






















Workforce shortages are starting to sound familiar, and not just in maternity services. SJOG blamed the closure of its maternity units on a drop in demand, highlighting the bite that cost-of-living pressures are putting on the private sector.
The demise of another maternity service, this time in regional WA, is bad news for young families, but nor does is bode well for the rest of the community.
St John of God Health has called time on private maternity services at its Bunbury Hospital, citing a chronic shortage of midwives and not enough obstetricians, GP-obstetricians, and paediatricians available locally.
Patients will be offered the choice of a transfer to Bunbury Regional Hospital or to SJOG facilities in Perth. I’m guessing the latter will be a fairly unsatisfactory option for families, so they will head straight to the public system.
It comes hot on the heels of the closure of three maternity units in Perth late last year, including at SJOG’s Mt Lawley hospital and the Ramsay-owned Glengarry hospital.
Workforce shortages are starting to sound familiar, and not just in maternity services. SJOG blamed the closure of its maternity units on a drop in demand, highlighting the bite that cost-of-living pressures are putting on the private sector.
Earlier this year, a State Government lifebuoy was thrown to the ailing mental health clinic in Cockburn, which was run by Bethesda until its abrupt closure before the paint on the walls had barely dried.
The Government has since signed a three-year agreement to lease the clinic to boost public mental health services in the southern suburbs.
Dr Shirley Bowen is no stranger to the private hospital system and has recently taken the helm as WA’s director-general of health – a role once dubbed the poisoned chalice (and there is no reason to think the challenges of the job have changed).
One of her first tasks might be to look at the fragile see-saw that exists between public and private health services in WA.
One cannot survive without the other, and right now both are struggling.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.

FEATURES
10 Cover story: Organ donation
18 GPs and ADHD
22 Close-up: Dr Ben McKernan
26 RSV the skyborne stowaway
LIFESTYLE
56 Art in the heart of Margs
57 Movie giveaway
58 Human skills coaching
59 Wine review: Below & Above – Dr Louis Papaelias




1 Editorial: More than babies to worry about – Cathy O’Leary
4 News & views
8 In brief
30 Local study sparks new bladder cancer treatment
39 Here we go again – Dr Joe Kosterich
Dr Ed Heydon is the lucky winner of our April doctors dozen from Frankland Estate. This month we have a great selection of wine from Below and Above to win, reviewed by Dr Louis Papaelias on page 59.
We continue our deep dive into this year’s foreign film festivals, with five double passes to the Spanish Film Festival, presented by Palace, which returns to Perth from June 13 to July 7.
We also have 10 double passes to the comedy romance Fly Me to the Moon, set against the historic Apollo 11 moon landing, which opens in cinemas on July 12.
To win this month’s doctors dozen or movie tickets, use the QR code on this page or go to www.mforum.com.au and hit the competitions tab.
PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au
Journalist Eric Martin 08 9203 5222 eric@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au















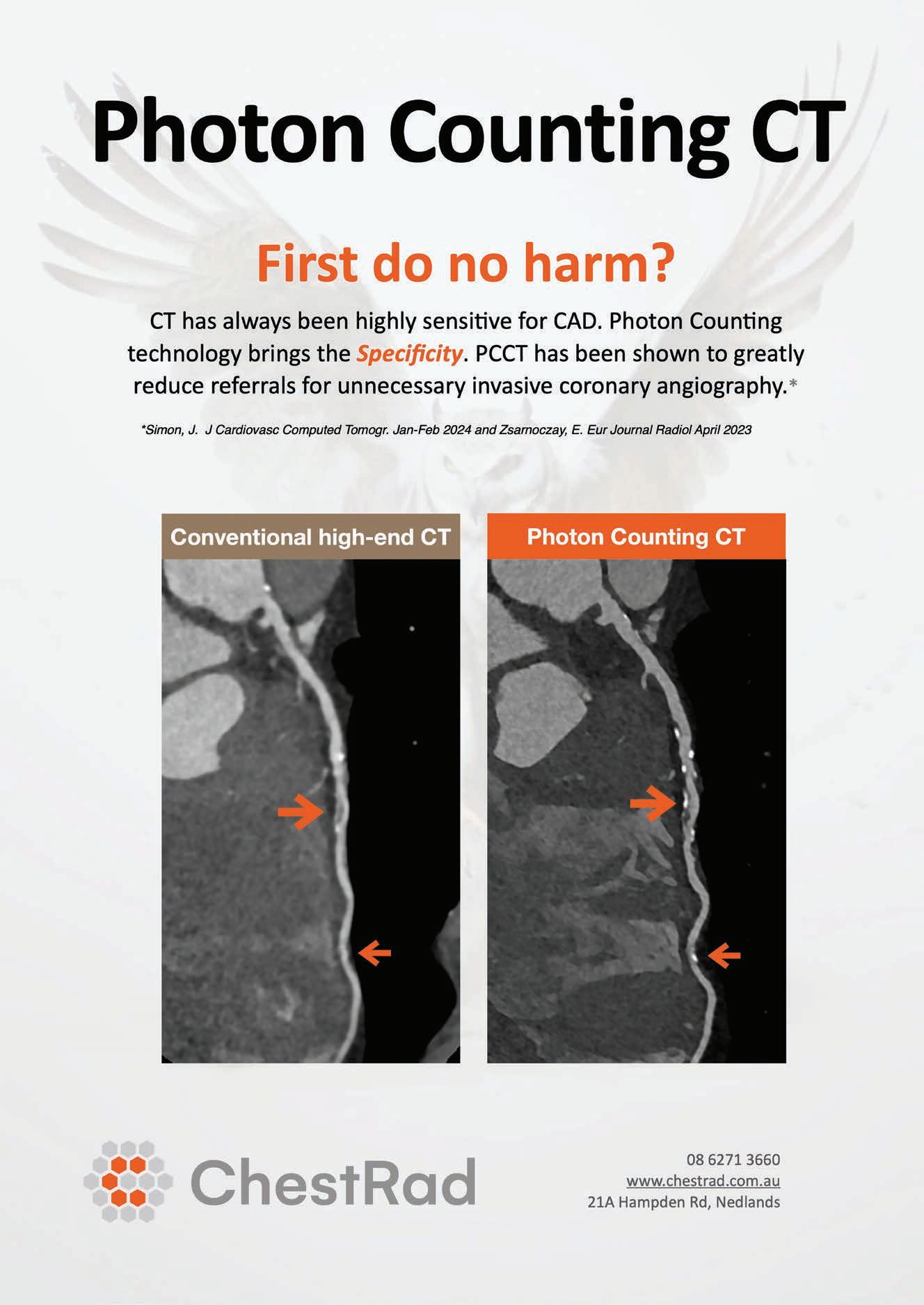
A revolutionary CT scanner was launched in Perth last month, the only machine of its kind in WA and offering a new way to check for heart and lung disease.
The photon-counting technology, designed by Siemens Healthineers and based at ChestRad in Nedlands, pictured right, has advantages over traditional scanners by emitting 50% less radiation while producing significantly higher definition images.
This is particularly useful for cancer patients needing multiple scans to minimise their radiation exposure.

In another first, doctors at Sir Charles Gairdner Hospital have carried out the first TricValve treatment in Australia on a 71-year-old heart patient.
The procedure involves having two self-expanding bioprosthetic valves implanted into the superior and inferior vena cava.
The treatment is used in heart failure patients who are unsuitable for surgical intervention, and the benefits include improvements in quality of life and exercise capacity, as well as alleviation of heart failure symptoms.
Edith Cowan University will become the first WA university to offer an osteopathy course when it starts at its School of Medicine and Health Sciences.
It will become one of only four osteopathy educators nationally, with a Bachelor of Medical Science (Osteopathy).
Osteopaths are registered healthcare practitioners, and the profession was one of the first 10 health professions registered when the Australian Health Professional Regulation Agency was established.
They provide direct manual therapy interventions, including exercise prescription and lifestyle advice to improve movement, reduce pain, and manage or treat a range of physical impairments.
Osteopathy treatment is recognised by Medicare, the Department of Veteran’s Affairs and the National Disability Insurance Scheme.
ECU will seek accreditation


TricValve is suitable for patients with functional tricuspid regurgitation and right heart disease who are not suitable for open heart surgery, and as an alternative to other transcatheter options.
And Hollywood Private Hospital recently notched up a heart surgery milestone, with 1000 cases in the four years since the opening of its purpose-built cardiac theatre.
Cardiothoracic surgeon Dr Pragnesh Joshi performed Hollywood’s first cardiac surgery, a beating heart bypass surgery in 2020, and this week performed the 1000th procedure.
from the Australian Osteopathic Accreditation Council, with a plan to offer the 3.5-year Bachelors’ degree in the first semester of 2026, and a four-year Honours degree to high-performing students.
Executive dean for the School of Medical and Health Sciences, Professor Moira Sim, said the ECU course was structured to ensure students could apply broad knowledge and theory of osteopathy in a range of clinical and practical situations, and to think critically to analyse and interpret skeletomuscular conditions and factors which would impact treatment.
“Osteopathy is the second fastest growing registered health professional in Australia and WA has the strongest workforce need,” Professor Sim said.
New research by Edith Cowan University and Fiona Stanley
Hospital is aiming to reduce noise levels in intensive care units by improving the acoustic design.
Up to 50% of patients in ICUs experience sleep disturbance because of noise and this can hinder their recovery.
ECU’S Adjunct Senior Research Fellow Dr Emil Jonescu and FSH Director of ICU Research Ed Litton did the study at a 40-bed ICU and involved clinicians, medical practitioners, academics and industry consultants.
The room acoustics analysis revealed that at times maximum noise levels in the ICU ranged from 60 to 90 dB(A), passing the thresholds for sleep disruption outlined by the World Health Organization guidelines.
Dr Jonescu said noise was primarily caused by alarms from medical equipment and discussions among clinical staff and was a common problem across all ICUs.





WA’s new Director-General of Health is Dr Shirley Bowen, most recently chief executive of the North Metropolitan Health Service and previously at St John of God Subiaco Hospital.
Two Telethon Kids Institute researchers were named finalists in the professions category of this year’s Western Australian of the Year Awards – paediatric oncologist Professor Nick Gottardo and paediatrician Professor Desiree Silva

Vale Dr Harry Cohen, who died in March at the age of 92, after a distinguished career as an obstetrician and gynaecologist at KEMH and active environmentalist.
Perth plastic surgeon Dr Brigid Corrigan has been appointed vice president of the Australian Society of Plastic Surgeons.

Perth Children’s Hospital paediatric endocrinologist Dr Mary Abraham is the inaugural winner of the PCH Foundation Stan Perron Charitable Foundation early career research award.
continued from Page 4
“In the ICU, there are a lot of beeps and alarms from machines and some of that noise can’t be mitigated because of the important information provided for clinicians,” he said.
“Our aim was to try and find the optimal balance of good information flow for clinicians and rest and recovery for patients, and we found there are certainly some design improvements that can be made.”
Part of the study investigated health professionals’ perceptions of noise impact on patient sleep and staff duties in the ICU. They reported ICU noise negatively impacted their work performance, patient connection and job satisfaction.
“They indicated that their biggest concern was the impact to patient sleep quality, however they also believe a quieter ICU would
improve clinicians thinking ability,” Dr Jonescu said.
While health statistics show 39% of hospitalisations for respiratory conditions are in regional WA, until now there has been no specific respiratory treatment available.
This has prompted Asthma WA to open its first regional hub in Bunbury to provide free lung function testing, and respiratoryspecific community education, support and health promotion for schools, community, and sporting groups.
Asthma WA CEO Anne Hallam said the respiratory hub was based on a model at Cockburn Integrated Care that was an Australian first –combining lung function testing, immediate review and consultation.
“Lung function testing is the service to accurately and comprehensively diagnose asthma and chronic
A Perth northern suburbs general practice is one of a growing number of clinics using a data tool to improve patient care and outcomes, including real-time medication alerts and care prompts.
The clinical decision support and data extraction tool known as Primary Sense was developed and now owned and operated by Primary Health Networks and is available free of charge to general practices.
It is currently used by 10 out of 31 PHNs nationally and accessed by almost 5000 GPs from over 1500 practices, supporting nearly 10 million patients.

WA Primary Health Alliance practice quality improvement coach Joe Staniszewski has helped the Wangara Medical Centre team to get the most out of the tool.
Perth-based Ear Science Institute Australia has signed a partnership with the National Acoustic Laboratories to bring together hearing researchers from across Australia.
Colin Smith has taken on the role of CEO of Lotterywest and Healthway, after a stint as chief operating officer at TKI.
He said the practice was running Primary Sense reports on chronic lung disease and asthma patients to identify those who have not undergone specialist evaluation or diagnostic testing and recall them for follow-up appointments.
The Wangara medical centre’s practice manager Anna Teki was initially hesitant to use the tool, but after seeing how the reporting functions could support practice audits, realised how it would improve patient care.
“When we started using Primary Sense reports, we focused on running easy reports such as identifying duplicate patients, checking patients who would be eligible for cardiovascular services, and finding reports like missing PIP QI measures with patients booked in the next two weeks,” Ms Teki said. She said the practice’s GPs were finding the patient care prompts and realtime medication alerts particularly helpful.
obstructive pulmonary disease and other respiratory conditions,” she said.
“Across our hubs, our free LFT service has led to a new diagnosis for 55% of our paediatric and adult consumers, significantly improving asthma and COPD care and management.
“Lung function testing can also be very expensive for people impacted by respiratory conditions and require GP referrals, testing and specialist appointments. We have respiratory specialists who review and analyse the results and then send them back to the regular doctor for ongoing management.”
Patients can be referred to the respiratory hub by their GP or can refer themselves by completing a form on Asthma WA’s website or by phoning Asthma WA.
The South-West Respiratory Hub is based at St John of God Specialist Centre in South Bunbury and will be open on Mondays and Tuesdays.
The WA Country Health Service is helping palliative care patients to get out and about without leaving their home or hospital room, thanks to an innovative virtual reality program.
Now available across regional WA, the new technology allows patients who are house- or hospital-bound to visit locations such as Kings Park, Broome and Perth Zoo.
The virtual reality headsets provide separate images for each eye, rendering a 3D virtual world, as well as a binaural audio system and real-time head tracking for virtual movement.
WACHS Executive Director Nursing and Midwifery Maria Flynn said patients receiving care for terminal and life-limiting conditions were able to experience sights and sounds they might not otherwise have the chance to see.
“Some of our patients are receiving 24/7 care and unable to leave their hospital room,” she said.
“This is a really innovative way of supporting patients at a difficult time in their life, giving them a chance to experience just a little bit of the outside world.”
St John of God Subiaco Eye Hospital has become the first private facility in WA to install a type of microscope that offers unparalleled vision for eye procedures.
The Zeiss Opmi Lumera 700 rescan microscope is suitable for all ophthalmic procedures and provides better accuracy.
Hospital ophthalmologist
Dr Olivia MacVie, far right, said ophthalmologists could use it to access optical coherence tomography – an emerging technology used to create highresolution cross-section images of tissue structure on the micron scale in real-time.

“OCT allows ophthalmologists to see the retina’s distinctive layers and map and measure their thickness,” she said.
“This helps to guide diagnosis and treatment for a range of conditions including cataracts, glaucoma and retinal disease such as age-related macular degeneration.
“Eye surgery requires an incredible amount of precision and through enhanced 3-dimensional images, we are better able to make quick and informed decisions during surgery.”
Rates of pre-term births in Australia have fallen by 10% since 2021 – a result linked to national initiatives backed by Perth doctors.
It comes as the Australian Preterm Birth Prevention Alliance and the ‘Every Week Counts’ national preterm birth prevention collaborative recently held a showcase event at Parliament House in Canberra.

