Helping kids to soar Child Health issue | Mental health, ENT, NIPT, Paediatric Sleep, Over-prescribing www.mforum.com.au
August 2020
DRAF
T
Is your practice covered for employment disputes? Employment disputes are more common than you think. At Avant, we’ve helped practices overcome disputes with or between staff, issues relating to employees’ use of social media and contractual arrangements. These employment issues can significantly affect the performance of your business, so it’s important your practice has the right protection and support to minimise their impact.
Avant Practice Medical Indemnity Insurance covers the legal costs to defend a claim against your practice. Our expert medico-legal team is also here to provide tailored advice so you can prevent disputes from escalating in the first instance. Employment disputes can significantly affect your business. Make sure your practice is covered with Avant Practice Medical Indemnity Insurance.
Avant Practice. By doctors, for doctors. 1800 128 268 avant.org.au/practices *IMPORTANT: Practice Medical Indemnity Policy is issued by Avant Insurance Limited, ABN 82 003 707 471, AFSL 238 765. The information provided here is general advice only. You should consider the appropriateness of the advice having regard to your own objectives, financial situation and needs before deciding to purchase or continuing to hold a policy with us. For full details including the terms, conditions, and exclusions that apply, please read and consider the policy wording which is available at avant.org.au or by contacting us on 1800 128 268. MJN220 03/20 (0811)
EDITORIAL BACK TO CONTENTS
Jan Hallam | Managing Editor
Listen and learn
It’s hard to think unemotionally about children, especially your own. There are plenty of people telling you what you, as parents, should do and what your children shouldn’t do. So much judgement is dressed up as advice and it can be exceedingly difficult to find enough detachment to separate the two. The results are feelings of hurt and resentment and the potential of dismissing useful information. Perhaps some of the solution lies by listening elsewhere.
The pandemic has made a lot of people economically and socially vulnerable, which will impact on our future generations in ways that haven’t even revealed themselves yet.
In the child health edition, we start by hearing from a non-clinician, the Commissioner for Children and Young People Colin Pettit, who describes some of the findings from his recent wellbeing survey. While the results are revealing, the most important element was the seeking of opinions from the very people everyone is concerned about – the kids! A sneak peek: Almost 5000 students from Years 4 to 12 were surveyed and while many reported they felt safe, supported and having their material needs met, there were a number of clear areas of concern: • 12% of survey participants rated their health as just fair or poor. • One-quarter of students say they cannot always access support for health worries when they need it. • 41% of females had sought help for mental health worries in the past year. • Half of Year 7 to 9 students and one quarter of Year 10 to 12 students feel they don’t know enough or are not sure about sexual health and pregnancy. • One in 10 students said they cannot achieve their goals or cope with life’s challenges.
It is a sobering list. But before we go half cocked with the judgement narrative – the one that seeks to apportion blame – let’s take a step back again and see what can be done about addressing them. The pandemic has made a lot of people economically and socially vulnerable, which will impact on our future generations in ways that haven’t even revealed themselves yet. More than ever our children need mature leadership from parents, teachers, health professionals and governments. Apart from being unable to guarantee the successful navigation of life’s challenges, we have it in our capacity right now to provide the tools to enable children and young people to give it a red-hot go.
SYNDICATION AND REPRODUCTION Contributors should be aware the publishers assert the right to syndicate material appearing in Medical Forum on the MedicalHub.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publishers for copyright permission. DISCLAIMER Medical Forum is published by HealthBooks as an independent publication for health professionals in Western Australia. The support of all advertisers, sponsors and contributors is welcome. Neither the publisher nor any of its servants will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the publisher or its contributors for the promoted product, service or treatment. Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Trades Practices Act 1974 as amended. All advertisements are accepted for publication on condition that the advertiser indemnifies the publisher and its servants against all actions, suits, claims, loss and or damages resulting from anything published on behalf of the advertiser. EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers.
MEDICAL FORUM | CHILD HEALTH ISSUE
AUGUST 2020 | 1
CONTENTS | AUGUST 2020 – CHILD HEALTH ISSUE
Inside this issue 8 12 24 14 Doctors Dozen...
INSIDE THIS ISSUE 8 Close-up: Dr David Atkinson
Emergency physician Dr Andrew Toffoli won last month’s Vasse Felix collection
12 Q&A with Dr Alex Thompson 14 ADHD: Attention to detail
For your chance to win a dozen bottles of premium
24 GPs? Hold the line please
Sandalford wines, see the review on Page 42 and go
NEWS & VIEWS
to the website www.mforum.com.au (click on the
1
competitions tab)
Editorial: Listen and learn – Jan Hallam
4 In the news 5
In brief
20 Remote patient monitoring LIFESTYLE
42 Wine Review: Sandalford – Dr Martin Buck
CONNECT WITH US /medicalforumwa
/MedicalForum_
2 | AUGUST 2020
/medical-forum-wa-magazine
www.mforum.com.au
info@mforum.com.au
MEDICAL FORUM | CHILD HEALTH ISSUE
CONTENTS
PUBLISHERS Karen Walsh – Director Chris Walsh – Director chris@mforum.com.au
Clinicals
ADVERTISING Advertising Manager Gary Sullivan (0403 282 510) mm@mforum.com.au EDITORIAL TEAM Managing Editor Ms Jan Hallam (0430 322 066) editor@mforum.com.au
29
Inconspicuous Penis Dr Japinder Khosa
31
Paediatric IBD – Crohn’s and colitis Dr Ajay Sharma
33
Non-invasive prenatal testing (NIPT) Dr Adeline Tan
34
Common paediatric ENT issues Dr George Sim
35
Undescended testis Dr Colin Kikiros
38
Temperament Dr David Roberts
39
Paediatric sleep disturbance and behavioural consequences Dr Veena Judge
40
Promises and problems of NIPT Prof Jan Dickinson & Ms Karen Harrop
Journalist James Knox (08 9203 5222) james@mforum.com.au Clinical Editor Dr Joe Kosterich (0417 998 697) joe@mforum.com.au Clinical Services Directory Editor Karen Walsh (0401 172 626) karen@mforum.com.au GRAPHIC DESIGN Thinking Hats studio@thinkinghats.net.au INDEPENDENT ADVISORY PANEL for Medical Forum John Alvarez (Cardiothoracic Surgeon), Astrid Arellano (Infectious Disease Physician), Peter Bray (Vascular Surgeon), Pip Brennan (Consumer Advocate), Joe Cardaci (Nuclear & General Medicine), Fred Chen (Ophthalmologist), Mark Hands (Cardiologist), Kenji So (Gastroenterologist), Alistair Vickery (General Practitioner: Academic), Olga Ward (General Practitioner: Procedural), Piers Yates (Orthopaedic Surgeon) CONTACT MEDICAL FORUM
Guest Columns
Suite 3/8 Howlett Street, North Perth WA 6006 Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
6
MEDICAL FORUM | CHILD HEALTH ISSUE
WA youth speak out Mr Colin Pettit
27
Exciting world of ePrescribing Mr Neil Keen
34
Rehabilitation medicine Dr Arti Fayers
AUGUST 2020 | 3
IN THE NEWS
BACK TO CONTENTS
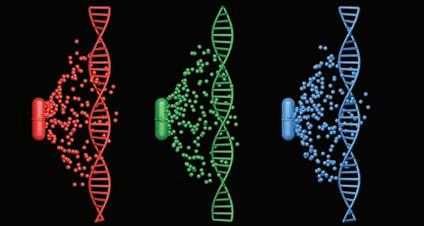
DNA and antidepressants WA psychiatrist and UWA head of psychiatry Professor Sean Hood and director of the Office of Population Health Genomics Kristen Nowak are part of a new $2.95 million project that will analyse a person’s genetic makeup to determine the best treatment for depression. The funding has been provided through the Commonwealth Government’s Medical Research Future Fund. Prof Hood said about half of patients with moderate to severe depression did not see a positive result from the first medication prescribed, with as many as two-thirds failing to achieve long-term relief.
“It’s difficult for doctors because they need to make important decisions about what antidepressants to prescribe, without having an understanding of how an individual’s chemistry might react to them.”
“It can often take weeks or months to get the right medication and dosage for a severely depressed patient and when the right medication is found it can also take weeks or months for it to take effect,” he said. “This is a risky time for severely depressed patients who might become really unwell and require hospitalisation. “Many could abandon their medication altogether if it is not effective or worsens their condition, and some may even attempt suicide.”
Charlie's ED upgrade COVID is making the money go around and SCGH can look forward to its spin of the wheel with the announcement that the state government would be spending $19m to expand and upgrade its Emergency Department. Part of the upgrade will include a new eightbed Behavioural Assessment Urgent Care Centre (BAUCC) for patients adversely affected by alcohol and/or drugs to be assessed safely. Charlie’s ED sees about 6000 patients a month so the waiting room and triage areas will be redesigned to minimise overcrowding and noise. The hospital's main entrance will be relocated from G Block to E Block. These upgrades are additional to the $23.8 hospital maintenance blitz.
Freo gets a share The WA government also announced $24.4m would go to Fremantle Hospital for an additional 20 mental health beds and supplement funding for the existing 20-bed expansion. The new unit will include a 10-bed older adult neurological behavioural unit with a shared model of care 4 | AUGUST 2020
The study will enrol 550 people including 275 from WA. The WA study will run through Sir Charles Gairdner and Hollywood Private hospitals. Study participants will undergo a brain scan and provide a swab for a pharmacogenomic (PG) test, which shows the biochemical process that affects the way individuals break down medications. Prof Hood said PG testing had been available for many years but until now it had been expensive and involved long turnaround times. The study also involves HBF Health Limited, mental health group Meeting for Minds and the Perron Institute.
between psychiatry and geriatrics. It is expected to open in 2023 and the government expects its 64-bed capacity to transform Fremantle Hospital into a key mental health hub in the South Metropolitan region.
Joondalup inches closer While the prep work continues for the major redevelopment of Joondalup Health campus to the tune of $256.7m ($158 from Canberra) the tender process is hotting up with four builders – Multiplex, Lendlease, Georgiou and Built – in the final stage. The tender is expected to be let in October and the build is scheduled to be completed by late 2025 (etch that date in stone). What the people of WA can expect is 90 extra regular and 30 mental health beds, a new operating theatre and cath lab and an expanded ED with a behavioural assessment urgent care clinic.
Alcohol warnings The Health Minister Roger Cook went to the Food Regulation Forum last month with a determined look in his eye. He flagged before the meeting he wanted national compliance of alcohol warnings for
pregnant women on drink labels. He succeeded with the warnings becoming mandatory across all states and territories. The labels will read ‘PREGNANCY WARNING Alcohol can cause lifelong harm to your baby’.
Wins for WIRF UWA researchers under the leadership of Senior Australian of the Year Professor John Newnham have published results which indicate that the rate of potentially fatal preterm births in Western Australian hospitals can be safely reduced by up to 20% when a coordinated series of interventions is applied to pregnant women. The paper, published in PLOS ONE, reveals a 7.6% reduction in preterm births across WA and a 20% reduction in WA’s major perinatal centre, King Edward Memorial Hospital, one year after introducing the WA Preterm Birth Prevention Initiative. John said the initiative was underpinned by seven main interventions including avoiding ending pregnancies before 39 weeks gestation, prescribing vaginal progesterone to women with a shortened cervix or a history of spontaneous preterm birth, and
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
IN BRIEF strongly discouraging smoking whilst pregnant. A new dedicated preterm birth prevention clinic was established at KEMH where all the interventions were promoted. He said the benefit was strongest in women who would not usually be identified as high risk, indicating that the program should be applied to the entire population of pregnant women, not just those with risk factors. The study also showed a significant reduction in preterm births in the Kimberley. “The reduction could be attributed to the introduction of free progesterone treatment – which is usually expensive – and the commencement of a midwifery continuity of care program which has been proven to prevent pregnancy complications,” John said.
Workers comp WA health workers will get special workers compensation protection as a result of the COVID-19 pandemic. The state government will introduce a Bill to ease the burden on health care workers who contract COVID-19 and require access to workers' compensation entitlements. The Act will be amended to establish a presumption of work-related injury for specified diseases suffered in specified classes of employment. Regulations will address health care workers suffering COVID-19 as a priority, this means workers will not be required to go through lengthy and costly claim investigations to prove they contracted the disease at work.
WA supports pill testing The Australian Institute of Health and Welfare’s (AIHW) annual national drug survey has been released with a state-bystate snapshot. Interesting, 55% West Australians supported pill testing at designated sites and 44% supported supervised drug consumption facilities. Nationally, fewer people are smoking (down to 11% in 2019 from 12.2% in 2016). However, this trend was bucked in WA with a slight increase in the number of daily smokers (11.9% from 11.5%). Fewer people in their 20s and Emerging topic: Medicinalwho cannabis 30s are smoking. Those are smoking are generally smoking less and more are rolling their own. Habitual e-cigarette use is up from 31% in 2016 to 39% in 2019. In WA 12.2% of vapers were smokers (from 6.6% to 12.2%) and 73% of WA people surveyed have consumed alcohol in the past 12 months. There were slight declines in the proportions of people drinking daily and weekly between 2016 and 2019.
Emerging topic: Medicinal cannabis
As for other drug use in WA, ecstasy and amphetamine use was slightly less (2.1% from 2.7% for amphetamine) and cocaine use is up (1.6% to 2.4%). The infograph below gives some interesting insight into medicinal cannabis use. In WA, illicit cannabis use has slightly declined from 11.6% to 11.2%.
