SPORTS MEDICINE: IT’S A PHILLY THING






SPRING 2023 Plus...
World
A Recognized
Center for Advancing Health Care through Science, Education & Technology A PhiladelphiaMedicineConversation on Digital Therapeutics
with Benjamin Alouf, MD, MBA, FAAP, Chief Medical Officer, Limbix
Interviews
with local physicians Medical Marijuana for Neuropathic Pain

4
Philadelphia County Medical Society
2100 Spring Garden Street, Philadelphia, PA 19130 (215) 563-5343
www.philamedsoc.org
EXECUTIVE COMMITTEE
Ricardo Morgenstern, MD PRESIDENT

John M.Vasudevan, MD
PRESIDENT ELECT
Stephen R. Permut, MD, JD

IMMEDIATE PAST PRESIDENT
Oneida Arosarena, MD, FACS
SECRETARY
Dale Mandel, MD
TREASURER
BOARD OF DIRECTORS
Dom Bucci, MD
Sharon Griswold, MD
Cadence A. Kim, MD
William King, MD
Harvey B. Lefton, MD
Max E. Mercado, MD, FACS
Natalia Ortiz-Torrent, MD, DFAPA
Anthony M. Padula, MD, FACS

Dhruvan Patel, MD
David A. Sass, MD, FACP
Katherine Sherif, MD
Walter Tsou, MD
Graeme Williams, MD
Rhea Trainson (Drexel)
FIRST DISTRICT TRUSTEE
Lynn Lucas Fehm, MD, JD
EXECUTIVE DIRECTOR
Mark C. Austerberry
Editor Tracy Hoffmann
7 Interview: Dr. Ted Christopher

Contents Spring 2023 Philadelphia Medicine is published by Hoffmann Publishing Group, Inc., Reading, PA HoffmannPublishing.com | (610) 685.0914 FOR ADVERTISING INFO CONTACT: Tracy Hoffmann • Tracy@Hoffpubs.com • 610-685-0914 x201 The opinions expressed in this publication are for general information only and are not intended to provide specific legal, medical or other advice or recommendations for any individuals. The placement of editorial opinions and paid advertising does not imply endorsement by the Philadelphia County Medical Society. All rights reserved. No portion of this publication may be reproduced electronically or in print without the expressed written consent of the publisher or editor.
Medical Society
Ricardo Morgenstern, MD, FRCPE, FACG, FCPP, the 161st President of The Philadelphia County
Working Toward Championship Years
5 Alexis Tingan Interview: We’re All
10 Interview: John Vasudevan, MD PCMS 162nd President Elect
Therapeutics
Limbix
Medical Marijuana for Neuropathic Pain
Inadequate Pain Management: A Suicidogen (Dr.
Kevorkian: Friend or Foe?)
American Medical Women’s Association 24 Facing the Health Effects of Increasing Exposures from Climate Change and Environmental Hazards 28 PCMS STUDENT INTERVIEW: Nicole V. Perry Bryce, Philadelphia College Osteopathic Medicine DO Class of 2023 30 Pennsylvania Venue Rule
12 A Philadelphia Medicine Conversation on Digital
with Benjamin Alouf, MD, MBA, FAAP, Chief Medical Officer,
16
18
Jack
22
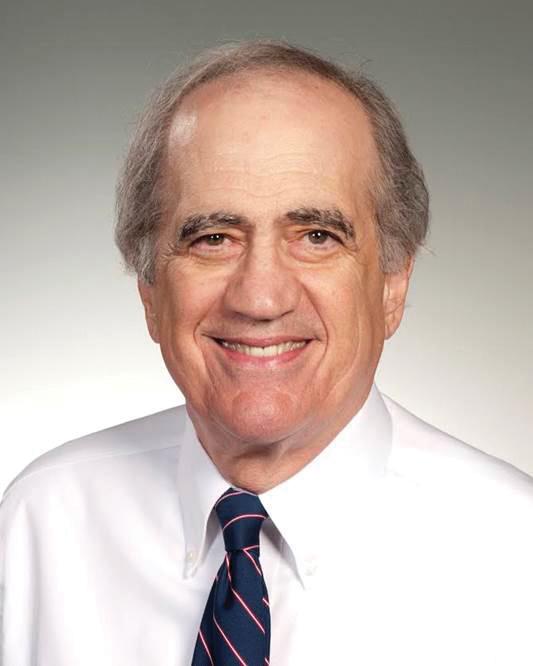
RICARDO MORGENSTERN, MD, FRCPE, FACG, FCPP, the 161st President of The Philadelphia County Medical Society
of Ibero Latin American Medical Professionals; past Secretary, InterAmerican Society for Digestive Endoscopy.
and Radnor campus and the Philadelphia Veterans Administration Hospital.
Born and raised in Oruro, Bolivia, he moved with his mother to Uruguay at the age of five. He completed grade school and high school in Uruguay and was always interested in a career in medicine. Dr. Morgenstern received his medical degree from the Universidad Mayor de San Simon School of Medicine in Bolivia; completed his residency at the Japanese-Bolivian Gastroenterology Institute in Bolivia; a fellowship at Western General Hospital and Royal Infirmary at the University of Edinburgh, Scotland.
Dr. Morgenstern is board certified in Gastroenterology. In 2004 Dr. Morgenstern came to the United States to work at Drexel/ Hahnemann University Hospital in the Gastroenterology Department and remained there until its closing in 2019.
It was also in 2004 that he became an active member of The Philadelphia and Pennsylvania Medical Societies, serving as Delegate to PAMED; serving on numerous PCMS House and Staff committees including the PCMS Board of Directors as Secretary and President Elect. Dr, Morgenstern has also been active in many organizations including: member of the American Medical Association; Fellow, American College of Gastroenterology; American Society for Gastrointestinal Endoscopy; British Society of Gastroenterology; Royal College of Physicians of Edinburgh; Delaware Valley Society of Gastrointestinal Endoscopy; Fellow, College of Physicians of Philadelphia; Vice President, 2022-2023 & President of the Society

Dr. Morgenstern has many goals and aspirations for PCMS including the continuation of their excellent educational programs currently being produced and education collaboration with our surrounding counties and professional organizations. He also hopes to search for opportunities so that more students gain access to medical careers by creating an atmosphere where students will want to go into medicine.
Dr. Morgenstern would also like to be of assistance to those physicians serving in the rural areas of Pennsylvania and for PCMS to be the voice for all Philadelphia physicians’ needs; to improve the quality of care and their quality of life.


Dr. Morgenstern is especially grateful to his wife, Tatiana, and their son Ariel and two daughters Monica and Michelle Morgenstern for their support, encouragement, and understanding. He has been married to his beautiful wife Tatiana for 32 years; Dr. Morgenstern states, “she is the pillar of the family.” He is also grateful to his parents, that through their hard work, they made it possible for him to reach his goals.
Dr. Morgenstern is grateful to his medical friends in Philadelphia who helped to make his dream of a medical career a reality; he further states, “to have a wonderful medical career and to work in this beautiful country, I am grateful to all my colleagues, teachers, mentors, including trainees, that through their example, they have inspired me to achieve higher goals.” Congratulations and good luck, Dr. Morgenstern! We look forward to a great year under your leadership as President of The Philadelphia County Medical Society. •
4 Philadelphia Medicine : Spring 2023
Alexis Tingan Interview: We’re All Working Toward Championship Years
a conversation with William King, MD, PCMS Boardmember
Alexis: I appreciate the opportunity to speak with the medical society. My background is in Physical Medicine and Rehab (PM&R). There are different names: there’s physical medicine, rehab medicine and PM&R, and the doctors who practice PM&R are called physiatrists. My residency training is in PM&R and then I did fellowship in primary care sports medicine. The best way to sum up is that we are physicians of function.
Physiatrists aren’t necessarily specialists of a particular part of the body; we’re specialists of function. When thinking about the function of our patient we may focus on a particular area of the body that may be affecting them, be it their hip, their knee, or in the case of a traumatic brain injury patient, their brain or a spinal cord injury. So, whether it be traumatic brain injuries, stroke rehab, spinal cord medicine, pain medicine, palliative care, sports medicine, or pain management, the core principle is that we are really assessing the function of the patient, seeing what the problem is, and creating a holistic treatment plan that gets them to where they want to be.
For athletes, we’re often looking holistically at the athlete. It’s not just the ankle sprain, the hamstring injury, the concussion; it’s how does that injury affect their entire lifestyle? And how does it affect their ability to compete and play and train at their optimal level? If working with non-athletes, we’re looking at how that particular problem affects their overall lifestyle to create a treatment plan that can optimize their function.

PCMS: In Philadelphia, we’re very much a sports city and in this past year we had this amazing experience of having three professional teams in their championship games; the Phillies in the World Series, the Philly Union in the
MLS championship, and then the Eagles in the Super Bowl. Unfortunately, we had the special experience of not winning any of those championship games. So, we wondered whether doctors on sports medicine could offer any advice in how to overcome our challenge of watching our home teams not quite get that championship trophy.
Alexis: I’ll just give one line: trust the process. That was the slogan for one team you didn’t mention, the Sixers. It’s going back to being a primary care physician and the holistic approach to patient care. Often, I think of myself as the primary care provider for my patient from a musculoskeletal standpoint, meaning I’m not just treating the one particular area of the body, I’m looking at the big picture. So, one year may be someone’s arm, and the next year it’s their shoulder. And because you’re looking at things holistically, you’re looking at things from a functional standpoint. There’s a process in getting back to your functional goals. And that’s often what I tell patients, whether it be some sort of chronic degenerative problem or an acute injury. I tell them, look, this is where we are, this is where we want to be, and this is the process that we’re going to have to go through to get there. And the process is important because sometimes it’s fast, but many times it’s slower than they desire. And when it’s slower, you have to trust the process to get to your destination.
But, very important in that, and this gets to the aspect of Philadelphia sports, is that the process itself is actually the purpose. The process is the purpose, meaning that there’s a lot that you can learn about yourself by going through processes to get to a particular destination. Like the Union, the Eagles, and the Phillies, they all wanted to win the
5 Spring 2023 : Philadelphia Medicine philamedsoc.org FEATURE
SPORTS MEDICINE: IT’S A PHILLY
THING
Alexis Tingan Interview: We’re All Working Toward Championship Years

