State of the Delaware Healthcare Workforce Report 2022 ACTION AND OPPORTUNITY





The purpose of this report is to provide an initial census of Delaware’s healthcare workforce contained in the Delaware Division of Professional Regulation (DPR) licensing database known as DELPROS and provide demographic and geographic information not readily available through DELPROS. The report also highlights key public health challenges related to common chronic disease states compiled from Delaware Health Information Network (DHIN) data on insurance claims. Finally, the report provides infor- mation on primary care, dental health, and behavioral health shortage areas as reported from Delaware’s Office of Primary Care and Rural Health.
Based upon June 2022 DELPROS data, this report contains information from the 19 distinct boards and commissions of practice within DPR which provide regulatory oversight of a majority of Delaware’s healthcare workforce personnel and some types of institutional licensing (which is not a focus of this report). These 19 boards and commissions in turn oversee about 200 types of professional and institutional licenses. This report does not contain information on Certified Nursing Assistants and Direct Service Pro- viders as they are not licensed by DPR nor Community Health Workers that are not registered or licensed in Delaware. Information on these professions is beyond the scope of this census data and report at this time.
As of June 2022, there were 63,123 active healthcare licenses in DELPROS. This number includes 3,529 institutional licenses (e.g., pharmacies and funeral establishments). There are also 7,760 additional licenses issued for prescribing controlled substances which are issued to both individuals and facilities. After accounting for institutions and certain duplications, there are 56,469 individual healthcare providers in DELPROS. This count includes: approximately 26,000 nursing licenses; 9,900 medical practice licenses, (e.g., physicians and physician assistants); 2,600 pharmacist licenses; 2,700 social work-related licenses; and 1,700 dentistry licenses (e.g., dentists and dental hygienists). The remaining boards each account for 1,100 or fewer licensees per board and are covered in detail in this report.
Overall, the licensed healthcare workforce in DELPROS is about 43,000 female (74%) and 15,000 male (26%). Gender is not reported for 4,566 licensees either because individuals did not disclose their gender or because the licensing database contains institutions which do not have a gender demographic. Based on year of birth (where individuals born in 1954 – 1955 are deemed by Social Security as age eligible for full Social Security benefits, we find that no less than 4,600 active licensed individuals are of full retirement age.
The purpose of this first report is not to provide recommendations. Rather this report provides the data and quantitative data analysis capacity to answer additional questions for policy makers and to begin to assess resource allocation to address health care workforce needs in our community. We thank the many institutions mentioned in this report, especially DPR, and look forward to further collaboration which will provide additional, robust information for future reports and a website dedicated to ongoing tracking of this critically important data.
Welcome Statements 6-13
Delaware Healthcare Workforce Vital Statistics 14
Boards and Commissions of the Division of Professional Regulation and notes 15
Board of Chiropractic 16-19
Board of Dentistry and Dental Hygiene 20-27
Board of Dietetics / Nutrition 28-33 Board of Funeral Services 34-39
Board of Massage and Bodywork 40-45
Board of Medical Licensure and Discipline Overview 46-53
ACGME Training 52-53
Acupuncture Detoxification Specialists 54-55
Eastern Medicine Practitioner 56-57
Genetic Counselors 58-59
Paramedics 60-61 Physician Assistants 62-63 Physicians – DO 64-65 Physicians – MD 66-67
Respiratory Practitioners 68-69
Acupuncture Practitioners 70-71 Administrative Medical 72-73 Polysomnographers 74-75
Certified Professional Midwife 76-77
Physician Licenses by Association of American Medical Colleges Specialty Overview 78-79 Association of American Medical Colleges Specialty Pathways Taxonomy 80-81
Addiction Medicine 82-83
Allergy and Immunology 84-85
Anesthesiology 86-87
Colon and Rectal Surgery 88-89
Dermatology 90-91 Diagnostic Radiology 92-93 Emergency Medicine 94-95 Family Medicine 96-97 General Surgery 98-99 Hospice and Palliative Care 100-101 Integrated Plastic Surgery 102-103 Integrated Thoracic Surgery 104-105 Integrated Vascular Surgery 106-107 Internal Medicine 108-109
Internal Medicine – Emergency Medicine 110-111 Internal Medicine – Pediatrics 112-113 Medical Genetics and Genomics 114-115
Neurological Surgery 116-117 Neurology 118-119 Nuclear Medicine 120-121 Obstetrics and Gynecology 122-123
Ophthalmology 124-125
Orthopaedic Surgery 126-127
Osteopathic Neuromusculoskeletal Medicine 128-129
Otolaryngology-Head and Neck Surgery 130-131 Pathology 132-133 Pediatric 134-135 Physical Medicine and Rehabilitation 136-137 Plastic Surgery 138-139
Preventive Medicine 140-141 Psychiatry 142-143 Sleep Medicine 144-145
Thoracic Surgery/Thoracic and Cardiac Surgery 146-147 Urology 148-149
Board of Nursing Overview 150-155
Acute Care Nurse Practitioners 156-157
Acute Care Certified Nurse Specialist 158-159
Adult Health Certified Nurse Specialist 160-161
Adult Nurse Practitioners 162-163
Certified Nurse Midwives 164-165
Certified Registered Nurse Anesthetists 166-167
Community Health Nursing Certified Nurse Specialist 168-169
Critical Care Certified Nurse Specialists 170-171
Family Nurse Practitioners 172-173
Board of Nursing, Continued
Gerontology Certified Nurse Specialists 174-175
Gerontology Nurse Practitioners 176-177
Health Promotion & Wellness Certified Nurse Specialists 178-179
Licensed Practical Nurse 180-181
Maternal Child Certified Nurse Specialists 182-183
Medical/Surgical Certified Nurse Specialists 184-185
Neonatal Nurse Practitioners 186-187
Oncology Certified Nurse Specialists 188-189
Pediatric Certified Nurse Specialists 190-191
Pediatric Nurse Practitioners 192-193
Perinatal Nurse Practitioners 194-195
Psych/Mental Health Certified Nurse Specialists 196-197
Psych/Mental Health Nurse Practitioners 198-199
Registered Nurses 200-201
Temporary Permit Registered Nurse 202-203
Women’s Health/Gender-Related Certified Nurse Specialist 204-205
Women’s Health/Gender-Related Nurse Practitioner 206-207
Adult/Gerontology Nurse Practitioners 208-209
Neonatal Certified Nurse Specialists 210-211
Adult/Gerontology Certified Nurse Specialists 212-213
Temporary Permit Graduate Nursing 214-215
BoardofNursingHomeAdministrators 216-219
BoardofOccupationalTherapyPractice 220-225
BoardofExaminersinOptometry 226-229
BoardofPharmacy 230-233
BoardofPhysicalTherapistsandAthleticTrainers 234-241
BoardofPodiatry 242-245
BoardofMentalHealthandChemicalDependencyProfessionals 246-261
BoardofExaminersofPsychologists 262-267
BoardofSocialWorkExaminers 268-275
BoardofSpeechPathologists,Audiologists,andHearingAidDispesers 276-287
BoardofVeterinaryMedicine 288-293
ControlledSubstanceAdvisoryCommittee 294-297
LongTermCareandSkilledNursingFacilities 298-304
PageLeftIntentionallyBlank 305
CompositionofIdealMedical CareTeam 306-310
Considerations forPatientPanelSize 311-315
ScopeandSpecializationinDentalCare 316
CompositionofanIdealDentalTeam 317-319
Delaware Primary Care Office 320-321
ExtraordinaryImpactsontheHealthcareWorkforce:COVID-19andAging 322-326
REPRINT:AddressingHealthDisparitiesinDelawarebyDiversifyingtheNextGenerationofDelaware’sPhysicians 327-329
Physician and Dentist Basic Demographics: Race and Ethnicity 330 Physician Statistics based on Allopathic (M.D.) and Osteopathic (D.O.) Education 331 Physician and Dentist Basic Demographics Age 332-333 Chronic Disease Management and the Healthcare Workforce 334-335 New Castle County Demographics 336-337
Kent County Demographics 338-339
Sussex County Demographics 340-341
Alzheimer’s and Dementia Data 342
Arthritis and Deteriorative Bone Disease Data 343-344 Cancer Data - Breast, Colorectal, Endometrial, Lung, and Prostate 345-346
Cardiovascular Disease Data - Acute Myocardial Infarction, Atrial Fibrillation, Heart Failure, Ishemic Heart Disease 347-349 Depression and Suicide Data 350
Diabetes Data 351
Endocrine Disease and Disorders Data 352
Systemic Illness Data - Anemia, Hyperlipidemia, Hypertension 353-354 Neurologic Disorders and Injury (Including Stroke) Data 355
Renal Disease Data 356
Respiratory Disease Data 357-358
Male Urology - Benign Prostatic Hyperplasia and Prostate Cancer 359 Vision Data - Cataract and Glaucoma 360 Appendices including Facility Maps 361
Methodology 362-363 Residency and Fellows as a Part of the Healthcare Workforce 364 Delaware Institutions Who Have OR Host Residents in Their Facilities 365 National and Delaware Fellowship Programs 366-367
Nursing Career Path 368-369
DELPROS License Types and Counts 370
Abbreviations 371
Select Facilities – Adult Day Care 372-373
Select Facilities – Dialysis 374-375
Select Facilities – Free-Standing Birthing Center 376-377
Select Facilities – Free Standing Surgical Care 378-379
Select Facilities – Home Healthcare Agencies 380-381
Select Facilities – Home Healthcare, Skilled 382-383
Select Facilities – Hospice 384-385
Select Facilities – Hospitals 386-38
Select Facilities – Personal Assistant Staffing Agencies 388-389
Select Facilities – Prescribed Pediatric Extended Care 390-391
Out of every crisis is borne an opportunity for change. Think back to the natural disasters, human conflicts and tragedies, and economic crises that have befallen our country. Each time, when the after-action report is written, an elected body examines the response, or the business community embraces reforms, we benefit as a society from the lessons learned. The COVID-19 pandemic is no different.
During the past two-and-a-half years, we have seen healthcare providers in our state stretched beyond their limits, dealing not only with the impacts brought on by a new and deadly respiratory virus, but also forced to embrace new ways of managing the chronic and acute conditions of their patients, unrelated to COVID-19. We know that this massive disruption to our healthcare system – and to the health of Delawareans – has taken a tremendous toll on our healthcare workforce, with many providers deciding to retire or leave the profession entirely.
And yet, we also are experiencing the opportunity. During the worst of the pandemic, providers across our state embraced telehealth as a way to see their patients for routine medical exams, to diagnose injuries or illnesses, or to continue regular psychiatric sessions. Regulators changed the rules, allowing insurers to reimburse for these services. The federal and state government provided funding to help advance providers’ transition to telehealth services. Patients no longer had to wait in reception areas or exam rooms when they didn’t feel well, because now their provider would call them back – in the comfort of their own home – when they were ready to see them virtually It all worked because the situation required it.
With the existing shortage of primary care providers exacerbated by the pandemic, patients, providers, employers and insurers all had to adapt to changes in primary care Often, primary care was delivered by nurse practitioners and physician assistants practicing at the top of their license
As practices and clinics evolve, we are likely to see this broadening of primary care and the use of telehealth increase. The state is investing in primary care practices, promoting person-centered care and advancing equity, and has embraced the new State Loan Repayment Program, all while continuing to support the Delaware Institute for Medical Education and Research (DIMER) to help grow the next generation of primary care providers We will continue to work with the General Assembly, healthcare providers, insurers and consumers to embrace additional changes that improve the patient and provider experience, improve overall health and help lower costs.
I am grateful to all of the Delaware stakeholders that are leaning into the workforce issue to help determine the best paths forward In this context, I especially want to thank the Academy of Medicine/the Delaware Public Health Association, the Health Workforce Subcommittee of the Delaware Healthcare Commission, the Delaware Health Sciences Alliance, and the Delaware Journal of Public Health for shining a light on the specific recommendations for Delaware’s workforce outlined in this report.
I look forward to joining stakeholders across our state in examining the recommendations in more detail, exploring the potential benefits, deter mining the policy changes that are needed, and embracing those changes that will have the most positive impact for the future of the healthcare system in our state – and the future health of Delawareans
Magarik, MS Secretary, Delaware Department of Health and Social ServicesIn 2019, the healthcare workforce was 22 million individuals strong. This sector was one of the largest and fastest-growing in the United States, accounting for 14% of all civilian, employed workers in the U.S. The majority worked in hospital settings—about 7 million healthcare workers to be exact. Another 4 million were in outpatient and physician offices, and 3.5 million were in Skilled Nursing Facilities and Home Care settings. All in all, the healthcare workforce was large, growing, and there was a steady amount of jobs that were open, making it a very employable sector overall
Then, the COVID-19 pandemic emerged As we now know, its impact on healthcare cannot be understated It changed care delivery and clearly demonstrated the need for sufficiently-sized and well-trained public health, healthcare, and health support workforces. Easy-entry, easy-exit occupations - the lowest-wage earners in healthcare - were the same groups whose employment was the most adversely impacted by COVID In 2020 alone, total injury and illness cases decreased or remained the same in all sectors except for healthcare, which saw a 4,000% increase in employer-reported respiratory illness.
The pandemic forced states to innovate to meet the needs of their populations, and at the center of that response was the workforce A number of strategies were implemented in response Many focused on creating state-level regulatory flexibilities, and engaging the public health workforce. Some states modified scope of practice r ules for health professionals, allowing for more autonomous practice. Others allowed health professionals licensed in other states to practice in their state Additionally, laws and regulations were changed to support greater use of telemedicine As our nation entered the 3rd year of the pandemic, issues surrounding health workforce capacity, resilience, training, education, and scope of practice have become front and center to moving forward from this phase of our history While the full impact on our health workforce will not be known for some time, a number of the resulting changes are likely to be long lasting
Despite the effects of the pandemic, there are several large, persistent policy issues that existed in 2019 and are still present today. These include: sufficiency of the workforce, mal-distribution, quality of healthcare training, and barriers to accessing ser vices. Additionally, there are population factors that have far reaching ramifications for our nation, impacting more than just the health workforce and employment in this sector First and foremost is the aging of our population. The current cohort of individuals ages 65 and older will continue to generate the majority of demand for healthcare and health support ser vices, and we will need a workforce of sufficient size and distribution to meet this demand However, this is juxtaposed against the fact that the U S birth rate has fallen by 20% since 2007, due to overall lower childbearing rates of current generations. Our population has shown zero growth for several years now, primarily because deaths (attributed to the aging population) exceed births (due to people not having children). Of course, these are issues affecting more than just healthcare in the U S
In a nutshell, the health workforce is in flux We are still understanding the impacts of the pandemic, while having to address previously existing problems. We know that addressing shortages and mal-distributions, continuing to try to improve access to services and train individuals in a way that improves the quality of patient and population outcomes needs to happen But we must also harness the power of this moment to address pandemic-exacerbated issues like burnout and equity in the workforce.
While it may seem like chaos, there is opportunity in times like this. Despite a low birthrate, demand from our aging population and the after-effects of the pandemic will cause employment in healthcare to grow faster than for other industries. This still allows for great opportunity to tackle the persistent policy issues, and if we follow the data, to craft a better health workforce for the future.
Michelle M Washko, PhD DirectorNational Center for Health Workforce Analysis Health Resources and Services Administration
As co-chairs of the Workforce Subcommittee of the Delaware Healthcare Commission, we are pleased to welcome you to the first “State of the Healthcare Workforce in Delaware: Action and Opportunity” Report. This report focuses on select components of the healthcare workforce, including primary care, dentistry, behavioral health, and others. It seeks a broader view of the entire healthcare sector, composed of physicians, dentists, nurses, physician assistants, the allied therapies, dental hygienists, and a vast ecosystem of providers.
We acknowledge and appreciate the work of others in this space. Work on this initiative was started by the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA) and the Delaware Health Sciences Alliance (DHSA) long before the COVID-19 pandemic changed our world, and the landscape of healthcare. As the reader knows, the pandemic directly and profoundly impacted both healthcare systems and individual providers.
Before the pandemic, there were tectonic workforce and demographic challenges facing almost every major industry in our State and our nation: the aging of our population, the related increase in the incidence and burden of chronic disease, and the concurrent aging of the healthcare workforce. And the financial impact is clear: the healthcare industry is rapidly approaching one-fifth of the United States Gross Domestic Product (GDP).
The contents of this report are based upon an unprecedented collaboration between multiple components of State government including the Delaware Healthcare Commission, the Division of Professional Regulation, the Delaware Institute for Medical Education and Research (DIMER), the Division of Public Health Primary Care Office, and the Departments of Finance and Labor. They are joined by the Academy/DPHA, DHSA, and the Delaware Health Information Network, and many other organizations playing essential smaller roles. This public-private partnership has gathered data on the healthcare workforce and analyzed the needs—both current and future—of the State of Delaware. The strategies within this report are based on hard data and analysis and recommend support for polices that will strengthen the healthcare workforce for years to come.
During the past two-years of the COVID-19 pandemic, we have experienced stress and crisis. We now have an extraordinary, federally-funded opportunity to take meaningful action to address the opportunities in our healthcare sector for employment throughout the workforce, as well as novel models (including telehealth and nurse-led health clinics) leading the way.
J. Geisenberger Nicholas A. Moriello, R.H.U.On behalf of the board and advisory council of the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA), we are pleased to be the lead institution in the public/private partnership named Delaware Health Force and the author of this report, which includes content from other experts in the field.
The Academy/DPHA started this initiative in early 2019, long before the COVID-19 Pandemic swept around the world and across our State. In the beginning, this effort focused on the State of Delaware’s DIMER (Delaware Institute for Medical Education and Research) program and its graduates for the 50th Anniversary Report of the program. As data was collected and analyzed, we realized we were pursing an important vein of data which, if related to other information, could supply policy makers and resource allocation alike.
We are informed by the Social Determinants of Health - in particular healthcare access and equity, components of the SDoH often overlooked due to their perceived, relatively minor role in health outcomes. Many scholarly articles have been written citing healthcare as only being responsible for 10-20% of health outcomes, however if an individual or community is medically underserved or has acute shortages of a variety of healthcare facilities, that 10% can become the single largest barrier to care for those who seek or need it.
We are also informed by the reality that the healthcare landscape is a complex one, and that simply looking at the physician component of the workforce, or the anchor institutions (hospitals) providing care, is not enough to truly understand the nature of opportunity for workforce enhancement. Today’s healthcare is a series of interlocking systems of care, and the better those connections, the strong the fabric of the safety net of care for our fellow Delawareans.
Several methodologies were considered before we settled on the approach used to generate this report. Some of those methodologies are used to great success by other researchers analyzing specific parts of the healthcare landscape, for instance, voluntary surveys. This report does not replace the high value of that research. Instead, it expands upon that research with additional data and analysis.
In a later section of this report our methodology is articulated in depth. For now, we extend sincere thanks to our institutional and individual partners: Delaware Division of Professional Regulation and Division Director, Geoff Christ; Delaware Health Information Network and executive director, Jan Lee, MD and staff; Agile Cloud Consulting and President and CEO, Sharif Shaalan and staff; TechImpact and Delaware Innovation Lab Director of Strategy and Operations, Ryan Harrington, and Director, Research Development & Analytics Data Lab, Héc Maldonado-Reis, and staff; Delaware Nurses Association Executive Director, Chris Otto; and the team at the Academy/DPHA including Kate Smith, MD, MPH; Matt McNeill, BS; Nicole Sabine, BS; and Caroline Harrington, M.S. and members of the board of directors.
S. John Swanson, MD President of the Board of Directors Timothy E. Gibbs, MPH Executive DirectorThe Delaware Health Sciences Alliance (DHSA) was established in 2009 with founding partners ChristianaCare, Nemours Children's Health, Thomas Jefferson University, and the University of Delaware. Since then, additional partners have joined including the Philadelphia College of Osteopathic Medicine, Bayhealth Medical Center, and the Delaware Academy of Medicine / Delaware Public Health Association.
The alliance enables partner organizations to collaborate and conduct cutting-edge research, to improve the health of Delawareans through access to services in the state and region, and to educate the next generation of healthcare professionals.
The DHSA’s unique, broad-based partnership focuses on establishing innovative collaborations among experts in medical education and practice, health economics and policy, population sciences, public health, and biomedical sciences and engineering.
This report, and the work behind it, is an example of the fruits of collaboration. In this case, through our partnership with the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA). In addition, the original work conducted by DHSA and the Academy/DPHA which was the basis for the DIMER 50th Anniversary Report and subsequent annual reports, continues in this report as reflected in key data as well as the recommendations section.
As mentioned elsewhere in this report, Delaware Health Source is comprised of four programmatic components; the core data and research initiative upon which this report is based, the expansion of Delaware Mini Medical School, the expansion of Student Financial Aid for Delawareans, and the expansion of key graduate education and fellowship programs. The DHSA is pleased to support all these programs, in particular those who directly address the pipeline of Delawareans pursuing a career in the health sciences generally, and in medicine and dentistry in particular.
Omar A. Khan, MD, MHS President and CEO Pamela Gardener Program ManagerThe mission of the Division of Professional Regulation (DPR) is to ensure protection of the public’s health, safety, and welfare. Our services benefit the citizens of Delaware, professional licensees, license applicants, other state and national agencies, and private organizations.
DPR provides regulatory oversight for 34 boards/commissions comprised of Governor-appointed public and professional members. Oversight activities include administrative, investigative, and fiscal support for 54 professions, trades and events with over 200 types of licenses and permits. License fees fund DPR and the expenditures related to each licensing board.
The following types of healthcare, and healthcare related services, are overseen by DPR:
- Acupuncture - Acupuncture Detoxification - Art Therapy - Athletic Trainers - Audiology - Chemical Dependency Professionals - Chiropractic - Controlled Substances - Counselors of Mental Health - Dental - Dietitians - Eastern Medicine - Genetic Counselors - Hearing Aid Dispensers - Marriage and Family Therapy - Massage and Bodywork - Medical Practice - Mental Health - Midwife (non-Nursing)
- Nursing - Nursing Home Administrators - Nutritionist - Occupational Therapy - Optometry - Paramedic - Pharmacy - Physical Therapy - Physician - Physician Assistant - Podiatry - Polysomnographer - Psychology - Respiratory Care - Social Workers - Speech Pathology - Tamper-Resistant Prescriptions - Veterinary Medicine
The Division is pleased to collaborate on this important initiative through the sharing of publicly available information. The Division looks forward to the findings that result from the information it shares through collaboration.
Geoffry Christ, RPh, J.D. DirectorThe Delaware Nurses Association (DNA) was established in 1911 in Claymont, DE and has served to advance the profession of nursing and our collective mission to improve the health of all Delawareans. We are the only professional association in Delaware representing all Licensed Practical Nurses, Registered Nurses, and Advanced Practice Registered Nurses We continue to advance health through the art and science of nursing supported by diverse members, advocacy, professional development, generation of new knowledge, effective communication, and community service.
In addition to our robust and inclusive membership , we also facilitate an organizational affiliate program . This program brings together state specialty nursing associations and health - related associations with nursing representation together The goal of the organizational affiliate program is to strengthen nursing ’ s and healthcare advocate’s voices in the reformation of healthcare delivery in Delaware.
In addition to sharing physical space, DNA has a long history of collaboration with the Delaware Academy of Medicine/Delaware Public Health Association (Academy/DPHA). This includes interprofessional education, removing scope of practice barriers and advancing public health Both organizations continue to partner with new endeavors. For example, the design and launch of Healthy Nurse Healthy Delaware, a program spearheaded by DNA to sup- port Delaware nurses’ mental health and overall wellbeing.
The DNA is proud to partner with the Academy/DPHA on Delaware Health Force and further inform efforts to grow, strengthen and advance Delaware ’ s healthcare workforce At DNA, we appreciate the importance of robust data and transparent reporting to further inform efforts that will support Delaware ’ s healthcare workforce and access to high-quality, equitable, affordable and convenient healthcare services for all Delawareans.
Christopher E. Otto, MSN, RN, CHFN, PCCN, CCRN Executive DirectorDelaware Nurses Association
The Society is one of the oldest institutions of its kind in the United States and rich in history. It was founded in 1776 and incorporated on February 3, 1789, only 12 days after President Washington took his oath of office. The first official meeting of the Society was held in Dover on May 12, 1789.
Today, the Apollo Youth in Medicine program provides opportunities for high school students who are interested in a physician career path to shadow practicing physicians and further pursue their interests in the medical profession. Please find below a summary for the Apollo Youth in Medicine Program, and the program logo attached.
With the support of The Medical Society of Delaware (MSD) and Delaware Youth Leadership Network (DYLN), the Apollo: Youth in Medicine program was founded by Sean Holly and Arjan Kahlon in the summer of 2018 with John Kepley joining the leadership team shortly after. Since then, the Apollo leadership team has grown to be led by several focused & resourceful students who are firmly supported by MSD and DYLN.
Together this team supports and coordinates opportunities and activities for Apollo students and their high schools with participating Apollo Physician Mentors.
Apollo was founded on the idea that high school students interested in the medical field need an outlet to connect them to opportunities present in the medical community, and that clinical shadowing provides valuable first-hand insight allowing exploration. Apollo has expanded its physician network to allow students across Delaware expansive access to shadowing in 17 medical disciplines.
The Apollo Program is Multistep
1.) Interested Delaware high school juniors and seniors are invited to apply every fall through our application.
2.) New students representing multiple Delaware high schools attend a fall education session that covers specific topics such as different specialties in medicine, and the academic pathway to becoming a doctor. Here, Students receive HIPAA training through Apollo, enabling them to shadow in physicians’ offices appropriately.
3.) Apollo gives students access to several shadowing slots offered by dozens of Delaware physicians across various specialties through ‘The Match’, which occurs multiple times per year. Students can choose as many or as few shadow slots as they’d like.
4.) In addition to shadowing opportunities, Apollo serves as a liaison to gain our students optional access to medical seminars and exclusive Apollo Enhanced Experiences.
Additional information can be found at their website, https://www.apolloprogram.org/.
Mark B. Thompson, MHSA Executive Director Medical Society of DelawareThis section’s data contains this vital statistics as collected in the DELPROS system. It is important to note that it does NOT cover the entire healthcare workforce, some of which is not licensed through this system, and others who are not directly licensed by any entity at this time. For instance, Certified Nursing Assistants (CNAs) are not licensed by DELPROS, nor are Community Health Workers (CHWs) or Direct Service Providers (DSPs).
Some types of facilities are licensed through DELPROS, while others are licensed through the Department of Health and Social Services Office Division of Healthcare Quality, Office of Health Facilities Licensing and Certification. We credit that office for providing a significant portion of facilities data found in this report.
The following is entirely based on the data contained within the DELPROS system, and therefore we make no claims to its accuracy or completeness except where noted. For instance, DELPROS does ask about gender when an individual registers, however it is not a required field, and therefore most sections will show a percent of persons who did not state their gender. DELPROS itself does not collect information regarding race and ethnicity - therefore this report does not contain that information. DELPROS does ask for date of birth, and we were supplied with year of birth only so provide a level of privacy to the licensees of the State licensing system. DELPROS does not collect information on languages spoken, therefore we do not report on that information. That said, race, ethnicity, languages spoken, and a variety of other characteristics of the healthcare workforce ARE essential data points to be considered in future reports as that information is collected.
The section is alphabetical by Division of Professional Regulation board name, which is then followed by information from the Office of Health Facilities Licensing and Certification. All information and tables contained in the following section is based on data from June 2022. Each section starts with objective of the Board which oversees a given area of licenses. Sometimes, but not always, this is followed by additional detail on the types of licensure granted under that board.
There will be a chart on active licenses; gender; year of birth and related conjecture one when individuals of a certain age may retire; and facing pages with numerical and visual distributions of providers by ZIP code. We use the primary license application ZIP code as the best available proxy for approximate location within Delaware, and acknowledge that a margin of error is inherent in this method. There are also a small number of providers who provided a ZIP code outside of the State of Delaware, which further compounds the absolute accuracy of our methodology.
Most of this report focuses on the healthcare workforce overseen by the following boards.
• Board of Chiropractic
• Board of Dentistry and Dental Hygiene
• Board of Dietetics/Nutrition
• Board of Funeral Services
• Board of Massage and Bodywork
• Board of Medical Licensure and Discipline
• Board of Nursing
• Board of Examiners of Nursing Home Administrators
• Board of Occupational Therapy Practice
• Board of Examiners in Optometry
• Board of Pharmacy
• Board of Physical Therapists and Athletic Trainers
• Board of Podiatry
• Board of Mental Health and Chemical Dependency Professionals
• Board of Examiners of Psychologists
• Board of Social Work Examiners
• Board of Speech Pathologists, Audiologists, and Hearing Aid Dispensers
• Board of Veterinary Medicine
• Controlled Substance Advisory Committee
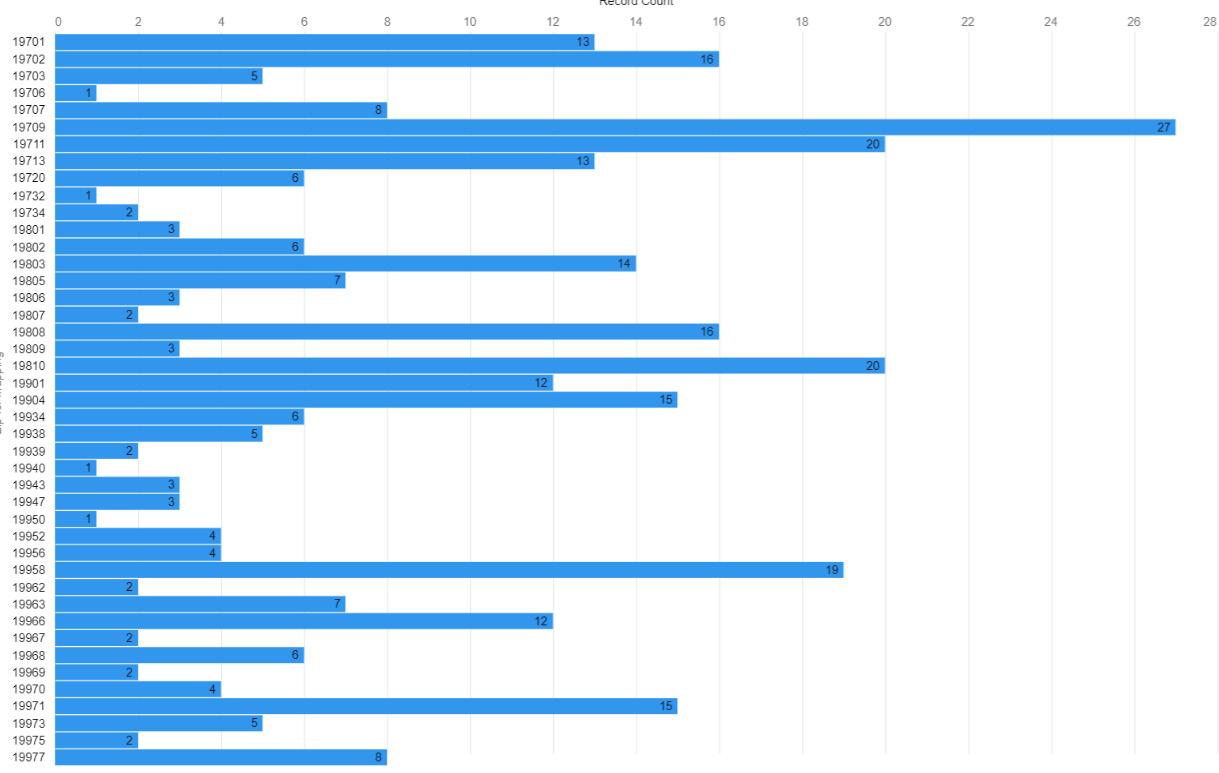
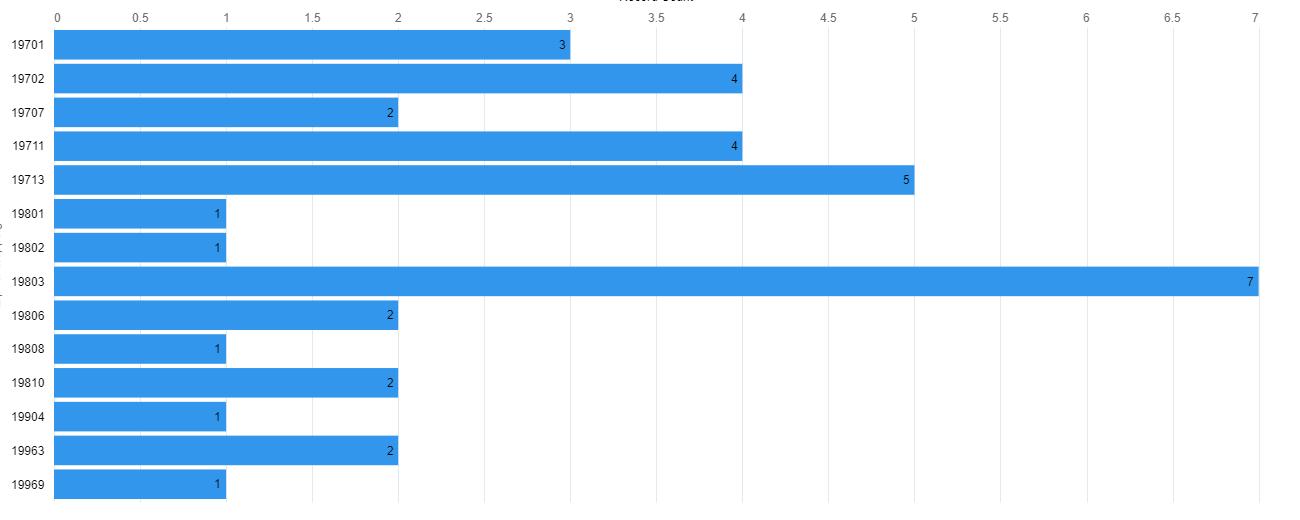
From page 16 to 271 we use charts created in Salesforce and maps created in ArcGIS. Please read the following so that you understand why they are configured as they are, and how to interpret them.
For the charts, to save space – a premium for many charts dense with information – we removed secondary labeling on the y-axis. For instance, on charts with ZIP codes, we removed the secondary label stating “ZIP code.” In doing so we freed up significant space to make some charts larger and more legible. The x-axis on all charts is always the number of licensed individuals or entities.
The bars on the charts are proportional to the number they represent, and therefore to each other. The Workforce Subcommittee Chairs and report writers reviewed a number of options for the maps used to represent where types of licensed individuals and facilities are located. By consensus we arrived at the decision to use a non-weighted heatmap.
The heatmaps are an exact representation of the data provided on the facing page. The maps are also subdivided by ZIP codes rather than census tracts to broaden they accessibility to a wide audience who many not be as familiar with census tract information. Counties are demarcated by different background colors. In all cases maps only look at the ZIP code level except later in the facilities section of the report. The location of the center of any ZIP code is solely determined by ArcGIS defaults, and in no manner implies actual location of any one (or more) individuals or facilities.
The size of the area representing licenses has no relation to the number of licenses or to their “reach” in that area. They only bring attention to the map and areas with, or without, licensed individuals or institutions. To restate, these maps are presented to give a sense, based on the primary ZIP code listed for each DELPROS license, of where licensed individuals and institutions are physically located.
IMPORTANT: ZIP codes are a proxy for provider or institution location and should not be considered definitive. For instance, while an institution can have one license per location, a provider (and especially physicians and nurses) may have multiple locations associated with their license. This was a limitation of the data provided for this first report which we hope to address in future reports as we become more granular in licensing information.
The primary objective of the Delaware Board of Chiropractic is to protect the public from unsafe chiropractic practice and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board:
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to chiropractic practitioners and approves preceptors.
The Board’s statutory authority is in 24 Del. C., Chapter 7.
Chiropractors focus on patients’ overall health. Chiropractors believe that malfunctioning spinal joints and other somatic tissues interfere with a person’s neuromuscular system and can result in poor health.
Some chiropractors use procedures such as massage therapy, rehabilitative exercise, and ultrasound in addition to spinal adjustments and manipulation. They also may apply supports, such as braces or shoe inserts, to treat patients and relieve pain.1
Figure 1
Active Chiropractic Licenses, N= 383
Figure 2
Active Chiropractic Licenses by Gender (when reported)

Note. An active license does not guarantee an individual is actively seeing patients.