Quick facts 6.8% of people who used cannabis only used it for medical purposes.
3.9% of those who used cannabis for medical purposes obtained it by prescription.
Older people were more likely than younger people to use cannabis only for medical purposes.
About 1 in 2 people who used cannabis for medical purposes had chronic pain.
People who did not use cannabis for medical purposes were twice as likely to use another illicit drug than a person who only used cannabis for medical purposes.
MEDICAL FORUM | CHILD HEALTH ISSUE
Dr Sophie Davison, who is currently deputy chief psychiatrist, has been appointed as Western Australia's first Chief Medical Officer, Mental Health. She will be acting in the role for the next six months. She will report directly to the Mental Health Commissioner and will play a key role in the newly created Mental Health Executive Committee. This group comprises chief executives and clinical leadership from the WA Health Service Providers and the WA Department of Health.
After a nine-month search Dr Matthew Miles has been appointed CEO of the RACGP. Dr Miles was previously MS Research Australia’s chief executive and a former recipient of the coveted Harvard Club of Australia not-for-profit (NFP) fellowship and shortlisted for the NFP CEO of the Year 2016 by CEO Magazine.
WA Department of Health has granted funding to UWA’s respiratory physician Dr Anna Tai to explore the use of convalescent plasma in early treatment of COVID-19 patients. A/Prof Roslyn Francis and her team will examine whether inflammation associated with COVID-19 persists in the lungs and blood vessels after a person has recovered from the virus.
Professor Barry Marshall’s team working on UWA’s Noisy Guts Project has been recognised at the inaugural Nature Spinoff Prize established by Nature Research and Merck. The project looks at a device that monitors and analyses gut noises to determine cause and severity of any gut disorders. Commercialisation of the device is in the wings.
AUGUST 2020 | 5
WA youth speak out Commissioner for Children and Young People Colin Pettit presents some startling insights about health and wellbeing of WA youth. Children and young people from across the state have shared their views on their wellbeing in WA’s first Speaking Out Survey – and their responses give the state’s health sector valuable insight for both now and into the future. Almost 5000 students from Years 4 to 12 were surveyed and while many reported they felt safe, supported and having their material needs met, there were a number of clear areas of concern: • 12% of survey participants rated their health as just fair or poor. • One-quarter of students say they cannot always access support for health worries when they need it. • 41% of females had sought help for mental health worries in the past year. • Half of Year 7 to 9 students and one quarter of Year 10 to 12 students feel they don’t know enough or are not sure about sexual health and pregnancy. • One in 10 students said they cannot achieve their goals or cope with life’s challenges. Physical and mental health are both critical to a child’s wellbeing, for both a healthy and happy childhood and as a building block for future life outcomes. While a doctor was the most commonly reported source of information for health worries, most students sought help from a friend for mental health concerns. There are positive signs of healthy behaviours, with most saying they had never tried smoking and that the majority of high school students think people their age should not use any substances. However, many Year 10 to 12 students are at risk
in terms of material needs, family stability and expectations for the future. Despite these findings, Aboriginal students have reported high levels of self-esteem and a strong sense of belonging in their community. Students in regional and remote areas fared less well on a number of health measures such as dental health, prevalence of long-term health conditions and weight.
of not getting enough sleep, 70% of female high school students worry about their weight, and one in five females report they often go without eating or sleeping because of their mobile phone use. Female students rated their wellbeing lower than male students and this was most evident in areas of mental health, their self-esteem, conflict, relationships, personal safety and independence. The gap between these female and male student perspectives widened with age. Too many children and young people said they do not always feel safe at home, at school or in their community and one in 10 WA children say there is not enough food for them at home. The challenges Aboriginal children and young people continue to face were evident in this survey, with those who took part faring less well than non-Aboriginal children
Too many children and young people said they do not always feel safe at home, at school or in their community.
6 | AUGUST 2020
The aim is to use this inaugural survey as a baseline. We are now preparing to undertake the next survey in 2021 – moving it forward by one year in light of the COVID-19 pandemic to give a clear indication of children and young people’s wellbeing both pre and post the events of this year. During the past few months I have been hearing from children and young people on how they have been impacted by the COVID-19 pandemic and what supports have helped them. Mental health is one of the main issues raised and while technology has helped many to maintain friend, family and school connections while at home, the long-term impacts of the COVID-19 pandemic on our children’s health and mental health are yet to be known. It is my aim that the views of our children and young people are used in shaping policy and service delivery. We cannot improve health outcomes for our youngest citizens without first understanding their needs. The findings from my Speaking Out Survey were tabled in Parliament and are available through my website. I encourage everyone working with children, young people and their families to consider the findings and the role we all play in shaping the lives of our children and young people.
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
GUEST COLUMN
A tailored banking experience. Bankwest Private Bank provides tailored banking services and access to Private Client Managers, dedicated to helping you reach your goals. Lisa is here to help. Lisa Hutchins Senior Strategic Partnership Manager 0467807662 lisa.hutchins@bankwest.com.au
HOSPITAL
A&E
MEDICAL FORUM | CHILD HEALTH ISSUE
Bankwest, a division of Commonwealth Bank of Australia ABN 48 123 123 124 AFSL/Australian credit licence 234945.
Parking
AUGUST 2020 | 7
BACK TO CONTENTS
CLOSE-UP
Hanging on the telephone A staunch advocate for improved Aboriginal health, Professor David Atkinson has spent much of his career in regional Western Australia. He tells Ara Jansen he wants to ensure the bush has well-trained, quality doctors.
David Atkinson never really made career plans. Turns out, he relied largely on the telephone because when it rang there was always an interesting offer on the other end. He thinks about it quite a bit – how did he end up in medicine? From David’s recollection it was a case of what seemed interesting, other students were planning to study medicine and it would get him a job. It was the 1970s and there was a family expectation that David would go to university. Hailing from ‘the other side of town’ and a not terribly affluent family, he suggests his expensive school probably helped open the doors. “Medicine interested me because of the complexity of what I learnt,” he said. “I have seriously eclectic interests when I can indulge them. I think mostly I enjoyed the clinical exposure. My parents died when I was in my second and third year. I met Sue, who became my wife, in fourth year and we took a year off, saved money and went overseas.” Sue and David have been married for 42 years and she recently retired from her career as a social worker. David is known for his decades-long work in Aboriginal health, particularly in training medical students and young doctors as well as doing research in areas of maternal and child health, chronic disease and aged care. He’s a staunch advocate for practical outcomes to improve the effectiveness of health services for Aboriginal people. When he was doing his internship at Fremantle Hospital, his sister was 8 | AUGUST 2020
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
CLOSE-UP teaching in remote Aboriginal communities. He visited her and something sparked.
Destination Darwin When it came time to finding a job after his internship, David accepted one in Darwin. With a wife and two young children in tow, the work kicked off a now life-long interest in Aboriginal health. “I jumped in and jumped in deep,” David said. “We had a lot of responsibility as junior doctors and learnt quickly. The consultants were also pretty young and I found that encouraging.” David spent a month in Gove, in the northeastern corner of Arnhem Land and then six months as a solo GP in Jabiru, inside Kakadu National Park. “I got involved in local politics there and had a lot to do with the locals working in the construction camp. I also had a number of patients who were the Asian wives of these older men who didn’t treat them very well. I got involved in helping them, made a bit of noise and became politically unpopular.” The Atkinsons ended up back in Perth and David didn’t want to work in a hospital, so he took on a series of GP-related jobs. Turns out, regional and outback life wasn’t finished with him. Over the years David said he stopped planning each time the phone rang, because it was usually an opportunity to consider. While in Perth, David also worked for the then Perth Aboriginal Medical Service, which left a lasting imprint on his career. With no long-term career plan in mind, a job at Fitzroy Crossing seemed the perfect answer and it became David’s formative career experience. The 29-year-old was GP to more than 2000 people spread across 50,000 square kilometres. The closest other doctors were in Halls Creek and Derby. “I spent three and a bit years there. That was the mid to late ’80s and Aboriginal health has improved quite a lot since those days, particularly for kids. “This work fostered a great interest in public health initiatives that made a difference, such as public housing.
Sue and David Atkinson
Learning from elders “One of my favourite activities was volunteering to talk about health at the Karrayili Adult Education Centre. I used to go there once a fortnight and have discussions with a group that included many of the local elders. That really developed my understanding of the place and its people. “We welcomed marban (traditional healers) at the hospital, so if someone wanted one, we went and found him. It was important for the patients to feel safe. “As the only doctor in town you have to understand where everyone comes from and who gets on with who. In Fitzroy Crossing I had to learn the local language groups, understand how to not get too close to one group as you had to be there for everyone.” The Atkinson children (a third son was born while there) had their formative years in Fitzroy Crossing and lived a different life from their city friends. The fact that they’ve gone into law, social work and medicine feels like a definite link to those regional experiences. Let’s not forget a doctor dad and a mother in social work. “I think it had an influence on them in different ways,” he said. “The youngest has ended up being a regional doctor in the Northern Territory.
MEDICAL FORUM | CHILD HEALTH ISSUE
“I think those experiences have had the greatest influence on my middle son – they have definitely influenced his personality and view of life. He’s always had a sense of social justice which I attribute to his outback experiences. “He used to walk home from school – 3km – and it was really hot. He’d walk via the Aboriginal community, chose not to take the bus and made his own way home. He was highly independent. It took him a while to adapt to being back in Perth. “My eldest son is a rural lawyer in a small town. His work supporting clients has many similarities to rural medical practice.” David eventually did a master’s in public health through UWA which led to research work and student supervision. He was the founding director of the Centre for Aboriginal Medical and Dental Health at UWA (1996-2002) recruiting and supporting Aboriginal people to study medicine and increasing Aboriginal health teaching in the medical course.
RCS is born In 2002, the opportunity to return to the Kimberley came as David became a founding member of the UWA Rural Clinical School, establishing the Kimberley branch continued on Page 10
AUGUST 2020 | 9
CLOSE-UP
BACK TO CONTENTS
Hanging on the telephone continued from Page 9 of the rural medical education program in collaboration with the Kimberley Aboriginal Medical Services (KAMS). As well as teaching medical students, it also led to him establishing the Kimberley GP training program for KAMS in partnership with Western Australian General Practice Education and Training (WAGPET). This program has led to a large increase in the number and skills of Australian training doctors working in remote Aboriginal health in the Kimberley. Eventually the phone rang again leading David to become the head of the Rural Clinical School of WA (RCSWA), now a combined program between UWA and Notre Dame. He held the job from 2015 to 2018. Along the way, David won the General Practice Education and Training (GPET) Ochre Recruitment Aboriginal and Torres Strait Islander Health Training Award in 2012 for his role in increasing the number of registrars taking up Aboriginal health posts in the Kimberley. He also received the GPET General Practitioner Supervisor of the Year Award in 2009. A longtime and reasonably permanent resident of Broome, David says part of his work now is to help make sure the Kimberley and regional Western Australia have well-trained and quality doctors living and working outside Perth. “We want to train and keep regional doctors here,” he says. “We want to do enough regional research to give them relevant information. “It’s also about setting up circumstances so doctors want to come and work regionally. For example, one of the first things you have to do is find them a place to live so they don’t have to fuss. You need to care for them from day one. You want to do all the little things which make someone feel welcome and wanted. That way, when issues arise, they feel supported.” 10 | AUGUST 2020
Sharing knowledge The 64-year-old currently splits his time between the Rural Clinical School, though he is no longer head, and works as a GP. He works with students in their second last year of medicine who are on rural placement for their first major clinical year. The hope is that the students enjoy the experience of living out of Perth enough to consider returning once they have qualified. While he has been in Broome for 18 years, David says he gets bored easily, which is why his CV has a lot of different positions on it. “At the moment, GP work is the most fulfilling part of my job as opposed to being on committees. That also has its rewards but I don’t want to do it all the time. The same goes for being in charge and making all the decisions. I think I’ve done my share of taking the responsibility.” That slight change of pace is giving David and Sue the chance to further enjoy what’s around Broome, which included a recent trip to the Bungle Bungles, spending time with their six grandchildren and growing their own vegetables.
“I love contributing to the gardening and eating the results.” Indulging a mutual love for bushwalking, particularly multi-day hikes, has seen the pair lace up their boots in Tasmania and Patagonia and on New Zealand’s Milford Track and Peru’s Inca Trail. Next trip will be to resurrect their recently cancelled walk along Scotland’s 154km long West Highland Way. “One of the things I love the most is genuinely working with younger people to help them do what they want to do. I like having students or doctor trainees. That’s really rewarding,” he said. “I feel the same about my patients. I want to be helpful. I’m in relationship with them and when that’s strong we can get into the issues. If you don’t have a good relationship with people or gel with them when they need something, they might not return. Particularly with adolescents and the disadvantaged – connecting with a 12-year-old can be quite a challenge. “It’s people I’m interested in – and I always have been. They’re probably my great fascination.”
MEDICAL FORUM | CHILD HEALTH ISSUE
You don’t buy a practice every week, but we do
It’s a big decision, Huge. For most, it’s a once in a lifetime proposition. We take this very seriously too. So much so, that over the last 25 years we’ve developed a process for medical professionals looking to go out on their own. But we don’t just look at you, we look at the business as a whole. We act as your partners in ensuring that it is a viable and profitable opportunity. We assess everything - location, competition, client-base and growth potential. Then, and only then, we tailor a loan to meet your needs. Forgive the pun, but we have a lot of practice when it comes to buying a practice. Visit us at boqspecialist.com.au or speak to your local finance specialist on 1300 131 141.
