Artificial intelligence (AI) is set to revolutionize the future of healthcare delivery, promising enhancements in quality, personalized medicine, and potential cost efficiency. However, achieving these benefits requires a transformative approach to hospital health IT, leveraging advanced third-party platforms to fully harness AI's potential.
Traditional IT systems are inadequate for the digital transformation. This transformation is needed to integrate AI tools into healthcare effectively. The future of healthcare demands sophisticated third-party AI deployment and management platforms that enable seamless, cost-effective, and timely integration of AI technologies.
These platforms are crucial for several reasons. They enable optimal selection of AI tools, ensuring that healthcare providers can implement the most effective solutions. Additionally, they form the foundation for adopting more advanced AI tools in the future, while also ensuring robust safety monitoring.
The transformative potential of AI in healthcare is already evident, with a growing number of FDA-cleared or classified medical AI applications, particularly in diagnostic medical imaging and radiology. These tools are set to multiply and evolve in complexity over the next five years, driven by rapid advancements in AI and technology. While the experimental applications of AI in medicine often make headlines, the real challenge lies in overcoming practical adoption and workflow barriers in clinical practice.
Early experiences with AI tools have highlighted significant challenges in timely and seamless integration within clinical settings. As healthcare operations
become increasingly digital and AI-supported, one of the most fundamental challenges will be the efficient deployment and management of a growing array of complex AI tools. This article delves into the limitations of traditional IT approaches and explores the potential of third-party AI deployment and orchestration platforms to support seamless, safe, and effective adoption of AI in healthcare.
We invite you to explore the future of healthcare with us in this edition of American Hospital & Healthcare Management magazine. Join us on a journey where AI turns possibilities into realities, transforming healthcare delivery for future generations. Thank you for being a vital part of the AmericanHHM community. We eagerly anticipate the continued exchange of ideas and knowledge as we navigate the ever-evolving global healthcare landscape together.
If you have a perspective, an idea, or a story to share, we welcome your contributions in our upcoming issues. Whether it's an article on emerging trends, an interview with a thought leader, or a unique insight into the healthcare ecosystem, your wisdom can guide others on their healthcare journey. We want to hear from you via email at editorial@americanhhm.com.
Stay tuned for more in upcoming editions!
N D Vijaya Lakshmi Editor
08 Promising Role of AI in Imaging Opportunities and Transformations
W. Alex Campbell, Division of Vascular and Interventional Radiology, Department of Radiology, University of Virginia
Mina S. Makary, Division of Vascular and Interventional Radiology, Department of Radiology, The Ohio State University Wexner Medical Center
14 Use of Cognitive Enhancers in Patients with Disorders of Consciousness
Benjamin Wai Yue Lo, MD PhD FRCSC, Queen Mary Hospital, Hong Kong Hospital Authority
18 Human Hearts Cannot Swim
Thomas N Muziani, President and CEO of HEMO-STAT Blood Management Consulting
26 Ex Vivo Lung Perfusion- ‘Lungs in a Box’
Anitha Chandrasekhar, Clinical Lead- Lung Bioengineering & Organ Procurement, Northwestern Medicine
34 Vascular Surgery in the Hybrid Age
Jakob Nowotny, Senior Vascular and Endovascular Surgeon, Department of Vascular surgery, Sha'are Tzedek Medical Center

42 The Evolution of Ultrasound Technology and the Rise of Point of Care
Ai Phi Thuy Ho, cardiology Specialist, Hospital Kalnes Trust

REZA FORGHANI MD, PhD, Prof of Radiology & Artificial Intelligence (AI) and Vice Chair of AI, Director, Radiomics & Augmented Intelligence Laboratory
46 A New Era in Patient Care AI Transforms Electronic Health Records Vijay Adapala, EVP & GM Global Supply Partners, Doceree
58 Enhancing Patient Care through Point of Care Ultrasound
Ai Phi Thuy Ho, Cardiology Specialist, Hospital Kalnes Trust











Andrey Andreevich Kapitonov
CEO
Oxygen Technologies LLC Belarus
Aung Pyae Kyaw
Executive Director Asia Royal Hospital Myanmar
Eiman Shafa
Medical Director, Spine Surgery
Abbott Northwestern Hospital USA
Gabe Rijpma
CEO
Aceso Health
New Zealand
James Doulgeris
Chairman
Population Health Advisory Board, RSDSA
United States
Likaa Najuib
Medical Marketing Operational Officer, Alfa Cure Oncology Center
Egypt
Pinheiro Neto Joao
Chief Executive Officer Meu Doutor Angola
Piyanun Yenjit
Managing Director APUK Co.,Ltd Thailand
Thitisak Kitthaweesin
Chief of Phramongkutklao Center of Academic and International Relations Administration, Thailand
Wanita Ramnath
CEO
International Pharmacy and Health Care Suriname
EDITOR
Vijaya Lakshmi N D
EDITORIAL TEAM
Sarah Richards
Debi Jones
Harry Callum
Supraja B R
ART DIRECTOR
M Abdul Hannan
PRODUCT MANAGER
Jeff Kenney
SENIOR PRODUCT ASSOCIATES
John Milton
Peter Thomas
BUSINESS EVENTS
Sussane Vincent
PRODUCT ASSOCIATE
Ethan Wade
CIRCULATION TEAM
Sam Smith
SUBSCRIPTIONS
Vijay Kumar Gaddam
HEAD-OPERATIONS
Sivala VNR

www.americanhhm.com


Congress dates 10 to 12
September 2024 Pre- & postcongress 9 and 13 September 2024
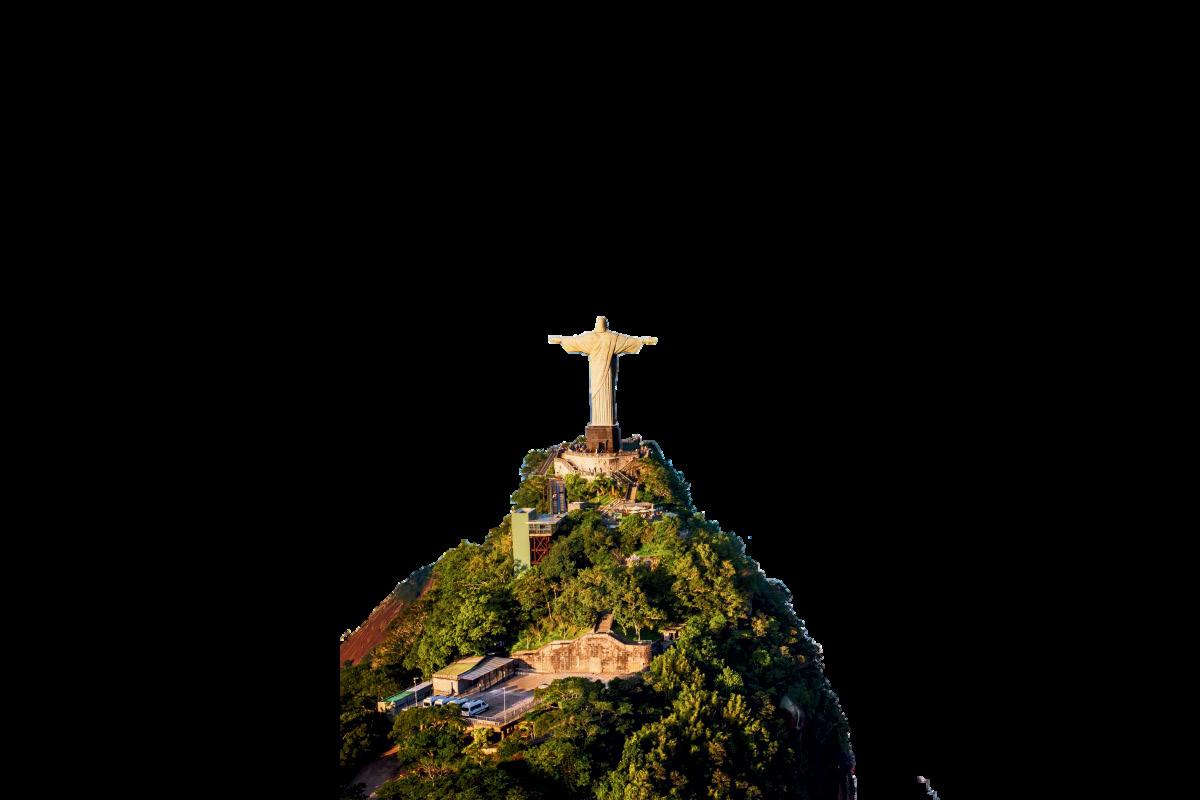




Dates: 10–12 September 2024 (Pre- and postcongress activities on 9 and 13 September)
Location: Windsor Convention & Expo Center, Rio de Janeiro, Brazil
Host: International Hospital Federation (IHF) and Brazilian Hospital Federation (FBH)
Theme: "Global learning, local action"
Overview:
The 47th World Hospital Congress is set to be a landmark event in the healthcare industry, bringing together leaders and decision-makers from hospitals and healthcare organizations worldwide. This year’s congress, hosted in the vibrant city of Rio de Janeiro, will focus on advancing leadership in the healthcare sector to be fit for the future.
Attendees will have the opportunity to:
• Share Knowledge: Gain insights into the latest leadership, management, and service delivery practices.
• Exchange Ideas: Discuss and explore new ideas and innovations in healthcare.
• Network: Connect with senior executives from the international healthcare community, building relationships and exploring collaboration opportunities.
The Scientific Committee has curated an exciting programme featuring:
• Plenary Sessions and Parallel Sessions: Led by industry experts.
• Workshops and Masterclasses: Offering hands-on learning experiences.
• Poster Presentations and the IHF Awards Ceremony: Showcasing cutting-edge research and recognizing excellence.
• i-to-i Innovation Hub: A space for innovative solutions and ideas.
• Industry Exhibition: Highlighting the latest products and services in healthcare.
• Hospital Visits and Networking Events: Facilitating in-depth learning and connections. Live translation services (English to Portuguese and Portuguese to English) will be available during the main Congress sessions.
The Congress offers a range of sponsorship opportunities, including:
• Symposia and Speaking Slots: Present your expertise to a global audience.
• Exhibition Spaces: Showcase your products and services.
• Branding and Digital Engagement: Enhance your organization's visibility.
Established in 1929 and headquartered in Geneva, Switzerland, the IHF is a global notfor-profit organization that supports healthcare leaders through knowledge exchange and networking. The IHF is dedicated to improving the standards, quality, and sustainability of healthcare services.
Don’t miss this unique opportunity to engage with healthcare leaders from around the world, gain insights into the latest trends, and showcase your solutions to a global audience.
W. Alex Campbell
Division of Vascular and Interventional
Radiology,
Department of Radiology, University of Virginia
Mina S. Makary
Division of Vascular and Interventional Radiology, Department of Radiology, The Ohio State University Wexner Medical Center
With the rapid development and innovations in machine learning, Artificial Intelligence (AI) has developed several meanings. While the general perception of the definition means a generalized understanding of a problem or process to be able suggest solutions that formerly required human input or cognition. This is more commonly
Recent advancements Artificial Intelligence (AI) advancements in machine learning have achieved tasks once reserved exclusively for human ability. Radiology is at the forefront of software tools to improve patient diagnosis and treatment of disease, including in AI. Despite initial fears that these more powerful tools will replace the role the radiologists, AI has become the next generation of tools to support a subspecialty under growing demand for increased medical imaging. AI technology--despite its limitations--may still be at the precipice of greater transformative opportunities, but with radiologists in control to potentiate their positive impact in patient care.
referred to as generalized AI. In practice, AI is about pattern recognition, and exposing or “training” an algorithm or network with a data set to be able to detect these patterns when introduced to novel data.
AI in radiology is no exception. The initial research implementing AI was on nodule detection in mammography to identify areas that represent a higher probability of
malignancy. The first FDA approved cloud based deep learning software tool for MR cardiovascular imaging in 2016. This decade is defined by an explosion of AI tools with the promise of exponential improvements in speed and performance with the potential to revolutionize radiology or even eliminate the need for the field entirely. Radiology was not the only specialty at risk of being replaced, as IBM’s AI Watson Health, having proven its language processing skills beating the world’s best jeopardy player in 2011, was showing promise in complex treatment recommendations in oncology to make individualized treatment plans at Memorial Sloan Kettering Cancer Center. Prominent computer scientist Geoffrey Hinton known for his contributions to neural networks once said,
“I think if you work as a radiologist, you are like the Wilie E Coyote in the cartoon. You are already over the edge of the cliff, but you have not looked down yet. There is no ground underneath. People should stop training as radiologists now. It’s just completely obvious that in five years, deep learning is going to do better than radiologists.”
This was said in November of 2016 at a “machine learning and Market for Intelligence seminar.” This warning was so powerful some
believe it partially contributed to the reduced training of radiologists for several years. Despite the AI hype, we still have human doctors and radiologists who are increasingly needed in the modern healthcare landscape. However, this does not mean Hinton’s predictions on radiology are principally incorrect, rather premature, and overstated. Transformer machine learning networks can perform better at more tasks than ever before. While the distant future of this technology in radiology is challenging to predict, over the next few years AI will offer exciting opportunities for radiologists to make transformative changes on how modern radiology is performed.
Machine learning tools have shown impressive capabilities in the fields of literature, education, interpretation, art, and data summarization. The initial challenge is the acquisition of training data containing sufficient imaging pathology for new pattern recognition. The data is manually curated to prevent exposure to poor quality data to reduce bias. The most expensive step is training the neural network to refine the prior correlation. Even if all this is done successfully, it must perform at a level that provides utility to the radiologist. Without effortless PACs integration and high sensitivity and specificity, the tools will go unused. The improvement process is not easy because the network nodes are a “black box,” and simple node modulations will not provide the desired

effect. Lastly, healthcare policy lags behind these technologies, further slowing down their implementation. The ethical implications and legal repercussions of AI-driven errors limits providers and companies willing to take on the risks with a lack of clear standards and precedents. Radiological AI progress is slower than anticipated, but steadily becoming more prevalent in radiological practice every year. AI now elicits excitement for how the role of the radiologist will transform throughout the years.
Current AI tools provide radiologist assistance in detection, surveillance, and workflow. Imaging tools are widely available in every
hospital system and are instrumental in numerous treatment and diagnostic evaluation algorithms. Furthermore, the accessibility of volumetric imaging studies has made their implementation more pervasive. As a result, the number of images per case continues to rise every year and increasing volume throughput demands of the available radiologist workforce. AI tools serve an immediate beneficial role as an additional auditor to reduce diagnostic errors and report variability.
The use of AI for interpretive assistance is present today, with the largest proportion of approved algorithms focusing on breast, lung, neurological, and musculoskeletal image interpretation. Breast and lung imaging focus on malignant detection and characterization from various imaging modalities, where neurological algorithms and MSK detect not only concerning masses but also other pathology such as hemorrhage and fractures. Their utility only exists as an aid, as radiologists are on average more sensitive and specific than the AI tool, but offer the most benefit to more junior and trainee radiologists.
Despite impressive computer vision for image interpretation, many are excited to automate the mundane task of protocolling studies. While Watson wasn’t the healthcare moonshot, its pattern detection has the potential to dynamically protocol studies to physician preference. While the correct study is context dependent, the limited number of potential protocol options helps improve the chances of successfully being first line. Furthermore,
AI may reduce the burden of documentation. Several institutions implement documentation templates to standardize reporting and encourage a complete search pattern. AI would take this aid a step further by communicating imaging findings automatically into these templates. These are some of the newest use cases being rolled out at academic medical centers due to the rapid advancement of machine learning to perform natural language processing tasks quickly and effectively.
In addition to improving the speed of work, AI prioritization can improve the quality of the radiologist’s work. AI scan prioritization helps the patient and primary care teams by first reading the scans with the most time sensitive findings. Preliminary screening and pattern recognition of ordering context can help reduce the time before communicating critical imaging findings to the primary team. It can also improve acquisition quality and time, with the approved algorithms that can upscale a lower quality pixelated image. When applied to positron emission tomography, shorter detection times reduces child and adult agitation with similar diagnostic capabilities.
The success of these software-based tools is their hyper focused scope. When targeted at niche tasks, they offer an advantage to the radiologist to generate quality image interpretation with improved efficiency. The nascent AI tools still offer significant potential to transform the field and allow the next generation of radiologists to take the reigns toward a bright future in an integral role of the healthcare team.
Similar to radiological images, image interpretation involves many grey areas requiring clinical correlation. Visualization alone can identify over 20,000 pathological states with over 50,000 causal relations to disease. This degree of variability and evolution of imaging technology changes the standards of practice and are in perpetual state of flux. AI must be similarly flexible, plastic, and responsive to increase the breath of its utility. The European Society of Radiology and the American College of Radiology conducted surveys to evaluate how AI tools are being integrated into clinical practice. The overwhelming majority of clinicians reported that these tools did not improve efficiency, performed inconsistently, and failed to be helpful in most cases. The most cited reason for this failure is that the algorithms are brittle, and crack under evolving clinical conditions and software environment. After training these models are static because of the risk of continuous training integration runs the risk of introducing erroneous and incorrect associations.
The AI machine learning networks, and the associated regulations, must evolve its adaptability standards to refine its capability over time in a way that does not introduce unnecessary risk to patients. The primary issue is that this requires significant manual labor to maintain a ground truth state without injecting any bias into an updated training set.
Integrating large language models, such as ChatGPT, can coordinate routine tasks such as patient referral, scheduling, procedural consent, research enrollment, outpatient monitoring, and follow-up.
The greatest immediate benefits can be quickly realized in non-interpretive tasks for clinic and procedures. Integrating large language models, such as ChatGPT, can coordinate routine tasks such as patient referral, scheduling, procedural consent, research enrollment, outpatient monitoring, and follow-up. This has a disproportionate impact on procedural focused subspecialties such as Interventional Radiology (IR) but can serve similar functions for radiologists in interdisciplinary teams as a consultant.
While interpretive AI functions exist now, it has not reached the envisioned potential of the synthetic radiologist to interpret and report on new images. For this to be achieved, there must be a concurrent ecosystem of AI algorithms to have access to and compare image interpretation. Their training exists in isolation and will become much stronger if able to competitively refine its interpretation
skills against other algorithms and experienced radiologists. Perhaps a public database of old and new radiological images grounded by experienced radiologist interpretation available for AI interpretation and re-evaluation will accelerate the rate at which these networks can read new images as fast and accurately as possible.
AI has captured the imagination of millions to perform tasks once thought impossible without human intervention, and that potential is no greater than in the field of Radiology. The private development of AI tools is fraught with overspeculation, fear mongering, false promises, and failures, but the resurgence of ever more skilled and agile AI software tools continues to fulfil this original promise of revolutionizing the field of radiology.
Current tools provide beneficial widgets to optimize workflow empower the next generation radiologist in an industry acquiring more images per capita than any time in history. The greatest opportunities are yet to come, and envisioning the distant role of this emerging technology is nebulous, the field is on the precipice of the greatest transformative changes to come. Ironically this transformation may actually free radiologists from ever growing tedium and complexity of the current working environment to once again focus on the fundamentals of the subspecialty—applying imaging tools to diagnose and treat disease.

