ISSUE 59 2023 www.asianhhm.com Building HealthcareSustainable Access in 2023 and Beyond How Asia can get ready? Patient-centric Models in Healthcare Systems Is Quality of Death as Important as Quality of Life?
Smart innovations to improve workflow: Baxter’s Connected Care Solutions

With patient acuity and complexity increasing, and patient-to-nurse ratios rising, connected care solutions support the changing needs of healthcare facilities - so you can deliver elevated care.
The Hillrom Centrella Smart+ Bed with Contact-Free, Continuous Monitoring helps:
Identify signs of patient deterioration. An integrated sensor detects heart and respiratory rates. The bed then alerts when the rates exceed a customisable threshold.


Initiate early intervention. Be notified via a SafeView+ System indicator light, GCI touchscreen alerts, and audible alarms. Alerts are sent to the nurse call system via dome lights, status boards, and mobile devices.
Promote patient safety. 86% reduction of code blue events, a 45% reduction in ICU days on patients transferred from med-surg, and a 9% reduction in length of stay.1

Explore our portfolio of solutions* to help you meet the challenges of a rapidly-evolving healthcare landscape. 1 Brown HV, et al. The American Journal of Medicine. 2014; 127:226-232. *The above products are not available in all the countries Baxter, Centrella Smart+, Hillrom and SafeView are trademarks of Baxter International Inc. or its subsidiaries. APR432801 Rev 1 1-Dec 2022-EN-APAC-ISEA
Hillrom Centrella Smart+ Bed
Making Healthcare Equitable and Accessible

Everyone deserves access to quality healthcare services without financial hardship. Consumers are spending more on health and wellness and increasingly demanding access to convenient, affordable care. Access to quality healthcare services is important for promoting and maintaining health, preventing and managing disease, reducing unnecessary disability and premature death, and achieving health equity.
The COVID-19 pandemic tested global healthcare systems like never before, highlighted long-standing inequalities in access for different groups the world over. The pandemic also brought to the fore how effective medical care has been out of reach for vulnerable populations showing its effect on the society and economy in particular. According to the World Health Organization (WHO), at least 50 per cent of the global population still lacks full coverage of essential health services.
Inadequate health insurance coverage and limited availability of healthcare resources are the main barriers that may reduce access to health services. Equity of access to health services is central to universal health coverage, particularly for the most vulnerable and marginalised people in our societies, owing to economic, geographic, epidemiological or cultural barriers. The WHO works with countries to identify the barriers and to provide evidence-based solutions to progressively expand access, while ensuring the highest possible quality of care. By working together, strong health systems can provide effective access to primary health care, as well as to timely secondary and tertiary care, reducing the burden of disease, while safe and effective surgery saves lives.
Even countries with a robust healthcare framework often have long waiting lists to consult a specialist or
get a simple surgery carried out. Some countries have systems in place that do not provide the best quality care due to lack of resources or budget constraints. And several countries have a limited number of facilities that are understaffed and under-resourced, with those living in rural or remote areas having to travel long distances to obtain the healthcare assistance they require.
In the cover story of this issue, Dr Joseph Saba, Chief Executive Officer and Co-founder, Axios International discusses how the healthcare community in Asia and worldwide became conscious of the existing gaps after the COVID-19 pandemic. He also discusses the current state of healthcare access within Asia — what has been the journey so far and what will be the trends in 2023 and beyond? He also shares insights on how the region should prepare itself for future health crises — how healthcare ecosystems can be made more resilient and how Asia can empower its people with sustainable access to healthcare.
Digital technologies have great potential to transform global health systems to be more accessible, affordable, scalable, and fit-for-purpose. Telehealth, in particular, could be helpful in increasing the accessibility of healthcare for underserved areas.
As we move towards the future, the focus on providing care is changing to health equity and making sure that no one is left behind in maintaining good health and well-being.
Prasanthi Sadhu Editor
1 www.asianhhm.com Foreword
CONTENTS
HEALTHCARE MANAGEMENT
06 Patient-centric Models in Healthcare Systems
Aaron Villaruz, Vice President, DePuy Synthes, Asia-Pacific, the Orthopaedics company of Johnson & Johnson
09 Prioritising the Mental Health and Well-being of Healthcare Workers
How to improve your mental health while sitting at the workplace
Tanjina Ashraf Khan Mou, CEO & Mental Health Practitioner
12 Healthcare Management Patient perspectives
Ratna Devi, CEO and Co-founder, DakshamA Health and Education
20 The Effects of Employee Mental Health on Organisational Health
Gurrit K Sethi, Founder, MIINDMYMIIND
24 Competency-based Medical Education
Shakti Kumar Gupta, Executive Director and CEO, AII India Institute of Medical Sciences Jammu
MEDICAL SCIENCES
27 Mechanical Circulatory Support
Historical perspective and management of advanced heart failure
Md. Anisuzzaman, Assistant Professor, Department of Cardiac Surgery, Chittagong Medical College
Nazmul Hossain, Professor & Head, Department of Cardiac Surgery, Chittagong Medical College
32 Precision Oncology
A revolutionary therapy for cancer
Harish Dave, Chief Medical Officer, AUM Biosciences
36 Is Quality of Death as Important as Quality of Life?
K Ganapathy, Member Board of Directors, Apollo Telemedicine Networking Foundation & Apollo Tele Health Services
Building HealthcareSustainable Access in 2023 and Beyond
How Asia can get ready?
Joseph Saba Chief Executive Officer and Co-founder

Axios International
18
40 The Wide Gap in Management of Aortic Stenosis and Tools to Narrow it
Prashanth Vallabhajosyula, Director of the aortic institute, Yale University
Sameh Yousef 1, Stuti Tank2, Chirag Ramachandra3, Aaron Pininti1, Raj Lingnurkar1, Brett Johnson1, Jin Young Park1, Franklin Burg1, Tul Maya Gurung1, Augustus Koch1, Prashanth Vallabhajosyula4
1 Division of General Surgery, Mercy Fitzgerald Hospital
2 Drexel University College of Medicine
3 Vanderbilt University School of Medicine
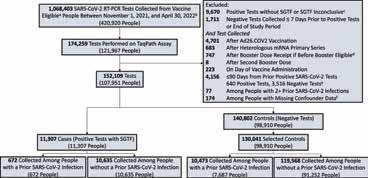
4 Division of Cardiac Surgery, Yale School of Medicine

FACILITIES & OPERATIONS MANAGEMENT
43 The Healthcare Sector Needs to Lead the way on Decarbonisation
Karan Thakur, Group Sustainability Lead &, Vice President – Public Affairs, Apollo Hospitals Group
INFORMATION TECHNOLOGY
46 Is Artificial Intelligence in Healthcare on the Wrong Track? Paulo Moreira, Editor in Chief, International Healthcare Review
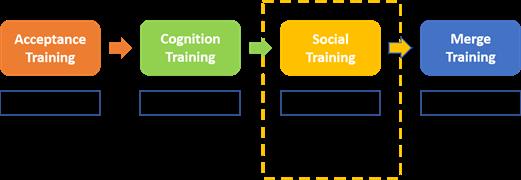
48 Virtual Reality (VR) Tools for Autism Spectrum Disorder (ASD)
Lei Fan1, Guangtao Zhai1 and Pradeep Ray2,3
1 School of Electronics, Information and Electrical Engineering, Shanghai Jiao Tong University, 2 University of Michigan-Shanghai Jiao Tong University Joint Institute
3 School of Population Health, UNSW Medicine and Health
SPECIAL FEATURES
35 Books
54 Research Insights
2 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
COVER STORY



Advisory Board
Beverly A Jensen President/CEO Women's Medicine Bowl, LLC

David A Shore Adjunct Professor, Organisational Development Business School, University of Monterrey

Eiman Shafa Medical Director Spine Surgery Abbott Northwestern Hospital

Gabe Rijpma Sr. Director Health & Social Services for Asia
EDITOR
Prasanthi Sadhu
EDITORIAL TEAM
Debi Jones
Grace Jones
Harry Callum
Rohith Nuguri
Swetha M
ART DIRECTOR
M Abdul Hannan
PRODUCT MANAGER

Jeff Kenney
SENIOR PRODUCT ASSOCIATES
Ben Johnson
David Nelson
Peter Thomas
Susanne Vincent
Gurrit K Sethi Founder, Miindmymiind
Imelda Leslie Vargas Regional Quality Assurance Director Zuellig Pharma



K Ganapathy Director
Apollo Telemedicine Networking Foundation & Apollo Tele health Services

Luzviminda Nietes Vice-President, Business Planning & Development, Metro Manila
Nicola Pastorello Data Analytics Manager Daisee


Microsoft Piyanun Yenjit Founder & Managing Director APUK Co.,Ltd.
Pradeep Chowbey Chairman

Minimal Access, Metabolic and Bariatric Surgery Centre, Sir Ganga Ram Hospital
Pradeep Kumar Ray Honorary Professor and Founder WHO Collaborating Centre on eHealth UNSW


Associate
Partner
PRODUCT ASSOCIATE
John Milton
CIRCULATION TEAM
Sam Smith
SUBSCRIPTIONS IN-CHARGE
Vijay Kumar Gaddam
HEAD-OPERATIONS
S V Nageswara Rao
Ochre Media Private Limited Media Resource Centre, #9-1-129/1,201, 2nd Floor, Oxford Plaza, S.D Road, Secunderabad - 500003, Telangana, INDIA, Phone: +91 40 4961 4567, Fax: +91 40 4961 4555
Email: info@ochre-media.com

© Ochre Media Private Limited. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, photocopying or otherwise, without prior permission of the publisher and copyright owner. Whilst every effort has been made to ensure the accuracy of the information in this publication, the publisher accepts no responsibility for errors or omissions.
The products and services advertised are not endorsed by or connected with the publisher or its associates. The editorial opinions expressed in this publication are those of individual authors and not necessarily those of the publisher or of its associates.
Copies of Asian Hospital & Healthcare Management can be purchased at the indicated cover prices. For bulk order reprints minimum order required is 500 copies, POA.
www.asianhhm.com | www.ochre-media.com Magazine Subscribe LinkedIn


5 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023 Four
year Every issue of AHHM magazine is a powerful dose of information and knowledge – filled with original and undiluted content. Written by the best brains in hospital and healthcare industry, the magazine offers timely business insights and articles on cutting-edge technologies. Subscribe now to get your doses regularly. Email: subscriptions@asianhhm.com Tel: +91 40 4961 4567 Fax +91 40 4961 4555 www.asianhhm.com
powerFul doses per
MANAGEMENT
PATIENTCENTRIC MODELS IN HEALTHCARE SYSTEMS
The healthcare sector has seen a seismic shift in models of care with an emphasis on patient centricity. The advancement of technology and the pandemic have been accelerating factors in the decentralisation of care models, seeing a rise in remote care management and patient voices. This is a time when MedTech innovations are playing an integral role in enabling the shift towards patient-centricity in the region, and how such digital transformations can support the optimisation of patient and surgical outcomes across every step of the healthcare journey.
Aaron Villaruz, Vice President,

HEALTHCARE
DePuy Synthes, Asia-Pacific, the Orthopaedics company of Johnson & Johnson
1. What is the importance of patient-centric models to healthcare systems in Asia-Pacific?
In Asia , the ageing population is expected to increase to 24 per cent by 2050, from 12 per cent in 2017. Patient demands are changing as this segment grows in the region, and they increasingly demand high-quality, integrated, and personalised care. Consumers are looking for a wider range of choices with more convenient, digitally driven solutions. So, as an industry, we need to evolve and adapt to meet these requirements.
Additionally, there are many upsides for healthcare systems to operate on truly patient-centric models. Going beyond traditional core offerings and proactively identifying unmet needs and pain points across the entire patient journey i.e., pre, during, and post-surgery can result in driving better outcomes and efficiencies along the patient care pathway, delivering value for patients, surgeons and hospitals. As a result, more patients can get the individualised care they need while supporting healthcare professionals to expand their knowledge and capabilities with the right technology.
2. What are the challenges in implementing new patient care models across Asia-Pacific? Markets across Asia-Pacific are rich veins of health data. We need a lot more engagement between government and industry to unleash the power of that health data to enable early detection, prevention, and intervention, and collaboration to produce efficiencies across health systems for the benefit of patients, surgeons, and the healthcare
systems. The most difficult thing, however, about new models is agreeing on the data or evidence required and being able to collect that data and demonstrate the outcome.
Governments and key stakeholders are still in the nascent stages of implementing and adapting to new models of care. Part of the reason is the increasing patient volume due to the ageing population and a backlog of elective surgeries post-pandemic, which makes it harder to look beyond traditional models. However, there is also a rising patient preference to minimise hospital stays and receive more of their care at home. This not only increases patient satisfaction but can also decrease medical costs. We need to ensure the system supports new care models rather than blocks them.
In Asia-Pacific, we are seeing curiosity and engagement from some governments in value-based care — Australia, Japan, and Singapore are notable in this region. We work closely with the Singapore Government to expand their understanding of these concepts and how to practically implement them in this market. This is more difficult in practice to implement than perhaps it needs to be, as it requires a fundamental rethink of how we fund and procure MedTech and needs willingness by all players to experiment and evolve.
Therefore, for true value-based care to create genuine and sustained efficiencies in the healthcare system, it is crucial to have an appetite for risk, curiosity and doing things differently for a greater return than the current systems allow. We need more trust and experimentation between government and industry, and greater access to the

7 www.asianhhm.com
HEALTHCARE MANAGEMENT
wealth of healthcare data we have in this region to deliver a better healthcare system.
3. What is MedTech's role in the shift towards patient-centricity?
As an industry, we need to focus on addressing the unmet needs through the entire patient journey i.e., pre-op, planning, post-operative monitoring, and recovery. Beyond developing medical devices to improve patient outcomes, MedTech companies must explore new ways to drive more personalisation and reproducibility throughout the continuum of care and develop new care models and programs that are supported by these technologies.
In Orthopaedic surgery, we are constantly striving to make surgery smarter and more personalised across the patient journey. We connect technologies that combine surgical knowledge and data insights to enhance the orthopaedic experience for patients, surgeons, and their teams.
By leveraging data for insights-driven decision-making, increased precision in treatment, and personalised care via robotic surgical tools and personalised post-operative care plans, we are improving patient outcomes and enabling surgeons to better serve their patients.
In terms of new care models, it’s more around healthcare systems having the right incentives in place to ensure efficiencies and outcomes. For hospital stays, often the system rewards a longer length of stay rather than getting a patient home to recover faster. We need to ensure the system supports new care models rather than blocks them. In Australia, for example, we have been working with hospitals to save costs by reducing the length of stay and enabling patients to recover faster at home. Within 18 months, based on a partnership with one hospital, we were able to deliver an average reduction in bed days of 1.5 days from an average of 4-5 days.
In a nutshell, innovation in MedTech should essentially address the question — how can we help patients recover faster and get back to living their best lives? When we do that, it will be hard to argue against a new standard of care.

AUTHOR BIO
AARON VILLARUZ is the Vice President of DePuy Synthes (DPS), Asia Pacific, the Orthopaedics company of Johnson & Johnson, where he oversees the delivery of a comprehensive orthopaedics portfolio in the region. With millions of people in Asia Pacific suffering from musculoskeletal conditions, Aaron is passionate about solving their healthcare challenges. He is focused on leveraging DePuy Synthes’ strong tradition in medical technologies and digital surgery to introduce innovation and drive meaningful collaboration in the region.
8 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
HEALTHCARE MANAGEMENT
Prioritising the Mental Health and Well-being of Healthcare Workers

The COVID-19 pandemic has had an extraordinary+- effect on the physical, mental and emotional health of the frontline healthcare workers across the globe. While discussions are on the rise, actions, particularly in regard to the mental health and well-being of healthcare professionals at the forefront, is still in its infancy. In recent years, mental health requirements of healthcare workers and professionals have drawn attention as a major global issue and it has also been talked about by the World Health Organization (WHO). These problems are projected to get worse as a result of the global pandemic or endemic response as they keep dealing with unprecedented challenges day in and day out. This article talks about three simple, every-day self-care strategies — gratitude, mindfuless that healthcare professionals can learn in order to minimise the potential risks to their mental health in their daily work life.
Tanjina Ashraf Khan Mou, CEO & Mental Health Practitioner
The COVID-19 pandemic has had tremendous effect on health systems in the majority of the world's nations, particularly in regard to the mental health and well-being of healthcare professionals working at the forefront of the pandemic response on a regular basis. Prior to the pandemic, topics related to the emotional and mental health of healthcare professionals were rarely addressed in appropriate depth. Healthcare professionals' mental health requirements have recently drawn attention as a significant concern and a challenge to the delivery of high-quality care. While awareness is better than it used to be, the measures taken to effectively address this issue are still not near
9 www.asianhhm.com
HEALTHCARE MANAGEMENT
How to improve your mental health while sitting at the workplace
sufficient. Healthcare professionals operate in an environment that exposes them to a variety of stressors, which can have adverse effects on their physical, mental, and emotional health. Anxiety has been reported to be a common symptom among this population as reported by the WHO in the year 2021. It estimates that by 2030, there will be a predicted shortage of 18 million health workers, primarily in low- and lowermiddle income nations. Hence, it is safe to predict that the workload in this sector will be on the rise in the coming years. Such issues are also evident at present, almost everywhere and whether all nations are well-equipped to combat these challenges are debatable. Now is a good time to talk about the detrimental impacts of this scenario on the mental health of these healthcare professionals.
Even before the pandemic, health workers were affected by stress, burnout, emotional discomfort, and other mental health problems, but this was not given the needed attention and was left at seasonal workshop level. We are all well-aware in this sector that healthcare professionals in many communities do not have easy access to mental health resources especially the ones working in remote areas. Also the long working hours leave no room for counselling, interventions or relaxation activities. While discussing the problems they are having may be simple, it is vital to rather concentrate on the solutions. The aim of this article to bring forth some simple but beneficial self-help activities that every professional must be wellequipped with in today’s world.
By examining the benefits of employing evidence-based self-care techniques, we need to find feasible solutions for overcoming these risks to their mental health. As a psychologist myself, the three most essential self-care skills that all professionals must possess include: skill of practising mindfulness as a method of relaxation; gratitude reflection in order to maintain a positive mindset; and resilience in order to
combat unpredicted situations.
Here are three quick activities to improve one’s mental health right away that has been tested in the CMMB mental health programme. These methods were created with psychologists and tested among midwives and nurses at a Peruvian healthcare facility supported by CMMB. These methods were also utilised and implemented among a team of psychologists and counsellors at MentCouch Psychology Centre based in Kuala Lumpur for a period on 3 months.
1.
Among the many effective solutions for stress, anxiety and burnout in healthcare settings, the practice of mindfulness has countless applications and proven benefits. For nurses, doctors and other providers, mindfulness eases such symptoms of stress, while improving the ability to navigate difficult conversations with patients, self and to feel more empathy. It also helps to not get too drained thinking about past or future situations and stay present in the work environment.
Every day after reaching office and before stepping out of office, set aside some time to reflect on the questions listed below. Each contemplation
should be finished with a long inhale and exhale. Pausing for Ten seconds is a recommended time-frame after each question, after which one may proceed to the next question:
• What can I hope for today that would make me a little happy?
• What am I willing to give others today?
• What aspect of my job currently makes me happy?
• What can I learn today?
- Can I aim to greet everyone with a smile today? / Can I aim to enjoy my lunch today?
At the end of day, repeat the same exercise with the following questions:
• What did I enjoy most today?
• What have I given and received?
• Why was today a good day despite all?
• What did I learn?
• What small win can I celebrate today?
2. Gratitude reflection
According to a team of researchers at the Indiana University, the more one focuses on that which they feel grateful for, the more one will notice to feel grateful for. If one feels down, overwhelmed, or stressed, it is a good practice to remind one’s self by quietly repeating in head that they are thankful, that they have