Car loans | Commercial property | Credit cards | Equipment finance | Fit-out finance | Foreign exchange | Home loans | Personal loans | Practice purchase | Practice set-up | Savings accounts | SMSF | Transaction accounts | Term deposits | Vehicle finance The issuer of these products and services is BOQ Specialist – a division of Bank of Queensland Limited ABN 32 009 656 740 AFSL no. 244616 (“BOQ Specialist”).
MEDICAL FORUM | CHILD HEALTH ISSUE
AUGUST 2020 | 11
Q&A with... Dr Alex Thompson, Consultant child and adolescent psychiatrist, CAMHS
12 | AUGUST 2020
MF: Tell us a bit about the mental health services at CAHS and your role in it?
consultant position in 2017 saw me working at the Bentley Adolescent Unit before the opening of PCH.
AT: The Child and Adolescent Health Service provide statewide and metropolitan mental health services in both community and hospital settings. Our 10 community clinics deliver services to children presenting with severe, complex and persistent mental health needs. Ward 5A at Perth Children’s Hospital is the state’s authorised mental health unit for children and young people aged 0-16 years, for inpatient mental health assessment, treatment and crisis intervention. We also provide a range of specialist outpatient and community-based services such as our Complex Attention Deficit Hyperactivity Disorder Service and our Eating Disorders Service. I am a Consultant Child and Adolescent Psychiatrist for Child and Adolescent Mental Health Services (CAMHS) at Perth Children’s Hospital (PCH). I provide advice and consultation for young people who present with mental health concerns to the Emergency Department and occasionally assist on Ward 5A. Most recently I am privileged to be heading up CAMHS’ Emergency Telehealth Service (ETS), based at PCH. No day is the same here – you never know what to expect and I enjoy that variety. I first came to CAMHS as part of my basic psychiatric training in 2013 and returned in 2015 as a senior registrar. My first
MF: How are services accessed? AT: Generally, by a referral from a GP, community nurse or psychologist, or from a school professional. Children and families can self-refer to some of our services as well. Children and young people experiencing acute concerns can present to the PCH ED without referral. MF: How and why did you choose to work in child and adolescent mental health? AT: This subspecialty is not for everyone. We have diagnoses that are largely derived from adult presentations and some would say forced on children and adolescents. We deal with very complex situations involving multiple parties and witness the suffering of very vulnerable young people. The treatment of children is not left to child psychiatrists alone. The function of the multidisciplinary team is vital, and the teamwork with nursing staff and allied health professionals is something I love about the field. The resilience of the children I meet is truly inspirational. Narratives that have been written for them by others are filled with adversity and trauma, but somehow, they find within themselves the spirit to survive. Child and adolescent psychiatrists are trained to provide expert, evidence-informed, individual and MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
Q&A
BACK TO CONTENTS
Q&A family-focused mental health care to infants, children, adolescents and their families. The subspecialty recognises the benefits of early intervention and prevention, as well as the clinical needs of young people with established severe and complex disorders. The second Australian Child and Adolescent Survey of Mental Health and Wellbeing (also known as the Young Minds Matter Survey), conducted by the Telethon Kids Institute at the University of WA in partnership with Roy Morgan Research demonstrated that, based on selfreported information, one in five adolescents are suffering from high to very high levels of psychological distress. I believe we have an important role in promoting their treatment and recovery. MF: What will the new helpline mean for the service? AT: The CAMHS ETS will enable us to better care for young people experiencing a mental health crisis in metro WA. It provides young people and their families with better access to urgent mental health assessments in their homes and communities instead of presenting to an ED – places which are continually busy, sensoryoverloading and not conducive to a young person’s mental wellbeing, particularly if they have to wait for an assessment. CAMHS ETS will provide virtual ‘in-reach’ to the young person and their carer, school or health professional and will provide a mental health assessment in a place they are comfortable with, and without delay. Health professionals are also able to call the ETS to speak to a mental health nurse or consult with a psychiatrist. This is going to improve the quality of clinical care and the experiences of WA young people accessing emergency mental health services. MF: Who will be on the phones? What will the clinical oversight be like? AT: The CAMHS ETS will be staffed by experienced senior mental health clinical nurse specialists who have clinical oversight by myself as Head of Service. Every child receiving an assessment will have their care plan developed in collaboration with either myself during business hours, or an on-call child and adolescent consultant psychiatrist outside of business hours.
MF: Children’s mental health and wellbeing has been put in sharp focus over the past few years and more keenly in the past several months. What are the particular worries for WA children and young people? AT: Suicide remains the leading cause of death for young people aged 13-17 in Australia – an unacceptable statistic. Investment in mental health services is urgently needed. There have been estimates of suicides increasing 30% across all demographic groups in Australia in the next year due to the pressures COVID-19 has created. If that prediction is right, we will see an impact on the child and adolescent population, too. The number of children who engage in self-harming behaviours continues to increase. We are seeing children injuring themselves at a younger age and more severely. This has a huge impact on families, and a ripple effect through the community. The CAMHS ETS is a step in the right direction and hopefully just the beginning of change with PCH CAMHS Emergency Services and child and adolescent mental health services within WA. MF: It has been a very disrupted year for everyone, how do you think that is impacting on kids’ mental health? AT: As the COVID-19 crisis continues, parents everywhere are struggling to keep children healthy and occupied. We saw a decline in children and families accessing our services at the start of the pandemic, and now we are seeing an increase compared to before the pandemic. There have been more mental health ED attendances to PCH in June than in any other month for the past year (263, an increase of 141 attendances since April and 102 on June last year, +63%). I believe the impact will be dependent on factors interrelated to the pandemic and also to a child’s systemic context. COVID19-associated mental health risks will disproportionately affect children and adolescents who are already disadvantaged and marginalised. Children in families where there is extreme financial hardship and an associated decline in parental mental health may experience a more detrimental impact on their own mental health. Other children who have experienced increased time with
MEDICAL FORUM | CHILD HEALTH ISSUE
secure and stable caregivers due to the pandemic may actually experience improved mental wellbeing outcomes. Parents (like all of us) are adjusting to this ‘new normal’, and that looks different for everyone. Understanding the mental health effects of social distancing and economic pressure, identifying risk and resilience factors, and preventing long-term consequences, including – but not restricted to – child maltreatment, are all necessary. MF: What facilities can you offer children and young people who may need more than a communitybased service? AT: Having the CAMHS ETS based at the PCH ED makes it easy for us to arrange admissions where necessary. If the ETS assessment shows a potential need for an inpatient admission, we will ask the family to present to the PCH and the staff who took the call will be able to hand over to the staff assessing in the ED. In cases where it makes more sense to refer to another inpatient service – for example one of the older youth units – CAMHS ETS will be able to share assessments and handover to the receiving hospital, which supports greater continuity of care during an acute presentation which is difficult for patients and their families. MF: The WA Government has recently appointed a Chief Medical Officer for mental health. Does that give you reassurance that public mental health policy – and especially children’s and young people’s mental health – will be given greater focus? AT: I think the COVID-19 pandemic has increased our awareness for the capability of our health and mental health services to deal with crises and subsequent demand escalations, which is a positive for the sector. The appointment of Dr Sophie Davison is welcomed and, alongside the implementation of other recommendations made by the Review of the Clinical Governance of Public Mental Health Services in Western Australia, I am confident that public mental health policy and young people’s mental health policy is higher on the agenda than ever before. Better representation for mental health at these higher levels is always welcome.
AUGUST 2020 | 13
Attention to detail ADHD kids are perhaps as misunderstood as the condition itself.
James Knox explores the road ahead in their treatment. There is something particularly polarising about adolescent attention deficit hyperactivity disorder (ADHD): be it the diagnostic criteria, the pharmaceutical interventions, the symptomology, even the disorder itself. In 1798, Scottish physician Sir Alexander Crichton published a series of books based on clinical cases of mental illness from observations during his clinical practice in hospitals throughout Western Europe. The result is the ‘succinctly’ titled series: An inquiry into the nature and origin of mental derangement: comprehending a concise system of the physiology and pathology of the human mind and a history of the passions and their effects. As part of this series, Crichton was the first to define an alteration of attention as, “the incapacity of attending with a necessary degree of constancy to any one object”, which is not too far removed from criteria found in the latest iteration of the Diagnostic and Statistical Manual of Mental Disorders (DSM), now in its firth edition. From Crichton’s initial observation of an alteration of attention to the latest definition, ADHD, the clinical understanding of inattentiveness evolved along this timeline: a defect of moral control (1902), postencephalitic behaviour disorder (1908), hyperkinetic disease of infancy (1932), minimal brain damage (1920s), minimal brain dysfunction (1960s), hyperkinetic reaction of childhood (1960s), attention deficit disorder – with and without hyperactivity – (1980s), 14 | AUGUST 2020
attention deficit hyperactivity disorder (1978, 1994, 2000, 2013).
effects from the pharmaceutical interventions.
There are two publications on which a mental health diagnosis is based – the International Classification of Diseases (ICD) published by the World Health Organisation or the DSM published by the American Psychiatric Association. The rationale for using these publications is diagnostic reliability and validity.
Beyond adolescence
The DSM is favoured over the ICD in Australia for a mental health diagnosis. If an individual is to be diagnosed with ADHD, their diagnosis will be based on the criteria in the latest version of DSM.
Prof Coghill is the Chair of Developmental Mental Health at The Royal Children’s Hospital, Melbourne, Vice President of the Australian ADHD Professionals Association and is one of the editors of the Oxford Textbook of Attention Deficit Hyperactivity Disorder.
The first edition of the DSM was published in 1952 with a remit to standardise the definitions of mental disorders, however, it was far from an ideal source, for instance, homosexuality was listed as symptomology of a sociopathic personality disturbance. As for ADHD and the DSM, it was initially termed hyperkinetic reaction of childhood in the second edition (1968), renamed to ADD, with or without hyperactivity, in the third edition (1980) and ADHD by the fourth edition (1994), which was carried over to the current fifth edition (2013). As the understanding of ADHD has developed since Crichton, some of the misunderstandings are still evident. However, instead of the clinical definition of the disorder being the source of consternation, the focus of debate is on the number of adolescents being diagnosed, the accuracy of these diagnoses and the long-term
As ADHD has become more widely understood, so, too, has the prevalence and longevity of the disorder according to Professor David Coghill, who has been involved in clinical care in his role as child and adolescent psychiatrist and researcher of ADHD for more than 20 years.
When Prof Coghill started to see cases, the general understanding of ADHD was that it was a disorder affecting primary school aged children, however, over time it became clear this was not the case. “Clinically, my understanding of ADHD in adolescents came from watching these kids grow up and realising that it did not just suddenly disappear when they went to high school. In many cases this was when the condition became more complicated. “We now realise that an awful lot of adolescents with ADHD will become adults who also have it. Not everyone, but many will continue to have problems. Even if they do not have the full set of ADHD symptoms, they will continue to have significant impairments,” Prof Coghill explained.
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
FEATURE
BACK TO CONTENTS
FEATURE
He said ADHD was both a mental health and neurodevelopmental disorder and attempting to make a distinction was difficult and not particularly helpful.
While ADHD presents as a diagnosis, the associated problems are what tends to interfere with individuals’ lives and development, Prof Coghill explained.
“ADHD is a constellation of difficulties in its classic form: poor attention, concentration, impulsivity and overactivity. Of course, all kids and all of us have problems in some of those domains over time, but those with ADHD have significant difficulties in inattention, concentration, impulsivity and hyperactivity that has caused problems across multiple parts of their lives.”
“The real issues come in the associated problems: Adolescents with ADHD have a higher risk of educational failure, trouble with the law and breaking rules, being victims of abuse, increased rates of self-harm and suicide, substance misuse and depression and anxiety.”
Prof Coghill explained that although ADHD symptomology is inherently heterogeneous and complex between individuals, in general, enough common themes, symptoms and problems will become apparent to make a reliable diagnosis. “These problems manifest themselves in very different ways, such as an interaction between the person and their environment, their family, their underlying strengths and difficulties,” he said. “ADHD is a complex condition and often becomes more complex the older someone becomes because they lose a lot of the supports, structures and scaffolding they had when they were younger.” By the end of adolescence, a quarter of diagnosed children will still meet the full criteria for ADHD, while about two thirds will still have considerable ADHD-associated impairments. “Adolescents with ADHD will develop, they will have better concentration when they are 14 compared to when they were five, but they are still falling behind the expected norms of development,” he said.
Diagnostic reliability Reliability and validity should be the foundations of an evidencebased diagnosis, yet unlike a physical morbidity that can be scanned or tested, an ADHD diagnoses is based on the clinician’s perception from an examination, the patient’s selfreported behaviours and the DSM criteria. None of which is as conclusive as an MRI or blood test. Nevertheless, ADHD is one of the most reliable diagnoses in the DSM, along with autism and severe cognitive difficulties, says Prof Coghill. “When you look at DSM disorders, the reliability of making the diagnosis depends on a good quality assessment and being trained to do such an assessment, but the reliability of an ADHD diagnosis when done properly is really good.”