Dr. Makary is a dual board-certified interventional and diagnostic radiologist, and serves as the director of radiology scholarly activity and research, director of the interventional radiology inpatient service, and director of the interventional radiology clerkship at the Ohio State University Wexner Medical Center, Columbus, OH, USA. He is also a prolific research, dedicated educator, and an active leader in the Society of Interventional Radiology and the American College of Radiology.

Dr. Campbell is an MSTP-trained physician with a PhD in the molecular mechanisms of neuroregeneration from The Ohio State University, Columbus, OH, USA. He is currently an Integrated Interventional Radiology resident at the University of Virginia Medical Center, Charlottesville, VA, USA. He has a diverse research background with published and presented works ranging from biophysics, bioengineering, bioinformatics, artificial intelligence, glial biology, and interventional radiology.

This article explores the use of cognitive enhancers in patients with disorders of consciousness. After intracranial injuries, these agents may support neuroplasticity and overall functional recovery. The discussion covers potential mechanisms of these pharmaceutical agents, along with their associated side effects.
Benjamin Wai Yue Lo MD PhD FRCSC, Queen Mary Hospital Hong Kong Hospital Authority
Cognitive enhancers may support neuroplasticity and overall functional recovery. They have been associated with neuronal sprouting, synaptogenesis and long term potentiation. Methylphenidate and modafinil are effective in restoring arousal in those with damaged reticular activating system (thalamus, brainstem) and bilateral hemispheres. Amantadine is effective in restoring arousal in those with lobar injuries, including after cerebrovascular accident, and post traumatic brain injury including diffuse axonal injury.
Of the five major monoaminergic pathways of the brain (dopamine, noradrenaline, adrenaline, sertonin, histamine), the catecholamines (dopamine, noradrenaline, adrenaline) are implicated in the mechanisms of cognitive enhancers. Catecholamines are derived from tyrosine (tyrosine --> dopa --> dopamine --> noradrenaline --> adrenaline).
Many dopaminergic cells are located in the midbrain including substantia nigra, pars compacta and ventral tegmentum. This large ascending projection system, mesotelencephalic dopaminergic system, carries input from the basal ganglia, extended amygdala, reticular formation (mesopontine tegmentum) and raphe nuclei. Fibers in this system traverse the internal capsule to the caudate and putamen to form the nigrostriatal dopamine pathway. Other fibers travel
through the lateral hypothalamus toward the accumbens and basal forebrain including the basolateral amygdala, septal and olfactory areas. Dopaminergic cells involved in neuroendocrine functions are located in the arcuate and periventricular nuclei of the tuberoinfundibular pathways projecting to the median eminence and posterior pituitary.
Noradrenaline is released from postganglionic sympathetic fibers. Noradrenergic fibers arise from the reticular formation especially pontine locus ceruleus and medullary intermediate reticular zone. Other structures containing high levels of noradrenaline include area postrema (medulla), dorsal nucleus of the vagus, solitary and ambiguus nuclei. Ascending noradrenergic fibers reach brainstem and basal forebrain. Locus ceruleus have widespread projections important in the sleep-wake cycle, wakefulness, attention and vigilance.
Cognitive enhancers have been safely used to support early neurorehabilition in those with intracranial injuries
Methylphenidate is a mild CNS stimulant. It inhibits re-uptake of noradrenaline and dopamine into pre-synaptic neurons, increasing monoamine concentrations in the extraneural space. It stimulates both cerebral cortex and subcortical structures, and is associated with increased sympathomimetic activity. Common side effects of methylphenidate may include anxiety, insomnia, GI upset, headache,

tachycardia, hypertension and euphoria. Methylphenidate is contraindicated in those with cardiac arrhythmias, cardiac structural abnormalities, severe hypertension, psychosis and hyperthyroidism.
Amantadine is a weak dopamine agonist with antimuscarinic properties. It is also a weak NDMA receptor antagonist. This medication inhibits presynaptic reuptake of catecholamines and increases dopamine release. Amantadine has been used in the treatment of Parkinson's disease, and also inhibits replication of influenza A virus. Common side effects of amantadine may include anxiety, agitation, orthostasis, hallucinations and breakthrough seizures. This agent is contraindicated in those with gastric ulceration, refractory epilepsy, severe renal impairment and lactation.
Memantine is a derivative of amantadine. It is
an NMDA receptor antagonist with potential inhibitory effects on excitotoxic cascades in secondary injury, NMDA-mediated calcium entry into neurons leading to cellular death. Memantine is a neuroprotective agent that also blocks the action of glutamate as a glutamate receptor antagonist. Glutamate may result in excitotoxicity and neuronal cell death, particularly in Alzheimer's disease. This agent has been used to treat moderate to severe Alzheimer's dementia. Common side effects of memantine may include headaches, dizziness, hypertension and impaired balance. This agent is used with caution in those with epilepsy disorder.
Modafinil is a central stimulant with wakefulness promoting effects that selectively inhibits the reuptake of dopamine and noradrenaline. This agent has been associated with stimulation of alpha nonadrenergic receptors, reduced GABA
release, increased glutamate or histamine release, as well as altered hypocretin activity. Common side effects of modafinil may include anxiety, headaches and nausea. This agent is contraindicated in those with uncontrolled hypertension, cardiac arrhythmias, mitral valve prolapse, cor pulmonale and pregnancy.
Piracetam is a nootropic cognitive enhancer that acts by improving blood flow, oxygen delivery and glucose utilization in the brain. This medication is a GABAergic agent that restores membrane fluidity and increases cellular levels of energy ATP. It increases acetylcholine levels in the brain. It has neuroprotective and anticonvulsant properties. It improves blood flow by enhancing red blood cell deformability, decreasing platelet aggregability, reducing capillary vasospasm and erythrocyte adhesion to blood vessel walls. Piracetam may be contraindicated in those with cerebral hemorrhage, Huntington's chorea and severe renal impairment.
Cognitive enhancers have been safely used as single agents or combination therapies to support early neurorehabilition in those with intracranial injuries. They have been associated with increased arousal and decreased number of ventilator dependent days in the neurocritical care unit. They promote overall enhanced neurological recovery.
AUTHOR BIO

Benjamin W Y Lo is a Neurosurgeon and Neuro-ICU specialist. His research focus characterizes brainbody interactions in neurocritical care patients. Dr. Lo’s qualifications include FRCSC certification in neurosurgery (2009), FRCSC certification in critical care medicine (2011), MSc and PhD degrees in clinical epidemiology and biostatistics from McMaster University, Canada. His clinical experience includes working as a licensed neurosurgeon and neuro-ICU specialist at St. Michael’s Hospital, University of Toronto, Canada, Montreal Neurological Institute & Hospital, McGill University, Canada, Northwell Health Lenox Hill Hospital, Manhattan, New York, and Queen Mary Hospital, Hong Kong Hospital Authority. He is licensed to practise medicine in these locations as well as the United Kingdom.
Gerald Buckberg, Professor Cardiac Surgery at University California Los Angeles was indeed a Renaissance Man. During the latter 1960’s, Dr. Buckberg envisioned a completely different approach in protecting the human heart during Cardiac Surgery. This was due to “Bucky” fully realizing this seldom discussed aspect of Cardiac Surgery that controlled the absolute key to life or death. No matter how adept or accomplished your Surgeon or the surgical procedure might be…if the heart does not resume beating toward the final portion of the procedure…the operation was for naught. Electrical pacing as standard is not considered Best Medicine.
Thomas N Muziani
President and CEO
HEMO-STAT
Blood Management Consulting
Up until World War I operating on the human heart was considered strictly off-limits. As has been selfevident since the dawn of history, the advent of war has demanded surgeons, nurses and staff become extremely creative. A spear, arrow, grenade or gunshot wound to the heart demanded at least an attempt at repair. The glorious nature of the military is…you could not be sued. Other than strong religious tenets, the conundrum was; In order to repair the Heart, you had to open it. Once opened by literally cracking the sternum (breastplate) apart with an axe and large hammer, the heart was fully exposed to air emboli and the possibility
Prior to this time in history, a cornucopia of techniques were advocated to stop and “protect the heart” to facilitate a repair and or replacement of a valve. Seldom, in the embryonic days, were operations performed on adults. The primary emphasis to accomplish a repair/replacement on the human heart was the necessity of stopping the myocardium completely in order for the Surgeons to perform the necessary operation. Stanford and Dr. Norman Shumway advocated the use of hypothermia for protection. A pericardial well (membrane sack surrounding the heart) was constructed in which ice-cold slush bathed the Heart and Lungs for periods of up to three hours plus. Unfortunately, it was discovered post-operatively that many patients developed atelectasis of the Lungs due to prolonged exposure to extreme cold.
The use of a fibrillator to jolt the heart out of beating regularly became highly popular until it was determined the heart was expending more energy acting like a “bag of worms” than beating in normal sinus rhythm.
UCLA thought completely outside the box. They envisioned Albert Einstein’s “Thought Experiment”; the idea of: “What if”. What if we not only produced quiescence (stilling) of the heart, but were able to protect the myocardium (heart muscle) during this rather traumatic period of literally starving the heart of oxygen and all necessary nutrients to thrive.
Since the earliest days when Man walked this Planet, the human heart has been held in great reverence. The earliest Shaman’s or Priests treated the heart as if it was the person’s spiritual center. On a cool South American evening, when a human sacrifice on your enemy was being carried out… opening the chest would allow the body to emit steam emanating from the heart. This provided a graphic visual to all worshipers attending the person’s essence was literally floating up to the God’s. Removing the heart from your enemy’s body (enucleation) meant you now had complete control of that person’s power.
From Stoicism to the earliest days of Catholicism the word pneuma has held that it was a mixture of air and fire held to be the divine principle of the universe. Early Christians used pneuma to refer to the-Holy Spirit. Pneuma according to ancient Greeks and Romans, was the driving force in the body, necessary for maintaining bodily functions.
of uncontrollable bleeding (exsanguination). Plus, when you are utilizing suture as thin as a human hair, it is almost impossible to operate while the heart is still beating. Lastly but certainly not least; If you got into trouble, and there was a very good chance of that, it was extremely difficult to extricate yourself out of the mess. A non-beating human heart over a period of hours meant a voyage to the entrance of Valhalla.
So, during the ensuing years a myriad of experiments were utilized on sometimes very unsuspecting and unfortunate patients. Everything from spreading Talcum powder all
over on top of the heart believing the abrasive nature of the powder would “re-vascularize” blood flow. To the idea of utilizing a Parent or sibling as a Heart-Lung machine. The parent would provide the circulation necessary to stop the patient’s heart and perform the necessary repair. Unfortunately, the procedure became very well known for all the wrong reasons. It was the one surgical procedure that ran a very high risk of killing two people from one operation. Having a father and son both die under one surgeons’ hand was not well received, and a blemish on a Surgeon he could never wipe clean.
In 1972, Drs’ Hearse and Bainbridge worked non-stop in their animal laboratory in London, England, next to Saint Thomas Hospital, formulating “the ideal cardioplegia”. Their experiments with different cocktails were producing very positive results, the
heart tolerating long period of ischemia (lack of blood supply). The formulation was predicated on the goal of deviating as little as possible from the normal extracellular ionic composition of the body and, in particular, to minimize the amount of potassium that was
A non-beating human heart over a period of hours meant a voyage to the entrance of Valhalla routinely used to ensure rapid and complete arrest.
The discovery of potassium as a “stilling agent” for the heart was a complete accident. The underground water pipes that supplied water for Dr, Hearse’s Laboratory and Saint Thomas Hospital were so foul and polluted, routine boiling was necessary. However, the Labs boiling system broke down one day and, unbeknownst to Dr, Hearse his assistants used the foul city water for their experiments. Suddenly, the animal hearts completely stopped. Upon extensive investigation, it was discovered that heavy amounts of potassium were contained in the putrid city water.
After the introduction of Saint Thomas’ Hospital cardioplegic solution No.1 numerous experimental testings’ continued with a view to improving efficacy. However, one persistent issue remained within the solution that most institutions attempted to minimize, but really had no work-around. Cardioplegia solution is 1000cc’s of crystalloid solution (water.) Compound the issue that many times a mechanical problem would occur (i.e. Aortic insufficiency, cross clamp not applied completely, open cardioplegia line) causing the heart to not stop. The frustrated surgeon would demand more potassium equaling more water, but the heart would continue to beat. Once the correction was made, the potassium would be way too high and the heart would be so swollen from the water infused. So much so, you could not close
the chest. The patient would have to go to Intensive Care Unit with a “wound towel” over his/her open chest. Nothing quite like the visual of a family member in ICU with a tube down their throat watching their wide open chest, their heart beating and lungs inflating/ deflating to cause constant nightmares. And this was not uncommon.
Now, you would think we could not make this visual any more frightening for family or patient. Well, we could and we did:
In the very early days (1950’s-1970’s) of “complex surgery” (craniotomies, cardiac surgery etc.) Intensive Care Units were nothing more than a glorified Recovery Room with more equipment. Patients were separated by nothing more than a pull drape. Therefore, when a patient went into cardiac arrest, which was quite often, fifteen to twenty people would show up…someone pumping on the patient’s chest, someone sticking a
tube down their throat to breathe…the yelling for drugs or where’s the Lab work? Then here is your father or mother in the next bed visualizing this Horror Show…panicking: “Is THAT going to happen to me??”
Gerald Buckberg knew there were many merits to the Saint Thomas’ Hospital Cardioplegia. He also witnessed the drawbacks. He became aware that by applying some very novel concepts, he would create a solution that could be utilized under all circumstances for three plus hours. He wanted to add blood to his cardioplegia to cut down on all the crystalloid solution. He wanted his solution to be administered not just once but during the entire time the cross clamp was applied. A collective decision was made to initially deliver the solution cold. Then his team discovered the marvelous benefit of warm delivery during induction and reanimation. Cold solution creates immediate
vasoconstriction, a primordial response to preserve life when encountering extreme cold. However, obvious logic dictates when you are confronted with a patient with severe coronary artery disease, you do not want to administer an extremely cold solution to still the beating heart. The heart is clamped down already from year’s long coronary artery disease. Attempting to reach the myocyte is virtually impossible with an 8°C solution. Plus, extreme cold has been documented to trigger atelectasis of the lungs if exposed to cold for two hours or more.
All of this effort was basically for one purpose; to prevent the onset of ischemia. Cardiac ischemia is analogous to dropping a pebble in a pond. It begins in one small area and travels out to all areas rather quickly. The onset can be rather quick or slow. No Lab experiment has yet to ascertain exactly when ischemia begins. Some patients at 10 minutes. Some patients at 1 hour. This was precisely why Dr. Buckberg believed reinfusion of cardioplegia should occur every 10 to 20 minutes.
Cardiac ischemia is analogous to dropping a pebble in a pond. It begins in one small area and travels out to all areas rather quickly.
We would joke the concept’s basic premise was to “Fool the Heart”.
In essence; “fooling the heart down to the myocyte” thinking nothing strange is happening. This was a Herculean task. In the dog lab at UCLA in Westwood, California, extensive testing had to be developed to ascertain exactly what triggered ischemia (lack of blood supply due to vasoconstriction). Vasoconstriction is an odd duck. A myriad
1970's – Major outbreak († 100's) septicemia from contaminated intravenous (IV) products
1984 – 11 patients received Pharmacy-prepared cardioplegia with Enterobacter cloacae - resulting in 5 deaths.
1990-2005 – 12 incidents contaminated Pharmacy-prepared sterile compounds nationally; involving >19,000 patients with 15 deaths
2012 – New England Compounding Center contaminated solution with over 800 cases fungal meningitis and 76 deaths
2013 – New England Compounding incident motivated Congress to change non-traditional compounding laws forever. FDA mandated the "Drug Quality and Security Act" on 13 Nov. 2013.
of issues will trigger it. From extreme cold, drugs, lower blood volume, shock and poor circulation. This is due to the fact it is front line defense to Preservation of Life. A primordial response to those myriad events in the effort for the animal to remain alive. Hypovolemia (lack of blood volume) is very common in the animal kingdom. Early HomoSapiens witnessed this first-hand and realized they would have to address this issue or die. As a result, UCLA produced a “Sea Change” of ideas on how best to protect the human heart from the insult of being stopped for the first time in this individual’s life. Normally this would mean “Enter Priest Stage Right”. UCLA had better ideas. Some would say magical. They threw the conventional wisdom of myocardial protection; primarily
a crystalloid cocktail with extreme cold… out the proverbial window.
1. Crystalloid no longer plays primary role. 2. Cardioplegia will hence be delivered as a ratio. Starting with 4:1. Four parts patients own blood and one part crystalloid. This would radically reduce hemodilution. Eventually, after extensive empirical utilization, the ratio was changed to 8:1.
3. Cardioplegia would be delivered Cold. The general consensus at the time was: “the colder the better”.
When Dr. Philippe Menasché, MD, PhD, Chief of Cardiovascular Surgery, Hôpital Lariboisière, Paris, France and his
In essence providing more oxygen to the myocardium than the heart is presently demanding. Now, you can tailor the exact amount of potassium and supporting drugs to the patient’s particular needs.
students dissected the overall structure of “Buckberg Solution” it became obvious they could create a simpler and equally, if not more, effective means for delivering warm blood cardioplegia. They accomplished this by utilizing pure patients’ blood, diverted from the arterial port of the Heart-Lung machine’s port on the oxygenator and only supplemented with arresting agents (undiluted potassium) and additives (magnesium). Dr. Menasché and his students called this solution “mini-cardioplegia” due to these arresting agents are concentrated in very small volumes continually replenished to the blood cardioplegia circuitry utilizing an electrically driven syringe pump. Initially the flow rate of the syringe pump was determined empirically. Subsequentially, a nomogram was developed that, based on the target potassium concentration (20mmol/L for induction, 10mmol/L for maintenance), the patient’s
pre-bypass serum potassium level, and the flow rate of the cardioplegia delivery pump, allowed an accurate determinization of the flow rate for the cardioplegia delivery pump. The flow rate on the cardioplegia pump was adjusted either up or down based on the heart remaining quiescent. If electromechanical activity resumed the syringe pumps could be easily adjusted.
“The magical power of Aerobic Arrest versus Ischemic Arrest”
Mini-cardioplegia, or as this author has discovered preferential “microplegia” technique provides for the creation of an aerobic environment. This is accomplished by the simple means of increasing oxygen supply. In essence providing more oxygen to the myocardium than the heart is presently demanding. Now, you can “tailor” the exact amount of potassium and supporting drugs to the patient’s particular needs. The years of “one size fits all” cardioplegia are effectively over. Utilizing the syringe pump to administer potassium and additives is preferential for several reasons:
1. All Hospitals have an abundance of syringe pumps
2. Extremely easy to switch out in case of malfunction
3. All syringe pumps have batteries for back-up power
4. May be utilized anywhere on this Planet
5. Extremely cost-effective and easily replaced
6. Very simple to operate and teach usage in 30 minutes.
Utilizing microplegia with the capacity to provide “on the fly” adjustment according to your patients’ needs totally avoids detrimental consequences of;
• Volume overload
• Over hemodilution
• Vasodilation, commonly associated with warm systemic perfusion
• Unintended high potassium’s
• Negate the need for ancillary drugs to mitigate high K+’s (Insulin)
• Overhead costs for disposables are minimal; 50cc syringe and syringe tubing.
Since the introduction of warm blood cardioplegia, despite the misperceptions and ongoing controversy regarding cold versus warm, there has been a slow but steady understanding that warm induction, cold maintenance and warm reanimation of cardioplegic solution holds a key to full restoration of normal sinus rhythm.
It has now become commonplace for many institutions to routinely begin warming the cardioplegia when approaching the last graft. The last dose may include warm cardioplegia or, as many institutions have discovered, just warm patients’ blood infused antegrade to start…then switch to retrograde and, if possible, flow the warm blood down all grafts. This will provide global protection while suffusing the myocardium with an aerobic environment facilitating an accelerated restoration back into normal sinus rhythm.
And the only issue it cost…is pride. I assure you; Monitor your patients in Intensive Care for one month. Witness how they respond. And then please provide me your thoughts.
Thomas Muziani began his career in medicine in 1968. In 1970 he entered military service with the United States Army, attending Physician’s Assistant training in 1974. Mr. Muziani is the author of: “The Utah Protocol”, a syllabus for providing micro-doses of cardioplegia for extremely ill adults. The protocol has been utilized in over 100,000 patients. Mr. Muziani is the author on a continuing series entitled: “Standing on Tall Shoulders; The History of Cardiac Surgery”.
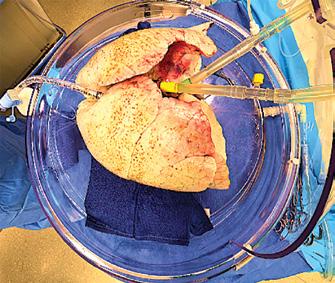
Lung transplantation has been established as the procedure of choice for end-stage lung disease patients with good survival benefits. However, the procedure is generally limited by the scarce availability of good-quality donor lungs. Ex vivo lung perfusion (EVLP) was developed to widen the pool of lung donors. This innovative technique provides the opportunity for extended assessment and the potential reconditioning of sub-optimal donor lungs.
Anitha Chandrasekhar
Clinical Lead- Lung Bioengineering & Organ Procurement, Northwestern Medicine
The most effective therapy for patients with end-stage disease is organ transplantation. Lung organ procurement rates from deceased donors for transplantation are significantly lower than those for other solid organs. This low rate is likely due to potential complications that may arise before or after brain death in the donor. These complications include aspiration, thoracic trauma, ventilator-associated barotrauma injury, ventilator-associated pneumonia, and

