Presence
A publication of Saint Francis Health System

Major Expansions at Saint Francis Hospital Muskogee and Saint Francis Hospital South
Summer 2023
ANNUAL COMMUNITY BENEFIT REPORT
Saint Francis Health System
Board of Directors
John-Kelly C. Warren, Chairman
Judy Kishner, Vice-Chair
Cliff Robertson, M.D.
Michael Case
Michael Cooke, J.D.
Tom Cooper
Reverend Gary Kastl
Laura Stuemky, M.D.
Sailatha Thomas, M.D.
Saint Francis Health System
Executive Leadership Team
Cliff Robertson, M.D.
President and Chief Executive Officer
Barry Steichen
Executive Vice President and Chief Operating Officer
Meridith Coburn
Chief Information Officer
Deborah Dage
Chief Financial Officer
Meg Duffy Chief Strategy Officer
Collin Henry, J.D. President, Warren Clinic
Michele
Sister
Lauren
Cindy Leathers
Mike
Finny
Brenda
Jamie
Scott
Todd

Doug
Keeling President, Saint Francis Hospital Muskogee
Marie Josepha Kluczny Vice President, Mission and Ministry
and Communications
Landwerlin Vice President, Strategy, Marketing
Chief Nursing Officer
Lissau, J.D.
Senior Vice President, General Counsel
OSU Medical Center
Mathew President,
President, Quality
Nance Vice
Payne Chief Human Resources Officer
Health Officer
Ptacnik Chief Population
Schuster President, Saint Francis Hospital South and Saint Francis Hospital Vinita
Singh, M.D. Chief Medical Officer
Reetu
Williams President, Saint Francis Hospital CONTENTS 6 2 14 18 20 34 36 40 44 49 38 30 28 22 Community Benefit Report Muskogee Expansion Features Iconic Patient Tower South Begins Construction Owasso Celebrates Opening of New Clinic and Urgent Care In Remembrance June 1, 2022 Values Award Winners MyChart Bedside Expands Technology for Inpatients Adult ECMO Saves Lifes for Patients in Respiratory Distress Human Trafficking Initiative Trains Staff to Offer Help to Victims Nursing Partnerships With Local Universities Champion Child: Super Preemie Now Donates Pajamas to Help Others Stroke Can Affect All Meet the Doctors New to Warren Clinic Heart Screenings Can Save Lives Learn more about the largest healthcare construction project in Muskogee's history. See page 12 Cover: Artist's rendering of Saint Francis Hospital Muskogee

A LETTER FROM President and
Cliff Robertson, M.D.
Chief Executive Officer
Each year we publish a special issue of Presence that features our community benefit report. This annual snapshot of our charitable and mission-focused endeavors is meant to serve as a testament to our commitment to meeting and exceeding the healthcare needs of the region we are proud to call home.
I am pleased to report that in the past fiscal year, Saint Francis Health System contributed $86.5 million back into the region. This number is smaller than last year, and one might see that as a negative. However, the primary reason for this decrease is due to Medicaid expansion in Oklahoma. Because of that legislation, more Oklahomans than ever had access to health benefits, which lessened the amount of uncompensated care historically provided by health systems like ours.
As you will see in the report, there are many facets of what we do that contribute to our total level of community benefit.
While it is not technically part of the equation, personally, I think the greatest benefit we provide to the community are the 11,000 women and men who make up the Saint Francis family. Our employees and volunteers are the heart, soul, hands and feet of our mission. It is their work, day in and day out, that makes our mission a reality.
To them, I say thank you. Thank you for making Saint Francis Health System the best place to work and receive care.
We are focused on being a good partner in the community and the region.
To the community, thank you for trusting us with your health and healthcare. We take our responsibility to you and your family’s health—and to the community as a whole— seriously because this is our home, too. Because of that we are proud to support local nonprofits whose mission and commitment to the community align with ours to address community needs such as food insecurity, housing and education.
In this issue of Presence, I hope you’ll see what I see every day: That Saint Francis is essential to our region. Our 24/7 trauma program is essential. So is our stroke program. So is The Children’s Hospital at Saint Francis. In all these ways and more, Saint Francis is showing we are essential to eastern Oklahoma, and I thank you for being an essential part of our Saint Francis community.
Thank you.
 Cliff Robertson, M.D. President and Chief Executive Officer Saint Francis Health System
Cliff Robertson, M.D. President and Chief Executive Officer Saint Francis Health System
1 Saint Francis Health System presence
REMEMBERING THOSE WE LOST JUNE 1, 2022
 STEPHANIE HUSEN, D.O.
STEPHANIE HUSEN, D.O.
On June 1, 2022, we lost four members of our community in a profoundly tragic event at Saint Francis. One year later, to honor the memory of Amanda Glenn, Dr. Stephanie Husen, William Love and Dr. Preston Phillips, the health system hosted a Mass of remembrance for family and employees.
Also on that date, Bishop David Konderla of the Diocese of Tulsa consecrated the health system to the Sacred Heart of Jesus to entrust our staff, patients and visitors—past, present and future— and all of our locations and work to God's blessings of mercy and healing.


 AMANDA GLENN
PRESTON PHILLIPS, M.D.
WILLIAM LOVE
AMANDA GLENN
PRESTON PHILLIPS, M.D.
WILLIAM LOVE

MASS OF REMEMBRANCE
June 1, 2023, was a solemn day of prayer and remembrance for Saint Francis Health System as staff members and the community marked one year since the shooting that took the lives of Dr. Stephanie Husen, Dr. Preston Phillips, medical assistant Amanda Glenn and family member William Love.
During the 24 hours leading up to the memorial Mass, employees and community friends participated in around-the-clock Eucharistic Adoration, a time of silent prayer, devotion and worship. As the Adoration concluded, hospital staff, family and friends attended a beautiful Mass said by Bishop Konderla to honor and remember those we lost on June 1, 2022. Special tribute was also paid to remember all health system employees who have died in the past year.
PROCESSION OF PRAYER
Following the Mass, those mourners who were closest to the tragedy—staff, family and members of security—were led on a Eucharistic Procession to the Natalie Medical Building.
There they gathered for a moment of silence and prayer in the building's lobby which is now home to a permanent memorial.

4 saintfrancis.com



SACRED HEART OF JESUS
A bronze crest with the image of the Sacred Heart of Jesus was installed as the centerpiece of the treed memorial to Dr. Husen, Mr. Love, Mrs. Glenn and Dr. Phillips.
This image, along with a verse from Matthew 11:28-29, reminds us that in times of suffering and loss, God's love for us is a place we can entrust all our hope.
“Come to me... for I am meek and lowly of heart, and you shall find rest for your souls.”
Matthew 11:28-29

$28,878,554 Charity Care

$8,500,379
FISCAL YEAR 2022
$86,569,365
essential adj. Of the utmost importance, necessary, indispensable.
ESSENTIAL: That word sums up the impact Saint Francis Health System has on eastern Oklahoma.
This means benefiting the community we serve in every way we can, in everything we do.
Our focus and fuel for this endeavor of essentiality stems from our mission: to extend the presence and healing ministry of Christ in all that we do. That, more than anything else, is what we see as essential. The opportunity and the ability to make a meaningful impact on the lives of the people we serve inspires our work and brings meaning to our mission.
$3,680,515
In the pages of this annual accounting of our of impact on the community, you will learn more about some of the ‘what’ and the ‘who’ behind our ‘why.’
You will read about the benefit that came from our $3.6 million support of Xavier Clinic that allowed their team to care for more than 1,500 men, women and children who are uninsured or underserved. You will read the story of a family who understands
why The Children’s Hospital at Saint Francis is essential—for the region and all of the kids and families who call it home. And you’ll learn more about our Meds to Beds program that helps to ensure our patients do not miss a step…or a dose…as they transition home from a hospital stay.
$2,854,190
Over the past 5 years, Saint
$628,735,450
$5,746,889
6 saintfrancis.com
SAINT FRANCIS HEALTH SYSTEM ANNUAL COMMUNITY BENEFIT REPORT
$36,101,173 Uncompensated
Community Contributions
Xavier Clinic Funding
Community Benefit
In-House Trauma Coverage
Francis Health System provided in community benefit to the region.
$28,878,554 Charity Care
36,101,173
Uncompensated Care
Providing free care for low- or no-income patients and families. This includes the charity care provided to patients who qualify for the Saint Francis Health System Financial Assistance Program.
What is Community Benefit?
COMMUNITY BENEFIT is defined as programs and services offered by healthcare providers that are designed to:
• improve the health of the community;
• increase access to healthcare services; and
• advance public knowledge on issues impacting health and wellness.
While providing community benefit is a core function of Catholic, not-for-profit healthcare and the basis of their tax-exempt status, Saint Francis Health System seeks not only to meet these core functions, but to exceed them whenever possible.
$807,665
$8,500,379
Med to Bed Program Subsidy
In-House Trauma Coverage
Providing comprehensive emergency services to the region, including the Saint Francis Trauma Institute—the region’s only trauma service that offers in-house, 24/7 coverage by surgical intensivists to meet the needs of the community.

$3,680,515 Xavier Clinic Funding
Supporting Xavier Medical Clinic—the free clinic operated by Saint Francis Health System to serve the needs of women, children and men who are uninsured or underserved.
$86,569,365 FISCAL YEAR 2022
$36,101,173
Uncompensated Care
Cost of uncompensated care related to the treatment of Medicaid patients
$2,854,190 Community Benefit
$5,746,889
Community Contributions
$807,665
Med to Bed Program Subsidy
Provides 30 to 90 days of medications to patients leaving the hospital needed to stay on the path to recovery.
Supporting local nonprofits whose values are aligned with Saint Francis Health System as well as assisting the uninsured enroll in a benefit plan.
7 Saint Francis Health System presence
The Children’s Hospital at Saint Francis
SERVES CRITICAL NEED FOR SICK AND INJURED KIDS
“Knowing that we have quality care for the children of Tulsa keeps me going.”
MICHELLE KEIL, CLINICAL QUALITY NURSE
One of the many ways that Saint Francis shows its commitment to the community is through The Children’s Hospital at Saint Francis.
Opened in 2008, the 162-bed hospital recently celebrated its 15th anniversary.
The children’s hospital was never meant to be a great business move. The families served typically couldn’t afford services, and before
Medicaid was expanded, most of the children had no insurance at all. Today, about 65% of the children served are on Medicaid, which usually does not cover all the costs associated with providing the medical services.
But making money was never the point. The point was serving children close to home and being an essential service for sick and injured children.

“If you’re going to work with children, this is the place to be.”
ANN WALLACE, CLINICAL QUALITY NURSE
“The children’s hospital was designed from the beginning to be a ministry to the City of Tulsa and the region,” said Kellie Brown, who at the time was the lead project manager for the opening of the children’s hospital and now works with adults in the main hospital. “It was never meant to be a revenue-generating endeavor.”
Since its official opening on a snowy day in February 2008, The Children’s Hospital at Saint Francis has had 3.8 million total patient encounters, including 187,000 patients admitted to the hospital. There have been more than 85,000 surgeries and more than 505,000 outpatient visits.
The 58-bed neonatal intensive care unit, named in honor of philanthropist Henry Zarrow, has admitted more than 12,000 premature and sick newborns.
The day the new children’s hospital opened, there were already 17 children being served in the pediatric intensive care unit in the main Saint Francis Hospital building plus more children on the general pediatrics floors.
Each of them would need to be moved quickly and safely to the new facility.
“I remember the day and the weeks leading up to the move as a very special time,” Brown said.
The move was the culmination of monthslong planning, from assigning phone numbers in the new facility to mapping out the path each critically ill child would take from one building to the next.
“Everybody met at the desk in the morning,” recalls nurse Ann Wallace. “One of the Sisters said a prayer for safety. And we took turns moving one patient at a time.”
Moving day started at 8 a.m., and it took six hours to move all 17 patients, Brown said.
Babies on ventilators had to be kept breathing by a respiratory therapist walking next to

the bed pumping a handheld air bag as the mechanical ventilator was unplugged and pushed behind the bed. Monitors were switched to battery power. Nurses checked vitals manually, and the most critical babies and children were saved for last.
Wallace recalls that she was assigned one of the most critical children, a twin with RSV who was on a ventilator.
The move was completed without any children injured during the transfer.
With the new, shiny hospital—complete with floor-to-ceiling windows in each room and animal murals on the walls—also came a new philosophy.
“Parents and caregivers were no longer visitors,” Brown said. “They were and continue to be part of the care, and they don’t ever leave. They became a part of rounds, of care and of planning. There used to be visiting hours, but no more.”
The philosophy continued to shift as more child life specialists—now nine—were added to the ranks. These staff members support children and families through the stress of illness or injury, often with toys, puppets and books.
“These kids deserve to be treated differently from adults,” Brown said. “They deserve for it to be kid-friendly and fun.”