continued from page 5
championship game. When you get to the final, you want to win. There’s still purpose in the process in terms of character building, learning again about yourself, and then being able to be a better person or better team in the future. My advice for Philadelphia fans is to trust the process. The teams have done very well to this point, but understand that it’s through that process that the teams have become very good, and it’s better to be in the playoffs and in the championship game than to be totally out of the game.
Philadelphia fans were obviously severely disappointed that we didn’t win the game, but they felt great about the team, and the teams felt good about the city, saying, “Hey, we were there, we were in the big game; we’ll get ‘em next time.”
PCMS: As doctors, we feel kind of like we’re coaches. We’re trying to coach our patients into winning at their goals, whether it’s recovering from illness, getting through a devastating illness, or changing their lifestyle to have a healthier outlook, leading to a healthier outcome. As primary care doctors, we often get discouraged with that process of motivating people to change. Do you have any advice for us in some of the primary scare care specialties with motivating our patients or helping them navigate through some of these challenges ?
Alexis: The one thing I can say is to celebrate and appreciate the small wins. Say, a primary care provider wants to help a patient get their weight to a certain level. The patient is saying, I’ve only lost one pound this week, and I want to lose 50 pounds. While the eye has to be on the prize and the destination, you really have to appreciate the process. So you need to have your patients focus on the small wins in the process.
Week to week or month to month, are you better? Have you gotten closer to your destination? And if you’ve gotten closer to your destination, that means you’re on the right trajectory. That’s important because that builds motivation and confidence towards getting towards your goal. If you can say, we lost three pounds this week, we’re three pounds lighter than we were the week before, that’s a win. We keep doing it one step or one foot in front of the other. And so, I would encourage primary care providers, when they’re counseling patients, to focus on what can you do in a short period of time to get a win. Then you get one win, another win, another win, and another win, eventually getting to your destination.
PCMS: In Philly, we’re facing a feeling that we’re losing. Whether it’s trying to stop violence in the community, trying to clean up litter, navigating traffic and the roads, or treating each other poorly. So, what can you tell those folks who are kind of feeling like they’re in a setback stage, maybe in their health or spirit?
Alexis: That’s really tough, and we all see it in our practices. Of course, the Covid pandemic has not been helpful regarding health-related matters. And we know that there’s a mind-body connection. So, we’re definitely facing an uphill battle. I counsel my patients when we’re in a setback mood by telling them to stabilize the emotions, and let’s just stop thinking worse. Again, we’re talking about setting up small wins.
They can’t start going the right way until they stop going the wrong way if you’re having a setback. It’s not like, tomorrow we’re going to get you back to where we want you to be. At some point, when you’re having a setback you just need to get back to neutral. And that becomes the new goal: to stop the negative thinking. It becomes the first step to getting back to neutral so we can move forward. That gives everyone a little better perspective.
PCMS: As physicians, we think we might be able to straighten out these gloomy attitudes and get back to helping our patients win. I think we sometimes forget what a great job we’re trying to do. As physicians, we might need to take some of your advice and philosophy, and apply it to not just our patients, but to ourselves.
Alexis: When we’re talking about goal setting and setbacks, both for patients and us as physicians, we occasionally want to blame somebody else, or something else, for the reasons we’re in this situation. One thing I do for a patient is to encourage them to take ownership. It’s not necessarily to blame the patient but for them to understand that much of their destiny and success is dependent on what they actually do. As physicians, we can complain about the government or the hospital, but at a certain point, we as physicians have to stand up and advocate for ourselves.
I grew up in Beaumont, Texas. I went to college at Princeton, then attended medical school at Emory, down in Atlanta before coming to Philadelphia, where I completed residency in physical medicine and rehabilitation and then followed with a fellowship in primary care sports medicine. •
6 Philadelphia Medicine : Spring 2023
philamedsoc.org FEATURE continued
Interview: Dr. Ted Christopher
a conversation with Mark Austerberry, PCMS Exec Director
PCMS: We are talking to doctors who had work experience with professional sports teams, and you fit that category. Philly recently had some great opportunities to “win it” all by having three professional teams – football, baseball and soccer – in their respective championship finals. Can you tell us about your experience when you worked with the Flyers back in the day?


Dr. Christopher: Yes. Over the course of my career here at Jefferson, we’ve been involved in many professional sports activities. We covered the Eagles on the sidelines for many years. Our residents and attendings currently cover Phillies games, although we’re there primarily for the fans, not so much for the team. And then again the most recent gig that we’ve had was with the Flyers, which was real medical coverage for any kind of acute emergency when the players were on the ice. We were around the players in the locker room, and were part of the Flyers medical team, led by a physician from the University of Pennsylvania. The Flyers medical team consisted of an orthopedic surgeon, an internist with additional training in head concussion, an oral surgeon, and an emergency physician. At times, the busiest physician of all was the oral surgeon, who treated not only all the dental injuries, but also the facial lacerations.

PCMS: So how many games did you handle? You used to go to many of the games. How did you cover 42 home games in a season?
Dr. Christopher: For the Flyers, we’d cover on-ice emergencies for every home game, for both the Flyers and the visiting team players…but it was not just me covering. I had a team of three or four emergency physicians from our staff who would cover the games. It turned out to be around 12 games a year for each of us, which was perfect.
PCMS: Is that a volunteer thing or did the Flyers pay you?
Dr. Christopher: We were paid.
PCMS: That’s a good gig. And the same with the Eagles and the Phillies?
Dr. Christopher: We were always paid for our professional services.
PCMS: Would you say that your experience with these competitive athletes has helped you as a physician and with your patients considering their health challenges?
Dr. Christopher: These are competitive athletes, right? So for their careers, which are their livelihoods, they are extremely motivated to stay healthy so they can play. That said, they often played through injuries. So I learned that if you really have a motivated patient, you can really do a lot more for that patient, and they’ll pay attention exactly to what you’re saying, and work with you. They’ll work hard because they want to get healed. They want to get better! In the case of
7 Spring 2023 : Philadelphia Medicine philamedsoc.org
FEATURE continued on next page SPORTS MEDICINE: IT’S A PHILLY THING
Interview: Dr. Ted Christopher

continued from page 7
passionate sports city. The fans are very involved in their athletes, and in how their teams perform. So, I think Philadelphia athletes realize that they’re representing a city that has an ethos around doing well and succeeding in sports. The city and the athletes take pride in that. All four of the major Philadelphia sports teams are usually up there in the standings. The Flyers had a rough year, but will come back for sure. The Sixers are likely to be in the playoffs again this year, playing for a championship. It just speaks to a Philadelphia culture of winning and competing hard. That’s what Philadelphia is known for. And as a Philadelphia athlete, if you don’t compete and don’t give one hundred percent, the fans see it and know it, and you will not have a good time here in Philadelphia!
I think of the many sports that are played – and I am not a football expert – but of all the teams, perhaps football is the one that needs everyone, all 11 men out there on the field doing their job, playing their role, going in the same direction.

You miss one block and it ruins the whole play. It truly is the ultimate team sport. So, I think the winning teams, and Philadelphia is in that category because they have teams that usually compete for championships, are those that establish a committed, winning team culture. The key is team owners and coaches selling this culture to the players they draft and hire, and the player’s willingness to buy in to that culture. It’s all about the team.
hockey players, and the Flyers, they really want to get back on the ice. So, they will listen to most of what the docs say because they’re very motivated.

I have gained perspective taking care of my patients from my work with the Flyers. But I have said that, in my experience, hockey players will do anything to stay on the ice, including playing injured or hurt. You wouldn’t want all your patients to do that necessarily, because you don’t want them to re-injure themselves or make the injury worse. I would say the key really is motivation. If you have a very motivated patient, you can do a lot more than with someone who’s not motivated. The motivated patient will, for example, not stop taking their medications and will make sure they return for follow-up visits. They will also follow your medical advice that you give them.
PCMS: Makes sense. So, on another sports topic, what does the experience of our three professional teams, competing in, but not winning, their championship game show about Philadelphians?
Dr. Christopher: You ask a Bostonian that question? I think the athletes who come to Philadelphia to play know it’s a very
PCMS: I know that Boston had a great run for years. You had the Red Sox, the Bruins, the Celtics, and the Patriots. My gosh. It was like a trifecta there. Were they all champions at the same time?
Dr. Christopher: There was a run of 10 years when all 4 major sports teams from Boston won a championship at least once. I think the Celtics won a couple, the Bruins once, the Red Sox won two or three times, and then, the Patriots…well, everyone knows they won six Super Bowls. I think it’s the Boston sports culture, especially with the Patriots most recently. Everyone knows about the Patriots’ culture.
PCMS: The final question is, what philosophical point of view can you give us in facing personal or health challenges?
Dr. Christopher: I’d say it depends on the health challenge, right? I mean, personal challenges and health challenges are kind of two different things. For personal challenges, I don’t know. It may be the way you were raised and how your parents taught you to live your life in establishing your value system. Personal challenges are more about integrity, doing the right thing, and having a moral compass and barometer.
For health challenges, much depends on the health issue. Obviously, if you strain
8 Philadelphia Medicine : Spring 2023 philamedsoc.org FEATURE continued
your ankle or bruise your finger, that’s a different kind of health challenge than being diagnosed with cancer or overcoming a serious illness. Most of the health challenges for athletes revolve around musculo-skeletal injuries. They can be serious, but ultimately, most of these injuries heal. In hockey, it’s all about “upper body” or “lower body” injuries. But in all sports, some injuries are more dangerous and concerning than others. The more serious? Internal bleeding, fractures of the spine and other major bones, head injuries and concussions. Again, it usually comes back to your motivation. If it’s a minor injury, you can wait and see what happens, as many of these minor items heal on their own or with little inconvenience. But if you’re an athlete, you will be motivated to heal as soon as possible. You don’t want to wait because the faster you heal or improve, the earlier you can get back on the floor, or field, or the ice to perform.

That said, you want to be fully healed to have longevity; it’s good for yourself, and it’s good for your team – high school, college, whatever! Regardless, persistent pain or symptoms need to be addressed. Knee pain from an old injury that developed into osteoarthritis – with bone grinding on bone – will need to be fixed most likely with a knee replacement.
PCMS: And for the average person?
Dr. Christopher: You must judge how much pain you’re willing to tolerate, or how much function you want in your life. If you want to go hiking up mountains, you’ll need to do something to fix your hips and your knees. If you have a rotator cuff injury on your shoulder, then you can probably live with that if you’re not raising your hand over your head, and have no plans to become a baseball pitcher! But much depends on your expectations and what flexibility you wish to have. My wife waited years for her hip replacements, but then it got to a point that she couldn’t walk without pain. Then you know it’s time to get your hip replaced. You won’t be running marathons, but you’ll have
We are proud to support Philadelphia County Medical Society by advising them for more than a decade.
Nash Wealth Management Group

Merrill Lynch Wealth Management
Two Bala Plaza Suite 601 Bala Cynwyd, PA 19004 610.668.6106
snash3@ml.com
Merrill Lynch, Pierce, Fenner & Smith Incorporated (also referred to as “MLPF&S” or “Merrill”) makes available certain investment products sponsored, managed, distributed or provided by companies that are affiliates of Bank of America Corporation (“BofA Corp.”). MLPF&S is a registered broker-dealer, registered investment adviser, Member SIPC and a wholly owned subsidiary of BofA Corp.
Investment products:
Are Not FDIC Insured Are Not Bank Guaranteed May Lose Value © 2023 Bank of America Corporation. All rights reserved. | MAP5448947 Vault-BA1IEJ | MLWM-243-AD
470945PM-0323 | 03/2023
function, so you must really set expectations depending on your age and just what you want to do with your life. This is where doctors come in, in all aspects of medicine. Not only do physicians treat their patients with medicines and surgery, but, more importantly, they also direct that medical and surgical treatment to help their patients evaluate and attain their specific personal targets and goals in life. •
philamedsoc.org 9 Spring 2023 : Philadelphia Medicine SPORTS MEDICINE: IT’S A PHILLY THING
When you’re ready to make a difference, we’re ready to help
Interview: John Vasudevan, MD