Increasing rates of diagnosis A common criticism of the increasing rates of ADHD diagnosis is a result of pathologising adolescent behaviour leading to over-diagnosing. Prof Coghill believes the reality is the opposite. “Although there has been an increase in the rate of diagnosis in Australia, it is much lower than the epidemiological rates suggest. The
MEDICAL FORUM | CHILD HEALTH ISSUE
estimated prevalence of ADHD in the community is about 7%, the global figure is about 5%, he said. Whilst the exact figures of ADHD diagnosis in Australia is difficult to know, Prof Coghill estimates the rate of diagnosis in Australia to be 2%, which would suggest about 40% of children with ADHD are being diagnosed. As to why so many adolescents go undiagnosed, he sees this partly as an issue of workforce capacity with most child and adolescent diagnoses being made by paediatricians, whilst the public mental health system is under significant pressure due to funding and resource limitations. “Child and adolescent mental health services have been seriously underfunded, with most of the funding coming from the state. Consequently, they have stepped back from working with ADHD,” he said. continued on Page 16
AUGUST 2020 | 15
Attention to detail continued from Page 15 “This has meant that most of the work in this space is conducted within the private system where there are many more paediatricians than there are child and adolescent psychiatrists. Access to these private services is more restricted for those with limited means. “It also means that those training and working within the public systems miss out on important learning about recognising and managing ADHD and when it presents in the public specialist mental health settings, it is often missed and untreated. “If we could bring together these fragmented systems, we would take a big step towards helping those with ADHD.”
Focused treatment The most contentious treatment for ADHD also happens to be the most effective: pharmacotherapy.
age, rather than they will not do something at all,” he said.
However, Prof Coghill emphasised it should not be the first intervention. “Certainly, the evidence base is much stronger for medication treatment, particularly in adolescents and adults, than it is for non-medical treatments, but we must be careful. The first treatment for ADHD should be psychoeducation, support and adjusting people's lives to allow them to function and manage better and to deal with their ADHD.” This type of approach focuses on the way parents organise their children’s days, activities outside of the home and how to manage them in classrooms. “These kinds of accommodations and support, along with clear psycho-education of the child, their parents, teachers and families to understand what ADHD is and to understand, for example, that many of the difficulties that a young person has is because they can't do something as well as others of their
“For example, when it comes to doing homework, it can be a real struggle for that young person to engage in that activity, to engage in less structured learning. So that is really the key beginning of treatment. However, support on its own is not usually enough to help people manage their ADHD.” When this support is not enough, pharmacotherapy is introduced, in conjunction with the accommodations and psychoeducation. “There is almost unanimous agreement amongst countries, along with national evidence-based guidelines, that for adolescents with ADHD, if the support is not helpful, then you should be thinking about medication as part of the treatment,” Prof Coghill said. “For younger children, parent training programs are good at reducing oppositional behaviour, improving cognitive parenting and reducing negative parenting. The interventions that we have got can provide important support to improve important parts of
Comprehensive Community Radiology Western Radiology, high quality imaging and intervention services available across Perth. With a focus on state of the art equipment, procedures and scans we deliver a higher standard of care in the community. Daily appointment availability at each branch, direct access to our clinical team and affordability set us apart. Catering for GPs and specialists with: • Comprehensive vascular, interventional and cardiac services. • Plus level-2 interventions: C-Spine, Epidural, Rhizotomy, P.R.P., plus oncology procedures daily. • Cardiac MRI, CT Coronary Angiogram & Calcium Scoring.
Staff are highly trained, experienced and service focussed. Results available online, with 24 hour turn‑around. A strong, growing list of radiologists and a policy to bulk‑bill all Medicare rebatable items rounds out a service that delivers more.
9200 2777
16 | AUGUST 2020
9200 2778
www.wradi.com.au
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
FEATURE
BACK TO CONTENTS
FEATURE their lives but are not particularly effective at reducing the ADHD symptoms and that is why the medications are used.” As to which medications are most effective, two classes of stimulants are most effective, methylphenidate and amphetamines, such as dexamphetamine. However, which drug is the most suitable will be individual, Prof Coghill explained. “We know that about 70% of people have a good response to methylphenidate and about 70% of people have a good response to amphetamines. Between 90 and 95% will have a good response to one or the other. It is not either one or the other, there are people who respond better to one or the other, but we cannot tell without trying, unfortunately.”
Kids will be kids This well-worn adage serves to normalise and generalise the mercurial, frenetic, and challenging behaviour of children during their development. Clinically, adages tend not to inform interventions, but in the case of ADHD diagnoses maybe they should, says Dr Martin Whitely.
Dr Whitely is a researcher at Curtin University and was a teacher and a former member of the Western Australian Parliament. Throughout his political and research careers, Dr Whitely has been a prominent critic of ADHD prescribing for children and adolescents.
Diagnosis by age Research led by Dr Whitely, published in the MJA in 2017, that found that the youngest children in Western Australian primary school classrooms (born in June) were twice as likely to be diagnosed with ADHD than their oldest classmates (born the previous July). 2019 research also led by Dr Whitely found similar relative age effects in 13 countries, including corresponding low (e.g. Finland, Sweden) and high (e.g. USA, Canada) rates of prescribing ADHD medications. Boys were also three to four times more likely to be medicated for ADHD than girls. “So, Oliver, one of the youngest boys in his class is many times more likely than Amy, one of Oliver’s oldest classmates, to be prescribed amphetamine-type stimulants,” Dr
MEDICAL FORUM | CHILD HEALTH ISSUE
Whitely told Medical Forum. “We treat Oliver’s perfectly normal age and gender-related immaturity as if it is a disease,” he added.
Broken system Is this a systemic failure of both the health care and education systems? According to Dr Whitely, the answer is yes. “We should expect younger children, particularly boys like Oliver, to be less mature – and frankly maybe a bit more annoying – than their older classmates. Our schools and health system should cater for this difference and not medicalise it.” Dr Whitely believes the fact that the ADHD late birthdate happens across the globe in both high and low prescribing countries makes a mockery of this claim that we just need to tackle over prescribing: “It indicates the diagnosis is fundamentally flawed.” “We have embraced this reductionist approach that says ADHD type behaviours are likely
continued on Page 19
AUGUST 2020 | 17
18 | AUGUST 2020
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
FEATURE
Attention to detail continued from Page 17 caused by a series of biochemical reactions requiring medication.” Dr Whitely concedes that could be true in some cases but argues this theory “is nothing more than an unproven hypothesis”. He believes there is too much emphasis on the use of medications for short-term behaviour management rather than on longterm outcomes: “What is missing in the ADHD debate is a systematic, independent, robust evaluation of the long-term outcomes associated with medications.” Dr Whitely says he would love to co-operate with researchers “on the other side of the ADHD debate” to develop long-term evidence of medication safety and efficacy “that could be trusted”. His interest in ADHD came from his years in the classroom, teaching at a private school which, according to him, there were high rates of children on ADHD medications. “I had 14-year-old medicated boys sitting unnaturally quietly and obediently in class. The medication made them subdued and easy to control but it did not seem to be helping them academically,” he said.
Dr Whitely said when he first became concerned about ADHD he had no medical training and didn’t feel he could challenge the experts. “But I soon came to realise there is no hard science in the DSM-based diagnostic process.” During his time in politics and after, as an academic, Dr Whitely has been a strong opponent of ADHD medication of children and is focused on the long-term harm associated with stimulants.
Problematic prescribing He has also recently co-authored research examining West Australia's history of amphetamine prescribing for ADHD and its diversion for illicit use. He said there was direct evidence of the illicit use of prescribed simulants, primarily dexamphetamine, by WA teenagers which he attributes to liberal prescribing of ADHD medications. His 2020 study found that in WA, in 2017, 3% of students aged 12 to 17 years reported they had used dexamphetamine for non-medical purposes. However, only 1.2% of this population was prescribed the drugs. “There is no doubt that we have a significant problem with prescription amphetamines being used illicitly by WA teenagers,” he said.
Dr Whitely said that this was particularly disappointing because regulatory moves he sponsored through state parliament when he was a member in 2003 have been weakened. “Back then, data showed a paediatrician prescribed ADHD medication to 2077 children over a 17-month period. This set off alarm bells so we acted and by 2010 the WA prescribing rates to children fell by 50%.” He said that in 2015, the last year for which individual clinician prescribing data was published, a single WA psychiatrist prescribed stimulants to 2074 patients. “It’s history repeating.” His 2020 study found that for at least two decades WA has had the highest rates of prescribing ADHD medications (primarily dexamphetamine) to adults in the country. The latest data indicates that in 2017 WA adults were 2.6 times more likely to take ADHD medications than elsewhere in Australia. “WA has also consistently reported high rates of illicit amphetamine use. Is it too much of a stretch to suggest the two facts are related?” Dr Whitely asked.
Read this story on mforum.com.au
WE HELP YOU GET ON TOP OF BUSINESS SO YOU CAN GET ON WITH CARING FOR THE COMMUNITY Talk to the ANZ Health Banking Specialist Team that understands your needs. Visit anz.com/health or contact your local State Health Director, Megan Carter, on 0411 140 781.
© Australia and New Zealand Banking Group Limited (ANZ) ABN 11 005 357 522.
MEDICAL FORUM | CHILD HEALTH ISSUE
AUGUST 2020 | 19
Hands off; Eyes ON In our wide-open land, or during an pandemic, monitoring patients remotely can save lives.
Jan Hallam reports. Everyone wants innovation, but no one wants to change. That old chestnut has been doing the rounds for a couple of decades now. And it has largely been true, until now. The coronavirus pandemic response is demanding faster, inclusive and accessible solutions and tech in Australia is no longer the crazy cousin in the room but a key to saving not only lives but livelihoods. We explore some of the impacts of telehealth on the delivery of care in the primary health space on Page 24. What telehealth has given GPs and their patients is accessibility where there have been regulatory and psychological barriers. But what happens to vulnerable patients once they hang up the phone or walk out the door? If the practitioner thought it desperate enough to know the answers to that question, it inevitably meant a return visit at best or a hospital admission at worst. Not necessarily, anymore. Remote patient monitoring is the next frontier of health technology that is being given a seat at the models-of-care table. At the recent From the Frontlines conference convened by the Australasian Institute of Digital Health, the chief technology officer of Wearable Health Tech, Ben Magid, offered some insight into the collaboration between his company and RPA Virtual Hospital (rpavirtual) in Sydney. 20 | AUGUST 2020
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
FEATURE
BACK TO CONTENTS
FEATURE
Oncology to COVID The rpavirtual models of virtual care have expanded from a limited number of patient cohorts at launch to being able to monitor COVID-19 positive patients while they are self-isolating, as well as virtual models of antenatal, paediatric, drug and alcohol, mental health and geriatric care for patients in hotel quarantine. TempTraq, an adhesive patch which continuously monitors body temperature, flagging dangerous spikes with the monitoring centre based at rpavirtual, is causing much excitement. Ben spoke to Medical Forum about its introduction and the country’s dawning realisation that technology is a help not a hindrance. “COVID-19 has broken down a lot of barriers within health systems. Voices that may have been drowned out a few months ago, have been heard as decisionmakers look for solutions to the current crisis in real time,” he said. “There has been a massive scaling up and it’s the simple things, which have been done laboriously for such a long time, that are changing.” Remote patient monitoring, given
the circumstances of the pandemic, is a no-brainer and Ben said that it had already been road-tested and worked effectively for oncology patients. For cancer patients and their carers, having post-chemotherapy temperature constantly monitored in their own home was a comfort and a relief. Evidence from US studies completed in April 2017 by University Hospital Seidman Cancer Center, in Cleveland, found that temperature rise, from a person’s own individual baseline, was detected quicker and antibiotics started 2.5 hours sooner than for people whose temperature was taken manually every four hours. US figures show that fever indicated infection in 53% of all hospitalised patients, and 78% of neutropenic patients. Every minute counts.
No time to waste “For each hour that treatment is delayed during septic shock, there is an approximate 8% increase in mortality,” Ben said. “So, having remote technology that can alert patients and hospitals, means proactive steps can be taken. It's a simple concept that has dramatic implications for patients.” The challenge now in Australia is the expansion of hospital capacity
MEDICAL FORUM | CHILD HEALTH ISSUE
to treat and monitor COVID-19 positive patients at home. “Countries around the world are going through the same problemsolving. There is enormous pressure to conserve hospital beds for seriously ill patients,” Ben said. “Broadly speaking, state health departments have traditionally had their own patient communication platforms that have stymied uniform information sharing. But in terms of remote patient monitoring for vital signs and physiological indicators, there wasn't so much guidance in that regard. “It’s been up to individual hospitals or hospital groups to identify what would work for them and then act on it quickly. “RPA Virtual Hospital in Sydney has been using TempTraq to manage its high-risk COVID positive patients at home or in hotel quarantine through the virtual hospital rather than a physical hospital. “The challenge for WH Tech has been sourcing the technology amid extreme worldwide demand. The manufacturers are typically in the US and Europe and have been overwhelmed with global demand. “So, lead times have been pushed out but we were lucky that one of the groups we partnered with early continued on Page 23
AUGUST 2020 | 21
DRUG & ALCOHOL Clinical Advisory Service Clinical advice for health professionals on issues relating to patient management of alcohol and other drug use. Information provided includes: • Management of withdrawal syndromes and intoxication • Appropriate substance detoxification advice • Management of medical, pain and psychiatric complications associated with alcohol and other drug use • Drug interaction information relating to alcohol and other drugs • Community treatment referral guidance The service is available to all metropolitan, regional and remote health professionals in Western Australia including GPs, public & private hospital emergency physicians and other health professionals.
