Saint Francis Health System Board of Directors
John-Kelly C. Warren, Chairman
Judy Kishner, Vice-Chair
Jake Henry Jr.
Michael Case
Michael Cooke, JD
Ashley Gable, MD
Reverend Gary Kastl
William R. Lissau
Charles McEntee, MD
Saint Francis Health System Executive Council
Jake Henry Jr.
President and Chief Executive Officer, Saint Francis Health System
Barry Steichen
Executive Vice President and Chief Operating Officer, Saint Francis Health System
Eric Schick
Executive Vice President and Chief Financial Officer, Saint Francis Health System
Mark Frost, MD
Senior Vice President, Medical Affairs, Saint Francis Health System
Mike Lissau, JD
Senior Vice President, General Counsel, Saint Francis Health System
Tom Neff
Senior Vice President, Strategic Planning and Corporate Business Development, Saint Francis Health System
Doug Williams
Senior Vice President, Saint Francis Health System and Administrator, Saint Francis Hospital
Collin Henry, JD
Vice President, Saint Francis Health System, Warren Clinic Operations and Physician Recruitment
Michele Keeling
Vice President, Saint Francis Health System and Administrator, Saint Francis Hospital Muskogee
Finny Mathew
Vice President, Saint Francis Health System and Administrator, OSUMC
Todd Schuster
Vice President, Saint Francis Health System and Administrator, Saint Francis Hospital South

a publication of
Health System 10 COVID-19: Saint Francis Health System’s Response One Year Later 22 Laureate Psychiatric Clinic and Hospital Healing the Mind and Renewing the Spirit 34 Pediatric Intensive Care at The Children’s Hospital at Saint Francis 32 Warren Clinic Continues Expansion of Virtual Care Services 28 Warren Clinic Primary Care Your Partner in Health–for Life 38 Children's Miracle Network 2021 Champion Child 44 The Rosary A Prayer for Our Times, and All Times 48 Stronger. Together. Again. Health Zone at Saint Francis Reopens with Ongoing Safety Measures 20 COVID-19 Vaccinations Contents Virtual Urgent Care Warren Clinic 24/7 Learn about easy access and emerging technologies on Page 28
Saint Francis
Letter from Jake Henry Jr.,
President
and Chief Executive Officer
There is little about providing healthcare today that is easy. Change is the new normal. Competition comes from all directions. Consumer needs are elusive and constantly evolving.
Change comes down to people designing better solutions for our patients. It is about seeing the world through a different lens, listening with a third ear and looking around corners. It is about Saint Francis innovating and transforming to meet patients where they are to make a lasting impact on their lives.
Happily, the Saint Francis Health System was both fortunate and grateful to receive a $10 million gift from the William K. Warren Foundation to establish the Institute for Emerging Technologies in health delivery. The Institute has as its virtual health objective the creation of a digital infrastructure within the Saint Francis Health System. This infrastructure will allow development of inpatient virtual health solutions that can be scaled across the health system and northeastern Oklahoma; will expand remote monitoring and other care models beyond the walls of Saint Francis; build a comprehensive digital front door that will allow easy navigation to all virtual and non-virtual health offerings; and develop an internal network of virtual health tools that can be expanded externally.
We had the good fortune to recruit Trey Bomier as the director of the Institute for Emerging Technologies. Trey had just completed the installation of an electronic health record in Denmark and we were pleased we were able to enlist him in this new Saint Francis enterprise.
Trey and his colleague, Brent Dennis, MD, a talented physician leader, have moved quickly since the Institute’s inception in the spring of 2020. Already the physician arm of Saint Francis, Warren Clinic, has seen 63,000 patients via video visits; 13,000 e-visits
have occurred since establishment of the service; the placement of a robot to assist with triage of patients and wayfinding missions in Muskogee has transpired; a virtual urgent care whereby patients can visit a local caregiver virtually around the clock seven days a week has been created; and virtual care clinics in neurology, diabetes education, dermatology and pain management counseling have been established. Artificial intelligence has been built into the Saint Francis electronic health record to predict patient falls and patient sepsis. And many more innovations are in the pipeline.
Healthcare organizations like Saint Francis face multiple new market entrants. It seems that every day ushers in another potential disruptor, whether it is a start-up, a new technology or another industry entering the healthcare realm and they are very different than traditional provider organizations. They are free from the brick-and-mortar facilities and payor contracts. Their unconventional backgrounds make these new entrants highly agile to test different products and service offerings until they find what resonates best with consumers.
So while it is easy for the consumer to become enamored by the latest advancement in digitalization, pursuing disconnected healthcare solutions is detrimental. Consequently, the value of our developing digital technology will center on end-to-end experiences that patients have as they move through the Saint Francis system of care.
Let me end by saying again how grateful the system is for the munificent gift of $10 million to start up the Institute for Emerging Technologies at Saint Francis. This gift enables the system to have the resources and leadership to improve the healthcare experience and ultimately, health outcomes of our patients. We are grateful!
Jake Henry Jr. President and Chief Executive Officer Saint Francis Health System

1 presence Saint Francis Health System
New Services for Patients in the Vinita Area
After more than a year of planning and renovations, a $2.5 million project comes to fruition and provides residents of Vinita and the Grand Lake area with access to new magnetic resonance imaging (MRI) services. The new scanner allows for a wide range of MRI procedures and the expanded scanning space can also accommodate bariatric patients, as well as patients who are claustrophobic.
“We are so pleased to bring this essential service closer to home for so many of our patients,” said Saint Francis Hospital Vinita executive director and administrator Melinda Culp. “A long commute can be a hardship sometimes, and now it won’t be necessary for patients who need this service.”
The new MRI suite is the latest in Saint Francis’ continuing efforts to update facilities and services at its Vinita hospital. In April, the hospital will open a new cardiac rehabilitation facility.
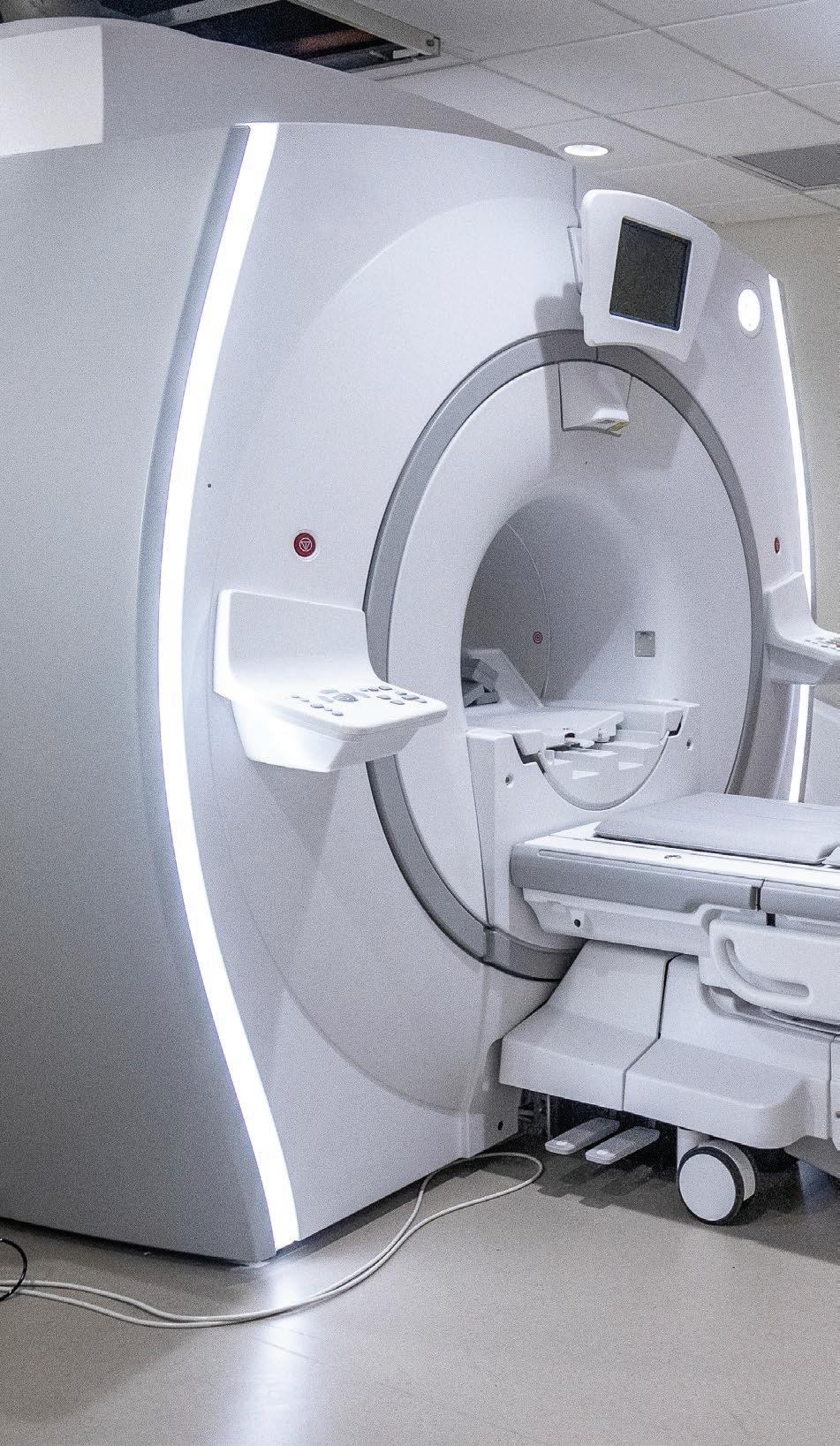
Since the acquisition of the Vinita hospital in 2016, Saint Francis Health System has invested more than $18 million in facility, infrastructure, equipment and technological updates as a part of the ongoing commitment to expand healthcare services to patients in Craig County and the surrounding area.
To learn more about Saint Francis Hospital Vinita, please visit saintfrancis.com/vinita.
2 saintfrancis.com 2 saintfrancis.com
presence in pictures


