June 2023 www.mforum.com.au Allied health taking off MAJOR PARTNERS Body & mind | Workers comp, endometriosis, gut microbiome, psychedelics
Be part of the WA mental health team.




WA Health is looking for skilled and experienced mental health professionals to strengthen its workforce. Be part of the team as we continue to provide world-class public health care for all Western Australians.


Be part of WA Health, where you belong.

belong.health.wa.gov.au





COM-014444 MAY’23
Competitors or collaborators?
It is not surprising that GPs have been wary of some of the enthusiasm for allied health professions playing a bigger role in primary health care.
Some might argue doctors are merely protecting their turf, refusing to give away any control, lest it affects their bottom line.
But those who have done a few laps around the block may be sceptical that it is not all about the oft-cited mantra of improving patient care.
They might question if the real goal is to find a way to shift some of the tasks performed by doctors to people who can be paid less.
And that comes back to the thorny issue of what GPs are paid. With poor remuneration that has failed to be indexed, who could blame them for feeling unloved and wary?
It is too cute to dismiss their concerns as protecting their turf. I doubt any GP has a problem with the smart use of allied health. There is plenty of sickness, disease and disability to keep everyone gainfully employed.
Trying to contain costs in the bottomless pit of Medicare is not a bad thing – in fact it is the government’s responsibility to question if taxpayers’ money can be spent more judiciously.
And where used appropriately, allied health practitioners can make the job of GPs easier – think diabetes educators, exercise physiologists, audiologists, psychologists and –probably the most contentious of all – pharmacists.

It is time to find a happy medium – a way to use allied health professionals carefully and cleverly – and not purely as a cost-cutting measure. That will involve some give-and-take from all parties.
This is somewhat of a segue to explain how Medical Forum is moving to recognise the role of allied health services in primary health care, with GPs still at the ship’s helm, but with more helping hands on deck.
Readers will see some changes in coming months, including clinical coverage of allied health topics, as well as a separate Clinical Services Directory.
As the only independent magazine in WA for the medical profession, we will always retain our core focus to inform, educate and entertain doctors. Now we hope to do that more comprehensively.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
JUNE 2023 | 1 MEDICAL FORUM | BODY & MIND EDITORIAL Cathy O’Leary | Editor
It is too cute to dismiss their concerns as protecting their turf. I doubt any GP has a problem with the smart use of allied health.
BACK TO CONTENTS
FEATURES
10 Allies in health

14 Close-up: Flying Physiotherapist Kennedy Lay

20 Dementia: Out of sight, out of mind

33 COVID – the long story
LIFESTYLE
54 Film: Bank of Dave
56 Rocky Horror’s 50th anniversary
57 Wine review: Cape Grace – Dr Craig Drummond
Cover picture: Physiotherapist Kennedy Lay and colleagues

WINNING TIMES
1
8
18
39
52
The happy winner of our April doctors dozen from Sandalford Wines is recently-retired Dr Peter Brockhoff, seen here collecting his wine from Medical Forum’s offices.

This month we have a superb selection of wine from small-batch Margaret River producer Cape Grace, reviewed by Dr Craig Drummond on page 57. And for the movie buffs, we have three double tickets to see Bank of Dave, based on the true story of one man’s efforts to fight the big banks.
To win the wine or movie tickets, use the QR code on this page or go to www.mforum.com.au and hit the competitions tab.
2 | JUNE 2023 MEDICAL FORUM | BODY & MIND
IN THE NEWS
Editorial: Competitors or collaborators?
Cathy O’Leary
News & views
–
4
In brief
Letters to the editor
13
HBF’s new gaps
Around and around we go
Dr Joe Kosterich
–
Happy parenting Inside
CONTENTS | JUNE 2023 – BODY & MIND 10 20 33
this issue
WINPREMIU M WINESFROM CA P E ECARG 14 CONNECT WITH US /medicalforumwa /MedicalForum_ /medical-forum-wa-magazine info@mforum.com.au www.mforum.com.au
PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au

EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au


Journalist Eric Martin 08 9203 5222 eric@mforum.com.au

Clinical Editor Dr Joe Kosterich 0417 998 697 joe@mforum.com.au


Marketing Rhiannon Arnold rhiannon@mforum.com.au






Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory

Andrew Bowyer 08 9203 5222 andrew@mforum.com.au


CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222
Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au
Guest Columns

JUNE 2023 | 3 MEDICAL FORUM | BODY & MIND
CONTENTS Clinicals 40 Diagnosis:
53 Childhood constipation
the
perspective
42 Workers
active
45
OUR PRINTER’S ACCREDITATIONS
Fear Dr Talia Steed
–
mother’s
Davina Houghton
comp – early and
intervention
Aaron McErlaine & Hadyn Sleeman
Endometriosis
update Dr Rose McDonnell
This magazine has been printed using solar electricity, and the paper from plantation-based timber has been manufactured and printed with ISO 14001 accreditation, the highest environmental standard. MAJOR PARTNERS 25 Physiotherapy for children Nicole Pates 27 New hope for pelvic pain sufferers Dr Andrew Leech 29 Keeping First Nations moving
31 Help to use digital mental health
50 Promise and perils of psychedelic-assisted therapy
Environment ISO 14001 46
49
Professor Andrew Maiorana
Dr Jan Orman
Dr Jeremy Tannenbaum
No health without mental health Dr Maxine
Hawkins
Better understanding the gut microbiome Charlene Grosse
Vision-impaired kids at risk
The institute was founded in 1983 by Professor Ian Constable, who was recruited from Boston and attracted to the role as he could see the need to improve eye health care in the State.
Eye surgery was not universally available, patients had to travel interstate for some conditions, and rural and remote services were very limited.
At the time, Perth-based Lions clubs were running a successful glaucoma detection clinic, operated from a now-iconic caravan. The clubs went on to form the Lions Save-Sight Foundation WA to expand on this work.

Over the years, the leadership baton for the institute has passed from Professor Constable to Professor David Mackey and then to the current managing director, Professor Bill Morgan.

Some of the institute’s biggest breakthroughs and treatments include inventing the first soft artificial cornea; discovering gene therapy to treat wet age-

RSV in the spotlight
The Immunisation Foundation of Australia is running the first Respiratory Syncytial Virus Awareness Week from June 4-10. RSV is an unpredictable and potentially dangerous virus that puts thousands of infants in hospital each year and can potentially cause serious long-term health issues.
The RSV and Me campaign aims to generate awareness of RSV and its impact on Australian children, particularly babies, by encouraging parents to tell their stories.
Perth vaccination campaigner Catherine Hughes said she was
related macular degeneration; and inventing the XEN gel stent, the most-used surgical glaucoma implant in the world.
Other developments were the Virna glaucoma drainage device, an affordable treatment for glaucoma used in Indonesia; the Barrett Universal II Formula used in cataract surgery; the central retinal vein occlusion bypass laser surgery procedure; and a significant scientific discovery into cytomegalovirus infections.
“Over the past 40 years, the Lions Eye Institute has discovered many new sight-saving treatments and therapies,” Professor Morgan said.
“This is largely due to the ability of our medical researchers to work closely with ophthalmologists, some of whom are researchers themselves, to ensure that patients receive the best possible and most advanced treatment available.”
Since its beginnings in the Queen Elizabeth II Medical Centre, the institute has opened clinics in Murdoch, Midland and Broome. In 2013, it introduced Lions Outback Vision to provide eye health care to the state’s remote, rural and Indigenous communities. It also partnered with the University of WA to establish the State’s first optometry school.
motivated to set up the event in part by her own experiences.
In the winter of 2016 – 18 months after her four-week-old baby boy Riley died from complications of whooping cough – her threeweek old baby Lucy was rushed to hospital with severe RSV. With prompt medical care, she fortunately recovered.
The foundation has information resources at www.ifa.org.au
Digging deeper
Child protection experts want doctors to broaden their duty of care to ensure that hidden trauma
is not overlooked by more obvious physical symptoms and illnesses. The move is aimed at reducing growing rates of chronic disease and mental health issues in Australia, some of which are believed to be underlined by deepseated trauma as a result of child abuse and neglect.
In a recent editorial published in the British Medical Journal, University of South Australia’s Professor Leonie Segal argued that a wholeof-person approach to medical care is vital to address poor health outcomes associated with child abuse and neglect.
continued on Page 8
4 | JUNE 2023 MEDICAL FORUM | BODY & MIND
NEWS & VIEWS
The Lions Eye Institute has one million reasons to celebrate this year, as it marks 40 years of operating in WA and one million patients treated.
BACK TO CONTENTS
Photo Credit: Arthur Nutt, City of Perth Lions Club



JUNE 2023 | 5 MEDICAL FORUM | BODY & MIND MAJOR PARTNER From sample collection to results, your patients are safe with us Prof. Catherine Cole Dr Clay Golledge Biochemistry & Toxicology Dr Jonathan Grasko Dr Yael Grasko Immunology Dr Martin Stuckey Dr Meilyn Hew Saturn Pathology | Level 2, 31 Cedric Street, Stirling 6021 | Phone: (08) 9253 4800 www.saturnpathology.com.au Laboratory Medicine Redefined BACK TO CONTENTS

BACK TO CONTENTS


MAJOR PARTNER BACK TO CONTENTS
Palliative Care WA has appointed Lenka Psar-McCabe as its CEO, with her most recent role being CEO of Perth Radiological Clinic, a position she held for almost 25 years.

Dr Vin Pushpalingam is the new director of the Rural Generalist Pathway at WA Country Health Service’s Medical Education Unit.
WA medicinal cannabis producer Cannaponics has appointed Perth cardiologist Dr Michael Nguyen as a non-executive director on its board.

Cyclowest has opened a $25 million cyclotron radiopharmaceutical manufacturing facility in Bayswater, using a $2.6 million grant awarded by the previous Federal Government’s Modern Manufacturing Initiative.
Perth Children’s Hospital immunology consultant Clinical Associate Professor Kristina Rueter has received Telethon Trust funding to allow children taking part in the SYMBA allergy study to be followed up at the age of three.
Newman’s new $61 million health facility was officially opened last month, housing an emergency department, inpatient beds, medical centre, consultation spaces and a dental clinic.
continued from Page 4
“There is sound evidence that child abuse and neglect is causally related to very poor health, including early death,” she said.
“Many chronic diseases, including severe mental illness, chronic pain, substance use, and physical health conditions, especially those with an inflammatory pathway such as gastrointestinal, respiratory, and autoimmune disease, are more common in victims of child abuse and neglect.
“Yet too often, patients present with physical symptoms that are treated, without sufficient consideration of possible underlying trauma.
“We know that people who have suffered child abuse and neglect are more likely to have chronic disease, so we need to encourage clinicians to extend their care
Better care for kids’ burns
A new 3D scanner is set to revolutionise the care of children’s burns in WA.

The handheld device generates high resolution 3D maps of scarring in just seconds, allowing doctors at Perth Children’s Hospital to better manage scar treatment.
Funded by the Perth Children’s Hospital Foundation, the scanner will allow clinicians to accurately measure and record details of scars during follow-up appointments, helping them to understand how the scar is changing over time and decide on the best course of treatment.
to consider possible underlying psychosocial causes.”
Thumbs up for downward dog
Many Australian psychologists are recommending complementary medicine, according to new research. The findings, published in the journal PLOS ONE, found that 90% of psychologists surveyed recommended complementary medicine products or practices to their clients, with the most common types being hypnotherapy, meditation and yoga.
The researchers from the University of Technology Sydney and Southern Cross University said policy and education development focusing upon this area of grassroots psychology practice would help ensure the care provided by all psychologists remained evidence-based, safe and optimal for their clients.
The WA Health Translation Network has been reaccredited as a NHMRC research translation centre for five years, while the WA Rural Research and Innovation Alliance has been recognised as an emerging research translation centre.
Burns surgeon Professor Fiona Wood, who is director of the Burns Service of WA, said that to the best of her knowledge, it was the first time in the world that a 3D scanner of this type had been used to generate an accurate measure of scarring.
“Having access to advanced technology like this is hugely exciting because it gives us the tools to improve clinical and research data. Ultimately, it will help WA to lead the way in burns care and scar reduction,” she said.
“At an individual patient level, having access to this data will also allow us to better understand those factors that influence scarring. This information can then be used to drive personalised treatment approaches and research to minimise scarring.”
Each year, about 500 children are admitted to PCH with a burn injury, with many requiring scar management. That can mean children wearing hot, uncomfortable pressure garments for 23 hours a day for up to two years, daily scar massage from parents, application of silicon products, and laser therapy or reconstructive surgery to release contractures as the child grows.
8 | JUNE 2023 MEDICAL FORUM | BODY & MIND NEWS & VIEWS
IN BRIEF BACK TO CONTENTS
Our contemporary courses offer personalised guidance to medical receptionists on how to provide excellent customer service to patients, families, and medical professionals while being aware of empathy, sensitivity, and confidentiality.


Our Courses include:
Introduction to various practice software

Online Claiming Masterclass Practice Policies & Procedures

Accounts Keeping
Understanding all types of billing Document Control
JUNE 2023 | 9 MEDICAL FORUM | BODY & MIND
your Receptionists need upskilling?
is a Reception Training Centre that offers specialised training and courses that equips medical receptionists with a range of skills from time
service to
entry, and communication skills.
Do
MediAcademy
management, organisation, and customer
problem-solving, data
About Us
Let's keep in touch More Information: P: 08 9301 1015 E: info@medibizz com au www medibizz com au 33/9 Vision Street Wangara WA 6065
MAJOR PARTNER BACK TO CONTENTS
Making allies in health
By Eric Martin
The Strengthening Medicare Taskforce Report and this year’s Federal Budget spelt out the need for improving primary care and reviving Australia’s general practice services using allied health professionals. Yet while funding has been allocated and the various doctor and allied health groups have been brought onboard, little has been revealed about the practical realities of how a more integrated general practice should operate, let alone the benefits for GPs.
Medical Forum caught up with paramedic and health care expert Professor David Reid , Associate Dean of Allied Health at ECU’s School of Medical and Health Sciences, to discuss the advantages and challenges facing GP clinics adopting the new model, as well as its impact on patients.
“The National Safety and Quality Standards put the patient at the centre of everything, but if it's going to benefit practitioners, it’s going to benefit the patient,” Professor Reid said.
“Ideally you have an integrated system that may be co-located in one building, or in buildings next door to each other, which is, for example, what ECU has done at Yanchep and Wanneroo, where we have a GP service with external allied health who come in and provide clinics.
“ECU is developing a health centre in Yanchep where there is not a huge amount of health services and the nearest hospital, Joondalup, is miles away. The GP clinic will be followed by a second building for the health hub containing allied health services such as exercise physiology, with sonography potentially coming in one day a week to do scans.
“Imagine being able to say, ‘you actually don't have to go all the way to Joondalup, they're going to be here next Wednesday, and I'll get I'll get them to book you in for an assessment’.