For more information visit mhc.wa.gov.au/DACAS
9442 5000 or 1800 198 024 (country callers). 22 | AUGUST 2020
MEDICAL FORUM | CHILD HEALTH ISSUE
MENT0246
For anyone concerned about their own or another person’s alcohol or drug use, refer to the 24-hour Alcohol and Drug Support Line.
Hands off; Eyes ON continued from Page 21 on have been able to ramp up their manufacturing.” So, how does TempTraq work? The flexible patch, which costs about $55 and works continuously for three days, is put under the arm and feeds data back to the patient’s mobile device and to a dashboard at the central monitoring point via Bluetooth and LTE. Ben said if the patient goes out of communication range, temperatures are internally stored so no data is lost.
Vitals in real time Being trialled elsewhere is the Lifetouch patch, which tracks heart rate and respiration rate, in combination with pulse oximetry and blood pressure; useful early warning detectors in COVID patients, though it also has indications post-surgery, for
infectious diseases, oncology, ICU and HDU. “Anywhere higher acuity patients are at greater risk of deterioration,” Ben added.
saving in terms of avoided hospital admissions is obvious but Ben said that because of the way the health system is structured, the costs accrue to the individual innovative hospital.
“Given that each person has a very different normal, being able to provide minute-by-minute data throughout the day and night, the system makes it easy for staff to identify trends and potentially act before a critical incident.
“We need a system-wide program and solution, which is why I'm excited about the recent National Health Reform Agreement because there are strong indications that innovative models of care will be funded in a different way,” he said.
“A nurses’ satisfaction survey was done about six months ago and the vast majority of nursing staff wanted to be doing more complex tasks. So, taking out some of those repetitive but absolutely critical tasks enables them to spend more time on some of those additional complex tasks which they've been trained to do.”
“There's not a whole lot of detail around but in speaking with hospital peak bodies, my understanding is that if hospitals want to propose an innovative model of care, they can work with their state health department and the Independent Hospital Pricing Authority to do that. And that is a huge step in the right direction in terms of breaking down those system barriers and driving sustained adoption of innovative models of care.”
While this is a standard model of care in the US, in Australia it has just found a beachhead at rpavirtual. The system-wide cost
It’s time to reconnect with breast health With coronavirus restrictions easing in WA, your patients can now reconnect with family and friends, but may not have thought about reconnecting with health service providers. BreastScreen WA is encouraging all eligible women 50 to 74 years, without breast symptoms to book in for a FREE screening mammogram. Clinic staff are aware that this continues to be an anxious time for many women and the safety and care of clients is of paramount importance. Making an appointment is contactless either online or over the phone and results can now be received via secure SMS. Having a mammogram is safe and can take as little as fifteen minutes for the whole appointment. Now is the right time to encourage your patients to be breast aware and to book an appointment with BreastScreen WA.
Women may book online www.breastscreen.health.wa.gov.au or phone 13 20 50 MEDICAL FORUM | CHILD HEALTH ISSUE
Mar ‘18
BACK TO CONTENTS
FEATURE
AUGUST 2020 | 23
GPs? Hold the line, please Telehealth opens up exciting frontiers of care but GPs want sound leadership to make it pay.
Jan Hallam reports.
Telehealth, that all-encompassing term that includes video, telephone, digital messaging and email, has transformed the primary care landscape in a few short months. While the catalyst was a pandemic, telehealth has shot rapidly onto the Medical Benefit Scheme and many GPs have been scrambling to find their digital feet ever since. While its reviews are variable depending on whose opinion is sought, its usefulness when confronted with a highly contagious disease is incontrovertible. The big question on everyone’s lips, will telehealth become a permanent fixture and be integral to general practice after September 30? Health Minister Greg Hunt indicated in June that this was his preferred position but he has already moved to appease growing GP concerns, advocated by the AMA and the RACGP about the so-called ‘popup’ telehealth services. The President of the AMA, Dr Tony Bartone, and President of the RACGP, Dr Harry Nespolon, 24 | AUGUST 2020
while both urging the retention of telehealth, welcomed the Health Minister regulating the use of telehealth by requiring GP providers to have an existing and continuous relationship with a patient in order to provide such services. “This will ensure patients continue to receive quality, ongoing care from a GP who knows their medical history and needs,” Minister Hunt said. He defined ‘relationship’ as “the patient having seen the same practitioner for a face-to-face service in the last 12 months, or having seen a doctor at the same practice for a face-to-face service during the same period”. In the AMA’s submission to a Senate select committee, Dr Bartone said with more than 30% of all consultations being done by telehealth, patients were clearly making a case for its retention. “Telehealth is not a substitute for face-to-face visits to the doctor, MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
FEATURE
BACK TO CONTENTS
FEATURE but it does provide a cost-effective option that can supplement traditional visits,” he told the committee hearing. “It has been an outstanding success that is supporting high-quality patient care from both GPs and non-GP specialists – and it should continue for the long term. We must now turn to the task of fully integrating telehealth into day-today medical practice according to best practice standards to ensure continuity of care. “Most GP telehealth consultations to date have been in circumstances where a patient has an existing relationship with a GP, but we have also seen the increasing emergence of ‘pop-up’ telehealth models and other models that are linked to pharmacies. “These arrangements fragment care and blur the important distinction between the prescribing and dispensing of medicines. They must be stopped. For telehealth in general practice, we need to build on what is key to our very successful primary care system – the relationship between a usual GP and a patient.” Dr Nespolon echoed those sentiments adding that ensuring quality care was critical. “We have been deeply concerned to see the rise of more and more ‘popup’ telehealth businesses offering low-value medical services. These businesses promise a ‘quick fix’ for patients but there is no commitment to the ongoing care of the patient,” he said. “These doctors have no connection to a patient’s usual clinic and won’t know their medical history. Increasing access to health services should never come at the cost of patient health and safety. “To ensure telehealth is not exploited and that the community receives the highest quality care, the RACGP has been calling on the Australian Government from the start to limit patient eligibility for telehealth. Telehealth services should only be accessible to patients through their regular GP, who can offer face-to-face consultations when needed.”
Of particular concern to the doctor groups are the pharmacysponsored services Instant Consult being promoted by the Chemist Warehouse chain and Scripts Now run through the Priceline pharmacy group. Business moving in on government funding is not a new story. One only has to cast back to GP afterhours when new, lucrative urgent GP after-hours item numbers were added to the MBS to encourage more doctor activity in an area of desperate need.
Earlier lesson The Health Minister was forced to turn off that particular tap after the proliferation of providers began threatening the Medicare bottom line and the chorus of complaint from bricks-and-mortar GP practices grew too loud to ignore. The pharmacy initiatives advertise themselves as “supplements to the traditional health care system”. While Instant Consult offers GPendorsed (the website specifies RACGP and ACRRM fellows) sick notes and referrals to specialists, radiology and pathology, it also offers prescriptions which can be sent direct to a pharmacy of the consumer’s choice. The Priceline service is less subtle. It describes Script Now as a selfservice prescription program accessible in participating Priceline pharmacies. After completing a range of questions, the survey is sent to a registered doctor for immediate review. If the doctor deems the prescription appropriate, the script is emailed directly to the store’s dispensary inbox. If the doctor requires further information, a virtual consultation will be requested before the script is approved. Consumers are told the process takes 15 minutes and costs the price of the medication plus a $22.99 service fee. Given the minister’s announcement, it is not certain how these businesses will now proceed. On the face of it, their business model may be in tatters. However, as reported in PulseIT, similar operations in the UK, Babylon Health is cited, have navigated around NHS restrictions. Babylon, through is GP on Hand group, has been accused similarly of picking the low hanging fruit
MEDICAL FORUM | CHILD HEALTH ISSUE
of general practice and leaving chronic disease management to bricks and mortar GPs. “They are correct in that – 94 per cent of GP at Hand's patients are under 45 – and Babylon has cleverly got around the NHS requirement that patients must be enrolled in a practice by offering that very capability. Babylon is also able to offer face-to-face consults through a few clinics in its target areas,” writes PulseIT’s Katie McDonald. In the minister’s mind, he hopes and intends for telehealth to be a “positive legacy of [the COVID-19] crisis and I am already engaged with the medical community in planning a long-term future for telehealth.” Practice owner Dr Jags Krishnan, who is also the WA representative of the practice owners’ group, Australian General Practice Alliance (AGPA), told Medical Forum while the initial telehealth experience for GPs was a shock, he would like to see telehealth stay as part of regular practice but he’d like GPs to have the opportunity to charge a co-payment. Currently, it’s bulk billing or nothing. “It has been a perfect storm. General practice was vulnerable before coronavirus and telehealth has put enormous pressure on some business owners,” he said. “Practices have had to significantly increase their technical investment as well as redraw and refit systems from reception to the consulting room. Many practices are now having to revert to bulk billing.”
More support “We are thankful to the government for doubling the QI PIP and also increasing the bulk billing incentive. We cannot underestimate what the government has done. It definitely helps, but it may not be enough to keep the doors open for some.” The most current MBS data indicates that there has been an increase in revenue of GP in-house and telehealth consultations in May.
continued on Page 23
AUGUST 2020 | 25
GPs? Hold the line, please continued from Page 21 Revenue for in-room consults showed an $11m increase from April from $328m to $339m but that figure is still $100m less than the $448m earned in March. Revenue from telehealth over the same period showed a steep increase from $45m in March to $219m in April and $261m in May. Overall, GP revenue, including mental health, after hours and aged care consults, rose to about $666m, the highest figure recorded in the past two years. While GP revenue has increased significantly, its distribution is not revealed and some speculate that bigger GP companies, which were equipped for telehealth before the COVID-19 restrictions, may have stolen the march on some of the smaller practices. Canberra GP and business owner Dr John Deery is chair of AGPA. He told Medical Forum that telehealth for a large number of his associates
meant telephone because it was the most accessible tool. “There are two factors that limit the effective use of telehealth. A lot of GP surgeries don't have the infrastructure in place, some don't have the NBN nor the bandwidth for several GPs at one time to do video consultations,” he said. “The flipside is that a lot of patients don't have the necessary tools or know-how, so the phone is easier. These consults are invariably quicker, so we can deal with more patients and it’s this that has been providing GPs with a financial buffer.
Phone default “However, video-consulting is now approaching a similar length of time as a normal consultation and we're forced to bulk bill every telehealth visit. It is an administrative nightmare. It's difficult to ask for financial consent when you're already on the phone with someone.” John acknowledges that the space has opened up for independent telehealth operators but urges his fellow GPs to be innovative themselves.
Support your patients with their diagnosis of dementia
Specialised support services available through:
» Home Care Packages » CHSP » NDIS
Call us today 1300 66 77 88 alzheimerswa.org.au
“You've got to figure out a way to make it work. There's always going to be face-to-face consultations because it's the gold standard. People want that. They want to go and see someone they know and trust. But it's different for different demographics. “I'm actually looking forward to telehealth if it's done well. It enables me to follow up with patients much more easily than I can now which doesn’t require them to get back in the car and come and visit me. Sometimes all that’s needed is a simple conversation over the phone and now I can get actually get paid for it. That’s wonderful. “I don't think the minister wants GPs to become call centre operators and I’m not sure there are many doctors who would want to become one. It wouldn’t be much fun.”
26 | AUGUST 2020
Dr Deery acknowledges that the so-called pop-up telehealth operators will challenge bricks-and mortar businesses initially, but he’s not fearful of them. “If people with infrastructure are going to be doing tricky and complicated stuff all the time, they need to start charging appropriately for the service,” he said. “There's a marketplace out there. If you want to get the easy stuff from one of these places, that’s fine, but when you want a doctor who knows you and knows what is appropriate for you, you are going to pay for it. That’s the service I provide now and patients keep turning up.
Scared to bill “GPs are their own worst enemies. Most of the doctors are terrified of not bulk billing someone. They are locked into this model of practice and so are their patients. “The poor indexation of Medicare rebates over the past 30 years has got us to where we're at. Bulk billing doctors are not bad doctors, some of them are awesome doctors. They just get paid really badly for the work they do. “And then you've got doctors who rush things through and provide poor service but get paid well for the work they do. Then there are the guys in the middle who are trying to provide a good service but they've got a limited time to spend with patients because, you know, they've got a mortgage. “Relying on a third party to set the fees is ridiculous.” John thinks there is a lack of leadership in medicine. “GPs are usually wonderful, caring individuals who want to share the journey with people and often aren't tough enough to ask a proper fee for their services. I see a lot of businesses run really poorly because there's no clear leadership. “I would encourage people to have business coaching. It will pay dividends.”
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
FEATURE
BACK TO CONTENTS
GUEST COLUMN
Exciting world of ePrescribing WA’s Chief Pharmacist Neil Keen walks through the process of ePrescriptions for doctors and their patients. Electronic prescribing refers to the use of wholly electronic means to prescribe and dispense medicines. The legal prescription only exists in electronic form and there is no paper-based prescription.
A prescription must be in either paper or electronic form, but cannot be both. Paper and electronic prescriptions are not interchangeable and cannot be converted from one form to another.
Any paper involved is for patient access purposes only, rather than having any legal standing.
The decision to use a paper or electronic prescription must be made at the point of prescribing and will depend on patient preference and preparedness, as well as the participation of the patient’s preferred pharmacy.
