
11 minute read
u Levator Ani muscle dimension changes with gestational and maternal age
Levator Ani muscle dimension changes with gestational and maternal age
Oreoluwa Odeniyi, Megan Routzong, B.S., Steven Abramowitch, Ph.D.
Department of Bioengineering
Oreoluwa Odeniyi Oreoluwa Odeniyi was raised in Poughkeepsie, NY. Her passion for women’s health motivates her to become an OB/GYN and embark on a path of advocacy/counseling for sexual assault survivors.
Dr. Abramowitch received his B.S. (1998) in Applied Mathematics and Ph.D. (2004) in Bioengineering from the University of Pittsburgh. Currently, he is an Associate Professor in the Department of Bioengineering and serves as the Director of the Translational Biomechanics Laboratory. Dr. Abramowitch’s research focuses on Steven Abramowitch, Ph.D. understanding the impact of pregnancy, delivery, and other life events (aging, menopause, etc.) on the structural integrity of the pelvic floor in women.
Significance Statement
The field of women’s health is underserved and research concerning pregnant women is especially important as issues with the mother may also affect the fetus. Approximately 3.7 million births occur per year in the US. Women who have had one or more vaginal births are at an increased risk of developing pelvic floor disorders [1]. The increase in M line, which represents the descent of the levator hiatus, is used to signify pelvic floor laxity and could be indicative of injury or some type of mechanical deficiency that would increase the risk of those women developing a pelvic floor disorder.
Category: Computational Research
Keywords: Levator Ani, M line, pelvic floor,
gestational age
Abbreviations: Gestational age – GA,
Maternal Age – MA, Pubococcygeal line – PCL, Levator Plate Angle – LPA, IRB – institutional review board
Abstract
The pelvic floor is a complex system of interconnected muscles that support the pelvic organs, such as the vagina, urethra, and rectum. The physical stress of pregnancy and childbirth can result in the weakening or permanent damage of the muscles of the pelvic floor, known as the levator ani muscles [2]. Large changes in the dimensions of the levator ani could be indicative of injury or remodeling and understanding these mechanisms could aid in the prevention or treatment of levator ani injury. Our goal was to quantify changes in the levator ani during pregnancy and with age by comparing MRI scans of women (age 20-49) at various timepoints during pregnancy. The use of four reference lines, M line, H line, Pubococcygeal line and Levator plate angle were measured from the midsagittal slice using Slicer (v. 4.11, slicer.org). These measurements were correlated with maternal and gestational age in order to define any significant relationships. There was a general increase in the M line, one of the levator ani muscle parameters, with respect to gestational age, leading to the conclusion of greater muscle laxity throughout gestation.
1. Introduction
1.1. Anatomical Background
Disruption of pelvic floor function serves as a factor that can affect a woman’s quality of life. The pelvic floor is a complex system of interconnected muscles and connective tissues that support the pelvic organs, such as the vagina, urethra, and rectum. The pelvis is divided into anterior, middle, and posterior compartments. The bladder and urethra compose the anterior compartment; the cervix and vagina compose the middle compartment; and the rectum, anus, and anal sphincters compose the posterior compartment. The levator ani muscles, the primary muscular support for the pelvic organs, attach to the sides of the lesser pelvis and unite posteriorly behind the rectum at the levator plate [2]. Three muscles are responsible for the composition of the levator ani; the iliococcygeus, pubococcygeus, and puborectalis, as shown in Figure 1.
Figure 1. Pelvic Floor muscles and other pelvic anatomy from an inferior view
The U-shaped puborectalis muscle wraps around the posterior wall of the rectum, defining the anorectal junction [3]. The anorectal junction and levator plate can be quantified by the H line, M line, and levator plate angle (Figure 2a and 2b).

Figure 2. a) An example of the PCL(green), H line(blue), M line(red), and b) Levator Plate Angle (LPA) measurements
Changes to the H line and M line are indicative of the degree of laxity or changes in material properties of the levator ani muscles [4]. With an increase in the degree of laxity, the levator ani muscles become elongated and when stretched may not provide resistance. This makes it more difficult for these muscles to perform their functions in holding up and supporting the pelvic organs. 1.2. Hypothesis and Reasoning for Experiment
The physical stress of pregnancy and childbirth can result in the weakening or permanent damage of these pelvic floor tissues, changing their mechanical properties and shape [2]. For example, during childbirth, the puborectalis muscle can be stretched to more than three times its original length, which is twice as much as a normal skeletal muscle can endure without injury [4]. Studies have confirmed that defects in levator ani muscles due to age, menopause, or trauma (i.e. childbirth) are risk factors for developing pelvic organ prolapse—a specific pelvic floor disorder in which compromised mechanical support results in the descent of pelvic organs into the vagina [2]. Large changes in levator ani dimensions could be indicative of injury or remodeling and understanding these mechanisms could aid in the prevention or treatment of levator ani injury. Our goal was to quantify changes in levator ani dimensions during pregnancy and with age by comparing MRI scans of women age 20-49 at different gestational ages. With an increase in gestational age (GA), where the fetal weight and size are increasing, there is likely an increase in tissue remodeling and/or stress being put on the levator ani, and with increased maternal age (MA) the muscles likely begin to weaken. Therefore, we hypothesize that there will be an increase in the M line and levator plate angle with increases in both GA and MA.