“When you know where you belong, you don’t go to work because it’s easy. You go because you know children need you. If I weren’t there, who would be? Some of us are meant to be there.”
BECKY REINHOLZ, CLINICAL MANAGER OF THE PEDIATRIC INTENSIVE CARE UNIT
Big Sam
USUALLY HEALTHY TEEN LANDS IN CHILDREN’S HOSPITAL TWICE IN SIX MONTHS
When Samual McKie woke up in December 2022 with a pain near his left shoulder, he assumed he had slept on it wrong. But the pain didn’t go away, so his family took him to their local doctor. A chest X-ray showed some cloudiness in his left lung, and the doctor sent him home on antibiotics. When he returned the following week, an X-ray revealed that the lung issue was worse instead of better, and the emergency room at W.W. Hastings Hospital in Tahlequah sent him by ambulance to The Children’s Hospital at Saint Francis.
The Children’s Hospital at Saint Francis is the only children’s hospital in eastern Oklahoma. It offers advanced services for children and has physicians and staff specially trained to treat young people—not as tiny adults, but as special patients with their own needs and concerns.
Each year, the children’s hospital cares for the spiritual, emotional and physical needs of more than 80,000 children and their families.
Usually a healthy teenager, the Kansas, Okla., high school senior is nicknamed “Big Sam” at school, where he is an offensive guard on the football team and a stateranked powerlifter. At 6 foot 2 inches and 270 pounds, Samual didn’t look much like some of his younger neighbors at the children’s hospital, but his condition was just as serious.
A CT scan showed a mass in his upper left lung, and the children’s hospital immediately started treating him with IV antibiotics.
He was inpatient for seven days and gradually started feeling better, had less pain, and regained some strength and

appetite. He was released and went home with a PICC line, a catheter that gives access to veins near the heart, and two more weeks of powerful antibiotics through the catheter.
Samual’s dad loves to sing the praises of The Children’s Hospital at Saint Francis because of the care his son received.
“Everybody was wonderful,” Jason McKie said. “For as horrible an experience as it was, everyone was super nice. Everyone entertained all of our questions. We are very grateful.”
Once Samual went home, he and his dad spent time together building Samual’s truck, starting with only a frame and adding a Cummins diesel engine, 37-inch wheels and parts from various trucks. The final step was a coat of victory red paint to complete the 1995 F-350, a one-ton dually truck.
What caused the lung infection is still a mystery, Samual’s dad said. At a followup appointment in May, Samual’s lung function was still normal, and the whole family was relieved that their hospital experience was behind them.
That seemed to be the end of the story until tragedy struck again just a few days later.
Over Memorial Day weekend, Samual was gathering wood for an outdoor fire when he was bitten on the hand by a snake. His dad turned the wood pile over, piece by piece, until he found the snake and identified it as a copperhead.

Samual’s mom rushed him to the local hospital, where he was stabilized and given the first dose of antivenin. The staff said he’d again need to be sent by ambulance to The Children’s Hospital at Saint Francis.
“When we found out we were going back to Saint Francis, I breathed a sigh of relief,” McKie said.
In all, Samual required 18 vials of antivenin during his two-day stay in the 20-bed Pediatric Intensive Care Unit, a Level 1 unit that treats respiratory conditions, trauma, cardiology and a variety of other conditions in critically ill children. The PICU is one of only two in the state fully equipped for pediatric critical care.
“He’s a kid, but he’s the size of a full-grown man,” McKie said.
No matter the size or age of the child, having a son or daughter in the hospital is a very stressful experience, he said.
“Everyone at the children’s hospital is on their A-game,” McKie said. “They’re all there to help the kids. As the parent of a sick kid, you feel helpless. But everyone cares so much at Saint Francis that they really take the edge off for families.”
The day after he left the hospital for the second time, Samual was again ready to get back to normal. He went to work at his summer job of cutting, baling and moving hay.
“We had nothing but good things to say after our first experience,” McKie said. “And our second experience was probably even better.”

“Everyone at the children’s hospital is on their A-game. They’re all there to help the kids. As the parent of a sick kid, you feel helpless. But everyone cares so much at Saint Francis that they really take the edge off for families.”
SAMUAL’S DAD, JASON MCKIE
Meds to Beds
Many patients at Saint Francis are uninsured or underinsured.
And that causes an issue when they are released from the hospital. Will they stop at a pharmacy on their way home and pay for a prescription? Or head home without their medication and hope for the best?
In 2018, Saint Francis started a program called Meds to Beds. This essential program provides 30 to 90 days of medications at discharge so that patients in need leaving the hospital have the insulin, blood thinner, heart medicines, steroids, antibiotics and other medicines they require to stay on the path to recovery.


“It really is a mission of service to patients who otherwise wouldn’t be able to get the medicine they need.”
JAY TIPPS, DIRECTOR OF RETAIL PHARMACY
“The idea is to have a bridge that hopefully helps the patient not get readmitted,” said David Donald, pharmacy director for Saint Francis Health System.
The number of patients benefitting from Meds to Beds has steadily increased and is projected to be more than 10,000 for the current year, up from 8,900 in 2022.
“It really is a mission of service to patients who otherwise wouldn’t be able to get the medicine they need,” said Jay Tipps, director of retail pharmacy. “It’s a wonderful feeling to know that we can help them stay healthy and not worry about the price.”
Xavier Clinic
Xavier Clinic was a gift from Saint Francis to the community so that some of the most forgotten residents could have essential medical care.
The clinic opened in 2001 across from St. Francis Xavier Catholic Church near Admiral Boulevard and Lewis Avenue, a location chosen because it was accessible to the community’s growing Hispanic population.
It set forth a mission to serve those without good access to healthcare services—adults and children. For many, language was also a barrier to seeking healthcare. Many had never seen a doctor in their entire lives. “Xavier Clinic truly is a special place, and I think that’s due to the people we have here,” said Dr. Rose Sloat, medical director. “Our staff and volunteers share a passion about what we do, and I believe that's something our patients can sense the minute they walk in the door.”
Originally, the clinic was open one day per week and run by retired doctors, plus a variety of volunteer nurses and social workers. On its first day, the clinic saw 21 patients. By the second week, the staff was seeing more than 40 patients a day. That number has continued to grow as have the services provided by the clinic to meet the needs of those seeking its care.
Fast forward to 2021 and the Xavier Clinic moved to its current location on 11th Street near Hwy. 169, a location again selected because of its proximity to the Hispanic community.
Still run by volunteers, the clinic is now open five days a week and uses the same online scheduling system as the rest of Saint Francis.
Volunteer doctors from across Warren Clinic had more than 3,500 visits in the last year.
More than 2,000 women had mammograms, and more than 18,000 prescriptions were filled.
Overall, in the past fiscal year, more than 1,500 patients accessed and received the care they need with the support of Saint Francis and the amazing staff and volunteers of the Xavier Clinic.
Its mission was to serve the poor, many who did not speak English or have documentation in order to have medical coverage. Many had never seen a doctor in their entire lives.


Saint Francis Begins Major Expansion for Healthcare Services in Muskogee

Saint Francis Hospital Muskogee has embarked on the largest healthcare construction project in the city’s history, and patients will be the real winners.
The over $200 million expansion and renovation project will have a focus on both functionality and ease of access, with the centerpiece, a new patient bed tower, being described as a new landmark for the region.
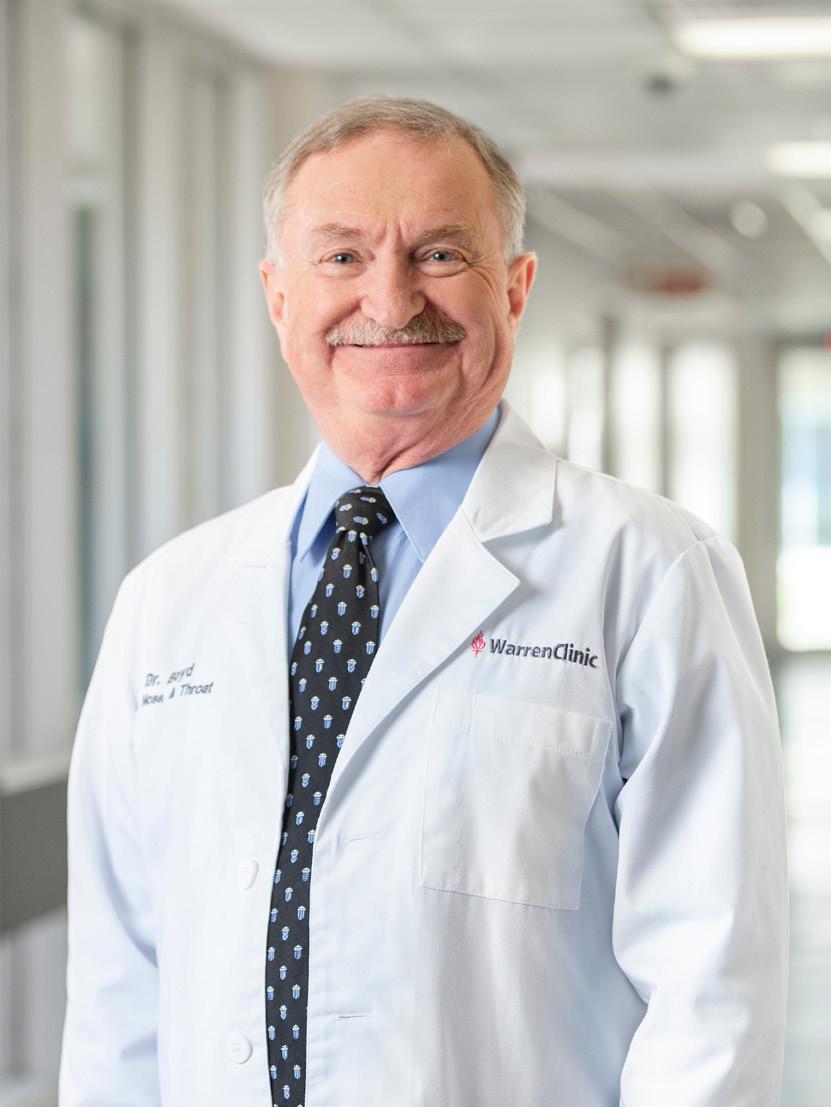
“We’re celebrating a big achievement,” said Dr. Edgar Boyd, who is a Warren Clinic ear, nose and throat specialist who has practiced in Muskogee for 20 years.
Currently licensed for 288 beds, much of the current hospital was built in the 1950s. Most patient rooms are small, and the patient bathrooms are a tight fit, many not able to accommodate wheelchairs and walkers.
With construction underway, the tower will measure approximately 290,000 square feet, which will be more than a 40% increase over the current 600,000-square-foot hospital.
The tower will house 158 new inpatient rooms that are 47% larger than current rooms, with bathrooms that are 70% larger and handicap-accessible. The critical care capacity will be expanded by 40%.
The project is expected to be completed in 2025.
There will be a striking new entrance with floor-to-ceiling windows in the lobby and a more streamlined way for visitors and patients to find their way around the facility.
New critical care units will increase Saint Francis Hospital Muskogee’s
14 saintfrancis.com
Dr. Edgar Boyd has practiced in Muskogee for 20 years.

critical care capacity, and a new hospital chapel will be available for staff, patients and families to pray and reflect.
“I pledge to you our commitment to provide the highest quality of care that your mother, your children, your family would be proud of,” said Saint Francis Hospital Muskogee president Michele Keeling during the ceremonial groundbreaking on December 3, 2022. “Our common goal in creating this new tower is that when complete, the care provided here will embody the spirit and soul of Saint Francis in eastern Oklahoma. We look forward to a long future of making Muskogee better together.”
The groundbreaking occurred about five and a half years after Saint Francis Health System acquired the Muskogee hospital in 2017. Now, at a time when community
hospitals are closing their doors, Saint Francis Hospital Muskogee is expanding in a big way.
“We are getting a brand new hospital in rural America during a time of economic uncertainty,” said Mayor Marlon Coleman. “While other parts of the economic sector are fearful of moving forward, Saint Francis is moving forward with Muskogee to build what others have only dreamed of. For the last decade, all I’ve heard from people is that we need a better healthcare system in Muskogee. Today, it’s time to smile and celebrate the fact that in Muskogee, we are getting a brand new bed tower, a brand new hospital and brand new healthcare for the residents of Muskogee.”

