world, including two other hospitals on the east coast of Australia.
“Not only have I been given a second chance at life, but now I don’t need to worry about my aorta tearing again. It’s life-changing,” Mr Tullock said.
Fundraising has helped to support the work by the Heart and Lung Research Institute. Back in April, it held its second annual Breaths and Beats cycling event, to raise funds for medical research into advanced heart and lung disease.
More than 230 cyclists led by 13 WA heart and lung transplant recipients raised over $255,000 for the institute.

Chemical pathologist Dr Michael Page has been re-elected for a second term as AMA WA president, with public health medicine trainee
Dr Katharine Noonan and consultant psychiatrist Dr Kyle Hoath taking on vice president roles.

In King’s birthday honours, former head of WAGPET
Dr Janice Bell and Goldfields paediatrician Dr Christine JeffriesStokes were among those awarded a Member (AM) of the Order of Australia.
The WA Country Health Service’s emergency telehealth service has reached a milestone, with the opening of its 100th site situated in Walpole.

Ear Science Institute Australia will develop the Australasian Hearing Registry and Biobank, the first centre of its kind to store tissue related to geneticassociated hearing loss. It has also made auditory neuroscientist
Dr Christo Bester head of implant innovation.
Perth researchers, including Professor Minghao Zheng from UWA and Perron Institute, have contributed to a big international discovery that bone cells 'feed' mitochondria to blood vessel cells.
Long-time Telethon Kids Institute staff member Mitch Messer was recognised at this year’s Western Australian of the Year Awards for his work to bridge the gap between consumers, the health system and policy makers.
In recognition of the telehealth service that Ms Shipway has been providing for CHF patients in regional WA, she was recently named the 2024 WA Pharmacist of the Year.
A survey of Australian workers has named Healthscope, St John of God Health and Sonic Healthcare as
the most attractive employers for people working in the health sector.
The annual independent analysis of more than 6000 Australians by recruitment and HR services company Randstad found that the three organisations were recognised for job security, financial health, career progression and a good reputation.
The survey found that over half of respondents identified transport and logistics as the most attractive sector to work for, tied with

A Perth neurologist has helped develop a global picture of the huge public health impact of 37 conditions affecting the nervous system.
Professor Graeme Hankey, the inaugural Perron Institute Chair in Stroke Research at UWA, contributed to the study published in The Lancet Neurology, which ranked neurological conditions as the top contributor to the global disease burden, followed by cardiovascular diseases.
Professor Hankey said that in 2021, two fifths of the world population (an estimated 3.4 billion people), had a condition affecting the nervous system.
“These disorders were diverse and included neurodevelopmental disorders, late-life neurodegeneration and emergent conditions, such as cognitive impairment following COVID-19,” he said.
“The 37 neurological conditions selected for the study were collectively the top contributors to ill-health and disability worldwide, measured as the sum of years of life lost to due to premature death and years lived with a disability.
“They led to the loss of the equivalent of 443 million years of full health globally in 2021.”
The top 10 conditions causing the greatest loss of years of healthy life were stroke, neonatal encephalopathy, migraine, Alzheimer's disease and other dementias, diabetic neuropathy, meningitis, epilepsy, neurological complications due to preterm birth, autism spectrum disorder and nervous system cancer.
The review found that 82% of deaths and 85% of illness and disability due to neurological conditions occurred in low-to middle-income countries.
construction, closely followed by health and social work activities.
Feedback included 88% of workers saying they did not believe they had been compensated for inflation, but unfavourable market conditions were stopping them from searching for better pay elsewhere.
There was also a downward shift from last year’s survey, when more people identified the public sector as the most attractive place to work.
Preventing hearing loss in children with cancer and revolutionising multiple sclerosis treatment are among the Curtin University health research projects awarded a total of $700,000 in WA Near Miss Awards Ideas Grants.
Seven Curtin projects will receive $100,000 from the State Government’s Future Health Research and Innovation Fund, which provides funding to WA researchers who miss out on National Health and Medical Research grants.
Deputy Vice-Chancellor, Research Professor Melinda Fitzgerald, said the grants would allow the projects to continue the search for new, innovative ways to improve people's health and wellbeing domestically and globally.
Curtin’s School of Population Health received funding for four projects, two of which are led by Dr Virginie Lam, who is also affiliated with the Curtin Health Innovation Research Institute and the Perron Institute.
Dr Lam is investigating a remyelination therapy aiming to restore myelin in people with MS, potentially improving symptoms and slowing or halting the progression of the disease.
Her other project aims to prevent cognitive issues caused by chemotherapy in breast cancer survivors, including memory lapses and difficulty concentrating, by using neuroprotective compounds developed by her team.
Medical Forum has a new advertising manager, Ross Bulman, who brings a wealth of experience in the advertising industry in Western Australia. He is looking forward to working with current and new clients.
Ross can be contacted on ross@mforum.com.au and phone 9203 5222 or mobile 0428 759 076


Edith Cowan University is using TikTok influencers to educate Aboriginal teenagers about the human papillomavirus.
WAFL players and brothers Sam and Ben Stubbs recently hosted a workshop to help create social media content about the dangers of HPV which, in the unvaccinated, can lead to deadly cancers.
The content creators, affectionately known as Stubbers, have amassed over 500,000 followers on TikTok and are trying to help young Aboriginal people aged 12 to 15 create their own social media content.
"At the end of the day we want all our families to live long and healthy lives, and to do that we have to learn to make healthy decisions," Sam said.
Associate Professor Natalie Strobel, a researcher in the Maladjiny Research Centre, said delivering health promotion through social media platforms could empower people to take ownership and control over their health.
Data from the National Centre for Immunisation Research and Surveillance show that many young Aboriginal and Torres Strait Islander people do not receive their HPV vaccine doses, resulting in missed opportunities to be protected from HPV and its related cancers.
"In the workshop, participants learnt how to develop and create TikTok messages for themselves that can inspire others to make good decisions when it comes to their health, like getting the HPV vaccination," she said.
Her research project, Improving HPV vaccination rates for Aboriginal young people through social media, received a National Health and Medical Research Council Ideas Grant to look at how combining co-created health promotion messages from young Aboriginal people with 'micro-influencers' could improve HPV vaccination rates.
"There is a HPV vaccine that children in Year 7 can get for free – it's a one-off vaccination – and the international evidence shows that deadly cancers like cervical cancer are declining significantly because of it," she said.
Doctors from the American College of Pediatricians and colleagues from other medical organisations across the US have signed the Doctors Protecting Children Declaration, calling on prominent medical institutions to halt protocols promoted for children and adolescents who are unhappy with their biological sex. WA Intensivist and anaesthetist Dr Luke Torre urges the same here.

I graduated from UWA School of Medicine in late 1999. Five of those graduates are now paediatricians and we are lucky to have them. I worked in paediatrics as a resident and training registrar for almost two years, meeting many impressive paediatricians and benefiting from their teaching and rapport.
Now, as a father of five children, I have needed the help of many paediatricians, in many subspecialities, to maintain the health of my young family. They have always provided accurate and exceptional care. The public of Western Australia is well served.
And, in part, I address this message to all WA paediatricians – puberty is a normal and essential part of every child’s development and progression to adulthood.
In medical history, we have never considered the primary cessation of puberty to be ethical or warranted. Puberty is not a medical disease. Precocious puberty is recognised, and we temporarily delay it, with the unquestionable intention of allowing a full natural puberty to occur. It is the exception that proves the rule.
Think of the medical scandal of the castrati in 16th and 17th century Italy. These young boys, with perfect soprano voices, singing in operas and choirs, were castrated to prevent the inevitable voice ‘crack’. Their puberty was
forcibly denied, aided and abetted by doctors. We see the ethical violations here and are horrified. Quite rightly this practice has long been consigned to antiquity.
But today there is a new paradigm. An idea has emerged that natural puberty can be blocked, and then chemically diverted to puberty of the opposite sex. This idea is new, it has only existed for about as long as I have been alive, and it has gone from obscurity to commonplace in one generation. The numbers of children on these treatments, particularly girls, has increased exponentially in a few short years.
Paediatrics now tells us that blocking testosterone and giving estrogen to a male child is good medical care. Despite knowing that this can cause a micropenis, testicular atrophy, infertility and sexual dysfunction, this is deemed appropriate.
Similarly, it believes blocking estrogen and giving testosterone to a female child is good medical care. Despite knowing this can cause atrophic vaginitis, dysmenorrhea, menstrual irregularities, infertility, sexual dysfunction, clitoral hypertrophy and hypersensitivity, this too is deemed appropriate.
Puberty blockers are also known to cause osteopaenia and idiopathic intracranial hypertension. Cross sex hormones also increase the likelihood of systemic diseases like obesity, atherosclerosis,
hypercholesterolaemia and thromboembolic events.
Finally, we recognise the effect of pubertal hormones on a child’s brain, altering their thoughts, emotions, desires, relationships and more. These natural hormonal effects are themselves treatment for the distress of puberty, a treatment now denied.
A male body does not respond healthily to a female puberty, nor a female body to a male puberty. Yet we are assured that these hybrid young adults will be healthier and happier with a life of chemical and then potentially surgical alteration. Can we truly accept that a child can fathom all of this, understand the lifelong consequences and provide consent to such a complex issue?
If those working in gender diversity services guaranteed that all children put on puberty blockers would have them stopped within a short time frame and allowed to undergo their natural programmed puberty, perhaps we could relax on this issue.
But the truth is starkly different. In gender diversity clinics around the world, most children who start puberty blockers transition to cross-sex hormones (64% in the Cass review, 98% in the UK early intervention study). They are denied their natural puberty, forced into one not fit for their sexual organs and consequently given lifelong complications and medical dependency.
In the WA parliament in April 2024, it was revealed the Perth Children’s Hospital Gender Diversity Service has 64 children on puberty blockers, and 41 on cross-sex hormones. These numbers increase year on year and include children as young as 10.
In my opinion, parents putting their children on puberty blockers and cross-sex hormones have consented under false pretences. They have been told that these drugs are fully reversible, safe and lifesaving. Yet we now know that children are harmed.
They are harmed in the name
of affirmation, in the name of empathy, in the name of diversity. This cannot be allowed to continue. The day of reckoning is upon us. The Cass review from the UK is evidence of the problems, and its recommendations are clear. Countries around the world are awakening to the dangers of interfering with puberty and are putting a stop to it.
Too often paediatricians and the wider medical community excuse themselves from this issue with comments such as “I don’t work in the gender clinics” or “I don’t prescribe those treatments”.
A WA study has helped unravel how parts of the immune system could be harnessed to treat multiple sclerosis.
The research, recently published in the journal Frontiers in Immunology, could help research on more targeted immunotherapies.
Joint author and postdoctoral researcher Dr Belinda Kaskow, from the Perron Institute, UWA and Murdoch University’s Centre for Molecular Medicine and Innovative Therapeutics, said that in MS, B cells played a key role in inflammation, either though pro-inflammatory signals or anti-inflammatory signals.
The study identified a subset of anti-inflammatory or regulatory B cells that could control inflammation caused by T cells. In people with MS, these regulatory B cells had lost their ability to control inflammation.
Those excuses no longer suffice. They rationalise the explosion of referrals of children, mainly girls, to gender clinics is due to a more accepting and inclusive society, ignoring the obvious evidence of a social contagion.
It is time to stand back and reflect on what exactly is happening here, why our children are not flourishing, and why we are not helping them. Time for the experts in puberty to stand up and speak out. Puberty requires little medical expertise and a lot of common sense. It must occur in every child, or we cannot have healthy adults.
Dr Kaskow said current treatments for MS worked by modifying the immune system to reduce inflammation in the central nervous system. A group of these immunomodulatory therapies target a protein called CD20, found on the surface of most B cells and a small subset of T cells.

“While anti-CD20 therapies deplete B cells, this effect is not permanent, and B cells reappear in the blood. When they do, they seem to be ‘reset’ and can restore immune balance,” she said.
“In our study, we found that these anti-inflammatory regulatory B cells were increased only in the blood of people who responded well to anti-CD20 therapy. These individuals showed improved symptoms, compared to those who did not respond to the therapy.”
GPs are in a special position to pick up subtle signs in patients that could indicate family abuse and violence, particularly at the hands of controlling men.

By Eric Martin
While the nation grapples with the issue of domestic violence, Western Australia has faced a spate of family killings that have claimed the lives of nine women in the first half of 2024. After the Northern Territory with 3.97 per 100,000 women killed this year, WA has the highest number, at 3.1 per 100,000, more than double that of NSW at 1.31.
And while the role of WA Police and their response to family requests for protection has been thrust into the spotlight by the allegations of the latest perpetrator’s daughter, it is often GPs who have the first glimpse of potential family violence and struggle with how to tackle such a sensitive yet crucial subject.
Why are men choosing to use extreme violence against their partners?
Professor Donna Chung , from Curtin University’s Faculty of Health Sciences, has worked on numerous research projects investigating family violence and consults government on related policies and programs. She pointed out that in the 1990s and 2000s, as more women entered the workforce, more men started to engage with parenting and had to renegotiate their place in the world.
“Everyone wants a good standard of living. But when it comes to the woman potentially earning more and being less available because of the hours she must work, that is often where there might be a tipping point, especially if there are children in the home.
“While the relationship dynamics might be split 50/50 when there are no kids, it often reverts to a more traditional role. That in turn is influenced by Australia having a very gender-segmented workforce, where the pay-gap is inherently skewed, such as plumbing getting paid more than hairdressing, for example.