It's Our Honor
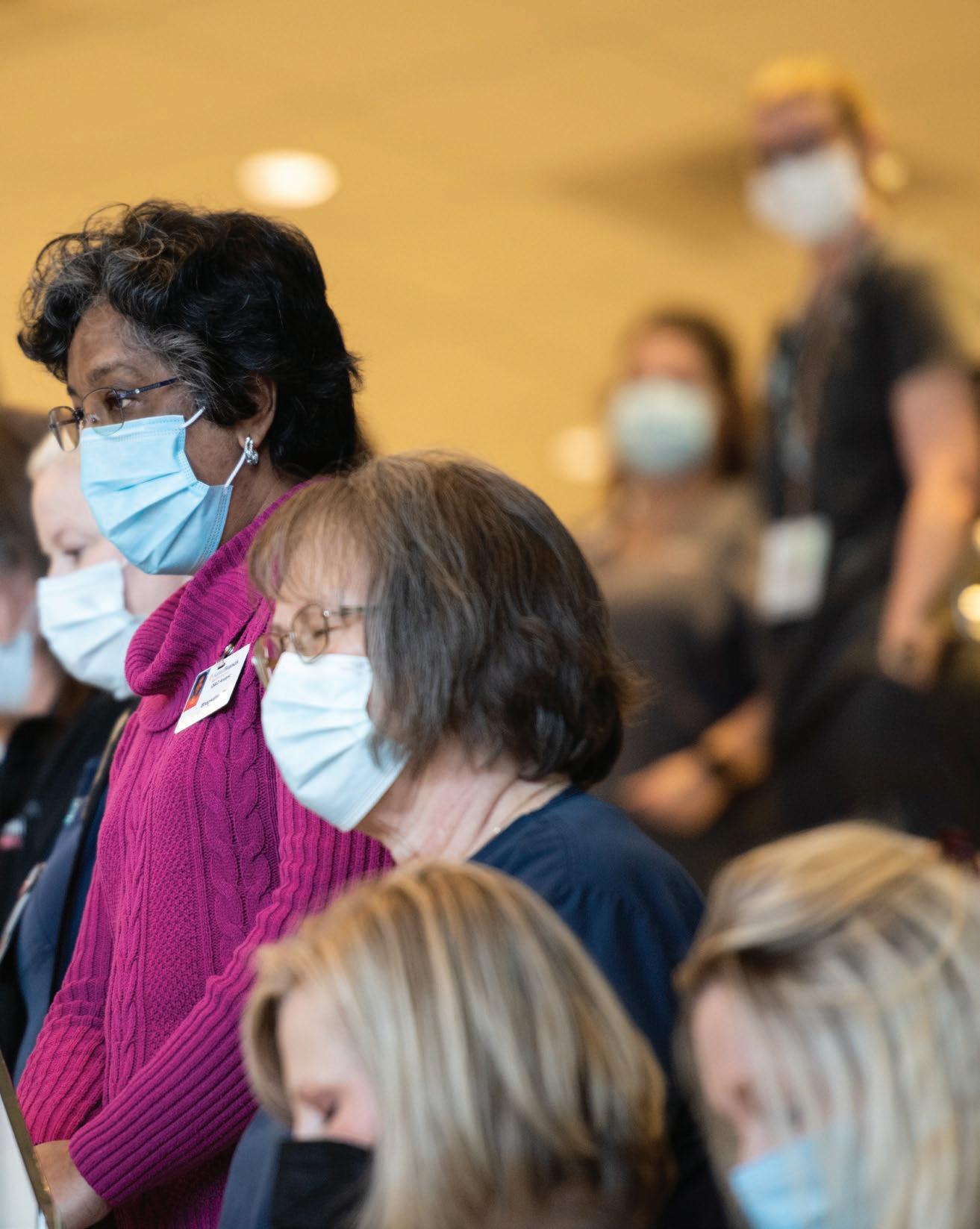
When COVID-19 vaccinations became available in Oklahoma, it was our privilege to serve as one of the first sites to partner with the Tulsa Health Department and the state to vaccinate healthcare workers and those in the Phase 1 stage of eligibility.
As more vaccine became available and the state expanded eligibility to more individuals, Saint Francis expanded its offerings with online scheduling capabilities and additional vaccination sites within the community.

As of late March, more than 50,000 doses of COVID-19 vaccine have been administered by Saint Francis Health System.
“Everyone has really come together to develop the infrastructures and processes to make this as easy as possible— and now, as vaccine availability has expanded, we’re excited to offer the vaccine to any eligible person in Oklahoma,” said Steve Davis, executive director, Warren Clinic.
For more information or to schedule the date, time and location for your firstdose COVID-19 vaccination, please visit saintfrancis.com/ getvaccinated. Appointments are required.
5 presence Saint Francis Health System
presence in pictures

Celebrating International Women’s Day
From all appearances, spring arrived early in Tulsa—and just in time to commemorate International Women’s Day.
On March 8, designated as International Women’s Day, the Lobeck Taylor Family Foundation (LTFF) and VEST (an organization committed to connecting and elevating women in the workplace) put its own spin on celebrating women with an interactive community art project.
These local projects involved abundant floral displays strategically placed at key locations within the community. One such location was at the statue of Mary Queen of Heaven at the south entrance of Saint Francis Hospital. This location was chosen as a salute to, and a celebration of, women in healthcare—as well as a beautiful sight to be enjoyed by hospital staff members, patients and guests.

7
presence in pictures
A Moment in Time
At noon on Monday, March 1, Saint Francis Health System staff members gathered for a moment of silence. This specific day and time were chosen as a somber acknowledgment of one year ago when Oklahoma’s first COVID-19 patient walked into a Warren Clinic Urgent Care location. This moment of silence was simultaneously observed at all Saint Francis Health System facilities—as well as at other organizations throughout the region, including area churches whose chapel bells tolled as a symbol of solidarity.
“Through this moment of silence, we honored those we have tragically lost while recognizing the sacrifices we have made together as a community,” said Tulsa Mayor, G.T. Bynum. “I want to share my profound gratitude to my fellow Tulsans for their perseverance and to our front line healthcare heroes and first responders for leading our community through this global pandemic.”
The past year witnessed many moments of silence—as well as many others of prayer, fear, compassion and hope. “We have been through a lot together over the past year and coming together for this moment of silence was very meaningful. It was a moment of sadness for all the people we have lost; but also, a moment of gratitude for how well we have worked together,” said Saint Francis cardiologist, Dr. Adam Karpman. “Now is a time for hope, but also a time for vigilance. It’s not over. By the time Tulsa marks the second anniversary of COVID-19, I hope we are back to normal. I hope we are all out doing the things we want to do.”

8 saintfrancis.com 8 saintfrancis.com
presence in pictures
COVID-19
SAINT FRANCIS HEALTH SYSTEM’S RESPONSE ONE YEAR LATER
With the arrival of COVID-19 in the U.S. and the first confirmed cases in Oklahoma, the physicians, nurses, leadership and staff across Saint Francis Health System have served on the front lines in the fight against the first global pandemic in more than a century.

There are so many Saint Francis stories of the pandemic. Stories of strength, loss, fear and courage under pressure. There are so many employees to thank for their tireless response, dedication to patients and grace under pressure.
Here are just a few voices from the pandemic.
10 saintfrancis.com
Saint Francis Health System is the largest healthcare provider in Oklahoma with a team of more than 10,500. Every employee was critical in the fight against COVID-19.

Marilynn Bartel, vice president, Saint Francis Health System, Ancillary Services: On March 2 of this year, I marked my 40th year with Saint Francis. I started my career with the lab and that's when I realized there was something different about this place.
Karen Njafuh, RN, COVID unit nurse: I was a hospice aide for five years, but I had been in healthcare for 10 years as a certified nurse assistant. I felt like I had a deeper calling to go further in my career. College was not a standard in my family, so I wanted to set new standards for my family. I graduated from Langston University in May 2018.
Cindy Leathers, NBA-HCM, BSN, RN, executive director, Patient Care Services/Chief Nurse Executive: I joined Saint Francis in February 2017. This is actually the third time I’ve worked for the health system. First right out of high school as a nurse assistant, then after some time out of healthcare, I went to nursing school later in life. I then returned to Saint Francis as a nurse, moved to Colorado for several years, and made my way back. Saint Francis was always the place for me in Tulsa.
Melinda Culp, BSN, executive director/ adminstrator, Saint Francis Hospital
Vinita: I’ve been with Saint Francis since 2001, but lived in Vinita and would drive to Tulsa every day. I took the director of nursing position at Vinita in 2018 and became executive director the next year. I bleed Saint Francis pink through and through, so it’s special to me that Saint Francis is in our community.
Roger Gallup, MD, pulmonary/critical care physician: This is my fourth year at Saint Francis. I’m a retired army colonel and I started my military career as a medic. When I was in Iraq and Afghanistan I was a theater surgeon. Before the pandemic, I had joked that my current job was supposed to be my retirement job. I am currently leading the pulmonary critical care unit.
Ryan Parker, MD, chief of Emergency Medicine, Saint Francis Health System: Originally, I wanted to go into social work because my dad was a police officer. I got an internship in an ER in Paris, Texas, and fell in love with emergency medicine and later worked in Dallas. Being in the ER gives me insight into what’s happening in the world.
Dr. Gallup: Being in the military prepared me a lot for the pandemic—how to prepare for various scenarios, go into new situations that didn’t have solutions and figure out how to meet those challenges. From the very start, our staff and leadership stayed calm and realized that COVID-19 was a marathon and we all had to pace ourselves to get through it.
11 presence Saint Francis Health System
”
“
“I never thought I’d see this in my lifetime.”
Roger Gallup, MD
From the very start, our staff and leadership stayed calm and realized that COVID-19 was a marathon and we all had to pace ourselves to get through it.
It was only a matter of time before COVID-19 arrived in our region. Saint Francis assembled a team representing many different disciplines and clinical specialties across the health system to prepare, but no one could have imagined what was to come.

Collin Henry, JD, vice president, Warren Clinic Operations and Physician
Recruitment: We started planning for COVID-19 in January 2020. We were hearing that Seattle had been hit hard with cases and New York was becoming a hotbed—we had to be ready for what could come our way.
Bartel: We prepared for the pandemic like we had for other outbreaks in the past, like swine flu or Ebola. It wasn’t a matter of if we’d see a case of COVID-19, but when.
Dr. Parker: I became chief of Emergency Medicine in January 2020. Just a short time later, Oklahoma confirmed its first few cases of COVID-19.
Leathers: We established a centralized 24/7 emergency command center for the entire health system. This way we could direct and monitor everything such as patient bed capacity, staffing, ICUs, ventilators, lab testing, pharmacy needs, PPE, emergency room capacity and so much more. At that time we really didn’t know the extent of how our community and health system would be impacted. That command center remains open today, more than one year later.
Dr. Gallup: It was a lot of work trying to get everything together and convert regular hospital units into units dedicated to the care of COVID patients. Everyone from engineering and environmental
services to nursing and epidemiology spent a number of days determining what was needed to make those units safe and ready.
Leathers: Ironically, our first confirmed COVID patient arrived on the day we were doing a preparedness drill. I remember working through the drill and we got a call, and the real scenario was the same as the drill.
Henry: We had a hypothetical scenario: A patient comes in with a cough who had just been to Italy. What do you do? Later that afternoon we had our first case at one of our Warren Clinic Urgent Care locations—it was a symptomatic patient who’d just come from Italy. It was almost divine intervention that we prepared for that exact scenario earlier that day.
Soon, COVID-19 cases and hospitalizations were increasing. All Saint Francis hospitals, ERs, clinics and departments worked quickly in response. Warren Clinic opened a drive-thru COVID testing site to meet the growing demand for testing in the community. More hospital units were converted to dedicated COVID units as more critically ill patients, young and old, were impacted by an invisible enemy.
Henry: Early on, the Warren Clinic Urgent Care locations got hit the hardest with the influx of patients. That’s where people who were symptomatic of COVID would walk in. Those Warren Clinic facilities were delivering care when we weren’t sure how to defend against the virus and when we had the most anxiety and fear. Seeing how the staff responded…those were moments where you’re really proud of your colleagues.
12 saintfrancis.com
“It was almost like divine intervention…”
“Lord, how can I help someone else?”
Karen Njafuh, RN
Njafuh: I was finishing up floor training as a part of my new nurse orientation at Saint Francis. We all heard that COVID was not overseas anymore, it was here. Then I heard our unit, 5 West, was going to be the first dedicated COVID unit. It was a shock. I’m just a week out of training and boom, I'm in a COVID unit.
Kim Walton, RN, CCRN, CEN, director, acute care services, Saint Francis Hospital Muskogee: Before rapid COVID tests, we designated patients as ‘PUI’, a person under investigation. It was how we discussed a patient who was symptomatic, but we didn’t know if they were positive or not. We had to stay in touch and keep track of the PUIs to make sure they weren’t spreading COVID-19 while we waited for the test results.