When using electronic prescribing, medical practitioners will not need to print or sign paper prescriptions. Similarly, pharmacists will not need to handle or store paper prescriptions. Electronic prescribing is expected to increase efficiency for health practitioners and reduce administrative burden. There will also be increased convenience and choice for health consumers. Using approved systems, prescriptions and patient information will remain private and secure. Advantages include efficiencies in areas such as aged care facilities, telehealth services and a potential reduction in prescribing and dispensing errors. The Australian model will make use of clinical systems already in place – the fundamental processes for prescribing and dispensing will not change. Existing medical practice systems will act as the Prescribing System, generating prescription information that can then be sent to a Prescription Delivery Service, where it will be securely held. The Prescribing System will also generate a ‘token’, provided to the patient or carer in the form of a unique QR barcode sent via email or SMS. This token is unique to a specific prescription, medicine and instance of supply. The patient or carer will be required to present the token to the pharmacy to dispense the medicine. In future stages of electronic prescribing, an Active Script List Registry will be available for patients as an alternative to the use of tokens.
An electronic prescription will be able to be dispensed at any pharmacy that has an approved Dispense System. Using the token, the pharmacy Dispense System will connect to an approved Prescription Delivery Service via a prescription exchange service. The medicine will be dispensed based on the electronic data supplied by the Delivery Service. The token is not reusable. If there are repeat supplies ordered by the prescriber on the prescription, a new token will be issued by the pharmacy. The repeat token can be used at the same pharmacy or taken to another pharmacy participating in electronic prescribing. All system components of the prescribing and dispensing process require approval. Prescribing, Dispensing and Delivery systems are currently undergoing required changes and seeking approval according to conformance requirements issued by the Australian Digital Health Agency (ADHA). To obtain necessary commonwealth and state and territory approvals these systems must first be registered on the Electronic Prescribing Register of Conformance. Paper prescriptions will remain valid and continue to exist alongside electronic prescribing for the foreseeable future.
MEDICAL FORUM | CHILD HEALTH ISSUE
Electronic prescriptions will be valid for both Pharmaceutical Benefits Scheme (PBS) and private prescriptions. Electronic prescriptions are required to contain all the usual information held in a paper prescription. Other normal requirements of prescriptions remain in place, for example, prescriptions continue to be valid for 12 months from the date of creation. Electronic prescribing capability is being progressively rolled out in Australia, with a number of approved systems in advance trials. For more information on the approval status of a system, anticipated start dates or to register interest in an advance trial, medical practices and pharmacies should contact their own software provider in the first instance. General information is available from the ADHA. To prepare for electronic prescribing, practices need to address requirements for a Healthcare Provider IdentifierOrganisation (HPI-O) and connect to an open Prescription Delivery Service, via a prescription exchange service. It is also recommended that practices ensure their patient and carer mobile phone and email contact details are updated and correct.
AUGUST 2020 | 27
MRI | CT | PET | Ultrasound | X-Ray | NucMed | Dental
Multiple Perth Children’s Hospital and overseas sub-specialty trained Radiologists Dedicated children’s ultrasound lists supervised by Paediatric Radiologists Wide bore MRI licensed for GP and Specialist paediatric conditions Low dose CT for every child, every time
Envision... much more than a picture. 178-190 Cambridge Street | Wembley | 6382 3888 | envisionmi.com.au 28 | AUGUST 2020
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
Inconspicuous penis: a conundrum By Dr Japinder Khosa, Paediatric Urologist, Joondalup The term ‘inconspicuous penis’ refers to a group of abnormalities in which the penis appears small for the age causing great concern and anxiety to both parents and the child.
commonly seen in older and obese adolescents. Most of these boys will lose their fat pad with growth and puberty. However, in obese individuals who are post pubertal, surgical correction may be needed to ensure psychological confidence and, in some cases, help in voiding standing up.
Micropenis is usually defined as a normally formed penis with a stretched penile length (SPL) of at least 2.5 SD below the mean for the patient’s age.
Inconspicuous penis is more common than is usually appreciated and a timely referral to a paediatric urologist or endocrinologist can alleviate parent and patient concerns.
SPL is defined as the maximum length of the penis when stretched and is measured from the base of the penis under the pubis symphysis to the tip of the glans. It usually results from hormonal abnormality during gestation and can present in isolation or as part of disorder of sexual differentiation (DSD).
Author competing interests – nil
An endocrinology referral and cultural circumcision should not be performed until assessed.
Concealed penis This is where a penis of normal size is hidden below the surface of prepubic skin, and has various causes. Congenital Megaprepuce is a condition characterised by poor fixation of the skin at the base of the penis, phimosis, deficiency of ventral shaft skin and a swollen large inner prepuce. This results in severe ballooning of the prepuce with inability to void completely. Parents are required to express urine manually from the foreskin of the baby, which is the clinch to the diagnosis. Visually the penis looks short, glans is located beneath the penoscrotal junction and the penis has a dome shaped appearance. This needs surgical correction. Webbed Penis results from a skin fold or a web that obscures the penoscrotal angle. Diagnosis is made by lifting the shaft of the penis and to see a cutaneous fold that extends from the ventral penile skin to the scrotal wall and sometimes there can be complete penoscrotal fusion, needing surgical correction.
Key messages
Inconspicuous penis can result in considerable concern for both parents and the child 9% of children presenting for circumcision have evidence of inconspicuous penis Differentiate true micropenis, which needs an endocrinology review, to a concealed penis, which needs a paediatric urology review.
Trapped penis is an acquired form where, following circumcision, the penile skin forms a circumferential scar distal to or at the level of the glans and traps the penis. It can happen after an overzealous neonatal circumcision or circumcision performed on a penis with moderate penoscrotal webbing. These boys can present with difficulty passing urine and UTI. It can be treated with topical steroids but if not responsive will need surgical correction. Excessive prepubic fat is more
MEDICAL FORUM | CHILD HEALTH ISSUE
For Lease
Brand New Medical Centre Suitable for a Variety of Medical Uses
Dianella 154 Wellington Road +300sqm* +Adjoining Wellington Village Shopping Centre +6 consulting rooms +Ample on site parking +Will be newly constructed Asking Rent: Contact Agent Tim Pittaway 0420 226 058 burgessrawson.com.au
Luke Randazzo 0417 181 309 *Approx
AUGUST 2020 | 29
30 | AUGUST 2020
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
Paediatric IBD – Crohn’s and colitis By Dr Ajay Sharma, Paediatric Gastroenterologist, Perth The incidence of Crohn’s disease (CD) and ulcerative colitis (UC), is increasing among children and impinges upon their growth, education and social wellbeing. Because high rates of IBD onset occur in childhood and adolescence, monitoring the incidence of paediatric IBD may reflect changing trends in IBD demographics. Environmental triggers, (e.g. dietary antigens, infections) combined with specific IBD genes (most are polygenic), can lead to a chronic activation of the mucosal immune system, recognised clinically as CD or UC. Growth failure, common in children and adolescents with CD, may be the only presenting symptom. The pathogenesis of growth failure in IBD includes malabsorption, increased caloric needs, suboptimal intake due to anorexia, and gastrointestinal losses. This affects growth. However, delayed puberty, corticosteroids, and proinflammatory cytokines such as TNFα and interleukin 6 are also responsible for growth failure in this patient population. IBD involving the colon (UC or CD) most commonly presents with diarrhoea and rectal bleeding. CD involving the ileum and/or cecum tends to present more subtly, with abdominal pain, weight loss, fatigue, and fever. Perianal fistulae and infections are seen in CD, but not UC. Extraintestinal
therapy, corticosteroids and enteral nutrition.
Key messages
The incidence of IBD is increasing in children Symptoms may be non-specific Treatment aims to optimise growth and quality of life.
manifestations (e.g. erythema nodosum, arthritis) are seen in both. Definitive diagnosis of IBD is established by a combination of radiography, endoscopy, and histology. Differentiating CD from UC can be difficult, especially if the IBD is limited to the colon.
Immunomodulators (e.g. Azathioprine, methotrexate) have a role in maintenance. Biologics (e.g. Anti TNF-Infliximab, and adalimumab) are approved for treatment of CD in children. Indications for surgery in CD include failure of medical therapy, intestinal complications (e.g. obstruction, perforation, intraabdominal abscess, fistula) growth failure in children, and carcinoma.
Over time, the natural history of the two diseases differs. Patients with CD will frequently develop complications such as strictures, abdominal abscesses, or perianal fistulae, whereas patients with UC continue to have bloody diarrhea as their principal manifestation.
5-ASA therapy is beneficial in inducing remission in UC and can be used in maintenance. AZA is effective maintenance therapy for those who have failed or cannot tolerate 5 ASA and those requiring repeated courses of steroids. Biologics are used in moderate to severe UC or failed steroids and AZA. Approximately third of patients with UC undergo surgery within the first 10 years of their illness.
Treatment goals are to maximise therapeutic response, adherence and psychological support, minimise toxicity, improve quality of life, promote physical growth and prevent complications.
Attention to emotional and family implications of chronic illness, and maximising the growth and nutrition, is an integral part of the long-term care of the paediatric patient.
Improved growth and development, without the side effects of steroid therapy, make exclusive enteral nutrition (EEN) a better first-line therapy in children with active CD. With mild-to-moderate levels of disease activity, therapy includes 5 ASA (amino salicylates), antibiotic
NEW SS RE ADD AME & N iously
Prevylands “Ma unding” po C om
Author competing interests – nil
‘Problem Solvers’ of Pharmaceuticals
We specialise in customised, compounded medicines Enquire about our Pick-up point pharmacies, all around the Metro area
BioHRT .Dental .Dermatology .Hospice .Nutrition .Paediatric .Pain .Sports www.clinicarecompounding.com.au MAYLANDS 245 Guildford Road, Maylands P: (08) 9370 4410 F: (08) 9471 7115 E: maylands@clinicarecompounding.com.au BALDIVIS Unit 1/7 Minden Lane, Baldivis (opp. Stockland Baldivis) P: (08) 9523 2274 E: baldivis@clinicarecompounding.com.au
MEDICAL FORUM | CHILD HEALTH ISSUE
AUGUST 2020 | 31
32 | AUGUST 2020
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
Non-invasive prenatal testing (NIPT) By Dr Adeline Tan, Gynaepathologist, Perth In recent years, there have been many advances in medical technology and women’s health. The connection between baby and mother begins from the very onset of conception, where fetal circulating free DNA (cfDNA) can be derived from the fetus and placenta within the maternal circulation. The ability to analyse the likelihood of a number of genetic disorders by ‘simply’ detecting fetal DNA or, more accurately, fetal fraction (the proportion of cfDNA) within maternal blood with non-invasive prenatal testing (NIPT) has been a welcomed addition in providing more information for patient management. NIPT is performed between 10 and 14 weeks of gestation, when there is sufficient fetal cfDNA in the maternal circulation for analysis (as early as 10 weeks of completed gestation). The test can assess the chance of Trisomy 21 (Down syndrome), Trisomy 18 (Edwards syndrome) and Trisomy 13 (Patau syndrome), plus 22q11.2 deletion (DiGeorge syndrome) and sex chromosome abnormalities.
Key messages
NIPT is performed between weeks 10 and 14
It is not a replacement for conventional screening
Specific chromosomal
abnormalities can be detected with NIPT. While many genetic conditions are familial, these conditions can occur in any pregnancy and its probability increases with age. If there is sufficient fetal DNA in the sample, NIPT can either confirm that the proportion of fragments is as expected (low-risk result) or detect a change in proportion (indicating that the fetal cfDNA is high risk for an abnormality). Any abnormal result will be correlated with ultrasound and other first trimester screening results. Referral to genetic counselling and further testing such as rapid FISH for aneupoloidy of chromosomes 13, 18, 21, X, Y or karyotyping on amniotic fluid and chorionic villous sampling (CVS) is required for confirmation.
Should a woman have conventional first trimester screening and ultrasound as well as NIPT testing? While NIPT is more accurate than conventional first trimester screening, conventional screening still has a place in patient care. It is important to note that NIPT is an optional screening test and not a diagnostic test. False positive and false negative results, although rare, can occur. NIPT is not able to test for fetal viability and may provide a valid result despite fetal demise (based on the analysis of any residual fetal DNA). Hence, an early ultrasound at 8-11 weeks is still required for dating and checking viability of the fetus (or detecting multiple gestation). The two tests measure two different things: NIPT evaluates cfDNA from specific chromosomes, while first trimester screening assesses anatomy and biochemical function. However, NIPT is highly accurate and may preclude the need for more invasive testing by minimising the risk of a false positive result. Author competing interest – nil
Professor Richard Naunton Morgan — General Surgeon MBBS FRCS AMC FRACS
South Perth Hospital is pleased to advise Professor Richard Naunton Morgan, General Surgeon, has commenced a General Surgical service. Professor Naunton Morgan consults at 72 South Terrace, South Perth. Consultation bookings: 0466 342 100 Postal address: PO Box 214, Como WA 6952 Professor Naunton Morgan and his anaesthetist are no gap providers.
