football medicine & performance
In this issue
Rehabilitation of Acute Ankle Sprain in Football
Location, Location, Location - A Key Consideration in Hamstring Rehabilitation
Role of the Sports Scientist in Elite Football & Being a Woman in the Football Industry
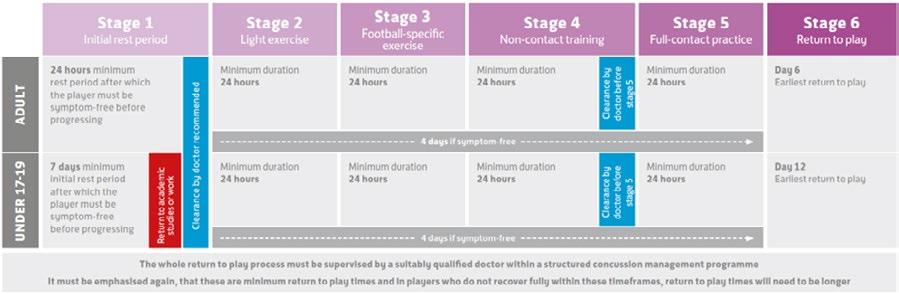
Protecting Players from the Effects of Concussion: A knee jerk reaction or better safe than sorry?

Legal • Education • Recruitment • Wellbeing www.fmpa.co.uk Issue 41 Winter 2022/23
The official magazine of the Football Medicine & Performance Association
Enigma Legal provides legal services and advice to managers, coaches and professionals working within the sports industry, its unique structure utilising a panel of expert barristers all with extensive experience of the sports industry, most notably their work with the League Managers Association.

Enigma Legal lawyers are tried and trusted to work in a flexible, agile and responsive way, demonstrating their understanding of the unique demands of the sports industry. A creative and pragmatic approach will ensure that Enigma Legal offers real value to the FMPA Membership.
www.enigmalegal.com admin@fmpa.co.uk
CEO MESSAGE
The uncertainty of life in professional football was highlighted once again in recent weeks with the appointment of a new manager at Wolverhampton Wanderers FC.
Such events always bring a sense of unease for staff but the announcement that the appointee was to be accompanied by at least seven staff no doubt sent shock waves through the medicine and performance departments. Predictably some staff were released with immediate effect while others faced the prospect of being offered alternative positions within the Club.
Football clubs operate a performance based culture where leaders at all levels focus on delivering results rather than focussing on safe and stable working conditions. The problem with this is that it creates a fear based working environment where leaders focus on self-preservation. At the same time, workers are less incentivised to innovate or take risks. The result is high employee burnout and turnover, which leads to poor organizational performance.
Clubs should adopt a growth culture encouraging continuous learning, experimentation and feedback but this takes time, commitment and long term stability in a workforce. While many heads of department will endeavour to provide just such an environment, can they really commit wholeheartedly, especially when they or their staff can literally be dismissed at the whim of a manager or Chairman?
The conversations that follow such events usually revolve around the idea that clubs should ring fence the medicine and performance sector so as to maintain some degree of continuity, but while this is an honourable intention it is also a scenario that falls at the first hurdle when a new manager is appointed. After all they are at their most powerful when a club is in need of their services.
Given that the tenure ship of managers averages around 18 months, the club will have to go through the process of reappointing new staff if/when things don’t work out. More disruption and the merry go round of new appointments, genuine endeavours, and sackings continues.
Perhaps a new model really does need to be found.
Salmon Eamonn
Chief Executive Officer Football Medicine & Performance Association

3
www.fmpa.co.uk

FROM THE EDITORS
The challenge has been set for the football medicine and science community by the findings of the most recent Football Research Group study. Hamstring injuries have almost doubled during the last 20 years, and now make up 24% of all injuries in men’s professional football. With training and match demands ever increasing, the pressure to improve the prevention, diagnosis, treatment and management of these injuries will continue to grow.
Committing to research and development may present the opportunity to innovate our way out of the hamstring crisis. Several clubs are now engaging in research, and Aston Villa’s recent study into hamstring injuries identified that ‘T-junction’ injuries present a particularly high risk of recurrence. In this edition of Football Medicine & Performance, Fearghal Kerin details the clinical challenges of this injury sub-type and presents potential solutions for its management.
Hamstring injuries are not the only muscle injury presenting problems in football, with quadricep injuries continuing to feature highly. We are delighted Dr Carles Pedret has given an in-depth insight into the importance of an accurate MRI diagnosis for these injuries in order to manage expectations with respect to prognosis and management.


With so many unknowns around what the impact of the timing of this year’s World Cup will be, it’s feared that the accumulation of fatigue will lead to even more muscle injuries in the new year. We hope the information in this edition may give you the tools to approach these problems with new insight, leading to better care for the players.
Enjoy reading the 41st edition of Football Medicine & Performance.
Sean Carmody Fadi Hassan Andrew Shafik
 Dr Sean Carmody Editor, FMPA Magazine
Dr Fadi Hassan Editor, FMPA Magazine
Dr. Andrew Shafik Editor, FMPA Magazine
Dr Sean Carmody Editor, FMPA Magazine
Dr Fadi Hassan Editor, FMPA Magazine
Dr. Andrew Shafik Editor, FMPA Magazine
5 www.fmpa.co.uk
Football Medicine & Performance Association.











All rights reserved.


The views and opinions of contributors expressed in Football Medicine & Performance are their own and not necessarily of the FMPA Members, FMPA employees or of the association. No part of this publication may be reproduced or transmitted in any form or by any means, or stored in a retrieval system without prior permission except as permitted under the Copyright Designs Patents Act 1988. Application for permission for use of copyright material shall be made to FMPA. For permissions contact admin@fmpa.co.uk




Football Medicine & Performance Association 43a Moor Lane, Clitheroe, Lancs, BB7 1BE T: 0333 456 7897 E: info@fmpa.co.uk W: www.fmpa.co.uk FMPA_Official Officialfmpa fmpa_official LinkedIn: Football Medicine & Performance Association Chief Executive Officer Eamonn Salmon eamonn.salmon@fmpa.co.uk Commercial Manager Angela Walton angela.walton@fmpa.co.uk Design Oporto Sports www.oportosports.com Photography Alamy, FMPA, Unsplash Cover Image Chelsea Women’s Kadeisha Buchanan receives medical attention after sustaining an injury. Photo: Alamy ABOUT FMPA_Register FMPARegister fmpa_register ASSOCIATE EDITORS Ian Horsley Lead Physiotherapist REVIEWERS Dr Jon Power Director of Sport & Exercise Medicine Dr Dáire Rooney Doctor Dr Andrew Butterworth Senior Lecturer Frankie Hunter Lead Sports Scientist Dr Manroy Sahni Medical Doctor Eleanor Trezise Medical Student Matthew Brown Academy Sports Scientist Callum Innes Medical Doctor Kevin Paxton Strength & Conditioning Coach
Avinash Chandran Director Mike Brown Head of Physical Performance Jake Heath Elite Sports Specialist Podiatrist Lisa Edwards Sports Therapist Dr Jose Padilla MD Sports Medicine Specialist Dr Daniela Mifsud Doctor & Physiotherapist Dr Danyaal Khan Academy Doctor
Dr









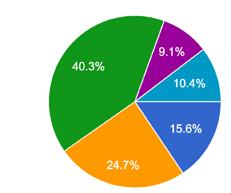
09 24 41 28 CONTENTS FEATURES 7 www.fmpa.co.uk 12 36 43 49 18 09 Defenders Run More in Formations with a Back Three Leon Forcher 12 Rehabilitation of Acute Ankle Sprain in Football Cian Gormley 18 Location, Location, Location: a Key Consideration in Hamstring Rehabilitation Ferghal Kerin 24 Role of the Sport Scientist in Elite Football & Being a Woman in the Football Industry Dr. Laura Bowen Interview by Elle Trezise 28 Understanding the Rectus Femoris: Anatomy, Diagnosis & Types of Injuries Carles Pedret, Iñigo Iriarte, Sandra Mechó 36 Protecting Players from the Effects of Concussion: A Knee Jerk Reaction or Better Safe than Sorry? Phillip Heritage 41 Understanding Recruitment of Backroom Talent in Elite Professional Football Dr. Dan Parnell 43 Medical Notekeeping Standards Across English Football: The Good, the Bad and the Athlete Passport App Dr. Ronnie Banerjee 49 Lessons Other Sports Can Learn from Formula 1 Dr. Daniela Mifsud

DEFENDERS RUN MORE IN FORMATIONS WITH A BACK THREE
/ LEON FORCHER1,2
Introduction
Alongside physical and technical elements, the performance of a professional soccer player is characterized by tactical aspects1 Moreover, playing position and tactical formations are well-known factors in soccer that have gained importance in research in recent years.

The physical, as well as the technical match performance of a professional soccer player, is highly affected by the playing position (i.e. central defender, wide defender, central/wide midfielder, striker)2,3. Contrary to this, the effects of the tactical formation (i.e. 4-4-2 vs. 3-5-2) on physical and technical match performance seem to be lower4,5. However, differences in match performance metrics between tactical formations were indicated earlier in the past6
Previous studies investigated the isolated effects of playing position and tactical formation on match performance and, therefore, the results are limited. To summarize, combining both tactical factors (formation & position) seem to provide further value 7,8
Therefore, we aimed to investigate the effects of playing positions in different tactical formations on physical and technical match performance in the German Bundesliga.
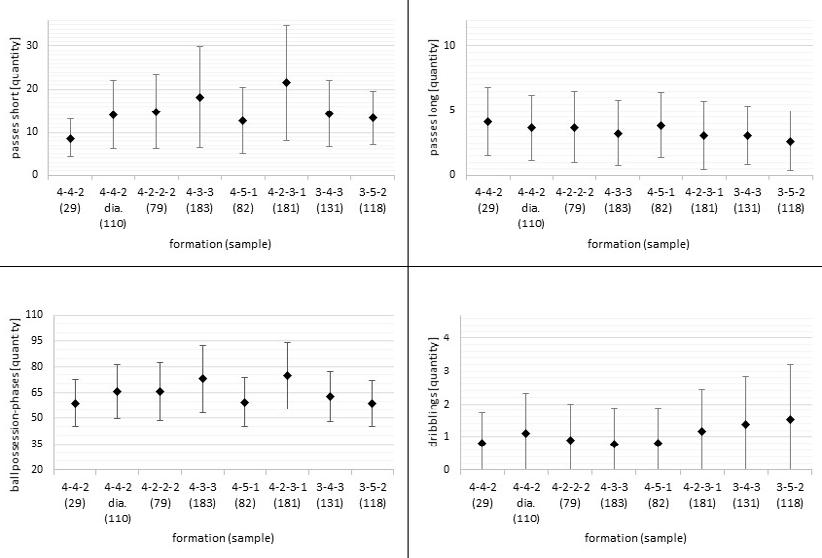
Physical Match Performance
In this chapter, the differences in physical match performance between the formations will be addressed for each playing position individually. Firstly, central defenders, wide defenders, and wide midfielders revealed significant and, therefore, decisive differences between formations. However, central midfielders and strikers showed less differences between formations.
Central defenders run the greatest distance in high intensity and sprinting speed zones in the 3-4-3 and 3-5-2 formations. These results are supported by a current review, analysing the impact of tactical formation on the match performance of male soccer players6 A possible explanation for this could be that wide defenders tend to be more offensive when being supported by three central defenders. Consequently, only three central defenders are left to prevent opposition scoring opportunities in defensive transition
phases. This situation might lead to higher physical performance for central defenders in formations with five defenders compared to formations with four defenders (e.g. 4-4-2).
Regarding the physical performance of wide defenders, a similar pattern was revealed. In detail, wide defenders cover the largest total, high-intensity, and sprinting distances in the 3-4-3 and 3-5-2 formations. Furthermore, wide defenders run less distance in total, high-intensity, and sprinting speed zones in the 4-4-2 and 4-5-1 formations. Concluding, wide defenders experience higher physical load (i.e. higher total distance, high-intensity distance, sprinting distance) in formations with a back three compared to formations with a back four (e.g. 4-4-2 or 4-5-1). Again, one can argue that wide defenders can be more offensive when supported by an additional central defender in formations with a back three (e.g. 3-5-2). Consequently, the wide defenders are more involved in offensive phases even though they still fulfill their original defensive duties. Potentially, this could explain the higher running output for wide defenders in formations with three central defenders.
FEATURE
9 feature www.fmpa.co.uk medicine & performance football
1Institute of Sports and Sports Science, Karlsruhe Institute of Technology, Karlsruhe, Germany 2TSG 1899 Hoffenheim, Zuzenhausen, Germany
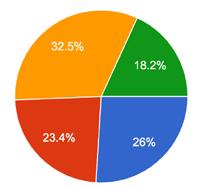
Figure 1: Example physical data for the position wide defender. The number in brackets indicates the number of observations.
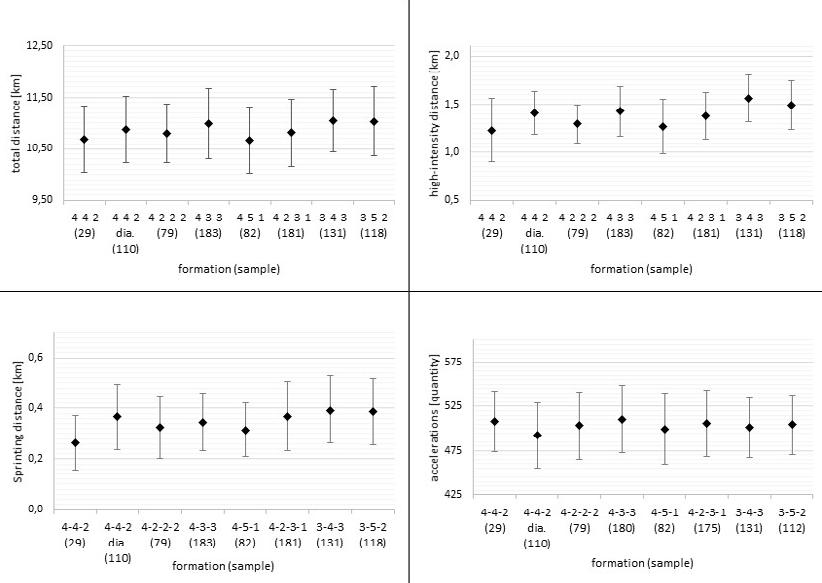
Figure 2: Example technical data for the position wide defender. The number in brackets indicates the number of observations.
feature 10 info@fmpa.co.uk
In contrast to the defenders, wide midfielders were less physically demanded in the 3-4-3 formation (i.e. lower total distance, high-intensity distance, sprinting distance, and number of accelerations). One explanation for this could be that the wide defender in the 3-4-3 formation (also known as the wing back) provides better offensive and defensive support for the wide midfielders and, therefore, wide midfielders are less physically demanded in this formation. Furthermore, in the 4-4-2 diamond formation wide midfielders sprinted less but indeed revealed higher total and high-intensity distances. A possible interpretation of this finding can be made with the linkage to the technical performance and is therefore found in the following section on technical performance.
Regarding central midfielders and strikers, fewer differences between formations were revealed. However, central midfielders are less physically pushed (i.e. total distance, high-intensity distance, sprinting distance) in the 4-4-2 diamond formation. Additionally, strikers sprinted further and revealed a higher maximum speed in the 4-4-2 diamond formation.
Technical Match Performance
The following section will discuss the effects of different formations on technical performance. While some interesting position dependant characteristics were revealed, the influence of contextual factors on technical performance was outstanding.
In 4-3-3 and 4-2-3-1 formations, central defenders, wide defenders, central midfielders, and wide midfielders revealed higher values for ball-possessions, short, and medium distance passes. In those formations (i.e. 4-3-3 & 4-2-3-1) the ball possession rate was higher compared to other formations. Therefore, one might assume that a higher percentage of ball possession in this particular formation leads to higher values for ball possessions for the players playing in those formations. Furthermore, a higher number of ball possessions is also related to a higher number of passes played, explaining the above mentioned findings. Solely strikers fell out of this observed influence of ball possession rates on technical match performance metrics. Since strikers are usually at the end of a ball relay or an attacking sequence, we suggested that they consequently do not benefit from a higher ball possession rate of their team.
Furthermore, there were few outstanding differences between formations regarding the technical match performance. Hence, only those will be addressed in the following. Wide defenders revealed more dribbles in 3-4-3 and 3-5-2 formations. As mentioned above, wide defenders in these formations are positioned in higher areas in offensive game phases more frequently, which could be a possible explanation for the increase in the number of dribbles.
Moreover, as addressed previously, wide midfielders revealed an alternating performance in the 4-4-2 diamond formation (i.e. more ball possessions, short, middle, and long passes; fewer dribbles). This divergent physical and technical match performance of wide midfielders in the 4-4-2 diamond formation is similar to the performance profile of central midfielders. A possible explanation for this finding could be the central positioning of the wide midfielders in the diamond formation.
Conclusion
• Central midfielders & strikers revealed less pronounced differences between tactical formations regarding physical and technical match performance.
• Central defenders, wide defenders, and wide midfielders revealed larger differences between tactical formations regarding physical and technical match performance.
• Most interesting examples: - central defenders and wide defenders revealed higher physical performance when playing in a tactical formation with a back three (i.e. 3-5-2) - wide midfielders in a 4-4-2 diamond revealed a match performance profile that is similar to central midfielders (i.e. possible explanation could be the central positioning of the wide midfielders in the diamond formation)
Practical implications/take home message
• Physical and technical match performance is influenced by a complex interaction of various tactical factors (e.g. playing position & tactical formation).
• Changes in the physical load and technical match performance that come with the switch of playing position or tactical formation can be anticipated.
• Training and recovery processes can be planned accordingly.
• More insights about this study can be found here: Center backs work hardest when playing in a back three: The influence of tactical formation
on physical and technical match performance in professional soccer | PLOS ONE
• Furthermore, a recent review analysed the impact of tactical formation on match performance: The influence of tactical formation on physical and technical match performance in male soccer: A systematic review - Leon Forcher, Leander Forcher, Hagen Wäsche, Darko Jekauc, Alexander Woll, Stefan Altmann, 2022 (sagepub.com)

