www.delamed.org | www.djph.org www.delamed.org | www.djph.org











Volu me 8 | Issue 5 December 2022 A publication of th eD el aw ar e Ac adem y of Me di ci ne / Del aw ar eP ublic He alth Associatio n
Delawa
Jour
Fo cus on Delaware’s Healthcare Workforce
Public Health
re
na l of
Delaware Academy of Medicine
OFFICERS
S. John Swanson, M.D. President
Lynn Jones, FACHE President-Elect
Professor Rita Landgraf Vice President
Jeffrey M. Cole, D.D.S., M.B.A. Treasurer
Stephen C. Eppes, M.D. Secretary
Omar A. Khan, M.D., M.H.S. Immediate Past President
Timothy E. Gibbs, M.P.H. Executive Director, Ex-officio
DIRECTORS
David M. Bercaw, M.D.
Lee P. Dresser, M.D.
Eric T. Johnson, M.D.
Erin M. Kavanaugh, M.D.
Joseph Kelly, D.D.S.
Joseph F. Kestner, Jr., M.D.
Brian W. Little, M.D., Ph.D.
Arun V. Malhotra, M.D.
Daniel J. Meara, M.D., D.M.D.
Ann Painter, M.S.N., R.N.
John P. Piper, M.D.
Charmaine Wright, M.D., M.S.H.P. EMERITUS
Barry S. Kayne, D.D.S.
Delaware Public Health Association
Advisory Council:
Omar Khan, M.D., M.H.S. Co-Chair
Professor Rita Landgraf Co-Chair
Timothy E. Gibbs, M.P.H. Executive Director
Louis E. Bartoshesky, M.D., M.P.H.
Gerard Gallucci, M.D., M.H.S.
Melissa K. Melby, Ph.D.
Mia A. Papas, Ph.D.
Karyl T. Rattay, M.D., M.S.
William J. Swiatek, M.A., A.I.C.P.
Delaware Journal of Public Health
Timothy E. Gibbs, M.P.H. Publisher
Omar Khan, M.D., M.H.S. Editor-in-Chief
Liz Healy, M.P.H.
Managing Editor
Kate Smith, M.D., M.P.H. Copy Editor
Suzanne Fields Image Director
ISSN 2639-6378
Public Health
In This Issue
Omar A. Khan, M.D., M.H.S.
Timothy E. Gibbs, M.P.H.
4 | Executive Summary
Richard J. Geisenberger
Nicholas A. Moriello, R.H.U.
5 | Delaware Department of Health and Social Services
Molly Magarik, M.S.
6 | U.S. Health Resources & Services Administration
Michelle M. Washko, Ph.D.
7 | Delaware Healthcare Commission Workforce Subcommittee
Richard J. Geisenberger
Nicholas A. Moriello, R.H.U.
8 | From the Delaware Academy of Medicine/ Delaware Public Health Association
S. John Swanson, M.D.
Timothy E. Gibbs, M.P.H.
10 | Welcome from the Delaware Health Sciences Alliance
Omar A. Khan, M.D., M.H.S. Pamela Gardner
11 | Delaware Division of Professional Regulation

Geoffry Christ, R.Ph., J.D.
12 | Delaware Nurses Association
Christopher E. Otto, M.S.N., R.N., C.H.F.N., P.C.C.N., C.C.R.N.
13 | Medical Society of Delaware
Mark B. Thompson, M.H.S.A.
18 | Origins of the PCP Shortage
Sharon Folkenroth Hess, M.A. 20 | Delaware Healthcare Workforce Vital Statistics 22 | Board of Chiropractic
| Board of Dentistry and Dental Hygiene
| Board of Dietetics / Nutrition
Board of Funeral Services
Board of Massage and Body
Board of Medical Licensure and Discipline
Board of Nursing
Board of Examiners of Nursing Home Administrators
Board of Occupational Therapy Practice
Board of Examiners in Optometry
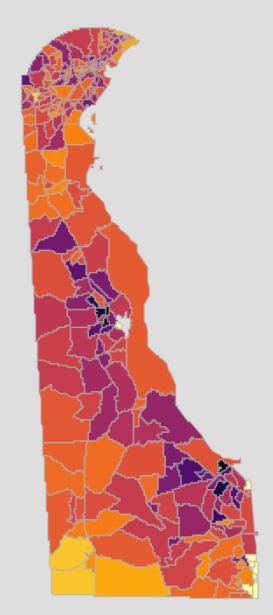
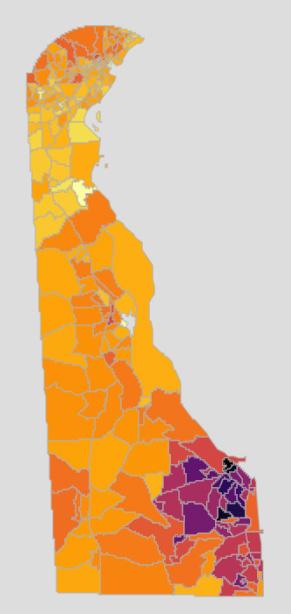
COVER
It is estimated that 20%, or more, of the social determinants of health are influenced by healthcare access and quality. While that number seems small, a lack of access through workforce shortages or weakness can disproportionately impact the provision of care to those who need it.
96 | Board of Pharmacy
102 | Board of Physical Therapists and Athletic Trainers 108 | Board of Podiatry 112 | Board of Mental Health and Chemical Dependency Professionals 118 | Board of Examiners of Psychologists 124 | Board of Social Work Examiners 128 | Board of Speech Pathologists, Audiologists, and Hearing Aid Dispersers 132 | Board of Veterinary Medicine 136 | Controlled Substance Advisory Committee 144 | Long Term Care and Skilled Nursing Facilities 150 | Composition of An Ideal Medical Care Team 154 | Considerations for Patient Panel Size 158 | Scope and Specialization in Dental Care 160 | Composition of Ideal Dental Team 162 | Delaware Health Provider Shortage Areas 164 | Extraordinary Impacts on the Healthcare Workforce:COVID-19 and Aging 168 | Addressing Health Disparities in Delaware by Diversifying the Next Generation of Delaware’s Physicians 172 | Physician and Dentist Basic Demographics: Race and Ethnicity
173 | Physician Statistics based on Allopathic (M.D.) and Osteopathic (D.O.) Education 174 | Physician and Dentist Basic Demographics Age 176 | Chronic Disease Management and the Healthcare Workforce 198 | Global Health Matters November/December 2022 210 | Methodology 212 | Health Care Database Comparisons by State 216 | Workforce In Training 221 | 2021 Delaware Institute for Medical Education and Research (DIMER) Annual Report: Abridged Executive Summary
222|AnEnvironmentalScanofHealthcarePathways ProgramsinDelaware 236|IndexofAdvertisers
The Delaware Journal of Public Health (DJPH), first published in 2015, is the official journal of the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA).

Submissions: Contributions of original unpublished research, social science analysis, scholarly essays, critical commentaries, departments, and letters to the editor are welcome. Questions? Write ehealy@delamed.org or call Liz Healy at 302-733-3989
Advertising: Please write to ehealy@delamed.org or call 302-733-3989 for other advertising opportunities. Ask about special exhibit packages and sponsorships. Acceptance of advertising by the Journal does not imply endorsement of products.
Copyright © 2022 by the Delaware Academy of Medicine / Delaware Public Health Association. Opinions expressed by authors of articles summarized, quoted, or published in full in this journal represent
only the opinions of the authors and do not necessarily reflect the official policy of the Delaware Public Health Association or the institution with which the author(s) is (are) affiliated, unless so specified.
Any report, article, or paper prepared by employees of the U.S. government as part of their official duties is, under Copyright Act, a “work of United States Government” for which copyright protection under Title 17 of the U.S. Code is not available. However, the journal format is copyrighted and pages June not be photocopied, except in limited quantities, or posted online, without permission of the Academy/ DPHA. Copying done for other than personal or internal reference use-such as copying for general distribution, for advertising or promotional purposes, for creating new collective works, or for resale- without the expressed permission of the Academy/DPHA is prohibited. Requests for special permission should be sent to ehealy@delamed.org
w.delamed.org w.djph.org
of Focus on Delaware’s Healthcare Workforce
pu Public Health Delaware Journal
3 |
28
34
40 |
46 |
52 |
70 |
82 |
86 |
90 |
Delaware Journal
of
December 2022 Volume 8 | Issue 5
A publication of the Delaware Academy of Medicine / Delaware Public Health Association
IN THIS ISSUE
Dear Reader,
This issue of the Delaware Journal of Public Health is a bit different from any issue published to date. As always, we share a lot of information we think you will find useful; however, this issue expands the idea of ‘a lot of content.’ Second, it links to a specific website for additional information. Finally, it is based upon research done by various colleagues and institutions in Delaware who have worked on healthcare workforce concerns.
Why have an issue dedicated to healthcare and healthcare access? Simply stated, it is one of the social determinants of health, and depending where you look, it is ranked as being accountable for 10%1 to over 27% 2 within the larger framework including genetic predisposition, behavioral patterns, social circumstances, and environment.3

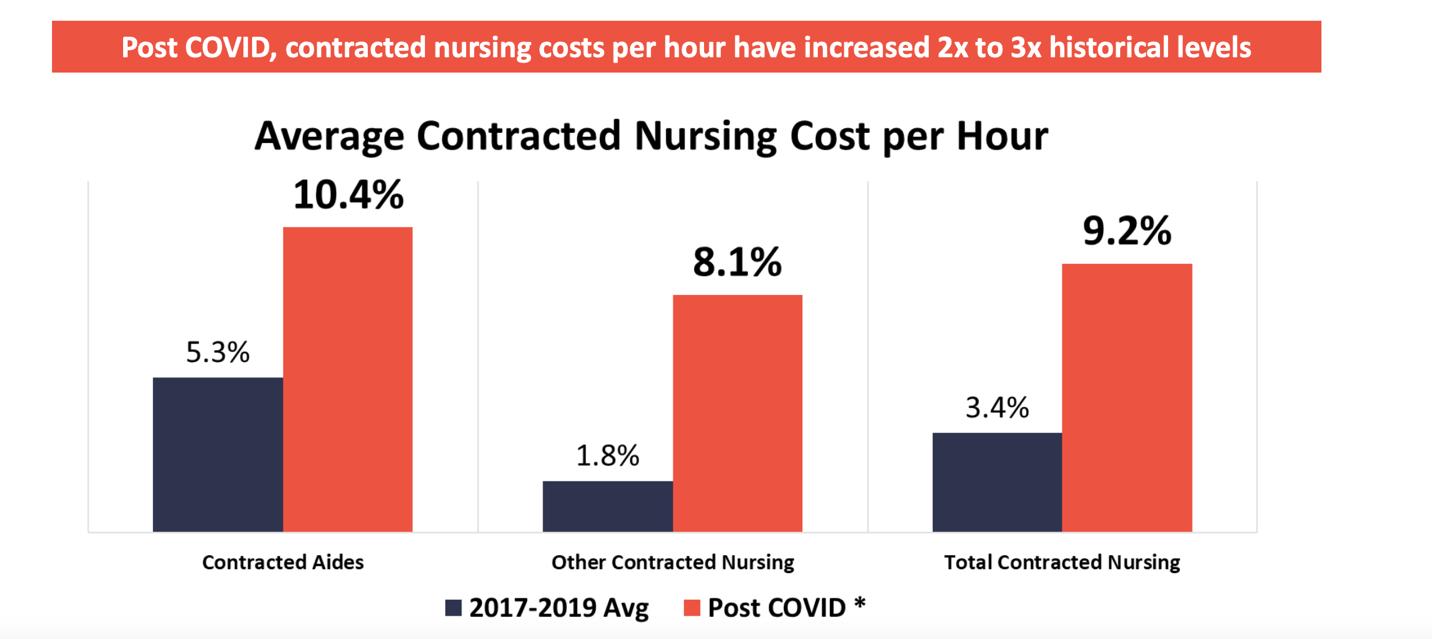
Those percentages, while informative, became even more important during the COVID-19 pandemic based upon the dramatic increase in need for services, the exodus of front line healthcare workers from the workforce, and the exacerbation of existing healthcare provider shortages and their impact on the provision of care, especially with respect to routine primary care and chronic disease management.
With startup funding from the Delaware Health Care Commission and American Rescue Plan Act funding from the United States Department of Treasury through the State of Delaware, we and our partners are engaged in a wide-ranging initiative. There are four components to the initiative:
1) To quantify the healthcare workforce in Delaware;
2) To expand pathways programs to encourage Delaware youth to pursue a career in healthcare;
3) To expand the graduate medical education capacity in Delaware for key practitioner disciplines; and

4) To expand our existing student financial aid program to include loans to nursing and physician assistant students, medical and dental technicians, and behavioral health providers who are residents of the State of Delaware, attend Delaware schools, and are willing to commit to practice in Delaware after graduation.
This issue of the Delaware Journal of Public Health focuses on our initial healthcare workforce analysis, based upon data from the Delaware Division of Professional Licensing and on data provided from the Delaware Health Information Network (DHIN) regarding healthcare utilization in Delaware and reflected in claims data. Numerous other sources of data have been brought to bear on this subject as well, which are too numerous to list here.
A website, https://dehealthforce.org has been built. You can find the complete (406 page!) 2022 Workforce Report there, and over time we will be enhancing the capacity of that website to bring you a series of dashboards and widgets to access additional, up-to-date workforce data.
Future issues of the DJPH will continue this dialog. We hope you enjoy this issue, and as always, we appreciate your input and suggestions on this and other public health topics.
REFERENCES
1. The Center for Health Affairs. (2017, May). Social determinants of health and their influence on health.
Retrieved from: https://www.neohospitals.org/healthcare-blog/2017/March/Social-Determinants-of-Health
2. Health Intelligence Network. (2017, Apr). What are the leading social determinants of health needs?
Retrieved from: http://www.hin.com/chartoftheweek/SDOH_domains_with_greatest_needs_printable.html#.Y5I5rnbMJPa
3. Schroeder, S. A. (2007, September 20). Shattuck Lecture. We can do better—Improving the health of the American people. The New England Journal of Medicine, 357(12), 1221–1228. https://doi.org/10.1056/NEJMsa073350 PubMed
DOI: 10.32481/djph.2022.12.001
Timothy E. Gibbs, M.P.H Publisher, Delaware Journal of Public Health
3
Omar A. Khan, M.D., M.H.S. Editor-in-Chief, Delaware Journal of Public Health
Executive Summary
Richard J. Geisenberger
Secretary of Finance, State of Delaware; Co-Chair, Workforce Subcommittee of the Delaware Healthcare Commission
Nicholas A. Moriello, R.H.U.
President, Highmark Blue Cross Blue Shield of Delaware; Co-Chair, Workforce Subcommittee of the Delaware Healthcare Commission
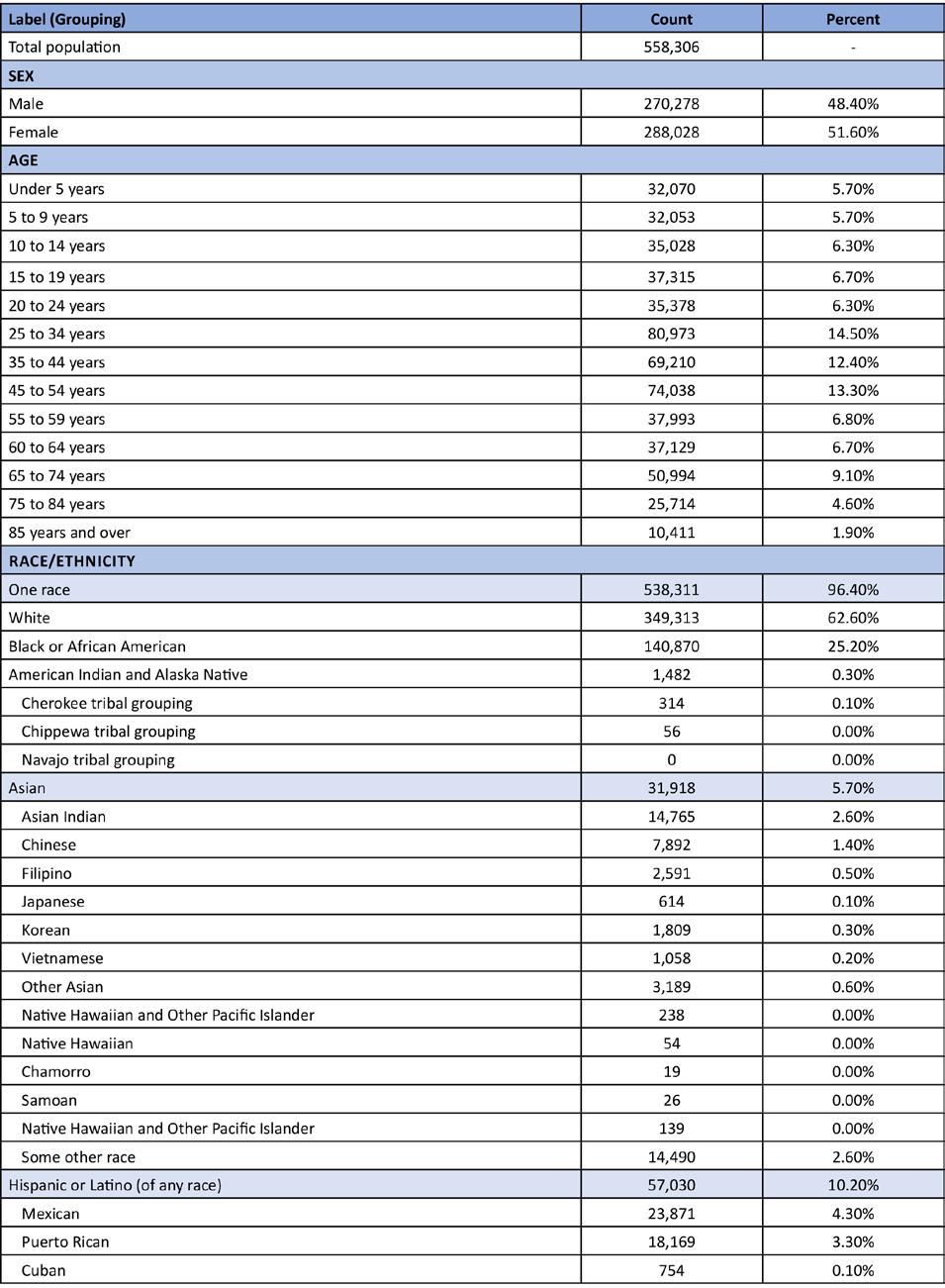
The purpose of this report is to provide an initial census of Delaware’s healthcare workforce contained in the Delaware Division of Professional Regulation (DPR) licensing database known as DELPROS and provide demographic and geographic information not readily available through DELPROS. The report also highlights key public health challenges related to common chronic disease states compiled from Delaware Health Information Network (DHIN) data on insurance claims. Finally, the report provides information on primary care, dental health, and behavioral health shortage areas as reported from Delaware’s Office of Primary Care and Rural Health. Based upon June 2022 DELPROS data, this report contains information from the 19 distinct boards and commissions of practice within DPR which provide regulatory oversight of a majority of Delaware’s healthcare workforce personnel and some types of institutional licensing (which is not a focus of this report). These 19 boards and commissions in turn oversee about 200 types of professional and institutional licenses. This report does not contain information on Certified Nursing Assistants and Direct Service Providers as they are not licensed by DPR nor Community Health Workers that are not registered or licensed in Delaware. Information on these professions is beyond the scope of this census data and report at this time.
As of June 2022, there were 63,123 active healthcare licenses in DELPROS. This number includes 3,529 institutional licenses (e.g., pharmacies and funeral establishments). There are also 7,760 additional licenses issued for prescribing controlled substances which are issued to both individuals and facilities. After accounting for institutions and certain duplications, there are 56,469 individual healthcare providers in DELPROS. This count includes: approximately 26,000 nursing licenses; 9,900 medical practice licenses, (e.g., physicians and physician assistants); 2,600 pharmacist licenses; 2,700 social work-related licenses; and 1,700 dentistry licenses (e.g., dentists and dental hygienists). The remaining boards each account for 1,100 or fewer licensees per board and are covered in detail in this report.
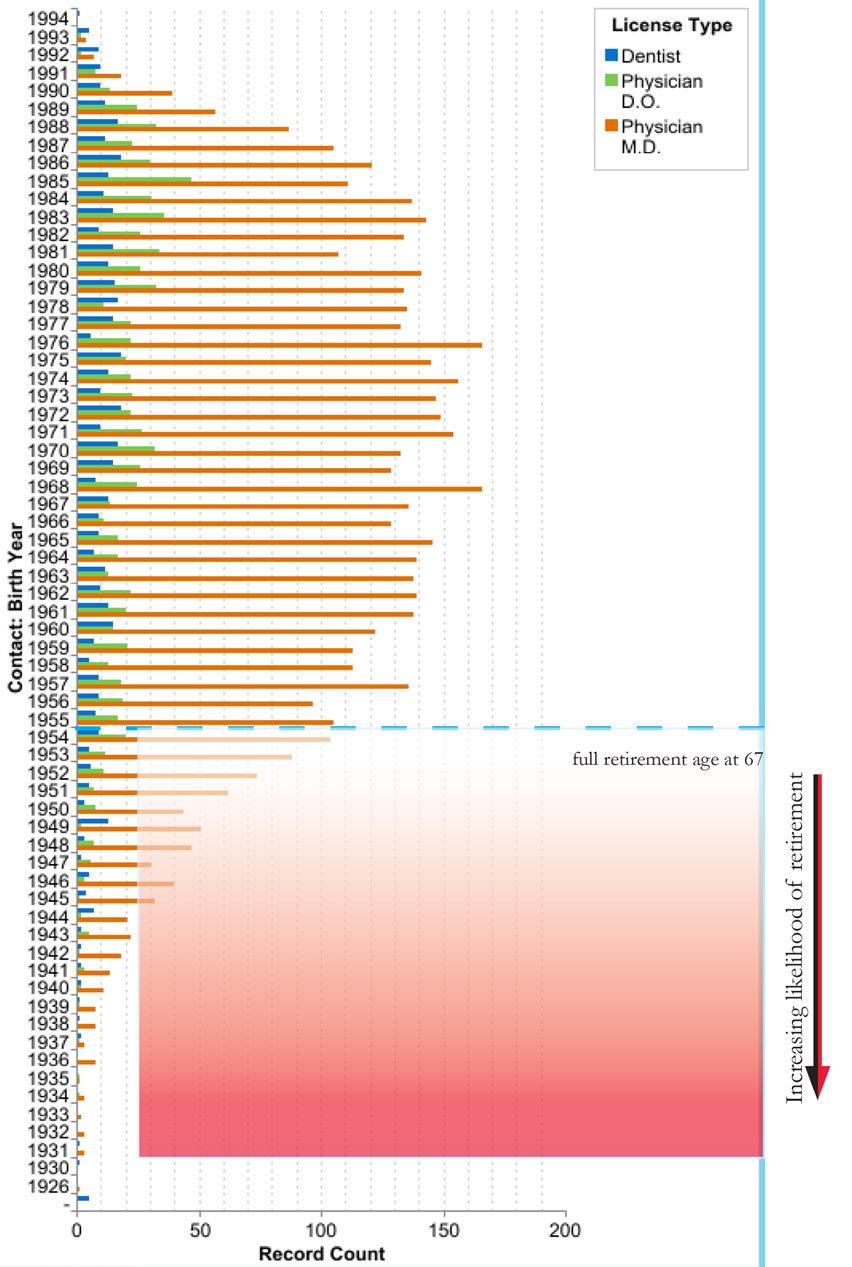
Overall, the licensed healthcare workforce in DELPROS is about 43,000 female (74%) and 15,000 male (26%). Gender is not reported for 4,566 licensees either because individuals did not disclose their gender or because the licensing database contains institutions which do not have a gender demographic. Based on year of birth (where individuals born in 1954 – 1955 are deemed by Social Security as age eligible for full Social Security benefits, we find that no less than 4,600 active licensed individuals are of full retirement age.
The purpose of this first report is not to provide recommendations. Rather this report provides the data and quantitative data analysis capacity to answer additional questions for policy makers and to begin to assess resource allocation to address health care workforce needs in our community. We thank the many institutions mentioned in this report, especially DPR, and look forward to further collaboration which will provide additional, robust information for future reports and a website dedicated to ongoing tracking of this critically important data.
DOI: 10.32481/djph.2022.12.002
4 Delaware Journal of Public Health - December 2022
Delaware Department of Health and Social Services
Molly Magarik, M.S. Secretary, Delaware Department of Health and Social Services
Out of every crisis is borne an opportunity for change. Think back to the natural disasters, human conflicts and tragedies, and economic crises that have befallen our country. Each time, when the after-action report is written, an elected body examines the response, or the business community embraces reforms, we benefit as a society from the lessons learned. The COVID-19 pandemic is no different.
During the past two-and-a-half years, we have seen healthcare providers in our state stretched beyond their limits, dealing not only with the impacts brought on by a new and deadly respiratory virus, but also forced to embrace new ways of managing the chronic and acute conditions of their patients, unrelated to COVID-19. We know that this massive disruption to our healthcare system – and to the health of Delawareans – has taken a tremendous toll on our healthcare workforce, with many providers deciding to retire or leave the profession entirely.
And yet, we also are experiencing the opportunity. During the worst of the pandemic, providers across our state embraced telehealth as a way to see their patients for routine medical exams, to diagnose injuries or illnesses, or to continue regular psychiatric sessions. Regulators changed the rules, allowing insurers to reimburse for these services. The federal and state government provided funding to help advance providers’ transition to telehealth services. Patients no longer had to wait in reception areas or exam rooms when they didn’t feel well, because now their provider would call them back – in the comfort of their own home – when they were ready to see them virtually. It all worked because the situation required it.
With the existing shortage of primary care providers exacerbated by the pandemic, patients, providers, employers and insurers all had to adapt to changes in primary care. Often, primary care was delivered by nurse practitioners and physician assistants practicing at the top of their license.
As practices and clinics evolve, we are likely to see this broadening of primary care and the use of telehealth increase. The state is investing in primary care practices, promoting person-centered care and advancing equity, and has embraced the new State Loan Repayment Program, all while continuing to support the Delaware Institute for Medical Education and Research (DIMER) to help grow the next generation of primary care providers. We will continue to work with the General Assembly, healthcare providers, insurers and consumers to embrace additional changes that improve the patient and provider experience, improve overall health and help lower costs.
I am grateful to all of the Delaware stakeholders that are leaning into the workforce issue to help determine the best paths forward. In this context, I especially want to thank the Academy of Medicine/the Delaware Public Health Association, the Health Workforce Subcommittee of the Delaware Healthcare Commission, the Delaware Health Sciences Alliance, and the Delaware Journal of Public Health for shining a light on the specific recommendations for Delaware’s workforce outlined in this report.
I look forward to joining stakeholders across our state in examining the recommendations in more detail, exploring the potential benefits, determining the policy changes that are needed, and embracing those changes that will have the most positive impact for the future of the healthcare system in our state – and the future health of Delawareans.
DOI: 10.32481/djph.2022.12.003
5
U.S. Health Resources & Services Administration
Michelle M. Washko, Ph.D. Director, National Center for Health Workforce Analysis, Health Resources and Services Administration, U.S. Department of Health and Human Services
In 2019, the healthcare workforce was 22 million individuals strong. This sector was one of the largest and fastest-growing in the United States, accounting for 14% of all civilian, employed workers in the U.S. The majority worked in hospital settings—about 7 million healthcare workers to be exact. Another 4 million were in outpatient and physician offices, and 3.5 million were in Skilled Nursing Facilities and Home Care settings. All in all, the healthcare workforce was large, growing, and there was a steady amount of jobs that were open, making it a very employable sector overall.
Then, the COVID-19 pandemic emerged. As we now know, its impact on healthcare cannot be understated. It changed care delivery and clearly demonstrated the need for sufficiently-sized and well-trained public health, healthcare, and health support workforces. Easy-entry, easy-exit occupations—the lowest-wage earners in healthcare—were the same groups whose employment was the most adversely impacted by COVID. In 2020 alone, total injury and illness cases decreased or remained the same in all sectors except for healthcare, which saw a 4,000% increase in employer-reported respiratory illness.
The pandemic forced states to innovate to meet the needs of their populations, and at the center of that response was the workforce. A number of strategies were implemented in response. Many focused on creating state-level regulatory flexibilities, and engaging the public health workforce. Some states modified scope of practice rules for health professionals, allowing for more autonomous practice. Others allowed health professionals licensed in other states to practice in their state. Additionally, laws and regulations were changed to support greater use of telemedicine. As our nation entered the 3rd year of the pandemic, issues surrounding health workforce capacity, resilience, training, education, and scope of practice have become front and center to moving forward from this phase of our history. While the full impact on our health workforce will not be known for some time, a number of the resulting changes are likely to be long lasting.
Despite the effects of the pandemic, there are several large, persistent policy issues that existed in 2019 and are still present today. These include: sufficiency of the workforce, mal-distribution, quality of healthcare training, and barriers to accessing services. Additionally, there are population factors that have far reaching ramifications for our nation, impacting more than just the health workforce and employment in this sector. First and foremost is the aging of our population. The current cohort of individuals ages 65 and older will continue to generate the majority of demand for healthcare and health support services, and we will need a workforce of sufficient size and distribution to meet this demand. However, this is juxtaposed against the fact that the U.S. birth rate has fallen by 20% since 2007, due to overall lower childbearing rates of current generations. Our population has shown zero growth for several years now, primarily because deaths (attributed to the aging population) exceed births (due to people not having children). Of course, these are issues affecting more than just healthcare in the U.S.
In a nutshell, the health workforce is in flux. We are still understanding the impacts of the pandemic, while having to address previously existing problems. We know that addressing shortages and mal-distributions, continuing to try to improve access to services and train individuals in a way that improves the quality of patient and population outcomes needs to happen. But we must also harness the power of this moment to address pandemic-exacerbated issues like burnout and equity in the workforce.
While it may seem like chaos, there is opportunity in times like this. Despite a low birthrate, demand from our aging population and the after-effects of the pandemic will cause employment in healthcare to grow faster than for other industries. This still allows for great opportunity to tackle the persistent policy issues, and if we follow the data, to craft a better health workforce for the future.
DOI: 10.32481/djph.2022.12.004
6 Delaware Journal of Public Health - December 2022
Delaware Healthcare Commission Workforce Subcommittee
Richard J. Geisenberger, M.G.A. Nicholas A. Moriello, R.H.U.
As co-chairs of the Workforce Subcommittee of the Delaware Healthcare Commission, we are pleased to welcome you to the first “State of the Healthcare Workforce in Delaware: Action and Opportunity” Report.
This report focuses on select components of the healthcare workforce, including primary care, dentistry, behavioral health, and others. It seeks a broader view of the entire healthcare sector, composed of physicians, dentists, nurses, physician assistants, the allied therapies, dental hygienists, and a vast ecosystem of providers.
We acknowledge and appreciate the work of others in this space. Work on this initiative was started by the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA) and the Delaware Health Sciences Alliance (DHSA) long before the COVID-19 pandemic changed our world, and the landscape of healthcare. As the reader knows, the pandemic directly and profoundly impacted both healthcare systems and individual providers.
Before the pandemic, there were tectonic workforce and demographic challenges facing almost every major industry in our State and our nation: the aging of our population, the related increase in the incidence and burden of chronic disease, and the concurrent aging of the healthcare workforce. And the financial impact is clear: the healthcare industry is rapidly approaching one-fifth of the United States Gross Domestic Product (GDP).
The contents of this report are based upon an unprecedented collaboration between multiple components of State government including the Delaware Healthcare Commission, the Division of Professional Regulation, the Delaware Institute for Medical Education and Research (DIMER), the Division of Public Health Primary Care Office, and the Departments of Finance and Labor. They are joined by the Academy/DPHA, DHSA, and the Delaware Health Information Network, and many other organizations playing essential smaller roles.
This public-private partnership has gathered data on the healthcare workforce and analyzed the needs—both current and future—of the State of Delaware. The strategies within this report are based on hard data and analysis and recommend support for polices that will strengthen the healthcare workforce for years to come.
During the past two-years of the COVID-19 pandemic, we have experienced stress and crisis. We now have an extraordinary, federally-funded opportunity to take meaningful action to address the opportunities in our healthcare sector for employment throughout the workforce, as well as novel models (including telehealth and nurse-led health clinics) leading the way.
DOI: 10.32481/djph.2022.12.005
7
From the Delaware Academy of Medicine/ Delaware Public Health Association
S. John Swanson, M.D.
President, Board of Directors, Delaware Academy of Medicine/Delaware Public Health Association
Timothy E. Gibbs, M.P.H.
Executive Director, Delaware Academy of Medicine/Delaware Public Health Association
On behalf of the board and advisory council of the Delaware Academy of Medicine / Delaware Public Health Association (Academy/ DPHA), we are pleased to be the lead institution in the public/private partnership named Delaware Health Force, and the author of this report, which includes content from other experts in the field.
The Academy/DPHA started this initiative in early 2019, long before the COVID-19 Pandemic swept around the world and across our State. In the beginning, this effort focused on the State of Delaware’s DIMER (Delaware Institute for Medical Education and Research) program and its graduates for the 50th Anniversary Report of the program. As data was collected and analyzed, we realized we were pursing an important vein of data which, if related to other information, could supply policy makers and resource allocation alike.
We are informed by the Social Determinants of Health (see Figure 1), in particular the healthcare access and equity components (often overlooked due to their perceived to be relatively minor role in health outcomes). Many scholarly articles have been written citing healthcare as being responsible for ten to twenty percent of health outcomes,2 however if an individual or community is medically underserved or has acute shortages of a variety of healthcare facilities, that 10% can become the single largest barrier to care for those who seek or need it.2
We are also informed by the reality that the healthcare landscape is a complex one, and that simply looking at the physician component of the workforce, or the anchor institutions (hospitals) providing care, is not enough to truly understand the nature of opportunity for workforce enhancement. Today’s healthcare is a series of interlocking systems of care, and the better those connections, the stronger the fabric of the safety net of care for our fellow Delawareans.
Several methodologies were considered before we settled on the approach used to generate this report. Some of those methodologies are used to great success by other researchers analyzing specific parts of the healthcare landscape (e.g., voluntary surveys). This report does not replace the high value of that research. Instead, it expands upon that research with additional data and analysis. Our methodology is articulated in depth in a later section of this report. For now, we extend sincere thanks to our institutional and individual partners:
• Delaware Division of Professional Regulation and Division Director, Geoff Christ;
• Delaware Health Information Network, Executive Director, Jan Lee, MD and staff;
• Agile Cloud Consulting and President and CEO, Sharif Shaalan and staff;
• TechImpact and Delaware Innovation Lab Director of Strategy and Operations, Ryan Harrington, and Director, Research Development & Analytics Data Lab, Héc Maldonado-Reis, and staff;
•Delaware Nurses Association Executive Director, Chris Otto; and
• The team at the Academy/DPHA including Kate Smith, MD, MPH; Matt McNeill, BS; Nicole Sabine, BS; Caroline Harrington, MS, and members of the Board of Directors.
REFERENCES
1. Healthy People 2030. (n.d.). Social determinants of health. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
2. Artiga, S., & Hinton, E. (2018, May). Beyond health care: The role of social determinants in promoting health and health equity. KFF.org.
https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/
10.32481/djph.2022.12.006
DOI:
8 Delaware Journal of Public Health - December 2022
Figure 1. The Social Determinants of Health1

9
Welcome from the Delaware Health Sciences Alliance
Omar A. Khan, M.D., M.H.S. President and CEO, Delaware Health Sciences Alliance
Pamela
Gardner, M.S.M. Program Manager, Delaware Health Sciences Alliance
The Delaware Health Sciences Alliance (DHSA) was established in 2009 with founding partners ChristianaCare, Nemours Children’s Health, Thomas Jefferson University, and the University of Delaware. Since then, additional partners have joined including the Philadelphia College of Osteopathic Medicine, Bayhealth Medical Center, and the Delaware Academy of Medicine / Delaware Public Health Association.

The alliance enables partner organizations to collaborate and conduct cutting-edge research, to improve the health of Delawareans through access to services in the state and region, and to educate the next generation of healthcare professionals.
The DHSA’s unique, broad-based partnership focuses on establishing innovative collaborations among experts in medical education and practice, health economics and policy, population sciences, public health, and biomedical sciences and engineering.
This report, and the work behind it, is an example of the fruits of collaboration. In this case, through our partnership with the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA). In addition, the original work conducted by DHSA and the Academy/DPHA which was the basis for the DIMER 50th Anniversary Report and subsequent annual reports, continues in this report as reflected in key data as well as the recommendations section.
As mentioned elsewhere in this report, Delaware Health Force is comprised of four programmatic components: the core data and research initiative upon which this report is based, the expansion of Delaware Mini Medical School, the expansion of Student Financial Aid for Delawareans, and the expansion of key graduate education and fellowship programs. The DHSA is pleased to support all these programs, in particular those which directly address the pipeline of Delawareans pursuing a career in the health sciences generally, and in medicine and dentistry in particular.
DOI: 10.32481/djph.2022.12.007
10 Delaware Journal of Public Health - December 2022
Delaware Division of Professional Regulation
Geoffry Christ, R.Ph., J.D.
Director, Delaware Division of Professional Regulation
The mission of the Division of Professional Regulation (DPR) is to ensure protection of the public’s health, safety, and welfare. Our services benefit the citizens of Delaware, professional licensees, license applicants, other state and national agencies, and private organizations.

DPR provides regulatory oversight for 34 boards/commissions comprised of Governor-appointed public and professional members. Oversight activities include administrative, investigative, and fiscal support for 54 professions, trades and events with over 200 types of licenses and permits. License fees fund DPR and the expenditures related to each licensing board.
The following types of healthcare, and healthcare related services, are overseen by DPR:
Acupuncture
Acupuncture Detoxification
Art Therapy
Athletic Trainers
Audiology
Chemical Dependency Professionals
Chiropractic
Controlled Substances
Counselors of Mental Health
Dental
Dietitians
Eastern Medicine
Genetic Counselors
Hearing Aid Dispensers
Marriage and Family Therapy
Massage and Bodywork
Medical Practice
Mental Health
Midwife (Nursing)
Midwife (non-Nursing)
Nutritionist
Occupational Therapy
Optometry
Paramedic
Pharmacy
Physical Therapy
Physician
Physician Assistant
Podiatry
Polysomnographer
Psychology
Respiratory Care
Social Workers
Speech Pathology
Tamper-Resistant Prescriptions
Veterinary Medicine
The Division is pleased to collaborate on this important initiative through the sharing of publicly available information. The Division looks forward to the findings that result from the information it shares through collaboration.
DOI: 10.32481/djph.2022.12.008
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
11
•
Delaware Nurses Association
Christopher E. Otto, M.S.N., R.N., C.H.F.N., P.C.C.N., C.C.R.N. Executive
Director, Delaware Nurses Association

The Delaware Nurses Association (DNA) was established in 1911 in Claymont, DE and has served to advance the profession of nursing and our collective mission to improve the health of all Delawareans. We are the only professional association in Delaware representing all Licensed Practical Nurses, Registered Nurses, and Advanced Practice Registered Nurses. We continue to advance health through the art and science of nursing supported by diverse members, advocacy, professional development, generation of new knowledge, effective communication, and community service.
In addition to our robust and inclusive membership, we also facilitate an organizational affiliate program. This program brings together state specialty nursing associations and health-related associations with nursing representation together. The goal of the organizational affiliate program is to strengthen nursing’s and healthcare advocate’s voices in the reformation of healthcare delivery in Delaware.
In addition to sharing physical space, DNA has a long history of collaboration with the Delaware Academy of Medicine/Delaware Public Health Association (Academy/DPHA). This includes interprofessional education, removing scope of practice barriers and advancing public health. Both organizations continue to partner with new endeavors. For example, the design and launch of Healthy Nurse Healthy Delaware, a program spearheaded by DNA to support Delaware nurses’ mental health and overall wellbeing.
The DNA is proud to partner with the Academy/DPHA on Delaware Health Force and further inform efforts to grow, strengthen and advance Delaware’s healthcare workforce. At DNA, we appreciate the importance of robust data and transparent reporting to further inform efforts that will support Delaware’s healthcare workforce and access to high-quality, equitable, affordable and convenient healthcare services for all Delawareans.
DOI: 10.32481/djph.2022.12.009
12 Delaware Journal of Public Health - December 2022
Mark B. Thompson, M.H.S.A.
Executive Director, Medical Society of Delaware

The Society is one of the oldest institutions of its kind in the United States and rich in history. It was founded in 1776 and incorporated on February 3, 1789, only 12 days after President Washington took his oath of office. The first official meeting of the Society was held in Dover on May 12, 1789.
Today, the Apollo Youth in Medicine program provides opportunities for high school students who are interested in a physician career path to shadow practicing physicians and further pursue their interests in the medical profession.
With the support of The Medical Society of Delaware (MSD) and Delaware Youth Leadership Network (DYLN), the Apollo: Youth in Medicine program (see Figure 1) was founded by Sean Holly and Arjan Kahlon in the summer of 2018, with John Kepley joining the leadership team shortly after. Since then, the Apollo leadership team has grown to be led by several focused & resourceful students who are firmly supported by MSD and DYLN.
Together this team supports and coordinates opportunities and activities for Apollo students and their high schools with participating Apollo Physician Mentors.
APOLLO: YOUTH IN MEDICINE
Apollo was founded on the idea that high school students interested in the medical field need an outlet to connect them to opportunities present in the medical community, and that clinical shadowing provides valuable first-hand insight allowing exploration. Apollo has expanded its physician network to allow students across Delaware expansive access to shadowing in 17 medical disciplines. The Apollo Program is Multistep
1.) Delaware high school juniors and seniors are invited to apply every fall through our application.
2.) New students representing multiple Delaware high schools attend a fall education session that covers specific topics such as different specialties in medicine, and the academic pathway to becoming a doctor. Here, Students receive HIPAA training through Apollo, enabling them to shadow in physicians’ offices appropriately.
3.) Apollo gives students access to several shadowing slots offered by dozens of Delaware physicians across various specialties through ‘The Match,’ which occurs multiple times per year. Students can choose as many or as few shadow slots as they’d like.
4.) In addition to shadowing opportunities, Apollo serves as a liaison to gain our students optional access to medical seminars and exclusive Apollo Enhanced Experiences.
Additional information can be found at their website, https://www.apolloprogram.org/
DOI: 10.32481/djph.2022.12.010
13
Figure 1. The Apollo Youth in Medicine Program Logo
Flu cases in Delaware soared to 1,404 laboratoryconfirmed cases as of November 12, according to the Division of Public Health (DPH). Of the total number of flu cases, 598 were reported between November 6 and 12
Slightly more than a quarter of the state’s population (26.2%) had received a flu vaccination as of November 12. DPH urges all Delawareans 6 months of age and older to get their annual flu vaccine as soon as possible to protect against flurelated illness, hospitalization, and death.

Flu vaccination also frees the state’s health care providers to address other respiratory viruses such as COVID-19 and Respiratory Syncytial Virus (RSV), which are especially dangerous to infants, young children under 2 and seniors
To find vaccine sites, use DPH’s Flu Vaccine Finder at flu.delaware.gov Uninsured and underinsured individuals can get flu vaccinations at Public Health Clinics and at community-based locations where DPH mobile units provide additional health services.
DPH launched its flu dashboard on My Healthy Community earlier this month.

The flu dashboard will share the state’s weekly and seasonal data on positive cases, hospitalizations, deaths, and for the first time, vaccinations. Updates will occur weekly on Thursdays for local data, and monthly for other geographies. Access the flu dashboard at https://myhealthycommunity.dhss.delaware.gov/home or click on the ‘Weekly Flu Data’ link at flu.delaware.gov.
flu.delaware.gov or call 1-800-282-8672.
Help Me Grow celebrates 10th anniversary
The Division of Public Health’s (DPH) Maternal Child Health (MCH) Bureau, Delaware 2-1-1, and other state and community organizations proudly recognized the 10th anniversary of the Help Me Grow Delaware program on November 9 at the Route 9 Library & Innovation Center in New Castle. Help Me Grow connects families with children at risk for developmental and behavioral challenges to community-based programs and services.

The MCH Bureau presented plaques to three individuals for their contributions to the program:
• Matthew Denn: During his tenure as Insurance Commissioner, Denn helped pass legislation that mandated insurance coverage of developmental screenings and provided funding to promote screenings in primary care, improving access across the state.

• Norma Everett: As the Early Childhood Comprehensive Systems Manager, Everett built community stakeholder relations to improve conditions for Delaware families and opened the door for collaboration that resulted in the passing of developmental screening legislation in 2009.
• Dr. Aguida Atkinson: She spent her career advocating for community health and, as Help Me Grow Physician Champion, continues to work toward improving Delaware's early childhood system through collaboration and innovation.
Of 19,693 calls to Delaware 2-1-1, a confidential, toll-free help hotline, 17,076 children were served. Learn more at DEThrives.com/Help-Me-Grow.


November 202
From the Delaware Division of Public Health
Delawareans urged to get vaccinated as 1,404 flu cases reported statewide
Three individuals were recognized for their contributions to the Help Me Grow program, now in its 10th year. From left: Paulina Gyan of the Division of Public Health’s Maternal and Child Health Bureau, Doug Tyan with Bryn Mawr Psychological Associates , and awardees Dr. Aguida Atkinson, Norma Everett, and Matthew Denn. Photos by Sharon Smith.
14 Delaware Journal of Public Health - December 2022
Telehealth: a new public health tool
Telehealth is the use of electronic information and telecommunication technologies to provide longdistance health care. Live videoconferencing, remote patient monitoring, streaming media, and land and wireless communications are examples of telehealth technologies.
Telehealth is a service delivery option that enables physicians and practitioners to provide health care throughout Delaware. Patients may be able to avoid lost wages, travel expenses, and childcare costs; overcome transportation barriers; and access services privately without worrying about any perceived stigma.
In Delaware:
• Telehealth services can be accessed, provided there is an established physician-patient relationship. This relationship can be established through previous in-person visits or through an initial telehealth visit.
• Informed consent is required and must comply with current HIPAA requirements.
• Prescriptions may be prescribed through a telehealth visit once the physician-provider relationship is established.
• Medicaid, Medicare, and private insurance carriers reimburse for telehealth services if those in-person services are covered.
• Telehealth appointments can occur through the use of audio-only technologies.

Visit the 2022 National Telehealth Conference Summary B and Telehealth.HHS.gov for how to use telehealth, prepare for a virtual visit, policies, reimbursement, and best practices.
Other sources are the Mid-Atlantic Telehealth Resource Center (https://www.matrc.org/) and the U.S. Health Resources & Services Administration’s Office for the Advancement of Telehealth: https://www.hrsa.gov/rural-health/topics/telehealth.
COVID-19 bivalent boosters advised
The Division of Public Health (DPH) recommends that all eligible Delawareans ages 5 years+ get vaccinated without delay for protection from severe COVID-19 disease, hospitalization, and death.
Individuals ages 5+ are eligible for the COVID-19 bivalent booster if they completed their primary series (gotten both doses of a two-dose vaccine) at least two months ago.
Bivalent boosters target both the original strain of COVID-19, and BA.4/BA.5 strains of the Omicron variant. They provide better and updated protection against the virus. The original boosters (monovalent) from Pfizer and Moderna are no longer available.
For bivalent booster information, visit de.gov/boosters. For vaccination sites, visit de.gov/getmyvaccine. For COVID-19 data, visit My Healthy Community. For COVID-19 information, visit https://coronavirus.delaware.gov/, email delaware211@uwde.org, or call Delaware 2-1-1. Individuals who are deaf or hard of hearing can text their ZIP code to 898-211 weekdays 8:00 a.m. to 9:00 p.m. and Saturdays 9:00 a.m. to 5:00 p.m.
Source: Centers for Disease Control and Prevention, https://www.cdc.gov/poxvirus
Monkeypox cases gradually decline
Only two new monkeypox (MPX) cases were reported to the Division of Public Health (DPH) between October 14 and November 16. As of November 18, DPH received reports of 43 MPX cases: 29 in New Castle County, five in Kent County, and nine in Sussex County. In the U.S., the Centers for Disease Control and Prevention reported 29,080 MPX cases as of November 18, with New Jersey, Pennsylvania, Maryland, and Washington, D.C. each having between 522 and 855 cases.
Visit de.gov/monkeypox for more information about MPX vaccination for at-risk individuals and health care workers who provide direct patient care to confirmed or suspected MPX cases. Email questions to DPHCall@delaware.gov

The DPH Bulletin – November 2022 Page 2 of 4
Getty Images
15
Daily Monkeypox Cases Reported and 7-Day Daily Average, U.S., May 17, 2022 - November 16, 2022
Caregiver Resource Centers offer support
Whether caring for a parent diagnosed with Alzheimer’s disease, a loved one who suffered a stroke, or a child with a disability, caregivers benefit from information, assistance, and support. They can find those things and more through the Delaware Caregiver Resource Center (CRC) Network.

CRCs in all three counties help caregivers navigate services systems, find solutions to individualized concerns, make appropriate referrals, conduct support groups, and provide specialized training to caregivers. Center coordinators understand the challenges that caregivers face. The CRCs are supported by the Delaware Department of Health and Social Services’ (DHSS) Division of Services for Aging and Adults with Physical Disabilities (DSAAPD)
The six CRC locations include: Easterseals Delaware & Maryland’s Eastern Shore (which operates a CRC in New Castle and Georgetown), the Wilmington Senior Center (with a Latino outreach specialist), Newark Senior Center, Modern Maturity Center in Dover, and the CHEER Community Center in Georgetown.
Caregivers seeking communication devices and modified items that support people with daily tasks, employment, and play can visit three assistive technology centers in person through the Delaware Assistive Technology Initiative’s (DATI) or in person and virtually at Easterseals’ demonstration center in New Castle. Caregivers can explore assistive devices such as medication reminders, adapted keyboards, smart devices, and other assistive technologies such as a smartphone application Search DATI’s lending inventory at www.dati.org/loan/search_inventory_new.php
For more information, visit Delaware's Aging and Disability Resource Center or call 1-800-223-9074.
November honors family caregivers
November is National Family Caregivers Month Caregiving is a physically and emotionally exhausting job According to National Today, most caregivers have additional jobs and most family caregiving is unpaid.
Easterseals’ respite voucher program, supported by the Delaware Department of Health and Social Services’ (DHSS) Division of Services for Aging and Adults with Physical Disabilities, gives family caregivers a much-needed temporary break. The DHSS Division of Developmental Disabilities Services, Division of Medicaid and Medical Assistance, and hospice agencies also offer respite. Adult day care programs offer activities for seniors, veterans, and adults with physical disabilities and individuals with dementia or Alzheimer’s disease. The DHSS Division of Health Care Quality provides a list of licensed adult day services
Caregiving resources
Delaware Department of Health and Social Services, Division of Services for Aging and Adults with Physical Disabilities (DSAAPD): Delaware's Aging and Disability Resource Center (ADRC), 1-800-223-9074, delawareadrc@delaware.gov. Caregiving information, including an Alzheimer’s toolkit and a legal handbook for relatives raising children
The Guide to Services for Older Delawareans and Persons with Disabilities
Assistive technology centers: The Resource and Technology Demonstration Center, 61 Corporate Circle, New Castle, Delaware 19720. Open Monday through Friday, 8:00 a.m. to 4:00 p.m.; or take a virtual tour at www.easterseals.com Contact them at 302-221-2087 or resources@esdel.org
Delaware Assistive Technology Initiative’s (DATI) lending libraries:
• University of Delaware Center for Disabilities Studies, 461 Wyoming Road, Newark, Delaware 19716-5901, Newcastle.atrc@dati.org, 302-831-0354
• Milford Wellness Village, 21 West Clarke Avenue, Suite 1200, Milford, Delaware, 19963, kent-sussex.atrc@dati.org, 302-739-6885.
The DPH Bulletin – November 2022 Page 3 of 4
16 Delaware Journal of Public Health - December 2022
Getty Images
Display address numbers
correctly
Can first responders quickly find your residence or business during an emergency?

New Castle County, Kent County, and Sussex County require structures and mailboxes to have legible address numbers that are visible from the street or road fronting the property. Structures that sit back from the road and/or are hidden are required to display address numbers on a pole, sign, monument placed where the driveway meets the street or road.
New Castle County Code requires residences to have Arabic or alphabetical characters that are at least 4” tall and a half-inch wide. They must contrast with their background and not be spelled out. Reflective numbers are not required. For more information, visit the New Castle County Department of Land Use or call 302-395-5572.
Kent County Code requires address residential numbers to contrast with their background, be either Arabic numbers or alphabetical letters, and be at least 4” tall and three-quarters of an inch wide Reflective numbers are not required. For more information, including commercial requirements, visit the Kent County Department of Planning Services or call 302-744-2451.
Sussex County Code requires address numbers on residences, townhouses, and businesses to be reflective, in block style, contrast with their background, and be visible from both sides of the street or road during day and nighttime hours. Numbers should be at least 3” tall on mailboxes and 4” tall on the side of residences, townhouses, and businesses. Apartment buildings and high-rises must display 6” reflective numbers above or to the side of the main entrance and above or to the side of the doorway of each unit. For more information, including industrial and commercial requirements, visit the Sussex County Geographic Information Office or call 302-855-1176.
Smoke detectors save lives
Your family only has four minutes or less to escape a house fire. Working smoke detectors reduce house fire deaths by as much as 70 percent.
Del. Code Title 16, Chapter 66, Section 6631 requires that smoke detectors be installed at each level of the home, including the basement, and outside each bedroom or group of bedrooms. The Delaware State Fire Marshal’s Office explains the law and includes placement diagrams; visit https://statefiremarshal.delaware.gov/specialprograms/smoke-detectors/.
Occupied residences constructed before July 8, 1993, are required to have individual, single station, battery-powered smoke detectors. Owners of occupied residences constructed after July 8, 1993 are required to have a licensed electrician install hard-wired smoke detectors powered by household electricity. Multiple smoke detectors must be wired so that if one smoke detector sounds, they all will sound. Most experts recommend that homes have hard-wired smoke detectors with a battery backup to provide protection with or without power. In rented or leased units, tenants are responsible for maintaining the smoke detector battery.
The Delaware State Fire School recommends following these fire protection steps:
• Every month, test a smoke detector by pushing its test button. It should loudly beep or chirp. Dust it regularly.

• Replace batteries whenever the smoke detector chirps or beeps and when changing the clocks to daylight savings time. Ten-year 10-year lithium batteries are good for 10 years from the date of manufacture, not 10 years from installation. Mark the date of manufacture on the outside of the smoke alarm to remind you when to replace it.
• The blind and deaf can purchase smoke detectors with a strobe-light feature and a vibration appliance placed beneath your pillow.
• If you cannot afford to purchase a new smoke detector, ask your local fire company if they distribute them.
For more information, visit the Delaware State Fire Marshal’s Office, the Delaware State Fire School or the National Fire Protection Association, which has fire safety information in different languages
The DPH Bulletin – November 2022 Page 4 of 4
17
Getty Images
Origins of the PCP Shortage
Sharon Folkenroth Hess, M.A. Collections Manager and Archivist, Delaware Academy of Medicine/Delaware Public Health Association
In John Thomas Scharf ’s History of Delaware: 1609 to 1888, the chapter “Medicine and Medical Men” concludes with a directory of all physicians registered with the clerk of the peace. The detailed list starts on page 507 and ends halfway down page 508 after just 230 names. He does not mention other healthcare providers, such as barbers, nurses, or unregistered doctors. With a population of ~146,608, Delaware doctors were outnumbered 638 to one.1 Though when bleeding, blistering, and purging are used as curatives, this ratio of providers-to-patients likely benefited many nineteenth-century patients and increased their chances of survival. However, even as medical science improved and the population increased, the number of doctors in the state remained roughly the same. In 1910, the state had grown to 202,322 inhabitants but added only 17 physicians— approximately 820 people for every doctor.2 Today, the ratio of primary care providers to patients in the state remains alarmingly high at 1,418 to one. While the COVID-19 pandemic has exacerbated the situation, our state has grappled with a healthcare workforce deficit for over a century.
THE WAY IT WAS
For most of human existence, healthcare happened at home. Generations of the sick or injured relied on the wisdom and support of family and community. Extra medical care came as a house call. With tools in tow, the doctor arrived ready to perform any number of treatments in any setting. Hospitals were few and primarily provided charitable care for the friendless and destitute. Medical training for rural doctors, such as it was, often happened ‘on the job’ with an apprenticeship. City physicians or those caring for wealthy families went to for-profit, proprietary medical schools. The professional training they provided was not much better— in two 16-week terms, a medical student read the required materials, attended lectures, and passed their exams, sometimes without touching a human patient.
To provide some oversight of the field, Delaware created a Board of Medical Examiners in 1802. Chief among their duties was to establish a system for issuing medical licenses. The requirements included “the presentation of a diploma conferred by a reputable college of medicine” or an examination by the Board, a thesis on a medical subject, and a $10 fee.3 However, even this bare-bones process was compromised within a few decades when the state legislature exempted homeopaths— allowing them to administer a separate self-regulated assessment system instead. Unfortunately, these competing systems decreased the state’s medical community’s reputation, rendering Delaware-issued licenses valid within her borders only.4
THE TIMES, THEY ARE A-CHANGIN’
By the end of the nineteenth century, the theory and practice of medicine in America began to change. With the growing acceptance of germ theory, centuries-old humoral and miasmal theories fell aside. Medicine quickly became a science rather than an art, requiring greater accountability from its practitioners. Sanitation, vaccination, and education became top public health priorities. Delaware’s General Assembly created the State Board of Health in 1879 to enforce the growing number of laws regarding contagious diseases and the duties of physicians in reporting them. Hospitals, too, transformed, becoming centers for clinical research and treatment of acute ailments.
In April 1899, the trustees of Delaware College (now the University of Delaware) provided space in the main building for a fully equipped pathological-biological laboratory, the Delaware Public Health Laboratory (DPHL). The lab continues to serve as an adjunct in diagnosing and controlling diseases. Physicians began to develop expertise in specialized areas like microscopy and infectious diseases, expanding opportunities in medicine beyond primary care.
In the last decades of the century, the face of medicine began to change as well. Western medicine had been a White man’s game for centuries. However as the field expanded, it began to open to previously excluded groups. Women were training at co-educational medical schools and newly-established women’s colleges. By the early 1900s, multiple medical schools opened for Black students.
This period of rapid expansion would soon end. In 1904, the largest professional organization of its kind, the American Medical Association, created the Council on Medical Education (CME) to evaluate the quality of training available in the US and Canada. The first order of business was to agree on what counted as a “medical education.” In addition to setting the minimum prior education required for admission to a medical school, they defined proper medical education as two years of human anatomy and physiology training followed by two years of clinical work in a teaching hospital.
Next, with funding from the Carnegie Foundation, they hired Abraham Flexner to examine the curricula offered by North American schools. Using the Johns Hopkins University School of Medicine as his standard for comparison, Flexner visited over 150 institutions for his evaluation. He published his findings in 1910 as Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching, generally referred to as the Flexner Report.5
Nearly half of American medical schools fell short of the report’s rubric. Flexner’s recommended reforms included increasing standards, partnering with hospitals for clinical training, and closing schools that could not afford to update and maintain facilities. He emphasized the need for curricula to adhere to the protocols of mainstream sciences in their teaching and research. Flexner additionally reported that too many medical schools were training too many doctors.
DOI: 10.32481/djph.2022.12.011
18 Delaware Journal of Public Health - December 2022
While Flexner and the CME did not have the power to enforce their recommendations, state licensing boards did, and they moved quickly to mitigate the perceived public health threat. Not long after the report’s publication, medical schools were legally required to refine admission standards and follow stricter curriculum requirements.
Though proprietary schools were already struggling financially, Flexner’s report sounded the death knell. Many schools derided in the report either merged or closed soon after publication. By 1915, ninety-six schools were training physicians; fifteen years later, there were only seventy-six.
With a standardized comprehensive course of study and stricter entrance requirements, medical education was available only to those from economically privileged backgrounds.6 The constriction of medical education to an elite few raised the social status of those granted access to the field and the price for their services.
Furthermore, the culling of the field reinforced race and gender segregation within the profession. Women were excluded to accommodate White men competing for spots at the remaining universities. Some opportunities remained for women within hospitals as nurses, though their role was limited. Many schools that dissolved were smaller rural and Black colleges. When these colleges disappeared, so too did the already small pool of doctors serving poor, working-class, rural, and Black communities. Few who graduated from the surviving medical schools moved away from cities and more populated areas, expanding the already large healthcare deserts throughout the county.
LASTING EFFECTS
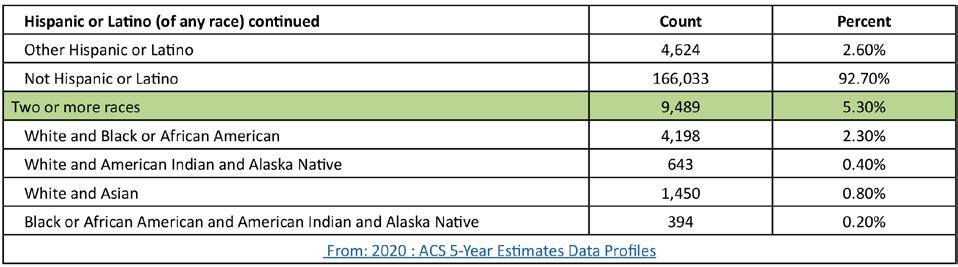
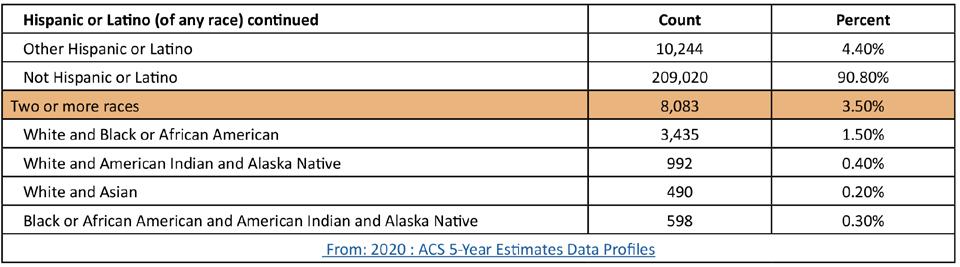
Black Delawareans comprise 23% of the population but only 6.6% of its doctors. In comparison, 66.7% of Delaware’s doctors are white, representing only 61.9% of the population. A 2020 study estimated that if all of the medical schools that educated Black physicians in the early 20th century remained open, there would have been an additional 35,315 Black physicians in the workforce between the 1910s and today.7
In 1900, six percent of practicing physicians were women, yet by 1940, they made up only four percent. Women started to raise that percentage in the 1960s, though they have yet to catch up to men in compensation, leadership positions, and research publications.8
Although Delaware has suffered from a lack of primary healthcare providers since the 1880s, racism and sexism have exacerbated the problem. The reforms ushered by the Flexner Report and the CME continue reverberating throughout the profession today.
REFERENCES
1. Scharf, J. T. (1888). History of Delaware: 1609 to 1888 (Vol. I). L.J. Richards.
2. Department of Health and Social Services. (1911). Annual Report. Department of Health and Social Services. https://www.google.com/books/edition/_/Ll9LAQAAMAAJ
3. Medical Society of Delaware. (n.d.). History of the Medical Society of Delaware. Retrieved from: https://www.medicalsocietyofdelaware.org/DELAWARE/assets/files/History%20of%20the%20Medical%20Society%20of%20Delaware.pdf
4. Conrad, H. C. (1908). History of the State of Delaware, from the Earliest Settlements to the Year 1907. Henry C. Conrad.
5. Duffy, T. P. (2011, September). The Flexner Report—100 years later. The Yale Journal of Biology and Medicine, 84(3), 269–276. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3178858/
6. Beck, A. H. (2004, May 5). STUDENTJAMA. The Flexner report and the standardization of American medical education. JAMA, 291(17), 2139–2140. Retrieved from: https://jamanetwork.com/journals/jama/article-abstract/198677 https://doi.org/10.1001/jama.291.17.2139
7. Campbell, K. M., Corral, I., Infante Linares, J. L., & Tumin, D. (2020, August 3). Projected estimates of African American medical graduates of closed historically black medical schools. JAMA Network Open, 3(8), e2015220. Retrieved from: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2769573 https://doi.org/10.1001/jamanetworkopen.2020.15220
8. Redford, G. (2020, November 17). AAMC renames prestigious Abraham Flexner award in light of racist and sexist writings. AAMC. Retrieved from: https://www.aamc.org/news-insights/aamc-renames-prestigious-abraham-flexner-award-light-racist-and-sexist-writings
19
Delaware Healthcare Workforce Vital Statistics
DATA
This section’s data contains workforce vital statistics as collected in the DELPROS system. It is important to note that it does NOT cover the entire healthcare workforce, some of which is not licensed through this system, and others who are not directly licensed by any entity at this time. For instance, Certified Nursing Assistants (CNAs) are not licensed by DELPROS, nor are Community Health Workers (CHWs) or Direct Service Providers (DSPs).
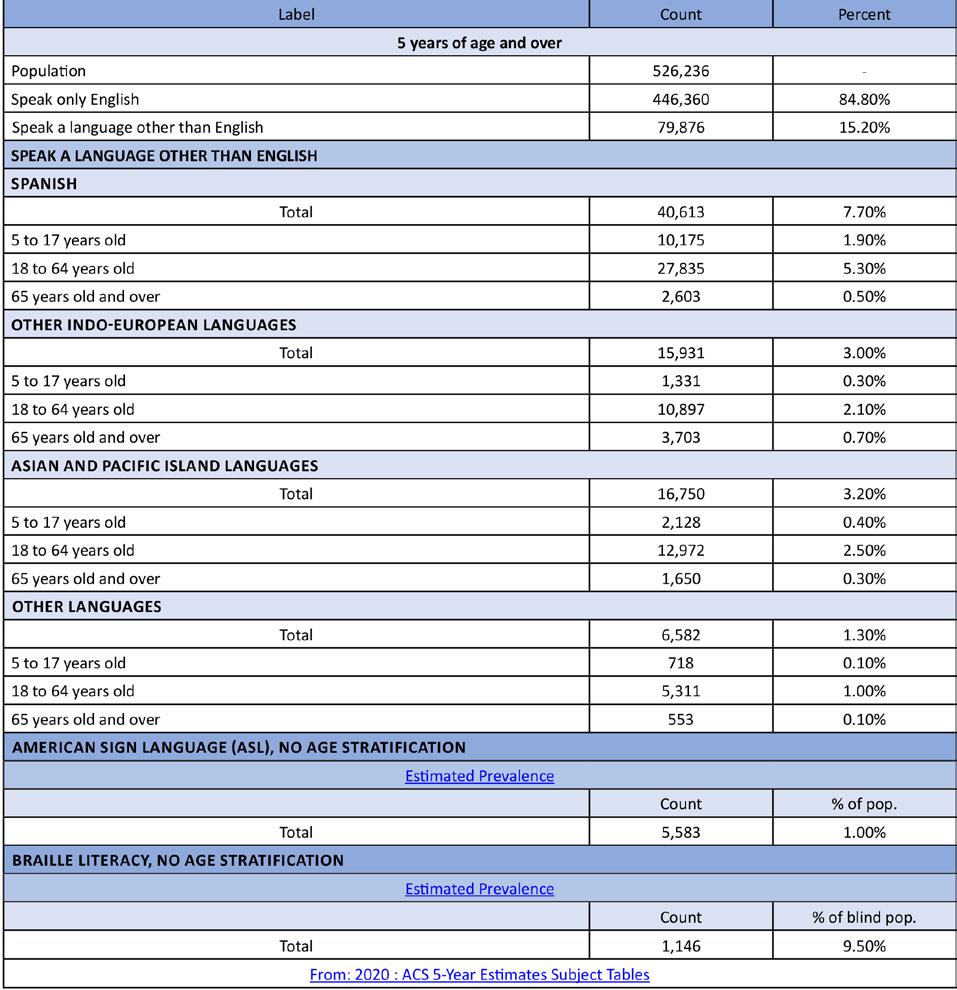
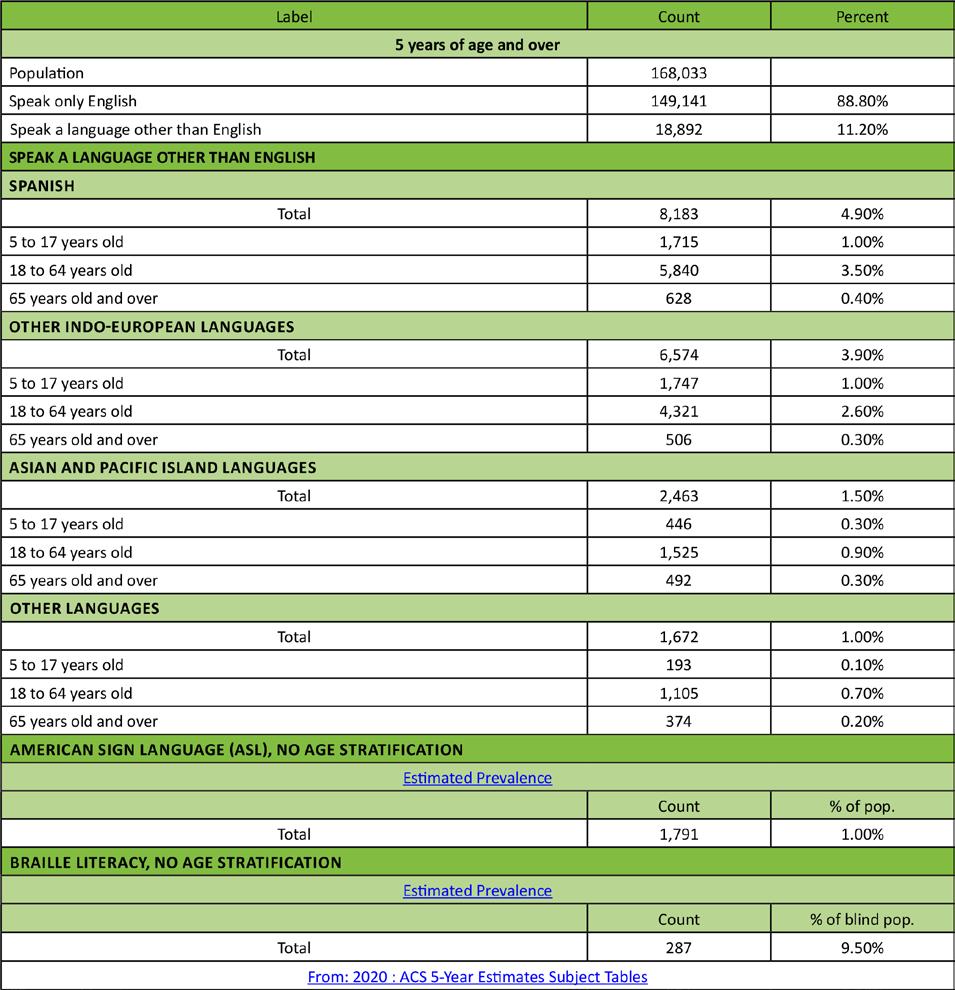
Some types of facilities are licensed through DELPROS, while others are licensed through the Department of Health and Social Services Office Division of Healthcare Quality, Office of Health Facilities Licensing and Certification. We credit that office for providing a significant portion of facilities data found in this report. The following is entirely based on the data contained within the DELPROS system, and therefore we make no claims to its accuracy or completeness except where noted. For instance, DELPROS does ask about gender when an individual registers, however it is not a required field, and therefore most sections will show a percent of persons who did not state their gender. DELPROS itself does not collect information regarding race and ethnicity, therefore this report does not contain that information. DELPROS does ask for date of birth, and we were supplied with year of birth only so provide a level of privacy to the licensees of the State licensing system. DELPROS does not collect information on languages spoken, therefore we do not report on that information. That said, race, ethnicity, languages spoken, and a variety of other characterizes of the healthcare workforce are essential data points to be considered in future reports as that information is collected.
The section is alphabetical by Division of Professional Regulation board name, which is then followed by information from the Office of Health Facilities Licensing and Certification. All information and tables contained in the following section is based on data from June 2022. Each section starts with objective of the Board which oversees a given area of licenses. Sometimes, but not always, this is followed by additional detail on the types of licensure granted under that board.
•Board of Chiropractic
• Board of Dentistry and Dental Hygiene
• Board of Dietetics/Nutrition
• Board of Funeral Services
• Board of Massage and Bodywork
• Board of Medical Licensure and Discipline
• Board of Nursing
• Board of Examiners of Nursing Home Administrators
• Board of Occupational Therapy Practice
• Board of Examiners in Optometry
METHODS
• Board of Pharmacy
• Board of Physical Therapists and Athletic Trainers
• Board of Podiatry
• Board of Mental Health and Chemical Dependency Professionals
• Board of Examiners of Psychologists
• Board of Social Work Examiners
• Board of Speech Pathologists, Audiologists, and Hearing Aid Dispensers
• Board of Veterinary Medicine
• Controlled Substance Advisory Committee
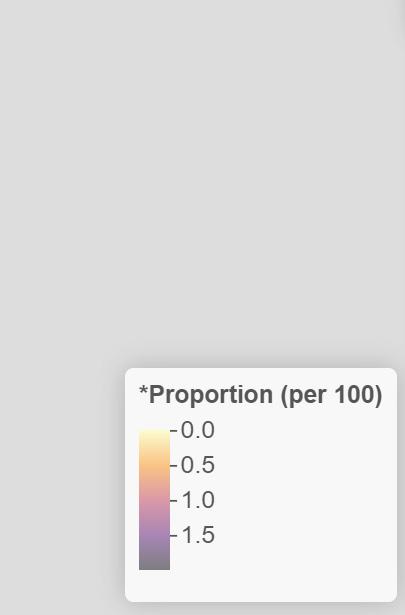
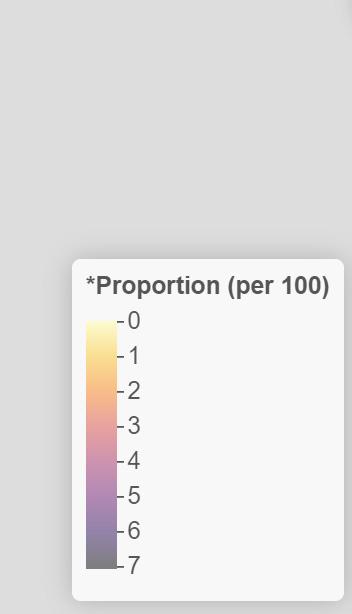
There are charts on active licenses, gender, year of birth and related conjecture one when individuals of a certain age may retire, and facing pages with numerical and visual distributions of providers by ZIP code. We use the primary license application ZIP code as the best available proxy for approximate location within Delaware, and acknowledge that a margin of error is inherent in this method. There are also a small number of providers who provided a ZIP code outside of the State of Delaware, which further compounds the absolute accuracy of our methodology.
Charts were created in Salesforce and maps created in ArcGIS.
CHARTS
To save space, we removed secondary labeling on the y-axis (i.e., “ZIP code”). In so doing, we freed up significant space to make some charts larger and more legible. The x-axis on all charts is always the number of licensed individuals or entities. The bars on the charts are proportional to the number they represent, and therefore to each other.
DOI: 10.32481/djph.2022.12.012
20 Delaware Journal of Public Health - December 2022
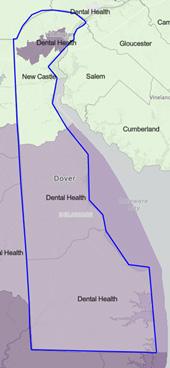
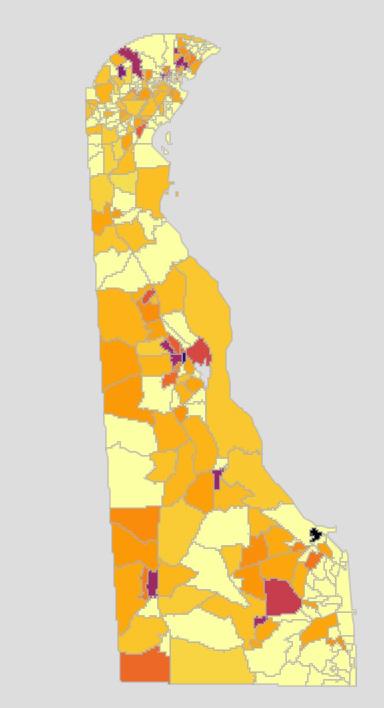
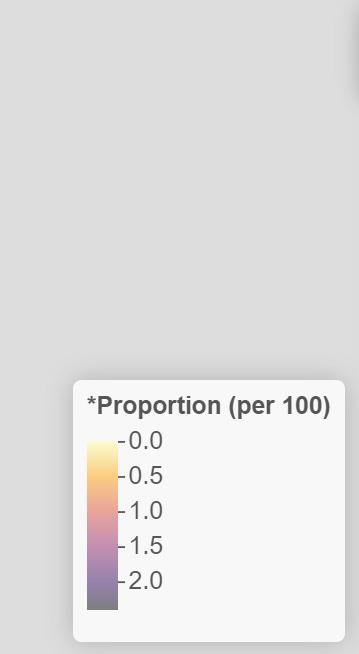
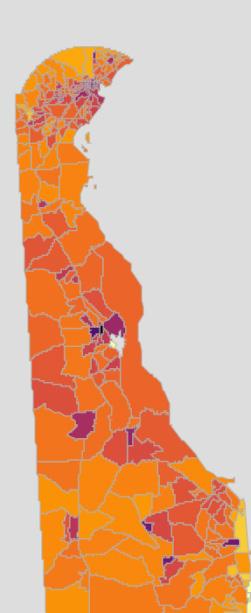
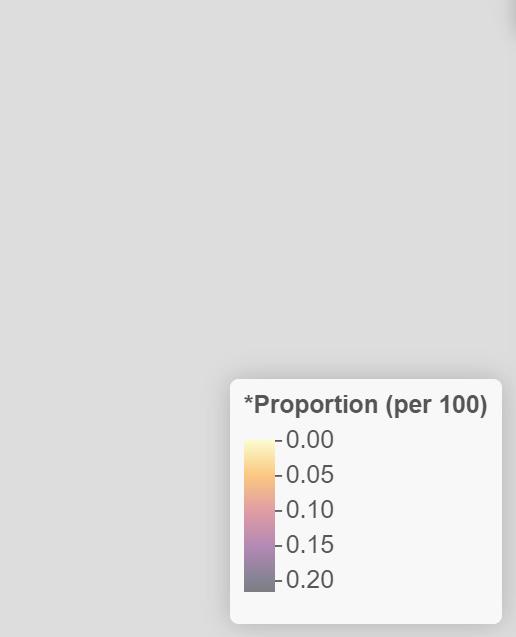
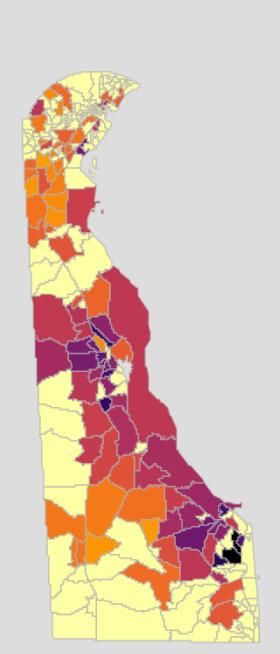
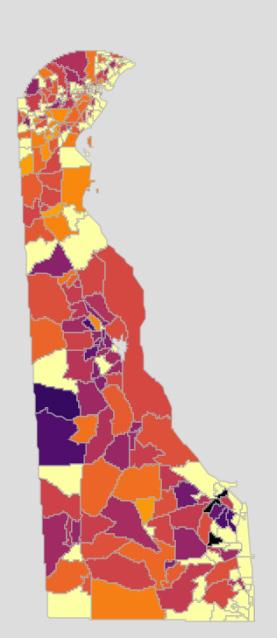
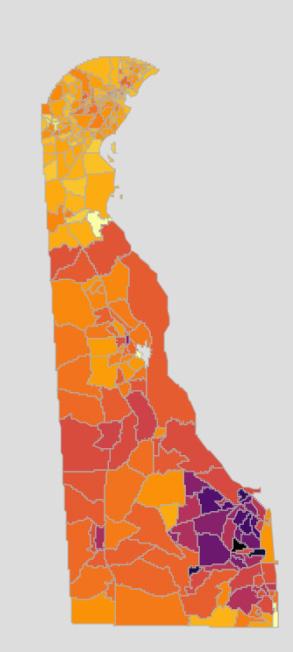
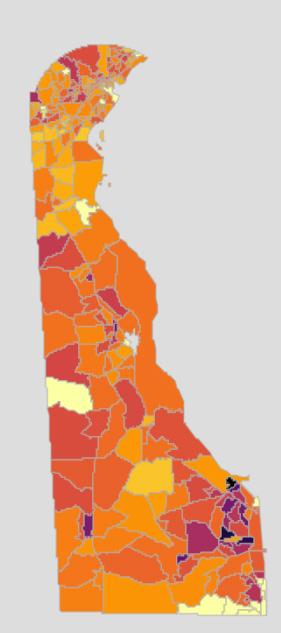
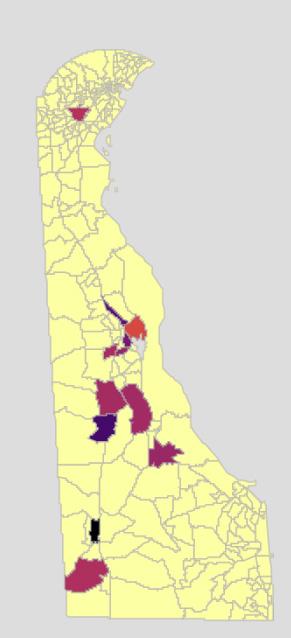
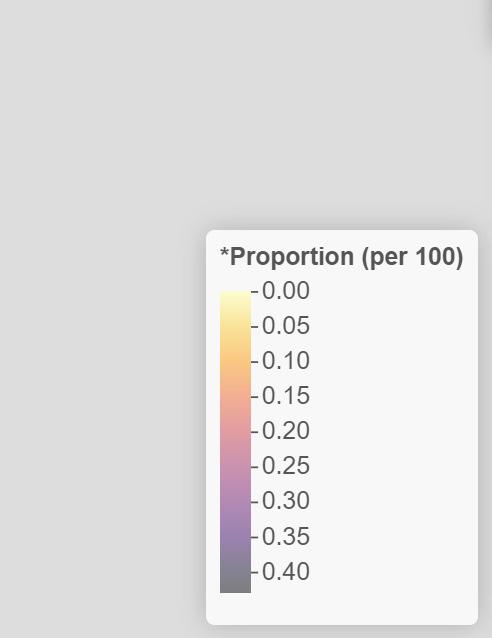
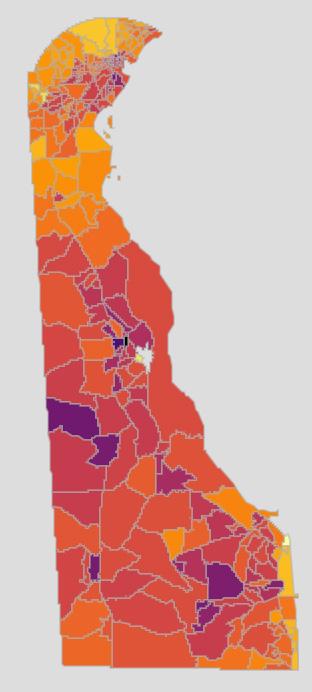
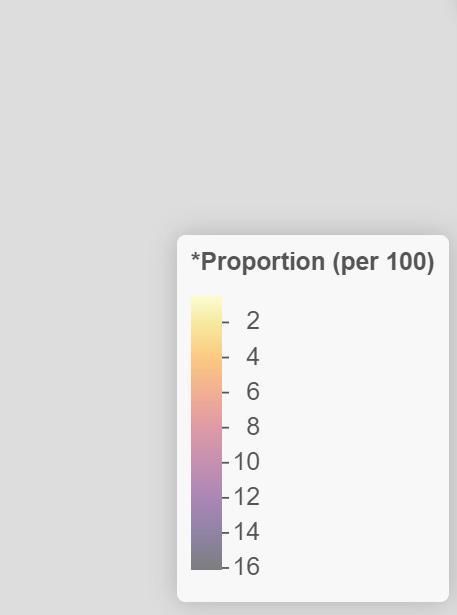
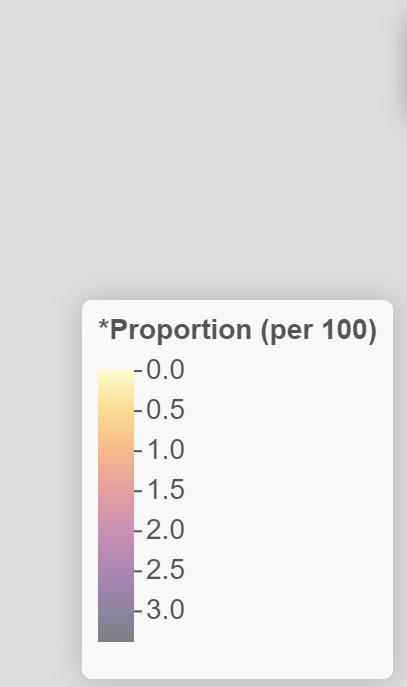
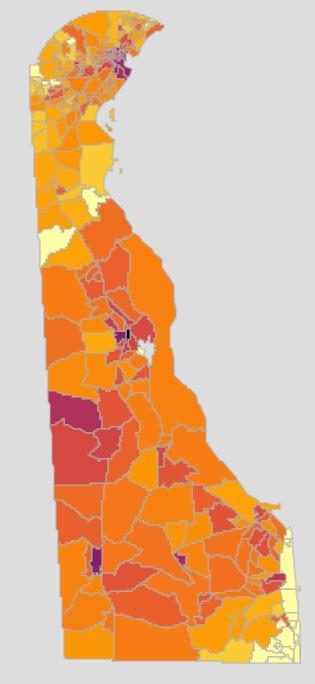
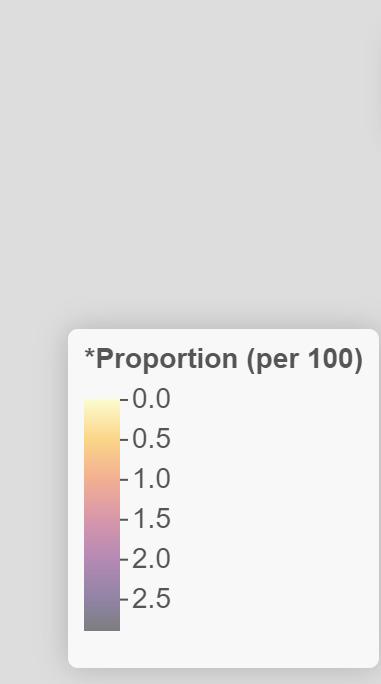
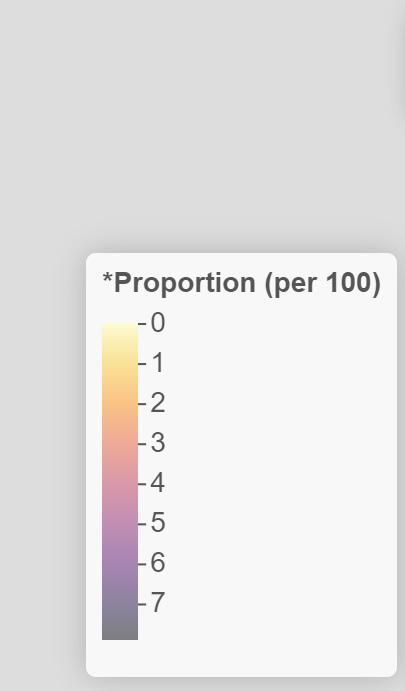
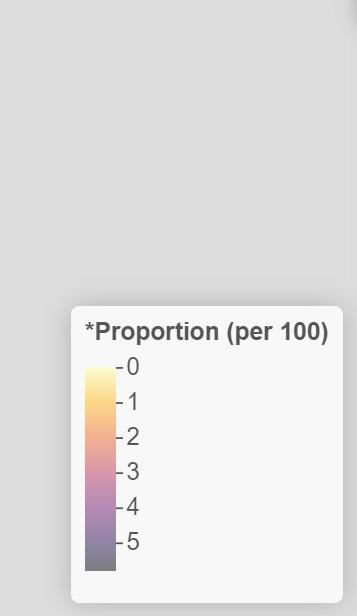
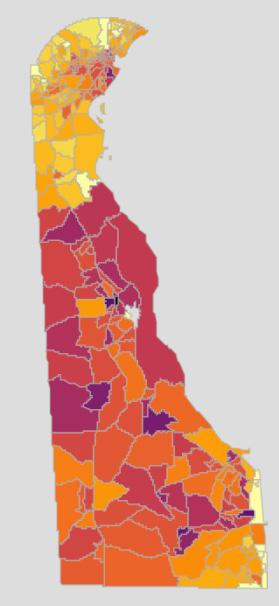
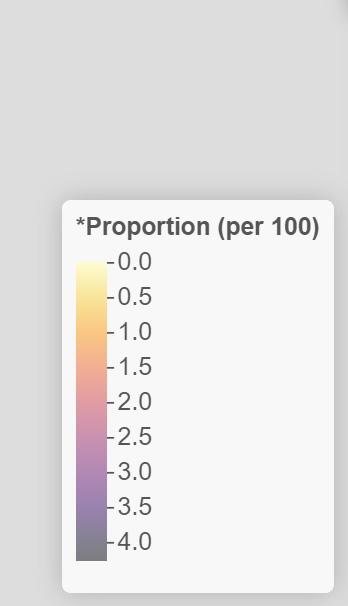
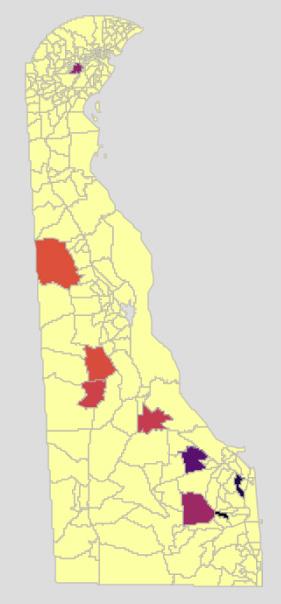
MAPS
The Workforce Subcommittee Chairs and report writers reviewed a number of options for the images used to represent where types of licensed individuals and facilities are located. By consensus we arrived at the decision to use a non-weighted heatmap. The heatmaps are an exact representation of the data provided on the facing page. The maps are also subdivided by ZIP codes rather than census tracts to broaden they accessibility to a wide audience who many not be as familiar with census tract information. Counties are demarcated by different background colors.
In all cases, maps only look at the ZIP code level (the exception is the facilities section of the report). The location of the center of any ZIP code is solely determined by ArcGIS defaults, and in no manner implies actual location of any one (or more) individuals or facilities. The size of the area representing licenses has no relation to the number of licenses or to their “reach” in that area. They only bring attention to the map and areas with, or without, licensed individuals or institutions.
These maps are presented to give a sense, based on the primary ZIP code listed for each DELPROS license, of where licensed individuals and institutions are physically located.
Please note that ZIP codes are being used as a proxy for provider or institution location and should not be considered definitive. For instance, while an institution can have one license per location, a provider (and especially physicians and nurses) may have multiple locations associated with their license. This was a limitation of the data provided for this first report which we hope to address in future reports as we become more granular in licensing information.
21
Board of Chiropractic
The primary objective of the Delaware Board of Chiropractic is to protect the public from unsafe chiropractic practice and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board:
• develops standards for professional competency, • promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to chiropractic practitioners and approves preceptors. The Board’s statutory authority is in 24 Del. C., Chapter 7.
CHIROPRACTOR
Chiropractors focus on patients’ overall health (see Figures 1-5). Chiropractors believe that malfunctioning spinal joints and other somatic tissues interfere with a person’s neuromuscular system and can result in poor health. Some chiropractors use procedures such as massage therapy, rehabilitative exercise, and ultrasound in addition to spinal adjustments and manipulation. They also may apply supports, such as braces or shoe inserts, to treat patients and relieve pain.1
Figure 1. Active Chiropractic Licenses, N= 383

DOI: 10.32481/djph.2022.12.013
22 Delaware Journal of Public Health - December 2022

Figure 2. Active
(when reported) 23
Chiropractic Licenses by Gender

Figure 3.
24 Delaware Journal of Public Health - December 2022
Active Chiropractic Licenses by Birth Year (when reported)

25
Figure 4. Numerical Distribution of Active Chiropractors by ZIP code
REFERENCES
1. US Bureau of Labor Statistics. (2022, Apr 18). What chiropractors do. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/chiropractors.htm#tab-2

Figure 5. Visual Distribution of Active Chiropractors by ZIP code
26 Delaware Journal of Public Health - December 2022
HIGHLIGHTS FROM
HEALTH
December 2022
Online-only news from The Nation’s Health newspaper
Pandemic takeaways being applied to broader public health practice: Pressures of pandemic spur innovation Mark Barna
Growing number of state, local measures undermining public health authority: Temple University researchers tracking laws, policies that limit public health protections Eeshika Dadheech
TGIF: How to make it a happy, healthy weekend Teddi Nicolaus
Climate change increasingly harming mental health: Resource-poor communities in US, across globe at high risk Teddi Nicolaus
Wanted: Advocates who speak up for climate justice, vulnerable people Kim Krisberg
In their own words: Advice from and for youth climate activists
APHA 2022 to rally around health equity, mark 150 years of progress


27
The NATION’S
A PUBLICATION OF THE AMERICAN PUBLIC HEALTH ASSOCIATION
Board of Dentistry and Dental Hygiene
The primary objective of the Delaware Board of Dentistry and Dental Hygiene is to protect the general public from unsafe and unprofessional practices. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to dentists, dentist academics, dental hygienists and dental residents. The Board also issues three types of permits to dentists and dentist academics who administer anesthesia.
The Board’s statutory authority is in 24 Del. C., Chapter 11.
The dental profession is the branch of healthcare devoted to maintaining the health of the teeth, gums and other tissues in and around the mouth.
WHAT IS A DENTIST?1
A dentist is a doctor, scientist and clinician dedicated to the highest standards of health through prevention, diagnosis and treatment of oral diseases and conditions (see Figures 1, 2, 3, and 4).
Dentists play a key role in the early detection of oral cancer and other systemic conditions of the body that manifest themselves in the mouth. They often identify other health conditions, illnesses, and other problems that sometimes show up in the oral cavity before they are identified in other parts of the body.
What does a Dentist do?
• Evaluates the overall health of their patients while advising them about oral health and disease prevention;
• Performs clinical procedures, such as exams, fillings, crowns, implants, extractions and corrective surgeries;
• Identifies, diagnoses and treats oral conditions; and
• Performs general dentistry or practices in one of nine dental specialties.
• Advances in dental research, including genetic engineering, the discovery of links between oral and systemic diseases, the development of salivary diagnostics and the continued development of new materials and techniques, make dentistry an exciting, challenging and rewarding profession.
WHAT IS A DENTAL HYGIENIST?2
Dental hygienists are preventive oral health professionals who have graduated from an accredited dental hygiene program in an institution of higher education, licensed in dental hygiene to provide educational, clinical, research, administrative and therapeutic services supporting total health through the promotion of optimum oral health.
In performing the dental hygiene process of care, the dental hygienist assesses the patient’s oral tissues and overall health determining the presence or absence of disease, other abnormalities and disease risks; develops a dental hygiene diagnosis based on clinical findings; formulates evidence-based, patient-centered treatment care plans; performs the clinical procedures outlined in the treatment care plan; educates patients regarding oral hygiene and preventive oral care; and evaluates the outcomes of educational strategies and clinical procedures provided.
Dental hygienists are preventive oral health professionals who have graduated from an accredited dental hygiene program in an institution of higher education, licensed in dental hygiene to provide educational, clinical, research, administrative and therapeutic services supporting total health through the promotion of optimum oral health.
In performing the dental hygiene process of care, the dental hygienist assesses the patient’s oral tissues and overall health determining the presence or absence of disease, other abnormalities and disease risks; develops a dental hygiene diagnosis based on clinical findings; formulates evidence-based, patient-centered treatment care plans; performs the clinical procedures outlined in the treatment care plan; educates patients regarding oral hygiene and preventive oral care; and evaluates the outcomes of educational strategies and clinical procedures provided.
Dental hygienists provide clinical services in a variety of settings such as private dental practice, community health settings, nursing homes, hospitals, prisons, schools, faculty practice clinics, state and federal government facilities and Indian reservations. In addition to clinical practice, there are career opportunities in education, research, sales and marketing, public health, administration and government. Some hygienists combine positions in different settings and career paths for professional variety. Working in education and clinical practice is an example.
DOI: 10.32481/djph.2022.12.014
28 Delaware Journal of Public Health - December 2022
WHAT IS A DENTIST ACADEMIC LICENSE?
A Delaware Dentist Academic license is given to practitioners who are full-time directors, chairpersons, or attending faculty members of a hospital-based dental, oral and maxillofacial surgery or other dental specialty residency program. The program must be:
• based in Delaware, and
• accredited by the Commission on Dental Accreditation of the American Dental Association (CODA) for the purposes of teaching, has received initial CODA accreditation or is in the process of establishing CODA accreditation
The academic license allows a practitioner to practice dentistry or oral and maxillofacial surgery only in the institution designated on the license and only on patients in an academic setting for teaching purposes.
WHAT ARE RESTRICTED PERMITS?
Restricted Permit I
A Restricted Permit I allows a practitioner to induce only conscious sedation by parenteral, enteral, or rectal routes, as well as nitrous oxide inhalation, at a specific location. (This does not prohibit the usual and customary pre-operative oral sedation.)
A Restricted Permit I does not allow induction using:
• deep sedation
• general anesthesia
Restricted Permit II
A Restricted Permit II allows induction of conscious sedation by nitrous oxide inhalation. It does not allow:
• deep sedation
• general anesthesia
Unrestricted Permit
An Unrestricted Permit applies only to one office location where anesthesia is administered. The two types of Unrestricted Permits are Individual and Facility. The type of permit selected determines who is allowed to administer anesthesia at that location:
An Unrestricted Permit-Individual allows the dentist to administer conscious sedation, general anesthesia and deep sedation, as defined by the Board’s Rules and Regulations governing anesthesia, at the location. If a certified registered nurse anesthetist (CRNA) is employed for deep sedation or general anesthesia at an office location, the facility must also have at least one individual with an Unrestricted Permit-Individual.
WHAT IS DENTIST-FQHC PROVISIONAL LICENSE?
This type of dental licensure is specific to dentists contracted to practice at a Federally Qualified Health Center (FQHC) in Delaware. The Dentist-FQHC Provisional license allows the practice of dentistry in Delaware…
• before the three examinations required for full Dentist licensure have been passed, • only at the FQHC named on the license, and • only under the general supervision of a Delaware-licensed dentist.
A Dental Resident is a license for dentists who will be starting a residency program in Delaware.
29
Figure 1. Active Dental Licenses by Type*, N=1,740
Note. An active license does not guarantee an individual is actively seeing patients.
Figure 2. Active Dental Licenses by Gender, all types (when reported)

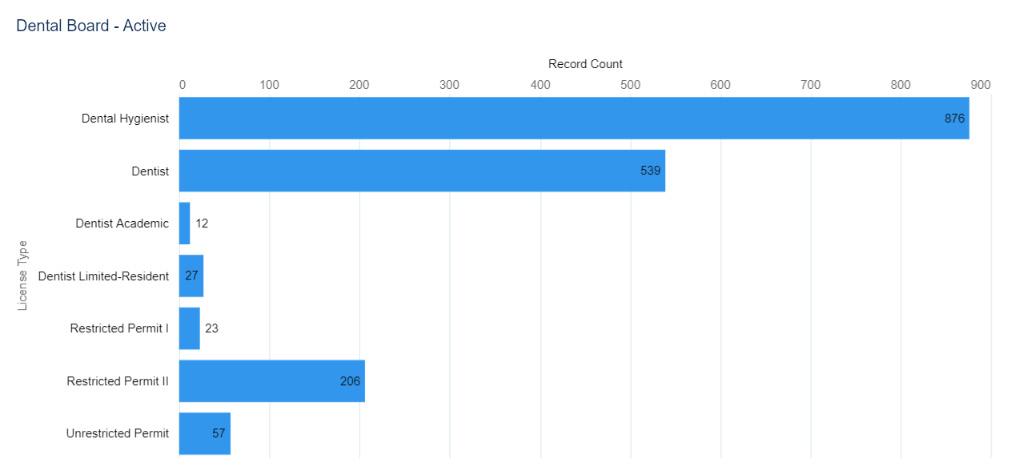
30 Delaware Journal of Public Health - December 2022
Note. Three individuals did not provide a year of birth.
*According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.‚

Figure 3. Dentists ONLY - Active Licenses by Birth Year (when reported)
31
Note. Map in Figure 4 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
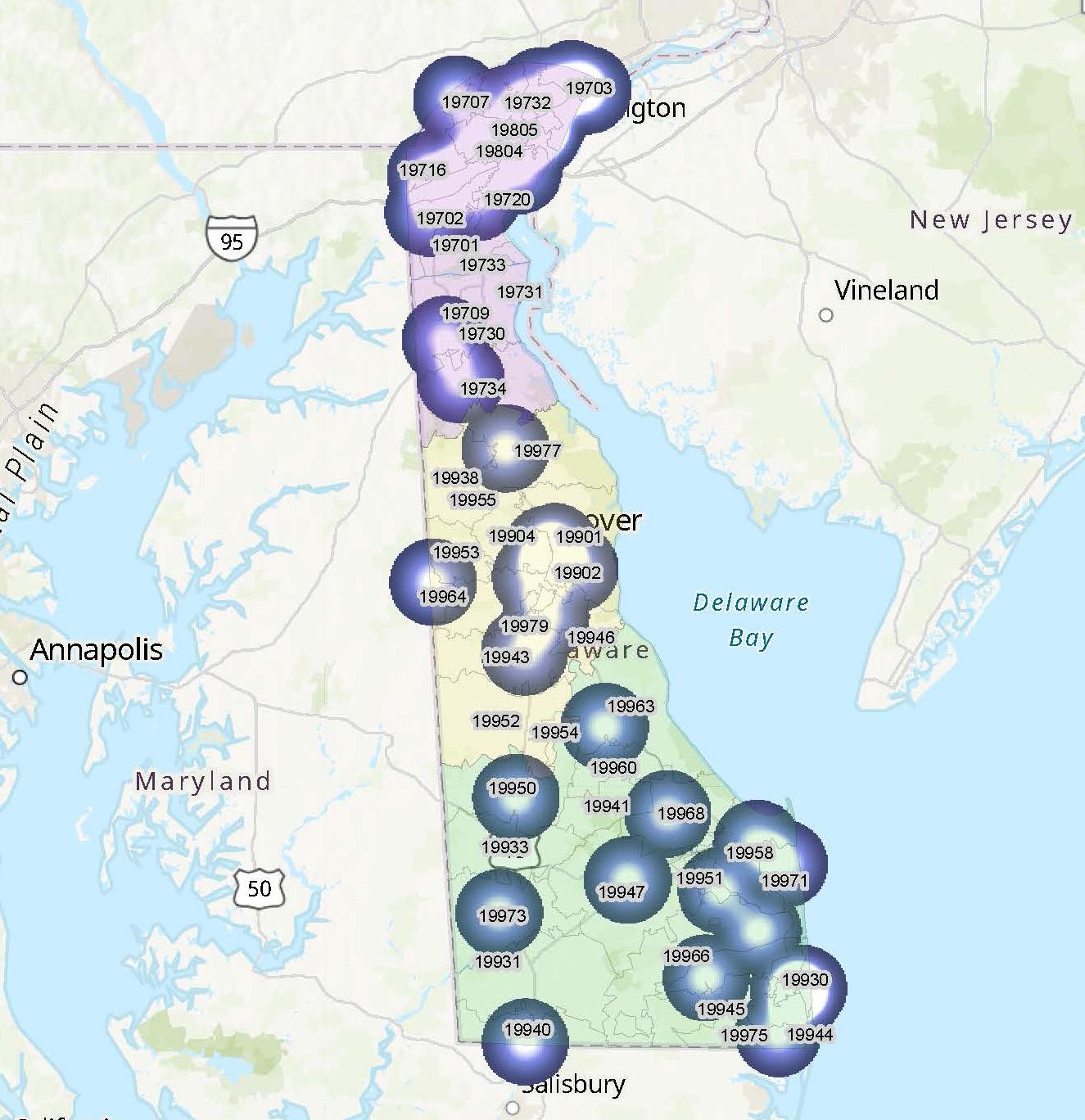
REFERENCES
1. American Dental Education Association. (n.d.). “Dentistry 101.” https://www.adea.org/GoDental/Dentistry_101.aspx
2. Explore Health Careers. (n.d.). Dental Hygienist. Retrieved from: https://explorehealthcareers.org/career/dentistry/dental-hygienist/
Figure 4. Numerical
Distribution of Active Dentists and Dental Academics by ZIP code
32 Delaware Journal of Public Health - December 2022




JOIN THE DELAWARE PUB LI C HEALT H IN STITUTE ON THE CHRONIC DISEASE PUBLIC HEALTH CONFERENCE: CONNECTING WITH PREVENTION FEBRUARY 15, 2023 EMBASSY SUITES 654 S COLLEGE AVE, NEWARK DE CLICK HERE to Register online 33
Board of Dietetics / Nutrition
The primary objective of the Delaware Board of Dietetics/Nutrition is to protect the health of the public by broadening access to appropriate dietetic and nutrition therapy. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• evaluates the credentials of persons applying for licensure,
• promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions. The Board issues licenses to dietitian/nutritionists. The Board’s statutory authority is in 24 Del. C., Chapter 38.
WHAT IS THE DIFFERENCE BETWEEN A DIETICIAN AND A NUTRITIONIST?
Although dietitians and nutritionists both help people find the best diets and foods to meet their health needs, they have different qualifications. In the United States, dietitians are certified to treat clinical conditions, whereas nutritionists are not always certified. In the U.S., dietitians must receive certification from the Academy of Nutrition and Dietetics in order to practice. Dietitians can treat specific health conditions, such as eating disorders, by providing food recommendations (see Figures 1-5 for Dietitians in Delaware). Some organizations also certify nutritionists, such as the Board for Certification of Nutrition Specialists (BCNS), however, nutritionist training can vary. Some states do not require certification, so it is possible for anyone in those states to offer nutrition advice. Nutritionists may also have different areas of focus to dietitians. For example, nutritionists can pursue advanced qualifications in specific health areas, such as sports nutrition, digestive disorders, and autoimmune conditions. The BCNS also offer Certified Ketogenic Nutrition Specialist qualifications for those who want to understand the keto diet in more detail. However, some nutritionists provide more general advice on healthful eating, weight loss, and reducing tiredness.1
WHAT IS A DIETICIAN?
Nutrition is a key element of good health. Registered dietitian nutritionists are the experts on good nutrition and the food choices that can make us healthy, whether it’s a proper diet or eating to manage the symptoms of a disease or chronic condition. Registered dietitian nutritionists design nutrition programs to protect health, prevent allergic reactions and alleviate the symptoms of many types of disease.
Clinical dietitians provide medical nutrition therapy for patients in institutions such as hospitals and nursing care facilities. They assess patients’ nutritional needs, develop and implement nutrition programs and evaluate and report the results. They confer with doctors and other healthcare professionals in order to coordinate medical and dietary needs. Some clinical dietitians specialize in the management of overweight and critically ill patients, such as those with renal (kidney) disease and diabetes. In addition, clinical dietitians in nursing care facilities, small hospitals, or correctional facilities may manage the food service department.
Community dietitians develop nutrition programs designed to prevent disease and promote health, targeting particular groups of people. Dietitians in this practice area may work in settings such as public health clinics, fitness centers, corporate wellness programs or home health agencies.
Corporate dietitians work in food manufacturing, advertising and marketing. In these areas, dietitians analyze foods, prepare literature for distribution, or report on issues such as the nutritional content of recipes, dietary fiber or vitamin supplements. Management dietitians oversee large-scale meal planning and preparation in healthcare facilities, company cafeterias, prisons and schools. They hire, train and direct other dietitians and food service workers; budget for and purchase food, equipment, and supplies; enforce sanitary and safety regulations; and prepare records and reports.
Consultant dietitians work under contract with healthcare facilities or in their own private practice. They perform nutrition assessments for their clients and advise them about diet-related concerns, such as weight loss or cholesterol reduction. Some work for wellness programs, sports teams, supermarkets and other nutrition-related businesses. They consult with food service managers, providing expertise in sanitation, safety procedures, menu development, budgeting and planning.2
DOI: 10.32481/djph.2022.12.015
34 Delaware Journal of Public Health - December 2022
*an active license does not guarantee an individual is actively seeing patients.
Figure 2. Active Dietician
Licenses
by Gender (when reported)


Figure
1. Active Dietician Licenses*, N=483
35
*According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.‚
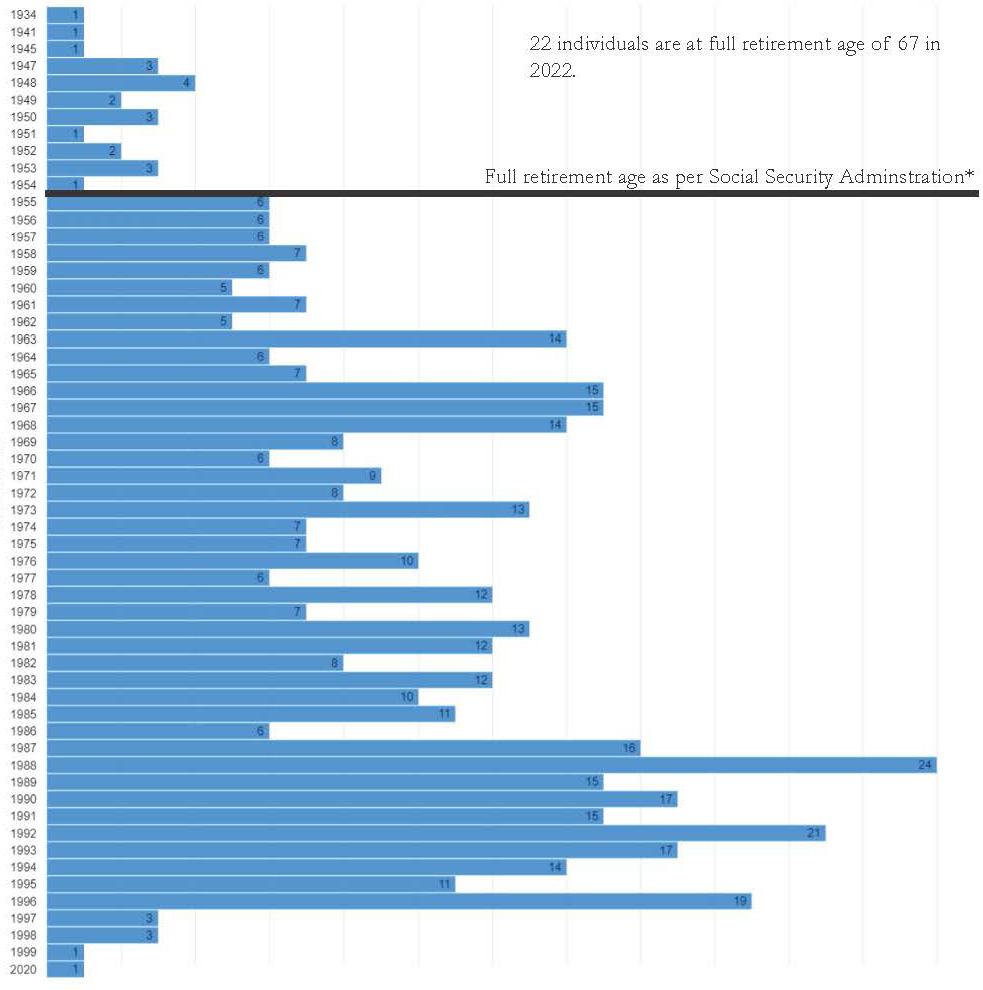
Figure 3. Active Dietician Licenses by Birth Year (when reported)
36 Delaware Journal of Public Health - December 2022

Figure 4. Numerical Distribution
by ZIP code 37
of Active Dieticians
REFERENCES
1. Medical News Today. (2020, Aug). What is the difference between nutritionists and dietitians? Retrieved from: https://www.medicalnewstoday.com/articles/nutritionist-vs-dietician#training
2. Healthcareers, E. (n.d.). Dietitian nutritionist. Retrieved from: https://explorehealthcareers.org/career/nutrition-dietetics/dietitian-nutritionist/

Figure 5. Visual Distribution of Active Dieticians & Nutritionists by ZIP code
38 Delaware Journal of Public Health - December 2022
Dear Public Health Partners,
The Mid-Atlantic Public Health Partnership is proud to bring its third annual and very first in-person conference to public health communities across Pennsylvania, Delaware, and Maryland. Extreme weather events in recent weeks are a reminder that climate change and public health are inextricably connected. Adapting public health policy to address the climate crisis is key to protecting and strengthening our communities.
The Delaware Academy of Medicine/Delaware Public Health Association (Academy/DPHA), Maryland Public Health Association (MdPHA), and Pennsylvania Public Health Association (PPHA) are bringing together regional experts through a two-day conference focused on the theme, “Public Health and Climate Change: Response, Policy and Implementation.”
Date: March 16 & 17, 2023
Location: The Sciences & Engineering Center and The Commons – West Chester University 155 University Ave, West Chester, PA 19383
Registration details to follow. Here is the link to the call for abstracts. Abstracts must be received by 5:00 p.m. on December 31, 2022.
This conference will provide public health students, professionals, and partners across our region with the opportunity to learn about and engage in conversations about innovative strategies to address climate issues in the region.