MEDICAL FORUM | CHILD HEALTH ISSUE
AUGUST 2020 | 33
Common paediatric ENT issues By Dr George Sim, Paediatric ENT Surgeon, Murdoch Acute otitis media causes pyrexia, fever and inflamed tympanic membrane. Occasionally the tympanic membrane can perforate leading to ear discharge. Usually the child will be irritable and unsettled both in the daytime and also at night. Sleep may also be disrupted. Treatment is usually symptomatic control with adequate pain relief with paracetamol and/or ibuprofen. If symptoms are persistent for two days or if pyrexic, antibiotics orally may be required. Acute otitis media may take up to one to two weeks to resolve. Recurrent otitis media being three or more episodes in six months may warrant further review and assessment. Common predisposing factors include children in day care; children with frequent upper respiratory tract infections/snorty noses; exposure to cigarette smoke. Otitis media with effusion or ‘glue ear’ is accumulation of fluid in the middle ear that is failing to resolve. Sometimes the effusions can be thick and therefore the term glue ear. Children with glue ear tend not have acute pain but rather some degree of hearing loss and possible speech delay, learning difficulties at school and imbalance. There
Key messages
Audiology and ENT input is needed for recurrent middle ear infections Guidelines indicate when ENT review is needed in tonsillitis Most paediatric anterior epistaxis are self-limiting.
may also cause mild ear aches that can keep the child awake. Some younger children will pull or poke at their ears frequently as a result. Often the care of a paediatric Ear, Nose and Throat surgeon will be involved in children with excessive middle ear issues. A hearing test including an audiology and tympanometry will usually be part of the ENT assessment.
review to determine its severity. There are guidelines as to the frequency of tonsillitis to warrant an ENT assessment. Also, there should be consideration for the frequency of use of antibiotics, time off school and also time taken off work by parents to look after the child with tonsillitis.
Epistaxis Anterior epistaxis is a common, usually self-limiting problem in children and settles with simple first aid measures. The anterior part of the septum (Little’s area) has a rich blood supply with anastomosis of blood vessels (Kiesselbach’s plexus) and bleeds most in children.
Tonsillitis
Trauma to Little’s area (e.g. nose picking, nasal trauma) is the commonest cause of epistaxis in children. Those with allergic rhinitis or dry noses may have increased risk of bleeding as well. It is also important to explore and ensure there is no family history of bleeding disorders needing further investigation.
Tonsillitis symptoms include sore throat, difficulty swallowing, bad breath, fever, cervical lymphadenopathy and also disrupted sleep from the discomfort.
Petroleum jelly or antibiotic ointment can be used as topical treatment initially. If the frequency or severity of epistaxis is excessive, silver nitrate cautery can be performed in the office.
If a child has recurrent tonsillitis, it will be recommended to have a GP
Author competing interests – nil
If necessary, surgical intervention will usually involve grommet insertion under anaesthetic.
Rehabilitation medicine stands up As health management shifts from acute to long-term conditions, the art of rehabilitation has taken on new significance, writes Dr Arti Fayers. The speciality of rehabilitation Medicine has been slowly growing in Western Australia. Its roots lay in RPH’s Shenton Park rehabilitation campus. By the late 1940s, it was at the forefront of polio rehabilitation and emerged as a centre for orthopaedic and spinal/paraplegia services. 34 | AUGUST 2020
Rehabilitation medicine has become a central feature in patient care in many states with large rehab hospitals providing care and optimising patients’ quality of life. With the emergence of the Australian Faculty of Rehabilitation Medicine within the Royal
Australian College of Physicians, a specialty training program is now producing rehabilitation medicine physicians. So, what is a rehabilitation physician? The four-year training program sees doctors manage inpatients,
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
BACK TO CONTENTS
CLINICAL UPDATE
Undescended testis By Dr Colin Kikiros, Paediatric Surgeon, Joondalup Differentiating between undescended and retractile testes is important for young males. Proper assessment can prevent unnecessary surgery on retractile testes. Timely referral and surgical correction of undescended testes (UDT) may improve fertility and can reduce the incidence of testicular cancer. Approximately 5% of boys have UDT at birth, reducing to around 1-2% by age one. Predisposing factors are prematurity, low birth weight and a family history of UDT. The testis may be in the abdomen, groin or upper scrotum. The diagnosis is made or suspected at birth and confirmed during the 6/8week check-up. UDT are more commonly unilateral rather than bilateral. Retractile testes are more commonly bilateral and can be brought down to the base of the scrotum without tension and, when released, remain in that location until the cremasteric muscle contracts and pulls the testis upwards. UDT cannot be brought down to the base of the scrotum. Discomfort occurs when attempting to do so, with brisk retraction towards the groin when released. The testis may
outpatients and community patients with medical, musculoskeletal, neurological and neuromuscular disorders, with an emphasis on maximising functional ability and quality of life. Ages range from paediatric, adolescent and young adulthood through to the elderly. Rehabilitation physicians may also play a role in a variety of programs such as early supported discharge, rehabilitation in the home, ambulatory care services, telehealth and other community rehabilitation care models. The typical rehabilitation patients are those affected by functional and mobility limitations and/
Key messages
Orchidopexy prior to 12 months of age is recommended for undescended testes Be aware of the acquired undescended testis in boys around 10 years of age Self-examination should be performed regularly in all adult males, especially in those who underwent orchidopexy in infancy for undescended testis. also be located in the perineum, which is classified as ectopic. A rare complication of UDT is torsion, which presents as pain, swelling and later redness of the area overlying the testis. UDT can be associated with a hernia sac, hence another complication may be obstructed inguinal hernia. Acquired UDT can occur later in childhood, usually after five years of age and peaking at around 10 years of age. This is more likely to occur in retractile testes. Therefore, it is wise to monitor boys with highly retractile testes regularly until teenage years.
surgeon is recommended if bilateral UDT are associated with ambiguous genitalia or penile abnormalities. Prompt referral is recommended for boys with bilateral UDT even if the penis is normal. Otherwise review of the patient is best done around three months of age. Just under half of UDT would have descended by this age. If UDT is suspected, this is an ideal time for referral to a surgeon. An ultrasound is not necessary before referral as they are not reliable in differentiating between retractile and UDT. In addition, up to 80% of UDT are palpable. Ultrasound can be ordered by the surgeon if the testis cannot be located. Surgery before six months is not required. To maximise fertility of UDT, surgery is best done before 12 months of age. UDT in the groin are approached by groin and scrotal incisions. Sometimes two stage surgery is required. Intra-abdominal testes are managed with two-stage laparoscopic-assisted surgery. Self-examination of the testis should be performed regularly in all adult males, especially those who underwent orchidopexy in infancy for undescended testis.
Urgent referral to a paediatric
Author competing interests – nil
or painful conditions involving the musculoskeletal system, the cardiopulmonary system and central, peripheral and autonomic nervous systems.
• Functional Neurological Disorder rehabilitation • Acute and persistent pain management • Management of patients with (upper and lower) limb amputations or limb deficiency; acquired brain injury; spinal cord impairment; spasticity and dystonia; rheumatological and other joint diseases and arthroplasty (pre- and postsurgery); pulmonary and cardiac conditions; oncological conditions; prolonged immobilisation.
Interdisciplinary training allows physicians to lead teams of allied health practitioners, nurses and other doctors (specialists or GPs) in the care of the patient requiring rehabilitation. As part of rehabilitation medicine speciality training, rehabilitation physicians are competent in: • Musculoskeletal and neurological assessment, diagnosis and rehabilitation
MEDICAL FORUM | CHILD HEALTH ISSUE
AUGUST 2020 | 35
P r e c i s i o n R A D I O L O G Y WA YOUR HEALTH - YOUR IMAGE - OUR COMMITMENT
dr. nadkarni & associates P - 08 9284 2900 I w - www.precisionradiology.com.au
Perth’s newest radiology service Providing Personalised care tailored to your needs
CT, ulTrasound & x-ray image guided proCedures Incorporating brand new, state of the art, low dose CT and ultrasound technology. Diagnostic imaging procedures offered include: • CT Scan 36 | AUGUST 2020
• Ultrasound
• Digital X-ray MEDICAL FORUM | CHILD HEALTH ISSUE
In addition to solution based diagnostic imaging, Dr. Nadkarni and his team offer vascular and pain management services, providing your patients the convenience of imaging and intervention all in the one location. Precision Radiology also offers patients the option of same day imaging and consulting.
your paTienTs are our prioriTy.
addiTional benefiTs inClude: • Over two decades of radiology experience • Bulk billing for diagnostic imaging without compromising service and quality • Easy electronic access to patient images • Free on-site parking 72 churchill ave. subiaco wa 6008 P - 08 9284 2900 I F - 08 9381 7346 E - office@virc.com.au w - www.precisionradiology.com.au MEDICAL FORUM | CHILD HEALTH ISSUE
Precision
R A D I O L O G Y WA
YOUR HEALTH - YOUR IMAGE - OUR COMMITMENT
AUGUST 2020 | 37
Temperament in Children By Dr David Roberts, Paediatrician, Joondalup The word temperament appears frequently in the literature of child psychology. Temperament effects mood and emotional intensity, security and exploration, social approach and reaction to perceived threats, resilience and perseverance, and tolerance of frustration. It is a characteristic peculiar to the individual, notwithstanding we all have one, and it appears to be stable and consistently expressed throughout the lifespan. It seems to arise de novo, but it can run in families; it can be at least in part inherited. It influences our affect and behaviour, both responsive and social, to an extent where it can shape life’s experience. And this particularly so in children. But exactly what temperament means depends on the context in which it is used. For example, it can be a near-synonym of personality or character; but in most people’s minds it is qualitatively different from both. The scientific study of temperament began in earnest in the early 20th century, rapidly expanding in the second half, particularly in the US. The pragmatic American approach displaced what was previously the most influential explanatory model, the Theory of the Bodily Humours. This was the Greek idea that air, water, fire and earth are the essential constituents of matter; that they are differentiated by the qualities of hot and cold, wet and dry, and they corelate with the seasons and the bodily fluids (the humours) of blood, phlegm, yellow bile and black bile. The Hippocratic corpus attributes disease to an imbalance between the humours. The Greek notion of balance (eucrasia) was central to their thinking and also modes of thinking of other ancient cultures. In medicine we still embrace that concept to this day, and not just by alternative therapists. Intensivists spend their days keeping 38 | AUGUST 2020
at different ages, temperament, itself, is subject to a developmental process. Secondly, we are wrong to conceive self-regulation along a single continuum from being poorly to being well-regulated. Reactivity and regulation are different entities, notwithstanding they have a relationship which is dynamic and reciprocal. They both develop and evolve in time.
Key messages
Temperament is an individual characteristic
Little has actually changed over the centuries
Parenting should adjust to suit the child’s temperament.
parameters within boundaries, in the hope that time will heal. Aristotle embraced the Theory of the Humours. It was the dominant concept of disease in Western medicine until the Age of Enlightenment. Galen extended the concept from disease to temperament, hence sanguine, phlegmatic, choleric and melancholic. This was the understanding of temperament until early last century. The theory persists and underpins the Rudolph Steiner educational system. The seminal figure in the modern study of temperament was Mary Rothbart. In 1981 she wrote “… we will define temperament as constitutional differences in reactivity and regulation, influenced over time by heredity, maturation and experience’. Her work has led to a change in the way we conceive temperament. First, she held that temperament is dynamic, not a static characteristic. It is not merely that the expression of a child’s temperament differs
For example, a very young child responds to a stimulus reactively. The ability to inhibit dominant reactive responses and perform subdominant ones, to detect errors and to engage in planning, concern aspects of regulation that are both conscious and voluntary. This is a regulatory function, not a fading of reactivity. It begins to emerge at about three years and develops rapidly soon thereafter. Rothbart called it Effortful Control. She proposed two other overarching factors in the development of temperament. Surgency/Extraversion is characterised by positive emotionality – activity, impulsivity and risk-taking; Negative Affectivity by negative emotionality – fear, anger and sadness. There is much correspondence between Rothbart’s factors and the characteristics of the humours. And like Galen, Rothbart proposed that temperamental problems develop when imbalance occurs between the three factors. Importantly, she held that because temperament emerges developmentally, day-to-day experience can modulate the imbalances when they occur. It then follows that temperamental outcome can be influenced by environmental experience. Parenting should be adjusted to suit the temperament of the individual child, at their age and stage. Subsequent research has shown this to be true many times. Everything old is new again. Author competing interests – nil
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
BACK TO CONTENTS
CLINICAL UPDATE
Paediatric sleep disturbance and behavioural consequences By Dr Veena Judge, Paediatric Respiratory & Sleep Physician, West Leederville Sleep problems, common in childhood and adolescence, have a significant association with daytime cognitive impairment, behavioural problems, poor school performance and inattention. Sleep disturbance or disorders in children may be the result of underlying medical conditions or psychological problems. Early diagnosis and treatment leads to the improvement of neuro-cognitive function and behavioural problems. Obstructive sleep apnoea (OSA) is by far the commonest diagnosed paediatric sleep disorder, affecting 2-5% of all children, with peaks in the preschool years. The commonest cause being adenotonsillar hypertrophy. The risk of OSA increases with obesity affecting up to 50% of overweight or obese children. Children with hypotonia, muscle weakness, craniofacial abnormalities (micro/retrognathia) and syndromes such as Trisomy 21, Pierre-Robin, achondroplasia are at increased risk. Allergic rhinitis and asthma are also risk factors. OSA is characterised Key messages by episodes of Snoring is common but should upper airway not be regarded as normal obstruction Paediatric sleep disorders (partial or are common and can cause complete) and neurocognitive deficit, poor blood-gas changes during school performance and sleep. The behavioural problems. Early most common treatment may prevent or presentation improve impairment is snoring Children with suspected ADHD and difficulty may have OSA. or pauses in breathing during sleep. These events (apnoeas) are terminated by arousal which is a protective mechanism that results in fragmented or disturbed sleep.