The event brought together participating hospital teams, health service executive leaders, state and federal Ministers, people who have experienced preterm birth and pregnancy loss, and leaders in maternity healthcare.
Alliance chair and Perth obstetrician Professor John Newnham, centre, said the world-first program had been a major success, with new data revealing a significant reduction in untimely early births since the program started in 2021.
“The latest data from the program on rates of early term birth suggest a reduction of at least 10%, which equates to 4000 fewer children each year being at increased risk of behavioural and learning problems at school age,” he said.
National data published by the Australian Institute for Health and Welfare show preterm rates have fallen by 6% since the alliance began its work in 2018, representing 1700 fewer babies each year and an estimated annual government saving of $90 million.
The figures on early term birth rates were released for the showcase event and are preliminary and yet to be published.
In Australia, the collaborative program included 54% of all public hospital births at 63 hospitals across the country from all states and territories.
The program has been led by the alliance in partnership with Women’s Healthcare Australasia, the Institute for Health Care Improvement, Safer Care Victoria, WA’s Women and Infants Research Foundation and state health departments.
Organ donation experts have a message for GPs – help them save more lives – while their call to the States is to bring back consent on driver’s licences.
By Cathy O’LearyOn a positive note, last year saw an improvement in Australia’s organ donation figures, with the highest rates of deceased organ, eye and tissue donation and transplantation since 2019.
But the good result is tempered by the reality check that many more lives could have been saved – or vastly improved – if more organs and tissue had made their way to the long list of would-be recipients.
Only 36% of Australia’s eligible population are registered as donors, and about 40% of families are unwilling to consent to their deceased family member becoming a donor if they are unsure of what their relative would want.
In April, a national webinar was held to try to encourage more GPs to get on board in the push to improve donation rates, with experts arguing that they hold a key role in being able to weave the conversation into routine consultations.
It was run ahead of an initiative which will see information kits specifically targeting GPs distributed to more than 3300 clinics nationally in July. The aim is to provide doctors with the facts about organ donation so they can help address myths and misconceptions in the community.
Some people are worried that if they become seriously ill and have registered as a donor, doctors will not work hard to keep them alive, while others believe their body will be badly disfigured if they end up having organ donor surgery.
According to Donatelife, there are 7.7 million people on the Australian Organ Donor Register, with about 180,000 more people registering last year.
This resulted in the highest rates of deceased organ, eye and tissue donation and transplantation since 2019.
Last year, there was a 13% increase in the number of living kidney donors compared to 2022, and 6% more than 2019. Of these, 55 kidney transplants were through the Australian and New Zealand Paired Kidney Exchange Program. This is a 31% increase over 2022 and the highest number of donors since the start of the exchange program.
Many more people became eye and tissue donors because donation can
happen in people who die outside a hospital and up to 24 hours after death.
While the national consent rate for last year sat at 55%, in WA it was slightly lower at 53%.
Generally, WA’s donor and transplant figures represent 8-9% of the national total, with 43 of the 513 deceased living donors; 126 of the 1396 transplant recipients; and 15,645 of the 179,813 new registrations last year.
Experts say there is still more work to do to increase consent for donation. A national consent rate of 70% would make Australia one of the world’s leading donation countries and see an extra 300 life-saving organ transplants every year.
But to reach the goal of having 50% registered by 2027, more needs to be done to increase options for large-scale registration, including through driver’s licences, and investing in public awareness campaigns.
Donatelife argues that registration and family
discussion have a direct impact on consent, with 80% of families saying yes to donation when their family member is on the register, dropping to 40% when families don’t know the intention.
The webinar for GPs in April –hosted by health commentator Dr Normal Swan – focused on the important role that family doctors can play in raising awareness and encouraging registration.
Key points included the many misconceptions, such as people believing they are too old, unhealthy, or have lifestyle choices that exclude them from donation, when in fact there are few conditions that would prevent someone from becoming a donor.
Dr Swan told the webinar that some doctors did not think that organ donation was part of the core business of general practice.

Associate Professor Helen Opdam, national medical director of the Organ and Tissue Authority, said many
continued from Page 11
more people could donate, and one of the biggest limiting factors is the consent rate of only 55% at the point when families are approached to offer consent in hospital. It
did not reflect survey findings of people’s general support for organ donation.
“The big problem is that people haven’t let their families know… so the biggest thing is talking to family, because we have 1800
You have limited time with your patients, and talking about organ and tissue donation at the right time is key. Many people think that their medical history will mean they’re not eligible to be a donor. It doesn’t matter how old you are, your lifestyle, what country you’re from or how healthy you are – you can still register as an organ and tissue donor. Preventive health consultations for screening, blood pressure, pathology, vaccinations, routine tests, annual health checks and other preventive health appointments could be suitable opportunities to discuss donation. MBS item numbers include: 701, 703, 705, 777, 715.
When taking a patient’s social history, you’ll ask questions about their lifestyle, which could include drugs and alcohol, smoking and vaping, work, family and home. You can use this point to discuss common myths about organ and tissue donation.
When advance care planning with older patients, you’ll likely ask questions about end-of-life decisions, which could include a discussion about enduring power of attorney. You can use this point to discuss organ and tissue donation.
Having the right facts about organ and tissue donation in Australia can help your patients consider it. Here are some common myths we hear from people who think they can’t register. Please help set the record straight.
MYTH: If I’m a registered donor, doctors won’t work hard enough to save my life.
FACT: The doctor’s priority is always to save your life. Organ and tissue donation will only be considered if you have died, or when death is inevitable.
MYTH: If I’m a registered donor, I’ll automatically become one when I die.
FACT: It’s unlikely. Only around 2% of people who die in Australian hospitals meet the criteria to become an organ donor. This is why every potential donor is precious. Your family also needs to give consent to donation. Many more people can become eye and tissue donors as death doesn’t need to occur in a hospital. Tissue donation saves
people on the waiting list for organ donation, and another 14,000 people on dialysis who could benefit,” she told webinar participants.
Professor Opdam said many people wrongly assumed there must be
and transforms lives in many ways including saving burns victims, restoring sight, repairing heart defects in babies and adults, rebuilding tendons and reconstructing bones.
MYTH: Donation will disfigure my body.
FACT: Donation surgery is conducted with the same care as any other operation. Your body will be treated with dignity and respect and your family can still have an open casket viewing if desired.
MYTH: I’m not healthy enough to donate because of my lifestyle choices or medical history.
FACT: If you smoke, drink, vape or have an unhealthy diet you can still register to be a donor. You don’t have to be in perfect health. There’s every chance that some of your organs and tissues may be suitable for donation. Only a few medical conditions may prevent you from being a donor. You can trust the medical team at the time of your death to assess if you can be a donor.
MYTH: I can’t be a donor because I lived in the UK.
FACT: You can donate your organs but not your tissues. If you lived in the UK between 1980 and 1996 for a period of six or more consecutive months, you can still donate your organs. You are not able to be a tissue donor due to the risk of transmitting variant CreutzfeldtJakob disease.
MYTH: I’m too old to be a donor.
FACT: Age is not a barrier - people over 80 have become organ and tissue donors. If you die in a way that gives you the opportunity to be considered for donation, leave it to the medical team to assess if you can become a donor, and if so, they will talk with your family.
MYTH: My religion doesn’t support donation.
FACT: All major religions support organ donation. This includes Islam, Buddhism, Hinduism, Judaism and Christianity.
If your patients want to be an organ and tissue donor at the end of their life, encourage them to register and talk to their family about donation. It’s easy and quick to register. It takes three taps to register on the Express Plus Medicare app, or one minute at donatelife.gov.au.
In South Australia, locals can also register via their driver licence, but this is currently not the case in other States and territories.
a lot of people dying who could be donors, but the limitation was that in order to have organs in the right condition so they could help people when donated after death, the death needed to occur on a ventilator in hospital.
Those circumstances of death occurred infrequently, in about 2% of people who die in hospital, or about 1500 people a year, while eye tissue could be donated later.
Professor Opdam said it could be a terrible dilemma for families when they did not know what their family member wanted in respect to organ donation, and in those circumstances only four out of 10 families said yes to donation. But if their family member had registered and particularly if they had that conversation, then consent rates were 80% or higher, because families wanted to honour the choices their loved one made.
She stressed it did not have to be an awkward conversation – it could be done while watching television. Young people could potentially donate to six or seven people.
“It can be extraordinary legacy to leave behind,” she said.
There were no major medical exclusions, as all the chronic medical conditions were not excluded, and probably the only condition that might prevent donation was metastatic cancer.
“Hepatitis C, hepatitis B, we’ve even had a HIV-infected person donating organs to another HIV-positive recipient,” she said.
“Smoking, drinking, drug use, none of those things are exclusions, but one of the reasons people don’t register or bother to say they’re willing to be a donor is because they assume their age, conditions or their lifestyle choices exclude them.
“GPs are in a position to dispel myths and not reinforce myths, and encourage people to talk about donation, and it doesn’t’ have to be a heavy or complex thing, it can be quick and easy, as is registering on a national register.
“It’s about looking for opportunities in regular consultations, particularly
when people are talking more generally about lifestyle, health or advanced care planning.
“And don’t restrict the conversation to older patients if there’s an opportunity to bring it up with younger patients too. GPs are so trusted, such leaders with respect to health in the community, and they’re really influential in (encouraging) people to be willing to donate and to understand that it’s quick and easy thing to register.”
When asked if organ donation could be part of the voluntary assisted dying process, Professor Opdam confirmed it had already happened in about half a dozen cases in Australia.
“But if people are dying from MND and other neuromuscular diseases, for example, they could donate but they might need to modify their experience of VAD, because it would need to occur within a hospital, usually in ICU,” she said.
“We’re really developing processes in Australia to support this, but it’s very important that any decisions
continued on Page 15
Ramsay Clinic Hollywood provides specialised inpatient and day patient services for patients struggling with eating disorders. Treatment comprises a mix of psychiatric interventions, psychological care, nutritional support and peer worker involvement.
• GP-referred (patient does not need own psychiatrist prior to admission)
• Patients are assessed prior to admission for the Day Program and admitted under the Consultant Psychiatrist, Dr Richard Clarke
• Inpatient Program Consultant Psychiatrist – Dr Leighton Chadwick
• Patients can enter the Day Program at any time
• An onsite support group is also available

Further information is available on the Ramsay Clinic Hollywood web site (see ‘For Doctors’ pages) or by contacting Wendy Henson E: hensonw@ramsayhealth.com.au
M: 0417 404 776
Referral:

• A Best Practice template or writable pdf referral is available
• Email to: rchbookings.hph@ramsayhealth.com.au
• Phone 9346 6850 to discuss pre-admission tests that may be required
Note: Private health insurance, DVA cover or self-funding required
Our new community clinic is conveniently located opposite Armadale Hospital on Albany Highway with plenty of free onsite parking. The clinic offers a warm welcoming space, catering for families with a dedicated children’s area and baby care facilities.

Armadale North services include: • MRI • CT including CTCA • X-ray • Ultrasound • DEXA • Interventional services
Location: 3043 Albany Highway, Kelmscott
Our sub-speciality reporting teams
continued from Page 13
regarding VAD is taken first, before any consideration of donation, so the two decisions don’t become conflated, but if people want to explore this, donation agencies can support that.
“In many ways, it’s the most informed consent process in any donation after death, because it’s the person themselves consenting and they understand the exact requirements which is quite different to when people simply say they’re willing to be a donor, or we get consent from families.”
GP Greg Stewart told the webinar about the life-saving transplant of his brother Paulie Stewart, from the pub rock band Painters and Dockers, who made life choices that were “not good for his liver” and went into liver failure.
After receiving a liver transplant 14 years ago, Paulie had been sober and now did a lot of volunteering.
“It’s a fantastic gift from someone,
and I try to encourage people to become donors, but there are a lot of competing interests you have to fit into a 15 or 20-minute consultation, such as diet, exercise, smoking and drugs, but organ donation is obviously a worthy cause,” Dr Stewart said.
“I think it’s a fantastic thing when it happens, and people can live many years of extra life. I’m all for it. There are ways to incorporate it into general practice, it can be part of what we do.
“Once you’ve registered, there’s nothing much more to do, other than to say to your spouse or family members every couple of years, ‘yep, I’m up for it’.”
Professor Opdam said there was still a myth you could register as a donor on your drivers’ licence, but in most States that was no longer the case, and people needed to go onto the register. [ED: in WA you cannot give consent on your driver’s licence.]
South Australia (which has driver’s

licence consent) had typically done well in donor rates, and there was now a push to get driver’s licence consent reinstated in other States.
Professor Opdam said organ donation staff would not go against the wishes of objecting families, and there was a need to normalise organ donation, rather than making it an extraordinary thing.
“We try to talk about donation in every end-of-life circumstance, even if it’s to say, just in case you were thinking about it, organ donation is not possible in these circumstances,” she said.
“The more we can normalise it, mention it, don’t make a big deal about it, the better, and I think GPs are so well regarded, and if it’s not (discussed) with their patients, maybe it’s within the community.
“That could influence people’s decisions and who knows how many lives you can save, outside of your GP clinic, just in your leadership in this area.”
A spokeswoman for the Organ and Tissue Authority told Medical Forum hard-copy kits were being mailed out to GPs next month, including a letter to the practice manager, a poster to display in waiting rooms, and a 12-page resource of facts about organ and tissue donation for GPs and community health professionals.
GPs were being asked to promote organ donation via communication channels such as practice newsletters or social media.
“Around 80% of Australians support organ and tissue donation, yet only 36% have registered. That’s why we’re asking GPs to help us spread the word,” she said.
Digital kits are also available on the website www.donatelife.gov.au/ gp-resources

As the Australian population ages and life expectancy increases, so too does the incidence of non-melanoma skin cancer (NMSC). Studies now indicate that nearly 70% of Australians are expected to have at least once NMSC excised in their lifetime.
The predominant NMSC, basal and squamous cell carcinoma (BCC/SCC), generally have a good prognosis if managed early. Excision or Mohs is the mainstay intervention for higher-risk lesions, achieving two-year complete response of 98%+. Fortunately, many other lesions can be managed through some form of ablative technique, such as cryotherapy or electro-desiccation, although long-term efficacy is generally lower.
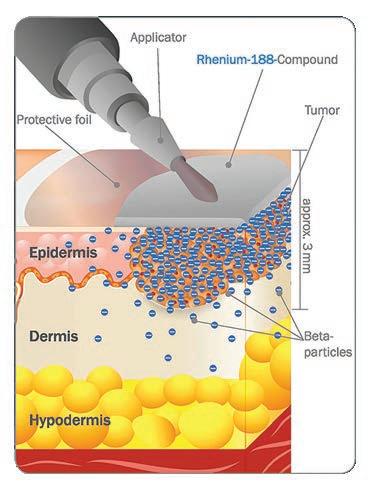
Patients with new or recurrent lesions where there are concerns for cosmetic or functional outcomes from surgery may be suitable for an innovative epidermal radioisotope therapy.
Rhenium-Skin Cancer Therapy (SCT)® is a singlesession, non-invasive treatment that achieves complete response rates of >95% out to two-years posttreatment. Rhenium-SCT is administered as a paste, allowing for conformal application to complex surfaces such as the nose, ear, lips, digits, genitals, or scalp. With lesion demarcation by skin specialists, Rhenium-SCT allows for precise treatment, minimising exposure of healthy tissue.
Rhenium-SCT offers patients:
• A non-surgical option
• An effective, single session treatment (30 to 180 minutes – depth dependent)
• A well-tolerated, painless treatment that spares underlying tissue.
Rhenium-SCT utilises beta particles emitted from the radioisotope rhenium-188. Like conventional radiotherapy (RT), Rhenium-SCT direct and indirect cell death responses, which cancer cells are traditionally more sensitive to. The beta particles penetrate up to 3mm into skin, reducing exposure to underlying healthy tissue and allowing treatment to be delivered in a single session. Longer-term data indicates favourable cosmesis, safety and patient-reported outcomes.
Rhenium-SCT may be an excellent option for patients who are not able to receive a fractionated course of RT.
Rhenium-SCT is a form of nuclear medicine, meaning that treatment is performed in specialised facilities by licensed practitioners, such as Nuclear Medicine Physicians or Radiation Oncologists. The radioisotope paste is made to order and shipped to the clinic on treatment day. Patients are treated comfortably in the specialist clinic for between 30 and 180 minutes, depending on the depth of the lesion. Following treatment, the patient can return to regular activities immediately without any downtime.
Post-treatment follow-up is simple, with patients and referring clinicians provided with tips to ensure the area heals without complications. Aftercare consists of keeping the area clean and avoiding cosmetic products.
Indications:
• BCC or SCC <3 mm deep (punch biopsy required).
• Treatment-naïve, refractory, or recurrent lesions.
• Lesions in areas with concerns for cosmetic or functional outcomes from conventional therapy.
• Lesions <3cm in diameter (larger considered in consultation with physicians).
Contraindications:
• Melanoma.
• Deep lesions (>3mm).
• Lesions with peri-neural invasion.
• Lesions on the eyelid.
• Pregnant patients.
All patients will develop a mildmoderate acute radiodermatitis reaction in the weeks following treatment with average healing time ~30 days. Common toxicities are itching and scabbing. Patient age and comorbidities, lesion depth and location will affect healing time.
Evolving face of skin cancer care
Rhenium-SCT is an excellent option for a subset of patients who are unsuitable for, or refuse, surgery or fractionated RT. The ability to effectively treat complex areas with minimal planning or downtime, makes Rhenium-SCT a valuable addition to the treatment portfolio. To ensure treatment access for suitable patients, public and private reimbursement will be important in the near future.
– References on request