neurogenic pulmonary edema. This results in a shortage of donor lungs leading to a 20% mortality in the lung transplant waiting list. Multiple methods are used to expand the donor pool with the use of extended criteria donors, donation after cardiac death (DCD), aggressive use of Extracorporeal Membrane Oxygenation (ECMO) post-transplantation for marginal lungs, lobar lung transplantations for small thoracic cavity patients, and the use of EVLP. EVLP is a groundbreaking therapy used to treat donor lungs outside the body (ex vivo) prior to transplantation. This process boosts organ quality and transforms previously unsuitable lungs into viable options for transplant.
The commonly used method for preserving and transporting lungs historically has been static cold storage (SCS). However, several limitations are associated with SCS. These include tissue damage from prolonged hypothermic preservation, challenges in assessing donor organ function and viability, the effects of ischemia-reperfusion injury (IRI), and limited opportunities for organ repair. EVLP not only serves as a great assessment tool but also enables graft repair, reconditioning, and immunomodulation. EVLP is transforming the landscape of lung transplantation through its ever-expanding applications by improving the transplantability of marginal donor lungs, prolongation of preservation, reconditioning of unsuitable lungs using therapeutics for the treatment of pulmonary emboli, bacterial colonization, pulmonary edema, aspiration injury, and further optimization of suitable lungs like blood group conversion, immunomodulation, virus inactivation, gene therapy, and tissue engineering.
The original method for preserving isolated organs before SCS began in the 1960s was machine perfusion using plasma or bloodbased solutions. Numerous preservation methods were attempted including hyperbaria, hypothermia, and hypothermic pulsatile or non-pulsatile perfusion. Organ preservation was revolutionized with the advent of SCS as scientists hypothesized that lower temperatures
could offer cytoprotection by lowering cellular metabolism. It then became the gold standard for preserving organs at hypothermic temperatures. The earliest concepts underwent numerous modifications and refinements, leading to the current practices of organ perfusion and preservation.
In 1935, Carrel and Lindbergh performed the first normothermic ex vivo organ perfusion by explanting the thyroid glands of cats and rabbits and perfusing them for up to a week. In the 1970s, EVLP was tested in various animal models like mice, rabbits, guinea pigs, dogs, and pigs. Hardesty attempted to study normothermic EVLP in the 1980s clinically but had to abandon it due to suboptimal outcomes. Steen et al. revisited EVLP in the mid-1990s to evaluate the transplant suitability of lungs procured from a non-beating heart donor. This trailblazing technique led to the first-in-human lung transplantation from a DCD donor in 2001, following successful evaluation ex vivo. Furthermore, in 2005, the same team went on to perform the first lung transplantation of a marginal lung which was initially rejected and then reconditioned using EVLP. In 2008, Cypel et al. took EVLP a step further and proposed extended EVLP up to 12 hours in a pre-clinical model using a new protocol.
Machine perfusion is an innovative method that optimizes organ condition by circulating a controlled flow of perfusate. This technique significantly enhances organ quality for
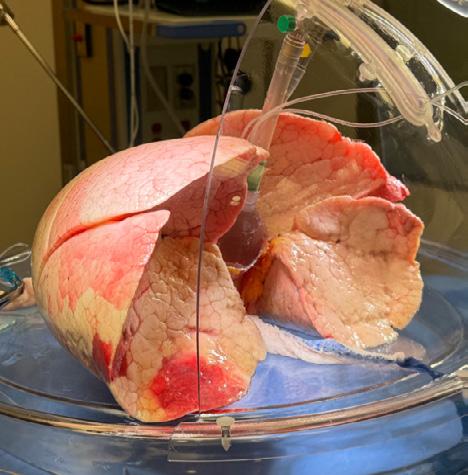
transplantation purposes. It ensures the delivery of oxygen and nutrients to support tissue metabolism and maintains the tone of the microvasculature in the organs while effectively removing toxic metabolic waste. Different temperatures have been explored for ex vivo machine perfusion. These include normothermic machine perfusion at 35–38 °C, sub-normothermic machine perfusion at 20–34 °C, controlled oxygenated rewarming at 8–20 °C, and hypothermic machine perfusion at 0–8 °C. Normothermic machine perfusion maintains the organ at body temperature under physiologic conditions to preserve metabolic activity and viability. (Figure 01)
Currently, there are no set standard guidelines for using EVLP. However, EVLP is commonly considered in cases where the PaO2/FiO2 ratio is ≤300 mmHg, there is an expected long period of ischemia, it involves DCD donors, or there are worrisome findings from bronchoscopic evaluation. Poor lung compliance, atelectasis, pulmonary edema, and pulmonary embolism are suitable lung conditions for EVLP. However, mechanical lung injury with air or blood leak, significant contusion, active infectious disease, major aspiration, and malignancy are contraindicated.
There are currently three EVLP protocols used globally- Lund protocol, Toronto protocol, and Organ Care System Lung. The original protocol is the Lund Protocol from Sweden which was further adapted into the currently widely used Toronto protocol. The third protocol involves the use of a portable device that effectively reduces the cold ischemic time. Currently, there are four commercially available EVLP devices in the US that use one of the three standard protocols or a hybrid of them. These devices are Lung Assist™ by Organ Assist®, XVIVO Perfusion System (XPS) ™ by XVIVO®(Figure 02), XVIVO LS™ by XVIVO®, and OCS™ by TransMedics®. In collaboration with Traferox Technologies Inc., the Toronto team successfully engineered the second generation of the TorEx Lung Perfusion System. This remarkable advancement specifically targets and resolves the engineering design limitations that were inherent in the original Toronto EVLP system. (Figure 02)

During the process of EVLP, the lungs are kept in a warm (37°C) environment, supplied with a cell-free perfusate solution,
and ventilated using a lung-protective ICU-type ventilator. Steen Solution™ is a precisely formulated solution, extensively utilized for EVLP and machine perfusion of various organs. This solution contains colloid components such as human serum albumin and Dextran 40, which help maintain oncotic pressure. Additionally, it includes specific physiological ion concentrations, which collectively play a crucial role in regulating osmolality to maintain fluid balance. Buffers help to stabilize and uphold normal pH levels, ensuring the organ's internal environment remains within the optimal pH range. Furthermore, the presence of glucose in the solution serves as a vital energy source to support various cellular functions and metabolic processes.
The EVLP system comprises various components in an enclosed and controlled unit to accede to the perfusion and respiratory requirements. The fundamental elements of an EVLP circuit consist of a pump, reservoir, perfusion solution, ventilator, oxygenator, endotracheal tube, air filter, and oxygen sensor. Additionally, the package consists of a container of deoxygenating gas, a set of tubing, and cannulae that need to be connected to both the pulmonary artery and the left atrial cuff.
The surgical part of EVLP consists of suturing the left atrial and pulmonary artery cannula (Figure 03), intubating the trachea, and connecting the cannulae to the lines in the XVIVO circuit after dividing and de-airing the tubings.

Lung monitoring currently involves assessing physiological parameters such as gas exchange, compliance, and airway pressure; biochemical factors like glucose, lactate levels, pH, and acid-base balance; imaging techniques such as radiographic images and bronchoscopy; and biological measurements including cytokines and chemokines.
The criteria for determining transplant suitability after EVLP usually include stability of lung function parameters, improvement in P/F ratio to more than 300 mmHg, and satisfactory lung examination. Conversion rates after EVLP have varied from 34% to 96% across studies.
The average overall conversion rate in the United States is 61.8%
Initially, the process of EVLP was limited to a short evaluation period after DCD to determine the suitability of the lungs for transplantation. However, advancements in techniques and technology have made it possible to extend the time for perfusing lungs outside the body, enabling a more thorough and objective assessment of lung quality. This extended evaluation period also allows for interventions to improve the function of the lungs before transplantation.
Different drugs have been delivered through the perfusate to prevent IRI. Inhalational gases (NO, CO, H2) have been used during EVLP to reduce inflammatory response and lung edema. Lung injury because of infection and endotoxins has been treated with mesenchymal stem cells. IL-10 gene therapy has made headway to mitigate IRI. When the specific types of injury are identifiable, utilizing injuryspecific treatments during EVLP can lead to more effective and targeted care. For example, the addition of high-dose, broad-spectrum anti-microbial agents to the perfusate helps to treat donor lung infection. In one study, acid aspiration-induced lung injury in pigs was effectively treated through lung lavage and surfactant replacement. Furthermore, pulmonary thrombolysis can be performed through EVLP to address pulmonary embolism, followed by a successful lung transplantation. (Figure 04)
During EVLP, targeted immunomodulation using RNA-based therapies can be specifically administered to modify the immune response of the donor lungs. This approach aims to reduce the recipient's immune system recognition and sensitization while potentially increasing tolerance markers. As a result, there is potential for a decrease in both acute and chronic rejection, which may lead to a decreased need for long-term immunosuppression.
EVLP has been linked to outstanding short-, mid-, and long-term survival in all studies. Data from retrospective studies conducted at individual institutions and post hoc analyses of clinical trials indicate that there is non-inferior 12-month allograft and patient survival following EVLP when compared to conventional transplantation. Recipients who
receive EVLP lungs experience comparable long-term survival without chronic lung allograft dysfunction (CLAD) when compared to recipients who receive conventional lungs.
EVLP is distinctly suitable for Artificial Intelligence (AI) and Machine Learning (ML) approaches because the ex vivo data is: (i) limited to an isolated organ and free of mixed signals from other organ systems; (ii) gathered longitudinally over several hours, allowing for a potential trajectory of improvement or deterioration in organ quality, and (iii) derived from numerous monitoring systems, resulting in a high volume of data. Although EVLP offers a potential solution to the organ shortage issue, its effectiveness is hindered by the absence of standardized criteria for determining when an organ is suitable for transplantation. The decision-making regarding EVLP is primarily subjective and involves numerous measurements during the perfusion, which can be overwhelming for inexperienced EVLP programs. To mitigate this, Keshavjee et al. from Toronto developed a machinelearning model in 2023, named InsighTx, to aid surgical decision-making and predict posttransplant outcomes, using clinical EVLP data collected over a decade. A sequential donorrecipient model was developed that could be used for evaluating donor lungs as a general model for any recipient or could be customized with specific recipient details to personalize predictions for individual patients.
The potential applications of EVLP are not limited to organ evaluation and the extension of ischemic time; they also encompass the integration of advanced diagnostic and therapeutic modalities. These may include improved transplant logistics (multi-day lung preservation pairing with 100C lung preservation with short cycles of EVLP), the opportunity to explore organ banking concepts, better immunological matching between donors and recipients, the opportunity to perform time-dependent therapeutics like blood group conversion, elimination of CMV pre-transplant, and further metabolic rehabilitation.
Cutting-edge research is currently exploring advanced imaging techniques like magnetic resonance imaging and ultrasound to provide a more comprehensive understanding beyond conventional chest radiography during EVLP. The assessment of perfusate samples in preclinical models has conclusively identified the presence of extracellular biomarkers and pro-inflammatory gene expression. Once validated, certain monitoring modalities could play a crucial role in evaluating organ response to ischemia, quantifying inflammation, and predicting future reperfusion injury and/or alloimmune response.
A promising approach to increase the availability of suitable lungs for transplantation involves bioengineering from a scaffold, which serves as a platform for the regeneration of new lungs. The creation of whole-lung extracellular matrix scaffolds involves perfusing cadaveric
organs with decellularizing detergents. The EVLP technique can be utilized as a bioreactor with vascular perfusion and liquid ventilation. This helps in repopulating the native lung matrix with endothelial and epithelial cells in the necessary numbers and appropriate anatomic locations, which are essential for enabling organ function. The rat and porcine transplantation models have shown exciting initial progress, demonstrating clear evidence of gas exchange after reperfusion. However, long-term functionality has yet to be attained due to the underdevelopment of the vascular bed and distal lung epithelia. The Toronto research group is currently exploring an innovative method involving the creation of a 3D-printed lung scaffold, known as Ulung. This scaffold has the potential to be infused with either allogeneic cells or a patient's cells. This neoterictechnique could pave the way for the creation of personalized and functional lung tissue for transplantation or regenerative medicine applications. It’s crucial to emphasize that much more additional basic and translational research is required before this method can be applied to humans clinically.
The widespread use of EVLP is limited due to costs. Incorporating EVLP into a lung transplant center's practice requires a significant investment of time and resources. Broadly, the components can be categorized into personnel costs, system costs (equipment and supplies), and physical space. Depending on the chosen
EVLP system, there may be a substantial initial capital investment for equipment and hands-on staff training. This requires a strong institutional commitment to the growth of the lung transplant program. It may be challenging for institutions to justify the use of a resourceintensive system that is only used sporadically. For institutions unable to make a large initial investment, outsourcing to a dedicated EVLP facility might be a more practical option. In some cases, a combination approach could offer the most flexibility for a program.
The remarkable advancements in Lung preservation research have greatly improved the success of clinical Lung transplantation for patients with end-stage lung disease. However, the high demand for Lungs surpasses the number of available donors.
The implementation of EVLP offers a promising strategy to utilize marginal donors by reducing IRI and supporting the repair and regeneration of less optimal grafts. It is also important to optimize current perfusion solutions by adding essential components to meet metabolic needs. Prolonged EVLP creates opportunities for organ repair and reprogramming,

highlighting the need for further study of new strategies to enhance the quality of donor grafts before transplantation. This approach contributes substantially to expanding the donor pool, increasing lung transplant volumes, and enhancing overall graft function posttransplantation. (Figure 05)

AUTHOR BIO
Dr. Anitha Chandrasekhar is a Cardiothoracic surgical professional with over two decades of involvement in cardiothoracic surgeries including the entire spectrum of congenital, coronary, valvular, aortic, heart and lung transplantation, and ventricular assist device implantation procedures. She has presented scientific papers extensively in national and international surgical conferences and published many articles in prestigious journals. She has held leadership positions in various associations and carved a unique pathway in the cardiothoracic surgical domain. As a passionate ‘Surgical Scientist’, she serves as Clinical Lead- Lung Bioengineering and Organ Procurement at Northwestern Medicine, Chicago, IL, USA.
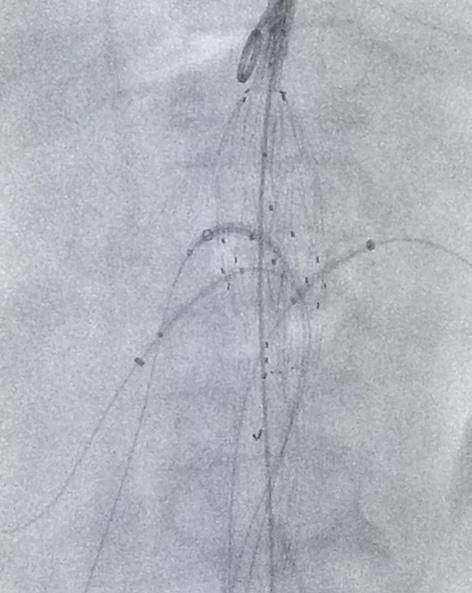
The first aortogram was performed in Lisbon in 1927. It was a long journey before Nicolai Volodos repaired the first aortic aneurysm endovascularly (EVAR) in 1987 followed by Parodi in 1990. Nowadays EVAR has become the gold standard. The evolution of new devices has enabled vascular surgeons to perform increasingly complicated pathologies in a minimally invasive manner, reducing operating time and patient morbidity and mortality. All fields of vascular surgery have undergone a remarkable transformation with a shift from open vascular to endovascular surgery, where a hybrid approach may just combine the best of both worlds.
Jakob Nowotny
MD, Senior Vascular and Endovascular Surgeon, the Department of Vascular Surgery, Sha’are Tzedek Medical Center
Over the past decades access to healthcare has improved worldwide. As a result, life expectancy has increased and with it the prevalence of vascular disease. Endovascular techniques have become the mainstay for vascular disease management over the past three decades. Traditional, open surgery continues to play a role in management of complex vascular disease and in developing countries. The forefront and future of vascular surgery lies in the field of hybrid procedures, where conventional open vascular operations meet cutting edge endovascular techniques, reducing operative time, time of hospitalization and improving patient outcomes.
The development of vascular surgery as a distinct specialty began in the early 20th century, with pioneering work by surgeons like Alexis Carrel, who was awarded the Nobel Prize in Medicine in recognition of his work on vascular suture and the transplantation of blood vessels and organs in 1912. The mid-20th century saw the introduction of the first successful arterial grafts, marking a turning point in the treatment of vascular diseases. Michael E. DeBakey was another pioneering figure in modern medicine, inventing countless surgical devices and spearheading the repair of aortic aneurysms and the introduction of
Dacron grafts for blood vessel replacement earning him prestigious awards such as the Presidential Medal of Freedom and the National Medal of Science.
The first "hybrid" vascular surgery, utilizing both open surgical and endovascular techniques simultaneously in a single setting, was reportedly performed in 1973, when an
iliac artery angioplasty was combined with a femoral-femoral bypass procedure for limb salvage.
The first endovascular repair of an abdominal aortic aneurysm in 1990 by Dr. Juan Parodi marked a significant milestone, establishing endovascular therapy as a standard of care in certain conditions.