“We saw the rise of the incel (voluntary celibacy) movement as a rejection of the dominant, sport-based, hyper-masculinity. But there's also a myth that these men don't have good communication skills, and that's why they use violence. Many give a good account of themselves. When you meet them online, in bars, or at work it's not, ‘hi, I'm John and I've got three VROs from three different women’. That's not the story, it's all their partner’s fault – ‘they're horrible, nasty women.’
money as a couple’ – meaning that financial abuse could be a more effective lever for control. Another potential target is a woman’s body image, ‘no one else would want to be with you’.”
While some relationships were not particularly healthy and may be uneven in their power dynamics, an abusive relationship could be defined as when one person was being intimidated all the time.
“There are moments when the victim in the relationship will snap back, they’ve had enough, and they could even throw a glass themselves. But that will be interpreted as reciprocal violence, whereas it’s just an expression of helplessness – there is a disregard for consequences in that moment because they have been pushed to the edge,” Professor Chung said.
“In a normal argument people can get into who was wrong and who was right, but no one feels fearful and intimidated. But in coercive relationships the other person is always walking on eggshells, dancing around trying to minimise potential triggers.
“Academics used talk about the ‘gender wars,’ yet it was not a war so much as everyone trying to work out their new identity,” she said. “While there is still an intergenerational pressure around masculine performance – such as my father was a good footballer or good surgeon – it's quite different to, for example, young African men from the first generation born in Australia, who are struggling with everyday microaggressions in terms of racism and finding their place in an Australian community that isn't necessarily that welcoming.
“Even though Australia is a very multicultural nation, our mainstream culture comes from that Western, Judeo-Christian breadwinner model where the man's had economic dominance and been the primary breadwinner or main provider. And I think that's been a challenge for some men.
“Women are caught up in that grooming, and once groomed, they can believe those accounts, drawing on those stereotypes. ‘She took me to the cleaners’ or ‘I came from an abusive family and don't have any contact with my family because of that.’ When in fact, years later, they discover the reason their partner has had no contact with the immediate nuclear family is because they've been deliberately ostracised.”
Professor Chung said that men with abusive tendencies would sometimes target people with low self-esteem or who have been through a tough time, enabling them to mark behaviours which could become the basis for coercive control.
“Much like a school bully will pick potential victims in the playground,” she said. “You target what you know will have the most crippling emotional effect. For example, ‘as a single mother for a long time you haven't had a lot of money, but now that I've come along, we have more
“It's not thoughtfulness so much as managing expectations: hyper-vigilance around keeping everything as calm as you can, which is exhausting. When women first leave and go to a refuge they will often sleep for the first few days. Their body takes over because they've been in overtime and probably haven't slept properly for years.
“We also have a more complex way of negotiating intimate partnerships and relationships: people aren't necessarily getting married at 20 and staying married till they're 90, like they used to. Research shows that people are often having two or three big relationships over their life and each time, it's generally a different type of negotiation.
“Paradoxically, many of our cultural rituals around courtship have changed as well and it’s also much easier to end up living together, which can be equally challenging for many older people entering relationships.
“Another exacerbating factor now is the housing crisis. Couples with separate houses and no plans to
continued from Page 13
move in together can be suddenly forced to live together if one partner loses their rental property. There's no sense of it being a stage of the relationship's development and commitment, it's a forced situation that brings its own associated stresses.
“Everything and everyone seem to be living on the edge and that can push people over the edge or hand an abusive partner another lever for control.”
While digital technology may have been a boon for communication, Professor Chung said it also
provided an effective tool that people could use to put their partner under constant surveillance.
“For example, texting 30 times a day and expecting a response within a few minutes – that’s another sign that GPs can watch for during consultations. While you don’t want to jump to conclusions, as we’re all relatively addicted to our phones, a patient occupied with their partner’s texts during the consultation could be a red flag for coercive control,” she said.
“Another flag, particularly if the relationship is abusive and is reaching its end is that the patient
might need something to deal with a high level of anxiety but could be reluctant to engage with treatment because of the fear that a mental health diagnosis could be used against them in the family court.”
Professor Chung said one of the particularly important factors for GPs to be aware of was the reluctance of perpetrators to have their children diagnosed with any sort of learning difficulties, disability, or stigmatised condition.
“Rather than support for the child, it’s used as another weapon in the relationship – ‘that's because you're a bad mother,’ or ‘that's from your side of the family, and I'm not
A new partnership between a community legal service and St John of God Midland Hospital is aimed at providing early responses to family and domestic violence.
Midland Information Debt and Legal Advocacy Services (MIDLAS), a not-for-profit centre which has been supporting victims and survivors of domestic violence for 35 years, has formed a health justice partnership with St John of God Midland public and private hospitals.
Supported with a $100,000 Impact100 WA grant, the partnership provides an early intervention response to the escalating family and domestic violence crisis as well as elder abuse in Western Australia.
Working in close liaison with health professionals, the partnership between MIDLAS and the Midland hospital provides onsite free legal support in a safe setting to victims and survivors of domestic violence.

MIDLAS chief executive officer Gaelle Gouillou said that with the potential to be replicated in other parts of WA, the initiative between the only community legal centre in the region and a major hospital provided an evidencebased early and primary prevention response to reduce rising rates of FDV.
According to figures reported in an Australian Bureau of Statistics Personal Safety Survey (2016), two out of five Australians would not know where to get help for a domestic violence issue and as few as 20% of victims contacted the police for assistance. But people experiencing FDV were known to be more likely to disclose abuse to healthcare providers.
Ms Gouillou said with the sharp rise in FDV-related deaths and WA Police reporting a 35% increase in family-related offences in 2022 and a 15% increase on that figure in the first nine months of 2023, early intervention solutions were needed more than ever.
The Midland Health Justice Partnership, which complemented screening by clinicians for FDV, had already provided help with 23 separate legal issues.
MIDLAS lawyer Anne-Marie Ricciardi said a high priority was to create greater awareness among victims and survivors of the options and types of support they could access.
“We can assist people to put legal protections in place to help keep them safe. We provide advice and assistance in relation to restraining orders, family law, criminal injuries compensation and tenancy matters,” she said.
Along with providing an early intervention response for the FDV crisis in WA, the service also offered an early intervention and prevention strategy for elder abuse and the protection of older people’s rights.

SJOG Midland chief executive officer Paul Dyer said the service would fill an identified gap, and health justice partnerships had a long history of delivering outcomes for the community across Australia.
The Midland program complements a similar service launched in October 2023 by the East Metropolitan Health Service.

supporting any treatment for that’,” she said.
“Even when a GP has referred the child to a paediatrician or a clinical child psychologist, the response is, ‘I'm not paying for any of that. There's nothing wrong with that kid. They need a kick up the arse and to go back to school.’
“Sometimes kids that seem overly socially withdrawn have been told to shut up all the time, ‘don't upset your father – everyone shut up.’ Other kids can be quite outspoken or seem overly familiar in social situations because they've worked out quickly that it's safe to actually push boundaries – like pushing a teacher to the limit because they know that adult can't hit them.
“However, even if GPs have a good relationship with the child or mother, they may still feel reluctant to talk about domestic violence as the source of the patient’s anxiety or depression. Unhealthy dynamics are built up in a relationship over time and it's hard for GPs to get to what the problem is in 15 minutes, it’s like opening Pandora’s box and is easily put in the too-hard basket.
“GPs can feel helpless, opening a conversation where there is a risk that the patient might go home and dwell on it, or leave the surgery in tears. But sometimes there are basic cues, and GP consultations often offer a brilliant entry point for wider discussions about relational issues.
“So, if it's about contraception, if it's about their sexuality or their gender identity, GPs can use that to initiate a conversation to discuss consent and equality in relationships in an informative manner.”
Professor Chung highlighted that the most recent guideline for GPs was the White Book, Abuse and violence - Working with our patients in general practice, published by the RACGP Vic and last updated with a fifth edition in 2022 by Dr Kelsey Hegarty, from the University of Melbourne’s Safer Family Centre.
“Dr Hegarty’s research has been some of the most forward thinking and it’s really the go-to-resource in Australia. It has webinars GPs can access and because it's NHMRC funded, everything must be publicly available,” she said.
“There is past and current research, and they are always adding to it. And as Dr Hegarty is still involved with general practice, she has firsthand experience to ensure the White Book is thoroughly grounded for GPs. She has been working alone for a long time on this topic before getting the funding for a team of people to pull it together and really amp up the volume of work.”
ED: The 430-page resource is divided into six topics, with levels of evidence and recommendations included: Domestic or intimate partner abuse/ violence; Trauma- and violence-informed care; Children and young people; Specific abuse issues for adults and older people; Specific populations; System issues.
The White Book is available online at https://www.racgp.org.au/ clinical-resources/clinical-guidelines/ key-racgp-guidelines/view-all-racgpguidelines/abuse-and-violence/ preamble
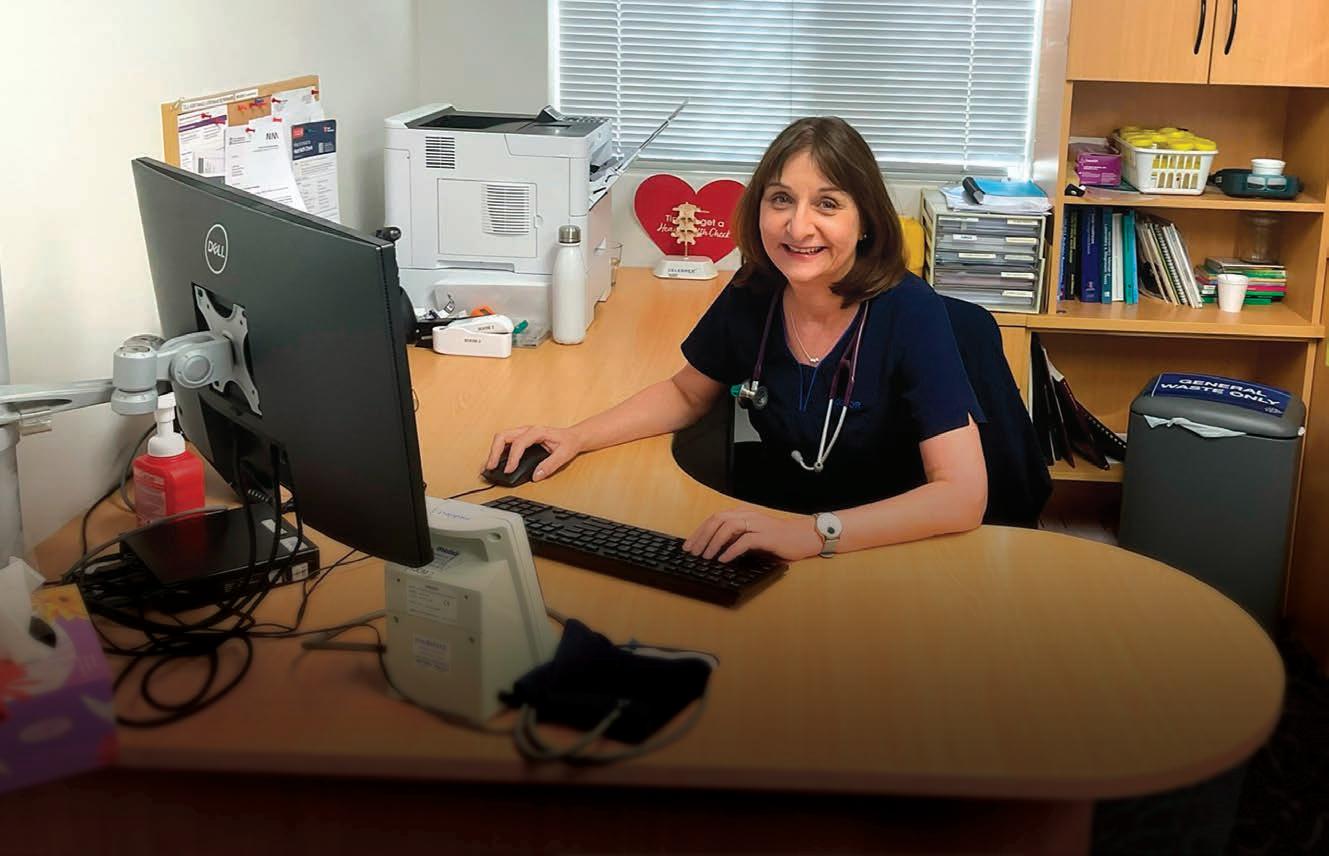
Dr Mariam Bahemia likes letting her work as a GP and advocate speak for itself rather than seeking the spotlight.
By Ara Jansen
She might consider herself low key when it comes to visibility, but Dr Mariam Bahemia’s work as a GP, volunteer and advocate makes plenty of noise.
“I enjoy making a contribution,” she says. “The groups I am involved with are an opportunity to provide advocacy, education and to make a difference to the lives of children in Mauritius and Rodrigues. There is a unique and special connection within our medical community in Perth. This provides many opportunities to network and find ways to make a contribution.
“It’s important to have member-based organisations to advocate for GPs and their patients. I’ve worked in three countries as a GP and wherever you go, you realise what a difference GPs make in their communities. It’s a very special relationship with a trusted doctor. There will never be anything that replaces the work of a GP. There’s so much we do to improve public and community health.”
Mariam’s parents – her father Mauritian and mother Irish – met at the Rotunda Hospital in Dublin, a maternity hospital. Mary was a midwife and Ally was a medical student at the Royal College of Surgeons. They connected when Mary took students on visits to do home births. It was the 1960s and a relationship which mixed culture and religion was quite unusual.
The pair married in London and Mariam and her two siblings were born there. Life in London wasn’t always comfortable in the 1970s and the pair were no strangers to racism. So, they decided to make a change.
Ally had a cousin who was a GP in Perth, so it became a choice of Western Australia or Canada. Mary wanted to move somewhere warm, so Perth won.
“I wasn’t particularly happy moving here,” says Mariam who was eight at the time. “I was extremely happy in London and loved it there. We travelled a lot to Mauritius and to the west of Ireland to visit family while I was a child.”
While being a doctor had always been on her radar, Mariam also had a talent for singing and had her own tutor. Before moving to Australia, she performed in Tchaikovsky’s opera The Queen of Spades
“I thought I would love to be an opera singer, but once we moved to Perth I didn’t continue with singing. There was a short time there where I wanted to be a pilot, after I went to an open day in Year 9. None of it was ever serious because I really always wanted to be a doctor, but not just a doctor, I wanted to be a GP.
“General practice was always something that interested me. I was inspired by my late father who knew something about everything. I worked as a receptionist in his

practice. I was touched by the way his patients trusted him and the very special relationship a GP has with their patients.
“After my years of studying at university I didn’t want to practise in a narrow field. As a GP and a medical receptionist, I realised what a privilege it was to care for people and be trusted by them.”
Unlike today’s proliferation of group practices, Ally started his practice in Perth as a solo GP, which wasn’t unusual at the time. As Mariam was readying herself to become a GP, she saw how difficult and challenging that was and not an easy choice.
Mariam studied medicine at UWA, but it wasn’t smooth sailing. In her
second year her father died of a heart attack. He was 52. Losing him so suddenly was “deeply traumatic”. While her friends and fellow students rallied around to help create some sense of normalcy, it was obviously a difficult time. Mariam failed her exams.
“This was a new experience for me. I still remember the telephone call from the university when they told me that after deliberation, they would grant me the opportunity to repeat the year and that I should consider myself extremely lucky. I told them I didn’t feel lucky.”
Mariam did seven years of medicine and made a new group of friends, many of them who are still her friends today.
“They have lasted a lifetime. Without them, things would have been even more difficult. I’m very grateful for them.”
She did her internship at Sir Charles Gairdner Hospital, then spent six months at PMH and did a diploma in child health. As part of her GP training program, she went to practices in Balga, Pinjarra and Whitfords.
On completing her fellowship, Mariam thought she would go back to the UK. An around-the-world ticket took her to New Zealand, Canada and eventually to London, where she worked as a GP. It didn’t take her long to decide she didn’t enjoy working in the NHS as a GP. She returned to Perth in her late 20s.
The GP went to work in the practice of the late Dr Mohan Singh. After
New clinic Armadale North now open

