


















You know how, once you’ve become interested in a thing, how suddenly you see that thing everywhere? Have you thought of a new car, or a pair of shoes, and now you spot them every day?
This year, my wife and I celebrated our 40th anniversary with a long-planned trip to Europe. One would think that walking around in centuries-old environs would draw me away from thinking about breathing and sleep. Instead, my eye spotted examples in museums and culture of all four countries to the value humans have placed on good sleep.
Billboards advertised sleep aids. Translations of tablets from ruins mention the value of sleep. Paintings and other artwork depict snoring as an irritant to another figure in the image. Medical terms are common enough that I was able to spot clinics that included sleep services. Meeting with professional friends in Denmark and Italy produced conversations about the state of sleep services in those countries and the US.
Happily for Midge and me, there were also plenty of other attractive distractions, so I was able to satisfy the spousal obligation of not thinking of work all the time. Life balance was a common theme in the museums and environs we were privileged to visit.
Then back to work – anyone who’s taken a vacation understands the need to emerge from the pile of work that awaits at the return to the ‘real world.’ A refreshed mind makes the work easier, and in some cases, possible!
Much like our sleep makes our daily lives possible. Today, we can assess our sleep in so many ways unavailable to our profession just a few years ago, much less at
the dawn of sleep medicine a few decades ago. It is energizing to see the many innovations that have arrived, or are shortly to be available, to allow us insight into sleep quality.
What happens next depends on our level of trust of the technology. We feel confident in polysomnography as a ‘gold standard’ test until we see studies that show night to night variability that erode the scientific support of one night’s evaluation. Can we trust the new rings, watches, and devices to gather biosignals that are ‘non-traditional,’ even though the tradition only started 40 years ago and has been constantly changing since then? Is ‘gold standard’ an appropriate label when innovation gives us a different way to look at the body responses?
Change within any profession is a slow process – but ours is a new part of medicine and may prove more nimble than most. Proper science is being done for these technological innovations for several admirable reasons: to answer the skeptics, for gaining a market edge, to satisfy the ethics of the engineers and doctors, and to meet FDA rules.
Together, these factors can indeed build trust in new ways to see the same problems artists from a thousand years ago depicted in their view of the human condition. We all want to be healthy, and to help others be healthy. Resting the mind on vacation and embracing new ways to see your work are two ways to move forward in healthcare.
Do you like what you are reading in DSP? Do you have ideas you want to share about what works in your practice? As Chief Dental Editor, I am happy to consider essays from any reader! Contact me at stevec@medmarkmedia.com.

Steve Carstensen, DDS Diplomate, American Board of Dental Sleep Medicine
Cover Story
The Mainstreaming of Oral Appliance Therapy by Wayne Wagner
Moving from a select group to everyday dentistry.


Continuing Education Is Your Mouthwash Putting You at Risk for Hypertension and Cardiovascular Disease? by
Nathan S. Bryan, PhD
New information requires challenging existing standards.


Medical Insight Insomnia and CBTi: Benefits for Patients and Opportunities for Dentists by Daniel Gartenberg, PhD
Insomnia often co-occurs with OSA; read about the new digital CBTi therapeutic options.

Medical Insight Breathless Nights: Tackling Expiratory Flow Limitation and Sleep Apnea in Lung Disease by
Saim S. Choundry, DO
Treating expiratory flow limitations intertwined with sleep apnea require adopting an integrated care approach.

2 CE CREDITS
Clinical Focus An OMD Assessment with TMD Muscle Pain: A Case Study by Judith Dember-Paige, BSOHP, COM® Transformation sometimes takes years, but it’s worth the effort.


Auto scoring available - perfect for scoring titration studies.

Nationwide network of RPSGT and Sleep Physicians for scoring, interpretation and telemed services.
The Zmachine Synergy provides accurate, EEG-based sleep staging on a web-based platform with auto-scoring capabilities and a nationwide network of RPSGT and Sleep physicians.
Battery - multi-night capable, perfect for titrations.
Most affordable Type 2 HST on the market.

6 Publisher’s Perspective
Weathering the Storms by Lisa
Moler, Founder/CEO, MedMark Media
12 Communications Corner Your Patients Aren’t Trying to be Difficult by Elizabeth Dooher-Anthony, RDH, OMT Empathy and creativity go a long way.
16 Communications Corner Why Some Quit and Others Never Start. Don’t Let It Be You! by Kalli Hale, DDS, MPH, D.ABDSM Make a brave choice and be persistant.
18 Cardio-Sleep Corner How Much Deep Sleep Do You Need? by Lee A. Surkin, MD, FACC, FCCP, FASNC, FAASM
Deep sleep is vital for optimal health; what is the magic number?
34 Technology & Innovation Empowering Dental Practitioners with AI to Expedite the Sleep Apnea Diagnosis to Therapy Pipeline by Steven Miller
Technology is giving us new ways to shorten the medical timeline.
37 Product Spotlight
The Next 5 years of Dental Sleep Medicine? by Steven Olmos, DDS
Keep your eye on what’s coming to prepare for new ways to help people.
38 Product Spotlight Accelerating MAD Treatment for OSA Patients through AHI Monitoring
AHI monitoring is a game-changer in the management of OSA with MADs.
40 Product Spotlight The Right Temporary Oral Appliance
We all need a ready to go, reliable backup device.
42 Product Spotlight The Top 3 Ways Dentists Can Stay Ahead of the EverChanging Sleep Industry Recognizing opportunities and moving forward is the key.
44 Product Spotlight Dry Mouth Needs a New Solution
A medical-grade xerostomia therapy may be the answer for your SRBD patients.
46 Practice Management Are You Using One of the Most Audited Codes? by Rose Nierman
Don’t risk your practice health using poor advice.
48 Sleep Humor Timing is Everything by David McCarty, MD, FAASM
Winter 2024
Publisher | Lisa Moler lmoler@medmarkmedia.com
Chief Dental Editor
Steve Carstensen, DDS, D.ABDSM stevec@medmarkmedia.com
Chief Medical Editor
Lee A. Surkin, MD, FACC, FCCP, FASNC drsurkin@n3sleep.com
Associate Editor | Lou Shuman, DMD, CAGS lou@medmarkmedia.com
Editorial Advisors
Jamila Battle, MD (Family/Sleep/Addiction)
Steven Bender, DDS
Jagdeep Bijwadia, MD (Pulmonary, Sleep)
Kevin Boyd, DDS
Saim Choudhry, DO (Internal Medicine, Sleep)
Alison Kole, MD, MPH, FCCP, FAASM (Sleep, Pulmonary, Critical Care)
Karen Parker Davidson, DHA, MSA, M.Ed., MSN, RN
Bertrand de Silva, MD, FCCP, D.ABSM
Daniel Gartenberg, PhD (Behavioral Sleep)
Kristie Gatto, MA, CCC-SLP, COM
Amalia Geller, MD (Neurology, Sleep)
William Hang, DDS, MSD
Steve Lamberg, DDS, D.ABDSM
Christopher Lettieri, MD (Pulmonary, Critical Care, Sleep)
Pat McBride, PhD, CCSH
Jyotsna Sahni, MD (Internal Medicine, Sleep)
Ed Sall, MD (ENT, Sleep)
Alan D. Steljes, MD (Cardiology, Sleep)
Laura Sheppard, CDT, TE
DeWitt Wilkerson, DMD
Scott Williams, MD (Psychiatry, Sleep)
Gy Yatros, DMD

National Account Manager
Adrienne Good | agood@medmarkmedia.com
Sales Assistant & Client Services
Melissa Minnick | melissa@medmarkmedia.com
Creative Director/Production Manager
Amanda Culver | amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury | amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius | emedia@medmarkmedia.com
Social Media
Felicia Vaughn | felicia@medmarkmedia.com
Website Support
Eileen Kane | webmaster@medmarkmedia.com
MedMark, LLC 15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260 Tel: (480) 621-8955 | Toll-free: (866) 579-9496
www.DentalSleepPractice.com


Lisa Moler Founder/CEO, MedMark Media
Droughts, heat waves, rain, hurricanes, blizzards, tornadoes, wildfires, and earthquakes, or beautiful sunshine — no matter where you live in the U.S., the weather can bring you the bliss of sitting by the pool or bring you scurrying into the safest windowless room for cover. It’s not just the weather’s fluctuations that we need to prepare for — hoping for the best while preparing for the worst is the best way to avoid storms in all aspects of life. Our focus at MedMark publications is to help you be prepared to face all of the issues that may pop up in your practice, to give you better control over your business and clinical decisions, less stress, and more success.
Here are three tips on keeping your head above water, when you feel that flood of anxiety from practice stress.
• Pinpoint your stressors: Define what in your practice is keeping you awake at night, and maybe even keep a journal of what is causing you stress at the end of each work day. Are you afraid that your computer systems aren’t secure from cyberattacks? Are you unsure that your equipment is providing the specific information you need to get the best diagnostics? Are you frustrated that you cannot offer the latest treatment opportunities? Before you can fix a problem, you have to be sure of what the problem actually is.
• Establish a practice culture: Make sure that your practice handbook specifically outlines what behaviors and attitudes are acceptable and which will not be tolerated. Have weekly or monthly team meetings to make sure everyone is on the same page. To head off problems before they grow, learn about conflict resolution skills or hiring-and-firing protocols. If you have an office manager, remember to include him/her in these learning opportunities, and make sure your team knows that you are available for the more complicated situations.
• Give yourself the edge over the competition: It is stressful to watch potential patients filling up other dentists’ appointment calendars. In this day of the Internet and technology, you need
to reassess your equipment to improve efficiency, accuracy, and increase patient care and options. Especially in this age of social media, you want your patients to see that you, rather than the clinician across the street, have the most up-to-date imaging, more painless protocols, or faster treatment options. MedMark publications can help you discover what innovations have been developed and how they pertain to your specialty. In our winter issue, the Cover Story, “The Mainstreaming of Oral Appliance Therapy,” tells the interesting evolution of the new K1027 billing code which was sparked by the design and manufacturing innovations of the Slow Wave DS8 oral appliance. In our CE, “Is Your Mouthwash Putting You at Risk for Hypertension and Cardiovascular Disease?” by Nathan S. Bryan, PhD, explores the role of nitric oxide protecting the body against inflammation and resulting diseases. Our Clinical Focus, “An OMD Assessment with TMD Muscle Pain: A Case Study,” shows how myofunctional therapy resulted in a patient’s ability to open his jaws with full range of motion and achieve his goal of being able to enjoy some of his favorite foods again.
In this last issue of 2024, we give you our “umbrella wish” for fair weather, a dedicated and efficient team, a growing loyal patient list, less stress, and more fulfillment of your goals in the coming year.
Remember, every storm passes, and you need to be prepared to make intentional, positive decisions for a stronger and more profitable future. To your best success!

12 modules cover both the medical and dental science of sleep medicine. Dentists who complete the coursework and pass the exam are qualified to submit cases for board review to achieve Diplomate status. The certificate is a prerequisite for ACSDD Fellow and Diplomate


by Wayne Wagner

Ten years ago, 80% of OSA sufferers were undiagnosed, and the same is true today.1,2 Ten years ago, oral appliance therapy had de minimis market share as a treatment for Obstructive Sleep Apnea. Today, even with the implosion of the CPAP industry due to the Philips recall and their subsequent exit from manufacturing the devices, Oral Appliance Therapy (OAT) still has an insignificant market share worldwide. Fortune Business Insights said the sleep apnea device market was worth $9.17 billion in 2023.3 Still, if you add all the revenue reported by oral appliance manufacturers, they don’t approach 5% of this number.
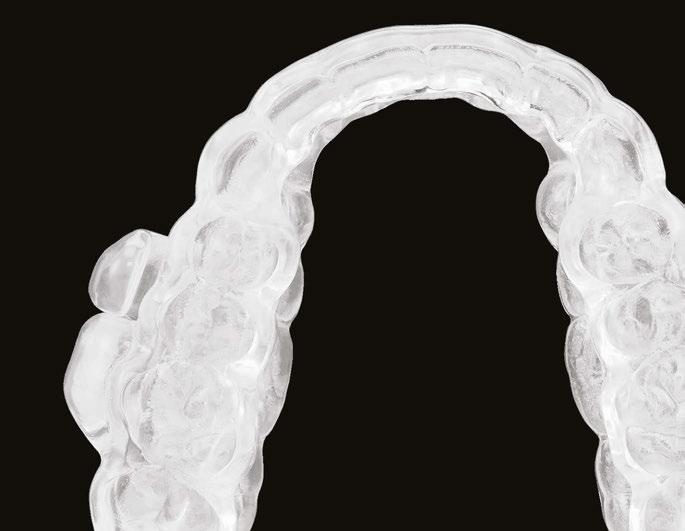
Before 2021, oral appliances treating OSA had to meet a strict, seven-bullet product definition established by the Centers for Medicare/Medicaid (CMS) for how Mandibular Advancement Devices (MAD) should operate4 to get insurance reimbursement. The last two requirements imposed rigid design specifications that did little to enhance patient choices or improve efficacy:
• Have a fixed mechanical hinge at the sides, front, or palate; and,
• Incorporate a mechanism that allows the mandible to be easily advanced by the beneficiary in increments of one millimeter or less.
The dental sleep medicine industry was unhappy about the billing code restrictions but did nothing in a coordinated fashion to try to change them. They just lived with the antiquated billing code and the low reimbursement rates that accompanied it.
In 2021, Slow Wave, Inc. did what the Dental Sleep Medicine industry could not do and gave CMS concrete reasons to introduce a new billing code. The introduction of the Slow Wave DS8 utilized a host of new design and manufacturing innovations that the dental community had embraced. CAD/ CAM, 3D printing, and milling have become pivotal technologies in digitization. This shift enabled highly accurate digital scanners to replace traditional impression molds that often-required time-consuming adjustments.
The materials used in the new production processes had already received FDA clearance and allowed for the fabrication of teeth, bridges, and custom oral appli-
ances with precision tolerances as tight as 1/100th of a millimeter. This digital revolution required a billing code that could evolve alongside technological advancements, and CMS agreed that the Slow Wave’s DS8 was ideal for launching the new K1027 billing code. Where the industry had failed to create change, a single product introduction succeeded. The product definition of K1027:
“Oral device/appliance used to reduce upper airway collapsibility, without fixed mechanical hinge, custom fabricated, includes fitting and adjustment.”
This more inclusive product definition has resulted in more than 27 products being approved under the new billing code in the three years since it was established by CMS.5
However, the fight for K1027 is far from over, and the industry needs to pull together to get CMS to issue both a benefit category and fee schedule so that both CMS and private insurers can reimburse the code. Until then, medical billing is not cost-effective, as the time and effort involved can exceed the appliance’s value. In addition, the reimbursement rate for billing code E0486, if applied to the new billing code K1027, will continue to suppress profitability in a historically highly unprofitable industry. This contrasts with Hypoglossal nerve surgery prescribed by physicians that gets reimbursed $50,000+ by CMS for a lower efficacy treatment.
The medical and dental communities have long suspected that both OSA and sleep bruxism may be concurrent in an individual. According to various research studies, OSA affects somewhere between 9% to 38% of the population.6 Sleep Bruxism (SB), a repetitive jaw muscle activity that manifests as clenching or grinding the teeth, is present in 5.5% to 8% of adults.7,8 The overlap between them is significant according to multiple studies, though. In one study of 147 patients, sleep bruxism was found to be present in 33.3% of the OSA patients studied. In another Japanese study, SB was found to be present in 48% of OSA patients.9 The question of why the overlap is still debated, but the Japanese study demonstrated positive correlations between “phasic-type sleep bruxism events and OSA desaturation, and microarousal event indices, suggesting that