Note. 18 individuals did not provide a year of birth
38 individuals are at full retirement age of 67 in 2022
age
per Social Security
Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















The primary objective of the Delaware Board of Dentistry and Dental Hygiene is to protect the general public from unsafe and unprofessional practices. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to dentists, dentist academics, dental hygienists and dental residents. The Board also issues three types of permits to dentists and dentist academics who administer anesthesia.
The Board’s statutory authority is in 24 Del. C., Chapter 11.
The dental profession is the branch of healthcare devoted to maintaining the health of the teeth, gums and other tissues in and around the mouth.
A dentist is a doctor, scientist and clinician dedicated to the highest standards of health through prevention, diagnosis and treatment of oral diseases and conditions.
Dentists play a key role in the early detection of oral cancer and other systemic conditions of the body that manifest themselves in the mouth. They often identify other health conditions, illnesses, and other problems that sometimes show up in the oral cavity before they are identified in other parts of the body.
• Evaluates the overall health of their patients while advising them about oral health and disease prevention;
• Performs clinical procedures, such as exams, fillings, crowns, implants, extractions and corrective surgeries;
• Identifies, diagnoses and treats oral conditions; and
• Performs general dentistry or practices in one of nine dental specialties.
• Advances in dental research, including genetic engineering, the discovery of links between oral and systemic diseases, the development of salivary diagnostics and the continued development of new materials and techniques, make dentistry an exciting, challenging and rewarding profession.
Dental hygienists are preventive oral health professionals who have graduated from an accredited dental hygiene program in an institution of higher education, licensed in dental hygiene to provide educational, clinical, research, administrative and therapeutic services supporting total health through the promotion of optimum oral health.
In performing the dental hygiene process of care, the dental hygienist assesses the patient’s oral tissues and overall health determining the presence or absence of disease, other abnormalities and disease risks; develops a dental hygiene diagnosis based on clinical findings; formulates evidence-based, patient-centered treatment care plans; performs the clinical procedures outlined in the treatment care plan; educates patients regarding oral hygiene and preventive oral care; and evaluates the outcomes of educational strategies and clinical procedures provided.
Dental hygienists are preventive oral health professionals who have graduated from an accredited dental hygiene program in an institution of higher education, licensed in dental hygiene to provide educational, clinical, research, administrative and therapeutic services supporting total health through the promotion of optimum oral health.
In performing the dental hygiene process of care, the dental hygienist assesses the patient’s oral tissues and overall health determining the presence or absence of disease, other abnormalities and disease risks; develops a dental hygiene diagnosis based on clinical findings; formulates evidence-based, patient-centered treatment care plans; performs the clinical procedures outlined in the treatment care plan; educates patients regarding oral hygiene and preventive oral care; and evaluates the outcomes of educational strategies and clinical procedures provided.
Dental hygienists provide clinical services in a variety of settings such as private dental practice, community health settings, nursing homes, hospitals, prisons, schools, faculty practice clinics, state and federal government facilities and Indian reservations.
In addition to clinical practice, there are career opportunities in education, research, sales and marketing, public
health, administration and government. Some hygienists combine positions in different settings and career paths for professional variety. Working in education and clinical practice is an example.
A Delaware Dentist Academic license is given to practioners who are full-time directors, chairpersons, or attending faculty members of a hospital-based dental, oral and maxillofacial surgery or other dental specialty residency program. The program must be:
• based in Delaware, and
• accredited by the Commission on Dental Accreditation of the American Dental Association (CODA) for the purposes of teaching, has received initial CODA accreditation or is in the process of establishing CODA accreditation
The academic license allows a practitioner to practice dentistry or oral and maxillofacial surgery only in the institution designated on the license and only on patients in an academic setting for teaching purposes.
What are Restricted Permits ?
Restricted Permit I
A Restricted Permit I allows a practitioner to induce only conscious sedation by parenteral, enteral, or rectal routes, as well as nitrous oxide inhalation, at a specific location. (This does not prohibit the usual and customary preoperative oral sedation.)
A Restricted Permit I does not allow induction using:
• deep sedation
• general anesthesia
Restricted Permit II
A Restricted Permit II allows induction of conscious sedation by nitrous oxide inhalation.
It does not allow:
• deep sedation
• general anesthesia
Unrestricted Permit
An Unrestricted Permit applies only to one office location where anesthesia is administered. The two types of Unrestricted Permits are Individual and Facility. The type of permit selected determines who is allowed to administer anesthesia at that location:
An Unrestricted Permit-Individual allows the dentist to administer conscious sedation, general anesthesia and deep sedation, as defined by the Board’s Rules and Regulations governing anesthesia, at the location. If a certified registered nurse anesthetist (CRNA) is employed for deep sedation or general anesthesia at an office location, the facility must also have at least one individual with an Unrestricted Permit-Individual.
This type of dental licensure is specific to dentists contracted to practice at a Federally Qualified Health Center (FQHC) in Delaware. The Dentist-FQHC Provisional license allows the practice of dentistry in Delaware…
• before the three examinations required for full Dentist licensure have been passed,
• only at the FQHC named on the license, and
• only under the general supervision of a Delaware-licensed dentist.
A Dental Resident is a license for dentists who will be starting a residency program in Delaware.
Figure 6
Active Dental Licenses by Type*, N=1,740

Note. An active license does not guarantee an individual is actively seeing patients.
Figure 7
Active Dental Licenses by Gender, all types (when reported)


80 individuals are at full retirement age of 67 in 2022.
Full retirement age as per Social Security Adminstration*
Note. Three individuals did not provide a year of birth
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















The primary objective of the Delaware Board of Dietetics/Nutrition is to protect the health of the public by broadening access to appropriate dietetic and nutrition therapy. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• evaluates the credentials of persons applying for licensure, • promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to dietitian/nutritionists.
The Board’s statutory authority is in 24 Del. C., Chapter 38
What is the difference between a dietician and a nutritionist?
Although dietitians and nutritionists both help people find the best diets and foods to meet their health needs, they have different qualifications.
In the United States, dietitians are certified to treat clinical conditions, whereas nutritionists are not always certified. In the U.S., dietitians must receive certification from the Academy of Nutrition and Dietetics in order to practice. Dietitians can treat specific health conditions, such as eating disorders, by providing food recommendations.
Some organizations also certify nutritionists, such as the Board for Certification of Nutrition Specialists (BCNS), however, nutritionist training can vary. Some states do not require certification, so it is possible for anyone in those states to offer nutrition advice.
Nutritionists may also have different areas of focus to dietitians. For example, nutritionists can pursue advanced qualifications in specific health areas, such as sports nutrition, digestive disorders, and autoimmune conditions. The BCNS also offer Certified Ketogenic Nutrition Specialist qualifications for those who want to understand the keto diet in more detail.
However, some nutritionists provide more general advice on healthful eating, weight loss, and reducing tiredness.1
Nutrition is a key element of good health. Registered dietitian nutritionists are the experts on good nutrition and the food choices that can make us healthy, whether it’s a proper diet or eating to manage the symptoms of a disease or chronic condition. Registered dietitian nutritionists design nutrition programs to protect health, prevent allergic reactions and alleviate the symptoms of many types of disease.
Clinical dietitians provide medical nutrition therapy for patients in institutions such as hospitals and nursing care facilities. They assess patients’ nutritional needs, develop and implement nutrition programs and evaluate and report the results. They confer with doctors and other healthcare professionals in order to coordinate medical and dietary needs. Some clinical dietitians specialize in the management of overweight and critically ill patients, such as those with renal (kidney) disease and diabetes. In addition, clinical dietitians in nursing care facilities, small hospitals, or correctional facilities may manage the food service department.
Community dietitians develop nutrition programs designed to prevent disease and promote health, targeting particular groups of people. Dietitians in this practice area may work in settings such as public health clinics, fitness centers, corporate wellness programs or home health agencies.
Corporate dietitians work in food manufacturing, advertising and marketing. In these areas, dietitians analyze foods, prepare literature for distribution, or report on issues such as the nutritional content of recipes, dietary fiber or vitamin supplements.
Management dietitians oversee large-scale meal planning and preparation in healthcare facilities, company cafeterias, prisons and schools. They hire, train and direct other dietitians and food service workers; budget for and purchase food, equipment, and supplies; enforce sanitary and safety regulations; and prepare records and reports.
Consultant dietitians work under contract with healthcare facilities or in their own private practice. They perform nutrition assessments for their clients and advise them about diet-related concerns, such as weight loss or cholesterol reduction. Some work for wellness programs, sports teams, supermarkets and other nutrition-related businesses. They consult with food service managers, providing expertise in sanitation, safety procedures, menu development, budgeting and planning.2
1. Medical News Today. (2020, Aug). What is the difference between nutritionists and dietitians? Retrieved from https://www.medicalnewstoday.com/ articles/nutritionist-vs-dietician#training
2. Explore Healthcareers. (n.d.). Dietitian nutritionist. Retrieved from: https://explorehealthcareers.org/career/nutrition-dietetics/dietitian-nutritionist/
Figure 13
Active Dietician Licenses*, N=483
* an active license does not guarantee an individual is actively seeing patients.
Figure 14
Active Dietician Licenses by Gender (when reported)



22 individuals are at full retirement age of 67 in 2022.
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















The primary objective of the Delaware Board of Funeral Services is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to funeral directors, interns, funeral establishments and crematory establishments. It also issues funeral director limited licenses to Maryland- or Pennsylvania-licensed funeral directors.
The Board’s statutory authority is in 24 Del. C., Chapter 31.
The Board of Funeral Services licenses both individuals and facilities which is somewhat different from many other board of the Division of Professional Regulation. Information on facilities is contained in the facilities section of this report.
All applicants, with the exception of the applicants who meet the experience requirement below to apply by reciprocity, must apply for a Funeral Resident Intern license and serve a one-year internship in Delaware, with the intention of later applying for Delaware licensure as a Funeral Director. A Delaware resident internship is required if a practitioner:
• does not hold a current Funeral Director license in any jurisdiction (state, U.S. territory or District of Columbia)
• holds a current Funeral Director license in another jurisdiction but has not practiced as a funeral director at least three of the past five years.
If a current Funeral Director license is current in another jurisdiction and an individual has practiced as a funeral director at least three of the past five years, they may submit the Funeral Director application.
The Funeral Director oversees, directs, and coordinates all aspects of funeral services including body preparation, visitation, services, burials, and cremations, while providing caring support and advice to families and friends of the deceased.1
Funeral Director Limited licensure is available only to funeral directors validly licensed by another jurisdiction (U.S. state, possession, territory or District of Columbia) provided that the jurisdiction where he or she is licensed grants a similar privilege to Delaware-licensed funeral directors (24 Del. C. §3108). Currently, Delaware only has limited licensure agreements with the States of Maryland and Pennsylvania.
Funeral Director Limited licensure allows a practitioner to:
• make a removal of a dead human body in Delaware,
• return the body to another state or country,
• return dead bodies from another state or country to Delaware for final disposition,
• complete the family history portion of the death certificate,
• sign the death certificate in the capacity of a licensed funeral director, and
• execute any other procedures necessary to arrange for the final disposition of a dead human body.
A valid Funeral Establishment Permit issued by the Board of Funeral Services is required to open or operate a funeral establishment in Delaware. This permit is required in addition to any business license issued by the Division of Revenue.
Please see the facilities section of this report for additional information.
A valid Crematory Establishment Permit issued by the Board of Funeral Services is required to open or operate a crematory in Delaware when crematory is not part of a Delaware-licensed Funeral Establishment’s operation. Section 13.2.13 of the Board’s Rules and Regulations more fully explains when a crematory does not need a permit.
Please see facilities section of this report for additional information.
1. Society for Human Resource Management. (2022). Funeral directors. Retrieved from https://www.shrm.org/ResourcesAndTools/tools-and-samples/ job-descriptions/Pages/Funeral-Director.aspx
Figure 18
Active Funeral Services Licenses by Type*, N=3


* an active license does not guarantee an individual is actively seeing patients.
Figure 19
Active Funeral Services Licenses by Gender, select license types (when reported)
* an active license does not guarantee an individual is actively seeing clients.
Figure
Birth
37 individuals are at full retirement age of 67 in 2022.
Note. Six individuals did not provide a year of birth

Full retirement age as per Social Security Adminstration*
(when reported) * According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















The primary objective of the Delaware Board of Massage and Bodywork is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board:
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to massage therapists, certifications to massage technicians and Massage Establishment licenses. It also issues temporary certifications to massage technicians.
The Board’s statutory authority is in 24 Del. C., Chapter 53.
The Board of Massage and bodywork licenses both individuals and facilities which is somewhat different from many other board of the Division of Professional Regulation. Information on facilities is contained in the facilities section of this report.
Massage therapists treat clients by using touch to manipulate the muscles and other soft tissues of the body. 1
Individuals holding a Delaware Massage Therapist license must be 18 years old, pass the National Certification Board for Therapeutic Massage and Bodywork (NCBTMB) exam and:
• not licensed by any other jurisdiction (state, District of Columbia, or U.S. territory), OR
• licensed by another jurisdiction but have not practiced continuously in that jurisdiction for at least two years, OR
• currently licensed as a Certified Massage Technician or Temporary Massage Technician in Delaware.
A “reciprocity” agreement can be made if a therapist is are currently licensed in another jurisdiction AND has practiced continuously in that jurisdiction for at least two years, AND has passed the NCBTMB exam.
Delaware Certified Massage Technicians must be 18 years old and:
• not licensed by any other jurisdiction (state, District of Columbia, or U.S. territory), OR
• licensed by another jurisdiction but have not practiced continuously in that jurisdiction for at least two years.
A “reciprocity” agreement can be made if a technician is currently licensed in another jurisdication AND has practiced continuously in that jurisdication for at least two years.
The purpose of a Temporary Massage Technician Certification is to allow an individual to practice while completing the educational requirements. They must be at least 18 years old, and have not yet completed the educational requirements for Massage Technician Certification.
The temporary certification is valid for one year only. It cannot be renewed, reissued or changed to inactive status.
An establishment license from the Board of Massage and Bodywork is required for each location operating as a
Massage Establishment as defined by 24 Del. C. §5302 and Section 12.0 of the Board’s Rules and Regulations. If any of the following occurs, a new application for licensure must be approved:
• An existing unlicensed massage/bodywork business with a first application for establishment licensure,
• Opening a new establishment,
• The ownership of an existing establishment is changing (regardless of whether the name is changing),
• The name of an existing establishment is changing (regardless of whether the owner is changing),
• The location of an existing establishment is changing.
The establishment may need other licenses and permits (such as a business license from the Division of Revenue or permit from the town/city where the establishment operates).
Please see facilities section of this report for additional information.
1. US Bureau of Labor Statistics. (2022, Aug). Massage therapists. Occupational outlook handbook. Retrieved from https://www.bls.gov/ooh/healthcare/massage-therapists.htm
Figure 23
Active Massage and Bodywork Licenses by Type*, N=1,197


* an active license does not guarantee an individual is actively seeing patients.
Figure 24
Active Certified Massage Technician & Massage Therapist Licenses by Gender (when reported)
Figure 25

55 individuals are at full retirement age of 67 in 2022.
Note. One individual did not provide a year of birth
Full retirement age as per Social Security Adminstration*
reported) * According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Figure 26
Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















The primary objectives of the Delaware Board of Medical Licensure and Discipline are to promote public health, safety and welfare and to protect the public from the unprofessional, improper, unauthorized, or unqualified practice of medicine and certain other healthcare professions. To meet these objectives, the Board:
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues physician (M.D. and D.O.) licenses and physician training licenses to residents, interns, fellows and house physicians.
The Board also issues for licenses these additional healthcare professions: physician assistants, respiratory care practitioners, acupuncture practitioners, acupuncture detoxification specialists, eastern medicine practitioners, genetic counselors, polysomnographers, midwifery practitioners and administrative medical. A Council for each of these healthcare professions advises and assists the Board on licensure and regulatory matters pertaining to its profession.
The Board also issues certifications to and has other responsibilities in regard to emergency medical technicians/ paramedics in collaboration with the Office of Emergency Medical Services.
The Board’s statutory authority is in 24 Del. C., Chapter 17. Additional statutory provisions on the Board’s responsibilities in connection with emergency medical technicians/paramedics are in 16 Del. C., Chapter 97 and Chapter 98.
Physicians and surgeons diagnose and treat injuries or illnesses and address health maintenance.
Physicians and surgeons work in both clinical and nonclinical settings. Clinical settings include physicians’ offices and hospitals; nonclinical settings include government agencies, nonprofit organizations, and insurance companies.1
There are two terminal degrees for physicians, Doctor of Osteopathic Medicine (D.O.) and Doctor of Medicine (M.D.) from the Latin Medicinae Doctor.
MDs are allopathic doctors. That means they treat and diagnose conditions using conventional medical tools like x-rays, prescription drugs, and surgery. Allopathic medicine is also called conventional or mainstream medicine.
MDs can choose to be broad practitioners and work as family medicine or primary care doctors. They can also specialize in several different areas requiring further education including:
• Surgery,
• Organ System Specific Specialty,
• Psychiatry,
• Geriatric Medicine, and
• Pediatrics
DO stands for doctor of osteopathic medicine. They use the same conventional medical techniques as MDs but with a few other methods. DOs tend to focus more on holistic health and prevention. In holistic health, all parts of a person, including their mind, body, and emotions, are considered during the treatment. They also use a system of physical manipulations and adjustments to diagnose and treat people.
Over half of DOs choose to work in primary care, but they can also choose to specialize in another area, just like MDs. DOs have all the same responsibilities and rights as MDs, including the abilities to perform surgery with proper training and prescribe medicine.
MDs and DOs follow similar educational routes. They must first earn a four-year undergraduate degree, and most will take pre-medicine courses during this time. After getting an undergraduate degree, they will attend either medical school or a college of osteopathic medicine.
After finishing four years of medical education, MDs and DOs must complete an internship and a residency. A residency is on-the-job training under the supervision of more experienced doctors. Some MDs and DOs will also go on to do fellowships to learn more about a specialty.
MDs and DOs often train side by side in residencies and internships, despite going to different types of schools.
Both MDs and DOs must also take a licensing exam in order to practice medicine professionally.2
An ACGME training license is required for that part of the education which all physicians, regardless of degree type (D.O. or M.D.), go through after medical school to prepare them for fully independent practice. Another section of this report examines these types of trainings and the Delaware institutions at which they are offered..
Physicians are employed in an ACGME-approved institution located in Delaware and are:
• a Resident, Intern or Fellow registered in a training program outside of Delaware who will rotate through a program in Delaware for over one month, or
• employed as a House Physician.
For more information about Training licensure, see Section 4.0 of the Board’s Rules and Regulations.
Physician assistants practice medicine on teams with physicians, surgeons, and other healthcare workers.
Physician assistants work in physicians’ offices, hospitals, outpatient clinics, and other healthcare settings. Most work full time.3
An Administrative Medical license allows physicians to use their medical and clinical knowledge, skill, and judgment only in an administrative capacity. These licensed cover physicians practicing administrative medicine and who do not provide any of the following medical or clinical services:
• examine, care for or treat patients;
• prescribe medications including controlled substances; or
• delegate medical acts or prescriptive authority to others
Respiratory therapists care for patients who have trouble breathing—for example, because of a chronic condition such as asthma.
Most respiratory therapists work full time. Because they may work in medical facilities that are always open, such as hospitals, they may have shifts that include nights, weekends, or holidays.4
• Acupuncture Practitioners have earned a Diplomate in Acupuncture from the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) or an equivalent organization.
• Eastern Medicine Practitioners have earned a Diplomate in Oriental Medicine from the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) or an equivalent organization. The Acupuncture Advisory Council may waive this Diplomate requirement under specific circumstances as outlined in 24 Del. C. §1798 (c)
Acupuncture/Oriental medicine (AOM) is an ancient and empirical system of medicine based on the concept of qi (pronounced “chee”), which is usually translated as energy.
AOM treatments identify a pattern of energetic imbalance within a patient and redress that disharmony through a variety of therapies that may include acupuncture needling, cupping, acupressure, exercises such as tai ji and qi gong and Chinese herbal preparations.
AOM is virtually free of the side effects that accompany many modern medical procedures. As a relatively inexpensive form of treatment, it is especially appropriate for reducing healthcare costs. The success of acupuncture today is due to its efficacy, remarkable safety record, cost-effectiveness and significant public demand.5
Individuals that have a current license or certificate, are in good standing in a healthcare related profession, are approved by the Acupuncture Advisory Council and the Medical Board are eligible for this additional level of specialization.6
The National Acupuncture Detoxification Association (NADA) protocol is a unique form of acupuncture. It specifically targets behavioral health, including addictions and co-occurring disorders. The protocol involves the bilateral insertion of 1Y5 needles into predetermined points on each ear (auricle).7
Genetic counselors assess individual or family risk for a variety of inherited conditions, such as genetic disorders and birth defects.
Genetic counselors work in university medical centers, private and public hospitals, diagnostic laboratories, and physicians’ offices. They work with families, patients, and other medical professionals. Most genetic counselors work full time.
Genetic counseling requires an original or provisional license from the American Board of Genetic Counselors or the American Board of Medical Genetics and Genomics. Genetic counselors typically need a master’s degree in genetic counseling or genetics, along with board certification.8
A Polysomnographer is an allied health professional who performs overnight sleep assessments used to diagnose various sleep disorders. In the evening the patient will arrive at a sleep laboratory in a hospital, medical facility, or hotel. Increasingly, physicians are prescribing at-home sleep tests to ensure the patient’s comfort and to reduce cost. The polysomnographer will attach various electrodes used to record the patient’s brain activity and will then monitor the patient throughout the night.
Work environments include:9
• Hospitals
• Medical facilities
• Hotels
• Patients’ homes
Midwifery encompasses the independent provision of care during pregnancy, childbirth, and the postpartum period; sexual and reproductive health; gynecologic health; and family planning services, including preconception care. 10
• Certified Professional Midwifes (CPM) receive certification by the North American Registry of Midwives (NARM) or its equivalent or successor.
• Certified Midwifes (CM) receive certification by the American Midwifery Certification Board (AMCB) or its equivalent or successor.
1. US Bureau of Labor Statistics. (2022, Aug). Physicians and surgeons. Occupational Outlook handbook. Retrieved from https://www.bls.gov/ooh/ healthcare/physicians-and-surgeons.htm
2. Web MD. (2021, Apr). Difference between MD and DO. Retrieved from: https://www.webmd.com/a-to-z-guides/difference-between-md-and-do
3. US Bureau of Labor Statistics. (2022, Aug). Physician assistants. Occupational Outlook handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/physician-assistants.htm
4. US Bureau of Labor Statistics. (2022, Aug). Respiratory therapists. Occupational Outlook handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/respiratory-therapists.htm
5. Explore Healthcareers. (n.d.). Acupuncture/oriental medicine practitioner. Retrieved from: https://explorehealthcareers.org/career/complementary-and-integrative-medicine/acupuncture-oriental-medicine-practitioner/
6. National Acupuncture Detoxification Association. (n.d.). Regulations. Retrieved from: https://acudetox.com/resources/regulations/
7. Carter, K., Olshan-Perlmutter, M. (2014). NADA protocol. Journal of Addictions Nursing, 25(4), 182-187. https://alliedhealth.ceconnection.com/files/ NADAProtocolIntegrativeAcupunctureinAddictions-1419263411853.pdf
8. US Bureau of Labor Statistics. (2022, Aug). Genetic counselors. Occupational Outlook handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/genetic-counselors.htm
9. Cleveland Clinic. (n.d.). Polysomnographer. Retrieved from: https://my.clevelandclinic.org/departments/health-sciences-education/careers/career-options/polysomnographer
10. American College of Nurse-Midwives. (n.d.). About the midwifery profession. Retrieved from: https://www.midwife.org/About-the-Midwifery-Profession
Figure 28
Active Medical Board Licenses by Type*, N=9,895 records across licenses
* an active license does not guarantee an individual is actively seeing patients.
Figure 29
Active Medical Board Licenses by Gender, select license types (when reported)



Not including 3 individuals listing no year of birth, 866 individuals are at full retirement age of 67 in 2022.
One record, at bottom of chart, indicates a birth year of 2020.
Full retirement age as per Social Security Adminstration*
Note. Three individuals did not provide a year of birth
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
19703 19702
19964
19720
19707 19732 19804 19730


19716 19731 19709 19734
19733
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19950 19960 19941 19973 19940
19931
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
Philadelphia 19944 19945
Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
19703 19702
19964
19720
19707 19732 19804 19730


19716 19731 19709 19734
19733
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19950 19960 19941 19973 19940
19931
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
Philadelphia 19944 19945
Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
19805
19703 19702
19964
19720
19707 19732 19804 19730


19716 19731 19709 19734
19733
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19950 19960 19941 19973 19940
19931
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
Philadelphia 19944 19945

Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.















Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
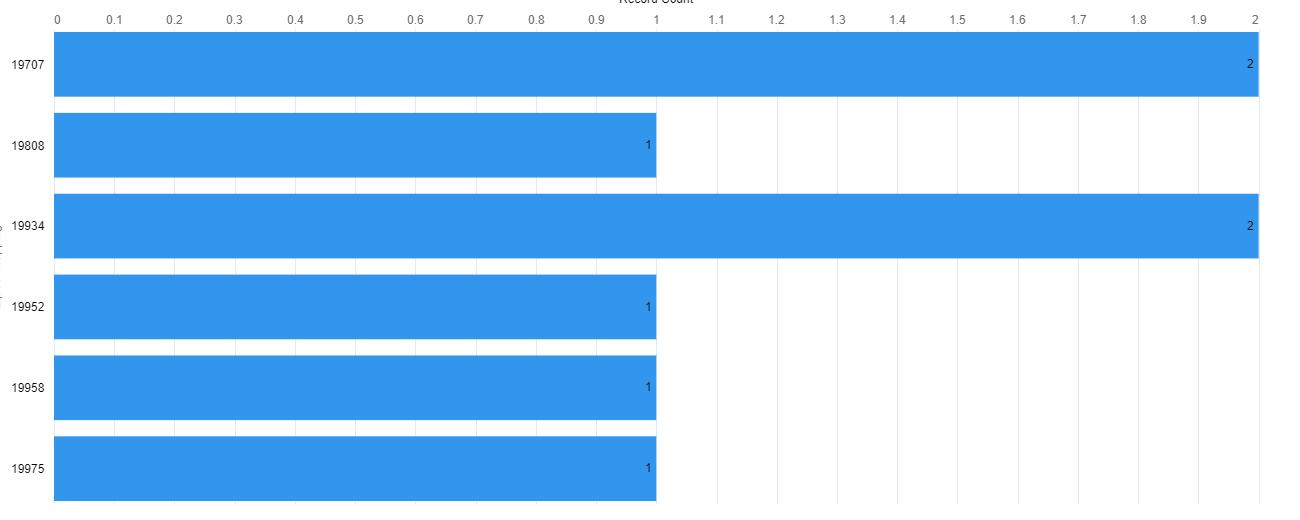
19805
19703 19702
19964
19720
19707 19732 19804 19730


19716 19731 19709 19734
19733
19977 19902
19938 19946
19955 19901 19943













19904
19953 19979 19954 19952
19950 19960 19941 19973 19940
19931
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
Philadelphia 19944 19945
Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.


19805
19703 19702
19707 19732 19804 19730

19964
19720
19733
19716 19731 19709 19734
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19950 19960 19941 19973 19940
19931
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
Philadelphia 19944 19945
Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Note. Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
19703 19702
19707 19732 19804 19730


19964
19720
19733
19716 19731 19709 19734
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19950 19960 19941 19973 19940
19931
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
Philadelphia 19944 19945
*At the time of data extraction, the DELPROS licensing system allowed for natural language submissions in the field “Specialty.” In over 1,600 instances no specialty was selected and those entries were researched. In the remaining records that did not have a listing which conformed to AAMC (Association of American Medical College) taxonomy, staff employed best reasoning possible in selecting an accurate category. This operation was overseen by a physician. Please see the following pages for the AAMC taxonomy detail with subspecialty information.
Future reports, pending adoption of a picklist system in DELPROS, will result in a more accurate number per specialty, and essential exercise to relate physician specialists to disease prevention and treatment.


803 individuals are at full retirement age of 67 in 2022.
Full retirement age as per Social Security Adminstration*
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
In a time of increasing specialization in medicine, we turned to the Assocation of American Medical Colleges for the taxonomy employed within this report. For the purposes of this report, we use values from the first, left-most column in BOLD.
Table 1
Addiction Medicine Allergy and Immunology Anesthesiology
Adult Cardiac Anesthesiology Pain Medicine Clinical Informatics Pediatric Anesthesiology Critical Care Medicine Pediatric Cardiac Anesthesiology Neurocritcial Care Regional Anesthesiology and Acute Pain Medicine Obstetric Anesthesiology Colon and Rectal Surgery Dermatology
Dermatopathology Pediatric Dermatology Micrographic Dermatologic Surgery Diagnostic Radiology
Abdominal Imaging Radiology Musculoskeletal Imaging Radiology Cardiothoracic Radiology Neuroradiology Clinical Informatics Nuclear Radiology Endovascular Surgical Neuroradiology Pain Medicine Interventional Radiology Pediatric Radiology Medical Physics Radiation Oncology Emergency Medicine
Anesthesiology Critical Care Medicine Pain Medicine Emergency Medical Services Pediatric Emergency Medicine Internal Medicine-Critical Care Medicine Sports Medicine Medical Toxicology Undersea and Hyperbaric Medicine Family Medicine/Family Practice Adolescent Medicine Pain Medicine Geriatric Medicine Sports Medicine General Surgery
Complex General Surgical Oncology Surgical Critical Care Hand Surgery Vascular Surgery Pediatric Surgery Hospice and Palliative Medicine Integrated Plastic Surgery Integrated Thoracic Surgery Integrated Vascular Surgery Internal Medicine
Adolescent Medicine Infectious Disease Adult Congenital Heart Disease Interventional Cardiology Advanced Heart Failure and Transplant Cardiology Medical Oncology Cardiovascular Disease Nephrology Clinical Cardiac Electrophysiology Neurocritical Care Critical Care Medicine Pulmonary Disease Endocrinology, Diabetes, and Metabolism Pulmonary Disease and Critical Care Medicine Gastroenterology Rheumatology Geriatric Medicine Sports Medicine Hematology Transplant Hepatology Hematology and Medical Oncology
Internal Medicine-Emergency Medicine Internal Medicine-Pediatrics
Medical Genetics and Genomics
Clinical Biochemical Genetics Medical Biochemical Genetics Clinical Genetics and Genomics Molecular Genetic Pathology Laboratory Genetics and Genomics Musculoskeletal Oncology Neurological Surgery
Endovascular Surgical Neuroradiology Neurocritical Care
Nuclear Medicine
Obstetrics and Gynecology
Brain Injury Medicine
Neurodevelopmental Disabilities Child Neurology/Pediatric Neurology Neuromuscular Medicine Clinical Neurophysiology Pain Medicine Epilepsy Vascular Neurology Neurocritical Care
Complex Family Planning Gynecologic Oncology Critical Care Medicine Maternal-Fetal Medicine Female Pelvic Medicine and Reconstructive Surgery Reproductive Endocrinology and Infertility Ophthalmology
Neuro-Ophthalmology Pediatric Ophthalmology Ophthalmic Pathology Uveitis and Ocular Immunology Ophthalmic Plastic and Reconstructive Surgery Orthopaedic Surgery
Adult Reconstructive Orthopaedic Surgery Orthopaedic Sports Medicine Foot and Ankle Orthopaedic Surgery Orthopaedic Surgery of the Spine Hand Surgery Orthopaedic Trauma Musculoskeletal Oncology Pediatric Orthopaedic Surgery Osteopathic Neuromusculoskeletal Medicine Otolaryngology-Head and Neck Surgery
Complex Pediatric Otolaryngology Plastic Surgery within the Head and Neck Neurotology
Pathology
Hematopathology/Hematology Chemical Pathology Medical Microbiology Pathology Clinical Informatics Molecular Genetic Pathology Cytopathology Neuropathology Dermatopathology Pediatric Pathology Forensic Pathology Selective Pathology Pediatrics
Blood Banking-Transfusion Medicine
Adolescent Medicine Pediatric Gastroenterology Child Abuse Pediatrics Pediatric Hematology-Oncology Developmental and Behavioral Pediatrics Pediatric Hospital Medicine Medical Toxicology Pediatric Infectious Disease Neonatal-Perinatal Medicine Pediatric Nephrology Pediatric Cardiology Pediatric Pulmonology Pediatric Critical Care Medicine Pediatric Rheumatology Pediatric Emergency Medicine Pediatric Sports Medicine Pediatric Endocrinology Pediatric Transplant Hepatology Physical Medicine and Rehabilitation
Brain Injury Medicine Pediatric Rehabilitation Medicine Neuromuscular Medicine Spinal Cord Injury Medicine Pain Medicine Sports Medicine Plastic Surgery
Craniofacial Surgery Plastic Surgery within the Head and Neck Hand Surgery
Preventive Medicine
Occupational Medicine Clinical Informatics Public Health and General Preventive Medicine Medical Toxicology Undersea and Hyperbaric Medicine Psychiatry
Aerospace Medicine
Consultation-Liaison Psychiatry/Psychosomatic Medicine Brain Injury Medicine Forensic Psychiatry Child and Adolescent Psychiatry Geriatric Psychiatry Sleep Medicine Thoracic Surgery/Thoracic and Cardiac Surgery Congenital Cardiac Surgery Urology
Addiction Psychiatry
Female Pelvic Medicine and Reconstructive Surgery Pediatric Urology
Figure 58
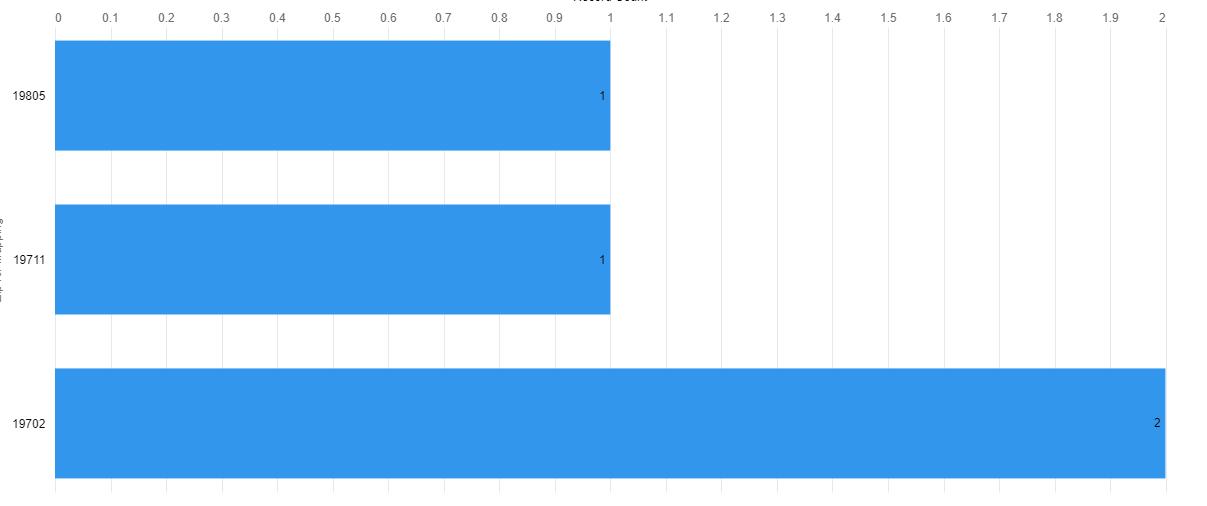
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Figure 60
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
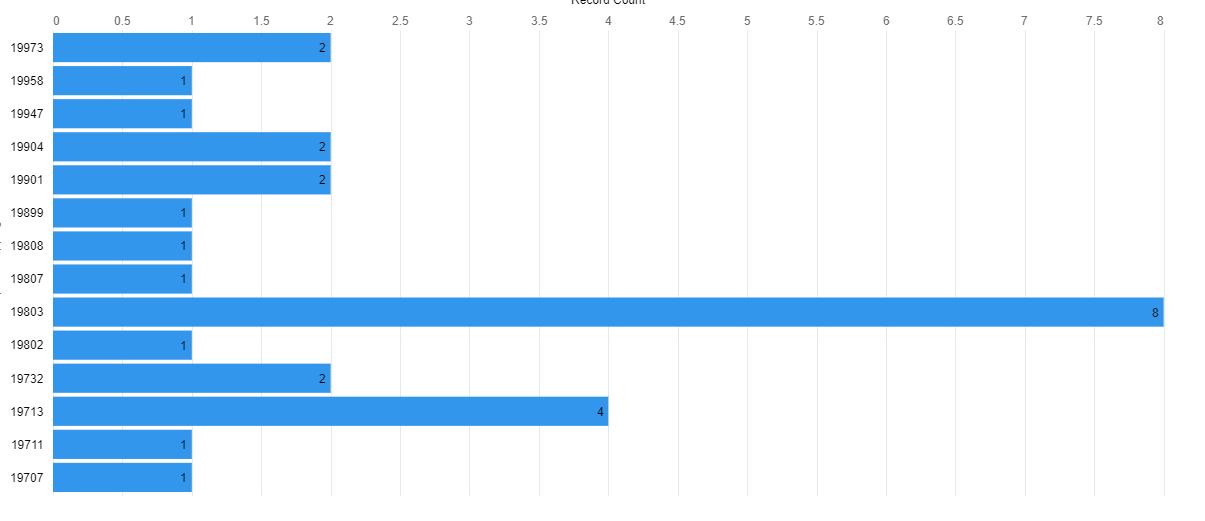















Figure 62
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.













Figure 64
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732
19801 19702
19733
19716 19709 19734


19904
19977 19902
19955 19943
19964 19979 19954














19963 19966
19933 19971
19951 19930
19944 19945 19931
19950 19960 19941 19973 19940
Figure 66
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.














Figure 68
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Figure 70
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Figure
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.













Figure 74
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.















Figure 76
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

Distribution
AAMC
19733 Fiure 77 Visual
19801 19702 of
Active Medicine Hospicea and Palliative Care Physicians by

and Palliative
19732 ZIP
19716 19709 19734 1:1,954,862
code
19964 19979 19954 0
19904 0
25 12.5














40 20
19955 19943 Medicine Delaware FirstMap, New Jersey Office of GIS, VGIN, Esri, FAO, NOAA, USGS, EPA, NPS, Esri, USGS
Figure 78
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
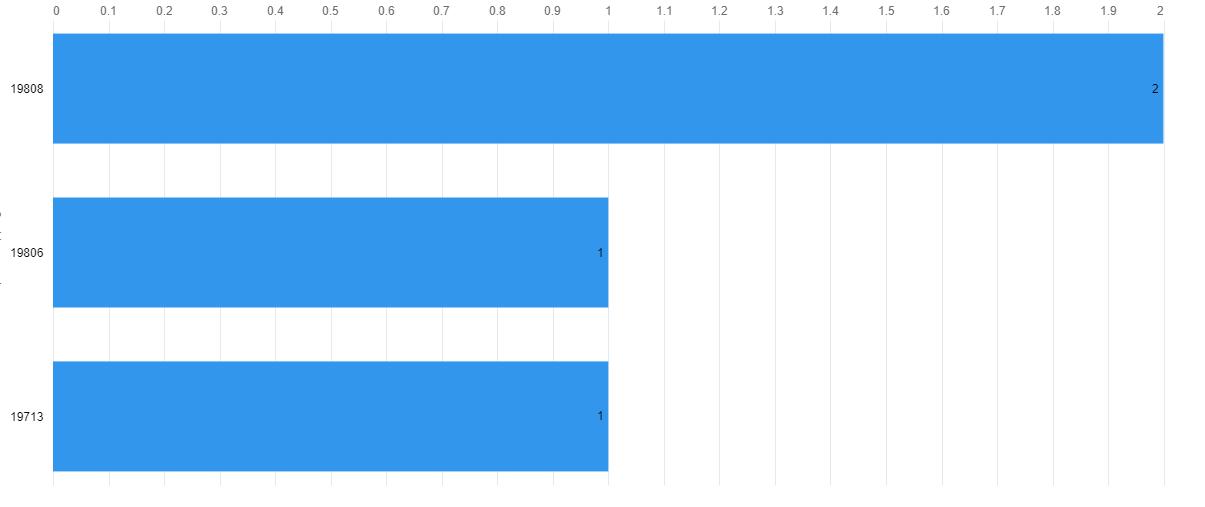















Figure 80
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Figure 82
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
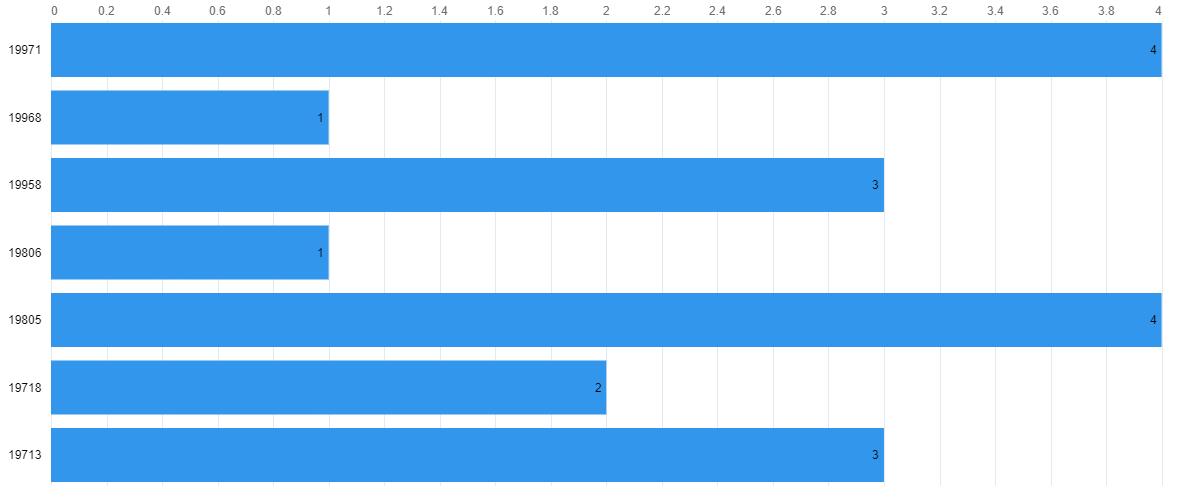















Figure 84
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Figure 86
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Figure 88
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Figure 90
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732
19801 19702
19733
19716 19709 19734


19904
19977 19902
19955 19943
19964 19979 19954














19963 19966
19933 19971
19951 19930
19944 19945 19931
19950 19960 19941 19973 19940
Figure 92
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
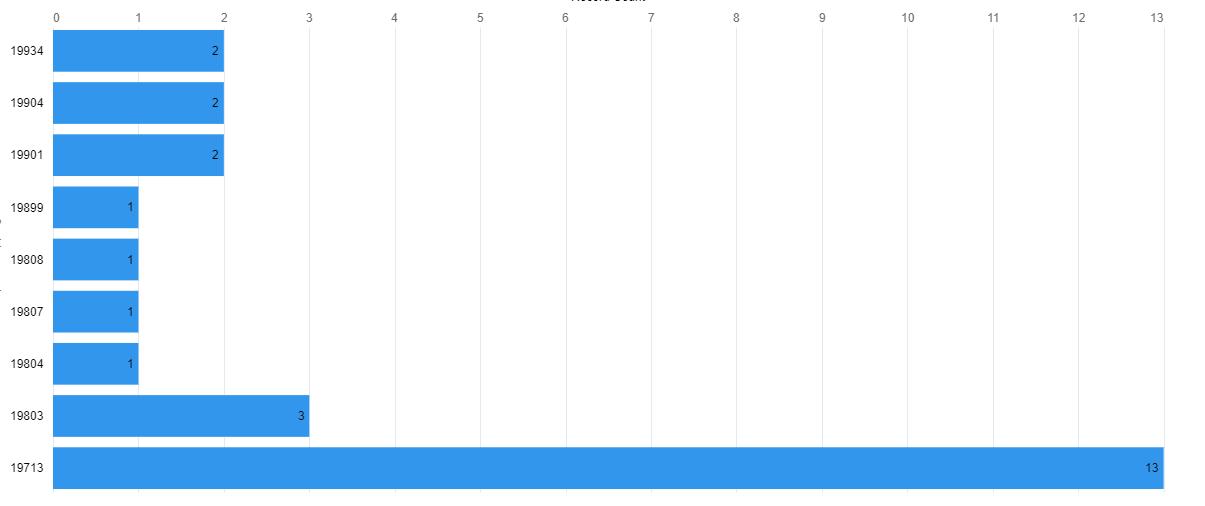
19732
19801 19702
19733
19716 19709 19734


19904
19977 19902
19955 19943
19964 19979 19954













19963 19966
19933 19971
19951 19930
19944 19945 19931
19950 19960 19941 19973 19940
Figure 94
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Figure 96
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Figure 98
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Figure 100
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Figure 102
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732 Figure 105 Visual














Distribution of Active Osteopathic Neuromusculoskeletal Medicine Physicians by ZIP code
AAMC Osteopathic Neuromusculo
19977 19902
19955 19943
19964 19979 19954
19801 19702 1:1,954,862

19716 19709 19734 0
19733 0
19950 19960 19941 19973 19940
19951 19930
25 12.5
40 20
19904 Delaware FirstMap, New Jersey Office of GIS, VGIN, Esri, FAO, NOAA, USGS, EPA, NPS, Esri, USGS

Figure 106
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Figure 110
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Figure 112
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.















Figure 114
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Figure 116
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732
19801 19702
19733
19716 19709 19734


19904
19977 19902
19955 19943
19964 19979 19954













19963 19966
19933 19971
19951 19930
19944 19945 19931
19950 19960 19941 19973 19940
Figure 118
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732
19801 19702
19733
19716 19709 19734


19904
19977 19902
19955 19943
19964 19979 19954














19963 19966
19933 19971
19951 19930
19944 19945 19931
19950 19960 19941 19973 19940
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732
19801 19702
19733
19716 19709 19734


19955 19943 19979 19954














19904
19977 19902
19933 19971
19931 19966
19950 19960 19941 19973 19940
19947 19930
19944
Figure 124
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.