15 Saint Francis Health System presence
The seven-story patient tower is described as an iconic structure in Muskogee.
Michele Keeling is the Saint Francis Hospital Muskogee president and was born in the hospital she now serves.

The City of Muskogee is no stranger to medical firsts. The first hospital in the State of Oklahoma was built in Muskogee in 1893 in Indian Territory. It had only 10 beds and was staffed by two doctors. After several small hospitals were outgrown, the City of Muskogee built Muskogee General Hospital, which opened in 1959 at the current site.
Additionally, the hospital achieved Primary Stroke Certification and now offers a certified cardiac and pulmonary rehabilitation program.
“Without Saint Francis, there’s no way we would be able to get the level of healthcare that we need here,” Dr. Boyd said.
Investment: Over $200 million
Height: Seven stories
Tower size: 290,000 square feet
Projected completion: 2025
Architect: GH2 Architects
Construction: JE Dunn Construction
Since Saint Francis acquired the Muskogee hospital, there have been $85 million in investments, many unseen, including the Epic electronic medical record system and infrastructure items such as air handlers, pumps and roof replacements. But other improvements have been very noticeable, such as $30 million in new radiology equipment and robotic surgical services. The da Vinci XI system is a state-of-the-art robotic-assisted surgery system, which handles colon and gallbladder surgeries, in addition to hysterectomies and hernia repairs.
With the new investment and construction project, administrators say that they’ll be able to recruit more physicians, nurses, therapists and technologists to keep Muskogee on the cutting edge of medical advancements.

For patients, the real benefit will be receiving care close to home. Research shows that treating people nearby is much more effective than forcing them to drive long distances.
 Mayor Marlon Coleman speaks at the groundbreaking in December 2022.
SAINT FRANCIS HOSPITAL MUSKOGEE
Seen in this artist’s rendering, construction is expected to be complete in 2025.
Mayor Marlon Coleman speaks at the groundbreaking in December 2022.
SAINT FRANCIS HOSPITAL MUSKOGEE
Seen in this artist’s rendering, construction is expected to be complete in 2025.

“In some ways in the United States, we have a two-tiered healthcare system,” said Saint Francis Health System President and CEO, Dr. Cliff Robertson. “There’s a certain healthcare that’s delivered in the metropolitan areas. But in the rural communities, it’s much harder for people to access the services they need, whether
it’s a brand-new hospital like we’re building or physician specialty services. That’s what Saint Francis is committed to. The best care we can deliver is the care that’s as close to home for the patient as possible.”
Dr. Boyd has seen many changes at the hospital during his 20 years practicing in Muskogee. One of the realities is that some patients prefer to travel to Tulsa to be treated in a newer facility with larger rooms and brighter environment, he said. And it’s hard for small towns to attract and keep providers when there are fancier facilities in larger cities.
Dr. Boyd says the best is yet to come because of the expansion project. Patients are going to want to come to Muskogee, and so will new doctors.
“I’m very proud to be part of this healthcare system,” Dr. Boyd said. “I live in Muskogee. I’m very proud that this is my hospital.”

The $200+ million expansion and renovation project will have a focus on both functionality and beauty, with the centerpiece, a new patient bed tower, being described as a new landmark for the region.
17 Saint Francis Health System presence
Officials from Saint Francis and Muskogee participate in the groundbreaking.
Saint Francis Hospital South Expands Toward Doubling the Size of the Facility
Construction has begun on a project that will add six stories, 90 beds and 10 additional operating rooms—nearly doubling the size of the current hospital. The new space will include a patient bed tower, central utility plant, plus an addition on the north side of Saint Francis Hospital South located near Highway 169 and 91st Street in Tulsa.
Additionally, 51,000 square feet will be renovated in the current hospital.
“We are thrilled to be able to offer even more services to our patients and families,” said Todd Schuster, president of Saint Francis Hospital South.
Work is almost complete on the first phase—a new central utility plant, which will support the growing campus with fuel, electricity, medical air and other services crucial to the hospital’s operation.
Once completed, the Saint Francis Hospital South campus will expand from 4 to 14 operating rooms, and intensive care capacity will double in size.
There will be a new cafeteria on the first floor, bringing more dining space to staff and visitors eating on campus.
Since it opened in 2008, Saint Francis Hospital South has gone through several renovations. As the population in south Tulsa, Bixby, Broken Arrow and the surrounding areas has grown, the facility has been growing, as well.
“To expand our mission and ministry, we have to grow, too,” Schuster said.
SAINT FRANCIS HOSPITAL SOUTH
Investment: $258 million
Height: Six stories
Total construction size: 283,600 square feet plus 51,000 square feet to be renovated in the current hospital
Projected completion: Late 2026
Architect: HOK
Construction: Crossland Construction

18 saintfrancis.com
The expansion project at Saint Francis Hospital South will add 90 additional beds, more critical care capacity and surgical space.


Warren Clinic Opens a New Facility and Urgent Care in Owasso
Earlier this year, Warren Clinic celebrated the opening of its newest location—a 48,000-square-foot outpatient facility in Owasso.
Located near U.S. 169 and Hwy. 20, this new $20 million facility houses Warren Clinic’s seventh urgent care in the region, as well as dedicated imaging services, outpatient rehabilitation services and a full-service laboratory.
The location is also home to Warren Clinic Owasso primary care services with family practice and pediatrics as well as specialty clinic services for cardiology, allergy/immunology and obstetrics/ gynecology.
Before his recent retirement, Dr. Gary Cannon was in practice for 42 years, with the last 27 years in Owasso. He always looked at Owasso, Collinsville and Skiatook as growing communities that needed more healthcare options. He was thrilled to see a beautiful, modern Warren Clinic facility come to Owasso just before he retired in March.
He was particularly happy about the urgent care clinic because “it will take a lot of burden off the emergency rooms, which are stacked full with cases that can be cared for here.”
The facility features a large lobby with a wall of windows and stone and wood accents, along with pink lotus flower lighting that adds an artistic flair.
“This is the nicest facility I’ve ever seen,” he said.
Owasso city councilor and Vice Mayor Alvin Fruga was so impressed by what he saw at the grand opening that he immediately made an appointment with his new doctor at the clinic.
The clinic is only five minutes from his house instead of having to drive all the way to Tulsa for care.
“My new physician also resides in Owasso,” he said. “That’s pretty cool.”



20 saintfrancis.com
Physicians, staff and community leaders take part in the ceremonial ribbon cutting for the new Warren Clinic Owasso.


With a design that provides plenty of natural lighting, the facility houses a new primary care clinic, a physical therapy center and a Warren Clinic Urgent Care site.


This new $20 million facility houses Warren Clinic’s seventh urgent care in the region, as well as dedicated imaging services, outpatient rehabilitation services and a full-service laboratory.
21 Saint Francis Health System presence
OUR VALUES
Excellence
Promoting high standards of service and performance Dignity
Respecting each person as an inherently valuable member of the human community and as a unique expression of life
Justice
Advocating for systems and structures that are attuned to the needs of the vulnerable and disadvantaged and that promote a sense of community among all persons
Integrity
Encouraging honesty, consistency and predictability in all relationships
Stewardship
Ensuring prudent use of talents and resources in a collaborative manner
SAINT FRANCIS HEALTH SYSTEM VALUES AWARDS
The values of excellence, dignity, justice, integrity and stewardship guide and support the work happening at Saint Francis as employees strive to extend the presence and healing ministry of Christ in all we do. These values guide how we treat patients, their family members and our coworkers.
It seems almost impossible to select five shining examples of our values from among the more than 11,000 employees.
But for the last 19 years, that’s exactly what has happened. Each year, staff members are encouraged to nominate a peer who exemplifies one of the five health system values. A committee of representatives from throughout the health system reviews the nominations and selects the winners for the Values Awards, which are the highest awards bestowed upon Saint Francis employees.
Nominated by their colleagues, the following five Values Award winners prove in their work each day that the values are alive and well, just as strong as when Saint Francis opened more than 60 years ago.
22 saintfrancis.com

CINDY RAY
NURSE TECHNICIAN
Nurse tech provides excellent care during the pandemic.
“Please give me a chance. I won’t disappoint you.”
Those words from Cindy Ray’s interview to become a nurse technician on 4 North resonated with Debbie Brown, the clinical manager who hired her.
Ray remembers going to the interview sure of her calling to be a caregiver, but unsure whether her age and inexperience would stand in her way.
When a relative in Mississippi needed aroundthe-clock care after being diagnosed with liver cancer, Ray headed there to help. She realized she had a gift for compassion and caring for the sick.
Eight months later, after her relative had died, Ray became a certified nursing assistant.
Her job interview at Saint Francis was her very first. She was nervous about the interview, and she also felt drained because of a cough. But she wouldn’t let anything stop her from the interview of a lifetime, she reasoned, certainly not a cold.
Shortly after the interview, she lost her sense of taste and smell, a symptom she thought was very strange.
Fortunately, her start date at Saint Francis was set three weeks after her interview, allowing her time to recover from what at that time was a mystery illness.
As she later found out from an antibody test, she had COVID a few weeks before the pandemic started making headlines. She was able to recover at home from the virus that soon would be consuming her days working at the hospital. As a new nursing assistant, she found herself working during one of the most crucial times in recent history—the start of the COVID-19 pandemic.
“I felt honored to be a part of healthcare at that time,” she said.
The pandemic, trying both physically and emotionally, allowed Ray’s commitment to excellence to shine.
One of the saddest parts of pandemic care was seeing patients, whether they had COVID or not, who were not allowed to have visitors. One patient in particular stole Ray’s heart.

A lady in her 80s had been living with her son and would be going to a nursing home as soon as the facility started accepting patients. Because of the pandemic, the patient’s hospital stay was extended. Her memory issues were heartbreaking, Ray said. And since she could have no visitors, she had no one to do her laundry.
Ray stepped in to take the patient’s clothes home to wash them. Plus, she bought her a few new items.
“We all fell in love with that lady,” Ray said.
Now past the pandemic, Ray has settled into a routine of taking vitals several times per shift. She sees the role as crucial because often she and the other nurse techs are the first ones to notice a change in the patient’s health, she said.
She also helps patients with meals. Often, she is the smiling face who brings snacks and ice.
“One of my favorite things to do is to put a warm blanket on patients,” she said.
Another of Ray’s specialties is getting to know her patients, asking about their families and friends. Sometimes she’ll share tidbits of her own life with them and endears herself to everyone she cares for.
“She’s an angel,” one of Ray’s patients said recently.
“She’s always happy and upbeat and compassionate. She’s a beautiful soul.”
Another patient said she would smile every time Ray came into her room.
“People come into our lives for a reason,” said Melissa Ethridge-Jack. “Cindy has touched my heart.”
23 Saint Francis Health System presence EXCELLENCE