A Hybrid Operating Room (OR) is an advanced procedural space that combines a traditional operating room with an imageguided interventional suite. This fusion enables clinicians to perform highly complex, advanced surgical procedures seamlessly. CT scans may be performed in some operating suites and advanced image guiding allows for
precise procedures with minimal contrast and radiation. This fusion enables clinicians to perform highly complex, advanced surgical procedures seamlessly. Patients typically experience shorter recovery times due to fewer surgeries, while hospitals benefit from improved staff efficiency and costeffectiveness.
Hybrid procedures allow more complex anatomy to be treated by less invasive procedures in medically higher risk patients.
Multimodal, multilevel vascular reconstructions or lesions which are difficult to approach or reach for anatomic lesions stand to be well suited for a hybrid approach.
It comes as no surprise that the first applications to gain wide acceptance in the surgical theaters of the 1990s involved aortoiliac disease, as open surgical reconstruction involves major surgery such as laparotomy or flank incision and often require aortic cross clamping resulting in high operative morbidity and mortality, which often precludes the use in the fragile, elderly population and those with high operative risk.
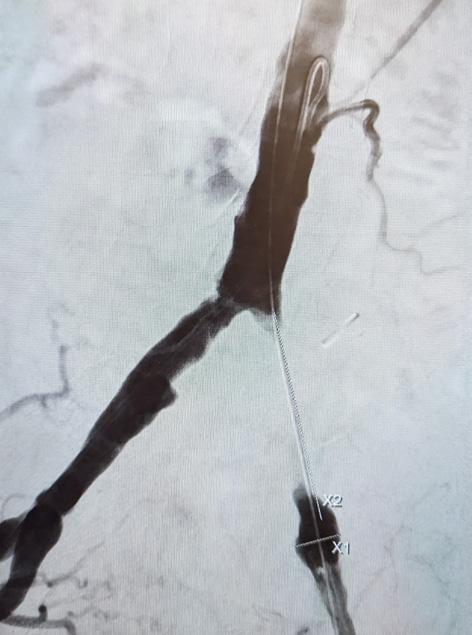
Particularly interventions that require a large dissection or insertion of synthetic grafts benefit from a hybrid approach. Bypass surgery, where the proximal intervention’s patency is dependent on the distal runoff or iliac PTA and common femoral endarterectomy with or without bypass, should be performed either simultaneously or soon thereafter to prevent thrombosis of the proximally treated artery or the bypass graft. Many centers have implemented the practice of completion angiography for all peripheral bypass surgeries to verify the patency of the inflow, outflow and the graft to prevent early occlusions of the graft. Upon identification of a technical defect immediate treatment can be performed by the operating physician at
the index procedure, such as revision of an anastomosis, excision of a retained valve or ballooning or stenting of a residual stenosis, dissection or tandem lesion.
Common femoral endarterectomy, combined with open iliac artery transluminal angioplasty and stent as well as Iinfrainguinal bypasses distal to either an iliac or superficial femoral artery (SFA) lesion are ideal candidates for a combined approach.
Particularly peripheral arterial disease has seen a rise in hybrid procedures.
Peripheral bypass surgery has become a last option nowadays. In most scenarios vascular surgeons and interventionalists chose an endovascular-first approach with peripheral arterial lesions. Several studies such as the BASIL trial have supported this approach, albeit with some reservations for long occlusions. Physicians are pushing the envelope to treat long lesions now using novel atherectomy devices, which physically remove atheromas and calcium using diamond blades with promising results.
Thrombectomy devices have replaced open thrombectomy in many acute conditions. Instead of open surgery and mechanical thrombectomy via a fogarty balloon of the dissected vessel, thrombectomy devices are inserted endovascularly via intruder sheaths. Fragmentation and aspiration of the clot material occurs mechanically or pharmaco- mechanically restoring blood flow to the affected limb/organ without incisions.
The hybrid OR represents a significant advancement in trauma medicine, offering a versatile environment that can adapt to the complex needs of critical patients
Drug coated balloons have recently made their way from the interventional cardiologists into the armamentarium of vascular surgeons and have improved long term results in several large randomized controlled studies. Many institutions have implemented DCBs for a majority of their peripheral cases and to treat restenosis in other parts of the vascular tree due to their favorable effect on vascular remodeling.
The Retrograde Open Mesenteric Stenting (ROMS) procedure is a hybrid technique used to treat mesenteric ischemia by combining open surgical and endovascular methods. It involves making an abdominal incision, placing a stent in the superior mesenteric artery against the blood flow direction, and using imaging to guide the process. This approach enables effective revascularization and potential bowel resection.
Transcarotid Artery Revascularization (TCAR) is a minimally invasive procedure to treat carotid artery blockages and reduce stroke risk. It involves a small neck incision, stent placement, and temporary blood flow reversal to prevent plaque from reaching the brain. TCAR is less invasive than traditional surgery.
Hybrid surgical approaches, combining elements of endovascular aneurysm repair (EVAR) and thoracic endovascular aortic repair (TEVAR), offer several advantages over traditional open surgery. These techniques are less invasive, reducing the need for large incisions and potentially decreasing the risk of complications associated with open surgery. Patients may benefit from shorter hospital stays and quicker recovery times, which can be particularly advantageous for those with complex medical conditions or advanced age. Additionally, hybrid surgeries can extend treatment options to patients who were previously considered unsuitable for conventional procedures due to anatomical constraints or other risk factors. Combining placement of a stent graft with open surgery decreases the morbidity and increases survival of these large procedures. When extensive dissections or aneurysms are treated via hybrid approach circulatory arrest may be avoided and operating time significantly reduced. With custom and physician- modified
fenestrated and branched devices anatomies can be treated and repaired that were previously off-limits to both open and endovascular intervention. While these methods may involve higher rates of reintervention compared to open repair, they do not significantly affect longterm survival, making them a viable option for many patients facing aortic aneurysms or dissections. (Figure 01)
Aorto-iliac occlusion has been traditionally treated by life-style modification and aortobifemoral bypass surgery when indicated. Since patency of this repair exceeds 90% over 10 years it was hailed as the holy grail of open vascular repair, specifically since a synthetic graft is used for this surgery. Skeptics questioned whether
endovascular treatment stood a chance against this gold standard treatment. Low and behold, the CERAB procedure, known as Covered Endovascular Reconstruction of the Aortic Bifurcation, entered the field and has replaced the traditional bypass surgery in many cases. This minimally invasive procedure involves the use of covered stents to reconstruct the aortic bifurcation without the significant morbidities associated with laparotomy, graft infection, graft-enteric fistula and incisional hernias or bowel obstruction. (Figure 02)
Trauma may be one of the areas where the fusion of open and endovascular surgery has saved the most lives. Studies have shown that
the use of a hybrid OR can reduce the mortality rate in severely injured patients from 50% to 16%, which is a substantial improvement in life-saving potential. When a trauma patient is immediately transferred to the hybrid OR, diagnostic imaging in the same space as surgery can lead to quicker decision-making and more targeted treatments, further enhancing the chances of survival for trauma patients. An intra-aortic balloon can be placed and the trauma surgeons can work side by side with the vascular surgeons, saving valuable time, resources and red-blood cells. Inaccessible injuries, such as the subclavian artery or the great vessels can be accessed via catheterization and immediate repair via covered stents or bleeding control via embolization or balloon occlusion can be achieved.
One of the last bastions of open vascular surgery lies in arteriovenous access. Long belittled as easy to access vessels with an overall low rate of complication and reimbursement cutting edge medical devices only recently made their impact. With the advent of AV access maintenance in the ever growing aging and diabetic population, angioplasty and stenting became one of the most frequent vascular procedures in the United States. A plethora of devices are nowadays available for maintenance of arteriovenous fistulas and grafts, but the revolution may lie in the endo-AVF creation. Two devices have caused a stir in the vascular community in recent years enabling creation
Staging hybrid lower extremity arterial surgery greatly increases healthcare costs adding to the total health burden of the often chronically and critically ill patients
of an AVF via endovascular means using radiofrequency to fuse fore-arm arteries and vein. Results are promising, but only time will tell whether the procedure will offer the same results and become economically feasible for most centers.
Hybrid procedures were initially implemented in the management of peripheral artery disease but are now being used in all parts of vascular surgery including cerebrovascular disease, aneurysm repair, mesenteric arterial disease and arterio-venous access procedures.
In light of rising health-care costs and limitations for providers and patients to undergo serial admissions for multiple interventions such as diagnostic angiography, bypass surgery and lastly endovascular intervention, many institutions have moved to from staged vascular interventions to a single hybrid procedure.
1. Decrease the invasiveness of open surgery, reducing physiological stress
2. Smaller incisions leading to lower compilation rate and re-admissions, specifically in the elderly diabetic population
3. Fewer procedures with lower requirement for anesthesia
4. Instant repair for multi-level disease
5. Prevention of continued symptoms, ischemic time and infection between procedures
6. Shortens ICU and hospital stays, contributing to lower 30-day perioperative mortality
7. Best option for high-risk patients who cannot tolerate an open operation.
8. Studies show an overall technical success rate of 99% for hybrid repair with lasting patency comparable to open surgery
The analysis of Ebaugh et al from 2008 elucidates how hospital systems and insurers can benefit from single hospitalization hybrid vascular procedures:
Excluding patients with confounders, hospital charges and length of stay (LOS) were compared. These results suggest that when performing elective hybrid procedures in patients without gangrene, ischemic rest pain, CHF or renal failure, performing both, the endovascular and open portions on the same day significantly reduces total hospital charges and LOS, by 78% and 133%, respectively.
The future of hybrid vascular surgery is poised for significant advancements, integrating stateof-the-art imaging systems with traditional surgical methods to enhance patient outcomes. The trend towards minimally invasive procedures, supported by real-time imaging and flexible imaging capabilities, is reshaping the landscape of vascular care. As hybrid operating theaters evolve, physicians will be able to treat patients with increasingly difficult anatomies and pathologies. Unmet needs for devices will lead to the development and integration of a variety of surgical and endovascular devices. Initial costs for new technologies and device development will be offset by shorter hospital stays and lower morbidity and mortality.
References are available at www.americanhhm.com

Dr. Jakob Nowotny is currently working as senior Vascular and Endovascular Surgeon at the Department of Vascular surgery, Sha'are Tzedek Medical Center, Jerusalem. He holds a medical degree from Ben Gurion University (Columbia Global Health Program), and trained at Mount Sinai In New York and Hadassah in Jerusalem. Following his academic journey, he gained extensive experience as a consultant in the field of Vascular Surgery. He is avidly involved in research, the development of medical devices, and as a tutor and mentor for students and residents. His expertise lies in performing hybrid vascular procedures where the endovascular realm meets vascular surgery.

Ultrasound technology has revolutionized patient care, transitioning from stationary, bulky machines to today's portable handheld devices. These devices provide flexibility in medical settings, enabling quicker diagnoses and enhancing patient care. This evolution highlights a trend towards more accessible and efficient healthcare diagnostics.

Ultrasound technology has undergone significant transformations since its inception. Originally, ultrasound machines were large, cumbersome, and expensive, typically housed in dedicated
Ai Phi Thuy Ho Cardiology Specialist, Hospital Kalnes Trust
imaging rooms within hospitals (figure 1). These early devices were stationary and required trained technicians to operate, limiting their use primarily to specialized departments and settings. Advances in microelectronics, battery technology, and medical imaging software have dramatically transformed these devices over the past few decades. The development of portable ultrasound machines marked a significant step forward, allowing for greater flexibility in where and how ultrasounds could be performed. However, the most ground-breaking evolution has been the introduction of handheld ultrasound devices. These pocket-sized tools, equipped with high-resolution imaging capabilities, have revolutionized the field by providing real-time, on-the-go diagnostic capabilities.
Handheld ultrasound devices offer several advantages over their larger predecessors (figure 2). The most obvious benefit is their size. Handheld devices can easily be carried in a doctor's pocket, making it possible to perform ultrasounds at the bedside, in emergency situations, or even in remote locations. Modern handheld devices are designed with user-friendly interfaces, often integrating touchscreen controls and intuitive software. This ease of use means that a broader range of healthcare professionals can operate the devices with minimal training. Handheld ultrasound devices are significantly less expensive than traditional machines. This lower cost can make ultrasound technology accessible to a wider range of healthcare settings, including small clinics and practices that might not have been able to afford traditional ultrasound machines.
Many studies show that portable handheld ultrasound devices are beneficial in different settings. This is where physicians use point of care ultrasound (POCUS). POCUS is an ultrasound examination performed by medical professionals at the bedside wherever a patient is being treated, whether that’s in a modern hospital, an ambulance, or a general practitioner’s office. The difference between a POCUS examiner and a radiologist is that medical professionals are answering yes or no questions: Is there the presence of pleural or pericardial effusion? Does the patient have heart failure? What about hydronephrosis? Does the

patient have gallstones or any signs of acute cholecystitis? Handheld ultrasound devices are not just for general practitioners and hospital doctors; paramedics are already using them to provide faster diagnostics and better patient care. In trauma cases, a handheld ultrasound device can detect or verify the presence of free fluid in the peritoneum or thorax, facilitating immediate investigation and improving patient prognosis.
Numerous articles in PubMed and other databases advocate the use of POCUS. For instance, one study encourages non-cardiologists to utilize heart ultrasound. Combining ultrasound with clinical expertise can expedite clarification, validate or challenge diagnoses, and facilitate swift interventions. Another study showed that targeted examinations conducted by skilled ultrasound doctors had diagnostic utility in nearly half of all patients examined, with almost one in five experiencing a change in diagnosis.
Other studies highlight that emergency doctors have high accuracy in performing POCUS for suspected deep venous thrombosis

(DVT) in the lower extremity, comparable to radiologists. They also performed assessments in an average time of three minutes. Ultrasound assessments for all lower extremity DVTs exhibited a sensitivity and specificity of 89%, while proximal lower extremity DVTs showed a sensitivity of 95% and specificity of 96%. Studies involving lung ultrasound and the kidney and urinary tract system show how medical professionals can confirm or negate conditions, reducing waiting times and delays in treatment.
For Focused Assessment with Sonography for Trauma (FAST) examinations, the primary goal in trauma patients is to identify intraperitoneal free fluid, allowing immediate transfer to higher levels of care. Various articles describe the advantages and disadvantages of this examination, with some studies showing no significant difference in diagnostic accuracy between radiologists and non-radiologists.
These studies underscore that ultrasound is a valuable tool for promptly diagnosing and implementing interventions, whether in a hospital or clinic setting. Quick access to ultrasound imaging can accelerate diagnosis and treatment, potentially saving lives.
POCUS is the use of ultrasound at the patient’s bedside for diagnostic and therapeutic purposes. The adoption of handheld ultrasound devices for POCUS offers numerous advantages. With handheld ultrasound, doctors can quickly gather critical information at the point of care, enhancing their diagnostic capabilities and improving patient outcomes. The immediacy and convenience of handheld ultrasound reduce the need for patient transport to imaging departments, increasing comfort and reducing wait times. By providing immediate visual information, POCUS enhances the clinician's ability to make timely and accurate decisions. For example, in trauma cases, POCUS can quickly identify internal bleeding or organ damage, guiding immediate intervention. The portable nature of POCUS devices, especially handheld ultrasound units, makes it possible to bring imaging capabilities to a wide range of settings, including remote locations, field hospitals, and during patient transport. Additionally, POCUS reduces the need for more expensive and time-consuming imaging modalities, such as CT scans or MRIs,
particularly in settings where rapid decisionmaking is critical. This cost-effectiveness is particularly beneficial in resource-limited environments.
Learning to use handheld ultrasound and perform POCUS can significantly enhance a doctor's skill set. It allows for better integration of imaging into everyday clinical practice, improving overall diagnostic accuracy and patient management. Handheld ultrasound can streamline workflows by reducing the need for referrals and follow-up imaging, thereby increasing efficiency and reducing healthcare costs.
POCUS has numerous clinical applications. In cardiology, it is used to assess cardiac function, detect pericardial effusion, and guide resuscitation in cardiac arrest situations. In pulmonology, it helps evaluate pleural effusions, pneumothorax, and pulmonary edema. In