Behavioural consequences Sleep fragmentation and hypoxemia results in neurocognitive and behavioural consequences. In children, this manifests as daytime hyperactivity, behavioural issues, poor school performance. continued on Page 41
MEDICAL FORUM | CHILD HEALTH ISSUE
LANGUAGE ACQUISITION – THE IMPORTANCE OF TWO EARS
Anne Gardner
Andre Wedekind
Post Dip. Aud., BSc
M.Clin.Aud., BHSc (Physiotherapy)
Language acquisition occurs within a critical period in the early years of life and requires hearing and practice to develop. Most infants begin producing speech-like sounds (babbling) at around seven months of age, but congenitally deaf infants show deficits in early vocalisations and fail to develop language if not provided with an early alternative (hearing aids, cochlear implants and/or sign language). If provided with an alternative by about six months and before 12months of age, then congenitally deaf infants begin to ‘babble’ and soon catch up to their normal-hearing peers. Children who have acquired speech but lose their hearing before puberty suffer a substantial decline in spoken language, which is thought to be due to the absence of an effective auditory feedback loop (the ability to hear, monitor and adjust their own speech). The effects of congenital unilateral deafness cannot be underestimated as studies have shown they demonstrate delays in speech and language comprehension as well as the likelihood of academic difficulty compared to normal-hearing peers. Unilateral hearing requires an increased effort to understand speech in noisy environments. Children with unilateral deafness are more likely to demonstrate attention fatigue, behaviour problems and academic weakness compared to bilaterally hearing peers. Neonatal hearing screening is very effective in identifying congenital hearing loss in newborns. Genetics is thought to be responsible for 50-60% of children with a hearing loss, with about 20% of those having a ‘syndrome’ (Down syndrome, Usher’s syndrome). For about 30% of babies with hearing loss, damage is caused by infections during pregnancy or complication at birth. Fourteen per cent of those exposed to CMV develop a sensorineural hearing loss of some degree. For young children and infants under three years of age, typical in-office hearing screening methods have poor reliability and may miss children with a unilateral loss, therefore referral to a paediatric audiologist is necessary. All children with an identified risk factor for hearing loss should be monitored closely. 51 COLIN STREET WEST PERTH WA 6005 P: 08 9321 7746 F: 08 9481 1917 W: www.medicalaudiology.com.au
AUGUST 2020 | 39
Promises and problems of NIPT By Professor Jan Dickinson, Maternal Fetal Medicine Specialist, and Ms Karen Harrop, Genetic Counsellor, Subiaco Prenatal screening is becoming more complex as technology expands the number of disorders potentially diagnosable prior to birth and as screening evolves to incorporate expanded genetic carrier screening and rarer chromosomal malformations. The options can be overwhelming for health care providers and women, potentially overshadowing the joy of pregnancy if not approached in a reasoned manner. Support and advice from trained genetic counsellors and specialists in prenatal diagnosis should be actively sourced when needed. Current obstetric practice guidelines in Australia advocate offering prenatal screening for fetal structural and genetic abnormalities, with the final decision for testing residing with the woman. The test performance characteristics of non-invasive prenatal testing (NIPT) for the common fetal aneuploidies are superior to combined First Trimester Screening (cFTS), although the expansion of NIPT into sex chromosome aneuploidy and microdeletion screening is associated with substantial false positive rates. NIPT has resulted in a significant reduction in amniocentesis and CVS. However, this reduction may be reversed if expanded NIPT panels become more widely used. Without a national policy, two main strategies have evolved for NIPT – to offer it as a first line test or after an increased risk cFTS.
Clinical considerations NIPT is not considered diagnostic for trisomy 21, 13 or 18. An increased probability result should be confirmed by a diagnostic test (e.g. CVS or amniocentesis). Sensitivity is lower in twin pregnancies. 40 | AUGUST 2020
be offered, but consider referral for expert ultrasound review.
If NIPT as a primary screen returns an increased probability for trisomy 13 or 18 but the fetus appears unremarkable to expert ultrasound, an amniocentesis (not CVS) is indicated to sample the fetal karyotype. If a cFTS demonstrates a large nuchal translucency (>3.5-4 mm), if the fetus displays structural malformations or if the cFTS result is >1:20 – NIPT is not an appropriate next step. Referral for advanced imaging and a diagnostic genetic test is required. In 1-3%, NIPT fails to provide a result (‘no-call’). This is usually due to a low fetal cell-free DNA fraction (which can be associated with factors like maternal obesity) or laboratory technical issues. Other reasons include fetal chromosomal abnormalities, maternal autoimmune disease or maternal heparin use. In the situation of a no-call result, a repeat NIPT should
Maternal chromosomal abnormalities, malignancies, recent blood transfusion and solid organ transplantation may produce difficulties in the interpretation of NIPT. Advanced NIPT is now available in the form of genome-wide (GW) cfDNA NIPT; with no additional cost, and no delay in turnaround time (3-5 working days). Genomewide NIPT reports on extra or missing whole chromosomes across all chromosomes, rare autosomal aneuploidies, copy number variations (CNVs) including duplication and deletions, and unbalanced translocations. Rare autosomal aneuploidies (RAAS) are the monosomies and trisomies not restricted to chromosomes 13, 18, 21 and frequently represent confined placental mosaicism (CPM) (e.g.
MEDICAL FORUM | CHILD HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
BACK TO CONTENTS
CLINICAL UPDATE
Key messages
NIPT is a sensitive and specific screening test for the detection of trisomy 21, 18 & 13, but less so for other chromosomal malformations A fetal abnormality on ultrasound should, in most cases, be regarded as a contraindication to NIPT A no-call result on NIPT may be the first indicator of increased obstetric risk.
trisomy 7). Identifying RAAS early in an ongoing pregnancy may assist in guiding management through the use of serial ultrasound to monitor for IUGR (although there is variance of opinion about this issue). Prenatal diagnosis via amniocentesis is required to identify true fetal mosaicism (TFM) and/or potential uniparental disomy (UPD) if imprinting chromosomes are involved CNV include deletions, duplications, unbalanced translocations and other complex changes which are screened for across all autosomes (excluding the sex chromosomes), with or without a family or personal history. One in 500 individuals carry a balanced reciprocal translocation and can experience subfertility, recurrent miscarriage, fetal loss or the birth of a baby with a severe disability. Most familial translocations are unique and occur across all chromosomes. Couples who are balanced translocation carriers, and/or
have experienced a fetal CNV in pregnancy (de novo or familial), report heightened anxiety in subsequent pregnancies. Many couples want an alternative to invasive testing, especially if they have a history of multiple miscarriage. A low probability screening result can provide early reassurance. A high probability screening result guides the appropriate use of diagnostic testing Genome wide NIPT provides most translocation carriers with a non-invasive screening option for their specific, and often unique chromosomal arrangement. It is an option for couples with prior fetal de novo duplication or deletion and low risk of recurrence but heightened
anxiety. It provides information to assist decision making regarding invasive diagnostic testing following a low or a high probability screening result. Early detection for rare aneuploidies may have implications for pregnancy and fetal wellbeing. For many it is an option for early and safe reassurance, altering the path and early bonding experience of a pregnancy, especially after previous fetal loss or infertility. – References available on request Author competing interests – nil
Paediatric sleep disturbances continued from Page 39
Learning and school performance Studies of primary schoolchildren demonstrated a higher proportion of OSA in those in the lowest 10% of academic performance, with subsequent improvement following treatment. The reciprocal has also been shown, that is children with poor academic performance are more likely to have sleep disturbances. As a child’s optimal academic performance is unknown, it is possible that there may still be
residual deficits. Teenagers who snored frequently in early childhood (compared to non-snorers) have been shown to be at increased risk for lower academic performance later in life well after snoring had resolved.
ADHD and sleep Children with OSA can have oppositional behaviour, cognitive problems, in attention and hyperactivity. Some of these children fulfil criteria for diagnosis of ADHD. Studies have reported that children with mild OSA demonstrate diminished selective and sustained attention compared with controls.
MEDICAL FORUM | CHILD HEALTH ISSUE
These deficits substantially improved following treatment (adenotonsillectomy). Hence careful evaluation of these children is vital to ensure correct diagnosis and treatment. Sleep disorders in children are common and can cause significant daytime disruption with behavioural and cognitive impairment. Early detection and treatment may prevent or improve behavioural and cognitive impairment. – References available on request Author competing interests – nil
AUGUST 2020 | 41
BACK TO CONTENTS
WINE REVIEW
Review by Dr Martin Buck
Sandalford legacy lives on John Septimus Roe was a very productive individual and after his long service to the Crown he was granted 4000 acres at Caversham. The first vintage at Sandalford was in 1842 and many varieties planted were brought from South Africa. These plantings were the dawn of the Swan Valley wine industry. This legacy
has given us not only the varieties of Shiraz and Chenin Blanc, which thrive in the Swan Valley, but also some of our great winemakers have passed through the estate. This tasting through the Sandalford wine stable was fascinating and we should all be grateful that John Septimus Roe saw the potential in the Swan Valley.
2017 Estate Reserve Cabernet Sauvignon
2017 Prendiville Reserve Shiraz
2018 Prendiville Reserve Chardonnay
The portfolio of red wine is extensive and I started with the 2017 Estate Reserve Cabernet Sauvignon which is also from the Wilyabrup vineyard. Although 2017 was a challenging season, this Cabernet shines with dark, ripe, wild berry flavours and fine tannins. It is certainly a more fruit-driven style of Cabernet but will age well. It is an exceptional wine with amazing deep purple hues in the glass and intense aromas of dark plums, spice and cloves. Maturation for 12 months in predominately new French oak barrels has given it great length and tannin structure. A wine for cellaring and enjoying over the next 15 years.
This Prendiville Reserve Shiraz is taking the premium Margaret River fruit and giving it very select, new French oak ageing for 12 months. As good a Shiraz as you can find in Western Australia with deep purple hues in the glass, intense berries, spice and nutmeg aromas. The palate is intense with deep fruit flavours, soft acid and subtle tannins that result in a long finish. Worth every cent and can be enjoyed now or in many years’ time.
The Chardonnay grapes in this wine are sourced from the Wilyabrup vineyard, hand-picked, whole-bunch pressed with only the free-run juice making its way into this premium wine. A generous wine with subtle oak influence from the 12 months in French barriques but soft fruit characters and lime. The clean acid finish and lean style makes this a perfect food wine.
'S EWER REVI
PICK
2017 Sandalford 1840 Shiraz
My favourite of the reds was the 1840 Shiraz as it is a reminder of how magnificent the Shiraz from the Swan Valley can be. Weighing in at 14.5% alcohol, this is a big wine from a challenging vintage and was made only using 10% of new French oak barrels. Deep purple in colour with aromas of fragrant blackberries, spice, violets and cigar-box oak. Fullbodied bold fruit flavours combine with soft, restrained tannins to give great length. A very stylish warm-climate Shiraz.
42 | AUGUST 2020
MEDICAL FORUM | CHILD HEALTH ISSUE
INSPIRATION, CAPTURED.
THE BMW X3 sDrive20i AT
FROM
$199
PER WEEK**.
4.99%
ON A P.A. COMPARISON RATE^.
60
MONTH BMW FINANCE CONTRACT+ WITH A GFV PAYMENT++.
Including 5 year/80,000km scheduled servicing#, 5 years BMW Roadside Assist~ and the benefit of paying no Finance set-up fees (govt. charges apply). Offer ends 30 September 2020, and applies to new vehicles only.
Test drive the BMW X3 sDrive20i today at your local BMW dealer. Auto Classic BMW 48 Burswood Road, Burswood. Ph (08) 9311 7533. Westcoast BMW 17 Luisini Road, Wangara. Ph (08) 9303 5888.
www.autoclassic.com.au DL2271 www.westcoastbmw.com.au DL2271
+Finance by BMW Finance, Australian Credit Licence no 392387. Restricted to approved customers (excl. fleet, government and rental buyers) for new BMW X3 (G01 sDrive20i) models with M Sports Package ordered and approved between 01.07.2020 & 30.09.2020 & delivered by 31.12.2020. Min. finance of $25,000 and min. term 24 months. Not available with other offers, and may be subject to change. Fees, charges and eligibility criteria apply. **Monthly payments apply. Weekly payments are estimated (annualised monthly payment/52). 60 monthly instalments of $859.68 and a total amount payable of $82,795.00 applies. ^ Annual percentage rate 4.99% p.a. Comparison rate based on a 5 year secured loan of $30,000. WARNING: This comparison rate is true only for the example given & may not include all fees and charges. Different terms, fees or other loan amounts might result in a different comparison rate. ++ Offer based on vehicle price of $69,900 & a Guaranteed Future Value (GFV) of $31,213.45 at 50,000km. On term expiry BMW will buy vehicle at GFV, subject to conditions for kms travelled and vehicle condition. See bmw.com.au/fullcircle. # BMW Service Inclusive - Basic is based on the vehicle's condition based service monitoring system for 5 years from the date of first registration or up to 80,000 kms, whichever occurs first. Normal wear & tear items & other exclusions apply. Scheduled servicing must be conducted by an authorised BMW dealer. ~ 5 years’ complimentary BMW Roadside Assistance & Accident Management service applies from the date of first registration of the vehicle. Terms & conditions apply. Please consult your participating BMW dealer for further details. Provided by AWP Australia Pty Ltd trading as Allianz Global Assistance ABN 52 097 227 177. Different service terms apply to the BMW GKL range and i range.