1. Sarmento H, Mercelino R, Teresa Anguera M, Campanico J, Matos N, Leitao JC. Match analysis in football: a systematic review. 2014;32(20):1831–43.
2. Dellal A, Wong DP, Moalla W, Chamari K. Physical and technical activity of soccer players in the French First League – with special reference to their playing position. 2010;11(2):278–90.
3. Rivilla-Garcia J, Calvo LC, Jimenez-Rubio S, Paredes-Hernandez V, Munoz A, van den Tillaar R, et al. Characteristics of very high intensity runs of soccer players in relation to their playing position and playing half in the 2013-14 Spanish La Liga season. J Hum Kinet. 2018;66(1):1–11.
4. Baptista I, Johansen D, Figueiredo P, Rebelo A, Pettersen SA. A comparison of matchphysical demands between different tactical systems: 1-4-5-1 vs 1-3-5-2. PLOS ONE. 2019;14(4):1–12.
5. Carling C. Influence of opposition team formation on physical and skill-related performance in a professional soccer team. Eur J Sport Sci. 2011;11(3):155–64.
6. Forcher L, Forcher L, Wäsche H, Jekauc D, Woll A, Altmann S. The influence of tactical formation on physical and technical match performance in male soccer: A systematic review. Int J Sports Sci Coach. 2022;1–30.
7. Aquino R, Palucci Vieira LH, Carling C, Martins GHM, Aves IS, Puggina EF. Effects of competitive standard, team formation and playing position on match running performance of brazilian professional soccer players. 2017;17(5):659–705.
8. Sarmento H, Clemente FM, Araujo D, Davids K, McRobert A, Figueiredo A. What Performance Analysts Need to Know About Research Trends in Association Football (20122016): A Systematic Review. Sports Med. 2018;48(4):799–836.
Leon Forcher M.Sc.
Email: leon.forcher@kit.edu
Twitter: @ForcherLeon
11 www.fmpa.co.uk
medicine & performance football
REHABILITATION OF ACUTE ANKLE SPRAIN IN FOOTBALL
FEATURE / CIAN GORMLEY
Introduction
Acute ankle sprains are one of the most commonly incurred musculoskeletal injuries in team sport athletes1. The Football Association Medical Research Programme conducted an audit of injuries in professional football across two seasons7. They found that ankle ligament sprains accounted for 11% of total injuries in football, with 77% of sprains involving the lateral ligament complex. Ankle inversion, with the foot in various degrees of plantar flexion, is the most common mechanism for Ankle Sprains 3
Mechanical stability of the ankle joint is provided by ligament integrity, while functional stability is maintained by ankle proprioception provided by muscles, tendons, ligaments, and capsular innervation3 Acute ankle sprains occur when there is an overreliance on the ankle’s mechanical stability, due to the shortcomings of the ankle’s functional stability.
Acute ankle sprains have the highest reinjury rate of all lower limb musculoskeletal injuries4. Athletes who suffer acute ankle sprains have a twofold increase in reinjury risk in the year after the initial injury5 Reinjury of the ankle is just one of the many symptoms that defines Chronic Ankle Instability (CIA)6. Other symptoms include pain, persistent swelling, feelings of
instability, “giving way” of the ankle and reduced functional capacity.
In footballers, acute ankle sprains can occur in both contact and non-contact scenarios, with the frequency influenced by playing position. Contact mechanisms (59%) were more common than non-contact mechanisms (39%) in outfield players, while the opposite was true for goal keepers where non-contact were more common than contact (79% vs. 21%, respectively)7
When looking at the most common mechanisms for contact injuries, tackling (36%) carried a greater risk than being tackled (18%). Alternatively, when analysing non-contact mechanisms, 77% of non-contact sprains were caused during landing, twisting, turning, and running. As practitioners, this information provides a great insight into areas that can be focused on to reduce the risk of both contact and non-contact acute ankle sprains. Tackling technique and landing mechanics, as well as running and change of direction mechanics should be incorporated into athletic development programs to reduce the initial injury risk and subsequent reinjury risk.
While 83% of ankle sprains had a rehabilitation period of less than one month, the research suggests that most
acute ankle sprains are not severe. However, due to the nature of the fixture list in football – particularly in the 2022/23 EFL Championship Season for example – there is a potential for a player in the starting 11 to miss 3 fixtures in 7-days and up to 9 fixtures in one-month which can be detrimental to a team’s standings in the league at the end of the season.

As practitioners it is important to address the high incidence and subsequent re-injury rates of acute ankle sprains and appropriately return athletes to full performance post-injury. To do this, a Return to Sport framework should be defined, and subsequently adapted, to maximise specificity for footballers. Similarly, by applying elements of this framework, and implementing them into a team’s athletic performance program, the initial injury risk can be reduced in the entire team.
Mechanosensory Impairments
Mechanosensory impairments are the dysfunction in the transduction of mechanical stimuli into neural signals. As practitioners, it is important to identify where these impairments are post-injury. To do this the qualities that are affected must be defined before they can be assessed.
feature 12 info@fmpa.co.uk
By assessing an athlete along the forcevelocity continuum, prior to assessing whether there is any apprehension in more football specific movements, a short- to long-term rehabilitation plan can be created to address the athlete holistically. This approach ensures the player isn’t rushed back by strapping their ankle or putting them on a course of anti-inflammatory medication, without addressing the underlying mechanosensory impairments. A robust testing strategy ultimately helps to reduce the risk of players developing chronic ankle instability.
So, what should be assessed?
In essence, it must be identified whether a player can: 1. Produce high levels of force 2. Produce high levels of force quickly 3. Produce high levels of force quickly in specific environments
side, or to baseline levels if the data is available. In addition to the quantitative data, an athlete’s qualitative symmetry should be assessed by analysing movement patterns across the controlchaos continuum8
Outlined below are some tests that assess the aforementioned areas. These can be used to identify any asymmetries caused by the mechanosensory impairments after an acute ankle sprain.
1. Producing Force
The purpose of the following assessments are to measure an athletes peak force and Rate of force development capabilities. This is the foundation of the functional stability discussed earlier.
In order to provide a holistic picture of where an athlete is at after an acute ankle sprain, the key muscles around the ankle must be assessed. The position of the foot during force production must also be noted – reducing over-pronation or over-
supination. This ensures the ankle is in the most mechanically advantageous position.
The calf muscles – the soleus and the gastrocnemius – are the two largest muscles in the lower leg. These muscles work most in a flexed and extended knee position, respectively. Their strength qualities should be tested accordingly. The two easiest ways to assess the strength of these muscles is through the use of Isokinetic Dynamometry (IKD) to assess isotonic strength or by using force plates to assess isometric strength.



Three common strength tests used are outlined below.
In addition to assessing the calf muscles, it is also important to assess an athlete’s eversion strength. The athlete can be tested in both a neutral foot position, as well as in a plantarflexed and inverted position, to replicate a position specific to the injury mechanism.
Neutral
Prone Ankle IKD @ 30deg/sec Standing Calf Isometric Seated Calf Isometric Warm Up Reps 5 (60-100%) 2 (80 & 90%) 2 (80 & 90%) Sets X Reps 2 X 5 1 X 3 (5sec PUSH) 1 X 3 (5sec PUSH) Target 180-200% (Peak Torque/BW) 2.5 X Bodyweight (N/kg) 1.5 X Bodyweight (N/kg) Table 1: Plantarflexion and Dorsiflexion Strength Assessments Eversion Isometric Warm Up Reps 2 (80 & 90%) Sets X Reps 1 X 3 (5sec PUSH) Target <10% difference compared to non-injured limb Table 2: Eversion Strength Assessment
The goal is to return a player’s injured ankle to within 10% difference of the uninjured Over-Pronation
Over-Supination
13 medicine & performance football www.fmpa.co.uk
2. Producing Force Quickly
Once an athlete is capable of producing high levels of force, the athlete’s explosive and reactive strength should be assessed as these qualities will be more applicable to the on-pitch demands during football training and games.
In addition to returning players to 90% limb symmetry in both explosive and reactive strength, it is also important to gradually reintroduce frontal plane plyometrics too. As previously discussed, 77% of noncontact sprains were caused during landing, twisting, turning, and running. Before reintroducing twisting and turning through both planned change of direction work and reactive agility work, ensuring athletes can both absorb and produce force in the sagittal plane, but most importantly – the frontal plane, due to the mechanism of the injury – should be assessed.
In the early stage of rehab, it is advantageous to expose players to sagittal plane hop and stick exercises before progressing to frontal plane variations. Initially, alternate leg variations can be used before progressing to unilateral variations.

In order to work the full SSC continuum, it is important to utilise both explosive strength through single jumps for height/distance while challenging the landing mechanics, however it is also important to work reactive strength in multiple planes too. By introducing repeated hops with a focus on reducing contact time, an athlete can be progressed towards more specific movements that they will be exposed to during training and matches.
Finally, by adding both visual and aural stimuli to replicate the psychological and ecological demands of the game, all bases can be covered to ensure a successful return to performance.
in RSI compared to
Image 2: Banded Single Leg Calf Raise – Peroneal Bias
Single Leg CMJ Single Leg DJ Repeated Hop Warm Up Reps 2 each leg (80 & 90%) 2 each leg (80 & 90%) 10 (80-90%) Sets X Reps 1 X 3 each leg 1 X 3 each leg 2 X 10 each leg Target >50% of Double Leg CMJ <10% difference compared to non-injured limb > 0.8 Reactive Strength Index <250ms
Time
limb
limb Table 3: Explosive and Reactive Strength Assessments Reactive Strength Level 1 Level 2 Level 3 Level 1 Linear Ankling Lateral Ankling Extensive Skater Hops (Focus –Reduce Contact Time) Level 2 Linear Penguin Taps Lateral Penguin Taps Intensive Skater Hops Level 3 Linear Double Leg Pogos Lateral Double Leg Pogos Repeated Double Leg Hurdle Hops (Medial & Lateral) Level 4 Linear Single Leg Pogos Medial/Lateral Single Leg Pogos Repeated Single Leg Hurdle Hops Table 4: Reactive Strength Progressions Explosive Strength Level 1 Level 2 Level 3 Level 1 Linear Alternate Leg Hop and Stick Lateral Alternate Leg Hop and Stick Multidirectional Leg Hop and Stick Level 2 Linear Alternate Leg Hurdle Hop and Stick Lateral Alternate Leg Hurdle Hop and Stick Multidirectional Leg Hop and Stick Level 3 Linear Single Leg Hop and Stick Lateral Single Leg Hop and Stick Alternate Leg Hop and Stick with Rotation Level 4 Linear Single Leg Hurdle Hop and Stick Lateral Single Leg Hurdle Hop and Stick Single Leg Hop and Stick with Rotation Table 5: Explosive Strength Progressions feature 14 info@fmpa.co.uk
Contact
>20cm Jump Height <10% difference compared to non-injured
<250ms Contact Times <10% difference
non-injured
3. Producing Force Quickly in Specific Environments
Once players have sufficient force production capabilities and both explosive and reactive strength capacities, their ability to utilise these qualities in football specific environments should be assessed.
Typically, with acute ankle sprains, once an athlete has achieved 85% limb symmetry on their single leg drop jumps and repeated hops, they can return to linear running. Once an athlete returns to linear running they can gradually return to match and supra-maximal match demands of both High-Speed Running Distance (>55% of Player’s Max Speed) and Sprint Distance (>85% of Player’s Max Speed). By exposing players to these running zones the risk of hamstring injuries upon their return to both training and matches can be mitigated.
More importantly however, when planning the end stage rehab for football players, is replicating both the positional demands of planned change of direction and reactive agility that each player is exposed to during a game. By gradually reintroducing both linear and multidirectional jumping into the program early on in the rehab, a player’s ability to absorb and produce force in multiple planes is sufficiently improved. This lays the foundation for more specific movements on the pitch.
Alongside the qualitative analysis of landing and change of direction mechanics, where a player’s ability to land in a hip dominant landing pattern is assessed, prior to exposing them to the more chaotic movements experienced in games, the number of accelerations – and particularly decelerations – that they must do in a game must also be quantified. These numbers will typically be dictated by both position and team tactical demands.
When looking at positions, typically, a centre-half will typically make more intense (>3metres/second/second) accelerations and decelerations than a striker. Alternatively, a team that employs a high-press strategy will be required to complete more intense accelerations and decelerations than teams that prefer to utilise a low-block for example.
Thankfully, with the availability of GPS units, an individual player’s typical game demands can be quantified – particularly focusing on both the count of accelerations and decelerations, as well as the distance covered during both of these movements. The latter is typically referred to as Explosive Distance by GPS companies (distance covered during accelerations and decelerations >3metres/ second/second). The intensity of these movements can be assessed by relating back to a per minute value, ie. Accelerations and Decelerations per minute. Finally, including a measure of density can also be utilised where the count of these accelerations and decelerations is measured as a distance per effort value.
The above GPS metrics can be influenced by pitch area and drill time. Similarly, they can be made more complex by adding players in. Due to the 360-degree nature of football, a player can be progressed through a box or rondo drill by starting them as an outside player where they are required to make lateral movements while challenging their passing accuracy, before progressing them to being an inside player where they are required to work both in possession and out of possession. The same principle can be applied to small sided games where the complexity of the drill is increased in line with the player’s return to performance plan.
To ensure specific movements are incorporated into the end-stage rehab, the Performance Analysis team can also be utilised if they are available to us, to look at movements that
the player is expected to undertake during the three moments of football games – attacking, defending and transitioning. This ensures the multidisciplinary team is utilised in the rehab process. This ensures all the player’s bases are covered and they can return fully to performance, while reducing the risk of the player experiencing reoccurrences and subsequently chronic ankle instability.
Conclusion
1. Can the player produce high levels of force?
• Ensure the player is strong and symmetrical in plantar flexion with both a flexed and extended knee, in addition to eversion in both a neutral and plantarflexed foot position.

2. Can the player produce high levels of force quickly?
• Assess and identify any deficits in both single leg explosive strength and reactive strength by analysing single leg countermovement jumps, drop jumps, and repeated hop tests.
3. Can the player produce high levels of force quickly in specific environments?
• Progress from planned change of direction drills to reactive agility drills in both attacking, transitioning and defending movements as appropriate.
1. Gribble PA, Bleakley CM, Caulfield BM, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med 2016;50:1496–505.
2. Nery, C., Raduan, F., & Baumfeld, D. (2016). Foot and ankle injuries in professional soccer players: diagnosis, treatment, and expectations. Foot and ankle clinics, 21(2), 391-403.
3. Hintermann, B. (1999). Biomechanics of the unstable ankle joint and clinical implications. Medicine and science in sports and exercise, 31(7 Suppl), S459-69.
4. Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med 2005;39:e14.
5. Verhagen EA, van Tulder M, van der Beek AJ, et al. An economic evaluation of a proprioceptive balance board training programme for the prevention of ankle sprains in volleyball. Br J Sports Med 2005;39:111–5.
6. Docherty CL, McLeod TC, Shultz SJ. Postural control deficits in participants with functional ankle instability as measured by the balance error scoring system. Clinical journal of sport medicine. 2006 May 1;16(3):203-8.
7. Woods, C., Hawkins, R., Hulse, M., & Hodson, A. (2003). The Football Association Medical Research Programme: an audit of injuries in professional football: an analysis of ankle sprains. British journal of sports medicine, 37(3), 233-238.
8. Taberner, M., Allen, T., & Cohen, D. D. (2019). Progressing rehabilitation after injury: consider the ‘control-chaos continuum’. British journal of sports medicine, 53(18), 1132-1136.
15
www.fmpa.co.uk
medicine & performance football