The primary objective of the Delaware Board of Nursing is to protect the public health, safety and welfare. To meet this objective to safeguard life and health, the Board
• develops standards for professional competency, • promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions
The Board issues licenses to registered nurses (RNs), practical nurses (LPNs) and advanced practice registered nurses (APRNs).
The Board’s statutory authority is in 24 Del. C., Chapter 19. Delaware is a member of the interstate nurse licensure compact covered in 24 Del. C., Chapter 19A.
Acute care nurse practitioners are advanced practice registered nurses who specialize in caring for patients with new acute conditions or exacerbated chronic conditions. ACNPs work in a variety of environments—from hospital emergency rooms to urgent-care clinics to operating rooms—and may focus on adults or children.1
A Clinical Nurse Specialist in Adult Health (ACNS) is an advanced nursing practitioner who participates in the advanced care of seriously ill, adult patients. This profession is involved with all aspects of adult care, from assessment to treatment and management of outcomes.2
Geriatric nurse practitioners (GNPs) provide medical services for older patients. They share skills common among all advanced nurse practitioners. Senior care institutions rely on GNPs to provide comprehensive healthcare services for aging patients. Geriatric nursing practitioners conduct physicals, evaluate well-being and devise care plans specifically for these individuals. GNPs educate senior clients and their caregivers on matters regarding geriatric well-being and also consult with senior patients and their caregivers. Geriatric nursing practitioners advance their discipline through involvement with the National Gerontological Nursing Association, which works with geriatric professionals to produce positive patient outcomes among the senior population.3
The Adult-Gerontological Clinical Nurse Specialists (AG CNS) cares for patients from wellness through acute care, with a specific focus on complex and vulnerable adult and older adult populations. The AG CNS is best described as the “nurses’ nurse” as the CNS is a resource and consultant to nurses and healthcare professionals. The AG CNS is involved in all levels of the healthcare system, spanning from the acute care setting to the home. The AG CNS engages in numerous direct care and leadership roles in the healthcare system including organizing and managing large scale programs, incorporating evidence into practice, coaching and mentoring nurses and serving as a consultant to healthcare professionals, organizations, patients and families.4
Provide general and preventative care, conduct check-ups, treat illnesses, order lab tests and prescribe medication for children and adults. A nurse practitioner is an advanced practice nurse that helps with all aspects of patient care, including diagnosis, treatments and consultations.5
Certified Nurse Midwife
A CNM is an advanced practice registered nurse who goes through comprehensive training, mainly providing care
to pregnant women from labor to delivery to postpartum care.6
A CRNA (certified registered nurse anesthetist or just “nurse anesthetist”) is an advanced practice registered nurse (APRN) who administers anesthesia and other medications. They also take care of and monitor people who receive or are recovering from anesthesia.7
Community Health Nursing Certified Nurse Specialist
The community health nurse clinical specialist (CHNCS) has been clearly delineated by the profession as having a responsibility to the community as client.8
Critical Care Certified Nurse Specialist
Provide direct care to acutely/critically ill adult patients regardless of their physical location. Nurses interested in this certification may work in areas such as intensive care units, cardiac care units, combined ICU/CCUs, medical/ surgical ICUs, trauma units or critical care transport/flight.9
Family Nurse Practitioner
Because of their high level of education, expertise and skill, family nurse practitioners (FNP) will often take on some of the roles of a physician. However, they will still generally work under the supervision of, or in close conjunction with, a physician. FNPs must be able to offer the care and support consistent with high-quality nursing to patients and families, diagnosing and treating patients across a wide variety of conditions.10
Gerontology Certified Nurse Specialist
Same as Adult/Gerontology Certified Nurse Specialist on facing page.
A Gerontological Nurse Practitioner is a multi-disciplined primary healthcare provider who helps patients manage the physical, mental, and social effects of aging.11
Health Promotion and Wellness Certified Nurse Specialist
Performing health assessments and health screenings such as physicals, checkups, or wellness visits with patients to identify problems and determine appropriate treatment plans. providing care to patients in hospitals and other settings who have been diagnosed with a chronic illness such as diabetes or cancer.12
The role of an LPN includes providing basic medical care to patients. In addition to helping patients eat, bathe and get dressed, LPNs also perform medical tasks such as changing bandages and inserting catheters. Another important aspect of the role is reporting changes in patient condition to supervisors such as RNs or physicians. Unlike RNs, LPNs do not set up care plans for patients.13
Maternal Child Certified Nurse Specialist
Provide individual care and monitoring and run educational programs to assist parents and enable them to develop supportive social networks. Maternal and child health nurses support the health and development of children from birth until school age and their parents.14
Medical-surgical nurses are registered nurses who provide care for primarily adult patients before and after surgical procedures. They coordinate healthcare plans with medical professionals, administer medications, and educate patients on surgical procedures. They may be employed at hospitals, clinics, physicians’ offices, or care facilities.15
The neonatal clinical nurse specialist is an advanced practice nurse who functions in the role of expert clinician, educator, consultant and researcher for the Neonatal Intensive Care Unit, NICU.16
The role of the NNP is to provide care to high-risk infants who need care due to low birth weights, complications of prematurity, heart abnormalities, infections or other conditions. However, some NNPs may care for infants with long-term health conditions until they reach two years of age.17
Oncology Certified Nurse Specialist
OCNSs are educationally prepared to provide advanced nursing care to meet the specialized physiologic and psychological needs of patients throughout the continuum of care, including cancer prevention and detection, cancer diagnosis and treatment, rehabilitation, survivorship, and end-of-life care.18
Pediatric Certified Nurse Specialist
clinical experts in pediatric nursing who, in addition to providing direct care, serve as leaders in education, research, quality improvement and outcome monitoring in consultation with other nurses. Pediatric clinical nurse specialists provide care to children and adolescents and their families within the context of the family, community and healthcare system.19
A PNP is an advanced practice registered nurse (APRN) who specializes in caring for newborns, infants, toddlers, adolescents and young adults. PNPs focus on well-child care and the prevention or management of common pediatric acute illnesses and chronic conditions.20
Perinatal Nurse Practitioner
Perinatal nurses care for pregnant patients and their newborns, usually from the early stages of pregnancy to just after giving birth.21
Psych/Mental Health Certified Nurse Specialist
PMH-CNSs are psychiatric-mental health advanced practice registered nurses (PMH-APRNs) with a Clinical Nurse Specialist certification. PMH-APRNs, whether CNS or NP, have received specialized graduate level education and are prepared to provide psychiatric and substance use assessments, diagnoses, and treatment, including medication interventions and psychotherapy.22
Psych/Mental Health Nurse Practitioner
PMHNPs combine a variety of nursing, psychosocial, and neurobiological expertise and methodologies to diagnose, treat, and improve the outcomes of patients facing psychiatric or mental health challenges.23
A registered nurse is a healthcare provider who has graduated from a nursing program and holds a nursing license. There are many types of registered nurses, mainly defined by their areas of specialization.24
A Temporary APRN Permit allows you to practice as an APRN in Delaware until your APRN license is issued.25
A Temporary RN Permit allows you to practice as an RN in Delaware until your RN license is issued.25
A women’s health nurse practitioner (WHNP) provides primary healthcare services to women of all ages, generally beginning at adolescence and continuing through pregnancy and menopause.26
Same as above, but as a certification rather than a degree focusing on the management of patient care. The WHCNS focus on complex cases and vulnerable populations.27
1. Nurse Journal. (2022, Jan 21). Acute care NP career overview. Retrieved from: https://nursejournal.org/careers/acute-care/
2. All Nursing Schools. (n.d.). What you’ll do as a clinical nurse specialist. Retrieved from: https://www.allnursingschools.com/clinical-nurse-specialist/ job-description/
3. Regis College. (2021, Oct 31). What does an adult geriatric nurse practitioner do. Retrieved from: https://online.regiscollege.edu/blog/what-does-anadult-geriatric-nurse-practitioner-do/
4. UCSF School of Nursing. (n.d.). Adult-gerontology clinical nurse specialist. Retrieved from: https://nursing.ucsf.edu/academics/programs/master-science-advanced-practice-programs/adult-gerontology-clinical-nurse-specialist-ag-cns
5. Community Clinic Association of Los Angeles County. (n.d.). Nurse practitioner job description. Retrieved from: https://ccalac.org/wordpress/ wp-content/uploads/gravity_forms/25-398983c110800ddd0c5c4e38d8739014/2017/03/Nurse-Practitioner-job des.pdf
6. Nursing License Map. (2021, Oct). Certified nurse-midwife (CNM). Retrieved from: https://nursinglicensemap.com/advanced-practice-nursing/certified-nurse-midwife-cnm/
7. Cleveland Clinic. (2022, Mar). Nurse anesthetist (CRNA). Retrieved from: https://my.clevelandclinic.org/health/articles/22561-nurse-anesthetist-crna
8. Mason, D.J., Knight, K., Toughill, E., DeMaio, D., Beck, T.L., Christopher, M.A. (1992). Promoting the community health clinical nurse specialist. Clin Nurse Spec, 6(1), 6-13. https://pubmed.ncbi.nlm.nih.gov/1559215/
9. American Association of Critical-Care Nurses. (n.d.). CCRN (Adult). Retrieved from: https://www.aacn.org/certification/get-certified/ccrn-adult
10. Nursing License Map. (n.d.). How to become a family nurse practitioner (FNP). Retrieved from: https://nursinglicensemap.com/advanced-practice-nursing/nurse-practitioner/family-nurse-practitioner/
11. Johnson&Johnson. (n.d.). Gerontological nurse practitioner. Retrieved from: https://nursing.jnj.com/specialty/gerontological-nurse-practitioner
12. Climb the Ladder. (2022, Mar). What does a wellness nurse do? Retrieved from: https://climbtheladder.com/wellness-nurse/
13. Nursing License Map. (n.d.). Nurse hierarchy. Retrieved from: https://nursinglicensemap.com/resources/nurse-hierarchy/
14. Nursing License Map. (n.d.). Fact sheet: Maternal Child Health Nurse. Retrieved from: http://www.education.vic.gov.au/Documents/about/careers/ factsheetmaternalchildhealthnurseaccessible.docx
15. Betterteam. (n.d.). Medical-surgical nurse job description. Retrieved from: https://www.betterteam.com/medical-surgical-nurse-job-description
16. Job Description and Resume Examples. (n.d.). Neonatal clinical nurse specialist job description, duties, and responsibilities. Retrieved from: https:// jobdescriptionandresumeexamples.com/neonatal-clinical-nurse-specialist-job-description-duties-and-responsibilities/.
17. American Association of Nurse Practitioners. (2020, Mar). Take a closer look at the role of a neonatal nurse practitioner (NNP). Retrieved from: https://www.aanp.org/news-feed/are-you-considering-a-career-as-neonatal-nurse-practitioner
18. Oncology Nursing Society. (n.d.). Oncology clinical nurse specialist competencies. Retrieved from: https://www.ons.org/oncology-clinical-nurse-specialist-competencies
19. University of Minnesota. (n.d.). Doctor of nursing practice. Retrieved from: https://nursing.umn.edu/academics/doctor-nursing-practice/specialty-areas/pediatric-clinical-nurse-specialist
20. American Association of Nurse Practitioners. (n.d.). Are you considering a career as a pediatric nurse practitioner? Retrieved from: https://www.aanp. org/news-feed/are-you-considering-a-career-as-a-pediatric-nurse-practitioner
21. Nurse Journal. (2022, Aug 5). Perinatal nurse career overview. Retrieved from: https://nursejournal.org/careers/perinatal-nurse/
22. American Psychiatric Nurses Association. (n.d.). Psychiatric-mental health clinical nurse specialists. Retrieved from: https://www.apna.org/pmh-cns/ 23. Nursing License Map. (n.d.). How to become a psychiatric-mental health nurse practitioner. Retrieved from: https://nursinglicensemap.com/advanced-practice-nursing/nurse-practitioner/psychiatric-and-mental-health-nurse-practitioner-pmhnp/
24. Nursing License Map. (n.d.). Types of nursing careers & specialties. Retrieved from: https://nursinglicensemap.com/nursing-specialties/ 25. Delaware Division of Professional Regulation. (n.d.). Temporary APRN permit. Retrieved from: https://dpr.delaware.gov/boards/nursing/apntemppermit/
26. American Association of Nurse Practitioners. (2020, Apr). Are you considering a career as a women’s health nurse practitioner? Retrieved from: https://www.aanp.org/news-feed/are-you-considering-a-career-as-a-womens-health-nurse-practitioner
28. Nurse Journal. (2022, Jun). NP vs. CNS: what’s the difference? Retrieved from: https://nursejournal.org/resources/np-vs-cns/
Figure 126
Active Nursing Licenses by Specialty, N=25,620

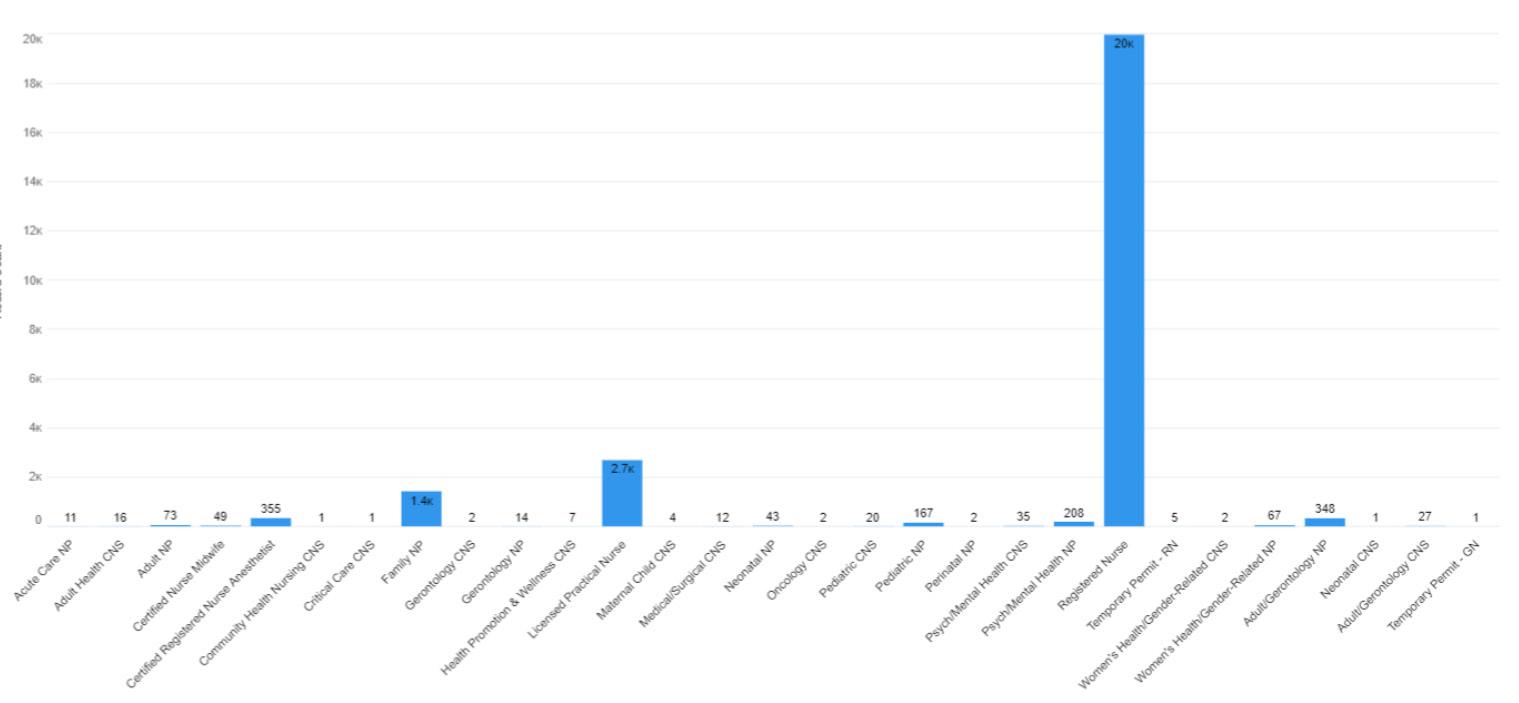
* an active license does not guarantee an individual is actively seeing patients.
Figure 127
Active Nursing Licenses by Gender, select license types (when reported)
Figure 128
Year (when reported)
1,193 individuals are at full retirement age of 67 in 2022.

Note. One individual did not provide a year of birth
Full retirement age as per Social Security Adminstration*
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

Reading Wilmington
19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19733
19977 19902
19938 19946
19964
19904
19953 19979 19954 19952
19955 19901 19943














19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732 19810
19805 19702














19716 19709 19734


19720
19733
19977 19902
19955 19901 19943 19946
19904
19964 19979 19954
19950 19960 19941 19973 19940
19933 19971
19931
19963 19966
19951 19947
19968 19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

Allentown
19732 19810
19805 19702














19716 19709 19734


19720
19733
19977 19902
19955 19901 19943 19946
19904
19964 19979 19954
19950 19960 19941 19973 19940
19933 19971
19931
19963 19966
19951 19947
19968 19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
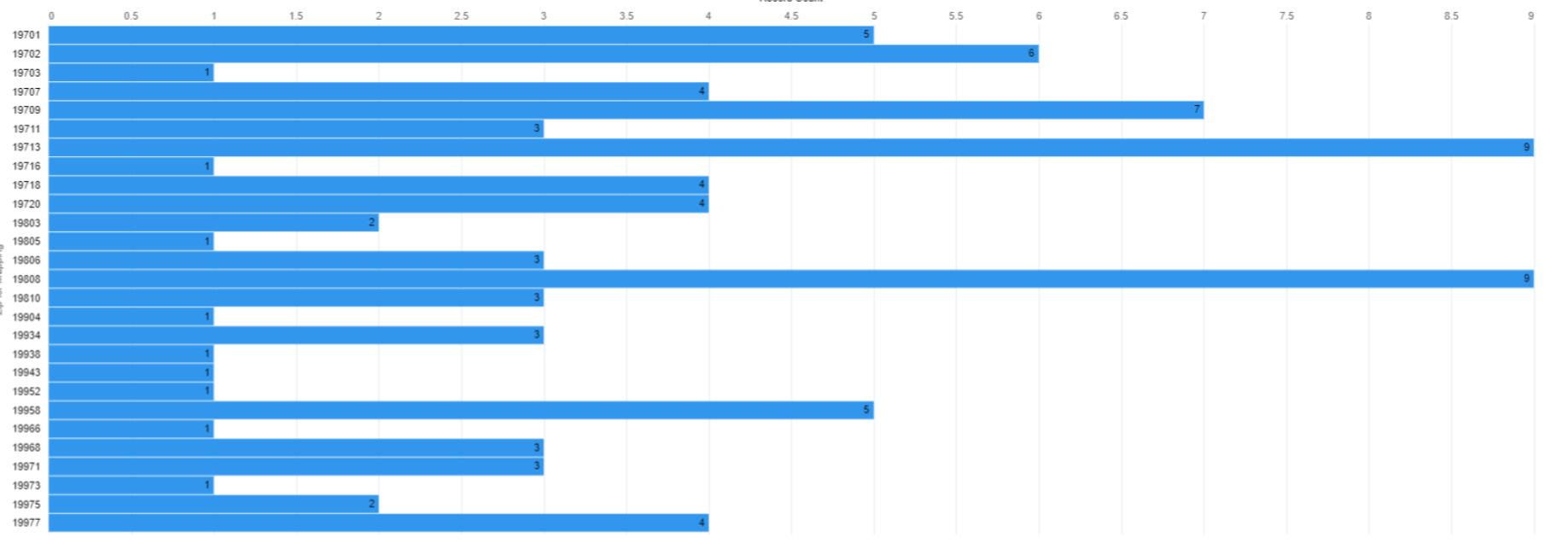
19707 19732


19805
19720
19703 19702
19977 19902
19938 19946
19964 19979 19954 19952
19955 19901 19943
19904
19950 19960 19941 19973 19940
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
19733 0
0 25 12.5













40 20 1:2,093,532
19716 19709 19734 Adult NP Delaware FirstMap, New Jersey Office of GIS, VGIN, Esri, FAO, NOAA, USGS, EPA, NPS, Esri, USGS
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943













19904
19953 19979 19954 19952
19950 19960 19941 19973 19940
19931
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
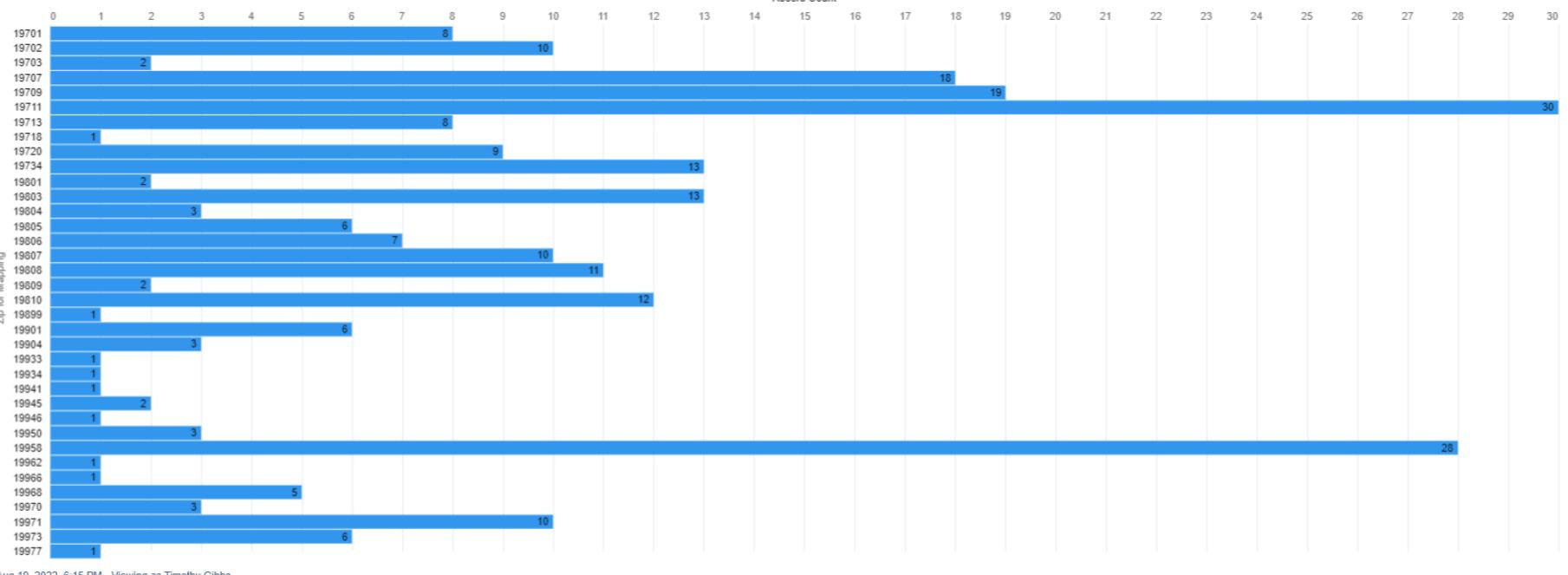
















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732
19805 19702














19977 19902
19955 19943
19964 19979 19954
19931
19950 19960 19941 19973 19940
19716 19709 19734 0 30 15 0 50 25

19933 19971
19951 19947
19733 1:2,532,654
19963 19966
19968 19958 19930
19904 Esri, USGS, Delaware FirstMap, Esri, HERE, Garmin, EPA, NPS

Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
Wilmington
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
Wilmington
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943












19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

Wilmington
19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943













19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

Wilmington
19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
Visual Distribution of Active Maternal Child Certified Nurse Specialists by ZIP code st
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.


Washington
19732 19810
19805 19702















19716 19709 19734
19720
19733
19977 19902
19955 19901 19943 19946
19904
19964 19979 19954
19950 19960 19941 19973 19940
19933 19971
19931
19963 19966
19951 19947
19968 19958 19930
19944 19945
Philadelphia P
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

Wilmington
19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943












19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
Wilmington
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732 19810
Philadelphia
P














19805 19702
19716 19709 19734
19720
19733
Visual Distribution of Active Pediatric Certified Nurse Specialists by ZIP code a

19904
19977 19902
19955 19901 19943 19946
Reading v Washington
19964 19979 19954
19950 19960 19941 19973 19940
19933 19971
19931
19963 19966
19951 19947
19968 19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.















Wilmington
19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943
19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

Reading
19703 19702
Wilmington
19805
19720
19701
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943












19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Figure 173
Numerical Distribution of Active Registered Nurses by ZIP code. n=19,992
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732 19810
Annapolis a
19805 19702















19716 19709 19734

19720
19733
19977 19902
19955 19901 19943 19946
19904
19964 19979 19954
19950 19960 19941 19973 19940
19933 19971
19931
19963 19966
19951 19947
19968 19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
Wilmington
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943













19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19703 19702
19805
19720
19701
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943
e














19904
19953 19979 19954 19952
19950 19960 19941 19973 19940
19931
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

Wilmington
19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.















Wilmington
19805
19703 19702
19701
19720
19707 19732 19804 19730

19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943
19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19732 19810
Annapolis a
19805 19702














19716 19709 19734

19720
19733
19977 19902
19955 19901 19943 19946
19904
19964 19979 19954
19950 19960 19941 19973 19940
19933 19971
19931
19963 19966
19951 19947
19968 19958 19930
19944 19945
The primary objective of the Delaware Board of Examiners of Nursing Home Administrators is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency
• promulgates rules and regulations
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues nursing home administrator and temporary nursing home administrator licenses. It also approves administrator-in-training programs.
The Board’s statutory authority is in 24 Del. C., Chapter 52.
Figure 189
Active Nursing Home Administrator Licenses by Type*
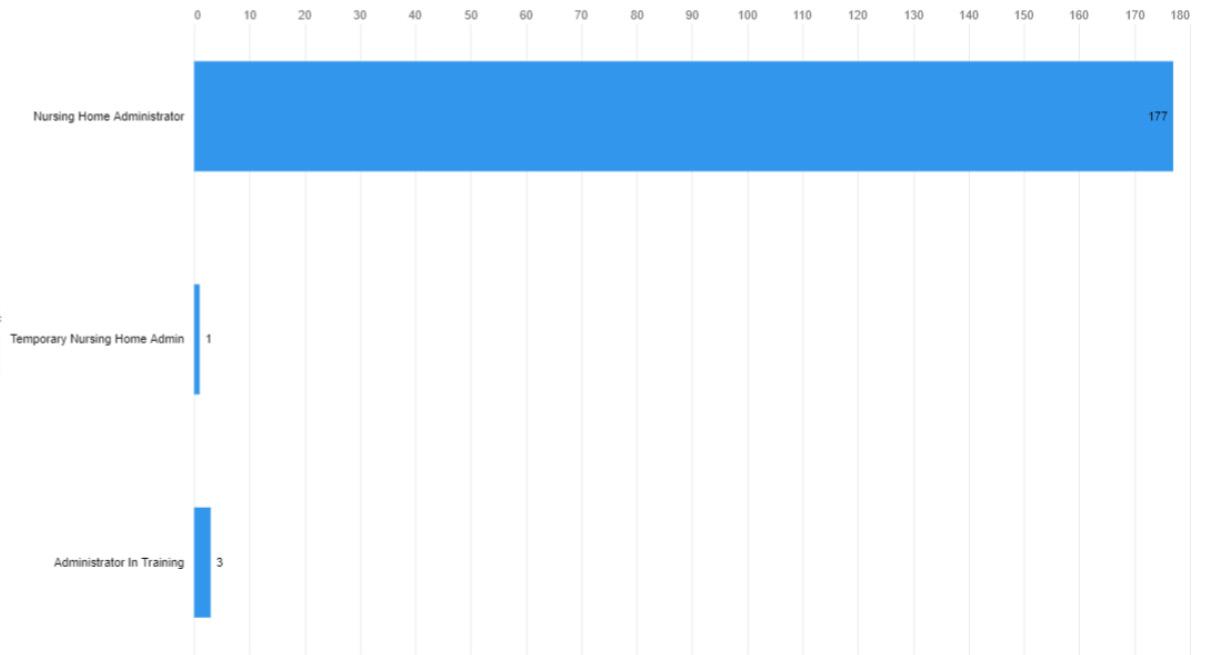
* an active license does not guarantee an individual is actively seeing patients.
Figure 190
Active Nursing Home Administrator Licenses by Gender, select license types (when reported)
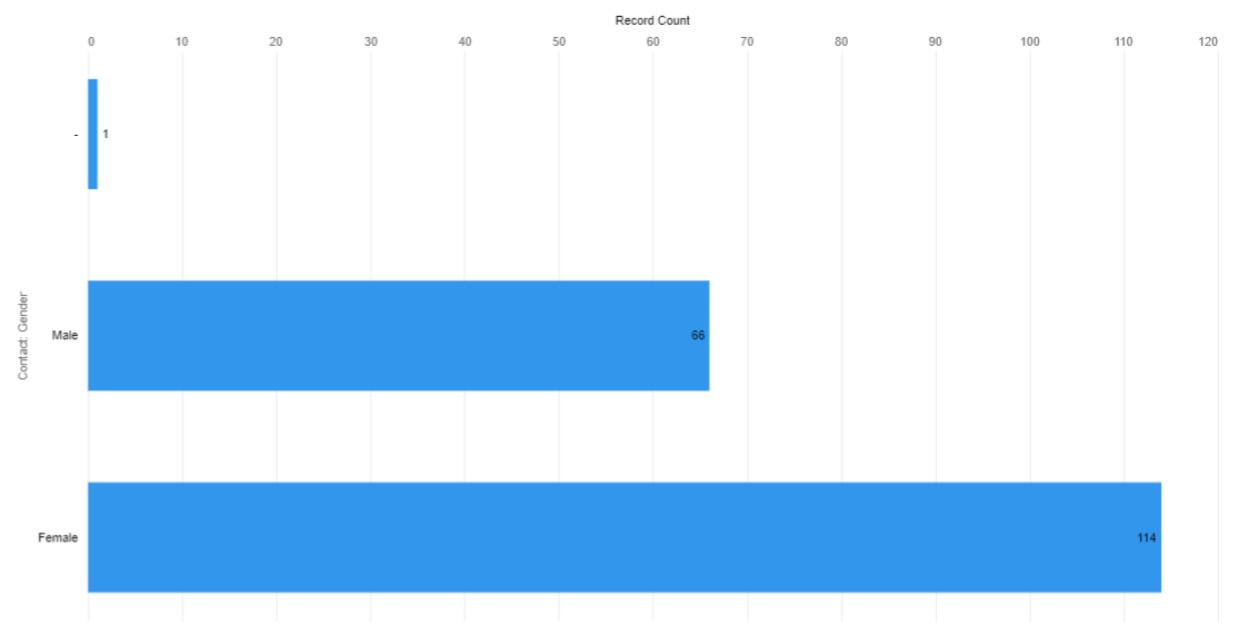

17 individuals are at full retirement age of 67 in 2022.
Full retirement age as per Social Security Adminstration*
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19703 19702
19805
19720
19701
19707 19732 19804 19730

19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19950 19960 19941 19973 19940
19931
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Note: Not shown on this map is one addition Temporary Nursing Home Administrator whose address is in New Jersey, and three Administrator’s in Training: one in Dover, 19904; one in Millsboro, 19966; and one in New Castle, 19720.

The primary objective of the Delaware Board of Occupational Therapy Practice is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to occupational therapists and occupational therapy assistants.
The Board’s statutory authority is in 24 Del. C., Chapter 20
Occupational therapists treat patients who have injuries, illnesses, or disabilities through the therapeutic use of everyday activities.
About half of occupational therapists work in offices of occupational therapy or in hospitals. Others work in schools, nursing homes, and home health services. Therapists may spend a lot of time on their feet while working with patients.1
Occupational Therapy Assistant
Occupational therapy assistants and aides help patients develop, recover, improve, as well as maintain the skills needed for daily living and working.
Occupational therapy assistants and aides work primarily in occupational therapists’ offices, in hospitals, and in nursing care facilities. Occupational therapy assistants and aides spend much of their time on their feet while setting up equipment and, in the case of assistants, providing therapy to patients.2
Figure 194
Active Occupational Therapy Practitioner Licenses by Type*, N=1,182
* an active license does not guarantee an individual is actively seeing patients.

Figure 195
Active Occupational Therapy Practitioner Licenses by Gender, select license types (when reported)
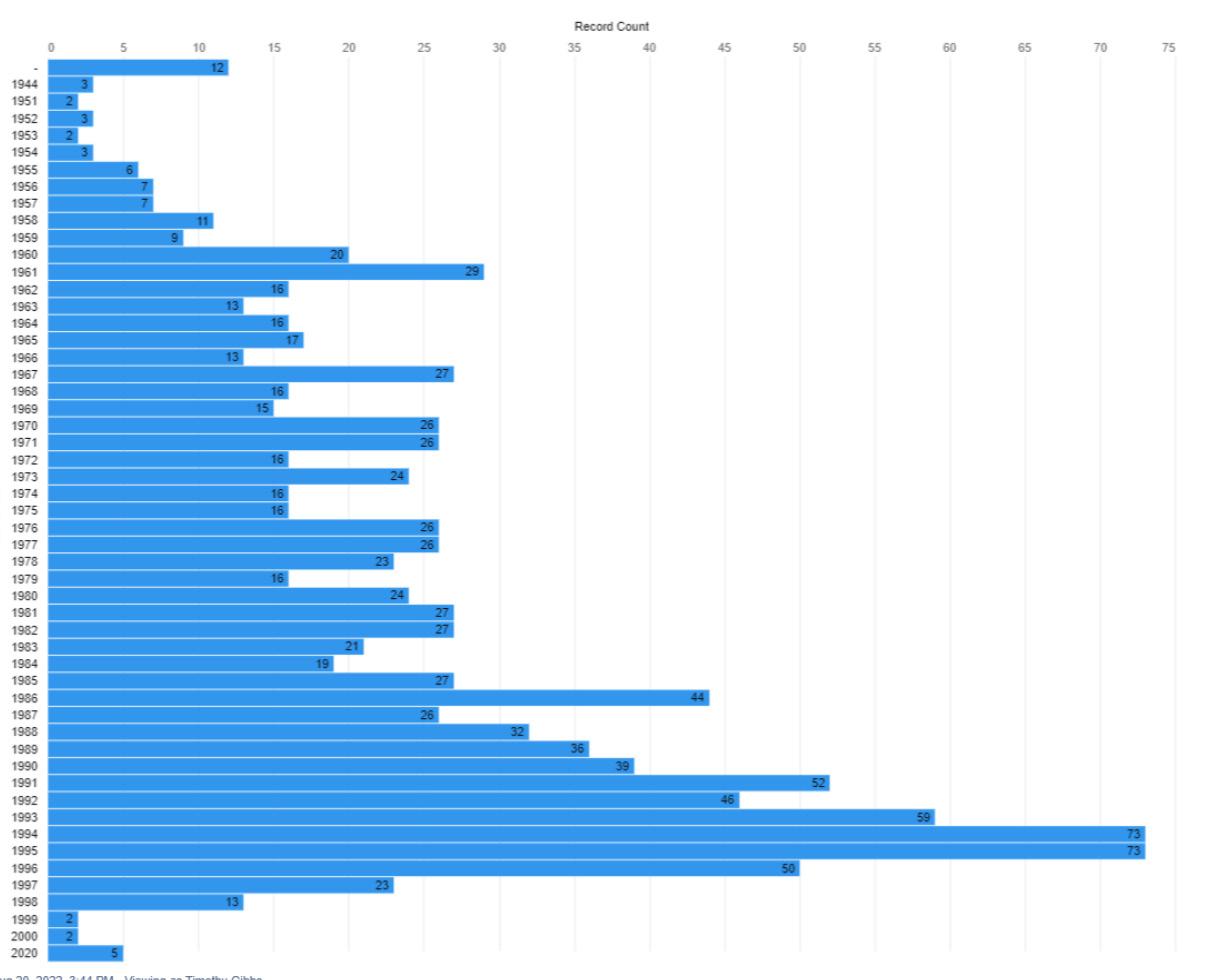

Figure 196
Active Occupational Therapy Practitioner Licenses by Birth Year
13 individuals are at full retirement age of 67 in 2022.
Full retirement age as per Social Security Adminstration*
Note. 12 individuals did not provide a year of birth
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















1. US Bureau of Laborr Statistics. (2022, Aug). Occupational therapists. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/ healthcare/occupational-therapists.htm
2. US Bureau of Labor Statistics. (2022, Aug). Occupational therapy assistants and aids. Occupational Outlook Handbook. Retrieved from: https://www. bls.gov/ooh/healthcare/occupational-therapy-assistants-and-aides.htm
The primary objective of the Delaware Board of Examiners in Optometry is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency, • promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to therapeutic optometrists and interns.
The Board’s statutory authority is in 24 Del. C., Chapter 21
Optometrists are healthcare professionals who provide primary vision care ranging from sight testing and correction to the diagnosis, treatment, and management of vision changes. An optometrist is not a medical doctor. An optometrist receives a doctor of optometry (OD) degree after completing four years of optometry school, preceded by three years or more years of college. They are licensed to practice optometry, which primarily involves performing eye exams and vision tests, prescribing and dispensing corrective lenses, detecting certain eye abnormalities, and prescribing medications for certain eye diseases.1
A therapeutic optometrist has undertaken at least one additional year of training and study, specifically in the diagnosis and management of eye diseases, in microbiology, pathology, ocular pharmacology, and in the treatment of eye conditions with Schedule 4 prescription-only medicines.
To be licensed as a Therapeutic Optometrist in Delaware one is required to complete a six-month internship.
Figure 201
Active Optometry Licenses by Type*, N=205
* an active license does not guarantee an individual is actively seeing patients.

Active Optometry Licenses by Gender select license types (when reported)


Figure 203
Active Optometry Licenses by Birth Year
20 individuals are at full retirement age of 67 in 2022.
Full retirement age as per Social Security Adminstration*

Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.














1. Hull, J. (2019, Feb). Difference between an ophthalmologist, optometrist and optician. American Association for Pediatric Ophthalmology and Strabismus. Retrieved from https://aapos.org/glossary/difference-between-an-ophthalmologist-optometrist-and-optician


The primary objective of the Delaware Board of Pharmacy is to promote, preserve, and protect the public health, safety, and welfare. To meet this objective, the Board
• maintains a registry of drug outlets that manufacture, produce, sell, and distribute drugs, medications, and other materials used to diagnose and prevent illness and disease and to treat injury,
• monitors the outlets to ensure safe practices,
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to pharmacists and pharmacy interns. It also licenses pharmacies (both in Delaware and elsewhere), pharmaceutical manufacturers and distributors, medical gas dispensers and retail businesses that sell non-controlled prescription drugs for veterinary use.
The Board’s statutory authority is in 24 Del. C., Chapter 25 Pharmacist
Pharmacists dispense prescription medications to patients and offer expertise in the safe use of prescriptions. Pharmacists work in pharmacies, including those in drug, general merchandise, and grocery stores. They also work in hospitals and other healthcare facilities.1
To be licensed as a Pharmacist in Delaware, a practitioner must provide proof they have completed 1,500 hours of pre-licensure experience. Interns must select a Delaware-licensed pharmacist to be a preceptor.2
Figure 206
Active Pharmacy Licenses by Type*, N=4,826
* an active license does not guarantee an individual is actively seeing patients.

Active Pharmacy Licenses by Gender, select license types (when reported)

Figure 208

104 individuals are at full retirement age of 67 in 2022.
Note. One individual did not provide a year of birth
Full retirement age as per Social Security Adminstration*
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.


1. US Bureau of Labor Statistics. (2022, Aug). Pharmacists. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/ pharmacists.htm
2. Delaware Division of Professional Regulation. (n.d.). Intern-US School. Retrieved from: https://dpr.delaware.gov/boards/pharmacy/newlicense/















The primary objective of the Delaware Examining Board of Physical Therapists and Athletic Trainers is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency, • promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to physical therapists, physical therapist assistants and athletic trainers, including temporary licenses.
The Board’s statutory authority is in 24 Del. C., Chapter 26.
Athletic trainers work with people of all ages and all skill levels, from young children to soldiers and professional athletes. Athletic trainers are usually one of the first healthcare providers on the scene when injuries occur on the field. They work under the direction of a licensed physician and with other healthcare providers, often discussing specific injuries and treatment options or evaluating and treating patients, as directed by a physician. Some athletic trainers meet with a team physician or consulting physician regularly.1
Physical therapists, sometimes called PTs, care for people of all ages who have functional problems resulting from back and neck injuries; sprains, strains, and fractures; arthritis; amputations; neurological disorders, such as stroke or cerebral palsy; injuries related to work and sports; and other conditions. Physical therapists use a variety of techniques to care for their patients. These techniques include exercises; training in functional movement, which may include the use of equipment such as canes, crutches, wheelchairs, and walkers; and special movements of joints, muscles, and other soft tissue to improve mobility and decrease pain.2
Physical therapist assistants, sometimes called PTAs, and physical therapist aides work under the direction and supervision of physical therapists. They help patients who are recovering from injuries and illnesses to regain movement and manage pain. Physical therapist assistants are involved in the direct care of patients. Physical therapist aides often have tasks that are indirectly related to patient care, such as cleaning and setting up the treatment area, moving patients, and doing clerical duties.3
Figure 211
Active License Physical Therapists and Athletic Trainers by Type*, N=2,604
* an active license does not guarantee an individual is actively seeing patients.