We look forward to an in-person exciting conference this time!
Sincerely,
Delaware Public Health Association
Maryland Public Health Association

Pennsylvania Public Health Association

39
Board of Funeral Services
The primary objective of the Delaware Board of Funeral Services is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to funeral directors, interns, funeral establishments and crematory establishments. It also issues funeral director limited licenses to Maryland- or Pennsylvania-licensed funeral directors.
The Board’s statutory authority is in 24 Del. C., Chapter 31
The Board of Funeral Services licenses both individuals and facilities which is somewhat different from many other board of the Division of Professional Regulation. Information on facilities is contained in the facilities section of this report.
FUNERAL RESIDENT INTERN
All applicants, with the exception of the applicants who meet the experience requirement below to apply by reciprocity, must apply for a Funeral Resident Intern license and serve a one-year internship in Delaware, with the intention of later applying for Delaware licensure as a Funeral Director. A Delaware resident internship is required if a practitioner:
• does not hold a current Funeral Director license in any jurisdiction (state, U.S. territory or District of Columbia)
• holds a current Funeral Director license in another jurisdiction but has not practiced as a funeral director at least three of the past five years.
If a current Funeral Director license is current in another jurisdiction and an individual has practiced as a funeral director at least three of the past five years, they may submit the Funeral Director application.
FUNERAL DIRECTOR
The Funeral Director oversees, directs, and coordinates all aspects of funeral services including body preparation, visitation, services, burials, and cremations, while providing caring support and advice to families and friends of the deceased.1
FUNERAL DIRECTOR LIMITED LICENSURE
Funeral Director Limited licensure (see Figures 1-5) is available only to funeral directors validly licensed by another jurisdiction (U.S. state, possession, territory or District of Columbia) provided that the jurisdiction where he or she is licensed grants a similar privilege to Delaware-licensed funeral directors (24 Del. C. §3108). Currently, Delaware only has limited licensure agreements with the States of Maryland and Pennsylvania.
Funeral Director Limited licensure allows a practitioner to:
• make a removal of a dead human body in Delaware,
• return the body to another state or country,
• return dead bodies from another state or country to Delaware for final disposition,
• complete the family history portion of the death certificate,
• sign the death certificate in the capacity of a licensed funeral director, and
• execute any other procedures necessary to arrange for the final disposition of a dead human body.
FUNERAL ESTABLISHMENT PERMIT
A valid Funeral Establishment Permit issued by the Board of Funeral Services is required to open or operate a funeral establishment in Delaware. This permit is required in addition to any business license issued by the Division of Revenue. Please see the facilities section of this report for additional information.
CREMATORY ESTABLISHMENT
A valid Crematory Establishment Permit issued by the Board of Funeral Services is required to open or operate a crematory in Delaware when crematory is not part of a Delaware-licensed Funeral Establishment’s operation. Section 13.2.13 of the Board’s Rules and Regulations more fully explains when a crematory does not need a permit. Please see facilities section of this report for additional information.
DOI: 10.32481/djph.2022.12.016
40 Delaware Journal of Public Health - December 2022
Figure 1. Active Funeral Services Licenses by Type*, N=307
* an active license does not guarantee an individual is actively seeing patients.
Figure 2. Active Funeral Services Licenses by Gender, select license types (when reported)
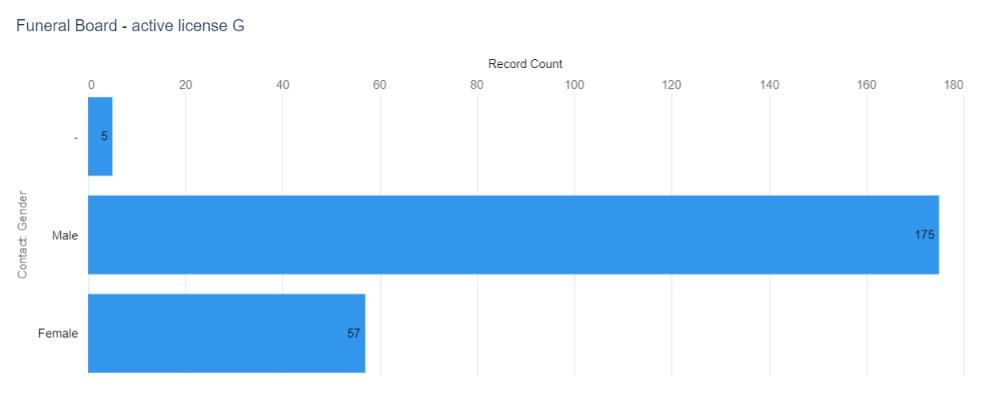
Figure 3. Active Funeral Services Licenses by Birth Year (when reported)

41
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.‚

42 Delaware Journal of Public Health - December 2022
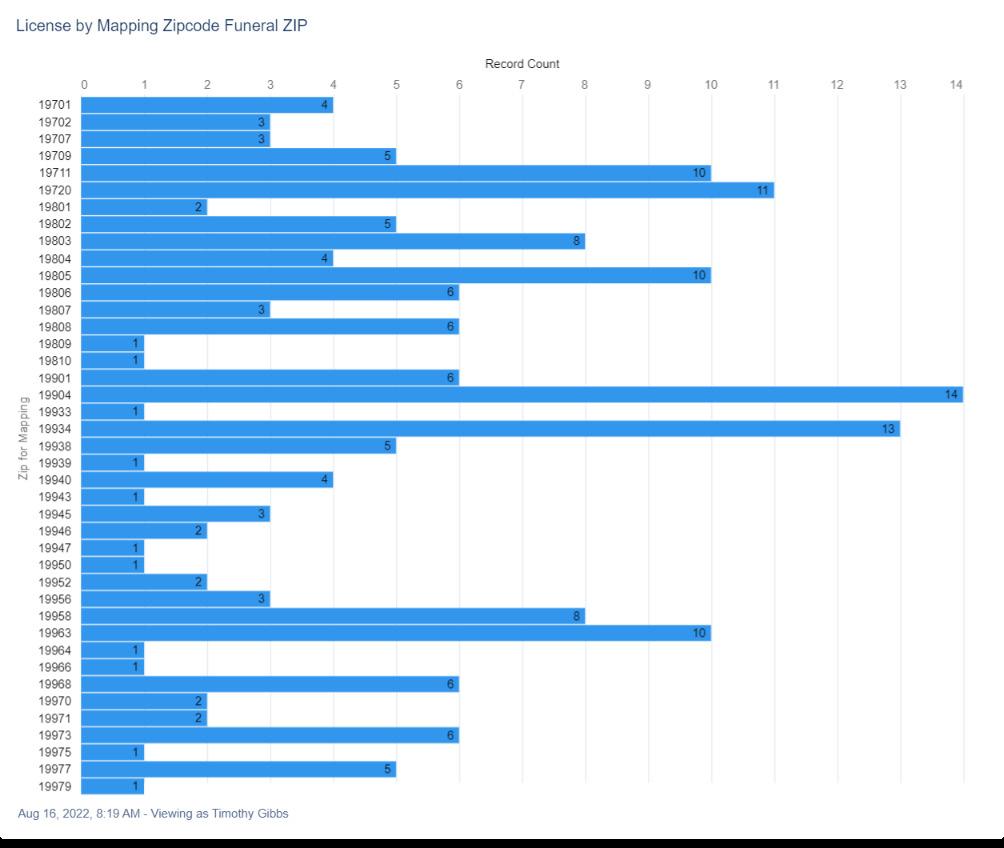
Figure 4. Numerical Distribution of Active Funeral Services Licenses by ZIP code 43
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 5. Visual Distribution of Active Funeral Services Licenses by ZIP Code

REFERENCES
1. Society for Human Resource Management. (2022). Funeral directors. Retrieved from: https://www.shrm.org/ResourcesAndTools/tools-and-samples/job-descriptions/Pages/Funeral-Director.aspx
44 Delaware Journal of Public Health - December 2022
45
Board of Massage and Bodywork
The primary objective of the Delaware Board of Massage and Bodywork is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board:
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to massage therapists, certifications to massage technicians and Massage Establishment licenses (see figures 1-5). It also issues temporary certifications to massage technicians.
The Board’s statutory authority is in 24 Del. C., Chapter 53
The Board of Massage and bodywork licenses both individuals and facilities which is somewhat different from many other board of the Division of Professional Regulation. Information on facilities is contained in the facilities section of this report.
MASSAGE THERAPIST
Massage therapists treat clients by using touch to manipulate the muscles and other soft tissues of the body.1
Individuals holding a Delaware Massage Therapist license must be 18 years old, pass the National Certification Board for Therapeutic Massage and Bodywork (NCBTMB) exam and:
• not licensed by any other jurisdiction (state, District of Columbia, or U.S. territory), OR
• licensed by another jurisdiction but have not practiced continuously in that jurisdiction for at least two years, OR
• currently licensed as a Certified Massage Technician or Temporary Massage Technician in Delaware.
A “reciprocity” agreement can be made if a therapist is are currently licensed in another jurisdiction AND has practiced continuously in that jurisdiction for at least two years, AND has passed the NCBTMB exam.
MASSAGE THERAPIST TECHNICIAN
Delaware Certified Massage Technicians must be 18 years old and:
• not licensed by any other jurisdiction (state, District of Columbia, or U.S. territory), OR
• licensed by another jurisdiction but have not practiced continuously in that jurisdiction for at least two years.
A “reciprocity” agreement can be made if a technician is currently licensed in another jurisdiction AND has practiced continuously in that jurisdiction for at least two years.
TEMPORARY MASSAGE TECHNICIAN CERTIFICATION
The purpose of a Temporary Massage Technician Certification is to allow an individual to practice while completing the educational requirements. They must be at least 18 years old, and have not yet completed the educational requirements for Massage Technician Certification.
The temporary certification is valid for one year only. It cannot be renewed, reissued or changed to inactive status.
MASSAGE ESTABLISHMENTS
An establishment license from the Board of Massage and Bodywork is required for each location operating as a Massage Establishment as defined by 24 Del. C. §5302 and Section 12.0 of the Board’s Rules and Regulations. If any of the following occurs, a new application for licensure must be approved:
• An existing unlicensed massage/bodywork business with a first application for establishment licensure,
• Opening a new establishment,
• The ownership of an existing establishment is changing (regardless of whether the name is changing),
• The name of an existing establishment is changing (regardless of whether the owner is changing),
• The location of an existing establishment is changing.
The establishment may need other licenses and permits (such as a business license from the Division of Revenue or permit from the town/city where the establishment operates). Please see facilities section of this report for additional information.
DOI: 10.32481/djph.2022.12.017
46 Delaware Journal of Public Health - December 2022
Figure 1. Active Massage and Bodywork Licenses by Type*, N=1,197
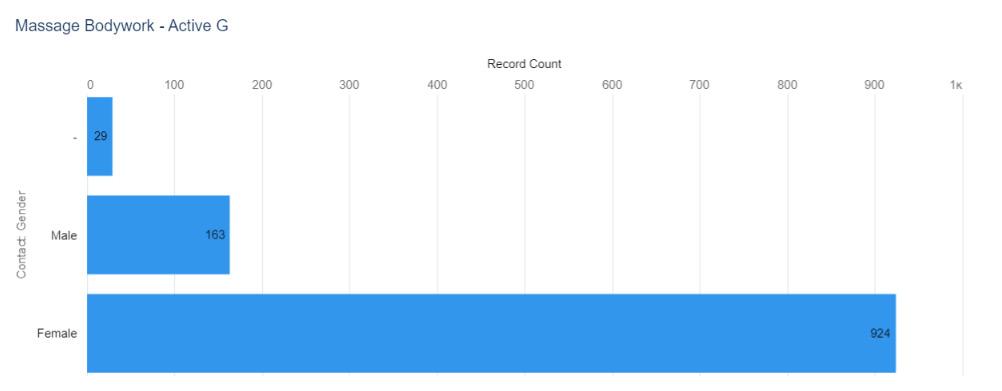
* an active license does not guarantee an individual is actively seeing patients.
Figure 2. Active Certified Massage Technician & Massage Therapist Licenses by Gender (when reported)
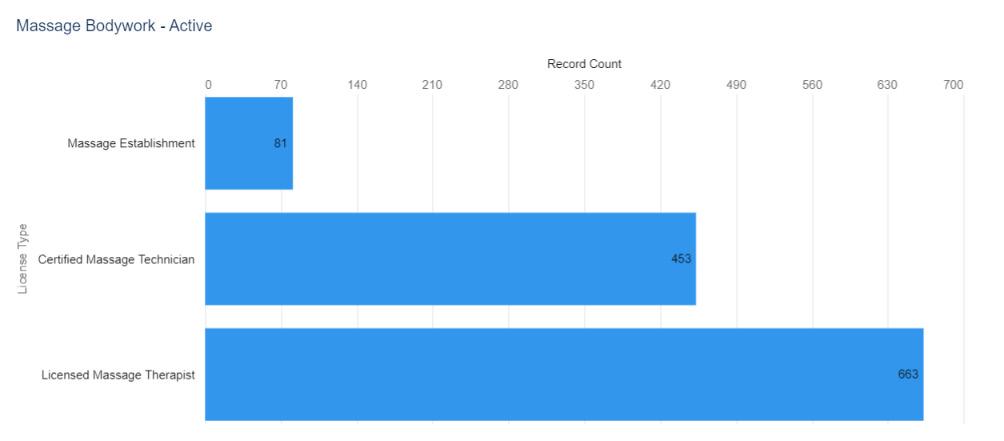
47
Note. One individual did not provide a year of birth
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.‚

Figure 3. Active Certified
& Massage Therapist Licenses by Birth Year
Massage Technician
(when reported)
48 Delaware Journal of Public Health - December 2022
Fig. 4 continued on next page.

 Figure 4. Numerical Distribution of Active Massage and Bodywork Licenses by ZIP code
Figure 4. Numerical Distribution of Active Massage and Bodywork Licenses by ZIP code
49


Figure 4. continued 50 Delaware Journal of Public Health - December 2022
REFERENCES
1. Bureau of Labor Statistics. (2022, Aug). Massage therapists. Occupational outlook handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/massage-therapists.htm
 Figure
Figure
5.
Visual Distribution of Active Massage and Bodywork Licenses by ZIP code
51
Board of Medical Licensure and Discipline
The primary objectives of the Delaware Board of Medical Licensure and Discipline are to promote public health, safety and welfare and to protect the public from the unprofessional, improper, unauthorized, or unqualified practice of medicine and certain other healthcare professions. To meet these objectives, the Board:
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues physician (M.D. and D.O.) licenses and physician training licenses to residents, interns, fellows and house physicians (see figures 1-3).
The Board also issues for licenses these additional healthcare professions: physician assistants, respiratory care practitioners, acupuncture practitioners, acupuncture detoxification specialists, eastern medicine practitioners, genetic counselors, polysomnographers, midwifery practitioners and administrative medical. A Council for each of these healthcare professions advises and assists the Board on licensure and regulatory matters pertaining to its profession.
The Board also issues certifications to and has other responsibilities in regard to emergency medical technicians/paramedics in collaboration with the Office of Emergency Medical Services.
The Board’s statutory authority is in 24 Del. C., Chapter 17. Additional statutory provisions on the Board’s responsibilities in connection with emergency medical technicians/paramedics are in 16 Del. C., Chapter 97 and Chapter 98.
Figure 1. Active Medical Board Licenses by Type*, N=9,895 records across licenses
* an active license does not guarantee an individual is actively seeing patients.
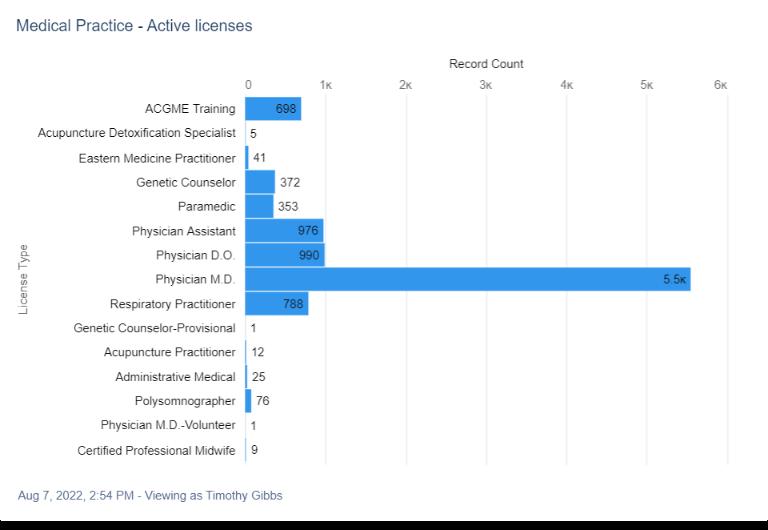
10.32481/djph.2022.12.018
DOI:
52 Delaware Journal of Public Health - December 2022

Figure 2. Active
53
Medical Board Licenses by Gender, select license types (when reported)
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.‚
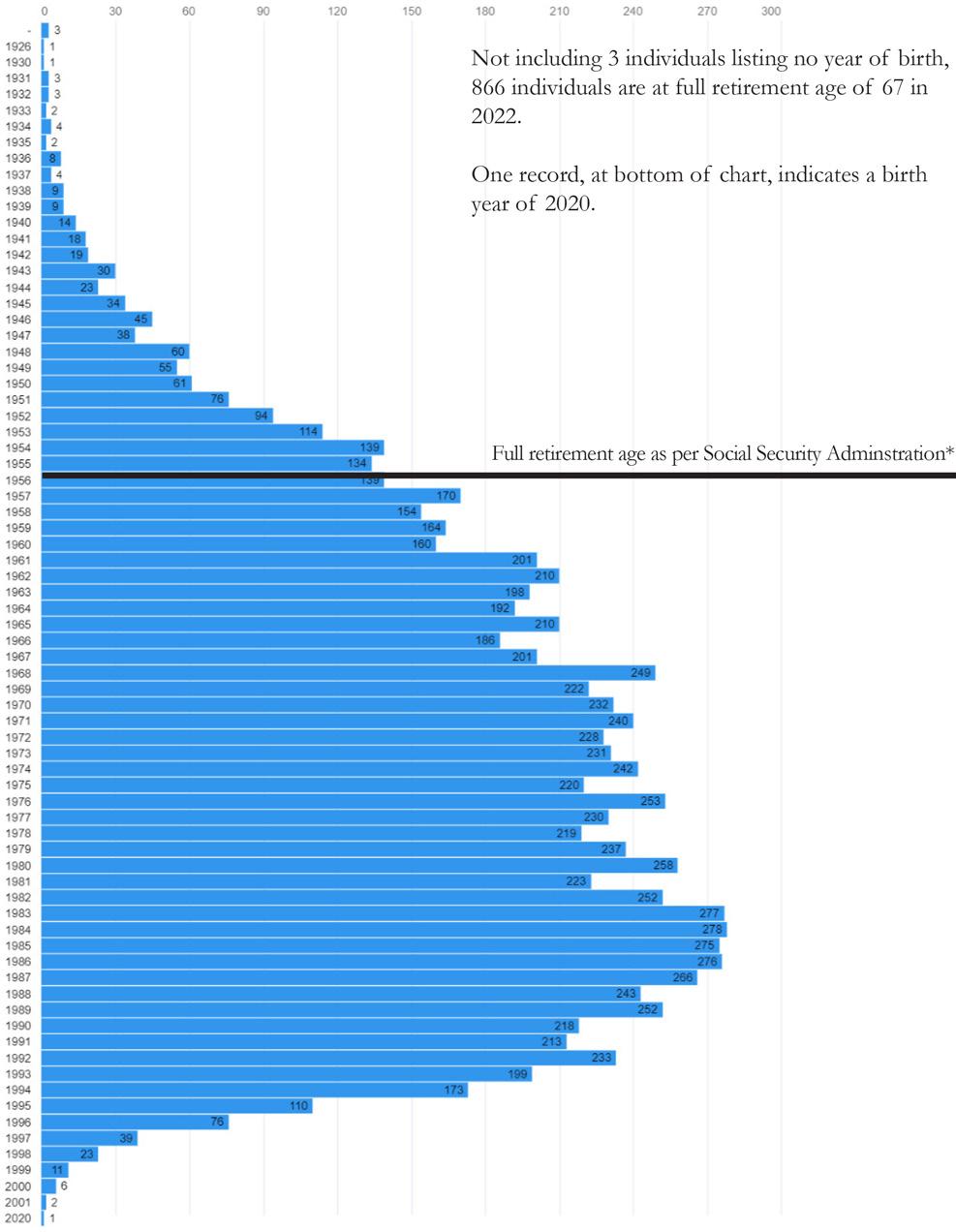
Figure 3. Active Physician Licenses by Birth Year
54 Delaware Journal of Public Health - December 2022
PHYSICIAN
Physicians and surgeons diagnose and treat injuries or illnesses and address health maintenance.
Physicians and surgeons work in both clinical and nonclinical settings. Clinical settings include physicians’ offices and hospitals; nonclinical settings include government agencies, nonprofit organizations, and insurance companies.1
There are two terminal degrees for physicians, Doctor of Osteopathic Medicine (D.O.) and Doctor of Medicine (M.D.) from the Latin Medicinae Doctor.
MDs are allopathic doctors. That means they treat and diagnose conditions using conventional medical tools like x-rays, prescription drugs, and surgery. Allopathic medicine is also called conventional or mainstream medicine see figure 4-5).
55

56 Delaware Journal of Public Health - December 2022
Figure 4. Numerical Distribution of Active Physician - MD by ZIP code
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in figure 4.
Figure 5. Visual Distribution of Active Physician - MD by ZIP code
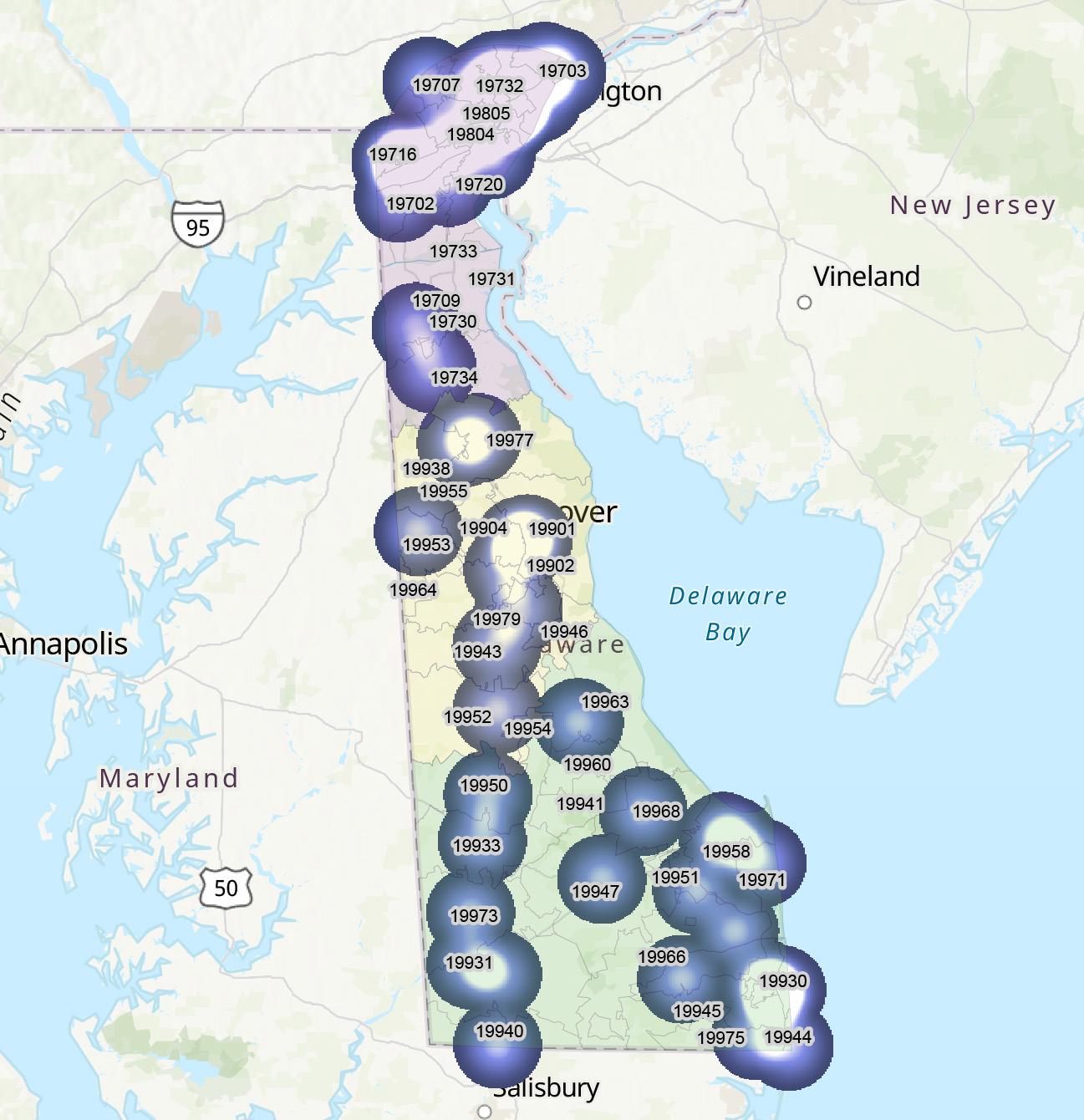
MDs can choose to be broad practitioners and work as family medicine or primary care doctors (see figures 6 & 7). They can also specialize in several different areas requiring further education (see figure 8) including:
• Surgery,
• Organ System Specific Specialty,
• Psychiatry,
• Geriatric Medicine, and • Pediatrics
57
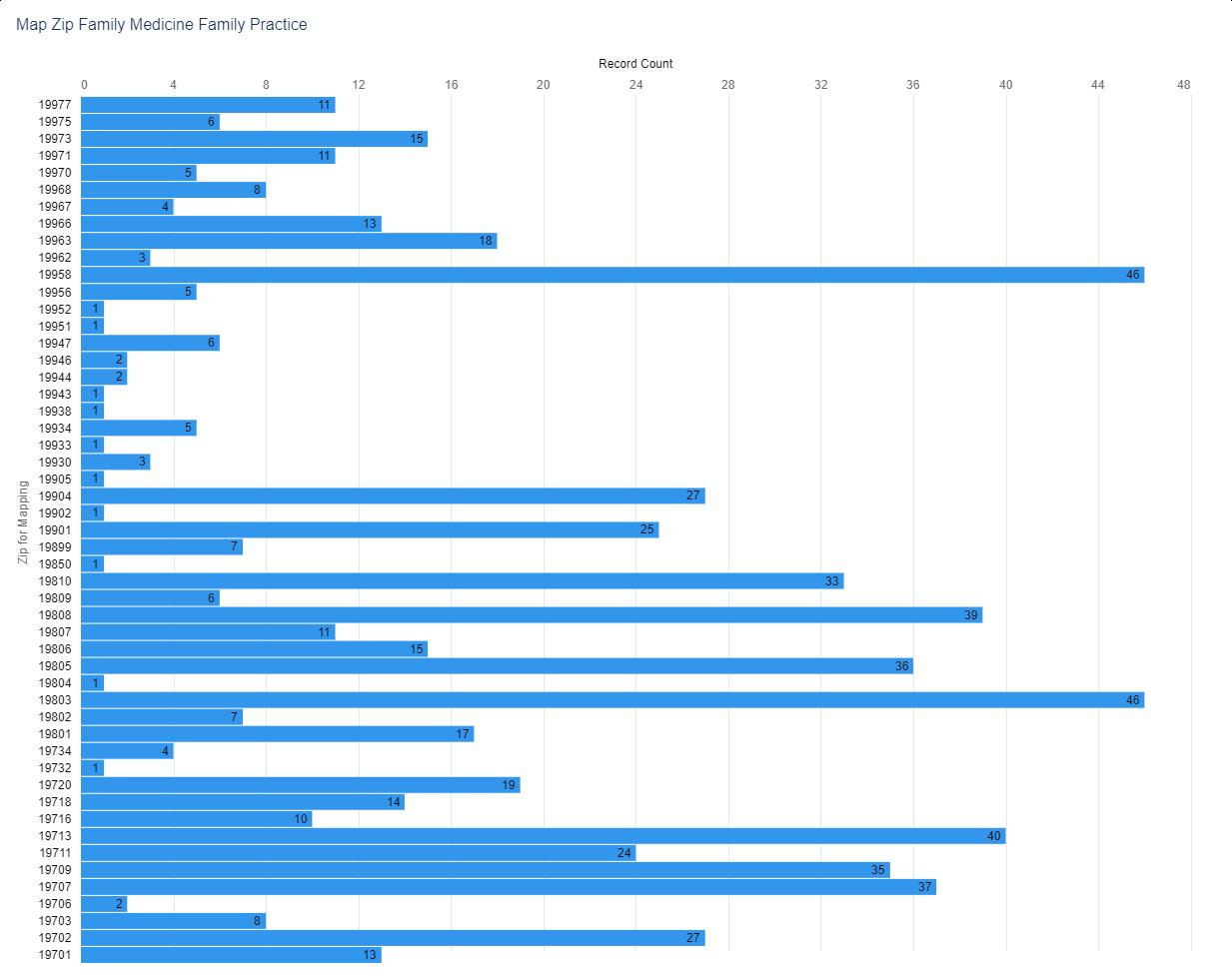
Figure 6. Numerical Distribution of Active Family Medicine Physicians by ZIP Code 58 Delaware Journal of Public Health - December 2022
Figure 7 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 7. Visual Distribution of Active Family Medicine Physicians by ZIP code

59
*At the time of data extraction, the DELPROS licensing system allowed for natural language submissions in the field “Specialty.‚ In over 1,600 instances no specialty was selected and those entries were researched. In the remaining records that did not have a listing which conformed to AAMC (Association of American Medical College) taxonomy, staff employed best reasoning possible in selecting an accurate category. This operation was overseen by a physician. Please see the following pages for the AAMC taxonomy detail with subspecialty information.

Future reports, pending adoption of a picklist system in DELPROS, will result in a more accurate number per specialty, and essential exercise to relate physician specialists to disease prevention and treatment.
DO stands for doctor of osteopathic medicine. They use the same conventional medical techniques as MDs but with a few other methods. DOs tend to focus more on holistic health and prevention. In holistic health, all parts of a person, including their mind, body, and emotions, are considered during the treatment. They also use a system of physical manipulations and adjustments to diagnose and treat people (see figures 9 & 10).
Figure 8. Physician Licenses by AAMC Specialty*
60 Delaware Journal of Public Health - December 2022

61
Figure 9. Numerical Distribution of Active Physician - DO by ZIP code
Figure 10 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 10. Visual Distribution of Active Physician - DO by ZIP code
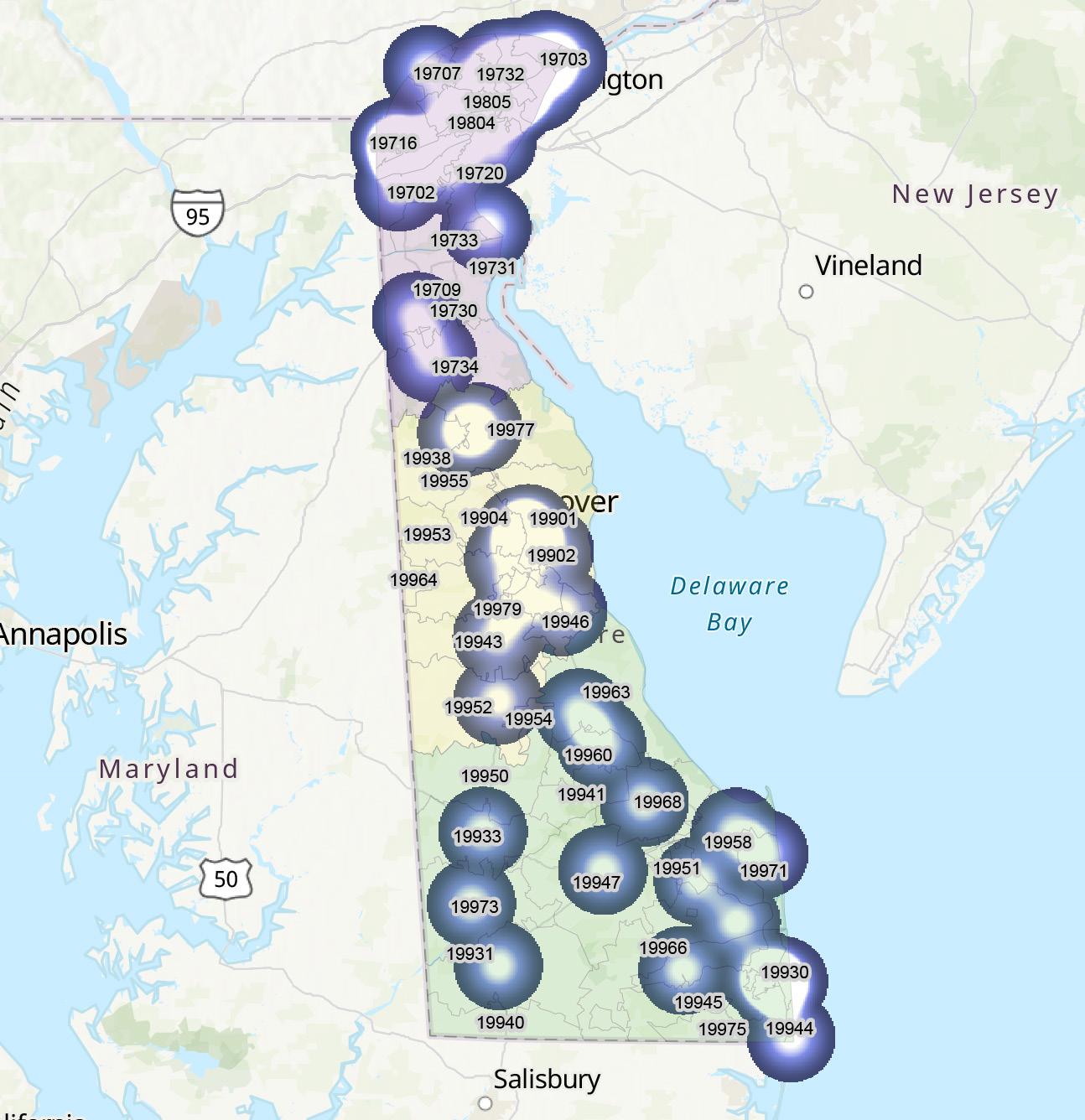
Over half of DOs choose to work in primary care, but they can also choose to specialize in another area, just like MDs. DOs have all the same responsibilities and rights as MDs, including the abilities to perform surgery with proper training and prescribe medicine.
HOW ARE MDS AND DOS SIMILAR?
MDs and DOs follow similar educational routes. They must first earn a four-year undergraduate degree, and most will take premedicine courses during this time. After getting an undergraduate degree, they will attend either medical school or a college of osteopathic medicine.
After finishing four years of medical education, MDs and DOs must complete an internship and a residency. A residency is on-the-job training under the supervision of more experienced doctors. Some MDs and DOs will also go on to do fellowships to learn more about a specialty.
MDs and DOs often train side by side in residencies and internships, despite going to different types of schools.
Both MDs and DOs must also take a licensing exam in order to practice medicine professionally.2
62 Delaware Journal of Public Health - December 2022
ACGME TRAINING LICENSE - PHYSICIAN TRAINING LICENSURE (RESIDENTS, INTERNS, FELLOWS, HOUSE PHYSICIANS)
An ACGME training license is required for that part of the education which all physicians, regardless of degree type (D.O. or M.D.), go through after medical school to prepare them for fully independent practice. Another section of this report examines these types of trainings and the Delaware institutions at which they are offered (see figures 11 & 12).
Figure 11. Numerical Distribution of Active ACGME Physicians by ZIP code
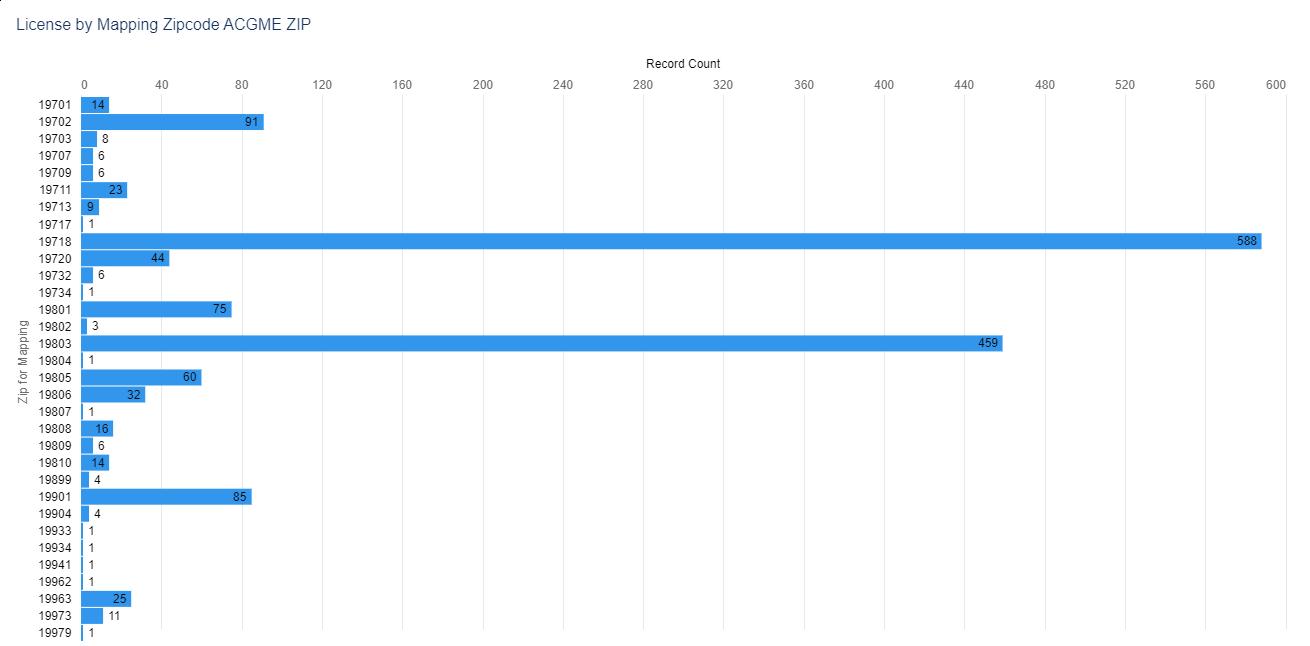
63
Figure 12 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 12. Visual Distribution of Active ACGME Physicians by ZIP code
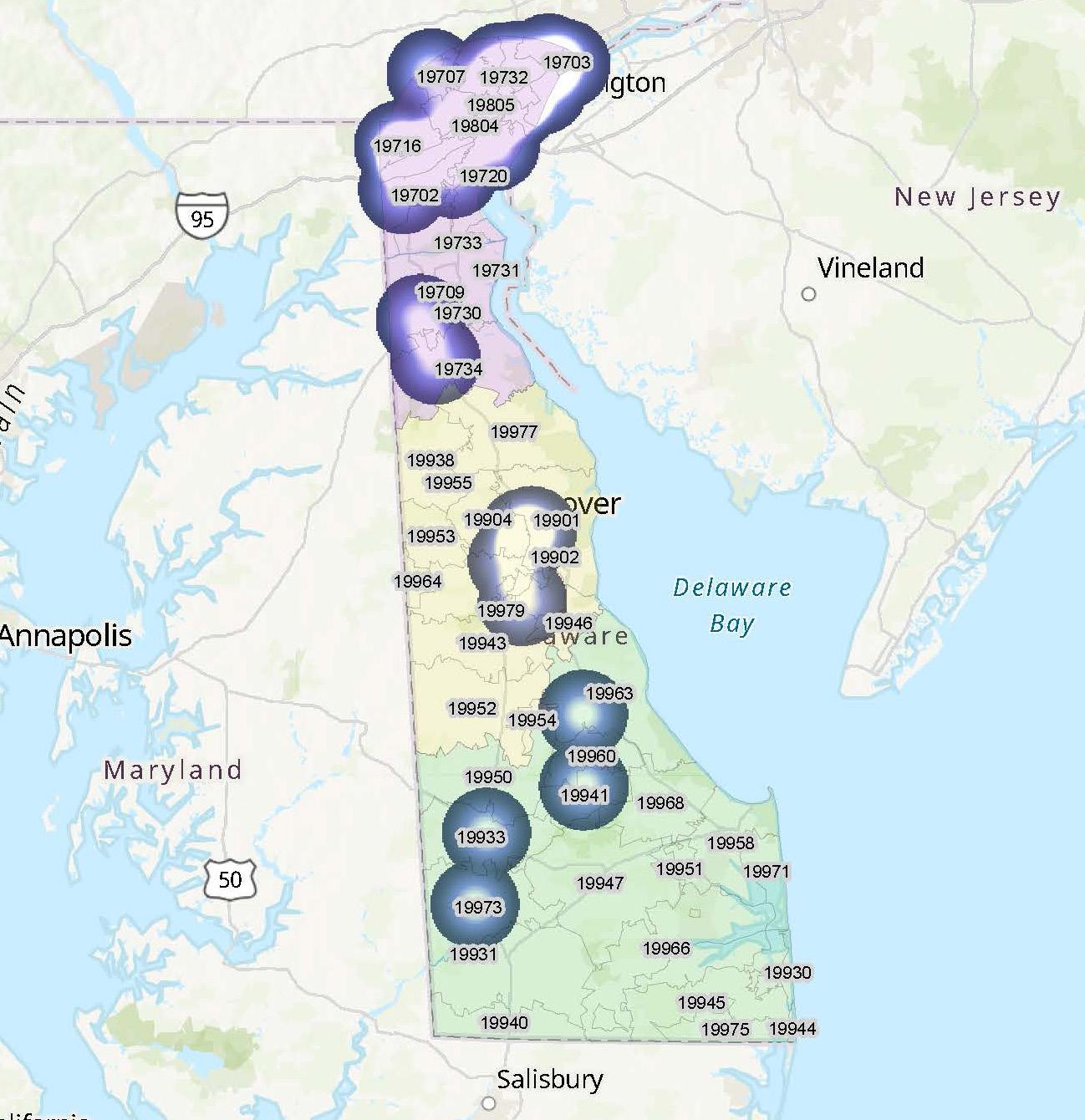
Physicians are employed in an ACGME-approved institution located in Delaware and are: • a Resident, Intern or Fellow registered in a training program outside of Delaware who will rotate through a program in Delaware for over one month, or • employed as a House Physician.
For more information about Training licensure, see Section 4.0 of the Board’s Rules and Regulations.
64 Delaware Journal of Public Health - December 2022
PHYSICIAN ASSISTANT
Physician assistants practice medicine on teams with physicians, surgeons, and other healthcare workers (see figures 13 & 14). Physician assistants work in physicians’ offices, hospitals, outpatient clinics, and other healthcare settings. Most work full time.3
Figure 13. Numerical Distribution of Active Physician Assistants by ZIP code
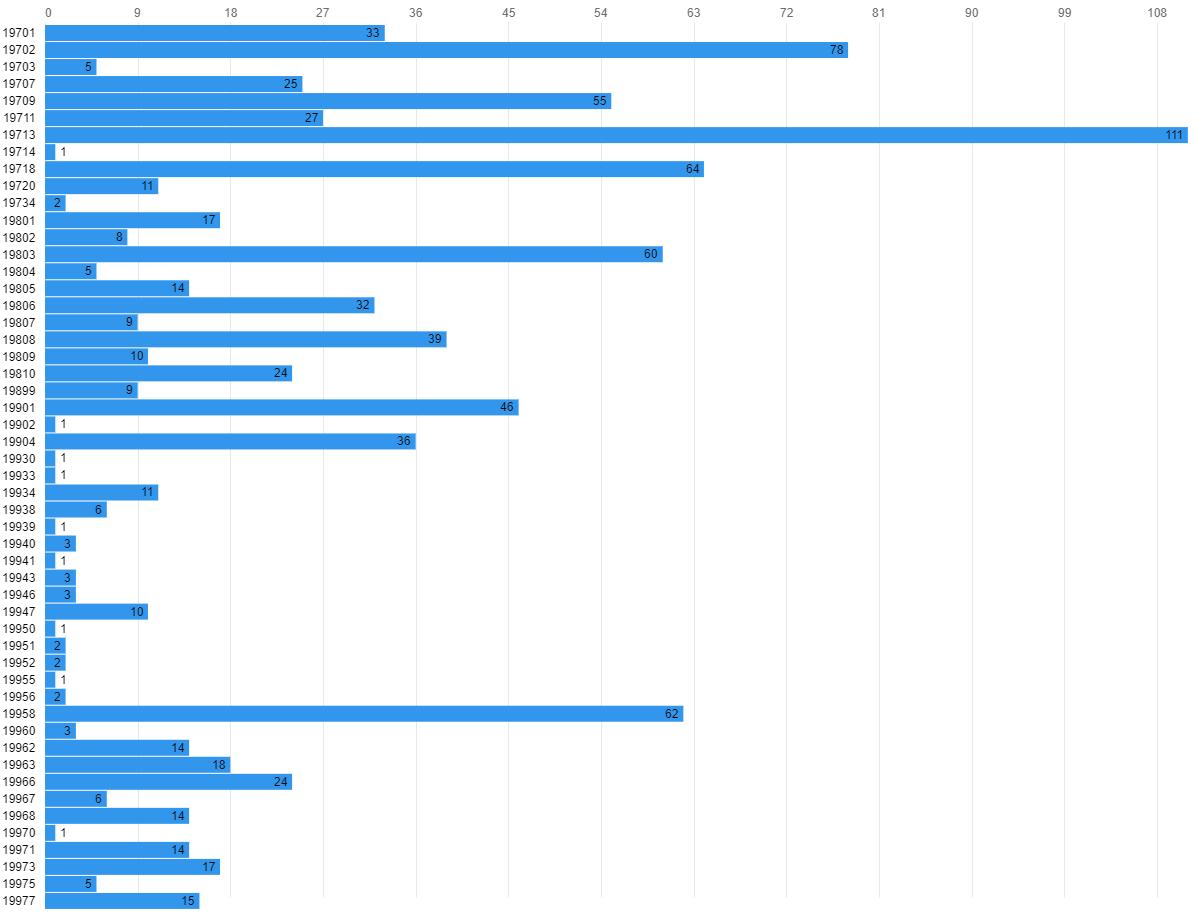
65
Figure 14 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 14. Visual Distribution of Active Physician Assistants by ZIP code

ADMINISTRATIVE MEDICAL
An Administrative Medical license allows physicians to use their medical and clinical knowledge, skill, and judgment only in an administrative capacity. These licensed cover physicians practicing administrative medicine and who do not provide any of the following medical or clinical services:
• examine, care for or treat patients;
• prescribe medications including controlled substances; or
• delegate medical acts or prescriptive authority to others
RESPIRATORY CARE PRACTITIONER
Respiratory therapists care for patients who have trouble breathing—for example, because of a chronic condition such as asthma. Most respiratory therapists work full time. Because they may work in medical facilities that are always open, such as hospitals, they may have shifts that include nights, weekends, or holidays.4
66 Delaware Journal of Public Health - December 2022
ACUPUNCTURE OR EASTERN MEDICINE PRACTITIONER
• Acupuncture Practitioners have earned a Diplomate in Acupuncture from the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) or an equivalent organization.
• Eastern Medicine Practitioners have earned a Diplomate in Oriental Medicine from the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) or an equivalent organization. The Acupuncture Advisory Council may waive this Diplomate requirement under specific circumstances as outlined in 24 Del. C. §1798 (c).
Acupuncture/Oriental medicine (AOM) is an ancient and empirical system of medicine based on the concept of qi (pronounced “chee”), which is usually translated as energy.
AOM treatments identify a pattern of energetic imbalance within a patient and redress that disharmony through a variety of therapies that may include acupuncture needling, cupping, acupressure, exercises such as tai ji and qi gong and Chinese herbal preparations. AOM is virtually free of the side effects that accompany many modern medical procedures. As a relatively inexpensive form of treatment, it is especially appropriate for reducing healthcare costs. The success of acupuncture today is due to its efficacy, remarkable safety record, cost-effectiveness and significant public demand.5
ACUPUNCTURE DETOXIFICATION SPECIALIST
Individuals that have a current license or certificate, are in good standing in a healthcare related profession, are approved by the Acupuncture Advisory Council and the Medical Board are eligible for this additional level of specialization.6
The National Acupuncture Detoxification Association (NADA) protocol is a unique form of acupuncture. It specifically targets behavioral health, including addictions and co-occurring disorders. The protocol involves the bilateral insertion of 1Y5 needles into predetermined points on each ear (auricle).7
GENETIC COUNSELOR
Genetic counselors assess individual or family risk for a variety of inherited conditions, such as genetic disorders and birth defects. Genetic counselors work in university medical centers, private and public hospitals, diagnostic laboratories, and physicians’ offices. They work with families, patients, and other medical professionals. Most genetic counselors work full time.
Genetic counseling requires an original or provisional license from the American Board of Genetic Counselors or the American Board of Medical Genetics and Genomics. Genetic counselors typically need a master’s degree in genetic counseling or genetics, along with board certification.8
POLYSOMNOGRAPHER
A Polysomnographer is an allied health professional who performs overnight sleep assessments used to diagnose various sleep disorders. In the evening the patient will arrive at a sleep laboratory in a hospital, medical facility, or hotel. Increasingly, physicians are prescribing at-home sleep tests to ensure the patient’s comfort and to reduce cost. The polysomnographer will attach various electrodes used to record the patient’s brain activity and will then monitor the patient throughout the night.
Work environments include:9
• Hospitals
• Medical facilities
• Hotels
• Patients’ homes
MIDWIFERY PRACTITIONER
Midwifery encompasses the independent provision of care during pregnancy, childbirth, and the postpartum period; sexual and reproductive health; gynecologic health; and family planning services, including preconception care. 10
• Certified Professional Midwifes (CPM) receive certification by the North American Registry of Midwives (NARM) or its equivalent or successor.
• Certified Midwifes (CM) receive certification by the American Midwifery Certification Board (AMCB) or its equivalent or successor.
67
REFERENCES
1. US Bureau of Labor Statistics. (2022, Aug). Physicians and surgeons. Occupational Outlook handbook. Retrieved from https://www.bls.gov/ooh/healthcare/physicians-and-surgeons.htm
2. Web, M. D. (2021, Apr). Difference between MD and DO. Retrieved from: https://www.webmd.com/a-to-z-guides/difference-between-md-and-do
3. US Bureau of Labor Statistics. (2022, Aug). Physician assistants. Occupational Outlook handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/physician-assistants.htm
4. US Bureau of Labor Statistics. (2022, Aug). Respiratory therapists. Occupational Outlook handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/respiratory-therapists.htm
5. Explore Healthcareers. (n.d.). Acupuncture/oriental medicine practitioner. Retrieved from: https://explorehealthcareers.org/career/complementary-and-integrative-medicine/acupuncture-oriental-medicine-practitioner/
6. National Acupuncture Detoxification Association. (n.d.). Regulations. Retrieved from: https://acudetox.com/resources/regulations/
7. Carter, K., & Olshan-Perlmutter, M. (2014, Oct-Dec). NADA protocol: Integrative acupuncture in addictions. Journal of Addictions Nursing, 25(4), 182–187. Retrieved from https://alliedhealth.ceconnection.com/files/NADAProtocolIntegrativeAcupunctureinAddictions-1419263411853.pdf
8. US Bureau of Labor Statistics. (2022, Aug). Genetic counselors. Occupational Outlook handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/genetic-counselors.htm
9. Cleveland Clinic. (n.d.). Polysomnographer. Retrieved from: https://my.clevelandclinic.org/departments/health-sciences-education/careers/career-options/polysomnographer
10. American College of Nurse-Midwives. (n.d.). About the midwifery profession. Retrieved from: https://www.midwife.org/About-the-Midwifery-Profession
LOWERING YOUR HIGH BLOOD PRESSURE IS EASIER THAN YOU THINK. There are FREE classes to help you get healthier and stay that way. HealthyDelaware.org/HealthyHeart 302-208-9097 68 Delaware Journal of Public Health - December 2022
Delaware Journal of
Public Health
Upcoming Issues
Each year, the Delaware Journal of Public Health publishes five different theme issues. Article submissions are accepted on a rolling basis, and the editorial board considers all submissions, both those connected directly to a theme issue, and non-thematic submissions. The editorial board reserves the right to include non-thematic submissions in each issue.
The working publishing calendar and thematic issues for 2023 are as follows:
Issue
Bio Tech/Research
Health Policy/Ethics
Submission Publication
February 2023 March 2023
April 2023 May 2023
Oral Health July 2023 September 2023
Neurological Impairment/Stroke September 2023 October 2023
Health Literacy and Communication November 2023 December 2023
If you have questions about submissions, ideas for an article, or suggestions for a future theme issue, please email Liz Healy: ehealy@delamed.org
All submissions can be submitted via the online submission portal: https://www.surveymonkey.com/r/2DSQN98
Submissions guidelines can be found at: https://djph.org

69
Board of Nursing
The primary objective of the Delaware Board of Nursing is to protect the public health, safety and welfare. To meet this objective to safeguard life and health, the Board
• develops standards for professional competency, • promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions The Board issues licenses to registered nurses (RNs), practical nurses (LPNs) and advanced practice registered nurses (APRNs) (see figures 1-3).
The Board’s statutory authority is in 24 Del. C., Chapter 19. Delaware is a member of the interstate nurse licensure compact covered in 24 Del. C., Chapter 19A
ACUTE CARE NURSE PRACTITIONER
Acute care nurse practitioners are advanced practice registered nurses who specialize in caring for patients with new acute conditions or exacerbated chronic conditions. ACNPs work in a variety of environments—from hospital emergency rooms to urgent-care clinics to operating rooms—and may focus on adults or children.1
ADULT HEALTH CERTIFIED NURSE SPECIALIST
A Clinical Nurse Specialist in Adult Health (ACNS) is an advanced nursing practitioner who participates in the advanced care of seriously ill, adult patients. This profession is involved with all aspects of adult care, from assessment to treatment and management of outcomes.2
ADULT/GERONTOLOGY NURSE PRACTITIONER
Geriatric nurse practitioners (GNPs) provide medical services for older patients. They share skills common among all advanced nurse practitioners. Senior care institutions rely on GNPs to provide comprehensive healthcare services for aging patients. Geriatric nursing practitioners conduct physicals, evaluate well-being and devise care plans specifically for these individuals. GNPs educate senior clients and their caregivers on matters regarding geriatric well-being and also consult with senior patients and their caregivers. Geriatric nursing practitioners advance their discipline through involvement with the National Gerontological Nursing Association, which works with geriatric professionals to produce positive patient outcomes among the senior population.3
ADULT/GERONTOLOGY CERTIFIED NURSE SPECIALIST
The Adult-Gerontological Clinical Nurse Specialists (AG CNS) cares for patients from wellness through acute care, with a specific focus on complex and vulnerable adult and older adult populations. The AG CNS is best described as the “nurses’ nurse” as the CNS is a resource and consultant to nurses and healthcare professionals. The AG CNS is involved in all levels of the healthcare system, spanning from the acute care setting to the home. The AG CNS engages in numerous direct care and leadership roles in the healthcare system including organizing and managing large scale programs, incorporating evidence into practice, coaching and mentoring nurses and serving as a consultant to healthcare professionals, organizations, patients and families.4
ADULT NURSE PRACTITIONER
Provide general and preventative care, conduct check-ups, treat illnesses, order lab tests and prescribe medication for children and adults. A nurse practitioner is an advanced practice nurse that helps with all aspects of patient care, including diagnosis, treatments and consultations.5
CERTIFIED NURSE MIDWIFE
A CNM is an advanced practice registered nurse who goes through comprehensive training, mainly providing care to pregnant women from labor to delivery to postpartum care.6
CERTIFIED REGISTERED NURSE ANESTHETIST
A CRNA (certified registered nurse anesthetist or just “nurse anesthetist”) is an advanced practice registered nurse (APRN) who administers anesthesia and other medications. They also take care of and monitor people who receive or are recovering from anesthesia.7
COMMUNITY HEALTH NURSING CERTIFIED NURSE SPECIALIST
The community health nurse clinical specialist (CHNCS) has been clearly delineated by the profession as having a responsibility to the community as client.8
DOI: 10.32481/djph.2022.12.019
70 Delaware Journal of Public Health - December 2022
Figure 1. Active Nursing Licenses by Specialty,
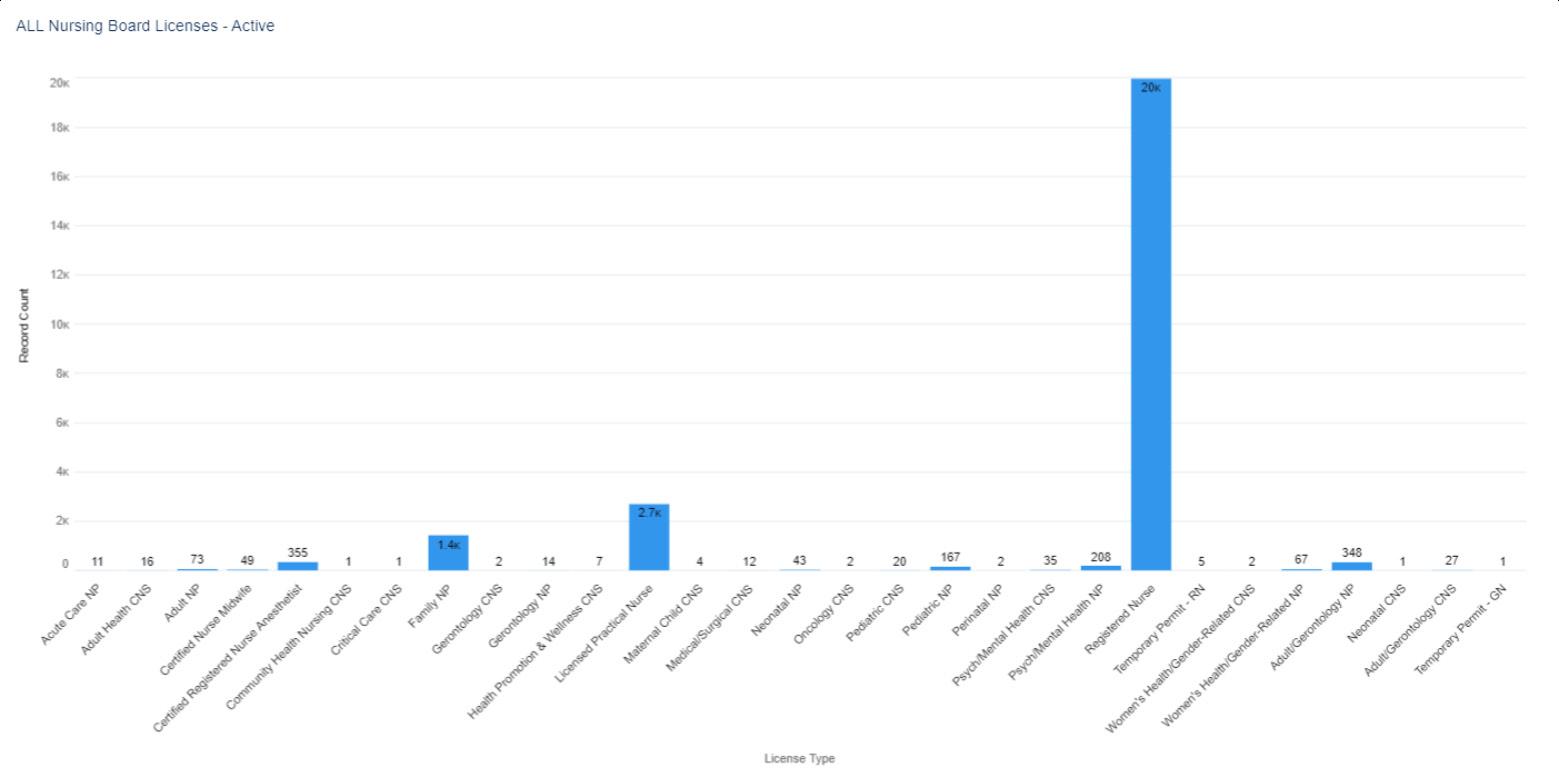 N=25,620
N=25,620
* an active license does not guarantee an individual is actively seeing patients.
71
Figure 2. Active Nursing Licenses by Gender, select license types (when reported)

72 Delaware Journal of Public Health - December 2022
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.‚

CRITICAL CARE CERTIFIED NURSE SPECIALIST
Provide direct care to acutely/critically ill adult patients regardless of their physical location. Nurses interested in this certification may work in areas such as intensive care units, cardiac care units, combined ICU/CCUs, medical/surgical ICUs, trauma units or critical care transport/flight.9
FAMILY NURSE PRACTITIONER
Because of their high level of education, expertise and skill, family nurse practitioners (FNP) will often take on some of the roles of a physician (see figures 4 & 5). However, they will still generally work under the supervision of, or in close conjunction with, a physician. FNPs must be able to offer the care and support consistent with high-quality nursing to patients and families, diagnosing and treating patients across a wide variety of conditions.10
GERONTOLOGY CERTIFIED NURSE SPECIALIST
Same as Adult/Gerontology Certified Nurse Specialist.
GERONTOLOGY NURSE PRACTITIONER
A Gerontological Nurse Practitioner is a multi-disciplined primary healthcare provider who helps patients manage the physical, mental, and social effects of aging.11
HEALTH PROMOTION AND WELLNESS CERTIFIED NURSE SPECIALIST
Performing health assessments and health screenings such as physicals, checkups, or wellness visits with patients to identify problems and determine appropriate treatment plans. providing care to patients in hospitals and other settings who have been diagnosed with a chronic illness such as diabetes or cancer.12
Figure 3. Active Nursing
by
Year
Licenses
Birth
(when reported)
73
Figure 4. Numerical Distribution of Active Family Nurse Practitioners by ZIP code

74 Delaware Journal of Public Health - December 2022
LICENSED PRACTICAL NURSE
The role of an LPN (see figures 6 & 7) includes providing basic medical care to patients. In addition to helping patients eat, bathe and get dressed, LPNs also perform medical tasks such as changing bandages and inserting catheters. Another important aspect of the role is reporting changes in patient condition to supervisors such as RNs or physicians. Unlike RNs, LPNs do not set up care plans for patients.13
MATERNAL CHILD CERTIFIED NURSE SPECIALIST
Provide individual care and monitoring and run educational programs to assist parents and enable them to develop supportive social networks. Maternal and child health nurses support the health and development of children from birth until school age and their parents.14
MEDICAL/SURGICAL CERTIFIED NURSE SPECIALIST
Medical-surgical nurses are registered nurses who provide care for primarily adult patients before and after surgical procedures. They coordinate healthcare plans with medical professionals, administer medications, and educate patients on surgical procedures. They may be employed at hospitals, clinics, physicians’ offices, or care facilities.15
NEONATAL CERTIFIED NURSE SPECIALIST
The neonatal clinical nurse specialist is an advanced practice nurse who functions in the role of expert clinician, educator, consultant and researcher for the Neonatal Intensive Care Unit, NICU.16
NEONATAL NURSE PRACTITIONER
The role of the NNP is to provide care to high-risk infants who need care due to low birth weights, complications of prematurity, heart abnormalities, infections or other conditions. However, some NNPs may care for infants with long-term health conditions until they reach two years of age.17
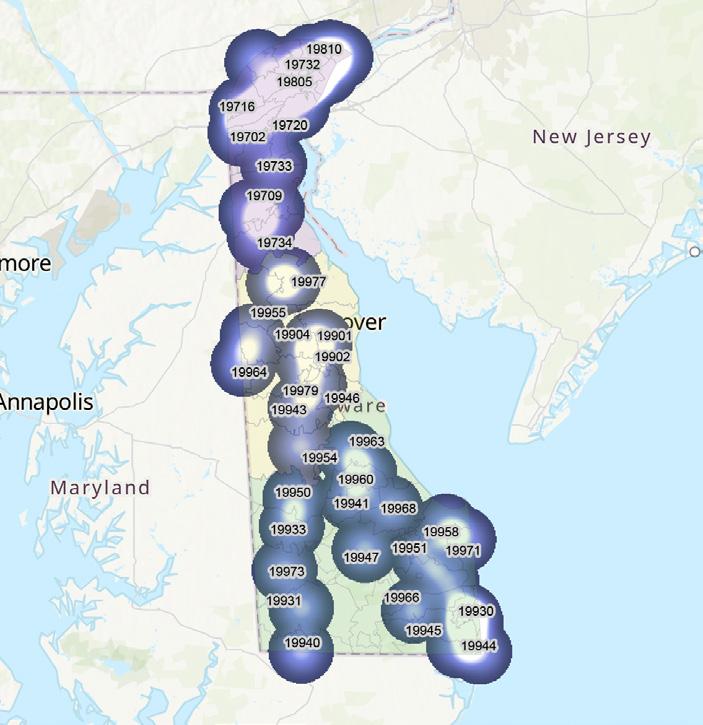
ONCOLOGY CERTIFIED NURSE SPECIALIST
OCNSs are educationally prepared to provide advanced nursing care to meet the specialized physiologic and psychological needs of patients throughout the continuum of care, including cancer prevention and detection, cancer diagnosis and treatment, rehabilitation, survivorship, and end-of-life care.18
Figure 5. Visual Distribution of Active Family Nurse Practitioners by ZIP code 75
Figure 6. Numerical Distribution of Active Licensed Practice Nurse by ZIP code

76 Delaware Journal of Public Health - December 2022
PEDIATRIC CERTIFIED NURSE SPECIALIST
Clinical experts in pediatric nursing who, in addition to providing direct care, serve as leaders in education, research, quality improvement and outcome monitoring in consultation with other nurses. Pediatric clinical nurse specialists provide care to children and adolescents and their families within the context of the family, community and healthcare system.19
PEDIATRIC NURSE PRACTITIONER
A PNP is an advanced practice registered nurse (APRN) who specializes in caring for newborns, infants, toddlers, adolescents and young adults. PNPs focus on well-child care and the prevention or management of common pediatric acute illnesses and chronic conditions.20
PERINATAL NURSE PRACTITIONER
Perinatal nurses care for pregnant patients and their newborns, usually from the early stages of pregnancy to just after giving birth.21
PSYCH/MENTAL HEALTH CERTIFIED NURSE SPECIALIST
PMH-CNSs are psychiatric-mental health advanced practice registered nurses (PMH-APRNs) with a Clinical Nurse Specialist certification. PMH-APRNs, whether CNS or NP, have received specialized graduate level education and are prepared to provide psychiatric and substance use assessments, diagnoses, and treatment, including medication interventions and psychotherapy.22
PSYCH/MENTAL HEALTH NURSE PRACTITIONER
PMHNPs combine a variety of nursing, psychosocial, and neurobiological expertise and methodologies to diagnose, treat, and improve the outcomes of patients facing psychiatric or mental health challenges.23
REGISTERED NURSE
A registered nurse is a healthcare provider who has graduated from a nursing program and holds a nursing license (see figures 8 & 9). There are many types of registered nurses, mainly defined by their areas of specialization.24
TEMPORARY PERMIT - ADVANCED PRACTICE NURSE PRACTITIONER
A Temporary APRN Permit allows you to practice as an APRN in Delaware until your APRN license is issued.25

Figure 7. Visual Distribution of Active Licensed Practical Nurses by ZIP code 77
TEMPORARY PERMIT - REGISTERED NURSE
Temporary RN Permit allows you to practice as an RN in Delaware until your RN license is issued.25
WOMEN’S HEALTH/GENDER-RELATED NURSE PRACTITIONER
A women’s health nurse practitioner (WHNP) provides primary healthcare services to women of all ages, generally beginning at adolescence and continuing through pregnancy and menopause.26
WOMEN’S HEALTH/GENDER-RELATED CERTIFIED NURSE SPECIALIST
Same as above, but as a certification rather than a degree focusing on the management of patient care. The WHCNS focus on complex cases and vulnerable populations.27

8.
78 Delaware Journal of Public Health - December 2022
Figure
Numerical Distribution of Active Registered Nurses by ZIP code. n=19,992
REFERENCES
1. Journal, N. (2022, Jan 21). Acute care NP career overview. Retrieved from: https://nursejournal.org/careers/acute-care/
2. Schools, A. N. (n.d.). What you’ll do as a clinical nurse specialist. Retrieved from: https://www.allnursingschools.com/clinical-nurse-specialist/job-description/
3. Regis College. (2021, Oct 31). What does an adult geriatric nurse practitioner do. Retrieved from: https://online.regiscollege.edu/blog/what-does-an-adult-geriatric-nurse-practitioner-do/
4. UCSF School of Nursing. (n.d.). Adult-gerontology clinical nurse specialist. Retrieved from: https://nursing.ucsf.edu/academics/programs/master-science-advanced-practice-programs/adult-gerontology-clinical-nurse-specialist-ag-cns
5. Community Clinic Association of Los Angeles County. (n.d.). Nurse practitioner job description. Retrieved from: https://ccalac.org/wordpress/wp-content/uploads/gravity_forms/25-398983c110800ddd0c5c4e38d8739014/2017/03/Nurse-Practitioner-job des.pdf
6. Map, N. L. (2021, Oct). Certified nurse-midwife (CNM). Retrieved from: https://nursinglicensemap.com/advanced-practice-nursing/certified-nurse-midwife-cnm/
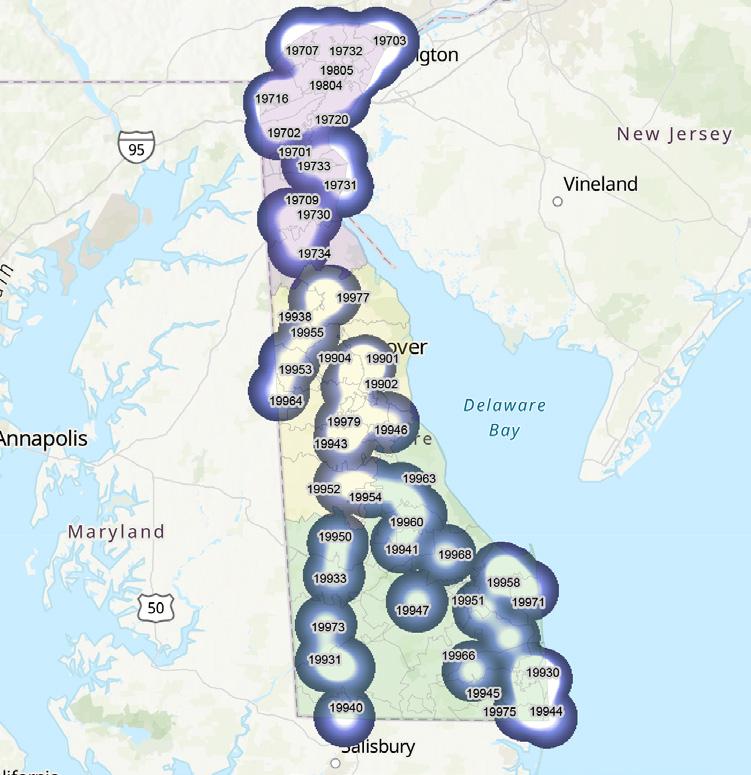
7. Cleveland Clinic. (2022, Mar). Nurse anesthetist (CRNA). Retrieved from: https://my.clevelandclinic.org/health/articles/22561-nurse-anesthetist-crna
8. Mason, D. J., Knight, K., Toughill, E., DeMaio, D., Beck, T. L., & Christopher, M. A. (1992, Spring). Promoting the community health clinical nurse specialist. Clinical Nurse Specialist CNS, 6(1), 6–13. Retrieved from https://pubmed.ncbi.nlm.nih.gov/1559215/ https://doi.org/10.1097/00002800-199200610-00004
9. American Association of Critical-Care Nurses. (n.d.). CCRN (Adult). Retrieved from: https://www.aacn.org/certification/get-certified/ccrn-adult
10. Map, N. L. (n.d.). How to become a family nurse practitioner (FNP). Retrieved from: https://nursinglicensemap.com/advanced-practice-nursing/nurse-practitioner/family-nurse-practitioner/
11. Johnson&Johnson. (n.d.). Gerontological nurse practitioner. Retrieved from: https://nursing.jnj.com/specialty/gerontological-nurse-practitioner
Figure 9. Visual
code 79
Distribution of Active Registered Nurses by ZIP
12 Climb the Ladder. (2022, Mar). What does a wellness nurse do? Retrieved from: https://climbtheladder.com/wellness-nurse/
13 Map, N. L. (n.d.). Nurse hierarchy. Retrieved from: https://nursinglicensemap.com/resources/nurse-hierarchy/
14. Map, N. L. (n.d.). Fact sheet: Maternal Child Health Nurse. Retrieved from: http://www.education.vic.gov.au/Documents/about/careers/factsheetmaternalchildhealthnurseaccessible.docx
15. Betterteam. (n.d.). Medical-surgical nurse job description. Retrieved from: https://www.betterteam.com/medical-surgical-nurse-job-description
16. Description, J., & Examples, R. (n.d.). Neonatal clinical nurse specialist job description, duties, and responsibilities. Retrieved from: https://jobdescriptionandresumeexamples.com/neonatal-clinical-nurse-specialist-job-description-duties-and-responsibilities/
17. American Association of Nurse Practitioners. (2020, Mar). Take a closer look at the role of a neonatal nurse practitioner (NNP). Retrieved from: https://www.aanp.org/news-feed/are-you-considering-a-career-as-neonatal-nurse-practitioner
18. Oncology Nursing Society. (n.d.). Oncology clinical nurse specialist competencies. Retrieved from: https://www.ons.org/oncology-clinical-nurse-specialist-competencies
19. University of Minnesota. (n.d.). Doctor of nursing practice. Retrieved from: https://nursing.umn.edu/academics/doctor-nursing-practice/specialty-areas/pediatric-clinical-nurse-specialist
20. American Association of Nurse Practitioners. (n.d.). Are you considering a career as a pediatric nurse practitioner? Retrieved from: https://www.aanp.org/news-feed/are-you-considering-a-career-as-a-pediatric-nurse-practitioner
21. Journal, N. (2022, Aug 5). Perinatal nurse career overview. Retrieved from: https://nursejournal.org/careers/perinatal-nurse/
22. American Psychiatric Nurses Association. (n.d.). Psychiatric-mental health clinical nurse specialists. Retrieved from: https://www.apna.org/pmh-cns/
23. Map, N. L. (n.d.). How to become a psychiatric-mental health nurse practitioner. Retrieved from: https://nursinglicensemap.com/advanced-practice-nursing/nurse-practitioner/psychiatric-and-mental-health-nurse-practitioner-pmhnp/
24. Map, N. L. (n.d.). Types of nursing careers & specialties. Retrieved from: https://nursinglicensemap.com/nursing-specialties/
25 Delaware Division of Professional Regulation. (n.d.). Temporary APRN permit. Retrieved from: https://dpr.delaware.gov/boards/nursing/apntemppermit/
26 American Association of Nurse Practitioners. (2020, Apr). Are you considering a career as a women’s health nurse practitioner? Retrieved from: https://www.aanp.org/news-feed/are-you-considering-a-career-as-a-womens-health-nurse-practitioner
27 Journal, N. (2022, Jun). NP vs. CNS: what’s the difference? Retrieved from: https://nursejournal.org/resources/np-vs-cns/
80 Delaware Journal of Public Health - December 2022
81
Board of Examiners of Nursing Home Administrators
The primary objective of the Delaware Board of Examiners of Nursing Home Administrators is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services (see figures 1-5). The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency
• promulgates rules and regulations
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues nursing home administrator and temporary nursing home administrator licenses. It also approves administrator-in-training programs. The Board’s statutory authority is in 24 Del. C., Chapter 52
Figure
1. Active Nursing Home Administrator Licenses by Type*
* an active license does not guarantee an individual is actively seeing patients.
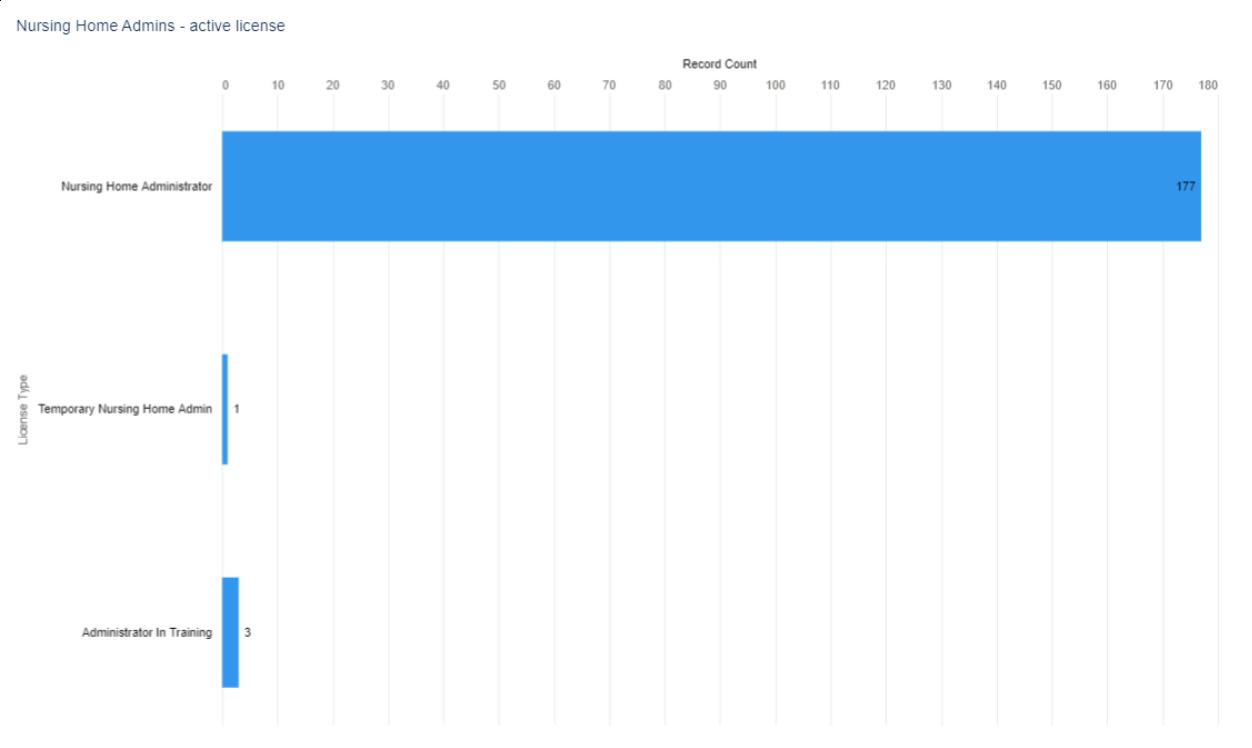
10.32481/djph.2022.12.020
DOI:
82 Delaware Journal of Public Health - December 2022
According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
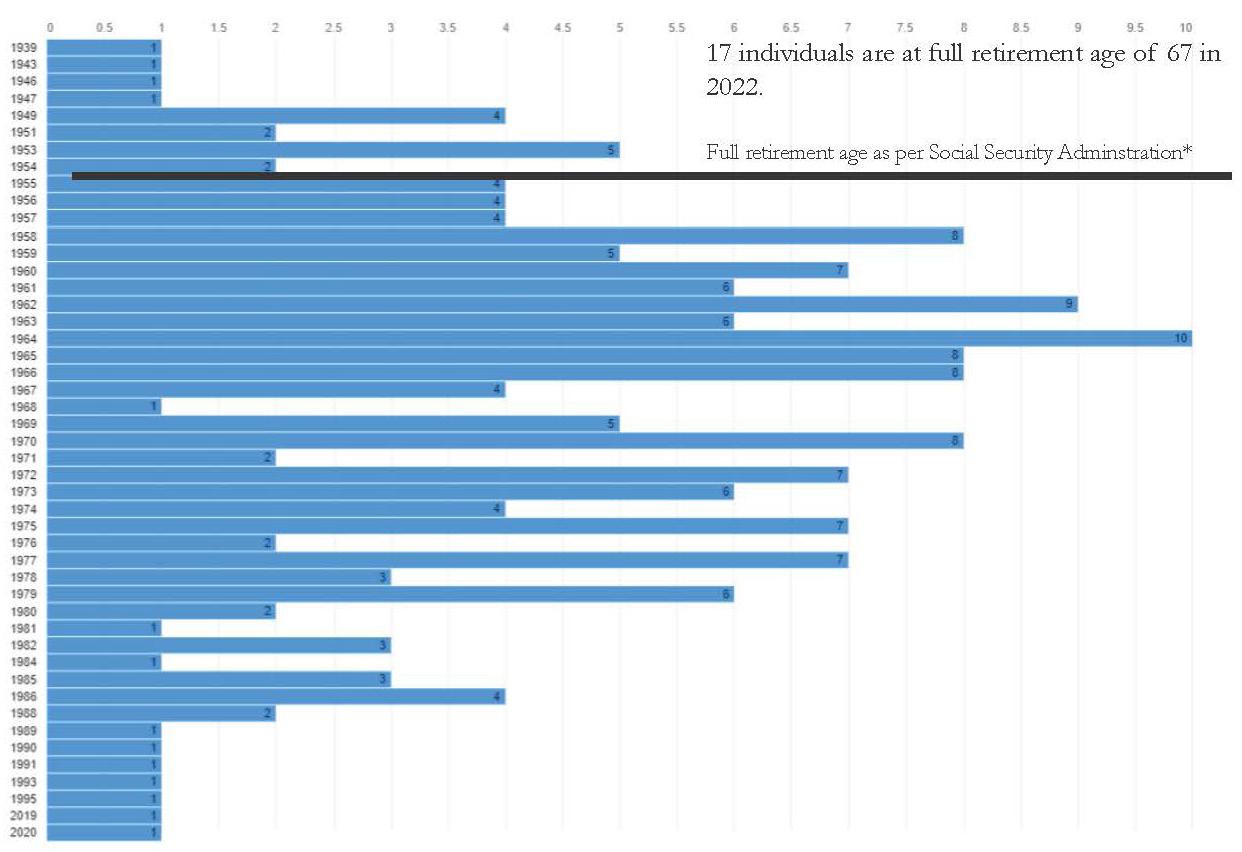
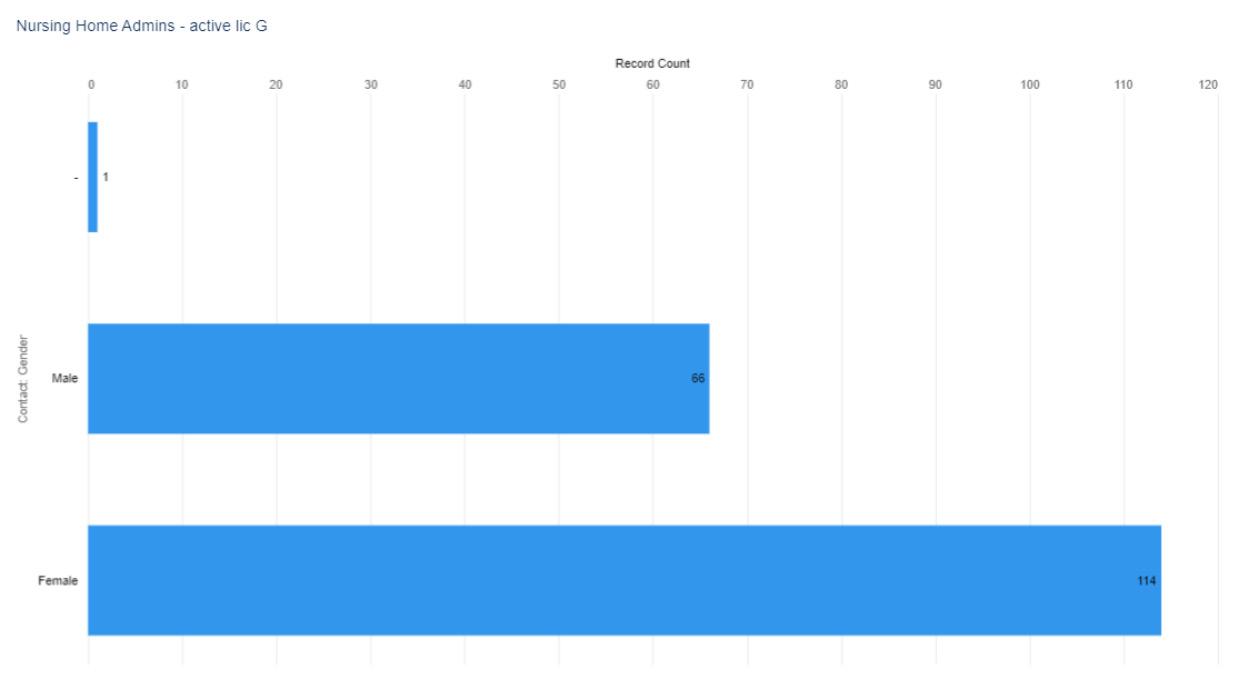 Figure 2. Active Nursing Home Administrator Licenses by Gender, select license types (when reported)
Figure 2. Active Nursing Home Administrator Licenses by Gender, select license types (when reported)
*
Figure 3. Active Nursing Home Administrator Licenses by Birth Year
83
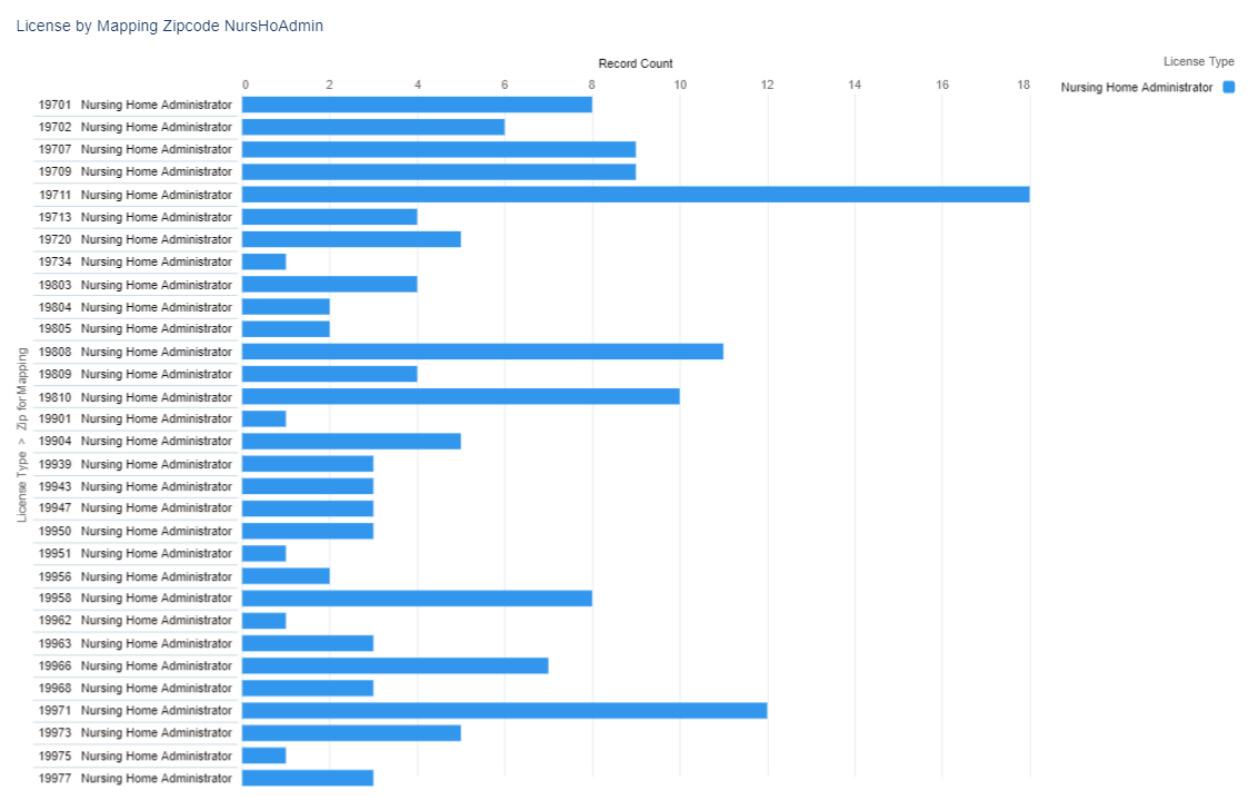
84 Delaware Journal of Public Health - December 2022
Figure 4. Numerical Distribution of Active Nursing Home Administrator Licenses by ZIP code
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 5. Visual Distribution of Active Nursing Home Administrator Licenses by ZIP code
Note: Not shown on this map is one addition Temporary Nursing Home Administrator whose address is in New Jersey, and three Administrator’s in Training: one in Dover, 19904; one in Millsboro, 19966; and one in New Castle, 19720.
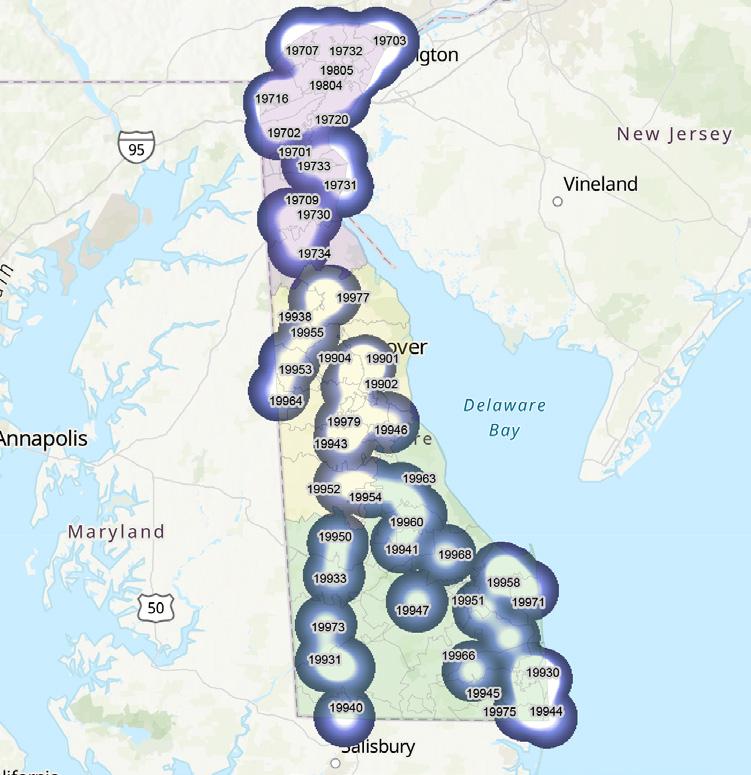
85
Board of Occupational Therapy Practice
The primary objective of the Delaware Board of Occupational Therapy Practice is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions. The Board issues licenses to occupational therapists and occupational therapy assistants (see figures 1-5). The Board’s statutory authority is in 24 Del. C., Chapter 20
Figure 1. Active Occupational Therapy Practitioner Licenses by Type*, N=1,182
* an active license does not guarantee an individual is actively seeing patients.
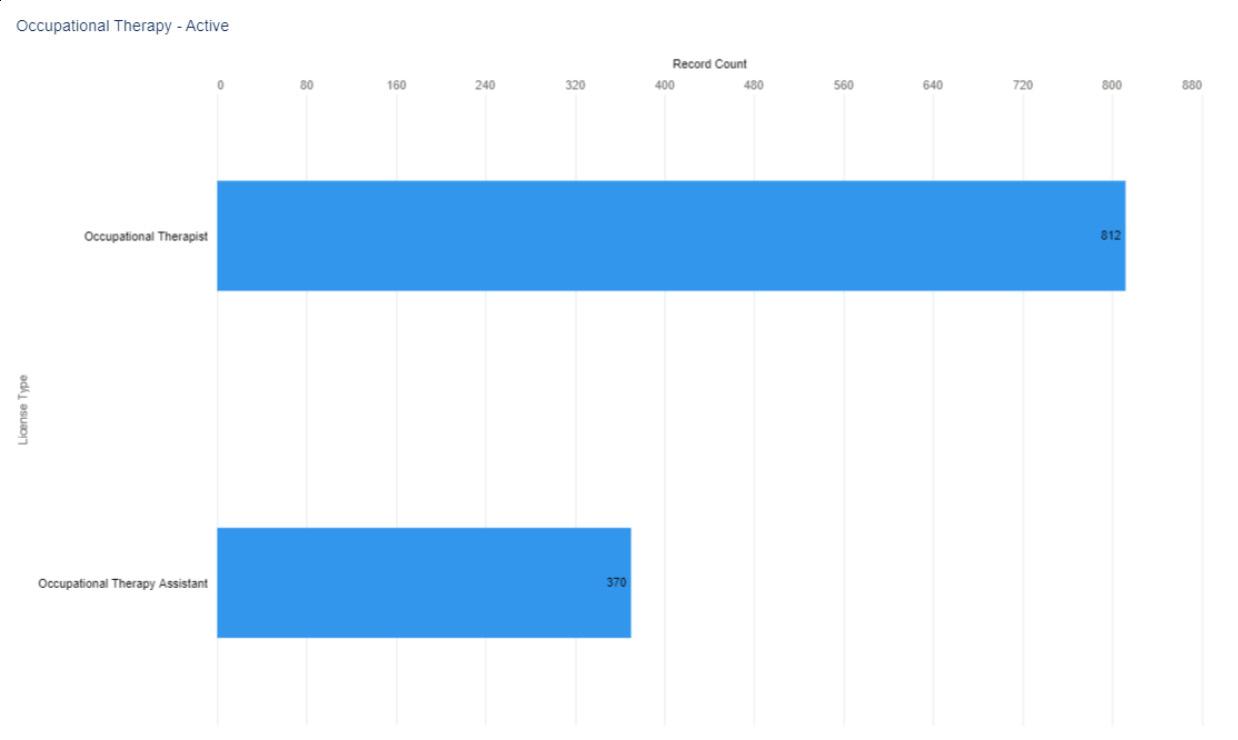
10.32481/djph.2022.12.021
DOI:
86 Delaware Journal of Public Health - December 2022
Figure 2. Active Occupational Therapy Practitioner Licenses by Gender, select license types (when reported)
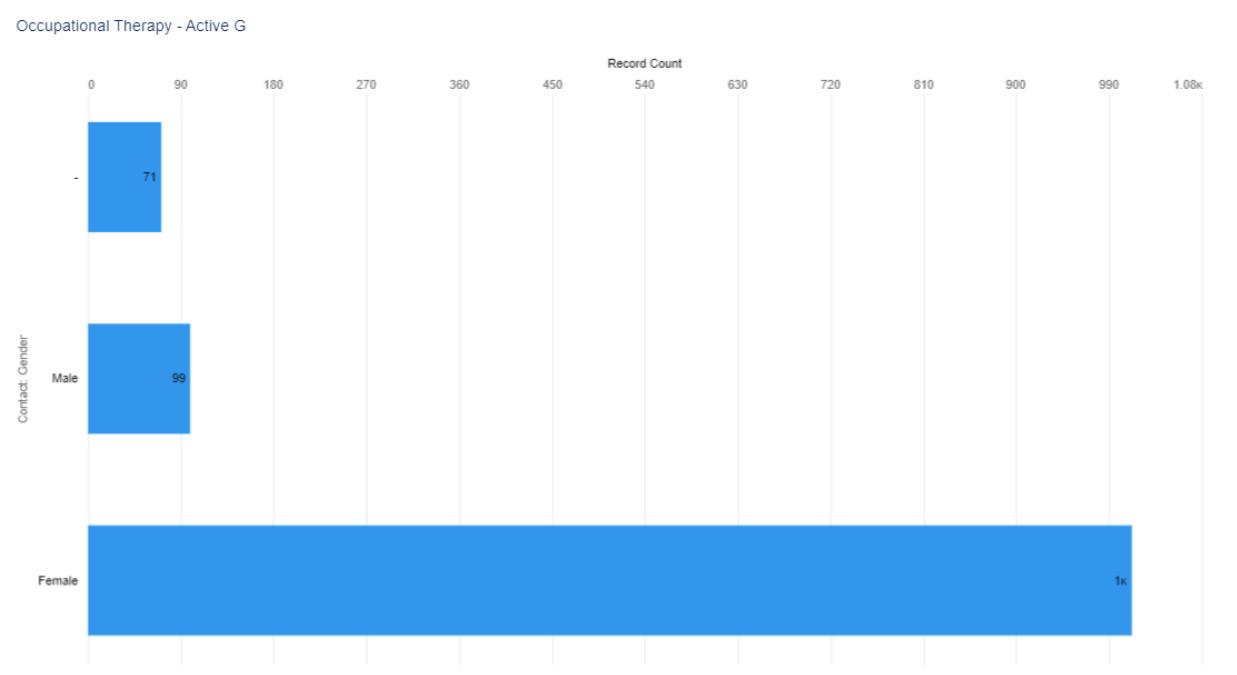
Figure
3. Active Occupational Therapy Practitioner Licenses by Birth Year

Note. 12 individuals did not provide a year of birth
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.‚
87

Figure 4.
ZIP code 88 Delaware Journal of Public Health - December 2022
Numerical Distribution of Active Occupational Therapists by
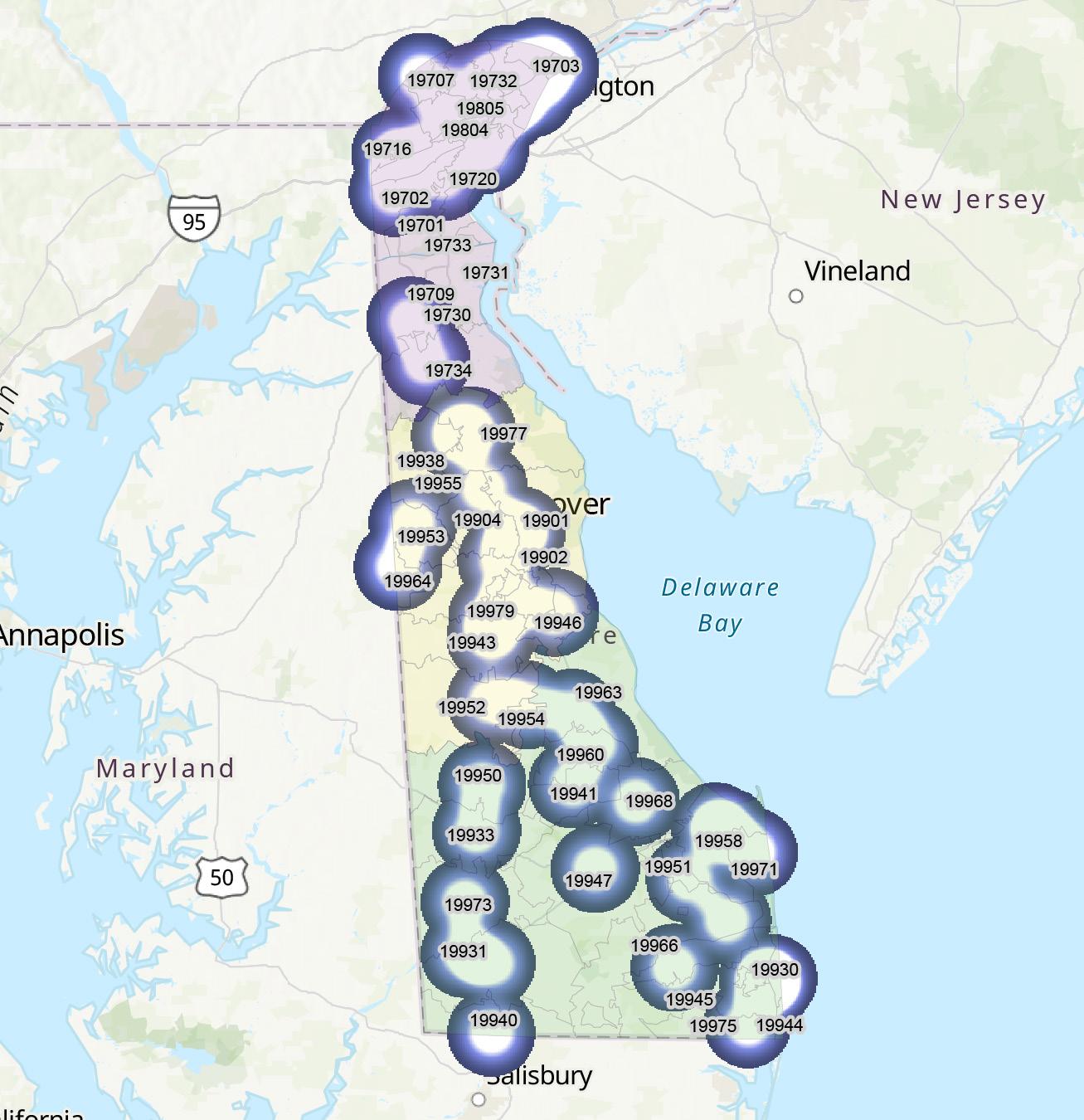
Figure 5. Visual
by ZIP code 89
Distribution of Active Occupational Therapists
Board of Examiners in Optometry
The primary objective of the Delaware Board of Examiners in Optometry is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions. The Board issues licenses to therapeutic optometrists and interns (see figures 1-5). The Board’s statutory authority is in 24 Del. C., Chapter 21
DIAGNOSTIC OPTOMETRIST
Optometrists are healthcare professionals who provide primary vision care ranging from sight testing and correction to the diagnosis, treatment, and management of vision changes. An optometrist is not a medical doctor. An optometrist receives a doctor of optometry (OD) degree after completing four years of optometry school, preceded by three years or more years of college. They are licensed to practice optometry, which primarily involves performing eye exams and vision tests, prescribing and dispensing corrective lenses, detecting certain eye abnormalities, and prescribing medications for certain eye diseases.1
THERAPEUTIC OPTOMETRIST
A therapeutic optometrist has undertaken at least one additional year of training and study, specifically in the diagnosis and management of eye diseases, in microbiology, pathology, ocular pharmacology, and in the treatment of eye conditions with Schedule 4 prescription-only medicines.
THERAPEUTIC OPTOMETRIST INTERNSHIP
To be licensed as a Therapeutic Optometrist in Delaware one is required to complete a six-month internship.
Figure 1. Active Optometry Licenses by Type*, N=205
* an active license does not guarantee an individual is actively seeing patients.