“There is a clear benefit to GPs if you've got an integrated service and you can immediately refer somebody to a dietician, to the physio, to the speech pathologist, to the psychologist, or to the community paramedic based

Allied health is increasingly seen as a key player in primary health care but what does it mean for general practice?
FEATURE BACK TO CONTENTS 10 | JUNE 2023 MEDICAL FORUM | BODY & MIND
in the GP surgery, who does the home visits and the follow ups.”
Finding trusted professionals

Professor Reid explained that the other big factor for GPs was having confidence in knowing which practitioner to refer to.
“One of the biggest issues for many doctors is trusting the clinicians that you are referring your patients to – it is a double-edged sword. But if you have that close relationship with them, you can be confident when saying, ‘Yes, I trust this person, I know what they're
doing, and I know they provide good service’,” he said.
“Allied health is becoming more specialised as well. Physios, for example, also differ in their areas of expertise – all of them can deal with anything essentially – but if you need a highly specialised one, it helps if you can ask other physios who to approach.”
Professor Reid highlighted that one of the first questions to ask when examining the new model was ‘what is good health care?’
“Is it the fact that you go into hospital and get discharged without an adverse event? Or is it the fact that you did not need to go
to hospital in the first place, because you have some good preventative care that meant you could stay at home? Which is the better metric?” he asked.
“They are hard to measure, and they are hard to define, but I think that having these wraparound services will be good for patients in the long run and probably take pressure off GPs as well. The model is moving into preventative medicine and will stop people from needing to see their GP in the first place.
“We all have different needs at different times: an individual is not going to need a GP all the time, it might be that they need to see a physio for a few months and can complete this aspect of their treatment before moving on to the dietician or the specialist.”
The second question was, ‘how many people want to stay in their own home and get the care they need there?’
Smarter use of resources
“It is a big focus in nursing homes, but with an ageing population, what does it mean for people staying at home? Is there going to be an increased use of allied health? I think allied health can play a big part in
continued on Page 12
FEATURE BACK TO CONTENTS JUNE 2023 | 11 MEDICAL FORUM | BODY & MIND
Making allies in health
continued from Page 11
saving GPs a physical visit in a lot of cases as well,” Professor Reid said.
“Especially by embracing technology such as the use of video consults and remote monitoring in aged care facilities, keeping track and touching base with the practice because somebody is sick or showing concerning symptoms.
“Nurses and paramedics know how to take the patient's vital signs, they know the patient's baseline, and they can electronically transmit it to the GP surgery or the care coordinator. There is the i-STAT machine where you can do basic bloods in the home, send it through and have a video consult.”
Professor Reid said it might be that the patient did not actually need clinical intervention, but it was important to look at their diet or get them to see a dentist.
It could be that this was their third fall in a week and the team knew that they needed a specialist to come in and look at what was needed to reduce the risk of falls.
“That is where the idea of allied health hubs and wraparound service can play a big part. Paying for a 15-minute consult is still a lot cheaper and a lot less resource intensive than paying $1250 for an ambulance trip to hospital as well as the cost of an ED presentation,” he said.
Enabling different clinicians to have efficient access to a patient’s medical records could also make a dramatic difference in terms of treatment options and outcomes.
“If you have a good wraparound service, there's clear sharing of information and you have got up to date, accurate feedback on the patient,” Professor Reid said.
“You can look at what has been happening with the patient and go, ‘Okay, they've been doing X, Y and Z as the clinician, I need to do A, B and C.’
GPs still the linchpins
“The ability in an integrated system to share records means the dietician can see what has been happening with the patient's blood pressure, they can see what the
physio's been doing, or what the OTs been doing, and equally, the GP can see what has been going on as well – this is a crucial feature of preventative healthcare.
“For example, if an individual suddenly has a spike in visits to his allied health practitioners, or they have suddenly seen the GP four times in the last two weeks, whereas in the last year they had seen the GP only once. That begs the question, is there something here that we need to put some extra support around for a few weeks or months?”
Professor Reid explained that he lived in the UK for eight years, where patients must be registered with a primary GP or practice.
GP as lead
“It meant that there was one source of truth, there was the longevity to build a solid history about that patient and that continuity of care, with the GP as the care lead for clinical staff, was crucial for patients over time, especially given the impact of chronic disease,” he said.
“Your GP has a long, established history of what has been happening in your life, and not just the clinical aspects but the social factors as well.
“There is a real challenge here as well in terms of the electronic medical records maintained within GP clinics. You may have your preferred GP within a clinic, but if they're busy, or it's something that you can see any doctor at the clinic for, then any GP should be able to access those records and continue treatment.
“Otherwise, you have got to try and draw it out of the patient and work out exactly what has happened.” Similarly, many patients going into hospital were frustrated when they had to tell their story to the triage nurse, then tell the first doctor who saw them, then the second doctor and the nurse who came to look after them.
“There are stories about patients turning to clinicians and going, ‘This is the sixth time I have told this story. Don't you talk to each other? Don't you read the notes that the last person made?’
“There's a level of relief when you have that primary care person coordinating your treatment, you don't have to repeat yourself over and over again and that provides for better care.”
Professor Reid said the other consideration when co-locating allied with health professionals was that health care in general has become increasingly specialised, providing more focused opportunities for businesses to pursue.
“Even within a GP practice you will find that a doctor may have a special interest in paediatrics, for example, mental health or dermatology, and you need to decide what the business model is going to be,” he said.
“Will it focus on a particular area, such as sporting injuries or diabetes, or will it remain a generalist service? Is it a group of people working together as employees, or will they all be independent practitioners?
“The other issue is timing. For example, do you want your paediatric services running during the day in school hours, or are you better off running them in the evening after school? Could that be an opportunity to have evening sessional rooms, for instance.”
He said the success or failure of the initiative could come down to the efficient, flexible use of space.
“Space in capital cities is expensive and you need to maximise its use, which is a skill that practice managers and GPs will evolve over time,” Professor Reid said.
“It will also come down to professional relationships and breaking down professional barriers, with all clinicians being prepared to let go of something they potentially think is only theirs.
“At the end of the day, if you're providing good care for your patients, it's going to be of benefit to other healthcare professionals as well.”
12 | JUNE 2023 MEDICAL FORUM | BODY & MIND
FEATURE BACK TO CONTENTS
Iron infusions and hypophosphataemia
Dear Editor,
The article ‘Iron Infusions and Hypophosphataemia’ in the May 2023 edition of Medical Forum highlighted hypophosphataemia as a potential and important complication of intravenous iron therapy with ferric carboxymaltose. This complication is relatively common and may currently be underappreciated. We assessed patient phosphate concentrations prior to, and approximately one month after iron infusion with 1g ferric carboxymaltose.
Of the 173 patients included, 47 of 173 patients (27%) had a low phosphate concentration (<0.75mmol/L) following the infusion. In four of these patients (2%), the hypophosphataemia was severe (<0.40 mmol/L); in 43 (25%) it was mild to moderate (0.40 to 0.75 mmol/L).
There was no pre-infusion phosphate concentration which predicted the development of hypophosphataemia. Nearly all patients in the study (169 of 172), including all four patients with severe hypophosphataemia, had normal serum phosphate concentrations prior to the infusion.
Other research has reported even higher incidence of hypophosphatemia (up to 75%) following infusion with ferric carboxymaltose, with peak incidence at 1-2 weeks following the infusion (Wolf et al, 2020).
We agree with the importance of measuring and monitoring phosphate concentrations in patients who experience symptoms post iron infusion, such as fatigue, bone pain or muscular weakness. It should be noted that management is not simple and phosphate
Medicare reform must continue
Dear Editor,
I am copying you in on my open letter to Federal Health Minister Mark Butler:
Congratulations on the first real initiatives to restore the primacy of general practice in the health system.
As you will be aware, the Morrison government set up a review of Medicare but their terms of reference refused to examine the following terms:
To demand a review of the Medicare schedule as applies to general practice with respect to changing the current time bands from 5 to 20 minutes and replace with 10-minute quintiles which better reflect the role of the holistic GP, reward high quality holistic care and return a better rebate to patients to preserve universal affordable access to primary health care.
Changes to Medicare bulk billing is the lifeboat general practice needed particularly in rural Australia where GPs could earn up to $150,000 more each year and preserve bulk billing for all those on a health care card.
Sadly, the working poor not on a health care card will be forced to pay Tony Abbott’s gap payment of $20 in the city and $40 in the country to get parity. Let’s hope next year’s budget will start building the Medicare ship of universal access to health care.
We must recognise the holistic GP who is more likely to be female and seeing the difficult female patient who comes in for a simple pill script but is suffering post-natal depression, she has breakthrough bleeding on the pill, she has doubts about her partner’s fidelity opening up issues of STDs.
supplementation may not be helpful.
In the setting of increased renal phosphate wasting mediated by FGF23, phosphate supplementation may actually increase urinary phosphate excretion and thus worsen or prolong hypophosphataemia (Schaefer et al. 2022). Treatment with activated vitamin D may be beneficial by mitigating secondary hyperaparathyroidism.
However, if subsequent iron infusions are required, choosing an alternative iron preparation such as ferric derisomaltose may be advisable in affected patients, in order to avoid complications such as osteomalacia.
Dr Rachel Dennis, Dr Aaron Simpson and Dr Ram Tampi Clinipath Pathology
Or the middle-aged male with early hypertension but is obese, has syndrome X with high triglycerides and truncal obesity. Low physical activity, drinks too much alcohol and pre-diabetic. Yes, we could just prescribe the blood pressure tablet and ‘kerching’, get the Medicare rebate, or allow this patient to see the pharmacist for a repeat script, or we could spend 15 minutes per consultation and start to address these issues.
Under current policies we encourage over-servicing and 6-minute medicine and totally ignore the productivity improvements that could be achieved by rewarding longer quality consultations. A bulk billing doctor now stands to earn up to 10x ($42 item 23 +$20 BB) = $620 per hour yet this government expects GPs to cope with the complicated patient with holistic care at a rebate to patients of just $42. No wonder GPs will charge a gap fee of $50, giving them an average net hourly rate of just $368.
Despite the obvious definition of stupidity (i.e. doing the same thing over and over and expecting a different result), when will the RACGP recognise that the current time bands are not fit for service and we must change to 10-minute quintiles?
The benefit is that it is revenue neutral to Treasury. Bulk billing clinics will still spend just 6 minutes per patient with no change to the budget. But quality GPs will be rewarded and patients will receive a higher rebate.
Dr Colin Hughes Former chair RACGPWA
JUNE 2023 | 13 MEDICAL FORUM | BODY & MIND LETTERS TO THE EDITOR
BACK TO CONTENTS
Flying right into health
Physiotherapist and commercial pilot Kennedy Lay has combined his two passions to create a business which takes allied health into the regions and has just made him a 40under40 award winner.
 By Ara Jansen
By Ara Jansen
What happens when you start your career and less than a handful of years in, feel burnt out and ready to try something else? It’s not easy to find something else you love just as much and are just as passionate about.
Kennedy Lay had a successful career as a physiotherapist, but like a lot of his colleagues, was burnt out and felt stagnant before he hit 30 and wondered what might come next.
“I was seeing about 60-70 patients a week,” says Kennedy, who found himself wanting to take a career sabbatical.
Born in Hong Kong, Kennedy moved to Melbourne when he was 13 and did his masters of physiotherapy at La Trobe University.
As he was feeling burnt out, generally just over it and wrestling with a lack of career progression, the 29-year-old started remembering a Hong Kong television series he loved as a teen called Triumph in the Skies screening in the early 2000s. It was a drama about the lives of pilots working for the fictional Solar Airways, which was based on Cathy Pacific Airways.
“One of the characters had a long distance romance with a girl in Rome,” he recalls. “That was a big deal in my head when I was young and I always wanted to be a pilot in some form or other.
14 | JUNE 2023 MEDICAL FORUM | BODY & MIND
CLOSE-UP BACK TO CONTENTS
“After four years of work as a physio I decided I wanted to pursue another pathway.”
He applied for flight school with Qantas in Queensland and after a series of tests, was accepted. It was a lot more work than he thought after his Triumph in the Skies romantic notions of flying collided with reality. While training to fly large commercial jets, Kennedy didn’t find a lot of magic in the way a commercial plane operated mostly on autopilot. But he still came away with a commercial pilots’ licence.

In a fortuitous conversation, one of Kennedy’s physio patients owned a sizable regional airline. When
they were talking about what he might do next, the client suggested Kennedy combine his two loves –flying and physiotherapy. It planted a seed and Kennedy started looking around for a problem or a need he might be able to solve using flying and physio.

After lots of research and business planning, 15 months ago, Kennedy founded Fly2Health Group, which flies allied health practitioners into rural and remote towns in small planes. Those practitioners work in areas such as physiotherapy, speech therapy, occupational therapy and psychology. They specialise in on-the-ground assessment and therapy but also have telehealth services.
Part of the Fly2Health business model is that staff fly out of Perth in the morning and return in the evening, which helps with retention.
Kennedy started with one light plane and seeing patients as a physio one day a week, while continuing to work in a clinic. Now there’s 50 staff and five planes ferrying people around the state on regular rotation across about 23 stops that include Albany, Kalgoorlie, Wiluna, Tjuntjuntjara and Carnarvon. There are more than 150 people on the list waiting to be seen and the highest area of demand is working with children with developmental barriers such
continued on Page 17

JUNE 2023 | 15 MEDICAL FORUM | BODY & MIND
CLOSE-UP
BACK TO CONTENTS
Kennedy with partner Carina, a doctor at RPH
Flying right into health
continued from Page 15
as autism, developmental delay or intellectual disability.
In September 2022, the Jandakot Airport-based business expanded into remote Queensland and the plan is to eventually start up hubs in other states as well.
As the business has grown so fast, its managing director doesn’t get to fly as often as he’d like, averaging about one flight every three weeks. His staff are usually younger practitioners who are attracted to the adventure of flying across the state to work. But it remains a challenge to find people. From his experience, Kennedy knows that the life span in allied health is about five to seven years and money tops out at about $150,000.
A former ski instructor on three continents who tries to hit the slopes once a year, Kennedy chooses golf as his way to unwind in Perth. He also likes to climb and says his 2017 adventure up Mt Kilimanjaro was one of the hardest things he has ever done. Doing some serious climbing around Mt Everest is on his bucket list. He’s started training, but doing it is still “way in the future”.

Kennedy lives with partner Carina, a doctor at Royal Perth Hospital. They met in Queensland while he was doing his flight training and he followed her to Perth. They both lead busy lives but find time to drive south for getaways and wine, fly to Rottnest and always make time for date night once a week. He’s a reader of business books and she likes fiction.
“Empathy, good communication and caring about other people forms a great cornerstone for our relationship,” he says.
Having a business of some sort was always part of his life plan. An only child, Kennedy’s mother has a real estate business in Melbourne and his dad is a business broker.
He describes himself as a chronic achiever of things, rather than a high achiever and while he has big goals, doesn’t consider himself ambitious.
“I reckon business might run in my
blood from my mum’s side. When I was 14, my dad left us, and mum and I were living in a friend’s spare room. She single-handedly made her own success. That was a really good example and lesson for me to create my own path.
“My mum is an amazing role model. She had nothing to lose so she created her own financial living.”
Having a higher purpose to his business also rings true. Kennedy says if you solve a problem or a need, the money will come. Indeed, Fly2Health has never taken external investment and cash flow has been positive from day one. The company’s goals include altruism and selflessness alongside having a positive culture and efficiency.
“Being able to make a difference in the lives and health of people is pretty special. Being able to help people who otherwise don’t have ready access to these services is also hugely satisfying.”
In early May, Kennedy was named a 40under40 award winner by
Business News. Journalist and chief judge Mark Pownall said the 2023 winners shared some unique qualities, including coming from difficult childhoods and facing health challenges.
The judge told Business News the panel was looking for “the entrepreneurs, the people who were willing to take a risk rather than follow the safe path, those who stepped outside their comfort zone”.
“Winning the 40under40 has made me reflect on how amazing the Fly2Health Group team has been to me,” says Kennedy. “I absolutely love what I do and thank my team for providing a platform for free conversation, trust and challenge.”
Now with more than 600 clients in WA and Queensland, Kennedy’s business is committed to rural and regional health and plans to continue to grow its services in WA, Queensland and South Australia.
JUNE 2023 | 17 MEDICAL FORUM | BODY & MIND
CLOSE-UP BACK TO CONTENTS
New compromise on medical payment reforms
Early last year, WA’s biggest health insurer HBF announced a major overhaul of how it pays doctors, to take effect from July 1, 2022.
Among the changes were plans to scrap the problematic Known Gap agreement, which it said was confusing and unfair, as well as the Limited Surgical Items List, which only pays patients benefits up to the MBS scheduled fee.
HBF also revealed it had revised all payments to doctors under its Full Cover agreement, with some increasing while others – including anaesthetist fees –decreasing.
But the health fund was forced to put the reforms on hold after strong pushback from several doctors’ groups, including the AMA.
This month, Dr Daniel Heredia, HBF’s Executive General Manager Insurance and Health Services, explains revised changes which he says will simplify medical gap arrangements.
HBF is redesigning its medical gap arrangements to provide clarity on out-of-pocket costs and to ensure a simpler experience for members, doctors and our frontline employees.
Currently, WA-based doctors can register with HBF in one of two ways.
They can be part of Full Cover and Specialist Anaesthetist agreements (chosen by 89% of HBF’s provider network).
The doctor agrees not to charge HBF members a gap for in-patient services covered by the Medicare Benefits Schedule. In exchange, HBF pays a premium above the MBS fee.
Alternatively, they can part of Known Gap agreements (chosen by 11% of HBF’s provider network).
They can opt in: the doctor charges our member a fee higher than the MBS but not exceeding the fees set out in our Full Cover schedule. HBF pays a benefit above what is legislatively required under the MBS and the member has a reduced or no out-of-pocket payment, depending on the fee charged by the doctor.
Or they can opt out: a provider can charge our member a fee above the MBS and above the fees set out in our Full Cover schedule. However, HBF will only cover the mandatory benefit (25% of the MBS), leaving the member with a large gap to make up the difference.
Under the Known Gap agreement, a doctor maintains the flexibility to choose either option (opt in or opt out) on a patient-by-patient basis.
HBF's Limited Surgical Items List, which accounts for 0.1% of services, also exists under our medical gap arrangements. Item numbers on this list are excluded from these arrangements and the doctor is free to set their own fees, with HBF paying benefits up to the MBS fee, regardless of the type of provider agreement.
Benefits for anaesthetic services associated with item numbers on this list are also excluded from the arrangements. It should be noted that no other insurer has such an offering.
In the 2022 financial year, HBF paid doctors on the Full Cover and Known Gap arrangements $95 million above what we were required to pay under the MBS, with the aim of reducing or eliminating out-of-pocket fees for our members.
Changes necessary
The Known Gap arrangement is a source of constant confusion and complaint from HBF members because there is nothing ‘known’ about the gap they may face. A member may have no gap, a modest gap, or a large gap when they see a Known Gap doctor.
The same can be said for the Limited Surgical Items List as it provides an exception to the requirements under the Full Cover arrangement.
18 | JUNE 2023 MEDICAL FORUM | BODY & MIND
NEWS
BACK TO CONTENTS
That is why we proposed changes in 2022 – our intent was to simplify our medical gap arrangements by removing both the Known Gap agreement and Limited Surgical Items List, while also addressing the disparity in fees across specialties under the Full Cover and Specialist Anaesthetist arrangement.
However, feedback from the profession was that doctors wanted to maintain the flexibility to charge a gap on a patient-by-patient basis. Additionally, doctors did not support the redistribution of fees under the Full Cover and Specialist Anaesthetist arrangement, so HBF paused to consider a different approach.