TRUDY TRENT
CLINICAL SECRETARY, PROGRESSIVE CARE UNIT
Clinical secretary shows honor to patients and families.
The fourth floor in the Saint Francis tower was a COVID intensive care unit for more than two years during the pandemic.
During that time, clinical secretary Trudy Trent did what she does best—comfort those who are hurting and tired.
“I’m like a mother hen to everyone, even the managers,” she said.
Although she usually doesn’t have much direct interaction with patients, during the pandemic she took on a new role—helping families, often when they were at the hospital to say their last goodbyes to their loved ones.
Trent helped families put on personal protective equipment, including gowns, gloves and masks. She allowed them to store their personal items underneath her desk while they made their visit. She often tried to prepare them for seeing their loved one on a ventilator.
And she was there to comfort them as well.
“I hugged plenty of people while they cried,” Trent said.
While she saw many sad situations, she also remembers happy times, such as the first patient who was on a ventilator for more than a month and was discharged from intensive care. The entire staff cheered for her as she was wheeled down the hallway.
While the word “dignity” never entered Trent’s mind as a guiding principle, she said she always has tried to put herself in the place of the patient, family member or staff member, then treats them the exact way she would want to be treated in that situation.
“She really does care about what’s going on in that person’s life,” said Mandy Meeks, clinical manager of 4 Tower.
In her own life, Trent had a relative who was in intensive care years ago, and she was moved by the compassion she saw at Saint Francis.
“I’ve seen what an awesome hospital this is and what amazing doctors we have,” she said.
Her care extends to her colleagues. If she sees someone who is too busy to stop for lunch, she often goes downstairs to buy them a sandwich. If she sees someone stressed, she is quick to bring a cup of coffee. She gives out hugs to anyone who seems down. And when she arrives for her morning shift, she greets the night shift with a cheerful, “I’m giving everybody joy this morning!”
“What keeps me going every day is that I get to come in and see the people I absolutely love to work with,” she said.
Now in her 23rd year at Saint Francis, Trent has seen many changes. She recalls that when she started, all charts were on paper, and doctors wrote their orders with a pen. Today, all charts are computerized, and doctors type their orders—a much smoother system than when she had to decipher doctors’ penmanship.
Now that the pandemic has subsided, 4 Tower has transitioned to a progressive care unit, which is an area for patients who need a high level of monitoring but who do not require intensive care. Her main duties include answering patient calls for assistance whenever they push their bedside button; answering the phone; and making a daily list of nurses, techs and phone numbers so that everyone on the floor knows how to reach other staff working that day.
At the stage in her career when many would be slowing down—not Trudy.
When anyone asks her when she’s retiring, she answers with a smile: “I can’t. I love my job.”
24 saintfrancis.com DIGNITY SAINT FRANCIS HEALTH SYSTEM VALUES AWARDS

SAHARI CAMACHO
Interpreter sees healthcare as a right for all people. CERTIFIED MEDICAL INTERPRETER, XAVIER CLINIC
Sahari Camacho starts every morning with a prayer before work.
“First, I talk to God,” she said. She starts to cry as she describes the vulnerable clients who often need a miracle.
“There are very sick people, very poor people that come to this clinic for help,” she said. “So I always ask God, ‘I hope we can help everybody that comes to the clinic that day.’”
Patients come to Xavier Clinic without money, without insurance, without the English skills to allow them to understand the doctor or nurse. That’s where Camacho comes in.
Camacho started volunteering for Xavier Clinic in 2006, a few years after the all-volunteer clinic started in a little frame house next door to St. Francis Xavier Catholic Church near Admiral and Lewis. She herself was a new immigrant to the United States, having been born and raised in San Luis Potosí, Mexico, and when she came to Tulsa, she was excited to learn that it was the Sister City to her hometown through the International Sister Cities Network.
Eventually her volunteer work turned into a job because the clinic’s reputation and clientele grew quickly. Camacho recalls that she would arrive at the little house at 6:30 a.m., and there already would be a line because patients started coming to the clinic door at 4:00 a.m.
She remembers giving out 30 tickets to the first 30 patients on any given Wednesday.
The rest of the patients would go home, determined to be the first in line the following week. For some, their wait would take three or four tries, but eventually they would be seen by volunteer doctors and nurses.
Today, the ticket system has been replaced by a computerized appointment system, and the once-a-week clinic has a new home in east Tulsa that sees patients five days per week.
When Camacho and her husband moved away from Tulsa briefly, she used the time to study to become a certified medical interpreter. When they returned to Tulsa, she went back to her old home at the Xavier Clinic with even more skills than before.
“I’ve known many of the patients for many years,” Camacho said. “They ask for me because we have known each other for so long.”
She says that her morning prayers are answered when patients get the help they need. Some middle-aged patients and senior citizens are seeing a doctor for the very first

time in their lives. Many have been suffering with serious conditions, such as diabetes, high blood pressure, kidney disease and sepsis.
She recalls a young boy who had colostomy surgery in Honduras when he was a newborn. Years later, the tubing never had been removed, and the boy was constantly suffering from infections.
Camacho made call after call on behalf of the family, finally locating a surgeon who agreed to take on the surgically complex case.
Today, the little boy runs to greet Camacho with a big hug every time he sees her.
“They were able to put everything together and take out the tubes,” she said. “That was a miracle.”
Another answered prayer was for a boy who was in a car accident, which severely injured his arm. Camacho found a specialist, helped the family set appointments, answer questions and fill out all the financial paperwork to get the surgery approved.
After the surgery, the boy’s father came in sobbing because he was so grateful that his son could use his arm again.
“She changed his life,” said Dr. Rose Sloat, medical director of Xavier Clinic.
Camacho, however, downplays any role she played in the boy’s outcome, giving all the credit to God for answering prayers.
“This is a miracle,” Camacho says.
For her work at Xavier Clinic, Camacho was nominated by her peers for the Value Award of Justice. Camacho sees healthcare not as a privilege for the rich, but as a right for all people.
“She’s allowing these patients the same quality of care, the same compassionate care, that we want to offer to anyone who walks through our doors,” said Sister Mary Gretchen Hoffman, M.D.
In a world of injustice, poverty and sickness, Camacho has made it her mission to make sure that the patients she sees experience justice at the clinic and wherever they are sent for specialty care.
“Everybody should be treated as equal, no matter what,” she said. “Everything always works out in this clinic, and our patients are so thankful to be here.”
25 Saint Francis Health System presence JUSTICE


MARALIE BARTEL
PHARMACY TECHNICIAN
Behind the scenes, pharmacy tech brings precision to every liquid medication.
The renowned physicist Stephen Hawking once said, “Quiet people have the loudest minds.”
That saying could not be any truer than for the winner of our Value Award for Integrity.
As she silently crushes tablets, pharmacy tech Maralie Bartel works to make liquid solutions for patients who are unable to swallow pills.
As she draws the batches into syringes, she precisely measures what each patient needs and labels each dose.
While she is reluctant to talk about herself, her coworkers line up to talk about what makes her so special. One jots down on his clipboard the words he would use to describe her: Thorough, dependable, accurate, diligent. He hands over the paper to a reporter to make sure she records the list.
“We’re taught in pharmacy school you have a 10% window,” said pharmacist Kristen Rowe.
“When Maralie compounds, it’s right on the money. She’ll take a picture of every step. Close enough is never good enough for her. If there is supposed to be 23 milliliters of water, it’s never 22 and a little bit. It’s always exact.”
As Rowe discusses Bartel’s many job duties, pharmacist Kyle Cohenour, the one who had written the list, comes back with a pen. He has more descriptors to add. Comforting. Perfect for her job. Perfect and beyond.
“She knows the value of precision,” Rowe continues. “It’s what makes her so good.”
In addition to making perfect oral solutions and measuring hundreds of doses for patients per day, Bartel also is in charge of tracking which medications need to be ordered for the month and estimating the hospital’s needs. If she notices a spike in demand for a particular drug, she is quick to make note of it so that it can be reordered sooner.
“She makes sure we never run out,” Rowe said. Bartel has won the hearts of the pharmacy staff not with her words but with her actions and her caring nature.
“She has a strong desire to help people,” said pharmacy supervisor Jacob Dunlap.
“She wanted a job in the pharmacy where she knew she could make a difference in people's lives.”
Bartel’s precision extends to her personal timeliness.
Her shift starts at 6:00 a.m. and ends at 2:30 p.m. The timecard is always punched precisely at 6:00 and 2:30, never 6:01 or 2:29. Never 5:59 or 2:31, Rowe said.
She never wastes a single minute.
“She’s always darting around,” said fellow pharmacy tech Barry Boley. “She has a very strong work ethic. She definitely has integrity in everything she does.”
So she stands in the lab, crushing, weighing, mixing, drawing up syringes, labeling for each patient. Despite her quiet nature, she was recognized by her peers because her integrity speaks louder than any words ever could.
“Her work can easily go unnoticed because she is so non-self-promoting,” said Tyler Metcalfe, pharmacy supervisor. “We need people who are regimented, but that is the least celebrated personality type. We wanted to make sure we noticed and celebrated everything Maralie does for Saint Francis.”
26 saintfrancis.com INTEGRITY
SAINT FRANCIS HEALTH SYSTEM VALUES AWARDS

JOHN TUTTLE
DIRECTOR, PLANT ENGINEERING
After 35 years, he never stops learning.
From supplemental oxygen traveling into patient rooms to the refrigerators keeping food cold in the cafeteria, from water lines serving the operating rooms to LED bulbs above the lobby’s art glass ceiling, one department oversees keeping hospital systems running smoothly.
While the engineering operations department may not have much direct contact with patients, John Tuttle always has patients on his mind.
“This isn’t an industrial plant or a construction site,” Tuttle said. “It’s much more important than that. People are depending on us to keep them safe, keep them comfortable and keep them alive.”
As he walks through Saint Francis Hospital, Tuttle recalls the many times a construction project has required shutting down various utilities in order to expand an area or move a department.
“I try to remind everyone of the effect that a shutdown will have on the entire complex,” he said. “And it may be one of their family members in a patient bed upstairs.”
Tuttle’s attention to the details of engineering and his dedication to keeping the hospital running at peak efficiency earned him the Saint Francis Value Award of Stewardship.
“I used to think of stewardship as saving money or spending it wisely,” Tuttle said. “But at Saint Francis it is so much more. We’re given a lot. It’s put in our hands, and we’re told to make it work as long as it possibly can, take care of it and keep it working efficiently. It’s a huge responsibility to take care of the hospital so the nursing staff doesn’t even have to think about whether things work. They can focus solely on taking care of their patients.”
One of Tuttle’s most challenging projects was at the start of the COVID-19 pandemic when rumblings of a new virus were making headlines. At the time, Saint Francis Hospital had only 45 negative-pressure rooms for patients in isolation. As he and engineering director Mike Mullins were watching the news, they realized they needed to quickly make some changes. Together, Tuttle and Mullins devised a strategy to modify air handlers and control systems to convert entire floors into negative-pressure rooms so that at the height of the pandemic, Saint Francis had 300 such rooms, allowing nurses and staff to be in the

hallways and nurses stations without any additional worry of contamination.
Another of Tuttle’s achievements has been ensuring that every system has at least one backup as well as testing systems regularly. Saint Francis has 15 diesel-powered generators that can provide power to critical systems in case of an electrical failure. Those 15 generators are set up in pairs so that if one of them were to go down, the backup also has a backup.
Nationally, all hospitals are required to have a backup power system that can activate within 10 seconds and enough fuel to run generators for 96 hours.
Few hospitals, though, have the multiple layers of redundant systems that Saint Francis does, Tuttle said.
“Not many hospitals have that luxury,” Tuttle said.
In addition to electricity, Tuttle oversees multiple medical air systems, vacuum systems, oxygen and pumps that keep anesthesia machines, ventilators and flowmeters running smoothly. However, he is reluctant ever to take credit for a team effort.
“He will say, ‘It’s not me; it’s my guys,’” Mullins said.
In his 35-year career at Saint Francis, Tuttle has never stopped learning. That carries over to his volunteer role of serving on the Kellyville Board of Education since 1993 and as the president of the National School Boards Association in 2015.
He says his work at the hospital and with schools complement each other because what he learns at work, he uses on the school board, and what he learns on the school board, he applies at the hospital.
“When I came to work here, it was mind boggling,” he said. “When I came, I was focusing on one trade. As I’ve grown to leadership positions, it’s taken on multiple trades and multiple facets of the building. It’s been a great learning experience for me.”
His philosophy is always one of growth and learning, plus his own version of the medical creed “do no harm.”
“I just try every day,” Tuttle said, “to leave things better than how I found them.”
27 Saint Francis Health System presence STEWARDSHIP
The Power of Information at Your Fingertips
Saint Francis Expands Use of MyChart Bedside for Patients
Being admitted to the hospital can sometimes feel like a waiting game: waiting for lab results, waiting to ask your care team a medication question and waiting to be discharged to go home. Now, real-time medical information is available during the hospital stay through the MyChart app.
DuringYourStay
Medications
PatientDining
TestResults
Education
BedsideSurvey
Toseeinformationfromoutsideyour hospitalstay,gotoyourMyChart homepage.
Gotohomepage