PCMS 162nd President Elect
PCMS: Please tell us a little about your background in medicine, and your long time involvement in sports medicine.
John: I’ve been working at Penn Sports Medicine for the past decade, through the physical medicine and rehabilitation practice. I work with Penn Athletics, specifically the sprint football team. I also take care of high school athletics at Archbishop Carroll High School in Radnor. I supervise several running events. I’m the medical director for the Broad Street Run and the Philadelphia Distance Run, and I am part of the medical team for the Penn Relays. I am the director of the Running and Endurance Sports Medicine Program and co-director of the Regenerative Sports Medicine Program at Penn Medicine. I came to sports medicine through physical medicine rehabilitation, which is a field that is often misunderstood. Part of the reason that I was drawn to it is because it looks beyond body systems to principally focus on the concept of function. Often, when we’re disabled, we have an impairment that keeps us from doing something, and it becomes quite obvious what we can’t do. The physical medicine field initially grew for the purpose of restoring ability or adapting to disability. Physical medicine is less about what you an fix, and more about helping people do the things they want to do despite their impairments. Sports medicine is a natural extension, focusing not only on regaining something that was lost but going beyond to push oneself even further. I use the same physiatric principles to ensure that anyone can achieve what they want in the body that they have.
PCMS: This year, Philadelphia has been a really interesting sports year for doctors as well as residents who are interested in how


people handle competition. We all watched our favorite teams, with all these elite athletes, try to bring home the championships in soccer, baseball and football. As the president of our medical society, you’re like our team captain. In the past year, our city has had three team captains that have each brought their teams to the championship game without capturing the elusive championship trophy. On a personal level, what did you see when you watched how the players and city reacted to the Phillies, the Union, the Eagles championship games?
John: After the Eagles lost, my daughter was crying at the end of the game…not because she likes football that much, but because she said, “everyone is going to be so sad tomorrow”. She understood the emotions that would flow in a city that goes up and won on a roller coaster ride through these kind of athletic events. But I think we saw something interesting. We’re in a special kind of city that can get to three championships in a hundred days and lose them all. That’s Philadelphia for you! Not many cities can claim to that. I told my daughter that first and foremost, success doesn’t come without hard work, but you can work as hard as you can and still have a bad day, and that’s just the way it goes sometimes. However, it doesn’t diminish all the hard work. I believe that’s one thing this town really recognizes in these three teams; it’s not the destination, it’s the journey. Of course, we want to win, but what we value the most, even more than a win, is hard work and consistent effort. If you focus on the pain of that single game that we lost, or if you just watched those final games, you’ve missed all of the joy of the ride through the entire season. I think life, like sports, is just full of ups and downs. It’s like a roller
10 Philadelphia Medicine : Spring 2023 FEATURE philamedsoc.org
a conversation with William King, MD, PCMS Boardmember
coaster ride but you have only real two choices. You ride it and take the ups and downs, or you stand on the platform and don’t go anywhere. I sometimes approach a patient who says, “I’m not an athlete. I don’t know what I’m doing at the Sports Medicine Center.” I explain that you don’t have to play a sport, but I’m encouraging a certain attitude. It’s anunderstanding that you are there because you have a level of performance you are seeking. You understand that it’s going to take consistent work, and that it won’t always lead to success, but that effort is more likely to get you there than if you didn’t try at all.
PCMS: We go by the Art Museum, and we see the Rocky statue. In Philly, Rocky I is our favorite movie. But in Rocky 1, Rocky Lost. What made it made him great was that he kept boxing, right? And so that is the Philly attitude. Do you think that your patients who are from this region bring some of that attitude? What, about the Philly attitude, can teach us how to succeed?
John: I grew up in the Midwest, so I’ve seen what both cultures offer. And one thing I like about Philly is that there’s a strong emphasis on being yourself, being genuine, and working hard. This town will call you out if you’re not being genuine. We know that these athletes make a lot of money, and most people don’t make what those athletes make, but we will respect the athletes if they work for every penny. We want to see the effort. When the Phillies lost, I thought more people would be disappointed, but instead they said “Hey, that was a heck of a ride!” An athlete like Bryce Harper, who we hated when he played for Washington, comes up here, and then we hated him again because we thought we paid too much. But then he helped us reach the championship level, and he never let up. He continually showed Philly what Philly wanted to see. And now we love him. He’s got hero status even if we didn’t win. He’s a winner in our books. Some of our greatest local champions, like Alan Iverson, never brought home the championship. Yet we still love him, you know? He looked like a guy who wanted to win. We relish being David to the Goliath.

PCMS: What can you tell us in terms of helping motivate our patients to put in that effort for their physical fitness.
John: The success that you celebrate when one wins a race or competition, or when you witness someone doing something great, is the culmination of discipline, consistency and effort. When you see someone who’s older, who has maintained a good quality of life, it’s not just because they were lucky. Often, they embraced health and wellness and self-enforced a habit for years. I see people who are younger, who aren’t as active, and aren’t choosing healthy habits. Fortunately, they still have some time, but every day they wait is a day less to make that change. The older we
get, the harder it is to change our habits. Even if we wish to change these habits, how will our body react? One thing I like about sports medicine is it tends to attract people, who realize that their bodies are no longer pristine. It’s a perfect opportunity to intervene and say, “let’s get you out of this mess and recalibrate your body so that you can keep up that good habit, so that you don’t find yourself in a ‘too little, too late’ situation.”
PCMS: Do you think there’s something about that physical activity that is helpful with that discipline?
John: It’s good to focus on physical health, but it’s also essential to focus on mental health. When I see someone who is having a hard time losing weight, or having a difficult time starting a running routine, I’ll ask about questions about their sleep patterns, and stresses in their life. In some cases, running or other exercise – as healthy as it may be – may be a way to compensate for a stress. When considering the whole health of the individual, to be well is to have more than the absence of disease. We are all missing out on our full potential if we’re not considering how the health of the physical, psychological, and social aspects of our lives. Furthermore, even though we think of athletes as being tough, they are as vulnerable as any of us. Athletes struggle just as much as anyone, but they benefit from sports that provide discipline, goals, and purpose. What really drives people, athletes and nonathletes alike, to my clinic, is not just that they have pain, but that their pain keeps them from performing for fitness, at work, or in their roles in life. When this happens, mental stress starts adversely influencing our physical stress.
PCMS: I think that a champion’s attitude is something we, as doctors, can use to help our patients. How does that translate to sports medicine?
John: I think sports teaches us all about life. Whether athletes or athletic pursuits are successful or not, it demonstrates the power of human relationships to fortify each other and create a common sense of purpose. This purpose drives us to gain, despite any pain, despite the losses, despite the pain in your muscles. It’s that kind of attitude that we should all embrace. We don’t all have to be athletes; we simply need relationships that fortify us, to discover what drives us, and to find what our mission is in life.
PCMS: That might be part of why this year, watching our teams give it their all, made us feel good in spite of not getting across that champions line. We still like being a part of their greatness and their effort. It felt like a relationship. It doesn’t need to stop at that season, and it doesn’t need to end in a perfect score. It just makes us all happy to see someone put in that kind of effort. That’s why we’re here on planet Earth. •
11 Spring 2023 : Philadelphia Medicine philamedsoc.org
SPORTS MEDICINE: IT’S A PHILLY THING
Broad Street Run Medical Crew
A PhiladelphiaMedicine Conversation on Digital Therapeutics with Benjamin Alouf,

PCMS: Dr. Alouf, you and I have had many years practicing primary care pediatrics in the Delaware Valley. Would you help us understand how you began working on solutions for mental health issues and developing tools in this new area of mental health digital therapeutics?

Dr. Alouf: Yes. I’m a pediatrician by trade. I’ve always been in primary care and did some hospitalist work as well in upstate New York, in north Philadelphia, which is where you and I met, and in Wilmington, Delaware. I was always working with an underserved community. One of the frustrating things we experienced back then is when we would see kids with depression, anxiety, other mental health conditions, there weren’t any good options for treatment, especially in the public payor sector.
There weren’t a lot of therapists available. The ones available had long waiting periods; there wasn’t much we could do in primary care for these patients. We gave them the support that we could, referred them to community resources if there were any, and tried to get them services through the schools. We were under-trained in mental health issues during medical school and residency, the communities were under-resourced, and there wasn’t much we could do. The current mental health crisis in America is not at all surprising. There are massive increases in
depression, anxiety, suicidal ideation that have disproportionately affected groups. The youth risk behavior surveillance survey from the CDC just came out showing that in 2021, almost 60% of female students experienced persistent feelings of sadness or hopelessness during the past year and nearly 25% made a suicide plan. Close to 70% of LGBQ+ students experienced persistent feelings of sadness or hopelessness during the past year and more than 50% had poor mental health during the past 30 days. Almost 25% attempted suicide during the past year.
When you think about it, with suicide being the number two cause of death in adolescents – if you told us that when we were practicing together 25 years ago, we wouldn’t believe it. Because we knew things were bad and getting worse, but I don’t think we anticipated it would be this severe. And really the ability to help and care for these kids has not changed. We still lack resources. A lot of people are leaving healthcare. The pandemic created a mass exodus. A lot of those people were mental health providers, so we’re in a crisis. They still need help and support. I don’t practice anymore but you do, so you can speak better to it, but from what I understand, you’re not seeing more colds, diarrhea, vomiting, and rashes. You’re seeing kids in mental health distress.
12 Philadelphia Medicine : Spring 2023 philamedsoc.org
a conversation with William King, MD, PCMS Boardmember
FEATURE
MD, MBA, FAAP, Chief Medical Officer, Limbix
The first digital treatment for adolescent depression is here!
PCMS: And we’re seeing the same strains on the adults. Parents are having untreated mental health crises. They’re facing anxiety from social isolation, strains of trying to parent kids at home, the chronic stress from job changes, switching from in-person, to remote, back to an in-person job, job losses, economic strains. There is the external load on families, whether it’s adults or youth, of domestic violence, the strain of neglect and abuse, violence in schools, and public violence. There are the strains of people being exposed to incidents of public violence, mass shootings or increased homicide rates, increased shooting rates in cities, and massive rates of suicide and self-harm in suburbs or rural communities. We are seeing healthcare providers in profound distress. When we try to schedule a patient, the waiting list might be nine months, twelve months, fifteen months.
Dr. Alouf: And guess what? They end up in the emergency rooms, in crisis. If they had been seen much earlier, that could have been averted and emergency rooms are packed. Hospitals are declaring states of emergency because acute beds and ED beds are filled with kids in acute behavioral and mental health crises. Once you’re in there, if they deem you unsafe to go home, you can spend days, weeks, living on a gurney in an emergency room waiting for placement.
PCMS: Even for people struggling with ongoing issues, like smoking cessation, overcoming addiction to cannabis, opiates, stimulants, or gambling, folks who are having chronic, interpersonal stresses and they need family counseling, those
services are even more unavailable.
I understand you’re working with a company trying to develop tools to bridge some therapy gaps, gaps between intensive inpatient environments, and time-intensive, and expensive, outpatient counseling. As a pediatrician, I do use some telemedicine tools to talk to families and I know psychiatrists and psychologists use telemedicine for remote counseling. But are there other tools?
Dr. Alouf: During the pandemic, seeing the crisis, witnessing horrific statistics we just discussed, I thought I needed to do something as a clinician, be true to my calling. I wanted to find out if there are innovative and scalable ways to provide care. I saw digital therapeutics as that answer.
The Digital Therapeutics Alliance put up a value statement and it states: digital therapeutics deliver to patients’ evidence-based therapeutic interventions that are driven by high quality software programs to treat, manage, or prevent a disease or disorder. They’re used independently or in concert with medications, devices, or other therapies to optimize patient care and health outcomes. They incorporate advanced technology best practices relating to design clinical evaluation, usability, and data security. They’re certified or cleared by a regulatory body as required to support the product claims regarding risk, efficacy, and intended use.
Being a provider and a health plan medical director, I had a lot of things pitched to me as solutions. I didn’t realize you can take software as a medical device that lives on your phone or tablet and
continued on next page