We’ve decided not to amend our Full Cover or Specialist Anaesthetist Schedules.
However, from October 1, 2023, Known Gap will be replaced with ‘Provider Choice,’ a simpler scheme under which a specialist can opt in or out case-by-case. If they opt in, they accept the HBF schedule fee as full payment for the service and a gap is not charged. If they opt out, a fee is charged above the HBF schedule, in which case payment to the provider defaults to the MBS schedule fee and the member is charged a gap.
The Limited Surgical Items List will be removed. A scheduled fee will instead be set for all items currently on the list, and those on Provider Choice can opt in or out of the agreement for those services as outlined above. Full Cover providers who wish to remain on this agreement must adhere to
the terms and conditions for these services but can choose to switch to the Provider Choice agreement. We believe this will drive value for members and flexibility and simplicity for providers.
Communication
HBF is sending tailored communications to our providers. We understand changes like this can trigger questions and we want to be transparent about how this may impact our providers to ensure they have time to find out more. Anyone who has queries should contact HBF.
Referrers and members are encouraged to use the Provider Search functionality on the HBF website to determine if a specialist is a participating provider. This information is also available through HealthShare.com.au and within GP practice software.
ED: What do you think of HBF's new plan? Give us your feedback at editor@mforum.com.au
JUNE 2023 | 19 MEDICAL FORUM | BODY & MIND
NEWS
BACK TO CONTENTS
In the 2022 financial year, HBF paid doctors on the Full Cover and Known Gap arrangements $95 million above what we were required to pay under the MBS.
Out of sight, out of mind
With dementia taking over as the biggest health issue for Australians aged 65 and over, it has given urgency to new research efforts underway in WA to stem the tide.
By Cathy O’Leary
Ask most people what they think are the two biggest causes of death among Australians and chances are their answer will be heart disease and cancer.
While one of those is correct – coronary heart disease claims the most lives of any condition – the second cause is a less visible and often down-played contributor.
Not only is dementia the second-leading cause of mortality among Australians – and the leading cause of death in women – it is also the top cause of disease burden among those aged 65 and over.
The increasing level of burden is largely due to the ageing population but also because the burden from other major causes such as heart disease has fallen.
The sobering statistics are part of a recent update to the Australian Institute of Health and Welfare’s compendium report Dementia in Australia, which shows that dementia was responsible for almost 230,000 years of healthy life lost among people aged 65 and over in 2022, a 62% increase since 2011.

In 2022, 401,300 Australians were estimated to be living with dementia – a 4% increase from the previous year. And without a medical breakthrough, the numbers are expected to more than double to 849,300 by 2058.
Getting in early
Dementia experts are warning that the accelerating numbers have big implications for GPs, current and future, because they are often the first point of contact for people with dementia and their families.
As such, they play a key role in the identification, assessment, provision of information, referral and ongoing management of dementia.
While early detection is considered crucial, often the disease develops slowly, with very subtle early signs. Challenges in detecting the transition between normal ageing and dementia onset, and the lack of a definitive diagnostic tool, can delay diagnosis.
Dementia’s link with ageing is complex too, because it perpetuates the belief that its onset is as inevitable as wrinkles as people get older.
It is that mythology around dementia – held not just by the broader community but also by some health professionals – that is part of the challenge facing Professor Blossom Stephan as she heads new research efforts in Perth.
Previously based at UK’s University of Nottingham where she was Professor of Neuroepidemiology and Global Ageing, the Sydney-born academic
20 | JUNE 2023 MEDICAL FORUM | BODY & MIND
FEATURE BACK TO CONTENTS
recently became the inaugural Chair of Dementia at Curtin University – a position jointly created with Dementia Australia.
Professor Stephan told Medical Forum that the new role would help to drive an ambitious research program in the prevention, detection and care of dementia – and she was excited to be based in Perth.
“The idea is to have a new centre for dementia excellence at Curtin that has both a national and international focus, and covers the whole course of dementia, from early diagnosis through to the care pathway, and how we plan for the individual and the carer’s journey, and improve that, all the way to end of life care,” she said.
“In terms of where I come in uniquely, I’m interested in risk factors for dementia, and how we identify those individuals at highest risk so we can mitigate that risk earlier in life.
Prevention
“We know that without a cure, prevention is going to be our best public health strategy, especially when you look at the Lancet Commission that came out in 2020 that said 40% of dementia cases are preventable.
“So, when you think of 40% of over 50 million cases, that’s a huge number that may be preventable.”
Professor Stephan said some simple strategies such as increasing education and awareness,
improving health and lifestyle, and reducing hearing loss could be readily implemented.
And while a cure might be the holy grail, prevention was the next best option, given the forecasted numbers.
Trial hope
“We’re seeing exciting results from clinical trials around being able to hold progression of the disease, so while we’re not seeing a cure, we’re hoping that within a decade there will be one,” she said.
“But in the meantime, prevention is so important, even if it’s to stop people progressing to advance disease stages where we know it’s very costly and has a greater impact on family carers.
“Hopefully, we can mitigate crisis situations and people progressing into care homes, and instead being able to live independently longer and at home longer, so there are a huge number of benefits that come with disease-modifying drugs.”
She concedes that a major challenge is the stubbornly persistent myth that dementia goes hand-in-hand with ageing.
“When people think about dementia, many think it’s just a disease of ageing. While it most certainly is – in that ageing is the highest risk factor – not everyone will develop the disease,” she said. “And that’s where it comes back to the fact that we need a lot more
education about the risk factors, and how people can mitigate them at a personal level.”
She said dementia had to be taken out of “such a negative perspective” and the stigma needed to be removed. There was a lot of bad publicity around it, and there were also different cultural perspectives around ageing and mental health.

“What we need to remember is that people can live to advanced old age free of dementia. In fact, that should be considered the norm –that their brain will age normally,” she said.
“We see different cognitive domains or types of cognitive processes across the life course. So, we see vocabulary and general knowledge increase and, as you would expect, as you get older and things slow down, the speed of information processing or executive function decreases.
“So, depending on the domain you’re testing at a given age, you might see differences in performance compared to an earlier or later age. We’re really looking at dementia from a lifecourse perspective.
“We know there’s a genetic contribution in dementia, but it’s important to give people, even those with a family history of dementia, the optimism that there are health and lifestyle risk factors that they can use to potentially moderate their overall risk, particularly if they can do it earlier rather than later in life.”
Professor Stephan said ongoing gaps in knowledge were highlighted in the results of a survey by Alzheimer’s Disease International which asked people the question ‘is dementia preventable?’. A substantial number of respondents said it wasn’t, despite simple health and lifestyle measures being known to make a real difference.
GPs sentinels
She said the role of GPs in dementia diagnosis and treatment remained integral.
“GPs are the first port of call for the patient, and we need to make sure they have appropriate education in terms of what dementia is, and how to diagnose it, and what the best referral pathways are,” she said.
continued on Page 23
JUNE 2023 | 21 MEDICAL FORUM | BODY & MIND
FEATURE BACK
TO CONTENTS
HBF launches Rehab in the Home with Life Ready Mobile
Enabling eligible HBF members* access to fully covered rehabilitation treatment at home following surgery for a joint replacement or fracture.
About Rehab in the Home:
Fully covered for eligible HBF members*
Eligible HBF members* can access the service at no additional cost when delivered by Life Ready Mobile.
Comfortable, private and convenient for patients
This service enables patients to recover in the privacy and familiarity of their own home with a personal and medical support network, instead of staying in a clinical setting. Exercises are practical and tailored to the member’s home environment.

Range of rehabilitation services offered
Physio, nursing, occupational therapy with consultation of a rehab physician.
Simple eligibility check for patients
As soon as the patient is admitted to hospital, the Life Ready Mobile team can carry out an eligibility check.
22 | JUNE 2023 MEDICAL FORUM | BODY & MIND
Refer a patient today Call 1300 730 852 or email hello@lifereadymobile.com *Rehab in the Home is fully covered for eligible members who hold eligible hospital covers. Excludes medication, appliances and dressings. Additional treatment may incur out-of-pocket costs. Waiting periods may apply before benefits are payable. Contact HBF to check cover eligibility on 133 423.
Out of sight, out of mind
continued from Page 21
“Depending on the patient’s symptoms, the GP needs to decide if they need a full work-up, or does it look like it’s a secondary complaint that can followed up in six or 12 months.”
Dementia Australia CEO Maree McCabe said Professor Stephan’s appointment as the inaugural Chair of Dementia presented big opportunities to improve care in dementia, which she described as the chronic disease of the 21st century.

“The creation of a Chair of Dementia presents an extraordinary opportunity – for dementia research, and for education and support for people living with dementia, their families and carers,” she said.
“We are extremely excited by the leadership and opportunities Professor Stephan brings to this role. Where similar positions have been created for other health conditions, we have seen positive advancements – and we are confident the same will occur for dementia.
Consumer input
“The insights of those living with dementia and the 1.5 million Australians involved in their care is critical to enabling and delivering better research, education and support.”
Ms McCabe said a key role of the university position was to elevate the voice of the consumer in dementia research, and ensure programs and services took into account their experiences and needs.
It was important to make people more aware that while there was nothing definitive they could to prevent dementia, there were many things that could reduce their risk.
“These include looking after your brain health, body health and heart health and it’s never too early or too late to start,” she said.
“While we cannot change getting older, genetics or family history, scientific research suggests that changing certain health and lifestyle habits may make a big difference to reducing or delaying the risk of developing dementia.”
Ms McCabe said dementia had many “touchpoints” across the healthcare system, so it was important the different parts of the system communicated with each other. Ideally an integrated healthcare system should offer more consistent experience of diagnosis, as well as access to support services across the trajectory of the disease to maintain the dignity and autonomy of the person impacted, as well as their families and carers.
And access to palliative care services to meet the needs of people with dementia also needed to be planned ahead of time.
Professor Bronwyn Myers, director of Curtin University’s enAble Institute – a research collaborative focused on helping people living with physical and mental health needs or facing the challenges of ageing – said the creation of the new position would promote a dedicated focus on dementia and research.
“Improving how we diagnose, treat and care for those living with dementia is critical to helping Australians age well,” she said.
Professor Stephan agreed that integration of care was important to ensure there was continuous care for a person, rather than receiving ad hoc, fragmented care.
“When you speak to consumer groups, they often say people go from one service to another and have to retell their story over and over again,” she said.
“Standardised education for carers is really important too, and then you can individualise it along the way. You want systems in place so
that individuals are diagnosed early enough – and GPs feel competent to do that, and they’re supported to do that, with clear referral paths, so they’re working within a holistic, multidisciplinary model.”
Planning ahead
The RACGP encourages doctors to help patients with dementia understand their condition and plan for the future, including choices they might need to make about their medical care.
GPs often had a long-term relationship with their patients, especially those with serious chronic disease and life-limiting illness such as Alzheimer’s disease and other forms of dementia.
The RACGP recommends that advance care planning be incorporated into routine general practice, to plan future medical treatment for a time when patients might not be competent to make, or communicate, decisions for themselves.
Dementia Training Australia also offers resources for GPs to help in recognising, diagnosing and managing dementia, at www.dta. com.au/general-practitioners
For general information and support, the National Dementia Helpline operates the hotline 1800 100 500 around the clock.
ED: Dementia Australia’s largest fundraising event – Memory Walk and Jog – will be held in Perth on Sunday June 11 at Victoria Gardens, East Perth. It hopes to raise $1.7 million across 20 events in Australia. For details go to www.memorywalk.com.au.
JUNE 2023 | 23 MEDICAL FORUM | BODY & MIND
FEATURE
BACK TO CONTENTS
Blossom Stephan (centre), Prof Myers (left), Maree McCabe (right)




Support and guidance whenever you need it, from the experts in medical indemnity insurance. For assistance call our friendly team on 1800 777 156 or visit www.miga.com.au ...we’re here for you Insurance policies available through MIGA are underwritten by Medical Insurance Australia Pty Ltd (AFSL 255906). Membership services are provided by Medical Defence Association of South Australia Ltd. Before you make any decisions about our policies, please read our Product Disclosure Statement and Policy Wording and consider if it is appropriate for you. Call MIGA for a copy or visit our website. 1 75,000 bonus Qantas Points offer only available to registered Australian medical practitioners who first insure with MIGA in a fully insured category, as a doctor in private practice, for cover commencing in the period between 30 June 2023 and 31 July 2023, and who pay in full by 31 July 2023 or enter into a direct debit arrangement with MIGA by 31 July 2023, and pay at least one instalment by 24 August 2023, who have not exercised their rights to cool off nor had their insurance cancelled by MIGA, as per the terms and conditions of the Policy. MIGA Terms and Conditions for bonus Qantas Points for Fully Insured are available at www.miga.com.au/qantas-bonus-tc-pp. 2 A business must be a Qantas Business Rewards Member and an individual must be a Qantas Frequent Flyer Member to earn Qantas Points with MIGA. Qantas Points are offered under the MIGA Terms and Conditions at www.miga.com.au/qantas-tc. Qantas Business Rewards Members and Qantas Frequent Flyer Members will earn 1 Qantas Point for every eligible $1 spent (GST exclusive) on payments to MIGA for Eligible Products. Eligible Products are Insurance For Doctors: Medical Indemnity Insurance Policy, Eligible Midwives in Private Practice: Professional Indemnity Insurance Policy, Healthcare Companies: Professional Indemnity Insurance Policy. Eligible spend with MIGA is calculated on the total of the base premium and membership fee (where applicable) and after any government rebate, subsidies and risk management discount, excluding charges such as GST, Stamp Duty and ROCS. Qantas Points will be credited to the relevant Qantas account after receipt of payment for an Eligible Product and in any event within 30 days of payment by You. Any claims in relation to Qantas Points under this offer must be made directly to MIGA by calling National Free Call 1800 777 156 or emailing clientservices@miga.com.au. © April 2023 Earn 75,000 bonus Qantas Points when you first insure with MIGA by 31 July 20231 Plus earn 1 Qantas Point per eligible $1 paid to MIGA for your medical indemnity insurance2 24 | JUNE 2023 MEDICAL FORUM | BODY & MIND
Getting kids on the right track … early
GPs play an important role in referring children with neuromuscular disorders for early help, explains paediatric physiotherapist Nicole Pates
Paediatric physiotherapists work with babies, children and adolescents experiencing a wide range of conditions, injuries, or developmental concerns. However, your regular private practice physio might not necessarily have paediatric experience or skills, as the entry level degrees in Australia have no standard for a paediatric curriculum.