Figure 212
Active License Physical Therapists and Athletic Trainers by Gender select license types (when reported)
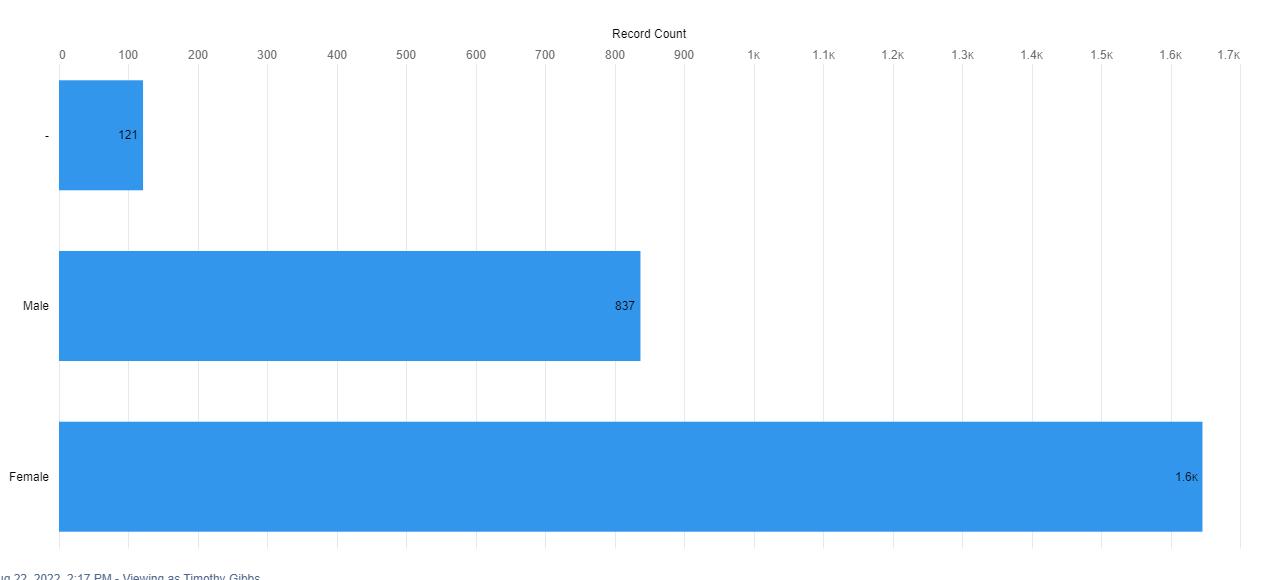
Figure 213
Active License Physical Therapists and Athletic Trainers by Birth Year

47 individuals are at full retirement age of 67 in 2022.
Full retirement age as per Social Security Adminstration*
Note. 35 individuals did not provide a year of birth
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Figure 214
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















1. US Burear of Labor Statistics. (2022, Aug). What athletic trainers do. Occupational Outlook Handbook Retrieved from: https://www.bls.gov/ooh/ healthcare/athletic-trainers.htm#tab-2

2. US Burear of Labor Statistics. (2022, Aug). What physical therapists do. Occupational Outlook Handbook Retrieved from:: https://www.bls.gov/ooh/ healthcare/physical-therapists.htm#tab-2
3. US Burear of Labor Statistics. (2022, Aug). What physical therapist assistants and aides do. Occupational Outlook Handbook Retrieved from:: https:// www.bls.gov/ooh/healthcare/physical-therapist-assistants-and-aides.htm#tab-2
The primary objective of the Delaware Board of Podiatry is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to podiatrists, including temporary licenses, and podiatrists-in-training.
The Board’s statutory authority is in 24 Del. C., Chapter 5
Podiatrists provide medical and surgical care for people with foot, ankle, and lower leg problems. They diagnose illnesses, treat injuries, and perform surgery involving the lower extremities.1
Most podiatrists work in offices of podiatry, either on their own or with other podiatrists. Some work in group practices with other physicians or specialists. Others work in private and public hospitals, in outpatient care centers, or for the government.
Podiatrist In-Training licensees are limited to the practice of medicine in the hospital where they are employed except for any outside medical duties that may be assigned as part of their residency program. They must perform outside duties under the supervision of a fully licensed podiatric physician.
A Temporary Podiatrist license may be issued to an out-of-state Podiatrist when he or she will be taking charge of the practice of a Delaware-licensed Podiatrist during the Delaware licensee’s temporary illness or absence from Delaware.
Figure 220
Active Podiatry Licenses by Type*, N=112
* an active license does not guarantee an individual is actively seeing patients.



Figure 222
Note. One individual did not provide a year of birth
Full retirement age as per Social Security Adminstration*
5 individuals are at full retirement age of 67 in 2022. * According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















1. US Burreau of Labor Statistics. (2022, Aug). What do podiatrists do? Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/ healthcare/podiatrists.htm#tab-2
The primary objective of the Delaware Board of Mental Health and Chemical Dependency Professionals is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency, • promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to professional counselors of mental health, associate counselors of mental health, chemical dependency professionals, marriage and family therapists and associate marriage and family therapists.
Art therapy is an integrative mental health and human services profession that enriches the lives of individuals, families, and communities through active art-making, creative process, applied psychological theory, and human experience within a psychotherapeutic relationship.1
Art therapy, facilitated by a professional art therapist, effectively supports personal and relational treatment goals as well as community concerns. Art therapy is used to improve cognitive and sensorimotor functions, foster self-esteem and self-awareness, cultivate emotional resilience, promote insight, enhance social skills, reduce and resolve conflicts and distress, and advance societal and ecological change.1
Associate Marriage and Family Therapists
Individuals licensed as associates are in the process of accumulating hours towards their full licensure.2
Marriage and family therapists work with individuals, couples, and families. They bring a family-centered perspective to treatment, even when treating individuals. They evaluate family roles and development, to understand how clients’ families affect their mental health.3
Chemical Dependency Counselor runs individual, family, and group counseling for patients in chemical dependency programs. Acts as mediator between patients, relatives, medical staff, and outside agencies if needed. Being a Chemical Dependency Counselor tracks patient progress and dispensation of treatment services.4
Associate Counselor of Mental Health Duties include leading individual and group therapy or interventions, administering medication, providing assistance to patients with their daily hygiene or self-care routines, and supervising recreational activities.5
Professional Counselor of Mental Health Counsels clients and patients, individually and in group sessions, to assist in overcoming dependencies, adjusting to life, and making changes. Maintains confidentiality of records relating to clients treatment. Guides clients in the development of skills and strategies to deal with their problems.6
Figure 225
Active Mental Health and Chemical Dependency Professional Licenses by Type*, N=1,036
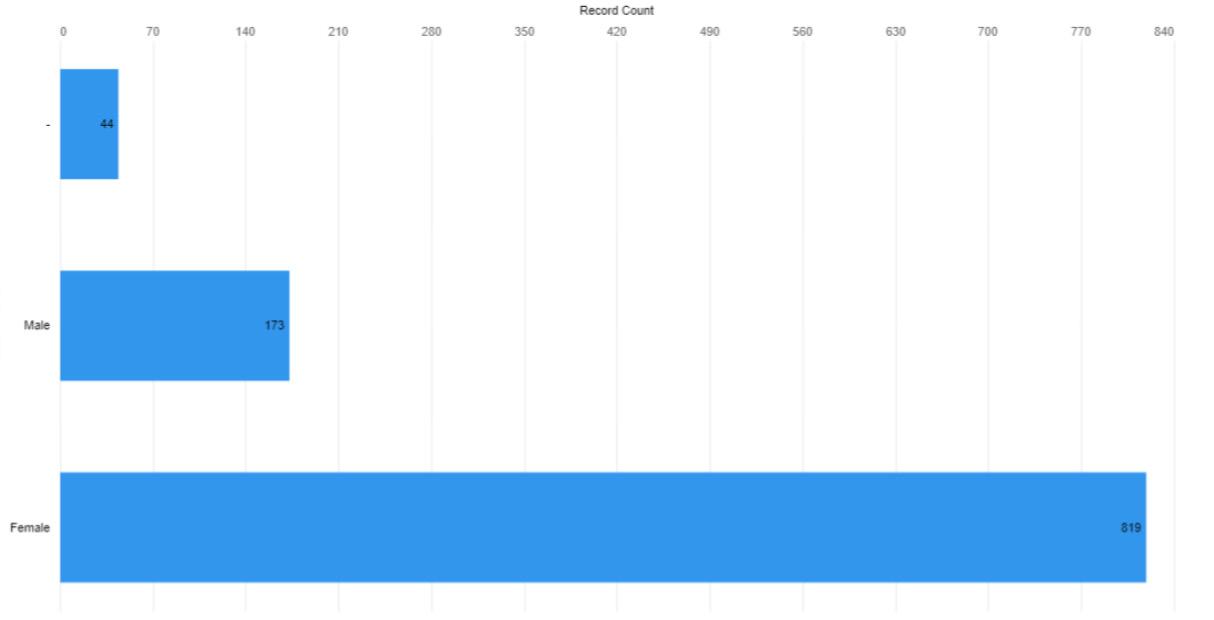

* an active license does not guarantee an individual is actively seeing patients.
Figure 226
Active Mental Health and Chemical Dependency Professional Licenses by Gender by select license types (when reported)

THIS PAGE LEFT INTENTIONALLY BLANK
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19707 19732
19805
19716 19709 19734
19720
19703 19702
19733
19977 19902
19938 19946
19964 19979 19954 19952
19955 19901 19943
19904
a
















19950 19960 19941 19973 19940
19931
19951 19947
19933 19971
19963 19966
19968 19975
19958 19930
i e ry 19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
Wilmington
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943













19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
1. American Art Therapy Association. (n.d.). About art therapy. Retrieved from: https://arttherapy.org/about-art-therapy/
2. American Association for Marriage and Family Therapy. (n.d.). Delaware state resources. Retrieved from: https://www.aamft.org/Advocacy/State_Resources/Delaware.aspx
3. US Bureau of Labor Statistics. (2022, Aug). Marriage and family therapists. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ ooh/community-and-social-service/marriage-and-family-therapists.htm
4. Salary.com. (n.d.). Chemical dependency counselor. Retrieved from: https://www.salary.com/research/job-description/benchmark/chemical-dependency-counselor-job-description
5. Zip Recruiter. (n.d.). What is a mental health associate and how to become one. Retrieved from: https://www.ziprecruiter.com/Career/Mental-Health-Associate/What-Is-How-to-Become
7. Society for Human Resource Management. (n.d.). Mental health counselor. Retrieved from: https://www.shrm.org/ResourcesAndTools/tools-andsamples/job-descriptions/Pages/Mental-Health-Counselor.aspx
The primary objective of the Delaware Board of Examiners of Psychologists is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to psychologists and psychological assistants.
The Board’s statutory authority is in 24 Del. C., Chapter 35
Psychologist
Psychologists study cognitive, emotional, and social processes and behavior by observing, interpreting, and recording how individuals relate to one another and to their environments.
Some psychologists work independently, conducting research, consulting with clients, or working with patients. Others work as part of a healthcare team, collaborating with physicians and social workers, or in school settings, working with students, teachers, parents, and other educators. Those in private practice often work evenings and weekends to accommodate clients.1
Psychological Assistant
Individuals who are in the process of obtaining post-doctoral hours under the supervising Psychologist’s supervision, and will apply for a Psychologist license after completing the post-doctoral hours.2
Figure 240
Active Psychologist Licenses by Type*, N=639
* an active license does not guarantee an individual is actively seeing patients.

Active Psychologist Licenses by Gender select license types (when reported)
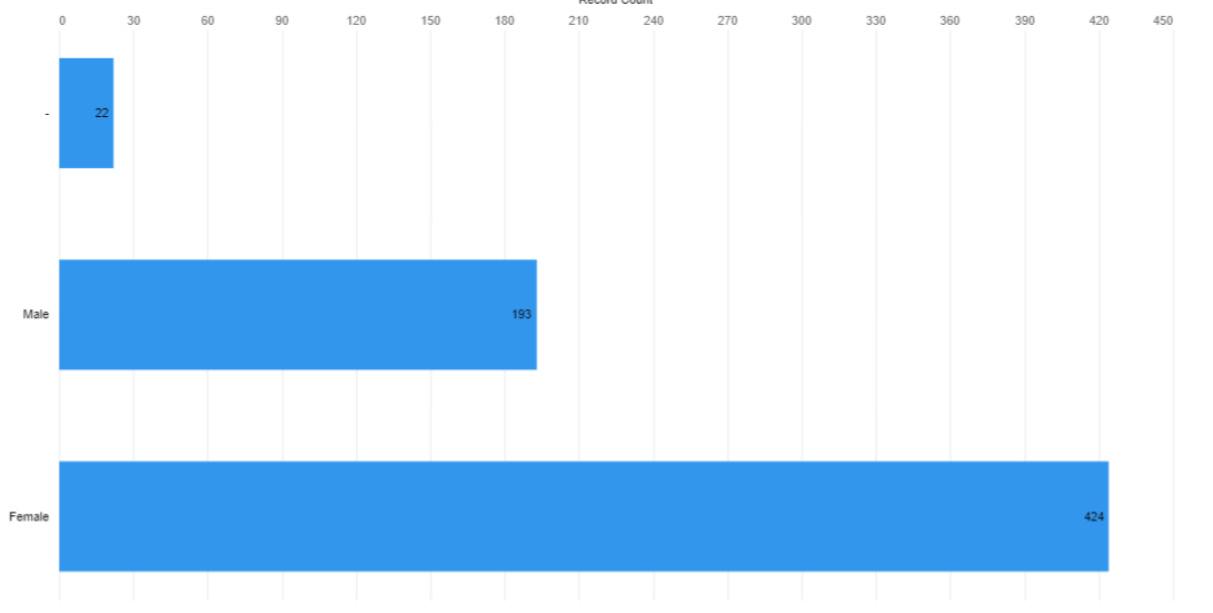
Figure 242

115 individuals are at full retirement age of 67 in 2022. * According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Full retirement age as per Social Security Adminstration*
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















1. US Bureau of Labor Statistics. (2022, Aug). Psychologists. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/life-physical-and-social-science/psychologists.htm
2. Delaware Division of Professional Regulation. (n.d.). Psychological assistant registration. Occupational Outlook Handbook. Retrieved from: https:// dpr.delaware.gov/boards/psychology/newassist/
The primary objective of the Delaware Board of Social Work Examiners is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to clinical social workers.
The Board’s statutory authority is in 24 Del. C., Chapter 39.
Clinical social work is a specialty practice area of social work which focuses on the assessment, diagnosis, treatment, and prevention of mental illness, emotional, and other behavioral disturbances. Individual, group and family therapy are common treatment modalities.1
While there are some social work jobs open to candidates with a bachelor’s degree in a related discipline, a bachelor’s in social work (BSW) is the minimum educational requirement for many positions. BSW program graduates can go on to work as community organizers, case managers, probation officers, and more.2
A Master of Social Work (MSW) degree is the standard requirement for the Licensed Clinical Social Worker (LCSW) credential. However, earning an MSW does not means a practitioner must become an LCSW. MSW graduates can also pursue non-clinical social work jobs or other careers in human services. The LCSW allows social workers to offer psychotherapy services and requires additional testing and experience that is not typically required in those other roles.3
Figure 247
Active License Social Work Practitioner Licenses by Type*, N=2,743
* an active license does not guarantee an individual is actively seeing patients.

Figure 248
Active License Social Work Practitioner Licenses by Gender select license types (when reported)

Note. 16 individuals did not provide a year of birth

Full retirement age as per Social Security Adminstration*
163 individuals are at full retirement age of 67 in 2022. * According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
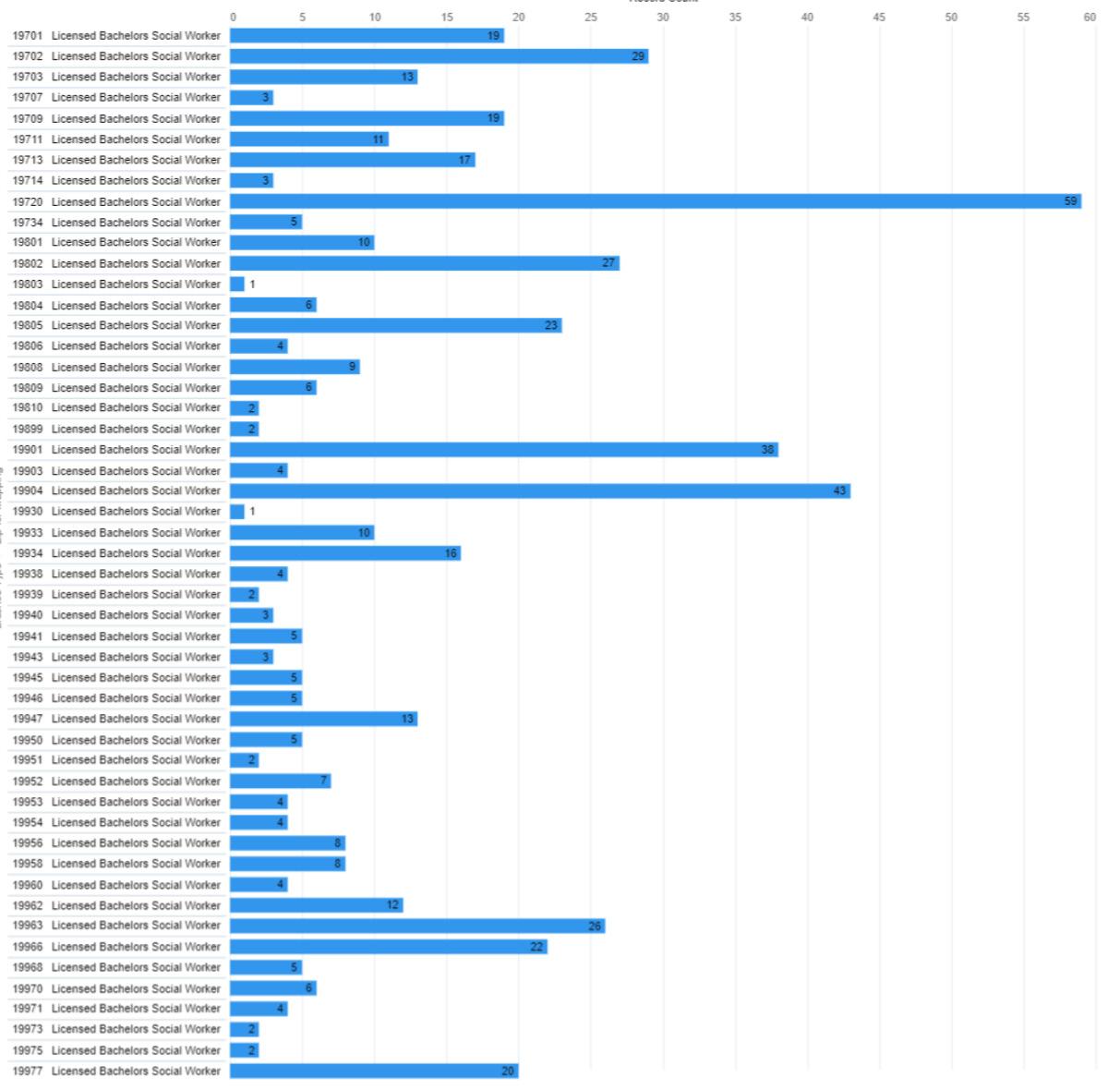















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.













1. National Association of Social Workers. (n.d.). Clinical social work. Retrieved from: https://www.socialworkers.org/Practice/Clinical-Social-Work
2. Social Work License Map. (n.d.). How to become a licensed clinical social worker (LCSW). Retrieved from: https://socialworklicensemap.com/social-work-careers/become-a-lcsw/
3. Wilson, S. (2021, Jun). LCSW vs. MSW (Master of social work). Human Services Edu. Retrieved from: https://www.humanservicesedu.org/ lcswvsmsw/


The primary objective of the Delaware Board of Speech Pathologists, Audiologists, and Hearing Aid Dispensers is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency, • promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to speech/language pathologists, audiologists and hearing aid dispensers.
The Board’s statutory authority is in 24 Del. C., Chapter 37 Audiologist
Audiologists are healthcare professionals who identify, assess and manage disorders of hearing, balance and other neural systems.1
Hearing Aid Dispenser
A hearing aid dispenser, or a hearing instrument specialist, is someone who is authorized by the state to measure hearing and to fit and sell hearing aids.2
Speech / Language Pathologist
Speech-language pathologists work with children and adults who have problems with speech and language, including related cognitive or social communication problems. They may be unable to speak at all, or they may speak with difficulty or have rhythm and fluency problems, such as stuttering.3
Temporary Hearing Aid Dispenser
If one wants to dispense hearing aids in Delaware, they must obtain a Delaware Hearing Aid Dispenser license, with the exception of Delaware-licensed Audiologists.4
Temporary Speech/Language Pathologist
Good for one year, this temporary license allows one to practice as a SLP while their Clinical Fellowship Plan is completed. There are additional requirements listed on the DELPROS website.5
Figure 256
Active Speech Pathology, Audiology, and Hearing Aid Dispenser Licenses by Type*, N=1,100
* an active license does not guarantee an individual is actively seeing patients.

Figure 257
Active License Speech Pathology, Audiology, and Hearing Aid Dispersers by Gender select license types
Figure 258
48 individuals are at full retirement age of 67 in 2022.

Full retirement age as per Social Security Adminstration*
Active License Speech Pathology, Audiology, and Hearing Aid Dispersers by Birth Year * According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”

Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

Reading Wilmington
19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943













19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19703 19702
19805
19720
19701
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.















Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.

19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943














19904
19953 19979 19954 19952
19931
19950 19960 19941 19973 19940
19963 19966
e y
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
1. Johns Hopkins Medicine. (n.d.). What is an audiologist? Retrieved from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/hearing-loss/what-is-an-audiologist
2. The Hearing Center. (2021, May). What is the difference between an audiologist and a hearing aid dispenser? Retrieved from: https://thehearingcentermcc.com/patient-resources/what-is-the-difference-between-an-audiologist-and-a-hearing-aid-dispenser/
3. US Bureau of Labor Statistics. (2022, Aug). Speech-language pathologists. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ ooh/healthcare/speech-language-pathologists.htm
4. Delaware Division of Professional Regulation. (n.d.). Hearing aid dispenser. Retrieved from: https://dpr.delaware.gov/boards/speechaudio/had/ 5. Delaware Division of Professional Regulation. (n.d.). Speech/language pathology licensurer. Retrieved from: https://dpr.delaware.gov/boards/ speechaudio/slpathology/
The primary objective of the Delaware Board of Veterinary Medicine is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to veterinarians and veterinary technicians, including temporary licenses.
The Board’s statutory authority is in 24 Del. C., Chapter 33
Veterinarians care for the health of animals and work to protect public health. They diagnose, treat, and research medical conditions and diseases of pets, livestock, and other animals.1
In addition to helping veterinarians during animal exams, veterinary technologists and technicians do a variety of clinical, care, and laboratory tasks. Veterinary technologists and technicians who work in research-related jobs ensure that animals are handled carefully and are treated humanely. They may help veterinarians or scientists on research projects in areas such as biomedical research, disaster preparedness, and food safety.2
Figure 269
Active Veterinary Practitioner Licenses by Type*, N=1,092
* an active license does not guarantee an individual is actively seeing patients.

Figure 270

Figure 271

70 individuals are at full retirement age of 67 in 2022.
Note. 6 individuals did not provide a year of birth
Full retirement age as per Social Security Adminstration*
Active Veterinary Practitioner Licenses by Birth Year * According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Figure 272
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.















Figure 274
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.













19805
19703 19702
19701
19720
19707 19732 19804 19730


19716 19731 19709 19734
19964
19733
19977 19902
19938 19946
19955 19901 19943
19904
19953 19979 19954 19952
19950 19960 19941 19973 19940
19931
19963 19966
19933 19971
19951 19947
19968 19975
19958 19930
19944 19945
1. US Bureau of Labor Statistics. (2022, Aug). What veterinarians do. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/ healthcare/veterinarians.htm#tab-2
2. US Bureau of Labor Statistics. (2022, Aug). What veterinary technologists and technicians do. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/veterinary-technologists-and-technicians.htm#tab-2
The primary objective of the Controlled Substance Advisory Committee is to promote, preserve and protect the public health, safety and welfare by regulating and monitoring use and abuse of controlled substances. To meet this objective, the Committee
• carries out a program of registration, inspection, investigation and education,
• recommends new/revised rules and regulations and disciplinary sanctions against registrants to the Secretary of State.
The Committee issues registrations to practitioners and facilities that prescribe, dispense, manufacture or distribute controlled substances. Practitioners include physicians, physician assistants, advanced practice registered nurses, podiatrists, dentists, optometrists, and veterinarians. Facilities include pharmacies, distributors, manufacturers, hospitals, clinics, researchers, laboratories and provider pharmacies.
To assist the Committee, the Drug Control Administrator for the Division of Professional Regulation is responsible for the Committee’s regular administrative functions.
The Committee’s authority is in 16 Del. C., Chapter 47 and the Uniform Controlled Substance Act Regulations.
The Controlled Substance Advisory Committee issues an additional license that has a prerequisite of an active practitioner license upon which to build. The following professional licenses may be supplemented with the CSR (Controlled Substances Registration) empowering these provides to prescribe certain classes of medicines which fall under the Uniform Controlled Substance Act Regulations as noted above. In addition, facilities may also be issued a CSR license.
• Advanced Practice Registered Nurse
• Dentist
• Facility
• Optometrist
• Pharmacist
• Physician Assistant
• Podiatrist
• Practitioner (Physicians)
• Veterinarian
Figure 276
Active CSR Licenses by Type*, N=7,760
* an active license does not guarantee an individual is actively seeing patients.

Figure 277

Figure 278

585 individuals are at full retirement age of 67 in 2022.
Note. Two individuals did not provide a year of birth
Full retirement age as per Social Security Adminstration*
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
One overall map is provided regarding the distribution of CSR licensed individuals as their location has already been disclosed in their section of the report for their primary license.
Map on facing page shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
















Long-term care (LTC) is experiencing a workforce crisis. For years this industry, including skilled nursing facilities (SNFs) and assisted living communities, has experienced workforce challenges that have needed to be addressed. The LTC workforce includes nurses and direct care workers. Certified nursing assistants (CNAs), licensed practical nurses (LPNs), and registered nurses (RNs) make up the nursing workforce in this industry. Personal care aides account for direct care workers. The COVID-19 pandemic only exacerbated the problem of retention and recruitment of SNF and assisted living community workers. The industry suffers from workforce shortages even though wages have increased, and bonuses have been offered. Facilities cannot maintain operational costs as the prices of goods and services have increased and hiring contract workers is more expensive than hiring employees. Additionally, there is a lack of qualified and interested candidates to fill open positions as many have left. Overall, the LTC industry lacks adequate funding. Still, the demand for LTC and SNFs is high and will likely increase as the population ages. Nationally, the population of adults 65 and older is expected to increase to 94.7 million by 2060.1 In Delaware, the proportion of adults aged 65 and older is estimated to increase by 48.6% by 2050. Additionally, the population of adults 85 and older will increase by 165%.2,3 The older population of the United States will lack access to and quality care without proper changes. Solutions must be implemented to enhance the workforce in this industry.
According to the Administration for Community Aging, “long-term care is services and supports necessary to meet health or personal care needs over an extended period of time.”4 Long-term care can be provided to anyone at any age, but older adults aged 65 and older who are unable to be independent use long-term care services and live in these facilities, where medical and personal care services are provided.5,6 Assistance with activities of daily living (ADLs), including help with dressing, bathing, eating, and moving around, is provided in multiple settings such as community settings like adult-day cares, assisted living communities, nursing homes, and continuing care retirement communities (CCRCs).4,6,7,8 Nurses, CNAs, and personal care aides provide services to these populations.6,9
According to the Centers for Medicare and Medicaid Services, a skilled nursing facility is “a facility (which meets specific regulatory certification requirements) which primarily provides inpatient skilled nursing care and related services to patients who require medical, nursing, or rehabilitative services but does not provide the level of care or treatment available in a hospital.”10 Individuals are discharged to a SNF when they no longer need care provided by a hospital but are unable to be sent home because they cannot get out of bed, move around, or use a wheelchair safely; have surgical wounds; or do not have adequate help at home. Like other long-term care facilities, SNFs provide assistance with activities of daily living, however SNFs also provide intravenous injections and physical therapy.10,11 These services are carried out by trained and licensed professionals (i.e. registered nurses and doctors). Personal care aides and CNAs are unable to perform these activities but assist with other duties. Other licensed professionals working at SNFs include physician assistants, nurse practitioners, physical therapists, occupational therapists, and speech language pathologists.12
The primary LTC and SNF workforce is composed of nurses and direct care workers. Nurses monitor residents’ and patients’ health conditions, provide education, give medicine, and perform wound care. According to the U.S. Bureau of Labor Statistics (BLS), six percent of nurses work in nursing and rehabilitation facilities.13 Nursing assistants take vital signs and assist with activities of daily living and are supervised by RNs. Most nursing assistants work in SNFs (37%) while some work in CCRCs or assisted living communities (11%).14 Personal care aides have
similar roles. Like nursing assistants, they help residents and patients with ADLs. However, they may also assist with cleaning and laundry, if needed. About 7% personal care aides work in CCRCs and assisted living facilities.15
Direct care aides are mainly women (87%), people of color (59%), and immigrants (27%).16 Generally, there is little training provided for direct care workers and little opportunity for these workers to advance in their career. However, in Delaware regulations are stronger than federal regulations and require not only initial training but on-going continuing education that is monitored by the Division of Healthcare Quality. Within the 24 month recertification period they need to have 24 hours of Continuing education, of which 6 hours must include dementia training, 2 hours residential/patient abuse prevention and they have to have had at least 64 hours of nursing related services for pay under the supervision of a nurse. In addition there is a competency exam with both a written and clinical portion. Seventy-five hours of training is required for CNAs, but no training is required for personal care aides.16
There have been LTC staffing issues prior to the pandemic, but COVID-19 highlighted the issues related to workers of LTC and SNFs. The rapid spread of COVID-19 put additional stress on care workers: these facilities are home to older residents who were likely to become ill, and residents lived close together, so it was difficult to follow distancing recommendations. Additionally, care workers were susceptible to getting sick, but did not always get paid time off, which influenced them to go into work.17 COVID-19 put undue stress on workers who were already burntout, so many left the workforce. Personal Assistance Services Agencies require an orientation, competency test, and training for their establishment.
There was a nursing shortage before the pandemic, but COVID-19 exacerbated the situation. In Indiana, 1,300 more nurses need to graduate every year until 2030 to meet the workforce demand for nurses in the State.18 As of March 2022, nursing staff accounted for the largest workforce shortage in nursing homes.19 In May 2020, 1,414 current and resigned direct care workers were surveyed to understand the challenges that these workers were facing. These workers reported external challenges like managing personal and family needs and financial circumstances; as well as staffing shortages, increased demands at work, and high risk of the virus being transmitted to and from residents.20 The nursing industry continued to suffer staffing shortages throughout the pandemic; by November 2021, 234,000 nursing home employees and 39,000 assisted living employees had left their jobs (Figure 257).21
Even as the pandemic has started to slow down, the industry has not fully recovered. 22,23 An Agency for Healthcare Administration (AHCA) survey of 759 nursing home providers showed that staffing problems have only been made worse for 60% of nursing homes since January 2022. Specifically, 87% of nursing homes have moderate to high levels of staffing shortages and hiring new staff has been challenging for 98% of nursing homes. These shortages could lead to facility closures: 73% of nursing homes are worried they will have to close.24 The National Center for Assisted Living (NCAL) surveyed 120 assisted living facilities and found similar—though less dramatic—results. According to the report from June 2022, staffing issues have only worsened for more than 50% of assisted living communities since the beginning of 2022. Sixty-three percent of facilities have moderate to high levels of staffing shortages, and it has been difficult for 87% of facilities to hire new staff. Some assisted living facilities (16%) are very worried about the possibility of having to close. Others (32%) are somewhat concerned about closing due to understaffing.25 “Lack of interested or qualified” workers is the top issue reported preventing nursing homes and assisted living facilities from hiring new staff (Figures 258 & 259). Due to understaffing, both facilities have asked workers to work overtime, hired staff from agencies, and reduced new admissions. Both types of facilities have even provided bonuses and benefits, increased wages, enhanced the workplace culture, and paid for staff trainings. Ninety percent of nursing home facilities have raised wages and proposed bonuses and over 90% of assisted living facilities have increased wages to entice workers.24,25

Figure 282
Obstacles to Hiring New Staff in Nursing Homes 24


In March of 2022, a total of 406,200 employees had left jobs in long-term care facilities since the beginning of the pandemic.23 Nursing homes lost 15.2% of their workforce or 241,000 employees (Figure 4). There has been an increase in assisted living jobs by 1.8% and CCRC jobs by 0.8%, but this sector has not fully recovered.22 Adequate labor in this industry is important as new residents cannot be admitted without proper employment levels. Facilities need an adequate number and type of staff to admit residents and patients, maintain quality care, and remain open. In July 2022, it was reported that greater than 60% of nursing homes in the United States have limited new admissions.26 Facilities are not closing admissions because they do not have enough beds. New patients are denied admission due to the lack of workers. The median occupancy rate for 2022 was estimated to be 77%, which is a lower occupancy rate than pre-COVID.27 In Oklahoma, a senior home closed due to staffing shortages. Another home in Pennsylvania had to close 61 beds out of 344 due to understaffing.28 Other states like New Hampshire and Massachusetts have closed new admissions due to worker shortages as well.26
These closures not only affect nursing homes but affect other sectors of the healthcare system: a hospital near a nursing home that closed twenty-two beds in Buffalo, New York due to staffing shortages was unable to discharge patients as efficiently because patients ready to be transferred to the nursing home had to wait for available space. This caused a backup at the hospital because patients in the emergency department could not be transferred to a hospital room due to capacity issues.28 In July 2022, 1,066 patients from various hospitals in Massachusetts were waiting to be discharged to a nursing home.26 Many facilities have had to fully close due to understaffing. Since the pandemic, 327 nursing homes have closed across the United States and in April 2022, more than 400 were estimated to close within the year.29 Many of these facilities even obtained 4 or 5-Star ratings from the Centers for Medicare and Medicaid Services (CMS).
Financial circumstances also hinder the industry. These circumstances were emphasized during the pandemic as facilities paid higher wages for employees and contracted workers, and the prices of goods and services increased. Specifically, in 2021, the average hourly wage doubled for nursing staff, like RNs, LPNs, and aides.27 Due to the staffing shortages, many facilities hired staff from agencies, which have higher rates. For contracted and agency nursing wage costs, the average wage per hour doubled to tripled post pandemic (Figure 261).27 In April 2022, hourly wages for SNF, assisted living, and CCRC employees increased again. SNF employees have experienced an
Figure 284
23

average hourly increase of $3.73 (18.2%). The total average hourly wage for SNF in April 2022 was $24.25. Assisted living employees’ wages have increased by 16% for a total average hourly wage of $20.72 and CCRC employees have received an average hourly increase of 17.1% for a total average hourly wage of $22.31.22 A survey of 330 SNFs show that nursing wages per hour and contracted work are still increasing in 2022.30 Retaining staff has been difficult for many facilities and this issue has forced them to hire staff from agencies. However, the cost to hire staff from these agencies further hinders the staffing problem. Contracted hourly rates are higher than hourly rates for employees. In May 2022, the average employee hourly wage for an RN was reported as $42.31 whereas the average contracted hourly rate for an RN was reported as $54.33 (a 28.4% difference).30 Similar differences were reported for LPNs and CNAs for employee versus contracted rates.
Costs of goods and services also increased during the pandemic. From 2020 to 2021, the average inflation rate was 6.9%.27 From March 2021 to March 2022, there was an overall inflation of goods and services of 8.5%.30 Inflation causes cost of care to rise. In June 2022, the average operational costs of nursing home facilities were reported to have increased by 41% in one year while the average operational costs for assisted living facilities were estimated to have increased by 40%.24,25 In May 2022, the number of SNFs at financial risk were estimated to increase to 47%. These facilities would include almost 417,000 residents, and many of the residents at these SNFs are of racial and ethnic minorities.30
Figure 285