10 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
Mindfulness meditation and reflection method
HEALTHCARE MANAGEMENT
accomplished a lot, and that they are capable of doing great things. Once done, it is recommended to sit quietly and say “thank you” to all the good people around. It is also important to thank own self for not giving up and thank whoever has contributed to the current good life. One can also be thankful for having a family, having good food, clean water, safe shelter, a job, public transport, the skillset to help others etc. Such reminders are powerful set of tools and this exercise must be done at least once a day.
3. Resilience: Turn anxiety into progress by reframing thoughts

Resilience is an essential lifeskill and adaptive behaviour to combat difficult situations and change. Resilience, like most self-care strategies, can be learnt, developed and improved over time. Most would have never experienced change so significantly as we have in the last two years during the COVID19 pandemic. Healthcare establishments and workforce have coped differently but majority have learnt the importance of this skill. Now, as we get back to new normal phase, it is important to acquire
this skill as a normal coping mechanism. Resilience heavily emphasises the importance of finding significance in one's surroundings (Buettner, 2005). People with a strong sense of purpose are thought to be more resilient (Boyle et. al, 2012). The protection of the brain from the damaging effects of stress provided by a sense of purpose in life helps to promote resilience. A crucial component of resilience is finding meaning in one's experiences, especially while dealing with difficulties.
Our brain’s plasticity is what trains is to be resilient during difficult times and to reassess situations in order to calm down and have a more positive perspective of something. Consider the below to reassess thoughts to something more meaningful:
ANGER can either hinder our capacity to focus and perform OR it can act as a reminder of what's important.
FEAR could trigger memories of past failures or future anxieties; OR it can make us more cautious when making decisions. It can also help us reflect and make positive changes by being extra prepared.
SADNESS could demotivate us, OR it could help us reprioritise. It could also be reminder that break is needed.
WORRY could hinder our progress, OR it could assist in fine-tuning our aim and help us become more realistic and goaloriented.
FRUSTRATION could give rise to emotional turmoil, OR it could challenge us to do better than before.
These comparisons may seem easy and simple, but regular practice along with self-talk can lead to tangible outcomes.
References are available at www.asianhhm.com
Tanjina Ashraf Khan Mou is an award winning, certified mental health professional, writer, entrepreneur and CEO of one of the leading private psychology centers in Kuala Lumpur, Malaysia. As an integrative therapist, she possesses a solid foundation in a wide variety of theoretical approaches and over time has developed her own way of working as a result. Tanjina specializes in positive psychology methods, resilience training, behavior analysis, mindfulness based therapies and has been actively advocating mental health and well-being for the past 4 years worldwide. Tanjina is an empathic and warm individual. She has been featured in prestigious platforms like FORBES, COSMOPOLITAN, The New Indian Express etc.
11 www.asianhhm.com
BIO
AUTHOR
Healthcare professionals' mental health requirements have recently drawn attention as a significant concern and a challenge to the delivery of high-quality care.
HEALTHCARE MANAGEMENT
HEALTHCARE MANAGEMENT PATIENT PERSPECTIVES

Co-creation and co-design of healthcare systems and delivery, with the patients and caregivers’ active participation can help to achieve better clinical outcomes. Healthcare providers and health workers need a paradigm shift in the way they have been taught to deliver healthcare, so that patient engagement becomes a reality and shared decision making and options for choice result in a more pleasant experience for care providers as well as patients.
Ratna Devi, CEO and Co-founder, DakshamA Health and Education
Healthcare has always been seen as delivered by doctors in a brick and mortar setting where the patient reaches the structure in times of sickness. Critical care has been the mainstay of medical teaching and learning, and the expectation is that those who are sick must seek healthcare from an expert. With the advent of long-term chronic diseases and more recently the
HEALTHCARE MANAGEMENT
Corona pandemic, delivery of healthcare has taken several other routes and home healthcare, community healthcare etc has become an accepted norm. With digital and technology adding value to access, healthcare is no longer seen in the traditional model of the patient traveling a long distance to see the doctor in his/her clinic or hospital. The changing models of receiving and delivering healthcare has also changed the relation between those who provide care and the recipients. The participation of sick people and the people who take care of them represents a significant change in the care model. The paternalistic and authoritarian model, centred on the illness and the authority of the professional, generated by the asymmetry of technical knowledge between patient and expert/ professional, is evolving towards a more deliberative model, centred on the rights and duties of the patient. Informing, consulting, involving, collaborating, and empowering are increasingly complex and comprehensive levels of participation and there are no standard criteria for approaching this participation. The importance of models of patient involvement in the health system can be understood by talking about the patient experience in its entirety. The patient experience covers the full range of interactions that patients have with the healthcare system and includes the care received from health programs
and health professionals, from doctors’ offices, care centres, as well as patients’ interactions with the fields of health research and education.

Advances in treatment modalities and personalised healthcare has also necessitated a deeper involvement of patients and caregivers. Person-centred care or people-centred care needs to shift to Collaborative Health (CH) to minimise the asymmetry between the professionals and the people under care and to meaningfully involve patients and caregivers in their healthcare journeys. The basic elements for building collaborative health would be A) Sharing information B) Accepting flexibility in the way decisions are made. C) Establish and build trust. D) Understanding the
key touch points and journeys. Acute and chronic conditions are influenced by the geographical conditions, health literacy, access, affordability, beliefs, cultural contexts, and healthcare infrastructure and journeys can significantly vary. Patient- and family-centred care expresses a vision of what healthcare should be in terms of a partnership between professionals, patients and families to ensure that decisions respect patients’ needs, wishes and preferences based on patients access to education, information and support they need to make decisions and participate in their own recovery. Involving patients in their healthcare decisions therefore is a complex and arduous experience and difficult in circumstances where
HEALTHCARE MANAGEMENT
healthcare providers are overburdened and short of time. However, journey mapping and key touchpoints can be advantageous in keeping patients engaged and involved and understand if the clinical outcomes are as expected by the patients and caregivers and help modify plans if outcomes are not as expected. This helps in adherence, timely revisits and refilling and minimising lost to follow up.
A patient journey is the sequence of steps beginning with a patient’s awareness that they are not well and reaching out to hospitals, healthcare professionals, or other stakeholders in healthcare. Insights into patient experience and the outcomes of their disease will be unravelled by understanding these journeys. In the context of patients suffering from non-communicable diseases, these interactions can be broadly categorised as (1) awareness of lifecycle and natural history of disease and knowledge of associated risk factors; (2) screening and risk assessment at an early stage; (3) early diagnosis and appropriate treatment decision; (4) treatment experience and access to care; and (5) adherence to treatment for longterm management. The examination of these patient journey touchpoints helpsto identify opportunities in noncommunicable disease management and helps in prioritizing interventions for improving prevention and control. Strategies to improve the patient journey must integrate the patients’1 perspective at each touchpoint.
A key question to be answered is: who represents the patients? Is it the person who is suffering from a disease, their caregivers, patient bodies and organisations or a combination of all? For a healthcare provider to decide this in a matter of few minutes of consultation is very difficult. It is, therefore, important to engage the patients and their families in the healthcare system as a whole and
1 https://link.springer.com/article/10.1007/s12325-02001519-3
not just in the consultation. For acute care and for immediate requirements the patients and families could offer a solution, for prevention, long term care and improving the experience of the therapy area, it might be more useful to engage patient bodies and associations that can bring the collective view of a number of patients. Participation at each touch point is dependent on several variables — the willingness to participate in a free and non-coercive way in an environment of trust and, at the same time, of a need to support those who have to make complex decisions2 3 Angela Coulter emphasizes collaboration between patients and healthcare providers to “promote and support the active participation of the patient and the
2 Gramberger M (editor). Citizens as Partners OECD Handbook on information, consultation and públic participation in policy-making. OECD, 2001. https://www. internationalbudget.org/wp-content/ uploads/Citizens-asPartners-OECD-Handbook.pdf
3 https://www.linkedin.com/pulse/what-do-wemean-patient-participation-shared-patient-experience?trk=organization-update-content_share-article
population in the healthcare system and enhance their influence on healthcare decisions, both individually and collectively”. James Conway developed the model of public participation at the Institute for Healthcare Improvement based on patient involvement during the care experience, within the microsystem of the clinic, care unit or healthcare institution. The Center for Advancing Health sets the framework for patient participation and involvement by focusing on behaviour, defining participation as “actions that people take for their health and to benefit from the healthcare they receive” and provides a list of participatory actions4. Another definition of patient involvement in health is: “patients, families, health representatives and health professionals working actively together at different levels of the health system to improve health and healthcare 5
Patient participation can have many dimensions depending on the maturity of participation. It usually starts with self in search of answers to unanswered questions and progresses to various levels of expertise. The various levels of engagement could be
A) Participation in their own health B) Participation in the improvement of services and the organisation of institutions C) Participation in the field of knowledge, research and teaching D) Participation in the field of health policy design. Co-production and Co-design of health systems and healthcare decisions ensure participation at all levels using the expertise of patients at a level they are comfortable with. A key element to this participation is the healthcare provider’s ability to communicate the right information and help the participant to feel comfortable and confident to participate. From the stage when the patient is informed of his diagnosis and
4 https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC7553852
5 https://www.linkedin.com/pulse/what-different-formsparticipation-shared-patient-experience
14 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
HEALTHCARE MANAGEMENT
The paternalistic and authoritarian model, centred on the illness and the authority of the professional, generated by the asymmetry of technical knowledge between patient and expert/professional, is evolving towards a more deliberative model, centred on the rights and duties of the patient.
understands it to the treatment decision process shared between the patient or his relatives and the professional health team, the provider should be able to communicate in simple non-threatening language, the essence of the treatment options and pathways and help the patient and family make a choice that is appropriate for them. Shared decision making would entail the professional determining how to leave sufficient space to understand and respect the patient’s values and preferences. More and more professionals believe that the paternalistic model of clinical practice is completely inappropriate and a deliberative model, where the physician and patients discuss what values are most appropriate for the patient in each specific circumstance can lead to better outcomes and enhanced patient satisfaction. Involving people and patients in the redesign of the services they receive enables adjustment of the services to real needs and is in turn a useful strategy to promote their implementation. People’s participation requires adequate tools and spaces to be effective and is a process that requires careful thought and sufficient investment in terms of time and resources. The European Patients Academy for Therapeutic Innovation (EUPATI) describes a pathway for involvement of patients and families in drug development research and clinical trials. In many parts of the world accessibility and perceived usefulness of existing research to the patient is very limited. Patient and public input can help to ensure that researchers clearly explain what their study is about, that they communicate more sensitively with the public, but also that studies are carried out to make research more effective, and that the communication of the results to citizens is improved helping better pooling of participants and increasing diversity of participation. Patient can contribute by offering their experiences, materials and design of protocols. The highest level of participation though is patient and patient groups led
research where patients and researchers systematically collaborate in all phases of the study, from defining the scope to disseminating the results, under the active participation of patients and caregivers or their representative organisation.
Another key area of participation is the design and delivery of medical and allied medical fields education — nursing, dentistry, pharmacy etc. The participation in this field is still evolving with a few universities developing models that believe that the patient experience can contribute to the professional’s scientific knowledge. Hearing patient stories and their lived experience reveals a different dimension to the textbook perception of the progression of disease that often misses the complex relationship between the individual’s psychological and societal dimensions of the lived experience and the clinical manifestation of the disease. The World Health organisation (WHO) has organised a series of consultations over the last two years with people with lived experience in non-Communicable diseases to inform policy and health system strengthening. The consultation report, scheduled to be released early 2023 emphasises the need to treat patients contributing to research and policy as experts and be
valued at par with any other expert. Titled “The WHO Framework for meaningful engagement of people living with noncommunicable diseases (NCDs) and mental health conditions” it lays down the norms/standards for engaging people with lived experience in the co-creation, implementation, monitoring, evaluation and governance process of related policies, programmes and services. It also emphasises the need to build capacities of patients and patient groups to meaningfully contribute to their healthcare journeys and decisionmaking process.
Conclusion
Co creation and Co-design of healthcare systems and delivery with the patients and caregivers’ active participation can help to achieve better clinical outcomes. Patient participation is one of the essential conditions to guarantee the Patient experience, but it is not sufficient on its own to change the organisational culture of an institution. Health care providers and health workers need a paradigm shift in the way they have been taught to deliver healthcare, so that patient engagement becomes a reality and shared decision making and options for choice result in a more pleasant experience for care providers as well as patients.
Ratna Devi is the CEO and Co-founder of DakshamA Health and Education, an organisation that is dedicated to working for access to health, patient education and advocacy. She leads a cross disease Patient Alliance in India called Indian Alliance of Patient Groups (IAPG) and is the Immediate past Chair of Board, IAPO (International Alliance of Patient Organisations, Chair ISPOR Patient Council, Board member HIA (Healthy India Alliance – the National NCD Alliance in India) and I – ORD (Indian Organisation for Rare Diseases).

15 www.asianhhm.com
AUTHOR BIO
HEALTHCARE MANAGEMENT
Building Sustainable Healthcare Access in 2023 and Beyond
How should Asia prepare?
In this in-depth interview, Dr. Joseph Saba, CEO of Axios International, discusses the current state of healthcare access within Asia – what has been the journey so far and what will be the trends in 2023 and beyond? He also shares insights on how the region should prepare itself for future health crises, how healthcare ecosystems can be made more resilient and how Asia can empower its people with sustainable access to healthcare.
Joseph Saba, Chief Executive Officer and Co-founder, Axios International

The disruption caused by COVID-19 has created a rallying cry to build sustainable healthcare access for the people. But, before we get into specifics, could you tell us how do you interpret the term ‘Sustainable healthcare access’?
I see it from the patients’ perspective as, ultimately, it is the patient’s health and medical outcomes that matter. COVID-19 overwhelmed hospitals and disrupted the management and treatment of patients who needed care. Patients with long and chronic diseases could not visit doctors or receive treatment. In hindsight, these were the people most vulnerable to developing severe COVID-19 infections. Sustainable healthcare access requires a resilient healthcare system. The world population is growing and ageing dramatically, increasing the prevalence of chronic diseases. Hospitals are unable to cope with this increase and face added global health threats like COVID-19, which overburdens them further. As a matter of fact, we realised that hospitals need help in connecting with patients, in following and managing them when they are outside the hospital space. This is what creates a resilient healthcare system.
Dr. Saba, you were instrumental in the fight against the HIV epidemic, with your work making antiretrovirals (ARVs) accessible to many vulnerable populations across the world. How would you compare that to vaccine accessibility during COVID-19?
Access to ARVs is a long and successful journey. I learned a key lesson that the availability of medicines and vaccines does not imply accessibility. There is more to access than just the availability of the product. During the HIV pandemic, we
16 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
HEALTHCARE MANAGEMENT
worked on the delivery of the products, patient records, training of physicians, and follow-up with patients. All these aspects improved patients’ accessibility when ARVs were made available. We seem to have forgotten these lessons. Access to COVID-19 vaccines was very challenging, especially in low-income countries. Initially, high-income countries were criticised for monopolising access to COVID-19 vaccines, but after the initial rush eased, vaccines were in high supply. Yet in March 2022, two years into the pandemic, only over 3 per cent of people in low-income countries were vaccinated.
COVID-19 elicited strong reactions from nations across the world. Many enforced stringent border restrictions and shut themselves off from the world. Do you think this was a justified emergency approach or could the pandemic have been handled better?
We closed borders and locked down populations because we could not do any better, and it didn’t really work. But ultimately, despite all these precautions, people continued to get infected until we began rolling out the vaccine. What could we have done better? In any epidemic or pandemic, we need to focus on protecting the most vulnerable people. In HIV, we began with mass prevention and later moved to targeted prevention, focusing on those most at risk of getting infected.
We knew from the beginning that the elderly and patients with chronic diseases were the most at risk of developing severe COVID-19 infections. These two populations are intertwined. We could have focused on these populations to protect them and ensure they are properly treated. But nearly all our healthcare systems are set up for the patients that come to the hospital or health facility. Once the patient leaves, there is no system to connect with the targeted prevention for COVID-19 as conducted with HIV.
Rising chronic diseases and an ageing population have caused healthcare costs in Asia to rise steeply over the years. How can the region ensure sustainable healthcare access for its people? Affordability needs to be addressed as a fundamental element in any access strategy to achieve sustainable healthcare access. Given the rising number of cases and the enormous scientific progress, no one person can address the issue of affordability alone. The affordability solutions to equitable healthcare access require multiple stakeholder collaboration between governments, multinational pharmaceutical companies, insurance companies, charities, and civil societies. Furthermore, lowering the price of a product alone does not and will not achieve sustainable access solutions because it does not look at the patient’s full course of treatment journey to achieve the best health outcomes. What is required is a more holistic solution than just price cuts to enable affordability. As we learned, with HIV and with COVID-19 vaccines, there is a lot more to consider when providing ‘equitable healthcare accessibility’ than the price.
How will sustainable healthcare access be defined in 2023 and beyond? How should Asia prepare itself?
In Asia, we must move our focus toward better health outcomes, starting by looking at the costs of accessibility and adherence to patient treatment from this perspective. More digitalisation and better connection with the patients will also help reduce costs and optimise medical outcomes. After the COVID-19 pandemic, the healthcare community in Asia and worldwide became conscious of the existing gaps. We are on the verge of a digital transformation in healthcare and more sustainable access solutions, but this journey to success will take longer than 2023.
What is the role of digital healthcare solutions in building sustainable healthcare access?
Modern healthcare requires a health ecosystem where hospitals and health facilities are at the centre but are not the only player. There need to be a multi-faceted approach and different stakeholders contributing to patient follow-up and treatment outside the healthcare facility to create sustainable healthcare access. In any ecosystem, connectivity is key. It facilitates patient outreach as a connection between healthcare providers and rapid response to health threats.
If we look around us, the banking, finance, and supply chain industries have embraced digital revolutions. Healthcare is still so much behind. Further, the world is now more interconnected, but healthcare systems are not. We need to transform healthcare accessibility by digitalising healthcare systems within and outside the healthcare facilities and be future-ready to face the next global health threats.
AUTHOR BIO
Dr. Joseph Saba is Co-Founder and Chief Executive Officer of Axios International, a global healthcare access company with 25 years of specialised experience developing practical and sustainable solutions to patient access challenges in emerging markets. Saba is a French Lebanese medical doctor specialised in infectious disease, healthmanagement and statistics. Saba has conducted numerous fieldworks and led various field teams in global health research projects, including a mother-to-child transmission prevention project in Tanzania, South Africa and Uganda, a female condom program in Thailand, and an epidemiologic survey on HIV patients in Rwanda.
17 www.asianhhm.com
HEALTHCARE MANAGEMENT
The Evolving Nature of Healthcare Management Education