LOCATION, LOCATION, LOCATION A KEY CONSIDERATION IN HAMSTRING REHABILITATION
FEATURE / FEARGHAL KERIN
Homogenising hamstrings
The evolution in the physical demands of football - challenging athletes to go faster and further, than ever beforecontinues unabated. As a result, despite all advances in technology, science, and rehabilitation, hamstring re-injury rates remain consistently high and remain a frustration to both athletes and medics charged with managing the injury quickly and safely back to the field of play. This challenge has perhaps been compounded by the post-pandemic fixture congestion over the past number of years.
UEFA injury study data have described reinjury rates of 13% in the first two months following return to play1. After such a re-injury, one of most difficult challenges is determining which component of the rehabilitation was to blame for the failure. The likes of muscle strength, neuromuscular control, or apparently

pathological running mechanics are often deemed the culprit.
However, the spotlight over the past decade has shifted somewhat from the functional diagnosis to the anatomy of the injury. This is due to the realisation that not all hamstring strain injuries are the same. Within the hamstring complex, there are three (or four if including short head) distinct muscles, each with proximal and distal components. In addition, the musculotendinous unit is made up of peripheral muscle fibres, the attachment of muscle to the intramuscular tendon (or musculotendinous junction) and the intramuscular tendon itself – the connective tissue that is analogous to the rachis of a feather. Within these, there are multiple potential locations for injury - each have their own appropriate timelines for return to play, and each benefitting from bespoke management.
Intramuscular Tendon Injuries
An analysis (currently under review) of the hamstring injuries at Leinster Rugby over 5 seasons found that 20% of hamstring strain injuries involved the intramuscular tendon. In a similar study predominantly involving footballers, van der Made, et al.2 found intramuscular tendon disruption in 39% of hamstring strain injuries. This suggests that this type of injury forms a significant proportion of the hamstring strain injuries seen by practitioners at clubs and warrants consideration.
This was highlighted in a review in the BJSM by Brukner and Connell3 where they named intramuscular tendon injuries as ‘a more serious type of thigh strain’ and this concept has evolved thereafter. Comin, et al.4 were the first to our knowledge to describe prolonged recovery in Australian Football players who had disrupted their intramuscular tendon. In 2014, Noel Pollock
feature 18 info@fmpa.co.uk
Leinster Rugby, Ireland University College Dublin, Ireland
of British Athletics published the British Athletics Muscle Injury Classification, which is now in almost ubiquitous use in elite football.5 The classification grades injury by their location within the musculotendinous unit in ascending severity - ‘a’ (peripheral myofascial injury), ‘b’ (musculotendinous junction) and the most severe, ‘c’ (intramuscular tendon injury). They later validated the scale when they demonstrated ‘c’ type injuries required prolonged rehabilitation and faced a 60% re-injury rate6
Given each sport is unique, with different demands and different potential mechanisms of injury, there has since been several welcome analyses to attempt to determine whether this BAMIC scale does indeed cause similar challenges in football as well as athletics. Shamji, et al. 7 reported intramuscular tendon disruption in 21.3% of all hamstring strain injuries. These injuries were seen to take significantly longer time (36 days versus 24 days) and risked higher recurrence rate (38.5% versus 12.5%) than ‘a’ and ‘b’ type injuries which though more frequent, are likely to be outnumbered by ‘c’ type.7 Research conducted at Liverpool FC, however, found no association with injury location and outcomes8
Another recent paper by Tears, et al. 9 at Sunderland AFC found a small difference between BAMIC grade and time to return to play.
What is certain is that track and field is not football and that it wouldn’t be appropriate to transpose the findings directly across regarding the BAMIC.
In addition, in a group of sub-elite athletes, van der Made, et al. 10 showed no difference in re-injury rate at 12 months. What is noteworthy about that work is that the clinicians and athletes were blinded to the imaging findings –raising the possibility that expectations of a difficult recovery following MRI may impact upon outcomes. However, there are pockets of evidence to support the hypothesis that ‘c’ type injuries are more severe. In truth, to expand our understanding of these injuries in the future, everyone would benefit from a collaborative approach to data sharing when cataloguing these injuries.
Bespoke Rehabilitation
In 2019, Macdonald, et al. 11 described the principles the British Athletics group had designed in respect of the high re-injury rates they were suffering following ‘c’ type injury. For ‘a’ type injury, though these may initially be quite painful due
to the highly innervated fascia, these were progressed quickly as the musculotendinous unit is largely intact. The authors continue to allow their athletes to train through some degree of pain in the first week for this reason, and running is re-introduced early. While ‘b’ type injuries may be considered ‘typical’ hamstring injuries, ‘c’ type injuries are argued to benefit from completely bespoke management. The authors advocate delayed running, delayed eccentrics, and delayed speed, to give respect to the slower healing process for tendons.
By utilising this approach, the authors were able to significantly reduce their recurrence rate for ‘c’ type injuries to 0%.8 It is critical to note that the approach used took similar time to return to play as previously, so it is not overly cautious in terms of holding the athletes out longer. The point of difference in this case is the structured rehabilitation which gives respect and attention to the specific tissues. These results are demonstrated in Table 1.
Table 1: Time to return to full training and number of reinjuries in the different BAMIC classes following a location specific approach to rehabilitation (reproduced from Pollock et al 2022)
Time to return to full training in the different BAMIC classes
BAMIC Number of Injuries Number of re-injuries Median TRFT (days (IQR, range))
0 16 9 (4.3, 4-17)
1a 6 1 12 (4.0, 9-16)
1b 19 17 (10.3, 8-32)
2a 4 19 (3.5, 14-21)
2b 11 1 19 (3.5, 11-36)
2c 7 35 (9.5, 25043)
3a 1 17
3c 6 51.5 (23.8, 28-70)
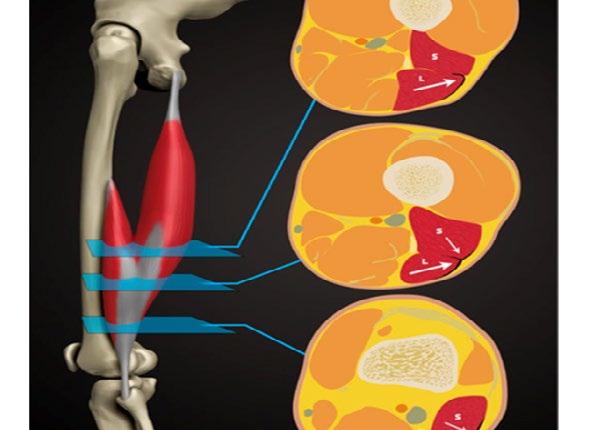
Figure 1: Reproduced from Entwisle et al. The anterolateral epimyseal surface of the long head (L) condenses to form the proximal portion of the distal musculotendinous junction. The opposing epimyseal condensations at the anterolateral aspect of the long head (L, large arrow) and the posterolateral aspect of the short head (S, small arrow) form the midportion of the distal musculotendinous junction that appears T-Shaped.
19 medicine & performance football www.fmpa.co.uk
T-Junction Injuries
It is not just intramuscular tendon injuries that have particularly high re-injury rates. Consideration needs to be given also to the distal hamstring, which may have its own characteristics. Kenneally-Dabrowski, et al. 12 noted that amongst a group of professional rugby players, distal hamstring injuries were the injuries typically classified as more severe. Entwisle, et al. 13 was the first to describe what is now known as the T-Junction of the distal hamstring. This is the confluence of the epimyseal surfaces of the biceps femoris long head and short head (Figure 1). These authors report re-injury rates for this sub-type of hamstring injury at 70% for the higher grade injuries, which must be the highest reported re-injury rate for any muscle injury. 13 Similarly, Kayani, et al. 14 noted 55% recurrence rates from conservatively managed injuries to this area. Shamji, et al. 7 in their group of professional footballers at Aston Villa found that most of the re-injuries they had, were indeed in the region of the T-Junction.
All in all, the existing data, and our experience, suggest that these are a particularly challenging injury tooperhaps even more challenging than intramuscular tendon injuries. These are not rare injuries – 18% of all hamstring injuries at Leinster Rugby over a 5-year period involved the T-Junction.
These injuries are difficult to diagnose without imaging. It is characteristic of T-Junction injuries that they present well early (perhaps due to limitations in clinical assessment in appropriately straining the T-Junction) and it is only when they progress through rehabilitation and reinjure that the severity becomes clear.
Thus, it is advocated that any acute distal hamstring injury should be treated with suspicion. The T-Junction confluence can be palpated in prone, located at the most distal component of long head where the short head condenses - usually 5cm (range 1.5-10) proximal to the knee joint space. A distal to proximal approach to palpation is advocated, to reach the thickening where the common insertion broadens to form two muscles, with short head the more lateral. While this is often a tender area even in an uninjured athlete, a side-to-side comparison should be a part of every hamstring assessment. In more severe injuries, an experienced practitioner may detect a defect.
While much of our understanding of the mechanism of hamstring injury comes from the likes of Thelen, et al. 15 who have described the kinematics of upright treadmill running, evasion sports such as football involve a mix of stretching and sprinting, in addition to stretching, reaching, changing direction and responding to opponents. Interestingly,
a recent study Gronwald, et al. 16 described using video analysis the mechanism of 52 hamstring injuries in elite German soccer. It was noteworthy that 27 of these were stretch type, and often occurred following contact from an opponent. This matches our own findings in rugby union, where trunk flexion and ipsilateral rotation were frequently associated with hamstring injury 17
In addition, while other authors have suggested that sprint type injuries tend to cause injury to the biceps femoris, and slow stretch type injuries to cause injury to semimembranosis, 18 19 our group have repeatedly detected a theme amongst athletes with T-Junction injuries (see Figure 2, reproduced from Kerin, et al. 17). Frequently these injuries occur during late swing phase (or early stance), with a rapid ipsilateral trunk rotation (often to catch a pass, make a tackle, reach for a ball or to look behind). If this is confirmed to be a pathognomic mechanism, it could be helpful in aiding clinicians and athletes in both detecting and optimally managing these challenging injuries. If this position is the position of injury, then we may consider ipsilateral trunk rotation in trunk flexion, hip flexion and knee extension a position of ‘end stage’ rehabilitation and periodise our exercise selection accordingly.

feature 20 info@fmpa.co.uk
Figure 2: Distal Biceps Femoris (T-Junction) injury during a braking and rotation task. Reproduced from Kerin et al. (2022)
Management of T-Junction Injuries
Pieters, et al. 17 (Figure 3) note that most athletes return to play following hamstring injury after 2-3 weeks, well before the optimal time point for healing. This time point is no doubt of particular importance in an injury like the T-Junction, with high re-injury rates, primarily in the early weeks. Respect must be given to pathology and healing time.

A strength of the tailored approach described by Macdonald, et al. 11 is that they were specific to the injured tissues
with consideration of intramuscular tendon versus other areas, but they did not differentiate between T-Junction and non-T-Junction injuries in their 2022 study. Nonetheless, they still achieved a miniscule re-injury rate, suggesting that this approach will work well for all injuries if consideration is given to BAMIC grading. It is still worthy of further consideration however, as to whether further modifications to the rehabilitation approach should be advocated given that the T-Junction has some unique characteristics, not least the contribution of the uniarticular short head muscle.
Rehabilitation
The return to sport process begins with the clinical assessment. Mechanisms associated with trunk rotation that present with symptoms in the distal half of the hamstring should be considered potential T-Junction injuries. Palpation of the confluence of the short and long head should be carried out, though sometimes it is generally a tender area even on the non-injured limb. In some more severe cases, the area can be boggy and swollen. Deep palpation may reveal a divot or loss of tension.
of
This should surely impact
some
of
Table 2: Specific exercise and running suggestions for a moderate to high grade T-Junction at 0-4, 4-6 and 6 weeks plus. Table 3: Suggested exercises at Early, Mid and Late Stages of rehabilitation of T-Junction injury Hip Dominant Knee Dominant Running 0-4 Moderate range isos and eccentrics - temp loading Moderate range isos and eccentrics - tempo loading Delayed - <70% linear only 4-6 Through range isos and eccentrics with multiplanar focus Through range isos and eccentrics <80% linear only 6+ Unanticipated and rapid focus Through range isos and eccentrics Curve, sport specific and 80%+ Early Stage Session Mid Strange Session Late Stage Session Knee Dominant Val Slide Curl to 3/4 range Single leg Natera Isometric - bent knee Prone Tempo Curl to 3/4 range Straight Leg Hamstring Bridge (load as appropriate) Single leg Natera Isometric weighted straight knee Seated Temp Hamstring Curl Cable eccentrics in hip flexion Single leg Isometric switches with trunk rotation Heavy eccentric tempo curls Hip Dominant GHR Isometric Rack Pull from above knees GHR through Range RDL/Rack Pull/SL RDL GHR with ball bounce or catch Bound to SL RDL Hip Extension Hip Thruster Hip Thruster Hip Thruster Glute Glute Work as Indicated Glute Work as Indicated Glute Work as Indicated Horizontal Force Heavy Sled Pushes Sled Acceleration Speed Linear Mechanics/ Angular Velocity Marching and Skipping OH A or B Skips 21
www.fmpa.co.uk
Figure 3: Reproduced from Pieters et al (2021). Following muscle injuries, footballers typically return after 2 to 3 weeks, several weeks before the end point
healing.
upon
aspects
load management, exercise selection and rehabilitation planning.
medicine & performance football
A major challenge of T-Junction injuries is that the initial examination may not reveal the extent of the injury, and the symptoms that do exist typically ease quickly. This may contribute to the high rate of early re-injuries, with athletes progressing too quickly as symptoms settle quickly and assessment normalises. It is possible that typical hamstring strength tests like single leg bridge and prone curl are simply not provocative enough to stress the T-Junction, either because they are not of sufficient rate of force development or because they are in a single plane. This is certainly one area for further research and conversation.
MRI is the probable imaging type of choice to confirm diagnosis, although dynamic ultrasound is also useful. Synchronous movement of the short and long heads during an isometric prone curl can be assessed and monitored as either a prognostic or progress indicator, though a reliable and valid protocol has yet to be described.
The suggested principles of a Grade 2 or 3 T-Junction injury are similar to those recommended by Macdonald, et al. 11 for intramuscular tendon injuries, and are described in Tables 2 and 3.
Regardless of clinical presentation, running is delayed for about two weeks, and subsequent running should be below 70% until 4 weeks post injury20 21. From 6 weeks, the athlete should gradually progress speed from 80 to 100% across several sessions, with the integration of curvilinear and reactive training (given the likely mechanism).
Hip and knee dominant exercises should be introduced early, using both isometric and eccentric exercises with the goal of maintaining eccentric strength and fascicle length to maintain the athlete’s hamstring conditioning in preparation for return to more challenging field-based activities. Suggestions for exercises across the stages are provided in Tables 2 and 3. In the early phase, range of motion should be capped in all exercises to avoid over stressing the healing area. Knee dominant exercises are likely to bias the distal hamstring and in particular the short head, so for this type of injury, these are considered high load 22. Slower, tempo-based exercises (both hip and knee dominant) are recommended to achieve time under tension and specific adaptation in both the proximal and distal hamstrings. Additional neuromuscular control, hip extension (thruster) and speed mechanics exercises should also
supplement the hamstring specific exercises throughout23 24
Given these injuries typically settle quickly, monitoring progression can be somewhat difficult. As a result, it is key to carry out a complete battery of assessment to guide progression, particularly ahead of the final phase of running (Figure 4). Strength deficits on the Nordic hamstring exercises or at outer range during isokinetic dynamometry have been noted following these injuries, while rate of force development during long lever bridges may be an area to further explore. Range of motion can sometimes be impacted, and the MHFAKE test should be monitored regularly25
Conclusion
• The anatomical location of hamstring injury (particularly the intramuscular tendon and distal T-Junction) may be associated with delayed return to play and higher re-injury rate
• Specific rehabilitation strategies have been shown by other authors to greatly reduce re-injury risk following intramuscular tendon injuries
• T-Junction injuries are a particular challenge to manage, given there is little evidence to guide conservative management
Indicators used to guide rehabilitation
T-Junction
Key Progression Indicators No tenderness Synchrony on Ultrasound Pain free bridge Nordic Split Stance Rack Pull Force on Force Plate IKDconcentric and eccentric SL Iso on Force Plate (Force and RFD) Speedmultiple exposures on curve and straight feature 22 info@fmpa.co.uk
Figure 4: Key Progression
of
injury
1. Ekstrand J, Walden M, Hagglund M. Hamstring injuries have increased by 4% annually in men’s professional football, since 2001: a 13-year longitudinal analysis of the UEFA Elite Club injury study. Br J Sports Med 2016;50(12):731-7. doi: 10.1136/bjsports-2015-095359 [published Online First: 2016/01/10]
2. van der Made AD, Almusa E, Reurink G, et al. Intramuscular tendon injury is not associated with an increased hamstring reinjury rate within 12 months after return to play. 2018(1473-0480 (Electronic))
3. Brukner P, Connell D. ‘Serious thigh muscle strains’: beware the intramuscular tendon which. Br J Sports Med 2016;50(4):205-8 LID - 10.1136/ bjsports-2015-095136 [doi].
4. Comin J, Malliaras P, Baquie P, et al. Return to competitive play after hamstring injuries involving disruption of the central tendon. Am J Sports Med 2013;41(1):111-5. doi: 10.1177/0363546512463679 [published Online First: 2012/11/01]
5. Pollock N, James SL, Lee JC, et al. British athletics muscle injury classification: a new grading system. Br J Sports Med 2014;48(18):1347-51. doi: 10.1136/bjsports-2013-093302 [published Online First: 2014/07/18]
6. Pollock N, Patel A, Chakraverty J, et al. Time to return to full training is delayed and recurrence rate is higher in intratendinous (‘c’) acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med 2016;50(5):305-10. doi: 10.1136/bjsports-2015-094657 [published Online First: 2016/02/19]
7. Shamji R, James SLJ, Botchu R, et al. Association of the British Athletic Muscle Injury Classification and anatomic location with return to full training and reinjury following hamstring injury in elite football. BMJ open sport & exercise medicine 2021;7(2):e001010. doi: 10.1136/ bmjsem-2020-001010 [published Online First: 2021/05/28]
8. McAuley S, Dobbin N, Morgan C, et al. Predictors of time to return to play and re-injury following hamstring injury with and without intramuscular tendon involvement in adult professional footballers: A retrospective cohort study. Journal of science and medicine in sport 2022;25(3):216-21. doi: 10.1016/j.jsams.2021.10.005 [published Online First: 2021/11/07]
9. Tears C, Rae G, Hide G, et al. The British Athletics Muscle Injury Classification grading system as a predictor of return to play following hamstrings injury in professional football players. Physical Therapy in Sport 2022;58:46-51. doi: https://doi.org/10.1016/j.ptsp.2022.08.002
10. van der Made AD, Almusa E, Reurink G, et al. Intramuscular tendon injury is not associated with an increased hamstring reinjury rate within 12 months after return to play. Br J Sports Med 2018;52(19):1261-66. doi: 10.1136/bjsports-2017-098725 [published Online First: 2018/04/15]
11. Macdonald B, McAleer S, Kelly S, et al. Hamstring rehabilitation in elite track and field athletes: applying the British Athletics Muscle Injury Classification in clinical practice. Br J Sports Med 2019;53(23):1464-73. doi: 10.1136/bjsports-2017-098971 [published Online First: 2019/07/14]
12. Kenneally-Dabrowski C, Serpell BG, Spratford W, et al. A retrospective analysis of hamstring injuries in elite rugby athletes: More severe injuries are likely to occur at the distal myofascial junction. Phys Ther Sport 2019;38:192-98. doi: 10.1016/j.ptsp.2019.05.009 [published Online First: 2019/06/09]
13. Entwisle T, Ling Y, Splatt A, et al. Distal Musculotendinous T Junction Injuries of the Biceps Femoris: An MRI Case Review. Orthop J Sports Med 2017;5(7):2325967117714998. doi: 10.1177/2325967117714998 [published Online First: 2017/08/11]
14. Kayani B, Ayuob A, Begum F, et al. Surgical Repair of Distal Musculotendinous T Junction Injuries of the Biceps Femoris. Am J Sports Med 2020;48(10):2456-64. doi: 10.1177/0363546520938679 [published Online First: 2020/08/02]
15. Thelen DG, Chumanov ES, Hoerth DM, et al. Hamstring muscle kinematics during treadmill sprinting. Med Sci Sports Exerc 2005;37(1):10814. doi: 10.1249/01.mss.0000150078.79120.c8 [published Online First: 2005/01/06]
16. Gronwald T, Klein C, Hoenig T, et al. Hamstring injury patterns in professional male football (soccer): a systematic video analysis of 52 cases. Br J Sports Med 2022;56(3):165-71. doi: 10.1136/bjsports-2021-104769 [published Online First: 2021/12/09]
17. Kerin F, Farrell G, Tierney P, et al. Its not all about sprinting: mechanisms of acute hamstring strain injuries in professional male rugby union-a systematic visual video analysis. Br J Sports Med 2022;56(11):608-15. doi: 10.1136/bjsports-2021-104171 [published Online First: 2022/01/21]
18. Askling CM, Tengvar M, Saartok T, et al. Acute first-time hamstring strains during slow-speed stretching: clinical, magnetic resonance imaging, and recovery characteristics. Am J Sports Med 2007;35(10):1716-24. doi: 10.1177/0363546507303563 [published Online First: 2007/06/15]
19. Askling CM, Tengvar M, Saartok T, et al. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med 2007;35(2):197-206. doi: 10.1177/0363546506294679 [published Online First: 2006/12/16]
20. Dorn TW, Schache AG, Pandy MG. Muscular strategy shift in human running: dependence of running speed on hip and ankle muscle performance. J Exp Biol 2012;215(Pt 11):1944-56. doi: 10.1242/jeb.064527 [published Online First: 2012/05/11]
21. Schache AG, Dorn TW, Blanch PD, et al. Mechanics of the human hamstring muscles during sprinting. Med Sci Sports Exerc 2012;44(4):64758. doi: 10.1249/MSS.0b013e318236a3d2 [published Online First: 2011/09/14]
22. Hegyi A, Csala D, Peter A, et al. High-density electromyography activity in various hamstring exercises. Scand J Med Sci Sports 2019;29(1):3443. doi: 10.1111/sms.13303 [published Online First: 2018/09/20]
23. Sugiura Y, Saito T, Sakuraba K, et al. Strength Deficits Identified With Concentric Action of the Hip Extensors and Eccentric Action of the Hamstrings Predispose to Hamstring Injury in Elite Sprinters. Journal of Orthopaedic & Sports Physical Therapy 2008;38(8):457-64. doi: 10.2519/jospt.2008.2575
24. Mendiguchia J, Edouard P, Samozino P, et al. Field monitoring of sprinting power-force-velocity profile before, during and after hamstring injury: two case reports. Journal of sports sciences 2016;34(6):535-41. doi: 10.1080/02640414.2015.1122207 [published Online First: 2015/12/10]
25. Whiteley R, van Dyk N, Wangensteen A, et al. Clinical implications from daily physiotherapy examination of 131 acute hamstring injuries and their association with running speed and rehabilitation progression. Br J Sports Med 2018;52(5):303-10. doi: 10.1136/bjsports-2017-097616 [published Online First: 2017/11/01]
23 medicine & performance football www.fmpa.co.uk
ROLE OF THE SPORT SCIENTIST IN ELITE FOOTBALL & BEING A WOMAN IN THE FOOTBALL INDUSTRY
This is a transcript of the FMPA Podcast episode of the same name that was released in April 2022. It has been edited for clarity and to improve readability. It was transcribed by the host.
If you’d prefer to listen, episodes can be found on the FMPA website, Apple Podcasts, SoundCloud and Spotify.
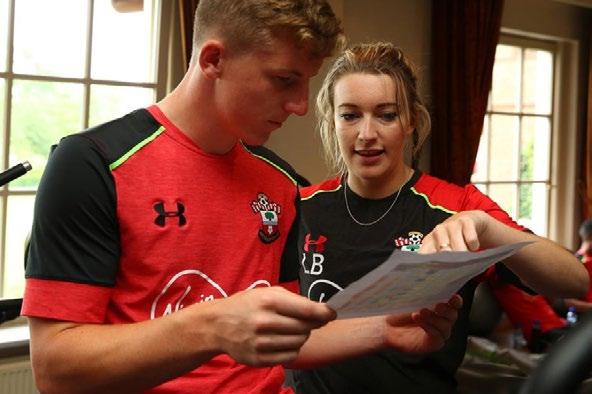
Elle
Welcome to this Football Medicine and Performance podcast. I’m Elle Trezise, a medical student in London and your host for today’s episode. Today I’m delighted to be joined by Dr Laura Bowen. Laura is the lead sport scientist for Southampton FC Women and Girls and in the past worked as a sport scientist with Southampton’s Men’s First Team. She also works as a consultant at FIFA. She has done a PhD on workloads and injury risk in Premier League football and has a bachelor’s degree in Sports and Exercise Sciences, both from the University of Birmingham. Thank you for joining us today, Laura.