DOI: 10.32481/djph.2022.12.022
90 Delaware Journal of Public Health - December 2022

Figure 2. Active
91
Optometry Licenses by Gender select license types (when reported)
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.‚

Figure 3. Active Optometry Licenses by Birth Year
92 Delaware Journal of Public Health - December 2022
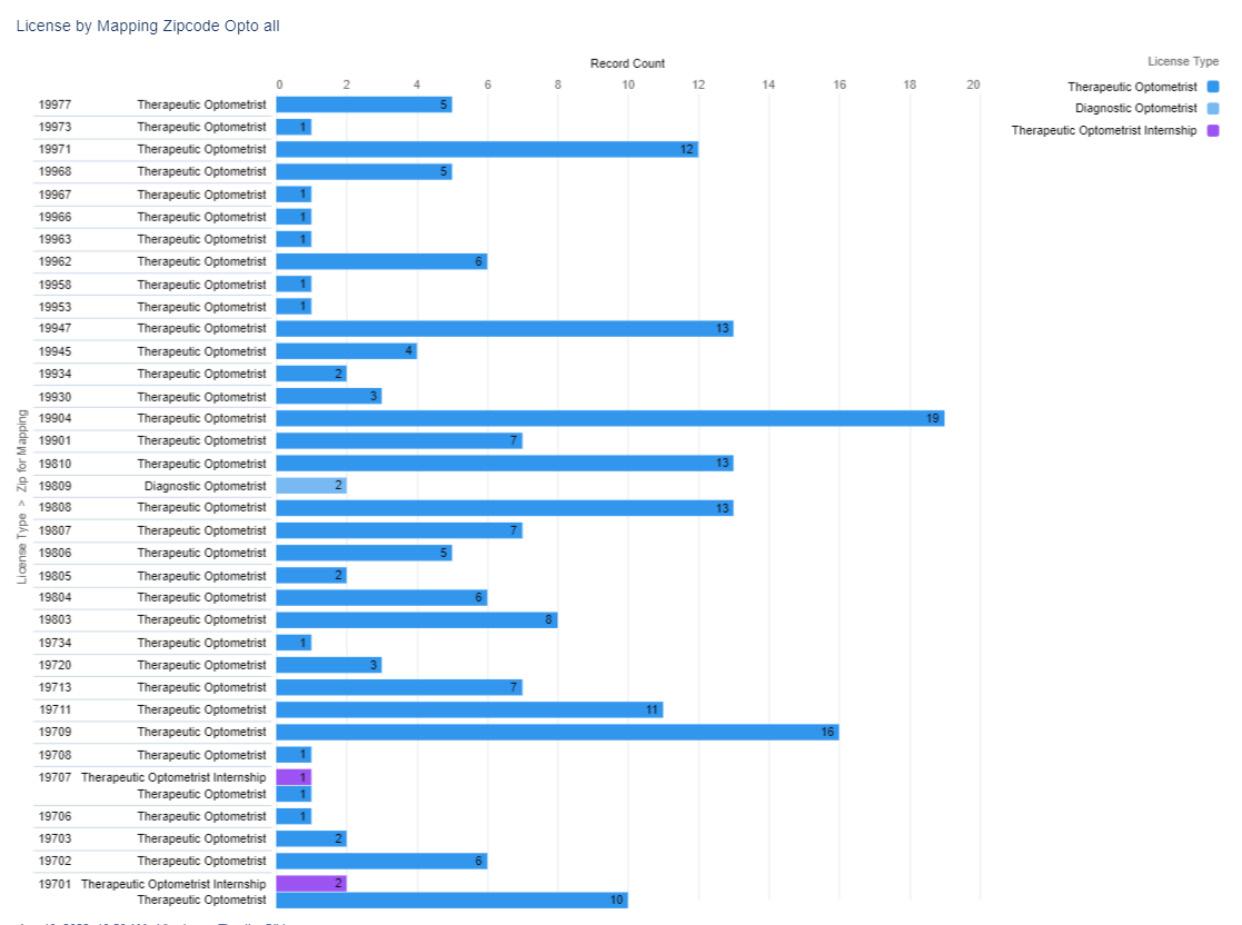
Figure 4. Numerical Distribution of Active
Licenses by ZIP code 93
Optometry
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 5. Visual Distribution of Active Optometry Licenses by ZIP code

REFERENCES
1. Hull, J. (2019, Feb). Difference between an ophthalmologist, optometrist and optician. American Association for Pediatric Ophthalmology and Strabismus.
Retrieved from https://aapos.org/glossary/difference-between-an-ophthalmologist-optometrist-and-optician
94 Delaware Journal of Public Health - December 2022
With
Everyone 6 months and older should get vaccinated, and those 5 years and older should get boosted when eligible.

STAY
The best way to stop the spread is to stay home if you don’t feel well.
It’s quick, and it gives you the answers you need.

STAY SMART. KEEP COVID-19 OUT OF SCHOOL. STAY SMART.
VACCINATED
BOOSTED
three simple steps, you can protect your child from serious illness caused by COVID-19 and help them have a healthy school year. GET FULLY
AND
SICK
EXPOSED
GET TESTED WHEN
OR
TO SOMEONE WITH COVID-19
HOME WHEN SICK
de.gov/youthvaccine 95
Board of Pharmacy
The primary objective of the Delaware Board of Pharmacy is to promote, preserve, and protect the public health, safety, and welfare. To meet this objective, the Board
• maintains a registry of drug outlets that manufacture, produce, sell, and distribute drugs, medications, and other materials used to diagnose and prevent illness and disease and to treat injury,
• monitors the outlets to ensure safe practices,
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to pharmacists and pharmacy interns (see figures 1-5). It also licenses pharmacies (both in Delaware and elsewhere), pharmaceutical manufacturers and distributors, medical gas dispensers and retail businesses that sell non-controlled prescription drugs for veterinary use. The Board’s statutory authority is in 24 Del. C., Chapter 25.
PHARMACIST
Pharmacists dispense prescription medications to patients and offer expertise in the safe use of prescriptions. Pharmacists work in pharmacies, including those in drug, general merchandise, and grocery stores. They also work in hospitals and other healthcare facilities.1
PHARMACY INTERN
To be licensed as a Pharmacist in Delaware, a practitioner must provide proof they have completed 1,500 hours of pre-licensure experience. Interns must select a Delaware-licensed pharmacist to be a preceptor.2
Figure 1. Active Pharmacy Licenses by Type*, N=4,826
* an active license does not guarantee an individual is actively seeing patients.
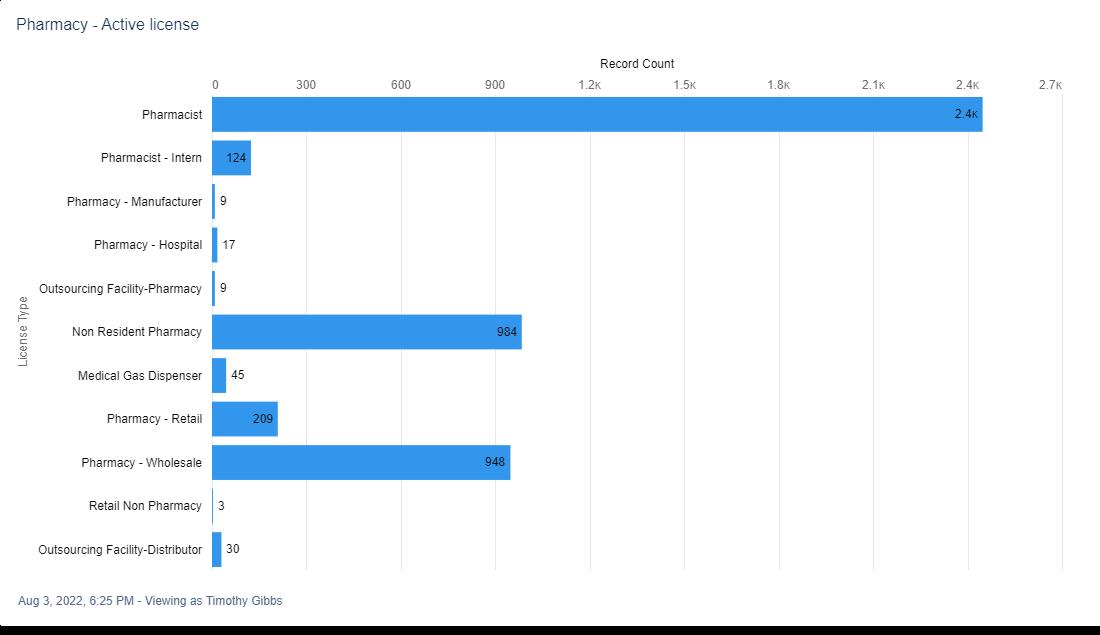
DOI: 10.32481/djph.2022.12.023
96 Delaware Journal of Public Health - December 2022

Figure 2. Active
97
Pharmacy Licenses by Gender, select license types (when reported)
Note. One individual did not provide a year of birth.
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.‚

Figure 3. Active Pharmacy Licenses by Birth Year*
98 Delaware Journal of Public Health - December 2022
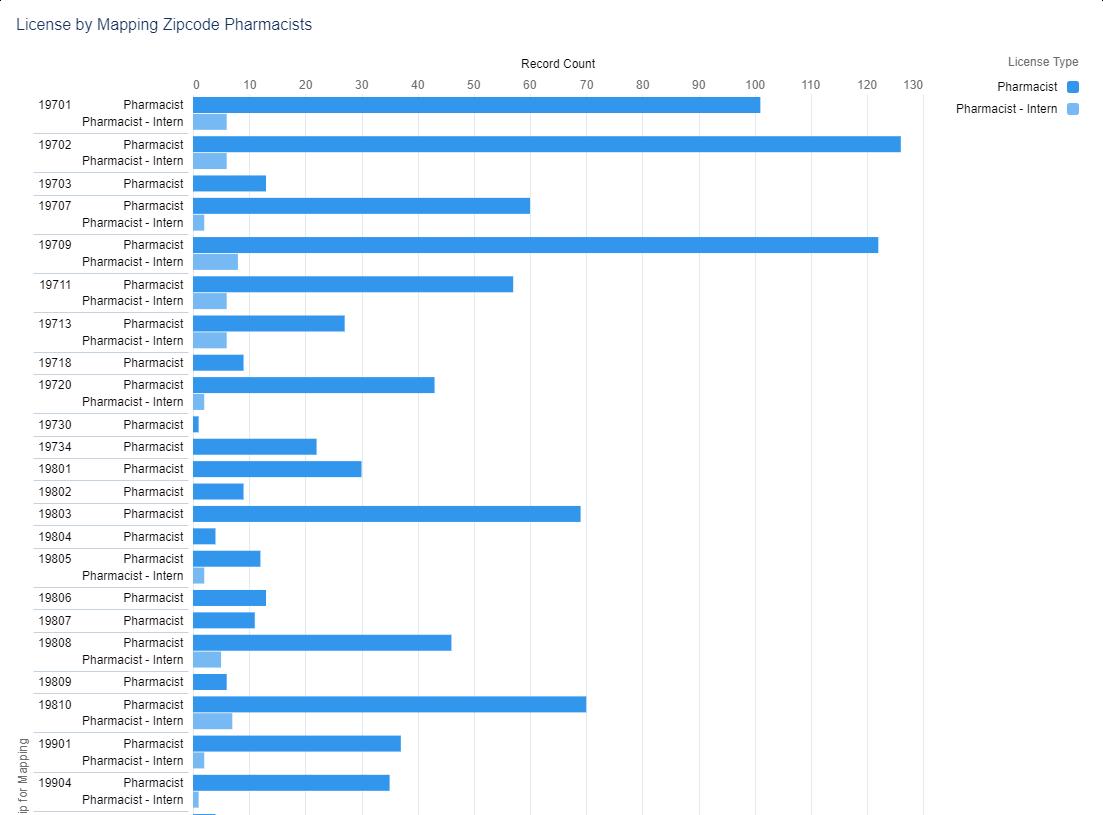

99
Figure 4. Numerical Distribution of Active Pharmacist and Pharmacy Intern Licenses by ZIP code
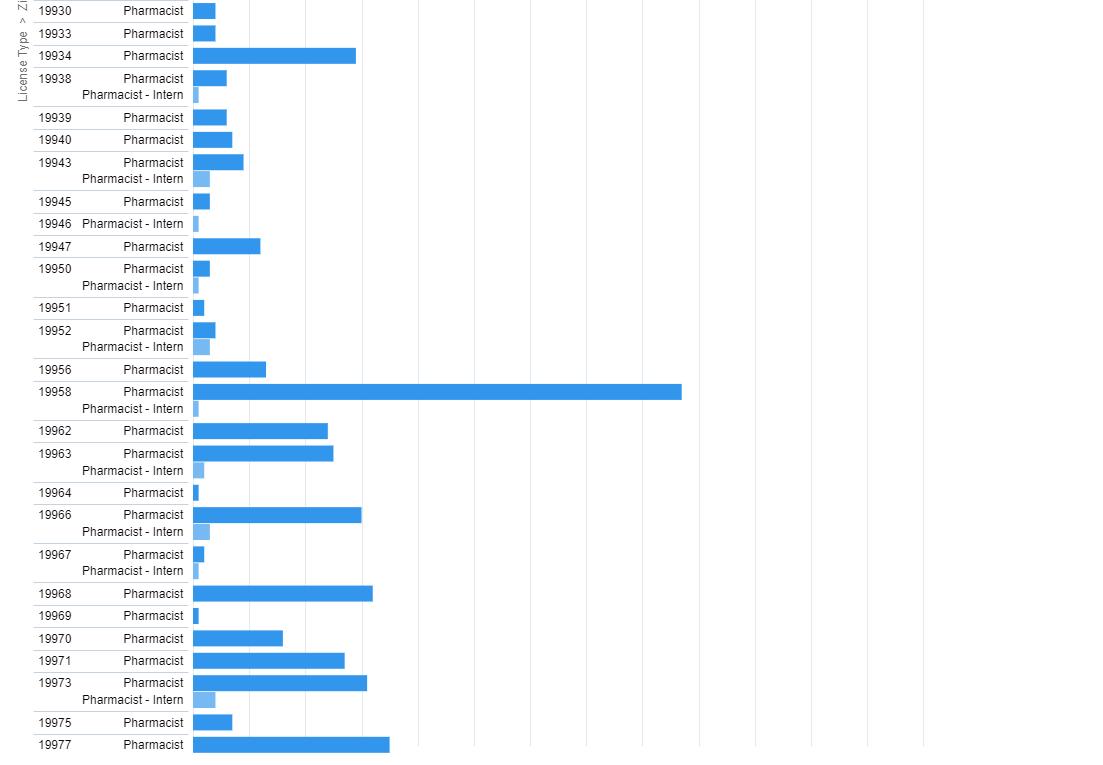

Figure 4. continued 100 Delaware Journal of Public Health - December 2022
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 5. Visual Distribution of Active Pharmacist and Pharmacy Intern Licenses by ZIP code
REFERENCES
1. US Bureau of Labor Statistics. (2022, Aug). Pharmacists. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/pharmacists.htm
2. Delaware Division of Professional Regulation. (n.d.). Intern-US School. Retrieved from: https://dpr.delaware.gov/boards/pharmacy/newlicense/
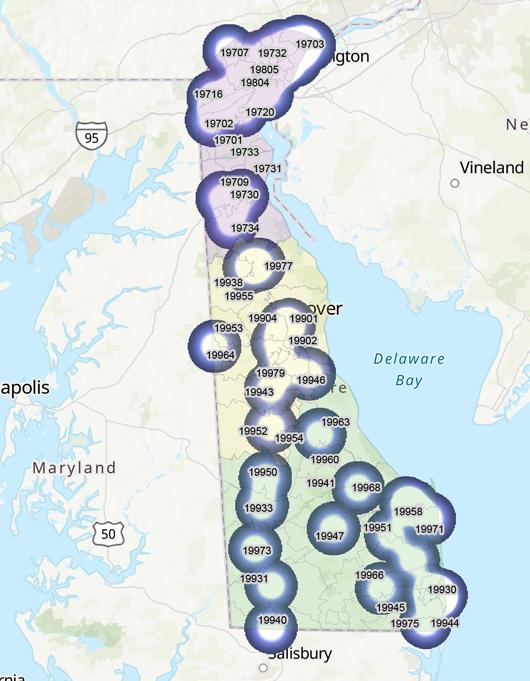
101
Board of Physical Therapists and Athletic Trainers
The primary objective of the Delaware Examining Board of Physical Therapists and Athletic Trainers is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to physical therapists, physical therapist assistants and athletic trainers, including temporary licenses (see figures 1-3). The Board’s statutory authority is in 24 Del. C., Chapter 26
Figure 1. Active License Physical Therapists and Athletic Trainers by Type*, N=2,604
* an active license does not guarantee an individual is actively seeing patients.
Figure 2. Active License Physical Therapists and Athletic Trainers by Gender select license types (when reported)
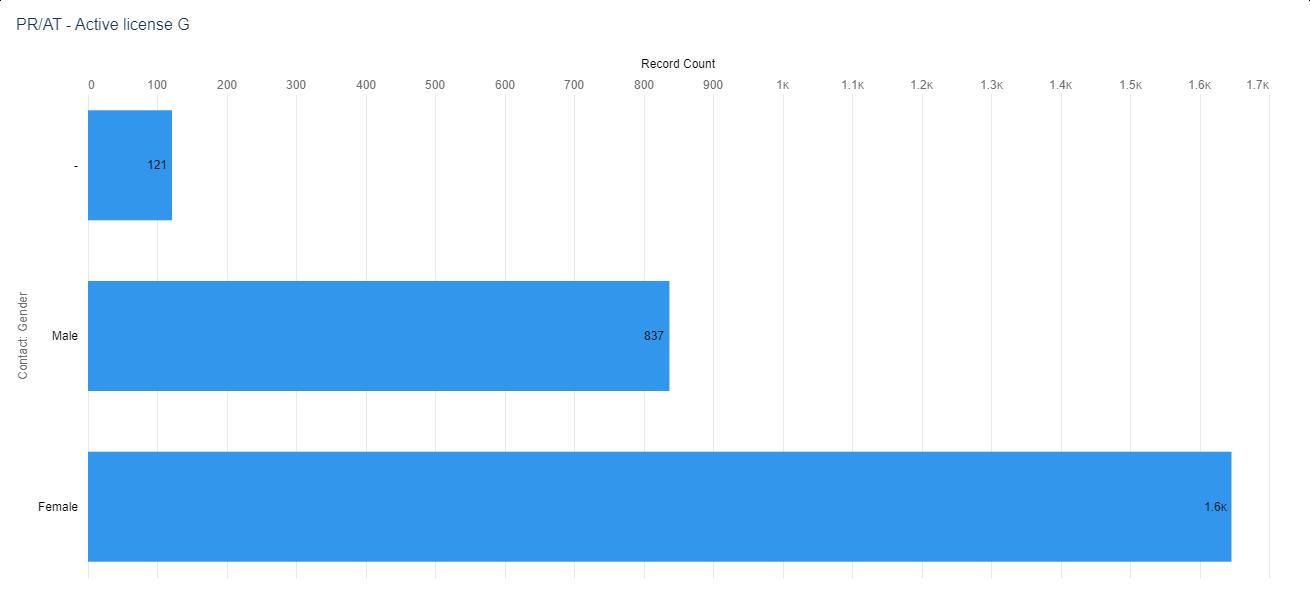

DOI: 10.32481/djph.2022.12.024
102 Delaware Journal of Public Health - December 2022
Note. 35 individuals did not provide a year of birth *
According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”

Figure 3. Active License Physical Therapists and Athletic Trainers by Birth Year
103
ATHLETIC TRAINER
Athletic trainers work with people of all ages and all skill levels, from young children to soldiers and professional athletes. Athletic trainers (see figures 4 & 5) are usually one of the first healthcare providers on the scene when injuries occur on the field. They work under the direction of a licensed physician and with other healthcare providers, often discussing specific injuries and treatment options or evaluating and treating patients, as directed by a physician. Some athletic trainers meet with a team physician or consulting physician regularly.1
Figure 4. Numerical Distribution of Active License Athletic Trainers by ZIP code

104 Delaware Journal of Public Health - December 2022
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 5. Visual Distribution of Active License Athletic Trainers by ZIP code
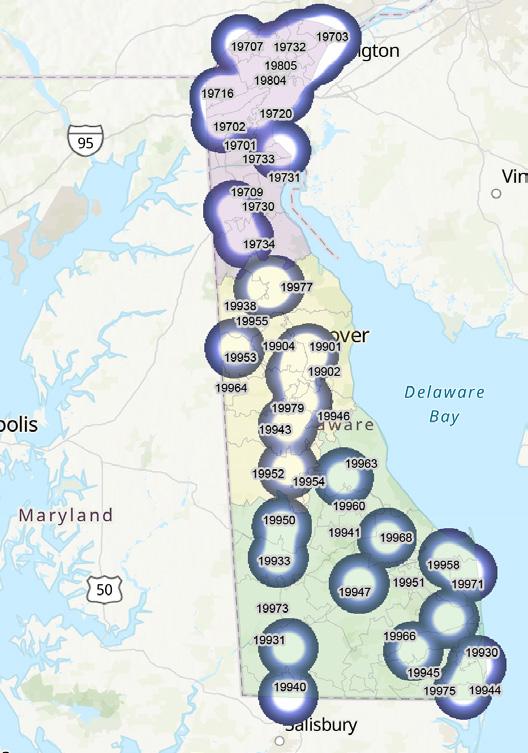
105
PHYSICAL THERAPIST (AND TEMPORARY)
Physical therapists (see figures 6 & 7), sometimes called PTs, care for people of all ages who have functional problems resulting from back and neck injuries; sprains, strains, and fractures; arthritis; amputations; neurological disorders, such as stroke or cerebral palsy; injuries related to work and sports; and other conditions. Physical therapists use a variety of techniques to care for their patients. These techniques include exercises; training in functional movement, which may include the use of equipment such as canes, crutches, wheelchairs, and walkers; and special movements of joints, muscles, and other soft tissue to improve mobility and decrease pain.2
PHYSICAL THERAPY ASSISTANT (AND TEMPORARY)
Physical therapist assistants, sometimes called PTAs, and physical therapist aides work under the direction and supervision of physical therapists. They help patients who are recovering from injuries and illnesses to regain movement and manage pain. Physical therapist assistants are involved in the direct care of patients. Physical therapist aides often have tasks that are indirectly related to patient care, such as cleaning and setting up the treatment area, moving patients, and doing clerical duties.3
Figure 6. Numerical Distribution of Active License Physical Therapists by ZIP code

106 Delaware Journal of Public Health - December 2022
Figure 7 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 7. Visual Distribution of Active License Physical Therapists by ZIP code

REFERENCES
1. US Burear of Labor Statistics. (2022, Aug). What athletic trainers do. Occupational Outlook Handbook Retrieved from: https://www.bls.gov/ooh/healthcare/athletic-trainers.htm#tab-2
2. US Burear of Labor Statistics. (2022, Aug). What physical therapists do. Occupational Outlook Handbook Retrieved from: https://www.bls.gov/ooh/healthcare/physical-therapists.htm#tab-2
3. US Burear of Labor Statistics. (2022, Aug). What physical therapist assistants and aides do. Occupational Outlook Handbook Retrieved from: https://www.bls.gov/ooh/healthcare/physical-therapist-assistants-and-aides.htm#tab-2
107
Board of Podiatry
The primary objective of the Delaware Board of Podiatry is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations, • adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions. The Board issues licenses to podiatrists, including temporary licenses, and podiatrists-in-training. The Board’s statutory authority is in 24 Del. C., Chapter 5
PODIATRIST
Podiatrists provide medical and surgical care for people with foot, ankle, and lower leg problems. They diagnose illnesses, treat injuries, and perform surgery involving the lower extremities (see figures 1-5).1 Most podiatrists work in offices of podiatry, either on their own or with other podiatrists. Some work in group practices with other physicians or specialists. Others work in private and public hospitals, in outpatient care centers, or for the government.
PODIATRIST IN TRAINING
Podiatrist In-Training licensees are limited to the practice of medicine in the hospital where they are employed except for any outside medical duties that may be assigned as part of their residency program. They must perform outside duties under the supervision of a fully licensed podiatric physician.
TEMPORARY PODIATRIST
A Temporary Podiatrist license may be issued to an out-of-state Podiatrist when he or she will be taking charge of the practice of a Delaware-licensed Podiatrist during the Delaware licensee’s temporary illness or absence from Delaware.
Figure 1. Active Podiatry Licenses by Type*, N=112 * an active license does not guarantee an individual is actively seeing patients.

DOI: 10.32481/djph.2022.12.025
108 Delaware Journal of Public Health - December 2022
Figure 2. Active Podiatry Licenses by Gender select license types (when reported)

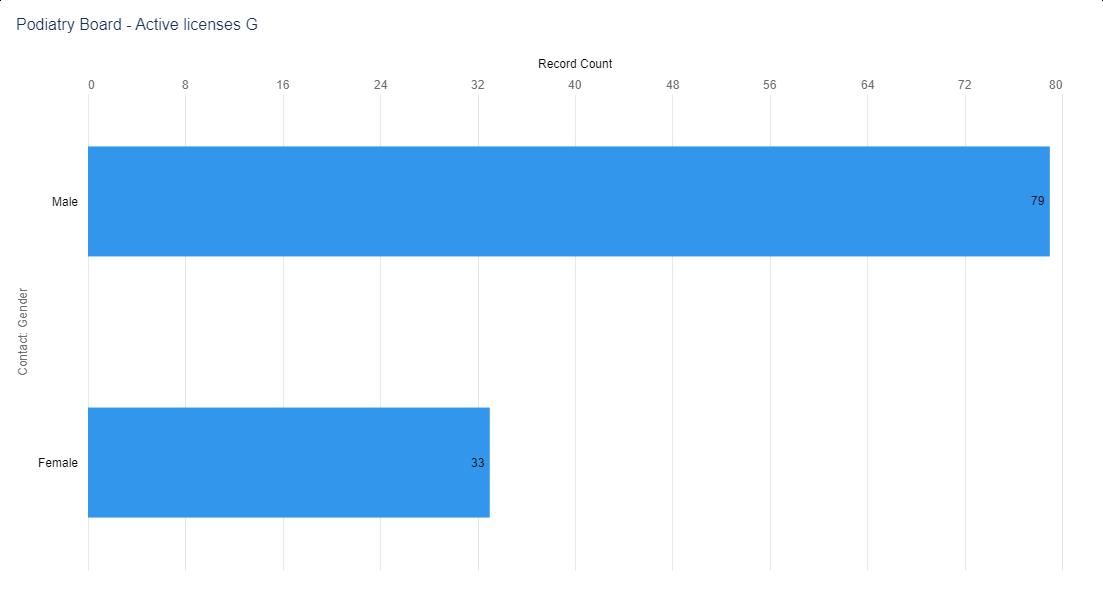
Figure 3. Active Podiatry Licenses by Birth Year
Note. One individual did not provide a year of birth * According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
109
REFERENCES
1. US Bureau of Labor Statistics. (2022, Aug). What do podiatrists do? Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/podiatrists.htm#tab2

 Figure 4. Numerical Distribution of Active Podiatrist and Podiatrist in Training License by ZIP code
Figure 5. Visual Distribution of Active Podiatrist and Podiatrist in Training License by ZIP code
Figure 4. Numerical Distribution of Active Podiatrist and Podiatrist in Training License by ZIP code
Figure 5. Visual Distribution of Active Podiatrist and Podiatrist in Training License by ZIP code
110 Delaware Journal of Public Health - December 2022
Feeling better starts with feeling

EMPOWERED.
If you have chronic pain, chronic illness, or diabetes, or are a cancer survivor, there are FREE workshops that can help you live better. You’ll meet others like you, learn skills to manage your illness, and start to redefine your life and your health.
Call 302-990-0522 or visit HealthyDelaware.org/SelfManagement to register or learn more. Chronic Disease | Diabetes | Chronic Pain

| Cancer
111
Board of Mental Health and Chemical Dependency Professionals
The primary objective of the Delaware Board of Mental Health and Chemical Dependency Professionals is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to professional counselors of mental health, associate counselors of mental health, chemical dependency professionals, marriage and family therapists and associate marriage and family therapists (see figures 1-3). The Board’s statutory authority is in 24 Del. C., Chapter 30
PROFESSIONAL ART THERAPISTS
Art therapy is an integrative mental health and human services profession that enriches the lives of individuals, families, and communities through active art-making, creative process, applied psychological theory, and human experience within a psychotherapeutic relationship.1 Art therapy, facilitated by a professional art therapist, effectively supports personal and relational treatment goals as well as community concerns. Art therapy is used to improve cognitive and sensorimotor functions, foster self-esteem and self-awareness, cultivate emotional resilience, promote insight, enhance social skills, reduce and resolve conflicts and distress, and advance societal and ecological change.1
ASSOCIATE MARRIAGE AND FAMILY THERAPISTS
Individuals licensed as associates are in the process of accumulating hours towards their full licensure.2
MARRIAGE AND FAMILY THERAPISTS
Marriage and family therapists work with individuals, couples, and families. They bring a family-centered perspective to treatment, even when treating individuals. They evaluate family roles and development, to understand how clients’ families affect their mental health.3
CHEMICAL DEPENDENCY PROFESSIONALS
Chemical Dependency Counselor runs individual, family, and group counseling for patients in chemical dependency programs. Acts as mediator between patients, relatives, medical staff, and outside agencies if needed. Being a Chemical Dependency Counselor tracks patient progress and dispensation of treatment services (see figures 4 & 5).4
ASSOCIATE COUNSELOR OF MENTAL HEALTH
Duties include leading individual and group therapy or interventions, administering medication, providing assistance to patients with their daily hygiene or self-care routines, and supervising recreational activities.5
PROFESSIONAL COUNSELOR OF MENTAL HEALTH
Counsels clients and patients, individually and in group sessions, to assist in overcoming dependencies, adjusting to life, and making changes. Maintains confidentiality of records relating to clients treatment. Guides clients in the development of skills and strategies to deal with their problems (see figures 6 & 7).6
DOI: 10.32481/djph.2022.12.026
112 Delaware Journal of Public Health - December 2022
Figure 1. Active Mental Health and Chemical Dependency Professional Licenses by Type*, N=1,036
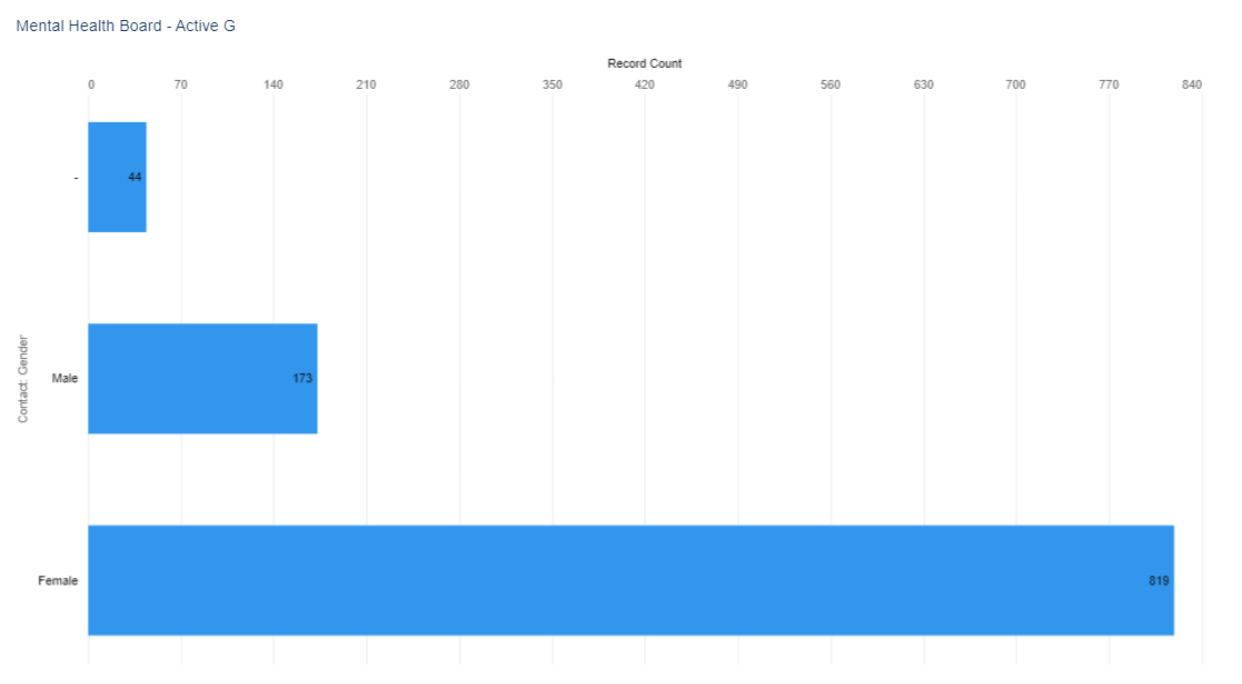
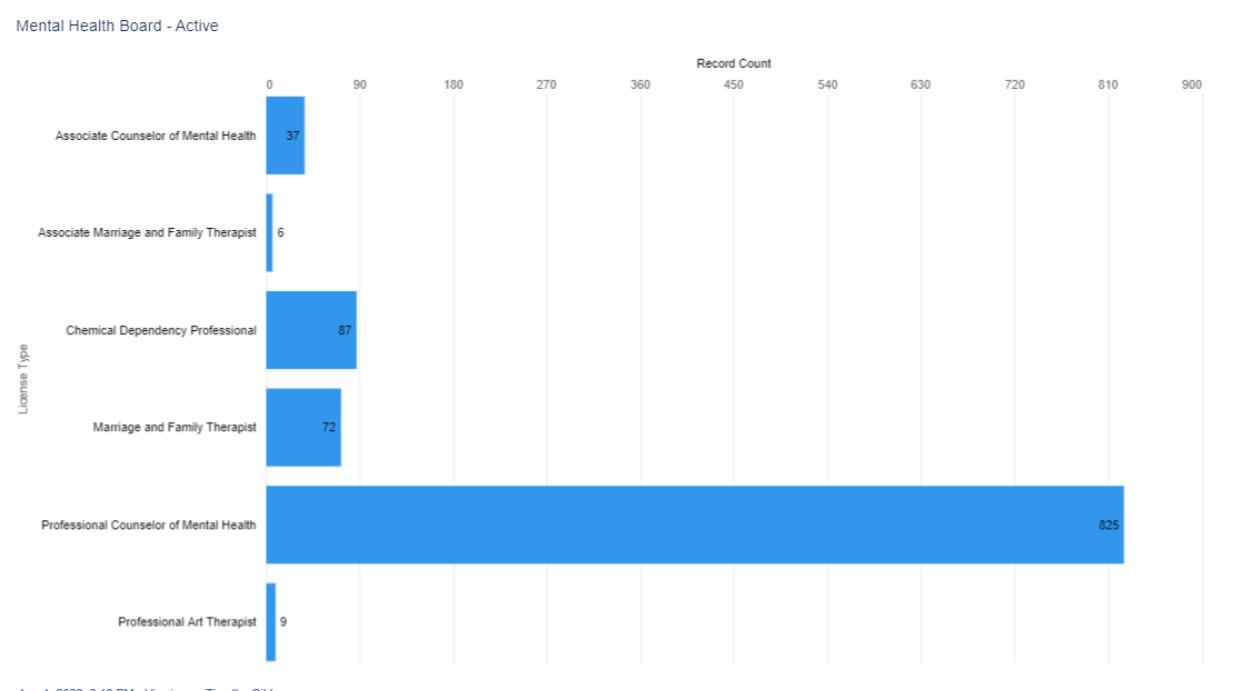
* an active license does not guarantee an individual is actively seeing patients.
Figure 2. Active Mental Health and Chemical Dependency Professional Licenses by Gender by select license types (when reported)
113
Figure 3. Active Mental Health and Chemical Dependency Professional Licenses by Birth Year
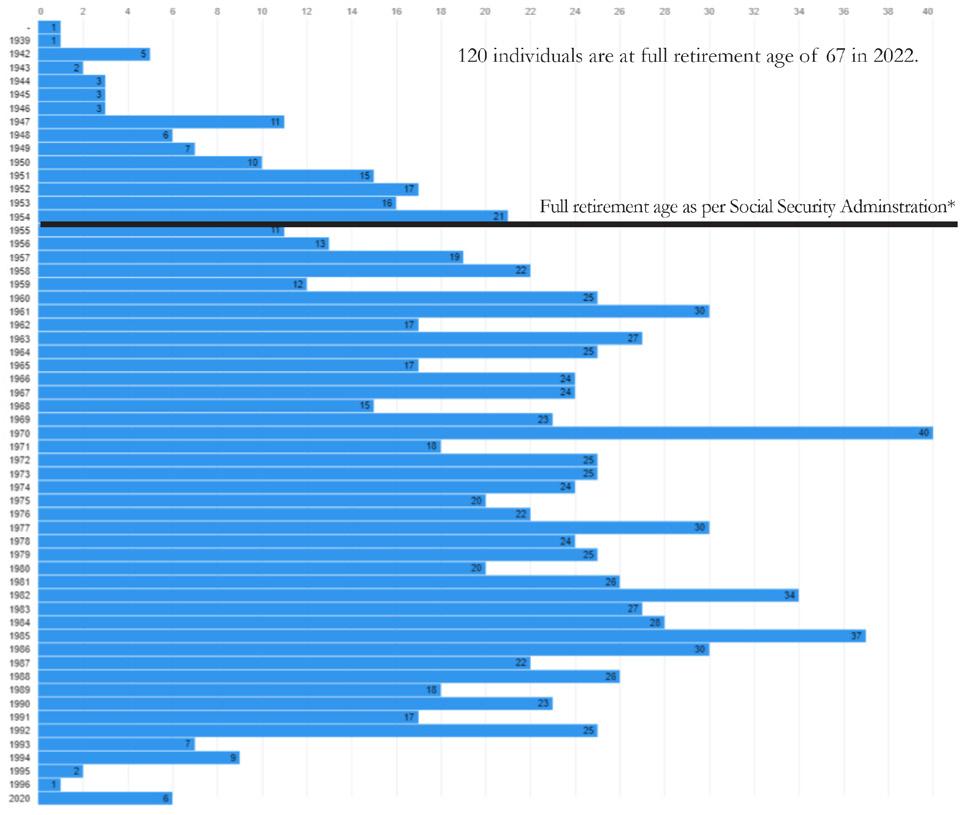
Note. One individual did not provide a year of birth
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
114 Delaware Journal of Public Health - December 2022
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
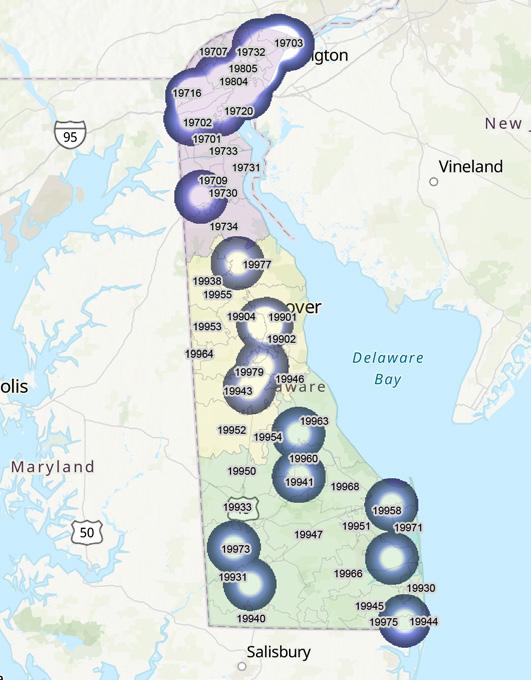
Figure 5. Visual Distribution of Active License Chemical Dependency Professionals by ZIP code
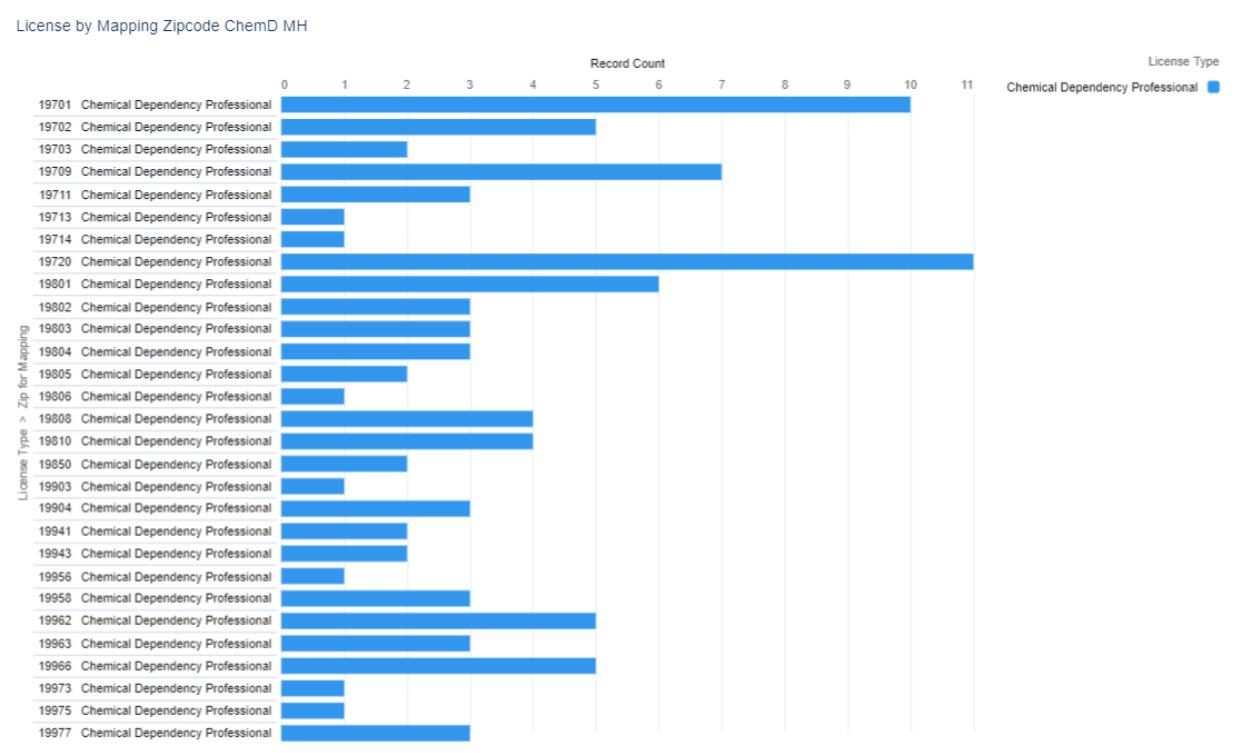
Figure 4. Numerical Distribution of Active License Chemical Dependency Professionals by ZIP code
115

Figure 6.
116 Delaware Journal of Public Health - December 2022
Numerical
Distribution of Active License Professional Counselors of Mental Health by ZIP code
Figure 7 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 7. Visual Distribution of Active License Professional Counselors of Mental Health by ZIP code
REFERENCES
1. American Art Therapy Association. (n.d.). About art therapy.
Retrieved from: https://arttherapy.org/about-art-therapy/
2. American Association for Marriage and Family Therapy. (n.d.). Delaware state resources.
Retrieved from: https://www.aamft.org/Advocacy/State_Resources/Delaware.aspx
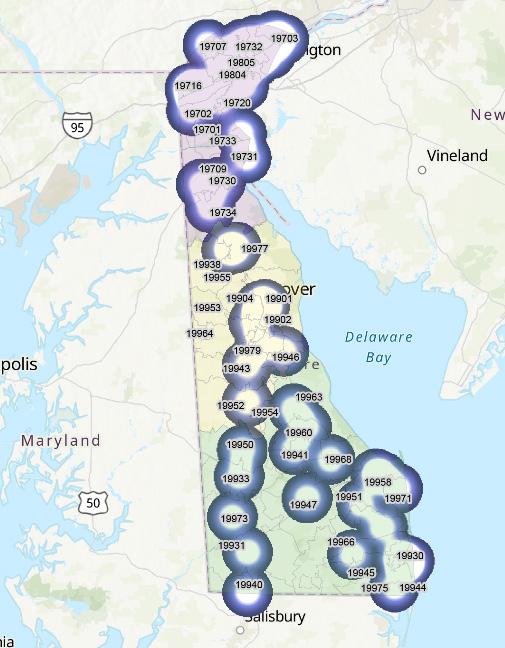
3. US Bureau of Labor Statistics. (2022, Aug). Marriage and family therapists. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/community-and-social-service/marriage-and-family-therapists.htm
4. Salary.com. (n.d.). Chemical dependency counselor.
Retrieved from: https://www.salary.com/research/job-description/benchmark/chemical-dependency-counselor-job-description
5. Recruiter, Z. (n.d.). What is a mental health associate and how to become one.
Retrieved from: https://www.ziprecruiter.com/Career/Mental-Health-Associate/What-Is-How-to-Become
6. Society for Human Resource Management. (n.d.). Mental health counselor.
Retrieved from: https://www.shrm.org/ResourcesAndTools/tools-and-samples/job-descriptions/Pages/Mental-Health-Counselor.aspx
117
Board of Examiners of Psychologists
The primary objective of the Delaware Board of Examiners of Psychologists is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
•develops standards for professional competency, •promulgates rules and regulations, •adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions. The Board issues licenses to psychologists and psychological assistants (see figures 1-3). The Board’s statutory authority is in 24 Del. C., Chapter 35
PSYCHOLOGIST
Psychologists study cognitive, emotional, and social processes and behavior by observing, interpreting, and recording how individuals relate to one another and to their environments (see figures 1-5).
Some psychologists work independently, conducting research, consulting with clients, or working with patients. Others work as part of a healthcare team, collaborating with physicians and social workers, or in school settings, working with students, teachers, parents, and other educators. Those in private practice often work evenings and weekends to accommodate clients.1
PSYCHOLOGICAL ASSISTANT
Individuals who are in the process of obtaining post-doctoral hours under the supervising Psychologist’s supervision, and will apply for a Psychologist license after completing the post-doctoral hours (see figures 6 & 7).2
Figure 1. Active Psychologist Licenses by Type*, N=639
* an active license does not guarantee an individual is actively seeing patients.
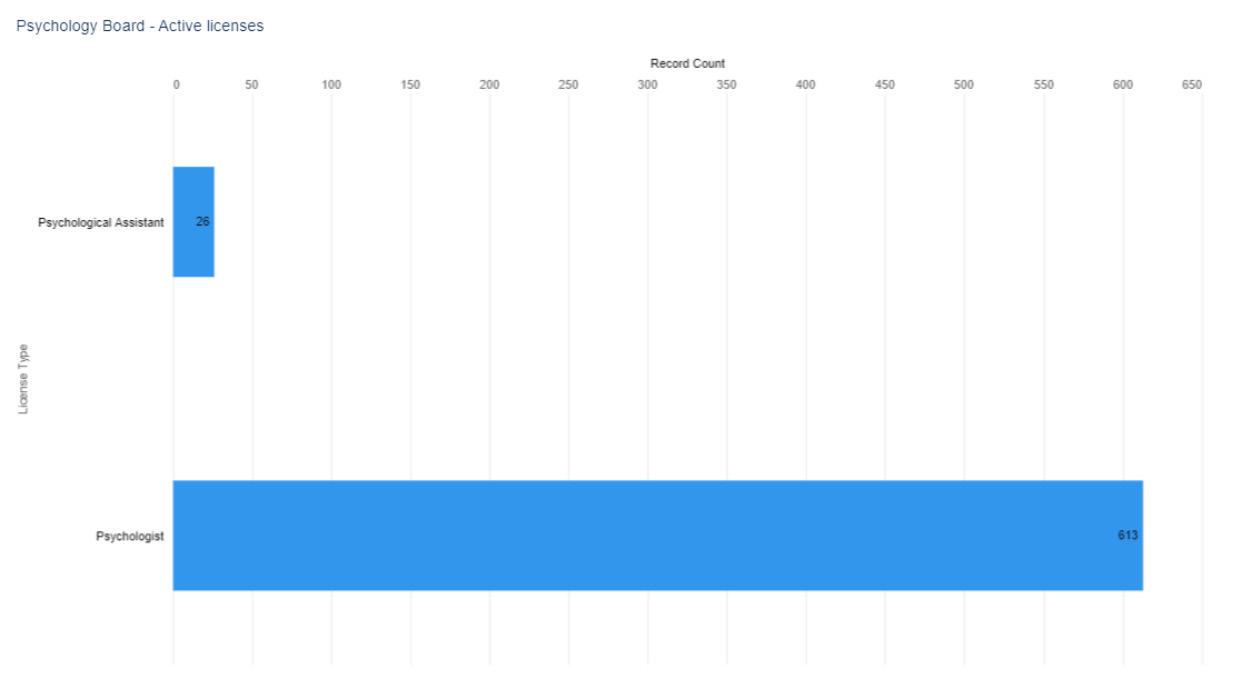
10.32481/djph.2022.12.027
DOI:
118 Delaware Journal of Public Health - December 2022
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”

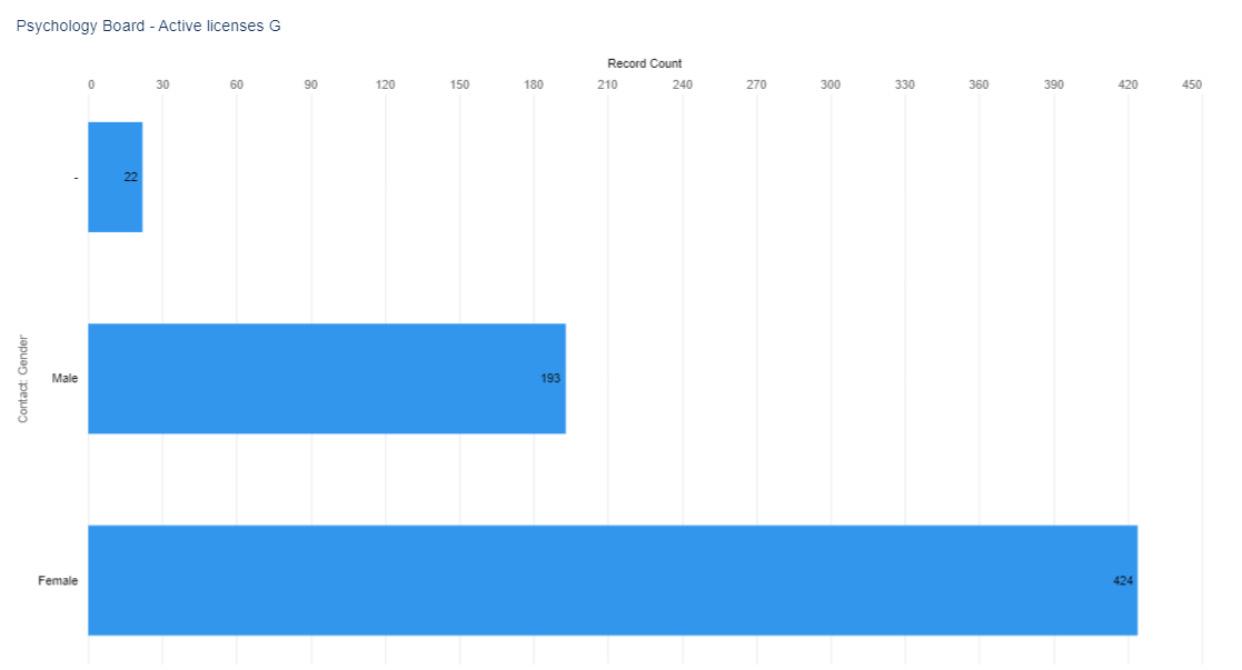 Figure 2. Active Psychologist Licenses by Gender select license types (when reported)
Figure 3. Active Psychologist Licenses by Birth Year
Figure 2. Active Psychologist Licenses by Gender select license types (when reported)
Figure 3. Active Psychologist Licenses by Birth Year
119
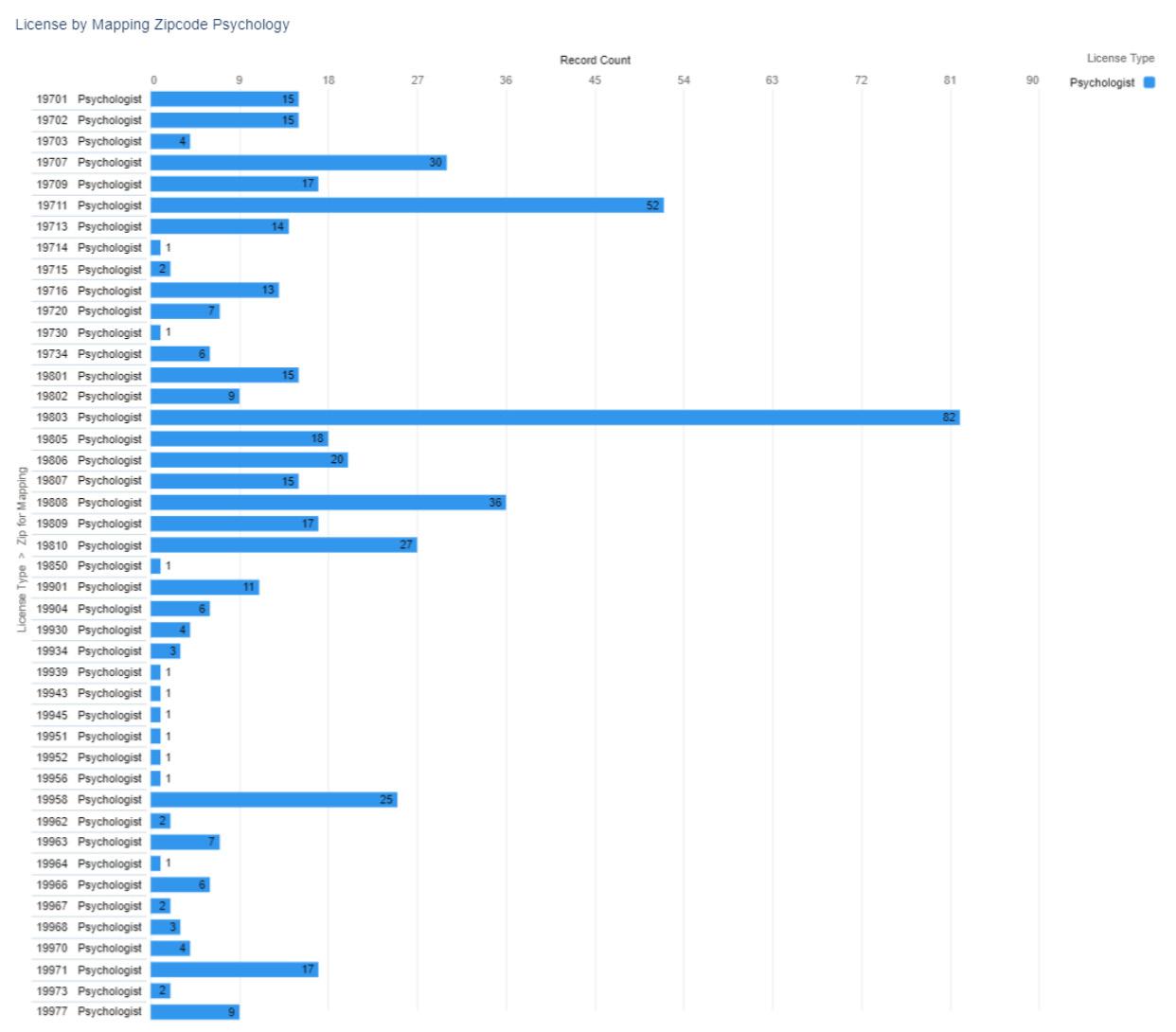
Figure 4. Numerical
Psychological
by ZIP code 120 Delaware Journal of Public Health - December 2022
Distribution of Active
Licenses
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 5. Visual Distribution of Active Psychological Licenses by ZIP code
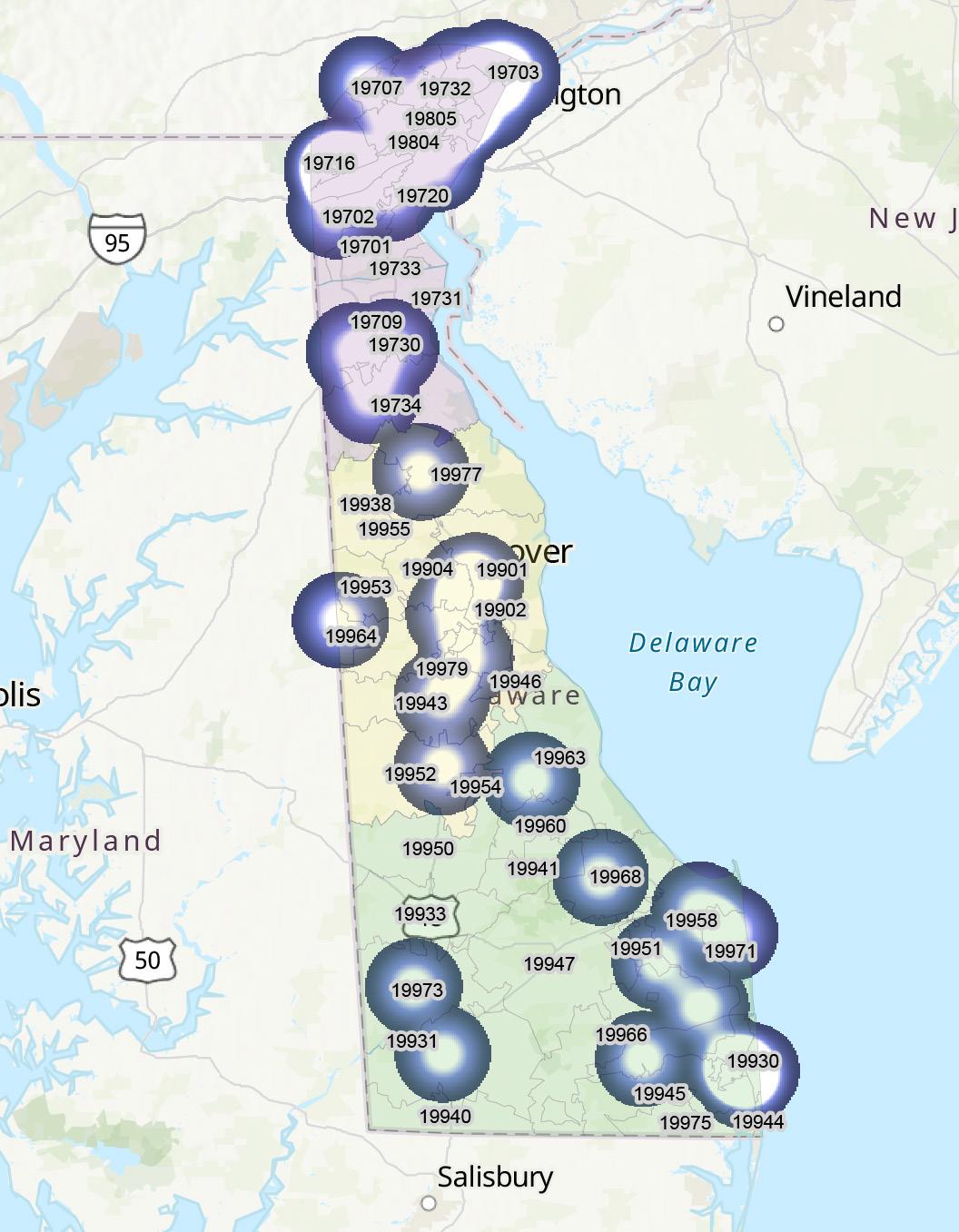
121
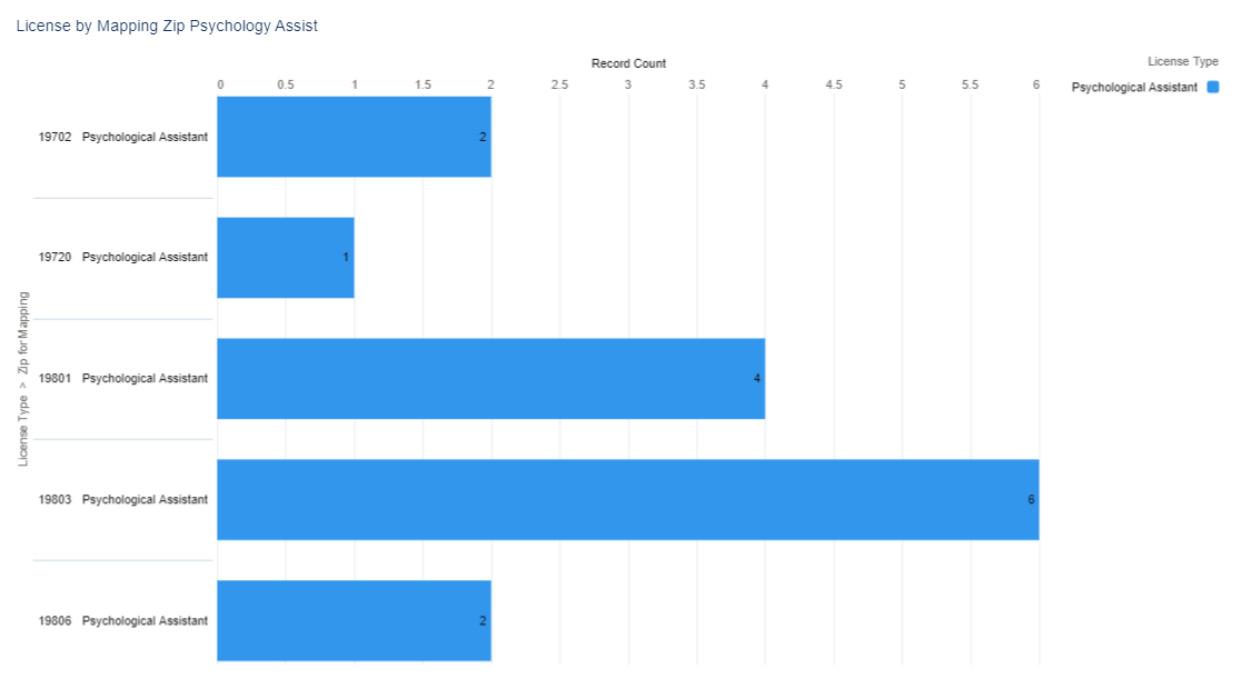
Figure 6. Numerical
ZIP code 122 Delaware Journal of Public Health - December 2022
Distribution of Active Psychologist Assistant Licenses by
Figure 7 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
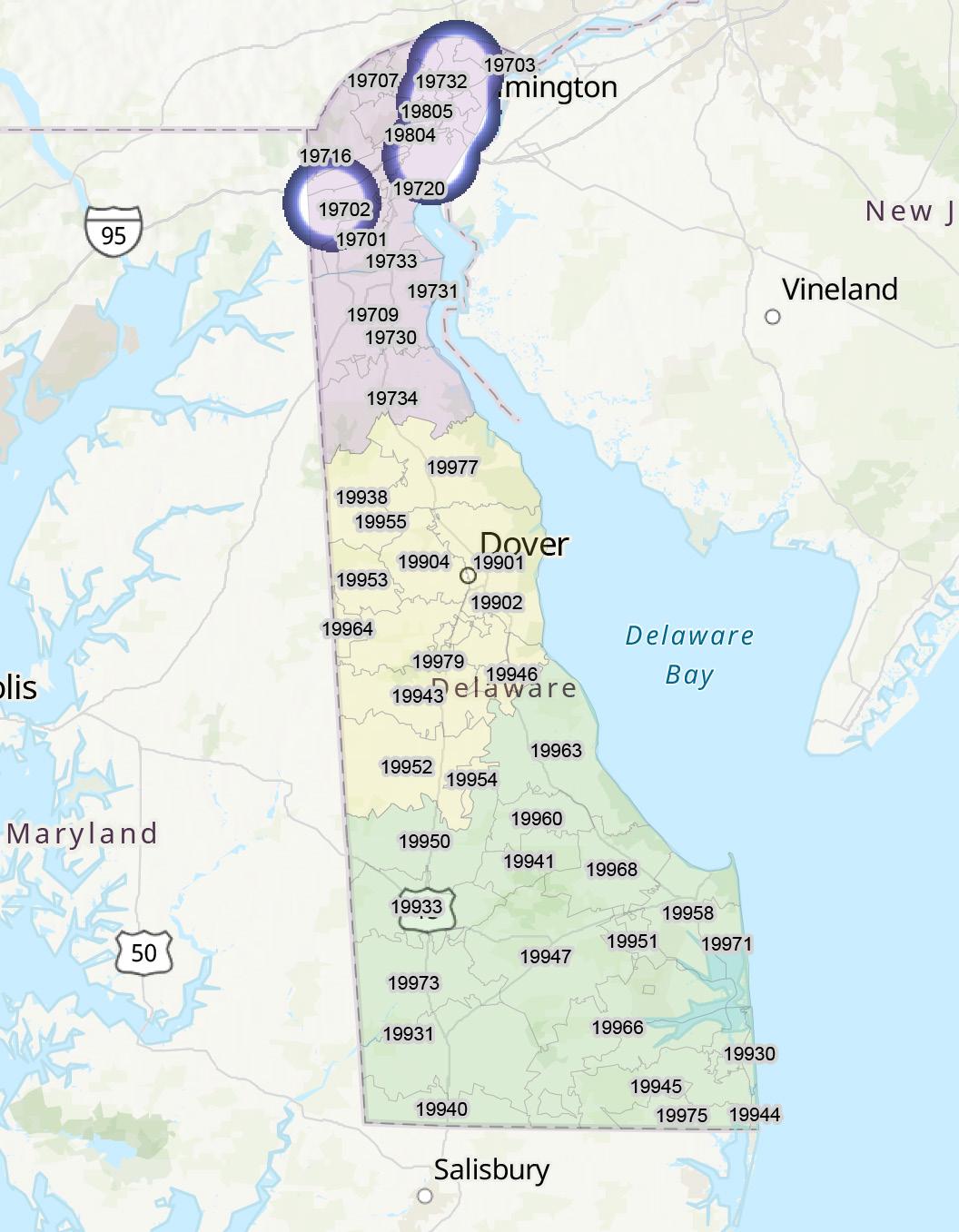
Figure 7. Visual Distribution of Active Psychologist Assistant Licenses by ZIP code
REFERENCES
1. US Bureau of Labor Statistics. (2022, Aug). Psychologists. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/life-physical-and-social-science/psychologists.htm
2. Delaware Division of Professional Regulation. (n.d.). Psychological assistant registration. Occupational Outlook Handbook. Retrieved from: https://dpr.delaware.gov/boards/psychology/newassist/
123
Board of Social Work Examiners
The primary objective of the Delaware Board of Social Work Examiners is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions. The Board issues licenses to clinical social workers (see figures 1-5). The Board’s statutory authority is in 24 Del. C., Chapter 39
CLINICAL SOCIAL WORKER
Clinical social work is a specialty practice area of social work which focuses on the assessment, diagnosis, treatment, and prevention of mental illness, emotional, and other behavioral disturbances. Individual, group and family therapy are common treatment modalities.1
BACHELOR AND MASTERS SOCIAL WORKERS
While there are some social work jobs open to candidates with a bachelor’s degree in a related discipline, a bachelor’s in social work (BSW) is the minimum educational requirement for many positions. BSW program graduates can go on to work as community organizers, case managers, probation officers, and more.2
A Master of Social Work (MSW) degree is the standard requirement for the Licensed Clinical Social Worker (LCSW) credential. However, earning an MSW does not means a practitioner must become an LCSW. MSW graduates can also pursue non-clinical social work jobs or other careers in human services. The LCSW allows social workers to offer psychotherapy services and requires additional testing and experience that is not typically required in those other roles.3
Figure 1. Active License Social Work Practitioner Licenses by Type*, N=2,743
* an active license does not guarantee an individual is actively seeing patients.
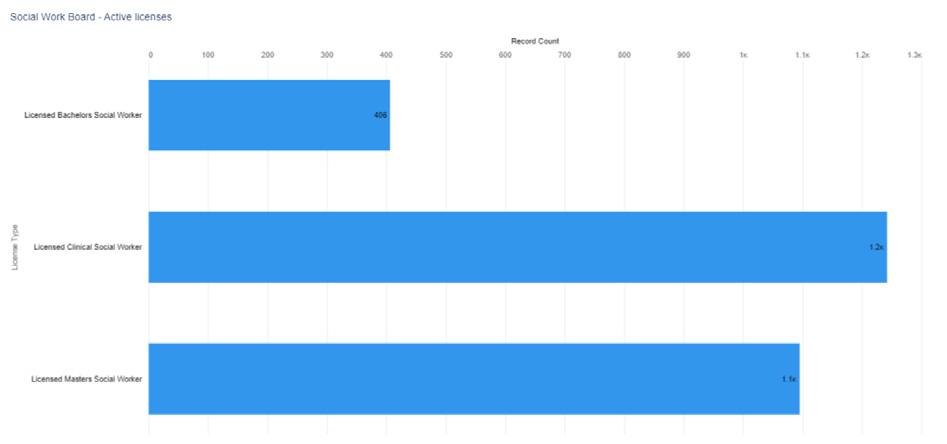
DOI: 10.32481/djph.2022.12.028
124 Delaware Journal of Public Health - December 2022
Figure 2. Active License Social Work Practitioner Licenses by Gender select license types (when reported)