OSA might be a high-risk factor for sleep bruxism.”
In 2017, the first oral appliance was dual cleared for OSA/Bruxism by the FDA. The LUCO Hybrid was initially cleared for bruxism in 2015 [510(k) # K16047] and, based on clinical data, cleared for OSA in 2017 [510(k) # K130797]. However, no one understood the implications of what this could do for the dental industry. In July 2024, the FDA dual cleared the Slow Wave DS8 for the treatment of OSA/Bruxism K191320 and K240463. The product, now marketed as BROSA (Bruxism, Retainer, OSA), is prescribed by dentists for a bruxism condition that shares a significant overlap with OSA.
Now, dentists can prescribe a product to treat a patient’s bruxism in just one visit and have treatment within days. The patient can also simultaneously monitor its impact on their sleep patterns. This new model makes it profitable for the dentist to make OAT a mainstream product.
Most existing oral appliances for bruxism are only on the top or bottom teeth and focus

Wayne Wagner is the founder and CEO of Slow Wave, Inc., an expert in 3D engineering, and a long-time OSA sufferer
on mitigating the effects of the condition –such as reducing teeth from being ground down – rather than addressing the condition itself. This means that most mouth guards can’t really help bruxism, let alone serve as a treatment for other sleep conditions like OSA.
But what makes devices like BROSA effective for both OSA and bruxism? Two key factors are the vertical opening of the mandible and making more room for the tongue.


Traditional devices advance the mandible forward in millimeter increments to open the airway. Still, research has shown that incorporating more vertical opening and making more room for the tongue allows for less forward movement of the mandible. This can reduce or eliminate the need for a morning repositioner, as the jaw remains in a more relaxed state during sleep. This relaxed state is not only beneficial for OSA but also ideal for treating bruxism.
A clinical trial in Chile provided further evidence of this. The study compared three groups, each fitted with an occlusal device that opened the jaw to varying degrees: 1mm, 4.25mm, and 8.25mm. The results showed a significant reduction in masseter muscle tension in the groups with 4.25mm and 8.25mm openings, with the best results in the 8.25mm group.11 This vertical opening helped relax the muscles responsible for bruxism events.
The Slow Wave BROSA device further enhances this relaxation thanks to how well the Formlabs material glides while using a ramp system that allows for a very smooth natural horizontal movement during sleep. The innovative ramp mechanism ensures that the more a patient bites down, the more the ramps gently advance the mandible forward. This system allows the body to find its ideal jaw position naturally during sleep. Initial use of the BROSA device in patients enabled 24 of 25 to achieve normal breathing levels of fewer than 5 AHI events per hour. These outcomes were observed across patients with mild, moderate, and severe OSA.
New technology allows dentists to treat bruxism and patients to monitor their OSA.
O2 rings from Wellue and SleepImage™ and watches from both Apple and Samsung mimic, with great accuracy, the oxygen and pulse readings from home sleep study devices. These devices can give some of the 80% undiagnosed their first clue that a formal sleep study might be warranted. In September 2024, the Apple Watch was even FDA cleared under new product code QZW as an “Over-the-counter Device to Assess the Risk of Sleep Apnea.”10 The SleepImage System is FDA-cleared to aid clinical diagnosis of sleep disordered breathing in children as young as 2 years-old, adolescents, and adults. For those previously diagnosed, nightly monitoring of their sleep provides clues when intervention from a sleep doctor might be warranted.
For Dr. Robert D’Alfanso, DDS, at Lakeway Cosmetic and Family Dentistry near Austin, Texas, innovation has drastically changed his 20-plus year dental practice. “I used to wait weeks or months for implants to come in from a dental lab. Now, I have a local lab, and my patients get better and more immediate service.” But like most general dentists, sleep dentistry is something that Dr. D’Alfonso has been reluctant to adopt. “Between the physician referrals and medical billing, treating OSA has been a non-starter for me. Chasing down medical insurance companies or checking on the status of a sleep study diagnosis is not productive time for our busy team.” Dr. D’Alfonso is not alone in his hesitancy. In a survey conducted by MedMark Media in December 2020, when dentists were asked what they see as the biggest challenges to sleep related practice growth, 81% replied medical billing/insurance.” 48% also reported “securing a medical diagnosis” as the second leading challenge. All too often, dental referrals for a sleep diagnosis result in a physician’s prescription for a CPAP or hypoglossal nerve surgery. As a result, sleep dentistry being practiced by about 1% of the general dentist population (2,000 American Academy of Dental Sleep Medicine certified out of 200,000+ dentists).
New CAD/CAM techniques can take
a closed-bite scan and digitally open the mouth. This process ensures no impact on the bite registration with skews of the midline or misalignment of the occlusal plane. Nor does it require special training for technicians. Closed-bite scans are how leading scanning manufacturers train dental technicians to scan for teeth aligners. The oral appliance market traditionally does open bite scans using a gauge to keep the teeth open during the scan. But For Dr. Mendy Ritchie, DDS of Braced Orthodontics in Marble Falls, Texas, the closed-bite scan helps her claw back valuable chair time. “I know that when I scan a closed bite for aligners or an oral appliance, I won’t have to worry about misalignment of the occlusal plane. No matter how practiced you are at using a gauge to create an open bite scan, the patient will invariably shift their jaw during the scan impacting the midline or occlusal plane. The usual result of this is a required adjustment on the finished product.” Dr. D’Alfonso agrees. “Refits and adjustments of improperly fitting devices take valuable chair time impacting the dentist and the entire staff.” Though closed bite scanning is not taught as a technique in most oral appliance design or continuing education courses, Slow Wave successfully uses it for all the products it makes. Another software innovation that complements closedbite scanning is the use of artificial intelligence (AI) which is helping to streamline the design process of both aligners and oral appliances. The result is an OAT product that requires only one visit, fits perfectly the first time, does not require adjustment, reduces the liability of the dentist, and has a dramatically higher compliance rate.


“I know that when I scan a closed bite for aligners or an oral appliance, I won’t have to worry about misalignment of the occlusal plane.”
– Dr. Mendy Ritchie, DDS
Braced Orthodontics in Marble Falls, Texas
Digital printing innovation is also advancing quickly. Formlabs 3D printers, with FDA cleared materials to produce dental products, could manufacture three oral appliances in a 5-hour print run in 2023. Today, the Formlabs Form4 can print the same three appliances in a quarter of the time without any loss of accuracy (1/100th of a mm), plus the design center can put the print job on a Formlabs printer anyplace in the world. It is just a matter of time before every dentist’s office is printing devices locally in office or at their local lab, regardless of where the design work is being accomplished.
These new FDA dual-cleared OAT products, innovations, technological advancements provide dentists and oral appliance suppliers with the market share growth opportunity that has eluded them thus far. The question now is whether the industry will take advantage of the opportunities it has been afforded. Will dentists quit looking at “sleep dentistry” as a forbidden fruit? Will bruxism devices finally help erode the “80% undiagnosed” talking point that has plagued the industry for decades? Will oral appliance therapy finally become a profitable mainstream product that every dentist prescribes for patients who walk in their doors?
1. https://www.ama-assn.org/delivering-care/public-health/what-doctors-wish-patients-knew-about-sleep-apnea
2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2727690/
3. https://www.fortunebusinessinsights.com/industry-reports/sleep-apnea-devices-market-100708
4. https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleid=52512
5. https://www4.palmettogba.com/pdac_dmecs/searchProductClassificationResults.do?manufacturer=&codeDecision=K1027&productName=&modelNumber=&classification=&producttable_length=10
6. Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of Obstructive sleep apnea in the general population. A systematic review. Sleep Med Rev 2017;34:70-81
7. Maluly M, Andersen ML, Dal-Fabbro C, et al. Polysomnographic study of the prevalence of sleep bruxism in a population sample. J Dent Res 2013;92(7 suppl);97S-103S
8. Manfredini D, winocur E, Guarda-Nardini L, Paesani D, Lobbezoo F. Epidemiology of bruxism in adults; A systemicreview of the literature. J Orofac Pain 2013; 27:99-110
9. Hoysosa H, Yamaguchi T, Mikami S, et al. Relationship between sleep bruxism and sleep respiratory events in patients with obstructive sleep apnea syndrome. Sleep Breath 2014;18:837-844
10. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpcd/classification.cfm?id=213
11. Manns A, D.D.S, Miralles R D.D.S, Cumsille F M.S, Vertical Dimension and EMG activity; Journal of Prosthetic Dentistry 1885;v53:243-247
by Elizabeth Dooher-Anthony, RDH, OMT
Ihave been a dental hygienist for more than 35 years. Early in my practice, I noticed there were some patients who were very difficult to work on. They were angry, belligerent. They seemed to be physically resisting my efforts by tightening their lips or cheeks. Their tongue was constantly in the way.
I realized there was a PTSD sort of response in these patients. I tried my best to make their experience less stressful by letting them know they were afraid for a reason, that I would not judge them. That I cared about them. I experimented with aromatherapy, soothing music, and facial massage. These generally worked well, and we both had a much more pleasant interaction.
I contemplated how patients reacted and concluded that their emotional perception of the appointment is what matters to them. How they felt they were treated was more important than the clinical parameters I was using.
I created a philosophy which I called Serdentity – a combination of serenity and dentistry. I realized it was my judgement of the situation that created my dissatisfaction. I tried to observe and respond instead of react. I told myself they were reacting to their fear

Elizabeth Dooher-Anthony, RDH, OMT, will tell you she became a dental hygienist by accident. She was supposed to be a rock star. She went to dental hygiene school after working in a dental office at the front desk. Before that, she got her BA in English with a minor in Theater Arts. Thirty-eight years later, she is still practicing and has not “burned out.” She developed a mindset toward her work that has sustained her and created positive patient experiences. She realized she could teach it to others and has found a way to use her performance skills to create a memorable, uplifting experience for her audiences. She has been presenting her seminar, Serdentity, since 2006. She published a book by the same name in 2013. Her articles have been published in RDH print and digital magazines. She hosted the “Serdentity Podcast” on the iLoveDentistry Facebook page, and is currently hosting it on her own Youtube channel. Elizabeth is from Rochester, New York, and lives there currently with her husband, Michael.

and that is why they were presenting with challenging attitudes and behaviors.
Once I became an Orofacial Myofunctional Therapist, I understood that patients were protecting their airway. This was the final piece in the puzzle. It took the mystery out of why. Now I could move forward with techniques that would truly address the root of the problem.
I helped patients understand that I knew their reactions were not in their conscious control. Particularly the gag reflex. So many patients expressed shame and related how they were made to feel guilty for it. I realized that the gag reflex is about the “in” breath. The patient can’t breathe in so the brain removes whatever is in the way. This makes sense considering many modern humans are mouth breathers.
I developed nasal breath coaching to help with getting radiographs. The gag reflex will not engage during the out breath. Having patients hold the breath and release during exposure helped many get through an experience they had always dreaded. They were pleasantly surprised. In a recent conversation with a fellow airway professional, we came up with the idea of having patients do a nose-clearing exercise prior to dental care. This would create better nasal breathing, making the procedure easier. Xylitol nasal spray and nasal dilators would also be helpful.
Non-judgement and positive communication are so important to creating a positive emotional experience for dental patients. I recently retired from clinical dental hygiene. I can honestly say I did not experience the burn-out, resentment, and other things I see my fellow professionals complaining about on social media. I want to help my colleagues understand there is a better way to practice. I figured it out, so it can’t be that hard!

by Judith Dember-Paige, BSOHP, COM®
tan was referred to my office by a TMD specialist. His chief complaints were he could not chew or open his mouth without pain. It seemed the less he chewed, the more pain he experienced. As a result, an Orofacial Myofunctional Therapy (OMT) program was created to help support his muscles of the TMJ and craniofacial respiratory complex. He used his splint as instructed by his specialist. However, his anterior open bite widened, and his teeth became more misaligned over time.
TMD and orofacial muscle pain is a problem that can start small and grow in magnitude and dysfunction. Sometimes the pain may be associated with Orofacial Myofunctional Disorders (OMDs). Therapy may be needed to address the muscle pain that accompanies the dysfunction
Stan was a 28-year-old male in a lot of pain. He had just come from his TMJ specialist where he received an oral orthotic splint to relieve his discomfort. He told me it all started after a long dental appointment where he received a root canal and a new crown on the upper right. After this procedure, his jaws felt tight so he gave it a good stretch by opening very wide. He heard a rip and a crunch. Opening his mouth was never the same after that. He presented with a set of symptoms: TMD muscle pain, he could no longer chew his food without pain (food had to be the soft consistency of tofu), daytime clenching and night time grinding of his teeth. In addition, he had daily headaches and ear ringing. He could not open his mouth very wide without experiencing sharp pain. He took acetaminophen for his discomfort and zolpidem nightly to help him fall asleep easier.