Laura
Thank you for having me. It’s exciting. Thank you for asking.
Elle
Good to have you on board. Today we’re going to discuss the work you do as a sport scientist in elite football, as well as your experience being a woman working in this industry.
Tell us a bit about your career to date. What got you interested in sport science and what drew you to working in elite football?
Laura
I played football from when I was a little kid. I grew up in an estate with boys. So, we’d just go out and play on the fields all afternoon and that’s how I got into football. When I got a little bit older, I realised I was never going to be a player. I’m not very good at playing and I think you’ll find most those of us that end up as sport scientists… it’s usually because we’re not good enough to play or we’ve played, and now retired.
As part of my dissertation at Uni we got the opportunity to work within a football club and that’s really where I jumped at the opportunity. I got into sport science because I love sport and it’s what made me confident and then I got the opportunity to work in a football club. So, I went to Villa and then I did my dissertation there and they offered me a job at the end of it because they needed a nerd to sit at a computer and crunch all the GPS numbers which was brand new at the time and that suited me perfectly. I saw it as a foot in the door.
Then I moved over to Southampton to do almost the same job in their academy there. I have been at SFC ever since, working with the academy first as a GPS analyst, then as a sport scientist before moving into the First Team. Again, started out crunching the numbers. Then was a bit more hands on, getting involved in rehabs and conditioning sessions. Then about a year ago I moved to the women’s team. It’s the first time I’ve led a squad as the lead sport scientist which is really nice too.
Elle
That’s really interesting. What does your typical day as a sport scientist look like?
Laura
At the moment or in the past?
Elle
It’d good to make the distinction actually. It’d be interesting to see how it does compare.
As we were discussing before we hit record when you were working with the men’s first team it was a very packed schedule. The women’s team’s schedule is not as packed at the moment because the team is in tier three
and so not yet full-time. So yeah, maybe give us some insight into how a typical day differs between the two.
Laura
With the men’s team I was in most days. You’d have a meeting first thing in the morning with all the backroom staff whether that be the doctors, physios, soft tissue therapists, sport science, strength conditioning. Everyone would map out the day and where you can all support each other best with a player-centred approach. From there, it would be potentially taking rehab sessions in the morning or getting things ready for the squad and then going out. Monitoring the training sessions for the ones that are in the squad or being out taking a rehab session, crunching all those numbers, making reports in the afternoon and then being in the gym, being around the team again, supporting in there. And then at the end of the day, you’d sort of bring it all together and plan for the next day. Quite fast paced and very reactive. But really a lot of planning, a lot of reacting to numbers and modifying things for the next day. In terms of my role anyway.
Now with the women’s team we train at night. So, I’ve been practising trying to turn my mornings into evenings and chill out [in the mornings]. From about 12 o’clock I go in. Again, sort of similar, we have a meeting amongst the staff but there’s less of us. It’s quite nice because within that meeting is the coaching team as well which is different from the men’s team where the backroom staff and coaching team are a bit more separate. Now it’s all together and we plan training as a group. From that point on, it’s making reports from the previous day,
FEATURE / DR. LAURA BOWEN INTERVIEW BY ELLE TREZISE
Eleanor Trezise
In this podcast episode host Elle Trezise, a medical student and member of the FMPA Education Team, speaks to Lead Sport Scientist for Southampton FC Women and Girls Dr. Laura Bowen.
Dr. Laura Bowen
feature 24 info@fmpa.co.uk
planning gym programmes and actually a lot of things that you wouldn’t necessarily expect to come under a sport science umbrella. So, making sure food is ordered for the weekend or making sure someone’s got the right size kit. It’s a lot of running around and doing jobs that sort of fit in as ad hoc duties. And then when the girls come in, especially because they have jobs as well, they come in at different times. So, being around for different gym and rehab slots that fit in around their other schedules. Then being around for a training session, taking warm-ups, taking conditioning sessions, advising the coach on, you know, “do we do one more small-sided game or do we come out?” Then more gym sessions after training. Then obviously being around on a matchday, supporting, taking warm-ups.
Elle
Thank you for that. I think that leads quite nicely into the next question.
I imagine it’s one thing to record the data and to analyse it, but quite another to
communicate it to coaching staff, other support staff, players, as well as to get buy in. So, in your experience what’s the best way to communicate the important metrics to players and other staff and what helps to get buy in?
Laura
I thought about this question because I think it’s something that took me longer than it should have to learn. The best way to get buy in and to get that information across is to ask them what they want. What do they want to know? What answers do they want from the data? For most coaches it’s “did we hit…?” Or “do we want to hit…? Are we preparing them for games?” and then using whatever metrics they’re comfortable with for answering their question.
Hopefully by now I have a reasonable experience of what the numbers actually mean. [The coaches] don’t need to know what they mean. It’s more around the conversation of, “today was extensive. Tomorrow we could maybe go a little bit
more intensive and make the pitch sizes smaller.” I think that conversation is really important.
And then with the players, again, I think it’s very important to have a conversation. Usually, they want to know who’s ran the most, who’s ran the fastest, who’s done the most accelerations. Whatever it is you’re looking at, I think it’s about giving them context behind that. Running the most doesn’t mean that you’ve performed the best. Running the fastest doesn’t mean you’ve performed the best. You might be sprinting max out because you’re out of position. It’s about having the conversation around the context and then, hopefully, building those relationships over time helps to build buy in.
Elle
Do you mind expanding a bit on the way that you have found you can build relationships to get buy in?
Laura
It’s different for everybody. For example, Marieanne who’s the head coach of the women’s team now, she’d much rather have a conversation that doesn’t involve a report. But learning that over time, you know. Getting into a position where you’re providing answers, where you’re open. You leave your ego at the door a little bit and do whatever is best for the players and show that that’s what you’re in it for.
I’ve worked with other coaches who were very interested in seeing the numbers. But they don’t always understand what they mean. They just like to see the numbers and then hopefully over time you can make little inroads into showing that you’re interested in just getting the best out of the players. Whatever they want, understanding how they want to play - I think it’s important.
I always try to understand what the coach wants out of the team rather than just being like, “I’m a sport scientist so I don’t need to know tactics”. Using the same terminology and understanding the way they want to play. Understanding where they see players fitting within the group. Understanding the player if they’ve just been dropped from the squad and then you tell them they’ve ran the least in the training session… understanding them as people, I think that’s what helps.
Elle
Yeah, that makes a lot of sense. So, in your opinion, at elite level, what’s the most effective way sport scientists and medics, physios, doctors, etc, can work together to optimise the physical performance of players and reduce their injury risk?
It’s about having the conversation around the context and then, hopefully, building those relationships over time helps to build buy in.
25
& performance
www.fmpa.co.uk
Photo: Southampton FC
medicine
football
 Laura
Laura
In a similar way, good communication and removing your own ego. Building trust as a team, understanding that everybody is there to get the best out of the players. So, if I suggest doing something and you suggest doing something and they’re against each other, they’re against each other but only because you’re doing what you think is best and I’m doing what I think is best. How can we reach a compromise? Or how can we at least understand where the other person is coming from?
Always have the players in the centre and not “I want to do this testing because it makes me look good.” Instead, more “what do the players actually need in this moment?”
I think the most success that I’ve ever seen is a team that actually works together and has each other’s backs because there’s lots of different ways of approaching things. I think you’re lying if you say there’s one answer but it’s at least just understanding that everyone is going for the same thing and where the benefits lie.
Elle
It sounds like you’re really saying to keep it player-centred and remember that you’ve all essentially got the same goal which is to support the players and the performance of that team.
Laura Yeah.
Elle
Moving on now to your experience being a woman working in the men’s professional game. What was that like? I ask because I imagine it is a different experience working with the Women and Girls programme, which you transferred across to just over a year ago, after previously working with the Men’s First Team at Southampton for a number of years.
Laura
Yeah. What was it like? Challenging is probably the best way that I can phrase it. Not necessarily in a bad way. It’s a professional environment and there’s very high standards. It is very fast paced. There’s a lot of experts so you learn a lot. Also challenging because in my opinion, as a female in that environment you have to prove yourself a lot. A lot more than maybe a man would. Because it’s so male dominated you instantly look out of place. If you’re one or two of the only females in the room and someone new walks in, it’s a bit of a shock especially if they’ve been at other clubs where there’s perhaps not females and you have to prove yourself over and over, I think.
I learnt a lot. The men’s game is ahead of the women’s game. It’s been going for longer. There’s a lot of experts in the field. There’s a lot of money. There’s a lot of experience. So, I got the opportunity to work with some incredible practitioners and some incredible athletes. I think being a woman in a male dominated environment, especially in football, it’s come a long way. But there’s still a long way to go. That’s probably the fairest way to put it.
Elle
Keeping that in mind, what advice would you have for women aspiring to have a successful career in elite football? In fact, anyone looking to achieve similar things to yourself regardless of gender?