Bartel: To manage the ever-changing situation in our hospitals, ICUs, outpatient clinics and laboratories, we had multiple daily briefings on numerous issues in the emergency command center. We put our problem-solving skills to the test. What tasks now required procedure masks? What required N95 masks? How do we get patients screened for COVID-19 and tested? We had a pretty robust supply of PPE and thankfully we never ran out.
Leathers: We had to change some pretty important policies in the beginning. It’s amazing that a place as big as Saint Francis, with all our locations, was able to quickly adapt, make changes and sustain them. A year later, everything we changed is still in place today.
Bartel: One key partnership was with the Tulsa Health Department (THD). They were embedded in our operations and we were in step with what they were advocating. We met with THD for weeks—every single day.
Dr. Parker: March and April allowed us some time to prepare. We saw what was happening in other cities and saw the horrible impact COVID-19 was having. Keeping that in mind, we properly managed our supplies and resources.
Culp: Tulsa was seeing the surges and supply demands, so here in Vinita, we kept an eye on what was happening there. When our first patient came in we were a step ahead in preparation because we were able to see what the hospital on Yale was doing.
Leathers: I've learned that if there's a crisis, I want the Saint Francis team to be there with me. This past year, we had some major challenges, but we came together and we worked through it.

Cindy Leathers, executive director, Patient Care Services/Chief Nurse Executive
I’ve learned that if there’s a crisis, I want the Saint Francis team to be there with me.
“
”
Culp: Even though people were educated, there was always the fear of the unknown: Who has it? Am I taking it home? As leadership, our role was to be very transparent. Things changed minute to minute, but we made sure our staff knew we were giving them everything we had.
Njafuh: Fear was my initial feeling. Some of us even had tears. In my unit we have staff with family members that are immunocompromised or at high risk. I had to really conquer that fear. I prayed: “Lord, how can I help someone else?” So I just had to surrender to God and He gave me help every day. The fear was lifted. I left it at God’s feet. I just trusted Him.”
Bartel: Misinformation was rampant, but the thing that is different about this disease is there is no cure and it spreads so easily.
Njafuh: We noticed that COVID-19 impacted people differently. You’re taught to look for symptoms, but not everybody has those same symptoms. Some people were in a bad way pretty quickly, and were going down fast.
Dr. Gallup: As pulmonologists and hospitalists we’re right at the heart of this. You have an enemy you can’t see, but you have to figure it out as you go how to fight this.
As Oklahoma’s COVID-19 cases increased, Saint Francis’ preparation turned to action. An internal mantra within Saint Francis Health System is: “We do crisis well.” That proved accurate during the challenging months that followed. But even though the health system prepared for what was ahead, at times it felt like COVID-19 was winning.
Dr. Parker: Biology follows patterns and we know how viruses tend to work. This was a new virus and it didn’t follow those typical patterns. In medicine you always want to have the correct, black-and-white answer. We’ve gotten better about saying medicine is a practice and it’s an art, we may not know everything, but we know a lot.
Walton: If a patient is in a life-threatening emergency, nurses are trained to rush in to save them. It was challenging for the emergency and ICU teams to relearn their protocols, to stop and don PPE
before running in the room. In the Saint Francis Hospital Muskogee ER at our peak, nurses pretty much had to be in PPE all the time.
Dr. Parker: When the big surge of COVID cases came in the winter, it was really scary for all of us, but we had good practices in place, we had efficiency. We were confident we could handle the tremendous influx of patients. I’m so thankful at that very difficult time, we were ready.

“You have an enemy that you can’t see.”
Karen Njafuh, RN
...I just had to surrender to God and He gave me help every day. The fear was lifted. I left it at God’s feet. I just trusted Him.
“ ”
Hospitalizations reached critical levels in the fall and winter months which put a significant strain on healthcare workers and hospitals throughout the region. In the face of increasing hospitalizations and battles over misinformation, Saint Francis published a full-page ad in local newspapers with the headline: “We’re Headed in the Wrong Direction.” While Saint Francis worked to inform the public about what was truly happening, the team was feeling the strain of working long hours away from their families, for the better part of a year. What kept the team going was a shared sense of mission—and each other.
Njafuh: The surges of COVID-19 patients we saw in the fall and winter were incredibly exhausting. Seeing so many people die, it really started to take a toll on all of us physically, mentally and emotionally.
Dr. Parker: My husband and I had a conversation early on in the pandemic about sending our family away to protect them. My husband said: “No, we’re sticking together.” My little girl would
get upset as I would leave for a shift in the ER. I had to remind her: ‘I’m not home with you because I’m helping other people.’ It was important for my kids to see and understand that.
Walton: At Saint Francis Hospital Muskogee we peaked with 61 COVID patients at our hospital. That means at that time about 50% of all our hospital beds were occupied by COVID patients. In December, almost 100% of our ICU cases were COVID.

Culp: Our peak in Vinita was nine. That doesn’t sound like a lot, but for a small community hospital with 15 medical/ surgical beds, it is.
Njafuh: This entire time has been a walk of faith for me. Fear was certainly a big deal. As healthcare workers, we see firsthand how bad things are and have been. You have to conquer that. I decided that I was not going to walk in fear—I’ll walk in faith instead.
Dr. Parker: Despite people’s fears, people took a deep breath and went to work. When bad things happen, you get together with people and you work together to solve a crisis.
Dr. Gallup: Numbers go up and down, but we have truly had so many critically ill patients with COVID-19. I feel like this war with COVID-19 never ends.

15 presence Saint Francis Health System
“I’m not home with you because I’m helping other people.”
Kim Walton, RN, director, acute care services, Saint Francis Hospital Muskogee
Newspaper ad published November, 2020
24/7
Command Center data SAINT FRANCIS HOSPITAL MUSKOGEE SAINT FRANCIS HOSPITAL VINITA SAINT FRANCIS BROKEN ARROW SAINT FRANCIS CANCER CENTER SAINT FRANCIS HOME CARE COMPANIES SAINT FRANCIS GLENPOOL SAINT FRANCIS HOSPITAL THE CHILDREN’S HOSPITAL AT SAINT FRANCIS WARREN CLINIC HEART HOSPITAL AT SAINT FRANCIS SAINT FRANCIS HOSPITAL SOUTH LAUREATE PSYCHIATRIC CLINIC AND HOSPITAL We were doing better when we were in this together. It’s not in our collective nature to back down from a challenge but we are losing ground to a common enemy. Like other health systems in our region, we’re at a critical capacity. We continue to work around the clock to protect our healthcare community so they can protect you, the community-at-large. We’re asking you to stay strong and committed to fighting this pandemic with us. Wear a mask, wash your hands and watch your distance Please do your part, so we can keep doing ours. Saint Francis Health System Daily Census of Inpatient Positive COVID-19 Admissions JULY THIS WEEK 129 55 97 MARCH WE’RE HEADED IN THE WRONG DIRECTION.
saintfrancis.com *Source: Saint Francis Health System
COVID
Dr. Parker: Watching my other colleagues, we all hit the wall at some point. There are several people who would stay at work in the ER for over 16 hours at a time. Just knowing there are human beings who are willing to do this makes me proud.
Walton: Our teams are tired. The COVID numbers were so high at our peak, but we’ve all been very flexible. Our thinking was: “How do we get this done as a group?” That’s how you survive—as a group.
Culp: When we had our surge in Craig County in November and December, we had to cross-train staff from other departments to help manage the situation. It was all hands on deck. We knew we needed to step up for our community, and we did.
Dr. Parker: Whether you’re a nurse tech, paramedic, building engineer, housekeeper, lab or pharmacy employee, on the supplies team, food services, pastoral care, radiology and so many more departments to name—I know everyone feels that same pride in what we were doing.

It was a harrowing experience that healthcare providers will carry with them forever.
Leathers: Our staff is used to taking care of very sick people. But this virus has caused a lot of death. I’ve heard from physicians that in a 12-hour shift they have ten conversations about end of life. It just weighs on you.
While the spirit of the statement is true, it hides an uncomfortable truth—many people have lost much more than others. Their jobs, their health, even their lives. Saint Francis’ team stood by patients in their darkest, loneliest hours and when family members were unable to even see their loved ones as they lay seriously ill or dying.
Dr. Gallup: Usually when a patient is critical, their family normally can be in the room, but with COVID the family can’t. Doctors, nurses and nurse techs had to help these patients, in even the most dire moments, to communicate with their loved ones via phone or iPad.
Dr. Parker: I recall a patient who was very sick and her family lived outside the area. On a phone call between her and her sister, I was able to hold the phone up for her. It’s humbling to bear witness
16 saintfrancis.com
“We show up for each other.”
“We’re all in this together.”
Ryan Parker,
MD, chief of Emergency Medicine, Saint Francis Health System
“
When we were scared of COVID-19, we showed up. You have to do that for your community. Whether it’s a pandemic, or flood or ice storm, we show up for each other.
”
to something so personal, knowing deep down that a patient may not survive this illness.
Dr. Gallup: There was an elderly COVID patient who was very critical. My nurse and I were there for her in her final moments. There were several moments like that I will never forget.
Walton: As a small-town hospital in Muskogee, we know many of our patients as friends and neighbors and really feel the impact of losing them. Just recently, we lost one of our own doctors to COVID-19. Dr. Yee Se Ong, one of our cardiologists, had been with this hospital for over 40 years. When he died it changed the tone, the morale. It was a significant event for our hospital and our community.
Njafuh: I had a patient who went on a ventilator. Some patients can’t communicate, but she could still write and communicate. She was really scared. So I sang and prayed with her. I believe a patient’s spiritual well-being is just as important as their medical care. When I sang to her, it gave her peace. If she was struggling, she could hear me singing and it would help keep her calm. She wound up improving and being discharged from the hospital. It gave me an extra boost of confidence to continue on in the fight.
Leathers: We have to stay positive for patients and their families. It’s so very emotional to be that person in the middle. Many times employees have sought support from our Pastoral Care department—priests, nuns and chaplains, to find comfort and solace as they face some very difficult moments.
Walton: I’m so inspired by the resiliency of our nurses, physicians and staff at the bedside. They’ve taken care of patients multiple shifts per week a month at a time, and then the patient doesn’t survive— that’s incredibly hard. But we’ve had
family members, despite losing loved ones, who have sent notes of appreciation, food or flowers to our staff for the care they provided.
Dr. Parker: We take care of everyone. When we were scared of COVID-19, we showed up. You have to do that for your community. Whether it’s a pandemic or flood or ice storm, we show up for each other.
Saint Francis’ local leadership in the war on COVID-19 cannot be measured or scaled. The health system’s across-the-board commitment to the community was critical in getting Oklahomans the care they needed.

Dr. Parker: I think that if we didn’t have the resources that we did, it would have looked much different for our region. I don’t think we’ll ever see the full impact of what we mitigated.
Leathers: We talk about being locally operated and that means we can make decisions in a matter of seconds. We have autonomy to make those decisions and make those things happen quickly. Because when there’s a crisis, everybody is all hands on deck to respond.
Henry: An example of this quick response was in testing, which has been such a key part in fighting the pandemic. If we didn’t have quick COVID testing, more people could potentially spread the virus. Being a part of Saint Francis allowed Warren Clinic to quickly establish a COVID testing site, which was testing 800 people a day at our peak. Anybody who wanted a test could get a test. Given our volume, knowing how many COVID tests we did per day, where else would those people go?
“Where else would these people go?”
Culp, BSN, executive director/ adminstrator, Saint Francis Hospital Vinita

Culp: Vinita is my home. These are my neighbors. They’re the people I go to church with, and the moms and dads of my children’s friends. We’ve seen what has happened to other rural clinics. To have the level of care that Saint Francis provides in Vinita, at this moment in our history, means the world to me.
Njafuh: Several rural hospitals didn’t have capabilities to care for people who were really sick. When patients needed a higher level of care, other hospitals sent them to us.
Leathers: Because of our size and critical care capabilities, Saint Francis Health System has cared for more COVID patients than most hospitals in the state. We’ve had a plan from the start to take care of them.
Dr. Parker: We know it’s important that the people who are making decisions for our health system are based here in our community. They understand and want to do right by their neighbors.
Culp: The Vinita community was so supportive. We’re in the middle of a neighborhood, so on nice days we’d take
walks when we had a minute of free time. People would see us and shout “Thank you.” People driving by would honk, wave and give a thumbs up. That was huge.
Saint Francis faced a global pandemic on a local level, but also worked to provide accurate information to the community. One year later, the health system—and the people who make it all possible—have emerged stronger.