Upon closer examination, there were contributing factors that led to his discomfort. Stan had been a stomach/face sleeper for years. He also bit his nails since childhood, had a smoking habit from his youth, and he was prone to ear infections. He had moderate tongue and buccal ties, obligate mouth breathing, aggravated by a deviated septum, narrow nares, low tongue resting posture, an



Judith Dember-Paige is a certified orofacial myologist, with 15 years in practice. Although retired from dental hygiene, she practiced for 35 years, and her license is current. Based in Westchester, New York, Judith now has a thriving practice specializing in both children and adults with orofacial myofunctional disorders. Beyond clinical practice, she is a respected lecturer/writer among dental professionals and parent groups. She is an avid saltwater fisherwoman and loves camping. Her site is www.oromyologist.com.
anterior open bite, a lower jaw that deviated upon opening, and bouts of acid reflux.
An orofacial therapy program was created to allow his tongue to give better support and function to his oral structures, especially the TMJ joint. When the tongue naturally rests in the palate, it removes the unwanted pressure off of the TMJ. As part of the course of his therapy, focus was made to reeducate his breathing to make his nose the primary way he breathes. Optimal breathing rate for an adult is slower than for a child. Good nasal breathing during the day supports good nasal breathing during the night for optimal sleep. When the tongue rests in the palate, it impacts facial development especially for children who are still growing. An adult, for example, like our friend Stan, the progress made is gradual but more likely to last a lifetime. Generally, therapy starts out once a week for about 2-3 months. Then therapy progresses to every other week for 2-3 months, and then changes to once a month for about 5 months for the rest of the year. The exercises are done a minimum of 2 times everyday. These exercises are designed to strengthen and tone the orofacial muscles, building brand new neuromuscular function. When the muscles of the face are well developed, it may favorably impact appearance and the overall integrity of the facial structures. The muscles of the face also include the tongue, lips, cheeks and neck. Although the therapy program is typically only a year, Stan really liked how good he felt and decided to continue with some of the exercises to this day. From the photos you can see how much the program has impacted his health and well-being.
During his therapy, there was a discussion about the possible benefits he may receive from having his jaws expanded, making more room for his tongue, then to be followed by a tongue and buccal frenums release. His intermolar width is 34 mm, and his intercanine width is 25 mm. I feel any expansion has a potential benefit.
After completing his course of myofunctional therapy, he was able to open his jaws with full range of motion and achieve his goal of being able to enjoy some of his favorite foods again. He was most excited about being able to bite into a juicy cheeseburger.
Stan has a very narrow external nasal valve and receives some benefit from using dilator nasal strips. There are a few more products on the market that may help make
nasal breathing easier for him.
To document any initial assessment, the midpoint of therapy, and when therapy has ended, it is important to take detailed photos, videos, plus full measurements of the face and teeth. This makes it possible to compare results while showing that your therapy works based on the evidence you gathered before, during, and after treatment.
In conclusion, Stan was very proud of how hard he worked during his myofunctional therapy and urged me to share his exceptional results.






“While your systems, screening, and patient conversations are foundations of success in dentistry, your mindset is what will ultimately determine the longevity of your sleep practice.”
by Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB
As 2024 comes to an end, I want to highlight the questions I am asked the most about dental sleep medicine and how to make this successful in your practice. While your systems, screening, and patient conversations are foundations of success in dentistry, your mindset is what will ultimately determine the longevity of your sleep practice. More on mindset later. Let me share what so many of you are asking, so together we can literally breathe life back into the patients in your practice.
1. I want to get started in “airway”, but I have no idea where to begin.
I’m not here to promote or tout any company or specific courses. There are many now and it’s overwhelming. But answering this question is obviously important and can only be answered with more questions: What demographic are you wanting to treat? What type of practice do you have? Do you see both kids and adults? Do you want to offer expansion orthodontics in your office, or traditional oral appliance therapy (OAT)? Once we uncover this together, it is much easier for me to guide you and help you avoid the pitfalls of ‘weekend CE’ that overpromises & under delivers. Additionally, having a clear picture of how you see yourself implementing sleep into your clinical practice allows you to incrementally move the needle forward in bite size steps.
2. I have spent thousands on sleep courses and know this is important for my patients, but I never implemented a thing…
I wish this message was not so common in my emails. I spoke with a dentist who was quoted over $200k for an “all-in-one” sleep education/practice management course, paid out monthly over a period of 2 years. I nearly fell over. Now, don’t get me wrong, I’ve got a hefty list of receipts from sleep CE myself, but from many credible sources. A
fee that high is an abuse to any dentist and directly affects the profitability of your office; that is to say, there are ways to spend $200k and get great value but diversification of modalities, ideas, diagnostics and administrative systems is what we should expect from something in that price range.
The implementation of these services is another barrier; after spending your money and time learning about how you can save patients’ lives and increase the arsenal of services in your practice, the excitement can wear off when you get to work that Monday to a note that your hygienist wants a raise. Or that your dental assistant is quitting. We get swept back into day-to-day dentistry and can forget to schedule time with our teams to excite them about what we just learned. One of the first things I recommend to doctors interested in taking CE? Invest in your teams too! Bring them to the conferences and make sure to schedule time with them to review what was learned & how to start screening your patients. Don’t forget, this is where you start! Here is where mentorship is critical in my opinion, because once you start screening, that’s when you need to know what to do next. If you have had a ‘failure to launch’ in your practice after training, it means something is missing. Be it a confidence problem on your part, or a leadership issue, it needs to be uncovered so you can make the right steps forward.
3. I really want to treat sleep apnea, but I’m concerned I’ll change the patient’s bite or cause TMD issues!
Good! I’m relieved you’re worried about that because it shows you care. It also identifies the lack of knowledge you have in oral appliance therapy, which is easily remedied by education. A mentor of mine once said, “if the fear of bite changes prevents you from offering this service, I guess the patient can have the prettiest occlusion in the graveyard.” How he humbled me!
What we have to realize is OSA is a chronic, progressive & life-threatening disease. Not fully understanding the gravity of hypoxemia, brain degeneration, hypertension, and general body inflammation will, not surprisingly, make you more concerned about TEETH… and begs the question, if your Mom or Dad stopped breathing 25 times per hour, and their oxygen dropped to 76%, would you care if they developed a slight gap in between #2 & #3?
Mindset here is important, you are no longer ‘just a dentist’, you are a doctor managing a chronic illness for a patient which, like everything in medicine, can have side effects. Do not let your lack of understanding be the reason you are held back from this life saving aspect of dentistry!
4. I would love to do what you do with pediatric sleep disordered breathing and expansion, but I can’t find enough support for these techniques?
Where are you looking? There are great articles coming out in support of dental expansion prior to surgery for tonsils/adenoids,
how we can resolve bedwetting issues by improving nasal breathing, how myofunctional therapy and expansion can permanently reduce a patient’s AHI, and the large effect we can have in a patient’s hypertension by treating their OSA. Reach out to me or find someone you trust that offers sleep services in your town. Those of us in the trenches doing this everyday love to talk about it to anyone who will listen!
I would also encourage you to start helping kids immediately. As slowly as literature progresses and as long as studies can take, so many kids are suffering and I refuse to wait until the world catches up. We have plenty of evidence that what we are doing is safe, effective, and life changing for our pediatric patients. Take the courses, learn the techniques, celebrate as what you do changes the trajectory of these kids’ lives. I promise you will never stop.
Lastly, discussing “mindset” as a dentist is critically important. You are not always going to win, and you are going to have days that make you question your abilities. Having a colleague to lean on who has gone before you and been through the trials and troubleshooting of OAT is the difference in how quickly you will gain confidence. You don’t learn as much when it all goes perfectly. You need someone to talk you off the ledge when you reach a limit in your understanding. Refer to my 2nd article in DSP magazine “The First Thing I Got Wrong”. Sleep apnea treatments couldn’t be more different from general dentistry, in both conversation & management. Don’t put unrealistic expectations on yourself and rest assured there is no one more qualified to help patients with this problem than you!

Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB, is passionate about how our teeth affect our systemic health – the link between chronic jaw infections, periodontal disease, and subsequent heart problems. Her training in obstructive sleep apnea has transformed both her personal and professional career. Dr. Hale is a Clinical Advocate for VIVOS Therapeutics and works with dentists around the country to develop clinical protocols for the treatment of mild to moderate obstructive sleep apnea and sleep-disordered breathing. Her work in pediatric expansion and sleep-disordered breathing catapulted her speaking career and she lives by the slogan “we have to stop getting it wrong, for our kids.” She is faculty for the Dental Success Network, a key-opinion leader for Candid, and the Chief Dental Officer for Toothpillow. She travels monthly across the U.S. and abroad to teach dentists about Obstructive Sleep Apnea. Learn more about her sleep mentorship program at https://sleepwelljourney.com/.
by Lee A. Surkin, MD, FACC, FCCP, FASNC, FAASM

Deep sleep, also known as slow-wave sleep or the third stage of non-REM sleep (stage N3), is vital for optimal health. It helps in repairing and restoring functions needed for day-to-day life. In short, deep sleep:
• Promotes feeling rested
• Supports memory consolidation
• Heals damaged tissue
• Strengthens the immune system
Due to its importance, a lack of deep sleep can lead to learning difficulties and frequent infections. Not getting enough deep sleep can even contribute to some serious health conditions like heart disease and Alzheimer’s disease.
Deep sleep occurs in the third stage of NREM (non-rapid eye movement) sleep. During deep sleep, heart rate, blood pressure, and breathing slow down and brain
activity appears in long slow waves, also referred to as delta waves.
In general, people fall into the deep sleep stage an hour after falling asleep. Initial periods of deep sleep are 20 to 40 minutes long, and become progressively shorter as the night wears on. Sleepers are typically hardest to wake up during deep sleep versus REM (rapid eye movement) sleep when they can be fast awakened. If awakened during slowwave sleep, people experience mental fogginess for up to an hour.
When it comes to non-REM, deep sleep versus REM sleep comparison, it is pretty obvious that we spend a lot more time during non-REM sleep – 75%, of which 13 to 23% are in deep sleep, whereas only 25% is spent in REM sleep.
However, our sleep requirements change with age. Precisely speaking, deep sleep reduces with age so a person under the age
of 30 may need 2 hours of deep sleep per night, whereas a person over the age of 65 may only need half an hour of deep sleep per night.
Making a difference between lack of deep sleep and sleep deprivation, in general, hasn’t been easy for researchers. Yet, they’ve found the following potential effects of lack of deep sleep:
• Sleep inertia – feeling groggy and disoriented for up to an hour after waking up.
• Impaired memory – forgetfulness and poor retention of memories.
• Higher risk of diabetes – lack of deep sleep reduces insulin sensitivity and leads to an increased risk of diabetes.
• Hypertension – during deep sleep blood pressure reduces and by losing deep sleep the risk of hypertension increases.
• Mood changes – staying positive during the day is difficult without getting the deep sleep needed at night.
Lack of deep sleep could also reduce sleep quality in general, thus leading to other sleep deprivation-related symptoms including:
• Poor focus and concentration
• Mood swings and irritability
• Slower reaction times
• Low energy levels
• Chronic health issues like obesity, depression, and heart disease
• Work, school, or social-life problems

Due to its importance, a lack of deep sleep can lead to learning difficulties and frequent infections. Not getting enough deep sleep can even contribute to some serious health conditions like heart disease and Alzheimer’s disease.
Finally, let’s see how you can increase the amount of deep sleep you get each night. Namely, even though there is no single solution to increasing deep sleep, certain steps can help improve your sleep hygiene which in turn would improve sleep quality and promote deep sleep. Here are some tips to follow:
• Do regular exercises – a half-an-hour work out a day, at least three hours before bed, is ideal for improving sleep.
• Don’t consume caffeine or alcohol before bedtime – avoid consuming these stimulants for at least several hours before going to bed.
• Increase sunlight exposure – to keep a healthy sleep schedule exposure to daylight is key, while lowering lights in your home before bed.
• Follow a strict sleep schedule – keeping a consistent schedule, i.e. going to bed and waking up at the same time every day, even during weekends, promotes better sleep.
1. Sleep physiology – sleep disorders and sleep deprivation
– NCBI bookshelf. (n.d.-b). https://www.ncbi.nlm.nih.gov/ books/NBK19956/
Lee A. Surkin, MD, is the Chief Medical Officer of Nexus Dental Systems. A private practitioner in cardiology, sleep medicine, and obesity medicine, he is one of a small group of physicians to be triple board certified in cardiology, sleep medicine, and nuclear cardiology. In 2009, he created Carolina Sleep – the only dedicated sleep medicine practice in eastern NC. Dr. Surkin has created a cardiovascular and sleep healthcare model that includes a multi-faceted diagnostic and treatment approach that is enhanced by a network of relationships with physicians, dentists, respiratory therapists, sleep technologists, and public officials who recognize the important role that sleep medicine has in our daily life. In 2012, Dr. Surkin founded the American Academy of Cardiovascular Sleep Medicine which is a not-for-profit academic organization dedicated to educating healthcare providers, supporting research, and increasing public awareness of the convergence between cardiovascular disease and sleep disorders. In 2014, Dr. Surkin created a new multi-specialty practice called Carolina Clinic for Health and Wellness which combines his specialties with primary care, gynecology, behavioral health and a medical spa. Dr. Surkin is married with three daughters and a golden retriever and resides in Greenville, NC.