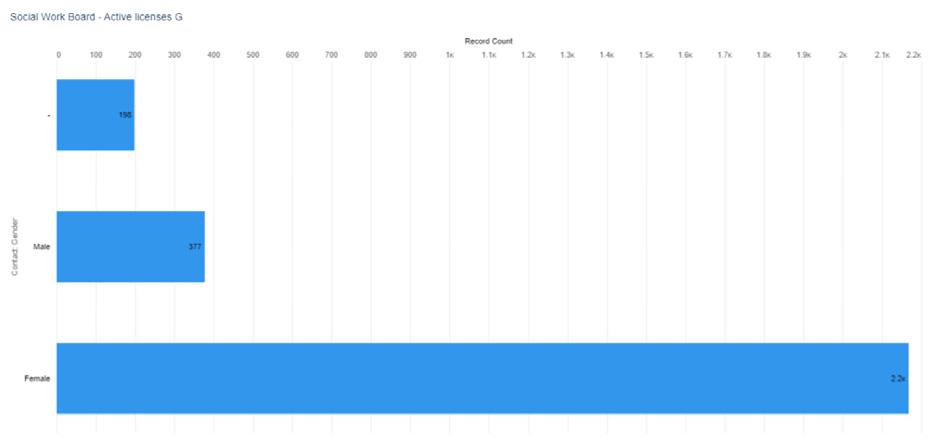
Figure 3. Active License Social Work Practitioner Licenses by Birth Year
Note. 16 individuals did not provide a year of birth
*According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
125
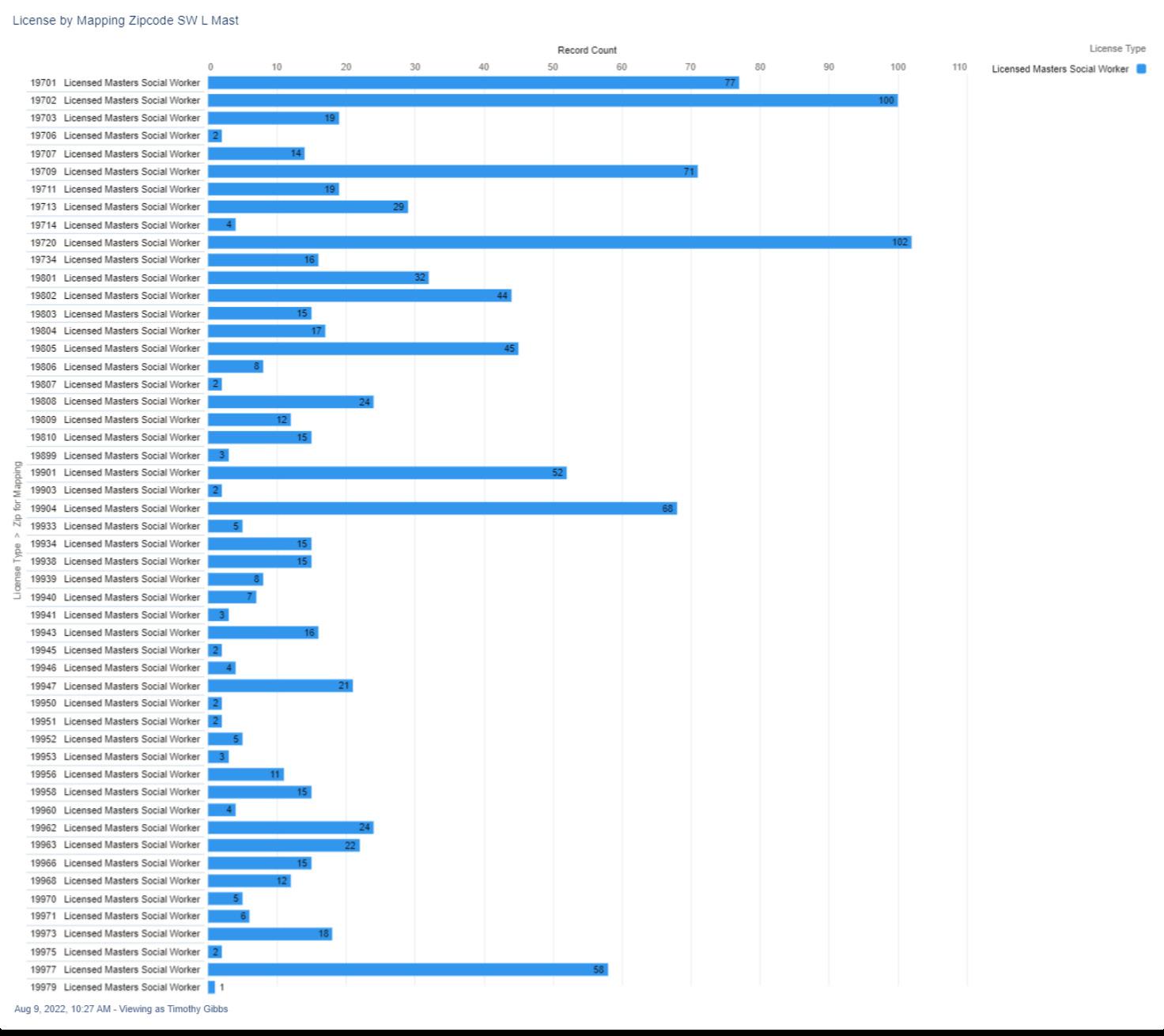
Figure 4. Numerical
ZIP code 126 Delaware Journal of Public Health - December 2022
Distribution of Active Master of Social Work License by
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 5. Visual Distribution of Active Master of Social Work License by ZIP code
REFERENCES
1. National Association of Social Workers. (n.d.). Clinical social work. Retrieved from: https://www.socialworkers.org/Practice/Clinical-Social-Work
2. Social Work License Map. (n.d.). How to become a licensed clinical social worker (LCSW). Retrieved from: https://socialworklicensemap.com/social-work-careers/become-a-lcsw/
3. Wilson, S. (2021, Jun). LCSW vs. MSW (Master of social work). Human Services Edu. Retrieved from: https://www.humanservicesedu.org/lcswvsmsw/
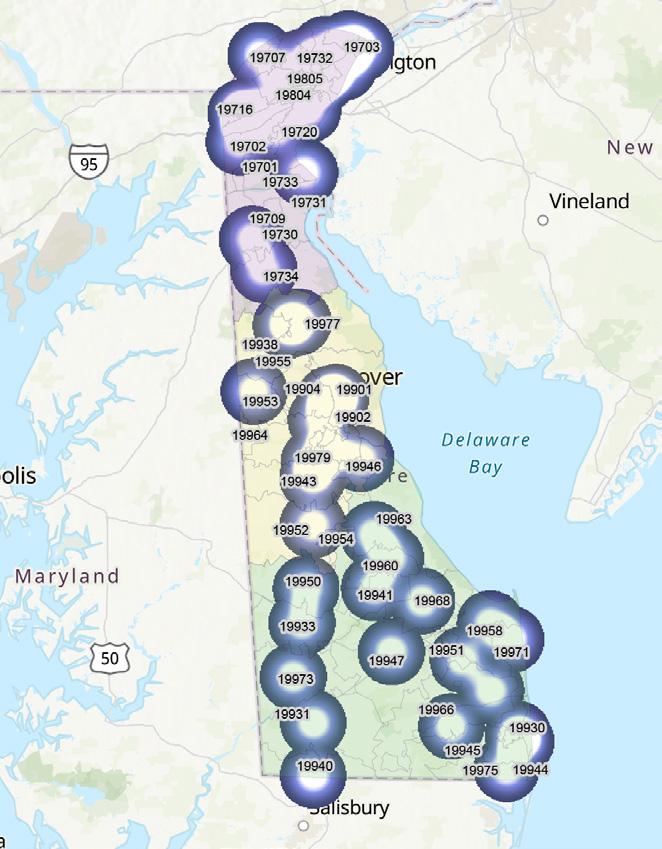
127
Board of Speech Pathologists, Audiologists, and Hearing Aid Dispersers
The primary objective of the Delaware Board of Speech Pathologists, Audiologists, and Hearing Aid Dispensers is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to speech/language pathologists, audiologists and hearing aid dispensers (see figures 1-3). The Board’s statutory authority is in 24 Del. C., Chapter 37
AUDIOLOGIST
Audiologists are healthcare professionals who identify, assess and manage disorders of hearing, balance and other neural systems.1
HEARING AID DISPENSER
A hearing aid dispenser, or a hearing instrument specialist, is someone who is authorized by the state to measure hearing and to fit and sell hearing aids.2
SPEECH / LANGUAGE PATHOLOGIST
Speech-language pathologists (see figures 1-5) work with children and adults who have problems with speech and language, including related cognitive or social communication problems. They may be unable to speak at all, or they may speak with difficulty or have rhythm and fluency problems, such as stuttering.3
TEMPORARY HEARING AID DISPENSER
If one wants to dispense hearing aids in Delaware, they must obtain a Delaware Hearing Aid Dispenser license, with the exception of Delaware-licensed Audiologists.4
TEMPORARY SPEECH/LANGUAGE PATHOLOGIST
Good for one year, this temporary license allows one to practice as a SLP while their Clinical Fellowship Plan is completed. There are additional requirements listed on the DELPROS website.5
Figure 1. Active Speech Pathology, Audiology, and Hearing Aid Dispenser Licenses by Type*, N=1,100
* an active license does not guarantee an individual is actively seeing patients.
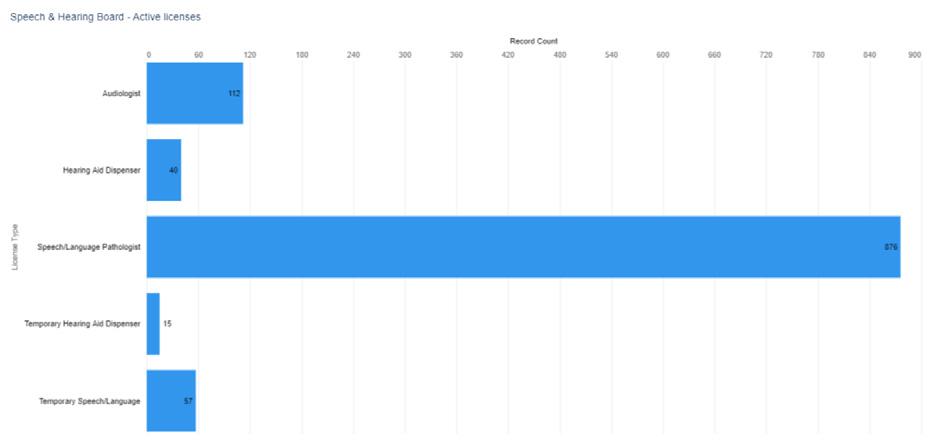
10.32481/djph.2022.12.029
DOI:
128 Delaware Journal of Public Health - December 2022
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
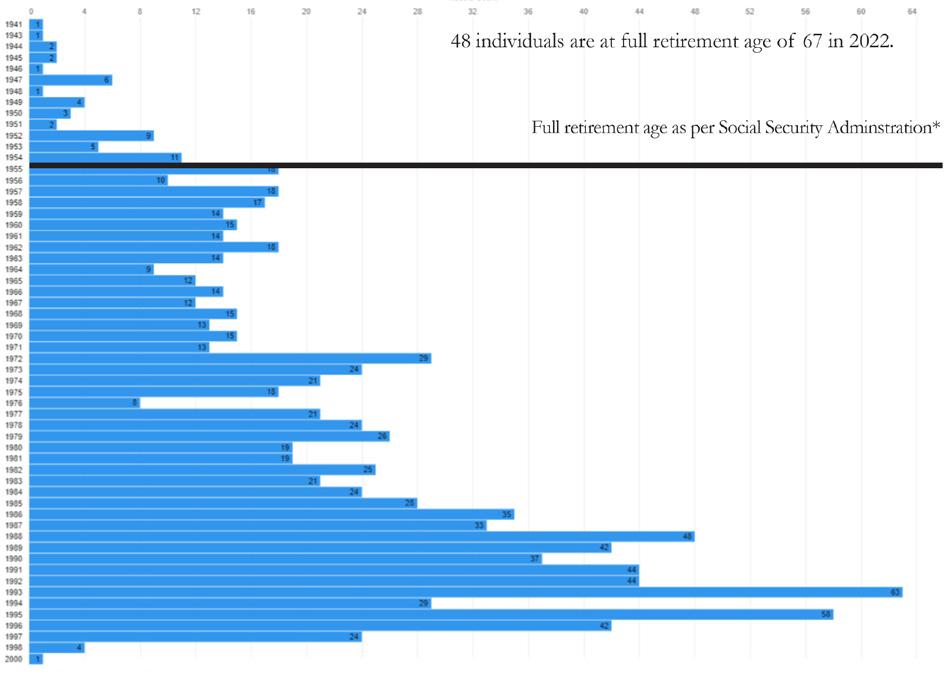
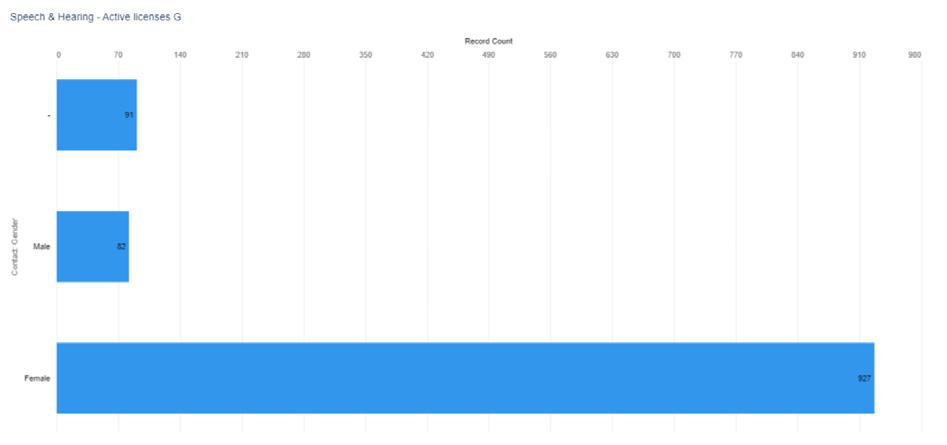 Figure 2. Active License Speech Pathology, Audiology, and Hearing Aid Dispersers by Gender select license types
Figure 3. Active License Speech Pathology, Audiology, and Hearing Aid Dispersers by Birth Year
Figure 2. Active License Speech Pathology, Audiology, and Hearing Aid Dispersers by Gender select license types
Figure 3. Active License Speech Pathology, Audiology, and Hearing Aid Dispersers by Birth Year
129
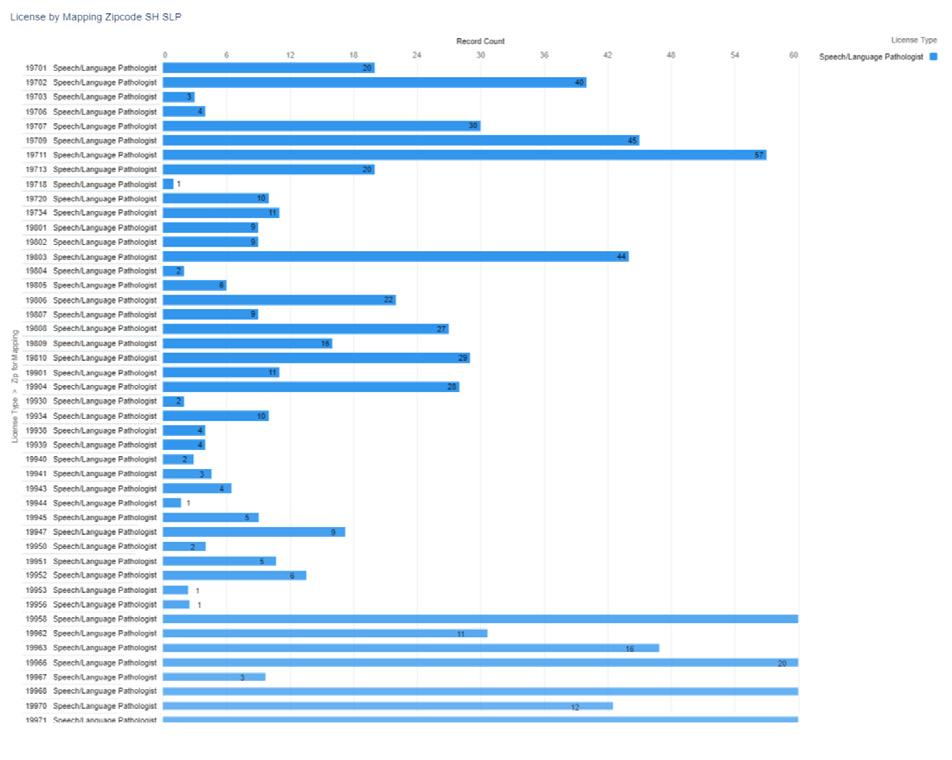
Figure 4. Numerical Distribution of Active Speech/Language Pathology Licenses by ZIP Code 130 Delaware Journal of Public Health - December 2022
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
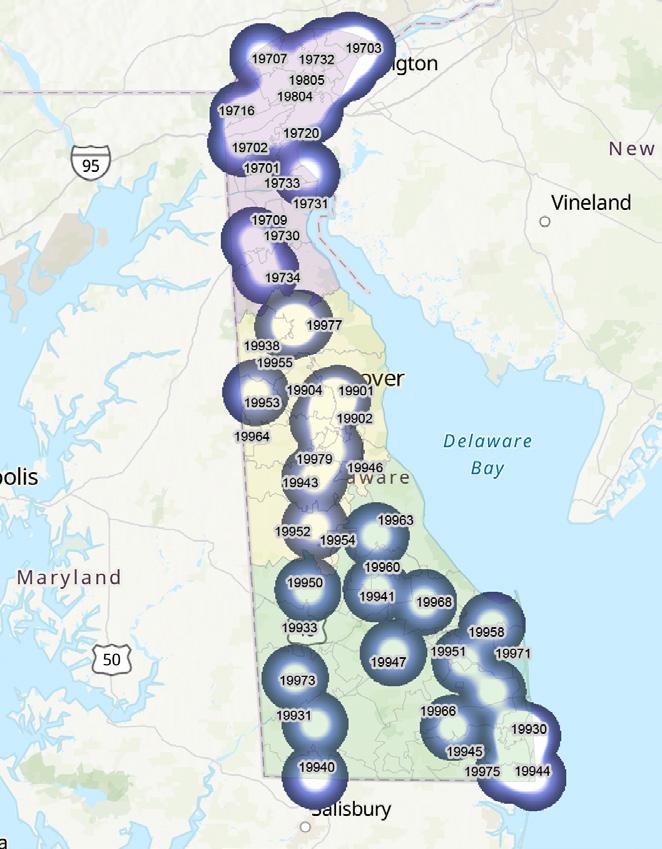
Figure 5. Visual Distribution of Active Speech/Language Pathology Licenses by ZIP Code
REFERENCES
1. Johns Hopkins Medicine. (n.d.). What is an audiologist?
Retrieved from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/hearing-loss/what-is-an-audiologist
2. The Hearing Center. (2021, May). What is the difference between an audiologist and a hearing aid dispenser?
Retrieved from: https://thehearingcentermcc.com/patient-resources/what-is-the-difference-between-an-audiologist-and-a-hearing-aid-dispenser/
3. US Bureau of Labor Statistics. (2022, Aug). Speech-language pathologists. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/speech-language-pathologists.htm
4. Delaware Division of Professional Regulation. (n.d.). Hearing aid dispenser.
Retrieved from: https://dpr.delaware.gov/boards/speechaudio/had/
5. Delaware Division of Professional Regulation. (n.d.). Speech/language pathology licensurer.
Retrieved from: https://dpr.delaware.gov/boards/speechaudio/slpathology/
131
Board of Veterinary Medicine
The primary objective of the Delaware Board of Veterinary Medicine is to protect the public from unsafe practices and practices which tend to reduce competition or fix prices for services. The Board must also maintain standards of professional competence and service delivery. To meet these objectives, the Board
• develops standards for professional competency,
• promulgates rules and regulations,
• adjudicates complaints against professionals and, when necessary, imposes disciplinary sanctions.
The Board issues licenses to veterinarians and veterinary technicians, including temporary licenses (see figures 1-5). The Board’s statutory authority is in 24 Del. C., Chapter 33
VETERINARIAN
Veterinarians care for the health of animals and work to protect public health. They diagnose, treat, and research medical conditions and diseases of pets, livestock, and other animals.1
VETERINARIAN TECHNICIAN
In addition to helping veterinarians during animal exams, veterinary technologists and technicians do a variety of clinical, care, and laboratory tasks. Veterinary technologists and technicians who work in research-related jobs ensure that animals are handled carefully and are treated humanely. They may help veterinarians or scientists on research projects in areas such as biomedical research, disaster preparedness, and food safety.2
Figure 1. Active Veterinary Practitioner Licenses by Type*, N=1,092
* an active license does not guarantee an individual is actively seeing patients.
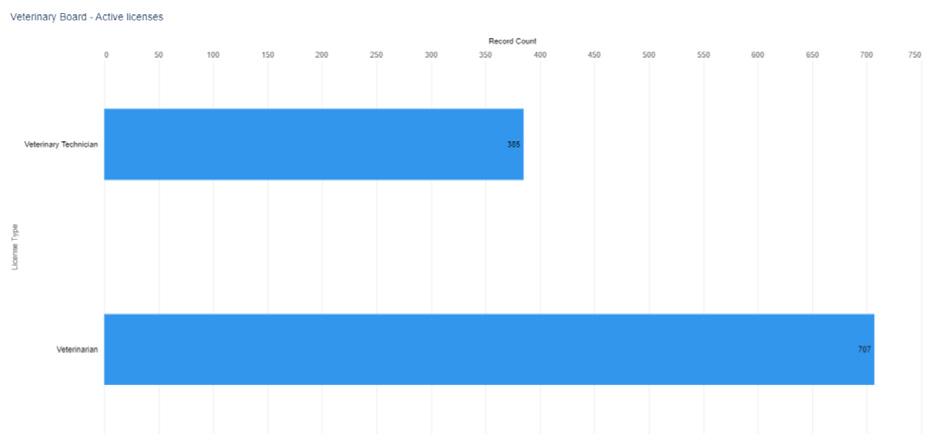
DOI: 10.32481/djph.2022.12.030
132 Delaware Journal of Public Health - December 2022
Note. Six individuals did not provide a year of birth
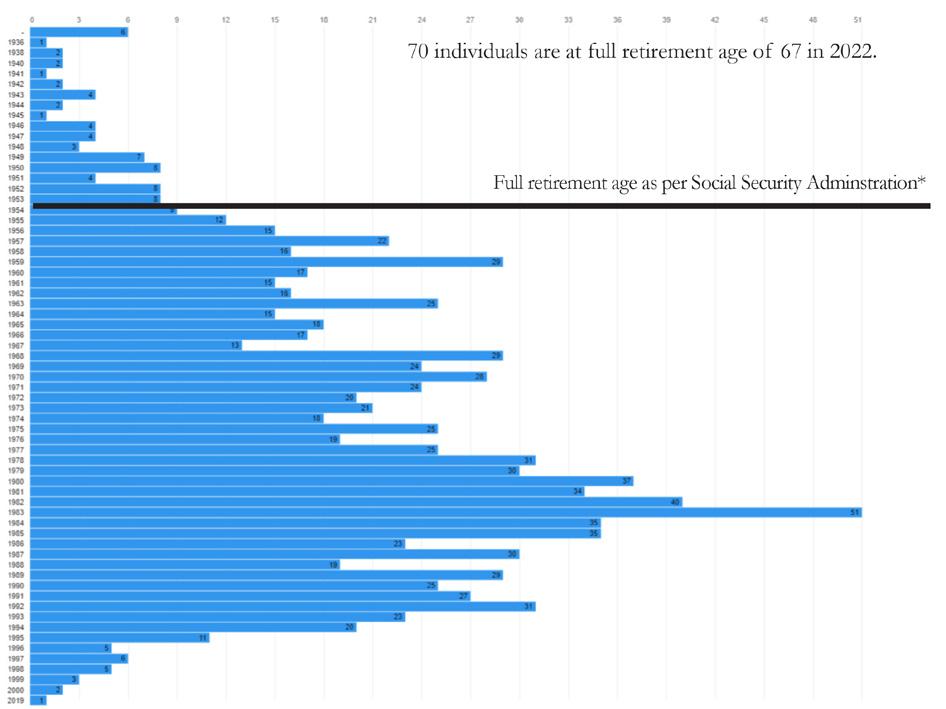
*According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
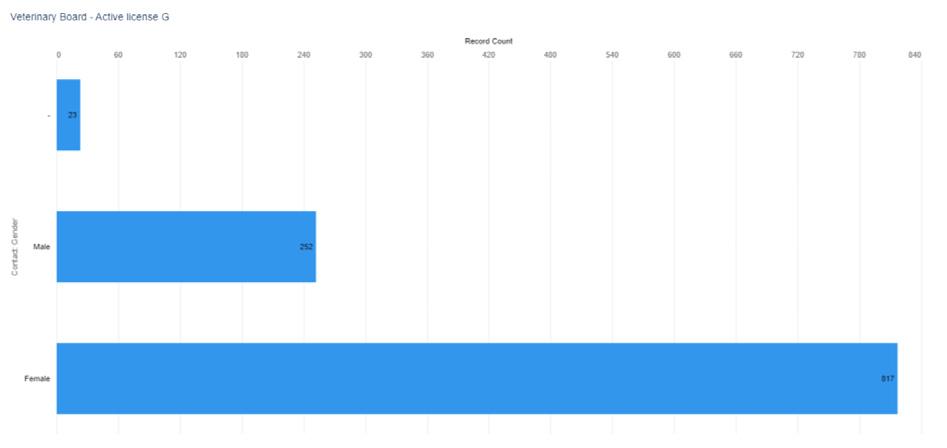
Figure 2. Active
Veterinary Practitioner Licenses by Gender
Figure 3. Active Veterinary Practitioner Licenses by Birth Year
133
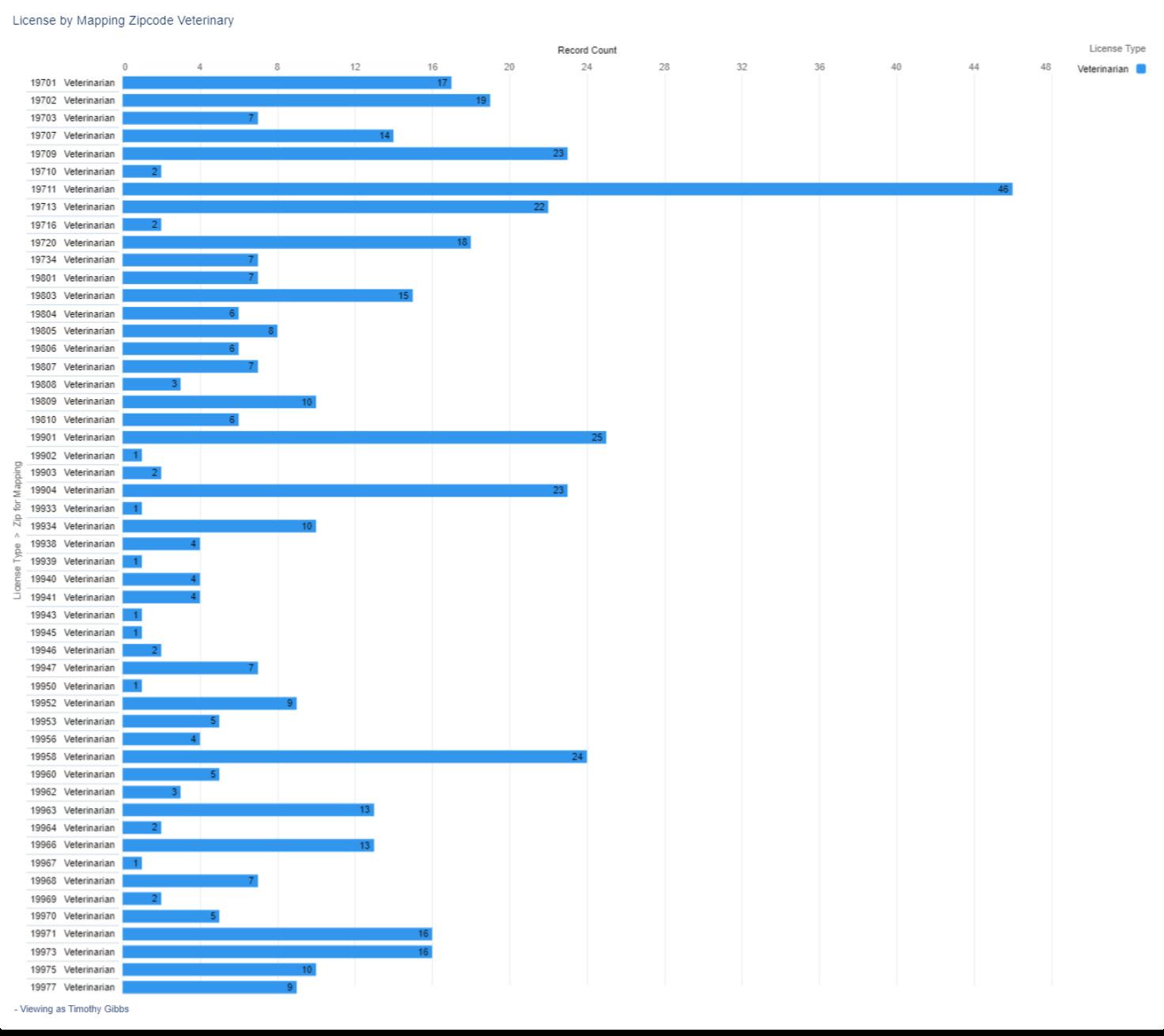
Figure 4. Numerical
ZIP code 134 Delaware Journal of Public Health - December 2022
Distribution of Active Veterinary Practitioner Licenses by
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
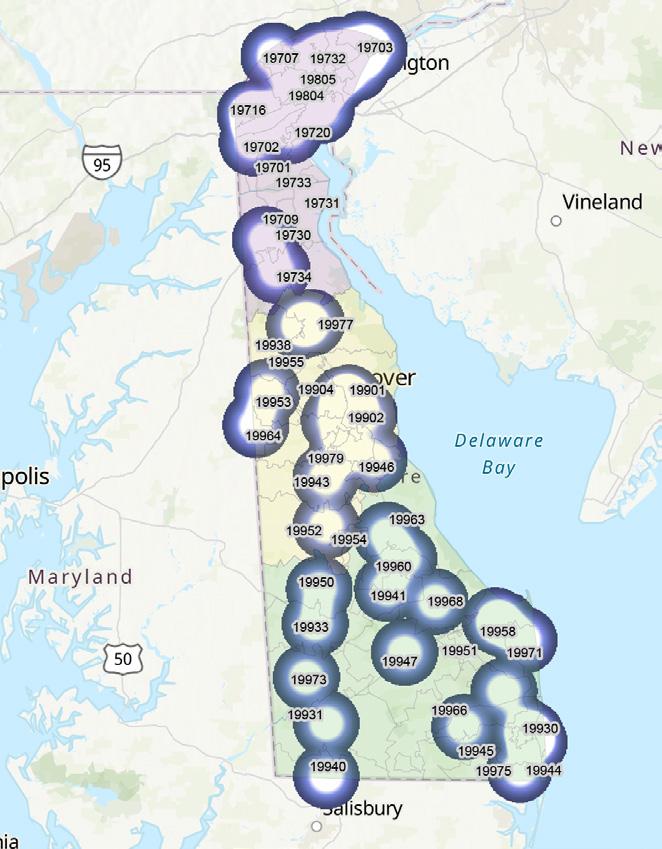
Figure 5. Visual Distribution of Active Veterinary Practitioner Licenses by ZIP code
REFERENCES
1. US Bureau of Labor Statistics. (2022, Aug). What veterinarians do. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/veterinarians.htm#tab-2
2. US Bureau of Labor Statistics. (2022, Aug). What veterinary technologists and technicians do. Occupational Outlook Handbook. Retrieved from: https://www.bls.gov/ooh/healthcare/veterinary-technologists-and-technicians.htm#tab-2
135
Controlled Substance Advisory Committee
The primary objective of the Controlled Substance Advisory Committee is to promote, preserve and protect the public health, safety and welfare by regulating and monitoring use and abuse of controlled substances. To meet this objective, the Committee
• carries out a program of registration, inspection, investigation and education,
• recommends new/revised rules and regulations and disciplinary sanctions against registrants to the Secretary of State.
The Committee issues registrations to practitioners and facilities that prescribe, dispense, manufacture or distribute controlled substances (see figures 1-5). Practitioners include physicians, physician assistants, advanced practice registered nurses, podiatrists, dentists, optometrists, and veterinarians. Facilities include pharmacies, distributors, manufacturers, hospitals, clinics, researchers, laboratories and provider pharmacies.
To assist the Committee, the Drug Control Administrator for the Division of Professional Regulation is responsible for the Committee’s regular administrative functions. The Committee’s authority is in 16 Del. C., Chapter 47 and the Uniform Controlled Substance Act Regulations.
The Controlled Substance Advisory Committee issues an additional license that has a prerequisite of an active practitioner license upon which to build. The following professional licenses may be supplemented with the CSR (Controlled Substances Registration) empowering these provides to prescribe certain classes of medicines which fall under the Uniform Controlled Substance Act Regulations as noted above. In addition, facilities may also be issued a CSR license.
• Advanced Practice Registered Nurse
• Dentist
• Facility
• Optometrist
• Pharmacist
• Physician Assistant
• Podiatrist
• Practitioner (Physicians)
• Veterinarian
Figure 1. Active CSR Licenses by Type*, N=7,760
* an active license does not guarantee an individual is actively seeing patients.
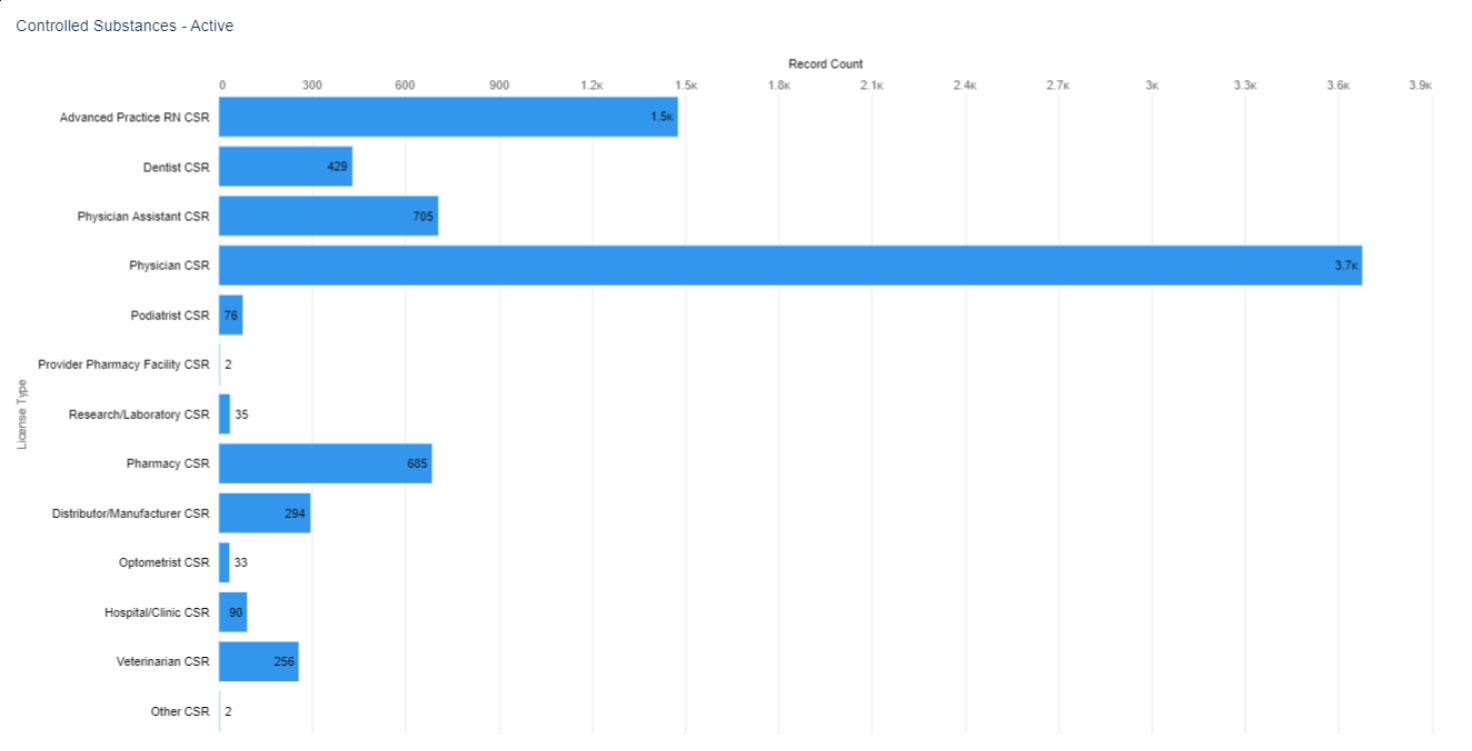
DOI: 10.32481/djph.2022.12.031
136 Delaware Journal of Public Health - December 2022
Figure 3. Active CSR Licenses by Birth Year


Note. Two individuals did not provide a year of birth
* According to the Social Security Administration “Full retirement age is the age when you can start receiving your full retirement benefit amount. The full retirement age is 66 if you were born from 1943 to 1954. The full retirement age increases gradually if you were born from 1955 to 1960, until it reaches 67. For anyone born 1960 or later, full retirement benefits are payable at age 67.”
Figure
2. Active CSR Licenses by Gender select license types
137
One overall map (figure 5) is provided regarding the distribution of CSR licensed individuals as their location has already been disclosed in their section of the report for their primary license.
Figure 4. Numerical Distribution of Active CSR Licenses by ZIP code
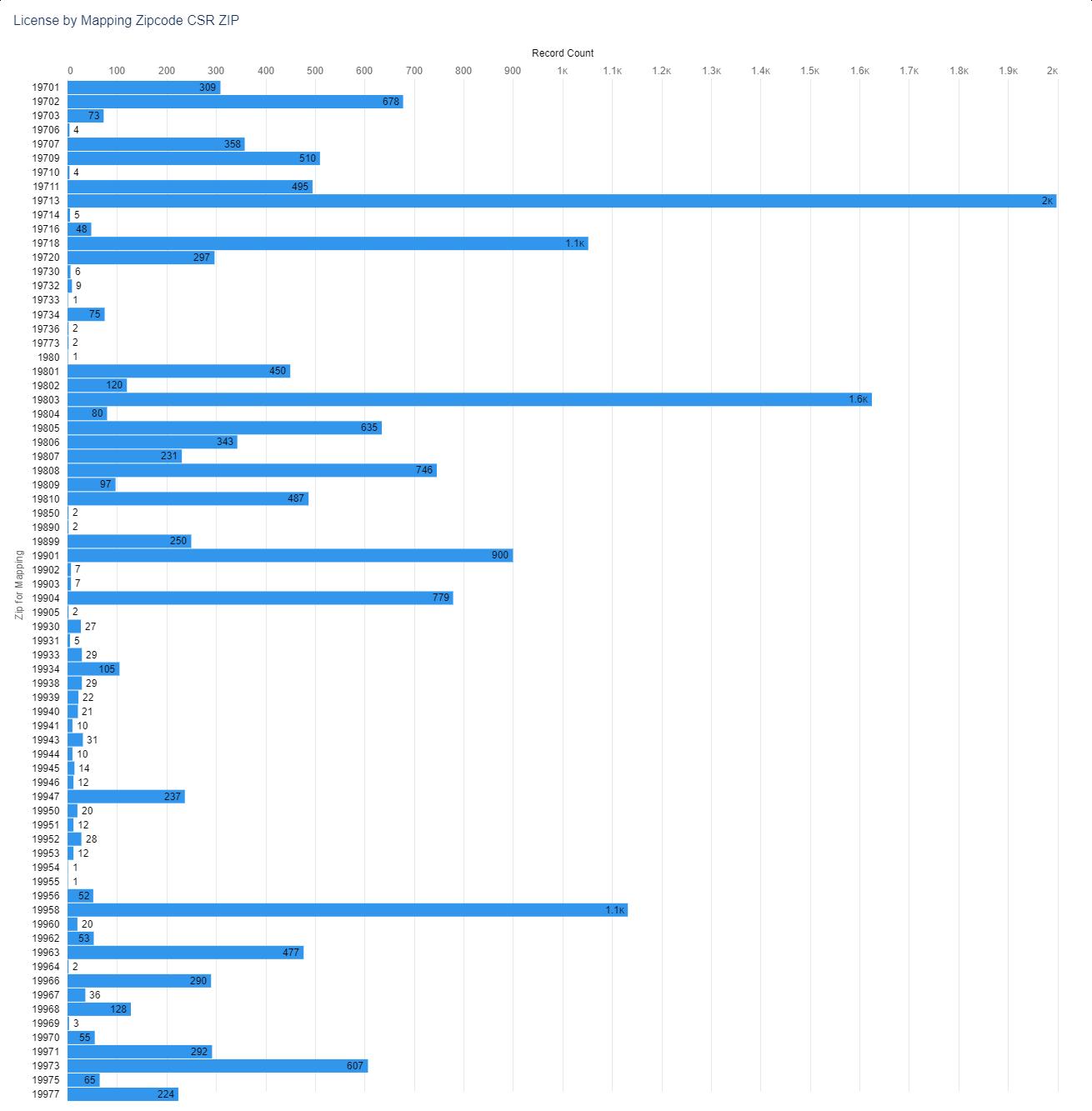
138 Delaware Journal of Public Health - December 2022
Figure 5 shows most, but not all, ZIP codes due to scaling limitations. Hot spots are employed to bring perspective to viewing the overall map and distribution of healthcare professionals and should not be interpreted has valuing value without referring to the numbers listed in the chart above.
Figure 5. Visual Distribution of Active CSR Licenses by ZIP code
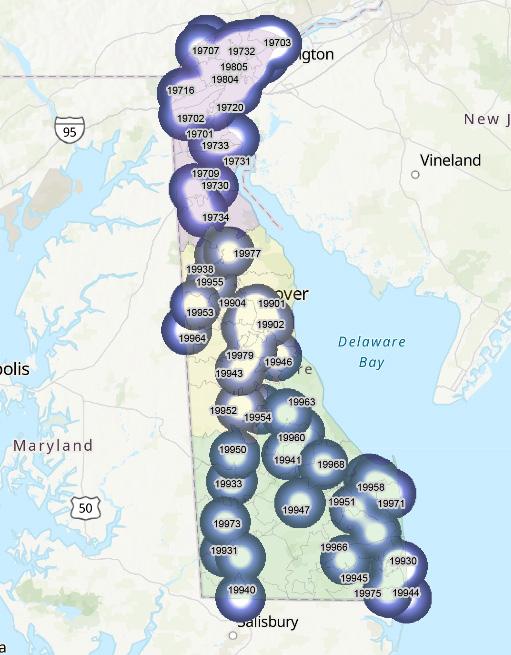
139
Protect loved ones and others from COVID-19 and flu this winter
Delawareans should remain vigilant this winter to protect their loved ones and fellow community members from COVID-19 and the flu. The Division of Public Health recommends following these prevention strategies:

• Get vaccinated and boosted for COVID-19, including the new bivalent booster if eligible. Visit de.gov/boosters and de.gov/getmyvaccine
• Delawareans age 6 months and older should get their annual flu shot to prevent illness, complications, hospitalization, and death. Visit flu.delaware.gov
• Get tested for COVID-19 (de.gov/gettested): – 1-2 days before a large gathering – If you have symptoms of COVID-19 (If you have symptoms and get a negative test result, take another test 2 days later.) – Five (5) days after being exposed to someone confirmed to have COVID-19.
• When sick, stay home to avoid spreading germs, especially to older, very young, or immunocompromised individuals.
• Avoid close contact with sick people.
• Wash hands often with soap and warm water for 20 seconds or longer or use hand sanitizer.
• Cover coughs and sneezes with a tissue or into your inner elbow. Immediately dispose of tissues and wash hands.
• Do not couch your eyes, nose, or mouth.
• Clean and disinfect frequently touched surfaces.
• After traveling, self-monitor for COVID19 symptoms, and isolate and get tested if symptoms develop.
Follow CDC ventilation guidance to reduce risk of airborne virus particles

The U.S. Centers for Disease Control and Prevention (CDC) website offers ventilation (air flow) guidance to prevent small, breathable virus particles from accumulating indoors. The fewer virus particles in the air, the less exposure individuals have to COVID-19, the flu, and other viruses
When guests visit, the CDC recommends ventilating your home or gathering space during the visit and for at least one hour after the visit. If it is safe to do so, bring fresh, outdoor air into the home by opening doors and windows Turn on kitchen and bathroom exhaust fans and ceiling fans Have window exhaust fans blow air outside. Use a portable highefficiency particulate air (HEPA) cleaner to trap particles that people exhale when breathing, talking, singing, coughing, and sneezing.

Use heating, ventilation, and air conditioning filters and change them frequently. Be sure that filters are properly fitted and provide higher filtration. The CDC suggests using portable high-efficiency particulate air (HEPA) cleaners. For continuous airflow and filtration, turn the thermostat to the “on” position instead of “auto. ”



The CDC website provides an easy-to-use interactive ventilation tool and ventilation guidance for buildings, schools, and childcare programs

GOOD VENTILATION
Improving ventilation can help reduce virus particles in your home and keep COVID-19, the flu, and other viruses from spreading. When guests visit and for at least one hour afterward, open windows, turn on ceiling fans, have window exhaust fans blow air outside, and use a portable high-efficiency particulate air (HEPA) cleaner to filter air.
Source: Centers for Disease Control and Prevention
December 202
From the Delaware Division of Public Health
140 Delaware Journal of Public Health - December 2022
Start planning for end of COVID-19 emergency housing and food benefits
Nearly 60,000 Delaware households will be profoundly impacted when they no longer receive emergency COVID-19 benefits for food, housing, and childcare benefits when federal and state governments lift the public health emergency. The Pandemic Emergency Shelter Program that provided motel housing ended September 30
“When these emergency benefits end, especially when enhanced food benefits go away, it will come as a shock to many households,” said Delaware Department of Health and Social Services (DHSS) Secretary Molly Magarik. “We are trying to connect these Delawareans to other services and urge them to prepare for the day when these additional benefits end.”
Delawareans should prepare now for the following temporary suspensions to end immediately or within 30 days after the COVID-19 public health emergency is lifted:
• SNAP food benefit work requirements
• TANF work requirements
• TANF time limit and sanction rules
• Temporary expansion of food benefits for eligible college students
• Waived Purchase of Care monthly childcare co-payments.
Since March 2020, the DHSS Division of Social Services (DSS) has issued monthly emergency benefits through the Supplemental Nutrition Assistance Program (SNAP), the Temporary Assistance for Needy Families (TANF)
program, and General Assistance program. In September, an estimated 59,367 Delaware households received emergency supplemental SNAP food benefits ranging from $95 to $250, and 185 households each received between $201 and $819 in TANF emergency benefits. Eligible General Assistance households received monthly emergency cash benefit checks ranging from $79 for one person to $239 for six people.
For more information, visit DSS's webpage of emergency benefit programs To screen for and apply for benefits, go to DHSS' online application portal Delaware ASSIST or call 1-866-843-7212.

Housing and other resources
Housing Alliance Delaware
www.housingalliancede.org
To find a bed, contact Centralized Intake Monday through Friday, 8:00 a.m.-5:00 p.m., by calling 1-833-FIND-BED (1-833-346-3233), texting the ZIP code to 898-211, or emailing intake@housingalliancede.org Clients may visit any State Service Center or local shelter or day center for help contacting Centralized Intake.
Delaware State Housing Authority
1-888-363-8808, www.destatehousing.com
DEHousingSearch.com 1-877-428-8844
DEHAP Rental Assistance 1-866-935-0407, decovidhousinghelp.com
Emergency Assistance Services
Provides eligible low-income persons up to $1,200 for rent, utilities, and emergency shelter. Division of State Service Centers www.dhss.delaware.gov/dhss/dssc 1-866-843-7212; DHSS_DSSC@delaware.gov
Veterans Multi-Service Center www.vmcenter.org 1-856-293-7321
Delaware Joining Forces Delaware.gov/djf
For military members, veterans, and families
Adult Behavioral Health 24/7 Mobile Crisis Services Northern Delaware: 1-800-652-2929 Southern Delaware: 1-800-345-6785
Youth Behavioral Health 24/7 Child Crisis Hotline 1-800-969-HELP (4357)
Youth Prevention Helpline 302-633-2680
PBHS_Prevention_Inquiries@delaware.gov
24/7 Delaware Hope Line 1-833-9-HOPEDE (1-833-946-7333)
Suicide and Crisis Lifeline 988
Help is Here Delaware HelpisHereDE.com/
The DPH Bulletin – December 2022 Page 2 of 3
141
How to help those less fortunate
Vulnerable families seek food, clothing, housing assistance, shelter, and charity medical and dental care from local food banks, charities, churches, and non-profit organizations. Here are ways to help:

• Support Delaware’s non-profit organizations this holiday season and beyond.
• Support local food banks, such as the Food Bank of Delaware, and community food pantries with food, money, grocery gift cards, or volunteer hours. Also support food drives.
• Clean out your pantry and donate unexpired food. Move foods with nearest expiration dates to the front of the pantry shelves to use them first.
• Eliminate food waste by planning meals ahead, eating leftovers, and freezing extra portions. Do not over-buy or over-order.
• Clip coupons for others. Put them in a recycled box and place in a common area. Someone short on change could use the help.
• Plant to share. Next spring, gardeners can plant extra vegetables to donate to neighbors or a local food pantry after you find out what they accept.
• Clean out your closets. Donate outgrown and unwanted clothes in good or excellent condition to local clothes closets and organizations.
• Give a needful gift. Consider gifting a week or more of childcare, rent, electricity, heating fuel, gas, or bus fare. Lend rides to and from work for those who must give up their car or to help them stretch their gas dollars.
• Be patient and understanding. Impacted individuals may be stressed as they try to provide basic needs for their families. Refer Delawareans in despair to the Suicide and Crisis Lifeline at 988 or the Delaware Hope Line at 1-833-946-7333.
DHSS hotline protects vulnerable adults
To protect vulnerable adults from neglect, abuse, and exploitation, the Delaware Department of Social Services’ Division of Services for Aging and Adults with Physical Disabilities launched a new 24-hour Adult Protective Services (APS) hotline: 888-APS-4302
Callers can remain anonymous and connect with free, voluntary services and resources. Victims can also report harm.
Concerned individuals should “Make the Call” to 888-APS-4302 if they suspect these forms of harm: Physical abuse – inflicting physical pain or injury on a senior

• Sexual abuse – non-consensual sexual contact of any kind
• Emotional abuse – inflicting mental pain, anguish, or distress on a vulnerable adult through verbal or nonverbal acts
• Neglect – the failure by those responsible to provide food, shelter, health care, or protection for a vulnerable adult
• Self-neglect – the failure of a person to perform essential, self-care tasks and that such failure threatens his/her own health or safety
• Exploitation – the illegal taking, misuse, or concealment of funds, property, or assets of a vulnerable adult for someone else’s benefit
• Abandonment – desertion of a vulnerable adult by anyone who has assumed the responsibility for care or custody of that person
• Additional forms of harm – mistreatment, intimidation, manipulation, or coercion.
Under Delaware law, a vulnerable adult is defined as a person 18 years of age or older who, because of isolation, sickness, debilitation, mental illness, or physical, mental, or cognitive disability, is easily susceptible to harm. In 2021, anonymous reports to APS helped protect 2,184 vulnerable adults
For more information, visit dhss.delaware.gov/dsaapd/aps
The DPH Bulletin – December 2022 Page 3 of 3
142 Delaware Journal of Public Health - December 2022





your
stay safe and
you’re
• Get vaccinated and
Get
gatherings. • Wear
when
Don’t let COVID-19 freeze your holiday season. For more information, visit de.gov/holidays. 143
COVID-19 doesn’t just crash holiday get-togethers — it cancels them. So whatever you’re celebrating this season, make sure you’ve gotten
bivalent booster and follow these other steps to
leave COVID out in the cold. Stay home if
sick.
boosted.
tested before and after
a mask
cases are high.
Long Term Care and Skilled Nursing Facilities
Cheryl Heiks, B.A./B.S. Executive Director, Delaware Health Care Facilities Association Nicole Sabine, B.S. Research Associate, Delaware Academy of Medicine/Delaware Public Health Association
INTRODUCTION
Long term care (LTC) is experiencing a workforce crisis. For years this industry, including skilled nursing facilities (SNFs) and assisted living communities, has experienced workforce challenges that have needed to be addressed. The LTC workforce includes nurses and direct care workers. Certified nursing assistants (CNAs), licensed practical nurses (LPNs), and registered nurses (RNs) make up the nursing workforce in this industry. Personal care aides account for direct care workers. The COVID-19 pandemic only exacerbated the problem of retention and recruitment of SNF and assisted living community workers. The industry suffers from workforce shortages even though wages have increased, and bonuses have been offered. Facilities cannot maintain operational costs as the prices of goods and services have increased and hiring contract workers is more expensive than hiring employees. Additionally, there is a lack of qualified and interested candidates to fill open positions as many have left. Overall, the LTC industry lacks adequate funding. Still, the demand for LTC and SNFs is high and will likely increase as the population ages. Nationally, the population of adults 65 and older is expected to increase to 94.7 million by 2060.1 In Delaware, the proportion of adults aged 65 and older is estimated to increase by 48.6% by 2050. Additionally, the population of adults 85 and older will increase by 165%.2,3 The older population of the United States will lack access to and quality care without proper changes. Solutions must be implemented to enhance the workforce in this industry.
LONG-TERM CARE VS. SKILLED NURSING FACILITIES
Long-Term Care
According to the Administration for Community Aging, “long-term care is services and supports necessary to meet health or personal care needs over an extended period of time.”4 Long-term care can be provided to anyone at any age, but older adults aged 65 and older who are unable to be independent use long-term care services and live in these facilities, where medical and personal care services are provided.5,6 Assistance with activities of daily living (ADLs), including help with dressing, bathing, eating, and moving around, is provided in multiple settings such as community settings like adult-day cares, assisted living communities, nursing homes, and continuing care retirement communities (CCRCs).4,6–8 Nurses, CNAs, and personal care aides provide services to these populations.6,9
Skilled Nursing Facilities
According to the Centers for Medicare and Medicaid Services, a skilled nursing facility is “a facility (which meets specific regulatory certification requirements) which primarily provides inpatient skilled nursing care and related services to patients who require medical, nursing, or rehabilitative services but does not provide the level of care or treatment available in a hospital.”10 Individuals are discharged to a SNF when they no longer need care provided by a hospital but are unable to be sent home because they cannot get out of bed, move around, or use a wheelchair safely; have surgical wounds; or do not have adequate help at home. Like other long-term care facilities, SNFs provide assistance with activities of daily living, however SNFs also provide intravenous injections and physical therapy.10,11 These services are carried out by trained and licensed professionals (i.e. registered nurses and doctors). Personal care aides and CNAs are unable to perform these activities but assist with other duties. Other licensed professionals working at SNFs include physician assistants, nurse practitioners, physical therapists, occupational therapists, and speech language pathologists.12
WORKFORCE LANDSCAPE AND DEMOGRAPHICS OF LTCS AND SNFS
The primary LTC and SNF workforce is composed of nurses and direct care workers. Nurses monitor residents’ and patients’ health conditions, provide education, give medicine, and perform wound care. According to the U.S. Bureau of Labor Statistics (BLS), six percent of nurses work in nursing and rehabilitation facilities.13 Nursing assistants take vital signs and assist with activities of daily living and are supervised by RNs. Most nursing assistants work in SNFs (37%) while some work in CCRCs or assisted living communities (11%).14 Personal care aides have similar roles. Like nursing assistants, they help residents and patients with ADLs. However, they may also assist with cleaning and laundry, if needed. About 7% personal care aides work in CCRCs and assisted living facilities.15
Direct care aides are mainly women (87%), people of color (59%), and immigrants (27%).16 Generally, there is little training provided for direct care workers and little opportunity for these workers to advance in their career. However, in Delaware regulations are stronger than federal regulations and require not only initial training but on-going continuing education that is monitored by the Division of Healthcare Quality. Within the 24 month recertification period they need to have 24 hours of Continuing education, of which 6 hours must include dementia training, 2 hours residential/patient abuse prevention and they have to have had at least 64 hours of nursing related services for pay under the supervision of a nurse. In addition there is a competency exam with both a written and clinical portion. Seventy-five hours of training is required for CNAs, but no training is required for personal care aides.16
DOI: 10.32481/djph.2022.12.032
144 Delaware Journal of Public Health - December 2022
CHANGES IN THE WORKFORCE DUE TO THE PANDEMIC
There have been LTC staffing issues prior to the pandemic, but COVID-19 highlighted the issues related to workers of LTC and SNFs. The rapid spread of COVID-19 put additional stress on care workers: these facilities are home to older residents who were likely to become ill, and residents lived close together, so it was difficult to follow distancing recommendations. Additionally, care workers were susceptible to getting sick, but did not always get paid time off, which influenced them to go into work.17 COVID-19 put undue stress on workers who were already burntout, so many left the workforce. Personal Assistance Services Agencies require an orientation, competency test, and training for their establishment.
Impact of COVID-19 on Nurses and Direct
Care Workers
There was a nursing shortage before the pandemic, but COVID-19 exacerbated the situation. In Indiana, 1,300 more nurses need to graduate every year until 2030 to meet the workforce demand for nurses in the State.18 As of March 2022, nursing staff accounted for the largest workforce shortage in nursing homes.19 In May 2020, 1,414 current and resigned direct care workers were surveyed to understand the challenges that these workers were facing. These workers reported external challenges like managing personal and family needs and financial circumstances; as well as staffing shortages, increased demands at work, and high risk of the virus being transmitted to and from residents.20 The nursing industry continued to suffer staffing shortages throughout the pandemic; by November 2021, 234,000 nursing home employees and 39,000 assisted living employees had left their jobs (Figure 1).21
Figure 1. Percent Change In Healthcare Sector Employment, February 2020 - March 202221

Sta ng Shortages
Even as the pandemic has started to slow down, the industry has not fully recovered.22,23 An Agency for Healthcare Administration (AHCA) survey of 759 nursing home providers showed that staffing problems have only been made worse for 60% of nursing homes since January 2022. Specifically, 87% of nursing homes have moderate to high levels of staffing shortages and hiring new staff has been challenging for 98% of nursing homes. These shortages could lead to facility closures: 73% of nursing homes are worried they will have to close.24 The National Center for Assisted Living (NCAL) surveyed 120 assisted living facilities and found similar—though less dramatic—results. According to the report from June 2022, staffing issues have only worsened for more than 50% of assisted living communities since the beginning of 2022. Sixty-three percent of facilities have moderate to high levels of staffing shortages, and it has been difficult for 87% of facilities to hire new staff. Some assisted living facilities (16%) are very worried about the possibility of having to close. Others (32%) are somewhat concerned about closing due to understaffing.25 “Lack of interested or qualified” workers is the top issue reported preventing nursing homes and assisted living facilities from hiring new staff (Figures 2 & 3). Due to understaffing, both facilities have asked workers to work overtime, hired staff from agencies, and reduced new admissions. Both types of facilities have even provided bonuses and benefits, increased wages, enhanced the workplace culture, and paid for staff trainings. Ninety percent of nursing home facilities have raised wages and proposed bonuses and over 90% of assisted living facilities have increased wages to entice workers.24,25
145
In March of 2022, a total of 406,200 employees had left jobs in long-term care facilities since the beginning of the pandemic.23 Nursing homes lost 15.2% of their workforce or 241,000 employees (Figure 4). There has been an increase in assisted living jobs by 1.8% and CCRC jobs by 0.8%, but this sector has not fully recovered.22 Adequate labor in this industry is important as new residents cannot be admitted without proper employment levels. Facilities need an adequate number and type of staff to admit residents and patients, maintain quality care, and remain open. In July 2022, it was reported that greater than 60% of nursing homes in the United States have limited new admissions.26 Facilities are not closing admissions because they do not have enough beds. New patients are denied admission due to the lack of workers. The median occupancy rate for 2022 was estimated to be 77%, which is a lower occupancy rate than pre-COVID.27 In Oklahoma, a senior home closed due to staffing shortages. Another home in Pennsylvania had to close 61 beds out of 344 due to understaffing.28 Other states like New Hampshire and Massachusetts have closed new admissions due to worker shortages as well.26 These closures not only affect nursing homes but affect other sectors of the healthcare system: a hospital near a nursing home that closed twenty-two beds in Buffalo, New York due to staffing shortages was unable to discharge patients as efficiently because patients ready to be transferred to the nursing home had to wait for available space. This caused a backup at the hospital because patients in the emergency department could not be transferred to a hospital room due to capacity issues.28 In July 2022, 1,066 patients from various hospitals in Massachusetts were waiting to be discharged to a nursing home.26 Many facilities have had to fully close due to understaffing. Since the pandemic, 327 nursing homes have closed across the United States and in April 2022, more than 400 were estimated to close within the year.29 Many of these facilities even obtained 4 or 5-Star ratings from the Centers for Medicare and Medicaid Services (CMS).
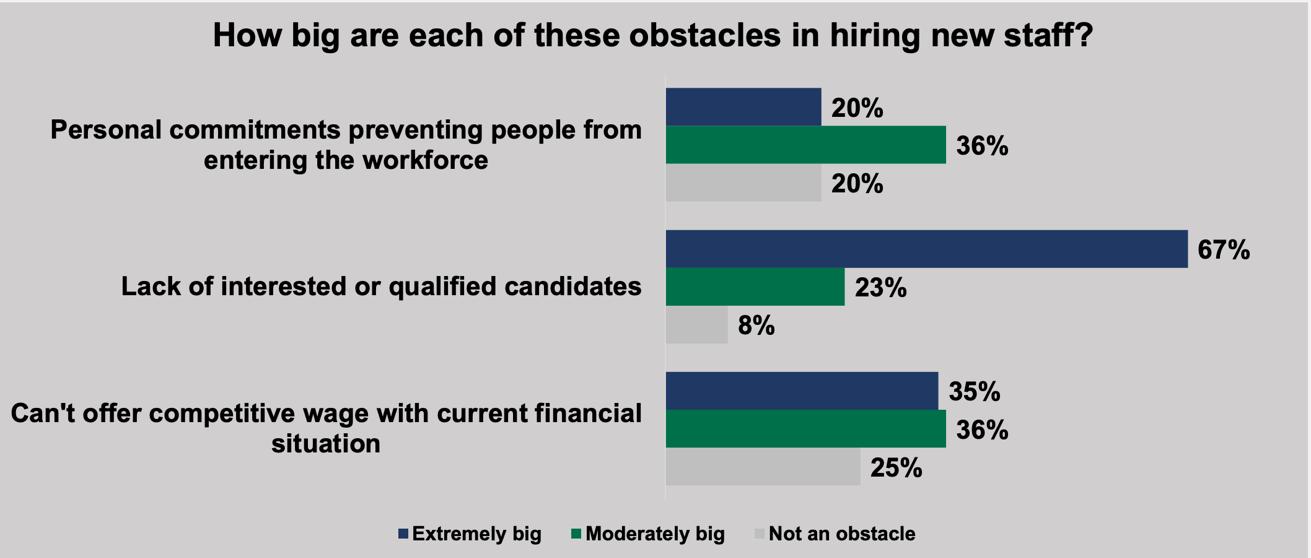
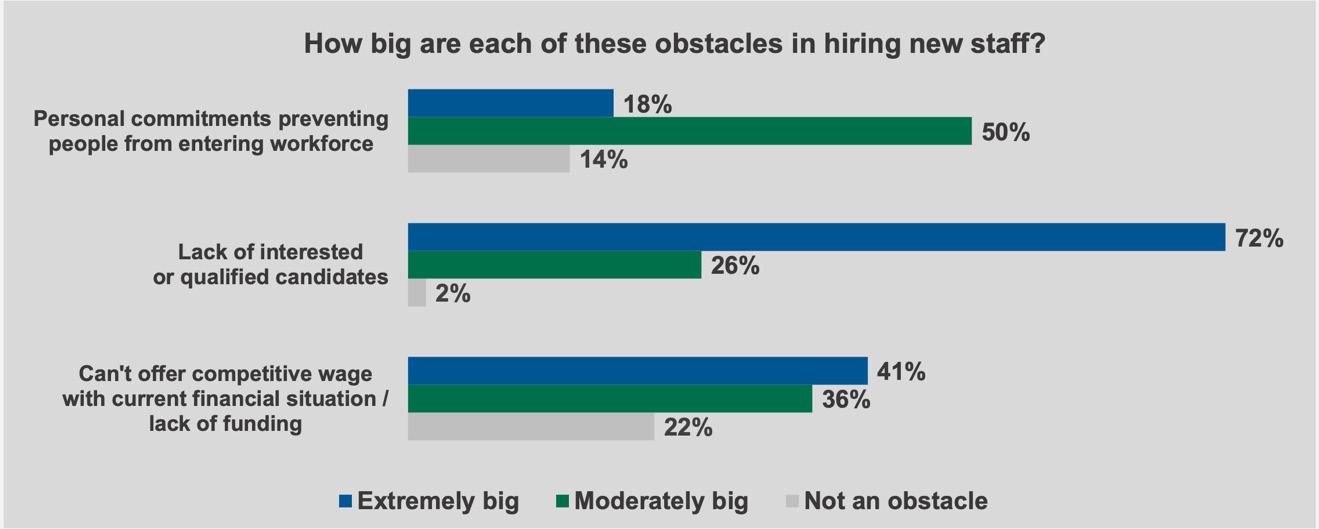 Figure 2. Obstacles to Hiring New Staff in Nursing Homes2
Figure 3. Obstacles to Hiring New Staff in Assisted Living Facilities25
Figure 2. Obstacles to Hiring New Staff in Nursing Homes2
Figure 3. Obstacles to Hiring New Staff in Assisted Living Facilities25
146 Delaware Journal of Public Health - December 2022
Financial Concerns
Financial circumstances also hinder the industry. These circumstances were emphasized during the pandemic as facilities paid higher wages for employees and contracted workers, and the prices of goods and services increased. Specifically, in 2021, the average hourly wage doubled for nursing staff, like RNs, LPNs, and aides.27 Due to the staffing shortages, many facilities hired staff from agencies, which have higher rates. For contracted and agency nursing wage costs, the average wage per hour doubled to tripled post pandemic (Figure 5).27 In April 2022, hourly wages for SNF, assisted living, and CCRC employees increased again. SNF employees have experienced an average hourly increase of $3.73 (18.2%). The total average hourly wage for SNF in April 2022 was $24.25. Assisted living employees’ wages have increased by 16% for a total average hourly wage of $20.72 and CCRC employees have received an average hourly increase of 17.1% for a total average hourly wage of $22.31.22 A survey of 330 SNFs show that nursing wages per hour and contracted work are still increasing in 2022.30 Retaining staff has been difficult for many facilities and this issue has forced them to hire staff from agencies. However, the cost to hire staff from these agencies further hinders the staffing problem. Contracted hourly rates are higher than hourly rates for employees. In May 2022, the average employee hourly wage for an RN was reported as $42.31 whereas the average contracted hourly rate for an RN was reported as $54.33 (a 28.4% difference).30 Similar differences were reported for LPNs and CNAs for employee versus contracted rates.

Figure 5. Average Contracted Nursing Cost per Hour
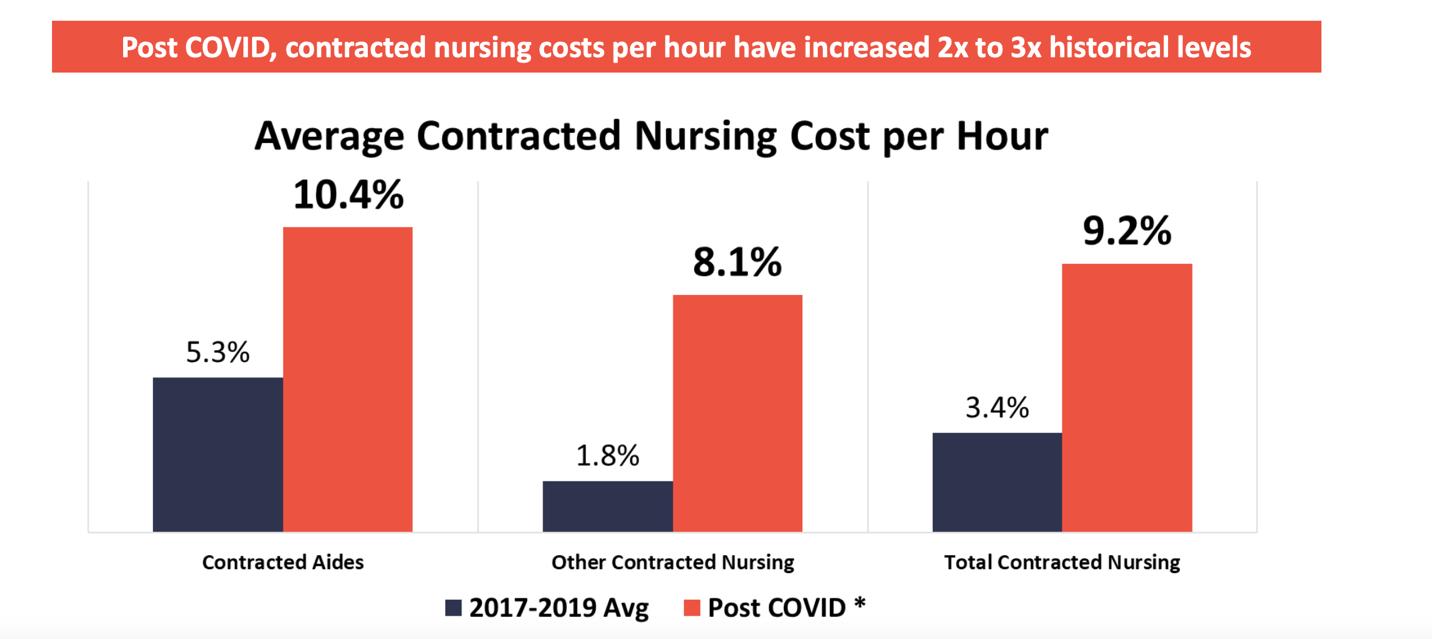
Figure 4. Nursing Home Jobs Lost, March 2020 to March 202223
147
Costs of goods and services also increased during the pandemic. From 2020 to 2021, the average inflation rate was 6.9%.27 From March 2021 to March 2022, there was an overall inflation of goods and services of 8.5%.30 Inflation causes cost of care to rise. In June 2022, the average operational costs of nursing home facilities were reported to have increased by 41% in one year while the average operational costs for assisted living facilities were estimated to have increased by 40%.24,25 In May 2022, the number of SNFs at financial risk were estimated to increase to 47%. These facilities would include almost 417,000 residents, and many of the residents at these SNFs are of racial and ethnic minorities.30
CHANGES IN LTC AND SNF INDUSTRY IN DELAWARE
According to the 2021 Delaware Nursing Home Utilization Statistical Report, there are 47 nursing homes with a total of 4,926 beds in the State of Delaware. During this time, two nursing homes were reported to have closed (Forward Manor Nursing Home and Foulk Manor South). In 2020, there were 8,238 nursing home admissions; this number increased in 2021 to 9,260. However, the 9,260 nursing home admissions is still 20% lower than before March 2020. From 2020 to 2021, the private nursing home occupancy rate reduced to 74% from 77.1%. Prior to COVID-19, occupancy rates for nursing homes were around 90%, and these occupancy rates have decreased for all three counties in the State of Delaware (New Castle, Kent, and Sussex).2 According to the 2021 Delaware Assisted Living Utilization Statistical Report, there are thirty-two assisted living facilities and two rest residential facilities providing long-term care in Delaware. No assisted living facility closures were reported for 2021. These facilities have a total of 2,003 units and 2,320 beds.3 These facilities are recovering at a faster rate than nursing homes in the State: in 2021, 809 new residents moved into these facilities, which was a 43.4% increase from 2020. Still, this sector has not fully recovered, this increase is 9.7% fewer than the number of residents who moved into these facilities prior to the pandemic.3
The LTC and SNF industry has not fully recovered from the effects of the pandemic, even with these increases in admissions and move-ins. The population of older adults is expected to increase exponentially from 2020 to 2050, emphasizing the need to improve this sector of healthcare and increase the number of staff recruited to work in LTC and SNFs.
CONCLUSION
The LTC and SNF industry needs improvement now more than ever. Unlike other sectors of healthcare, this industry has not been able to fully recover from the pandemic. Staffing shortages have existed prior to the pandemic, but the rapid spread of COVID-19 made the issue worse. Workers became stressed and burnt out in times of increasing workload demand. Workers leaving the industry exacerbated the stress felt from the employees who stayed. Understaffing influenced facilities to increase wages and offer bonuses and forced them to use contract agencies. Contract workers cost facilities more money but do not always deliver the same level of care as nursing employees. Contract staff do not work at the same facilities every day, leading to inconsistent care for residents and patients. The supply of long-term care workers needs to be increased as other healthcare facilities, like hospitals need to hire similar staff such as nurses. In February 2022, the Biden Administration suggested a minimum nursing home staff requirement. With such a limited pool of qualified and interested workers this requirement would cause many nursing homes (94%) to have to hire more staff, increasing costs for facilities.31,32
Of note, DELPROS does not collect information on CNAs. The Division of Healthcare Quality is responsible for the training and testing program for CNAs and for the CNA Registry. At the time of this report, we were unable access their database, thus the lack of essential CNA information in this report.
REFERENCES
1. Administration on Aging. (2021). 2020 profile older Americans. U.S. Department of Health and Human Services, Administration for Community Aging. https://acl.gov/sites/default/files/Profile%20of%20OA/2020ProfileOlderAmericans_RevisedFinal.pdf
2. Delaware Health and Social Services & Delaware Healthcare Commission. (2022, May). 2021 Delaware nursing home utilization statistical report. https://dhss.delaware.gov/dhcc/hrb/files/nursinghomeutilization2021.pdf
3. Delaware Health and Social Services & Delaware Healthcare Commission. (2022, May). 2021 Delaware assisted living utilization statistical report. https://dhss.delaware.gov/dhcc/hrb/files/2021alrrpt.pdf
4. Administration for Community Aging. (2020, March). Glossary. U.S. Department of Health and Human Services. https://acl.gov/ltc/glossary#long-term-care
5. Centers for Disease Control and Prevention. (2020). Nursing homes and assisted living (Long-term Care Facilities [LTCFs]). U.S. Department of Health and Human Services. https://www.cdc.gov/longtermcare/index.html
6. National Institute on Aging. (n.d.). What is long term care? U.S. Department of Health and Human Services, National Institutes of Health. https://www.nia.nih.gov/health/what-long-term-care
7. Administration for Community Living. (2020, Feb). Where can you receive care? U.S. Department of Health and Human Services. https://acl.gov/ltc/basic-needs/where-can-you-receive-care
8. U.S. Centers for Medicare and Medicaid Services. (n.d.). Long-term care. U.S. Department of Health and Human Services. https://www.healthcare.gov/glossary/long-term-care/
9. Administration for Community Living. (2020, Feb). Who will provide your care? U.S. Department of Health and Human Services. https://acl.gov/ltc/basic-needs/who-will-provide-your-care
10. Centers for Medicare and Medicaid Services. (n.d.). Glossary. https://www.cms.gov/glossary
148 Delaware Journal of Public Health - December 2022
11. Centers for Medicare and Medicaid Services. (n.d.). Skilled nursing facility care. U.S. Department of Health and Human Services. https://www.healthcare.gov/glossary/skilled-nursing-facility-care/
12. National Library of Medicine. (2021, July). Skilled nursing or rehabilitation facilities. U.S. Department of Health and Human Services, National Institutes of Health. https://medlineplus.gov/ency/patientinstructions/000435.htm
13. U.S. Bureau of Labor Statistics. (2022, April). Occupational outlook handbook, Registered nurses. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/registered-nurses.htm
14. U.S. Bureau of Labor Statistics. (2022, April). Occupational outlook handbook, Nursing Assistants and orderlies. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/nursing-assistants.htm#tab-2
15. U.S. Bureau of Labor Statistics. (2022, April). Occupational outlook handbook, Home health and personal care aides. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/home-health-aides-and-personal-care-aides.htm
16. Stone, R. I., & Bryant, N. (2021). Feeling valued because they are valued. [White Paper]. LeadingAge LTSS Center. https://leadingage.org/sites/default/files/Workforce%20Vision%20Paper_FINAL.pdf
17. Barnett, M. L., & Grabowski, D. C. (2020, March 2). Nursing homes are ground zero for COVID-19 pandemic. JAMA Health Forum, 1(3), e200369. 10.1001/jamahealthforum.2020.0369 https://pubmed.ncbi.nlm.nih.gov/36218601
18. Quinton, S. (2022). As nurses quit, states seek to train more. Pew. https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2022/03/17/as-nurses-quit-states-seek-to-train-more
19. Musumeci, M., Childress, E., & Harris, B. (2022, May). State actions to address nursing home staffing during COVID-19. Kaiser Family Foundation.
https://www.kff.org/medicaid/issue-brief/state-actions-to-address-nursing-home-staffing-during-covid-19/
20. Cimarolli, V., & Bryant, N. (2021). COVID-19: Experiences of direct care workers in aging services. LeadingAge LTSS Center. https://www.ltsscenter.org/wp-content/uploads/2021/02/COVID-Brief-LTSS-Feb-2021_FINAL.pdf
21. American Healthcare Association / National Center for Assisted Living. (2021). BLS November jobs report: Nursing homes. [Fact sheet].
https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/AHCA%20NCAL%20Report_BLS%20Data%20on%20Staffing%20Shortages%2012.10.21.pdf
22. Zahraoui, O. (2022, Jun). Workforce contraction and recovery varies across healthcare sectors. National Investment Center. https://blog.nic.org/workforce-contraction-and-recovery-varies-across-healthcare-sectors
23. American Healthcare Association / National Center for Assisted Living. (2022). BLS March 2022 jobs report. [Fact sheet]. https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/BLS-MARCH2022-JOBS-REPORT.pdf
24. American Healthcare Association. (2022). State of the nursing home industry: Survey of 759 nursing home providers show industry still facing major staffing and economic crisis. [Slides].
https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/SNF-Survey-June2022.pdf
25. National Center for Assisted Living. (2022). State of the assisted living industry: Survey of 120 assisted living providers show industry still facing major staffing and economic crisis. [Slides].
https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/AL-Survey-June2022.pdf
26. American Healthcare Association / National Center for Assisted Living. (2022, July 14). Historic staffing shortages continue to force nursing homes to limit new admissions, creating bottlenecks at hospitals and reducing access to care for seniors [Press release]. https://www.ahcancal.org/News-and-Communications/Press-Releases/Pages/Historic-Staffing-Shortages-Continue-To-Force-Nursing-Homes-ToLimit-New-Admissions,-Creating-Bottlenecks-at-Hospitals-and-.aspx
27. CliftonLarsonAllen LLP. (2022). State of skilled nursing facility (SNF) industry. [Slides] American Healthcare Association/ National Center for Assisted Living.
https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/2022%20State%20of%20the%20SNF%20Industry%20Report.pdf
28. B ernstein, L., & Van Dam, A. (2021, Dec). Nursing home staff shortages are worsening problems at overwhelmed hospitals. The Washington Post. https://www.washingtonpost.com/health/2021/12/28/nursing-home-hospital-staff-shortages/
29. American Healthcare Association / National Center for Assisted Living. (2022). Nursing home closures: By the numbers. https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/SNF-Closures-Report.pdf
30. CliftonLarsonAllen LLP. (2022). State of skilled nursing facility industry: In-depth analysis on increasing cost and local impact. [Slides] American Healthcare Association/ National Center for Assisted Living.
https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/AHCA%20-%20State%20of%20Skilled%20Nursing%20Facility%20 Industry%20-%20In-Depth%20Analysis%20on%20Increasing%20Costs%20and%20Local%20Impact.pdf
31. American Healthcare Association / National Center for Assisted Living. (2022, July 19). Report: Increasing nursing home staffing minimums estimated at $10 billion annually [Press release].
https://www.ahcancal.org/News-and-Communications/Press-Releases/Pages/Report-Increasing-Nursing-Home-Staffing-Minimums-Estimated-at-$10-Billion-Annually.aspx
32. CliftonLarsonAllen LLP. (2022, July). Staffing mandates analysis in-depth analysis on minimum nurse staffing levels and local impact. [Slides] American Healthcare Association/ National Center for Assisted Living. https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/CLA-Staffing-Mandate-Analysis.pdf
149
Composition of An Ideal Medical Care Team
Caroline Harrington, M.S., C.H.E.S. Intern, Delaware Academy of Medicine/Delaware Public Health Association
INTRODUCTION
Team-based care is becoming increasingly important as the health system changes. There is currently a physician shortage issue in the United States. A report from the Association of American Medical Colleges predicts that there will be a shortage of 17,800 to 48,000 primary care physicians and a shortage of 21,000 and 77,100 of non-primary care physicians by 2034.1 Ensuring that other healthcare professionals can collaborate, and delegating tasks away from the physician might improve the physician shortage problem. The population of the U.S. is aging, and disease states are becoming more complex.2 These issues will require the expertise of various care team members so that the patient receives the most effective care to optimize outcomes. Team-based care involves two or more health professionals working with the patient to achieve shared goals.3 Health professionals from multiple disciplines work together to inform decision-making that also includes families in the care plan.4 The professionals involved on the care team will vary depending on the population, type of disease, and healthcare setting.3,5 For instance, a mix of registered nurses, medical assistants, nurse aides, technologists, nutritionists, genetic counselors, social workers, and chaplains along with primary care providers could make up a cardiovascular care team.2 However, allergists or immunologists should be a part of a team that provides care for patients with asthma.6
Although team-based care is needed in the United States to address healthcare system issues, care teams need to be effective to improve patient health outcomes. An effective healthcare team will embody multiple characteristics, such as shared goals, explicitly stated roles, clear and prompt communication, respect, and a positive attitude.7,8 Healthcare team members need to work together with the patient and family to address shared goals. Roles and responsibilities for each care member should be clearly stated and each care member needs to know what is expected of each other. If problems arise, then team members should be open and honest about any mistakes or uncertainties.2
The purpose of this review is to identify the primary members of a care team and determine what characteristics make an effect care team. This review seeks to answer the following questions:
1.What is the ideal care team?
2.What are the characteristics of an effective care team?
Understanding the composition of the ideal healthcare team will assist healthcare leaders, healthcare settings, and policy makers, among others, to create care teams that are effective to improve patient health outcomes.
WHAT IS THE IDEAL CARE TEAM?
Patients
Patients along with their families are the most important member of the healthcare team. Patients contribute to the care plan and collaborate with the care team on shared health goals.2,4,9 It is essential that care teams factor in the preferences of patients and their families to achieve desired health results. When patients are included on the care team, they experience higher satisfaction and achieve better self-management skills and adhere to treatment more (Biederman, 2021).10
Primary Care Providers
Primary care providers such as physicians, advanced practice nurses (APNs), nurse practitioners (NPs), and physician assistants (PAs) should be involved in all care teams, especially related to cardiac care, cancer, HIV/AIDs, and asthma teams.2,10–16 Physicians are highly trained health professionals with a large scope of practice. Primary care physicians are most likely the first health professional that a patient will visit before being diagnosed with a health condition. However, other advanced practice providers, like APNs, NPs and PAs, are suitable to care for patients with chronic conditions. These healthcare professionals should assist patients within their scope of practice but can help delegate tasks away from the physician. APNs can provide education and chronic disease management services while PAs roles directly align with physicians.2 In a study that examined how A1c, LDL, and systolic blood pressure measures related to new onset disease differed between solo and team-based care teams, teams had more patients who brought their A1c, LDL, and systolic blood pressure under control. Teams included physicians-only teams, non-physician teams of NPs and PAs, and mixed teams of physician and non-physicians. All teams had the same effect on patients lowering their A1c and LCL levels. However, physician-only teams and mixed teams showed patients with better management of hypertension compared to the other types of teams.11 Providers who have expertise in the health condition of concern, such as HIV care, will have patients who experience better HIV outcomes. Primary care providers should then refer out to other providers on the team if they are less familiar with HIV.15 Referral to specialists will be need for numerous diseases. Overall, primary care providers can enhance the care of patients due to their autonomy, expertise, and skill.2,10
Specialists
Specialists will be required on care teams for most chronic diseases, as primary care providers do not have the full expertise on chronic conditions related to cardiac diseases, cancer, HIV/AIDS, and asthma. Exercise specialists may be on the cardiac team as they can
DOI: 10.32481/djph.2022.12.033
150 Delaware Journal of Public Health - December 2022
provide behavioral counseling and it is recommended that behavioral counseling is offered to individuals eighteen years or older with hypertension and multiple risk factors for heart.17 For cancer, there are several types of cancer teams due to the prevalence of various forms of cancer. Other cancer teams that need to be included in cancer care can include radiology, pulmonology, and palliative care among others.9,12,13 In a systematic review, it was shown that multidisciplinary cancer care teams improved patient’s adherence to pain medication. Additionally, palliative care teams decreased hospitalizations and increased quality of life for those with cancer.18 Due to the aging population, geriatricians are an important aspect to HIV/AIDS care. In fact, any team member should be familiar with regular HIV care as well as geriatric approaches to HIV.14 Geriatricians may also be important team members for other chronic illnesses because the population of the U.S. is aging. Finally, allergists and immunologists, physician specialists, are a part of asthma care teams. These health professionals can confirm asthma diagnoses, provide additional recommendations, and assist with controlling more difficult symptoms.6
Nurses and Pharmacists
Nurses and pharmacists add additional expertise to primary care providers roles and teams. For years, nurses have shown that they can improve chronic disease management, especially if they are trained in the disease that their patient is experiencing. In an intervention for thyroid cancer, nurses had a comprehensive role by being involved in the reveal of biopsy results and providing support. Results of the intervention revealed that thyroid patients consider nurses an essential part of their care.19 Additionally, nurses assist primary care providers by communicating with them regularly and assisting with medication management by contacting pharmacists in the interest of physicians.8,20
A pharmacist is crucial to have on the team as they have also been shown to improve chronic disease management outcomes and can assist physicians with medication responsibilities.8,20 Pharmacists assist with medication management, adherence, and education.2,21 A hypothetical intervention using modeling examined the impact of a care team involving a pharmacist on health and cost in the U.S. It was found that pharmacists on a care team prevented uncontrolled blood pressure, heart attacks, strokes, and cardiovascular deaths over five years.21 A review of 54 studies conducted by the Community Preventive Services Task Force shows that nurses and pharmacists working together provide strong evidence for hypertension management.22 Specifically, blood pressure control and systolic blood pressure improved more when a nurse and pharmacist were on a team together and when they had the ability to control hypertension medication with and without physician approval.
Community Health Workers
Community health workers (CHWs) add significant assistance to care teams. Community health workers, also referred to as lay health workers, peer educators, patient navigators, among others, are trusted members of communities and provide support and resources to community members.23,24 Over the years, lay health workers have been shown to be effective on care teams to improve chronic disease management.8 For heart disease, community health workers have been associated with decreases in cardiovascular risks and reduction of blood pressure, cholesterol, and blood sugar levels.23 For HIV, community health workers have been able to commonly refer individuals to STI testing and health education during a street-based outreach intervention. The CHWs in this intervention referred ten individuals with HIV, to HIV medical care, twenty individuals who injected drugs to syringe service programs, and nineteen individuals who were at risk for HIV infections to a medical visit for PreP.23
Social Workers
Social workers team members of multiple care teams. During a multidisciplinary care team intervention, a team of a social worker along with a nurse and pharmacist resulted in improved antiretroviral therapy (ART) adherence.23 This adherence even occurred when nonHIV specialists were on the care team. Social workers who have led teams and have had shared responsibilities on teams have improved health outcomes related to asthma, maternal and child health, and hospitalized patients. These teams included nurses, physicians, PAs, pharmacists, counselors, and administrative staff. Patients with asthma had increased symptom-free days, NICU admission rates decreased, and mortality rates for patients who were frequently hospitalized decreased with the inclusion of social workers.24
Dietitians
Registered Dietitians show improved health outcomes on teams as well. A retrospective cohort study showed that high-risk adults had greater improvements in HbA1c and greater weight loss than the group only seen by a primary care physician.25 The study resulted in long-term improvements at six, twelve, and twenty-four months. Although the improvement related to weight loss was not significant at six or twenty-four months. The decrease in HbA1c was significant at twelve and twenty-four months. Dietitians are experts in nutritional counseling and a systematic review of randomized controlled trials examining the effects of dietitians in primary care environments showed that the effect of dietitians on weight management and blood sugar control to be positive. The same review showed fewer positive effects on cholesterol, blood pressure, and triglycerides but this could be because this review did not include multidisciplinary care team studies.26 If dietitians are not on the care team, then physicians and primary care providers can refer their patients to a nutrition professional.27
CHARACTERISTICS OF EFFECTIVE HEALTHCARE TEAMS
It is just as important to have teams that are effective than it is to have a team composed of certain professionals with specific expertise. Leadership is important to any team. Most healthcare teams will be led by physicians. If fact, the American Medical Association believes that physicians should lead all teams due to physicians’ high level of expertise and scope of practice.28 In contrast, the American College of Cardiology states that the leadership role of care teams should be dependent on the task that needs to be completed. The leader of the team should be a flexible role.2
151
Team roles need to be clarified and clearly stated.2,7,18 Explicitly defined roles help inform all team members of each member’s responsibilities and duties so that there is no confusion. Team members who are aware of their roles can then take accountability for their actions. Confusion can be avoided with proper communication between and within teams as well. Communication should be clear and prompt.7,8 Regular team meetings can enhance team communication.5
DISCUSSION
Health care teams are now more than ever becoming imperative as the physician shortage problem worsens, the U.S. population ages, and disease severity increases. The patient is at the forefront of all healthcare teams while other members can vary. Most often, primary care providers, nurses, pharmacists, community health workers, social workers, dietitians, and specialists should collaborate with the patient. Other members on care teams will depend on the type of illness, patient characteristics, and setting. Health professionals can delegate tasks away from each other so that other members can practice at their full capacity. Though, no matter what, team members must work within their scope of practice.5
Effective teams are just as important as the composition of teams. Effective teams improve patient outcomes and enhance how teams interact with one another. A survey of primary care providers and staff from primary care clinics in San Francisco found that a positive team culture improves burnout in primary care. Team culture was found to have more benefit in decreasing burnout than team structure.29
CONCLUSION
Implementing effective care teams is imperative as the nature of primary care changes and the physician shortage issue continues. Patients, primary care providers, nurses, pharmacists, community health workers, social workers, dietitians, and specialists should be involved on all teams to encompass all aspects of care and enhance patient outcomes. The composition of care teams will vary slightly depending on the patient needs and care environment. Care teams should be trained to work together effectively.
REFERENCES
1. IHS Markit LTd. (n.d.). The complexities of physician supply and demand: Projections from 2019 to 2034. Association of American Medical Colleges. https://www.aamc.org/media/54681/download
2. Brush, J. E., Jr., Handberg, E. M., Biga, C., Birtcher, K. K., Bove, A. A., Casale, P. N., . . . Wyman, J. F. (2015, May 19). 2015 ACC health policy statement on cardiovascular team-based care and the role of advanced practice providers. Journal of the American College of Cardiology, 65(19), 2118–2136. https://doi.org/10.1016/j.jacc.2015.03.550
3 Hupke, C. (2014, May 16). Team-based care: optimizing primary care for patients and providers. Institute for Healthcare Improvement. http://www.ihi.org/communities/blogs/team-based-care-optimizing-primary-care-for-patients-and-providers-
4. Arnett, D. K., Blumenthal, R. S., Albert, M. A., Buroker, A. B., Goldberger, Z. D., Hahn, E. J., . . . Ziaeian, B. (2019, September 10). 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation, 140(11), e596–e646. https://doi.org/10.1161/CIR.0000000000000678
5. Institute for Healthcare Improvement. (n.d.). Optimize the care team. http://www.ihi.org/resources/Pages/Changes/OptimizetheCareTeam.aspx
6. American Academy of Allergy Asthma and Immunology. (n.d). Consultation and referral guidelines: How the allergist/ immunologist can help. https://www.aaaai.org/Allergist-Resources/Statements-Practice-Parameters/consultation-and-referral-guidelines
7. Safford, B. H., & Manning, C. (2012, May-June). Six characteristics of effective practice teams. Family Practice Management, 19(3), 26–30. https://www.aafp.org/pubs/fpm/issues/2012/0500/p26.html
8. Wagner, E. H. (2000, February 26). The role of patient care teams in chronic disease management. BMJ (Clinical Research Ed.), 320(7234), 569–572. https://doi.org/10.1136/bmj.320.7234.569
9. Osarogiagbon, R. U., Rodriguez, H. P., Hicks, D., Signore, R. S., Roark, K., Kedia, S. K., . . . Krasna, M. J. (2016, November). Deploying team science principles to optimize interdisciplinary lung cancer care delivery: Avoiding the long and winding road to optimal care. J Oncol Pract, 12(11), 983–991. https://doi.org/10.1200/JOP.2016.013813
10. U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Primary Healthcare. (2017). Integrating HIV care, treatment & prevention services into primary care – a toolkit for health centers. https://bphc.hrsa.gov/sites/default/files/bphc/technical-assistance/p4c-toolkit-2018.pdf
11. Pany, M. J., Chen, L., Sheridan, B., & Huckman, R. S. (2021, March). Provider teams outperform solo providers in managing chronic disease and could improve the value of care. Health affairs (Project Hope), 40(3), 435–444. https://doi.org/10.1377/hlthaff.2020.01580
152 Delaware Journal of Public Health - December 2022
12. Institute of Medicine. (2013). Delivering high-quality cancer care: Charting a new course for a system in crisis. The National Academies Press. https://nap.nationalacademies.org/read/18359/chapter/6
13. Verhoeven, D. C., Chollette, V., Lazzara, E. H., Shuffler, M. L., Osarogiagbon, R. U., & Weaver, S. J. (2021, April 6). The anatomy and physiology of teaming in cancer care delivery: A conceptual framework. Journal of the National Cancer Institute, 113(4), 360–370.
https://doi.org/10.1093/jnci/djaa166
14. Health Resources and Services Administration. (n.d.). Optimizing HIV care for people aging with HIV: Putting together the best healthcare team. U.S. Department of Health and Human Services. https://ryanwhite.hrsa.gov/sites/default/files/ryanwhite/grants/aging-guide-best-team.pdf
15. Goldschmidt, R. H., & Chu, C. (2016, November 1). Primary care for patients with HIV infection: It’s not who should provide it, it’s how to provide it. American Family Physician, 94(9), 687–688. Retrieved from https://www.aafp.org/afp/2016/1101/p687.html
16. Asthma and Allergy Foundation of America. (n.d.). healthcare professionals. https://www.aafa.org/about-aafa/our-partners/health-care-professionals.aspx
17. U.S. Preventive Services Task Force. (2020, November). Healthy diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: Behavioral counseling interventions. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/healthy-diet-and-physical-activity-counseling-adults-with-high-risk-of-cvd
18. Taplin, S. H., Weaver, S., Salas, E., Chollette, V., Edwards, H. M., Bruinooge, S. S., & Kosty, M. P. (2015, May). Reviewing cancer care team effectiveness. J Oncol Pract, 11(3), 239–246. https://doi.org/10.1200/JOP.2014.003350
19. Henry, M., Frenkiel, S., Chartier, G., MacDonald, C., Payne, R. J., Black, M. J., . . . Hier, M. P. (2018, March). Thyroid cancer patients receiving an interdisciplinary team-based care approach (ITCA-ThyCa) appear to display better outcomes: Program evaluation results indicating a need for further integrated care and support. Psycho-Oncology, 27(3), 937–945. https://doi.org/10.1002/pon.4590
20. Smith, M. A. (2018, March). Primary care teams and pharmacist staffing ratios: Is there a magic number? The Annals of Pharmacotherapy, 52(3), 290–294. https://doi.org/10.1177/1060028017735119
21. Overwyk, K. J., Dehmer, S. P., Roy, K., Maciosek, M. V., Hong, Y., Baker-Goering, M. M., . . . Ritchey, M. D. (2019, November). Modeling the health and budgetary impacts of a team-based hypertension care intervention that includes pharmacists. Medical Care, 57(11), 882–889. https://doi.org/10.1097/MLR.0000000000001213
22. The Community Preventive Services Task Force. (2020, December). Heart disease and stroke prevention: Team-based care to improve blood pressure control. https://www.thecommunityguide.org/content/tffrs-heart-disease-and-stroke-prevention-team-based-care-improve-blood-pressure-control
23. Centers for Disease Control and Prevention. (2020, June). Integrating community health workers on clinical care teams and in the community. U.S. Department of Health & Human Services. https://www.cdc.gov/dhdsp/pubs/guides/best-practices/chw.htm
24. Centers for Disease Control and Prevention. (2016, January). CHW job titles. https://www.cdc.gov/dhdsp/chw_elearning/s1_p6.html
25. Zeman, H., Cavanaugh, E., Metallinos-Katsaras, E., Ireland, K., & Pojednic, R. (2021). Improved long-term outcomes in high-risk patients receiving registered dietitian nutritionist care. Endocrine and Metabolic Science, 2(31). https://doi.org/10.1016/j.endmts.2021.100078
26. Mitchell, L. J., Ball, L. E., Ross, L. J., Barnes, K. A., & Williams, L. T. (2017, December). Effectiveness of dietetic consultations in primary healthcare: A systematic review of randomized controlled trials. Journal of the Academy of Nutrition and Dietetics, 117(12), 1941–1962.
https://doi.org/10.1016/j.jand.2017.06.364
27. Ellis, E. (2021). Nutrition tips to keep the immune system strong for people with HIV-AIDS. Eat Right. https://www.eatright.org/health/diseases-and-conditions/hiv-aids/nutrition-tips-to-keep-the-immune-system-strong-for-people-with-hiv-aids
28. American Medical Association. (2022). What is scope of practice?
https://www.ama-assn.org/practice-management/scope-practice/what-scope-practice
29. Willard-Grace, R., Hessler, D., Rogers, E., Dubé, K., Bodenheimer, T., & Grumbach, K. (2014, March-April). Team structure and culture are associated with lower burnout in primary care. J Am Board Fam Med, 27(2), 229–238. https://doi.org/10.3122/jabfm.2014.02.130215
153
Considerations for Patient Panel Size
Caroline Harrington, MS, CHES Intern, Delaware Academy of Medicine/Delaware Public Health Association
INTRODUCTION
The prevalence of chronic disease remains high in the United States. In the U.S., six in ten adults experience a chronic illness while four in ten adults have two or more.1 Those that experience chronic conditions visit primary care physicians and specialists. Primary care enhances the health of populations, reduces health costs, and improves quality of life. By 2034 there will be a shortage of between 17,800 to 48,000 primary care physicians and a shortage of between 21,000 and 77,100 of non-primary care physicians.2 To ensure that proper patient care is provided, it is imperative that physicians and providers deliver adequate patient care to optimize health outcomes. Adequate patient care can be delivered by focusing on patient panel sizes for physicians, providers, and the organization of healthcare.
Patient panel size refers to the number of patients that a physician cares for during a specified period, usually 12 or 18 months. The standard patient panel size has often been determined to be 2500 patients. However, according to the Journal of the American Board of Family Medicine, this number is not feasible for a primary care physician to provide adequate patient interaction for all patients. At a panel size of 2500, a physician would have to work 21.7 hours per day to provide proper care to each patient.3,4 Calculating the ideal patient panel size is important to ascertain the number of patients seeking consultations and treatments, as well as the provider’s workload. It is important that providers on the same level share similar workloads, especially if they are earning similar salaries.5
Many factors affect what the patient panel size for a physician should be, including the organizational set up of practices, how the physician prefers to care for their patient, the type of patient population that the physician cares for, and the number and type of health professionals who work with physicians.3 Due to these changing factors, it can be just as important to manage patient panel sizes as it is to know the proper patient panel size.
The purpose of this review is to identify the number patients that should be on a provider’s panel to provide adequate patient interaction and determine how to manage patient panels for optimal outcomes. This review seeks to answer the following questions:
1.What is the ideal patient panel size based on disease (or wellness) state?
2.What factors affect patient panel size and how can panel sizes be managed correctly?
Answering these questions can provide guidance to primary care providers and team members to help providers have enough time to care for patients that need services. Optimizing care will improve patient health outcomes.
PATIENT PANEL SIZE
How to Determine Patient Panel Size?
Establishing a patient panel for providers ensures that the patient is given a provider with whom they can build a relationship and trust.5 Patients deserve adequate care to optimize their health outcomes and determining patient panel sizes can ensure that practices are making enough revenue. In the past, the ideal patient panel size has been calculated by determining the current panel size, not necessarily what the panel size should be for optimal care.5,6 Determining the current panel size has previously been completed by using the “four-cut method.”6
First, the patient panel for the practice must be identified. In 2007, the Family Practice Management Journal suggested that the patient panel for a practice was determined by identifying the patients who have seen a provider in the last 18 months, since many patients do not visit providers within a one year timeframe.7 More recently, the active panel has been suggested to be the patients seen by a physician or primary care provider within the last 12 months.6 It is unclear which period of time is correct, and practices may use different timeframes depending on what is best for them.
Second, the patient panel per provider is calculated by assigning a patient on the practice’s panel to the provider that they have visited the most. Sometimes, a patient on the practice’s panel has seen more than one provider. Certain guidelines can assist to determine what provider’s panel the patient should be on. If the patient has seen providers equally, then the patient is assigned to the provider who they saw first, last, or for their most recent health check.5,6
Another way to calculate patient panel size is using a supply and demand equation, like panel size multiplied by visits per patient per year (demand) which equals provider visits per day multiplied by provider days per year (supply). The number of patients needing an appointment must equal the number of appointment slots that a provider has available.7 Lack of appointments create high demand and may cause inadequate care. Too few patients needing to be seen causes practice revenue to decrease.
A systematic review to determine the patient panel size for the Veterans’ Administration (VA) showed that some of these older methods can be updated.8 The “right-sized” process can be used to determine what the panel should be for providers:6 this process factors in patient and workload complexity.6 Severity of patient illness, reporting and patient charting guidelines, refilling prescriptions, and conducting visits via telehealth while checking patients in-person throughout the workday will decrease physician capacity to conduct appointments.
DOI: 10.32481/djph.2022.12.034
154 Delaware Journal of Public Health - December 2022
In order to “right size” the patient panel, the Family Practice Management Journal created a spreadsheet. First, practices should use the “four-cut method to assign patients to providers. This information goes into the spreadsheet, which includes the current panel, visit rate, physician days worked, and visits per day so that the current panel and right-sized panel can be compared. The right-sized panel is calculated by dividing clinician visit capacity by the panel visit rate. The equation is days worked per year multiplied by visits per day divided by visit rate.6 No evidence was found that this equation determines the ideal patient panel size; numerous factors impact the capacity that physicians have to see patients, other factors influence the need for patients to receive services, and these factors can constantly evolve.
Factors A ecting Patient Panel Size / Supply and Demand Changing Primary Care System
Balancing patient demand and provider supply is important to create the ideal patient panel size, however the organization of healthcare affects demand and supply. Primary care in the U.S. is changing rapidly.9 Understanding primary care is important as populations in the U.S. visit primary care services more than any other type of healthcare service. The American Medical Association’s Physician Practice Benchmark Surveys assist in understanding the change in primary care. These surveys have been conducted every even year starting in 2012.10 From 2012 to 2018, the percentage of physicians practicing in large practices (at least 50 physicians) increased.11 In 2020, the number of physicians switching from working in private practice to working in hospitals increased.12,13 Although limited evidence shows that practice size is associated with quality of care, one review showed that some larger practices are associated with better quality of care while some smaller practices (five physicians or fewer) are related to improved patient outcomes, like satisfaction.14 The change from physicians working in larger practices compared to smaller practices may affect patient panel sizes. More physicians in the practice could allow for increased patient panels as physicians have the largest scope of practice. Still, no literature was found to support this relationship.
Physician Preferences and Characteristics
How a physician manages their patient affects patient panel size and supply of appointments. Some physicians may prefer to have fewer patients so that they can spend more time consulting with each patient. Longer and more in-depth visits increase the length of appointments which will impact how many patients can be seen per day.7
Types of physicians like residents and supervising physicians also affect panel size. Residents require a certain number of visits, but their panel is usually smaller than physicians. Supervising physicians and physicians who have academic responsibilities may also need an adjusted panel size to account for other duties.
Patient Characteristics
Patient population affects panel sizes. Age, failing to keep appointments, and disease complexity will impact demand and supply.7–9,15 In 2014, the youngest (0-4) and oldest (65-100) patients visited primary care physicians most often,9 but not all these patients will require the same amount of appointment time. Patients who fail to keep appointments affect the supply of physician visits per day: no shows make physicians unable to see any patient during an appointment slot.7 Patients with more severe illnesses may require longer visits.8
Future Supply
The supply of physicians is changing. Physicians in the United States are getting older. One reason for the shift away from smaller practices is that physicians are retiring but not being replaced by younger physicians.13 Many primary care physicians start in their 20s and work for around 40 years. In 2017, more than 25% of primary care physicians were 60 years of age or older.9 Many of these physicians are of retiring age. As physicians retire the supply of providers reduces, and the data shows that younger physicians are not necessarily taking the place of retiring physicians, especially ones who work in smaller practices. Older physicians may have decreased activity levels affecting their speed and type of care performed.15 Younger physicians may have higher activity levels and be more motivated to treat patients causing younger physicians to be able to see more patients.
Advanced Practice Providers
Physicians are primary care providers, but nurse practitioners and physician assistants provide primary care as well. As physicians retire and the physician shortage problem intensifies, it will be important to take a team-based approach and introduce more nurse practitioners and physician assistants into the healthcare workforce. In 2017, about 50% of nurse practitioners and 40% of physician assistants were practicing in primary care.9 Integrating additional primary care providers into practice environments positively affects patient panel size and supply and demand. NPs and PAs can increase the supply of provider appointments by increasing physicians’ scope of practice.16,17 A retrospective cross-sectional analysis was conducted using the National Sample of Survey of Nurse Practitioners to understand the productivity of nurse practitioners. Of the nurse practitioners included in the survey, some had their own patient panel (64%) while others did not. The average patient panel size for NPs with patient panels was 567. The average number of patients seen per week for NPs was around 80 patients, and this average did not differ between NPs who had a panel and those who did not: NPs who had their own patient panels provided a higher proportion of specific services to patients than NPs who did not have their own panels. Additionally, having a physician on site compared to not having one was associated with an increase in patients seen and greater chance of NPs having a patient panel.17
Team care can help with productivity. When physicians work with NPs as well as PAs, physicians can offer more services.16 NPs and PAs are advanced practice providers who have similar skill levels to physicians. Data from a survey from the American Board of Family Medicine Certification Examination showed that PAs had a larger effect on primary care physician panels and scope of practice than NPs and PAs and NPs together: the mean panel size was 2,263.16
155
MANAGING PATIENT PANEL SIZES
Managing patient panel sizes can be helpful since many different factors affect the ideal patient panel size per provider. Provider panels have limits: if providers are assigned too many patients, then wait times, no-shows, and scheduling increases. However, avoiding too small of patient panels is just as important. Costs of practices cannot be covered when panel sizes are too small.7
Practices can close provider panels to new patients if a provider has too many patients on their list.5,6,18 The panel can remain open for providers that have lower patient panels unless the whole practice needs to close to new patients. Hiring new team members can help limit patient panel sizes to avoid closing provider panels.19 Assigning other staff members to assist physicians can help optimize patient panel size, as can assigning nurses or physician assistants to patient appointments.19
Practices and physicians can also optimize the visit length, which then affects the number of patients seen.7 Practices should ensure that patients see the same doctor regularly so that relationships can be built. Reducing visit interruptions by ensuring all equipment needs are in the room and tests and labs are completed can reduce visit length. Finally, team members can limit visit length by supporting the primary care provider and limiting physician responsibilities that other staff can accomplish.
DISCUSSION
Research is needed to calculate the ideal patient panel size for any disease or wellness sate. Angstman et al could not identify their primary objective of determining the ideal panel size for their practice,20 and the strongest evidence shows that a panel size of 2500 patients per provider is not feasible.3,4 Higher panel sizes may negatively affect patient health outcomes, and may be associated with poorer clinical quality, patient experience, and burnout of providers.21
Determining a proper patient panel size is important for practices and providers to establish patient provider relationships, ensure providers are sharing workloads, and confirm that costs of practices are being covered. It may be as equally important to focus on other aspects of care—like the factors affecting panel sizes—to ensure that providers are providing the most cost effective and adequate care.8,20–22
CONCLUSION
Large patient panels per provider are likely not feasible, but determining the optimal patient panel per provider is challenging. Demand for appointments and supply of providers are ever evolving. Assigning patients to providers should be done so that provider-patient relationships can be formed. Limiting visit length, and preparing for changes in primary care and supply by utilizing other healthcare providers may provide efficient care and reduce physician patient panel sizes as needed.
REFERENCES
1. Centers for Disease Control and Prevention. (2022). Chronic diseases in America. U.S. Department of Health and Human Services. https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm
2. IHS Markit LTd. (2021, Jun). The complexities of physician supply and demand: Projections from 2019 to 2034. Association of American Medical Colleges. https://www.aamc.org/media/54681/download
3. Raffoul, M., Moore, M., Kamerow, D., & Bazemore, A. (2016, July-August). A primary care panel size of 2500 is neither accurate nor reasonable. J Am Board Fam Med, 29(4), 496–499. https://doi.org/10.3122/jabfm.2016.04.150317
4. Minemyer, P. (2016). Study discredits industry standard panel size for primary care physicians. https://www.fiercehealthcare.com/practices/study-discredits-industry-standard-panel-size-for-primary-care-physicians
5. Murray, M., Davies, M., & Boushon, B. (2007, April). Panel size: How many patients can one doctor manage? Family Practice Management, 14(4), 44–51. Retrieved from https://www.aafp.org/fpm/2007/0400/p44.html
6. Weber, R., & Murray, M. (2019, November/December). The right-sized patient panel: A practical way to make adjustments for acuity and complexity. Family Practice Management, 26(6), 23–29. Retrieved from https://www.aafp.org/fpm/2019/1100/p23.html
7. Murray, M., Davies, M., & Boushon, B. (2007, November-December). Panel size: Answers to physicians’ frequently asked questions. Family Practice Management, 14(10), 29–32.
Retrieved from https://www.aafp.org/fpm/2007/1100/p29.html
8. Shekelle, P. G., Paige, N. M., Apaydin, E. A., Goldhaber-Fiebert, J. D., Mak, S. S., Miake-Lye, I. M., . . . Boroes-Severin, J.M. (2019). What is the optimal panel size in primary care? A systematic review. U.S. Department of Veterans Affairs. https://www.hsrd.research.va.gov/publications/esp/panel-size-primary-care.pdf
9. Petterson, S., McNellis, R., Klink, K., Meyers, D., & Bazemore, A. (2018). The state of primary care in the United States: A chartbook of facts and statistics. https://www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/PrimaryCareChartbook.pdf
156 Delaware Journal of Public Health - December 2022
10. American Medical Association. (n.d.). Physician practice benchmark survey. https://www.ama-assn.org/about/research/physician-practice-benchmark-survey
11. Kane, C. K. (2019). Updated data on physician practice arrangements: For the first time, fewer physicians are owners than employees. American Medical Association.
https://www.ama-assn.org/system/files/2019-07/prp-fewer-owners-benchmark-survey-2018.pdf
12. American Medical Association. (2021, May 5). AMA analysis shows most physicians work outside of private practice. [Press release].
https://www.ama-assn.org/press-center/press-releases/ama-analysis-shows-most-physicians-work-outside-private-practice
13. Kane, C. K. (2021). Recent changes in physician practice arrangements: Private practice dropped to less than 50 percent of physicians in 2020. American Medical Association. https://www.ama-assn.org/system/files/2021-05/2020-prp-physician-practice-arrangements.pdf
14. Ng, C. W., & Ng, K. P. (2013, September). Does practice size matter? Review of effects on quality of care in primary care. Br J Gen Pract, 63(614), e604–e610. https://doi.org/10.3399/bjgp13X671588
15. Finarelli, H. J. (2009). How many physicians make a health system? The hospital executive‘s guide to physician staffing. (pp. 103123). HealthLeaders Media. https://store.healthleadersmedia.com/aitdownloadablefiles/download/aitfile/aitfile_id/1672.pdf/
16. Dai, M., Ingham, R. C., & Peterson, L. E. (2019, April). Scope of practice and patient panel size of family physicians who work with nurse practitioners or physician assistants. Family Medicine, 51(4), 311–318. Retrieved from https://journals.stfm.org/familymedicine/2019/april/dai-2018-0146/ https://doi.org/10.22454/FamMed.2019.438954
17. Xue, Y., & Tuttle, J. (2017, March - April). Clinical productivity of primary care nurse practitioners in ambulatory settings. Nursing Outlook, 65(2), 162–171. https://doi.org/10.1016/j.outlook.2016.09.005
18. Institute for Healthcare Improvement. (n.d.). Decrease demand for appointments. http://www.ihi.org/resources/Pages/Changes/DecreaseDemandforAppointments.aspx
19. Institute for Healthcare Improvement. (n.d.). Manage panel size and scope of the practice. http://www.ihi.org/resources/Pages/Changes/ManagePanelSizeandScopeofthePractice.aspx
20. Angstman, K. B., Horn, J. L., Bernard, M. E., Kresin, M. M., Klavetter, E. W., Maxson, J., . . . Thacher, T. D. (2016, July-August). Family medicine panel size with care teams: Impact on quality. J Am Board Fam Med, 29(4), 444–451. https://doi.org/10.3122/jabfm.2016.04.150364
21. Paige, N. M., Apaydin, E. A., Goldhaber-Fiebert, J. D., Mak, S., Miake-Lye, I. M., Begashaw, M. M., . . . Shekelle, P. G. (2020, February 4). What is the optimal primary care panel size? A systematic review. Annals of Internal Medicine, 172(3), 195–201. Retrieved from https://doi-org.udel.idm.oclc.org/10.7326/M19-2491 https://doi.org/10.7326/M19-2491
22. Robeznieks, A. (2020, March). What’s the right panel size for your physician private practice? https://www.ama-assn.org/practice-management/private-practices/whats-right-panel-size-your-physician-private-practice
157
Scope and Specialization in Dental Care
Caroline Harrington, M.S., C.H.E.S.
Jeffrey Cole, D.D.S., M.B.A.
Joseph Kelly, D.D.S.
Oral health is an important, and often overlooked, aspect of general health. Simple oral care—regular tooth brushing, flossing, avoiding smoking, and decreasing the intake of sugary foods and drinks—and visiting a dentist for regular cleanings and dental exams can greatly reduce the chances of suffering from various oral health problems.1 The American Dental Association (ADA) states that oral health is an essential part of healthcare due to its role in evaluating, diagnosing, preventing and/or treating oral diseases, which can affect systemic health.2
In addition to general dentistry, the National Commission on Recognition of Dental Specialties and Certifying Boards (NCRDSCB) recognizes twelve specialties, where advanced knowledge and skills greater than those taught in graduate dental education programs are taught: dental anesthesiology; dental public health; endodontics, oral and maxillofacial pathology, radiology, and surgery; oral medicine; orofacial pain; orthodontics and dentofacial orthopedics; pediatric dentistry; periodontics; and prosthodontics.3
The ADA estimates that 100 million Americans do not visit a dentist on a yearly basis, despite the fact that preventative care and good oral hygiene can prevent most dental disease.4 The most prevalent dental problem world-wide is tooth decay (dental caries or cavities). According to the Centers for Disease Control and Prevention (CDC), almost 90% of adults have some degree of tooth decay.5 Other major dental problems, like gingivitis (gum disease), tooth sensitivity, and oral cancer can be alleviated or cured with early diagnosis and treatment.4
Adults of working-age and seniors are more likely to face financial barriers to obtaining dental care than children, perhaps in part due to the inclusion of pediatric dental care in the Affordable Care Act of 2010, and the mandatory Early and Periodic Screening, Diagnostic, and Treatment benefit of Medicaid.1 As with any type of healthcare, having a sufficient number and distribution of providers is essential to ensuring access to care. In 2020, there were 201,117 practicing dentists in the US, or approximately 60 dentists per 100,000 population, and is expected to increase somewhat until 2040.6 In 2016, there were 437 dentists in Delaware, of which 352 were general/pediatric dentists, or 1 dentist to every 3,128 persons.7 (We should acknowledge that Delaware borders New Jersey, Maryland and Pennsylvania, and patients may seek care in the adjacent states due to proximity. An example would be patients in western Sussex County seeking care in Salisbury, Maryland.) Sussex County was the only Delaware county considered underserved (exceeding the threshold of 5,000 patients to one dentist).7
REFERENCES
1. Vujicic, M., & Fosse, C. (2022, Jan). Time for dental care to be considered essential in US healthcare policy. AMA Journal of Ethics. https://journalofethics.ama-assn.org/article/time-dental-care-be-considered-essential-us-health-care-policy/2022-01
2. American Dental Association. (2020). Current policies. https://www.ada.org/about/governance/current-policies
3. NCRDSCB. (n.d.). Specialty definitions. NCRDSCB. https://ncrdscb.ada.org/en/dental-specialties/specialty-definitions
4. Medical News Today. (n.d.). What to know about dental problems and oral health. https://www.medicalnewstoday.com/articles/dental-problems
5. CDC. (2019). Dental caries among adults and older adults. https://www.cdc.gov/oralhealth/publications/OHSR-2019-dental-carries-adults.html
6. Munson, B., & Vujicic, M. (2021, May). Projected supply of dentists in the United States, 2020-2040. Health Policy Institute. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/hpibrief_0521_1.pdf
7. Tóth, T. (2017, May). Dentists in Delaware-2016. Center for Applied Demography & Survey Research, University of Delaware. https://dhss.delaware.gov/dph/hsm/files/dentistsinde2016.pdf
DOI: 10.32481/djph.2022.12.03.035
158 Delaware Journal of Public Health - December 2022
TRAPPED BY TOBACCO? WE HAVE A WAY OUT.
Call the Delaware Quitline and free yourself from tobacco. Free counseling, cessation aids, and medications are available to help you get on the path to living tobacco-free. Stop getting pulled back in. Let us help you quit for good.
QuitSupport.com