Perth Radiological Clinic offers a comprehensive range of men’s imaging services including:
Multi-parametric MRI for early detection and staging of prostate cancer
MRI guided prostate biopsy
PET-CT PMSA studies
Penile ultrasound
Scrotal ultrasound—adult and paediatric
Urethrograms
Scrotal interventional procedures
Cross sectional imaging including MRI for diagnosis and staging of male genitourinary malignancy
All imaging reported by PRC’s expert sub-specialist urogenital and nuclear medicine reporting teams
Armadale North services include:
• MRI • CT including CTCA
• X-ray • Ultrasound • DEXA • Interventional services
3043 Albany Highway, Kelmscott
continued from Page 17
she became a parent, he was hugely supportive of Mariam having flexible work hours.
“His approach was that your family should come first. He passed away suddenly in 2010 of a heart attack and the practice closed. I had already watched my father’s practice close. That really brought home to me how important a GP is to a community and the farreaching effects that are felt when a doctor passes away.”
Mariam herself had the same GP for 36 years in Dr Stephan Hellmuth, who retired last year. He was the first person she rang after she passed her final medical exams. She also sat in with him as a student.
“He showed me it’s really important for every doctor to have their own GP. I encourage every doctor to have a GP of their own. Many of us are happy to see other doctors as patients. It’s very rewarding. He was also one of four GPs who has inspired and mentored me – I am grateful for the support they have given me.”
Another GP who is both a mentor and friend is Dr Serge Toussaint. He is a founding member of COMMSSA – the Children of Mauritius Medical and Surgical Support Association which was started in 1991. It’s a group very dear to Mariam’s heart.
“He approached me when I was a medical student when he recognised my surname as being Mauritian. I became involved with COMMSSA as an intern. It’s one of the most fulfilling things I have done in my life. Working with a team of volunteers we raise money and facilitate the treatment of disadvantaged children from Mauritius and Rodrigues. There are also many non-GP specialists in Perth who have assisted in the care of these children and given their time and expertise to make a difference. We are deeply grateful to them.”
Mariam – currently the group’s president – has travelled to Mauritius and Rodrigues with members of the committee numerous times over the years on self-funded trips to facilitate specialist nurse education programs in stoma and wound care.

The high incidence of Hirschsprung disease in Mauritius brought the group’s attention to the need for specialised nursing and wound care. They ran a stoma course for student nurses in Mauritius earlier this year.
Mariam is also active locally in the medical community including being co-deputy chair of RACGP WA and was a UWA clinical tutor for nine years. She currently works in a group practice in Bedford, where she has been since 2012. She has been working part-time since the early 2000s, after she had her first child.
“I do my best work part-time and continue being a doctor because I really enjoy everything about it. It gives me time to do other things in my life as well. I like combining being a doctor, teaching and with my Mauritian background, getting to meet and mix with people as part of fundraising. That’s how I can mix medicine with my time off, volunteering and giving my time to groups related to medicine.”
Married to obstetrician and gynaecologist Dr Michael Gannon, the pair have two teenage children.
In perhaps the closing of a circle, Dr Gannon’s fellowship in 2004 took the pair to Dublin and back to the Rotunda Hospital, where their daughter was born.
“Neither of my children are interested in medicine. I want them to be happy in whatever
they choose to do. Medicine is a challenging career. You have to really want to do it. It’s important to do what makes you happy and fulfilled.
“I grew up in a house with medical and nursing parents, my spouse is also medical. We both feel proud to be doctors, have a sharp understanding of what it takes and feel fortunate and lucky to be able to practise medicine and look after patients. I don’t know any different.”
When she’s not working, Mariam is an avid reader and enjoys spending time with family and friends. She has a deep interest in English literature and history.
“Growing up, my parents took us to see all the museum and art galleries – castles, Tower of London, Hampton Court, Hatfield House. History has always intrigued me and still does. I do miss that, living in Perth, so I travel and that fulfills my interest in history.”
When she’s in need of something less cerebral and more of a rush, it comes in the form of zip-lining. Mariam has zip-lined in Busselton, England, Ireland, Mauritius and the Otway ranges in Victoria. Her latest jump was off Matagarup Bridge on her birthday earlier this year. If there’s a zip-line, Mariam says she’ll give it a go.

A sharp rise in the number of people accessing some diabetes medications off-label in a bid to shed kilos is prompting governments and private health insurers to tighten access.
By Cathy O’Leary
The widespread use of weight-busting drugs such as Ozempic is a phenomenon that continues to polarise the community, governments and doctors.
And caught in the middle of the surging demand in people wanting to lose weight with the injectables are patients using it for diabetes control, who are struggling to access their essential medicines amid a global shortage.
On the one hand, patients who have struggled to lose weight for years swear by drugs such as Ozempic, which contains semaglutide.
But in the other corner are private health funds which have been stung by soaring costs in pharmaceutical claims, and health officials and doctors worried about the risks associated with the rising ‘back door access’ using compounded replicas.
Recent data suggests that at least 20,000 Australian patients are injecting these compounded replicas, and the majority are using them to lose weight.
Although originally developed to help people with type 2 diabetes, Ozempic has exploded in popularity as a weight loss drug since it came on the market in 2021. It is from the class of drugs known as glucagon-like peptide 1 receptor agonists, or GLP-1 RAs,
Although it is only approved for the treatment of diabetes in Australia, its off-label prescribing for weight loss is driving shortages which the Therapeutic Goods Administration believes will last until next year.
To manage these shortages, Australian doctors and pharmacies are being asked not to start new patients on Ozempic and to prioritise it for patients with type 2 diabetes who are already stabilised on the medicine.
However, the TGA says it does not have the power to regulate the clinical decisions of health professionals and is unable to prevent doctors from using their clinical judgment to prescribe Ozempic for other health conditions.
Meanwhile the pharmacycompounded versions of the drug are not identical to Ozempic (semaglutide) or Mounjaro (tirazapetide) nor are they TGAapproved. There are increasing reports of patients coming to harm from these drugs, including the hospitalisation of a patient in Australia due to a serious adverse event.
Internationally, the US Food and Drug Administration has warned consumers about the safety risks of injecting some compounded products following an increase in adverse events.
Here, the Federal Government recently moved to stamp out the compounded replicas, with new regulations from October that will remove GLP-1 RAs from the pharmacy compounding exemption. The Government says it has broad support of the crackdown from many health groups including the Royal Australian College of General Practitioners, the medical and pharmacy boards.
But there have also been financial implications from the surging demand, because people who take Ozempic for weight loss are prescribed it off-schedule, which
means they cannot get it PBSsubsidised.
A month's supply of Ozempic, or its counterpart Wegovy, on a private prescription, costs about $130 to $200 in Australia, while some of the sting is taken out for patients who can claim it on their private health insurance extras cover.
But research so far suggests that people tend to regain weight after they stop using the medications, leaving health funds with the prospect of potentially having to fund the treatment for life.
Whether to cover the drugs or not has divided insurers. WA’s biggest health fund, HBF, has moved to cut benefits significantly, arguing the rise in claims has become unsustainable.
From this month, rebates for Wegovy, which contains semaglutide, and several other pre-manufactured medications such as Saxenda will be cut, while benefits for other medications containing semaglutide will be halved. Compounded medications containing semaglutide will not be covered at all.
continued on Page 22
No benefits will be payable for these pre-manufactured medications.
• Saxenda
• Contrave
• Duromine
• Wegovy
• Other medication listed on the Australian Register of Therapeutic Goods with an approved use of weight management/reduction.
No benefits will be payable for compounded medications containing any of these active ingredients.
• Semaglutide
• Estradiol
• Minoxidil
• Liraglutide
• Tadalafil

• Finasteride
• Phentermine
• Alprostadil
• Drospirenone
• Naltrexone hydrochloride and Bupropion hydrochloride (when compounded together)
Benefits will be reduced for pre-manufactured medications containing any of these active ingredients. The new benefit will depend on the level of cover you hold.
• Semaglutide
• Dulaglutide
• Exanatide
• Liraglutide
• Tirzepatide
continued from Page 21
But HBF’s decision, which was announced in May, is at odds with how some of the country's other major insurers are treating Ozempic, with some making it more affordable under certain coverage plans.
HBF Executive General Manager Insurance and Health Services, Dr Daniel Heredia , said the fund had always paid out about the double the industry average on pharmaceuticals, but in the past three years alone, its pharmacy spend had almost doubled, with most of that growth coming from the GLP-1 medications.
“We drilled down on what is a significant deviation from the longterm trend in this claim size and we saw that a very small proportion of policyholders, about 3% of the 900,000 people who are eligible for a pharmacy benefit, were claiming on this medication, the GLP-1s,” he said.
“And when you take into account that a diabetic person, as long as they meet the relevant criteria, can access these medications on the PBS, that would lead you to the conclusion that of the people who are claiming it against their policy, probably the majority are doing it for weight loss, while there will be some who have type 2 diabetes but perhaps don’t meet the PBS criteria.”
Dr Heredia said he accepted the argument that the cost of the medications had to weighed up against the expense of other weight-loss treatments such as bariatric surgery, which could be expensive and claimed on private health insurance.
But he said that with the weightloss medications there were many unknowns, because the drugs were relatively new, and the weight loss was initially a side effect of the medications designed to treat type 2 diabetes.
“We don’t have a lot of experience with these medications, but we do know that for a number of people they are seen to have quite significant weight loss,” he said.

“Ultimately, as a not-for-profit insurer, our interest in terms of the health and wellbeing of the membership is sustainable, longterm weight loss.”
another one of the unknowns when it comes to the GLP-1s because what we’re tending to see is that once they’re stopped, weight is put back on.”
Dr Heredia said the fund offered health management programs that were focused on weight in one form or another, and they were more holistic in terms of diet, exercise and lifestyle change. They also had a proven track record when it came to people keeping the weight off.
“What we don’t know are the medium and long-term impacts of taking them, and so that needs to be factored into any analysis.
“It might prevent or avoid people needing to have bariatric surgery, but what we don’t know yet is what, if any, damage the medications do in the medium to long term, and what are the side effects.
“Ultimately, as a not-for-profit insurer, our interest in terms of the health and wellbeing of the membership is sustainable, longterm weight loss. And that is
He said that while he was comfortable with the new policy, the fund would continue to monitor medical practice and medications, so current decisions were not set in stone.
“The average price of Ozempic at the moment is $155, so there are big dollars attached to it, and it does get expensive,” he said.
“However, each insurer is very different, and so where we’ve seen a 40% growth in pharmaceuticals spend, others might have seen a much smaller growth.
“And even after these changes, when you look at something like Ozempic, the rebate that our members will get is still one of the highest compared to other funds.”

Dr Heredia also pointed out that there were other commercial factors that might affect insurers, with at least one of the other health funds involved in a business that prescribed those medications.
“We have to make decisions that are in the interests of the broader membership, so it’s always a challenge where you want to offer everyone everything. But we have to think of those who are eligible for pharmaceutical benefits and are not claiming for these medications but end up having to crosssubsidise the other 3%.
“It’s about balancing premiums, which is our biggest focus now because of the cost-of-living pressures and the need to keep premiums as low as possible, against the potential benefits, as well as potential risks and side effects that would ultimately end up costing the system.”
Dr Heredia said the fund had not specifically consulted with doctors on its change of policy, but they seemed to be divided on GLP-1s and the off-label use.
“There are those who are active proponents and prescribers, but similarly there are many who are
very cautious, and they see a more limited use for these medications,” he said.
“This is also one of the first examples of social media really driving demand,” he said.
“We’ve seen it a bit in bariatrics and cosmetic surgery, but the social media impact in terms of the GLP-1s is unprecedented and to the point where people with diabetes can’t even access these medications.
“This was part of our considerations, and that is one of the reasons that in the changes we’ll continue to pay benefits for medications that are TGA-approved for diabetes because the intent of these changes is not to stop funding diabetic medications – it’s for medications that are solely being used for weight loss.”
Dr Heredia said the fund also wanted to close the compounding loophole, similar to the recent Federal Government move.
“We have rules where there are certain medications we won’t fund, such as for weight loss, erectile dysfunction and hair loss, but
people could go to a compounding pharmacist and get it made up and we would end up paying,” he said.
“So, we’re closing that loophole at the same time, saying if we don’t pay for a medication, we can’t pay for it if it’s compounded because that defeats the purpose.”
Dr Heredia said that while there had been some feedback from members, it was mostly questions about how the new rules would work.
“We haven’t had a flood of people grossly upset about the changes, although there are obviously people who are disappointed, but it’s been measured feedback,” he said.
Dr Heredia said he was keen to make doctors aware of the new rules, which broadly meant that medications solely approved for weight loss were not covered. Nor were compounded medications for a certain list such as weight loss, erectile dysfunction and hair loss. Medications that were TGA-approved for diabetes would continue to be covered but the benefits would reduce in line with the member’s cover.
For the
past few years, a
highly respected former educator in the mining industry has been a regular and valued contributor to
Medical Forum.

