BACK TO CONTENTS
CLINICAL UPDATE
Oral manifestations of inflammatory bowel disease By Dr Amanda Phoon Nguyen, Oral Medicine Specialist, Perth Inflammatory bowel disease (IBD) is a broad term that consists of conditions with recurring and chronic inflammation of the gastrointestinal tract, represented mainly by the disease entities Crohn’s disease (CD) and ulcerative colitis (UC). There is an approximate equal distribution of the two clinically definable entities, although in 15% of patients with UC, the distinction is not clear, and these patients are classified as having indeterminate colitis. The distribution of the inflammation in the gastrointestinal tract involves only the large bowel in UC, and most commonly the ileum and colon in CD. IBD is more common in males and is seen increasingly in children. Australia has more than 80,000 Australians living with these conditions, with numbers expected to increase to more than 100,000 by 2022. It is not uncommon for patients with IBD to describe a long
Key messages
Oral manifestations of IBD may precede gastrointestinal symptoms. It may be the only presenting sign of IBD. IBD may have negative effects on oral and dental health. diagnostic process taking months or even years. Oral manifestations are not uncommon with an estimated prevalence rate of between 20% and 50%, (more common in CD than UC). In adults, the oral symptoms appear less often than in children, and a higher degree of perianal involvement in patients with oral symptoms has been reported. In a minority of cases, oral involvement may precede the intestinal lesions. The oral manifestations may also be the only presenting sign in a small percentage of affected patients.
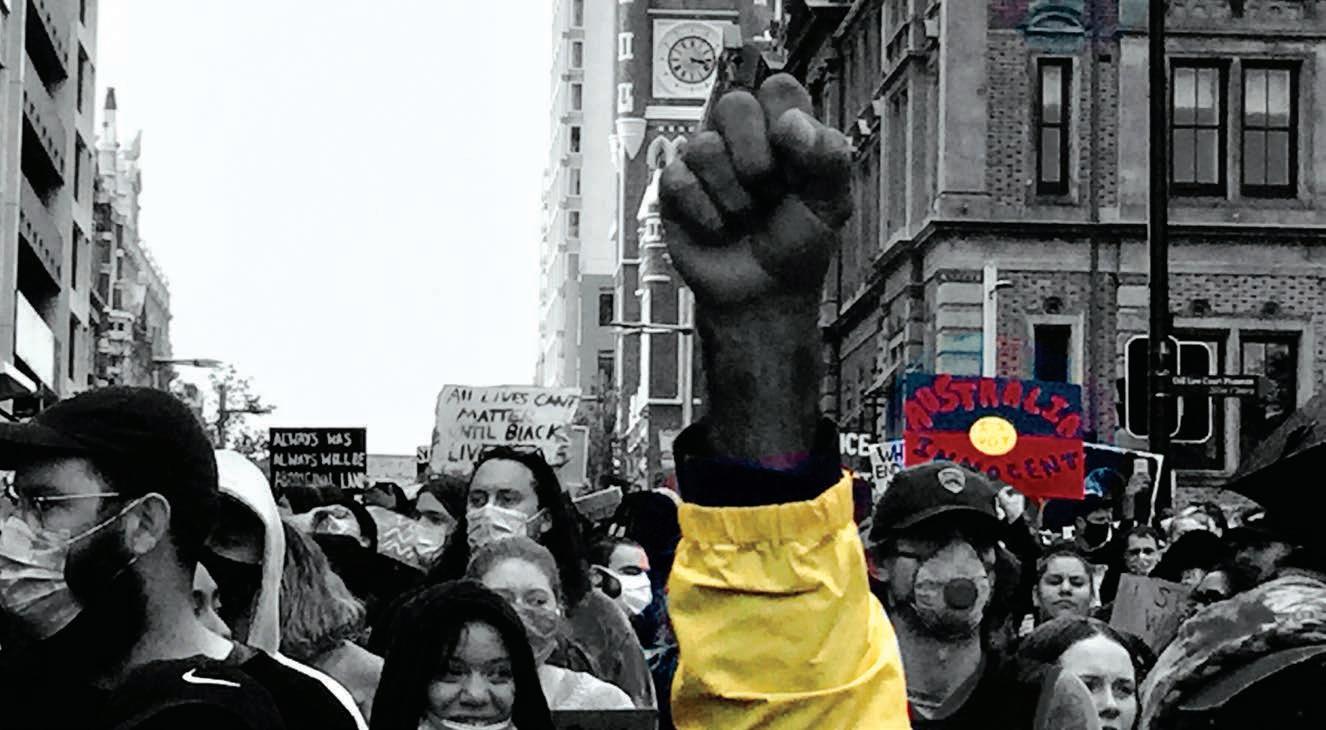
17-year-old female with a 4 week history of a lower lip swelling (a), which was accompanied by: (b) Lip fissuring (c) Mucosal cobblestoning (d) “Staghorning”
A
While oral lesions might be more severe during active intestinal disease, approximately 30% of patients may continue to manifest oral lesions despite intestinal disease activity being controlled.
Specific oral lesions Mucogingivitis (gingival swelling, erythema and there may be ulceration present) is the most common. Others include mucosal tags (small, localised, firm nodules which are often asymptomatic), cobblestoning of the buccal mucosa (mucosal nodularity where the mucosa can appear hyperplastic with corrugation), oral ulceration (which is usually linear, running the length of the buccal sulcus or alveolar mucosa), firm lip swelling (usually the lower lip) and vertical fissures involving the lip. Non-specific oral lesions include aphthous-like ulceration, ‘staghorn sign’ (swelling in the floor of mouth), pyostomatitis vegetans, angular cheilitis, persistent submandibular lymphadenopathy, gingival hyperplasia, taste changes and oral candidiosis. Orofacial granulomatosis may present a diagnostic challenge, as it can present very similarly to the above. Besides the above, there is also increased risk of dental decay, periodontitis and oral infection.
B
Patients at risk should be encouraged to maintain frequent preventive and routine dental care. Gingival bleeding is common, occurring in about 20% of patients. Oral lesions associated with IBD generally resolve once the gastrointestinal disease is under control. If symptomatic, the use of topical anaesthetics such as lidocaine, topical and/or systemic corticosteroid therapy may be indicated, however, liaison with the patient’s gastroenterologist is recommended.
C
D
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
Author competing interests – nil
SEPTEMBER 2020 | 47