Bartel: I can’t tell you how many of my friends have asked: “Don’t you wish you retired in March of last year?” I can’t put it into words really. I tear up thinking about this past year, seeing the impact we have made as a health system and ending my career with Saint Francis.
(See side-bar on page 19.)
Walton: We had to manage this crisis and so far, we’ve done it. The people of Muskogee saw that. They know we were there when they needed us, and we always will be.
“We came together like a family.”
Melinda
Dr. Parker: I told my team once this gets better, we’ll tell our children and grandchildren: “Yeah, we did that.”
Henry: I think we are honestly more confident because when a challenge presented itself and there wasn’t a playbook; we now know what we’re capable of when we work together. We have the resolve to tackle what might come our way.
Dr. Parker: We rose to the occasion. It really inspires you. We knew this is what we trained for. One of my doctors sent me a quote from St. Joan of Arc to sum up what we do as healthcare workers: “I am not afraid. I am made for this.”
Njafuh: I have no regrets and no second thoughts about joining Saint Francis and the respiratory care unit. It was an honor to walk through this experience. It has molded me into a better nurse. I pray we don’t experience anything like this again, but if we do, I know all of us will come together like a family.

Honoring Marilynn Bartel on her 40-year career with
Saint Francis Health System
“I never thought I’d work this long, but you know, I just keep loving to work here,” said Marilynn Bartel, vice president of Saint Francis Health System Ancillary Services. “Not everyone gets to wake up every morning wanting to go to work, and going home knowing you did something to make a difference. That’s most days.”
This year, Marilynn Bartel will retire from her 40-year career at Saint Francis Health System. Her retirement comes after the most difficult year of her career, in which her leadership and experience were pivotal in the health system’s response to COVID-19.

Saint Francis was Bartel’s fifth hospital job, and her last. She worked her way up from the lab to her leadership position the old-fashioned way: Hard work, passion and a commitment to helping patients and empowering her colleagues.
“When I got here, I realized Saint Francis was not like any other place and this is where I wanted to retire from,” said Bartel. “We have values that aren’t just words on a wall. How great is it to be able to go to work and live out your faith?”
While friends and family have asked Bartel if she wished she had retired in March of last year, before the pandemic, she says she is proud to have made a contribution. That’s putting it mildly. The work Bartel did this past year, and her entire career, has helped save countless lives. For that we are forever grateful.
“I am glad I stayed this past year, and I know we’re in a good spot,” said Bartel. “I can retire and go off into the sunset and know I’m leaving everything in good hands.”
19 presence Saint Francis Health System
VACCINE PROVIDES NEW HOPE IN THE FIGHT AGAINST COVID-19
“Hero” has been used a lot during this pandemic. Who, exactly, is a hero? To us, a hero helps others. Period. So it is only appropriate that we thank all those who have so far chosen to get their first COVID-19 vaccination with this simple message: Thank you for being a hero.
Make no mistake, by receiving the COVID-19 vaccine you are not only protecting yourself, but stopping the spread of a virulent plague that has claimed more than 8,000 lives in Oklahoma and a halfmillion lives nationwide. That makes you a hero and a part of something much bigger.

“It’s super exciting to be a part of history,” said Matzali Medina. As an ICU nurse tech, she helps care for those with COVID-19. She was among the first healthcare workers at Saint Francis to get the vaccine back in December. “I’m so proud to get the vaccine and get things changing for everyone.”
Kellie Brewer, RN, shares Medina’s enthusiasm. As the clinical manager of two COVID-19 inpatient units at Saint Francis Hospital, Brewer was also one of the first people to receive the vaccine in Tulsa. “That was probably one of the best days of my life,” said Brewer. “We’ve seen the horrible things this disease has done to people. This is our opportunity to stop it.”
From the start of the pandemic here in our area, Saint Francis and Warren Clinic quickly mobilized to help public health officials lead the fight against COVID-19 in the community.
20 saintfrancis.com
“We’ve seen the horrible things this disease has done to people. This is our opportunity to stop it.”
Kellie Brewer, RN
“In March 2020, we immediately opened up a 24/7 call center to answer people’s questions about COVID-19 symptoms and testing; we have now received more than 113,000 calls,” said Collin Henry, JD, vice president, Warren Clinic. “Our health system has tested more than 110,000 people. So far we have given just over 50,000 doses of vaccine.” When the COVID-19 vaccine became available, Saint Francis partnered with the Tulsa Health Department to vaccinate front line workers, first responders and physicians, both within the health system and from other hospitals and healthcare facilities in the area.
Despite being Oklahoma’s largest health system, with a workforce of 10,500 people, Saint Francis has remained creative, innovative, adaptable and nimble. These attributes have been essential during an ever-evolving, year-long health crisis. “During flu season last fall, we needed a convenient way to get people the flu vaccine but also keep patients and providers safe from COVID-19. So we built drive-thru flu clinics at Warren Clinic and at Saint Francis Hospital Muskogee,” said Henry.

“But then we realized with just a few modifications these clinics would work perfectly for administering the COVID-19 vaccine. So we installed central heat and air to keep our staff comfortable, but also have the right cold temperatures to safely prepare the vaccine. We’ve been able to help so many people thanks to our drivethru clinics.”
Thanks to healthcare workers in general, our community—our world—is experiencing something we have not in what seems like forever: Hope.

“There’s been a shift from anxiety to hope. In February, for the first time we vaccinated more people for COVID-19 in one day than we tested,” said Henry. “We’re building on the energy of coming together, pulling through the hard times, and finally we see light at the end of the tunnel.”
But the Saint Francis team is not just seeing light at the end of the tunnel—Our people are helping carry that torch that is guiding the way. “Getting vaccinated has a special meaning,” said Brewer. “It’s moving toward a new beginning for all of us.”
21 presence Saint Francis Health System
Schedule your first COVID-19 vaccine online today. C H O O S E YO U R DAT E , TIM E A N D LOC ATIO N eligible under the Oklahoma State Department of Health’s vaccine distribution plan. Visit saintfrancis.com/getvaccinated to schedule your vaccination online. An appointment is required. saintfrancis.com/getvaccinated
Healing the mind and renewing the spirit.
To say the human brain is nothing more than just a part of the body that controls biological functions does not do it justice.
The mind is the seat of consciousness, the singular characteristic which St. Augustine believed is what made us in the image and likeness of God. Your mind is a divine gift, which should be appreciated, protected, and most of all, loved. For as miraculous as it may be, it is not invincible.
A year into the COVID-19 pandemic and the disruption that came with it, people of all ages have dealt with various negative emotions—among them stress, anxiety, loneliness, uncertainty and fear. The situation is even worse for those who have lost loved ones to the pandemic or the millions who have lost their jobs and had their lives upended.
Thankfully, COVID-19 cases are dropping and millions are getting
vaccinated, generating a renewed sense of hope and optimism for the future.
However, negative emotions did not start with the pandemic and they will not go away once it is over. Last year was not the beginning of our mental health crisis; it was only the latest chapter. For years, we have been living in a stew of mental health triggers: comparing our lives to the so-called “perfect lives'' we often see on social media; feeling the pressure to be perfect in our careers and relationships; negative news fatigue; social isolation…the list goes on.
“We saw the demand for behavioral healthcare services growing even before COVID-19. I do believe the way we now interact digitally is increasing that demand,” said Brandon Keppner,
 Laureate Psychiatric Clinic and Hospital
Laureate Psychiatric Clinic and Hospital
executive director and administrator of Laureate Psychiatric Clinic and Hospital. “Losing those social skills and losing that personal connection has an impact. The more we drift in that direction as a culture, the more damaging the emotional consequences of how people see themselves. You have the social media context and then you have a pandemic that has pulled people away socially. Then you have the fear…and it’s just a perfect storm.”
Times have been tough, but during these times, and at all times, Laureate’s message is simple: It’s OK to not be OK. You are not alone. There is value in seeking care and advice from a professional counselor to help you build emotional resiliency in your own life and seeking care when you need it the most.
Besides being a full-time therapist, George is also a mom to two little girls, so she can relate to what parents have been going through in the past year. She says her family started a new tradition during the pandemic: Friday movie nights followed by a dance party. While of course that may not be your thing, George encourages people to “fill their bowls with pink M&M’s,” in whatever that means to them. “If there’s a movie you like, or a friend you wanted to connect with, or a hobby you enjoyed before COVID-19, make sure you’re still enjoying those,” said George. “Refill your life with things that are really positive for you.”
Hannah George, MA, LMFT, a licensed therapist with Laureate describes the brain in an uncomplicated and colorful way. “If you think of your brain as a bowl of M&M’s, the negativity, stress and anxiety are like filling your bowl with black M&M’s. It’s damaging,” said George. “Doing what you enjoy is putting in a brighter color, so I tell my patients to ‘fill your bowls with pink M&M’s’ since pink is my favorite color.”

While it may be necessary take care of yourself first, we must never forget the needs of others, especially at this time. “If you notice your loved ones seem really worried or don’t seem like themselves, just check in and ask how they’re doing,” said George. “Don’t assume or accuse. Just reach out and ask what you can do for them. Sometimes just showing up with flowers, or taking a meal to a friend or a neighbor is enough.”

23 presence Saint Francis Health System
“Fill your life with pink M&M’s.”
“Refill your life with things that are really positive for you.”
Hannah George, MA, LMFT licensed therapist Laureate Psychiatric Clinic and Hospital
The weight of negative emotions
While trying to stay positive is important, running away from negative emotions is not possible. Nor, for that matter, is it healthy.
“It’s OK to feel difficult emotions— especially those that have emerged during the past year,” said Rebecca Brumm, MA, LPC, CEDS-S, clinical director at Laureate Psychiatric Clinic and Hospital. “Our natural tendency is to run away from them, but that’s just about the worst thing you can do with emotions.”
“It’s not like putting your hand on a hot burner, where you have to quickly pull it away,” said Brumm. “What we have to do with emotional pain is move toward it. If a dog were to bite your hand, your natural tendency is to pull away. But the dog only sinks its teeth in deeper. You have to jam your hand in the dog’s mouth, which is counterintuitive, but the dog gags and releases. Emotions are the same way.”
Brumm tells her patients that when you are experiencing negative emotions, whether it is loneliness, sadness, resentment or stress, do not ignore or bury those emotions; that only allows them to grow and fester. Instead, acknowledge your emotions, experience them and recognize that it comes and goes in waves. “I have so much compassion for running away,” said Brumm, “but we have to train ourselves to face it.”
“Life is uncertain,” said George. “We like to think we have control over it, but people get tripped up when they try to control things. The more you try to force things, the more you miss opportunities to be happy.”
The value of seeking care

While it is important to build emotional resiliency, you do not have to face hard times alone. There is nothing wrong with reaching out for help if you need it.
As a part of Saint Francis Health System, Laureate has a broad range of services for patients in need of various levels of care. This includes people who are facing a first-time emotional crisis, such as depression or anxiety, a traumatic event or the death of a loved one. Services are also available for outpatients who simply want someone to talk with about their concerns and obstacles.
“If things feel like they’re piling up or hard to manage, or you have low motivation, are struggling to concentrate, are down and depressed, can’t control your worrying or can’t sleep, those are big markers that you may need to seek some support,” said George.
“Don’t run faster than you are able. You have to check in with yourself,” said Keppner. “We all have stress, but how does it affect everything? Does your depression, anxiety or stress affect your daily life or your eating or sleeping? That’s a sign it’s time to have a conversation.”
“It’s OK to feel difficult emotions— especially those that have emerged during the past year.”
24 saintfrancis.com
Rebecca Brumm, MA, LPC, CEDS-S, clinical director at Laureate Psychiatric Clinic and Hospital
Keppner equates Laureate’s outpatient services to Christ’s “teach a man to fish” edict in Matthew 4:19. “Laureate is about teaching patients key coping skills. It’s patients learning what behaviors or thoughts are triggering issues. If you can help people with that chain of events, you can help them change their path,” said Keppner. “Therapy helps people slow down, look at themselves and how they’re reacting so they can find better solutions.”
Laureate’s purpose to uplift and empower patients is even reflected on its campus.