2. Methods
This IRB approved, retrospective study consisted of 31 pregnant patients between the ages of 21 and 45 who underwent pelvic MRI at their physician’s request—most frequently due to right lower quadrant pain or suspected appendicitis. Using an open source software called 3D Slicer v4.11, displayed in Figure 3, the midsagittal slice in the sagittal view was identified for each patient and four levator ani measurements were taken using definitions from previous literature, shown in Figure 2a and 2b [3].
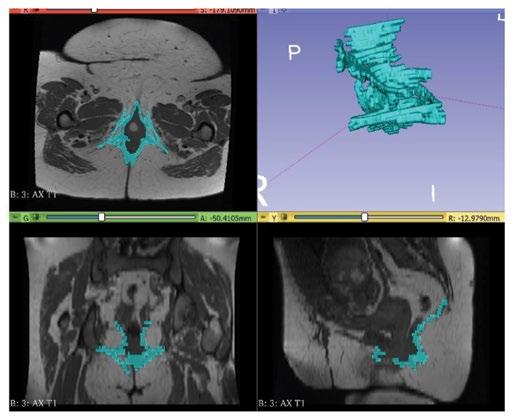
Figure 3. A screenshot of the segmentation software with representative coronal (bottom left), sagittal (bottom right), and axial (top left) slices shown with the 3D segmentation (top right)
The pubococcygeal line (PCL) runs from the inferior border of the pubic symphysis to the last coccygeal joint. The H line runs from the inferior border of the pubic symphysis to the posterior wall of rectum at anorectal junction. The M line is the perpendicular line from the anorectal junction to the PCL representing the vertical descent of the levator hiatus. The levator plate angle (LPA) is the angle between horizontal and the levator plate best fit line, as shown in Figure 2b [3]. Partial Correlations were performed between the PCL, M line, H line, LPA, GA, and MA using SPSSTM v25 while controlling for parity (the number of times a woman has given birth) by including it as a covariate. A p-value of less than 0.05 indicated a significant correlation.
3. Results
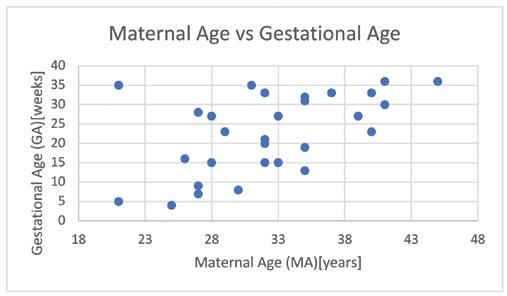
All correlational coefficients between variables are shown in Table 1. The H line was significantly correlated with the M line (ρ=0.575, p=0.001). In Figure 4, we see a positive correlation between the M line and GA (ρ=0.391, p=0.036). Additionally, as displayed in Figure 5, there is a
positive correlation between GA and MA (ρ=0.428, p=0.018). However, there is a lack of correlation between the M line and MA, as displayed in Figure 6. Lastly, the PCL and LPA were not significantly correlated with any variables.

Figure 4. M line (mm) and Gestational Age were positively correlated (ρ=0.391, p=0.036).
Figure 5. Maternal Age and Gestational Age were positively correlated (ρ=0.428, p=0.018).
Figure 6. M line and Maternal Age were not significantly correlated (ρ =-0.104)

4. Discussion
The positive correlation observed between the levator hiatus descent (M line) and GA demonstrated a laxity in the levator ani muscles with increasing gestational age. Due to the increasing descent of the levator hiatus with GA, the levator ani muscles are more elongated. This could be the result of a maternal adaptation whereby these tissues remodel to minimize the risk of injury during delivery or it could indicate a response to increased intra-abdominal pressure that is known to occur with GA [3].