Just like in medicine, physiotherapists undergo extensive post graduate paediatric training to become a paediatric physiotherapist. The Australian College of Physiotherapists recognises these physiotherapists with expertise through titling and specialisation, and it is possible to find these professionals in local areas.
However, it gets a bit trickier still. Paediatrics is a broad age range, covering 0-18 years. We can work in the city and the country, in hospitals and in the community, in private practice, in not-for-profit organisations and in the disability sectors. Just like in medicine, there are generalist paeds physios who see a little bit of everything and paediatric physiotherapists with expertise in particular areas.
So, what are these areas?
Paediatric physiotherapists work across a range of areas including neuromuscular disorders such as muscular dystrophy, neurological conditions such as cerebral palsy, injuries to the spinal cord, respiratory conditions such as cystic fibrosis, congenital issues such as spina bifida and developmental delay, rheumatological issues such as chronic pain, CRPS and Ehlers Danlos Syndrome and of course orthopaedics/musculoskeletal practice.
One thing that all paediatric physios have in common is we work in a family-centred practice model
of care. We are working with the child in the context of their family and their community to build their physical skills and participation, to help them do the things they love doing.
So how can a paediatric physiotherapist help you and the families you see?
Across all ages we work with children with disabilities in the NDIS, more often than not in multidisciplinary teams.
Paediatric physiotherapists can make a big difference in the first few years of a baby’s life, providing assessment and management for:
• Gross motor delay
• Asymmetrical movement patterns
• Plagiocephaly/brachycephaly –referral prior to 12 weeks is ideal
• Developmental dysplasia of the hip
• Foot shape concerns such as talipes and metatarsus adductus.
As children grow, we can help in the assessment and management of gross motor skill development, walk, run, jump, hop, skip and ball skills, as well as playground confidence; balance and coordination, including developmental coordination disorder assessments; in-toeing, out-toeing, toe walking, knock knees and bow legs; and growing pains.
Towards and into the adolescent years we can help with musculoskeletal concerns such as apophysitis – the wait and see approach is no longer evidencebased and early intervention is key to prevent ongoing pain and maximise participation; rehab after injury or surgery, sports participation, sports performance and post-fracture rehabilitation.
Working with GPs
We are so grateful to GPs for their use of Medicare-funded MRI scans for children under 15 to rule out significant ligamentous or bony trauma.
For rheumatological and pain conditions such as hypermobility, connective tissue disorders such as Ehlers Danlos Syndrome, juvenile idiopathic arthritis, CRPS, chronic fatigue and chronic pain – usually these paediatric physios will work in a multidisciplinary team with psychologists and occupational therapists.
One of the most common reasons a child is seen in private practice for physiotherapy is pain.
Experienced paediatric physiotherapists are adept at understanding and assessing the possible red flags in this cohort and work with you as the child’s GP to minimise the risk of missing pertinent diagnoses, which if not caught early can lead to both unfavourable outcomes and missed opportunities for intervention.
The earlier we can see kids in pain, the more efficient and effective care we can provide.
The moral of the story is to refer early and refer to a paediatric physiotherapist with expertise in the area you need.
ED: Nicole Pates is a paediatric physiotherapist and managing director of Western Kids Health.

JUNE 2023 | 25 MEDICAL FORUM | BODY & MIND
GUEST COLUMN
BACK TO CONTENTS
GP Urology Masterclass 2023
The Westin, East Perth
Saturday 10th June 2023
Please book a place for the conference at gpurologymasterclass.com.au
RACGP CPD Hours - Approval Pending As Per New CPD Requirements
Grants available for rural GPs to attend
You may be eligible for funding through the Health Workforce Scholarship Program (HWSP) to attend the GP Urology Masterclass.
To apply for HWSP funding, you must meet the eligibility requirements: ruralhealthwest.com.au/ programs/health-workforce-scholarship-program
Dr Shane La Bianca
Dr Andrew Tan
Dr Jeff Thavaseelan
Dr Trent Barrett
Dr Matt Brown
Dr Akhil Hamid
Dr Manmeet Saluja
Dr Alarick Picardo
Dr Steve McCombie
Dr Sarah O’Neill
With the largest partnership of Urologists in Western Australia, Perth Urology Clinic can manage all urological conditions, offering a wide range of treatment options.

For urgent referrals or queries, use our GP Hotline on 1800 487 656 (Press 9). refer@perthurologyclinic.com.au
Healthlink: puclinic
Hollywood Clinic | Wexford Clinic
26 | JUNE 2023 MEDICAL FORUM | BODY & MIND
6 TH ANNUAL
Feel at ease. Expert urological care and surgical management.
New hope for pelvic pain sufferers
A Murdoch medical centre is one of 20 GP clinics across Australia selected to support patients with endometriosis and chronic pelvic pain. Dr Andrew Leech explains the concept.

Our current experience is that patients with chronic pelvic pain and endometriosis generally struggle for significant periods of time without a clear diagnosis.

Symptoms can be misdiagnosed because testing modalities such as ultrasound or pathology are not always helpful. Other issues such as infertility, mental health, pain and suffering are significant.
Patients are often lost to follow-up and may lose hope that anything can be done. We recognise that endometriosis and pelvic pain can be complex. There can be difficult conversations around trauma, sexual health and fertility that doctors may not always have time to approach.
Services are also disjointed across the public and private sectors and may not collaborate on how they are managing patients.
Our vision for this new service is to provide care with a focus on physical, mental, and spiritual wellbeing. The staff involved in the Pelvic Pain Clinic will support and work with patients to tailor an individualised treatment plan, recognising the complex interplay of factors that can lead to pelvic pain, and the significant impact it can have on all areas of a woman’s life.
Through advertising and social media, we will increase community awareness of pelvic pain and encourage patients to seek treatment.
And there will be regular training and education in the management of pelvic pain, including medical management, physiotherapy, psychological factors, dietary and lifestyle factors.
We plan to use the multidisciplinary team to bring knowledge and wisdom together, with the patient and their needs always at the centre. The aim is to include the patient
in setting realistic and achievable goals and regularly review her progress towards those goals, adjusting the plan when necessary, in collaboration with the patient and other providers.
We will have a focus on gathering feedback from patients to improve the service to women and contribute to ongoing research. The Commonwealth Government recently announced funding for 20 GP clinics across Australia to offer improved services for patients experiencing endometriosis and chronic pain. The goal of these clinics is to improve accessibility to care and streamline the process. The average time for a diagnosis of endometriosis in Australia is 10 years. We aim to not only improve this wait time, but also improve the quality of care patients receive during the process. This is an area that has many facets, and it is important we consider not only the physical nature of the problem, but also the psychological impacts on patients.
We will use the funding to build our existing service through increased training and upskilling of doctors and nurses, recruitment of additional nursing team members who will help triage, screen and support patients, workshops and education for patients and purchasing of essential equipment such as gynaecology examination beds.
We have also considered more broader opportunities that we would not normally have had. Ideas from our team have included trialling a Tens machine, training in acupuncture, purchasing VR goggles for pain management during procedures and for mindfulness, running regular zoom education sessions and improving our online resources.
Most of the clinics involved are mixed billing practices and will continue this model for consultations with patients. However, we are looking at ideas around how to offer some of the grant funding towards allied health, diagnostic imaging and specialists so that these services are not unaffordable for patients.
We also hope to value-add to the service we already provide through funding the education workshops and resources so that patients are not out of pocket for these.
An additional benefit is the link between the 20 clinics. We have already met together and discussed how we will share our resources and run our service, and we are setting up a community of practice so that the experiences we each have can lead to better outcomes.
We have already connected with local specialists including several gynaecologists who have additional training and skills in dealing with endometriosis. We have also linked with local women’s health allied health and women’s imaging services. We have had initial meetings with Endometriosis WA and connected with Endometriosis Australia. WAPHA has helped us to navigate how to use the funding appropriately and will also be seeking our feedback on improving the Health Pathways for endometriosis.
continued on Page 29
JUNE 2023 | 27 MEDICAL FORUM | BODY & MIND
GUEST COLUMN
BACK TO CONTENTS
Supporting you and your patients to navigate WA’s Mental Health system
Peer Pathways is coordinated by Consumers of Mental Health WA (CoMHWA) where all staff have a lived experience of mental health challenges and recovery. Being Peer run, our Peer Pathways staff use their own personally acquired knowledge to help your patients to identify and link with supports and services that fit their own personal definition of wellbeing.
People accessing our service can choose to do so anonymously if they wish.

Our operating hours are 9:00am to 5:00pm, Monday to Friday.
Call: (08) 9477 2809
Email: info@peerpathways.org.au
Peer Pathways can assist with:
• Individualised service navigation for you and your patients
• Investigation into suitable supports and services most appropriate to your patients’ mental health and wellbeing
• Explaining access pathways and referrals to services and programs, including non-clinical and social support, and support for people ineligible for the NDIS

• Making detailed enquiries on your behalf around waitlists, cost of services, and accessibility requirements
• Tailored resources on service pathways and support options.
Peer Pathways is an initiative of Consumers of Mental
a
(08) 9477 2809
peerpathways.org.au
28 | JUNE 2023 MEDICAL FORUM | BODY & MIND
Health WA (CoMHWA), the WA State Peak organisation for people with
lived experience of mental issues, and is supported by WA Primary Health Alliance under the Australian Government’s Primary Health Networks Program.
Keeping First Nations moving
Community leadership is vital when developing health initiatives with Aboriginal communities, according to Professor Andrew Maiorana
Self-determination is an important, but often neglected consideration when developing health and lifestyle programs for Aboriginal people. Historically, such programs have often been developed by central bureaucracies, without the input and guidance of the community the program is designed to benefit.
As the nation prepares for a referendum on an Indigenous Voice to Parliament, it is imperative to recognise the importance of an Aboriginal ‘voice’ in developing health initiatives designed for Aboriginal communities.
Health inequalities for Aboriginal people are well recognised and underpin the 10-year life expectancy gap experienced by Aboriginal people, compared with the nonAboriginal population. However, much of the chronic disease burden experienced by Aboriginal people is preventable.
Improving access to health services that are culturally appropriate and are guided by Aboriginal ways of knowing, being and doing are critical to helping address the gap.
Sport and physical activity are important to reducing the risk of chronic disease, maintaining good mental health and strengthening social engagement.
Many Aboriginal communities are well supported by organisations that provide sporting initiatives for children and youth, however,
culturally appropriate physical activity programs for adults are much less available. This likely contributes to reduced levels of physical activity in Aboriginal adults.
Talking Together, Walking Together is a research project designed to address this inequity. Recently funded by the Medical Research Future Fund, the project will run in three diverse Aboriginal communities – the Watjuk Noongar community of the Perth region, the Yamatji community of the Geraldton/ Mid West region and the Martu community in the Eastern Pilbara.
It is important that Aboriginal communities have the opportunity to lead the project. At its core, Talking Together, Walking Together is about establishing physical activity programs that are led by the community.
Our research team will provide support for the community to do this, but the ownership of the programs will remain with the community. The communities’ guidance in developing the programs will ensure they meet their needs and expectations.
Some of the physical activity initiatives the project will explore include ‘on-country’ walking programs, peer-led walking programs, modified sporting activities for older participants (such as walking football and basketball), dance-based physical activity programs, and improving
.
community resources to improve access to physical activity.
While improving access to physical activity is the primary objective of the project, sport and physical activity will be employed as a vehicle for increasing awareness about healthy lifestyle more broadly, such as nutrition, smoking cessation, and alcohol and drug avoidance. Knowledge sharing is an important aspect of the project.
The project will embrace the concept of ‘both ways learning’. This involves the researcher team and Aboriginal community learning with and from one another. This will involve using traditional knowledge and ways of learning including locally meaningful metaphors, empowerment through critical thinking and community ownership of knowledge.
An important outcome of the study will be training local community members to deliver the physical activity programs that are developed, so that these are sustainable beyond the duration of the project.
The health benefits of physical activity are only maintained as long as people remain active, so we are mindful that we need to develop programs that the community embraces and can continue to run once the project concludes.
ED: Professor Andrew Maiorana is from Curtin University’s School of Allied Health, and Fiona Stanley Hospital’s Exercise Physiology Department.
New hope for pelvic pain sufferers
continued from Page 27
The stronger we make our networks, the more successful this project will be. A collaborative team approach, with regular multidisciplinary team meetings and
education is a crucial part of the pilot.
It is also important that we offer patients a summary of their outcomes with us, including a clear, comprehensive management plan to take back to their regular GPs.
We feel it is important to involve the patients’ regular GP, especially given patients may be visiting us from regional and remote areas of WA.
ED: Dr Andrew Leech is from The Garden Family Medical Clinic in Murdoch. The second pelvic pain clinic is in Albany.

JUNE 2023 | 29 MEDICAL FORUM | BODY & MIND
GUEST COLUMN
BACK TO CONTENTS
Dermatologist-led cosmetic medicine service

Doctor-delivered treatments, for GP-referred patients
EXPERT LASER, INJECTABLES
Laser modalities for
Rosacea
Acne
Hyperpigmentation
Lentigos, melasma etc.
Vascular Lesions
Tattoo removal
Hair removal
&
HAIR LOSS SERVICES:
Hair loss service
Comprehensive medical service for alopecia and patterned hair loss
Injectables for medical indications
Wrinkle relaxers
Fillers for loss of facial volume
Birthmarks (pigmented & vascular)
Rejuvenation/ageing
Emphasis on ‘natural look’
Axillary Hyperhidrosis
Referrals accepted by Healthlink, Email, Fax, Post or Phone
Post: Karrinyup Dermatology, 5 Cheddar Place, Karrinyup WA 6018
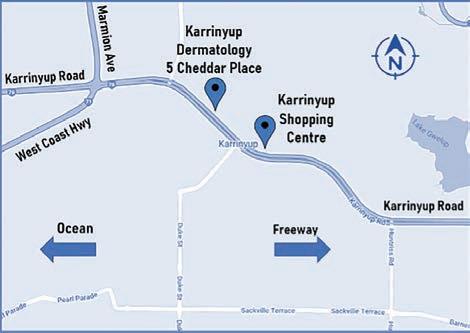
Phone: (08) 9245 3376 Fax: (08) 9245 5033
Healthlink: karrinyd
Email: admin@karrinyupdermatology.com.au
As a specialist Dermatology Clinic, we continue to accept GP referrals for all general dermatology presentations.
30 | JUNE 2023 MEDICAL FORUM | BODY & MIND
Find out more at
www.karrinyupderm.com.au
Help at hand to use digital mental health
There is a need to do better when it comes
to ready access to mental health support, argues Dr Jan Orman from the Black Dog Institute.

Contrary to expectations, we have not had a digital mental health revolution.
Yes, we have developed any number of useful digital tools, some of them with a good body of evidence to support their efficacy, but we are still struggling to have them accepted by patients and practitioners alike, and we continue to struggle to work out how to use them in our practices.
Australia has led the way in the development of evidence-based digital resources and treatment programs. We live and work in a vast country, often with huge distances between patients and their professional care.
GPs in both metropolitan and rural and remote areas (if there are GPs there at all) struggle to find mental health support for their patients. And, as is happening everywhere else in the world, the need for mental health care is rising as the prevalence of psychological distress and mental illness rises in the community post-pandemic.
Telehealth boon
These days, thanks to the pandemic, we have telepsychology and telepsychiatry, and it’s been a great step forward. But these services remain expensive, often with long wait times and, while many with mental health issues benefit from them, not everybody needs or can afford the intensity of treatment they provide.
The rising rates of psychological distress tell us that there is something missing.
Do we need another layer of professional support in our communities? A big injection of well-trained mental health nurses, for example, who can live and work in communities providing skilled care and support. Or do we need GPs with better training in mental health and a better understanding of how to use the available resources?
Since 2001, when MoodGYM burst onto the scene with a promise of a revolutionary way of helping people build their psychological resilience, the way we think about digital resources has changed. Therapy programs, once considered to be stand-alone self-help programs with excellent results in research trials for people suffering mild to moderate anxiety and depression, have been difficult to sell (even for free) in the real world.
Initial engagement and continuing adherence have been major problems. Recent research has shown that most people need a person involved to kick start their use of these programs and to coach them through to the point where they are benefiting from the content.
We are now moving away from “online self-help” to a model of “blended care” where online resources are incorporated into face-to-face care.
There’s plenty of room for GPs to be involved in their patient’s use of digital mental health resources. If we can find an efficient way to incorporate digital resources into our care of people in distress, maybe we can be helpful to them without burning ourselves out. We just need to do a little bit of work to acquaint ourselves with what’s available and how to use it.
The trouble for most GPs is that getting acquainted with the use of digital mental health resources requires time and effort – initially about what is available in the way of evidence-based digital therapy, then to think about which of their patients would benefit from these programs. Most GPs find that it is time well spent in terms of efficiency, confidence and patient outcomes.
Aiming to raise health practitioner awareness and knowledge of digital mental health, the Australian Government in 2013 funded the
eMHPrac (e-Mental Health in Practice) initiative. As part of this project, Black Dog Institute provides training and resources to support health professionals in the use of digital mental health.
The institute has recently launched a new free Health Professional Resource & Education Hub – a custom-built platform providing health professionals with access to evidence-based digital resources, including training modules, webinars, podcasts and e-Mental Health in Practice content.
There is also a highly engaged online Community of Practice in which practitioners can connect with peers and share their knowledge and experience of working in mental health care.
There to use
It is imperative to make use of all the resources available if we are going to meet demand and provide high quality information for both patients and practitioners. Online portals can direct you to resources appropriate for a range of ages, disorder and cultures. You can refer to the Guide to Digital Mental Health Resources available at https://www.emhprac.org.au/ resource/a-guide-to-digital-mentalhealth-resources/ for information. These resources make a reliable and valuable addition to the practitioner toolbox.
ED: The Black Dog Institute Health Professional Resource and Education Hub is available for free for AHPRAregistered health professionals. Visit blackdog.org.au/cop to register
JUNE 2023 | 31 MEDICAL FORUM | BODY & MIND
GUEST COLUMN
BACK TO CONTENTS
Timely mental health care for your patients