The Healthcare sector is undergoing enormous change post Covid-19 pandemic. The development of institutional infrastructure and technological advancements has led to an increased demand for qualified healthcare professionals. The Healthcare Management education in business schools attempts to bridge the gap between clinical and allied functions in healthcare ecosystem. The niche Healthcare Management MBA Programme provides a competitive advantage to young managers to be future ready to serve the dynamic Healthcare Sector.
&
COVID-19 posed unique challenges to higher education as our university adapted to on-line/ digital platforms for all the activities from delivering lectures, presentations, organising competition, hackathons, events to a range of administrative pursuits. As India rolled out a successful vaccination drive, we deliberated over the risk to start classes in person. We initiated hybrid classes maintaining COVID protocols and gradually opened the campus. There is renewed enthusiasm for peer learning in physical classrooms. Student confidence has increased and engagement has improved. Post pandemic there is more focus on preventive healthcare and wellness. The wearables, trackers, sensors and m-health solutions are being adopted at unprecedented pace.
1. The COVID-19 outbreak was one of the biggest challenges the healthcare sector has ever faced. Do you see any trends emerging that might change how your B-school operates in the wake of the pandemic?
Poonam Chauhan Faculty – Marketing
International Business Programme Co-cordinator - MBA Healthcare Management K J Somaiya Institute of Management
2. How does digital technology impact healthcare?
Digital technology helps in preventive care and lowering the overall healthcare cost. It improves efficiency and helps both the healthcare providers and patients. Virtual consulting, Telemedicine and Telehealth makes healthcare affordable and accessible for rural masses. Health apps empower the users to monitor their health, get real time feedback and quick test results on their health condition. Healthcare providers and service organisations, Hospitals, Diagnostic labs are taking design thinking approach to integrate digital solutions for improved user experience and care outcomes. The advancement in digital technologies will be able to offer personalised care and improve wellbeing.
3. K J Somaiya Institute of Management (KJSIM) offers


covers healthcare sector in a very holistic manner which covers Hospital, Pharma Companies, Biotech, Diagnostics, Health Insurance, Fitness and Wellness. It has a good blend of managerial and technical subjects. The technical courses are facilitated by global industry experts from Healthcare sector. The programme encourages experiential learning by organising field trips and international immersion in healthcare sector. The programme intends to build managerial competencies along with imparting comprehensive knowledge in Healthcare sector which is growing at an unprecedented rate. The programme aims to integrate healthcare delivery and operations along with finance, innovation and entrepreneurship. It instills social and ethical responsibility among budding managers, a crucial requirement for healthcare sector. The students are typically Doctors, Dentists, candidates who have worked in healthcare or pharma companies or someone who is keen on pursuing a career in Healthcare sector.
4. What are the potential career paths in this area?
Healthcare is one of the fastest growing sector and offers immense opportunities in Hospital administration, Telemedicine, Digital healthcare, Digital marketing & Sales and marketing of healthcare products & services, Human Resources Management in healthcare sector, Operations and supply chain management in healthcare, Managing Healthcare Chains, Data analytics and informatics in healthcare, Quality management, Consultancy in healthcare, New business development in healthcare and Health insurance.
KJSIM offers MBA in Healthcare Management with Imperial College Health Partners, UK and K J Somaiya Hospital and Research Centre, Mumbai as its academic partners. The teaching learning process lays emphasis on leadership and integrative thinking. MBA HCM
With over 20 years of experience in teaching and research at post graduate degree level, Dr. Poonam Chauhan is an Associate Professor in the area of Marketing & International Business at K J Somaiya Institute of Management. She is also the Programme Co-coordinator for MBA Healthcare Management at the institute. She holds a Ph.D. from SNDT University (Mumbai) in the area of ‘Role of Women Cooperatives in Economic Empowerment of Indian Women’. Her core areas include International Business, International Marketing and Marketing Strategy. Her endeavour is to strengthen and build excellence for the Healthcare Management Programme at K J Somaiya Institute of Management.
19 www.asianhhm.com
a niche MBA in Healthcare Management (HCM), could you give us a general understanding of MBA HCM and the background required for them? Also what distinguishes it from others?
The Effects of Employee Mental Health on Organisational Health
The effects of poor mental health of an employee on the productivity of the organisation are subtle and often go unnoticed. More so in larger organisations, as the effects could be infectious and viral out as an unwanted and unwarranted imprint on the culture of an organisation.
Gurrit K Sethi, Founder, MIINDMYMIIND
Poor employee mental health costs India Inc around US$14 billion yearly. Around 80 per cent of the Indian workforce has reported mental health issues over the past year’, reveals a recent survey by Deloitte.

If these statistics are to be believed, it is indeed high time that we understand what this means for businesses on ground!
How often do we hear these or similar statements?
• I was unable to sleep last night so need a strong coffee
• I am not feeling too well – have a constant headache, unable to concentrate
• I have a back issue
• I have a migraine
• Oh I am having a panic attack!
• Colleagues complaining of muscle aches, blood pressure, fatigue, acidity
• I was unable to sleep so I am not feeling very bright. And the list goes on… Ask any medical specialist and they will brush these aside
as not really medical issues and probably resulting out of over thinking. Then there is a different set of statements one hears:
• I am wondering why I have been entrusted this responsibility. I do not think I am good enough for it
• Because of issues at home, I do not have any peace of mind there. When I come to work, I get to gossip with my colleagues
• There is too much work!
• I am stretched! And stressed!
• This is how it works here! Get used to it!
These have become commonplace jargons of the corporate goers. How many of us are not guilty for having said at least a few of these?
What do these utterances tell us? Because, how an individual manifests
issues and concerns like these, or even experiences these, invariably gets shaped by the environment one is in. It is reflective of the atmosphere and belief systems of the workplace. And on the rebound, these also end up shaping the environment around the naysayers. Negative thought processes always have a higher ripple effect than the positive.
These also point to poor mental health and to poor coping skills of common place issues and problems perhaps. It is the same persona that one has in the personal space that we carry to the workplace. And the tensions and effects of one does carry forward to the other. This is a pointer to how we perceive health as well — physical and mental, how we seek to treat the concerns and create coping skills. The generic health statistics of both mental
20 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
HEALTHCARE MANAGEMENT
and physical health say a lot about this — we bear 30% of the world’s mental health burden, we are third highest in obesity, we are the diabetes capital of the world and similar for cardiac diseases! It is a no brainer that the work place will be affected! A healthy body and a healthy mind go hand-in-hand.
In essence, the examples of the utterances, also point to the culture of the organisation. To put it in a more common place language — these reflect if it is a happy workplace environment or not. Are people wasting their time in such expressions or are they driven to find solutions. Are people motivated enough to perform well? Are they able to overcome daily workplace issues? Is there a way that enables them to cultivate their skills to do better?
Workplace achievements fuel a sense of growth and well-being. The cheer is not merely because the people are happy, but a lot more goes into creating this positive environment. And creating this is indeed the responsibility of the leadership and leadership at every level and rung of the organisation, not just the HR. As the organisation size goes up, this needs to be a more structured approach to overcome the various complexities of a business environment.
Do reflect back on the instances when you achieved your target. Did the motivation to achieve play a role in the achievement? For that matter, reflect back on our childhood instances of achievements. What motivates us to expand our capabilities?
Unfortunately, such statements are now commonplace. And no, this is not just the outcome of COVID. Yes, COVID did expound it to a degree, but the problem has been brewing for long and is finally showing up in the statistics. In the eagerness for growth, we have been pushing the targets higher, we have been focussing on ‘performance’ albeit without the environment for
Footnotes
performance. The pink slip culture seeped in and did take away the security of survival thus converting this to a deed for survival itself.
The health issues — physical or mental — do also show up in forms of absenteeism, insurance costs etc. These have been well researched in some countries around the world. While these are more tangible aspects of the costs incurred, the culture of negative whispers across the corridors can be worse because of the infective nature of negativity! Loss of productivity in terms of quality output is difficult to measure.
A work environment is like setting the temperature of the room. Too cold and you are inactive, too hot and you are again in a not so active situation. To thrive, the right environment is critical. And we have pushed ourselves probably in the wrong direction. Is it not surprising to have seen the year of the great resignation? Or the number of people now choosing to set up their own shop, happy to survive on lesser?
Each one of us thinks of ourselves as a good manager, a good person. However, how many times do we hear of people talking about their good managers? Very few! Should this be a reality check for those of us who consider ourselves super bosses? Yes, the two statistics do not add up!
So, what can we do? Yes, we do have Employee Assistance Programmes
AUTHOR
(EAPs) working in our organisations. Are these enough? Because most of these are a tick in the box as a necessary HR activity to be done! This journey of the turnaround has to start with every CEO / COO / C -suite employee across organisations.
Can we create an environment where these can be addressed from a ‘ground up’ approach and re-establish a culture of growth and achievement and rectify and address behaviours that are counterproductive? After all, a working person spends most time of the productive day at the workplace. In many instances today, where the workplace has encroached the home, the problems can be different, and, also need a solution. The right environment can in fact be used to erase the negativity of the system by implanting the right perception and the right treatment / problem solving behaviours.
There is a huge need to infuse positivity, security and cheer to churn these numbers around. This also means earning more! So, a little spend on the right programmes to build awareness on health, a little handholding with the right learning and development programs and well-defined fruitful support for health needs is the need of the hour. And this would differ from organisation to organisation given the nature of the industry and the work profiles.
Gurrit K Sethi, Founder, MIINDMYMIIND, contributes to healthcare by bringing to life new concepts which enhance accessibility, helps providers re-engineer businesses, works with Global Challenges Forum (a Swiss Foundation) on sustainable health initiatives. An avid traveller and voracious reader, these attributes provide her with incisive insights about people and systems and what drives them.
https://www.peoplematters.in/article/employee-relations/unhealthy-cost-poor-employee-mental-health-costs-india-inc-around-14-billion-yearly-35231
https://businessconnectindia.in/employees-poor-mental-health-costs-employers-14-billion/

21 www.asianhhm.com
BIO
HEALTHCARE MANAGEMENT
VACUETTE® BLOOD COLLECTION SYSTEM ALL IN ONE
Greiner Bio-One offers a whole product line for venous blood collection. The closed system enables a hygienic and simple sample collection. All VACUETTE® products are compatible with all common analysis equipment.

VACUETTE® Blood Collection Tubes
The innovative VACUETTE® Blood Collection Tubes made out of virtually unbreakable PET plastic have set the standard on today‘s market. They provide improved safety and hygiene during specimen collection procedures with the advantage of being as clear as glass.
VACUETTE® tubes can be changed quickly and hygienically during blood collection, without any risk of coming into contact with specimen material. Most tubes contain chemical additives, which in combination with the pre-determined vacuum ensure the correct mixing ratio for the blood sample. The cap
colours of the tubes are based on the internationally recommended colour code so that different tube types can be recognised at first glance. The unique screw thread of the VACUETTE® PREMIUM Tube ensures effortless manual opening of the tube and it is perfect for automated decapping too. If necessary, the tube can be easily opened with one hand.
Make needlestick injuries history
A large number of all infectious diseases acquired at work in the healthcare sector can be attributed to injuries with medical sharps. Needlestick injuries pose by far the highest risk of infection. More than 50% of all registered cases concern nursing staff, followed by doctors and laboratory staff. However, this does not mean that needlestick injuries represent an unavoidable occupational risk. The correct use of VACUETTE® safety products can virtually eliminate this risk. VACUETTE® safety products comply with the EU Directive (EU 2010/32).
22 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
For daily blood collection routines: VACUETTE® QUICKSHIELD Safety Tube Holder
The VACUETTE® QUICKSHIELD Safety Tube Holder by Greiner Bio-One can be used either with VACUETTE® Multiple Use Drawing Needles or with VACUETTE® VISIO PLUS Needles. With our VACUETTE® QUICKSHIELD Complete and VACUETTE® QUICKSHIELD Complete PLUS, the needles are already assembled. The protective shield is attached directly to the holder. Thanks to the one-handed activation of the protective shield with the aid of a stable surface or the finger or thumb, this product is a winner with its easy handling and extensive protection against injury and infection.
The VACUETTE® QUICKSHIELD Safety Tube Holder offers protection against needlestick injuries with no change to collection technique.

The First Step into Safety: VACUETTE® SAFETY Winged Set
The VACUETTE® SAFETY Winged Set is a sterile, plastic winged blood collection set. The set consists of a stainless steel needle, colour-coded wings according to needle size, flexible tubing and a plastic safety cover. The version without Luer Adapter as well as the SAFETY Winged Set + Luer Adapter is also suitable
for the single-use short-term infusion of intravenous fluids.1 Each product is equipped with a safety mechanism to reduce the risk of needlestick injuries. After blood collection is completed, the needle is carefully removed from the patient's vein and the safety mechanism is activated immediately afterwards.
The gentle touch: VACUETTE® EVOPROTECT SAFETY Blood Collection Set
The safety mechanism with a semi-automatic spring mechanism protects you from the risk of a needlestick injuryand makes your daily work easier. Any needlestick injury is one too many. The VACUETTE® EVOPROTECT Safety Blood Collection Set is exceptionally comfortable and intuitive to use. It consists of a winged needle with a safety mechanism, which is suitable for one-handed activation thanks to the special design. Activating the safety mechanism while the needleis still in the vein largely eliminates the risk of needlestick injuries. Extra-thin needle walls of the 21G and 23G cannulas have a positive effect on the flow rate and thus also on the duration of blood collection and infusion. For further information on our products, please visit our website www.gbo.com

23 www.asianhhm.com
1 Note: for some product versions, minimum order quantities and lead-up times apply.
Advertorial
Competency-based Medical Education


Medical education aims to train graduates to take care of the health needs of the society. The existing curriculum is subject-centered and time-based. Most evaluations are summative & focus more on knowledge than on attitude and skills. Thus, graduates lack the basic required skills. CBME is targeted to achieve this paradigm shift in Medical education.
Shakti Kumar Gupta, Executive Director and CEO, AII India Institute of Medical Sciences Jammu
Medical education is metamorphosing into objectivity and every detail needs to be captured and replicated. To achieve the national goal of “health for all,” it is an inescapable need to understand the felt needs of the society they serve in. Medical education in India, however, has lot to be desired to meet this expectation. It is time to reengineer the traditional medical education to competency based education. There is a huge challenge in
24 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
HEALTHCARE MANAGEMENT
converting it to deliverables. The aim of imparting medical education is to train graduates to efficiently take care of the health needs of the society. The current medical education system is based on a curriculum that is subject-centred and time-based. Most evaluations are summative, with little opportunity for feedback. The teaching–learning activities and the assessment methods focus more on knowledge than on attitude and skills. Thus, graduates may have extraordinary knowledge, but may lack the basic clinical skills required in practice. In addition, they may also lack the soft skills related to communication, doctor–patient relationship, ethics, and professionalism (EPA’s). Change is inevitable and more so the management of change is a huge issue.
The need of the hour is to allay this apprehension and address the key issues that are hindering the implementation of CBME. There are three Components of CBME, Competency, Entrustable Professional Activity (EPA) and Milestones.
The term “competency” refers to a combination of skills, attributes and behaviours that are directly related to successful performance on the job. Core competencies are the skills, attributes and behaviours which are considered important for all staff of the organisation, regardless of their function or level. Managerial competencies are the skills, attributes and behaviours which are considered essential for staff with managerial or supervisory responsibilities.
This refers to the application of skills in an actual setting, and an individual who is able to do so is considered competent. The Medical Council of India (MCI) (Presently National Medical Commission, NMC) has also suggested that competencybased learning must be implemented in all the medical colleges. It would include designing and implementing a curriculum that would focus on the