13 Spring 2023 : Philadelphia Medicine philamedsoc.org
CBT-based digital therapeutic for adolescents ages 13-22 Interactive self-guided programs designed with clinical experts No costs to patients or providers Built-in safety features To learn more vist: www.sparkrx.com Important Safety Information: SparkRx is a digital therapeutic intended to provide a neurobehavioral (Cognitive Behavioral Therapy - Behavioral Activation) in patients 13 to 22 years of age as adjunct treatment for symptoms of depression SparkRx has not been cleared or approved by the U.S. Food and Drug Administration. SparkRx is not for emergency use. SparkRx is not meant to be used as treatment without supervision of a health care provider. SparkRx is not meant to be a substitution for any treatment or medication. SparkRx does not address concerns of active suicidal ideation with intent. SparkRx is not intended for the prevention of suicide attempts or self-harm behaviors. For more safety information about SparkRx, visit sparkrx.com to learn more. Complete SparkRx safety information can be found at sparkrx.com. Rev 11,2022-09-28
A Philadelphia Medicine Conversation on Digital Therapeutics continued
from page 13
have it be a regulated therapy and meet the standards of the FDA. There are a lot of wellness or health apps, about 300,000 with about 250 that come to market daily at last reading. They’re not necessarily regulated. Are they following HIPAA regulations? Do they have strict privacy and security regulations? What do they do with data? I didn’t realize that you can develop a device that follows FDA regulatory pathways, and you can offer it to your patient through a prescriptive mechanism.
PCMS: My dad is in his eighties and his providers have tried to help him manage his diabetes by having reminders or text messages. Folks use software for smoking cessation so they can log their successes. Diet management companies have software based behavioral health tools such as diet management. Instead of sending food to you, they’re sending therapeutic messages. Is that what we’re talking about?
D. Alouf: It depends, different digital therapeutics are designed differently based on diagnosis and patient needs. Some are standalone software as a medical device that sits as an app or video game and takes you through structured therapy. Some are connected to a physical device. They may treat psychiatric conditions directly or help with associated comorbid conditions. The critical component is that they use software, that they’re regulated, and that they must back up their claims by the rigor of scientific studies and the FDA has to say yes, your claims are true.
PCMS: Physicians are skeptical of the attempts by industries thinking they can replace the therapeutic relationship built between patient and provider. In the wellness area and some unregulated environments, we worry about chatbots and things that are running with their own algorithms. We’ve watched in the news about things like chatbots and some AI tools going rogue. Do you think digital tools have a place in our instrument bags?
Dr. Alouf: The intention is not for these to replace us; a lot of them are adjunct therapy. The relationship between patient and provider is sacred, and especially as pediatricians, we have this relationship. We are possessive. If somebody starts treating them for something and we don’t know about it, we get upset.
PCMS: That’s true of many primary care providers.
Dr. Alouf: We believe in longitudinal care and want to treat the whole person. We want to know them. These devices are intended to help you manage your patients through some of the more difficult diagnoses and conditions at a time when access to therapy for these conditions is quite limited. Many of these products you can use yourself and see what your patient’s going through. You can actually see what your patients are doing with it and you can counsel your patients through it. Also, these devices are frequently connected to portals or dashboards where you can monitor how your patient is doing, how they’re engaging.
You can see a patient, diagnose them, and, in some instances, have them download the software right in your office. You talk them through and with a dashboard that can be built into your EMR, you can track how they’re doing. It allows you to spend more time with your patient. It’s never intended to be an alternative though.
We don’t want people to come in and I’ve tried five different apps for my condition. We’re hearing a lot more about teenagers self-diagnosing. I’m wondering how many self-treating, and with what they see on social media or TikTok. Somebody’s saying they have ADD and this is what they use and now a teenager starts using it. There’s a lot of overdiagnosis but at least it brings them to the office. And are they also self-treating with things that may not necessarily be best for them? Now you can say, ‘if you like this digital stuff, I have something for you that’s FDA-cleared. I’ve tried it and I think this will work for you. I can monitor how you’re doing on it virtually’.
PCMS: We know in primary care where the rubber hits the road is lifestyle change. Do you think that these tools are going to get good enough so they can help with primary care?
We struggle with this in primary care. A lot of these questions: Did you lose any weight? No. Did you stop drinking sodas? No. Did you quit smoking? No. Then we say, okay. Come back in a month. How about now? No. How can I try to convince you this time? We don’t know what tools we have besides monthly persuasion.
Dr. Alouf: A lot of these products have built-in proven therapies and methods, ‘nudges’, reminders of getting people to do those things and allow for providers to monitor progress. That’s more than just having them remember that my doc told me last week I need to eat better.
PCMS: Do you think some of these technologies or techniques are going to be part of the solution? I’m afraid if we doctors don’t learn some of these tools, the business world and supplement world, the non-scientific world of commercial products will overwhelm our ability to have any voice in helping change lifestyles. There are a million YouTube videos and a billion TikTok videos and a million memes that are influencing our patients.
Dr. Alouf: I’m convinced these digital therapeutics are going to become a standard of care to help providers with their patients. With dermatitis, depression, or diabetes, you’re going to see a doctor and they’re not going to just send you home and say check your sugar or here’s a prescription or follow up with a psychologist. There will be a digital attachment to it, so you are interacting with it.
But yes, education is key and separating these devices from the other unregulated products out there is part of that education. This is not just new for the providers to learn. It’s difficult for the
FEATURE continued philamedsoc.org
14 Philadelphia Medicine : Spring 2023
patients. ‘I thought you were going to write me a prescription’, or ‘just gimme a referral.’ Well, I am. Also, I’m going to give you this app and you’re going to download it, and this is how you’re going to use it, and I’ll be monitoring you.

PCMS: There are a million apps. Are we in the age of digital quackery? Everything is unregulated, so doctors need to get moving. A hundred years ago, there were all these patent remedies, and anybody could just slap together a tonic, or a potion, and they built whole empires off them.
We need to certify and license things. We need things to be studied, we need them to be cleared. We develop these whole protocols to avoid quackery.
Do you think that government institutions and policy and insurance regulators are going to be on board or are they going to be dragged along? How are the doctors going to get the framework around us so this makes sense, and we can use digital therapeutics in the same way that we do with medicines? So, we can say ‘I’m prescribing it because I know, first of all, it is not built to do harm, and it’s been tested to be more helpful than harmful’.
Dr. Alouf: We’re working on getting bills passed. The Access to Prescription Digital Therapeutics Act will be an act of Congress to create a product or benefit category for these products under specific criteria, then for CMS to start paying for them for Medicare beneficiaries. It’s the hope that will trickle down to Medicaid, commercial payers.
Then it’s getting providers to learn about them, use the ones that are out, and really participate in development, then that trickles to professional societies. It’s incumbent on professional societies to look at these products, talk about them, learn about them, and educate members.
Until government says this is something you must cover, until patients are saying why am I paying you premiums when you don’t have this as a benefit, and until professional societies are saying these are tools our doctors need to take better care of their patients, the health plans are going to be the last to accept these.
PCMS: So, providers need to get up to speed if we want to get in front instead of being the last to learn about these tools and solutions? With medical and surgical techniques, we have a hundred years of moving along, but even with the information age and using digital techniques, doctors may feel that their trade is an old art, a medieval art, a colonial art, a pre-industrial art.
Using digital tools, many industries have revolutionized their businesses, but it sounds like doctors are going to be caught
flat-footed. We really saw with electronic medical records that instead of being a tool that helps us increase our productivity, it became a tool to take more of our time to document things for payers and regulators. In terms of enhancing our work, letting us do more, and reach our patients better, it sounds like digital therapeutics are not that ominous thing we saw with EMR.
Dr. Alouf: I think there’s mistrust, and I point to your comment about EMR as a prime example. There’s trepidation by doctors because historically technology has not been something that they were included in. It was something that they were told to do. And here you have devices that are meant to help you treat your patients and help your life be easier. We are constantly requesting doctors to give us information and have gotten great advice from providers. Let’s take this opportunity to have doctors participate in the development of this new industry as opposed to what’s happened before, when by the time it was created and put into your office, it was too late.
PCMS: Thanks, Dr. Alouf. I really think that this will help our members understand an emerging area of treatment. And, who knew that these computers that we’ve been using could actually help patients? •
philamedsoc.org
15 Spring 2023 : Philadelphia Medicine
Medical Marijuana for Neuropathic Pain
 by Frederick J. Goldstein, PhD, FCP* Professor of Clinical Pharmacology Philadelphia College of Osteopathic Medicine
by Frederick J. Goldstein, PhD, FCP* Professor of Clinical Pharmacology Philadelphia College of Osteopathic Medicine
Marijuana for pain? Who does that? Actually, many Americans do across all ages even into the geriatric range.
Opioids have been among the most widely used drugs to relieve acute and chronic pain but there are issues with long-term use. In 2022, the Departments of Veterans Affairs and of Defense issued their Clinical Practice Guideline for pain management. As stated therein, “The guideline development group does not recommend use of opioid analgesics in the daily management of chronic pain. The benefits that opioids can provide are small and are outweighed by the risks to the patient.”1
Is marijuana a good substitute? In my opinion, it is.
However, what is missing are well-designed clinical studies to provide greater understanding of this beneficial effect.
As a medical scientist, I have been conducting clinical research for decades to improve analgesia in patients with cancer and/or neuropathic pain as well as in the immediate post-op period of those recovering from surgery. Currently, I have two preliminary (pilot) studies in progress.
One of my current investigations is at the Philadelphia College of Osteopathic Medicine (PCOM). Along with my clinical colleague, Katherine Galluzzi, DO, I administer THC to those presenting with chronic neuropathic pain. Our patients have diverse etiologies, e.g., multiple sclerosis, diabetic peripheral neuropathy, temporomandibular joint disorder, but all have suffered from nerve pain for at least two months. The insurance classification for chronic pain coverage is three months but as a medical scientist I can start treating patients earlier. Funding is from the PCOM Division of Research, and there is no cost to any patient.
THC is the main psychoactive ingredient in marijuana but also provides analgesia. We use Marinol-CIII, an FDA-approved drug, but is officially sanctioned only for treatment of nausea and vomiting from cancer chemotherapy, and as an appetite stimulant in those suffering from a lack of appetite such that their lives are in danger, e.g., AIDS patients.
The use of THC for analgesia is not banned in the USA but is considered an ‘Off’-Label’ use, that is, one that does not have FDA authorization. To receive approval, I – as the Principal Investigator – submitted our study for evaluation by the PCOM Institutional Review Committee (IRB). Permission was granted, and the project began.
We carefully evaluate all patients who wish to participate since entrance is not automatic. Some of the criteria for admission are age 18 to 75 years old, and having neuropathic pain for at least two months. Participation is not permitted for several reasons including those with cardiovascular or liver problems, epilepsy, depression or substance use disorders.
This is a seven-week study. Patients are seen every week. For the first two, patients complete a pain diary three times a day, using an 11-point scale from ‘0’ [“I have no pain”] to ‘10’ [“This is the worst pain I ever had”]. They also list how many of their usual pain medications they take each day. If there are no problems in this important record-keeping aspect, they are given, in Week 3, capsules containing 5 mg of THC; one is to be taken at night at lights-out time. Patients continue to be seen each week, and decide at that time if they wish to go up to the next doses, i.e., increasing by 5 mg up to 20 mg in Week 6, the last week.
16 Philadelphia Medicine : Spring 2023 FEATURE philamedsoc.org
* Fellow in Clinical Pharmacology
investigation involves a limited number if there are any reductions in pain, and true benefit from placebo that is actually does. Therefore, the placebo effect is real,
score drops by at least 2 points. However, subjects have reported not only less pain – which is the most important – but other benefits as well. My patients always ask about weight gain having heard that marijuana increases appetite (a/k/a/ the ‘munchies’). Good news! While two did have a slight increase, the other five lost weight! Why? Well, they reported being able to sleep better so they had less stress and did not seek comfort food (e.g., ice cream) as often. With less pain they were able to be more active, e.g., greater distances in walking their dogs.
There were some side effects. We had to remove two patients from the study because they were experiencing dizziness; at night, when going to the bathroom, this serious side effect could cause a fall with a severe outcome like a bone fracture.
As mentioned, this is a limited investigation but recruitment is still occurring. If any person with chronic neuropathic pain for a duration of at least two months is interested in more information, please contact me: fredg@pcom.edu.