gastroenterology, POCUS is used to identify free fluid in the abdomen, assess the gallbladder for cholecystitis, and guide procedures such as paracentesis. In obstetrics and gynecology, it is valuable for monitoring fetal development, assessing early pregnancy viability, and evaluating gynecological emergencies. In emergency medicine, POCUS is essential for the rapid assessment of trauma patients, diagnosing abdominal aortic aneurysms, and guiding vascular access.
The use of POCUS is expected to continue growing as more clinicians recognize its value in enhancing patient care. Technological advancements, such as the development of more affordable, high-quality handheld ultrasound devices, and the integration of artificial intelligence for image interpretation, are likely to further expand its applications and accessibility.
AUTHOR BIO
Dr. Ai Phi Thuy Ho is a cardiology specialist and fellow in Norway who is passionate about POCUS and its transformative impact on medicine. As the founder of NorVue, she provides online POCUS training to healthcare professionals worldwide. Her mission is to enhance diagnostic skills and improve patient care through innovative ultrasound technology.
Ultrasound technology has evolved significantly from large, stationary machines to today's portable handheld devices. POCUS further enhances this technology, allowing clinicians to perform ultrasound exams at the patient's bedside, providing immediate diagnostic information crucial for emergency and critical care settings. POCUS improves diagnostic accuracy, patient outcomes, and clinical workflows, making it an indispensable tool in modern medicine due to its portability, cost-effectiveness, and broad range of applications.
Moving health records into digital systems revolutionised patient care, and now another revolution in patient data is happening with the integration of artificial intelligence (AI) inside electronic health records (EHRs). Adding these computer science breakthroughs into the daily workflows of healthcare professionals (HCPs) has a vast impact on patient outcomes, reducing burnout, and cutting costs. While there are concerns with AI integration into EHRs, such as data quality and privacy challenges, bias, and transparency, the successful implementation of these tools must be pursued. This article focuses on how AI enhances EHRs.
Vijay Adapala
EVP & GM Global Supply Partners, Doceree
With the adoption of EHRs and other digital healthcare solutions, came an explosion of clinical data to analyse. Data is vital for HCPs to make informed decisions about patient care and to uncover treatment trends, but now there is simply too much health information to process for most humans – especially during record levels of HCP burnout. With 73% of patients in a recent survey reporting that the healthcare system fails to meet their needs,
and 64% saying HCPs should understand their health journey better, there are obvious gaps between the information available and using it effectively to treat patients.
HCPs in a recent study identified critical areas of care that can be improved by implementing AI: predictive analysis, clinical decision support, data visualisation, and patient monitoring. Not only do patients and providers see room for improvement, but also the majority of healthcare executives agree
that these technologies can positively impact global health challenges.
Integrating AI into EHRs can revolutionize data discovery, offering healthcare providers real-time personalised recommendations, patient satisfaction, and risk prediction analytics, equipping HCPs to understand the individual patient’s journey better. The market for AI inside healthcare was valued at $11 billion in 2021, and by 20230, it is projected to be at $187 billion, indicating that the industry will continue to invest in these technologies.
HCPs and patients manage healthcare data within EHRs, and these platforms bring together data from medical records, multiple providers, test results, and pharmaceutical orders. Bringing AI technology into EHR systems would unlock the potential of this data to reduce HCP burnout and improve patient outcomes. By improving the accessibility of patient data, AI can reduce the risk of human error and facilitate personalised treatment recommendations.
The average hospital produces roughly 50 petabytes of data each year, and a staggering 97% of that health data goes unused. Harnessing the power of AI to connect this fragmented data and enhance the quality of care can ultimately improve patient outcomes. Here are five ways AI can change the way HCPs interact with data inside of an EHR:
1. AI inside of an EHR can create patient
overviews for their HCP by summarising test results, and patient history, and recommending diagnostic testing.
2. AI algorithms can interpret medical data more accurately and faster than HCPs alone. By analysing information available inside of an EHR, such as medical history, lifestyle, social factors, and genetics, these programs can improve test ordering and diagnosis.
3. AI tools can provide personalised care recommendations in real time using AI-triggered messaging.
4. These algorithms can simplify data input, reduce errors, and provide much-needed reliability to improve healthcare delivery.
5. Using predictive modelling, patient adherence can be predicted, and HCPs can proactively intervene by offering support and resources.
Patients often fail to adhere to a treatment protocol prescribed by their HCP, and this can be a barrier to improved health outcomes. Big data and AI can be used to discover these issues. One study found that 70% of patients fail to administer their insulin correctly. An AI monitoring system was developed to monitor patient drug administration and alert providers to errors.
Working with Google Health, Meditech uses AI to answer patient questions, auto-generate clinical notes, and create AI virtual assistance to search chart notes and place orders. Meditech sees these programs as ways to reduce physician burnout and improve the patient experience.
Many clinical trials struggle to recruit the right participants needed to determine a drug’s efficacy. Because patient data is disparate and siloed, HCPs struggle to connect the patients with the latest research that can improve not only that patient’s health outcomes, but thousands of patients who can benefit from a drug once it is fully developed. AI can be used to find potential patients and inform HCPs when patients qualify for clinical trials.
Using AI to identify suitable candidates based on individual health profiles and conditions creates a personalized approach to trial recruitment. This improved accuracy adds efficiency which can ensure access to the latest breakthrough treatments. With AI identification of participants, the HCPs who would otherwise need to manually search for clinical trials available to their patients can use their time to better inform patients about the trial process, and drug testing and development can be expedited.
Across the globe, the effectiveness of treatment plans is impacted by healthcare affordability. One in four Americans skipped necessary medical treatments because of the high cost in 2022. Yet only 15% of co-pay dollars aimed to lower patient costs for brand prescriptions are utilised.
Often the biggest hurdle to accessing these programs is awareness. More than 40% of HCPs self-report limited awareness of support programs for patient prescriptions, and this affordability gap has a direct impact on treatment adherence and therefore patient outcomes.
Utilizing data about pharmacy benefits coverage, pharmaceutical co-pay assistance programs, and the individual patient, AI-triggered technology can connect prescribers to details financial programs available to their patient. By using AI to connect HCPs to this information in real time, EHRs can help patients save on healthcare expenses and empower HCPs to improve patient engagement through personalised recommendations.
The advanced data analysis of AI tools creates opportunities to improve healthcare costs outside of connecting patients to affordability programs as well. According to the CDC, chronic health conditions account for 90% of annual healthcare costs. Helping patients with chronic conditions manage their health can reduce overall healthcare costs. With AI assistance, providers can examine factors from economic status to social support and predict which patients are most likely to miss scheduled treatments and intervene. Harvard’s School of Public Health found that diagnoses made with AI reduced treatment costs by up to 50%.
When implementing an AI tool within an EHR system it is important to think through
Integrating AI into EHRs can revolutionize data discovery, offering healthcare providers real-time personalised recommendations, patient satisfaction, and risk prediction analytics, equipping HCPs to understand the individual patient’s journey better.
specific use cases. Consider which tasks are time-consuming, repetitive, and causing burnout, and prioritize AI solutions that can clearly demonstrate value. EHR software managers should create governance teams to oversee AI software solutions and ensure the ethical execution of these tools, protect patient information, and optimize program deployment.
Many existing EHR partners may offer AI solutions that can be easily adapted or developed to meet a specific need. Look for partners who are excited about the potential of AI and understand the need for human oversight.
As EHRs add AI functionality to their software offering, challenges can and will surface. Here are five key concerns to consider when developing or integrating an AI-powered solution:
1. AI tools rely on quality data and the lack of standardization between tools can impact the
functionality and output of these algorithms. To effectively integrate an AI solution, highquality, consistent, and interoperable data must be accessible. When data is complex or ambiguous, it can be difficult for today’s AI algorithms to understand.
2. Keeping sensitive patient data secure is not only a concern for complying with regulations like the Health Insurance Portability and Accountability Act (HIPAA), but it is also important for building trust with health systems and HCPs. When training AI software or adding an AI-powered integration, EHR systems must follow robust security and privacy protocols to reduce the risk of data misuse or breaches. HIPAA applies to protected health information (PHI), and AI software that learns from this data requires consent and enhanced security measures.
3. Beyond HIPAA concerns, EHR leadership should consider other regulatory processes and understand that this is an evolving space where regulatory guidelines are trying to keep up with technological breakthroughs. The FDA may need to approve AI tools that make diagnosis recommendations. Gaining FDA approval can be a lengthy process, and to stay on the forefront EHRs should look for partners who have successfully launched AI tools to provide guidance.
4. While HCPs will ultimately benefit from AI-enhanced EHRs, many have not been trained on these tools or fully understand how to use the new functionality. EHR leadership teams should work with hospitals and health
systems to provide the right training and messaging to end users to ensure tools are used effectively.
5. Outside of training, EHR systems will also need to inform HCPs and health systems about how AI tools work to build trust and ensure transparency. Concerns about bias and legal implications require collaboration between the EHR system and the health systems using these tools. When AI tools provide diagnosis recommendations, there’s potential for liability risks particularly when there are errors or adverse effects. Highlighting the importance of human oversight and intervention.
Clearly, advancements in AI are driving the core goal of the healthcare industry: Delivering superior treatment outcomes. These technologies enhance how physicians interact with data, reshape the EHR ecosystem, and improve patient outcomes. From enhanced access to tests, medical histories, and treatment recommendations, AI-powered technology is assisting diagnoses, treatment recommendations, and risk assessments.
By taking on the tasks of transcribing patient conversations, AI tools allow HCPs to focus on their patients. This EHR enhancement can reduce provider burnout and burdens on understaffed teams. By creating summaries and intuitive visualisations of complex data, AI can help HCPs identify important trends in health data.
With trend recognition power, AI systems can connect patients to affordability programs and connect researchers to clinical trial participants to improve drug discovery.
From personalised medication recommendations to improved test ordering, there is no limit to the EHR enhancements now available through AI. As patient outcomes improve and HCP burnout improves, the entire healthcare system will feel relief.

AUTHOR BIO
Adapala is a seasoned executive with 25 years of experience in healthcare marketing, ad tech, digital media, and consumer tech. At Doceree, Adapala oversees the end-to-end global supply partnerships with healthcare platforms and publishers. Prior to joining Doceree, Adapala served as the GM at Amazon Publisher Services for web and mobile app publishers, where he led the strategic vision, successfully launched and scaled Amazon's ad tech solutions, and spearheaded global expansion strategies. Prior to Amazon, he held leadership positions at Yahoo and Motorola. He holds an MBA from Kellogg School of Management, Northwestern University, and a BSEE from Purdue University.

Artificial intelligence (AI) is likely to transform healthcare delivery of the future, increasing quality, personalized medicine, and potentially cost efficiency. However, successful deployment, orchestration, and safety monitoring of this technology will likely require rethinking of hospital health IT and leveraging of third-party platforms for AI to achieve its full potential.
Reza Forghani
MD, PhD, Prof of Radiology & Artificial Intelligence (AI) and Vice Chair of AI, Director, Radiomics & Augmented Intelligence Laboratory
Artificial Intelligence (AI) is likely to transform the healthcare practice of the future. There are steadily increasing FDA cleared or classified medical AI applications, and currently over half of these tools are based on diagnostic medical imaging
or radiological images. These are furthermore likely to multiply in the next 5 years. They are also likely to increase in complexity and sophistication, fueled by the rapidly evolving AI landscape and technological advances, most recently exemplified by large language and

Traditional or legacy IT approaches for AI tool adoption are not cost-effective and unlikely to be able to effectively support the anticipated digital transformation and adoption of multiple AI tools for leading-edge and competitive healthcare organizations in the future
There are increasingly sophisticated thirdparty AI deployment and management platforms that enable seamless, costeffective, and timely AI deployment and facilitate optimal AI tool selection; these are also likely to form the foundation for future more advanced AI tool adoption and safety monitoring
Healthcare leaders should become familiar and consider adoption of AI deployment platforms as part of their digital transformation roadmap and future AI infrastructure planning
other emerging multimodal foundation models. While there are many interesting and headline grabbing applications of AI tools in medicine in experimental preclinical settings, the practical adoption and workflow barriers that must be overcome for successful adoption of such tools in clinical practice are frequently overlooked. Notwithstanding the potential of this technology, early experience with AI tools has revealed significant challenges for timely and seamless AI adoption in the clinical. In an increasingly digital and AI-supported healthcare operation, one of the most basic foundational challenges for healthcare organizations will be seamless and timely deployment and management
of an increasing number of complex AI tools. In this article, the challenges with traditional or legacy information technology (IT) approaches and the potential utility of third-party AI deployment and orchestration platforms will be discussed for empowering and supporting seamless deployment, orchestration, and safe adoption of this technology in the healthcare environment.
It is fair to state that traditionally, hospital IT systems are frequently under-resourced. If the healthcare of the future is going to be truly revolutionized and transformed using digital technologies and AI, the status quo will no longer be sustainable or acceptable. Under the current legacy health IT paradigm, AI software such as those used in radiology are procured and technically deployed one at a time. This is repeated over and over every time a new AI tool is acquired. The process is painstakingly slow, laborious, and costly to the organization, both from the perspective of resources utilized for procurement and implementation of each AI tool as well as the opportunity cost of hindering trials to determine the optimal tool for the organization and delaying the adoption of potentially transformative technology. Even in the traditional setting, this legacy approach has not been optimal and its negative impact on the organization’s progress and competitive edge is likely underestimated. However, in a potential future world where hospitals may have to adopt and manage tens if not hundreds
of AI tools, the legacy approach will simply not be sustainable. In addition to resources required for deployment and management of these tools, at some point, the complexity may exceed what can be reasonably expected of a hospital IT department. Afterall, hospitals are not IT companies, and the point may come when they have neither the resources nor the full complement of necessary technical expertise in order to effectively manage and increasingly complex AI landscape. One likely solution that is increasingly being considered for these fundamental challenges is the strategic use of third-party AI deployment and orchestration platforms that help mitigate these problems.
Over the past few years, an increasing number of platforms have become available that can facilitate the deployment and orchestration of AI tools. These platforms are becoming increasingly sophisticated and can represent a solution and a fundamental framework facilitating seamless, timely, and cost-effective adoption of multiple AI applications in the healthcare setting. It is neither the intention nor within the scope of this article to discuss individual platforms, their advantages, and pitfalls. Rather, the purpose of this article is to provide an overview and bring these platforms and their importance to the attention of key stakeholders within the healthcare organization’s leadership as part of their necessary infrastructure planning for the future
Increasingly sophisticated thirdparty AI deployment platforms enable seamless, cost-effective, and timely AI adoption, providing one important cornerstone for digital AI transformation of future healthcare organizations.
digital transformation and adoption of AI in their respective organizations.
There are currently several different vendors providing advanced platforms that can be used to deploy, manage and orchestrate AI tools. Currently, the primary focus of many of these platforms is the deployment of diagnostic imaging AI applications but these have the potential, and their functionalities can be expanded in the future, in order to integrate other modalities and data types. These platforms come with different configurations, but all of the major ones have the core functionality of being able to host and effortlessly deploy multiple AI algorithms from the standpoint of the healthcare institution. Depending on the platform, they can also have other key functionalities that range from image routing to sophisticated abilities to orchestrate and integrate various applications that form the foundation for effective deployment and
use of increasingly sophisticated AI tools, including multi-modal applications. For the purposes of this article, the focus will be on the basic but fundamental advantages of these platforms in facilitating cost effective and timely adoption of multiple AI applications and empowering the organization to try and select the optimal AI application that serves its unique needs, followed by a brief overview of other current and potential future fundamental advantages of these platforms.
Timely deployment of AI tools remains a major challenge under the current legacy healthcare IT paradigm. It is not unusual for the process of procuring and making an AI application available to clinician providers to take 3 to 6 months, if not more. From an implementation cost perspective, ballpark estimates are that the resources required to get each AI tool through this process, including security review and integration of the tool, can cost an organization in the range of 15,000 to 20,000$ or more per application. There are in addition indirect and opportunity costs for such delays. One negative downstream effect is the delay in deploying cutting edge tools that can improve healthcare processes and patient care. There are also other negative effects, including friction within the organization that arises from such delays and an overall contribution to staff and provider dissatisfaction. The costs and challenges are compounded and multiply
with an increasing number of AI tools, making the legacy approach unsustainable. All of this can have a substantially negative impact an organization’s operations and competitive edge. When using a platform, on the other hand, the “heavy lifting” is done once. Once a platform is reviewed and securely integrated and adopted by an organization, deploying individual AI software can be as seamless as tuning on an App, making a tool immediately available and avoiding the repetitive, laborious, and costly approach of legacy one at a time, standalone AI tool adoption. This will enable the competitive organization to lead in technology adoption.
AI tool performance can vary at different hospital sites. Furthermore, for a given tool performing a similar task, there are unique aspects both from a diagnostic performance and operational/workflow standpoint that can make a given tool more or less desirable depending on the specific hospital/organization’s unique needs. One important direct benefit of enabling effortless AI application deployment through a platform is that it empowers the organization and providers to try different applications, providing them with first-hand knowledge and exposure to functionality of a given tool within that organization. Using legacy approaches, trials (even if provided at no cost by the vendor) are resource intensive and costly to the organization, essentially requiring the same degree resources that is
required for full adoption of a standalone software discussed earlier. This disincentivizes trials, especially when multiple applications are being considered, and ultimately may lead to procurement of a less-than-optimal tool. By making application trials effortless and less resource intensive, AI deployment platforms enable seamless evaluation of multiple applications, ultimately enabling the organization to select the tool that is best suited to the needs of the organization and its providers.
Although a detailed discussion is beyond the scope of this article, the ideal platform can have many additional advantages that support technology adoption and transformation of a healthcare organization. Platforms support interoperability and have the potential to make AI applications more effective using sophisticated image/date routing. They facilitate management and integration of multiple applications and can potentially support multimodal applications that include both image analysis and language or reporting tasks. Lastly, with increasingly complex AI applications, including development of biomarker tools that perform tasks such as predicting a molecular phenotype or treatment response, there will be a requirement for more robust quality monitoring tools. One can envisage platforms playing a fundamental role in this essential requirement of future advanced AI models. These are few
among a range of potential possible benefits of using platforms for safe and effective AI deployment and management.
Digital technologies and AI are likely to play an essential role in the healthcare of the future. Although much attention has been paid to specific applications and clinical or healthcare process-related tasks they perform, the essential infrastructure investments and planning that form the foundation and are required for successful adoption of these technologies in clinical practice does not always get the necessary attention. To ensure that a healthcare organization is competitive and leads
in technology adoption, it is imperative that its leaders make the necessary infrastructure planning and investments that will facilitate successful future digital transformation and AI tool adoption. In that regard, legacy IT approaches for AI tool deployment may not be viable or satisfactory for leading clinics and hospital systems. AI deployment and orchestration platforms can provide the necessary infrastructure to make seamless, effective and timely AI tool adoption possible in clinical practice. Healthcare organization leaders would benefit from familiarizing themselves and considering adoption of such platforms as part of their digital transformation and AI roadmap.
Dr. Reza Forghani is a radiologist and researcher with medical Artificial Intelligence (AI) expertise. He is Professor of Radiology & AI and Vice Chair of AI at the Department of Radiology, University of Florida College of Medicine where he is also the director of Radiomics & Augmented Intelligence Laboratory (RAIL).