Cost:
• Cost dependent on lesion size and determined during consultation.
• Currently not covered by Medicare.
• Some private health funds consider treatment coverage (pre-approval required following consideration of request by treating physician).
Referrals
To refer patients or for more information, please contact:
A/Prof Joe Cardaci (Diagnostic Nuclear Imaging, Hollywood Private Hospital): admin@dni.com.au , or medical@oncobeta.com.au www.oncobeta.com





Long waiting lists for patients to be assessed and treated for ADHD by specialists is fuelling frustration among GPs, prompting some to speak out.
By Cathy O’LearyThe referral system is accepted as a fundamental part of medical practice and a way of keeping GPs as the gatekeepers of patients’ sometimes complex health profiles and with some medical conditions such as ADHD, the referrals are essential to get a diagnosis and treatment.
However, patients hoping to be assessed are sitting on waiting lists for 12 months or more, or worst still, their referrals are rejected by specialists who have closed their books.
For some GPs, the growing frustration of not being able to help patients has bubbled over into the mainstream media, as some speak out about the lack of support and funding from governments.
Unlike in Queensland and NSW, WA GPs cannot provide a diagnosis or prescription of stimulant medication to any patient, no matter their age. The State’s public ADHD clinic treats only children, forcing adults seeking ADHD assessment and diagnosis into the private sector.
With no public pathway to diagnosis and even private psychiatry waitlists ballooning, some patients have resorted to going interstate to see specialists, while others have faced sharply increased fees to see a WA psychiatrist – a move which has raised eyebrows among GPs.
Earlier this year, a survey on wellbeing and job satisfaction by the Royal Australian and New Zealand College of Psychiatrists found that 93% of psychiatrists believed the current workforce crisis was negatively affecting patient care.
Across all states and territories, many psychiatrists responded that they had experienced burnout, with the highest rate in WA, with 80%.
The State Government says it is working to fix the problem of the unprecedented demand for children’s health services across WA, and in April this year announced a near-$40 million funding injection.
Part of the plans include expanding the Child Development Service to increase staff including paediatricians, clinical nurse specialists, speech pathologists, occupational therapists, psychologists and audiologists in metropolitan and regional areas.
Support group ADHD WA welcomed the investment but said children were facing unacceptably long wait times for both diagnosis and treatment, with some primary aged children waiting about two years to see a paediatrician.
Dr Andrew Leech – RACGP WA’s GP of the Year for 2023 – is one of those challenging the status quo and looking for new ways to deal with demand and changing expectations from patients.
He says hundreds of GPs like him are battling issues around poor or unwieldy Medicare rebates, and increasingly high demand from families seeking an ADHD diagnosis.
to be bit louder,” he told Medical Forum
Part of the change in how Dr Leech works at The Garden Family Medical Clinic, based in Murdoch and Piara Waters, is to have a full-time child health nurse with a background in working at the Child Development Service, who can do a lot of the pre- and post-legwork for appointments.
Chloe Barber has only been working with Dr Leech for a few months but said families appreciated the continuity of care from a health professional who was familiar with their situation when they were feeling lost.
Dr Leech said this approach might not be for everyone, but it was how he had decided to manage a difficult situation for now. But his new model of care was not funded, so came at a cost.
“We know the families well and we’re able to do the standard screening tools and take a good history and speak to the schools if we have to, or to family members, and the NDIS and the Education Department are allowing more GP input in the revisions in autism,” he said.
“But with ADHD there is still this roadblock where GPs are not recognised as being able to even diagnose let alone prescribe.
“We’re seeing a lot of complex patients and some families going through really difficult times, with a wide variety of neurodevelopmental problems like the trend in ADHD and autism, as well as mental health challenges in families and children.

“With anxiety being at the top of that – traumabased problems, issues around school bullying and social media, and we’re seeing a bit of eating disorders too.”
Dr Leech said everyone could be working to make the system more streamlined because there was not going to be an increasing medical workforce or a sudden change in the number of graduate paediatricians or GPs who were interested in this field.
to avoid having silos across different sectors.
“Otherwise, patients become confused about who they’re meant to be seeing, and they get rejected by referrals, then they come back to us, and the whole thing starts again. It’s so much effort to get the help they need,” he said.
“Unfortunately, we’re in that cycle of not very good care at the moment.”
Dr Leech said GPs did not have time for longer consults and more complex paediatrics, so they had to refer, and not everyone was interested in this work anyway.
“The big issue is getting the support from the specialists and the hospitals, and while the government has announced funding for the Child Development Service, which is hopefully going to help, it will be medium to long-term before the benefits from the money are going to show up,” he said.
“We’ve advocated for GPs to be able to initiate stimulants, and I think that would be a gamechanger, and I know it’s very controversial because psychiatrists and paediatricians would generally feel that it is in their domain to be doing that, around safety, but we’re in different era now.
“We have a lot of people coming through wanting to know if they have a diagnosis of autism or ADHD, and GPs can do that, it’s not that hard to do that assessment and decide for them. For the more complicated cases, that’s when we need specialists, and we need them to be available to help those people.
“But now, whether they’re coming for an initial diagnosis or coming for a lot of different things, we can’t get any specialists for anyone, and most of the referrals are rejected.”
Dr Leech said there was also a problem of patient expectations, because a lot of families came in expecting a referral to a paediatrician based on what their child’s school had told them, creating a fear of missing out.
“It’s been good to have a platform to advocate, because when you go straight to the government it doesn’t always lead to any change, so sometimes it’s a case of having
GPs needed to be smarter in how they used nurses, for example, as well as the way they worked collaboratively with paediatricians
“They say ‘we need that referral, we need to get on a list, the school says there’s trouble going on with
continued from Page 19
the child’s learning’. We need to be cleverer in approaching that by doing other things and not just jumping on a referral.
“We definitely need education for GPs who are going to work in this role, who would potentially be doing this work in straight-forward cases and know when to refer. So there needs to be a bit of a shift in how we manage this area to reduce the burden on the tertiary sector and the specialists.”
Dr Leech said that GPs needed to be more empowered to help, just as they already have when dealing with conditions such as diabetes and chronic pain.
His practice has run a small pilot ADHD program with a paediatrician, doing a lot of the work-up and follow-up at the GP clinic. “What we were able to do with 20 patients, with the ongoing reviews, was done a lot quicker than the paediatrician could have been able to do,” he said.
Dr Leech and colleagues had put in a funding proposal to the WA Government several months ago to expand the program but had not heard back.
“I don’t think we’re going to become a ‘Stimulant State’, which is one of the comments I’ve heard from paediatricians, with Safe Script WA crosschecking our scripts with the State database to make sure we’re not overprescribing, or that patients are not abusing their medication, so the protections are there,” Dr Leech said.
ADHD, or not?
But he was concerned that some children were being sent in because they did not fit into the typical school model of sitting still, listening, focusing, and keeping up.
“Schools are also not coping with that style of learning, because they have large classes, so on the education side there are issues around the way they’re able to handle busy children, or those that don’t listen, and maybe disobedient children,” he said.
“The pressure builds for them to
send the children in for funding and treatment and a label, so they can cope. This is some of the pressure on getting a diagnosis to help with learning, and it makes it a bit confusing sometimes, and we need to be careful about who gets treatment and look at what other options there are for improved learning for kids who might need more one-to-one support and different learning environments.
“The rise in ADHD is still unknown, and we don’t know exactly why we’re seeing it, and yes there are responsibilities around making a diagnosis, but some paediatricians make a very quick diagnosis and label a child.
“Part of my assessment now is not jumping to a referral, I’m not doing that anymore, this is a different way of doing it. We just spend a lot of time observing and reviewing each term and getting a feel for what is happening over time.
“And for children in pre-primary and Year 1, there’s a lot of normal development at that age, with busy brains and kids who just can’t keep still, so the child needs a full assessment of their health. There are blood and iron tests that need to be done, and they need their eyes and ears checked, and that takes a while.
“A big problem is sleep. Many kids have very bad sleep apnoea so we can go ahead and treat it, and
there’s nothing more rewarding than finding that they can regulate better, they’re concentrating better, and their energy is back.
“We have the ability as GPs to do that, to really tick off things.”
The way ahead
Dr Leech said GPs needed more support and funding options from the Government because many could not afford to hire a nurse to make it work better.
“We need education and funding for us to train large cohorts of GPs who are interested in this work and get them onboard. And those longer item numbers are helpful, but obviously Medicare is still behind, and out-of-pocket costs are still higher for patients,” he said.
“But these are the solutions, including the regulations for prescribing, and they’re achievable quickly – even just a relaxing of the rules.
“It doesn’t have to be a free for all that everyone can prescribe – just something that gives us a bit of room to work with families while they’re waiting, even a starter script to get them on their way.”
Dr Ben McKernan has an insatiable curiosity and medicine offers the rural generalist the perfect opportunity to put it into action.
 By Ara Jansen
By Ara Jansen
Endlessly curious, Dr Ben McKernan likes to explore things just for their own sake. It’s how he’ll find himself going down a rabbit hole exploring something medical that he finds interesting.
“I think I have always been like that,” says the rural generalist. “I have a natural curiosity which definitely manifests in my day-to-day. As I’m learning something, questions will pop up and off I go on these massive explorations.
“I’m a reader. I read more fiction growing up and really like science fiction. Over the years, and with my studies, I’ve ended up reading more non-fiction. Maybe that’s because I have found that there’s a utility in my day-to-day at work. I can read and learn something in medicine and as I’m doing anaesthesiology, I’m learning more about physics and how gasses diffuse across barriers.
“I love being able to read about things and then going to work and seeing that information being applied, used and put to work. There’s something hugely satisfying, addictive and exciting about that. I feel like a wizard sometimes, being able to read about it and then do it. It’s like doing magic out of Harry Potter some days.”
Ben is training to become a rural generalist as part of the Rural Generalist Pathway WA (RGPWA).

Currently living and working in Albany, he has three jobs – working at a group practice as a GP and in the Albany Health Campus Emergency Department furthering his advanced skills in emergency medicine and anaesthesiology.
“I have found a career that is copacetic with my temperament and personality, and which is intellectually challenging enough to keep me interested. Medicine is the tool I’m allowed to use to satisfy

my curiosity and it gives me great insight into a patient’s life. I don’t take that for granted.”
Ben’s dad works in mining and his mum is a math’s teacher. After Ben was born in Gosnells, the family moved around spending time in Newman, Port Hedland and Boddington before he finished high school in Australind.
Post-school, a cousin who was doing podiatry sparked Ben’s interest to follow suit. He thought the combination of science and sport-related work would be interesting and began his degree at UWA.
His first job placement was in Albany, most of his patients were in their 50s and 60s and he did enjoy interacting with them. Unfortunately, podiatry didn’t challenge Ben as much as he had hoped. What his podiatry studies did do though was expose him to units in a medical degree.
“The podiatry side didn’t capture me as much as I thought it was going to. But it gave me a thorough medical introduction and good background. My brother was studying medicine at that stage. We were coming back from a surfing trip in Yallingup and he suggested I do some research and consider medicine.”
continued from Page 23
After four years of podiatry study, Ben went back to university and did his medical degree at Notre Dame for another four years.
“Medicine made more sense,” says Ben. “The cogs were better fitted with medicine. Podiatry was a bit underpowered for giving me what I wanted. I felt more intellectually stimulated and it was a better application of my education.
“I find human beings fascinating most of the time – and infuriating sometimes. I wanted to have an opportunity and the privilege and unique vantage point to see into their worlds and to watch, to help. There’s lots of ways to do medicine and that’s one of its blessings.”
Another one of those blessings he says is that Australia has a well-established rural generalist program where he can do both his GP training and advanced classes. He says from a training perspective,

more sparsely populated regional centres (compared with Perth) mean he’s exposed to more opportunities because there are fewer doctors and specialist skills. He’s already spent time working in the Kimberley.
“Illness doesn’t respect geography so I can be involved in removing a gall bladder or helping stabilise someone who has been in a car accident. I have a passion for critical care and being able to do that in a remote area. I like being at the pointy end of the stick.”
At 33, Ben reckons over the past decade his studies and work have
taught him to be a little more laid back but working in an ED has also taught him more about staying calm and collected under pressure. When looking after critically ill patients, the SEAL mantra of “slow is smooth and smooth is fast” often comes to mind.
Working in the ED has given Ben his first advanced skill in emergency medicine. He has completed his Diploma in Rural Generalist Anaesthesia and is finishing the general practice part of his rural generalist training. There are three anaesthetists in Albany and a cohort of about a dozen who

have advanced skills in the area. Ben is the youngest doctor of the group.
Growing up around WA, Ben says living and working in the regions is where he’s likely to stay and why he’s found the rural generalist pathway perfect for him. He likes the utility and pragmatism of rural and remote medicine and says it makes for a flexible and handy
doctor with a broad range of skills.
“I feel like my blood pressure normalises, particularly when I’m in coastal country areas, so those coastal country towns are my favourite places. I grew up along the coast, learnt to surf in Bunbury and Yallingup and learnt to fish. I have a great love of the water.”
Ben remains a surfer, loves to get out when the swell is good and tags
Esperance as one of his favourite spots to swim or ride a board.
A close friend, who is also Ben’s emergency medicine mentor, often says “you can’t have systole without diastole” which reminds the junior doctor that working hard – at the moment about 60 hours a week –requires down time as well.
Outside and fishing, he also likes to play guitar, enjoys video games, swimming, seeing friends and doesn’t mind the odd glass of red. Ben has recently taken up trail running as a way of keeping fit and getting out into nature, making the most of the Great Southern’s extensive trail network.
“I love living here and I love my job. My brother lives in Denmark and my other brother is studying medicine in Perth. Three brothers in medicine – my parents valued learning and reading. They are kind and caring people, from both a philosophical and practical perspective. They taught us to think quite broadly across areas like civics in terms of being responsible to fellow man. They are solid role models.”
Our treatment services include:
• Intensive Treatment Program (ITP) and a NEW Adolescent Intensive Treatment Program (AITP).
• Private Health Funded Day Programs including Schema Therapy, Teen DBT Skills, DBT Skills, RO-DBT, as well as Binge Eating Disorder (BED) and Post-bariatric surgery BED groups.
• Coordinated and collaborative individual and family outpatient treatment with Psychiatrists, Psychologists, Dietitians, Occupational Therapists, Physiotherapists and Specialist GPs.
For more information about our programs and services visit www.esuscentre.au
Esus Centre, 588 Hay Street Subiaco WA 6008 T 08 6255 9900 F 08 6255 9920

Understanding how respiratory syncytial virus behaves is the first step in discovering how to stop its nasty impact on the young and not-so-young.
Vaccine research is ramping up but this tricky ‘quiet one’ will need vigilance and caution.
By Eric MartinAn unexpected outcome of the interruption of global travel during the COVID pandemic was that shut borders and geographic isolation led to a complete absence of Australian cases of RSV during the winter of 2020.
“In fact, we were we were one of the first countries to report that RSV (respiratory syncytial virus) was disappearing,” according to WA vaccine expert Professor Peter Richmond
He heads the Vaccine Trials Group at the Wesfarmers Centre of Vaccines and Infectious Diseases based at the Telethon Kids Institute, as well as being head of paediatrics at UWA and head of immunology at Perth Children’s Hospital.
use both in pregnancy and older adults, which could spread quite quickly and limit the impact of those vaccines. It also explains the unexpected results that we saw during the pandemic, when RSV suddenly went away and came back the way it did once air travel returned.
“The most surprising thing when we did the modelling was that we could trace the predominant spread along frequently flown air traffic routes. Five years ago, I would not have said that was the case.