“Laureate’s campus is beautiful—a bit like a college campus,” said Keppner. “There’s something about nature that brings a sense of peace that sits in harmony with your soul.”
However, in-person sessions at Laureate may not be an option for many patients during COVID-19. For patients unable to come to Laureate, Laureate can come to them through telehealth.
“Video visits have been great for me as a therapist, because most of our clients are far away,” said George. “It has opened up opportunities to help people that might not have been there beforehand.”
“In the past year, our demand has gone straight up, and we’ve been creative and thoughtful for using our resources,” said Brumm. “Being able to condense our new appointment wait times has been critical.”
“Christ is asking us to be His hands.”
While technology is important to expanding patient access to mental healthcare, the most important part for Laureate will always be the team doing the work. This goes beyond the staff’s esteemed credentials or evidence-based therapeutic practices; it comes down to shared purpose.
“Everyone who works here, who is drawn here, is drawn to excellence,” said
“We all have stress, but how does it affect everything? Does your depression, anxiety or stress affect your daily life or your eating or sleeping? That’s a sign it’s time to have a conversation.”
Brandon Keppner, executive director and administrator of Laureate Psychiatric Clinic and Hospital
thing to be quarantined and isolated when you have several people in your home. If


separate from their parents. “Think of ways your teen can safely be with friends. They can go on a walk, hang out, volunteer, get

26 saintfrancis.com
Never hesitate to reach out and help others, but never be afraid to ask for help either.
a job or find other ‘COVID-conscious’ activities that provide independence and structure. Just as long as they’re being extra cautious.”
Older adults: “I think the pandemic has hit hardest for seniors,” said George, who mentions how her grandmother “has made a conscious decision to choose joy. She’s not letting negative things keep her from what she loves.” Even as COVID vaccinations become more available, it is important to remember that many older adults have suffered from social isolation for quite some time. Both George and Brumm recommend children and grandchildren reach out to the seniors in their lives.
“Reach out to an older adult, even if it’s just dropping a card,” said George. “Little small acts, as much as you can do things for them, and help them out, mean a lot.”
Laureate Depression and Anxiety Program
Laureate offers a comprehensive range of services, from outpatient visits with a therapist, to intensive outpatient and inpatient care. The Depression and Anxiety Program is designed for adults who need short-term support, mood stabilization or help dealing with a situational crisis. The program includes:
Inpatient Care: short-term treatment and stabilization in a safe, structured environment. Following inpatient treatment, patients are encouraged to extend treatment through our Intensive Outpatient Program.
Intensive Outpatient Program (IOP): provides intensive outpatient services with options for individual therapy after completion. Programs offered within IOP:
Mental Health Intensive Outpatient Program (MH IOP): provides structured care with frequent treatment sessions that address and treat depression, anxiety, panic and mood disorders. With the provider’s encouragement and support, people learn new coping skills to deal with life’s situations.
Chemical Dependency Intensive Outpatient Program (CD IOP): provides structured care with frequent treatment sessions. Through education, encouragement and support, patients can work to break the cycle of substance abuse and improve their quality of life.
If you would like more information about Laureate’s programs and services, please call 918-481-4000 or visit saintfrancis.com/laureate.
In case of a mental health emergency and if you are worried you might harm yourself or others, please call 911 or the National Suicide Prevention Hotline at 1-800-273-8255.
27 presence Saint Francis Health System
Kyle Rock, MD

“I was hugely influenced by my own pediatrician, Dr. Patrick Hughes,” Dr. Rock said about the long-serving Warren Clinic pediatrician. “His influence, his calming presence, his rapport and the way my parents spoke so fondly of him, was inspiring to me.”
Dr. Rock even got to work with Dr. Hughes before his retirement several years ago.

Warren Clinic is bringing the physician-patient connection into the future. Your Partner in Health Warren Clinic Primary Care:
saintfrancis.com 28
Dr. Rock’s opportunity to work with his pediatrician was unique, but his experience of building a connection with his doctor was not. In fact, it is the point of primary care.
“Your doctor provides the foundation for overall good health,” said Chitralekha Kathuria, MD, a Warren Clinic Family Medicine physician. “Having a primary care doctor allows patients to become comfortable, not only with their own health, but with seeking care when they need it.”

“I’ve just felt so blessed to be able to touch so many lives and help people lead better, healthier lives,” said Dr. Kathuria. “It’s very rewarding and very humbling to know you helped make a difference in somebody’s life. It’s a different realm of happiness.”
A passion for their profession.
A sense of purpose is a common refrain among the adult and pediatric primary care providers throughout eastern Oklahoma who call Warren Clinic home.

“I could not be happier,” said Bradley D. Hardy, DO, Family medicine is family business for Dr. Hardy, a third-generation primary care physician.
His father and grandfather were also long-time Tulsa physicians and Dr. Hardy is proud to be a part of Warren Clinic’s 32year legacy. “This is home. It truly does feel like an honor,” he said.
The bond between patient and physician is alive and well at Saint Francis, and is what inspires each provider’s passion for his or her profession.
“I have taken care of five generations of the same family,” said Dr. Kathuria. “I get the opportunity to know families, to direct health, to pick up on health concerns and help lead patients to live long, happy lives. I feel that is my calling.”
“It is the good Lord’s presence that helps and sustains all of us,” said Dr. Kathuria. “My job is to bring that to people’s lives.”
29 presence Saint Francis Health System
Health
Chitralekha Kathuria, MD
Establishing a relationship with your primary care physician is vitally important for your lifelong health and well-being. Yet far too many patients simply do not do it.
“Some people think it’s unnecessary until something goes wrong,” said Dr. Kathuria. “We don’t want something bad to happen. That’s why you see the doctor.”
Avoiding primary healthcare services is not just a problem in Oklahoma; it’s a nationwide epidemic and is especially prevalent among men. According to a survey by the American Academy of Family Physicians, men are three times less likely to have seen a doctor in the past 12 months


than women, while a 2019 Cleveland Clinic study found that only 50 percent of men ages 18-years or older feel getting a check-up is important. While women are more likely to visit the doctor than men, 45 percent of the women surveyed in a study by the Journal of the American College of Cardiology admitted to canceling or postponing appointments for reasons that included wanting to lose weight first.
“It is imperative to have a primary care physician because we are your medical home,” said Dr. Kathuria.
“You’re not going to know anything is wrong if you don’t get checked,” said Dr. Hardy. “I would love to see my patients on an annual basis just to see and talk to them,
know their medical hopes and dreams, know how they’re doing emotionally, just making sure we’re doing everything right for them.”
“It’s incredibly important to see your doctor, especially the older you get,” said Dr. Hardy. “If you don’t have a primary care physician, if you don’t have a record on file, nobody is going to know your medical history, and how that translates into the care you want to receive.”
If you’re a parent of a younger child or teenager, establishing a baseline of health is just as important for your child’s pediatrician.
30 saintfrancis.com
“We are your medical home.”
“Life’s too short to have a poor quality of life. We’re here to be your advocate.”
DO
Bradley D. Hardy,
“There’s nuance and guidelines for children that may not be relevant for adults and vice-versa,” said Dr. Rock. “My experience as a pediatrician helps me minimize unnecessary treatments and focus on appropriate testing.” Dr. Rock also says consistency is key. “Sometimes I’ll see kids a couple of years after they’re sick, and if I had seen them earlier, we could have handled the issue, but now it requires surgery.”
Pretty much every primary care physician has a story about critical problems that a patient could have been ameliorated or even avoided simply by scheduling regular checkups.
“We've found cancers early, and the vast majority of those patients end up with good outcomes,” said Dr. Kathuria. “But there are cases that break my heart and make me wish they came in earlier. We see a lot of sad outcomes that would have been preventable if the patient came in. We want every person to achieve the best health and the best health outcomes that we can.”
Primary Care: The best investment of your life.
Being eastern Oklahoma’s largest, locally governed and operated health system gives Saint Francis and Warren Clinic unique insight into the needs of the community.

“Just like I need to put a hand on a patient to take their pulse, the local leadership feels the pulse of the community,” said Dr. Kathuria. “That’s how we can determine the needs and seek solutions.”
Beyond a shared commitment to serving the community, everyone at Saint Francis is driven to help each patient get the most out of life—during every stage of life. This mission starts with primary care.
“Life’s too short to have a poor quality of life,” said Dr. Hardy. “We’re here to be your advocate.”
“If something is wrong and my patients don’t know what to do, I am there for them,” said Dr. Kathuria. “To tell them: ‘This is your medical home and we’ll hold your hand. With God’s grace, we’ll get you to the best path.’”
31 presence Saint Francis Health System
Warren Clinic 24/7 Virtual Urgent Care:
On-demand care
provided by local physicians
Saint Francis is helping patients access healthcare services and achieve better health outcomes by leveraging emerging technologies that expand access to primary care like never before.


The nostalgic image of the family physician going on house calls is making a comeback. However, the leather medical satchel filled with stethoscopes and otoscopes is being replaced by a more state-of-the-art toolkit.
“Since the start of the pandemic, our job was to explore and adopt solutions to address the new challenges faced by our patients,” said Trey Bomier, director of the Saint Francis Institute of Emerging Technologies. “This solution included virtual visits, which have increased dramatically in the past year.”
“Virtual care was originally something that was two to three years on the horizon,” said Chris Abshere, MD. “Then COVID-19 comes along and forces your hand, because you need to take care of people, but we have been limited on face-to-face contact.”
“Saint Francis’ pre-COVID investments paid off. We’ve done more than 100,000 video visits with over 60,000 patients across the system in under a year,” said Bomier.
32 saintfrancis.com
Chris Abshere, MD
The latest addition to services available for patients is Warren Clinic 24/7 Virtual Urgent Care which launched in December 2020. These video visits allow patients to receive on-demand care from a Saint Francis provider from wherever they are in the state of Oklahoma. “Before, patients had to make tough choices like missing work or going to the ER. This helps remove barriers for patients to get the care they need, when they need it.”
“This is a local service,” said Bomier. “We connect you to a Saint Francis provider who can reference your electronic medical record through our system. This is as much like going to visit the doctor as possible.”
Next up, the Saint Francis Care Kit, a supplement to Warren Clinic video visits, is being piloted with Saint Francis employees now. Bomier says these kits will be available to patients later this year. This groundbreaking technology is an all-inone device that attaches to a smartphone, and includes a thermometer, stethoscope and otoscope. With a Saint Francis Care
Kit, your doctor can listen to your heart and lungs, utilize camera images look into your mouth and ears and take your vital signs, all while you are comfortably at home or in your office.