desired and observable ability in real life situations. The criteria of change is in changing people’s behavior.
Entrustable Professional Activity (EPA)
EPA helps bridge the gap between the theory and practice of CBME. While competencies are the abilities of a physician, EPAs are descriptors of work that define a profession. The process and outcomes of EPAs are observable and measurable. They require multiple competencies in an integrative, holistic
nature. For example, let us consider Oncological assessment as the EPA. It would require a definite set of knowledge (the clinical presentation, the investigations needed, and the treatment protocol), skill (clinical interviewing, general and systemic examination, and interpretation of the reports), and attitude (communicating with empathy, inviting questions, and offering appropriate guidance and advice). The core competencies reflected here would be those of a clinician, a communicator, and a professional.
25 www.asianhhm.com
HEALTHCARE MANAGEMENT
Milestones
A competency is achieved gradually, step-by-step. These steps are designated as milestones. The Dreyfus model as applied to education would have five such steps or milestones. These are a novice, advanced beginner, competent, proficient, and expert.
CBME will help today’s learners to become better physicians of tomorrow by providing a holistic experience. Radical educational thinking and new medical program accreditation process in India provides us an opportunity to reconsider existing approaches to medical education.
CBME will focus on individualised customisation and level playing field of teaching. Individualised learning facilitated through CBME will ensure that competencies are being met for each stage. Students will receive more personal supervision, mentorship and day-today assessment. Increased flexibility may provide additional opportunities for enrichment of knowledge during electives. Students will get equal opportunity of learning and performing the task at their own pace without being compared to other fellow learners avoiding peer pressure in particular. Mastering essential clinical skills will provide necessary impetus by enhancing preparedness for practice.
Faculty will see and feel the paradigm shift in their role while implementing CBME. They will help the teachers to handhold and be a part of the teaching learning process rather than just deliver lectures. The incorporation of different instructional methods, namely small group discussions, early clinical exposures and linkers allows the teachers to facilitate active learning. Teaching will be based on well-defined learning outcomes; hence, they can focus on specific observable competencies. Thus, teacher centered approach will be properly aligned with student centred teaching without replacing each other.
CBME has been suggested and tried to tackle these concerns. This means that teaching–learning and assessment would focus on the development of competencies and would continue till
the desired competency is achieved. The training would continue not for a fixed duration, but till the time the standard of desired competency is attained. Assessments would be frequent and formative in nature, and feedback would be inbuilt in the process of training. Furthermore, each student would be assessed by a measurable standard which is objective and independent of the performance of other students. Thus, it is an approach in which the focus of teaching–learning and assessment is on real-life medical practice.
Despite the broad endorsement of CBME as a core strategy to educate and assess the next generation of physicians, major concern is about reductionist approaches in CBME, lack of standardisation and assessments. We have to take little steps towards this change in education system. CBME remains the best possible solution for most of the problems inherent to conventional system of medical education in India. Hence, a systemic collaborative approach and dedicated involvement of all the stakeholders; medical educators, students and policy makers will ensure successful implementation of CBME.
Shakti Kumar Gupta hails from a border Village Ari (LOC), Dist. Poonch, J&K. Commencing his medical career at grass-root levels as an Assistant Surgeon in J&K Health Services, he provided curative, preventive, promotive and rehabilitative services at dispensary and primary healthcare centres. His quest for achieving professional excellence propelled him to relocate to AIIMS New Delhi where he joined as a faculty. He was Medical Superintendent at Doctor RP Centre for Ophthalmic Sciences, New Delhi for fifteen years. He is Fellow of National Academy of Medical Sciences, International Medical Sciences Academy, Academy of Hospital Administration, and Institute of Hospital Engineering. He has been the recipient of WHO Fellowship to study accident and emergency services at USA, and Management Development Programme of National University, Singapore. He is presently ED & CEO of AIIMS, Jammu.

26 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
AUTHOR BIO
HEALTHCARE MANAGEMENT
CBME will help today’s learners to become better physicians of tomorrow by providing a holistic experience. CBME will focus on individualised customization and level playing field of teaching.
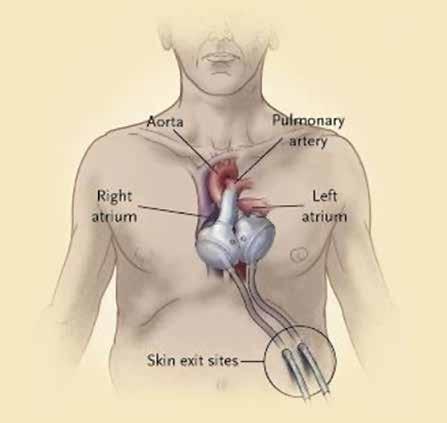
MECHANICAL CIRCULATORY SUPPORT
Historical perspective and management of advanced heart failure
Effort to develop successful mechanical circulatory support started at the same time with the development of cardiopulmonary bypass for safe open heart surgery in 1950s. After the beginning of heart transplantation, necessity of mechanical circulatory support (MCS) become evident because patient need a bridge time support up to the availability of donor organ. Contraindications to heart transplantation and lack of donor heart further stimulated the development of long term mechanical circulatory support. But it is very important to select the device for a particular patient, whether need a temporary device or permanent.
Md. Anisuzzaman Assistant Professor, Department of Cardiac Surgery, Chittagong Medical College
Nazmul Hossain Professor & Head, Department of Cardiac Surgery, Chittagong Medical College
Advanced heart failure patients are severely ill and have exertional dyspnea on minimal effort or even at rest. Hemodynamic instability is so severe that need multiple inotropic support, mechanical circulatory support or even heart transplantation.
Most of these patients are in the hospital on support. Many of the patients have to wait for a long times for heart transplantation. Patients who are
ineligible for heart transplantation due to underlying medical conditions may take the service of MCS for the beneficial effects of it.
Decades of research has enabled durable mechanical circulatory support devices that are widely available now. The recent advancement in pump technology produced the left ventricular assist system and reduces the burden of advanced heart failure management.
Candidate selection for MCS service, risk stratification, and management strategies change with the development of new pump technology. As do profiles of patients according to MCS device.
History of mechanical circulatory assist device
After the first human heart transplant by Cristiaan Barnard in December 3, 1967, artificial ventricle technology began to be used as a mechanical bridge to support patients with post-cardiotomy shock until a donor organ could be available. In 1969, Cooley et al., reported the first use of a total artificial heart as a bridge to transplant (BTT).
In the early 1970s, heart transplantation faced a difficult period of high mortality due to transplant rejection due to inadequate immunosuppression. That accelerated the development of MCS.
However, the first generation LVADs of the 1970s could only support for a matter of days. For these limitations the NIH authority of USA had to issue another series of initiatives in the late 1970s to develop durable implantable assist devices intended for use in chronic heart failure (Figure 1).
27 www.asianhhm.com
MEDICAL SCIENCES
The interest of mechanical circulatory assist technology came in 1982 after Barney Clark, a Seattle dentist, received the Jarvik-7 total artificial heart (TAH). But TAH development almost stopped because of high rates of infection, pump thrombosis, and stroke.

At the same time, cardiac transplantation experienced a renaissance after the US FDA approved cyclosporine in 1983. Improved immunosuppression featuring a calcineurin inhibitor contributed to a sharp increase in graft survival and a rapid expansion in the number of heart transplant programs in the United States.
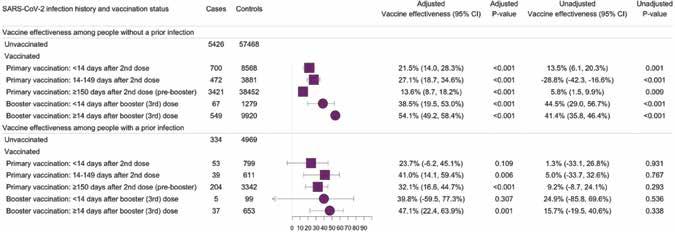
Pulsatile versus continuous flow pump
Continuous flow pumps started replacing previous pulsatile technology in 2008 and covered completely by 2010 due to more complication rate. With this shift of pulsatile to continuous flow pump, another development occurred at the same time and that is small pump profile to allow easy intrapericardial implantation.
Complications of MCS Technology
Device durability increased with continuous flow left ventricular assist device (LVADs) but risks of bleeding, stroke, infection remains together with device malfunction or failure.
For patients with irreversible biventricular failure TAH can help in this regard. But same type of problems of LVADs accompany the TAH technology (Figure 2).
Benefits of smaller pump design
Another important trend in pump development has been miniaturization, even at the expense of flow rate. HeartMate III heart pump (weight 200g, measuring 50.3mm in diameter and 55.8mm in height, including inflow cannula) has bearing less motor using magnetic levitation (Full MagLevTM Flow Technology), able to fit intrapericardially and has less chance of pump failure.
Smaller pump design can be used in both acute insult or cardiogenic shock and chronic heart failure. So, it can help
the heart to recover ventricular function in case of acute insult and to provide durable assistance in chronic failure.
Every therapy designed to increase survival must be judged in part not only by those events or complications that diminish survival but also by those that help define the quality of life anticipated. For device therapy, the critical adverse events include device malfunction or failure, neurologic events, and infections. From the early analyses, about 10 per cent of patients developed significant device malfunction within the first six months. Cardiovascular failure, central nervous system events, infection, liver failure, and respiratory failure were the most frequent causes of death. It is hoped that the precision and consensus underlying this effort will level the playing field and accelerate the reduction of complications for current and future device development.
In case of advanced heart failure patient, it is observed that few pathology of the patient are predictors of high mortality even if we use more than one modality of treatment. As for example, pulmonary hypertension increases risk of mortality in medical therapy
28 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
The first implantation of durable left ventricular assist device (LVAD) in Bangladesh happened recently in United Hospital Dhaka on the 2nd of March 2022.
MEDICAL SCIENCES
Figure 1: Left ventricular assist device (LVAD)
and also in heart transplantation. In patient with right ventricular failure, mortality increases with medical therapy and mechanical ventricular assist. If advanced heart failure patient has renal dysfunction, there is chance of more complication during management and also more mortality even with all modality of medical and surgical approach.
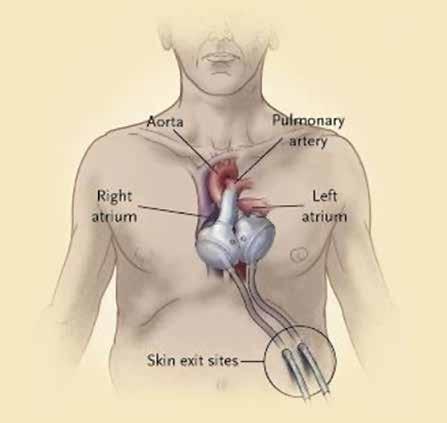
Actually current and future research should focus to fix the clinical indicators of advanced heart failure patient that can predict the poor survival with standard heart failure therapies. So, ventricular assist technology can be considered in appropriate time and patient can get maximum benefit from this treatment modality.
Bangladesh perspective
In Bangladesh, circulatory support devices have little application. National Institute of Cardio-Vascular Diseases (NICVD) had a Datascope IABP machine since the 1990s. This device
was first used in 1997. Off Pump CABG was demonstrated in Bangladesh for the first time by a French surgeon
AUTHOR BIO
Dr Akter Ali Rama at that time. One of the patient developed low output syndrome and he used IABP then. Now IABP is available in all cardiac centres. The first use of ECMO in Bangladesh was in 2013. Now it is available only in four centres (three in Dhaka and one in Sylhet district). A CentriMag device also ready for use in a hospital of Dhaka. The first implantation of durable LVAD in Bangladesh happened recently in United Hospital Dhaka on the 2nd of March 2022. A HeartMate III device was successfully implanted in a 42-yearold patient.
Conclusion:
In recent years, the rapid progress of MCS technology has increased survival and improved quality of life for selective patients with advanced heart failure. And there is a meaningful option generated for lifelong support even in patients who are not candidates for transplantation. With these advances have come new challenges and opportunities.
References are available at www.asianhhm.com
Md Anisuzzaman specialised in cardiovascular and thoracic surgery from Bangabandhu Sheikh Mujib Medical University in 2007. He has got fellowship FACS(USA) from American College of Surgeons in 2020. Now he is working as an Assistant Professor of Cardiac Surgery in Chittagong Medical College, Chittagong, Bangladesh. He has around 50 publications in different national and international journals and author of two books of cardiovascular science. He has been serving as a reviewer of several reputed journals.

Professor Nazmul Hosain is a Bangladeshi surgeon, author and research scholar. He is the founder of cardiac surgery in Chittagong, the second biggest city of Bangladesh. Hosain has91 publications and has presented 39 scientific presentations in international medical conferences. He participates in humanitarian activities including prevention of poverty amongthe socio-economically disadvantageous patients.

29 www.asianhhm.com
Figure 2: Total Artificial Heart (TAH)
MEDICAL SCIENCES
Working Smarter: Reducing the burden of work through connected care solutions.
Digital transformation has long been coming. Paper-based systems have been replaced by electronic health records (EHR), and telehealth has gained traction. But the pandemic accelerated all that - advancing the adoption of connected care solutions and changing the conversation on the future of healthcare. COVID-19 compounded the greater demands from healthcare workers worldwide,1 leading to elevated psychological symptoms such as depression, somatic symptoms, anxiety, and burnout1. To get the latest updates, Hospital Management Asia recently held the “Tackling The New Healthcare Crisis: Healthcare Worker Burnout” webinar, sponsored by Baxter.
Lightening the impossible load: Protocols and Digital Solutions
At the webinar, Dr Ananth Rao, Chief Operating Officer, IHH Healthcare India,
shared a holistic approach to mitigating burnout by allowing employees to be active crafters of their work, providing stress management interventions, and cultivating and encouraging social support2
Connected care solutions also helped keep healthcare workers safe and improve efficiency. At the webinar, Ms Png Gek Kheng, Chief Nurse and Advanced Practice Nurse, Changi General Hospital, shared the implementation of2:
∫ Nurse-led pre-anesthesia assessment via the Health Buddy app
∫ Wearable medical sensors for vital signs monitoring
∫ A hub and spoke distribution model made shared supplies easily accessible
∫ Telepresence with Temi Bot facilitated remote interactions with inpatients
Studies from the McKinsey Global Institute also revealed that 15% of the
work hours in healthcare is expected to be automated with AI, helping to minimise time spent on routine administrative tasks, which can take up to 70% of a healthcare practitioner’s time.3 As we move forward, the greater demands on healthcare will continue to catapult connected care further.
Connected Care Solutions: Improving workflow efficiency and minimising the burden of care.

Technology is critical in reducing healthcare workers’ care burden. It touches almost every point of patient care, from electronic health records (EHRs) to continuous patient monitoring, and intelligent medical devices. When connected to care teams, these technologies create a system that can help reduce errors, enhance collaboration, and accelerate response time.4-6
With almost 95% of hospitals using EHRs, many have taken the first step to introduce connected systems into their workflow.7 Hospitals can build on this foundation, integrate more products and technologies, and reach end-to-

30 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
30 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
end connected care.
Select continuous monitoring technologies can also wirelessly detect a patient’s heart and respiratory rate in real time and alert the appropriate healthcare providers if those rates go outside predefined thresholds.11 Patient issues may be identified sooner, allowing acceleration of treatment and recovery times.
Because 70–80% of patients show vital sign changes at least six hours before a critical event, 12,13 continuous monitoring can help identify patient deterioration before crisis.11 Continuous monitoring has been shown to facilitate appropriate treatment, which may lead to quicker recovery.11
Progressa Bed
Many hospitals also utilise connected products and technologies, like smart bed surfaces and communication solutions, to collect and transmit patient information. When these devices are part of a connected care environment, patient care teams may be significantly improved.4–6,11

63% reduction in falls with injury14,15
86% reduction in code blue events16
20% reduction in days on ventilator17


16% reduction in length of stay with early mobilization19
85% reduction in skins exposure to moisture18
77% reduction in time for more effective turn19
Modern connected care solutions are highly beneficial in easing healthcare providers’ burdens. But only with a committed and proactive approach can we ensure the sustainability and future of our industry.
At Baxter, we continue to seize opportunities to expand global access to our medically essential product portfolio to support more patients through every point of their journey.
72 min time savings
40to1 minute reduction
Sign-up
Learn more about Hillrom products and solutions* at www.hillrom.com

per round by automating vital signs documentation8 per round by automating vital signs documentation10
of vital signs data latency in the EMR after connection9
20%to1% documentation errors
New Healthcare
Webinar. Online. December 29, 2022. Available from: https://www.hospitalmanagementasia.com/webinar/watch-on-demand-video-from-our-webinar-tackling-
A., Hieronimus, S., & Jenkins, J. (2021, July 1). Transforming healthcare with ai: The impact on the workforce and Organizations. McKinsey & Company. Retrieved December 12, 2022, from https://www.mckinsey.com/industries/healthcare-systems-and-services/ our-insights/transforming-healthcare-with-ai 4. Meccariello M, Perkins D, Quigley LG, Rocak A, Qui J. Vital time savings: Evaluating the use of an automated vital signs documentation system on a medical/surgical unit. J Healthc Inf Manag. 2010;24(4):46-51.
5. CareAware VitalsLink Prepared by Cerner Corporation. 2013.
6. Fieler VK, Jaglowski T, Richards K. Eliminating errors in vital signs documentation. Comput Informatics Nurs. 2013;31(9):422-427. 7. Parasrampuria S, Henry J. Hospitals’ use of electronic health records data, 2015–2017. Onc Data Brief, no 46. 2019. Office of the National Coordinator for Health Information Technology; Washington, DC. Available at: https://www.healthit.gov/sites/default/files/page/2019-04/AHAEHRUseDataBrief.pdf. Accessed January 23, 2020. 8. JHIM FALL 2010 Volume 24:Number 4, Vital Time Savings: Evaluating the Use of an Automated Vital Signs Documentation System on a Medical/Surgical Unit based on 30-bed unit with 6:1 staffing ratio
9. CareAware VitalsLink: Eliminating Data Latency & Manual Documentation at Naples Hospital. Prepared by Cerner, 2013 10. CIN: Computers, Informatics, Nursing: Eliminating Errors in Vital Signs Documentation, FIELER, VICKIE K. PhD, RN, AOCN; JAGLOWSKI, THOMAS BSN, RN; RICHARDS, KAREN DNP, RN, NE-BC, 2013. The paper vital signs recording had an error rate of 18.75%. 11. Brown H, Terrence J, Vasquez P, Bates DW, Zimlichman E. Continuous monitoring in an inpatient medical-surgical unit: A controlled clinical trial. Am J Med. 2014;127(3):226-232. 12. Rose MA, Hanna LA, Nur SA, Johnson CM. Utilization of electronic modified early warning score to engage rapid response team early in clinical deterioration. J Nurses Prof Dev. 2015;31(3):E1-E7. 13. Subbe CP, Kruger M, Rutherfor P, Gemmel L. Validation of a modified early warning score in medical admissions. QJM. 2001;94(10):521-526. 14. Hill-Rom Customer. Oncology Falls Study. OVU. 2015 -2016. 15. Cuttler, et al. Beyond the Falling Star: Sustained Decrease in Falls and Injuries with Targeted Bed Exit Alarm, Staff Education Icons, and Patient Education Video. Collaborative Alliance for Nursing Outcomes. 2015. 16. Brown, et al. Continuous Monitoring in an Inpatient Medical-Surgical Unit: A Controlled Clinical Trial, AJM Mar. 2014 (127:3). 17. Hill-Rom Services, Inc. Medical/Surgical ICU Reduces Length of Stay by 16%, Total Ventilator Days by 20% and Saves an Estimated $508,000. 198672 rev 2. Jan 2017. 18. Abbott C, et al. Incontinence Management System Use Significantly Reduces Incontinence Exposure Time. 2019 American College of Wound Healing and Tissue Repair Conference. 19. Wiggerman N. 2017. Data on file
*The above products are not available in all the countries. Baxter, Connex, Hillrom, Progressa and Welch Allyn are trademarks of Baxter International Inc. or its subsidiaries. Any other trademarks, product names or brand images appearing herein are the property of their respective owners. APR432801 Rev 1 5-Dec-2022 ENG-APAC-ISEA
31 www.asianhhm.com
1.
Zhou, T., Xu, C., Wang, C. et al. Burnout and well-being of healthcare workers in the post-pandemic period of COVID-19: a perspective from the job demands-resources model. BMC Health Serv Res 22, 284 (2022). https://doi.org/10.1186/s12913-022-07608-z 2. Sigari et al. 2022.Tackling
the
Crisis: Healthcare Worker Burnout
the-new-healthcare-crisis-healthcare-worker-burnout/ 3. Spatharou,
to our newsletter.
31 www.asianhhm.com
Welch Allyn Connex Vital Signs Monitor
Precision Oncology