Emeritus Professor Ifan Odwyn Jones began his mining career in Wales, later moving to WA and becoming principal of the Western Australian School of Mines at Kalgoorlie for 15 years.
He has been a longstanding member of the Minerals Research Institute of WA, and in 2006 was awarded the Order of Australia for service to the mining industry and the Kalgoorlie-Boulder community.
Odwyn has written several books on mining, as well as a collection of poetry and prose, and has several
Mitigation strategies are needed to safeguard the community from the ravages of air pollution in our cities and urban areas, according to E/Prof Odwyn Jones.
Much is currently known about the health impacts of air pollution on the health of those living in our cities and populated urban areas. They include cardiovascular, respiratory and neuronal diseases, with each disease affected by its own range of pollutants, whether it be pollutants from vehicular transport or specific work-related environments, or indeed, both.
Consequently, mitigation strategies are urgently required to improve the awareness of the public about these health hazards and what the city and urban planners and members of the public can do to reduce such unwanted exposures to poisonous ambient air.
It is generally acknowledged that air pollution is worsening in many cities and urban areas worldwide, leading to adverse health impacts for the populace. According to the World Health Organization (WHO), more than 80% of people living in urban areas are subjected to air pollution levels exceeding the prevailing emission standards.
It is worthwhile referring briefly to the stark facts revealed by Dr Tedros Adhanom Ghebreyesus, Director General, WHO, at its Global Conference in 2018:
• Air pollution kills some 7 million people annually.
• Estimates show that up to one-third of deaths from heart attack, stroke, lung cancer and

respiratory diseases are due to air pollution.
• Some of our children will not achieve their full potential due to their exposure to air pollution, and in many parts of the world the situation is worsening.
The WHO is doing its best to empower health professionals to explain the health risks of air pollution to parents and how best to reduce those risks
The WA Government’s Public Health Act 2016 is a risk-based proactive framework embodying regulations for controlling any specific risk to public health. Local
governments are the enforcement agencies, who have ‘authorised officers’ available to investigate any public health issue, such as atmospheric pollution.
The Act’s chief features include:
• Promotion of public health,
• Assisting to prevent disease, injury, disability and premature death, and
• Informing individuals and communities regarding public health risks.
Unfortunately, the current system of regulating and policing the quality of the air we breathe is failing the general public in our polluted cities and towns. Surely, there is an urgent need to inform
mining scholarships named in his honour. Together with his respected peer, the late respiratory diseases expert Professor Bill Musk, Odywn has written for us on a variety of issues, from the need for more rigorous oversight of the health of mine workers including the rise of silicosis in engineered stone workers, to broader concerns about the impact of climate change and pollution.
This month, he has penned his final piece for Medical Forum, calling for more to be done to garner support for climate action and measures to reduce pollution.
and educate Perth’s populace about the “impact of air pollution on their health and wellbeing”.
Not only is it important to measure and record the PM2.5 levels at carefully selected registered locations within our cities, it’s also important to measure levels of CO2 , since it not only affects the climate, but it also clouds our thinking. Indeed, it is claimed by researchers from Beijing University and Yale School of Public Health, that at levels of 1000 ppm of CO2 , human cognitive ability is reduced by about 21%.
As reported by the researcher, PN Bierwirth, Australian National University, (2018), “there is general agreement that levels of CO2 in 20-50% of classrooms commonly exceed 1000 ppm, and are often much higher, sometimes reaching levels as high as 6000 ppm for extended periods”.
These facts should be passed on to the public in an appropriate way, as a precursor to suggesting mitigation strategies.
Unfortunately, there is too little being done to keep the general populace informed of current knowledge about the health hazards associated with breathing polluted air as well as too little action being taken by public officers, government agencies and local authorities in, for example, doing something to minimise the effects of polluted air on children and youths in child care centres, schools, and colleges currently located near major freeways and/or busy roads.
This topic is covered in a recent article (Sofia, D., et al, Environmental Science and Research, 2020). It highlights the need to pay particular attention to the air quality in and around schools and colleges, including the time spent in traffic jams moving students to and from childcare centres and schools.
It is also worthwhile exploring how people, companies and committees can contribute to minimising air pollution by getting involved in proenvironmental programs.
Following is a list of some recommendations worthy of consideration by governments, local authorities and business enterprises:
• More use of public transport to reduce the number of cars on the major roads leading to the CBD.
• Reducing the number of fossil fuel powered vehicles on the urban and city roads, by car owners sharing their cars with other car owners and the increasing use of electricalpowered vehicles
• Improving the combustion efficiency of household solid fuels thereby reducing the release of unwanted products due to incomplete combustion.
• Using available technologies for improving the energy efficiency of buildings e.g. external wall insulation and painting outside walls in lighter colours.
• Improving the air quality control in buildings, with particular attention being paid to childcare
centres, schools and colleges, where children and youths are particularly susceptible to air pollutants due to their age.
As we know, industrial enterprises are one of the major contributors to global air pollution, and their pollutants are often easily transported into urbanised areas. Consequently, they need to adopt all available anti-pollution strategies to minimise the release of fine particulates and toxic gases into the ambient air.
Establishing effective vegetative and/or solid barriers for reducing the impact of localised ambient air pollution at or near major freeways and busy urban roads.
It is important that the public is kept aware of the extent of air pollution prevailing in their neighbourhoods and the health effects of breathing air pollution. Like any large city, Perth has its air pollution challenges, and perhaps it is time to organise a regional conference highlighting these issues and what can be done to mitigate their health effects.
Such a conference being organised in Perth by a small group of individuals representative of interested organisations and agencies such as Medical Forum, WA Health, the RAC and local universities, and led by experts in the field, with the local media in attendance, will ensure members of the public are well-informed of the issues being discussed and mitigation strategies.
A WA Health Department report has warned of a significant rise in heat-related deaths in Perth by the middle of this century, with people aged over 75 and those with heart disease most likely to be affected.
The analysis investigates the escalating heat-related health impacts within the context of climate change.
In earlier studies, extreme heat exposure has been closely associated with an increase in mortality and morbidity, particularly from ischemic heart disease, stroke, respiratory diseases, renal diseases and mental health conditions.
Building on this research, the WA
report analyses a broader period of historical data and a wider range of health outcomes, including cause-specific mortality, hospital admissions, emergency department presentations and health care costs. It then projects the potential health impacts and costs relating to heat exposure up until the middle of the century, finding that heat-related deaths are set to increase by 61.4% in the 2050s from the 2010s, with healthcare costs projected to increase by $30.6 million over that period.
The analysis reveals heat-related deaths will increase from 5.29 deaths per 100,000 in the 2010s
to 8.54 deaths per 100,000 in the 2050s, with people over 75 and those susceptible to cardiovascular diseases impacted most.
“Heat-sensitive hospital admissions and ED presentations are expected to rise by 33.8% and 29.8% respectively,” according to the report.
“Additionally, extreme heat-related mortality during summer (more than 11.5 deaths per 100,000) is expected to shift from a one in 50-year event under the climate of 2020 to nearly one in 10-year event by 2050.
“These results align with similar studies, reinforcing the urgency


for adaptive measures as recommended in the Australian National Health and Climate Strategy.”
The report concedes that establishing direct causality and the uncertainties in extrapolating current health impacts to future unobserved temperature extremes meant caution was needed when interpretating the results.
“Ongoing monitoring is essential to accurately understand and mitigate the evolving health impacts of rising temperatures in the region,” it said.
But the increase in pressure on hospitals was a particularly concerning finding, considering bed occupancy was already limited at Perth hospitals. Population growth was deliberately excluded from
the central cost projection of the report to isolate the impact of rising temperatures.
It warned that the evolving health impacts of rising temperatures required continuous monitoring.
“The projected increase in heat-related health impacts in Perth underscores the need for adaptation to mitigate these effects,” it found.
“The recently published Australian National Health and Climate Strategy outlines a range of measures that could help manage the health impacts of heat including heatwave warning systems, effective risk communication and targeted outreach for at-risk populations.”
Measures such as widespread tree planting could offset the increases in heat-attributable deaths in Australian cities, with tree canopies mitigating the additional heat that comes from increasing density and urbanisation.
Our treatment services include:
• Intensive Treatment Program (ITP) and a NEW Adolescent Intensive Treatment Program (AITP).
• Private Health Funded Day Programs including Schema Therapy, Teen DBT Skills, DBT Skills, RO-DBT, as well as Binge Eating Disorder (BED) and Post-bariatric surgery BED groups.
• Coordinated and collaborative individual and family outpatient treatment with Psychiatrists, Psychologists, Dietitians, Occupational Therapists, Physiotherapists and Specialist GPs.
For more information about our programs and services visit www.esuscentre.au
Esus Centre, 588 Hay Street Subiaco WA 6008 T 08 6255 9900 F 08 6255 9920

Medical breakthroughs don’t stop at ‘Eureka’. To be useful they need to be brought to market, and scientists now have somewhere to turn to for commercial help.
By Eric Martin
Producing a groundbreaking medical product or drug that has the potential to meaningfully improve patients’ lives is the holy grail for many independent researchers.
It is also the culmination of years of study, creativity, design and experimentation in a specific field.
Yet once the goal has been realised, many medical researchers struggle to make the next step to commercialisation and launch – a process that can be as legally and financially challenging as the initial research and development. It requires business acumen and entrepreneurial skills.
Rather than enrolling in an MBA or hiring consultants, Perth’s Centre for Entrepreneurial Research and Innovation (CERI) offers another avenue for building the commercial knowledge required to convert a medical innovation into the centrepiece of a viable business.
CEO Toby Swingler told Medical Forum that since opening its doors in 2016, CERI had assisted numerous medical startups and that Perth was well positioned to become a leader in this space, thanks to the number, energy, and expertise of West Australian research organisations.
“Western Australia has a strong life sciences research community: there are six medical research institutions within proximity of Sir Charles Gairdner Hospital, such as Harry Perkins, Telethon Kids and the Perron Institutes, with another cluster around Fiona Stanley Hospital. And there is world class research coming out of those organisations, a lot of people within that community have developed things that they see as having commercial potential,” Mr Swingler said.
“CERI has supported people that are developing medical devices, genetic tests, and even potential solutions to antimicrobial resistance, which is a global issue seeing serious treatment options being discovered in Perth labs.”
Lixa Revolutionary Antimicrobial Technologies, led by CEO Dr Maud Eijkenboom, has targeted biofilms based on a series of experiments conducted by researchers at the University of Western Australia that has led to the isolation of a potent naturally occurring antibiofilm molecule. The researchers had been working with clinicians and patients with chronic respiratory infections and limited antibiotic options. Their new technology platform, called NeoX, can break down the biofilm and is compatible with existing antimicrobials. The new technology is also expected to be scalable ‘regardless of economic environments and living standards.’
Another resident, Gene S, has released a new pharmacogenomic test that uses a cheek swab or blood test to determine whether a patient’s DNA is likely to affect their suitability for a particular medication being prescribed.
“This is about removing the guesswork for doctors so they’re able to prescribe the right drug at the right dose straight away,” Gene S co-founder Dr Suzanna LindseyTemple said.
“We know that 70% of medications are either not effective or cause adverse drug reactions because individual genetics impacts how the body metabolises and responds to medication. This simple test will be able to be requested by GPs and they’ll receive results back in a couple of days to help them know which drug to prescribe.”
The first test will be available for
most medications used to treat mental health conditions such as depression, anxiety, post-traumatic stress disorder and bi-polar.
“We typically look for people and products that are in the high knowledge, high value, probably deeper technology space. So, we involve people that have been in the throes of research, but they don't really speak the language of business,” Mr Swingler said.
“Through our programs we teach them skills such as marketing and branding, how to raise capital, protecting intellectual property, how to engage with the marketplace and potential customers. Some of these concepts can often be foreign to researchers, but they're critical when it comes to forming a successful business.”
One of CERI’s residents, Isopogen, led by Dr Marian Sturm, highlights the crucial nature of intellectual property rights, when the East Metropolitan Health Service took the former boss of Royal Perth Hospital’s cell and tissue therapies facility to court on the day of her retirement in 2021, claiming she had breached her contract by commercialising an innovative cell therapy, which used several patents developed by Dr Sturm during her tenure.
The stoush over the IP for improved manufacturing of mesenchymal stromal cells lasted three years, only ending earlier this year when a confidential settlement was reached in March.
“I think one of the challenges in the medical space is that a lot of them have quite long time-horizons and are often quite expensive to back, and these groups need patient investors. They need organisations like ours that can give them several years to develop and test their concepts,” Mr Swingler said.
“We are all so used to software startups that can scale rapidly within the space of six to 12 months and start trading revenues. Many of these companies don't fall into that boat, but they have the potential to be transformational companies within the medical sector. Genetic technology is certainly one of those areas and, as such, the IP is highly valuable and well-guarded.
“Particularly in medicine, where you need the necessary approvals, if
you require animal and/or human trials that can take a long period of time, and typically for companies in that space, you might be looking at two or three years of development at a minimum, but it will usually be more like five to 10.
“And that certainly creates challenges for people who are looking at creating a medical startup, because, frankly, a lot of investors will baulk at the time frames and the complexity involved with commercialising either a medical device or a medical service.
“We wrap services around our teams, so if they're struggling with various aspects, such as capital raising or grant writing, we can help them with that.”
Mr Swingler said it was about providing people with access to services in an affordable way.
“Even though a lot of startups don't have access to a lot of capital to begin with, we don't take equity in the startups we support, as we want to support the team to generate successful businesses and diversify,” he said.
“We also try to connect our organisations with the relevant people interstate and overseas. All our organisations work in a global marketplace and look globally not only for customers, but also for investors.
“One of our startups did two capital raisings in Singapore because they felt that the capital market there was more conducive to their style of business. Much of the technology coming out of WA is globally relevant and I think that the world is the oyster for many of these West Australian companies.”
In addition to hosting events with guest speakers, CERI also runs courses in each half of the year, with another round of the Entrepreneurial Mindset Bootcamp beginning in August, followed by the Concept Creation Course in September.
“If people are interested in the entrepreneurial journey, I'd encourage them to reach out to CERI and find out more,” Mr Swingler said.

Dr Shane La Bianca
Dr Andrew Tan
Dr Jeff Thavaseelan
Dr Trent Barrett
Dr Matt Brown
Dr Manmeet Saluja
Dr Alarick Picardo
Dr Steve McCombie
Dr Sarah O’Neill
The diagnosis and treatment of people with ADHD remains a hot topic in WA, with some doctors warning about the rise of rapid and potentially inaccurate ‘quick fixes’ that offer swift diagnosis and prescriptions.
Despite patients facing long wait times, a group of healthcare professionals and ADHD experts are urging people to avoid fastturnaround telehealth, or same-day appointments being offered at high cost.
The doctors, including consulting psychiatrist and recently elected AMA WA vice president Dr Kyle Hoath, have also renewed calls for the Federal Government to publish its now overdue response to the 2023 Senate inquiry.
By Cathy O’Leary
Victorian ADHD expert Professor David Coghill was among those in Perth last month for a community forum to highlight concerns, with a panel discussion including Dr Hoath and Dr Tim Leahy, a GP and member of the ADHD WA Professional Advisory Body.

The event was organised by Oqea, a WA-based digital platform providing ADHD support, of which Dr Hoath is a director.