MyChart Bedside is an extension of SaintFrancis MyChart, a secure online app accessible on a tablet or smartphone to help you review and manage your medical care and information. Currently, more than 395,000 health system patients have used Saint Francis MyChart as a health management tool for things such as scheduling appointments, using the portal for virtual visits, reviewing lab and test results, seeing vaccination records or medication management and refills.
Rolled out in mid-December, that same convenience can follow you if you’re admitted to Saint Francis Hospital, Saint Francis Hospital South, Saint Francis Hospital Muskogee and Saint Francis Hospital Vinita. Once you’re admitted to
the hospital, MyChart Bedside is enabled within your Saint Francis MyChart account, giving you access to many features including your hospital care team, medications, test results and dining options.
Parents of pediatric patients who have MyChart proxy on their child can also access MyChart Bedside at The Children’s Hospital at Saint Francis. Labor and delivery patients can utilize the system and establish proxy for their newborns while they are in postpartum care.
“MyChart Bedside is a relatively simple app to use with secure, patient-friendly features,” said Meridith Coburn, Chief Information Officer for Saint Francis Health System.
“It’s powerful because it’s giving patients autonomy in their care and some control,” said Dan Hall, executive director of patient care services at Saint Francis Hospital South. “The patient can already start formulating questions for the physician or surgeon or whoever might be caring for them.”
Features include:
• Taking Care of You: Information about your immediate care team, including names and pictures of your doctor, nurse and nurse tech, with a description of their roles in your care.
• Medications: Medications prescribed during your hospital stay and your existing medications.
28 saintfrancis.com
D
YourHospitalStay Home TakingCareofYou
KarenJones,DO AttendingProvider SeeAll

“… a patient who is more engaged during their stay can result in better outcomes and better interaction with providers.”
Tammy Bagby, Web Application Development Supervisor
Manage Your Health with MyChart
To register for a Saint Francis MyChart account, please visit mychart.saintfrancis.com.
This free tool offers secure and convenient access to your Saint Francis appointments, test results and immunization record. An active MyChart account also allows you to communicate with your Saint Francis healthcare team, request prescription refills and access ondemand 24/7 virtual urgent care services.
In a survey of MyChart Bedside users, patients said:
“Everything was easy to operate and everyone was helpful. I appreciate the team of Saint Francis Hospital South.”
• Patient Dining: View hospital dining menus and order meals from the app.
• Test Results: View your most current health information, latest lab tests and imaging results.
• Education: Looking for more information? A variety of educational resources and videos are available.
• Bedside Survey: Provide feedback using MyChart Bedside.
“Having a patient who is more engaged during their stay can result in better outcomes and better interaction with providers,” said Tammy Bagby, who has worked on the MyChart rollout since 2014 and implementation of MyChart Bedside since 2021.
If Saint Francis MyChart proxy access for a spouse, parent or adult child was already authorized before hospital admission, the medical proxy is sent a message when the patient is admitted, and the proxy will be kept updated via MyChart, said Nabeel Mahfooz, Epic applications manager.
Once the patient is discharged, the MyChart Bedside feature transitions back to the Saint Francis MyChart outpatient application, and the information from your hospital stay—including discharge instructions and medication information—remains available.
“I felt kept in the loop on my own healthcare without the need to rely solely on my care team.”
“I really liked being able to see lab results and knowing what to expect.”
“It was very nice to be able to see everything while almost being bedridden and having the schedule available.”
29 Saint Francis Health System presence
Download the MyChart Mobile App!

Saint Francis Adult ECMO Program
The machine may not look like much, but it is one of the most sophisticated devices available that helps keep patients in respiratory distress alive while allowing their lungs time to rest and heal.
The extracorporeal membrane oxygenation machine, or ECMO for short, acts as an artificial heart and lung. It pumps blood outside the body, adds oxygen, removes carbon dioxide, warms the blood and pumps it back into the patient. During the COVID-19 epidemic, Saint Francis Hospital staff realized that many more respiratory patients could be helped with ECMO rather than being transferred as previously there was only one other
program in the region. This prompted hospital leadership to embark on the process to start an ECMO program at Saint Francis Hospital.
Saint Francis Hospital’s four new ECMO machines, each costing around $500,000, will allow highly critical patients to receive this specialized care when all other options have failed. The program was launched in late September 2022, and the first patient was put on ECMO in early December. The team, led by Dr. Naziha Malik, has more than 50 specially trained experts that include critical care nurses, respiratory therapists, physicians and pharmacists. By supporting the lungs and heart, the ECMO

30 saintfrancis.com
Top image: An ECMO machine keeping a patient alive as the lungs heal.
Bottom image: Dr. Roger Gallup and Dr. Naziha Malik review the ECMO settings.
ECMO acts as an artificial heart and lungs. It pumps blood outside the body through a tube, adds oxygen, removes carbon dioxide, warms the blood and pumps it back into the patient.


machine stabilizes patients so that their body has more time to fight the COVID virus, pneumonia or other pulmonary or cardiac issues. The machine does not fix any condition; rather, it buys the patient time while their lungs heal on their own and with the help of medications.
ECMO is the most advanced form of life support available for adults and children and the patients on ECMO are usually among the sickest in the hospital.
“This brings up the high end of our critical care abilities,” said Roger Gallup, M.D., a pulmonology/critical care specialist on the ECMO team. “It extends what we can do here and will certainly save lives.”
What makes ECMO different?
Unlike a ventilator, which acts as bellows, moving air in and out of the lungs when patients are unable to get enough oxygen on their own, ECMO allows the lungs to rest. The patient’s blood is removed through a vein in the neck. The blood circulates through an oxygenation machine to remove carbon dioxide and deliver oxygen. Therefore, the body is receiving oxygen while the lungs are resting and healing. With ECMO, the patient can still breathe on their own, as much as their fluid-filled or infected lungs are able, and their heart still beats, but the lungs are assisted in a way that a traditional ventilator cannot.
Typically, an ECMO patient is on the ventilator first. The ventilator forces air into the lungs through a tube in the throat and windpipe. The air from the ventilator causes the lungs to expand and contract, and the patient usually is sedated because of the tubes.
“We want the lungs to heal,” Dr. Gallup said. “With a ventilator, we are limited by the damage in the lungs.”
Sometimes the lungs are so damaged that even a ventilator on its highest settings cannot get enough oxygen into the body.
Long-term use of the ventilator itself can often put stress on the lungs because of the air being forced inside. Also, ventilated patients can develop pneumonia because they cannot cough while on the ventilator and because there is also risk for infection.
“With a ventilator, you’re giving maximum oxygen and maximum support,” said nurse Kellie Brown, manager of the Adult ECMO Program. “Over time, if you have to stay at those very high ventilator settings, that can cause trauma to the sensitive lung tissue, so you don’t want to leave a patient on the vent too long.”
31 Saint Francis Health System presence

“It’s exciting to keep patients close to home,”
Malik said, “and provide additional services we’ve never had before.”
Another big advantage of ECMO:
Patients are conscious and can talk—both impossible on a ventilator.
“The biggest difference is being awake and able to communicate,” Dr. Malik said. Patients on a ventilator usually are sedated, she said, while patients on ECMO can be awake, only needing a little pain medicine.
The first Saint Francis patient to be on ECMO in December, for example, asked for a drink of water and answered simple questions from her medical team.
She came to the Saint Francis Hospital Trauma Emergency Center because of mild shortness of breath after Thanksgiving. She had been exposed to influenza and RSV at a
recent gathering. Within a day, her oxygen levels had dipped to dangerous levels, and she was on a ventilator because of her rapid decline. However, the ventilator could only get her oxygen levels up to 55% instead of the goal level in the 90th percentile—far too low to sustain life. With no other options, she became the first patient to utilize the new adult ECMO machines at Saint Francis.
A nurse monitors the machine 24 hours a day, adjusting how much oxygen and carbon dioxide goes in and out, watching for clots, and adjusting tubing.
 Dr. Naziha Malik talks with her patient who is awake and able to communicate while on ECMO.
Dr. Naziha Malik talks with her patient who is awake and able to communicate while on ECMO.

A long history of ECMO technology
ECMO was developed in the 1970s by Dr. Robert Bartlett, a thoracic surgeon, while he was at the University of California, Irvine School of Medicine. His research started on adults, but attention quickly turned to newborns with breathing problems. His first successful case was in a newborn named Esperanza, a baby in California who was blue from lack of oxygen. With the baby on the brink of death, Dr. Bartlett connected her to the ECMO machine, and within a few days, her lungs were healed, and she was ready to be disconnected.
Dr. Malik met both Dr. Bartlett and baby Esperanza, who is now in her late 40s, as
they were featured speakers at the 2022 Extracorporeal Life Support Conference in Boston, which Dr. Malik and Brown attended as they prepared to launch the Saint Francis program.
Because of Esperanza’s recovery, ECMO for years has focused on pediatric and neonatal patients. The Children’s Hospital at Saint Francis has had a successful ECMO program since the late 1980s. In fact, Kelly Brown, the adult ECMO program manager, worked with the pediatric team for decades prior to taking on her new role. “We are thankful we can offer this lifesaving therapy to our patients. Our pediatric ECMO team is driven by the ‘best of the best’ nurses— many who’ve been doing this for 30+ years. And, as a result, our ECMO outcomes
in the children’s hospital are consistently among the best in the country,” said Becky Reinholz, Pediatric Intensive Care Unit Clinical Manager. But it wasn’t until the COVID epidemic that attention shifted to helping adult patients who suddenly had acute respiratory failure so severe that ventilation was not enough.
As patients improve, doctors gradually wean them off ECMO support, transitioning them back to a ventilator before they start breathing on their own again.
“It’s exciting to keep patients close to home,” Dr. Malik said, “and provide additional services we’ve never had before.”

 Nurses Heather Spears and Sarah Arp meet with Dr. Roger Gallup and Dr. Naziha Malik.
Nurses Heather Spears and Sarah Arp meet with Dr. Roger Gallup and Dr. Naziha Malik.
Saint Francis Implements Initiative to Help Victims of HumanTrafficking
Training healthcare staff to spot the signs of those in dire need of help
During a bioethics class, a professor assigned a young nun a research project that would open her eyes to a vulnerable population. That project has led to a new initiative that can improve the lives of countless patients in the Saint Francis Health System.
The case she investigated in school involved a woman who went to the same hospital multiple times to give birth without ever receiving prenatal care. Each time, the baby was born on drugs. Each time, the local human services agency was summoned. And each time, the baby was removed from the mother’s custody. It was suspected the patient was a victim of human trafficking.
Eventually, with the hospital staff seeing no alternative but to intervene, the patient was sterilized; a decision that caused that hospital to lose its Catholic affiliation. This case, tragic in every way, was what Sister Brigid Mary Meeks studied for a master of science in bioethics at the University of Mary in Bismarck, N.D. Her conclusion: The hospital staff was not equipped to adequately care for the patient’s many psychosocial and spiritual needs. Frustrated at their inability to achieve a comprehensive healing, Sister Brigid Mary reasoned, the staff fell victim to despair and thought that doing something— anything— was better than doing nothing.
When Sister Brigid Mary was sent by the Religious Sisters of Mercy to study law at Villanova Law School, this case never left her mind. As a legal intern to Mike Lissau, senior vice president and general counsel for Saint Francis, they began discussing how the health system could better serve this vulnerable population.
The answer became clear: Saint Francis needed a program to help victims of human trafficking. The goal of the program is not a new one for the health system. At the founding of the health system, William K. and Natalie Warren prayed “that all those, ordained by God, seeking
admittance here…will find life.” The program at Saint Francis seeks just that: to provide the patient with an encounter of the presence and healing ministry of Christ, who is Life.
“It’s a pervasive enough issue that every staff member needs to know the signs,” said Sister Marie Josepha Kluczny, a nurse midwife and vice president of mission and ministry. “We want every staff member to be the potential touch point with Christ.”
34 saintfrancis.com
Sister Marie Josepha Kluczny, RSM, APRN-CNM, MSN (left), vice president of mission and ministry, and Sister Brigid Mary Meeks, RSM, JD, are Religious Sisters of Mercy at Saint Francis. Both are involved in the initiative to educate employees on how to recognize and help patients who may be victims of human trafficking.