A revolutionary therapy for cancer
Precision oncology is a novel approach that aims to reverse cancer resistance and transform patient outcomes. Given the rising incidence of cancer cases in Asia, innovations within precision oncology is paramount in tackling the region's cancer burden. This article explores the benefits of precision oncology in comparison to traditional therapies, and the way forward for this promising space.
The global burden of cancer is increasing at an alarming rate. Cancer is the second leading cause of death globally, accounting for over 9.6 million deaths, or one in six deaths in 2018. Lung, prostate, colorectal, stomach, and liver cancer are the most widespread forms of cancer in men, whereas breast, colorectal, lung, cervical and thyroid cancer are the most
frequent among women. It is predicted that by 2030, there will be nearly 26 million new cancer cases and 17 million cancer deaths each year. Some of the contributing factors to this rise include increasingly ageing populations as well as shifts in the prevalence and spreading of key risk factors of cancer such as harmful lifestyle changes and environmental exposures.
Asia accounts for nearly half the global burden of cancer. Moreover, the incidence of cancer cases is estimated to reach 10.6 million in 2030. There are 3.6 million males and 4 million females battling cancer in Asian countries. In South-Eastern and Eastern Asia, infection-related cancers such as liver and stomach cancers remain among the most diagnosed cancers and top causes of cancer death among males. Cancer prevalence has also been growing within the female population, with Korea, Japan and Kuwait showing the most substantial rise in the past decade. In 2020, there were nearly 159,000 new cases of breast cancer in Southeast Asia alone. A lack of awareness may increase the cancer burden over and above the current estimates.
32 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
Harish Dave, Chief Medical Officer, AUM Biosciences
MEDICAL SCIENCES
Along with this, most cancer treatment modalities, barring a few exceptions, are not efficacious in curing the disease. Once the disease is widespread (metastatic), more often than not, all we can do is offer palliative care. Moreover, the ongoing financial burden borne by cancer patients and their families takes a huge emotional, mental, and physical toll. A cancer diagnosis can rapidly bring about catastrophic expenses for a household, where a disproportionate amount of income is spent on cancer treatment. Moreover, patients may not be able to continue working due to their symptoms, treatment, and/or side-effects, leading to weaker economic conditions. A recent study has shown that there is a significant prevalence of anxiety and depression among patients suffering from various types of cancers in Southeast Asia.
There are several methods for treating cancer, depending on the cancer type and stage, and the desired patient outcomes. For example, if a cure is not available, the patient’s treatment regime is largely focused on shrinking the cancer or slowing the growth of the cancer cells to allow the patient to live symptom-free for as long as possible. There are local treatments such as surgery and radiation therapy, which are used to treat a specific tumour or area of the body. Meanwhile, systemic treatments like chemotherapy can affect the entire body. However, these traditional therapeutic approaches have their own significant share of challenges. The side-effects and longterm consequences of chemotherapy remain major causes of concern for both patients and doctors. Gastrointestinal side-effects are common and can be both troubling and potentially even fatal for some patients. In addition, radiation therapy not only kills or reduces the growth of cancer cells but can also harms adjacent healthy cells. Some common possible side-effects of radiation therapy include dry mouth, fatigue, loss of appetite, hair loss, nausea, and vomiting. Both chemotherapy and
radiation therapy, even when effective, increase the risk of secondary cancers developing some years after the first cancer due to the damage caused by the treatment itself. The complexity of cancer treatment is increased by the fact that cancer cells can develop resistance to traditional therapies, leading to a rise in drug-resistant types which necessitate further research and development to discover novel therapies.
Precision oncology: the future of cancer care
Though modern medicine has achieved important milestones, there are still many concerns that need to be addressed to improve cancer therapy. In this direction, research in oncology continuously endeavours to find new, advanced, and efficient treatments which can reduce the serious side-effects and drug resistance triggered by conventional treatments. Doctors are switching from generalised, one-size-fits-all therapies to tailored treatments and disease interventions. One such innovation is precision oncology. Cancer development can vary from patient to patient and this form of treatment is exclusively designed and directed towards a patient’s unique cancer characteristics.
While genetic variations impact our physical characteristics such as height and hair colour, they also influence the probability of getting certain diseases like cancer. Some genetic variations shield us from certain diseases, while others make us more prone to diseases. Tumours have genetic variations that affect the growth and spread of cancer. These changes are different for different people. Precision oncology uses each patient’s distinct genetic profile to diagnose cancer, create personalised treatment plans, monitor the response to treatment, or make a prognosis. Examples of precision medicine consist of targeted therapies that are used to treat certain types of cancer cells, like HER2-positive breast cancer cells or be utilised for tumour marker or biomarker testing to help
in the diagnosis of cancer. Precision oncology holds the promise of better efficiency, improved care, and reduction of treatment costs. Currently, it is still in the nascent stages of development for the treatment of several cancers.
Importance of precision oncology
Due to the heterogeneity of the disease, standard cancer treatments such as radiotherapy or chemotherapy are efficacious only in certain subsets of patients. Well-designed and accurate cancer treatments like precision oncology can give patients and physicians the opportunity for better therapy selection and improve treatment success rates, thereby increasing the chances of survival. These therapies also result in reduced exposure to ineffective drugs and their negative side-effects.
While conventional treatment like chemotherapy kills cancer cells by generally “poisoning” the cells’ metabolic processes, targeted therapies treat cancer by blocking specific proteins that facilitate the growth and spread of malignant tumours. Precision therapeutics builds upon a better understanding of the fundamental mechanisms of the occurrence of various diseases and also offers an improved capacity to identify which treatments will yield positive results for certain patients. Moreover, precision treatment is less harmful to healthy cells and generally has more tolerable side-effects in patients as compared to traditional cancer treatments like chemotherapy. The ultimate goal of this treatment is to recognise and provide the ideal therapy for patients to boost their chances of survival and improve their quality of life. There have been multiple stories of success exhibiting the potential of targeted therapy in precision oncology. For example, when patients with breast cancer, metastatic gastric adenocarcinoma, and salivary ductal adenocarcinoma with HER2 magnification are given the combination of trastuzumab (monoclonal antibody)
33 www.asianhhm.com
MEDICAL SCIENCES
with chemotherapy, it has shown improved clinical results compared to chemotherapy alone. Precision oncology is therefore bringing about a paradigm shift in the treatment approach of doctors treating cancer patients.
In this regard, biotechnology firms like AUM Biosciences are pushing new frontiers in the field of precision oncology by developing a pipeline of therapeutics designed to overturn cancer resistance through multi-faceted inhibition strategies. They have cited optimistic results of their cancer drug, AUM001, a mitogen-activated protein kinaseinteracting kinases (MNK) inhibitor. It has completed two Phase I trials and has demonstrated good safety, tolerability, and target engagement. A global phase II trial has been initiated for patients with colorectal cancer. Among the different roles in the body, MNKs are also involved in tumorigenesis. Inhibition of MNKs is a newer area of precision medicine acting at the chokepoint of selective translation inhibition (where RNA messages are converted to proteins) in cells. This allows AUM001 to potentially overcome drug resistance in the cancer cells, as well as having the ability to target “undruggable” pathways.
Novel trial designs have also been adopted to identify patients who are most likely to benefit from a treatment, thereby reducing drug development time and costs. As the role of biomarkers in the early detection and monitoring of cancers as well as the development of cancer therapeutics is important, biotech companies such as AUM also mandate use of biomarkers to enhance patient selection and conduct trials to increase the prospect of success over conventional approaches.
Challenges in the field of precision oncology

Over the last decade, there has been continuous progress in the field of precision oncology across multiple tumour histology and biomarker-based trials. However, some critical challenges
persist. Since precision oncology is a growing field, many of the technologies that are necessary to meet the goals have only recently been developed. For example, databases are needed to store large amounts of patient data efficiently. Cost is also a concern with precision oncology. Clinical trials of precision oncology require millions of dollars of funding over several years. Technologies like DNA sequencing, which are an integral part of the research, are expensive to carry out. It is vital that the potential participants get a holistic idea of the risks and benefits of participating in this research. There is also a need to promote inclusivity to overcome the inherent limitations in current studies which primarily include the western or European population. Since these modern therapeutics are based on patient data, there is a growing concern about ethical, social, and legal issues. Additionally, standardisation and harmonisation of the collected clinical and genomic data and its accurate interpretation to enable best practices remains a challenge. Moreover, according to a report, 70 per cent of oncologists agree that precision oncology is promising, while 29 per cent admit that it is still not widely applied in their daily practice.
Additionally, there is also the problem of providing sufficient evidence of safety and efficacy which hinders approval processes. Regulators struggle
AUTHOR BIO
to accommodate new innovations in this field due to smaller trial designs which create statistical complications in terms of understanding a drug’s risk-benefit profile.
What the future holds
Researchers are continuously trying to make the latest and the best cancer treatments more accessible to patients. Precision oncology has the potential to become one of the most successful therapies for cancer and much progress has been made in this field. However, transforming cancer care with precision medicine remains a major challenge due to still-evolving technology, specific infrastructural requirements, need for extensive and standardised database development, lack of inclusive trial data and significant financial implications.
Precision oncology can bring groundbreaking changes in cancer treatment and transform the approval process for new therapeutics. This coupled with the introduction of molecular data in electronic health records will improve the timeliness of patient screening and treatment, thereby improving their health outcomes. With collaboration among the various stakeholders such as clinical, diagnostic, pharmaceutical and academic communities, we can dream of living in a world where cutting-edge cancer treatments are accessible to all. References are available at www.asianhhm.com
Harish Dave is the Co-Founder & Chief Medical Officer of AUM Biosciences and is Boardcertified in Internal Medicine, Medical Oncology and Hematology. He has more than 35 years of experience in basic science, academia and industry and has conducted over 100 studies with a focus on hematology, oncology and transplantation. Dr. Dave has also had extensive interactions with the FDA and submitted multiple IND’s. He has a lengthy publication record and has spoken extensively both nationally and internationally. Dr. Dave also has experience in the finance sector.
34 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
MEDICAL SCIENCES
Liquid Biopsy: New Challenges in the era of Immunotherapy and

Precision Oncology
Editors: Antonio Russo, Ettore Capoluongo, Antonio Galvano, Antonio Giordano
Date of Publishing: 3 November 2022
No of Pages: 205
Book Description: New Challenges in the era of Immunotherapy and Precision Oncology aims to describe links between cancer, precision oncology, and liquid biopsy, focusing on their participation to immunotherapy management. The book provides updated information on the main applications of liquid biopsy and immunotherapy as well as interesting aspects useful for planning basic and translational research activities. It helps readers understand the central aspects of precision medicine in oncology, including the use of new generation technologies for translational and diagnostic settings and the main clinical trials in this area that may be useful during their research.
Artificial Intelligence and Precision Oncology: Bridging Cancer Research and Clinical Decision Support
Editors: Zodwa Dlamini
Date of Publishing: 21 January 2023
No of Pages: 550
Book Description: This book highlights the use of artificial intelligence (AI), big data and precision oncology for medical decision making in cancer screening, diagnosis, prognosis and treatment. Precision oncology has long been thought of as ideal for the management and treatment of cancer. This strategy promises to revolutionize the treatment, control, and prevention of cancer by tailoring tests, treatments and predictions to specific individuals or population groups. In order to accomplish these goals, vast amounts of patient or population group specific data needs to be integrated and analysed to be able to identify key patterns or features which can be used to define or characterize the disease or the response to the disease in these individuals. These patterns or features can be as varied as molecular patterns or features in medical images. This level of data analysis and integration can only be achieved through the use of AI.

Precision Medicine in Cancer Therapy: 178 (Cancer Treatment and Research)
Editors: Daniel D.Von Hoff, aiyong Han
Date of Publishing: 15 August 2020
No of Pages: 283
Book Description: This book presents the latest advances in precision medicine in some of the most common cancer types, including hematological, lung and breast malignancies.

35 www.asianhhm.com
BOOKS
Is Quality of Death as Important as Quality of Life?
The author, with over a 40-year period of active neurosurgical practice (1975-2015) has personally certified over 2,500 deaths in a government, trust, and corporate hospital in Chennai, India. Retrospectively, the author wonders if, the importance he paid to Quality of Life should have been supplemented with equal importance to good quality of death. This is even more important in 2023. This future ready article will emphasise that the radical transformation of healthcare due to unprecedented growth and development of technology brings with it dangers of dehumanisation. Exposure to end of life and palliative care is even more important now.
This article is to sensitise the readers that in 2023, facilitating a good Quality of Death is as important, as what doctors are normally taught — to ensure a good quality of life. Until six decades ago, death was considered a specific point in time — the moment at which life ends. Today, it is accepted that death is an ongoing process — a series of events culminating in irreversible cardiac arrest. Perceptions of a healthcare Provider towards death, changes as he/she ages. Initially, the emphasis is to prevent death in every patient taking every possible measure. After all saving lives is the raison d’etre for our existence. How often did we then ask ourselves “but at what cost?” With time a

36 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
MEDICAL SCIENCES
K Ganapathy, Member Board of Directors, Apollo Telemedicine Networking Foundation & Apollo Tele Health Services
major constraint, did we spend quality time with the caregivers of an individual, whose passing away was imminent. Did we discuss End of Life scenarios? We were so engrossed in providing intensive critical care, in adjusting ventilator settings, correcting electrolytes, repeating imaging studies, protecting ourselves by getting multiple second opinions that we hardly ruminated on the Quality of Death. Understanding psychological, social and spiritual needs at this time is as critical, as developing skills in grief counselling.
Personal clinical illustrations from neurosurgical practice
How does one discuss “good death” with a just married wife, when her husband has had a devastating bleed in the brain? How does one inform a retired Professor of Surgery that he has multiple secondaries not only in the brain but elsewhere and any therapy will at the best only postpone the inevitable. A 92-year-old woman with stroke on both sides is strongly encouraged to be taken home. She also has multiple hip fractures secondary to the trivial fall. Two months elapse. Patient is in coma for four weeks.
Death asked life,
Morphine patches are being used for analgesia. The 70-year-old son cannot withstand her suffering. After discussion, Ryles tube feeding is also stopped with the hope and prayers that an irreversible cardiac arrest would occur. Alas, the lady has not read text books of medicine. The heart goes on beating for another 48 hours with the elderly children going through an agonising time.
What is Good Death?

The term Good Death was introduced in the nineteen sixties. A Good Death implies that treatment preferences,
quality of life and maintenance of dignity have been as per patient’s desires. There has been no distress or suffering for patient, family and caregivers. There has been little or no pain. The death is consistent with prevailing clinical, cultural and ethical standards. Excessive or futile treatments are not used just to prolong life. There is total trust, support and comfort with the doctor and the nurse. There is an opportunity to frankly discuss all beliefs and fears and to bid farewell to near and dear. When end-oflife is inevitable and patients or their families consent, aggressive therapies, medications and interventions are stopped but care is never withdrawn. Death and process of dying play an important role in all societies and cultures. Notions of good death are specific, unique, and different. Advances in medicine and technology have resulted in longer end-of-life periods often making the process of dying more protracted. A Good Death is not a single final event, but a series of social events. End-of-life support and care should continually respond in flexible and dynamic ways to the wishes of the dying person. Dying needs to be understood as a process that can be influenced. Though dying is inextricably tied to life, there is a general reluctance to speak about death. A study in 2017, revealed that seven in 10 Americans preferred to die at home, an important component of Good Death. Costs also needs to be factored.
37 www.asianhhm.com
Why does everyone love you, but hate me.
MEDICAL SCIENCES
Life replied, Because I'm the beautiful lie and you're the painful truth.
Interventions to improve end-of-life care have important ramifications for dying patients and spouses. Sudden events precludes time to discuss end-of-life issues with family members. Terminal illnesses offers time for discussion and resolution of "unfinished" psychological and practical business. Good Death includes not being a burden to the family, leaving affairs in order and having a sense of fulfilment.
What is Bad Death?
A bad death is one in which there is violence, pain, torture, dying alone, being kept alive against one’s wishes, loss of dignity, and inability to communicate one’s wishes. Proper communication makes a difference between good and bad death. Excessive use of technology, with patient and family wishes ignored, contributes to a bad death.
Assisted dying
Choosing assisted dying is an incredibly difficult decision for all involved. Judging quality of death is very personal. Assisted dying laws allow patients and families some measure of control over time and manner of death. Switzerland’s law permitting assisted death has been in force since 1942. In 2014, Belgium included children in its 2002 euthanasia law, the same year when the Netherlands legalized assisted suicide and euthanasia. Oregon in the USA has permitted selfadministered doctor prescribed lethal medications since 1997, under the Death With Dignity Act (DWDA). Washington passed a similar law in 2008, as did Vermont in 2013. Eight states in the USA have passed laws allowing doctor-assisted death In February 2015, Canada’s Supreme Court ruled that
adults suffering extreme, unending pain would have the right to doctor-assisted death. The South Korean government implemented the "well-dying law" in 2018, which enables patients to refuse futile life-sustaining treatment (LST) after being determined as terminally ill. In a landmark judgement delivered on 9th March 2018, a 5-judge bench of the Supreme Court of India recognising ‘living wills’ made by terminally ill patients, held that the right to die with dignity is a fundamental right.
Legalising passive euthanasia Justice Chandrachud had remarked, “Life and death are inseparable. Every moment our bodies undergo change… life is not disconnected from death. Dying is a part of the process of living.”
Death cafés
Palliative care extends beyond medical treatment. In many countries, Death Cafés, offers meetings over tea and cakes where participants can hold open conversations on death, sharing ideas and concerns. The Death over Dinner movement suggests groups of friends host dinner parties to process how they feel about death. “How we want to die,” the movement’s website prompts, “represents the most important and costly conversation America isn’t having.”