by Daniel Gartenberg, PhD

Insomnia is the most pervasive sleep disorder in the United States, impacting roughly 1 in 5 adults.1 This physiological and psychological disorder often co-occurs with obstructive sleep apnea, where 39-58% of sleep apnea patients also have insomnia.2-4 But the problem of poor sleep health in general is even larger than this. About 1 in 2 Americans suffer from poor sleep health due to a combination of sleep disorders, sleep deprivation, and poor sleep quality. Poor sleep health is a primary cause of chronic disease, including heart disease, Alzheimer’s and related dementia, cancer, and diabetes.5-12 As William Dement stated, the father of sleep medicine, “We are a sleep sick society.” Dentists may hold the keys to solving this public health crises of poor sleep health, for both insomnia and sleep apnea.
The first line treatment for insomnia is Cognitive Behavioral Therapy for Insomnia (CBTi), recommended by both the American College of Physicians (ACP) and the American Academy of Sleep Medicine.13 CBTi is typically administered by a sleep medicine specialist or a psychologist certified in behavioral sleep medicine. The main components of CBTi include sleep restriction, stimulus control, cognitive training, relaxation, and sleep hygiene. By focusing on cognitive, behavioral, and emotional-based strategies to change sleep, CBTi is designed to get at the root causes of sleep challenges. Sleep restriction, or the gentler method of sleep compression, involves reducing time in bed until ideal sleep efficiency of ~85% is reached. Sleep logs are typically kept to inform the recommended sleep schedule. Stimulus control refers to using the bed for only
sleep (with sex being the exception), to reestablish the association between bed and sleep. Cognitive training involves psychoeducation about normal sleep and skills to challenge and cope with unhelpful thoughts, including those about sleep. Finally, relaxation includes behavioral techniques to decrease hyperarousal, which is thought to be a primary contributor to insomnia. Relaxation training includes breathing exercises, progressive muscle relaxation, and mindfulness skills.
Yet the medical community has failed at addressing the public health issue of poor sleep health with this proven solution. Most people who have sleep disorders remain undiagnosed and untreated.14 This failure is due to issues of access, cost, and adherence. Medical doctors typically only receive about two hours of didactic training in sleep health and there are only ~7,500 MDs board certified in sleep medicine. Psychologists certified in Behavioral Sleep Medicine (BSM) can also administer CBTi, but again, there is an issue of access. In 2023, the New York Times reported that in the United States there are less than 700 providers trained in BSM. Many communities completely lack effective care, given that 58% of BSM providers reside in only twelve U.S. states.15 Cost is another major limiting factor because CBTi treatment involves at least six consultations, typically ranging from weekly to monthly, with a clinician, at a potential cost up to as much as $3000. This treatment can be onerous and time consuming for patients, with homework assignments and changes to typical habits. This makes adherence another major challenge of CBTi.16,17
As a result of access, cost, and adherence limitations, few people receive the gold-stan-
dard treatment of CBTi and often turn to risky alternatives (i.e. drugs and alcohol). The most common treatment for insomnia is sedating anti-depressant and hypnotic medications. However, these solutions are not as effective in the long-term as CBTi,18 can negatively impact sleep quality,19 cause falls in the elderly,19 and have other negative side effects, such as doubling the risk of developing dementia.20,21 Recently, FDA approved digital therapeutics for CBTi (dCBTi) solutions, such as Somryst and Sleepio, have improved the cost, access, scalability, and ease of dissemination for CBTi, in addition to demonstrating efficacy.22-25 However, these solutions are still currently not accepted by insurance and are costly for most Americans, ranging in price from $450-$850. Additionally, adherence to these solutions is poor,26 which negatively impacts the effectiveness of these interventions. There is currently no easy and affordable way for patients to access dCBTi, and when they do, they are unlikely to complete treatment.
Recently, FDA approved digital therapeutics for CBTi (dCBTi) solutions, such as Somryst and Sleepio, have improved the cost, access, scalability, and ease of dissemination for CBTi, in addition to demonstrating efficacy.22-25 However, these solutions are still currently not accepted by insurance and are costly for most Americans, ranging in price from $450-$850. Additionally, adherence to these solutions is poor,26 which negatively impacts the effectiveness of these interventions. There is currently no easy and affordable way for patients to access dCBTi, and when they do, they are unlikely to complete treatment.
Building on the work of prior dCBTi solutions, and through funding from the National Institutes of Health (NIH) and major venture capitalists, SleepSpace.com was developed. SleepSpace is a software platform that activates the sensors available in any smart phone to track sleep, includes a digital version of the consensus sleep diary, sounds and meditations to help with sleep, and automated notifications and content based on cognitive behavioral therapy for insomnia. SleepSpace can be either fully automated or administered by a trained sleep specialist.
Along with collaborators Professor Orfeu Buxton at the Pennsylvania State University and Professor Daniel Taylor at the University of Arizona, a randomized controlled trial was performed showing that an Internet of
Things (IoT) solution like SleepSpace, when administered by a trained BSM psychologist, can more effectively treat insomnia.27-30 The study showed that when a BSM trained psychologist used the SleepSpace system alongside 6-weeks of telehealth administered CBTi, compared to treatment-as-usual and a sleep hygiene control that also involved 6-weekly sessions with a clinician, there was increased remission of insomnia.29,30 This was based on the Insomnia Severity Index (ISI), the gold standard measure of insomnia, in addition to improvements across other sleep statistics. The SleepSpace system was built off of proven CBTi-based interventions and designed to increase adherence, which was shown to be an effective and safe solution for individuals suffering from insomnia. This technology is currently available on all iPhone and Android platforms to improve at an affordable price ($49.99 / year) that includes a 7-day free trial. Such dCBTi or dCBTi-based solutions can be made more efficacious when combined with safe and effective pharmacological interventions.31 Therefore, SleepSpace was recently combined with a pharmacological solution called MDbio - The Doctors Brand™. MDbio ran the largest non-melatonin randomized, double-blind, placebo-controlled trial showing that this nutraceutical significantly reduced symptoms of insomnia.32 The formulation, called MDsleep, has a mechanism of

Daniel Gartenberg, PhD, is a world-renowned sleep scientist and the founder and CEO of SleepSpace, a company that develops innovative solutions for improving sleep quality and health. He has a PhD in cognitive psychology from George Mason University and more than 15 years of experience in sleep research and technology. He is also an Adjunct Assistant Professor at Penn State University’s Department of Biobehavioral Health. He is a scientific consultant for a number of sleep related companies including MDbio - The Doctors Brand, Wesper, CPAP.com, Perfectly Snug, and Biostrap. Dr. Gartenberg is at the forefront of sleep science innovation. His work, supported by over $3.5 million in grants from the National Science Foundation and the National Institute of Aging, focuses on developing cutting-edge technologies and strategies to address the global challenge of poor sleep health. As a biohacker who founded the DC chapter of the Quantified Self, a former insomniac, and a sleep apnea patient, improving sleep is deeply personal to him. Yet sleep is also still a mystery. Scientists have made great strides in understanding sleep, but there is still a ton we don’t know about when we close our eyes for the night. Dr. Gartenberg has more than 20 peer-reviewed publications and a viral TED Talk with over 5 million views.


action that utilizes GABA, L-theanine, and botanicals, which are non-psychoactive and do not have risks like addiction or falls. The benefit of combining dCBTi-based solutions with nutraceuticals is that they can compound one-another’s effects on reducing the activation of the sympathetic nervous system. An overactive fight-or-flight response is a primary driver of both insomnia and sleep apnea. GABA is the most common inhibitory neurotransmitter, which is why it plays a key role in reducing the stress response physiologically, while CBTi-based solutions act on addressing the root causes of stress and anxiety, reducing the likelihood of excessive rumination and staying up with insomnia.
This combined dCBTi and nutraceutical solution was recently coined the “Sleep Corner,” which is currently being piloted with a number of dental offices and longevity centers. Dentists can play an important role in increasing access for these new technologies for addressing the public health issue of poor sleep. To provide a complete and holistic solution for society’s sleep health crises, at-home-sleepapnea testing is also optionally included in the Sleep Corner to evaluate breathing health when appropriate. This solution can pivot into a fully reimbursable medical diagnosis for sleep apnea that includes a treatment plan with reliable referrals to develop a Mandibular Advancement Device when appropriate. The solution can be a medical or non-medical sleep health tool administered by coaches, members of the dental team, or licensed sleep specialists. Only 2-hours of virtual training is needed to activate to sleep corner in dental practices. Digital and physical assets for identifying what sleep solutions are right for the patient and driving the purchase of this comprehensive product offering are also provided to help get more people’s sleep health under control. As many as 80% of people with sleep apnea remain undiagnosed and untreated. A dentist can now easily incorporate CBTi-based solutions, nutraceuticals, and an at-home-apnea-test with a medical diagnosis into their practice through signage and digital assets. This provides a turnkey and comprehensive sleep health solution for the 1 in 2 patients that suffer from poor sleep.
Dentists have access to more patient time than any other doctor. They are therefore best positioned to deal with the issue of poor sleep health. Identifying issues like bruxism, snor-
ing, daily fatigue, and problems falling asleep and staying asleep can be easily screened for. The next logical step is to then get patients quick access to sleep solutions and a pathway to get diagnosed and treated. The Sleep Corner can be a first step in dental practices becoming more acquainted with sleep medicine before engaging in more extensive training in sleep medicine. Once certified in dental sleep medicine by accredited organizations like Nexus Dental Systems, practices can play an important role in treating sleep apnea with MADs. Such training can further improve the positive healthcare footprint of dental practices and finally solve the public health issue of poor sleep. For more information on how to incorporate Sleep Corner to your practice today, contact dan@sleepSpace.com.
1. Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J. The Economic Burden of Insomnia: Direct and Indirect Costs for Individuals with Insomnia Syndrome, Insomnia Symptoms, and Good Sleepers. 2009;32(1):10.
2. Grandner MA, Perlis ML. Insomnia as a cardiometabolic risk factor. Sleep. 2013;36(1):11-12. doi:10.5665/sleep.2288
3. Grandner MA, Jackson NJ, Pak VM, Gehrman PR. Sleep disturbance is associated with cardiovascular and metabolic disorders. J Sleep Res. 2012;21(4):427-433. doi:10.1111/j.1365-2869.2011.00990.x
4. Laugsand LE, Strand LB, Platou C, Vatten LJ, Janszky I. Insomnia and the risk of incident heart failure: a population study. Eur Heart J. Published online March 5, 2013. doi:10.1093/eurheartj/eht019
5. Pandey A, Williams N, Donat M, et al. Linking sleep to hypertension: greater risk for blacks. Int J Hypertens. 2013;2013.
6. Bamimore A, Olafiranye O, Demede M, et al. High Prevalence of Hypertension and Other Cardiometabolic Risk Factors in US- and Caribbean-Born Blacks with Chest Pain Syndromes. Cardiorenal Med. 2012;2(3):163-167. doi:10.1159/000337716
7. St-Onge MP, Grandner MA, Brown D, et al. Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement From the American Heart Association. Circulation. 2016;134(18):e367-e386. doi:10.1161/ CIR.0000000000000444
8. Liu Y, Wheaton AG, Chapman DP, Croft JB. Sleep duration and chronic diseases among U.S. adults age 45 years and older: evidence from the 2010 Behavioral Risk Factor Surveillance System. Sleep. 2013;36(10):1421-1427. doi:10.5665/sleep.3028
9. Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863-867.
10. Lu C, Sun H, Huang J, et al. Long-Term Sleep Duration as a Risk Factor for Breast Cancer: Evidence from a Systematic Review and Dose-Response Meta-Analysis. Biomed Res Int. 2017;2017.
11. Truong KK, Lam MT, Grandner MA, Sassoon CS, Malhotra A. Timing Matters: Circadian Rhythm in Sepsis, Obstructive Lung Disease, Obstructive Sleep Apnea, and Cancer. Ann Am Thorac Soc. 2016;13(7):1144-1154. doi:10.1513/AnnalsATS.201602-125FR
12. Alcantara C, Biggs ML, Davidson KW, et al. Sleep Disturbances and Depression in the Multi-Ethnic Study of Atherosclerosis. Sleep. 2016;39(4):915-925. doi:10.5665/sleep.5654
13. Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD, for the Clinical Guidelines Committee of the American College of Physicians. Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2016;165(2):125. doi:10.7326/M15-2175
14. Liao WJ, Song LJ, Yi HL, et al. Treatment choice by patients with obstructive sleep apnea: data from two centers in China. J Thorac Dis. 2018;10(3):1941-1950. doi:10.21037/jtd.2018.03.135
15. Thomas A, Grandner M, Nowakowski S, Nesom G, Corbitt C, Perlis
Science-backed sleep protocol for real results

Offer the most comprehensive sleep solution in your clinic, complete with an OSA diagnosis


Sleep quality aid
Sleep tracking & protocols
Sleep stages, sleep efficiency, HRV, sleep time stress, CBTi

sleep test
Your one stop solution for restful nights. Our 30-day clinical program is designed to uncover the root causes of your sleeplessness and provide the most comprehensive, personalized sleep solutions. Our kit includes: clinically proven sleep supplements, at-home sleep test, Cognitive Behavioral Therapy, consultations with board certified sleep physicians, and 30 day personalized programming from world renowned sleep experts.
Learn more about Sleep Corner™ for dental sleep medicine.

ML. Where are the Behavioral Sleep Medicine Providers and Where are They Needed? A Geographic Assessment. Behav Sleep Med. 2016;14(6):687-698. doi:10.1080/15402002.2016.1173551
16. Vincent NK, Hameed H. Relation between adherence and outcome in the group treatment of insomnia. Behav Sleep Med. 2003;1(3):125-139.
17. Harvey L, Inglis SJ, Espie CA. Insomniacs’ reported use of CBT components and relationship to long-term clinical outcome. Behav Res Ther. 2002;40(1):75-83.
18. Morin CM, Vallières A, Guay B, et al. Cognitive Behavioral Therapy, Singly and Combined With Medication, for Persistent Insomnia: A Randomized Controlled Trial. JAMA. 2009;301(19):2005. doi:10.1001/jama.2009.682
19. Chen TY, Lee S, Buxton OM. A Greater Extent of Insomnia Symptoms and Physician-Recommended Sleep Medication Use Predict Fall Risk in Community-Dwelling Older Adults. Sleep. 2017;40(11). doi:10.1093/sleep/zsx142
20. Chen PL, Lee WJ, Sun WZ, Oyang YJ, Fuh JL. Risk of Dementia in Patients with Insomnia and Long-term Use of Hypnotics: A Population-based Retrospective Cohort Study. Forloni G, ed. PLoS ONE. 2012;7(11):e49113. doi:10.1371/journal.pone.0049113
21. Lee J, Jung SJ, Choi J won, Shin A, Lee YJ. Use of sedative-hypnotics and the risk of Alzheimer’s dementia: A retrospective cohort study. Romigi A, ed. PLOS ONE. 2018;13(9):e0204413. doi:10.1371/journal.pone.0204413
22. Ritterband LM, Thorndike FP, Ingersoll KS, et al. Effect of a WebBased Cognitive Behavior Therapy for Insomnia Intervention With 1-Year Follow-up: A Randomized Clinical Trial. JAMA Psychiatry. 2017;74(1):68-75. doi:10.1001/jamapsychiatry.2016.3249
23. Ritterband LM, Thorndike FP, Morin CM, et al. Real-world evidence from users of a behavioral digital therapeutic for chronic insomnia. Behav Res Ther. 2022;153:104084. doi:10.1016/j.brat.2022.104084