“Love is powerful, and if we can provide just one memory to this patient of being genuinely loved, then, that’s a win.” Sister Brigid Mary Meeks
The federal definition of human trafficking is “the recruitment, harboring, transportation, provision, obtaining, patronizing or soliciting of a person for the purpose of a commercial sex act, in which the commercial sex act is induced by force, fraud or coercion.”
Why should this issue interest hospitals? Statistics show that 88% of victims of human trafficking seek medical attention, yet most are never identified, and
most providers have never been trained to identify victims.
Why should the issue be so close to the Sisters’ hearts at Saint Francis? Sister Brigid Mary explains that the Religious Sisters of Mercy were founded in 1831 by Venerable Catherine McAuley primarily to respond to distressed women. At the time, Ireland faced massive poverty, and women were being forced into sex labor. The Foundress wanted the women to have a real opportunity at life.
“Not many programs respond to sex trafficking with the Christian world view that we at Saint Francis believe is necessary for healing,” Sister Brigid Mary said. “Who understands these women better than Christ, who was betrayed with a kiss for 30 pieces of silver, bound in a dark cell, beaten, tortured, forced to walk the streets and stripped naked? Christ has taken on everything they have experienced.”
The signs can be subtle, such as a simple medical issue becoming serious due to lack
of care. Through the new program, all staff will have an indicator tool to identify red flags in patients. These red flags include hypervigilance, gaps in care, signs of abuse and evidence of dominating relationships.
Because human trafficking is a long-term issue with many societal causes and many medical comorbidities, the Sisters realize that one visit at the hospital often won’t be enough to get women to a place of safety. But they remain hopeful.
“Love is powerful, and if we can provide just one memory to this patient of being genuinely loved,” says Sister Brigid Mary, “then, that’s a win.”
“If, however, through the experience of being safe and loved, they’re ready to get out, we will be prepared to assist them to a safe environment,” Sister Marie Josepha said. “As a health system, in time we’ll start to see how we can continue to follow and help these women through the healing process.”
But the important work will have begun: the identification of a victim and the start of a relationship that can help save someone’s life.
35 Saint Francis Health System presence
Saint Francis Partners with Local Universities for Nursing Education

During a nationwide nursing shortage that is expected to intensify, Saint Francis Health System is committed to finding creative ways to recruit and retain nurses.
As the largest health system in the state, Saint Francis registered nurses make up more than 20% of our workforce. Each year, we need to hire more than 600 nurses to keep up with retirements and growth within departments.
One of our newest initiatives is a partnership to educate nursing students from Rogers State University.
Saint Francis will be an extended campus of RSU, and Rogers State University will award the Bachelor of Science degree in nursing upon students’ graduation.
The extended campus will open in the fall of 2023 for students who have been accepted into the Rogers State University
nursing program. Applications for the spring 2024 semester are currently open.
The Saint Francis extended campus has been generously underwritten for the first three years by a grant from The William K. Warren Foundation.
To be eligible for the program, students should have applied and been accepted to the Rogers State University nursing program and completed 58 hours of prerequisite classes. As juniors, students will be able to choose either nursing classes in Claremore on the Rogers State University campus or at Saint Francis Hospital. Classroom instruction at Saint Francis will be presented via video simulcast with instructors in Claremore and live with facilitators in Tulsa.
Saint Francis is renovating a 6,000-squarefoot area within the hospital that will house a state-of-the-art simulation center and
classrooms. A new simulation center will include four high-fidelity simulation suites designed to replicate Saint Francis inpatient rooms. The suites will include medical/ surgical nursing, critical care, labor and delivery, trauma and pediatrics settings complete with sophisticated manikins that simulate breathing, sweating, talking and even giving birth.
The Saint Francis extended campus will accept 16 juniors in fall 2023 and add 16 more each semester, ultimately with 64 nursing students—32 juniors and 32 seniors—each year at Saint Francis. The new partnership allows Rogers State to expand its nursing graduates by more than 50%.
“Saint Francis has a strategic initiative to recruit registered nurses by developing academic partnerships with area nursing programs,” said Chief Nursing Officer
36 saintfrancis.com
Cindy Leathers. “The RSU extended campus at Saint Francis will increase enrollment, enhance learning with the culture of Saint Francis, and help the students engage in our vision, mission and values. Our goal is for these students to become career nurses at Saint Francis.”
In addition to the RSU program, Saint Francis has several ongoing partnerships with local colleges so that nursing students can learn clinical skills at Saint Francis. Currently, there are nursing cohorts with the University of Oklahoma, University of Tulsa, Northern Oklahoma College, Rogers State and Connors State. By 2025, Saint Francis will have up to 188 nursing students in clinical rotations, with 124 graduating per year.
Currently, Saint Francis employs 13 master’s and doctorate-level nurses who serve as adjunct faculty for the clinical
rotations that nursing students do at Saint Francis.
For the new RSU program, the health system will be hiring two coordinators for the Saint Francis extended campus and simulation center and two full-time nursing instructors who will have an academic appointment at Rogers State University.
In addition to educating the next generation of nurses, Saint Francis also has programs to recruit experienced nurses, including Coffee Connection, a free coffee event that is held monthly, and Walk-In Wednesday, an opportunity for nurses to have same-day interviews.
For more information about nursing opportunities at Saint Francis, please visit jointeampink.com.










Screening for HEART DISEASE

38 saintfrancis.com
We sat down with Dr. Stephen Dixon, an interventional cardiologist with Saint Francis Heart and Vascular Institute, to discuss the benefits of heart screenings.
He said that there has been growing interest in screening tests in the last five to six years, and now that COVID-19 is not such a threat, more people are exploring cardiovascular testing after a lull during the pandemic.
Most of the time patients aren’t diagnosed with a life-threatening condition through a screening, although that is possible, Dr. Dixon said. Usually, the tests reveal the need for a person to modify risk factors by improving their diet, exercising more or taking a statin.
“Some people may need a little extra motivation,” Dr. Dixon said. “And seeing the results of a screening may be just the encouragement they need.”
Typically, the $99 cost is paid out of pocket, rather than being covered by insurance.
Any adult can schedule a screening without a physician referral, but Dr. Dixon recommends them for people with a family history of heart disease—especially if a mother or father had a heart attack or stroke in their 40s or 50s, then their adult children could be at higher risk, too—or if a person has other risk factors, such as diabetes, smoking and high blood pressure.
“Even if the results are abnormal, it’s all about lifestyle and making modifications,” he said. “No one needs to be alarmed, but the screenings are tools to prevent future heart attacks and strokes. It’s a number to let us know how aggressive we need to be.”
CARDIAC CALCIUM SCREENING - $99
The cardiac calcium screening measures the calcified plaque in the arteries that supply blood to the heart. This non-invasive CT scan helps calculate your risk of a heart attack.
SET OF THREE CARDIOVASCULAR SCREENINGS - $99
• Carotid Disease—This simple ultrasound helps detect plaque in arteries that can cause stroke.
• Abdominal Aortic Aneurysm—This test checks for enlargement of the part of the abdominal aorta that suggests a risk for rupture.
• Peripheral Arterial Disease—This condition of the arteries in the legs is related to an increased risk of heart attack or stroke. This test will record blood pressure in both legs to evaluate blood circulation.
to watch the video

For more details about this series of cardiovascular screenings, scan here or visit saintfrancis.com/heartscreening
Each test takes about 15 minutes, and results typically are available the same day through MyChart. If there is a significant finding, that information will be assigned to the patient’s primary care physician for follow-up.
To schedule a screening for heart disease, call 918-494-6900.
39 Saint Francis Health System presence
SCAN HERE
Heart of a Champion
One of the smallest babies born at Saint Francis makes a mission of giving back

As she plays veterinarian with her stuffed animals, Ella Gruenberg points out that most of them are quite a bit larger than she was when she was born.
“I was a tiny baby,” Ella says, as she holds her fingers together to show just how little she was.
Born extremely premature—also called a super preemie—she weighed only 470 grams, which equals 1 pound and less than 1 ounce. She was only 10 inches long.
Today, she is an energetic 7-year-old who loves to swing; build with blocks; and arrange and rearrange her collection of toy bunnies, puppies and cats.
Ella was selected as the 2023 Children’s Miracle Network Champion Child for the Tulsa area, representing The Children’s Hospital at Saint Francis, where she spent the first three months of her life.
Her mother, Amanda Gruenberg, was 23 weeks pregnant when she went to work as an elementary school teacher feeling dizzy. The school nurse took her blood pressure, and it was high enough that she recommended Amanda leave immediately to get treatment.
“I was aware of preeclampsia and thought I’d be going home on bed rest,” she said. “Never did I dream I’d be having a baby that week.”
At Saint Francis, she and her husband heard the news they dreaded. Her baby would be delivered by cesarean section, and doctors listed a variety of potential complications—blindness, heart defects, brain bleeds and more.
“It was a pretty grim outlook,” Ella’s dad, Ross Gruenberg, said.
At 24 to 25 weeks, babies are considered to be extremely preterm—three to four months shy of their due date. They need the support of medical equipment because their heart, lungs, kidneys and other organs have not developed enough for them to stay alive without medical support, said Dr. Margaret Donahue, a neonatologist in the Neonatal Intensive Care Unit at The Children’s Hospital at Saint Francis.
“There is never a point when a baby born that early is out of the woods,” Dr. Donahue said. “There is truly never a period of time when you can say, ‘I can guarantee you that your baby is going to make it out of the NICU.’”
Ella, Dr. Donahue recalls, was one of the smallest newborns she had ever seen. Usually a small preemie would weigh 650 to 700 grams—about a pound and a half. Since Ella was so much smaller, “just getting medical equipment to fit was a challenge.” Years ago, a baby born so early and so small would not have had a chance at survival. The technology just was not advanced enough, Dr. Donahue said. But being born in 2016 and living close to a Level 4 NICU gave Ella a chance.
“It gave me a comfort knowing that the place we were at Saint Francis was the best place for her,” Ross said.
When Ella was born, she let out a cry. That was a great sign because the parents and the medical team were prepared for her to be completely quiet. For a while, she was breathing on her own, and everyone was impressed with her strength to survive.
On Easter Sunday, three days after she was born on Good Friday, Ella’s mom received a terrifying call that she was needed in the NICU immediately. Still recovering from the C-section, Amanda had not been out of her hospital bed. While her husband had visited Ella in the NICU, Amanda had not been able to.
When she arrived in her wheelchair, she realized that Ella’s situation was critical because the baby was surrounded by 15 hospital staff members. Her lung had collapsed, causing her oxygen level and heart rate to drop. Within 30 seconds, Ella had become critically ill and needed ventilation.
“They wanted me to see her because they didn’t know if she was going to make it,” Amanda said, wiping away tears.
That was the first time she had been able to touch her baby, and she worried it may be her last.
Ross noticed that Ella’s skin, usually red and translucent, had become gray due to the breathing issue.
That most critical hour turned into the next morning, and little Ella was still fighting for survival.
The medical team sought to make their tiniest equipment work for an even tinier patient. The smallest breathing tubes were too big and had to be forced to fit.
At two weeks of age, she had to have heart surgery for patent ductus arteriosus, a heart defect that affects the way blood flows through the lungs. Her tiny heart was only the size of a grape, and the vessel next to it that surgeons were operating on was as narrow as a piece of spaghetti.
“Every part of her needed TLC and a lot of technology,” Dr. Donahue said.
For the first month, Ella stayed in the dark, tucked in tightly. On day 30, Amanda held Ella for the first time through kangaroo care, a process for allowing skin-to-skin contact between mother and baby.
Amanda also maintained her bond with Ella by reading her books quietly in the dark.
About Children’s Miracle Network Hospitals
More than 10 million kids enter a children’s hospital like The Children’s Hospital at Saint Francis across North America every year. To provide the best care, children’s hospitals rely on donations and community support, as Medicaid and insurance programs do not fully cover the cost of care. Since 1983, Children’s Miracle Network Hospitals has helped fill those funding gaps by raising more than $7 billion, most of it $1 at a time through Miracle Balloon icon campaigns. Its various fundraising partners and programs support the nonprofit’s mission to save and improve the lives of as many children as possible.
You’ll have a chance to give at Sam’s Club, Walmart, Costco, Panda Express, ACE Hardware, Love’s and Dairy Queen. We hope you’ll consider giving a gift at the register during checkout to help The Children’s Hospital at Saint Francis. Those gifts stay local.
Scan here to give!