“As a paediatrician who has seen our hospitals full every year, we always assumed that it was circulating within older children and that it would simply continue and wouldn't be affected by shutting our borders,” he said. “But instead, we saw this complete absence.”
The subsequent RSV epidemic came out of season – instead of occurring in the middle of winter, it happened over Christmas.
“And that particular outbreak, which occurred in WA and in the eastern states, was due to one strain of the virus, whereas previously from, our studies, we knew there were multiple strains circulating all the time,” he said.
“We looked at the strains across different countries over a threeyear period and it was really quite detailed molecular epidemiology: sequencing the genome of these viruses, examining how they related to each other, and what might explain how they tracked across the globe.
“It appeared that like influenza, RSV is spread in part through air travel – that's why we're getting this introduction of new strains that arise by ‘chance’ in countries around the world. I think we are all aware this also occurs with SARSCoV-2, and it does have significant implications.
“We have the emergence of strains that may be resistant to one or more of the monoclonal antibodies that have been developed for
“The other thing was understanding that RSV actually does change, and we need to be aware of how we can track this efficiently as part of our public health programs.
“RSV is not as diverse as SARSCoV-2 or influenza, so it tends to be a bit more stable, yet it is clearly changing from time to time, and we still haven't had a highly effective drug treatment. It’s important research that we need to keep doing and having the local ability to do this, while tracking the results globally, enables us to look at the bigger picture and reveal these novel findings.”
Professor Richmond said his team had been working on several prevention strategies for RSV infections, particularly focusing on studies in children and infants, using a monoclonal antibody and nirsevimab, a new drug still in the last phases of clinical trials.
“Our new understanding of clades has helped us track them with greater certainty and we can identify where they're first appearing and then where they might go – much like bird-flu.”
“One of the important parts of protection, particularly for monoclonal antibodies, is that small changes in the critical binding site can render the antibody unviable. This has certainly been well described for COVID, but it is also the case for some RSV monoclonal antibodies that looked very promising – where a mutation meant they were ineffective.
“A global consortium has been established to search for these mutations that might predict whether we have circulating strains that will be harder to prevent through vaccination, and to try and decrease the severity of infection. That work has been going on for several years.
“Our new understanding of clades has helped us track them with greater certainty and we can identify where they're first appearing and then where they might go – much like bird-flu.
“In some tropical countries we see that RSV seems to circulate all year round and similarly in northern Australia. The Northern Territory, Kimberley and far North Queensland – even greater parts of Queensland – seem to have a much longer RSV season. This is important knowledge when you're going to target children being born throughout the year. We might have an effective intervention, then suddenly it becomes more complicated to work out the best way to prevent a new strain of RSV.”
Professor Richmond explained that the F-protein (or fusion protein) was critical for the initial cell entry and infectivity of the RSV, akin to the spike protein in a coronavirus.
“The protein structure also changes shape significantly when it binds to a cell – forming the elongated shape unique to RSV – which is why we talk about prefusion F-protein or pre-F-protein, and post-fusion protein or post-F-protein,” he said.
“Understanding that was one of the reasons we were able to develop effective vaccines and monoclonal antibodies, because the earlier vaccines used the postfusion construct, yet the better the F-protein can be conserved in that prefusion structure, the more effective it will be.
We’re supporting HBF members to better manage chronic health conditions, such as cardiovascular disease and diabetes.
We’re supporting members
We’re supporting members to
We’re supporting members to better manage chronic health conditions, such as cardiovascular disease and diabetes.
manage chronic health conditions, such as cardiovascular disease and diabetes.
We’re

We’re supporting members to better manage chronic health conditions, such as cardiovascular disease and diabetes.
The COACH program is telehealth based coaching delivered by qualified health professionals.
The COACH program is telephone based health coaching delivered by qualified health professionals.
The COACH program is telephone based health coaching delivered by qualified health professionals.
The COACH program is telephone based health coaching delivered by qualified health professionals.
The
The COACH program is telephone based health coaching delivered by qualified health professionals.
Fully covered for eligible HBF members with HBF hospital cover.*
Fully covered for eligible HBF members with HBF hospital cover.*
Fully covered for eligible HBF members with HBF hospital cover.*
Fully covered for eligible HBF members with HBF hospital cover.*
Fully covered for eligible HBF members with HBF hospital cover.*
Fully
Tailored to your needs.
Tailored to your needs.
Tailored to your needs.
Tailored to an individual’s needs.
Each coaching session is customised to help you identify and achieve your goals.
Each coaching session is customised to help identify and achieve goals.
Tailored to your needs.
Each coaching session is customised to help you identify and achieve your goals.
Each coaching session is customised to help you identify and achieve your goals.
Tailored to your needs.
Each coaching session is customised to help you identify and achieve your goals.
Complements existing care and support.
Complements existing care and support.
Complements existing care and support.
Each coaching session is customised to help you identify and achieve your goals.
Complements existing care and support.
This flexible program can enhance your interaction with your existing health care team.
This flexible program can enhance your interaction with your existing health care team.
Complements existing care and support.
This flexible program can enhance your interaction with your existing health care team.
This flexible program can enhance the interaction with the participant’s existing health care team.
This
Complements existing care and support.
1 to 1 practical health advice.
This flexible program can enhance your interaction with your existing health care team.
1 to 1 practical health advice.
1 to 1 practical health advice.
Reliable and easy to digest information that helps you understand and take control of your health.
Reliable and easy to
1 to 1 practical health advice.
1 to 1 practical health advice.
Reliable
1 to 1 practical health advice.
Reliable
Convenient and easy to access.
Reliable and easy to digest information that helps individuals understand and take control of their health.
Convenient and easy to access.
Reliable and easy to digest information that helps you understand and take control of your health.
Convenient and easy to access.
Telephone support at a time that suits you.
Convenient and easy to access.
Convenient and easy to access.
Convenient and easy to access.
Telephone support at a time that suits you.
Telephone support at a time that suits you.
Call 1300 886 513
Telephone support at a time that suits you. Call 1300 886 513
Telehealth support at a time that suits the participant.
Call 1300 886 513
Telephone support at a time that suits you. Call 1300 886 513
Refer a patient today
Call 1300 886 513
Email hbfhealthprograms@hbf.com.au *HBF
email hbfhealthprograms@hbf.com.au
continued from Page 27
“The G-protein tends to be more variable and has a slightly different role in the pathogenesis of RSV and may be the reason for overall viral variation. There have been several people developing vaccines that include the G-protein, or adjust against it, but they have not been able to progress to advanced-stage efficacy trials yet.”
Professor Richmond pointed out that a downside of less variability within RSV’s structure was that it was less likely that mutations, which have resulted in higher rates of transmission but less severe symptoms in the coronaviruses, would occur with RSV.
“Because it has been around for such a long time, it's in a relatively steady state, but we don't know for sure. These viruses are very good at adapting and finding new ways to spread,” Professor Richmond said.
“It is important that we don't start to say this type of research is of ‘academic interest’ only – and that applies to infectious disease much more broadly, not just respiratory diseases. We need to invest in a population health strategy that endeavours to understand what is circulating in our particular part of the world and that will help us identify the next outbreak of a virus or bacteria that's going to cause global problems.
“This type of research needs to become a bigger part of our public health approach to reduce the burden of infectious diseases and the technology is such that the cost of doing it has come down rapidly.”
Professor Richmond said there were several other key healthcare principles that the team drew from the study, based on the discovery that RSV was spread primarily through droplets rather than pure airborne transmission – making it somewhat less likely to spread throughout a plane.
“You need to have closer contact and, as such, it appears that preschool and primary schoolaged children are probably the population most responsible for dissemination of new strains in the community,” he said.

“If your child is unwell with a new cold, particularly if you've just returned from overseas, dropping them off at daycare or at primary school to share it with their classmates is probably not the best thing to do.
“And that's an important message for the parents of small children who can't wear masks – if your child is sick and you've just come back from overseas or had contact with other children who have been unwell, don't send them to school to spread the new strain of the virus.
“And, somewhat controversially, wearing a mask while traveling on airplanes may be a much more frequent event. And it's not pleasant. I'm not one who loves putting on a mask and wearing it for a 20-hour flight to the Northern Hemisphere.
“But I do know that it is the time you are most likely to be exposed and contract one of these viruses. When putting yourself at risk by traveling overseas, you need to think about masking up.”
Professor Richmond said that while the original study used the defined context of children hospitalised with RSV, his team was already looking at conducting broader studies on transmission in daycare centres and the community.
“We need more understanding to identify the most important groups
to vaccinate to try and stop the spread of RSV because the mAb monoclonal antibody that we're currently using won't necessarily stop transmission of the virus,” he said.
“Other vaccines, like pneumococcal for infants, actually stop babies and toddlers from spreading them to the rest of the community. That's perfect, and we think that with newer RSV vaccines coming down the line, that might be possible.
“But, for now, it's vital to understand how RSV spreads. It can be difficult to tell the difference between RSV, influenza and COVID, but the good news for GPs is that we now have a range of tests that can target multiple viruses with a single swab. We're very lucky in WA that we have the capacity for these viruses to be sequenced.
“The most important thing to remember is that we have a very effective RSV prevention strategy for young children that's currently provided free by the WA government. We need to use this to its fullest extent to make sure as many children as possible can be protected against RSV in early childhood.”
There are some promising results from a Perth study into the treatment of bladder cancer by delivering drugs in a new way.
By Eric MartinA world-first research trial led by Perth urologist Professor Dickon Hayne has shown that a new potential treatment for bladder cancer is feasible and safe.
The SUBDUE-1 trial was run at Fiona Stanley Hospital to investigate administering immunotherapy drug durvalumab via sub-urothelial injection or directly into the bladder wall.

the surface lining of the bladder, so that we know the drug has been administered to the area where the action is occurring.
“We also know that bladders are a very immune competent environments, and because of the changes that we saw in populations of immune cells, we knew that it had an effect that could potentially be addressed by incrementally increasing the dose as well.”
In fact, management of NMIBC has hardly changed in three decades and radical cystectomy is still the preferred treatment for patients with BCG-unresponsive tumours –even though it has a high morbidity rate and may be overtreating many patients.
Durvalumab is commonly used to treat several cancers including bladder cancer by injection into a vein.
Results from the Australian and New Zealand Urogenital and Prostate Cancer Trials Group SUBDUE-1 trial on the safety and immunological implications of the treatment in patients suffering from muscle-invasive bladder cancer were recently published in BJU International
Professor Hayne said the study concluded that the sub-urothelial injection of durvalumab was both feasible and safe, without immune related adverse events, and provided evidence for the establishment of a localised immunological response.
“Durvalumab, a human monoclonal anti-PD-L1 antibody, blocks the PD1/PD-L1 interaction, with systemic administration showing benefit in various cancer types. Systemic durvalumab for nonmuscle invasive bladder cancer (NMIBC) has been delivered in a multi-arm trial, although few patients received durvalumab alone making efficacy assessment difficult,” he explained.
“The problem is that these immune checkpoint inhibitors (ICIs) are big antibodies and the urothelium is a watertight layer designed to keep toxins and fluid from being reabsorbed through its surface.
“Given what we know about chemotherapy drugs that are administered intravesically, we hypothesised that the durvalumab is probably just going to wash around for a bit, before ending up as a very expensive way of pouring it down the toilet.
“What we have done is cystoscopic – we injected the drug around the bladder, just like you would under the skin, but into and under
Bladder cancer features among the 10 most prevalent cancers worldwide. At diagnosis, 75% of patients have NMIBC, but these patients experience high rates of disease recurrence and progression to muscle-invasive bladder cancer. According to the Cancer Council:
• In NMIBC, cancer cells are found only in the inner lining of the bladder (urothelium) or the next layer of tissue (lamina propria) and have not grown into the deeper layers of the bladder wall.
• In muscle-invasive bladder cancer (MIBC), the cancer has spread beyond the urothelium and lamina propria into the layer of muscle (muscularis propria), or sometimes through the bladder wall into the surrounding fatty tissue. These cancers can also sometimes spread to lymph nodes close to the bladder.
• Advanced bladder cancer has metastasised outside of the bladder into distant lymph nodes or other organs of the body.
• Bladder cancer sub-typing is well established with core luminal, basal, and mixed sub-types, with basal sub-types often associated with lower overall and diseasespecific survival.
“I think there have been big advantages for patients realised from the developments in the metastatic and advanced bladder cancer settings,” Professor Hayne said. “Drugs like enfortumab vedotin and other advances in immunotherapy in general have had a big impact systemically.
“But there has been little change until recently in the NMIBC space and that is why it's such an obvious and interesting concept to try and introduce these effective agents in the advanced metastatic setting earlier on in the treatment paradigm.”
According to the Cancer Council, the Bacillus Calmette-Guérin (BCG) vaccine was originally used to prevent tuberculosis but can also be used to stimulate a person’s immune system for low- to medium-risk non-muscleinvasive bladder cancer to prevent recurrence.
The combination of BCG and TURBT (a transurethral resection of bladder tumour, done under general anaesthetic using a rigid cystoscope) is clinically considered the most effective treatment for high-risk NMIBC.
For most people with high-risk NMIBC, the initial course of six BCG treatments is followed by ‘maintenance’ BCG to reduce the risk of metastasis. Maintenance treatment can last for one to three years, but according to the American Cancer Society, BCG can cause a wide range of side effects such as fever, aches, chills, and fatigue. It also commonly results in a burning feeling in the bladder, the need to urinate often, and even blood in the urine.
As this method of treatment cannot reach cancer cells outside the bladder lining, or in other parts of the body, SUBDUE-1 wanted to explore whether there were benefits (and minimal side effects) to sub-urothelial durvalumab injection for NMIBC patients, and investigate its impact on tissue and circulating immune cell populations.
“Sub-urothelial injection of ICIs is untested but could prove beneficial for several reasons: a sub-urothelial administration route would facilitate maximal urothelial penetrance; the procedure does not require surgical upskilling; local ICI administration may be safer than systemic delivery with less immune-related AEs (IRAEs); and it may be effective in BCG-unresponsive bladder cancer,” Professor Hayne said.
The study wanted to determine what was a reasonable dose of this drug – in terms of body mass, when you are just trying to treat the
continued on Page 33
35 years!

Opened first BreastScreen WA clinic in Cannington.

BreastScreen WA is mobile! By 1995 there are 4 mobile units travelling around WA.
BreastScreen WA extends North by welcoming a Mirrabooka clinic.
Service continues to expand with a Midland clinic.
Perth City clinic opens and BreastScreen WA becomes first state service to go statewide.
BreastScreen WA achieves full accreditation with BreastScreen Australia.

Launch of website.
BreastScreen WA
Consumer Reference Group is formed.
Cannington clinic relocates.
One million screens!
Online bookings, new website and social media is launched. Cockburn clinic opens. 2015
Wanneroo clinic opens. New breast assessment centre at Fiona Stanley Hospital.
2016

Mandurah clinic opens. Introduction of electronic GP notifications.
2017

performs its 2 millionth screen!
Assessment comes under the BreastScreen WA umbrella - Sir Charles Gairdner and Royal Perth Hospitals. GP Advisory committee is convened.
“Screening Saves Lives” partnership with National Cervical and Bowel Screening Programs to promote screening in the LGBTQIA+ community. 1990
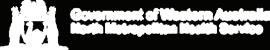
Padbury clinic opens.

The digital revolution begins. 2012
New mobile screening units are launched. David Jones Rose Clinic opens in Perth City store. Health Promotion team can make opportunistic bookings at events.
A secure client result portal is launched.
2020
COVID-19 Pandemic causes 2 month suspension of services. Clients can now receive

East Perth- Mardalup Clinic opens, first to be Aboriginal co-named.

screening units are launched.