38 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
"I am not afraid of death. I just don't want to be there when it happens."
MEDICAL SCIENCES
- Woody Allen, 1975
Quality of Death Index
India has been ranked 67 out of 80 countries on the 2015 Quality of Death Index, lower than South Africa (34), Brazil (42), Russia (48), Indonesia (53) and Sri Lanka (65) but above China (71). People in the United Kingdom get the best end-of-life care, according to the index; calculated by the Economist Intelligence Unit. In recent years policy interventions and public engagement to improve quality of death through provision of high-quality palliative care have gained impetus. Recent legislative changes, have made it easier for doctors in India to prescribe morphine. Recognising that most individuals are uncomfortable to talk about death, it has been stressed that Quality of Life ‘Die-logues’ Needs to Include Quality of Death and End-of-Llife care discussions to increase public awareness.
Execution of a Living Will in India
Though the Supreme Court of India in 2018 ruled that “the right to die with dignity is a fundamental right” the implementation and execurion of a Living Will (LW) is still mired in controversy. At present a LW has to be written by the Executor with 2 independent attesting witnesses. This is then countersigned by a Judicial Magistrate First Class (JMFC). The jurisdictional JMFC supplies the LW to the concerned authorities and informs immediate family members. The Hospital Medical Board where the patient is admitted certifies the instructions, informs the Collector who constitutes an independent Medical Board (MB) . This MB visits the hospital and if concurring with the previous MB, endorses the certificate to implement the LW instructions. This MB then informs the JMFC who after visiting the patient and examining all aspects, authorises implementation of the MB’s decision. If life support is withdrawn, JMFC will inform the High Court who shall maintain requisite records in digital format. If there is
a difference of opinion between the MB and family members, parties can prefer a writ petition in the concerned High Court decision shall be final and binding. The Supreme Court of India on Nov 23 2022 heard a petition on these ‘unworkable guidelines’. The case has been adjourned to Jan 17th 2023
Conclusion
The last two decades have witnessed an unprecedented deployment of technology in Healthcare. Younger clinicians are super-efficient in what they have been trained to do, but somewhere along the line are we missing the wood for the trees. Is it not in their ‘job profile’, to also be responsible to ensure a good death for patients, when death is inevitable. Are we too busy, to commiserate with the family, empathise, sympathise with the individual who has placed his/her life in our hands.
Textbooks, journals, clinical meetings and group discussions can give us guidelines and scientifically valid statistics of different outcomes with different management plans. How often do we factor in the specific desire of the patient? Are we totally transparent during our counselling sessions. Unconsciously, inadvertently is our approach influenced because we are on a ‘fee for service’ or on a salary. Should society's healthcare resources be directed primarily for ‘curing,’ or ‘caring,’? When is enough enough for the terminally ill? Who decides? Should decisions always be based on irrefutable scientific evidence and available technology? Do increased ‘options’ only compound the issue. Having been involved in hundreds of deaths during a full professional career, one sometimes becomes less sensitive. We forget that for the aggrieved family it is often the first experience.
Working in a public hospital in the late seventies the author has on several occasions encouraged the family to take a sick moribund patient home so that the septuagenarian would have a good death. Influencing factors
included logistics of transporting a dead body across interstate check posts and the costs. Do treatment protocols, algorithms and flow charts give adequate weightage to what the patient and the family wants. Even if “Primum non nocere” is considered, it is generally about the physical body. Do no harm rarely extends to the emotional and economic domains. Discussion of end-of-life management scenarios often has to be initiated within days or even hours of admission. The situation is more complex as the moribund patients were probably in good health before a totally unexpected catastrophe struck. Discussing death should not be considered macabre, ghoulish and in morbid taste. As clinicians, it behoves us to strive to achieve at least a Good Death for all those who have placed their trust in us.
On January 25th 2023 the Supreme Court of India, accepting the appeal that the earlier guidelines were “ unworkable” and that in the preceding four years there was not a single request for passive euthanasia in spite of the 2018 ruling, have relaxed some of the requirements. Hopefully the implementation and execution will now be less cumbersome.
AUTHOR BIO
K Ganapathy Former Secretary and Past President Neurological Society of India, Telemedicine Society of India & Indian Society for Stereotactic & Functional Neurosurgery Distinguished Visiting Professor IIT Kanpur, Distinguished Professor The TamilNadu Dr. MGR Medical University, Emeritus Professor, National Academy of Medical Sciences, Formerly Member Roster of Experts Digital Health WHO. Director, Apollo Telemedicine Networking Foundation & Apollo Tele Health Services, India.
URL: https:kganapathy.in
Mail: drganapathy@apollohospitals.com
39 www.asianhhm.com
MEDICAL SCIENCES
The Wide Gap in Management of Aortic Stenosis and Tools to Narrow it

Misunderstanding of the natural history of the disease, lack of screening programmes, and reliance on the degree of stenosis as the sole determinant of intervention are important factors contributing to a wide gap in the management of aortic stenosis. We present tools to narrow this gap through series of studies conducted on a large cohort of patients.
Aortic stenosis (AS) is the most common valvular heart disease in Western countries and is expected to become a larger healthcare concern as populations continue to age and the burden of atherosclerotic risk factors concurrently increases. Prevalence of moderate or severe AS in patients 75 or older is 2.8 per cent, and the number of patients with AS in the United States is projected to more than double by 2050. AS carries a high risk of morbidity and mortality even in early stages of the disease, and the only available treatment is aortic valve replacement (AVR).
40 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
Prashanth Vallabhajosyula, Director of the aortic institute, Yale University
Sameh Yousef 1, Stuti Tank2, Chirag Ramachandra3, Aaron Pininti1, Raj Lingnurkar1, Brett Johnson1, Jin Young Park1, Franklin Burg1, Tul Maya Gurung1, Augustus Koch1, Prashanth Vallabhajosyula4
1 Division of General Surgery, Mercy Fitzgerald Hospital 2 Drexel University College of Medicine 3 Vanderbilt University School of Medicine 4 Division of Cardiac Surgery, Yale School of Medicine
MEDICAL SCIENCES
AS initially develops by endothelial injury and dysfunction, inflammation, progressive remodelling, and calcification. This process stiffens or fuses the valve leaflets, which inhibits their separation during systole. The stenosis impedes left ventricular ejection and increases left ventricular systolic pressure, resulting in compensatory adaptive changes such as concentric hypertrophy. Initially, ejection fraction, cardiac output, and left ventricular end-diastolic volume are maintained, and patients may have a prolonged asymptomatic period. However, as the degree of stenosis and hypertrophy worsens, AS becomes clinically significant. Common symptoms include dyspnea, decreased exercise tolerance, dizziness or syncope, and angina pectoris.
AS can be stratified into mild, moderate, and severe through haemodynamic staging. Although patients with moderate and severe AS experience high morbidity and mortality, AVR is typically reserved for patients with severe AS, when the risk of death of AS outweighs the risk of surgical mortality. The current definition of severe AS is based on studies showing that a maximum flow (Vmax) > 4 m/s aligns with the onset of symptoms in 70-80 per cent of patients. While onset of symptoms marks a significant increase in mortality, up to 50 per cent of patients with AS are asymptomatic and still have high mortality. Because AVR has been shown to increase longevity and improve quality of life, studying patient risk factors in conjunction with echocardiographic findings can help inform decisions on the timing of intervention.
In our experience, we found that all degrees of AS are associated with higher mortality risk compared to subjects with no AS. We studied 37,131 patients over six years period. These patients were then stratified into five groups (A-E) according to Vmax percentile (Group A: Vmax<75th percentile,
Group B: Vmax between 75th and 90th percentile, Group C: Vmax between 90th and 97.5th percentile, Group D: Vmax between 97.5th and 99th percentile, Group E: Vmax≥ 99th percentile). There was a steady increase in mortality rates in Groups B-D, which an exponential increase in mortality in Group E. This pattern was also accompanied by an increasing frequency of end-organ comorbidities (dementia, chronic kidney disease, peripheral arterial disease, and heart failure) and cardiac functional and structural changes.
These results are supported by studies demonstrating that two major factors affect survival in AS: comorbidity and cardiac changes. Patients with more comorbid conditions are at a higher risk of being in conditions where supraphysiologic cardiac output is needed, placing additional stress on the already-strained heart. One of the cardiac structural changes caused by the chronic pressure overload in AS is an increase in left ventricular mass. This leads to higher filling pressure, resulting in diastolic dysfunction, which often precedes systolic dysfunction, and onset of symptoms in most patients.
Traditionally, an ejection fraction (EF) < 50 per cent or symptom development have been used to define cardiac dysfunction, but these may represent later stages of AS. Because AVR has typically been restricted to symptomatic patients with severe AS, intervention in this later stage may have reduced benefit. Irreversible myocardial damage may have already been established. The results of this large study support considerations for earlier intervention in AS patients with Vmax≥ 3.2 m/sec consistent with moderate AS.
Thereafter, we developed a risk prediction model for mortality in patients with AS using a subgroup analysis of the aforementioned cohort. We calculated the risk of 1- and 5-year mortality for patients who have moderate or severe AS. The models included only patients with complete follow-up (3966 in the 1-year, and 816 in the 5-year model) and encompassed variables related to patient characteristics, degree of AS, and AVR. Amongst the 13 variables included in the final models, AVR was the strongest predictor associated with decreased mortality and improved longevity. Yet, a large fraction of patients did not undergo intervention (97.2 per cent of patients with moderate and 57 per cent of patients with severe AS). This underscores the existing gap in management of AS. In a contemporary report, 74 per cent of patients with severe AS who did not undergo AVR, were not referred for evaluation. Hence, tools such as this individualised risk calculator can help patients and providers understand the risks of mortality associated with medical management of moderate and severe AS over the short and long terms. This may eventually lead to expeditious referral to specialized centers.
On the other hand, there are currently no screening algorithms to diagnose AS, and so many patients are diagnosed later in the disease process based on symptom onset, which occurs
41 www.asianhhm.com
MEDICAL SCIENCES
Prevalence of moderate or severe AS in patients 75 or older is 2.8 per cent, and the number of patients with AS in the United States is projected to more than double by 2050.
after a long period of asymptomatic AS. As a result, there is a need to develop tools for screening programmes for earlier diagnosis. In another large crosssectional study conducted by our group, we developed an algorithm for early diagnosis of AS. Using echocardiographic results and data from the electronic health records, we developed a prediction model to identify patients with moderate and severe AS-based on readily available demographic and comorbidity information. Compared to patients with no AS, patients with moderate or severe AS were more likely to be older (mean age 76.6 ±11.3 years vs. 66.4 ±13.3 years), male, and Caucasian. They also had a higher prevalence of hypertension, dyslipidemia, coronary artery disease, pulmonary hypertension, heart block, atrial fibrillation, cerebral infarction, peripheral vascular disease, chronic kidney disease, diabetes mellitus, dementia, inability to walk, heart failure, dilated cardiomyopathy, pacemaker, defibrillator, percutaneous coronary
interventions, and coronary artery bypass graft. Additionally, they were more likely to be taking beta-blockers, calcium-channel blockers, angiotensin - converting enzyme inhibitors, and diuretics. This model has the potential to be used clinically because it relies on readily available data from patient charts and is simplified to a point coring system that is translated into the probability of a patient having moderate or severe AS. Identification at the moderate stage of disease can prompt future diagnostic assessments, such as echocardiogram,
AUTHOR BIO
Prashanth Vallabhajosyula, MD, MS, is the director of both Yale aortic institute and Yale pulmonary thromboendarterectomy programs. He performs the entire spectrum of cardiac surgeries with special expertise in complex endovascular repairs of thoracic and throacoabdominal aortic aneurysms and dissections.

with the goal of timely intervention aiming to increase survival and improve quality of life of patients with AS.
References are available at www.asianhhm.com

42 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
MEDICAL SCIENCES
The Healthcare Sector Needs to Lead the way on Decarbonisation
Given that India has committed to a net-zero target by 2070, and international health systems like the UK’s NHS and the US’ Department of Health and Human Services department giving clear reduction and net zero targets, the need for concerted action on decarbonisation by the Indian healthcare sector has become an imperative.
Karan Thakur, Group Sustainability Lead &, Vice President – Public Affairs, Apollo Hospitals Group
The recent Lancet Countdown report on Climate Change highlighted the impact of the healthcare sector in global emissions. The report indicates that the total emissions footprint of the global health sector is 5.2 per cent or 2.7 GtCO2e of the total global emissions, while contributing to 10 per cent of global GDP. As per Health Care
Without Harm, the Indian health sector’s contribution of the country’s total emissions is approximately 2 per cent. While this may seem like a small contribution towards the total, the fact that it continues to increase at a rate of approximately 5 per cent every year is a cause for concern. Additionally, the extensive use of anaesthetic gases, single use plastics, generation of

43 www.asianhhm.com
FACILITIES & OPERATIONS MANAGEMENT
biomedical waste and a poor substitution uptake of renewables makes the issue more germane. Given that India has committed to a net-zero target by 2070, and international health systems like the NHS and the US’ Health and Human Services department given clear reduction and net zero targets, the need for concerted action on decarbonisation by the Indian healthcare sector has become an imperative.
As we begin this journey of decarbonisation, it is important to understand the key contributors to the emissions inventory in a typical hospital. Studies by the UK’s NHS indicate that 24 per cent of emissions are through delivery of care, which includes energy use, procurement of pharmaceuticals and chemicals, use of medical equipment and materials like anaesthetic gases and metered dose inhalers. Add to that another 10 per cent of emissions are contributed by patient and visitor travel to hospitals and through staff commutes. Most of the emissions however, come from the supply chain, averaging at 62 per cent of the total carbon footprint. Of this, pharmaceuticals, chemicals, and medical devices make the majority of the emissions inventory, with non-medical equipment, food and catering and business services like indemnity insurance bringing up the rear.
Indian healthcare offers slight variations but is broadly in line with global peers. As per a 2019 report by Health Care Without Harm and ARUP, on an average 8 per cent of total emissions in Indian healthcare is attributable to direct emissions, i.e. those generated through operational emissions. A further 11 per cent of emissions come from indirect emissions of those from purchased energy sources for a hospital or health centre. 81 per cent of emissions are through the supply chain which includes emissions on account of manufacturing, transport and storage of pharmaceuticals, medical devices and chemicals, transport and business services. As Indian healthcare
becomes more mature in the years ahead, it may start to mirror the emissions inventory of the rest of the world, but the skew towards a majority of emissions coming from the supply chain are likely to remain.
As with any data sets, it is easy to postulate and take positions. It can be argued that till the supply chain emissions, largely beyond the scope of healthcare providers, are not reduced, any meaningful progress towards decarbonisation will remain futile. Others could argue that the onus remains on the decarbonisation efforts by power generators and equipment manufacturers to ensure the health sector meets its carbon neutrality and net zero ambitions. The merits of these arguments aside, the onus remains on the sector to implementing measures to that impact direct and indirect emissions. Not only does this make economic and ecological sense, it is critical in order to reduce the climate related disease burden that one is witnessing over the past decade.
First, the health sector needs to conduct an analysis of their actual carbon footprint. An emissions inventory framework for all hospitals
and health institutions needs to find priority in amongst policymakers and health administers. Only with real and credible data can the sector make targets and affirm to actions that are measurable and impactful. Multiple solutions based on the UN’s Greenhouse Gas (GHG) Protocol are available for ready use by healthcare institutes. Second, the sector needs to create emission and consumption reduction targets that look at fossil fuel consumption, waste generation and water consumption and effluents generated. This is a critical step towards the sector making consequential progress towards reducing its carbon footprint with eventual attainment of net zero ambitions. Third, the need to move en-masse to renewable sources of energy is the need of the hour. The marketplace mechanism of power purchase in many jurisdictions allows for judicious decisions to be taken on sourcing of energy for the health sector. This move towards cleaner fuels should have adjuncts including increasing self-generation through solar energy and exploring new technologies like renewables-based power back-ups and enhanced battery storage to meet critical
44 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
FACILITIES & OPERATIONS MANAGEMENT
operational needs of a hospital. Fourth, the generation of biomedical waste has seen an exponential rise in the Covid years. While unavoidable, the levels of biomedical waste generation needs to see a commensurate reduction as we emerge in the post-Covid clinical world. This will only be possible with a significant reduction in the use of masks, gloves and single use plastics for clinical procedures that do not require these. Keep in mind, as Indian healthcare becomes more specialised and tertiary care facilities grow across India, the commensurate generation of biomedical waste is expected to rise. The sector, therefore, needs a clear roadmap on defining the appropriate, safe and required use of masks, gloves and single use plastics that ensure harmonisation between high quality care, staff safety and the carbon footprint. Given that net zero to landfill for biomedical waste is a challenge, given the health risks and toxicity of this type of waste, local and state governments needs to prioritise increased capacity waste to energy units that are aligned towards biomedical waste.
In addition to the above, the healthcare build will need to be aligned with principles of carbon neutrality and energy efficiencies. Building energy efficiency certifications like LEED go a long way in ensuring lowering of the carbon footprint and should be taken up in a concerted manner within the broader health sector. Also, the introduction of new low embodied carbon materials and greater use of smart building technologies that lower the footprint need prioritisation. These measures can help the sector make progress on carbon neutrality, but it will continue to depend on the broader ecosystem to help attain net zero status. The decarbonisation of the supply chain needs partnerships, incentives, and regulatory measures. While the health sector must use its purchasing power, the lack of alternatives or fiscal and regulatory motivations for manufacturers to decarbonise will impede progress. Therefore, industry
participation in developing alternatives and embarking on a net-zero journey will need to go hand-in-hand as the sector decarbonises.
Governments and regulatory agencies too will need to play their part in this journey. Healthcare accrediting bodies need to have measurable standards on consumption, waste reduction targets
AUTHOR BIO
and decarbonisation in place to provide regulatory nudges. Similarly, access to funding and incentives that aligns with progress on healthcare decarbonisation needs broader deliberation. The use of carbon offsets finds discussion within healthcare decarbonisation, given that involuntary and unavoidable residual emissions will continue to persist even in the most decarbonised systems. However, just like with any other sector, offsets should be the port of last call, rather than the first off-the-shelf approach. And given the tortuous history of offsets currently, the health sector would be best advised to pursue other strategies more vigorously.
The Covid-19 pandemic reaffirmed the role of the health sector in forefronting a national cause and response. It builds on the tremendous work done by the sector previously as India made admirable progress on various health indicators and continues to do so. And therefore, the onus on facing the perpetual pandemic that is climate change requires the same fervent response from the sector to decarbonise. The route to the planet getting back to the pink of health is through greener healthcare.
References are available at www.asianhhm.com
Karan Thakur serves as the Group Sustainability Lead &Vice President – Public Affairs for the Apollo Hospitals Group, Asia’s largest integrated healthcare provider. Thakur is a seasoned healthcare administrator with wide experience in the field of health policy, hospital operations, projects, health communications and healthcare sustainability.
In his current role, Thakur is part of the Group’s expansion initiatives, public policy engagement & sustainability initiatives.