Ai Phi Thuy Ho Cardiology Specialist, Hospital Kalnes Trust

Have you heard about point of care ultrasound (POCUS)? Could this be the next-generation tool, replacing the stethoscope? This interview explores how POCUS is revolutionizing medical practice. It highlights the many benefits of POCUS, showing how it not only enhances patient care but also boosts doctors' confidence and efficiency. By providing immediate diagnostic insights, POCUS cuts down the waiting time for traditional imaging results, reducing anxiety and frustration. Physicians can turn the knowledge gained from POCUS into practical skills, allowing them to make quicker, more informed decisions for their patients. The discussion will emphasize that every doctor, regardless of specialty, should embrace this technology, positioning POCUS as an essential skill for the future of medicine.
1. Could you share your journey and motivation for specializing in cardiology, and what led you to incorporate Point of Care Ultrasound (POCUS) into your practice?
Back during my internship, guess which specialty I absolutely didn't want to go into? Cardiology. Cardiology was nowhere on my radar!
For many, cardiology is prestigious, but for me, it wasn't about that. I chose it for the challenge, to push my limits and manage really sick patients. Plus, I met this amazing
cardiologist who inspired me. So, during my internship, I made up my mind: cardiology it is. And you know what? I've never looked back.
My journey has been filled with highs and lows, but it's where I found my purpose. In 2019, I discovered ultrasound, which fascinated me. Despite struggles and moments of doubt, a life-saving diagnosis in 2020 reaffirmed why I became a doctor. I remember telling my mother about this event. Her words has always stayed with me ever since: “Ai Phi, it’s great that you saved this patient with ultrasound.
But everyone should know and understand the use of ultrasound. Help your fellows and share your knowledge so everyone can give and receive the best care.”
Those words make my heart sing. This is for my parents, so they will always be safe in the hands of a doctor and as patients if they ever need help. That's why I incorporate POCUS into my practice – to make a difference and help others learn this invaluable skill.
2. What were the key challenges you faced in integrating POCUS into your clinical workflow, and how did you overcome them?
Integrating POCUS into my clinical workflow was a journey filled with challenges. I remember feeling isolated, with limited resources and guidance available. Understanding ultrasound basics was daunting, and I felt lost in deciphering which transducer to use and when. It seemed like a mystery.

I tried various resources but made little progress. Then, a pivotal moment came when I diagnosed massive pericardial effusion, which changed everything.
After a heartfelt talk with my mom, I made a promise to persist. I sought learning opportunities, traveled to learn from experts, and even conducted late-night teaching sessions. I refused to give up.
Overcoming these challenges required discipline and resilience. Every challenge I faced in life helped me grow stronger. Once I grasped POCUS, it became transformative. Despite challenges, POCUS is the future of medicine, empowering us to change lives.
3. What specific advantages have you observed in patient outcomes when using POCUS compared to traditional diagnostic methods?
POCUS has revolutionized patient care by complementing clinical assessment and offering a more comprehensive picture. One of my earliest experiences with POCUS, about 7.5 years ago, stands out. Traditional methods failed to detect massive pericardial effusion in a patient, but POCUS did, ultimately saving her life.
In the emergency ward, POCUS drastically reduces waiting times. For instance, when suspecting deep venous thrombosis, I can perform the ultrasound myself. Detecting a clot means immediate treatment, saving crucial time and improving patient satisfaction.
Using POCUS for cardiac exams guides further diagnostic tests like coronary angiograms. It helps assess heart function, identify conditions like pulmonary embolism or acute cholecystitis, accelerating diagnosis
- crucial in fast-paced emergency settings where conditions deteriorate rapidly.
Being proficient in POCUS enables faster, more accurate decisions, ultimately improving patient outcomes. Sometimes, it's the difference between life and death.
4. How does POCUS help reduce the frustration and insecurity doctors often feel while waiting for diagnostic results from traditional imaging methods?
POCUS is a game-changer for us doctors. Waiting for traditional imaging results can be nerve-wracking and feel like an eternity, leading to doubts about patient management. With POCUS, we get immediate answers right at the bedside.
In critical situations, instead of waiting for hours or days, POCUS provides real-time information, boosting our confidence to act promptly. I recall a case where POCUS helped diagnose cardiac tamponade swiftly, allowing for immediate intervention.
POCUS gives us more control and reduces reliance on other departments, minimizing delays and stress. Getting crucial answers on the spot allows us to make informed decisions quickly, leading to better patient care. It's incredibly satisfying and makes our job more efficient.
5. What are the most significant barriers to the widespread adoption of POCUS in various medical specialties, and how can they be addressed?
Widespread adoption of POCUS faces several challenges. Firstly, not every doctor is trained to use it effectively. Improved train-
ing programs tailored to various specialties are essential to address this gap.
Cost remains a significant hurdle despite decreasing device prices. Initiatives such as grants or bulk buying deals could make POCUS more accessible to medical facilities.
Resistance to change is another barrier. Some doctors are skeptical about incorporating POCUS into practice. We need to demonstrate its benefits through success stories and research findings, highlighting faster diagnostics and improved outcomes.
Integrating POCUS into workflow seamlessly is crucial. Clear protocols and guidelines are needed to ensure its effective use without disrupting routine clinical practice.
By investing in better training, providing financial support, fostering mindset shifts, and ensuring smooth integration into workflow, we can make POCUS a standard tool across all medical specialties.
6. What are the key components of your NorVue training program that make it effective for both new and experienced practitioners in mastering POCUS?
Learning ultrasound can be a daunting journey, especially when you're unsure where to begin. I made every mistake imaginable when I first delved into POCUS. Months passed with little progress, feeling lost and frustrated.
I know many others face similar struggles. Some expect a single workshop to teach them everything, only to forget most of it without practice. I remember the overwhelm, the hours spent trying to learn, and I don't want anyone else to experience that.
That's why I created NorVue – to simplify learning. My courses cover the basics in an
easy-to-follow format. What sets them apart? They save you time. Knowledge leads to better decisions. Investing in my courses saves you from endless searching through free resources. Time is precious, and I want to help you make the most of it.
I want you to thrive and enjoy the journey. Keep going, even when it's tough. POCUS is the future of medicine – it can change lives, including yours.
7. How do you envision the role of POCUS evolving in the next decade within the field of cardiology and beyond?
I believe POCUS will revolutionize cardiology and beyond in the next decade. In cardiology, POCUS will become indispensable for quick bedside heart assessments, enabling immediate evaluations of cardiac function and abnormalities, leading to more efficient and effective patient care.
Beyond cardiology, POCUS will become a standard tool in many specialties. In emergency medicine, it will expedite trauma assessments and guide procedures. In primary care, it will aid in routine checkups, early issue identification, and reducing specialist referrals.
I envision POCUS becoming more userfriendly and integrating with advanced technologies like AI. Portable devices with improved image quality and AI-assisted features will aid interpretation. Many ultrasound companies are already developing AI tools, which I’m optimistic about.
However, it's crucial for users to be proficient in performing scans and evaluating images themselves to support AI findings. AI
POCUS isn´t just another gadget; it´s like having superpowers in the medical world.
can assist beginners, guiding them to obtain optimal views and understand anatomical structures. Given the lack of supervision in learning POCUS, AI can be immensely helpful here.
Increased use of POCUS in medical training will be significant. As more students and residents become proficient, it will become a standard practice. This new generation of doctors will be more comfortable and innovative with POCUS, ultimately improving patient care.
8. What has been the most rewarding aspect of incorporating POCUS into your practice, and what advice would you give to healthcare providers considering its adoption?
The most rewarding aspect of incorporating POCUS into my practice has been the immediate impact it brings to patient care. Being able to diagnose on the spot and start treatment right away is incredibly satisfying. It boosts my confidence as a physician and strengthens my connection with patients.
If you're considering adopting POCUS, my advice is to jump right in! Start with the basics, don't be afraid to ask for help, and integrate it into your daily practice. The more you use it, the more proficient you'll become. Remember, it's not just about diagnoses; it's about making patient care smoother and more fulfilling. Embrace it, and you'll see how much of a difference it can make!
9. What message would you like to convey to the medical community about the importance and potential of POCUS in transforming patient care and empowering healthcare professionals?
POCUS isn't just another gadget; it's like having superpowers in the medical world. Imagine having the ultrasound right at the patient's bedside, like having x-ray vision! With POCUS, we can diagnose things faster than ever, and in emergencies, those quick seconds can save lives. It's like having a secret weapon against time.
But it's not just about speed; it's about accuracy too. POCUS helps us pinpoint problems precisely for the best treatment, and it's not just for one type of doctor. From ERs to ICUs, orthopedics to cardiology, POCUS is everywhere, making a big difference.
And the best part? It's not just for experienced doctors. Nurses, paramedics – everyone can use it. Imagine being able to see inside a patient right away – it's empowering and makes our jobs even cooler. Plus, it's an amazing learning tool, like having a tiny ultrasound lab wherever you are.
I truly believe POCUS is the future of medicine. It's making healthcare more
patient-centered too. Patients can see what we see, understand better, and be part of decisions about their care.
10. What steps can the medical community take to accelerate the adoption of POCUS, and how can interested practitioners learn more about your work and the training programs offered by NorVue?
To establish POCUS as a standard in patient care, early education is crucial. Imagine if students had hands-on POCUS experience from day one of med school! We also need continuous support: workshops, online courses, and mentoring for all levels. Hospitals must invest in accessible equipment.
At NorVue, we're dedicated to this cause. Our courses at www.norvueas.com are practical for beginners and pros alike. We provide video tutorials, interactive modules, and mentorship, focusing not only on technical skills but also on mindset and resilience.
Exciting news: We're launching a YouTube podcast sharing real-life doctor experiences. Follow me on Instagram and LinkedIn for updates!
AUTHOR BIO
Dr. Ai Phi Thuy Ho is a cardiology specialist and fellow in Norway who is passionate about POCUS and its transformative impact on medicine. As the founder of NorVue, she provides online POCUS training to healthcare professionals worldwide. Her mission is to enhance diagnostic skills and improve patient care through innovative ultrasound technology.

Hassan Mostafa Quality Manager DEEF Pharmaceutical
QMS Healthcare significantly evolved, driven by various factors including advancements in technology, changes in regulatory frameworks, and a growing emphasis on patient-centered care. QM frameworks and methodologies address patient safety and care quality through various mechanisms such as standardizing processes, utilizing data for decision-making, promoting a culture of safety and engaging staff in continuous improvement. Balancing rigorous QM with cost-efficiency is a critical challenge for healthcare organizations. Achieving this balance requires the implementation of strategies and practices that enhance quality and controlling or reducing costs. To sustain QMS over the long term HCPs need to implement strategic planning, commitment from leadership, and a culture of continuous improvement ingrained throughout the organization.
1. In your experience, how has the concept of quality management evolved in the healthcare industry over the past decade, and what key factors have driven these changes?
QMS Healthcare significantly evolved, driven by various factors including advancements in technology, changes in regulatory frameworks, and a growing emphasis on patient-centered care. Some key aspects as follow:
QM via using EHRs enabling data collection, analysis, facilitate real-time monitoring of patient outcomes and streamline processes, leading to enhance clinical decision-making and improving patient care. Encourage patients to focus on their own care using tools such as patient portals, mobile health apps, and shared decision-making models to play an active role in managing their health, engaged in their treatment plans to improve the outcomes. Adapt measuring clinical outcomes to weigh the effectiveness of care.
Adapting and using continuous quality improvement (CQI) programs, such as Lean and Six Sigma, in healthcare settings. Theses advanced methodologies help streamline processes, reduce waste, and improve patient care.
2. Could you discuss the primary quality management frameworks and methodologies that are currently being implemented in healthcare organizations? How do these frameworks address patient safety and care quality?
QM frameworks and methodologies aiming to improve organization operations, reduce errors, and enhance overall patient outcomes.
A data-driven methodology aimed at reducing variability and defects in processes. It uses the DMAIC (Define, Measure, Analyze, Improve, and Control) cycle to improve processes. Reduces medical errors and adverse events by identifying root causes and implementing corrective measures.
Enhances safety by reducing unnecessary steps that can lead to errors. Improves
efficiency and effectiveness in delivering care, such as optimizing supply chains and improving surgical procedures. Promotes a culture of safety where all staff are engaged in identifying and solving safety issues.
Encourages leadership commitment to safety and systematic processes to manage risks. Identifies and addresses the root causes of safety incidents to prevent recurrence. Improves processes by understanding and mitigating the fundamental issues affecting care quality.
3. What role does data analytics play in enhancing quality management practices in healthcare? Can you provide examples of how data-driven insights have led to improvements in patient outcomes?
Data analytics plays a critical role in improving quality management practices in healthcare through: Empowering more informed decision-making, recognizing patterns and trends, Envisaging outcomes, and enabling the implementation of evidence-based practices.
Identify factors affect the contribution of high readmission rates, e.g.: certain conditions, treatment styles, and discharge procedures, via healthcare providers through patient data analysis. Adapting the usage of “MLA” Machine learning algorithms that used in analyzing patients’ vital signs, patients’ lab results, and other patients’ clinical data help to predict and/or define which patients are at risk of deteriorating.
Optimizing operating room schedule through analyzing historical data on surgery durations, patient flow, and resource utilization. Identification of patients with chronic
diseases, at high risk for complications and hospitalizations can be done via analyzing the population health historical data. Through regular monitoring and patient education, HCPs can improve health outcomes.
4. How do healthcare organizations balance the need for rigorous quality management with the demand for cost-efficiency? Are there any specific strategies or practices that have proven effective in achieving this balance?
Balancing rigorous quality management with cost-efficiency is a critical challenge for healthcare organizations. Achieving this balance requires the implementation of strategies and practices that enhance quality while also controlling or reducing costs.
Encouraging efficiency and coordinated care Providers using a single payment for all services related to a treatment or condition. Focus on eliminating waste, reducing variability, and improving processes to enhance efficiency and quality. Using Electronic Health Records (EHRs) and data analytics, supports quality management and cost-efficiency. Streamlines documentation, reduces duplication of tests, and enhances communication among providers.
Take action to prevent the beginning of diseases via detection their conditions early. Establish training program to educate and support patients to manage their conditions such as diabetes and hypertension, lead to reducing hospitalizations rates and reducing emergency visits. Ensure that patients receive the most effective treatments, reducing unnecessary interventions and associated costs. Improve patients’ adherence to care
Ensuring
patient-centered care is a fundamental aspect of healthcare delivery. Leading to improved patient satisfaction, better health outcomes, and a more responsive healthcare system
plans and reduce unnecessary utilization of healthcare services. Support patients with easy access to their health information and resources to manage their health.
5. In what ways do regulatory requirements influence quality management systems in healthcare? How do organizations stay compliant while continuously striving for quality improvement?
Through implementing health and robust QMS, Healthcare organizations stay compliant and continuously improve quality, conducting regular audits, leveraging data analytics, engaging patients, and fostering a culture of education and continuous improvement.
Adapt the QMS frameworks such as ISO 9001 and Six Sigma to structure QMS, ensuring processes align with regulatory standards while promoting continuous improvement. Define and track key performance indicators (KPIs) relevant to patient safety, clinical outcomes, and operational efficiency. Perform the required trending for data analysis to identify improvement areas. Plan for “CPD”
continuous personnel Development, deliver ongoing education and training to ensure staff are knowledgeable with regulatory requirements updates and quality improvement methodologies.
Conduct regular risk assessments to identify potential areas of non-compliance and implement preventive measures. Train personnel on clear and precise incident reporting, analyzing, and addressing incidents and their adverse events. Adapt CAPA usage of Quality tools, root cause analysis, implement CA, and PA to prevent incident recurrence and improve safety.
6. Patient-centered care is a cornerstone of quality healthcare. How do quality management initiatives ensure that patient perspectives and feedback are integrated into care delivery processes?
QM design and adapt a variety of strategies and practices to: Actively involve patients in their own care. Ensuring patient-centered care is a fundamental aspect of healthcare delivery. Leading to improved patient satisfaction, better health outcomes, and a more responsive healthcare system.
Collect standardized patient feedback on their hospital experiences. Use results to identify strengths and areas for improvement. Involve patients in developing their care plans, ensuring that their goals and preferences are prioritized.
Use patient portals that allow patients to provide real-time feedback, communicate with their healthcare team, and access their health information. Monitor patient feedback continuously and address concerns
promptly to improve the patient experience. Provide training for healthcare providers on empathy, active listening, and effective communication to improve interactions with patients. Develop programs that empower patients with knowledge and skills to manage their health, understand their treatment options, and advocate for their care preferences.
7. Can you share insights on the challenges and barriers healthcare providers face when implementing quality management systems? How can these challenges be effectively addressed?
HCPS should effectively address these challenges with strategic planning, stakeholder engagement, and continuous improvement efforts.
Leadership should encourage the sense of ownership and responsibility through HC staff involvement in the planning and implementation processes. Implementing QMS requires significant investment [time, money, measurement, method, materials, Mother Nature, implement safety and personnel] specify and focus on the high-impact to demonstrate quick wins and justify further investments. Deliver training regarding quality culture importance and contributions.
Managing costs of high-quality care while managing is a significant challenge. Adopt value-based care models that align financial incentives with quality outcomes. Develop long-term strategic plans that include quality management as a core component. Maintain ongoing engagement with all stakeholders to secure continued support and resources.
8. Technology and innovation are transforming healthcare delivery. How are new technologies, such as AI and IoT, being leveraged to enhance quality management practices?
Using AI algorithms help in vast analysis of patient data to predict patient outcomes e.g.: readmissions, disease progression, and potential complications. e.g.: AI models can identify patients at high risk of sepsis, enabling prompt treatment and reducing mortality rates.
HCPs can use AI to analyze genetic data to identify personalized treatment plans for patients, especially in fields like oncology. This leads to more effective treatments with fewer side effects. Using AI systems can support in analyzing medical images such as X-rays, MRIs, and CT scans.
Supply patient with wearable devices such as smart watches and fitness trackers to monitor vital signs like heart rate, blood pressure, and glucose levels in real-time. IoT-enabled medical devices, such as infusion pumps and ventilators, can be monitored and controlled remotely, ensuring optimal performance, and reducing the risk of malfunctions.
HCPs can track the location and status of medical equipment and supplies, reducing the risk of errors and ensuring that critical resources are available when needed.
9. How important is staff training and engagement in maintaining highquality care standards? What strategies are employed to ensure continuous education and involvement of healthcare professionals in quality initiatives?