A recent Federal Health Department report on ADHD medications in Australia up to September 2023 found an overall rise in prescribing rates of about 25% for ADHD across different ages.
ADHD medication levels more than doubled in the past five years from 1.4 million prescriptions given to 186,000 people in 2018, to 3.2 million prescriptions to 414,000 people in 2022.
Quick fixes for ADHD were becoming increasingly popular... which raises concerns over the quality of care received by patients.
Those at the forum advocated that assessment for ADHD be comprehensive, with a two-to-threehour clinician interview conducted by trained professionals such as psychiatrics, psychologists and paediatricians.
Professor Coghill said quick fixes for ADHD were becoming increasingly popular, with offers of swift diagnosis and prescriptions, which he claimed raised concerns over the quality of care received by patients.
The Professor of Child and Youth Mental Health at the University of Melbourne and president of the Australasian ADHD Professionals Association said a lack of comprehensive assessment could lead to inaccurate ADHD diagnoses.
“While there is still an important discussion about improving access to services, we also need to ensure the quality of services that are provided,” Professor Coghill said. “We need greater oversight and regulation of these ‘quick fix’ options to ensure individuals with ADHD receive the comprehensive care they deserve.”
“However, it is difficult for any level of government to take action on this important issue until the
Federal Government’s response to the Senate inquiry into ADHD has been published.”
One of the key recommendations of the Senate inquiry was that all levels of government consider investing in the implementation of the Australasian ADHD Professionals Association’s evidencebased clinical practice guideline for ADHD. The guideline recommends that ADHD assessments need to be thorough and based on in depth clinical interviews.
Dr Hoath said he supported Professor Coghill’s call for an urgent response to the inquiry, saying the over-reliance on medication as a stand-alone solution for ADHD was a worrying trend that could have long-term implications for patients’ health and well-being.
“It is crucial to promote evidencebased practices and holistic approaches to diagnosis and treatment to address the complex needs to individuals with ADHD in Australia,” Dr Hoath said. “This should include non-medication approaches to support people with ADHD and those around them.
“Policy makers, healthcare professionals and community members need to work together to advocate for a comprehensive approach to addressing the challenges associated with this complex disorder.”
Last month, Perth GP Dr Andrew Leech – the RACGP WA’s GP of the Year for 2023 – spoke out in Medical Forum about the frustration faced by GPs not being able to diagnose or treat people for ADHD.
Dr Leech said some patients were waiting 12 months or more to see a specialist or were even having their referrals from GPs rejected outright.

The field of RNA therapeutics has expanded over the past 40 years, and mRNA-based COVID-19 vaccines are just the start, according to researchers Drs Emily Pilkington (pictured) and Rekha Shandre Mugan
It was a case of perfect timing. Scientists had been researching how to use RNA for medical purposes for more than 40 years when the COVID-19 pandemic hit in 2020.
They had already had some success with an RNA therapeutic approved in 2018 to treat people with the rare hereditary disease familial amyloid polyneuropathy, but the use of RNA in the widely used Pfizer-BioNTech and Moderna COVID vaccines put the molecule on a much bigger stage.
RNA – ribonucleic acid – can be thought of as the spin-off of the more well-known DNA or deoxyribonucleic acid. All humans have naturally occurring RNA in their cells as the molecule is vital to the everyday upkeep of healthy cells and acts as the cell's internal messaging system.
The field of RNA-based therapeutics lets scientists write their own set of instructions for cells to follow and different types of RNA allows for different types of therapeutics to be developed.
Arguably, the type of RNA that people are most familiar with is messenger RNA, or mRNA, which is a type of coding RNA. Think of it like an instruction manual that teaches a cell to build a specific protein.
MRNA therapeutics include the COVID vaccines from Moderna and Pfizer-BioNTech, which give cells a blueprint to make their own copy of the SARS-CoV-2 spike protein in order to train people's immune systems to recognise and defend against the virus.
Why mRNA vaccines have been so lauded is that they are often cheaper and faster to make than traditional vaccines, and are generally safer and more efficient at producing an immune response.
However, mRNA vaccines are
not limited to battling infectious diseases. Basically, a vaccine is anything that trains the immune system to fight something.
In cancer, mRNA vaccines provide instructions to make proteins that teach the immune system how to find and destroy cancer cells without hurting the healthy cells around them.
These vaccines can be both prophylactic — given to healthy people to prevent certain cancers — or therapeutic — given to cancer patients to assist the body in fighting particular cancers. This is because unlike with other diseases, cancer patients sometimes can't mount a sufficient immune response on their own.
Despite the complexity of cancer, there are multiple mRNA-based vaccines currently in human trials.
This includes Moderna's mRNA vaccine against melanoma — currently in phase III clinical trials for use in combination with Merck's approved cancer drug Keytruda — which teaches the immune system to selectively take down tumour cells.
BioNTech, in collaboration with Genentech, has an mRNA vaccine in phase II human trials to treat colorectal cancer. And the University of Florida is undertaking a phase I clinical trial for an mRNA vaccine to tackle the most common type of brain tumour.
If even one of these vaccines is successful, it will mark the beginning of a new generation of cancer treatments which will hopefully improve patient survival rates.
Beyond vaccines, mRNA can have as many functions as can be written into their biological coding.
One application for which mRNA is being developed is protein replacement therapy.
Sometimes cells may naturally lack
the capacity to make their own mRNA for a specific protein in-house or the instructions they have are faulty, leading to nonfunctional or toxic forms of the protein mistakenly being built.
This is the case for certain genetic disorders such as cystic fibrosis, where cells produce a faulty copy of a protein called cystic fibrosis transmembrane conductance regulator, or CFTR, which causes unhealthy levels of mucus to build up in the lungs.
By providing regular deliveries of the correct mRNA to the cells, they can start making the normal protein instead.
RCT2100, a cystic fibrosis mRNA drug developed by ReCode Therapeutics, is one of multiple mRNA drugs currently in human trials for this application.
Here, an inhaled form of mRNA is introduced to the lung cells to help them produce healthy CFTR proteins, with the aim of reducing the build-up of thick mucus and alleviating the symptoms experienced by cystic fibrosis patients.
If successful, such mRNA therapeutics can address unmet clinical needs and the lack of effective treatments, particularly for people diagnosed with rare genetic disorders.
Another type of RNA is silencing or small interfering RNA, abbreviated to siRNA. This is a type of noncoding RNA, which means it can't instruct a cell to build a protein.
Instead, siRNA is like a gag order — designed to put a halt to the production of faulty or undesirable proteins – and it instructs cellular machinery to seek out and intercept any copies of a specific mRNA out for delivery, and then tear them in half before they can be read by the cell's manufacturing systems.
The state of men's oral health has surprising effects on the body, according to restorative dentist Dr Adrian Kat.
What seems to be forgotten in the treatment of men’s oral health is the direct connection between their mouth and the rest of their body.
Dental issues can escalate into broader medical problems, affecting more than just the mouth. Simply brushing teeth and caring for the gums can go a long way to preventing potential systemic health conditions such as cardiovascular disease and respiratory complications.
Men with serious gum disease, or periodontal disease, have two to three times the risk of having a heart attack, stroke or some other serious cardiovascular event.
Understanding how the mouth can affect men’s health begins with knowing what can go wrong.
When men don’t brush their teeth regularly, bacteria can build up in the mouth and on teeth, making their gums susceptible to infection. This can trigger an immune reaction to attack the infection, which leaves the gums inflamed and often bleeding.
Without dental attention, inflammation remains, and the infection worsens. Over time, the inflammation and the chemicals it
releases eat away at the gums and the jawbone structure that hold the teeth in place.
This long-term inflammation is a key contributor to many health problems. The most obvious issue being that without teeth, it is difficult to maintain a healthy diet and further compounds health risks.
Serious gum disease can compromise the immune system and lower the body’s ability to fight infections.
Oral health can also influence surgical treatments and decisions. If bacteria in the mouth travels through the bloodstream to the surgery site, there’s a risk it may cause complications such an endocarditis.
Health problems from severe gum disease may not be obvious but they can leave people exposed to cardiovascular problems, gastrointestinal issues, type 2 diabetes, and respiratory complications.
For men, who statistically are less likely to seek preventive health care, including dental treatment, understanding these connections is crucial. For instance:
• Diabetes complications – the
This leaves the cell with unfinished instructions which it cannot build from, and so it discards the mRNA.
Patisiran, for example, is an siRNA therapeutic approved in 2018 to treat the rare hereditary disease familial amyloid polyneuropathy, by instructing cells to stop making a faulty, toxic form of the protein transthyretin.
Over the past 30 years, scientists have faced and overcome multiple challenges in the development of RNA therapeutics.
One of the major breakthroughs has
been the development of the lipid nanoparticle delivery system — a synthetic 'envelope' for the RNA instructions, protecting it from the harsh conditions in the body and allowing more precise delivery to targeted cells.
As a result, the field of RNA therapeutics has expanded incredibly. As of late 2023, there are more than 80 mRNA therapeutics in human trials, with at least five new clinically approved mRNA drugs coming to market and many more in the registration process.
This doesn’t include the myriad

risk of developing periodontitis is greater in men with diabetes. Inflammation that starts in the mouth weakens the body’s ability to control blood sugar.
• Cardiovascular disease –research indicates that if men show signs of gum disease, they are twice as likely to have heart disease. Inflammation caused by periodontitis has been linked to other cardiovascular conditions such clogged arteries and stroke.
• Respiratory issues – bacteria that causes gum disease can also affect the lungs, especially in men with pre-existing respiratory conditions. If bacteria in the periodontal tissues is inhaled by patients or travels through their bloodstream, it can potentially lead to respiratory infections, pneumonia or exacerbation of COPD.
• Dry mouth – as men get older, the salivary glands produce less saliva, a natural mouth cleanser, and a dry mouth with little saliva allows bad bacteria to grow.
• Bruxism – certain medications, misaligned teeth, airway issues, jaw, sleep problems or stress and anxiety can be the cause of grinding and clenching.
therapeutics in preclinical stages being developed by hundreds of companies and academic institutes worldwide, and medicines being developed using other types of RNA.
While there is still room for improvement, with RNA therapeutics the future looks bright.
ED: Dr Emily Pilkington and Dr Rekha Shandre Mugan are research fellows at Monash Institute of Pharmaceutical Sciences, and project managers for mRNA Core. This article was originally published under Creative Commons by 360info.


• Advara HeartCare is pleased to offer CV risk assessment clinics from our centre at St John of God Murdoch Hospital, with access to our inhouse cardiac CT scanner to perform calcium scores or CT coronary angiography scans where appropriate.
• Our CV risk assessment clinic is designed to provide patients at risk of cardiovascular disease with access to expert cardiologist assessment and investigation in a timely manner.
• Patients referred for a CV risk assessment will undergo Cardiologist review, and if clinically appropriate referred for a CTCA directly.
• This reduces delay in their diagnostic process and enables specialist review and management, resulting in continuity of care and world-class patient experience.
• To refer a patient, select CV risk assessment clinic on our referral form requesting this pathway.*

Scan the QR code to access our referral form or go to advaraheartcare.com/locations/murdoch to learn more

What's a man now? What's a man mean? Is he rough or is he rugged? Is he cultural and clean? Now it's all changed, it's got to change more 'Cause we think it's getting better But nobody's really sure
– Singer-songwriter Joe Jackson, 1982
Sometimes a statistic causes one to really question assumptions and to ask why? The winter edition of Horizons (RAC member magazine) has data on road fatalities. What was staggering is that 80% of fatalities were male.
This seems very disproportionate and the immediate question is why? Do men spend more time in vehicles? Does this reflect a rural versus metro effect? Are men worse drivers? Nobody knows. And here is the kicker – it would appear (and I am happy to stand corrected) that nobody cares or feels any need to investigate reasons. Call me whatever but if 80% of fatalities were female there would be a myriad of government initiatives designed to address it. Where else are there gender gaps that we never hear about?
AIHW data shows that in 2022, 75% of suicides were men. This pattern is consistent from 1910! Some 73% of homicide victims are male. Again this is a consistent number. Industrial injuries and deaths are predominately in males. All this contributes to the fact that males have a lower life expectancy.
Having gone down the rabbit hole there are other remarkable statistics – this time from the US, although likely similar here. Fatherless homes account for 63% of youth suicides, 80% of rapists, 71% of high school dropouts and 75% of those admitted to drug abuse centres.
The dominant narrative has become ‘toxic’ masculinity and, yes, this is a problem. But it does not apply to 50% of the world’s population. In no other circumstance is it deemed that an entire group of people who share an immutable characteristic with the perpetrator of a crime are all equally culpable.
But it is not PC to either talk about it and certainly not to do anything about it. I am generally disposed to proposing solutions rather than just highlight problems. On this occasion the best I can suggest is that we need to re-examine societal attitudes to males and masculinity. Throwing the proverbial baby out with the bathwater is not working. In 2024, we remain unsure what a man is and we don’t really seem to care. We need to!


By Dr William Ormiston, Interventional Radiologist, Nedlands
Prostate artery embolisation (PAE) is a minimally invasive interventional radiology procedure that has gained increasing attention as a promising treatment option for benign prostatic hyperplasia (BPH), a common condition affecting aging men.
BPH, characterised by the nonmalignant enlargement of the prostate gland, often leads to bothersome lower urinary tract symptoms (LUTS) and can significantly impact quality of life. PAE offers an alternative to traditional surgical interventions such as transurethral resection of the prostate (TURP), HoLEP, Urolift or (in severe cases) prostatectomy, providing symptomatic relief while avoiding some of the potential risks and complications associated with surgery.
PAE involves the selective catheterisation and embolisation of the prostatic arteries, which are responsible for supplying blood to the prostate gland. By occluding these arteries with embolic agents, PAE aims to induce ischemic necrosis and subsequent shrinkage of the prostate gland, thereby alleviating urinary symptoms. The procedure is typically performed by an interventional radiologist under local anaesthesia and conscious sedation, with guidance from fluoroscopy and angiography.
PAE is minimally invasive, typically performed as an outpatient procedure, and patients can often return to their normal activities within a few days. Additionally, PAE preserves sexual function and urinary continence, making it an attractive option for men concerned about the potential side effects of surgery.
Clinical studies evaluating the efficacy and safety of PAE have demonstrated promising results in relieving LUTS associated with BPH. Several randomised controlled trials and prospective cohort studies have reported significant improvements in International