41 Saint Francis Health System presence
Weeks turned into months, and on July 1, 2016, Ella was ready to be released from the hospital, 10 days before her original due date.
“It was just amazing how strong she was through all of this,” Dr. Donahue said.
So many parts of Ella’s story were unusual. Since her parents thought they were 16 weeks away from having a baby, they hadn’t decided on a name. The family also had not had a baby shower or started decorating a nursery.
Another difficult situation—buying clothes. She was so tiny, so frail, and her condition seemed so perilous that shopping felt a bit presumptuous.
“I just couldn’t bring myself to buy her pajamas,” Amanda said.
So Ella’s first onesie was one that had been donated to the hospital. Once Ella was released, Amanda had an idea. She would make an annual donation of preemie clothes to The Children’s Hospital at Saint Francis to help other families of preemies.
As Ella got older, she took on the project herself, collecting preemie clothes for her birthday, folding each little outfit and commenting on how much a baby and mom would love it. Ella makes a stack of onesies with zippers, a stack for pajamas with long sleeves, a stack of those with short sleeves. Stacks for boys and stacks for girls, each one folded and gushed over by their 7-year-old curator.
“It is my goal to show love and support to families in the NICU,” Amanda says. “It is an amazing thing to remind others, even those we will never meet, that there is someone rooting for them. Someone who cares. Someone who knows they are hurting and chooses to do something to make their day a little better.”
Now in the fourth year, Ella’s Preemie Pajama Project brought in 436 pajamas and blankets plus 221 books—well over of her goal of 178 pajamas, one for each of the 98 days Ella spent in NICU and one for each month she has been at home since graduating the NICU.
When Ella delivers the pajamas to the hospital, one of her biggest fans— Dr. Donahue—always plans to be there to welcome one of her strongest, toughest patients back to the place where she spent her first three months.
“Watching her as she grows and seeing that she can do everything that she needs to do as a happy, healthy 7-year-old,” Dr. Donahue said, “it’s extremely rewarding.”
Scan here to watch a video of Ella’s story!




43 Saint Francis Health System presence 2019 206 ITEMS 2021 240 ITEMS 2022 233 ITEMS 2023 436 PAJAMAS & BLANKETS PLUS 221 BOOKS
Preemie Pajama
Ella’s
Project
No Such Thing as Too Young
STROKE
KNOW THE SYMPTOMS, BECAUSE STROKE CAN HAPPEN AT ANY AGE
When Monica Bein’s right eye stopped seeing correctly and she could not read the words on her phone, she had already worked with several stroke patients that day, helping them with speech and swallowing.
That put her in a pretty good position to recognize her own stroke as it was happening while she was cooking dinner.
“What I was seeing was a crescent-shaped figure in the upper right quadrant of my right eye, and the crescent was made up of smaller geometric shapes,” she said. “It was so bright and illuminated, and no matter where I looked, the crescent was there.”
Her first inclination was to lie on the couch and watch TV for a bit. Then she wondered if she could read. “I picked up my phone and could not read any of it,” Bein said. “I was trying to say, ‘I can’t read,’ but it wouldn’t come out.”
This Saint Francis Hospital physical medicine and rehab supervisor, who has a master’s degree in speech pathology, realized quickly what was happening and went into diagnosis mode. Was it an occipital stroke because her vision was impaired? Was it parietal because her speech was impaired?
She motioned for her husband to take a video of her trying to read so that she would have proof of what was happening in case the symptoms resolved quickly and so that she would have documented what time the troubles started.
“I was actually praying in my head, too, but I didn’t have the words for it,” the 49-year-old Bein said. “I remember thinking that I hope God knew I was praying even though I didn’t have the words.”
Although strokes are more common in people over 60, about 10% of strokes happen to those younger than 50, according to the Centers for Disease Control.
A study in the journal Stroke, a publication of the American Heart Association, revealed that younger

Meet Monica Bein
Age: 49
Stroke date: August 16, 2022
Profession: Physical medicine supervisor at Saint Francis Hospital. Works with stroke and trauma patients who need speech or swallowing therapy.
Symptoms: Vision impaired, speech slurred, couldn’t understand words she tried to read.
Advice: “Even if you suspect you’re having a stroke or see any sign, go to the hospital immediately because the worst-case scenario is that it’s not a stroke. You’ll never regret being too safe, and nobody is too young. It can happen at any age.”
44 saintfrancis.com
STROKE
patients don’t get to the hospital as quickly as older patients, probably because they are less likely to perceive stroke symptoms as serious.
A study published in the journal Neurology revealed that adolescents and young adults are less likely to call 911 for stroke-like symptoms because they do not realize they are at risk.
Those are statistics Bein wants to change. She credits early recognition, early emergency care and early access to a clot-busting drug as the reasons she recovered thoroughly. Her husband called 911, and within 25 minutes of her first symptom, she was at the Saint Francis Trauma and Emergency Center.
Now, her mission is to spread the word about stroke symptoms and what to do if you experience even one of them.
“I want everyone to know,” she said. “I want the word out. Stroke can happen to anyone.”
Experts agree that stroke can happen at any age and any health.
“It isn’t just middle age and older or those with numerous risk factors,” said Cameron Richardson, stroke program manager at Saint Francis Hospital. “We see marathon runners and football players. Children and young adults have strokes every year and often do not get treatment because they arrive to the hospital after 24 hours.”
The mayor of Muskogee found out that younger people can have a stroke. In April 2022, just one month after he turned 50, he experienced numbness and weakness in one leg, and his speech was slurred. Also, he noticed his breakfast tasted funny—like it had been drowned in salt.
Without the urging of a persistent friend at a board meeting, Mayor Marlon Coleman said he might have ignored the symptoms and continued dragging his leg.
“Don’t assume you’re just having a bad day,” he said. “Know the symptoms and take them seriously. I knew the stroke-like symptoms and would have told someone
Meet
Marlon Coleman
Age: 51
Stroke date: April 25, 2022
Profession: Mayor of Muskogee and pastor of Temple of Hope Church
Symptoms: Numbness in leg, weakness in leg, strange taste of food, slurred speech
Advice: “If you’re having the symptoms, you don’t have time to wait. I believe God is a healer. But what more healing would he have had to do for me if I was more debilitated? That’s why you cannot wait.”

else they were having a stroke, but it was harder to see in myself.”
Another young stroke patient is Donovan Cotner, a 54-year-old business owner from Kiefer. Before his stroke in July 2022, he was a runner and worked out at the gym several times a week. He was in a CrossFit class the evening he collapsed.
“He fell over, and they saw him laying in the floor,” said Cotner’s wife, Janna. “At first, they thought he was just being silly. They instantly realized he wasn’t joking and called 911.”
Within minutes, he was being treated in the Saint Francis Hospital Trauma Emergency Center. Doctors could see blood clots on the CT scan, and a neurologist performed a thrombectomy, which is a surgery to remove a clot from a vessel in the brain. Because the ambulance was called immediately and he was at the hospital quickly, Cotner was also able to receive a clot-dissolving medication to dissolve the smaller clots.
45 Saint Francis Health System presence

Help close to home
Like Bein and Coleman, Cotner had an ischemic stroke, which means that blood supply to part of the brain was cut off because of a blood clot in a vessel. This is the most common type of stroke, accounting for 87% of cases. Hemorrhagic stroke, which is caused by a blood vessel rupturing and bleeding inside the brain, accounts for the other 13%.
Saint Francis Hospital has been recognized as a Certified Comprehensive Stroke Center, which means it delivers the highest quality of care to the most complex stroke cases.
Saint Francis Hospital Muskogee has been designated as a Primary Stroke Center, a designation signifying it has the necessary staffing, infrastructure and programs to stabilize and treat most emergent stroke patients.
SCAN HERE
to watch the video

Saint
Francis Hospital
Additionally, Saint Francis Hospital has been recognized by the American Heart Association as having a Gold Plus rating for stroke care, which signifies that the hospital can care for very complex strokes and that at least 85% of patients eligible for a clotdissolving medication receive it quickly.
“It’s a huge priority for Saint Francis because we have a very sick population,” Richardson said. “Hypertension, diabetes, overweight, high cholesterol—all of those have a higher incidence of stroke. It’s important that those patients get the highest quality care close to home without being sent to Oklahoma City or Dallas.”
has been recognized as a Certified Comprehensive Stroke Center
Saint Francis Hospital Muskogee has been designated a Primary Stroke Center
The warning signs: BE FAST
As a part of the stroke center certification process, every hospital employee, even those in non-clinical settings, is trained to recognize stroke warning signs. The acronym BE FAST is used as a reminder about balance, eyes, face, arms and speech. The T stands for time because getting care quickly saves brain cells. It also stands for terrible headache because some strokes, especially those that involve bleeding in the brain, can be marked by a sudden headache.
“Roughly 1.9 million brain cells die each minute during a stroke,” Richardson said. “That’s about 31,600 brain cells each second. To think of it another way, having a stroke not only reduces your overall life expectancy but severely changes the quality of your life relative to the area of the brain affected.”
Put simply, a person who is having a stroke needs to call 911 immediately or have someone around them call 911. Richardson says that the 911 system notifies the hospital that a possible stroke patient is on the way, which allows stroke centers to activate their stroke team, decreasing the time to treatment. That doesn’t happen if someone drives a car to the emergency room.
46 saintfrancis.com
Cameron Richardson, stroke program manager at Saint Francis Hospital
BE FAST
The signs of a stroke are usually very sudden and are not always obvious or dramatic. It is important to recognize subtle stroke symptoms because early treatment is the key to a successful recovery.
Signs of a stroke include:
B | Balance. Is there a sudden loss of balance or coordination?
(Ask the person to walk in a straight line or touch their finger to their nose.)
E | Eyes. Are there sudden vision changes?
(Ask if the person has double vision or cannot see out of one eye.)
F | Face. Does one side of the face droop? (Ask the person to smile.)
A | Arm. Does one arm drift downward? (Ask the person to raise both arms.)
S | Speech. Are words slurred? Is speech confused? (Ask the person to repeat a sentence.)
T | Time. What time did the symptoms begin? When was the person last seen looking or acting normally? Also, the T can stand for terrible headache. While the majority of strokes don’t have any pain, the most deadly type of stroke (hemorrhagic, specifically subarachnoid hemorrhage) are commonly associated with a sudden terrible headache.
During a stroke, every second counts. If you see someone experiencing these stroke symptoms, call 911 immediately.
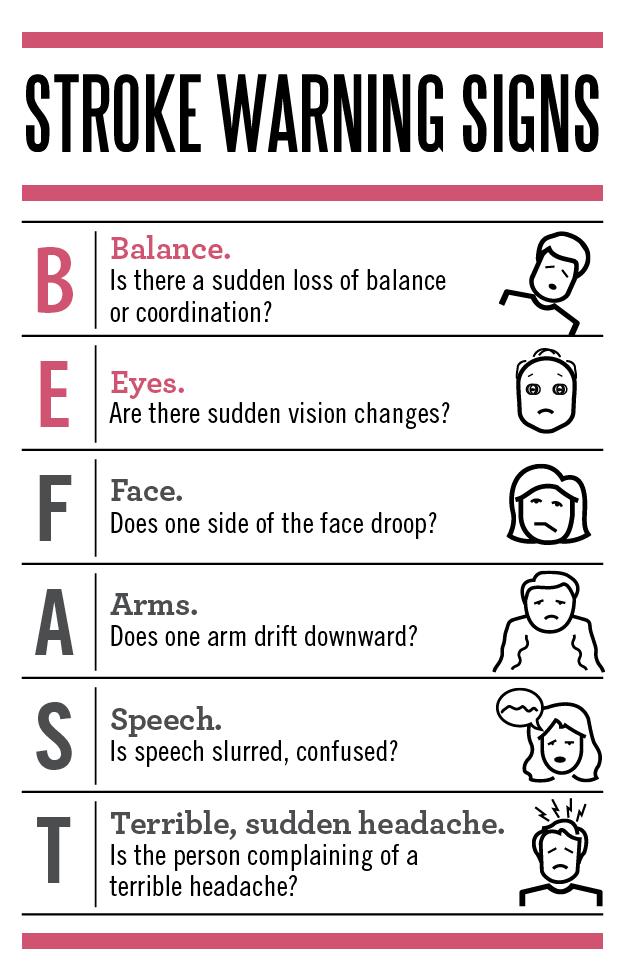
Risk factors
The most common cause of stroke is high blood pressure, which the American Stroke Association calls the “silent killer” because it has no symptoms, and many people don’t realize they have it.
High blood pressure was Coleman’s number one risk factor, he said.
The TIA, or transient ischemic attack, also called a mini stroke, was just the wake-up
call Coleman needed to take his blood pressure medicine regularly, improve his diet and begin exercising regularly. He also is being more careful with his health because he realizes that as an African American, he is at a higher risk of stroke. Black Americans have a higher prevalence of stroke and the highest death rate from stroke of any racial group.
He has started a diet of mostly salad, fruit and vegetables, and he goes to Champions
Fitness several times a week to work out.
Prior to his stroke, he used the gym mostly as a social outlet rather than a place to be on the treadmill. Since his stroke, Coleman has lost about 30 pounds and says he is in much better shape physically. He also is working to lower his stress, especially trying not to take his work home with him.
For Bein, she found out she had two blood clotting disorders that she never knew she had until the stroke.
47 Saint Francis Health System presence
She now takes blood thinner to control the disorders, and she also is having her children tested for them.
For Cotner, there were no definitive answers about why he had a stroke, his wife said.
He never smoked and was a fitness fanatic, having run a 50K the month before his stroke and even ran a 100-mile endurance race through the Mark Twain Forest in 2017. He worked every day as the owner of Cotner Transport, a trucking company.
After a week in the intensive care unit and four weeks in inpatient rehab at Saint Francis Hospital, Cotner was released Aug. 24, 2022. Every day, he gains more mobility and is still working on his speech, although he understands almost everything and can even help his wife with questions about their business, Janna Cotner said.
Meet Donovan Cotner
Age: 54
Stroke date: July 19, 2022
Profession: Owner of Cotner Transport
Symptoms: Loss of mobility on right side and loss of speech
From his wife: “He ran a 50K in Arkansas last June, so this really can happen to anybody. We give God the glory for his recovery, but also are thankful for his physical strength and determination.”
In March 2023, he competed in a 16-kilometer trail run at Turkey Mountain. He walked much of it, Janna Cotner said, and was tremendously proud to be back to his hobby of running.
“He gets steadier and steadier,” she said. “He stays in good spirits all the time, which is his personality. We are still believing in a full recovery.”
Each of the patients is grateful for receiving a clot-buster, which dissolves clots, allowing blood to start flowing again, but it’s only given if patients arrive at the hospital within a few short hours of the first symptom.
For Bein, she says she could actually feel the medication take effect. She recalls trying to read the white board in her emergency room bay. During her typical shift working at the hospital, she’d see those signs several times—nurse’s name, pain scale, doctor’s