25. Morin CM. Profile of Somryst Prescription Digital Therapeutic for Chronic Insomnia: Overview of Safety and Efficacy. Expert Rev Med Devices. 2020;17(12):1239-1248. doi:10.1080/17434440.2020.18 52929
26. Nwosu A, Boardman S, Husain MM, Doraiswamy PM. Digital therapeutics for mental health: Is attrition the Achilles heel? Front Psychiatry. 2022;13:900615. doi:10.3389/fpsyt.2022.900615
27. Gartenberg D. Can smart lights improve your sleep quality. Medium. https://medium.com/@dangartenberg/can-smart-lights-improveyour-sleep-quality-7fc7894446ca. June 25, 2023.
28. Emert SE, Taylor DJ, Gartenberg D, et al. A non-pharmacological multi-modal therapy to improve sleep and cognition and reduce mild cognitive impairment risk: Design and methodology of a randomized clinical trial. Contemp Clin Trials. Published online June 2023:107275. doi:10.1016/j.cct.2023.107275
29. Schade, M. M., Roberts, D. M., Gartenberg D, et al. Randomized controlled trial of telehealth: Technology-assisted CBTi+, CBTi, and sleep hygiene in older adults. 38th Annu Meet Assoc Prof Sleep Soc APSS. Published online (submitted).
30. Schade, M. M., Roberts, D. M., Gartenberg D, et al. Randomized controlled trial of telehealth: Technology-assisted CBTi+, CBTi, and sleep hygiene in older adults. J Clin Sleep Med. Published online (in prep).
31. Vallim JRDS, Pires GN, Bonaldi RR, et al. Effectiveness of digital cognitive-behavioral therapy for insomnia alone or combined with sleep medication: A real-world evidence study. Sleep Epidemiol. 2023;3:100061. doi:10.1016/j.sleepe.2023.100061
32. Kolobaric A, Hewlings SJ, Bryant C, et al. A Randomized, Double-Blind, Placebo-Controlled Decentralized Trial to Assess Sleep, Health Outcomes, and Overall Well-Being in Healthy Adults Reporting Disturbed Sleep, Taking a Melatonin-Free Supplement. Nutrients. 2023;15(17):3788. doi:10.3390/nu15173788
24. Seyffert M, Lagisetty P, Landgraf J, et al. Internet-Delivered Cognitive Behavioral Therapy to Treat Insomnia: A Systematic Review and Meta-Analysis. Ferri R, ed. PLOS ONE. 2016;11(2):e0149139. doi:10.1371/journal.pone.0149139

Air is designed to quickly and easily set therapeutic bite for optimal airflow. With 7 levels of vertical and 8 levels of horizontal adjustment in 1mm increments, this precise system is easy to understand and fast to administer.
Air is also 3D printed to an accuracy of under 50 microns.



by Saim S. Choudhry, DO
Expiratory flow limitation (EFL) is a common feature in patients with obstructive lung diseases such as COPD and asthma. EFL not only impacts daytime respiratory function but also significantly affects sleep quality and the severity of sleep apnea. Understanding the relationship between EFL and sleep apnea is crucial for the effective management of sleep-related breathing disorders in these patients.
Expiratory Flow Limitation and Sleep Apnea: The Connection
1. Mechanisms Linking EFL and Sleep Apnea: EFL occurs when the maximum flow rate during expiration is reached and cannot be increased by further respiratory effort. This limitation is due to airway obstruction, which is exacerbated during sleep when muscle tone decreases, leading to increased airway resistance and collapse. In patients with obstructive lung disease, this can result in the worsening of obstructive sleep apnea.
2. Dynamic Hyperinflation During Sleep: Dynamic hyperinflation, a consequence of EFL, leads to increased lung volumes and reduced inspiratory capacity. During sleep, this can cause a higher intrathoracic pressure, increasing the

likelihood of upper airway collapse and apneic events. The combination of EFL and reduced airway muscle tone during sleep can significantly worsen sleep apnea severity.
3. Increased Work of Breathing: Patients with EFL experience increased work of breathing, which can carry over into sleep. This increased effort can lead to frequent arousals and fragmented sleep, contributing to poor sleep quality and exacerbation of daytime symptoms such as fatigue and cognitive impairment.
Clinical Implications of EFL in Sleep Apnea
1. Symptom Severity and Quality of Life: EFL is associated with more severe symptoms of sleep apnea, including


higher AHI scores, increased nocturnal desaturation, and more pronounced daytime sleepiness. This can significantly impact the patient’s quality of life, leading to increased morbidity and healthcare utilization.
2. Challenges in PAP Therapy: Patients with both EFL and OSA may find PAP therapy more challenging due to the higher pressures required to keep the airways open. This can lead to discomfort, reduced adherence, and the need for specialized PAP devices or settings.
3. Assessment and Monitoring: Proper assessment of EFL in patients with obstructive lung disease and sleep apnea is crucial. Techniques such as spirometry, body plethysmography, and overnight polysomnography can help quantify the extent of airway obstruction and sleep apnea severity, guiding personalized treatment plans.
1. Optimizing PAP Therapy: For patients with both EFL and OSA, optimizing PAP therapy is essential. Auto-titrating PAP devices that adjust pressure in response to respiratory events can be particularly beneficial. Additionally, BPAP therapy,

Dr. Saim Choudhry, based at the Haven Health Care Medical Group in Woodhaven, Michigan, is a distinguished sleep medicine specialist renowned for his expertise and board certification in internal medicine. With advanced training from the Detroit Medical Center, Dr. Choudhry is at the forefront of diagnosing and treating a broad spectrum of sleep disorders, including sleep apnea, restless legs syndrome, narcolepsy, and various sleep movement disorders. Dr. Choudhry’s practice is centered on the belief that sleep is a critical pillar of health, alongside diet, exercise, and mental well-being. His approach is holistic, ensuring that treatment plans are not only focused on alleviating symptoms but also on integrating healthy sleep habits to improve overall life quality. His work extends beyond the clinic as he actively engages in sleep medicine advancements to bring the latest and most effective treatments to his patients. At Haven Health Care Medical Group, Dr. Choudhry emphasizes a patient-centered approach, tailoring treatments to each individual’s needs and lifestyle. His dedication to his patients’ well-being is evident in the compassionate care he provides and his commitment to educating patients about their conditions and treatment options. For those seeking expert care in sleep medicine and a path to better overall health, Dr. Choudhry offers a blend of specialized knowledge, innovative treatment solutions, and a deeply empathetic approach to patient care.
which provides different pressures for inhalation and exhalation, can help reduce the work of breathing and improve comfort.
2. Pharmacological Interventions: Bronchodilators, such as LABAs and LAMAs, can reduce airway resistance and improve expiratory flow. These medications can be used in conjunction with PAP therapy to enhance overall respiratory function and sleep quality.
3. Non-Pharmacological Approaches: Pulmonary rehabilitation, including exercise training and breathing techniques, can improve respiratory muscle function and reduce the impact of EFL. Weight management and positional therapy may also help reduce the severity of sleep apnea.
4. Integrated Care Approach: An integrated care approach that involves pulmonologists, sleep specialists, and respiratory therapists can provide comprehensive management for patients with EFL and OSA. Coordinated care ensures that both the respiratory and sleep-related aspects of the patient’s condition are addressed.
Expiratory flow limitation significantly impacts the severity and management of sleep apnea in patients with obstructive lung diseases. Understanding the interplay between EFL and sleep apnea is essential for providing effective treatment and improving patient outcomes. By optimizing PAP therapy, utilizing pharmacological and non-pharmacological interventions, and adopting an integrated care approach, healthcare providers can help patients achieve better sleep quality and overall health. Continued research and innovation in this field will lead to more effective treatments and improved management strategies for this complex patient population.
1. Pepin, J. L., Guillot, M., Tamisier, R., & Lévy, P. (2012). The Role of Expiratory Flow Limitation in Obstructive Sleep Apnea. European Respiratory Journal, 40(6), 1513-1520. Available at: https://erj.ersjournals.com
2. Owens, R. L., & Malhotra, A. (2010). Sleep-disordered Breathing and COPD: The Overlap Syndrome. Respiratory Care, 55(10), 1333-1344. Available at: https://rc.rcjournal.com
3. McNicholas, W. T., & Bonsignore, M. R. (2007). Sleep Apnea as an Independent Risk Factor for Cardiovascular Disease: Current Evidence, Basic Mechanisms and Research Priorities. European Respiratory Journal, 29(1), 156-178. Available at: https://erj.ersjournals.com
4. Fletcher, E. C., & Miller, J. (2007). Role of Respiratory Muscle Function and Control in the Pathogenesis of Obstructive Sleep Apnea. American Journal of Respiratory and Critical Care Medicine, 175(8), 823-830. Available at: https://www.atsjournals.org

• Whole-Team Training
• Ongoing Coaching
• Streamlined Protocols
• Precision Bite Technology
• Patient Education
• In-Network Medical Billing

by Nathan S. Bryan, PhD
Chronic disease starts in the mouth. Dental medicine practitioners are the most important and most impactful practitioners in medicine. The discovery and elucidation of the human microbiome project has led to a new understanding into the potential mechanism of human disease. This self-instructional course for dentists reveals the role of the oral microbiome in producing nitric oxide and protecting from hypertension, inflammation, and cardiovascular disease. There must be a balance between eradicating known oral pathogens while maintaining and supporting a healthy and diverse oral microbiome.
Dental Sleep Practice subscribers can answer the CE questions online at https:// dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
1. Understand the role of the oral microbiome in producing nitric oxide.
2. Discuss how nitric oxide protects against inflammation and resulting diseases.
3. Provide recommendations on how to improve a patient's nitric oxide production.
Oral health is absolutely essential for systemic health. The notion that oral bacteria may contribute to disease in other parts of the body has been discussed since at least the end of the 19th century. William Hunter in 1900 first described “oral sepsis” as a cause of human disease.1 This started a wave of research into the role of oral health and the development of systemic disease. Today we certainly have an appreciation for the oral systemic link that describes how poor oral hygiene leads to an increased risk of conditions such as cardiovascular diseases, diabetes, respiratory disorders, osteoporosis, and even adverse pregnancy outcomes. There are known bacterial pathogens that have been shown to contribute to periodontal disease and gingivitis. Rightfully so, these pathogens are often times targeted by dentists in patients that have known oral pathogens. Use of stringent antiseptics such as chlorhexidine has been used in dental medicine since the 1970s. Data have shown that the use of chlorhexidine can reduce gingival plaque by killing oral bacteria thereby improving the progression of periodontal disease.2 However, there is always collateral damage due to the complete destruction of the human oral microbiome. These antiseptics kill the pathogens, but they also destroy the non-pathogenic commensal bacteria. Science now reveals this may cause more harm than good.
The human microbiome is made up of hundreds of different bacterial species, which outnumber our human cells ten to one and provide functions that are essential for our survival. There exists a human nitrogen cycle which is now well elucidated that provides a source of bioactive nitric oxide through the activity of specific oral bacteria. This pathway, termed the entero-salivary nitrate-nitrite-nitric oxide pathway, can positively contribute nitric oxide based signaling throughout the human host.3,4 It is now recognized that the oral commensal bacteria provide an important metabolic function in human physiology by contributing a nitric oxide synthase (NOS)-independent source of NO. Human nitrate reduction requires the presence of oral nitrate-reducing bacteria as mammalian cells cannot effectively reduce this anion. The two-electron reduction of nitrate forms nitrite in the saliva and then when we swallow our own saliva, in the acid environment of the stomach, nitric oxide is produced. The nitric oxide that is produced in the acid stomach enhances gastric mucosal blood flow,5 protects from gastric ulcerations from chronic non-steroidal anti-inflammatory drugs (NSAIDS)6 and from ulcer causing bacteria Helicobacter pylori.7 Obviously, this pathway serves as a critical and fundamental source of nitric oxide. The process of bacterial nitrate reduction to nitrite and nitric oxide is illustrated below. Nitric oxide derived from nitrite is known to regulate blood pressure, improve insulin signaling, and inhibit inflammation.8-10 Without the right oral bacteria
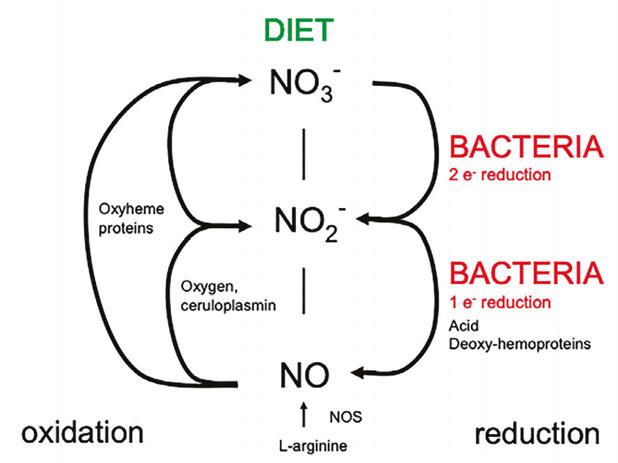
present and without stomach acid production, this pathway cannot be effective at producing nitric oxide and providing any benefit to the human host.
An increase in blood pressure puts you at an increased risk for heart disease and stroke, which are leading causes of death in the United States and worldwide. Two out of every three Americans has an unsafe elevation in blood pressure. Despite aggressive treatment with medications, sometimes multiple medications, only about half of those medicated have managed blood pressure. The Systolic Blood Pressure Intervention Trial (SPRINT) showed that among adults with hypertension but without diabetes, lowering systolic blood

Nathan S. Bryan, PhD, earned his undergraduate Bachelor of Science degree in Biochemistry from the University of Texas at Austin and his doctoral degree from Louisiana State University School of Medicine in Shreveport where he was the recipient of the Dean’s Award for Excellence in Research. He pursued his post-doctoral training as a Kirschstein Fellow at Boston University School of Medicine in the Whitaker Cardiovascular Institute. After a two year post-doctoral fellowship, in 2006 Dr. Bryan was recruited to join faculty at the University of Texas Health Science Center at Houston by Ferid Murad, MD, PhD, 1998 Nobel Laureate in Medicine or Physiology. Dr. Bryan has been involved in nitric oxide research for the past 20 years and has made many seminal discoveries in the field. His many seminal discoveries have resulted in dozens of issued US and International patents and the product technology resulting from his discoveries and inventions has improved patient care worldwide. Dr. Bryan is a successful entrepreneur and Founder, Chairman, and CEO of Bryan Therapeutics, Inc., a privately-held, clinical-stage biotechnology company that is actively engaged in the discovery and development of nitric oxide-based therapies. BTI has active drug development programs in heart disease, Alzheimers’ Disease, and topical drugs for diabetic ulcer and non-healing wounds. Dr. Bryan is an international leader in molecular medicine and nitric oxide biochemistry.
pressure to a target goal of less than 120 mm Hg, as compared with the standard goal of less than 140 mm Hg, resulted in significantly lower rates of fatal and nonfatal cardiovascular events and death from any cause.11 Because blood pressure remains elevated in ≈50% of all treated hypertensive patients despite polypharmacy,12,13 perhaps focusing on a healthy oral microbiome that can provide a source of nitric oxide may provide additional blood pressure lowering effects.
The presence or absence of select and specific bacteria may determine steady state blood pressure levels.14
In various animal models and in humans, dietary nitrate supplementation has shown numerous beneficial effects, including a reduction in blood pressure, protection against ischemia-reperfusion damage, restoration of NO homeostasis with associated cardioprotection, increased vascular regeneration after chronic ischemia, and a reversal of vascular dysfunction in the elderly.15-18 However, all of these effects were reduced or completely abolished when the oral microbiota were abolished with an antiseptic mouthwash.15,19 Plasma and salivary nitrite levels are abolished after a dietary nitrate load in healthy subjects taking an antiseptic mouthwash.20 It has been reported that dietary nitrate reduces blood pressure in healthy volunteers,21,22 and that the effects are abolished after rinsing with oral antiseptic mouthwash.23 Both strong and weak antibacterial agents suppress the rise in plasma nitrite observed following the consumption of a high nitrate diet and stronger antiseptics can influence