45 www.asianhhm.com
The total emissions footprint of the global health sector is 5.2 per cent or 2.7 GtCO2e of the total global emissions, while contributing to 10 per cent of global GDP.
FACILITIES & OPERATIONS MANAGEMENT
The recent Lancet Countdown report says.
TECHNOLOGY
Is Artificial Intelligence in Healthcare on the Wrong Track?
A recent article published in a leading international journal specialised in healthcare management describes developments in artificial intelligence (AI) for healthcare in the past ten years. The article identified serious gaps between the priorities defined for healthcare and nursing management and the actual developments developed by AI solutions for healthcare.
Paulo Moreira, Editor in Chief, International Healthcare Review
The article here briefly discussed outlined the contrast between priorities for nursing management proposed in 2011 and the parallel developments on AI for healthcare and nursing management since then. The article describes a clear gap between the focus of Artificial Intelligence developers and the priorities for healthcare management.
AI research is expected to identify innovative approaches to supporting health professionals’ clinical decision-making and

INFORMATION
support on tasks not related to patient interaction, namely administrative activities and patient records.
However, the article demonstrates that in 2022 it is still unclear to what extent the priorities of Healthcare and Nursing Management have been adopted by AI solutions.
The article’s reasoning evolved from identifying three priorities for healthcare management identified in 2011 and goes on to identify recent evidence concerning the past ten years of AI applications development.
Overall, the article identified a serious conceptual gap between both worlds. That is to say the real world of healthcare management and the world of conceptual and programming in AI solutions for healthcare., While admitting that there have been positive developments in AI for healthcare, the key finding of this article is that the previously defined priorities for healthcare management, as perceived by health professionals, have been taken into consideration by AI developers.
What are the gaps?

There seems to be a gap when we set prime concerns of both sides. Healthcare management priorities, as proposed in 2011, focussed on three key ideas. One, would be evolving human resources management from staff satisfaction to staff retention namely through revised workload, enhancing group cohesion and social support. Second priority was developing the support and access to sources of evidence-based-practice (EBP) promoting impacts on the quality of healthcare. Also, adapt research resources for those purposes via more efficient knowledge transfer to improve clinical supervision. A third priority established in 2011 was the expectation of the advancement of competencies on financial responsibility practiced by health professionals and contributing to health organisations sustainability, budgetary control for healthcare added value and accountable care.
The article argues that these priorities have not been taken into consideration by AI developments.
To back up this argument, the authors worked around major scientific evidence available till 2021 and the main areas of development devised by Artificial Intelligence applied to healthcare. Thus, evidence suggests that AI contributions have adopted a clear focus on hospitals and independent living at home complemented with a focus on patient tracking and monitoring, classification of activity and broad care coordination. Additionally, published research on AI shows that a major topic in the past ten years has been image and signal processing and machine learning (ML) systems.
In this sense, while exploring contributions of AI to patient care, evidence suggests a focus on patient fall detection as well as predicting and classifying pressure ulcers (on a rare emphasis on specific healthcare management issues).
In short, the article puts in contrast the evolution between 2011 and 2021 and argues that the gap between the proposed priorities for the improvement of healthcare management and the actual developments of AI applications is quite clear.
The evidence explored in the article raises important questions for the international debate:
• Where are the AI applications to support the evolution from staff satisfaction to staff retention? Namely, AI solutions that contribute to revising workload, balance hours of work aimed at enhancing group cohesion and social support?
• How has AI contributed to developing the practice and quality of healthcare care, through the support and access to sources of evidence-basedpractice or more efficient knowledge transfer to improve clinical supervision?
• How have AI applications contributed to the advancement of
competencies on financial budgetary and management control for healthcare value; and accountable care?
The article does not deny the value and interest of AI applications for healthcare care. It has, however, identified a set of gaps that needs to be discussed internationally.
Additionally, a further critical problem signalled in the article concerns the limitations of the clinical storage systems, noise removal methods and multi-disease prediction models, these being related to innovation system performance.
Overall, the article contributes to the international debate on research priorities for health systems and the application of innovative solutions namely those stemming from technological developments. A closer relation between commercial developers and all professions involved in healthcare management is fundamental.
References are available at www.asianhhm.com
47 www.asianhhm.com
INFORMATION TECHNOLOGY
PAULO MOREIRA holds a Ph.D. from the Faculty of Biology, Medicine and Health (ex-HSMU) at the University of Manchester, UK and currently the Editor-in-Chief of the International Healthcare Review. He is the Founding Editor-in-Chief or the International Journal of Healthcare Management (2007 -2021), based in Oxford, UK and currently published by Taylor & Francis.
AUTHOR BIO
Virtual Reality (VR) Tools for Autism Spectrum Disorder (ASD)
Autism or autistic spectrum disorder (ASD) is a neurodevelopmental condition (affecting nearly 1 per cent of the population) characterised by core differences in social communication, interaction and repetitive behaviours across a variety of contexts (American Psychological Association, 2013). Virtual Reality (VR) includes some interactive video gaming, virtual environments, and, commonly, a multisensory experience. Virtual reality (VR) technologies can provide authentic ‘real world’ contexts that target social and life skills training in safe, controllable and repeatable virtual environments. This article presents some recent work in the development of VR tools for the education of autistic children in Shanghai, China.
Lei Fan1, Guangtao Zhai1 and Pradeep Ray2,3
1 School of Electronics, Information and Electrical Engineering, Shanghai Jiao Tong University,
2 University of Michigan-Shanghai Jiao Tong University Joint Institute
3 School of Population Health, UNSW Medicine and Health
“Autism spectrum disorder (ASD), hereafter referred to as Autism (which includes Asperger’s Disorder and Pervasive Developmental Disorder — not Otherwise Specified [PDD-NOS]), is a complex, lifelong developmental condition that typically appears during early childhood and can impact a person’s social skills, communication, relationships, and self-regulation. The autism experience is different for different ASD affected people. It is defined by a certain set of behaviours and is often referred to as a “spectrum condition” that affects people differently and to varying degrees.”1
1 Autism Society, see https://autismsociety.org/the-autism-experience/, accessed Jan 2022
Virtual reality (VR) is defined as “an artificial environment which is experienced through sensory stimuli (such as sights and sounds) provided by a computer and in which one’s actions partially determine what happens in the environment”1 VR uses many different technologies: monoscopic or stereoscopic displays, user tracking technologies, augmented reality (AR) to merge real and virtual worlds, etc.
VR has emerged as an effective new treatment approach in different areas of the health field, such as rehabilitation, promotion of emotional wellbeing in inpatients, diagnosis, surgery training and mental health treatment. With regard to mental health treatment, VR is used in the treatment of a wide range of disorders: Phobias, post-traumatic stress disorders, obsessive-compulsive disorders, and, of course, ASD. Specifically, in this intervention area, VR has shown some advantages, allowing ASD patients to be trained in a realistic environment that could be manipulated and adapted to the characteristics and capabilities of the subject .2
1 Merriam-Webster. Available online: https://www. merriam-webster.com/dictionary/virtual%20reality (accessed on 20 February 2018).
2 P. Mesa-Gresa et al.,Effectiveness of Virtual Reality for Children and Adolescents with Autism Spectrum Disorder:
48 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
INFORMATION TECHNOLOGY
AR is a technology where digital information (images, audio, text) is superimposed on the real world, either with mobile devices or headsets and glasses. AR is emerging as a promising technology to help those with ASD understand the world more fully by bridging the physical and digital worlds. AR can encourage play and improve language, communication, emotion identification, and vocabulary. Results also indicate benefits like increased motivation, attention, and the learning of new tasks.
This article presents the work led by Prof Guangtao Zhai at Shanghai Jiao Tong University, China on the development and assessment of VR tools (apps) for the education of autistic children. The article starts with the characterisation of VR in three dimensions, namely interaction, immersion and imagination to address
An Evidence-Based Systematic Review, Sensors 2018, 18(8), 2486; https://doi.org/10.3390/s18082486

the ASD triad of communication, interaction and imagination. This is followed by a historical roadmap of VR (superimposed with that of ASD treatment) and a simple conceptual model based on four stages (acceptance, cognition, social, merge) to help guide the development of VR tools. Finally, the article provides a simple example of how
to teach an autistic child the idea of safe road crossing, using VR means involving cartoon and robotic characters to attract the attention of autistic children. This is followed by a summary of the test results.

1. Three dimensions of VR superimposed with the ASD Triad The interactive three-dimensional

49 www.asianhhm.com
Interaction Immersion Imagination
Interaction Communication Imagination ASD INFORMATION TECHNOLOGY
Figure 1: Three I's components of VR & ASD triangle
Three I's of VR
interface of the virtual world allows users to directly participate in and explore the role and changes of simulated objects in their environment, creating a sense of immersion, and then gaining freedom of thinking and imagination. Regarding the basic characteristics of virtual reality technology, American scientists Grigore Burdea and Philippe Coiffet proposed the three most prominent characteristics of virtual reality at the 1993 World Electronic Conference: interactivity, immersion, and imagination3, which is the 3I characteristics of virtual reality. This kind of virtual world is generated by a computer and can be a reproduction of the real world or a conceived world. The user can use various sensing channels such as vision, hearing and touch to communicate with the virtual world. (Figure 1)
ASD triangle of lack of communication, interaction and imagination (in the middle) just matches Virtual Reality's Three I dimensions: interactivity, immersion and imagination4 (Figure 1). This strong correlation above led to the idea to apply VR tech on the applications of ASD early
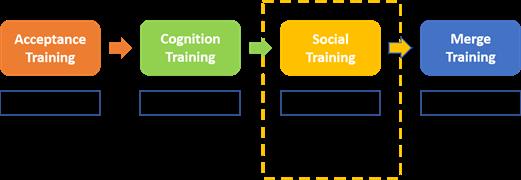
3 P. Richard, G. Burdea, and P. Coiffet, “Performances Humaines dans des Taches Impliquant des Objets Virtuells avec Retour d'Effort,” Interface to Real and Virtual Worlds Conference, pp. 229-238, Montpellier, France, March, 1993.
4 A. P. Association, “Diagnostic and statistical manual of mental disorders (DSM-IV®),” American Psychiatric Pub, 1994.
Traditionally Difficult to achieve Difficult to generalise
training and the R & D on this direction in recent years by Prof. Guangtao Zhai.
The world interacts naturally. INTERACTIVITY refers to the interaction between participants and the virtual environment in a natural way. Users can interact with dedicated interactive devices (such as HMDs, handle controllers, data gloves, position
The interactive threedimensional interface of the virtual world allows users to directly participate in and explore the role and changes of simulated objects in their environment, creating a sense of immersion, and then gaining freedom of thinking and imagination. ASD triangle of lack of communication, interaction and imagination just matches Virtual Reality's Three I dimensions: interactivity, immersion and imagination.
trackers and other sensing devices). The HMD is a display device that provides users with a sense of visual immersion. The handle controller and data glove are the main input devices for virtual reality applications. It is used as a virtual hand or control to simulate interaction in a VR scene.
IMMERSION refers to the degree of reality that users feel as a subject in a virtual environment, and is a direct measure of the performance of a VR system. The main reasons for the user's immersion are as follows: multiperception, the ideal virtual reality should have a variety of visual-based perception functions that humans have; autonomy, the objects in the virtual environment are made according to the laws of physics. Feedback that corresponds to the subject's actions. In addition, the factors that affect immersion include image quality, depth information, field of view, and time delay.
IMAGINATION means that in a virtual environment, users can use various information acquired and their own behaviour in the system, through thought processes such as association, reasoning, and logical judgment, as the operating state of the system changes to affect the future of system movement. Imagine progress in order to acquire more knowledge and understand the deep-level movement mechanisms and regularities of complex systems. With the improvement of related technologies
50 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
INFORMATION TECHNOLOGY
in the virtual reality industry, the capital-driven industry's explosive point is approaching. Some supporting technologies required by virtual reality itself have gradually matured, and the user experience created has begun to gradually reach a level accepted by the public and consumers.
2. Four stage model (acceptance, cognition, social and merge) to develop VR tools for ASD (Figure 2)
As a large proportion of children with ASD are afraid of hair-washing, haircut, braiding and other different levels of head contact sensitivity, guiding children to accept VR helmets is the key to the following social training. The problem of contact sensitivity in
a high proportion of children with ASD has become the biggest obstacle restricting the application of VR technology to ASD research, diagnosis and treatment. After experiments and discussions over 3 months in early 2017, the process of reducing children's insecurity and attracting children to participate in VR training voluntarily has come into being. The overall procedure of the VRASD training includes 4 steps (Figure 2), resolving ASD child’s acceptance of the training interface and system, cognition basis for social contact, social experience and skill training, and merge training for further training in next stage5.
ACCEPTANCE TRAINING: The most important assumption in this stage is the understanding and supporting from the parents, who manage to understand that the key of VRASD startup is ASD children’s free will during VRASD training. We have to wait for ASD children’s interest in VRASD app from inside other than forced by outside. This gains them the sense of security, willing to the steps following. And the performance assessment in this step could well percept the style and speed of the 3 steps of training later6
COGNITION TRAINING: As the basis of social training, cognition training provides the ASD children with the elements of objects, relationships between objects, the procedure how we operate them, which as the raw materials for information assimilation and integration later.
SOCIAL TRAINING: After the preparation in the previous 2 steps, social training could be much smoother than
5 P. T. Shattuck et al., "Timing of Identification Among Children With an Autism Spectrum Disorder: Findings From a Population-Based Surveillance Study," Journal of the American Academy of Child Adolescent Psychiatry, vol. 48, no. 5, pp. 474-483, 2009.
11%
26%
63%
ever, otherwise this key stage would be full of masses of blackbox without resolution and internal details to the ASD children. All the elements during cognition training are integrated in different scenes in a virtual large shopping-mall (Figure 3) for case study and training. VR could provide practices with quality wellcontrolled in low cost7

51 www.asianhhm.com
Reject
Figure 3: Scenes integrated in a virtual large shopping-mall
Reject Accept Unstable
Figure 4: Acceptance rate by 355 ASD kids in age 5-8 at the first 3-time trainings
6 H. Duan, G. Zhai, X. Min, Y. Fang, Z. Che, X. Yang, C. Zhi, H. Yang, and N. Liu, “Learning to Predict where the Children with ASD Look”. IEEE International Conference on Image Processing (ICIP). 704–708, Athens, Greece, 2018.
INFORMATION TECHNOLOGY
7 A. P. Association, “Diagnostic and statistical manual of mental disorders (DSM-5®),” American Psychiatric Pub, 2013.
Lei Fan is a researcher in the ASD lab led by Prof Guangtao Zhai in Shanghai Jiao Tong University. His research mainly focuses on VR applications for Autism Spectrum Disorder (ASD). He has been directly involved in the development of VR systems for education of children with ASD in Shanghai.





Guangtao Zhai is a Professor of Electronics Engineering at Shanghai Jiao Tong University, China. His research interests are theories and applications of perceptual signal processing. He has published over 500 research papers. He has received 7 best paper awards of international conferences and journals, including the IEEE Multimedia Prize Paper Award.
Pradeep Ray is an Honorary Professor and Founder of the WHO Collaborating Centre on eHealth at the UNSW Medicine and Health (University of New South Wales, Australia). He founded the Centre for Entrepreneurship at the University of Michigan-SJTU Joint Institute-China. Pradeep is particularly interested in the role of entrepreneurship in healthcare, leading to three recent books; Technology Entrepreneurship and Sustainable Development (Springer Nature-Singapore 2022), Digital Methods and Tools for Healthy Ageing (IET Press-UK 2021) and Mobile Technologies for Delivering Healthcare in Remote, Rural or Developing Regions (IET Press-UK 2020).
MERGE TRAINING. Merge means the ability of independence, and reliable relationship with others. Therefore, as the last step for this VR training system, VR would show its great advantages on feedback processing and progress assessing, and as the final target to encourage the ASD children with the will and courage to leave VR for more active interactions with real people in the real world. (Figure 3 & 4)
During the software development test with ASD children, we created this operation procedure to help about 89 per cent of ASD children accept VR HMD device within 3-time trainings. In the practical operation, if the child hesitates or withdraws before accepting the VR headset, it is helpful to give the child the "right to refuse".
In the large virtual shopping-mall, VRASD integrates 10 grades of scenes with space large enough for indoor navigation training and performance assessment. And the 5-7 levels in each grade provide totally 55 levels to locate ASD child's status and dynamic progress by time. Different scenes emphasis on different aspects, while the scene of crossing road in the last scene of Hello Home is used for exit mechanics after the core mechanics of all the other trainings, which is unique from most of ASD training app around
52 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
AUTHOR BIO
Figure 5: Grade 10, Hello Home, scene for exit mechanics
3. Safe Road Crossing Example with description, Screenshots and Test results.
INFORMATION TECHNOLOGY
the world. It mainly covers the abilities of reaction in middle level, locating in the urban street, outsides the shopping mall with the movement mechanism of portal (Figure 5). As the last scene, an exit mechanism is applied to reduce the challenge and complexity in this scene greatly from the top challenges in the previous Grade of Find Friend, in order to provide better subjective experience of sense of achievement for ASD children, and encourage them to interact with real people in the real world. (Figure 5)
Here is an interesting example during the experiments: a 5-year-old volunteer ASD child who participated in the experiment had certain language barriers. At the beginning, he could only speak two words. He did not suffer from color blindness, but he could not distinguish colours. He could not use a smart phone or iPad, or complete tasks such as reading and writing on paper. After 3 times VR-ASD experiments, he accepted it. After 3-6 months of
systematic VR training once a week, the number of words spoken gradually increased to around 10. He learned more words, and learned the corresponding expressions of various colors and shapes through scene experiments, and began to actively request the time of electronic devices such as smart phones and iPad. This project suffered substantially from the COVID-19 pandemic since 2020, as it required continuous training lasting for years for process evaluation.
Considering that most of the children participating in the ASD test are at the age of intellectual development, and the parents and the school also carry out a lot of training and hard work simultaneously, it cannot be taken for granted that VR adjuvant therapy is the only or the main reason leading to similar obvious effects, however, this type of continuous observation of the phenomenon deserve further experiments in the future and analysis will help to discover more rules for ASD training, thereby providing more clues
for the research on the pathogenicity and treatment mechanism of ASD, and then guiding the in-depth research and development of related VR.