Ongoing training/development programs and engaging staff in QMS and implementing continuous education along with involvement of HCPs will deliver better patient care and contribute to a more motivated, skilled, and satisfied workforce.
Utilize e-learning platforms to provide flexible, accessible training options for staff, allowing them to learn at their own pace. Conduct webinars and interactive workshops on emerging healthcare topics and innovations. Provide leadership training programs to develop the next generation of healthcare leaders who can drive quality improvement initiatives. Provide regular updates on quality improvement initiatives, progress, and outcomes to keep staff informed and engaged.
Develop and regularly update SOPs that integrate quality standards into daily
practices, ensuring consistency and reliability in care delivery. Use performance dashboards to provide real-time feedback on quality metrics, helping staff understand their impact on care quality. Employ predictive analytics to identify areas for improvement and tailor training programs accordingly.
10. In the context of a global healthcare landscape, how do quality management practices vary across different regions? Are there any best practices or lessons learned that can be universally applied?
Using effective QMS along with adapting new technologies will attain higher standards of care, improved patient outcomes, and greater equity in healthcare delivery. Focus on efficiency metrics such as wait times and patient outcomes. Focus on patient satisfaction and financial performance, with variations in access based on insurance coverage. Patients’ Engagement in decisionmaking, respect cultural preferences, and provide clear communication about treatment options and care plans. Implement mechanisms for collecting patient feedback to improve service delivery and care experiences.
Adapt methodologies to streamline processes, reduce waste, and enhance efficiency in resource-constrained settings. Foster a culture of continuous improvement by testing changes on a small scale before full implementation. Define and measure key performance indicators (KPIs) relevant to local priorities and healthcare goals, using data analytics to drive improvements.
Encourage collaboration among healthcare professionals to optimize care delivery,
improve patient outcomes, and reduce medical errors. Facilitate knowledge exchange and capacity-building through conferences, workshops, and international collaborations.
11. Can you provide examples of successful quality management projects or initiatives within your organization that have led to significant improvements in patient care and operational efficiency?
Focusing on evidence-based practices, leveraging technology, engaging staff, and continuously monitoring outcomes, healthcare providers can drive meaningful change and deliver higher standards of care to their patient populations.
Implementing a comprehensive infection prevention and control program focused on reducing hospital-acquired infections (HAIs). Implement electronic monitoring systems and regular training sessions to improve hand hygiene practices among staff.
Implemented a comprehensive EHR system that allows for seamless sharing of patient information across departments and facilities. Conducted thorough process mapping to identify inefficiencies and waste in clinical and administrative workflows. Use data-driven approaches like root cause analysis to identify and address underlying issues affecting patient care quality. Implement continuous improvement projects focused on reducing wait times, enhancing discharge processes, and improving medication management. Enhanced patient safety, satisfaction, and clinical outcomes through standardized processes and error reduction.
12. How do healthcare organizations measure and benchmark their quality management performance? What key performance indicators (KPIs) are most commonly used, and how are they tracked?
KPIs help organizations assess their performance, identify areas for improvement, and compare their outcomes with industry benchmarks or internal targets.
Measure the number of deaths within a specific population or condition, often adjusted for risk factors. Track the occurrence of complications during or after procedures or treatments. Monitor patient re-addition rate to the hospital within a specified period after discharge. Track incidents of patient falls and associated injuries within healthcare facilities. Monitor Medication errors related to medication administration or prescription. Measure adverse events such as allergic reactions or surgical errors.
Assess patient satisfaction through surveys or feedback mechanisms. Measure patient likelihood to recommend the healthcare organization to others. Track the average duration patients spend in the hospital for specific procedures or conditions. Measure hospital beds turn over time after patient is charge. Monitor patients wait times in emergency department before receiving care. Track the average cost of care per patient, factoring in direct and indirect costs.
13. With the increasing focus on personalized medicine, how are quality management systems adapting to support individualized patient care plans and treatments?
QMS in healthcare enhance treatment efficacy, minimize adverse effects, and optimize patient outcomes. And support individualized patient care plans and treatments. Integrating genetic and clinical data from electronic health records (EHRs) enables comprehensive patient profiles, facilitating personalized treatment decisions.
QMS Promot shared decision-making between patients and healthcare providers ensures alignment with patient preferences and values in developing care plans. QMS establish feedback mechanisms to evaluate patient responses to treatments, adjusting plans based on outcomes and patient-reported experiences. Adhering to regulatory guidelines and ethical standards in managing personalized medicine data, ensuring patient privacy and confidentiality. QMS support informed consent processes for genetic testing and personalized treatments, ensuring patients understand risks, benefits, and implications.
14. How do healthcare organizations ensure that quality management practices are sustainable over the long term? What role does leadership play in fostering a culture of continuous quality improvement?
To sustain QMS over the long term in healthcare organizations, HCPs need to implement strategic planning, commitment from leadership, and a culture of continuous improvement ingrained throughout the organization. Establish key performance indicators (KPIs) to measure quality outcomes and regularly monitor performance against benchmarks. Implement systems for collecting feedback
from patients, staff, and stakeholders to identify areas for improvement. Incorporate patient feedback and perspectives into quality improvement efforts to ensure care is aligned with patient needs and preferences. Allocate resources, including financial investments and technological infrastructure, to support quality management efforts. Ensure adequate staffing levels and expertise in quality improvement methodologies and data analytics. Adapt quality management practices in response to changes in healthcare delivery models, technological advancements, and patient
15. Finally, looking ahead, what do you envision as the future of quality management in healthcare? What emerging trends or innovations do you believe will shape the next generation of quality improvement practices?
Healthcare QMS next generation of quality improvement practices will likely to be shaped with several emerging trends and innovations .AI-powered tools will support clinicians in making evidence-based decisions, reducing diagnostic errors, and optimizing treatment pathways. AI-driven automation will streamline administrative processes, optimize resource allocation, and reduce healthcare delivery costs.
Telemedicine platforms will integrate with EHR systems for seamless data sharing and care coordination across healthcare settings. Remote monitoring devices and wearable technology will enable continuous data collection, allowing for proactive interventions and personalized care plans. Implementing real-time feedback mechanisms to monitor quality metrics, patient outcomes, and opera-
tional efficiency, enabling rapid adjustments and improvements. Integration of research findings, best practices, and patient data into clinical practice will facilitate continuous learning and improvement across the healthcare continuum.
In brief:
QMS in healthcare is a dynamic and driven by technological innovation, data-driven insights, patient-centered care models, and a commitment to improving outcomes while controlling costs.
HCPs can deliver higher quality, more efficient, and personalized care to patients through involving these emerging trends and innovations, eventually, improving health outcomes and enhancing the overall healthcare experience.

AUTHOR BIO
Dr. Hassan Mostafa Mohamed, Chairman & Chief Executive Officer at ReyadaPro is an entrepreneurial and growth-driven executive with more than 25 years of experience in pharmaceutical industries, including, Technical, sales & marketing, Production, Supply chain, Engineering/ utilities, Quality, and regulatory issues. Mr. Hassan is an expert in driving pharmaceutical facilities to accomplish corporate goals, Building and leading technical & quality aspects with market consideration for rapid Growth, and efficient operational excellence.
Internal politics and power dynamics in healthcare significantly impact policy outcomes, resource allocation, and care quality. Leadership requires political acumen to navigate these complexities effectively, influencing patient care and technological advancements. However, recruitment practices that prioritize alignment over merit can undermine organizational integrity, stifle innovation and growth.
Salman Pervaiz Butt
MBA MSc MPHYS, Healthcare Leader, Interim Manager Perfusion Services, Cleveland Clinic Abu Dhabi
Healthcare leadership faces a myriad of unique challenges as it endeavors to balance clinical objectives with administrative efficiency and the intricacies of political dynamics within healthcare systems. The ability of leaders to skilfully manage and harness power dynamics is paramount in promoting equitable resource allocation and fostering the advancement of healthcare technologies. This leadership complexity is heightened by the pressing need to navigate
through fast-evolving healthcare policies, technological innovations, and patient care standards that demand both agile and strategic responses.
Effective leadership in healthcare is not merely about managing resources but also involves steering complex human interactions and ethical considerations that affect patient outcomes. Leaders are tasked with making critical decisions that can have profound impacts on patient health and organizational sustainability. This requires a deep understanding of the healthcare landscape, including regulatory requirements, financial constraints, and the evolving needs of patient populations.

Furthermore, the process of selecting and developing healthcare leaders is crucial. Ethical recruitment practices ensure that the most capable individuals, who possess both the technical skills and the moral compass necessary to lead, are placed in these roles. This is vital to maintain the integrity of healthcare institutions and to foster a culture that values continuous improvement and excellence in patient care.
Leaders must also cultivate a robust understanding of political acumen to effectively navigate the sector's inherent complexities. This involves engaging with various stakeholders, from government bodies and insurers to patient advocacy groups, to align
on common goals and work collaboratively towards enhancing healthcare delivery.
“In healthcare leadership, political acumen is not merely advantageous—it's crucial."
In essence, healthcare leadership is about creating a vision for the future of healthcare, one that integrates clinical excellence with efficient management practices and ethical governance. The leaders' role is to instill a proactive culture within healthcare organizations, champion
innovation, and ensure that systems are responsive to the needs of both patients and healthcare professionals.
Power and politics within healthcare systems has a profound impact on both the internal dynamics and the overarching goals of healthcare organizations. Leaders in healthcare are required to possess a high degree of political acumen to effectively navigate these complex waters, advocating for necessary resources and implementing reforms that can handle diverse, and often conflicting, stakeholder interests.
However, the influence of power and politics can also manifest negatively, affecting the overall vision and integrity of healthcare services. Leadership power struggles often lead to internal divisions, affecting small to large departments and even at the highest

levels of organizational leadership. Such conflicts may result in a culture where ideas and contributions are evaluated not on their merit or empirical basis but rather on the origin or affiliation of the idea presenter. This can stifle innovation and hinder effective decisionmaking processes.
"Mastering healthcare's complexities demands a compass of political skill guided by the map of moral integrity."
Moreover, these power dynamics often extend into the domains of employment and promotion, where decisions may be influenced by non-performance related factors such as race, origin, or religion. This not only undermines meritocracy but also affects morale and equity within the organization, potentially leading to decreased job satisfaction and increased turnover.
Addressing these issues requires a concerted effort to foster an organizational culture that prioritizes transparency, meritocracy, and inclusiveness. Leaders must be trained not just in the technical aspects of healthcare management, but also in ethical leadership and conflict resolution, to ensure that power and politics are used positively to advance the goals of healthcare institutions rather than detract from them.
Political skills are critical for effective leadership in healthcare, a field characterized by complex interactions among a wide array of stakeholders including patients, healthcare professionals, regulatory bodies, and insurance companies. Developing these skills enables leaders to understand and balance these diverse motivations and to act with strategic acumen in a highly regulated and emotionally charged environment.
Understanding the motivations of various stakeholders is foundational. Healthcare leaders must grasp not only the explicit needs such as quality patient care and compliance with regulations but also the implicit drives like job security for staff, institutional reputation, and financial sustainability. This comprehensive understanding allows leaders to anticipate reactions and tailor their strategies accordingly.
Effective leverage of influence is another crucial political skill. Healthcare leaders must navigate between competing interests and limited resources, using their influence to advocate for necessary changes and resources. This might involve lobbying for policy adjustments, negotiating with suppliers, or persuading stakeholders to adopt new technologies or methods, all while maintaining trust and credibility.
"Leadership extends beyond choices; it's about impacting change and guiding through power dynamics to ensure fair and equitable culture."
Negotiation and compromise are equally essential, as leaders often find themselves mediating between conflicting interests within the healthcare facility. The ability to find common ground and build consensus is vital, particularly when decisions affect patient care, staff welfare, and organizational viability. Moreover, these skills can indeed be enhanced through targeted training programs that focus on areas such as conflict resolution, ethical decision-making, and strategic communication. Real-world experience also plays a pivotal role, providing leaders with practical insights and adaptive strategies that are crucial for navigating the healthcare landscape effectively.
Ethical recruitment practices in healthcare are essential to building effective leadership that is capable of addressing the multifaceted challenges of modern healthcare systems. These practices should prioritize merit and capability over political alignment to ensure a diverse leadership team that can bring varied perspectives and innovative solutions to the
table. Emphasizing political alignment over skill and experience can lead to a homogenous leadership structure, which stifles creativity and may not adequately represent the interests of all stakeholders.
Diversity in leadership is not just a moral imperative but also a strategic one. Research shows that organizations with diverse leadership teams are more innovative and better equipped to navigate the complexities of the healthcare industry. These teams are likely to consider a wider range of strategies and more effectively address the needs of a diverse patient population.
Furthermore, the negative consequences of recruitment practices that focus too heavily on political alignment can be profound. Such strategies can undermine the integrity of healthcare organizations, leading to biased decisions that favor certain groups over the broader needs of the community. This not only affects the quality of patient care but also the morale of the healthcare workforce, as decisions may be perceived as unfair or exclusionary.
Case studies in healthcare settings have highlighted that when recruitment is aligned with broader organizational goals rather than political agendas, institutions are more successful at implementing effective change and improving patient outcomes. Leaders who are chosen based on their qualifications, experience, and alignment with ethical standards are more likely to foster trust and cooperation among their teams and facilitate a culture of accountability and continuous improvement.
Therefore, it is imperative for healthcare organizations to adopt and rigorously maintain recruitment practices that are fair, transparent, and based on the principles of equity and inclusivity. This approach not only enhances the capability of healthcare systems to adapt and innovate but also upholds the ethical standards essential to patient care and community trust.
"Ethical recruitment forms the bedrock of effective leadership, ensuring that merit and integrity are the core pillars of healthcare excellence."
Healthcare, leadership is profoundly influenced by the ability to navigate the complex interaction of power and politics, which significantly impacts organizational outcomes and patient care. Research highlights that political astuteness, a critical facet of leadership, is essential for the effective implementation of strategic health system changes. Leaders who are politically astute can effectively manage and leverage power dynamics, enhancing their ability to secure resources, foster collaboration, and implement necessary reforms.
The importance of these skills has led to the incorporation of political astuteness in healthcare leadership development programs, where leaders are trained to understand and utilize power and authority ethically and effectively. Such programs focus on building the capacity of leaders to handle power dynamics and anticipate political issues that may arise during the execution of healthcare initiatives. This training is critical as it prepares leaders to navigate the often informal politics that can dominate healthcare organizations, ensuring that strategic changes are not only implemented but are sustainable and aligned with the broader goals of healthcare provision. Furthermore, the recruitment practices within healthcare organizations are beginning to reflect an awareness of the need for political skills in potential leaders. Assessments that evaluate a candidate’s political skills during the hiring or promotion processes are becoming more common. This shift underscores an acknowledgment of the importance of political savvy in achieving

effective leadership in healthcare settings, where leaders must often negotiate, influence, and align various stakeholders with diverse and sometimes conflicting interests.
Effective healthcare leadership hinges on navigating complex power dynamics and political nuances with acumen and ethical foresight. The development of political skills is essential for leaders to influence healthcare policy, manage resources efficiently, and drive technological advancements. However, ethical recruitment practices are paramount to ensure that leadership is based on merit rather than political alignment, preserving organizational integrity and promoting innovation. Leaders equipped with both technical skills and a deep understanding of political landscapes can better serve their organizations and patients. As healthcare continues to evolve, fostering a leadership culture that values ethical practices, inclusivity, and adaptability will be crucial in meeting the challenges and opportunities of the future.
References are available at www.americanhhm.com
AUTHOR BIO
Salman is a renowned healthcare leader with 25 years in Clinical Perfusion, Research, and Medical Device Management. His leadership is marked by his international recognition as a speaker, his 30 peer-reviewed publications, and his dedication to charitable work. His awards highlight his contributions across risk management, patient safety, and policy development.
September 05 -07, 2024 | Madrid, Spain
https://cardiologyworldconference.com/
About Event: The summit will unravel recent trends and breakthroughs in cardiology, inviting prominent researchers, cardiologists, cardiothoracic surgeons, healthcare professionals, students, professors, nurses, scientists, and business professionals. Join this convergence to explore topics ranging from Heart Diseases, Clinical Cardiology, Pediatric Cardilology, Sports Cardiology, Cardiac Surgery, Cardiac Nursing, and many more.
Listed Under: Surgical Speciality
September 11-12, 2024 | Basel, Switzerland
https://intelligenthealth.ai/
About Event: Intelligent Health hosts the world’s largest healthtech community dedicated to saving lives with AI. CPD accredited and aligned with the UN Sustainable Development Goals, we are committed to advancing pivotal conversations on AI in medicine and fostering global collaboration across the healthcare sector.
Listed Under: Technology, Equipment & Devices

Healthcare Technology & AI Transformation Assembly
September 17-18, 2024 | Miami, USA
https://mill-all.com/assemblies/healthcaretechnology-ai-transformation-assemblyseptember-2024/
About Event: Healthcare AI Transformation Assembly is set to be a groundbreaking opportunity for C-Level Healthcare Officers to meet face-to-face and connect on the current trends & challenges the industry is facing.
Listed Under: Information Technology
Public Health and Preventive Medicine
September 19-21, 2024 | Prague, Czech Republic
https://www.publichealthsummit2024.com/
About Event: The meeting brings together World Class participants and young researchers looking for opportunities for exchanges that cross the traditional discipline boundaries and allows them to resolve multidisciplinary challenging problems that only a venue of this nature can offer.
GSPHPM2024 Conference provides a platform of international standards where you can discuss and share persuasive key advances in Public Health.
Listed Under: Medical Sciences
October 7-9, 2024 | Boston Marriott Cambridge, Massachusetts
https://worldbigroup.com/digital-healthsummit-2024/
About Event: Attend the Digital Health & AI Innovation Summit to meet world-class experts and thought leaders who are shaping the future of digital health and AI.
Listed Under: Information Technology