159
Caroline Harrington, M.S.,
Jeffrey Cole, D.D.S., M.B.A.
Joseph Kelly, D.D.S.
Composition of Ideal Dental Team
C.H.E.S.
INTRODUCTION
Oral health is essential to individuals’ overall health and quality of life, so it is important that dental professionals are considered in the healthcare workforce. Poor oral health can lead to tooth decay (cavities), gum disease (periodontal disease), or oral cancer. Cavities are a common condition that can occur from childhood to adulthood.1 Individuals with oral cancers have a five-year survival rate of 61%. Stained teeth, cavities, mouth cancers, gum disease, and canker sores can develop when an individual engages in smoking.2,3 Smokeless tobacco causes the same conditions. Cavities can also develop from consuming foods high in sugar. The food that an individual consumes affects oral health and the condition of the mouth affects what a person can eat.4 Oral health is not only related to smoking and eating habits. Oral health is associated with other chronic conditions such as heart disease and diabetes.1 Early detection of these chronic and oral conditions is crucial to ensure an individual’s quality of life remains. Unfortunately, oral health problems affect populations disproportionately. Older adults, non-Hispanic Black Americans, and Mexican Americans experience tooth decay that goes untreated more than non-Hispanic White Americans.5,6 Healthy People 2030 focuses on oral health with the goals to decrease oral health issues and increase access to oral care services as not all Americans have equal access to care.7 In 2020, sixty million Americans resided in Dental Health Professional Shortage Areas (DHPSA).8 There are various dental professionals in the workforce and understanding the composition of the dental team can lead to better quality care and improved access to dental services.
DENTAL TEAM
General Dentists and Dental Specialists
Dentists act as the leader of the dental care team and supervise other members of the dental profession, like dental hygienists and dental assistants.9 Dentists include general dentists, oral and maxillofacial surgeons, orthodontists, and prosthodontists, among other specialties, and they are required to be licensed.10,11 Dentists diagnose and treat problems of the mouth and teeth. They examine the gums, teeth and mouth, fill cavities and refer individuals to other healthcare professionals when needed.11,12 Dentists also provide education about proper nutrition, smoking cessation and proper oral health behaviors.3,11–13 Dentists are encouraged to educate their patients about healthy eating behaviors such as limiting sugar sweetened beverages due to the association between nutrition and oral health.13 Dentists are also encouraged to provide patients who smoke with resources, information and education about quitting smoking because of the affects that smoking has on oral health problems and health.3 Dentists inform patients of oral health behaviors like flossing, brushing teeth twice a day, and seeing a dentist regularly as well.12,13
Dental Hygienists, Dental Assistants, and Dental Laboratory Technicians
Dental hygienists, dental assistants and dental laboratory technicians are supervised by dentists. All states require licensure for dental hygienists.10,14 Teeth cleanings and taking x-rays are common responsibilities of a dental hygienist.12,14,15 Like dentists, dental hygienists provide oral health education, including how to floss and what toothbrushes to use.14 A dental hygienist also reviews oral health histories and can conduct oral health screenings.12 Dental hygienists can screen for diabetes, oral cancer, and hypertension, among other conditions.16-18 Screening for chronic diseases is important in the dental field since oral health is linked to many different conditions. Screening also allows for early detection and treatment of diseases. However, not all dental hygienists screen for such diseases. A cross-sectional survey of dental hygienists who practiced in the U.S. and Canada showed that 56% of dental hygienist state screening for diabetes is their responsibility but many do not screen due to of lack of time, education, and awareness of state rules and regulations related to screenings. Ninety-five percent did report that they provide education about the association between diabetes and oral health.16 Similar results occurred for oral cancer. A systematic review showed that dental hygienists feel that they are knowledgeable about oral cancer risks factors, like tobacco but that they lack the education to perform certain screenings, like palpation of lymph nodes.17 Overall, a survey of three thousand one hundred thirty-three dental hygienists showed that 85% of dental hygienists feel it is important to screen for conditions, especially hypertension and diabetes. Training, time, and dentist and owner support were reported to be factors that affect dental hygienists’ likelihood of conducting medical screening.18 Dental assistants work directly with dentists, assisting them during procedures.12,19 These dental professionals may also perform x-rays and provide education after surgery.15,19 Scheduling patient appointments and keeping records are other tasks dental assistants perform.12 Dental laboratory technicians work closely with dentists but do not have as much contact with patients as dental hygienists and dental assistants. Dental laboratory technicians follow dentists’ instructions to create dental appliances, like dentures, crowns, veneers and bridges.12,15,20
Community Dental Health Coordinators
Community dental health coordinators (CDHDs) are dental professionals that have been recently integrated into the field of dentistry. Community dental health coordinators improve dental care as well. These professionals act as community health workers and patient navigators to connect individuals struggling to access dental care to dental services in their area.15,21 CDHCs were first introduced in the United States through a program that the American Dental Association piloted. The program improved oral health outcomes and access to dental care. Results reported from the pilot program showed that one hundred eighty-four children aged zero to three years old were set up with dental care by one CDHC in Virginia, and in New Jersey, HPV vaccine rates increased by 19% due to the incorporation of CDHCs. Overall, the pilot program connected six thousand patients to dental services.22
DOI: 10.32481/djph.2022.12.03.036
160 Delaware Journal of Public Health - December 2022
CONCLUSION
Dentists, dental hygienists, dental assistants, dental laboratory technicians, and community dental health coordinators account for the dental care team. These healthcare professionals improve oral health problems and impact other health conditions. CDHCs are not common among dental professionals throughout the United States.23
REFERENCES
1. Centers for Disease Control and Prevention. (2022). Oral health conditions. U.S. Department of Health and Human Services. https://www.cdc.gov/oralhealth/conditions/index.html
2. Centers for Disease Control and Prevention. (2020). Dental Professionals: Help your patients quit. U.S. Department of Health and Human Services. https://www.cdc.gov/oralhealth/publications/features/dental-pros-help-your-patients-quit-tobacco.html
3. American Dental Association. (2022) Tobacco use and cessation. https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/tobacco-use-and-cessation
4. American Dental Association. (2021). Nutrition and oral health. https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/nutrition-and-oral-health
5. Centers for Disease Control and Prevention. (2021). Disparities in oral health. U.S. Department of Health and Human Services. https://www.cdc.gov/oralhealth/oral_health_disparities/index.htm
6. Office of Disease Prevention and Health Promotion. (n.d.) Oral health workgroup. U.S. Department of Health and Human Services. https://health.gov/healthypeople/about/workgroups/oral-health-workgroup
7. Office of Disease Prevention and Health Promotion. (n.d.) Oral conditions. U.S. Department of Health and Human Services. https://health.gov/healthypeople/objectives-and-data/browse-objectives/oral-conditions
8. County Health Rankings. (n.d.) Dentists. University of Wisconsin Population Health Institute School of Medicine and Public Health. https://www.countyhealthrankings.org/explore-health-rankings/measures-data-sources/county-health-rankings-model/health-factors/clinical-care/access-to-care/dentists
9. U.S. Bureau of Labor Statistics. (2022). Dentists. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/dentists.htm
10. Torpey, E. (2020). Dental work: Careers in oral care. U.S. Department of Labor. https://www.bls.gov/careeroutlook/2020/article/dental-careers.htm
11. U.S. Bureau of Labor Statistics. (2022). Dentists. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/dentists.htm
12. National Institute of Dental and Craniofacial Research. (2021). Oral health in America: Advances and challenges. U.S. Department of Health and Human Services, National Institutes of Health. https://www.nidcr.nih.gov/sites/default/files/2021-12/Oral-Health-in-America-Advances-and-Challenges.pdf#page=495
13. American Dental Association. (2016). Diet and nutrition. https://www.ada.org/about/governance/current-policies#dietnutrition
14. U.S. Bureau of Labor Statistics. (2022). Dental hygienists. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/dental-hygienists.htm
15. American Dental Association. (n.d.). Dental team careers. https://www.ada.org/resources/careers/dental-team-careers
16. DeBiase, C., Giblin-Scanlon, L., Boyd, L. D., & Vineyard, J. (2020, April). Knowledge, attitudes and practices of dental hygienists regarding diabetes risk assessments and screenings. J Dent Hyg, 94(2), 37–44. https://pubmed.ncbi.nlm.nih.gov/32354850
17. Coppola, N., Rivieccio, I., Blasi, A., Ferrigno, R., Baldares, S., Mignogna, M. D., & Leuci, S. (2022, May). Current knowledge, attitude and practice among dental hygienists in oral cancer awareness: Systematic review. International Journal of Dental Hygiene, 20(2), 249–261. https://doi.org/10.1111/idh.12575
18. Greenberg, B. L., Kantor, M. L., & Bednarsh, H. (2017, November). American dental hygienists’ attitudes towards chairside medical screening in a dental setting. International Journal of Dental Hygiene, 15(4), e61–e68. https://doi.org/10.1111/idh.12217
19. U.S. Bureau of Labor Statistics. (2022). Dental assistants. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/dental-assistants.htm
20. U.S. Bureau of Labor Statistics. (2022). Dental and Ophthalmic Laboratory Technicians and Medical Appliance Technicians. U.S. Department of Labor.
https://www.bls.gov/ooh/production/dental-and-ophthalmic-laboratory-technicians-and-medical-appliance-technicians.htm#tab-2 – 5
21. American Dental Association. (n.d.). Community dental health coordinator. https://www.ada.org/resources/community-initiatives/action-for-dental-health/community-dental-health-coordinator
22. American Dental Association. (n.d.). The value of community dental health coordinators [Fact Sheet]. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/communityinitiatives/action-for-dental-health/community-dental-health-coordinator/ada_cdhc_value_infographic. pdf?rev=77b553b44e324ec281873256b52f64bb&hash=5CBBD0E0BCFBBA5F83C0A7D622FDD4D6
23. Community Health Rankings. (2016). Allied dental health professional scope of practice. University of Wisconsin Population Health Institute School of Medicine and Public Health.
https://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health/strategies/allied-dental-professional-scope-of-practice
161
Delaware Health Provider Shortage Areas
Nichole Moxley, B.S. Director, Primary Care Office, Delaware Department of Health and Social Services
There are State Primary Care Offices (PCO) programs located in every state and territory of the United States. The PCO program is funded by the Health Resources and Services Administration (HRSA). In Delaware, the PCO program is located within the Bureau of Health Planning and Resources Management of the Division of Public Health. The PCO program facilitates the coordination of activities to assess the need for primary care, dental health, and mental health providers and services, promote recruitment and retention of providers to fulfill identified needs, work to identify Health Professional Shortage Area designations, and reduce healthcare provider shortages.
One of the key aspects of the PCO program is Health Professional Shortage Area (HPSA) designations. HPSA designations denote geographic areas, populations, and facilities without adequate providers and services (shortages) in the disciplines of primary care, dental health, and mental health. The purpose of HPSA designations is to improve healthcare service delivery and workforce availability, in each of the disciplines, to meet the needs of underserved populations in the designated areas. Determining which areas should be shortage designations is central to prioritizing and focusing resources to the areas of highest need.
To determine if an area is experiencing a shortage of health professionals, the PCO reviews several data elements that are sourced from the American Community Survey, Centers for Disease Prevention and Control, Census Tiger Geometry Data, ESRI 2020 ArcGIS, Uniform Data System, and the National Provider Identifier data file. These data elements are assigned a point value and combined to determine an overall score – the higher the score the higher the need. The data elements and their point values for each of the disciplines is outlined in table 1 below.
Table 1. HPSA Scoring
DOI: 10.32481/djph.2022.12.03.037
Data
Primary Care Dental Health Mental Health Rational Service Area Census Tract(s) County Census Tract(s) County Census Tract(s) County
Provider Ratio 10 10 7 Percent
Area 5 10 5 Travel Time
Source of Care 5 5 5 Infant
Rate) 5 0 0 Water Fluoridation
0 1 0 Elderly
0 0 3
0 0 3
0 0 1 Alcohol
0 0 1 HRPA Score 25 26 25 162 Delaware Journal of Public Health - December 2022
Elements HPSA Disciplines
Population to
of Population below 100% Federal Poverty
to the Nearest
Health Index (Low birth weight or Infant Mortality
Status
Ratio (percent of people over age 65)
Youth Ratio (percent of people under age 18)
Substance Abuse Prevalence
Abuse Prevalence
Once the analysis is complete for each of the rational service areas and disciplines, the information is submitted to the HRSA for review and approval. If the request is denied, the PCO and HRSA work together to determine if the information can be revised to obtain a designation and if a designation is not possible – the request is denied. If the request for designation is approved, the HRSA issues a formal notice approving the designation and the designation is valid for a minimum of one year or until the data sources are updated with new information to request a designation update. Delaware has HPSA designations for primary care (figure 1), dental health (figure 2), and mental health (figure 3).
Figure
1. Delaware HPSA Designations Primary Care

Figure 2. Delaware HPSA Designations Dental Health
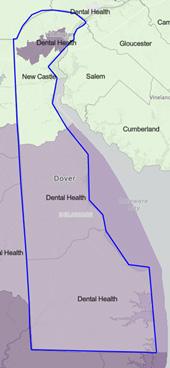
3. Delaware HPSA Designations Mental Health

Figure
HPSAs are prerequisites for various Federal and State programs. Providers rendering service in HPSA designated areas are eligible to participate in medical education loan repayment programs; National Health Service Corps (NHSC) Loan Repayment Programs; Traditional, Substance Use Disorder, and Rural Community; NHSC Scholarship Program; Delaware State Loan Repayment and Healthcare Provider Loan Programs; Nurse Corps and Nurse Scholar Programs; and the j1 Visa Waiver Program. And there is potential for grants residency and training programs across the primary care, dental health, and mental health disciplines, public health projects, and nurse training and education programs.
163
Extraordinary Impacts on the Healthcare Workforce: COVID-19 and Aging
Matt McNeill, B S Research Associate, Delaware Academy of Medicine/Delaware Public Health Association
INTRODUCTION
The COVID-19 pandemic has created challenges in just about every facet of everyday life, for everyone across the world. Offices closing, restaurants closing, zoom meetings and online classes all became the new normal. Our population faced a challenge it has not seen since 1918, when the Spanish Influenza rampaged throughout the world, killing an estimated 50 million people.1 While COVID-19 may not have the same lethality as the Spanish Influenza, it put a strain on our modern medical system. The pandemic pulled apart the fibers of the global healthcare ecosystem and exposed some major shortcomings in pandemic preparedness, which has caused ripple effects throughout the world.
COVID-19 AND HEALTHCARE
During the first wave of the pandemic, COVID-19 patients were being admitted to hospitals at such a rapid pace that it was difficult to keep them isolated from the rest of the patient population. The pressure on healthcare workers and engineers to develop controls for a safe working environment led to some exceptional innovation in minimizing the transferability of airborne illness in efficient and cost-effective ways. Due to the limited number of negative pressure isolation units, regular heating, ventilation, and air conditioning (HVAC) systems could continue to circulate the disease to uninfected units of the hospital.2,3 In a study conducted at a skilled nursing facility (SKF) in Lancaster, Pennsylvania, negative air pressure isolation of individual rooms using modified HVAC systems seemed to keep airborne disease from escaping the negative pressure space.2 A similar system was used in South Korea, where existing HVAC systems were adapted to create negative pressure zones in existing hospital units that were turned into isolation units, with a dressing room outside of the individual isolation units as well as a buffer room between the isolation room and the hallway.3 This process of creating negative pressure spaces could also be used to turn non-hospital buildings like warehouses into temporary COVID-19 units.3 Despite innovations in patient isolation, the drastic increase in hospitalizations meant that nurses, who perform much of the direct patient care in a hospital setting, had more dangerous and psychologically taxing work than ever before.4 A 2020 edition of “The Exchange” notes that “COVID-19 has presented healthcare with a unique set of challenges: constrained resources, a highly infectious, novel pathogen that poses a significant threat to the health of providers and support staff, large numbers of critically ill patients and deaths—often with only the caregivers to accompany the patient in their final moments—limited [personal protective equipment] PPE and therapeutics, restricted social interactions, and a protracted timeline with no clear end in sight. These challenges have contributed to unprecedented mental health impacts among healthcare workers.”5
SYSTEM BURNOUT AND LOSS
The Office of the Inspector General of the U.S. Department of Health and Human Services contacted over 300 hospitals asking what challenges they faced because of the pandemic, to which the overwhelming response was a lack of staff and critical care equipment, causing difficulties in resuming routine hospital care.4 In a meta-analysis paper detailing the impacts of COVID-19 on the nursing workforce specifically, Michelle Cleary of Central Queensland University indicated that the increased workload and inflexibility of hours—as well as significant lack of mental health treatment for nurses—has led to tremendous burnout and an exodus from the profession.6 The increase in demand for nursing care, coupled with the seemingly ever-decreasing supply due to burnout from inadequate mental healthcare for providers and a significant lack of hospital resources like PPE and critical care equipment, have led to a nursing shortage that extends across the globe.
Nurses were not the only people who felt burnt out or nervous about contracting COVID-19; a 2021 article from Bloomberg suggests as many as three million Americans may have retired early across the job market.7 Another 2021 article by CNBC quotes a figure of around 3.2 million more Baby Boomers retired in late 2020 than expected, and the number of Americans planning to work past age 67 dropped 32.9%.8 For the first time in history, healthcare workforce jobs were not recession-proof, and employment rates fell along with other job sectors.9 A recent AMA study found “20% of physicians said they were likely to leave their current practice within two years, while one third planned to reduce their work hours in the next 12 months.”10 Nurses are leaving the profession at an unprecedented rate due to burnout and aging medical professionals are seeking to reduce their hours or outright retire early due to pandemic fears.4,7,8,10
While the outbreak of COVID-19 has certainly impacted the burnout rates both in the U.S. and abroad, excess healthcare worker deaths are also causing shortages across the globe. A 2021 Working Paper by The WHO claims that the 6,633 reported healthcare worker deaths due to the pandemic falls embarrassingly short of reality, which they estimate could be anywhere between 83,000 and 115,000.11 The WHO states that much of the underreporting comes from their African, South-East Asia, Eastern Mediterranean and Western Pacific regions, where it is reasonable to assume that the excess deaths are contributing to stress and burnout in those
DOI: 10.32481/djph.2022.12.038
164 Delaware Journal of Public Health - December 2022
healthcare workers that have survived, as well as disparities in access to care across those regions most heavily impacted by the loss.11
AN AGING POPULATION
The impact of the reduction in the healthcare workforce is being compounded by an overall aging population. A Chinese study conducted on patients with COVID-19 found that the elderly [60+] were more likely to have comorbidities that influence the outcome of COVID-19 infection than those who are not elderly [<60].12 This study also indicates that the proportion of severe cases was higher in the elderly than in the non-elderly. Addressing the Health Needs of an Aging America states “[b]y 2050, adults over the age 65 will make up 20 percent of the U.S. population.”13 The surge in retirees, not just from the healthcare workforce but from the overall population, has left the tenability of certain social programs, such as Social Security and Medicare, questionable at best. The National Academy of Social Insurance predicts that social security will face significant challenges by the year 2030, as more adults age 65+ will be taking benefits from Social Security than there are adults in the workforce paying into it.14 These figures indicate a growing shortage of healthcare providers that is expected to keep growing, as well as an aging population that will inevitably require increased care in the coming years, with high potential for limited availability of social programs, greatly exacerbating the growing shortage of providers in the healthcare workforce.
SHORTAGES AND DISPARITIES
In the United States, the shortage within the primary care workforce and the disparities in available primary care both between and within different states have been a known issue for over a decade. As stated previously, the U.S. also faces the challenge of an aging population that will require increased primary care. In 2014, the Stern Center for Evidence-Based Policy at the University of Pittsburgh contends that “[w]hile the U.S. population of adults aged 65 and older currently account for only 13% of the population, this cohort consumes more 34% of national health expenditures.”13 A 2013 review conducted by the Robert Graham Center estimated that, by 2030, Delaware would need an additional 177 primary care physicians—a 27% increase from 2010.15 This review only considered physicians, and not the significant number of physicians assistants, nurse practitioners, specialists (e.g. obstetricians, gynecologists, cardiologists), and mental health professionals who also either practice primary care or are deemed a primary care provider by patients. Data sourced from the Delaware Professional Regulatory Online Services (DELPROS) in March 2020 indicated there are an additional 709 adult, family, or gerontological nurse practitioners actively practicing in Delaware.
Primary care disparities exist not just between states but also within states. In Delaware, more than half of the land area is federally designated as a healthcare shortage area (HAS).16 Of the three counties in Delaware, the entirety of Kent and Sussex Counties are designated HSAs with large rural populations that lack access healthcare. Even parts of New Castle County are designated as HSAs, despite the more urban/suburban landscape.16 However, these designations are based on studies that fail to assess the importance of physicians assistants, nurse practitioners, and other types of primary care that do not fall under the “physician” category.
SEEKING PRIMARY CARE
While the trend in hospitalizations over the past two years increased, fewer people sought necessary medical treatment, and elective procedures were deferred. Even now that significant mitigation measures have been put in place, preventative care is being put off.9 A study conducted by the Australian Institute of Health Innovation revealed that “[a]n estimated 1.3 million (13.2%) fewer manual therapy services, with a total cost of AUD 84 million, were provided within the Australian private healthcare setting during the first half of 2020.”17 Another study conducted by the U.S. Centers for Disease Control and Prevention (CDC) estimated that 41% of Americans deferred necessary healthcare, including a 12% reduction in emergency care and a 32% deferral of routine medical care.18 Emergency department visits were down 40%, while office visits were cancelled in favor of telehealth appointments, and elective procedures were delayed indefinitely.19 Despite decreased use of medical services across the board, a December 2021 press release from the Centers for Medicare and Medicaid Services (CMS) stated that 2020 saw a 9.7% overall increase in healthcare spending due to the pandemic.20 With an aging population and their chronic diseases in mind, these delays in routine and emergency care will likely lead to worsening overall health outcomes, increased healthcare costs, and worsening of chronic conditions.
DELAWARE HEALTH CARE WORKFORCE DATABASE
The challenges faced during the COVID-19 pandemic exposed significant flaws in the current medical systems’ ability to provide adequate care for those in need during times of exacerbated strain. From severe lack of PPE and critical care equipment (CCE), to nursing shortages and fears of accessing care during a pandemic, hospitals and other critical care facilities were woefully unprepared. While the U.S. has taken significant measures to shore up hospital reserves of PPE and CCE, every state is taking its own precautions and putting measures in place to prevent another such epic disaster. Delaware has chosen to create a Health Force Database, to include every licensed and unlicensed healthcare practitioner in the state, from chiropractors to dentists to physicians and more. This database provides a clear picture of what access to different types of healthcare looks like across the state, and will help to inform decisions on workforce development.
PRACTITIONER DEMOGRAPHICS
The development of the database began in early 2020, using Excel to capture licensing information on all the existing practitioners listed in the Delaware Division of Professional Regulation (DELPROS). This initial picture of active and inactive practitioners across
165
various healthcare sectors in the state was limited to a name, a general profession (e.g., nursing, dentistry, occupational therapy), a license type (e.g., Registered Nurse, Dentist, Occupational Therapist), and the activity status of that license (e.g., Active, Inactive, Expired, Deceased).
The lack of available information was a major challenge, for a project that would include demographic information, schooling or higher education information, Medicare & Medicaid acceptance, and several other data points. Since the beginning of the project, a data use agreement has been established with DELPROS that provides a slightly more detailed picture of each practitioner. Some data acquired through this agreement, such as birth year, is instrumental in determining which practitioners are likely to retire in the coming year(s). This data is also strictly unavailable through any other means of data collection: the DELPROS provided data is the one source of truth for the ages of the practitioner population in Delaware. Early attempts were made to “scrape” internet sources (WebMD, Healthcare4ppl, Doximity, etc.) using several different third party applications that specialized in collecting large amounts of data from web sources and compiling them into excel files. This process was used to gather publicly available information on thousands of practitioners, although much work was needed to be done to remove duplicate practitioner profiles, combine information for individual practitioners, and correct or refine the information gathered (e.g. incomplete addresses, separating combined fields). After data refinement, it was found that not all practitioners were captured and not all profiles were complete. Despite this, there is a considerable amount of usable data concerning schooling and higher education data points that are not available through other, more robust data sources.
After evaluating the data from the scraped websites and the data from DELPROS, it was apparent that another major data source would be necessary to gather specialty and sub-specialty information. The National Provider Identifier (NPI) Registry contains a highly detailed and organized taxonomical structure of profession, specialty, and sub-specialties, as well as practitioners whose profession may not require a license (e.g. home health-aides, technicians). The NPI Registry is a service of the Centers for Medicaid and Medicare Service which operates on a national level. In the future, access to information about the neighboring regions of Philadelphia, Baltimore, Atlantic City, and Ocean City, Maryland. This report do not rely on or include NPI Registry data, but future work will after data integration hurdles have been overcome. It should be noted that the NPI Registry data is only as up to date as providers maintain their own records, so this is a limitation of that source.
In addition to DELPROS, the scraped websites, and the NPI Registry, claims data is also being collected from the Delaware Health Information Network (DHIN) as a way of verifying practitioners are in fact practicing some form of medicine in Delaware. This information also helps validate specialty information gathered from the NPI Registry.
DATASET
With so many different data sources, Excel became inadequate as a data storage and aggregation tool. The Health Force Database moved to Salesforce, a cloud-based data storage and computing software, which can handle significantly larger data sets and organize them in drastically shorter time frames than are possible in Excel. Of equal importance, the DELPROS system is also based in the Salesforce environment, making data transfer between systems easier once all components are configured and reconciled. The creation of the Salesforce database required adjustments as the team learned how the aggregate inputs came together to form an individual practitioner profile. A contract was given to a third-party to build out the database, however it did not adequately meet the needs of the project, and the contract was terminated after a year of work with no system implemented. The contract was instead given to a new third-party system, Agile Cloud Consulting (ACC), which has a better understanding of the Salesforce system and how to leverage existing components of the system to best meet the needs of the project. The desired output of the Health Force Database is a structural system that includes a profile of all Delaware practitioners and their specialties as individual practitioners, as well as a profile of all practice locations in Delaware (e.g. Nemours Children’s HospitalDelaware) with a full list of practitioners providing care at these locations.
To accompany the individual and institutional profiles, two statistical analysis tools will be used to better understand the data. Geopointe, a mapping tool, will provide a visual display of how many practitioners of a given type are in a geographic area as well as the demographic breakdown of the population of that area. This will provide an understanding of where the Delaware health workforce is practicing, the populations they are serving, and whether the healthcare needs of that population are being adequately met. The second statistical tool, Tableau, will use practitioner age data acquired from DELPROS to help to predict future changes to the healthcare workforce due to provider retirement, and help determine locations and specialties that may need to be filled in the future.
REFERENCES
1. Centers for Disease Control and Prevention. (2019, Mar 20). 1918 pandemic (H1N1 virus). Centers for Disease Control and Prevention. https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html
2. Miller, S. L., Mukherjee, D., Wilson, J., Clements, N., & Steiner, C. (2020, Oct 3). Implementing a negative pressure isolation space within a skilled nursing facility to control SARS-COV-2 transmission. Science Direct. https://www.sciencedirect.com/science/article/pii/S0196655320308944
3. Alberico, J., & Phillips, D. (n.d.). Creating temporary isolation zones with emergency retrofits of ... - RWDI. RWDI. https://rwdi.com/assets/factsheets/RWDI-COVID19-ISOLATION-ZONES.pdf
166 Delaware Journal of Public Health - December 2022
4. Grimm, C. A. (2021, Mar). Hospitals reported that the COVID-19 pandemic has significantly strained healthcare delivery. Office of Inspector General Department of Health and Human Services. https://oig.hhs.gov/oei/reports/OEI-09-21-00140.pdf
5. Herrman, J. (2020). COVID-19 and healthcare professional stress and resilience. ASPR TRACIE. https://files.asprtracie.hhs.gov/documents/aspr-tracie-the-exchange-issue12-final.pdf
6. Lopez, V., Anderson, J., West, S., & Cleary, M. (2021, Sep 29). Does the COVID-19 pandemic further impact nursing shortages? Taylor & Francis. https://www.informahealthcare.com/doi/full/10.1080/01612840.2021.1977875
7. Tanzi, A., & Sasso, M. (2021, Oct 22). COVID early retirees top 3 million in U.S., Fed research shows. Bloomberg.com https://www.bloomberg.com/news/articles/2021-10-22/covid-early-retirees-top-3million-in-u-s-fed-research-show
8. Dore, K. (2021, May 9). The pandemic drove these Americans into early retirement. what to know before making the leap. CNBC. https://www.cnbc.com/2021/05/09/the-pandemic-drove-these-americans-into-early-retirement.html
9. Wager, E., Amin, K., Cox, C., & Hughes-Cromwick, P. (2022, Feb 1). What impact has the coronavirus pandemic had on health employment? Health System Tracker. https://www.healthsystemtracker.org/chart-collection/what-impact-has-the-coronavirus-pandemic-had-on-healthcare-employment/
10. Robeznieks, A. (2022, Apr 6). How an aging nation, COVID-19 stretch the doctor workforce thin. American Medical Association. https://www.ama-assn.org/practice-management/sustainability/how-aging-nation-covid19-stretch-doctor-workforce-thin
11. World Health Organization. (2021, Sep). The impact of COVID-19 on health and care workers: a closer look at deaths. WHO. https://apps.who.int/iris/bitstream/handle/10665/345300/WHO-HWF-WorkingPaper-2021.1-eng.pdf
12. Dai, S.-P., Zhao, X., & Wu, J.-H. (2020, Oct 12). Effects of comorbidities on the elderly patients with COVID-19: Clinical characteristics of elderly patients infected with COVID-19 from Sichuan, China - The Journal of Nutrition, Health & Aging. https://link.springer.com/article/10.1007/s12603-020-1486-1
13. Bellon, J., Coley, K., Coulthart, S., Degenholtz, H., Delitto, A., Driessen, J., . . . Wessel, C. B. (n.d.). Addressing the health needs of an aging America. University of Pittsburgh. https://www.healthpolicyinstitute.pitt.edu/sites/default/files/SternCtrAddressingNeeds.pdf
14. National Academy of Social Insurance. (2021, Dec 30). How will boomers affect social security? National Academy of Social Insurance. https://www.nasi.org/learn/social-security/how-will-boomers-affect-social-security/
15.Petterson, S.M., Cai, A., Moore, M., Bazemore, A. (2013, Sep). State-level projections of primary care workforce, 2010-2030. Robert Graham Center, Washington, D.C.
16. Malayala, S. V., Vasireddy, D., Atluri, P., & Alur, R. S. (2021, Feb 10). Primary care shortage in medically underserved and health provider shortage areas: Lessons from Delaware, USA. Journal of primary care & community health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7882751/
17. Lystad, R. P., Brown, B. T., Swain, M. S., & Engel, R. M. (2020, Dec 13). Impact of the COVID-19 pandemic on manual therapy service utilization within the Australian private healthcare setting. MDPI. https://www.mdpi.com/2227-9032/8/4/558
18. Czeisler, M. É., Marynak, K., Clarke, K. E. N., Salah, Z., Shakya, I., Thierry, J. A. M., . . . Howard, M. E. (2020, Sep 10). Delay or avoidance of medical care because of COVID-19–related concerns - United States, June 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/mmwr/volumes/69/wr/mm6936a4.htm
19. Department of Health and Human Services. (2021, Apr). COVID-19 healthcare delivery impacts (summary). https://files.asprtracie.hhs.gov/documents/covid-19-healthcare-delivery-impacts-quick-sheet.pdf
20. Office of the Actuary. (2021, Dec 15). National health spending in 2020 increases due to impact of COVID-19 pandemic. CMS. https://www.cms.gov/newsroom/press-releases/national-health-spending-2020-increases-due-impact-covid-19-pandemic
167
Addressing Health Disparities in Delaware by Diversifying the Next Generation of Delaware’s Physicians
Kristyn Mitchell
ChristianaCare, Harrington Value Institute Translational Research Intern
Franklin Iheanacho
ChristianaCare, Harrington Value Institute Translational Research Intern
Jacqueline Washington, Ed.D.
ChristianaCare, Program Manager of the Harrington Value Institute Community Partnership Fund
Marshala Lee, M.D., M.P.H.
ChristianaCare, Director of the Harrington Value Institute Community Partnership Fund
The COVID-19 pandemic has shined a light on health disparities in the United States and the impact of the social determinates of health (SDOH). Black Americans have a mortality rate 2.4 times that of whites and this disproportionality is more widespread throughout the United States compared to any other racial/ethnic group.1 COVID-19 disparities are also manifesting in the State of Delaware. As of May 24, 2020, both Non-Hispanic Black and Hispanic/Latino Americans have the highest rate of COVID-19 cases, with a rate of 111.3 and 281.6 cases, respectively, while non-Hispanic Whites have a rate of 38.5.2 These disparities, although startling, are not surprising considering that before the COVID-19 outbreak health disparities were already persistent. For the top ten leading causes of death, when compared to non-Hispanic White Delawareans, non-Hispanic Black Delawareans lead with the highest adjusted mortality rate for seven of the causes of deaths between 2014 and 2018 (see Table 1). The most common comorbidities associated with COVID-19 are hypertension, obesity, and diabetes, all of which disproportionately impact Black and Hispanic/Latin Americans in the United States and Delaware.4,5 Effective strategies must be deployed in the short-term to reduce COVID-related health disparities while simultaneously investing in long-term strategies such as improving workforce diversity to completely eliminate future health disparities.
Table 1. Five year age adjusted mortality rate of the top 10 leading causes of death (2014-2018)3 LEADING CAUSES OF DEATH NON-HISPANIC White
10.32481/djph.2022.12.039
DOI:
neoplasms 169.1 181.2 Diseases of the heart 159.4 179.0 Chronic lower respiratory diseases 44.8 32.7 Cerebrovascular diseases 39.2 55.1
35.7 41.0
This
is
168 Delaware Journal of Public Health - December 2022
Black Malignant
Dementia
Accidents (unintentional injuries) 65.5 44.8 Diabetes mellitus 16.0 32.5 Alzheimer’s disease 25.2 28.4 Nephritis, nephrotic syndrome, and nephrosis13.3 31.1 Influenza and pneumonia 13.9 12.3
article
a reprint from DJPH, August 202, Vol 6, Issue 3
STRATEGIES: HEALTH WORKFORCE DIVERSITY PIPELINE INVESTMENTS
One strategic approach for improving the SDOH for minority communities and reducing health disparities is to invest in the recruitment of a diverse healthcare workforce. Diverse healthcare workers are uniquely positioned to tackle these dimensional problems for several reasons. For one, a diverse healthcare workforce increases the likelihood that high quality care will be provided to underserved populations and people of color. For example, physicians who self-identified as belonging to an underrepresented minority (URM) group were more likely than their colleagues to practice in high-need areas.6 In a Stanford Study, Black men in Oakland, California were paired with either Black or non-Black physicians. The men seen by Black physicians were more likely to engage with them, and even consent to preventive services like immunizations. Additionally, the Black physicians were more inclined to write detailed notes about their Black patients.7 A diverse health workforce will also strengthen cultural competence throughout the health system. The U.S. healthcare system has largely been built upon the practices of Western medicine. Many healthcare systems are currently poorly equipped to provide culturally competent care to patients from underrepresented backgrounds and to those who believe in nontraditional concepts of illness and treatment. Diversity in our healthcare workforce is an effective strategy to increase patient satisfaction, decease health workforce shortages, improve the cultural competence of health systems, and ultimately decrease health disparities. Although a diverse healthcare workforce is crucial for achieving health equity thus reducing health disparities, there persists an underrepresentation of certain racial/ethnic groups in the United States and Delaware. The Association of American Medical Colleges (AAMC) historically classified four racial/ethnic groups as underrepresented in medicine: Black Americans, Mexican Americans, Native Americans (which include American Indians, Alaska Natives, and Native Hawaiians) and mainland Puerto Ricans.8 The state of Delaware suffers from an underrepresentation of minority physicians similar to most other states in the United States (see Table 2). These disparities are consistent within the medical school applicant pool, with far less URM students applying to and matriculating into medical school even after Liaison Committee of Medical Education diversity accreditation guidelines were established in 2009.12 As the United States becomes more diverse, action must be taken now to better address health disparities by ensuring that the future physician workforce is more diverse and better reflects the makeup of the communities that they serve.
Table 2: Percentages of active physicians in USA by race/ethnicity compared to the percentage of US population by race/ethnicity and the percentage of primary care physicians by race/ethnicity in Delaware compared to percentage of Delawareans by race/ethnicity
United States
Race/Ethnicity
Percentage of active physicians in the USA (2018)9 Percentage of USA population10
Non-Hispanic Black 5% 13% Hispanic/Latin 5.8% 18.3% American Indian, Alaskan native, Native Hawaiian, and pacific Islander 0.4% 1.5% Asian 17.1% 5.9% Non-Hispanic White 56.2% 60.4% Delaware
Race/Ethnicity
Percentage of primary care physicians in Delaware11
Total population of Delaware by percentage10
Non-Hispanic Black 6.6% 23% Hispanic/Latin 4.4% 9.5% Asian 22.6% 5.9% White 66.7% 61.9%
169
CURRENT HEALTH WORKFORCE PIPELINE DIVERSITY EFFORTS IN DELAWARE
There are increasing efforts from the government, healthcare organizations, and academic institutions nationwide to address the underrepresentation of minorities in health professions and foster strategies for workforce diversification. According to the Institute of Medicine, pipeline programs that support the needs and success of minorities are pivotal for improving healthcare workforce diversity.13 For example, the Human Resources and Services Administration (HRSA) has grant funding for academic institutions to promote recruitment and retention of minorities in the field of nursing. The funding provides academic and financial support, mentorship, community engagement, and clinical and research opportunities.14 Similarly, the Health Sciences Camp at the University of Delaware provides high schoolers from underrepresented backgrounds and first-generation college families with a free college immersion experience in the health sciences. Students can engage with faculty and researchers, and also gain exposure to nursing, biotechnology, exercise science, and other health specialties.15
For students particularly interested in pursuing medicine, the Harrington Value Institute Community Partnership (VICP) Fund sponsors a yearlong research internship to support URM students in their pursuit to medical school. Established in 2015, The Harrington Value Institute Community Partnership Fund was established by a donation from the estate of Charles J. Harrington, Ph.D. Dr. Harrington was deeply committed to advancing scholarship and supporting innovative projects that help reduce health care disparities for underserved and disadvantaged populations. The Harrington Value Institute Translational Research Internship prepares recently graduated college students for careers in medicine and translational research by providing enriching research opportunities, clinical shadowing, mentorship, and a curriculum tailored to academic and professional development. The internship is primarily housed at ChristianaCare’s Value Institute, where students engage with physicians, nurses, researchers, community leaders, and other healthcare professionals throughout the health system to enhance their understanding of translational research, public health, the social determinants of health, and medicine. Upon completing the internship, many interns have successfully matriculated into accredited medical schools and left the internship with added confidence and skills that will better prepare them for medical school and clinical research careers.
FUTURE HEALTH WORKFORCE PIPELINE DIVERSITY EFFORTS IN DELAWARE
The Harrington VICP Fund plans to expand this opportunity to more underrepresented students in the upcoming years. Additionally, the Harrington VICP Fund also understands the vast array of other common barriers affecting the URM medical school pipeline and has recently created an MCAT Prep Program for students to receive quality preparation for the Medical College Admissions Test (MCAT). According to the AAMC, minority students traditionally do not perform as well as white students on the MCAT, and a major factor contributing to this disparity is lack of financial support for test preparation materials.16,17 Furthermore, the current COVID-19 pandemic and its threats to many underserved communities have intensified students’ financial challenges. Students enrolled in the MCAT Prep Program will have access to a 6-week online Kaplan MCAT course as well as mentoring and peer support during their medical school application process. These students will also be introduced to the concepts of health disparities, social determinants of health, and the importance of cultural competence in caring for their future patients. Upon completing the program, program participants will not only be better prepared candidates for medical school, but they will also be equipped with skills to become culturally humbled leaders in their community.
While there are a few strategies in place to increase diversity of the healthcare workforce, there is still much work to be done. Substantial investments are needed to build robust physician pipeline programs for URM students in K-12 and undergraduate levels to ensure a diverse healthcare workforce. Delaware is presented with a unique challenge to its physician pipeline because the state does not have its own medical school. The Harrington VICP is optimistic that many of its program participants will return to practice in Delaware after completing their medical training and commit to careers committed to reducing health disparities. As Delaware’s population continues to diversify, the programs implemented by the Harrington Fund can serve as a guideline for the development of additional URM physician pipeline programs.
170 Delaware Journal of Public Health - December 2022
REFERENCES
1. APM Research Lab. (n.d.). COVID-19 deaths analyzed by race and ethnicity. Retrieved from https://www.apmresearchlab.org/covid/deaths-by-race
2. My Healthy Community. (n.d.). Coronavirus (COVID-19) Data Dashboard State of Delaware. Retrieved from https://myhealthycommunity.dhss.delaware.gov/locations/state
3. Delaware Division of Public Health. (2020, Feb). Delaware Vital Statistics Annual Report 2018. Retrieved from: https://dhss.delaware.gov/dph/hp/files/ar2018_net.pdf
4. Richardson, S., Hirsch, J. S., Narasimhan, M., Crawford, J. M., McGinn, T., Davidson, K. W., ... Zanos, T. P., & the and the Northwell COVID-19 Research Consortium. (2020, April 22). Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA, 323(20), 2052–2059. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32320003&dopt=Abstract
5. Centers for Disease Control and Prevention. (n.d.). BRFSS Prevalence & Trends Data. Retrieved from https://www.cdc.gov/brfss/brfssprevalence/
6. Goodfellow, A., Ulloa, J. G., Dowling, P. T., Talamantes, E., Chheda, S., Bone, C., & Moreno, G. (2016, September). Predictors of primary care physician practice location in underserved urban and rural areas in the United States: A systematic literature review. Acad Med, 91(9), 1313–1321. https://doi.org/10.1097/ACM.0000000000001203
7. Alsan, M., Garrick, O., & Graziani, G. (2019). Does diversity matter for health? Experimental evidence from Oakland. The American Economic Review, 109(12), 4071–4111. https://doi.org/10.1257/aer.20181446
8. American Association of Medical Colleges. (n.d.). Underrepresented in medicine definition. Retrieved from https://www.aamc.org/what-we-do/mission-areas/diversity-inclusion/underrepresented-in-medicine
9. American Association of Medical Colleges. (2019). Diversity in Medicine: Facts and Figures 2019. Retrieved from: https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018
10. US Census Bureau. (n.d.). United States: Quick Facts. Retrieved from: https://www.census.gov/quickfacts/fact/table/US/PST045219
11. Delaware Department of Health and Social Services. (2018). Primary Care Physicians in Delaware, 2018. Retrieved from: https://dhss.delaware.gov/dhss/files/primarycarestudy.pdf
12. Lett, L. A., Murdock, H. M., Orji, W. U., Aysola, J., & Sebro, R. (2019, September 4). Trends in racial/ethnic representation among US medical students. JAMA Network Open, 2(9), e1910490–e1910490. https://doi.org/10.1001/jamanetworkopen.2019.10490
13. Altman, S. (2016, Feb 22). Promoting diversity. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK350167/
14. Kukich, D. (2014, Nov 18). Nursing workforce diversity. Retrieved from http://www1.udel.edu/udaily/2015/nov/nursing-diversity-111814.html
15. B enjamin, A. (n.d.). Pipeline program: Health sciences: University of Delaware. Retrieved from https://www.chs.udel.edu/pipeline-program/
16. American Association of Medical Colleges. (2019, Oct 16). MCAT Scores and GPAs for Applicants and Matriculants to U.S. Medical Schools by Race/Ethnicity, 2019-2020. Retrieved from https://www.aamc.org/system/files/2019-10/2019_FACTS_Table_A-18.pdf
17. American Association of Medical Colleges. (2018, Jun). Using MCAT® Data in 2019 Medical Student Selection. (2018, June). Retrieved from https://www.aamc.org/system/files/c/2/462316-mcatguide.pdf
171
Matt
Physician and Dentist Basic Demographics: Race and Ethnicity
McNeill, B.S. Research Associate, Delaware Academy of Medicine/Delaware Public Health Association
At the writing of this report, data on race and ethnicity of Delaware Healthcare Providers (including physicians and dentists), was not readily available. However, in a study published by Mitchell et al1 we obtain a glimpse at this information juxtaposed against that of the total population of Delaware when looking at primary care physicians (see tables 1 & 2).
Table 1. Race and Ethnicity of Delaware Primary Care Physicians
Percentage of Primary Care Physicians in Delaware
Total Population of Delaware by Percentage
Non-Hispanic Black 6.6% 23% Hispanic/Latin 4.4% 9.5% Asian 22.6% 5.9% White 66.7% 61.9%
While generalization from this focused examination is difficult, it does suggest a larger trend where Non-Hispanic Black and Hispanic/ Latin physicians are underrepresented relative to population percentages. On the other hand, White and Asian primary care physicians are both represented at higher rates than in population percentages.
The authors go on to state “[t]hese disparities are consistent within the medical school applicant pool, with far less URM (underrepresented minority) students applying to and matriculating into medical school even after Liaison Committee of Medical Education diversity accreditation guidelines were established in 2009. As the United States becomes more diverse, action must be taken now to better address health disparities by ensuring that the future physician workforce is more diverse and better reflects the makeup of the communities that they serve … [d]iversity in our healthcare workforce is an effective strategy to increase patient satisfaction, decease health workforce shortages, improve the cultural competence of health systems, and ultimately decrease health disparities.”1
Table 2. Gender of Delaware Dentists and Physicians, Compared to Demographics1,2
License Type Gender Record Count Percentage
Dentist (N=540)
No Data 3 0.55% Male 340 62.96% Female 197 36.48% Physician (DO) (N=933) No Data 21 2.25% Male 543 58.2% Female 369 39.55% Physician (MD) (N=5,308) No Data 87 1.64% Male 3,265 61.51% Female 1,956 36.85% Total 6,781 Delaware Population (N=998,619) Male 483,332 48.4% Female 515,287 51.6%
REFERENCES
1. Mitchell, K., Iheanacho, F., Washington, J., & Lee, M. (2020, Aug). Addressing health disparities in Delaware by diversifying the next generation of Delaware’s physicians. Dela J Public Health, 6(3), 26-38. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8389095/
2. Delaware Population. 2022. (n.d.) World Population Review. Retrieved from https://worldpopulationreview.com/states/delaware-population
DOI: 10.32481/djph.2022.12.040
172 Delaware Journal of Public Health - December 2022
Physician Statistics based on Allopathic (M.D.) and Osteopathic (D.O.) Education
Note: The following is reprinted from a 2021 American Medical Association article.1
In the U.S., there are two types of degrees in which physicians can practice medicine: an MD, a doctor of medicine, or a DO, a doctor of osteopathic medicine. The two degrees reflect different types of medical school training. MDs attend allopathic medical schools, while DOs attend osteopathic medical schools.
THE SIMILARITIES
About one-quarter of U.S. medical students train at osteopathic medical schools. That number has grown significantly in recent years, with the American Association of Colleges of Osteopathic Medicine reporting first year enrollment at osteopathic medical schools rising by more than 40% over the past decade. That spike is, at least, in part due to additional DO-granting medical schools opening.
In terms of the requirements to apply to MD and DO programs, the criteria are virtually the same, with both osteopathic and allopathic programs weighing grade-point average and Medical College Admission Test (MCAT) scores heavily. The curriculum is largely the same structure, with students in both types of programs typically spending much of their first 12-24 months in the classroom and the majority of their training beyond that in a clinical setting.
SINGLE ACCREDITATION, RESIDENCY TRAINING
In the past, graduates from osteopathic and allopathic medical schools have generally matched with residency programs through separate processes.
In an effort to simplify the graduate medical education (GME) accreditation system in the United States, the organizations that accredit GME—the Accreditation Council for Graduate Medical Education and the American Osteopathic Association (AOA)—have changed how they do things. The 2020 Main Residency Match marked the completion of the transition to a single accreditation system and the consolidation to one Match for U.S. DO and MD seniors.
Those changes also affect licensing. Most residency programs will accept the Comprehensive Osteopathic Medical Licensing Examination taken by DO graduates, as well as the United States Medical Licensure Exam which is taken by MD graduates and can be taken by DO graduates.
MIND, BODY, SPIRIT
Historically, DO programs have touted their methods as more holistic. One aspect of that is the osteopathic manipulative treatment, defined by the AOA as a “set of hands-on techniques used by osteopathic physicians ... to diagnose, treat, and prevent illness or injury.”
Those skills typically mean that osteopathic medical students spend an additional 200-plus hours training on the musculoskeletal system in the curriculum.
“If a student is somebody who really enjoys that patient-centered approach and really is of the mindset that medicine is a mindbody-spirit relationship, a DO program will serve them well,” said John D. Schriner, PhD, associate dean for admissions and student affairs at Ohio University Heritage College of Osteopathic Medicine, one of 37 member schools of the AMA Accelerating Change in Medical Education Consortium.
MOST DOS CHOOSE PRIMARY CARE
The 2021 Match, the second fully combined Match for DOs and MDs, yielded positive results for graduates from both types of schools. About 6,300 U.S. DO seniors submitted rank order lists of programs, and 89.1% of them matched. That percentage is a bit lower than the 92.8% Match percentage posted by graduates of U.S. MD-granting medical schools.1
REFERENCES
1. Murphy, B. (2021, Oct). DO vs. MD: How much does the medical school degree type matter? American Medical Association. Retrieved from: https://www.ama-assn.org/residents-students/preparing-medical-school/do-vs-md-how-much-does-medical-school-degree-type
DOI: 10.32481/djph.2022.12.041
173
Physician and Dentist Basic Demographics Age
Matt McNeill, B.S Research Associate, Delaware Academy of Medicine/Delaware Public Health Association
In a 2016 article, “A systematic review of physician retirement planning” by Silver et al, both expected and actual retirement ages appear to have occurred between 50-59 years of age (see table 1). A smaller number of physicians across studies predicted a later retirement age between 60-69 years of age.1
In a study by the American Dental Association’s Health Policy Institute, 49.8% of dentists aged 65-74 were projected to retire. That number increases to a projected 79.2% for those aged 75-84.2
Delaware data show on the facing page shows a steady increase in the number of physicians (both M.D., and D.O.) retiring starting at age 57 (individuals born in 1965). It appears that dentists follow a similar trend starting five years later (individuals born in 1960).
In figure 1, the blue dashed line between 1954 and 1955 roughly illustrates retirement age for those born in that range who can retire with full social security benefit when they turn 67 sometime in 2022. The red gradient box illustrates the increasing likelihood of end of career. The data does indicate that there are both physicians and dentists who maintain a license and practice significantly longer that their peers.
Future data will aid in development of a projection model for retirement of physicians and dentists as well as other types of healthcare providers.
Table 1. Expected and Actual Physician Retirement Age1
Expected Retirement Age
50-59 Years 60-69 Years>70 Years “Never”
Burke [76]
Eagles [30] Luce [7] Fletcher [38] Mears [41] Goldberg [57] Sansom [28] French [36] French [23] Gee [82] Pit [45] Rayburn [31] Shanafelt [[53] Smith [91] Wakeford [18]
Actual retirement age Baker [52]
Eagles [30] Sansom [28] Farley [39] Fletcher [38] French [36] Jonasson [84] Meghea [54] Luce [7] Orkin [34] Rayburn [31] Rowe [90] Van Greuningen [17] Wakeford [18]
Anderson [37] Dietch [48] Dodds [46] Farley [39] Florence [81] Grondin [61] Mears [41]
Batchelor [22]Draper [40]
Joyce [42] Rayburn [31] –
DOI: 10.32481/djph.2022.12.042
Anderson [37] Austrom [58] Batchelor [22] 174 Delaware Journal of Public Health - December 2022
REFERENCES
1. Silver, M. P., Hamilton, A. D., Biswas, A., & Warrick, N. I. (2016, November 15). A systematic review of physician retirement planning. Human Resources for Health, 14(1), 67. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5109800/ PubMed https://doi.org/10.1186/s12960-016-0166-z
2. Munson, B., & Vuujicic, M. (2021, May). Projected supply of dentists in the United States, 2020-2040. Health Policy Institute. Retrieved from: https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/hpibrief_0521_1.pdf
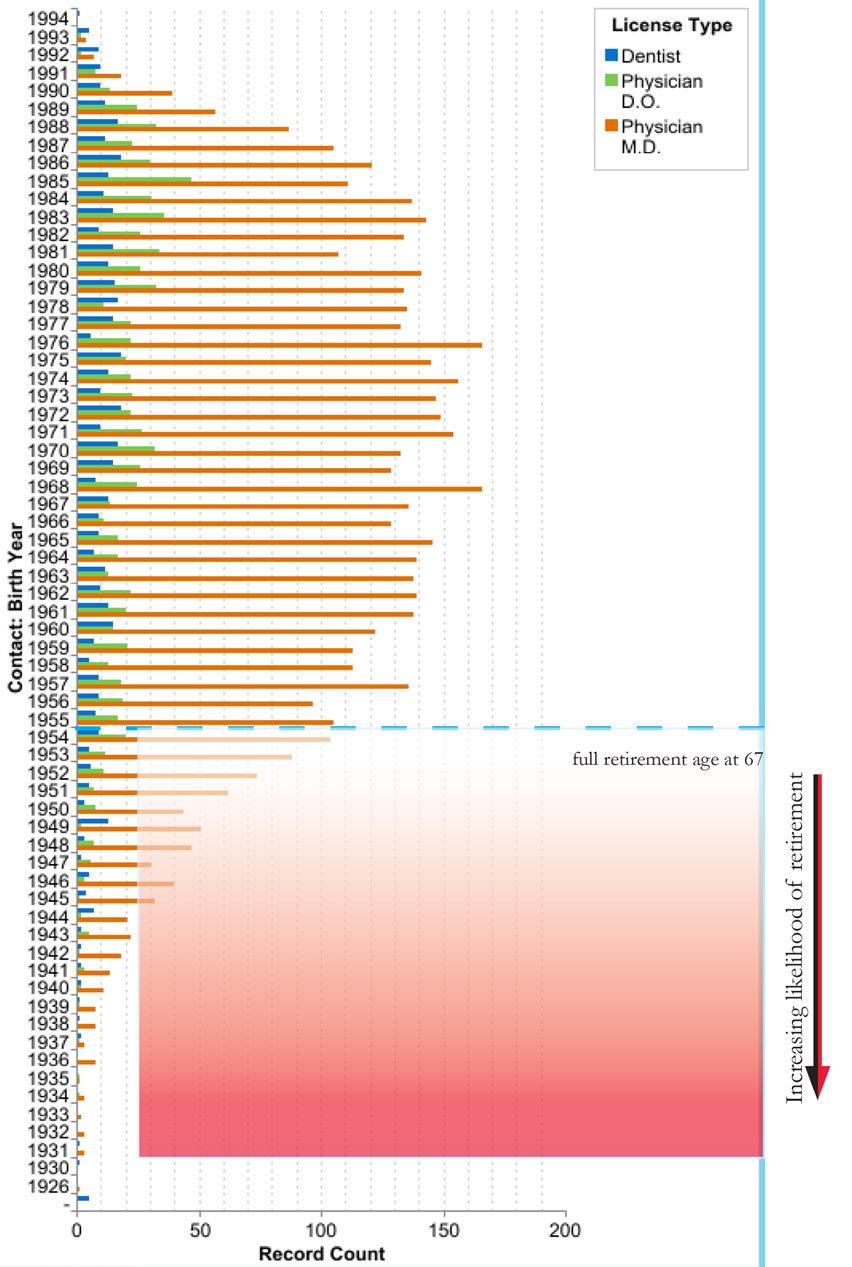
Figure 1. Delaware Active License Physician and Dentist Age Demographics
175
Chronic Disease Management and the Healthcare Workforce
Tim Gibbs, M.P.H. Nicole Sabine, B.S.
While this report is about the healthcare workforce, it is difficult to talk about capacity, demand for services, and growth potential without a discussion of the disease and wellness management. To that end, the next section of the report looks at the healthcare workforce through the lens of key chronic diseases, their prevention and management. We look at Chronic Disease because “currently, some 50% of the US population has a chronic disease, creating an epidemic, and 86% of healthcare costs are attributable to chronic disease.”1 Furthermore, according to the CDC “90% of the nation’s $4.1 trillion in annual healthcare expenditures are for people with chronic and mental health conditions.”2 The differences between acute and chronic disease are numerous and are illustrated in Table 1. 2
Table 1. Differences Between Acute and Chronic Disease
Acute Disease Chronic Disease
Sudden Onset Gradual Onset Cure Usual Cure Rare Course Short Course Lengthy Patient Passive Patient Active, Caregiver Physician Dominant Team Care, Patient Included Return to Normal Likely Return to Normal Unlikely Future Uncertainty Rare Future Uncertainty Common
The capacity of medical practice to address acute disease and injury has dramatically reduced the incidence of death from these diseases, and increased life expectancy for the population overall. This increase is not consistent across demographics, nonetheless, it is a population wide change. In its place, chronic disease has grown to replace acute disease and injury as the leading cause of death and disability, and an aging population (see Table 2) is more likely to develop chronic disease as a natural result of the aging process.
Table 2. Population Projections for Persons Aged 60 and Older State of Delaware.3
Year20162017201820192020202520302035204020452050
60 -6460,23762,23164,21966,16566,64968,92164,32259,97160,29966,918 70,051 65 -6954,91557,05756,76457,12456,77064,19666,80162,60058,62459,10565,576
70 -74 40,41541,63145,05247,52348,41252,27059,41262,14158,41555,02155,727
75 -7928,36729,49031,08733,14333,92242,38245,82852,34254,93451,85749,235
80 -8419,57820,05620,56621,54522,23627,65634,68937,53142,96445,25942,983 85 +20,41021,20621,91222,55222,48226,46032,70941,21847,61754,47259,584
Totals223,922231,671239,600248,052250,471281,885303,761315,803322,853332,632343,156
The next section of this report uses the following format.
•1) Sections are alphabetical by chronic disease name.
•2) State level data is presented first, and are based on CDC, Behavioral Risk Factor Surveillance System, 2020 data.
•3) Additional information as compiled by County Health Rankings, US Census Data, and other sources are located immediately below State data.
•4) The first group of pages will contain three sections representing New Castle, Kent, and Sussex County disease prevalence among adults aged 18 years and older (see figures 1-6). The data source will be identified at the top of each table and is not uniform from one chronic disease to another as there is no single source for all diseases.
•5) The next group of pages looks at the number of individuals, by census tract per 100 persons, with the given chronic disease.
•6) The following pages also contain health claims data for all publicly and privately insured Delawareans as reported to and captured by the Delaware Health Information Network (DHIN). The information is displayed based on census tract per 100 persons. This section looks specifically at healthcare utilization, which brings disease management into alignment against demands on the healthcare workforce.
DOI: 10.32481/djph.2022.12.043
176 Delaware Journal of Public Health - December 2022
An important limitation of this data is that an estimated 15% of transactions are not captured in the DHIN as some providers are not yet aligned with the DHIN. It is also important to note that data is not captured on self-insured & uninsured individuals, so any conclusions based upon this data must be carefully considered.
Figure 1. New Castle County Basic Demographics
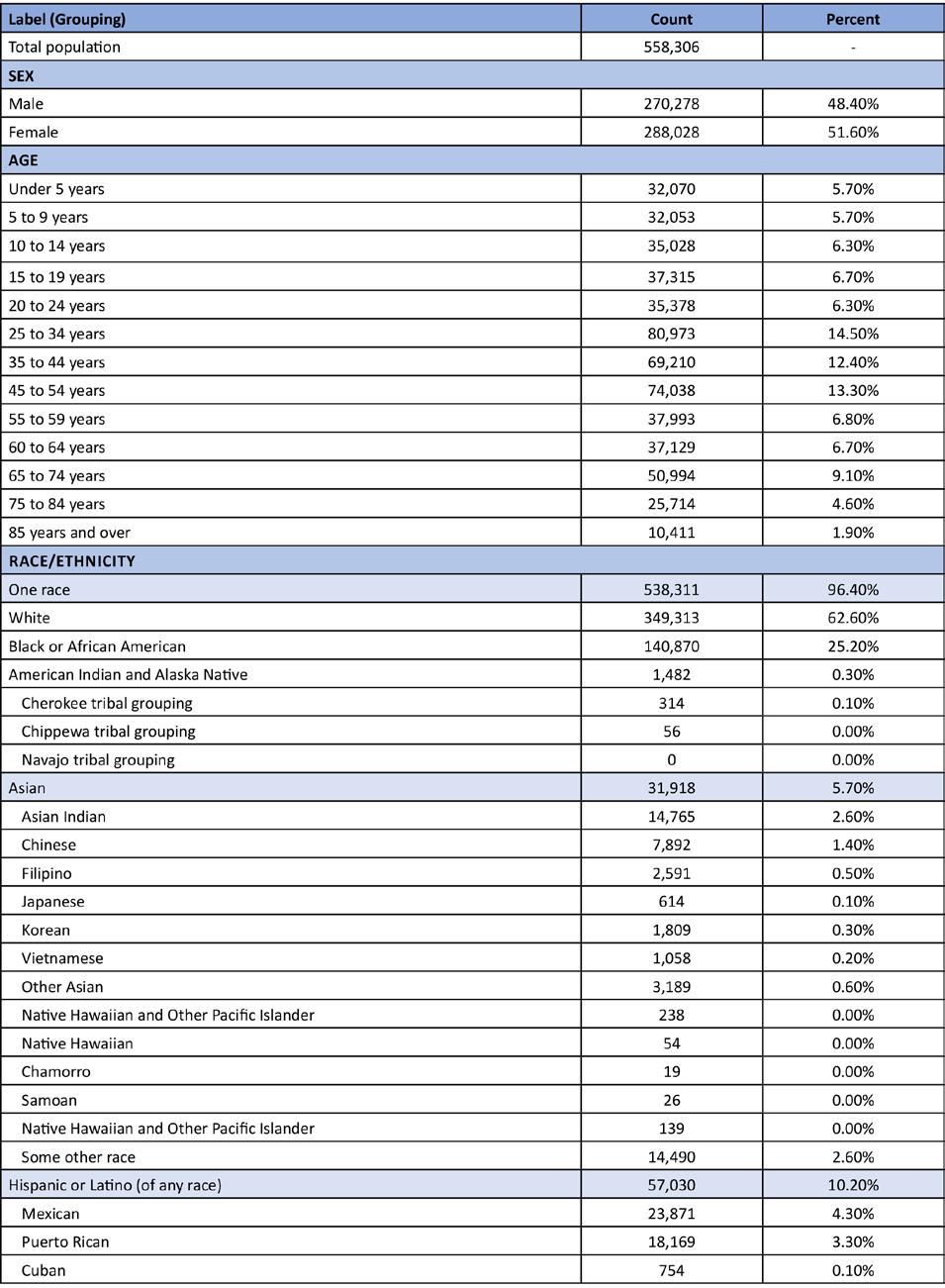
177
Figure 2. New Castle County Language Stratified by Age Groupings
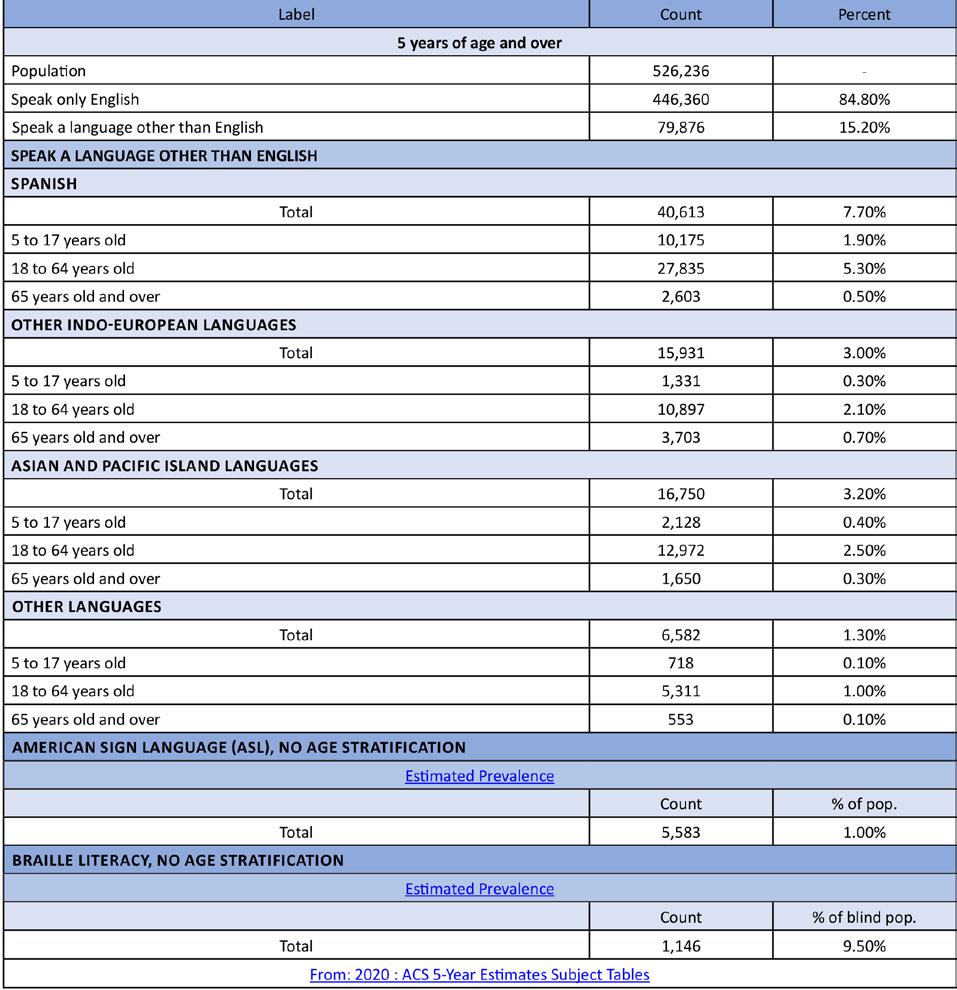

178 Delaware Journal of Public Health - December 2022

Figure 3. Kent County Basic Demographics 179
Figure 4. Kent County Language Stratified by Age Groupings
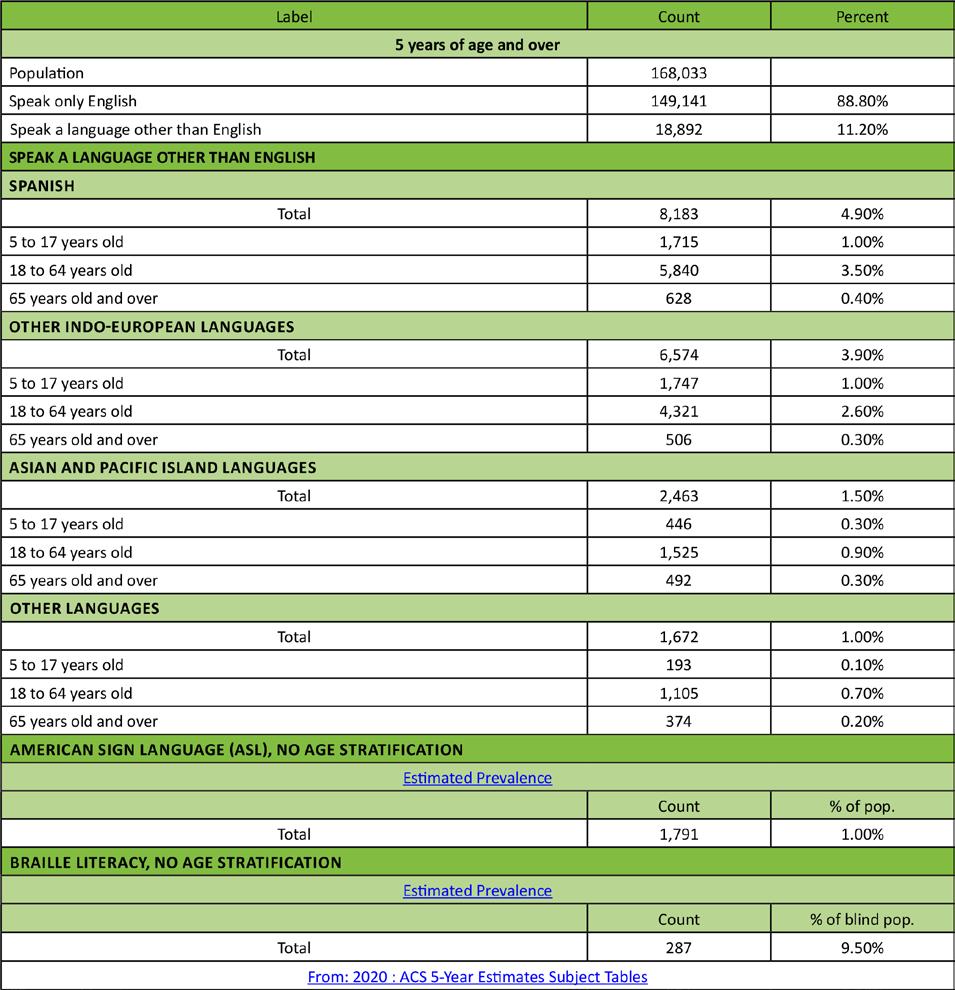
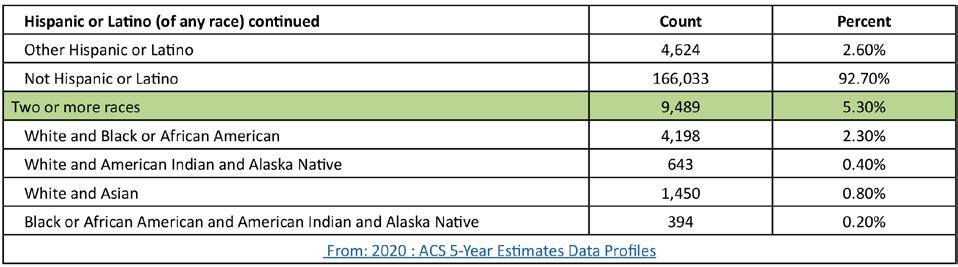
180 Delaware Journal of Public Health - December 2022

Figure 5. Sussex County Basic Demographics 181
Figure 6. Sussex County Language Stratified by Age Groupings

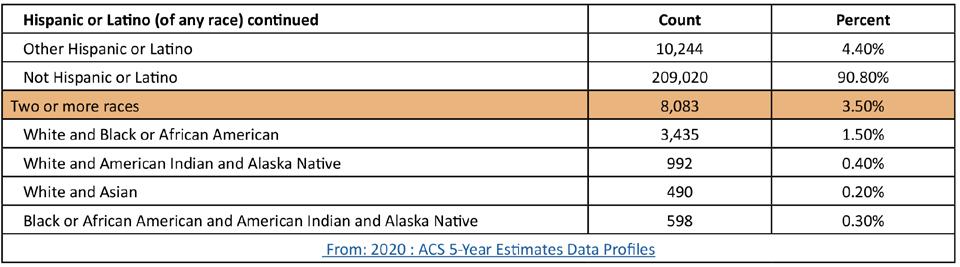
182 Delaware Journal of Public Health - December 2022
ALZHEIMER’S AND DEMENTIA DATA
The data indicates that there are areas of an increased incidence of Alzheimer’s and other dementia disease in each of Delaware’s three counties. Interestingly, these areas seem to correlate with the areas in which Delaware’s healthcare institutions are located (Wilmington Hospital and Christiana Hospital in New Castle County, Bayhealth in Kent County, Tidal Health and Beebe in Sussex County (see figures 7 & 8). This suggests an increased reporting due to the increased number of healthcare providers in these areas. Individuals living with Alzheimer’s and/or dementia may live elsewhere, and travel to the major healthcare institutions for care. The data suggest that keeping a workforce of providers specializing in Alzheimer’s and other dementias in these areas would be prudent to the continuation of care for these individuals. Specialists in neurology and neuropsychology (specific to the type of dementia), geriatrics, psychiatry and/or psychology are likely warranted. Allied health professionals in the fields of speech and language, physical, and occupational therapy and memory may also be included.
Figure 7. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Alzheimers Disease, Related Disorders, or Senile Dementia
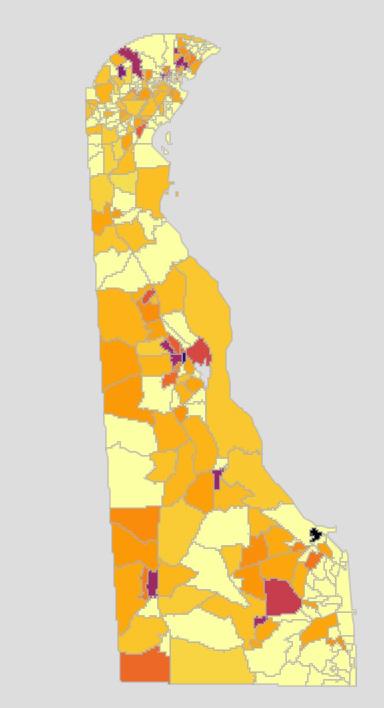

183
ARTHRITIS
AND DETERIORATIVE BONE DISEASE DATA


Figure 8 shows that the incidence of osteoporosis, a degenerative bone disease, is higher in the beach town communities, which are well known for their higher population of older Delawareans and retirees. Rheumatoid arthritis is an autoimmune disease, and has similar risk for all populations (figure 9). The incidence of rheumatoid arthritis is lower in New Castle County, and higher in Kent and Sussex Counties. Despite the low numbers of individuals living with these diseases, there is a need for specialists in all three counties due to complications like fractures of the hip (figure 10).

Figure 8. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Osteoporosis
Figure 9. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Rheumatoid Arthritis or Ostoarthritis
Figure 10. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Pelvic Hip Fracture
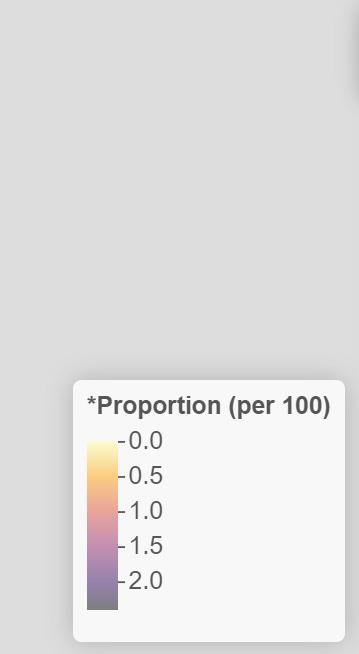
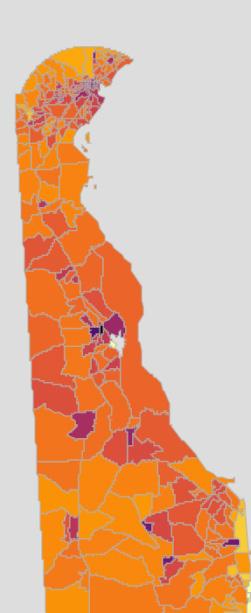


184 Delaware Journal of Public Health - December 2022
CANCER DATA



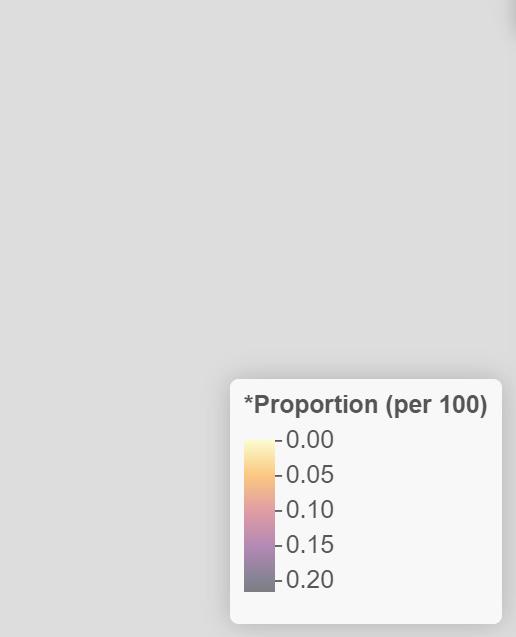

The data for the incidence of breast cancer (figure 11) indicates that there is no geographical component to a breast cancer diagnosis, although there are greater numbers of individuals with this diagnosis living in or around Delaware’s healthcare institutions. The data also shows a very low incidence of colorectal cancer (figure 12) in Delaware. Increased incidence of breast cancer may be due in part to increased screening (breast exams and mammograms) and thus, increased positive cases. In the same fashion, increased use of colonoscopy to screen for colon cancer may have led to Delaware’s low numbers of cases. Prostate cancer incidence higher in those areas known for retirement communities and an older population are indicative of the slow growth of prostate cancers, and the increased screening and testing for this cancer with age (figure 13). While it is important for oncologists and other cancer specialists to practice in all three counties and provide cancer care, it is equally important for primary care physicians and medical homes to be available to assist these individuals with their ongoing healthcare. Healthcare specialists who work with people with cancer include a general oncologist, an oncologist specializing in the type of cancer, surgical and radiation oncologists, social workers, patient navigators, psychiatrists, dieticians, home health aides, and a pharmacist.
Figure 11. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Breast Cancer
Figure 12. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Colorectal Cancer
Figure 13. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Prostate Cancer
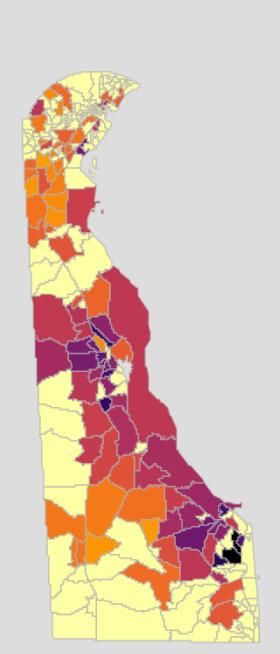


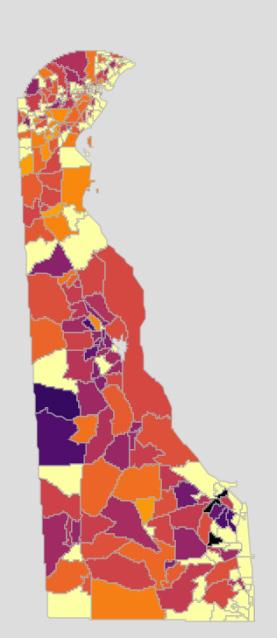
185
CARDIOVASCULAR DISEASE DATA



A cardiovascular team will likely consist of specialists in cardiovascular disease, nephrology, and/or neurology (depending on the mechanism of action of the disease) to treat cardiovascular diseases like acute myocardial infarction (figure 14), atrial fibrillation (figure 15), heart failure (figure 16), and ischemic heart disease (figure 17). Community health workers (for blood pressure maintenance and tracking), allied health professionals, radiologists, and medical technicians may also be appropriate.
Figure 14. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Acute Myocardial Infarction
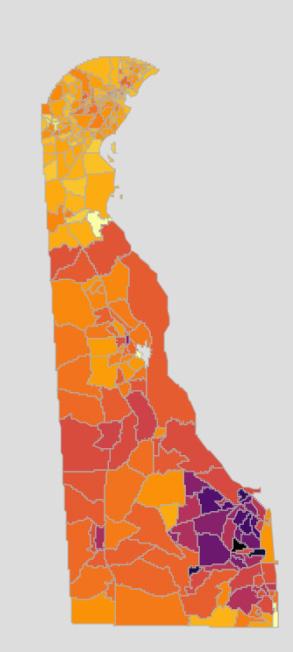
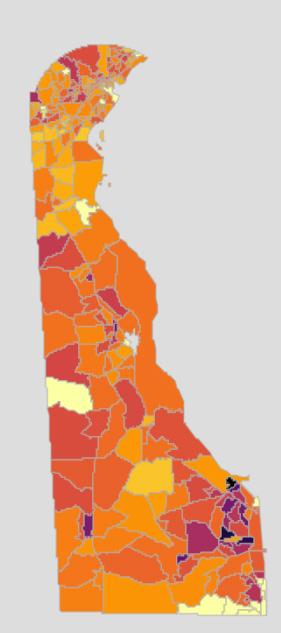
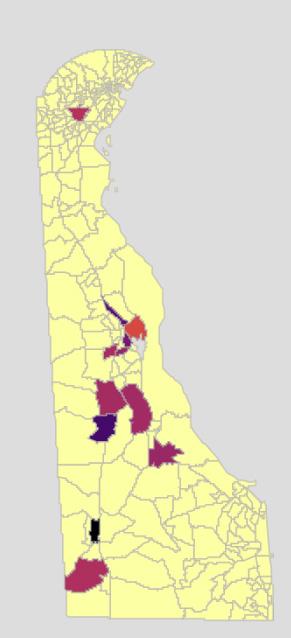

Figure 15. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Atrial Fibrillation
Figure 16. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Heart Failure

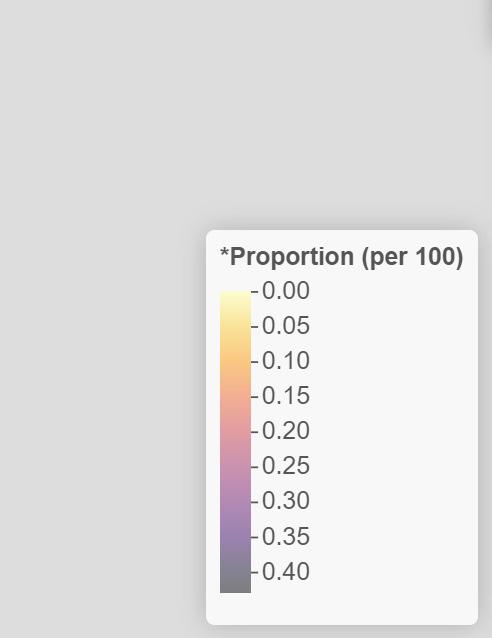
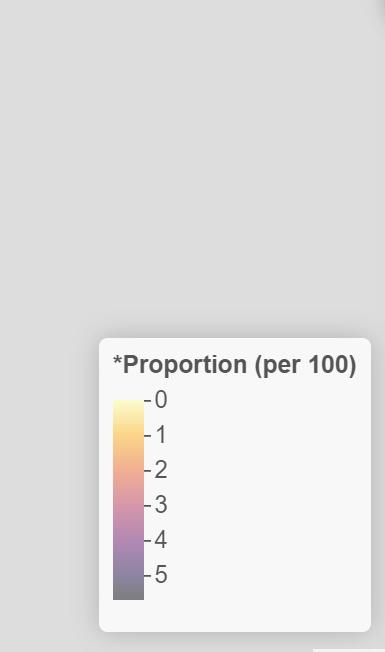
Figure 17. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Ischemic Heart Disease
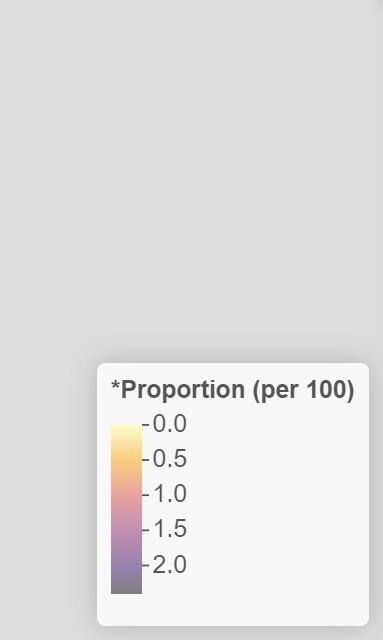
186 Delaware Journal of Public Health - December 2022
DEPRESSION AND SUICIDE DATA


According to the data, the incidence of depression (figure 18) and suicide does not follow any kind of geographical border. There are more cases in urban areas, which may in part be due to an increased population, and highlights the need for mental health professionals throughout the state.
Mental health diagnoses are complex, and require a multidisciplinary team including a psychiatrist and/or psychologist, social workers and therapists. Other professionals may be called upon for assistance as needed (i.e. long-term care nurses, pharmacists, community health workers).

187
Figure 18. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Depression
DIABETES DATA

Diabetes (figure 19) is ubiquitous throughout the state and may be due to an auto-immune disorder (type I, seen in children and adolescents); due to obesity, poor diet, or other chronic disease (type II); or due to pregnancy (gestational diabetes). Despite the reason, the data proves the need for diabetes specialists, care teams, and education throughout the state.
Managing diabetes requires a multi-disciplinary approach, and includes endocrinologists, dieticians, and community health workers like diabetes care and education specialists. It may also require the use of podiatrists, dermatologists, ophthalmologists and/or optometrists, long term care nurses, home health aides, dentists, fitness professionals, mental health workers, and pharmacists.
Figure 19. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Diabetes
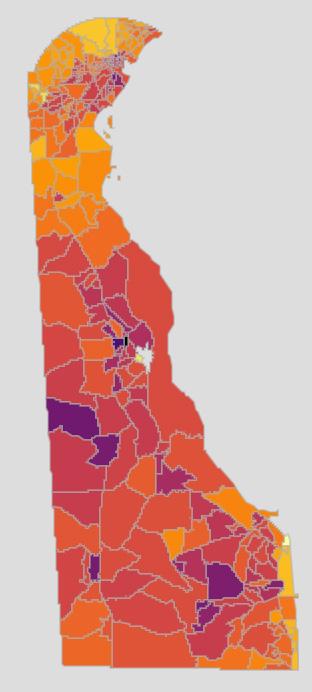

188 Delaware Journal of Public Health - December 2022
ENDOCRINE DISEASE AND DISORDERS DATA

As evidenced in the data showing the incidence of hypothyroidism (figure 20) in Delaware, endocrine disease does not follow any geographical border. There is an increased risk of being diagnosed with an endocrine disease as a person ages, particularly hypothyroidism. Other disorders of the endocrine system (i.e., diseases of the pituitary, diabetes) may be more likely seen in children and young adults. This indicates the need for endocrine specialists.
Endocrinologists will work with various specialties to give the appropriate care, based on the specific disorder. These specialists may include geneticists, orthopedists, dieticians and nutritionists, gastroenterologists, fertility specialists, mental health providers, renal specialists, ophthalmologists and/or optometrists.
Figure 20. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Acquired

Hypothyroidism
189
SYSTEMIC ILLNESS DATA
Anemia can be seen throughout the State of Delaware, with pockets of increased incidence in some communities (figure 21). Anemia is generally managed by primary care physicians and continuity of care is important.