Laura
I would say be passionate about it. Show who you are as a person and don’t lose that. Stay true to your values. I would like to think that the environment is changing but the biggest changes are made when there is a shift in mindset. It is not about anybodymale or female - belonging or not belonging in that environment. It’s about the mindset of everyone that is professional within a professional environment. So be yourself. Stay true to your values and be passionate because there’s a lot of people who want these jobs but it’s a lot of time and a lot of commitment. You have to really love it. And you have to keep showing it.
Elle
That’s great. Now for the last question.
Some say there is a bias in football and it is a barrier to women getting certain positions. In fact, a previous guest who came on the pod, Rachel Davis who is head of physiotherapy at Harrogate Town FC, said this in her episode
with us. Do you agree with this? If so, do you have any views about how this could be addressed?
Laura
You know, I do agree with it. I think probably one of the best ways to address it is to be open and upfront about it. It’s not just in football. Lots of industries will talk about how women don’t apply to roles or they have a lot less females applying to roles than males. You can see from the environment that football is very male dominated still. So, you can’t say there’s not that issue there.
I think, again, it’s about changing mindset. The old school mindset might be that women in football are a distraction, but it’s actually about professionals being professionals and treating each other that way. I think everybody deserves respect and to be valued for whoever they are. I think most companies are striving for that now and it is getting there. You’re only narrowing your talent pool otherwise, right?
Elle
Yeah, that’s fair. Well, thank you so much, Laura. Thank you for coming on the podcast today and for giving up your time. I found that really interesting and insightful. I’m sure the listeners have too.
Laura
Thank you very much for having me. Elle
Listeners, if you enjoyed today’s episode, please subscribe to the FMPA podcast on Spotify, SoundCloud or Apple Podcasts. Alternatively, please check out the podcast section of the FMPA website. Thank you for listening to the Football Medicine and Performance Podcast. Have a great day.
27 medicine & performance football www.fmpa.co.uk
Photo: Southampton FC
UNDERSTANDING THE RECTUS FEMORIS ANATOMY, DIAGNOSIS & TYPES OF INJURIES
FEATURE / CARLES PEDRET1, IÑIGO IRIARTE2, SANDRA MECHÓ3
Rectus Femoris anatomy
The rectus femoris is a long and fusiform muscle that is part of the femoral quadriceps group. It is located at the most superficial and anterior position. It is the only one that crosses two joints (hip and knee) and has a high proportion of type II muscle fibers, being both circumstances related to a greater tendency to injure1. The distribution of the muscular and connective components of the rectus femoris is key to understand its injuries and will be reviewed here.
The rectus femoris has a proximal and a distal myoconnective junction. At the proximal one, which is the most commonly injured, the rectus femoris originates from 2 tendons mainly. A direct (straight) tendon that originates from the anteroinferior iliac spine (AIIS) and an indirect (reflected) tendon that originates from the acetabular margin and hip capsule. Recently Mechó et al reported a third component, a connective membrane originating from the anterosuperior iliac spine reaching the conjoint tendon2. Both tendons merge a few centimetres distal to its origin, forming the conjoint tendon with the direct tendon located anterior and superficial and the indirect deep and posterior3. The muscular component initiates at this level below the direct tendon and lateral to the indirect tendon (Figure 1).
Most of the fibers of the direct tendon will continue superficial to the muscle, conforming an aponeurotic expansion that becomes broader and thinner covering the proximal third of the muscle´s length, and eventually fusing with the anterior fascia.
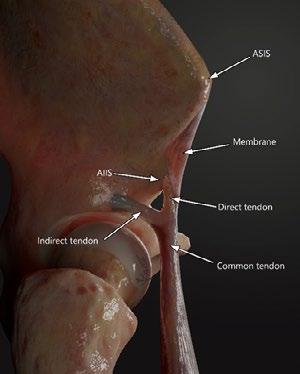
On the other side, the indirect tendon, is located medially to the muscular component. Its oval shape progressively changes as it goes distal, getting thinner and longer in a sagittal plane adopting a coma shape at first and flat at the end. It also changes its relative muscular position from medial to the centre forming the called intramuscular central tendon. Finally, it ends at the distal third of the muscle.
The distal myotendinous junction arises in the proximal third of the rectus femoris on
Figure 1. Illustration of a lateral overview of a right thigh showing the tendinous origin of the rectus femoris. AIIS: Antero inferior iliac spine; ASIS: Antero superior iliac spine
its posterior face. The connective tissue thickens as it advances distally forming the posterior aponeurosis. The muscular component ends quite proximally, about 15 cm from the superior border of the patella, leaving a free tendon that forms the superficial layer of the quadricipital tendon, the intermediate layer being formed by the vastus medialis and lateralis, and the deep layer being formed by the vastus intermedius. They all insert on the superior border of the patella.
Introduction and epidemiology
Muscle injuries are the most common injuries in sports, accounting for more than 30% of injuries in football players. The hamstring muscle group injuries are the most frequent non-contact injuries according to epidemiologic studies4–7 with an increasing incidence and a really high reinjury risk. Rectus femoris (RF) injuries are approximately 4.6% of all football injuries and have a reinjury incidence of about 15,6% 8–10
An early and accurate diagnosis is essential to determine the most appropriate course
of treatment. For that purpose imaging tests are gold standard, specifically magnetic resonance imaging (MRI) which can accurately identify the exact anatomical location of the injuries, the presence or absence of oedema, its type and its extension and the amount of connective tissue involved (intramuscular tendon injuries)11–15. It is known that tendon involvement (as a free tendon or as a intramuscular tendon/aponeurosis) is associated with a longer return to play (RTP) and with a higher reinjury risk16–18
As we have seen, the anatomy of the RF is highly complex and given this complexity of its anatomy and its connective tissue distribution, different types of injuries can occur. Classification of such injuries is challenging as many injuries cannot be classified with the traditional muscle strain classification systems19
Diagnosis
As in any muscle injury, it is essential to have a diagnosis as early as possible including imaging tests (MRI and/or ultrasound scan) and clinical assessment to accurately prepare for the RTP decision-making process, which allows medical staff to support the athlete’s RTP as soon as possible with a reasonable re-injury risk.
If we understand the injury mechanism and the biomechanics of the RF, and the clinical assessment suspects a RF injury, MRI is required in the first 48-72 hours to confirm the diagnosis. MRI provides details that ultrasound can’t, especially small transversal gaps or longitudinal splits in connective tissue structures (i.e. in the proximal region of the RF where ultrasound is limited due to the different trajectories and disposition of the RF direct tendon, the reflected tendon or the conjoint tendon)20. Once the correct diagnosis has been stablished, the most appropriate treatment is decided, depending on the injury type and specifically on the amount and location of connective tissue affected21–23. Ultrasound scan can also be used in the initial diagnosis and also for follow-up as it provides useful information about the injury, but it is important to note it doesn’t reach the detail level of an MRI.
1. Sports Medicine and Imaging department. Clínica Diagonal. Barcelona
2. Physical Medicine and Rehabilitation department. Clínicas Ars Médica. Bilbao
3. Radiology department Hospital de Barcelona-SCIAS. Barcelona
feature 28 info@fmpa.co.uk
Types of injuries in the Rectus femoris
Most injuries affecting the RF muscle can be managed with rehabilitation and physiotherapy treatment normally based in a progressive exercise protocol tailored individually for every case. But for that, we need to define the different types of injuries that could occur in the RF.
Proximal injuries
In this region we can consider injuries affecting the proximal tendons complex. As we have seen in the anatomy section injuries in the proximal part of the RF can be located in the direct tendon (DT), the indirect tendon (IT), the conjoint tendon or any kind of combination.
Due to its particular anatomy, severe injuries affecting the DT and the IT require, normally, surgical treatment especially in professional players22 in order to avoid loss of function and also to decrease the incidence of reinjuries.
In childhood, avulsion of the anterior inferior iliac spine is not uncommon. The weakest point in the muscle-tendon-bone chain in very young athletes is the unfused physis. Fusion of the secondary ossification centre of AIIS occurs at 16 years of age 23, so children under 16 years of age are at greater risk of suffering a bone avulsion than a tendon injury. In subacute or chronic lesions, the healing process can produce images heterogeneous characteristics that can mimic with some aggressive pathologies and could misinterpreted as a tumour lesion, but the location and the traumatic history help to avoid misinterpretation 17

In case of tendinous injuries, in order to decide the treatment we need to consider if there is a complete transversal rupture of any of these tendons and/or if there is loss of tension or retraction24. It is important to understand that the proximal region of the RF is subjected to high workloads and functional stress, especially in football players.
There is another injury located in the proximal region of the RF which is the rupture of the anterior and superficial aponeurotic expansion (coming from the DT). This concrete injury
is well tolerated by players (sometimes is completely underdiagnosed because they don’t complain about it). The treatment is conservative, and the prognosis is good with a fast RTP. But there is an exception; injuries that occur close to the border of the anterior aponeurosis with the central septum (Figure 3) have a high rate of reinjury. It is possible that the divided distribution of the transmission of forces is the cause of the high tendency to reinjury. It is important not to confuse them with conjoint tendon injuries (sometimes similar in terms of imaging).
 Figure 2. Coronal Proton Density Fat Saturated images of different injuries in the proximal region of the rectus femoris. A) Complete transversal tear of the DT in its preinsertional portion (arrow). B) Partial longitudinal tear of the IT in its insertional portion (arrow). In this case the IT shows as variant of normality an inferior band with a tear (arrowhead). C) Complete transversal tear of the conjoint tendon (arrow) with longitudinal extension to the DT
Figure 3. Axial Proton Density Fat Saturated image of a tear of the anterior aponeurotic expansion of the DT (arrow). Injury close to the junction with the central tendon.
Figure 2. Coronal Proton Density Fat Saturated images of different injuries in the proximal region of the rectus femoris. A) Complete transversal tear of the DT in its preinsertional portion (arrow). B) Partial longitudinal tear of the IT in its insertional portion (arrow). In this case the IT shows as variant of normality an inferior band with a tear (arrowhead). C) Complete transversal tear of the conjoint tendon (arrow) with longitudinal extension to the DT
Figure 3. Axial Proton Density Fat Saturated image of a tear of the anterior aponeurotic expansion of the DT (arrow). Injury close to the junction with the central tendon.
29 medicine & performance football www.fmpa.co.uk
Injuries affecting the central tendon
The central tendon is the most common site of RF injury in football20, 25. Injuries affecting the intramuscular aponeurosis of the RF are one of the injuries with more peculiarities and controversies that exist in sport.
The central tendon of the RF is one of the most important structures in the quadriceps muscle group and it’s an intramuscular expansion of the IT that conditions completely the function and biomechanics of this muscle. It acts like a whip when kicking, recruiting fibres all along its trajectory and releasing them abruptly to generate more power (also when accelerating, sprinting and decelerating). The presence of the central tendon conditions the bipennate aspect of the inner part of the RF and develops also a myoconnective junction that is significantly overloaded (especially during pre-season in kicking sports, e.g., football).
Injuries at this location are severe, especially in football players. Its treatment is initially with rehabilitation but there are some factors to consider. Injuries affecting the proximal part of the central tendon have worse prognosis than those affecting the distal part23. Also, injuries with extension to the conjoint tendon, with loss of tension or reinjuries, should be considered for surgical treatment21
Another important concept is if the injury affects the central tendon itself or if it is a myoconnective (myotendinous) injury. The first group of injuries can be seen as a complete transversal gap (named “bull’s-eye” lesions) or longitudinal splits (Figure 4A, 5A). Myotendinous injuries are those that produce a rupture of the muscle fibres attached to the central tendon but without affection of the latter (Figure 4B, 5B). Usually this type of injury occurs within an overloaded muscle8 They imply a better prognosis than those affecting the central tendon.
Finally, the degloving injury that involves the indirect myotendinous complex of the RF whereby the inner bipennate muscle belly is separated and dissociated from the superficial unipennate muscle. Such dissociation may lead to retraction of the inner muscle belly25. This injury is the explanation of why, colloquially, we speak about the RF as a muscle within a muscle (Figure 4C, 5C). In those cases where there is no retraction of the inner muscle belly, signs of muscle rupture in the distal portion of the myotendinous junction can be identified by MRI, but the dynamic study by ultrasound ends up being the most optimal diagnostic test at the time of demonstrating a muscle gap26
Figure 4. Coronal Proton Density Fat Saturated images of different injuries in the central tendon. A) Complete transversal tear of the central tendon in its middle portion (arrow). There is tendon retraction and extensive interstitial oedema. B) Myotendinous injury. Rupture of the muscle fibers attached to the central tendon (arrows) without affection of the central tendon itself. C) Degloving injury. Distal muscular fibers tear, with paraseptal muscle tears that extend cranially. Severe retraction of the central tendon myoconnective junction.

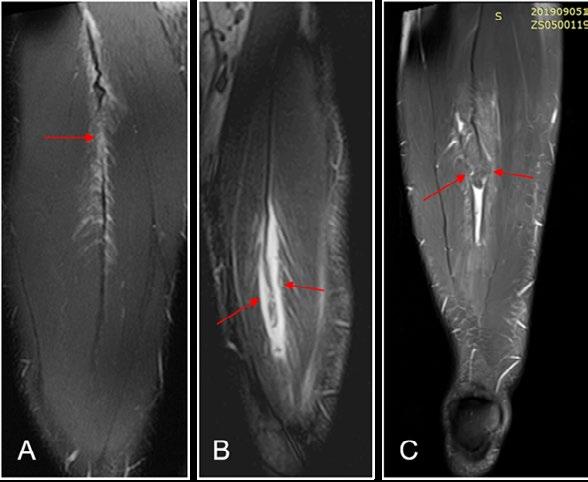
If we try to classify injuries affecting the central tendon of the RF in terms of prognosis, we can say that the worst prognosis is for those affecting the central tendon itself followed by the myotendinous injuries with central tendon retraction and finally the degloving injuries. This is in general, as always there is the need to individualise and contextualise every injury.
Myofascial injuries of the RF
Myofascial or fascial injuries affecting the RF are the clearest example to understand what exactly a myofascial injury is. They are normally located in the
proximal, posterior and lateral region of the RF and are very well tolerated clinically and have a good prognosis20. The treatment is with progressive rehabilitation protocols depending on player subjective feedback, clinical tests and strength tests. The RTP time will vary depending if the injury is myofascial (without affecting the fascia itself) or fascial (with a rupture of the fascia). In case of fascia rupture, bleeding is in the intermuscular space and large haemorrhages can occur, whereas in case of no rupture, bleeding is contained in the intramuscular compartment12. In both cases, the RTP time is normally less than 3 weeks (Figure 6).
Figure 5. Ultrasound transverse images of different injuries in the central tendon. A) Partial central tendon tear in the posterior portion with interstitial oedema of the myotendinous junction (arrow). B) Myotendinous injury. There is a muscular fibre tear (arrow) and muscular oedema related to overload status. The central tendon is normal. C) Degloving injury. Paraseptal tears surrounding the myotendinous junction of the central tendon.
31 medicine & performance football www.fmpa.co.uk
Distal injuries. Posterior aponeurosis of the RF
In the distal part of the RF we can find injuries that affect the posterior aponeurosis of the RF which can mimic the injuries affecting the distal myotendinous junction (MTJ) of the medial gastrocnemius (MG)27 This injury produces a rupture in the posterior aponeurosis of the RF. It is very close to the quadriceps tendon (in fact there is a continuity between the RF posterior aponeurosis and the quadriceps tendon). Depending on how much the posterior aponeurosis is affected, a variable amount of intermuscular haematoma between RF and vastus intermedius can be found. If there is a complete rupture of the posterior aponeurosis, a proximal retraction of the RF muscle could be seen (the clinical image is a stump in the middle of the anterior thigh with a RF contraction). As in the MG this injury can have an extension to the fibres of the quadriceps tendon corresponding to the RF component. All of these factors influence the injury prognosis. Initially this injury is considered to have a rehabilitation protocol as the main treatment (ultrasound guided drainage of the intermuscular haematoma could be necessary) but, in cases where there is a severe retraction or after some reinjuries where the tissue is completely degenerated, surgical treatment can be also considered (Figure 7).


Conclusions
There is a wide range of injuries that can affect RF and they have a great variation in terms of prognosis and treatment options depending on the exact structure affected.
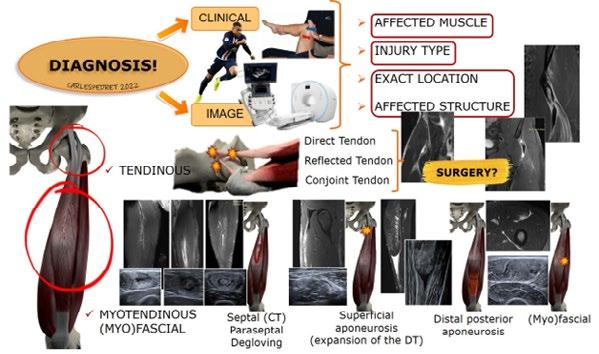
The main objective when suspecting a musculotendinous RF injury is to plan the RTP process in the most correct and individualized way. For that purpose, it is essential to have a diagnosis as early and accurate as possible to know which exact injury we are facing.
Once the diagnosis is confirmed, the treatment options are much clearer and planning the RTP process becomes “easier” (you can’t treat what you don’t know). The decision between rehabilitation or surgical treatment should be made depending on the injury type and the affected structure.
It is also important to consider other key points during the RTP process that are not only clinical tests, strength test or imaging tests. These include individual internal risk factors (genetics, age, previous injuries etc), external risk factors (overload or overtraining during the RTP process, training or technical mistakes, fatigue…), lumbo-pelvic stability control or other factors such as recovery, sleep and nutrition.
Figure 6. Axial proton density fat saturated image (A) and transversal ultrasound corresponding image(B) of a myofascial injury. Myofascial injury with rupture of the fascia, there is interstitial oedema and intermuscular fluid (arrowhead)
feature 32 info@fmpa.co.uk
Figure 7. Sagittal STIR (short tau inversion recovery) image (A) and longitudinal ultrasound (B) of distal portion of the RF. Complete rupture of the posterior aponeurosis with proximal retraction of the RF and moderate intermuscular haematoma (arrow). Usually these injuries go with an extensive interstitial oedema in the distal myoaponeurotic junction (arrowhead).
1. Johnson MA, Polgar J, Weightman D, Appleton D. Data on the distribution of fibre types in thirty-six human muscles. An autopsy study. J Neurol Sci. 1973 Jan;18(1):111–29.
2. Mechó S, Iriarte I, Pruna R, Pérez-Andrés R, Rodríguez-Baeza A. A newly discovered membrane at the origin of the proximal tendinous complex of the rectus femoris. Surg Radiol Anat. 2022 Jun;44(6):835–43.
3. Hasselman CT, Best TM, Hughes C, Martinez S, Garrett WE. An Explanation for Various Rectus Femoris Strain Injuries Using Previously Undescribed Muscle Architecture. Am J Sports Med. 1995;23(4):493–9.
4. Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–32.
5. Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football: The UEFA injury study. Br J Sports Med. 2011;45(7):553–8.
6. Hägglund M, Waldén M, Ekstrand J. UEFA injury study - An injury audit of European Championships 2006 to 2008. Br J Sports Med. 2009;43(7):483–9.
7. Ekstrand J, Waldén M, Hägglund M. Hamstring injuries have increased by 4% annually in men’s professional football, since 2001: A 13-year longitudinal analysis of the UEFA Elite Club injury study. Br J Sports Med. 2016;50(12):731–7.
8. de Visser HM, Reijman M, Heijboer MP, Bos PK. Risk factors of recurrent hamstring injuries: a systematic review. Br J Sports Med [Internet]. 2012 Feb 1;46(2):124 LP – 130. Available from: http://bjsm.bmj.com/content/46/2/124.abstract
9. Ekstrand J, Healy JC, Waldén M, Lee JC, English B, Hägglund M. Hamstring muscle injuries in professional football: The correlation of MRI findings with return to play. Br J Sports Med. 2012;46(2):112–7.
10. Rudisill SS, Kucharik MP, Varady NH, Martin SD. Evidence-Based Management and Factors Associated With Return to Play After Acute Hamstring Injury in Athletes: A Systematic Review. Orthop J Sport Med. 2021;9(11):1–14.
11. Isern-Kebschull J, Mechó S, Pruna R, Kassarjian A, Valle X, Yanguas X, et al. Sports-related lower limb muscle injuries: pattern recognition approach and MRI review. Insights Imaging. 2020;11(1).
12. Patel A, Chakraverty J, Pollock N, Chakraverty R, Suokas AK, James SL. British athletics muscle injury classification: A reliability study for a new grading system. Clin Radiol [Internet]. 2015;70(12):1414–20. Available from: http://dx.doi.org/10.1016/j.crad.2015.08.009
13. Valle X, Mechó S, Pruna R, Pedret C, Isern J, Monllau JC, et al. The MLG-R muscle injury classification for hamstrings. Examples and guidelines for its use. Apunt Med l’Esport [Internet]. 2019 Apr 1 [cited 2020 Sep 14];54(202):73–9. Available from: https://linkinghub.elsevier. com/retrieve/pii/S1886658118300422
14. Baldock J, Wright S, Mcnally E, Wedatilake T. Intratendinous hamstring injuries: Sequential MRIs as a tool to reduce the risk of reinjury in elite sport. BMJ Case Rep. 2021;14(11):1–5.
15. Traumatology SG of the M and TS from the SS of S, Balius R, Blasi M, Pedret C, Alomar X, Peña-Amaro J, et al. A Histoarchitectural Approach to Skeletal Muscle Injury: Searching for a Common Nomenclature. Orthop J Sport Med [Internet]. 2020 Mar 20;8(3):2325967120909090–2325967120909090. Available from: https://pubmed.ncbi.nlm.nih.gov/32232071
16. Pollock N, Patel A, Chakraverty J, Suokas A, James SLJ, Chakraverty R. Time to return to full training is delayed and recurrence rate is higher in intratendinous (‘c’) acute hamstring injury in elite track and field athletes: Clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med. 2016;50(5):305–10.
17. Macdonald B, Mcaleer S, Kelly S, Chakraverty R, Johnston M, Pollock N. Hamstring rehabilitation in elite track and field athletes: applying the British Athletics Muscle Injury Classification in clinical practice. Br J Sports Med [Internet]. 2019;bjsports-2017-098971. Available from: http:// bjsm.bmj.com/lookup/doi/10.1136/bjsports-2017-098971
18. Shamji R, James SLJ, Botchu R, Khurniawan KA, Bhogal G, Rushton A. Association of the British Athletic Muscle Injury Classification and anatomic location with return to full training and reinjury following hamstring injury in elite football. BMJ Open Sport Exerc Med. 2021;7(2).
19. Balius R, Pedret C, Kassarjian A. Muscle Madness and Making a Case for Muscle-Specific Classification Systems: A Leap from Tissue Injury to Organ Injury and System Dysfunction. Sport Med [Internet]. 2021;51(2):193–7. Available from: https://doi.org/10.1007/s40279-020-01387-5
20. Kassarjian A, Rodrigo RM, Santisteban JM. Current concepts in MRI of rectus femoris musculotendinous (myotendinous) and myofascial injuries in elite athletes. Eur J Radiol. 2012 Dec;81(12):3763–71.
21. Lempainen L, Kosola J, Valle X, Puigdellivol J, Ranne J, Orava S, et al. Chronic and Recurrent Rectus Femoris Central Tendon Ruptures in Athletes: Clinical Picture, MRI Findings, and Results of Surgical Treatment. Orthop J Sport Med. 2021;9(2).
22. Lempainen L, Kosola J, Pruna R, Puigdellivol J, Ranne J, Orava S. Operative Treatment of Proximal Rectus Femoris Injuries in Professional Soccer Players: A Series of 19 Cases. Orthop J Sport Med. 2018 Oct;6(10):2325967118798827.
23. Balius R, Maestro A, Pedret C, Estruch A, Mota J, Rodríguez L, et al. Central aponeurosis tears of the rectus femoris: Practical sonographic prognosis. Br J Sports Med. 2009;
24. Lempainen L, Mechó S, Valle X, Mazzoni S, Villalon J, Freschi M, et al. Management of anterior thigh injuries in soccer players: practical guide. BMC Sports Sci Med Rehabil [Internet]. 2022;14(1):1–9. Available from: https://doi.org/10.1186/s13102-022-00428-y
25. Kassarjian A, Rodrigo RM, Santisteban JM. Intramuscular degloving injuries to the rectus femoris: Findings at MRI. Am J Roentgenol. 2014;202(5):475–80.
26. Iriarte I, Pedret C, Balius R CL. Ultrasound of the Musculoskeletal System Anatomical exploration and pathology [Internet]. 2021. 570 p. Available from: https://mskroom.com/books.php
27. Pedret C, Balius R, Blasi M, Dávila F, Aramendi JF, Masci L, et al. Ultrasound classification of medial gastrocnemious injuries. Scand J Med Sci Sport. 2020;30(12):2456–65.
33 medicine & performance football www.fmpa.co.uk