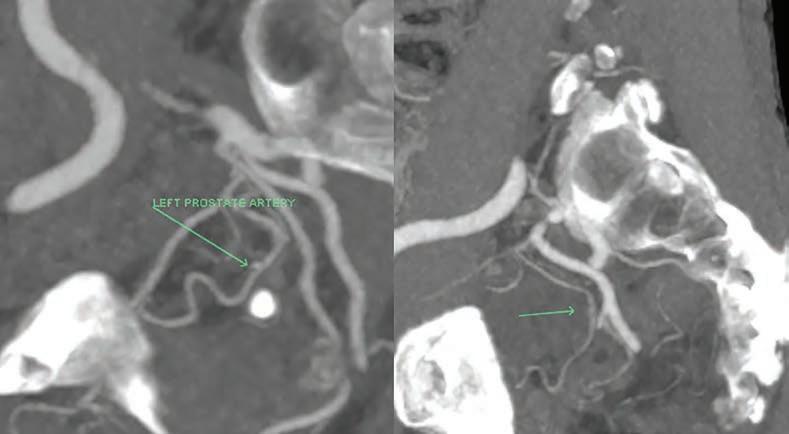
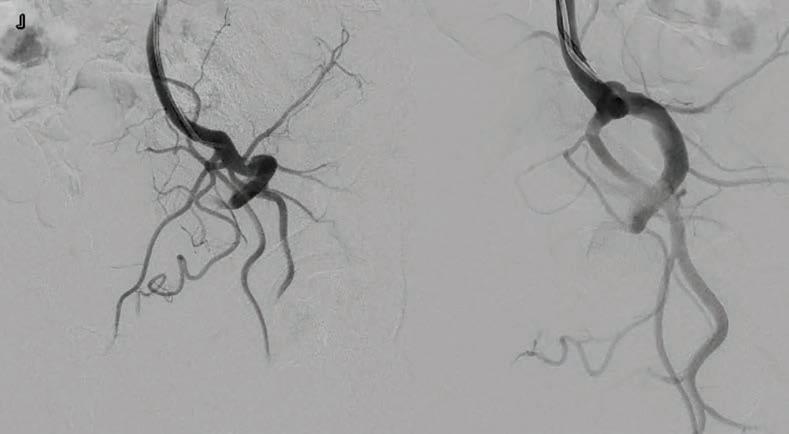
Prostate Symptom Score (IPSS), peak urinary flow rate (Qmax), and quality of life following PAE.
These improvements are sustained over long-term follow-up, with many patients experiencing durable symptomatic relief for up to five years or more. Additionally, PAE can be safely repeated if necessary, offering a potential alternative for patients who experience recurrence of symptoms following initial treatment.
While PAE has demonstrated efficacy in improving urinary symptoms and quality of life, patient selection remains crucial for optimising outcomes. Ideal candidates for PAE are typically men with moderate to severe LUTS
secondary to BPH who have failed conservative management or are not candidates for surgery.
Moreover, PAE has been shown to be effective in treating large prostates and patients with severe urinary symptoms who may not be suitable candidates for surgery. Unlike surgical interventions, PAE does not involve a general anaesthetic, making it particularly well-suited for men with significant comorbidities.
Men with BPH and also on anticoagulation can undergo a PAE without ceasing their blood thinners, and the potential bleeding complications associated with anticoagulation and surgery are also avoided.
Prostate artery embolisation is a minimally invasive endovascular option for treatment of LUTS and BPH
It is effective especially in non-candidates for surgical interventions, but also in men wanting to avoid TURP or other transurethral procedures
It is an awake day-case procedure, with preservation of sexual function and urinary continence.
Pre-procedural evaluation, including urological assessment, prostate imaging, and prostatespecific antigen (PSA) testing, helps identify suitable candidates and ensure that PAE is performed safely and effectively. As with any medical procedure, PAE carries certain risks and potential complications, including urinary retention, urinary tract infection, and post-embolisation syndrome (flu-like symptoms).
However, serious adverse events are rare, and the overall safety

profile of PAE is favourable compared to surgical interventions. Close monitoring and followup care are essential to identify and manage any potential complications promptly.
Prostate artery embolization represents a promising minimally invasive treatment option for men with benign prostatic hyperplasia and bothersome lower urinary tract symptoms.
With its proven efficacy, safety, and minimal impact on sexual function, PAE offers a valuable alternative to
traditional surgical interventions. Continued research and clinical experience will further refine patient selection criteria, optimise procedural techniques, and expand the role of PAE in the management of BPH, ultimately improving outcomes for men seeking relief from urinary symptoms.
Author competing interests – nil


Paul is a locally trained surgeon who brings with him experience gained from several years of interstate and overseas fellowships, and specialises in:
Hip & Knee replacement
Robotic-assisted joint replacement
Sports knee
Foot & Ankle
Upper & Lower limb trauma
Perth Hip and Knee are a specialist practice focused on the treatment of all aspects of hip and knee pathology. From arthroscopy to complex joint replacement and revision surgery, we deliver excellence in care utilising state-of-art surgical techniques and cutting-edge technologies to achieve optimal outcomes for our patients. We are delighted to have Paul join Perth Hip & Knee and he is a valued addition to our group of experienced hip & knee surgeons. You can contact his rooms direct at rebgetz@hipnknee.com.au or on 08 6489 1766
Perth Hip & Knee
Suite 1/1 Wexford Street
Subiaco WA 6008
PHONE: 6489 1700
EMAL: admin@hipnknee.com.au www.hipnknee.com.au
By Dr Jan Orman, GP Services Consultant, Black Dog Institute
As GPs, we are often short of both time and resources, and when it comes to providing mental health care, many of us feel inadequately prepared for the task. We are also often isolated and undersupported.
However, there is a wide range of evidence-based resources available to support us in caring for patients experiencing mental health issues, so why don’t we make use of them?
The trouble is, using online resources is not as simple as prescribing a medication or making a referral. To have our patients get the best out of digital mental health resources we need to get to know these resources and learn to use them appropriately. On top of that initial investment, we also need to convince our patients that using an app or working through an online

treatment program is likely to help. Then we need to support them while they do the work.
Perhaps it sounds like too much effort but, given the lengthy wait times for specialist mental health services, isn’t it worth a try?
I am talking specifically here about online mental health treatment
Heel pain is a frequent problem that presents to the general practitioner. Plantar fasciitis is the most common cause of under the heel pain. Most patients will improve with non-operative treatment but not all.
Surgery is a very effective form of treatment for this condition in patients with long standing refractory symptoms.
Before being considered for surgery patients should undergo at least six months of non-operative treatment that includes the following (in the appropriate order):
• Rest, avoidance of activity
• NSAIDs, stretching exercise program
• Orthotics: off the shelf or custom
• Cortisone injection (one only)
• Shockwave therapy

Surgery can be open or endoscopic. The principle part of the procedure is release of the plantar fascia near its origin on the heel. Historically only the medial half was released but recent literature supports more complete release.

programs such as THISWAYUP, MindSpot. MoodGYM and myCompass (mycompass.org.au). All of these are Australian-made programs with a solid evidence base behind them.
These online treatment programs are largely based on Cognitive Behavioural Therapy and are designed to give users skills to monitor mood, thoughts and behaviours, and to reduce mild to moderate symptoms of depression, anxiety and stress. The programs can be used as a standalone resource but are likely to have greater adherence and better results if you introduce them yourself with enthusiasm and see your patients regularly to enhance their commitment to the program and their understanding of its content.

Open surgery is performed through a 3cm incision in the proximal arch and allows not just plantar fascia release but also decompression of the tarsal tunnel and Baxters nerve which is often implicated in heel pain.
Endoscopic plantar fascia release is indicated for those without nerve compression symptoms and is done through a much smaller incision using a camera assisted cutting device much like a carpal tunnel release.
Both open and endoscopic releases are performed as day cases and require approximately two weeks on crutches. Recovery is slightly quicker for endoscopic patients as you would expect. Patients can expect an 8090% chance of a good result from surgery. Complications are rare.


St John of God Medical Centre
Suite 10, 100 Murdoch Drive, Murdoch WA 6150
Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301
www.murdochorthopaedic.com.au
Murdoch Orthopaedic Clinic
GPs are often short of mental health resources
Digital tools are easily accessed and generally free
Blended care is use of in person and online/therapies/tools.
Integrating the content of online treatment programs into your therapeutic conversations is known as ‘blended care’.
Case example
Edward is 54 and has been troubled by low mood and anxiety for some years. He is taking some medications but their value to him is dubious. Despite the impact on his life, work and relationships, he has refused to accept there is anything anyone can do to help him and he is unwilling to talk to anyone but me.
Ed feels very strongly that seeking help for his mental health is a sign of weakness. Ed is very inflexible in his thinking and it is hard to make a difference beyond that
which comes with listening with an empathic ear.
Recently, I talked to Ed about possibly doing some work on his mental health online. I used my laptop in session to show Ed the Men’s module in myCompass, a modular CBT program from Black Dog Institute. myCompass is structured so that users do not need to work linearly through the program as they do with many others, they simply register then choose the modules they think might suit them best.
Ed agreed to look at a module designed especially for men and to check back with me in a week, when he could reasonably be expected to have finished the first set of activities.
On review, Ed told me excitedly about what he had learned. He was also keen to tell me there were other modules in the program that he might benefit from and he would like to get on with them.
Ed is now working through the modules and learning about skills he can use to improve his mental health. He likes the online
Perth’s comprehensive vascular and vein treatment destination, with fully accredited integrated vascular ultrasound.
environment (rather than in-person therapy), but he still has me there as his GP to discuss any difficulties he is having or gains he has made.
You can help make blended care in mental health work by:
• learning about what online resources are available (check out the Guide to Digital Mental Health Resources and other resources available through the e-Mental Health in Practice program and on Black Dog Institute’s website).
• recommending digital resources enthusiastically and appropriately.
• showing them to people so they are familiar with them before leaving your consulting room.
• helping your patient download the resource or program you recommend so it is ready to use on their own device when they get home.
• continuing to see them regularly while they are using the online resource or program and discussing their progress.
Author competing interests – nil
All surgeons at Perth Reconstructive Urology – Dr James Chen, Dr David Sofield and Dr Mikhail Lozinskiy – have dual expertise in prostate cancer surgery and management of post-prostatectomy incontinence & erectile dysfunction. No matter where patients are on their journey, we are here to help.
We accept referral for all forms of urological conditions and offer rapid access for new patients and direct access cystoscopy with GP referral.

All surgeons consult at 4 Antony St, Palmyra 6157
Dr James Chen: reception@drjameschen.com.au
Dr David Sofield: reception@sofield.com.au
Dr Mikhail Lozinskiy: info@southwesturology.com.au
Dr James Chen also consults at SJOG Subiaco Sessional Suite at Level 2, 2 McCourt Street, West Leederville 6007
Phone number: (08)6363 5688 Fax: (08)9339 1832
By James L. Nuzzo, PhD, Edith Cowan University
Muscle strength is an indicator of human vitality. It fluctuates throughout the day, following a circadian pattern, and it also changes across a lifespan. Muscle strength increases until about 25-35 years of age after which it plateaus and then declines at a rate of about 10% per decade after the fifth decade of life. The rate of decline can differ based on patient’s sex and assessed muscle group.
Loss of muscle strength with aging is due primarily to reduced muscle mass (sarcopenia). Reduced muscle strength correlates with earlier mortality, increased risk of falls, and greater difficulty in performing activities of daily living. Thus, increasing or maintaining muscle strength is critical for living a long, healthy life.
The most effective way to increase or maintain muscle mass and strength is by participating in resistance exercise, such as weight training, or other musclestrengthening activities. Resistance exercise is safe, and it creates many

health benefits, including improved cardiovascular profiles, better walking and sit-to-stand ability, reduced anxiety and depression, and better quality of life.
For these reasons, professional exercise organisations in Australia and abroad have published position statements on resistance exercise participation for healthy aging and for inclusion in treatment plans for conditions such as diabetes, cardiovascular disease, cancer, and
Promising findings from an international clinical trial have offered hope for patients with high-risk, localised soft tissue sarcoma of the limb.
The results, released at the recent American Society of Clinical Oncology conference in Chicago, came from a multicentre trial led by the Sarcoma Alliance Research Collaboration in the US and the Australia and New Zealand Sarcoma Association. The meeting was told that the randomised controlled trial SARC032 marked a significant advancement in the treatment.
Soft tissue sarcoma, a rare aggressive cancer originating in connective tissues, can affect both
children and adults. It is particularly challenging to conduct clinical trials due to its rarity. Patients with sarcoma are best managed at the few specialised sarcoma centres in Australia.
SARC032 is the first completed randomised clinical trial of its kind, with compelling evidence to integrate immunotherapy –specifically pembrolizumab – with the standard treatment regimen of radiotherapy and surgery for patients with grade 2 or 3, stage III soft tissue sarcoma of the limb. It showed significant improvement in disease-free survival, with the addition of pembrolizumab resulting in an 18% reduction in recurrence of the sarcoma or death.

motor impairments like multiple sclerosis and spinal cord injury.
Public health bodies recommend that adults participate in resistance exercise or other musclestrengthening activities two or more days a week. Professional exercise organisations then further specify that exercise sessions include multiple sets of 8-10 different exercises that target all major muscle groups.
Nevertheless, a significant number of Australians – roughly 60% – do not meet recommended guidelines for participation in muscle-strengthening activities. Similar results are observed in other countries.
Multiple factors contribute to low participation in resistance exercise. Key intrapersonal barriers include perceived lack of time, lack of exercise knowledge or confidence, not enjoying or prioritising exercise, and being ill or having a disability. Common social or environmental barriers include family and work obligations, financial costs, lack
Professor Angela Hong, Australia’s principal trial investigator, believes the results will be beneficial for patients for this specific stage of sarcoma, with pembrolizumab emerging as a new potential option for patients grappling with high-risk sarcoma of the limb.
“The integration of immunotherapy into standard treatment protocols heralds a new era in sarcoma management, offering patients and clinicians a potent tool against this formidable disease.”
Adequate muscle strength is important for daily life
Resistance exercise, even in minimal doses, improves muscle strength
Patients should be encouraged to participate in resistance exercise.
of access to exercise facilities or programs, and transportation and exercise location challenges.
Clinicians can help patients overcome some of these barriers by informing them that there is no single resistance exercise script that everyone must follow. Some script specifications are based on the patient’s preferences and circumstances. For example, muscles can be strengthened by using different types of resistance, including dumbbells, weight machines, elastic bands, and one’s own body weight. Also, resistance exercise can be performed in various locations such as at home, at the gym, at the park, and at treatment facilities.
Ideally, patients would achieve the recommended guidelines for resistance exercise each week. However, these guidelines should not preclude clinicians from also informing patients that ‘doing something is better than doing nothing’ when it comes to the exercise volume on the patient’s muscle-strengthening script.
Health and fitness benefits derived from physical exercise generally follow a dose-response relationship, whereby more weekly exercise causes greater benefits. However, fitness benefits still occur at the low end of the exercise volume spectrum. In fact, given that perceived lack of time is one of the most frequently reported barriers to exercise participation, and many individuals do not participate in any muscle-strengthening activities, researchers have started to explore the scientific credibility of minimal dose resistance exercise.
Minimal dose resistance exercise refers to a volume of exercise that does not meet recommended guidelines but that might still improve muscle strength. “Weekend Warrior” is one example. With this
approach, training frequency is minimised. All weekly resistance exercise volume is completed in one session, often on a Saturday or Sunday, if an individual works fulltime during the week.
Another example is resistance exercise ‘snacking’. Snacks reduce session duration. They are brief bouts of exercise (5-10 minutes) performed once or more daily on most, if not all, days of the week. Snacks would suit, for example, patients who work from home and own equipment like dumbbells or elastic bands.
Current evidence suggests that when these and other types of minimal dose programs are performed regularly over a few weeks, they improve muscle strength and some other outcomes of health and fitness. This is especially true for individuals who have no previous experience with resistance exercise.
Thus, resistance exercise is medicine…even in small doses.
Author competing interests – nil