“You can even record things, which adds a whole new dimension to what you can look at and document,” said Dr. Abshere. “For me it’s almost easier to deliver the personalized care because we’re actually in their home. You really get more of a sense of who the patient is, where they live and what their situation is.”
“Think of it as an at-home, self-care kit,” said Bomier. “One Saint Francis Care Kit can be used for an entire family.”
“There’s still that art of medicine that comes with seeing patients in the office, and the communication that goes with that,” said Dr. Abshere. “Technology has opened up so many opportunities for healthcare that did not exist before, but the doctor-patient relationship still comes down to empathy, compassion and trust.”
33 presence Saint Francis Health System
“Think of it as an at-home, self-care kit.
One Saint Francis Care Kit can be used for an entire family.”
– Trey Bomier, director of the Saint Francis Institute of Emerging Technologies
Pediatric Intensive Care at The Children’s
Hospital at Saint Francis
As the only dedicated children’s hospital in eastern Oklahoma, The Children’s Hospital at Saint Francis provides a variety of specialized services coupled with family-centered care for infants, children and teens. Among those services, and one of the most critical, is the Pediatric Intensive Care Unit (PICU).
Doctors say that children are generally healthy. By that they mean that unlike adults, they haven’t acquired some of the habits that can have a negative impact on health and well-being. In fact, they say it is unusual for a child to become critically ill in the first place. But when they do, it happens quickly. Whether it is due to illness, chronic disease or trauma, if a child’s condition escalates to a critical level of severity, a Level 1 Pediatric Intensive Care Unit (PICU) can provide the highest level of care.
Level 1 Care
A Level 1 PICU is certified to provide specialized care for highly acute patients. This means that children can receive the critical care they need—while family members receive the guidance and support services they desperately want.

The Children’s Hospital at Saint Francis PICU is the only unit of its kind in the Tulsa area and one of two in the state that is fully equipped for pediatric-specific critical care.
“It’s so important for families within the region to know they have close access to a Level 1 PICU,” said Phil Barton, MD, pediatric intensivist. “A pediatric intensive care environment is unique in that every staff member—physicians, nurses, respiratory therapists—must be specially trained to provide care for a wide range of patients that require vastly different modes of care—ranging from a two-day-old infant, to a 21-year-old young adult. Pediatric intensive care is the only type of intensive care setting that requires staff members to have such diverse knowledge and skill base. In our world, each day is different, and we must be flexible and ready for anything… and we are.”
34 saintfrancis.com
The PICU provides a total of 23 beds. In addition to five, full-time, board-certified pediatric intensivist physicians, the unit staff also includes pediatric intensive care nurses, social workers, child life specialists, a specially trained pharmacist, dietitian and case manager.
“The PICU team is extremely engaged in the work they do and honestly takes care of each patient as if they were their own child. They have a fantastic ‘can do’ attitude and regardless of the challenges they face, they do all they can to get to ‘yes,’” said Kristi Baker, executive director, Women’s and Children’s Services at Saint Francis. “Providing care for our sickest patients on a daily basis can be emotionally draining— and it is remarkable to see how this team is there not only for each patient, but for each other, as well. What’s more, the PICU team at Saint Francis is also there to support and collaborate with referring physicians within the health system as well as those throughout the region.”

Among the more common conditions treated in the pediatric intensive care unit:

• sepsis and other major infections;
• major surgery;
• breathing or lung conditions;
• cancer and blood disorders;
• diabetic ketoacidosis;
• accidental and traumatic injuries;
• near-drowning;
• child abuse;
• accidental poisoning;
• craniofacial conditions;
• neurologic/brain disorders;
• epilepsy and other conditions of the nervous system;
• genetic and chromosomal conditions;
• metabolic disturbances and imbalances;
• certain heart conditions; and
• complications of chronic health conditions.
Highly-advanced, lifesaving therapies provided at The Children’s Hospital at Saint Francis include:
• Extracorporeal Membrane Oxygenation (ECMO): a form of heart and lung bypass designed as critical support for infants and children.
• Neurally Adjusted Ventilation Assist (NAVA): an advanced mode of mechanical ventilation that delivers assistance in proportion to and in synchrony with the patient’s respiratory efforts.
• Continuous Renal Replacement Therapy (CRRT): a type of blood purification therapy used with patients who are experiencing acute kidney injury.
“Time matters when an infant or child becomes critically ill. For instance, infants and children who receive ECMO therapy are those whose bodies are experiencing multi-system failure—primarily of the heart and lungs,” said Becky Reinholz, RN, clinical manager. “When we walk in to talk with a family about ECMO, their child just became the most critical patient in the entire health system.”
“A word that often comes to mind when I try to describe our team is ‘fortitude.’”
Becky Reinholz, RN, clinical manager
Saint Francis Health System 35 presence
Kristi Baker, executive director of Saint Francis Women's and Children's Services meets with pediatric nurse managers.
“We are thankful we can offer these lifesaving therapies to our patients. Our ECMO team is driven by the ‘best of the best’ nurses—many who’ve been doing this for 30-plus years. And as a result, our ECMO outcomes are consistently among the best in the country. With each patient and in every situation, the PICU team provides care for a family’s most prized possession. The magnitude of this responsibility is never lost on us.”
A Constant Reminder
Regardless of a medical team’s extensive skills and intense level of dedication; and despite their access to the most advanced medical technology available anywhere, it is inevitable that there are times when the PICU team cannot send a family home intact.

“When this happens, our team’s entire focus shifts to the family—mom, dad, siblings,
grandparents—we are there to support each family member in any way and for as long as is needed,” Reinholz said.
Dr. Barton added, “When we are able to help a family navigate through the process of finding their way again, it helps us too. Every person on our staff has the heart and the compassion needed for this kind of work. What we do here stands as a constant reminder to live in the present and to be there for others in need.”
36 saintfrancis.com
24/7 pediatric emergency center Adolescent medicine Allergy/Immunology Cardiology Child abuse pediatrics Critical care Dental Surgery Dermatology Eating disorders Endocrinology/ Diabetes care Gastroenterology General pediatrics General surgery Genetics Hematology/Oncology via the St. Jude Affiliate Clinic Infectious disease Neonatal transport team Neonatology Neurology Neurosurgery Oculoplastic surgery Ophthalmology Oral/Maxillofacial surgery Orthopedic surgery Otolaryngology (ENT) Palliative care Pathology Pediatric stroke team Physical medicine and rehabilitation Plastic and reconstructive surgery Psychiatry (child and adolescent) Pulmonology Radiology SAFE Kids program Sports medicine Trauma care Urology As the only Children’s Hospital in Eastern Oklahoma, The Children’s Hospital at Saint Francis offers specialized services in a family-centered environment. Pediatric healthcare services provided include the following:
Children’s Hospital at Saint Francis: Pediatric Specialties
Services
The
and
Phil Barton, MD, pediatric critical care intensivist

Fortitude and a Heart for Kids
So, what is it that binds the PICU staff together as they care for some of the most critically ill or injured patients?
“A word that often comes to mind when I try to describe our team is ‘fortitude’— which is defined as ‘strength of mind that enables a person to encounter danger or bear pain or adversity with courage,’” said Reinholz. “Strength of mind—along with a certain heart for kids—are reasons why no matter what the day holds, we hold each other to the highest standards.”
Elisabeth Case, RN, has been a pediatric critical care nurse at Saint Francis since 2006. “It was the first job I had following nursing school, so I guess you could say this place has raised me. From the minute I walked into the PICU, I just knew this is where I needed to be. Every day is a challenge; but every day is also an opportunity to learn something new. No words can describe the feeling I get every time I watch a child—who was so, so sick upon arrival— later smiling and waving goodbye as they leave the hospital,” she said. “It’s also difficult to put into words how I feel about our PICU team. We are not just co-workers; we are family. We laugh together. We cry together and we take excellent care of our young patients together.”

A Wealth of Wisdom
Despite being comparatively small, the PICU at The Children’s Hospital at Saint Francis is indeed mighty.
“For some time now, we’ve been a member of a consortium comprised of approximately 300 PICUs throughout the country. All 300 members are required to enter quality data in key categories and I’m proud to say our unit is consistently in the top five percent in all categories— foremost being good patient outcomes,” Dr. Barton said. “We have an incredibly talented team and I have always been very proud to be part of it.”
“It takes extraordinary people to provide this level of pediatric critical care,” Baker said. “Even though they already function at a very high level, the PICU team continually strives for quality improvement and consistently tries to see if they can do things better. It is clear this entire group is fully invested on both a professional and an emotional level.”
For more information about The Children’s Hospital at Saint Francis, please visit saintfrancis.com/ childrenshospital or call 918-502-6000.
37 presence Saint Francis Health System
“What we do here stands as a constant reminder to live in the present and to be there for others in need.”
Elisabeth Case, RN
“We are not just co-workers; we are family.”
Pediatric Intensive Care
One Child’s Remarkable Recovery from a Critical Illness

A Remarkable Journey
Friday, August 24, 2019, marked the end of the first week back at preschool for Francie VanTrease, the youngest in a family of seven children. Shortly after picking up her fouryear-old daughter that Friday afternoon, her mother Jill VanTrease knew something wasn’t quite right.
Out of Nowhere
“Once we got admitted to The Children’s Hospital at Saint Francis, Francie’s entire system crashed…seemingly out of nowhere. Before I knew it, we were surrounded by a medical team who hooked her up to many machines,” Jill said. “My first thought was, ‘how could I ever have wanted anything else in this world other than healthy children?’”
Francie in the PICU in the early days of her hospitalization
“Francie just wasn’t her usual effervescent self,” Jill said. “Once we got home, I discovered she had a slight fever; but it was so much more than that…suddenly she couldn’t even walk to the bathroom.”

Jill phoned the pediatrician who advised her to immediately bring Francie to the Pediatric Emergency Center at Saint Francis Hospital. “Our pediatrician later told me ‘something in my voice’ was the reason he directed us to Saint Francis, rather than to an urgent care or a smaller hospital. I believe if he hadn’t done that, we wouldn’t be here today telling this story,” Jill said.
Minutes later, pediatric critical care physician, Dr. Roopa Thukaram, arrived in the room to help stabilize and evaluate Francie’s condition. “When I first observed Francie, her body was very cold; and her skin was mottled and appeared blue. It was clear her body was undergoing severe cardiovascular dysfunction,” Dr. Thukaram said.

 Francie VanTrease
The Children’s Hospital at Saint Francis Children’s Miracle Network 2021 Champion Child
Francie VanTrease
The Children’s Hospital at Saint Francis Children’s Miracle Network 2021 Champion Child
Shortly thereafter, Francie’s dad, Phil, arrived at the children’s hospital. “Looking back, one of the moments I’ll never forget is when Dr. Thukaram first told us our daughter had tested positive for E. coli and that she was in septic shock. Everything was intense and became critical so fast that I kept asking myself, ‘did this really just happen?’ Yet, the severity of Francie’s condition was undeniably real,” Phil said. Upon being admitted to the Pediatric Intensive Care Unit (PICU) within the children’s hospital, Francie’s parents stayed alongside their daughter and prepared to await the indeterminate path ahead.
Day Two
The next morning at 2:00 a.m. in Francie’s hospital room, her path took a terrifying turn. When her parents were abruptly awakened, they knew instinctively what was happening—their daughter was experiencing cardiac arrest.


Within seconds, PICU team members were at Francie’s bedside performing chest compressions, resuscitating and stabilizing her. “Something else I’ll never forget is how we all froze for about 15 seconds and then breathed a collective sigh of relief as her vitals kicked back in,” Phil said. “But, unfortunately the sense of relief was short-lived. We learned we were still deep in the woods.”
Despite the successful resuscitation and the profusion of intensive care she had been receiving, Francie’s condition continued spiraling downward.