Hypertension (high blood pressure) is one of the leading causes of morbidity and mortality throughout the nation and in Delaware (figure 22). All three counties in Delaware show high incidence rate of hypertension, with increased numbers in and around the major urban areas.
Although the incidence of hyperlipidemia (high blood pressure) are not quite as high, they also spike around the urban areas in the State (figure 23). This suggests a need for cardiovascular specialists in the major healthcare institutions, and primary care physicians throughout the state to provide timely check-ups and ongoing care.
Figure 21. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Anemia
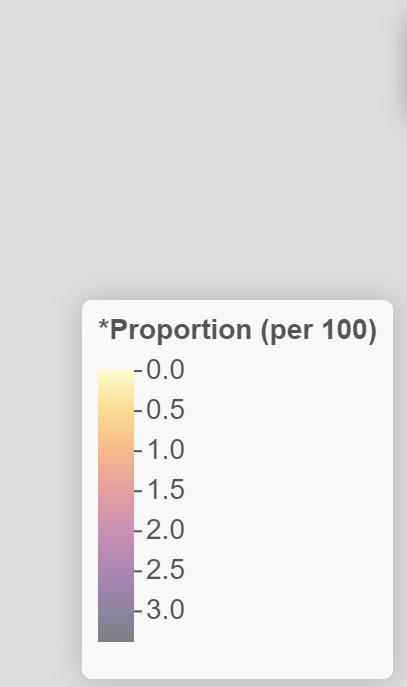
Figure 22. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Hypertension
Figure 23. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Hyperlipidemia

190 Delaware Journal of Public Health - December 2022
NEUROLOGIC DISORDERS AND INJURY (INCLUDING
STROKE) DATA
As shown in Figure 24, the incidence of stroke is higher in Delaware’s urban areas, which may be due to an increased population. Although the greatest risk factor for a stroke is age, high blood pressure, high cholesterol, obesity, and kidney disease can all contribute to increased risk. This map illustrates the need for both acute stroke treatment at healthcare institutions as well as ongoing post-stroke care throughout the state.
Stroke care teams will likely consist of specialists in cardiovascular disease (including atherosclerosis, heart disease); cardiovascular surgery, pharmacy, and radiology; and neurology immediately after a stroke occurs. Once a patient has been treated, a care team consisting of allied health professionals (occupational, physical, and speech language therapy) and psychiatrists and/or psychologists will likely be added.
Figure 24. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Stroke / Transient Ischemic Attack
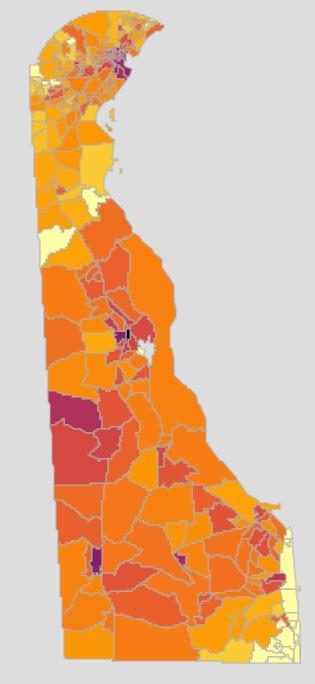
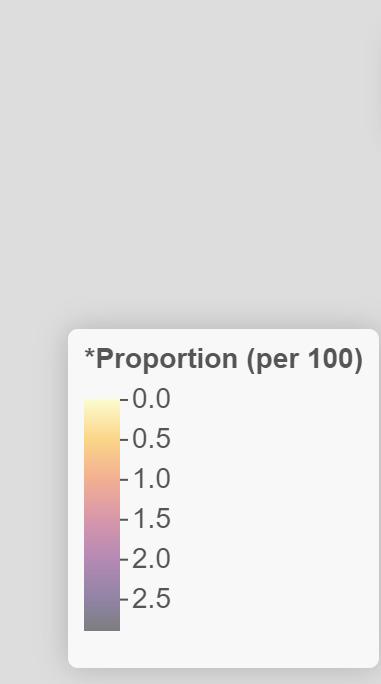
191
RENAL DISEASE DATA
According to the data (figure 25), the incidence of renal disease is higher in Kent County than New Castle and Sussex County. There are also areas of high incidence around the urban areas of Delaware. Not only does this show the need for renal specialists throughout the state, it also illustrates the need for dialysis centers, home care providers, and other renal specialists throughout the state. If renal disease progresses, an individual will also need the skills of transplant surgeons.
Individuals with chronic kidney disease or end stage renal disease will probably have a care team that includes a nephrologist, a nephrology nurse, a dietitian, and potentially a social worker. If a patient is placed on dialysis, their care team will expand to include patient care technicians and renal technologists. If a patient is matched with a kidney transplant, the care team will expand again to include a transplant surgeon, transplant coordinator, and a donor coordinator.
Figure 25. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Chronic Kidney Disease

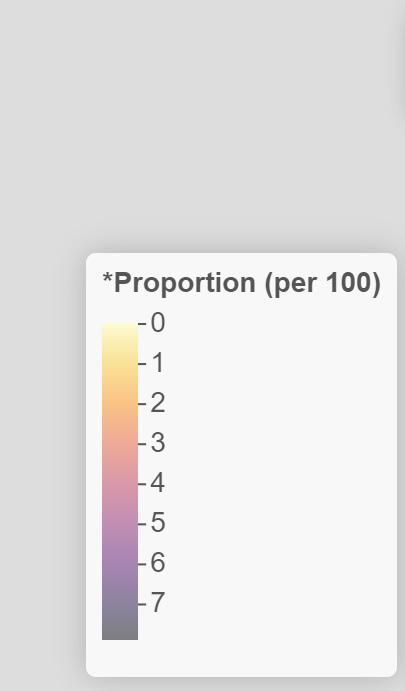
192 Delaware Journal of Public Health - December 2022
RESPIRATORY DISEASES DATA
Asthma can be diagnosed at any age. As seen in Figure 26, incident rates increase in urban areas, perhaps due to increased air pollution due to traffic and industry. Chronic Obstructive Pulmonary Disease (COPD) incidence in Delaware is lower in New Castle County than in Kent or Sussex Counties (figure 27). This could be due to a lack of pulmonary specialists in these counties, increased risk of COPD with age, or a difference in air pollutants in these counties. The data illustrates the need for pulmonary specialists in these areas, as well as care teams specializing in COPD.
Data on lung cancer has only been reported in a few census tracts (figure 28). These areas may contain larger populations of individuals at increased risk for lung cancer (i.e., history of smoking, increased age), and thus have an increased screening rate. There may also be an association with cancer treatment centers and their reporting.
Allergies
Individuals with food allergies will require a care team consisting of an allergist and a dietitian. Those with respiratory allergies may create a team of pulmonologists, respiratory therapists, and pharmacists.
Asthma
Asthma care teams may include a pulmonologist, an allergist, pharmacists, exercise physiologists, respiratory therapists, and mental health providers.
Chronic Obstructive Pulmonary Disease
Individuals with COPD will likely include a pulmonologist, a pulmonary rehabilitation therapist, pharmacists, mental health providers, and a nutritionist on their care team. Depending on the severity of their COPD, the team may also include a thoracic surgeon and/or a palliative care provider.
Figure 26. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Asthma

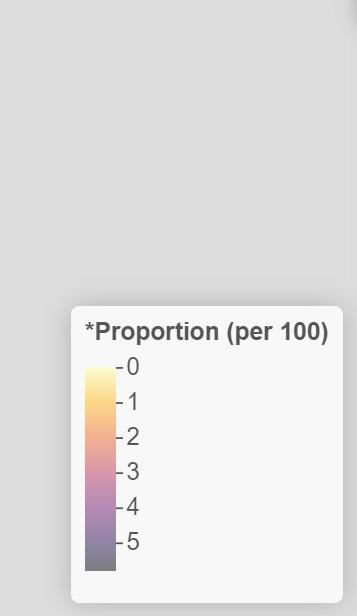
193
Figure 27. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Chronic Obstructive Pulmonary Disease
Figure 28. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Lung Cancer
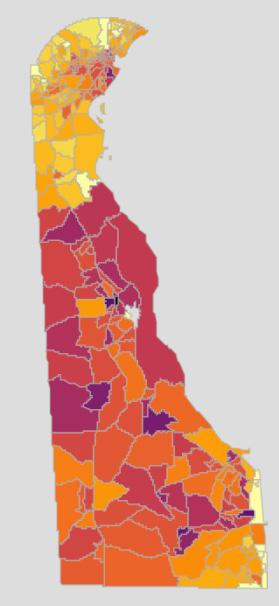
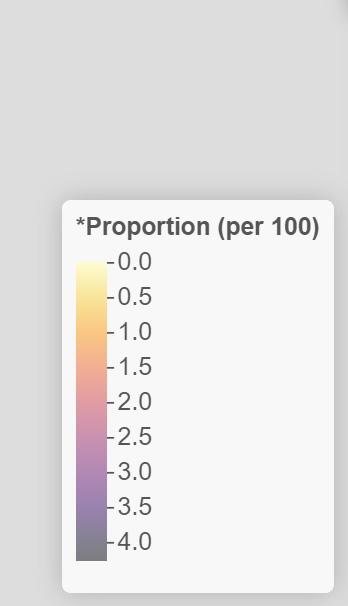

194 Delaware Journal of Public Health - December 2022
MALE UROLOGY
Incidence of benign prostate hyperplasia and prostate cancer increase with age, as shown in figures 29 and 13. These data illustrate the need for urologists and prostate specialists throughout the state, but especially in areas with older populations.
Figure 29. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Benign Prostatic Hyperplasia

195
VISION DATA
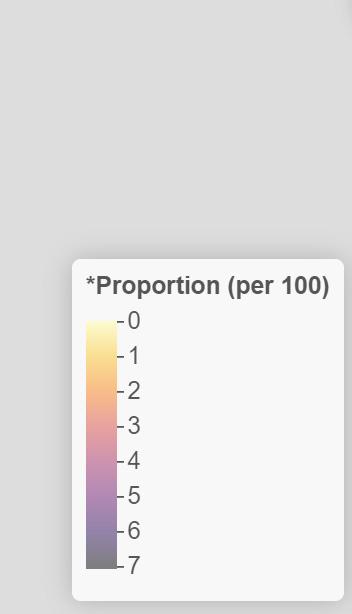
The risk of cataracts increases with age, as the data in figure 30 shows. Glaucoma is more ubiquitous, and can affect individuals at any age, although it is more likely seen in adults. Figure 31 shows that there is an increased incidence of glaucoma in areas of increased populations. There is a need for healthcare providers specializing in ophthalmology and optometry to assist these individuals with their vision needs.
Figure 30. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Cataracts
Figure 31. 2020 Proportion of the Total Insured Delawarean Population by Census Tract (per 100 persons) with Glaucoma
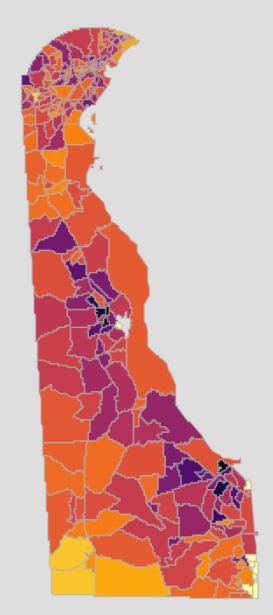

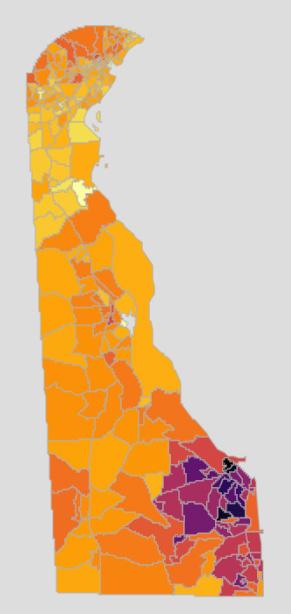
REFERENCES
1. Holman, H. R. (2020, March). The relation of the chronic disease epidemic to the healthcare crisis. ACR Open Rheumatology, 2(3), 167–173. Epub2020Feb19. https://doi.org/10.1002/acr2.11114
2. Council on Aging. (2020, Mar 9). Chronic vs. acute medical conditions: What’s the difference? Retrieved from: https://www.ncoa.org/article/chronic-versus-acute-disease
3. Office of State Planning Coordination. (n.d.). Demographic Information. Retrieved from: http://www.stateplanning.delaware.gov/demography/documents/dpc/DPC-2021v0-report.xls
196 Delaware Journal of Public Health - December 2022
Take the flu out of the season. Get your flu vaccine. Put the flu in its place — get the flu vaccine. If you’re eligible, you can get your COVID-19 bivalent booster at the same time. Visit flu.delaware.gov for more info and locations to get your vaccine. 197
GLOBAL HEALTH MATTERS
GLOBAL HEALTH MATTERS
GLOBAL HEALTH MATTERS
GLOBAL HEALTH MATTERS
NOV/DEC 2022
NOV/DEC 2022
NOV/DEC 2022
Tackling tobacco, TB, and mental health in South Africa…p. 4
Tackling tobacco, TB, and mental health
Tackling tobacco, TB, and mental health in South Africa…p. 4
in South Africa…p. 4
Tackling tobacco, TB, and mental health in South Africa…p. 4
Capacity building leads to pandemic preparedness
Capacity building leads to pandemic preparedness
Capacity building leads to pandemic preparedness
“Research capacity is a critical element of pandemic preparedness.” With these words, Fogarty Deputy Director Dr. Peter Kilmarx began a symposium at the annual meeting of the American Society of Tropical Medicine & Hygiene (ASTMH) in November. The panel was moderated by Kilmarx and Karen Goraleski, ASTMH CEO and a Fogarty board member, and featured speakers from Africa, South Asia, Latin America, and the Caribbean. Each speaker related how establishing research capacity before the pandemic at their respective institutions with support from Fogarty and other NIH institutes aided their national and regional response to COVID-19.
Capacity building leads to pandemic preparedness








“Research capacity is a critical element of pandemic preparedness.” With these words, Fogarty Deputy Director Dr. Peter Kilmarx began a symposium at the annual meeting of the American Society of Tropical Medicine & Hygiene (ASTMH) in November. The panel was moderated by Kilmarx and Karen Goraleski, ASTMH CEO and a Fogarty board member, and featured speakers from Africa, South Asia, Latin America, and the Caribbean. Each speaker related how establishing research capacity before the pandemic at their respective institutions with support from Fogarty and other NIH institutes aided their national and regional response to COVID-19.
“Research capacity is a critical element of pandemic preparedness.” With these words, Fogarty Deputy Director Dr. Peter Kilmarx began a symposium at the annual meeting of the American Society of Tropical Medicine & Hygiene (ASTMH) in November. The panel was moderated by Kilmarx and Karen Goraleski, ASTMH CEO and a Fogarty board member, and featured speakers from Africa, South Asia, Latin America, and the Caribbean. Each speaker related how establishing research capacity before the pandemic at their respective institutions with support from Fogarty and other NIH institutes aided their national and regional response to COVID-19.
“Research capacity is a critical element of pandemic preparedness.” With these words, Fogarty Deputy Director Dr. Peter Kilmarx began a symposium at the annual meeting of the American Society of Tropical Medicine & Hygiene (ASTMH) in November. The panel was moderated by Kilmarx and Karen Goraleski, ASTMH CEO and a Fogarty board member, and featured speakers from Africa, South Asia, Latin America, and the Caribbean. Each speaker related how establishing research capacity before the pandemic at their respective institutions with support from Fogarty and other NIH institutes aided their national and regional response to COVID-19.
Dr. Christian Happi, Director of the African Centre of Excellence for Genomics of Infectious Diseases (ACEGID), highlighted how conducting genomic sequencing of Ebola during the 2014-2016 West African outbreak prepared them for COVID-19. “We were years ahead of the WHO because we were trying to use genomics to guide the public health response,” he said. This progressive thinking meant ACEGID, based at Redeemer’s University, Nigeria, was equipped to respond to COVID. During the pandemic, ACEGID trained more than 1,300 scientists in 42 African countries.
Dr. Christian Happi, Director of the African Centre of Excellence for Genomics of Infectious Diseases (ACEGID), highlighted how conducting genomic sequencing of Ebola during the 2014-2016 West African outbreak prepared them for COVID-19. “We were years ahead of the WHO because we were trying to use genomics to guide the public health response,” he said. This progressive thinking meant ACEGID, based at Redeemer’s University, Nigeria, was equipped to respond to COVID. During the pandemic, ACEGID trained more than 1,300 scientists in 42 African countries.
Dr. Christian Happi, Director of the African Centre of Excellence for Genomics of Infectious Diseases (ACEGID), highlighted how conducting genomic sequencing of Ebola during the 2014-2016 West African outbreak prepared them for COVID-19. “We were years ahead of the WHO because we were trying to use genomics to guide the public health response,” he said. This progressive thinking meant ACEGID, based at Redeemer’s University, Nigeria, was equipped to respond to COVID. During the pandemic, ACEGID trained more than 1,300 scientists in 42 African countries.
Dr. Christian Happi, Director of the African Centre of Excellence for Genomics of Infectious Diseases (ACEGID), highlighted how conducting genomic sequencing of Ebola during the 2014-2016 West African outbreak prepared them for COVID-19. “We were years ahead of the WHO because we were trying to use genomics to guide the public health response,” he said. This progressive thinking meant ACEGID, based at Redeemer’s University, Nigeria, was equipped to respond to COVID. During the pandemic, ACEGID trained more than 1,300 scientists in 42 African countries.
In Pakistan, the Aga Khan University (AKU) was able to mobilize research scientists trained in whole genome sequencing of diseases like dengue, West Nile Virus, and tuberculosis to aid in the government’s response, said Dr. Erum Khan, Professor in Microbiology at AKU Hospital. She noted, “If we hadn’t been able to move people from the research side [of the university] to the clinical side, it would not have been possible to identify COVID variants and run diagnostics” at the pace of up to 2,000 cases per day.
In Pakistan, the Aga Khan University (AKU) was able to mobilize research scientists trained in whole genome sequencing of diseases like dengue, West Nile Virus, and tuberculosis to aid in the government’s response, said Dr. Erum Khan, Professor in Microbiology at AKU Hospital. She noted, “If we hadn’t been able to move people from the research side [of the university] to the clinical side, it would not have been possible to identify COVID variants and run diagnostics” at the pace of up to 2,000 cases per day.
In Pakistan, the Aga Khan University (AKU) was able to mobilize research scientists trained in whole genome sequencing of diseases like dengue, West Nile Virus, and tuberculosis to aid in the government’s response, said Dr. Erum Khan, Professor in Microbiology at AKU Hospital. She noted, “If we hadn’t been able to move people from the research side [of the university] to the clinical side, it would not have been possible to identify COVID variants and run diagnostics” at the pace of up to 2,000 cases per day.
In Pakistan, the Aga Khan University (AKU) was able to mobilize research scientists trained in whole genome sequencing of diseases like dengue, West Nile Virus, and tuberculosis to aid in the government’s response, said Dr. Erum Khan, Professor in Microbiology at AKU Hospital. She noted, “If we hadn’t been able to move people from the research side [of the university] to the clinical side, it would not have been possible to identify COVID variants and run diagnostics” at the pace of up to 2,000 cases per day.
The Jamaican Ministry of Health wanted to use nextgeneration sequencing for COVID surveillance. They knew of Dr. John Lindo’s laboratory at University of the West Indies (UWI), which, through a Fogarty-funded partnership
The Jamaican Ministry of Health wanted to use nextgeneration sequencing for COVID surveillance. They knew of Dr. John Lindo’s laboratory at University of the West Indies (UWI), which, through a Fogarty-funded partnership
The Jamaican Ministry of Health wanted to use nextgeneration sequencing for COVID surveillance. They knew of Dr. John Lindo’s laboratory at University of the West Indies (UWI), which, through a Fogarty-funded partnership
The Jamaican Ministry of Health wanted to use nextgeneration sequencing for COVID surveillance. They knew of Dr. John Lindo’s laboratory at University of the West Indies (UWI), which, through a Fogarty-funded partnership




ments during the COVID-19 pandemic at the 2022 ASTMH meeting.
Dr. Erum Khan,
with the State University of New York at Buffalo, runs a program focused on emerging and chronic viral infections. The ministry reached out and eventually enabled UWI to set up a genomic center. Prior to that, Lindo explained, “we’d have to send samples to Trinidad and wait quite a while for results.”
with the State University of New York at Buffalo, runs a program focused on emerging and chronic viral infections. The ministry reached out and eventually enabled UWI to set up a genomic center. Prior to that, Lindo explained, “we’d have to send samples to Trinidad and wait quite a while for results.”
with the State University of New York at Buffalo, runs a program focused on emerging and chronic viral infections. The ministry reached out and eventually enabled UWI to set up a genomic center. Prior to that, Lindo explained, “we’d have to send samples to Trinidad and wait quite a while for results.”
with the State University of New York at Buffalo, runs a program focused on emerging and chronic viral infections. The ministry reached out and eventually enabled UWI to set up a genomic center. Prior to that, Lindo explained, “we’d have to send samples to Trinidad and wait quite a while for results.”
Before COVID, the Centro Internacional de Entrenamiento e Investigaciones Médicas (CIDEIM) in Colombia, did not focus on virology at all but on parasitic and bacterial diseases. Yet their “know-how in diagnostic tests”—some of it developed via their Fogarty-funded training program focusing on emerging infectious diseases—allowed them to lend support for case identification and validation, according to Dr. Nancy Gore Saravia, director of CIDEIM.
Before COVID, the Centro Internacional de Entrenamiento e Investigaciones Médicas (CIDEIM) in Colombia, did not focus on virology at all but on parasitic and bacterial diseases. Yet their “know-how in diagnostic tests”—some of it developed via their Fogarty-funded training program focusing on emerging infectious diseases—allowed them to lend support for case identification and validation, according to Dr. Nancy Gore Saravia, director of CIDEIM.
Before COVID, the Centro Internacional de Entrenamiento e Investigaciones Médicas (CIDEIM) in Colombia, did not focus on virology at all but on parasitic and bacterial diseases. Yet their “know-how in diagnostic tests”—some of it developed via their Fogarty-funded training program focusing on emerging infectious diseases—allowed them to lend support for case identification and validation, according to Dr. Nancy Gore Saravia, director of CIDEIM.
Before COVID, the Centro Internacional de Entrenamiento e Investigaciones Médicas (CIDEIM) in Colombia, did not focus on virology at all but on parasitic and bacterial diseases. Yet their “know-how in diagnostic tests”—some of it developed via their Fogarty-funded training program focusing on emerging infectious diseases—allowed them to lend support for case identification and validation, according to Dr. Nancy Gore Saravia, director of CIDEIM.
Finally, Dr. Sikhulile Moyo discussed how studying HIV viral evolution prepared him for COVID. The former Fogarty Fellow and current Laboratory Director at the BotswanaHarvard AIDS Institute Partnership said that having built systems and networks in response to HIV/AIDS over the years allowed his team in Botswana to pivot and establish systematic pathogen surveillance early in the pandemic. This was critical for identifying and tracking variants, and eventually led to Moyo’s discovery of omicron.
Finally, Dr. Sikhulile Moyo discussed how studying HIV viral evolution prepared him for COVID. The former Fogarty Fellow and current Laboratory Director at the BotswanaHarvard AIDS Institute Partnership said that having built systems and networks in response to HIV/AIDS over the years allowed his team in Botswana to pivot and establish systematic pathogen surveillance early in the pandemic. This was critical for identifying and tracking variants, and eventually led to Moyo’s discovery of omicron.
Finally, Dr. Sikhulile Moyo discussed how studying HIV viral evolution prepared him for COVID. The former Fogarty Fellow and current Laboratory Director at the BotswanaHarvard AIDS Institute Partnership said that having built systems and networks in response to HIV/AIDS over the years allowed his team in Botswana to pivot and establish systematic pathogen surveillance early in the pandemic. This was critical for identifying and tracking variants, and eventually led to Moyo’s discovery of omicron.
Finally, Dr. Sikhulile Moyo discussed how studying HIV viral evolution prepared him for COVID. The former Fogarty Fellow and current Laboratory Director at the BotswanaHarvard AIDS Institute Partnership said that having built systems and networks in response to HIV/AIDS over the years allowed his team in Botswana to pivot and establish systematic pathogen surveillance early in the pandemic. This was critical for identifying and tracking variants, and eventually led to Moyo’s discovery of omicron.
www.fic.nih.gov
Inside this issue FOCUS
Konzo
• The
•Bitter
•A
Read more on pages 6 – 9
FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES
NOV/DEC 2022
and the children of Kahemba
researchers trying to save them
cassava, bitter irony
quest for solutions
Professor in Microbiology at AKU Hospital, presents key achievements during the COVID-19 pandemic at the 2022 ASTMH meeting.
www.fic.nih.gov
Courtesy of ASTMH
FOCUS
FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES
Inside this issue
Konzo
• The
• Bitter
• A
Read more on pages 6 – 9
and the children of Kahemba
researchers trying to save them
cassava, bitter irony
quest for solutions
www.fic.nih.gov
Courtesy of ASTMH
Inside
issue FOCUS
FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES
this
•The
•
•
Read more on pages 6 – 9
Konzo and the children of Kahemba
researchers trying to save them
Bitter cassava, bitter irony
A quest for solutions
Dr. Erum Khan, Professor in Microbiology at AKU Hospital, presents key achievements during the COVID-19 pandemic at the 2022 ASTMH meeting.
www.fic.nih.gov
Courtesy of ASTMH
Inside
FOCUS
•The
•
•
Read more on pages 6 – 9
FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES
this issue
Konzo and the children of Kahemba
researchers trying to save them
Bitter cassava, bitter irony
A quest for solutions
Dr. Erum Khan, Professor in Microbiology at AKU Hospital, presents key achievements during the COVID-19 pandemic at the 2022 ASTMH meeting.
201 Read More on pages 203-206 • The 198 Delaware Journal of Public Health - December 2022
Courtesy of ASTMH
Addressing mental health abroad helps US communities
Addressing mental health abroad helps US communities
As the U.S. population becomes increasingly diverse, it is more important than ever to ensure that providers can serve their patients in a culturally responsive way. A recent educational case report published in Academic Psychiatry highlights how global collaborations in mental health research can help providers better reach underserved communities in the United States.
As the U.S. population becomes increasingly diverse, it is more important than ever to ensure that providers can serve their patients in a culturally responsive way. A recent educational case report published in Academic Psychiatry highlights how global collaborations in mental health research can help providers better reach underserved communities in the United States.
The report came from a study co-funded by Fogarty and the National Institute for Mental Health (NIMH). Authors Dr. Kristina Korte, Assistant Professor of Psychology at Harvard Medical School and Clinical Psychologist at Massachusetts General Hospital, and Dr. Kimberly Hook, Research Fellow at Harvard T.H. Chan School of Public Health, described a long-standing program led by senior author, Dr. David Henderson, Chief of Psychiatry at the Boston University School of Medicine. He and his colleagues supported the Liberian Ministry of Health in developing that nation's first mental health strategic plan. They surveyed Liberians to better understand mental health needs, specifically focusing on children and adolescents and patterns of substance abuse associated with mental illness.
The report came from a study co-funded by Fogarty and the National Institute for Mental Health (NIMH). Authors Dr. Kristina Korte, Assistant Professor of Psychology at Harvard Medical School and Clinical Psychologist at Massachusetts General Hospital, and Dr. Kimberly Hook, Research Fellow at Harvard T.H. Chan School of Public Health, described a long-standing program led by senior author, Dr. David Henderson, Chief of Psychiatry at the Boston University School of Medicine. He and his colleagues supported the Liberian Ministry of Health in developing that nation's first mental health strategic plan. They surveyed Liberians to better understand mental health needs, specifically focusing on children and adolescents and patterns of substance abuse associated with mental illness.
While in the U.S., the team enlisted the help of the Liberian immigrant community in Massachusetts through a local church congregation. These volunteers helped translate and transcribe the survey results from Liberia to ensure researchers captured linguistic nuances and cultural differences they might have otherwise missed. With the volunteers’ input, researchers could identify inefficiencies, restructure their initial survey, and develop a more culturally relevant questionnaire for future study
While in the U.S., the team enlisted the help of the Liberian immigrant community in Massachusetts through a local church congregation. These volunteers helped translate and transcribe the survey results from Liberia to ensure researchers captured linguistic nuances and cultural differences they might have otherwise missed. With the volunteers’ input, researchers could identify inefficiencies, restructure their initial survey, and develop a more culturally relevant questionnaire for future study
participants in Liberia. The volunteers who helped the researchers also recognized similar mental health issues in their community in the U.S. One church member was quoted as saying, “Even though we are here in America, we are still the same Africans. We still have the same beliefs. We still handle mental and emotional health issues the same way.”
participants in Liberia. The volunteers who helped the researchers also recognized similar mental health issues in their community in the U.S. One church member was quoted as saying, “Even though we are here in America, we are still the same Africans. We still have the same beliefs. We still handle mental and emotional health issues the same way.”


Ultimately the project not only supported Liberia's Mental Health Policy and Strategic Plan, but in Massachusetts, the Health and Mental Health Education and Awareness for Africans in Lowell or HEAAL initiative was established between the church and the Department of Psychiatry at Boston University School of Medicine with the goal of better understanding the nature, characteristics, scope, and magnitude of health and mental health issues in this faith community of primarily immigrants and refugees.
Ultimately the project not only supported Liberia's Mental Health Policy and Strategic Plan, but in Massachusetts, the Health and Mental Health Education and Awareness for Africans in Lowell or HEAAL initiative was established between the church and the Department of Psychiatry at Boston University School of Medicine with the goal of better understanding the nature, characteristics, scope, and magnitude of health and mental health issues in this faith community of primarily immigrants and refugees.
While this global-local paradigm has clear positive implications for the patient population, this work also creates new training opportunities for mental health professionals in U.S. and global settings. As trainees work with diverse populations through global-local collaboration or community engagement, their cultural competency and humility grows, enabling providers to address potential cultural barriers to care. With the growing recognition of mental health as a global issue, it is increasingly important to help bridge the gap and provide culturally responsive care for the diverse communities of the U.S. The report notes that while this study focused on Liberia, the lessons learned can be implemented in other LMICs and their respective diaspora communities in the West.
While this global-local paradigm has clear positive implications for the patient population, this work also creates new training opportunities for mental health professionals in U.S. and global settings. As trainees work with diverse populations through global-local collaboration or community engagement, their cultural competency and humility grows, enabling providers to address potential cultural barriers to care. With the growing recognition of mental health as a global issue, it is increasingly important to help bridge the gap and provide culturally responsive care for the diverse communities of the U.S. The report notes that while this study focused on Liberia, the lessons learned can be implemented in other LMICs and their respective diaspora communities in the West.
Save the date: Global Health Fellows & Scholars 20th Anniversary
Save the date: Global Health Fellows & Scholars 20th Anniversary
Fogarty’s flagship Global Health Fellows and Scholars program, now known as LAUNCH, will celebrate its 20th Anniversary in 2023. To mark the occasion, Fogarty invites program alums to join us for a commemorative event at NIH in April 2023.
Fogarty’s flagship Global Health Fellows and Scholars program, now known as LAUNCH, will celebrate its 20th Anniversary in 2023. To mark the occasion, Fogarty invites program alums to join us for a commemorative event at NIH in April 2023.




The event will be an opportunity to celebrate alumni accomplishments and share our hopes for future cohorts. Attendees will also have the opportunity to network and hear from directors from several NIH Institutes and Centers about the impact of Fogarty Fellows and Scholars in the global health workforce.
The event will be an opportunity to celebrate alumni accomplishments and share our hopes for future cohorts. Attendees will also have the opportunity to network and hear from directors from several NIH Institutes and Centers about the impact of Fogarty Fellows and Scholars in the global health workforce.
The Fellows and Scholars program, established in 2003, aims to foster the next generation of global health scientists by providing trainees, early in their careers, a one-year mentored research training experience at established biomedical and behavioral research institutions and project sites in low- and middle-income countries (LMICs) as well as opportunities for postprofessional trainees from the U.S. and LMICs.
The Fellows and Scholars program, established in 2003, aims to foster the next generation of global health scientists by providing trainees, early in their careers, a one-year mentored research training experience at established biomedical and behavioral research institutions and project sites in low- and middle-income countries (LMICs) as well as opportunities for postprofessional trainees from the U.S. and LMICs.
More information about the agenda and hybrid options for attendance will be shared in the coming months.
More information about the agenda and hybrid options for attendance will be shared in the coming months.
NOVEMBER/DECEMBER 2022 2
Community-based training, such as this session in Sinoe County, Liberia, provides health practitioners with the skills to be able to recognize symptoms of mental illness.
NOVEMBER/DECEMBER 2022 2
Photo courtesy of WHO/Alison Brunier
Community-based training, such as this session in Sinoe County, Liberia, provides health practitioners with the skills to be able to recognize symptoms of mental illness.
199
Photo courtesy of WHO/Alison Brunier
Climate change accelerates outbreak frequency
The frequency of Ebola outbreaks in Uganda has been increasing due to climate change and this is likely happening in other African nations as well, according to Dr. Sam Okware, director general of the Uganda National Health Research Organization. Central Africa has suffered 28 large Ebola outbreaks, and, since 2000, Uganda has experienced seven of these, including the most recent declared in September. Managing fear and rumors is crucial to an effective outbreak response, given the negative impacts of social media seen in some places, noted Okware, who spoke at a November 25 webinar sponsored by the African Forum for Research and Education in Health (AFREHealth), an interdisciplinary group seeking to improve the quality of health care in Africa.
Lieutenant Colonel Dr. Henry Kyobe Bosa, incident commander, provided a status update for the current outbreak of Sudan ebolavirus, for which there is no proven vaccine. Tallies for the ninth week include 141 total cases, 55 deaths, 79 recoveries, and 22 probable cases (where samples could not be taken). The highest recovery rate has been in Kampala, where 83% of infected people have survived the illness. Lowest recovery has been seen in Mubende and Kassanda, the epicenters of illness, where 73% of infected children under age 9 have died. The movement from rural epicenter to Uganda’s capital city was rapid, taking just two weeks and resulting in 10 independent clusters, Bosa noted. “Rural tools for contact tracing are ineffective in cities.” Developing better response tools for an urban setting is a priority.
This current outbreak has been a disease of children and women, signaling household transmission, noted Bosa. While the initial outbreak affected children, now there is mainly illness among young adults. “Since November 12, we haven’t had any new cases,” stated Bosa, adding that this is considered a real “remission” given surveillance systems are running well.
Dr. Jean-Jacques Muyembe TamFum, a member of the team that investigated the first known Ebola outbreak at Yambuku Mission in 1976, recounted lessons learned from past Zaire ebolavirus outbreaks in the Democratic Republic of Congo (DRC). Of the 318 total infected patients, 280 died during the Yambuku outbreak, which lasted less than 11 weeks—an 88% case fatality rate (CFR). Muyembe, a microbiologist, recalls lacking even basic personal protective equipment, including gloves, so he carefully washed his hands with soap and water after handling patient samples. He credits this practice with his personal survival.
In 1995, the first outbreak after Yambuku occurred in Kikwit, also in DRC, recounted Muyembe who is now director of the country's National Institutes of Bio-Medical Research. Researchers recorded 317 total cases and 250 deaths there, a 78% CFR.
Eight patients were treated with blood from survivors, and, in a paper published in The Journal of Infectious Diseases, “we concluded that Ebola antibodies were protective,” said Muyembe. Yet this experiment “remained a mere anecdote for a long time” because the observational study lacked a control arm and had a small sample size.

Still Muyembe believed in the protective qualities of antibodies, and, with help from other scientists, “the dream of my life is now a reality.” That dream is EBANGA, a therapy based on a single monoclonal antibody isolated from a human survivor of the outbreak in Kikwit. Today, EBANGA is used to treat children and adults who've been infected with Zaire ebolavirus.
Africa needs to develop more mobile and local laboratory capacity if it is to become more effective in rapidly addressing outbreaks of the deadly hemorrhagic fever in the future, concluded Muyembe.
The webinar can be viewed on the AFREHealth website.
3 NOVEMBER/DECEMBER 2022
Photo courtesy of NIAID
200 Delaware Journal of Public Health - December 2022
An artist’s rendering based on electron micrography of filamentous Ebola virus particles
PROFILE
PROFILE
Tackling tobacco, TB, and mental health in South Africa
Tackling tobacco, TB, and mental health in South Africa
Dr. Richard van-Zyl Smit comes from a family of physicians: His parents were physicians, his sister, who is currently practicing, married a physician, his uncle is a physician, and his aunt is a nurse. Before he applied to become a Fogarty Global Health Fellow, his cousin and fellow medical doctor, Jacqueline Firth, was accepted into the inaugural Fogarty Global Health Fellows & Scholars cohort.
Dr. Richard van-Zyl Smit comes from a family of physicians: His parents were physicians, his sister, who is currently practicing, married a physician, his uncle is a physician, and his aunt is a nurse. Before he applied to become a Fogarty Global Health Fellow, his cousin and fellow medical doctor, Jacqueline Firth, was accepted into the inaugural Fogarty Global Health Fellows & Scholars cohort.
A consultant pulmonologist at Groote Schuur Hospital in Cape Town, South Africa, and a deputy head of the division of pulmonology at the University of Cape Town Lung Institute, van-Zyl Smit credits his Fogarty Fellowship as the starting point for his current career. “The Fogarty program was instrumental in my career, launching me and pushing me in the direction I went. It was just a fantastic immersion into research and an opportunity I don’t think anyone should pass up,” van Zyl-Smit said.
A consultant pulmonologist at Groote Schuur Hospital in Cape Town, South Africa, and a deputy head of the division of pulmonology at the University of Cape Town Lung Institute, van-Zyl Smit credits his Fogarty Fellowship as the starting point for his current career. “The Fogarty program was instrumental in my career, launching me and pushing me in the direction I went. It was just a fantastic immersion into research and an opportunity I don’t think anyone should pass up,” van Zyl-Smit said.
For his Fogarty project, he exposed TB-infected macrophages to tobacco smoke and nicotine to test their immune responses. He found that this exposure significantly reduced the production of cytokines key in the defense against tuberculosis during infection. He later replicated his results using vaping products, suggesting a potential mechanism to explain the epidemiological link between tobacco smoking and the risk of TB infection.
For his Fogarty project, he exposed TB-infected macrophages to tobacco smoke and nicotine to test their immune responses. He found that this exposure significantly reduced the production of cytokines key in the defense against tuberculosis during infection. He later replicated his results using vaping products, suggesting a potential mechanism to explain the epidemiological link between tobacco smoking and the risk of TB infection.
Since his fellowship, van Zyl-Smit has been actively involved in poverty-related respiratory health issues in South Africa and has made it central to his research and career. South Africa has some of the highest rates of tuberculosis, chronic obstructive pulmonary disease (COPD) and several other chronic respiratory illnesses in the world. He has co-authored publications on TB, COPD, smoking cessation programs, and the interplay between tobacco use and diseases such as HIV/AIDS and COVID-19.
Since his fellowship, van Zyl-Smit has been actively involved in poverty-related respiratory health issues in South Africa and has made it central to his research and career. South Africa has some of the highest rates of tuberculosis, chronic obstructive pulmonary disease (COPD) and several other chronic respiratory illnesses in the world. He has co-authored publications on TB, COPD, smoking cessation programs, and the interplay between tobacco use and diseases such as HIV/AIDS and COVID-19.
“The intersection of poverty and respiratory disease is not unique to South Africa,” said van Zyl-Smit. “However, I fear that unless we address poverty, we will be ineffective at treating all the other components related to these high rates.”
“The intersection of poverty and respiratory disease is not unique to South Africa,” said van Zyl-Smit. “However, I fear that unless we address poverty, we will be ineffective at treating all the other components related to these high rates.”
Richard van-Zyl Smit, MD, PhD
Richard van-Zyl Smit, MD, PhD
Fogarty Fellow: 2009-2011
Fogarty Fellow: 2009-2011
U.S. institution: Vanderbilt University
U.S. institution: Vanderbilt University
Foreign institution: University of Cape Town
Foreign institution: University of Cape Town
Research topic: The interaction of tobacco smoke and pulmonary defenses against tuberculosis
Research topic: The interaction of tobacco smoke and pulmonary defenses against tuberculosis
Van Zyl-Smit currently serves as president of the South African Thoracic Society, co-chair of the American Thoracic Society International Health committee, and as a global ambassador for the Global Initiative for Asthma. He presented his Fogarty data at an American Thoracic Society meeting in 2008 and was awarded an international trainee scholarship from that presentation. Today he runs the American Thoracic Society’s international scholarship program.
Van Zyl-Smit currently serves as president of the South African Thoracic Society, co-chair of the American Thoracic Society International Health committee, and as a global ambassador for the Global Initiative for Asthma. He presented his Fogarty data at an American Thoracic Society meeting in 2008 and was awarded an international trainee scholarship from that presentation. Today he runs the American Thoracic Society’s international scholarship program.
“My Fogarty project gave me access to an entirely new network outside of my region, and I would not be in the position I am today without those connections.”
“My Fogarty project gave me access to an entirely new network outside of my region, and I would not be in the position I am today without those connections.”
In addition to his work as a pulmonologist, in recent years van Zyl-Smit has become an advocate for mental health.
In addition to his work as a pulmonologist, in recent years van Zyl-Smit has become an advocate for mental health.
During his inaugural lecture at the University of Cape Town in 2022, van Zyl-Smit shared his personal struggles with mental health. After being diagnosed with stressinduced anxiety in 2016, he began writing his first book titled “They Don’t Award Nobel Prizes to Dead People.” The book, which helped him process his anxiety, advocates for a culture change with a stronger emphasis on worklife balance. He later went on to author another book, “Thoughts on a Saturday Morning: A collection of essays on life, work and relationships during COVID-19,” in which he wrote about the stress he and his fellow health care workers suffered at the hands of the pandemic in South Africa.
During his inaugural lecture at the University of Cape Town in 2022, van Zyl-Smit shared his personal struggles with mental health. After being diagnosed with stressinduced anxiety in 2016, he began writing his first book titled “They Don’t Award Nobel Prizes to Dead People.” The book, which helped him process his anxiety, advocates for a culture change with a stronger emphasis on worklife balance. He later went on to author another book, “Thoughts on a Saturday Morning: A collection of essays on life, work and relationships during COVID-19,” in which he wrote about the stress he and his fellow health care workers suffered at the hands of the pandemic in South Africa.


As part of the closing remarks of his inaugural lecture, he reminded his colleagues to care for themselves and each other noting, “we are of greater value alive and functional than dead or dysfunctional.”
As part of the closing remarks of his inaugural lecture, he reminded his colleagues to care for themselves and each other noting, “we are of greater value alive and functional than dead or dysfunctional.”
4
4
201
LOLA KOLA, PHD
Dr. Lola Kola is a senior research fellow at University of Ibadan's WHO Collaborating Centre for Research and Training in Mental Health, Neurosciences and Drug and Alcohol Abuse. She also serves as adjunct associate professor at Lead City University, Nigeria. Prior to this, she earned master's and doctoral degrees in Medical Sociology at University of Ibadan. Kola partners on projects with the Behavioral Research in Technology and Engineering (BRiTE) Center at the University of Washington (UW) in Seattle and the Centre for Child and Adolescent Mental Health at University of Ibadan. Most recently she’s a Visiting Researcher in the Centre for Global Mental Health Department of Kings College London.

Tell us about your work.
I developed a mobile phone app as an adjunct treatment to routine primary care for adolescent mothers with depression. In Nigeria—and in many places—young mothers don’t want to go to clinics because the nurses seem unkind: “You're pregnant but not married. Your mates are in school.” Because these teen mothers have depression, they may also have problems with personal care. Others shame them as “sluggish” or “lazy.” Not only do they feel social stigma from family members, nurses, neighbors and friends, they’ve disappointed themselves and feel self-stigma. Generally, they experience very low social support.
Seeing this, I thought, How do I reach these girls? Originally, I planned in-depth interviews, but adolescents are sometimes not so trusting. They did not talk. Next, I brought them together in focus group discussions and then they couldn’t stop talking! There, I noticed nine out of 10 had mobile phones and I asked what they liked to do on them. They all liked watching short videos—funny skits, you know? This struck me as a possible area for innovation for my Emerging Global Leader award, which is supported by the National Institute of Mental Health (NIMH). So, applying usercentered design, my team created 14 short videos (with music the girls chose) to help them increase their engagement with care, while teaching them how to take care of their mental and physical health.
My evaluations showed that this adjunct treatment (adjunct to face-to-face clinical care) delivered through a mobile phone app helped the young mothers overcome problems related to stigma and improved treatment outcomes. We also found that relatives played an important role in supporting teen mothers’ uptake of digital tools.
What is Nigeria’s most urgent health issue?


Nigeria has an outdated mental health law known as the Lunacy Act of 1958. First enacted in 1916, this legislation was later amended in 1958, but it hasn’t been updated since then, despite several attempts by the mental health community. It is archaic! It uses the derogatory term “lunatics” to refer to mentally ill patients and it only acknowledges asylum-type care—it does not include rehabilitation of mentally ill patients within communities. I would go so far as to say that Nigeria faces a human rights emergency in mental health.
What’s ahead?
I worked with the WHO country office in Abuja, Nigeria, from 2011-2014 as a National Consultant for mental health and I coordinated the rollout of the WHO’s Mental Health Gap Action Programme (mhGAP) in the country. The mhGAP provides a framework for scaling up health interventions in non-specialist settings and this informs my own research today. I focus on developing digital psychosocial tools to increase patient access and to strengthen health systems. I’m currently designing (with help from young mothers) an electronic magazine to provide health education to address the impact of climate change on mental health in pregnancy. I’m also part of a new project, supported by NIMH and co-led by my mentor, UW Professor Dror Ben-Zeev. WADMA or the West Africa Digital Mental Health Alliance aims to grow the next generation of regional researchers and clinicians designing tools for mental health care. Finally, I’m building my own team and increasing my international collaborative network so that I can move deeper into public health and apply for more competitive grants.
5 202 Delaware Journal of Public Health - December 2022
A&Q
FOCUS FOCUS
Konzo and the children of Kahemba
Konzo and the children of Kahemba
All researchers of konzo, a paralyzing disease that can occur in impoverished regions where bitter cassava is a food staple, share at least one thing in common: utter shock when first encountering the disease. Dr. Desire Tshala, who grew up in a modern, urban area of the Democratic Republic of Congo (DRC), said, “I couldn’t believe that in my own country, just 600 miles from the capital city, Kinshasa, people were living in such a high degree of poverty and malnutrition. In the villages in and near Kahemba, DRC, about two out of 10 people” are affected.
All researchers of konzo, a paralyzing disease that can occur in impoverished regions where bitter cassava is a food staple, share at least one thing in common: utter shock when first encountering the disease. Dr. Desire Tshala, who grew up in a modern, urban area of the Democratic Republic of Congo (DRC), said, “I couldn’t believe that in my own country, just 600 miles from the capital city, Kinshasa, people were living in such a high degree of poverty and malnutrition. In the villages in and near Kahemba, DRC, about two out of 10 people” are affected.
The Yaka tribe’s word “konzo,” referring to an antelope tethered at its knees, was used to describe cases seen in the Belgian Congo in 1928. Later, this term was adopted by Dr. Hans Rosling, the late Swedish physician and epidemiologist, who began characterizing the disease in 1989. At that time, no one understood what caused konzo: Was it a virus? Mutations? Rosling identified the cassava plant, a tuberous root containing toxic cyanide that also happens to be the world's fourth most consumed food staple.
The Yaka tribe’s word “konzo,” referring to an antelope tethered at its knees, was used to describe cases seen in the Belgian Congo in 1928. Later, this term was adopted by Dr. Hans Rosling, the late Swedish physician and epidemiologist, who began characterizing the disease in 1989. At that time, no one understood what caused konzo: Was it a virus? Mutations? Rosling identified the cassava plant, a tuberous root containing toxic cyanide that also happens to be the world's fourth most consumed food staple.
Specifically, Rosling showed that cyanide poisoning from cassava, when it coincides with a diet lacking in sulfurbased amino acids, can damage upper motor neuron pathways within an individual's brain. The result is sudden,
Specifically, Rosling showed that cyanide poisoning from cassava, when it coincides with a diet lacking in sulfurbased amino acids, can damage upper motor neuron pathways within an individual's brain. The result is sudden,
Kahemba residents gather near the health center. Even as Dr. Desire Tshala worked in the lab to find answers to konzo, the people of Kahemba remained foremost in his thoughts.


Kahemba residents gather near the health center. Even as Dr. Desire Tshala worked in the lab to find answers to konzo, the people of Kahemba remained
non-progressive and non-reversible paralysis of the lower and/or upper extremities in severely affected people. So a child—usually those affected are malnourished children or mothers of child-bearing age—who has been eating cassava lifelong will wake up one morning either limping or needing a stick to walk or only able to crawl. This condition will remain unchanged throughout the child’s life. (In rare cases, another meal of improperly processed, toxic cassava will worsen the paralysis.)
non-progressive and non-reversible paralysis of the lower and/or upper extremities in severely affected people. So a child—usually those affected are malnourished children or mothers of child-bearing age—who has been eating cassava lifelong will wake up one morning either limping or needing a stick to walk or only able to crawl. This condition will remain unchanged throughout the child’s life. (In rare cases, another meal of improperly processed, toxic cassava will worsen the paralysis.)
Because konzo happens in isolated, rural areas, the exact number of cases remains unknown, though scientists estimate hundreds of thousands of affected people, most of them living in the DRC. The disease usually occurs as an outbreak triggered by crisis situations, such as drought, civil wars or famine.
Because konzo happens in isolated, rural areas, the exact number of cases remains unknown, though scientists estimate hundreds of thousands of affected people, most of them living in the DRC. The disease usually occurs as an outbreak triggered by crisis situations, such as drought, civil wars or famine.
Dr. Julie Cliff, a physician and epidemiologist who worked with Rosling in Mozambique, explained, “Everybody says, ‘Once you’ve seen konzo, you have to do something, you cannot stop.’ It’s just a horrifying sight to see so many people paralyzed. And in rural areas, paralyzed people cannot walk to their fields, yet they still crawl. I find that particularly moving.”
Dr. Julie Cliff, a physician and epidemiologist who worked with Rosling in Mozambique, explained, “Everybody says, ‘Once you’ve seen konzo, you have to do something, you cannot stop.’ It’s just a horrifying sight to see so many people paralyzed. And in rural areas, paralyzed people cannot walk to their fields, yet they still crawl. I find that particularly moving.”
Dr. Matthew Bramble, a genetic medicine researcher who is exploring connections between konzo and the gut microbiome, said, “You can read all you like about cassavaassociated paralysis, but when you go to the village and the kids are greeting you on all fours and people have canes and, later, the person you’re eating with is on the ground, well…. The community is completely used to it, and that is the most unusual component of konzo.”
Dr. Matthew Bramble, a genetic medicine researcher who is exploring connections between konzo and the gut microbiome, said, “You can read all you like about cassavaassociated paralysis, but when you go to the village and the kids are greeting you on all fours and people have canes and, later, the person you’re eating with is on the ground, well…. The community is completely used to it, and that is the most unusual component of konzo.”
Dr. Michael Boivin, a neuropsychology specialist whose research in the Democratic Republic of Congo began in the 1980s, credits one man as the driving force behind much of the konzo research happening today: “Desire Tshala. He’s at the center of it all.”
Dr. Michael Boivin, a neuropsychology specialist whose research in the Democratic Republic of Congo began in the 1980s, credits one man as the driving force behind much of the konzo research happening today: “Desire Tshala. He’s at the center of it all.”
Spearheading prevention
Spearheading prevention
Dr. Desire Tshala was 31 when he first confronted konzo. Dr. Thorkild Tylleskar, a former Rosling student, suggested
Dr. Desire Tshala was 31 when he first confronted konzo. Dr. Thorkild Tylleskar, a former Rosling student, suggested
FOCUS FOCUS
Photo courtesy of Neerja Vashist
203
Photo courtesy of Neerja Vashist
Tshala work with him in the field. That was 1996. Tshala’s neuro-epidemiological characterization of konzo, a project for his Ph.D. thesis, involved transporting villagers in remote, konzo-affected areas to cities and conducting “electrophysiology investigations with equipment brought from Sweden.” This early research sparked his passion and resulted in a logical progression towards increasing scientific understanding of konzo’s effects.
Eventually, his projects received funding from Fogarty, the National Institute of Environmental Health Sciences (NIEHS), and the National Institute of Neurological Disorders and Stroke (NINDS), enabling him to develop an experimental lab model and explore his most pressing questions. “In the same village or family, you’d see that some children are more susceptible than others, so I was looking for a biomarker.” By 2016, his experiments on rodents had suggested that cyanate, a chemical relative of cassava cyanide, may be associated with konzo.
The value of konzo research extends far beyond African villages, he explained. “Our models and what we are learning from the various studies—including epigenetic, microbiome, and toxicology studies—is very helpful in terms of understanding all motor neuron diseases, including ALS.” His research is also relevant in terms of studying the toxicity itself. “We work on cyanide, an important toxin in chemical warfare, and our understanding of it benefits the counterterrorism program at NINDS.”
The wetting method
Though his research grew more sophisticated, the villagers of Kahemba remained foremost in Tshala’s thoughts. Seeing the prevalence of paralysis, he decided his team could no longer continue observational studies. “We needed to start an intervention to prevent the disease.” He collaborated with Dr. James Howard Bradbury's team to introduce the wetting method in Kahemba (with added help from the DRC’s National Nutrition Program at the Ministry of Health).
The wetting method removes the toxic components of cassava from cassava flour, according to a study coauthored by Bradbury and Cliff. A food preparer mixes cassava flour with water and creates a thin layer of mixture which is left to dry in the sun for two hours or five in the shade. During this time, the chemicals break down, producing hydrogen cyanide gas, which harmlessly dissipates into the atmosphere.
Dr. Julie Cliff helped field-test the wetting method in Mozambique. “It should work to prevent konzo, it doesn’t take too long, and the rural women find it easy to use.”
Though hopeful, Tshala knows he faces an uphill battle.
A child who has been eating cassava lifelong will wake up one morning either limping or needing a stick to walk or only able to crawl. This condition will remain unchanged throughout the child’s life.

“While the wetting method works, it’s difficult for people to change the way they’ve been processing food.” Also, Tshala expects that natural catastrophes, like droughts or flooding, and climate variations, will likely increase the prevalence of konzo in the African countries already affected: DRC, Angola, Zambia, Tanzania, Mozambique, Uganda, Cameroon, and Nigeria.
The poorest of the poor Cliff’s own global health career stretches back to the 1970s. After a stint in Tanzania, the Australian native began working in Mozambique, where, in 1981, she faced her first konzo epidemic as a Ministry of Health physician. “We had a huge epidemic—hundreds of cases of paralyzed children, women of reproductive age and a few men. It was overwhelming.” Rosling, who had been working in the district, and Anders Molin, a Swedish doctor, investigated. This led to subsequent publications and a landmark epidemiological case history.
In the years following, Cliff continued to research konzo and the wetting method, while making significant contributions to the development of the Mozambique health system. She also contributed to a data report on konzo sponsored by the WHO. While the UN health agency has shown some interest, it hasn’t been enough, she explained. “We, the konzo workers, have felt continually frustrated because we’ve never managed to get this issue onto the agenda of the big organizations.”
This is because konzo is a problem among the poorest of the poor, she said. “The solution is development. Put resources into these poor, rural areas. Give them agricultural support.”
FOCUS ON COVID AWARDS 7 FOCUS ON KONZO – CHILDREN OF KAHEMBA
Photo courtesy of Michael Boivin
That characterization for his Ph.D. areas
204 Delaware Journal of Public Health - December 2022
National that his experiments with helpful neuron including research terms “We
Bitter cassava, bitter irony
Bitter cassava, bitter irony
Bitter cassava, bitter irony
To get to Kahemba, site of Dr. Michael Boivin's konzo research program in the Democratic Republic of Congo (DRC), you begin in Kinshasa, DRC’s capital city, and drive for two days until you reach a rural region near the Angolan border. Over the years, depending on economic and political conditions, people have moved back and forth between the two countries, Boivin explained: “It’s with this movement and instability, if you will, that people fail to ferment, dry and process cassava sufficiently to eliminate the cyanide contained within it.”
To get to Kahemba, site of Dr. Michael Boivin's konzo research program in the Democratic Republic of Congo (DRC), you begin in Kinshasa, DRC’s capital city, and drive for two days until you reach a rural region near the Angolan border. Over the years, depending on economic and political conditions, people have moved back and forth between the two countries, Boivin explained: “It’s with this movement and instability, if you will, that people fail to ferment, dry and process cassava sufficiently to eliminate the cyanide contained within it.”
To get to Kahemba, site of Dr. Michael Boivin's konzo research program in the Democratic Republic of Congo (DRC), you begin in Kinshasa, DRC’s capital city, and drive for two days until you reach a rural region near the Angolan border. Over the years, depending on economic and political conditions, people have moved back and forth between the two countries, Boivin explained: “It’s with this movement and instability, if you will, that people fail to ferment, dry and process cassava sufficiently to eliminate the cyanide contained within it.”
Failure to detoxify cassava places children at risk of konzo; malnourishment escalates the danger. “It’s the perfect storm of toxic cassava flour as a food staple and no beans or animal protein sources for sulfur-based amino acids so that, if cyanide levels build up sufficiently within a short period of time, the poison penetrates the blood-brain barrier, causing permanent and irreversible neurological injury,” said Boivin.
described konzo as an upper motor neuron disease that did not affect cognition. “We suspected otherwise," said Boivin. The team set out to prove it, but before they could begin, civil conflict in the region forced them to evacuate. Boivin turned his attention to cerebral malaria. Sometime later, at a scientific conference, he presented his research of school-age children affected by that disease, when “a tall, formidable Congolese neurologist came up to me and said, ‘We need this kind of work on our konzo project, would you write up a grant with me?’”
described konzo as an upper motor neuron disease that did not affect cognition. “We suspected otherwise," said Boivin. The team set out to prove it, but before they could begin, civil conflict in the region forced them to evacuate. Boivin turned his attention to cerebral malaria. Sometime later, at a scientific conference, he presented his research of school-age children affected by that disease, when “a tall, formidable Congolese neurologist came up to me and said, ‘We need this kind of work on our konzo project, would you write up a grant with me?’”
described konzo as an upper motor neuron disease that did not affect cognition. “We suspected otherwise," said Boivin. The team set out to prove it, but before they could begin, civil conflict in the region forced them to evacuate. Boivin turned his attention to cerebral malaria. Sometime later, at a scientific conference, he presented his research of school-age children affected by that disease, when “a tall, formidable Congolese neurologist came up to me and said, ‘We need this kind of work on our konzo project, would you write up a grant with me?’”
And so began Boivin’s collaboration with Desire Tshala.
And so began Boivin’s collaboration with Desire Tshala.
Failure to detoxify cassava places children at risk of konzo; malnourishment escalates the danger. “It’s the perfect storm of toxic cassava flour as a food staple and no beans or animal protein sources for sulfur-based amino acids so that, if cyanide levels build up sufficiently within a short period of time, the poison penetrates the blood-brain barrier, causing permanent and irreversible neurological injury,” said Boivin.
Failure to detoxify cassava places children at risk of konzo; malnourishment escalates the danger. “It’s the perfect storm of toxic cassava flour as a food staple and no beans or animal protein sources for sulfur-based amino acids so that, if cyanide levels build up sufficiently within a short period of time, the poison penetrates the blood-brain barrier, causing permanent and irreversible neurological injury,” said Boivin.
Damage to the upper motor neuron pathways in the brain results in paralysis. Boivin's recent research reveals that konzo has more extensive, if less visible, cognitive effects.
Damage to the upper motor neuron pathways in the brain results in paralysis. Boivin's recent research reveals that konzo has more extensive, if less visible, cognitive effects.
Damage to the upper motor neuron pathways in the brain results in paralysis. Boivin's recent research reveals that konzo has more extensive, if less visible, cognitive effects.
And so began Boivin’s collaboration with Desire Tshala.
Developmental delays
Developmental delays
Developmental delays
In 2011, parts of DRC became stable enough for the pair to begin “a multi-faceted research program” in Kahemba. Through 2017, Tshala and Boivin’s team documented konzo’s effects on development, constructing a portrait of affected, school-aged children.
In 2011, parts of DRC became stable enough for the pair to begin “a multi-faceted research program” in Kahemba. Through 2017, Tshala and Boivin’s team documented konzo’s effects on development, constructing a portrait of affected, school-aged children.
In 2011, parts of DRC became stable enough for the pair to begin “a multi-faceted research program” in Kahemba. Through 2017, Tshala and Boivin’s team documented konzo’s effects on development, constructing a portrait of affected, school-aged children.

Colonial legacy
Colonial legacy
“Bitter cassava is not indigenous to the Congo basin. The Portuguese brought it from the Amazon in 1558 and it just thrived in Congolese soil,” explained Boivin.” And, today, what’s the option for millions of poor people who face famine due to drought or war? Starve… or eat bitter cassava and risk konzo.”
Colonial legacy
“Bitter cassava is not indigenous to the Congo basin. The Portuguese brought it from the Amazon in 1558 and it just thrived in Congolese soil,” explained Boivin.” And, today, what’s the option for millions of poor people who face famine due to drought or war? Starve… or eat bitter cassava and risk konzo.”
“Bitter cassava is not indigenous to the Congo basin. The Portuguese brought it from the Amazon in 1558 and it just thrived in Congolese soil,” explained Boivin.” And, today, what’s the option for millions of poor people who face famine due to drought or war? Starve… or eat bitter cassava and risk konzo.”
Continuing work in the region pioneered by Jean-Pierre Banea in the DRC Ministry of Health and Nutrition, Tshala and Boivin’s team, in partnership with Esperance KashalaAbotnes at the University of Bergen in Norway, was the first to document overall cognitive delays in addition to motor delays from poorly processed cassava in infants and very young children.
Continuing work in the region pioneered by Jean-Pierre Banea in the DRC Ministry of Health and Nutrition, Tshala and Boivin’s team, in partnership with Esperance KashalaAbotnes at the University of Bergen in Norway, was the first to document overall cognitive delays in addition to motor delays from poorly processed cassava in infants and very young children.
Continuing work in the region pioneered by Jean-Pierre Banea in the DRC Ministry of Health and Nutrition, Tshala and Boivin’s team, in partnership with Esperance KashalaAbotnes at the University of Bergen in Norway, was the first to document overall cognitive delays in addition to motor delays from poorly processed cassava in infants and very young children.
Boivin has witnessed the effects of konzo since 1990, when a Fulbright scholarship brought him to DRC. He later revisited the country to complete an ecological analysis of konzo. “Then in May of 1993, I planned to return to the DRC for an assignment with Thorkild Tylleskar, Hans Rosling, and their colleagues from Uppsala University in Sweden.” At that time, the WHO
Boivin has witnessed the effects of konzo since 1990, when a Fulbright scholarship brought him to DRC. He later revisited the country to complete an ecological analysis of konzo. “Then in May of 1993, I planned to return to the DRC for an assignment with Thorkild Tylleskar, Hans Rosling, and their colleagues from Uppsala University in Sweden.” At that time, the WHO
Boivin has witnessed the effects of konzo since 1990, when a Fulbright scholarship brought him to DRC. He later revisited the country to complete an ecological analysis of konzo. “Then in May of 1993, I planned to return to the DRC for an assignment with Thorkild Tylleskar, Hans Rosling, and their colleagues from Uppsala University in Sweden.” At that time, the WHO
These disturbing results raised an urgent question: How can konzo be prevented? “The only practical way is the wetting method," said Boivin. It was clear, though, that mothers who learned the method only practiced it for a time before returning to familiar tradition.
These disturbing results raised an urgent question: How can konzo be prevented? “The only practical way is the wetting method," said Boivin. It was clear, though, that mothers who learned the method only practiced it for a time before returning to familiar tradition.
Caregiver intervention
These disturbing results raised an urgent question: How can konzo be prevented? “The only practical way is the wetting method," said Boivin. It was clear, though, that mothers who learned the method only practiced it for a time before returning to familiar tradition.
Caregiver intervention
Previously, with funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Boivin’s team had adapted a caregiver training intervention for Ugandan mothers living with HIV. The Mediational Intervention for Sensitizing Caregivers (MISC) teaches mothers how to better care for their children, leading to improved developmental outcomes and survival rates for the children.
Previously, with funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Boivin’s team had adapted a caregiver training intervention for Ugandan mothers living with HIV. The Mediational Intervention for Sensitizing Caregivers (MISC) teaches mothers how to better care for their children, leading to improved developmental outcomes and survival rates for the children.
Caregiver intervention
Previously, with funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Boivin’s team had adapted a caregiver training intervention for Ugandan mothers living with HIV. The Mediational Intervention for Sensitizing Caregivers (MISC) teaches mothers how to better care for their children, leading to improved developmental outcomes and survival rates for the children.
Boivin hypothesized that it might encourage mothers towards sustainable use of the wetting method. Preliminary results show the program is making a difference.
Boivin hypothesized that it might encourage mothers towards sustainable use of the wetting method. Preliminary results show the program is making a difference.
Boivin hypothesized that it might encourage mothers towards sustainable use of the wetting method. Preliminary results show the program is making a difference.


“We’re preventing konzo, a permanent, irreversible neurological disease, in the most abject impoverished setting you can imagine,” said Boivin. If some mothers become peer leaders-trainers for the wetting method with MISC, the benefits could extend exponentially—to her family, her community, and beyond.
“We’re preventing konzo, a permanent, irreversible neurological disease, in the most abject impoverished setting you can imagine,” said Boivin. If some mothers become peer leaders-trainers for the wetting method with MISC, the benefits could extend exponentially—to her family, her community, and beyond.
“We’re preventing konzo, a permanent, irreversible neurological disease, in the most abject impoverished setting you can imagine,” said Boivin. If some mothers become peer leaders-trainers for the wetting method with MISC, the benefits could extend exponentially—to her family, her community, and beyond.
Nutritionist Dr. Nicole Mashukano (right) teaches the wetting method to village women in Kahemba.
FOCUS ON KONZO –
Photo courtesy Neerja Vashist
CHILDREN OF KAHEMBA
Nutritionist Dr. Nicole Mashukano (right) teaches the wetting method to village
FOCUS ON KONZO – CHILDREN OF KAHEMBA
Photo courtesy Neerja Vashist
Nutritionist Dr. Nicole Mashukano (right) teaches the wetting method to village women in Kahemba.
FOCUS ON KONZO – CHILDREN OF KAHEMBA
Photo courtesy Neerja Vashist
205
A quest for solutions to prevent konzo
While working on an Ebola project in the Democratic Republic of Congo (DRC), Dr. Matthew Bramble—a staff scientist at Children’s National Medical Center—met Dr. Desire Tshala, who convinced him to work on konzo, a disease he’d never heard of. Over the next two years, Bramble helped analyze data collected by Tshala’s team without once meeting anyone affected by the disease. Eventually, Bramble found time to make the long trek to Kahemba. “You get to know the kids, and, well, the story changes. It’s no longer just interesting science. Now I’d like to solve it.”
Bramble’s Fogarty-funded project aims to reveal connections between konzo and the gut microbiome— the trillions of bacteria and other microbes living in our gastrointestinal tracts. The human body cannot metabolize linamarin (a toxic, cyanide-related chemical in cassava), so it eliminates it instead. “If linamarin is going through you, it’s still got to be acted on by intestinal microflora,” explained Bramble. The gut microbiome, then, may play a significant role in konzo’s genesis.
Big data applications
In Kahemba, there are many households where one sibling gets konzo but another doesn’t, despite sharing the same lifestyle and food, said Bramble. “Why that exists we still don't know." To find answers, his team assembled a hundred sibling pairs—one hundred konzo-affected children plus a hundred unaffected siblings—collected samples, and then performed 50 million DNA reads. Data analysis is not yet complete, but early findings have shown “some very interesting metabolic differences between affected and unaffected children.”
Neerja Vashist, co-author and a graduate student researcher in the Department of Genomics and Precision Medicine at George Washington University, said they knew a “big data component” would be needed to answer the most pressing questions about konzo. “Big data allows you to get a lot of information out, and the data we get from the gut microbiome can possibly be applied, in a laboratory setting, to test other hypotheses.”
Introducing a new strain
either.
Historically, the villagers have seen konzo as random and sporadic, said Bramble. “But I don’t think it’s either There is a variable enabling this to happen to some but not all the kids. This is what the newest konzo research is trying to identify.” Bramble noted that outbreaks of konzo always follow an environmental stressor that interferes with the processing of cassava. He hopes his research elucidates the factors determining which children are affected.

It’s likely that not all answers will be found in hard molecular science, said Bramble, who also conducts research in the Philippines. There, he discussed konzo with Professor Vivian Topor, an agricultural expert. “Over her 30-year career, she’s bred various strains of cassava and, based on the color, you can estimate the cyanide content in some varieties.” He plans to introduce cassava from the Philippines to DRC, monitoring the crop to see how it behaves. “Cassava toxicity is very dependent on the environment. So poor soil and/or low water can make the plant more poisonous, but this new strain doesn't fluctuate nearly as much as others.”
An agricultural solution to prevent konzo “inherently makes sense,” said Vashist. “Change the crop, fix the problem permanently.” Yet, research conducted by Tshala, Cliff, and others show proven benefits when using the wetting method and nutritional rehabilitation. Until scientists gather evidence-based results for a new crop-swap solution, these older methods may best protect the children against konzo.
9 FOCUS ON KONZO – CHILDREN OF KAHEMBA
Dr. Matthew Bramble spends time with the children of Kahemba. “You get to know the kids, and, well, the story changes. It’s no longer just interesting science.”
Photo courtesy of Matthew Bramble
“It’s likely that not all answers will be found in hard molecular science.”
206 Delaware Journal of Public Health - December 2022
By Dr. Roger I. Glass, Director, Fogarty International Center


Let’s not forget our pandemic achievements as we prepare for a new year
It’s not yet time to declare victory over COVID-19, even if most nations have learned to live side-by-side with the pandemic. Still, events over the past two years reveal how global health impacts individual well-being and national security. As you know, the Fogarty International Center helps each of the other institutes at NIH become engaged with global health research. For more than 50 years, Fogarty has been building partnerships between institutions in the U.S. and abroad, while training the next generation of scientists focused on universal health needs. These collaborative ventures include investigations of the dual burden of infectious and noncommunicable diseases, while encompassing data science, economics, genetics, climate change science, and many other disciplines.
Contributions made by Fogarty trainees Throughout the pandemic, researchers trained by our programs have made scientific discoveries that have contributed to international security. Take Dr. Jessica Manning, a former Fogarty fellow who now conducts malaria research in Phnom Penh. Her team at the Ministry of Health sequenced the viral strain infecting the first Cambodian COVID-19 patient and documented early spread of pandemic disease outside of China.
Similarly, Dr. Christian Happi, director of the African Centre of Excellence for Genomics of Infectious Diseases, sequenced the first SARS-CoV-2 genome in Africa by adapting sequencing and analytical pipelines he’d created back when he was a Fogarty grantee studying Ebola. In Botswana, Dr. Sikhulile Moyo leveraged the skills he’d acquired while supported by a Fogarty HIV research training grant to track COVID-19 mutations for his country’s Ministry of Health. Last November, he alerted the world of a new omicron variant, which within six weeks became the dominant global strain, challenging the ability of COVID vaccines to control its spread. In the Dominican Republic, Dr. William Duke, a national commission member, used what he’d learned as a Fogarty trainee to help create a COVID-19 intervention plan to prevent and control the disease.
An enduring legacy
As we prepare to begin 2023, I want to share additional news about Fogarty’s Global Brain and Nervous System Disorders Research across the Lifespan program. In 2023, this “brainchild” of Dr. Kathy Michels, a Fogarty veteran who retired earlier this year, will be 20 years old! The program’s exploratory and developmental research grants help investigators build research capacity, research collaborations and research networks within institutions, countries and regions.
Global Brain studies address a range of conditions. I’d like to bring two unique projects, both targeting fetal alcohol spectrum disorders, to your attention. Psychologist Tatiana Balachova of the University of Oklahoma has designed an intervention for women in Russia, while Drs. Sandra and Joseph Jacobson, a research team from Wayne State University, conducted the first-ever prospective longitudinal study of the syndrome in South Africa. Findings from both projects are ripe for translation within an American context.
Other examples of Global Brain program investigations with broad implications in our own country include a psychobiological study of early psychosis in China; schizophrenia research capacity building in Macedonia; a planning grant to reduce the burden of chronic psychotic disorders in Tanzania; an exploration of the family consequences of Zika in Brazil; an investigation of maternal traumatic stress and child development in South Africa; a study of internet-based treatment for common mental disorders in Latin America; an exploration of the genetics of psychosis in Africa; and a study on dementia and related health and social challenges in Lebanon. The program has supported collaborating scientists working in Shanghai Mental Health Center in China, Macedonia Academy of Sciences and Arts, Muhimbili University of Health and Allied Sciences in Tanzania, Altino Ventura Foundation in Brazil, the National Institute of Psychiatry in Mexico City, and Addis Ababa University in Egypt, among many other institutes.
Once again, I thank Kathy Michels for generously endowing Fogarty with a substantial legacy. Best wishes to her and to each of you in 2023.
OPINION
10
207
HEALTH Briefs Global PEOPLE
University of Lagos names first female vice-chancellor
Dr. Folasade Ogunsola was named Vice Chancellor of the University of Lagos, the first woman to hold the position. A principal investigator on the MEPI Jr project, Ogunsola was a founding member of the Nigerian Society for Infection Control and served as team lead for Infection Prevention and Control during the 2014-2016 Ebola outbreak.

Infectious disease leader Lee Riley passes away
Dr. Lee W. Riley, a pioneer in global health, died on October 19, 2022, at 73. An expert in molecular epidemiology, Riley was director of the Global Health Equity Scholars Program at UC Berkeley School of Public Health, one of the consortia in Fogarty’s Global Health Fellows & Scholars/LAUNCH program.
RAPIDD program co-founder awarded Kyoto Prize

Dr. Brian Grenfell, co-founder of Fogarty’s Research and Policy for Infectious Disease Dynamics (RAPIDD) modeling program, was awarded the 2022 Kyoto prize in basic sciences for his research in phylodynamics, a methodology that predicts the dynamics of RNA viruses in wildlife.

Fogarty grantees elected to National Academy

Three Fogarty grantees were recently named to the National Academy of Medicine.
Dr. Marleen Temmerman, principal investigator on a Fogarty Global Infectious Diseases grant, was recognized for being a penholder of the U.N. Global Strategy for Women’s, Children’s, and Adolescents’ Health and founding director of the International Center for Reproductive Health at Ghent University.

Dr. Gagandeep Kang, a professor in the Division of Gastrointestinal Sciences at Christian Medical College in Vellore, India, and recipient of multiple Fogarty grants, was recognized for her contributions to understanding and improving child health during the SARS-CoV-2 pandemic.

Dr. Wafaie Fawzi, principal investigator for the Fogarty-funded Partnership for Global Health Research Training Program, was recognized for advancing the science of safety and efficacy of nutritional interventions in the prevention and management of major global health threats.
Dashboard aims to aid food crisis response
The Global Alliance for Food Security (GAFS), convened by the Group of Seven (G7) and the World Bank, launched the Global Food and Nutrition Security Dashboard in early November. The dashboard includes global and country-level data on food crisis severity, global food security financing, and innovative research to strengthen crisis response and resilience.
GMU launches public health college
George Mason University has renamed its College of Health and Human Services to the College of Public Health, a first for Virginia according to the university. The college includes the School of Nursing and the Departments of Global and Community Health, Health Administration and Policy, Nutrition and Food Studies, and Social Work.
White House expands global health security partnerships
The Biden Administration announced new and enhanced health security partnerships with six countries and a strengthening of existing partnerships in 19 more, with a goal of directly supporting at least 50 countries, by 2025. The administration hopes to strengthen and achieve capacity in five critical areas in order to prevent, detect, and respond to infectious disease threats.
TDR releases research skills curriculum
The Special Programme for Research and Training in Tropical Diseases (TDR) and the Global Health Network (TGHN) have developed a curriculum to provide knowledge and skills in health research to those with limited or no previous experience in order to deliver a safe, ethical, and accurate study.
WHO holds school on refugee health
The third annual Global School on Refugee and Migrant Health was held in Dhaka, Bangladesh, in late November/early December. The virtual program focused on capacity-building for health systems response, addressing gender, culturally pertinent health care, the role of universities, and global and regional cooperation.
11
208 Delaware Journal of Public Health - December 2022
Funding Opportunity Announcement Deadline Details
Interventions for Stigma Reduction to Improve HIV/AIDS Prevention, Treatment and Care in LMIC Countries

R01 Clinical Trial Optional https://bit.ly/HIV_AIDS_StigmaReduction Dec 20, 2022
Japanese Research Fellowships (JSPS)
International Research Scientist Development Award (IRSDA)
K01 Independent Clinical Trial Required
Feb 17, 2023
http://bit.ly/JSPSforUS
K01 Independent Clinical Trial Not Allowed http://bit.ly/IRSDAK01 Mar 8, 2023
International Bioethics Training
D43 Clinical Trial Optional
R25 Clinical Trial Not Allowed
For more information, visit www.fic.nih.gov/funding
Global Health Matters
November/December 2022
Volume 21, No. 6 ISSN: 1938-5935
Fogarty International Center National Institutes of Health Department of Health and Human Services
Managing editor: Judy Coan-Stevens Judith.Coan-Stevens@nih.gov
Writer/editor: Mariah Felipe Mariah.Felipe@nih.gov
Writer/editor: Susan Scutti Susan.Scutti@nih.gov
Digital analyst: Merrijoy Vicente Merrijoy.Vicente@nih.gov
Designer: Carla Conway
All text produced in Global Health Matters is in the public domain and may be reprinted. Please credit Fogarty International Center. Images must be cleared for use with the individual source, as indicated.
Scan

SUBSCRIBE: www.fic.nih.gov/subscribe
http://bit.ly/BioethicsTraining Jun 6, 2023
Revised NIH data requirements start Jan 25
Starting January 25, 2023, NIH will require a data management plan in grant applications. The NIH Data Management & Sharing (DMS) Policy applies to all research, funded or conducted in whole or in part by NIH, that results in the generation of scientific data, regardless of funding level.
Scientific data is defined as data commonly accepted in the scientific community as of sufficient quality to validate and replicate research findings, regardless of whether the data are used to support scholarly publications.
Refer to the Funding Opportunity Announcement to determine if the DMS Policy applies to your application. NIH has also compiled a complete list of NIH activity codes subject to the DMS Policy.
Current NIH policies specific to certain types of research (e.g., clinical trials, research generating large-scale genomic data) continue to apply. In the event that another applicable policy has more detailed expectations than that of the DMS Policy, those expectations should be followed in addition to the DMS Policy.
Policies related to data sharing vary across countries. Investigators from foreign institutions and U.S. investigators collecting data in other countries should familiarize themselves with the policies governing data sharing in the countries in which they plan to work and address any specific limitations in the data sharing plan in their application.
NOVEMBER/DECEMBER 2022
Photo courtesy of CDC/ Nicholas S. Tenorio
and read this issue online
The revised policy applies to all research that generates scientific data.
209
Methodology
The Delaware Health Force (DHF) team imports data on licensed healthcare providers and institutions in Delaware. This data is collected under a data use agreement established with the Delaware Division of Professional Regulation and comes from their DELPROS system.
Once the data import for the license types of interest is complete, analysts prepare the data following these steps:
1.Data scrubbing is undertaken to normalize the data, and to catch variation in, for instance, how a person’s name is listed, or degree information is recorded.
2.Duplicates are removed or merged. Duplicates can occur within the data for a variety of reasons, and they are merged into a single record after record by record review.
3.Addresses are prepared geocoding. This may involve editing typos, correcting street directionals, replacing PO boxes with physical addresses, and making similar corrections to maximize the accuracy of the automated geocoding process.
4.Address data is geocoded. Providers’ county, ZIP code, census tract, and other geofenced areas are identified as needed.
COUNTING PROVIDERS AND FACILITIES
DELPROS data gives us a total count of the licensed providers within a given profession, and is further delineated into Active, Cancelled, Closed, Expired, and “Other” status categories.
Providers with out–of–state practice addresses. Within each profession, some share of licensees report out–of–state practice addresses. Often, but not always, these addresses are in states that border Delaware: Maryland, New Jersey, and Pennsylvania. Some providers with out-of-state addresses may in fact be practicing in Delaware. Some providers treat patients via telehealth; others may practice in Delaware for part of the year; still others may work in Delaware as well as a border state. Currently, there is no way to know with certainty how many providers with out-of-state addresses are actually treating patients in Delaware. This is an enhancement planned for the future.
Providers with no clearly identified practice address.
In its present form, DELPROS allows new and renewing applicants to list addresses without defining their attribute. As a result an address may be home, office, institution, main office, branch location, etc. Similarly, some smaller share of licensees report no practice address at all. Often this is because they are no longer practicing. A future enhancement based upon the USPS “Residential Delivery Indicator” (RDI) will be employed to verify addresses, validate addresses, standardize addresses, and provide both RDI and Delivery Point Validation (DPV). Two such applications are the API Tool SmartyStreet and Lob.
When considering the broad range of disciplines that the entire caregiver team encompasses, we realize that at any point in time some number of licensed professionals of all types may be in administration and not seeing patients in any capacity. Others may be un- or underemployed at any point in time as well. At this time, there is no effective way to differentiate and isolate them from the larger workforce, and so a margin of error is implied. Further study will be necessary to determine what that margin of error is in arithmetic terms. Facilities provide their own challenges in counting including whether or not that are actually open for business, have closed to never be reopened, or are newly licensed but not yet seeing clients.
NORMALIZING SELF-REPORTED SPECIALTY AND SUBSPECIALTY
How physicians self-cateogorize their specialty practice is subject to the vagarities of natural language input. For this report, we have chosen to use the Association of American Medical College’s Specialty Pathway architecture shown on the following two pages. While imperfect as some speciality / subspeciality destinations can be achieved via various pathways, this does provide us with a consistent framework.
NORMALIZING SELF-REPORTED EDUCATIONAL LEVEL
Similar to self-reported specialty and subspecialty, there are numerous self-reported terms referring to what year of education a physician is in. This is compounded by the date of the data in question as what month of the year the data is being viewed from as internships and residency start dates do not follow the calendar year. Further more, the length of residency varies by specialty. We utilized the Accreditation Council for Graduate Medicine Education pipeline matrix, shown in table 1, to adjust for these significant differences. It should be further noted that not all residency types are offered at Delaware locations.
DOI: 10.32481/djph.2022.12.044
210 Delaware Journal of Public Health - December 2022
Table 1. Accreditation Council for Graduate Medicine Education Pipeline Specialty Matrix 1
Internal Medicine
Medical Genetics and Genomics
Three Years
Three to Four Years (depending on program)
Osteopathic Neuromusculoskeletal Medicine (up to 5 years) Pediatrics
Preventive Medicine
Emergency Medicine
Family Medicine
Neurology Pathology (anatomic and clinical)
Anesthesiology
Internal Medicine-Pediatrics
Nuclear Medicine
Four Years
Obstetrics and Gynecology
Ophthalmology
Dermatology
Psychiatry
Child Neurology
Diagnostic Radiology
Orthopaedic Surgery
Five Years
Six Years
Seven Years
FUTURE ENHANCEMENTS
Otolaryngology – Head and Neck Surgery
Radiation Oncology General Surgery Urology
Vascular Surgery
Plastic Surgery – Integrated Interventional Radiology (up to 7 years, depending on the program) Thoracic Surgery (up to 7 years, depending on the program)
Neurological Surgery
In the near future, this data will be cross-referenced against the NPI Registry in the Delaware Health Force system. The NPI Registry is a service of the US Centers for Medicare and Medicaid Services, which, in many cases, provides additional information not captured within the DELPROS system. Information is also imported from the Delaware Health Information Network for those professionals who have both a Delaware license and an NPI number to further refine data on active practitioners.
REFERENCES
1. Murphy, B. (2020, Nov 19). Medical specialty choice: Should residency training length matter? American Medical Association. Retrieved from: https://www.ama-assn.org/residents-students/specialty-profiles/medical-specialty-choice-should-residency-training-length
211
Health Care Database Comparisons by State
Matt McNeill, B.S. Research Associate, Delaware Academy of Medicine / Delaware Public Health Association
The Delaware Health Force (DHF) database created by the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA) includes a list of every licensed healthcare provider actively practicing in Delaware, as well as those who have ever practiced in the state, regardless of whether they now practice somewhere else, are retired, have had their license suspended or revoked, or are deceased. The list of provider names used to create the database was populated from DELPROS, the Delaware Division of Professional Regulations online public database.
Whenever possible, the DHF database lists the following information by provider NPI number:
• License Number(s),
• License Type(s),
• License Status,
• Practitioner Specialty
• Practice Location,
• Medical School and/or Residency Location (when applicable),
• Graduation Year and Years of Practice,
• Medicare/Medicaid Acceptance,
• Practice Proprietorship, and
• Contact Information.
This data will then be integrated with health outcomes, demographics, and other data to allow for real-time and predictive data modeling to inform decision and policy.
Below is a list of similar local and national databases, with bullet point information about the information available and comparisons to the DHCW database.
CONNECTICUT
Connecticut Healthcare Workforce Scan http://www.healthreform.ct.gov/ohri/lib/ohri/sim/work_force/ct_healthcare_workforce_scan.pdf
• Detailed description of how healthcare workforce data was collected and analyzed
• Limited types of practitioners – Similar to Maryland, not as in depth as Delpros
–Significant portions of the data are estimates based on national data
–Data sources contradict one another
–Double counted physicians who practiced in multiple locations
MARYLAND
Maryland Medical Programs
https://encrypt.emdhealthchoice.org/searchable/main.action
• Requires search to find providers – all searches include hospitals/locations unless a provider’s name is searched, or if the “only PCP” option is selected, however this limits the search options and doesn’t include other HCP’s.
• Provider search engine for patients
• Greater focus on access to care for individuals and less focus on compiling provider info
[Maryland] Medical Care Database
https://mhcc.maryland.gov/mhcc/pages/apcd/apcd_data_release/apcd_data_release_mcdb.aspx
• Stringent process for accessing data- not much information could be obtained
• Cost prohibitive for small organizations that could benefit from this data
–$4,000/year for nonprofits + $1,000/year for re-use rights
• Based on claims data
Maryland Healthcare Workforce Study Phase II
https://mhcc.maryland.gov/mhcc/pages/apc/apc_workforce/documents/MD_Health_Workforce_Study_Phase_2_Report_pdf.pdf
• Detailed description of how healthcare workforce data was collected and analyzed
• Limited types of practitioners – Physicians (Family Medicine, Geriatrics, Internal Medicine, Pediatrics), Psychiatrists, Psychologists, Counselors, Social Workers, Physician Assistants, Pharmacists, Nurses, Dentists
–Record detail is not equivalent to Delpros
• Detailed population level data / assessment of healthcare workforce shortages by county
DOI: 10.32481/djph.2022.12.045
212 Delaware Journal of Public Health - December 2022
NEW JERSEY
New Jersey Healthcare Profile https://www.njdoctorlist.com/
• Only includes physicians
• Provider search engine for patients
• No broad search for county/zip available to create lists of doctors for data collection
• No data files
New Jersey Hospital Association https://www.njha.com/membership/list-of-nj-providers/hospitals/
• Full roster of hospitals, medical centers, and rehab facilities, and their locations/phone numbers
• Provider search engine for patients
• Links to individual websites for each facility
• No data files
NEW YORK
New York State Health Care Reform Act https://www.health.ny.gov/regulations/hcra/provider/provhosp.htm
• Full roster of General Hospitals
– Population health data files but no provider data files
The New York State Health Care Provider Database: A Framework for Action https://www.nyspma.org/aws/NYSPMA/asset_manager/get_file/103473
• Nearly identical in concept to the DHF, completed in 2014
• Created a database of all licensed physicians in the state and included location/specialty/age/etc.
–Helped predict future shortages from aging practitioner populations
–Helped increase access to care through state sponsored programs in healthcare shortage areas
–Created links to community organizations serving the same patient populations
• Used data collection during licensure, and many other sources to compile data
• Fully Detailed blueprint of how to build a healthcare database
PENNSYLVANIA
Pennsylvania Department of Human Services [Physician] Provider Directory https://provider.directory.dpw.state.pa.us/ProviderSearch.aspx
• Provider search engine for patients
• Only includes physicians – searchable by specialty
Pennsylvania Department of Human Services – Human Services Provider Directory https://www.humanservices.state.pa.us/HUMAN_SERVICE_PROVIDER_DIRECTORY/
• Provider search engine for patients
–Includes lists of organizations/services for various social service providers
–Not searchable by individual providers, does not include medical care
Pennsylvania Licensing System Verification Service https://www.pals.pa.gov/#/page/search
• Provider search engine for licenses
–Does not include practice location street address, only city/state/ZIP
–Includes out-of-state practice locations
–Does not include practitioner specialties
Pulse of Pennsylvania’s Workforce https://www.health.pa.gov/topics/Health-Planning/Pages/Reports.aspx
• Individualized data reports on various categories of healthcare provision
–Limited selection of healthcare provider categories
• Data is old (2011-2015 data from 2012-2018 reports)
• Reports are not generated annually
–The 2018 Report only reported 2015 Dentist/Dental Hygienist data
–The 2017 Report only reported 2014 Physician/Physician Assistant data
• No new data since 2015
• No new reports since 2018
213
VIRGINIA
Virginia Healthcare Workforce Data Center
https://www.dhp.virginia.gov/PublicResources/HealthcareWorkforceDataCenter/ProfessionReports/MedicineReports/
• Profession specific workforce data reports
• Uses self-report survey data to compile information for each report
• High response rate on survey when administered during license registration
• Data include ethnicity, age, location/population served, Virginia residency, specialties, and current work status (license status), as well as income/debt figures
• Includes many of the same categories as DELPROS
Virginia Board of Medicine Practitioner Information http://www.vahealthprovider.com/search.asp http://www.vahealthprovider.com/
• Provider search engine for licenses/information
• Required information includes location/phone, education, number of years in active practice, board certifications, hospital affiliations, academic appointments, publications, Medicaid info, actions, felony convictions, paid claims in last 10 years
• Information that is not required includes insurance plans, honors/awards, Medicare acceptance, and continuing education credits
• Information is limited to physicians (MD, DO) and Doctors of Podiatric Medicine (DPM)
WEST VIRGINIA
West Virginia Health Data Portal http://portals.ncahd.org/wvhdp/
• Map overlay tool with aggregate totals for county/zip of various types of healthcare practitioners
–Includes food resources like farmers markets, food deserts, fast food
–Includes healthcare locations, workforce trends, patient demographic information
• Each map layer has several different stratifications to pick from
NATIONAL
National Practitioner Database https://www.npdb.hrsa.gov/analysistool/ Contains unnamed data on each of the states licensed healthcare providers
• Inaccurate information for Delaware
–NPDB total = 2,652 // DHF total = 50,422
• Does contain the same categories as the DHF database
–Only gives raw number of each type of provider
–Counts are inaccurate
–Does not specify specific license types (i.e. Family Nurse Practitioner, Paramedic, etc.)
–Categories are not matchable with Delpros CarePrecise https://www.careprecise.com/state/delaware_healthcare_providers.htm
• Contains named data on 6.7m providers across the country
–Includes named data on over 20,000 providers in DE (6,000 less than HCW)
–Includes NPI number, practice location, specialty information, Medicare acceptance, and wealth level of population in area served
• Does not include Medical school/residency information, or years of practice/graduation year
• Only includes those actively practicing in Delaware
• Updated monthly (subscription service costs approximately $900/year for national data) Centers for Medicare & Medicaid https://data.cms.gov/provider-data/search?theme=Doctors%20and%20clinicians
• Data file with over 1 million records (only 2,400 from Delaware – very limited)
• Includes NPI number, practice location, specialty information, medical school and year of graduation, some phone numbers
United States Health Workforce State Profiles
https://bhw.hrsa.gov/data-research/review-health-workforce-research/state-profiles
• Individual PDF files for each state, with total number of each type of provider and per capita
• Includes most of the same categories as Delpros
• Data is inaccurate
–Delaware is missing several categories
–Data wass not updated from 2011-2015
214 Delaware Journal of Public Health - December 2022