New screening and assessment centre opened in Joondalup. clinic reopens after a


continued from Page 31
bladder – injecting the drug directly into the bladder wall through the urothelium.
Researchers did not know how much of the injected drug was going to stay localised, and whether it would have an immune impact when administered this way.
“Though you are already giving quite a high dose to the bladder, hopefully, because the overall dose is low and the systemic absorption is relatively less, the patient will not be impacted by those nasty immune-related side effects that we can often see with high doses of these drugs,” Professor Hayne said.
The success of the trial had now opened the way for further studies of treatment options for nonmuscle-invasive bladder cancer, with the potential to change how the disease is managed globally.
“Whether local administration by injection is the preferable approach
remains unknown but the potential advantages of less toxicity, greater efficacy and lower cost are selfevident. Further trials are now necessary to further explore this exciting development.
“For someone who's facing losing their bladder, it can be very motivating for them to realise that they might help other people to have their bladder cancer managed without cystectomy, which is such an impactful and unpleasant procedure. It is an operation no one would choose to have quite frankly, but obviously, if there's not a better option to treat a more aggressive and muscle invasive disease, then that's all you are left with.
“Our application is still more invasive than having a needle in a vein, but the needle in the vein is delivering high doses of the drug all around your body with the risk of hepatitis, myositis, dermatitis, colitis, encephalitis, etc. We saw none of these really concerning immune-related side effects.
“We can’t forget that this is a small study, and it may be that we just got lucky, and no one had any systemic immune-related side effects, but nonetheless out of 11 patients, there were none.”
Professor Hayne said that potentially, the new approach could become a standard therapy for difficult to treat NMIBC and as clinicians increased their aptitude with the procedure, patients could progress to having it performed while awake, using a flexible cystoscope.
“It's not a new thing injecting drugs into the bladder, but now physicians can do so using a flexible cystoscope under local anaesthetic. By placing a telescope into the bladder while the patient is awake, you can put what are essentially little bee stings of durvalumab around the bladder. They are aware of a little bit of discomfort when it is going on, but it is very well tolerated by most people,” he said.
Living Diabetes & Endocrinology is WA’s first integrated, comprehensive care centre for people living with diabetes and other endocrine and metabolic conditions delivered by a team of experienced endocrinologists and skilled allied health professionals including:
Endocrinologists
Diabetes educators
Dieticians
Exercise physiologists
Podiatrists
Psychologists and other allied health professionals
Centrally located in Osborne Park with free parking, Living Diabetes is the vision of one of Perth’s most experienced diabetes specialists, Dr Joey Kaye, providing care for adult patients with all forms of diabetes including GDM, pre-diabetes and cardiometabolic dysfunction.
We are also accepting referrals for all forms of general endocrine conditions.

Conversational
It is no secret that Australia's mental health system is under immense strain.
According to recent statistics from 2022, two-thirds of Australian patients had waiting times of more than 12 weeks before receiving their initial consultations, with nearly half failing to receive any psychiatric evaluation during the 2022-23.
Additionally, a report by the Australian Institute of Health and Welfare revealed that 58% of students under the age of 65 faced challenges in their educational pursuits due to long-standing mental health conditions.
This vicious cycle has a ripple effect on the Australian economy, with
estimates suggesting that up to $39 billion is lost annually due to reduced productivity and lower workforce participation rates, as of 2021.
Health Minister Mark Butler has admitted the sector is in the worst shape it has been in its 40-year history, and the Federal Government has set up a $750 million task force to improve Medicare.
Enhancing accessibility to mental health professionals could be a viable strategy to streamline patient evaluations during the initial diagnostic phases and provide continuous support throughout their treatment process.
Since the COVID-19 pandemic,

there has been a marked increase in telehealth usage, with 69% of Australians using such services in 2022, and 70% indicating their openness to continuing with virtual healthcare systems in the future.
The growing prominence of artificial intelligence is propelling virtual healthcare through the implementation of conversational digital human AI. These 'digital humans' go beyond conventional chatbots by leveraging sophisticated AI algorithms that can be feed data to each patient's unique treatment needs.
Compared to conventional technologies, the use of conversational digital human AI in mental health services
Develop



offers several benefits for both professionals and patients:
• Providing 24/7 support: Unlike medical personnel who can assist one patient at a time, digital humans can support an unlimited number of patients simultaneously and are available at any time and from any device.
• Saving costs and healthcare professional time: Patients don't incur travel costs to and from clinics by using digital humans from home. Healthcare professionals save time and better streamline patients by using digital humans to answer a set series of initial screening
questions, therefore introducing cost savings throughout the system.
• Providing reminders for medication and prevention: Digital humans can utilise patient data to provide reminders about medications to take by collecting data that helps professionals make more informed and effective decisions, identifying risks, behaviour patterns, and recommending healthy habits for good mental health.
• Non-judgmental support: Digital humans offer a non-judgmental space for individuals to express themselves without fear of
stigma or criticism. This can be particularly beneficial for those who may feel uncomfortable sharing their thoughts and feelings with another human.
• Skills development: Digital humans can provide guidance and support for developing coping skills, managing stress, practising mindfulness, and improving emotional regulation. These tools can empower individuals to take an active role in managing their mental health and well-being.
By providing people with the necessary tools and resources to support their mental health, digital humans can help decrease the prevalence of mental illnesses and enhance overall well-being.
While conversational digital human AI cannot replace the invaluable work of on-the-ground mental health professionals, they are designed to complement their efforts by assuming a supportive role that provides improved initial comfort and assistance to patients.
ED: Idan Schmorak is chief executive of Ai technology company UNITH


Paul is a locally trained surgeon who brings with him experience gained from several years of interstate and overseas fellowships, and specialises in:
Hip & Knee replacement Sports knee Upper & Lower limb trauma
Robotic-assisted joint replacement Foot & Ankle
Perth Hip and Knee are a specialist practice focused on the treatment of all aspects of hip and knee pathology. From arthroscopy to complex joint replacement and revision surgery, we deliver excellence in care utilising state-of-art surgical techniques and cutting-edge technologies to achieve optimal outcomes for our patients. We are delighted to have Paul join Perth Hip & Knee and he is a valued addition to our group of experienced hip & knee surgeons. You can contact his rooms direct at rebgetz@hipnknee.com.au or on 08 6489 1766
Perth Hip & Knee
Suite 1/1 Wexford Street
Subiaco WA 6008
PHONE: 6489 1700
EMAL: admin@hipnknee.com.au www.hipnknee.com.au

Dermatologist supervised total body photography and sequential digital dermoscopic imaging for high risk patients with multiple naevi and melanoma.
Urgent Lesion Clinic for suspected melanoma diagnoses or any urgent lesion (private health insurance rebates apply in our day procedure centre).
Personalised melanoma risk assessment to determine surveillance intervals and educate patients on risk factors.
Confocal microscopy for diagnosis and pre-surgical mapping of lentigo maligna (in situ melanoma) at complex and cosmetically sensitive sites (Dr Collgros).
Management of cutaneous toxicities related to medical oncology treatments.


Grief in young people is more common than you might think, according to Perth clinical psychologist
When we think about grief, it is usually around older adults. But by the time they turn 10, 60% of children have lost a loved one.
Grief is a normal and universal experience. Not everyone who experiences grief has significant issues because of grief. However, for up to a quarter of young people, grief can be linked to mental health problems.
Grief refers to our thoughts, feelings, and behaviours in response to loss. Usually, people think of grief as relating to bereavement through the death of a close person.
But young people have told us in our research that they think grief should be considered broader than bereavement of a person, to also include the death of a pet, parental separation and relationship breakup.
Young people have also talked about how information on the ‘stages of grief’ or advice to ‘move on’ is unhelpful during grief. We know the stages of grief model is outdated and does not have evidence to support it. People do not move through ‘stages’ of grief. Young people who experience bereavement are at an increased risk of mental health problems, including anxiety, depression, and poorer physical health. Losing a parent in childhood through death


or parental separation, is also a known risk factor for depression in adulthood.
In a meta-analysis we conducted in 2023, that included 28 psychological intervention studies in 14 to 24-year-olds, cognitive behaviour therapy (CBT) for grief was found to be the most effective treatment for grief, anxiety and depression.
We have recently developed an online CBT program to improve access to treatment, given most young people will never have access to see a psychologist for CBT, or one who is trained specifically in grief. CBT for grief includes addressing the cognitive and behavioural processes that maintain anxiety and depression related to grief.
Key aspects of CBT for grief involve education about normalising grief, decreasing avoidance, e.g., visiting a grave, looking at photos of the person who died that have been avoided, challenging negative thinking, and increasing enjoyable activities.
It is important that young people understand that grief is a normal experience.
The CBT program we have developed, together with a group of 15 young people with lived experience of grief, is a brief, fourweek online self-help program comprised of two short modules each week. The modules include videos of young people talking about ways to improve their mental health and wellbeing during grief, exercises, worksheets, and text.
We are recruiting for adolescents aged 13-17 who live in Australia. To participate, young people can enrol in the self-help online program Project Sail at www.sailgrief.org. There are also resources at Grief Australia at www.grief.org.au.
ED: Professor Sarah Egan is from Curtin University’s School of Population Health and enAble Institute. The project is supported by Telethon 7.

Although we sometimes pretend that money doesn’t matter –it does! Doctors are not immune to inflationary pressures.
Australia is again facing a shortage of doctors. This happened in the mid-1980s and in early 2000s. This time it is more severe. The solution being proposed is a throwback to the ’80s – bring in more doctors from overseas.
On April 30 the Medical Board announced that “A new process to safely fast track internationally trained medical specialists into the Australian health system is coming. GPs, anaesthetists, obstetricians and gynaecologists, and psychiatrists are the priority specialties identified by jurisdictions.”
Funny how in the real world we still reap what we sow. This shortage was predictable.
We are not alone. Projections are that the US will have a shortage of 124,000 doctors (almost the entire Australian medical workforce) by 2034 with 48,000 of this being in primary care. Closer to home, New Zealand is grappling with the same problem as we are. The UK is losing doctors fast!
Although we sometimes pretend that money doesn’t matter – it does! Doctors are not immune to inflationary pressures. This is where economics shows us that human beings will behave in ways that are in their best interests. At a deep level, it is about survival.
So people will look to ways to get best reward for time and effort. The increase in sub-specialised clinics and treatment specific (e.g. semaglutide) telehealth clinics reflects doctors seeing better reward for effort. Please note I am not opining on the morals but the actions.
The Federal Government plans to open 29 more urgent care clinics. Politicians love opening buildings, but when I last checked, no building ever provided medical care. This is essentially the plot of the hospital episode in Yes Minister. The existing ones already struggle to comply with the onerous opening requirements due to, you guessed it, lack of doctors. But don’t expect any action to be taken for breach of contract. Another 29 buildings won’t magically create more doctors.
With state and federal elections due within 12 months, the words of Ronald Regan are truer than ever. The nine most dangerous words in the English language are “I’m from the government and I’m here to help.”



Psychiatric medication deprescribing has gained significant attention in recent years as healthcare professionals recognise the importance of optimising medication use and minimising potential harms associated with long-term use. Historically, there has been little attention paid to deprescribing in psychiatry, and the focus of research had been on prescribing.
Psychotropic medications play a crucial role in managing mental health conditions. While these medications can be effective in alleviating symptoms and improving quality of life, they also come with potential side effects, especially with long-term use.
Deprescribing psychiatric medications involves a careful and gradual reduction in dosage or discontinuation of medications with the goal of minimising adverse effects, optimising therapeutic outcomes, and promoting overall well-being. This process requires a collaborative approach between doctors and patients to ensure safe and effective deprescribing.
A variety of clinical scenarios warrant deprescribing. For example, a patient’s medication regimen comprising high doses of medication and polypharmacy with associated drug interactions leading to medical risk, patient preference, risk of continuing medications outweighing benefits (although this may not have been the case when the medication was initially instituted), or the condition has remitted.
Some adverse effects of psychotropic medications that lead to considerations of deprescribing include weight gain and other metabolic consequences, impaired capacity for feeling (emotional flattening), sexual side effects (anorgasmia and delayed arousal), effects on memory and concentration (cognitive fogginess), and extrapyramidal side effects, particularly from first-generation antipsychotics, and tremor from lithium.

Deprescribing involves an individualised approach based on factors such as patient diagnosis, treatment history, current symptoms and shared decisionmaking
Risk-benefit evaluation is essential in deprescribing with a focus on the patient quality of life
A gradual reduction rather than an abrupt discontinuation is preferred to minimise risk of withdrawal symptoms and to monitor any risk of relapse of symptoms.
Furthermore, as the patient’s age increases, the psychotropic medication side effect profile may increase due to impacts on drug metabolism, leading to reduced tolerance.
The Maudsley Deprescribing Guidelines 2024 provides evidencebased recommendations and practical guidance for deprescribing psychiatric medications. These guidelines are designed to assist healthcare providers in making informed decisions about when and how to deprescribe medications based on individual patient factors, medication characteristics, and treatment goals.
Key Principles of Deprescribing include:
• Patient-centred care - where patients are actively involved in shared decision-making regarding their medications to ensure that patient preferences, values, and

goals are considered, coupled with detailed psychoeducation regarding the deprescribing process and potential risks.
• Risk-benefit assessment of each medication considering efficacy, side effects, potential drug interactions, and the patient's psychological status.
• Gradual reduction in dosage over time to minimise withdrawal symptoms and monitor for any recurrence of symptoms.
• Monitoring and support for patients during the deprescribing process.
While psychiatric medication deprescribing offers significant benefits, it also presents challenges and considerations that must be addressed such as:
• Withdrawal symptoms during the deprescribing process, including rebound anxiety, insomnia, mood fluctuations, and physical discomfort.
• Relapse risk of illness recurrence when reducing psychiatric medications.
It is also important to distinguish deprescribing-related withdrawal symptoms from a relapse of a psychiatric condition. Withdrawal symptoms (including poor mood, anxiety and insomnia) can sometimes be mistaken as a relapse of the underlying disorder. A careful history can help distinguish withdrawal from a relapse of illness.
Key points of the history include the re-onset of symptoms, the presence of distinctive (physical and psychological) symptoms of discontinuation, and a response of those symptoms after a reinstatement of the previous dose for a short period of time.
Therefore, medication deprescribing is an important part of psychiatric pharmacology, and the approach of listening to the patient’s concerns and proceeding cautiously with appropriate rationale in deprescribing is in keeping with good clinical practice.
Author competing interests – nil

Dr Gayatri Borude
Clinical Director (WA), Fertility Specialist, Obstetrician & Gynaecologist
MBBS, MD, DNB, FRANZCOG, FACOG, M Rep Med


Dr Mahalakshmi Ragunath
Fertility Specialist, Obstetrician & Gynaecologist
MBBS, DGO, MRCOG, MSc, FRCOG, FRANZCOG

Dr Shanthi Srinivasan
Fertility Specialist, Obstetrician & Gynaecologist
MBBS, MD, DNB, FNB (Rep Medicine), FRANZCOG
Adora Fertility has helped create over 11,000 babies through IVF since 2014. We provide affordable IVF without compromising on quality. By referring your patient to one of our highly qualified specialists, they will receive a tailored approach to their fertility treatment plans with medications sensitive to their needs. We bulk-bill the majority of Medicare eligible expenses resulting in out-of-pocket costs which are typically around $2,000 for a fully stimulated IVF cycle. We now offer IVF with a known donor allowing us to help more people grow their families in more ways. Give your patients the best chance of conception without the financial sacrifice.
Pain is the most common presentation in the shoulder. After 15 years of consultant practice, I would like to share some tips and pearls learnt, sometimes through bitter experience. As the saying goes, ‘Good judgment comes from experience, experience comes from bad judgment.’
To begin, use the anatomic paradigm. We are all taught and use the tried-and-tested approach of history, examination, investigation then coming up with a differential diagnosis. I have found it useful to run an anatomic approach parallel to this – running through the different anatomic structures which may be the pain generator(s) for the patient and think whether the pain relates to:
• the glenohumeral joint (e.g. capsulitis, arthritis)
• the subacromial region (e.g. cuff tear, calcific tendinitis, bursitis)
• the biceps tendon (tears, tendinopathy)
• the acromioclavicular (AC) joint (e.g. arthritis, bone oedema)
• teferred pain from the cervical spine or brachial neuritis
From the opening questions in the history taking, we can ask to follow up focused questions related to the different structures, such as the exact location of the pain (e.g. superior over the AC joint), provoking factors, responses to injections, acuity versus chronicity of the pain, and the presence or not of stiffness.
Instead of performing a generic examination, we then do a focused examination to help confirm or refute our working diagnosis. We can do a slightly different examination for glenohumeral pathology versus the AC joint, versus one for instability etc., considering the nuances of the patient’s presentation.
Many patients are referred with an ultrasound of the shoulder and perhaps a subacromial injection. Radiographs are a safe, efficient and useful tool for aiding in the