The adaptation/remodeling hypothesis is supported by research that has shown increases in hormones with GA that influence the muscles responsible for holding up the organs of the pelvis. The hormonal influence is likely driven by estrogen and progesterone, which both increase as gestational age increases. In literature it has been demonstrated that the levator ani muscles are activated by these two steroid hormones [5]. While it is unclear whether these are the sole cause of the decent observed in this study, the concomitant descent observed here and in other studies along with is a reported decrease in levator ani muscle contractions is suggestive [7]. Indeed, it has been observed that prolonged duration of high progesterone levels can lead to hypotonia, weak muscle tone [7]. Additionally, increases in other hormones lead to an increased ability for the levator ani muscles and connective tissue to stretch [7]. Thus, it would be speculated that these changes would correspond with changes in mechanical properties and shape of these tissues.
This increase in M line is normal during gestation, however a large M line post-delivery or M line measurements that do not return to pre-pregnancy levels could be indicative of injury or an increased risk of developing a pelvic floor disorder. After the baby is delivered the steroid hormones decrease drastically. These two hormones help in reproducing the vascularity and proliferation of the cells in the muscle [5,6]. When injury occurs during vaginal delivery, the post pregnancy drop in hormones may make it harder for the muscles to recover and lead to atrophy instead of recovery. While the exact mechanisms and effects of specific hormones are not definitive, this study helps to establish the bounds for the normal changes that occur during pregnancy that can be useful for comparisons to post-delivery measurements in the future.
As stated in the Results, there was no significant correlation between any variables and LPA. In past studies, the LPA has been correlated with an increase in gestational age and an increase in the M line [4]. The LPA is positively correlated in literature with the displacement of the perineal body, which is correlated with levator hiatus descent, and small bowel prolapse [4]. However, the lack of significance concerning the levator plate angle (LPA) in the current study is conflicting with the results in other literature, which could be due to the subjectivity of the definition of the horizontal line [3]. A repeat of this measurement will be done in a more objective manner in the future by measuring the LPA with respect to the PCL rather than the horizontal.
One major limitation that existed within this study was correlation between GA and MA, meaning our younger patients tended to be imaged earlier in pregnancy and older women tended to be imaged later in pregnancy, which is not representative of pregnancy in general. Due to the retrospective and cross-sectional study design, there was no control over when the scans were taken and we only have one timepoint for each woman. In a prospective study we could control for maternal age and gestational age, where in our retrospective study these variables were random. In the future, a larger sample size and longitudinal study design should be considered.
5. Conclusions
There was a positive correlation between the levator hiatus descent (M line) and gestational age (GA), suggesting that levator ani muscle laxity increases with increasing gestational age. Due to the retrospective nature of this study, a correlation between GA and MA existed and served as a limitation. This study supported that as gestational age increases and hormones are released to prepare for childbirth, the muscles responsible for holding up the organs of the pelvic floor begin to change in their mechanical properties and shape likely in preparation for vaginal delivery.
6. Acknowledgements
The Swanson School of Engineering undergraduate research grant and NSF GRFP Grant #1747452 are acknowledged for supporting this research.
7. References
[1] “FastStats - Births and Natality.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 20 Jan. 2017, www.cdc.gov/nchs/fastats/ births.htm. [2] JO. Ashton-Miller, JA. Delancey. “On the Biomechanics of Vaginal Birth and Common Sequelae.” Annual Review of Biomedical Engineering, U.S. National Library of Medicine, 2009, pubmed.ncbi.nlm.nih.gov/19591614/. [3] JC. Salvador, MP. Coutinho. “Dynamic Magnetic Resonance Imaging of the Female Pelvic Floor-a Pictorial Review.” Insights into Imaging, SpringerOpen, 28 Jan. 2019, insightsimaging.springeropen.com/articles/10.1186/ s13244-019-0687-9. [4] Fielding, Julia R., et al. “Practical MR Imaging of Female Pelvic Floor Weakness.” RadioGraphics, 1 Mar. 2002, pubs.rsna.org/doi/10.1148/radiographics.22.2.g02mr25295. [5] Smith P, Heimer G, Norgren A, Ulmsten U. Steroid hormone receptors in pelvic muscles and ligaments in women. Gynecol Obstet Invest. 1990;30(1):27-30. doi: 10.1159/000293207. PMID: 2227608. [6] Marzieh Saei Ghare Naz, Fahimeh Ramezani Tehrani, Tahereh Behroozi-Lak, Farnaz Mohammadzadeh, Farhnaz Kholosi Badr and Giti Ozgoli. Journal: Research and Reports in Urology, 2020, Volume Volume 12, Page 179. DOI: 10.2147/RRU.S249611 [7] Jacobus Wijma, Annemarie E. Weis Potters, Ben T.H.M. de Wolf, Dick J. Tinga, Jan G. Aarnoudse, Anatomical and functional changes in the lower urinary tract during pregnancy, British Journal of Obstetrics and Gynaecology, Volume 108, Issue 7,2001, Pages 726-732, ISSN 03065456, https://doi.org/10.1016/S0306-5456(00)00123-6.