These programs allow patients to address mental health issues with minimal wait time or disruption to their everyday lives.
Structured, therapeutic group sessions tailored to the specific needs of patients experiencing:
• Depression
• Anxiety
• Bi-polar disorder
• Personality disorder
• Trauma
• Eating disorders
• Substance dependency
For more information visit ramsaymentalhealth.com.au/hollywood
• Refer directly to Ramsay Clinic Hollywood, no psychiatrist referral necessary
• Cost covered under private health insurance (top cover in psychiatric)
For a GP information pack, please contact Wendy Henson HensonW@ramsayhealth.com.au
People
ramsaymentalhealth.com.au
Ramsay
Hollywood Day
Clinic
Programs
caring for people
COVID: a never-ending story
It is fair to say the emergence of long COVID has been an enigma for researchers, health care professionals and governments.
The Federal Government’s parliamentary inquiry found that GPs would continue to provide most of the care needed by long COVID patients, and therefore needed more education and support. In response, it has pledged to do more, including allocating $50 million for research.
And as our pandemic-fatigued population focuses on normal life without restrictions, Australians continue to be infected by SARS-CoV-2 at a rate of almost 4000 a day.
By April this year, there have been 11,352,930 COVID cases in Australia – almost half the population – and even if just 5% go on to develop long COVID, the addition of more than half a million patients would have a significant impact on demand for Australian healthcare providers.
Yet according to WHO, 10-20% of people infected will also acquire long COVID, and though estimates vary, “the highest percentage of the 65 million global diagnoses were between the ages of 36 and 50 years among nonhospitalised patients with a mild acute illness.”
In WA, 1,308,433 people (also nearly 50% of the population) have contracted COVID and just six months ago, on October 31, 2022, four days before Premier Mark McGowan ended WA’s Public Health State of Emergency, the Department of Health launched Perth’s first long COVID clinic, a pilot-program at Bentley Health Service.
A survey exploring the impacts of long COVID on West Australians was also announced and Senior Medical Adviser for Communicable Disease Control, Dr Paul Effler, explained at the time that the study would help shape WA’s response to long COVID, noting the need to gain “a better understanding of the risk factors and potential causes.”
“WA’s high vaccination rate when we were hit by the Omicron variant means information about long-COVID from other countries with lower vaccination rates, and which experienced different variant waves, is not likely to be applicable to us,” Dr Effler said.
The move followed the Australian Government’s launch of an official inquiry into the impacts of long-COVID and repeated COVID infections, chaired by paediatrician Dr Mike Freelander.
continued on Page 35

JUNE 2023 | 33 MEDICAL FORUM | BODY & MIND
Long COVID remains largely a mystery and GPs are at the front line yet again. Eric Martin looks at why it is proving to be such a headache.
FEATURE
BACK TO CONTENTS
GUARANTEED ACCESS TO A SURGEON ALL YEAR ROUND







34 | JUNE 2023 MEDICAL FORUM | BODY & MIND
Dr Paul Taylor A/Prof Greg Cunningham
Specialising in Spine Surgeons Neurosurgeons Pain Specialist Minimally invasive spine surgery √ √ √ √ Complex spinal surgery including fusion and motion preserving disc replacement surgery √ √ √ √ Lumbar artificial disc replacement √ √ Anterior lumbar fusion surgery √ √ √ √ Cervical disc replacement surgery √ √ √ √ Complex revision deformity spinal surgery √ √ Cervical spine surgery √ √ √ √ Sciatica and radiculopathy spine surgery √ √ √ √ Adult Neurosurgery √ √ Intracranial & spinal cord tumours √ √ Scoliosis surgery √ √ Chronic spine pain management √ √ √ Pain injection procedures √ √ √ Spinal conditions in athletes √ Adult acute and chronic pain management √ APPOINTMENTS P 1800 NEUROSPINE (1800 638 767) F (08) 6147 8200 | W nsiwa.com.au E info@nsiwa.com.au | Healthlink EDI: neurospn MURDOCH | MOUNT (PERTH) | WEMBLEY | CARINE | MANDURAH | VASSE (BUSSELTON) | ALBANY A multi-disciplinary specialist practice offering advice and treatment across the full range of spine and brain conditions, for privately insured and workers’ compensation patients. Privately Insured & Workers’ Compensation patients seen within 3 working days who meet clinical criteria* Referral Criteria: *Neck and back pain in isolation is not suitable for this service Acute – sudden onset of pain (within 30 days) √ Severe leg (Sciatica) or arm pain (Brachalgia) in a radiculopathic (nerve) pattern WITH proven nerve compression (on MRI or CT) √ Plus √ Leg weakness, arm weakness or numbness Or
Dr Andrew Miles Dr Michael Kern Dr David Hamilton
Email referrals to: acutedisc@nsiwa.com.au OR mark your usual referral with ACUTE DISC SERVICE Acute Disc Priority Service
OFFERING:
Physiotherapy Treatment Service for patients in need of treatment for back and neck pain, rehabilitation or recovery following injury or spinal surgery. NeuroSpine Institute is an AO Spine Certified Centre
ALSO
Spine Focused
COVID: a never-ending story
continued from Page 33
An unknown quantity
According to the inquiry, “the cause or causes of long-COVID are unknown” and the condition has remained as equally difficult to diagnose as define.
“There is apparent and significant overlap between long COVID and some other chronic health conditions, such as chronic fatigue syndrome. However, the nature of any relationship between long COVID and other chronic health conditions remains unclear,” the committee reported.
This was highlighted in March, when Australian researchers from UNSW, Western Sydney University, and the University of Sydney published research in JAMA Network Open
The team clinically examined a cohort aged 12-25, six months after they took a COVID test – 382 who tested positive and 85 who tested negative – and while 48.5% of the group who had been infected had long COVID symptoms, 47.1% of the COVID negative group presented with symptoms too.
The researchers noted that other factors, including psychosocial ones, could be behind the persistent symptoms and disability some young people were experiencing, and suggested that the WHO’s definition of long COVID, which has been adopted by most State healthcare systems, may not be accurate.
The latest round of consultation saw the Inquiry meet with federal bodies and Australians living with long-COVID at a public hearing on 17 February 2023 at Parliament House, followed by another in Melbourne on 20 February 2023.
At Malvern’s Cabrini Hospital, the Burnet Institute’s Director and Chief Executive, Professor Brendan Crabb, unpacked the latest information on long COVID and repeat COVID infections, and the hearing listened to peak bodies, medical researchers, and ventilation experts about the impact on patients, health workers and schools.
Dr Freelander noted at the time that it was also important to
see how long COVID and repeat COVID infections were impacting Australia’s primary care capability. While the committee acknowledged that primary care would “play an important and central role in supporting people with long COVID”, in the Issues paper, it also noted that serious challenges still existed in terms of implementation and integration.
Role of GPs
“The committee has heard about different approaches to managing long COVID, including through GPs, specialist long COVID clinics, and via multidisciplinary approaches involving allied health services,” it said.
“There is currently a lack of consistency in relation to the long COVID clinics between how they operate, including the referral processes, how they are funded, the services they provide, and their existence and accessibility across Australia.
“There also appears to be ambiguity as to whether and/or how these should be integrated into the healthcare system. Some submitters have also reported challenges seeking help from GPs, partly due to limited GP knowledge and/or acceptance of long-COVID as a condition, or lack of access to a GP in a timely manner.”
RACGP president Dr Jacqueline Small said that the consequences of repeated infection were still unknown, so doctors’ ability to provide effective treatment was hampered.
“There could be as many as 500,000 Australians living with long-COVID and yet we still do not have all the answers that we need to properly diagnose and treat it,” she said.
“And once diagnosed, the pathway to recovery is still unclear and there is an urgent need for research into long-COVID and its impacts – for some doctors, managing patients with long-COVID can feel like putting together the puzzle pieces without always having the full picture.”
The National COVID-19 Health Management Plan for 2023, released in December, acknowledged that “an important aspect of Australia’s COVID recovery will be management of long-COVID,” with the Government committing an additional $2.9 billion dollars in special measures and research in 2023.
“We need to investigate the Australia-specific, longer-term effects of the COVID pandemic. Research is required into the causes and impacts of long-COVID on individuals and the health system, particularly in the context of high vaccination rates and lower severity variants,” the National Plan stated, in agreement with WA’s Dr Effler.

“Understanding the effect on mental health, chronic disease management and cancer screening as well as delayed elective surgery will also be important.”
Significantly, the plan also noted
continued on Page 37
JUNE 2023 | 35 MEDICAL FORUM | BODY & MIND
FEATURE
BACK TO CONTENTS
“We have had twelve fit-out contract companies at the St John Of God - Wexford Centre site, and without doubt Medifit Design & Construction stands head & shoulders above the rest for professionalism & quality, I have no problem recommending Medifit for any future works”.
Martin
Manager
Best Practices
Since 2002, Medifit has helped hundreds of healthcare providers create their dream practices. Our award winning design and construction service will deliver a practice that will enhance your working life and we do it with integrity and transparency from our Perth Head Office. As Australia’s premier healthcare design and construction provider, we know what it takes to create a beautiful, productive working environment.


If you are considering space at Murdoch, contact Medifit today for a no obligation consultation.

36 | JUNE 2023 MEDICAL FORUM | BODY & MIND
AWARD WINNING INDUSTRY PIONEER DESIGN & CONSTRUCTION HEALTHCARE FITOUTS ARCHITECTURAL INTERIORS WA HEAD OFFICE MASTER BUILDERS WA WINNERS - 2022 BEST BUILDING FITOUT UP TO $1.5m & BEST INTERIOR FITOUT MEDICAL PROFESSIONAL SUITES | 2021 BEST HEALTHCARE BUILDING UP TO $1.5m 2020/22 IFA BEST INTERIOR FITOUT HEALTH & BEAUTY | BEST INTERIOR FITOUT MEDICAL PROFESSIONAL SUITES | 2017/18 IFA BEST MEDICAL FITOUT | 2017/18 & 2018/19 IFA BEST PROFESSIONAL SUITE DESIGN Contact Medifit today for a no obligation consultation and get the practice you deserve. 1300 728 133 www.medifit.com.au
Johnson - Development Construction
ST JOHN OF GOD WEXFORD CENTRE - MURDOCH
COVID: a never-ending story
continued from Page 35
that “infection with the Omicron variant was less likely to lead to long COVID than the Delta variant,” an observation supported by findings presented to the European Congress of Clinical Microbiology and Infectious Diseases in Copenhagen in April 2023.
The Swiss study, from the Cantonal Hospital St Gallen, found that while 67% of healthcare workers with Delta indicated long COVID symptoms, those first infected with Omicron were no more likely to report symptoms than healthcare workers who had never caught COVID.
Indeed, international and Australian studies published in 2023 have already started to answer some of the big questions posed by the committee – a crucial development given that leading Australian long COVID resources, such as the NSW COVID-19 Critical Intelligence Unit and National Clinical Evidence Taskforce on COVID-19, depend on weekly updates in research to inform doctors and clinical practice.
Complex signs
One of the most comprehensive reviews from 2023, Long COVID: major findings, mechanisms, and recommendations, published 13 January revealed that “hundreds of biomedical findings have been documented, with many patients experiencing dozens of symptoms across multiple organ systems.”
The analysis, led by Professor Eric Topol, Director of Genomics at the US Scripps Research Translational Science Institute, highlighted that common new-onset conditions included cardiovascular, thrombotic and cerebrovascular disease, type 2 diabetes (where risk stayed elevated by 27% for up to 12 weeks), myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), and dysautonomia.
“Long COVID is associated with all ages and acute phase disease severities, with the highest percentage of diagnoses between the ages of 36 and 50 years, and most long-COVID cases are in nonhospitalised patients with a mild acute illness,” Professor Topol said.
Significantly, the review showed
that the incidence rate was estimated at 10-30% for nonhospitalised cases, 50-70% for hospitalised cases, and 10-12% for vaccinated cases, giving further impetus to the investigation of vaccine-based interventions.
Vaccination was associated with an overall 43% reduction in the risk of developing long COVID, and on Professor Topol highlighted that Paxlovid had just reported a 26% efficacy rate in initial long-COVID tests, with another study about to commence.
The greatest increase in healthcare use was attributable to just 1% of people who developed long COVID.
Solid data on recovery time also emerged from Israel in research published in January in BMJ, which found that people who developed long-COVID after a mild infection took an average of 12 months to recuperate, with most symptoms more prominent during the first six months.
Hair loss, chest pain, cough, muscle aches and pains, and respiratory disorders were usually resolved between six to 12 months, yet infection was “significantly associated with increased risk of loss of smell and taste, concentration, memory impairment, breathing difficulties, weakness, palpitations, streptococcal tonsillitis and dizziness throughout the study.
“The overall burden of conditions after infection across the 12-month study period was highest for weakness (an additional 136 people per 10,000) and breathing difficulties (107 per 10,000),” Dr Maytal Bivas-Benita from the KI Research Institute said.
Vax protection
“Importantly, the risk for lingering dyspnoea was reduced in vaccinated patients with breakthrough infection compared with unvaccinated people, while risks of all other outcomes were comparable.”
Evidence from other investigations also indicated the potential impact of other case severities and paths of infection on prolonging longCOVID’s impact.
“Symptoms can last for years, and particularly in cases of new onset
ME/CFS and dysautonomia are expected to be lifelong,” Professor Topol clarified, and the review noted that the “overwhelming diagnostic similarity” between long-COVID and ME/CFS was highlighted by numerous studies. Australian researchers from Griffith University confirmed this in March using an ultra-high field 7 Tesla MRI to map the physiological similarities between long COVID and ME/CFS. Their study, published in Frontiers in Neuroscience, revealed that the brainstem was significantly larger in ME/CFS and long-COVID patients.
Complications
“We also discovered smaller midbrain volumes were associated with more severe breathing difficulty in ME/CFS and long COVID patients,” lead author Dr Kiran Thapaliya said.
“Brainstem dysfunction in ME/CFS and long-COVID patients could contribute to their neurological, cardiorespiratory symptoms and movement disorder.”
In addition to dysfunctional signalling in the brainstem and/ or vagus nerve, 2023 also reinforced findings that longCOVID could be attributed to multiple, overlapping causes, including “immune dysregulation, impacts on microbiota and virome, autoimmunity and priming of the immune system from molecular mimicry, and microvascular blood clotting with endothelial dysfunction.
A key discovery, however, was that “persisting reservoirs” of SARSCoV-2 were identified in different tissues of patients with longCOVID.
Multiple reports following gastrointestinal biopsies also indicated the presence of SARSCoV-2, along with an increased number of cytotoxic T cells.
One of the key themes to emerge was that researchers have consistently warned that governments should prepare for sustained healthcare demand thanks to the global impact of long-COVID.
JUNE 2023 | 37 MEDICAL FORUM | BODY & MIND
FEATURE BACK TO CONTENTS
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
52 | APRIL 2021 MEDICAL FORUM | CARDIOVASCULAR HEALTH
Cycles and reflections
The Federal Budget threw a few shekels at general practice. It is a sign of having been around a while when you can see cycles repeat. Falling rates of direct billing create a political problem which leads to money been thrown. This increases direct billing. Over ensuing years, the value drops and the cycle repeats. It happened in the early 1990s and mid-2000s. COVID delayed it this time.
My Medicare resembles the defunct Health Care Homes which was going to “revolutionise” primary care. My prediction is that the renamed version will also eventually disappear without trace. There is a renewed emphasis on team care. Realistically, with changing disease patterns from acute to mainly chronic, this makes sense. Care needs of an ageing population require input from multiple disciplines. However, like a sports team, there needs to be a captain and this role must be retained by GPs. Each team member can make a valuable contribution but to quote Don Lucchesi from Godfather III – “our ships must sail in the same direction”.
Medical Forum must have had a premonition as we are highlighting Allied Health in this edition and going forward will be expanding the Clinical Service Directory at the back of the magazine to include more of these services. The other theme is Body & Mind. I saw an interesting statistic form the US Surgeon General claiming that loneliness and lacking social connection is worse than smoking 15 cigarettes a day when it comes to impact on premature mortality.
Interviewed by Vox, former surgeon general Vivek Murthy claimed the USA faced a loneliness epidemic. The article states: “The coronavirus pandemic has created a loneliness epidemic. Social distancing, while necessary from a public health standpoint, has caused a collapse in social contact among family, friends, and entire communities – one that is particularly hard on populations already most vulnerable to isolation.”
Side effects are real in any medical intervention. Ignoring them has not changed that. Australia is not dissimilar. There are no medical solutions, but the problems will be seen in medical practice.
Lastly, it is worth noting the passing of Jerry Springer in April. This is the show that everyone watched but few admitted to. As one pundit noted he paved the way for today’s reality shows such as MAFS. At the end of each program, he delivered the same line “Till next time, take care of yourselves, and each other”. In times of stress, or any time – this is good advice for all of us.