According to the 2021 Delaware Nursing Home Utilization Statistical Report, there are 47 nursing homes with a total of 4,926 beds in the State of Delaware. During this time, two nursing homes were reported to have closed (Forward Manor Nursing Home and Foulk Manor South). In 2020, there were 8,238 nursing home admissions; this number increased in 2021 to 9,260. However, the 9,260 nursing home admissions is still 20% lower than before March 2020. From 2020 to 2021, the private nursing home occupancy rate reduced to 74% from 77.1%. Prior to COVID-19, occupancy rates for nursing homes were around 90%, and these occupancy rates have decreased for all three counties in the State of Delaware (New Castle, Kent, and Sussex).2 According to the 2021 Delaware Assisted Living Utilization Statistical Report, there are thirty-two assisted living facilities and two rest residential facilities providing long-term care in Delaware. No assisted living facility closures were reported for 2021. These facilities have a total of 2,003 units and 2,320 beds.3 These facilities are recovering at a faster rate than nursing homes in the State: in 2021, 809 new residents moved into these facilities, which was a 43.4% increase from 2020. Still, this sector has not fully recovered, this increase is 9.7% fewer than the number of residents who moved into these facilities prior to the pandemic.3
The LTC and SNF industry has not fully recovered from the effects of the pandemic, even with these increases in admissions and move-ins. The population of older adults is expected to increase exponentially from 2020 to 2050, emphasizing the need to improve this sector of healthcare and increase the number of staff recruited to work in LTC and SNFs.
The LTC and SNF industry needs improvement now more than ever. Unlike other sectors of healthcare, this industry has not been able to fully recover from the pandemic. Staffing shortages have existed prior to the pandemic, but the rapid spread of COVID-19 made the issue worse. Workers became stressed and burnt out in times of increasing workload demand. Workers leaving the industry exacerbated the stress felt from the employees who stayed. Understaffing influenced facilities to increase wages and offer bonuses and forced them to use contract agencies. Contract workers cost facilities more money but do not always deliver the same level of care as nursing employees. Contract staff do not work at the same facilities every day, leading to inconsistent care for residents and patients. The supply of long-term care workers needs to be increased as other healthcare facilities, like hospitals need to hire similar staff such as nurses. In February 2022, the Biden Administration suggested a minimum nursing home staff requirement. With such a limited pool of qualified and interested workers this requirement would cause many nursing homes (94%) to have to hire more staff, increasing costs for facilities.31,32
Of note, DELPROS does not collect information on CNA’s. The Division of Healthcare Quality is responsible for the training and testing program for CNAs and for the CNA Registry. At the time of this report, we were unable access their database, thus the lack of essential CNA information in this report.
1. Administration on Aging. (2021). 2020 profile older Americans. U.S. Department of Health and Human Services, Administration for Community Aging. https://acl.gov/sites/default/files/Profile%20of%20OA/2020ProfileOlderAmericans_RevisedFinal.pdf
2. Delaware Health and Social Services & Delaware Healthcare Commission. (2022, May). 2021 Delaware nursing home utilization statistical report. https://dhss.delaware.gov/dhcc/hrb/files/nursinghomeutilization2021.pdf
3. Delaware Health and Social Services & Delaware Healthcare Commission. (2022, May). 2021 Delaware assisted living utilization statistical report. https://dhss.delaware.gov/dhcc/hrb/files/2021alrrpt.pdf
4. Administration for Community Aging. (2020, March). Glossary. U.S. Department of Health and Human Services. https://acl.gov/ltc/glossary#longterm-care
5. Centers for Disease Control and Prevention. (2020). Nursing homes and assisted living (Long-term Care Facilities [LTCFs]). U.S. Department of Health and Human Services. https://www.cdc.gov/longtermcare/index.html
6. National Institute on Aging. (n.d.). What is long term care? U.S. Department of Health and Human Services, National Institutes of Health. https:// www.nia.nih.gov/health/what-long-term-care
7. Administration for Community Living. (2020, Feb). Where can you receive care? U.S. Department of Health and Human Services. https://acl.gov/ltc/
basic-needs/where-can-you-receive-care
8. U.S. Centers for Medicare and Medicaid Services. (n.d.). Long-term care. U.S. Department of Health and Human Services. https://www.healthcare.gov/ glossary/long-term-care/
9. Administration for Community Living. (2020, Feb). Who will provide your care? U.S. Department of Health and Human Services. https://acl.gov/ltc/ basic-needs/who-will-provide-your-care
10. Centers for Medicare and Medicaid Services. (n.d.). Glossary. https://www.cms.gov/glossary
11. Centers for Medicare and Medicaid Services. (n.d.). Skilled nursing facility care. U.S. Department of Health and Human Services. https://www. healthcare.gov/glossary/skilled-nursing-facility-care/
12. National Library of Medicine. (2021, July). Skilled nursing or rehabilitation facilities. U.S. Department of Health and Human Services, National Institutes of Health. https://medlineplus.gov/ency/patientinstructions/000435.htm
13. U.S. Bureau of Labor Statistics. (2022, April). Occupational outlook handbook, Registered nurses. U.S. Department of Labor. https://www.bls.gov/ ooh/healthcare/registered-nurses.htm
14. U.S. Bureau of Labor Statistics. (2022, April). Occupational outlook handbook, Nursing Assistants and orderlies. U.S. Department of Labor. https:// www.bls.gov/ooh/healthcare/nursing-assistants.htm#tab-2
15. U.S. Bureau of Labor Statistics. (2022, April). Occupational outlook handbook, Home health and personal care aides. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/home-health-aides-and-personal-care-aides.htm
16. Stone, R.I. & Bryant, N. (2021). Feeling valued because they are valued. [White Paper]. LeadingAge LTSS Center. https://leadingage.org/sites/default/ files/Workforce%20Vision%20Paper_FINAL.pdf
17. Barnett, M.L. & Grabowski, D.C. (2020). Nursing homes are ground zero for COVID-19 pandemic. JAMA Health Forum, 1(3), e200369. https://doi. org/10.1001/jamahealthforum.2020.0369
18. Quinton, S. (2022). As nurses quit, states seek to train more. Pew. https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2022/03/17/ as-nurses-quit-states-seek-to-train-more
19. Musumeci, M., Childress, E. & Harris, B. (2022, May). State actions to address nursing home staffing during COVID-19. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/state-actions-to-address-nursing-home-staffing-during-covid-19/
20. Cimarolli, V. & Bryant, N. (2021). COVID-19: Experiences of direct care workers in aging services. LeadingAge LTSS Center. https://www.ltsscenter. org/wp-content/uploads/2021/02/COVID-Brief-LTSS-Feb-2021_FINAL.pdf
21. American Healthcare Association / National Center for Assisted Living. (2021). BLS November jobs report: Nursing homes. [Fact sheet]. https:// www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/AHCA%20NCAL%20Report_BLS%20Data%20on%20Staffing%20 Shortages%2012.10.21.pdf
22. Zahraoui, O. (2022, Jun). Workforce contraction and recovery varies across healthcare sectors. National Investment Center. https://blog.nic.org/ workforce-contraction-and-recovery-varies-across-healthcare-sectors
23. American Healthcare Association / National Center for Assisted Living. (2022). BLS March 2022 jobs report. [Fact sheet]. https://www.ahcancal.org/ News-and-Communications/Fact-Sheets/FactSheets/BLS-MARCH2022-JOBS-REPORT.pdf
24. American Healthcare Association. (2022). State of the nursing home industry: Survey of 759 nursing home providers show industry still facing major staffing and economic crisis. [Slides]. https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/SNF-Survey-June2022.pdf
25. National Center for Assisted Living. (2022). State of the assisted living industry: Survey of 120 assisted living providers show industry still facing major staffing and economic crisis. [Slides]. https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/AL-Survey-June2022.pdf
26. American Healthcare Association / National Center for Assisted Living. (2022, July 14). Historic staffing shortages continue to force nursing homes to limit new admissions, creating bottlenecks at hospitals and reducing access to care for seniors [Press release]. https://www.ahcancal.org/Newsand-Communications/Press-Releases/Pages/Historic-Staffing-Shortages-Continue-To-Force-Nursing-Homes-To-Limit-New-Admissions,-CreatingBottlenecks-at-Hospitals-and-.aspx
27. CliftonLarsonAllen LLP. (2022). State of skilled nursing facility (SNF) industry. [Slides] American Healthcare Association/ National Center for Assisted Living. https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/2022%20State%20of%20the%20SNF%20Industry%20 Report.pdf
28. Bernstein, L. & Van Dam, A. (2021, Dec). Nursing home staff shortages are worsening problems at overwhelmed hospitals. The Washington Post. https://www.washingtonpost.com/health/2021/12/28/nursing-home-hospital-staff-shortages/
29. American Healthcare Association / National Center for Assisted Living. (2022). Nursing home closures: By the numbers. https://www.ahcancal.org/ News-and-Communications/Fact-Sheets/FactSheets/SNF-Closures-Report.pdf
30. CliftonLarsonAllen LLP. (2022). State of skilled nursing facility industry: In-depth analysis on increasing cost and local impact. [Slides] American Healthcare Association/ National Center for Assisted Living. https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/AHCA%20 -%20State%20of%20Skilled%20Nursing%20Facility%20Industry%20-%20In-Depth%20Analysis%20on%20Increasing%20Costs%20and%20Local%20 Impact.pdf
31. American Healthcare Association / National Center for Assisted Living. (2022, July 19). Report: Increasing nursing home staffing minimums estimated at $10 billion annually [Press release]. https://www.ahcancal.org/News-and-Communications/Press-Releases/Pages/Report-Increasing-Nursing-HomeStaffing-Minimums-Estimated-at-$10-Billion-Annually.aspx
32. CliftonLarsonAllen LLP. (2022, July). Staffing mandates analysis in-depth analysis on minimum nurse staffing levels and local impact. [Slides] American Healthcare Association/ National Center for Assisted Living. https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/CLAStaffing-Mandate-Analysis.pdf
THIS PAGE LEFT INTENTIONALLY BLANK
Team-based care is becoming increasingly important as the health system changes. There is currently a physician shortage issue in the United States. A report from the Association of American Medical Colleges predicts that there will be a shortage of 17,800 to 48,000 primary care physicians and a shortage of 21,000 and 77,100 of non-primary care physicians by 2034.1 Ensuring that other healthcare professionals can collaborate, and delegating tasks away from the physician might improve the physician shortage problem. The population of the U.S. is aging, and disease states are becoming more complex.2 These issues will require the expertise of various care team members so that the patient receives the most effective care to optimize outcomes.
Team-based care involves two or more health professionals working with the patient to achieve shared goals.3 Health professionals from multiple disciplines work together to inform decision-making that also includes families in the care plan.4 The professionals involved on the care team will vary depending on the population, type of disease, and healthcare setting.3,5 For instance, a mix of registered nurses, medical assistants, nurse aides, technologists, nutritionists, genetic counselors, social workers, and chaplains along with primary care providers could make up a cardiovascular care team.2 However, allergists or immunologists should be a part of a team that provides care for patients with asthma.6
Although team-based care is needed in the United States to address healthcare system issues, care teams need to be effective to improve patient health outcomes. An effective healthcare team will embody multiple characteristics, such as shared goals, explicitly stated roles, clear and prompt communication, respect, and a positive attitude.7,8 Healthcare team members need to work together with the patient and family to address shared goals. Roles and responsibilities for each care member should be clearly stated and each care member needs to know what is expected of each other. If problems arise, then team members should be open and honest about any mistakes or uncertainties.2
The purpose of this review is to identify the primary members of a care team and determine what characteristics make an effect care team. This review seeks to answer the following questions:
1. What is the ideal care team?
2. What are the characteristics of an effective care team?
Understanding the composition of the ideal healthcare team will assist healthcare leaders, healthcare settings, and policy makers, among others, to create care teams that are effective to improve patient health outcomes.
Patients along with their families are the most important member of the healthcare team. Patients contribute to the care plan and collaborate with the care team on shared health goals.2,4,9 It is essential that care teams factor in the preferences of patients and their families to achieve desired health results. When patients are included on the care team, they experience higher satisfaction and achieve better self-management skills and adhere to treatment more (Biederman, 2021).15
Primary care providers such as physicians, advanced practice nurses (APNs), nurse practitioners (NPs), and physician assistants (PAs) should be involved in all care teams, especially related to cardiac care, cancer, HIV/AIDs, and asthma teams.2,10-16 Physicians are highly trained health professionals with a large scope of practice. Primary care physicians are most likely the first health professional that a patient will visit before being diagnosed with a health
condition. However, other advanced practice providers, like APNs, NPs and PAs, are suitable to care for patients with chronic conditions. These healthcare professionals should assist patients within their scope of practice but can help delegate tasks away from the physician. APNs can provide education and chronic disease management services while PAs roles directly align with physicians.2 In a study that examined how A1c, LDL, and systolic blood pressure measures related to new onset disease differed between solo and team-based care teams, teams had more patients who brought their A1c, LDL, and systolic blood pressure under control. Teams included physicians-only teams, non-physician teams of NPs and PAs, and mixed teams of physician and non-physicians. All teams had the same effect on patients lowering their A1c and LCL levels. However, physician-only teams and mixed teams showed patients with better management of hypertension compared to the other types of teams.10 Providers who have expertise in the health condition of concern, such as HIV care, will have patients who experience better HIV outcomes. Primary care providers should then refer out to other providers on the team if they are less familiar with HIV.14 Referral to specialists will be need for numerous diseases. Overall, primary care providers can enhance the care of patients due to their autonomy, expertise, and skill.2,15
Specialists will be required on care teams for most chronic diseases, as primary care providers do not have the full expertise on chronic conditions related to cardiac diseases, cancer, HIV/AIDS, and asthma. Exercise specialists may be on the cardiac team as they can provide behavioral counseling and it is recommended that behavioral counseling is offered to individuals eighteen years or older with hypertension and multiple risk factors for heart.17 For cancer, there are several types of cancer teams due to the prevalence of various forms of cancer. Other cancer teams that need to be included in cancer care can include radiology, pulmonology, and palliative care among others.9,11,12 In a systematic review, it was shown that multidisciplinary cancer care teams improved patient’s adherence to pain medication. Additionally, palliative care teams decreased hospitalizations and increased quality of life for those with cancer.18 Due to the aging population, geriatricians are an important aspect to HIV/AIDS care. In fact, any team member should be familiar with regular HIV care as well as geriatric approaches to HIV.13 Geriatricians may also be important team members for other chronic illnesses because the population of the U.S. is aging. Finally, allergists and immunologists, physician specialists, are a part of asthma care teams. These health professionals can confirm asthma diagnoses, provide additional recommendations, and assist with controlling more difficult symptoms.6
Nurses and Pharmacists
Nurses and pharmacists add additional expertise to primary care providers roles and teams. For years, nurses have shown that they can improve chronic disease management, especially if they are trained in the disease that their patient is experiencing. In an intervention for thyroid cancer, nurses had a comprehensive role by being involved in the reveal of biopsy results and providing support. Results of the intervention revealed that thyroid patients consider nurses an essential part of their care.19 Additionally, nurses assist primary care providers by communicating with them regularly and assisting with medication management by contacting pharmacists in the interest of physicians. 8,20
A pharmacist is crucial to have on the team as they have also been shown to improve chronic disease management outcomes and can assist physicians with medication responsibilities.8,20 Pharmacists assist with medication management, adherence, and education.2,21 A hypothetical intervention using modeling examined the impact of a care team involving a pharmacist on health and cost in the U.S. It was found that pharmacists on a care team prevented uncontrolled blood pressure, heart attacks, strokes, and cardiovascular deaths over five years.21 A review of 54 studies conducted by the Community Preventive Services Task Force shows that nurses and pharmacists working together provide strong evidence for hypertension management.22 Specifically, blood pressure control and systolic blood pressure improved more when a nurse and pharmacist were on a team together and when they had the ability to control hypertension medication with and without physician approval.
Community health workers (CHWs) add significant assistance to care teams. Community health workers, also referred to as lay health workers, peer educators, patient navigators, among others, are trusted members of communities and provide support and resources to community members.23,24 Over the years, lay health workers
have been shown to be effective on care teams to improve chronic disease management.8 For heart disease, community health workers have been associated with decreases in cardiovascular risks and reduction of blood pressure, cholesterol, and blood sugar levels.23 For HIV, community health workers have been able to commonly refer individuals to STI testing and health education during a street-based outreach intervention. The CHWs in this intervention referred ten individuals with HIV, to HIV medical care, twenty individuals who injected drugs to syringe service programs, and nineteen individuals who were at risk for HIV infections to a medical visit for PreP.23
Social workers team members of multiple care teams. During a multidisciplinary care team intervention, a team of a social worker along with a nurse and pharmacist resulted in improved antiretroviral therapy (ART) adherence.23 This adherence even occurred when non-HIV specialists were on the care team. Social workers who have led teams and have had shared responsibilities on teams have improved health outcomes related to asthma, maternal and child health, and hospitalized patients. These teams included nurses, physicians, PAs, pharmacists, counselors, and administrative staff. Patients with asthma had increased symptom-free days, NICU admission rates decreased, and mortality rates for patients who were frequently hospitalized decreased with the inclusion of social workers.48
Registered Dietitians show improved health outcomes on teams as well. A retrospective cohort study showed that high-risk adults had greater improvements in HbA1c and greater weight loss than the group only seen by a primary care physician.27 The study resulted in long-term improvements at six, twelve, and twenty-four months. Although the improvement related to weight loss was not significant at six or twenty-four months. The decrease in HbA1c was significant at twelve and twenty-four months. Dietitians are experts in nutritional counseling and a systematic review of randomized controlled trials examining the effects of dietitians in primary care environments showed that the effect of dietitians on weight management and blood sugar control to be positive. The same review showed fewer positive effects on cholesterol, blood pressure, and triglycerides but this could be because this review did not include multidisciplinary care team studies.28 If dietitians are not on the care team, then physicians and primary care providers can refer their patients to a nutrition professional.29
It is just as important to have teams that are effective than it is to have a team composed of certain professionals with specific expertise. Leadership is important to any team. Most healthcare teams will be led by physicians. If fact, the American Medical Association believes that physicians should lead all teams due to physicians’ high level of expertise and scope of practice.30 In contrast, the American College of Cardiology states that the leadership role of care teams should be dependent on the task that needs to be completed. The leader of the team should be a flexible role.2
Team roles need to be clarified and clearly stated.2,7,18 Explicitly defined roles help inform all team members of each member’s responsibilities and duties so that there is no confusion. Team members who are aware of their roles can then take accountability for their actions. Confusion can be avoided with proper communication between and within teams as well. Communication should be clear and prompt.7,8 Regular team meetings can enhance team communication.5
Team care now more than ever is becoming imperative as the physician shortage problem worsens, the U.S. population ages, and disease severity increases. The patient is at the forefront of all healthcare teams while other members can vary. Most often, primary care providers, nurses, pharmacists, community health workers, social workers, dietitians, and specialists should collaborate with the patient. Other members on care teams will depend on the type of illness, patient characteristics, and setting. Health professionals can delegate tasks away from each other so that other members can practice at their full capacity. Though, no matter what, team members must work within
their scope of practice.5
Effective teams are just as important as the composition of teams. Effective teams improve patient outcomes and enhance how teams interact with one another. A survey of primary care providers and staff from primary care clinics in San Francisco found that a positive team culture improves burnout in primary care. Team culture was found to have more benefit in decreasing burnout than team structure.31
Implementing effective care teams is imperative as the nature of primary care changes and the physician shortage issue continues. Patients, primary care providers, nurses, pharmacists, community health workers, social workers, dietitians, and specialists should be involved on all teams to encompass all aspects of care and enhance patient outcomes. The composition of care teams will vary slightly depending on the patient needs and care environment. Care teams should be trained to work together effectively.
1. IHS Markit LTd. (n.d.). The complexities of physician supply and demand: Projections from 2019 to 2034. Association of American Medical Colleges. https://www.aamc.org/media/54681/download
2. Brush, J.E., Handberg, E.M., Biga, C., Birtcher, K.K., Bove, A.A., Casale, P.N., …, Wyman, J.F. (2015). 2015 ACC health policy statement on cardiovascular team-based care and the role of advanced practice providers. Journal of the American College of Cardiology, 65(19), 2118-2136. https:// doi.org/10.1016/j.jacc.2015.03.550
3. Hupke, C. (2014, May 16). Team-based care: optimizing primary care for patients and providers. Institute for Healthcare Improvement. http://www.ihi. org/communities/blogs/team-based-care-optimizing-primary-care-for-patients-and-providers-
4. Arnett, D.K., Blumenthal, R.S., Albert, M.A., Buroker, A.B., Goldberger, Z.D., Hahn, E.J., …, Ziaeian, B. (2019). 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation, 140(11), e596–e646. https://doi.org/10.1161/CIR.0000000000000678
5. Institute for Healthcare Improvement. (n.d.). Optimize the care team. http://www.ihi.org/resources/Pages/Changes/OptimizetheCareTeam.aspx
6. American Academy of Allergy Asthma and Immunology. (n.d). Consultation and referral guidelines: How the allergist/immunologist can help. https:// www.aaaai.org/Allergist-Resources/Statements-Practice-Parameters/consultation-and-referral-guidelines
7. Safford, B. & Manning, C.A. (2012). Six characteristics of effective practice teams. Family Practice Management, 19(3), 26-30. https://www.aafp.org/ pubs/fpm/issues/2012/0500/p26.html
8. Wagner, E. (2000). The role of patient care teams in chronic disease management. BMJ, 320(7234), 569-572. https://doi.org/10.1136/bmj.320.7234.569
9. Osarogiagbon, R.U., Rodriguez, H.P., Hicks, D., Signore, R.S., Roark, K., Kedia, S.K., …, & Krasna, M.J. (2016). Deploying team science principles to optimize interdisciplinary lung cancer care delivery: Avoiding the long and winding road to optimal care. Journal of Oncology Practice, 12(11), 983-991. https://doi.org10.1200/JOP.2016.013813
10. Pany, M.J., Chen, L., Sheridan, B., & Huckman, R.S. (2021). Provider teams outperform solo providers in managing chronic disease and could improve the value of care. Health Affairs, 40(3), 435-444. https://doi.org10.1377/hlthaff.2020.01580.
11. Institute of Medicine. (2013). Delivering high-quality cancer care: Charting a new course for a system in crisis. The National Academies Press. https:// nap.nationalacademies.org/read/18359/chapter/6
12. Verhoeven, D.C., Chollette, V., Lazzara, E.H., Shuffler, M.L., Osarogiagbon, R.U., & Weaver, S.J. (2021). The anatomy and physiology of teaming in cancer care delivery: A conceptual framework. Journal of the National Cancer Institute, 113(4), 360-370. https://doi.org/10.1093/jnci/djaa166
13. Health Resources and Services Administration. (n.d.). Optimizing HIV care for people aging with HIV: Putting together the best healthcare team. U.S. Department of Health and Human Services. https://ryanwhite.hrsa.gov/sites/default/files/ryanwhite/grants/aging-guide-best-team.pdf
14. Goldschmidt, R.H. & Cu, C. (2016). Primary care for patients with HIV infection: It’s not who should provide it, it’s how to provide it. American Family Physician, 94(9), 687-688. https://www.aafp.org/afp/2016/1101/p687.html
15. U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Primary Healthcare. (2017). Integrating HIV care, treatment & prevention services into primary care – a toolkit for health centers. https://bphc.hrsa.gov/sites/default/files/bphc/technicalassistance/p4c-toolkit-2018.pdf
16. Asthma and Allergy Foundation of America. (n.d.). healthcare professionals. https://www.aafa.org/about-aafa/our-partners/health-care-professionals. aspx
17. U.S. Preventive Services Task Force. (2020, November). Healthy diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: Behavioral counseling interventions. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/healthy-diet-andphysical-activity-counseling-adults-with-high-risk-of-cvd
18. Taplin, S.H., Weaver, S., Salas, E., Chollette, V., Edwards, H.M., Bruinooge, S.S., & Kosty, M.P. (2015). Reviewing cancer care team effectiveness. Journal of Oncology Practice, 11(3), 239-246. https://doi.org/10.1200/JOP.2014.003350
19. Henry, M., Frenkiel, S., Chartier, G., MacDonald, C., Payne, R.J., Black, M.J., …, & Hier, M.P. (2018). Thyroid cancer patients receiving an interdisciplinary team-based care approach (ITCA-ThyCa) appear to display better outcomes: Program evaluation results indicating a need for further integrated care and support. Psycho-Oncology, 27(3), 937-945. https://doi.org/10.1002/pon.4590
20. Smith, M.A. (2018). Primary care teams and pharmacist staffing ratios: Is there a magic number? Annals of Pharmacotherapy, 52(3), 290-294. https:// doi.org/10.1177/1060028017735119
21. Overwyk, K.J., Dehmer, S.P., Roy, K., Maciosek, M.V., Hong, Y., Baker-Goering, M.M., …, & C. Ritchey, M.D. (2019). Modeling the health and budgetary impacts of a team-based hypertension care intervention that includes pharmacists. Medical Care, 57(11), 882-889. https://doi.org/10.1097/ MLR.0000000000001213
22. The Community Preventive Services Task Force. (2020, December). Heart disease and stroke prevention: Team-based care to improve blood pressure control. https://www.thecommunityguide.org/content/tffrs-heart-disease-and-stroke-prevention-team-based-care-improve-blood-pressure-control
23. Centers for Disease Control and Prevention. (2020, June). Integrating community health workers on clinical care teams and in the community. U.S. Department of Health & Human Services. https://www.cdc.gov/dhdsp/pubs/guides/best-practices/chw.htm
24. Centers for Disease Control and Prevention. (2016, January). CHW job titles. https://www.cdc.gov/dhdsp/chw_elearning/s1_p6.html
25. Hammack, A.Y., Bickham, J.N., Gilliard, I., & Robinson, W.T. (2021). A community health worker approach to ending the HIV epidemic. American Journal of Preventive Medicine, 61(5), S26-S31. https://doi.org/10.1016/j.amepre.2021.06.008
26. Horberg, M.A., Hurley, L.B., Towner, W.J., Allerton, M.W., Ting-Ting Tang, B., Catz, S.L. ,…, & Quesenberry, C.P. (2012). Determination of optimized multidisciplinary care team for maximal antiretroviral therapy adherence. Journal of Acquired Immune Deficiency Syndromes, 60(2), 183-190. https://doi. org/10.1097/QAI.0b013e31824bd605
27. Zeman, H., Cavanaugh, E., Metallinos-Katsaras, E., Ireland, K., Pojednic, R. (2021). Improved long-term outcomes in high-risk patients receiving registered dietitian nutritionist care. Endocrine and Metabolic Science, 2(31), https://doi.org/10.1016/j.endmts.2021.100078
28. Mitchell, L.J., Ball, L.E., Ross, L.J., Barnes, K.A., Williams, L.T. (2017). Effectiveness of dietetic consultations in primary healthcare: A systematic review of randomized controlled trials. Journal of the Academy of Nutrition and Dietetics, 117(12), 1941-1962.
29. Ellis, E. (2021). Nutrition tips to keep the immune system strong for people with HIV-AIDS. Eat Right. https://www.eatright.org/health/diseasesand-conditions/hiv-aids/nutrition-tips-to-keep-the-immune-system-strong-for-people-with-hiv-aids
30. American Medical Association. (2022). What is scope of practice? https://www.ama-assn.org/practice-management/scope-practice/what-scopepractice
31. Willard-Grace, R., Hessler, D., Rogers, E., Dubé, K., Bodenheimer, T., & Grumbach, K. (2014). Team structure and culture are associated with lower burnout in primary care. The Journal of the American Board of Family Medicine, 27(2), 229-238. https://doi.org/10.3122/jabfm.2014.02.130215
The prevalence of chronic disease remains high in the United States. In the U.S., six in ten adults experience a chronic illness while four in ten adults have two or more.1 Those that experience chronic conditions visit primary care physicians and specialists. Primary care enhances the health of populations, reduces health costs, and improves quality of life. By 2034 there will be a shortage of between 17,800 to 48,000 primary care physicians and a shortage of between 21,000 and 77,100 of non-primary care physicians.2 To ensure that proper patient care is provided, it is imperative that physicians and providers deliver adequate patient care to optimize health outcomes. Adequate patient care can be delivered by focusing on patient panel sizes for physicians, providers, and the organization of healthcare.
Patient panel size refers to the number of patients that a physician cares for during a specified period, usually 12 or 18 months. The standard patient panel size has often been determined to be 2500 patients. However, according to the Journal of the American Board of Family Medicine, this number is not feasible for a primary care physician to provide adequate patient interaction for all patients. At a panel size of 2500, a physician would have to work 21.7 hours per day to provide proper care to each patient.3,4 Calculating the ideal patient panel size is important to ascertain the number of patients seeking consultations and treatments, as well as the provider’s workload. It is important that providers on the same level share similar workloads, especially if they are earning similar salaries.5
Many factors affect what the patient panel size for a physician should be, including the organizational set up of practices, how the physician prefers to care for their patient, the type of patient population that the physician cares for, and the number and type of health professionals who work with physicians.3 Due to these changing factors, it can be just as important to manage patient panel sizes as it is to know the proper patient panel size.
The purpose of this review is to identify the number patients that should be on a provider’s panel to provide adequate patient interaction and determine how to manage patient panels for optimal outcomes. This review seeks to answer the following questions:
1. What is the ideal patient panel size based on disease (or wellness) state?
2. What factors affect patient panel size and how can panel sizes be managed correctly?
Answering these questions can provide guidance to primary care providers and team members to help providers have enough time to care for patients that need services. Optimizing care will improve patient health outcomes.
Establishing a patient panel for providers ensures that the patient is given a provider with whom they can build a relationship and trust.5 Patients deserve adequate care to optimize their health outcomes and determining patient panel sizes can ensure that practices are making enough revenue. In the past, the ideal patient panel size has been calculated by determining the current panel size, not necessarily what the panel size should be for optimal care.5,6 Determining the current panel size has previously been completed by using the “four-cut method.”6
First, the patient panel for the practice must be identified. In 2007, the Family Practice Management Journal suggested that the patient panel for a practice was determined by identifying the patients who have seen a provider
in the last 18 months, since many patients do not visit providers within a one year timeframe.7 More recently, the active panel has been suggested to be the patients seen by a physician or primary care provider within the last 12 months.6 It is unclear which period of time is correct, and practices may use different timeframes depending on what is best for them.
Second, the patient panel per provider is calculated by assigning a patient on the practice’s panel to the provider that they have visited the most. Sometimes, a patient on the practice’s panel has seen more than one provider. Certain guidelines can assist to determine what provider’s panel the patient should be on. If the patient has seen providers equally, then the patient is assigned to the provider who they saw first, last, or for their most recent health check.5,6
Another way to calculate patient panel size is using a supply and demand equation, like panel size multiplied by visits per patient per year (demand) which equals provider visits per day multiplied by provider days per year (supply). The number of patients needing an appointment must equal the number of appointment slots that a provider has available.7 Lack of appointments create high demand and may cause inadequate care. Too few patients needing to be seen causes practice revenue to decrease.
A systematic review to determine the patient panel size for the Veterans’ Administration (VA) showed that some of these older methods can be updated.8 The “right-sized” process can be used to determine what the panel should be for providers:6 this process factors in patient and workload complexity. 6 Severity of patient illness, reporting and patient charting guidelines, refilling prescriptions, and conducting visits via telehealth while checking patients inperson throughout the workday will decrease physician capacity to conduct appointments.
In order to “right size” the patient panel, the Family Practice Management Journal created a spreadsheet. First, practices should use the “four-cut method to assign patients to providers. This information goes into the spreadsheet, which includes the current panel, visit rate, physician days worked, and visits per day so that the current panel and right-sized panel can be compared. The right-sized panel is calculated by dividing clinician visit capacity by the panel visit rate. The equation is days worked per year multiplied by visits per day divided by visit rate.6 No evidence was found that this equation determines the ideal patient panel size; numerous factors impact the capacity that physicians have to see patients, other factors influence the need for patients to receive services, and these factors can constantly evolve.
Balancing patient demand and provider supply is important to create the ideal patient panel size, however the organization of healthcare affects demand and supply. Primary care in the U.S. is changing rapidly.9 Understanding primary care is important as populations in the U.S. visit primary care services more than any other type of healthcare service. The American Medical Association’s Physician Practice Benchmark Surveys assist in understanding the change in primary care. These surveys have been conducted every even year starting in 2012.10 From 2012 to 2018, the percentage of physicians practicing in large practices (at least 50 physicians) increased.11 In 2020, the number of physicians switching from working in private practice to working in hospitals increased.12,13 Although limited evidence shows that practice size is associated with quality of care, one review showed that some larger practices are associated with better quality of care while some smaller practices (five physicians or fewer) are related to improved patient outcomes, like satisfaction.14 The change from physicians working in larger practices compared to smaller practices may affect patient panel sizes. More physicians in the practice could allow for increased patient panels as physicians have the largest scope of practice. Still, no literature was found to support this relationship.
How a physician manages their patient affects patient panel size and supply of appointments. Some physicians may prefer to have fewer patients so that they can spend more time consulting with each patient. Longer and more indepth visits increase the length of appointments which will impact how many patients can be seen per day.7
Types of physicians like residents and supervising physicians also affect panel size. Residents require a certain number of visits, but their panel is usually smaller than physicians. Supervising physicians and physicians who have academic responsibilities may also need an adjusted panel size to account for other duties.
Patient population affects panel sizes. Age, failing to keep appointments, and disease complexity will impact demand and supply.7-9,15 In 2014, the youngest (0-4) and oldest (65-100) patients visited primary care physicians most often,9 but not all these patients will require the same amount of appointment time. Patients who fail to keep appointments affect the supply of physician visits per day: no shows make physicians unable to see any patient during an appointment slot.7 Patients with more severe illnesses may require longer visits.8
The supply of physicians is changing. Physicians in the United States are getting older. One reason for the shift away from smaller practices is that physicians are retiring but not being replaced by younger physicians.13 Many primary care physicians start in their 20s and work for around 40 years. In 2017, more than 25% of primary care physicians were 60 years of age or older.9 Many of these physicians are of retiring age. As physicians retire the supply of providers reduces, and the data shows that younger physicians are not necessarily taking the place of retiring physicians, especially ones who work in smaller practices. Older physicians may have decreased activity levels affecting their speed and type of care performed.15 Younger physicians may have higher activity levels and be more motivated to treat patients causing younger physicians to be able to see more patients.
Physicians are primary care providers, but nurse practitioners and physician assistants provide primary care as well. As physicians retire and the physician shortage problem intensifies, it will be important to take a team-based approach and introduce more nurse practitioners and physician assistants into the healthcare workforce. In 2017, about 50% of nurse practitioners and 40% of physician assistants were practicing in primary care.9 Integrating additional primary care providers into practice environments positively affects patient panel size and supply and demand. NPs and PAs can increase the supply of provider appointments by increasing physicians’ scope of practice.16,17 A retrospective cross-sectional analysis was conducted using the National Sample of Survey of Nurse Practitioners to understand the productivity of nurse practitioners. Of the nurse practitioners included in the survey, some had their own patient panel (64%) while others did not. The average patient panel size for NPs with patient panels was 567. The average number of patients seen per week for NPs was around 80 patients, and this average did not differ between NPs who had a panel and those who did not: NPs who had their own patient panels provided a higher proportion of specific services to patients than NPs who did not have their own panels. Additionally, having a physician on site compared to not having one was associated with an increase in patients seen and greater chance of NPs having a patient panel.17
Team care can help with productivity. When physicians work with NPs as well as PAs, physicians can offer more services.16 NPs and PAs are advanced practice providers who have similar skill levels to physicians. Data from a survey from the American Board of Family Medicine Certification Examination showed that PAs had a larger effect on primary care physician panels and scope of practice than NPs and PAs and NPs together: the mean panel size was 2,263.16
Managing patient panel sizes can be helpful since many different factors affect the ideal patient panel size per provider. Provider panels have limits: if providers are assigned too many patients, then wait times, no-shows, and scheduling increases. However, avoiding too small of patient panels is just as important. Costs of practices cannot be covered when panel sizes are too small.7
Practices can close provider panels to new patients if a provider has too many patients on their list.5,6,18 The panel can remain open for providers that have lower patient panels unless the whole practice needs to close to new patients. Hiring new team members can help limit patient panel sizes to avoid closing provider panels.19 Assigning other staff members to assist physicians can help optimize patient panel size, as can assigning nurses or physician assistants to patient appointments.19
Practices and physicians can also optimize the visit length, which then affects the number of patients seen.7 Practices should ensure that patients see the same doctor regularly so that relationships can be built. Reducing visit interruptions by ensuring all equipment needs are in the room and tests and labs are completed can reduce visit length. Finally, team members can limit visit length by supporting the primary care provider and limiting physician responsibilities that other staff can accomplish.
More research is needed to calculate the ideal patient panel size for any disease or wellness sate. Angstman et al could not identify their primary objective of determining the ideal panel size for their practice,20 and the strongest evidence shows that a panel size of 2500 patients per provider is not feasible.3,4 Higher panel sizes may negatively affect patient health outcomes, and may be associated with poorer clinical quality, patient experience, and burnout of providers.21
Determining a proper patient panel size is important for practices and providers to establish patient provider relationships, ensure providers are sharing workloads, and confirm that costs of practices are being covered. It may be as equally important to focus on other aspects of care—like the factors affecting panel sizes—to ensure that providers are providing the most cost effective and adequate care.8,20-22
Large patient panels per provider are likely not feasible, but determining the optimal patient panel per provider is challenging. Demand for appointments and supply of providers are ever evolving. Assigning patients to providers should be done so that provider-patient relationships can be formed. Limiting visit length, and preparing for changes in primary care and supply by utilizing other healthcare providers may provide efficient care and reduce physician patient panel sizes as needed.
1. Centers for Disease Control and Prevention. (2022). Chronic diseases in America. U.S. Department of Health and Human Services. https://www.cdc. gov/chronicdisease/resources/infographic/chronic-diseases.htm
2. IHS Markit LTd. (2021, Jun). The complexities of physician supply and demand: Projections from 2019 to 2034. Association of American Medical Colleges. https://www.aamc.org/media/54681/download
3. Raffoul, M., Moore, M. Kamerow, D., & Bazemore, A. (2016). A primary care panel size of 2500 is neither accurate nor reasonable. Journal of the American Board of Family Medicine, 29(4). https://doi.org/10.3122/jabfm.2016.04.150317
4. Minemyer, P. (2016). Study discredits industry standard panel size for primary care physicians. https://www.fiercehealthcare.com/practices/studydiscredits-industry-standard-panel-size-for-primary-care-physicians
5. Murray, M., Davies, M., & Boushon, B. (2007). Panel size: How many patients can one doctor manage? Family Practice Management, 14(4), 44-51. https://www.aafp.org/fpm/2007/0400/p44.html
6. Weber, R. & Murray, M. (2019). The right-sized patient panel: A practical way to make adjustments for acuity and complexity. Family Practice Management, 26(6), 23-29. https://www.aafp.org/fpm/2019/1100/p23.html
7. Murray, M. Davies, M. & Boushon, B. (2007). Panel size: Answers to physicians’ frequently asked questions. Family Practice Management, 14(10), 29-32. https://www.aafp.org/fpm/2007/1100/p29.html
8. Shekelle, P.G., Paige, N.M., Apaydin, E.A., Goldhaber-Fiebert, J.D., Mak, S.S., Miake-Lye,I.M., …, Boroes-Severin, J.M. (2019). What is the optimal panel size in primary care? A systematic review. U.S. Department of Veterans Affairs. https://www.hsrd.research.va.gov/publications/esp/panel-sizeprimary-care.pdf
9. Petterson, S., McNellis, R., Klink, K., Meyers, D., & Bazemore, A. (2018). The state of primary care in the United States: A chartbook of facts and statistics. https://www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/PrimaryCareChartbook.pdf
10. American Medical Association. (n.d.). Physician practice benchmark survey. https://www.ama-assn.org/about/research/physician-practice-benchmarksurvey
11. Kane, C.K. (2019). Updated data on physician practice arrangements: For the first time, fewer physicians are owners than employees. American Medical Association. https://www.ama-assn.org/system/files/2019-07/prp-fewer-owners-benchmark-survey-2018.pdf
12. American Medical Association. (2021, May 5). AMA analysis shows most physicians work outside of private practice. [Press release]. https://www.amaassn.org/press-center/press-releases/ama-analysis-shows-most-physicians-work-outside-private-practice
13. Kane, C.K. (2021). Recent changes in physician practice arrangements: Private practice dropped to less than 50 percent of physicians in 2020. American Medical Association. https://www.ama-assn.org/system/files/2021-05/2020-prp-physician-practice-arrangements.pdf
14 .Ng, C.W. & Ng, K.P. (2013). Does practice size matter? Review of effects on quality of care in primary care. British Journal of General Practice, 63(614), e605-e610. https://doi.org/10.3399/bjgp13X671588
15. Finarelli, H.J. (2009). How many physicians make a health system? The hospital executive‘s guide to physician staffing. (pp. 103-123). HealthLeaders Media. https://store.healthleadersmedia.com/aitdownloadablefiles/download/aitfile/aitfile_id/1672.pdf/
16. Dai, M., Ingram, R.C., & Peterson, L.C. (2019). Scope of practice and patient panel size of family physicians who work with nurse practitioners or physician assistants. Family Medicine, 51(4), 311-318. https://journals.stfm.org/familymedicine/2019/april/dai-2018-0146/
17. Xue, Y. & Tuttle, J. (2017). Clinical productivity of primary care nurse practitioners in ambulatory settings. Nursing Outlook, 65(2), 162-171. https:// doi.org/10.1016/j.outlook.2016.09.005
18. Institute for Healthcare Improvement. (n.d.). Decrease demand for appointments. http://www.ihi.org/resources/Pages/Changes/ DecreaseDemandforAppointments.aspx
19. Institute for Healthcare Improvement. (n.d.). Manage panel size and scope of the practice. http://www.ihi.org/resources/Pages/Changes/ ManagePanelSizeandScopeofthePractice.aspx
20. Angstman, K.B., Horn, J.L., Bernard, M.E., Kresin, M.M., Klavetter, E.W., Maxon, J. …, Thacher, T.D. (2016). Family medicine panel size with care teams: Impact on quality. Journal of the American Board of Family Medicine, 29(4), 444-451. https://doi.org/10.3122/jabfm.2016.04.150364
21. Paige, N.M., Apaydin, E.A., Goldhaber-Fiebert, J.D., Mak, S., Miake-Lye, I.M., Begashaw, M.M., …, & Shekelle, P.G. (2020). What is the optimal primary care panel size? A systematic review. Annals of Internal Medicine, 172(3), 195-201. https://doi-org.udel.idm.oclc.org/10.7326/M19-2491
22. Robeznieks, A. (2020, March). What’s the right panel size for your physician private practice? https://www.ama-assn.org/practice-management/ private-practices/whats-right-panel-size-your-physician-private-practice
Oral health is an important, and often overlooked, aspect of general health. Simple oral care—regular tooth brushing, flossing, avoiding smoking, and decreasing the intake of sugary foods and drinks—and visiting a dentist for regular cleanings and dental exams can greatly reduce the chances of suffering from various oral health problems.1 The American Dental Association (ADA) states that oral health is an essential part of healthcare due to its role in evaluating, diagnosing, preventing and/or treating oral diseases, which can affect systemic health.2
In addition to general dentistry, the National Commission on Recognition of Dental Specialties and Certifying Boards (NCRDSCB) recognizes twelve specialties, where advanced knowledge and skills greater than those taught in graduate dental education programs are taught: dental anesthesiology; dental public health; endodontics, oral and maxillofacial pathology, radiology, and surgery; oral medicine; orofacial pain; orthodontics and dentofacial orthopedics; pediatric dentistry; periodontics; and prosthodontics.3
The ADA estimates that 100 million Americans do not visit a dentist on a yearly basis, despite the fact that preventative care and good oral hygiene can prevent most dental disease.4 The most prevalent dental problem world-wide is tooth decay (dental caries or cavities). According to the Centers for Disease Control and Prevention (CDC), almost 90% of adults have some degree of tooth decay.5 Other major dental problems, like gingivitis (gum disease), tooth sensitivity, and oral cancer (I would defer to Dan on the oral cancer statement. Oral cancer can have a poor outcome.) can be alleviated or cured with early diagnosis and treatment.4
Adults of working-age and seniors are more likely to face financial barriers to obtaining dental care than children, perhaps in part due to the inclusion of pediatric dental care in the Affordable Care Act of 2010, and the mandatory Early and Periodic Screening, Diagnostic, and Treatment benefit of Medicaid.1 As with any type of healthcare, having a sufficient number and distribution of providers is essential to ensuring access to care. In 2020, there were 201,117 practicing dentists in the US, or approximately 60 dentists per 100,000 population, and is expected to increase somewhat until 2040.6 In 2016, there were 437 dentists in Delaware, of which 352 were general/pediatric dentists, or 1 dentist to every 3,128 persons.7 (We should acknowledge that Delaware borders New Jersey, Maryland and Pennsylvania, and patients may seek care in the adjacent states due to proximity. An example would be patients in western Sussex County seeking care in Salisbury, Maryland.) Sussex County was the only Delaware county considered underserved (exceeding the threshold of 5,000 patients to one dentist).7
1. Vujicic, M. & Fosse, C. (2022, Jan). Time for dental care to be considered essential in US healthcare policy. AMA Journal of Ethics. https:// journalofethics.ama-assn.org/article/time-dental-care-be-considered-essential-us-health-care-policy/2022-01
2. American Dental Association. (2020). Current policies. https://www.ada.org/about/governance/current-policies
3. NCRDSCB. (n.d.). Specialty definitions. NCRDSCB. https://ncrdscb.ada.org/en/dental-specialties/specialty-definitions
4. Medical News Today (n.d.). What to know about dental problems and oral health. https://www.medicalnewstoday.com/articles/dental-problems
5. CDC. (2019). Dental caries among adults and older adults. https://www.cdc.gov/oralhealth/publications/OHSR-2019-dental-carries-adults.html
6. Munson, B. & Vujicic, M. (2021, May). Projected supply of dentists in the United States, 2020-2040. Health Policy Institute. https://www.ada.org/-/ media/project/ada-organization/ada/ada-org/files/resources/research/hpi/hpibrief_0521_1.pdf
7. Tóth, T. (2017, May). Dentists in Delaware-2016. Center for Applied Demography & Survey Research, University of Delaware. https://dhss.delaware. gov/dph/hsm/files/dentistsinde2016.pdf
Oral health is essential to individuals’ overall health and quality of life, so it is important that dental professionals are considered in the healthcare workforce. Poor oral health can lead to tooth decay (cavities), gum disease (periodontal disease), or oral cancer. Cavities are a common condition that can occur from childhood to adulthood.1 Individuals with oral cancers have a five-year survival rate of 61%. Stained teeth, cavities, mouth cancers, gum disease, and canker sores can develop when an individual engages in smoking.2,3 Smokeless tobacco causes the same conditions. Cavities can also develop from consuming foods high in sugar. The food that an individual consumes affects oral health and the condition of the mouth affects what a person can eat.4 Oral health is not only related to smoking and eating habits. Oral health is associated with other chronic conditions such as heart disease and diabetes.1 Early detection of these chronic and oral conditions is crucial to ensure an individual’s quality of life remains. Unfortunately, oral health problems affect populations disproportionately. Older adults, non-Hispanic Black Americans, and Mexican Americans experience tooth decay that goes untreated more than non-Hispanic White Americans.5,6 Healthy People 2030 focuses on oral health with the goals to decrease oral health issues and increase access to oral care services as not all Americans have equal access to care.7 In 2020, sixty million Americans resided in Dental Health Professional Shortage Areas (DHPSA).8 There are various dental professionals in the workforce and understanding the composition of the dental team can lead to better quality care and improved access to dental services.
General Dentists and Dental Specialists
Dentists act as the leader of the dental care team and supervise other members of the dental profession, like dental hygienists and dental assistants.9 Dentists include general dentists, oral and maxillofacial surgeons, orthodontists, and prosthodontists, among other specialties, and they are required to be licensed.10,11 Dentists diagnose and treat problems of the mouth and teeth. They examine the gums, teeth and mouth, fill cavities and refer individuals to other healthcare professionals when needed.11,12 Dentists also provide education about proper nutrition, smoking cessation and proper oral health behaviors.3,11-13 Dentists are encouraged to educate their patients about healthy eating behaviors such as limiting sugar sweetened beverages due to the association between nutrition and oral health.13 Dentists are also encouraged to provide patients who smoke with resources, information and education about quitting smoking because of the affects that smoking has on oral health problems and health.3 Dentists inform patients of oral health behaviors like flossing, brushing teeth twice a day, and seeing a dentist regularly as well.12,13
Dental Hygienists, Dental Assistants, and Dental
Dental hygienists, dental assistants and dental laboratory technicians are supervised by dentists. All states require licensure for dental hygienists.10,14 Teeth cleanings and taking x-rays are common responsibilities of a dental hygienist.12,14,15 Like dentists, dental hygienists provide oral health education, including how to floss and what toothbrushes to use.14 A dental hygienist also reviews oral health histories and can conduct oral health screenings.12 Dental hygienists can screen for diabetes, oral cancer, and hypertension, among other conditions.16-18 Screening for chronic diseases is important in the dental field since oral health is linked to many different conditions. Screening also allows for early detection and treatment of diseases. However, not all dental hygienists screen for such diseases. A cross-sectional survey of dental hygienists who practiced in the U.S. and Canada showed that 56% of dental hygienist state screening for diabetes is their responsibility but many do not screen due to of lack of time, education, and awareness of state rules and regulations related to screenings. Ninety-five percent did report that they provide education about the association between diabetes and oral health.16 Similar results occurred for oral cancer. A systematic review showed that dental hygienists feel that they are knowledgeable about oral cancer risks
factors, like tobacco but that they lack the education to perform certain screenings, like palpation of lymph nodes.17 Overall, a survey of three thousand one hundred thirty-three dental hygienists showed that 85% of dental hygienists feel it is important to screen for conditions, especially hypertension and diabetes. Training, time, and dentist and owner support were reported to be factors that affect dental hygienists’ likelihood of conducting medical screening.18
Dental assistants work directly with dentists, assisting them during procedures.12,19 These dental professionals may also perform x-rays and provide education after surgery.15,19 Scheduling patient appointments and keeping records are other tasks dental assistants perform.12 Dental laboratory technicians work closely with dentists but do not have as much contact with patients as dental hygienists and dental assistants. Dental laboratory technicians follow dentists’ instructions to create dental appliances, like dentures, crowns, veneers and bridges.12,15,20
Community Dental Health Coordinators
Community dental health coordinators (CDHDs) are dental professionals that have been recently integrated into the field of dentistry.
Community dental health coordinators improve dental care as well. These professionals act as community health workers and patient navigators to connect individuals struggling to access dental care to dental services in their area.15,23 CDHCs were first introduced in the United States through a program that the American Dental Association piloted. The program improved oral health outcomes and access to dental care. Results reported from the pilot program showed that one hundred eighty-four children aged zero to three years old were set up with dental care by one CDHC in Virginia, and in New Jersey, HPV vaccine rates increased by 19% due to the incorporation of CDHCs. Overall, the pilot program connected six thousand patients to dental services.24
Dentists, dental hygienists, dental assistants, dental laboratory technicians, and community dental health coordinators account for the dental care team. These healthcare professionals improve oral health problems and impact other health conditions. CDHCs are not common among dental professionals throughout the United States.25
1. Centers for Disease Control and Prevention. (2022). Oral health conditions. U.S. Department of Health and Human Services. https://www.cdc.gov/ oralhealth/conditions/index.html
2. Centers for Disease Control and Prevention. (2020). Dental Professionals: Help your patients quit. U.S. Department of Health and Human Services. https://www.cdc.gov/oralhealth/publications/features/dental-pros-help-your-patients-quit-tobacco.html
3. American Dental Association. (2022) Tobacco use and cessation. https://www.ada.org/resources/research/science-and-research-institute/oral-healthtopics/tobacco-use-and-cessation
4. American Dental Association. (2021). Nutrition and oral health. https://www.ada.org/resources/research/science-and-research-institute/oral-healthtopics/nutrition-and-oral-health
5. Centers for Disease Control and Prevention. (2021). Disparities in oral health. U.S. Department of Health and Human Services. https://www.cdc.gov/ oralhealth/oral_health_disparities/index.htm
6. Office of Disease Prevention and Health Promotion. (n.d.) Oral health workgroup. U.S. Department of Health and Human Services. https://health. gov/healthypeople/about/workgroups/oral-health-workgroup
7. Office of Disease Prevention and Health Promotion. (n.d.) Oral conditions. U.S. Department of Health and Human Services. https://health.gov/ healthypeople/objectives-and-data/browse-objectives/oral-conditions
8. County Health Rankings. (n.d.) Dentists. University of Wisconsin Population Health Institute School of Medicine and Public Health. https://www. countyhealthrankings.org/explore-health-rankings/measures-data-sources/county-health-rankings-model/health-factors/clinical-care/access-to-care/ dentists
9. U.S. Bureau of Labor Statistics. (2022). Dentists. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/dentists.htm
10. Torpey, E. (2020). Dental work: Careers in oral care. U.S. Department of Labor. https://www.bls.gov/careeroutlook/2020/article/dental-careers.htm
11. U.S. Bureau of Labor Statistics. (2022). Dentists. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/dentists.htm
12. National Institute of Dental and Craniofacial Research. (2021). Oral health in America: Advances and challenges. U.S. Department of Health and Human Services, National Institutes of Health. https://www.nidcr.nih.gov/sites/default/files/2021-12/Oral-Health-in-America-Advances-andChallenges.pdf#page=495
13. American Dental Association. (2016). Diet and nutrition. https://www.ada.org/about/governance/current-policies#dietnutrition
14. U.S. Bureau of Labor Statistics. (2022). Dental hygienists. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/dental-hygienists.htm
15. American Dental Association. (n.d.). Dental team careers. https://www.ada.org/resources/careers/dental-team-careers
16. DeBiase, C., Giblin-Scanlon, L., Boyd, L.D. & Vineyard, J. (2020). Knowledge, attitudes and practices of dental hygienists regarding diabetes risk assessments and screenings. Journal of Dental Hygiene, 94(2).
17. Coppola, N., Rivieccio, I., Blasi, A., Ferrigno, R., Baldares, S., Mignogna, M.D. & Leuci, S. (2021). Current knowledge, attitude and practice among dental hygienists in oral cancer awareness: Systematic review. International Journal of Dental Hygiene, 20, 249-261.
18. Greenberg, B.L., Kantor, M.L. & Bednarsh, H. (2017). American dental hygienists’ attitudes towards chairside medical screening in a dental setting. International Journal of Dental Hygiene, 15, e61-e68. https://doi.org/10.1111/idh.12217
19. U.S. Bureau of Labor Statistics. (2022). Dental assistants. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/dental-assistants.htm
20. U.S. Bureau of Labor Statistics. (2022). Dental and Ophthalmic Laboratory Technicians and Medical Appliance Technicians. U.S. Department of Labor. https://www.bls.gov/ooh/production/dental-and-ophthalmic-laboratory-technicians-and-medical-appliance-technicians.htm#tab-2 – 5
21. Mertz, E., Kottek, A., Werts, M., Langelier, M., Surdu, S. & Moore, J. (2021). Dental therapists in the United States. Medical Care, 59(10), S441-S448. https://doi.org/10.1097/MLR.0000000000001608
22. Friedman, J.W. & Mathu-Muju, K.R. (2014). Dental therapists: Improving access to oral healthcare for underserved children. American Journal of Public Health, 104(6), 1005-1009. https://doi.org/10.2105/AJPH.2014.301895
23. American Dental Association. (n.d.). Community dental health coordinator. https://www.ada.org/resources/community-initiatives/action-for-dentalhealth/community-dental-health-coordinator
24. American Dental Association. (n.d.). The value of community dental health coordinators [Fact Sheet]. https://www.ada.org/-/media/project/ ada-organization/ada/ada-org/files/resources/community-initiatives/action-for-dental-health/community-dental-health-coordinator/ada_cdhc_value_ infographic.pdf?rev=77b553b44e324ec281873256b52f64bb&hash=5CBBD0E0BCFBBA5F83C0A7D622FDD4D6
25. Community Health Rankings. (2016). Allied dental health professional scope of practice. University of Wisconsin Population Health Institute School of Medicine and Public Health. https://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health/strategies/allied-dentalprofessional-scope-of-practice
There are State Primary Care Offices (PCO) programs located in every state and territory of the United States. The PCO program is funded by the Health Resources and Services Administration (HRSA). In Delaware, the PCO program is located within the Bureau of Health Planning and Resources Management of the Division of Public Health. The PCO program facilitates the coordination of activities to assess the need for primary care, dental health, and mental health providers and services, promote recruitment and retention of providers to fulfill identified needs, work to identify Health Professional Shortage Area designations, and reduce healthcare provider shortages.
One of the key aspects of the PCO program is Health Professional Shortage Area (HPSA) designations. HPSA designations denote geographic areas, populations, and facilities without adequate providers and services (shortages) in the disciplines of primary care, dental health, and mental health. The purpose of HPSA designations is to improve healthcare service delivery and workforce availability, in each of the disciplines, to meet the needs of underserved populations in the designated areas. Determining which areas should be shortage designations is central to prioritizing and focusing resources to the areas of highest need.
To determine if an area is experiencing a shortage of health professionals, the PCO reviews several data elements that are sourced from the American Community Survey, Centers for Disease Prevention and Control, Census Tiger Geometry Data, ESRI 2020 ArcGIS, Uniform Data System, and the National Provider Identifier data file. These data elements are assigned a point value and combined to determine an overall score – the higher the score the higher the need. The data elements and their point values for each of the disciplines is outlined in the table below:
Table 2
Primary Care Dental Health Mental Heatlh
Rational Service Area Census Tract(s) County Census Tract(s) County Census Tract(s) County
Population to Provider Ratio 10 10 7
Percent of Population below 100% Federal Provety Area 5 10 5
Travel Time to the Nearst Source of Care 5 5 5 Infant Health Index (Low birth weight or Infant Mortality Rate) 5 0 0
Water Fluoridation Status 0 1 0
Elderly Ratio (percent of people over age 65) 0 0 3 Youth Ratio (percent of people under age 18) 0 0 3
Substance Abuse Prevalence 0 00 1 Alcohol Abuse Prevalence 0 1 HRPA Score 25 26 25
Once the analysis is complete for each of the rational service areas and disciplines, the information is submitted to the HRSA for review and approval. If the request is denied, the PCO and HRSA work together to determine if the information can be revised to obtain a designation and if a designation is not possible – the request is denied. If the request for designation is approved, the HRSA issues a formal notice approving the designation and the designation is valid for a minimum of one year or until the data sources are updated with new information to request a designation update.

