BACK TO CONTENTS
CLINICAL UPDATE
Reflux-induced respiratory disease By Dr Michael Prichard, Respiratory Physician, Perth Reflux of gastric contents into the oesophagus may occur during intermittent relaxation of the lower oesophageal sphincter (LOS). Occasionally there is free reflux through an incompetent LOS, sometimes associated with a hiatus hernia. Reflux into the lower oesophagus when upright is cleared readily by swallowing, peristalsis, gravity. Local mucosal factors help protect against intermittent acid injury (epithelial lining fluid and saliva, carbonic anhydrase). Reflux symptoms (regurgitation, belching, heartburn) are common and not necessarily pathological. However, recurrent reflux can result in chronic aerodigestive disease. Gastro-oesophageal reflux disease (GORD) is usually considered an oesophageal disease, affecting about 20% of the population, but may also present with upper and lower respiratory manifestations (Table 1). Most reflux-induced airway and lung injury occurs as a result of high reflux and micro-aspiration during sleep. While sleeping, there is reduced oesophageal sphincter tone, increased evening acid production, delayed gastric emptying, impaired oesophageal
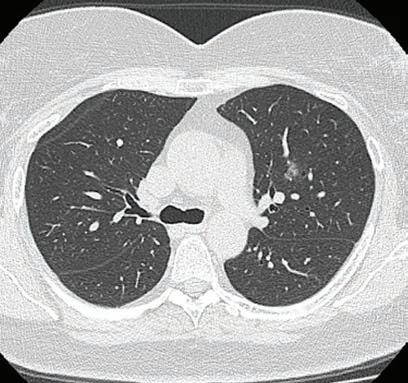
Anecdotally, single interventions tend to be less effective than combination therapy, however, there are no randomised controlled trials. Combination therapy includes proton pump inhibitors (PPI) at night, H2R blocker, promotility agent, dietary modification (avoid eating late, small evening meal, avoid certain food groups), raised head of bed, weight loss. Fig 1. Penetrated PA chest x-ray demonstrating a retrocardiac opacity with air fluid level (blue arrow): moderate hiatus hernia.
clearance of acid and reduced swallowing and saliva production. Obstructive sleep apnoea (OSA) is a key risk factor for nocturnal reflux due to increased transdiaphragmatic pressure. Acid and pepsin are additive in causing respiratory mucosal injury. Barium swallow and upper GI endoscopy are useful when positive but have limited sensitivity. Oesophageal pH studies are more useful for oesophageal disease. Measurement of pepsin or bile acids in respiratory secretions are generally diagnostic, but not yet readily available. The best ‘diagnostic test’ is response to combination therapy.
Table 1: Extra-oesophageal disorders secondary to gastro-oesophageal reflux. Location
Disorders
Oropharyngeal
dental erosion postnasal irritation chronic rhinitis
otalgia sleep disordered breathing
Laryngeal
Globus sensation Frequent throat clearing Dysphonia
Paroxysmal reflex laryngospasm Subglottic stenosis Laryngeal carcinoma
Bronchopulmonary
Chronic cough Chronic bronchitis Recurrent respiratory infections
Chronic bronchiolitis Community-acquired pneumonia Aspiration pneumonia, abscess Acute lung injury Exacerbation of chronic lung disease
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
Case study A 45-year-old woman has a fiveyear history of gradually increasing cough, initially dry, and more recently productive of mucoid sputum. Her cough tended to be worse in the morning, sometimes caused sleep disturbance and, rarely, she woke from sleep with a choking sensation. Weight increased 18kg in the past decade, recently her voice was hoarse, and she noted wheeze and shortness of breath, unresponsive to overthe-counter salbutamol. She complained of waking unrefreshed in the morning and daytime sleepiness. There was a history of snoring but not asthma. On examination, she was overweight (BMI = 32), had noticeable dysphonia, mild pharyngeal erythema and reduced pharyngeal volume (Malampatti class IV). Respiratory examination: wheeze on forced expiration. Spirometry demonstrated moderate volume loss with no bronchodilator response. Chest x-ray showed a moderate hiatus hernia (Fig 1). This is a typical presentation of reflux induced cough and asthmalike symptoms in an adult. A sleep study demonstrated severe OSA which responded to CPAP. Prior to commencing CPAP, she was treated with PPI, pro-motility agent at night and dietary modification and her cough, wheeze and dysphonia resolved over three weeks. Author competing interests – nil
SEPTEMBER 2020 | 35