4. Conclusion
This article has presented some initial work in the use of VR for children with ASD in China, which is among the few countries with highest number of children with ASD. For example, VR-ASD helps in improving the attention of ASD children in a stepby-step method. So these children can gradually improve their learning like climbing stairs in a ladder.
The encouraging test results may motivate other countries in the world to deploy VR for the education of children with ASD. However, this VR method requires more research with large number of test subjects and more focused experimentation to help specialists in recommending VR based learning to the appropriate group of children with ASD.
53 www.asianhhm.com
INFORMATION TECHNOLOGY
Association between primary or booster COVID-19 mRNA vaccination and Omicron lineage BA.1 SARS-CoV-2 infection in people with a prior SARS-CoV-2 infection: A test-negative case–control analysis?

The benefit of primary and booster vaccination in people who experienced a prior Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection remains unclear. The objective of this study was to estimate the effectiveness of primary (two-dose series) and booster (third dose) mRNA vaccination against Omicron (lineage BA.1) infection among people with a prior documented infection.
Methods and findings
We conducted a test-negative case–control study of reverse transcription PCRs (RT-PCRs) analyzed with the TaqPath (Thermo Fisher Scientific) assay and recorded in the Yale New Haven Health system from November 1, 2021, to April 30, 2022. Overall, 11,307 cases (positive TaqPath analyzed RT-PCRs with S-gene target failure [SGTF]) and 130,041 controls (negative TaqPath analyzed RT-PCRs) were included (median age: cases: 35 years, controls: 39 years). Among cases and controls, 5.9% and 8.1% had a documented prior infection (positive SARS-CoV-2 test record ≥90 days prior to the included test), respectively. We estimated the effectiveness of primary and booster vaccination relative to SGTF-defined Omicron (lineage BA.1) variant infection using a logistic regression adjusted for date of test, age, sex, race/ethnicity, insurance, comorbidities, social venerability index, municipality, and healthcare utilization. The effectiveness of primary vaccination 14 to 149 days after the second dose was 41.0% (95% confidence interval (CI): 14.1% to 59.4%, p 0.006) and 27.1% (95% CI: 18.7% to 34.6%, p < 0.001) for people with and without a documented prior infection, respectively. The effectiveness of booster vaccination (≥14 days after booster dose) was 47.1% (95% CI: 22.4% to 63.9%, p 0.001) and 54.1% (95% CI: 49.2% to 58.4%, p < 0.001) in people with and without a documented prior infection, respectively. To test whether booster vaccination reduced the risk of infection beyond that of the primary series, we compared the odds of infection among boosted (≥14 days after booster dose) and booster-eligible people (≥150 days after second dose). The odds ratio (OR) comparing boosted and booster-eligible people with a documented prior infection was 0.79 (95% CI: 0.54
to 1.16, p 0.222), whereas the OR comparing boosted and booster-eligible people without a documented prior infection was 0.54 (95% CI: 0.49 to 0.59, p < 0.001). This study’s limitations include the risk of residual confounding, the use of data from a single system, and the reliance on TaqPath analyzed RT-PCR results.
Conclusions
In this study, we observed that primary vaccination provided significant but limited protection against Omicron (lineage BA.1) infection among people with and without a documented prior infection. While booster vaccination was associated with additional protection against Omicron BA.1 infection in people without a documented prior infection, it was not found to be associated with additional protection among
30, 2022.
TaqPath COVID-19 (Thermo Fisher Scientific) confirmed SARS-CoV-2 infections among vaccine-eligible individuals. Infections were classified as Omicron (lineage BA.1) based on presence of SGTF. COVID-19, Coronavirus Disease 2019; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2; SGTF, S-gene target failure; YNHH, Yale New Haven Health System.
https://doi.org/10.1371/journal.pmed.1004136.g001
54 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
RESEARCH INSIGHTS
Fig 1. Daily Omicron lineage BA.1 (SGTF) and other variant (non-SGTF) SARS-CoV-2 infections identified during TaqPath testing at the YNHH between November 1, 2021 and April
people with a documented prior infection. These findings support primary vaccination in people regardless of documented prior infection status but suggest that infection history may impact the relative benefit of booster doses.
Author summary
Why was this study done?
• mRNA COVID-19 vaccines provide lower levels of protection against Omicron (BA.1 lineage) infections than previously circulating variants.
• Prior to the emergence of the Omicron variant, primary vaccination (first two mRNA vaccine doses) afforded protection against reinfection among people with prior infections.
• The benefit of primary and booster vaccination against Omicron (BA.1 lineage) infections remains unclear among people with prior infections.
What did the researchers do and find?
• We evaluated the benefit of primary series and booster mRNA vaccine doses against Omicron (BA.1 lineage, defined by S-gene target failure) infection among people with and without documented prior infections.
• We found that primary vaccination was associated with statistically significant but low levels of protection against Omicron (BA.1 lineage) infection among people with and without a documented prior infection.
• Booster vaccination was found to be associated with protection beyond that afforded by the primary series among people without a documented prior infection, but we did not observe a significant increase in protection among people with a documented prior infection.
What do these findings mean?
• Primary vaccination provides limited but significant protection against Omicron (BA.1 lineage) infection regardless of prior infection history.
• The relative benefits of a booster dose may be affected by a person’s history of prior SARSCoV-2 infection.
Citation: Lind ML, Robertson AJ, Silva J, Warner F, Coppi AC, Price N, et al. (2022) Association
Fig 2. Selection of tests for the case–control analysis.
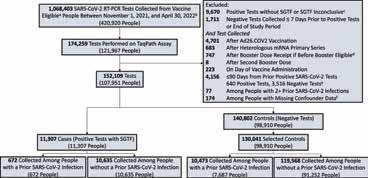
The sample was limited to RT-PCRs run on the TaqPath COVID-19 (Thermo Fisher Scientific) assay among vaccine-eligible individuals. Case status was defined based on the reflex results. We included all positive tests (cases) and up to three negative tests (controls) per person. Cases and controls were stratified by presence of a documented prior infection (a positive RT-PCR or rapid antigen test at least 90 days before the included test). aVaccine eligibility was defined as age ≥5 years. bThe first SGTF defined Omicron (BA.1 lineage) variant infection in the study population was identified on November 11, 2021. cSamples with a positive reflex RT-PCR but that did not meet our SGTF definition (an ORF1ab Ct value of <30 and S-gene Ct–ORF1ab Ct value ≥5; or 2] ORF1ab Ct value <30 and S-gene Ct value ≥40. dExcluded tests that were performed after a person was given a booster dose before FDA authorization or that was given less than 150 days after primary vaccination completion. eThe median time between the 640 dropped positives and the prior positive was 5 days (first-third quartiles: 3 to 7 days). fThere were 134 people with missing SVI data, 40 people with missing sex data and none with missing age data. People were allowed to contribute up to three negative tests to the control sample. If they had more than three negative tests over the study period, three tests were randomly selected. If a person had more than one negative test within a 7-day period, one test performed within that period was randomly selected. COVID-19, Coronavirus Disease 2019; RT-PCR, reverse transcription PCR; SGTF, S-gene target failure.
https://doi.org/10.1371/journal.pmed.1004136.g002
55 www.asianhhm.com
between primary or booster COVID-19 mRNA vaccination and Omicron lineage BA.1 SARS-CoV-2 infection in people with a prior SARS-CoV-2 infection: A test-negative case–control analysis. PLoS Med 19(12): e1004136. https://doi.org/10.1371/journal. pmed.1004136
Academic Editor: Elvin Hsing Geng, Washington University in St Louis School of Medicine, UNITED STATES
Received: May 27, 2022; Accepted: October 26, 2022; Published: December 1, 2022
Copyright: © 2022 Lind et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data used in this analysis cannot be shared publicly because of the presence of potentially identifiable health information. However, to aid in future research, we have provided an aggregated form of the data from which researchers can conduct future analyses. The provided data is aggregated by year of SARS-CoV-2 testing, age (><40 years – mean age in population rounded up), sex, race/ethnicity, Charlson comorbidity score categorized as 0 or 1+, number of non-emergent YNHH encounters in the year prior to vaccine rollout in CT categorized as 0 or 1+, insurance status (insured, uninsured), SVI of zip code (><0.50), and vaccine status at time of testing (received 1 mRNA dose, received 2 mRNA doses, received 3 mRNA doses). The aggregated data along with a data dictionary can be found: https://github.com/lindm89/SUCCESS_ Published.git . Requests for access to the unaggregated data can be directed to the Yale Human Research Protection Program (hrpp@yale.edu).
Funding: Funding for the Studying COVID19 Outcomes after SARS-CoV-2 Infection and Vaccination (SUCCESS) Study was provided by the Beatrice Kleinberg Neuwirth (https://medicine.yale. edu/intmed/medonc/events/neuwirth/) to AIK and the Yale Schools of Public Health and Medicine (https:// ysph.yale.edu/) to AIK and WS. Some of the study results were obtained with the support of a research
grant from the Investigator-Initiated Studies Program of Merck Sharp & Dohme Corp (Title: Harnessing Large Cohorts and a Rapid Knowledge Pipeline to Elucidate Immunity to SARS-CoV-2 Infection; MISP Database No. 60487; https://www.merck.com/) given to AIK and WS. Finally, some of the funding for this study was provided by the Sendas Family Fund to AIK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: I have read the journal’s policy and the authors of this manuscript have the following competing interests: A.I.K serves as an expert panel member for Reckitt Global Hygiene Institute, scientific advisory board member for Revelar Biotherapeutics and a consultant for Tata Medical and Diagnostics and Regeneron Pharmaceuticals, and has received grants from Merck, Regeneron Pharmaceuticals and Tata Medical and Diagnostics for research related to COVID-19. W.L.S. was an investigator for a research agreement, through Yale University, from the Shenzhen Center for Health Information for work to advance intelligent disease prevention and health promotion; collaborates with the National Center for Cardiovascular Diseases in Beijing; is a technical consultant to Hugo Health, a personal health information platform, and co-founder of Refactor Health, an AI-augmented data management platform for healthcare; and has received grants from Merck and Regeneron Pharmaceutical for research related to COVID-19. Other authors declare no conflict of interest. M.O.F had past stock ownership in GlaxoSmithKline. MDTH reports a contract (to the University of Florida) from Merck, Sharp and Dohme to perform research unrelated to this project.
Abbreviations: CI, confidence interval; COVID-19, Coronavirus Disease 2019; EMR, electronic medical record; OR, odds ratio; RT-PCR, reverse transcription PCR; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2; SGTF, S-gene target failure; SVI, social vulnerability index; TNCC, test-negative case–control; YNHH, Yale New Haven Health System
Please use six figures from this link: Association between primary or booster COVID-19 mRNA vaccination and Omicron lineage BA.1 SARS-CoV-2 infection in people with a prior SARS-CoV-2 infection: A test-negative case–control analysis | PLOS Medicine
56 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
RESEARCH INSIGHTS

57 www.asianhhm.com
Table 1. Characteristics of SARS-CoV-2 tests included as cases or controls between November 1, 2021 and April 30, 2022.
Table
Risk of SARS-CoV-2
(BA.1
variant infection among people who received booster vaccination relative to booster-eligible people, according to history of a documented prior SARS-CoV-2 infection.

Table
Risk of
variant infection among people who received booster vaccination relative to booster-eligible peoplea, according to time after receiving a booster vaccine dose.

58 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
2.
Omicron
lineage)
RESEARCH INSIGHTS
3.
SARS-CoV-2 Omicron (BA.1 lineage)
Fig 3. Effectiveness of primary and booster vaccination with COVID-19 mRNA vaccines against SARS-CoV-2 Omicron (BA.1 lineage) variant infections, stratified by the history of a documented prior SARS-CoV-2 infection.
Forest plot depicting vaccine effectiveness against Omicron (lineage BA.1) infections for US-approved mRNA vaccines (BNT162b2 and mRNA-1273) among people with and without a documented prior infection. A documented prior infection was defined as a positive RT-PCR or rapid antigen test at least 90 days before the included test. Omicron (lineage BA.1) infection was defined as the presence of SGTF defined as ORF1ab Ct <30 and S-gene–ORF1ab ≥ 5, or ORF1ab <30 and S-gene ≥ 40. Vaccine effectiveness was estimated as one minus the OR from a model adjusted for date of test, age, sex, race/ethnicity, Charlson comorbidity score, number of nonemergent visits in the year prior to the vaccine rollout in Connecticut, insurance status, municipality, and SVI of residential zip code in all analyses and time between testing and last documented prior infection in analyses of people with a documented prior infection. COVID-19, Coronavirus Disease 2019; OR, odds ratio; RT-PCR, reverse transcription PCR; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2; SGTF, S-gene target failure; SVI, social vulnerability index. https://doi.org/10.1371/journal.pmed.1004136.g003
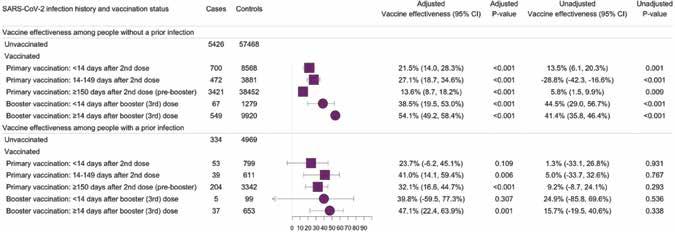
PRODUCTS & SERVICES
59 www.asianhhm.com
COMPANY PAGE NO.
COMPANY PAGE NO. To receive more information on products & services advertised in this issue, please fill up the "Info Request Form" provided with the magazine and fax it. 1.IFC: Inside Front Cover 2.IBC: Inside Back Cover 3.OBC: Outside Back Cover HEALTHCARE MANAGEMENT Hillrom IFC, 30-31 K J Somaiya Institute of Management ......................................... 03, 18-19 DIAGNOSTICS Greiner Bio-One 22-23 TECHNOLOGY, EQUIPMENT & DEVICES Greiner Bio-One 22-23 Hillrom IFC, 30-31 K J Somaiya Institute of Management 03, 20-21 FACILITIES & OPERATIONS MANAGEMENT Greiner Bio-One 22-23 K J Somaiya Institute of Management 03, 18-19 INFORMATION TECHNOLOGY K J Somaiya Institute of Management 03, 18-19 Greiner Bio-One ............................................................................... 22-23 www.gbo.com Hillrom ...................................................................................... IFC, 30-31 www.hillrom.com K J Somaiya Institute of Management 03, 18-19 https://simsr.somaiya.edu/
SUPPLIERS GUIDE
WE ARE ONLINE TOO!
In addition to advertising in AHHM magazine, our clients benefit from cost-effective online options for branding and promotion campaigns through www. asianhhm.com. With large number of visitors and huge database that we built over the years, we help you to devise and execute targeted promotion campaigns.


For more details:
Email: advertise@asianhhm.com
Tel: +91 40 4961 4567
Fax +91 40 4961 4555
www.asianhhm.com
60 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
E-NEWSLETTER
DIRECT MARKETING
BANNER ADVERTISING
STRATEGY
EXCLUSIVE WEBINAR
SERVICES
Hosting Promotions Lead Generation
Engage people to your business Gain Market Confidence Be an Authority
Use the webinar as a platform to launch new products and services
Grow your audience with increased reach, impact and user-friendliness
Rise above geographical boundaries
Generate new business
Gain the strong web presence differentiating yourself from competitors
Connect and engage with your target audience

Give more exposure to industry specific people
Increase your brand profile and share your capabilities with leading industry professionals
61 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023
the true “Digital Transformation” be the base of all your marketing campaigns Email: advertise@asianhhm.com Tel: +91 40 4961 4567 Fax +91 40 4961 4555
UPGRADE
Let
www.asianhhm.com
YOUR MARKETING

62 ASIAN HOSPITAL & HEALTHCARE MANAGEMENT ISSUE - 59, 2023 Introducing Advent of NEW-AGE HEALTHCARE REPORTING From the house of Ochre Media: Automotive-technology.com | Defence-industries.com | Hospitals-management.com | Packaging-labelling.com Pharmaceutical-tech.com | Plantautomation-technology.com | Plastics-technology.com | Pulpandpaper-technology.com Sportsvenue-technology.com | Steel-technology.com | Asianhhm.com | Pharmafocusasia.com Aspiring to be leading journals in the B2B landscape of Healthcare-Industry covering Medical Science, Business & Technology and all the latest innovations. Introducing a group of highly focused magazines for the American and European markets. Poised for bi-annual issuance, our new magazines bring a fresh outlook towards insightful and pragmatic Healthcare-Industry reporting. Scan to check websites Scan to check websites www.ochre-media.com