JUNE 2023 | 39 MEDICAL FORUM | BODY & MIND
OPINION
| Clinical Editor
Dr Joe Kosterich
My Medicare resembles the defunct Health Care Homes which was going to “revolutionise” primary care. My prediction is that the renamed version will also eventually disappear without trace.
BACK TO CONTENTS
Diagnosis: Fear
By Dr Talia Steed, Holistic Doctor, Perth

Going through a journey of chronic symptoms in the body is no easy feat! It tests your resilience and perseverance, while activating a shedding process helping you let go of the parts of your personality that contributed to the development of the symptoms in the first place.
Just a few major lessons on my journey have been about developing patience, acceptance, learning to self-soothe my emotions and to sit with uncertainty, while surrendering the illusion of control. It started with an event or series of events. Traumatic. Stressful. Disruptive to the nervous system, putting it into a state of activation and constant fight or flight. But then the events resolved. Time passed. The external world shifted in positive directions. Yet still the symptoms remained.
For me it showed up in the bowel, but as Dan Buglio calls them, “perceived danger” pain or symptoms can show up anywhere in the body (e.g. back pain, migraines, fibromyalgia, the list goes on). Anything chronic, nonstructural seeming to follow an unpredictable and erratic course that is ill-defined is likely to fall under this umbrella.
The root cause of all these symptoms is exactly this, a perceived danger that something is wrong, fear. Fear of the symptoms, fear of them never going away, fear of daily life being negatively affected, fear that there is actually something wrong.
And it is this fear cycle that keeps them stuck in the body. For 10 years I dealt with relentless erratic constipation, reflux, bloating, pain, classically diagnosed as a simple case of Irritable Bowel Syndrome. However, in my experience this was anything but simple. Even jealousy can arise when others are given a “proper diagnosis” for their ailments, as the feeling is that at least they can do something about
it or know what’s going on.
Over time I discovered that I did know what was going on. The diagnosis was FEAR.
After so many years of judging the day ahead as good or bad based on whether or not I had a bowel motion and the degree of bloating and reflux present, with an extreme fixation and preoccupation on this area of my body through every moment of the day, I reached
a point at which it was time to address the core of what was really at play.
It was time to tell my brain a new message. That I was safe. My body was safe. That there was really nothing physically wrong with my gut (which deep down I had always known), no food sensitivity, bacterial imbalance or leaky walls. That when a symptom showed up it wasn’t a big deal. It would pass.
40 | JUNE 2023 MEDICAL FORUM | BODY & MIND
CLINICAL UPDATE BACK TO CONTENTS
Key messages
The mind and body are not separate.
Symptoms may manifest in any body system.
Asking key questions may unmask the underlying issue.

And my body would take care of the automatic process of digestion if my mind got out of its way.
It was then that the true healing began.
It wasn’t the body I had to direct my attention to, it was time to shine the light on the activation of fear in my mind and my soul. The fear that had got stuck, if you like, in the crevices of my being and had remained so activated that it had been limiting my autonomic nervous system’s ability to do its job.
After all the years of seeing doctors, integrative and specialist, naturopaths, acupuncturists, body talk practitioners, the list goes on, it was time to find the true specialist for these issues showing up in my body. Me!
The journey through chronic symptoms is a journey of awakening. It is awakening to the fears lying dormant in our mind and soul. It is awakening to the ways in which we are living our lives that no longer serve us. It is letting go people, circumstances and places that no longer resonate with the person we are becoming.
It was never really about the gut.
My gut was my saviour. My gut had shown me all the ways my ego and personality had been keeping me stuck. My gut helped me see, through a physical manifestation, where I needed to shed something externally or within, through the years the symptoms infiltrated my life.
Perhaps when you next encounter a patient with chronic symptoms that don’t seem to fit a classic pattern, you might like to think twice before dismissing them with a generic explanation for their symptoms. It is important even amidst the pressures of a busy day and patient load to hold a level of empathy for the complex journey they might be on, which will validate their experience and facilitate improved
is now MindSpot GP
outcomes. By taking the time to ask these questions:
1. What was happening in your life at the time these symptoms first showed up in your body?
2. What is your relationship to the symptoms? Do they activate fear within you?
3. Do the symptoms impact your mood or daily functioning with your attention fixated on what’s happening in your body?
You might even diagnose fear and save that person years or a lifetime of unnecessary suffering.
– References available on request. Author competing interests – nil.
To refer a patient, visit: mindspot.org.au/mindspot-gp
JUNE 2023 | 41 MEDICAL FORUM | BODY & MIND
CLINICAL UPDATE An accessible mental health clinic MindSpot GP is an expansion of the PORTS referral service for general practitioners. We provide free, clinically-validated mental health assessment and treatment. Our support is therapist-guided and accessible online or by telephone.
BACK TO CONTENTS
Key to workers compensation = early and active intervention
 By Aaron McErlaine, Exercise Physiologist & Hadyn Sleeman, Physiotherapist
By Aaron McErlaine, Exercise Physiologist & Hadyn Sleeman, Physiotherapist



In Western Australia, there continues to be an increase in the use of active therapies such as exercise physiology for managing workers compensation claims. This falls in line with the overwhelming evidence for use of exercise therapy as a primary treatment for a multitude of health conditions, both physical and psychological. Early referral of compensable patients to a trusted network of good quality allied health professionals with experience in the scheme will maximise the chances of a positive clinical outcome for patients.
Injured workers have symptoms, restrictions and functional deficits which directly affect their quality of life. Just like anyone that sustains an injury, they have goals that include reduced symptoms and a return to meaningful employment. A patient’s return to health and work should be viewed as a continuum, not as isolated silos of intervention.
The evidence strongly suggests that the following approach gives the best chance of a successful return to pre-injury function, and quality of life – injury seen by a GP for assessment and medical management, then acute
symptomatic treatment overlapping with early active-based therapies, progressing to gym-based and jobspecific strength and conditioning. All health professionals involved in a claim are to provide comprehensive and coordinated care, requiring regular, open and clear communication to all other parties involved in the treatment of the patient. This creates a truly patient-centred approach, an approach which addresses the physical, emotional, psychological,
and social needs of the patient. The known positive outcomes of a truly collaborative approach are comprehensive and effective care to patients; improved patient satisfaction and outcomes; reduced burden and time on the GP; and reduced overall length and cost of the workers compensation claim.
Active therapy benefits
Exercise physiology is one of the primary allied health options available early in a workers compensation claim for GPs and specialists. The benefit of early intervention with exercise physiology is it will empower the patient to have a self-management mindset with regards to their treatment.
Passive therapies may offer the patient temporary symptomatic relief, but there is minimal functional or long-term benefit after the initial two-to-six week acute phase of a musculoskeletal injury has passed.
Early reliance on passive therapies can also result in the patient being reluctant and apprehensive to move on to active therapies with the feeling that ‘exercise’ may
42 | JUNE 2023 MEDICAL FORUM | BODY & MIND
CLINICAL UPDATE BACK TO CONTENTS
Key messages
Have a multi-disciplinary team that works well together to get the best outcome for the patient
Refer early for exercise physiology as an active treatment within a workers compensation claim
Establish an allied health team that specialises in workers compensation.
increase pain and discomfort as opposed to the more relaxed and dependant nature of passive therapies such as massage and dry needling.
The reality is that exercise-based therapies will help in the following ways: individualised specific programs that improve functional capacity and promote a quicker return to work and activities of daily living, faster recovery, pain relief, reduced risk of reinjury through improved strength and education, and improved mental health associated with exercise and routine
As a GP, what should you expect from your accredited exercise physiologist for your workers compensation patients?
• Regular and easy to understand functional capacity updates to make filling in medical certificates easy. Spending less time on paperwork will provide you with more time to focus on patient care and developing the best strategy for your patient.
• Attendance at medical case conferences to provide real-time feedback on patient progress as well as an opportunity to address any barriers to recovery including any biopsychosocial flags.
• Individualised, job-specific and evidence-based exercise programming should be provided to get optimal outcomes in the quickest time frames. Completing work specific conditioning provides you and the patient with confidence in progressing their return to work.
• A deep understanding of the WA workers compensation system and the roles of different stakeholders that work within the system including insurers and vocational rehabilitation consultants. Specialists within workers compensation can speed up the treatment approval process with insurers and provide guidance on any questions you may have about a claim.
• Fully mobile to reduce any barriers that patients may have with travelling to a clinic, particularly if their current capacity may inhibit their ability to travel.
• All the tools should be provided to your patient to empower them to take control of their rehabilitation and self-manage their condition. This should include their individualised program on an app, a printout or other resource that provides visual support and clear guidance on how to complete their program, both supervised and independently. Access should also be set up to a gym or pool facility close to home to promote self-management.
– References available on request
Author competing interests – nil
By Mr Peter Ammon Foot Ankle & Knee Surgery




JUNE 2023 | 43 MEDICAL FORUM | BODY & MIND
CLINICAL UPDATE
PETER AMMON St John of God Medical Centre Suite 10, 100 Murdoch Drive Murdoch WA 6150 Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301 www.murdochorthopaedic.com.au Murdoch Orthopaedic Clinic Pty Ltd ACN 064 146 774 ABN 23 070 745 210
MR
BACK
Plantar fascia origin
TO CONTENTS
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
52 | APRIL 2021 MEDICAL FORUM | CARDIOVASCULAR HEALTH
Endometriosis update
By Dr Rose McDonnell, Obstetrician & Gynaecologist, Claremont

Endometriosis is characterised by the presence of tissue similar to the lining of the uterus that grows outside of the uterus, most commonly on the ovaries, fallopian tubes, and pelvic cavity. This tissue responds to hormonal changes in the menstrual cycle and can cause a range of symptoms, including pelvic pain, infertility and painful menstrual periods.
While there is no cure for endometriosis, there have been significant advancements in our understanding and treatment of this condition in recent years. The exact prevalence of endometriosis is unknown, but estimates range from 2-10% within the general female population but up to 50% in infertile women.
One of the most significant developments in the field of endometriosis research has been recognising the role of the immune system in the development and progression of the disease. One promising approach is the use of immunomodulatory drugs, which work by altering the activity of the immune system to reduce inflammation, scarring and pain associated with endometriosis.
While hormonal therapies and immunomodulatory drugs have shown promise in treating endometriosis, surgical intervention remains an important treatment option for many women.
Laparoscopic surgery is most commonly performed to treat endometriosis, involving the removal of endometriotic lesions and adhesions from the pelvic cavity.
Biobank projects are currently underway to collect samples of endometriotic lesions in patients who have undergone laparoscopy for confirmed or suspected endometriosis to better understand the pathophysiological disease process and how this correlates with metabolic markers.
One such biobank exists locally, Endoorigins, supported by the University of Western Australia. In
Key messages
Endometriosis affects 2-10% of women and up to 50% of infertile women
The immune system may play a bigger role than previously thought
Diagnosis remains challenging. Biomarkers are a promising diagnostic tool.
time, subgroups of endometriosis sufferers may be characterised and allow us to understand why some people have slow growing lesions and others have lesions that are fast growing with a tendency for deep infiltration of surrounding tissue and organs. This will allow the creation of models that will help determine disease progression and novel drug targets and potentially delineate specific immune dysfunction markers and cellular anomalies.
Diagnosing endometriosis can be challenging due to its varied clinical presentations and lack of specific symptoms. Biomarkers have emerged as promising tools in the diagnosis and management of endometriosis, providing valuable insights into disease pathogenesis, aiding in early detection and monitoring treatment response.
A biomarker is a unique protein fingerprint in the blood and can be used as a screening test. Proteomics International recently presented results at the international conference for the Society of Reproductive Investigation at their 70th Annual Scientific Meeting held in Brisbane. They showed that their biomarker test for endometriosis was able to correctly identify up to 90% of patients with moderate or severe endometriosis in a study of over 900 participants.
The European Society of Human Reproduction and Embryology (ESHRE) 2022 guideline on Endometriosis does not recommend biomarker testing for diagnosis of
endometriosis. They suggest that large, multi-centre prospective studies with independent validation sample sets are needed to investigate the potential benefit of biomarkers in the detection and prognosis of endometriosis.
These recommendations were largely based on a Cochrane database systematic review, which looked at the diagnostic potential of biomarkers for the diagnosis of endometriosis. So far, no reliable biomarkers are available for clinical use but it is thought that an effective biomarker may reduce the number of laparoscopies done for assessment of the pelvis for endometriosis. For now, laparoscopy remains the gold standard for diagnosis of endometriosis.
The Australian government has recently announced funding for two general practices, Garden Family Medical Clinic in Murdoch, and Pioneer Health in Albany to develop endometriosis and pelvic pain clinics. According to media statements these clinics will provide expert, multidisciplinary primary care for women living with one or both conditions. Funding has been provided to improve provision of diagnosis, treatment and management of endometriosis and pelvic pain with an ability to link to relevant primary and tertiary care services in the public and private sector.
It is expected that the introduction of such clinics will reduce the average time to diagnosis, which is currently 6.5 years. Both conditions are known to have a devastating impact on the daily lives of women who suffer from these conditions with long-term mental, physical, financial, and social costs. With an overstretched public service, it would be desirable to see further clinics open to improve access to services which could provide medical, nursing, and allied health support to women who suffer from endometriosis and pelvic pain.
– References available on request
Author competing interests – nil
JUNE 2023 | 45 MEDICAL FORUM | BODY & MIND
CLINICAL UPDATE
BACK TO CONTENTS
No health without mental health
By Dr Maxine Hawkins, Psychologist, Mt Lawley


“There is no health without mental health”. I love this quote for so many reasons. Physical health and emotional health are intimately intertwined in what’s known as the mind-body connection. While this statement is widely acknowledged, how each person experiences and address their mind body connection varies.
Some people have the tenacity to push themselves to superhuman levels and their ‘health’ holds out. However, we then see them with low mood and anxiety symptoms. For some, their resentment builds, or they struggle to find joy in life. They may turn to food, alcohol or other substances to cope with emotions. For others, their physical health (chest pain, migraines, fatigue) declines first and their
Key messages
“There is no health without mental health.”
Our feelings are trying to talk to us. Learning to listen to them is a skill.
Slowing down is vital.
mental health follows. A decline can present in many ways such as fatigue, feeling numb, somatic or cognitive anxiety symptoms, difficulty with relationships and irritability.
The words or care shown by a GP will make people do things they won’t normally do! A health professional advocating to their patients to take action to improve the way they feel is a gift. A referral
to a psychologist from a GP validates they have a real issue and gives the patient permission to seek support and hope for change.
A skilled psychologist has been trained how to conduct an extensive assessment. There is no point in assisting someone to manage anxiety better or improve their mood when the root causes of some of their issues remain unaddressed. Slowing things down in an assessment phase is important for the psychologists to understand the patient, as well as the opportunity for golden therapy moments – when the client better understands themselves to promote action within their own lives.
Melbourne University (where I studied) taught us how to conduct
Perth’s comprehensive vascular and vein treatment destination
46 | JUNE 2023 MEDICAL FORUM | BODY & MIND
Hollywood Consulting Centre T: 08 9386 6200 F: 08 9689 2222 HL: stponosh ponoshvascular.com.au
BACK TO CONTENTS CLINICAL UPDATE
Mr Stefan Ponosh Vascular & Endovascular Surgeon
a comprehensive assessment, create a formulation, focuses on the treatment goals then discharge. Post my doctoral training I was lucky to work closely with a psychiatrist in psycho-oncology. Together we would conduct the assessments and I would continue with the therapy.
It wasn’t until I was working with people over the years, did I realise the value of the long-term therapeutic relationship. For a client knowing they can return at any time is very containing and helps them work on their health (mind and body connection) as a way of life not just for a period in time. Being aware of triggers or symptoms and taking steps (such as returning to a psychologist) towards promoting mental health is a good life plan.
Studies show that the mindful movement and breathing done in yoga activates the relaxation response via the vagus nerve. For some patients, mentioning the word mindfulness or meditation would make them run out of the room! Instead, even a few simple breathing exercises can help people see the value of breathing deeply

to slow our motors and be aware of what our body is doing.
I often use the analogy that you are more likely to crash the car driving 100km/h than 20km/h. Yes, you may get to your destination later, but you will be more likely to get there and you can enjoy the ride. Slowing down and being aware of our emotions and feelings can save us from ‘crashing’ our mental and physical health. Prevention is better than the cure!
Our chemistry and biology impact our mood and emotions, as well as
GenesisCare, Hollywood
100% patient satisfaction rating achieved*
GenesisCare at Hollywood offers access to radiation oncology consultations, treatment, and access to allied health support services. We offer modern evidence-based techniques and technology combined with compassionate care – aiming to deliver the best possible patient experience and outcomes.
We offer patients:

• Personalised treatment plans, striving for minimal wait times
• Tattoo-free technology
• Access to a wide range of allied health services (including exercise physiology), accommodation, and transportation packages
• For patients who are eligible for Medicare, approximately 80 to 90% of radiation therapy treatment costs are often covered by Medicare rebates

• Private health insurance is not required for radiation therapy
• A multidisciplinary team of supportive clinical professionals
*For radiation treatment patients. Based on patient survey results Oct 2021–2022.
genesiscare.com
thoughts and beliefs. If you’ve ever felt your stomach tighten up when you were anxious, you experienced the mind-body connection. Physical or emotional symptoms are great; it's the body trying to tell us something and we need to learn to listen and take steps.
At times a patient may come through via a Mental Health Care Plan or through an Employee Assistance Program. Both have the potential to address current issues and promote awareness and opportunity to seek further help if required. Finding the right psychologist can be a personal thing and different for everyone. Sometimes it's a perfect fit and at other times it needs a few attempts. The key is to find someone who supports but also challenges you to be your best and thrive.
– References available on request
Author competing interests – nil
JUNE 2023 | 47 MEDICAL FORUM | BODY & MIND
CLINICAL UPDATE
100% Hollywood Consulting Centre, Ground Floor, Unit 1 91 Monash Avenue Nedlands WA 6009 Where to find us Scan the QR code for more information Tel: (08) 9286 8800 | Fax: (08) 9286 8810 receptiononcologyhollywood@genesiscare.com Contact us 3357_O_MEDcon advertising for Hollywood_Medical Forum_185x125mm_V1.indd 1 22/5/2023 4:00 pm BACK TO CONTENTS
CSAT score
A new specialist sexual health clinic for Perth’s northern suburbs
Sexual Health North, in Joondalup, we offer a wide range of services for our patients from the diagnosis and management of STIs, HIV, PrEP, Hepatitis B & C, trans and gender diverse health care for those over 18 years old, genital skin conditions and vulvovaginal medicine. Newer services include the provision of long acting reversible contraception (LARC) including intrauterine devices- hormonal and non hormonal, erectile dysfunction, premature ejaculation and menopausal symptoms.
As our service grows, we will expand and offer further services. Our clinic strives to create a friendly and knowledgeable service in an open-minded atmosphere. We aim to work with our colleagues in primary care and specialist settings for the total wellbeing of our mutual patients. We would also be happy to take calls about your patients.
Dr Christine Dykstra
MBChB (U. of Auckland), FAChSHM
Dr Christine Dykstra trained and completed her fellowship at Royal Perth Hospital, where she has been a specialist sexual health physician for over a decade. With a keen interest in improving sexual health care in Perth, Christine has provided sexual health medical education at various universities and postgraduate programs in Perth.
Her most recent role in research was as the principal investigator for the Royal Perth Hospital site of the WA PrEPIT trial for the provision of HIV pre-exposure prophylaxis in Western Australia. Having lived in Perth’s northern suburbs for many years, Christine is happy to finally bring specialist sexual health care to the Joondalup and Wanneroo regions.

Dr Michelle Yong

MBChB (U. of Liverpool, UK), FAChSHM, MRCP (UK), DIP G-U-MED, DFSRH
Dr Michelle Yong initially gained her experience in sexual health and HIV management at Royal Liverpool University Hospital, UK. Moving to Perth in 2012, she continues to develop her clinical skills at Royal Perth Hospital including transgender medicine.
Sexual health issues can feel embarrassing for many patients. Michelle excels at putting patients at ease with her non-judgmental and empathetic manner along with a healthy dose of humour. She would like to put her expertise to good use by setting up specialist sexual health service to serve the communities of the Northern suburbs.
In order to help reduce the rates of STIs in our community, we offer our patients the opportunity for on-site consultation, pathology / investigations , and medication dispensing with many acute STI treatments. For acute STIs, we try to keep fees to a minimum. You can contact our friendly team to discuss your patient’s needs.
48 | JUNE 2023 MEDICAL FORUM | BODY & MIND 3/5 Regents Park Rd, Joondalup WA 6027 Phone (08) 6119 9140 Email enquiries@sexualhealthnorth.com.au Healthlink EDI: shealthn (preferred for secure contact) www.sexualhealthnorth.com.au
Better understanding the gut microbiome
By Charlene Grosse, Advanced Accredited Practising Dietitian, Subiaco

The role of the gut microbiome (also called ‘microbiota’) in health and disease is an area of intensive research, which has shown that it plays a critical role in many aspects of physical and mental health, including mood, cognition and behaviour.
The gut and brain are intimately connected forming what is known as the gut-brain axis. This axis allows for bidirectional communication between the two organs via the vagus nerve with signals being transmitted from the gut to the brain and vice versa.
Individuals with depression and anxiety have alterations in their gut microbiome, including changes in the abundance and diversity of certain bacterial species. Alterations in the gut microbiome can lead to increased inflammation throughout the body.
Lack of exercise, stress, poor sleep, smoking and an unhealthy diet can all contribute to chronic inflammation. While counselling and medications have been key treatments in managing mental health problems, we are now discovering what we eat can also have an important role.
Diet has a big influence on our gut microbiota composition through influencing the effect on inflammation. Some researchers suggest today’s typically low-fibre, Western-style diet as a reason for a loss of diversity in the gut microbiome. Our gut microbial profile will be different if we eat, for example, a diet based on plant foods or one rich in animal foods, due to corresponding changes in the bacteria involved in metabolising the nutrients in these foods (whether that be carbohydrates or protein).
In 2020, the Australian and New Zealand College of Psychiatrists updated their clinical practice guidelines for mood disorders with a specific recommendation around diet and other positive lifestyle habits such as exercise. While there
Key messages
The role of the gut microbiome is subject to intensive research
Alterations in the gut microbiome are associated with a number of medical conditions
Exercise and a healthy diet can make a difference.
is no single diet that is considered the best way to eat for mental health, a Mediterranean-style diet is has been associated with a reduced risk of depression. There are two key principles for the Mediterranean diet.
1. Eat plenty of vegetables, fruits, wholegrains, fish and seafood.
2. Eat less red meat and less highly processed foods and added sugars.
Healthy eating means a well-fed and more diverse population of microbes in the gut. Aim for a healthy, balanced and varied diet, based around whole foods, and rich in fibre. Resistant starch is
also important for gut health, and consider probiotic and prebiotic foods, which are considered safe to eat.
Exercise has also been shown to be beneficial for gut health through increasing the diversity and abundance of beneficial gut bacteria, while reducing the abundance of harmful bacteria. Additionally exercise can have a positive effect on mood and cognitive function through its effects on the gut-brain axis.
While the gut microbiome is complex, improving gut health through diet and exercise may be an effective way to promote better mental health and wellbeing.
Autor competing interests – nil
JUNE 2023 | 49 MEDICAL FORUM | BODY & MIND
CLINICAL UPDATE
BACK TO CONTENTS
The promise and perils of psychedelic-assisted therapy
By Dr Jeremy Tannenbaum, Pain Specialist & Psychiatrist, West Perth

Psychiatric research has seen a resurgence of interest in psychedelic-assisted therapy (PAT) over the past two decades. The US Food and Drug Administration designated MDMA and psilocybin as ‘breakthrough therapies’ for post-traumatic stress disorder (PTSD) and treatment-resistant depression (TRD), respectively, in 201819, in a field where response and remission rates have been stagnant for decades.
From the 1950s until criminalisation and the ‘War on Drugs’ in 1970, over a thousand clinical papers on the therapeutic uses of psychedelics (mainly LSD and psilocybin) were published, and several international conferences held. Psychiatrists prescribed and often conducted treatment, including group therapies. Common indications were ‘neurosis’, OCD and alcoholism. Many psychiatrists had personal experience with psychedelics as part of their training.
In February 2023, the TGA surprised the clinical and research communities as it responded to lobbyists and rescheduled MDMA and psilocybin, going against the recommendations of leading experts in the field and undermining the scientific process. There are widespread concerns about the role lobbying, political and community interests played in the decision.
Rescheduling allows authorised psychiatrists to prescribe MDMA and psilocybin, in conjunction with psychotherapy; so-called MDMAassisted therapy (MDMA-AT) and psilocybin-assisted therapy (PsilAT). MDMA-AT will be indicated for PTSD and Psil-AT for TRD and must be supervised by the psychiatrist and conducted in controlled clinical settings.
From July 1, psychiatrists can apply, on a case-by-case basis, to a human research ethics committee and then the TGA to become an authorised prescriber. Authorised
Key messages
Research in psychedelics has been resurgent
From July 1st 2023, psychiatrists can apply to be authorised prescribers of MDMA and psilocybin
Hype needs to be tempered but there is genuine promise.
therapy. However, there are concerns regarding the potential risks of MDMA, including neurotoxicity, medication interactions and cardiovascular effects. Concerningly, there have already been reports of patient-therapist boundary violations in clinical trials.
Psil-AT for TRD has also shown promise in recent clinical trials, with some studies showing significant improvements in symptoms lasting up to six or more months posttreatment.
prescribers must have experience, which at this stage is likely only accessible through participation in clinical trials. Therapists must also have additional training. New groups are vying to be the first to establish professional standards and accredited training organisations.
Several phase 3 randomised control trials of MDMA-AT for PTSD have been conducted in recent years, with initial results indicating higher rates of response and remission compared to placebo. MDMA, a ‘serotonergic amphetamine’, induces mood elevation, fear extinction and pro-affiliative social behaviour, which can enhance the patient-therapist relationship.
MDMA may reduce adverse physiological, cognitive and affective responses in patients with PTSD, enabling them to revisit and work through traumatic experiences in
Partial or full agonism at the post-synaptic 5-HT2A receptor, characteristic of psilocybin and the other ‘classic’ psychedelics, induces neuroplastic changes and may destabilise the usually rigid, negative thought patterns characteristic of depression (and perhaps other mental disorders). Psychotherapy may harness transient neuroplasticity and cognitive shifts to allow patients to develop insights, change behaviour and hopefully enable recovery. Ketamine, a dissociative anesthetic, is increasingly used off-label for TRD and acute suicidality. Many trials are underway investigating ketamineassisted therapy (KAT) for psychiatric and non-psychiatric indications. Ketamine’s antidepressant effects have been attributed to NMDA receptor antagonism and other multimodal effects of the r and s-ketamine entantiomers and various active metabolites.
Unfortunately, relapse typically occurs after 7-10 days following a single dose, so repeated dosing may be required to see a benefit and to maintain effectiveness. The widespread emergence of unregulated ketamine clinics managed by health professionals without psychiatric expertise raises many concerns.
Psychological risks of psychedelics include 'bad trips’, flashbacks, and deterioration of mental state, for example, psychosis, or complications from withdrawing medications due to a potential

50 | JUNE 2023 MEDICAL FORUM | BODY & MIND
CLINICAL UPDATE
BACK TO CONTENTS
drug interaction with psychedelics. Medical risks may include cardiovascular toxicity (MDMA and ketamine), and hepatotoxicity, bladder injury and cognitive impairment with ketamine.
Many of these risks are established in long-term recreational users, although the risks within therapeutic contexts are poorly understood. These risks may be minimised with robust screening, psychotherapy, safety and monitoring processes.
PAT trial results must be interpreted cautiously in confronting unrealistic expectations amplified by media hype. PAT trials are typically limited in size, scope, and duration. Participants may not be representative of clinical populations, and maintaining the blinding of participants and researchers has been challenging, introducing significant bias. Further, PAT trial therapy protocols are unrealistically intensive and usually involve two clinicians.
Crucially, significant challenges remain in translating PAT trial protocols into clinical services. These protocols are incompatible
with the conventional, individual psychiatric/psychotherapy practice, and most other existing clinical services and funding models. There is no clarity on training requirements for clinicians. We have already seen the exploitation of vulnerable patients in clinical trials, and there are significant medicolegal risks for clinicians. Rigorous safety protocols and clinical guidelines do not exist, and peak bodies are yet to release updated position statements.
Having two therapists per patient in a dosing session is not feasible from a workforce or payer perspective and, therefore, is not viable as a business model. Dosing sessions alone can last half a day or more, which is exhausting for patients and therapists. This would reduce therapy access for other patients, and is a financial opportunity cost for therapists, and psychiatrists depending on the level of supervision required of them by regulators.
In my opinion, MDMA and psilocybin rescheduling was premature. Nevertheless, this reality is fast approaching.
While PAT offers exciting opportunities for treating psychiatric disorders, it is important to approach these treatments with cautious optimism, given the potential risks and challenges involved in translating these therapies into clinical services. This will require large-scale accredited training and education programs, the development of clinical guidelines, clinical service restructuring and digital transformation, a national framework for monitoring and outcome evaluation, and a commitment from payers to develop adequate funding models. Despite these challenges, I remain hopeful that person-centred care principles are compatible with sustainable and accessible PAT programs and that we will see these treatments integrated safely and effectively into mental health services.
– References provided on request. Author competing interests - Dr Tannenbaum has consulted for Emyria and Reset Mind Sciences and is engaged in several industry-sponsored clinical trials of psychedelic-assisted psychotherapy.
JUNE 2023 | 51 MEDICAL FORUM | BODY & MIND
CLINICAL UPDATE
BACK TO CONTENTS
Happy parenting – prevention is better than cure