has HPSA designations for primary care, dental health, and mental health
HPSAs are prerequisites for various Federal and State programs. Providers rendering service in HPSA designated areas are eligible to participate in medical education loan repayment programs: National Health Service Corps (NHSC) Loan Repayment Programs: Traditional, Substance Use Disorder, and Rural Community; NHSC Scholarship Program, Delaware State Loan Repayment and Healthcare Provider Loan Programs; Nurse Corps and Nurse Scholar Programs; and the j1 Visa Waiver Program. And there is potential for grants residency and training programs across the primary care, dental health, and mental health disciplines, public health projects, and nurse training and education programs.
Nichole MoxleyDirector, Primary Care Office
Delaware Department of Health and Social Services


The COVID-19 pandemic has created challenges in just about every facet of everyday life, for everyone across the world. Offices closing, restaurants closing, zoom meetings and online classes all became the new normal. Our population faced a challenge it has not seen since 1918, when the Spanish Influenza rampaged throughout the world, killing an estimated 50 million people.1 While COVID-19 may not have the same lethality as the Spanish Influenza, it put a strain on our modern medical system. The pandemic pulled apart the fibers of the global healthcare ecosystem and exposed some major shortcomings in pandemic preparedness, which has caused ripple effects throughout the world.
During the first wave of the pandemic, COVID-19 patients were being admitted to hospitals at such a rapid pace that it was difficult to keep them isolated from the rest of the patient population. The pressure on healthcare workers and engineers to develop controls for a safe working environment led to some exceptional innovation in minimizing the transferability of airborne illness in efficient and cost-effective ways. Due to the limited number of negative pressure isolation units, regular heating, ventilation, and air conditioning (HVAC) systems could continue to circulate the disease to uninfected units of the hospital.2,3 In a study conducted at a skilled nursing facility (SKF) in Lancaster, Pennsylvania, negative air pressure isolation of individual rooms using modified HVAC systems seemed to keep airborne disease from escaping the negative pressure space.2 A similar system was used in South Korea, where existing HVAC systems were adapted to create negative pressure zones in existing hospital units that were turned into isolation units, with a dressing room outside of the individual isolation units as well as a buffer room between the isolation room and the hallway.3 This process of creating negative pressure spaces could also be used to turn non-hospital buildings like warehouses into temporary COVID-19 units.3
Despite innovations in patient isolation, the drastic increase in hospitalizations meant that nurses, who perform much of the direct patient care in a hospital setting, had more dangerous and psychologically taxing work than ever before.4 A 2020 edition of “The Exchange” notes that “COVID-19 has presented healthcare with a unique set of challenges: constrained resources, a highly infectious, novel pathogen that poses a significant threat to the health of providers and support staff, large numbers of critically ill patients and deaths—often with only the caregivers to accompany the patient in their final moments—limited [personal protective equipment] PPE and therapeutics, restricted social interactions, and a protracted timeline with no clear end in sight. These challenges have contributed to unprecedented mental health impacts among healthcare workers.”5
The Office of the Inspector General of the U.S. Department of Health and Human Services contacted over 300 hospitals asking what challenges they faced because of the pandemic, to which the overwhelming response was a lack of staff and critical care equipment, causing difficulties in resuming routine hospital care.4 In a metaanalysis paper detailing the impacts of COVID-19 on the nursing workforce specifically, Michelle Cleary of Central Queensland University indicated that the increased workload and inflexibility of hours—as well as significant lack of mental health treatment for nurses—has led to tremendous burnout and an exodus from the profession.6 The increase in demand for nursing care, coupled with the seemingly ever-decreasing supply due to burnout from inadequate mental healthcare for providers and a significant lack of hospital resources like PPE and critical care equipment, have led to a nursing shortage that extends across the globe.
Nurses were not the only people who felt burnt out or nervous about contracting COVID-19; a 2021 article from Bloomberg suggests as many as three million Americans may have retired early across the job market.7 Another 2021 article by CNBC quotes a figure of around 3.2 million more Baby Boomers retired in late 2020 than expected, and the number of Americans planning to work past age 67 dropped 32.9%.8 For the first time in history, healthcare workforce jobs were not recession-proof, and employment rates fell along with other job sectors.9 A recent AMA study found “20% of physicians said they were likely to leave their current practice within two years, while one third planned to reduce their work hours in the next 12 months.”10 Nurses are leaving the profession at an unprecedented rate due to burnout and aging medical professionals are seeking to reduce their hours or outright retire early due to pandemic fears.4,7,8,10
While the outbreak of COVID-19 has certainly impacted the burnout rates both in the U.S. and abroad, excess healthcare worker deaths are also causing shortages across the globe. A 2021 Working Paper by The WHO claims that the 6,633 reported healthcare worker deaths due to the pandemic falls embarrassingly short of reality, which they estimate could be anywhere between 83,000 and 115,000.11 The WHO states that much of the underreporting comes from their African, South-East Asia, Eastern Mediterranean and Western Pacific regions, where it is reasonable to assume that the excess deaths are contributing to stress and burnout in those healthcare workers that have survived, as well as disparities in access to care across those regions most heavily impacted by the loss.11
The impact of the reduction in the healthcare workforce is being compounded by an overall aging population. A Chinese study conducted on patients with COVID-19 found that the elderly [60+] were more likely to have comorbidities that influence the outcome of COVID-19 infection than those who are not elderly [<60].12 This study also indicates that the proportion of severe cases was higher in the elderly than in the non-elderly. Addressing the Health Needs of an Aging America states “[b]y 2050, adults over the age 65 will make up 20 percent of the U.S. population.”13 The surge in retirees, not just from the healthcare workforce but from the overall population, has left the tenability of certain social programs, such as Social Security and Medicare, questionable at best. The National Academy of Social Insurance predicts that social security will face significant challenges by the year 2030, as more adults age 65+ will be taking benefits from Social Security than there are adults in the workforce paying into it.14 These figures indicate a growing shortage of healthcare providers that is expected to keep growing, as well as an aging population that will inevitably require increased care in the coming years, with high potential for limited availability of social programs, greatly exacerbating the growing shortage of providers in the healthcare workforce.
In the United States, the shortage within the primary care workforce and the disparities in available primary care both between and within different states have been a known issue for over a decade. As stated previously, the U.S. also faces the challenge of an aging population that will require increased primary care. In 2014, the Stern Center for Evidence-Based Policy at the University of Pittsburgh contends that “[w]hile the U.S. population of adults aged 65 and older currently account for only 13% of the population, this cohort consumes more 34% of national health expenditures.”13 A 2013 review conducted by the Robert Graham Center estimated that, by 2030, Delaware would need an additional 177 primary care physicians—a 27% increase from 2010.15 This review only considered physicians, and not the significant number of physicians assistants, nurse practitioners, specialists (e.g. obstetricians, gynecologists, cardiologists), and mental health professionals who also either practice primary care or are deemed a primary care provider by patients. Data sourced from the Delaware Professional Regulatory Online Services (DELPROS) in March 2020 indicated there are an additional 709 adult, family, or gerontological nurse practitioners actively practicing in Delaware.
Primary care disparities exist not just between states but also within states. In Delaware, more than half of the land area is federally designated as a healthcare shortage area (HAS).16 Of the three counties in Delaware, the entirety of Kent and Sussex Counties are designated HSAs with large rural populations that lack access healthcare. Even parts of New Castle County are designated as HSAs, despite the more urban/suburban landscape.16 However, these designations are based on studies that fail to assess the importance of physicians assistants, nurse practitioners, and other types of primary care that do not fall under the “physician” category.
While the trend in hospitalizations over the past two years increased, fewer people sought necessary medical treatment, and elective procedures were deferred. Even now that significant mitigation measures have been put in place, preventative care is being put off.9 A study conducted by the Australian Institute of Health Innovation revealed that “[a]n estimated 1.3 million (13.2%) fewer manual therapy services, with a total cost of AUD 84 million, were provided within the Australian private healthcare setting during the first half of 2020.”17 Another study conducted by the U.S. Centers for Disease Control and Prevention (CDC) estimated that 41% of Americans deferred necessary healthcare, including a 12% reduction in emergency care and a 32% deferral of routine medical care.18 Emergency department visits were down 40%, while office visits were cancelled in favor of telehealth appointments, and elective procedures were delayed indefinitely.19 Despite decreased use of medical services across the board, a December 2021 press release from the Centers for Medicare and Medicaid Services (CMS) stated that 2020 saw a 9.7% overall increase in healthcare spending due to the pandemic.20 With an aging population and their chronic diseases in mind, these delays in routine and emergency care will likely lead to worsening overall health outcomes, increased healthcare costs, and worsening of chronic conditions.
The challenges faced during the COVID-19 pandemic exposed significant flaws in the current medical systems’ ability to provide adequate care for those in need during times of exacerbated strain. From severe lack of PPE and critical care equipment (CCE), to nursing shortages and fears of accessing care during a pandemic, hospitals and other critical care facilities were woefully unprepared. While the U.S. has taken significant measures to shore up hospital reserves of PPE and CCE, every state is taking its own precautions and putting measures in place to prevent another such epic disaster. Delaware has chosen to create a Health Force Database, to include every licensed and unlicensed healthcare practitioner in the state, from chiropractors to dentists to physicians and more. This database provides a clear picture of what access to different types of healthcare looks like across the state, and will help to inform decisions on workforce development.
The development of the database began in early 2020, using Excel to capture licensing information on all the existing practitioners listed in the Delaware Division of Professional Regulation (DELPROS). This initial picture of active and inactive practitioners across various healthcare sectors in the state was limited to a name, a general profession (e.g., nursing, dentistry, occupational therapy), a license type (e.g., Registered Nurse, Dentist, Occupational Therapist), and the activity status of that license (e.g., Active, Inactive, Expired, Deceased).
The lack of available information was a major challenge, for a project that would include demographic information, schooling or higher education information, Medicare & Medicaid acceptance, and several other data points. Since the beginning of the project, a data use agreement has been established with DELPROS that provides a slightly more detailed picture of each practitioner. Some data acquired through this agreement, such as birth year, is instrumental in determining which practitioners are likely to retire in the coming year(s). This data is also strictly unavailable through any other means of data collection: the DELPROS provided data is the one source of truth for the ages of the practitioner population in Delaware.
Early attempts were made to “scrape” internet sources (WebMD, Healthcare4ppl, Doximity, etc.) using several different third party applications that specialized in collecting large amounts of data from web sources and compiling them into excel files. This process was used to gather publicly available information on thousands of practitioners, although much work was needed to be done to remove duplicate practitioner profiles, combine information for individual practitioners, and correct or refine the information gathered (e.g. incomplete addresses, separating combined fields). After data refinement, it was found that not all practitioners were captured and not all profiles were complete. Despite this, there is a considerable amount of usable data concerning schooling and higher education data points that are not available through other, more robust data sources.
After evaluating the data from the scraped websites and the data from DELPROS, it was apparent that another major data source would be necessary to gather specialty and sub-specialty information. The National Provider Identifier (NPI) Registry contains a highly detailed and organized taxonomical structure of profession, specialty, and sub-specialties, as well as practitioners whose profession may not require a license (e.g. home health-aides, technicians). The NPI Registry is a service of the Centers for Medicaid and Medicare Service which operates on a national level. In the future, access to information about the neighboring regions of Philadelphia, Baltimore, Atlantic City, and Ocean City, Maryland. This report do not rely on or include NPI Registry data, but future work will after data integration hurdles have been overcome. It should be noted that the NPI Registry data is only as up to date as providers maintain their own records, so this is a limitation of that source.
In addition to DELPROS, the scraped websites, and the NPI Registry, claims data is also being collected from the Delaware Health Information Network (DHIN) as a way of verifying practitioners are in fact practicing some form of medicine in Delaware. This information also helps validate specialty information gathered from the NPI Registry.
With so many different data sources, Excel became inadequate as a data storage and aggregation tool. The Health Force Database moved to Salesforce, a cloud-based data storage and computing software, which can handle significantly larger data sets and organize them in drastically shorter time frames than are possible in Excel. Of equal importance, the DELPROS system is also based in the Salesforce environment, making data transfer between systems easier once all components are configured and reconciled. The creation of the Salesforce database required adjustments as the team learned how the aggregate inputs came together to form an individual practitioner profile. A contract was given to a third-party to build out the database, however it did not adequately meet the needs of the project, and the contract was terminated after a year of work with no system implemented. The contract was instead given to a new third-party system, Agile Cloud Consulting (ACC), which has a better understanding of the Salesforce system and how to leverage existing components of the system to best meet the needs of the project.
The desired output of the Health Force Database is a structural system that includes a profile of all Delaware practitioners and their specialties as individual practitioners, as well as a profile of all practice locations in Delaware (e.g. Nemours Children’s Hospital-Delaware) with a full list of practitioners providing care at these locations. To accompany the individual and institutional profiles, two statistical analysis tools will be used to better understand the data. Geopointe, a mapping tool, will provide a visual display of how many practitioners of a given type are in a geographic area as well as the demographic breakdown of the population of that area. This will provide an understanding of where the Delaware health workforce is practicing, the populations they are serving, and whether the healthcare needs of that population are being adequately met. The second statistical tool, Tableau, will use practitioner age data acquired from DELPROS to help to predict future changes to the healthcare workforce due to provider retirement, and help determine locations and specialties that may need to be filled in the future.
1. Centers for Disease Control and Prevention. (2019, Mar 20). 1918 pandemic (H1N1 virus). Centers for Disease Control and Prevention. https://www. cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html
2. Miller, S. L., Mukherjee, D., Wilson, J., Clements, N., & Steiner, C. (2020, Oct 3). Implementing a negative pressure isolation space within a skilled nursing facility to control SARS-COV-2 transmission. Science Direct. https://www.sciencedirect.com/science/article/pii/S0196655320308944
3. Alberico, J., & Phillips, D. (n.d.). Creating temporary isolation zones with emergency retrofits of - RWDI. RWDI. https://rwdi.com/assets/ factsheets/RWDI-COVID19-ISOLATION-ZONES.pdf
4. Grimm, C. A. (2021, Mar). Hospitals reported that the COVID-19 pandemic has significantly strained healthcare delivery. Office of Inspector General Department of Health and Human Services. https://oig.hhs.gov/oei/reports/OEI-09-21-00140.pdf
5. Herrman, J. (2020). COVID-19 and healthcare professional stress and resilience. ASPR TRACIE. https://files.asprtracie.hhs.gov/documents/asprtracie-the-exchange-issue12-final.pdf
6. Lopez, V., Anderson, J., West, S., & Cleary, M. (2021, Sep 29). Does the COVID-19 pandemic further impact nursing shortages? Taylor & Francis. https://www.informahealthcare.com/doi/full/10.1080/01612840.2021.1977875
7. Tanzi, A., & Sasso, M. (2021, Oct 22). COVID early retirees top 3 million in U.S., Fed research shows. Bloomberg.com. https://www.bloomberg.com/ news/articles/2021-10-22/covid-early-retirees-top-3million-in-u-s-fed-research-show
8. Dore, K. (2021, May 9). The pandemic drove these Americans into early retirement. what to know before making the leap. CNBC. https://www.cnbc. com/2021/05/09/the-pandemic-drove-these-americans-into-early retirement.html
9. Wager, E., Amin, K., Cox, C., & Hughes-Cromwick, P. (2022, Feb 1). What impact has the coronavirus pandemic had on health employment? Health System Tracker. https://www.healthsystemtracker.org/chart-collection/what-impact-has-the-coronavirus-pandemic-had-on-healthcare-employment/ 10. Robeznieks, A. (2022, Apr 6). How an aging nation, COVID-19 stretch the doctor workforce thin. American Medical Association. https://www.amaassn.org/practice-management/sustainability/how-aging-nation-covid19-stretch-doctor-workforce-thin
11. World Health Organization. (2021, Sep). The impact of COVID-19 on health and care workers: a closer look at deaths. WHO. https://apps.who.int/ iris/bitstream/handle/10665/345300/WHO-HWF-WorkingPaper-2021.1-eng.pdf
12. Dai, S.-P., Zhao, X., & Wu, J.-H. (2020, Oct 12). Effects of comorbidities on the elderly patients with COVID-19: Clinical characteristics of elderly patients infected with COVID-19 from Sichuan, China - The Journal of Nutrition, Health & Aging. https://link.springer.com/article/10.1007/s12603020-1486-1
13. Bellon, J., Coley, K., Coulthart, S., Degenholtz, H., Delitto, A., Driessen, J., & Wessel, C. B. (n.d.). Addressing the health needs of an aging America. University of Pittsburgh. https://www.healthpolicyinstitute.pitt.edu/sites/default/files/SternCtrAddressingNeeds.pdf
14. National Academy of Social Insurance. (2021, Dec 30). How will boomers affect social security? National Academy of Social Insurance. https://www. nasi.org/learn/social-security/how-will-boomers-affect-social-security/
15. Petterson, S.M., Cai, A., Moore, M., Bazemore, A. (2013, Sep). State-level projections of primary care workforce, 2010-2030. Robert Graham Center, Washington, D.C.
16. Malayala, S. V., Vasireddy, D., Atluri, P., & Alur, R. S. (2021, Feb 10). Primary care shortage in medically underserved and health provider shortage areas: Lessons from Delaware, USA. Journal of primary care & community health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7882751/
17. Lystad, R. P., Brown, B. T., Swain, M. S., & Engel, R. M. (2020, Dec 13). Impact of the COVID-19 pandemic on manual therapy service utilization within the Australian private healthcare setting. MDPI. https://www.mdpi.com/2227-9032/8/4/558
18. Czeisler, M. É., Marynak, K., Clarke, K. E. N., Salah, Z., Shakya, I., Thierry, J. A. M., & Howard, M. E. (2020, Sep 10). Delay or avoidance of medical care because of COVID-19–related concerns - United States, June 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/ mmwr/volumes/69/wr/mm6936a4.htm
19. Department of Health and Human Services. (2021, Apr). COVID-19 healthcare delivery impacts (summary). https://files.asprtracie.hhs.gov/ documents/covid-19-healthcare-delivery-impacts-quick-sheet.pdf
20. Office of the Actuary. (2021, Dec 15). National health spending in 2020 increases due to impact of COVID-19 pandemic. CMS. https://www.cms. gov/newsroom/press-releases/national-health-spending-2020-increases-due-impact-covid-19-pandemic
Kristyn Mitchell, 1 Franklin Iheanacho, 2 Jacqueline Washington, EdD, 3 and Marshala Lee, MD, MPH 4
The COVID-19 pandemic has shined a light on health disparities in the United States and the impact of the social determinates of health (SDOH). Black Americans have a mortality rate 2.4 times that of whites and this disproportionality is more widespread throughout the United States compared to any other racial/ethnic group.1 COVID-19 disparities are also manifesting in the State of Delaware. As of May 24, 2020, both Non-Hispanic Black and Hispanic/Latino Americans have the highest rate of COVID-19 cases, with a rate of 111.3 and 281.6 cases, respectively, while non-Hispanic Whites have a rate of 38.5.2 These disparities, although startling, are not surprising considering that before the COVID-19 outbreak health disparities were already persistent. For the top ten leading causes of death, when compared to non-Hispanic White Delawareans, non-Hispanic Black Delawareans lead with the highest adjusted mortality rate for seven of the causes of deaths between 2014 and 2018 (see Table 1). The most common comorbidities associated with COVID-19 are hypertension, obesity, and diabetes, all of which disproportionately impact Black and Hispanic/Latin Americans in the United States and Delaware.4,5 Effective strategies must be deployed in the short-term to reduce COVID-related health disparities while simultaneously investing in long-term strategies such as improving workforce diversity to completely eliminate future health disparities.
Table 1
Five year age adjusted mortality rate of the top 10 leading causes of death (2014-2018)3
Malignant neoplasms 169.1 181.2 Diseases of the heart 159.4 179.0
Chronic lower respiratory diseases 44.8 32.7 Cerebrovascular diseases 39.2 55.1 Dementia 35.7 41.0 Accidents (unintentional injuries) 65.5 44.8
Diabetes mellitus 16.0 32.5 Alzheimer’s disease 25.2 28.4 Nephritis, nephrotic syndrome, and nephrosis 13.3 31.1 Influenza and pneumonia 13.9 12.3
One strategic approach for improving the SDOH for minority communities and reducing health disparities is to invest in the recruitment of a diverse healthcare workforce. Diverse healthcare workers are uniquely positioned to tackle these dimensional problems for several reasons. For one, a diverse healthcare workforce increases the likelihood that high quality care will be provided to underserved populations and people of color. For example, physicians who self-identified as belonging to an underrepresented minority (URM) group were more likely than their colleagues to practice in high-need areas.6 In a Stanford Study, Black men in Oakland, California were paired with either Black or non-Black physicians. The men seen by Black physicians were more likely to engage with them, and even consent to preventive services like immunizations. Additionally, the Black physicians were more inclined to write detailed notes about their Black patients.7 A diverse health workforce will also strengthen cultural competence throughout the health system. The U.S. healthcare system has largely been built upon the practices of Western medicine. Many healthcare systems are currently poorly equipped to provide culturally competent care to patients from underrepresented backgrounds and to those who believe in nontraditional concepts of illness and treatment. Diversity in our healthcare workforce is an effective strategy to increase patient satisfaction, decease health workforce shortages, improve the cultural competence of health systems, and ultimately decrease health disparities.
Although a diverse healthcare workforce is crucial for achieving health equity thus reducing health disparities, there persists an underrepresentation of certain racial/ethnic groups in the United States and Delaware. The Association of American Medical Colleges (AAMC) historically classified four racial/ethnic groups as underrepresented in medicine: Black Americans, Mexican Americans, Native Americans (which include American Indians, Alaska Natives, and Native Hawaiians) and mainland Puerto Ricans.8 The state of Delaware suffers from
an underrepresentation of minority physicians similar to most other states in the United States (see Table 2). These disparities are consistent within the medical school applicant pool, with far less URM students applying to and matriculating into medical school even after Liaison Committee of Medical Education diversity accreditation guidelines were established in 2009.12 As the United States becomes more diverse, action must be taken now to better address health disparities by ensuring that the future physician workforce is more diverse and better reflects the makeup of the communities that they serve.
Table 2
Percentages of active physicians in USA by race/ethnicity compared to the percentage of US population by race/ethnicity and the percentage of primary care physicians by race/ethnicity in Delaware compared to percentage of Delawareans by race/ethnicity
United States
Race/Ethnicity
Percentage of active Percentage of USA population10 physicians in the USA (2018)9
Non-Hispanic Black 5% 13% Hispanic/Latin 5.8% 18.3% Indiginous Persons* 0.4% 1.5% Asian 17. 1% 5.9% Non-Hispanic White 56.2% 60.4%
* American Indian, Alaskan native, Native Hawaiian, and pacific Islander
Delaware
Percentage of primary care Total population of physicians in Delaware11 Delaware by percentage10
Non-Hispanic Black 6.6% 23% Hispanic/Latin 4.4% 9.5% Asian 22.6% 5.9% White 66.7% 61.9%
There are increasing efforts from the government, healthcare organizations, and academic institutions nationwide to address the underrepresentation of minorities in health professions and foster strategies for workforce diversification. According to the Institute of Medicine, pipeline programs that support the needs and success of minorities are pivotal for improving healthcare workforce diversity.13 For example, the Human Resources and Services Administration (HRSA) has grant funding for academic institutions to promote recruitment and retention of minorities in the field of nursing. The funding provides academic and financial support, mentorship, community engagement, and clinical and research opportunities.14 Similarly, the Health Sciences Camp at the University of Delaware provides high schoolers from underrepresented backgrounds and first-generation college families with a free college immersion experience in the health sciences. Students can engage with faculty and researchers, and also gain exposure to nursing, biotechnology, exercise science, and other health specialties.15
For students particularly interested in pursuing medicine, the Harrington Value Institute Community Partnership (VICP) Fund sponsors a yearlong research internship to support URM students in their pursuit to medical school. Established in 2015, The Harrington Value Institute Community Partnership Fund was established by a donation from the estate of Charles J. Harrington, Ph.D. Dr. Harrington was deeply committed to advancing scholarship and supporting innovative projects that help reduce healthcare disparities for underserved and disadvantaged populations. The Harrington Value Institute Translational Research Internship prepares recently graduated college students for careers in medicine and translational research by providing enriching research opportunities, clinical shadowing, mentorship, and a curriculum tailored to academic and professional development. The internship is primarily housed at ChristianaCare’s Value Institute, where students engage with physicians, nurses, researchers, community leaders, and other healthcare professionals throughout the health system to enhance their understanding of translational research, public health, the social determinants of health, and medicine. Upon completing the internship, many interns have successfully matriculated into accredited medical schools and left the internship with
added confidence and skills that will better prepare them for medical school and clinical research careers.
The Harrington VICP Fund plans to expand this opportunity to more underrepresented students in the upcoming years. Additionally, the Harrington VICP Fund also understands the vast array of other common barriers affecting the URM medical school pipeline and has recently created an MCAT Prep Program for students to receive quality preparation for the Medical College Admissions Test (MCAT). According to the AAMC, minority students traditionally do not perform as well as white students on the MCAT, and a major factor contributing to this disparity is lack of financial support for test preparation materials.16,17 Furthermore, the current COVID-19 pandemic and its threats to many underserved communities have intensified students’ financial challenges. Students enrolled in the MCAT Prep Program will have access to a 6-week online Kaplan MCAT course as well as mentoring and peer support during their medical school application process. These students will also be introduced to the concepts of health disparities, social determinants of health, and the importance of cultural competence in caring for their future patients. Upon completing the program, participants will not only be better prepared candidates for medical school, but they will also be equipped with skills to become culturally humbled leaders in their community.
While there are a few strategies in place to increase diversity of the healthcare workforce, there is still much work to be done. Substantial investments are needed to build robust physician pipeline programs for URM students in K-12 and undergraduate levels to ensure a diverse healthcare workforce. Delaware is presented with a unique challenge to its physician pipeline because the state does not have its own medical school. The Harrington VICP is optimistic that many of its program participants will return to practice in Delaware after completing their medical training and commit to careers committed to reducing health disparities. As Delaware’s population continues to diversify, the programs implemented by the Harrington Fund can serve as a guideline for the development of additional URM physician pipeline programs.
1. APM Research Lab. (n.d.). COVID-19 deaths analyzed by race and ethnicity. Retrieved from https://www.apmresearchlab.org/covid/deaths-by-race
2. My Healthy Community. (n.d.). Coronavirus (COVID-19) Data Dashboard State of Delaware. Retrieved from https://myhealthycommunity.dhss. delaware.gov/locations/state
3. Delaware Division of Public Health. (2020, Feb). Delaware Vital Statistics Annual Report 2018. Retrieved from: https://dhss.delaware.gov/dph/hp/ files/ar2018_net.pdf
4. Richardson, S., Hirsch, J. S., Narasimhan, M., Crawford, J. M., McGinn, T., Davidson, K. W., . . .. Zanos, T. P., & the and the Northwell COVID-19 Research Consortium. (2020, April 22). Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA, 323(20), 2052–2059. [PMC free article] [PubMed]
5. Centers for Disease Control and Prevention. (n.d.). BRFSS Prevalence & Trends Data. Retrieved from https://www.cdc.gov/brfss/brfssprevalence/
6. Goodfellow, A., Ulloa, J. G., Dowling, P. T., Talamantes, E., Chheda, S., Bone, C., & Moreno, G. (2016, September). Predictors of primary care physician practice location in underserved urban and rural areas in the United States: A systematic literature review. Acad Med, 91(9), 1313–1321. 10.1097/ ACM.0000000000001203 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
7. Alsan, M., Garrick, O., & Graziani, G. (2019). Does diversity matter for health? Experimental evidence from Oakland. The American Economic Review, 109(12), 4071–4111. 10.1257/aer.20181446 [CrossRef] [Google Scholar]
8. American Association of Medical Colleges. (n.d.). Underrepresented in medicine definition. Retrieved from https://www.aamc.org/what-we-do/ mission-areas/diversity-inclusion/underrepresented-in-medicine
9. American Association of Medical Colleges. (2019). Diversity in Medicine: Facts and Figures 2019. Retrieved from: https://www.aamc.org/datareports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018#:~:text=race%2Fethnicity%2C%202018-,New%20 section,as%20Black%20or%20African%20American
10. US Census Bureau. (n.d.). United States: Quick Facts. Retrieved from: https://www.census.gov/quickfacts/fact/table/US/PST045219
11. Delaware Department of Health and Social Services. (2018). Primary Care Physicians in Delaware, 2018. Retrieved from: https://dhss.delaware.gov/ dhss/files/primarycarestudy.pdf
12. Lett, L. A., Murdock, H. M., Orji, W. U., Aysola, J., & Sebro, R. (2019, September 4). Trends in racial/ethnic representation among US medical students. JAMA Network Open, 2(9), e1910490–e1910490. 10.1001/jamanetworkopen.2019.10490 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
13. Altman, S. (2016, Feb 22). Promoting diversity. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK350167/
14. Kukich, D. (2014, Nov 18). Nursing workforce diversity. Retrieved from http://www1.udel.edu/udaily/2015/nov/nursing-diversity-111814.html
15. Benjamin, A. (n.d.). Pipeline program: Health sciences: University of Delaware. Retrieved from https://www.chs.udel.edu/pipeline-program/
16. American Association of Medical Colleges. (2019, Oct 16). MCAT Scores and GPAs for Applicants and Matriculants to U.S. Medical Schools by Race/ Ethnicity, 2019-2020. Retrieved from https://www.aamc.org/system/files/2019-10/2019_FACTS_Table_A-18.pdf
17. American Association of Medical Colleges. (2018, Jun). Using MCAT® Data in 2019 Medical Student Selection. (2018, June). Retrieved from https:// www.aamc.org/system/files/c/2/462316-mcatguide.pdf
At the writing of this report, data on race and ethnicity of Delaware Healthcare Providers (including physicians and dentists), was not readily available. However, in a study published by Mitchell et al1 we obtain a glimpse at this information juxtaposed against that of the total population of Delaware when looking at primary care physicians.
Percentage of primary care physicians in Delaware Total population of Delaware by percentage
Non-Hispanic Black 6.6% 23% Hispanic/Latin 4.4% 9.5% Asian 22.6% 5.9% White 66.7% 61.9% While generalization from this focused examination is difficult, it does suggest a larger trend where Non-Hispanic Black and Hispanic/Latin physicians are underrepresented relative to population percentages. On the other hand, White and Asian primary care physicians are both represented at higher rates than in population percentages.
The authors go on to state “These disparities are consistent within the medical school applicant pool, with far less URM (underrepresented minority) students applying to and matriculating into medical school even after Liaison Committee of Medical Education diversity accreditation guidelines were established in 2009. As the United States becomes more diverse, action must be taken now to better address health disparities by ensuring that the future physician workforce is more diverse and better reflects the makeup of the communities that they serve.” “Diversity in our healthcare workforce is an effective strategy to increase patient satisfaction, decease health workforce shortages, improve the cultural competence of health systems, and ultimately decrease health disparities.”
Table 4 Gender1
License Type ↑ Contact: Gender ↑ Record Count Percentage
Dentist No Data 3 0.55 Male 340 62.96 Female 197 36.48 Subtotal 540 100.00
Physician D.O. No Data 21 2.25 Male 543 58.20 Female 369 39.55 Subtotal 933 100.00
Physician M.D. No Data 87 1.64 Male 3,265 61.51 Female 1,956 36.85 Subtotal 5,308 100.00 Total 6,781
Delaware Population2 Male 483,332 48.40 Female 515,287 51.60 Total 998,619 100.00
References
1. From https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8389095/ 2. From https://worldpopulationreview.com/states/delaware-population
“In the U.S., there are two types of degrees in which physicians can practice medicine: an MD, a doctor of medicine, or a DO, a doctor of osteopathic medicine. The two degrees reflect different types of medical school training. MDs attend allopathic medical schools, while DOs attend osteopathic medical schools.
About one-quarter of U.S. medical students train at osteopathic medical schools. That number has grown significantly in recent years, with the American Association of Colleges of Osteopathic Medicine reporting first year enrollment at osteopathic medical schools rising by more than 40% over the past decade. That spike is, at least, in part due to additional DOgranting medical schools opening.
In terms of the requirements to apply to MD and DO programs, the criteria are virtually the same, with both osteopathic and allopathic programs weighing grade-point average and Medical College Admission Test (MCAT) scores heavily. The curriculum is largely the same structure, with students in both types of programs typically spending much of their first 12-24 months in the classroom and the majority of their training beyond that in a clinical setting.
In the past, graduates from osteopathic and allopathic medical schools have generally matched with residency programs through separate processes.
In an effort to simplify the graduate medical education (GME) accreditation system in the United States, the organizations that accredit GME—the Accreditation Council for Graduate Medical Education and the American Osteopathic Association (AOA)—have changed how they do things. The 2020 Main Residency Match marked the completion of the transition to a single accreditation system and the consolidation to one Match for U.S. DO and MD seniors.
Those changes also affect licensing. Most residency programs will accept the Comprehensive Osteopathic Medical Licensing Examination taken by DO graduates, as well as the United States Medical Licensure Exam which is taken by MD graduates and can be taken by DO graduates.
Historically, DO programs have touted their methods as more holistic. One aspect of that is the osteopathic manipulative treatment, defined by the AOA as a “set of hands-on techniques used by osteopathic physicians to diagnose, treat, and prevent illness or injury.”
Those skills typically mean that osteopathic medical students spend an additional 200-plus hours training on the musculoskeletal system in the curriculum.
“If a student is somebody who really enjoys that patient-centered approach and really is of the mindset that medicine is a mind-body-spirit relationship, a DO program will serve them well,” said John D. Schriner, PhD, associate dean for admissions and student affairs at Ohio University Heritage College of Osteopathic Medicine, one of 37 member schools of the AMA Accelerating Change in Medical Education Consortium.
The 2021 Match, the second fully combined Match for DOs and MDs, yielded positive results for graduates from both types of schools. About 6,300 U.S. DO seniors submitted rank order lists of programs, and 89.1% of them matched. That percentage is a bit lower than the 92.8% Match percentage posted by graduates of U.S. MD-granting medical schools.1
1. Murphy, B. (2021, Oct). DO vs. MD: How much does the medical school degree type matter? American Medical Association. Retrieved from: https:// www.ama-assn.org/residents-students/preparing-medical-school/do-vs-md-how-much-does-medical-school-degree-type
In a 2016 article, “A systematic review of physician retirement planning” by Silver et al, both expected and actual retirement ages appear to have occurred between 50-59 years of age. A smaller number of physicians across studies predicted a later retirement age between 60-69 years of age. 1
In a study by the American Dental Association’s Health Policy Institute, 49.8% of dentists aged 65-74 were projected to retire. That number increases to a projected 79.2% for those aged 75-84.2
Delaware data show on the facing page shows a steady increase in the number of physicians (both M.D., and D.O.) retiring starting at age 57 (individuals born in 1965). It appears that dentists follow a similar trend starting 5 years later (individuals born in 1960).
The blue dashed line between 1954 and 1955 roughly illustrates retirement age for those born in that range who can retire with full social security benefit when they turn 67 sometime in 2022. The red gradient box illustrates the increasing likelihood of end of career. The data does indicate that there are both physicians and dentists who maintain a license and practice significantly longer that their peers.
Future data will aid in development of a projection model for retirement of physicians and dentists as well as other types of healthcare providers.
50–59 years 60–69 years >70 years “Never” Expected retirement age Burke [76] Anderson [37] Batchelor [22] Draper [40] Eagles [30] Dietch [48] Luce [7] Dodds [46]
Fletcher [38] Farley [39] Mears [41] Florence [81] Goldberg [57] Grondin [61] Sansom [28] Mears [41] French [36] French [23] Gee [82] Pit [45] Rayburn [31] Shanafelt [53] Smith [91] Wakeford [18]
Actual retirement age Baker [52] Anderson [37] Joyce [42] –Eagles [30] Austrom [58] Rayburn [31] Sansom [28] Batchelor [22] Farley [39]
Fletcher [38] French [36] Jonasson [84] Meghea [54] Luce [7] Orkin [34] Rayburn [31] Rowe [90] Van Greuningen [17] Wakeford [18]