Pain, the most common presentation in the shoulder, can come from multiple structures
A systematic, comprehensive and nuanced approach is key Investigations, whilst very useful have pitfalls.
diagnosis. Stiff and painful shoulder with a normal X-ray? Think frozen shoulder. But one must rule out osteoarthritis. Look out for sclerosis of the greater tuberosity and enthesopathic changes which suggest cuff tears or AC joint arthritis. Calcifications may be present. There may be a high riding humeral head consistent with chronic and extensive cuff tears.
Injecting a shoulder with arthritis or cuff deficiency where a joint replacement might be the end game, could complicate matters with an infection compromising the patient’s treatment. Or worse, one may miss a metastasis or malign problem. It is critical to treat the patient and not the investigation.
Investigations are a useful tool to aid the diagnosis, however, there

are some pitfalls to look out for. For example, it is very common in the middle-aged patient and older, that AC joint arthritis is present on the X-ray. This should be confirmed on the history and examination as to whether it is likely to be the patient’s pain generator or not.
One thing I have found useful is to use local anaesthetic injections, only to aid diagnosis. This is a good way of confirming if an anatomic area is the pain generator without the ‘feel good’ effects of the steroid with a diagnostic injection into the structure of interest.
An MRI is a highly sensitive test and will often show multiple pathologies. Our job is to marry these up with the patient’s presentation and separate out agerelated changes versus pathology. There may be multiple pain generators as the shoulder is a complex of joints and soft tissue structures - the biceps, cuff and AC joints can all contribute. This is where a nuanced and careful history, examination and diagnostic injections can help in identifying the precise pain generators.
Watch for frozen shoulder, which is the great mimicker in the shoulder. I’m sure I am not alone in having misdiagnosed a patient’s source of pain as being cuff tears or other pathologies when the underlying cause was an evolving frozen shoulder. Loss of motion can be subtle and only be present a few months after the onset of pain. Always be on the lookout for this condition. Sometimes, observation after ruling out malign causes is the best way to arrive at this diagnosis, where the condition will declare itself.
Author competing interests – nil
Illicit drug use in young females has increased from 27% in 2019 to over 35% in 2023. Risky alcohol consumption has increased in young females from 28% (2019) to 35% (2023). Females are still seeking AOD treatment at lower rates than males despite these changes in behaviour.
Women often face greater discrimination and stigma for their AOD use than men, particularly in relation to pregnancy and parenting. This is often influenced by traditional gender-based roles and values placed on women.
Risk factors for Substance use Disorders:
Recurrent and easy access to substances
Stress and financial difficulties
Any mental illness or impairment
PTSD and trauma.
Signs & symptoms of a substance use disorder:
Frequent requests for early prescription refills
Social withdrawal or neglecting responsibilities
Physical changes; weight, poor hygiene or skin problems
Taking higher doses or more frequently than prescribed
Patient requesting prescriptions on first visit, “doctor shopping”
Changes in mood or behaviour; agitation, irritability and mood swings
Defensive or evasive when questioned about medications or drug use.
We can help...
If you think that a patient may have a substance use disorder, please refer them to Fresh Start, or a suitable specialist.
Referral forms can be found on our website www.freshstart.org.au or call our clinic on 08 9381 1333
Incidence of posttraumatic stress disorder (PTSD) varies across population, countries and trauma types, with rough estimates suggesting about 3.5% of the population experience PTSD at some point in their lifetime.
PTSD involves four clusters of symptoms being 1) re-experiencing symptoms (intrusive thoughts); 2) hyperarousal (irritable/ startled response); 3) avoidance of reminders of the event; and 4) numbing/negative moods cognition.
The most common events leading to PTSD are sexual violence, childhood abuse, military combat and deployment, motor vehicle accidents, exposure to violence, mass shooting/knifing and natural disaster. I have seen PTSD in teachers, aged care and DCP workers, prison and police officers, lifesavers, park rangers and defense personnel.
Group-based intervention can offer effective ways to reduce PTSD symptoms. It can be more cost and time effective than individual treatment as multiple people can be treated at once by one or more facilitators who lead the sessions.
Group-based psychological treatment for PTSD can offer benefit for wellbeing through sense of belonging and social support. The provision of social support is particularly important for people who have experienced trauma as often the experience of trauma leads to social withdrawal and identity loss.
Social isolation in turn can affect severity of PTSD symptoms as a lack of social support can impair a person’s ability to regulate distress leading to poor clinical outcome.
Group-based treatment can put people in contact with others “like them”. Identification with others can help mitigate the effects of trauma and reduce PTSD symptoms. It is preferable to begin treatment for PTSD as soon as possible after the
Key messages
PTSD can affect a wide variety of people
Group therapy can produce positive outcomes
Local research is ongoing.
diagnosis is made by a psychiatrist.
The goals of treatment include maintaining safety of the patient and others, reduce distressing symptoms, reduce avoidant behaviours, diminish anxiety, improve adaptive and psychosocial functioning, and lessen the risk of relapse. SSRIs are an appropriate alternative to psychotherapy and are preferred in patients with comorbid depression or other anxiety disorder, particularly if their symptoms interfere with psychotherapy.
Specific populations which require careful consideration of treatment include substance use disorders, personality disorders and moderate-to-severe traumatic brain injury.
For individuals with PTSD who experience significant sleep disturbance, typically nightmares, an option will be Prazosin. This can be used as an augmenting agent with serotonin reuptake inhibitors or in some cases as monotherapy or combined with trauma-focused therapy.
For individuals with PTSD who have

prominent psychotic symptoms, treatment with a combination SSRI and second-generation antipsychotic (SGA) medication.
Medications that are effective for PTSD are continued for at least six months to one year in order prevent relapse or recurrence.
<subhead>Group therapy in Perth
In 2021, the community-based WA Centre for Trauma Treatment and Research was established launching a series of programs.
An intensive four-week Trauma Recovery and Growth Program tailored for first responders and uniformed personnel showed significant improvements across all measures compared to existing programs. This was extended to WA Police (WAPOL), Department of Fire and Emergency Services (DFES), DVA Veterans, and Insurance Commission of WA Approved Claims (ICWA).
Building on this, gaps were identified in treatment options for workers' compensation, third-party insurance, the mining industry, and government workers. These individuals often found conventional treatments ineffective and sought alternative solutions.
The four-week group therapy course offered 100 hours of therapy, focusing not only on trauma recovery but also on personal growth. Participants gained insights into the psychological and physiological effects of trauma, often overlooked or misunderstood.
A holistic approach was adopted, encompassing psychiatric and psychological assessments, as well as advice from an exercise physiologist and a nutritionist. Participants were prescribed appropriate medications before beginning therapy to optimise their outcomes.
All doctors will eventually experience a medical emergency. Complex, important decisions are required urgently, often with inadequate information. To manage an emergency well, a clinician needs both technical competence (medical knowledge, procedural skill), and the socalled ‘soft’ skills (communication, leadership and decision-making).
These skills are teachable. Doctors in acute-care specialties have focused training on management of medical emergencies and have more frequent exposure, resulting in greater confidence and competence in those situations. Doctors in other specialties may receive minimal or no such training.
Current training is often hospitalfocused and can be rigid in structure and content. However, a spectrum of needs should be recognised. A general practitioner in the Kimberley has very different needs to a Perth teaching hospital registrar. Furthermore, maintenance of professional standards is now under detailed scrutiny, recognising the need for lifelong learning. Evidence-based medicine is required to ensure patient safety, so appropriate training in emergency management is a pressing need.


Adult learners have specific needs in acquiring new knowledge and skills. Existing knowledge must be recognised to get the best out of the learner. Content must align with adult learning goals and be presented in a manner relevant to the learner, fostering autonomy in developing durable knowledge and skills. The focus for adult learning should be practical and problemcentred and should relate to the learners’ professional lives.
As with other professions, doctors benefit from multidisciplinary and multimodal teaching environments, providing perspectives from all members of the healthcare team. Diversity enhances problem solving
continued from Page 45
The program structure included:
• 20 days of group work from 9am to 3pm, Monday to Friday, supervised by a consulting psychiatrist, along with four individual trauma-focused therapy sessions
• A five-hour relapse prevention session held four weeks after program completion
• Follow-up assessments at one month and three months postcompletion, along with two
three-hour support sessions for partners and significant others
• Comprehensive intake assessments and discharge reports by clinical lead
• All necessary materials, including catering, stationary, workbooks and manuals.
Since inception, 25 program cycles, each with four or five participants have been concluded with positive feedback from both participants and referring organisations. The camaraderie developed during sessions and the trust in therapists
and improves decision making. It helps develop communication skills, with a positive impact on adaptability, teamworking and patient safety.
Given this background, we must examine whether the educational opportunities available meet doctors needs and societal expectations. Medical schools have advocated for inclusion of the Australian Resuscitation Council (ARC) accredited Advanced Life Support 1 (ALS1) course into their curricula. ALS1 provides expertise beyond Basic Life Support, including the skills to recognise and intervene in clinical deterioration, and inhospital cardiac arrest management.
have led to sustained benefits for participants.
The centre also emphasises its research component, focusing on report writing and statistical analysis. Positive effects were observed three months postprogram, and participants often maintained connections due to the shared journey they experienced.
– References available on request
Author competing interests – the author is clinical lead and company director for WA Centre for Trauma Treatment and Research
Emergency skills are necessary and teachable
Current courses while very useful can be rigid
Bespoke offerings focusing on the needs of target audience are needed.
The ARC also provides the more advanced ALS2 course. ALS2 providers can lead a cardiac arrest team, can deal with special circumstances (e.g. pregnancy), and consider post-resuscitation care and end-of-life decisionmaking. Standardised ALS1 and ALS2 training is available in WA from various providers listed on the ARC website.
The ALS courses focus on inhospital deterioration and provide an excellent, standardised and evidence-based approach. Among doctors, ALS1 and ALS2 are the most popular training choice. Many other standardised courses (e.g. Advanced Paediatric Life Support and Emergency Management of Severe Trauma) all have an
important role in training. Some colleges require these qualifications for specialist training.
For non-specialist healthcare providers and others in firstresponder settings, there are a variety of ‘off the shelf’ courses in first aid and basic life support, generally delivered by TAFE and RTO providers.
Despite the assortment of courses on offer, some difficulties are apparent. Most courses are structured without the ability to modify the teaching to suit the audience. However, doctors work in a variety of nuanced settings, with major differences in location, populations, resources and backup.
In order to meet proscribed training standards, a medical practitioner may not receive training that is actually relevant or tailored to their needs. As previously discussed, adult learning is predicated on the relevance and applicability of content to the learners’ actual role.
Regional health services deserve special consideration. Limited access to training presents a particular challenge, with
Heel pain is a frequent problem that presents to the general practitioner. Plantar fasciitis is the most common cause of under the heel pain. Most patients will improve with non-operative treatment but not all.
Surgery is a very effective form of treatment for this condition in patients with long standing refractory symptoms.
Before being considered for surgery patients should undergo at least six months of non-operative treatment that includes the following (in the appropriate order):
• Rest, avoidance of activity
• NSAIDs, stretching exercise program
• Orthotics: off the shelf or custom
• Cortisone injection (one only)
• Shockwave therapy

Surgery can be open or endoscopic. The principle part of the procedure is release of the plantar fascia near its origin on the heel. Historically only the medial half was released but recent literature supports more complete release.
demand currently outstripping supply. Most courses provide certification for a limited time only, so clinicians subject to mandatory recertification must often travel to metropolitan centres, which is costly and places demand upon stretched regional services. The delivery of regional courses should be considered by existing public and commercial providers, tailored to local circumstance.
Although multiple providers are delivering high-quality training in WA, the environment could be enhanced by introducing modifiable content into existing courses.
The delivery of a bespoke educational offering, co-designed for the target audience, is a necessity moving forward. This will align education with adult learning requirements, improving learning outcomes. Tailored education caters for diverse learning styles, provides relevant content, and allows the flexibility, inclusivity and scalable education that medical practitioners need. This can be achieved with existing expertise but requires a change in education mindset.
Author competing interests – nil

Open surgery is performed through a 3cm incision in the proximal arch and allows not just plantar fascia release but also decompression of the tarsal tunnel and Baxters nerve which is often implicated in heel pain.
Endoscopic plantar fascia release is indicated for those without nerve compression symptoms and is done through a much smaller incision using a camera assisted cutting device much like a carpal tunnel release.
Both open and endoscopic releases are performed as day cases and require approximately two weeks on crutches. Recovery is slightly quicker for endoscopic patients as you would expect. Patients can expect an 8090% chance of a good result from surgery. Complications are rare.


St John of God Medical Centre
Suite 10, 100 Murdoch Drive, Murdoch WA 6150
Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301
www.murdochorthopaedic.com.au
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
General practitioners play a crucial role in guiding patients through various stages of medical care, including post-joint replacement recovery.
Joint replacement surgeries offer tremendous relief and mobility improvements for individuals suffering from chronic joint pain and dysfunction. However, optimising the outcomes of these surgeries often requires comprehensive rehabilitation strategies, with physiotherapy standing as a cornerstone in this process.
As advocates for patients' wellbeing, it is imperative to recognise the integral role of physiotherapy in joint replacement recovery. One of the primary objectives of physiotherapy following joint replacement is to facilitate early mobilisation and functional independence. Through targeted exercises, manual therapy techniques and assistive devices, when necessary, physiotherapists empower patients to regain strength and mobility.
In the context of total knee replacement (TKR) recovery, facilitating patients to regain their range of motion is vital to satisfactory, long-term outcome. Rehabilitation of TKR patients is simple but not easy, as the methods for achieving an improved range of motion are established and straight forward, but the process can be physically painful for the patient. Through manual therapy techniques, appropriate load management principles and education, physiotherapists are well placed to optimise what patients can achieve, despite their pain.
Usually, when pain is experienced, it is associated with damage. Thorough education on the difference between hurt and harm in this setting is vital to ensuring patients can optimally approach the challenge of stretching a healing knee incision. Time is a pertinent factor here as if stretching is avoided following

Knee replacement recovery is simple, not easy. The goals of rehabilitation are non-ambiguous but can be painful to achieve Education by physiotherapists on pain during healing (hurt not meaning harm) should be prioritised early in the recovery process. Painful stretching is eased by physiotherapy input Early engagement with physiotherapy is key – input is always easier to dial back when not required. Patients are often reluctant to increase physio input once they start to fall behind.
the TKR procedure, proliferating scar tissue at the incision site can become mature, adhering the quadriceps to the femur reducing potential for later range of motion improvements.
Following this timeframe (8-12 weeks), not only is physiotherapy going to be far less effective, but also the window of opportunity for specialist intervention (via manipulation under anaesthetic) is rapidly closing. Care needs to be taken here to ensure the patient balances their loading of the knee – too much forceful, aggressive rehabilitation (common in younger, more active individuals undergoing TKR surgery) can be counterproductive and put patients at risk of complications like arthrofibrosis.

Timely intervention and continuity of care are essential elements in achieving optimal patient recovery and long-term joint health. Incorporating physiotherapy referrals as standard practice postjoint replacement surgery is always in the patients’ best interest. In the event a patient is progressing at a satisfactory rate, it is far easier to reduce input from physiotherapy than convince a patient to increase their involvement with physiotherapy later in recovery.
If physiotherapy is not encouraged from the outset, later introduction of physiotherapy can be seen by the patient as an indication they are ‘failing’ their rehab. Patients are also more inclined to be returning to normal activities later in the rehab process, meaning they have less time available for physiotherapy input and the attitude that ‘they have gotten themselves through so far’.
By encouraging patients to seek physio from the outset of recovery, its importance in rehabilitation is implied and compliance is much greater among patients.
Collaborative care between GPs and physiotherapists (especially joint replacementspecific physiotherapists) ensures comprehensive management, improving patient outcomes and reducing the risk of complications or setbacks.
Orthopaedic physiotherapy stands as a cornerstone in the rehabilitation journey following joint replacement surgery. By acknowledging its significance and fostering interdisciplinary collaboration, general practitioners can contribute significantly to the holistic care and well-being of their patients undergoing arthroplasty procedures.
Author competing interests – nil.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
Rhinoplasty is one of the most common cosmetic procedures performed globally. The advent of social media and video conferencing platforms such as Zoom have increased the number of people interested in aboveshoulder surgery, with rhinoplasty being the most common.
During the COVID pandemic this trend exploded.
Social media usage is known to contribute to concerns about appearance and consequently leads to cosmetic surgery. The ‘selfie’ social media phenomenon resulted in an increase in patients reviewing their facial features at different angles, highlighting potential imperfections, and has also contributed to an increased awareness of plastic surgery and patients seeking treatment, especially male patients.
According to surveys carried out in the United Kingdom in 2017, approximately 55% of facial plastic surgeons stated that patients in their cosmetic practice were motivated by a desire to appear better in selfies, compared with 13% in 2016.