I am also starting another pilot study on the pain-relieving benefit of a combination of THC plus cannabidiol (CBD) for chronic pain which will be described in a subsequent article. •



17 Spring 2023 : Philadelphia Medicine
1. Sandbrink F et al. The Use of Opioids in the Management of Chronic Pain: Synopsis of the 2022 Updated U.S. Department of Veterans Affairs and U.S. Department oF Defense Clinical Practice Guideline Ann Intern Med. doi:10.7326/M22-2917
A Suicidogen (Dr. Jack Kevorkian: Friend or Foe?)
by Frederick J. Goldstein, PhD, FCP* Professor of Clinical Pharmacology Philadelphia College of Osteopathic Medicine
In a recent statement carried on national television in late September of 1996, the lawyer for Dr. Jack Kevorkian reported that his client had assisted in another suicide for a patient in “excruciating pain” (in this case, from prostate cancer). What made this announcement different was the victim: Not only was he a “doctor” but he had been a “psychiatrist.” The message from Dr. Kevorkian and his attorney was, in my opinion, very clear: They believe that if a doctor who specialized in treating psychic pain could benefit from this death service, then those of us who are just ordinary folks with no medical specialty—but in severe pain—could certainly call on old Doc Kevorkian to terminate our suffering. Their attitude is that there is no need to disturb your physician to demand an improved analgesic regimen—just be a good patient and allow Dr. Kevorkian to help you die.
If you have continued to read this far, you know that I strongly disapprove of Dr. Kevorkian’s approach to pain control, which I will refer to as “Kevorkianism” or the use of physician-assisted suicide to relieve pain. More to the point, as a neuropharmacologist who has conducted many preclinical and clinical studies designed to improve drug-induced analgesia, I believe that Dr. Kevorkian is starting to have a negative impact on our major national effort to improve pain relief in patients with terminal cancer.
NATIONAL SUMMIT ON CANCER PAIN CONTROL
I was given the honor of representing the American College of Clinical Pharmacology at the National Summit on Cancer Pain Control on September 7 and 8, 1996, in Reston, Virginia. This major meeting was planned and conducted by the American Cancer Society, Oncology Nursing Society, and American
Alliance of Cancer Pain Initiatives, organizations that recognize the need of all health professions to expand and improve the delivery of both pharmacologic and nonpharmacologic methods of analgesia to the patient in pain. This Summit was designed to expand professional collaboration—and to develop a national plan—for better management of cancer pain. In addition to the American College of Clinical Pharmacology, there were 45 other national organizations in attendance including the American Hospital Association, American Nurses Association, American Pain Society, American Pharmaceutical Association, American Society of Clinical Oncology, American Society of HealthSystem Pharmacists, American Society of Law, Medicine and Ethics, American Pain Society, City of Hope National Medical Center, Hospice Nurses Association, Leukemia Society of America, National Cancer Institute, and the National Hospice Organization.
Although the requisite luncheon and dinner were held, this was not a social gathering; it was a very intensive event with all participants working hard over a day and a half in both small groups and large seminars. Valuable clinical information was presented on barriers encountered by health professionals who try to provide adequate analgesia for their patients. At our conclusion, I found many issues about which there was general agreement among Summit participants, which I have organized into national, state, and institutional concerns as follows:
A. National
1. the notoriety of Dr. Jack Kevorkian has increased attention and discussion of pain control;

2. because of pain that is poorly relieved, some patients request physician-assisted suicide;

18 Philadelphia Medicine : Spring 2023
philamedsoc.org FEATURE
:
Inadequate
* Fellow in Clinical Pharmacology
3. many patients underreport their pain;
4. many health professionals still undertreat pain;
5. pain management can be advanced immediately if all health professionals would make full use of existing clinical pharmacologic agents;
6. nonpharmacologic therapies need to be more fully incorporated in managing cancer pain;
7. to reduce opiophobia (i.e., unwarranted fear of addiction):
a. more education is needed for health care professionals, managed care organizations, and patients;
b. this educational presentation must include an extensive discussion of narcotic use and the difference between addiction (i.e., psychological dependence, which is rare in patients with cancer) and physical dependence (which always occurs during long-term use of opioids).
B. State
1. certain states have regulations (e.g., triplicate prescription forms) for prescribing and dispensing narcotics that are so strict that some of their residents are deprived of adequate pain control;

2. state-wide Cancer Pain Initiatives, a group typically composed of all types of health professionals plus other interested persons (e.g., attorneys, legislators), have been successful in reducing some barriers (especially legislative) to proper pain control.
C. Institutional
1. assessment tools for pain (i.e., pain scales) should be used in pain management and charted (e.g., as fifth vital sign);
2. the pain assessment tool should be of a standard type, and one of the most widely used for adult patients is a 0-to-10 scale with only two verbal descriptors—‘‘no pain” at 0 and “this is the worst pain I ever had” at 10;
3. a health care institution should use the same pain scale in all of its separate units;
4. for pediatric use—and for impaired adults—a five-point descriptor scale with faces is widely used. For additional timely and important information on pain management, I recommend the excellent article entitled “Quality Improvement Guidelines for the Treatment of Acute Pain and Cancer Pain” prepared by the American Pain Society Quality of Care Committee.1
ACTION PLAN TO COMBAT KEVORKIANISM
As a result of attending the National Summit—and recognizing that we have to deal with Kevorkianism—I expanded my efforts to improve treatment of patients in pain by:
• presenting a proposal at an affiliate hospital to have a uniform pain scale on every hospital form that currently has a space for assessment of pain by our staff;
• establishing this pain assessment tool on a scale from 0 to 10 (I am pleased to report that my proposal was enthusiastically and rapidly approved);
• developing a position statement from the Philadelphia College of Osteopathic Medicine (PCOM) Cancer Pain Research Center for the lay public on currently accepted and proper approaches to pain control; for example:
• most cancer patients can be provided with a significant degree of analgesia;
• for cancer patients with excruciating pain, analgesia can be achieved, but it takes a team approach to accomplish this objective;
• all patients have a right to receive adequate analgesia;
• a patient should consult with other doctors—especially those specializing in pain management—if the current physician is unable or unwilling to provide adequate analgesia;
• distributing this position statement to local media and being personally available to discuss it.
Of course, I will continue to teach my medical students the importance of proper pain management (which involves a discussion of all points identified in this article) and about how a team approach may be helpful with the difficult cases. With a good initial presentation and repeated attention to this matter during their training, the opinions of medical students can be altered. Recently, with the assistance of two colleagues (Anthony Errichetti and Dee Bill-Harvey), I presented the following case to first-year medical students before they had any of my lectures in pharmacology and to second-year medical students after they had many of my presentations, for example, on narcotics, pain control, and differentiation of addiction from physical dependence. The case was as follows: “A 62-year-old male patient who you have been seeing on occasion for the past 20 years has developed lung cancer. Your patient has had three different jobs in his 30 years of working. He is not an alcoholic nor does he have a history of drug abuse. He has been married for 26 years and has four children ranging in age from 12 to 25 years.
continued on next page
19 Spring 2023 : Philadelphia Medicine philamedsoc.org
Inadequate Pain Management: A Suicidogen continued from page 19
“You are given the responsibility to manage his pain, which is now severe, with narcotics.” Please answer the following:
In Regard to his Narcotic Therapy, I Believe that:
CONCLUSION
Adequate analgesia is not a privilege; it is a right. Every patient in pain should expect to receive it. All health professionals need to recognize this important issue of good pain control—even in patients with advanced cancer-and know how to break through barriers (e.g., Kevorkianism) that impede such therapy. •
REFERENCES
1. American Pain Society Quality of Care Committee: Quality improvement guidelines for the treatment of acute pain and cancer pain. JAMA 1995;274:1874-1880.
D.
These results show that attitudes of medical students can be shifted toward the correct approach to using narcotics in patients with cancer. Hopefully, they will continue to hold this opinion when they graduate and become directly responsible for patient care.

20 Philadelphia Medicine : Spring 2023
4.0% 3.3%
A. he will become addicted
28.7% 9.0%
B. he has a great chance of
becoming addicted
48.9% 14.8%
C. he has a moderate chance
of becoming addicted
16.1% 54.1%
he has an extremely small
chance of becoming addicted
2.3% 18.9%
E. he will not become addicted
FEATURE continued philamedsoc.org
First-Year Medical Student (n = 174) Second-Year Medical Student (n = 122)


21 Spring 2023 : Philadelphia Medicine philamedsoc.org FOR ADVERTISING INFORMATION CONTACT: Tracy Hoffmann • Tracy @Hoffpubs.com • 610-685-0914 x201 The Official Magazine of the Philadelphia County Medical Society. Locally-Written Health Care News That Impacts Your Community Your advertisement in Philadelphia Medicine will be read by more than 10,000 Philadelphia physicians, 25,000 affiliated health care practitioners, 1000 business, education and community leaders, and 100,000 engaged community residents throughout the Greater Philadelphia region. Read by More Than 100,000 Health-Conscious, Civic-Minded Philadelphians Advertise in Read online at pm.hoffmannpublishing.com SPRING 2022 A Recognized World Center for Advancing Health Care through Science, Education & Technology You can help end the HIV epidemic CLINICIANS: Riding theWaves of Burnout CRC SCREENING: GUIDING OUR PATIENTS THROUGH THE OPTIONS
American Medical Women’s Association (AMWA)
For over a century, the vision and voice of women in medicine

The American Medical Women’s Association (AMWA) is the oldest, national multi-specialty association for women in medicine. It was founded in 1915 by Dr. Bertha Van Hoosen at a time when women physicians numbered less than 6% of the physician population. From the outset, some questioned the need for a separate organization for women, but when World War I broke out and women physicians were turned away for service by the U.S. military, AMWA became a platform for the unified voice of women physicians. This work laid the foundation for the American Women’s Hospitals Service (AWHS), AMWA’s longest lasting program. AWHS began as humanitarian relief efforts in the war-ravaged areas of Europe and has continued since to provide aid most recently through raising funds for Ukraine, Pakistan, and Turkey relief efforts. Learn more about the founding of AWHS through the short documentary, At Home and Over There, American Women Physicians in WWI.
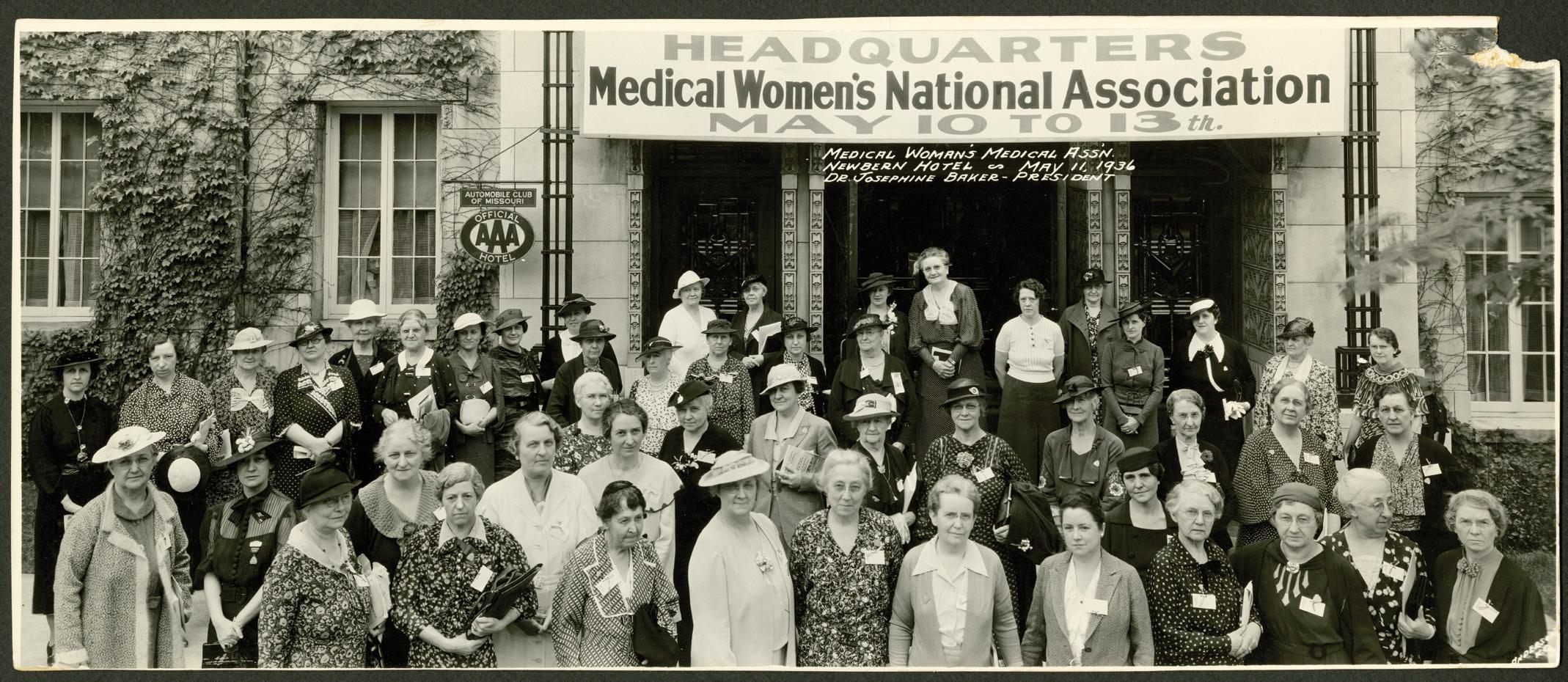
Over the next few decades, AMWA would grow as an organization and advocate for equitable opportunities for women in
medicine. Because many hospitals would not take on women for post-graduate practice, AMWA published lists of female-friendly programs. AMWA also worked to improve women’s health, including support of the 1921 Sheppard Towner Act that would lay the foundation for maternal and prenatal care programs which still exist to this day.
Throughout this time, AMWA’s mission was to advance women in medicine and improve women’s health. As such, AMWA played a key role in the 1990s in promoting women’s health as a specialty and ensuring the integration of women’s health education within medical school curricula. In more recent years, this focus has broadened to encourage an approach to medical care within a sex and gender lens.
With the increasing numbers of women entering the medical profession, now comprising just over 50% of matriculating students, one might assume that the work of AMWA is finished. But in fact, organizations like AMWA are needed more than ever before.
22 Philadelphia Medicine : Spring 2023
FEATURE philamedsoc.org
Then: AMWA Meeting 1936
Photo credit: Legacy Center Archives, Drexel University College of Medicine
Take leadership. For over two decades, there has been not been significant change in the leadership gender gap within the top tiers of academic medicine. Likewise, women attain less than 30% of the top positions in healthcare leadership overall, and the number of women from underrepresented groups is far lower. There is still much to be done to address pay disparities, gender and sexual harassment, implicit bias, and occupational gender segregation.
AMWA’s goal is to support women in medicine at every stage of their career, by providing mentorship, sponsorship, advocacy, education, and mentoring. In addition, AMWA works with a broad coalition of strategic partners ranging from academic institutions, government agencies, industry, and media—with a goal of uniting women physician leaders across all sectors. AMWA’s current initiatives have also expanded to include public health campaigns against gun violence, human trafficking, opioid addiction, nutrition, and obesity prevention—in addition to our signature leadership development programs, AMWA Elevate and AMWA Evolve, and our