At this point, doctors made the decision to place her on extracorporeal membrane oxygenation (ECMO). ECMO is a form of heart and lung bypass designed as a temporary support for infants and children who are failing all other conventional methods of life support.
“We were ushered out of the room as the team prepared to place Francie on ECMO. I looked out the window just as the sun was coming up on what appeared to be a gloomy day. We are people of faith and so I started praying to God. I didn’t know what answer I’d get, but I knew He was there,” Jill said. “Suddenly the doctors
Did This Really Just Happen?
“We are so happy Francie is again her happy, ‘chirpy’ self.”
Roopa Thukaram, MD, pediatric critical care intensivist
came around the corner with smiles of relief on their faces and I knew it was going to be OK. They told us when they’d just slightly shifted Francie’s body while getting her ready for ECMO, her vitals inexplicably kicked back in—which negated the need for ECMO.”
While it was indeed good news that Francie’s vitals had improved, it became evident that her kidneys were now of critical concern.
“Francie’s kidneys were very sick and were completely shutting down. We were seeing necrosis of her kidneys, which essentially means her kidneys were dying,” Dr. Thukaram said. “Kidney removal is a serious step to take. We were determined to do what we could to avoid the need to perform a nephrectomy (kidney removal)—despite the fact there was a greater than 50 percent chance she could lose them. We began implementing a conservative approach which included antibiotics, ventilation, dialysis support and epinephrine—and then hoped and prayed her body would respond.”
And, respond she did.
Slowly, but surely, Francie began to turn the corner toward improving. Due to the highly specialized, 24/7 care she received in the PICU, it became clear this busy threeyear-old was on her way to recovery.


“All told, we ended up spending about a week in the PICU, followed by four additional weeks on another floor in the children’s hospital,” Phil said. “Despite being so critical and coming so near to the edge, Francie had a miraculous turnaround!”
Dr. Thukaram adds: “We are so happy Francie is again her happy, ‘chirpy’ self— fully engaged in all the activities she enjoys. In light of the number—as well as the severity—of afflictions she battled, her turnaround was all the more remarkable. In addition to being a story about this little girl’s amazing recovery, I believe it is also a testament to the PICU’s incredible teamwork and to the countless young lives they save.”
Francie with her parents, Jill and Phil
41 presence Saint Francis Health System
Children’s Miracle Network Champion Child
As a former patient, Francie represents The Children’s Hospital at Saint Francis as the 2021 Children’s Miracle Network Hospitals (CMNH) Champion Child—helping to raise awareness for eastern Oklahoma’s only children’s hospital.

As a group, CMNH Champions represent the millions of children treated at pediatric hospitals around the U.S. and Canada. Every year, 170 local Children's Miracle Network Hospitals identify a “Champion” in each of their local communities to serve as the representative for all children treated at their local pediatric healthcare facility.
The Children’s Hospital at Saint Francis is the eastern Oklahoma affiliate hospital for Children’s Miracle Network Hospitals. All of the funds raised by CMNH sponsors stay in the area in order to help sick and injured kids in eastern Oklahoma.
Children's Miracle Network Hospitals


Eastern Oklahoma Partners include:
For more information about becoming a Children’s Miracle Network Hospitals partner in the Tulsa, Oklahoma area, please call The Children’s Hospital Foundation at Saint Francis at 918-502-6762.
42 saintfrancis.com
Fundraising Records
Tulsa-area Panda Express Locations Set for Children’s Miracle Network Hospitals
Could it be a happy coincidence that P.J. Panda (The Children’s Hospital at Saint Francis’ loyal and lovable mascot) and Panda Express share a heartfelt commitment for kids? Judging from the recent fundraising success exhibited by the Panda Express teams at locations in the Tulsa area, the answer is a definitive yes.
Following a year of fundraising for the annual Children’s Miracle Network Hospitals (CMNH) campaign, ten local Panda Express locations raised an amazing $109,500 last year to benefit The Children’s Hospital at Saint Francis. For the team at the 21st and Yale location in particular, their team of 30 associates raised $20,837—an accomplishment that resulted in the most funds raised by a single Panda Express location in the area.
“Since the beginning of this campaign, our team’s mission has been to communicate with those in our community about children in need of quality healthcare,” said Pau Sang, manager of the 21st and Yale Panda Express location. “We have an extra source of inspiration since one of our associates was actually a patient at the children’s hospital years ago. Hearing his personal story made our enthusiasm catch on even more. We are inspired
by these stories and the care children receive at Saint Francis. We feel it is our duty to do all we can to help.”
A Recipe for Success
The 21st and Yale Panda Express team’s recipe for fundraising success has been relatively simple, remarkably effective and straight from the heart.

“Of course, we never apply pressure, but with every single food order and with each guest we ask if they would like to donate to The Children’s Hospital at Saint Francis. Most of our guests are more than happy to donate and express a desire to be part of our mission,” Sang said. “I’d like to thank our guests for their generosity—and also my co-workers for working together and inspiring each other every day. We are proud to be making a difference as a team.”
Panda Love
“We are so grateful to Panda Express, as well as to our other wonderful CMNH partners,” said Morgan Johnson, Children’s Miracle Network coordinator of The Children’s Hospital at Saint Francis. “Despite recent and changing circumstances, their devotion remains constant and unwavering in support of Children’s Miracle Network Hospitals and directly benefits the well-being of our young patients.”
– Morgan Johnson, Children’s Miracle Network coordinator of The Children’s Hospital at Saint Francis.
43 presence Saint Francis Health System
“We are so grateful to Panda Express, as well as to our other wonderful CMNH partners.”
in the life of Jesus Christ. Praying each decade is a pondering of these mysteries together with His mother Mary who pondered these things in


44 saintfrancis.com
Donald Prudlo, PhD, Warren Chair for Catholic Studies at The University of Tulsa.
her heart. In a world filled with noise, praying the Rosary encourages blissful silence, inviting “the words to sink into us as we touch the beads and sink into us deeper the more we say them,” said Dr. Prudlo.
While the Rosary is “a training ground for deeper Christian prayer,” Dr. Prudlo notes. “It is so simple, so direct, small children can learn it, and yet people at the heights of the spiritual journey, saints, still pray it.”
What religion preaches, science confirms, with numerous studies demonstrating prayer’s positive impact on well-being. Like the Rosary itself, the reason is simple: humans yearn for God.
“Our hearts are restless until they rest in You,” Saint Augustine wrote around 400 A.D. More than 1,200 years later, Catholic mathematician Blaise Pascal said there was “…a God-shaped vacuum…” in the heart of each person.
What was true then is even more so now. People hunger for meaning and purpose. The material world leaves us famished; prayer satisfies.
“Anthropologists define humans as ‘the ritual animal,’” said Dr. Prudlo. “In order to live an authentically human life we need ritual. People are going to default to ritual. Binging a show is a ritualized behavior, but the absence of a deeply well-functioning ritual is damaging. We need our rituals to be grounded in the reality of who we are as humans.”
Community and connection are also key to who we are as humans, yet both have been stripped away in the past year by a pandemic. The Rosary is a remedy not just for emptiness, but loneliness. The Rosary is one of the most popular prayers in history. Even when you pray it in solitude, you are never alone.
“One of the issues with modernity is individualism. When we add forced isolation it becomes a very difficult way of living,” said Dr. Prudlo. “The Rosary connects us to other people around the world praying the prayer, as well as other people praying it throughout history.”
The Rosary is meant for Catholics and non-Catholics alike, so Dr. Prudlo encourages people interested to get a Rosary, study manuals (see page 47, “How To Pray The Rosary”), and feel free to ask a Catholic friend or clergyman for guidance.

“The tender image of the human Christ and His mother, allied with the simplicity of the prayer, coupled with having that tactile feedback, and the fact it can be said anywhere, makes the Rosary a powerful prayer for everyone,” said Dr. Prudlo. “Once you get into the habit, you’ll never want to break it.”

45 presence Saint Francis Health System
“It is so simple, so direct, small children can learn it, and yet people at the heights of the spiritual journey, saints, still pray it.”
Donald Prudlo, PhD, Warren Chair for Catholic Studies at The University of Tulsa
Prayers of the Rosary

The Apostles’ Creed
I believe in God, the Father almighty, Creator of heaven and earth, and in Jesus Christ, His only Son, our Lord, who was conceived by the Holy Spirit, born of the Virgin Mary, suffered under Pontius Pilate, was crucified, died and was buried; He descended into hell; on the third day He rose again from the dead; He ascended into heaven, and is seated at the right hand of God the Father almighty; from there He will come to judge the living and the dead.
I believe in the Holy Spirit, the holy catholic Church, the communion of saints, the forgiveness of sins, the resurrection of the body, and life everlasting.
Amen.
The Our Father
Our Father, who art in heaven, hallowed be Thy name; Thy kingdom come; Thy will be done on earth as it is in heaven. Give us this day our daily bread; and forgive us our trespasses as we forgive those who trespass against us; and lead us not into temptation, but deliver us from evil.
Amen.
The Hail Mary
Hail Mary, full of grace, the Lord is with thee. blessed art thou amongst women, and blessed is the fruit of thy womb, Jesus. Holy Mary, Mother of God, pray for us sinners now and at the hour of our death.
Amen.
The Glory Be (The Doxology)
Glory be to the Father, to the Son, and to the Holy Spirit; as it was in the beginning, is now, and ever shall be, world without end.
Amen.
The Fatima Prayer
Oh My Jesus, forgive us our sins, save us from the fires of Hell, lead all souls to Heaven, especially those in most need of Thy mercy.
The Hail Holy Queen (The Salve Regina)
Hail, holy Queen, Mother of mercy, our life, our sweetness, and our hope. To thee do we cry, poor banished children of Eve; to thee do we send up our sighs, mourning and weeping in this valley of tears. Turn, then, most gracious advocate, thine eyes of mercy toward us; and after this, our exile, show unto us the blessed fruit of thy womb, Jesus. O clement, O loving, O sweet Virgin Mary.
Pray for us, O holy Mother of God, that we may be made worthy of the promises of Christ.
The Final Prayer
O God, whose only-begotten Son, by His life, death, and resurrection, has purchased for us the rewards of eternal life; grant, we beseech You, that we who meditate upon these mysteries of the most holy Rosary of the Blessed Virgin Mary, may imitate what they contain and obtain what they promise. We ask this through Christ our Lord.
Amen.
46 saintfrancis.com
How to pray the Rosary
The Rosary is a prayer that invites us to draw closer to Christ by reflecting on the mysteries of His life. The physical Rosary itself is a spiritual compass that guides you through the prayer, though you can still pray it without one.
1. Make the Sign of the Cross and say the “Apostles Creed.”
2. Say the “Our Father.”
3. Say three “Hail Marys” for Faith, Hope, and Charity.
4. Say the “Glory Be.”
5. Announce the First Mystery and say the “Our Father.”
6. Say ten “Hail Marys” while meditating on the Mystery.
7. Say the “Glory Be” and “The Fatima Prayer.”
8. Announce the next Mystery and say the “Our Father.”
Repeat steps 6 through 8 as you complete the Mysteries.
9. Say the “Hail Holy Queen” and “Final Prayer.”
10. Make the Sign of the Cross.
The Mysteries
Joyful Mysteries Monday and Saturday
• The Annunciation to Mary
• The Visitation of Mary
• The Birth of our Lord Jesus Christ
• The Presentation of the Child Jesus in the Temple
• The Finding of Our Lord in the Temple
Sorrowful Mysteries Tuesday and Friday
• The Agony of Christ in the Garden
• The Scourging at the Pillar
• The Crowning with Thorns
• The Carrying of the Cross
• The Crucifixion and Death of Our Lord on the Cross
Glorious Mysteries Wednesday and Sunday
• The Resurrection
• The Ascension
• The Descent of the Holy Spirit
• The Assumption of Mary
• The Coronation of the Virgin
Luminous Mysteries Thursday
• The Baptism of Jesus in the Jordan
• The Wedding at Cana
• Jesus’ Proclamation of the Kingdom of God
• The Transfiguration
• The Institution of the Eucharist
This guide comes from the United States Conference of Catholic Bishops and The Rosary Center. More information may be found at usccb.org or rosarycenter.org.
If you are interested in receiving a complimentary Rosary, please email us at events@saintfrancis.com.
47 presence Saint Francis Health System
st nd rd th th
STRONGER. TOGETHER. AGAIN. Health Zone at Saint Francis Reopens with



After temporarily closing in the fall of 2020 during the region’s COVID-19 surge, the Health Zone at Saint Francis reopened its doors for exercise and wellness activities on March 8.