In some cases, using mouthwash for only one week caused a more than 25 mmHg increase in blood pressure.
the blood pressure response during low-intensity exercise.24 Additionally, it was recently shown that in the absence of any dietary modifications, a seven-day period of antiseptic mouthwash treatment to disrupt the oral microbiota reduced both oral and plasma nitrite levels in healthy human volunteers, and was associated with a sustained increase in both systolic and diastolic blood pressure.23 Oral nitrite exerts antihypertensive effects in the presence of antiseptic mouthwash that disrupts the enterosalivary circulation and reduction of nitrate.25 Altogether, these studies firmly establish the role for oral nitrate-reducing bacteria in making a physiologically relevant contribution to host nitrite and thus NO levels, with measureable physiological effects. It appears that providing nitrite can overcome the absence of microbial nitrate reduction.
Eradication of oral bacteria through anti-septic mouthwash or over-use of antibiotics causes blood pressure to increase. Allowing recolonization of nitrate and nitrite reducing bacteria can normalize blood pressure. Management of systemic hypertension through maintenance of the oral microbiome is a completely new paradigm in cardiovascular medicine. In some cases, using mouthwash for only one week caused a more than 25 mmHg increase in blood pressure. The results and implications from this study are life changing. For the first time, we may have an explanation for the hypertension epidemic and why prescription drugs don’t always work to reduce blood pressure. This study demonstrates that we have missed the target and have focused on the wrong scientific pathways for answers.
Cardiovascular disease remains the number one killer of men and women worldwide. Every year approximately 610,000 people die from cardiovascular related events in the US alone. That’s one out of every 4 deaths. High blood pressure is the number one modifiable risk factor for the development of cardiovascular disease. Two out of three people in the US have an elevation in blood pressure.26 This is over 200,000,000 people. For every 1 mmHg increase in blood pressure starting at 110 mmHg in systolic blood pressure, this increases your risk of heart disease by 1%. So, if your systolic pressure or top number is 140, you have increased your chance of heart disease by 30%. Ac-
cording to the American Heart Association, only about half of the people who take blood pressure medicine have their blood pressure normalized and many of these people are taking 2-4 different prescription medications.
The microbiome has been a major story in science and medicine for the past 20 years. We now know that many diseases are caused by dysbiosis or disruption of good bacterial communities in the body. However, most of these studies and information comes from studying our gut bacteria. We have only recently begun to focus on oral bacteria. We have known for decades the importance of oral bacteria. Poor oral hygiene, people with periodontitis and gingivitis have an increased risk of dying from heart disease. In fact, oral bacteria have been found in the plaque of arteries of people who have died of heart attack. This led dentists and other health care practitioners to recommend using antiseptic mouthwash to kill the oral bacteria. The use of fluoride toothpaste has increased. Recommendations to use antiseptic mouthwash were pushed by dentists and consumer product makers. Over prescribing antibiotics began to occur. All of these now common practices have now caused a serious problem. We know that along with the bad bacteria, there are good bacteria that are necessary for normal human metabolism. Killing the bad bacteria leads to the collateral damage and killing of the good bacteria. The consequences may be more damaging than we ever imagined.
We need nitrate reducing bacteria in the mouth in order to utilize the nitrate we get from eating green leafy vegetables in our diet. Without these bacteria, we do not get the cardiovascular benefits of eating a healthy diet.27 The nitrate reducing bacteria generate nitrite and nitric oxide which are both cardioprotective, reduce blood pressure, and maintain normal cardiovascular function. At least 50% of our daily nitric oxide production comes from our diet and oral bacteria. Loss of nitric oxide production is the first step in the onset and development of cardiovascular disease. Therefore, anything that disrupts or interrupts nitric oxide puts our body at risk for hypertension and cardiovascular disease.28
This is our problem today. Every single day, over 200,000,000 Americans get up and use an antiseptic mouthwash. Most people are using a fluorinated toothpaste. Fluoride
is a stringent antiseptic that kills most oral bacteria. There are over 250,000,000 million prescriptions written every year for antibiotics. Are these practices causing unintended problems with oral dysbiosis and a lack of nitric oxide production? It is time to re-evaluate our daily practices. The risks of using antiseptic mouthwash far outweigh the benefits. Doctors are too eager to prescribe antibiotics even for prophylactic reasons rather than let our own immune system do its job.
If you use mouthwash or use fluorinated toothpaste, then this completely eliminates the nitric oxide producing effects of eating a plant-based diet.20 Using antiseptic mouthwash can actually prevent the cardioprotective benefits of exercise.29 As we try to live longer and better lives, many of us try to eat better, including more green leafy vegetables, and try to get exercise. However, if we use mouthwash or any oral antiseptic, we lose the benefits of our diet and of our exercise regimen.
What is becoming increasingly clear is how critical and important nitric oxide is for our health and well-being. There is a clear and beneficial role of oral nitrate reducing bacteria to produce nitric oxide inside our bodies. Getting rid of these bacteria disrupts nitric oxide production and therefore disrupts every function in the body that is dependent upon nitric oxide. This includes maintaining normal blood pressure, maintaining normal sexual function, cognition, memory, reducing inflammation, and making sure every cell in our body gets the oxygen and nutrients it needs to survive and do its job.
It is important to remember to do the good things that are proven to improve nitric oxide production such as moderate physical exercise, eating a balanced diet enriched in green leafy nitrate rich vegetables, and deep breathing. Perhaps just as or more important, we must stop doing the things that disrupt our body’s ability to produce nitric oxide and this includes using antiseptic mouthwash, overusing antibiotics as well as antacids. The human body is much smarter than we are. If we give the body what it needs, it heals itself. If we remove the barriers that disrupt how the body works, it begins to heal itself.
I think sometimes we have become too sophisticated in our daily practices. There is nothing more important to your health and well-being than making sure your body can
We now know that many diseases are caused by dysbiosis or disruption of good bacterial communities in the body.
produce nitric oxide. We should get out of our own way and let the body do what it is designed to do. Heal thyself. The good news is that you do not have to rely on your physician to get you started. You can actually take control of your own health. Start improving your nitric oxide production today. There are a few simple steps:
• If you use antiseptic mouthwash or fluoride toothpaste, you must stop. Mouthwash and fluoride kill essential bacteria in the mouth responsible for production of nitric oxide.
• If you use antacids, you should consult with your physician to wean off. Antacids shut down nitric oxide production and increase your risk of heart attack and stroke by 40%.
• Avoid sugary foods, gummies, and
chews that disrupt the oral microbiome.
• Eat more green leafy vegetables and less processed food.
• Get at least 20-30 minutes of physical activity per day.
• Take a nitric oxide supplement to restore normal levels.
These simple steps will have a profound impact on your personal health. I have witnessed this over the past 20 years. Consult with your dentist or find a dentist that understands the importance of a healthy and diverse oral microbiome. Advancements in dental medicine are dependent upon continuous research and new discoveries. Once we learn and understand new mechanisms, we must integrate those into clinical practice. This is innovation and improvement in patient care.
1. Hunter, W., Oral sepsis as a cause of disease. Br Med J, 1900. 1: p. 215-216.
2. Chye, R.M.L., et al., Effectiveness of Different Commercial Chlorhexidine-Based Mouthwashes After Periodontal and Implant Surgery: A Systematic Review. Implant Dent, 2019. 28(1): p. 74-85.
3. Lundberg, J.O., E. Weitzberg, and M.T. Gladwin, The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Discov, 2008. 7(8): p. 156-167.
4. Lundberg, J.O., et al., Nitrate, bacteria and human health. Nat Rev Microbiol, 2004. 2(7): p. 593-602.
5. Bjorne, H.H., et al., Nitrite in saliva increases gastric mucosal blood flow and mucus thickness. J Clin Invest, 2004. 113(1): p. 106-14.
6. Jansson, E.A., et al., Protection from nonsteroidal anti-inflammatory drug (NSAID)-induced gastric ulcers by dietary nitrate. Free Radic Biol Med, 2007. 42(4): p. 510-8.
7. Dykhuizen, R.S., et al., Helicobacter pylori is killed by nitrite under acidic conditions. Gut, 1998. 42(3): p. 334-7.
8. Stokes, K.Y., et al., Dietary nitrite prevents hypercholesterolemic microvascular inflammation and reverses endothelial dysfunction. Am J Physiol Heart Circ Physiol, 2009. 296(5): p. H1281-8.
9. Jiang, H., et al., Dietary nitrite improves insulin signaling through GLUT4 translocation. Free Radic Biol Med, 2014. 67: p. 51-7.
10. Bryan, N.S., Functional Nitric Oxide Nutrition to Combat Cardiovascular Disease. Curr Atheroscler Rep, 2018. 20(5): p. 21.
11. Wright, J.T., Jr., et al., A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med, 2015. 373(22): p. 2103-16.
12. Wang, Y.R., G.C. Alexander, and R.S. Stafford, Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Arch Intern Med, 2007. 167(2): p. 141-7.
13. Cutler, J.A., et al., Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988-1994 and 1999-2004. Hypertension, 2008. 52(5): p. 818-27.
14. Bryan, N.S., G. Tribble, and N. Angelov, Oral Microbiome and Nitric Oxide: the Missing Link in the Management of Blood Pressure. Curr Hypertens Rep, 2017. 19(4): p. 33.
15. Petersson, J., et al., Gastroprotective and blood pressure lowering effects of dietary nitrate are abolished by an antiseptic mouthwash. Free Radic Biol Med, 2009. 46(8): p. 1068-75.
16. Webb, A., et al., Reduction of nitrite to nitric oxide during ischemia protects against myocardial ischemia-reperfusion damage. Proc Natl Acad Sci USA, 2004. 101(13683-13688).
17. Bryan, N.S. and J. Loscalzo, eds. Nitrite and Nitrate in Human Health and Disease. Nutrition and Health, ed. A. Bendich. 2011, Humana Press: New York.
18. Bryan, N.S. and J.L. Ivy, Inorganic nitrite and nitrate: evidence to support consideration as dietary nutrients. Nutr Res, 2015. 35(8): p. 643-54.
19. Hendgen-Cotta, U.B., et al., Dietary nitrate supplementation improves revascularization in chronic ischemia. Circulation, 2012. 126(16): p. 1983-92.
20. Woessner, M., et al., A stepwise reduction in plasma and salivary nitrite with increasing strengths of mouthwash following a dietary nitrate load. Nitric Oxide, 2016. 54: p. 1-7.
21. Larsen, F.J., et al., Effects of dietary nitrate on blood pressure in healthy volunteers. N Engl J Med, 2006. 355(26): p. 2792-3.
22. Webb, A.J., et al., Acute blood pressure lowering, vasoprotective, and antiplatelet properties of dietary nitrate via bioconversion to nitrite. Hypertension, 2008. 51(3): p. 784-90.
23. Kapil, V., et al., Physiological role for nitrate-reducing oral bacteria in blood pressure control. Free Radic Biol Med, 2013. 55: p. 93-100.
24. McDonagh, S.T., et al., The Effects of Chronic Nitrate Supplementation and the Use of Strong and Weak Antibacterial Agents on Plasma Nitrite Concentration and Exercise Blood Pressure. Int J Sports Med, 2015. 36(14): p. 1177-85.
25. Pinheiro, L.C., et al., Oral nitrite circumvents antiseptic mouthwash-induced disruption of enterosalivary circuit of nitrate and promotes nitrosation and blood pressure lowering effect. Free Radic Biol Med, 2016. 101: p. 226-235.
26. Wang & Wang, The Prevalence of Prehypertension and Hypertension Among US Adults According to the New Joint National Committee Guidelines. New Challenges of the Old Problem. Archives of Internal Medicine. Volume 164 Issue 19 Page 2126-2134
27. Kapil et al Physiological role for nitrate-reducing oral bacteria in blood pressure control. Free Radical Biology and Medicine. 55 (2013) 93–100
28. Bryan, NS. Nitric oxide deficiency is a primary driver of hypertension. Biochem Pharmacol. 2022 Dec;206:115325.
29. Cutler, C., et al., Post-exercise hypotension and skeletal muscle oxygenation is regulated by nitrate-reducing activity of oral bacteria. Free Radic Biol Med, 2019. 143: p. 252-259.
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 8 CE credits for only $149 by visiting https://dentalsleeppractice.com/subscribe/.
AGD Code: 730
Date Published: November 10, 2024 Course Expires: November 10, 2027
Legal disclaimer: Course expires 3 years after publication date. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
n To receive credit: Go online to dentalsleeppractice.com/continuing-education/, click on the article, then click on the take quiz button, and enter your test answers
To provide feedback on this article and CE, email us at education@medmarkmedia.com.
by Nathan S. Bryan, PhD
1. How does the human body produce nitric oxide?
a. From the oxidation of L-arginine by the nitric oxide synthase enzyme
b. From the reduction of inorganic nitrate by oral bacteria
c. Deep nasal breathing
d. All of the above
2. What is the physiological half-life of nitric oxide?
a. 10 seconds
b. 2 hours
c. 8 hours
d. 1 millisecond
3. What state of matter is nitric oxide when produced in the human body?
a. Liquid
b. Solid
c. Gas
d. Plasma
4. Nitric oxide production declines with age.
a. True
b. False
5. What of the following can interfere or disrupt nitric oxide production?
a. Antibiotics
b. Oral antiseptics
c. Antacids
d. All of the above
6. What role do oral bacteria play in the production of nitric oxide?
a. Oxidation of L-arginine
b. 2-electron reduction of salivary nitrate
c. Production of acid
d. None of the above
7. Oral dysbiosis, periodontal disease, and gingivitis increase risks of cardiovascular disease.
a. True
b. False
8. What percent of people who are prescribed blood pressure medication still have an unsafe elevation in blood pressure?
a. 5%
b. 25%
c. 50%
d. 80%
9. Which of the below can help improve or stimulate nitric oxide production?
a. Green leafy vegetables enriched in nitrate
b. High carbohydrate diet that acidifies saliva
c. Fluoride rinses
d. None of the above
10. Oral dysbiosis can lead to hypertension.
a. True
b. False

Innovative AI and study management tools enhance your ability to impact community health while improving the bottom line of your practice by
Steven Miller
Imagine you stop breathing throughout the night, multiple times, for periods of time that stretch out to full minutes, and this happens every single night. That’s sleep apnea, and it affects millions of people worldwide. Despite its high prevalence – estimated globally at 22.6% – sleep apnea goes undiagnosed nearly 80% of the time.