longstanding work in gender equity.
As an association within the Medical Women’s International Association (MWIA), AMWA promotes awareness of global health issues. During the COVID-19 pandemic, AMWA hosted a series of webinars bringing together women physicians from around the globe to discuss strategies for COVID-19 mitigation and prevention. AMWA membership confers membership in MWIA and access to a global network of professional colleagues.
For over a century, AMWA has been the vision and voice of women in medicine. We work at the forefront of women’s health, reproductive rights, sex and gender specific medicine, and women’s leadership, equity, and advancement. A growing portion of our membership also includes our allies in this work—and as such, membership is open to all genders. Learn more at amwa-doc.org. •


23 Spring 2023 : Philadelphia Medicine philamedsoc.org
Now: AMWA Interim Leadership Meeting 2018
Now: AMWA Hosts the 100th Anniversary Congress of the Medical Women’s International Association
Facing the Health Effects of Increasing Exposures from Climate Change and Environmental Hazards
 by Julie Becker, MA, PhD, MPH Pouné Saberi, MD, MPH
by Julie Becker, MA, PhD, MPH Pouné Saberi, MD, MPH
Introduction
Pennsylvania residents are facing the health effects of increasing exposures from climate change and environmental hazards like contaminated drinking water supplies from per- and polyfluoroalkyl substances (PFAS). While these hazards are common to other parts of the United States, in the state of Pennsylvania there are added environmental exposure hazards from shale gas operations. Many illnesses with environmental etiologies present with non-specific symptoms and are overlooked. Alternatively, clinicians are often asked about environmental health issues but may not feel confident in addressing them. The purpose of this paper is to outline the health implications of these emerging problems and what role clinicians can play from medical and advocacy perspectives by offering tools for strengthening environmental history taking and assessment.
Climate Change
Background: According to the PA Department of Environmental Protection (PA DEP) 2021 Climate Impact Assessment (2021 Climate Impact Assessment, 2023), health will be extremely impacted by increasing temperatures, heat waves, and precipitation, primarily through rain. They predict there will be more days above 90oF; temperature has increased 1.8oF over the last century and is expected to rise 5.9oF by 2050. Pennsylvanians are experiencing a rise in precipitation by at least 80% by 2050. In Philadelphia, just like the state, climate change is projected to create hotter temperatures with prolonged heat waves; more precipitation in the form of rain, although snow events are inevitable. These weather and temperature events can lead to worsening of air and water quality, flooding, landslides, blizzards and creating challenging health effects for Pennsylvania residents. Figure 1 is a summary of the predicted risks on different climate-caused events by 2050 for the state.
Heavy precipitation and inland flooding Heat waves
Landslides Sea level rise
Severe tropical and extra-tropical cyclones
FEATURE philamedsoc.org 24 Philadelphia Medicine : Spring 2023
Figure 1: Risks associated from climate events by 2050
Increasing average temperatures
key Low Medium High Extreme Human health Environmental justice and equity Agriculture
Risk
Recreation and tourism Energy and other economic activity Forests, ecosystems, and wildlife Built infrastructure Adapted from the Pennsylvania Climate Assessment 2021.
F A S T
Climate change affects health in three key ways: medical and physical health, mental health, and community health (Figure 2). Philadelphians, like all people across the United States, will be tested by climate change. Clinicians will be vital in addressing these challenges to health.

through forests, ecosystems, and wildlife has been shown to mitigate mental health problems, therefore an increase in temperature will influence access to this resource. The health consequences will not affect all Pennsylvanians equally. Some may be more at risk because of the Social Determinants of Health (SDoH) relating to their location, income, housing, health, work, or other factors, as part of environmental justice and equity. (About Social Determinants of Health (SDOH), 2021) Populations at higher risk include older adults, children, pregnant women, individuals with pre-existing conditions, outdoor workers, low-income communities, and communities of color.
Role of clinicians linking climate to health

Source: U.S. Global Change Research Program. 2016. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. https://health2016.globalchange.gov/
Medical and physical health will be challenged directly as described above. Indirectly, the challenge will be reduction of access to resources. For example, there will be issues in accessing food from heavy precipitation or extreme temperatures. Or exposure to nature

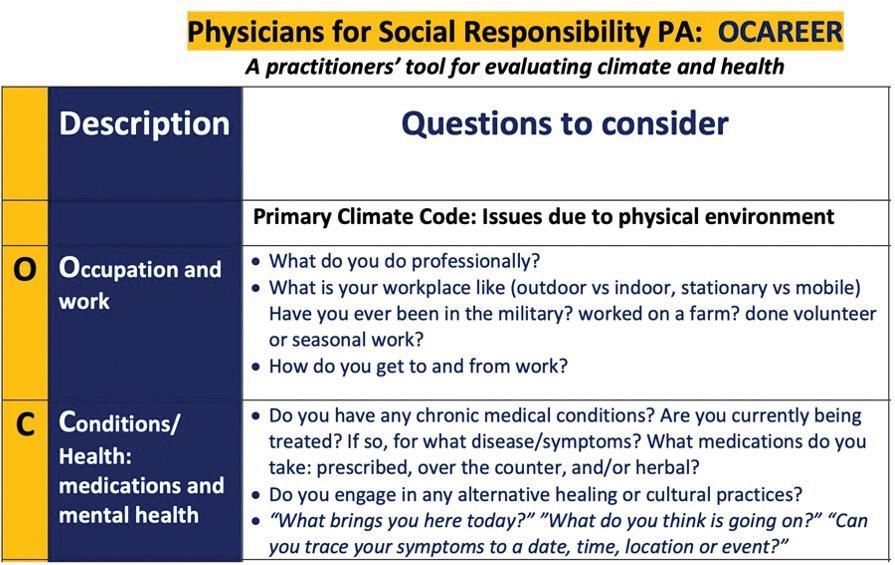
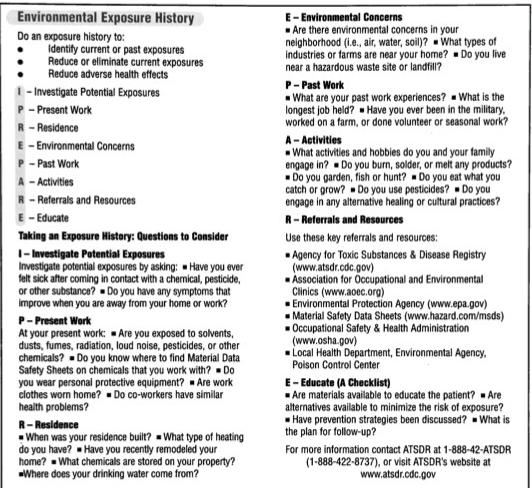
Climate change will alter treatments and recommendations that clinicians provide for their patients. To facilitate this, Physicians for Social Responsibility Pennsylvania (PSR PA) has created a climate history taking mnemonic to help clinicians ask their patients how climate change is influencing their health, through an SDoH lens. OCAREER [Occupation; Conditions; Activities; Residence; Environment; Education; and Resources] is a tool for examining the links between climate and health. It is an outgrowth of certain gaps that were identified. Surveys have revealed that many clinicians are concerned about climate change as it relates to health, but they do not feel that they have the tools or the knowledge necessary to assess the people they work with. (Samano-Martin-Del-Campo D, 2020) Clinicians often use mnemonics such as PET-MAC to quickly assess chest pain and we modeled OCAREER similarly. (PETMAC continued on next page