PROTECTING PLAYERS FROM THE EFFECTS OF CONCUSSION: A KNEE JERK REACTION OR BETTER SAFE THAN SORRY?
 FEATURE / PHILLIP HERITAGE
FEATURE / PHILLIP HERITAGE
Introduction
Through the iconic image of Terry Butcher’s bloodied, bandaged head fans and players alike have been aware of the dangers that football can hold when it comes to head injuries. But long-term neurological disease seemed to be the reserve of higher contact sports as chronic traumatic encephalopathy, dementia and Alzheimer’s disease became associated with participation with American Football and more recently, rugby1. However, recent analysis of health data in Scotland has concluded that footballers may similarly face increased risk of developing these diseases , with ex-players three times more likely to be diagnosed with Dementia or Alzheimer’s than their non-playing equivalents2,3. The increased risk, associated with repeated impacts of the head, has been associated with player-to-player, player-to-ground, and playerto-ball contact and led to some proactive initiatives and temporary rule changes aimed at enhancing player protection in the professional game. While concussion injuries are mainly associated with unexpected
head contact with other surfaces causing greater cranial acceleration5, long-term risks including the development of Dementia and Alzheimer’s have been associated more with sub-concussive effects of heading the ball4
How big is the problem?
This is a hard question to answer from outside of the football world. As a former performance analyst in the sport, I know how secretive clubs are about performance and medical data. There are also potential impacts of player data being freely available when transfer dealings and wages may be put at risk through awareness of players’ exposure to repeated head injuries. On an acute level, injury surveillance data is collected by the Football Association but is not published publicly in the way seen by its equivalent governing body for Rugby Union in England (RFU) or the International Olympic and Paralympic Committees.
Relying on published data alone raises a variety of issues with data sets coming
from a broad selection of playing levels and environments, with incidence commonly based on collegiate statistics in the United States. Reporting processes and inclusion criteria are also inconsistent between studies, and this means often reporting on head injury incidence generally rather than concussions specifically.
Despite this, some data has been published reporting longitudinal injury surveillance statistics across men’s and women’s international competitions6,7. These studies reflect the research that shows women are at greater risk of concussion than men, with women experiencing one concussion for every 1080 playing minutes versus every 3025 in their male equivalents. However, this only represents the very top of the game and more information is needed on all playing levels. These studies also reported concussions accounted for just 2% of all injuries on average in the competitions covered. Due to variances in assessment between medical staff (e.g. physicians,
Human Performance Lead and Senior Lecturer at AECC University College, Bournemouth
feature 36 info@fmpa.co.uk
(a) Standard (b) Enhanced
physiotherapists, sports therapists) and the lack of a definitive diagnostic test it is difficult to draw any conclusions from these numbers .
The greater health concern appears to be in the longer-term impacts of players suffering concussions and sub-concussive injuries 1,2,3. As explained in the introduction, recent research highlights an associated risk with playing football and developing neurodegenerative disease in later life. These studies observed a three-fold increase in the risk for professional footballers developing a neurodegenerative disease compared to the general population2 and that outfield players are at a significantly greater risk than goalkeepers3
What has the response been?
The response from the Football Association involves a combination of developing educational materials and implementing new rules restricting the volume of heading in training , with a phased increase to the professional level. The publication of the Football Association’s Concussion
Age Group
Heading should not be introduced in training sessions at this age
Heading remains a low priority – 1 session per month & max 5 headers
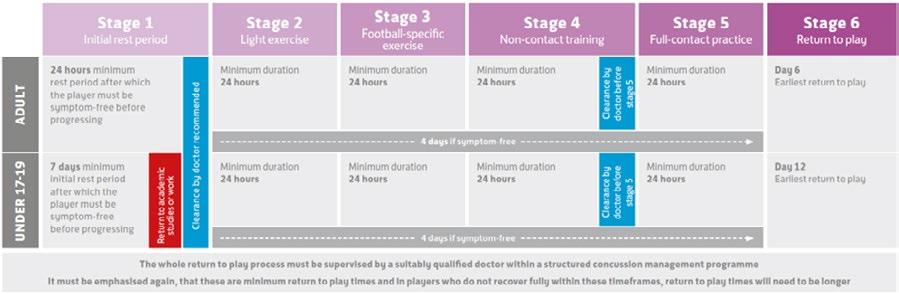
Heading remains a low priority – 1 session per week & max 5 headers
Heading remains a low priority – 1 session per week & max 10 headers
Heading drills should be reduced as far as possible, taking into consideration the heading exposure in matches
Guidelines: ‘If in doubt sit them out ’ is aimed at offering guidance on identifying signs and symptoms of concussion, more severe brain injury and the use of graduated return-to-play protocols (Figure 1).

They have also restricted heading for all age groups shown in Figure 2 to reduce the previously reported risk associated with developing neurodegenerative diseases in the future.
Meanwhile, the Premier League has acted to also restrict the volume of heading exposure in training to “a maximum of 10 higher force headers are carried out in any training week”. This has been based on research conducted by the Premier League, which has observed cranium force exposures due to heading exceeding those seen in activities of daily living, and greater forces observed in youth and female footballers than their adult male counterparts.
Figure 1. Graphic depicting the timelines for Graduated Return to Play from the FAs Concussion Guidelines (updated 2019) for players after concussion. (a) Standard, (b) Enhanced8
Heading frequency U7, U8, U9, U10, U11
U12
U13
U14, U15, U16
U18
37 medicine & performance football www.fmpa.co.uk
Figure 2. The FA Heading Guidance (updated 2020-21)9
The question of heading is one raised regularly with various factors requiring further exploration. Recent criticism has commented that while published data on neurocognitive disease risk in ex-players shows a compelling association, it lacks adequate evidence of causality4:
• Is heading a ball enough to cause a concussion?
- This seems unlikely and is unsupported by literature, but research has been restricted by issues with accelerometer accuracy. It is hoped that new gum-shield mounted accelerometers could change this as they provide a solid fixing to the cranium. However, research on amateur footballers has shown that heading a ball just 15 times causes transient electrophysiological and cognitive impairment, a potential effect of sub-concussive injury10
• Does removing heading in children benefit them in older age?
- This question is impossible to answer until we see the effects of these recent changes by the Football Association.
• Will the lack of time training at heading reduce the strength of neck musculature which protects the head from the accelerations and decelerations that cause concussive and sub-concussive injury?
- This has become a more common part of training in a variety of sports and professions to protect the cranium from high forces in people such as Formula 1 drivers, Rugby Union players and jet pilots.
• Should other neck strengthening exercises be included at all levels where heading is limited?
Additionally, a temporary change in the rules was trialled to allow up to two additional permanent substitutions where a player is believed to have suffered a to lessen the competitive impact of removing a player from the field of play. A recent survey of professional football medical professionals highlighted they would like to see the introduction of replacements to allow an assessment, such as the Head Injury Assessment process in Rugby Union to be conducted, the player returned to the pitch upon receiving an all-clear or substituted should they fail11

This research also found that 5% and 10% of medical professionals felt under pressure from players and technical staff respectively not to remove a player with a suspected concussion. This highlights to me a lack of awareness of the potential medium- to long-term health repercussions of playing on after suffering a concussion. This is reflected in past research in Italian football , which shows poor knowledge of the signs and symptoms of concussion in football players, and coaches and medical staffs’ reliance on self-reporting to assess players for the injury12. However, more recent research has not been conducted on knowledge and understanding in the English game, or whether playing level affects the quality of care a player is likely to receive.
What more can we do?
The concussion discussion is complicated by timeframes related to mild-traumatic brain injury. The injury presents through a variety of short-term signs and symptoms which can influence player performance and health for days to weeks. Additionally, more sinister health related changes in the brains structure and chemistry that affect quality of life and life expectancy post-career could occur. It is also important to consider medium-term health complications associated with mental health in active and retired players. While this is starting to be researched, current findings have found no greater associated risk so far13,14
To improve our capacity to better understand the scale of the issue and existing practices in place to protect player health, we need to better understand the following:
• How heading affects brain structure and chemistry in the short- to medium-term and how does this influence long-term health?
• In the absence of a definitive test for concussion, what assessments are being used most widely and effectively to monitor and protect player neurocognitive health and diagnose concussion?
• How the demands of professional sport influence short-term behaviour towards player welfare.
• How medical teams design their diagnostic and monitoring protocols for concussion.
feature 38 info@fmpa.co.uk
Better understanding of these key themes, in my opinion, and the use of longitudinal research to measure how player monitoring, diagnosis and return to play affect neurocognitive health in the short, medium, and long-term is crucial to us gaining a better understanding of the impact of repetitive head injury on player health.
Research is currently being conducted to better understand player monitoring, diagnostic and return to play practises in professional football in England. Additionally, it aims to better understand knowledge of concussion and its associated signs and symptoms along with attitudes and behaviours related to player welfare in relation to concussion. You can contribute by scanning this QR code and completing the 10–15-minute survey.

How can we protect our players?
While no definitive test exists to diagnose a concussion, battery tests that measure a variety of physical and cognitive factors do and are widely used and supported by research. As a minimum, clubs must:
• Educate staff and players yearly on the risks of playing with a concussion
• Educate staff and players on the signs and symptoms of concussion
• Perform baseline assessment of a physical-cognitive test battery (e.g. SCAT-5)
• Regularly re-test physical-cognitive performance to ensure changes in performance are compared to up-to-date results
• Implement a Graduate Return to Play protocol that protects their players
• Remove any player from training or competition who there is concern has suffered a concussion. If in doubt, sit them out.
Where possible, clubs should also:
• Involve an independent physician/ neurologist in the decision-making process when diagnosing a concussion
• Utilising video footage as part of the decision-making process to remove a player from training or competition
1. Lee EB, Kinch K, Johnson VE, Trojanowski JQ, Smith DH, Stewart W. Chronic Traumatic Encephalopathy is a common co-morbidity, but less frequent primary dementia in former soccer and rugby players. Acta Neuropathologica.2019;138: 389-399
2. Russell ER, Mackay DF, Stewart K, MacLean JA, Pell JP, Stewart W. Association of Field Position and Career Length with Risk of Neurodegenerative Disease in Male Former Professional Soccer Players. Journal of the American Medical Association. 2021;78(8):1057-1063
3. Mackay DF, Russell ER, Stewart K, Maclean JA, Pell JP, Stewart W. Neurodegenerative Disease Mortality Among Former Professional Soccer Players. New England Journal of Medicine.2019;381(19): 1801-1808
4. Gouttebarge V. Is the Call to Reduce Heading Exposure in Professional Football to Prevent Dementia Evidence-based? British Medical Journal Open Sport and Exercise Medicine. 2021;7.
5. Mooney J, Self M, ReFaey K. Elsayed G, Chagoya G, Bernstock JD, Johnston JM. Concussion in Soccer: A Comprehensive Review of the Literature. Concussion. 2020;5(3).
6. Junge A, Dvorak J. Injury Surveillance in the World Football Cup Tournaments 1998-2012. British Journal of Sports Medicine. 2013;47: 782-788

7. Junge A, Dvorak J. Football Injuries During the 2014 FIFA World Cup. British Journal of Sports Medicine. 2015;49: 599-602
8. Football Association. The FAs Concussion Guidelines. 2019. https://www.thefa.com/get-involved/ fa-concussion-guidelines-if-in-doubt-sit-them-out [Accessed 3.9.2022]
9. Football Association. English Football Introduces New Guidance for Heading Ahead of 2021-2 Season. 2021. https://www.thefa.com/news/2021/jul/28/20210728-new-heading-guidance-published [Accessed 3.9.2022]
10. Di Virgilio TG, Hunter A, Wilson L, Stewart W, Goodall S, Howatson G, Donaldson DI, Ietswaart, M. Evidence for Acute Electrophysiological and Cognitive Changes Following Routine Soccer Heading. EBioMedicine. 2016;13: 66-71
11. Gouttebarge V, Ahmad I, Iqbal Z, Orhant E, Rosenbloom C, Sas K, Kerkhoffs GMMJ. Concussion in European Professional Football: A view of team physicians. British Medical Journal Open Sport and Exercise Medicine. 2021;7.
12. Broglio SP, Vagnozzi R, Sabin M, Signoretti S, Tavazzi B, Lazzarino G. Concussion occurrence and knowledge in Italian football (soccer). Journal of Sports Science and Medicine. 2010;9: 418-430
13. Taioli E. All Causses Mortality in Male Professional Soccer Players. European Journal of Public Health. 2007;17(6): 600-604
14. Russell ER, McCabe T, Mackay DF, Stewart K, MacLean JA, Pell JP, Stewart W. Mental Health and Suicide in Former Professional Soccer Players. Neuropsychiatry. 2020:91; 1256-1260
39 medicine &
performance football www.fmpa.co.uk

UNDERSTANDING RECRUITMENT OF BACKROOM TALENT IN ELITE PROFESSIONAL FOOTBALL
FEATURE / DR. DAN PARNELL
In this article, Dr Dan Parnell and colleagues examine some of the important factors for sporting directors in England when they are recruiting backroom staff and middle-managers. It raises important questions on the value based on human capital or merit.
Parnell is an Associate Professor in Sport Business at the University of Liverpool, however he is deeply immersed within industry to ensure he can deliver an enriched teaching and learning environment for his students through undertaking high quality research. This involves undertaking public engagement roles to build relationships with and access to usually closed environments. One such role, is CEO of the Association of Sporting Directors.
Through unprecedented access to 25 Sporting Directors in England, Parnell’s and colleagues recent research examines their guarded recruitment processes. The research explicitly looks at the recruitment of nonplaying staff rather than players.
Read the open access research by searching for ‘recruitment in elite football: a network approach’ online or clicking here
The research focuses on the process of recruitment and how Sporting Directors are able to find middle-managers, such as heads of department. Through the lens of network theory the research identifies how the Sporting Directors established relationships with similar people heavily influence their decisions.
Naturally, recruitment decisions in elite football are constrained by tight timeframes and high pressure from club boards, fans and the media. As such, any leader under these pressures require people ‘they know’.
People you ‘know’ often know how you think, what you need and when you need it. Communication is easier, faster and more effective. Importantly, trust is high. These are all important for high performing teams.
This is also important is the culture of high employee turnover, especially in relation to
middle-management-level positions, in the football industry. Roles including the Head of Recruitment, Head of Academy, Head of Sport Science, Loans Manager, Club Doctor, First Team Head Coach and other backroomstaff are all susceptible to this culture.
Despite ‘knowing someone’ being generally favoured over an objective assessment of a candidate’s human capital and merit, there can be constraints in this approach. This approach can have a limiting impact upon existing practices and can influence the clubs’ levels of diversity, problem-solving, creativity and innovation.
The insights collected from 25 English Premier League and Championship Sporting Directors helps better understand these recruitment decisions in the football industry.
The data evidences that, whilst normally in recruitment, weak ties (i.e. more removed connections) are essential for getting a job, in football, trust and knowing people (i.e. strong ties) are the most critical aspects.
Hiring from within an existing closed network is often the default position for recruiters, which triggers a process of homophily, where people cluster with others who share similar characteristics.