Increasing use of social media and video conferencing platforms has led to patients being more socially conscious of their appearance
Preservation rhinoplasty is a new technique offering patients a potentially scarless and more natural result
While the techniques continue to improve the philosophy remains the same – to preserve and to reshape existing nasal structures.
In this context, a total of 64% of individuals who had rhinoplasty between 2015 and 2020 were wholly or partially motivated to do so by social media, which accordingly has been shown to have a significant impact on surgical procedure participation. Interestingly, men made up 58% of those influenced by social media sites.
As to whether social media usage by rhinoplasty patients has led to a recourse to rhinoplasty has been questioned, with observers





stating higher rates of social media addiction in patients seeking rhinoplasty. No evidence supports this view. However, a study by Furnham and Levitas found increasing media exposure, poor self-esteem and life satisfaction increased the likelihood of patients undergoing cosmetic surgery.
Since its founding in October 2012, Instagram has grown to over 1.4 billion users. Many surgeons worldwide use social media to raise public awareness, interact with colleagues, attract new patients and establish careers and reputations. Instagram can also function as a patient-centric platform, where prospective patients can review aesthetic surgery results and previous patients can communicate their results, outcomes, and perspectives of the procedure.
Essentially, Instagram can act as a powerful customer-review site, which can affect prospective patients’ desire to undergo aesthetic procedures with specific surgeons. Recently AHPRA has amended the guidelines for Australian practitioners and surgeons using these platforms, clamping down on the rogue use of social media. It has focused on controlling testimonials, reposts and comments, ensuring that standardised medical photos are used and reducing the number of sites which portray unreasonable expectations to the patient.
New AHPRA guidelines state that all patients seeking rhinoplasty surgery must first have a GP referral before seeing a specialist plastic surgeon. All these measures have been implemented to improve patient safety and transparency of care. However, rates of cosmetic tourism to countries such as Turkey, where the most rhinoplasty surgeries in the world are performed and where plastic surgeons do not have to adhere to regulations relating to social media use, have increased exponentially.
Late last year, I was stuck. Lost. Feeling uncertain about my career direction. Isolated. Examining deeper existential questions related to my life purpose and what I was doing here on earth. Being an emotional person, this manifested as heightened emotions – anxiety, tears, feeling restless, with nowhere to go.
One afternoon amid this state it was quiet at work and I was able to finish early. But where to go? I had so much time to myself that it had become a source of anxiety. Many people in this overly busy world perhaps could not fathom such a state of being. Yet on my life path, alone time was a familiar state. I had time for exercise, hobbies, to see family and friends and spend quality time with my husband, a luxury many yearn for and wish to create. Perhaps there are subconscious reasons why they don’t. Maybe the questions that might arise when alone with oneself for too long. The emotions that might surface. The thoughts that may enter.
Our society is based on a model where outrunning oneself is the key to staying afloat, but sometimes the universe calls us to stop and really look within. But that afternoon was not a day for self-reflection. For connection to my deeper truths or


higher self. I was in panic. I needed to connect. To be heard. To be seen by another. To feel understood. And so I did what so many people often do when needing the very same things. I made a last-minute appointment with the GP. Not a GP I had seen before, but another at the practice I attended.
As I entered the consult, I was acutely aware of how it felt to be in her shoes having worked in similar situations before. Often as the doctor, we feel as if we must do something to fix whatever it is that the person in front of us has presented with.
So, I said from the outset, in
continued from Page 51
Australians now spend around $1 billion on cosmetic surgery annually, making it more popular per capita than the United States. Turkey is visited most for cosmetic surgery and rhinoplasty the most common surgical procedure.
Preservation rhinoplasty, a surgical philosophy developed in Turkey, championed by Teoman Dogan and
Baris Cakir (both plastic surgeons), has improved results for rhinoplasty patients.
Preservation rhinoplasty is a scarless endonasal approach to reshape and preserve as much anatomy of the nose as possible. It reduces the number of dissection planes resulting in less post-operative swelling and maintains the natural contours of the dorsum of the nose to give a more natural look.
No splints are used externally or internally, and patients are discharged on the day of surgery. It is the no-scar, minimal postoperative swelling and natural look that is attracting rhinoplasty patients in 2024.
Author competing interests – nil
Key messages
Emotions are human and perhaps we can hold off on our medical model of diagnose, label and treat until it is necessary
Remember patient is person, and doctor is patient too.
Often what someone really needs when going through issues of the heart or mind is someone to see them. To validate their experience. Not to “fix” them, but to connect with another human being in a time of need.
attempt to make her job easier, that I just needed someone to talk to. I became emotional, hurriedly expressing my feelings due to being aware of the time pressure she was under. Delving straight into the deeper emotions and existential questions that had been on my mind. Just wanting someone to tell me that it would all be okay.
But instead she pulled out the K10. Or perhaps it was the DASS21, my memory eludes me, but either
way it had the same effect. It was the point at which I knew the appointment had been a mistake. That I was not going to get what I was looking for. She then proceeded to tell me, albeit the first time she had ever met me, that I was probably depressed. That perhaps medication was required. Straight into diagnose, label, treatment.
Which made me wonder, at what point as doctors did we become so detached? So uncomfortable dealing with very normal human emotions. So quick to label, not for the sake of the person sitting in front of us, but to feel like we have done something. Solved something. Fixed something.
And that sometimes instead of seeing a patient, perhaps we could see a person, realising that emotions are normal. Even big emotions. And really if we were honest with ourselves, have we not felt anxiety, flatness, loneliness, or any other of the myriad emotions that are a normal part of the human experience?
And perhaps, even more so, given the fact that doctors’ mental health is often a lot worse than that of the general population. So surely many of us know how it feels to have these thoughts and feelings running though us, and very much not wanting to rush into a diagnosis. Label. Treatment.
So perhaps it is time to shift the way we view mental health. I am not saying that the diagnosis and treatment of ongoing symptoms can’t be of value. There is a role for this. However, we need to be less hasty in trying to move a person from where they are at in a given moment, to try to fix it. The question we really need to ask ourselves in these situations is, who are we really trying to fix it for?
The patient, who just wants to talk and be heard and feel seen, or ourselves?
Author competing interests – nil



Consulting at:
SJOG Murdoch Medical Centre Suite 27 St John of God Medical Centre Murdoch, 100 Murdoch Drive, Murdoch WA 6150
Garden City Specialist Centre 537 Marmion St, Booragoon WA
Surgeons House 162 Cambridge St, West Leederville WA 6007
St John of God House 117 Anstruther Rd, Mandurah, WA 6210
Office Phone: (08) 9332 0066 | Mobile Phone: 0401809255 | Fax: (08) 9463 6202






We offer a wide range of fertility services including: New referrals welcome
• Fertility Evaluation
• Assisted Reproduction
• Freezing & Storage
• Genetic Testing
• Surrogacy
• Fertility Counselling
• Dedicated Donor program
Concept Fertility Centre 218 Nicholson Road SUBIACO WA 6008
Phone: 08 9382 2388
Fax: 08 9381 3603
Email: referral@conceptfertility.com.au
Find out more at conceptfertility.com.au
Work contributes to a significant component of an individual’s life; hence ongoing efforts are made to ensure safety protocols protect employees from physical and mental harm. Despite these strategies, more than a quarter of a million Australians lodged a workers compensation claim between 2022 and 2023.
Often overlooked in the management of these claims is the complex interplay between mental and physical health.
During a patient’s rehabilitation, accredited exercise physiologists play a significant role in managing these factors to facilitate early work engagement, not only for the injured worker’s benefit, but also for employers and society as a whole.
Key Statistics in Australian Claims 2021/22 show that 127,756 serious claims were lodged with the median time lost being eight weeks. Some 9.2% of claims were directly due to mental health conditions
Work-related injuries can have an impact on employees’ mental health. Workplace injuries can lead to prolonged pain, which can disrupt neurochemical pathways, alter mood regulation, and increase vulnerability to psychiatric conditions such as depression, anxiety and other psychological disorders.
The relationship between pain and mental health is bidirectional, each influencing the other. For instance, mental health conditions can amplify the perception of pain and reduce pain tolerance, while chronic pain can contribute to psychological distress, creating a cycle of mutual reinforcement.
Mental health conditions have also been linked with lower selfefficacy and an external locus of control, which refers to an individual’s lack of confidence in their ability, alongside a belief that they are not in control of their own outcome. This can lead to feelings of helplessness, powerlessness,



Key messages
Poor mental health negatively impacts return to work outcomes
Exercise aids mental health and promotes positive return-to-work outcomes.
and inadequacy, which in turn can further exacerbate symptoms of mental health, which has been supported in occupational settings. Work is often accompanied by a sense of self-worth and can form a substantial part of a person’s identity. Following a workplace injury, the impacts of work-absence may include depression, decreased income and social status, loss of support networks, decreased confidence and self-efficacy
Mental health can also impact return-to-work outcomes. The presence of biopsychosocial factors can prolong recovery times and impact positive returnto-work outcomes. Commonly reported problems such as stress, depression and anxiety lead to delays in an individual’s returnto-work, with a median of 34 weeks off for psychological claims. Research shows that 45 days off work (median time off in Australian models) can lead to a 50% return rate, alongside the worker being less likely to return to the same employer. This rate continues to decrease the longer a person is absent from work.
Exercise is important to reverse the bidirectional relationship between mental health and physical health. Exercise stimulates the release of endorphins, dopamine, serotonin, and other neurotransmitters, which are known as ‘feel-good’ chemicals that help regulate mood, reduce stress and alleviate symptoms of anxiety and depression. By improving mental health through exercise, return-to-work outcomes improve and help transition injured workers back to meaningful employment.
Accredited exercise physiologists can empower individuals to selfmanage their rehabilitation, which can enhance independence and self-efficacy. This can promote participation in community-led exercise, with research showing that these individuals are less likely to experience psychological distress, which can lead to greater return-to-work outcomes.
Setting and achieving exerciserelated goals promotes an internal locus of control while also increasing self-efficacy. When workers experience these improvements, it leads to increased engagement in return-to-work programs, which leads to efficient and effective outcomes.
– References available on request Author competing interests – nil

Known for its art, a building in Margaret River has had a face-lift and boasts an exciting new collection of works.
One of the grand dames of the Margaret River’s main street has been given a new lease on life thanks to a couple who have holidayed in the region for decades.
The recently opened REDSEA Gallery in the historic building of 83 Bussell Highway, has new owners in Chris and Charlie Churcher.
“The response has been amazing, and people have been generally quite wide-eyed to see what changes have been made,” says gallerist Charlie Churcher. “People are talking a lot about the quality of the art and how it is curated.”
Starting in 1974, Margaret River’s first art and craft group, which had 80 members, rented the space for 13 years. The building was then sold to a group of 15 local artists who refurbished the buildings. It has remained an art gallery ever since. The Churchers acquired the
By Ara Jansenbuilding in 2022 – exactly 100 years after it was built.
The original timber and the charm of the heritage building have been retained in an extensive and sympathetic renovation which began in the middle of last year. Clean lines and light-filled spaces ensure the art has been given the reverence and space to breathe.
REDSEA features a diverse range of paintings, sculpture, glass, ceramics and even cutting-edge x-ray art from local and global artists, thoughtfully and carefully curated by its experienced owners.
Originally from the UK, Charlie Churcher and her husband Chris have holidayed in the Margaret River region for the past 20 years while living and working in Singapore. On New Year’s Day in 2002, while looking in a real estate window, they saw a block of land for sale in Prevelly and fell in love.
They acquired it and built the house in which they are now living.
It probably seemed like fate that the historic building came up for sale just as the family were deciding on their next move. “We’ve been holidaying here with our children for years,” says Charlie. “We wanted to give both ourselves and them a different experience to Asia and were looking around for where to live next.”
They haven’t totally abandoned Singapore as the original REDSEA Gallery still operates there. The bonus of having two galleries allows exhibitions and artworks to travel between Singapore and Margaret River and expands the exposure of local, national and international REDSEA artists in both markets.
Charlie says they are excited to be able to share and showcase the artists they discovered globally and are equally keen to take local

WA artists into Asia. The galleries represent more than 50 artists. Local artists exhibiting in REDSEA Margaret River include Leon Pericles, Alice Linford Forte, Sam Broadhurst, David Wroth, Lauren Wilhelm, Leigh Hewson Bower and Jason Wooldridge, as well as Shaun Atkinson, one of the buildings initial original artist owners.
“What is really positive is that we are bringing our international artists – whom we have been representing for years – to WA and Australia. We’re also able to bridge the gap for WA artists by taking them overseas to give them international exposure, including some artists local to Margaret River.
“We’ve been representing Australian artists for quite some time, so it’s great to be able to have them in both galleries. That’s exciting for both us and them.”
A couple of years ago, the Churchers heard that the Bussell Highway property was for sale and once they secured it, started making plans for a second gallery. In mid-last year renovations started and the sister gallery opened a couple of months ago.
“It seemed like a wonderful opportunity. We also really wanted
to keep the space going as a gallery because historically it has been a hub for art for so long. We saw a good business opportunity and we’re pleased we have been able to keep the space as a gallery.
“We wanted to renovate the building tastefully. The frontages are so gorgeous – it has a nostalgic feel that relates to the history of the building; we have given the frontage and outside a new look with the chosen paint colours. The work we’ve done has also brightened the inside, which is sympathetic to the art being displayed.”
Between the renovations, moving countries and getting their girls settled into new schools, Charlie says it has been a whirlwind, but they’re excited to be living in Margaret River. She’s hoping once things settle, she’ll be able to find
a studio to instal a kiln and start making ceramics.
“I am a teacher of early years but have taught art as a specialist as well. We ran an art school at the gallery in Singapore for many years. I haven’t had a lot of time to play and create for myself though. I’m looking forward to finding the time to do something creative. Having space to do those kinds of things is great for mental wellbeing. Chris and I are finding the environment where we live now provides us with chances to wind down, relax and enjoy the glorious natural environment.
“There’s lots of creative people in the area and we have made good friends here. I am looking forward over time to meeting more people and making new friends, both through the gallery and through local groups.”

Get ready to “Viva la fiesta!” as the Spanish Film Festival, presented by Palace, returns to Perth from June 13 to July 7. Films from Spain and Latin America will grace the screens of Palace Cinemas Raine Square, Luna Leederville, and Luna on SX Fremantle. From the latest Spanish drama to uproarious comedies, the festival delves into a retrospective showcasing the early masterpieces of Isabel Coixet and a special tribute marking the 120th anniversary of Salvador Dali. Visit www. spanishfilmfestival.com for more details.
Thanks to Palace, we have five double passes to give away, valid for any festival screening at Palace Cinemas Raine Square (excluding special events).
This month we also have 10 double passes to Fly Me to the Moon, in cinemas from July 12.
To win tickets, use the QR code on this page or go to www.mforum.com.au and hit the competitions tab.