philamedsoc.org 25 Spring 2023 : Philadelphia Medicine
Figure 2: Climate Impacts on Health
Face Arm Speech Time
Facing the Health Effects of Increasing Exposures from Climate Change and Environmental Hazards
continued from page 25
as a mnemonic for the 6 deadly causes of chest pain, 2022) And lastly, while health effects of climate change are not billable through ICDS-10 codes, they could be documented as secondary or tertiary codes. This would provide measurable information about the linkages between extreme weather/temperatures and their health impacts through a consistent set of codes. Figure 3 is an example of part of the tool. For each letter, there are associated ICD-10 codes.
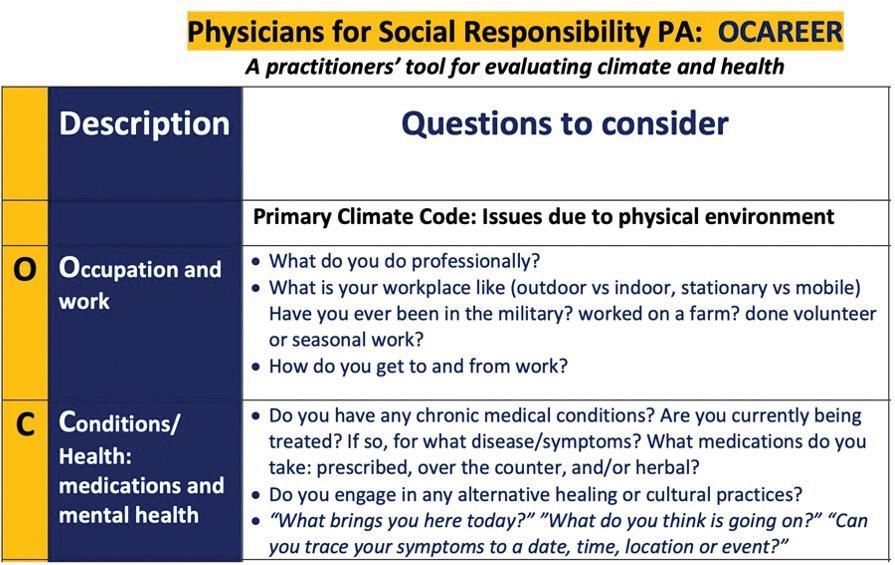
activities; and people are making the connection between exposure and their health issues, looking to clinicians to identify and treat their symptoms. While it is hard to measure these increases, let’s consider three examples of environmental hazards: contaminated water supplies from PFAS, contacts with chemicals from military service and those particularly present in this region, and shale gas operations from unconventional oil and gas development.
Examples of Hazards
Shale oil and gas are produced extensively in Pennsylvania, including fracking (as high-volume hydraulic fracturing method of shale gas extraction is referred to by popular media) and liquified natural gas (LNG). Much of the research about health hazards of fracking including cancers, asthma, respiratory diseases, skin rashes, heart problems, and mental health problems identifies living in proximity to shale oil and gas operations as the risk factor. (CHPNY, April 2022) Philadelphia does not lie atop of Marcellus Shale and therefore fracking operations such as extraction and processing do not happen in its metropolitan region. However, the transportation of the fossil fuels in the form of LNG has been approved by city council to go through the city. (Bate, 2019)
If interested in OCAREER, please contact: ocareer@psrpa.com
During extreme heat or prolonged heat waves, heart failure patients will need to be counseled about spending time outdoors and activities to prevent heat stroke, accessing food and medications to limit strain on the heart, and potential changes in medications, like diuretics, to address dehydration. The need to apply common sense solutions to these types of issues will be incumbent upon clinicians. Clinicians may also need to advocate on behalf of their patients to get services reflecting changes in climate. Continuing with extreme heat or prolonged heat waves as an example, air conditioning should be considered as part of a treatment plan. Since paying for electricity is a major concern, clinicians will need to advocate for their patients to receive services like Low Income Home Energy Assistance Program (LIHEAP), such as energy vouchers, in order for them to use air conditioning. This type of advocacy is an upstream approach to address SDoH that impact health from climate change.
Environmental Hazards
Background: With the rise of acknowledged environmental hazards, the medical knowledge of threats to people’s health is increasing. These include sources from air pollution, chemical contamination, and emerging disasters. More environmental hazards are being identified and linked to negative health outcomes because of several factors: technology is better able to detect lower levels of contaminants in the air, water, and land; information about the health impacts of contaminants is more complete through research
LNG is a highly flammable product, making it a security threat but it can also flash freeze human flesh creating a public health hazard. The process of liquefaction is a source of toxic air pollutants and the production process emits 30 percent higher greenhouse gases than conventional gas. (CHPNY, April 2022) In many parts of the state, families seek medical attention as they are experiencing health symptoms they associate with proximity to and length of exposure to nearby fracking operations. Physicians in Philadelphia who may find themselves in the role of a specialty consultant and frontline clinicians in other parts of the state are often at a loss as to how to mitigate the sources of exposures for these families and as such end up downplaying the exposure concerns. The section on role of clinician is aimed to help with history taking and documentation of these concerns as the first step in addressing the exposures.
PFAS, nicknamed the “forever chemical,” are human-made chemicals used in many industries and consumer products. They are resistant to heat, water and oil, and persist in the environment and the human body. PFAS are not found naturally in the environment. Since the 1950s they have been applied to manufacture cookware, carpets, clothing, fabrics for furniture and packaging for food. They are also used in firefighting foams and in a number of industrial processes. In the Philadelphia region, the former Willow Grove Naval Air Station in Horsham has demonstrated high levels of PFAS, contaminating public wells. In a publication by the Agency of Toxic Substances and Disease registry (What are the health effects of PFAS?, 2022), a number of health effects were associated with PFAS exposure, including increased cholesterol levels, decreased vaccine response in children, changes in liver enzymes, increased risk of pre-eclampsia in pregnant women, decreases in infant birth weights and increased risk of kidney or testicular cancer. In November
26 Philadelphia Medicine : Spring 2023
Figure 3: Sample of the climate health assessment mnemonic OCAREER
FEATURE continued philamedsoc.org
2022, the PA department of health released a public health advisory highlighting these findings. (2022– PAHAN –674 – 11-15 – ADV Per- and Polyfluoroalkyl Substances (PFAS) Exposure, 2022) To read more about the impacts on the pediatric population and what patients can do, you may refer to a blog by pediatrician Dr. Ned Ketyer. (Ketyer, 2022)
A third environmental exposure that has increasingly been discussed occurred in the course of many veterans’ military deployments. Pennsylvania has the 4th largest veteran population in the nation. During the military operation in Southwest Asia Theater, in countries such as Iraq and Afghanistan, trash, human waste, and other military items such as batteries and equipment were burned in open pits using gasoline and fuels. Other airborne hazards also existed, such as the fire of oil wells in Kuwait in early 1991. While these exposures occurred in the past, many veterans have expressed significant concern about their current health problems in relation to these and other environmental exposures. In August of 2022 President Biden signed the PACT (Promising to Address Comprehensive Toxics) Act into law. While the Veteran Health Administration (VHA) has historically pioneered the incorporation of assessment of environmental exposures into clinical care by creating environmental health registries, this act is among the first instances where the importance of environmental exposures has been highlighted throughout the healthcare system. Many veterans seek care with non-VA clinicians, especially in more rural areas of Pennsylvania and as such, these clinicians may find themselves needing to assess military exposures. VHA offers extensive informational training and clinicians are encouraged to take advantage of these educational resources. (Department of Veteran Affair Public Health, 2022)
Role of clinicians in Assessing Environmental Exposures
Clinicians need to identify and diagnose environmental exposures. Similar to climate change, they are faced with the need to assess them without possessing the tools to do so. To assist clinicians, the I-PREPARE (Paranzino GK, 2005) tool is a mnemonic developed in the late 1990s by public health and nursing professionals to take an environmental history. I PREPARE is: I - Investigate Potential Exposures; P - Present Work; R – Residence; E - Environmental Concerns; P - Past Work; R - Referrals and Resources; E - Educate (Figure 4).
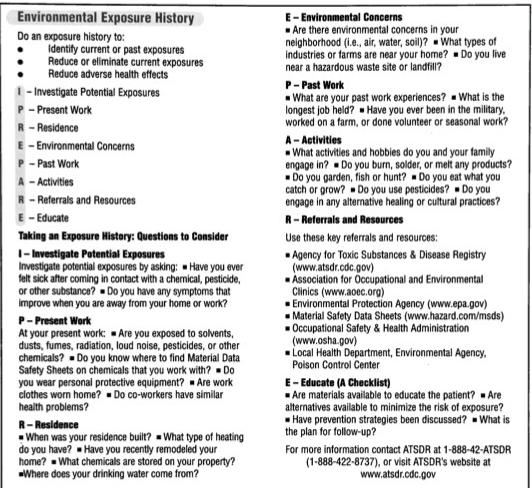
In an evaluation of this tool, 80% of the participants said that they would be more likely to ask patients environmental health history questions if they had a mnemonic card. Two-thirds would use at least part if not all the questions on the tool. Overall, the response for use of this mnemonic was very positive and helpful for clinicians.
As environmental medicine experts, we recognize the difficulty facing clinicians in assessing environmental hazards and addressing the concerns of the patients. Often front-line healthcare workers conduct the preliminary assessments and then proceed to refer to specialists when more complex evaluations and/or treatment regimens are called for. The dearth of specialists in environmental medicine and related fields such as toxicology limit the ability of clinicians to refer their patients when environmental exposures arise. Furthermore, the lack of comprehensive treatments especially for past exposures may be sources of frustration for both the clinician and patient alike. (Ryan EC, 2020) In outlining these mnemonic aides, we hope to increase the repertoire of tools available to clinicians to elicit histories that lead to accurate documentation, applicable medical evaluation and ideally possible solutions for treatment and at the very least management of environmental exposures. It is paramount to end on the importance of clinicians advocating for what can be done to lessen the hazards of the impact of climate change and other environmental exposures on the health of their patients, as well as offering social and educational resources to their patients so that they can be their own advocates. •
Works Cited
2021 Climate Impact Assessment. (2023). Retrieved from PA Department of Environmental Protection (PA DEP): http://www.depgreenport.state.pa.us/elibrary/GetDocument?docId=3667348&DocName=PENNSYLVANIA%20CLIMATE%20IMPACTS%20 ASSESSMENT%202021.PDF
2022– PAHAN –674 – 11-15 – ADV Per- and Polyfluoroalkyl Substances (PFAS) Exposure. (2022). Retrieved from PENNSYLVANIA DEPARTMENT OF HEALTH : https://www.health.pa.gov/topics/Documents/HAN/2022-674-11-15-ADV-PFAS.pdf
About Social Determinants of Health (SDOH). (2021, March 10). Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/socialdeterminants/about.html
Bate, D. (2019, June 13). WHYY. Retrieved from https://whyy.org/articles/ philadelphia-city-council-approves-pgws-60-million-liquified-natural-gas-plant/ CHPNY. (April 2022). Compendium of Scientific, Medical, and Media Findings
Demonstrating Risks and Harms of Fracking and Associated Gas and Oil Infrastructure. Retrieved from https://concernedhealthny.org/wp-content/uploads/2022/04/CHPNY-Compendium-8-FINAL.pdf
Department of Veteran Affair Public Health. (2022). Retrieved from https://www. publichealth.va.gov/exposures/index.asp
Ketyer, N. (2022). Retrieved from The PediaBlog: http://www.thepediablog.com/2022/12/15/ pa-health-advisory-pfas/
Paranzino GK, B. P. (2005). I Prepare: Development and Clinical Utility of an Environmental Exposure History Mnemonic. AAOHN Journal, 53(1):37-42.
PETMAC as a mnemonic for the 6 deadly causes of chest pain. (2022, june 23). Retrieved from https://canadiem.org/tiny-tips-petmac-mnemonic-for-6-deadly-causes-of-chest-pain/ Ryan EC, D. R. (2020). Medical, nursing, and physician assistant student knowledge and attitudes toward climate change, pollution, and resource conservation in health care. BMC Med Educ, 20(1):200.
Samano-Martin-Del-Campo D, S. C. (2020 , October ). Climate change expertise, knowledge, attitudes, and behaviors: An assessment of the apha community. Retrieved from APHA’s 2020 VIRTUAL Annual Meeting and Expo (Oct 24-28): https://apha.conf
What are the health effects of PFAS? (2022). Retrieved from Agency for Toxic Substances and Disease Registry: https://www.atsdr.cdc.gov/pfas/health-effects/index.html
27 Spring 2023 : Philadelphia Medicine philamedsoc.org
Figure 4: “ I-Prepare” mnemonic card
PCMS STUDENT INTERVIEW:

Nicole V. Perry Bryce Philadelphia College Osteopathic Medicine DO Class
of 2023
Formal Name: Nicole V. Perry Bryce
Everyone calls me: Nikki
As a PCOM leader, delegate to the PAMED House of Delegates, Student Representative on the PAMED Women’s Section, member of numerous medical organizations, how has organized medicine impacted your career in medicine?