Donovan Cotner and his wife, Janna, completed a 16K trail run at Turkey Mountain less than a year after his stroke.
name and room number. But as she lay in the bed the night she had the stroke, she couldn’t make sense of anything on the board that she had seen hundreds of times previously. That is, until she received the clot buster through an IV in her arm.
“As it was infusing, I could read,” Bein said. “I was amazed because I could actually feel it working, and I was able to read more and more.”
All three patients are grateful that they were around others when they had a stroke so that they could get help quickly.
But even Bein, who sees stroke patients professionally, almost did the wrong thing—wait to see if some rest would help.
“I have a new understanding of why people would wait or take a nap because you really cannot believe that it would be a stroke,” she said.
Now, as a stroke survivor, she has a newfound camaraderie with her patients.
“I’ve easily had good relationships with my patients through the years,” Bein said. “But this has given me a connection with them. I understand what it’s like to be scared and not know if they’ll get better or get worse. Now I have a much better understanding of being on that side of not knowing what the outcome will be.”
48 saintfrancis.com
New Providers
SINCE SUMMER 2022
For more information, or to find a Warren Clinic physician, specialist or Urgent Care location, please call Saint Francis HealthLink at 918-488-6688 or visit saintfrancis.com.








49 Saint Francis Health System presence
Rebecca Abraham, MD Family Medicine North Peoria
Tanushree Agrawal, MD Cardiology (Non-Invasive) Saint Francis Heart and Vascular Institute
Neil Agrawal, MD Cardiology (Non-Invasive) Saint Francis Heart and Vascular Institute
Madison Beckman, DO Family Medicine Tulsa
Barry Berch, MD Pediatric Surgery Tulsa
Mark Walter Boomer, MD Outpatient Pulmonology Tulsa
Casey Butler, MD Pain Management Tulsa
Amy Dunn, DO Family Medicine Tulsa
Andre Fallot, MD Pediatric Intensive Care Medical Director
The Children’s Hospital at Saint Francis
John Fell, DO Family Medicine Fort Gibson
Melissa Frandsen, MD Physical Medicine and Rehabilitation Medical Director Tulsa
Yinan Fu, MD Pediatric Gastroenterology The Children's Hospital at Saint Francis
New Providers








50 saintfrancis.com
Hee Won Kim, MD Pediatric Intensive Care The Children's Hospital at Saint Francis
Clifford Kissling, MD Physical Medicine and Rehabilitation Muskogee
Chris Klotz, MD Family Medicine Owasso
Jason Keith Miles, DO Family Medicine Owasso
Bilal Muzaffar, MD OBGYN Saint Francis Hospital South
Charles Fullenwider, MD Neurosurgery Muskogee
Santhi Gokaraju, MD Nephrology Tulsa
Benjamin Greiner, DO Internal Medicine Tulsa
Jonathan Israel, MD Urology Tulsa
Rohit Josyabhatla, MD Pediatric Gastroenterology
The Children's Hospital at Saint Francis
Stewart Katz, MD Cardiology Saint Francis Heart and Vascular Institute
Ahmad Khattab, DO Pain Management Saint Francis Hospital South
New Providers
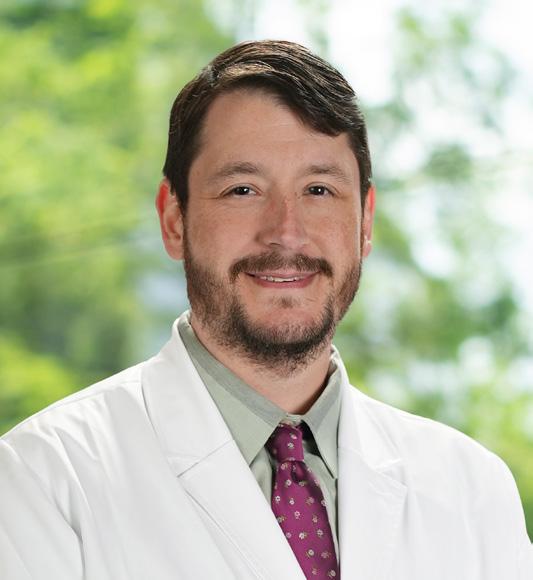









51 Saint Francis Health System presence
Daniel Ostmo, DO Internal Medicine Tulsa
Pooja Parmar, MD Pediatrics Owasso
Cassandra Riddle, DO General Surgery Saint Francis Hospital South
Jason Riffe, DO Family Medicine Broken Arrow
Richard Saint, MD Urology Saint Francis Hospital South
Donald Schleicher, DO Neurosurgery Tulsa
Tiffany Sibley, DO Urgent Care Sand Springs
Lakshmi Uppaluru, MD Hematology/Oncology Saint Francis Cancer Center
Richard Vigh, MD Maternal Fetal Medicine Tulsa
Amanda Whytal, DO OBGYN Tulsa
Presence
A publication of Saint Francis Health System
MISSION
To extend the presence and healing ministry of Christ in all we do
VISION
Inspired to create a sustainable and just healthcare system, Saint Francis will be the technology-enabled health ministry that delivers integrated, market-leading, high-quality, affordable care through engaged caregivers to the people of eastern Oklahoma.
VALUES
EXCELLENCE
Promoting high standards of service and performance
DIGNITY
Respecting each person as an inherently valuable member of the human community and as a unique expression of life
JUSTICE
Advocating for systems and structures that are attuned to the needs of the vulnerable and disadvantaged and that promote a sense of community among all persons
INTEGRITY
Encouraging honesty, consistency and predictability in all relationships
STEWARDSHIP
Ensuring prudent use of talents and resources in a collaborative manner
6161 South Yale Avenue • Tulsa, Oklahoma 74136
SAINT FRANCIS HOSPITAL | THE CHILDREN’S HOSPITAL AT SAINT FRANCIS | WARREN CLINIC | SAINT FRANCIS HEART AND VASCULAR INSTITUTE | SAINT FRANCIS HOSPITAL SOUTH | LAUREATE PSYCHIATRIC CLINIC AND HOSPITAL SAINT FRANCIS HOSPITAL MUSKOGEE | SAINT FRANCIS HOSPITAL VINITA | SAINT FRANCIS CANCER CENTER | SAINT FRANCIS HOME CARE COMPANIES | SAINT FRANCIS GLENPOOL



 Cliff Robertson, M.D. President and Chief Executive Officer Saint Francis Health System
Cliff Robertson, M.D. President and Chief Executive Officer Saint Francis Health System

 STEPHANIE HUSEN, D.O.
STEPHANIE HUSEN, D.O.


 AMANDA GLENN
PRESTON PHILLIPS, M.D.
WILLIAM LOVE
AMANDA GLENN
PRESTON PHILLIPS, M.D.
WILLIAM LOVE



















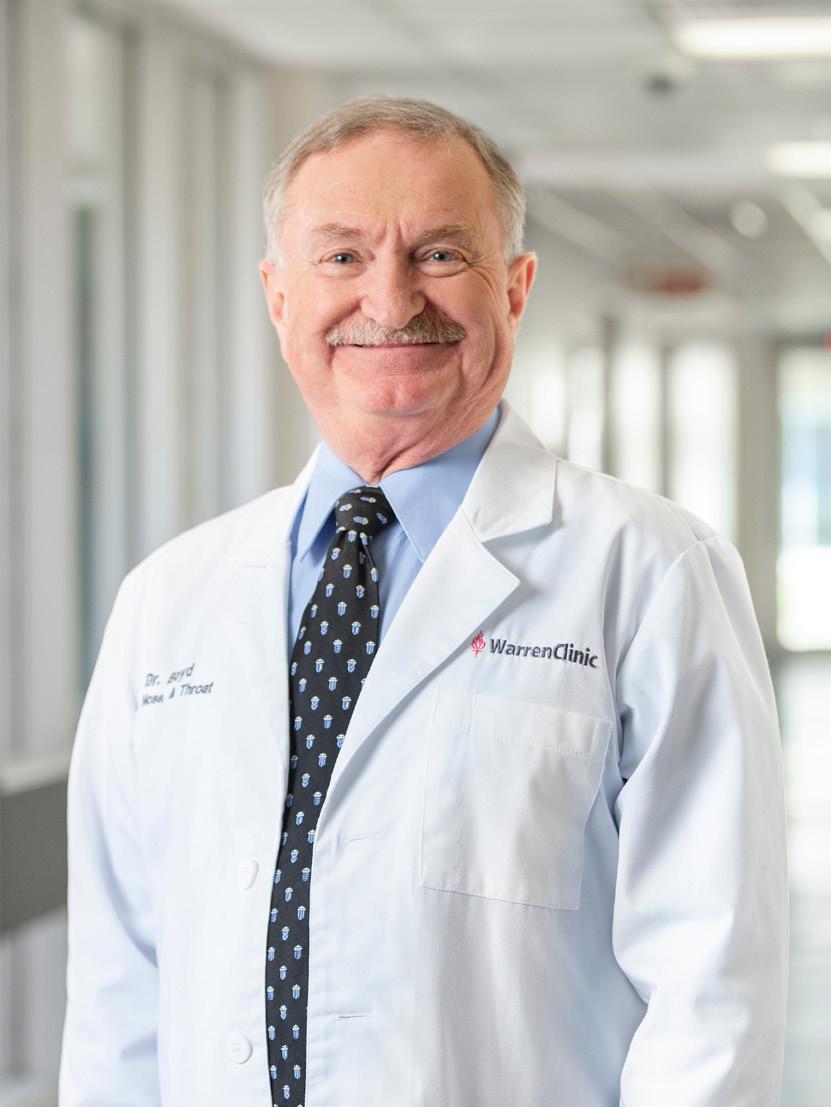




 Mayor Marlon Coleman speaks at the groundbreaking in December 2022.
SAINT FRANCIS HOSPITAL MUSKOGEE
Seen in this artist’s rendering, construction is expected to be complete in 2025.
Mayor Marlon Coleman speaks at the groundbreaking in December 2022.
SAINT FRANCIS HOSPITAL MUSKOGEE
Seen in this artist’s rendering, construction is expected to be complete in 2025.




























 Dr. Naziha Malik talks with her patient who is awake and able to communicate while on ECMO.
Dr. Naziha Malik talks with her patient who is awake and able to communicate while on ECMO.


 Nurses Heather Spears and Sarah Arp meet with Dr. Roger Gallup and Dr. Naziha Malik.
Nurses Heather Spears and Sarah Arp meet with Dr. Roger Gallup and Dr. Naziha Malik.