“I have recruited someone I trust, who I know can do the job, even if they have never done the role before. I need to know that if I say do X, it gets done. You need that quick trust to get things going”
English Premier League Sporting Director
“When you join a club, you don’t know how much time you have. You need people who can hit the ground running. People you can trust. So you need people you know. This could be someone you have worked with, or someone who has worked with someone you trust. But the main thing is you trust them.”
English Championship Sporting Director
Potential impact on club culture, innovation and performance
Although the study does not focus on the consequences of recruitment practices,
41 feature www.fmpa.co.uk
medicine & performance football
lack of meritocracy may create a dangerous precedent in the football industry.
Homophily can be damaging to football clubs, as it can promote a toxic culture, where individuals are fearful of those deemed as ‘outsiders’.
Although unintentionally, this has the potential to create non-diverse and inequal organisations, as it is easier to discriminate against people whose gender and ethnicity make them less likely to access existing networks.
Most importantly, homophily raises player welfare, safety, and performance questions concerning the recruitment of Head of Sport Science and Medicine or staff supporting playing squads.
While hiring known people speeds up recruitment and future workflows, overreliance on tight connections may damage creativity, innovation and access to knowledge, by blocking professionals who might be ahead of the learning curve in these areas.
Weak ties and ‘network entrepreneurs’ as sources of competitive advantage
Although the issue of homophily remains, the study findings point at alternative strategies which could help optimise the recruitment decision making process.
While reliance on strong ties is the norm, reaching out to people outside their network helps recruiters gather information on potential candidates, especially in areas outside of their expertise (e.g. medicine, periodisation, coaching).
“My background is in [player] recruitment, so when it comes to stuff outside my direct expertise, such as medicine, periodisation or coaching, I know I need to be clever. Of course, I know a lot of be topics and know a lot of people who can do the job[s], but I know people who might be ahead of [learning] curve. If I am looking for Head of Performance, I will speak with people I know, who will know who the next best thing is. I would speak to colleagues universities and people who are the heads of performance even if they are in other sports. This will give me a start.”
English Championship Sporting Director
“If I am looking for Head of Performance, I will speak with people I know, who will know who the next best thing is. I would speak to colleagues, universities and people who are the heads of performance, even if they are in other sports. This will give me a start.”
English Premier League Sporting Director
English Championship Sporting Director
English Premier League Sporting Director
Likewise, clubs can take advantage of ‘network entrepreneurs’ (e.g. agents, loan managers) or people who can connect multiple networks by introducing people or organisations, and facilitating the flow of information and opportunities.
“We have a number of strategies for finding backroom staff [i.e. Heads of Departments]. We usually have a few names that we know could fit in and hit the ground running. Then we speak to other execs (executives), agents, consultants, existing staff and when applicable, players. To get a better understand of the quality of the candidate.”
English Championship Sporting Director
“Our loans manager has to work with other teams. He feeds information on good practice and people into me directly, and if we like someone, then we have a route to get a sense of whether they are interested in joining us.”
English Premier League Sporting Director
Impacting recruitment in elite football
At present the study is the most viewed empirical research within the ABS Journal European Sport Management Quarterly, with 12,000+ views since December 2021.
The impact of the study goes beyond academia, as it has been shared with some of the most influential decision makers in the UK and worldwide.
The research team have engaged in extensive knowledge exchange with the technical leaders globally, including the Association of Sporting Directors, global football leagues (i.e., Major League Soccer, United Soccer League, Korea League), The Football Association and Abex Futebol in Brazil.
Through this article we hope further leaders in football can utilise the findings to discuss the questions it raises and begin to influence and improve recruitment and performance in football.
Acknowledgements:
We would like to thank Ana Alvarez (Marketing Officer – Marketing, Recruitment, Communications and Events, Management School, University of Liverpool, UK) for her support in this article.
Research paper:
Daniel Parnell, Alexander John Bond, Paul Widdop, Ryan Groom & David Cockayne (2021).
Recruitment in elite football: a network approach, European Sport Management Quarterly, DOI: 10.1080/16184742.2021.2011942
You need people who can hit the ground running. People you can trust.
So you need people you know.
I would speak to colleagues, universities and people who are the heads of performance, even if they are in other sports.
feature 42 info@fmpa.co.uk

MEDICAL NOTEKEEPING STANDARDS ACROSS ENGLISH FOOTBALL:
THE GOOD, THE BAD AND THE ATHLETE PASSPORT APP
FEATURE / DR. RONNIE BANERJEE
THE PROBLEM
After being involved in a ground-breaking legal case where there was a failure to disclose crucial medical information at a medical, I wanted to know current notekeeping standards across English football and rugby league.
Abstract Objective
To evaluate notekeeping in athletes across football and rugby league in England to see if current guidelines are met and appropriate care is being provided.
Design
Researched across teams to see if there is effective handover of data internally and externally. A comparative study was undertaken to see what electronic medical record (EMR) systems are currently being used. Then using the Delphi method, a questionnaire was completed.
Data sources
Doctors across Premier League, English Football League (EFL) and Rugby Football League (RFL)
Eligibility criteria for selecting studies This had to be completed by a doctor currently working in the sport. This ranged from head first team, academy to matchday only doctors. They were selected by being the named team doctor online and through EPL, EFL and RFL chat groups.
Results
See infographic. In 2021, an anonymous Google questionnaire (Figure 1) was completed by 77 respondents out of 92 football clubs (26% Premier League, 23.4% Championship, 32.5% League 1 and 18.2% League 2 - Figure 2). In rugby league there were 28 respondents (46.4% Super League, 28.6% Championship, 10.7% League 1 and 14.3% covering multiple teams).
Conclusion
Data is fragmented across different siloed systems. There is poor transferability between teams and healthcare sectors.
There are currently no standardised guidelines for medical notekeeping or handovers apart from follow General Medical Council (GMC) recommendations, which is not occurring.
Solutions are needed to make health data more accessible and interoperable for daily care and medicals. An integrated athlete passport app will help manage injuries and illness better and have huge financial and time implications for all stakeholders.
Current Issues
Multiple silos of information negate the excellent care provided by clinicians across sport. If several clubs do not pass on all the pertinent clinical data, the player is left with a poorly summarised record over their career. The outcome is duplication, increased cost, delays in diagnosis and treatment and potentially fatal consequences.
Figure 1. Notekeeping questions
1. For your doctor consultations do you use paper notes or an online system? This refers to history/exam findings of primary care complaints, medication prescribing, medical screening, scans (MSK and non MSK), bloods, specialist letters.
2. What division is your team?
3. What is your role in the club?
4. As the team doctor are you classed as the players and staff’s ‘GP?’
5. In the vast majority how are they registered with a GP?
6. Which online system if applicable do you enter all of your doctor notes?
7. Who files/uploads the medical notes (specialist letters, scans, bloods) whether online or paper?
8. Do you generally get previous team doctor records on signing? Please tick all relevant boxes.
9. Generally do medicals happen after the signing has already taken place?
10. Generally does a doctor perform the ‘doctor’ part of the medical (medical screen, non-MSK exam, maybe bloods)
11. What do you do with the notes when a player leaves the club? Please tick all relevant boxes.
12. How much doctor coverage is there at the training ground through the week excluding fixtures?
13. How are issued medications generally documented at the training ground and on matchday?
14. Hepatitis B blood screening. are players tested and offered vaccination if no immunity?
15. Any additional comments?
POOR RECORDING + COMMUNICATION POORLY INFORMED DECISIONS DANGER TO HEALTH & PERFORMANCE KNOWLEDGE COST TIME LITIGATION POOR DECISION MAKING
feature 44 info@fmpa.co.uk
Hull City Training Ground, Millhouse Woods Lane, Hull Leeds Rhinos Training Ground, Bridge Road, Leeds
Litigation
Lawsuits for medical negligence in sport are becoming increasingly common and recent times has seen brain injury, cardiac problems and COVID-19 take the headlines. Even if you have a notekeeping system it doesn’t necessarily translate to good medicine. The 2021 anonymous Google questionnaire (Figure 1) completed by 77 football doctors shows more than 10 different systems are in use. To view the questions in further detail please visit this link
The number of systems is problematic when 49% of doctors are not handing over information when a player exits their club. In addition, 50% do not know if their players are registered with a GP. Consequently, doctors are oblivious to important data if there is a mix of private and NHS care; for example vaccination history, emergency care and chronic disease management.
a) Thought provoking comments from doctors across the leagues:
Premier league: ‘If other clubs are as poor as we have been then it’s time that there was a consensus within sports to have workable and cost-effective solutions. Ideally these would mirror the common GP systems.’
Championship: ‘System used not particularly useful for non-orthopaedic medical issues.’ ‘Players should be registered with a GP in my humble opinion.’
League 1: ‘Way way below GP standards. Signing we request notes, exiting nothing. No cross linking with academy notes.’

League 2: ‘No idea when players leave club. No notes exchanged. Nobody requests them. No online system at club. No governance system in place.
b) Current governing bodies and medical insurer recommendations:
Sempris: All medical teams need to ensure appropriate patient handover and continuity of care as per the overriding duties under Good Medical Practice which states that you must ‘work with colleagues in the ways that best serve patients’ interests.’
MPS: A lack of clear documentation can make defence of a claim, for example, very difficult.
FSEM(UK) Position Statement: ‘Doctors giving medical advice and treatment at any level of sport are required, under the GMC’s Good Medical Practice 2013, to keep medical records. These records must be made at the time of the event or as soon as possible after the event.’
ATMMiF: “if it isn’t written down, it didn’t happen”.
Your duty of care ends when you have passed the player onto another healthcare professional (HCP) and not on leaving your club. If their career has come to an end, the GP should be informed with permission.
Chronic disease management
Players who suffer with chronic conditions like epilepsy, asthma and diabetes are not followed up well in the private sector due to moving clubs and not being registered with a local GP. They will see expert specialists but it is difficult to coordinate annual reviews and know if these are adequate or appropriate.
Emergency care and practice abroad
In A&E or care abroad, medical information is difficult to manage. These doctors will not have access to important information as it is currently not all in one place, which wastes unnecessary resources. On discharge the player may be given a letter. More commonly team doctors are trying to claw back information which is time consuming and often futile. Weiler et al (2021) recognise challenges in medical handover between national and club teams and suggest a standardised medical handover checklist.
Outside the normal clinic setting
Another challenge is when primary and emergency care advice is given in places like a corridor or pitchside. This is notoriously not documented well. The questionnaire showed that prescribed medications are not documented in 22% of cases.
Retirement
There is a huge volume of medical information
accumulated over a career like data on injuries, cardiac and blood screens. This needs to be handed over and be easily accessible when transitioning away from sport to continue good healthcare and save resources. Carmody et al (2022) found osteoarthritis of the lower limb, musculoskeletal pain and mental health problems to be common amongst retired players. Risk can be lowered by being proactive during a player’s career.
Third party clinicians
A team doctor in the higher leagues is more likely to have a good EMR system, however there are multiple clinicians involved including the GP, orthopaedics, medical specialists, tournament and matchday doctor. In most circumstances these clinicians are not on the same system and will be unaware of the entire medical presentation; as they are reliant on the athlete’s recollection or a phone or email handover.
Medicals and handover
The Google questionnaire states 49% of doctors do not pass on information, whereas 39% get information through a phone call with the previous doctor.
An inadequate medical handover can lead to a waste of time, manpower and financial resources whilst potentially delaying diagnoses and management of health conditions.
Clinicians must protect themselves by keeping good records and giving a satisfactory handover of pertinent medical information with the athlete’s consent. A comment a colleague once made still resonates with me... ’what you don’t know you can’t help.’
Figure 2. Doctors involved in the questionnaire by division and role.
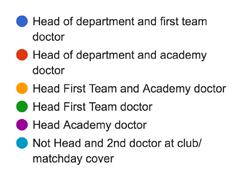
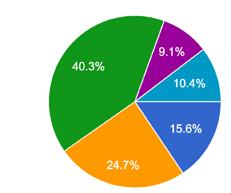
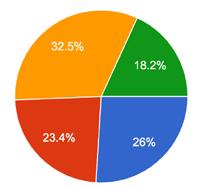
45 medicine & performance football www.fmpa.co.uk
Key messages
• 77 doctors across the elite football pyramid and 28 RFL doctors completed questionnaires.
• There are currently no specific standardised guidelines for notekeeping or handovers.
• Multiple silos undo the excellent care provided by clinicians across sport. If several clubs do not pass all the pertinent clinical data, the player is left with a poorly summarised record over their career. The outcome is duplication, increased cost, and delays in diagnosis and treatment.
RECOMMENDATIONS
A more accessible, standardised and interoperable record is needed across a career into retirement to benefit all stakeholders, but most importantly the athlete’s health and welfare.
A) A standardised approach
• Football and rugby league need to adopt a standardised approach regardless of the system used.

• English elite club and national rugby union and cricket teams are on the same EMR system. This allows all private healthcare such as screenings, injuries, scans and specialist letters to be in one place when a player moves between clubs in this country.
B) An interoperable record
• Unfortunately, a standardised approach alone does not solve the lack of information and handover from third party clinicians like:
- matchday and tournament doctors
- international care – national teams and emergency treatment abroad
- NHS care from the GP, A&E or specialists.
• A system is needed which allows clinicians to immediately see other professionals medical input as this might influence the care they deliver. There are currently delays in correspondence or nothing is received at all.
• This allows better documentation of consultations and prescribed medication by all clinicians.
C) Better accessibility and portability for the athlete
• Points A and B still do not give the athlete readily available access to their own record. Better accessibility and portability are the athlete’s right under the Data Protection Act 2018.
• They might be struggling to recount multiple injuries or potentially complex medical presentations in scenarios such as in an emergency, care abroad, retirement, or insurance purposes.
D) A template for medicals
• Medicals will be transformed if a system exists incorporating points A to C.
• It will remove non-medical disclosure disputes
• With the athlete’s consent it will allow quicker risk stratification when time might be of the essence.
• It will help teams with financial constraints or limited medical provisions to see historic radiology, blood tests or mandatory cardiac screens and stop unnecessary duplication.
• It will allow transparency and remove the stigma associated with certain conditions.
E) Easier transition into retirement
The athlete should have a seamless handover to NHS or abroad. Carmody et al (2017) discuss the role of an ‘exit health examination’ to minimise the risk of poor long term health outcomes.
THE SOLUTION FOR A > E = AN ATHLETE MEDICAL PASSPORT APP
• Any of the multiple EMR systems currently used can solve point A by being standardised across the sport, however this would only be in this country.
• Current EMR systems do not account for points B and C, increasing the risk of missing important information and making medicals and retirement more complicated.
• The read only passport allows better accessibility and portability of medical notes, following GDPR.
• A standardised clinician dashboard for the team doctor syncs with a patient’s app and populates it throughout a career.
• A simple user interface with 24/7 access will empower athletes to better understand their injuries, illness and screening; improve data quality and consequently health needs.
• With consent, any clinician can be shown all the right medical information immediately, whatever the club, country or healthcare sector. Major life-threatening problems, consultations, letters, scans and medications are some of the instantaneous history visible.
• By having features like in built forms or audio dictation, third party clinicians can now directly add to a truly interoperable system so that the regular team clinician gets immediate handover. This protects these clinicians by giving them as much relevant information as possible and the ability to record notes.
• Lessons can be learnt from the strengths and weaknesses of the NHS patient app used in the public sector. Eventually unique identifiers can allow full merging of the records.
feature 46 info@fmpa.co.uk
Next steps
The research questionnaire helped create the AB3 Medical athlete passport app as a possible solution. No current EMR system or passport tackles points A to E. Figure 3 shows how AB3 aims to benefit the athlete with additional features to make their medical passport as interactive and educational as possible. Figure 4 demonstrates the app homepage and its simple user interface.