Once diagnosed, the gold standard treatment is CPAP, with dental practices often getting more involved when patients are trying oral appliance therapy (OAT). Until recently, monitoring for patient compliance was largely an arduous, manual process. But now, a new wave of technology-focused tools is giving organizations the ability to better manage patients and improve patient outcomes and the bottom line of their practice.
Expedited Patient Diagnosis and Reporting with EnsoSleep PPG Home Sleep Testing
Testing backlogs for OSA are lengthy, so the ability to expand home sleep testing with novel solutions – like EnsoData’s FDA-cleared EnsoSleep PPG AI diagnostic algorithm – is crucial to improving patient care. EnsoSleep PPG leverages data collected from pulse ox devices and provides a determination of the AHI on single-channel photoplethysmography (PPG). And this matters, because pulse oximeters are becoming one of the most ubiquitously deployed devices across healthcare settings for diagnostic testing, bedside monitors, and consumer wearables. Pulse oximeters can be as simple to wear as a ring, like the BodiMetrics Circul, or watch, like the Nonin WristOx2® Model










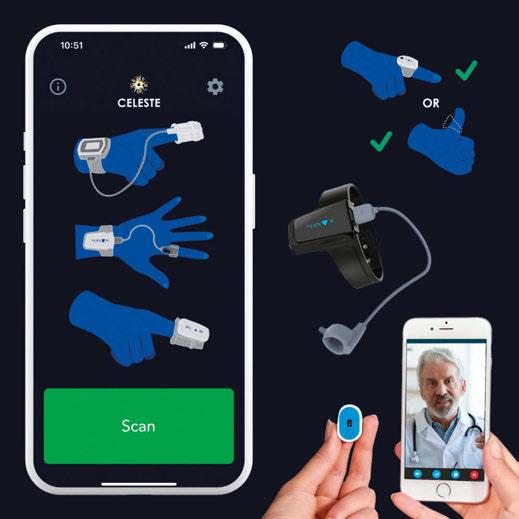
3150, and record physiological data related to sleep and breathing, including the photoplethysmogram (PPG) signal, pulse, and oxygen saturation levels. EnsoSleep PPG uses AI to analyze these data points and outputs a number of important metrics, including but not limited to eAHI, heart rate variability (HRV), flow and effort signals, sleep efficiency (SE), sleep latency (SL), and wake after sleep onset (WASO).
In order to treat patients, clinicians need a simple, easy way to manage patients who might fit into the dental sleep medicine pathway. New options like VirtuOx’s Sleepifi Dental platform help dentists easily manage every step of the dental sleep medicine work-

flow, from patient screening and diagnosis, through the patient journey to treatment selection, prescription management, and ultimately billing documentation.
The Sleepifi Dental platform offers custom workflows and patient e-communications, while also providing automated titration testing, reducing the time a patient spends struggling with their device while also alleviating dental staff burden
How else does it provide this support to clinicians? Patient testing and diagnosis is accomplished with the new Sleepifi Dream home sleep test. The wrist-based Dream device uses high-resolution pulse oximetry and EnsoSleep PPG AI analysis to identify sleep stages and detect sleep-disordered breathing events.
As Jon Fedele, a founder at VirtuOx, noted in Sleep Review: “VirtuOx is thrilled to collaborate with EnsoData on the Dream project. Their AI-driven analysis software is highly regarded within the sleep community.”
The combination of AI and innovative platforms designed with ease-of-use in mind allow dental clinicians and practices a seamless way to deploy affordable, accessible screening and diagnostic support for OSA, improving patient health outcomes and increasing the bottom line.
Adopting pulse oximetry home sleep testing with Sleepifi Dream, EnsoSleep PPG AI, and Sleepifi Dental can revolutionize sleep apnea diagnosis in dental practices boosting therapy patient outcomes, and practice revenue. This integration enables dental practices to play a key role in addressing sleep apnea, benefiting both patients and the practice
Steven Miller is a graduate of the nationally ranked School of Journalism and Mass Communication of the University of Wisconsin-Madison. He has more than 15 years of experience across various marketing areas of expertise. He is the Senior Marketing Manager at EnsoData, an innovative company impacting sleep labs in health systems and private labs with powerful, FDA-cleared AI SaaS products. He also serves on the Sleep Research Society Communications Committee and the Social Media Subcommittee, helping the society advance the state of sleep medicine with cutting edge research.
by Steven Olmos, DDS, Founder of TMJ Sleep & Therapy Centre
Awareness of sleep breathing disorders for adults and children will continue to grow. A recently completed research study validating a visual screening tool for pediatric OSA has been submitted to the Journal of Evidence-Based Dental Practice. Judith Owens, MD, MPH, of Boston Children’s Hospital was the principal investigator for this project which was funded by the American Academy of Craniofacial Pain (AACP) and the Board of Craniofacial Pain & Dental Sleep Medicine (ABCDSM). Adoption of this tool will ensure early treatment for children with OSA. The most common craniofacial features, in order: forward head posture, narrow vaulted palate, open bite, tongue thrust, tongue tie, and heart-shaped tongue.
Education for physicians and dentists will improve and become more comprehensive. Screening will be ubiquitous for all health care practitioners. Improved interpretation of sleep studies will allow the dentist to triage the specific phenotypic traits of OSA (PCrit, muscle responsiveness, loop gain, and arousal threshold). Lowering the cost of sleep studies by evaluation of other biomarkers such as fractional exhaled nitric oxide, which has been found to be correlated to OSA in snorers, with higher levels in uncontrolled asthma.1 In addition to lowering the cost of sleep studies will be the routine evaluation of jaw movements and giving a more accurate understanding of sleep bruxism. Mandibular jaw movement biosignal evaluation depicts the muscular trigeminal respiratory drive and is a highly effective tool for differentiating between central and obstructive sleep apnea episodes, including hypopneas. This provides clinicians valuable insights into wake/sleep states, arousals, and sleep stages.2
Oral appliances have been our entry to treating OSA. Their design and function have changed greatly. Appliances have changed from acrylic to more biofriendly materials such as 3D printed type 12 nylon or ethyl-methacrylate. Printed Hybrid appliances (Shirazi Hybrid/ Diamond Orthotic Lab) allows nasal delivery to address claustrophobia, and the absence of straps prevents aggravation of headaches and head pain. The frequency of use will increase to insure all patients have an optimal outcome.
The nose accounts for 50% of airway resistance so evaluating nasal function will increase in dental offices. Measuring volume and flow rate by utilizing rhinometry and rhinomanometry equipment will help to triage those patients needing nasal surgery or therapy for better treatment outcomes. Accounting for the starling resistor model of increased extra-luminar pressure of the pharyngeal airway (PCrit) with nasal obstruction or narrowing of the nasal valve is more precise medicine.
A reduction in morbidity of surgery for hypertrophied tonsils and adenoids, as well as pharyngeal soft tissue and tethered oral tissues, can be accomplished utilizing CO2 laser systems (Deka/BioResearch Inc). A study at
the University of Manitoba Canada is headed by Enoch Ng, DDS. PhD utilizing CO2 lasers for tonsil reduction in children. Dentists of the future will take over this role routinely after FDA approval.
Orthopedic development techniques will be routine for properly trained dentists that are specific for pediatric OSA. The psychosocial pathology associated with OSA is less discussed. Untreated OSA impacts affective disorders such as depression and anxiety, and often leads to decline of cognitive functions or permanent brain damage.3 Attention-deficit/hyperactivity disorder (ADHD) is among the neurobehavioral sequelae associated with OSA. A study review found that children with OSA had a high rate of attentional deficits (95%), and up to 20-30% of children with ADHD had OSA.4 ADHD and Autism Spectrum Disorder (ASD) in children are highly comorbid with prevalence rates of ADHD in ASD being 39.4% ages (6-11) and 38% ages (12-17).5 Suicide is the second leading cause of death for 10 to 24-year-olds in the US. Individuals with neurodevelopmental disorders, including attention-deficit/ hyperactivity disorder, learning disabilities, and autism spectrum disorder, are at higher risk for suicide attempts.6 For education and training in chronic pain and sleep breathing disorders, contact www.tmjtherapycentre.com.
1. Kiaer E, Ravn A, Jennum P, Pretorius C, et al. Fractional exhaled nitric oxide-a possible risk of obstructive sleep apnea in snorers. J Clin Sleep Med. 2024;20(1):85-92.
2. Malhorta A, Martinot JB, Pepin JL. Insights on mandibular jaw movements during polysomnography in obstructive sleep apnea. J Clin Sleep Med. 2024;20(1):151-163.
3. Vanek J, Prasko J, Genzor S, Ociskova M, et al. Obstructive sleep apnea, depression and cognitive impairment. Sleep Med. 2020 Aug:72:50-58.
4. Ivanov I, Miraglia B, Prodanova D, Newcorn JH. Sleep disordered breathing and risk for ADHD: review of supportive evidence and proposed underlying mechanisms. J Atten Diord. 2024;28(5):686-698.
5. Jones Piltz V, Halldner L, Markus J-F, Fridell A, et al. Symptom similarities and differences in social interaction between autistic children and adolescents with and without ADHD. Curr Psychol. 2024;43:3503-3513.
6. Hua LL, Lee J, Rahmandar MH, Sigel EJ. Suicide and Suicide Risk in Adolescents. Pediatrics Jan 2024;153(1).
Obstructive Sleep Apnea (OSA) is a prevalent and serious sleep disorder that affects millions of Americans. Mandibular Advancement Devices (MADs) are an effective treatment option, especially for those who cannot tolerate Continuous Positive Airway Pressure (CPAP) therapy. However, the titration process – where the device is adjusted to find the optimal advancement that effectively reduces the Apnea-Hypopnea Index (AHI) – can be time-consuming and challenging.
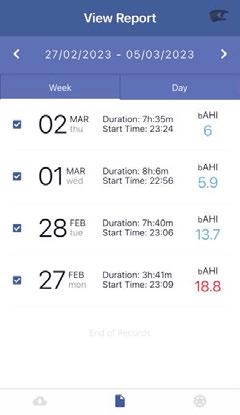

Traditionally, the titration of MADs has relied on periodic sleep studies or follow-up appointments, often spaced weeks or months apart. During this time, patients may continue to experience poor sleep quality, daytime fatigue, and associated health risks due to insufficient control of their OSA. The intermittent nature of monitoring makes it difficult for dentists to quickly determine if adjustments are effectively lowering the AHI, leading to a prolonged titration period and delayed therapeutic outcomes.
The Solution: Daily AHI Monitoring
Integrating AHI monitoring into the treatment process can revolutionize the titration of MADs, offering a faster and more precise approach. By utilizing Belun Ring, the advanced home sleep monitoring device, which can track AHI on a nightly basis, dentists can obtain real-time data on the effectiveness of the current MAD settings.
1. Real-Time Feedback: Dentists can access AHI data, allowing them to make timely adjustments to the MAD. This continuous feedback loop accelerates the titration process by quickly identifying the optimal device settings.
2. Increased Patient Engagement: Patients become active participants in their treatment by monitoring their own AHI. This engagement can improve adherence to
therapy and encourage patients to report back on their comfortability and any residual symptoms.
3. Reduced Time to Optimal Therapy: By identifying the correct titration settings sooner, patients can achieve therapeutic AHI levels more quickly, reducing the duration of ineffective treatment periods. This leads to faster symptom relief and improved overall health outcomes.
4. Customized Treatment Plans: Daily* monitoring allows for highly individualized treatment. Dentists can finetune the MAD to each patient’s specific needs, improving the overall treatment outcomes.
5. Improved Clinical Efficiency: For the dental practice, daily* AHI monitoring reduces the need for frequent in-person follow-up visits solely for MAD adjustments. This efficiency allows for better resource allocation and more focused patient care.
6. Mobile app BelunPro X*: To collect the daily AHI data, Healthcare professionals make the decision if the optional mobile app will be used to get the data remotely. BelunPro X is available at both Apple App Store or Google Play
AHI monitoring is a game-changer in the management of OSA with MADs. Data empowers dentists to accelerate the titration process, ensuring that patients receive the most effective treatment in the shortest possible time. This approach not only enhances treatment outcomes but also improves the overall efficiency of OSA management in dental practices across the U.S. Adopting Belun Sleep System in the titration process of MAD treatment could mark a significant advancement in the standard of care for OSA patients, offering a faster path to better sleep and health.
* Daily monitoring requires the use of the BelunPro X mobile app.




BelunSleepPlatformisanAI-enabledFDA510(k)clearedsystemforOSAdiagnosis withsleepstages.It’susedforbothHSAT& MADtreatmentcalibrationfor multi-nighttestingandhasreusablecapability.

Manufactured by the French company Newsom, BluePro® has transformed the way snoring and mild to moderate obstructive sleep apnea (OSA) are managed. Since receiving FDA clearance in December 2016, this groundbreaking device has been helping patients worldwide with a fast, effective, same-day solution.
BluePro is a prefabricated, adjustable appliance made from high-quality thermoplastic materials. The fitting process is quick and easy, performed chair-side by a dentist in just 7 minutes. The two splints are heated in boiling water, molded directly onto the patient’s dental arches, and assembled into a monobloc that gently advances the lower jaw to an optimal position. The advancement can be adjusted millimeter by millimeter, thanks to the graduated splints allowing precise customization for each patient.
BluePro acts as a temporary appliance, offering professional same-day treatment to trial how patients respond to mandibular advancement. It also provides a way to finetune the optimal advancement level through

Retention issues are rare with BluePro. However, patients may occasionally experience tightness or dental discomfort. This can be easily addressed by trimming excess material from the splint during the fitting process. Two independent studies have confirmed the efficacy of BluePro in treating OSA. In the U.S., BluePro is primarily used as a trial or transitional appliance, serving as a backup device once a custom-made solution is delivered. Its sleek design, affordability (150 USD), easy adjustability, and potential lifespan of up to one year (with regular cleaning) make it a pragmatic choice for many patients. Additionally, it offers an affordable alternative for patients without access to custom devices or those who need a spare appliance for travel.