We’ll meet you where you are. Get personal support for those who have a disability. We provide information on how the vaccine works, how to get it, and how to separate the myths from the facts. I want to be sure that the COVID-19 vaccine is safe for me. Emmanuel, Sussex County, DE 1-833-643-1715 VaccineAccessDE.com 215
Workforce In Training
Katherine W. Smith, M.D., M.P.H. Program Manager, Delaware Academy of Medicine/Delaware Public Health Association
Timothy
E. Gibbs, M.P.H. Executive Director, Delaware Academy of Medicine/Delaware Public Health Association
Omar Khan, M D , M H S Editor-in-Chief, Delaware Journal of Public Health
In the “Frequently Asked Questions” section of Harvard Health, the question was posed, “In the hospital recently, a ‘resident’ cared for me. Should I ask for a more experienced doctor?”
The answer goes a long way to explaining why we must count those in-training (physicians, dentists, pharmacists, and others) as a key part of our healthcare workforce: “Residents are doctors-in-training. They have graduated from medical school, been awarded an M.D. degree, and now are training to be a particular type of doctor – such as a pediatrician or pediatric specialist, or a type of surgeon. In their first year of such training, residents are sometimes called interns. All residents are supervised by a legally responsible senior physician. For over 40 years, I have been such a supervising physician. The residents typically have more time to spend with a patient than the supervising physician does. At major teaching hospitals, like those here at Harvard, the competition to be selected for a residency is fierce. Those chosen are extraordinarily intelligent and knowledgeable. I’ve seen many residents save many lives. In fact, a recent study found that the quality of care was better in teaching hospitals. In short, you generally are in very good hands with a resident. But if you are concerned about the way a resident is handling your care, you always have the right to speak to the supervising physician.”1
Residents account for a large proportion of the active healthcare workforce in major teaching institutions like ChristianaCare, Nemours, and Bayhealth. These physicians, while still training in their chosen specialty, care for patients, order labs and tests, examine results, and create treatment plans for patients on a daily basis.
PHYSICIAN TRAINING
In order to become board-certified in a medical specialty, all physicians (M.D.s and D.O.s) must complete additional education after graduating from medical school. The first year of post graduate work (Post-Graduate Year 1, or PGY-1) is traditionally called internship (or first year of residency) and begins on July 1 every year. The recently graduated physician trains in a hospital setting with oversight by board certified attending physicians. Before beginning their second year of residency, physicians must have passed four national exams. Upon passing the final exam, they are eligible to apply for an independent medical license. In their second year (PGY-2) after medical school graduation, the resident physician is still supervised by an attending physician (someone who has completed residency training), and they take on progressively more responsibilities in patient care. Depending on the specialty, residency programs can last from three to seven years. At the end of these residencies, all physicians will have taken three parts of the US Medical Licensing Examination (USMLE, parts 1-3), in order to obtain licensure to practice. In addition, many physicians take another set of examinations set by their particular specialty; upon passing, they are considered board-certified in that specialty area. Once their residency is complete, a physician may continue working in a hospital (inpatient) or clinic (outpatient) setting as an attending physician. Many types of employment models are available, such as being employed by a health system, or in a private practice. Some physicians may choose to undergo further training known as a fellowship. Physicians in fellowship programs seek training in an area for which they wish additional specialization (and usually, certification). They are supervised by other licensed physicians in that specialty, participate in patient care, and assist in the training of residents. Delaware enjoys many residency and fellowship programs in the teaching hospitals throughout the state, with more opening every year (see Tables 1 and 2). United States residency and fellowship programs can be seen in Table 3. Delaware programs are highlighted in blue and underlined.
DOI: 10.32481/djph.2022.12.046
Table 1. Accredited Residency Programs Hosted by Delaware Healthcare Institutions Bayhealth https://bayhealthgme.org/graduate-medical-education/ Beebehealthcare.org https://www.beebehealthcare.org/medical-education/graduate/family-medicine-residency ChristianaCare https://residency.christianacare.org/ Nemours https://www.nemours.org/education/gme.html St. Francis https://www.trinityhealthma.org/healthcare-professionals/gme/ Delaware Psychiatric Center https://dhss.delaware.gov/dhss/dsamh/residency/ 216 Delaware Journal of Public Health - December 2022
Table 2. Delaware Institutions Who Have OR Host Residents In Their Facilities 090007 ABC Pediatrics 238081 Armed Forces Medical Examiner System 098081 Armed Forces Medical Examiner System 090002 Bayhealth Hospital – Sussex Campus 090248 Bayhealth Medical Center 090009 Beebe Healthcare 098082 Beebe Medical Center 090019 Brandywine Counseling and Community Services Inc 098020 Christiana Care Center for Urogynecology and Pelvic Surgery 090247 Christiana Care Health Services Inc 098085 Christiana Hospital 090004 CNMRI - Milford O ce 098004 Community Mental Health Clinic - Dover 098005 Community Mental Health Clinic - Wilmington 090297 Delaware Division of Substance Abuse and Mental Health 090005 Delaware Eye Care Center 090022 Delaware Hospice 090021 DSAMH Bridge Clinic New Castle 098017 Fresenius Brandywine Home Therapies 098014 Fresenius Medical Care (Wilmington) 090008 Infusion Solutions of Delaware LLD - Dover O ce 098086 Kent Sussex Counseling Services 090006 Kids and Teens Pediatrics 098009 Mid Atlantic Pain Institute PA 098010 Milton & Hattie Kutz Home Inc 098022 Morgan Kalman Clinic 090340 Nemours Children’s Health Wilmington 098013 Nephrology Associates PA 090018 Norman Broudy MD & Associates 098007 O ce of the Chief Medical Examiner (OCME) 098083 Planned Parenthood of Delaware Inc 090011 Psychiatry & Neurology 090015 Psychiatry Delaware LLC 090010 RI International - Restart Newark 098012 Rockford Center 098021 Roxana Cannon Arsht Surgicenter 090024 Seasons Hospice and Palliative Care Facility 090014 Serene Minds LLC 098006 Silver Lake Treatment Consortium 090709 St Francis Hospital 098003 Terry Children’s Psychiatric Center 098087 Thresholds Inc 090013 TidalHealth Nanticoke 098016 University of Delaware - Student Health Center 098002 Veterans A airs Medical Center (Elsmere) 090462 Veterans A airs Medical Center (Wilmington) 098011 West Side Health 217
Fellowship Type
Number of Programs
Nationally
Delaware Programs
Abdominal Radiology (DR) 14 0
Addiction Psychiatry (P) 57 0
Adolescent Medicine (PD) 32 0
Adult Cardiothoracic Anesthesiology 71 0
Adult Reconstructive Orthopaedics (ORS) 28 0
Advanced Heart Failure and Transplant Cardiology 81 1
Blood banking-transfusion medicine (PTH) 51 0
Cardiovascular Disease (IM) 267 1
Chemical Pathology (PTH) 5 0
Child abuse pediatrics (PD) 31 0
Child and Adolescent Psychiatry (P) 143 0
Child Neurology (N) 77 1
Clinical Cardiac Electrophysiology (IM) 116 0
Clinical Informatics (PD) 1 0
Clinical Neurophysiology (N) 91 0
Complex Surgical Oncology (GS) 30 0
Congenital cardiac surgery (TS) 14 0
Craniofacial Surgery (PS) 9 0
Critical Care Medicine (AN) 64 0
Critical Care Medicine (IM) 49 0
Dermatopathology (D and PTH) 57 0
Developmental-Behavioral Pediatrics (PD) 44 0
Endocrinology, Diabetes, and Metabolism (IM) 155 0
Endovascular Surgical Neuroradiology (DR) 4 0
Endovascular Surgical Neuroradiology (N) 2 0
Endovascular surgical neuroradiology (NS) 2 0
Foot and Ankle Orthopaedics (ORS) 8 0
Forensic Pathology (PTH) 48 0
Forensic Psychiatry (P) 50 0
Gastroenterology (IM) 219 0
Geriatric Medicine (FM) 51 0
Geriatric Medicine (IM) 114 0
Geriatric Psychiatry (P) 63 0
Hand Surgery (GS) 1 0
Hand Surgery (ORS) 74 0
Hand Surgery (PS) 16 0
Hematology (IM) 2 0
Hematology (PTH) 87 0
Hematology and Oncology (IM) 174 0
Infectious Disease (IM) 158 0
Interventional Cardiology (IM) 183 1
Medical Microbiology (PTH) 15 0
Medical Toxicology (EM) 27 0
Medical Toxicology (GPM) 2 0
Molecular Genetic Pathology (MG and PTH) 42 0
Musculoskeletal Oncology (ORS) 12 0
Musculoskeletal Radiology (DR) 18 0
Neonatal-Perinatal Medicine (PD) 102 0
Table 3. National and Delaware Fellowship Programs2
218 Delaware Journal of Public Health - December 2022
Nephrology (IM) 152 0
Neurodevelopmental Disabilities (N) 8 0
Neuromuscular Medicine (N) 1 0
Neuropathology (PTH) 36 0
Neuroradiology (DR) 89 0
Neurotology (OTO) 24 0
Nuclear Radiology (DR) 18 0
Obstetric Anesthesiology (AN) 38 0
Oncology (IM) 7 0
Orthopaedic Sports Medicine (ORS) 96 0
Orthopaedic Surgery of the Spine (ORS) 16 0
Orthopaedic Trauma (ORS) 12 0
Pain Medicine (AN) 1 0
Pediatric Anesthesiology (AN) 63 1
Pediatric Cardiology (PD) 62 1
Pediatric Critical Care Medicine (PD) 74 1
Pediatric Emergency Medicine (EM) 29 0
Pediatric Emergency Medicine (PD) 59 1
Pediatric Endocrinology (PD) 73 0
Pediatric Gastroenterology (PD) 65 1
Pediatric Hematology Oncology (PD) 74 1
Pediatric Infectious Diseases (PD) 65 0
Pediatric Nephrology (PD) 47 0
Pediatric Orthopaedics (ORS) 25 1
Pediatric Otolaryngology (OTO) 31 1
Pediatric Pathology (PTH) 29 0
Pediatric Pulmonology (PD) 56 1
Pediatric Radiology (DR) 47 1
Pediatric Rehabilitation (PM) 22 0
Pediatric Rheumatology (PD) 35 1
Pediatric Sports Medicine (PD) 17 0
Pediatric Surgery (GS) 54 0 Pediatric Urology (U) 26 0
Procedural Dermatology (D) 1 0
Psychosomatic Medicine (P) 64 0
Pulmonary Disease (IM) 24 0
Pulmonary Disease and Critical Care Medicine (IM) 193 0
Rheumatology (IM) 125 0
Selective Pathology (PTH) 99 0
Spinal Cord Injury Medicine (PM) 24 0
Sports Medicine (EM) 9 0
Sports Medicine (FM) 154 1
Sports medicine (PM) 21 0
Surgical Critical Care (GS) 142 1
Transplant hepatology (IM) 60 0
Undersea and Hyperbaric Medicine (EM) 8 0
Undersea and Hyperbaric Medicine (GPM) 2 0
Vascular and Interventional Radiology (DR) 90 1
Vascular Neurology (N) 106 0
Vascular Surgery (GS) 117 0
Table 3, continued. 219
NURSE TRAINING
There are many levels of nurse certification, and nurses with these certifications can be seen at all levels and departments in healthcare institutions throughout Delaware. These levels follow a model of academic progression, based on bridge or ladder programs (called stacking) where one degree or certification provides the prerequisite for the next level. There are generally three categories of nursing education related to licensure and scope of practice, although there are variations in the names of the equivalent levels of nursing throughout the country.
Unlicensed Assistive Personnel/Pre-Licensure
A certified nursing assistant (CNA) has completed a 4-12 week program and received a certificate of their training. They are eligible to sit for a national certification test.
Entry to Nursing Practice/Licensure
Licensed Practical or Vocational Nurses (LPN or LVN) have completed a one-year, non-degree program. They are eligible to sit for a national LPN licensure which will allow them to obtain licensure in all fifty U.S. states and U.S. territories. LPNs and LVNs who wish to progress academically in nursing can complete an LPN-RN program, most of which will terminate in an Associate Degree in Nursing. Some U.S. colleges offer LPN to Bachelors of Science in Nursing programs.
Registered nurses (RN) have completed a 2-year, non-academic degree program. They have received a diploma in nursing and are eligible to sit for a national RN licensure which will allow them to be licensed in all 50 US states and territories and obtain specialty nursing certifications.
Individuals with an associate degree in nursing (ADN) have completed 2-3 years of training before obtaining their degree. RNs and ADNs can complete RN-BSN academic programs, and typically take 1-2 years to complete. Nurses with a Bachelors of Science in Nursing (BSN) have completed a 4-year academic degree. ADNs, RNs, and BSNs are also eligible to sit for the national RN exam.
Graduate and Advanced Nursing Practice
Nurses with a Master of Science in Nursing have completed a 2-4 year degree program. Their specialty is further defined by the attainment of an Advanced Practice Registered Nurse (APRN) certification and the potential for licensure.
An APRN has completed a 2-4 year program, and may be a certified nurse practitioner (CNP), a certified nurse midwife (CNM), a clinical nurse specialist (CNS), and/or a certified registered nurse anesthetist (CRNA).
Non-APRNs with a MSN degree may have a selection of focus areas including nurse leaders, nurse educators, public health nurses, and clinical nurse leaders.
Post-Masters certifications are available, and nurses may obtain licensure for specialties within the field. They may also go on to obtain a doctorate of nursing practice or doctor of philosophy in nursing (DNP/PhD), which typically take from 6-8 years.
PHYSICIAN, HEAL THY COMMUNITY
Research shows that medical students who grow up in small communities far from urban centers are more likely to return to them to practice.2 For this reason, many communities are working to place physicians and training programs in rural communities and communities which may not have a large healthcare workforce. Training in these areas provide hands-on experience in scope of practice and primary care in communities with few specialists with whom to consult.
Local training programs and schools allow young people who are seeking a career in the health sciences to see and interact with experts working within their community. They allow for newly graduated physicians and providers in training to return to the communities of their youth and bring with them a wealth of knowledge of medicine and healthcare, and apply that medicine to their knowledge of their community.
These also allow an influx of health care providers and specialists in communities which might not otherwise have these options close by. They allow new physicians to learn about continuity of care and work closely within the community. They also learn about the specific needs of underserved communities and the roles of medical providers working with these groups, and can lead to employment within these communities and the eventual increase in physicians working within these communities.
REFERENCES
1. Harvard Health Publishing. (2017, Aug 1). Should I see a “resident” doctor?
Retrieved from: https://www.health.harvard.edu/healthcare/should-i-see-a-resident-doctor
2. Freida. (n.d.). Institution directory.
Retrieved from https://freida.ama-assn.org/institution?page=2&filter=D
220 Delaware Journal of Public Health - December 2022
2021 Delaware Institute for Medical Education and Research (DIMER) Annual Report: Abridged Executive Summary
HISTORY AND BACKGROUND
The Delaware Institute of Medical Education and Research (DIMER) was founded in 1969, as an alternative to an in-state medical school, to address the concern of access to high-quality medical education for Delaware residents. Upon creation, DIMER formalized a relationship with Thomas Jefferson University for 20 admission slots for Delawareans at Jefferson Medical College (now Sidney Kimmel Medical College (SKMC)). In 2000, DIMER expanded its education relationships to also include the Philadelphia College of Osteopathic Medicine (PCOM), further increasing access to medical education for Delawareans. Upon creation, PCOM held five admission slots for qualified Delaware applicants and in 2019, the number of admission slots was increased to 10. DIMER is incredibly grateful to both institutions, who continue to exceed their commitments in accepting highly qualified Delawareans into their respective medical education programs and provide the highest quality training to future physicians.
THE DIMER ADVANTAGE
Delaware is one of four states that does not offer an in state medical school. This would ordinarily present a disadvantage for Delaware residents seeking medical education and future careers in medical professions. However, through its innovative relationships with SKMC and PCOM, Delaware has secured a minimum number of slots for highly qualified Delaware applicants. In recent years, SKMC and PCOM have each seen an increase in annual applications received to an estimated 12,000 applications for ultimately no more than 280 slots per respective institution. As a DIMER applicant, Delaware resident applications are pulled from the overall 12,000 applications received and evaluated against Delaware only applicants. This significantly improves the odds, to being one of ultimately 30 or more slots out of approximately 90-100 Delaware applicants. DIMER therefore provides one of the best medical education admission advantages in the country for qualified applicants from the First State.
DELAWARE BRANCH CAMPUS AND RESIDENCY
DIMER is not only focused on providing medical education opportunities for Delawareans but also on the retention of Delaware physicians to serve our communities. DIMER’s relationships extend beyond its education partners and into Delaware’s health systems and Delaware Health Sciences Alliance (DHSA) partners. DIMER Medical students at SKMC and PCOM have an opportunity to conduct their third- and fourth-year rotations at the Delaware Branch Campus. The Delaware Branch Campus provides medical students clinical training at ChristianaCare, Nemours, and the Wilmington VA Medical Center. In addition, PCOM clinical rotations also include Bayhealth’s Kent and Sussex Campuses as well as recently adding opportunities for rotation at Beebe Healthcare also in Sussex County. The opportunities for residency training in Delaware are numerous and expanding. ChristianaCare and Nemours offer an array of residency opportunities. Delaware residency match opportunities are not limited to Delaware Branch Campus partners as St. Francis also has a residency program and Bayhealth launched its family medicine and internal medicine residency programs in 2021. Beebe Healthcare is also currently planning for a launch of its family medicine residency program in 2023. Bayhealth also has plans to launch its general surgery residency program in 2022 and an emergency medicine program in 2023. Recruitment and retention of Delaware physicians is enhanced with the increased opportunities for Delawareans to complete their medical training and serve their community in their home state.
The DIMER Board recognizes the high cost for medical education and enormous debt students face upon graduation. The DIMER Board continued to advocate and work closely with the Heath Care Commission, Delaware Legislators, and partners such as the Delaware Health Sciences Alliance, in support of the now passed legislature for a new robust State of Delaware Student Loan Repayment Program. This program will provide for increased participation and funding support for those physicians with Primary Care focused specialties, serving geographic areas of need throughout the First State. DIMER leadership looks forward to continued engagement and advocacy as the new loan repayment program is implemented increasing opportunities to support returning physicians to Delaware. DIMER has a rich tradition of extending its activities beyond its mission to ensure access to quality medical education for Delaware residents. DIMER and its partners are committed to providing a network of support for its students and engage students throughout the academic year in a variety of ways. In collaboration with DHSA, DIMER provided care packages to each student; co-hosted virtual receptions with PCOM and SKMC for DIMER students to network with DIMER and institutional leadership; and conducted virtual awareness events in every county with prospective students and families to discuss the many benefits of DIMER.
CONCLUSION
The DIMER program continues to represent an incredible value for Delawareans’ medical education. The full annual report contains detailed information on the demographics and data relative to DIMER’s 2021 incoming and graduating classes, as well as personal stories from state and institution leadership, including DIMER students. DIMER’s approach to partnering with the DHSA, health systems and others has resulted in a robust array of services intended to facilitate Delawareans’ pathway to medical school and improved chances of returning to Delaware to practice medicine in geographic and specialty areas of need. We express our gratitude for all who have supported DIMER over its 50-year plus history and look forward to even greater achievements in the future.
DOI: 10.32481/djph.2022.12.047
221
An Environmental Scan of Healthcare Pathways Programs in Delaware
Nicole Sabine, B.S.
INTRODUCTION
In order to better understand the programing landscape of Delaware for individuals interested in going on to careers in the sciences, The Delaware Academy of Medicine | Delaware Public Health Association (Academy/DPHA) has conducted an environmental scan to identify the available programs for youth and young adults throughout the state. The programs of particular interest were those that engaged in activities in the fields of Science, Technology, Engineering, and Mathematics (STEM), with a special focus in the health sciences.
The environmental scan identified 52 different youth and undergraduate programs. Data on these programs were compiled and categorized using several factors:
•By hosting organization;
•Program Life;
•Duration and frequency of program sessions;
•Participation eligibility;
•Current demographic composition;
•Location of program; and
•Program cost to participants.
To achieve research objectives, the Academy/DPHA contacted each program in order to generate the most accurate depiction. It is important to note that not all programs responded, and thus data compiled was that of public availability (i.e. program website).
STATEWIDE PROGRAMS
Delaware Mini Medical School
Delaware Mini Medical School (Mini Med) was created in 2009 as a way for adults and high school students to gain insight to current trends in medicine. Participants learn the process by which health care providers diagnose and treat illnesses by attending in-depth lectures. From 2009 to 2021, the program was held in person every spring, in partnership with the Delaware Academy of Medicine/ Delaware Public Health Association and ChristianaCare. Beginning in 2021, Mini Med switched to entirely virtual and expanded to six cohorts per year. The six-week program has no cost to the participant. Participants who attend all six session are given a Certificate of Achievement
There is no specification of recent demographic composition; however, the majority of participants are either aged 16-19 or over 50 years. Participants are made up of all races and ethnicities, men and women, and two participants listed as “other” gender since option became available.
Delaware Institute for Medical Education and Research
Since 1969, the Delaware Institute for Medical Education and Research (DIMER) has provided an alternative to an in-state medical school for Delawareans. DIMER initially offered 20 admission slots for Delawarean medical students at Jefferson Medical College— now the Sidney Kimmel Medical College (SKMC) at Jefferson University. In 2000, the program expanded to the Philadelphia College of Osteopathic Medicine (PCOM) with five admission slots. As of 2021, both medical schools had increased the number of available admission slots: SKMC to 31 and PCOM to 18.1
DIMER offers a unique advantage as Delaware resident applications are pulled from the general medical school application pool and evaluated only against other Delaware applicants. This process proves fruitful: compared to all the 2021 SKMC and PCOM applicants, DIMER students had a higher acceptance rate than the general application pool (see Table 1). At SKMC, 35% of DIMER applicants were accepted in comparison to the 4.4% of the general pool. The difference in acceptance rates is even more evident at PCOM, as DIMER applicants had a 61.01% acceptance rate and the general pool was only 5.06%.
10.32481/djph.2022.12.048
DOI:
222 Delaware Journal of Public Health - December 2022
In addition to admission slot program, DIMER partners with the Delaware Health Sciences Alliance (DHSA) in creating health panel events. Each event is curated to engage high school and undergraduate students with an interest in the health and medical professions. Panelists consist of experts among DIMER leadership, DIMER program alum, current medical students, medical education partners, and DHSA members. Attendees are provided information on the DIMER program, and the medical school application process. Discussions on loan opportunities and financing medical school are also available.
Delaware Pathways
Delaware Pathways is an education and workforce partnership that provides opportunities for youth to gain work experience and hone their academic and technical skills. Currently, Delaware Pathways offers 89 different middle and high school pathway programs with a total enrollment of 23,009 students. All programs are free, however students may be expected to purchase extra expenses (i.e. new scrubs, shoes), depending on the program. To view all available health science programs, please see Appendix A.
Girl Scouts of the Chesapeake Bay
Open to all girls in grades K-12, the Girl Scouts of the Chesapeake Bay (GSCB) offers a variety of activities to develop life and technical skills. Participants are divided intro groups by grade level: Daisies (K-1), Brownies (2-3), Juniors (4-5), Cadettes (6-8), Seniors (910), and Ambassadors (11-12) (see Table 2). GSCB serves 14 counties throughout Delaware and the eastern shores of Maryland and Virginia. Membership to GSCB costs $40 per year, with an extra $0-60 fee depending on the program. Summer camp program registrations range from $215-650. Financial aid is available to those who qualify.
Table 1. 2021 DIMER Matriculant Demographics Count % of Total Total # of participants 49 100 Sex Female 30 61.22 Male 18 36.74 Not
1 2.04 Race/Ethnicity Caucasian/White 20 40.82 African American/Black 6 12.24 Asian 22 44.9 Not Disclosed 1 2.04 Participants by County New Castle 39 79.6 Kent 6 12.24 Sussex 4 8.16
Disclosed
223
All groups are eligible to participate in “Journeys,” which consists of earning three to four related badges and then creating a “Take Action Project.” Through the project, participants identify a problem, create a sustainable solution and team plan, and then put their plan into action. Finally, they present what they learned and what future steps they may take. The Girl Scout Leadership Experience is an annual one weekend-long program, open to girls in grades 6-12. The program begins on a Friday at 7pm and ends on Sunday at 10 am. Throughout the weekend, participants will engage in four key activity areas: STEM, outdoors, life skills, and entrepreneurship.
Another program of interest is the GSCB’s Program on the Move. This program is entirely free to the participants and is a mobile program that brings all the necessary materials to a location of the troop’s choosing. The troop also may choose any topic from the available list: circuits, robotics, color exploration, content creation leadership basics, environmental stewardship 101, and virtual reality/ augmented reality. Every scout will receive one free patch per year of participation. Each session is approximately one hour and a half and is available October—December and February—May.
Million Women Mentors Delaware
Million Women Mentors Delaware (MWM-DE) is a program designed to connect girls and young women with female leaders in STEM across the state. MWM-DE partners with many Delaware corporations on community events and mentoring programs. Some programs of note are The Future is Female: Girls in STEM camp, DigiGirlz Day, the Science and Technology Career Fair, and Engineering Your Tomorrow. MWM-DE runs throughout the year and has no cost to the participant.
Table 2. Current Participant Demographics
Count % of Population
Girl Scout/ Grade Level
White
African American/ Black
Asian
American Indian or Alaskan Native 12
Hawaiian or Pacific Islander
Two or More Races
Other Races
Choose Not to Share
Daisies (K-1) 563 17.02 Brownies (2-3) 850 25.71 Juniors (4-5) 761 23.01 Cadettes (6-8) 675 20.41 Seniors (9-10) 232 7.02 Ambassadors (11-12) 221 6.68 Unknown 5 0.15 Total youth membership 3,307 100 Race/Ethnicity
4398 62.32
733 10.39
90 1.275
0.17
5 0.07
208 2.95
229 3.245 I
784 11.11 Not Reported 598 8.47 Total membership (youth, adult & lifetime) 7057 100
224 Delaware Journal of Public Health - December 2022
Delaware HOSA
Delaware HOSA- Future Health Professionals is a student-led program that provides opportunities for students to gain knowledge and skills related to the health sciences. Through various competitive events and workshops, students are able to develop, practice, and refine their leadership and teamwork skills. Participants are also prepared for higher education and entry level certification (i.e. EMT, CNA, etc.). HOSA is open to students in grades 6-12 and meets approximately once a month throughout the year (see Table 3). Prior to the COVID-19 pandemic, 1400-1500 students participated in the program throughout the state. The total cost of program membership is $150: $10 national fee, $40 state conference, and $100 for the national conference.
Table 3. National HOSA Participant Demographics
% of Total Population
Sex
Female 81 Male 19
Race/Ethnicity
White 49
Non-white 51
Delaware HOSA also heads the Fusion Program which is open to students in grades 9-12. Fusion is a student organization geared towards students not enrolled in a health science program of study but demonstrate interest in a healthcare career. The total cost of program membership is $200: $10 national fee, $90 state fee, and $100 for registration into the state conference.
Delaware Department of Education & TeenSHARP
Since 2009, TeenSHARP has been dedicated to serving the low-income, unrepresented student population in Delaware. Every year, the Delaware Department of Education and TeenSHARP partners to host the Delaware Goes to College Academy. This week-long program is open to students in grades 9-11. Participants are educated about the process of applying to college and financial aid through several workshops. The program also offers the opportunity to meet with representatives from many in and out-of-state colleges. The program is entirely virtual and has no cost to the participants.
Del-Mar-Va Council’s Boy Scouts of America (BSA)
The Del-Mar-Va Council’s BSA is open to both boys and girls aged 5-20 years. BSA is divided into three main groups: Cub Scouts (ages 5-10), Scouts BSA (ages 11-17), and Venturing & Exploring (ages 13-20) (see Table 4). All sections include the opportunity to earn STEM-related badges and engage in STEM activities. The annual membership fee for Scouts BSA is $148 for new scouts, and $123 for returning scouts. Extra costs for uniforms, activities, and camping trips are included but may be alleviated through fundraising initiatives.
Venturing is a youth-led program aimed to improve leadership and teamwork skills. Through venturing, young adults are able to advance their skills in various areas including but not limited to: arts, religion, sports, outdoors, hobbies, and Sea Scouting. Exploring is a work site-based program where youth and young adults learn about the day-to-day activities and responsibilities of various careers (see Table 5). Del-Mar-Va Council’s BSA currently offers exploring opportunities in law enforcement, fire & emergency services, and health care. Other programs such as aviation and engineering are in development and may become open in the future. Generally, the exploring programs meet once a month and cost $45 per participant annually.
The ChristianaCare Explorer Post 2613 is a Co-Ed program which is open to high school and college students aged 14-20 years (see Table 6). The program is a part of the Learning for Life section of the Del-Mar-Va Council, Boy Scouts of America Exploring Program. For 35 years, the program has offered volunteer and shadowing opportunities along with leadership and life skills development at both Christiana Hospital and Wilmington Hospital. The program meets every second Sunday of the month and each session is two hours long. Program fees are free to the participant.
225
Table 5. Exploring Program Demographic Composition as of January 2020 Count % of Total Total # of participants 250 100 Sex Female 172 68.8 Male 78 31.2 Race/Ethnicity Caucasian/White 112 44.8 African American/Black 35 14 Asian 28 11.2 Hispanic 9 3.6 Other 10 4 Not provided 56 22.4 Table 4. Del-Mar-Va Council BSA Participant Demographics as of October 2022: Count % of Total Total # of participants 3,964 100 Sex Female 570 14.38 Male 3,394 85.62 Race/Ethnicity Caucasian/White 3,136 79.11 African American/Black 217 5.47 Asian 141 3.56 Hispanic 205 5.17 Native American 9 0.22 Pacific Islander 8 0.20 Alaska Native 1 0.03 Other 148 3.73 Not provided 99 2.5 Program Participation Cub Scouts 1,916 48.34 Scouts BSA 1,966 49.6 Explorers 29 0.73 Venturers 22 0.55 Sea Scouts 31 0.78 Table 6. Current Explorer Post 2613 Participant Demographics Race/Ethnicity Sex Total FemaleMale Asian 55 10 African American/Black 50 5 White 21 3 Total participants 18 226 Delaware Journal of Public Health - December 2022
DELAWARE INBRE SUMMER SCHOLARS PROGRAM
The Delaware IDeA Network of Biomedical Research Excellence (INBRE) Summer Scholars Program is a 10-week, summer research program open to full-time undergraduate rising sophomores or above. Participants must be a Delaware resident or attend a Delaware college/university. Each participant creates an independent research project while studying full-time under a mentor and learning about research techniques. All Delaware INBRE events are mandatory and participants must participate in an oral or poster presentation of their findings at the Research Symposium. Program participants are given stipends ranging from $4300 to $5600, depending on the institution where the mentor is located.
From 2002 to 2020, Delaware INBRE has served a total of 811 students. Of the past participants, 85% of them are currently employed in science or health-related fields. Over 300 of all participants have gone on to pursue graduate degrees. In 2020, there were 74 participants, 30 of whom were categorized as an underrepresented minority (URM) in biomedical fields.2
United Way of Delaware
The United Way of Delaware (UWDE) is an organization dedicated to maximizing educational resources in Delaware communities. During the COVID-19 pandemic, UWDE opened 27 learning pods—after-school programs geared toward improving reading and math scores. Additionally, the organization gave away 70,000 free books and 6,000 literacy kits to 14 different elementary schools across the state. UWDE also leads the Career & College Success program which works in partnership with Delaware Pathways.
Stand By Me
United Way of Delaware and the State of Delaware are judiciary partners of financial coaching program Stand By Me (SBM). Stand By Me NexGen is a school-based program available to Delaware high school students who want to improve financial literacy and seek support in completing college financial aid applications. NexGen offers two sub-programs: College, Careers & Cash (CCC) and the College Funding Project (CFP). All SBM programs are entirely free as they are underwritten by a grant from the Delaware Department of Education Higher Education Office.
The CCC program is open to ninth and tenth graders and provides them with a custom-designed curriculum. Participants engage in classroom workshops that help to improve financial literacy and build connections between higher education and career pathways. Financial literacy is tested through student-developed budget plans and understanding of credit and its consequences. In the 2021-2022 period, CCC served 22 public and charter schools and a total of 3,500 students.
Through the CFP program, participants are educated on how to complete Free Application for Federal Student Aid (FAFSA) and apply for scholarships. Participants may also utilize personal step-by-step coaching, with each session ranging from 30 minutes to one hour. In 2021, the program hosted 190 in-school and virtual events and 380 FAFSA completion appointments.
227
NEW CASTLE COUNTY PROGRAMS
University of Delaware Student Clubs
Of the total 52 programs acknowledged, 19 are student-led clubs available to undergraduate students at the University of Delaware. All clubs run throughout the academic year (September to June). Program participation fees range from $0 to $12. Program demographic composition is varied, and similar to the make-up of the University of Delaware. Please see Appendix B for a list of the programs and their related information.
Medical Society of Delaware (MSD) & the Delaware Youth Leadership Network (DYLN): Apollo: Youth in Medicine
The Apollo: Youth in Medicine (YIM) program is an entirely student-led non-profit that exposes high school juniors and seniors to the medical profession. Since 2018, the program has offered in-person physician shadowing along with special education sessions involving information on medical pathways, and hands-on medical education such as cadaver labs. Students are admitted in the fall and given access to 4-hour shadowing slots offered by the program during three seasonal sessions (Fall, Spring, and Summer) throughout each year, each lasting for 2- to 6-weeks. Apollo offers shadowing in 17 different specialties: students are required to take one slot in primary care during their first session in the program, and are encouraged to explore a breadth of specialties of their choosing during future slots. Apollo has offered 1,082 shadowing slots since its inception.
To date, the program has served 32 high schools and a total of 189 students, both matriculating and graduated. Apollo is an applicationbased program and, over the last 5 years, it has enrolled more female than male participants. Fully supported by the work of student volunteers and grant funding from Delaware Medical Education Founation (DMEF), the program is free to the participating students.
Walnut Street YMCA
The Walnut Street YMCA located in Wilmington, DE offers many programs for youth engagement and building life skills. Two programs of note are the Black Achiever program and the Teen Workforce Development.
Since 1989, the Black Achiever Program has provided college readiness and career awareness to African American teens aged 1418 years. The teens meet with African American mentors from various career fields who prepare the participants for future success. The program meets every Saturday except for holiday weekends, and each session is two hours long. The program has no cost to the participants. The program currently comprises of 60% females and 40% males, all of whom identify as African American/Black.
The Teen Workforce Development Program engages teens aged 15-18 in workshops designed to improve job readiness and the associated life skills. Workshop topics may include financial literacy, public speaking, resume writing, and more. Each session is two hours long and has no cost to the participant. The program has run since 2017, and offers four cohorts per year. The current demographic composition is 50% females and 50% males, all of mixed-race backgrounds.
Junior Achievement of Delaware
Junior Achievement (JA) of Delaware offers a variety of programs open to grades K-12. Programs offered include financial literacy, entrepreneurship, and career readiness. Although there is no specific health science program, JA students have the opportunity to learn from role models who work in the health sciences and their experiences in said career. Program cost varies from $15-65 per participant and experience; however, costs are usually covered through public and private contributions.
Year Up Wilmington
Year Up is a 3-step training program that takes up to one year to complete. The program has provided opportunities for internship placement, and the development of professional and personal skills since 2017. Additionally, participants may utilize staff guidance throughout the program. The program has no cost to the participant.
Dawn Career Institute
The Dawn Career Institute (DCI) is a private, post-secondary educational institution. In 2002, DCI began offering two health sciencerelated programs: The Nursing Assistant and Medical Assisting Diploma Programs, both of which are available to ages 17 and up (see Table 7). Both programs have a rolling enrollment and include career success coaching.
228 Delaware Journal of Public Health - December 2022
The Nursing Assistant Diploma Program includes a combination of qualified instruction and relevant medical equipment and instruments. The program has seven to eight cohorts per year, with each cohort running for six weeks. The total for tuition and fees is $3,213; however, tuition-free grants are available based on eligibility.
The Medical Assisting Diploma Program teaches participants the technical knowledge required to perform key medical office procedures and protocols. The program is 36 weeks long, and includes a six-week externship. This program is offered both in-person and virtually. The total program cost is $16,352.61 before financial aid.
Table 7. Dawn Career Institute Student Body Demographics Data Collection Report July
2020 thru June
2021 Total Served Percent of Demographic Served Sex Male 40 17 Female 202 83 Did Not Self Identify 0 0 Age 14-21 39 16 22-29 151 62 30-54 51 21 55+ 1 1 Race/ Ethnicity American Indian/Alaskan Native 0 0 Asian 0 0 African American 117 49 Pacific Islander 0 0 White 66 27 Did not
Identify 0 0 *More than one Race 59 24 All Hispanic Hispanic 38 16 Not Hispanic 204 84 Did Not Self
0 0 All Disability Disabled 0 0 Not Disabled 242 100 Participant Did Not Disclose 0 0
1,
30,
Self
Identify
229
Charter School of Wilmington
The Charter School of Wilmington (CSW) (see Table 8) opened in 1997 and is one of the first independent public charter schools in the United States. In addition to a traditional high school curriculum, CSW offers a college preparatory program with a special focus in STEM. Once students reach their junior year, they are required to participate in the Junior Research Program. Through this program, students acquire knowledge and skills in experimental design, data collection, and data analysis. Students are then required to present their findings to their mentors and judges at a final symposium. Overall, the school consistently ranks in the top 1% of math and reading proficiency, and testing rank among Delaware schools.3
Table 8. 2021 Charter School of Wilmington Student Body Demographics
Conrad Schools of Science
Opened in 2001, the Conrad Schools of Science is a life science magnet school for grades 6-12 (see Table 9). Students are able to take advanced placement and dual enrollment courses throughout their time at the school. Various career pathways and programs are offered at Conrad including, but not limited to nurse technology, physical therapy, and athletic health care. Students are also given the opportunity to earn certification and licensing in CPR/First Aid, Nurse Assistants (CNA), and ACSM Certified Personal Training.4
Table 9. 2021 Conrad Schools of Science Student Body Demographics Count Percent of Total
Total
Race/Ethnicity
Caucasian/White
African
American Indian/Alaska Native 3 0.3
Student: Teacher Ratio 19:1
FAME, Inc.
FAME Incorporated of Delaware has a variety of STEM programs open to grades K-12. Programs include the STEMulate® Change Outreach Initiative, Core STEM Initiative, Summer Enrichment Program, School Year Program, and the Talent Engagement Connection (TEC) initiative. FAME is also currently in development of The Learning Lab which will be located in Wilmington, Delaware. The Learning Lab will be a multi-level building with study/work spaces, classrooms, laboratories, and a rooftop garden and lounge. The Learning Lab will only admit students under the age of 18 years.
The STEMulate® Change Outreach Initiative encourages interest in STEM among grades K-6. Classes are project-based and explore cross-curricular topics through experiments and engineering problem-solving prototypes. Additionally, students are exposed to various STEM careers through each project.
Count Percent of Total
965 100
502 52
463 48
504 52.2
71 7.4
286 29.6
65 6.7
35 3.6
4
20:1
Total # of students
Sex Female
Male
Race/Ethnicity Caucasian/White
African American/Black
Asian
Hispanic
Two or More Races
American Indian/Alaska Native
0.4 Student: Teacher Ratio
# of students 1,178 100 Sex Female 589 50 Male 589 50
663 56.3
American/Black 139 11.8 Asian 74 6.3 Hispanic 263 22.3 Two or More Races 36 3.06
230 Delaware Journal of Public Health - December 2022
The Core STEM Initiative is a four to six-week summer curriculum that includes over 220 hours of exhaustive, innovative STEM instruction for grades 7-12. Students in grades 7-10 take classes at John Dickinson High School for six weeks. Students in grades 11 and 12 live on-campus at University of Delaware for four weeks. Through the program, students are exposed to robotics and offered test awareness, college prep, peer counseling, and job readiness.
The School Year Program is an extension program of the CoreSTEM Initiative that takes place at John Dickinson High School. The program meets the first and third Saturday of each month, October through May. In addition to CoreSTEM activities, participants will engage in academic planning, test taking, and maintenance. The program fee is $500 per student, with a discount of $250 for a sibling in the same household.
The Summer Enrichment Program is an intensive six-week program open to students in grades 1-12. The program runs Monday through Thursday from 8:00 a.m. to 3:00 p.m. The first half of the day is geared toward STEM and Communication/English skills, and the second half includes business and cultural tours along with group-based engineering/STEM projects for grades 1-10. Eleventh and twelfth grade students are offered the opportunity to experience college life in a four-week fast-paced program at the University of Delaware. High school juniors take course work in Algebra II, Pre-Calculus, Geometry, Chemistry, and Engineering. Seniors take two college-level courses in Pre-Calculus/Calculus and Physics and have two additional courses in computers and engineering research design.
The Talent Engagement Connection (TEC) Initiative connects high school and college students with Delaware colleges and companies. TEC utilizes the Tallo platform to create a workforce pipeline for employers to track and communicate with qualified talent. Students are also able to view eligibility for scholarships along with direct messaging and easy application to job opportunities.
KENT COUNTY
Delaware State University
The Howard Hughes Medical Institute (HHMI) Inclusive Excellence (IE) Initiative emphasizes first generation and “nontraditional” college student engagement in STEM. Non-traditional students are those who:
• Did not enroll high school;
• Attend college part-time;
• Work full time;
• Are financially independent;
• Are a single parent;
• Have a GED;
• Are a veteran;
• Transferred from a 2-year college; and/or
• Have dependents other than a spouse.
HHMI activities include 24/7 free online tutoring, student-centered learning, and support for degree completion and career preparation. Degree completion options consist of Advanced Placement (AP), College-Level Examination Programs (CLEP), and Defense Activity for Non-traditional Education Support (DANTES). Students are also assisted in finding STEM internships and jobs.
The Undergraduate Research Training Initiative for Student Enhancement (U-RISE) program goal is to develop a diverse pool of undergraduate students who earn their bachelor’s degree and pursue higher education. The program is open to sophomores who meet the following minimum criteria:
•Full-time student at DSU, with enough credits to reach upper division standing by the following fall (30 or more credits accumulated);
•At least two summers remaining before planned graduation date;
•Underrepresented minority (as defined in NIH Notice NOT-OD-18-129);
•US citizen or permanent resident;
•Demonstrated potential and interest in pursuing a graduate degree (Ph.D.) in biomedical or behavioral science;
•Both STEM and overall GPA of 3.2 or better; and
•Commitment to complete the program and related activities.
U-RISE comprises of a series of activities, course, and workshops to support the transition and success in graduate school. Additionally, participants will complete an online mentoring course and participate in implicit bias interventions.
231
SUSSEX COUNTY
Sussex County STEM Alliance
The Sussex County STEM Alliance is a non-profit organization committed to advocating for STEM awareness and involvement in Sussex County youth. According to the organization’s mission statement, there is no official dissemination of STEM related information in Sussex County for kindergarten through higher education. In order to alleviate this issue, the organization promotes three specific programs: the Sussex County K-5 STEM Fair, Virtual STEM Socials, and Engineering Your Tomorrow.
Starting November 2022, the Sussex County K-5 STEM Fair will be held annually at the Lewes Public Library due to the support of the Carl M. Freeman Foundation FACES Grant. All children in grades K-5 are encouraged to participate regardless of schooling status (public, private, home-schooled, etc.). Participants may enter their projects as an individual or a group. Submitted projects will be judged by local STEM professionals and awarded prizes.
Virtual STEM Socials connect Sussex County stakeholders with the public while engaging in STEM-related discussions. Topics range from building inclusivity and equality in STEM to how the COVID-19 pandemic shaped innovation. This program is entirely virtual and at no cost to the participant.
Engineering Your Tomorrow (EYT) is a program that has been going on for 29 years in New Castle County thanks to its sponsors DuPont, Girls Inc and the Girl Scouts. In April 2019, EYT was brought to Sussex County through the support of the Delaware Foundation for Science and Math Education, Mountaire Farms, Delaware Technical and Community College, and the Sussex County STEM Alliance. Participants engage in hands-on STEM activities and work with female scientists to test scientific hypotheses. Parents of the participants are provided with information to guide them in preparing their daughters for higher education and careers in STEM. Engineering Your Tomorrow is open to girls in grades 6-8 and has no cost to the participant.
DISCUSSION
The environmental scan detailed 52 youth and undergraduate programs throughout the state. Of the 52 programs, there are 15 statewide initiatives with the other 37 divided among the three counties in Delaware. Excluding statewide programs, New Castle County (NCC) houses the most programs out of all the counties with 32 programs—19 of them being student-led clubs at the University of Delaware. The other two counties are largely underserved in comparison, with two programs in Kent and three in Sussex respectively.
Although the scan was conducted with the intent to pinpoint health science programs, any programs open to middle school to undergraduate students were considered. The breakdown of number of programs by type is:
•29 health science-related programs, •17 STEM programs, and •17 programs for college and career readiness. It is important to note that some programs are multi-faceted and may cover more than one program area. From the available demographics, there is a relatively even distribution of program participants that are people of color (POC) and those that are White. This is likely attributed to the programs that are specifically designed for POC youth such as those at the YMCA Walnut Street.
Recommendations for future programming include an increase in programs within Kent and Sussex County. Furthermore, providing the means for attendance and affordability should be considered especially in areas of low socioeconomic status. The majority of the programs were of little to no cost to participants, with a few exceptions. Programs with high fees may benefit from exploring funding avenues such as grant and public fundraising to alleviate the burden on participants.
REFERENCES
1. DIMER. (2021). DIMER annual report.
Retrieved from https://dhss.delaware.gov/dhcc/files/2021dimerannualrpt.pdf
2. Lessard, L., & Dixon, K. L. (2021). 2021 Student success report.
Retrieved from http://de-inbre.org/wp-content/uploads/2021/09/DE-INBRE-STUDENT-SUCCESS-Report-2021.pdf
3. U.S. News. (n.d.). Charter School of Wilmington.
Retrieved from https://www.usnews.com/education/best-high-schools/delaware/districts/charter-school-of-wilmington/charter-school-of-wilmington-4580W
4. U.S. News. (n.d.). Conrad Schools of Science.
Retrieved from https://www.usnews.com/education/k12/delaware/conrad-schools-of-science-4628#data
232 Delaware Journal of Public Health - December 2022

APPENDIX A. DELAWARE PATHWAYS: HEALTH SCIENCE PROGRAM OFFERINGS 233
B.
UNIVERSITY OF DELAWARE STUDENT CLUBS
Program Name Program Description
University of Delaware Pre-Student Osteopathic Medical Association (PreSOMA) Society
University of Delaware American Medical Student Association (AMSA)
student-led; promote and inform the public about osteopathic medical education, to increase the number of applicants to osteopathic medical schools; o er volunteering, shadowing, medical school application opportunities
student-led; create an open forum of discussion about the track that pre-med students follow, both in academic and extracurricular settings; host speakers and events that allow greater exposure to the medical field
Health Professions Councilstudent-led; hosts events that will allow the students in organization to connect with upperclassmen in a mentee-mentor program; events with guest speakers from all di erent specialties in health care
Making Doctors student-led; guides students in preparing and applying to medical school, provides volunteer opportunities
Medical and Molecular Sciences Club promote the majors of the department, academic betterment, and o er networking opportunities for its members
Men in Nursing to create well-rounded, proficient and professional male nurses; have skill labs, service opportunities, and more ways to be involved
Minority Association of Pre-Med Students at UD (MAPS at UD)
Program Link
https://studentcentral.udel.edu/organization/pre-somasociety
https://studentcentral.udel.edu/organization/ americanmedicalstudentassociation
https://studentcentral.udel.edu/organization/healthprofessionscouncil
https://studentcentral.udel.edu/organization/makingdoctors
https://studentcentral.udel.edu/organization/ medicalandmolecularsciencesclub
https://studentcentral.udel.edu/organization/meninnursing
student-led; mphasizes the importance of diversity in the health professional field through educating and building a community; includes volunteer and service events, informing admission processes, MCAT tips and tricks
skill tricks
Multicultural Student Nurses Organization includes supporting, empowering, and networking all minority nursing students; volunteer opportunities & educational tips
Nutrition & Dietetics Clubevents, opportunities to help out in the community, and listen to guest speakers come in to talk about possible career paths in dietetics
oSTEM at UD identify, address, and advocate for the needs of LGBTQ+ students in the fields of STEM; fulfill student needs through mentorship connections, networking opportunities, strategic collaborations, and professional/leadership development
Phi Delta Epsilon International Medical Fraternity (PhiDE) at UD
Physical Therapy Interest Club
speakers relating to the medical profession, and community service; fundraise for the Children’s Hospital of Philadelphia via the Children’s Miracle Network.
student-led; exposing and preparing students for careers in Physical Therapy; work closely with UD’s STAR Campus, listen to guest speakers such as therapists and grad students, form ties with surrounding PT facilities and help prepare students for the grad school application process
https://studentcentral.udel.edu/organization/maps
https://studentcentral.udel.edu/organization/ multiculturalstudentnursesorganization
https://studentcentral.udel.edu/organization/nutritiondieteticsclub
https://studentcentral.udel.edu/organization/ostem
https://studentcentral.udel.edu/organization/ phideltaepsiloninternationalmedicalfraternity
https://studentcentral.udel.edu/organization/physicaltherapyinterestclub
Physician Assistant Club
AssistantClub
informational meetings, CASPA prep, panels with PA students and practicing PAs, and advice on courses/majors at UD; provide volunteer, shadowing, and patient contact hour opportunities for undergraduate students
Pre-Dental Society dental school prep, admissions presentations by dental schools, panels with current dental students, expert presentations
Pre-Pharmacy Society learning about drug related issues; help students with PCAT prep, get information on how to maximize opportunities to get into pharmacy school, discuss general and specific pharmaceutical interventions
Student Nurses Organization (SNO) fundraising events, volunteer opportunities; linking students to parttime/temp nursing jobs
UD Student Chapter of Doctors without Borders raising awareness and knowledge about MSF’s work in the field and about humanitarian issues, encouraging students to consider working with non-governmental organizations, post-graduation, supporting MSF in advocacy campaigns, and raising money for MSF, our work in the field, and specific campaigns
Lori’s Hands at UD student volunteers provide in-home support to people with chronic illnesses like cancer, MS, Lou Gehrig’s Disease (ALS), and heart failure; assist community members with grocery shopping, yard work and other tasks, while gaining valuable insight into the human experience of chronic illness.; gain a understanding of the social determinants of health
Black Student Nurse Association (BSNA)
https://studentcentral.udel.edu/organization/physicianassistantclub
https://studentcentral.udel.edu/organization/predentalsociety
https://studentcentral.udel.edu/organization/prepharmacysociety
https://studentcentral.udel.edu/organization/studentnursesorganization
https://studentcentral.udel.edu/organization/doctorswithoutborders
https://studentcentral.udel.edu/organization/lorishands
forAfrican/African-American/Black challenges
establish a safe space for African/African-American/Black nursing students; provide a social and academic support system to black nursing students as they endure the challenges of the nursing profession.
https://studentcentral.udel.edu/organization/blackstudentnurseassociation
APPENDIX
234 Delaware Journal of Public Health - December 2022
Duration & Frequency
2016throughout the academic year (September- June), 1 hour sessions
throughout the academic year (September- June)
2020throughout the academic year (September- June); 30 mins to 1 hour sessions
Eligibility
Undergraduate students 10 members (all 20-22, 2 Asian, 1 African American, restare Caucausian, all females) $0 per participant
Undergraduate students on pre-med track
Undergraduate students
rest are
throughout the academic year (September- June)
Undergraduate students throughout the academic year (September- June)
Undergraduate students throughout the academic year (September- June) Male undergraduate nursing students throughout the academic year (September- June) pre-medicine/pre-health professional undergraduate students
2006throughout the academic year (September- June) all nursing undergraduate students throughout the academic year (September- June) undergraduate students throughout the academic year (September- June) undergraduate students throughout the academic year (September- June) undergraduate students throughout the academic year (September- June) undergraduate students
201110 meetings per academic year (September- June); each session varies from 45 mins to 3 hours undergraduate students no specification, similar to UD student body $0 per participant
201110
throughout the academic year (September- June) undergraduate students throughout the academic year (September- June) undergraduate students
throughout the academic year (September- June) undergraduate nursing students throughout the academic year (September- June) undergraduate students
2019continuous/throughout the year (college session during academic year)
throughout the academic year (September- June) African/African-American/Black nursing undergraduate students
Program Inception
Demographic Composition Program cost
“18+, males/females, predominately white but a mix of most ethnicities and races” $5.00 one time membership fee
Race: 74% white, 12% Asian, 7% Black, 7% other Gender: 86% female, 13% male, 1% other Age: 97% 17 - 22, 3% 23+ $10-12
undergraduate and graduate students
per participant for criminal background check; financial aid available
235
Index of Advertisers
The DPH Bulletin - November 2022 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
Delaware Division of Public Health
The Nation's Health . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27
American Public Health Association
Chronic Disease Public Health Conference . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33
Delaware Public Health Institute
Mid-Atlantic Partnership Regional Conference . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39
Delaware Public Health Association
The DPH Bulletin - December 2022 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 140
Delaware Division of Public Health
Submission Guidelines . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 238
Delaware Journal of Public Health
236 Delaware Journal of Public Health - December 2022
Share love, not germs.
Get your
flu vaccine.
237
Put the flu in its place — get the flu vaccine. If you’re eligible, you can get your COVID-19 bivalent booster at the same time. Visit flu.delaware.gov for more info and locations to get your vaccine.
Public Health Delaware Journal of Submission Guidelines
updated April, 2020
About the Journal
Established in 2015, e Delaware Journal of Public Health is a bi-monthly, peer-reviewed electronic publication, created by the Delaware Academy of Medicine/Delaware Public Health Association. e publication acts as a repository of news for the medical, dental, and public health communities, and is comprised of upcoming event announcements, past conference synopses, local resources, peer-reviewed content ranging from manuscripts and research papers to opinion editorials and personal interest pieces, relating to the public health sector. Each issue is largely devoted to an overarching theme or current issue in public health.
e content in the Journal is informed by the interest of our readers and contributors. If you have an event coming up, would like to contribute an Op-Ed, would like to share a job posting, or have a topic in public health you would like to see covered in an upcoming issue, please let us know.
If you are interested in submitting an article to the Delaware Journal of Public Health, or have any additional inquiries regarding the publication, please contact DJPH Deputy Editor Elizabeth Healy at ehealy@delamed.org, or the Executive Director of e Delaware Academy of Medicine and Delaware Public Health Association, Timothy Gibbs, at tgibbs@delamed.org
Information for Authors
Submission Requirements
e DJPH accepts a wide variety of submission formats including brief essays, opinion editorials pieces, research articles and ndings, analytic essays, news pieces, historical pieces, images, advertisements pertaining to relevant, upcoming public health events, and presentation reviews. If there is an additional type of submission not previously mentioned that you would like to submit, please contact a sta member.
e initial submission should be clean and complete, without edits or markups, and contain both the title and author(s) fulls name(s). Submissions should be 1.5 or double spaced with a font size of 12. Initial submissions must also contain a cover letter with concise text (maximum 150 words). Once completed, articles should be submitted via email to Elizabeth Healy at ehealy@delamed.org as an attachment. Graphics, images, info-graphics, tables, and charts, are welcome and encouraged to be included in articles. Please ensure that all pieces are in their nal format, and all edits and track changes have been implemented prior to submission.
Cover Letters must address the following four article requirements:
1. A description of what the paper adds to current knowledge, in particular with respect to material previously published in DJPH, and if systematic reviews exist on the topic.
2. e public health importance of the paper.
3. One sentence summarizing the main message(s) of the paper, which may be used to disseminate the paper on social media.
4. For individual or group randomized trials, provide the date of trial registration and the NCT number from www.Clinicaltrials.gov or other approved registry. In the cover letter only, not in the paper. Do NOT include the trial registration or NCT number in the abstract or the body of the manuscript during the initial submission.
All manuscripts must be submitted via email to Elizabeth Healy at ehealy@delamed.org.
238 Delaware Journal of Public Health - December 2022
To view additional information for online submission requirements, please refer to the website for the Delaware Journal of Public Health: https://djph.org/sample-page/submit-an-article/

Submission Length
While there is no prescribed word length, full articles will generally be in the 2500-4000-word range, and editorials or brief reports will be in the 1500-2500-word range. If you have any questions regarding the length of a submission, or APA guidelines, please contact a sta member.
Copyright
Opinions expressed by contributors and authors do not necessarily re ect the opinions of the DJPH or a liated institutions of authors. Copying for uses other than personal reference or interest without the consent of the DJPH is prohibited. All material submitted alongside written work, including graphics, charts, tables, diagrams, etc., must be referenced properly in accordance with APA formatting.
Con icts of Interest
Any con icts of interest, including political, nancial, personal, or academic con icts, must be declared prior to the submission of the article, or in conjunction with a submission. Con icts of interest are any competing interests that may leave readers feeling misled or deceived, and/or alter their perception of subject matter. Declared con icts of interest may be published alongside articles in the nal electronic publication.
Nondiscriminatory Language
Use of nondiscriminatory language is required in all DJPH submissions. e DJPH reserves the right to reject any submission found to be using sexist, racist, or heterosexist language, as well as unethical or defamatory statements.
Additional Documents and Information for Authors
Please Note: All authors and contributors are asked to submit a brief personal biography (3 sentences maximum) and a headshot along submissions. ese will be published alongside nal submissions in the nal electronic publication. For pieces with multiple authors, these additional documents are requested for all contributors.
Abstracts
Authors must submit a structured or unstructured abstract along with their article.
e word limit is 200 words, including headings. A title page should be submitted with this abstract as well.
Structured abstracts should employ 4-5 headings: Objectives (begins with “To…”) Methods Results Conclusions
A fth heading, Policy Implications, may be used if relevant to the article.
Trial Registration information is required for clinical trials and must be included in the nal version abstract
All abstracts should provide the dates(s) and location(s) of the study is applicable.
Note: ere is no Background heading.
239
The Delaware Academy of Medicine is a private, nonprofit organiz ation foun de d in 1930 Our mission is to enhance the well bein g of our community through medical education an d the promotio n of public health. Our edu cational initiative s span the spectr um fr om consumer health education tocontinuing medical education conferences an d symposia
The Delaware Public Health Association wa s of ficially reborn at the 141st Annual Meetin g of the American Public Health Association (A HPA) held in Boston , MA in November, 2013 At this meeting, af filiation of the DPHA wa s transferred to the Delaware Academy of Medicine of ficially on November 5, 2013 by action of the APHA Governing Council. The Delaware Academy of Medicine, who’ s mission statemen t is “t o promot e the well-being of our communit y through education an d the promotio n of public health,” is honore d to take on this respon sibility in the First State.
ISSN 2639-6378
Delaware Academy of Medicine / DPHA P.O. Box 89 Historic New Castle, DE 19720 www.dela med.org | www.djph.org Follow Us:






































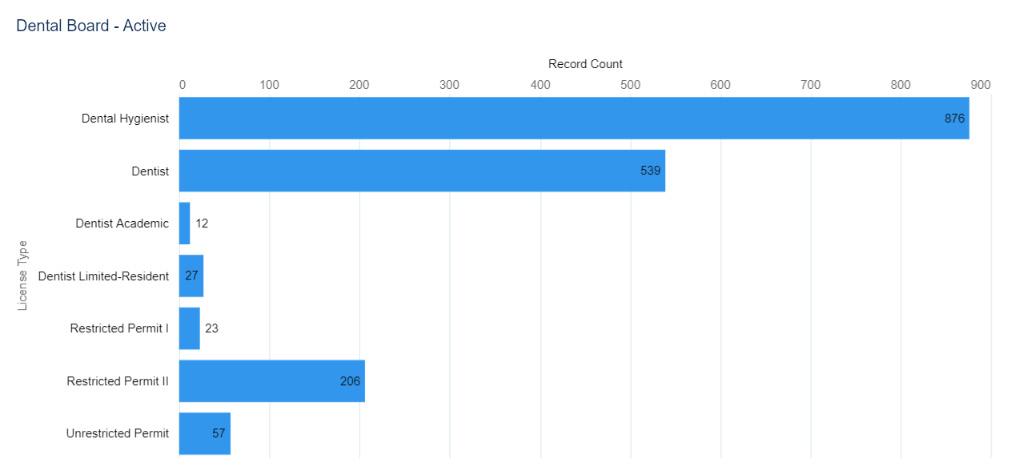

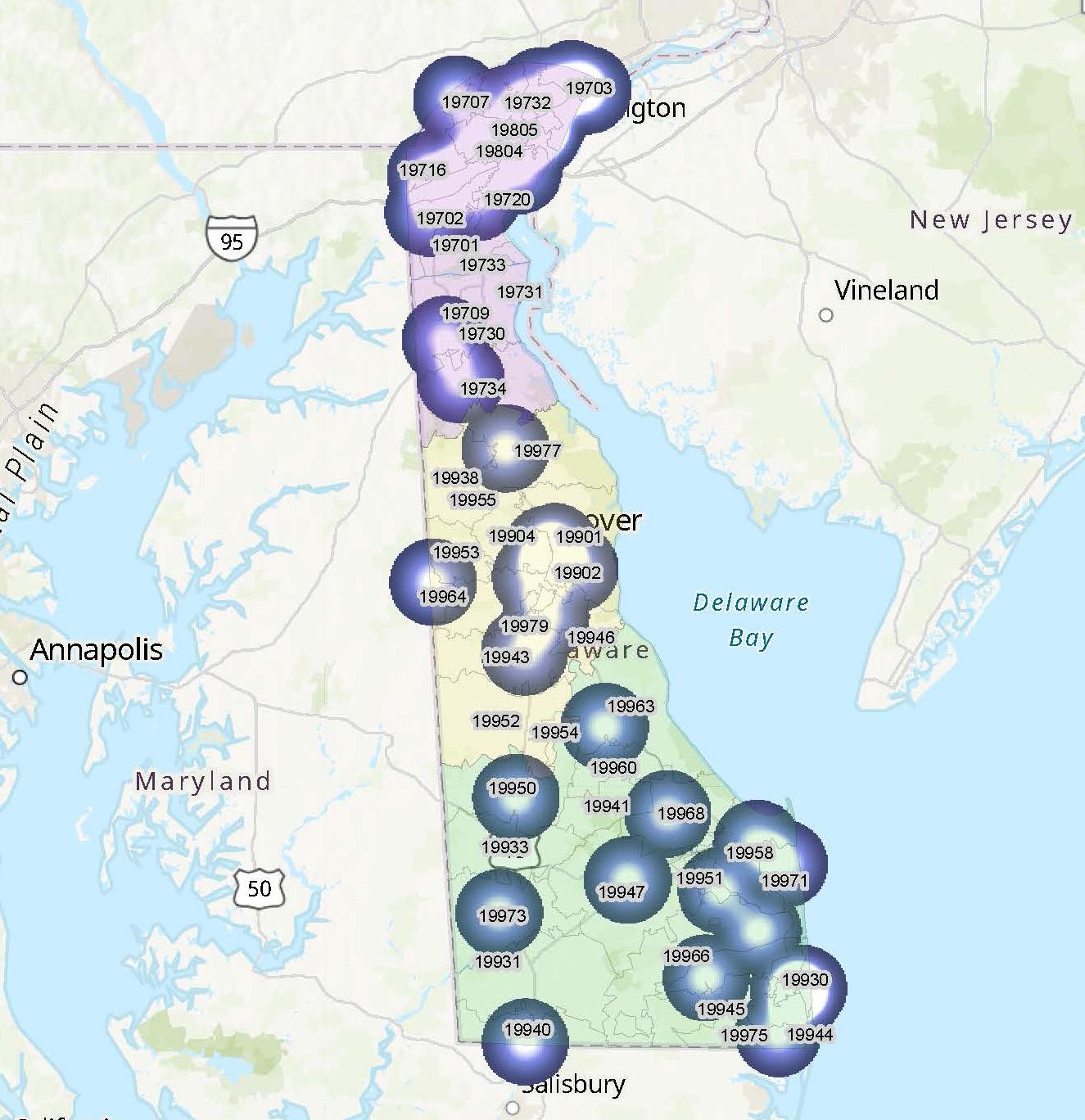






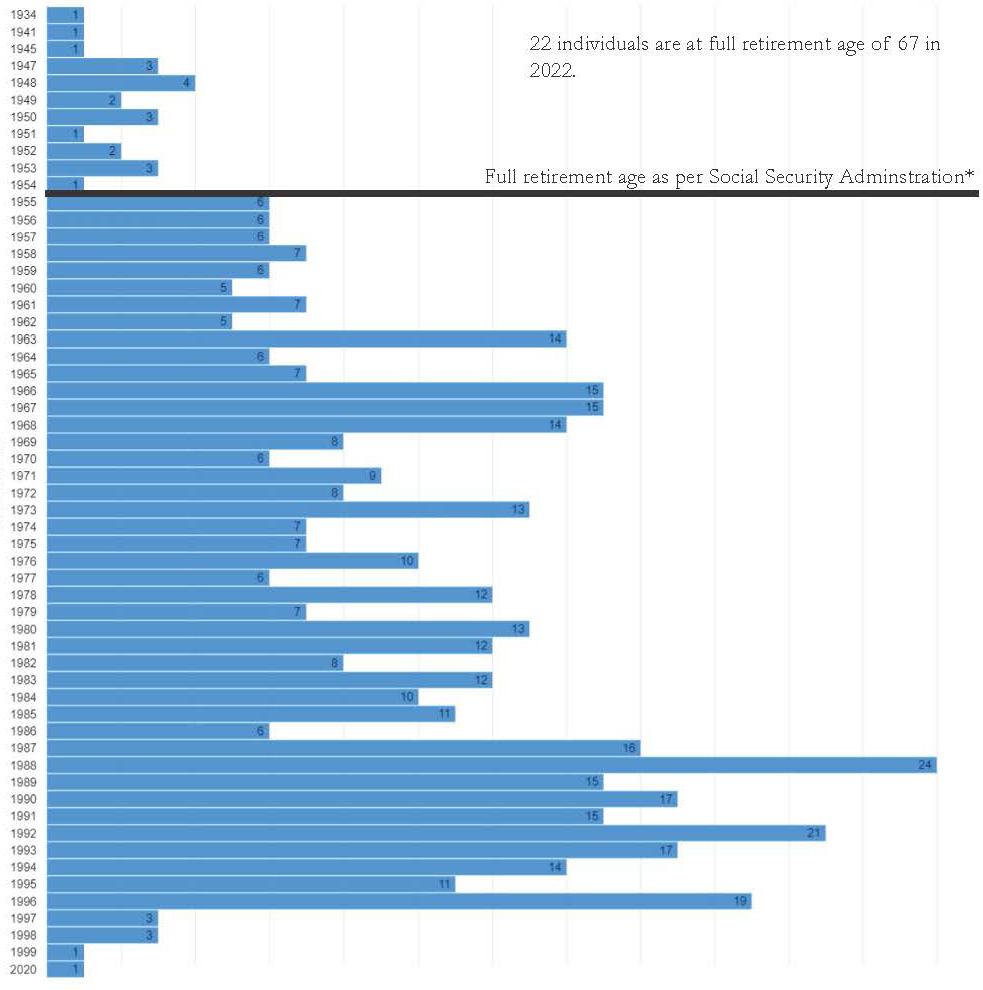





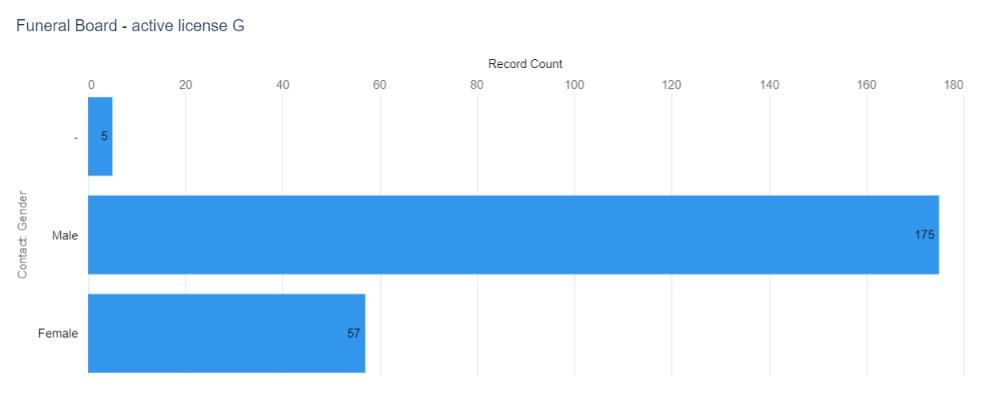


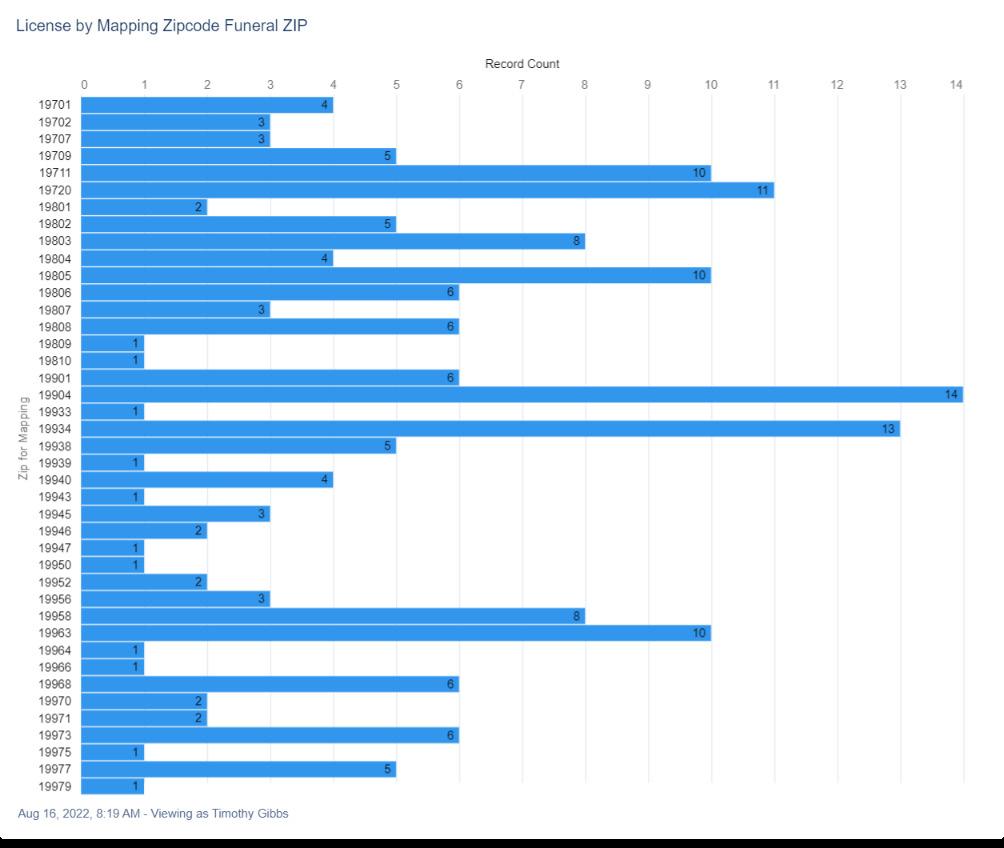

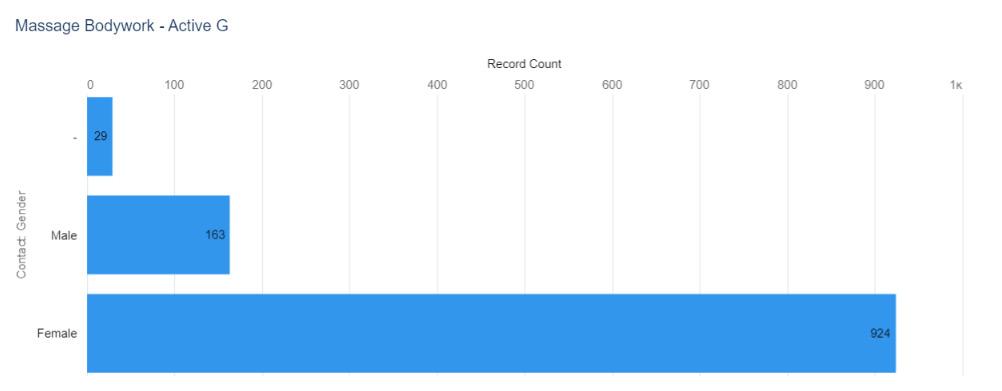
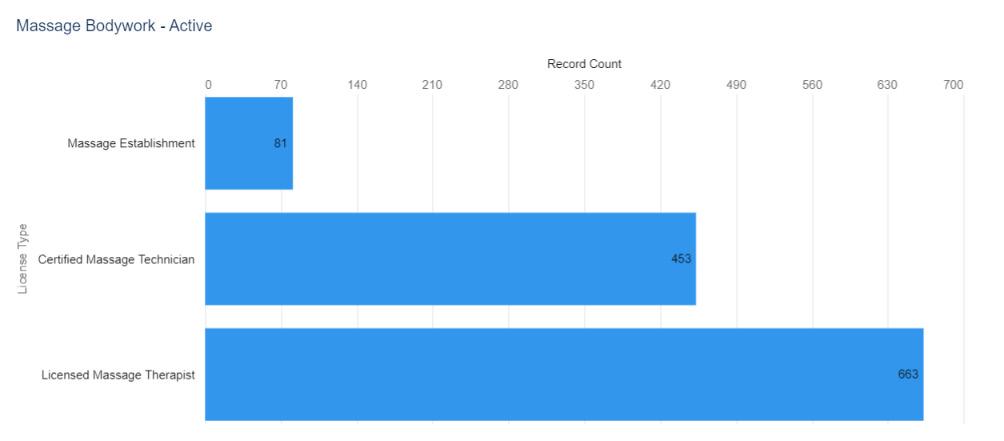

 Figure 4. Numerical Distribution of Active Massage and Bodywork Licenses by ZIP code
Figure 4. Numerical Distribution of Active Massage and Bodywork Licenses by ZIP code

 Figure
Figure
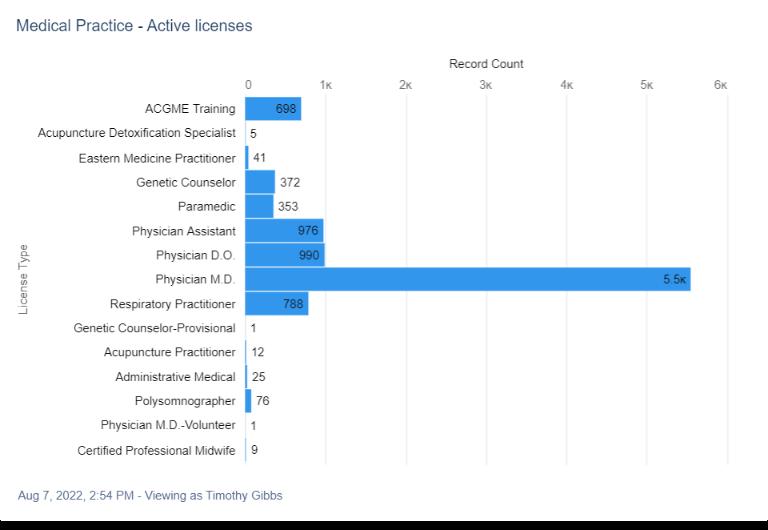

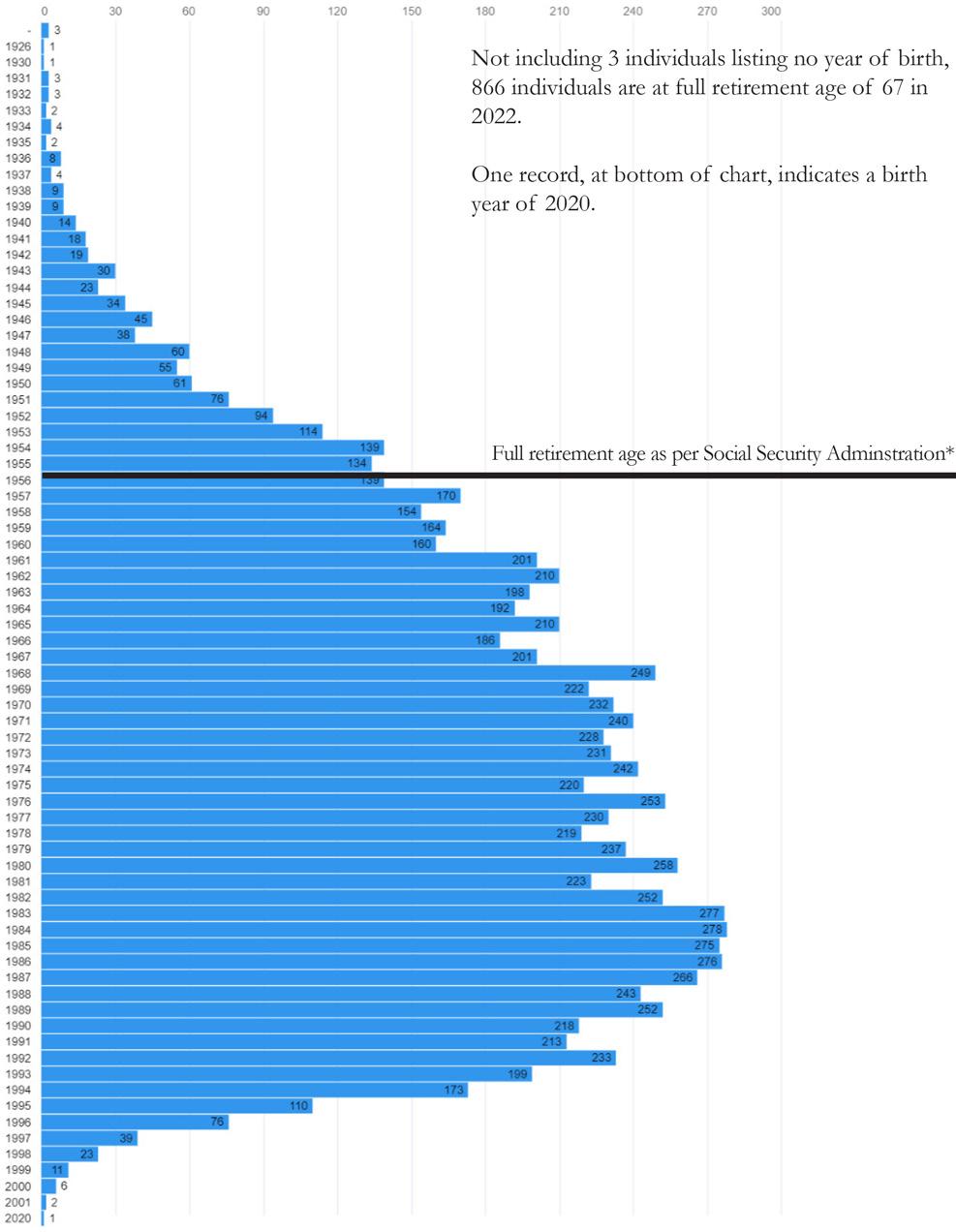

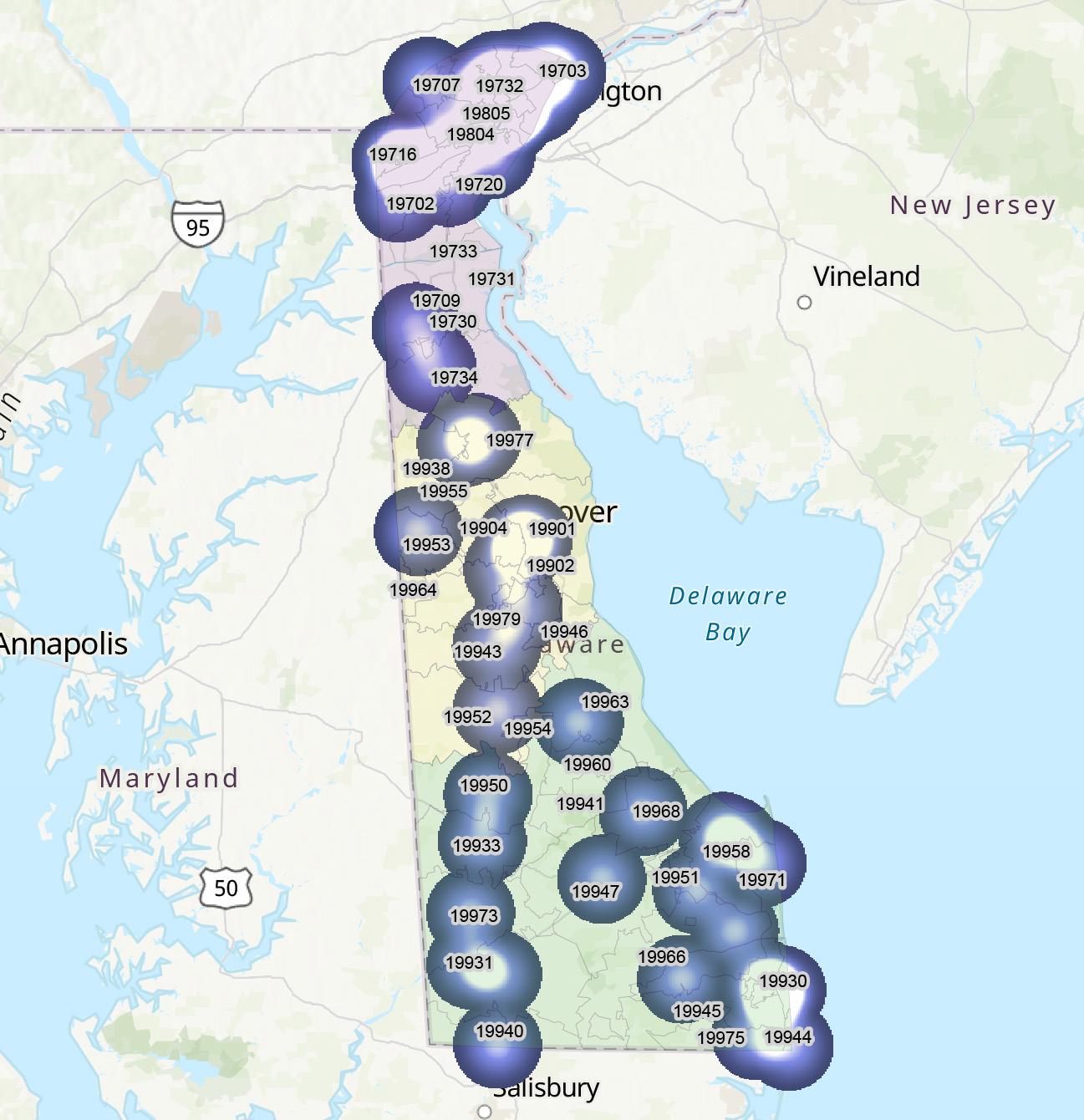
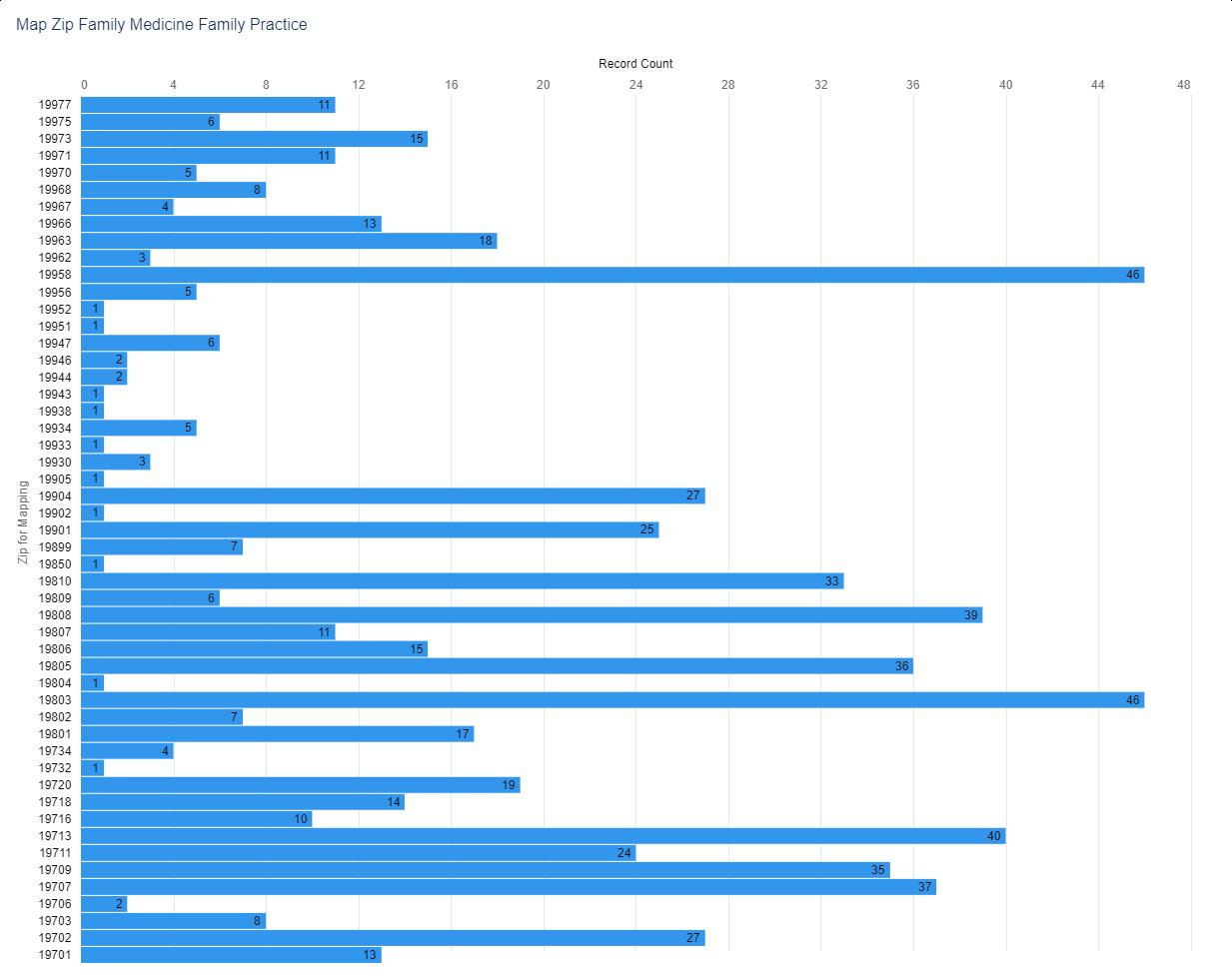



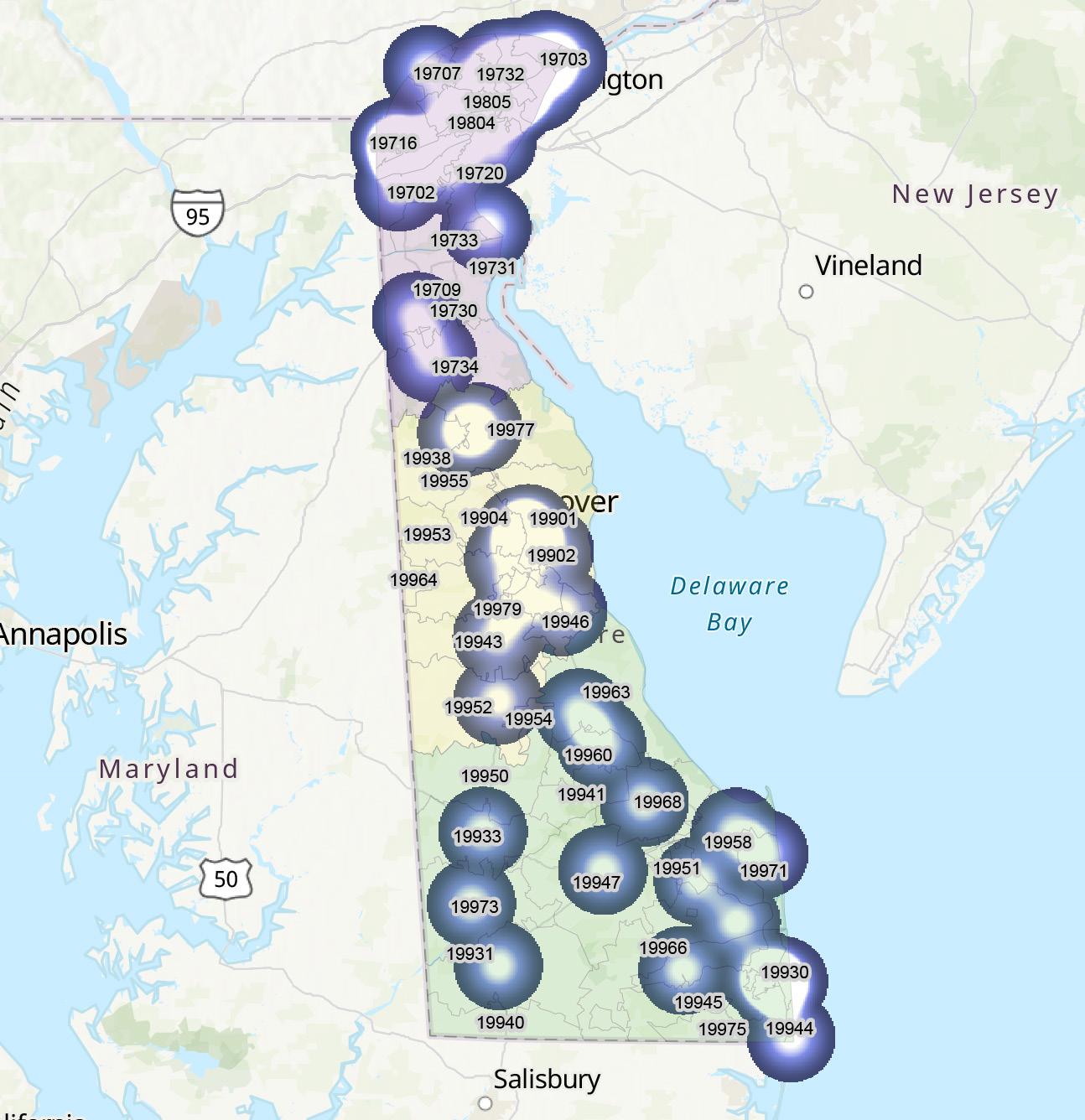
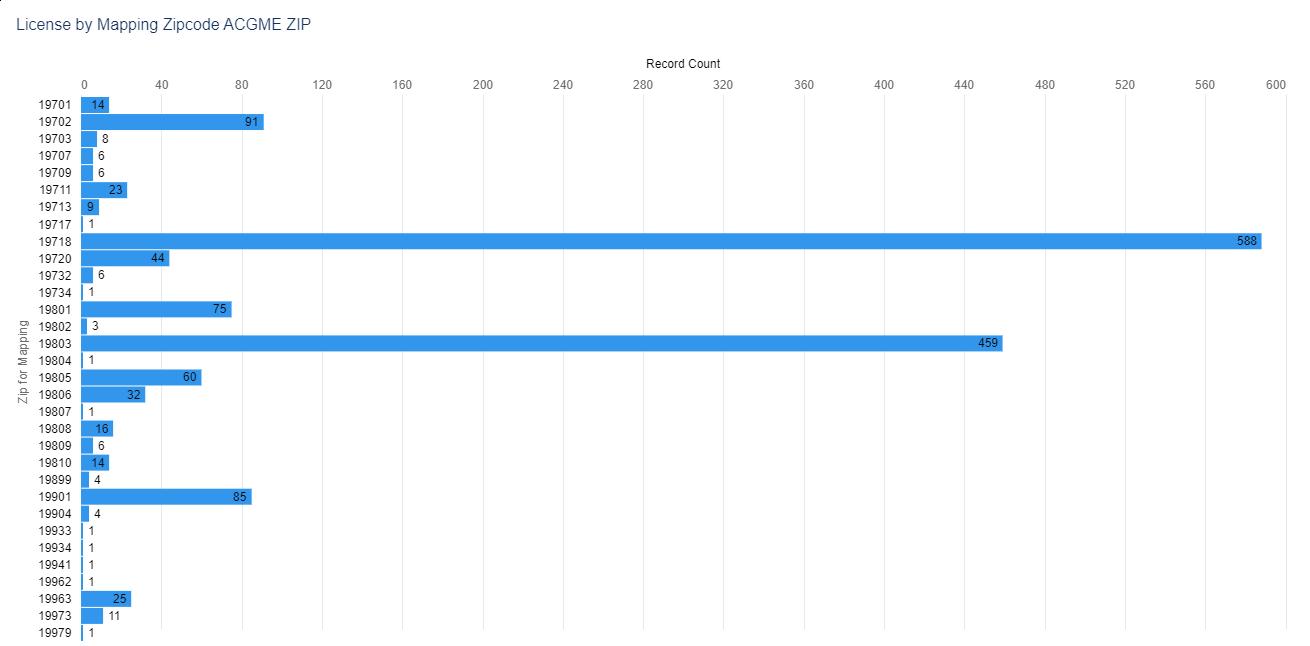
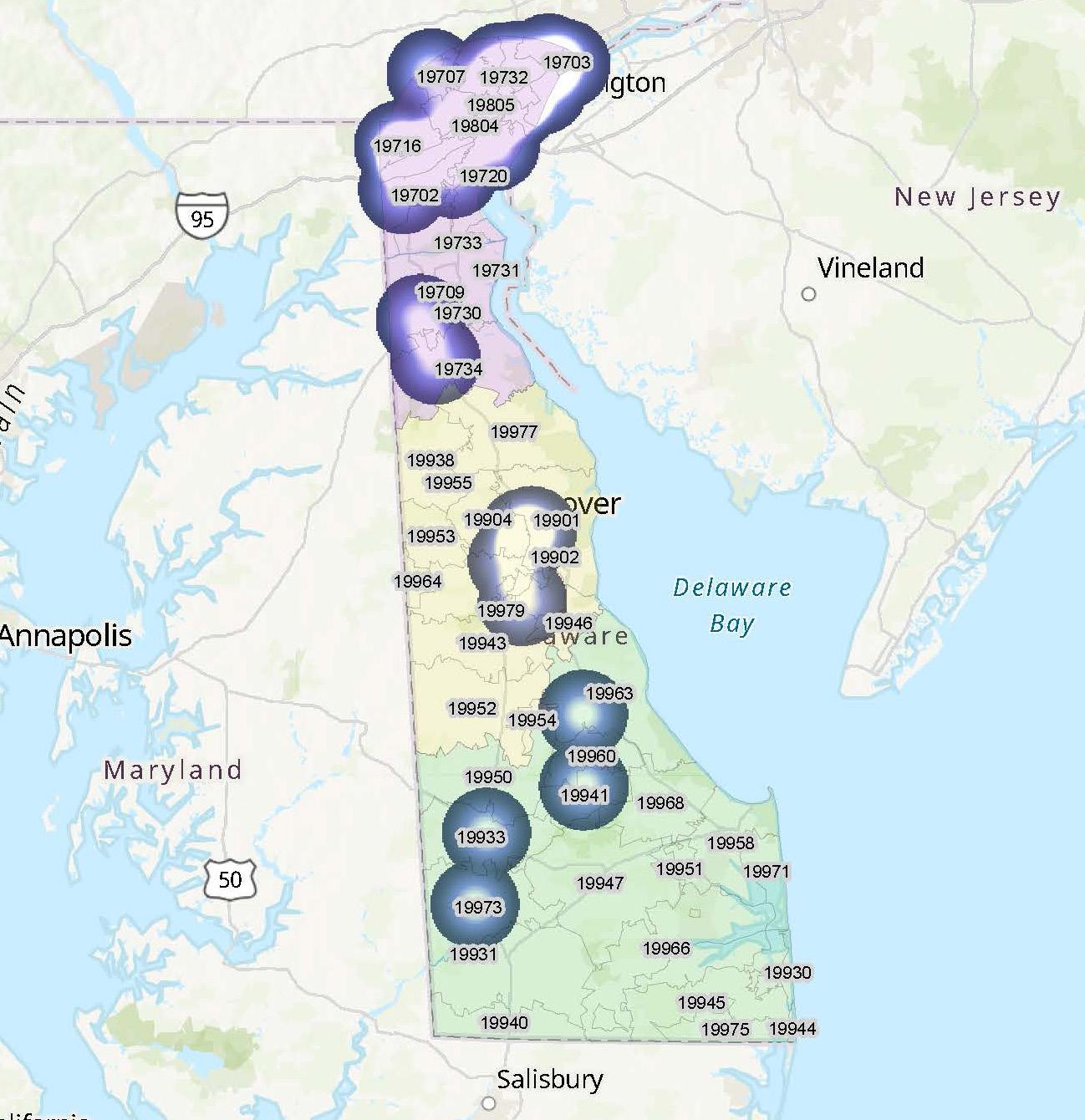
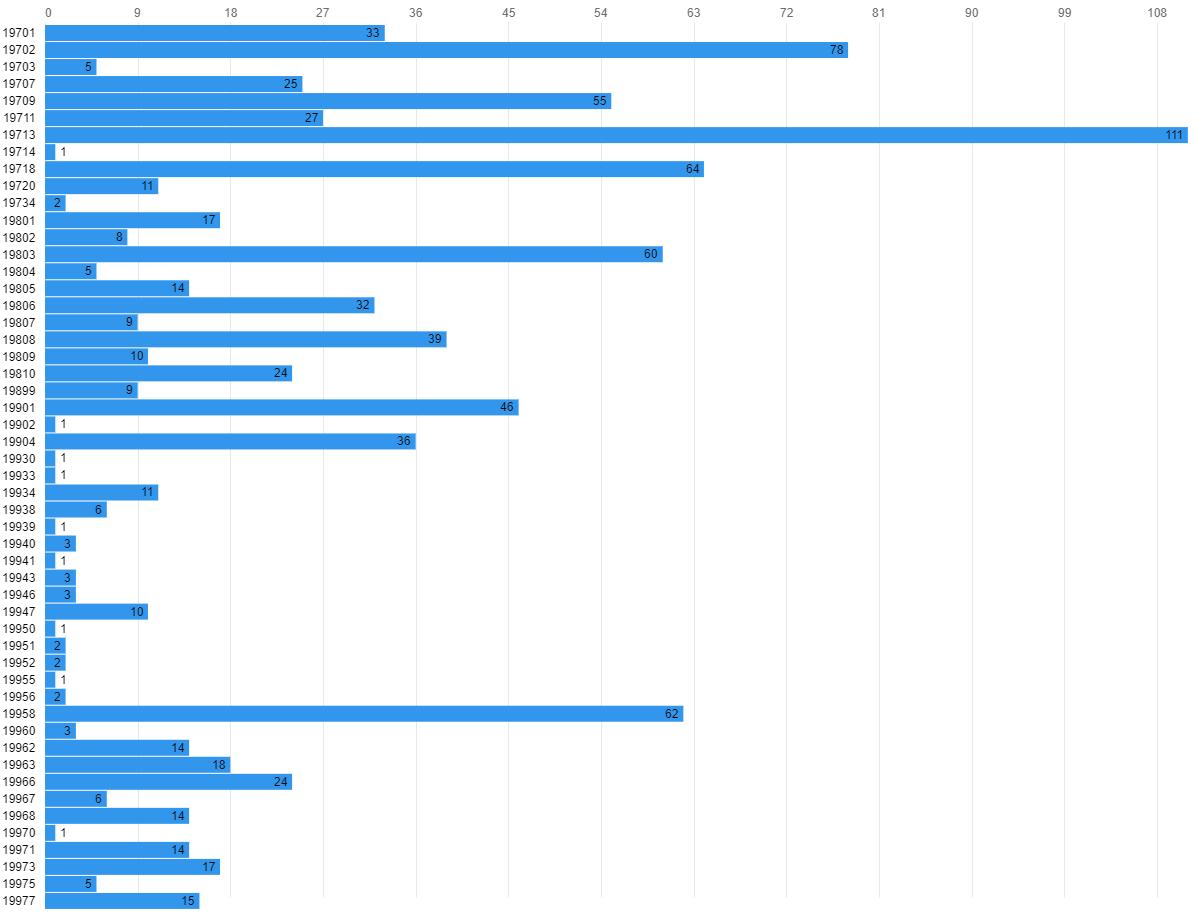


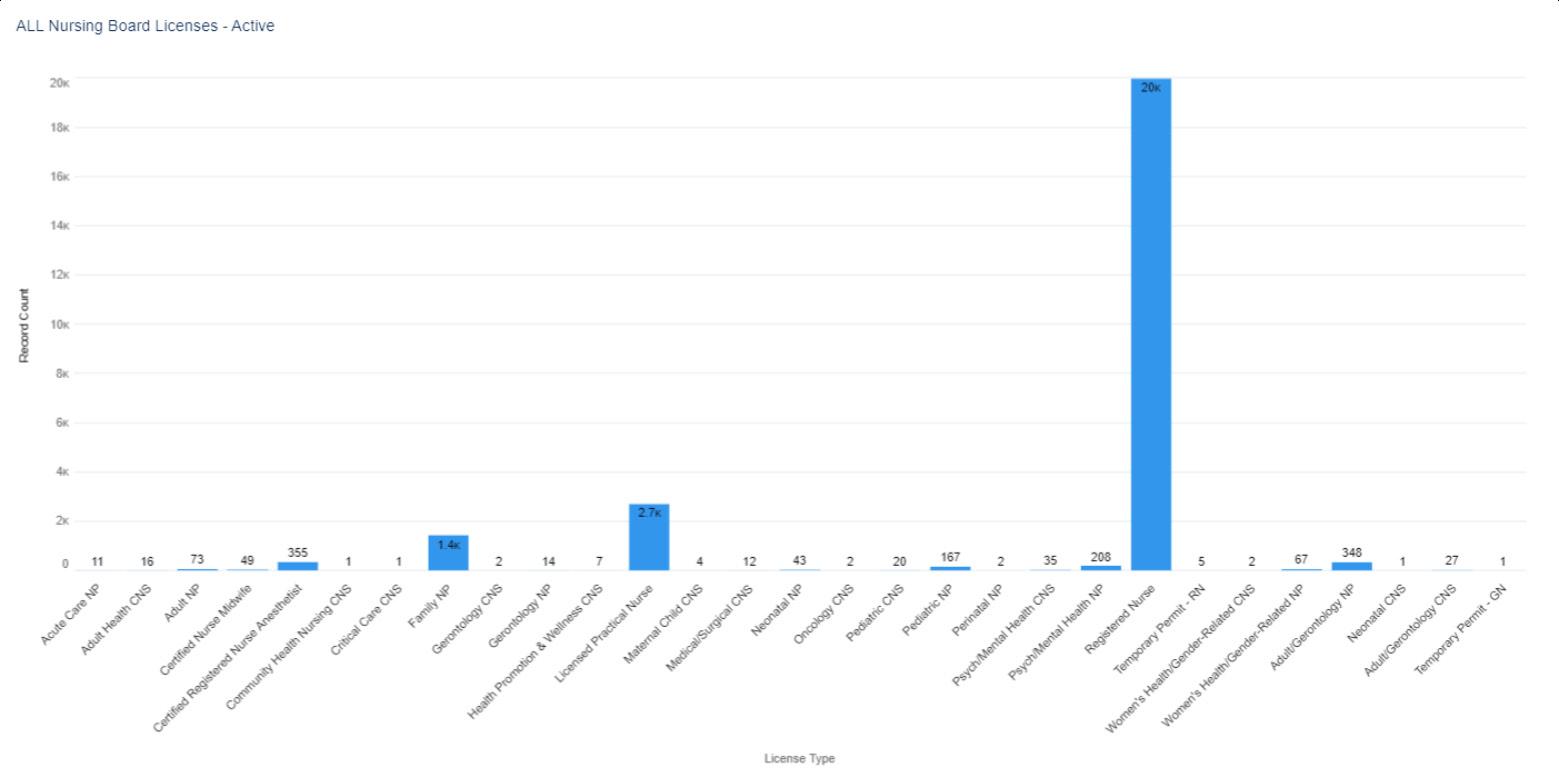 N=25,620
N=25,620



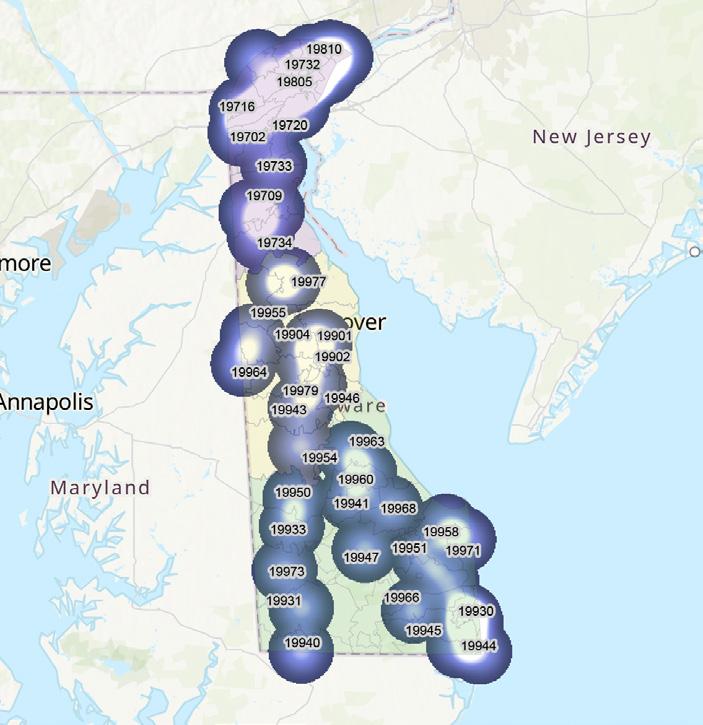



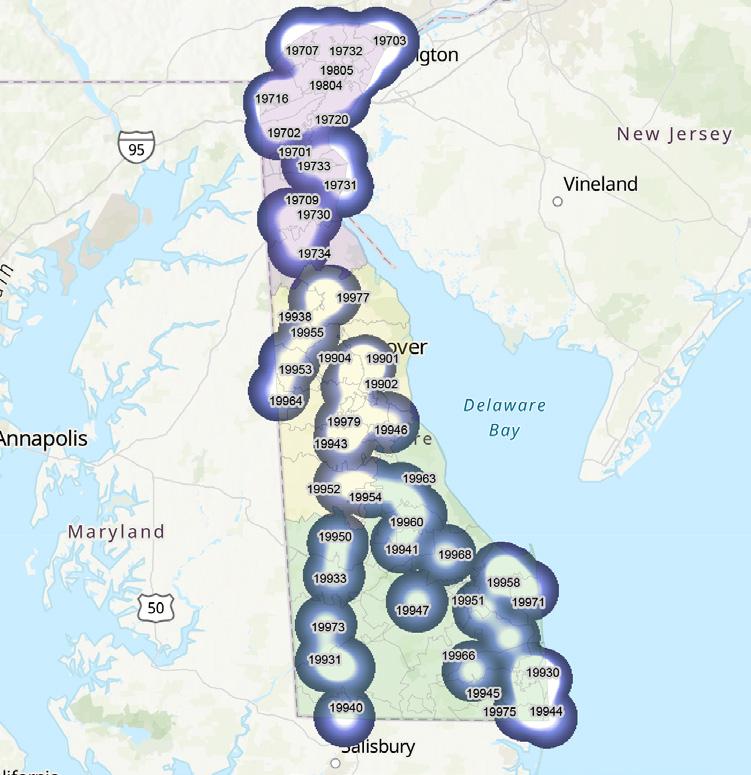
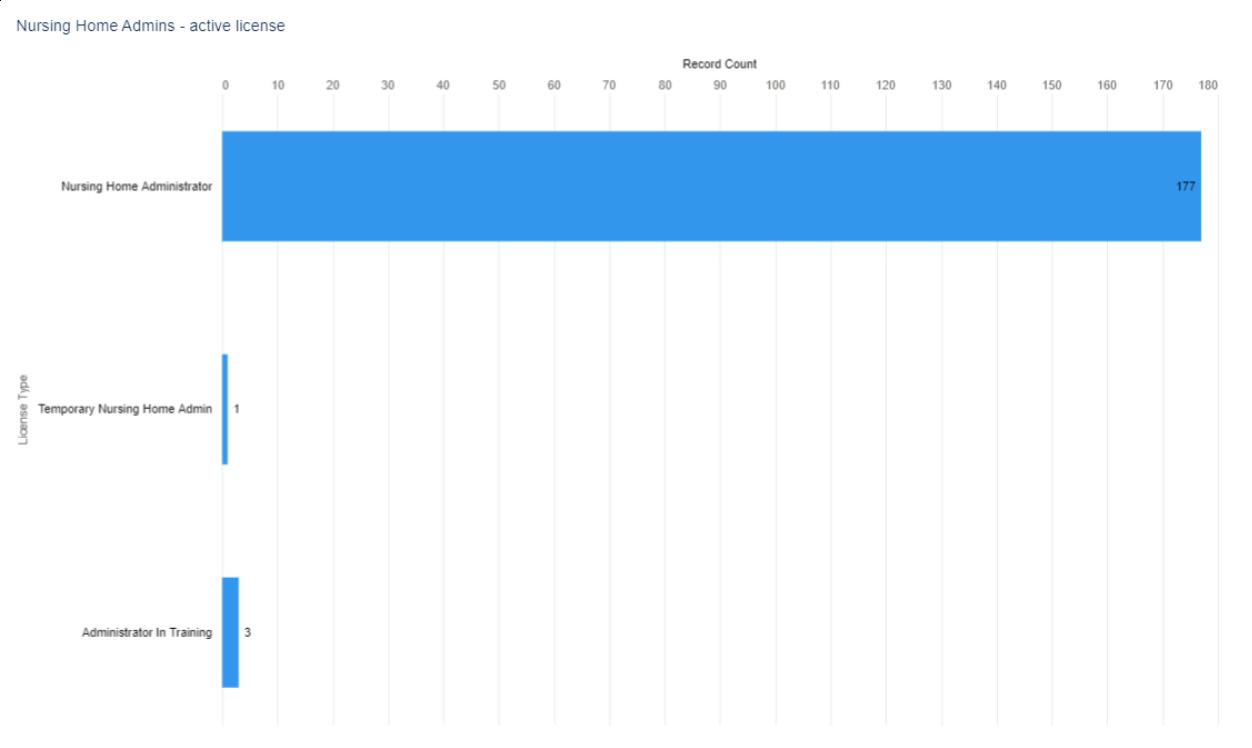
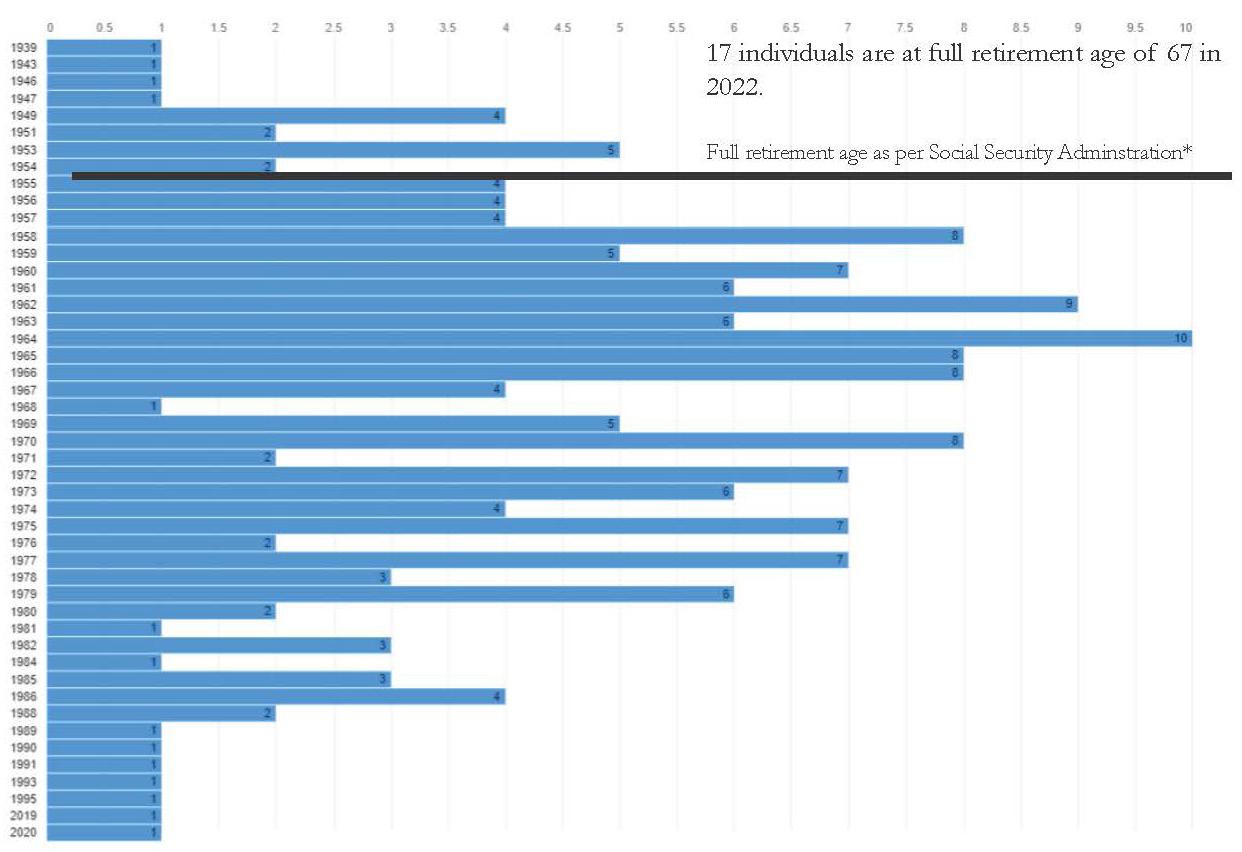
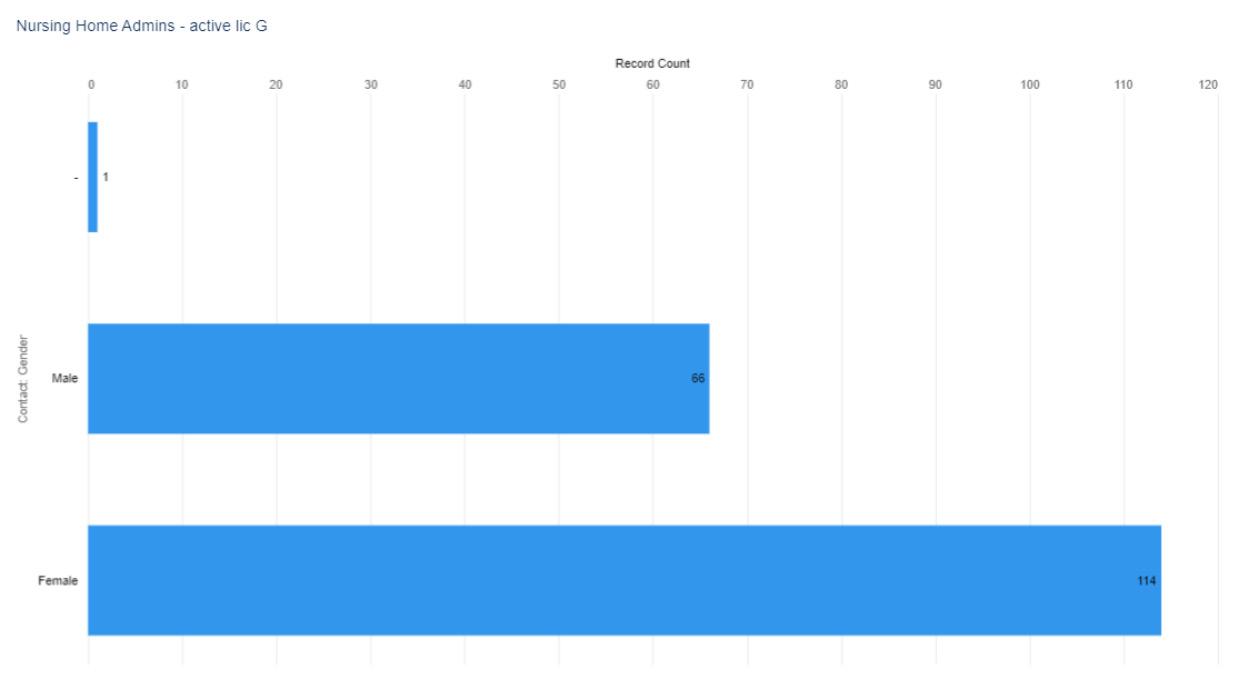 Figure 2. Active Nursing Home Administrator Licenses by Gender, select license types (when reported)
Figure 2. Active Nursing Home Administrator Licenses by Gender, select license types (when reported)
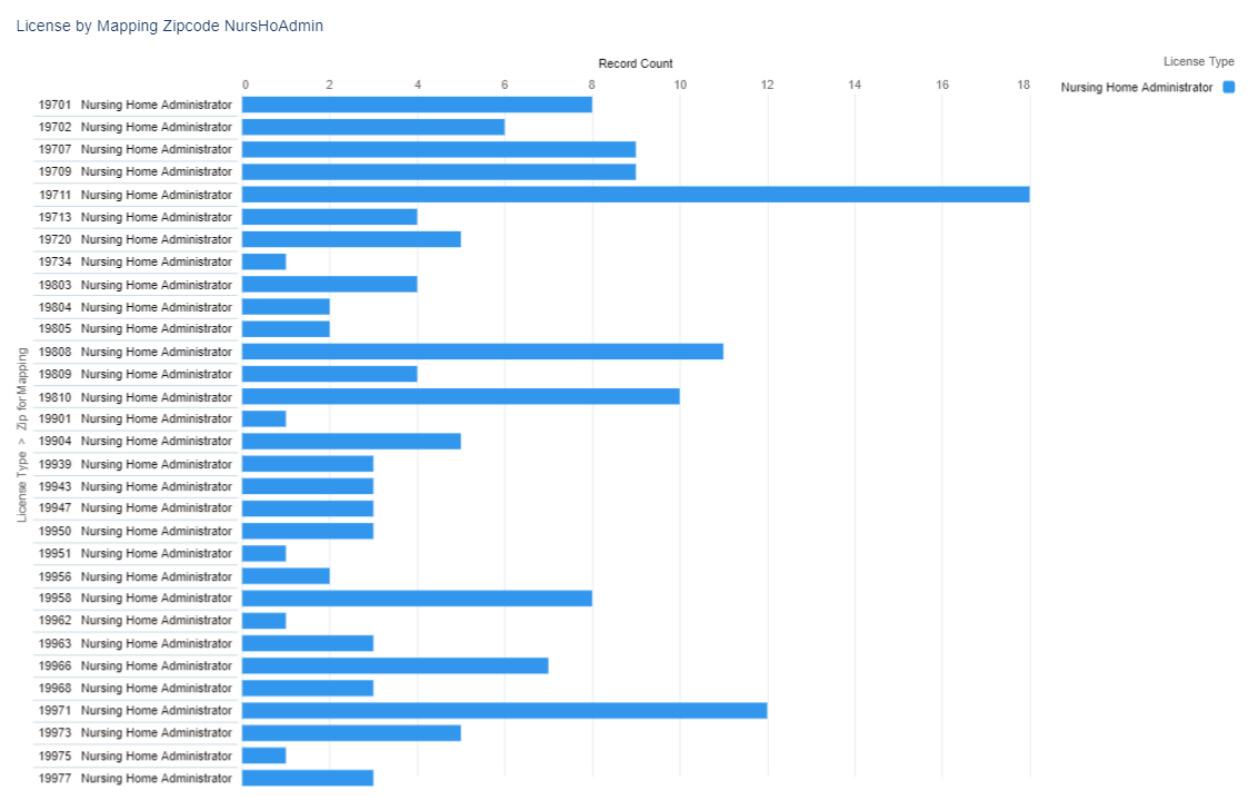
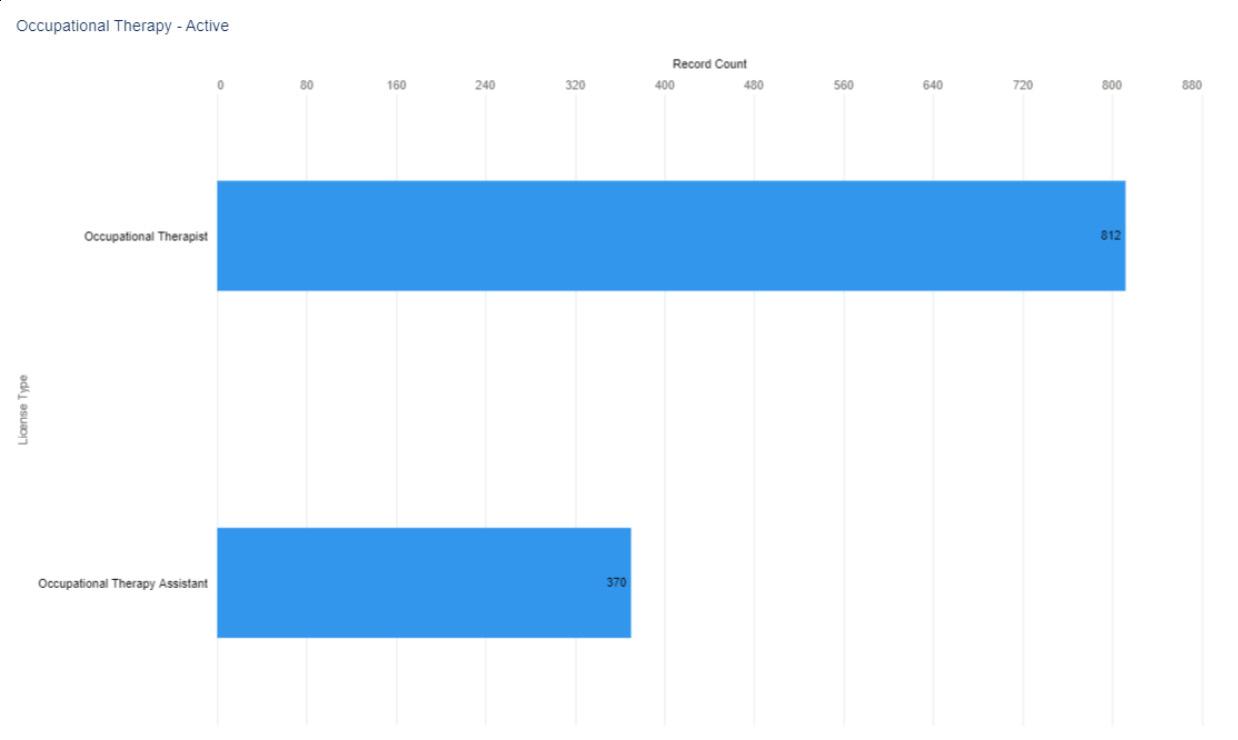
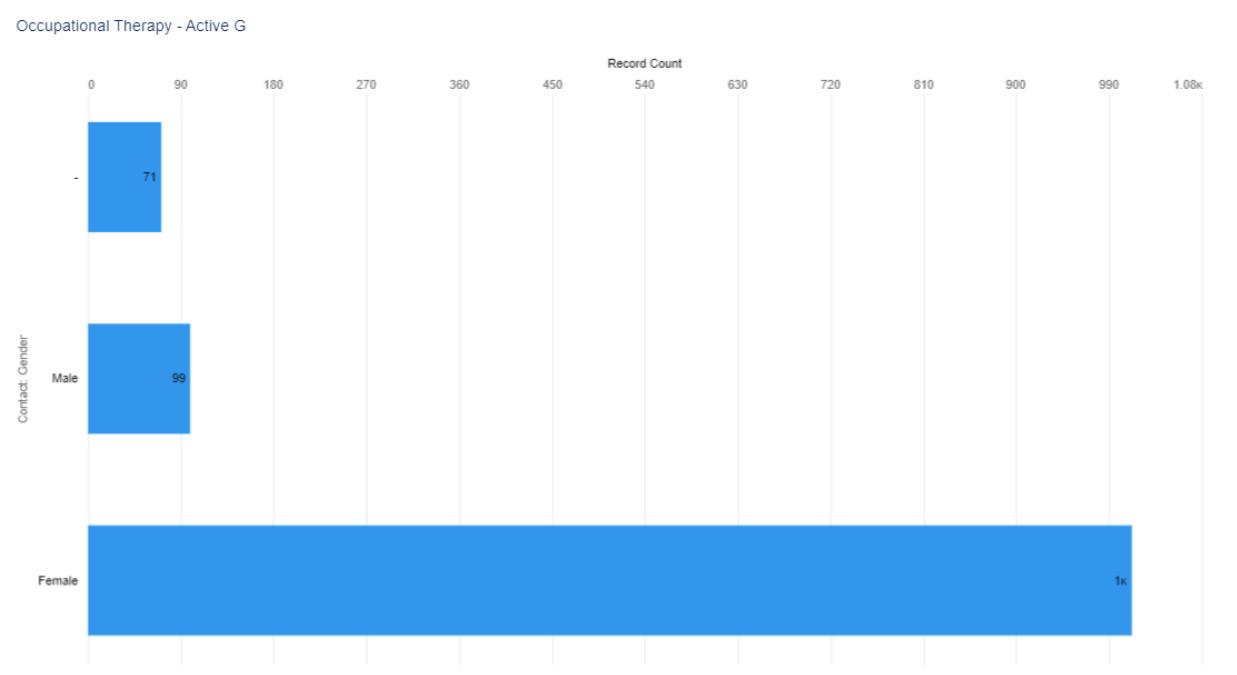