Many parenting interventions emphasise skills training after problems develop, as opposed to establishing a strong parentchild relationship from early on. For young children, growing up with a good relationship with their parents may help prevent longterm health issues.
An important part of healthy child development is learning how to cope with mild stressful events, which trigger physiological effects. When young children experience stress in the context of supportive relationships with their parents, these effects are cushioned and return to normal levels relatively quickly. The result is the development of healthy stress response systems.
However, if a young child is living in a chronically high stress environment without a safe and dependable relationship with their caregiver, the result can be very different. Healthy development can be affected, resulting in detrimental influences on learning, behaviour and well-being.
Stressed new parents
The first year of a child’s life can be particularly stressful for new parents. It’s a time of many challenges: sleeping, teething, starting solid foods, rapid development and more. Supporting families early in their parenting journey can help parents develop a dependable relationship with their children and help the family navigate stressful periods.
This is particularly important for children from economically disadvantaged households, where stress levels of both parents and children are persistently higher.
Our current research is investigating a distinctive style of early parenting known as the Respectful Approach. Originally designed for institutional care in Eastern Europe and introduced to the US by world-renowned
child specialist, and leader in the field of early childhood education, Magda Gerber.
The approach focuses on developing a dependable and cooperative relationship with the child from infancy. Caregivers are guided to treat their infants as capable and independent, with emphasis on sensitive observation and attention to cues.
This approach aims to empower parents with a new mindset and strategies to develop a respectful and collaborative relationship with their children. Workshops include infants as well as parents, so parents can see the approach modelled and practise it directly with their children.
Our workshops focus on six key principles for parents to incorporate while caring for their infants. These are trust, respect, sensitive observation, intentional quality caregiving, safe uninterrupted play and consistency.
As an example, quality caregiving is a technique that engages the infant in basic daily tasks by speaking to them and explaining actions, while also allowing for active participation, such as saying: ‘it’s time to put a bib on for lunch’, and then letting them point to which bib they would like to wear. Feeding infants on the parent’s lap rather than in a highchair helps parents better tune into cues and gives infants the opportunity to have their parent’s full attention.
As another example, safe uninterrupted play involves childled play, allowing children the freedom to explore at their own pace within a safe area without disturbance from older siblings or pets, or direction from parents. Parents often like to jump in and show infants the ‘right’ way to play
with a toy (“push this button and then that happens, look how I do it!”) but infants are likely to stay more engaged when they discover things for themselves.
Play with everyday household objects is encouraged (like small bowls, boxes, spoons, small cotton napkins) – these items are openended and infants love interacting with them. Gerber is attributed to the saying that passive toys create active children, while active toys create passive children.
Our preliminary work has indicated that our Respectful Approach parent-child education significantly lowers parents stress levels, with parents reporting they felt calmer and better understood their children which resulted in increased confidence in their own parenting. For our new project, the Happy Parenting Program, we want to discover whether the intervention can also improve children’s health – particularly their stress levels, behaviour and development. Further, we aim to determine whether children from disadvantaged families benefit more from the intervention than children from advantaged families. For this program, we are currently recruiting families with babies up to six months of age to take part in weekly parenting workshops, for two sets of eight-week blocks. The workshops are free and held in locations both north and south of Perth. Parents who are interested in taking part with their babies can find more information at the Happy Parenting Program homepage.
This project is sponsored by Channel 7 Telethon Trust and the Royal Perth Hospital Research Foundation.
ED: A/Prof Therese O’Sullivan is Discipline Lead, Nutrition & Dietetics at Edith Cowan University.
52 | JUNE 2023 MEDICAL FORUM | BODY & MIND
GUEST COLUMN
BACK TO CONTENTS
A strong parent-child relationship from infancy can help set up children for long-term success, says ECU’s Assoc/Prof Therese O’Sullivan.
Living with a child with constipation – the mother’s perspective
By Davina Houghton, School of Nursing & Midwifery, ECU Joondalup
Despite increasing knowledge and evidence being acquired on the subject of idiopathic childhood constipation (ICC), we are no further forward in reducing the burdens for (in this case) the mother caring for a child with this common childhood condition. Research has been undertaken in WA on this subject and preliminary results are available.
ICC affects up to 32.2% of all children in the world and has been described as a “growing global public health problem”. With no underlying medical cause, ICC often goes unrecognised by the child or parent/carer, which increases the risk for chronicity if it lasts two months or more.
It can be easily diagnosed and well-managed within the primary health care setting with the aid of several evidence-based constipation guidelines (e.g. clinical guideline developed by the National Institute for Health and Care Excellence).
The aim is to investigate the range of ICC health education provided to families by primary care practitioners and the formats in which it is delivered, the aspects of the health education that families use, and what other health education and/or resources families feel might help them.
Preliminary findings
The last question of the online questionnaire invited the participants (all mothers) to share anything else in relation to their child’s constipation. The information shared included:
“We were told that she will possibly grow out of it.”
“More awareness of constipation in children and how common. I was at a total loss as to what/ how/treatment/prevention of constipation for this child.”
“She [the child] tells school she feel sick a lot, especially nausea, and then I get called to fetch her resulting in missed school and time off work a lot. I explained to them about her constipation but doesn't
Key messages
Idiopathic childhood constipation is common
Mothers often feel unsupported Use of evidence-based guidelines is strongly advised.
seem to help. I am at a loss as to how to help my daughter and it makes me very sad.”
“Constipation is so tricky!!! GPs have been useless and very dismissive. I have had to guide care and interventions ourselves over many years which at times has been so distressing for the whole family. We still do not have solutions”.
“I feel very discarded when attending medical appointments regarding constipation and feel I am always told the same thing, ‘take Movicol’, ‘take up to 7 adult Movicol a day’.”
“I would like more information on how to manage constipation, prevent it from occurring again and possible causes for it. Dietary advice will be appreciated as well.”
The burdens for these mothers in caring for their child with ICC is both evident and well-documented. It appears to result from primary care practitioners being unaware of the evidence-based guidelines, lacking ICC-specific knowledge, having short consultation times, and providing irregular or short-term follow-up.
Mothers state that they feel they are not being taken seriously, their concerns are often dismissed, or that they are frequently told their child will grow out of ICC. Mothers also feel sadness and distress for their child; guilt, shame and embarrassment that may cause them to question their competence as a mother; and frustration and isolation from the perceived ‘taboo’ nature of ICC.
Furthermore, mothers experience stress from having to administer regular laxative medication, resolve
conflict with partners and siblings, and from having to negotiate care needs with schoolteachers and employers. Often the arduous ICC journey lasts for years, and this diminishes the motivation to adhere to treatment regimens, which can then result in significant adverse effects for the child, their family, society, and the economy of health services.
While there is no quick-fix for curing ICC, ideally primary care practitioners would always use evidence-based constipation guidelines to:
(a) provide a timely diagnosis;
(b) initiate aggressive pharmacological treatment (laxative medication) to disimpact the child, followed by a regular maintenance dose of medication, titrated according to stool consistency as per the Bristol Stool Scale;
(c) demystify ICC through providing collaborative oral, and written non-pharmacological health education to both the child and the mother/parent/ carer, which is individualised according to the family’s educational and cultural needs;
(d) suggest evidence-based dietary and behavioural strategies for managing ICC;
(e) secure regular follow-up consultations to monitor progress, and provide on-going health education and support; and to
(f) refer children unresponsive to the treatment regimen to an expert within three months.
– References available on request
Author competing interests – the author is involved in the research quoted

JUNE 2023 | 53 MEDICAL FORUM | BODY & MIND
CLINICAL UPDATE
BACK TO CONTENTS
For the love of Dave
Dave Fishwick started a bank to help his community and big banking fought him all the way. Now his story is told in a feel-good movie Bank of Dave, in cinemas this month.
 By Ara Jansen
By Ara Jansen
Dave Fishwick’s story is a perfect David versus Goliath tale. How does the owner of a minibus business, who wants to open a community bank, take on the English banking system and win?
What had spurred this seemingly crazy idea was that during the global financial crisis of 2007, locals had started asking Dave for small loans – an amplifier for the local busker, help with a catering company, IVF and funeral expenses.
Over that time, he lent out about one million pounds and says no one defaulted and this gave him an idea. He went up against the London establishment to open a community bank in his hometown of Burley (near Manchester) where all the profits go to local charities.
He won and ended up setting up Bank of Dave in 2011, which is officially called Burley Savings and Loans.
Now his story has been made into a mostly true movie called, you guessed
54 | JUNE 2023 MEDICAL FORUM | BODY & MIND
MOVIES
BACK TO CONTENTS
Actor Rory Kinnear plays Dave Fishwick in Bank of Dave
it, Bank of Dave. It’s an inspiring and feel-good tale of how the little guy (Dave played by Rory Kinnear) took on the suits (Hugh Bonneville) and won with help from a struggling London lawyer (Joel Fry), a local doctor (Phoebe Dynevor) and a concert by Def Leppard.
“It’s totally bonkers,” says Dave, 51, about both his success and the movie coming out in Australia. “Rory Kinnear looks more like me than I do. So maybe as he’s playing in the next Bond movie, I can be his double!”

Bank of Dave is filmed mainly in and around Burnley, which was important to Dave, including in his own home and the pub where he does karaoke. The father of two admits he’s a bit rubbish at karaoke but he’s got plenty of heart and that’s what counts.
Dave recently got a letter from the nurses in the gynae wing of a local hospital near his hometown. They said 200 people jostled daily for the use of one microwave at lunch and could Dave help them buy another one. For Dave it was an easy answer: of course. Through the profits of Bank of Dave – which all go to charity – the nurses have received not only a new microwave but an oven.
These are the kinds of requests Dave gets all the time. Other recent requests include a kitchen and a year’s supply of food for a local school because kids were starting class hungry and a year’s worth of milk for a church’s soup kitchen.
Since 2012, Bank of Dave has given away 31 million pounds to charity and helped thousands of people. Dave has become commentator and pundit on the big banks (he calls them “financial weapons of mass destruction”), a newspaper columnist on financial issues, penned a book and made a number of shows about his story.
“The big banks really do want to get rid of me. They’ve offered me a lot of money to sell and they can’t believe there isn’t a number I will sell for,” he says with great satisfaction. “The Bank of Dave has a worldwide following, people love what it stands for. I’m frightened of nothing and no one.”
Not bad for a kid who left school at 15 with no money or skills. He worked as a labourer until he
decided it was time to experiment with his passion for cars. He asked a local garage to let him fix up and sell one of their old cars and take a cut. He made 30 pounds, kept going from there and always had two of three jobs on the go. Now he has a number of successful businesses, David Fishwick Minibus Sales operates internationally and is the head of a community bank.
“I would love it if the movie inspires people in Australia and New Zealand to start their own banks to help people who are struggling. While I can’t start those banks myself, I’m happy to give people free advice on how to do it.”
Dave says it might well be time to change his name, as in the streets of his hometown no one calls him Dave anymore, they all call him Bank of Dave. He ponders out loud whether “of” is a decent middle name. Yup, it’s another thing which is totally bonkers about his life.
Bank of Dave opens in cinemas this month.
We have three double tickets to give away. To enter go to www.mforum.com.au and hit the competitions tab.

JUNE 2023 | 55 MEDICAL FORUM | BODY & MIND
Win...
MOVIES BACK TO CONTENTS
It’s just a jump to the left…
By Ara Jansen
“It’s a chance to be a rock star,” laughs David Bedella about the fourth time he’ll be playing the notoriously sexy and strange Dr Frank’n’Furter for the Rocky Horror Show ’s 50th anniversary tour.

“You don’t get that often in musical theatre and you get to sing everything from raunchy numbers to beautiful ballads,” he says. “Plus, stepping through the doors and seeing the audience leap to their feet is an amazing feeling.”
He also feels embarrassingly comfortable in the suspenders and platform shoes, which are an essential part of Frank’n’Furter’s costume. “I have to dance and run and hop in them and it was never a problem for me. At least they are platforms and not stilettos!”
David – who turns 61 this year –admits it’s exciting to be his age and playing such an iconic and energetic role. While he can no longer party like it’s 1999, it is a perfect opportunity to be highly conscious about how he treats himself. David makes sure he gets to the gym, stays well hydrated, doesn’t drink and party all night and limits long phone calls to his sisters to preserve his voice.
An American who relocated to England early on in his career, David has spent his life in the theatre,
winning awards for his work in Jerry Springer – The Opera, In the Heights and & Juliet. Over the past decade has also moved into film and TV, appearing in numerous shows including Tom Clancy’s Jack Ryan, Deep State and All the Old Knives
Now he’s thrilled to be part of the touring show for Rocky Horror ’s 50th anniversary which opens in Perth in August. Written and created by Richard O’Brien, Rocky Horror Show is one of the world’s favourite musicals and a classic of musical theatre. It’s currently the only contemporary rock musical to celebrate 50 years on stage.
Since first opening in London in 1973 at the Royal Court’s Theatre Upstairs to 63 people, the show has been continuously on stage somewhere in the world. Stars who have appeared in the show over the years include Russell Crowe, Tim Curry, Susan Sarandon, Meat Loaf, Jerry Springer, Adam Lambert, Emma Bunton, Stephen Fry, Bert Newton, Gretel Killeen, Derryn Hinch, Jason Donovan and Shane Jacobsen.
Let’s not forget the 1975 movie The Rocky Horror Picture Show, which has made more than $135 million and continues to be screened around the world.
David believes the show has become part of the pop culture lexicon for
numerous reasons, including having a great story and songs that have stood the test of time.
“Part of it is also the audience getting so excited at the shows. We’re living in a world where people have so many restrictions and societal norms. Coming to this show lets people live how they want to live, granted within some parameters. People can put on their heels, dress up, come along and have fun and for a little while, forget their problems.”
Tim Curry still sets the bar for Frank’n’Furter, so David tries to bring something different to each performance, drawing from his life and experience.
“You feed the machine of the character each time and see what comes out. Sometimes it’s a surprise to me as well as the audience. I love that. What makes the role so interesting is that constant change. Sometimes he can be shorttempered and stroppy or more congenial, remembering what best serves the story. The art is to always do it with the character in mind.”
The Rocky Horror Show is at Crown Theatre from August 6 – 13. Tickets from Ticketmaster.
56 | JUNE 2023 MEDICAL FORUM | BODY & MIND
THEATRE
The Rocky Horror Show comes to Perth in August and celebrates 50 years of madness taking its toll.
BACK TO CONTENTS
Wines of grace and finesse

It is again a pleasure to review the wines of this high quality, small-volume Margaret River producer, Cape Grace. My last review was in 2016, and the wines continue to grow in stature. Production is so small that I have noted the volumes of each wine. They certainly pertain to the ‘small is beautiful' concept. Robert and Karen Karri-Davies planted their 6ha of vines in Wilyabrup in 1996.
All wines are produced from estate-grown fruit, and certainly compare with their high-profile neighbouring vineyards. In fact, Dr Tom Cullity wanted their site for his pioneering 1967 Vasse Felix vineyard, but the land was not for sale then.

Robert's family history in the region dates back to 1875, when his great grandfather built the Leeuwin Lighthouse and founded the township of Margaret River. Cape Grace’s vines are low yielding and this, combined with their current maturity, is behind the excellent quality of wines produced. With production so small, wines are predominantly sold through cellar door and mail order (www.capegracewines.com.au).
Cape Grace 2022 Margaret River Chenin Blanc (RRP $26)
An enjoyable wine. Tropical fruit aromas with pineapple and guava. Fruit driven flavours – ripe red apples, rock melon, pineapple. Nice weight and texture, and a slightly 'funky' character from a portion of wild ferment in barrel. A 'zingy' acidity gives this wine crispness and clean finish. Great to drink now, though the 'Chenin acidity' will give it medium-term longevity (production 290 dozen).
A 50/50 blend of Cabernet Sauvignon and Shiraz, not common in Margaret River, but a recognised Aussie style. Displays attractive aromas of blackberry and allspice. A medium-bodied wine. A harmonious amalgam of Cabernet and Shiraz characters as evidenced by flavours of blackberry, mulberry, pepper and spice. Bright fruit, supple tannins, mellow and easy drinking now and for a further few years (production 555 dozen).
Attractive in the glass with a youthful green tinged mid-gold colour. Nose is inviting with nectarine, nutty oak/cashew, a touch of brioche. Slightly reductive (which protects the wine in its youth). Palate shows peach, grapefruit and honeydew melon. Quality French oak is integrating. Texture from lees stirring and partial malolactic fermentation, balanced by a fine mineral core. Needs time to express its inherent quality and should evolve over 6-8 years into a complex rewarding wine (production 296 dozen).
Cab Franc is often considered secondary to Cab Sav, but often shows its best in cooler vintages when Cab Sav may show more herbal, unripe characters as it ripens a week or two later. This wine displays beautiful aromatics — fragrant, perfumed with redcurrant, leafy elements and a touch of spice. Flavours of blood plums, a touch of licorice and herbal nuances. Good acidity for this variety in a warmish vintage. Tannins are velvety, finish is fruity and refreshing. Enjoy now, or up to seven years cellaring (production 56 dozen).
REVIEWER'S PICK
Cape Grace 2019 Margaret River Basket Pressed Cabernet Sauvignon (RRP $58)
A wonderful expression of Margaret River Cabernet. A cooler vintage, but this wine has achieved optimal ripeness due to low-yield concentrated fruit from mature vines. Youthful purple/red colour for its four years, which suggests a wine of longevity. Vibrant, enticing nose — blackcurrant and cigar box from quality French oak barriques. Palate refined and elegant. Flavours of blackcurrant and black olives with the Margaret River gravelly trademark in the background. Fine grained tannins glide across the palate. Integrated oak. Beautiful balance. Long flavours. A wonderful wine in the Margaret River mould. Delightful current drinking but will reward cellaring for another 15 years (production 415 dozen).

JUNE 2023 | 57 MEDICAL FORUM | BODY & MIND
Cape Grace 2020 Margaret River Basket Pressed Cabernet Franc (RRP $45)
Cape Grace 2020 Margaret River Basket Pressed Cabernet Shiraz (RRP $28)
Cape Grace 2022 Margaret River Chardonnay (RRP $42)
WINE REVIEW
Review by Dr Craig Drummond Master of Wine
WINPREMIU M WINESFROM CA P E ECARG BACK TO CONTENTS
ACHIEVE YOUR VISION WITH ONE TEAM, FROM CONCEPT TO COMPLETION.

We respect your time is precious. Humphrey Homes’ integrated model of architecture, building and interior design ensures you realise your vision with unrivalled efficiency, construction quality and budget control. To learn how our approach makes the process seamless and enjoyable, contact Dean Humphrey for an informal chat

BC 12003 | ABWA Lic 2601 H U M PH R E YHOM E S COM AU OFFICE: 52 FLORENCE STREET (CNR CU RTIN AVEN U E) COT TESLOE | 92 8 4 544 4
Winner 2022 HIA Perth Peter Overman Award for Innovation in Housing
















































































 By Ara Jansen
By Ara Jansen


















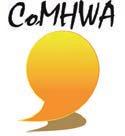


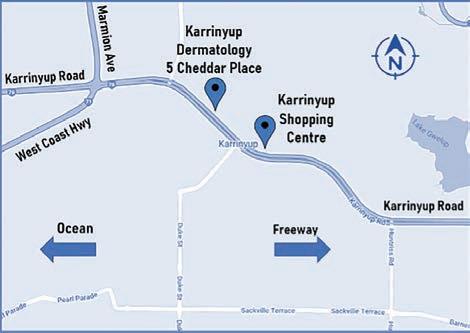
















 By Aaron McErlaine, Exercise Physiologist & Hadyn Sleeman, Physiotherapist
By Aaron McErlaine, Exercise Physiologist & Hadyn Sleeman, Physiotherapist




















 By Ara Jansen
By Ara Jansen