717-961-9017
np7437@pcom.edu
she/her/hers
I was brought into organized medicine by my mentors, Drs. John Mantione and Joe Answine. Each time I asked how to find mentors, research, or advocacy opportunities the answer was always organized medicine. Through the PAMED House of Delegates I was able to network with many physicians also interested in supporting and uplifting women in medicine. This year I was able to work with medical students across the state to craft new resolutions and bring to the HOD floor.
Tell us a little about your road to Medicine. Why did you choose PCOM and what drew you to Philadelphia?
My road to medical school was a pretty winding path with many starts and stops. My
first real exposure to medicine was in fourth grade. My mom was pregnant with twins and my favorite show and tell was ultrasound pictures of my baby brothers. At the anatomic scan my parents were given a devastating diagnosis of trisomy 18. My parents made the difficult decision to have a selective reduction. When I joined my mom at some of her appointments afterwards, I saw how the physicians supported her without judgment regardless of whether or not they agreed with her choices. I knew then I wanted to be just like them. I wanted to be there for people in times of great joy and also great sorrow. I attended Dickinson College with the plan to then apply to medical school. Little did I know that first curve in my road to medical school would happen. Instead of applying to medical school, I applied to nursing school instead. I attended Lancaster General School of Nursing, then I worked as an ER nurse with the plan to apply to NP school. As a nurse I would ask questions and the nurse educator would say “oh you don’t need to know that” or “the doctors knows all about that, so you don’t need to know that.” While the doctors would patiently answer all my questions, even in a busy ER. Eventually one of the physicians saw me looking at NP programs and said “You’re smart. Why not
28 Philadelphia Medicine : Spring 2023 philamedsoc.org FEATURE
Nikki Perry Bryce
Philadelphia College Osteopathic Medicine DO Class of 2023
medical school?” That got me thinking about the dreams I had as a small child of becoming a physician. I soon realized that in order to provide my patients with the high quality health care I want to provide, the only way to do that was to get the education and training that I could only receive as a physician. I reached out to my pre-health advisor at Dickinson, who reminded me that my gen Eds were now 10 years or older. So I repeated all my gen Eds in 10 calendar months taking my last final on a Wednesday and the MCAT that Saturday. I applied to medical schools and was accepted to PCOM. I applied to medical schools and was accepted to PCOM. I am happy to say that I will be graduating in May and will be starting my residency at PCOM in July.
What do you like most about medical school?
I love showing my kids that with hard work and dedication you can achieve all your dreams. I love watching my friends achieve their dreams and goals. I love watching how each of us has grown. We went from struggling in the anatomy lab to discussing how we are caring for critical patients on our rotations.
What would you tell someone that is interested in going into Medicine?
Medicine is beyond rewarding. Everyday we have the privilege to care for patients on the best days of their lives and the worst. It will be your greatest honor to step into your patients’ lives even for the briefest of moments. These moments will make all the hardships worthwhile. Medicine ins’t perfect. The system is on the verge of breaking. Cling to those moments. Use the amazing advocacy and social media skills to be the change we want to see in medicine. I can’t wait to work alongside you!
Tell us about your goals for your Residency and beyond.
I am looking forward to working as a general practice OBGYN, and continuing to advocate for my patients and colleagues on the local, state, and federal levels.
Are you involved in any community, or non-profit organizations? If so, please list the groups:
Mid-Atlantic Babywearing - Board of Directors
Period Project Harrisburg - Board of Advisors
Le Leche League - volunteer and working toward becoming a leader
Delta Nu Alumni Advisory Board - Risk and Wellness Co-Chair
Being a full time Mom in Medical School, Any Tips, and What are your interests when you’re not working?
My husband, Brandon, and I have four children. I have been either pregnant or nursing every year of nursing school. Colton is 14. Robbie was born in May before M1. Rory was born the Saturday before our last finals week of M1. Freya was born during the last week of my EM rotation of M4. Sometime I feel like Dory. “Just keep swimming, swimming. Just keep swimming.” Any parent will tell you are never ready to have kids. Do whatever works for you and your family. Having a career prior to medicine meant either having children in medical school or not having any more kids. I know that I am not a typical medical student or mom. I love leaning into both. You can figure it. We do amazing, hard, challenging things everyday. I believe in you!
My husband grew up on a farm in Arizona and he is slowly converting me from a city girl into a country girl. I love our chickens. When I’m not working I love taking the kids out to our barn to help feed and take care of them. We love Hershey Park. It was not uncommon for Brandon, who is an emergency medicine physician, to help review whatever I was studying as we floated on lazy river. We love spending time together not only as a family, but also as a couple. It’s really important to prioritize that time together.
What do you value most about your membership in PCMS PAMED?
I value the opportunity to shape the future of medicine in Pennsylvania and beyond. There are a lot of challenges in medicine and I look forward to being a part of the solution.
Any Final Comments
Please continue to talk to your colleagues and especially your trainees about the importance of participating in PAMED and AMA. While being a member of your specialty group, we must come together as the house of medicine to advocate for our profession and our patients. •
29 Spring 2023 : Philadelphia Medicine philamedsoc.org
Pennsylvania Venue Rule Medical Malpractice
March 14, 2023
Introduction
Since 2003, medical malpractice cases in Pennsylvania had to be filed in the county (venue) where care was rendered. This “rule” (it was never law) was reversed by the Supreme Court of Pennsylvania on August 25, 2022, and this reversal took effect January 1, 2023.
History
Pennsylvania has long been a difficult state to underwrite predictable medical malpractice insurance coverage. Philadelphia, in particular, has consistently been named a “judicial hellhole” by the American Tort Reform Foundation.
Twenty years ago, several reforms were enacted in order to make the state more attractive from a medical malpractice standpoint. A significant action was the “venue rule” by which plaintiffs could no longer “venue shop” for more favorable jurisdictions. This change helped decrease the number of claims both statewide and in the state’s two largest cities: Philadelphia (Philadelphia County) and Pittsburgh (Allegheny County).
Conversely, some counties in proximity to larger cities or more plaintiff-friendly venues saw significant increases:
Impact
• According to The Philadelphia Inquirer, Philadelphia filings in January and February 2023 almost tripled compared to the same time last year.
• Premiums in some areas could rise as high as 25%

PA Malpractice 2000 to 2002 2018 to 2020 Case Filings Average Average Impact Pennsylvania Statewide 2,733 1,541 -44% Philadelphia County 1,204 390 -68% Allegheny County 396 256 -35%
County 2000 to 2002 2018 to 2020 Case Filings Average Average Impact Montgomery County 22 111 +500% Lancaster County 7 105 +1,500% Washington County 7 26 +370%
Risk & Insurance | Employee Benefits | Retirement & Private Wealth www.hubinternational.com Pat Nolen 484-620-0440 pat.nolen@hubinternational.com Mike Nolen 610-322-0930 mike.nolen@hubinternational.com 30 Philadelphia Medicine : Spring 2023 FEATURE philamedsoc.org

We understand that starting, running, and expanding a practice is no small feat. Our team of Relationship Managers offers years of experience partnering with medical professionals to develop custom strategies that address their distinct healthcare business needs.



CitadelBanking.com/ Medical WELCOME TO BETTER Built for Your Practice BUSINESS BANKING
Citadel is recognized as a Forbes 2022 Best-in-State Credit Union. Federally Insured by NCUA.































 by Frederick J. Goldstein, PhD, FCP* Professor of Clinical Pharmacology Philadelphia College of Osteopathic Medicine
by Frederick J. Goldstein, PhD, FCP* Professor of Clinical Pharmacology Philadelphia College of Osteopathic Medicine
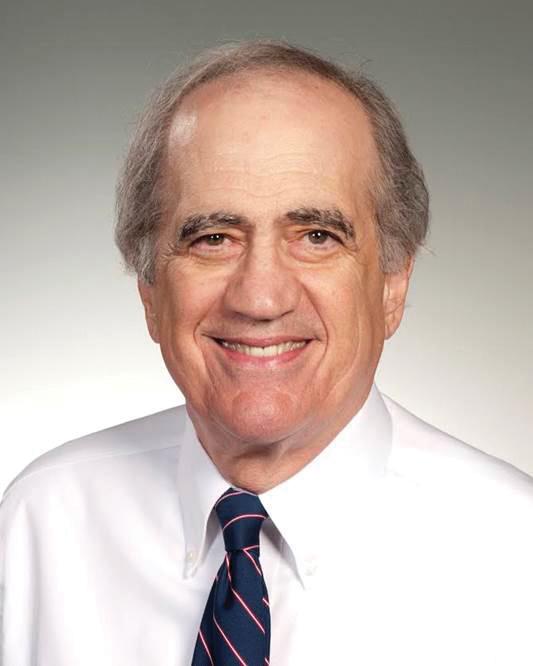










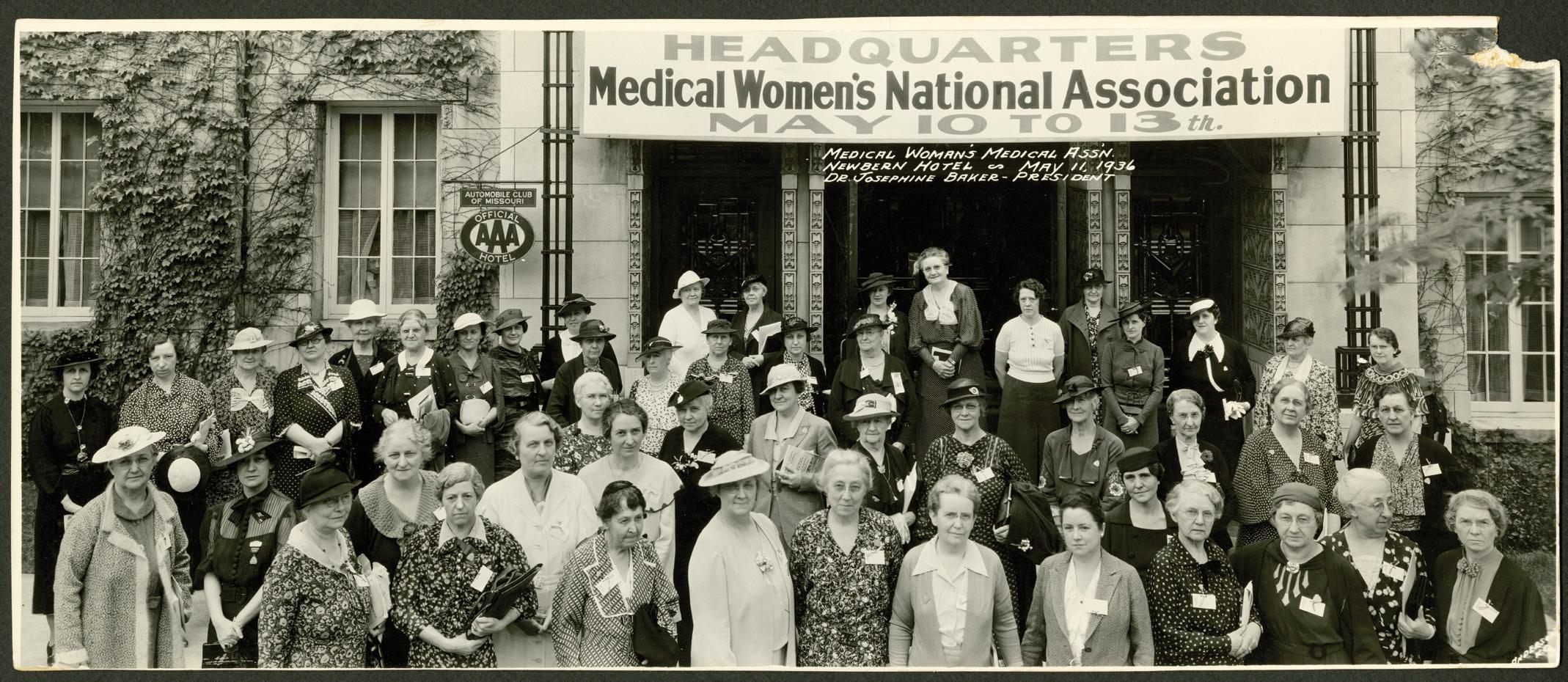



 by Julie Becker, MA, PhD, MPH Pouné Saberi, MD, MPH
by Julie Becker, MA, PhD, MPH Pouné Saberi, MD, MPH