Since the beginning of the pandemic, Saint Francis Health System has been a loud advocate for COVID-19 precautions, safety and prevention. And while other “fitness” facilities in town stayed open during the record-setting surge of COVID-19 cases and hospitalizations in our area, for the safety of our members and staff, the difficult decision was made to temporarily close. “As part of Saint Francis Health System, the Health Zone is more than just a gym—it is a partner in health,” said Graydon Yohe, director of Health Zone. “In early March as COVID numbers declined, and after consultation with our infection control department, the Tulsa Health Department and medical staff leadership, Health Zone was allowed to reopen with strict safety and prevention protocols in place.”

48 saintfrancis.com
Ongoing Safety Measures
Health Zone has the following safety policies in effect:
• temperatures taken at check-in to the facility;
• masks are mandatory at all times throughout the building (regardless of vaccination status);
• monitored capacity limits;

• enhanced pandemic-guided sanitation measures;
• increased air exchanges within ventilation system;
• exercise floor arranged for social distancing;

• fitness class capacity limits to allow for social distancing;



• locker room arranged for social distancing;

• members asked to wash and sanitize their hands frequently;
• equipment should be wiped down before and after each use;
• members are asked to stay home if they are sick.
To learn more about Health Zone, class schedules and membership information, please visit saintfrancis.com/healthzone, call 918-494-1660 or email hzone@saintfrancis.com.
49 presence Saint Francis Health System
a publication of Saint Francis Health System
MISSION
To extend the presence and healing ministry of Christ in all we do
VISION
Inspired to create a sustainable and just healthcare system, Saint Francis will be the technology-enabled health ministry that delivers integrated, market-leading, highquality, affordable care through engaged caregivers to the people of eastern Oklahoma.
VALUES
EXCELLENCE
Promoting high standards of service and performance
DIGNITY
Respecting each person as an inherently valuable member of the human community and as a unique expression of life
JUSTICE
Advocating for systems and structures that are attuned to the needs of the vulnerable and disadvantaged and that promote a sense of community among all persons
INTEGRITY
Encouraging honesty, consistency and predictability in all relationships
STEWARDSHIP
Ensuring prudent use of talents and resources in a collaborative manner
50 saintfrancis.com
6161 South Yale Avenue • Tulsa, Oklahoma 74136
SAINT FRANCIS HOSPITAL | THE CHILDREN’S HOSPITAL AT SAINT FRANCIS | WARREN CLINIC | HEART HOSPITAL AT SAINT FRANCIS | SAINT FRANCIS HOSPITAL SOUTH | LAUREATE PSYCHIATRIC CLINIC AND HOSPITAL SAINT FRANCIS HOSPITAL MUSKOGEE | SAINT FRANCIS HOSPITAL VINITA | SAINT FRANCIS BROKEN ARROW | SAINT FRANCIS CANCER CENTER | SAINT FRANCIS HOME CARE COMPANIES | SAINT FRANCIS GLENPOOL




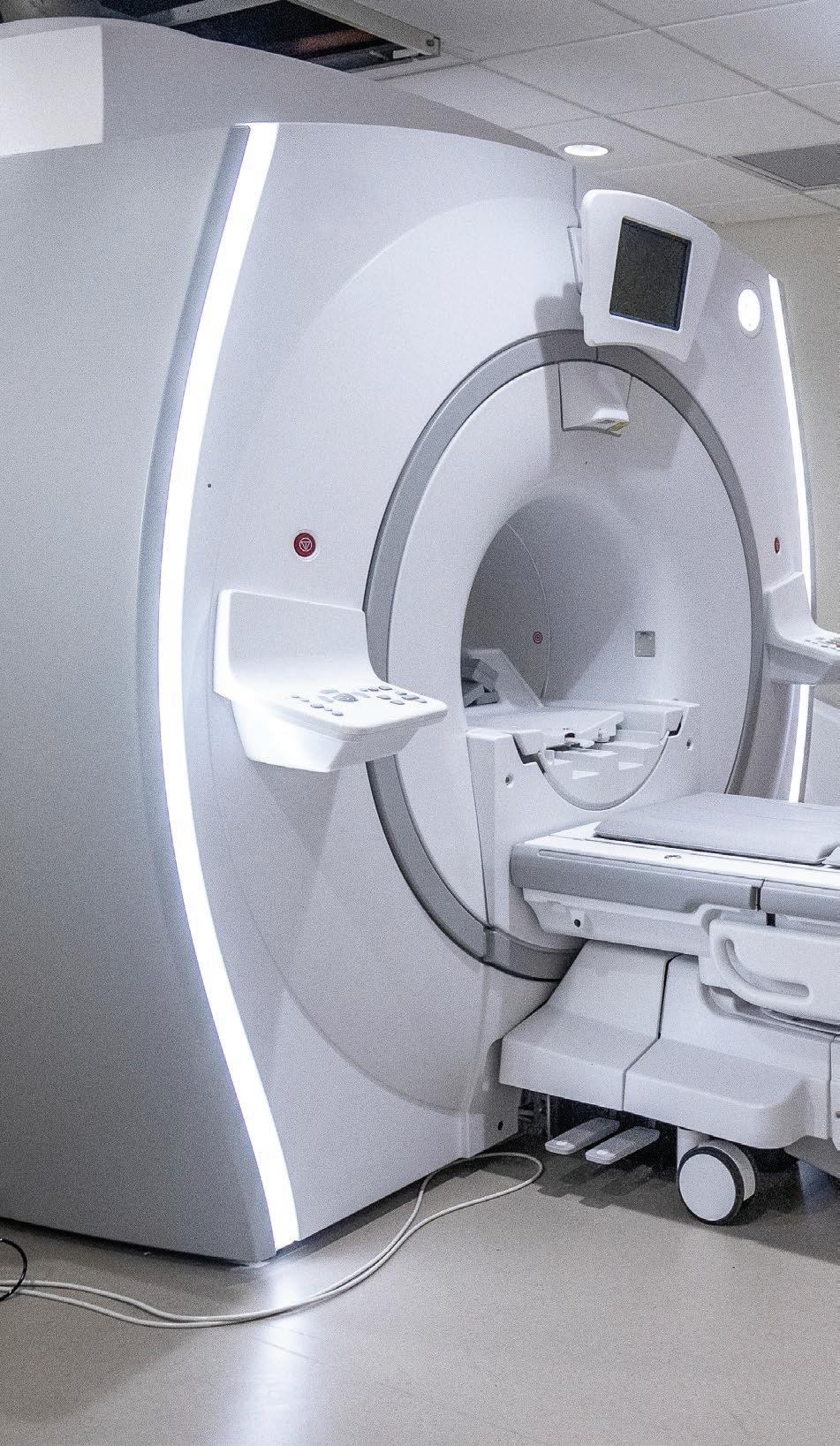






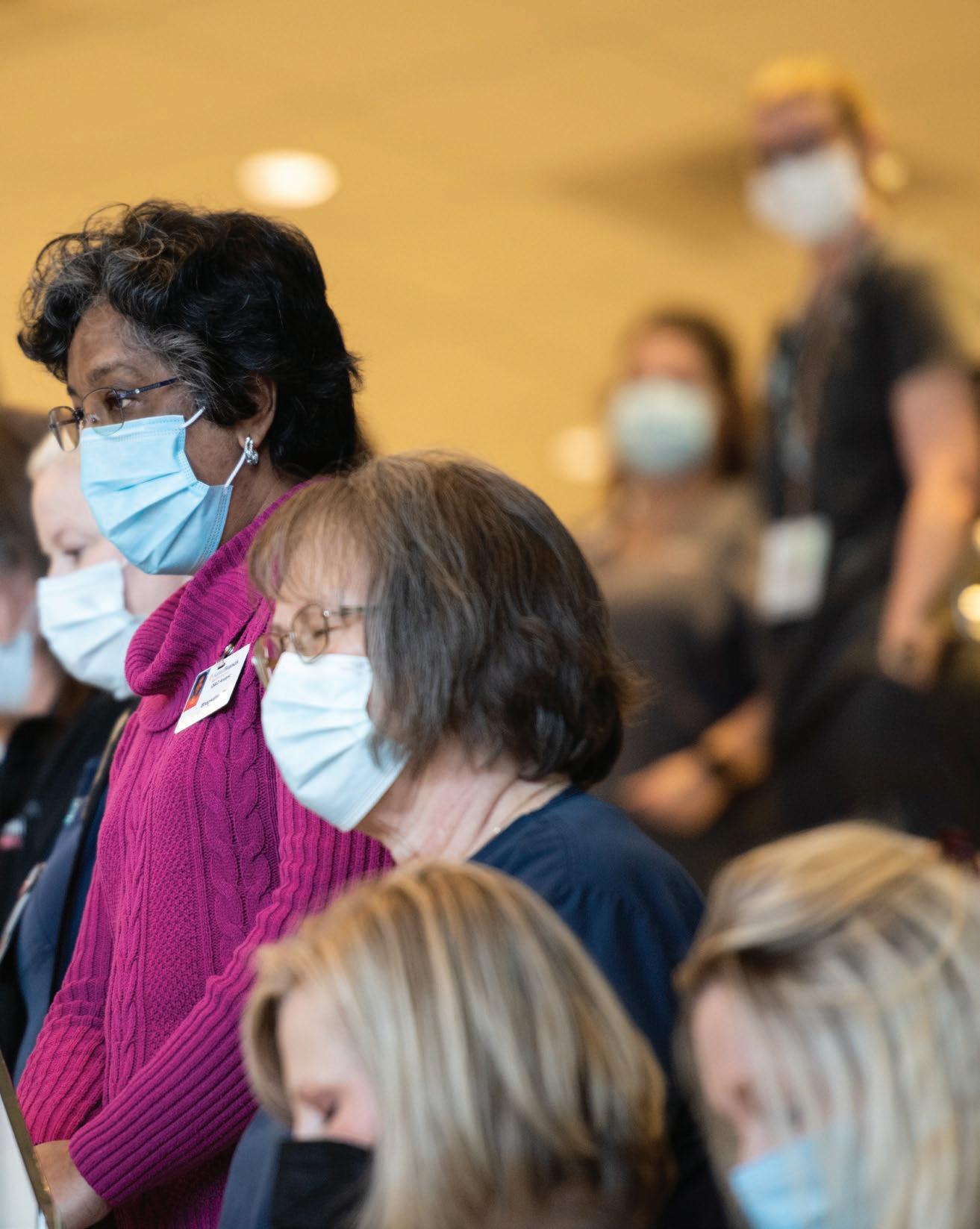

















 Laureate Psychiatric Clinic and Hospital
Laureate Psychiatric Clinic and Hospital




























 Francie VanTrease
The Children’s Hospital at Saint Francis Children’s Miracle Network 2021 Champion Child
Francie VanTrease
The Children’s Hospital at Saint Francis Children’s Miracle Network 2021 Champion Child