October 16-17 2024 | Konstanz, Germany
https://www.diagnostics4future.org/
About Event: Diagnostics-4-Future Conference is the international meeting-place for users and providers from industry and science. Based on questions in medical care, clinics and laboratories, innovative solutions for new diagnostics are discussed including research and development. The focus is also on solutions for rural areas (point-of-care).
Listed Under: Diagnostics
November 19-21, 2024 | London, UK
https://www.micad.org/
About Event: 5th International Conference on Medical Imaging and Computer-Aided Diagnosis is dedicated to fostering a dynamic forum where researchers, academics, and industry experts can connect and exchange insights on the leading-edge developments in medical imaging and computer-aided diagnosis.
Listed Under: Diagnostics
November 18-19, 2024 | Rome, Italy
https://scisynopsisconferences.com/neurology/about-us
About Event: This conference offers a perfect opportunity for Plenary, Keynote, Exhibitor, Research Analysts, Authors, Physicians, Medical Service providers, Academicians, Industrialists, Teaching Professionals, and Students in the fields of Neurology, Neuroscience, Psychiatry, and Brain Disorders to exchange knowledge and ideas
Listed Under: Medical Sciences
December 9-11, 2024 | Scottsdale, AZ
https://events.cdmmedia.com/event/ea252f11-071c-47eda6f8-7cf0a672bb39/summary
About Event: In this dynamic scenario, the role of technology leaders such as Chief Information Officers (CIOs), Chief Data Officers (CDOs), and Chief Medical Information Officers (CMIOs) has become pivotal in steering healthcare institutions toward successful digital transformation, harnessing the power of information technology and data management. As healthcare organizations navigate the complexities of cybersecurity, interoperability, and digital health solutions, establishing meaningful connections with these executives becomes essential for staying informed and forging partnerships that can drive positive change in the healthcare ecosystem.
Listed Under: Healthcare Management
December 02 - 04, 2024 | Westin Rancho Mirage, Palm Springs, CA
https://patientexperience.wbresearch.com/
About Event: NGPX is a community that unites America's best and brightest patient experience leaders to connect, inspire and transform healthcare. Through intimate networking events, inspiring idea exchanges, and unparalleled story-telling, NGPX reinvigorates and breathes new life into the world of patient experience.
Listed Under: Facilities & Operations

Dates: 12 September - 13 September 2024
Location: Four Seasons Hotel, Westlake Village, CA, USA
The Healthcare CMO Summit 2024 is set to be an exclusive, high-level event designed to bring together Chief Medical Officers (CMOs) and innovative suppliers and solution providers. This invitation-only summit will address the most pressing clinical healthcare challenges and explore relevant market developments through practical and progressive ideas and strategies adopted by industry pioneers.
Key Topics for 2024:
1. Building Collaborative Hospital Teams: Learn how to foster teamwork and enhance communication among hospital leaders while preparing the physician leaders of tomorrow.
2. Unlocking the Potential of AI and Virtual Health:
Discover how virtual care delivery, artificial intelligence, and machine learning are revolutionizing the healthcare industry.
3. Empowering Physician Well-Being: Explore practical tactics to combat burnout and enhance well-being among the healthcare workforce.
4. Thriving in Value-Based Care: Master quality care and delve into strategies for successful value-based care implementation and compliance.
5. Staffing the Modern Hospital: Address healthcare staffing shortages and explore innovative solutions to meet modern hospital needs.
6. Sustainable Financial Strategies: Navigate fiscal stability amidst fluctuating economies, regulatory demands, and an evolving healthcare landscape.
Summit Partners:
Strategic Connections | Powerful Alliances
The Healthcare CMO Summit offers a unique platform for America's Chief Medical Officers to evaluate and partner with relevant suppliers and solution providers. The summit facilitates the connection between innovative healthcare companies and Chief Medical strategists.
Chief Medical Officers:
Representing America's healthcare organizations, CMOs will find the summit to be an essential resource for professional intelligence and business catalysis. The summit's annual assessments focus on their strategic goals and needs, introducing effective products and solutions to streamline the vendor selection process.
Service Providers:
Selected from across North America, innovative healthcare organizations are carefully aligned with the needs of CMOs. This ensures a collaborative approach that matches the value propositions of service providers with the specific needs of prospective clients.
Connectors:
As experienced outsourced sales partners, the mission of Marcus Evans is to modernize outdated sales processes, creating efficient and cost-effective partnerships between leaders in the clinical healthcare community. Their role adds value to the decision-making of CMOs and facilitates the search for qualified prospects for suppliers and service provider clients.
Esteemed Collaborators:
Leading Voices | Indispensable Insights
Join us at the Healthcare CMO Summit 2024 to be part of an event that promises to be both enlightening and transformative for the healthcare industry.

The Healthcare CEO & Executive Strategy Summit, set for October 21-22, 2024, at the luxurious Encore Boston Harbor in Boston, MA, is an exclusive, invitation-only gathering designed to bring together top-tier healthcare executives and forward-thinking suppliers. This premier summit focuses on addressing the most pressing challenges and opportunities within the healthcare sector.
• Reimagining Healthcare Workforce Management: Delve into innovative approaches to attract, retain, and nurture top talent in the healthcare industry.
• Technological Innovation: Explore the latest emerging technologies and learn proven strategies for seamlessly integrating them into existing healthcare workflows.
• Achieving Financial Sustainability: Examine evidence-based methods to optimize operations, control costs, and maintain high-quality patient care.
• The Changing Reimbursement Landscape: Navigate the shift towards value-based care, understand changes in payment models, and the impact of government regulations on revenue streams.
• The Future of Healthcare: Assess the major trends revolutionizing healthcare in 2024 and identify opportunities to enhance the future of care.
• Creating Safe Workplaces: Prioritize staff mental health and well-being, fostering a culture of safety to protect healthcare workers and patients alike.
Strategic Connections and Powerful Alliances
The summit serves as a crucial platform for senior healthcare executives to evaluate and partner with relevant suppliers and solution providers. It also connects innovative healthcare facilities with strategic leaders in the industry.
Representing America's largest hospitals and healthcare systems, these senior-level healthcare executives view the summit as an essential resource for professional intelligence and business strategies. Through annual assessments focused on their strategic goals, the summit introduces effective products and solutions to streamline their vendor selection processes.
As your experienced outsourced sales partner, Marcus Evans aims to modernize outdated sales processes by fostering partnerships within the healthcare community. Their mission is to add value to decision-making processes for senior healthcare executives while identifying qualified prospects for suppliers and solution providers.
Attendees will experience a dynamic program featuring visionary keynote presentations, reallife case studies, and interactive forums led by compelling speakers and expert moderators. The Healthcare CEO & Executive Strategy Summit promises to be an invaluable event for those looking to stay ahead in the rapidly evolving healthcare landscape.

Dates: October 21-22, 2024
Venue: Encore Boston Harbor, Boston, MA, USA
The Healthcare CFO, Financial Strategy & Revenue Cycle Summit is a distinguished, invitation-only event that unites senior-level healthcare finance executives with leading suppliers and service providers. This premium summit offers a strategic platform for addressing pivotal healthcare finance issues, exploring market developments, and sharing progressive strategies from industry pioneers.
Regenerative AI, Machine Learning, and Automation
Harnessing advanced technology to enhance operations and drive transformational changes.
Staff Shortages & Labor Costs
Tackling the ongoing healthcare worker shortage and escalating labor expenses.
Cyber Security
Implementing best practices to safeguard against unauthorized access and cyber threats.
Revenue Cycle Management
Developing strategies to improve denial management and optimize revenue streams.
Payer Relations
Collaborating effectively with payers to maximize revenue and minimize denials and underpayments.
Navigating financial challenges and ensuring steady cash flow within healthcare institutions.
Alliances: The summit facilitates meaningful connections between America’s senior healthcare finance executives and innovative
suppliers and service providers. By fostering these strategic alliances, the event aims to enhance the capabilities and efficiencies of participating healthcare facilities.
The Executives: Senior healthcare finance executives representing America’s foremost hospitals and healthcare systems regard this summit as an essential resource for professional intelligence and business strategy. Through annual assessments focused on their strategic needs, the summit introduces tailored products and solutions, streamlining their vendor selection process.
The Service Providers: Partnering only with the most innovative healthcare organizations from across North America, the summit ensures that the offerings of these suppliers and service providers align with the needs of senior healthcare finance executives. This selective and collaborative approach guarantees that the value propositions meet the strategic goals of prospective clients.
The Connectors: Marcus Evans, the summit organizer, aims to modernize outdated sales processes by fostering efficient, cost-effective partnerships within the healthcare community. Their mission is to support the decisionmaking of senior healthcare finance executives while identifying qualified prospects for suppliers and service provider clients.
Participants at the Healthcare CFO, Financial Strategy & Revenue Cycle Summit can expect a dynamic program filled with visionary keynote presentations, practical case studies, and interactive forums led by expert speakers and moderators.

Dates: September 12-13, 2024
Venue: Four Seasons Hotel, Westlake Village, CA, USA
The Healthcare CNO Summit is an exclusive, invitation-only event designed to bring together Chief Nursing Officers and leading suppliers and solution providers. The summit aims to address key clinical challenges, explore relevant market developments, and share innovative strategies from industry leaders.
CNO Leadership Role
Focus: Developing the essential skill set for impactful CNO leadership.
Workforce Resiliency and Attractiveness
Focus: Rebranding the nursing profession to appeal to future generations.
Securing Multi-Generational Workforce Satisfaction
Focus: Creating HR plans that cater to the needs of nurses from different generations.
Critical to Healthcare Reform
Focus: Navigating regulations, policies, and legislation critical to healthcare reform.
Digital Integration
Focus: Understanding leadership dynamics crucial for successful digital implementation.
Quality Safety Controls
Focus: Implementing strategies to ensure quality patient safety.
The summit provides a vital platform for America’s leading Chief Nursing Executives to connect with innovative healthcare facilities
and relevant suppliers. This event is crucial for evaluating potential partnerships and finding solutions tailored to their strategic goals.
• Audience: Chief Nursing Executives from America's largest hospitals and healthcare systems.
• Role: Acting as essential resources for professional intelligence and business strategy.
• Process: Annual assessments help introduce effective products and streamline vendor selection.
• Profile: Innovative healthcare companies from across North America.
• Selection: Only those whose offerings align with the needs of Chief Nursing Executives.
• Approach: A collaborative process to match value propositions with client needs.
• Mission: Modernizing outdated sales processes for efficient, cost-effective partnerships.
• Value: Adding significant value to the decision-making process for CNOs and assisting suppliers in finding qualified prospects.
Participants will experience a dynamic program featuring visionary keynote presentations, practical case studies, and interactive forums led by compelling speakers and expert moderators. The Healthcare CNO Summit promises invaluable insights and strategies to navigate the evolving landscape of nursing leadership.
Oticon Medical has announced that the U.S. Food and Drug Administration (FDA) has approved its new hearing system, the Sentio System. This system is the company's first active bone conduction hearing system that works through the skin.
The Sentio System includes two parts: the Sentio 1 Mini, an external sound processor, and the Sentio Ti Implant, which is placed under the skin. It is the smallest system of its kind available today.

Unlike the older Ponto system and other similar devices that require parts sticking out through the skin, the Sentio System keeps the skin intact, providing a new option for patients. This aligns with Oticon Medical’s commitment to offering patients more choices.
The Sentio 1 Mini is designed to be comfortable and easy to use. It is 26% lighter than other similar devices and provides a full 360-degree sound experience with a wide bandwidth of 9.5kHz.
The Sentio Ti implant is very powerful, designed to support patients with worsening hearing loss without needing additional surgeries. It is built to handle stronger sound processors, ensuring reliable performance. Surgeons will find the implant easy to place, making the procedure simple.
The Sentio System is for patients aged 12 and older who have conductive hearing loss, mixed hearing loss, or single-sided deafness.
This new launch is a big step for Oticon Medical, continuing their mission to provide innovative hearing solutions to help people live their lives to the fullest.

Philips has strengthened its leadership in digital pathology with the FDA’s approval of the latest version of its IntelliSite Pathology Solution.
Diagnosing cancer and providing personalized treatments is a collaborative effort involving various specialists, and Philips’ digital pathology solution helps streamline this process. Philips was the first to market an FDA-approved digital pathology solution in 2017 and is now the most widely used solution for primary diagnosis globally.
Their latest version, Philips IntelliSite Pathology Solution 5.1, has just received 510(k) clearance from the FDA. This solution helps pathologists work together remotely, boosts productivity, addresses staff shortages, and reduces costs. It includes hardware, software, storage, analysis tools, and enterprise-wide connectivity, providing an integrated digital workflow for pathologists to deliver accurate diagnoses and improve patient outcomes.
The Philips IntelliSite Pathology Solution shortens the time needed to review, report, and sign off on cases, and allows pathologists to work remotely, improving efficiency by up to 21% compared to traditional workflows. This helps address the shortage of trained pathologists and reduce costs. It enables pathologists to collaborate remotely for second opinions and use the latest AI applications, leading to timely and precise diagnoses that improve patient outcomes.
Synchron, a company that creates brain-computer interfaces (BCIs) to help people with motor impairments, has announced a new chat feature for its BCI platform using OpenAI's advanced AI technology.

This new feature allows people with severe paralysis, who cannot move their upper limbs, to interact with the digital world using only their thoughts. The chat feature, powered by OpenAI, is simple to use and learn. It can generate automated prompts for texting and chatting based on the user’s emotions and other contextual inputs, making communication easier for them. Importantly, Synchron ensures that users’ brain data is not shared with OpenAI.
OpenAI’s technology, which can create content in both text and audio, allows for more natural and real-time interactions between humans and AI. This is especially helpful for people with neurological disorders who may have difficulty forming complex responses. Synchron continues to explore the best AI models to meet the needs of its BCI users.
The Synchron BCI is implanted through a minimally invasive procedure that places it in the blood vessel on the surface of the motor cortex of the brain. Once implanted, it detects and wirelessly transmits motor intent from the brain, enabling people with severe paralysis to control personal devices without using their hands.
With OpenAI’s AI models, the updated BCI platform lets user’s text more efficiently, with faster response times and natural conversational speeds. These improvements will benefit users with upper limb mobility impairments and other neurological diseases.
MicroVention, Inc., a global neurovascular company and part of Terumo Corporation, announced the publication of the SOFAST study. This study evaluated the SOFIA™ Flow Plus Aspiration Catheter (SOFIA 6F) for treating acute ischemic stroke caused by large vessel blockage. The study involved 108 patients in the U.S. and aimed to confirm the catheter’s safety, speed, and effectiveness.

Key results from the study include:
• Speed: It took a median of 12 minutes from groin puncture to clot contact and 17 minutes to restore blood flow.
• Efficacy: 75% of patients had successful revascularization on the first try using SOFIA 6F.
• Safety: There were no cases of new blood clots forming in other areas or symptomatic brain bleeding within 24 hours.
• Clinical Outcomes: 66.7% of patients had good functional outcomes after 90 days.
MicroVention also celebrated a decade of innovation with SOFIA™ and SOFIA™ Flow Plus Aspiration Catheters, having been used in over half a million procedures in 170 countries and featured in over 30 articles worldwide. The SOFIA Flow Plus Aspiration Catheter is known for its speed, reliability, and effectiveness in treating acute ischemic stroke.
MicroVention offers a comprehensive range of stroke solutions, including SOFIA™, SOFIA™ Flow Plus Aspiration Catheters, ERIC™ Retrieval Device, BOBBY™ Balloon Guide Catheter, WEDGE™ Microcatheter, HEADWAY™ Microcatheters, and TRAXCESS™ Guidewires.
Carestream Health has announced new upgrades to its ImageView Software and DRX-Evolution Plus System, enhancing its range of top-notch imaging solutions.

The latest version, ImageView Software 2.1, includes new Smart Room Options like Virtual Long-Length Imaging, Virtual Collimation, Patient-Position Monitoring, Patient Picture, Positioning Overlay, and Align Assist. These features help radiographers quickly confirm accurate positioning for consistent image capture, leading to faster diagnosis and treatment.
Additionally, the new software includes tools to quickly check the detector position in non-bucky environments, ensuring proper alignment between the tube and detector. This boosts radiographer confidence and reduces the risk of grid cutoff.
Carestream also announced new features for its DRXEvolution Plus Digital Radiography System, which now includes the latest ImageView 2.1 features. Other enhancements include new grid frames for the wall stand, bi-directional audio assist, a patient picture option, and an AEC edge location on the console screen.
These innovations join Carestream’s wide range of imaging solutions, including Tube Line Visualization, Pneumothorax Visualization, low-dose dual-energy bone suppression, Digital Tomosynthesis, and AIbased Smart Noise Cancellation.
QuantHealth, a top company using AI to design clinical trials, has announced a partnership with OMNY Health. OMNY Health is known for its healthcare ecosystem that facilitates compliant cross-industry health data sharing.
This collaboration aims to use OMNY Health's large network of de-identified data to discover new insights and opportunities for clinical trials, benefiting QuantHealth’s clients, including four of the five largest pharmaceutical companies in the world.
OMNY Health organizes diverse Electronic Health Records (EHRs) into research-ready, de-identified data products. This gives researchers and providers detailed information to address disparities in clinical trials and fill significant gaps in demographic data for drug discovery and development.
OMNY's vast data resources support various analytic needs in life sciences innovation. By partnering with QuantHealth, they aim to unlock insights that will speed up life-changing medical advancements, highlighting the critical role of data in powering AI companies.
QuantHealth’s AI, trained on data from 350 million patients, improves clinical trial timelines, reduces trial risks, and identifies patient sub-groups likely to respond to treatments. This partnership will help QuantHealth’s pharmaceutical partners speed up drug development through simulated clinical trials informed by real-world evidence, predicting clinical trial outcomes, drug effectiveness, and patient responses.
The partnership also highlights OMNY Health's commitment to enhancing participation in diverse clinical trials and strengthening its real-world data ecosystem. By enabling secure data sharing, OMNY supports companies like QuantHealth in simulating trials on a large scale, expediting, de-risking, and optimizing drug development to provide effective medications faster.
This collaboration comes after QuantHealth’s recent investment from Accenture Ventures and a leading Contract Research Organization (CRO), bringing their Series A funding to US$17 million.
Dawn Health, a company focused on digital health solutions, is teaming up with Merck, a major pharmaceutical company, to create a new digital platform for people with Growth Hormone Disorders (GHD).

Over the next two years, they will work together to develop this advanced platform, aiming to help thousands of patients in over 40 countries.
The new platform will use the latest AI technologies to include features like growth predictions and personalized support. This will enhance the user experience, improve treatment adherence, and provide better outcomes for patients. The platform is designed to support children and young adults with GHD, as well as their caregivers, both at home and in clinical settings.
Dawn Health and Merck are committed to making the platform patient-friendly and engaging. They are talking to patients, caregivers, and healthcare professionals to understand their needs and ensure the platform provides the best possible support throughout the treatment journey.
The collaboration has started well, with productive workshops and discussions between Dawn Health and Merck teams.
Together, they aim to launch a cutting-edge platform that will significantly improve the lives of people living with Growth Hormone Disorders globally.