Helping people think critically and connect better are a focus for the work Bethan Winn does.
In a world where we’re so connected, we’ve also lost so many skills around connecting, especially in person. When Perth educator Bethan Winn was starting out in her career, she discovered that if she was going to learn life and business skills, she was going to have to figure it out.
“I didn’t have a great manager in my first job, and I had to figure a lot of these skills out for myself,” she says. “I was burnt out, crying all the time and thought I was depressed. I wasn’t getting any support or training in my workplace. I was also so busy, not eating lunch and living on marshmallows and beer.”
Twenty years later, the mother of two has drawn on her early career experiences to create Human Skills, courses for young professionals in areas such as difficult conversations, critical thinking and establishing a rapport with new people.
“In some professions, like medicine, it’s important to be able to establish a rapport with someone else pretty quickly, in order to get a good outcome,” says Bethan. “You can have a lot of other skills but not being able to talk to others might well hinder your progress.”
By Ara JansenShe says compared with 30 years ago, when people were likely to learn such skills from a mentor or manager in their workplace, it’s not the same today. Those people also had more time, space and capacity to be able to help younger members of staff.
Decades later, many young professionals have missed out on that hard-fought wisdom and Bethan says they are scared of making mistakes.
“People are complex, and we have to make mistakes in order to learn. But I’ve noticed there’s a fear in young professionals – especially high achievers – around making those mistakes. If you’re smart, you don’t want to look stupid, which can make you scared to try things. I realise we’re all doing our best, trying to figure things out and more willing to say ‘I don’t know’.”
She argues that a complete focus on academics in high school for example, means kids might miss out on the socialisation and benefits of playing team sport, while getting a part-time job in a shop or in hospitality teaches young people how to talk to others, learn customer service and leadership skills.
“It’s these sorts of situations that mean younger generations aren’t comfortable talking on the telephone. I see this creeping into a number of age groups.”
Bethan works with corporate groups, individuals in person and online where she addresses many of these types of deficits through frameworks which people can use to guide them through uncomfortable situations.
“That scaffolding allows a jumping off point. Telling someone just to go and have more conversations to practise isn’t necessarily going to help them. Showing them how to approach that, offering tips and ways to try it will be a lot more helpful.
“It’s still important to make mistakes but we also don’t want to set people up for failure. I suggest people find their own version and use the course as an exercise in opportunity. If you’re trying to talk to more people, you could actually tell them that you’re doing a course about it. People love to be asked their opinions.”
www.humanskills.com.au
Vines above. Truffles below. Images of karri forest, cool-cimate misty mornings, open fires spring to mind. Thella Estate is both a serious truffle grower and a premium wine producer. The truffles are actually grown in Manjimup, while the vines are in Pemberton located off the Vasse Highway on Eastbrook Road. If my memory serves me well, in the late 1980s a very large farm owned by the Littlefair family was broken up into smaller lots which became vineyards. Those were Salitage, Picardy, Eastbrook and a vineyard owned by Drs Raad and Samaha. It is from the doctors’ vineyard that Below and Above came into being. Since 2013, the current owners, John and Evdokia Klepec, have made significant improvements in the vineyard replanting 7.8ha to premium clones of Chardonnay, Pinot Noir and Merlot. Of the 34ha of vines, only the top 5% make it into the Below and Above range – the aim being to produce small-batch premium wines. The wines are made by Bruce Dukes, who as usual shows a deft hand in raising these wines to a very high standard. All in all, a lovely set of wines. I couldn’t really separate the pinot and the chardonnay Both were exemplary and well worth seeking out.

2020 Below and Above Chardonnay
From a warm, dry vintage, this Gingin clone chardonnay was fermented and matured in French oak barrels for 10 months. At four years of age, it shows youthful fragrances of pear and nectarine, with a touch of flint and savory. In the mouth it springs to life with layers of spice, savoury oak and intense fruitiness that treads with elegance. The acidity is fine and clean. The finish is long and satisfying. Excellent now but will age (13.2% alcohol. $48)
2020 Below and Above Pinot Noir
From the fifth vintage of the newly planted pinot clones there is real complexity here. Perfumed cherry fruit and spice have developed nicely, flowing into the mouth with intensity of flavour and pleasing tannins. Clean, lively acidity carries through to a generous lingering aftertaste. An excellent Pinot, highlighting the quality possible from Pemberton (13.9% alcohol. $55)
2019 Below and Above Merlot
From a cooler vintage this Merlot came from new clones that were closely planted after the French practice. Made in the Bordeaux style, this is a quality wine with length and power. Spicy fruit tobacco and coffee aromas. Generous texture fine tannins, a touch of earth and integrated oak make for a very fine drink that will improve for a few more years beyond its current age. (13.8% alcohol $45)



SOUTH LAKE
Medical Rooms Available for Specialists and Allied Health
Lakes Shopping Centre, Shop 2, 620 Northlake Rd, South Lake WA 6164
•Available for ALL Specialists
•These consulting suites are situated on the ground floor of the medical practice, Featuring; -Reception area and patient waiting rooms -Staff kitchen and toilet.
Asking Rent: $30/Hour + GST, Annal rent $25,000 + GST (Per room) For Further details and enquiries
please contact p.manager@southlakefamilypractice.com.au or 08 9417 1009
Hollywood Medical Centre
Suite 36, First Floor, 85 Monash Avenue, Nedlands
87sq m – fully fitted, large reception, 2 consulting, 2 treatment & 2 store rooms.
Contact: Irene 0409 688 339

JOONDALUP
87 McLarty Avenue – 2 units
Opportunities to secure 37m2 or 78m2 in this convenient location between the Health Campus and the CBD.
Contact Jackie Skubevski 0428 820 052 or visit Xceedre.com.au


MURDOCH
SJOG Murdoch –
Consulting Suite for Sale
–TWO GENEROUS CONSULTING SUITES
–FURNISHED SUITE AT SJOG MURDOCH
Sterling Property is delighted to offer 47 / 100 Murdoch Drive, SJOG Murdoch for Sale.
This generously proportioned furnished consulting suite comprises of 97 sqm, configured with two large consulting rooms, reception and waiting area. Onsite on SJOG Murdoch and a short walk to Fiona Stanley Hospital.
Asking Price : $880,000 + GST (Includes Leased Car Bay)
Contact Simon Brady from Sterling Property on 0407 486 401 sbrady@sterlingproperty.au

The RFDS WA Strategy 2024 – 2028 strives to make a positive difference to the health and well-being of people living and working in regional WA. One of the focus areas will be to expand Primary Health Care services for a bigger community impact, with an initiative to establish an inaugural RFDS GP Clinic in Kalgoorlie, partnered with the Kalgoorlie Campus of the Curtin Goldfields University Department of Rural Health.
We are looking for a Clinical Lead General Practitioner, who will provide clinical leadership for the RFDS General Practice Clinic supporting the delivery of highquality care to patients and the community.
Please contact Lauren.Dawe@rfdswa.com.au

Queens Road Surgery is a busy GP owned general practice located in Mount Pleasant.
We are looking for a VR GP to join our well established practice. We offer a supportive team based culture, experienced administrative staff and quality full time nursing support. Queens Road Surgery is a fully equipped accredited practice. For a confidential discussion please contact our Practice Manager Narelle 0412 113 584 or narelle@queensroadsurgery.com.au

Niche, Boutique Medical Centre looking for PART-TIME OR FULL-TIME VR GP
Our practice is situated in the Golden Triangle in the Western Suburbs.
Standard consult 23 - $100, 36 - $180 Practice nurse, and an outstanding administration support.
One Saturday per month (AM only) with higher rates.
Please send through your EOI to: manager@nedlandsmedicalcentre.com.au
75% OF BILLINGS!!
GP positions available in accredited mixed-billing clinics in Burswood and Claremont.
Looking for VR GPs and non-VR GP’s on a full time/part-time basis for weekday and Saturday afternoon sessions. Fully computerised with on-site pathology and RN support.
Please contact Dr Ang on 9472 9306 or Email: info@thewalkingp.com.au

We are looking for experience GPs with a passion to make a difference for people seeking help for substance use disorders to join our team at Fresh Start Clinic in Subiaco.
Fresh Start Clinic is the entry point for all clients and patients at Fresh Start. Our doctor’s perform general health checks, and create informed care plans for patient’s recovery.
•Fully bulk billed clinic
•Onsite Pathology
•Best Practice Software
•Nursing support
•Encourage special interest of addiction
•Immediate start
•Free parking
Business hours 9am – 5pm
Monday to Friday
For a confidential discussion please email Jeff Claughton ceo@freshstart.org.au

VR GP - Mount Lawley WA - Privately billed After Hours practice
GP After Hours Mount Lawley is a well-established, community-based after-hours practice. We privately bill and are GP owned and run.
We are looking for an experienced VR GP to join our team of clinicians in providing quality after hours care to our patients.
Our practice offers:
•Modern facilities with a fully equipped treatment room
•Fully computerised practice using Best Practice software
•Percentage of the billings with a minimum hourly rate guarantee
•All sessions are 4 hours in duration
•Opportunity for weekend / public holiday sessions
For all enquiries, please email Gina at gpahmtlawley@3rdave.com.au or call 0412760871
VR GP POSITION – Full time/Part time
•A busy, well equipped, fully computerized and AGPAL Accredited
GP Practice in Perth, WA is looking for a VR Doctor
•Flexible days and hours tailored to your need
•Excellent RN and reception team as well as managerial support and onsite pathology
•Clinical full autonomy guaranteed
•Mixed Billings, using Best Practice Software
•GP private ownership
•Good income potential and emuneration at 72%, negotiable.
•$150 hourly minimum for the first three months.
The practice provides general GP services including skin check and many more.
For enquiries,
Email: highwycombemc@bigpond.com
Phone: 08 9454 6987

KALAMUNDA/ HIGH WYCOMBE
•Well established and regarded medical practice, about to celebrate 60th year, offers a unique opportunity for a VR General Practitioner
•Long history of being a training practice, both GP Registrars and Medical Students.
•Main surgery in Kalamunda, with a further two surgeries in High Wycombe and second satellite surgery in Kalamunda
•Mixed billing (or private billing if preferred)
•Well organized for Chronic Disease Management and Care of the Elderly, with Primary Care (CDM) Nursing Staff at all four surgeries
•Very nurturing practice, empathic to patients and staff. Supportive of clinical team members with individual special interests (such as cosmetic and skin lesion skills, mental health, LGBTIQA+…)
•Excellent schools in the fantastic Perth Hills area, very welcoming community
•Work life balance a major priority that is respected by the team at Stirk
•Have the best of both worlds; country living with the city only 30 minutes away
Please forward a CV and any enquiries to either Karin Tatnell (0438 211 240) or Dr Mike Civil (0419 965 377 ) or email : manager@stirkmedicalgroup.com
P/T GP required for our friendly practice in the heart of Fremantle. Young demographic with lots of student health, sexual health, women’s health and mental health. Fully equipped, accredited practice with full time practice nurse and onsite pathology, 2-3 days/week, days negotiable.
Contact Stephen on 0411 223 120 or at stephen@westendmed.com.au

Opening for VR GP - F/time or P/time
Full Private List available now from retiring GPs
FRACGP essential
Up to 70% private billings
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs.
Enjoy working for a doctor-owned, non-corporate, well supported, and accredited practice.
Please contact the Practice Manager on 6165 2444 or email: reception@comogp.com.au

Exciting opportunity with a leading medical research institute. Attractive salary packaging benefits. Previous clinical research experience is not essential.
RESPONSIBILITIES
Clinical assessments of research participants. Obtaining informed consent. Perform study activities as required by the protocol and regulations.
Interpretation of laboratory results, ECG, imaging. Monitor and evaluate study participants for the duration of the study.
Documentation of clinical care and research findings.
REQUIREMENTS
Current unconditional AHPRA Medical Practitioner Registration. Knowledge of ICH/GCP guidelines, MA Code of Conduct, National Statement is desirable.
TO APPLY
For full details and to apply, please go to seek.com.au CONTACT: yasmin@zesthr.au


Join the Soleil Health Team –Your Gateway to Exceptional Healthcare!
Soleil Health, the future hub of unparalleled medical care and holistic well-being, is on the lookout for passionate and skilled General Practitioners to join our dynamic team in Cottesloe. As we prepare to open our doors in August 2024, we invite you to be a part of a healthcare revolution that prioritises clinical excellence, patient well-being, and a collaborative work environment.
About the Role: As a General Practitioner at Soleil Health, you’ll experience clinical autonomy, allowing you to practice on your own terms. Our commitment to providing the best healthcare is reflected in the use of Best Practice Software, ensuring streamlined and efficient processes. Embrace a collegial and collaborative culture where teaching and education are at the forefront of our mission. GPs working for the practice also have the opportunity to provide home visit service to the neighbouring aged care residences.
Key Highlights:
Clinical Autonomy: Have the freedom to practice medicine focusing on your special interest.
Best Practice Software: Utilise cutting-edge tools to enhance the efficiency of your practice.
Collegial Culture: Engage in a collaborative environment, emphasising teaching and education.
Private Billing: Be a part of a practice that values your expertise with a private billing model.
About the Requirements:
Current unrestricted registration with the Medical Board of Australia / AHPRA VR status with Medicare AHPRA Registration
Valid working rights in Australia
Phone 0493 977 301 Email Manpreet.kaur@soleilhealth.com au soleilhealth.com.au


We have six consulting rooms and it is a lovely calm, caring environment with a great patient base.
We are close to all amenities including shopping, cafes, beaches and river.
This can be a full-time or part-time position with scope for all GP areas of interest.
Our team of friendly receptionists is complemented by two experienced practice nurses at all times.

For more information please contact admin@mosmanparkmedicalcentre.com.au

Gosnells Healthcare Centre has a great opportunity for General Practitioner to join a very well-established practice.
The role would suit a new Fellow or GP who wants to curate their own patient base with a guaranteed minimum offered for 6 months.
Wonderful, friendly practice
Experienced Doctors
Very Large existing and loyal patient base
Mixed billing practice
Enjoy an innovative, modern practice with the latest equipment and software (Best Practice)
70% of billings- plus attractive relocation package
Choose your hours, Our Clinic is open from 8am-5pm Monday-Friday.
On-site services include Pathology, Physiotherapy, Podiatry, Dietician
Fully Accredited practice
DPA Replacement Provider Number available
Safety Net of $150 per hour for 6 months
If you are interested in the exciting opportunity please contact Phil at ceo@spectrumhealth.net.au
Gosnells HealthCare Centre
2227A Albany Highway, Gosnells WA 6110
Join our team at Bullsbrook Medical Centre where you will enjoy every aspect of general practice. We are a well-established clinic with a strong and loyal patient base.
• Value driven, innovative, non-corporate GP owned medical centre with a highly competent administrative and nursing team, supporting the practice and allowing you to focus on servicing the patient demand.
• Large patient base with broad demographics.
• Team of GPs providing high quality care with a strong focus on comprehensive chronic disease management
• Fantastic opportunity for GP’s with special interests
• Friendly working environment of mutual support
• On-site Practice Manager, pathology and allied health.
• Fully computerised (Best Practice).
• AGPAL accredited.
• Training Practice for GP Registrars.
• Independent Contractor Agreement with high income potential
• Incentivised opportunity for FRACGPs interested in providing supervision to training GP’s.
Requirements: Unrestricted AHPRA registration, VR/FRACGP
For a confidential discussion please contact Dr Raf Francikiewicz on 0424436663 or email raf@bullsbrookmedicalcentre.com.au

Are you a GP seeking an exceptional opportunity in Perth’s bustling CBD? Look no further! Doctor Northbridge, a private doctor-owned practice, is offering a dynamic VR GP position in one of the city’s most sought-after locations. Our state-of-the-art medical centre, nestled within heritage-listed buildings, boasts top-notch facilities and a supportive environment.
Enjoy the perks of:
High-earning potential with private billing
Highly-trained administrative team
Private billing practice with excellent earning potential
On-site parking and convenient proximity to Perth CBD
Strong nursing support and low Did Not Attend (DNA) rate
With over 100 new patients a week and effective marketing strategies driving growth, Doctor Northbridge is the perfect place to advance your career. Join us and be part of a collegial environment dedicated to excellence in patient care.
Contact us today to learn more and schedule a visit!
Dr Yoon Low | Phone: 0431299328 Email: careers@drnorthbridge.com.au www.drnorthbridge.com.au











Spectrum Health has a team of professional and skilled managers with many years of industry experience who ensure the seamless and successful operation of medical practices.
Dr Vishnu Gopalan, the Chairman of Spectrum Health helms an expansive network of medical centres with a
strong intent to build genuine partnership with
The Spectrum Health team welcomes the opportunity to partner with you in general practice.