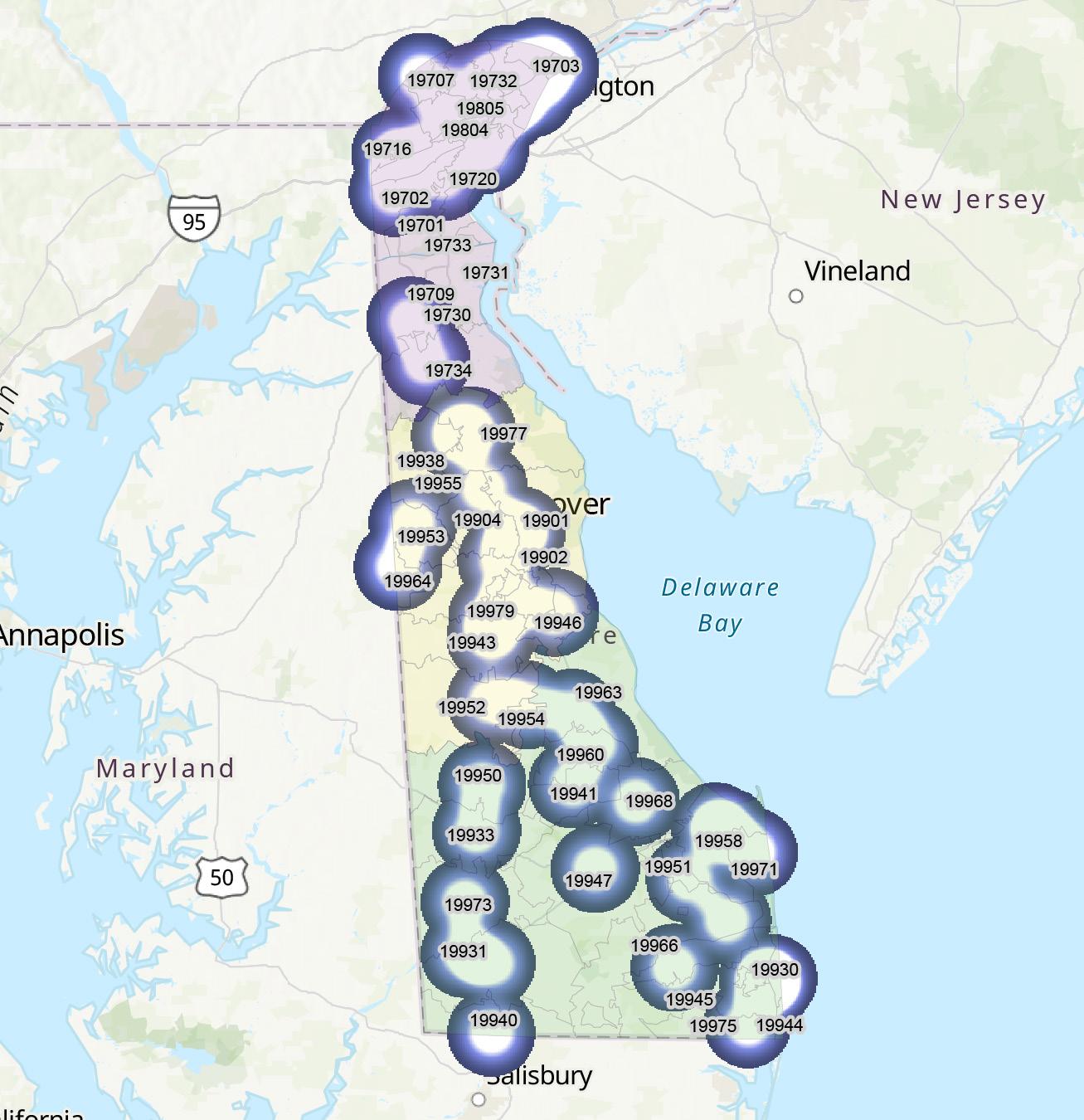



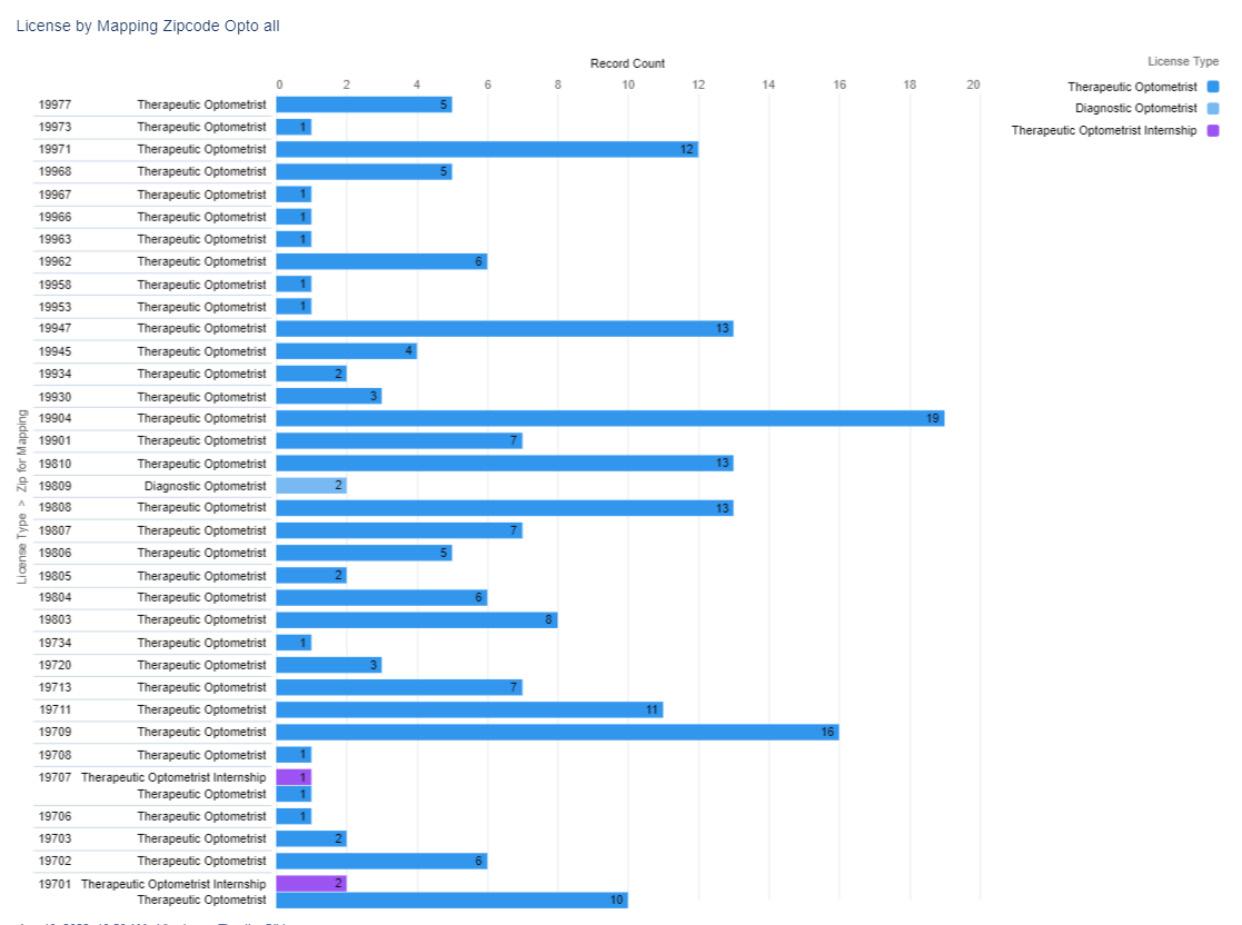



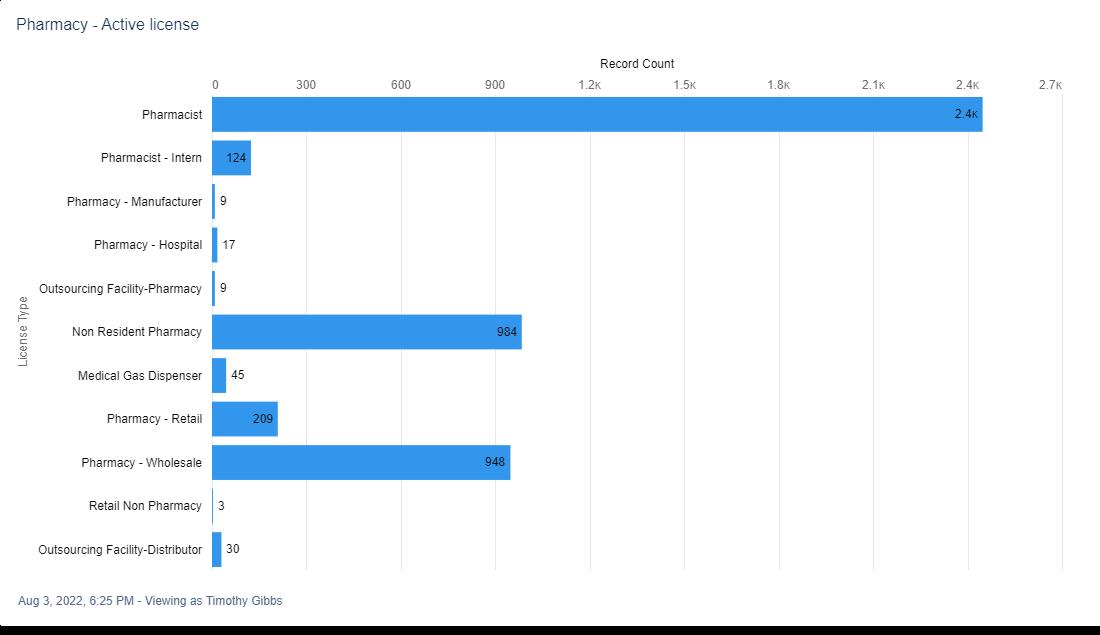


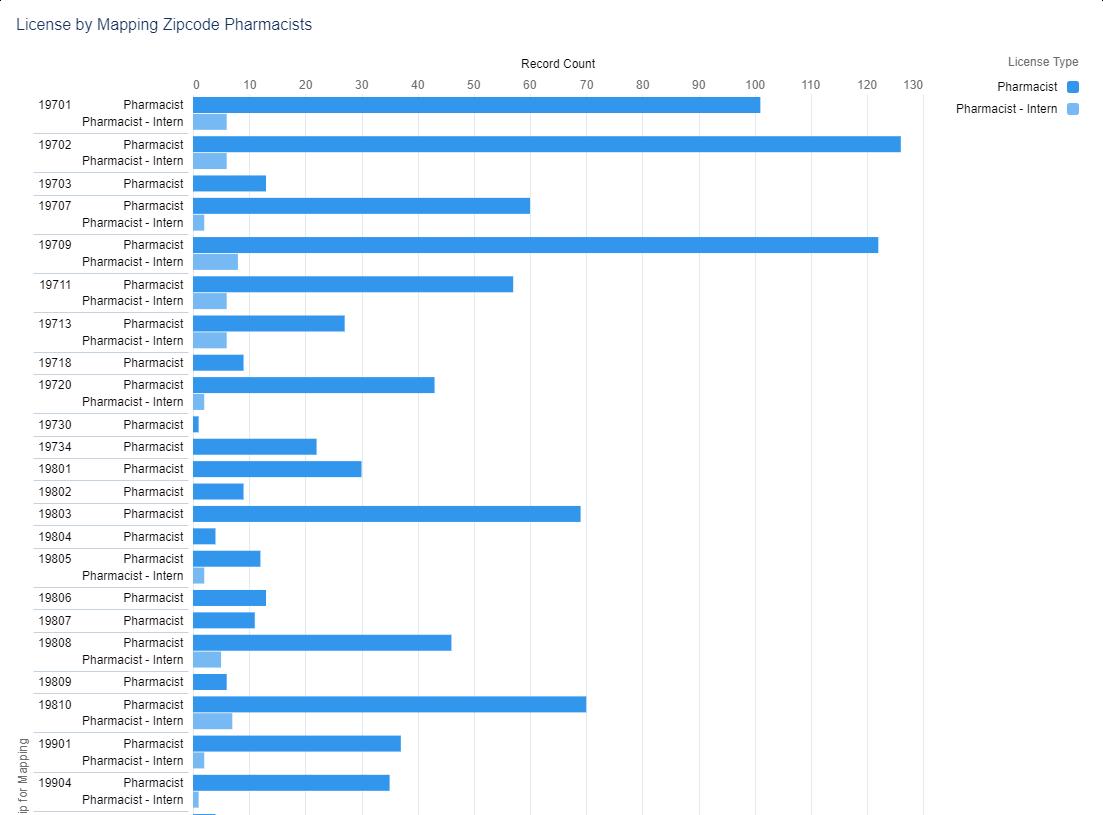
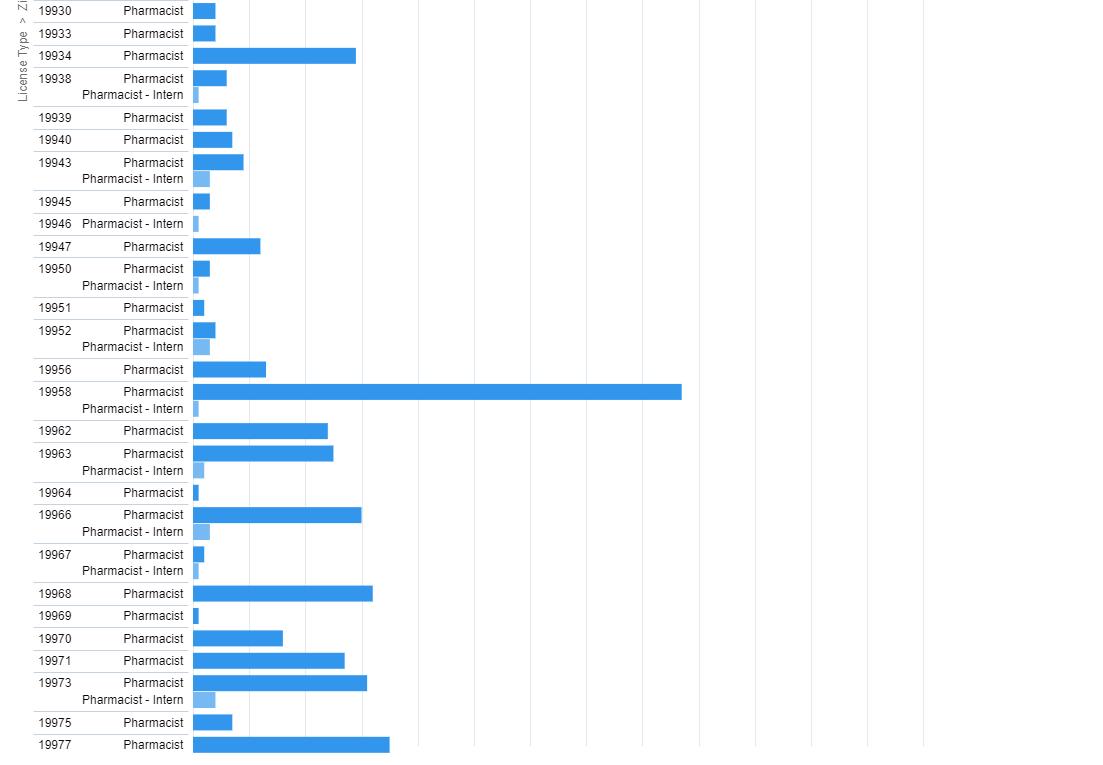
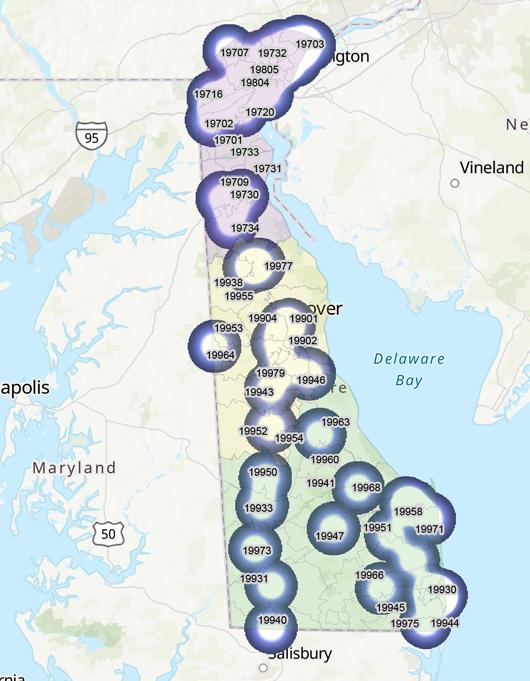
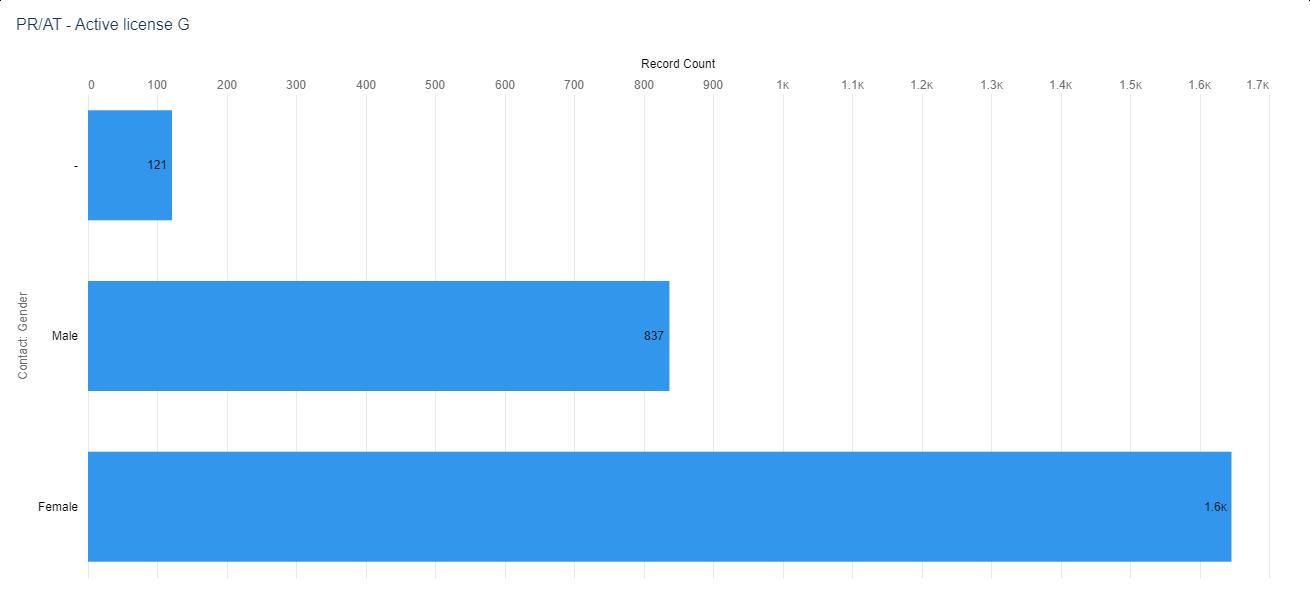



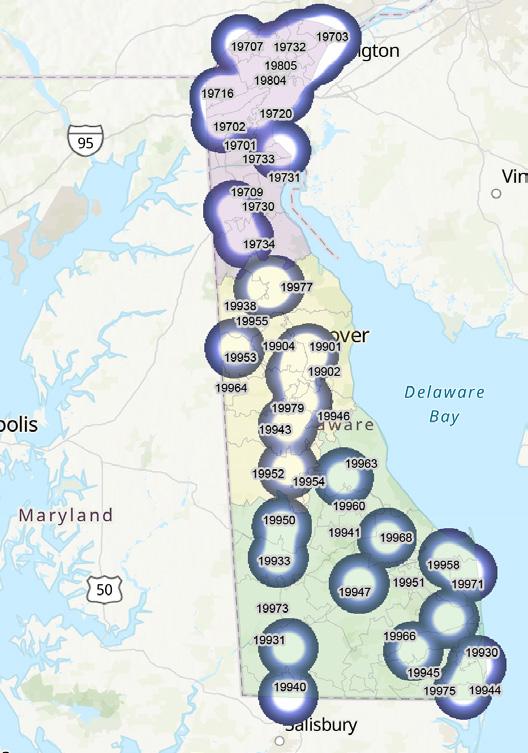




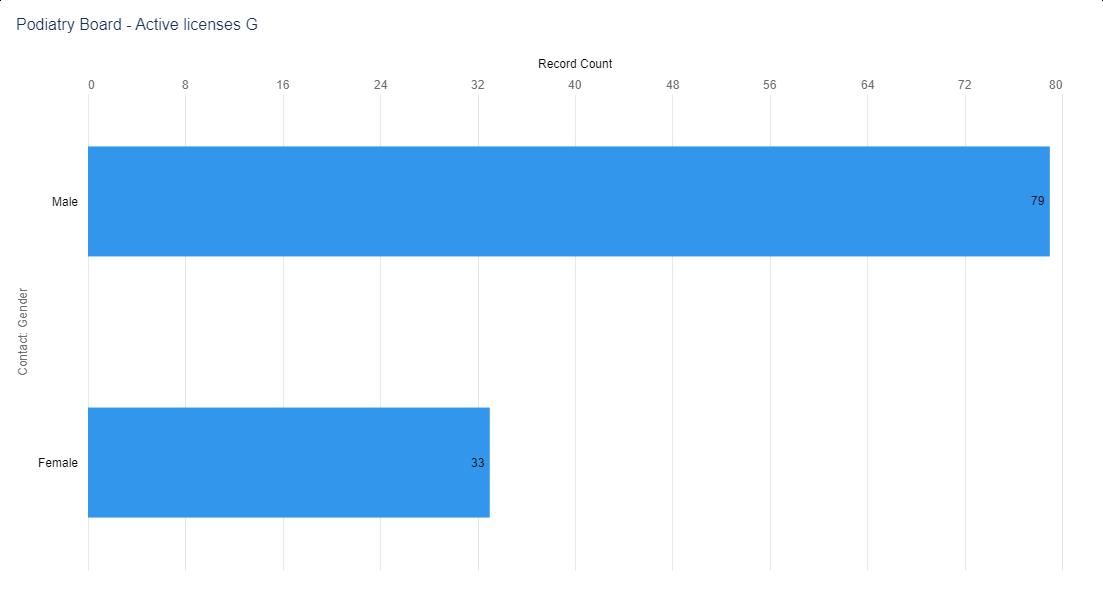

 Figure 4. Numerical Distribution of Active Podiatrist and Podiatrist in Training License by ZIP code
Figure 5. Visual Distribution of Active Podiatrist and Podiatrist in Training License by ZIP code
Figure 4. Numerical Distribution of Active Podiatrist and Podiatrist in Training License by ZIP code
Figure 5. Visual Distribution of Active Podiatrist and Podiatrist in Training License by ZIP code


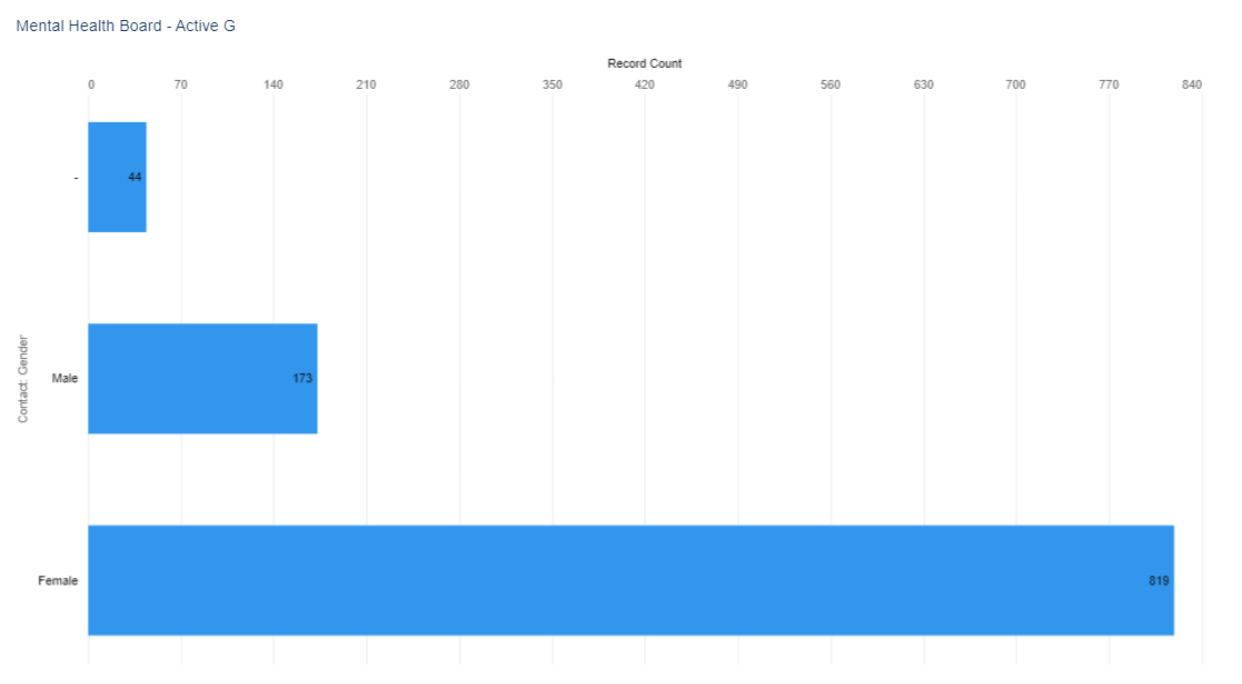
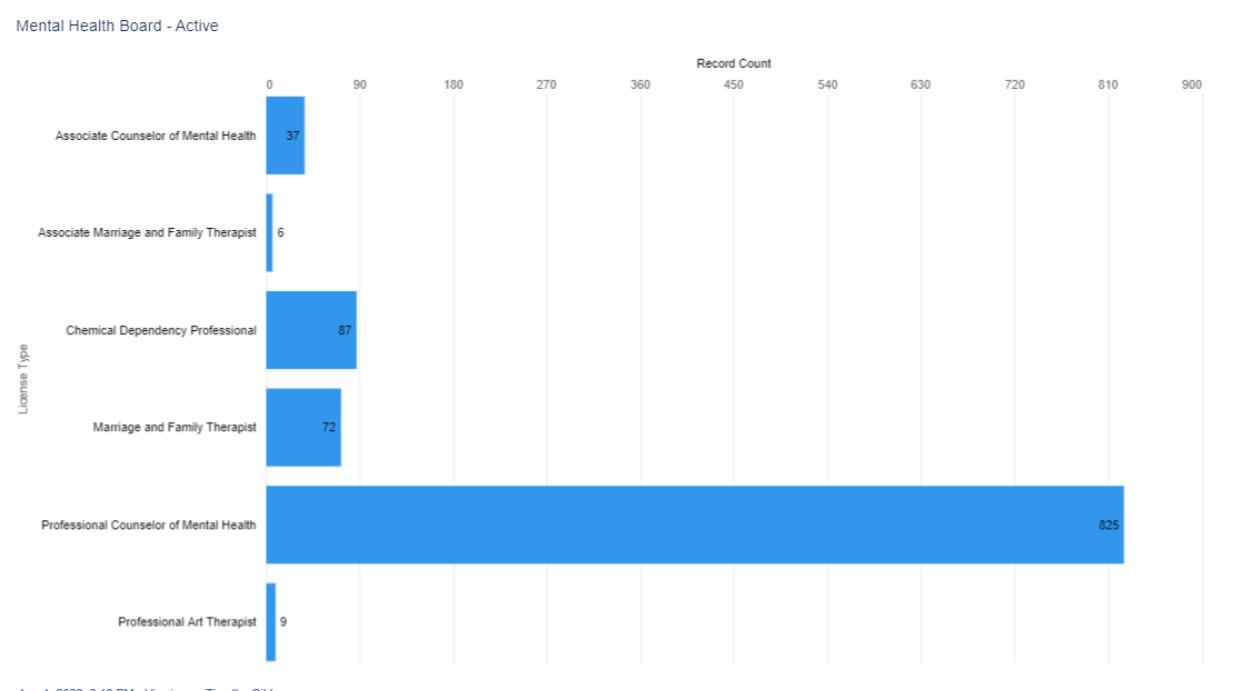
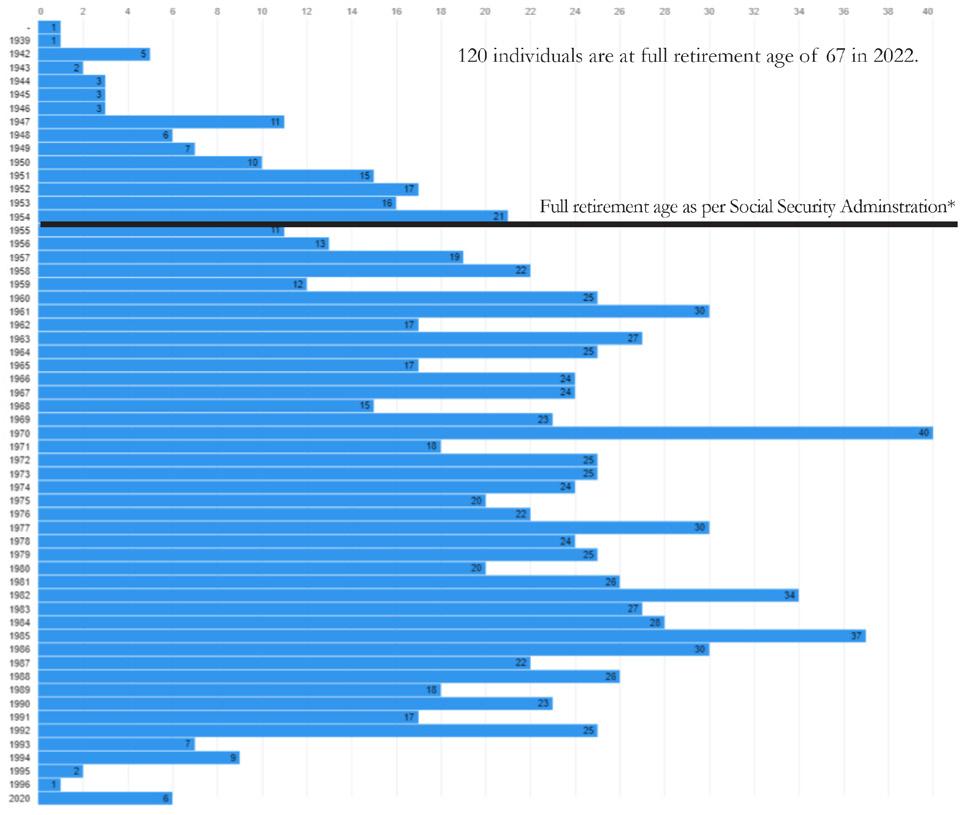
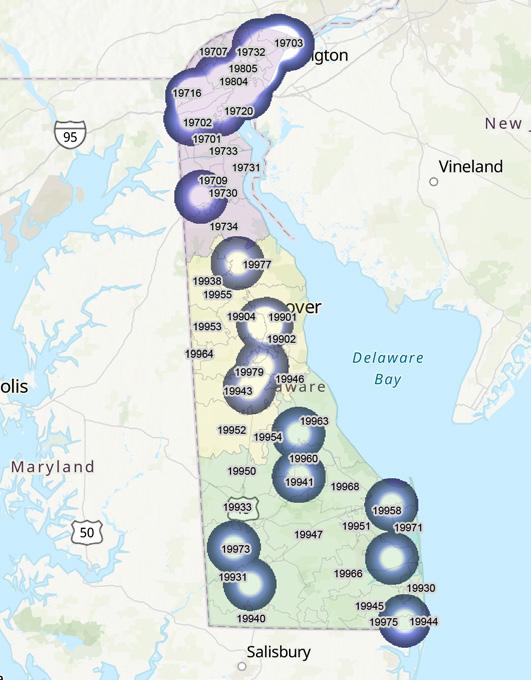
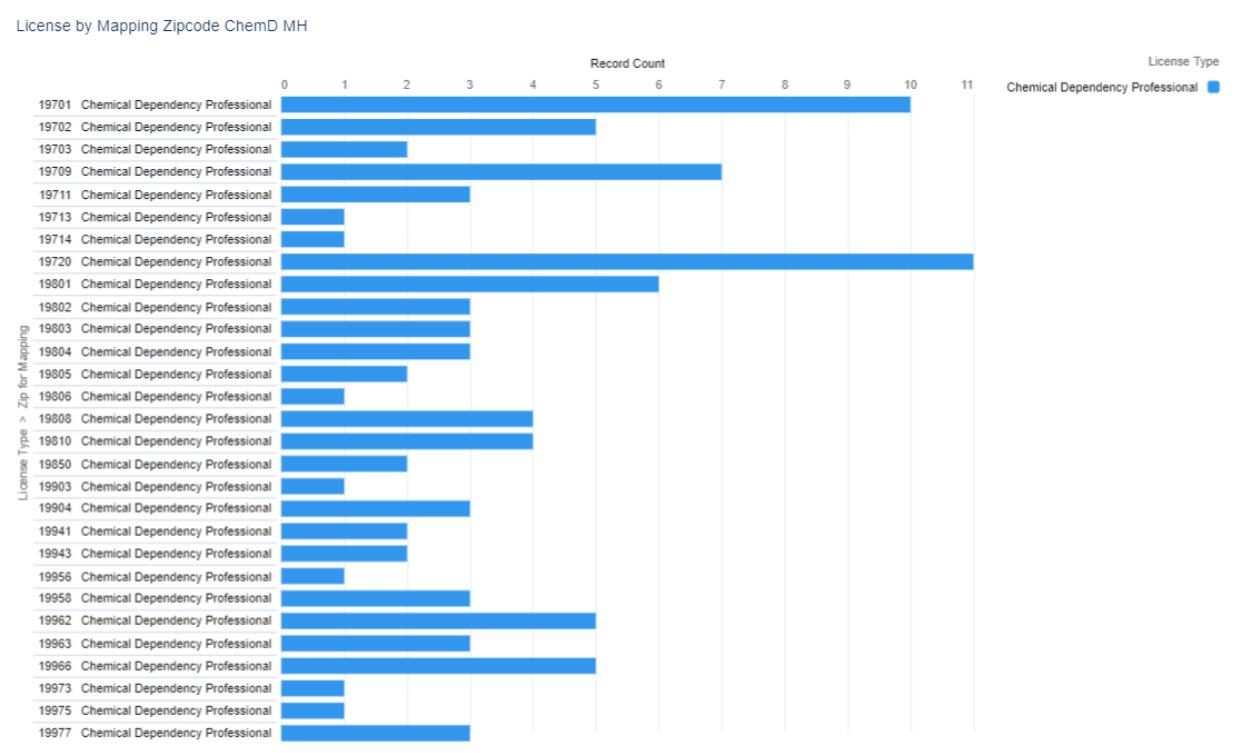

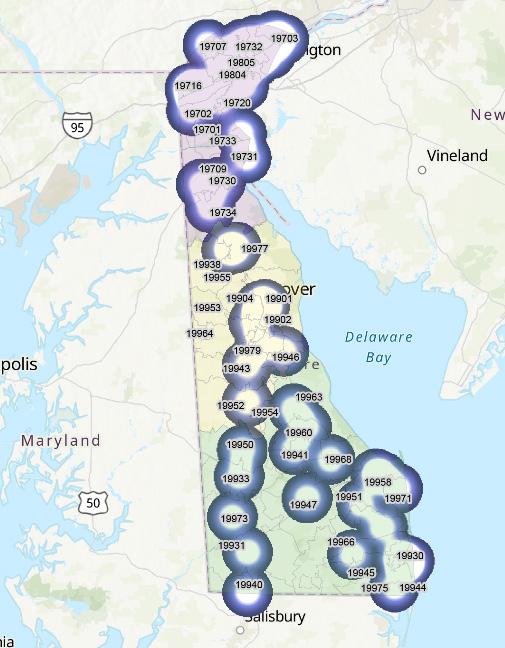
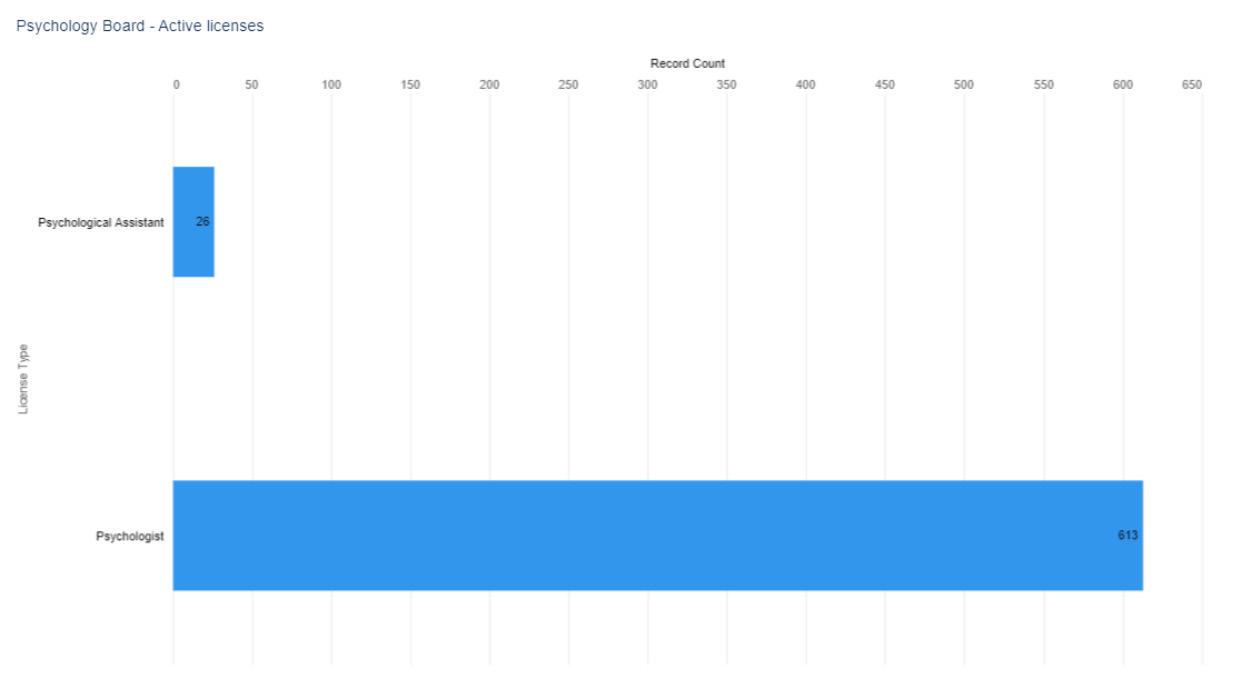

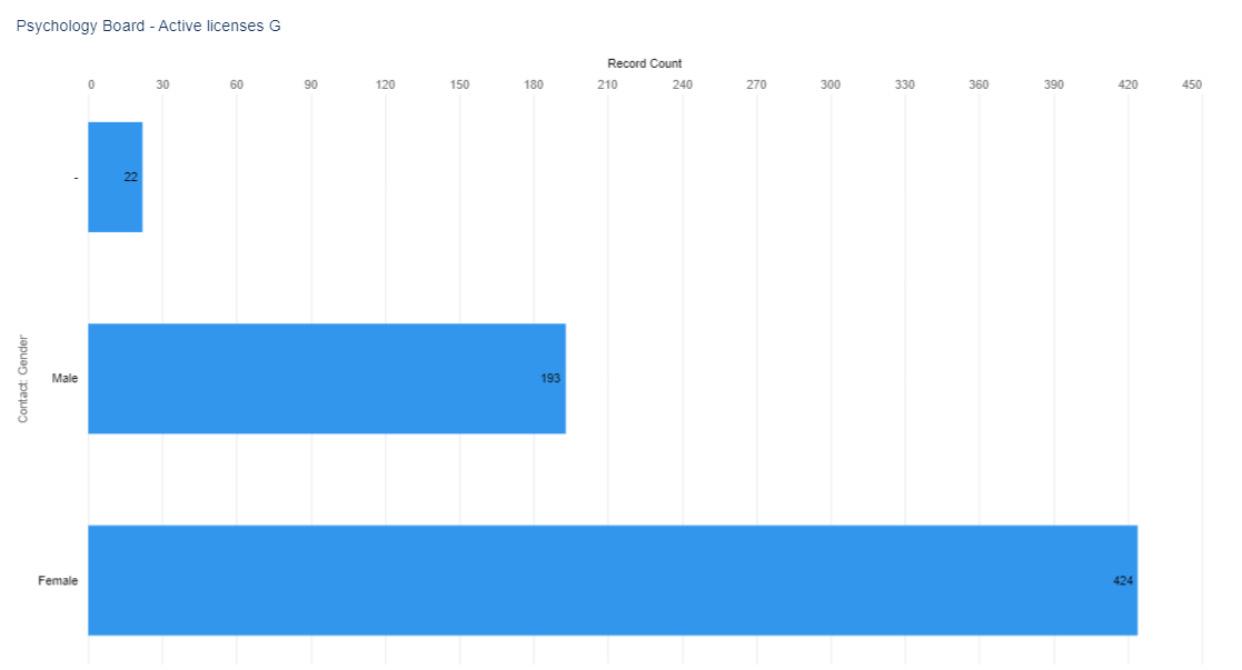 Figure 2. Active Psychologist Licenses by Gender select license types (when reported)
Figure 3. Active Psychologist Licenses by Birth Year
Figure 2. Active Psychologist Licenses by Gender select license types (when reported)
Figure 3. Active Psychologist Licenses by Birth Year
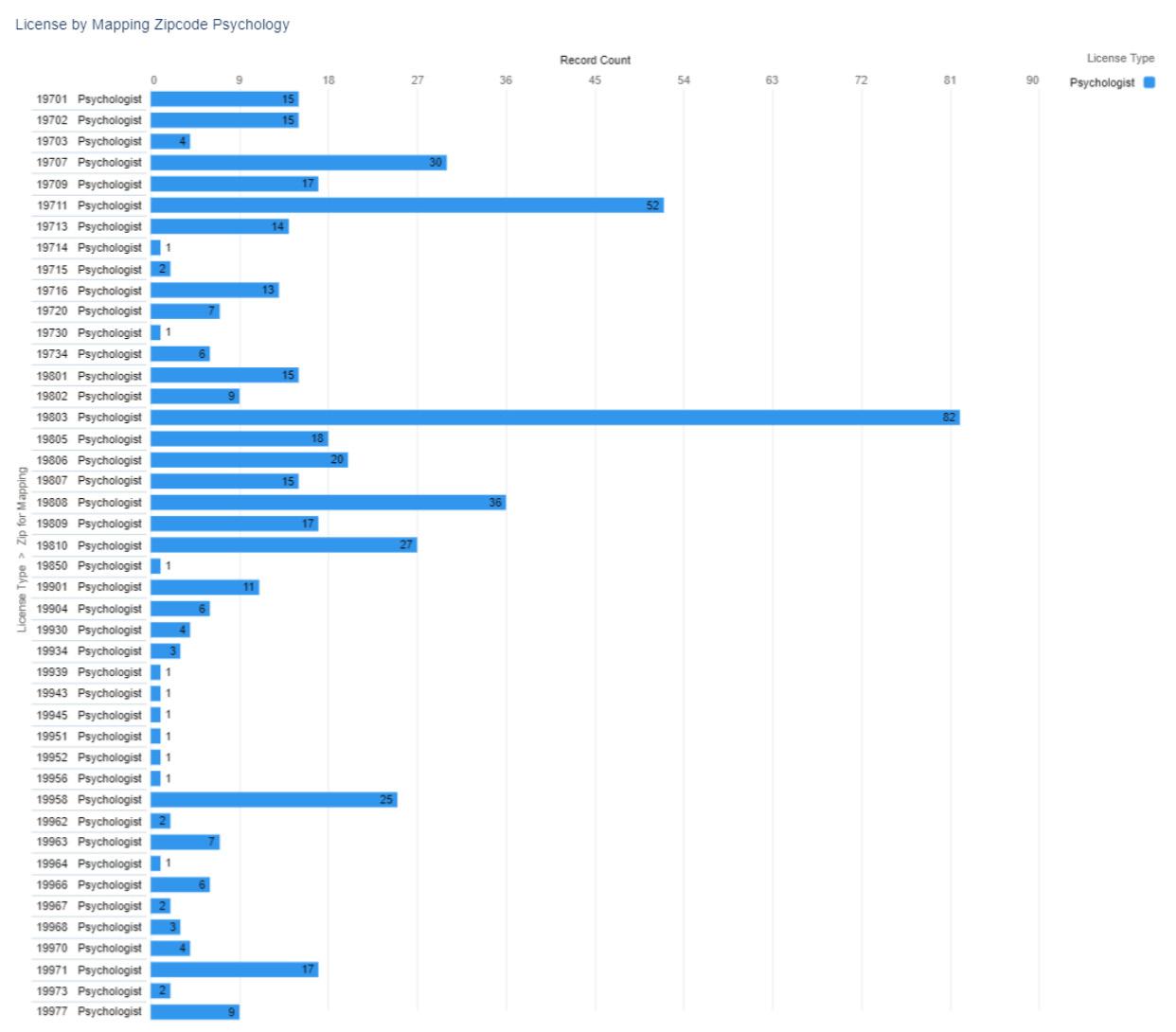
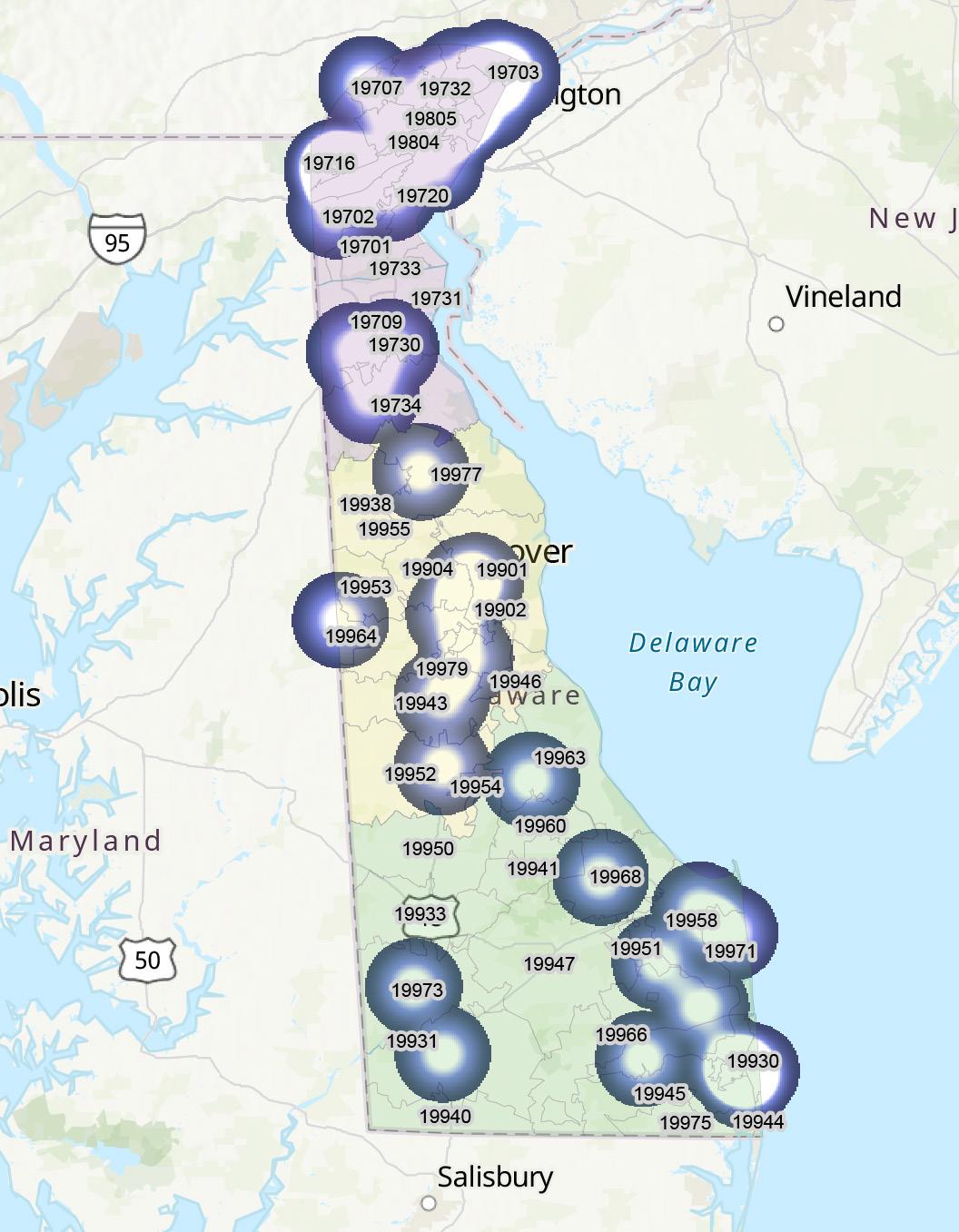
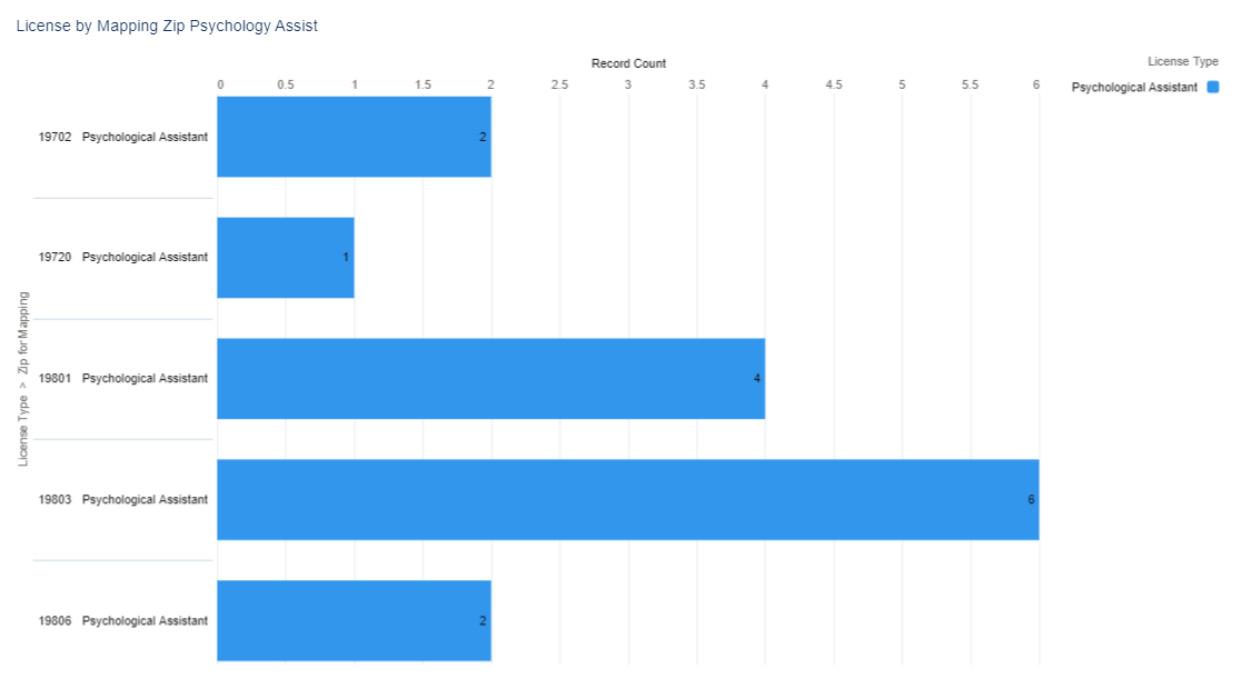
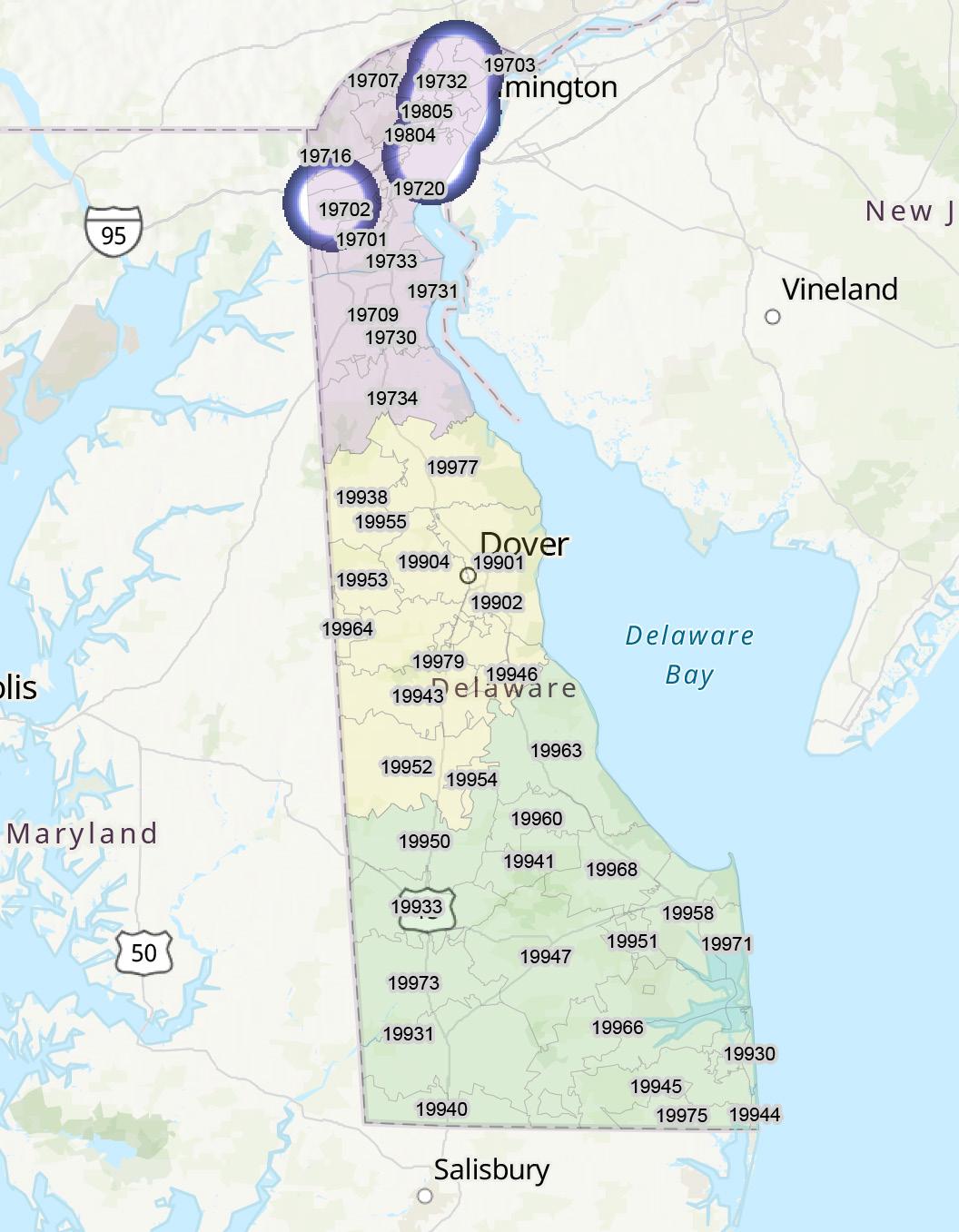
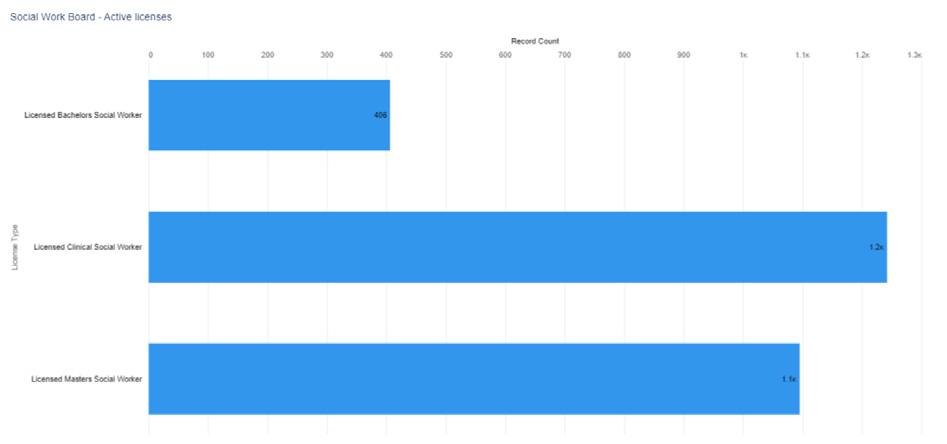

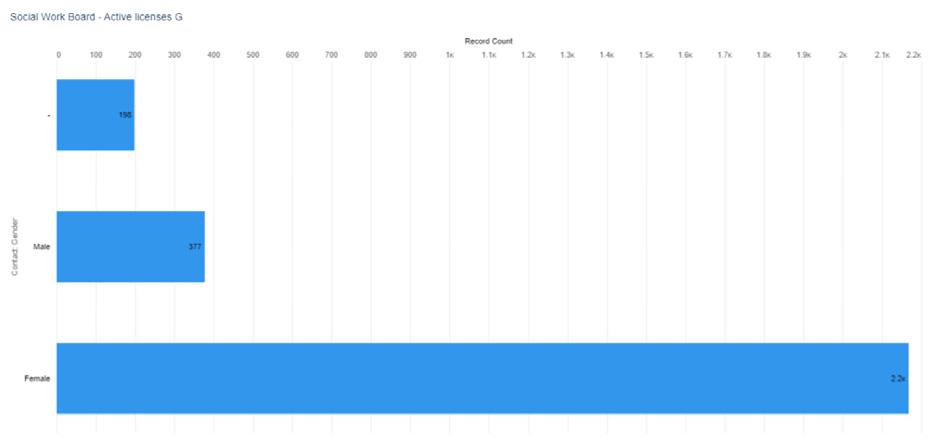
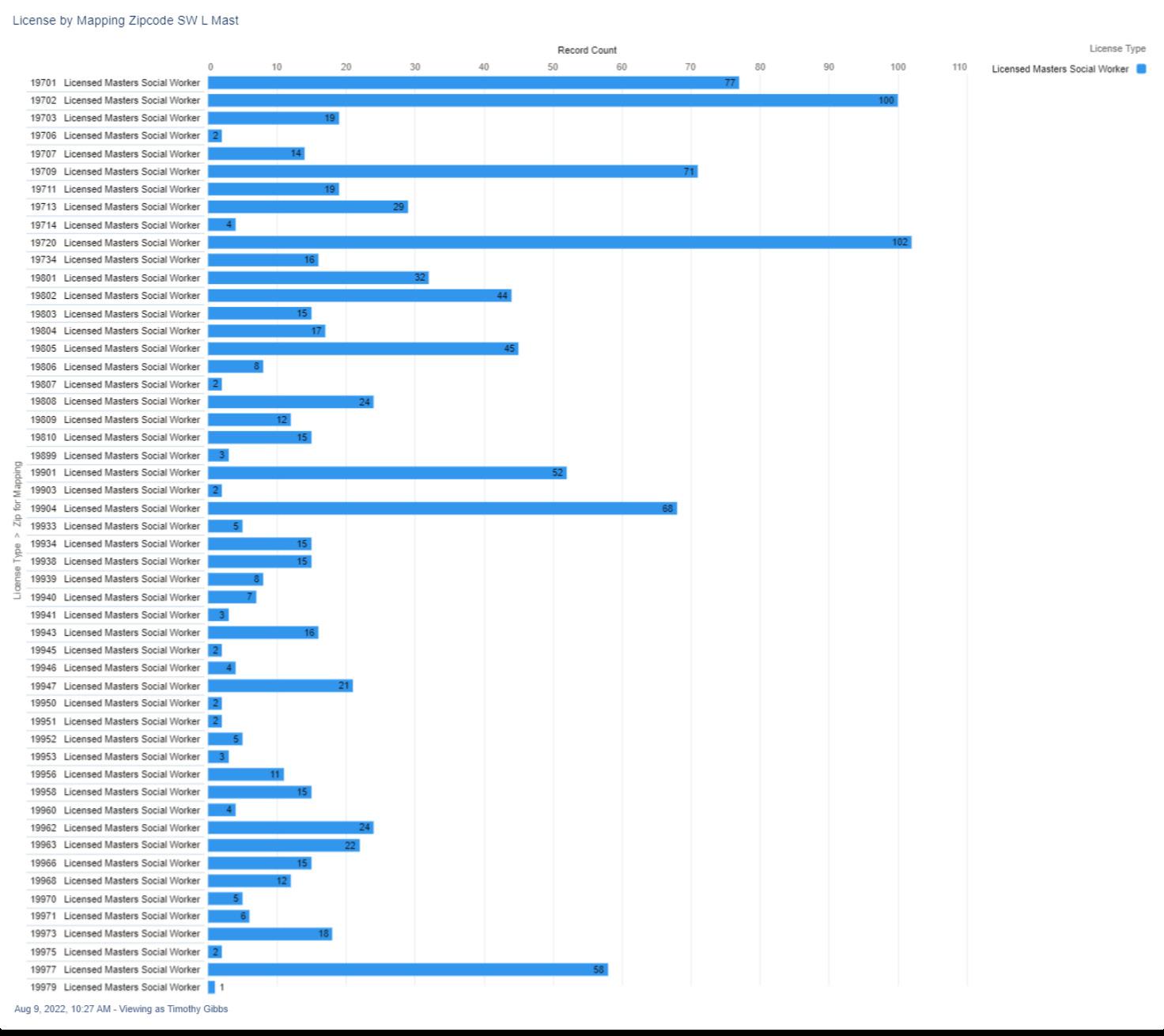
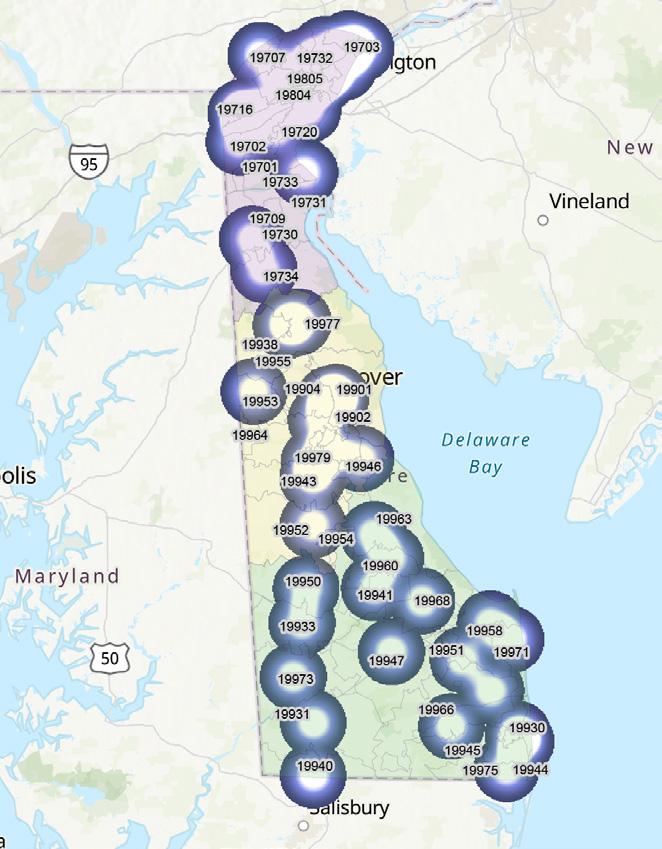
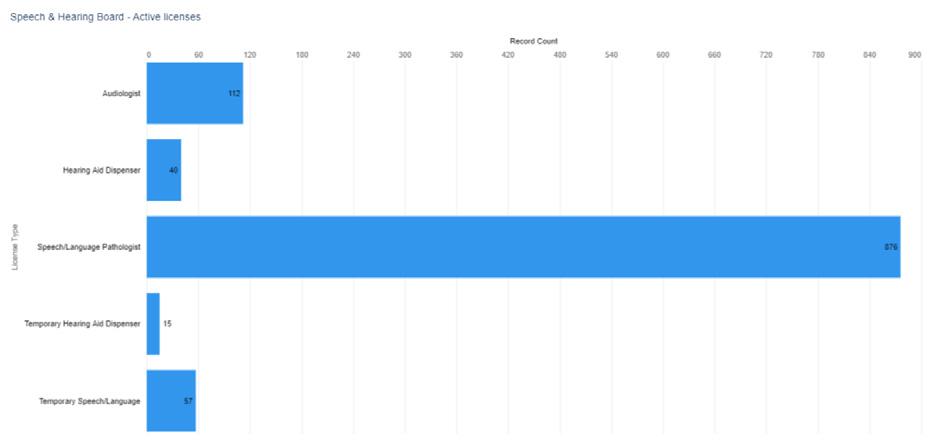
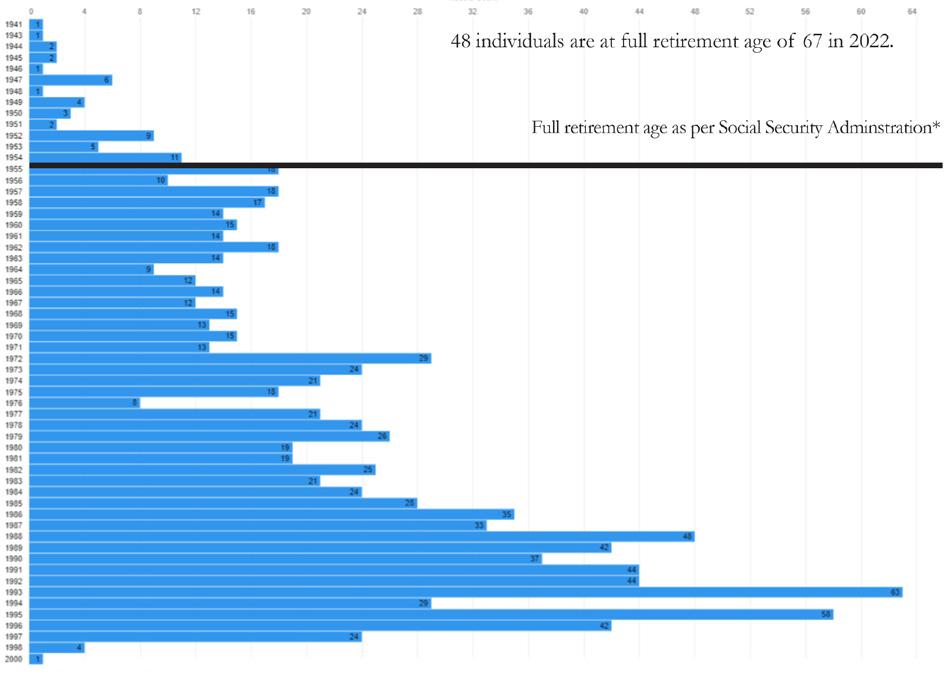
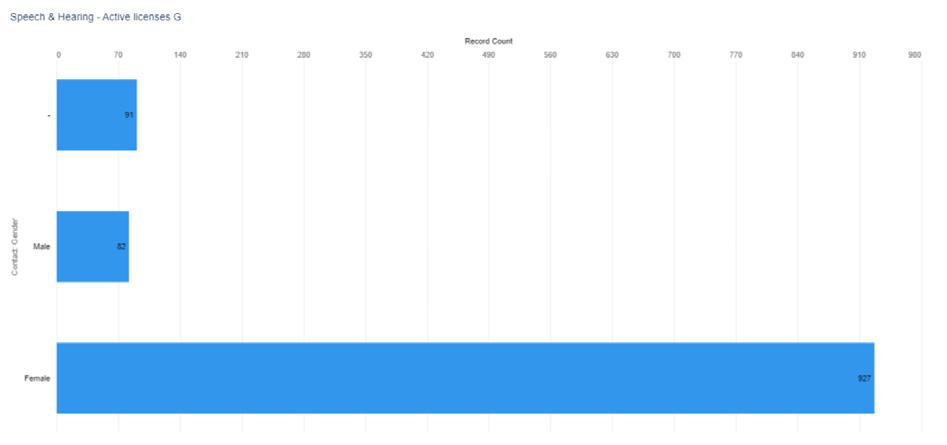 Figure 2. Active License Speech Pathology, Audiology, and Hearing Aid Dispersers by Gender select license types
Figure 3. Active License Speech Pathology, Audiology, and Hearing Aid Dispersers by Birth Year
Figure 2. Active License Speech Pathology, Audiology, and Hearing Aid Dispersers by Gender select license types
Figure 3. Active License Speech Pathology, Audiology, and Hearing Aid Dispersers by Birth Year
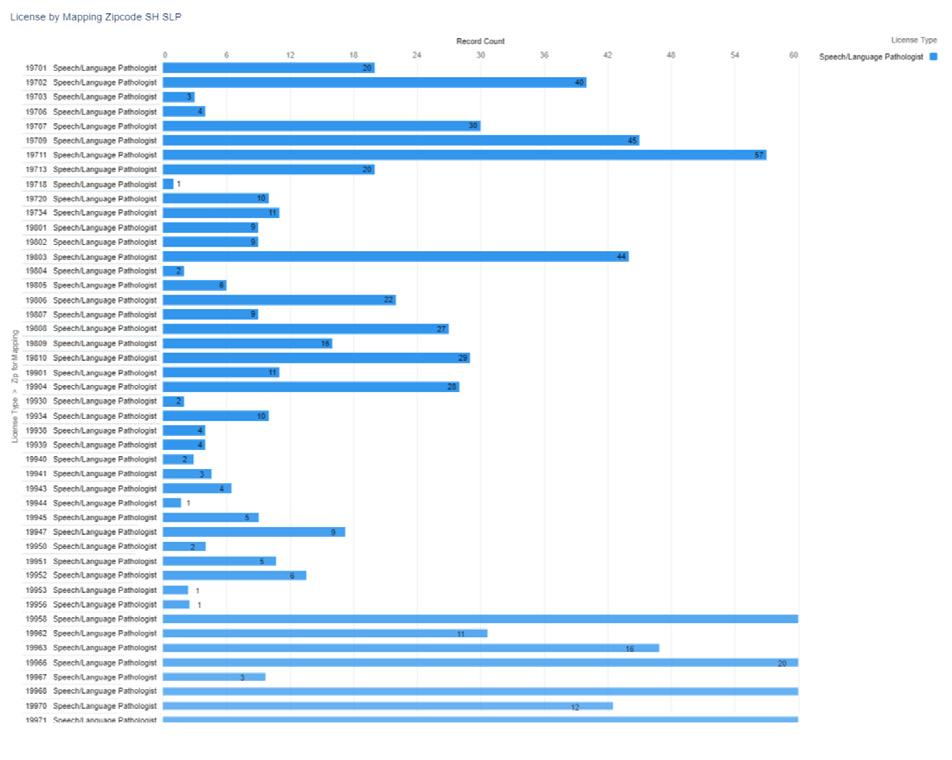
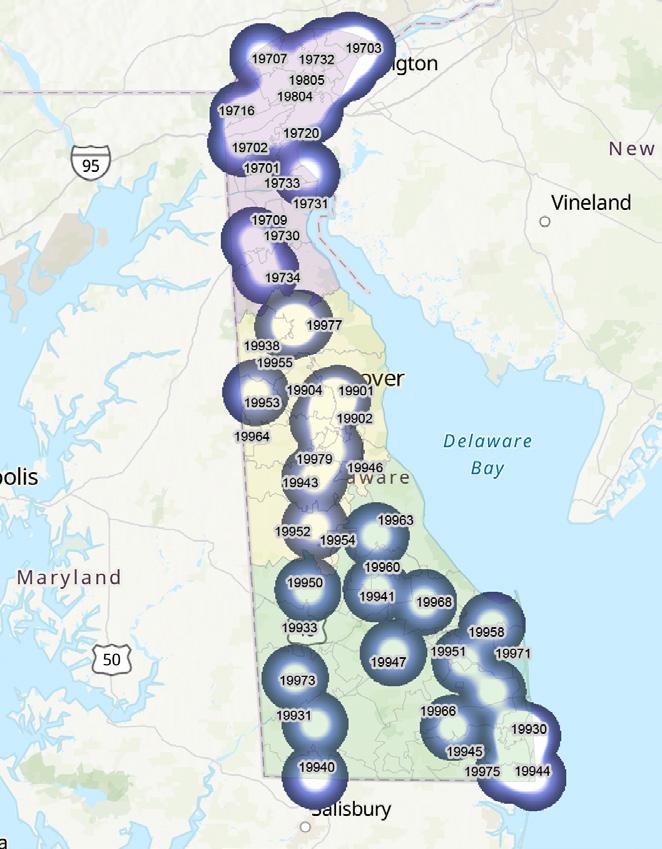
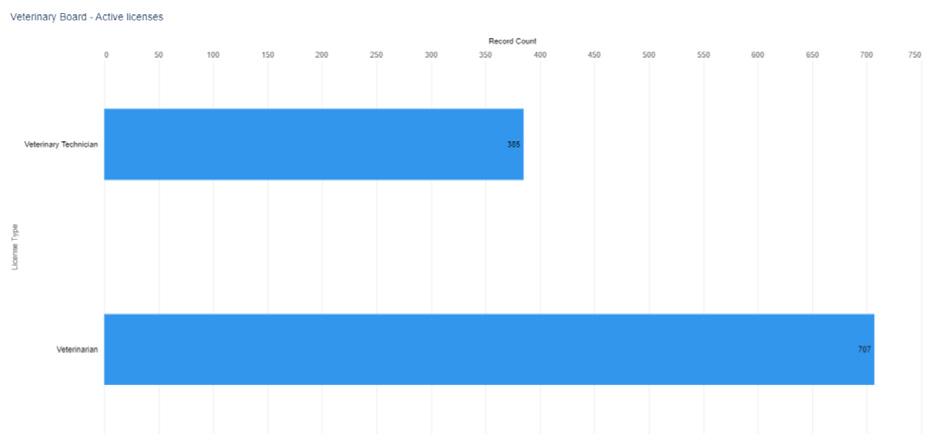
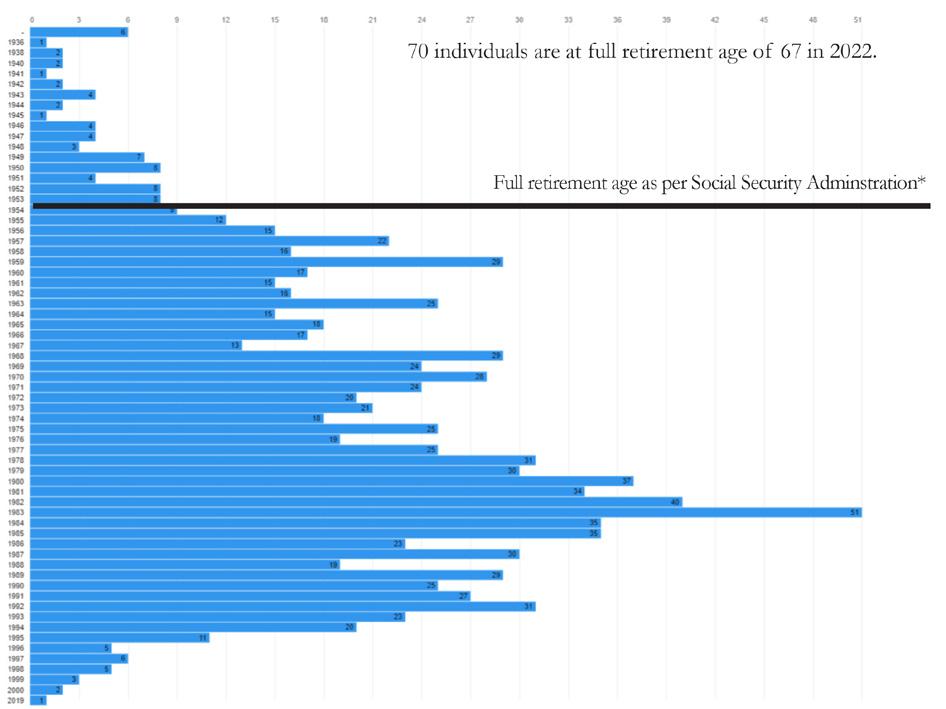
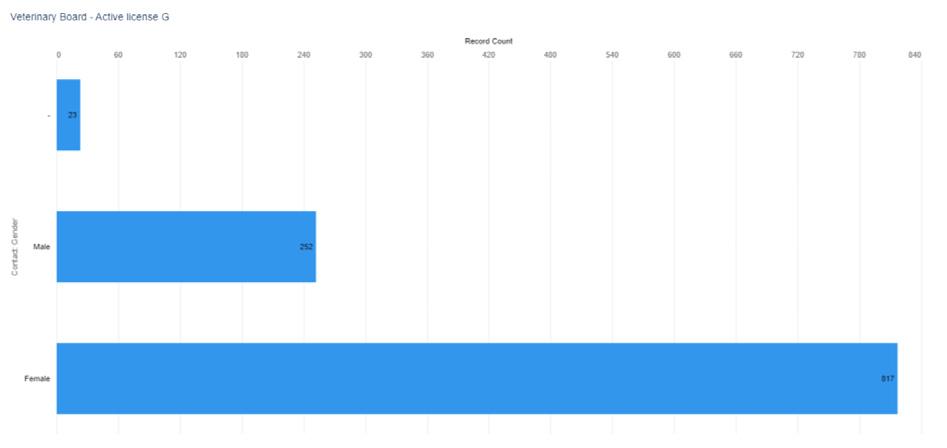
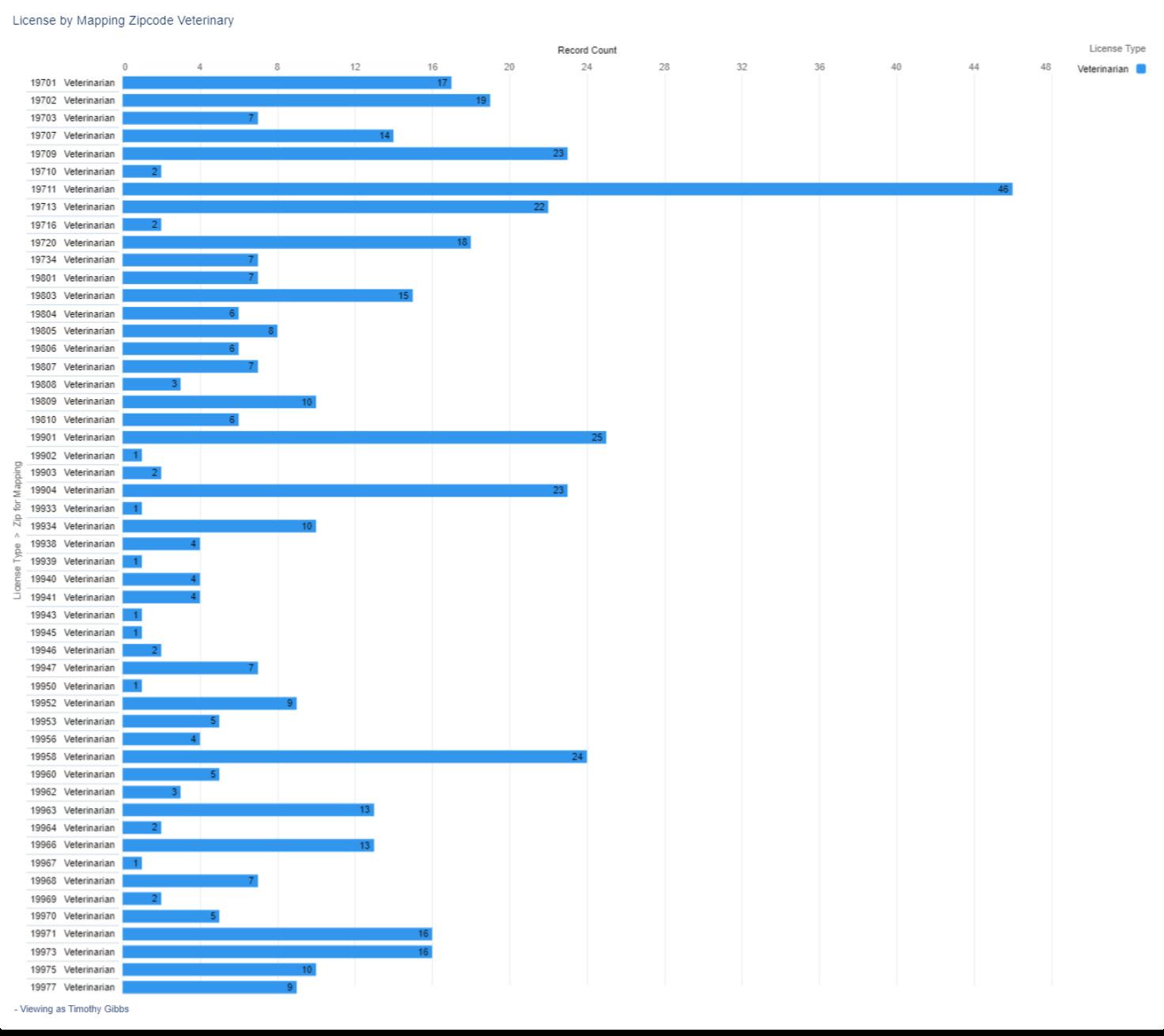
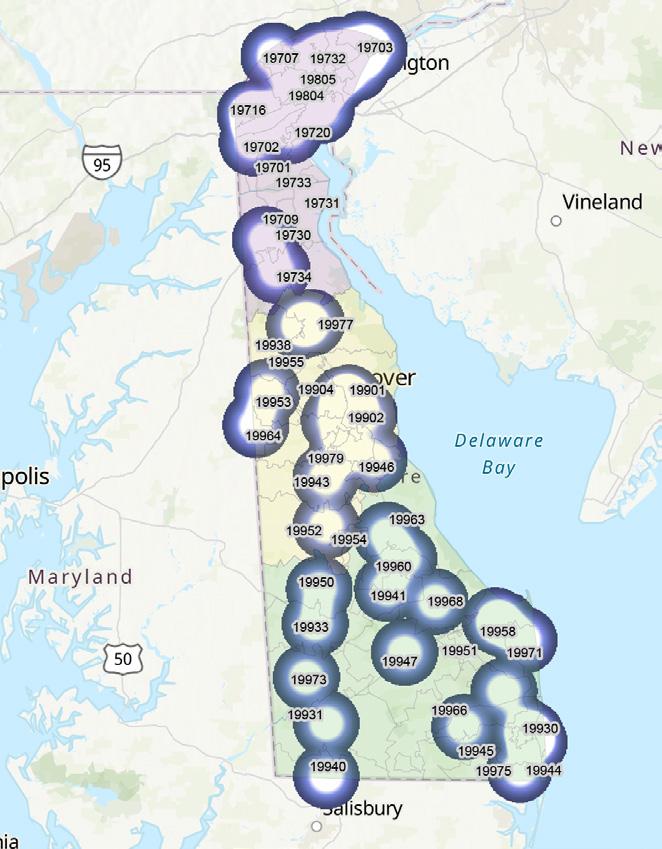
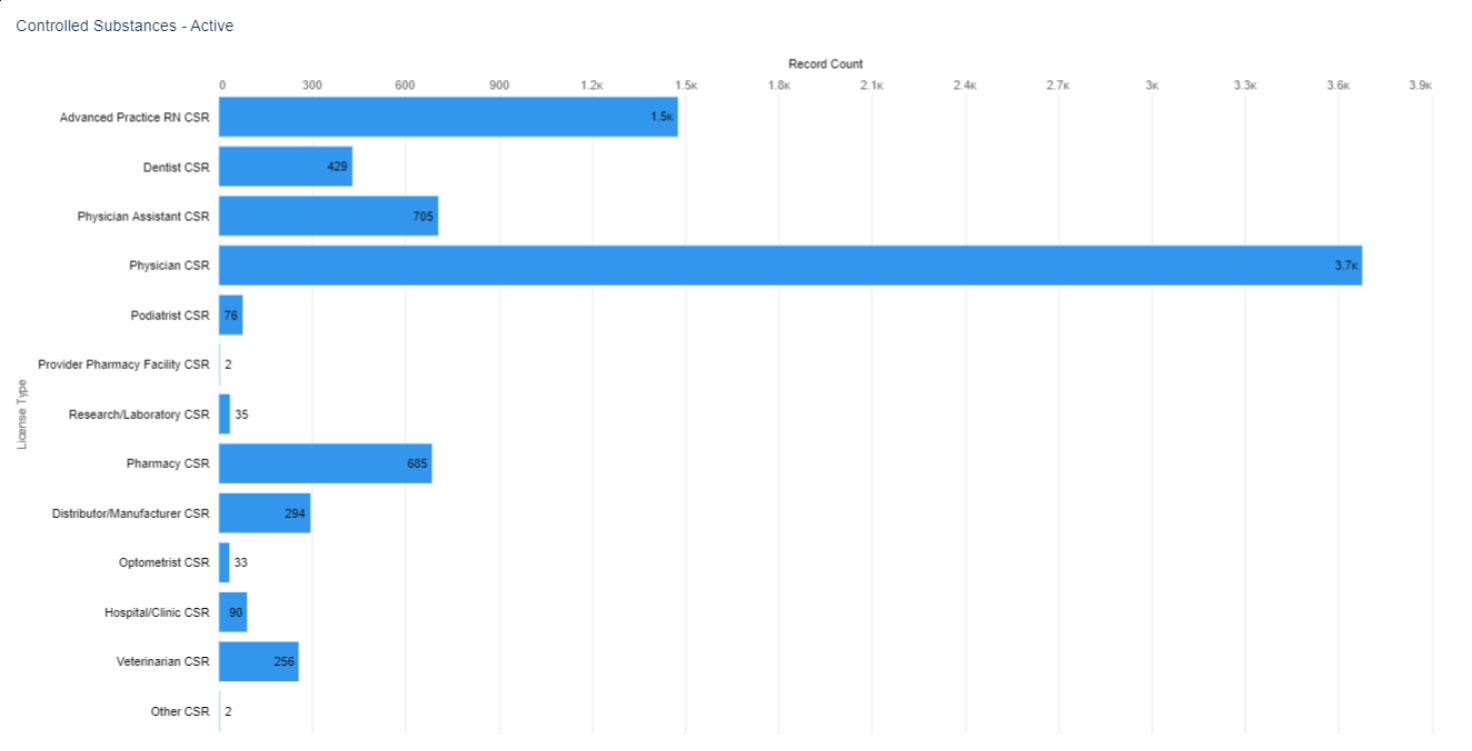


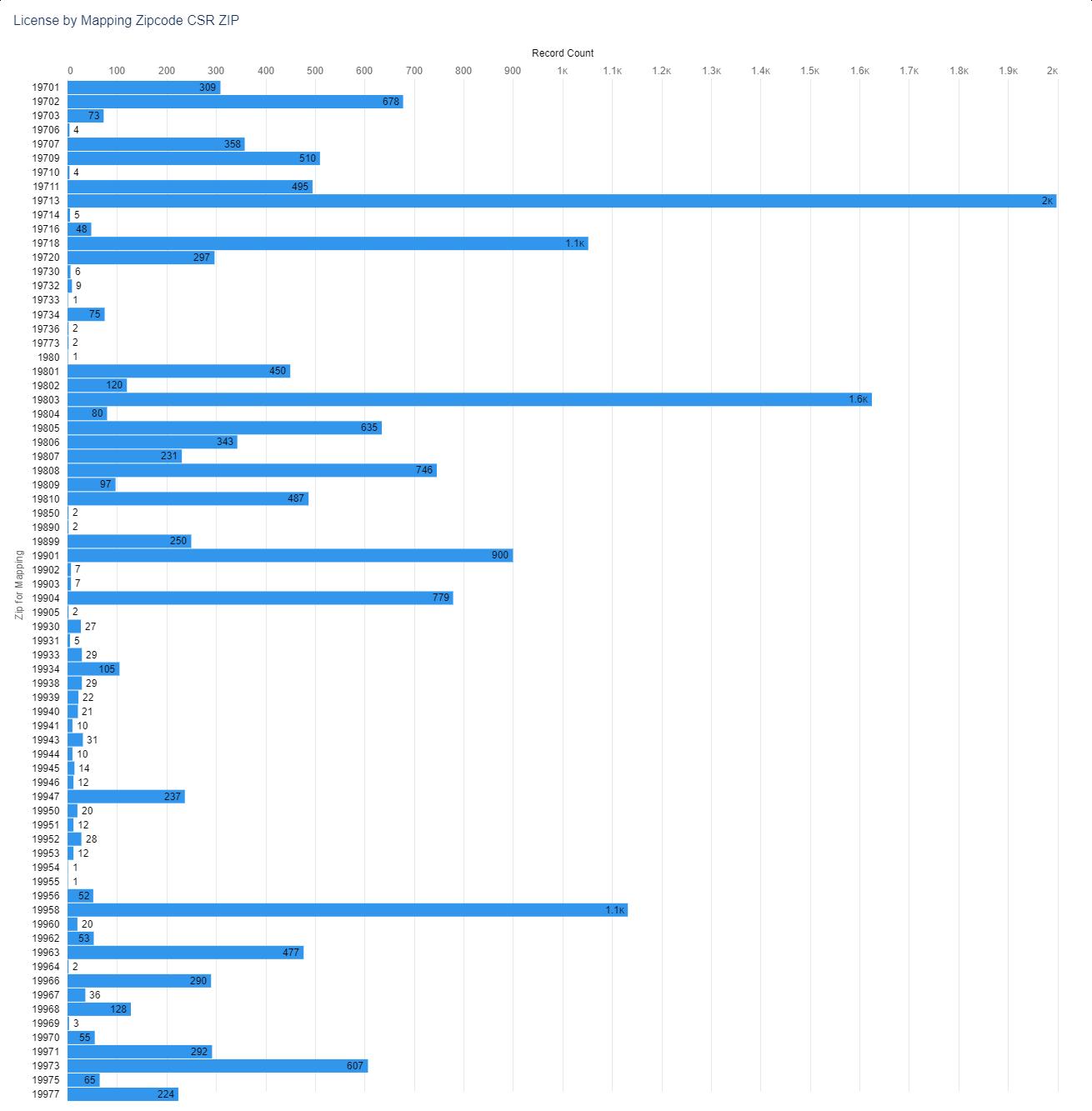
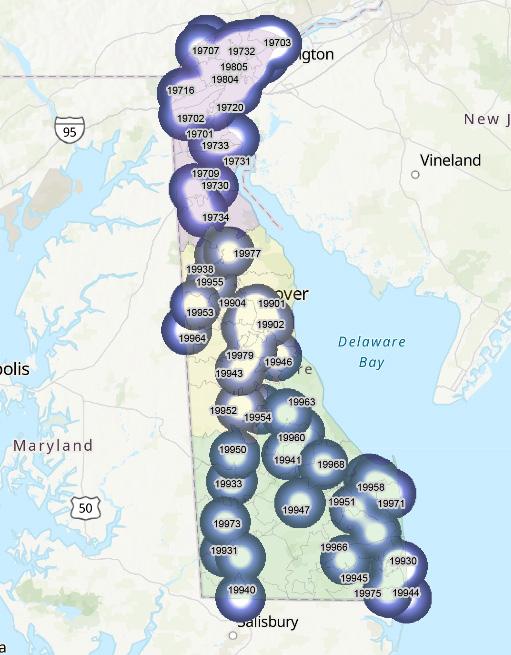















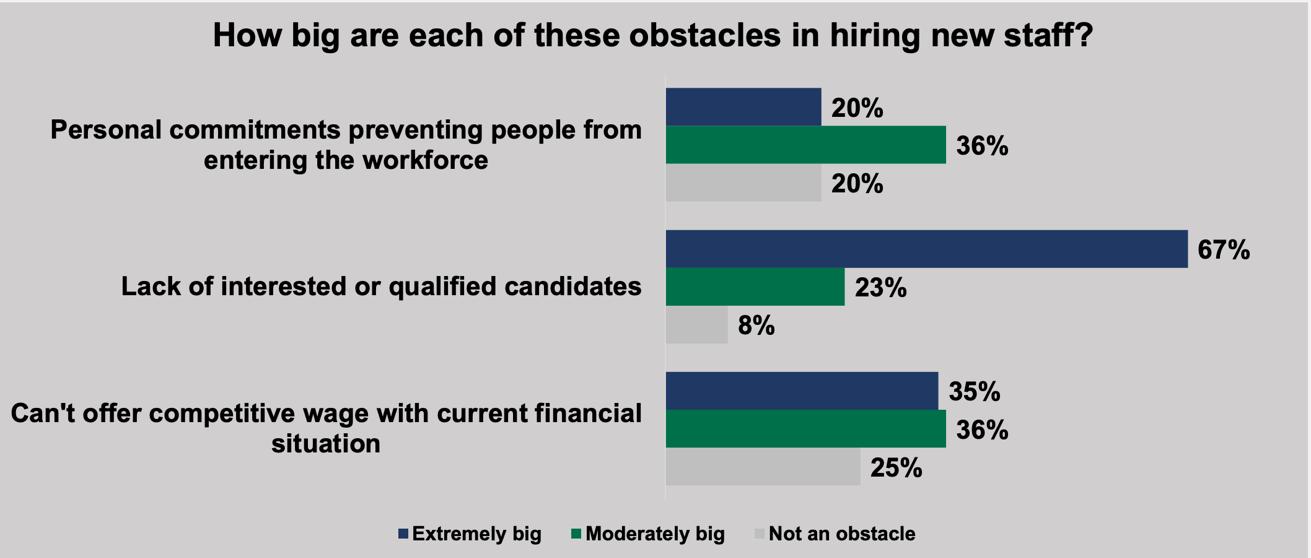
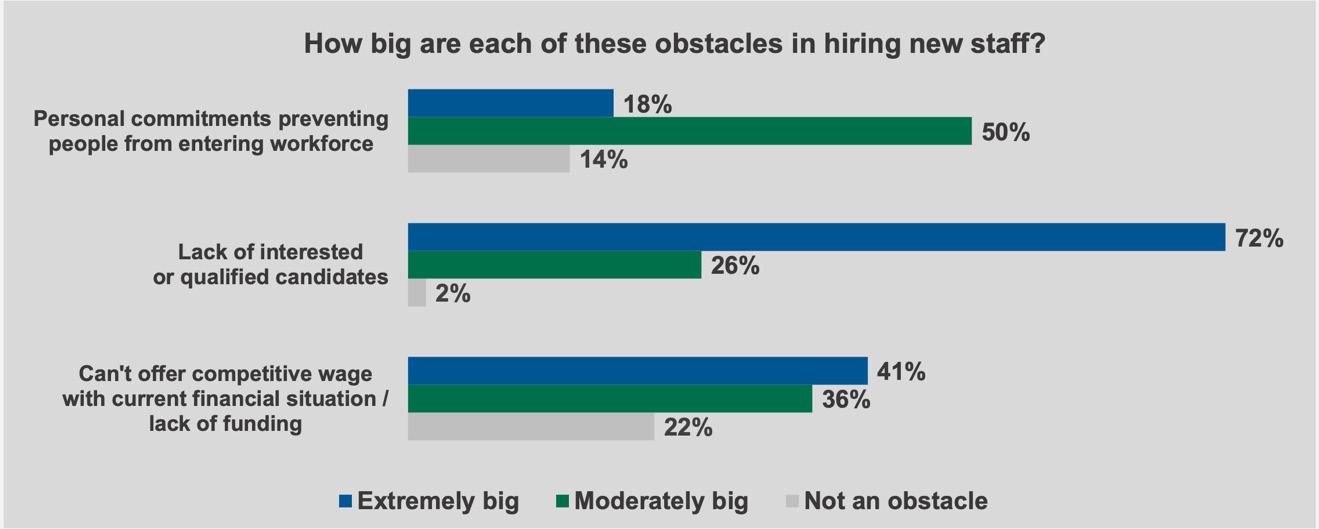 Figure 2. Obstacles to Hiring New Staff in Nursing Homes2
Figure 3. Obstacles to Hiring New Staff in Assisted Living Facilities25
Figure 2. Obstacles to Hiring New Staff in Nursing Homes2
Figure 3. Obstacles to Hiring New Staff in Assisted Living Facilities25