full retirement age at 67
1. Silver, M.P., Hamilton, A.D., Biswas, A., & Warrick, N.I. (2016). A systematic review of physician retirement planning. Hum Resour Health, 14, 67. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5109800/
2. Munson, B. & Vuujicic, M. (2021, May). Projected supply of dentists in the United States, 2020-2040. Health Policy Institute. Retrieved from: https:// www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/hpibrief_0521_1.pdf
While this report is about the healthcare workforce, it is difficult to talk about capacity, demand for services, and growth potential without a discussion of the disease and wellness management. To that end, the next section of the report looks at the healthcare workforce through the lens of key chronic diseases, their prevention and management. We look at Chronic Disease because “currently, some 50% of the US population has a chronic disease, creating an epidemic, and 86% of healthcare costs are attributable to chronic disease.”1 Furthermore, according to the CDC “90% of the nation’s $4.1 trillion in annual healthcare expenditures are for people with chronic and mental health conditions.”2
The differences between acute and chronic disease are numerous and are illustrated below.2
Acute Disease Chronic Disease Sudden onset Gradual onset Cure usual Cure rare Course short Course lengthy Patient passive Patient active, caregiver Physician dominant Team care, patient included Return to normal likely Return to normal unlikely Future uncertainty rare Future uncertainty common
The capacity of medical practice to address acute disease and injury has dramatically reduced the incidence of death from these diseases, and increased life expectancy for the population overall. This increase is not consistent across demographics, nonetheless, it is a population wide change. In its place, chronic disease has grown to replace acute disease and injury as the leading cause of death and disability, and an aging population is more likely to develop chronic disease as a natural result of the aging process.
Table 6
Population Projections for Persons Aged 60 and Older State of Delaware.3
Year 2016 2017 2018 2019 2020 2025 2030 2035 2040 2045 2050 60 -64 60,237 62,231 64,219 66,165 66,649 68,921 64,322 59,971 60,299 66,918 70,051 65 -69 54,915 57,057 56,764 57,124 56,770 64,196 66,801 62,600 58,624 59,105 65,576 70 -74 40,415 41,631 45,052 47,523 48,412 52,270 59,412 62,141 58,415 55,021 55,727 75 -79 28,367 29,490 31,087 33,143 33,922 42,382 45,828 52,342 54,934 51,857 49,235 80 -84 19,578 20,056 20,566 21,545 22,236 27,656 34,689 37,531 42,964 45,259 42,983 85 &up 20,410 21,206 21,912 22,552 22,482 26,460 32,709 41,218 47,617 54,472 59,584
Totals 223,922 231,671 239,600 248,052 250,471 281,885 303,761 315,803 322,853 332,632 343,156
The next section of this report uses the following format.
1) Sections are alphabetical by chronic disease name.
2) State level data is presented first, and are based on CDC, Behavioral Risk Factor Surveillance System, 2020 data.
3) Additional information as compiled by County Health Rankings, US Census Data, and other sources are located immediately below State data.
4) The first group of pages will contain three sections representing New Castle, Kent, and Sussex County disease prevalence among adults aged 18 years and older. The data source will be identified at the top of each table and is not uniform from one chronic disease to another as there is no single source for all diseases.
5)The next group of pages looks at the number of individuals, by census tract per 100 persons, with the given chronic disease.
6) The following pages also contain health claims data for all publicly and privately insured Delawareans as reported to and captured by the Delaware Health Information Network. The information is displayed based on census tract per 100 persons. This section looks specifically at healthcare utilization, which brings disease management into alignment against demands on the healthcare workforce.
An important limitation of this data is that an estimated 15% of transactions are not captured in the DHIN as some providers are not yet aligned with the DHIN. It is also important to note that data is not captured on selfinsured & unisured individuals, so any conclusions based upon this data must be carefully considered.
Immediately before the chronic disease pages are basic demographics for the three counties.
1. Holman, H.R. (2020, Feb 19). The relation of the chronic disease epidemic to the healthcare crisis. ACR Open Rheumatol, 2(3), 167-173. doi: 10.1002/ acr2.11114. Epub 2020 Feb 19. PMID: 32073759; PMCID: PMC7077778.
2. National Council on Aging. (2020, Mar 9). Chronic vs. acute medical conditions: What’s the difference? Retrieved from: https://www.ncoa.org/article/ chronic-versus-acute-disease
3. Delaware Office of State Planning Coordination. (n.d.). Demographic Information. Retrieved from: http://www.stateplanning.delaware.gov/demography/documents/dpc/DPC-2021v0-report.xls
Count Percent
Total population 558,306SEX
Male 270,278 48.40%
Female 288,028 51.60%
Under 5 years 32,070 5.70% 5 to 9 years 32,053 5.70% 10 to 14 years 35,028 6.30% 15 to 19 years 37,315 6.70% 20 to 24 years 35,378 6.30% 25 to 34 years 80,973 14.50% 35 to 44 years 69,210 12.40% 45 to 54 years 74,038 13.30% 55 to 59 years 37,993 6.80% 60 to 64 years 37,129 6.70% 65 to 74 years 50,994 9.10% 75 to 84 years 25,714 4.60% 85 years and over 10,411 1.90%
One race 538,311 96.40%
White 349,313 62.60% Black or African American 140,870 25.20%
American Indian and Alaska Native 1,482 0.30%
Cherokee tribal grouping 314 0.10%
Chippewa tribal grouping 56 0.00%
Navajo tribal grouping 0 0.00%
Asian 31,918 5.70%
Asian Indian 14,765 2.60% Chinese 7,892 1.40% Filipino 2,591 0.50%
Japanese 614 0.10%
Korean 1,809 0.30%
Vietnamese 1,058 0.20%
Other Asian 3,189 0.60%
Native Hawaiian and Other Pacific Islander 238 0.00%
Native Hawaiian 54 0.00%
Chamorro 19 0.00%
Samoan 26 0.00%
Native Hawaiian and Other Pacific Islander 139 0.00%
Some other race 14,490 2.60%
Hispanic or Latino (of any race) 57,030 10.20%
Mexican 23,871 4.30%
Puerto Rican 18,169 3.30%
Cuban 754 0.10%
Hispanic or Latino (of any race) continued
Count Percent
Other Hispanic or Latino 14,236 2.50%
Not Hispanic or Latino 501,276 89.80%
Two or more races 19,995 3.60%
White and Black or African American 7,402 1.30%
White and American Indian and Alaska Native 1,147 0.20%
White and Asian 2,320 0.40%
Black or African American and American Indian and Alaska Native 643 0.10%
From: 2020 : ACS 5-Year Estimates Data Profiles
Table 8
New Castle County Language Stratified by Age Groupings
Label
Count Percent
5 years of age and over
Population 526,236 -
Speak only English 446,360 84.80%
Speak a language other than English 79,876 15.20%
SPEAK A LANGUAGE OTHER THAN ENGLISH
SPANISH
Total 40,613 7.70%
5 to 17 years old 10,175 1.90% 18 to 64 years old 27,835 5.30% 65 years old and over 2,603 0.50%
OTHER INDO-EUROPEAN LANGUAGES
Total 15,931 3.00%
5 to 17 years old 1,331 0.30% 18 to 64 years old 10,897 2.10% 65 years old and over 3,703 0.70%
ASIAN AND PACIFIC ISLAND LANGUAGES
Total 16,750 3.20%
5 to 17 years old 2,128 0.40% 18 to 64 years old 12,972 2.50% 65 years old and over 1,650 0.30%
OTHER LANGUAGES
Total 6,582 1.30%
5 to 17 years old 718 0.10% 18 to 64 years old 5,311 1.00% 65 years old and over 553 0.10%
AMERICAN SIGN LANGUAGE (ASL), NO AGE STRATIFICATION
Estimated Prevalence
Count % of pop.
Total 5,583 1.00%
BRAILLE LITERACY, NO AGE STRATIFICATION
Estimated Prevalence
Count % of blind pop.
Total 1,146 9.50%
From: 2020 : ACS 5-Year Estimates Subject Tables
Label (Grouping)
Count Percent
Total population 179,124 -
SEX
Male 270,278 48.20%
Female 288,028 51.80%
Under 5 years 32,070 6.20% 5 to 9 years 32,053 6.60% 10 to 14 years 35,028 6.30% 15 to 19 years 37,315 6.70% 20 to 24 years 35,378 7.10% 25 to 34 years 80,973 13.50% 35 to 44 years 69,210 11.70% 45 to 54 years 74,038 12.00% 55 to 59 years 37,993 6.90% 60 to 64 years 37,129 5.80% 65 to 74 years 50,994 10.10% 75 to 84 years 25,714 5.40% 85 years and over 10,411 1.70%
One race 169.635 94.70%
White 116,704 65.20%
Black or African American 45,803 25.60%
American Indian and Alaska Native 1,167 0.70%
Cherokee tribal grouping 123 0.10%
Chippewa tribal grouping 5 0.00%
Navajo tribal grouping 0 0.00%
Asian 3.756 2.10%
Asian Indian 998 0.60% Chinese 858 0.50%
Filipino 794 0.40% Japanese 174 0.10% Korean 308 0.20%
Vietnamese 151 0.10%
Other Asian 473 0.30%
Native Hawaiian and Other Pacific Islander 36 0.00%
Native Hawaiian 4 0.00%
Chamorro 15 0.00%
Samoan 12 0.00%
Native Hawaiian and Other Pacific Islander 5 0.00%
Some other race 2,169 1.20%
Hispanic or Latino (of any race) 13,091 7.30%
Mexican 2,596 1.40%
Puerto Rican 5,615 0.10%
Cuban 256 0.10%
Hispanic or Latino (of any race) continued Count Percent
Other Hispanic or Latino 4,624 2.60%
Not Hispanic or Latino 166,033 92.70%
Two or more races 9,489 5.30%
White and Black or African American 4,198 2.30%
White and American Indian and Alaska Native 643 0.40%
White and Asian 1,450 0.80%
Black or African American and American Indian and Alaska Native 394 0.20%
From:
Table 10
Population 168,033 Speak only English 149,141 88.80% Speak a language other than English 18,892 11.20% SPEAK A LANGUAGE OTHER THAN ENGLISH SPANISH
Total 8,183 4.90%
5 to 17 years old 1,715 1.00% 18 to 64 years old 5,840 3.50% 65 years old and over 628 0.40%
OTHER INDO-EUROPEAN LANGUAGES
Total 6,574 3.90%
5 to 17 years old 1,747 1.00% 18 to 64 years old 4,321 2.60% 65 years old and over 506 0.30%
ASIAN AND PACIFIC ISLAND LANGUAGES
Total 2,463 1.50%
5 to 17 years old 446 0.30% 18 to 64 years old 1,525 0.90% 65 years old and over 492 0.30% OTHER LANGUAGES
Total 1,672 1.00%
to 17 years
to 64 years
years
Label (Grouping)
Count Percent
Total population 230,249SEX
Male 111,129 48.30%
Female 119,120 51.70%
Under 5 years 11,613 5.00% 5 to 9 years 11,375 4.90% 10 to 14 years 12,800 5.60% 15 to 19 years 10,822 4.70% 20 to 24 years 10,365 4.50% 25 to 34 years 23,512 10.20% 35 to 44 years 21,815 9.50% 45 to 54 years 26,317 11.40% 55 to 59 years 18,459 8.00$ 60 to 64 years 18,931 8.20% 65 to 74 years 39,970 17.40% 75 to 84 years 18,886 8.20% 85 years and over 5,384 2.30%
One race 222,166 96.50%
White 186,570 81.00%
Black or African American 26,122 11.30%
American Indian and Alaska Native 911 0.40%
Cherokee tribal grouping 65 0.00%
Chippewa tribal grouping 0 0.00%
Navajo tribal grouping 0 0.00%
Asian 2,854 1.20%
Asian Indian 415 0.20% Chinese 462 0.20%
Filipino 480 0.20%
Japanese 37 0.00% Korean 316 0.10%
Vietnamese 523 0.20%
Other Asian 621 0.30%
Native Hawaiian and Other Pacific Islander 431 0.20%
Native Hawaiian 33 0.00%
Chamorro 368 0.20%
Samoan 0 0.00%
Native Hawaiian and Other Pacific Islander 30 0.00%
Some other race 5,278 2.30%
Hispanic or Latino (of any race)
21,229 9.20%
Mexican 7,551 3.30%
Puerto Rican 3,124 1.40%
Cuban 310 0.10%
Hispanic or Latino (of any race) continued Count Percent
Other Hispanic or Latino 10,244 4.40%
Not Hispanic or Latino 209,020 90.80%
Two or more races 8,083 3.50%
White and Black or African American 3,435 1.50%
White and American Indian and Alaska Native 992 0.40%
White and Asian 490 0.20%
Black or African American and American Indian and Alaska Native 598 0.30%
From: 2020 : ACS 5-Year Estimates Data Profiles
Table 12
Population 218,636
Speak only English 194,740 89.10%
Speak a language other than English 23,896 10.90%
SPANISH
Total 16,036 89.10%
5 to 17 years old 4,999 10.90% 18 to 64 years old 10,003 89.10% 65 years old and over 1,034 10.90%
OTHER INDO-EUROPEAN LANGUAGES
Total 5,354 2.40%
5 to 17 years old 688 0.30% 18 to 64 years old 3,368 1.50% 65 years old and over 1,298 0.60%
ASIAN AND PACIFIC ISLAND LANGUAGES
Total 2,036 0.90%
5 to 17 years old 209 0.10% 18 to 64 years old 1,328 0.60% 65 years old and over 499 0.20%
OTHER LANGUAGES
Total 470 0.20%
5 to 17 years old 43 0.00% 18 to 64 years old 347 0.20% 65 years old and over 80 0.00%
From:
The data indicates that there are areas of an increased incidence of Alzheimer’s and other dementia disease in each of Delaware’s three counties. Interestingly, these areas seem to correlate with the areas in which Delaware’s healthcare institutions are located (Wilmington Hospital and Christiana Hospital in New Castle County, Bayhealth in Kent County, Tidal Health and Beebe in Sussex County, see Figure 264). This suggests an increased reporting due to the increased number of healthcare providers in these areas. Individuals living with Alzheimer’s and/or dementia may live elsewhere, and travel to the major healthcare institutions for care. The data suggest that keeping a workforce of providers specializing in Alzheimer’s and other dementias in these areas would be prudent to the continuation of care for these individuals.
Specialists in neurology and neuropsychology (specific to the type of dementia), geriatrics, psychiatry and/or psychology are likely warranted. Allied health professionals in the fields of speech and language, physical, and occupational therapy and memory may also be included.
Figure 288
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Alzheimers Disease, Related Disorders, or Senile Dementia

Figure 265 shows that the incidence of osteoporosis, a degenerative bone disease, is higher in the beach town communities, which are well known for their higher population of older Delawareans and retirees. Rheumatoid arthritis is an autoimmune disease, and has similar risk for all populations. The incidence of rheumatoid arthritis is lower in New Castle County, and higher in Kent and Sussex Counties. Despite the low numbers of individuals living with these diseases, there is a need for specialists in all three counties.
Figure 289
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Osteoporosis
Figure 290
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Osteoporosis.


Figure 291
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Rheumatoid Arthritis/Osteoarthritis
Figure 292
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Pelvic Hip Fracture


The data for the incidence of breast cancer (Figure 269) indicates that there is no geographical component to a breast cancer diagnosis, although there are greater numbers of individuals with this diagnosis living in or around Delaware’s healthcare institutions. The data also shows a very low incidence of colorectal cancer (Figure 270) in Delaware. Increased incidence of breast cancer may be due in part to increased screening (breast exams and mammograms) and thus, increased positive cases. In the same fashion, increased use of colonoscopy to screen for colon cancer may have led to Delaware’s low numbers of cases. Prostate cancer incidence higher in those areas known for retirement communities and an older population are indicative of the slow growth of prostate cancers, and the increased screening and testing for this cancer with age (Figure 271). While it is important for oncologists and other cancer specialists to practice in all three counties and provide cancer care, it is equally important for primary care physicians and medical homes to be available to assist these individuals with their ongoing healthcare.
Healthcare specialists who work with people with cancer include a general oncologist, an oncologist specializing in the type of cancer, surgical and radiation oncologists, social workers, patient navigators, psychiatrists, dieticians, home health aides, and a pharmacist.
Figure 293
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Breast Cancer

Figure 294
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Colorectal Cancer
Figure 295
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Prostate Cancer.

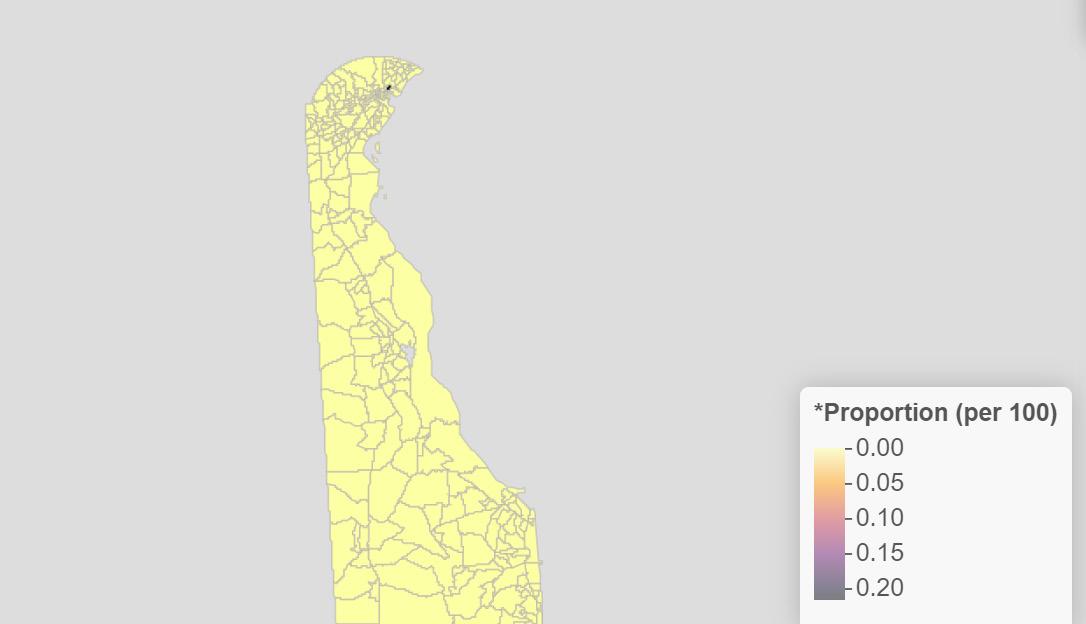
A cardiovascular team will likely consist of specialists in cardiovascular disease, nephrology, and/or neurology (depending on the mechanism of action of the disease). Community health workers (for blood pressure maintenance and tracking), allied health professionals, radiologists, and medical technicians may also be appropriate.
Figure 296 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Acute Myocardial Infarction.

Figure 297
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Atrial Fibrillation

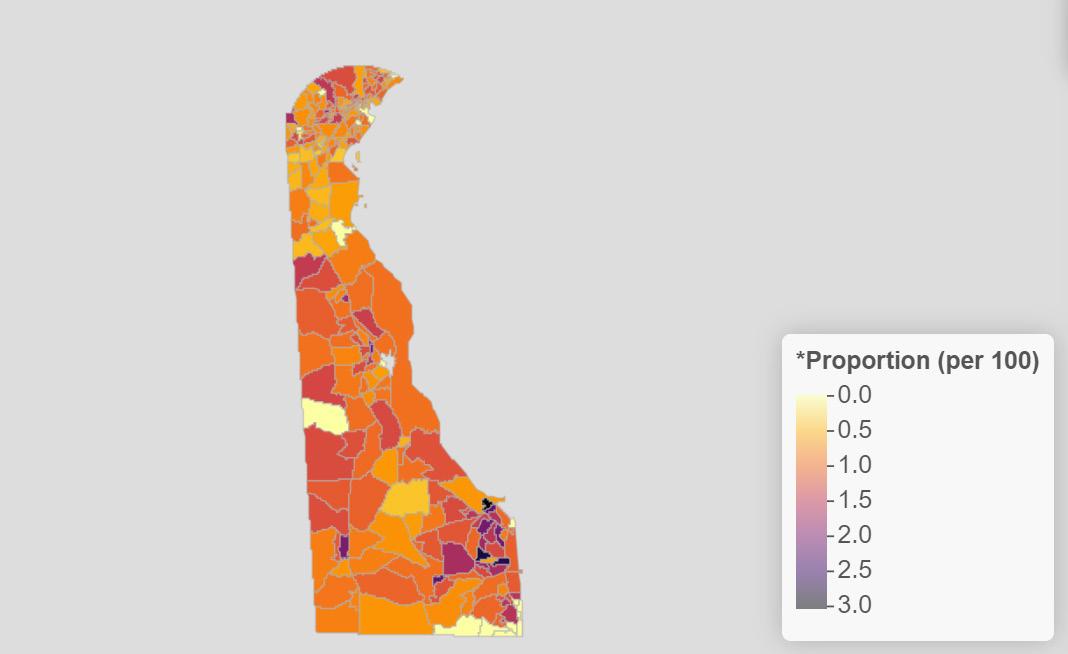
Figure 298
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Heart Failure.
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Ischemic Heart Disease
Also see Systemic Diseases section for Hyperlipidemia and Hypertension, page 238

According to the data, the incidence of depression and suicide does not follow any kind of geographical border. There are more cases in urban areas, which may in part be due to an increased population, and highlights the need for mental health professionals throughout the state.
Mental health diagnoses are complex, and require a multidisciplinary team including a psychiatrist and/or psychologist, social workers and therapists. Other professionals may be called upon for assistance as needed (i.e. long-term care nurses, pharmacists, community health workers).
Figure 300
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Depression

Diabetes is ubiquitous throughout the state and may be due to an auto-immune disorder (type I, seen in children and adolescents); due to obesity, poor diet, or other chronic disease (type II); or due to pregnancy (gestational diabetes). Despite the reason, the data proves the need for diabetes specialists, care teams, and education throughout the state.
Managing diabetes requires a multi-disciplinary approach, and includes endocrinologists, dieticians, and community health workers like diabetes care and education specialists. It may also require the use of podiatrists, dermatologists, ophthalmologists and/or optometrists, long term care nurses, home health aides, dentists, fitness professionals, mental health workers, and pharmacists.
Figure 301
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Diabetes

As evidenced in the data showing the incidence of hypothyroidism in Delaware, endocrine disease does not follow any geographical border. There is an increased risk of being diagnosed with an endocrine disease as a person ages, particularly hypothyroidism. Other disorders of the endocrine system (i.e., diseases of the pituitary, diabetes) may be more likely seen in children and young adults. This indicates the need for endocrine specialists.
Endocrinologists will work with various specialties to give the appropriate care, based on the specific disorder. These specialists may include geneticists, orthopedists, dieticians and nutritionists, gastroenterologists, fertility specialists, mental health providers, renal specialists, ophthalmologists and/or optometrists.
Figure 302
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Acquired Hypothyroidism

Anemia can be seen throughout the State of Delaware, with pockets of increased incidence in some communities (Figure 279). Anemia is generally managed by primary care physicians and continuity of care is important.
Hypertension (high blood pressure) is one of the leading causes of morbidity and mortality throughout the nation and in Delaware (Figure 280). All three counties in Delaware show high incidence rate of hypertension, with increased numbers in and around the major urban areas.
Although the incidence of hyperlipidemia (high blood pressure) are not quite as high, they also spike around the urban areas in the State (Figure 281). This suggests a need for cardiovascular specialists in the major healthcare institutions, and primary care physicians throughout the state to provide timely check-ups and ongoing care.
Figure 303
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Anemia

Figure 304
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Hypertension

Figure 305
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Hyperlipidemia

As shown in Figure 282, the incidence of stroke is higher in Delaware’s urban areas, which may be due to an increased population. Although the greatest risk factor for a stroke is age, high blood pressure, high cholesterol, obesity, and kidney disease can all contribute to increased risk. This map illustrates the need for both acute stroke treatment at healthcare institutions as well as ongoing post-stroke care throughout the state.
Stroke care teams will likely consist of specialists in cardiovascular disease (including atherosclerosis, heart disease); cardiovascular surgery, pharmacy, and radiology; and neurology immediately after a stroke occurs. Once a patient has been treated, a care team consisting of allied health professionals (occupational, physical, and speech language therapy) and psychiatrists and/or psychologists will likely be added.
Figure 306
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Stroke / Transient Ischemic Attack

According to the data (Figure 283), the incidence of renal disease is higher in Kent County than New Castle and Sussex County. There are also areas of high incidence around the urban areas of Delaware. Not only does this show the need for renal specialists throughout the state, it also illustrates the need for dialysis centers, home care providers, and other renal specialists throughout the state. If renal disease progresses, an individual will also need the skills of transplant surgeons.
Individuals with chronic kidney disease or end stage renal disease will probably have a care team that includes a nephrologist, a nephrology nurse, a dietitian, and potentially a social worker. If a patient is placed on dialysis, their care team will expand to include patient care technicians and renal technologists. If a patient is matched with a kidney transplant, the care team will expand again to include a transplant surgeon, transplant coordinator, and a donor coordinator.
Figure 307
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Chronic Kidney Disease

Asthma can be diagnosed at any age. As seen in Figure 284, incident rates increase in urban areas, perhaps due to increased air pollution due to traffic and industry. Chronic Obstructive Pulmonary Disease (COPD) incidence in Delaware is lower in New Castle County than in Kent or Sussex Counties (Figure 285). This could be due to a lack of pulmonary specialists in these counties, increased risk of COPD with age, or a difference in air pollutants in these counties. The data illustrates the need for pulmonary specialists in these areas, as well as care teams specializing in COPD.
Data on lung cancer has only been reported in a few census tracts (Figure 286). These areas may contain larger populations of individuals at increased risk for lung cancer (i.e., history of smoking, increased age), and thus have an increased screening rate. There may also be an association with cancer treatment centers and their reporting.
Individuals with food allergies will require a care team consisting of an allergist and a dietitian. Those with respiratory allergies may create a team of pulmonologists, respiratory therapists, and pharmacists.
Asthma care teams may include a pulmonologist, an allergist, pharmacists, exercise physiologists, respiratory therapists, and mental health providers.
Individuals with COPD will likely include a pulmonologist, a pulmonary rehabilitation therapist, pharmacists, mental health providers, and a nutritionist on their care team. Depending on the severity of their COPD, the team may also include a thoracic surgeon and/or a palliative care provider.
Figure 308
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Asthma

Figure 309
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Chronic Obstructive Pulmonary Disease
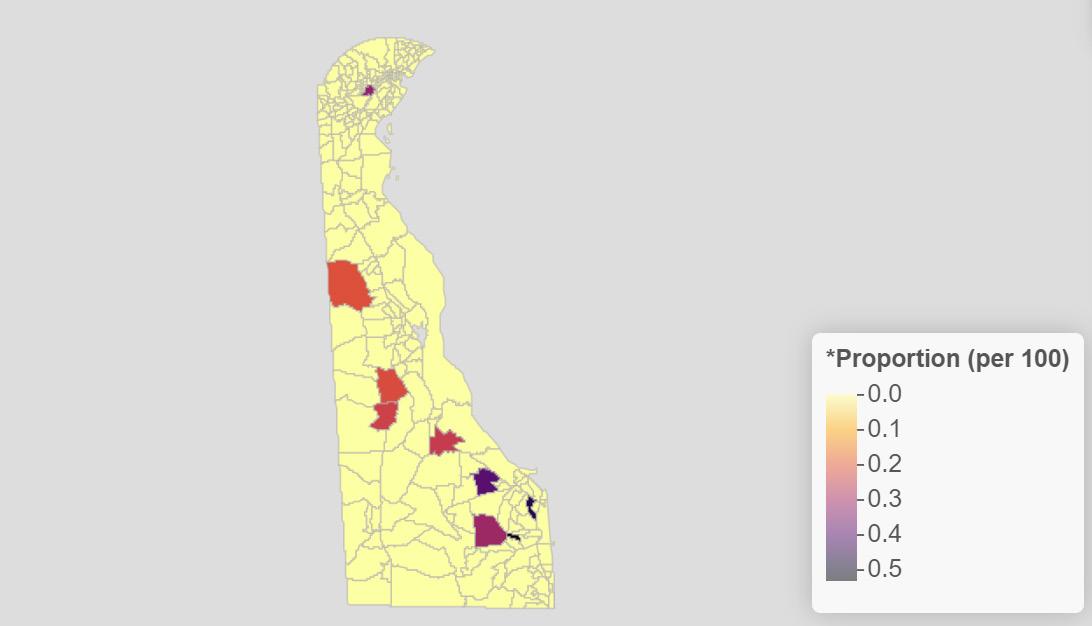
Figure 310
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Lung Cancer

Incidence of benign prostate hyperplasia and prostate cancer increase with age, as shown in figures x and x. These data illustrate the need for urologists and prostate specialists throughout the state, but especially in areas with older populations.
Figure 311
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Benign Prostatic Hyperplasia
Figure 312
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Prostate Cancer


The risk of cataracts increases with age, as the data in figure x shows. Glaucoma is more ubiquitous, and can affect individuals at any age, although it is more likely seen in adults. Figure x shows that there is an increased incidence of glaucoma in areas of increased populations. There is a need for healthcare providers specializing in ophthalmology and optometry to assist these individuals with their vision needs.
Figure 313
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Cataracts
Figure 314
2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Glaucoma