By Dr Kim Farrington, Forensic Physician, Sexual Assault Resource Centre
With nearly 41% of Australians experiencing violence before adulthood, it is important to understand the impact of trauma on a patient’s healthcare journey.
Trauma-informed care recognises the widespread incidence and impact of trauma on patients. A trauma-informed environment is one where a patient feels safe, experiences choice in their treatment options and is empowered in their relationship with their health care providers.
Trauma-informed care is a type of ‘universal precaution’ that presumes that most people have experienced some form of trauma in their life.
Physical, sexual and emotional abuse, witnessing violence, having a family member with a substance use disorder, experiencing a serious accident or the sudden or violent loss of a loved one are all examples of trauma.
Trauma can be defined by three Es: the event, how it’s experienced, which is affected by age and the context in which it was experienced, and the effect on the person, their family and their life.
Experiencing trauma, especially during childhood, is now recognised as common. It is linked to significant increases in the risk of health problems in adulthood such as mental health issues and cardiovascular co-morbidities.
Two key studies were influential in the development of trauma-informed care. The Adverse Childhood Experiences (ACE) study published in 1998 revealed ACEs as risk factors for physical and mental illness and early death. The greater the number of adverse childhood experiences, the higher the prevalence of negative outcomes. Physical and sexual abuse in childhood is associated with significantly higher rates of depression, suicide, substance use disorders and PTSD than other ACEs. The Women, Co-Occurring Disorders and Violence study in 2005 focused
41% of Australians experience trauma before adulthood
Trauma-informed care recognises the impact of trauma in a patient presentation
Start from the premise that every patient has experienced trauma.
on the role of interpersonal violence and traumatic stressors in women with mental health disorders and substance abuse issues. Further studies have found that 90% of public mental health clients have been exposed to multiple physical or sexual abuse traumas.
A trauma-informed approach does not see trauma as a past event but as one which can contribute to the patient’s current state. The focus is shifted from ‘What’s wrong with you?’ to ‘What’s happened to you?’.
Consider a young boy whose father suddenly dies and he and his mother must move to an apartment. His mother begins working at night, leaving him with his aunt whose boyfriend physically and sexually abuses him. Later as a young man, he suffers from anxiety and abuses illicit drugs. If his treatment focuses only on his symptoms and behaviours, the impact of the earlier childhood trauma will remain unrecognised.
A trauma informed approach aims to:
1. Realise the widespread impact of trauma.
2. Recognise the signs and symptoms of trauma in individuals, families, and staff.
3. Respond by integrating knowledge about trauma into policies, procedures and practices.
4. Resist re-traumatisation by not inadvertently triggering a person’s traumatic experiences.
In a trauma-informed organisation. all services are designed with an awareness of trauma and its impact. Becoming a trauma-informed

organisation begins with being ‘trauma aware’ and progresses to a cultural shift at the systemic level with leaders, managers and all staff working together in a traumainformed way.
Six core principles of traumainformed care are:
1. Safety: Understanding that a ‘sense of safety’ must be experienced and is determined only by the patient.
2. Trustworthiness: Decisionmaking is transparent. Processes are designed to build and maintain the trust of patients, families and staff.
3. Choice: Informing patients regarding treatment options so they can choose the options they prefer.
4. Collaboration: Among health care staff, patients, and their families, collaboration is prioritised in treatment planning.
5. Empowerment: Using individuals’ strengths to empower them in their treatment.
6. Cultural and gender issues: The organisation offers gender responsive services which recognise cultural stereotypes and address historical trauma.
A place to start is to behave as if every patient has experienced trauma. For example asking a patient “Is there anything I can do to make your consultation easier?” Provide explanations as to why certain questions need to be asked and be sensitive that undergoing a physical examination may be difficult for a patient.
Being aware of the potential impact of trauma on a patient allows health care professionals to improve their delivery of care and enhance patient outcomes.
– References available on request Author competing interests – nil
By Dr Amit Saha, Paediatric Gastroenterologist, Hollywood
It is common for babies to cry. A 2017 systematic review identified that newborns cry about two hours a day, peaking to an average of three hours by six weeks age, eventually decreasing to one hour a day by age four months.
Mostly it has a benign underlying cause. In acute cases, it is prudent to rule out a medical cause. The presence of any red flags (e.g. decreased feeding, fever, vomiting, rash) should prompt urgent medical assessment. However, the majority will have a few weeks history of persistent, excessive crying, and the sleepless and distressed parents will present for help.
Is this colic?
Infantile colic is a symptom-based diagnosis following the ‘rule of three’ – excessive, inconsolable crying for at least three hours a day, for at least three days a week, for at least three weeks. It usually presents at the same time of the day, commonly late afternoons, and can start and stop quite abruptly.
Its incidence is reported to be as high as 40% of all infants, typically peaking at six weeks and resolving by six months of age. It is benign and self-limiting, and its etiology remains elusive.
Recent studies found that
Probiotic drops containing L. reuteri DSM 17938 can be used to treat colic in breastfed but not formula-fed babies
Distinguish infant dyschesia from constipation, to avoid unnecessary use of laxatives
In diagnostic uncertainty between GOR and CMPA, change formula before trialling PPIs. Lactose intolerance in uncommon in babies. Treat as CMPA if suspected.
administration of probiotic drops containing L. reuteri DSM 17938 significantly decreased colic in breastfed infants, but actually increased crying in bottle-fed babies. Simethicone, present in infant colic drops, is safe although a recent systematic study showed it is no better than placebo. Simple soothing techniques such as swaddling, skin-to skin contact, warm bath, massage etc and parental reassurance remain the mainstay of management.
Constipation is far less common in babies than in older children, with notable peaks with any dietary changes (e.g. changing formula,


weaning onto solids). Stooling can be as frequent as with every feed or as infrequent as a couple of times a week, depending on the age and other factors. Hence stooling frequency is not a reliable indicator for infant constipation.
However, consistently painful bowel movements with hard pellet like stools can be safely treated with easily available Poloxamer based osmotic laxatives that can be administered as drops. Lactulose is an alternative but can have side effects such as flatulence and abdominal cramps, and a plateauing effect with higher doses. Extra water (boiled and cooled) may be safely given.
Dyschesia is often mistreated as constipation, and its recognition by health-care professionals remains suboptimal. It is defined (Rome IV) as straining and crying for at least 10 minutes, often associated with infants turning red or purple in the face, before successful passage of soft stools.
It is thought to be due to incoordination between increased intra-abdominal pressure preceding defecation and relaxation of the pelvic floor muscles. It usually starts in the first months of life and resolves spontaneously after a few weeks, and always characterised by passage of soft stools. Parental reassurance is the key, and laxatives avoided.
Gastro-oesophageal reflux (GOR) and cow’s milk protein allergy (CMPA) are relatively common in the first year of life, presenting with symptoms such as food refusal, irritability, vomiting, crying, back arching, poor appetite, slow weight gain and sleep disturbances. That both conditions have similar symptoms, coupled with no reliable diagnostic tests, makes the diagnosis challenging. Blood and/or
By Dr Guillaume Walters-du Plooy, Clinical Psychologist, Nedlands
With over one million Australians experiencing an eating disorder, and prevalence rates continuing to rise, the recently released National Eating Disorders Strategy 2023-2033 (Strategy) arrives at a crucial stage. Released by the National Eating Disorders Collaboration (NEDC), it identifies key components and actions needed to achieve an effective and coordinated system of care for those living with, or at risk of developing, eating disorders.
The Strategy emphasises the pivotal role GPs will play in its successful implementation. As a comprehensive and extensive plan, it should be considered in its entirety, but we are all time poor so let’s consider four of its key points.
The Strategy calls for a shift away from the historical view of eating disorders as exclusively the domain of specialists, rather to a whole-ofhealth system response, integrating medical and mental health services for all eating disorder diagnoses. It
classifies that eating disorders are not solely a specialist clinical area, but rather a mainstream health concern requiring coordinated response across multiple care settings.
Under this new approach, it is planned that GPs will become an integral part of the eating disorder care system, with clearly defined roles, accountabilities, and resources.
Thus, one key action is ensuring GPs have access to training and resources to support the management of eating disorders, including tailored online training modules and tools to assist with medical monitoring, treatment planning, and referrals. This aims to equip professionals with the knowledge and tools to conduct initial assessments, make preliminary diagnoses, and provide psychoeducation to patients and their families.
Another key focus area is enhancing early intervention and
continued from Page 43
mucous in stool, chronic diarrhoea or atopic risk factors makes CMPA more likely.
Where there is diagnostic uncertainty, the current recommendation is to change formula before acid suppression. The recommended formula change is to an extensively hydrolysed formula (eHF), hydrolysed rice formula (HRF) or amino acid based formula (AAF), there is no role for hydrolysed formula only, and soy milk is not recommended due to cross-reactivity. If mother is keen to breast feed, a strict maternal dairy and soy free diet is
recommended. Acid suppression with proton pump inhibitors (PPIs) are safe and effective in babies, and a trial of 6-8 weeks is prudent if there is a suboptimal response to formula change. Refractory cases warrant referral to a paediatrician or paediatric gastroenterologist.
Although not all reactions to cow’s milk are due to CMPA, lactose intolerance is uncommon in babies. If symptomatic, babies should be treated as CMPA. This is because lactose intolerance only manifests later in life with the gradual decline in production of the enzyme lactase.
However, some babies can be born

community-based treatment options. It acknowledges that eating disorders often have their roots in sub-clinical concerns or risk factors, and that early, lowerintensity interventions can prevent escalation and improve long-term outcomes. The Strategy states GPs will play a vital role in identifying warning signs and facilitating access to initial responses, such as guided self-help programs, brief interventions, or longer courses of community-based treatments for eating disorders.
The Strategy also focuses on addressing weight stigma and promoting inclusive, personcentred care, which sometimes serves as barriers for patients accessing treatment. The strategy calls for a shift away from weightcentric approaches and towards inclusive, person-centred care that celebrates body diversity and focuses on health-promoting behaviours.
As a GP, the Strategy encourages examining your own attitudes and practices to ensure you are
with congenital lactase deficiency, and they present since birth with profuse diarrhoea and failure to thrive. If strongly suspected, it is usually transient, and breastfeeding should be continued. If formula fed, a change to a lactose free formula can be trialled, with resolution of symptoms within 2-3 days (as opposed to CMPA wherein it can take 4-6 weeks for symptoms to resolve).
Author competing interests – nil
Implementation of the National Eating Disorders Strategy will create clearer care pathways and enhanced integration of care
More educational opportunities will be available
GPs will be able to better contribute to the care and support of those with eating disorders and their families.
providing compassionate, nonjudgmental care to patients of all body sizes and shapes. The Strategy also advocates for policy changes that prohibit weight-based discrimination and promoting more inclusive language and imagery within healthcare settings and public health campaigns.
Recognising the workforce challenges in addressing eating disorders, the Strategy prioritises the development of a skilled and diverse healthcare workforce, including expanding the lived experience workforce.
It emphasises the importance of interdisciplinary collaboration, with GPs working alongside mental health professionals, dietitians, and other specialists to provide comprehensive care. This multidisciplinary approach ensures that patients receive holistic support, addressing both the physical and psychological aspects of their condition.
For GPs, the Strategy calls for increased eating disorder content in medical education and professional development opportunities to improve overall patient care and outcomes.
The Strategy outlines a comprehensive system of care, ranging from community-based treatment to intensive inpatient services. It tries to move away from a predominant focus on acute treatment services, to a well-developed stepped system of care including community-based treatment and support delivered as early in illness presentation as possible. This stepped approach ensures that patients with diverse presentations are well matched
to their treatment needs, whether their care calls for guided selfhelp, outpatient therapy, or more intensive interventions.
The Strategy aims to increase the availability of community-based treatment options, including in rural and remote areas of WA. This means patients will have better access to local services, reducing the need for travel and supporting their recovery within their community.
The Strategy emphasises collaboration between primary care and specialised eating disorder services, ensuring seamless transitions and clear communication throughout the treatment journey. GPs will play a pivotal role in referring patients to the appropriate level of care based on their needs.
By staying informed and engaged with the strategy's initiatives you can contribute to the development of a robust and responsive healthcare system that supports individuals with eating disorders and their families.
Author competing interests


Local independent publisher Night Parrot Press has released its latest book – 100 short memoirs which explore the human condition in all its glory and pain.
A Perth-based publisher has captured 100 slices of life in an anthology which reveals true stories from local writers.
Night Parrot Press has released a book called Ourselves: 100 Micro Memoirs, small but meaningful life stories revealed in 750 words.
Drawn from personal and true-life experiences, these moments might at first seem insignificant, but when written with care and imagination can reveal large insights into life and identity. In the independent publisher’s fourth anthology, the
By Ara Jansen
book mixes new and established voices who tell short, sharp, memorable true stories in this exciting genre.
From school and childhood moments, to love and heartbreak, siblings and family, to grief and loss, co-editor and Night Parrot Press publisher Laura Keenan says the voices in the collection offer beautiful threads of shared experience that resonate across cultures and generations.

“There’s a large spectrum of themes and topics – everything from people writing about their school swimming carnival to personal loss,” says Laura. “It covers the spectrum of human experience which we can all relate to, which is what is making the book resonate with so many people.”