By standardising care across a sport and empowering the athlete there are massive implications for all stakeholders in player handover and medicals.
*Visit ab3medical.com or @ab3medical for further information
Acknowledgements:
I would like to acknowledge all the Premier League, EFL and RFL doctors for taking part in the anonymised questionnaire, in order to improve medical notekeeping standards across the sports.
References:
• ATTMiF manual
• Carmody S, Jones C, Malhotra A, Gouttebarge V, Ahmad I (2017). Br J Sports Med 53(13). Put out to pasture: what is our duty of care to the retiring professional footballer? Promoting the concept of the ‘exit health examination’ (EHE).
• Carmody S, Anemaat K, Massey A et al (2022). Br J Sports Med 8(2). Health conditions among retired professional footballers: a scoping review.
• Data Protection Act (2018). Available at https://www.gov.uk/data-protection#: (Accessed 25 January 2022)
• General Medical Council (2013) GMC Good Medical Practice, ‘Record your work clearly, accurately and legibly’ Domain 1, (19 – 21)
• Medical Protection (2017) An essential guide to medical records. Available at https://www.medicalprotection.org/ uk/articles/an-mps-essential-guide-tomedical-records (Accessed 25 January 2022)
• Sempris (2018) Contract risk and the football transfer window. Available at https://www.sempris.co.uk/2018/12/21/ contract-risk-and-the-football-transferwindow/ (Accessed 25 January 2022)
• Weiler R, Collinge R, Ewens J et al (2021). Br J Sports Med December 2021 55(24). Club, country and clinicians united: ensuring collaborative care in elite sport medical handovers.
Figure 3. AB3 Medical Passport benefits to the athlete
47 medicine & performance
www.fmpa.co.uk
Figure 4. AB3 Medical app homepage
football
FMPA

Business Directory FMPA Business Directory is now available on the FMPA site to give members quick access to products/services. VIEW THE DIRECTORY www.fmpa.co.uk/fmpa-directory
LESSONS OTHER SPORTS CAN LEARN FROM FORMULA 1

Lessons other sports can learn from Formula 1 was the topic for the first FA Medical Society evening lecture of this 2022/23 season.
Current developments and future innovations in Motorsports Medicine
Dr James McBride - Chief Medical Officer,
Abu Dhabi Desert Challenge
The Abu Dhabi Desert Challenge is an event that occurs over 5 days and runs over 2000km in distance. There are two classes of vehicles within the events which are cars and motorbikes with approximately 40 teams per class. Given the nature of such a huge event, a support team consisting of doctors, nurses, physiotherapists, and chiropractors are required to be on standby. There are also 3 search and rescue aircrafts with four medical personnel on board.
The rally control can access the GPS device of each vehicle. This shows up as green if they are moving and yellow when stationary. However, if they hit their SOS button it will show as red, and an alarm will also sound.
The usual response time is ten minutes from the initiation of alarm to ‘wheels down’ for the helicopter. Furthermore, self-extraction is preferable due to the time demands and dangers of being on a live rally course. Penthrox is the drug routinely used to offer quick analgesia and is usually deemed to be effective after around 6-8 breaths.
One of the main concerns in this event is that the risk of injury increases as the event goes on due to dehydration and fatigue. To mitigate risks, a compulsory 15-minute rehydration stop for the motorcycle riders were put in place. Another concern is the sudden vertical drops from dunes which predispose the drivers to lower thoracic or lumbar spine fractures. For this reason, it is essential to have knowledgeable and experienced medical personnel on standby in such events.
Smooth running and pitfalls in the Pits Andrea Skyring – Pit Lane Chief, Abu Dhabi Formula 1
Motorsport is dangerous which is why trained officials and marshals are present in the
pitlane and on the start grid to ensure safety and discipline of the pits, paddock, and grid (PPG). The best way to ensure a smoothrunning race weekend is to work with an expert PPG marshal team who can be relied on to professionally deal with any pitlane/ startline incidents. Pitlane marshals not only deal with the competitors but also deal with team personnel, media, and guests.
Some pitfalls commonly dealt with include unsafe releases (collisions between cars entering and leaving their pit boxes or car parts flying off), speeding, fire and burns, conflict and paddock club mishaps related to smoking and drinking. The pitlane/ garages have many flammable/combustible materials which means the pitlane/grid is designated a no smoking areas (and this includes e-cigarettes).
Startline marshals play a significant part before the start of the race, making sure that cars are all correctly lined up on the grid. They then wave a yellow flag if any driver stalls or struggles to get off the line when the race begins and recovers any disabled cars
WEBINAR TRANSCRIPTION / DR. DANIELA MIFSUD
49 feature www.fmpa.co.uk medicine & performance football
from the grid. It is very important for PPG marshals and officials to stay alert and know what is going on around them to help avoid incidents.
For Formula One, pitlane speeds were trialed in 1993 and introduced in 1994 and most circuits have a pitlane speed of 80km/h, whilst others that are smaller have a 60km/h (such as Zandvoort and Singapore). The speed limit helps protect the marshals, teams, and the media. For every km/h a driver exceeds there is a €100 penalty (up to €1000). Other race series (F2, 24H etc.) have their own prescribed pit lane speeds. At some circuits pit marshals are equipped with a speed gun to make sure drivers are not exceeding the permitted speed when travelling down the pitlane.
Performance and optimising recovery in drivers

Paul Cheung – President, National Chiropractic Sports Council UAE at Emirates Chriopractic Association, Former Red Bull F1 Chiropractor
Drivers must be able to withstand high gravitational force (up to 6G) which can result in stress and strain. The role of a chiropractor within a F1 team is to analyse the symmetry of the drivers to ensure there
is nothing that predisposes them to stress. High loads are required to break the car which results in high force loading on the core and the pelvis. Before getting into the car the drivers usually get an assessment. Myofascial techniques and mobilization techniques are useful at this stage.
Post-race recovery is essential as around 2kg of fluid is lost after a race. Therefore hydration, electrolyte supplementation and taking a snack is essential.
Managing emergencies during the race
Mr Mansoor Khan – Trauma Surgeon
It is important to keep in mind that anybody and everybody can get injured and not just the athletes themselves. The team at the Grand Prix is composed of orthopaedic and trauma surgeons, GPs, EMTs, and paramedics amongst others. There are 2 sets of teams. One takes care of the perimeter and general population whilst another team takes care of the athletes and staff. The ambulances and extrication team are strategically placed to get quickly to the incident place. There are also aircrafts which have full prehospital capability manned by experienced paramedics.
All of the medical teams will have completed a large number of scenarios which means that whenever the situations occur they will already know exactly what needs to be done as they have done it all before. In cases where interventions were done in pit, the prehospital center is the point where doctors ensure they didn’t miss anything prior transfer to a hospital. The medical facility in motor sport is a high turnover facility and thus, in cases where there is doubt the patient should be immediately transferred to a nearby hospital.
There are three types of extrications. Self-extrication is when the driver comes out of the race car on his/her own. Controlled extrication is when the casualty must be pulled out of the car. The final type of extrication is rapid extrication which is used in cases of an unconscious racer and requires a lot of training to be done beforehand by the medical team.
If there is a conscious athlete then there is no need for a collar to protect the c-spine while if the driver is unconscious, a rapid extrication should be carried out and a collar should be applied.
50 info@fmpa.co.uk medicine & performance football feature
LEGAL
Compromise agreement
“...I took your advice and have been working with the FMPA lawyer on the conclusion of my contract. Martin from his swift response on day one has been a real rock on my side and he has stayed in contact with me at regular intervals. His professionalism and knowledge of the football contract has helped me to be both realistic and hopeful regarding my case. We are now at the final stages of discussions with the club and the financial and emotional support I have has come through my contact with Martin. I am also immensely grateful to the FMPA for your help and support at this difficult time. At a low point in my life both the FMPA and Martin have helped me get the contractual situation sorted with as little fuss as possible and that’s been important to me and my family.”
Head of Medicine, League 2
Contract review
“...I just wanted to drop you an email to let you know how helpful Martin has been this last week. Although away, and with poor signal, he consistently made the effort to respond quickly to my questions when the club came back with updated terms. I believe his guidance has been fundamental to my negotiations.”
Head Physiotherapist, Premier League
“...Thank you so much. Really appreciate your help with this, it’s brilliant that the FMPA offer this service to its members. This stuff can be a minefield.”
Lead Sports Scientist, Premier League
TODAY
JOIN
www.fmpa.co.uk/legal Tel: 0333 4567897


TEL: 0333 4567897 EMAIL: CONFERENCE@FMPA.CO.UK TWITTER: @FMPA_OFFICIAL FACEBOOK: @OFFICIALFMPA INSTAGRAM: @FMPA_OFFICIAL WWW.FMPA.CO.UK #fmpa2023 2023 THURSDAY 1 ST JUNE SCAN FOR MORE DETAILS The Rehab T E A M Together Everyone Achieves More







 Dr Sean Carmody Editor, FMPA Magazine
Dr Fadi Hassan Editor, FMPA Magazine
Dr. Andrew Shafik Editor, FMPA Magazine
Dr Sean Carmody Editor, FMPA Magazine
Dr Fadi Hassan Editor, FMPA Magazine
Dr. Andrew Shafik Editor, FMPA Magazine




























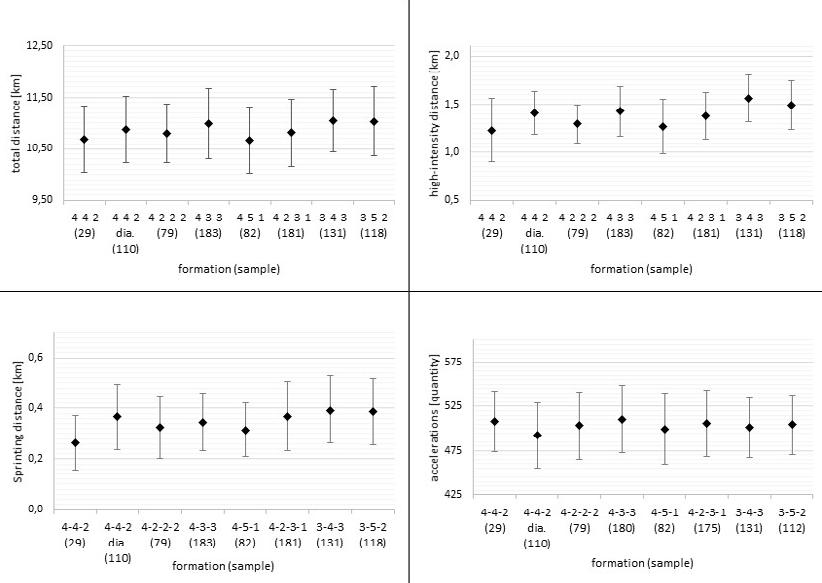








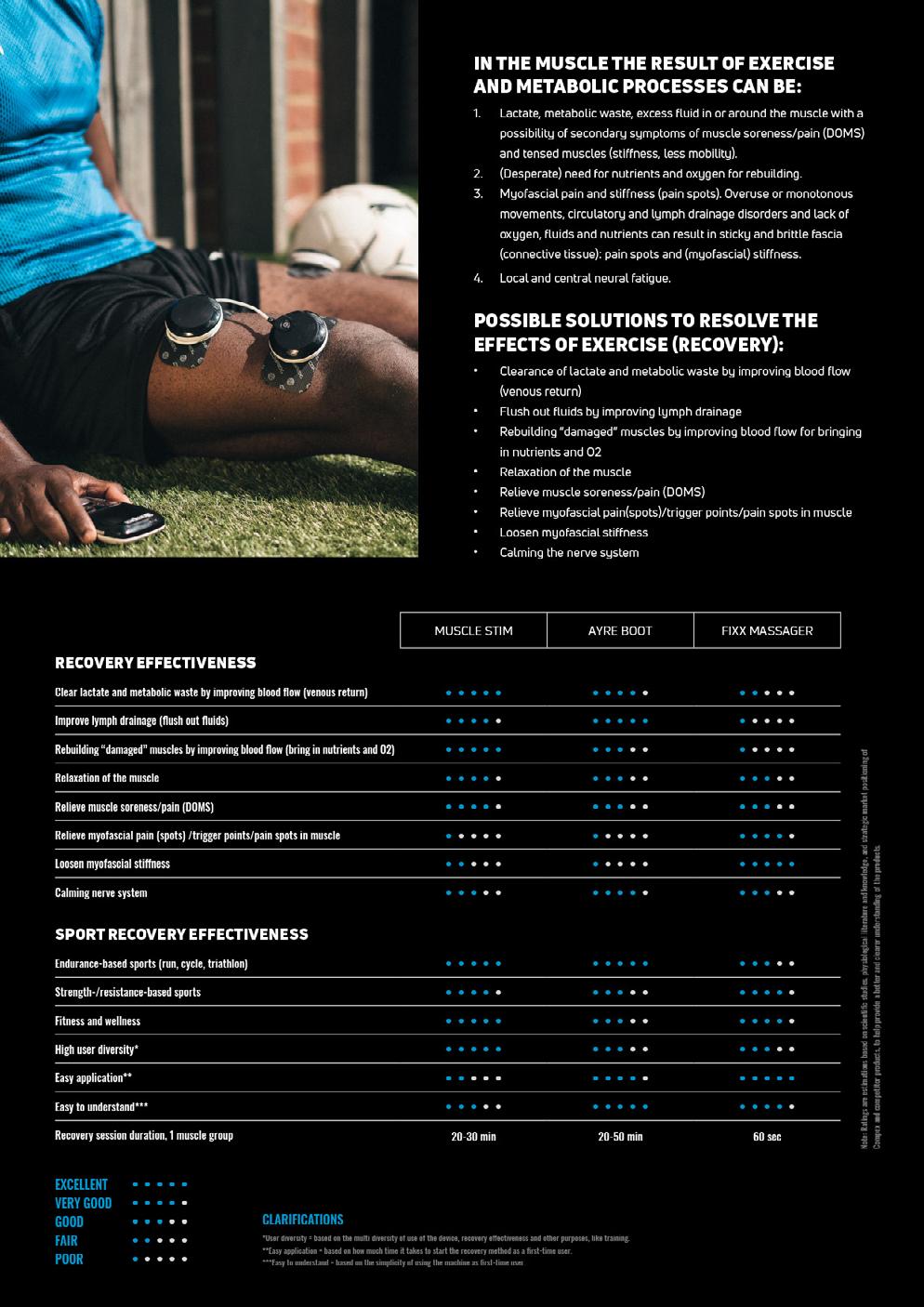

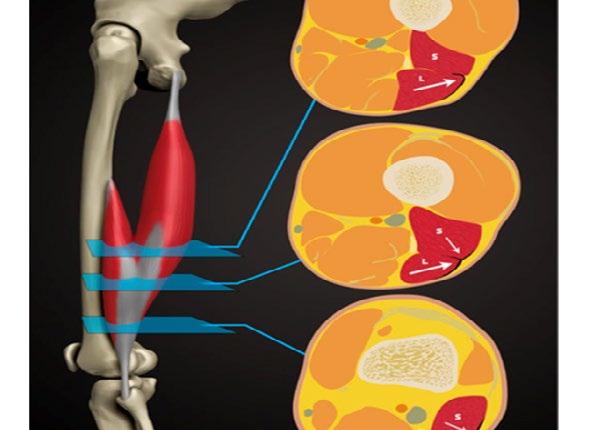




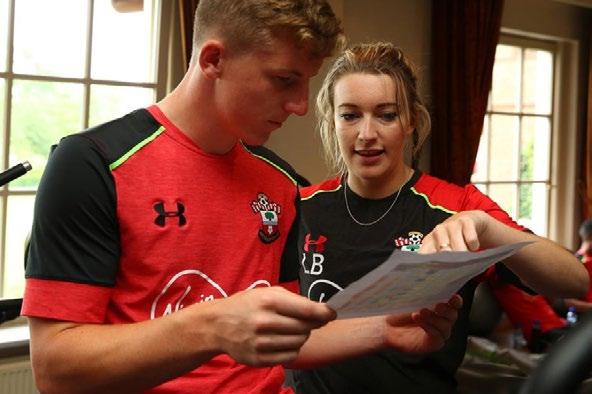
 Laura
Laura

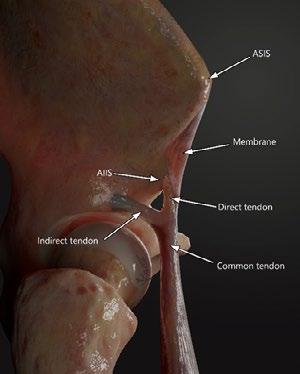

 Figure 2. Coronal Proton Density Fat Saturated images of different injuries in the proximal region of the rectus femoris. A) Complete transversal tear of the DT in its preinsertional portion (arrow). B) Partial longitudinal tear of the IT in its insertional portion (arrow). In this case the IT shows as variant of normality an inferior band with a tear (arrowhead). C) Complete transversal tear of the conjoint tendon (arrow) with longitudinal extension to the DT
Figure 3. Axial Proton Density Fat Saturated image of a tear of the anterior aponeurotic expansion of the DT (arrow). Injury close to the junction with the central tendon.
Figure 2. Coronal Proton Density Fat Saturated images of different injuries in the proximal region of the rectus femoris. A) Complete transversal tear of the DT in its preinsertional portion (arrow). B) Partial longitudinal tear of the IT in its insertional portion (arrow). In this case the IT shows as variant of normality an inferior band with a tear (arrowhead). C) Complete transversal tear of the conjoint tendon (arrow) with longitudinal extension to the DT
Figure 3. Axial Proton Density Fat Saturated image of a tear of the anterior aponeurotic expansion of the DT (arrow). Injury close to the junction with the central tendon.

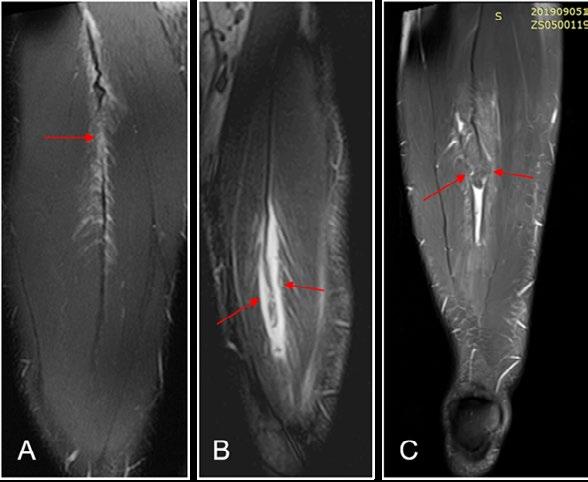


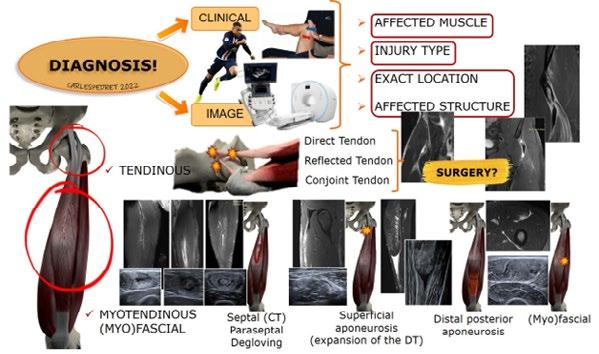






 FEATURE / PHILLIP HERITAGE
FEATURE / PHILLIP HERITAGE