BACK TO CONTENTS
CLINICAL UPDATE
Video thoracoscopy in empyema By Clin A/Prof Parshotam Gera, Paediatric Surgeon, West Leederville Pneumonic infection and the associated inflammation of the pleural lining leads to an exudative uncomplicated parapneumonic pleural effusion. This effusion becomes complicated if there is invasion of the pleural space by bacteria. The term ‘empyema’ is derived from the Greek words pyon, meaning pus, and empyein, meaning pusproducing. Thus, the presence of pus in the pleural space is consistent with the diagnosis of empyema. Empyema complicates pneumonia (incidence 1.0-4.5 cases/100 children) in around 0.6% of children and can result in significant morbidity. There are three stages of empyema. These are exudative phase (early empyema), fibrinopurulent phase (loculations) and organising phase (thick
Key messages
Empyema: pus in pleural cavity Chest drain with Fibrinolysis and VATS are accepted interventions in paediatric empyema VATS is a preferable to open thoracotomy in empyema.
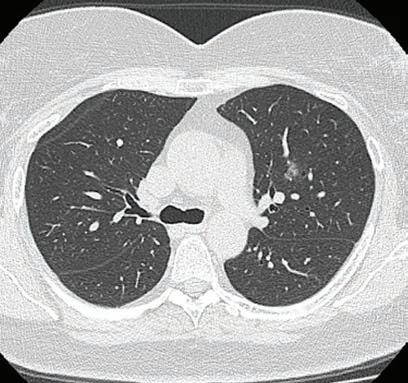
Fibrinous peel in empyema.
fibrinous peel, presence of peel may hinder lung re-expansion). Various therapeutic options are available. Medical management (antibiotics) and surgical interventions. These include percutaneous aspiration and chest drain insertion (with or without intra-pleural fibrinolytic agents) ,video-assisted thoracoscopic surgery (VATS) and thoracotomy with decortication Surgical intervention is indicated when sepsis and infected fluid are not effectively controlled with antibiotics alone. Both VATS and chest drain with fibrinolysis (CDF) are accepted surgical interventions in a paediatric age group. In most paediatric centres VATS is considered only after treatment failure with CDF. VATS was described by Kern et al. in 1993 and provides access to the entire pleural space offering direct video-controlled imaging for visceral and parietal pleural debridement and decortication. Anaesthetic airway management is critical during VATS to prevent endobronchial aspiration and intraoperative hypoxaemia in lateral decubitus position.
other two ports are placed in accordance with triangularisation (ergonomics). The procedure involves disrupting all loculated fluid collections and to make multilocular empyema into a single communicating space. After aspirating the liquified exudate, the fibrin deposits/ peel is removed with grasper. Intermittent irrigation is useful to allow improved visualisation of pleural space. A small-bore chest tube is inserted at the end of the procedure. The lung is mobilised from apical pleural region, posterior costomediastinal gutter, anterior pulmonomediastinal recess and the entire diaphragmatic surface of the lung. Conversion to open thoracotomy might be required in advanced phase or with complications such as bleeding. VATS require surgical expertise which may not be available in all centres particularly non-tertiary hospitals. Contraindications to VATS include an inability to develop a pleural window to access the pleural cavity. Furthermore, VATS has several advantages over open thoracotomy including less postoperative pain, shorter hospital stay and better cosmetic result. Author competing interests – nil
VATS is performed by three (5mm) port incisions; one for 30-degree scope and the other two for instrumentation (laparoscopic graspers, suction).
Fibrinous peel.
The initial camera port is inferior most mid-axillary level and the
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 45