The publishers received more than 300 submissions and the final 100 stories feature writing by new and established writers including Zoe Deleuil, Barry Divola, Seth Malacari, Tracy Peacock, Scott-Patrick Mitchell, Rashida Murphy, Gillian O’Shaughnessy and Ros Thomas.
The collection also features the work of six First Nations writers and was co-edited by First Nations editor Casey Mulder.
“Bringing all these writers together has been exciting,” says Laura.
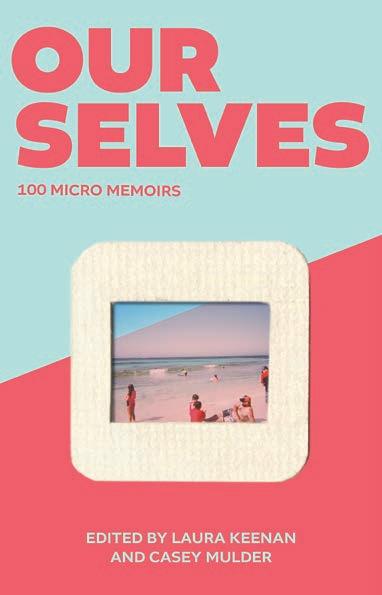
“Quite a few of these authors have written novels, so this is a different form for them. It’s a creative challenge trying to distil what you want to say into so few words, but I’ve found that a lot of journalists are amazing at this form because they have the skill of writing short pieces. It’s a great writing challenge for any writer or anyone who wants to write in this style.”
As far as a theme was concerned, they didn’t set one. What was interesting though was that as the micro memoirs were collected, common threads linked many of them – like a connected consciousness shining through. In Ourselves, a lot of people wrote about the ocean and the water, though Laura says given where we live, that is perhaps unsurprising. The ocean, the Swan River and other bodies of water are very much part of the West Australian psyche.
“Even if you’re not thinking about it, water is often in our sightlines where we live and work. For myself, when I need to decompress or find a moment for myself, I will go to the river or the ocean. I feel buoyed by the ocean. It’s like an immediate reset.”
Night Parrot Press has been teaching this exciting form of writing in workshops and at universities and festivals over the past few years and now, for the first time, these micro memoirs have been published in a groundbreaking anthology.
The growing-in-popularity micro memoir is perfect way to drop into a collection. With Ourselves, Laura says it’s a perfect book to read on your daily commute or while sitting in a waiting room. In a short amount of time, you get the complete satisfaction of a whole story.
“Micro memoirs also don’t have the same rules as a traditional short story, so you can find yourself going anywhere with it. With Ourselves, you don’t need to read the collection from the beginning.
“One of the things I like most about this book is that it has brought a community together. About 80 of
the authors turned up to the launch and it was lovely to see them all talking to each other, meeting each other for the first time. I loved that they were signing each other’s stories in the book. It’s now a community in itself, which feels very special.”
ED: Ourselves: 100 Micro Memoirs is available in paperback (RRP $27.99) online through Night Parrot Press and across WA in select bookstores.

Nordic gems to warm the winter chill
With a lineup set to warm the hearts and minds of cinemagoers, the 2024 Saxo Scandinavian Film Festival returns to Palace Cinemas Raine Square, Luna Leederville and Luna on SX this winter.
Running from July 25 to August 14, the festival features films from Sweden, Norway, Finland, Denmark and Iceland and includes a selection of epic dramas, sweeping romances and stunning visuals.
Festival centrepiece The Tundra Within Me from Norway is a powerful drama exploring community, heritage and identity, as Sámi artist Lena returns to her hometown in northern Norway where she finds an unexpected new love and is forced to confront her past.
Danish box office hit Boundless is a gripping thriller that follows Detective Mørck and his team who become embroiled in a cold case on the remote Danish Island of Bornholm.
We have five Scandi double passes to give away.
And for romantics, we have 10 double tickets to It Ends With Us, the first Colleen Hoover novel adapted for the big screen, which stars Blake Lively and starts in cinemas on August 11.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.

The Revelation Perth International Film Festival once again pushes boundaries and buttons to enlighten, entertain and enthral.
A dollop of horror, a dose of kickass sci-fi, some big tent pole films to win the box office and lots of local flavour.
While it’s not that simple a success recipe when programming a film festival, the Revelation Perth International Film Festival will definitely have a bit of all that.
Running from July 3-14, this year’s screen fest features more than 30 feature films and over 80 short films. The selections cross styles and genres including Kid Snow, which was shot in Perth and Kalgoorlie and stars Billy Howle as a washed-up Irish boxer in the sweat-drenched world of 1970s tent boxing.
There’s an absurdly stylish and chaotic psychological drama called Birdeater where a bride-to-be is invited to join her own fiancé’s bachelor party on a remote outback property. Aimed at children aged three to five years, Pencilheads – Safari So Good is based on the educational online series and colour books.
Art lovers can see documentaries on musicians Red Kross, Stuart Gray, Mogwai and Perth’s own Wayne Green as well as Canadian photojournalist Larry Towell, artist Blak Douglas, an ode to early Australian surf culture and
By Ara Jansen
the exploration of how a beloved NYC video store’s contents ended up in Sicily.
Just one of the ways Revelation takes film to the people this year, rather than the other way around, are the screenings of timeless classics such as First Men in the Moon (1964) and 2001: A Space Odyssey (1968), at the WA Museum Boola Bardip, with entry for the To the Moon exhibition included. Other film events will happen at Scitech and the State and Perth Library, as well as Industrial Revelations, explorations for emerging and established practitioners.
“We wanted to find exciting places for film lovers to go and to attract audiences that went to those spaces,” says festival director Richard Sowada. “The festival did start in a bar after all. We’re taking film to audiences, which made us nimble and flexible.”
Now in its 27th year, that push to move the boundaries and explore is something that has never felt forced. It’s an authentic and natural part of the festival’s character.
“We’ve always experimented and never been complacent,” says Richard who lives in Melbourne and has a team scattered across Australia and overseas. “When a lot of our
industry vaporised during COVID, we used it as an opportunity to do things like produce short films, make VR content, integrate music and dance, and collaborate – so we came out of it strong. While lots of festivals came back and didn’t change, we pushed the boat out creatively.”
Once again, West Australian filmmakers make a big impact on the festival. Richard says there are a lot of indie films and shorts being made in WA on not a lot of money, many of them self-financed.
“There’s a whole local movement in WA of self-funded films. Many of them are made by young people just out of their teens. Their experiences of coming of age are very immediate and there’s a real sense of urgency in the films. They have a great creative spirit. They want to work together and support each other and are very active and aware. There’s a lot of energy there.”
See the full program at www.revelationfilmfest.org and get tickets from www.lunapalace.com.au Access many past festival films and shorts for free at www.revstream.com.au


SJOG Murdoch –
Consulting Suite for Sale
–TWO GENEROUS CONSULTING SUITES
–FURNISHED SUITE AT SJOG MURDOCH
Sterling Property is delighted to offer 47 / 100 Murdoch Drive, SJOG Murdoch for Sale.
This generously proportioned furnished consulting suite comprises of 97 sqm, configured with two large consulting rooms, reception and waiting area. Onsite on SJOG Murdoch and a short walk to Fiona Stanley Hospital.
Asking Price : $880,000 + GST (Includes Leased Car Bay)
Contact Simon Brady from Sterling Property on 0407 486 401 sbrady@sterlingproperty.au

Treendale Medical Group
– GP Positions
•DPA Area’s and MMM5 Available
•FSP GP’s are welcome to apply
•Busy & well established Medical Group with 4 Location in the South West of WA
•Full time & Part Time GP Positions in Treendale & Harvey
•Fully computerized and accredited modern practice with nursing and admin support
•Well supported with large team of experienced GP’s
•Situated in the beautiful South West Region surrounded by coast and forest and close to tourist areas in the south of WA
•Only 1 ½ hrs from Perth
•Family friendly working hours and no on call or hospital cover required
•65 – 70% of billings depending on experience
Please forward CV and enquiries to Kylie Wilson kyliew@harveymed.com.au

The RFDS WA Strategy 2024 – 2028 strives to make a positive difference to the health and well-being of people living and working in regional WA. One of the focus areas will be to expand Primary Health Care services for a bigger community impact, with an initiative to establish an inaugural RFDS GP Clinic in Kalgoorlie, partnered with the Kalgoorlie Campus of the Curtin Goldfields University Department of Rural Health.
We are looking for a Clinical Lead General Practitioner, who will provide clinical leadership for the RFDS General Practice Clinic supporting the delivery of highquality care to patients and the community.
Please contact Lauren.Dawe@rfdswa.com.au
P/T GP required for our friendly practice in the heart of Fremantle. Young demographic with lots of student health, sexual health, women’s health and mental health. Fully equipped, accredited practice with full time practice nurse and onsite pathology, 2-3 days/week, days negotiable.
Contact Stephen on 0411 223 120 or at stephen@westendmed.com.au

Queens Road Surgery is a busy GP owned general practice located in Mount Pleasant.
We are looking for a VR GP to join our well established practice.
We offer a supportive team based culture, experienced administrative staff and quality full time nursing support.
Queens Road Surgery is a fully equipped accredited practice.
For a confidential discussion please contact our Practice Manager Narelle 0412 113 584 or narelle@queensroadsurgery.com.au

Opening for VR GP - F/time or P/time Full Private List available now from retiring GPs FRACGP essential Up to 70% private billings
Contact Ross, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs. Enjoy working for a doctor-owned, non-corporate, well supported, and accredited practice.
Please contact the Practice Manager on 6165 2444 or email: reception@comogp.com.au


Mosman Park Medical Centre is a GP owned practice. We are looking for another GP to join us.
We have six consulting rooms and it is a lovely calm, caring environment with a great patient base.
We are close to all amenities including shopping, cafes, beaches and river.
This can be a full-time or part-time position with scope for all GP areas of interest.
Our team of friendly receptionists is complemented by two experienced practice nurses at all times.

For more information please contact admin@mosmanparkmedicalcentre.com.au

Soleil Health, the future hub of unparalleled medical care and holistic well-being, is on the lookout for passionate and skilled General Practitioners to join our dynamic team in Cottesloe. As we prepare to open our doors in August 2024, we invite you to be a part of a healthcare revolution that prioritises clinical excellence, patient well-being, and a collaborative work environment.
About the Role: As a General Practitioner at Soleil Health, you’ll experience clinical autonomy, allowing you to practice on your own terms. Our commitment to providing the best healthcare is reflected in the use of Best Practice Software, ensuring streamlined and efficient processes. Embrace a collegial and collaborative culture where teaching and education are at the forefront of our mission.
GPs working for the practice also have the opportunity to provide home visit service to the neighbouring aged care residences.
Key Highlights:
Clinical Autonomy: Have the freedom to practice medicine focusing on your special interest.
Best Practice Software: Utilise cutting-edge tools to enhance the efficiency of your practice.
Collegial Culture: Engage in a collaborative environment, emphasising teaching and education.
Private Billing: Be a part of a practice that values your expertise with a private billing model.
About the Requirements:
Current unrestricted registration with the Medical Board of Australia / AHPRA VR status with Medicare
AHPRA Registration
Valid working rights in Australia

Wheatbelt Health Network







Emmba b k rk on t thhe e neexxt t phasse e o of f your G GP P caare r er witth Wh Wheaeattbbeelt t He Healalth th Netetwwoork rk in No Nortrthhamm. Diisscocovever r e exxceeptptioona n l su supp p orrtt, , inntetegrgraatted e hea e ltthccarare se serv v r i icces e , an and p prroospeectts in n emmeerggeency y mediccine. Do Don’ n t m miiss s thi h s op oppo p r rtununity contntacct t th the e CE C O Ca Caththerrin i e M Millinner r at c o ceo@whheeat a belt .coom.aau @
Are you a GP seeking an exceptional opportunity in Perth’s bustling CBD? Look no further! Doctor Northbridge, a private doctor-owned practice, is offering a dynamic VR GP position in one of the city’s most sought-after locations. Our state-ofthe-art medical centre, nestled within heritage-listed buildings, boasts top-notch facilities and a supportive environment.
Enjoy the perks of:
High-earning potential with private billing
Highly-trained administrative team
Private billing practice with excellent earning potential
On-site parking and convenient proximity to Perth CBD
Strong nursing support and low Did Not Attend (DNA) rate
65% of Billing with a Minimum Guarantee of $200 per hour for 3 months
Part-time or full-time opportunities available



I am retiring in October after 38 years as a GP. I have a loyal following of patients and am always fully booked.
I have special interests in mens and women’s health, sexual health, mental health and skin cancer surgery.
West End Medical is a boutique practice in the heart of old Fremantle. It is fully equipped and computerised (BP) with experienced staff and on-site pathology. The practice is accredited, private billing and non-corporate.
This is a huge opportunity for a VR GP to take over an established patient list with high earning potential with an opportunity to become a co-practice owner. I am happy to offer mentoring to anyone interested in developing their sexual health skills.
For further information contact Stephen Adams on 0411223120 or stephen@westendmed.com.au or Dovida Hickey on dovida@westendmed.com.au westendmed.com.au
With over 100 new patients a week and effective marketing strategies driving growth, Doctor Northbridge is the perfect place to advance your career. Join us and be part of a collegial environment dedicated to excellence in patient care.
Contact us today to learn more and schedule a visit!
Dr Yoon Low | Phone: 0431299328 Email: careers@drnorthbridge.com.au www.drnorthbridge.com.au



Join our Busy Mixed-Billing Medical Centre in Perth’s Northern Suburbs Start Immediately and Be Busy from Day One!
We are seeking a skilled and dedicated GP to join our dynamic team in Perth’s northern suburbs. As a valued member of our medical centre, you will:
Key Responsibilities:
Provide a full range of GP services, including health assessments, chronic disease management, and minor surgical procedures
Collaborate with our multidisciplinary team to achieve the best patient outcomes
Utilize our on-site specialized Mole & Skin Cancer Clinic, Allied Health Services, and Pathology
Work in a fully computerized environment with the latest technology (Best Practice)
Training practice for GP Registrar.
Requirements:
AHPRA registration
FRACGP or equivalent and VR.
What We Offer:
Flexible working hours with full-time and part-time options
Competitive remuneration with percentage earnings
Supportive and friendly team environment
Modern facility with state-of-the-art equipment
Fabulous career opportunities for experienced GPs.
Get in Touch:
Call Nash on 0433 400 792 or Julius on 0400 016 257 for a discreet and confidential chat. Alternatively, email nash.qamar@gmail.com to learn more.
Let’s work together to provide exceptional patient care!
Located on the lands and waters of the Whadjuk peoples of the Noongar nation, Murdoch University’s South Street Campus is a young, innovative, and enterprising university committed to helping people discover how to make a difference, through education and research endeavours
With more than 23,000 students and 1,700 staff, Murdoch University is one of the most inclusive universities in the country with a strong commitment to sustainability, equity, diversity and inclusion, and first nations.
Working as a General Practitioner, supported by a team of highly experienced nurses and administrative staff, you will be providing clinical care to predominantly young adults, including persons from Aboriginal and Torres Strait Islander, CALD, and LGBTIQ A+ communities. Experience and interest in mental health, sexual health, gender diversity, and public health will be highly regarded.
This is a great opportunity to work in a dynamic environment with a unique and diverse population, including domestic and international students, and staff.
Vocationally registered and AHPRA registration is essential.

Full-time preferred, part-time and/or flexible sessions considered
Mixed billing practice (GP retains 85% billing for 0.8FTE+, negotiable)
Opening hours Monday to Friday, 0830 to 1630
No on-call or af ter-hours required
Free on-campus reserved parking
Access to campus amenities, including childcare, gym, veterinary hospital, and chiropractic clinic
Working within the Access, Wellbeing & Equity directorate provides access to, and support from on-campus Counsellors, Clinical Psychologists, Social Worker, and Disability Specialists
Potential to support research projects
Please email your resume to Lisa Cranfield on l.cranfield@murdoch.edu.au or phone 08 360 2293 for more information.
Please note, applications will only be accepted from candidates who have either permanent residency or Australian citizenship, unrestricted medical board registration and no restrictions on their Medicare provider number.