As dentistry becomes more competitive due to consolidation and saturation, dentists have turned to dental sleep medicine (DSM) to differentiate themselves from their peers; and as recently as 2022, the National Library of Medicine (NIH) reported 66% of responding dentists were involved in DSM. While some have found success in treating sleep disorders, most dentists find the shift to sleep challenging. While most dentists have taken a basic sleep course, few have delivered a successful appliance. Still, fewer have ever been paid for any of their work in sleep. So what’s the solution?
Here are our 3 top strategies to secure a thriving dental sleep practice.
One of the most frustrating challenges sleep dentists face is getting properly reimbursed for their treatments, resulting in lost
revenue from incomplete reimbursements or denials altogether. 99 times out of 100 when we audit credentials with Restfull BI, we typically see the following two things: usually they aren’t credentialled appropriately and their payer portals aren’t set up correctly. Commonly, it’s the likely combination of both so it’s important you go through the right processes to avoid any losses. You could be the best sleep dentist in the world, but without getting properly reimbursed, your practice won’t be successful.


Some of the most successful players in the stock market amassed their wealth by diversifying their portfolios, and the same concept applies to dentistry. Although implementing sleep is one way to diversify your income streams, you can take it further with medical billing. Gaining a comprehensive, operational grasp of medical billing can enable you to maintain a profitable practice by maximizing your reimbursements both legally and quickly.
Restfull is an all-in-one solution for your dental sleep practice that encompasses patient communications, office management, sleep test orders, and more. Combined with our Billing Intelligence service, Restfull BI, you’ll be guided through the proper process to getting your reimbursements approved. The platform was designed with failsafes, ensuring there’s no way you can incorrectly complete your reimbursements.
Get started with dental sleep medicine with these 3 strategies by booking a demo now so you can see just what Restfull can do for you and your practice! Visit restfull.com. Or reach out to team@restfull.com to book a call!



Your patients often complain about xerostomia (they don’t use that word) – what do you say? Have you been happy with results from OTC mouth moisturizer products? The same ones dentists have been recommending for decades?
The reasons why people suffer from xerostomia become more numerous every day. We’ve long known about the mouth-drying effects of some medications like antihistamines. There are over one thousand drugs that create problems and the list grows every day, along with diseases, radiation therapy, some foods, even anxiety and simply being dehydrated.
In our field, the major culprit is mouth breathing. When we apply PAP or oral appliance therapy, dry air can pass through the mouth and create enough discomfort to interfere with therapy. Hence, recommendations for water by the bed, lozenges, rinses, and sprays applied before sleep. None of which work all that well, or for very long.

Your patient is frustrated and blames the device that critically supports their airway. They don’t feel the apnea, but they sure feel that dry tongue!
When patients undergo invasive, serious medical care such as cancer therapy, prescription solutions to xerostomia are often applied. To create a solution and gain FDA approval specifically for medically-induced xerostomia, formulations must meet more stringent criteria than an OTC rinse. The effect must be robust and persistent, lasting several hours even in awake patients.
Thinking about our sleep patients, if we prescribe a medical-grade xerostomia therapy for our relatively simple sleep related breathing disorder patients, it will improve their quality of life and enhance commitment to therapy. How many patients do dentists see who complain about PAP therapy being unacceptable because of dry mouth? If their jaw configuration doesn’t allow for full lip closure with a mandibular advancement device, what do you do? Recommend lip tape or SomnoSeal? Good solutions, but what if they don’t want or cannot use those methods?
Aquoral Protective Oral Spray is a medical-grade xerostomia solution that has many applications for our dental practices. Its patented, clinically proven, lipid-based formula provides a protective coating of the oral mucosa, offering relief for as long as 6 hours and helping to aid our prevention efforts –xerostomia creates perfect conditions for rampant caries, especially root caries.
As a prescription item, Aquoral is available by mail-order pharmacy, just like most medications these days, and the company has a program for stocking it in the professional office as well. Patients can use HSA benefits to help with the cost, not something an OTC product is eligible for.
Don’t continue to recommend products that fail to solve problems. Relief of suffering from dry mouth, whatever the reason, goes a long way to improving the quality of life your patients will feel.
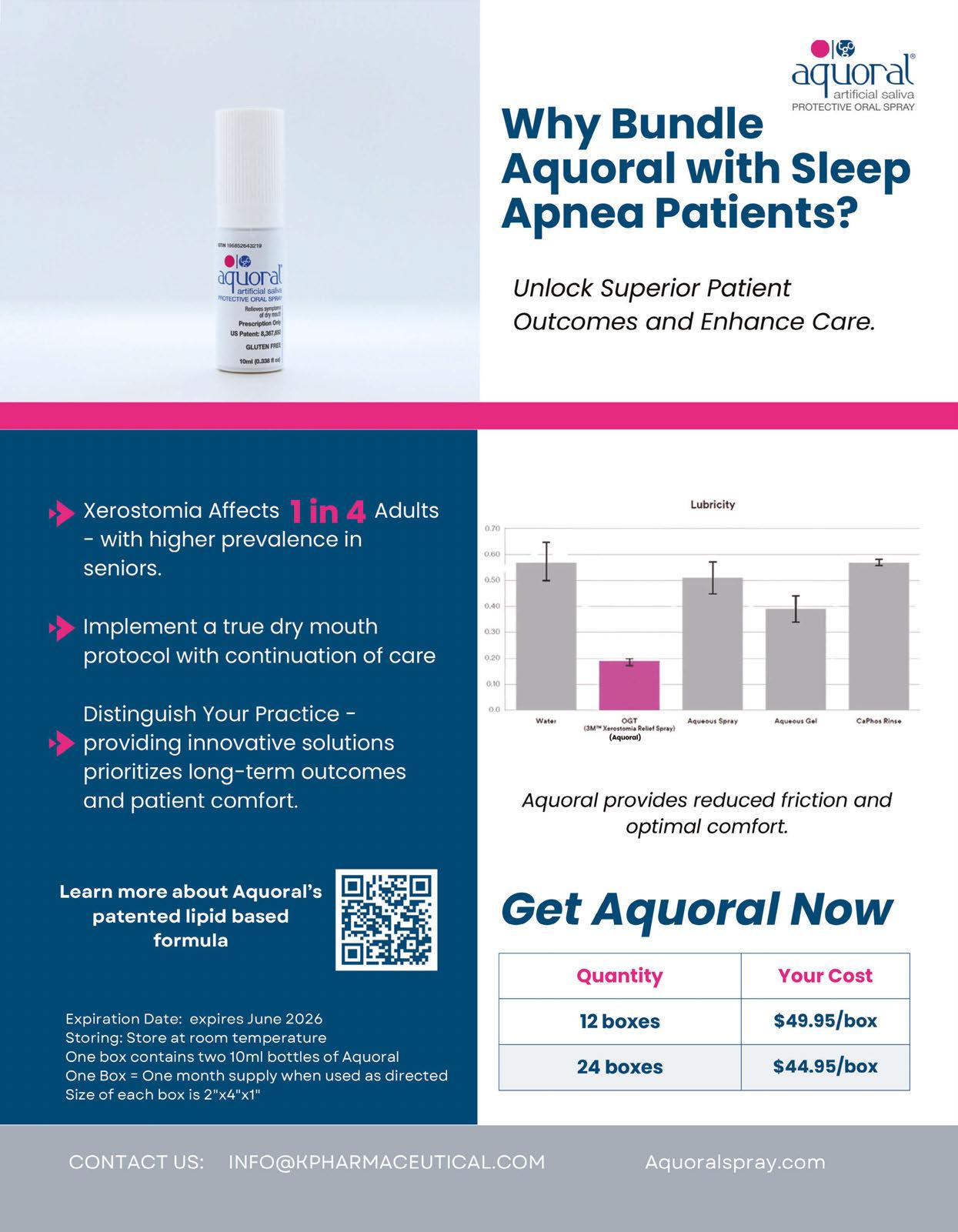
by Rose Nierman, CEO Nierman Practice Management
Unlocking the code to dental sleep medicine can be confusing, especially when it comes to correct coding. Not to worry – I’ve already covered oral appliance codes E0486 and K1027 in the fall issue of Dental Sleep Practice. In this edition, we’re tackling a frequently misunderstood code: CPT 21085, which is often mistakenly applied to morning repositioners used to restore the jaw to its previous position to prevent bite changes.
Q: What is CPT 21085, and when should it be used?
A: CPT 21085 is for “Impression and custom preparation of an oral surgical splint.” The splint is designed to support the patient’s facial structures during orthognathic reconstruction or other oral surgeries, such as when the mandible has been removed due to trauma or ablative surgery. It often involves an impression of the face and must be constructed in the office, not by an outside lab.
Q: Why does CPT 21085 need attention?
A: CPT 21085 is particularly prone to audits due to its classification as a surgical code, often submitted incorrectly for nonsurgical services. Misuse of this code can lead to claim denials, compliance issues, and increased scrutiny from private carriers and Medicare.
Q: What are other common errors with CPT 21085?
A: Utilizing CPT 21085 for impressions, TMJ orthotics and morning repositioners.
Q: If we can’t use CPT 21085, is there another code for impressions for morning repositioners?
A: There isn’t a specific code for morning repositioners. Recent policy updates from Aetna and United Healthcare now explicitly exclude these devices from separate coverage. Some practices attempt Miscellaneous DME or

A pioneer of medical billing in dentistry, Rose Nierman is the CEO of Nierman Practice Management (NPM) and creator of DentalWriter Plus Software. For more than 30 years, Rose has taught dental practices successful and ethical medical billing through the iconic Successful Medical Insurance in Dentistry seminars. Contact NPM at 1-800879-6468 or at Coding@dentalwriter.com.
Supplies and Materials codes, but these rarely succeed when the policy excludes them.
Q: Does this mean we are limited to billing only for the oral appliance?
A: No, many private carriers also cover services like exams, radiographs, and other related treatments. We encourage you to bill for all covered services – don’t leave any reimbursement on the table!
Q: Are there other codes that raise red flags?
A: Yes. CPT 21110 (Interdental Fixation Device), which involves wiring of the teeth or jaw, should be avoided for removable devices or nonsurgical appliances.
Q: Is it okay to list the date of service as the next day for a morning repositioner?
A: The date of service for any custom oral appliance or morning repositioner should always be the delivery date, not when the patient starts using it – even if that’s the next day.
Q: We want to do everything right. How can we stay compliant?
A: When outsourcing billing, request the codes billed on your behalf to ensure they are accurate. Conducting regular internal audits can help catch issues early. Documentation is essential for success and for your practice to maintain compliance. Finally, remain alert to organizations that manipulate codes or documentation. Fortunately, many reputable mentors and organizations are dedicated to supporting the dental sleep community and sharing best practices to guide you on an ethical and compliant path to success.
Tip: Request “Codes that Raise Red Flags for Dental Sleep Medicine” by emailing Coding@dentalwriter.com.




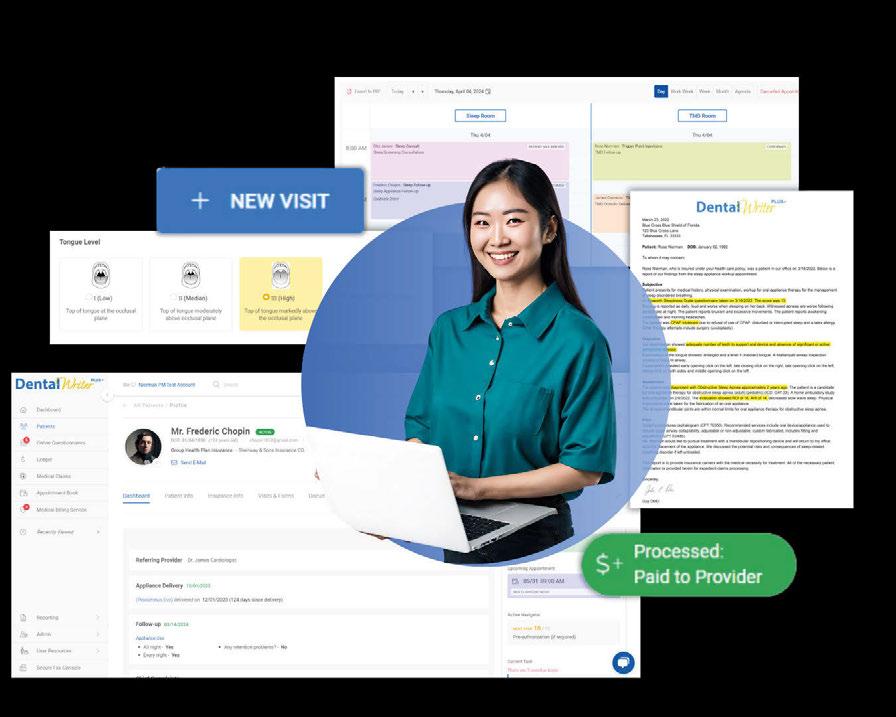


Cartoon reprinted with permission. Originally published June 14, 2022 in “The Story of My Friend Doug and the Problem of Time” (https://bit.ly/40dp2kS) on “Dave’s Notes” blog which is part of the Empowered Sleep Apnea project website. More info at www.EmpoweredSleepApnea.com.

• Offer FDA-cleared therapeutic procedures that provide pain relief and rehabilitate force imbalances for new and existing patients
• Provide medically necessary dentistry using tested technologies including ultrasound, photobiomodulation, microcurrent, and muscle manipulation.
• Precisely diagnose and deliver state-of-the-art treatment for chronic migraines and headaches, tinnitus, and other neck/jaw/face pain
• Address an individual patient’s symptoms with a drug-free, needle-free treatment plan that has a 95%-100% clinical success rate
• Receive clinical training along with ongoing implementation assistance
• Add a revenue stream to your practice, increasing your non-doctor revenue
• See nearly 389% ROI and only 30 minutes of doctor chair time per case.