The Delaware Health Force (DHF) team imports data on licensed healthcare providers and institutions in Delaware. This data is collected under a data use agreement established with the Delaware Division of Professional Regulation and comes from their DELPROS system.
Once the data import for the license types of interest is complete, analysts prepare the data following these steps:
1. Data scrubbing is undertaken to normalize the data, and to catch variation in, for instance, how a person’s name is listed, or degree information is recorded.
2. Duplicates are removed or merged. Duplicates can occur within the data for a variety of reasons, and they are merged into a single record after record by record review.
3. Addresses are prepared geocoding. This may involve editing typos, correcting street directionals, replacing PO boxes with physical addresses, and making similar corrections to maximize the accuracy of the automated geocoding process.
4. Address data is geocoded. Providers’ county, ZIP code, census tract, and other geofenced areas are identified as needed.
DELPROS data gives us a total count of the licensed providers within a given profession, and is further delineated into Active, Cancelled, Closed, Expired, and “Other” status categories.
Providers with out–of–state practice addresses. Within each profession, some share of licensees report out–of–state practice addresses. Often, but not always, these addresses are in states that border Delaware: Maryland, New Jersey, and Pennsylvania. Some providers with out-of-state addresses may in fact be practicing in Delaware. Some providers treat patients via telehealth; others may practice in Delaware for part of the year; still others may work in Delaware as well as a border state. Currently, there is no way to know with certainty how many providers with outof-state addresses are actually treating patients in Delaware. This is an enhancement planned for the future.
Providers with no clearly identified practice address. In its present form, DELPROS allows new and renewing applicants to list addresses without defining their attribute. As a result an address may be home, office, institution, main office, branch location, etc. Similarly, some smaller share of licensees report no practice address at all. Often this is because they are no longer practicing. A future enhancement based upon the USPS “Residential Delivery Indicator” (RDI) will be employed to verify addresses, validate addresses, standardize addresses, and provide both RDI and Delivery Point Validation (DPV). Two such applications are the API Tool SmartyStreet and Lob.
When considering the broad range of disciplines that the entire caregiver team encompasses, we realize that at any point in time some number of licensed professionals of all types may be in administration and not seeing patients in any capacity. Others may be un- or underemployed at any point in time as well. At this time, there is no effective way to differentiate and isolate them from the larger workforce, and so a margin of error is implied. Further study will be necessary to determine what that margin of error is in arithmetic terms. Facilities provide their own challenges in counting including whether or not that are actually open for business, have closed to never be reopened, or are newly licensed but not yet seeing clients.
How physicians self-cateogorize their specialty practice is subject to the vagarities of natural language input. For this report, we have chosen to use the Association of American Medical College’s Specialty Pathway architecture shown on the following two pages. While imperfect as some speciality / subspeciality destinations can be achieved via various pathways, this does provide us with a consistent framework.
Similar to self-reported specialty and subspecialty, there are numerous self-reported terms referring to what year of education a physician is in. This is compounded by the date of the data in question as what month of the year the data is being viewed from as internships and residency start dates do not follow the calendar year. Further more, the length of residency varies by specialty. We utilized the Accreditation Council for Graduate Medicine Education pipeline matrix, shown in table 10, to adjust for these significant differences. It should be further noted that not all residency types are offered at Delaware locations.
Table 10
Three years:
• Internal medicine
• Medical genetics and genomics
• Osteopathic neuromusculoskeletal medicine—up to five years depending on program.
• Pediatrics
• Preventive medicine
Three–four years (depending on program):
• Emergency medicine
• Family medicine
• Neurology
• Pathology—anatomic and clinical
Four years:
• Anesthesiology
• Internal medicine-pediatrics
• Nuclear medicine Obstetrics and gynecology
• Ophthalmology
• Dermatology
• Psychiatry
1
Five years:
• Child neurology
• Diagnostic radiology
• Orthopaedic surgery
• Otolaryngology—head and neck surgery
• Radiation oncology
• General surgery
• Urology
• Vascular surgery
Six years:
• Plastic surgery—integrated
• Interventional radiology (up to seven years depending on program)
• Thoracic surgery (up to seven years depending on program)
7 years:
• Neurological surgery
In the near future, this data will be cross-referenced against the NPI Registry in the Delaware Health Force system. The NPI Registry is a service of the US Centers for Medicare and Medicaid Services, which, in many cases, provides additional information not captured within the DELPROS system. Information is also imported from the Delaware Health Information Network for those professionals who have both a Delaware license and an NPI number to further refine data on active practitioners.
1. Murphy, B. (2020, Nov 19). Medical specialty choice: Should residency training length matter? American Medical Association. Retrieved from: https://www.ama-assn.org/residents-students/specialty-profiles/medical-specialty-choice-should-residency-training-length
In the “Frequently Asked Question” section of Harvard Health the question is posed
“
In the hospital recently, a “resident” cared for me. Should I ask for a more experienced doctor?”
The answer, in it entirety below, goes a long way to explaining why we must count medical (and, for that matter, dental providers, pharmacists, and others) as a part of our healthcare workforce.
“Residents are doctors in training. They have graduated from medical school, been awarded an M.D. degree, and now are training to be a particular type of doctor — such as a pediatrician or pediatric specialist, or a type of surgeon. In their first year of such training, residents are sometimes called interns. All residents are supervised by a legally responsible senior physician. For over 40 years, I have been such a supervising physician. The residents typically have more time to spend with a patient than the supervising physician does. At the major teaching hospitals, like those here at Harvard, the competition to be selected for a residency is fierce. Those chosen are extraordinarily intelligent and knowledgeable. I’ve seen many residents save many lives. In fact, a recent study found that the quality of care was better in teaching hospitals. In short, you generally are in very good hands with a resident. But if you are concerned about the way a resident is handling your care, you always have the right to speak to the supervising physician.”1
Similarly, physicians who have progressed to where they are pursuing a fellowship, have all completed their residency. Delaware enjoys multiple residency and fellowship programs, with new slots being opened at a brisk pace. This information was gathered from institutional websites by the report authors, and it as up-to-date as of the time of publication.
For the advanced training which a fellowship provides, please see the list on page 340-341 which reviews ALL United States fellowship programs2 or thru the American Medical Associations FREIDATM Service.3
Bayhealth: https://bayhealthgme.org/graduate-medical-education/ Beebehealthcare.org: https://www.beebehealthcare.org/medical-education/graduate/family-medicine-residency ChristianaCare: https://residency.christianacare.org/ Nemours: https://www.nemours.org/education/gme.html St. Francis: https://www.trinityhealthma.org/healthcare-professionals/gme/ Delaware Psychiatric Center https://dhss.delaware.gov/dhss/dsamh/residency/
090007 - ABC Pediatrics
238081 - Armed Forces Medical Examiner System
098081 - Armed Forces Medical Examiner System
090002 - Bayhealth Hospital-Sussex Campus
090248 - Bayhealth Medical Center 090009 - Beebe Healthcare 098082 - Beebe Medical Center
090019 - Brandywine Counseling and Community Services Inc 098020 - Christiana Care Center for Urogynecology and Pelvic Surgery 090247 - Christiana Care Health Services Inc 098085 - Christiana Hospital 090004 - CNMRI-Milford Office
098004 - Community Mental Health Clinic-Dover 098005 - Community Mental Health Clinic-Wilmington
090297 - Delaware Division of Substance Abuse and Mental Health 090005 - Delaware Eye Care Center 090022 - Delaware Hospice 090021 - DSAMH Bridge Clinic New Castle 098017 - Fresenius Brandywine Home Therapies 098014 - Fresenius Medical Care (Wilmington) 090008 - Infusion Solutions of Delaware LLD-Dover Office 098086 - Kent Sussex Counseling Services 090006 - Kids and Teens Pediatrics 098009 - Mid Atlantic Pain Institute PA
098010 - Milton & Hattie Kutz Home Inc 098022 - Morgan Kalman Clinic 090340 - Nemours Children’s Health Wilmington 098013 - Nephrology Associates PA 090018 - Norman Broudy MD & Associates 098007 - Office of the Chief Medical Examiner (OCME) 098083 - Planned Parenthood of Delaware Inc 090011 - Psychiatry & Neurology 090015 - Psychiatry Delaware LLC 090010 - RI International-Restart Newark 098012 - Rockford Center
098021 - Roxana Cannon Arsht Surgicenter 090024 - Seasons Hospice and Palliative Care Facility 090014 - Serene Minds LLC
098006 - Silver Lake Treatment Consortium
090709 - St Francis Hospital
098003 - Terry Children’s Psychiatric Center 098087 - Thresholds Inc
090013 - TidalHealth Nanticoke 098016 - University of Delaware-Student Health Center 098002 - Veterans Affairs Medical Center (Elsmere) 090462 - Veterans Affairs Medical Center (Wilmington) 098011 - West Side Health
Abdominal Radiology (DR): 14 fellowships 0
Addiction Psychiatry (P): 57 fellowship programs 0
Adolescent Medicine (PD): 32 fellowships 0
Adult Cardiothoracic Anesthesiology (AN): 71 fellowships 0
Adult Reconstructive Orthopaedics (ORS): 28 fellowship programs 0
Advanced Heart Failure and Transplant Cardiolog...: 81 fellowships 1
Blood banking-transfusion medicine (PTH): 51 fellowship programs 0
Cardiovascular Disease (IM): 267 fellowship programs 1
Chemical Pathology (PTH): 5 fellowship programs 0
Child abuse pediatrics (PD): 31 fellowship programs 0
Child and Adolescent Psychiatry (P): 143 fellowships 0
Child Neurology (N): 77 fellowships 1
Clinical Cardiac Electrophysiology (IM): 116 fellowship programs 0
Clinical Informatics (PD): 1 fellowship 0
Clinical Neurophysiology (N): 91 fellowship programs 0
Complex Surgical Oncology (GS): 30 fellowships 0
Congenital cardiac surgery (TS): 14 fellowship programs 0
Craniofacial Surgery (PS): 9 fellowships 0
Critical Care Medicine (AN): 64 fellowship programs 0
Critical Care Medicine (IM): 49 fellowship programs 0
Dermatopathology (D and PTH): 57 fellowships 0
Developmental-Behavioral Pediatrics (PD): 44 fellowship programs 0
Endocrinology, Diabetes, and Metabolism (IM): 155 fellowships 0
Endovascular Surgical Neuroradiology (DR): 4 fellowships 0
Endovascular Surgical Neuroradiology (N): 2 fellowships 0
Endovascular surgical neuroradiology (NS): 2 fellowship programs 0
Foot and Ankle Orthopaedics (ORS): 8 fellowships 0
Forensic Pathology (PTH): 48 fellowships 0
Forensic Psychiatry (P): 50 fellowships 0
Gastroenterology (IM): 219 fellowships 0
Geriatric Medicine (FM): 51 fellowship programs 0
Geriatric Medicine (IM): 114 fellowships 0
Geriatric Psychiatry (P): 63 fellowship programs 0
Hand Surgery (GS): 1 fellowship 0
Hand Surgery (ORS): 74 fellowships 0
Hand Surgery (PS): 16 fellowship programs 0
Hematology (IM): 2 fellowship programs 0
Hematology (PTH): 87 fellowships 0
Hematology and Oncology (IM): 174 fellowships 0
Infectious Disease (IM): 158 fellowships 0
Interventional Cardiology (IM): 183 fellowship programs 1
Medical Microbiology (PTH): 15 fellowship programs 0
Medical Toxicology (EM): 27 fellowship programs 0
Medical Toxicology (GPM): 2 fellowships 0
Molecular Genetic Pathology (MG and PTH): 42 fellowships 0
Musculoskeletal Oncology (ORS): 12 fellowships 0
Musculoskeletal Radiology (DR): 18 fellowships 0
Neonatal-Perinatal Medicine (PD): 102 fellowship programs 0
Nephrology (IM): 152 fellowship programs 0
Neurodevelopmental Disabilities (N): 8 fellowships 0
Neuromuscular Medicine (N): 1 fellowship program 0
Neuropathology (PTH): 36 fellowship programs 0
Neuroradiology (DR): 89 fellowship programs 0
Neurotology (OTO): 24 fellowships 0
Nuclear Radiology (DR): 18 fellowship programs 0
Obstetric Anesthesiology (AN): 38 fellowships 0
Oncology (IM): 7 fellowship programs 0
Orthopaedic Sports Medicine (ORS): 96 fellowships 0
Orthopaedic Surgery of the Spine (ORS): 16 fellowships 0
Orthopaedic Trauma (ORS): 12 fellowships 0
Pain Medicine (AN): 1 fellowship program 0
Pediatric Anesthesiology (AN): 63 fellowship programs 1
Pediatric Cardiology (PD): 62 fellowships 1
Pediatric Critical Care Medicine (PD): 74 fellowship programs 1
Pediatric Emergency Medicine (EM): 29 fellowships 0
Pediatric Emergency Medicine (PD): 59 fellowships 1
Pediatric Endocrinology (PD): 73 fellowships 0
Pediatric Gastroenterology (PD): 65 fellowships 1
Pediatric Hematology Oncology (PD): 74 fellowships 1
Pediatric Infectious Diseases (PD): 65 fellowships 0
Pediatric Nephrology (PD): 47 fellowship programs 0
Pediatric Orthopaedics (ORS): 25 fellowship programs 1
Pediatric Otolaryngology (OTO): 31 fellowships 1
Pediatric Pathology (PTH): 29 fellowship programs 0
Pediatric Pulmonology (PD): 56 fellowship programs 1
Pediatric Radiology (DR): 47 fellowships 1
Pediatric Rehabilitation (PM): 22 fellowships 0
Pediatric Rheumatology (PD): 35 fellowship programs 1
Pediatric Sports Medicine (PD): 17 fellowship programs 0
Pediatric Surgery (GS): 54 fellowship programs 0
Pediatric Urology (U): 26 fellowships 0
Procedural Dermatology (D): 1 fellowship program 0
Psychosomatic Medicine (P): 64 fellowships 0
Pulmonary Disease (IM): 24 fellowship programs 0
Pulmonary Disease and Critical Care Medicine (IM): 193 fellowships 0
Rheumatology (IM): 125 fellowships 0
Selective Pathology (PTH): 99 fellowship programs 0
Spinal Cord Injury Medicine (PM): 24 fellowships 0
Sports Medicine (EM): 9 fellowship programs 0
Sports Medicine (FM): 154 fellowship programs 1
Sports medicine (PM): 21 fellowships 0
Surgical Critical Care (GS): 142 fellowships 1
Transplant hepatology (IM): 60 fellowship programs 0
Undersea and Hyperbaric Medicine (EM): 8 fellowships 0
Undersea and Hyperbaric Medicine (GPM): 2 fellowships 0
Vascular and Interventional Radiology (DR): 90 fellowships 1
Vascular Neurology (N): 106 fellowships 0
Vascular Surgery (GS): 117 fellowship programs 0
1. Harvard Health Publishing. (2017, Aug 1). Should I see a “resident” doctor? Retrieved from: https://www.health.harvard.edu/healthcare/should-i-see-aresident-doctor
2. Resident Swap. (n.d.). Residency and fellowship programs. Retrieved from: https://www.residentswap.org/view_specialties.php
3. Freida. (n.d.). Institution directory. Retrieved from https://freida.ama-assn.org/institution?page=2&filter=D
The profession of nursing follows a model of academic progression, accounting for the personal and professional decision(s) of the individual. Generally, nursing education is based upon bridge or ladder programs (also known as stacking) where one degree or certification provides the prerequisite for the subsequent level. There are generally three categories of nursing education that are related to licensure and scope of practice: unlicensed assistive personnel/pre-licensure, entry to practice/licensure and graduate/advanced nursing practice. Around the United States there is variation in what equivalent levels of nursing are called, and the path outlined below is a US model that is broadly applicable.
CNA (Certified Nursing Assistant): 4 - 12-week programs; result in a certificate and eligibility to sit for a national certification test
LPN/LVN (Licensed Practical/Vocational Nurse): 1 year program; non-degree program; eligible to sit for national LPN licensure exam and obtain licensure in all 50 states and U.S. territories.
*LPN/LVNs seeking to progress academically in nursing complete a LPN-RN program. Most LPN-RN programs result in an Associate Degree in Nursing, however, some U.S. colleges offer LPN to Bachelor of Science in Nursing programs.
Diploma (Registered Nurse): 2-year program; non-academic degree program; eligible to sit for national RN licensure exam, obtain licensure in all 50 states and U.S. territories, and obtain specialty nursing certification.
ADN (Associate Degree in Nursing): 2 - 3 Years; result in academic degree; eligibility to sit for national RN licensure exam and obtain licensure in all 50 states and U.S. territories, and obtain specialty nursing certification.
*RN-BSN academic progression programs can be completed by the Diploma or ADN nurse and typically take 1-2 years to complete.
BSN (Bachelor of Science in Nursing): 4 Years; results in academic degree; eligibility to sit for national RN licensure exam, obtain licensure in all 50 states and U.S. territories, and obtain specialty nursing certification; can be attained by a LPN, Diploma, or ADN.
Graduate/Advanced Nursing Practice
MSN (Master of Science in Nursing): 2 - 4 Years
Graduate/MSN is further defined based on the attainment of an Advanced Practice Registered Nurse (APRN) certification and licensure or not.
Advanced Practice Registered Nurse (APRN) 2 – 4 Years
Certified Nurse Practitioner (CNP)
Certified Nurse Midwife (CNM)
Clinical Nurse Specialist (CNS)
Certified Registered Nurse Anesthetist (CRNA)
An RN or APRN possessing an MSN may elect to return to a post-Masters certificate program to continue their academic progression. Again, this may result in the attainment of an APRN certification and licensure or not. For example, an RN with an MSN in Nursing Leadership may complete a post-Masters certificate program and sit for certification and licensure as a CNS or CNP. Additionally, an APRN with an MSN, certification, and licensure as a Family Nurse Practitioner may complete a post-Masters certificate program and sit for certification as an Acute Care Adult-Gerontology Nurse Practitioner.
DNP/PhD (Doctor of Nursing Practice/Doctor of Philosophy in Nursing) 6 - 8 Years
Registered Nurse 19577 Physician M.D. 5308 Physician CSR 3566 Licensed Practical Nurse 2595 Pharmacist 2423 Physical Therapist 1681 Advanced Practice RN CSR 1435 Family NP 1342 Licensed Clinical Social Worker 1175 Licensed Masters Social Worker 1039 Non Resident Pharmacy 985 Physician Assistant 944 Pharmacy - Wholesale 940 Physician D.O. 933 Dental Hygienist 874 ACGME Training 849 Speech/Language Pathologist 842 Occupational Therapist 782 Professional Counselor of Mental Health 774 Respiratory Practitioner 774 Physician Assistant CSR 680 Pharmacy CSR 677 Psychologist 607
Physical Therapist Assistant 578 Dentist 540 Dietitian/Nutritionist 461 Dentist CSR 422 Licensed Bachelors Social Worker 381 Chiropractor 379 Occupational Therapy Assistant 366 Genetic Counselor 348 Certified Registered Nurse Anesthetist 344 Paramedic 343 Adult/Gerontology NP 326 Athletic Trainer 310 Distributor/Manufacturer CSR 292 Veterinarian CSR 253 Pharmacy - Retail 212 Restricted Permit II 200 Therapeutic Optometrist 199 Psych/Mental Health NP 182 Pediatric NP 165 Pharmacist - Intern 123 Podiatrist 108 Audiologist 106 Hospital/Clinic CSR 89 Chemical Dependency Professional 82 Podiatrist CSR 76 Adult NP 73 Polysomnographer 73 Marriage and Family Therapist 68 Women’s Health/Gender-Related NP 65
Temporary Speech/Language 61 Unrestricted Permit 57 Certified Nurse Midwife 48 Medical Gas Dispenser 45 Neonatal NP 43 Eastern Medicine Practitioner 41 Hearing Aid Dispenser 38 Psych/Mental Health CNS 34 Research/Laboratory CSR 34 Optometrist CSR 33 Associate Counselor of Mental Health 29 Outsourcing Facility-Distributor 29 Adult/Gerontology CNS 27 Psychological Assistant 26 Restricted Permit I 23 Administrative Medical 23 Dentist Limited-Resident 21 Pediatric CNS 20 Pharmacy - Hospital 17 Adult Health CNS 16 Gerontology NP 14 Dentist Academic 12 Medical/Surgical CNS 12 Acupuncture Practitioner 12 Acute Care NP 11 Temporary Hearing Aid Dispenser 11 Pharmacy - Manufacturer 9 Professional Art Therapist 9 Certified Professional Midwife 9 Outsourcing Facility-Pharmacy 9 Health Promotion & Wellness CNS 7 Associate Marriage and Family Therapist 6 Acupuncture Detoxification Specialist 5
Temporary Permit - RN 5 Maternal Child CNS 4 Podiatrist In-Training 4 Diagnostic Optometrist 3 Retail Non Pharmacy 3 Therapeutic Optometrist Internship 3 Gerontology CNS 2 Oncology CNS 2 Perinatal NP 2 Women’s Health/Gender-Related CNS 2 Provider Pharmacy Facility CSR 2 Genetic Counselor-Provisional 2 Other CSR 2
Community Health Nursing CNS 1 Critical Care CNS 1 Physical Therapist Temporary 1 Temporary Permit - GN 1 Physician M.D.-Volunteer 1 Neonatal CNS 1
Total 58799
ACGME Training - a Resident, Intern or Fellow registered in a training program outside of Delaware who will rotate through a program in Delaware for over one month, or employed as a House Physician.
Acupuncture Practitioners - not all certified acupuncturists are physicians. However an AOM (Acupuncture/ Oriental Medicine) has its own unique training and terminal degree.
CNS - Clinical Nurse Specialist, individuals must maintain an RN license simultaneously
CSR - Controlled Substances Registration. Practitioners include physicians, physician assistants, advanced practice registered nurses, podiatrists, dentists, optometrists, and veterinarians. Facilities include pharmacies, distributors, manufacturers, hospitals, clinics, researchers, laboratories and provider pharmacies. CSR is a secondary license. For instance, there are a total of 6,241 Physicians (M.D. and D.O.) of whom 3,566 are additionally licensed to prescribe controlled substances.
GN - Graduate Nurse. A graduate nurse (GN) is someone who has graduated from a nursing degree program but has not yet earned state licensure. Depending on the employer, GNs may work in clinical settings pending licensure.
NP - Nurse Practitioner, individuals must maintain an RN license simultaneously
Ophthalmologist - are medical doctors
Optometrists - are not medical doctors, instead they have an OD (doctor of optometry) degree.
Podiatrists - are medical doctors with specialized training who go thru specialized training that results in a DPM, (doctor of podiatric medicine) degree.
Restricted Permit I - A Restricted Permit I allows the license holder to induce only conscious sedation by parenteral, enteral, or rectal routes, as well as nitrous oxide inhalation, at a specific location. (This does not prohibit the usual and customary pre-operative oral sedation.) If one holds a Restricted Permit I, they are not allowed to induce: deep sedation or general anesthesia.
Restricted Permit II - A Restricted Permit II allows the license holder to induce conscious sedation by nitrous oxide inhalation. If one holds a Restricted Permit II, they are not allowed to induce the following: deep sedation or general anesthesia.
RN - Registered Nurse
Number Facility Name A-Z
License ID
1 Cheer/Sand Hill Adult Day Program ADC-018
2 Day Break Mature Adult Care ADC-001
3 Delaware Adult Daycare LLC ADC-020
4 Easter Seals Delaware & Maryland's Eastern Shore ADC-010 5 Easter Seals Delaware & Maryland's Eastern Shore ADC-011 6 Elwyn of Pennsylvania and Delaware ADC-007
7 Evergreen Center I: Alzheimer's Adult Day Care ADC-003
8 Gilpin Hall Adult Day Program ADC-014 9 Messiah's Angels ADC-019
10 Smyrna Adult Day Care ADC-013
11 Weston Adult Day Care Center ADC-015

Number Facility Name A-Z License ID Street Address
City Zip Code
1 Alfred I duPont Hospital for Children Dialysis Unit DC-007 1600 Rockland Rd Wilmington 19803
2 American Kidney Care Dover DC-001 107 Mont Blanc Blvd Ste 100 Dover 19904
3 American Kidney Care Hockessin DC-010 5936 Limestone Rd Suite 101 Hockessin 19707
4 American Kidney Care Middletown DC-034 601 Tower Lane, Suite 100 Middletown 19709
5 American Kidney Care Newark DC-006 1415 Pulaski Hwy Suite B Newark 19702
6 Bayhealth Medical Center Kent Campus Dialysis Unit DC-009 640 South State St Dover 19901
7 Christiana Care Newark Campus Dialysis Center DC-014 4755 Ogletown-Stanton Rd Newark 19713
8 Christiana Care Wilmington Campus Dialysis Center DC-015 501 West 14th St Wilmington 19801
9 FKC Bridgeville DC-016 9115 Antique Alley Bridgeville 19933
10 FKC First State DC-002 608 Ferry Cut-Off Rd New Castle 19720
11 FKC Lantana DC-020 214 Lantana Dr Hockessin 19707
12 FKC Main Street DC-028 230 East Main St Suite 325 Newark 19711
13 FKC North Dover DC-024 80 Salt Creek Dr Dover 19904
14 FKC Talleyville DC-030 1417 Foulk Rd Suite 100 Wilmington 19803
15 FMC Brandywine Home Therapies DC-025 4923 Ogletown-Stanton Rd Ste 210 Newark 19713
16 FMC Central Delaware DC-023 655 S Bay Rd Ste 4M Blue Hen Corp Ctr Dover 19901
17 FMC Dover Home Dialysis Center DC-017 1198 S Governors Ave Bldg B Ste 100 Dover 19904
18 FMC Fox Run DC-029 2520 Wrangle Hill Rd Bear 19701
19 FMC Green Tree DC-019 97 Commerce Way Ste 104 Dover 19904
20 FMC Mid-Sussex DC-026 34 Georgetown Plaza Georgetown 19947
21 FMC Milford DC-013 656D North DuPont Hwy Milford 19963
22 FMC Millsboro DC-027 30164 Commerce Dr Peninsula Crossing Millsboro 19966
23 FMC Newport Pike DC-021 605 W Newport Pk Wilmington 19804
24 FMC North Wilmington DC-012 4000 Washington St Wilmington 19802
25 FMC of Brandywine DC-031 303 A St Wilmington 19801
26 FMC of Christiana DC-018 63 University Plaza Newark 19702
27 FMC of Middletown DC-022 104 Sleepy Hollow Dr Middletown 19709
28 FMC Rehoboth DC-003 19339 Coastal Hwy Suite 100 Rehoboth Beach 19971
29 FMC Riverside Park DC-032 700 W Lea Blvd Unit G-2 Wilmington 19802
30 FMC Smyrna DC-008 210 Stadium St Gateway North Shopping Ctr Smyrna 19977
31 FMC Wilmington DC-033 701 North Clayton St Suite 404 Wilmington 19805
32 US Renal Care Laurel Dialysis DC-005 30214 Sussex Hwy Unit 4 Laurel Sq Shopping Ctr Laurel 19958
33 US Renal Care Seaford Dialysis DC-011 600 Health Services Dr Seaford 19973
34 US Renal Care Wilmington Dialysis DC-004 913 Delaware Ave Wilmington 19806

Number Facility NameSorted Ascending License ID Street Address City Zip Code 1 The Birth Center: Holistic Women's Health Care LLC FSBC-001 620 Churchmans Rd Newark 19713

Number Facility Name A-Z License ID Street Address
1 Advance Endoscopy Center LLC
City Zip Code
FSSC-028 742 S Governors Ave Suite 2 Dover 19904
2 American Surgery Center FSSC-007A 900 Foulk Rd Wilmington 19803
3 Bayhealth Surgery Center FSSC-022A 100 Scull Ter Dover 19901
4 Beebe Outpatient Surgery Center FSSC-012 18941 John J Williams Hwy Rehoboth Beach 19971
5 Cataract and Laser Center FSSC-004A 4102 Ogletown-Stanton Rd Suite 1 Newark 19713
6 Center for Advanced Surgical Arts FSSC-021A 2710 Centerville Rd Suite 100 Wilmington 19808
7 Central Delaware Endoscopy Unit LLC FSSC-025 644 S Queen St Dover 19904
8 Christiana Spine Ambulatory Surgery Center FSSC-032 1101 Twin C Lane Suite 102 Newark 19713
9 CTS Surgical Associates LLC FSSC-006 32711 Long Neck Rd Millsboro 19966
10 Delaware Eye Surgery Center FSSC-010 18791 John J Williams Hwy Suite 2 Rehoboth 19971
11 Delaware Outpatient Center for Surgery FSSC-013A 774 Christiana Rd Suite 2 Newark 19713
12 Delaware Surgery Center LLC FSSC-009 200 Banning St Suite 110 Eden Hill Medical Center Dover 19904
13 Delaware Surgical Arts (C&S Medical) FSSC-018 537 Stanton-Christiana Rd Suite 109 Newark 19713
14 Endoscopy Center of Delaware FSSC-029 1090 Old Churchman's Rd Newark 19713
15 First State Surgery Center LLC FSSC-008 1000 Twin C La Suite 200 Newark 19713
16 Glasgow Ambulatory Surgery Center FSSC-003 2600 Glasgow Ave Suite 226 Newark 19702
17 Lewes Surgery Center FSSC-020A 17015 Old Orchard Rd Unit 4 Lewes 19958
18 Limestone Surgery Center FSSC-001A 1941 Limestone Rd Suite 113 Wilmington 19808
19 Mid-Atlantic Endoscopy Center LLC FSSC-031 4923 Ogletown-Stanton Rd Newark 19713
20 Orthopaedic Specialists Surgi-Center LLC FSSC-019 1096 Old Churchman's Rd Newark 19713
21 Seaford Endoscopy Center LLC FSSC-026 13 Fallon Ave Seaford 19973
22 Seaside Endoscopy Center LLC FSSC-030 34444 Kings St Row Lewes 19958
23 SpineCare Delaware LLC FSSC-027 4102 Ogletown-Stanton Rd Newark 19711

Number Facility Name A-Z
1 Bayada Home Health Care Inc (Wilmington)
License ID Street Address
City Zip Code
HHAAO-064B 4250 Lancaster Pike Suite 310 Wilmington 19805
2 Bayada Home Health Care Inc. (Milford) HHAAO-070 100 Silicato Parkway Suite 104 Milford 19963
3 CarpeVITA Home Care
4 Coastal Home Care
5 Comfort Care at Home
6 Comfort Keepers
7 Cornerstone Health Partners LLC
8 Four Seasons Healthcare LLC
HHAAO-022A 240 S James St Suite 107 Newport 19804
HHAAO-025A 20771 Professional Park Blvd Suite 2 Georgetown 19947
HHAAO-017A 260 Chapman Rd Suite 200A Newark 19702
HHAAO-011A 92 Reads Way Suite 207 New Castle 19720
HHAAO-066 920 Justison Street Wilmington 19801
HHAAO-021A 229 N Main Street Suite 204 Smyrna 19977
9 Guardian Angel Home Health Care Agency LLC HHAAO-069 30 Prestbury Square Suite 301 Newark 19713
10 Home Helpers & Direct Link of Wilmington
11 Ingleside Home Health Care
12 PRN Staffers Home Healthcare Agency
13 Senior Home Help LLC
14 Shorecare of Delaware
15 Solution On-Call Services LLC
HHAAO-024 3301 Green St Ste 231 Claymont Community Center Claymont 19703
HHAAO-015 1005 N Franklin St Wilmington 19806
HHAAO-067 1400 Peoples Plaza Suite 200 Newark 19702
HHAAO–065A 11550 Willow Grove Rd Suite B Camden 19934
HHAAO-019 874 Walker Rd Suite D-1 Dover 19904
HHAAO-020 19 Lambsons Lane Suite 108B New Castle 19720

Number Facility Name A-Z
1 Addus Health Care
License ID Street Address
City Zip Code
HHAS-013A 1675 S State St Suite 4C Dover 19901
2 Affinity Home Care Services LLC HHAS-070 1040 South State St Suite A Dover 19901
3 Amedisys Delaware LLC (Kent) HHAS-010A 1201 College Park Drive Suite 101 Dover 19904
4 Amedisys Delaware LLC (Sussex) HHAS-028A 20093 Office Circle Unit 205 Georgetown 19947
5 Aston Home Health Care Inc HHAS-032 1021 Gilpin Ave Suite 202 Wilmington 19806
6 At Home Care Agency LLC HHAS-053 57 Saulsbury Rd Dover 19904
7 Aveanna Health Services (DE) LLC (Milford) HHAS-017B 20093 Office Circle Unit 205 Georgetown 19947
8 Aveanna Health Services (DE) LLC (Newark) HHAS-039B 56 W Main St Suite 211 Plaza 273 Newark 19702
9 Aveanna Home Health Care (Milford) f/k/a Millenium Home Healthcare HHAS-034B 1017 Mattlind Way Milford 19963
10 Aveanna Home Health Care (Newark) HHAS-079 262 Chapman Road Suite 102 Newark 19702
11 BAYADA Home Health Care at Bayhealth HHAS-003A 655 South Bay Rd Suite K-1 Dover 19901
12 Bayada Home Health Care Inc (Dover) HHAS-062B 655 South Bay Rd Ste 1G Dover 19901
13 Bayada Home Health Care Inc (Milford) HHAS-040B 1016 North Walnut St Milford 19963
14 Bayada Home Health Care Inc (New Castle) HHAS-041B 15 Reads Way Suite 205 New Castle 19720
15 Bayada Home Health Care Inc (Newark) HHAS-043B 200 Biddle Ave Suite 111 Newark 19702
16 Bayada Home Health Care Inc (Wilmington) HHAS-011B 4250 Lancaster Pike Suite 300 Wilmington 19805
17 Bayada Home Health Care Inc (Wilmington) HHAS-042B 4250 Lancaster Pike Suite 304 & 312 Wilmington 19805
18 Beebe Home Health Agency HHAS-002 232 Mitchell St Suite 200 Millsboro 19966
19 Care at Home of Delaware LLC HHAS-072 20 Montchanin Road Suite 50 Wilmington 19807
20 Caring n' Action Nursing Agency HHAS-060 30 Prestbury Square Suite 314 Newark 19713
21 Caritas Home Health Services HHAS-051 15 Prestbury Square Suite 15 Newark 19713
22 ChristianaCare HomeHealth (Kent) HHAS-007 2116 S DuPont Hwy Suite 2 Camden 19934
23 ChristianaCare HomeHealth (NCC) HHAS-006 One Reads Way Suite 100 New Castle 19720
24 Edlyncare LLC HHAS-066 821 Seymour Rd Bear 19701
25 Grace Miracle Home Care LLC HHAS-075 3604 Miller Road Wilmington 19802
26 IJN Health Systems LLC HHAS-069 603 Parkman Ct Bear 19701
27 Interim Healthcare of Delaware LLC HHAS-029A 100 S Main St Suite 203 Smyrna 19977
28 Maxim Healthcare Services (Kent) HHAS-035 671 S. Carter Road Suites 5 & 6 Smyrna 19977
29 Mirage Health Services LLC HHAS-077 1575 McKee Road Suite 203 Dover 19904
30 Neuro-care/Total Care HHAS-008 34 Germay Dr Wilmington 19804
31 Patriot Home Care HHAS-068 1225 N King St Suite 300 Wilmington 19801
32 Peninsula Home Care at Nanticoke HHAS-031B 501 Health Services Dr Herring Run Prof Center Seaford 19973
33 Preferred Home Health Care & Nursing Services Inc HHAS-071 3529-31 Philadelphia Pike Claymont 19703
34 Saint Francis Hospital Home Care HHAS-001 100 Commerce Dr Suite 100 Newark 19713
35 Shepherds Healthcare Services HHAS-078 278 Jordan Drive Suite A-9 Dover 19904
36 Silver Lining Home Healthcare (f/k/a Nurse Next Door) HHAS-055 24 Hiawatha Lane Dover 19901
37 Steps Homecare Services HHAS-073 915 N. Madison Street Wilmington 19801
38 Summit Orthopaedic Home Care LLC (Kent) HHAS-058 490 N DuPont Hwy Dover 19901
39 Summit Orthopaedic Home Care LLC (Sussex) HHAS-067 1632 Savannah Rd Suite 8 Lewes 19958
40 Trinity Home Health Care Corp HHAS-045A 1400 Peoples Plaza Suite 215 Newark 19702
41 Trinity Home Health LLC HHAS-074 707 Pinewood Drive Middletown 19709
42 Unity Healthcare Services HHAS-076 2131 South DuPont Highway Suite 4 Dover 19901
43 Vicdania Health Services LLC HHAS -057 1006 College Road Suite 101 Dover 19904

Number Facility Name A-Z
License ID Street Address City Zip Code
1 ACTS Signature Hospice HSPC-018 726 Loveville Rd Suite 3000 Hockessin 19707
2 Aveanna Hospice f/k/a Millenium Hospice HSPC-020 1101 Mattlind Way Milford 19963
3 Bayada Hospice HSPC-019B 4250 Lancaster Pike, Suite 308 Wilmington 19805
4 ChristianaCare-AccentCare Millsboro HSPC-014B 30265 Commerce Dr Suite 205 Millsboro 19966
5 ChristianaCare-AccentCare Newark HSPC-010C 220 Continental Dr Suite 407 Newark 19713
6 ChristianaCare-AccentCare Newark (IPU) HSPC-010C 4755 Ogletown Statnton Rd Newark 19713
7 ChristianaCare-AccentCare Newark (Wilm IPU) HSPC-010C 504 West 14th St Wilmington 19801
8 Compassionate Care Hospice (office location) HSPC-004A 405 East Marsh La Suite 4 Newport 19804
9 Compassionate Care Hospice of the Delmar Peninsula LLC HSPC-011A 20165 Office Cir Unit 2 North Building Georgetown Professional Park Georgetown 19947
10 Delaware Hospice Inc Dover HSPC-002 911 S duPont Hwy Lotus Plaza Dover 19901
11 Delaware Hospice Inc Milford IPU HSPC-003 100 Patriots Way Milford 19963
12 Delaware Hospice Inc Newark HSPC-001 16 Polly Drummond Center 2nd Floor Polly Drummond Shopping Ctr Newark 19711
13 Heartland Hospice Services HSPC-008 750 Prides Crossing Suite 110 Newark 19713
14 Millenium Hospice HSPC-020 1017 Mattlind Way Suite B Milford 19963
15 ProMedica Hospice Services HSPC-008 750 Prides Crossing Suite 110 Newark 19713
16 Seasons Hospice & Palliative Care of Delaware Millsboro HSPC-014 30265 Commerce Dr Suite 205 Millsboro 19963
17 Seasons Hospice & Palliative Care of Delaware LLC Newark HSPC-010A 220 Continental Dr Suite 407 Christiana Executive Campus Newark 19713
18 Seasons Hospice & Palliative Care of Delaware LLC (Newark Inpatient Unit) HSPC-010A 4755 Ogletown Stanton Rd 6th Floor Newark 19718
19 Vitas Healthcare Corporation (NCC) HSPC-009 100 Commerce Dr Suite 302 Newark 19713
20 Vitas Healthcare Corporation (Sussex) HSPC-012 30265 Commerce Dr Suite 202 & 203 Millsboro 19966
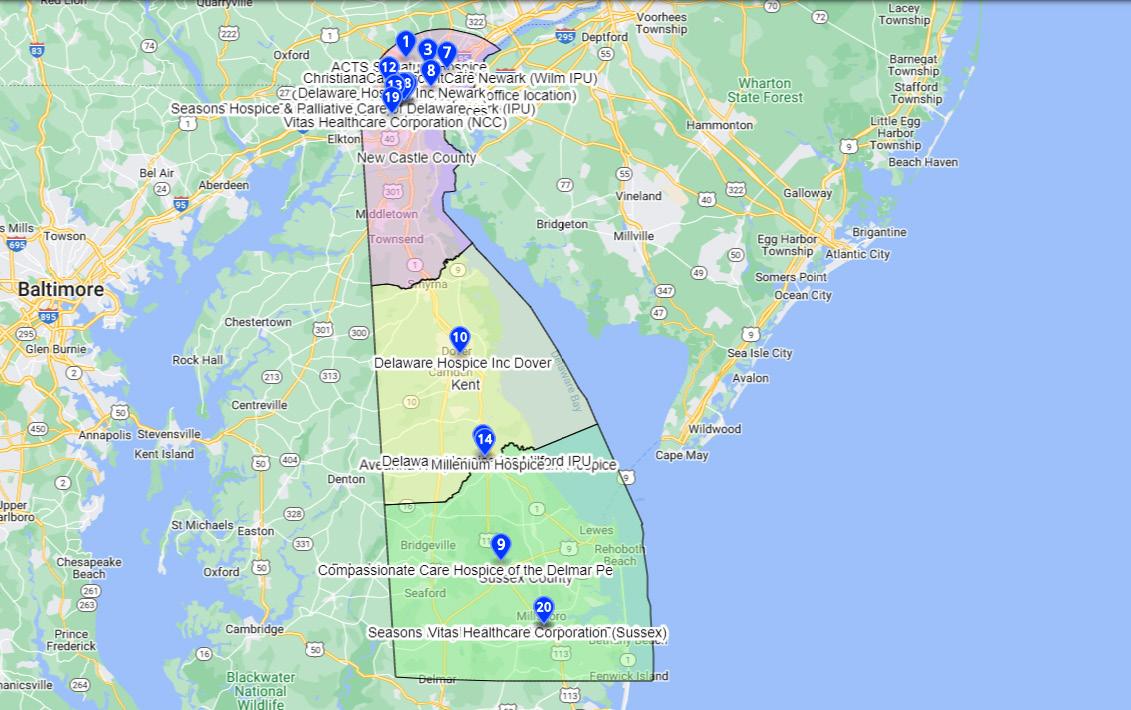
Number Facility Name A-Z
1 A I duPont Hospital for Children
License ID Street Address
City Zip Code # of Licensed Beds
HSPTL-003 1600 Rockland Rd PO Box 269 Wilmington 19803 206
2 Bayhealth Hospital, Kent Campus HSPTL-005 640 South State St Dover 19901 266
3 Bayhealth Hospital, Sussex Campus HSPTL-006 100 Wellness Way Milford 19963 128
4 Beebe Medical Center HSPTL-007 424 Savannah Rd Lewes 19958 210
5 Christiana Care Health Services - Christiana Hospital HSPTL-002 4755 Ogletown-Stanton Rd PO Box 6001 Newark 19718 906
6 Christiana Care Health Services - Wilmington Hospital HSPTL-001 501 West 14th St PO Box 1668 Wilmington 19899 321
7 Delaware Psychiatric Center HSPTL-009 1901 North duPont Hwy New Castle 19720 200
8 Dover Behavioral Health System HSPTL-013 725 Horsepond Rd Dover 19901 104
9 Encompass Health Rehabilitation Hospital of Middletown HSPTL-014 250 East Hampden Rd Middleton 19709 40
10 MeadowWood Behavioral Health System HSPTL- 010C 575 South duPont Hwy New Castle 19720 120
11 PAM Rehab Hospital of Dover HSPTL-016 1240 McKee Rd Dover 19904 34
12 Rockford Center HSPTL-011 100 Rockford Dr Newark 19713 138
13 Select Specialty Hospital of Wilmington HSPTL-012 701 N Clayton St Fifth Floor Wilmington 19805 35
14 St Francis Healthcare HSPTL-004 701 N Clayton St Wilmington 19805 395
15 Sun Behavioral Delaware LLC HSPTL-015 21655 Biden Ave Georgetown 19947 90
16 Tidal Health Nanticoke HSPTL-008 801 Middleford Road Seaford 19973 139

Number Facility Name A-Z
1 Acclaim Home Care of Delaware
License ID Street Address City Zip Code
PASA-030A 17527 Nassau Commons Blvd Suite 210 Lewes 19958
2 ACTS Home Care and Senior Services - Delaware PASA-069 726 Loveville Road Suite 3000 Hockessin 19707
3 Addus Home Care Delaware PASA-028 1675 South State Street Suite 4C Dover 19901
4 Age Advantage Senior Care Services PASA-037 2634 Capitol Trail Meadowood Shopping Center II Newark 19771
5 Always Best Care (NCC) PASA-050 1905 North Market Street Wilmington 19802
6 Always Best Care (Sussex) PASA-058 624 Mulberry St Milton 19968
7 Amada Senior Care Solutions Delaware Inc PASA-063 1 Ashford Drive Lewes 19958
8 Amazing Home Care Agency PASA-070 1012 College Road Suite 101 Dover 19904
9 Americare Home Solutions PASA-032 32 West Loockerman St Suite 104 Dover 19904
10 Blue Ridge Home Care Inc PASA-056 9 East Loockerman Street Suite 211 Dover 19901
PASA-047 838 Walker Rd Ste 22-3 Dover 19904
11 Caring Hearts Home Care LLC
12 Cheer Personal Assistant Services Program PASA-045 546 South Bedford Street Georgetown, 19947
13 Compassionate Angels
14 Delaware Caregivers
PASA-064 200 Continental Drive, Suite 401 Newark 19713
PASA-072 260 Chapman Road Suite 104D Newark 19702
15 Dependable Community Home Care LLC PASA-077 260 Chapman Road Suite 200F Newark 19702
16 Edlyncare LLC
17 Empathy Home Care LLC
PASA-026 821 Seymour Rd Bear 19701
PASA-071 57 Anglin Drive Newark 19713
18 Family Benefit Homecare PASA-017 3322 Englewood Rd Wilmington 19810
19 Greater Works Companion Care PASA-018 5574 Kirkwood Hwy Wilmington 19808
20 Griswold Home Care (Kent & Sussex)
PASA-006A 18335 Coastal Hwy Suite 200A Lewes 19958
21 Griswold Home Care (NCC) PASA-005A 5145 W Woodmill Drive Suite 22 Wilmington 19808
22 Home Instead (formerly Homewatch Caregivers of Delaware (Sussex)
23 Home Instead Senior Care (Kent & Sussex)
PASA-029 17527 Nassau Commons Blvd Suite 204 Lewes 19958
PASA-044 17577 Nassau Commons Blvd Lewes 19958
24 Home Instead Senior Care (NCC & Kent) PASA-003 30 South American Ave Dover 19901
25 Home Instead Senior Care (NCC)
26 Homewatch Caregivers of Delaware (NCC)
PASA-001 1701 Shallcross Avenue Suite A Wilmington 19806
PASA-015 5560 Kirkwood Hwy Wilmington 19808
27 Homewatch Caregivers of Delaware (Sussex) (JP Nacchia & Associates Inc) PASA-029 17527 Nassau Commons Blvd Suite 204 Lewes 19958
28 HomeWell Care Services
PASA-068 142 East Market Street Georgetown 19947
29 Incredible Home Care PASA-061 1224 North King St Wilmington 19801
30 Interim Personal Care and Support LLC PASA-054 100 South Main St Ste 203 Smyrna 19977
PASA-055 555 East Loockerman St Suite 100 Dover 19901
31 Kaleidoscope Family Solutions Inc
32 Lean on Me Caregiving PASA-073 1277 South Governors Avenue Dover 19904
33 Life Force Caregivers Inc PASA-007 127 East Glenwood Avenue Smyrna 19977
34 Macklyn Home Care (NCC)
PASA-043 5179 West Woodmill Drive Wilmington 19808
35 Macklyn Home Care (Sussex) PASA-053 111 South Race Street Georgetown 19947
36 Neighborly Home Care (NCC) PASA-057 1213 North King St Wilmington 19801
37 Neighborly Home Care (Sussex) PASA-078 208 North Bedford Street Suite 201 Georgetown 19947
38 Nurturing Angels Home Care
39 Open Heartz Care LLC
40 Open Systems
PASA-075 3826 Kennett Pike Suite 206 Greenville Suite
PASA-066 3640 Kirkwood Hwy Suite 111 Wilmington 19808
PASA-038 3 Mill Rd Suite 303 Wilmington 19806
41 Patriot Home Care PASA-074 1225 North King Street Suite 300 Wilmington 19801
42 Radnon Home Care LLC PASA-060 3906 Concord Pike Suite E1 Wilmington 19803
43 Reliable Aid Inc PASA-052 2 Commonwealth Blvd New Castle 19720
44 Right at Home PASA-004 1500 N French St Wilmington 19801
45 Senior Helpers (Kent)
46 Senior Helpers (NCC)
PASA-013 9 East Loockerman St Suite 3B Dover 19901
PASA-016A 630 Churchmans Rd Suite 107 Newark 19702
47 Seniors Helping Seniors (Sussex) PASA-040 26279 Bayside Drive Long Neck 19966
48 Synergy HomeCare of MOT PASA-067 364 East Main Street Suite 344 Middletown 19709
49 Tailored Care LLC PASA-065 85 Point Landing La Magnolia 19962
50 Visiting Angels Dover PASA-076 1050 Industrial Hwy Suite 120 Middletown 19709
51 Visiting Angels New Castle County PASA-023 3101 Limestone Rd Wilmington 19808
52 Visiting Angels of Sussex County PASA-019B 28350 Lewes-Georgetown Hwy Milton 19968
53 We Care Home Care of Delaware Inc PASA-062 2706 Kirkwood Hwy 3rd Fl Wilmington 19805
54 Your Own Home LLC PASA-009 17 Brandywine Blvd Wilmington 19803

Number Facility Name A-Z License ID Street Address City Zip Code
1 Nurses 'n Kids Inc New Castle
PPECC-001A 904 Churchmans Road Ext New Castle 19720
2 Nurses 'n Kids of Milford Inc PPECC-002A 705 North St Ext Milford 19963
3 Pediatric Health Choice at The Children's Secret Garden PPECC-004A 717 Hatchery Rd Dover 19901
